User login
Official Newspaper of the American College of Surgeons
Peer pressure moves dial on restricting RBC transfusions
LAKE BUENA VISTA, FLA. – A multimodal intervention founded on prompt peer-to-peer review increased adherence to restrictive red blood cell transfusion guidelines without increasing mortality.
During the intervention, if patients were transfused outside of established hospital guidelines, all clinicians taking care of the patient received an e-mail notification within 72 hours of transfusion. This included the ICU staff, primary team, intern, resident, fellow, nurse practitioner, and attending, said Dr. Daniel Yeh, a trauma and critical care surgeon at Massachusetts General Hospital in Boston whose signature appears on the e-mail along with the endorsement of the surgeon-in-chief, anesthetist-in-chief, director of the MGH Critical Care Center, codirector of blood transfusion services, and the urology chief.
The e-mail blast was coupled with a 1-hour educational lecture during surgery grand rounds on the potential harms of and indications for blood transfusion, a surgical ICU didactic lecture, and monthly division-wide reports.
Prior to the intervention, providers felt they were probably doing pretty well in terms of using a more restrictive transfusion strategy, Dr. Yeh said. After all, there are strong guidelines in all the professional societies and 15 years of high-quality, level 1 evidence from the pivotal 1999 TRICC (Transfusion Requirements in Critical Care) trial to last year’s data in traumatic brain injury (TBI) patients (JAMA 2014;312:36-47) showing that a lower transfusion threshold is noninferior, if not superior, to a higher transfusion threshold.
“Yet, anecdotally in my own practice and objectively in observational data, we see what can only be euphemistically described as a knowledge-practice gap,” he said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST). “Basically, we weren’t practicing what we were preaching.”
A record review of 144 patients from January to June 2013 found that fully 25% of all transfusions in stable, low-risk ICU patients had a pretransfusion hemoglobin (Hb) trigger > 8.0 g/dL.
Further, 5% of patients received the old standby 2-unit transfusion without an intervening hemoglobin measurement, which has been recommended against by all major medical societies, Dr. Yeh said.
The overtransfusion rate, defined as a post-transfusion level > 10 g/dL, was 11%. Most of this was accounted for by these 2-unit patients, he added.
Stable, low-risk patients comprised 33% of all transfusions during the review period and were identified using liberal exclusion criteria including anyone with visible bleeding or suspected internal bleeding, hemodynamic instability, ischemia (myocardial, intestinal, or peripheral vascular), or who were high risk (defined by a history of coronary artery disease, coronary artery bypass grafting, or congestive heart failure).
After the October 2013 to March 2014 intervention, the percentage of stable, low-risk patients with a Hb trigger of > 8.0 g/dL declined from 25% to 2% (P < .001), with a 1-month audit of 15 patients showing a rebound up to 17% 6 months after the intervention ended, Dr. Yeh said.
“There was no difference in the patients who got a single transfusion; however, the ones who got multiple transfusions during their hospital stay decreased, so that is where we believe most of the decline came from,” he explained.
Among the 137 postintervention patients, the average pretransfusion trigger decreased significantly (7.6 g/dL vs. 7.1 g/dL; P < .001), before rising to 7.3 g/dL 6 months post intervention.
The number of monthly transfusions declined 35% from 47 units to 31 units (P = NS) and the overtransfusion rate fell from 11% to 3% (P = .004).
There were no significant differences in maximum lactate, maximum troponin, median ICU or hospital length of stay, although ICU discharge Hb (8.6 g/dL vs. 8.2 g/dL; P = .087) and hospital discharge Hb (9.0 g/dL vs. 8.6 g/dL; P = .006) were lower in the intervention period, Dr. Yeh said.
No significant differences were seen post intervention in 30-day readmission (23% vs. 16%; NS) or overall mortality (4% vs. 9%; NS).
“Transfusions were not really temporally related to the death nor did we attribute any of these deaths to symptomatic anemia,” he said.
Limitations of the intervention include the possibility of a Hawthorne effect, use of crude clinical outcomes, and the lack of concomitant control in the ICU, although the partial regression seen 6 months after the intervention suggests something about the intervention was working, Dr. Yeh observed.
Discussant Dr. Laura J. Moore of the University of Texas Health Science Center at Houston, congratulated the authors on an interesting and pertinent study, but questioned why they utilized a Hb threshold of 8 g/dL when the transfusion trigger was set at 7 g/dL in TRICC and in the Villanueva et al. study in acute upper gastrointestinal bleeders (N. Engl. J. Med. 2013;368:11-21).
“Certainly in my institution, we utilize a trigger of 7 [g/dL] and some of us might even push that down to 6 [g/dL],” she said.
Some of the landmark studies including FOCUS and TRACS used a trigger of 8 g/dL and the investigators wanted to give the clinicians a bit of a benefit of doubt, Dr. Yeh responded.
Results of the intervention were met with surprise, but were quickly reinforced with the publication of the TBI and Villanueva studies and an accompanying editorial (N. Engl. J. Med. 2014;371:1459-61) arguing that a transfusion threshold of 7 g/dL is the new normal, he noted.
“We’ve continued on daily rounds to really focus on that [trigger]. We’ve become empowered as the ICU team to say ‘No,’ to argue and at least put up roadblocks when the primary teams are requesting transfusions and ask them to justify why patients need the additional oxygen carrying capacity when they’re waiting on the floor for 3 days and doing totally fine,” Dr. Yeh said.
As for how they deal with offending providers or outliers, electronic records identify who signed each transfusion order, even if it’s in the dead of night, and simply showing physicians where they stack up with their peers can be the biggest driver of practice change. The team no longer performs monthly audits due to time constraints, but hopes to resume e-mail interventions once MGH’s transition to a new electronic medical system is complete, Dr. Yeh said in an interview.
LAKE BUENA VISTA, FLA. – A multimodal intervention founded on prompt peer-to-peer review increased adherence to restrictive red blood cell transfusion guidelines without increasing mortality.
During the intervention, if patients were transfused outside of established hospital guidelines, all clinicians taking care of the patient received an e-mail notification within 72 hours of transfusion. This included the ICU staff, primary team, intern, resident, fellow, nurse practitioner, and attending, said Dr. Daniel Yeh, a trauma and critical care surgeon at Massachusetts General Hospital in Boston whose signature appears on the e-mail along with the endorsement of the surgeon-in-chief, anesthetist-in-chief, director of the MGH Critical Care Center, codirector of blood transfusion services, and the urology chief.
The e-mail blast was coupled with a 1-hour educational lecture during surgery grand rounds on the potential harms of and indications for blood transfusion, a surgical ICU didactic lecture, and monthly division-wide reports.
Prior to the intervention, providers felt they were probably doing pretty well in terms of using a more restrictive transfusion strategy, Dr. Yeh said. After all, there are strong guidelines in all the professional societies and 15 years of high-quality, level 1 evidence from the pivotal 1999 TRICC (Transfusion Requirements in Critical Care) trial to last year’s data in traumatic brain injury (TBI) patients (JAMA 2014;312:36-47) showing that a lower transfusion threshold is noninferior, if not superior, to a higher transfusion threshold.
“Yet, anecdotally in my own practice and objectively in observational data, we see what can only be euphemistically described as a knowledge-practice gap,” he said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST). “Basically, we weren’t practicing what we were preaching.”
A record review of 144 patients from January to June 2013 found that fully 25% of all transfusions in stable, low-risk ICU patients had a pretransfusion hemoglobin (Hb) trigger > 8.0 g/dL.
Further, 5% of patients received the old standby 2-unit transfusion without an intervening hemoglobin measurement, which has been recommended against by all major medical societies, Dr. Yeh said.
The overtransfusion rate, defined as a post-transfusion level > 10 g/dL, was 11%. Most of this was accounted for by these 2-unit patients, he added.
Stable, low-risk patients comprised 33% of all transfusions during the review period and were identified using liberal exclusion criteria including anyone with visible bleeding or suspected internal bleeding, hemodynamic instability, ischemia (myocardial, intestinal, or peripheral vascular), or who were high risk (defined by a history of coronary artery disease, coronary artery bypass grafting, or congestive heart failure).
After the October 2013 to March 2014 intervention, the percentage of stable, low-risk patients with a Hb trigger of > 8.0 g/dL declined from 25% to 2% (P < .001), with a 1-month audit of 15 patients showing a rebound up to 17% 6 months after the intervention ended, Dr. Yeh said.
“There was no difference in the patients who got a single transfusion; however, the ones who got multiple transfusions during their hospital stay decreased, so that is where we believe most of the decline came from,” he explained.
Among the 137 postintervention patients, the average pretransfusion trigger decreased significantly (7.6 g/dL vs. 7.1 g/dL; P < .001), before rising to 7.3 g/dL 6 months post intervention.
The number of monthly transfusions declined 35% from 47 units to 31 units (P = NS) and the overtransfusion rate fell from 11% to 3% (P = .004).
There were no significant differences in maximum lactate, maximum troponin, median ICU or hospital length of stay, although ICU discharge Hb (8.6 g/dL vs. 8.2 g/dL; P = .087) and hospital discharge Hb (9.0 g/dL vs. 8.6 g/dL; P = .006) were lower in the intervention period, Dr. Yeh said.
No significant differences were seen post intervention in 30-day readmission (23% vs. 16%; NS) or overall mortality (4% vs. 9%; NS).
“Transfusions were not really temporally related to the death nor did we attribute any of these deaths to symptomatic anemia,” he said.
Limitations of the intervention include the possibility of a Hawthorne effect, use of crude clinical outcomes, and the lack of concomitant control in the ICU, although the partial regression seen 6 months after the intervention suggests something about the intervention was working, Dr. Yeh observed.
Discussant Dr. Laura J. Moore of the University of Texas Health Science Center at Houston, congratulated the authors on an interesting and pertinent study, but questioned why they utilized a Hb threshold of 8 g/dL when the transfusion trigger was set at 7 g/dL in TRICC and in the Villanueva et al. study in acute upper gastrointestinal bleeders (N. Engl. J. Med. 2013;368:11-21).
“Certainly in my institution, we utilize a trigger of 7 [g/dL] and some of us might even push that down to 6 [g/dL],” she said.
Some of the landmark studies including FOCUS and TRACS used a trigger of 8 g/dL and the investigators wanted to give the clinicians a bit of a benefit of doubt, Dr. Yeh responded.
Results of the intervention were met with surprise, but were quickly reinforced with the publication of the TBI and Villanueva studies and an accompanying editorial (N. Engl. J. Med. 2014;371:1459-61) arguing that a transfusion threshold of 7 g/dL is the new normal, he noted.
“We’ve continued on daily rounds to really focus on that [trigger]. We’ve become empowered as the ICU team to say ‘No,’ to argue and at least put up roadblocks when the primary teams are requesting transfusions and ask them to justify why patients need the additional oxygen carrying capacity when they’re waiting on the floor for 3 days and doing totally fine,” Dr. Yeh said.
As for how they deal with offending providers or outliers, electronic records identify who signed each transfusion order, even if it’s in the dead of night, and simply showing physicians where they stack up with their peers can be the biggest driver of practice change. The team no longer performs monthly audits due to time constraints, but hopes to resume e-mail interventions once MGH’s transition to a new electronic medical system is complete, Dr. Yeh said in an interview.
LAKE BUENA VISTA, FLA. – A multimodal intervention founded on prompt peer-to-peer review increased adherence to restrictive red blood cell transfusion guidelines without increasing mortality.
During the intervention, if patients were transfused outside of established hospital guidelines, all clinicians taking care of the patient received an e-mail notification within 72 hours of transfusion. This included the ICU staff, primary team, intern, resident, fellow, nurse practitioner, and attending, said Dr. Daniel Yeh, a trauma and critical care surgeon at Massachusetts General Hospital in Boston whose signature appears on the e-mail along with the endorsement of the surgeon-in-chief, anesthetist-in-chief, director of the MGH Critical Care Center, codirector of blood transfusion services, and the urology chief.
The e-mail blast was coupled with a 1-hour educational lecture during surgery grand rounds on the potential harms of and indications for blood transfusion, a surgical ICU didactic lecture, and monthly division-wide reports.
Prior to the intervention, providers felt they were probably doing pretty well in terms of using a more restrictive transfusion strategy, Dr. Yeh said. After all, there are strong guidelines in all the professional societies and 15 years of high-quality, level 1 evidence from the pivotal 1999 TRICC (Transfusion Requirements in Critical Care) trial to last year’s data in traumatic brain injury (TBI) patients (JAMA 2014;312:36-47) showing that a lower transfusion threshold is noninferior, if not superior, to a higher transfusion threshold.
“Yet, anecdotally in my own practice and objectively in observational data, we see what can only be euphemistically described as a knowledge-practice gap,” he said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST). “Basically, we weren’t practicing what we were preaching.”
A record review of 144 patients from January to June 2013 found that fully 25% of all transfusions in stable, low-risk ICU patients had a pretransfusion hemoglobin (Hb) trigger > 8.0 g/dL.
Further, 5% of patients received the old standby 2-unit transfusion without an intervening hemoglobin measurement, which has been recommended against by all major medical societies, Dr. Yeh said.
The overtransfusion rate, defined as a post-transfusion level > 10 g/dL, was 11%. Most of this was accounted for by these 2-unit patients, he added.
Stable, low-risk patients comprised 33% of all transfusions during the review period and were identified using liberal exclusion criteria including anyone with visible bleeding or suspected internal bleeding, hemodynamic instability, ischemia (myocardial, intestinal, or peripheral vascular), or who were high risk (defined by a history of coronary artery disease, coronary artery bypass grafting, or congestive heart failure).
After the October 2013 to March 2014 intervention, the percentage of stable, low-risk patients with a Hb trigger of > 8.0 g/dL declined from 25% to 2% (P < .001), with a 1-month audit of 15 patients showing a rebound up to 17% 6 months after the intervention ended, Dr. Yeh said.
“There was no difference in the patients who got a single transfusion; however, the ones who got multiple transfusions during their hospital stay decreased, so that is where we believe most of the decline came from,” he explained.
Among the 137 postintervention patients, the average pretransfusion trigger decreased significantly (7.6 g/dL vs. 7.1 g/dL; P < .001), before rising to 7.3 g/dL 6 months post intervention.
The number of monthly transfusions declined 35% from 47 units to 31 units (P = NS) and the overtransfusion rate fell from 11% to 3% (P = .004).
There were no significant differences in maximum lactate, maximum troponin, median ICU or hospital length of stay, although ICU discharge Hb (8.6 g/dL vs. 8.2 g/dL; P = .087) and hospital discharge Hb (9.0 g/dL vs. 8.6 g/dL; P = .006) were lower in the intervention period, Dr. Yeh said.
No significant differences were seen post intervention in 30-day readmission (23% vs. 16%; NS) or overall mortality (4% vs. 9%; NS).
“Transfusions were not really temporally related to the death nor did we attribute any of these deaths to symptomatic anemia,” he said.
Limitations of the intervention include the possibility of a Hawthorne effect, use of crude clinical outcomes, and the lack of concomitant control in the ICU, although the partial regression seen 6 months after the intervention suggests something about the intervention was working, Dr. Yeh observed.
Discussant Dr. Laura J. Moore of the University of Texas Health Science Center at Houston, congratulated the authors on an interesting and pertinent study, but questioned why they utilized a Hb threshold of 8 g/dL when the transfusion trigger was set at 7 g/dL in TRICC and in the Villanueva et al. study in acute upper gastrointestinal bleeders (N. Engl. J. Med. 2013;368:11-21).
“Certainly in my institution, we utilize a trigger of 7 [g/dL] and some of us might even push that down to 6 [g/dL],” she said.
Some of the landmark studies including FOCUS and TRACS used a trigger of 8 g/dL and the investigators wanted to give the clinicians a bit of a benefit of doubt, Dr. Yeh responded.
Results of the intervention were met with surprise, but were quickly reinforced with the publication of the TBI and Villanueva studies and an accompanying editorial (N. Engl. J. Med. 2014;371:1459-61) arguing that a transfusion threshold of 7 g/dL is the new normal, he noted.
“We’ve continued on daily rounds to really focus on that [trigger]. We’ve become empowered as the ICU team to say ‘No,’ to argue and at least put up roadblocks when the primary teams are requesting transfusions and ask them to justify why patients need the additional oxygen carrying capacity when they’re waiting on the floor for 3 days and doing totally fine,” Dr. Yeh said.
As for how they deal with offending providers or outliers, electronic records identify who signed each transfusion order, even if it’s in the dead of night, and simply showing physicians where they stack up with their peers can be the biggest driver of practice change. The team no longer performs monthly audits due to time constraints, but hopes to resume e-mail interventions once MGH’s transition to a new electronic medical system is complete, Dr. Yeh said in an interview.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: Peer-to-peer review improves the use of restrictive transfusion guidelines without increasing mortality.
Major finding: The percentage of stable, low-risk patients with a hemoglobin trigger > 8 g/dL decreased from 25% to 2% post intervention (P < .001).
Data source: Prospective interventional study of 137 stable, low-risk patients with 144 retrospective controls.
Disclosures: Dr. Yeh, his coauthors, and Dr. Moore reported having no disclosures.
Jury still out on survival benefit of resecting primary in mCRC
SAN FRANCISCO – Resecting the primary tumor in patients with metastatic colon or colorectal cancer may prolong survival. But then again, it may not.
This was the overarching take-home message from a trio of cohort studies presented at the Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. Results were reported in a poster session.
“Whereas surgery is the primary treatment of localized colorectal cancer, resection of the primary tumor in patients with incurable metastatic disease is usually recommended for palliative purposes to manage obstruction, perforation, or bleeding,” Dr. Shahid Ahmed, lead investigator of one of the studies, noted in comments provided by e-mail. “The role of surgical resection of the primary tumor in patients with newly diagnosed incurable stage IV colorectal cancer remains controversial.”
In earlier research, he and colleagues found a survival benefit of primary resection among Canadian patients whose cancer was diagnosed between 1992 and 2005 (Cancer 2014;120:683-91). But the majority did not receive systemic therapy, and those who did were often given older regimens.
In a new study aimed at testing the association in the contemporary treatment era, the researchers analyzed data from 569 patients with stage IV colorectal cancer diagnosed between 2006 and 2010 who had a median follow-up of 11 months. Overall, 55% had resection of the primary tumor.
Among the 57% of patients who received systemic therapy, 91% received FOLFIRI or FOLFOX, 65% received bevacizumab (Avastin), and 10% received cetuximab (Erbitux) or panitumumab (Vectibix), according to Dr. Ahmed, professor of medicine, University of Saskatchewan, Canada.
Results for the entire cohort showed that median overall survival was 18 months in patients who had resection of their primary versus 4 months in those who did not (multivariate hazard ratio, 0.44; P less than .001).
Among the subgroup of patients who received chemotherapy, median survival was 27 months with primary resection versus 14 months without it (P less than .0001). And among the subgroup that specifically received FOLFIRI or FOLFOX and a biologic agent, it was 35 months with primary resection and 23 months without it (P less than .001).
“Surgical resection of primary tumor improves survival of patients with stage IV colorectal cancer, independent of other prognostic variables including age, performance status, comorbid illness, and chemotherapy,” maintained Dr. Ahmed. “The current study validates our findings and supports surgical resection of primary tumor in patients with stage IV colorectal cancer who are treated with modern chemotherapy and biologics.
“A well-designed prospective randomized trial is warranted to confirm the survival benefit conferred by the primary tumor resection,” he added, noting that two such trials in Europe – SYNCHRONOUS and CAIRO4 – are underway.
“If the magnitude of survival benefit is confirmed in these future randomized studies, surgical resection of the primary tumor could potentially be a more cost-effective intervention compared with novel systemic therapy in the management of metastatic colorectal cancer,” he concluded.
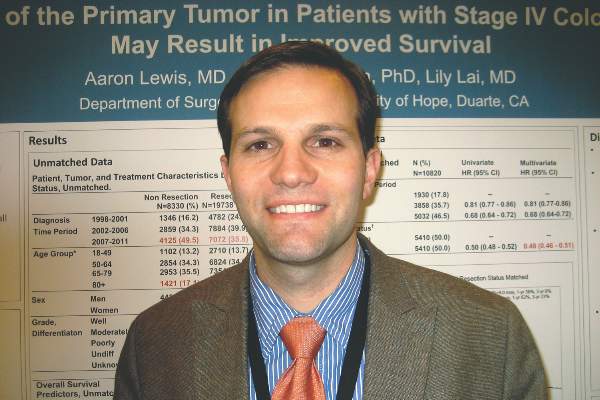
In a second study, Dr. Aaron Lewis, a surgical oncology fellow at the City of Hope, Duarte, Calif., and colleagues analyzed data from patients with stage IV colon cancer in the Surveillance, Epidemiology, and End Results (SEER) database for the years 1998 through 2011. They excluded those who died within 30 days of diagnosis or had resection of metastases. Overall, 70% of the 28,068 included patients had resection of their primary.
In multivariate analyses, patients who underwent resection had half the risk of death when compared with peers who did not have this surgery (hazard ratio, 0.49), reported Dr. Lewis.
Findings were essentially the same when the analysis was repeated in a subset of matched patients: Median survival was 17 months with resection versus 9 months without it (hazard ratio, 0.48; P less than .0001). Estimated 3-year survival was 23% and 6%, respectively.
“There are limitations, factors that we couldn’t completely control for. For example, there is no chemotherapy data in the SEER database. We didn’t know the timing of surgery in relation to chemotherapy. And we didn’t know whether these patients were asymptomatic or symptomatic,” Dr. Lewis noted in an interview. “But analysis of this huge group of patients in the United States that are getting treated shows that there is a survival benefit.”
Possible reasons why surgery might prolong life in this setting are unknown but may include the effects of tumor debulking or some enhancement of the immune response, he proposed.
To definitively confirm a survival benefit, a randomized controlled trial is needed, he agreed. “This seems to be a popular question in the literature in the last couple of years, so maybe somebody will be willing to take it on.”
In a third study, a team led by Dr. Zeinab Alawadi, a surgeon and postdoctoral fellow at the University of Texas MD Anderson Cancer Center, Houston, analyzed data from 14,399 patients in the National Cancer Data Base. They had been diagnosed with stage IV colon cancer between 2003 and 2005. The researchers excluded patients who had nonelective resection or surgery at other sites, such as metastasectomy.
The primary tumor was resected in 55% of all patients studied and in 74% of patients included in a 1-year landmark analysis done to account for early deaths related to comorbidity or disease burden, reported Dr. Alawadi.
In the entire cohort, primary resection conferred a significant survival benefit after standard multivariate adjustment (hazard ratio, 0.39) that persisted after propensity score weighting to account for treatment selection bias (hazard ratio, 0.41). The benefit was also significant, but much attenuated, in an instrumental variable analysis, another method for accounting for treatment selection bias (relative mortality rate, 0.88).
In the 1-year landmark population, primary resection conferred a smaller significant survival benefit after standard multivariate adjustment (hazard ratio, 0.60) that persisted after propensity score weighting (hazard ratio, 0.59). But there was no longer a significant benefit in the instrumental variable analysis here.
“Among the entire cohort of patients with stage 4 colon cancer, primary tumor resection offered no survival benefit over systemic chemotherapy alone when the [instrumental variable] method was applied at the 1 year landmark,” the investigators write.
“Subject to selection and survivor treatment bias, standard regression analysis may overestimate the benefit of [primary tumor resection],” they concluded.
SAN FRANCISCO – Resecting the primary tumor in patients with metastatic colon or colorectal cancer may prolong survival. But then again, it may not.
This was the overarching take-home message from a trio of cohort studies presented at the Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. Results were reported in a poster session.
“Whereas surgery is the primary treatment of localized colorectal cancer, resection of the primary tumor in patients with incurable metastatic disease is usually recommended for palliative purposes to manage obstruction, perforation, or bleeding,” Dr. Shahid Ahmed, lead investigator of one of the studies, noted in comments provided by e-mail. “The role of surgical resection of the primary tumor in patients with newly diagnosed incurable stage IV colorectal cancer remains controversial.”
In earlier research, he and colleagues found a survival benefit of primary resection among Canadian patients whose cancer was diagnosed between 1992 and 2005 (Cancer 2014;120:683-91). But the majority did not receive systemic therapy, and those who did were often given older regimens.
In a new study aimed at testing the association in the contemporary treatment era, the researchers analyzed data from 569 patients with stage IV colorectal cancer diagnosed between 2006 and 2010 who had a median follow-up of 11 months. Overall, 55% had resection of the primary tumor.
Among the 57% of patients who received systemic therapy, 91% received FOLFIRI or FOLFOX, 65% received bevacizumab (Avastin), and 10% received cetuximab (Erbitux) or panitumumab (Vectibix), according to Dr. Ahmed, professor of medicine, University of Saskatchewan, Canada.
Results for the entire cohort showed that median overall survival was 18 months in patients who had resection of their primary versus 4 months in those who did not (multivariate hazard ratio, 0.44; P less than .001).
Among the subgroup of patients who received chemotherapy, median survival was 27 months with primary resection versus 14 months without it (P less than .0001). And among the subgroup that specifically received FOLFIRI or FOLFOX and a biologic agent, it was 35 months with primary resection and 23 months without it (P less than .001).
“Surgical resection of primary tumor improves survival of patients with stage IV colorectal cancer, independent of other prognostic variables including age, performance status, comorbid illness, and chemotherapy,” maintained Dr. Ahmed. “The current study validates our findings and supports surgical resection of primary tumor in patients with stage IV colorectal cancer who are treated with modern chemotherapy and biologics.
“A well-designed prospective randomized trial is warranted to confirm the survival benefit conferred by the primary tumor resection,” he added, noting that two such trials in Europe – SYNCHRONOUS and CAIRO4 – are underway.
“If the magnitude of survival benefit is confirmed in these future randomized studies, surgical resection of the primary tumor could potentially be a more cost-effective intervention compared with novel systemic therapy in the management of metastatic colorectal cancer,” he concluded.
In a second study, Dr. Aaron Lewis, a surgical oncology fellow at the City of Hope, Duarte, Calif., and colleagues analyzed data from patients with stage IV colon cancer in the Surveillance, Epidemiology, and End Results (SEER) database for the years 1998 through 2011. They excluded those who died within 30 days of diagnosis or had resection of metastases. Overall, 70% of the 28,068 included patients had resection of their primary.
In multivariate analyses, patients who underwent resection had half the risk of death when compared with peers who did not have this surgery (hazard ratio, 0.49), reported Dr. Lewis.
Findings were essentially the same when the analysis was repeated in a subset of matched patients: Median survival was 17 months with resection versus 9 months without it (hazard ratio, 0.48; P less than .0001). Estimated 3-year survival was 23% and 6%, respectively.
“There are limitations, factors that we couldn’t completely control for. For example, there is no chemotherapy data in the SEER database. We didn’t know the timing of surgery in relation to chemotherapy. And we didn’t know whether these patients were asymptomatic or symptomatic,” Dr. Lewis noted in an interview. “But analysis of this huge group of patients in the United States that are getting treated shows that there is a survival benefit.”
Possible reasons why surgery might prolong life in this setting are unknown but may include the effects of tumor debulking or some enhancement of the immune response, he proposed.
To definitively confirm a survival benefit, a randomized controlled trial is needed, he agreed. “This seems to be a popular question in the literature in the last couple of years, so maybe somebody will be willing to take it on.”
In a third study, a team led by Dr. Zeinab Alawadi, a surgeon and postdoctoral fellow at the University of Texas MD Anderson Cancer Center, Houston, analyzed data from 14,399 patients in the National Cancer Data Base. They had been diagnosed with stage IV colon cancer between 2003 and 2005. The researchers excluded patients who had nonelective resection or surgery at other sites, such as metastasectomy.
The primary tumor was resected in 55% of all patients studied and in 74% of patients included in a 1-year landmark analysis done to account for early deaths related to comorbidity or disease burden, reported Dr. Alawadi.
In the entire cohort, primary resection conferred a significant survival benefit after standard multivariate adjustment (hazard ratio, 0.39) that persisted after propensity score weighting to account for treatment selection bias (hazard ratio, 0.41). The benefit was also significant, but much attenuated, in an instrumental variable analysis, another method for accounting for treatment selection bias (relative mortality rate, 0.88).
In the 1-year landmark population, primary resection conferred a smaller significant survival benefit after standard multivariate adjustment (hazard ratio, 0.60) that persisted after propensity score weighting (hazard ratio, 0.59). But there was no longer a significant benefit in the instrumental variable analysis here.
“Among the entire cohort of patients with stage 4 colon cancer, primary tumor resection offered no survival benefit over systemic chemotherapy alone when the [instrumental variable] method was applied at the 1 year landmark,” the investigators write.
“Subject to selection and survivor treatment bias, standard regression analysis may overestimate the benefit of [primary tumor resection],” they concluded.
SAN FRANCISCO – Resecting the primary tumor in patients with metastatic colon or colorectal cancer may prolong survival. But then again, it may not.
This was the overarching take-home message from a trio of cohort studies presented at the Gastrointestinal Cancers Symposium cosponsored by the AGA Institute, the American Society of Clinical Oncology, ASTRO, and the Society of Surgical Oncology. Results were reported in a poster session.
“Whereas surgery is the primary treatment of localized colorectal cancer, resection of the primary tumor in patients with incurable metastatic disease is usually recommended for palliative purposes to manage obstruction, perforation, or bleeding,” Dr. Shahid Ahmed, lead investigator of one of the studies, noted in comments provided by e-mail. “The role of surgical resection of the primary tumor in patients with newly diagnosed incurable stage IV colorectal cancer remains controversial.”
In earlier research, he and colleagues found a survival benefit of primary resection among Canadian patients whose cancer was diagnosed between 1992 and 2005 (Cancer 2014;120:683-91). But the majority did not receive systemic therapy, and those who did were often given older regimens.
In a new study aimed at testing the association in the contemporary treatment era, the researchers analyzed data from 569 patients with stage IV colorectal cancer diagnosed between 2006 and 2010 who had a median follow-up of 11 months. Overall, 55% had resection of the primary tumor.
Among the 57% of patients who received systemic therapy, 91% received FOLFIRI or FOLFOX, 65% received bevacizumab (Avastin), and 10% received cetuximab (Erbitux) or panitumumab (Vectibix), according to Dr. Ahmed, professor of medicine, University of Saskatchewan, Canada.
Results for the entire cohort showed that median overall survival was 18 months in patients who had resection of their primary versus 4 months in those who did not (multivariate hazard ratio, 0.44; P less than .001).
Among the subgroup of patients who received chemotherapy, median survival was 27 months with primary resection versus 14 months without it (P less than .0001). And among the subgroup that specifically received FOLFIRI or FOLFOX and a biologic agent, it was 35 months with primary resection and 23 months without it (P less than .001).
“Surgical resection of primary tumor improves survival of patients with stage IV colorectal cancer, independent of other prognostic variables including age, performance status, comorbid illness, and chemotherapy,” maintained Dr. Ahmed. “The current study validates our findings and supports surgical resection of primary tumor in patients with stage IV colorectal cancer who are treated with modern chemotherapy and biologics.
“A well-designed prospective randomized trial is warranted to confirm the survival benefit conferred by the primary tumor resection,” he added, noting that two such trials in Europe – SYNCHRONOUS and CAIRO4 – are underway.
“If the magnitude of survival benefit is confirmed in these future randomized studies, surgical resection of the primary tumor could potentially be a more cost-effective intervention compared with novel systemic therapy in the management of metastatic colorectal cancer,” he concluded.
In a second study, Dr. Aaron Lewis, a surgical oncology fellow at the City of Hope, Duarte, Calif., and colleagues analyzed data from patients with stage IV colon cancer in the Surveillance, Epidemiology, and End Results (SEER) database for the years 1998 through 2011. They excluded those who died within 30 days of diagnosis or had resection of metastases. Overall, 70% of the 28,068 included patients had resection of their primary.
In multivariate analyses, patients who underwent resection had half the risk of death when compared with peers who did not have this surgery (hazard ratio, 0.49), reported Dr. Lewis.
Findings were essentially the same when the analysis was repeated in a subset of matched patients: Median survival was 17 months with resection versus 9 months without it (hazard ratio, 0.48; P less than .0001). Estimated 3-year survival was 23% and 6%, respectively.
“There are limitations, factors that we couldn’t completely control for. For example, there is no chemotherapy data in the SEER database. We didn’t know the timing of surgery in relation to chemotherapy. And we didn’t know whether these patients were asymptomatic or symptomatic,” Dr. Lewis noted in an interview. “But analysis of this huge group of patients in the United States that are getting treated shows that there is a survival benefit.”
Possible reasons why surgery might prolong life in this setting are unknown but may include the effects of tumor debulking or some enhancement of the immune response, he proposed.
To definitively confirm a survival benefit, a randomized controlled trial is needed, he agreed. “This seems to be a popular question in the literature in the last couple of years, so maybe somebody will be willing to take it on.”
In a third study, a team led by Dr. Zeinab Alawadi, a surgeon and postdoctoral fellow at the University of Texas MD Anderson Cancer Center, Houston, analyzed data from 14,399 patients in the National Cancer Data Base. They had been diagnosed with stage IV colon cancer between 2003 and 2005. The researchers excluded patients who had nonelective resection or surgery at other sites, such as metastasectomy.
The primary tumor was resected in 55% of all patients studied and in 74% of patients included in a 1-year landmark analysis done to account for early deaths related to comorbidity or disease burden, reported Dr. Alawadi.
In the entire cohort, primary resection conferred a significant survival benefit after standard multivariate adjustment (hazard ratio, 0.39) that persisted after propensity score weighting to account for treatment selection bias (hazard ratio, 0.41). The benefit was also significant, but much attenuated, in an instrumental variable analysis, another method for accounting for treatment selection bias (relative mortality rate, 0.88).
In the 1-year landmark population, primary resection conferred a smaller significant survival benefit after standard multivariate adjustment (hazard ratio, 0.60) that persisted after propensity score weighting (hazard ratio, 0.59). But there was no longer a significant benefit in the instrumental variable analysis here.
“Among the entire cohort of patients with stage 4 colon cancer, primary tumor resection offered no survival benefit over systemic chemotherapy alone when the [instrumental variable] method was applied at the 1 year landmark,” the investigators write.
“Subject to selection and survivor treatment bias, standard regression analysis may overestimate the benefit of [primary tumor resection],” they concluded.
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Data are mixed regarding an overall survival benefit of resecting the primary tumor.
Major finding: Two studies found a halving of the risk of death, whereas one study found lesser or even no benefit.
Data source: A trio of cohort studies in 569 patients, 28,068 patients, and 14,399 patients with metastatic colon or colorectal cancer.
Disclosures: Dr. Ahmed, Dr. Lewis, and Dr. Alawadi disclosed that they had no conflicts of interest.
More donated hearts rejected, even as wait list grows
Only about one in three available hearts was accepted for transplant in the United States in 2010, down from 44% 2 decades ago, researchers reported online Feb. 9 in the American Journal of Transplantation.
The decline stems in part from transplant centers rejecting “marginal” donor hearts, belying a growing need for heart transplants, longer waiting times, and multiple campaigns to expand the use of organs donated for transplantation, said Dr. Kiran Khush of Stanford (Calif.) University and her associates.
The researchers analyzed data on 82,053 potential donor hearts from the Organ Procurement and Transplantation Network. In 1995, 44% of available hearts were accepted for transplant, compared with only 29% in 2006 and 32% in 2010, they found. Meanwhile, rejection rates for donor hearts rose from 37% in 1995 to 52% in 2010, they reported (Am. J. Transplant. 2015 Feb. 10 [doi:10.1111/ajt.13055]).
Several factors might explain the trends, the investigators said. Potential heart donors tended to be older and more often had hypertension and diabetes by the final years of the study period, and transplant centers were less likely to accept hearts from such individuals. Also, mechanical circulatory devices were more commonly used, and centers might hesitate to transplant “marginal” hearts into “stable” recipients of such devices, Dr. Khush and her associates said. Furthermore, government scrutiny of post-transplant outcomes might make centers more conservative when evaluating potential donors, they added.
The study also uncovered regional variations in acceptance rates for donor hearts, with the lowest – about 25%-28% – found primarily in the southeastern United States. “Unfortunately, there are no standard guidelines for donor heart evaluation and acceptance, resulting in considerable inconsistencies in the types of donor hearts that are accepted by different transplant centers, and likely resulting in nonrecovery of potentially useful organs,” the investigators said. The findings “lend support to research and policy efforts aimed at establishing evidence-based criteria for donor heart evaluation and acceptance,” they added.
The work was supported by the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; and the Health Resources and Services Administration. The authors reported having no conflicts of interest.
Only about one in three available hearts was accepted for transplant in the United States in 2010, down from 44% 2 decades ago, researchers reported online Feb. 9 in the American Journal of Transplantation.
The decline stems in part from transplant centers rejecting “marginal” donor hearts, belying a growing need for heart transplants, longer waiting times, and multiple campaigns to expand the use of organs donated for transplantation, said Dr. Kiran Khush of Stanford (Calif.) University and her associates.
The researchers analyzed data on 82,053 potential donor hearts from the Organ Procurement and Transplantation Network. In 1995, 44% of available hearts were accepted for transplant, compared with only 29% in 2006 and 32% in 2010, they found. Meanwhile, rejection rates for donor hearts rose from 37% in 1995 to 52% in 2010, they reported (Am. J. Transplant. 2015 Feb. 10 [doi:10.1111/ajt.13055]).
Several factors might explain the trends, the investigators said. Potential heart donors tended to be older and more often had hypertension and diabetes by the final years of the study period, and transplant centers were less likely to accept hearts from such individuals. Also, mechanical circulatory devices were more commonly used, and centers might hesitate to transplant “marginal” hearts into “stable” recipients of such devices, Dr. Khush and her associates said. Furthermore, government scrutiny of post-transplant outcomes might make centers more conservative when evaluating potential donors, they added.
The study also uncovered regional variations in acceptance rates for donor hearts, with the lowest – about 25%-28% – found primarily in the southeastern United States. “Unfortunately, there are no standard guidelines for donor heart evaluation and acceptance, resulting in considerable inconsistencies in the types of donor hearts that are accepted by different transplant centers, and likely resulting in nonrecovery of potentially useful organs,” the investigators said. The findings “lend support to research and policy efforts aimed at establishing evidence-based criteria for donor heart evaluation and acceptance,” they added.
The work was supported by the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; and the Health Resources and Services Administration. The authors reported having no conflicts of interest.
Only about one in three available hearts was accepted for transplant in the United States in 2010, down from 44% 2 decades ago, researchers reported online Feb. 9 in the American Journal of Transplantation.
The decline stems in part from transplant centers rejecting “marginal” donor hearts, belying a growing need for heart transplants, longer waiting times, and multiple campaigns to expand the use of organs donated for transplantation, said Dr. Kiran Khush of Stanford (Calif.) University and her associates.
The researchers analyzed data on 82,053 potential donor hearts from the Organ Procurement and Transplantation Network. In 1995, 44% of available hearts were accepted for transplant, compared with only 29% in 2006 and 32% in 2010, they found. Meanwhile, rejection rates for donor hearts rose from 37% in 1995 to 52% in 2010, they reported (Am. J. Transplant. 2015 Feb. 10 [doi:10.1111/ajt.13055]).
Several factors might explain the trends, the investigators said. Potential heart donors tended to be older and more often had hypertension and diabetes by the final years of the study period, and transplant centers were less likely to accept hearts from such individuals. Also, mechanical circulatory devices were more commonly used, and centers might hesitate to transplant “marginal” hearts into “stable” recipients of such devices, Dr. Khush and her associates said. Furthermore, government scrutiny of post-transplant outcomes might make centers more conservative when evaluating potential donors, they added.
The study also uncovered regional variations in acceptance rates for donor hearts, with the lowest – about 25%-28% – found primarily in the southeastern United States. “Unfortunately, there are no standard guidelines for donor heart evaluation and acceptance, resulting in considerable inconsistencies in the types of donor hearts that are accepted by different transplant centers, and likely resulting in nonrecovery of potentially useful organs,” the investigators said. The findings “lend support to research and policy efforts aimed at establishing evidence-based criteria for donor heart evaluation and acceptance,” they added.
The work was supported by the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; and the Health Resources and Services Administration. The authors reported having no conflicts of interest.
FROM THE AMERICAN JOURNAL OF TRANSPLANTATION
Key clinical point: Acceptance rates of hearts donated for transplantation have declined substantially in the United States.
Major finding: Only 32% of donated hearts were accepted for transplant in 2010, compared with 44% in 1995.
Data source: Analysis of 82,053 potential donor hearts from the Organ Procurement and Transplantation Network.
Disclosures: The study was supported by the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; and the Health Resources and Services Administration. The authors reported having no conflicts of interest.
Transcarotid angioplasty device approved; reverses blood flow to capture embolic debris
The Food and Drug Administration has approved a minimally invasive angioplasty system that enters the carotid artery adjacent to a blockage, and captures embolic debris by extracorporeal filtration of blood near the blockage.
The ENROUTE Transcarotid Neuroprotection System (ENROUTE TNS) is inserted into the artery near the stenotic region. As the stent is deployed, the system draws blood down the tube, away from the brain, under high pressure. An extracorporeal filter traps any emboli, and the filtered blood is returned via the femoral vein.
ENROUTE TNS was approved on the basis of the successful ROADSTER trial (Safety and Efficacy Study for Reverse Flow Used During Carotid Artery Stenting Procedure). In this study, there was a 3.5% rate of stroke, heart attack, and death among patients treated with the device – significantly lower than the study’s primary outcome goal of 11%. The rate of adverse events was about 14%; these included excessive bleeding or injury at the device insertion site, hypotension, and thrombosis.
The system’s benefits include its minimally invasive approach and the ability to successfully navigate severe carotid tortuosity. It also may be more successful than traditional arterial angioplasty for patients with difficult anatomy of the aortic arch, according to an FDA statement.
Manufactured by Silk Road, Sunnyvale, Calif., the ENROUTE TNS device was approved through a 510(k) submission, which provides an approval pathway for low- to moderate-risk devices that are substantially equivalent to a legally marketed device. According to the FDA statement, ENROUTE TNS is equivalent to a currently marketed flow-reversal system that uses similar technology and has the same intended use, but is designed to be introduced through the groin.
On Twitter @alz_gal
The Food and Drug Administration has approved a minimally invasive angioplasty system that enters the carotid artery adjacent to a blockage, and captures embolic debris by extracorporeal filtration of blood near the blockage.
The ENROUTE Transcarotid Neuroprotection System (ENROUTE TNS) is inserted into the artery near the stenotic region. As the stent is deployed, the system draws blood down the tube, away from the brain, under high pressure. An extracorporeal filter traps any emboli, and the filtered blood is returned via the femoral vein.
ENROUTE TNS was approved on the basis of the successful ROADSTER trial (Safety and Efficacy Study for Reverse Flow Used During Carotid Artery Stenting Procedure). In this study, there was a 3.5% rate of stroke, heart attack, and death among patients treated with the device – significantly lower than the study’s primary outcome goal of 11%. The rate of adverse events was about 14%; these included excessive bleeding or injury at the device insertion site, hypotension, and thrombosis.
The system’s benefits include its minimally invasive approach and the ability to successfully navigate severe carotid tortuosity. It also may be more successful than traditional arterial angioplasty for patients with difficult anatomy of the aortic arch, according to an FDA statement.
Manufactured by Silk Road, Sunnyvale, Calif., the ENROUTE TNS device was approved through a 510(k) submission, which provides an approval pathway for low- to moderate-risk devices that are substantially equivalent to a legally marketed device. According to the FDA statement, ENROUTE TNS is equivalent to a currently marketed flow-reversal system that uses similar technology and has the same intended use, but is designed to be introduced through the groin.
On Twitter @alz_gal
The Food and Drug Administration has approved a minimally invasive angioplasty system that enters the carotid artery adjacent to a blockage, and captures embolic debris by extracorporeal filtration of blood near the blockage.
The ENROUTE Transcarotid Neuroprotection System (ENROUTE TNS) is inserted into the artery near the stenotic region. As the stent is deployed, the system draws blood down the tube, away from the brain, under high pressure. An extracorporeal filter traps any emboli, and the filtered blood is returned via the femoral vein.
ENROUTE TNS was approved on the basis of the successful ROADSTER trial (Safety and Efficacy Study for Reverse Flow Used During Carotid Artery Stenting Procedure). In this study, there was a 3.5% rate of stroke, heart attack, and death among patients treated with the device – significantly lower than the study’s primary outcome goal of 11%. The rate of adverse events was about 14%; these included excessive bleeding or injury at the device insertion site, hypotension, and thrombosis.
The system’s benefits include its minimally invasive approach and the ability to successfully navigate severe carotid tortuosity. It also may be more successful than traditional arterial angioplasty for patients with difficult anatomy of the aortic arch, according to an FDA statement.
Manufactured by Silk Road, Sunnyvale, Calif., the ENROUTE TNS device was approved through a 510(k) submission, which provides an approval pathway for low- to moderate-risk devices that are substantially equivalent to a legally marketed device. According to the FDA statement, ENROUTE TNS is equivalent to a currently marketed flow-reversal system that uses similar technology and has the same intended use, but is designed to be introduced through the groin.
On Twitter @alz_gal
PORT boosts survival in N2 NSCLC patients
Modern postoperative radiotherapy, or PORT, appears to provide an additional overall survival advantage in patients with N2 non–small cell lung cancer treated with complete resection and adjuvant chemotherapy, according to a review of the National Cancer Database.
The median survival was 45.2 months in 1,850 patients treated with PORT at a dose of at least 45 Gy (median 54 Gy over 43 days), compared with 40.7 months in 2,633 who were not treated with PORT. The 3- and 5-year survival rates were 59.3% vs. 55.2% and 39.3% vs. 34.8% in the groups, respectively, and on multivariable analysis, PORT was an independent predictor of improved overall survival (hazard ratio, 0.886), as was younger age, female sex, urban population, lower Charlson score, smaller tumor size, multiagent chemotherapy, and resection with at least a lobectomy, Dr. Clifford G. Robinson and his colleagues at Washington University, St. Louis, reported online Feb. 9 in the Journal of Clinical Oncology.
Patients included in the review had pathologic stage IIIA (N2) NSCLC, underwent complete resection and adjuvant chemotherapy between 2006 and 2010, and were followed for median of 22 months. Those who received neoadjuvant chemotherapy or radiotherapy, were missing data on adjuvant therapy timing, had evidence of metastatic disease, were treated with palliative intent, or had incomplete resection were excluded (J. Clin. Oncol. 2015 Feb. 9 [doi:10.1200/JCO.2014.58.5380]).
Although studies of PORT in the 1960s and 1970s showed a lack of benefit in patients with NSCLC, this was felt to be due in large part to competing cardiac and pulmonary toxicity from outdated equipment, techniques, and dosing; patients in the current study were likely treated with modern techniques, including computed tomography, simulation, and at least linear accelerator–based, three-dimensional, conformal radiotherapy, the investigators said, noting that the finding of a possible survival advantage with PORT underscores the importance of enrolling patients in randomized trials such as LungART.
Dr. Robinson is on the speakers’ bureau for ViewRay, which has paid for travel, accommodations, and other expenses. Several of his coauthors also reported receiving research funding, honoraria, and expenses, or serving as a consultant or advisor for a number of companies, including ViewRay, Varian, Traxxsson, Agennix, Lilly, Pfizer, Daiichi Sankyo, Spectrum Pharmaceuticals, Astex Therapeutics, Novartis, Genentech, Transgene, Eisai, New Link Genetics Corp., Merck, Puma, Roche, Incyte, Boehringer Ingelheim, Celgene, Wyeth, ImClone Systems, Merrimack, Bristol-Meyers Squibb, Onocyte, Astex Therapeutics, Onyx, GlaxoSmithKline, Bayer, Covidien, and Ethicon.
Modern postoperative radiotherapy, or PORT, appears to provide an additional overall survival advantage in patients with N2 non–small cell lung cancer treated with complete resection and adjuvant chemotherapy, according to a review of the National Cancer Database.
The median survival was 45.2 months in 1,850 patients treated with PORT at a dose of at least 45 Gy (median 54 Gy over 43 days), compared with 40.7 months in 2,633 who were not treated with PORT. The 3- and 5-year survival rates were 59.3% vs. 55.2% and 39.3% vs. 34.8% in the groups, respectively, and on multivariable analysis, PORT was an independent predictor of improved overall survival (hazard ratio, 0.886), as was younger age, female sex, urban population, lower Charlson score, smaller tumor size, multiagent chemotherapy, and resection with at least a lobectomy, Dr. Clifford G. Robinson and his colleagues at Washington University, St. Louis, reported online Feb. 9 in the Journal of Clinical Oncology.
Patients included in the review had pathologic stage IIIA (N2) NSCLC, underwent complete resection and adjuvant chemotherapy between 2006 and 2010, and were followed for median of 22 months. Those who received neoadjuvant chemotherapy or radiotherapy, were missing data on adjuvant therapy timing, had evidence of metastatic disease, were treated with palliative intent, or had incomplete resection were excluded (J. Clin. Oncol. 2015 Feb. 9 [doi:10.1200/JCO.2014.58.5380]).
Although studies of PORT in the 1960s and 1970s showed a lack of benefit in patients with NSCLC, this was felt to be due in large part to competing cardiac and pulmonary toxicity from outdated equipment, techniques, and dosing; patients in the current study were likely treated with modern techniques, including computed tomography, simulation, and at least linear accelerator–based, three-dimensional, conformal radiotherapy, the investigators said, noting that the finding of a possible survival advantage with PORT underscores the importance of enrolling patients in randomized trials such as LungART.
Dr. Robinson is on the speakers’ bureau for ViewRay, which has paid for travel, accommodations, and other expenses. Several of his coauthors also reported receiving research funding, honoraria, and expenses, or serving as a consultant or advisor for a number of companies, including ViewRay, Varian, Traxxsson, Agennix, Lilly, Pfizer, Daiichi Sankyo, Spectrum Pharmaceuticals, Astex Therapeutics, Novartis, Genentech, Transgene, Eisai, New Link Genetics Corp., Merck, Puma, Roche, Incyte, Boehringer Ingelheim, Celgene, Wyeth, ImClone Systems, Merrimack, Bristol-Meyers Squibb, Onocyte, Astex Therapeutics, Onyx, GlaxoSmithKline, Bayer, Covidien, and Ethicon.
Modern postoperative radiotherapy, or PORT, appears to provide an additional overall survival advantage in patients with N2 non–small cell lung cancer treated with complete resection and adjuvant chemotherapy, according to a review of the National Cancer Database.
The median survival was 45.2 months in 1,850 patients treated with PORT at a dose of at least 45 Gy (median 54 Gy over 43 days), compared with 40.7 months in 2,633 who were not treated with PORT. The 3- and 5-year survival rates were 59.3% vs. 55.2% and 39.3% vs. 34.8% in the groups, respectively, and on multivariable analysis, PORT was an independent predictor of improved overall survival (hazard ratio, 0.886), as was younger age, female sex, urban population, lower Charlson score, smaller tumor size, multiagent chemotherapy, and resection with at least a lobectomy, Dr. Clifford G. Robinson and his colleagues at Washington University, St. Louis, reported online Feb. 9 in the Journal of Clinical Oncology.
Patients included in the review had pathologic stage IIIA (N2) NSCLC, underwent complete resection and adjuvant chemotherapy between 2006 and 2010, and were followed for median of 22 months. Those who received neoadjuvant chemotherapy or radiotherapy, were missing data on adjuvant therapy timing, had evidence of metastatic disease, were treated with palliative intent, or had incomplete resection were excluded (J. Clin. Oncol. 2015 Feb. 9 [doi:10.1200/JCO.2014.58.5380]).
Although studies of PORT in the 1960s and 1970s showed a lack of benefit in patients with NSCLC, this was felt to be due in large part to competing cardiac and pulmonary toxicity from outdated equipment, techniques, and dosing; patients in the current study were likely treated with modern techniques, including computed tomography, simulation, and at least linear accelerator–based, three-dimensional, conformal radiotherapy, the investigators said, noting that the finding of a possible survival advantage with PORT underscores the importance of enrolling patients in randomized trials such as LungART.
Dr. Robinson is on the speakers’ bureau for ViewRay, which has paid for travel, accommodations, and other expenses. Several of his coauthors also reported receiving research funding, honoraria, and expenses, or serving as a consultant or advisor for a number of companies, including ViewRay, Varian, Traxxsson, Agennix, Lilly, Pfizer, Daiichi Sankyo, Spectrum Pharmaceuticals, Astex Therapeutics, Novartis, Genentech, Transgene, Eisai, New Link Genetics Corp., Merck, Puma, Roche, Incyte, Boehringer Ingelheim, Celgene, Wyeth, ImClone Systems, Merrimack, Bristol-Meyers Squibb, Onocyte, Astex Therapeutics, Onyx, GlaxoSmithKline, Bayer, Covidien, and Ethicon.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Patients with N2 NSCLC may have better overall survival if they receive PORT in addition to surgery and adjuvant chemotherapy.
Major finding: The 3- and 5-year survival rates were 59.3% vs. 55.2% and 39.3% vs. 34.8% in the PORT and non-PORT patients, respectively.
Data source: A review of 4,483 cases from the National Cancer Data Base.
Disclosures: Dr. Robinson is on the speakers’ bureau for ViewRay, which has paid for travel, accommodations, and other expenses. Several of his coauthors also reported receiving research funding, honoraria, and expenses, or serving as a consultant or advisor for a number of companies.
NASH on the rise as a cause of liver transplants
Since 2004, there’s been almost a tripling of the number of nonalcoholic steatohepatitis patients waiting for liver transplants; the condition is now the second leading reason to be put on the waiting list in the United States, according to a study published in the March issue of Gastroenterology.*
Even so and for reasons that are not fully clear, adults with nonalcoholic steatohepatitis (NASH) are less likely to survive for 90 days on the wait list than are patients with alcoholic liver disease (ALD), and less likely to get a new liver within 90 days than are patients with ALD, hepatitis C virus (HCV), or a blend of both. For now, HCV remains the No. 1 reason for liver transplants in the United States (Gastroenterology 2014 Nov. 24 [doi: 10.1053/j.gastro.2014.11.039]).
“Our study provides valuable information about the changing epidemiology of chronic liver disease among wait-listed patients, and adds greatly to our understanding of the epidemiology of NASH in the United States,” the researchers wrote. The rapid rise in the prevalence of NASH is “a direct consequence of the worldwide obesity epidemic” as well as greater awareness of the condition. An expected decline in HCV-related cirrhosis due to effective antiviral therapy “will further contribute to the changing epidemiology of patients awaiting liver transplants in the United States,” said the authors, led by Dr. Robert Wong of the division of gastroenterology and hepatology at Highland Hospital, Oakland, Calif.
“Given the expected continued rise in the number of NASH patients awaiting liver transplant, additional research is needed to improve wait-list survival and ... outcomes among this cohort. In addition, the projection that overall donor availability will significantly diminish in the next 15-20 years emphasizes the need for additional research to improve liver transplant opportunities for NASH patients, including the option of living donor[s],” they said.
The researchers analyzed data from the United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174; those with ALD increased by 45% from 1,400 to 2,024; and those with HCV increased by 14% from 2,887 to 3,291. Registrants with both HCV and ALD decreased by 9% from 880 to 803. NASH became the second-leading disease among liver transplant wait-list registrants in 2013.
Patients with ALD had a significantly higher Model for End-Stage Liver Disease (MELD) score at the time of registration than did others. However, after adjustment for MELD and other variables, patients with ALD were less likely to die within 90 days than were NASH patients (OR 0.77; 95% CI 0.67–0.89; P < .001). No difference was seen in wait-list mortality between NASH and HCV and HCV/ALD patients.
Compared with NASH, patients with HCV (OR 1.45; 95% CI 1.35–1.55; P < .001), ALD (OR 1.15; 95% CI: 1.06–1.24; P < .001), and HCV/ALD (OR 1.29; 95% CI 1.18–1.42; P < .001) were all significantly more likely to receive a liver after 3 months on the wait list.
A “potential explanation for these observations might be etiology-specific differences in disease progression, such that more aggressive etiologies (e.g., HCV or HCV/ALD) can have a more rapid rise in MELD score, receive liver transplant, and have lower wait-list mortality, and etiologies with less rapid progression (e.g., NASH) can have slower rise in MELD score over time, lower rates of LT, but no significant increase in wait-list mortality,” the investigators said.
Overall 1-year wait-list survival among NASH patients decreased from 42.8% in 2004-2008 to 25.6% in 2009-2013, and overall 1-year probability of receiving liver transplant among NASH patients also decreased from 42.1% in 2004-2008 to 39.6% in 2009-2013. The trends were similar for other etiologies, perhaps in part because there are more people waiting for a liver.
The authors said they have no financial conflicts to disclose.
*A change was made to the text on 3/12/2015.
Since 2004, there’s been almost a tripling of the number of nonalcoholic steatohepatitis patients waiting for liver transplants; the condition is now the second leading reason to be put on the waiting list in the United States, according to a study published in the March issue of Gastroenterology.*
Even so and for reasons that are not fully clear, adults with nonalcoholic steatohepatitis (NASH) are less likely to survive for 90 days on the wait list than are patients with alcoholic liver disease (ALD), and less likely to get a new liver within 90 days than are patients with ALD, hepatitis C virus (HCV), or a blend of both. For now, HCV remains the No. 1 reason for liver transplants in the United States (Gastroenterology 2014 Nov. 24 [doi: 10.1053/j.gastro.2014.11.039]).
“Our study provides valuable information about the changing epidemiology of chronic liver disease among wait-listed patients, and adds greatly to our understanding of the epidemiology of NASH in the United States,” the researchers wrote. The rapid rise in the prevalence of NASH is “a direct consequence of the worldwide obesity epidemic” as well as greater awareness of the condition. An expected decline in HCV-related cirrhosis due to effective antiviral therapy “will further contribute to the changing epidemiology of patients awaiting liver transplants in the United States,” said the authors, led by Dr. Robert Wong of the division of gastroenterology and hepatology at Highland Hospital, Oakland, Calif.
“Given the expected continued rise in the number of NASH patients awaiting liver transplant, additional research is needed to improve wait-list survival and ... outcomes among this cohort. In addition, the projection that overall donor availability will significantly diminish in the next 15-20 years emphasizes the need for additional research to improve liver transplant opportunities for NASH patients, including the option of living donor[s],” they said.
The researchers analyzed data from the United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174; those with ALD increased by 45% from 1,400 to 2,024; and those with HCV increased by 14% from 2,887 to 3,291. Registrants with both HCV and ALD decreased by 9% from 880 to 803. NASH became the second-leading disease among liver transplant wait-list registrants in 2013.
Patients with ALD had a significantly higher Model for End-Stage Liver Disease (MELD) score at the time of registration than did others. However, after adjustment for MELD and other variables, patients with ALD were less likely to die within 90 days than were NASH patients (OR 0.77; 95% CI 0.67–0.89; P < .001). No difference was seen in wait-list mortality between NASH and HCV and HCV/ALD patients.
Compared with NASH, patients with HCV (OR 1.45; 95% CI 1.35–1.55; P < .001), ALD (OR 1.15; 95% CI: 1.06–1.24; P < .001), and HCV/ALD (OR 1.29; 95% CI 1.18–1.42; P < .001) were all significantly more likely to receive a liver after 3 months on the wait list.
A “potential explanation for these observations might be etiology-specific differences in disease progression, such that more aggressive etiologies (e.g., HCV or HCV/ALD) can have a more rapid rise in MELD score, receive liver transplant, and have lower wait-list mortality, and etiologies with less rapid progression (e.g., NASH) can have slower rise in MELD score over time, lower rates of LT, but no significant increase in wait-list mortality,” the investigators said.
Overall 1-year wait-list survival among NASH patients decreased from 42.8% in 2004-2008 to 25.6% in 2009-2013, and overall 1-year probability of receiving liver transplant among NASH patients also decreased from 42.1% in 2004-2008 to 39.6% in 2009-2013. The trends were similar for other etiologies, perhaps in part because there are more people waiting for a liver.
The authors said they have no financial conflicts to disclose.
*A change was made to the text on 3/12/2015.
Since 2004, there’s been almost a tripling of the number of nonalcoholic steatohepatitis patients waiting for liver transplants; the condition is now the second leading reason to be put on the waiting list in the United States, according to a study published in the March issue of Gastroenterology.*
Even so and for reasons that are not fully clear, adults with nonalcoholic steatohepatitis (NASH) are less likely to survive for 90 days on the wait list than are patients with alcoholic liver disease (ALD), and less likely to get a new liver within 90 days than are patients with ALD, hepatitis C virus (HCV), or a blend of both. For now, HCV remains the No. 1 reason for liver transplants in the United States (Gastroenterology 2014 Nov. 24 [doi: 10.1053/j.gastro.2014.11.039]).
“Our study provides valuable information about the changing epidemiology of chronic liver disease among wait-listed patients, and adds greatly to our understanding of the epidemiology of NASH in the United States,” the researchers wrote. The rapid rise in the prevalence of NASH is “a direct consequence of the worldwide obesity epidemic” as well as greater awareness of the condition. An expected decline in HCV-related cirrhosis due to effective antiviral therapy “will further contribute to the changing epidemiology of patients awaiting liver transplants in the United States,” said the authors, led by Dr. Robert Wong of the division of gastroenterology and hepatology at Highland Hospital, Oakland, Calif.
“Given the expected continued rise in the number of NASH patients awaiting liver transplant, additional research is needed to improve wait-list survival and ... outcomes among this cohort. In addition, the projection that overall donor availability will significantly diminish in the next 15-20 years emphasizes the need for additional research to improve liver transplant opportunities for NASH patients, including the option of living donor[s],” they said.
The researchers analyzed data from the United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174; those with ALD increased by 45% from 1,400 to 2,024; and those with HCV increased by 14% from 2,887 to 3,291. Registrants with both HCV and ALD decreased by 9% from 880 to 803. NASH became the second-leading disease among liver transplant wait-list registrants in 2013.
Patients with ALD had a significantly higher Model for End-Stage Liver Disease (MELD) score at the time of registration than did others. However, after adjustment for MELD and other variables, patients with ALD were less likely to die within 90 days than were NASH patients (OR 0.77; 95% CI 0.67–0.89; P < .001). No difference was seen in wait-list mortality between NASH and HCV and HCV/ALD patients.
Compared with NASH, patients with HCV (OR 1.45; 95% CI 1.35–1.55; P < .001), ALD (OR 1.15; 95% CI: 1.06–1.24; P < .001), and HCV/ALD (OR 1.29; 95% CI 1.18–1.42; P < .001) were all significantly more likely to receive a liver after 3 months on the wait list.
A “potential explanation for these observations might be etiology-specific differences in disease progression, such that more aggressive etiologies (e.g., HCV or HCV/ALD) can have a more rapid rise in MELD score, receive liver transplant, and have lower wait-list mortality, and etiologies with less rapid progression (e.g., NASH) can have slower rise in MELD score over time, lower rates of LT, but no significant increase in wait-list mortality,” the investigators said.
Overall 1-year wait-list survival among NASH patients decreased from 42.8% in 2004-2008 to 25.6% in 2009-2013, and overall 1-year probability of receiving liver transplant among NASH patients also decreased from 42.1% in 2004-2008 to 39.6% in 2009-2013. The trends were similar for other etiologies, perhaps in part because there are more people waiting for a liver.
The authors said they have no financial conflicts to disclose.
*A change was made to the text on 3/12/2015.
FROM GASTROENTEROLOGY
Key clinical point: As the epidemiology of liver transplantation changes in the United States, more needs to be done to ensure good outcomes in NASH patients.
Major finding: From 2004 to 2013, new wait-list registrants with NASH increased by 170% from 804 to 2,174.
Data source: The United Network for Organ Sharing and Organ Procurement and Transplantation Network registry.
Disclosures: The authors said they have no relevant disclosures.
Physical signs indicate impending death in cancer patients
Several physical symptoms may signal upcoming death in advanced cancer patients, said Dr. David Hui and his colleagues in the department of palliative care and rehabilitation medicine at the University of Texas MD Anderson Cancer Center, Houston.
In a study of 357 advanced cancer patients in palliative care, 203 of whom died, eight specific symptoms were associated with death within 3 days. These physical signs were nonreactive pupils (positive likelihood ratio [LR], = 16.7), decreased response to verbal stimuli (LR, 8.3), decreased response to visual stimuli (LR, 6.7), inability to close the eyelids (LR, 13.6), drooping of the nasolabial fold (LR, 8.3), hyperextension of the neck (LR, 7.3), grunting of vocal chords (LR, 11.8), and upper gastrointestinal bleeding (LR, 10.3), the authors reported.
“The use of these bedside physical signs individually or in combination may assist clinicians in making the diagnosis of impending death,” Dr. Hui and his associates wrote.
Read the full article in Cancer at doi:10.1002/cncr.29048.
Several physical symptoms may signal upcoming death in advanced cancer patients, said Dr. David Hui and his colleagues in the department of palliative care and rehabilitation medicine at the University of Texas MD Anderson Cancer Center, Houston.
In a study of 357 advanced cancer patients in palliative care, 203 of whom died, eight specific symptoms were associated with death within 3 days. These physical signs were nonreactive pupils (positive likelihood ratio [LR], = 16.7), decreased response to verbal stimuli (LR, 8.3), decreased response to visual stimuli (LR, 6.7), inability to close the eyelids (LR, 13.6), drooping of the nasolabial fold (LR, 8.3), hyperextension of the neck (LR, 7.3), grunting of vocal chords (LR, 11.8), and upper gastrointestinal bleeding (LR, 10.3), the authors reported.
“The use of these bedside physical signs individually or in combination may assist clinicians in making the diagnosis of impending death,” Dr. Hui and his associates wrote.
Read the full article in Cancer at doi:10.1002/cncr.29048.
Several physical symptoms may signal upcoming death in advanced cancer patients, said Dr. David Hui and his colleagues in the department of palliative care and rehabilitation medicine at the University of Texas MD Anderson Cancer Center, Houston.
In a study of 357 advanced cancer patients in palliative care, 203 of whom died, eight specific symptoms were associated with death within 3 days. These physical signs were nonreactive pupils (positive likelihood ratio [LR], = 16.7), decreased response to verbal stimuli (LR, 8.3), decreased response to visual stimuli (LR, 6.7), inability to close the eyelids (LR, 13.6), drooping of the nasolabial fold (LR, 8.3), hyperextension of the neck (LR, 7.3), grunting of vocal chords (LR, 11.8), and upper gastrointestinal bleeding (LR, 10.3), the authors reported.
“The use of these bedside physical signs individually or in combination may assist clinicians in making the diagnosis of impending death,” Dr. Hui and his associates wrote.
Read the full article in Cancer at doi:10.1002/cncr.29048.
Trio of risk factors predict gangrenous cholecystitis
LAKE BUENA VISTA, FL. – Older age, diabetes, and elevated bilirubin were significant risk factors for acute gangrenous cholecystitis in a retrospective study of 489 patients undergoing cholecystectomy.
Patients with acute gangrenous cholecystitis (AGC) were on average 15 years older than those with cholecystitis without necrosis (CN) were (55.8 vs. 40.8 years; P value ≤ .001), almost five times more likely to have comorbid diabetes (32% vs. 6.7%; P≤ .05), and had significantly higher bilirubin levels (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
The findings are consistent with previous studies showing that all three risk factors are strongly associated with gangrenous cholecystitis, Seda Bourikian reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
“Future studies may explore how the pathophysiology of diabetes, or the duration of illness in each patient, plays a role in the development of AGC,” the authors suggested in the poster presentation.
The chart review included 489 patients admitted to an emergency general surgery service who underwent cholecystectomy between January 2009 and April 2014. Retrospectively evaluated pathological specimen reports identified 464 patients with CN and 25 patients with AGC.
Male patients had a significantly higher incidence of AGC than CN (56% vs. 26%; P≤ .05), whereas women were less likely to have AGC (44% vs. 74%; NS), Ms. Bourikian and her colleagues at Virginia Commonwealth University in Richmond wrote.
Previous studies also have shown that acute cholecystitis is more common in men and patients over the age of 50 years.
Notably, lactate, obesity, and systolic blood pressure below 100 mm Hg were not different between groups.
As expected, patients with AGC were significantly more likely to die than their counterparts with cholecystitis without necrosis (16% vs. 0.86%; P≤ .05), the authors reported.
People with diabetes with AGC were almost five times more likely to die than were diabetics with CN (32% vs. 6.7%; P≤ .05). according to the authors.
Mortality, however, was nearly identical between AGC and CN patients with a systolic BP ≤ 100 mm Hg (0% vs. 0.02%; NS).
Logistic regression analysis showed that increased age (P≤ .001) and male gender (P≤ .05) were strongly associated with the development of AGC. The failure of more risk factors to pan out in logistic regression is likely because of the small number of patients with gangrenous cholecystitis, senior author and colleague Dr. Paula Ferrada of Virginia Commonwealth University suggested.
“This is not a common disease,” she said in an interview. “That’s why it’s so hard to diagnose and triage. Clinicians need to have a higher suspicion” of AGC.
LAKE BUENA VISTA, FL. – Older age, diabetes, and elevated bilirubin were significant risk factors for acute gangrenous cholecystitis in a retrospective study of 489 patients undergoing cholecystectomy.
Patients with acute gangrenous cholecystitis (AGC) were on average 15 years older than those with cholecystitis without necrosis (CN) were (55.8 vs. 40.8 years; P value ≤ .001), almost five times more likely to have comorbid diabetes (32% vs. 6.7%; P≤ .05), and had significantly higher bilirubin levels (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
The findings are consistent with previous studies showing that all three risk factors are strongly associated with gangrenous cholecystitis, Seda Bourikian reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
“Future studies may explore how the pathophysiology of diabetes, or the duration of illness in each patient, plays a role in the development of AGC,” the authors suggested in the poster presentation.
The chart review included 489 patients admitted to an emergency general surgery service who underwent cholecystectomy between January 2009 and April 2014. Retrospectively evaluated pathological specimen reports identified 464 patients with CN and 25 patients with AGC.
Male patients had a significantly higher incidence of AGC than CN (56% vs. 26%; P≤ .05), whereas women were less likely to have AGC (44% vs. 74%; NS), Ms. Bourikian and her colleagues at Virginia Commonwealth University in Richmond wrote.
Previous studies also have shown that acute cholecystitis is more common in men and patients over the age of 50 years.
Notably, lactate, obesity, and systolic blood pressure below 100 mm Hg were not different between groups.
As expected, patients with AGC were significantly more likely to die than their counterparts with cholecystitis without necrosis (16% vs. 0.86%; P≤ .05), the authors reported.
People with diabetes with AGC were almost five times more likely to die than were diabetics with CN (32% vs. 6.7%; P≤ .05). according to the authors.
Mortality, however, was nearly identical between AGC and CN patients with a systolic BP ≤ 100 mm Hg (0% vs. 0.02%; NS).
Logistic regression analysis showed that increased age (P≤ .001) and male gender (P≤ .05) were strongly associated with the development of AGC. The failure of more risk factors to pan out in logistic regression is likely because of the small number of patients with gangrenous cholecystitis, senior author and colleague Dr. Paula Ferrada of Virginia Commonwealth University suggested.
“This is not a common disease,” she said in an interview. “That’s why it’s so hard to diagnose and triage. Clinicians need to have a higher suspicion” of AGC.
LAKE BUENA VISTA, FL. – Older age, diabetes, and elevated bilirubin were significant risk factors for acute gangrenous cholecystitis in a retrospective study of 489 patients undergoing cholecystectomy.
Patients with acute gangrenous cholecystitis (AGC) were on average 15 years older than those with cholecystitis without necrosis (CN) were (55.8 vs. 40.8 years; P value ≤ .001), almost five times more likely to have comorbid diabetes (32% vs. 6.7%; P≤ .05), and had significantly higher bilirubin levels (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
The findings are consistent with previous studies showing that all three risk factors are strongly associated with gangrenous cholecystitis, Seda Bourikian reported at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
“Future studies may explore how the pathophysiology of diabetes, or the duration of illness in each patient, plays a role in the development of AGC,” the authors suggested in the poster presentation.
The chart review included 489 patients admitted to an emergency general surgery service who underwent cholecystectomy between January 2009 and April 2014. Retrospectively evaluated pathological specimen reports identified 464 patients with CN and 25 patients with AGC.
Male patients had a significantly higher incidence of AGC than CN (56% vs. 26%; P≤ .05), whereas women were less likely to have AGC (44% vs. 74%; NS), Ms. Bourikian and her colleagues at Virginia Commonwealth University in Richmond wrote.
Previous studies also have shown that acute cholecystitis is more common in men and patients over the age of 50 years.
Notably, lactate, obesity, and systolic blood pressure below 100 mm Hg were not different between groups.
As expected, patients with AGC were significantly more likely to die than their counterparts with cholecystitis without necrosis (16% vs. 0.86%; P≤ .05), the authors reported.
People with diabetes with AGC were almost five times more likely to die than were diabetics with CN (32% vs. 6.7%; P≤ .05). according to the authors.
Mortality, however, was nearly identical between AGC and CN patients with a systolic BP ≤ 100 mm Hg (0% vs. 0.02%; NS).
Logistic regression analysis showed that increased age (P≤ .001) and male gender (P≤ .05) were strongly associated with the development of AGC. The failure of more risk factors to pan out in logistic regression is likely because of the small number of patients with gangrenous cholecystitis, senior author and colleague Dr. Paula Ferrada of Virginia Commonwealth University suggested.
“This is not a common disease,” she said in an interview. “That’s why it’s so hard to diagnose and triage. Clinicians need to have a higher suspicion” of AGC.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: Older age, diabetes and elevated bilirubin were risk factors for acute gangrenous cholecystitis.
Major finding: Patients with acute gangrenous cholecystitis vs. cholecystitis without necrosis were older (55.8 vs. 40.8 years; P value ≤ .001), more likely to have diabetes (32% vs. 6.7%; P≤ .05) and an elevated bilirubin (1.96 mg/dL vs. 0.89 mg/dL; P≤ .001).
Data source: Retrospective analysis of 489 patients undergoing cholecystectomy.
Disclosures: The authors reported having no relevant financial disclosures.
Medicare now covers low-dose CT screen for lung cancer
Effective immediately, Medicare will cover annual lung cancer screening with low-dose CT for certain beneficiaries, according to a Feb. 5 national coverage determination.
To qualify, beneficiaries must be 55-77 years old, have a smoking history of at least a 30 pack-years, exhibit no signs or symptoms of lung cancer, and currently smoke or have quit within 15 years. They also must have a written screening order from their provider.
Coverage includes a counseling visit for shared decision-making, so patients know beforehand the “benefits and harms of screening, follow-up diagnostic testing, over-diagnosis, false positive[s], and total radiation exposure,” among other things, according to the decision memo from the Centers for Medicare & Medicaid Services.
Imaging centers are required to collect data on each screening and submit it to a CMS-approved registry.
The decision has been in the works for a while. In 2011, the National Cancer Institute–sponsored National Lung Screening Trial (NLST) showed that people aged 55-74 years with a history of heavy smoking are 20% less likely to die from lung cancer if they are screened with low-dose helical CT instead of standard chest x-ray (N. Engl. J. Med. 2011;365:395-409). Previous studies had shown that screening with standard chest x-rays does not reduce mortality from lung cancer.
Results from NLST and other studies prompted the U.S. Preventive Services Task Force in 2013 to recommend annual low-dose CT screening for adults aged 55-80 years with a 30 pack-year history; the recommendation in turn led to formal requests to CMS for coverage. In proposing coverage, the task force received almost 500 public comments “generally supportive of [expanding] Medicare coverage to include lung cancer screening,” it said.
Low-dose CT is performed at acquisition settings to minimize radiation exposure. For lung cancer screening, CMS is requiring a volumetric CT dose index (CTDIvol) of ≤ 3.0 mGy for standard-size patients – defined to be 5 feet 7 inches tall and approximately 155 pounds – with appropriate reductions or increases for smaller or larger patients.
Effective immediately, Medicare will cover annual lung cancer screening with low-dose CT for certain beneficiaries, according to a Feb. 5 national coverage determination.
To qualify, beneficiaries must be 55-77 years old, have a smoking history of at least a 30 pack-years, exhibit no signs or symptoms of lung cancer, and currently smoke or have quit within 15 years. They also must have a written screening order from their provider.
Coverage includes a counseling visit for shared decision-making, so patients know beforehand the “benefits and harms of screening, follow-up diagnostic testing, over-diagnosis, false positive[s], and total radiation exposure,” among other things, according to the decision memo from the Centers for Medicare & Medicaid Services.
Imaging centers are required to collect data on each screening and submit it to a CMS-approved registry.
The decision has been in the works for a while. In 2011, the National Cancer Institute–sponsored National Lung Screening Trial (NLST) showed that people aged 55-74 years with a history of heavy smoking are 20% less likely to die from lung cancer if they are screened with low-dose helical CT instead of standard chest x-ray (N. Engl. J. Med. 2011;365:395-409). Previous studies had shown that screening with standard chest x-rays does not reduce mortality from lung cancer.
Results from NLST and other studies prompted the U.S. Preventive Services Task Force in 2013 to recommend annual low-dose CT screening for adults aged 55-80 years with a 30 pack-year history; the recommendation in turn led to formal requests to CMS for coverage. In proposing coverage, the task force received almost 500 public comments “generally supportive of [expanding] Medicare coverage to include lung cancer screening,” it said.
Low-dose CT is performed at acquisition settings to minimize radiation exposure. For lung cancer screening, CMS is requiring a volumetric CT dose index (CTDIvol) of ≤ 3.0 mGy for standard-size patients – defined to be 5 feet 7 inches tall and approximately 155 pounds – with appropriate reductions or increases for smaller or larger patients.
Effective immediately, Medicare will cover annual lung cancer screening with low-dose CT for certain beneficiaries, according to a Feb. 5 national coverage determination.
To qualify, beneficiaries must be 55-77 years old, have a smoking history of at least a 30 pack-years, exhibit no signs or symptoms of lung cancer, and currently smoke or have quit within 15 years. They also must have a written screening order from their provider.
Coverage includes a counseling visit for shared decision-making, so patients know beforehand the “benefits and harms of screening, follow-up diagnostic testing, over-diagnosis, false positive[s], and total radiation exposure,” among other things, according to the decision memo from the Centers for Medicare & Medicaid Services.
Imaging centers are required to collect data on each screening and submit it to a CMS-approved registry.
The decision has been in the works for a while. In 2011, the National Cancer Institute–sponsored National Lung Screening Trial (NLST) showed that people aged 55-74 years with a history of heavy smoking are 20% less likely to die from lung cancer if they are screened with low-dose helical CT instead of standard chest x-ray (N. Engl. J. Med. 2011;365:395-409). Previous studies had shown that screening with standard chest x-rays does not reduce mortality from lung cancer.
Results from NLST and other studies prompted the U.S. Preventive Services Task Force in 2013 to recommend annual low-dose CT screening for adults aged 55-80 years with a 30 pack-year history; the recommendation in turn led to formal requests to CMS for coverage. In proposing coverage, the task force received almost 500 public comments “generally supportive of [expanding] Medicare coverage to include lung cancer screening,” it said.
Low-dose CT is performed at acquisition settings to minimize radiation exposure. For lung cancer screening, CMS is requiring a volumetric CT dose index (CTDIvol) of ≤ 3.0 mGy for standard-size patients – defined to be 5 feet 7 inches tall and approximately 155 pounds – with appropriate reductions or increases for smaller or larger patients.
GOP lawmakers offer ACA alternative that includes tort reform
Three Republican lawmakers are proposing an alternative to the Affordable Care Act that would undo the controversial individual and employer mandates, cap medical liability damages, and offer a slimmed-down set of consumer insurance protections.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee; Rep. Fred Upton (R-Mich.), chairman of the House Energy and Commerce Committee; and Sen. Richard Burr (R-N.C.), a member of the Senate Finance Committee, proposed on Feb. 5 the Patient Choice, Affordability, Responsibility, and Empowerment (CARE) Act to repeal and replace the current health law.
“Our nation’s health care system was broken before Obamacare, and the President’s health care debacle has only made things worse,” Sen. Burr said in a statement. “The Patient CARE Act repeals Obamacare and addresses the fundamental cost drivers that Obamacare failed to address. We can lower costs and expand access to quality coverage and care by empowering individuals and their families to make their own health care decisions, rather than having the federal government make those decisions for them.”
The proposal – which came in the form of a 9-page outline – was unveiled just days after the House passed a bill to repeal the ACA by a vote of 239 to 186. While the House has voted numerous times to repeal the health law, this is the first time that the bill might actually be considered in the Senate, since control of that chamber has shifted to the Republicans.
Sen. Hatch and other GOP lawmakers offered a similar replacement proposal last year.
The Patient CARE Act outlines some federal medical liability reforms, including a cap on noneconomic damages and limits on attorneys’ fees. It also seeks to encourage new models for resolving disputes on the state level, such as expert panels to evaluate injury claims and administrative health courts.
The proposal offers a more limited range of consumer insurance protections than does the ACA, including:
• Adopting an age rating ratio of 5-1 for premiums, which would limit plans from charging older individuals any more than five times what a younger person pays. Under the ACA, the age rating ratio is 3-1.
• Banning the use of lifetime dollar limits on health coverage.
• Allowing states to opt out of the ACA’s dependent coverage provision, which lets younger adults stay on their parents’ health plans up to age 26.
• Providing guaranteed renewability of health plans regardless of an individual’s health status. Health plans would be able to cancel coverage only in cases of fraud, misrepresentation by a consumer, or failure to pay premiums.
• Banning denials of coverage based on preexisting medical conditions as long as the individual has been continuously covered with at least a catastrophic plan for 18 months. The proposal includes a one-time open enrollment for people currently uninsured.
The Patient CARE Act would provide federal tax subsidies to purchase insurance to individuals with annual incomes of up to 300% of the federal poverty level. The amount of the tax credit would decrease between 200% and 300% percent of poverty and would be age-adjusted with older individuals receiving a larger subsidy.
The proposal would change the tax treatment of employer-sponsored health insurance by capping the tax exclusion for health benefits at $12,000 for individuals and $30,000 for families. That means that workers would pay federal income taxes on benefits above those thresholds.
Within the Medicaid program, the Patient CARE Act seeks to provide states with a capped amount of federal funds that would “follow the patient” based on health status, age, and life circumstances. Some Medicaid participants would also have the option of using their federal tax credits to purchase private coverage.
On Twitter @maryellenny
Dr. Michael Nelson, FCCP, comments: With a new Congress controlled by Republicans, and given the prior attempts to overturn the Patient Protection and Affordable Care Act (a.k.a. "Obamacare"), it is not surprising that early in this legislative session an alternative plan has been proposed. One could argue some of the points of the proposal but not the accuracy of the statement made by one of the bills authors that "our nation's health care system was broken before Obamacare."
While this bill does address some issues of importance to physicians, it is certainly disappointing that this bill does not address the Sustainable Growth Rate formula (SGR). This looming threat of a 20% or more cut in physician reimbursement will do more harm to patient access and care than any other aspect addressed in this bill. Unfortunately, physicians rarely advocate at the federal level for themselves or their patients. Perhaps, with the introduction of this bill, it is the time to start.
Dr. Michael Nelson, FCCP, comments: With a new Congress controlled by Republicans, and given the prior attempts to overturn the Patient Protection and Affordable Care Act (a.k.a. "Obamacare"), it is not surprising that early in this legislative session an alternative plan has been proposed. One could argue some of the points of the proposal but not the accuracy of the statement made by one of the bills authors that "our nation's health care system was broken before Obamacare."
While this bill does address some issues of importance to physicians, it is certainly disappointing that this bill does not address the Sustainable Growth Rate formula (SGR). This looming threat of a 20% or more cut in physician reimbursement will do more harm to patient access and care than any other aspect addressed in this bill. Unfortunately, physicians rarely advocate at the federal level for themselves or their patients. Perhaps, with the introduction of this bill, it is the time to start.
Dr. Michael Nelson, FCCP, comments: With a new Congress controlled by Republicans, and given the prior attempts to overturn the Patient Protection and Affordable Care Act (a.k.a. "Obamacare"), it is not surprising that early in this legislative session an alternative plan has been proposed. One could argue some of the points of the proposal but not the accuracy of the statement made by one of the bills authors that "our nation's health care system was broken before Obamacare."
While this bill does address some issues of importance to physicians, it is certainly disappointing that this bill does not address the Sustainable Growth Rate formula (SGR). This looming threat of a 20% or more cut in physician reimbursement will do more harm to patient access and care than any other aspect addressed in this bill. Unfortunately, physicians rarely advocate at the federal level for themselves or their patients. Perhaps, with the introduction of this bill, it is the time to start.
Three Republican lawmakers are proposing an alternative to the Affordable Care Act that would undo the controversial individual and employer mandates, cap medical liability damages, and offer a slimmed-down set of consumer insurance protections.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee; Rep. Fred Upton (R-Mich.), chairman of the House Energy and Commerce Committee; and Sen. Richard Burr (R-N.C.), a member of the Senate Finance Committee, proposed on Feb. 5 the Patient Choice, Affordability, Responsibility, and Empowerment (CARE) Act to repeal and replace the current health law.
“Our nation’s health care system was broken before Obamacare, and the President’s health care debacle has only made things worse,” Sen. Burr said in a statement. “The Patient CARE Act repeals Obamacare and addresses the fundamental cost drivers that Obamacare failed to address. We can lower costs and expand access to quality coverage and care by empowering individuals and their families to make their own health care decisions, rather than having the federal government make those decisions for them.”
The proposal – which came in the form of a 9-page outline – was unveiled just days after the House passed a bill to repeal the ACA by a vote of 239 to 186. While the House has voted numerous times to repeal the health law, this is the first time that the bill might actually be considered in the Senate, since control of that chamber has shifted to the Republicans.
Sen. Hatch and other GOP lawmakers offered a similar replacement proposal last year.
The Patient CARE Act outlines some federal medical liability reforms, including a cap on noneconomic damages and limits on attorneys’ fees. It also seeks to encourage new models for resolving disputes on the state level, such as expert panels to evaluate injury claims and administrative health courts.
The proposal offers a more limited range of consumer insurance protections than does the ACA, including:
• Adopting an age rating ratio of 5-1 for premiums, which would limit plans from charging older individuals any more than five times what a younger person pays. Under the ACA, the age rating ratio is 3-1.
• Banning the use of lifetime dollar limits on health coverage.
• Allowing states to opt out of the ACA’s dependent coverage provision, which lets younger adults stay on their parents’ health plans up to age 26.
• Providing guaranteed renewability of health plans regardless of an individual’s health status. Health plans would be able to cancel coverage only in cases of fraud, misrepresentation by a consumer, or failure to pay premiums.
• Banning denials of coverage based on preexisting medical conditions as long as the individual has been continuously covered with at least a catastrophic plan for 18 months. The proposal includes a one-time open enrollment for people currently uninsured.
The Patient CARE Act would provide federal tax subsidies to purchase insurance to individuals with annual incomes of up to 300% of the federal poverty level. The amount of the tax credit would decrease between 200% and 300% percent of poverty and would be age-adjusted with older individuals receiving a larger subsidy.
The proposal would change the tax treatment of employer-sponsored health insurance by capping the tax exclusion for health benefits at $12,000 for individuals and $30,000 for families. That means that workers would pay federal income taxes on benefits above those thresholds.
Within the Medicaid program, the Patient CARE Act seeks to provide states with a capped amount of federal funds that would “follow the patient” based on health status, age, and life circumstances. Some Medicaid participants would also have the option of using their federal tax credits to purchase private coverage.
On Twitter @maryellenny
Three Republican lawmakers are proposing an alternative to the Affordable Care Act that would undo the controversial individual and employer mandates, cap medical liability damages, and offer a slimmed-down set of consumer insurance protections.
Sen. Orrin Hatch (R-Utah), chairman of the Senate Finance Committee; Rep. Fred Upton (R-Mich.), chairman of the House Energy and Commerce Committee; and Sen. Richard Burr (R-N.C.), a member of the Senate Finance Committee, proposed on Feb. 5 the Patient Choice, Affordability, Responsibility, and Empowerment (CARE) Act to repeal and replace the current health law.
“Our nation’s health care system was broken before Obamacare, and the President’s health care debacle has only made things worse,” Sen. Burr said in a statement. “The Patient CARE Act repeals Obamacare and addresses the fundamental cost drivers that Obamacare failed to address. We can lower costs and expand access to quality coverage and care by empowering individuals and their families to make their own health care decisions, rather than having the federal government make those decisions for them.”
The proposal – which came in the form of a 9-page outline – was unveiled just days after the House passed a bill to repeal the ACA by a vote of 239 to 186. While the House has voted numerous times to repeal the health law, this is the first time that the bill might actually be considered in the Senate, since control of that chamber has shifted to the Republicans.
Sen. Hatch and other GOP lawmakers offered a similar replacement proposal last year.
The Patient CARE Act outlines some federal medical liability reforms, including a cap on noneconomic damages and limits on attorneys’ fees. It also seeks to encourage new models for resolving disputes on the state level, such as expert panels to evaluate injury claims and administrative health courts.
The proposal offers a more limited range of consumer insurance protections than does the ACA, including:
• Adopting an age rating ratio of 5-1 for premiums, which would limit plans from charging older individuals any more than five times what a younger person pays. Under the ACA, the age rating ratio is 3-1.
• Banning the use of lifetime dollar limits on health coverage.
• Allowing states to opt out of the ACA’s dependent coverage provision, which lets younger adults stay on their parents’ health plans up to age 26.
• Providing guaranteed renewability of health plans regardless of an individual’s health status. Health plans would be able to cancel coverage only in cases of fraud, misrepresentation by a consumer, or failure to pay premiums.
• Banning denials of coverage based on preexisting medical conditions as long as the individual has been continuously covered with at least a catastrophic plan for 18 months. The proposal includes a one-time open enrollment for people currently uninsured.
The Patient CARE Act would provide federal tax subsidies to purchase insurance to individuals with annual incomes of up to 300% of the federal poverty level. The amount of the tax credit would decrease between 200% and 300% percent of poverty and would be age-adjusted with older individuals receiving a larger subsidy.
The proposal would change the tax treatment of employer-sponsored health insurance by capping the tax exclusion for health benefits at $12,000 for individuals and $30,000 for families. That means that workers would pay federal income taxes on benefits above those thresholds.
Within the Medicaid program, the Patient CARE Act seeks to provide states with a capped amount of federal funds that would “follow the patient” based on health status, age, and life circumstances. Some Medicaid participants would also have the option of using their federal tax credits to purchase private coverage.
On Twitter @maryellenny