User login
Official Newspaper of the American College of Surgeons
Mesh erosion less likely in prior vaginal prolapse repair
CHICAGO – The presence of scar tissue may protect against synthetic mesh erosion following vaginal prolapse repair, according to findings from a retrospective case-control study.
The findings provide further support for the existing American College of Obstetricians and Gynecologists recommendation that vaginal mesh repair should be reserved for women with recurrent prolapse, and may be helpful for preoperative counseling in these patients, according to Dr. Nicholas Kongoasa of Saint Peter’s University Hospital, New Brunswick, N.J.
"Women are four times less likely to have mesh erosion if they have previously undergone prolapse repair, and that mesh should be reserved for those who fail primary repair," Dr. Kongoasa said in an interview.
Dr. Kongoasa was unable to make his presentation at the scheduled session at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Patients in the study included all those who underwent mesh-augmented pelvic floor repair between June 1, 2008, and Dec. 31, 2011. All surgeries were performed by a single surgeon using polypropylene mesh. Of 810 mesh-augmented pelvic floor repair surgeries, 688 involved no prior vaginal prolapse surgery and 142 were in patients with a prior vaginal prolapse repair.
The two groups did not differ with respect to mean operating time, intraoperative complications, postoperative complications, hospital stay, or prolapse recurrence. Also, they were similar in terms of demographics and pelvic organ prolapse quantification staging with the exception of prior hysterectomy in the prior surgery group.
During follow-ups of 1-4.5 years, mesh erosion occurred in 10.6% of those with no prior vaginal prolapse surgery, and in 2.8% of those with prior vaginal prolapse surgery (odds ratio, 4.1).
Among those with mesh erosion, no differences were seen between those with and without prior surgery with respect to time to diagnosis or location and size of erosion.
"The large number of cases and the high odds ratio warrant that this subject be further investigated by future prospective studies," he said.
The study was limited by its retrospective nature and the fact that some patients who experienced complications may have sought care elsewhere.
As for why previous surgery may protect against mesh erosion, "my personal theory is that there is generally less blood supply to the previously operated area, and this may lead to less inflammation and reaction to the foreign body," he said.
Dr. Kongoasa reported having no disclosures.
CHICAGO – The presence of scar tissue may protect against synthetic mesh erosion following vaginal prolapse repair, according to findings from a retrospective case-control study.
The findings provide further support for the existing American College of Obstetricians and Gynecologists recommendation that vaginal mesh repair should be reserved for women with recurrent prolapse, and may be helpful for preoperative counseling in these patients, according to Dr. Nicholas Kongoasa of Saint Peter’s University Hospital, New Brunswick, N.J.
"Women are four times less likely to have mesh erosion if they have previously undergone prolapse repair, and that mesh should be reserved for those who fail primary repair," Dr. Kongoasa said in an interview.
Dr. Kongoasa was unable to make his presentation at the scheduled session at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Patients in the study included all those who underwent mesh-augmented pelvic floor repair between June 1, 2008, and Dec. 31, 2011. All surgeries were performed by a single surgeon using polypropylene mesh. Of 810 mesh-augmented pelvic floor repair surgeries, 688 involved no prior vaginal prolapse surgery and 142 were in patients with a prior vaginal prolapse repair.
The two groups did not differ with respect to mean operating time, intraoperative complications, postoperative complications, hospital stay, or prolapse recurrence. Also, they were similar in terms of demographics and pelvic organ prolapse quantification staging with the exception of prior hysterectomy in the prior surgery group.
During follow-ups of 1-4.5 years, mesh erosion occurred in 10.6% of those with no prior vaginal prolapse surgery, and in 2.8% of those with prior vaginal prolapse surgery (odds ratio, 4.1).
Among those with mesh erosion, no differences were seen between those with and without prior surgery with respect to time to diagnosis or location and size of erosion.
"The large number of cases and the high odds ratio warrant that this subject be further investigated by future prospective studies," he said.
The study was limited by its retrospective nature and the fact that some patients who experienced complications may have sought care elsewhere.
As for why previous surgery may protect against mesh erosion, "my personal theory is that there is generally less blood supply to the previously operated area, and this may lead to less inflammation and reaction to the foreign body," he said.
Dr. Kongoasa reported having no disclosures.
CHICAGO – The presence of scar tissue may protect against synthetic mesh erosion following vaginal prolapse repair, according to findings from a retrospective case-control study.
The findings provide further support for the existing American College of Obstetricians and Gynecologists recommendation that vaginal mesh repair should be reserved for women with recurrent prolapse, and may be helpful for preoperative counseling in these patients, according to Dr. Nicholas Kongoasa of Saint Peter’s University Hospital, New Brunswick, N.J.
"Women are four times less likely to have mesh erosion if they have previously undergone prolapse repair, and that mesh should be reserved for those who fail primary repair," Dr. Kongoasa said in an interview.
Dr. Kongoasa was unable to make his presentation at the scheduled session at the annual meeting of the American Congress of Obstetricians and Gynecologists.
Patients in the study included all those who underwent mesh-augmented pelvic floor repair between June 1, 2008, and Dec. 31, 2011. All surgeries were performed by a single surgeon using polypropylene mesh. Of 810 mesh-augmented pelvic floor repair surgeries, 688 involved no prior vaginal prolapse surgery and 142 were in patients with a prior vaginal prolapse repair.
The two groups did not differ with respect to mean operating time, intraoperative complications, postoperative complications, hospital stay, or prolapse recurrence. Also, they were similar in terms of demographics and pelvic organ prolapse quantification staging with the exception of prior hysterectomy in the prior surgery group.
During follow-ups of 1-4.5 years, mesh erosion occurred in 10.6% of those with no prior vaginal prolapse surgery, and in 2.8% of those with prior vaginal prolapse surgery (odds ratio, 4.1).
Among those with mesh erosion, no differences were seen between those with and without prior surgery with respect to time to diagnosis or location and size of erosion.
"The large number of cases and the high odds ratio warrant that this subject be further investigated by future prospective studies," he said.
The study was limited by its retrospective nature and the fact that some patients who experienced complications may have sought care elsewhere.
As for why previous surgery may protect against mesh erosion, "my personal theory is that there is generally less blood supply to the previously operated area, and this may lead to less inflammation and reaction to the foreign body," he said.
Dr. Kongoasa reported having no disclosures.
AT THE ACOG ANNUAL CLINICAL MEETING
Key clinical point: Vaginal mesh repair should be reserved for women with recurrent prolapse.
Major finding: Mesh erosion occurred in 10.6% of those without and 2.8% of those with prior vaginal prolapse surgery (OR, 4.10).
Data source: A retrospective case-control study involving 810 repairs.
Disclosures: Dr. Kongoasa reported having no disclosures.
New ICD-10 deadline: Oct. 1, 2015
The new deadline for making the switch to the ICD-10 coding system is Oct. 1, 2015, the Centers for Medicare & Medicaid Services announced.
On April 1, President Obama signed legislation that delayed the start of ICD-10 from Oct. 1, 2014, until at least a year later. The law did not specify a new start date, leaving the physicians and health care providers wondering how long they would have to prepare for the new code set.
CMS officials said they will release an interim final rule in the "near future" with more details about the compliance date. But the rule will require physicians to continue to use ICD-9 through Sept. 30, 2015.
On Twitter @maryellenny
The new deadline for making the switch to the ICD-10 coding system is Oct. 1, 2015, the Centers for Medicare & Medicaid Services announced.
On April 1, President Obama signed legislation that delayed the start of ICD-10 from Oct. 1, 2014, until at least a year later. The law did not specify a new start date, leaving the physicians and health care providers wondering how long they would have to prepare for the new code set.
CMS officials said they will release an interim final rule in the "near future" with more details about the compliance date. But the rule will require physicians to continue to use ICD-9 through Sept. 30, 2015.
On Twitter @maryellenny
The new deadline for making the switch to the ICD-10 coding system is Oct. 1, 2015, the Centers for Medicare & Medicaid Services announced.
On April 1, President Obama signed legislation that delayed the start of ICD-10 from Oct. 1, 2014, until at least a year later. The law did not specify a new start date, leaving the physicians and health care providers wondering how long they would have to prepare for the new code set.
CMS officials said they will release an interim final rule in the "near future" with more details about the compliance date. But the rule will require physicians to continue to use ICD-9 through Sept. 30, 2015.
On Twitter @maryellenny
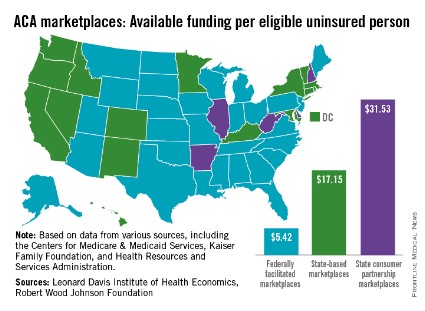
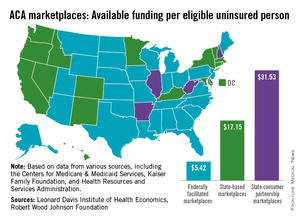
ACA exchanges most expensive in state-based systems
States that opted to run their own Affordable Care Act–mandated health insurance marketplace spent more than three times as much per uninsured person to assist consumers than did states with federally run exchanges.
An analysis by the Leonard Davis Institute of Economics and the Robert Wood Johnson Foundation showed that the 17 state-based marketplaces (SBMs) spent an average of $17.15/eligible uninsured person, compared with $5.42/eligible uninsured person in the 29 federally facilitated marketplaces (FFMs). The five states that use a state-consumer partnership to run their marketplaces spent $31.53/uninsured person.
"SBMs accounted for 50% of total consumer assistance funds, although they have just 31% of all uninsured. In contrast, 63% of the uninsured live in FFM states, which accounted for 33% of the funding. The five partnership states in charge of consumer assistance functions were home to just 6% of the uninsured, but garnered 17% of the funding," the report noted.
The District of Columbia, grouped among the SBM states, spent $163.93/uninsured person, which was higher than any state. The highest-spending state was Hawaii (SBM) at $87.86, and the lowest-spending state was Georgia (FFM), which spent $4.24 per uninsured person, according to the report.
The joint study used data from the Centers for Medicare & Medicaid Services, the Kaiser Family Foundation, and the Health Resources and Services Administration. The Leonard Davis Institute is a cooperative venture between the University of Pennsylvania and the Children’s Hospital of Philadelphia.
States that opted to run their own Affordable Care Act–mandated health insurance marketplace spent more than three times as much per uninsured person to assist consumers than did states with federally run exchanges.
An analysis by the Leonard Davis Institute of Economics and the Robert Wood Johnson Foundation showed that the 17 state-based marketplaces (SBMs) spent an average of $17.15/eligible uninsured person, compared with $5.42/eligible uninsured person in the 29 federally facilitated marketplaces (FFMs). The five states that use a state-consumer partnership to run their marketplaces spent $31.53/uninsured person.
"SBMs accounted for 50% of total consumer assistance funds, although they have just 31% of all uninsured. In contrast, 63% of the uninsured live in FFM states, which accounted for 33% of the funding. The five partnership states in charge of consumer assistance functions were home to just 6% of the uninsured, but garnered 17% of the funding," the report noted.
The District of Columbia, grouped among the SBM states, spent $163.93/uninsured person, which was higher than any state. The highest-spending state was Hawaii (SBM) at $87.86, and the lowest-spending state was Georgia (FFM), which spent $4.24 per uninsured person, according to the report.
The joint study used data from the Centers for Medicare & Medicaid Services, the Kaiser Family Foundation, and the Health Resources and Services Administration. The Leonard Davis Institute is a cooperative venture between the University of Pennsylvania and the Children’s Hospital of Philadelphia.
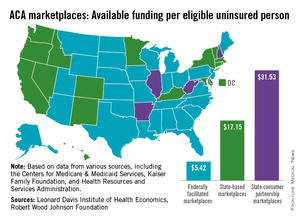
States that opted to run their own Affordable Care Act–mandated health insurance marketplace spent more than three times as much per uninsured person to assist consumers than did states with federally run exchanges.
An analysis by the Leonard Davis Institute of Economics and the Robert Wood Johnson Foundation showed that the 17 state-based marketplaces (SBMs) spent an average of $17.15/eligible uninsured person, compared with $5.42/eligible uninsured person in the 29 federally facilitated marketplaces (FFMs). The five states that use a state-consumer partnership to run their marketplaces spent $31.53/uninsured person.
"SBMs accounted for 50% of total consumer assistance funds, although they have just 31% of all uninsured. In contrast, 63% of the uninsured live in FFM states, which accounted for 33% of the funding. The five partnership states in charge of consumer assistance functions were home to just 6% of the uninsured, but garnered 17% of the funding," the report noted.
The District of Columbia, grouped among the SBM states, spent $163.93/uninsured person, which was higher than any state. The highest-spending state was Hawaii (SBM) at $87.86, and the lowest-spending state was Georgia (FFM), which spent $4.24 per uninsured person, according to the report.
The joint study used data from the Centers for Medicare & Medicaid Services, the Kaiser Family Foundation, and the Health Resources and Services Administration. The Leonard Davis Institute is a cooperative venture between the University of Pennsylvania and the Children’s Hospital of Philadelphia.
Eight million enroll in ACA plans; 28% are young adults
With the official figures in, the federal government reported that more than 8 million Americans enrolled in private health plans through either state- or federally run insurance marketplaces between Oct. 1 and April 19.
A month after the close of the Affordable Care Act’s first open enrollment period, the Health & Human Services department released a detailed accounting of enrollment through the marketplaces. The final number for private plans was 8,019,763, including individuals who enrolled during the special enrollment extension ending April 19.
HHS officials still could not say how many of the individuals who signed up for coverage had paid their premiums. That information won’t be available until later this year, they said.
It’s also still unclear how many of those who signed up for health plans through the marketplaces gained coverage for the first time. Among the 5.18 million individuals who selected plans in the federal marketplaces and also applied for financial assistance, only 13% said they had coverage at the time of their application. But HHS officials said that number is probably not reliable because it only includes a subset of enrollees and they were asked a narrow question about coverage, which did not take into account whether individuals had recently lost their coverage.
According to federal officials, an additional 4.8 million people gained insurance coverage via Medicaid and the Children’s Health Insurance Program, an additional 3 million adults under age 26 gained coverage by staying on their parents’ health plans, and an estimated 5 million people gained coverage by buying ACA-compliant plans outside of the marketplaces.
The report also sheds some light on who the newly insured are.
The majority of those who signed up for coverage on the ACA marketplaces were women (54%). About a third were under age 35, with 28% between the ages of 18 and 34 years. The largest number of sign-ups were among individuals aged 45-54 years (23%) and 55-64 years (25%).
Most who signed up (85%) qualified for financial assistance. The most popular type of health plan was the "silver" plan, with 65% selecting that plan and another 20% opting for the "bronze" plans.
Race/ethnicity was reported by 69% of enrollees. Of those, nearly 63% reported their race/ethnicity as white, 17% were African American, 11% were Latino, 8% were Asian, 1% were multiracial, and less than 1% were American Indian/Alaska Native and Native Hawaiian/Pacific Islander.
Republican lawmakers on the House Energy and Commerce Committee contend that only 67% of those who have selected a health plan in the federal marketplaces had paid their first month’s premium as of April 15. The committee said their information came from asking the insurance companies participating in the marketplaces for their enrollment data.
On Twitter @maryellenny
With the official figures in, the federal government reported that more than 8 million Americans enrolled in private health plans through either state- or federally run insurance marketplaces between Oct. 1 and April 19.
A month after the close of the Affordable Care Act’s first open enrollment period, the Health & Human Services department released a detailed accounting of enrollment through the marketplaces. The final number for private plans was 8,019,763, including individuals who enrolled during the special enrollment extension ending April 19.
HHS officials still could not say how many of the individuals who signed up for coverage had paid their premiums. That information won’t be available until later this year, they said.
It’s also still unclear how many of those who signed up for health plans through the marketplaces gained coverage for the first time. Among the 5.18 million individuals who selected plans in the federal marketplaces and also applied for financial assistance, only 13% said they had coverage at the time of their application. But HHS officials said that number is probably not reliable because it only includes a subset of enrollees and they were asked a narrow question about coverage, which did not take into account whether individuals had recently lost their coverage.
According to federal officials, an additional 4.8 million people gained insurance coverage via Medicaid and the Children’s Health Insurance Program, an additional 3 million adults under age 26 gained coverage by staying on their parents’ health plans, and an estimated 5 million people gained coverage by buying ACA-compliant plans outside of the marketplaces.
The report also sheds some light on who the newly insured are.
The majority of those who signed up for coverage on the ACA marketplaces were women (54%). About a third were under age 35, with 28% between the ages of 18 and 34 years. The largest number of sign-ups were among individuals aged 45-54 years (23%) and 55-64 years (25%).
Most who signed up (85%) qualified for financial assistance. The most popular type of health plan was the "silver" plan, with 65% selecting that plan and another 20% opting for the "bronze" plans.
Race/ethnicity was reported by 69% of enrollees. Of those, nearly 63% reported their race/ethnicity as white, 17% were African American, 11% were Latino, 8% were Asian, 1% were multiracial, and less than 1% were American Indian/Alaska Native and Native Hawaiian/Pacific Islander.
Republican lawmakers on the House Energy and Commerce Committee contend that only 67% of those who have selected a health plan in the federal marketplaces had paid their first month’s premium as of April 15. The committee said their information came from asking the insurance companies participating in the marketplaces for their enrollment data.
On Twitter @maryellenny
With the official figures in, the federal government reported that more than 8 million Americans enrolled in private health plans through either state- or federally run insurance marketplaces between Oct. 1 and April 19.
A month after the close of the Affordable Care Act’s first open enrollment period, the Health & Human Services department released a detailed accounting of enrollment through the marketplaces. The final number for private plans was 8,019,763, including individuals who enrolled during the special enrollment extension ending April 19.
HHS officials still could not say how many of the individuals who signed up for coverage had paid their premiums. That information won’t be available until later this year, they said.
It’s also still unclear how many of those who signed up for health plans through the marketplaces gained coverage for the first time. Among the 5.18 million individuals who selected plans in the federal marketplaces and also applied for financial assistance, only 13% said they had coverage at the time of their application. But HHS officials said that number is probably not reliable because it only includes a subset of enrollees and they were asked a narrow question about coverage, which did not take into account whether individuals had recently lost their coverage.
According to federal officials, an additional 4.8 million people gained insurance coverage via Medicaid and the Children’s Health Insurance Program, an additional 3 million adults under age 26 gained coverage by staying on their parents’ health plans, and an estimated 5 million people gained coverage by buying ACA-compliant plans outside of the marketplaces.
The report also sheds some light on who the newly insured are.
The majority of those who signed up for coverage on the ACA marketplaces were women (54%). About a third were under age 35, with 28% between the ages of 18 and 34 years. The largest number of sign-ups were among individuals aged 45-54 years (23%) and 55-64 years (25%).
Most who signed up (85%) qualified for financial assistance. The most popular type of health plan was the "silver" plan, with 65% selecting that plan and another 20% opting for the "bronze" plans.
Race/ethnicity was reported by 69% of enrollees. Of those, nearly 63% reported their race/ethnicity as white, 17% were African American, 11% were Latino, 8% were Asian, 1% were multiracial, and less than 1% were American Indian/Alaska Native and Native Hawaiian/Pacific Islander.
Republican lawmakers on the House Energy and Commerce Committee contend that only 67% of those who have selected a health plan in the federal marketplaces had paid their first month’s premium as of April 15. The committee said their information came from asking the insurance companies participating in the marketplaces for their enrollment data.
On Twitter @maryellenny
Medicare projects $241M drop in hospital payments
General acute care hospitals are likely to see their Medicare payments drop slightly next year because of penalties for readmissions and hospital-acquired conditions, as well as other proposed payment cuts.
The Centers for Medicare & Medicaid Services released a proposed rule with new payment policies for fiscal year 2015 under the Inpatient Prospective Payment System and the Long-Term Care Hospital Prospective Payment System April 30. The proposal would provide a 1.3% payment increase for general acute care hospitals for fiscal year 2015 and a 0.8% increase for long-term care hospitals.
But the agency estimates that general acute care hospitals will actually see a 0.8% pay cut because of reductions from the Hospital Readmissions Reduction Program, the Hospital-Acquired Condition Reduction Program, cuts to disproportionate share hospitals, and the expiration of some temporary payment increases.
Overall, the CMS estimates that Medicare spending on inpatient hospital services will drop by about $241 million in the next fiscal year, while payments to long-term care hospitals are projected to increase by $44 million.
The proposal also places new requirements on hospitals to be open with their patients about prices. Under the rule, the CMS is requiring hospitals to either make a list of their standard charges publicly available or publicize their policies for allowing the public to view a list of charges upon request.
"This proposed rule is geared toward improving hospital performance while creating an environment for improved Medicare beneficiary care and satisfaction," CMS Administrator Marilyn Tavenner said in a statement.
The proposal also increases the penalties for some quality improvement programs: For example, the CMS will reduce the base operating diagnosis-related group payment amounts for all hospitals 1.5%, up from 1.25% this year. Overall, the CMS estimates that $1.4 billion will be available to fund incentive payments through the program in the next fiscal year.
The proposal also calls for increasing penalties* for hospital readmissions from 2% to 3% starting in October. Hospitals will be evaluated based on how well they do in reducing readmissions due to myocardial infarction, heart failure, pneumonia, chronic obstructive pulmonary disease, and hip/knee arthroplasty.
The CMS is also proposing to launch the Hospital Acquired Condition Reduction Program in October. This Affordable Care Act program will reduce Medicare inpatient payments by 1% for hospitals with the poorest record of preventing hospital-acquired conditions.
The public can comment on the proposal until June 30 at regulations.gov. The CMS said a final rule will be issued by Aug. 1.
On Twitter @maryellenny
*CORRECTION, 5/2/2014: An earlier version of this story incorrectly stated that there would be increased payments for hospital readmissions
General acute care hospitals are likely to see their Medicare payments drop slightly next year because of penalties for readmissions and hospital-acquired conditions, as well as other proposed payment cuts.
The Centers for Medicare & Medicaid Services released a proposed rule with new payment policies for fiscal year 2015 under the Inpatient Prospective Payment System and the Long-Term Care Hospital Prospective Payment System April 30. The proposal would provide a 1.3% payment increase for general acute care hospitals for fiscal year 2015 and a 0.8% increase for long-term care hospitals.
But the agency estimates that general acute care hospitals will actually see a 0.8% pay cut because of reductions from the Hospital Readmissions Reduction Program, the Hospital-Acquired Condition Reduction Program, cuts to disproportionate share hospitals, and the expiration of some temporary payment increases.
Overall, the CMS estimates that Medicare spending on inpatient hospital services will drop by about $241 million in the next fiscal year, while payments to long-term care hospitals are projected to increase by $44 million.
The proposal also places new requirements on hospitals to be open with their patients about prices. Under the rule, the CMS is requiring hospitals to either make a list of their standard charges publicly available or publicize their policies for allowing the public to view a list of charges upon request.
"This proposed rule is geared toward improving hospital performance while creating an environment for improved Medicare beneficiary care and satisfaction," CMS Administrator Marilyn Tavenner said in a statement.
The proposal also increases the penalties for some quality improvement programs: For example, the CMS will reduce the base operating diagnosis-related group payment amounts for all hospitals 1.5%, up from 1.25% this year. Overall, the CMS estimates that $1.4 billion will be available to fund incentive payments through the program in the next fiscal year.
The proposal also calls for increasing penalties* for hospital readmissions from 2% to 3% starting in October. Hospitals will be evaluated based on how well they do in reducing readmissions due to myocardial infarction, heart failure, pneumonia, chronic obstructive pulmonary disease, and hip/knee arthroplasty.
The CMS is also proposing to launch the Hospital Acquired Condition Reduction Program in October. This Affordable Care Act program will reduce Medicare inpatient payments by 1% for hospitals with the poorest record of preventing hospital-acquired conditions.
The public can comment on the proposal until June 30 at regulations.gov. The CMS said a final rule will be issued by Aug. 1.
On Twitter @maryellenny
*CORRECTION, 5/2/2014: An earlier version of this story incorrectly stated that there would be increased payments for hospital readmissions
General acute care hospitals are likely to see their Medicare payments drop slightly next year because of penalties for readmissions and hospital-acquired conditions, as well as other proposed payment cuts.
The Centers for Medicare & Medicaid Services released a proposed rule with new payment policies for fiscal year 2015 under the Inpatient Prospective Payment System and the Long-Term Care Hospital Prospective Payment System April 30. The proposal would provide a 1.3% payment increase for general acute care hospitals for fiscal year 2015 and a 0.8% increase for long-term care hospitals.
But the agency estimates that general acute care hospitals will actually see a 0.8% pay cut because of reductions from the Hospital Readmissions Reduction Program, the Hospital-Acquired Condition Reduction Program, cuts to disproportionate share hospitals, and the expiration of some temporary payment increases.
Overall, the CMS estimates that Medicare spending on inpatient hospital services will drop by about $241 million in the next fiscal year, while payments to long-term care hospitals are projected to increase by $44 million.
The proposal also places new requirements on hospitals to be open with their patients about prices. Under the rule, the CMS is requiring hospitals to either make a list of their standard charges publicly available or publicize their policies for allowing the public to view a list of charges upon request.
"This proposed rule is geared toward improving hospital performance while creating an environment for improved Medicare beneficiary care and satisfaction," CMS Administrator Marilyn Tavenner said in a statement.
The proposal also increases the penalties for some quality improvement programs: For example, the CMS will reduce the base operating diagnosis-related group payment amounts for all hospitals 1.5%, up from 1.25% this year. Overall, the CMS estimates that $1.4 billion will be available to fund incentive payments through the program in the next fiscal year.
The proposal also calls for increasing penalties* for hospital readmissions from 2% to 3% starting in October. Hospitals will be evaluated based on how well they do in reducing readmissions due to myocardial infarction, heart failure, pneumonia, chronic obstructive pulmonary disease, and hip/knee arthroplasty.
The CMS is also proposing to launch the Hospital Acquired Condition Reduction Program in October. This Affordable Care Act program will reduce Medicare inpatient payments by 1% for hospitals with the poorest record of preventing hospital-acquired conditions.
The public can comment on the proposal until June 30 at regulations.gov. The CMS said a final rule will be issued by Aug. 1.
On Twitter @maryellenny
*CORRECTION, 5/2/2014: An earlier version of this story incorrectly stated that there would be increased payments for hospital readmissions
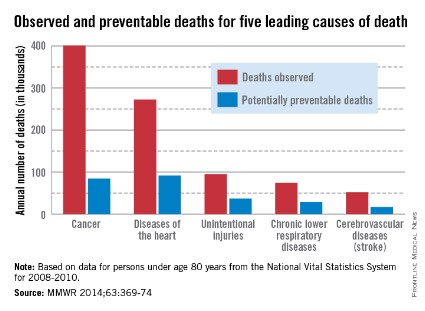
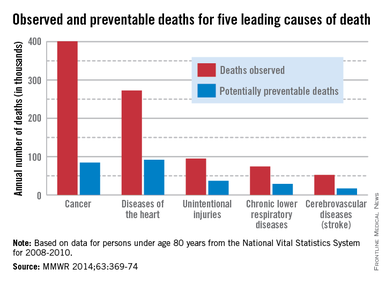
CDC: Policy changes could prevent 100,000 deaths a year
About one-third of heart disease deaths and one-fifth of cancer deaths could be prevented if overall U.S. death rates were the same as those in the states with the lowest rates, the Centers for Disease Control and Prevention reported May 1.
By using an average of the three states with the lowest death rates as a benchmark for each of the five causes, the analysis showed that 91,757 deaths from heart disease could be prevented each year. For cancer, 84,443 deaths could be prevented annually, according to the CDC report (MMWR 2014;63:369-74).
The total number of potentially preventable deaths is around 100,000, because the figures for each cause cannot be added together because someone who doesn’t die of heart disease may die of cancer or stroke, CDC Director Tom Frieden noted in a press briefing. For the rest of the top five causes of death, the numbers of avoidable deaths were 36,836 for unintentional injuries, 28,831 for chronic lower respiratory disease, and 16,973 for cerebrovascular disease.
The report highlights "the enormous variability among states" when it comes to public health policy, he said, with deaths for all five causes highest in the Southeast.
"In this country, your health and safety are determined more by your ZIP code than your genetic code," Dr. Frieden said. "We need to move the needle on policy change and programmatic change."
The analysis used mortality data from 2008 to 2010 for those younger than age 80 years from the National Vital Statistics System.
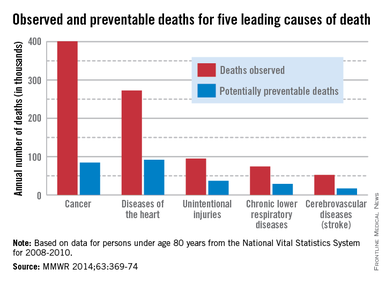
About one-third of heart disease deaths and one-fifth of cancer deaths could be prevented if overall U.S. death rates were the same as those in the states with the lowest rates, the Centers for Disease Control and Prevention reported May 1.
By using an average of the three states with the lowest death rates as a benchmark for each of the five causes, the analysis showed that 91,757 deaths from heart disease could be prevented each year. For cancer, 84,443 deaths could be prevented annually, according to the CDC report (MMWR 2014;63:369-74).
The total number of potentially preventable deaths is around 100,000, because the figures for each cause cannot be added together because someone who doesn’t die of heart disease may die of cancer or stroke, CDC Director Tom Frieden noted in a press briefing. For the rest of the top five causes of death, the numbers of avoidable deaths were 36,836 for unintentional injuries, 28,831 for chronic lower respiratory disease, and 16,973 for cerebrovascular disease.
The report highlights "the enormous variability among states" when it comes to public health policy, he said, with deaths for all five causes highest in the Southeast.
"In this country, your health and safety are determined more by your ZIP code than your genetic code," Dr. Frieden said. "We need to move the needle on policy change and programmatic change."
The analysis used mortality data from 2008 to 2010 for those younger than age 80 years from the National Vital Statistics System.
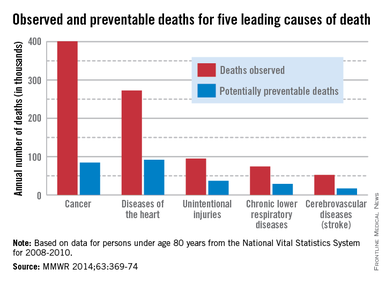
About one-third of heart disease deaths and one-fifth of cancer deaths could be prevented if overall U.S. death rates were the same as those in the states with the lowest rates, the Centers for Disease Control and Prevention reported May 1.
By using an average of the three states with the lowest death rates as a benchmark for each of the five causes, the analysis showed that 91,757 deaths from heart disease could be prevented each year. For cancer, 84,443 deaths could be prevented annually, according to the CDC report (MMWR 2014;63:369-74).
The total number of potentially preventable deaths is around 100,000, because the figures for each cause cannot be added together because someone who doesn’t die of heart disease may die of cancer or stroke, CDC Director Tom Frieden noted in a press briefing. For the rest of the top five causes of death, the numbers of avoidable deaths were 36,836 for unintentional injuries, 28,831 for chronic lower respiratory disease, and 16,973 for cerebrovascular disease.
The report highlights "the enormous variability among states" when it comes to public health policy, he said, with deaths for all five causes highest in the Southeast.
"In this country, your health and safety are determined more by your ZIP code than your genetic code," Dr. Frieden said. "We need to move the needle on policy change and programmatic change."
The analysis used mortality data from 2008 to 2010 for those younger than age 80 years from the National Vital Statistics System.
FROM MMWR
Liver transplant exceptions deserve fresh look
Room air hypoxemia was associated with greater post–liver transplant mortality in hepatopulmonary syndrome patients, according to Dr. David S. Goldberg and his colleagues.
On the other hand, HPS transplant candidates had overall decreased pretransplantation mortality compared with non-HPS patients, suggesting that "current exception policy might overprioritize waitlisted HPS patients," they wrote.
The report appears in the May 1 issue of Gastroenterology (doi:10.1053/j.gastro.2014.01.005).
Dr. Goldberg of the University of Pennsylvania, Philadelphia, looked at all 973 liver transplant candidates from the United Network for Organ Sharing database who had at least one exception application for HPS approved between Feb. 27, 2002, and Dec. 14, 2012.
For comparison, the authors assessed 59,619 non-HPS adult waitlist candidates who registered for their first liver transplantation on or after Feb. 27, 2002.
Overall, there was a 1-year posttransplant survival rate of 91%, a 3-year survival rate of 81%, and a 5-year rate of 76% among the HPS cohort, the authors wrote. Those rates were comparable with the 1-year, 3-year, and 5-year posttransplant rates for non-HPS patients of 89%, 81%, and 74%.
However, looking at pretransplant survival, the authors found that a significantly greater proportion of non-HPS transplant candidates died on the waitlist, compared with HPS patients (20% vs. 9%; P less than .001). That translated to a hazard ratio of 0.82 among HPS patients for dying on the waitlist, compared with non-HPS patients (95% confidence interval, 0.70-0.96).
Next, the authors assessed the relationship between pretransplant room air oxygenation among HPS patients on posttransplant survival rates. They found that patients with pretransplant PaO2 (partial pressure of oxygen in arterial blood) levels of less than 50 mm Hg had a significantly higher posttransplant mortality, compared with patients with PaO2 levels between 50 and 59 mm Hg (HR = 1.56; 95% CI, 1.02-2.38).
Similarly, in a cubic spline model, transplant recipients with a PaO2 of less than 44.0 mm Hg had significantly increased posttransplantation mortality compared with recipients with a PaO2 of 44.1-54.0 mm Hg (HR = 1.58; 95% CI, 1.15-2.18).
"These data must be taken in context, as the 5-year posttransplantation patient survival in HPS patients with the lowest values of PaO2 is still at or above a threshold many would consider acceptable for a transplant recipient," the authors cautioned. "Therefore, the transplant community must decide what degree of hypoxemia makes a patient too high risk," they added.
The authors conceded several limitations. "First, we were unable to employ the strict criteria defining HPS used in prospective multicenter studies," they wrote.
"However, we are confident that most, if not all, of the patients had HPS based on the data documenting hypoxemia and shunting in nearly 90% of patients."
Nevertheless, "excellent posttransplantation outcomes in those with less severe hypoxemia suggest that it might be possible to optimize posttransplantation outcomes for patients with HPS without disadvantaging the broader transplant population," they wrote.
This could be accomplished by a review of current exception algorithms, and "by decreasing the initial number of exception points for HPS patients, while offering additional priority to those whose PaO2 values decline toward higher-risk values," they wrote.
Given the fact that this would increase the overall waitlist time, "an increase rather than decrease in data collected regarding these patients is needed to guide policy," they concluded.
The authors disclosed no conflicts of interest. Dr. Goldberg reported receiving funding from the National Institutes of Health, and the study was partially supported by the Health Resources and Services Administration.
This study is an important reminder of the need for ongoing evidence-based revision of the MELD-based liver allocation system. It has been clear since the adoption of MELD for the purpose of organ allocation that there are patients for whom the laboratory components of the MELD score do not accurately portray their disease-associated risk of death. Thus, there is widespread petitioning for MELD exception points for a number of conditions, including hepatopulmonary syndrome (HPS). While criteria for some such conditions are clearly defined, most prominently including hepatocellular carcinoma, for most other conditions practices vary by region and criteria are not always strictly adhered to.
The initial number of points granted for most conditions, including HPS, is arbitrary rather than based on objective analysis. This study suggests that while posttransplant outcomes are similar between patients with HPS exception points and those without points, pretransplant survival is superior in the HPS group, suggesting that perhaps a lower MELD score should be assigned to these patients.
While exceptions are currently a fundamental part of MELD-based liver allocation, greater standardization of MELD exception point criteria is urgently needed. Additional analysis of wait list survival and survival benefit models will be required to ensure that individual groups of patients are not being unjustly overprioritized.
Dr. Elizabeth C. Verna is assistant professor of medicine, Center for Liver Disease and Transplantation, Division of Digestive and Liver Diseases, Columbia University College of Physicians and Surgeons, New York. She disclosed no conflicts of interest.
This study is an important reminder of the need for ongoing evidence-based revision of the MELD-based liver allocation system. It has been clear since the adoption of MELD for the purpose of organ allocation that there are patients for whom the laboratory components of the MELD score do not accurately portray their disease-associated risk of death. Thus, there is widespread petitioning for MELD exception points for a number of conditions, including hepatopulmonary syndrome (HPS). While criteria for some such conditions are clearly defined, most prominently including hepatocellular carcinoma, for most other conditions practices vary by region and criteria are not always strictly adhered to.
The initial number of points granted for most conditions, including HPS, is arbitrary rather than based on objective analysis. This study suggests that while posttransplant outcomes are similar between patients with HPS exception points and those without points, pretransplant survival is superior in the HPS group, suggesting that perhaps a lower MELD score should be assigned to these patients.
While exceptions are currently a fundamental part of MELD-based liver allocation, greater standardization of MELD exception point criteria is urgently needed. Additional analysis of wait list survival and survival benefit models will be required to ensure that individual groups of patients are not being unjustly overprioritized.
Dr. Elizabeth C. Verna is assistant professor of medicine, Center for Liver Disease and Transplantation, Division of Digestive and Liver Diseases, Columbia University College of Physicians and Surgeons, New York. She disclosed no conflicts of interest.
This study is an important reminder of the need for ongoing evidence-based revision of the MELD-based liver allocation system. It has been clear since the adoption of MELD for the purpose of organ allocation that there are patients for whom the laboratory components of the MELD score do not accurately portray their disease-associated risk of death. Thus, there is widespread petitioning for MELD exception points for a number of conditions, including hepatopulmonary syndrome (HPS). While criteria for some such conditions are clearly defined, most prominently including hepatocellular carcinoma, for most other conditions practices vary by region and criteria are not always strictly adhered to.
The initial number of points granted for most conditions, including HPS, is arbitrary rather than based on objective analysis. This study suggests that while posttransplant outcomes are similar between patients with HPS exception points and those without points, pretransplant survival is superior in the HPS group, suggesting that perhaps a lower MELD score should be assigned to these patients.
While exceptions are currently a fundamental part of MELD-based liver allocation, greater standardization of MELD exception point criteria is urgently needed. Additional analysis of wait list survival and survival benefit models will be required to ensure that individual groups of patients are not being unjustly overprioritized.
Dr. Elizabeth C. Verna is assistant professor of medicine, Center for Liver Disease and Transplantation, Division of Digestive and Liver Diseases, Columbia University College of Physicians and Surgeons, New York. She disclosed no conflicts of interest.
Room air hypoxemia was associated with greater post–liver transplant mortality in hepatopulmonary syndrome patients, according to Dr. David S. Goldberg and his colleagues.
On the other hand, HPS transplant candidates had overall decreased pretransplantation mortality compared with non-HPS patients, suggesting that "current exception policy might overprioritize waitlisted HPS patients," they wrote.
The report appears in the May 1 issue of Gastroenterology (doi:10.1053/j.gastro.2014.01.005).
Dr. Goldberg of the University of Pennsylvania, Philadelphia, looked at all 973 liver transplant candidates from the United Network for Organ Sharing database who had at least one exception application for HPS approved between Feb. 27, 2002, and Dec. 14, 2012.
For comparison, the authors assessed 59,619 non-HPS adult waitlist candidates who registered for their first liver transplantation on or after Feb. 27, 2002.
Overall, there was a 1-year posttransplant survival rate of 91%, a 3-year survival rate of 81%, and a 5-year rate of 76% among the HPS cohort, the authors wrote. Those rates were comparable with the 1-year, 3-year, and 5-year posttransplant rates for non-HPS patients of 89%, 81%, and 74%.
However, looking at pretransplant survival, the authors found that a significantly greater proportion of non-HPS transplant candidates died on the waitlist, compared with HPS patients (20% vs. 9%; P less than .001). That translated to a hazard ratio of 0.82 among HPS patients for dying on the waitlist, compared with non-HPS patients (95% confidence interval, 0.70-0.96).
Next, the authors assessed the relationship between pretransplant room air oxygenation among HPS patients on posttransplant survival rates. They found that patients with pretransplant PaO2 (partial pressure of oxygen in arterial blood) levels of less than 50 mm Hg had a significantly higher posttransplant mortality, compared with patients with PaO2 levels between 50 and 59 mm Hg (HR = 1.56; 95% CI, 1.02-2.38).
Similarly, in a cubic spline model, transplant recipients with a PaO2 of less than 44.0 mm Hg had significantly increased posttransplantation mortality compared with recipients with a PaO2 of 44.1-54.0 mm Hg (HR = 1.58; 95% CI, 1.15-2.18).
"These data must be taken in context, as the 5-year posttransplantation patient survival in HPS patients with the lowest values of PaO2 is still at or above a threshold many would consider acceptable for a transplant recipient," the authors cautioned. "Therefore, the transplant community must decide what degree of hypoxemia makes a patient too high risk," they added.
The authors conceded several limitations. "First, we were unable to employ the strict criteria defining HPS used in prospective multicenter studies," they wrote.
"However, we are confident that most, if not all, of the patients had HPS based on the data documenting hypoxemia and shunting in nearly 90% of patients."
Nevertheless, "excellent posttransplantation outcomes in those with less severe hypoxemia suggest that it might be possible to optimize posttransplantation outcomes for patients with HPS without disadvantaging the broader transplant population," they wrote.
This could be accomplished by a review of current exception algorithms, and "by decreasing the initial number of exception points for HPS patients, while offering additional priority to those whose PaO2 values decline toward higher-risk values," they wrote.
Given the fact that this would increase the overall waitlist time, "an increase rather than decrease in data collected regarding these patients is needed to guide policy," they concluded.
The authors disclosed no conflicts of interest. Dr. Goldberg reported receiving funding from the National Institutes of Health, and the study was partially supported by the Health Resources and Services Administration.
Room air hypoxemia was associated with greater post–liver transplant mortality in hepatopulmonary syndrome patients, according to Dr. David S. Goldberg and his colleagues.
On the other hand, HPS transplant candidates had overall decreased pretransplantation mortality compared with non-HPS patients, suggesting that "current exception policy might overprioritize waitlisted HPS patients," they wrote.
The report appears in the May 1 issue of Gastroenterology (doi:10.1053/j.gastro.2014.01.005).
Dr. Goldberg of the University of Pennsylvania, Philadelphia, looked at all 973 liver transplant candidates from the United Network for Organ Sharing database who had at least one exception application for HPS approved between Feb. 27, 2002, and Dec. 14, 2012.
For comparison, the authors assessed 59,619 non-HPS adult waitlist candidates who registered for their first liver transplantation on or after Feb. 27, 2002.
Overall, there was a 1-year posttransplant survival rate of 91%, a 3-year survival rate of 81%, and a 5-year rate of 76% among the HPS cohort, the authors wrote. Those rates were comparable with the 1-year, 3-year, and 5-year posttransplant rates for non-HPS patients of 89%, 81%, and 74%.
However, looking at pretransplant survival, the authors found that a significantly greater proportion of non-HPS transplant candidates died on the waitlist, compared with HPS patients (20% vs. 9%; P less than .001). That translated to a hazard ratio of 0.82 among HPS patients for dying on the waitlist, compared with non-HPS patients (95% confidence interval, 0.70-0.96).
Next, the authors assessed the relationship between pretransplant room air oxygenation among HPS patients on posttransplant survival rates. They found that patients with pretransplant PaO2 (partial pressure of oxygen in arterial blood) levels of less than 50 mm Hg had a significantly higher posttransplant mortality, compared with patients with PaO2 levels between 50 and 59 mm Hg (HR = 1.56; 95% CI, 1.02-2.38).
Similarly, in a cubic spline model, transplant recipients with a PaO2 of less than 44.0 mm Hg had significantly increased posttransplantation mortality compared with recipients with a PaO2 of 44.1-54.0 mm Hg (HR = 1.58; 95% CI, 1.15-2.18).
"These data must be taken in context, as the 5-year posttransplantation patient survival in HPS patients with the lowest values of PaO2 is still at or above a threshold many would consider acceptable for a transplant recipient," the authors cautioned. "Therefore, the transplant community must decide what degree of hypoxemia makes a patient too high risk," they added.
The authors conceded several limitations. "First, we were unable to employ the strict criteria defining HPS used in prospective multicenter studies," they wrote.
"However, we are confident that most, if not all, of the patients had HPS based on the data documenting hypoxemia and shunting in nearly 90% of patients."
Nevertheless, "excellent posttransplantation outcomes in those with less severe hypoxemia suggest that it might be possible to optimize posttransplantation outcomes for patients with HPS without disadvantaging the broader transplant population," they wrote.
This could be accomplished by a review of current exception algorithms, and "by decreasing the initial number of exception points for HPS patients, while offering additional priority to those whose PaO2 values decline toward higher-risk values," they wrote.
Given the fact that this would increase the overall waitlist time, "an increase rather than decrease in data collected regarding these patients is needed to guide policy," they concluded.
The authors disclosed no conflicts of interest. Dr. Goldberg reported receiving funding from the National Institutes of Health, and the study was partially supported by the Health Resources and Services Administration.
FROM GASTROENTEROLOGY
Major finding: Liver transplant recipients with hepatopulmonary syndrome have success similar to that of other transplant candidates, unless severe hypoxemia is present.
Data source: A retrospective cohort study of data submitted to the United Network for Organ Sharing.
Disclosures: The authors disclosed no conflicts of interest. Dr. Goldberg reported receiving funding from the National Institutes of Health, and the study was partially supported by the Health Resources and Services Administration.
RFA ablation and resection avoids esophagectomy in dysplastic Barrett’s and intramucosal adenocarcinoma
TORONTO – Radiofrequency ablation with or without endoscopic mucosal resection resulted in complete remission of high-grade dysplasia in 79% of patients and Barrett’s esophagus in 49%, and none of the patients required esophagectomy, according to Dr. Michal J. Lada.
"Endoscopic treatment of early neoplasia is a safe and effective modality," said Dr. Lada. "The use of esophagectomy for high-grade dysplasia has been eliminated since 2008 in our center and has been significantly decreased for intramucosal disease as primary therapy."
Early neoplasia is increasingly being identified because of better surveillance of known Barrett’s esophagus. Once Barrett’s is identified, it carries a 0.4% risk of progression to adenocarcinoma. For the year 2014, it is estimated that 18,100 people will be diagnosed with esophageal cancer, and 15,450 will die of the disease.
While esophagectomy was once advocated as the optimal treatment for high-grade dysplasia or intramucosal adenocarcinoma, it is associated with significant morbidity and impaired long-term alimentary outcomes. Radiofrequency ablation coupled with endoscopic mucosal resection (EMR) has emerged as the standard of care in the management of these patients, said Dr. Lada of the University of Rochester (N.Y.) Medical Center.
The 57 patients in this retrospective study (45 with high-grade dysplasia and 12 with intramucosal adenocarcinoma) underwent a total of 181 ablation procedures (mean of 3.2 per patient) between 2007 and 2012. EMR prior to ablation was applied liberally for any mucosal irregularities or nodules, being used in 61% of patients overall, and as a first procedure in 49%, for a total of 58 EMR procedures. With surveillance endoscopies every 2 months throughout treatment included, patients underwent a total of 753 procedures, averaging 13.2 procedures per patient.
"When we proposed this therapy to patients for high-grade dysplasia or intramucosal disease, we offered the option of esophagectomy, with the full disclosure that endoscopic treatment is a lifelong commitment rather than a single event," said Dr. Lada. "Esophagectomy can really be viewed as kind of a radical prophylaxis."
The mean age of treated patients was 66.2 years and 88% were male. Most patients had gastroesophageal reflux disease (89%) and were taking proton pump inhibitors (89%) on a long-term basis, Dr. Lada reported at the annual meeting of the American Association for Thoracic Surgery.
Complete remission of dysplasia was achieved in 79% of patients (45 of 57), with a median time of remission of 11.5 months. Complete remission of Barrett’s esophagus was achieved in 49% (28 of 57 patients), within a median of 18.4 months. All patients without complete remission continued endoscopic treatment.
The recurrence of dysplasia was observed in 21% of patients, with a time to recurrence of 29.1 months, and a return of Barrett’s esophagus was seen in only 7%, during a median of 14.8 months. Seven percent of patients progressed from high-grade dysplasia to intramucosal adenocarcinoma over a median of 12.6 months, but all of them were treated endoscopically. No patients required esophagectomy or developed metastatic disease.
There were six deaths during follow-up, none from esophageal cancer. There were also no major complications of treatment and only two minor complications.
"The use of endoscopic therapies appears justified as the new standard of care in the majority of patients with Barrett’s and early esophageal neoplasia," said Dr. Lada.
"Endoscopic therapy, using combinations of endoscopic resection and ablation, has revolutionized the treatment of patients with high-grade dysplasia and superficial adenocarcinomas. This strategy represents a major paradigm shift in the management of this disease, and I applaud the authors for being early adopters of this approach," commented Dr. Steven R. Demeester, a professor in the department of cardiothoracic surgery at the University of Southern California, Los Angeles, and an invited discussant on the paper.
"It’s an interesting paradox that while we now have endoscopic, organ-preserving techniques to treat these patients, at the same time there seems to be an increasing nihilism among our gastroenterology colleagues about the benefits of surveillance for Barrett’s esophagus," Dr. Demeester said.
Dr. Lada countered that, as an established referral center for reflux disease, the center’s referral numbers continue to increase.
Dr. Lada reported no financial disclosures. Dr. Demeester is a consultant for C2 Therapeutics, Bard/Davol, and Novadaq.
TORONTO – Radiofrequency ablation with or without endoscopic mucosal resection resulted in complete remission of high-grade dysplasia in 79% of patients and Barrett’s esophagus in 49%, and none of the patients required esophagectomy, according to Dr. Michal J. Lada.
"Endoscopic treatment of early neoplasia is a safe and effective modality," said Dr. Lada. "The use of esophagectomy for high-grade dysplasia has been eliminated since 2008 in our center and has been significantly decreased for intramucosal disease as primary therapy."
Early neoplasia is increasingly being identified because of better surveillance of known Barrett’s esophagus. Once Barrett’s is identified, it carries a 0.4% risk of progression to adenocarcinoma. For the year 2014, it is estimated that 18,100 people will be diagnosed with esophageal cancer, and 15,450 will die of the disease.
While esophagectomy was once advocated as the optimal treatment for high-grade dysplasia or intramucosal adenocarcinoma, it is associated with significant morbidity and impaired long-term alimentary outcomes. Radiofrequency ablation coupled with endoscopic mucosal resection (EMR) has emerged as the standard of care in the management of these patients, said Dr. Lada of the University of Rochester (N.Y.) Medical Center.
The 57 patients in this retrospective study (45 with high-grade dysplasia and 12 with intramucosal adenocarcinoma) underwent a total of 181 ablation procedures (mean of 3.2 per patient) between 2007 and 2012. EMR prior to ablation was applied liberally for any mucosal irregularities or nodules, being used in 61% of patients overall, and as a first procedure in 49%, for a total of 58 EMR procedures. With surveillance endoscopies every 2 months throughout treatment included, patients underwent a total of 753 procedures, averaging 13.2 procedures per patient.
"When we proposed this therapy to patients for high-grade dysplasia or intramucosal disease, we offered the option of esophagectomy, with the full disclosure that endoscopic treatment is a lifelong commitment rather than a single event," said Dr. Lada. "Esophagectomy can really be viewed as kind of a radical prophylaxis."
The mean age of treated patients was 66.2 years and 88% were male. Most patients had gastroesophageal reflux disease (89%) and were taking proton pump inhibitors (89%) on a long-term basis, Dr. Lada reported at the annual meeting of the American Association for Thoracic Surgery.
Complete remission of dysplasia was achieved in 79% of patients (45 of 57), with a median time of remission of 11.5 months. Complete remission of Barrett’s esophagus was achieved in 49% (28 of 57 patients), within a median of 18.4 months. All patients without complete remission continued endoscopic treatment.
The recurrence of dysplasia was observed in 21% of patients, with a time to recurrence of 29.1 months, and a return of Barrett’s esophagus was seen in only 7%, during a median of 14.8 months. Seven percent of patients progressed from high-grade dysplasia to intramucosal adenocarcinoma over a median of 12.6 months, but all of them were treated endoscopically. No patients required esophagectomy or developed metastatic disease.
There were six deaths during follow-up, none from esophageal cancer. There were also no major complications of treatment and only two minor complications.
"The use of endoscopic therapies appears justified as the new standard of care in the majority of patients with Barrett’s and early esophageal neoplasia," said Dr. Lada.
"Endoscopic therapy, using combinations of endoscopic resection and ablation, has revolutionized the treatment of patients with high-grade dysplasia and superficial adenocarcinomas. This strategy represents a major paradigm shift in the management of this disease, and I applaud the authors for being early adopters of this approach," commented Dr. Steven R. Demeester, a professor in the department of cardiothoracic surgery at the University of Southern California, Los Angeles, and an invited discussant on the paper.
"It’s an interesting paradox that while we now have endoscopic, organ-preserving techniques to treat these patients, at the same time there seems to be an increasing nihilism among our gastroenterology colleagues about the benefits of surveillance for Barrett’s esophagus," Dr. Demeester said.
Dr. Lada countered that, as an established referral center for reflux disease, the center’s referral numbers continue to increase.
Dr. Lada reported no financial disclosures. Dr. Demeester is a consultant for C2 Therapeutics, Bard/Davol, and Novadaq.
TORONTO – Radiofrequency ablation with or without endoscopic mucosal resection resulted in complete remission of high-grade dysplasia in 79% of patients and Barrett’s esophagus in 49%, and none of the patients required esophagectomy, according to Dr. Michal J. Lada.
"Endoscopic treatment of early neoplasia is a safe and effective modality," said Dr. Lada. "The use of esophagectomy for high-grade dysplasia has been eliminated since 2008 in our center and has been significantly decreased for intramucosal disease as primary therapy."
Early neoplasia is increasingly being identified because of better surveillance of known Barrett’s esophagus. Once Barrett’s is identified, it carries a 0.4% risk of progression to adenocarcinoma. For the year 2014, it is estimated that 18,100 people will be diagnosed with esophageal cancer, and 15,450 will die of the disease.
While esophagectomy was once advocated as the optimal treatment for high-grade dysplasia or intramucosal adenocarcinoma, it is associated with significant morbidity and impaired long-term alimentary outcomes. Radiofrequency ablation coupled with endoscopic mucosal resection (EMR) has emerged as the standard of care in the management of these patients, said Dr. Lada of the University of Rochester (N.Y.) Medical Center.
The 57 patients in this retrospective study (45 with high-grade dysplasia and 12 with intramucosal adenocarcinoma) underwent a total of 181 ablation procedures (mean of 3.2 per patient) between 2007 and 2012. EMR prior to ablation was applied liberally for any mucosal irregularities or nodules, being used in 61% of patients overall, and as a first procedure in 49%, for a total of 58 EMR procedures. With surveillance endoscopies every 2 months throughout treatment included, patients underwent a total of 753 procedures, averaging 13.2 procedures per patient.
"When we proposed this therapy to patients for high-grade dysplasia or intramucosal disease, we offered the option of esophagectomy, with the full disclosure that endoscopic treatment is a lifelong commitment rather than a single event," said Dr. Lada. "Esophagectomy can really be viewed as kind of a radical prophylaxis."
The mean age of treated patients was 66.2 years and 88% were male. Most patients had gastroesophageal reflux disease (89%) and were taking proton pump inhibitors (89%) on a long-term basis, Dr. Lada reported at the annual meeting of the American Association for Thoracic Surgery.
Complete remission of dysplasia was achieved in 79% of patients (45 of 57), with a median time of remission of 11.5 months. Complete remission of Barrett’s esophagus was achieved in 49% (28 of 57 patients), within a median of 18.4 months. All patients without complete remission continued endoscopic treatment.
The recurrence of dysplasia was observed in 21% of patients, with a time to recurrence of 29.1 months, and a return of Barrett’s esophagus was seen in only 7%, during a median of 14.8 months. Seven percent of patients progressed from high-grade dysplasia to intramucosal adenocarcinoma over a median of 12.6 months, but all of them were treated endoscopically. No patients required esophagectomy or developed metastatic disease.
There were six deaths during follow-up, none from esophageal cancer. There were also no major complications of treatment and only two minor complications.
"The use of endoscopic therapies appears justified as the new standard of care in the majority of patients with Barrett’s and early esophageal neoplasia," said Dr. Lada.
"Endoscopic therapy, using combinations of endoscopic resection and ablation, has revolutionized the treatment of patients with high-grade dysplasia and superficial adenocarcinomas. This strategy represents a major paradigm shift in the management of this disease, and I applaud the authors for being early adopters of this approach," commented Dr. Steven R. Demeester, a professor in the department of cardiothoracic surgery at the University of Southern California, Los Angeles, and an invited discussant on the paper.
"It’s an interesting paradox that while we now have endoscopic, organ-preserving techniques to treat these patients, at the same time there seems to be an increasing nihilism among our gastroenterology colleagues about the benefits of surveillance for Barrett’s esophagus," Dr. Demeester said.
Dr. Lada countered that, as an established referral center for reflux disease, the center’s referral numbers continue to increase.
Dr. Lada reported no financial disclosures. Dr. Demeester is a consultant for C2 Therapeutics, Bard/Davol, and Novadaq.
AT THE AATS ANNUAL MEETING
Major finding: Radiofrequency ablation with or without endoscopic mucosal resection eradicated early neoplasia in 79% of patients and Barrett’s esophagus in 49%.
Data source: A review of 57 patients with high-grade dysplasia or intramucosal adenocarcinoma treated from January 2007 through December 2012.
Disclosures: Dr. Lada reported no financial disclosures.
Lap surgery not to blame for post-appy infection in children
BOSTON – Operative approach, as previously suggested, was not a significant predictor of postappendectomy organ space infection in children, according to a large, national database analysis.
Instead, organ space infection appears to be associated with largely nonmodifiable factors of disease severity, preoperative sepsis, and long operative duration, Dr. Fergal J. Fleming said at the annual meeting of the American Surgical Association.
"It would appear that the die is cast with respect to the risk of organ space infection at the time of presentation," he said. "This would suggest that our focus, in terms of quality improvement, should be on identifying patients at highest risk for complications."
The study findings are important because laparoscopic appendectomy has become widely accepted in children and adults, but has also been associated with increased odds of intra-abdominal abscess formation in adults (Ann. Surg. 2010;252:895-900), said Dr. Fleming, a colorectal surgeon at the University of Rochester (N.Y.) Medical Center.
To determine the effect of surgical approach on organ space infection (OSI) in children, Dr. Fleming and his associates analyzed 5,097 children, aged 2-18 years, undergoing open or laparoscopic appendectomy for acute appendicitis in the 2012 ACS National Surgical Quality Improvement Program (ACS NSQIP) pediatric database. The approach was laparoscopic in 4,514 patients (88.5%) and open in 583 patients.
OSI occurred in only 155 children (3%), but accounted for more than half of reoperations and nearly two-thirds of readmissions at 30 days, Dr. Fleming reported.
The unadjusted OSI rate was 0.9% (31/3,613) for uncomplicated appendicitis and 8.4% (124/1,484) for complicated appendicitis, which was a significant difference (P less than .001).
OSI rates did not differ significantly between laparoscopic and open surgery for uncomplicated appendicitis (0.8% vs. 1.7%; P = .160) and complicated appendicitis (8.7% vs. 7.3%; P = .415), defined by abscess, perforation, or sepsis.
In multivariable logistic regression analysis, complicated appendicitis was again the major factor associated with OSI (adjusted odds ratio, 4.85), he said. Other significant drivers were wound class III/IV (OR, 4.17), preoperative sepsis (OR, 2.19), and operative time of 60 minutes or more (OR, 2.15).
The model, which controlled for age, sex, pulmonary comorbidity, obesity, and emergency operations, had excellent predictive ability, with a c-statistic of 0.837, Dr. Fleming said.
He acknowledged that baseline differences between the two groups suggested that sicker children may have been selected as candidates for open surgery. Compared with the laparoscopic group, the open surgery group had significantly higher rates of preoperative sepsis/septic shock (24.7% vs. 14.7%), complicated appendicitis (58.8% vs. 25.3%), and emergency surgery (74.4% vs. 62%; all P values less than .001).
"Now that your group has identified these perioperative risk factors for children undergoing emergency appendectomy, do you have any guidelines for pediatric surgeons on how to follow their patients postop to identify organ space infections earlier?" asked discussant Dr. Paul Colombani, Children’s Surgeon-in Charge, Johns Hopkins Hospital, Baltimore.
Dr. Fleming suggested a bundle for high-risk patients that could include predischarge education for parents and patients, an early clinic visit before postoperative day 9, and a structured telephone call on day 2 or 3 post discharge to run through risk factors such as low-grade fever, malaise, and diarrhea. He noted that high-risk patients represented less than 15% of the cohort, but 80% of OSI events.
Dr. Fleming reported having no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, is anticipated to be published in Annals of Surgery, pending editorial review.
BOSTON – Operative approach, as previously suggested, was not a significant predictor of postappendectomy organ space infection in children, according to a large, national database analysis.
Instead, organ space infection appears to be associated with largely nonmodifiable factors of disease severity, preoperative sepsis, and long operative duration, Dr. Fergal J. Fleming said at the annual meeting of the American Surgical Association.
"It would appear that the die is cast with respect to the risk of organ space infection at the time of presentation," he said. "This would suggest that our focus, in terms of quality improvement, should be on identifying patients at highest risk for complications."
The study findings are important because laparoscopic appendectomy has become widely accepted in children and adults, but has also been associated with increased odds of intra-abdominal abscess formation in adults (Ann. Surg. 2010;252:895-900), said Dr. Fleming, a colorectal surgeon at the University of Rochester (N.Y.) Medical Center.
To determine the effect of surgical approach on organ space infection (OSI) in children, Dr. Fleming and his associates analyzed 5,097 children, aged 2-18 years, undergoing open or laparoscopic appendectomy for acute appendicitis in the 2012 ACS National Surgical Quality Improvement Program (ACS NSQIP) pediatric database. The approach was laparoscopic in 4,514 patients (88.5%) and open in 583 patients.
OSI occurred in only 155 children (3%), but accounted for more than half of reoperations and nearly two-thirds of readmissions at 30 days, Dr. Fleming reported.
The unadjusted OSI rate was 0.9% (31/3,613) for uncomplicated appendicitis and 8.4% (124/1,484) for complicated appendicitis, which was a significant difference (P less than .001).
OSI rates did not differ significantly between laparoscopic and open surgery for uncomplicated appendicitis (0.8% vs. 1.7%; P = .160) and complicated appendicitis (8.7% vs. 7.3%; P = .415), defined by abscess, perforation, or sepsis.
In multivariable logistic regression analysis, complicated appendicitis was again the major factor associated with OSI (adjusted odds ratio, 4.85), he said. Other significant drivers were wound class III/IV (OR, 4.17), preoperative sepsis (OR, 2.19), and operative time of 60 minutes or more (OR, 2.15).
The model, which controlled for age, sex, pulmonary comorbidity, obesity, and emergency operations, had excellent predictive ability, with a c-statistic of 0.837, Dr. Fleming said.
He acknowledged that baseline differences between the two groups suggested that sicker children may have been selected as candidates for open surgery. Compared with the laparoscopic group, the open surgery group had significantly higher rates of preoperative sepsis/septic shock (24.7% vs. 14.7%), complicated appendicitis (58.8% vs. 25.3%), and emergency surgery (74.4% vs. 62%; all P values less than .001).
"Now that your group has identified these perioperative risk factors for children undergoing emergency appendectomy, do you have any guidelines for pediatric surgeons on how to follow their patients postop to identify organ space infections earlier?" asked discussant Dr. Paul Colombani, Children’s Surgeon-in Charge, Johns Hopkins Hospital, Baltimore.
Dr. Fleming suggested a bundle for high-risk patients that could include predischarge education for parents and patients, an early clinic visit before postoperative day 9, and a structured telephone call on day 2 or 3 post discharge to run through risk factors such as low-grade fever, malaise, and diarrhea. He noted that high-risk patients represented less than 15% of the cohort, but 80% of OSI events.
Dr. Fleming reported having no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, is anticipated to be published in Annals of Surgery, pending editorial review.
BOSTON – Operative approach, as previously suggested, was not a significant predictor of postappendectomy organ space infection in children, according to a large, national database analysis.
Instead, organ space infection appears to be associated with largely nonmodifiable factors of disease severity, preoperative sepsis, and long operative duration, Dr. Fergal J. Fleming said at the annual meeting of the American Surgical Association.
"It would appear that the die is cast with respect to the risk of organ space infection at the time of presentation," he said. "This would suggest that our focus, in terms of quality improvement, should be on identifying patients at highest risk for complications."
The study findings are important because laparoscopic appendectomy has become widely accepted in children and adults, but has also been associated with increased odds of intra-abdominal abscess formation in adults (Ann. Surg. 2010;252:895-900), said Dr. Fleming, a colorectal surgeon at the University of Rochester (N.Y.) Medical Center.
To determine the effect of surgical approach on organ space infection (OSI) in children, Dr. Fleming and his associates analyzed 5,097 children, aged 2-18 years, undergoing open or laparoscopic appendectomy for acute appendicitis in the 2012 ACS National Surgical Quality Improvement Program (ACS NSQIP) pediatric database. The approach was laparoscopic in 4,514 patients (88.5%) and open in 583 patients.
OSI occurred in only 155 children (3%), but accounted for more than half of reoperations and nearly two-thirds of readmissions at 30 days, Dr. Fleming reported.
The unadjusted OSI rate was 0.9% (31/3,613) for uncomplicated appendicitis and 8.4% (124/1,484) for complicated appendicitis, which was a significant difference (P less than .001).
OSI rates did not differ significantly between laparoscopic and open surgery for uncomplicated appendicitis (0.8% vs. 1.7%; P = .160) and complicated appendicitis (8.7% vs. 7.3%; P = .415), defined by abscess, perforation, or sepsis.
In multivariable logistic regression analysis, complicated appendicitis was again the major factor associated with OSI (adjusted odds ratio, 4.85), he said. Other significant drivers were wound class III/IV (OR, 4.17), preoperative sepsis (OR, 2.19), and operative time of 60 minutes or more (OR, 2.15).
The model, which controlled for age, sex, pulmonary comorbidity, obesity, and emergency operations, had excellent predictive ability, with a c-statistic of 0.837, Dr. Fleming said.
He acknowledged that baseline differences between the two groups suggested that sicker children may have been selected as candidates for open surgery. Compared with the laparoscopic group, the open surgery group had significantly higher rates of preoperative sepsis/septic shock (24.7% vs. 14.7%), complicated appendicitis (58.8% vs. 25.3%), and emergency surgery (74.4% vs. 62%; all P values less than .001).
"Now that your group has identified these perioperative risk factors for children undergoing emergency appendectomy, do you have any guidelines for pediatric surgeons on how to follow their patients postop to identify organ space infections earlier?" asked discussant Dr. Paul Colombani, Children’s Surgeon-in Charge, Johns Hopkins Hospital, Baltimore.
Dr. Fleming suggested a bundle for high-risk patients that could include predischarge education for parents and patients, an early clinic visit before postoperative day 9, and a structured telephone call on day 2 or 3 post discharge to run through risk factors such as low-grade fever, malaise, and diarrhea. He noted that high-risk patients represented less than 15% of the cohort, but 80% of OSI events.
Dr. Fleming reported having no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, is anticipated to be published in Annals of Surgery, pending editorial review.
AT THE ASA ANNUAL MEETING
Major finding: OSI rates did not differ significantly between laparoscopic and open surgery for uncomplicated appendicitis (0.8% vs. 1.7%, respectively) and complicated appendicitis (8.7% vs. 7.3%), defined by abscess, perforation, or sepsis.
Data source: A retrospective analysis of 5,097 children undergoing appendectomy in the NSQIP database.
Disclosures: Dr. Fleming reported having no financial disclosures.
Shortage of general surgeons ups probability of ruptured appendix
Patients with appendicitis who live in areas having a critical shortage of general surgeons are at increased risk for appendiceal rupture, finds a cross-sectional, observational study published in the Annals of Surgery.
Investigators used discharge data to identify 29,403 patients with acute appendicitis seen in acute care and ambulatory surgery facilities in North Carolina between 2007 and 2009. Diagnostic codes indicated that 24.6% overall had experienced rupture.
In multivariate analyses, the probability of rupture was a significant 4.8 percentage points higher for patients in surgical service areas having a critical shortage of general surgeons (fewer than 3 per 100,000 people) than for patients in areas not having any shortage (at least 5 per 100,000 people), the investigators report (Ann Surg. 2014;259:910-15). Patients living in areas having lesser shortages did not have significantly elevated risk.
In contrast, the primary care physician supply in a given surgical service area did not predict rupture on its own, although it did show an interaction with area, with greater supply increasing the probability of rupture in some areas having a general surgeon shortage and decreasing it in others.
"Although rupture risk also depends on several other determinants of access, the density of the local general surgery workforce may be the most important determinant of access for timely appendicitis care. The independent effect of living in a critical surgery shortage area was greater than that of race, insurance status, rural status, and admission source," the investigators note.
"Enhancing supply in critical shortage areas could reduce appendiceal rupture and improve surgical access more generally," they maintain.
At the same time, the findings regarding primary care physician supply also have implications for policies aimed at improving general surgeon supply, according to the investigators.
"These results underscore the need for an effectively targeted HPSA (health professional shortage area) surgical incentive payments policy," which currently provides a 10% bonus payment to general surgeons operating in primary care health professional shortage areas, they note. "The current rule for designation of a surgical HPSA assumes that they coincide with current primary care HPSAs and designates them accordingly. This assumption is not supported by our analysis."
The investigators disclosed no relevant conflicts of interest.
Patients with appendicitis who live in areas having a critical shortage of general surgeons are at increased risk for appendiceal rupture, finds a cross-sectional, observational study published in the Annals of Surgery.
Investigators used discharge data to identify 29,403 patients with acute appendicitis seen in acute care and ambulatory surgery facilities in North Carolina between 2007 and 2009. Diagnostic codes indicated that 24.6% overall had experienced rupture.
In multivariate analyses, the probability of rupture was a significant 4.8 percentage points higher for patients in surgical service areas having a critical shortage of general surgeons (fewer than 3 per 100,000 people) than for patients in areas not having any shortage (at least 5 per 100,000 people), the investigators report (Ann Surg. 2014;259:910-15). Patients living in areas having lesser shortages did not have significantly elevated risk.
In contrast, the primary care physician supply in a given surgical service area did not predict rupture on its own, although it did show an interaction with area, with greater supply increasing the probability of rupture in some areas having a general surgeon shortage and decreasing it in others.
"Although rupture risk also depends on several other determinants of access, the density of the local general surgery workforce may be the most important determinant of access for timely appendicitis care. The independent effect of living in a critical surgery shortage area was greater than that of race, insurance status, rural status, and admission source," the investigators note.
"Enhancing supply in critical shortage areas could reduce appendiceal rupture and improve surgical access more generally," they maintain.
At the same time, the findings regarding primary care physician supply also have implications for policies aimed at improving general surgeon supply, according to the investigators.
"These results underscore the need for an effectively targeted HPSA (health professional shortage area) surgical incentive payments policy," which currently provides a 10% bonus payment to general surgeons operating in primary care health professional shortage areas, they note. "The current rule for designation of a surgical HPSA assumes that they coincide with current primary care HPSAs and designates them accordingly. This assumption is not supported by our analysis."
The investigators disclosed no relevant conflicts of interest.
Patients with appendicitis who live in areas having a critical shortage of general surgeons are at increased risk for appendiceal rupture, finds a cross-sectional, observational study published in the Annals of Surgery.
Investigators used discharge data to identify 29,403 patients with acute appendicitis seen in acute care and ambulatory surgery facilities in North Carolina between 2007 and 2009. Diagnostic codes indicated that 24.6% overall had experienced rupture.
In multivariate analyses, the probability of rupture was a significant 4.8 percentage points higher for patients in surgical service areas having a critical shortage of general surgeons (fewer than 3 per 100,000 people) than for patients in areas not having any shortage (at least 5 per 100,000 people), the investigators report (Ann Surg. 2014;259:910-15). Patients living in areas having lesser shortages did not have significantly elevated risk.
In contrast, the primary care physician supply in a given surgical service area did not predict rupture on its own, although it did show an interaction with area, with greater supply increasing the probability of rupture in some areas having a general surgeon shortage and decreasing it in others.
"Although rupture risk also depends on several other determinants of access, the density of the local general surgery workforce may be the most important determinant of access for timely appendicitis care. The independent effect of living in a critical surgery shortage area was greater than that of race, insurance status, rural status, and admission source," the investigators note.
"Enhancing supply in critical shortage areas could reduce appendiceal rupture and improve surgical access more generally," they maintain.
At the same time, the findings regarding primary care physician supply also have implications for policies aimed at improving general surgeon supply, according to the investigators.
"These results underscore the need for an effectively targeted HPSA (health professional shortage area) surgical incentive payments policy," which currently provides a 10% bonus payment to general surgeons operating in primary care health professional shortage areas, they note. "The current rule for designation of a surgical HPSA assumes that they coincide with current primary care HPSAs and designates them accordingly. This assumption is not supported by our analysis."
The investigators disclosed no relevant conflicts of interest.
FROM ANNALS OF SURGERY
Major finding: The probability of rupture was 4.8 percentage points higher for patients in surgical service areas having fewer than 3 general surgeons per 100,000 people versus those in areas having at least 5 general surgeons per 100,000 people.
Data source: A cross-sectional observational study of 29,403 patients with acute appendicitis.
Disclosures: The investigators disclosed no relevant conflicts of interest.