User login
Official Newspaper of the American College of Surgeons
Congress to doctors: How can we pay for SGR fix?
WASHINGTON – Legislators on the Health Subcommittee looked to physicians and health care providers for ways to pay for a repeal of the Medicare Sustainable Growth Rate formula at a hearing Jan. 22.
The subcommittee is looking “at opportunities for pay-fors” to fund the already-agreed-upon bipartisan legislation to permanently repeal and replace the SGR, according to Rep. Joseph Pitts (R-Pa.), Health Subcommittee chairman. The panel’s ranking member, Rep. Gene Green, (D-Tex.), noted that he didn’t mind looking outside of health care to cover the estimated $140 billion cost of repeal.
Dr. Barbara L. McAneny, chair of the American Medical Association Board of Trustees, said that her organization needed more guidance from the subcommittee before leaders could recommend specific offsets.
The issue “is a very difficult one because, within the health care sector, so many people are struggling now just to keep their doors open to their patients, that for us from within the health care sector to really come up with a specific pay-for may not be as useful until there are some guidelines set up by Congress,” Dr. McAneny testified. “What are the rules of this particular budgetary process? How do we fit those things within that? I think the AMA stands ready to assist and help by weighing in on any given suggestions, but I think we are very uneasy and feel that we don’t really have the ability to give you specific pay-fors.”
Her testimony drew sharp criticism from Rep. Larry Bucshon, (R-Ind.).
“I would just implore you to really reconsider that and the AMA reconsider and maybe help us rather than waiting for other options and coming out and saying up or down, we disagree or we agree,” Rep. Bucshon said. “If you are going to offer an opinion at the end, then you should be part of the offering solutions on the front side. … If you are just going to wait and be a critic and not offer solutions yourself, to me that’s not very helpful.”
Others testifying before the subcommittee noted that despite the committee being open to all avenues to finance the SGR bill, Medicare would likely bear some of those costs.
“The [American Hospital Association] cannot support any proposal to fix the physician payment problem at the expense of funding for services provided by other caregivers,” AHA President and CEO Richard Umbdenstock testified, adding that the organization “cannot simply oppose payment cuts without supporting other solutions.”
Mr. Umbdenstock highlighted four solutions that the AHA supports: combining Medicare Part A and Part B with a unified deductible and coinsurance; higher premiums for beneficiaries coming into Medicare as well as means-testing for premiums; altering incentives to first-dollar coverage for Medigap so that beneficiaries will be more aware of how they are choosing the health care they need; and medical liability reform.
Mr. Umbdenstock added that these suggestions have general bipartisan support and “would not only generate savings, but also put the Medicare program on firmer financial footing for years to come.”
Eric Schneidewind, president-elect of AARP, also offered a number of solutions to the committee and suggested that maybe Congress does not need to fully fund the SGR bill.
“In light of current and future savings in the Medicare program, Congress would be justified in not fully offsetting the cost of a permanent repeal at this time,” Mr. Schneidewind said. He also added that legislators could consider expansion of competitive bidding for durable medical equipment, equalize payments based on physician site of services, be more aggressive in collecting overpayments to Medicare Advantage plans, increasing transitional care and chronic care management, and encourage the use of all highly skilled clinicians.
But what likely would be considered more controversial were Mr. Schneidewind’s suggestions related to drugs.
“AARP believes that any discussion of budget offsets for Medicare reimbursement reform should include savings from prescription drugs,” he said. “We urge you to give strong consideration to the following prescription drug proposals that could save at least $150 billion.”
Those proposals included offering Medicaid-level drug rebates to beneficiaries who are eligible for both Medicare and Medicaid, giving the secretary of Health and Human Services the power to negotiate drug prices, reduce the exclusivity period for biologics, prohibit pay-for-delay agreements (when a brand-name drug manufacturer pays to delay the launch of a generic equivalent), and prohibit the use of Risk Evaluation and Mitigation Strategies (REMS) to block generic and biosimilar drug development.
WASHINGTON – Legislators on the Health Subcommittee looked to physicians and health care providers for ways to pay for a repeal of the Medicare Sustainable Growth Rate formula at a hearing Jan. 22.
The subcommittee is looking “at opportunities for pay-fors” to fund the already-agreed-upon bipartisan legislation to permanently repeal and replace the SGR, according to Rep. Joseph Pitts (R-Pa.), Health Subcommittee chairman. The panel’s ranking member, Rep. Gene Green, (D-Tex.), noted that he didn’t mind looking outside of health care to cover the estimated $140 billion cost of repeal.
Dr. Barbara L. McAneny, chair of the American Medical Association Board of Trustees, said that her organization needed more guidance from the subcommittee before leaders could recommend specific offsets.
The issue “is a very difficult one because, within the health care sector, so many people are struggling now just to keep their doors open to their patients, that for us from within the health care sector to really come up with a specific pay-for may not be as useful until there are some guidelines set up by Congress,” Dr. McAneny testified. “What are the rules of this particular budgetary process? How do we fit those things within that? I think the AMA stands ready to assist and help by weighing in on any given suggestions, but I think we are very uneasy and feel that we don’t really have the ability to give you specific pay-fors.”
Her testimony drew sharp criticism from Rep. Larry Bucshon, (R-Ind.).
“I would just implore you to really reconsider that and the AMA reconsider and maybe help us rather than waiting for other options and coming out and saying up or down, we disagree or we agree,” Rep. Bucshon said. “If you are going to offer an opinion at the end, then you should be part of the offering solutions on the front side. … If you are just going to wait and be a critic and not offer solutions yourself, to me that’s not very helpful.”
Others testifying before the subcommittee noted that despite the committee being open to all avenues to finance the SGR bill, Medicare would likely bear some of those costs.
“The [American Hospital Association] cannot support any proposal to fix the physician payment problem at the expense of funding for services provided by other caregivers,” AHA President and CEO Richard Umbdenstock testified, adding that the organization “cannot simply oppose payment cuts without supporting other solutions.”
Mr. Umbdenstock highlighted four solutions that the AHA supports: combining Medicare Part A and Part B with a unified deductible and coinsurance; higher premiums for beneficiaries coming into Medicare as well as means-testing for premiums; altering incentives to first-dollar coverage for Medigap so that beneficiaries will be more aware of how they are choosing the health care they need; and medical liability reform.
Mr. Umbdenstock added that these suggestions have general bipartisan support and “would not only generate savings, but also put the Medicare program on firmer financial footing for years to come.”
Eric Schneidewind, president-elect of AARP, also offered a number of solutions to the committee and suggested that maybe Congress does not need to fully fund the SGR bill.
“In light of current and future savings in the Medicare program, Congress would be justified in not fully offsetting the cost of a permanent repeal at this time,” Mr. Schneidewind said. He also added that legislators could consider expansion of competitive bidding for durable medical equipment, equalize payments based on physician site of services, be more aggressive in collecting overpayments to Medicare Advantage plans, increasing transitional care and chronic care management, and encourage the use of all highly skilled clinicians.
But what likely would be considered more controversial were Mr. Schneidewind’s suggestions related to drugs.
“AARP believes that any discussion of budget offsets for Medicare reimbursement reform should include savings from prescription drugs,” he said. “We urge you to give strong consideration to the following prescription drug proposals that could save at least $150 billion.”
Those proposals included offering Medicaid-level drug rebates to beneficiaries who are eligible for both Medicare and Medicaid, giving the secretary of Health and Human Services the power to negotiate drug prices, reduce the exclusivity period for biologics, prohibit pay-for-delay agreements (when a brand-name drug manufacturer pays to delay the launch of a generic equivalent), and prohibit the use of Risk Evaluation and Mitigation Strategies (REMS) to block generic and biosimilar drug development.
WASHINGTON – Legislators on the Health Subcommittee looked to physicians and health care providers for ways to pay for a repeal of the Medicare Sustainable Growth Rate formula at a hearing Jan. 22.
The subcommittee is looking “at opportunities for pay-fors” to fund the already-agreed-upon bipartisan legislation to permanently repeal and replace the SGR, according to Rep. Joseph Pitts (R-Pa.), Health Subcommittee chairman. The panel’s ranking member, Rep. Gene Green, (D-Tex.), noted that he didn’t mind looking outside of health care to cover the estimated $140 billion cost of repeal.
Dr. Barbara L. McAneny, chair of the American Medical Association Board of Trustees, said that her organization needed more guidance from the subcommittee before leaders could recommend specific offsets.
The issue “is a very difficult one because, within the health care sector, so many people are struggling now just to keep their doors open to their patients, that for us from within the health care sector to really come up with a specific pay-for may not be as useful until there are some guidelines set up by Congress,” Dr. McAneny testified. “What are the rules of this particular budgetary process? How do we fit those things within that? I think the AMA stands ready to assist and help by weighing in on any given suggestions, but I think we are very uneasy and feel that we don’t really have the ability to give you specific pay-fors.”
Her testimony drew sharp criticism from Rep. Larry Bucshon, (R-Ind.).
“I would just implore you to really reconsider that and the AMA reconsider and maybe help us rather than waiting for other options and coming out and saying up or down, we disagree or we agree,” Rep. Bucshon said. “If you are going to offer an opinion at the end, then you should be part of the offering solutions on the front side. … If you are just going to wait and be a critic and not offer solutions yourself, to me that’s not very helpful.”
Others testifying before the subcommittee noted that despite the committee being open to all avenues to finance the SGR bill, Medicare would likely bear some of those costs.
“The [American Hospital Association] cannot support any proposal to fix the physician payment problem at the expense of funding for services provided by other caregivers,” AHA President and CEO Richard Umbdenstock testified, adding that the organization “cannot simply oppose payment cuts without supporting other solutions.”
Mr. Umbdenstock highlighted four solutions that the AHA supports: combining Medicare Part A and Part B with a unified deductible and coinsurance; higher premiums for beneficiaries coming into Medicare as well as means-testing for premiums; altering incentives to first-dollar coverage for Medigap so that beneficiaries will be more aware of how they are choosing the health care they need; and medical liability reform.
Mr. Umbdenstock added that these suggestions have general bipartisan support and “would not only generate savings, but also put the Medicare program on firmer financial footing for years to come.”
Eric Schneidewind, president-elect of AARP, also offered a number of solutions to the committee and suggested that maybe Congress does not need to fully fund the SGR bill.
“In light of current and future savings in the Medicare program, Congress would be justified in not fully offsetting the cost of a permanent repeal at this time,” Mr. Schneidewind said. He also added that legislators could consider expansion of competitive bidding for durable medical equipment, equalize payments based on physician site of services, be more aggressive in collecting overpayments to Medicare Advantage plans, increasing transitional care and chronic care management, and encourage the use of all highly skilled clinicians.
But what likely would be considered more controversial were Mr. Schneidewind’s suggestions related to drugs.
“AARP believes that any discussion of budget offsets for Medicare reimbursement reform should include savings from prescription drugs,” he said. “We urge you to give strong consideration to the following prescription drug proposals that could save at least $150 billion.”
Those proposals included offering Medicaid-level drug rebates to beneficiaries who are eligible for both Medicare and Medicaid, giving the secretary of Health and Human Services the power to negotiate drug prices, reduce the exclusivity period for biologics, prohibit pay-for-delay agreements (when a brand-name drug manufacturer pays to delay the launch of a generic equivalent), and prohibit the use of Risk Evaluation and Mitigation Strategies (REMS) to block generic and biosimilar drug development.
AT A HOUSE ENERGY AND COMMERCE HEALTH SUBCOMMITTEE HEARING
Guidelines for drug treatment of obesity unveiled
For the first time, a task force of experts has assembled clinical practice guidelines dedicated to the medical treatment of obesity.
The development, spearheaded by the Endocrine Society with support from the Obesity Society and the European Society of Endocrinology, comes after four new anti-obesity drugs hit the market in the past 2 years: lorcaserin (Belviq), phentermine/topiramate (Qsymia), naltrexone/bupropion (Contrave) and liraglutide (Saxenda). The new guidelines expand on guidelines for managing overweight and obesity in adults that were released in 2013 by the Obesity Society, the American Heart Association, and the American College of Cardiology.
“Medications used for the management of conditions other than obesity can contribute to or exacerbate weight gain in susceptible individuals,” the eight-member task force wrote online Jan. 15 in the Journal of Clinical Endocrinology and Metabolism (doi:10/1210/jc.2014-3415).” Many of these conditions are also associated with obesity. Health care providers can help patients prevent or attenuate weight gain by appropriately prescribing medications that would promote weight loss or minimize weight gain when treating these conditions.”
The task force, chaired by Dr. Caroline M. Apovian professor of medicine at Boston University, recommends that diet, exercise, and behavioral modifications be part of all obesity management approaches. “Drugs may amplify adherence to behavior change and may improve physical functioning such that increased physical activity is easier in those who cannot exercise initially,” they wrote. “Patients who have a history of being unable to successfully lose and maintain weight and who meet label indications are candidates for weight-loss medications.”
Another recommendation based on high-quality evidence is that if a patient responds well to a weight-loss medication and loses 5% or more of his or her body weight after 3 months, the medication should be continued. If the medication is ineffective or the patient experiences side effects, “we recommend that the medication be discontinued and alternative medications or referral for alternative treatment approaches be considered the prescription should be stopped and an alternative medication or approach considered.”
In a recommendation based on moderate quality evidence, the task force suggests that patients with diabetes who are obese or overweight should be given medications that promote weight loss or have no effect on weight as first-and second-line treatments. “In obese patients with T2DM requiring insulin therapy, we suggest adding at least one of the following: metformin, pramlintide (Symlin), or GLP-1 (glucagonlike peptide-1 receptor) agonists to mitigate associated weight gain due to insulin,” they noted.
Furthermore, the task force advises that ACE inhibitors, angiotensin receptor blockers, and calcium channel blockers should be used as a first-line treatment for high blood pressure in obese people with type 2 diabetes.
The task force also recommends that when patients need medications that can have an impact on weight, such as antidepressants, antipsychotic drugs, and medications for treating epilepsy, they should be fully informed and provided with estimates of each option’s anticipated effect on weight. Clinicians and patients should engage in a shared-decision making process to evaluate the options.
Another recommendation is that phentermine and diethylpropion (Tenuate) should not be used in patients with uncontrolled high blood pressure or a history of heart disease.
“Although there is abundant evidence for the value of shared decision making across several clinical scenarios, specific evidence for obesity management is scant,” the task force members acknowledged. “This highlights a limitation of the existing literature and poses a challenge for implementing a specific strategy for shared decision making in managing obesity.”
The Endocrine Society funded development of the guidelines. Dr. Apovian disclosed that she has a financial and/or leadership position with Zafgen, MYOS Corp., Eisai, Vivus, Orexigen Therapeutics, and Takeda. Other members of the task force disclosed numerous relevant financial conflicts.
On Twitter @dougbrunk
The recommendations emphasize the importance of treating obesity as a disease and, with that, the use of pharmacotherapy to manage obesity. The guidelines also discuss ways clinicians can avoid using medications that may contribute to obesity. This is usually overlooked in many clinician’s minds when choosing medications – especially in those patients with obesity – and the task force should be commended for doing so.
Unfortunately, the guidelines do not provide a pathway for how to choose among the various antiobesity medications. This would have been helpful for clinicians. The guidelines follow the FDA-approved use of obesity medications (i.e., in those with a body mass index of greater than 30 kg/m2 or in those with a BMI of greater than 27 kg/m2 plus a comorbid condition). However, this approach will not benefit certain ethnic populations, including Asians, whose cardiovascular complications associated with obesity are linked to a lower BMI.
Dr. Felice A. Caldarella is and endocrinologist at the Center for Advanced Weight Loss in Clinton, N.J. He is a member of the speakers bureau for Novo Nordisk, Takeda, and Salix.
The recommendations emphasize the importance of treating obesity as a disease and, with that, the use of pharmacotherapy to manage obesity. The guidelines also discuss ways clinicians can avoid using medications that may contribute to obesity. This is usually overlooked in many clinician’s minds when choosing medications – especially in those patients with obesity – and the task force should be commended for doing so.
Unfortunately, the guidelines do not provide a pathway for how to choose among the various antiobesity medications. This would have been helpful for clinicians. The guidelines follow the FDA-approved use of obesity medications (i.e., in those with a body mass index of greater than 30 kg/m2 or in those with a BMI of greater than 27 kg/m2 plus a comorbid condition). However, this approach will not benefit certain ethnic populations, including Asians, whose cardiovascular complications associated with obesity are linked to a lower BMI.
Dr. Felice A. Caldarella is and endocrinologist at the Center for Advanced Weight Loss in Clinton, N.J. He is a member of the speakers bureau for Novo Nordisk, Takeda, and Salix.
The recommendations emphasize the importance of treating obesity as a disease and, with that, the use of pharmacotherapy to manage obesity. The guidelines also discuss ways clinicians can avoid using medications that may contribute to obesity. This is usually overlooked in many clinician’s minds when choosing medications – especially in those patients with obesity – and the task force should be commended for doing so.
Unfortunately, the guidelines do not provide a pathway for how to choose among the various antiobesity medications. This would have been helpful for clinicians. The guidelines follow the FDA-approved use of obesity medications (i.e., in those with a body mass index of greater than 30 kg/m2 or in those with a BMI of greater than 27 kg/m2 plus a comorbid condition). However, this approach will not benefit certain ethnic populations, including Asians, whose cardiovascular complications associated with obesity are linked to a lower BMI.
Dr. Felice A. Caldarella is and endocrinologist at the Center for Advanced Weight Loss in Clinton, N.J. He is a member of the speakers bureau for Novo Nordisk, Takeda, and Salix.
For the first time, a task force of experts has assembled clinical practice guidelines dedicated to the medical treatment of obesity.
The development, spearheaded by the Endocrine Society with support from the Obesity Society and the European Society of Endocrinology, comes after four new anti-obesity drugs hit the market in the past 2 years: lorcaserin (Belviq), phentermine/topiramate (Qsymia), naltrexone/bupropion (Contrave) and liraglutide (Saxenda). The new guidelines expand on guidelines for managing overweight and obesity in adults that were released in 2013 by the Obesity Society, the American Heart Association, and the American College of Cardiology.
“Medications used for the management of conditions other than obesity can contribute to or exacerbate weight gain in susceptible individuals,” the eight-member task force wrote online Jan. 15 in the Journal of Clinical Endocrinology and Metabolism (doi:10/1210/jc.2014-3415).” Many of these conditions are also associated with obesity. Health care providers can help patients prevent or attenuate weight gain by appropriately prescribing medications that would promote weight loss or minimize weight gain when treating these conditions.”
The task force, chaired by Dr. Caroline M. Apovian professor of medicine at Boston University, recommends that diet, exercise, and behavioral modifications be part of all obesity management approaches. “Drugs may amplify adherence to behavior change and may improve physical functioning such that increased physical activity is easier in those who cannot exercise initially,” they wrote. “Patients who have a history of being unable to successfully lose and maintain weight and who meet label indications are candidates for weight-loss medications.”
Another recommendation based on high-quality evidence is that if a patient responds well to a weight-loss medication and loses 5% or more of his or her body weight after 3 months, the medication should be continued. If the medication is ineffective or the patient experiences side effects, “we recommend that the medication be discontinued and alternative medications or referral for alternative treatment approaches be considered the prescription should be stopped and an alternative medication or approach considered.”
In a recommendation based on moderate quality evidence, the task force suggests that patients with diabetes who are obese or overweight should be given medications that promote weight loss or have no effect on weight as first-and second-line treatments. “In obese patients with T2DM requiring insulin therapy, we suggest adding at least one of the following: metformin, pramlintide (Symlin), or GLP-1 (glucagonlike peptide-1 receptor) agonists to mitigate associated weight gain due to insulin,” they noted.
Furthermore, the task force advises that ACE inhibitors, angiotensin receptor blockers, and calcium channel blockers should be used as a first-line treatment for high blood pressure in obese people with type 2 diabetes.
The task force also recommends that when patients need medications that can have an impact on weight, such as antidepressants, antipsychotic drugs, and medications for treating epilepsy, they should be fully informed and provided with estimates of each option’s anticipated effect on weight. Clinicians and patients should engage in a shared-decision making process to evaluate the options.
Another recommendation is that phentermine and diethylpropion (Tenuate) should not be used in patients with uncontrolled high blood pressure or a history of heart disease.
“Although there is abundant evidence for the value of shared decision making across several clinical scenarios, specific evidence for obesity management is scant,” the task force members acknowledged. “This highlights a limitation of the existing literature and poses a challenge for implementing a specific strategy for shared decision making in managing obesity.”
The Endocrine Society funded development of the guidelines. Dr. Apovian disclosed that she has a financial and/or leadership position with Zafgen, MYOS Corp., Eisai, Vivus, Orexigen Therapeutics, and Takeda. Other members of the task force disclosed numerous relevant financial conflicts.
On Twitter @dougbrunk
For the first time, a task force of experts has assembled clinical practice guidelines dedicated to the medical treatment of obesity.
The development, spearheaded by the Endocrine Society with support from the Obesity Society and the European Society of Endocrinology, comes after four new anti-obesity drugs hit the market in the past 2 years: lorcaserin (Belviq), phentermine/topiramate (Qsymia), naltrexone/bupropion (Contrave) and liraglutide (Saxenda). The new guidelines expand on guidelines for managing overweight and obesity in adults that were released in 2013 by the Obesity Society, the American Heart Association, and the American College of Cardiology.
“Medications used for the management of conditions other than obesity can contribute to or exacerbate weight gain in susceptible individuals,” the eight-member task force wrote online Jan. 15 in the Journal of Clinical Endocrinology and Metabolism (doi:10/1210/jc.2014-3415).” Many of these conditions are also associated with obesity. Health care providers can help patients prevent or attenuate weight gain by appropriately prescribing medications that would promote weight loss or minimize weight gain when treating these conditions.”
The task force, chaired by Dr. Caroline M. Apovian professor of medicine at Boston University, recommends that diet, exercise, and behavioral modifications be part of all obesity management approaches. “Drugs may amplify adherence to behavior change and may improve physical functioning such that increased physical activity is easier in those who cannot exercise initially,” they wrote. “Patients who have a history of being unable to successfully lose and maintain weight and who meet label indications are candidates for weight-loss medications.”
Another recommendation based on high-quality evidence is that if a patient responds well to a weight-loss medication and loses 5% or more of his or her body weight after 3 months, the medication should be continued. If the medication is ineffective or the patient experiences side effects, “we recommend that the medication be discontinued and alternative medications or referral for alternative treatment approaches be considered the prescription should be stopped and an alternative medication or approach considered.”
In a recommendation based on moderate quality evidence, the task force suggests that patients with diabetes who are obese or overweight should be given medications that promote weight loss or have no effect on weight as first-and second-line treatments. “In obese patients with T2DM requiring insulin therapy, we suggest adding at least one of the following: metformin, pramlintide (Symlin), or GLP-1 (glucagonlike peptide-1 receptor) agonists to mitigate associated weight gain due to insulin,” they noted.
Furthermore, the task force advises that ACE inhibitors, angiotensin receptor blockers, and calcium channel blockers should be used as a first-line treatment for high blood pressure in obese people with type 2 diabetes.
The task force also recommends that when patients need medications that can have an impact on weight, such as antidepressants, antipsychotic drugs, and medications for treating epilepsy, they should be fully informed and provided with estimates of each option’s anticipated effect on weight. Clinicians and patients should engage in a shared-decision making process to evaluate the options.
Another recommendation is that phentermine and diethylpropion (Tenuate) should not be used in patients with uncontrolled high blood pressure or a history of heart disease.
“Although there is abundant evidence for the value of shared decision making across several clinical scenarios, specific evidence for obesity management is scant,” the task force members acknowledged. “This highlights a limitation of the existing literature and poses a challenge for implementing a specific strategy for shared decision making in managing obesity.”
The Endocrine Society funded development of the guidelines. Dr. Apovian disclosed that she has a financial and/or leadership position with Zafgen, MYOS Corp., Eisai, Vivus, Orexigen Therapeutics, and Takeda. Other members of the task force disclosed numerous relevant financial conflicts.
On Twitter @dougbrunk
Permanent SGR fix faces funding hurdle
WASHINGTON – With bipartisan agreement to repeal and replace the Medicare Sustainable Growth Rate formula already on the table, the next battle facing passage of the legislation will be how to pay for it.
Republican leadership of the House Energy and Commerce Health Subcommittee made it clear at a Jan. 21 hearing that a permanent SGR fix would not move forward without offsets to cover the estimated $140 billion price tag for the current agreement.
Finding the offsets “will not be easy, but it is a task we must embrace,” Subcommittee Chairman Joseph Pitts, (R-Pa.), said in opening the first of two days of hearings on SGR repeal. “Some argue that SGR reform does not need to be paid for. I respectfully disagree.”
Rep. Pitts noted that 98% of enacted SGR patches, spanning 120 of the 123 months worth of so-called “doc-fix” legislation, have been paid for with offsets.
Democrats on the subcommittee were critical of that hard line, noting that the House recently passed a bill to change definition of full-time employment in the Affordable Care Act to 40 hours a week, a bill estimated to cost more than $50 billion, without any cost offsets. They also suggested to look elsewhere in government to find the offsets.
“But a fix to the SGR that harms Medicare beneficiaries because of the insistence of offsets that reduce benefits and limit access is not an acceptable tradeoff,” said the subcommittee’s ranking member, Rep. Gene Green, (D-Tex.).
Witnesses who testified on Jan. 21 agreed that it should not be passed without offsets, though the common message was not to put the burden on beneficiaries through higher premiums or reduction of services.
Alice Rivlin, Ph.D., director of the Engelberg Center for Health Care Reform at the Brookings Institution and cochair of the delivery system reform initiative at the Bipartisan Policy Center, offered a number of potential cost-saving reforms, including income-adjusting premiums, accelerating of payment reform, rewarding seniors for choosing generic drugs, more competitive bidding, and accelerating the time frame for higher payments to providers participating in alternative payment mechanisms highlighted in the legislation to 2018 and offering those incentives to all Medicare providers.
“They would move to make Medicare a more efficient program,” Dr. Rivlin, founding director of the Congressional Budget Office, said.
Dr. Rivlin also suggested that strengthening accountable care organizations (ACOs) would help with finding savings offsets, including setting longer-term savings goals rather than resetting baselines every year or eliminating historical or “after-the-fact” attribution of beneficiaries to ACOs.
“The long-term promise of these models won’t be realized if unrealistic short-term pressures for savings make it unlikely that many providers can succeed,” she said. “These are all fixable problems that can be addressed as part of SGR reform.”
Better care coordination also could save Medicare money and contribute to SGR reform funding, according to Marilyn Moon, Ph.D., a fellow at the American Institutes for Research.
Dr. Moon said that there should be incentives that emphasize performing the right care at the right place and at the right time. To that end, she said the notion of bundled payments needs to be carefully examined because of the influence the entity in charge of payments might have.
For example, if a hospital is the lead organization in charge of distributing bundled payments in a coordinated care system, it might be inclined to keep patients in house rather than send them to a more appropriate setting.
There are “a lot of things that need to be worked out,” she said, adding that the SGR legislation could be a good vehicle for it.
On Jan. 22, the Health Subcommittee will hear testimony on SGR reform from a panel of representatives of physician organizations.
WASHINGTON – With bipartisan agreement to repeal and replace the Medicare Sustainable Growth Rate formula already on the table, the next battle facing passage of the legislation will be how to pay for it.
Republican leadership of the House Energy and Commerce Health Subcommittee made it clear at a Jan. 21 hearing that a permanent SGR fix would not move forward without offsets to cover the estimated $140 billion price tag for the current agreement.
Finding the offsets “will not be easy, but it is a task we must embrace,” Subcommittee Chairman Joseph Pitts, (R-Pa.), said in opening the first of two days of hearings on SGR repeal. “Some argue that SGR reform does not need to be paid for. I respectfully disagree.”
Rep. Pitts noted that 98% of enacted SGR patches, spanning 120 of the 123 months worth of so-called “doc-fix” legislation, have been paid for with offsets.
Democrats on the subcommittee were critical of that hard line, noting that the House recently passed a bill to change definition of full-time employment in the Affordable Care Act to 40 hours a week, a bill estimated to cost more than $50 billion, without any cost offsets. They also suggested to look elsewhere in government to find the offsets.
“But a fix to the SGR that harms Medicare beneficiaries because of the insistence of offsets that reduce benefits and limit access is not an acceptable tradeoff,” said the subcommittee’s ranking member, Rep. Gene Green, (D-Tex.).
Witnesses who testified on Jan. 21 agreed that it should not be passed without offsets, though the common message was not to put the burden on beneficiaries through higher premiums or reduction of services.
Alice Rivlin, Ph.D., director of the Engelberg Center for Health Care Reform at the Brookings Institution and cochair of the delivery system reform initiative at the Bipartisan Policy Center, offered a number of potential cost-saving reforms, including income-adjusting premiums, accelerating of payment reform, rewarding seniors for choosing generic drugs, more competitive bidding, and accelerating the time frame for higher payments to providers participating in alternative payment mechanisms highlighted in the legislation to 2018 and offering those incentives to all Medicare providers.
“They would move to make Medicare a more efficient program,” Dr. Rivlin, founding director of the Congressional Budget Office, said.
Dr. Rivlin also suggested that strengthening accountable care organizations (ACOs) would help with finding savings offsets, including setting longer-term savings goals rather than resetting baselines every year or eliminating historical or “after-the-fact” attribution of beneficiaries to ACOs.
“The long-term promise of these models won’t be realized if unrealistic short-term pressures for savings make it unlikely that many providers can succeed,” she said. “These are all fixable problems that can be addressed as part of SGR reform.”
Better care coordination also could save Medicare money and contribute to SGR reform funding, according to Marilyn Moon, Ph.D., a fellow at the American Institutes for Research.
Dr. Moon said that there should be incentives that emphasize performing the right care at the right place and at the right time. To that end, she said the notion of bundled payments needs to be carefully examined because of the influence the entity in charge of payments might have.
For example, if a hospital is the lead organization in charge of distributing bundled payments in a coordinated care system, it might be inclined to keep patients in house rather than send them to a more appropriate setting.
There are “a lot of things that need to be worked out,” she said, adding that the SGR legislation could be a good vehicle for it.
On Jan. 22, the Health Subcommittee will hear testimony on SGR reform from a panel of representatives of physician organizations.
WASHINGTON – With bipartisan agreement to repeal and replace the Medicare Sustainable Growth Rate formula already on the table, the next battle facing passage of the legislation will be how to pay for it.
Republican leadership of the House Energy and Commerce Health Subcommittee made it clear at a Jan. 21 hearing that a permanent SGR fix would not move forward without offsets to cover the estimated $140 billion price tag for the current agreement.
Finding the offsets “will not be easy, but it is a task we must embrace,” Subcommittee Chairman Joseph Pitts, (R-Pa.), said in opening the first of two days of hearings on SGR repeal. “Some argue that SGR reform does not need to be paid for. I respectfully disagree.”
Rep. Pitts noted that 98% of enacted SGR patches, spanning 120 of the 123 months worth of so-called “doc-fix” legislation, have been paid for with offsets.
Democrats on the subcommittee were critical of that hard line, noting that the House recently passed a bill to change definition of full-time employment in the Affordable Care Act to 40 hours a week, a bill estimated to cost more than $50 billion, without any cost offsets. They also suggested to look elsewhere in government to find the offsets.
“But a fix to the SGR that harms Medicare beneficiaries because of the insistence of offsets that reduce benefits and limit access is not an acceptable tradeoff,” said the subcommittee’s ranking member, Rep. Gene Green, (D-Tex.).
Witnesses who testified on Jan. 21 agreed that it should not be passed without offsets, though the common message was not to put the burden on beneficiaries through higher premiums or reduction of services.
Alice Rivlin, Ph.D., director of the Engelberg Center for Health Care Reform at the Brookings Institution and cochair of the delivery system reform initiative at the Bipartisan Policy Center, offered a number of potential cost-saving reforms, including income-adjusting premiums, accelerating of payment reform, rewarding seniors for choosing generic drugs, more competitive bidding, and accelerating the time frame for higher payments to providers participating in alternative payment mechanisms highlighted in the legislation to 2018 and offering those incentives to all Medicare providers.
“They would move to make Medicare a more efficient program,” Dr. Rivlin, founding director of the Congressional Budget Office, said.
Dr. Rivlin also suggested that strengthening accountable care organizations (ACOs) would help with finding savings offsets, including setting longer-term savings goals rather than resetting baselines every year or eliminating historical or “after-the-fact” attribution of beneficiaries to ACOs.
“The long-term promise of these models won’t be realized if unrealistic short-term pressures for savings make it unlikely that many providers can succeed,” she said. “These are all fixable problems that can be addressed as part of SGR reform.”
Better care coordination also could save Medicare money and contribute to SGR reform funding, according to Marilyn Moon, Ph.D., a fellow at the American Institutes for Research.
Dr. Moon said that there should be incentives that emphasize performing the right care at the right place and at the right time. To that end, she said the notion of bundled payments needs to be carefully examined because of the influence the entity in charge of payments might have.
For example, if a hospital is the lead organization in charge of distributing bundled payments in a coordinated care system, it might be inclined to keep patients in house rather than send them to a more appropriate setting.
There are “a lot of things that need to be worked out,” she said, adding that the SGR legislation could be a good vehicle for it.
On Jan. 22, the Health Subcommittee will hear testimony on SGR reform from a panel of representatives of physician organizations.
AT A HOUSE ENERGY AND COMMERCE HEALTH SUBCOMMITTEE HEARING
Medicine grapples with physician suicide
One day in 1986, a medical school classmate handed Dr. Robert P. Bright a gun that she intended to use to kill herself. She asked him to hold on to it for her and to keep quiet about her sense of hopelessness.
“She didn’t want anybody in the medical school to know; it was all hidden and hush-hushed,” recalled Dr. Bright, who is now a psychiatrist at the Mayo Clinic, Scottsdale, Ariz. “I was trying to juggle that with the issue of safety.”
He honored his classmate’s request for confidentiality, but he sought advice from the medical school dean about what to do. Before long, his classmate sought help from a psychiatrist and got better with medication and psychotherapy. “It turned out well, thank goodness,” Dr. Bright said.
Similar stories of despair among medical students and physicians don’t always end well. The American Foundation for Suicide Prevention estimates that 300-400 U.S. physicians commit suicide each year, about one per day. Suicide deaths are 250%-400% higher among female physicians, compared with women in other professions, and 70% higher among male physicians, compared with men in other professions. Major depression is a common risk factor, along with bipolar disorder and substance abuse.
Depression and other mood disorders may be underrecognized and inadequately treated in physicians because they may be reluctant to seek treatment, may attempt to diagnose and treat themselves, or may seek and receive “VIP treatment” from health care providers, according to a review article coauthored by Dr. Bright (Current Psych. 2011;10:16-30).
“Physicians struggling with these things are very much in the closet about it,” he said. “It’s a sad reflection on the stigma that’s still in our country that people can’t come forth and say, ‘I’m struggling with depression or anxiety.’ ”
Researchers led by Dr. Katherine J. Gold at the University of Michigan used data from the National Violent Death Reporting System to evaluate suicide among physicians and found that job stressors “may impact physician identity and be a particular risk factor for which more attention is warranted” (Gen. Hosp. Psychiatry 2013;35:45-9).
Work dissatisfaction sent Dr. Pamela Wible into a tailspin early in her career. In 2004 she found herself in a suicidal state for about 6 weeks, “I stayed at home, crying myself into my pillow and I never sought help from my colleagues,” recalled Dr. Wible, a family physician in Eugene, Ore., who currently leads training sessions in medical student and physician suicide prevention. “I was not depressed before entering the medical profession, but [I had developed] constant thoughts of ‘Can I just disappear? What’s the easiest way to do this?’ I got to a place of complete surrender but I didn’t have the gun. I didn’t have the stockpile of pills. I didn’t have a follow-through on the plan.”
Instead of taking her own life, she “had an epiphany” and changed the way she practiced medicine. She said that owning her own clinic empowered her to “become the doctor I had originally described on my personal statement when I entered medical school.”
According to Dr. Charles F. Reynolds III, a psychiatrist at the University of Pittsburgh, reluctance to seek treatment can also be driven by concerns about the amount of time that treatment could take.
“As physicians, we often don’t appropriately take care of ourselves when it comes to issues like depression,” said Dr. Reynolds, who also directs the National Institute of Mental Health–sponsored Center of Excellence in the Prevention and Treatment of Late Life Mood Disorders. “We may still see it as a character weakness rather than as a medical illness that can be diagnosed and appropriately treated. Concerns about privacy also figure into the concerns of some physicians as well.”
Practicing in a rural area or small community can also be an obstacle to treatment, not only because of limited access to psychiatrists, but because the “patient” may be the only physician in town.
“As much as there’s stigma for everybody being voluntarily or involuntarily admitted [for suicidal ideation], it’s a little different when you’re a provider within the hospital where you’re seeking care,” Dr. Bright noted.
He said that if he had the opportunity to counsel physicians experiencing suicidal thoughts, he would “remind them of the medical nature of depression, that the brain is just another organ and the organ is not making chemicals just like the pancreas doesn’t make insulin in diabetes,” he said. “I’d also encourage them to get the treatment that they need. I would encourage compassion for themselves that they would give to anybody else in the same situation.”
He said that he would advise them to find a mental health provider “that they trust with confidentiality, and to reach out to other people for support. I would also let them know about the physician assistance programs that are available. There’s one through Vanderbilt (the Vanderbilt Center for Professional Health) and several others that specialize in working with physicians who are struggling with mental health or substance abuse or disruptive behavior.”
Dr. Reynolds’ core message to distressed physicians is that “you’re a better doctor for your patients, and a better father or mother for your family, if you’re taking good care of yourself,” he said. “It’s hard for you to take care of your patients if you’re not also taking care of yourself, if you’re burning out. Get help. Treatment works.”
Dr. Christine Moutier, chief medical officer of the American Foundation for Suicide Prevention, added that troubled physicians “should feel no shame for the fact that they’re in distress. Any of us can get there through a whole variety of different pathways that life presents. There’s science and data to support this experience as commonplace and having underpinnings that are of no fault to anyone. That’s the reality.”
Dr. Wible, who has lost several colleagues and physician friends to suicide, said that she hopes for a more transparent discussion of the topic by the medical profession. She presented on the topic at the 2014 annual scientific assembly of the American Academy of Family Physicians.
“The talk before mine was on Ebola, and every seat was taken” in the 900-seat room. When it came time for her presentation, “I maybe had 100 people in the room. Now, are physicians more likely to die from Ebola or from suicide? We are in a state of denial. If we don’t talk about suicide, we will continue to lose one or two medical students or doctors every day. The sooner we talk about this and connect with each other outside of a PowerPoint presentation, the sooner we’re going to solve this.”
After a physician in a large clinical department at the University of Pittsburgh took his own life several years ago, the chair of that department invited Dr. Reynolds to speak with his staff. The meeting “was primarily educational in nature, so we talked about the topic, to try to destigmatize and to educate people about the need for appropriate help-seeking,” recalled Dr. Reynolds, who is a former president of the American College of Psychiatrists. “If the leadership of a medical institution appropriately sanctions help-seeking behavior and treatment of mental disorders like depression, that’s going to make it okay for people to reach out and seek help rather than pushing it under the rug, so to speak. If the leadership says ‘this is a key thing and we don’t think you can function adequately as a medical student or as a physician if you’re not taking appropriate care of yourself,’ that helps to shift the culture.”
The ripple effect of that kind of message from health care administrators can’t be underestimated, said Dr. Moutier, who helped launch a suicide and depression awareness program at the University of California, San Diego (Acad. Med. 2012;87:320-6). She encouraged health care leaders to stage periodic grand rounds and lectures for their medical staff about physician well-being, burnout, and the risk of suicide. “If the leader is uncomfortable talking about these things, that’s a sign they should get a little education for themselves about [these topics],” she said.
Dr. Reynolds noted that certain state medical licensure boards including those for Arkansas and Pennsylvania have incorporated destigmatizing language into relicensure exams. “Some of them previously would ask questions such as whether the applicants had a history of a mental disorder like depression,” he said. “What you’re beginning to see now increasingly is that the state medical board will ask more generic questions, like ‘Do you have any conditions that would interfere with the practice of your specialty in medicine?’ This is a good thing.”
He said that he is optimistic about future of physician well-being, noting that the University of Pittsburgh and other medical schools have incorporated wellness principles into first-year curriculum. “We underscore the importance of students becoming sensitive to one another, learning how to recognize depression in each other and creating a culture in which students can encourage each other to engage in appropriate help-seeking,” Dr. Reynolds explained. “I think we are witnessing a shift in the culture of institutional medicine as we bring along new generations of physicians who are better educated about mental disorders and their treatment and issues related to suicide as we reach out to students, make counseling services available to them, educate them about these issues. That supports a cultural shift that gradually erodes the issue of stigma that has so long plagued appropriate help-seeking in medical institutions.”
Still, Dr. Wible said that she worries about the disaffected colleagues who reach out to her almost every day. “Just yesterday I got an e-mail from a physician in Oklahoma who told me they just lost three physicians to suicide in 1 month who were on probation with the medical board,” she said. “These are not defective physicians. These people need to be helped.”
Dr. Wible said that she favors holding periodic panel discussions on the topics of depression and physician suicide for medical students and physicians alike. “Let other physicians who’ve been depressed and suicidal sit in front of the room on the first week of medical school, or in a hospital once in a while, mandatory, where you listen to other well-respected physicians say, ‘yeah. I cried myself to sleep after I lost this patient,’ or ‘I had suicidal thoughts during a malpractice case.’ There are lots of reasons why physicians could be sad. They need to start talking about it publicly. Other medical students and physicians would then feel comfortable to raise their hands in the audience and say, ‘I felt the same way.’ ”
Suggested resources for help
American Foundation for Suicide Prevention (www.afsp.org/).
24-hour crisis line: 1-800-273-TALK (8255).
In 2008 the AFSP released a documentary about the problem of physician depression and suicide titled “Struggling in Silence,” which aired on public television stations nationwide and is available on DVD for $24.99.
Center for Patient and Professional Advocacy (www.mc.vanderbilt.edu/centers/cppa/index.php)
Depression and Bipolar Support Alliance (www.dbsalliance.org).
Federation of State Physician Health Programs Inc. (www.fsphp.org).
Vanderbilt Center for Professional Health (www.mc.vanderbilt.edu/cph).
The Mayo Clinic Program on Physician Well-Being (http://www.mayo.edu/research/centers-programs/physician-well-being-program/overview).
ePhysicianHealth.com, a program of the Ontario Medical Association (http://php.oma.org/ePhysicianHealth.html)
The Academic Medicine Handbook: A Guide to Achievement and Fulfillment for Academic Faculty, New York: Springer, 2013 (http://www.springer.com/medicine/internal/book/978-1-4614-5692-6)
[email protected]
On Twitter @dougbrunk
As a specialist in physician health, I shout out that we can never have too many articles on this heartbreaking tragedy that claims so many lives each year - and leaves so many devastated people in its wake.

|
| Dr. Michael F. Myers |
It is sobering and frightening that despite the excellent institutional and systemic changes outlined by Dr. Reynolds and Dr. Moutier and the moving first-hand testimonials of Dr. Bright and Dr. Wible, despairing doctors continue to die by their own hands. The loss of so many intelligent, highly trained, and compassionate caregivers is mind-numbing and unconscionable. We cannot afford to let down our guard.
As part of my research for a book in progress "When Physicians Kill Themselves: The Voices of Those They Leave Behind," I have been interviewing the family members and medical colleagues of doctors who have died by suicide.
One theme that is ascendant is how commonly the ailing physician has fallen through the cracks. Initially, he may not recognize or accept that he is burned out, depressed, or abusing alcohol and other drugs. When she does begin to understand what her symptoms suggest, the internalized stigma is so harsh and relentless that seeking help is out of the question. This drives self-medicating, but even when this does not occur and he consults a psychiatrist, punishing shame colors and works against forming a therapeutic alliance, accepting the diagnosis, keeping appointments, disclosing dangerous suicidality, adhering to medication, engaging in lifesaving psychotherapy and maintaining (or regaining) hope.
What makes matters worse is when the treating professional cuts corners (or enables self-defeating behaviors in the patient) and does not use the same judgment, monitoring, and vigilance that she uses with her nonphysician patients.
What I have found most disturbing in these narratives of my interviewees is how often their attempts to access their loved one's caregiver have fallen on deaf ears. This has to stop.
Dr. Wible says that she "had an epiphany" and changed the way she practiced medicine. It is our duty to reach out and help more physicians find their epiphany.
Dr. Michael F. Myers is professor of clinical psychiatry at SUNY Downstate Medical Center in Brooklyn, N.Y. He also is the coauthor (with Carla Fine) of "Touched by Suicide: Hope and Healing After Loss" and (with Dr. Glen O. Gabbard) of "The Physician as Patient: A Clinical Handbook for Mental Health Professionals."
As a specialist in physician health, I shout out that we can never have too many articles on this heartbreaking tragedy that claims so many lives each year - and leaves so many devastated people in its wake.

|
| Dr. Michael F. Myers |
It is sobering and frightening that despite the excellent institutional and systemic changes outlined by Dr. Reynolds and Dr. Moutier and the moving first-hand testimonials of Dr. Bright and Dr. Wible, despairing doctors continue to die by their own hands. The loss of so many intelligent, highly trained, and compassionate caregivers is mind-numbing and unconscionable. We cannot afford to let down our guard.
As part of my research for a book in progress "When Physicians Kill Themselves: The Voices of Those They Leave Behind," I have been interviewing the family members and medical colleagues of doctors who have died by suicide.
One theme that is ascendant is how commonly the ailing physician has fallen through the cracks. Initially, he may not recognize or accept that he is burned out, depressed, or abusing alcohol and other drugs. When she does begin to understand what her symptoms suggest, the internalized stigma is so harsh and relentless that seeking help is out of the question. This drives self-medicating, but even when this does not occur and he consults a psychiatrist, punishing shame colors and works against forming a therapeutic alliance, accepting the diagnosis, keeping appointments, disclosing dangerous suicidality, adhering to medication, engaging in lifesaving psychotherapy and maintaining (or regaining) hope.
What makes matters worse is when the treating professional cuts corners (or enables self-defeating behaviors in the patient) and does not use the same judgment, monitoring, and vigilance that she uses with her nonphysician patients.
What I have found most disturbing in these narratives of my interviewees is how often their attempts to access their loved one's caregiver have fallen on deaf ears. This has to stop.
Dr. Wible says that she "had an epiphany" and changed the way she practiced medicine. It is our duty to reach out and help more physicians find their epiphany.
Dr. Michael F. Myers is professor of clinical psychiatry at SUNY Downstate Medical Center in Brooklyn, N.Y. He also is the coauthor (with Carla Fine) of "Touched by Suicide: Hope and Healing After Loss" and (with Dr. Glen O. Gabbard) of "The Physician as Patient: A Clinical Handbook for Mental Health Professionals."
As a specialist in physician health, I shout out that we can never have too many articles on this heartbreaking tragedy that claims so many lives each year - and leaves so many devastated people in its wake.

|
| Dr. Michael F. Myers |
It is sobering and frightening that despite the excellent institutional and systemic changes outlined by Dr. Reynolds and Dr. Moutier and the moving first-hand testimonials of Dr. Bright and Dr. Wible, despairing doctors continue to die by their own hands. The loss of so many intelligent, highly trained, and compassionate caregivers is mind-numbing and unconscionable. We cannot afford to let down our guard.
As part of my research for a book in progress "When Physicians Kill Themselves: The Voices of Those They Leave Behind," I have been interviewing the family members and medical colleagues of doctors who have died by suicide.
One theme that is ascendant is how commonly the ailing physician has fallen through the cracks. Initially, he may not recognize or accept that he is burned out, depressed, or abusing alcohol and other drugs. When she does begin to understand what her symptoms suggest, the internalized stigma is so harsh and relentless that seeking help is out of the question. This drives self-medicating, but even when this does not occur and he consults a psychiatrist, punishing shame colors and works against forming a therapeutic alliance, accepting the diagnosis, keeping appointments, disclosing dangerous suicidality, adhering to medication, engaging in lifesaving psychotherapy and maintaining (or regaining) hope.
What makes matters worse is when the treating professional cuts corners (or enables self-defeating behaviors in the patient) and does not use the same judgment, monitoring, and vigilance that she uses with her nonphysician patients.
What I have found most disturbing in these narratives of my interviewees is how often their attempts to access their loved one's caregiver have fallen on deaf ears. This has to stop.
Dr. Wible says that she "had an epiphany" and changed the way she practiced medicine. It is our duty to reach out and help more physicians find their epiphany.
Dr. Michael F. Myers is professor of clinical psychiatry at SUNY Downstate Medical Center in Brooklyn, N.Y. He also is the coauthor (with Carla Fine) of "Touched by Suicide: Hope and Healing After Loss" and (with Dr. Glen O. Gabbard) of "The Physician as Patient: A Clinical Handbook for Mental Health Professionals."
One day in 1986, a medical school classmate handed Dr. Robert P. Bright a gun that she intended to use to kill herself. She asked him to hold on to it for her and to keep quiet about her sense of hopelessness.
“She didn’t want anybody in the medical school to know; it was all hidden and hush-hushed,” recalled Dr. Bright, who is now a psychiatrist at the Mayo Clinic, Scottsdale, Ariz. “I was trying to juggle that with the issue of safety.”
He honored his classmate’s request for confidentiality, but he sought advice from the medical school dean about what to do. Before long, his classmate sought help from a psychiatrist and got better with medication and psychotherapy. “It turned out well, thank goodness,” Dr. Bright said.
Similar stories of despair among medical students and physicians don’t always end well. The American Foundation for Suicide Prevention estimates that 300-400 U.S. physicians commit suicide each year, about one per day. Suicide deaths are 250%-400% higher among female physicians, compared with women in other professions, and 70% higher among male physicians, compared with men in other professions. Major depression is a common risk factor, along with bipolar disorder and substance abuse.
Depression and other mood disorders may be underrecognized and inadequately treated in physicians because they may be reluctant to seek treatment, may attempt to diagnose and treat themselves, or may seek and receive “VIP treatment” from health care providers, according to a review article coauthored by Dr. Bright (Current Psych. 2011;10:16-30).
“Physicians struggling with these things are very much in the closet about it,” he said. “It’s a sad reflection on the stigma that’s still in our country that people can’t come forth and say, ‘I’m struggling with depression or anxiety.’ ”
Researchers led by Dr. Katherine J. Gold at the University of Michigan used data from the National Violent Death Reporting System to evaluate suicide among physicians and found that job stressors “may impact physician identity and be a particular risk factor for which more attention is warranted” (Gen. Hosp. Psychiatry 2013;35:45-9).
Work dissatisfaction sent Dr. Pamela Wible into a tailspin early in her career. In 2004 she found herself in a suicidal state for about 6 weeks, “I stayed at home, crying myself into my pillow and I never sought help from my colleagues,” recalled Dr. Wible, a family physician in Eugene, Ore., who currently leads training sessions in medical student and physician suicide prevention. “I was not depressed before entering the medical profession, but [I had developed] constant thoughts of ‘Can I just disappear? What’s the easiest way to do this?’ I got to a place of complete surrender but I didn’t have the gun. I didn’t have the stockpile of pills. I didn’t have a follow-through on the plan.”
Instead of taking her own life, she “had an epiphany” and changed the way she practiced medicine. She said that owning her own clinic empowered her to “become the doctor I had originally described on my personal statement when I entered medical school.”
According to Dr. Charles F. Reynolds III, a psychiatrist at the University of Pittsburgh, reluctance to seek treatment can also be driven by concerns about the amount of time that treatment could take.
“As physicians, we often don’t appropriately take care of ourselves when it comes to issues like depression,” said Dr. Reynolds, who also directs the National Institute of Mental Health–sponsored Center of Excellence in the Prevention and Treatment of Late Life Mood Disorders. “We may still see it as a character weakness rather than as a medical illness that can be diagnosed and appropriately treated. Concerns about privacy also figure into the concerns of some physicians as well.”
Practicing in a rural area or small community can also be an obstacle to treatment, not only because of limited access to psychiatrists, but because the “patient” may be the only physician in town.
“As much as there’s stigma for everybody being voluntarily or involuntarily admitted [for suicidal ideation], it’s a little different when you’re a provider within the hospital where you’re seeking care,” Dr. Bright noted.
He said that if he had the opportunity to counsel physicians experiencing suicidal thoughts, he would “remind them of the medical nature of depression, that the brain is just another organ and the organ is not making chemicals just like the pancreas doesn’t make insulin in diabetes,” he said. “I’d also encourage them to get the treatment that they need. I would encourage compassion for themselves that they would give to anybody else in the same situation.”
He said that he would advise them to find a mental health provider “that they trust with confidentiality, and to reach out to other people for support. I would also let them know about the physician assistance programs that are available. There’s one through Vanderbilt (the Vanderbilt Center for Professional Health) and several others that specialize in working with physicians who are struggling with mental health or substance abuse or disruptive behavior.”
Dr. Reynolds’ core message to distressed physicians is that “you’re a better doctor for your patients, and a better father or mother for your family, if you’re taking good care of yourself,” he said. “It’s hard for you to take care of your patients if you’re not also taking care of yourself, if you’re burning out. Get help. Treatment works.”
Dr. Christine Moutier, chief medical officer of the American Foundation for Suicide Prevention, added that troubled physicians “should feel no shame for the fact that they’re in distress. Any of us can get there through a whole variety of different pathways that life presents. There’s science and data to support this experience as commonplace and having underpinnings that are of no fault to anyone. That’s the reality.”
Dr. Wible, who has lost several colleagues and physician friends to suicide, said that she hopes for a more transparent discussion of the topic by the medical profession. She presented on the topic at the 2014 annual scientific assembly of the American Academy of Family Physicians.
“The talk before mine was on Ebola, and every seat was taken” in the 900-seat room. When it came time for her presentation, “I maybe had 100 people in the room. Now, are physicians more likely to die from Ebola or from suicide? We are in a state of denial. If we don’t talk about suicide, we will continue to lose one or two medical students or doctors every day. The sooner we talk about this and connect with each other outside of a PowerPoint presentation, the sooner we’re going to solve this.”
After a physician in a large clinical department at the University of Pittsburgh took his own life several years ago, the chair of that department invited Dr. Reynolds to speak with his staff. The meeting “was primarily educational in nature, so we talked about the topic, to try to destigmatize and to educate people about the need for appropriate help-seeking,” recalled Dr. Reynolds, who is a former president of the American College of Psychiatrists. “If the leadership of a medical institution appropriately sanctions help-seeking behavior and treatment of mental disorders like depression, that’s going to make it okay for people to reach out and seek help rather than pushing it under the rug, so to speak. If the leadership says ‘this is a key thing and we don’t think you can function adequately as a medical student or as a physician if you’re not taking appropriate care of yourself,’ that helps to shift the culture.”
The ripple effect of that kind of message from health care administrators can’t be underestimated, said Dr. Moutier, who helped launch a suicide and depression awareness program at the University of California, San Diego (Acad. Med. 2012;87:320-6). She encouraged health care leaders to stage periodic grand rounds and lectures for their medical staff about physician well-being, burnout, and the risk of suicide. “If the leader is uncomfortable talking about these things, that’s a sign they should get a little education for themselves about [these topics],” she said.
Dr. Reynolds noted that certain state medical licensure boards including those for Arkansas and Pennsylvania have incorporated destigmatizing language into relicensure exams. “Some of them previously would ask questions such as whether the applicants had a history of a mental disorder like depression,” he said. “What you’re beginning to see now increasingly is that the state medical board will ask more generic questions, like ‘Do you have any conditions that would interfere with the practice of your specialty in medicine?’ This is a good thing.”
He said that he is optimistic about future of physician well-being, noting that the University of Pittsburgh and other medical schools have incorporated wellness principles into first-year curriculum. “We underscore the importance of students becoming sensitive to one another, learning how to recognize depression in each other and creating a culture in which students can encourage each other to engage in appropriate help-seeking,” Dr. Reynolds explained. “I think we are witnessing a shift in the culture of institutional medicine as we bring along new generations of physicians who are better educated about mental disorders and their treatment and issues related to suicide as we reach out to students, make counseling services available to them, educate them about these issues. That supports a cultural shift that gradually erodes the issue of stigma that has so long plagued appropriate help-seeking in medical institutions.”
Still, Dr. Wible said that she worries about the disaffected colleagues who reach out to her almost every day. “Just yesterday I got an e-mail from a physician in Oklahoma who told me they just lost three physicians to suicide in 1 month who were on probation with the medical board,” she said. “These are not defective physicians. These people need to be helped.”
Dr. Wible said that she favors holding periodic panel discussions on the topics of depression and physician suicide for medical students and physicians alike. “Let other physicians who’ve been depressed and suicidal sit in front of the room on the first week of medical school, or in a hospital once in a while, mandatory, where you listen to other well-respected physicians say, ‘yeah. I cried myself to sleep after I lost this patient,’ or ‘I had suicidal thoughts during a malpractice case.’ There are lots of reasons why physicians could be sad. They need to start talking about it publicly. Other medical students and physicians would then feel comfortable to raise their hands in the audience and say, ‘I felt the same way.’ ”
Suggested resources for help
American Foundation for Suicide Prevention (www.afsp.org/).
24-hour crisis line: 1-800-273-TALK (8255).
In 2008 the AFSP released a documentary about the problem of physician depression and suicide titled “Struggling in Silence,” which aired on public television stations nationwide and is available on DVD for $24.99.
Center for Patient and Professional Advocacy (www.mc.vanderbilt.edu/centers/cppa/index.php)
Depression and Bipolar Support Alliance (www.dbsalliance.org).
Federation of State Physician Health Programs Inc. (www.fsphp.org).
Vanderbilt Center for Professional Health (www.mc.vanderbilt.edu/cph).
The Mayo Clinic Program on Physician Well-Being (http://www.mayo.edu/research/centers-programs/physician-well-being-program/overview).
ePhysicianHealth.com, a program of the Ontario Medical Association (http://php.oma.org/ePhysicianHealth.html)
The Academic Medicine Handbook: A Guide to Achievement and Fulfillment for Academic Faculty, New York: Springer, 2013 (http://www.springer.com/medicine/internal/book/978-1-4614-5692-6)
[email protected]
On Twitter @dougbrunk
One day in 1986, a medical school classmate handed Dr. Robert P. Bright a gun that she intended to use to kill herself. She asked him to hold on to it for her and to keep quiet about her sense of hopelessness.
“She didn’t want anybody in the medical school to know; it was all hidden and hush-hushed,” recalled Dr. Bright, who is now a psychiatrist at the Mayo Clinic, Scottsdale, Ariz. “I was trying to juggle that with the issue of safety.”
He honored his classmate’s request for confidentiality, but he sought advice from the medical school dean about what to do. Before long, his classmate sought help from a psychiatrist and got better with medication and psychotherapy. “It turned out well, thank goodness,” Dr. Bright said.
Similar stories of despair among medical students and physicians don’t always end well. The American Foundation for Suicide Prevention estimates that 300-400 U.S. physicians commit suicide each year, about one per day. Suicide deaths are 250%-400% higher among female physicians, compared with women in other professions, and 70% higher among male physicians, compared with men in other professions. Major depression is a common risk factor, along with bipolar disorder and substance abuse.
Depression and other mood disorders may be underrecognized and inadequately treated in physicians because they may be reluctant to seek treatment, may attempt to diagnose and treat themselves, or may seek and receive “VIP treatment” from health care providers, according to a review article coauthored by Dr. Bright (Current Psych. 2011;10:16-30).
“Physicians struggling with these things are very much in the closet about it,” he said. “It’s a sad reflection on the stigma that’s still in our country that people can’t come forth and say, ‘I’m struggling with depression or anxiety.’ ”
Researchers led by Dr. Katherine J. Gold at the University of Michigan used data from the National Violent Death Reporting System to evaluate suicide among physicians and found that job stressors “may impact physician identity and be a particular risk factor for which more attention is warranted” (Gen. Hosp. Psychiatry 2013;35:45-9).
Work dissatisfaction sent Dr. Pamela Wible into a tailspin early in her career. In 2004 she found herself in a suicidal state for about 6 weeks, “I stayed at home, crying myself into my pillow and I never sought help from my colleagues,” recalled Dr. Wible, a family physician in Eugene, Ore., who currently leads training sessions in medical student and physician suicide prevention. “I was not depressed before entering the medical profession, but [I had developed] constant thoughts of ‘Can I just disappear? What’s the easiest way to do this?’ I got to a place of complete surrender but I didn’t have the gun. I didn’t have the stockpile of pills. I didn’t have a follow-through on the plan.”
Instead of taking her own life, she “had an epiphany” and changed the way she practiced medicine. She said that owning her own clinic empowered her to “become the doctor I had originally described on my personal statement when I entered medical school.”
According to Dr. Charles F. Reynolds III, a psychiatrist at the University of Pittsburgh, reluctance to seek treatment can also be driven by concerns about the amount of time that treatment could take.
“As physicians, we often don’t appropriately take care of ourselves when it comes to issues like depression,” said Dr. Reynolds, who also directs the National Institute of Mental Health–sponsored Center of Excellence in the Prevention and Treatment of Late Life Mood Disorders. “We may still see it as a character weakness rather than as a medical illness that can be diagnosed and appropriately treated. Concerns about privacy also figure into the concerns of some physicians as well.”
Practicing in a rural area or small community can also be an obstacle to treatment, not only because of limited access to psychiatrists, but because the “patient” may be the only physician in town.
“As much as there’s stigma for everybody being voluntarily or involuntarily admitted [for suicidal ideation], it’s a little different when you’re a provider within the hospital where you’re seeking care,” Dr. Bright noted.
He said that if he had the opportunity to counsel physicians experiencing suicidal thoughts, he would “remind them of the medical nature of depression, that the brain is just another organ and the organ is not making chemicals just like the pancreas doesn’t make insulin in diabetes,” he said. “I’d also encourage them to get the treatment that they need. I would encourage compassion for themselves that they would give to anybody else in the same situation.”
He said that he would advise them to find a mental health provider “that they trust with confidentiality, and to reach out to other people for support. I would also let them know about the physician assistance programs that are available. There’s one through Vanderbilt (the Vanderbilt Center for Professional Health) and several others that specialize in working with physicians who are struggling with mental health or substance abuse or disruptive behavior.”
Dr. Reynolds’ core message to distressed physicians is that “you’re a better doctor for your patients, and a better father or mother for your family, if you’re taking good care of yourself,” he said. “It’s hard for you to take care of your patients if you’re not also taking care of yourself, if you’re burning out. Get help. Treatment works.”
Dr. Christine Moutier, chief medical officer of the American Foundation for Suicide Prevention, added that troubled physicians “should feel no shame for the fact that they’re in distress. Any of us can get there through a whole variety of different pathways that life presents. There’s science and data to support this experience as commonplace and having underpinnings that are of no fault to anyone. That’s the reality.”
Dr. Wible, who has lost several colleagues and physician friends to suicide, said that she hopes for a more transparent discussion of the topic by the medical profession. She presented on the topic at the 2014 annual scientific assembly of the American Academy of Family Physicians.
“The talk before mine was on Ebola, and every seat was taken” in the 900-seat room. When it came time for her presentation, “I maybe had 100 people in the room. Now, are physicians more likely to die from Ebola or from suicide? We are in a state of denial. If we don’t talk about suicide, we will continue to lose one or two medical students or doctors every day. The sooner we talk about this and connect with each other outside of a PowerPoint presentation, the sooner we’re going to solve this.”
After a physician in a large clinical department at the University of Pittsburgh took his own life several years ago, the chair of that department invited Dr. Reynolds to speak with his staff. The meeting “was primarily educational in nature, so we talked about the topic, to try to destigmatize and to educate people about the need for appropriate help-seeking,” recalled Dr. Reynolds, who is a former president of the American College of Psychiatrists. “If the leadership of a medical institution appropriately sanctions help-seeking behavior and treatment of mental disorders like depression, that’s going to make it okay for people to reach out and seek help rather than pushing it under the rug, so to speak. If the leadership says ‘this is a key thing and we don’t think you can function adequately as a medical student or as a physician if you’re not taking appropriate care of yourself,’ that helps to shift the culture.”
The ripple effect of that kind of message from health care administrators can’t be underestimated, said Dr. Moutier, who helped launch a suicide and depression awareness program at the University of California, San Diego (Acad. Med. 2012;87:320-6). She encouraged health care leaders to stage periodic grand rounds and lectures for their medical staff about physician well-being, burnout, and the risk of suicide. “If the leader is uncomfortable talking about these things, that’s a sign they should get a little education for themselves about [these topics],” she said.
Dr. Reynolds noted that certain state medical licensure boards including those for Arkansas and Pennsylvania have incorporated destigmatizing language into relicensure exams. “Some of them previously would ask questions such as whether the applicants had a history of a mental disorder like depression,” he said. “What you’re beginning to see now increasingly is that the state medical board will ask more generic questions, like ‘Do you have any conditions that would interfere with the practice of your specialty in medicine?’ This is a good thing.”
He said that he is optimistic about future of physician well-being, noting that the University of Pittsburgh and other medical schools have incorporated wellness principles into first-year curriculum. “We underscore the importance of students becoming sensitive to one another, learning how to recognize depression in each other and creating a culture in which students can encourage each other to engage in appropriate help-seeking,” Dr. Reynolds explained. “I think we are witnessing a shift in the culture of institutional medicine as we bring along new generations of physicians who are better educated about mental disorders and their treatment and issues related to suicide as we reach out to students, make counseling services available to them, educate them about these issues. That supports a cultural shift that gradually erodes the issue of stigma that has so long plagued appropriate help-seeking in medical institutions.”
Still, Dr. Wible said that she worries about the disaffected colleagues who reach out to her almost every day. “Just yesterday I got an e-mail from a physician in Oklahoma who told me they just lost three physicians to suicide in 1 month who were on probation with the medical board,” she said. “These are not defective physicians. These people need to be helped.”
Dr. Wible said that she favors holding periodic panel discussions on the topics of depression and physician suicide for medical students and physicians alike. “Let other physicians who’ve been depressed and suicidal sit in front of the room on the first week of medical school, or in a hospital once in a while, mandatory, where you listen to other well-respected physicians say, ‘yeah. I cried myself to sleep after I lost this patient,’ or ‘I had suicidal thoughts during a malpractice case.’ There are lots of reasons why physicians could be sad. They need to start talking about it publicly. Other medical students and physicians would then feel comfortable to raise their hands in the audience and say, ‘I felt the same way.’ ”
Suggested resources for help
American Foundation for Suicide Prevention (www.afsp.org/).
24-hour crisis line: 1-800-273-TALK (8255).
In 2008 the AFSP released a documentary about the problem of physician depression and suicide titled “Struggling in Silence,” which aired on public television stations nationwide and is available on DVD for $24.99.
Center for Patient and Professional Advocacy (www.mc.vanderbilt.edu/centers/cppa/index.php)
Depression and Bipolar Support Alliance (www.dbsalliance.org).
Federation of State Physician Health Programs Inc. (www.fsphp.org).
Vanderbilt Center for Professional Health (www.mc.vanderbilt.edu/cph).
The Mayo Clinic Program on Physician Well-Being (http://www.mayo.edu/research/centers-programs/physician-well-being-program/overview).
ePhysicianHealth.com, a program of the Ontario Medical Association (http://php.oma.org/ePhysicianHealth.html)
The Academic Medicine Handbook: A Guide to Achievement and Fulfillment for Academic Faculty, New York: Springer, 2013 (http://www.springer.com/medicine/internal/book/978-1-4614-5692-6)
[email protected]
On Twitter @dougbrunk
State of the Union: Obama announces Precision Medicine Initiative
President Obama has announced a new initiative that aims to improve medical treatments for many diseases by tailoring treatments to a patient’s unique genetic makeup.
During his Jan. 20 State of the Union address, the president unveiled the Precision Medicine Initiative, a plan to increase physicians’ ability to take a patient’s individual genetic makeup and molecular subtypes of diseases into account to improve the chances of successful treatment.
“I want the country that eliminated polio and mapped the human genome to lead a new era of medicine – one that delivers the right treatment at the right time,” President Obama said in his speech. “In some patients with cystic fibrosis, this approach has reversed a disease once thought unstoppable. Tonight, I’m launching a new Precision Medicine Initiative to bring us closer to curing diseases like cancer and diabetes – and to give all of us access to the personalized information we need to keep ourselves and our families healthier.”
“Physicians have been at the forefront of accelerating genomic discoveries and rapidly driving these innovations into daily clinical practice,” said Dr. Robert M. Wah, president of the American Medical Association. “We believe that all of the Administration’s policies should advance and build on the incredible progress that physicians are making to apply genetic and genomic breakthroughs into clinical decision-making and health promotion that can ease substantial disease burden and cost in this country.”
American College of Cardiology President Patrick T. O’Gara called the announcement an important step for continuing medical progress.
“Incredible advances have already been made in cardiovascular research, and I hope initiatives like this will lead to even more important discoveries, treatments, and cures that can be directed to patients more quickly,” Dr. O’Gara said in a statement. “The promise of precision medicine is within our grasp.”
Few details on the initiative were released during the State of the Union address; however, research into precision medicine, also known as personalized medicine, is already underway. In August 2014, the National Institutes of Health launched the Adjuvant Lung Cancer Enrichment Marker Identification and Sequencing Trials, or ALCHEMIST, a 3-part clinical trial to identify early-stage lung cancer patients with tumors that harbor certain uncommon genetic changes. The research will evaluate whether drug treatments targeted against those changes can lead to improved survival. The project adds to research by the Cancer Genome Atlas, a collaboration between the National Cancer Institute and the National Human Genome Research Institute, both divisions of NIH.
Additionally, in 2013, the American Heart Association set aside a 5-year, $30 million research fund to dig deeper into two large national studies in hopes of finding more clues to personalized treatment and prevention of cardiovascular disease. The AHA and its two main collaborators, the University of Mississippi and Boston University, said their goal is to expand population studies by adding more research subjects and more genetic analysis.
Although much of the president’s address focused on nonmedical issues, he did take the opportunity to let legislators in the Republican-led Congress know that he would veto any bill that seeks to undo progress gained under the Affordable Care Act.
“We can’t put the security of families at risk by taking away their health insurance, or unraveling the new rules on Wall Street, or refighting past battles on immigration when we’ve got a system to fix,” President Obama said. “And if a bill comes to my desk that tries to do any of these things, it will earn my veto.”
The president also urged Congress to pass the Healthy Families Act, a bill that would require businesses to provide employees up to 7 paid sick days per year. His administration also plans to help more states adopt sick leave laws of their own, he said.
“Since paid sick leave won where it was on the ballot last November, let’s put it to a vote right here in Washington. Send me a bill that gives every worker in America the opportunity to earn 7 days of paid sick leave,” he said.
On Twitter @legal_med
President Obama has announced a new initiative that aims to improve medical treatments for many diseases by tailoring treatments to a patient’s unique genetic makeup.
During his Jan. 20 State of the Union address, the president unveiled the Precision Medicine Initiative, a plan to increase physicians’ ability to take a patient’s individual genetic makeup and molecular subtypes of diseases into account to improve the chances of successful treatment.
“I want the country that eliminated polio and mapped the human genome to lead a new era of medicine – one that delivers the right treatment at the right time,” President Obama said in his speech. “In some patients with cystic fibrosis, this approach has reversed a disease once thought unstoppable. Tonight, I’m launching a new Precision Medicine Initiative to bring us closer to curing diseases like cancer and diabetes – and to give all of us access to the personalized information we need to keep ourselves and our families healthier.”
“Physicians have been at the forefront of accelerating genomic discoveries and rapidly driving these innovations into daily clinical practice,” said Dr. Robert M. Wah, president of the American Medical Association. “We believe that all of the Administration’s policies should advance and build on the incredible progress that physicians are making to apply genetic and genomic breakthroughs into clinical decision-making and health promotion that can ease substantial disease burden and cost in this country.”
American College of Cardiology President Patrick T. O’Gara called the announcement an important step for continuing medical progress.
“Incredible advances have already been made in cardiovascular research, and I hope initiatives like this will lead to even more important discoveries, treatments, and cures that can be directed to patients more quickly,” Dr. O’Gara said in a statement. “The promise of precision medicine is within our grasp.”
Few details on the initiative were released during the State of the Union address; however, research into precision medicine, also known as personalized medicine, is already underway. In August 2014, the National Institutes of Health launched the Adjuvant Lung Cancer Enrichment Marker Identification and Sequencing Trials, or ALCHEMIST, a 3-part clinical trial to identify early-stage lung cancer patients with tumors that harbor certain uncommon genetic changes. The research will evaluate whether drug treatments targeted against those changes can lead to improved survival. The project adds to research by the Cancer Genome Atlas, a collaboration between the National Cancer Institute and the National Human Genome Research Institute, both divisions of NIH.
Additionally, in 2013, the American Heart Association set aside a 5-year, $30 million research fund to dig deeper into two large national studies in hopes of finding more clues to personalized treatment and prevention of cardiovascular disease. The AHA and its two main collaborators, the University of Mississippi and Boston University, said their goal is to expand population studies by adding more research subjects and more genetic analysis.
Although much of the president’s address focused on nonmedical issues, he did take the opportunity to let legislators in the Republican-led Congress know that he would veto any bill that seeks to undo progress gained under the Affordable Care Act.
“We can’t put the security of families at risk by taking away their health insurance, or unraveling the new rules on Wall Street, or refighting past battles on immigration when we’ve got a system to fix,” President Obama said. “And if a bill comes to my desk that tries to do any of these things, it will earn my veto.”
The president also urged Congress to pass the Healthy Families Act, a bill that would require businesses to provide employees up to 7 paid sick days per year. His administration also plans to help more states adopt sick leave laws of their own, he said.
“Since paid sick leave won where it was on the ballot last November, let’s put it to a vote right here in Washington. Send me a bill that gives every worker in America the opportunity to earn 7 days of paid sick leave,” he said.
On Twitter @legal_med
President Obama has announced a new initiative that aims to improve medical treatments for many diseases by tailoring treatments to a patient’s unique genetic makeup.
During his Jan. 20 State of the Union address, the president unveiled the Precision Medicine Initiative, a plan to increase physicians’ ability to take a patient’s individual genetic makeup and molecular subtypes of diseases into account to improve the chances of successful treatment.
“I want the country that eliminated polio and mapped the human genome to lead a new era of medicine – one that delivers the right treatment at the right time,” President Obama said in his speech. “In some patients with cystic fibrosis, this approach has reversed a disease once thought unstoppable. Tonight, I’m launching a new Precision Medicine Initiative to bring us closer to curing diseases like cancer and diabetes – and to give all of us access to the personalized information we need to keep ourselves and our families healthier.”
“Physicians have been at the forefront of accelerating genomic discoveries and rapidly driving these innovations into daily clinical practice,” said Dr. Robert M. Wah, president of the American Medical Association. “We believe that all of the Administration’s policies should advance and build on the incredible progress that physicians are making to apply genetic and genomic breakthroughs into clinical decision-making and health promotion that can ease substantial disease burden and cost in this country.”
American College of Cardiology President Patrick T. O’Gara called the announcement an important step for continuing medical progress.
“Incredible advances have already been made in cardiovascular research, and I hope initiatives like this will lead to even more important discoveries, treatments, and cures that can be directed to patients more quickly,” Dr. O’Gara said in a statement. “The promise of precision medicine is within our grasp.”
Few details on the initiative were released during the State of the Union address; however, research into precision medicine, also known as personalized medicine, is already underway. In August 2014, the National Institutes of Health launched the Adjuvant Lung Cancer Enrichment Marker Identification and Sequencing Trials, or ALCHEMIST, a 3-part clinical trial to identify early-stage lung cancer patients with tumors that harbor certain uncommon genetic changes. The research will evaluate whether drug treatments targeted against those changes can lead to improved survival. The project adds to research by the Cancer Genome Atlas, a collaboration between the National Cancer Institute and the National Human Genome Research Institute, both divisions of NIH.
Additionally, in 2013, the American Heart Association set aside a 5-year, $30 million research fund to dig deeper into two large national studies in hopes of finding more clues to personalized treatment and prevention of cardiovascular disease. The AHA and its two main collaborators, the University of Mississippi and Boston University, said their goal is to expand population studies by adding more research subjects and more genetic analysis.
Although much of the president’s address focused on nonmedical issues, he did take the opportunity to let legislators in the Republican-led Congress know that he would veto any bill that seeks to undo progress gained under the Affordable Care Act.
“We can’t put the security of families at risk by taking away their health insurance, or unraveling the new rules on Wall Street, or refighting past battles on immigration when we’ve got a system to fix,” President Obama said. “And if a bill comes to my desk that tries to do any of these things, it will earn my veto.”
The president also urged Congress to pass the Healthy Families Act, a bill that would require businesses to provide employees up to 7 paid sick days per year. His administration also plans to help more states adopt sick leave laws of their own, he said.
“Since paid sick leave won where it was on the ballot last November, let’s put it to a vote right here in Washington. Send me a bill that gives every worker in America the opportunity to earn 7 days of paid sick leave,” he said.
On Twitter @legal_med
Justices grill attorneys on right to sue states over Medicaid payments
Some Supreme Court justices appear skeptical about whether physicians and other health providers have the right to sue states over low Medicaid reimbursement.
During oral arguments Jan. 20 in Armstrong v. Exceptional Child Center Inc., Chief Justice John G. Roberts Jr. questioned whether letting providers challenge state-set payment rates would lead to a wave of litigation and force federal judges to make state budgetary decisions.
“There are dozens of different types of providers under the [Social Security] Act,” Justice Roberts said during oral arguments. “Now, what do you do if each of those providers bring a lawsuit similar to yours? The effect, it seems to me, will be putting the setting of budget priorities in the hands of dozens of different federal judges, and I just don’t know what the practical significance of that’s going to be.”
In Armstrong v. Exceptional Child Center Inc., the high court justices are weighing whether the U.S. Constitution’s Supremacy Clause – which establishes the Constitution and federal law as the law of the land – gives health care providers under Medicaid a private “right of action” to enforce Medicaid funding conditions against states. The case originates from a 2009 lawsuit by Exceptional Child Center Inc., of Twin Falls, Idaho, and four other residential habilitation centers against Richard Armstrong, director of the Idaho Department of Health and Welfare.
The centers claimed the state was violating Medicaid’s equal access provision by refusing to raise its payment rates. Under the equal access provision, states that accept federal Medicaid funding are required to set reimbursement rates at levels sufficient to retain enough providers and make sure patients have proper access to care. The Idaho Department of Health and Welfare and its Medicaid division conducted yearly cost studies between 2006 and 2009, developed a new rate-setting methodology, and recommended substantial increases in reimbursement rates for supported living services, according to court documents. However, the new methodology and rate increases were not enacted for budgetary reasons.
A district court ruled in favor of the centers, and the 9th U.S. Circuit Court of Appeals affirmed the ruling. The state petitioned the Supreme Court to resolve the issue.
During arguments, Idaho deputy attorney general Carl J. Withroe argued the courtroom is an incorrect avenue for Medicaid providers to dispute pay rates. If displeased, physicians and other health providers should issue an administrative challenge to the Centers for Medicare & Medicaid Services over its approval of the state’s Medicaid plan. He noted that such state plans – known as waivers – must be approved by the CMS every 5 years.
But Justice Sonia Sotomayor called this pathway an ineffective remedy.
“Let’s assume inflation is going up constantly. What happens 2 years into the plan when providers can’t work for what the state is giving or the state is imposing a tremendous hardship on them, which is happening to a lot of providers who are being underpaid. Where do they go? ... What do they do?”
Other panelists, such as Justice Ruth Bader Ginsberg, expressed doubt that the centers’ case against the state has merit, namely that Idaho is violating Medicaid’s equal access provision.
“According to the district court, all eligible recipients received the services that they needed,” Justice Ginsberg said. “So again, there was no waiting list; nobody’s being kept waiting. These providers, while they say they’re not getting enough, are still providing the service. So where is the [equal access] violation?”
Attorney James M. Piotrowski, who represented the centers, countered that the equal access provision imposes both procedural and substantive requirements. The substantive requirement mandates there must be enough providers to allow access and generate quality care, Mr. Piotrowski said. The procedural requirement entails that the rates be set based upon factors that Congress considers important.
“The violation of [the equal access provision] here was that the state gave no consideration whatsoever to the federal factors,” he said. “They relied only on their own factors.”
The Armstrong case is being closely watched by states, physicians, and patient advocates alike. Twenty-seven states have reached out to the high court in support of Idaho. The states saidthey have been subject to numerous, unwarranted lawsuits because of misguided interpretations of the Supremacy Clause. A number of physician and patient advocacy associations joined a friend-of-the-court brief in support of the centers, including the American Academy of Family Physicians and the American Medical Association. The AMA and other organizations said ongoing violations of Medicaid’s equal access provision by states continue to drive doctors from the program and harm access to care.
A decision by the high court is expected by June.
On Twitter @legal_med
Some Supreme Court justices appear skeptical about whether physicians and other health providers have the right to sue states over low Medicaid reimbursement.
During oral arguments Jan. 20 in Armstrong v. Exceptional Child Center Inc., Chief Justice John G. Roberts Jr. questioned whether letting providers challenge state-set payment rates would lead to a wave of litigation and force federal judges to make state budgetary decisions.
“There are dozens of different types of providers under the [Social Security] Act,” Justice Roberts said during oral arguments. “Now, what do you do if each of those providers bring a lawsuit similar to yours? The effect, it seems to me, will be putting the setting of budget priorities in the hands of dozens of different federal judges, and I just don’t know what the practical significance of that’s going to be.”
In Armstrong v. Exceptional Child Center Inc., the high court justices are weighing whether the U.S. Constitution’s Supremacy Clause – which establishes the Constitution and federal law as the law of the land – gives health care providers under Medicaid a private “right of action” to enforce Medicaid funding conditions against states. The case originates from a 2009 lawsuit by Exceptional Child Center Inc., of Twin Falls, Idaho, and four other residential habilitation centers against Richard Armstrong, director of the Idaho Department of Health and Welfare.
The centers claimed the state was violating Medicaid’s equal access provision by refusing to raise its payment rates. Under the equal access provision, states that accept federal Medicaid funding are required to set reimbursement rates at levels sufficient to retain enough providers and make sure patients have proper access to care. The Idaho Department of Health and Welfare and its Medicaid division conducted yearly cost studies between 2006 and 2009, developed a new rate-setting methodology, and recommended substantial increases in reimbursement rates for supported living services, according to court documents. However, the new methodology and rate increases were not enacted for budgetary reasons.
A district court ruled in favor of the centers, and the 9th U.S. Circuit Court of Appeals affirmed the ruling. The state petitioned the Supreme Court to resolve the issue.
During arguments, Idaho deputy attorney general Carl J. Withroe argued the courtroom is an incorrect avenue for Medicaid providers to dispute pay rates. If displeased, physicians and other health providers should issue an administrative challenge to the Centers for Medicare & Medicaid Services over its approval of the state’s Medicaid plan. He noted that such state plans – known as waivers – must be approved by the CMS every 5 years.
But Justice Sonia Sotomayor called this pathway an ineffective remedy.
“Let’s assume inflation is going up constantly. What happens 2 years into the plan when providers can’t work for what the state is giving or the state is imposing a tremendous hardship on them, which is happening to a lot of providers who are being underpaid. Where do they go? ... What do they do?”
Other panelists, such as Justice Ruth Bader Ginsberg, expressed doubt that the centers’ case against the state has merit, namely that Idaho is violating Medicaid’s equal access provision.
“According to the district court, all eligible recipients received the services that they needed,” Justice Ginsberg said. “So again, there was no waiting list; nobody’s being kept waiting. These providers, while they say they’re not getting enough, are still providing the service. So where is the [equal access] violation?”
Attorney James M. Piotrowski, who represented the centers, countered that the equal access provision imposes both procedural and substantive requirements. The substantive requirement mandates there must be enough providers to allow access and generate quality care, Mr. Piotrowski said. The procedural requirement entails that the rates be set based upon factors that Congress considers important.
“The violation of [the equal access provision] here was that the state gave no consideration whatsoever to the federal factors,” he said. “They relied only on their own factors.”
The Armstrong case is being closely watched by states, physicians, and patient advocates alike. Twenty-seven states have reached out to the high court in support of Idaho. The states saidthey have been subject to numerous, unwarranted lawsuits because of misguided interpretations of the Supremacy Clause. A number of physician and patient advocacy associations joined a friend-of-the-court brief in support of the centers, including the American Academy of Family Physicians and the American Medical Association. The AMA and other organizations said ongoing violations of Medicaid’s equal access provision by states continue to drive doctors from the program and harm access to care.
A decision by the high court is expected by June.
On Twitter @legal_med
Some Supreme Court justices appear skeptical about whether physicians and other health providers have the right to sue states over low Medicaid reimbursement.
During oral arguments Jan. 20 in Armstrong v. Exceptional Child Center Inc., Chief Justice John G. Roberts Jr. questioned whether letting providers challenge state-set payment rates would lead to a wave of litigation and force federal judges to make state budgetary decisions.
“There are dozens of different types of providers under the [Social Security] Act,” Justice Roberts said during oral arguments. “Now, what do you do if each of those providers bring a lawsuit similar to yours? The effect, it seems to me, will be putting the setting of budget priorities in the hands of dozens of different federal judges, and I just don’t know what the practical significance of that’s going to be.”
In Armstrong v. Exceptional Child Center Inc., the high court justices are weighing whether the U.S. Constitution’s Supremacy Clause – which establishes the Constitution and federal law as the law of the land – gives health care providers under Medicaid a private “right of action” to enforce Medicaid funding conditions against states. The case originates from a 2009 lawsuit by Exceptional Child Center Inc., of Twin Falls, Idaho, and four other residential habilitation centers against Richard Armstrong, director of the Idaho Department of Health and Welfare.
The centers claimed the state was violating Medicaid’s equal access provision by refusing to raise its payment rates. Under the equal access provision, states that accept federal Medicaid funding are required to set reimbursement rates at levels sufficient to retain enough providers and make sure patients have proper access to care. The Idaho Department of Health and Welfare and its Medicaid division conducted yearly cost studies between 2006 and 2009, developed a new rate-setting methodology, and recommended substantial increases in reimbursement rates for supported living services, according to court documents. However, the new methodology and rate increases were not enacted for budgetary reasons.
A district court ruled in favor of the centers, and the 9th U.S. Circuit Court of Appeals affirmed the ruling. The state petitioned the Supreme Court to resolve the issue.
During arguments, Idaho deputy attorney general Carl J. Withroe argued the courtroom is an incorrect avenue for Medicaid providers to dispute pay rates. If displeased, physicians and other health providers should issue an administrative challenge to the Centers for Medicare & Medicaid Services over its approval of the state’s Medicaid plan. He noted that such state plans – known as waivers – must be approved by the CMS every 5 years.
But Justice Sonia Sotomayor called this pathway an ineffective remedy.
“Let’s assume inflation is going up constantly. What happens 2 years into the plan when providers can’t work for what the state is giving or the state is imposing a tremendous hardship on them, which is happening to a lot of providers who are being underpaid. Where do they go? ... What do they do?”
Other panelists, such as Justice Ruth Bader Ginsberg, expressed doubt that the centers’ case against the state has merit, namely that Idaho is violating Medicaid’s equal access provision.
“According to the district court, all eligible recipients received the services that they needed,” Justice Ginsberg said. “So again, there was no waiting list; nobody’s being kept waiting. These providers, while they say they’re not getting enough, are still providing the service. So where is the [equal access] violation?”
Attorney James M. Piotrowski, who represented the centers, countered that the equal access provision imposes both procedural and substantive requirements. The substantive requirement mandates there must be enough providers to allow access and generate quality care, Mr. Piotrowski said. The procedural requirement entails that the rates be set based upon factors that Congress considers important.
“The violation of [the equal access provision] here was that the state gave no consideration whatsoever to the federal factors,” he said. “They relied only on their own factors.”
The Armstrong case is being closely watched by states, physicians, and patient advocates alike. Twenty-seven states have reached out to the high court in support of Idaho. The states saidthey have been subject to numerous, unwarranted lawsuits because of misguided interpretations of the Supremacy Clause. A number of physician and patient advocacy associations joined a friend-of-the-court brief in support of the centers, including the American Academy of Family Physicians and the American Medical Association. The AMA and other organizations said ongoing violations of Medicaid’s equal access provision by states continue to drive doctors from the program and harm access to care.
A decision by the high court is expected by June.
On Twitter @legal_med
Residents looking to work in larger cities
Since 2008, residents’ preference for their future practice location has shifted from smaller cities and rural areas to large population centers, according to findings reported by physician recruitment firm Merritt Hawkins.
In a survey of residents who completed their training in 2014, 24% said that they wanted to practice in a community with a population of more than 1 million, compared with 6% in 2008, while 23% of residents chose the next-highest level of population – 500,001 to 1 million – compared with 15% in 2008, according to Merritt Hawkins.
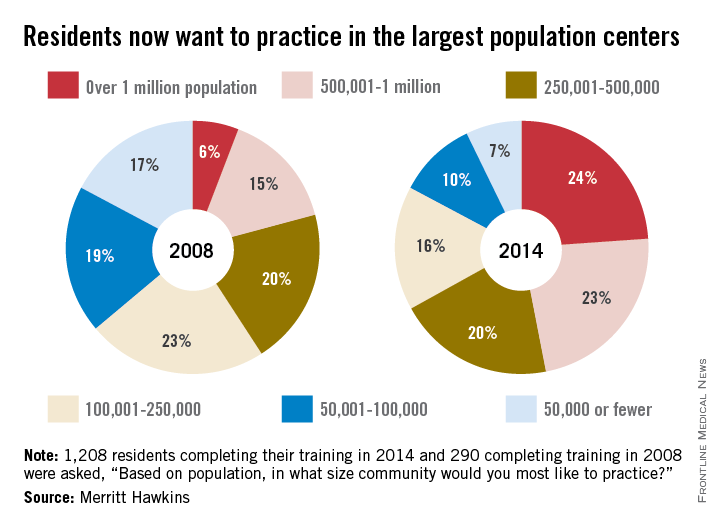
As for the smaller communities, residents who wanted to practice in a area of 50,000 or fewer dropped from 17% in 2008 to 7% in 2014. Support for communities of 50,001-100,000 fell from 19% in 2008 to 10% in 2014, the company said. Only 1% of residents wanted to practice in a community of 10,000 people or fewer in 2014.
Residents’ reservations about practicing in rural areas more often are related to their “concerns about being on a clinical ‘island’ without specialty support, information technology, and other resources than they may be about the amenities of rural communities,” Merritt Hawkins said in its analysis of the 1,208 survey responses.
Since 2008, residents’ preference for their future practice location has shifted from smaller cities and rural areas to large population centers, according to findings reported by physician recruitment firm Merritt Hawkins.
In a survey of residents who completed their training in 2014, 24% said that they wanted to practice in a community with a population of more than 1 million, compared with 6% in 2008, while 23% of residents chose the next-highest level of population – 500,001 to 1 million – compared with 15% in 2008, according to Merritt Hawkins.
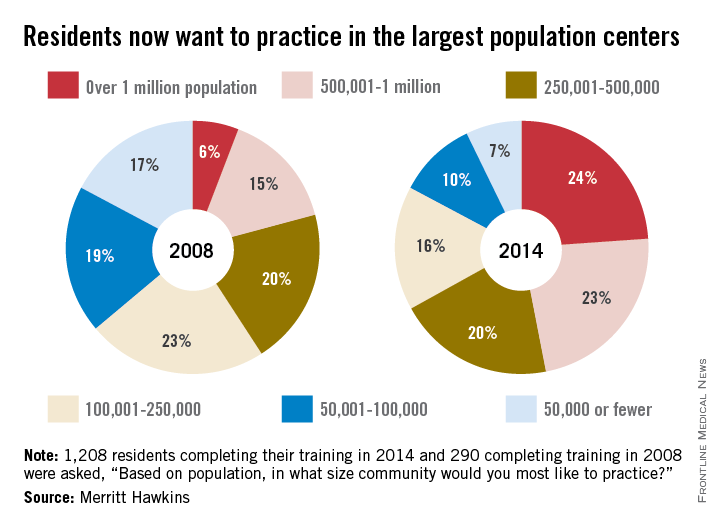
As for the smaller communities, residents who wanted to practice in a area of 50,000 or fewer dropped from 17% in 2008 to 7% in 2014. Support for communities of 50,001-100,000 fell from 19% in 2008 to 10% in 2014, the company said. Only 1% of residents wanted to practice in a community of 10,000 people or fewer in 2014.
Residents’ reservations about practicing in rural areas more often are related to their “concerns about being on a clinical ‘island’ without specialty support, information technology, and other resources than they may be about the amenities of rural communities,” Merritt Hawkins said in its analysis of the 1,208 survey responses.
Since 2008, residents’ preference for their future practice location has shifted from smaller cities and rural areas to large population centers, according to findings reported by physician recruitment firm Merritt Hawkins.
In a survey of residents who completed their training in 2014, 24% said that they wanted to practice in a community with a population of more than 1 million, compared with 6% in 2008, while 23% of residents chose the next-highest level of population – 500,001 to 1 million – compared with 15% in 2008, according to Merritt Hawkins.
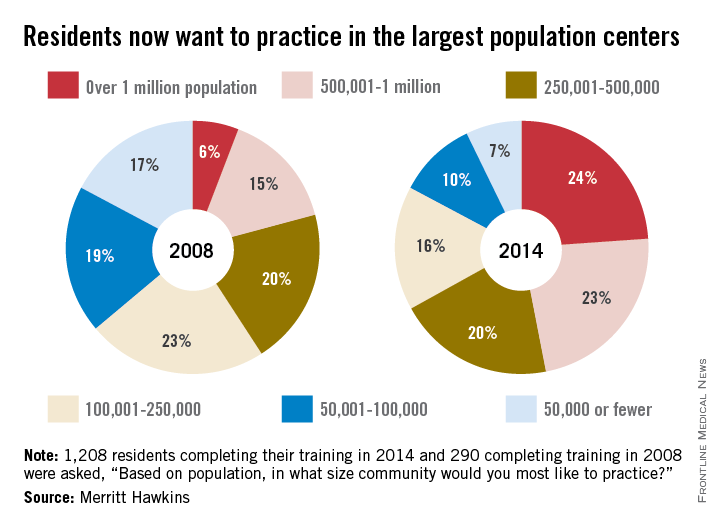
As for the smaller communities, residents who wanted to practice in a area of 50,000 or fewer dropped from 17% in 2008 to 7% in 2014. Support for communities of 50,001-100,000 fell from 19% in 2008 to 10% in 2014, the company said. Only 1% of residents wanted to practice in a community of 10,000 people or fewer in 2014.
Residents’ reservations about practicing in rural areas more often are related to their “concerns about being on a clinical ‘island’ without specialty support, information technology, and other resources than they may be about the amenities of rural communities,” Merritt Hawkins said in its analysis of the 1,208 survey responses.
Preoperative hepatic, regional arterial chemo nets better outcomes in early CRC
SAN FRANCISCO – Giving preoperative chemotherapy directly into the tumor-feeding artery and prophylactically into the common hepatic artery to target any liver micrometastases improves outcomes in patients with early colorectal cancer undergoing curative resection. But benefit is seen mainly in patients with stage III disease.
These were among the key findings of the randomized multicenter phase III PHRAC trial (Preoperative Hepatic and Regional Arterial Chemotherapy) conducted among 688 patients in China with stage II or III colorectal cancer.
Compared with curative resection alone, followed by adjuvant systemic chemotherapy with the modified FOLFOX6 regimen, the addition of preoperative arterial chemotherapy reduced the 5-year estimated risks of disease-free survival events by 40%, of liver metastases by 61%, and of death by 41% in the trial population overall, according to data reported at the annual Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. But stratified analyses showed that these benefits were significant only among the patients with stage III disease.
“Preoperative hepatic and regional arterial chemotherapy had no effect on colorectal cancer surgery or postoperative morbidity,” commented lead investigator Jianmin Xu, an oncologist at the Zhongshan Hospital, Fudan University, in Shanghai. This therapy “is safe and feasible and can reduce liver metastasis and improve disease-free survival and overall survival, especially for the stage III patients.”
“Dr. Xu’s study was a positive study, but we have no description of the catheter problems or the number of patients who could be treated,” commented invited discussant Dr. Nancy E. Kemeny of Memorial Sloan-Kettering Cancer Center, New York. Additionally, outcomes in the control group fell short of those seen in patients treated with FOLFOX historically.
Despite accumulating evidence of benefit, the procedure is not yet ready for incorporation into routine care, according to Dr. Kemeny. “Since we don’t have a lot of information about the problems with the catheters or other problems like that, we need a larger, international study. I think one should be done because if you can prevent recurrences right away, which is what this study is suggesting, then that’s very good for these patients. We have ways of dealing with this afterwards, but it would be nice to prevent it right way. So given the fact that we already have five studies suggesting some benefit with this type of treatment, we should move into a large randomized study,” she recommended.
A session attendee noted that although colon cancer most commonly recurs in the liver, rectal cancer most commonly recurs in the pelvis. “Therefore, chemoradiotherapy is the standard of care now [for rectal cancer]. So infusional arterial chemotherapy should be used in patients with colon cancer, I think,” he said.
The patients with rectal cancer received radiation therapy after surgery if needed, Dr. Xu replied. “In the future, we will do subgroup analyses for colon cancer and for rectal cancer,” he added.
In the trial, patients from five hospitals in China were randomized to immediate curative primary surgery or to hepatic and regional arterial chemotherapy – floxuridine (FUDR), mitomycin C, and oxaliplatin delivered to both the main tumor-supplying artery and to the common hepatic artery – followed by curative primary surgery a week later. All patients received the same adjuvant therapy.
In the intention-to-treat population, estimated 5-year disease-free survival, the trial’s primary endpoint, was 75% with preoperative arterial chemotherapy versus 61% without it (hazard ratio, 0.60; P less than .001), reported Dr. Xu, who disclosed no relevant conflicts of interest. Subgroup analyses indicated that the benefit was significant in patients with stage III disease (68% vs. 51%; HR, 0.62; P = .017) but showed only a trend in patients with stage II disease (84% vs. 74%; HR, 0.64; P = .068).
Patients in the arterial chemotherapy group also were less likely to develop liver metastases (8% vs. 18%; HR, 0.39; P less than .001) and had better overall survival (81% vs. 72%, HR, 0.59; P = .003). But subgroup analyses again showed that benefit was significant only in the stage III patients.
Efficacy findings were similar in the trial’s eligible population, which excluded patients who were found to have pathologic stage I or IV disease at surgery and patients who developed metastases within 6 months of surgery.A total of 25% of patients in the arterial chemotherapy group experienced grade 3 toxicity from the procedure. However, the rate of postoperative complications did not differ significantly between the arterial chemotherapy and control groups.
SAN FRANCISCO – Giving preoperative chemotherapy directly into the tumor-feeding artery and prophylactically into the common hepatic artery to target any liver micrometastases improves outcomes in patients with early colorectal cancer undergoing curative resection. But benefit is seen mainly in patients with stage III disease.
These were among the key findings of the randomized multicenter phase III PHRAC trial (Preoperative Hepatic and Regional Arterial Chemotherapy) conducted among 688 patients in China with stage II or III colorectal cancer.
Compared with curative resection alone, followed by adjuvant systemic chemotherapy with the modified FOLFOX6 regimen, the addition of preoperative arterial chemotherapy reduced the 5-year estimated risks of disease-free survival events by 40%, of liver metastases by 61%, and of death by 41% in the trial population overall, according to data reported at the annual Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. But stratified analyses showed that these benefits were significant only among the patients with stage III disease.
“Preoperative hepatic and regional arterial chemotherapy had no effect on colorectal cancer surgery or postoperative morbidity,” commented lead investigator Jianmin Xu, an oncologist at the Zhongshan Hospital, Fudan University, in Shanghai. This therapy “is safe and feasible and can reduce liver metastasis and improve disease-free survival and overall survival, especially for the stage III patients.”
“Dr. Xu’s study was a positive study, but we have no description of the catheter problems or the number of patients who could be treated,” commented invited discussant Dr. Nancy E. Kemeny of Memorial Sloan-Kettering Cancer Center, New York. Additionally, outcomes in the control group fell short of those seen in patients treated with FOLFOX historically.
Despite accumulating evidence of benefit, the procedure is not yet ready for incorporation into routine care, according to Dr. Kemeny. “Since we don’t have a lot of information about the problems with the catheters or other problems like that, we need a larger, international study. I think one should be done because if you can prevent recurrences right away, which is what this study is suggesting, then that’s very good for these patients. We have ways of dealing with this afterwards, but it would be nice to prevent it right way. So given the fact that we already have five studies suggesting some benefit with this type of treatment, we should move into a large randomized study,” she recommended.
A session attendee noted that although colon cancer most commonly recurs in the liver, rectal cancer most commonly recurs in the pelvis. “Therefore, chemoradiotherapy is the standard of care now [for rectal cancer]. So infusional arterial chemotherapy should be used in patients with colon cancer, I think,” he said.
The patients with rectal cancer received radiation therapy after surgery if needed, Dr. Xu replied. “In the future, we will do subgroup analyses for colon cancer and for rectal cancer,” he added.
In the trial, patients from five hospitals in China were randomized to immediate curative primary surgery or to hepatic and regional arterial chemotherapy – floxuridine (FUDR), mitomycin C, and oxaliplatin delivered to both the main tumor-supplying artery and to the common hepatic artery – followed by curative primary surgery a week later. All patients received the same adjuvant therapy.
In the intention-to-treat population, estimated 5-year disease-free survival, the trial’s primary endpoint, was 75% with preoperative arterial chemotherapy versus 61% without it (hazard ratio, 0.60; P less than .001), reported Dr. Xu, who disclosed no relevant conflicts of interest. Subgroup analyses indicated that the benefit was significant in patients with stage III disease (68% vs. 51%; HR, 0.62; P = .017) but showed only a trend in patients with stage II disease (84% vs. 74%; HR, 0.64; P = .068).
Patients in the arterial chemotherapy group also were less likely to develop liver metastases (8% vs. 18%; HR, 0.39; P less than .001) and had better overall survival (81% vs. 72%, HR, 0.59; P = .003). But subgroup analyses again showed that benefit was significant only in the stage III patients.
Efficacy findings were similar in the trial’s eligible population, which excluded patients who were found to have pathologic stage I or IV disease at surgery and patients who developed metastases within 6 months of surgery.A total of 25% of patients in the arterial chemotherapy group experienced grade 3 toxicity from the procedure. However, the rate of postoperative complications did not differ significantly between the arterial chemotherapy and control groups.
SAN FRANCISCO – Giving preoperative chemotherapy directly into the tumor-feeding artery and prophylactically into the common hepatic artery to target any liver micrometastases improves outcomes in patients with early colorectal cancer undergoing curative resection. But benefit is seen mainly in patients with stage III disease.
These were among the key findings of the randomized multicenter phase III PHRAC trial (Preoperative Hepatic and Regional Arterial Chemotherapy) conducted among 688 patients in China with stage II or III colorectal cancer.
Compared with curative resection alone, followed by adjuvant systemic chemotherapy with the modified FOLFOX6 regimen, the addition of preoperative arterial chemotherapy reduced the 5-year estimated risks of disease-free survival events by 40%, of liver metastases by 61%, and of death by 41% in the trial population overall, according to data reported at the annual Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. But stratified analyses showed that these benefits were significant only among the patients with stage III disease.
“Preoperative hepatic and regional arterial chemotherapy had no effect on colorectal cancer surgery or postoperative morbidity,” commented lead investigator Jianmin Xu, an oncologist at the Zhongshan Hospital, Fudan University, in Shanghai. This therapy “is safe and feasible and can reduce liver metastasis and improve disease-free survival and overall survival, especially for the stage III patients.”
“Dr. Xu’s study was a positive study, but we have no description of the catheter problems or the number of patients who could be treated,” commented invited discussant Dr. Nancy E. Kemeny of Memorial Sloan-Kettering Cancer Center, New York. Additionally, outcomes in the control group fell short of those seen in patients treated with FOLFOX historically.
Despite accumulating evidence of benefit, the procedure is not yet ready for incorporation into routine care, according to Dr. Kemeny. “Since we don’t have a lot of information about the problems with the catheters or other problems like that, we need a larger, international study. I think one should be done because if you can prevent recurrences right away, which is what this study is suggesting, then that’s very good for these patients. We have ways of dealing with this afterwards, but it would be nice to prevent it right way. So given the fact that we already have five studies suggesting some benefit with this type of treatment, we should move into a large randomized study,” she recommended.
A session attendee noted that although colon cancer most commonly recurs in the liver, rectal cancer most commonly recurs in the pelvis. “Therefore, chemoradiotherapy is the standard of care now [for rectal cancer]. So infusional arterial chemotherapy should be used in patients with colon cancer, I think,” he said.
The patients with rectal cancer received radiation therapy after surgery if needed, Dr. Xu replied. “In the future, we will do subgroup analyses for colon cancer and for rectal cancer,” he added.
In the trial, patients from five hospitals in China were randomized to immediate curative primary surgery or to hepatic and regional arterial chemotherapy – floxuridine (FUDR), mitomycin C, and oxaliplatin delivered to both the main tumor-supplying artery and to the common hepatic artery – followed by curative primary surgery a week later. All patients received the same adjuvant therapy.
In the intention-to-treat population, estimated 5-year disease-free survival, the trial’s primary endpoint, was 75% with preoperative arterial chemotherapy versus 61% without it (hazard ratio, 0.60; P less than .001), reported Dr. Xu, who disclosed no relevant conflicts of interest. Subgroup analyses indicated that the benefit was significant in patients with stage III disease (68% vs. 51%; HR, 0.62; P = .017) but showed only a trend in patients with stage II disease (84% vs. 74%; HR, 0.64; P = .068).
Patients in the arterial chemotherapy group also were less likely to develop liver metastases (8% vs. 18%; HR, 0.39; P less than .001) and had better overall survival (81% vs. 72%, HR, 0.59; P = .003). But subgroup analyses again showed that benefit was significant only in the stage III patients.
Efficacy findings were similar in the trial’s eligible population, which excluded patients who were found to have pathologic stage I or IV disease at surgery and patients who developed metastases within 6 months of surgery.A total of 25% of patients in the arterial chemotherapy group experienced grade 3 toxicity from the procedure. However, the rate of postoperative complications did not differ significantly between the arterial chemotherapy and control groups.
AT THE 2015 GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Preoperative arterial chemotherapy improves outcomes, but mainly for stage III patients.
Major finding: Five-year disease-free survival was 75% with preoperative arterial chemotherapy vs. 61% without it.
Data source: A randomized phase III trial among 688 patients undergoing curative resection of stage II or III colorectal cancer.
Disclosures: Dr. Xu disclosed that he had no relevant conflicts of interest.
Post-lumpectomy radiotherapy benefits good-risk DCIS patients
The ipsilateral local failure rate in women with good-risk ductal carcinoma in situ was low with observation after breast-conserving surgery, but was significantly lower with the addition of radiotherapy, according to findings from a prospective, randomized, Radiation Therapy Oncology Group trial.
Failure occurred in 19 of 298 patients in the observation group, compared with 2 of 287 patients in the radiotherapy group; the cumulative rates of ipsilateral local failure at 7 years were 6.7% and 0.9% in the groups, respectively (hazard ratio, 0.11), Dr. Beryl McCormick of Memorial Sloan Kettering Cancer Center, New York, and her colleagues reported online Jan. 19 in the Journal of Clinical Oncology.
Local failures were invasive in 42% of cases in the observation arm and in one of the two patients in the radiotherapy arm. The 7-year cumulative mastectomy incidence was 2.8% in the observation arm and 1.5% in the radiotherapy arm. Survival was excellent and did not differ between the arms, the investigators said (J. Clin. Oncol. 2015 Jan. 19 [doi:10.1200/JCO.2014.57.9029]).
Study subjects were women with a mean age of 58 years and mammographically detected low- or intermediate-grade ductal carcinoma in situ (DCIS) that measured less than 2.5 cm with margins of at least 3 mm. Those assigned to the radiotherapy group underwent whole-breast radiotherapy at a dose of 50 Gy in 25 fractions, 50.4 Gy in 28 fractions, or 42.5 Gy in 16 fractions, and most received tamoxifen, which was required in both arms when the study opened before being made optional in 2001.
The women were followed for a median of 7.2 years.
Grade 1 and 2 toxicities occurred more often in the radiotherapy group (30% vs. 76%), but grade 3 and 4 toxicities occurred in 4% of women in both groups. Late toxicity in the radiotherapy patients was grade 1 in 30%, grade 2 in 4.6%, and grade 3 in 0.7% of subjects, the investigators said.
Breast-conserving surgery and radiation have been shown to produce results that are equivalent to mastectomy in patients with DCIS, and in four large prospective trials, radiation therapy reduced the risk of local failure by at least 50%. About half of the recurrences in those trials were DCIS and half were invasive breast cancer, but survival was excellent regardless of local treatment, the investigators explained.
“More recently, an understanding of DCIS as not just one disease but a group of related subtypes of cancers has emerged, with a spectrum of local failure risk. Is there a low-risk DCIS for which the benefit of radiotherapy would not be seen?” they wrote.
The current study was designed to address the question of radiotherapy benefit in a good-risk DCIS subset. Although it didn’t meet the targeted accrual of 1,790 patients and was thus closed early, the findings – along with those from an Eastern Cooperative Oncology Group trial, “imply that clinical pathologic criteria can be used to define a cohort of patients with DCIS who can be expected to have a much lower rate of in-breast recurrence without radiotherapy in the first 7 years after lumpectomy than previously reported in past randomized trials,” they said.
These data may support decisions to forego adjuvant radiotherapy after breast-conserving surgery, particularly given the low mastectomy rate, but they also confirm that radiotherapy provides significant benefit with respect to further reducing local failure risk, they added.
However, given historic patterns of increasing local failure rates over 10 to 15 years, longer follow-up of these patients is needed to fully realize the rates of local failure, they said.
This study was supported by grants from the National Institutes of Health. Dr. McCormick reported having no disclosures.
The ipsilateral local failure rate in women with good-risk ductal carcinoma in situ was low with observation after breast-conserving surgery, but was significantly lower with the addition of radiotherapy, according to findings from a prospective, randomized, Radiation Therapy Oncology Group trial.
Failure occurred in 19 of 298 patients in the observation group, compared with 2 of 287 patients in the radiotherapy group; the cumulative rates of ipsilateral local failure at 7 years were 6.7% and 0.9% in the groups, respectively (hazard ratio, 0.11), Dr. Beryl McCormick of Memorial Sloan Kettering Cancer Center, New York, and her colleagues reported online Jan. 19 in the Journal of Clinical Oncology.
Local failures were invasive in 42% of cases in the observation arm and in one of the two patients in the radiotherapy arm. The 7-year cumulative mastectomy incidence was 2.8% in the observation arm and 1.5% in the radiotherapy arm. Survival was excellent and did not differ between the arms, the investigators said (J. Clin. Oncol. 2015 Jan. 19 [doi:10.1200/JCO.2014.57.9029]).
Study subjects were women with a mean age of 58 years and mammographically detected low- or intermediate-grade ductal carcinoma in situ (DCIS) that measured less than 2.5 cm with margins of at least 3 mm. Those assigned to the radiotherapy group underwent whole-breast radiotherapy at a dose of 50 Gy in 25 fractions, 50.4 Gy in 28 fractions, or 42.5 Gy in 16 fractions, and most received tamoxifen, which was required in both arms when the study opened before being made optional in 2001.
The women were followed for a median of 7.2 years.
Grade 1 and 2 toxicities occurred more often in the radiotherapy group (30% vs. 76%), but grade 3 and 4 toxicities occurred in 4% of women in both groups. Late toxicity in the radiotherapy patients was grade 1 in 30%, grade 2 in 4.6%, and grade 3 in 0.7% of subjects, the investigators said.
Breast-conserving surgery and radiation have been shown to produce results that are equivalent to mastectomy in patients with DCIS, and in four large prospective trials, radiation therapy reduced the risk of local failure by at least 50%. About half of the recurrences in those trials were DCIS and half were invasive breast cancer, but survival was excellent regardless of local treatment, the investigators explained.
“More recently, an understanding of DCIS as not just one disease but a group of related subtypes of cancers has emerged, with a spectrum of local failure risk. Is there a low-risk DCIS for which the benefit of radiotherapy would not be seen?” they wrote.
The current study was designed to address the question of radiotherapy benefit in a good-risk DCIS subset. Although it didn’t meet the targeted accrual of 1,790 patients and was thus closed early, the findings – along with those from an Eastern Cooperative Oncology Group trial, “imply that clinical pathologic criteria can be used to define a cohort of patients with DCIS who can be expected to have a much lower rate of in-breast recurrence without radiotherapy in the first 7 years after lumpectomy than previously reported in past randomized trials,” they said.
These data may support decisions to forego adjuvant radiotherapy after breast-conserving surgery, particularly given the low mastectomy rate, but they also confirm that radiotherapy provides significant benefit with respect to further reducing local failure risk, they added.
However, given historic patterns of increasing local failure rates over 10 to 15 years, longer follow-up of these patients is needed to fully realize the rates of local failure, they said.
This study was supported by grants from the National Institutes of Health. Dr. McCormick reported having no disclosures.
The ipsilateral local failure rate in women with good-risk ductal carcinoma in situ was low with observation after breast-conserving surgery, but was significantly lower with the addition of radiotherapy, according to findings from a prospective, randomized, Radiation Therapy Oncology Group trial.
Failure occurred in 19 of 298 patients in the observation group, compared with 2 of 287 patients in the radiotherapy group; the cumulative rates of ipsilateral local failure at 7 years were 6.7% and 0.9% in the groups, respectively (hazard ratio, 0.11), Dr. Beryl McCormick of Memorial Sloan Kettering Cancer Center, New York, and her colleagues reported online Jan. 19 in the Journal of Clinical Oncology.
Local failures were invasive in 42% of cases in the observation arm and in one of the two patients in the radiotherapy arm. The 7-year cumulative mastectomy incidence was 2.8% in the observation arm and 1.5% in the radiotherapy arm. Survival was excellent and did not differ between the arms, the investigators said (J. Clin. Oncol. 2015 Jan. 19 [doi:10.1200/JCO.2014.57.9029]).
Study subjects were women with a mean age of 58 years and mammographically detected low- or intermediate-grade ductal carcinoma in situ (DCIS) that measured less than 2.5 cm with margins of at least 3 mm. Those assigned to the radiotherapy group underwent whole-breast radiotherapy at a dose of 50 Gy in 25 fractions, 50.4 Gy in 28 fractions, or 42.5 Gy in 16 fractions, and most received tamoxifen, which was required in both arms when the study opened before being made optional in 2001.
The women were followed for a median of 7.2 years.
Grade 1 and 2 toxicities occurred more often in the radiotherapy group (30% vs. 76%), but grade 3 and 4 toxicities occurred in 4% of women in both groups. Late toxicity in the radiotherapy patients was grade 1 in 30%, grade 2 in 4.6%, and grade 3 in 0.7% of subjects, the investigators said.
Breast-conserving surgery and radiation have been shown to produce results that are equivalent to mastectomy in patients with DCIS, and in four large prospective trials, radiation therapy reduced the risk of local failure by at least 50%. About half of the recurrences in those trials were DCIS and half were invasive breast cancer, but survival was excellent regardless of local treatment, the investigators explained.
“More recently, an understanding of DCIS as not just one disease but a group of related subtypes of cancers has emerged, with a spectrum of local failure risk. Is there a low-risk DCIS for which the benefit of radiotherapy would not be seen?” they wrote.
The current study was designed to address the question of radiotherapy benefit in a good-risk DCIS subset. Although it didn’t meet the targeted accrual of 1,790 patients and was thus closed early, the findings – along with those from an Eastern Cooperative Oncology Group trial, “imply that clinical pathologic criteria can be used to define a cohort of patients with DCIS who can be expected to have a much lower rate of in-breast recurrence without radiotherapy in the first 7 years after lumpectomy than previously reported in past randomized trials,” they said.
These data may support decisions to forego adjuvant radiotherapy after breast-conserving surgery, particularly given the low mastectomy rate, but they also confirm that radiotherapy provides significant benefit with respect to further reducing local failure risk, they added.
However, given historic patterns of increasing local failure rates over 10 to 15 years, longer follow-up of these patients is needed to fully realize the rates of local failure, they said.
This study was supported by grants from the National Institutes of Health. Dr. McCormick reported having no disclosures.
Key clinical point: Foregoing adjuvant radiotherapy after breast-conserving surgery is a reasonable choice, but radiotherapy provides significant benefit with respect to reducing the local failure risk.
Major finding: The cumulative rates of ipsilateral local failure at 7 years were 6.7% and 0.9% in the observation and radiotherapy groups, respectively (HR, 0.11)
Data source: A prospective randomized trial involving 585 women.
Disclosures: This study was supported by grants from the National Institutes of Health. Dr. McCormick reported having no disclosures.
Promising new therapy for critical limb ischemia
CHICAGO– A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
CHICAGO– A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
CHICAGO– A single set of intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia showed safety as well as evidence of efficacy through 12 months of follow-up in the STOP-CLI trial.
“Patients treated with JVS-100 demonstrated dose-dependent improvement across multiple patient-centered outcomes, including pain, quality of life, and wound healing, with less change in macrovascular objective measures in this small study,” Dr. Melina R. Kibbe reported at the American Heart Association scientific sessions. JVS-100 is a nonviral plasmid encoding human stromal cell–derived factor-1 (SDF-1), a natural chemokine protein that promotes angiogenesis by recruiting endothelial progenitor cells from the bone marrow to ischemic sites, explained Dr. Kibbe, professor and vice chair of surgical research and deputy director of the Simpson Querrey Institute for BioNanotechnology at Northwestern University, Chicago.
STOP-CLI was an exploratory, phase IIa, double-blind, first-in-humans study involving 48 patients with Rutherford classification 4 or 5 critical climb ischemia (CLI). All had an ankle-brachial index of 0.4 or lower, an ankle systolic blood pressure of 70 mm Hg or less or a toe systolic blood pressure of 50 or less, and were poor candidates for surgical revascularization. None had Buerger’s disease.
Participants were randomized to one of four study arms, and within each study arm further randomized 3:1 to stromal cell–derived factor-1 (SDF-1) or placebo injections. The patients received either 8 or 16 injections, each containing either 0.5 or 1.0 mg of SDF-1 or placebo. The injections, given in a single session, were placed at least 0.5 cm apart throughout the ischemic area of the affected limb.
By chance, most patients randomized to the placebo group were Rutherford 4, a category of CLI defined by rest pain, while the majority in the active treatment arms were Rutherford 5, a more severe disease manifestation characterized by ulcers. As a consequence, the SDF-1 recipients also had far larger nonhealing wounds, with an average area of 6.4 cm2, compared with 1.5 cm2, in controls.
The SDF-1 injections proved safe and were well tolerated, with no treatment-related serious adverse events and no safety signals evident in the laboratory results.
Turning to efficacy endpoints, Dr. Kibbe said self-rated visual analog scale pain scores showed clear, dose-dependent improvement over time in the SDF-1 treatment cohorts and no change in controls.
Similarly, the active treatment groups showed improved quality of life scores on all domains of the Short Form-36: physical functioning, bodily pain, general health, social functioning, energy/fatigue, emotional well-being, and overall physical and mental health, the surgeon continued.
Wound area decreased significantly in the SDF-1-treated groups, with the biggest reduction – more than 8 cm2 – being noted in the three patients who received eight 1-mg injections. That was also the group with the largest wounds at baseline, with an average area of 11.4 cm2.
Of note, the major limb amputation rate was “remarkably low” for patients with such severe CLI, according to Dr. Kibbe. The rate was less than 10% over the course of 12 months, with one patient in each of the four active treatment arms having a major amputation at time intervals of 58-112 days post injection. No major limb amputations occurred in the control group.
There was a hint of improvement with SDF-1 therapy over placebo in ankle-brachial index and transcutaneous oxygen pressure, but the between-group differences were too narrow in this study to allow for any conclusions. That must await planned much larger phase III trials, according to Dr. Kibbe.
Audience members, citing the numerous failures of once-promising stem cell therapies for CLI at phase III testing over the last 10-15 years, wondered why Dr. Kibbe thinks SDF-1 will fare any better.
“This is much debated and discussed among all the people involved in these kinds of trials,” she replied. “I’d say, briefly, that a lot of it has to do with patient selection. I think when you have a mixed bag of patients in a trial, including patients with Buerger’s disease, treated in multiple different countries, using different definitions of when to amputate, all those things come into play and could account for why those phase III trials were not successful.”
“Having been involved in lots of the different gene- and cell-based therapy trials, I think one of the unique benefits of this therapy is that it kind of bridges between the two. SDF-1 basically homes your endothelial progenitor cells to the site of ischemic injury for enhanced vasculogenesis. But SDF-1 also has direct effects on endothelial cells, including stimulating proliferation and preventing apoptosis,” she added.
JVS-100 has also successfully completed a phase II clinical trial for the treatment of heart failure. In addition, the agent is being developed as a treatment for acute MI, chronic angina, and for muscle regeneration.
The STOP-CLI study was sponsored by Juventas Therapeutics. Dr. Kibbe reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Intramuscular injections of stromal cell–derived factor-1 in patients with critical limb ischemia demonstrated safety and efficacy; the therapy is moving forward to phase III testing.
Major finding: The major limb amputation rate was less than 10% during 12 months of follow-up after a single dose of the novel therapy.
Data source: The STOP-CLI trial was a phase IIa, 12-month, randomized, double-blind, placebo-controlled, six-center trial including 48 patients with critical limb ischemia.
Disclosures: The STOP-CLI trial was sponsored by Juventas Therapeutics. The presenter reported serving as a consultant to Johnson & Johnson/Cordis and Pluristem.