User login
Official Newspaper of the American College of Surgeons
Corticosteroids didn’t help pediatric septic shock
SAN FRANCISCO – Adjunctive corticosteroid therapy for pediatric septic shock was associated with increased risks for a complicated course or death within 28 days in a retrospective study of data on 496 patients.
The investigators hypothesized that any potential benefit from adjunctive corticosteroids might depend on the patient’s initial risk of death, but they found no significant differences in outcomes between subgroups of patients that were rated as low risk, intermediate risk, or high risk at baseline using the Pediatric Sepsis Biomarker Risk Model (PERSEVERE) and received corticosteroids.
Among the 252 patients who received corticosteroids, 17% died within 38 days and 32% had a complicated course, defined as persistence of two or more organ failures at day 7 of septic shock or death within 28 days. Those rates were significantly higher than among the 244 patients who did not get corticosteroids, 8% of whom died within 28 days and 22% of whom had a complicated course, Dr. Sarah J. Atkinson and her associates reported.
The PERSEVERE-based mortality probability at baseline did not differ significantly between patients who did or did not get corticosteroids, though those who got corticosteroids had higher risk scores at baseline when assessed using the Pediatric Risk of Mortality score (PRISM).
Patients who got corticosteroids were twice as likely to die and nearly twice as likely to have a complicated course, compared with the no-corticosteroid group, she said at the annual clinical congress of the American College of Surgeons. The risks of death or complicated course did not differ significantly based on steroid use, however, in the 323 patients deemed to be low risk, the 117 intermediate-risk patients, or the 56 high-risk patients as rated by PERSEVERE. “Even in high-risk patients, the sickest patients, we do not even see a trend for benefit” from the use of corticosteroids, she said.
Because the corticosteroid group had a higher rate of comorbidity (42%), compared with the no-corticosteroid group (29%), the investigators conducted a sensitivity analysis of data on a subset of 321 patients without any comorbidities. Steroid use was associated with a 2.6 odds ratio for dying within 28 days and a doubling in odds for a complicated course, reported Dr. Atkinson of the University of Cincinnati.
“Risk-stratified analysis failed to demonstrate any benefit associated with corticosteroid use as adjunctive therapy for pediatric septic shock and suggests the possibility for harm in some patients,” Dr. Atkinson said. A randomized, controlled trial would be needed to identify any efficacy of corticosteroids as adjunct therapy in children with septic shock, she added.
Use of steroids in septic shock remains heavily debated, with no consensus and varying practices among physicians, she said. The 2012 update of Surviving Sepsis guidelines suggests “timely hydrocortisone therapy in children with fluid-refractory, catecholamine-resistant shock and suspected or proven absolute [classic] adrenal insufficiency,” Dr. Atkinson noted.
The current study analyzed data from a database of 27 pediatric centers on children who received corticosteroids within 7 days of ICU admission. In the corticosteroid group, 79% received hydrocortisone, 15% got methylprednisolone, and 6% received dexamethasone. Fluticasone, budesonide, or less than 48 hours of dexamethasone were classified as no steroids. Corticosteroids were administered for a median of 5 days starting on the day patients met criteria for septic shock.
Dr. Atkinson reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Adjunctive corticosteroid therapy for pediatric septic shock was associated with increased risks for a complicated course or death within 28 days in a retrospective study of data on 496 patients.
The investigators hypothesized that any potential benefit from adjunctive corticosteroids might depend on the patient’s initial risk of death, but they found no significant differences in outcomes between subgroups of patients that were rated as low risk, intermediate risk, or high risk at baseline using the Pediatric Sepsis Biomarker Risk Model (PERSEVERE) and received corticosteroids.
Among the 252 patients who received corticosteroids, 17% died within 38 days and 32% had a complicated course, defined as persistence of two or more organ failures at day 7 of septic shock or death within 28 days. Those rates were significantly higher than among the 244 patients who did not get corticosteroids, 8% of whom died within 28 days and 22% of whom had a complicated course, Dr. Sarah J. Atkinson and her associates reported.
The PERSEVERE-based mortality probability at baseline did not differ significantly between patients who did or did not get corticosteroids, though those who got corticosteroids had higher risk scores at baseline when assessed using the Pediatric Risk of Mortality score (PRISM).
Patients who got corticosteroids were twice as likely to die and nearly twice as likely to have a complicated course, compared with the no-corticosteroid group, she said at the annual clinical congress of the American College of Surgeons. The risks of death or complicated course did not differ significantly based on steroid use, however, in the 323 patients deemed to be low risk, the 117 intermediate-risk patients, or the 56 high-risk patients as rated by PERSEVERE. “Even in high-risk patients, the sickest patients, we do not even see a trend for benefit” from the use of corticosteroids, she said.
Because the corticosteroid group had a higher rate of comorbidity (42%), compared with the no-corticosteroid group (29%), the investigators conducted a sensitivity analysis of data on a subset of 321 patients without any comorbidities. Steroid use was associated with a 2.6 odds ratio for dying within 28 days and a doubling in odds for a complicated course, reported Dr. Atkinson of the University of Cincinnati.
“Risk-stratified analysis failed to demonstrate any benefit associated with corticosteroid use as adjunctive therapy for pediatric septic shock and suggests the possibility for harm in some patients,” Dr. Atkinson said. A randomized, controlled trial would be needed to identify any efficacy of corticosteroids as adjunct therapy in children with septic shock, she added.
Use of steroids in septic shock remains heavily debated, with no consensus and varying practices among physicians, she said. The 2012 update of Surviving Sepsis guidelines suggests “timely hydrocortisone therapy in children with fluid-refractory, catecholamine-resistant shock and suspected or proven absolute [classic] adrenal insufficiency,” Dr. Atkinson noted.
The current study analyzed data from a database of 27 pediatric centers on children who received corticosteroids within 7 days of ICU admission. In the corticosteroid group, 79% received hydrocortisone, 15% got methylprednisolone, and 6% received dexamethasone. Fluticasone, budesonide, or less than 48 hours of dexamethasone were classified as no steroids. Corticosteroids were administered for a median of 5 days starting on the day patients met criteria for septic shock.
Dr. Atkinson reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Adjunctive corticosteroid therapy for pediatric septic shock was associated with increased risks for a complicated course or death within 28 days in a retrospective study of data on 496 patients.
The investigators hypothesized that any potential benefit from adjunctive corticosteroids might depend on the patient’s initial risk of death, but they found no significant differences in outcomes between subgroups of patients that were rated as low risk, intermediate risk, or high risk at baseline using the Pediatric Sepsis Biomarker Risk Model (PERSEVERE) and received corticosteroids.
Among the 252 patients who received corticosteroids, 17% died within 38 days and 32% had a complicated course, defined as persistence of two or more organ failures at day 7 of septic shock or death within 28 days. Those rates were significantly higher than among the 244 patients who did not get corticosteroids, 8% of whom died within 28 days and 22% of whom had a complicated course, Dr. Sarah J. Atkinson and her associates reported.
The PERSEVERE-based mortality probability at baseline did not differ significantly between patients who did or did not get corticosteroids, though those who got corticosteroids had higher risk scores at baseline when assessed using the Pediatric Risk of Mortality score (PRISM).
Patients who got corticosteroids were twice as likely to die and nearly twice as likely to have a complicated course, compared with the no-corticosteroid group, she said at the annual clinical congress of the American College of Surgeons. The risks of death or complicated course did not differ significantly based on steroid use, however, in the 323 patients deemed to be low risk, the 117 intermediate-risk patients, or the 56 high-risk patients as rated by PERSEVERE. “Even in high-risk patients, the sickest patients, we do not even see a trend for benefit” from the use of corticosteroids, she said.
Because the corticosteroid group had a higher rate of comorbidity (42%), compared with the no-corticosteroid group (29%), the investigators conducted a sensitivity analysis of data on a subset of 321 patients without any comorbidities. Steroid use was associated with a 2.6 odds ratio for dying within 28 days and a doubling in odds for a complicated course, reported Dr. Atkinson of the University of Cincinnati.
“Risk-stratified analysis failed to demonstrate any benefit associated with corticosteroid use as adjunctive therapy for pediatric septic shock and suggests the possibility for harm in some patients,” Dr. Atkinson said. A randomized, controlled trial would be needed to identify any efficacy of corticosteroids as adjunct therapy in children with septic shock, she added.
Use of steroids in septic shock remains heavily debated, with no consensus and varying practices among physicians, she said. The 2012 update of Surviving Sepsis guidelines suggests “timely hydrocortisone therapy in children with fluid-refractory, catecholamine-resistant shock and suspected or proven absolute [classic] adrenal insufficiency,” Dr. Atkinson noted.
The current study analyzed data from a database of 27 pediatric centers on children who received corticosteroids within 7 days of ICU admission. In the corticosteroid group, 79% received hydrocortisone, 15% got methylprednisolone, and 6% received dexamethasone. Fluticasone, budesonide, or less than 48 hours of dexamethasone were classified as no steroids. Corticosteroids were administered for a median of 5 days starting on the day patients met criteria for septic shock.
Dr. Atkinson reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Key clinical point: Adjunctive corticosteroid therapy didn’t offer benefits to pediatric patients with septic shock, regardless of initial mortality risk.
Major finding: With steroids, 17% died and 32% had a complicated course, versus 8% and 22% without steroids, respectively.
Data source: A retrospective analysis of multicenter data on 496 cases of pediatric septic shock.
Disclosures: Dr. Atkinson reported having no financial disclosures.
CMS proposes new network, formulary standards for 2016 ACA plans
The Obama administration is proposing to widen provider networks and increase access to prescription drugs in health plans that participate in marketplace plans in 2016.
“It is one of our many goals to strengthen the integrity of programs that fall under the Affordable Care Act to ensure the delivery of quality care with affordable options,” said Centers for Medicare & Medicaid Services Administrator Marilyn Tavenner, in a statement. “CMS is working to improve the consumer experience and promote accountability, uniformity and transparency in private health insurance.”
According to the proposal, issued on Nov. 21, the administration “continues to take great interest in ensuring strong network access.” The CMS is proposing that only hospitals and physicians that are in-network can be considered part of the network. Out-of-network providers cannot be included to demonstrate adequacy.
For now, insurers will have to follow standards issued by the agency in March, but changes could come by the time the 2016 proposal is made final.
The agency says it is waiting to see the final results of a model law on network adequacy that’s being developed by the National Association of Insurance Commissioners. A draft of that proposal was recently released and comments are due by Jan. 12.
The CMS also is proposing that new enrollees be given 30 days to transition from current physicians or hospitals to the new plan’s network.
Health plans also will be required to publish an up-to-date, accurate, and complete provider directory, including information on which providers are accepting new patients, the provider’s location, contact information, specialty, medical group, and any institutional affiliations. The guide has to be easily accessible – without having to create an account or use a policy number – to plan enrollees, prospective enrollees, states, and marketplace plans. It should be updated at least once a month, said the CMS.
The agency also is proposing changes to how marketplace plans cover prescription drugs. Currently, plans are required to cover at least one drug in each class.
But plans have had trouble meeting that requirement, and there were other problems, including that the criteria did not exactly encourage newly approved drugs to be included, according to the agency.
Instead, it is proposing that plans use pharmacy and therapeutics committees – following specific standards set out by the CMS – to review and approve drugs, and that it be an adequate amount in each class.
Drug formularies also should be easily accessible to the general public, without having to create and account or give a policy number, and it should be up to date, according to the proposal.
The proposal is open for comment until Dec. 21.
On Twitter @aliciaault
The Obama administration is proposing to widen provider networks and increase access to prescription drugs in health plans that participate in marketplace plans in 2016.
“It is one of our many goals to strengthen the integrity of programs that fall under the Affordable Care Act to ensure the delivery of quality care with affordable options,” said Centers for Medicare & Medicaid Services Administrator Marilyn Tavenner, in a statement. “CMS is working to improve the consumer experience and promote accountability, uniformity and transparency in private health insurance.”
According to the proposal, issued on Nov. 21, the administration “continues to take great interest in ensuring strong network access.” The CMS is proposing that only hospitals and physicians that are in-network can be considered part of the network. Out-of-network providers cannot be included to demonstrate adequacy.
For now, insurers will have to follow standards issued by the agency in March, but changes could come by the time the 2016 proposal is made final.
The agency says it is waiting to see the final results of a model law on network adequacy that’s being developed by the National Association of Insurance Commissioners. A draft of that proposal was recently released and comments are due by Jan. 12.
The CMS also is proposing that new enrollees be given 30 days to transition from current physicians or hospitals to the new plan’s network.
Health plans also will be required to publish an up-to-date, accurate, and complete provider directory, including information on which providers are accepting new patients, the provider’s location, contact information, specialty, medical group, and any institutional affiliations. The guide has to be easily accessible – without having to create an account or use a policy number – to plan enrollees, prospective enrollees, states, and marketplace plans. It should be updated at least once a month, said the CMS.
The agency also is proposing changes to how marketplace plans cover prescription drugs. Currently, plans are required to cover at least one drug in each class.
But plans have had trouble meeting that requirement, and there were other problems, including that the criteria did not exactly encourage newly approved drugs to be included, according to the agency.
Instead, it is proposing that plans use pharmacy and therapeutics committees – following specific standards set out by the CMS – to review and approve drugs, and that it be an adequate amount in each class.
Drug formularies also should be easily accessible to the general public, without having to create and account or give a policy number, and it should be up to date, according to the proposal.
The proposal is open for comment until Dec. 21.
On Twitter @aliciaault
The Obama administration is proposing to widen provider networks and increase access to prescription drugs in health plans that participate in marketplace plans in 2016.
“It is one of our many goals to strengthen the integrity of programs that fall under the Affordable Care Act to ensure the delivery of quality care with affordable options,” said Centers for Medicare & Medicaid Services Administrator Marilyn Tavenner, in a statement. “CMS is working to improve the consumer experience and promote accountability, uniformity and transparency in private health insurance.”
According to the proposal, issued on Nov. 21, the administration “continues to take great interest in ensuring strong network access.” The CMS is proposing that only hospitals and physicians that are in-network can be considered part of the network. Out-of-network providers cannot be included to demonstrate adequacy.
For now, insurers will have to follow standards issued by the agency in March, but changes could come by the time the 2016 proposal is made final.
The agency says it is waiting to see the final results of a model law on network adequacy that’s being developed by the National Association of Insurance Commissioners. A draft of that proposal was recently released and comments are due by Jan. 12.
The CMS also is proposing that new enrollees be given 30 days to transition from current physicians or hospitals to the new plan’s network.
Health plans also will be required to publish an up-to-date, accurate, and complete provider directory, including information on which providers are accepting new patients, the provider’s location, contact information, specialty, medical group, and any institutional affiliations. The guide has to be easily accessible – without having to create an account or use a policy number – to plan enrollees, prospective enrollees, states, and marketplace plans. It should be updated at least once a month, said the CMS.
The agency also is proposing changes to how marketplace plans cover prescription drugs. Currently, plans are required to cover at least one drug in each class.
But plans have had trouble meeting that requirement, and there were other problems, including that the criteria did not exactly encourage newly approved drugs to be included, according to the agency.
Instead, it is proposing that plans use pharmacy and therapeutics committees – following specific standards set out by the CMS – to review and approve drugs, and that it be an adequate amount in each class.
Drug formularies also should be easily accessible to the general public, without having to create and account or give a policy number, and it should be up to date, according to the proposal.
The proposal is open for comment until Dec. 21.
On Twitter @aliciaault
Careful screening catches sarcomas before morcellation
VANCOUVER, B.C.– A thorough preop work-up can just about eliminate the risk of accidentally morcellating an occult uterine sarcoma, according to a prospective series of 2,824 women referred for minimally invasive myomectomy to a French university hospital from 2002 to 2013.
The message came just days before the Food and Drug Administration’s Nov. 24 advice not to use power morcellationin the majority of women undergoing hysterectomy or myomectomy for uterine fibroids because “there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma” that morcellation could spread. The agency estimated that about 1 in 350 fibroid patients actually have an occult sarcoma.
That’s close to the 1 in 400 incidence investigators at the Lariboisière Hospital in Paris found; the difference is that the French investigators detected all but one of the seven sarcomas in their series before entering the operating room, using a heightened screening protocol. “That’s the major difference between our series and the other series that the” FDA relied on for their advice, said lead investigator and gynecologic surgeon Dr. Afshin Fazel, an assistant professor of obstetrics and gynecology at Lariboisière Hospital.
Physicians at the hospital go further than some to rule out sarcomas prior to fibroid surgery. “Every single patient with a pelvic mass gets an MRI,” as well as a clinical exam and pelvic ultrasound. “If the endometrium is thicker than 4 mm, every patient older than 40 [years old] has endometrial sampling, and if there’s bleeding, every single patient has an office hysteroscopy.” A multidisciplinary team – oncologists, radiologists, gynecologists, and surgeons – review the results and select the appropriate surgical approach, Dr. Fazel said at a meeting sponsored by AAGL.
The screening protocol caught five of the seven sarcomas before surgery. A sixth case, a ruptured uterine sarcoma, presented emergently. All seven women had open surgeries, most had a hysterectomy as their initial operation, and none were morcellated. “The take-home message is that you need all the cards in your hand” to rule out sarcomas before myomectomy. No one screening test is sufficient. Some sarcomas, for instance, don’t have the usual MRI signs; of the three sarcomas the team had detected so far in 2014 – not included in the reported series – just one was found on MRI; the other two were found by endometrial sampling. “Preoperative diagnosis is the key to preventing [accidental] morcellation,” Dr. Fazel said.
The second message is that although “1 out of 400 fibroids in our series were actually sarcomas,” the extra screening meant that “the undiagnosed rate of sarcoma was” 0.035% (or 1 in 2,824), he said.
One of the sarcoma patients was from Taiwan, another was African, and the rest were French. Their age ranged from 38 to 78 years, with a mean age 50 years; two were postmenopausal. They had heavy bleeding and pain, and two had multiple masses. The average size of the uterus was 1,136 cc, and the average size of the mass 891 cc. Four of the seven patients died within 2 years of their surgery.
Among all 2,824 women, two-thirds had minimally invasive approaches, including 743 laparoscopic, 510 hysteroscopic, and 336 vaginal procedures; 262 had uterine artery embolization, which was pioneered by Lariboisière in the late 1980s.
Dr. Fazel said he has no disclosures.
VANCOUVER, B.C.– A thorough preop work-up can just about eliminate the risk of accidentally morcellating an occult uterine sarcoma, according to a prospective series of 2,824 women referred for minimally invasive myomectomy to a French university hospital from 2002 to 2013.
The message came just days before the Food and Drug Administration’s Nov. 24 advice not to use power morcellationin the majority of women undergoing hysterectomy or myomectomy for uterine fibroids because “there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma” that morcellation could spread. The agency estimated that about 1 in 350 fibroid patients actually have an occult sarcoma.
That’s close to the 1 in 400 incidence investigators at the Lariboisière Hospital in Paris found; the difference is that the French investigators detected all but one of the seven sarcomas in their series before entering the operating room, using a heightened screening protocol. “That’s the major difference between our series and the other series that the” FDA relied on for their advice, said lead investigator and gynecologic surgeon Dr. Afshin Fazel, an assistant professor of obstetrics and gynecology at Lariboisière Hospital.
Physicians at the hospital go further than some to rule out sarcomas prior to fibroid surgery. “Every single patient with a pelvic mass gets an MRI,” as well as a clinical exam and pelvic ultrasound. “If the endometrium is thicker than 4 mm, every patient older than 40 [years old] has endometrial sampling, and if there’s bleeding, every single patient has an office hysteroscopy.” A multidisciplinary team – oncologists, radiologists, gynecologists, and surgeons – review the results and select the appropriate surgical approach, Dr. Fazel said at a meeting sponsored by AAGL.
The screening protocol caught five of the seven sarcomas before surgery. A sixth case, a ruptured uterine sarcoma, presented emergently. All seven women had open surgeries, most had a hysterectomy as their initial operation, and none were morcellated. “The take-home message is that you need all the cards in your hand” to rule out sarcomas before myomectomy. No one screening test is sufficient. Some sarcomas, for instance, don’t have the usual MRI signs; of the three sarcomas the team had detected so far in 2014 – not included in the reported series – just one was found on MRI; the other two were found by endometrial sampling. “Preoperative diagnosis is the key to preventing [accidental] morcellation,” Dr. Fazel said.
The second message is that although “1 out of 400 fibroids in our series were actually sarcomas,” the extra screening meant that “the undiagnosed rate of sarcoma was” 0.035% (or 1 in 2,824), he said.
One of the sarcoma patients was from Taiwan, another was African, and the rest were French. Their age ranged from 38 to 78 years, with a mean age 50 years; two were postmenopausal. They had heavy bleeding and pain, and two had multiple masses. The average size of the uterus was 1,136 cc, and the average size of the mass 891 cc. Four of the seven patients died within 2 years of their surgery.
Among all 2,824 women, two-thirds had minimally invasive approaches, including 743 laparoscopic, 510 hysteroscopic, and 336 vaginal procedures; 262 had uterine artery embolization, which was pioneered by Lariboisière in the late 1980s.
Dr. Fazel said he has no disclosures.
VANCOUVER, B.C.– A thorough preop work-up can just about eliminate the risk of accidentally morcellating an occult uterine sarcoma, according to a prospective series of 2,824 women referred for minimally invasive myomectomy to a French university hospital from 2002 to 2013.
The message came just days before the Food and Drug Administration’s Nov. 24 advice not to use power morcellationin the majority of women undergoing hysterectomy or myomectomy for uterine fibroids because “there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma” that morcellation could spread. The agency estimated that about 1 in 350 fibroid patients actually have an occult sarcoma.
That’s close to the 1 in 400 incidence investigators at the Lariboisière Hospital in Paris found; the difference is that the French investigators detected all but one of the seven sarcomas in their series before entering the operating room, using a heightened screening protocol. “That’s the major difference between our series and the other series that the” FDA relied on for their advice, said lead investigator and gynecologic surgeon Dr. Afshin Fazel, an assistant professor of obstetrics and gynecology at Lariboisière Hospital.
Physicians at the hospital go further than some to rule out sarcomas prior to fibroid surgery. “Every single patient with a pelvic mass gets an MRI,” as well as a clinical exam and pelvic ultrasound. “If the endometrium is thicker than 4 mm, every patient older than 40 [years old] has endometrial sampling, and if there’s bleeding, every single patient has an office hysteroscopy.” A multidisciplinary team – oncologists, radiologists, gynecologists, and surgeons – review the results and select the appropriate surgical approach, Dr. Fazel said at a meeting sponsored by AAGL.
The screening protocol caught five of the seven sarcomas before surgery. A sixth case, a ruptured uterine sarcoma, presented emergently. All seven women had open surgeries, most had a hysterectomy as their initial operation, and none were morcellated. “The take-home message is that you need all the cards in your hand” to rule out sarcomas before myomectomy. No one screening test is sufficient. Some sarcomas, for instance, don’t have the usual MRI signs; of the three sarcomas the team had detected so far in 2014 – not included in the reported series – just one was found on MRI; the other two were found by endometrial sampling. “Preoperative diagnosis is the key to preventing [accidental] morcellation,” Dr. Fazel said.
The second message is that although “1 out of 400 fibroids in our series were actually sarcomas,” the extra screening meant that “the undiagnosed rate of sarcoma was” 0.035% (or 1 in 2,824), he said.
One of the sarcoma patients was from Taiwan, another was African, and the rest were French. Their age ranged from 38 to 78 years, with a mean age 50 years; two were postmenopausal. They had heavy bleeding and pain, and two had multiple masses. The average size of the uterus was 1,136 cc, and the average size of the mass 891 cc. Four of the seven patients died within 2 years of their surgery.
Among all 2,824 women, two-thirds had minimally invasive approaches, including 743 laparoscopic, 510 hysteroscopic, and 336 vaginal procedures; 262 had uterine artery embolization, which was pioneered by Lariboisière in the late 1980s.
Dr. Fazel said he has no disclosures.
AT THE AAGL GLOBAL CONFERENCE
Key clinical point: It’s possible to catch most sarcomas before fibroid morcellation.
Major finding: One in 400 women with fibroids have an occult sarcoma; preoperative MRI, pelvic ultrasound, endometrial sampling, and hysteroscopy reduces the chance that they will undergo morcellation to 0.035%.
Data source: Prospective case series of 2,824 women referred for minimally invasive myomectomy to a university hospital in Paris.
Disclosures: Dr. Fazel said he has no financial conflicts.
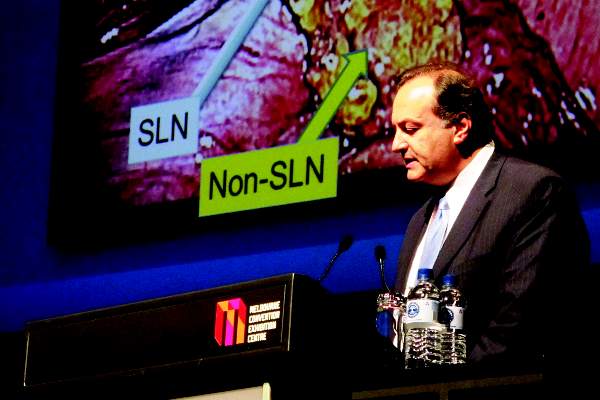
Sentinel lymph node mapping effective for staging early endometrial cancer
MELBOURNE – Staging endometrial cancer using sentinel lymph node mapping reduces side effects for patients, and enables selection of lymph nodes for pathology that are more likely to have disease in them, an investigator reported at the biennial meeting of the International Gynecologic Cancer Society.
The procedure results in fewer lymph nodes being removed – usually two to three on each side, and no more than ten – which meant less side effects such as lymphedema, and potentially avoided the need for pelvic lymphadenectomy said Dr. Nadeem Abu-Rustum, chief of the gynecology service at Memorial Sloan Kettering Cancer Center, New York.
“One, you are removing fewer lymph nodes so there’s less radicality in surgery and less side effects; two, it makes the operating time faster, and three, you give the pathologist fewer lymph nodes but they can work on them in more depth to try to find low-volume metastases,” Dr. Abu-Rustum said in an interview.
“It’s a win-win situation for the patient.”
Dr. Abu-Rustum and colleagues at Memorial Sloan-Kettering have developed a sentinel lymph node mapping algorithm for stage I cervical or endometrial cancers.
“It is applicable for any women who has endometrial cancer where the surgeon feels that the cancer is contained, and you need staging information,” he said.
However he stressed it was not applicable in patients with obvious metastases or with abnormal lymph nodes.
“This is for normal-appearing lymph nodes, clinical stage I, and the algorithm checklist really protects you because it will exclude those patients [with abnormal lymph nodes].”
While there was ongoing debate about where to inject the dye to best identify the sentinel node, Dr. Abu-Rustum told the conference that he and his colleagues believed injecting into the cervix at the three o’clock and nine o’clock positions was the most reasonable option.
He also commented on the different dyes used, saying that while methylene blue or lymphazurin had been the traditional choice – with or without technetium-99 – the near-infrared fluorescing indocyanine green and use of a laser significantly improved accuracy of the procedure.
“Now you’re able to increase the chance of finding the lymph node from 80% to almost 100%, and finding it on the right and the left was 60%, now it’s 80%,” he said.
In another presentation, a speaker reported an overall sentinel lymph node detection rate of 92%, and a 74% rate of bilateral detection, using a combination of methylene blue, technetium-99, and indocyanine green, in 100 patients who underwent sentinel lymph node mapping for endometrial cancer.
Among the 10 patients in the prospective study who had metastatic disease, 9 had a positive sentinel lymph node. The sentinel node was found to be the only positive node in 66% of these patients, suggesting that this was the most clinically relevant node. There was one case of a false negative for a sentinel lymph node, reported Dr. Jeffrey How, obstetrics and gynecology resident at the McGill University Health Centre, Montreal.
The addition of indocyanine green increased the precision of in vivo detection of sentinel lymph nodes, aiding detection of the highest-yield lymph nodes for pathology, he said.
No conflicts of interest were declared.
MELBOURNE – Staging endometrial cancer using sentinel lymph node mapping reduces side effects for patients, and enables selection of lymph nodes for pathology that are more likely to have disease in them, an investigator reported at the biennial meeting of the International Gynecologic Cancer Society.
The procedure results in fewer lymph nodes being removed – usually two to three on each side, and no more than ten – which meant less side effects such as lymphedema, and potentially avoided the need for pelvic lymphadenectomy said Dr. Nadeem Abu-Rustum, chief of the gynecology service at Memorial Sloan Kettering Cancer Center, New York.
“One, you are removing fewer lymph nodes so there’s less radicality in surgery and less side effects; two, it makes the operating time faster, and three, you give the pathologist fewer lymph nodes but they can work on them in more depth to try to find low-volume metastases,” Dr. Abu-Rustum said in an interview.
“It’s a win-win situation for the patient.”
Dr. Abu-Rustum and colleagues at Memorial Sloan-Kettering have developed a sentinel lymph node mapping algorithm for stage I cervical or endometrial cancers.
“It is applicable for any women who has endometrial cancer where the surgeon feels that the cancer is contained, and you need staging information,” he said.
However he stressed it was not applicable in patients with obvious metastases or with abnormal lymph nodes.
“This is for normal-appearing lymph nodes, clinical stage I, and the algorithm checklist really protects you because it will exclude those patients [with abnormal lymph nodes].”
While there was ongoing debate about where to inject the dye to best identify the sentinel node, Dr. Abu-Rustum told the conference that he and his colleagues believed injecting into the cervix at the three o’clock and nine o’clock positions was the most reasonable option.
He also commented on the different dyes used, saying that while methylene blue or lymphazurin had been the traditional choice – with or without technetium-99 – the near-infrared fluorescing indocyanine green and use of a laser significantly improved accuracy of the procedure.
“Now you’re able to increase the chance of finding the lymph node from 80% to almost 100%, and finding it on the right and the left was 60%, now it’s 80%,” he said.
In another presentation, a speaker reported an overall sentinel lymph node detection rate of 92%, and a 74% rate of bilateral detection, using a combination of methylene blue, technetium-99, and indocyanine green, in 100 patients who underwent sentinel lymph node mapping for endometrial cancer.
Among the 10 patients in the prospective study who had metastatic disease, 9 had a positive sentinel lymph node. The sentinel node was found to be the only positive node in 66% of these patients, suggesting that this was the most clinically relevant node. There was one case of a false negative for a sentinel lymph node, reported Dr. Jeffrey How, obstetrics and gynecology resident at the McGill University Health Centre, Montreal.
The addition of indocyanine green increased the precision of in vivo detection of sentinel lymph nodes, aiding detection of the highest-yield lymph nodes for pathology, he said.
No conflicts of interest were declared.
MELBOURNE – Staging endometrial cancer using sentinel lymph node mapping reduces side effects for patients, and enables selection of lymph nodes for pathology that are more likely to have disease in them, an investigator reported at the biennial meeting of the International Gynecologic Cancer Society.
The procedure results in fewer lymph nodes being removed – usually two to three on each side, and no more than ten – which meant less side effects such as lymphedema, and potentially avoided the need for pelvic lymphadenectomy said Dr. Nadeem Abu-Rustum, chief of the gynecology service at Memorial Sloan Kettering Cancer Center, New York.
“One, you are removing fewer lymph nodes so there’s less radicality in surgery and less side effects; two, it makes the operating time faster, and three, you give the pathologist fewer lymph nodes but they can work on them in more depth to try to find low-volume metastases,” Dr. Abu-Rustum said in an interview.
“It’s a win-win situation for the patient.”
Dr. Abu-Rustum and colleagues at Memorial Sloan-Kettering have developed a sentinel lymph node mapping algorithm for stage I cervical or endometrial cancers.
“It is applicable for any women who has endometrial cancer where the surgeon feels that the cancer is contained, and you need staging information,” he said.
However he stressed it was not applicable in patients with obvious metastases or with abnormal lymph nodes.
“This is for normal-appearing lymph nodes, clinical stage I, and the algorithm checklist really protects you because it will exclude those patients [with abnormal lymph nodes].”
While there was ongoing debate about where to inject the dye to best identify the sentinel node, Dr. Abu-Rustum told the conference that he and his colleagues believed injecting into the cervix at the three o’clock and nine o’clock positions was the most reasonable option.
He also commented on the different dyes used, saying that while methylene blue or lymphazurin had been the traditional choice – with or without technetium-99 – the near-infrared fluorescing indocyanine green and use of a laser significantly improved accuracy of the procedure.
“Now you’re able to increase the chance of finding the lymph node from 80% to almost 100%, and finding it on the right and the left was 60%, now it’s 80%,” he said.
In another presentation, a speaker reported an overall sentinel lymph node detection rate of 92%, and a 74% rate of bilateral detection, using a combination of methylene blue, technetium-99, and indocyanine green, in 100 patients who underwent sentinel lymph node mapping for endometrial cancer.
Among the 10 patients in the prospective study who had metastatic disease, 9 had a positive sentinel lymph node. The sentinel node was found to be the only positive node in 66% of these patients, suggesting that this was the most clinically relevant node. There was one case of a false negative for a sentinel lymph node, reported Dr. Jeffrey How, obstetrics and gynecology resident at the McGill University Health Centre, Montreal.
The addition of indocyanine green increased the precision of in vivo detection of sentinel lymph nodes, aiding detection of the highest-yield lymph nodes for pathology, he said.
No conflicts of interest were declared.
AT IGCS 2014
Shoulder morbidity common after thyroid cancer surgery
CORONADO, CALIF. – More than 50% of patients who underwent surgery for differentiated thyroid cancer experienced shoulder morbidity up to 10 years after the procedure, results from a Dutch study showed.
“What’s causing the pain?” Dr. Romana T. Netea-Maier asked in an interview at the annual meeting of the American Thyroid Association. “It may be that the spinal accessory nerve or other nerves have been injured during the surgery. We don’t know.”
In what she said is the first study of its kind, Dr. Netea-Maier and her associates compared the prevalence of shoulder morbidity and its relation to clinical characteristics and quality of life in 109 patients who underwent surgery for differentiated thyroid cancer at Radboud University Medical Center, Nijmegen, the Netherlands, with a group of 81 healthy controls and a group of 59 patients who underwent surgery for benign thyroid pathology. Main outcome measures were the prevalence of shoulder complaints based on results of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and the European Organization for Research and Treatment of Cancer, Quality of Life Questionnaire-C-30 (EORTC QLQ-C30).
Dr. Netea-Maier, of the department of medicine at the university, reported that the mean age of patients in the two surgery groups was 46 years, and 73% were women. During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01). The chief complaints among patients in the thyroid cancer group were pain (25%), muscle weakness (8%), and tingling (8%), while the main complaints among those with benign thyroid pathology were pain (38%), and tingling (7%).
Compared with healthy controls, patients in the thyroid cancer group scored worse on all subscales of the DASH and the EORTC QLQ-C30. On bivariate analysis, level V neck dissection, spinal accessory nerve damage, and employment status were associated with the prevalence of shoulder complaints and DASH scores, while the prevalence of shoulder complaints and DASH scores correlated significantly with EORTC QLQ-C30 scores.
The researchers found that only 12% of patients in the thyroid cancer group received preoperative information on the potential for shoulder morbidity and 35% received additional care for postoperative shoulder complaints.
“The take-home message would be to inform your patients of the potential for shoulder comorbidity, because what we have shown here is that patients do not recall being informed about this possible complication before the surgery,” Dr. Netea-Maier said. “If they have complaints, start with physiotherapy early on.”
Dr. Netea-Maier reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – More than 50% of patients who underwent surgery for differentiated thyroid cancer experienced shoulder morbidity up to 10 years after the procedure, results from a Dutch study showed.
“What’s causing the pain?” Dr. Romana T. Netea-Maier asked in an interview at the annual meeting of the American Thyroid Association. “It may be that the spinal accessory nerve or other nerves have been injured during the surgery. We don’t know.”
In what she said is the first study of its kind, Dr. Netea-Maier and her associates compared the prevalence of shoulder morbidity and its relation to clinical characteristics and quality of life in 109 patients who underwent surgery for differentiated thyroid cancer at Radboud University Medical Center, Nijmegen, the Netherlands, with a group of 81 healthy controls and a group of 59 patients who underwent surgery for benign thyroid pathology. Main outcome measures were the prevalence of shoulder complaints based on results of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and the European Organization for Research and Treatment of Cancer, Quality of Life Questionnaire-C-30 (EORTC QLQ-C30).
Dr. Netea-Maier, of the department of medicine at the university, reported that the mean age of patients in the two surgery groups was 46 years, and 73% were women. During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01). The chief complaints among patients in the thyroid cancer group were pain (25%), muscle weakness (8%), and tingling (8%), while the main complaints among those with benign thyroid pathology were pain (38%), and tingling (7%).
Compared with healthy controls, patients in the thyroid cancer group scored worse on all subscales of the DASH and the EORTC QLQ-C30. On bivariate analysis, level V neck dissection, spinal accessory nerve damage, and employment status were associated with the prevalence of shoulder complaints and DASH scores, while the prevalence of shoulder complaints and DASH scores correlated significantly with EORTC QLQ-C30 scores.
The researchers found that only 12% of patients in the thyroid cancer group received preoperative information on the potential for shoulder morbidity and 35% received additional care for postoperative shoulder complaints.
“The take-home message would be to inform your patients of the potential for shoulder comorbidity, because what we have shown here is that patients do not recall being informed about this possible complication before the surgery,” Dr. Netea-Maier said. “If they have complaints, start with physiotherapy early on.”
Dr. Netea-Maier reported having no financial disclosures.
On Twitter @dougbrunk
CORONADO, CALIF. – More than 50% of patients who underwent surgery for differentiated thyroid cancer experienced shoulder morbidity up to 10 years after the procedure, results from a Dutch study showed.
“What’s causing the pain?” Dr. Romana T. Netea-Maier asked in an interview at the annual meeting of the American Thyroid Association. “It may be that the spinal accessory nerve or other nerves have been injured during the surgery. We don’t know.”
In what she said is the first study of its kind, Dr. Netea-Maier and her associates compared the prevalence of shoulder morbidity and its relation to clinical characteristics and quality of life in 109 patients who underwent surgery for differentiated thyroid cancer at Radboud University Medical Center, Nijmegen, the Netherlands, with a group of 81 healthy controls and a group of 59 patients who underwent surgery for benign thyroid pathology. Main outcome measures were the prevalence of shoulder complaints based on results of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and the European Organization for Research and Treatment of Cancer, Quality of Life Questionnaire-C-30 (EORTC QLQ-C30).
Dr. Netea-Maier, of the department of medicine at the university, reported that the mean age of patients in the two surgery groups was 46 years, and 73% were women. During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01). The chief complaints among patients in the thyroid cancer group were pain (25%), muscle weakness (8%), and tingling (8%), while the main complaints among those with benign thyroid pathology were pain (38%), and tingling (7%).
Compared with healthy controls, patients in the thyroid cancer group scored worse on all subscales of the DASH and the EORTC QLQ-C30. On bivariate analysis, level V neck dissection, spinal accessory nerve damage, and employment status were associated with the prevalence of shoulder complaints and DASH scores, while the prevalence of shoulder complaints and DASH scores correlated significantly with EORTC QLQ-C30 scores.
The researchers found that only 12% of patients in the thyroid cancer group received preoperative information on the potential for shoulder morbidity and 35% received additional care for postoperative shoulder complaints.
“The take-home message would be to inform your patients of the potential for shoulder comorbidity, because what we have shown here is that patients do not recall being informed about this possible complication before the surgery,” Dr. Netea-Maier said. “If they have complaints, start with physiotherapy early on.”
Dr. Netea-Maier reported having no financial disclosures.
On Twitter @dougbrunk
AT THE ATA ANNUAL MEETING
Key clinical point: Postoperative shoulder morbidity is highly prevalent in patients who undergo surgery for thyroid cancer.
Major finding: During an average of 10 years following surgery, 59% of patients in the thyroid cancer group and 49% of patients in the benign thyroid pathology group reported shoulder morbidity, compared with 14% of controls (P < .01).
Data source: A Dutch study of 109 patients who underwent surgery for differentiated thyroid cancer, compared with 81 healthy controls and 59 patients who underwent surgery for benign thyroid pathology.
Disclosures: Dr. Netea-Maier reported having no financial disclosures.
VIDEO: AMA president talks meaningful use, ICD-10, and Ebola
WASHINGTON – The recent deadline extensions for meaningful use attestation are encouraging, but not enough. The process must be more user-friendly and clinically meaningful.
That’s according to Dr. Robert Wah, president of the American Medical Association. Dr. Wah discussed the AMA’s concerns about meaningful use and health information technology in a video interview – including whether there is enough of a focus on interoperability of electronic health records.
He also touched on the transition to the ICD-10 code set, again questioning whether the move is clinically useful and ultimately helps improve patient care.
Recently, Dr. Karen DeSalvo, National Coordinator for Health Information Technology, was given an additional appointment as the acting assistant secretary for health to help with the effort to combat the Ebola epidemic. That caused concern among physicians that there could be a leadership vacuum at the Office of the National Coordinator at a time when so much is happening in health IT. Although it was later clarified that she would remain in charge of the effort, there are still some worries, Dr. Wah said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @aliciaault
WASHINGTON – The recent deadline extensions for meaningful use attestation are encouraging, but not enough. The process must be more user-friendly and clinically meaningful.
That’s according to Dr. Robert Wah, president of the American Medical Association. Dr. Wah discussed the AMA’s concerns about meaningful use and health information technology in a video interview – including whether there is enough of a focus on interoperability of electronic health records.
He also touched on the transition to the ICD-10 code set, again questioning whether the move is clinically useful and ultimately helps improve patient care.
Recently, Dr. Karen DeSalvo, National Coordinator for Health Information Technology, was given an additional appointment as the acting assistant secretary for health to help with the effort to combat the Ebola epidemic. That caused concern among physicians that there could be a leadership vacuum at the Office of the National Coordinator at a time when so much is happening in health IT. Although it was later clarified that she would remain in charge of the effort, there are still some worries, Dr. Wah said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @aliciaault
WASHINGTON – The recent deadline extensions for meaningful use attestation are encouraging, but not enough. The process must be more user-friendly and clinically meaningful.
That’s according to Dr. Robert Wah, president of the American Medical Association. Dr. Wah discussed the AMA’s concerns about meaningful use and health information technology in a video interview – including whether there is enough of a focus on interoperability of electronic health records.
He also touched on the transition to the ICD-10 code set, again questioning whether the move is clinically useful and ultimately helps improve patient care.
Recently, Dr. Karen DeSalvo, National Coordinator for Health Information Technology, was given an additional appointment as the acting assistant secretary for health to help with the effort to combat the Ebola epidemic. That caused concern among physicians that there could be a leadership vacuum at the Office of the National Coordinator at a time when so much is happening in health IT. Although it was later clarified that she would remain in charge of the effort, there are still some worries, Dr. Wah said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @aliciaault
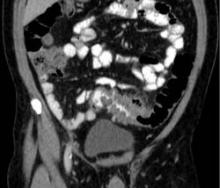
Nonoperative management okay after draining diverticular-associated abscess
SAN FRANCISCO – Patients who did not undergo elective surgical resection after successful percutaneous drainage of a diverticular-associated abscess had low rates of recurrent diverticulitis in a retrospective study, a finding that suggests nonoperative management is a reasonable option in such patients, Dr. Tarek K. Jalouta said.
Percutaneous drainage of diverticular-associated abscess resolved symptoms in 118 of 165 (72%) patients who underwent the procedure at two teaching hospitals in 2001-2013. Sixty of the patients with successful drainage did not undergo elective surgical resection, and eight of these died within a year of the drainage procedure.
Among the remaining 52 patients who had nonoperative management, 72% remained free of diverticulitis after 5 years, Dr. Jalouta and his associates reported at the annual clinical congress of the American College of Surgeons.
“A significant number of patients successfully recover from complicated diverticulitis following percutaneous drainage,” Dr. Jalouta said. “Subsequent nonoperative management carries an acceptable risk for recurrent episodes and may be considered as a reasonable management option.”
All patients diagnosed with diverticular-associated abscess received IV antibiotics within 24-48 hours of diagnosis. The decision to perform percutaneous drainage was at the discretion of the consulting surgeon and the interventional radiologist.
Practice parameters issued by the American Society of Colon and Rectal Surgeons in 2014 suggest that elective colectomy “should typically be advised” following successful medical treatment of diverticular-associated abscess with or without percutaneous drainage, noted Dr. Jalouta of Spectrum Health System, Grand Rapids, Mich. Separate guidelines from the Association of Coloproctology of Great Britain and Ireland state that there is not sufficient evidence to make a formal recommendation on this topic, he added.
For the cohort of 165 patients, the abscesses averaged 6 cm in diameter and were pelvic in 73% of patients, abdominal in 22%, and in both locations in 5%. Multiple abscesses were present in 17%. Patients had a mean age of 61 years and a mean body mass index of 21 kg/m2, and 52% were female.
The patients who did not undergo surgery after successful percutaneous drainage were significantly older than those who had surgery – 62 years vs. 55 years. Those subgroups did not differ in other respects.
An estimated 130,000 U.S. hospitalizations each year are due to diverticulitis, with 10%-20% of cases complicated by an associated intra-abdominal abscess, he said. Most diverticular-associated abscesses smaller than 5 cm in diameter will respond to antibiotic therapy, but patients with larger abscesses or associated sepsis often get percutaneous drainage.
The results were slightly better than those seen in two previous studies. In one study of 511 patients admitted for acute diverticulitis in 1994-2003, 5 of 12 patients (42%) who did not undergo surgery after percutaneous drainage of abscesses averaging 7 cm in size had a recurrence of diverticulitis (Am. J. Gastroenterol. 2005;100:910-7), Dr. Jalouta said. A separate study of 32 patients managed without surgery after percutaneous drainage of diverticular-associated abscesses found a recurrence-free survival rate of 58% after 7 years (Dis. Colon Rectum 2013;56:622-6).
Dr. Jalouta reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Patients who did not undergo elective surgical resection after successful percutaneous drainage of a diverticular-associated abscess had low rates of recurrent diverticulitis in a retrospective study, a finding that suggests nonoperative management is a reasonable option in such patients, Dr. Tarek K. Jalouta said.
Percutaneous drainage of diverticular-associated abscess resolved symptoms in 118 of 165 (72%) patients who underwent the procedure at two teaching hospitals in 2001-2013. Sixty of the patients with successful drainage did not undergo elective surgical resection, and eight of these died within a year of the drainage procedure.
Among the remaining 52 patients who had nonoperative management, 72% remained free of diverticulitis after 5 years, Dr. Jalouta and his associates reported at the annual clinical congress of the American College of Surgeons.
“A significant number of patients successfully recover from complicated diverticulitis following percutaneous drainage,” Dr. Jalouta said. “Subsequent nonoperative management carries an acceptable risk for recurrent episodes and may be considered as a reasonable management option.”
All patients diagnosed with diverticular-associated abscess received IV antibiotics within 24-48 hours of diagnosis. The decision to perform percutaneous drainage was at the discretion of the consulting surgeon and the interventional radiologist.
Practice parameters issued by the American Society of Colon and Rectal Surgeons in 2014 suggest that elective colectomy “should typically be advised” following successful medical treatment of diverticular-associated abscess with or without percutaneous drainage, noted Dr. Jalouta of Spectrum Health System, Grand Rapids, Mich. Separate guidelines from the Association of Coloproctology of Great Britain and Ireland state that there is not sufficient evidence to make a formal recommendation on this topic, he added.
For the cohort of 165 patients, the abscesses averaged 6 cm in diameter and were pelvic in 73% of patients, abdominal in 22%, and in both locations in 5%. Multiple abscesses were present in 17%. Patients had a mean age of 61 years and a mean body mass index of 21 kg/m2, and 52% were female.
The patients who did not undergo surgery after successful percutaneous drainage were significantly older than those who had surgery – 62 years vs. 55 years. Those subgroups did not differ in other respects.
An estimated 130,000 U.S. hospitalizations each year are due to diverticulitis, with 10%-20% of cases complicated by an associated intra-abdominal abscess, he said. Most diverticular-associated abscesses smaller than 5 cm in diameter will respond to antibiotic therapy, but patients with larger abscesses or associated sepsis often get percutaneous drainage.
The results were slightly better than those seen in two previous studies. In one study of 511 patients admitted for acute diverticulitis in 1994-2003, 5 of 12 patients (42%) who did not undergo surgery after percutaneous drainage of abscesses averaging 7 cm in size had a recurrence of diverticulitis (Am. J. Gastroenterol. 2005;100:910-7), Dr. Jalouta said. A separate study of 32 patients managed without surgery after percutaneous drainage of diverticular-associated abscesses found a recurrence-free survival rate of 58% after 7 years (Dis. Colon Rectum 2013;56:622-6).
Dr. Jalouta reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Patients who did not undergo elective surgical resection after successful percutaneous drainage of a diverticular-associated abscess had low rates of recurrent diverticulitis in a retrospective study, a finding that suggests nonoperative management is a reasonable option in such patients, Dr. Tarek K. Jalouta said.
Percutaneous drainage of diverticular-associated abscess resolved symptoms in 118 of 165 (72%) patients who underwent the procedure at two teaching hospitals in 2001-2013. Sixty of the patients with successful drainage did not undergo elective surgical resection, and eight of these died within a year of the drainage procedure.
Among the remaining 52 patients who had nonoperative management, 72% remained free of diverticulitis after 5 years, Dr. Jalouta and his associates reported at the annual clinical congress of the American College of Surgeons.
“A significant number of patients successfully recover from complicated diverticulitis following percutaneous drainage,” Dr. Jalouta said. “Subsequent nonoperative management carries an acceptable risk for recurrent episodes and may be considered as a reasonable management option.”
All patients diagnosed with diverticular-associated abscess received IV antibiotics within 24-48 hours of diagnosis. The decision to perform percutaneous drainage was at the discretion of the consulting surgeon and the interventional radiologist.
Practice parameters issued by the American Society of Colon and Rectal Surgeons in 2014 suggest that elective colectomy “should typically be advised” following successful medical treatment of diverticular-associated abscess with or without percutaneous drainage, noted Dr. Jalouta of Spectrum Health System, Grand Rapids, Mich. Separate guidelines from the Association of Coloproctology of Great Britain and Ireland state that there is not sufficient evidence to make a formal recommendation on this topic, he added.
For the cohort of 165 patients, the abscesses averaged 6 cm in diameter and were pelvic in 73% of patients, abdominal in 22%, and in both locations in 5%. Multiple abscesses were present in 17%. Patients had a mean age of 61 years and a mean body mass index of 21 kg/m2, and 52% were female.
The patients who did not undergo surgery after successful percutaneous drainage were significantly older than those who had surgery – 62 years vs. 55 years. Those subgroups did not differ in other respects.
An estimated 130,000 U.S. hospitalizations each year are due to diverticulitis, with 10%-20% of cases complicated by an associated intra-abdominal abscess, he said. Most diverticular-associated abscesses smaller than 5 cm in diameter will respond to antibiotic therapy, but patients with larger abscesses or associated sepsis often get percutaneous drainage.
The results were slightly better than those seen in two previous studies. In one study of 511 patients admitted for acute diverticulitis in 1994-2003, 5 of 12 patients (42%) who did not undergo surgery after percutaneous drainage of abscesses averaging 7 cm in size had a recurrence of diverticulitis (Am. J. Gastroenterol. 2005;100:910-7), Dr. Jalouta said. A separate study of 32 patients managed without surgery after percutaneous drainage of diverticular-associated abscesses found a recurrence-free survival rate of 58% after 7 years (Dis. Colon Rectum 2013;56:622-6).
Dr. Jalouta reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients can do well without elective surgical resection following successful percutaneous drainage of diverticular-associated abscess.
Major finding: No recurrent diverticulitis was seen at 5 years in 37 of 52 patients who did not have surgery.
Data source: A retrospective review of all 165 patients who underwent percutaneous drainage of diverticular-associated abscesses in 12 years at two hospitals.
Disclosures: Dr. Jalouta reported having no financial disclosures.
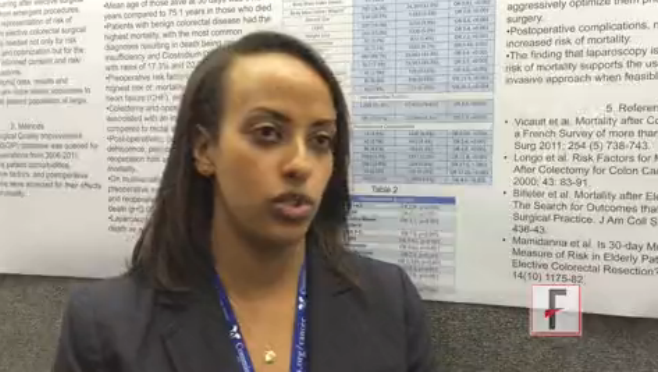
VIDEO: Mortality rate after elective colorectal surgery hits 2%
SAN FRANCISCO– Patients undergoing elective colorectal surgery had an overall mortality rate of 1.7% after 30 days, an analysis of data from 65,716 patients showed.
Patients with significant preoperative morbidity had a significantly higher risk of dying after the surgery, Dr. Alodia Gabre-Kidan and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview, Dr. Gabre-Kidan discusses the results of the retrospective study, including the especially high risk for patients with preoperative renal failure or heart failure. The findings should help clinicians better counsel patients who are considering elective colorectal surgery, said Dr. Gabre-Kidan of Columbia University, New York.
Dr. Gabre-Kidan reporting having no financial disclosures.
On Twitter @sherryboschert
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Patients undergoing elective colorectal surgery had an overall mortality rate of 1.7% after 30 days, an analysis of data from 65,716 patients showed.
Patients with significant preoperative morbidity had a significantly higher risk of dying after the surgery, Dr. Alodia Gabre-Kidan and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview, Dr. Gabre-Kidan discusses the results of the retrospective study, including the especially high risk for patients with preoperative renal failure or heart failure. The findings should help clinicians better counsel patients who are considering elective colorectal surgery, said Dr. Gabre-Kidan of Columbia University, New York.
Dr. Gabre-Kidan reporting having no financial disclosures.
On Twitter @sherryboschert
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Patients undergoing elective colorectal surgery had an overall mortality rate of 1.7% after 30 days, an analysis of data from 65,716 patients showed.
Patients with significant preoperative morbidity had a significantly higher risk of dying after the surgery, Dr. Alodia Gabre-Kidan and her associates reported at the annual clinical congress of the American College of Surgeons.
In a video interview, Dr. Gabre-Kidan discusses the results of the retrospective study, including the especially high risk for patients with preoperative renal failure or heart failure. The findings should help clinicians better counsel patients who are considering elective colorectal surgery, said Dr. Gabre-Kidan of Columbia University, New York.
Dr. Gabre-Kidan reporting having no financial disclosures.
On Twitter @sherryboschert
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
Nitinol stent maintained patency of hemodialysis access routes
PHILADELPHIA – A covered nitinol stent graft effectively restored and maintained patency of hemodialysis access routes that had been impaired by in-stent restenosis.
The combination of a stent graft plus angioplasty was significantly more effective than angioplasty alone at keeping the access routes open, Dr. Alexander Yevzlin reported at Kidney Week 2014.
Maintaining healthy vascular access is key for effective dialysis; this is usually accomplished by bare metal stenting. However, in-stent restenosis is so common that patients may need angioplasty every 3-6 months to maintain access patency.
In comparison, coronary angioplasty is usually sustained for at least 5 years, said Dr. Yevzlin, director of interventional nephrology at the University of Wisconsin, Madison. “This places a very large extra burden of morbidity on patients, and a large burden of cost on society.”
The ongoing RESCUE study is examining the Fluency Plus cardiovascular stent graft for in-stent restenosis. Fluency is a nitinol stent covered with a plastic graft of expanded polytetrafluoroethylene. Dr. Yevzlin reported preliminary 6-month data.
The study has randomized 265 patients with in-stent restenosis of a dialysis access circuit to treatment with either balloon angioplasty alone, or angioplasty plus the stent graft. The primary endpoints are access circuit primary patency at 6 months and 30-day safety. Safety endpoints are any additional interventions including surgery, hospitalization, or prolongation of an existing hospitalization; or death. The secondary endpoint is postintervention lesion patency (defined as the interval after the index intervention until the next reintervention at the original treatment site or until the extremity is abandoned for permanent access).
There were no safety issues, Dr. Yevzlin said; by 30 days, 97% of patients in both groups were still free of any adverse event.
By 6 months, access circuit patency was significantly higher among those who received stent grafts than those who had angioplasties alone. Postintervention lesion patency was 65% in the stent graft group and 10% in the angioplasty group – a significant difference.
The stent graft performed well in both arteriovenous grafts and fistulas. In a subgroup of those with an arteriovenous graft, the postinterventional lesion patency rate was 58% in the stent graft group and 5% in the angioplasty group. In the fistula subgroup, the rates were 72% and 15%, respectively.
The meeting was sponsored by the American Society of Nephrology. Dr. Yevzlin disclosed financial relationships with Bard Peripheral Vascular, the manufacturer of the stent graft; Phraxis; CytoPherx; and Covidien.
PHILADELPHIA – A covered nitinol stent graft effectively restored and maintained patency of hemodialysis access routes that had been impaired by in-stent restenosis.
The combination of a stent graft plus angioplasty was significantly more effective than angioplasty alone at keeping the access routes open, Dr. Alexander Yevzlin reported at Kidney Week 2014.
Maintaining healthy vascular access is key for effective dialysis; this is usually accomplished by bare metal stenting. However, in-stent restenosis is so common that patients may need angioplasty every 3-6 months to maintain access patency.
In comparison, coronary angioplasty is usually sustained for at least 5 years, said Dr. Yevzlin, director of interventional nephrology at the University of Wisconsin, Madison. “This places a very large extra burden of morbidity on patients, and a large burden of cost on society.”
The ongoing RESCUE study is examining the Fluency Plus cardiovascular stent graft for in-stent restenosis. Fluency is a nitinol stent covered with a plastic graft of expanded polytetrafluoroethylene. Dr. Yevzlin reported preliminary 6-month data.
The study has randomized 265 patients with in-stent restenosis of a dialysis access circuit to treatment with either balloon angioplasty alone, or angioplasty plus the stent graft. The primary endpoints are access circuit primary patency at 6 months and 30-day safety. Safety endpoints are any additional interventions including surgery, hospitalization, or prolongation of an existing hospitalization; or death. The secondary endpoint is postintervention lesion patency (defined as the interval after the index intervention until the next reintervention at the original treatment site or until the extremity is abandoned for permanent access).
There were no safety issues, Dr. Yevzlin said; by 30 days, 97% of patients in both groups were still free of any adverse event.
By 6 months, access circuit patency was significantly higher among those who received stent grafts than those who had angioplasties alone. Postintervention lesion patency was 65% in the stent graft group and 10% in the angioplasty group – a significant difference.
The stent graft performed well in both arteriovenous grafts and fistulas. In a subgroup of those with an arteriovenous graft, the postinterventional lesion patency rate was 58% in the stent graft group and 5% in the angioplasty group. In the fistula subgroup, the rates were 72% and 15%, respectively.
The meeting was sponsored by the American Society of Nephrology. Dr. Yevzlin disclosed financial relationships with Bard Peripheral Vascular, the manufacturer of the stent graft; Phraxis; CytoPherx; and Covidien.
PHILADELPHIA – A covered nitinol stent graft effectively restored and maintained patency of hemodialysis access routes that had been impaired by in-stent restenosis.
The combination of a stent graft plus angioplasty was significantly more effective than angioplasty alone at keeping the access routes open, Dr. Alexander Yevzlin reported at Kidney Week 2014.
Maintaining healthy vascular access is key for effective dialysis; this is usually accomplished by bare metal stenting. However, in-stent restenosis is so common that patients may need angioplasty every 3-6 months to maintain access patency.
In comparison, coronary angioplasty is usually sustained for at least 5 years, said Dr. Yevzlin, director of interventional nephrology at the University of Wisconsin, Madison. “This places a very large extra burden of morbidity on patients, and a large burden of cost on society.”
The ongoing RESCUE study is examining the Fluency Plus cardiovascular stent graft for in-stent restenosis. Fluency is a nitinol stent covered with a plastic graft of expanded polytetrafluoroethylene. Dr. Yevzlin reported preliminary 6-month data.
The study has randomized 265 patients with in-stent restenosis of a dialysis access circuit to treatment with either balloon angioplasty alone, or angioplasty plus the stent graft. The primary endpoints are access circuit primary patency at 6 months and 30-day safety. Safety endpoints are any additional interventions including surgery, hospitalization, or prolongation of an existing hospitalization; or death. The secondary endpoint is postintervention lesion patency (defined as the interval after the index intervention until the next reintervention at the original treatment site or until the extremity is abandoned for permanent access).
There were no safety issues, Dr. Yevzlin said; by 30 days, 97% of patients in both groups were still free of any adverse event.
By 6 months, access circuit patency was significantly higher among those who received stent grafts than those who had angioplasties alone. Postintervention lesion patency was 65% in the stent graft group and 10% in the angioplasty group – a significant difference.
The stent graft performed well in both arteriovenous grafts and fistulas. In a subgroup of those with an arteriovenous graft, the postinterventional lesion patency rate was 58% in the stent graft group and 5% in the angioplasty group. In the fistula subgroup, the rates were 72% and 15%, respectively.
The meeting was sponsored by the American Society of Nephrology. Dr. Yevzlin disclosed financial relationships with Bard Peripheral Vascular, the manufacturer of the stent graft; Phraxis; CytoPherx; and Covidien.
AT KIDNEY WEEK 2014
Key clinical point: A covered nitinol stent combined with angioplasty effectively maintained patency in hemodialysis access circuits impaired by in-stent restenosis.
Major finding: By 6 months, access circuit patency was significantly higher among the stent grafts than the angioplasties (17% vs. 3%).
Data source: The randomized study comprised 265 patients.
Disclosures: The meeting was sponsored by the American Society of Nephrology. Dr. Yevzlin disclosed financial relationships with Bard Peripheral Vascular, the manufacturer of the stent graft; Phraxis; CytoPherx; and Covidien.
Mismatch seen between trends in elective, emergent colectomies for diverticulitis
SAN FRANCISCO – Performance of more elective colectomies for diverticulitis in recent years does not seem to be preventing the need for emergent or urgent colectomies, investigators reported at the annual clinical congress of the American College of Surgeons.
The investigators analyzed data from the Comprehensive Hospital Abstract Reporting System (CHARS), a Washington State inpatient database, for the years 1987-2012.
Results showed that the age- and sex-adjusted rate of elective colectomies for diverticulitis increased from about 7 per 100,000 people to more than 20 per 100,000 people. But the rate of nonelective (emergent or urgent) colectomies for this indication remained fairly stable, if anything, increasing slightly.
“Despite 15 years of evolving guidelines to operate less, we are actually seeing a threefold increase in elective colectomy for diverticulitis. We did not see a decrease in emergency surgery during the same time,” commented lead investigator Dr. Vlad V. Simianu, a research fellow in the department of surgery, University of Washington, Seattle.
Several hypotheses might explain this disconnect, he proposed: a rising incidence of diverticulitis, increasing severity of disease (although data do not support this), or surgeons’ adoption of a lower threshold for elective colectomy. “In fact, if you look at where the biggest climb in elective surgery was, it was sort of in the early 2000s, which was the time contemporaneous to when the first laparoscopic colorectal randomized trials were being published, and training programs were incorporating laparoscopy into their training. That’s really where we see the biggest jump. So it may be that what we are seeing is an increase in this procedure [laparoscopic colectomy], the same as what we saw with laparoscopic cholecystectomy.”
“Whatever you choose ... to believe about what’s driving this, what remains certain going forward is that routine elective colectomy is not supported by the most recent guidelines [from the American Society of Colon and Rectal Surgeons], and actually these guidelines are for the first time recommending that the decision to offer elective surgery be individualized,” Dr. Simianu noted.
“Our group is actually doing some neat work in this space trying to identify which metrics should be used to individualize surgery, so we look forward to sharing that with you in the future,” he added.
Session comoderator Dr. James J. Mezhir of the University of Iowa, Iowa City, asked, “It may be difficult, but are you able to look at general surgeons versus those who are colorectal trained?”
The database does not specify surgeon training, according to Dr. Simianu, who disclosed that he had no relevant conflicts of interest. “What is interesting is that in Washington State, about half the surgery is done laparoscopically, in recent years at least. Whether laparoscopy is lowering the threshold, we know that colorectal surgeons are trained to do more laparoscopic colectomy maybe than their general surgeon counterparts.”
Another state database has provided some additional relevant information, he noted. “When laparoscopy first started being adopted, we saw a spike in right-sided colon surgery, which was previously a pretty rare colectomy for diverticulitis. So it is hard to know who is sort of driving this.”
Dr. Mezhir also wanted to know, “How generalizable is this across the United States? Have you looked at something like the nationwide inpatient sample or some other data set to say whether this is something you are seeing in Washington or is this something across the U.S.?”
Similar national trends have been reported in studies using that database, according to Dr. Simianu. “One of the things they point out is that there is a spike in diverticulitis in the younger population, which is something we are seeing in Washington State as well,” he noted.
Another session attendee noted that patients with acute diverticulitis sometimes have immediate procedures, such as drainage, but then go on to have colectomy not long afterward. Thus, he wondered about misclassification, asking, “Are you capturing it as elective although it’s sorted out as an acute episode?”
“That’s a great question, said another way, are we actually just delaying things into the elective category, as opposed to operating on them emergently?” Dr. Simianu replied. “It’s a little hard to tell. We do know that during this time, rates of percutaneous drainage have gone up. So it’s sort of the same conclusion that we are doing more elective surgery but we are not really preventing complications. But I think the crux of that is when these patients have complications and have emergency surgery, they have it on their first episode, 80%-90% of them. So offering a delayed operation ... to prevent [complications] where the likelihood is highest of having a complication, doesn’t seem to bear out in the data.”
SAN FRANCISCO – Performance of more elective colectomies for diverticulitis in recent years does not seem to be preventing the need for emergent or urgent colectomies, investigators reported at the annual clinical congress of the American College of Surgeons.
The investigators analyzed data from the Comprehensive Hospital Abstract Reporting System (CHARS), a Washington State inpatient database, for the years 1987-2012.
Results showed that the age- and sex-adjusted rate of elective colectomies for diverticulitis increased from about 7 per 100,000 people to more than 20 per 100,000 people. But the rate of nonelective (emergent or urgent) colectomies for this indication remained fairly stable, if anything, increasing slightly.
“Despite 15 years of evolving guidelines to operate less, we are actually seeing a threefold increase in elective colectomy for diverticulitis. We did not see a decrease in emergency surgery during the same time,” commented lead investigator Dr. Vlad V. Simianu, a research fellow in the department of surgery, University of Washington, Seattle.
Several hypotheses might explain this disconnect, he proposed: a rising incidence of diverticulitis, increasing severity of disease (although data do not support this), or surgeons’ adoption of a lower threshold for elective colectomy. “In fact, if you look at where the biggest climb in elective surgery was, it was sort of in the early 2000s, which was the time contemporaneous to when the first laparoscopic colorectal randomized trials were being published, and training programs were incorporating laparoscopy into their training. That’s really where we see the biggest jump. So it may be that what we are seeing is an increase in this procedure [laparoscopic colectomy], the same as what we saw with laparoscopic cholecystectomy.”
“Whatever you choose ... to believe about what’s driving this, what remains certain going forward is that routine elective colectomy is not supported by the most recent guidelines [from the American Society of Colon and Rectal Surgeons], and actually these guidelines are for the first time recommending that the decision to offer elective surgery be individualized,” Dr. Simianu noted.
“Our group is actually doing some neat work in this space trying to identify which metrics should be used to individualize surgery, so we look forward to sharing that with you in the future,” he added.
Session comoderator Dr. James J. Mezhir of the University of Iowa, Iowa City, asked, “It may be difficult, but are you able to look at general surgeons versus those who are colorectal trained?”
The database does not specify surgeon training, according to Dr. Simianu, who disclosed that he had no relevant conflicts of interest. “What is interesting is that in Washington State, about half the surgery is done laparoscopically, in recent years at least. Whether laparoscopy is lowering the threshold, we know that colorectal surgeons are trained to do more laparoscopic colectomy maybe than their general surgeon counterparts.”
Another state database has provided some additional relevant information, he noted. “When laparoscopy first started being adopted, we saw a spike in right-sided colon surgery, which was previously a pretty rare colectomy for diverticulitis. So it is hard to know who is sort of driving this.”
Dr. Mezhir also wanted to know, “How generalizable is this across the United States? Have you looked at something like the nationwide inpatient sample or some other data set to say whether this is something you are seeing in Washington or is this something across the U.S.?”
Similar national trends have been reported in studies using that database, according to Dr. Simianu. “One of the things they point out is that there is a spike in diverticulitis in the younger population, which is something we are seeing in Washington State as well,” he noted.
Another session attendee noted that patients with acute diverticulitis sometimes have immediate procedures, such as drainage, but then go on to have colectomy not long afterward. Thus, he wondered about misclassification, asking, “Are you capturing it as elective although it’s sorted out as an acute episode?”
“That’s a great question, said another way, are we actually just delaying things into the elective category, as opposed to operating on them emergently?” Dr. Simianu replied. “It’s a little hard to tell. We do know that during this time, rates of percutaneous drainage have gone up. So it’s sort of the same conclusion that we are doing more elective surgery but we are not really preventing complications. But I think the crux of that is when these patients have complications and have emergency surgery, they have it on their first episode, 80%-90% of them. So offering a delayed operation ... to prevent [complications] where the likelihood is highest of having a complication, doesn’t seem to bear out in the data.”
SAN FRANCISCO – Performance of more elective colectomies for diverticulitis in recent years does not seem to be preventing the need for emergent or urgent colectomies, investigators reported at the annual clinical congress of the American College of Surgeons.
The investigators analyzed data from the Comprehensive Hospital Abstract Reporting System (CHARS), a Washington State inpatient database, for the years 1987-2012.
Results showed that the age- and sex-adjusted rate of elective colectomies for diverticulitis increased from about 7 per 100,000 people to more than 20 per 100,000 people. But the rate of nonelective (emergent or urgent) colectomies for this indication remained fairly stable, if anything, increasing slightly.
“Despite 15 years of evolving guidelines to operate less, we are actually seeing a threefold increase in elective colectomy for diverticulitis. We did not see a decrease in emergency surgery during the same time,” commented lead investigator Dr. Vlad V. Simianu, a research fellow in the department of surgery, University of Washington, Seattle.
Several hypotheses might explain this disconnect, he proposed: a rising incidence of diverticulitis, increasing severity of disease (although data do not support this), or surgeons’ adoption of a lower threshold for elective colectomy. “In fact, if you look at where the biggest climb in elective surgery was, it was sort of in the early 2000s, which was the time contemporaneous to when the first laparoscopic colorectal randomized trials were being published, and training programs were incorporating laparoscopy into their training. That’s really where we see the biggest jump. So it may be that what we are seeing is an increase in this procedure [laparoscopic colectomy], the same as what we saw with laparoscopic cholecystectomy.”
“Whatever you choose ... to believe about what’s driving this, what remains certain going forward is that routine elective colectomy is not supported by the most recent guidelines [from the American Society of Colon and Rectal Surgeons], and actually these guidelines are for the first time recommending that the decision to offer elective surgery be individualized,” Dr. Simianu noted.
“Our group is actually doing some neat work in this space trying to identify which metrics should be used to individualize surgery, so we look forward to sharing that with you in the future,” he added.
Session comoderator Dr. James J. Mezhir of the University of Iowa, Iowa City, asked, “It may be difficult, but are you able to look at general surgeons versus those who are colorectal trained?”
The database does not specify surgeon training, according to Dr. Simianu, who disclosed that he had no relevant conflicts of interest. “What is interesting is that in Washington State, about half the surgery is done laparoscopically, in recent years at least. Whether laparoscopy is lowering the threshold, we know that colorectal surgeons are trained to do more laparoscopic colectomy maybe than their general surgeon counterparts.”
Another state database has provided some additional relevant information, he noted. “When laparoscopy first started being adopted, we saw a spike in right-sided colon surgery, which was previously a pretty rare colectomy for diverticulitis. So it is hard to know who is sort of driving this.”
Dr. Mezhir also wanted to know, “How generalizable is this across the United States? Have you looked at something like the nationwide inpatient sample or some other data set to say whether this is something you are seeing in Washington or is this something across the U.S.?”
Similar national trends have been reported in studies using that database, according to Dr. Simianu. “One of the things they point out is that there is a spike in diverticulitis in the younger population, which is something we are seeing in Washington State as well,” he noted.
Another session attendee noted that patients with acute diverticulitis sometimes have immediate procedures, such as drainage, but then go on to have colectomy not long afterward. Thus, he wondered about misclassification, asking, “Are you capturing it as elective although it’s sorted out as an acute episode?”
“That’s a great question, said another way, are we actually just delaying things into the elective category, as opposed to operating on them emergently?” Dr. Simianu replied. “It’s a little hard to tell. We do know that during this time, rates of percutaneous drainage have gone up. So it’s sort of the same conclusion that we are doing more elective surgery but we are not really preventing complications. But I think the crux of that is when these patients have complications and have emergency surgery, they have it on their first episode, 80%-90% of them. So offering a delayed operation ... to prevent [complications] where the likelihood is highest of having a complication, doesn’t seem to bear out in the data.”
AT THE ACS CLINICAL CONGRESS
Key clinical point: An increase in elective colectomies has not been accompanied by a decrease in emergent/urgent colectomies.
Major finding: The adjusted rate of elective colectomies tripled, but the rate of emergent/urgent colectomies remained stable.
Data source: A cohort study of colectomies for diverticulitis in Washington State between 1987 and 2012.
Disclosures: Dr. Simianu disclosed that he had no relevant conflicts of interest.