User login
Official Newspaper of the American College of Surgeons
Even mild preop sepsis boosts postop thrombosis risk
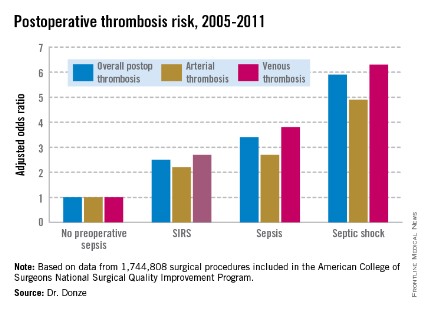
WASHINGTON – Preoperative sepsis proved to be an important independent risk factor for both arterial and venous thrombosis during or after surgery in an analysis of nearly 1.75 million U.S. surgical procedures.
The take-home message here is that the risk-benefit assessment of surgical procedures should take into account the presence of sepsis. And if the surgery can’t be delayed, prophylaxis against arterial as well as venous thrombosis should be employed, Dr. Jacques Donze said at the annual meeting of the American College of Cardiology.

Another key finding in this study was that the risk of postoperative thrombosis varied according to the severity of preoperative sepsis. Even the early form of sepsis known as systemic inflammatory response syndrome, or SIRS, was associated with a 2.5-fold increased risk.
"Include even early signs of sepsis as a risk factor," urged Dr. Donze of Brigham and Women’s Hospital, Boston.
Also, preoperative sepsis was a risk factor for postoperative thrombosis in connection with outpatient elective surgery as well as inpatient operations, he added.
Dr. Donze presented an analysis of 1,744,808 surgical procedures performed during 2005-2011 at 314 U.S. hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program. This large, prospective, observational registry is known for its high-quality data.
Within 48 hours prior to surgery, 7.8% of patients – totaling more than 136,000 – had SIRS, sepsis, or septic shock. Their postoperative thrombosis rate was 4.2%, compared with a 1.2% rate in patients without sepsis. In a multivariate regression analysis adjusted for potential confounding factors, the postoperative thrombosis risk climbed with increasing severity of preoperative sepsis.
SIRS was defined on the basis of temperature, heart rate, respiratory rate, WBC count, and/or the presence of anion gap acidosis. "Sepsis" was defined as SIRS plus infection. And septic shock required the presence of sepsis plus documented organ dysfunction, such as hypotension.
The importance of recognizing this newly spotlighted sepsis/postoperative thrombosis connection is that most of the other known risk factors for thrombosis in surgical patients, including age, cancer, renal failure, and immobilization, are nonmodifiable, Dr. Donze observed.
Among the factors known to contribute to thrombosis are a hypercoagulable state, a proinflammatory state, hypoxemia, hypotension, and endothelial dysfunction. "All of these factors can be triggered by sepsis," Dr. Donze noted.
He reported having no financial conflicts regarding this study.
WASHINGTON – Preoperative sepsis proved to be an important independent risk factor for both arterial and venous thrombosis during or after surgery in an analysis of nearly 1.75 million U.S. surgical procedures.
The take-home message here is that the risk-benefit assessment of surgical procedures should take into account the presence of sepsis. And if the surgery can’t be delayed, prophylaxis against arterial as well as venous thrombosis should be employed, Dr. Jacques Donze said at the annual meeting of the American College of Cardiology.

Another key finding in this study was that the risk of postoperative thrombosis varied according to the severity of preoperative sepsis. Even the early form of sepsis known as systemic inflammatory response syndrome, or SIRS, was associated with a 2.5-fold increased risk.
"Include even early signs of sepsis as a risk factor," urged Dr. Donze of Brigham and Women’s Hospital, Boston.
Also, preoperative sepsis was a risk factor for postoperative thrombosis in connection with outpatient elective surgery as well as inpatient operations, he added.
Dr. Donze presented an analysis of 1,744,808 surgical procedures performed during 2005-2011 at 314 U.S. hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program. This large, prospective, observational registry is known for its high-quality data.
Within 48 hours prior to surgery, 7.8% of patients – totaling more than 136,000 – had SIRS, sepsis, or septic shock. Their postoperative thrombosis rate was 4.2%, compared with a 1.2% rate in patients without sepsis. In a multivariate regression analysis adjusted for potential confounding factors, the postoperative thrombosis risk climbed with increasing severity of preoperative sepsis.
SIRS was defined on the basis of temperature, heart rate, respiratory rate, WBC count, and/or the presence of anion gap acidosis. "Sepsis" was defined as SIRS plus infection. And septic shock required the presence of sepsis plus documented organ dysfunction, such as hypotension.
The importance of recognizing this newly spotlighted sepsis/postoperative thrombosis connection is that most of the other known risk factors for thrombosis in surgical patients, including age, cancer, renal failure, and immobilization, are nonmodifiable, Dr. Donze observed.
Among the factors known to contribute to thrombosis are a hypercoagulable state, a proinflammatory state, hypoxemia, hypotension, and endothelial dysfunction. "All of these factors can be triggered by sepsis," Dr. Donze noted.
He reported having no financial conflicts regarding this study.
WASHINGTON – Preoperative sepsis proved to be an important independent risk factor for both arterial and venous thrombosis during or after surgery in an analysis of nearly 1.75 million U.S. surgical procedures.
The take-home message here is that the risk-benefit assessment of surgical procedures should take into account the presence of sepsis. And if the surgery can’t be delayed, prophylaxis against arterial as well as venous thrombosis should be employed, Dr. Jacques Donze said at the annual meeting of the American College of Cardiology.

Another key finding in this study was that the risk of postoperative thrombosis varied according to the severity of preoperative sepsis. Even the early form of sepsis known as systemic inflammatory response syndrome, or SIRS, was associated with a 2.5-fold increased risk.
"Include even early signs of sepsis as a risk factor," urged Dr. Donze of Brigham and Women’s Hospital, Boston.
Also, preoperative sepsis was a risk factor for postoperative thrombosis in connection with outpatient elective surgery as well as inpatient operations, he added.
Dr. Donze presented an analysis of 1,744,808 surgical procedures performed during 2005-2011 at 314 U.S. hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program. This large, prospective, observational registry is known for its high-quality data.
Within 48 hours prior to surgery, 7.8% of patients – totaling more than 136,000 – had SIRS, sepsis, or septic shock. Their postoperative thrombosis rate was 4.2%, compared with a 1.2% rate in patients without sepsis. In a multivariate regression analysis adjusted for potential confounding factors, the postoperative thrombosis risk climbed with increasing severity of preoperative sepsis.
SIRS was defined on the basis of temperature, heart rate, respiratory rate, WBC count, and/or the presence of anion gap acidosis. "Sepsis" was defined as SIRS plus infection. And septic shock required the presence of sepsis plus documented organ dysfunction, such as hypotension.
The importance of recognizing this newly spotlighted sepsis/postoperative thrombosis connection is that most of the other known risk factors for thrombosis in surgical patients, including age, cancer, renal failure, and immobilization, are nonmodifiable, Dr. Donze observed.
Among the factors known to contribute to thrombosis are a hypercoagulable state, a proinflammatory state, hypoxemia, hypotension, and endothelial dysfunction. "All of these factors can be triggered by sepsis," Dr. Donze noted.
He reported having no financial conflicts regarding this study.
AT ACC 14
Major finding: Preoperative sepsis is a strong independent risk factor for postoperative arterial and venous thrombosis; the more severe the sepsis, the greater the thrombosis risk.
Data source: This was an analysis of nearly 1.75 million surgical procedures at 314 U.S. hospitals detailed in the American College of Surgeons National Quality Improvement Program registry.
Disclosures: The presenter reported having no financial conflicts.
Antitrust issues in health care (Part I)
This article introduces United States antitrust laws and discusses their application in health care. Part 2 will summarize major court decisions covering that subject.
Question: Antitrust laws:
A. Are based in part on the physician-patient trust relationship.
B. Prohibit anticompetitive behavior.
C. Regulate business activities but not professional services.
D. A, B, and C are correct.
E. B and C are correct.
Answer: B. Economic interests are best served in a freely competitive marketplace. Trade restraints such as price fixing and monopolization tend to promote inefficiency and increase profit for the perpetrators, at the expense of consumer welfare.
Accordingly, Congress enacted the Sherman Antitrust Act way back in 1890 to promote competition and outlaw unreasonable restraint of trade. Additional laws prohibit mergers that substantially lessen competition, price discrimination, and unfair trade practices. Collectively, these are known as the antitrust laws, the term reflecting their initial purpose to prevent commercial traders from forming anticompetitive groups or "trusts."
The Department of Justice (DOJ), the Federal Trade Commission (FTC), and their state counterparts enforce these laws, which have nothing whatsoever to do with the doctor-patient trust relationship.
Section I of the Sherman Act, the paramount antitrust statute, declares that "Every contract, combination in the form of trust or otherwise, or conspiracy, in restraint of trade or commerce among the several States, or with foreign nations, is declared to be illegal." Section II stipulates, "Every person who shall monopolize, or attempt to monopolize, or combine or conspire with any other person or persons, to monopolize any part of the trade or commerce among the several States, or with foreign nations, shall be deemed guilty of a felony."
Other important laws are Sections 4 and 7 of the Clayton Antitrust Act and Section 5(a)(1) of the Federal Trade Commission Act, which outlaws "unfair methods of competition in or affecting commerce ... " Additionally, all states have their own antitrust statutes, which in some cases may be more restrictive than the federal laws are.
These laws initially targeted anticompetitive business practices. In 1975, the U.S. Supreme Court declared that there was to be no "learned profession" exemption, although special considerations may apply.1 However, activities of state government officials and employees are exempt from antitrust scrutiny under the so-called "state action doctrine," which confers immunity if an exemption is clearly articulated and affirmatively expressed as state policy, and there is active state supervision of the conduct in question.
Antitrust issues are ubiquitous in health care, and fall into seven major categories: 1) price fixing; 2) boycotts; 3) market division; 4) monopolization; 5) joint ventures; 6) exclusive contracts, and 7) peer review.
1. Price fixing. An agreement to fix prices is the most egregious example of anticompetitive conduct, so much so that the courts will use a per se analysis, i.e., without need to consider other factors, to arrive at its decision. Price fixing does not require any party to show market dominance or power, and its presence can be inferred from circumstances and agreements, which can be either oral or written.
For example, physician fee schedules or guidelines by a medical association would constitute price fixing. Even an agreement to fix maximum prices, as opposed to minimum prices, has been ruled illegal. At a practical level, physicians should avoid sharing pricing information with anyone, especially with colleagues, unless strict FTC "safety zone" criteria are satisfied.
2. Boycotts. Group boycotts are usually per se illegal, but in the health care industry, a rule of reason analysis is frequently used. Courts will look at the circumstances and purpose of the boycott, its pro- and anti-competitive effects, and whether there are other less restrictive ways to achieve the purported goal.
Affiliating physicians face this risk when forming alliances, as boycott questions may arise when a doctor is inappropriately excluded, which deprives him/her from earning a living in the relevant market.
A related controversial issue is the unionization of doctors. Unionization protects labor rights, especially those of medical residents, and offers greater parity in collective bargaining. On the other hand, the danger is in tying a physician’s obligations to the interests of other workers who may not share the same ethical commitment to patients.2
Strikes by doctors are likely to interfere with patient care, raise serious ethical questions, and may also be in violation of antitrust laws although boycotts for sociopolitical and noncommercial reasons are not specifically prohibited.
3. Market division. Agreements to restrict competition by dividing or allocating territories or patients are illegal per se under the Sherman Act.
4. Monopolization. Section 2 of the Sherman Act prohibits monopolization and attempts to monopolize. Examples are predatory pricing, long-term exclusive contracts, and refusal to deal. Mergers and acquisitions may substantially lessen competition with the tendency to create a monopoly, and they are subject to Section 7 of the Clayton Act. Proof of monopolization requires an inquiry into the relevant product and geographic markets (usually greater than 50%-60% market share), and regularly requires an economist’s expertise at trial.
As a general proposition, restraint of trade and monopolistic charges are difficult to prove. Monopoly through "the exercise of skill, foresight, and industry" does not constitute monopolizing conduct.
5. Joint ventures. The two main ways physicians form network joint ventures are: 1) join together in an entity with shared financial risks and clinical integration, and 2) join a looser network without integration to simply facilitate the flow of information for contracting purposes between physicians and other payers, the so-called messenger method.
Many health delivery systems involve joint venture agreements among practitioners or groups of health professionals and health care institutions, e.g., physician hospital organizations (PHOs), independent practice associations (IPAs), and preferred physician organization (PPOs). Physicians and physician practice groups may become targets if their attempted efforts at joint ventures are deemed to be a pretext for price fixing or otherwise anticompetitive.
The DOJ and FTC have promulgated guidelines regarding joint venture structures and will perform a review of the proposal upon request.3
However, under Obamacare, which promotes the efficient integration of health services through competition such as accountable care organizations, these guidelines are likely to be revised in the near future.
6. Exclusive contracts. Many hospitals have exclusive contracts with health professionals such as radiologists, anesthesiologists, and pathologists. Patients using the facility may be forced to use the services of these providers ("tying arrangement"). If the hospital does not possess requisite market power, or force the acceptance of the service, such agreements may pass antitrust scrutiny.
7. Peer review. The Health Care Quality Improvement Act (42 U.S.C. §§ 1101 et seq.) immunizes physicians and others performing peer review activities from federal antitrust claims so long as peer review was carried out: 1) in reasonable belief that the action was in furtherance of quality health care; 2) after reasonable effort to obtain the facts; 3) after an adequate notice and hearing procedure; 4) in reasonable belief that the action was warranted; and 5) any adverse outcome was reported to the National Practitioners’ Data Bank.
A doctor who is judged wanting in peer review occasionally asserts a discriminatory or anticompetitive intent, and may file a retaliatory lawsuit. One caveat: Peer review deliberations are always held in strict confidence. Disparaging a doctor under review in an unrelated forum constitutes a violation of the peer review process, which risks nullification of discovery protection and antitrust immunity.
Antitrust problems are highly fact dependent and analytically complex, and therefore require counsel with special expertise and experience. Issues are surprisingly prevalent and may be counterintuitive, affecting not only parties in joint ventures and mergers, but also the solo office or hospital practitioner. Matters of medical staffing, joint purchasing, information exchange, managed care negotiation, peer review and price agreements are some examples.
Penalties are severe, and may cover more than simple cease and desist orders. Some behavior constitutes criminality punishable by prison terms, though this is rare in the health care arena.
More often, the guilty parties face heavy monetary fines from both governmental officials as well as private litigants who can join in the lawsuit and stand to benefit from awards of treble damages and attorneys’ fees.
References:
1. Goldfarb v. Virginia State Bar 421 U.S. 773, 1975.
2. Code of Medical Ethics, AMA, 9.025, 2012-2013 edition.
3. Statements of Antitrust Enforcement Policy in Health Care. Department of Justice and Federal Trade Commission (1996).
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, "Medical Malpractice: Understanding the Law, Managing the Risk," and his 2012 Halsbury treatise, "Medical Negligence and Professional Misconduct." For additional information, readers may contact the author at [email protected].
This article introduces United States antitrust laws and discusses their application in health care. Part 2 will summarize major court decisions covering that subject.
Question: Antitrust laws:
A. Are based in part on the physician-patient trust relationship.
B. Prohibit anticompetitive behavior.
C. Regulate business activities but not professional services.
D. A, B, and C are correct.
E. B and C are correct.
Answer: B. Economic interests are best served in a freely competitive marketplace. Trade restraints such as price fixing and monopolization tend to promote inefficiency and increase profit for the perpetrators, at the expense of consumer welfare.
Accordingly, Congress enacted the Sherman Antitrust Act way back in 1890 to promote competition and outlaw unreasonable restraint of trade. Additional laws prohibit mergers that substantially lessen competition, price discrimination, and unfair trade practices. Collectively, these are known as the antitrust laws, the term reflecting their initial purpose to prevent commercial traders from forming anticompetitive groups or "trusts."
The Department of Justice (DOJ), the Federal Trade Commission (FTC), and their state counterparts enforce these laws, which have nothing whatsoever to do with the doctor-patient trust relationship.
Section I of the Sherman Act, the paramount antitrust statute, declares that "Every contract, combination in the form of trust or otherwise, or conspiracy, in restraint of trade or commerce among the several States, or with foreign nations, is declared to be illegal." Section II stipulates, "Every person who shall monopolize, or attempt to monopolize, or combine or conspire with any other person or persons, to monopolize any part of the trade or commerce among the several States, or with foreign nations, shall be deemed guilty of a felony."
Other important laws are Sections 4 and 7 of the Clayton Antitrust Act and Section 5(a)(1) of the Federal Trade Commission Act, which outlaws "unfair methods of competition in or affecting commerce ... " Additionally, all states have their own antitrust statutes, which in some cases may be more restrictive than the federal laws are.
These laws initially targeted anticompetitive business practices. In 1975, the U.S. Supreme Court declared that there was to be no "learned profession" exemption, although special considerations may apply.1 However, activities of state government officials and employees are exempt from antitrust scrutiny under the so-called "state action doctrine," which confers immunity if an exemption is clearly articulated and affirmatively expressed as state policy, and there is active state supervision of the conduct in question.
Antitrust issues are ubiquitous in health care, and fall into seven major categories: 1) price fixing; 2) boycotts; 3) market division; 4) monopolization; 5) joint ventures; 6) exclusive contracts, and 7) peer review.
1. Price fixing. An agreement to fix prices is the most egregious example of anticompetitive conduct, so much so that the courts will use a per se analysis, i.e., without need to consider other factors, to arrive at its decision. Price fixing does not require any party to show market dominance or power, and its presence can be inferred from circumstances and agreements, which can be either oral or written.
For example, physician fee schedules or guidelines by a medical association would constitute price fixing. Even an agreement to fix maximum prices, as opposed to minimum prices, has been ruled illegal. At a practical level, physicians should avoid sharing pricing information with anyone, especially with colleagues, unless strict FTC "safety zone" criteria are satisfied.
2. Boycotts. Group boycotts are usually per se illegal, but in the health care industry, a rule of reason analysis is frequently used. Courts will look at the circumstances and purpose of the boycott, its pro- and anti-competitive effects, and whether there are other less restrictive ways to achieve the purported goal.
Affiliating physicians face this risk when forming alliances, as boycott questions may arise when a doctor is inappropriately excluded, which deprives him/her from earning a living in the relevant market.
A related controversial issue is the unionization of doctors. Unionization protects labor rights, especially those of medical residents, and offers greater parity in collective bargaining. On the other hand, the danger is in tying a physician’s obligations to the interests of other workers who may not share the same ethical commitment to patients.2
Strikes by doctors are likely to interfere with patient care, raise serious ethical questions, and may also be in violation of antitrust laws although boycotts for sociopolitical and noncommercial reasons are not specifically prohibited.
3. Market division. Agreements to restrict competition by dividing or allocating territories or patients are illegal per se under the Sherman Act.
4. Monopolization. Section 2 of the Sherman Act prohibits monopolization and attempts to monopolize. Examples are predatory pricing, long-term exclusive contracts, and refusal to deal. Mergers and acquisitions may substantially lessen competition with the tendency to create a monopoly, and they are subject to Section 7 of the Clayton Act. Proof of monopolization requires an inquiry into the relevant product and geographic markets (usually greater than 50%-60% market share), and regularly requires an economist’s expertise at trial.
As a general proposition, restraint of trade and monopolistic charges are difficult to prove. Monopoly through "the exercise of skill, foresight, and industry" does not constitute monopolizing conduct.
5. Joint ventures. The two main ways physicians form network joint ventures are: 1) join together in an entity with shared financial risks and clinical integration, and 2) join a looser network without integration to simply facilitate the flow of information for contracting purposes between physicians and other payers, the so-called messenger method.
Many health delivery systems involve joint venture agreements among practitioners or groups of health professionals and health care institutions, e.g., physician hospital organizations (PHOs), independent practice associations (IPAs), and preferred physician organization (PPOs). Physicians and physician practice groups may become targets if their attempted efforts at joint ventures are deemed to be a pretext for price fixing or otherwise anticompetitive.
The DOJ and FTC have promulgated guidelines regarding joint venture structures and will perform a review of the proposal upon request.3
However, under Obamacare, which promotes the efficient integration of health services through competition such as accountable care organizations, these guidelines are likely to be revised in the near future.
6. Exclusive contracts. Many hospitals have exclusive contracts with health professionals such as radiologists, anesthesiologists, and pathologists. Patients using the facility may be forced to use the services of these providers ("tying arrangement"). If the hospital does not possess requisite market power, or force the acceptance of the service, such agreements may pass antitrust scrutiny.
7. Peer review. The Health Care Quality Improvement Act (42 U.S.C. §§ 1101 et seq.) immunizes physicians and others performing peer review activities from federal antitrust claims so long as peer review was carried out: 1) in reasonable belief that the action was in furtherance of quality health care; 2) after reasonable effort to obtain the facts; 3) after an adequate notice and hearing procedure; 4) in reasonable belief that the action was warranted; and 5) any adverse outcome was reported to the National Practitioners’ Data Bank.
A doctor who is judged wanting in peer review occasionally asserts a discriminatory or anticompetitive intent, and may file a retaliatory lawsuit. One caveat: Peer review deliberations are always held in strict confidence. Disparaging a doctor under review in an unrelated forum constitutes a violation of the peer review process, which risks nullification of discovery protection and antitrust immunity.
Antitrust problems are highly fact dependent and analytically complex, and therefore require counsel with special expertise and experience. Issues are surprisingly prevalent and may be counterintuitive, affecting not only parties in joint ventures and mergers, but also the solo office or hospital practitioner. Matters of medical staffing, joint purchasing, information exchange, managed care negotiation, peer review and price agreements are some examples.
Penalties are severe, and may cover more than simple cease and desist orders. Some behavior constitutes criminality punishable by prison terms, though this is rare in the health care arena.
More often, the guilty parties face heavy monetary fines from both governmental officials as well as private litigants who can join in the lawsuit and stand to benefit from awards of treble damages and attorneys’ fees.
References:
1. Goldfarb v. Virginia State Bar 421 U.S. 773, 1975.
2. Code of Medical Ethics, AMA, 9.025, 2012-2013 edition.
3. Statements of Antitrust Enforcement Policy in Health Care. Department of Justice and Federal Trade Commission (1996).
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, "Medical Malpractice: Understanding the Law, Managing the Risk," and his 2012 Halsbury treatise, "Medical Negligence and Professional Misconduct." For additional information, readers may contact the author at [email protected].
This article introduces United States antitrust laws and discusses their application in health care. Part 2 will summarize major court decisions covering that subject.
Question: Antitrust laws:
A. Are based in part on the physician-patient trust relationship.
B. Prohibit anticompetitive behavior.
C. Regulate business activities but not professional services.
D. A, B, and C are correct.
E. B and C are correct.
Answer: B. Economic interests are best served in a freely competitive marketplace. Trade restraints such as price fixing and monopolization tend to promote inefficiency and increase profit for the perpetrators, at the expense of consumer welfare.
Accordingly, Congress enacted the Sherman Antitrust Act way back in 1890 to promote competition and outlaw unreasonable restraint of trade. Additional laws prohibit mergers that substantially lessen competition, price discrimination, and unfair trade practices. Collectively, these are known as the antitrust laws, the term reflecting their initial purpose to prevent commercial traders from forming anticompetitive groups or "trusts."
The Department of Justice (DOJ), the Federal Trade Commission (FTC), and their state counterparts enforce these laws, which have nothing whatsoever to do with the doctor-patient trust relationship.
Section I of the Sherman Act, the paramount antitrust statute, declares that "Every contract, combination in the form of trust or otherwise, or conspiracy, in restraint of trade or commerce among the several States, or with foreign nations, is declared to be illegal." Section II stipulates, "Every person who shall monopolize, or attempt to monopolize, or combine or conspire with any other person or persons, to monopolize any part of the trade or commerce among the several States, or with foreign nations, shall be deemed guilty of a felony."
Other important laws are Sections 4 and 7 of the Clayton Antitrust Act and Section 5(a)(1) of the Federal Trade Commission Act, which outlaws "unfair methods of competition in or affecting commerce ... " Additionally, all states have their own antitrust statutes, which in some cases may be more restrictive than the federal laws are.
These laws initially targeted anticompetitive business practices. In 1975, the U.S. Supreme Court declared that there was to be no "learned profession" exemption, although special considerations may apply.1 However, activities of state government officials and employees are exempt from antitrust scrutiny under the so-called "state action doctrine," which confers immunity if an exemption is clearly articulated and affirmatively expressed as state policy, and there is active state supervision of the conduct in question.
Antitrust issues are ubiquitous in health care, and fall into seven major categories: 1) price fixing; 2) boycotts; 3) market division; 4) monopolization; 5) joint ventures; 6) exclusive contracts, and 7) peer review.
1. Price fixing. An agreement to fix prices is the most egregious example of anticompetitive conduct, so much so that the courts will use a per se analysis, i.e., without need to consider other factors, to arrive at its decision. Price fixing does not require any party to show market dominance or power, and its presence can be inferred from circumstances and agreements, which can be either oral or written.
For example, physician fee schedules or guidelines by a medical association would constitute price fixing. Even an agreement to fix maximum prices, as opposed to minimum prices, has been ruled illegal. At a practical level, physicians should avoid sharing pricing information with anyone, especially with colleagues, unless strict FTC "safety zone" criteria are satisfied.
2. Boycotts. Group boycotts are usually per se illegal, but in the health care industry, a rule of reason analysis is frequently used. Courts will look at the circumstances and purpose of the boycott, its pro- and anti-competitive effects, and whether there are other less restrictive ways to achieve the purported goal.
Affiliating physicians face this risk when forming alliances, as boycott questions may arise when a doctor is inappropriately excluded, which deprives him/her from earning a living in the relevant market.
A related controversial issue is the unionization of doctors. Unionization protects labor rights, especially those of medical residents, and offers greater parity in collective bargaining. On the other hand, the danger is in tying a physician’s obligations to the interests of other workers who may not share the same ethical commitment to patients.2
Strikes by doctors are likely to interfere with patient care, raise serious ethical questions, and may also be in violation of antitrust laws although boycotts for sociopolitical and noncommercial reasons are not specifically prohibited.
3. Market division. Agreements to restrict competition by dividing or allocating territories or patients are illegal per se under the Sherman Act.
4. Monopolization. Section 2 of the Sherman Act prohibits monopolization and attempts to monopolize. Examples are predatory pricing, long-term exclusive contracts, and refusal to deal. Mergers and acquisitions may substantially lessen competition with the tendency to create a monopoly, and they are subject to Section 7 of the Clayton Act. Proof of monopolization requires an inquiry into the relevant product and geographic markets (usually greater than 50%-60% market share), and regularly requires an economist’s expertise at trial.
As a general proposition, restraint of trade and monopolistic charges are difficult to prove. Monopoly through "the exercise of skill, foresight, and industry" does not constitute monopolizing conduct.
5. Joint ventures. The two main ways physicians form network joint ventures are: 1) join together in an entity with shared financial risks and clinical integration, and 2) join a looser network without integration to simply facilitate the flow of information for contracting purposes between physicians and other payers, the so-called messenger method.
Many health delivery systems involve joint venture agreements among practitioners or groups of health professionals and health care institutions, e.g., physician hospital organizations (PHOs), independent practice associations (IPAs), and preferred physician organization (PPOs). Physicians and physician practice groups may become targets if their attempted efforts at joint ventures are deemed to be a pretext for price fixing or otherwise anticompetitive.
The DOJ and FTC have promulgated guidelines regarding joint venture structures and will perform a review of the proposal upon request.3
However, under Obamacare, which promotes the efficient integration of health services through competition such as accountable care organizations, these guidelines are likely to be revised in the near future.
6. Exclusive contracts. Many hospitals have exclusive contracts with health professionals such as radiologists, anesthesiologists, and pathologists. Patients using the facility may be forced to use the services of these providers ("tying arrangement"). If the hospital does not possess requisite market power, or force the acceptance of the service, such agreements may pass antitrust scrutiny.
7. Peer review. The Health Care Quality Improvement Act (42 U.S.C. §§ 1101 et seq.) immunizes physicians and others performing peer review activities from federal antitrust claims so long as peer review was carried out: 1) in reasonable belief that the action was in furtherance of quality health care; 2) after reasonable effort to obtain the facts; 3) after an adequate notice and hearing procedure; 4) in reasonable belief that the action was warranted; and 5) any adverse outcome was reported to the National Practitioners’ Data Bank.
A doctor who is judged wanting in peer review occasionally asserts a discriminatory or anticompetitive intent, and may file a retaliatory lawsuit. One caveat: Peer review deliberations are always held in strict confidence. Disparaging a doctor under review in an unrelated forum constitutes a violation of the peer review process, which risks nullification of discovery protection and antitrust immunity.
Antitrust problems are highly fact dependent and analytically complex, and therefore require counsel with special expertise and experience. Issues are surprisingly prevalent and may be counterintuitive, affecting not only parties in joint ventures and mergers, but also the solo office or hospital practitioner. Matters of medical staffing, joint purchasing, information exchange, managed care negotiation, peer review and price agreements are some examples.
Penalties are severe, and may cover more than simple cease and desist orders. Some behavior constitutes criminality punishable by prison terms, though this is rare in the health care arena.
More often, the guilty parties face heavy monetary fines from both governmental officials as well as private litigants who can join in the lawsuit and stand to benefit from awards of treble damages and attorneys’ fees.
References:
1. Goldfarb v. Virginia State Bar 421 U.S. 773, 1975.
2. Code of Medical Ethics, AMA, 9.025, 2012-2013 edition.
3. Statements of Antitrust Enforcement Policy in Health Care. Department of Justice and Federal Trade Commission (1996).
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, "Medical Malpractice: Understanding the Law, Managing the Risk," and his 2012 Halsbury treatise, "Medical Negligence and Professional Misconduct." For additional information, readers may contact the author at [email protected].
High-dose steroids tame post-EVAR inflammation
BOSTON – Preoperative high-dose methylprednisolone dramatically reduced inflammation and enhanced recovery after endovascular aortic repair without increased morbidity in a prospective, double-blinded randomized study.
The primary outcome of modified systemic inflammatory response syndrome (SIRS) developed in 92% on placebo and 27% given methylprednisolone (relative risk, 0.29; P less than .001).
The effect was particularly striking in patients with three or more SIRS criteria, with an overall number needed to treat of 1.5, Dr. Henrik Kehlet said at the annual meeting of the American Surgical Association.
Tempering the postoperative inflammatory response with methylprednisolone also significantly trimmed hospital stays from 3 to 2 days (P less than .001) and morphine requirements from 10 mg to 0 mg (P less than .001).
Medical morbidity was reduced in the methylprednisolone group, but not significantly (23% vs. 36%; P = .1), as was surgical morbidity (20% vs. 21%; P = 1.0).
Importantly, there was no sign of an increase in diagnosed (23% vs. 17%) or treated (1% vs. 3%) endoleaks on computed tomography scan among 146 patients evaluable at 3 months’ follow-up, said Dr. Kehlet, professor of perioperative therapy and head of the surgical pathophysiology section at Rigshospitalet, Copenhagen University, and the oft-described "father" of rapid recovery.
About 40%-60% of patients undergoing endovascular aortic repair (EVAR) will develop postoperative SIRS. Although there is limited surgical injury with the minimally invasive procedure, there is still a stress response because the prosthesis releases proinflammatory mediators from the thrombus in the aortic aneurysm, he explained.
Invited discussant Dr. Basil Pruitt of the division of trauma at the University of Texas Health Science Center, San Antonio, observed that the findings take on added import in light of a 7,500-patient study presented at the recent American College of Cardiology meeting showing that methylprednisolone conferred no significant benefit and was associated with a 15% increased risk of postoperative heart attack plus death when given during cardiac surgery with cardiopulmonary bypass. He also questioned whether the glucocorticosteroid lowered the metabolic rate, as this would impair wound healing, or induced hypoglycemia or glucose intolerance.
"Do those findings and the concerns noted above simply define patient groups in whom methylprednisolone should not be infused preoperatively or, alternatively, do they define a threshold of physiologic or operative insult beyond which the effect of methylprednisolone is outweighed by the magnitude of injury and the associated systemic inflammatory response syndrome?" he asked.
Dr. Kehlet responded that he was unable to determine why that particular abstract found increased morbidity, but noted that the same authors previously published a systematic review (Eur. Heart J. 2008;29:2592-600) supporting reduced morbidity with steroid use in cardiopulmonary bypass.
He added, "The effect may depend on the type of injury, as you mention; cardiopulmonary bypass [is] a very special injury with many mediators of the stress response, compared to other surgical operations. We need more studies. And, finally, if you want to find out about the real outcomes, you must integrate the pharmacologic intervention with an optimized, fast-track setup."
Dr. Kehlet said they did not measure metabolic rate, but that no clinical problem was observed in the limited number of diabetics (n = 22) in their study. This finding is also supported by a huge, multicenter Dutch trial, in which intraoperative high-dose dexamethasone was associated with higher postoperative glucose levels in cardiopulmonary bypass patients, but had no effect on diabetes in subgroup analyses or on the primary endpoint of major morbidity at 30 days (JAMA 2012;308:1761-7).
For Dr. Kehlet's single-center, double-blinded study, 153 patients undergoing EVAR for abdominal aortic aneurysm were randomly assigned to receive a preoperative single dose of placebo or what was described as a single "old-fashioned sepsis dose of methylprednisolone" at 30 mg/kg. The two groups were similar at baseline with respect to age, comorbidities, aneurysm size, thrombus volume, EVAR procedures, and blood loss.
A modified version of SIRS was assessed during the first 4 days after surgery and defined by two or more of the following criteria: fever of more than 38° C (100.4° F) or less than 36° C (96.8° F), heart rate of more than 90 beats per minute, respiratory rate of more than 20 breaths per minute or arterial carbon dioxide tension of less than 4.3 kPa (32.25 mm Hg), and a C-reactive protein (CRP) level of more than 75 mg/L. The traditional fourth SIRS criterion of leukocytosis was replaced with CRP level because glucocorticoids always lead to leukocytosis, Dr. Kehlet noted.
Among 150 evaluable patients, high-dose methylprednisolone almost completely eliminated the proinflammatory activities of interleukin (IL)-6 (186 pg/mL vs. 20 mg/dL; P less than .001), IL-8, and CRP.
Among other inflammatory parameters, methylprednisolone reduced soluble tumor necrosis factor receptor 1 levels, but did not modify the d-dimer response, metalloproteinase-9, or myeloperoxidase, he said.
By 3 months, mortality was similar at 3% in the methylprednisolone group and 1% in the placebo group (P less than .5).
"What we don’t know is what the optimal dose-response relationship is because we used a very high dose and, of course, this was only 150 patients, so the safety issues cannot be answered based on this study, but the results are promising for future large-scale studies in this interesting operation," Dr. Kehlet concluded.
Dr. Kehlet and his coauthors reported no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
BOSTON – Preoperative high-dose methylprednisolone dramatically reduced inflammation and enhanced recovery after endovascular aortic repair without increased morbidity in a prospective, double-blinded randomized study.
The primary outcome of modified systemic inflammatory response syndrome (SIRS) developed in 92% on placebo and 27% given methylprednisolone (relative risk, 0.29; P less than .001).
The effect was particularly striking in patients with three or more SIRS criteria, with an overall number needed to treat of 1.5, Dr. Henrik Kehlet said at the annual meeting of the American Surgical Association.
Tempering the postoperative inflammatory response with methylprednisolone also significantly trimmed hospital stays from 3 to 2 days (P less than .001) and morphine requirements from 10 mg to 0 mg (P less than .001).
Medical morbidity was reduced in the methylprednisolone group, but not significantly (23% vs. 36%; P = .1), as was surgical morbidity (20% vs. 21%; P = 1.0).
Importantly, there was no sign of an increase in diagnosed (23% vs. 17%) or treated (1% vs. 3%) endoleaks on computed tomography scan among 146 patients evaluable at 3 months’ follow-up, said Dr. Kehlet, professor of perioperative therapy and head of the surgical pathophysiology section at Rigshospitalet, Copenhagen University, and the oft-described "father" of rapid recovery.
About 40%-60% of patients undergoing endovascular aortic repair (EVAR) will develop postoperative SIRS. Although there is limited surgical injury with the minimally invasive procedure, there is still a stress response because the prosthesis releases proinflammatory mediators from the thrombus in the aortic aneurysm, he explained.
Invited discussant Dr. Basil Pruitt of the division of trauma at the University of Texas Health Science Center, San Antonio, observed that the findings take on added import in light of a 7,500-patient study presented at the recent American College of Cardiology meeting showing that methylprednisolone conferred no significant benefit and was associated with a 15% increased risk of postoperative heart attack plus death when given during cardiac surgery with cardiopulmonary bypass. He also questioned whether the glucocorticosteroid lowered the metabolic rate, as this would impair wound healing, or induced hypoglycemia or glucose intolerance.
"Do those findings and the concerns noted above simply define patient groups in whom methylprednisolone should not be infused preoperatively or, alternatively, do they define a threshold of physiologic or operative insult beyond which the effect of methylprednisolone is outweighed by the magnitude of injury and the associated systemic inflammatory response syndrome?" he asked.
Dr. Kehlet responded that he was unable to determine why that particular abstract found increased morbidity, but noted that the same authors previously published a systematic review (Eur. Heart J. 2008;29:2592-600) supporting reduced morbidity with steroid use in cardiopulmonary bypass.
He added, "The effect may depend on the type of injury, as you mention; cardiopulmonary bypass [is] a very special injury with many mediators of the stress response, compared to other surgical operations. We need more studies. And, finally, if you want to find out about the real outcomes, you must integrate the pharmacologic intervention with an optimized, fast-track setup."
Dr. Kehlet said they did not measure metabolic rate, but that no clinical problem was observed in the limited number of diabetics (n = 22) in their study. This finding is also supported by a huge, multicenter Dutch trial, in which intraoperative high-dose dexamethasone was associated with higher postoperative glucose levels in cardiopulmonary bypass patients, but had no effect on diabetes in subgroup analyses or on the primary endpoint of major morbidity at 30 days (JAMA 2012;308:1761-7).
For Dr. Kehlet's single-center, double-blinded study, 153 patients undergoing EVAR for abdominal aortic aneurysm were randomly assigned to receive a preoperative single dose of placebo or what was described as a single "old-fashioned sepsis dose of methylprednisolone" at 30 mg/kg. The two groups were similar at baseline with respect to age, comorbidities, aneurysm size, thrombus volume, EVAR procedures, and blood loss.
A modified version of SIRS was assessed during the first 4 days after surgery and defined by two or more of the following criteria: fever of more than 38° C (100.4° F) or less than 36° C (96.8° F), heart rate of more than 90 beats per minute, respiratory rate of more than 20 breaths per minute or arterial carbon dioxide tension of less than 4.3 kPa (32.25 mm Hg), and a C-reactive protein (CRP) level of more than 75 mg/L. The traditional fourth SIRS criterion of leukocytosis was replaced with CRP level because glucocorticoids always lead to leukocytosis, Dr. Kehlet noted.
Among 150 evaluable patients, high-dose methylprednisolone almost completely eliminated the proinflammatory activities of interleukin (IL)-6 (186 pg/mL vs. 20 mg/dL; P less than .001), IL-8, and CRP.
Among other inflammatory parameters, methylprednisolone reduced soluble tumor necrosis factor receptor 1 levels, but did not modify the d-dimer response, metalloproteinase-9, or myeloperoxidase, he said.
By 3 months, mortality was similar at 3% in the methylprednisolone group and 1% in the placebo group (P less than .5).
"What we don’t know is what the optimal dose-response relationship is because we used a very high dose and, of course, this was only 150 patients, so the safety issues cannot be answered based on this study, but the results are promising for future large-scale studies in this interesting operation," Dr. Kehlet concluded.
Dr. Kehlet and his coauthors reported no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
BOSTON – Preoperative high-dose methylprednisolone dramatically reduced inflammation and enhanced recovery after endovascular aortic repair without increased morbidity in a prospective, double-blinded randomized study.
The primary outcome of modified systemic inflammatory response syndrome (SIRS) developed in 92% on placebo and 27% given methylprednisolone (relative risk, 0.29; P less than .001).
The effect was particularly striking in patients with three or more SIRS criteria, with an overall number needed to treat of 1.5, Dr. Henrik Kehlet said at the annual meeting of the American Surgical Association.
Tempering the postoperative inflammatory response with methylprednisolone also significantly trimmed hospital stays from 3 to 2 days (P less than .001) and morphine requirements from 10 mg to 0 mg (P less than .001).
Medical morbidity was reduced in the methylprednisolone group, but not significantly (23% vs. 36%; P = .1), as was surgical morbidity (20% vs. 21%; P = 1.0).
Importantly, there was no sign of an increase in diagnosed (23% vs. 17%) or treated (1% vs. 3%) endoleaks on computed tomography scan among 146 patients evaluable at 3 months’ follow-up, said Dr. Kehlet, professor of perioperative therapy and head of the surgical pathophysiology section at Rigshospitalet, Copenhagen University, and the oft-described "father" of rapid recovery.
About 40%-60% of patients undergoing endovascular aortic repair (EVAR) will develop postoperative SIRS. Although there is limited surgical injury with the minimally invasive procedure, there is still a stress response because the prosthesis releases proinflammatory mediators from the thrombus in the aortic aneurysm, he explained.
Invited discussant Dr. Basil Pruitt of the division of trauma at the University of Texas Health Science Center, San Antonio, observed that the findings take on added import in light of a 7,500-patient study presented at the recent American College of Cardiology meeting showing that methylprednisolone conferred no significant benefit and was associated with a 15% increased risk of postoperative heart attack plus death when given during cardiac surgery with cardiopulmonary bypass. He also questioned whether the glucocorticosteroid lowered the metabolic rate, as this would impair wound healing, or induced hypoglycemia or glucose intolerance.
"Do those findings and the concerns noted above simply define patient groups in whom methylprednisolone should not be infused preoperatively or, alternatively, do they define a threshold of physiologic or operative insult beyond which the effect of methylprednisolone is outweighed by the magnitude of injury and the associated systemic inflammatory response syndrome?" he asked.
Dr. Kehlet responded that he was unable to determine why that particular abstract found increased morbidity, but noted that the same authors previously published a systematic review (Eur. Heart J. 2008;29:2592-600) supporting reduced morbidity with steroid use in cardiopulmonary bypass.
He added, "The effect may depend on the type of injury, as you mention; cardiopulmonary bypass [is] a very special injury with many mediators of the stress response, compared to other surgical operations. We need more studies. And, finally, if you want to find out about the real outcomes, you must integrate the pharmacologic intervention with an optimized, fast-track setup."
Dr. Kehlet said they did not measure metabolic rate, but that no clinical problem was observed in the limited number of diabetics (n = 22) in their study. This finding is also supported by a huge, multicenter Dutch trial, in which intraoperative high-dose dexamethasone was associated with higher postoperative glucose levels in cardiopulmonary bypass patients, but had no effect on diabetes in subgroup analyses or on the primary endpoint of major morbidity at 30 days (JAMA 2012;308:1761-7).
For Dr. Kehlet's single-center, double-blinded study, 153 patients undergoing EVAR for abdominal aortic aneurysm were randomly assigned to receive a preoperative single dose of placebo or what was described as a single "old-fashioned sepsis dose of methylprednisolone" at 30 mg/kg. The two groups were similar at baseline with respect to age, comorbidities, aneurysm size, thrombus volume, EVAR procedures, and blood loss.
A modified version of SIRS was assessed during the first 4 days after surgery and defined by two or more of the following criteria: fever of more than 38° C (100.4° F) or less than 36° C (96.8° F), heart rate of more than 90 beats per minute, respiratory rate of more than 20 breaths per minute or arterial carbon dioxide tension of less than 4.3 kPa (32.25 mm Hg), and a C-reactive protein (CRP) level of more than 75 mg/L. The traditional fourth SIRS criterion of leukocytosis was replaced with CRP level because glucocorticoids always lead to leukocytosis, Dr. Kehlet noted.
Among 150 evaluable patients, high-dose methylprednisolone almost completely eliminated the proinflammatory activities of interleukin (IL)-6 (186 pg/mL vs. 20 mg/dL; P less than .001), IL-8, and CRP.
Among other inflammatory parameters, methylprednisolone reduced soluble tumor necrosis factor receptor 1 levels, but did not modify the d-dimer response, metalloproteinase-9, or myeloperoxidase, he said.
By 3 months, mortality was similar at 3% in the methylprednisolone group and 1% in the placebo group (P less than .5).
"What we don’t know is what the optimal dose-response relationship is because we used a very high dose and, of course, this was only 150 patients, so the safety issues cannot be answered based on this study, but the results are promising for future large-scale studies in this interesting operation," Dr. Kehlet concluded.
Dr. Kehlet and his coauthors reported no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
AT ASA 2014
Major finding: Systemic inflammatory response syndrome developed in 92% on placebo and 27% given methylprednisolone (relative risk, 0.29; P less than .001).
Data source: A single-center, randomized double-blinded study in 153 patients undergoing EVAR for abdominal aortic aneurysm.
Disclosures: Dr. Kehlet and his coauthors reported no financial disclosures.
Affordable Care Act sign-ups hit 8 million
In the Affordable Care Act’s first open enrollment period, 8 million Americans signed up for private health insurance through the state and federal health marketplaces.
President Obama announced the latest figures on April 17, more than 2 weeks after the close of the first open enrollment period. Though March 31 was the deadline for signing up, individuals who had started the process by the deadline were given until April 15 to complete the process. During that time, nearly 1 million additional people signed up for health plans.
More young people have signed up for coverage as well. President Obama reported that in the federally run marketplaces, 35% of the sign-ups were from individuals under age 35, including children. About 28% of sign-ups were from young adults aged 18-34 years. That’s similar to the percentage of young adults who signed up for insurance in Massachusetts during the first year of its health reform effort, according to the White House.
"The Affordable Care Act is working," President Obama said during a White House press conference.
He once again called on the ACA’s opponents to stop trying to repeal it.
Rep. Fred Upton (R- Mich.), chairman of the House Energy and Commerce Committee, said the law has disrupted health care for millions of Americans, limited access to physicians, and caused insurance premiums to skyrocket.
"The administration still has not answered basic questions about enrollment and why it will not support fairness for all," Rep. Upton said in a statement.
On Twitter @maryellenny
In the Affordable Care Act’s first open enrollment period, 8 million Americans signed up for private health insurance through the state and federal health marketplaces.
President Obama announced the latest figures on April 17, more than 2 weeks after the close of the first open enrollment period. Though March 31 was the deadline for signing up, individuals who had started the process by the deadline were given until April 15 to complete the process. During that time, nearly 1 million additional people signed up for health plans.
More young people have signed up for coverage as well. President Obama reported that in the federally run marketplaces, 35% of the sign-ups were from individuals under age 35, including children. About 28% of sign-ups were from young adults aged 18-34 years. That’s similar to the percentage of young adults who signed up for insurance in Massachusetts during the first year of its health reform effort, according to the White House.
"The Affordable Care Act is working," President Obama said during a White House press conference.
He once again called on the ACA’s opponents to stop trying to repeal it.
Rep. Fred Upton (R- Mich.), chairman of the House Energy and Commerce Committee, said the law has disrupted health care for millions of Americans, limited access to physicians, and caused insurance premiums to skyrocket.
"The administration still has not answered basic questions about enrollment and why it will not support fairness for all," Rep. Upton said in a statement.
On Twitter @maryellenny
In the Affordable Care Act’s first open enrollment period, 8 million Americans signed up for private health insurance through the state and federal health marketplaces.
President Obama announced the latest figures on April 17, more than 2 weeks after the close of the first open enrollment period. Though March 31 was the deadline for signing up, individuals who had started the process by the deadline were given until April 15 to complete the process. During that time, nearly 1 million additional people signed up for health plans.
More young people have signed up for coverage as well. President Obama reported that in the federally run marketplaces, 35% of the sign-ups were from individuals under age 35, including children. About 28% of sign-ups were from young adults aged 18-34 years. That’s similar to the percentage of young adults who signed up for insurance in Massachusetts during the first year of its health reform effort, according to the White House.
"The Affordable Care Act is working," President Obama said during a White House press conference.
He once again called on the ACA’s opponents to stop trying to repeal it.
Rep. Fred Upton (R- Mich.), chairman of the House Energy and Commerce Committee, said the law has disrupted health care for millions of Americans, limited access to physicians, and caused insurance premiums to skyrocket.
"The administration still has not answered basic questions about enrollment and why it will not support fairness for all," Rep. Upton said in a statement.
On Twitter @maryellenny
Data derail dogma of elective diverticulitis surgery
BOSTON – The risks of readmission and emergency surgery are low for patients with acute diverticulitis initially managed nonoperatively, a population-based, competing risk analysis found.
At a median of 3.9 years (range, 1.7-6.4 years) after discharge among 14,124 patients, only 8% required urgent readmission. Of these, 22% went on to urgent surgery and 20%, to elective surgery after additional episodes.
Among the remaining 12,981 patients with no urgent readmissions, 9% went on to elective surgery, 13% died of other causes, and 78% had no events in follow-up, Dr. Debbie Li said at the annual meeting of the American Surgical Association.
The 5-year cumulative incidence was 9% for readmission, 1.9% for emergency surgery, and 14.1% for all-cause mortality.
"Elective colectomy may not be warranted for the majority of patients in the absence of chronic symptoms or multiple frequent recurrences," she said.
Elective colectomy has traditionally been recommended for patients at high risk for future recurrence and emergency surgery based on the indications of age less than 50 years, complicated disease including perforation and abscess, and two or more episodes of uncomplicated disease. Evidence is building, however, to challenge these indications, and guidelines are evolving, said Dr. Li, a general surgery resident at the University of Toronto.
The current study used administrative data to identify all patients in Ontario, Canada, treated nonoperatively at first hospitalization for diverticulitis from 2002 to 2012. Time-to-event and competing-risk regression analyses were performed, with data adjusted for such potential confounders as sex, medical comorbidity, neighborhood income quintile, rural residency, and calendar year of index admission.
Data are limited on the natural history of diverticulitis, and the few population-based studies that have been conducted have not accounted for competing risks such as elective colectomy or death, Dr. Li said.
The patients’ median age was 59 years, 79% had uncomplicated index disease, 18% had complicated disease (abscess, fistula, and perforation) with no abscess drain, and 3% had complicated disease with an abscess drain.
Young patients had more readmissions than those 50 years and older (10.5% vs. 8.4%; P less than .001), but not more emergency surgery (1.8% vs. 2.0%; P = .52), she said.
For patients older than 50 years, the risk of death by other causes was 10 times the risk of an emergency surgery for diverticulitis (19.5% vs. 2%).
Patients with complicated rather than uncomplicated index disease had more readmissions (12% vs. 8.2%; P less than .001) and urgent surgery (4.3% vs. 1.4%; P less than .001).
In adjusted analyses, young age was associated with more readmissions (hazard ratio, 1.24), but not subsequent emergency surgery (HR, 0.83). Complicated disease (HR, 3.15) and multiple recurrences (HR, 2.41) predicted an increased risk for emergency surgery.
"Young age, complicated disease, and multiple recurrences do infer increased relative risk, but the vast majority (85%) of such patients remain recurrence free," Dr. Li said.
Invited discussant Dr. David Schoetz, professor of surgery, Tufts University, Boston, said, "While it’s reassuring that even complicated diverticulitis can be safely managed without subsequent operation, there still must be a subgroup who should be offered early surgery."
With disease severity more common in younger patients and overall mortality less than 1%, perhaps aggressive surgery would be justified in those younger than 50 years, he suggested.
Dr. Li responded that an administrative database is unable to capture clinical nuances such as which patients had ongoing symptoms, chronic persistent disease, or reduced quality of life, and that a prospective trial would be needed to identify which subgroup of patients will need aggressive surgery.
Older patients, those with more complicated disease, and those with greater medical comorbidities are more likely to undergo urgent surgery, according to ongoing analyses of roughly 4,000 patients, treated during the same time period, but excluded from the current analysis because they underwent surgery at index admission. Previously published work also suggests that patients with a higher body mass index have poorer outcomes.
A recent systematic review of diverticulitis surgery (JAMA Surg. 2014;149:292-303) reported that complicated recurrence after an episode of uncomplicated diverticulitis is rare, occurring in less than 5% of cases. The authors called for existing guidelines to be updated and said that decisions to proceed with elective surgery should be based instead on patient-reported frequency and severity of symptoms.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
Dr. Li and her coauthors reported no relevant financial disclosures.
urgent surgery, elective surgery, Dr. Debbie Li, American Surgical Association, colectomy, abscess, fistula, perforation, abscess drain, Young patients,
BOSTON – The risks of readmission and emergency surgery are low for patients with acute diverticulitis initially managed nonoperatively, a population-based, competing risk analysis found.
At a median of 3.9 years (range, 1.7-6.4 years) after discharge among 14,124 patients, only 8% required urgent readmission. Of these, 22% went on to urgent surgery and 20%, to elective surgery after additional episodes.
Among the remaining 12,981 patients with no urgent readmissions, 9% went on to elective surgery, 13% died of other causes, and 78% had no events in follow-up, Dr. Debbie Li said at the annual meeting of the American Surgical Association.
The 5-year cumulative incidence was 9% for readmission, 1.9% for emergency surgery, and 14.1% for all-cause mortality.
"Elective colectomy may not be warranted for the majority of patients in the absence of chronic symptoms or multiple frequent recurrences," she said.
Elective colectomy has traditionally been recommended for patients at high risk for future recurrence and emergency surgery based on the indications of age less than 50 years, complicated disease including perforation and abscess, and two or more episodes of uncomplicated disease. Evidence is building, however, to challenge these indications, and guidelines are evolving, said Dr. Li, a general surgery resident at the University of Toronto.
The current study used administrative data to identify all patients in Ontario, Canada, treated nonoperatively at first hospitalization for diverticulitis from 2002 to 2012. Time-to-event and competing-risk regression analyses were performed, with data adjusted for such potential confounders as sex, medical comorbidity, neighborhood income quintile, rural residency, and calendar year of index admission.
Data are limited on the natural history of diverticulitis, and the few population-based studies that have been conducted have not accounted for competing risks such as elective colectomy or death, Dr. Li said.
The patients’ median age was 59 years, 79% had uncomplicated index disease, 18% had complicated disease (abscess, fistula, and perforation) with no abscess drain, and 3% had complicated disease with an abscess drain.
Young patients had more readmissions than those 50 years and older (10.5% vs. 8.4%; P less than .001), but not more emergency surgery (1.8% vs. 2.0%; P = .52), she said.
For patients older than 50 years, the risk of death by other causes was 10 times the risk of an emergency surgery for diverticulitis (19.5% vs. 2%).
Patients with complicated rather than uncomplicated index disease had more readmissions (12% vs. 8.2%; P less than .001) and urgent surgery (4.3% vs. 1.4%; P less than .001).
In adjusted analyses, young age was associated with more readmissions (hazard ratio, 1.24), but not subsequent emergency surgery (HR, 0.83). Complicated disease (HR, 3.15) and multiple recurrences (HR, 2.41) predicted an increased risk for emergency surgery.
"Young age, complicated disease, and multiple recurrences do infer increased relative risk, but the vast majority (85%) of such patients remain recurrence free," Dr. Li said.
Invited discussant Dr. David Schoetz, professor of surgery, Tufts University, Boston, said, "While it’s reassuring that even complicated diverticulitis can be safely managed without subsequent operation, there still must be a subgroup who should be offered early surgery."
With disease severity more common in younger patients and overall mortality less than 1%, perhaps aggressive surgery would be justified in those younger than 50 years, he suggested.
Dr. Li responded that an administrative database is unable to capture clinical nuances such as which patients had ongoing symptoms, chronic persistent disease, or reduced quality of life, and that a prospective trial would be needed to identify which subgroup of patients will need aggressive surgery.
Older patients, those with more complicated disease, and those with greater medical comorbidities are more likely to undergo urgent surgery, according to ongoing analyses of roughly 4,000 patients, treated during the same time period, but excluded from the current analysis because they underwent surgery at index admission. Previously published work also suggests that patients with a higher body mass index have poorer outcomes.
A recent systematic review of diverticulitis surgery (JAMA Surg. 2014;149:292-303) reported that complicated recurrence after an episode of uncomplicated diverticulitis is rare, occurring in less than 5% of cases. The authors called for existing guidelines to be updated and said that decisions to proceed with elective surgery should be based instead on patient-reported frequency and severity of symptoms.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
Dr. Li and her coauthors reported no relevant financial disclosures.
BOSTON – The risks of readmission and emergency surgery are low for patients with acute diverticulitis initially managed nonoperatively, a population-based, competing risk analysis found.
At a median of 3.9 years (range, 1.7-6.4 years) after discharge among 14,124 patients, only 8% required urgent readmission. Of these, 22% went on to urgent surgery and 20%, to elective surgery after additional episodes.
Among the remaining 12,981 patients with no urgent readmissions, 9% went on to elective surgery, 13% died of other causes, and 78% had no events in follow-up, Dr. Debbie Li said at the annual meeting of the American Surgical Association.
The 5-year cumulative incidence was 9% for readmission, 1.9% for emergency surgery, and 14.1% for all-cause mortality.
"Elective colectomy may not be warranted for the majority of patients in the absence of chronic symptoms or multiple frequent recurrences," she said.
Elective colectomy has traditionally been recommended for patients at high risk for future recurrence and emergency surgery based on the indications of age less than 50 years, complicated disease including perforation and abscess, and two or more episodes of uncomplicated disease. Evidence is building, however, to challenge these indications, and guidelines are evolving, said Dr. Li, a general surgery resident at the University of Toronto.
The current study used administrative data to identify all patients in Ontario, Canada, treated nonoperatively at first hospitalization for diverticulitis from 2002 to 2012. Time-to-event and competing-risk regression analyses were performed, with data adjusted for such potential confounders as sex, medical comorbidity, neighborhood income quintile, rural residency, and calendar year of index admission.
Data are limited on the natural history of diverticulitis, and the few population-based studies that have been conducted have not accounted for competing risks such as elective colectomy or death, Dr. Li said.
The patients’ median age was 59 years, 79% had uncomplicated index disease, 18% had complicated disease (abscess, fistula, and perforation) with no abscess drain, and 3% had complicated disease with an abscess drain.
Young patients had more readmissions than those 50 years and older (10.5% vs. 8.4%; P less than .001), but not more emergency surgery (1.8% vs. 2.0%; P = .52), she said.
For patients older than 50 years, the risk of death by other causes was 10 times the risk of an emergency surgery for diverticulitis (19.5% vs. 2%).
Patients with complicated rather than uncomplicated index disease had more readmissions (12% vs. 8.2%; P less than .001) and urgent surgery (4.3% vs. 1.4%; P less than .001).
In adjusted analyses, young age was associated with more readmissions (hazard ratio, 1.24), but not subsequent emergency surgery (HR, 0.83). Complicated disease (HR, 3.15) and multiple recurrences (HR, 2.41) predicted an increased risk for emergency surgery.
"Young age, complicated disease, and multiple recurrences do infer increased relative risk, but the vast majority (85%) of such patients remain recurrence free," Dr. Li said.
Invited discussant Dr. David Schoetz, professor of surgery, Tufts University, Boston, said, "While it’s reassuring that even complicated diverticulitis can be safely managed without subsequent operation, there still must be a subgroup who should be offered early surgery."
With disease severity more common in younger patients and overall mortality less than 1%, perhaps aggressive surgery would be justified in those younger than 50 years, he suggested.
Dr. Li responded that an administrative database is unable to capture clinical nuances such as which patients had ongoing symptoms, chronic persistent disease, or reduced quality of life, and that a prospective trial would be needed to identify which subgroup of patients will need aggressive surgery.
Older patients, those with more complicated disease, and those with greater medical comorbidities are more likely to undergo urgent surgery, according to ongoing analyses of roughly 4,000 patients, treated during the same time period, but excluded from the current analysis because they underwent surgery at index admission. Previously published work also suggests that patients with a higher body mass index have poorer outcomes.
A recent systematic review of diverticulitis surgery (JAMA Surg. 2014;149:292-303) reported that complicated recurrence after an episode of uncomplicated diverticulitis is rare, occurring in less than 5% of cases. The authors called for existing guidelines to be updated and said that decisions to proceed with elective surgery should be based instead on patient-reported frequency and severity of symptoms.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston, is anticipated to be published in the Annals of Surgery, pending editorial review.
Dr. Li and her coauthors reported no relevant financial disclosures.
urgent surgery, elective surgery, Dr. Debbie Li, American Surgical Association, colectomy, abscess, fistula, perforation, abscess drain, Young patients,
urgent surgery, elective surgery, Dr. Debbie Li, American Surgical Association, colectomy, abscess, fistula, perforation, abscess drain, Young patients,
AT ASA 2014
Key clinical point: As recurrence is very rare, conservative nonoperative treatment should be considered first.
Major finding: The 5-year cumulative incidence was 9% for readmission, 1.9% for emergency surgery, and 14.1% for all-cause mortality.
Data source: A population-based, competing risk analysis of 14,124 patients with initial nonoperative management of diverticulitis.
Disclosures: Dr. Li and her coauthors reported no relevant financial disclosures.
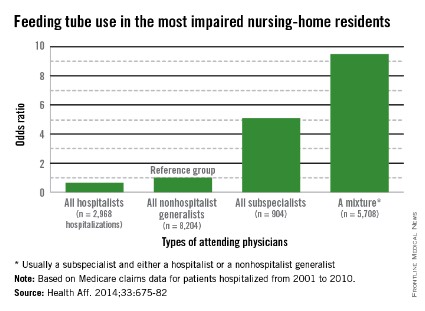
Some providers quicker to tube feed end-of-life elderly
Hospitalists who care for dementia patients near the end of life are much less likely to introduce a feeding tube than other physicians who follow such patients.
Compared with nonhospital generalists, hospitalists were 22% less likely to tube-feed hospitalized nursing home residents – and even less likely to tube-feed patients who were the most severely impaired (35%). In contrast, subspecialists were five times more likely to insert a tube. When a mixed group of physicians was on the case, rates were even higher, with a 9-fold increase overall and a 9.5-fold increase for severely demented patients.
The findings clearly illustrate that nonhospitalists could benefit from some education about the most appropriate interventions when patients near the end of life enter a hospital, Dr. Joan Teno and her associates reported in the April issue of Health Affairs (Health Aff. April 2014;33:675-82).
"It may be that subspecialists do not have adequate knowledge about the risks and benefits of using feeding tubes in people with advanced dementia," said Dr. Teno of Brown University, Providence, R.I., and her coauthors. "Hospitals should educate physicians about the lack of efficacy of PEG [percutaneous endoscopic gastrostomy] feeding tubes, compared with hand feeding, in prolonging survival and preventing aspiration pneumonias and pressure ulcers in people with advanced dementia. In addition, hospitals should examine how they staff the role of attending physician and ensure coordination of care when patient hand-offs are made between different types of attending physicians."
Such education would bring all physicians up to speed with position statements against tube feeding for this group of patients. The issue sits atop the Choosing Wisely lists of both the American Academy of Hospice and Palliative Medicine and the American Geriatrics Society. The American Academy of Hospice and Palliative Medicine states that "feeding tubes do not result in improved survival, prevention of aspiration pneumonia, or improved healing of pressure ulcers. Feeding tube use in such patients has actually been associated with pressure ulcer development, use of physical and pharmacological restraints, and patient distress about the tube itself."
Internal medicine physician Eric G. Tangalos of the Alzheimer’s Disease Research Center at Mayo Clinic, Rochester, Minn., works closely with hospitalists. He agrees with the concept that tube feeding can impose even more distress on both these patients and their families. "As a medical profession and a society, we have yet to accept some of the futility of our actions and continue to ignore the burdens tube feedings place on patients, families, and the health care system once a hospitalization has come to its conclusion," he said in an interview.
Dr. Teno and her team looked at the rate of feeding tube insertion in fee-for-service Medicare patients with advanced dementia who were within 90 days of death and hospitalized with a diagnosis of urinary tract infection, sepsis, pneumonia, or dehydration. The study examined decisions made by four groups of physicians who cared for these patients: hospitalists, nonhospitalist generalists (geriatricians, general practitioners, internists, and family physicians), subspecialists, and mixed groups that included a subspecialist and either a hospitalist or nonhospitalist generalist.
The cohort comprised 53,492 patients hospitalized from 2001 to 2010. The patients’ mean age was 85 years. About 60% had a do not resuscitate order, and 10% had an order against tube feeding.
The rate of hospitalists as attending physicians increased from 11% in 2001 to 28% in 2010. The portion of patients seen by a mixture of attending physicians increased from 29% in 2001 to 38% in 2010.
The rates of tube feeding were lowest when a hospitalist or nonhospitalist generalist was the attending physician (1.6% and 2.2%, respectively). Subspecialists had significantly higher rates (11%). The highest rate occurred when there were mixed groups of physicians involved in the patient’s care (15.6%).
Using the nonhospitalist generalists as a reference group, the researchers found that hospitalists were 22% less likely to insert a tube overall and 35% less likely to do so when the patient had very severe cognitive and physical impairment.
Conversely, subspecialists were five times more likely to commence tube feeding for all patients and for very severely impaired patients. The mixed groups were the most likely to begin tube feeding – almost 9 times more likely overall and 9.5 times more likely for the most severely impaired patients.
"Our finding that subspecialists had a higher rate of insertions of PEG feeding tubes might reflect their lack of experience in providing care for people with advanced dementia," the authors wrote.
The mixed-physician group could be seen as a proxy for discontinuity of care among the attending physicians, they noted. Prior studies have found that such discontinuity was associated with longer hospital stays.
"There may be a lack of care coordination during patient hand offs between attending physicians that begins a cascade of events, ending with the insertion of a PEG feeding tube."
Dr. Diane E. Meier, professor of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and director of the Center to Advance Palliative Care, agreed that group care without a leader creates confusion. "One of the hallmarks of modern medicine in the U.S. is fragmentation. It is typical for a person with dementia to have a different specialist for every organ system, a problem compounded in the hospital when a completely new group of specialists is brought into the care team. The problem with this abundance of doctors is that no one is really in charge of the whole patient and what makes the most sense for the patient as a person. Organ- and specialty-specific decision making leads to bad practices – including trying to ‘solve’ a feeding difficulty as if it is an isolated problem when the real issue is progressive brain failure – a terminal illness that cannot be fixed with a feeding tube."
The study not only questions the feeding tube issue, but also the wisdom of repeatedly hospitalizing elderly patients with severe dementia who could be in the last phase of life – especially for conditions that are expected complications of severe dementia. The authors suggested that there may be financial motives to admit fee-for-service patients.
"The fee-for-service system provides incentives to hospitalize nursing home residents with severe dementia because such hospitalizations qualify the patients for skilled nursing home services. Bundling of payments and institutional special needs plans that reverse these financial incentives may reduce health care expenditures and improve the quality of care for nursing home residents with advanced dementia by avoiding burdensome transitions between facilities and the stress of relocation."
The National Institute on Aging funded the study. Dr. Teno made no financial declarations.
Hospitalists who care for dementia patients near the end of life are much less likely to introduce a feeding tube than other physicians who follow such patients.
Compared with nonhospital generalists, hospitalists were 22% less likely to tube-feed hospitalized nursing home residents – and even less likely to tube-feed patients who were the most severely impaired (35%). In contrast, subspecialists were five times more likely to insert a tube. When a mixed group of physicians was on the case, rates were even higher, with a 9-fold increase overall and a 9.5-fold increase for severely demented patients.
The findings clearly illustrate that nonhospitalists could benefit from some education about the most appropriate interventions when patients near the end of life enter a hospital, Dr. Joan Teno and her associates reported in the April issue of Health Affairs (Health Aff. April 2014;33:675-82).
"It may be that subspecialists do not have adequate knowledge about the risks and benefits of using feeding tubes in people with advanced dementia," said Dr. Teno of Brown University, Providence, R.I., and her coauthors. "Hospitals should educate physicians about the lack of efficacy of PEG [percutaneous endoscopic gastrostomy] feeding tubes, compared with hand feeding, in prolonging survival and preventing aspiration pneumonias and pressure ulcers in people with advanced dementia. In addition, hospitals should examine how they staff the role of attending physician and ensure coordination of care when patient hand-offs are made between different types of attending physicians."
Such education would bring all physicians up to speed with position statements against tube feeding for this group of patients. The issue sits atop the Choosing Wisely lists of both the American Academy of Hospice and Palliative Medicine and the American Geriatrics Society. The American Academy of Hospice and Palliative Medicine states that "feeding tubes do not result in improved survival, prevention of aspiration pneumonia, or improved healing of pressure ulcers. Feeding tube use in such patients has actually been associated with pressure ulcer development, use of physical and pharmacological restraints, and patient distress about the tube itself."
Internal medicine physician Eric G. Tangalos of the Alzheimer’s Disease Research Center at Mayo Clinic, Rochester, Minn., works closely with hospitalists. He agrees with the concept that tube feeding can impose even more distress on both these patients and their families. "As a medical profession and a society, we have yet to accept some of the futility of our actions and continue to ignore the burdens tube feedings place on patients, families, and the health care system once a hospitalization has come to its conclusion," he said in an interview.
Dr. Teno and her team looked at the rate of feeding tube insertion in fee-for-service Medicare patients with advanced dementia who were within 90 days of death and hospitalized with a diagnosis of urinary tract infection, sepsis, pneumonia, or dehydration. The study examined decisions made by four groups of physicians who cared for these patients: hospitalists, nonhospitalist generalists (geriatricians, general practitioners, internists, and family physicians), subspecialists, and mixed groups that included a subspecialist and either a hospitalist or nonhospitalist generalist.
The cohort comprised 53,492 patients hospitalized from 2001 to 2010. The patients’ mean age was 85 years. About 60% had a do not resuscitate order, and 10% had an order against tube feeding.
The rate of hospitalists as attending physicians increased from 11% in 2001 to 28% in 2010. The portion of patients seen by a mixture of attending physicians increased from 29% in 2001 to 38% in 2010.
The rates of tube feeding were lowest when a hospitalist or nonhospitalist generalist was the attending physician (1.6% and 2.2%, respectively). Subspecialists had significantly higher rates (11%). The highest rate occurred when there were mixed groups of physicians involved in the patient’s care (15.6%).
Using the nonhospitalist generalists as a reference group, the researchers found that hospitalists were 22% less likely to insert a tube overall and 35% less likely to do so when the patient had very severe cognitive and physical impairment.
Conversely, subspecialists were five times more likely to commence tube feeding for all patients and for very severely impaired patients. The mixed groups were the most likely to begin tube feeding – almost 9 times more likely overall and 9.5 times more likely for the most severely impaired patients.
"Our finding that subspecialists had a higher rate of insertions of PEG feeding tubes might reflect their lack of experience in providing care for people with advanced dementia," the authors wrote.
The mixed-physician group could be seen as a proxy for discontinuity of care among the attending physicians, they noted. Prior studies have found that such discontinuity was associated with longer hospital stays.
"There may be a lack of care coordination during patient hand offs between attending physicians that begins a cascade of events, ending with the insertion of a PEG feeding tube."
Dr. Diane E. Meier, professor of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and director of the Center to Advance Palliative Care, agreed that group care without a leader creates confusion. "One of the hallmarks of modern medicine in the U.S. is fragmentation. It is typical for a person with dementia to have a different specialist for every organ system, a problem compounded in the hospital when a completely new group of specialists is brought into the care team. The problem with this abundance of doctors is that no one is really in charge of the whole patient and what makes the most sense for the patient as a person. Organ- and specialty-specific decision making leads to bad practices – including trying to ‘solve’ a feeding difficulty as if it is an isolated problem when the real issue is progressive brain failure – a terminal illness that cannot be fixed with a feeding tube."
The study not only questions the feeding tube issue, but also the wisdom of repeatedly hospitalizing elderly patients with severe dementia who could be in the last phase of life – especially for conditions that are expected complications of severe dementia. The authors suggested that there may be financial motives to admit fee-for-service patients.
"The fee-for-service system provides incentives to hospitalize nursing home residents with severe dementia because such hospitalizations qualify the patients for skilled nursing home services. Bundling of payments and institutional special needs plans that reverse these financial incentives may reduce health care expenditures and improve the quality of care for nursing home residents with advanced dementia by avoiding burdensome transitions between facilities and the stress of relocation."
The National Institute on Aging funded the study. Dr. Teno made no financial declarations.
Hospitalists who care for dementia patients near the end of life are much less likely to introduce a feeding tube than other physicians who follow such patients.
Compared with nonhospital generalists, hospitalists were 22% less likely to tube-feed hospitalized nursing home residents – and even less likely to tube-feed patients who were the most severely impaired (35%). In contrast, subspecialists were five times more likely to insert a tube. When a mixed group of physicians was on the case, rates were even higher, with a 9-fold increase overall and a 9.5-fold increase for severely demented patients.
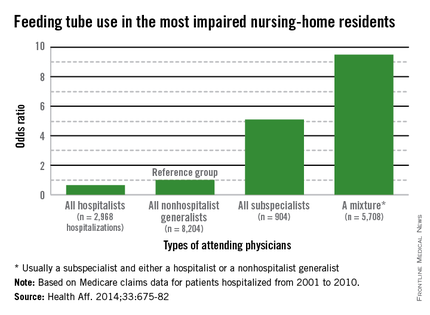
The findings clearly illustrate that nonhospitalists could benefit from some education about the most appropriate interventions when patients near the end of life enter a hospital, Dr. Joan Teno and her associates reported in the April issue of Health Affairs (Health Aff. April 2014;33:675-82).
"It may be that subspecialists do not have adequate knowledge about the risks and benefits of using feeding tubes in people with advanced dementia," said Dr. Teno of Brown University, Providence, R.I., and her coauthors. "Hospitals should educate physicians about the lack of efficacy of PEG [percutaneous endoscopic gastrostomy] feeding tubes, compared with hand feeding, in prolonging survival and preventing aspiration pneumonias and pressure ulcers in people with advanced dementia. In addition, hospitals should examine how they staff the role of attending physician and ensure coordination of care when patient hand-offs are made between different types of attending physicians."
Such education would bring all physicians up to speed with position statements against tube feeding for this group of patients. The issue sits atop the Choosing Wisely lists of both the American Academy of Hospice and Palliative Medicine and the American Geriatrics Society. The American Academy of Hospice and Palliative Medicine states that "feeding tubes do not result in improved survival, prevention of aspiration pneumonia, or improved healing of pressure ulcers. Feeding tube use in such patients has actually been associated with pressure ulcer development, use of physical and pharmacological restraints, and patient distress about the tube itself."
Internal medicine physician Eric G. Tangalos of the Alzheimer’s Disease Research Center at Mayo Clinic, Rochester, Minn., works closely with hospitalists. He agrees with the concept that tube feeding can impose even more distress on both these patients and their families. "As a medical profession and a society, we have yet to accept some of the futility of our actions and continue to ignore the burdens tube feedings place on patients, families, and the health care system once a hospitalization has come to its conclusion," he said in an interview.
Dr. Teno and her team looked at the rate of feeding tube insertion in fee-for-service Medicare patients with advanced dementia who were within 90 days of death and hospitalized with a diagnosis of urinary tract infection, sepsis, pneumonia, or dehydration. The study examined decisions made by four groups of physicians who cared for these patients: hospitalists, nonhospitalist generalists (geriatricians, general practitioners, internists, and family physicians), subspecialists, and mixed groups that included a subspecialist and either a hospitalist or nonhospitalist generalist.
The cohort comprised 53,492 patients hospitalized from 2001 to 2010. The patients’ mean age was 85 years. About 60% had a do not resuscitate order, and 10% had an order against tube feeding.
The rate of hospitalists as attending physicians increased from 11% in 2001 to 28% in 2010. The portion of patients seen by a mixture of attending physicians increased from 29% in 2001 to 38% in 2010.
The rates of tube feeding were lowest when a hospitalist or nonhospitalist generalist was the attending physician (1.6% and 2.2%, respectively). Subspecialists had significantly higher rates (11%). The highest rate occurred when there were mixed groups of physicians involved in the patient’s care (15.6%).
Using the nonhospitalist generalists as a reference group, the researchers found that hospitalists were 22% less likely to insert a tube overall and 35% less likely to do so when the patient had very severe cognitive and physical impairment.
Conversely, subspecialists were five times more likely to commence tube feeding for all patients and for very severely impaired patients. The mixed groups were the most likely to begin tube feeding – almost 9 times more likely overall and 9.5 times more likely for the most severely impaired patients.
"Our finding that subspecialists had a higher rate of insertions of PEG feeding tubes might reflect their lack of experience in providing care for people with advanced dementia," the authors wrote.
The mixed-physician group could be seen as a proxy for discontinuity of care among the attending physicians, they noted. Prior studies have found that such discontinuity was associated with longer hospital stays.
"There may be a lack of care coordination during patient hand offs between attending physicians that begins a cascade of events, ending with the insertion of a PEG feeding tube."
Dr. Diane E. Meier, professor of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and director of the Center to Advance Palliative Care, agreed that group care without a leader creates confusion. "One of the hallmarks of modern medicine in the U.S. is fragmentation. It is typical for a person with dementia to have a different specialist for every organ system, a problem compounded in the hospital when a completely new group of specialists is brought into the care team. The problem with this abundance of doctors is that no one is really in charge of the whole patient and what makes the most sense for the patient as a person. Organ- and specialty-specific decision making leads to bad practices – including trying to ‘solve’ a feeding difficulty as if it is an isolated problem when the real issue is progressive brain failure – a terminal illness that cannot be fixed with a feeding tube."
The study not only questions the feeding tube issue, but also the wisdom of repeatedly hospitalizing elderly patients with severe dementia who could be in the last phase of life – especially for conditions that are expected complications of severe dementia. The authors suggested that there may be financial motives to admit fee-for-service patients.
"The fee-for-service system provides incentives to hospitalize nursing home residents with severe dementia because such hospitalizations qualify the patients for skilled nursing home services. Bundling of payments and institutional special needs plans that reverse these financial incentives may reduce health care expenditures and improve the quality of care for nursing home residents with advanced dementia by avoiding burdensome transitions between facilities and the stress of relocation."
The National Institute on Aging funded the study. Dr. Teno made no financial declarations.
FROM HEALTH AFFAIRS
Major finding: Primary care doctors and subspecialists were up to 9 times more likely to initiate tube feeding in hospitalized patients with severe dementia.
Data source: Data are from a review of more than 53,000 Medicare fee-for-service nursing home patients.
Disclosures: The National Institute on Aging sponsored the study. Dr. Teno had no financial disclosures.
Negotiation: Priceless in good communication
The Society of Hospital Medicine held its annual meeting recently in Las Vegas, and Stephen had the opportunity to speak on the topic of "Family Meetings: The Art and the Evidence." As a special edition of Palliatively Speaking, we thought we would highlight one aspect of this subject, with other elements forthcoming in future pieces.
As a hospitalist, I stumbled and stuttered through many family meetings until I eventually found myself on more comfortable ground. Overall, I found them rewarding when they went well but stressful and deflating when they did not. The latter sensation was enough to create some avoidant behavior on my part.
After a few years of practice, my hospitalist group began shadowing one another periodically on rounds to provide feedback to our colleagues in the hope of improving the quality of our communication skills. It was then that I noticed that one of my partners was a master at these meetings. A real Rembrandt. He had the ability to deliver bad or difficult news without the dynamic in the room becoming inflammatory or out of control.
I will never forget watching him mediate a disagreement between a nurse and a patient suspected of using illicit substances while hospitalized. He flipped an antagonistic, heated situation into one where the patient, nurse, and physician all agreed on putting the past to rest and forging ahead with his proposed plan. We all left the room with a genuine sense that we had mutual purpose. In my admiration I realized that some of these skills must be teachable.
While I didn’t act on learning those communication techniques immediately after that encounter, I would eventually be formally exposed to them during my palliative medicine training. As it turns out, I still have some uncomfortable meetings with patients and families, but they come around much less frequently and when they do I now have a variety of tools to deal with challenges.
My appreciation of these tools doesn’t stop when I walk through the hospital doors each evening. I have found them to be invaluable in my personal life. In fact, learning to communicate better has been a source of renewal for me at work and staves off burnout. These techniques include active listening, motivational interviewing, demonstration of empathy, conflict resolution, and also negotiation. For the Society of Hospital Medicine meeting audience, I dissected negotiation, citing how it and the other skills can inject vitality into your interactions.
In any negotiation, it’s all about the other party. You are the smallest person in the room, the least important.
This is counterintuitive. Oftentimes at work we are trying to convince everyone how important we are. The readmissions committee should implement your plan to reduce recurrent hospitalizations. Your fellow hospitalists should recognize your value and make you the leader of the group. Patients show their appreciation for you making the right diagnosis and averting a medical calamity for them. But when you enter a family meeting, the patient and his or her loved ones are the center stage. To be successful you have to listen more and talk less. Get to understand the pictures in their heads and then summarize those thoughts and ideas back to them to show you’ve listened.
Make emotional payments. I don’t get into the meat of the meeting until I’ve done that with the patient and every family member in the room. No one holds family meetings for patients who are thriving and have outstanding outcomes. We have family meetings to figure out goals in the face of terrible diseases, when elder abuse is a possibility, when insurance-funded resources are depleted, and for a host of other difficult reasons.
This means that everyone in the room is suffering, sacrificing, scared, confused, or worried. Acknowledge them. Hold them up. Thank them. Reflect on similar moments in your life and demonstrate empathy. Apologize when things haven’t gone right for them at your hospital. These payments will pay handsome dividends as your relationship evolves.
Not manipulation. The term negotiation might bring up images of used car salespeople. I strongly disagree. In manipulation, one side wins and the other doesn’t. In negotiation, the goal is improved communication and understanding. Manipulation is about one side of the equation having knowledge that the other side is lacking and using that to achieve its means. Negotiators hope everyone at the table has the same knowledge.
This leads to two key principles of negotiations: transparency and genuineness. Patients and families are excellent at taking the temperature of the room when you sit down to meet with them. Share knowledge. Don’t have any hidden agendas. Following this principle builds trust.
Be incremental. Taking patients from comfortable, familiar territory into that which is uncomfortable or unfamiliar should not be done in one giant leap. Let’s use code status (CS) as an example because of the frequency with which it comes up (though I rarely talk about CS without first understanding the patient’s goals and hopes).
Some patients refuse to talk about CS, so I think incrementally. I ask that they consider talking about CS with me in the future. Very few people refuse to consider something. Two or three days later I ask, "Have you considered talking to me about CS?" That by itself opens up the topic for conversation. In the extremely unusual case where they still won’t engage, I then ask them, "What would it take for you to consider talking to me about this?" More incrementalism.
While this is not nearly an exhaustive list of negotiation techniques, we hope it is stimulating enough that you might be curious enough to learn more on your own and try incorporating this into your practice. If you’re motivated to do so, please feel free to contact us for reading suggestions: E-mail [email protected].
Dr. Bekanich and Dr. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern Residency Programs in Austin.
The Society of Hospital Medicine held its annual meeting recently in Las Vegas, and Stephen had the opportunity to speak on the topic of "Family Meetings: The Art and the Evidence." As a special edition of Palliatively Speaking, we thought we would highlight one aspect of this subject, with other elements forthcoming in future pieces.
As a hospitalist, I stumbled and stuttered through many family meetings until I eventually found myself on more comfortable ground. Overall, I found them rewarding when they went well but stressful and deflating when they did not. The latter sensation was enough to create some avoidant behavior on my part.
After a few years of practice, my hospitalist group began shadowing one another periodically on rounds to provide feedback to our colleagues in the hope of improving the quality of our communication skills. It was then that I noticed that one of my partners was a master at these meetings. A real Rembrandt. He had the ability to deliver bad or difficult news without the dynamic in the room becoming inflammatory or out of control.
I will never forget watching him mediate a disagreement between a nurse and a patient suspected of using illicit substances while hospitalized. He flipped an antagonistic, heated situation into one where the patient, nurse, and physician all agreed on putting the past to rest and forging ahead with his proposed plan. We all left the room with a genuine sense that we had mutual purpose. In my admiration I realized that some of these skills must be teachable.
While I didn’t act on learning those communication techniques immediately after that encounter, I would eventually be formally exposed to them during my palliative medicine training. As it turns out, I still have some uncomfortable meetings with patients and families, but they come around much less frequently and when they do I now have a variety of tools to deal with challenges.
My appreciation of these tools doesn’t stop when I walk through the hospital doors each evening. I have found them to be invaluable in my personal life. In fact, learning to communicate better has been a source of renewal for me at work and staves off burnout. These techniques include active listening, motivational interviewing, demonstration of empathy, conflict resolution, and also negotiation. For the Society of Hospital Medicine meeting audience, I dissected negotiation, citing how it and the other skills can inject vitality into your interactions.
In any negotiation, it’s all about the other party. You are the smallest person in the room, the least important.
This is counterintuitive. Oftentimes at work we are trying to convince everyone how important we are. The readmissions committee should implement your plan to reduce recurrent hospitalizations. Your fellow hospitalists should recognize your value and make you the leader of the group. Patients show their appreciation for you making the right diagnosis and averting a medical calamity for them. But when you enter a family meeting, the patient and his or her loved ones are the center stage. To be successful you have to listen more and talk less. Get to understand the pictures in their heads and then summarize those thoughts and ideas back to them to show you’ve listened.
Make emotional payments. I don’t get into the meat of the meeting until I’ve done that with the patient and every family member in the room. No one holds family meetings for patients who are thriving and have outstanding outcomes. We have family meetings to figure out goals in the face of terrible diseases, when elder abuse is a possibility, when insurance-funded resources are depleted, and for a host of other difficult reasons.
This means that everyone in the room is suffering, sacrificing, scared, confused, or worried. Acknowledge them. Hold them up. Thank them. Reflect on similar moments in your life and demonstrate empathy. Apologize when things haven’t gone right for them at your hospital. These payments will pay handsome dividends as your relationship evolves.
Not manipulation. The term negotiation might bring up images of used car salespeople. I strongly disagree. In manipulation, one side wins and the other doesn’t. In negotiation, the goal is improved communication and understanding. Manipulation is about one side of the equation having knowledge that the other side is lacking and using that to achieve its means. Negotiators hope everyone at the table has the same knowledge.
This leads to two key principles of negotiations: transparency and genuineness. Patients and families are excellent at taking the temperature of the room when you sit down to meet with them. Share knowledge. Don’t have any hidden agendas. Following this principle builds trust.
Be incremental. Taking patients from comfortable, familiar territory into that which is uncomfortable or unfamiliar should not be done in one giant leap. Let’s use code status (CS) as an example because of the frequency with which it comes up (though I rarely talk about CS without first understanding the patient’s goals and hopes).
Some patients refuse to talk about CS, so I think incrementally. I ask that they consider talking about CS with me in the future. Very few people refuse to consider something. Two or three days later I ask, "Have you considered talking to me about CS?" That by itself opens up the topic for conversation. In the extremely unusual case where they still won’t engage, I then ask them, "What would it take for you to consider talking to me about this?" More incrementalism.
While this is not nearly an exhaustive list of negotiation techniques, we hope it is stimulating enough that you might be curious enough to learn more on your own and try incorporating this into your practice. If you’re motivated to do so, please feel free to contact us for reading suggestions: E-mail [email protected].
Dr. Bekanich and Dr. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern Residency Programs in Austin.
The Society of Hospital Medicine held its annual meeting recently in Las Vegas, and Stephen had the opportunity to speak on the topic of "Family Meetings: The Art and the Evidence." As a special edition of Palliatively Speaking, we thought we would highlight one aspect of this subject, with other elements forthcoming in future pieces.
As a hospitalist, I stumbled and stuttered through many family meetings until I eventually found myself on more comfortable ground. Overall, I found them rewarding when they went well but stressful and deflating when they did not. The latter sensation was enough to create some avoidant behavior on my part.
After a few years of practice, my hospitalist group began shadowing one another periodically on rounds to provide feedback to our colleagues in the hope of improving the quality of our communication skills. It was then that I noticed that one of my partners was a master at these meetings. A real Rembrandt. He had the ability to deliver bad or difficult news without the dynamic in the room becoming inflammatory or out of control.
I will never forget watching him mediate a disagreement between a nurse and a patient suspected of using illicit substances while hospitalized. He flipped an antagonistic, heated situation into one where the patient, nurse, and physician all agreed on putting the past to rest and forging ahead with his proposed plan. We all left the room with a genuine sense that we had mutual purpose. In my admiration I realized that some of these skills must be teachable.
While I didn’t act on learning those communication techniques immediately after that encounter, I would eventually be formally exposed to them during my palliative medicine training. As it turns out, I still have some uncomfortable meetings with patients and families, but they come around much less frequently and when they do I now have a variety of tools to deal with challenges.
My appreciation of these tools doesn’t stop when I walk through the hospital doors each evening. I have found them to be invaluable in my personal life. In fact, learning to communicate better has been a source of renewal for me at work and staves off burnout. These techniques include active listening, motivational interviewing, demonstration of empathy, conflict resolution, and also negotiation. For the Society of Hospital Medicine meeting audience, I dissected negotiation, citing how it and the other skills can inject vitality into your interactions.
In any negotiation, it’s all about the other party. You are the smallest person in the room, the least important.
This is counterintuitive. Oftentimes at work we are trying to convince everyone how important we are. The readmissions committee should implement your plan to reduce recurrent hospitalizations. Your fellow hospitalists should recognize your value and make you the leader of the group. Patients show their appreciation for you making the right diagnosis and averting a medical calamity for them. But when you enter a family meeting, the patient and his or her loved ones are the center stage. To be successful you have to listen more and talk less. Get to understand the pictures in their heads and then summarize those thoughts and ideas back to them to show you’ve listened.
Make emotional payments. I don’t get into the meat of the meeting until I’ve done that with the patient and every family member in the room. No one holds family meetings for patients who are thriving and have outstanding outcomes. We have family meetings to figure out goals in the face of terrible diseases, when elder abuse is a possibility, when insurance-funded resources are depleted, and for a host of other difficult reasons.
This means that everyone in the room is suffering, sacrificing, scared, confused, or worried. Acknowledge them. Hold them up. Thank them. Reflect on similar moments in your life and demonstrate empathy. Apologize when things haven’t gone right for them at your hospital. These payments will pay handsome dividends as your relationship evolves.
Not manipulation. The term negotiation might bring up images of used car salespeople. I strongly disagree. In manipulation, one side wins and the other doesn’t. In negotiation, the goal is improved communication and understanding. Manipulation is about one side of the equation having knowledge that the other side is lacking and using that to achieve its means. Negotiators hope everyone at the table has the same knowledge.
This leads to two key principles of negotiations: transparency and genuineness. Patients and families are excellent at taking the temperature of the room when you sit down to meet with them. Share knowledge. Don’t have any hidden agendas. Following this principle builds trust.
Be incremental. Taking patients from comfortable, familiar territory into that which is uncomfortable or unfamiliar should not be done in one giant leap. Let’s use code status (CS) as an example because of the frequency with which it comes up (though I rarely talk about CS without first understanding the patient’s goals and hopes).
Some patients refuse to talk about CS, so I think incrementally. I ask that they consider talking about CS with me in the future. Very few people refuse to consider something. Two or three days later I ask, "Have you considered talking to me about CS?" That by itself opens up the topic for conversation. In the extremely unusual case where they still won’t engage, I then ask them, "What would it take for you to consider talking to me about this?" More incrementalism.
While this is not nearly an exhaustive list of negotiation techniques, we hope it is stimulating enough that you might be curious enough to learn more on your own and try incorporating this into your practice. If you’re motivated to do so, please feel free to contact us for reading suggestions: E-mail [email protected].
Dr. Bekanich and Dr. Fredholm are codirectors of Seton Palliative Care, part of the University of Texas Southwestern Residency Programs in Austin.
Short CAM-S delirium scale predicted clinical outcomes
A new delirium scoring system has shown excellent correlation with clinical outcomes in hospitalized elderly patients, including length of stay, functional decline, and death, investigators report.
In both short and long form, the Confusion Assessment Methods-S (CAM-S) is designed to complement the existing CAM, Dr. Sharon Inouye and her colleagues reported in the April 14 issue of Annals of Internal Medicine (2014;160:526-33).
"The short form (5-minute completion and scoring time), which is based on the CAM diagnostic algorithm alone, is quicker and simpler to rate; however, the long form (10-minute completion and scoring time) provides a broader range of severity scores in delirium and no-delirium groups," wrote Dr. Inouye of the Institute for Aging Research, Boston, and her coauthors.
"Unlike the Delirium Rating Scale, a clinician rater is not required for the CAM-S. Instead, well-trained research assistants can reliably conduct the assessments," the researchers wrote.
Both the short-form and long-form CAM-S instruments were validated in a group of 919 patients aged 70 years or older, who were scheduled for major surgery. The cohort was drawn from two extant study groups: the ongoing SAGES (Successful Aging After Elective Surgery) study,and Project Recovery, which ran from 1995 to 1998. Delirium was first rated by the existing CAM, and then according to the two versions of CAM-S.
The short-form CAM-S rates patients on four features of the CAM: symptom fluctuation, inattention, disorganized thinking, and altered level of consciousness. The most severe score is a 7. The longer form is based on 10 features, which also include disorientation, memory impairment, perceptual disturbances, psychomotor agitation, and sleep-wake cycle disturbance. The most severe score is a 19.
The measures had excellent correlation with each other, and with several clinical outcomes, the investigators said.
Length of hospital stay increased with increasing delirium severity across both forms, with an adjusted mean stay of 6.5 days for no delirium to almost 13 days with high severity in the short form. In the long form, length of stay increased from about 6 days to 12 days.
Hospital costs also tracked severity, ranging from an adjusted mean of $5,100 for no delirium to $13,200 for severe delirium in the short form. A similar pattern emerged in the long form, ranging from $4,200 to $11,400.
Functional decline was also highly correlated with score. On the short form, it occurred in 36%-68% of patients, depending on severity. In the long form, the range was 25%-61%. Cognitive decline showed a similar pattern.
In the short form, the cumulative adjusted rates of death within 90 days ranged from 7% to 27%, depending on severity. In the long form, the range was 7%-22%.
In the composite outcome of death or nursing home placement, results on the short form ranged from 15% to 51%, depending on severity. In the long form, the range was 13%-48%
While the Project Recovery data are more than 16 years old, the researchers said that this time lapse is not an issue because their primary interest is in comparison of outcomes among severity groups, which minimizes the importance of the internal values.
Also, "there may be inherent dependencies between CAM-S score and adverse outcomes," investigators wrote. "For example, patients with longer lengths of stay may have had higher CAM-S scores because of more opportunities for measurement."
The CAM-S score requires validation in groups younger than the age 70-plus patients addressed in the current study, researchers noted.
The National Institute on Aging funded the study. None of the authors reported having any financial declarations.
On Twitter @alz_gal
A new delirium scoring system has shown excellent correlation with clinical outcomes in hospitalized elderly patients, including length of stay, functional decline, and death, investigators report.
In both short and long form, the Confusion Assessment Methods-S (CAM-S) is designed to complement the existing CAM, Dr. Sharon Inouye and her colleagues reported in the April 14 issue of Annals of Internal Medicine (2014;160:526-33).
"The short form (5-minute completion and scoring time), which is based on the CAM diagnostic algorithm alone, is quicker and simpler to rate; however, the long form (10-minute completion and scoring time) provides a broader range of severity scores in delirium and no-delirium groups," wrote Dr. Inouye of the Institute for Aging Research, Boston, and her coauthors.
"Unlike the Delirium Rating Scale, a clinician rater is not required for the CAM-S. Instead, well-trained research assistants can reliably conduct the assessments," the researchers wrote.
Both the short-form and long-form CAM-S instruments were validated in a group of 919 patients aged 70 years or older, who were scheduled for major surgery. The cohort was drawn from two extant study groups: the ongoing SAGES (Successful Aging After Elective Surgery) study,and Project Recovery, which ran from 1995 to 1998. Delirium was first rated by the existing CAM, and then according to the two versions of CAM-S.
The short-form CAM-S rates patients on four features of the CAM: symptom fluctuation, inattention, disorganized thinking, and altered level of consciousness. The most severe score is a 7. The longer form is based on 10 features, which also include disorientation, memory impairment, perceptual disturbances, psychomotor agitation, and sleep-wake cycle disturbance. The most severe score is a 19.
The measures had excellent correlation with each other, and with several clinical outcomes, the investigators said.
Length of hospital stay increased with increasing delirium severity across both forms, with an adjusted mean stay of 6.5 days for no delirium to almost 13 days with high severity in the short form. In the long form, length of stay increased from about 6 days to 12 days.
Hospital costs also tracked severity, ranging from an adjusted mean of $5,100 for no delirium to $13,200 for severe delirium in the short form. A similar pattern emerged in the long form, ranging from $4,200 to $11,400.
Functional decline was also highly correlated with score. On the short form, it occurred in 36%-68% of patients, depending on severity. In the long form, the range was 25%-61%. Cognitive decline showed a similar pattern.
In the short form, the cumulative adjusted rates of death within 90 days ranged from 7% to 27%, depending on severity. In the long form, the range was 7%-22%.
In the composite outcome of death or nursing home placement, results on the short form ranged from 15% to 51%, depending on severity. In the long form, the range was 13%-48%
While the Project Recovery data are more than 16 years old, the researchers said that this time lapse is not an issue because their primary interest is in comparison of outcomes among severity groups, which minimizes the importance of the internal values.
Also, "there may be inherent dependencies between CAM-S score and adverse outcomes," investigators wrote. "For example, patients with longer lengths of stay may have had higher CAM-S scores because of more opportunities for measurement."
The CAM-S score requires validation in groups younger than the age 70-plus patients addressed in the current study, researchers noted.
The National Institute on Aging funded the study. None of the authors reported having any financial declarations.
On Twitter @alz_gal
A new delirium scoring system has shown excellent correlation with clinical outcomes in hospitalized elderly patients, including length of stay, functional decline, and death, investigators report.
In both short and long form, the Confusion Assessment Methods-S (CAM-S) is designed to complement the existing CAM, Dr. Sharon Inouye and her colleagues reported in the April 14 issue of Annals of Internal Medicine (2014;160:526-33).
"The short form (5-minute completion and scoring time), which is based on the CAM diagnostic algorithm alone, is quicker and simpler to rate; however, the long form (10-minute completion and scoring time) provides a broader range of severity scores in delirium and no-delirium groups," wrote Dr. Inouye of the Institute for Aging Research, Boston, and her coauthors.
"Unlike the Delirium Rating Scale, a clinician rater is not required for the CAM-S. Instead, well-trained research assistants can reliably conduct the assessments," the researchers wrote.
Both the short-form and long-form CAM-S instruments were validated in a group of 919 patients aged 70 years or older, who were scheduled for major surgery. The cohort was drawn from two extant study groups: the ongoing SAGES (Successful Aging After Elective Surgery) study,and Project Recovery, which ran from 1995 to 1998. Delirium was first rated by the existing CAM, and then according to the two versions of CAM-S.
The short-form CAM-S rates patients on four features of the CAM: symptom fluctuation, inattention, disorganized thinking, and altered level of consciousness. The most severe score is a 7. The longer form is based on 10 features, which also include disorientation, memory impairment, perceptual disturbances, psychomotor agitation, and sleep-wake cycle disturbance. The most severe score is a 19.
The measures had excellent correlation with each other, and with several clinical outcomes, the investigators said.
Length of hospital stay increased with increasing delirium severity across both forms, with an adjusted mean stay of 6.5 days for no delirium to almost 13 days with high severity in the short form. In the long form, length of stay increased from about 6 days to 12 days.
Hospital costs also tracked severity, ranging from an adjusted mean of $5,100 for no delirium to $13,200 for severe delirium in the short form. A similar pattern emerged in the long form, ranging from $4,200 to $11,400.
Functional decline was also highly correlated with score. On the short form, it occurred in 36%-68% of patients, depending on severity. In the long form, the range was 25%-61%. Cognitive decline showed a similar pattern.
In the short form, the cumulative adjusted rates of death within 90 days ranged from 7% to 27%, depending on severity. In the long form, the range was 7%-22%.
In the composite outcome of death or nursing home placement, results on the short form ranged from 15% to 51%, depending on severity. In the long form, the range was 13%-48%
While the Project Recovery data are more than 16 years old, the researchers said that this time lapse is not an issue because their primary interest is in comparison of outcomes among severity groups, which minimizes the importance of the internal values.
Also, "there may be inherent dependencies between CAM-S score and adverse outcomes," investigators wrote. "For example, patients with longer lengths of stay may have had higher CAM-S scores because of more opportunities for measurement."
The CAM-S score requires validation in groups younger than the age 70-plus patients addressed in the current study, researchers noted.
The National Institute on Aging funded the study. None of the authors reported having any financial declarations.
On Twitter @alz_gal
FROM ANNALS OF INTERNAL MEDICINE
Major finding: Two versions of the CAM-S delirium scale were predictive of major clinical outcomes in the elderly, including death within 30 days of surgery (7%-27%, depending on severity scores).
Data source: CAM-S was validated in a group of 919 patients.
Disclosures: The National Institute on Aging funded the study. Neither Dr. Inouye nor any of the coauthors had any financial disclosures.
VIDEO: The don'ts of social media for physicians
ORLANDO — If you’re on social media sites such as Twitter and Facebook, or considering joining one, there’s one type of post you should absolutely refrain from making.
In an interview at the American College of Physicians annual meeting, Dr. Matthew DeCamp, assistant professor at the Johns Hopkins Berman Institute of Bioethics and in the Johns Hopkins division of general internal medicine, revealed the type of post that poses greatest danger for clinicians, and outlined other tips for safely navigating social media as a physician.
On Twitter @naseemmiller
ORLANDO — If you’re on social media sites such as Twitter and Facebook, or considering joining one, there’s one type of post you should absolutely refrain from making.
In an interview at the American College of Physicians annual meeting, Dr. Matthew DeCamp, assistant professor at the Johns Hopkins Berman Institute of Bioethics and in the Johns Hopkins division of general internal medicine, revealed the type of post that poses greatest danger for clinicians, and outlined other tips for safely navigating social media as a physician.
On Twitter @naseemmiller
ORLANDO — If you’re on social media sites such as Twitter and Facebook, or considering joining one, there’s one type of post you should absolutely refrain from making.
In an interview at the American College of Physicians annual meeting, Dr. Matthew DeCamp, assistant professor at the Johns Hopkins Berman Institute of Bioethics and in the Johns Hopkins division of general internal medicine, revealed the type of post that poses greatest danger for clinicians, and outlined other tips for safely navigating social media as a physician.
On Twitter @naseemmiller
AT ACP INTERNAL MEDICINE 2014
Budget chief Burwell tapped for HHS
Sylvia Mathews Burwell, best known in Washington for managing last fall’s government shutdown, has been tapped to head the Department of Health & Human Services.
On April 11, President Obama announced that Kathleen Sebelius has resigned after 5 years as HHS secretary. The president will nominate Ms. Burwell, the current director of the White House Office of Management and Budget (OMB), to replace Ms. Sebelius.
Ms. Burwell faces confirmation by the Senate, but new rules mean that she will need only a majority of senators to vote in her favor.
Ms. Burwell, a Rhodes Scholar from Hinton, W.Va., was confirmed unanimously by the Senate last year to head the OMB. Before coming to the White House, she served as president of the Walmart Foundation and as president of the global development program at the Bill & Melinda Gates Foundation.
During the Clinton administration, Ms. Burwell worked as deputy director of OMB, as well as in other roles at the White House.
President Obama praised Ms. Burwell as "experienced" and "competent" and said she will bring common sense to the HHS job. "She knows how to deliver results," he said.
President Obama also commended the work done by Ms. Sebelius, saying that she turned around the struggling healthcare.gov website and helped to get 7.5 million Americans signed up for health insurance during the Affordable Care Act’s first open enrollment period.
"The final score speaks for itself," he said.
Ms. Sebelius will remain at the HHS helm until her successor is confirmed.
On Twitter @maryellenny
Sylvia Mathews Burwell, best known in Washington for managing last fall’s government shutdown, has been tapped to head the Department of Health & Human Services.
On April 11, President Obama announced that Kathleen Sebelius has resigned after 5 years as HHS secretary. The president will nominate Ms. Burwell, the current director of the White House Office of Management and Budget (OMB), to replace Ms. Sebelius.
Ms. Burwell faces confirmation by the Senate, but new rules mean that she will need only a majority of senators to vote in her favor.
Ms. Burwell, a Rhodes Scholar from Hinton, W.Va., was confirmed unanimously by the Senate last year to head the OMB. Before coming to the White House, she served as president of the Walmart Foundation and as president of the global development program at the Bill & Melinda Gates Foundation.
During the Clinton administration, Ms. Burwell worked as deputy director of OMB, as well as in other roles at the White House.
President Obama praised Ms. Burwell as "experienced" and "competent" and said she will bring common sense to the HHS job. "She knows how to deliver results," he said.
President Obama also commended the work done by Ms. Sebelius, saying that she turned around the struggling healthcare.gov website and helped to get 7.5 million Americans signed up for health insurance during the Affordable Care Act’s first open enrollment period.
"The final score speaks for itself," he said.
Ms. Sebelius will remain at the HHS helm until her successor is confirmed.
On Twitter @maryellenny
Sylvia Mathews Burwell, best known in Washington for managing last fall’s government shutdown, has been tapped to head the Department of Health & Human Services.
On April 11, President Obama announced that Kathleen Sebelius has resigned after 5 years as HHS secretary. The president will nominate Ms. Burwell, the current director of the White House Office of Management and Budget (OMB), to replace Ms. Sebelius.
Ms. Burwell faces confirmation by the Senate, but new rules mean that she will need only a majority of senators to vote in her favor.
Ms. Burwell, a Rhodes Scholar from Hinton, W.Va., was confirmed unanimously by the Senate last year to head the OMB. Before coming to the White House, she served as president of the Walmart Foundation and as president of the global development program at the Bill & Melinda Gates Foundation.
During the Clinton administration, Ms. Burwell worked as deputy director of OMB, as well as in other roles at the White House.
President Obama praised Ms. Burwell as "experienced" and "competent" and said she will bring common sense to the HHS job. "She knows how to deliver results," he said.
President Obama also commended the work done by Ms. Sebelius, saying that she turned around the struggling healthcare.gov website and helped to get 7.5 million Americans signed up for health insurance during the Affordable Care Act’s first open enrollment period.
"The final score speaks for itself," he said.
Ms. Sebelius will remain at the HHS helm until her successor is confirmed.
On Twitter @maryellenny