User login
Official Newspaper of the American College of Surgeons
Laparoscopic splenectomy underutilized in the U.S.
LAS VEGAS – Laparoscopic splenectomy has become the preferred surgical approach in the literature, but the number of such procedures performed in the United States remains relatively low, according to Dr. John Afthinos.
National data for 2005-2010 showed a total of 37,006 elective total splenectomies were performed. Only 4,938 of them, or 13.3%, began as laparoscopic procedures, of which 40% had to be converted to open splenectomies, he reported at the annual Minimally Invasive Surgery Week.
“Laparoscopic splenectomy remains underutilized,” Dr. Afthinos commented. “This is one of the lowest recorded rates of laparoscopic completion of any advanced procedure that we know of.”
For example, other investigators have demonstrated that laparoscopic colectomies and bariatric surgical procedures are typically completed laparoscopically in 85%-95% of cases, noted Dr. Afthinos of Staten Island (N.Y.) University Hospital.
The laparoscopic approach has convincingly been shown to result in less pain, shorter hospital length of stay, faster recovery, and improved cosmetic results, compared with the open surgical versions of various operations.
“In the U.S., laparoscopic splenectomy is not well incorporated into the armamentarium of the average general surgeon. We can speculate that the underutilization of this approach around the country prevents development of the familiarity and skill that you need to perform the operation safely without conversion,” he said at the meeting, presented by the Society of Laparoscopic Surgeons and affiliated societies.
Dr. Afthinos’s data were drawn from the Nationwide Inpatient Sample maintained by the U.S. Agency for Healthcare Research and Quality. In this database, patients who had a laparoscopic splenectomy had the shortest average hospital length of stay: 5.6 days, compared with 7.5 in those who underwent open splenectomy and 7.1 for conversion procedures. The overall morbidity rate was significantly lower in the laparoscopic group, too: 7.4%, compared with 10.4% in the open splenectomy group.
In a multivariate analysis, he and his coworkers identified three independent risk factors for conversion from laparoscopic to open splenectomy: hemorrhage, with a 3.23-fold increased risk; splenomegaly, with a 1.3-fold increased risk; and autoimmune hemolytic anemia, with an associated 1.36-fold elevated risk of conversion.
Dr. Catalin Vasilescu of Carol Davila University in Bucharest, Romania, rose from the audience to voice his incredulity at the American data: “I am really surprised at your national conversion rate of well over 30%. That is really a problem. Earlier at this meeting, we presented 520 laparoscopic splenectomy patients with a conversion rate over 20 years of 4%-5%,” the Romanian general surgeon said.
“How do you explain this? I have a hypothesis: Perhaps there are so many surgeons each performing very few of these procedures, instead of referring patients to an experienced center,” he said.
“It was surprising to us, too,” Dr. Afthinos replied. “I mean, I was expecting the conversion rate to be high, but not that high.”
He said Dr. Vasilescu was right on the mark. In addition, he explained, it’s important to understand that there are vast rural areas of the United States, and some rural patients are reluctant to travel hundreds of miles to undergo laparoscopic splenectomy at a large experienced center, especially in the winter or if their family can’t come along for support. And a rural general surgeon is not going to risk a patient’s life if he or she isn’t comfortable with a laparoscopic approach.
There is hope that the situation will improve, however, as more fellowship-trained minimally invasive surgeons enter clinical practice, according to Dr. Afthinos. He cited a recent report from a Columbus, Ohio, general surgery practice that after a fellowship-trained minimally invasive surgeon joined the practice, the group – excluding their fellowship-trained recent hire – increased its rate of various advanced procedures being performed laparoscopically from 12% to 48%. The five established surgeons indicated they found mentoring by a colleague with minimally invasive surgery training was a better way to learn the procedures than via weekend courses, videos, traveling proctors, and other methods (Surg. Endosc. 2013;27:1267-72).
Dr. Afthinos reported having no relevant financial conflicts.
LAS VEGAS – Laparoscopic splenectomy has become the preferred surgical approach in the literature, but the number of such procedures performed in the United States remains relatively low, according to Dr. John Afthinos.
National data for 2005-2010 showed a total of 37,006 elective total splenectomies were performed. Only 4,938 of them, or 13.3%, began as laparoscopic procedures, of which 40% had to be converted to open splenectomies, he reported at the annual Minimally Invasive Surgery Week.
“Laparoscopic splenectomy remains underutilized,” Dr. Afthinos commented. “This is one of the lowest recorded rates of laparoscopic completion of any advanced procedure that we know of.”
For example, other investigators have demonstrated that laparoscopic colectomies and bariatric surgical procedures are typically completed laparoscopically in 85%-95% of cases, noted Dr. Afthinos of Staten Island (N.Y.) University Hospital.
The laparoscopic approach has convincingly been shown to result in less pain, shorter hospital length of stay, faster recovery, and improved cosmetic results, compared with the open surgical versions of various operations.
“In the U.S., laparoscopic splenectomy is not well incorporated into the armamentarium of the average general surgeon. We can speculate that the underutilization of this approach around the country prevents development of the familiarity and skill that you need to perform the operation safely without conversion,” he said at the meeting, presented by the Society of Laparoscopic Surgeons and affiliated societies.
Dr. Afthinos’s data were drawn from the Nationwide Inpatient Sample maintained by the U.S. Agency for Healthcare Research and Quality. In this database, patients who had a laparoscopic splenectomy had the shortest average hospital length of stay: 5.6 days, compared with 7.5 in those who underwent open splenectomy and 7.1 for conversion procedures. The overall morbidity rate was significantly lower in the laparoscopic group, too: 7.4%, compared with 10.4% in the open splenectomy group.
In a multivariate analysis, he and his coworkers identified three independent risk factors for conversion from laparoscopic to open splenectomy: hemorrhage, with a 3.23-fold increased risk; splenomegaly, with a 1.3-fold increased risk; and autoimmune hemolytic anemia, with an associated 1.36-fold elevated risk of conversion.
Dr. Catalin Vasilescu of Carol Davila University in Bucharest, Romania, rose from the audience to voice his incredulity at the American data: “I am really surprised at your national conversion rate of well over 30%. That is really a problem. Earlier at this meeting, we presented 520 laparoscopic splenectomy patients with a conversion rate over 20 years of 4%-5%,” the Romanian general surgeon said.
“How do you explain this? I have a hypothesis: Perhaps there are so many surgeons each performing very few of these procedures, instead of referring patients to an experienced center,” he said.
“It was surprising to us, too,” Dr. Afthinos replied. “I mean, I was expecting the conversion rate to be high, but not that high.”
He said Dr. Vasilescu was right on the mark. In addition, he explained, it’s important to understand that there are vast rural areas of the United States, and some rural patients are reluctant to travel hundreds of miles to undergo laparoscopic splenectomy at a large experienced center, especially in the winter or if their family can’t come along for support. And a rural general surgeon is not going to risk a patient’s life if he or she isn’t comfortable with a laparoscopic approach.
There is hope that the situation will improve, however, as more fellowship-trained minimally invasive surgeons enter clinical practice, according to Dr. Afthinos. He cited a recent report from a Columbus, Ohio, general surgery practice that after a fellowship-trained minimally invasive surgeon joined the practice, the group – excluding their fellowship-trained recent hire – increased its rate of various advanced procedures being performed laparoscopically from 12% to 48%. The five established surgeons indicated they found mentoring by a colleague with minimally invasive surgery training was a better way to learn the procedures than via weekend courses, videos, traveling proctors, and other methods (Surg. Endosc. 2013;27:1267-72).
Dr. Afthinos reported having no relevant financial conflicts.
LAS VEGAS – Laparoscopic splenectomy has become the preferred surgical approach in the literature, but the number of such procedures performed in the United States remains relatively low, according to Dr. John Afthinos.
National data for 2005-2010 showed a total of 37,006 elective total splenectomies were performed. Only 4,938 of them, or 13.3%, began as laparoscopic procedures, of which 40% had to be converted to open splenectomies, he reported at the annual Minimally Invasive Surgery Week.
“Laparoscopic splenectomy remains underutilized,” Dr. Afthinos commented. “This is one of the lowest recorded rates of laparoscopic completion of any advanced procedure that we know of.”
For example, other investigators have demonstrated that laparoscopic colectomies and bariatric surgical procedures are typically completed laparoscopically in 85%-95% of cases, noted Dr. Afthinos of Staten Island (N.Y.) University Hospital.
The laparoscopic approach has convincingly been shown to result in less pain, shorter hospital length of stay, faster recovery, and improved cosmetic results, compared with the open surgical versions of various operations.
“In the U.S., laparoscopic splenectomy is not well incorporated into the armamentarium of the average general surgeon. We can speculate that the underutilization of this approach around the country prevents development of the familiarity and skill that you need to perform the operation safely without conversion,” he said at the meeting, presented by the Society of Laparoscopic Surgeons and affiliated societies.
Dr. Afthinos’s data were drawn from the Nationwide Inpatient Sample maintained by the U.S. Agency for Healthcare Research and Quality. In this database, patients who had a laparoscopic splenectomy had the shortest average hospital length of stay: 5.6 days, compared with 7.5 in those who underwent open splenectomy and 7.1 for conversion procedures. The overall morbidity rate was significantly lower in the laparoscopic group, too: 7.4%, compared with 10.4% in the open splenectomy group.
In a multivariate analysis, he and his coworkers identified three independent risk factors for conversion from laparoscopic to open splenectomy: hemorrhage, with a 3.23-fold increased risk; splenomegaly, with a 1.3-fold increased risk; and autoimmune hemolytic anemia, with an associated 1.36-fold elevated risk of conversion.
Dr. Catalin Vasilescu of Carol Davila University in Bucharest, Romania, rose from the audience to voice his incredulity at the American data: “I am really surprised at your national conversion rate of well over 30%. That is really a problem. Earlier at this meeting, we presented 520 laparoscopic splenectomy patients with a conversion rate over 20 years of 4%-5%,” the Romanian general surgeon said.
“How do you explain this? I have a hypothesis: Perhaps there are so many surgeons each performing very few of these procedures, instead of referring patients to an experienced center,” he said.
“It was surprising to us, too,” Dr. Afthinos replied. “I mean, I was expecting the conversion rate to be high, but not that high.”
He said Dr. Vasilescu was right on the mark. In addition, he explained, it’s important to understand that there are vast rural areas of the United States, and some rural patients are reluctant to travel hundreds of miles to undergo laparoscopic splenectomy at a large experienced center, especially in the winter or if their family can’t come along for support. And a rural general surgeon is not going to risk a patient’s life if he or she isn’t comfortable with a laparoscopic approach.
There is hope that the situation will improve, however, as more fellowship-trained minimally invasive surgeons enter clinical practice, according to Dr. Afthinos. He cited a recent report from a Columbus, Ohio, general surgery practice that after a fellowship-trained minimally invasive surgeon joined the practice, the group – excluding their fellowship-trained recent hire – increased its rate of various advanced procedures being performed laparoscopically from 12% to 48%. The five established surgeons indicated they found mentoring by a colleague with minimally invasive surgery training was a better way to learn the procedures than via weekend courses, videos, traveling proctors, and other methods (Surg. Endosc. 2013;27:1267-72).
Dr. Afthinos reported having no relevant financial conflicts.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: American general surgeons lag far behind their foreign colleagues in their rate of laparoscopically completed splenectomies.
Major finding: Only 13.3% of elective splenectomies performed in the United States started out as laparoscopic procedures – and of those, 40% were converted to open splenectomy.
Data source: A retrospective study of the Nationwide Inpatient Sample for 2005-2010, during which 37,006 elective total splenectomies were performed.
Disclosures: The presenter reported having no relevant financial conflicts.
Many will be automatically re-enrolled in ACA plans
WASHINGTON – Unless patients actively choose a new plan before Dec. 15, those who paid for a health insurance plan through the federal marketplace in 2014 will be automatically re-enrolled in the same plan for 2015, federal officials said.
The goal is to ensure there will be no gaps in coverage, Kevin Counihan, CEO of the federal health insurance marketplace, said at the Health Insurance Exchanges Forum held by America’s Health Insurance Plans.
Mr. Counihan did not give an estimate on how many people might be automatically re-enrolled, but he did say that some 7.3 million Americans had selected and paid for a health plan through the federal marketplace.
Mr. Counihan was appointed in late August to oversee the operations of healthcare.gov, the web portal for the federal health insurance marketplace. He is also director of the Centers for Medicare & Medicaid Services Center for Consumer Information and Insurance Oversight.
Open enrollment for health plans offered under the Affordable Care Act begins Nov. 15.
The CMS is starting to send notices to patients who either enrolled in a plan in 2014, or had been determined to be eligible but did not enroll, reminding them that they can start the renewal process on Nov. 15. The notices will arrive by mail or e-mail, depending on what the patient indicated as a preference.
At the same time, patients will receive notices from their current insurers, letting them know whether there are network or benefits changes, or if there is an increase or decrease in the premiums or other costs.
Patients have until Dec. 15 to enroll in a plan for coverage that starts on Jan. 1.
If they do not renew a current plan or elect a new plan by Dec. 15, they will be automatically re-enrolled in the existing plan, said Ben Walker, director of open enrollment for the federal marketplace at the CCIIO.
They will get the same amount of advance payment of the premium tax credit and same subsidies as in 2014. Those credits and cost-sharing reductions are subject to change, depending on a patient’s updated eligibility information.
Even if they’ve been auto-enrolled, they can eventually go back and select a different plan, as long as they do it by Feb. 15, when open season ends, Mr. Walker said at the meeting. The coverage in the new plan will start on the first day of the next or second month depending on when the patient enrolled.
The National Governors Association is somewhat concerned about the automatic re-enrollments, Esther Krofah, program director in the NGA’s health division, said at the meeting. “We have to make sure consumers are aware of their options and are taking the steps they need to protect themselves,” she said.
Rachel Klein, organizational strategy and enrollment program director for Families USA, said that patients could be confused, or potentially harmed, by the automatic re-enrollment. In some cases, they might want to stay with the plan, especially if they’ve developed a relationship with a physician in that plan’s network, she said.
But they may also have gotten a new diagnosis that requires them to see a particular doctor, who might not be in the plan, said Ms. Klein. For that reason, it will be especially important for patients to be able to “compare in much greater detail the plans available,” she said.
To help increase awareness of the re-enrollment process, the CMS on Oct. 15 launched the “Five Steps to Staying Covered” campaign, urging patients to review their current plans, and then, starting on Nov. 15, to update their income and other information, compare the current plan with other plans, choose a plan, and enroll.
The CMS has been testing the healthcare.gov website and is encouraged by what it has seen so far, Mr. Counihan told health plan representatives.
“We feel confident we’re going to have a successful 2015,” he said.
On Twitter @aliciaault
WASHINGTON – Unless patients actively choose a new plan before Dec. 15, those who paid for a health insurance plan through the federal marketplace in 2014 will be automatically re-enrolled in the same plan for 2015, federal officials said.
The goal is to ensure there will be no gaps in coverage, Kevin Counihan, CEO of the federal health insurance marketplace, said at the Health Insurance Exchanges Forum held by America’s Health Insurance Plans.
Mr. Counihan did not give an estimate on how many people might be automatically re-enrolled, but he did say that some 7.3 million Americans had selected and paid for a health plan through the federal marketplace.
Mr. Counihan was appointed in late August to oversee the operations of healthcare.gov, the web portal for the federal health insurance marketplace. He is also director of the Centers for Medicare & Medicaid Services Center for Consumer Information and Insurance Oversight.
Open enrollment for health plans offered under the Affordable Care Act begins Nov. 15.
The CMS is starting to send notices to patients who either enrolled in a plan in 2014, or had been determined to be eligible but did not enroll, reminding them that they can start the renewal process on Nov. 15. The notices will arrive by mail or e-mail, depending on what the patient indicated as a preference.
At the same time, patients will receive notices from their current insurers, letting them know whether there are network or benefits changes, or if there is an increase or decrease in the premiums or other costs.
Patients have until Dec. 15 to enroll in a plan for coverage that starts on Jan. 1.
If they do not renew a current plan or elect a new plan by Dec. 15, they will be automatically re-enrolled in the existing plan, said Ben Walker, director of open enrollment for the federal marketplace at the CCIIO.
They will get the same amount of advance payment of the premium tax credit and same subsidies as in 2014. Those credits and cost-sharing reductions are subject to change, depending on a patient’s updated eligibility information.
Even if they’ve been auto-enrolled, they can eventually go back and select a different plan, as long as they do it by Feb. 15, when open season ends, Mr. Walker said at the meeting. The coverage in the new plan will start on the first day of the next or second month depending on when the patient enrolled.
The National Governors Association is somewhat concerned about the automatic re-enrollments, Esther Krofah, program director in the NGA’s health division, said at the meeting. “We have to make sure consumers are aware of their options and are taking the steps they need to protect themselves,” she said.
Rachel Klein, organizational strategy and enrollment program director for Families USA, said that patients could be confused, or potentially harmed, by the automatic re-enrollment. In some cases, they might want to stay with the plan, especially if they’ve developed a relationship with a physician in that plan’s network, she said.
But they may also have gotten a new diagnosis that requires them to see a particular doctor, who might not be in the plan, said Ms. Klein. For that reason, it will be especially important for patients to be able to “compare in much greater detail the plans available,” she said.
To help increase awareness of the re-enrollment process, the CMS on Oct. 15 launched the “Five Steps to Staying Covered” campaign, urging patients to review their current plans, and then, starting on Nov. 15, to update their income and other information, compare the current plan with other plans, choose a plan, and enroll.
The CMS has been testing the healthcare.gov website and is encouraged by what it has seen so far, Mr. Counihan told health plan representatives.
“We feel confident we’re going to have a successful 2015,” he said.
On Twitter @aliciaault
WASHINGTON – Unless patients actively choose a new plan before Dec. 15, those who paid for a health insurance plan through the federal marketplace in 2014 will be automatically re-enrolled in the same plan for 2015, federal officials said.
The goal is to ensure there will be no gaps in coverage, Kevin Counihan, CEO of the federal health insurance marketplace, said at the Health Insurance Exchanges Forum held by America’s Health Insurance Plans.
Mr. Counihan did not give an estimate on how many people might be automatically re-enrolled, but he did say that some 7.3 million Americans had selected and paid for a health plan through the federal marketplace.
Mr. Counihan was appointed in late August to oversee the operations of healthcare.gov, the web portal for the federal health insurance marketplace. He is also director of the Centers for Medicare & Medicaid Services Center for Consumer Information and Insurance Oversight.
Open enrollment for health plans offered under the Affordable Care Act begins Nov. 15.
The CMS is starting to send notices to patients who either enrolled in a plan in 2014, or had been determined to be eligible but did not enroll, reminding them that they can start the renewal process on Nov. 15. The notices will arrive by mail or e-mail, depending on what the patient indicated as a preference.
At the same time, patients will receive notices from their current insurers, letting them know whether there are network or benefits changes, or if there is an increase or decrease in the premiums or other costs.
Patients have until Dec. 15 to enroll in a plan for coverage that starts on Jan. 1.
If they do not renew a current plan or elect a new plan by Dec. 15, they will be automatically re-enrolled in the existing plan, said Ben Walker, director of open enrollment for the federal marketplace at the CCIIO.
They will get the same amount of advance payment of the premium tax credit and same subsidies as in 2014. Those credits and cost-sharing reductions are subject to change, depending on a patient’s updated eligibility information.
Even if they’ve been auto-enrolled, they can eventually go back and select a different plan, as long as they do it by Feb. 15, when open season ends, Mr. Walker said at the meeting. The coverage in the new plan will start on the first day of the next or second month depending on when the patient enrolled.
The National Governors Association is somewhat concerned about the automatic re-enrollments, Esther Krofah, program director in the NGA’s health division, said at the meeting. “We have to make sure consumers are aware of their options and are taking the steps they need to protect themselves,” she said.
Rachel Klein, organizational strategy and enrollment program director for Families USA, said that patients could be confused, or potentially harmed, by the automatic re-enrollment. In some cases, they might want to stay with the plan, especially if they’ve developed a relationship with a physician in that plan’s network, she said.
But they may also have gotten a new diagnosis that requires them to see a particular doctor, who might not be in the plan, said Ms. Klein. For that reason, it will be especially important for patients to be able to “compare in much greater detail the plans available,” she said.
To help increase awareness of the re-enrollment process, the CMS on Oct. 15 launched the “Five Steps to Staying Covered” campaign, urging patients to review their current plans, and then, starting on Nov. 15, to update their income and other information, compare the current plan with other plans, choose a plan, and enroll.
The CMS has been testing the healthcare.gov website and is encouraged by what it has seen so far, Mr. Counihan told health plan representatives.
“We feel confident we’re going to have a successful 2015,” he said.
On Twitter @aliciaault
AT THE AHIP HEALTH INSURANCE EXCHANGES FORUM
Study finds lap approach to bariatric revision safe, effective
LAS VEGAS– As the volume of bariatric surgery climbs sharply in response to the obesity epidemic, the need for revision procedures due to weight regain is also on the rise.
Laparoscopic revision bariatric surgery, while more technically challenging, is safe and effective, and it entails less morbidity than typically seen with open revisions, Dr. Rana M. Ballo said at the annual Minimally Invasive Surgery Week.
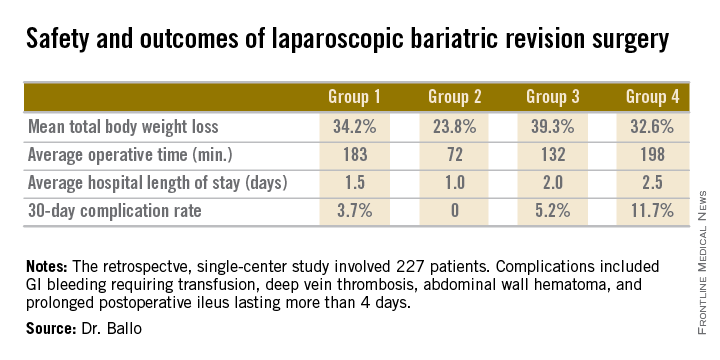
Dr. Ballo, a fifth-year general surgery resident at Rush University Medical Center in Chicago, presented a retrospective single-center study involving 227 patients who during 2001-2011 underwent laparoscopic revision of bariatric procedures that had failed because of weight regain. The goal of the revision bariatric surgery was to restore the restrictive component and/or add a malabsorptive component in order to improve long-term weight loss.
The patients fell into four groups. Group 1 consisted of 53 patients who initially had a laparoscopic adjustable gastric band procedure which was converted to a gastric bypass. Group 2, the largest group, initially had a Roux-en-Y gastric bypass in which the pouch eventually became dilated, which is the No. 1 cause of failure of this operation in the literature; their revision surgery entailed laparoscopic pouch reduction. The 38 patients who comprised Group 3 had a Roux-en-Y gastric bypass with subsequent pouch reduction and elongation of the biliopancreatic limb. Group 4 consisted of 17 patients who initially had a vertical banded gastroplasty – a procedure with a restrictive component only – and subsequently underwent laparoscopic conversion to a gastric bypass.
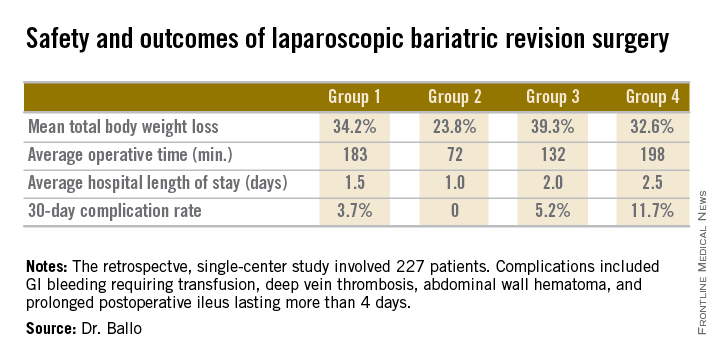
After a median follow-up of 3.9 years, Group 2 had significantly less total body weight loss than the rest of the groups, all of which had similar weight losses. On the other hand, Group 2 also had a shorter operative time and briefer average hospital length of stay than the other three groups, and it was the only group with zero complications. Still, the lengths of stay and 30-day morbidity rates across the board in this laparoscopic revision series were impressively low in comparison to those previously reported in series involving open revision, Dr. Ballo noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
There was no mortality in this study. This is one of the largest series reported to date of laparoscopic revision of failed bariatric surgery. Most prior studies have involved 30-100 patients, according to Dr. Ballo.
In the 1990s, roughly 13,000 bariatric procedures were performed annually in the United States. Today that figure is in excess of 200,000 annually.
Dr. Ballo reported having no financial conflicts with regard to this study.
LAS VEGAS– As the volume of bariatric surgery climbs sharply in response to the obesity epidemic, the need for revision procedures due to weight regain is also on the rise.
Laparoscopic revision bariatric surgery, while more technically challenging, is safe and effective, and it entails less morbidity than typically seen with open revisions, Dr. Rana M. Ballo said at the annual Minimally Invasive Surgery Week.
Dr. Ballo, a fifth-year general surgery resident at Rush University Medical Center in Chicago, presented a retrospective single-center study involving 227 patients who during 2001-2011 underwent laparoscopic revision of bariatric procedures that had failed because of weight regain. The goal of the revision bariatric surgery was to restore the restrictive component and/or add a malabsorptive component in order to improve long-term weight loss.
The patients fell into four groups. Group 1 consisted of 53 patients who initially had a laparoscopic adjustable gastric band procedure which was converted to a gastric bypass. Group 2, the largest group, initially had a Roux-en-Y gastric bypass in which the pouch eventually became dilated, which is the No. 1 cause of failure of this operation in the literature; their revision surgery entailed laparoscopic pouch reduction. The 38 patients who comprised Group 3 had a Roux-en-Y gastric bypass with subsequent pouch reduction and elongation of the biliopancreatic limb. Group 4 consisted of 17 patients who initially had a vertical banded gastroplasty – a procedure with a restrictive component only – and subsequently underwent laparoscopic conversion to a gastric bypass.
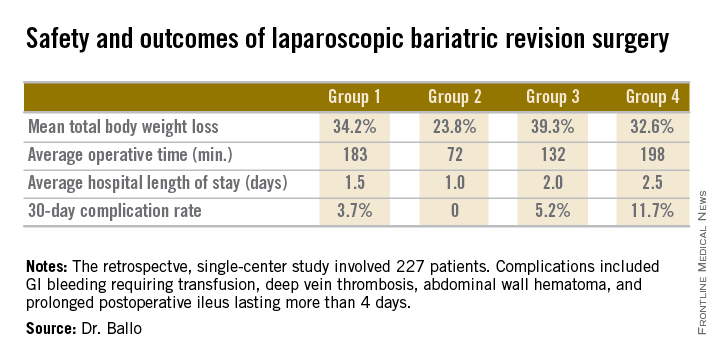
After a median follow-up of 3.9 years, Group 2 had significantly less total body weight loss than the rest of the groups, all of which had similar weight losses. On the other hand, Group 2 also had a shorter operative time and briefer average hospital length of stay than the other three groups, and it was the only group with zero complications. Still, the lengths of stay and 30-day morbidity rates across the board in this laparoscopic revision series were impressively low in comparison to those previously reported in series involving open revision, Dr. Ballo noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
There was no mortality in this study. This is one of the largest series reported to date of laparoscopic revision of failed bariatric surgery. Most prior studies have involved 30-100 patients, according to Dr. Ballo.
In the 1990s, roughly 13,000 bariatric procedures were performed annually in the United States. Today that figure is in excess of 200,000 annually.
Dr. Ballo reported having no financial conflicts with regard to this study.
LAS VEGAS– As the volume of bariatric surgery climbs sharply in response to the obesity epidemic, the need for revision procedures due to weight regain is also on the rise.
Laparoscopic revision bariatric surgery, while more technically challenging, is safe and effective, and it entails less morbidity than typically seen with open revisions, Dr. Rana M. Ballo said at the annual Minimally Invasive Surgery Week.
Dr. Ballo, a fifth-year general surgery resident at Rush University Medical Center in Chicago, presented a retrospective single-center study involving 227 patients who during 2001-2011 underwent laparoscopic revision of bariatric procedures that had failed because of weight regain. The goal of the revision bariatric surgery was to restore the restrictive component and/or add a malabsorptive component in order to improve long-term weight loss.
The patients fell into four groups. Group 1 consisted of 53 patients who initially had a laparoscopic adjustable gastric band procedure which was converted to a gastric bypass. Group 2, the largest group, initially had a Roux-en-Y gastric bypass in which the pouch eventually became dilated, which is the No. 1 cause of failure of this operation in the literature; their revision surgery entailed laparoscopic pouch reduction. The 38 patients who comprised Group 3 had a Roux-en-Y gastric bypass with subsequent pouch reduction and elongation of the biliopancreatic limb. Group 4 consisted of 17 patients who initially had a vertical banded gastroplasty – a procedure with a restrictive component only – and subsequently underwent laparoscopic conversion to a gastric bypass.
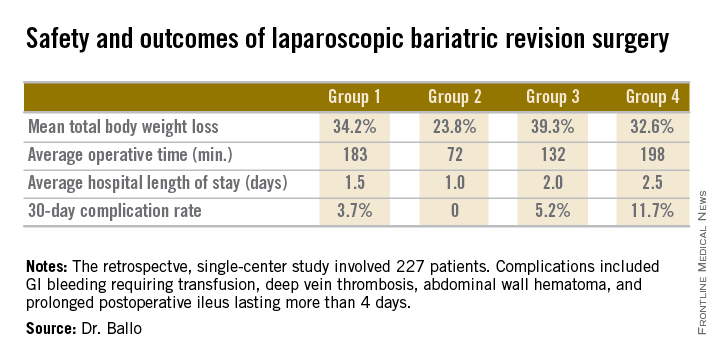
After a median follow-up of 3.9 years, Group 2 had significantly less total body weight loss than the rest of the groups, all of which had similar weight losses. On the other hand, Group 2 also had a shorter operative time and briefer average hospital length of stay than the other three groups, and it was the only group with zero complications. Still, the lengths of stay and 30-day morbidity rates across the board in this laparoscopic revision series were impressively low in comparison to those previously reported in series involving open revision, Dr. Ballo noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
There was no mortality in this study. This is one of the largest series reported to date of laparoscopic revision of failed bariatric surgery. Most prior studies have involved 30-100 patients, according to Dr. Ballo.
In the 1990s, roughly 13,000 bariatric procedures were performed annually in the United States. Today that figure is in excess of 200,000 annually.
Dr. Ballo reported having no financial conflicts with regard to this study.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Laparoscopic revision of failed bariatric surgery is safe and effective.
Major finding: Patients experienced a mean total body weight loss of 24%-39% at a median of 3.9 years after laparoscopic revision of failed bariatric surgery. The weight loss depended upon the primary procedure and type of revision.
Data source: This was a retrospective single-center series involving 227 patients who underwent laparoscopic revisional bariatric surgery in response to weight regain.
Disclosures: The presenter reported having no financial conflicts regarding this study.
Intraoperative evaluation may be best for predicting AVF success
CORONADO, CALIF. – Intraoperative vessel assessment, not preoperative vein mapping, was more accurately associated with maturation and cumulative functional patency rates of arteriovenous fistulas, results from a 5-year, single-center retrospective study showed.
“The prevalence of chronic kidney disease has increased over the last 3 decades, and efforts by the Centers for Medicare & Medicaid Services and the National Kidney Foundation have sought to increase the use of fistulas,” Dr. Khanh P. Nguyen said at the annual meeting of the Western Vascular Society.
“Since 2003, the incidence and prevalence of fistulas have increased. More recently, even higher goals have been set. Arteriovenous fistulas are the preferred procedures due to higher patency rates, reduced rates of reintervention, and lower costs, compared with central venous catheters or grafts.”
Dr. Nguyen, formerly of Loma Linda (Calif.) Medical Center who is now a vascular surgery fellow at Oregon Health and Science University, noted that while many studies as well as the Society for Vascular Surgery have advocated the use of routine preoperative ultrasound in predicting the success of arteriovenous fistulas (AVFs), its use varies among vascular surgeons. “Given the additional costs and time of preoperative ultrasound, this study was undertaken to examine the use of this technique and compare it to intraoperative assessment,” she said.
The researchers examined all autologous AVFs created for patients with end-stage-renal disease at the Veterans Affairs Loma Linda Health System between February 2007 and July 2012. Preoperative ultrasound mapping of upper-extremity veins occurred, and patients were divided into two groups: those with veins less than 3 mm in size and those with veins 3 mm or greater in size. Subjective intraoperative evaluation was conducted by the operative surgeon, who rated the vein as either “good” or “poor” because of factors such as inadequate diameter, sclerosis, and calcification. Kaplan-Meier analysis was used to calculate maturation and patency rates.
Over the 5-year period, 387 fistulas were created in 361 patients. Of these, 198 had preoperative vein mapping; 36% were less than 3 mm in size, and 64% were 3 mm or greater in size.
By intraoperative assessment, 14% of patients were determined to have had poor vessels, and 86% were found to have good vessels. About half of the fistulas (51%) were created at the wrist. The average age of patients was 65 years, their mean body mass index was 28 kg/m2, and their mean time on dialysis was 84 years. The majority (97%) were male.
Among patients with preoperative veins less than 3 mm in size or 3 mm in size or greater, the maturation and overall failure rates were similar at 71% vs. 75% (P = .61) and 68% vs. 58% (P = .15). However, among patients with assessments of poor or good veins at the time of operation, the maturation and overall failure rates were 42% vs. 82% (P < .001) and 86% vs. 54% (P < .001).
Subgroup analysis revealed that patients with good intraoperative evaluation, regardless of preoperative ultrasound findings, had higher maturation rates. “Likewise, patients with good intraoperative assessment, regardless of preoperative ultrasound findings, had higher cumulative functional patency rates. Of note, no patient who had both poor preoperative ultrasound and intraoperative assessments had a functional fistula at the time of last follow-up.”
Dr. Nguyen and her associates concluded that intraoperative vessel assessment, and not preoperative ultrasound, was more accurately associated with maturation and cumulative functional patency rates. “Even in patients with inadequate preoperative ultrasound vein mapping, intraoperative assessment may still be warranted,” she said. “If both preoperative and intraoperative assessments conclude that vessels are inadequate, do not create an AVF at that site.”
Dr. Nguyen reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Intraoperative vessel assessment, not preoperative vein mapping, was more accurately associated with maturation and cumulative functional patency rates of arteriovenous fistulas, results from a 5-year, single-center retrospective study showed.
“The prevalence of chronic kidney disease has increased over the last 3 decades, and efforts by the Centers for Medicare & Medicaid Services and the National Kidney Foundation have sought to increase the use of fistulas,” Dr. Khanh P. Nguyen said at the annual meeting of the Western Vascular Society.
“Since 2003, the incidence and prevalence of fistulas have increased. More recently, even higher goals have been set. Arteriovenous fistulas are the preferred procedures due to higher patency rates, reduced rates of reintervention, and lower costs, compared with central venous catheters or grafts.”
Dr. Nguyen, formerly of Loma Linda (Calif.) Medical Center who is now a vascular surgery fellow at Oregon Health and Science University, noted that while many studies as well as the Society for Vascular Surgery have advocated the use of routine preoperative ultrasound in predicting the success of arteriovenous fistulas (AVFs), its use varies among vascular surgeons. “Given the additional costs and time of preoperative ultrasound, this study was undertaken to examine the use of this technique and compare it to intraoperative assessment,” she said.
The researchers examined all autologous AVFs created for patients with end-stage-renal disease at the Veterans Affairs Loma Linda Health System between February 2007 and July 2012. Preoperative ultrasound mapping of upper-extremity veins occurred, and patients were divided into two groups: those with veins less than 3 mm in size and those with veins 3 mm or greater in size. Subjective intraoperative evaluation was conducted by the operative surgeon, who rated the vein as either “good” or “poor” because of factors such as inadequate diameter, sclerosis, and calcification. Kaplan-Meier analysis was used to calculate maturation and patency rates.
Over the 5-year period, 387 fistulas were created in 361 patients. Of these, 198 had preoperative vein mapping; 36% were less than 3 mm in size, and 64% were 3 mm or greater in size.
By intraoperative assessment, 14% of patients were determined to have had poor vessels, and 86% were found to have good vessels. About half of the fistulas (51%) were created at the wrist. The average age of patients was 65 years, their mean body mass index was 28 kg/m2, and their mean time on dialysis was 84 years. The majority (97%) were male.
Among patients with preoperative veins less than 3 mm in size or 3 mm in size or greater, the maturation and overall failure rates were similar at 71% vs. 75% (P = .61) and 68% vs. 58% (P = .15). However, among patients with assessments of poor or good veins at the time of operation, the maturation and overall failure rates were 42% vs. 82% (P < .001) and 86% vs. 54% (P < .001).
Subgroup analysis revealed that patients with good intraoperative evaluation, regardless of preoperative ultrasound findings, had higher maturation rates. “Likewise, patients with good intraoperative assessment, regardless of preoperative ultrasound findings, had higher cumulative functional patency rates. Of note, no patient who had both poor preoperative ultrasound and intraoperative assessments had a functional fistula at the time of last follow-up.”
Dr. Nguyen and her associates concluded that intraoperative vessel assessment, and not preoperative ultrasound, was more accurately associated with maturation and cumulative functional patency rates. “Even in patients with inadequate preoperative ultrasound vein mapping, intraoperative assessment may still be warranted,” she said. “If both preoperative and intraoperative assessments conclude that vessels are inadequate, do not create an AVF at that site.”
Dr. Nguyen reported having no relevant financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – Intraoperative vessel assessment, not preoperative vein mapping, was more accurately associated with maturation and cumulative functional patency rates of arteriovenous fistulas, results from a 5-year, single-center retrospective study showed.
“The prevalence of chronic kidney disease has increased over the last 3 decades, and efforts by the Centers for Medicare & Medicaid Services and the National Kidney Foundation have sought to increase the use of fistulas,” Dr. Khanh P. Nguyen said at the annual meeting of the Western Vascular Society.
“Since 2003, the incidence and prevalence of fistulas have increased. More recently, even higher goals have been set. Arteriovenous fistulas are the preferred procedures due to higher patency rates, reduced rates of reintervention, and lower costs, compared with central venous catheters or grafts.”
Dr. Nguyen, formerly of Loma Linda (Calif.) Medical Center who is now a vascular surgery fellow at Oregon Health and Science University, noted that while many studies as well as the Society for Vascular Surgery have advocated the use of routine preoperative ultrasound in predicting the success of arteriovenous fistulas (AVFs), its use varies among vascular surgeons. “Given the additional costs and time of preoperative ultrasound, this study was undertaken to examine the use of this technique and compare it to intraoperative assessment,” she said.
The researchers examined all autologous AVFs created for patients with end-stage-renal disease at the Veterans Affairs Loma Linda Health System between February 2007 and July 2012. Preoperative ultrasound mapping of upper-extremity veins occurred, and patients were divided into two groups: those with veins less than 3 mm in size and those with veins 3 mm or greater in size. Subjective intraoperative evaluation was conducted by the operative surgeon, who rated the vein as either “good” or “poor” because of factors such as inadequate diameter, sclerosis, and calcification. Kaplan-Meier analysis was used to calculate maturation and patency rates.
Over the 5-year period, 387 fistulas were created in 361 patients. Of these, 198 had preoperative vein mapping; 36% were less than 3 mm in size, and 64% were 3 mm or greater in size.
By intraoperative assessment, 14% of patients were determined to have had poor vessels, and 86% were found to have good vessels. About half of the fistulas (51%) were created at the wrist. The average age of patients was 65 years, their mean body mass index was 28 kg/m2, and their mean time on dialysis was 84 years. The majority (97%) were male.
Among patients with preoperative veins less than 3 mm in size or 3 mm in size or greater, the maturation and overall failure rates were similar at 71% vs. 75% (P = .61) and 68% vs. 58% (P = .15). However, among patients with assessments of poor or good veins at the time of operation, the maturation and overall failure rates were 42% vs. 82% (P < .001) and 86% vs. 54% (P < .001).
Subgroup analysis revealed that patients with good intraoperative evaluation, regardless of preoperative ultrasound findings, had higher maturation rates. “Likewise, patients with good intraoperative assessment, regardless of preoperative ultrasound findings, had higher cumulative functional patency rates. Of note, no patient who had both poor preoperative ultrasound and intraoperative assessments had a functional fistula at the time of last follow-up.”
Dr. Nguyen and her associates concluded that intraoperative vessel assessment, and not preoperative ultrasound, was more accurately associated with maturation and cumulative functional patency rates. “Even in patients with inadequate preoperative ultrasound vein mapping, intraoperative assessment may still be warranted,” she said. “If both preoperative and intraoperative assessments conclude that vessels are inadequate, do not create an AVF at that site.”
Dr. Nguyen reported having no relevant financial disclosures.
On Twitter @dougbrunk
AT THE WESTERN VASCULAR SOCIETY ANNUAL MEETING
Key clinical point: Routine preoperative ultrasound is not reliable for predicting the success of arteriovenous fistulas.
Major finding: Among patients with assessments of poor or good veins at the time of operation, the maturation and overall failure rates were 42% vs. 82% (P < .001) and 86% vs. 54% (P < .001).
Data source: A retrospective study of 387 AVFs created in 361 patients at the VA Loma Linda Health System between February 2007 and July 2012.
Disclosures:Dr. Nguyen reported having no relevant financial disclosures.
FDA approves budesonide rectal foam for distal UC
A rectal foam formulation of 2% budesonide has been approved by the Food and Drug Administration for treating distal ulcerative colitis, the manufacturer, Salix Pharmaceuticals, has announced.
The approved indication is for the induction of remission in patients with mild to moderate distal ulcerative colitis extending up to 40 cm from the anal verge. The foam is administered rectally and “overcomes treatment limitations associated with currently approved therapies which are often ineffective due to insufficient distribution of active drug to the distal colon,” the company said in a statement announcing the final approval on Oct. 8.
The company will be marketing the product as Uceris.
The company also markets budesonide oral extended-release tablets under the same name.
A rectal foam formulation of 2% budesonide has been approved by the Food and Drug Administration for treating distal ulcerative colitis, the manufacturer, Salix Pharmaceuticals, has announced.
The approved indication is for the induction of remission in patients with mild to moderate distal ulcerative colitis extending up to 40 cm from the anal verge. The foam is administered rectally and “overcomes treatment limitations associated with currently approved therapies which are often ineffective due to insufficient distribution of active drug to the distal colon,” the company said in a statement announcing the final approval on Oct. 8.
The company will be marketing the product as Uceris.
The company also markets budesonide oral extended-release tablets under the same name.
A rectal foam formulation of 2% budesonide has been approved by the Food and Drug Administration for treating distal ulcerative colitis, the manufacturer, Salix Pharmaceuticals, has announced.
The approved indication is for the induction of remission in patients with mild to moderate distal ulcerative colitis extending up to 40 cm from the anal verge. The foam is administered rectally and “overcomes treatment limitations associated with currently approved therapies which are often ineffective due to insufficient distribution of active drug to the distal colon,” the company said in a statement announcing the final approval on Oct. 8.
The company will be marketing the product as Uceris.
The company also markets budesonide oral extended-release tablets under the same name.
Rethinking the postop patient-surgeon visit
LAS VEGAS– Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a possible alternative to the traditional surgeon-patient clinic visit, a pilot study indicates.
“It is feasible and seems effective. It is well received by patients, and it’s especially attractive for patients traveling long distances to receive their medical care. It may well prove to be the most efficient method for follow-up after laparoscopic inguinal hernia repair. It frees up clinic time: More than 80% of patients in our study were spared a clinic visit, and this allowed us to increase the number of our outpatient encounters,” Dr. Dan Eisenberg said at the annual Minimally Invasive Surgery Week.
He presented a prospective study of 62 consecutive patients who underwent laparoscopic inguinal hernia repair at the Veterans Affairs Palo Alto (Calif.) Health Care System and agreed to follow-up by a physician assistant 2-3 weeks after surgery in lieu of the traditional face-to-face clinic visit with the surgeon. The phone interview involved a predetermined nine-question script. A single “yes” answer prompted an appointment for a clinic visit.
Of the 62 patients, 3 were lost to follow-up. Because of a scheduling error, another four showed up at the VA clinic for a follow-up visit before the planned phone call. Of the remaining 55 patients, 50 (91%) were satisfied with their telephone follow-up experience.
Five patients were seen face to face at the clinic as a result of their telephone follow-up. Three did so because of self-limited groin discomfort, one for a large seroma, and one for early hernia recurrence treated by the total extraperitoneal approach, reported Dr. Eisenberg, a general surgeon at the Palo Alto VA.
Session chair Vincenzo Neri voiced a misgiving about the study.
“The only problem I see is that it contributes to the dehumanization of surgery,” commented Dr. Neri, professor and director of the division of general surgery at the University of Foggia (Italy). “The follow-up contact that you have in the clinic when you actually see the patient can be important because so many things can happen to the patient that he has no awareness of. Your way, the follow-up is basically gone.”
Dr. Eisenberg was quick to concur that the patient-surgeon relationship is basic to clinical medicine, and that the postop clinic visit is a fundamental part of this relationship.
“It is unfortunate to see that in the U.S., external constraints are changing the way we practice medicine,” he added, “but these external pressures are demanding more time efficiency and more resource efficiency, ultimately culminating, hopefully, in cost efficiency. The VA system is single payer. At the Palo Alto VA, we’ve noticed an increase in resource constraint limiting clinic access, and financial constraints going along with it.”
The Palo Alto VA Health Care System serves an enormous geographic area running north to the Oregon border and east into Nevada. The average roundtrip distance to the VA hospital for the study participants was 122 miles, and they were happy to forgo the journey.
“In Bay Area traffic, that corresponds to 3 to 3 1/2 hours on the road,” Dr. Eisenberg noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
His future research plans include randomizing patients to telephone follow-up or a face-to-face clinic visit after laparoscopic inguinal hernia repair in order to quantify the impact of the novel alternative on clinic flow and patient satisfaction. He also plans to extend the practice of telephone follow-up by a midlevel provider to other surgical procedures. He and his coworkers have already applied it to patients after laparoscopic cholecystectomy, where it also appears to be safe and efficient.
“It raises the question of how much further we can push this. Maybe it doesn’t have to be just for outpatient surgery,” according to Dr. Eisenberg.
Dr. Eisenberg reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
The nine yes/no telephone follow-up questions
Do you feel unwell?
Are you requiring frequent analgesics?
Are you having trouble returning to your normal activities?
Do you have fever or chills?
Is there increasing redness or swelling at the incision site?
Do you have testicular swelling or pain?
Are you having trouble tolerating a regular diet?
Do you have any concerns?
Would you like a face-to-face clinic visit?
A “yes” answer to any of the above triggers a clinic visit.
Source: Dr. Eisenberg
LAS VEGAS– Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a possible alternative to the traditional surgeon-patient clinic visit, a pilot study indicates.
“It is feasible and seems effective. It is well received by patients, and it’s especially attractive for patients traveling long distances to receive their medical care. It may well prove to be the most efficient method for follow-up after laparoscopic inguinal hernia repair. It frees up clinic time: More than 80% of patients in our study were spared a clinic visit, and this allowed us to increase the number of our outpatient encounters,” Dr. Dan Eisenberg said at the annual Minimally Invasive Surgery Week.
He presented a prospective study of 62 consecutive patients who underwent laparoscopic inguinal hernia repair at the Veterans Affairs Palo Alto (Calif.) Health Care System and agreed to follow-up by a physician assistant 2-3 weeks after surgery in lieu of the traditional face-to-face clinic visit with the surgeon. The phone interview involved a predetermined nine-question script. A single “yes” answer prompted an appointment for a clinic visit.
Of the 62 patients, 3 were lost to follow-up. Because of a scheduling error, another four showed up at the VA clinic for a follow-up visit before the planned phone call. Of the remaining 55 patients, 50 (91%) were satisfied with their telephone follow-up experience.
Five patients were seen face to face at the clinic as a result of their telephone follow-up. Three did so because of self-limited groin discomfort, one for a large seroma, and one for early hernia recurrence treated by the total extraperitoneal approach, reported Dr. Eisenberg, a general surgeon at the Palo Alto VA.
Session chair Vincenzo Neri voiced a misgiving about the study.
“The only problem I see is that it contributes to the dehumanization of surgery,” commented Dr. Neri, professor and director of the division of general surgery at the University of Foggia (Italy). “The follow-up contact that you have in the clinic when you actually see the patient can be important because so many things can happen to the patient that he has no awareness of. Your way, the follow-up is basically gone.”
Dr. Eisenberg was quick to concur that the patient-surgeon relationship is basic to clinical medicine, and that the postop clinic visit is a fundamental part of this relationship.
“It is unfortunate to see that in the U.S., external constraints are changing the way we practice medicine,” he added, “but these external pressures are demanding more time efficiency and more resource efficiency, ultimately culminating, hopefully, in cost efficiency. The VA system is single payer. At the Palo Alto VA, we’ve noticed an increase in resource constraint limiting clinic access, and financial constraints going along with it.”
The Palo Alto VA Health Care System serves an enormous geographic area running north to the Oregon border and east into Nevada. The average roundtrip distance to the VA hospital for the study participants was 122 miles, and they were happy to forgo the journey.
“In Bay Area traffic, that corresponds to 3 to 3 1/2 hours on the road,” Dr. Eisenberg noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
His future research plans include randomizing patients to telephone follow-up or a face-to-face clinic visit after laparoscopic inguinal hernia repair in order to quantify the impact of the novel alternative on clinic flow and patient satisfaction. He also plans to extend the practice of telephone follow-up by a midlevel provider to other surgical procedures. He and his coworkers have already applied it to patients after laparoscopic cholecystectomy, where it also appears to be safe and efficient.
“It raises the question of how much further we can push this. Maybe it doesn’t have to be just for outpatient surgery,” according to Dr. Eisenberg.
Dr. Eisenberg reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
The nine yes/no telephone follow-up questions
Do you feel unwell?
Are you requiring frequent analgesics?
Are you having trouble returning to your normal activities?
Do you have fever or chills?
Is there increasing redness or swelling at the incision site?
Do you have testicular swelling or pain?
Are you having trouble tolerating a regular diet?
Do you have any concerns?
Would you like a face-to-face clinic visit?
A “yes” answer to any of the above triggers a clinic visit.
Source: Dr. Eisenberg
LAS VEGAS– Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a possible alternative to the traditional surgeon-patient clinic visit, a pilot study indicates.
“It is feasible and seems effective. It is well received by patients, and it’s especially attractive for patients traveling long distances to receive their medical care. It may well prove to be the most efficient method for follow-up after laparoscopic inguinal hernia repair. It frees up clinic time: More than 80% of patients in our study were spared a clinic visit, and this allowed us to increase the number of our outpatient encounters,” Dr. Dan Eisenberg said at the annual Minimally Invasive Surgery Week.
He presented a prospective study of 62 consecutive patients who underwent laparoscopic inguinal hernia repair at the Veterans Affairs Palo Alto (Calif.) Health Care System and agreed to follow-up by a physician assistant 2-3 weeks after surgery in lieu of the traditional face-to-face clinic visit with the surgeon. The phone interview involved a predetermined nine-question script. A single “yes” answer prompted an appointment for a clinic visit.
Of the 62 patients, 3 were lost to follow-up. Because of a scheduling error, another four showed up at the VA clinic for a follow-up visit before the planned phone call. Of the remaining 55 patients, 50 (91%) were satisfied with their telephone follow-up experience.
Five patients were seen face to face at the clinic as a result of their telephone follow-up. Three did so because of self-limited groin discomfort, one for a large seroma, and one for early hernia recurrence treated by the total extraperitoneal approach, reported Dr. Eisenberg, a general surgeon at the Palo Alto VA.
Session chair Vincenzo Neri voiced a misgiving about the study.
“The only problem I see is that it contributes to the dehumanization of surgery,” commented Dr. Neri, professor and director of the division of general surgery at the University of Foggia (Italy). “The follow-up contact that you have in the clinic when you actually see the patient can be important because so many things can happen to the patient that he has no awareness of. Your way, the follow-up is basically gone.”
Dr. Eisenberg was quick to concur that the patient-surgeon relationship is basic to clinical medicine, and that the postop clinic visit is a fundamental part of this relationship.
“It is unfortunate to see that in the U.S., external constraints are changing the way we practice medicine,” he added, “but these external pressures are demanding more time efficiency and more resource efficiency, ultimately culminating, hopefully, in cost efficiency. The VA system is single payer. At the Palo Alto VA, we’ve noticed an increase in resource constraint limiting clinic access, and financial constraints going along with it.”
The Palo Alto VA Health Care System serves an enormous geographic area running north to the Oregon border and east into Nevada. The average roundtrip distance to the VA hospital for the study participants was 122 miles, and they were happy to forgo the journey.
“In Bay Area traffic, that corresponds to 3 to 3 1/2 hours on the road,” Dr. Eisenberg noted at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
His future research plans include randomizing patients to telephone follow-up or a face-to-face clinic visit after laparoscopic inguinal hernia repair in order to quantify the impact of the novel alternative on clinic flow and patient satisfaction. He also plans to extend the practice of telephone follow-up by a midlevel provider to other surgical procedures. He and his coworkers have already applied it to patients after laparoscopic cholecystectomy, where it also appears to be safe and efficient.
“It raises the question of how much further we can push this. Maybe it doesn’t have to be just for outpatient surgery,” according to Dr. Eisenberg.
Dr. Eisenberg reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
The nine yes/no telephone follow-up questions
Do you feel unwell?
Are you requiring frequent analgesics?
Are you having trouble returning to your normal activities?
Do you have fever or chills?
Is there increasing redness or swelling at the incision site?
Do you have testicular swelling or pain?
Are you having trouble tolerating a regular diet?
Do you have any concerns?
Would you like a face-to-face clinic visit?
A “yes” answer to any of the above triggers a clinic visit.
Source: Dr. Eisenberg
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Scripted telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair is a safe, effective, and resource-sparing alternative to the traditional face-to-face surgeon-patient follow-up visit.
Major finding: Fifty of 55 patients who underwent laparoscopic inguinal hernia repair were safely able to be spared a follow-up clinic visit as a result of telephone follow-up by a physician assistant several weeks after surgery.
Data source: This was a prospective observational study in which patients who had laparoscopic repair of an inguinal hernia agreed to a scripted telephone follow-up by a physician assistant instead of returning to the clinic for the traditional surgeon-patient face-to-face encounter.
Disclosures: The presenter reported having no financial conflicts with regard to the study, which was funded by the Department of Veterans Affairs.
Malpractice premiums remained flat in 2014
Malpractice premiums for physicians stayed mostly the same in 2014, with 65% of liability insurance rates remaining steady nationwide, according to the Medical Liability Monitor’s annual survey and analysis of premiums nationwide.
Ongoing trends of slow lawsuit frequency and low plaintiff payouts are contributing to the steady market, said Chad C. Karls, editor of the 2014 Annual Rate Survey and a principal and consulting actuary for Milliman in Brookfield, Wis.
“We certainly do see those very large verdicts in the industry, but when we take it across all claims, the vast majority don’t have a verdict attached to them,” Mr. Karls said in an interview. “The vast majority get settled. That average claim has remained relatively stable.”
Unchanging insurance rates, however, can mean payment misery or relief depending on where physicians practice. Internists in southern Florida will pay a high of $47,707 for malpractice insurance this year, while their counterparts in South Dakota will pay just $3,697. For ob.gyns., malpractice insurance is priciest in the New York counties of Nassau and Suffolk, where they will pay $214,999 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240. General surgeons in southern Florida will dish out $190,829 in premiums in 2014, while Wisconsin surgeons will pay $10,868.
Premiums did increase in some areas in 2014. Indiana physicians saw the highest increase at 4.5%. Nevada doctors experienced a 34.8% decrease in premiums, by far the largest drop among states. (See map.) Nevada’s average percent change was driven by two companies that reported high rate decreases, the survey noted. (Acquisitions by some Nevada insurers may have affected the numbers.)
In general, Nevada’s large rate decline is not surprising, said Dr. Warren Volker, trustee-at-large for the Clark County (Nev.) Medical Society and chair of Premiere Physician Insurance Company in Nevada. Doctors in the state have experienced a stable medical liability climate for the last decade, he said.
“Our premiums have gone down dramatically, across the board,” Dr. Volker said in an interview. “Physicians have enjoyed cost savings as long as they have a good history.”
He attributed the declines to tort reform passed in 2002, including a $350,000 noneconomic damages cap in medical malpractice cases. Since then, the number of lawsuit filings has gone down and competition among liability insurers has increased, he said.
Legal reforms such as Nevada’s have probably contributed to the overall decrease in lawsuit frequency and payout severity across the country, Mr. Karls said. Patient safety initiatives and better risk management within medical practices also may be having an impact.
It remains to be seen how the Affordable Care Act will affect medical liability premiums. So far, industry analysts have not seen a definitive impact on medical malpractice insurance rates from the law, Mr. Karls said. The law could ultimately help lower liability claims if the ACA results in more proactive, preventive approaches to medical errors and less acute care, but in the short term, more patients covered under the ACA could mean a rise in lawsuits and, thus, premiums.
There are “more people getting care from the same number of health providers,” he said. “That puts additional pressure on an already strained system. Short term, the impact of the ACA could lead to additional [malpractice] claims.”
As for states with extremely high insurance rates, Dr. Volker does not see premium relief any time soon. He expects the trend of practice mergers and acquisitions to continue as more physicians seek to escape high premium costs and regulatory burdens.
“I think what you’re going to see in the hotbeds is more migration,” said Dr. Volker, who is licensed to practice in Nevada, California, Florida, and Arizona. “More doctors [will be] giving up their individual practices and joining larger groups.”
The MLM survey, published in October, gathered July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
Malpractice premiums for physicians stayed mostly the same in 2014, with 65% of liability insurance rates remaining steady nationwide, according to the Medical Liability Monitor’s annual survey and analysis of premiums nationwide.
Ongoing trends of slow lawsuit frequency and low plaintiff payouts are contributing to the steady market, said Chad C. Karls, editor of the 2014 Annual Rate Survey and a principal and consulting actuary for Milliman in Brookfield, Wis.
“We certainly do see those very large verdicts in the industry, but when we take it across all claims, the vast majority don’t have a verdict attached to them,” Mr. Karls said in an interview. “The vast majority get settled. That average claim has remained relatively stable.”
Unchanging insurance rates, however, can mean payment misery or relief depending on where physicians practice. Internists in southern Florida will pay a high of $47,707 for malpractice insurance this year, while their counterparts in South Dakota will pay just $3,697. For ob.gyns., malpractice insurance is priciest in the New York counties of Nassau and Suffolk, where they will pay $214,999 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240. General surgeons in southern Florida will dish out $190,829 in premiums in 2014, while Wisconsin surgeons will pay $10,868.
Premiums did increase in some areas in 2014. Indiana physicians saw the highest increase at 4.5%. Nevada doctors experienced a 34.8% decrease in premiums, by far the largest drop among states. (See map.) Nevada’s average percent change was driven by two companies that reported high rate decreases, the survey noted. (Acquisitions by some Nevada insurers may have affected the numbers.)
In general, Nevada’s large rate decline is not surprising, said Dr. Warren Volker, trustee-at-large for the Clark County (Nev.) Medical Society and chair of Premiere Physician Insurance Company in Nevada. Doctors in the state have experienced a stable medical liability climate for the last decade, he said.
“Our premiums have gone down dramatically, across the board,” Dr. Volker said in an interview. “Physicians have enjoyed cost savings as long as they have a good history.”
He attributed the declines to tort reform passed in 2002, including a $350,000 noneconomic damages cap in medical malpractice cases. Since then, the number of lawsuit filings has gone down and competition among liability insurers has increased, he said.
Legal reforms such as Nevada’s have probably contributed to the overall decrease in lawsuit frequency and payout severity across the country, Mr. Karls said. Patient safety initiatives and better risk management within medical practices also may be having an impact.
It remains to be seen how the Affordable Care Act will affect medical liability premiums. So far, industry analysts have not seen a definitive impact on medical malpractice insurance rates from the law, Mr. Karls said. The law could ultimately help lower liability claims if the ACA results in more proactive, preventive approaches to medical errors and less acute care, but in the short term, more patients covered under the ACA could mean a rise in lawsuits and, thus, premiums.
There are “more people getting care from the same number of health providers,” he said. “That puts additional pressure on an already strained system. Short term, the impact of the ACA could lead to additional [malpractice] claims.”
As for states with extremely high insurance rates, Dr. Volker does not see premium relief any time soon. He expects the trend of practice mergers and acquisitions to continue as more physicians seek to escape high premium costs and regulatory burdens.
“I think what you’re going to see in the hotbeds is more migration,” said Dr. Volker, who is licensed to practice in Nevada, California, Florida, and Arizona. “More doctors [will be] giving up their individual practices and joining larger groups.”
The MLM survey, published in October, gathered July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
Malpractice premiums for physicians stayed mostly the same in 2014, with 65% of liability insurance rates remaining steady nationwide, according to the Medical Liability Monitor’s annual survey and analysis of premiums nationwide.
Ongoing trends of slow lawsuit frequency and low plaintiff payouts are contributing to the steady market, said Chad C. Karls, editor of the 2014 Annual Rate Survey and a principal and consulting actuary for Milliman in Brookfield, Wis.
“We certainly do see those very large verdicts in the industry, but when we take it across all claims, the vast majority don’t have a verdict attached to them,” Mr. Karls said in an interview. “The vast majority get settled. That average claim has remained relatively stable.”
Unchanging insurance rates, however, can mean payment misery or relief depending on where physicians practice. Internists in southern Florida will pay a high of $47,707 for malpractice insurance this year, while their counterparts in South Dakota will pay just $3,697. For ob.gyns., malpractice insurance is priciest in the New York counties of Nassau and Suffolk, where they will pay $214,999 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240. General surgeons in southern Florida will dish out $190,829 in premiums in 2014, while Wisconsin surgeons will pay $10,868.
Premiums did increase in some areas in 2014. Indiana physicians saw the highest increase at 4.5%. Nevada doctors experienced a 34.8% decrease in premiums, by far the largest drop among states. (See map.) Nevada’s average percent change was driven by two companies that reported high rate decreases, the survey noted. (Acquisitions by some Nevada insurers may have affected the numbers.)
In general, Nevada’s large rate decline is not surprising, said Dr. Warren Volker, trustee-at-large for the Clark County (Nev.) Medical Society and chair of Premiere Physician Insurance Company in Nevada. Doctors in the state have experienced a stable medical liability climate for the last decade, he said.
“Our premiums have gone down dramatically, across the board,” Dr. Volker said in an interview. “Physicians have enjoyed cost savings as long as they have a good history.”
He attributed the declines to tort reform passed in 2002, including a $350,000 noneconomic damages cap in medical malpractice cases. Since then, the number of lawsuit filings has gone down and competition among liability insurers has increased, he said.
Legal reforms such as Nevada’s have probably contributed to the overall decrease in lawsuit frequency and payout severity across the country, Mr. Karls said. Patient safety initiatives and better risk management within medical practices also may be having an impact.
It remains to be seen how the Affordable Care Act will affect medical liability premiums. So far, industry analysts have not seen a definitive impact on medical malpractice insurance rates from the law, Mr. Karls said. The law could ultimately help lower liability claims if the ACA results in more proactive, preventive approaches to medical errors and less acute care, but in the short term, more patients covered under the ACA could mean a rise in lawsuits and, thus, premiums.
There are “more people getting care from the same number of health providers,” he said. “That puts additional pressure on an already strained system. Short term, the impact of the ACA could lead to additional [malpractice] claims.”
As for states with extremely high insurance rates, Dr. Volker does not see premium relief any time soon. He expects the trend of practice mergers and acquisitions to continue as more physicians seek to escape high premium costs and regulatory burdens.
“I think what you’re going to see in the hotbeds is more migration,” said Dr. Volker, who is licensed to practice in Nevada, California, Florida, and Arizona. “More doctors [will be] giving up their individual practices and joining larger groups.”
The MLM survey, published in October, gathered July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
‘Prehabilitation’ cut postoperative care costs for total hip and knee replacements
Physical therapy before joint replacement surgery cut the predicted use of postoperative care by 29%, saving an estimated $1,215 in health care costs per patient, according to a Medicare claims analysis.
“These data are clinically relevant and can be used in the development of cost-effective and value-based total joint replacement programs,” said Dr. Richard Snow at OhioHealth in Columbus and his associates. The study is the first to evaluate the real-world link between preoperative physical therapy and use of postoperative care, the researchers said.
Numbers of total hip and knee replacements are projected to increase by 1.7 and 6.7 times, respectively, in the United States between 2005 and 2030, Dr. Snow and his coauthors noted. And while average length of hospital stay after these surgeries has dropped by more than 50%, there has been a substantial rise in per-patient costs of skilled nursing facilities, home health agencies, and inpatient rehabilitation, they said (J. Bone Joint Surg. 2014 Oct. 1 [doi:10.2106/JBJS.M.01285]).
The researchers analyzed 4,733 hip and knee replacement cases within a 39-county cluster of Medicare referral hospitals, and looked at the association between preoperative physical therapy (or “prehabilitation”) and use of postoperative care services in the 90 days after hospital discharge. Because of the skewed distribution of payments, the investigators looked only at cases that fell below the 95th percentile (or $41,113) for cost of care, they said.
In all, 79.7% of patients who did not undergo prehabilitation used acute care services after surgery, compared with 54.2% of patients who did (P < .0001). After controlling for comorbidities and demographic variables, prehabilitation was linked to an absolute reduction of 29% from the predicted to the observed rate of post-acute care use, saving an estimated average of $1,215 per patient, they said. Reductions in use of skilled nursing facilities, home health care services, and inpatient rehabilitation were the main drivers of the cost reduction, the researchers reported.
The findings support prior work indicating that prehabilitation can improve the value of care for patients undergoing total joint replacements, said Dr. Snow and his associates. “As the volume of arthroplasties expands within the framework of increasing health care costs, providers are under mounting pressure to identify the most cost-effective method of delivering high-quality, value-based health care,” they said.
Future studies should look at optimal ways to balance preoperative and postoperative care in specific populations of patients, the investigators said.
The research was partially supported by OhioHealth Research Institute. One or more authors reported financial relationships with biomedical entities deemed to possibly influence the research.
Physical therapy before joint replacement surgery cut the predicted use of postoperative care by 29%, saving an estimated $1,215 in health care costs per patient, according to a Medicare claims analysis.
“These data are clinically relevant and can be used in the development of cost-effective and value-based total joint replacement programs,” said Dr. Richard Snow at OhioHealth in Columbus and his associates. The study is the first to evaluate the real-world link between preoperative physical therapy and use of postoperative care, the researchers said.
Numbers of total hip and knee replacements are projected to increase by 1.7 and 6.7 times, respectively, in the United States between 2005 and 2030, Dr. Snow and his coauthors noted. And while average length of hospital stay after these surgeries has dropped by more than 50%, there has been a substantial rise in per-patient costs of skilled nursing facilities, home health agencies, and inpatient rehabilitation, they said (J. Bone Joint Surg. 2014 Oct. 1 [doi:10.2106/JBJS.M.01285]).
The researchers analyzed 4,733 hip and knee replacement cases within a 39-county cluster of Medicare referral hospitals, and looked at the association between preoperative physical therapy (or “prehabilitation”) and use of postoperative care services in the 90 days after hospital discharge. Because of the skewed distribution of payments, the investigators looked only at cases that fell below the 95th percentile (or $41,113) for cost of care, they said.
In all, 79.7% of patients who did not undergo prehabilitation used acute care services after surgery, compared with 54.2% of patients who did (P < .0001). After controlling for comorbidities and demographic variables, prehabilitation was linked to an absolute reduction of 29% from the predicted to the observed rate of post-acute care use, saving an estimated average of $1,215 per patient, they said. Reductions in use of skilled nursing facilities, home health care services, and inpatient rehabilitation were the main drivers of the cost reduction, the researchers reported.
The findings support prior work indicating that prehabilitation can improve the value of care for patients undergoing total joint replacements, said Dr. Snow and his associates. “As the volume of arthroplasties expands within the framework of increasing health care costs, providers are under mounting pressure to identify the most cost-effective method of delivering high-quality, value-based health care,” they said.
Future studies should look at optimal ways to balance preoperative and postoperative care in specific populations of patients, the investigators said.
The research was partially supported by OhioHealth Research Institute. One or more authors reported financial relationships with biomedical entities deemed to possibly influence the research.
Physical therapy before joint replacement surgery cut the predicted use of postoperative care by 29%, saving an estimated $1,215 in health care costs per patient, according to a Medicare claims analysis.
“These data are clinically relevant and can be used in the development of cost-effective and value-based total joint replacement programs,” said Dr. Richard Snow at OhioHealth in Columbus and his associates. The study is the first to evaluate the real-world link between preoperative physical therapy and use of postoperative care, the researchers said.
Numbers of total hip and knee replacements are projected to increase by 1.7 and 6.7 times, respectively, in the United States between 2005 and 2030, Dr. Snow and his coauthors noted. And while average length of hospital stay after these surgeries has dropped by more than 50%, there has been a substantial rise in per-patient costs of skilled nursing facilities, home health agencies, and inpatient rehabilitation, they said (J. Bone Joint Surg. 2014 Oct. 1 [doi:10.2106/JBJS.M.01285]).
The researchers analyzed 4,733 hip and knee replacement cases within a 39-county cluster of Medicare referral hospitals, and looked at the association between preoperative physical therapy (or “prehabilitation”) and use of postoperative care services in the 90 days after hospital discharge. Because of the skewed distribution of payments, the investigators looked only at cases that fell below the 95th percentile (or $41,113) for cost of care, they said.
In all, 79.7% of patients who did not undergo prehabilitation used acute care services after surgery, compared with 54.2% of patients who did (P < .0001). After controlling for comorbidities and demographic variables, prehabilitation was linked to an absolute reduction of 29% from the predicted to the observed rate of post-acute care use, saving an estimated average of $1,215 per patient, they said. Reductions in use of skilled nursing facilities, home health care services, and inpatient rehabilitation were the main drivers of the cost reduction, the researchers reported.
The findings support prior work indicating that prehabilitation can improve the value of care for patients undergoing total joint replacements, said Dr. Snow and his associates. “As the volume of arthroplasties expands within the framework of increasing health care costs, providers are under mounting pressure to identify the most cost-effective method of delivering high-quality, value-based health care,” they said.
Future studies should look at optimal ways to balance preoperative and postoperative care in specific populations of patients, the investigators said.
The research was partially supported by OhioHealth Research Institute. One or more authors reported financial relationships with biomedical entities deemed to possibly influence the research.
FROM JOURNAL OF BONE & JOINT SURGERY
Key clinical point: Physical therapy before total knee or total hip replacement surgeries can improve the value of care.
Major finding: In all, 79.7% of patients who did not undergo presurgical physical therapy used acute care services after surgery, compared with 54.2% of patients who underwent “prehabilitation” (P < .0001).
Data source: Medicare claims analysis of 4,733 total hip or knee replacement surgeries.
Disclosures: The research was partially supported by OhioHealth Research Institute. One or more authors reported financial relationships with biomedical entities deemed to possibly influence the research.
AMA study: Wellpoint dominates the insurance market
In many areas of the country, only one or two health insurers dominate the market, leaving physicians and patients with few choices when it comes to dealing with health plans, according to a new analysis from the American Medical Association.
In 41% of metropolitan areas examined in the AMA’s study, a single health insurer holds half or more of the market share. And the AMA found that 72% of the markets they analyzed would be considered “highly concentrated” under guidelines developed by the U.S. Department of Justice and the Federal Trade Commission to assess market competition.
Wellpoint Inc. stood out among insurers as the most dominant across the country. As of Jan. 1, 2012, Wellpoint had the greatest market share in 82 of 388 metropolitan areas analyzed by the AMA, giving it the top market share in more than double the number of areas as the next two insurers (Health Care Service Corp. and UnitedHealth Group).
The lack of competition puts physicians and patients at risk, the AMA said, because it gives health plans the power to raise premiums without increasing benefits, while also cutting payments to providers. The AMA is calling on state and federal regulators to take the lack of competition into account when considering future insurance mergers.
“The dominant market power of big health insurers increases the risk of anticompetitive behavior that harms patients and physicians and presents a significant barrier to the market success of smaller insurance rivals,” Dr. Robert M. Wah, AMA president, said in a statement.
The 10 states with the least competition in their commercial health insurance markets were: Alabama, Hawaii, Michigan, Delaware, Louisiana, South Carolina, Alaska, Illinois, Nebraska, and North Dakota.
On Twitter @maryellenny
In many areas of the country, only one or two health insurers dominate the market, leaving physicians and patients with few choices when it comes to dealing with health plans, according to a new analysis from the American Medical Association.
In 41% of metropolitan areas examined in the AMA’s study, a single health insurer holds half or more of the market share. And the AMA found that 72% of the markets they analyzed would be considered “highly concentrated” under guidelines developed by the U.S. Department of Justice and the Federal Trade Commission to assess market competition.
Wellpoint Inc. stood out among insurers as the most dominant across the country. As of Jan. 1, 2012, Wellpoint had the greatest market share in 82 of 388 metropolitan areas analyzed by the AMA, giving it the top market share in more than double the number of areas as the next two insurers (Health Care Service Corp. and UnitedHealth Group).
The lack of competition puts physicians and patients at risk, the AMA said, because it gives health plans the power to raise premiums without increasing benefits, while also cutting payments to providers. The AMA is calling on state and federal regulators to take the lack of competition into account when considering future insurance mergers.
“The dominant market power of big health insurers increases the risk of anticompetitive behavior that harms patients and physicians and presents a significant barrier to the market success of smaller insurance rivals,” Dr. Robert M. Wah, AMA president, said in a statement.
The 10 states with the least competition in their commercial health insurance markets were: Alabama, Hawaii, Michigan, Delaware, Louisiana, South Carolina, Alaska, Illinois, Nebraska, and North Dakota.
On Twitter @maryellenny
In many areas of the country, only one or two health insurers dominate the market, leaving physicians and patients with few choices when it comes to dealing with health plans, according to a new analysis from the American Medical Association.
In 41% of metropolitan areas examined in the AMA’s study, a single health insurer holds half or more of the market share. And the AMA found that 72% of the markets they analyzed would be considered “highly concentrated” under guidelines developed by the U.S. Department of Justice and the Federal Trade Commission to assess market competition.
Wellpoint Inc. stood out among insurers as the most dominant across the country. As of Jan. 1, 2012, Wellpoint had the greatest market share in 82 of 388 metropolitan areas analyzed by the AMA, giving it the top market share in more than double the number of areas as the next two insurers (Health Care Service Corp. and UnitedHealth Group).
The lack of competition puts physicians and patients at risk, the AMA said, because it gives health plans the power to raise premiums without increasing benefits, while also cutting payments to providers. The AMA is calling on state and federal regulators to take the lack of competition into account when considering future insurance mergers.
“The dominant market power of big health insurers increases the risk of anticompetitive behavior that harms patients and physicians and presents a significant barrier to the market success of smaller insurance rivals,” Dr. Robert M. Wah, AMA president, said in a statement.
The 10 states with the least competition in their commercial health insurance markets were: Alabama, Hawaii, Michigan, Delaware, Louisiana, South Carolina, Alaska, Illinois, Nebraska, and North Dakota.
On Twitter @maryellenny
Physician candidates playing key role in midterm elections
Two candidates are playing a role in the GOP push to take control of the U.S. Senate and potentially hamper the further implementation of the Affordable Care Act – and they’re both doctors.
Rep. Bill Cassidy (R-La.) is a physician and congressman who is giving incumbent Sen. Mary Landrieu (D-La.) the fight of her career. And in Oregon, Dr. Monica Wehby, a pediatric neurosurgeon, is challenging Sen. Jeff Merkley (D-Ore.), though she still trails by double digits in the polls.
Both Dr. Wehby and Rep. Cassidy have made their opposition to the Affordable Care Act (ACA) a major component of their campaigns.
Rep. Cassidy, whose wife Laura is also a physician, favors a system that focuses on consumer-driven options such as health savings accounts, as well as moving forward on medical liability reform.
Dr. Wehby, who wants to repeal and replace the ACA, has also called for a federal investigation of the Cover Oregon insurance marketplace.
“It’s not brain surgery; Obamacare is bad for Oregon,” Dr. Wehby said in one of her political ads, which features footage of her in the hospital.
All U.S. Senate races are getting close attention this year because the upper chamber is so closely divided. The GOP needs a net gain of only 6 seats to win control.
Dr. Steve Shogan, a neurosurgeon from Denver, seeks one of Colorado’s Senate seats as an independent, though he’s not considered a contender in the race. Dr. Shogan has also been critical of the ACA, but says that he would prefer to replace it with a two-tiered approach that combines government-provided basic health care coverage with supplemental private insurance.
Several other doctors – mostly Republicans – lost primary bids for the Senate earlier this year.
But while the Senate is getting a lot of attention, there are plenty of physicians who are vying for seats in the House this year. At least 6 doctors are looking to become first-time lawmakers, and another 13 physicians are seeking reelection to the House, according to the American Medical Association.
Currently there are 20 physicians serving in Congress, including 4 Democrats and 16 Republicans.
While the physician candidates come from both parties, the majority are running as Republicans, and their platforms specifically call for repealing the ACA.
Dr. Jane Orient, an internist and executive director of the Association of American Physicians and Surgeons, said that she isn’t surprised. Not only do most physicians tend to be conservative, she said, but frustration with the ACA and other health care regulations is bubbling over.
“Physicians are seeing that their profession is being destroyed,” she said. “If they don’t fight for our rights to practice medicine according to our best judgment and according to our professional ethics, and without constantly being clerks for the third-party payers and the government, then we really have to get politically active.”
The ACA has prompted more physicians to get engaged in politics this year, according to Mark A. Peterson, Ph.D., professor of public policy and political science at the University of California, Los Angeles. While Dr. Peterson said that he agrees that most physicians identify with the Republican party, he added that there are still plenty of physicians who favor the ACA or even single-payer approaches, but they seem to have largely stayed out of politics.
“I don’t know why more of them haven’t taken up the charge to run for office, but it certainly didn’t help Democrats in recruitment that 2014 has been long perceived as a Republican year,” he said.
On Twitter @maryellenny
Two candidates are playing a role in the GOP push to take control of the U.S. Senate and potentially hamper the further implementation of the Affordable Care Act – and they’re both doctors.
Rep. Bill Cassidy (R-La.) is a physician and congressman who is giving incumbent Sen. Mary Landrieu (D-La.) the fight of her career. And in Oregon, Dr. Monica Wehby, a pediatric neurosurgeon, is challenging Sen. Jeff Merkley (D-Ore.), though she still trails by double digits in the polls.
Both Dr. Wehby and Rep. Cassidy have made their opposition to the Affordable Care Act (ACA) a major component of their campaigns.
Rep. Cassidy, whose wife Laura is also a physician, favors a system that focuses on consumer-driven options such as health savings accounts, as well as moving forward on medical liability reform.
Dr. Wehby, who wants to repeal and replace the ACA, has also called for a federal investigation of the Cover Oregon insurance marketplace.
“It’s not brain surgery; Obamacare is bad for Oregon,” Dr. Wehby said in one of her political ads, which features footage of her in the hospital.
All U.S. Senate races are getting close attention this year because the upper chamber is so closely divided. The GOP needs a net gain of only 6 seats to win control.
Dr. Steve Shogan, a neurosurgeon from Denver, seeks one of Colorado’s Senate seats as an independent, though he’s not considered a contender in the race. Dr. Shogan has also been critical of the ACA, but says that he would prefer to replace it with a two-tiered approach that combines government-provided basic health care coverage with supplemental private insurance.
Several other doctors – mostly Republicans – lost primary bids for the Senate earlier this year.
But while the Senate is getting a lot of attention, there are plenty of physicians who are vying for seats in the House this year. At least 6 doctors are looking to become first-time lawmakers, and another 13 physicians are seeking reelection to the House, according to the American Medical Association.
Currently there are 20 physicians serving in Congress, including 4 Democrats and 16 Republicans.
While the physician candidates come from both parties, the majority are running as Republicans, and their platforms specifically call for repealing the ACA.
Dr. Jane Orient, an internist and executive director of the Association of American Physicians and Surgeons, said that she isn’t surprised. Not only do most physicians tend to be conservative, she said, but frustration with the ACA and other health care regulations is bubbling over.
“Physicians are seeing that their profession is being destroyed,” she said. “If they don’t fight for our rights to practice medicine according to our best judgment and according to our professional ethics, and without constantly being clerks for the third-party payers and the government, then we really have to get politically active.”
The ACA has prompted more physicians to get engaged in politics this year, according to Mark A. Peterson, Ph.D., professor of public policy and political science at the University of California, Los Angeles. While Dr. Peterson said that he agrees that most physicians identify with the Republican party, he added that there are still plenty of physicians who favor the ACA or even single-payer approaches, but they seem to have largely stayed out of politics.
“I don’t know why more of them haven’t taken up the charge to run for office, but it certainly didn’t help Democrats in recruitment that 2014 has been long perceived as a Republican year,” he said.
On Twitter @maryellenny
Two candidates are playing a role in the GOP push to take control of the U.S. Senate and potentially hamper the further implementation of the Affordable Care Act – and they’re both doctors.
Rep. Bill Cassidy (R-La.) is a physician and congressman who is giving incumbent Sen. Mary Landrieu (D-La.) the fight of her career. And in Oregon, Dr. Monica Wehby, a pediatric neurosurgeon, is challenging Sen. Jeff Merkley (D-Ore.), though she still trails by double digits in the polls.
Both Dr. Wehby and Rep. Cassidy have made their opposition to the Affordable Care Act (ACA) a major component of their campaigns.
Rep. Cassidy, whose wife Laura is also a physician, favors a system that focuses on consumer-driven options such as health savings accounts, as well as moving forward on medical liability reform.
Dr. Wehby, who wants to repeal and replace the ACA, has also called for a federal investigation of the Cover Oregon insurance marketplace.
“It’s not brain surgery; Obamacare is bad for Oregon,” Dr. Wehby said in one of her political ads, which features footage of her in the hospital.
All U.S. Senate races are getting close attention this year because the upper chamber is so closely divided. The GOP needs a net gain of only 6 seats to win control.
Dr. Steve Shogan, a neurosurgeon from Denver, seeks one of Colorado’s Senate seats as an independent, though he’s not considered a contender in the race. Dr. Shogan has also been critical of the ACA, but says that he would prefer to replace it with a two-tiered approach that combines government-provided basic health care coverage with supplemental private insurance.
Several other doctors – mostly Republicans – lost primary bids for the Senate earlier this year.
But while the Senate is getting a lot of attention, there are plenty of physicians who are vying for seats in the House this year. At least 6 doctors are looking to become first-time lawmakers, and another 13 physicians are seeking reelection to the House, according to the American Medical Association.
Currently there are 20 physicians serving in Congress, including 4 Democrats and 16 Republicans.
While the physician candidates come from both parties, the majority are running as Republicans, and their platforms specifically call for repealing the ACA.
Dr. Jane Orient, an internist and executive director of the Association of American Physicians and Surgeons, said that she isn’t surprised. Not only do most physicians tend to be conservative, she said, but frustration with the ACA and other health care regulations is bubbling over.
“Physicians are seeing that their profession is being destroyed,” she said. “If they don’t fight for our rights to practice medicine according to our best judgment and according to our professional ethics, and without constantly being clerks for the third-party payers and the government, then we really have to get politically active.”
The ACA has prompted more physicians to get engaged in politics this year, according to Mark A. Peterson, Ph.D., professor of public policy and political science at the University of California, Los Angeles. While Dr. Peterson said that he agrees that most physicians identify with the Republican party, he added that there are still plenty of physicians who favor the ACA or even single-payer approaches, but they seem to have largely stayed out of politics.
“I don’t know why more of them haven’t taken up the charge to run for office, but it certainly didn’t help Democrats in recruitment that 2014 has been long perceived as a Republican year,” he said.
On Twitter @maryellenny