User login
After POEM, FLIP matches HRM for measuring patient response
LAS VEGAS – Functional lumen imaging probe (FLIP) was equivalent to high-resolution manometry (HRM) in predicting clinical response by Eckardt score 6 months or more after per oral endoscopic myotomy (POEM) for achalasia or esophagogastric junction (EGJ) outlet obstruction (EGJOO).
Measures for clinical response following lower esophageal sphincter myotomy procedures include Eckardt Score, timed barium esophagram, HRM, and FLIP. However, since FLIP is a relatively new technique, there are few clinical data comparing its efficacy versus HRM in patients who have a positive response to POEM measured by the Eckardt score, according to John DeWitt, MD, who presented the research at the annual meeting of the American College of Gastroenterology.
FLIP can be performed during a follow-up endoscopy while a patient is sedated, while HRM requires the patient to be awake. Some patients find the procedure intolerable, and Dr. DeWitt estimates that 10%-20% of patients don’t return for follow-up assessments because of the discomfort.
“[FLIP] is a relatively new technology, the role of which is still being discovered. We have a lot more information on the diagnosis side of things. The role in follow-up, particularly after myotomy, is really not defined well. This is the first study to my knowledge that has evaluated manometry and FLIP head-to-head to compare patient-reported outcomes,” said Dr. DeWitt in an interview. He is a professor of medicine and the director of endoscopic ultrasound at Indiana University Medical Center, in Indianapolis.
Going head-to-head
The researchers conducted a retrospective, single-center study of 265 consecutive patients who underwent POEM for achalasia or EGJOO from 2016 through 2020. A clinical response was defined as an Eckardt score ≤3, EGJ distensibility index (EGJ-DI) higher than 2.8 mm2/mm Hg, maximum integrated relaxation pressure (IRP) <15 mm Hg, or a maximum EGJ diameter greater than 14 mm at any balloon distension.
In all, 126 patients returned for follow-up and completed an upper endoscopy with FLIP, HRM, and Eckardt scores within a 6-12 month period after the POEM procedure.
With respect to HRM, an IRP measurement <15 mm Hg predicted post-POEM Eckardt score with a sensitivity of 86.7% (95% confidence interval, 79.3-92.2) and a specificity of 33.3% (95% CI, 4.3-77.7), with an area under the curve of 0.60 (95% CI, 0.39-0.81). A maximum EJG diameter ≥ 14 mm had a sensitivity of 77.5% (95% CI, 69.0-84.6) and a specificity of 33.3% (95% CI, 4.3-77.7), with an AUC of 0.55 (95% CI, 0.34-0.76).
The performance was similar with FLIP: EGJ-DI > 2.8 mm2/mm Hg at any balloon setting had a sensitivity of 95.0% (95% CI, 89.4-98.1) and a specificity% of 0.0, and an AUC of 0.53 (95% CI, 0.51-0.55). A similar measurement at 40 mL or 50 mL distension had a sensitivity of 93.3% (95% CI, 87.3-97.1) and a specificity of 16.7% (95% CI, 0.4-64.1), with an AUC of 0.55 (95% CI, 0.39-0.72). Receiver operator characteristic analysis showed no significant difference between ability of FLIP and HRM to predict a normal Eckardt score.
If the study is repeated in other patient populations, Dr. DeWitt hopes that it could eliminate manometry altogether in a large majority of patients. “That would be potentially a game changer for bringing patients back to see how well they’re doing,” said Dr. DeWitt.
Not all patients who undergo POEM would be good candidates for FLIP, said Dr. DeWitt. The study was limited to patients with hypertension in the lower esophageal sphincter. Other disorders such as diffuse esophageal spasm, jackhammer esophagus, and type III achalasia would not likely be candidates for FLIP. “Those patients are going to probably still need manometry because if the esophageal body abnormalities are still present, then repeat testing might need to be performed,” said Dr. DeWitt. Still, he estimated about 80% of patients could be eligible for FLIP instead.
Impact on patients
“I think it’s interesting new data,” said Patrick Young, MD, who comoderated the session where the research was presented. He noted that the treatment of achalasia is evolving away from surgery, and the techniques to measure response are evolving along with it. “As we progress in that technology and using that procedure, we need to understand better how to follow those people up. I think adding this new device may help us to understand who’s going to respond well, and who’s not going to respond well. This is an early investigation, so I think we’ll need to do trials, but I think this is a good first step,” said Dr. Young, who is a professor of medicine at the Uniformed Services University of the Health Sciences, Bethesda, Md.
Comoderator Mohammad Yaghoobi, MD, also praised the study, but noted that the cost of FLIP could be a concern. “We want to have a reasonable ratio of the cost versus the effectiveness,” said Dr. Yaghoobi, who is an associate professor of medicine at McMaster University in Hamilton, Ont.
Dr. DeWitt, Dr. Young, and Dr. Yaghoobi had no relevant disclosures.
LAS VEGAS – Functional lumen imaging probe (FLIP) was equivalent to high-resolution manometry (HRM) in predicting clinical response by Eckardt score 6 months or more after per oral endoscopic myotomy (POEM) for achalasia or esophagogastric junction (EGJ) outlet obstruction (EGJOO).
Measures for clinical response following lower esophageal sphincter myotomy procedures include Eckardt Score, timed barium esophagram, HRM, and FLIP. However, since FLIP is a relatively new technique, there are few clinical data comparing its efficacy versus HRM in patients who have a positive response to POEM measured by the Eckardt score, according to John DeWitt, MD, who presented the research at the annual meeting of the American College of Gastroenterology.
FLIP can be performed during a follow-up endoscopy while a patient is sedated, while HRM requires the patient to be awake. Some patients find the procedure intolerable, and Dr. DeWitt estimates that 10%-20% of patients don’t return for follow-up assessments because of the discomfort.
“[FLIP] is a relatively new technology, the role of which is still being discovered. We have a lot more information on the diagnosis side of things. The role in follow-up, particularly after myotomy, is really not defined well. This is the first study to my knowledge that has evaluated manometry and FLIP head-to-head to compare patient-reported outcomes,” said Dr. DeWitt in an interview. He is a professor of medicine and the director of endoscopic ultrasound at Indiana University Medical Center, in Indianapolis.
Going head-to-head
The researchers conducted a retrospective, single-center study of 265 consecutive patients who underwent POEM for achalasia or EGJOO from 2016 through 2020. A clinical response was defined as an Eckardt score ≤3, EGJ distensibility index (EGJ-DI) higher than 2.8 mm2/mm Hg, maximum integrated relaxation pressure (IRP) <15 mm Hg, or a maximum EGJ diameter greater than 14 mm at any balloon distension.
In all, 126 patients returned for follow-up and completed an upper endoscopy with FLIP, HRM, and Eckardt scores within a 6-12 month period after the POEM procedure.
With respect to HRM, an IRP measurement <15 mm Hg predicted post-POEM Eckardt score with a sensitivity of 86.7% (95% confidence interval, 79.3-92.2) and a specificity of 33.3% (95% CI, 4.3-77.7), with an area under the curve of 0.60 (95% CI, 0.39-0.81). A maximum EJG diameter ≥ 14 mm had a sensitivity of 77.5% (95% CI, 69.0-84.6) and a specificity of 33.3% (95% CI, 4.3-77.7), with an AUC of 0.55 (95% CI, 0.34-0.76).
The performance was similar with FLIP: EGJ-DI > 2.8 mm2/mm Hg at any balloon setting had a sensitivity of 95.0% (95% CI, 89.4-98.1) and a specificity% of 0.0, and an AUC of 0.53 (95% CI, 0.51-0.55). A similar measurement at 40 mL or 50 mL distension had a sensitivity of 93.3% (95% CI, 87.3-97.1) and a specificity of 16.7% (95% CI, 0.4-64.1), with an AUC of 0.55 (95% CI, 0.39-0.72). Receiver operator characteristic analysis showed no significant difference between ability of FLIP and HRM to predict a normal Eckardt score.
If the study is repeated in other patient populations, Dr. DeWitt hopes that it could eliminate manometry altogether in a large majority of patients. “That would be potentially a game changer for bringing patients back to see how well they’re doing,” said Dr. DeWitt.
Not all patients who undergo POEM would be good candidates for FLIP, said Dr. DeWitt. The study was limited to patients with hypertension in the lower esophageal sphincter. Other disorders such as diffuse esophageal spasm, jackhammer esophagus, and type III achalasia would not likely be candidates for FLIP. “Those patients are going to probably still need manometry because if the esophageal body abnormalities are still present, then repeat testing might need to be performed,” said Dr. DeWitt. Still, he estimated about 80% of patients could be eligible for FLIP instead.
Impact on patients
“I think it’s interesting new data,” said Patrick Young, MD, who comoderated the session where the research was presented. He noted that the treatment of achalasia is evolving away from surgery, and the techniques to measure response are evolving along with it. “As we progress in that technology and using that procedure, we need to understand better how to follow those people up. I think adding this new device may help us to understand who’s going to respond well, and who’s not going to respond well. This is an early investigation, so I think we’ll need to do trials, but I think this is a good first step,” said Dr. Young, who is a professor of medicine at the Uniformed Services University of the Health Sciences, Bethesda, Md.
Comoderator Mohammad Yaghoobi, MD, also praised the study, but noted that the cost of FLIP could be a concern. “We want to have a reasonable ratio of the cost versus the effectiveness,” said Dr. Yaghoobi, who is an associate professor of medicine at McMaster University in Hamilton, Ont.
Dr. DeWitt, Dr. Young, and Dr. Yaghoobi had no relevant disclosures.
LAS VEGAS – Functional lumen imaging probe (FLIP) was equivalent to high-resolution manometry (HRM) in predicting clinical response by Eckardt score 6 months or more after per oral endoscopic myotomy (POEM) for achalasia or esophagogastric junction (EGJ) outlet obstruction (EGJOO).
Measures for clinical response following lower esophageal sphincter myotomy procedures include Eckardt Score, timed barium esophagram, HRM, and FLIP. However, since FLIP is a relatively new technique, there are few clinical data comparing its efficacy versus HRM in patients who have a positive response to POEM measured by the Eckardt score, according to John DeWitt, MD, who presented the research at the annual meeting of the American College of Gastroenterology.
FLIP can be performed during a follow-up endoscopy while a patient is sedated, while HRM requires the patient to be awake. Some patients find the procedure intolerable, and Dr. DeWitt estimates that 10%-20% of patients don’t return for follow-up assessments because of the discomfort.
“[FLIP] is a relatively new technology, the role of which is still being discovered. We have a lot more information on the diagnosis side of things. The role in follow-up, particularly after myotomy, is really not defined well. This is the first study to my knowledge that has evaluated manometry and FLIP head-to-head to compare patient-reported outcomes,” said Dr. DeWitt in an interview. He is a professor of medicine and the director of endoscopic ultrasound at Indiana University Medical Center, in Indianapolis.
Going head-to-head
The researchers conducted a retrospective, single-center study of 265 consecutive patients who underwent POEM for achalasia or EGJOO from 2016 through 2020. A clinical response was defined as an Eckardt score ≤3, EGJ distensibility index (EGJ-DI) higher than 2.8 mm2/mm Hg, maximum integrated relaxation pressure (IRP) <15 mm Hg, or a maximum EGJ diameter greater than 14 mm at any balloon distension.
In all, 126 patients returned for follow-up and completed an upper endoscopy with FLIP, HRM, and Eckardt scores within a 6-12 month period after the POEM procedure.
With respect to HRM, an IRP measurement <15 mm Hg predicted post-POEM Eckardt score with a sensitivity of 86.7% (95% confidence interval, 79.3-92.2) and a specificity of 33.3% (95% CI, 4.3-77.7), with an area under the curve of 0.60 (95% CI, 0.39-0.81). A maximum EJG diameter ≥ 14 mm had a sensitivity of 77.5% (95% CI, 69.0-84.6) and a specificity of 33.3% (95% CI, 4.3-77.7), with an AUC of 0.55 (95% CI, 0.34-0.76).
The performance was similar with FLIP: EGJ-DI > 2.8 mm2/mm Hg at any balloon setting had a sensitivity of 95.0% (95% CI, 89.4-98.1) and a specificity% of 0.0, and an AUC of 0.53 (95% CI, 0.51-0.55). A similar measurement at 40 mL or 50 mL distension had a sensitivity of 93.3% (95% CI, 87.3-97.1) and a specificity of 16.7% (95% CI, 0.4-64.1), with an AUC of 0.55 (95% CI, 0.39-0.72). Receiver operator characteristic analysis showed no significant difference between ability of FLIP and HRM to predict a normal Eckardt score.
If the study is repeated in other patient populations, Dr. DeWitt hopes that it could eliminate manometry altogether in a large majority of patients. “That would be potentially a game changer for bringing patients back to see how well they’re doing,” said Dr. DeWitt.
Not all patients who undergo POEM would be good candidates for FLIP, said Dr. DeWitt. The study was limited to patients with hypertension in the lower esophageal sphincter. Other disorders such as diffuse esophageal spasm, jackhammer esophagus, and type III achalasia would not likely be candidates for FLIP. “Those patients are going to probably still need manometry because if the esophageal body abnormalities are still present, then repeat testing might need to be performed,” said Dr. DeWitt. Still, he estimated about 80% of patients could be eligible for FLIP instead.
Impact on patients
“I think it’s interesting new data,” said Patrick Young, MD, who comoderated the session where the research was presented. He noted that the treatment of achalasia is evolving away from surgery, and the techniques to measure response are evolving along with it. “As we progress in that technology and using that procedure, we need to understand better how to follow those people up. I think adding this new device may help us to understand who’s going to respond well, and who’s not going to respond well. This is an early investigation, so I think we’ll need to do trials, but I think this is a good first step,” said Dr. Young, who is a professor of medicine at the Uniformed Services University of the Health Sciences, Bethesda, Md.
Comoderator Mohammad Yaghoobi, MD, also praised the study, but noted that the cost of FLIP could be a concern. “We want to have a reasonable ratio of the cost versus the effectiveness,” said Dr. Yaghoobi, who is an associate professor of medicine at McMaster University in Hamilton, Ont.
Dr. DeWitt, Dr. Young, and Dr. Yaghoobi had no relevant disclosures.
AT ACG 2021
Dupilumab shows long-term efficacy in EoE
LAS VEGAS –Data from the 28-week extension of the Liberty EoE TREET phase 3 clinical trial showed that the anti–interleukin-4/IL-13 antibody dupilumab led to long-term improvement in eosinophil count, histology, and patient-reported symptoms of eosinophilic esophagitis (EoE) out to 28 weeks. Dupilumab is Food and Drug Administration approved for the treatment of atopic dermatitis, asthma, and chronic rhinosinusitis with nasal polyposis.
Many patients don’t respond to the standard therapies of proton pump inhibitors, steroids, or diet. Some evidence suggests that EoE might be driven by type 2 inflammation, and dupilumab’s effect on the shared receptor of IL-4 and IL-13 directly counters that pathway.
“The current treatments are [proton pump inhibitors], steroids, or diet – a good proportion of patients don’t respond to them. And they’re also not targeted,” Evan Dellon, MD, professor of medicine and epidemiology at the University of North Carolina at Chapel Hill, said in an interview. Dr. Dellon presented the research at the annual meeting of the American College of Gastroenterology.
“The bottom line is that people who responded up front to dupilumab maintain that response to a year, and the people on placebo gained a similar response as the people who were treated. It looked good. It was histologic, symptomatic, and endoscopic outcomes,” said Dr. Dellon.
Many of the patients in the new study were steroid refractory, making it a difficult population to treat, according to Dr. Dellon. “You can’t compare to the steroid-treated patients, but the 6-month data showed about a 60% response rate histologically, which is right up there with where steroids and diet are for easier to treat patients. So the fact that it’s a harder to treat cohort is pretty impressive from that standpoint,” said Dr. Dellon.
Data from the first 24 weeks was previously reported at UEG Week 2020 and showed that dupilumab outperformed placebo in EoE patients aged 12 years and older, with dupilumab producing better outcomes in peak esophageal intraepithelial eosinophil count and change in Dysphagia Symptom Questionnaire (DSQ) Score at 24 weeks.
At ACG 2021, Dr. Dellon reported on 52-week results, where all patients from both treated and placebo groups received dupilumab after the initial 24-week phase. Dupilumab reduced dysphagia symptoms as measured by the absolute change in DSQ score at 24 weeks (–21.9 vs. –9.6; P < .001). At 52 weeks, the dupilumab group showed a change of –23.4 from the start of the study, and the placebo-to-dupilumab group had a DSQ score change of –21.7. Dupilumab also led to a greater percentage reduction in DSQ score by 24 weeks (69.2% versus 31.7%; P < .001); at 52 weeks, the dupilumab group had a 75.9% reduction and the placebo-to-dupilumab group had a 65.9% reduction (no significant difference).
The dupilumab group had a greater proportion of patients who achieved peak esophageal eosinophil count of 6 eosinophils or less per high power field at 24 weeks (59.5% vs. 5.1%); at 52 weeks, 55.9% had achieved this measure, versus 60.0% of the placebo-to-dupilumab group. At 24 weeks, the dupilumab group had a 71.2% reduction in peak eosinophil count from baseline versus –3.0% in placebo (P < .001). At week 52, the reductions were 88.6% and 83.8%, respectively.
Histology features were improved with dupilumab. At week 24, the absolute change in histology scoring system mean grade score (histologic severity) from initial baseline was greater in the dupilumab group (least squares mean, –0.761 vs. –0.001; P < .001). The improvement continued at week 52 (LS mean, –0.87) and occurred in the placebo-to-dupilumab group (LS mean, –0.87). The dupilumab group had a greater absolute change in mean stage score at 24 weeks (histologic extent, LS mean, –0.753 vs. –0.012; P < .001) and 52 weeks (LS mean, –0.89), while the placebo-to-dupilumab group achieved a similar change at 52 weeks (LS mean, –0.87).
Endoscopic features improved in the dupilumab group as measured by endoscopic reference score at 24 weeks (LS mean, –3.2 versus –0.3; P <.001) and at 52 weeks (LS mean, –4.1). The placebo-to-dupilumab group had a similar outcome at 52 weeks (LS mean, –3.9).
Dupilumab was well tolerated, with the only significant difference in treatment-emergent adverse events being injection-site reactions and injection-site erythema.
“I thought the data was really impressive and compelling,” said Amy Oxentenko, MD, chair of medicine at the Mayo Clinic in Phoenix, who comoderated the session. “It’d be nice to have something like this that is a targeted therapy that clearly shows improvement in not only some of the symptoms and histology, but also having an impact possibly on that fibrotic piece, which I think is really the area of morbidity in these patients long term.”
If approved, dupilumab could improve compliance among patients, who sometimes struggle with taking topical steroids properly, said comoderator David Hass, MD, who is an associate clinical professor at Yale University, New Haven, Conn. He also agreed that the potential for remodeling would be a significant benefit over steroids.
One concern with dupilumab would be any potential for immune suppression. “It’s always something to think about,” Dr. Hass said.
LIBERTY EoE TREET was funded by Sanofi and Regeneron. Dr. Dellon has consulted and received research support from numerous pharmaceutical companies. Dr. Oxentenko and Dr. Hass have no relevant financial disclosures.
This article was updated Nov. 4, 2021.
LAS VEGAS –Data from the 28-week extension of the Liberty EoE TREET phase 3 clinical trial showed that the anti–interleukin-4/IL-13 antibody dupilumab led to long-term improvement in eosinophil count, histology, and patient-reported symptoms of eosinophilic esophagitis (EoE) out to 28 weeks. Dupilumab is Food and Drug Administration approved for the treatment of atopic dermatitis, asthma, and chronic rhinosinusitis with nasal polyposis.
Many patients don’t respond to the standard therapies of proton pump inhibitors, steroids, or diet. Some evidence suggests that EoE might be driven by type 2 inflammation, and dupilumab’s effect on the shared receptor of IL-4 and IL-13 directly counters that pathway.
“The current treatments are [proton pump inhibitors], steroids, or diet – a good proportion of patients don’t respond to them. And they’re also not targeted,” Evan Dellon, MD, professor of medicine and epidemiology at the University of North Carolina at Chapel Hill, said in an interview. Dr. Dellon presented the research at the annual meeting of the American College of Gastroenterology.
“The bottom line is that people who responded up front to dupilumab maintain that response to a year, and the people on placebo gained a similar response as the people who were treated. It looked good. It was histologic, symptomatic, and endoscopic outcomes,” said Dr. Dellon.
Many of the patients in the new study were steroid refractory, making it a difficult population to treat, according to Dr. Dellon. “You can’t compare to the steroid-treated patients, but the 6-month data showed about a 60% response rate histologically, which is right up there with where steroids and diet are for easier to treat patients. So the fact that it’s a harder to treat cohort is pretty impressive from that standpoint,” said Dr. Dellon.
Data from the first 24 weeks was previously reported at UEG Week 2020 and showed that dupilumab outperformed placebo in EoE patients aged 12 years and older, with dupilumab producing better outcomes in peak esophageal intraepithelial eosinophil count and change in Dysphagia Symptom Questionnaire (DSQ) Score at 24 weeks.
At ACG 2021, Dr. Dellon reported on 52-week results, where all patients from both treated and placebo groups received dupilumab after the initial 24-week phase. Dupilumab reduced dysphagia symptoms as measured by the absolute change in DSQ score at 24 weeks (–21.9 vs. –9.6; P < .001). At 52 weeks, the dupilumab group showed a change of –23.4 from the start of the study, and the placebo-to-dupilumab group had a DSQ score change of –21.7. Dupilumab also led to a greater percentage reduction in DSQ score by 24 weeks (69.2% versus 31.7%; P < .001); at 52 weeks, the dupilumab group had a 75.9% reduction and the placebo-to-dupilumab group had a 65.9% reduction (no significant difference).
The dupilumab group had a greater proportion of patients who achieved peak esophageal eosinophil count of 6 eosinophils or less per high power field at 24 weeks (59.5% vs. 5.1%); at 52 weeks, 55.9% had achieved this measure, versus 60.0% of the placebo-to-dupilumab group. At 24 weeks, the dupilumab group had a 71.2% reduction in peak eosinophil count from baseline versus –3.0% in placebo (P < .001). At week 52, the reductions were 88.6% and 83.8%, respectively.
Histology features were improved with dupilumab. At week 24, the absolute change in histology scoring system mean grade score (histologic severity) from initial baseline was greater in the dupilumab group (least squares mean, –0.761 vs. –0.001; P < .001). The improvement continued at week 52 (LS mean, –0.87) and occurred in the placebo-to-dupilumab group (LS mean, –0.87). The dupilumab group had a greater absolute change in mean stage score at 24 weeks (histologic extent, LS mean, –0.753 vs. –0.012; P < .001) and 52 weeks (LS mean, –0.89), while the placebo-to-dupilumab group achieved a similar change at 52 weeks (LS mean, –0.87).
Endoscopic features improved in the dupilumab group as measured by endoscopic reference score at 24 weeks (LS mean, –3.2 versus –0.3; P <.001) and at 52 weeks (LS mean, –4.1). The placebo-to-dupilumab group had a similar outcome at 52 weeks (LS mean, –3.9).
Dupilumab was well tolerated, with the only significant difference in treatment-emergent adverse events being injection-site reactions and injection-site erythema.
“I thought the data was really impressive and compelling,” said Amy Oxentenko, MD, chair of medicine at the Mayo Clinic in Phoenix, who comoderated the session. “It’d be nice to have something like this that is a targeted therapy that clearly shows improvement in not only some of the symptoms and histology, but also having an impact possibly on that fibrotic piece, which I think is really the area of morbidity in these patients long term.”
If approved, dupilumab could improve compliance among patients, who sometimes struggle with taking topical steroids properly, said comoderator David Hass, MD, who is an associate clinical professor at Yale University, New Haven, Conn. He also agreed that the potential for remodeling would be a significant benefit over steroids.
One concern with dupilumab would be any potential for immune suppression. “It’s always something to think about,” Dr. Hass said.
LIBERTY EoE TREET was funded by Sanofi and Regeneron. Dr. Dellon has consulted and received research support from numerous pharmaceutical companies. Dr. Oxentenko and Dr. Hass have no relevant financial disclosures.
This article was updated Nov. 4, 2021.
LAS VEGAS –Data from the 28-week extension of the Liberty EoE TREET phase 3 clinical trial showed that the anti–interleukin-4/IL-13 antibody dupilumab led to long-term improvement in eosinophil count, histology, and patient-reported symptoms of eosinophilic esophagitis (EoE) out to 28 weeks. Dupilumab is Food and Drug Administration approved for the treatment of atopic dermatitis, asthma, and chronic rhinosinusitis with nasal polyposis.
Many patients don’t respond to the standard therapies of proton pump inhibitors, steroids, or diet. Some evidence suggests that EoE might be driven by type 2 inflammation, and dupilumab’s effect on the shared receptor of IL-4 and IL-13 directly counters that pathway.
“The current treatments are [proton pump inhibitors], steroids, or diet – a good proportion of patients don’t respond to them. And they’re also not targeted,” Evan Dellon, MD, professor of medicine and epidemiology at the University of North Carolina at Chapel Hill, said in an interview. Dr. Dellon presented the research at the annual meeting of the American College of Gastroenterology.
“The bottom line is that people who responded up front to dupilumab maintain that response to a year, and the people on placebo gained a similar response as the people who were treated. It looked good. It was histologic, symptomatic, and endoscopic outcomes,” said Dr. Dellon.
Many of the patients in the new study were steroid refractory, making it a difficult population to treat, according to Dr. Dellon. “You can’t compare to the steroid-treated patients, but the 6-month data showed about a 60% response rate histologically, which is right up there with where steroids and diet are for easier to treat patients. So the fact that it’s a harder to treat cohort is pretty impressive from that standpoint,” said Dr. Dellon.
Data from the first 24 weeks was previously reported at UEG Week 2020 and showed that dupilumab outperformed placebo in EoE patients aged 12 years and older, with dupilumab producing better outcomes in peak esophageal intraepithelial eosinophil count and change in Dysphagia Symptom Questionnaire (DSQ) Score at 24 weeks.
At ACG 2021, Dr. Dellon reported on 52-week results, where all patients from both treated and placebo groups received dupilumab after the initial 24-week phase. Dupilumab reduced dysphagia symptoms as measured by the absolute change in DSQ score at 24 weeks (–21.9 vs. –9.6; P < .001). At 52 weeks, the dupilumab group showed a change of –23.4 from the start of the study, and the placebo-to-dupilumab group had a DSQ score change of –21.7. Dupilumab also led to a greater percentage reduction in DSQ score by 24 weeks (69.2% versus 31.7%; P < .001); at 52 weeks, the dupilumab group had a 75.9% reduction and the placebo-to-dupilumab group had a 65.9% reduction (no significant difference).
The dupilumab group had a greater proportion of patients who achieved peak esophageal eosinophil count of 6 eosinophils or less per high power field at 24 weeks (59.5% vs. 5.1%); at 52 weeks, 55.9% had achieved this measure, versus 60.0% of the placebo-to-dupilumab group. At 24 weeks, the dupilumab group had a 71.2% reduction in peak eosinophil count from baseline versus –3.0% in placebo (P < .001). At week 52, the reductions were 88.6% and 83.8%, respectively.
Histology features were improved with dupilumab. At week 24, the absolute change in histology scoring system mean grade score (histologic severity) from initial baseline was greater in the dupilumab group (least squares mean, –0.761 vs. –0.001; P < .001). The improvement continued at week 52 (LS mean, –0.87) and occurred in the placebo-to-dupilumab group (LS mean, –0.87). The dupilumab group had a greater absolute change in mean stage score at 24 weeks (histologic extent, LS mean, –0.753 vs. –0.012; P < .001) and 52 weeks (LS mean, –0.89), while the placebo-to-dupilumab group achieved a similar change at 52 weeks (LS mean, –0.87).
Endoscopic features improved in the dupilumab group as measured by endoscopic reference score at 24 weeks (LS mean, –3.2 versus –0.3; P <.001) and at 52 weeks (LS mean, –4.1). The placebo-to-dupilumab group had a similar outcome at 52 weeks (LS mean, –3.9).
Dupilumab was well tolerated, with the only significant difference in treatment-emergent adverse events being injection-site reactions and injection-site erythema.
“I thought the data was really impressive and compelling,” said Amy Oxentenko, MD, chair of medicine at the Mayo Clinic in Phoenix, who comoderated the session. “It’d be nice to have something like this that is a targeted therapy that clearly shows improvement in not only some of the symptoms and histology, but also having an impact possibly on that fibrotic piece, which I think is really the area of morbidity in these patients long term.”
If approved, dupilumab could improve compliance among patients, who sometimes struggle with taking topical steroids properly, said comoderator David Hass, MD, who is an associate clinical professor at Yale University, New Haven, Conn. He also agreed that the potential for remodeling would be a significant benefit over steroids.
One concern with dupilumab would be any potential for immune suppression. “It’s always something to think about,” Dr. Hass said.
LIBERTY EoE TREET was funded by Sanofi and Regeneron. Dr. Dellon has consulted and received research support from numerous pharmaceutical companies. Dr. Oxentenko and Dr. Hass have no relevant financial disclosures.
This article was updated Nov. 4, 2021.
AT AGC 2021
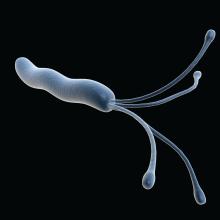
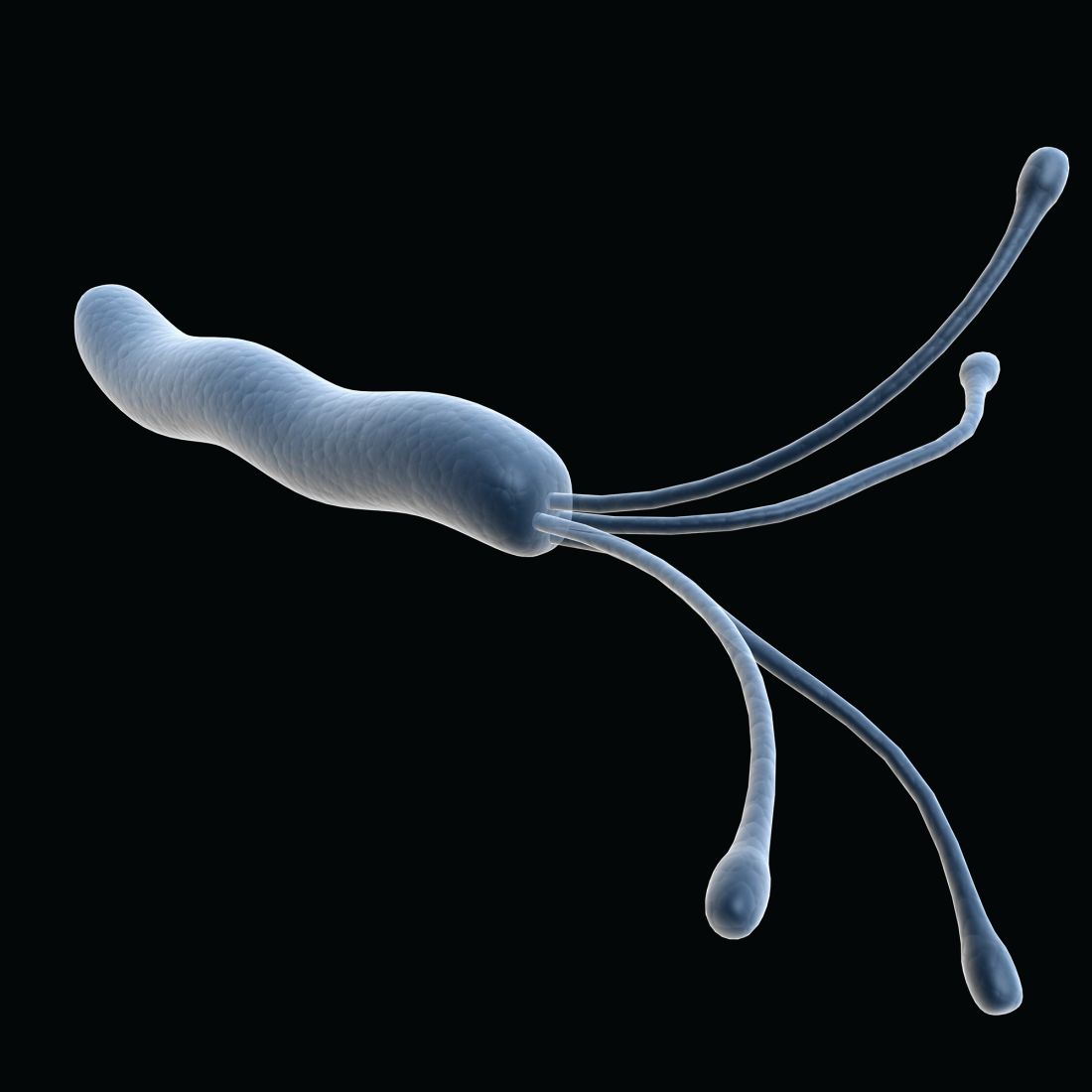
Stool samples meet gastric biopsies for H. pylori antibiotic resistance testing
Using stool samples to test for Helicobacter pylori antibiotic resistance provides highly similar results to those of gastric biopsy samples, which suggests that stool testing may be a safer, more convenient, and more cost-effective option, according to investigators.
Head-to-head testing for resistance-associated mutations using next-generation sequencing (NGS) showed 92% concordance between the two sample types, with 100% technical success among polymerase chain reaction (PCR)–positive stool samples, lead author Steven Moss, MD, of Brown University, Providence, R.I., and colleagues reported.
“H. pylori eradication rates have declined largely due to rising antimicrobial resistance worldwide,” Dr. Moss said at the annual meeting of the American College of Gastroenterology. “There is therefore a need for rapid, accurate, reliable antibiotic resistance testing.”
According to Dr. Moss, molecular resistance testing of gastric biopsies yields similar results to culture-based testing of gastric biopsies, but endoscopic sample collection remains inconvenient and relatively costly, so “it is not commonly performed in many GI practices.
“Whether reliable resistance testing by NGS is possible from stool samples remains unclear,” Dr. Moss said.
To explore this possibility, Dr. Moss and colleagues recruited 262 patients scheduled for upper endoscopy at four sites in the United States. From each patient, two gastric biopsies were taken, and within 2 weeks of the procedure, prior to starting anti–H. pylori therapy, one stool sample was collected.
For gastric biopsy samples, H. pylori positivity was confirmed by PCR, whereas positivity in stool samples was confirmed by both fecal antigen testing and PCR. After confirmation, NGS was conducted, with screening for resistance-associated mutations to six commonly used antibiotics: clarithromycin, levofloxacin, metronidazole, tetracycline, amoxicillin, and rifabutin.
Out of 262 patients, 73 tested positive for H. pylori via stool testing; however, 2 of these patients had inadequate gastric DNA for analysis, leaving 71 patients in the evaluable dataset. Within this group, samples from 50 patients (70.4%) had at least one resistance-association mutation.
Among all 71 individuals, 65 patients (91.5%) had fully concordant results between the two sample types. In four out of the six discordant cases, there was only one difference in antibiotic-associated mutations. Concordance ranged from 89% for metronidazole mutations to 100% for tetracycline, amoxicillin, and rifabutin mutations.
“It is now possible to rapidly obtain susceptibility data without endoscopy,” Dr. Moss concluded. “Using NGS to determine H. pylori antibiotic resistance using stool obviates the cost, inconvenience, and risks of endoscopy resistance profiling.”
Dr. Moss noted that the cost of the stool-based test, through study sponsor American Molecular Laboratories, is about $450, and that the company is “working with various insurance companies to try to get [the test] reimbursed.”
For cases of H. pylori infection without resistance testing results, Dr. Moss recommended first-line treatment with quadruple bismuth–based therapy; however, he noted that “most gastroenterologists, in all kinds of practice, are not measuring their eradication success rate ... so it’s really difficult to know if your best guess is really the appropriate treatment.”
According to Lukasz Kwapisz, MD, of Baylor College of Medicine, Houston, the concordance results are “encouraging,” and suggest that stool-based testing “could be much easier for the patient and the clinician” to find ways to eradicate H. pylori infection.
Dr. Kwapisz predicted that it will take additional successful studies, as well as real-world data, to convert clinicians to the new approach. He suggested that the transition may be gradual, like the adoption of fecal calprotectin testing.
“I don’t know if it’s one singular defining study that will tell you: ‘Okay, we all have to use this [stool-based resistance testing],’ ” he said. “It kind of happens over time – over a 2- or 3-year stretch, I would think, with positive results.”
The study was supported by American Molecular Labs. The investigators disclosed additional relationships with Takeda, Phathom, and Redhill. Dr. Kwapisz reported no conflicts of interest.
Using stool samples to test for Helicobacter pylori antibiotic resistance provides highly similar results to those of gastric biopsy samples, which suggests that stool testing may be a safer, more convenient, and more cost-effective option, according to investigators.
Head-to-head testing for resistance-associated mutations using next-generation sequencing (NGS) showed 92% concordance between the two sample types, with 100% technical success among polymerase chain reaction (PCR)–positive stool samples, lead author Steven Moss, MD, of Brown University, Providence, R.I., and colleagues reported.
“H. pylori eradication rates have declined largely due to rising antimicrobial resistance worldwide,” Dr. Moss said at the annual meeting of the American College of Gastroenterology. “There is therefore a need for rapid, accurate, reliable antibiotic resistance testing.”
According to Dr. Moss, molecular resistance testing of gastric biopsies yields similar results to culture-based testing of gastric biopsies, but endoscopic sample collection remains inconvenient and relatively costly, so “it is not commonly performed in many GI practices.
“Whether reliable resistance testing by NGS is possible from stool samples remains unclear,” Dr. Moss said.
To explore this possibility, Dr. Moss and colleagues recruited 262 patients scheduled for upper endoscopy at four sites in the United States. From each patient, two gastric biopsies were taken, and within 2 weeks of the procedure, prior to starting anti–H. pylori therapy, one stool sample was collected.
For gastric biopsy samples, H. pylori positivity was confirmed by PCR, whereas positivity in stool samples was confirmed by both fecal antigen testing and PCR. After confirmation, NGS was conducted, with screening for resistance-associated mutations to six commonly used antibiotics: clarithromycin, levofloxacin, metronidazole, tetracycline, amoxicillin, and rifabutin.
Out of 262 patients, 73 tested positive for H. pylori via stool testing; however, 2 of these patients had inadequate gastric DNA for analysis, leaving 71 patients in the evaluable dataset. Within this group, samples from 50 patients (70.4%) had at least one resistance-association mutation.
Among all 71 individuals, 65 patients (91.5%) had fully concordant results between the two sample types. In four out of the six discordant cases, there was only one difference in antibiotic-associated mutations. Concordance ranged from 89% for metronidazole mutations to 100% for tetracycline, amoxicillin, and rifabutin mutations.
“It is now possible to rapidly obtain susceptibility data without endoscopy,” Dr. Moss concluded. “Using NGS to determine H. pylori antibiotic resistance using stool obviates the cost, inconvenience, and risks of endoscopy resistance profiling.”
Dr. Moss noted that the cost of the stool-based test, through study sponsor American Molecular Laboratories, is about $450, and that the company is “working with various insurance companies to try to get [the test] reimbursed.”
For cases of H. pylori infection without resistance testing results, Dr. Moss recommended first-line treatment with quadruple bismuth–based therapy; however, he noted that “most gastroenterologists, in all kinds of practice, are not measuring their eradication success rate ... so it’s really difficult to know if your best guess is really the appropriate treatment.”
According to Lukasz Kwapisz, MD, of Baylor College of Medicine, Houston, the concordance results are “encouraging,” and suggest that stool-based testing “could be much easier for the patient and the clinician” to find ways to eradicate H. pylori infection.
Dr. Kwapisz predicted that it will take additional successful studies, as well as real-world data, to convert clinicians to the new approach. He suggested that the transition may be gradual, like the adoption of fecal calprotectin testing.
“I don’t know if it’s one singular defining study that will tell you: ‘Okay, we all have to use this [stool-based resistance testing],’ ” he said. “It kind of happens over time – over a 2- or 3-year stretch, I would think, with positive results.”
The study was supported by American Molecular Labs. The investigators disclosed additional relationships with Takeda, Phathom, and Redhill. Dr. Kwapisz reported no conflicts of interest.
Using stool samples to test for Helicobacter pylori antibiotic resistance provides highly similar results to those of gastric biopsy samples, which suggests that stool testing may be a safer, more convenient, and more cost-effective option, according to investigators.
Head-to-head testing for resistance-associated mutations using next-generation sequencing (NGS) showed 92% concordance between the two sample types, with 100% technical success among polymerase chain reaction (PCR)–positive stool samples, lead author Steven Moss, MD, of Brown University, Providence, R.I., and colleagues reported.
“H. pylori eradication rates have declined largely due to rising antimicrobial resistance worldwide,” Dr. Moss said at the annual meeting of the American College of Gastroenterology. “There is therefore a need for rapid, accurate, reliable antibiotic resistance testing.”
According to Dr. Moss, molecular resistance testing of gastric biopsies yields similar results to culture-based testing of gastric biopsies, but endoscopic sample collection remains inconvenient and relatively costly, so “it is not commonly performed in many GI practices.
“Whether reliable resistance testing by NGS is possible from stool samples remains unclear,” Dr. Moss said.
To explore this possibility, Dr. Moss and colleagues recruited 262 patients scheduled for upper endoscopy at four sites in the United States. From each patient, two gastric biopsies were taken, and within 2 weeks of the procedure, prior to starting anti–H. pylori therapy, one stool sample was collected.
For gastric biopsy samples, H. pylori positivity was confirmed by PCR, whereas positivity in stool samples was confirmed by both fecal antigen testing and PCR. After confirmation, NGS was conducted, with screening for resistance-associated mutations to six commonly used antibiotics: clarithromycin, levofloxacin, metronidazole, tetracycline, amoxicillin, and rifabutin.
Out of 262 patients, 73 tested positive for H. pylori via stool testing; however, 2 of these patients had inadequate gastric DNA for analysis, leaving 71 patients in the evaluable dataset. Within this group, samples from 50 patients (70.4%) had at least one resistance-association mutation.
Among all 71 individuals, 65 patients (91.5%) had fully concordant results between the two sample types. In four out of the six discordant cases, there was only one difference in antibiotic-associated mutations. Concordance ranged from 89% for metronidazole mutations to 100% for tetracycline, amoxicillin, and rifabutin mutations.
“It is now possible to rapidly obtain susceptibility data without endoscopy,” Dr. Moss concluded. “Using NGS to determine H. pylori antibiotic resistance using stool obviates the cost, inconvenience, and risks of endoscopy resistance profiling.”
Dr. Moss noted that the cost of the stool-based test, through study sponsor American Molecular Laboratories, is about $450, and that the company is “working with various insurance companies to try to get [the test] reimbursed.”
For cases of H. pylori infection without resistance testing results, Dr. Moss recommended first-line treatment with quadruple bismuth–based therapy; however, he noted that “most gastroenterologists, in all kinds of practice, are not measuring their eradication success rate ... so it’s really difficult to know if your best guess is really the appropriate treatment.”
According to Lukasz Kwapisz, MD, of Baylor College of Medicine, Houston, the concordance results are “encouraging,” and suggest that stool-based testing “could be much easier for the patient and the clinician” to find ways to eradicate H. pylori infection.
Dr. Kwapisz predicted that it will take additional successful studies, as well as real-world data, to convert clinicians to the new approach. He suggested that the transition may be gradual, like the adoption of fecal calprotectin testing.
“I don’t know if it’s one singular defining study that will tell you: ‘Okay, we all have to use this [stool-based resistance testing],’ ” he said. “It kind of happens over time – over a 2- or 3-year stretch, I would think, with positive results.”
The study was supported by American Molecular Labs. The investigators disclosed additional relationships with Takeda, Phathom, and Redhill. Dr. Kwapisz reported no conflicts of interest.
FROM ACG 2021
GERD: Composite pH impedance monitoring better identifies treatment escalation need
Combinations of abnormal pH-impedance metrics better predicted nonresponse to proton pump inhibitor therapy, as well as benefit of treatment escalation, than individual metrics in patients with gastroesophageal reflux disease (GERD) on twice-daily PPI.
The researchers found a higher proportion of nonresponders to PPI in a group of patients that had combinations of abnormal reflux burden, characterized as acid exposure time greater than 4%, more than 80 reflux episodes, and/or mean nocturnal baseline impedance (MNBI) less than 1,500 ohms, with 85% of these patients improving following initiation of invasive GERD management such as antireflux surgery or magnetic sphincter augmentation.
Not only does the combination of metrics offer more value in identifying responders to PPI than individual metrics, but the combination also offer greater value in “subsequently predicting response to escalation of antireflux management,” study authors C. Prakash Gyawali, MD, of Washington University, St. Louis, and colleagues wrote in Gastroenterology.
Currently in question is the applicability of thresholds for metrics from pH impedance monitoring for studies performed on PPI. According to Dr. Gyawali and colleagues, thresholds from the Lyon Consensus may be too high and likewise lack optimal sensitivity for detecting refractory acid burden in patients on PPI, while thresholds based on pH-metry alone, as reported in other publications, may also lack specificity.
To determine which metrics from “on PPI” pH impedance studies predict escalation therapy needs, the researchers analyzed deidentified pH impedance studies performed in healthy volunteers (n=66; median age, 37.5 years) and patients with GERD (n = 43; median age, 57.0 years); both groups were on twice-daily PPI. The investigators compared median values for pH impedance metrics between healthy volunteers and patients with proven GERD using validated measures.
Data were included from a total of three groups: tracings from European and North American healthy volunteers who received twice-daily PPI for 5-7 days; tracings from European patients with heartburn-predominant proven GERD with prior abnormal reflux monitoring off PPI who subsequently received twice-daily PPI; and tracings from a cohort of patients with regurgitation-predominant, proven GERD and prior abnormal reflux monitoring off PPI who subsequently received twice-daily PPI.
A improvement in heartburn of at least 50%, as recorded on 4-point Likert-type scales, defined PPI responders and improvements following antireflux surgery in the European comparison group. Additionally, an improvement of at least 50% on the GERD Health-Related Quality of Life scale also characterized PPI responders and improvements following magnetic sphincter augmentation in the North American comparison group.
There was no significant difference between PPI responders and nonresponders in terms of individual conventional and novel reflux metrics. The combinations of metrics associated with abnormal reflux burden and abnormal mucosal integrity (acid exposure time >4%, >80 reflux episodes, and MNBI <1,500 ohms) were observed in 32.6% of patients with heartburn and 40.5% of patients with regurgitation-predominant GERD, but no healthy volunteers. The combinations were also observed in 57.1% and 82.4% of nonresponders, respectively.
The authors defined a borderline category (acid exposure time, >0.5% but <4%; >40 but <80 reflux episodes), which accounted for 32.6% of patients with heartburn-predominant GERD and 50% of those regurgitation-predominant GERD. Nonresponse among these borderline cases was identified in 28.6% and 81%, respectively.
“Performance characteristics of the presence of abnormal reflux burden and/or abnormal mucosal integrity in predicting PPI nonresponse consisted of sensitivity, 0.50; specificity, 0.71; and AUC, 0.59 (P = .15),” the authors explained. “Performance characteristics of abnormal and borderline reflux burden categories together in predicting PPI nonresponse consisted of sensitivity, 0.86; specificity, 0.36; and AUC, 0.62 (P = .07).”
Limitations of this study included its retrospective nature, small sample sizes for the healthy volunteer and GERD populations, and the lack of data on relevant clinical information, including body mass index, dietary patterns, and PPI types and doses. Additionally, the findings may lack generalizability because of the inclusion of only patients with GERD who underwent surgical management.
Despite these limitations, the researchers wrote that the findings and identified “thresholds will be useful in planning prospective outcome studies to conclusively determine when to escalate antireflux therapy when GERD symptoms persist despite bid PPI therapy.”
The study researchers reported conflicts of interest with several pharmaceutical companies. No funding was reported for the study.
The management of gastroesophageal reflux disease (GERD) is the most common referral for a gastroenterologist; however, metrics to determine dose-escalation for persistent symptoms in patients with proven GERD is an unmet need. The Lyon consensus aimed to standardize abnormal pH parameters but used similar thresholds for off– and on–proton pump inhibitor testing; these thresholds for on-PPI testing are likely too high to detect refractory reflux on PPI therapy. The use of pH-impedance testing is an optimal test for patients with persistent symptoms in the setting of proven GERD to determine escalation of antireflux therapy. In this multicenter, international cohort study, Gyawali and colleagues rigorously challenged the definition of abnormal pH-impedance testing with an evaluation of pH impedance parameters comparing controls (n = 66) versus proven GERD (n = 43) on twice-daily PPI dosing to define pH-impedance parameters.
Rishi D. Naik, MD, MSCI, is an assistant professor in the department of medicine in the section of gastroenterology & hepatology at the Esophageal Center at Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
The management of gastroesophageal reflux disease (GERD) is the most common referral for a gastroenterologist; however, metrics to determine dose-escalation for persistent symptoms in patients with proven GERD is an unmet need. The Lyon consensus aimed to standardize abnormal pH parameters but used similar thresholds for off– and on–proton pump inhibitor testing; these thresholds for on-PPI testing are likely too high to detect refractory reflux on PPI therapy. The use of pH-impedance testing is an optimal test for patients with persistent symptoms in the setting of proven GERD to determine escalation of antireflux therapy. In this multicenter, international cohort study, Gyawali and colleagues rigorously challenged the definition of abnormal pH-impedance testing with an evaluation of pH impedance parameters comparing controls (n = 66) versus proven GERD (n = 43) on twice-daily PPI dosing to define pH-impedance parameters.
Rishi D. Naik, MD, MSCI, is an assistant professor in the department of medicine in the section of gastroenterology & hepatology at the Esophageal Center at Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
The management of gastroesophageal reflux disease (GERD) is the most common referral for a gastroenterologist; however, metrics to determine dose-escalation for persistent symptoms in patients with proven GERD is an unmet need. The Lyon consensus aimed to standardize abnormal pH parameters but used similar thresholds for off– and on–proton pump inhibitor testing; these thresholds for on-PPI testing are likely too high to detect refractory reflux on PPI therapy. The use of pH-impedance testing is an optimal test for patients with persistent symptoms in the setting of proven GERD to determine escalation of antireflux therapy. In this multicenter, international cohort study, Gyawali and colleagues rigorously challenged the definition of abnormal pH-impedance testing with an evaluation of pH impedance parameters comparing controls (n = 66) versus proven GERD (n = 43) on twice-daily PPI dosing to define pH-impedance parameters.
Rishi D. Naik, MD, MSCI, is an assistant professor in the department of medicine in the section of gastroenterology & hepatology at the Esophageal Center at Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Combinations of abnormal pH-impedance metrics better predicted nonresponse to proton pump inhibitor therapy, as well as benefit of treatment escalation, than individual metrics in patients with gastroesophageal reflux disease (GERD) on twice-daily PPI.
The researchers found a higher proportion of nonresponders to PPI in a group of patients that had combinations of abnormal reflux burden, characterized as acid exposure time greater than 4%, more than 80 reflux episodes, and/or mean nocturnal baseline impedance (MNBI) less than 1,500 ohms, with 85% of these patients improving following initiation of invasive GERD management such as antireflux surgery or magnetic sphincter augmentation.
Not only does the combination of metrics offer more value in identifying responders to PPI than individual metrics, but the combination also offer greater value in “subsequently predicting response to escalation of antireflux management,” study authors C. Prakash Gyawali, MD, of Washington University, St. Louis, and colleagues wrote in Gastroenterology.
Currently in question is the applicability of thresholds for metrics from pH impedance monitoring for studies performed on PPI. According to Dr. Gyawali and colleagues, thresholds from the Lyon Consensus may be too high and likewise lack optimal sensitivity for detecting refractory acid burden in patients on PPI, while thresholds based on pH-metry alone, as reported in other publications, may also lack specificity.
To determine which metrics from “on PPI” pH impedance studies predict escalation therapy needs, the researchers analyzed deidentified pH impedance studies performed in healthy volunteers (n=66; median age, 37.5 years) and patients with GERD (n = 43; median age, 57.0 years); both groups were on twice-daily PPI. The investigators compared median values for pH impedance metrics between healthy volunteers and patients with proven GERD using validated measures.
Data were included from a total of three groups: tracings from European and North American healthy volunteers who received twice-daily PPI for 5-7 days; tracings from European patients with heartburn-predominant proven GERD with prior abnormal reflux monitoring off PPI who subsequently received twice-daily PPI; and tracings from a cohort of patients with regurgitation-predominant, proven GERD and prior abnormal reflux monitoring off PPI who subsequently received twice-daily PPI.
A improvement in heartburn of at least 50%, as recorded on 4-point Likert-type scales, defined PPI responders and improvements following antireflux surgery in the European comparison group. Additionally, an improvement of at least 50% on the GERD Health-Related Quality of Life scale also characterized PPI responders and improvements following magnetic sphincter augmentation in the North American comparison group.
There was no significant difference between PPI responders and nonresponders in terms of individual conventional and novel reflux metrics. The combinations of metrics associated with abnormal reflux burden and abnormal mucosal integrity (acid exposure time >4%, >80 reflux episodes, and MNBI <1,500 ohms) were observed in 32.6% of patients with heartburn and 40.5% of patients with regurgitation-predominant GERD, but no healthy volunteers. The combinations were also observed in 57.1% and 82.4% of nonresponders, respectively.
The authors defined a borderline category (acid exposure time, >0.5% but <4%; >40 but <80 reflux episodes), which accounted for 32.6% of patients with heartburn-predominant GERD and 50% of those regurgitation-predominant GERD. Nonresponse among these borderline cases was identified in 28.6% and 81%, respectively.
“Performance characteristics of the presence of abnormal reflux burden and/or abnormal mucosal integrity in predicting PPI nonresponse consisted of sensitivity, 0.50; specificity, 0.71; and AUC, 0.59 (P = .15),” the authors explained. “Performance characteristics of abnormal and borderline reflux burden categories together in predicting PPI nonresponse consisted of sensitivity, 0.86; specificity, 0.36; and AUC, 0.62 (P = .07).”
Limitations of this study included its retrospective nature, small sample sizes for the healthy volunteer and GERD populations, and the lack of data on relevant clinical information, including body mass index, dietary patterns, and PPI types and doses. Additionally, the findings may lack generalizability because of the inclusion of only patients with GERD who underwent surgical management.
Despite these limitations, the researchers wrote that the findings and identified “thresholds will be useful in planning prospective outcome studies to conclusively determine when to escalate antireflux therapy when GERD symptoms persist despite bid PPI therapy.”
The study researchers reported conflicts of interest with several pharmaceutical companies. No funding was reported for the study.
Combinations of abnormal pH-impedance metrics better predicted nonresponse to proton pump inhibitor therapy, as well as benefit of treatment escalation, than individual metrics in patients with gastroesophageal reflux disease (GERD) on twice-daily PPI.
The researchers found a higher proportion of nonresponders to PPI in a group of patients that had combinations of abnormal reflux burden, characterized as acid exposure time greater than 4%, more than 80 reflux episodes, and/or mean nocturnal baseline impedance (MNBI) less than 1,500 ohms, with 85% of these patients improving following initiation of invasive GERD management such as antireflux surgery or magnetic sphincter augmentation.
Not only does the combination of metrics offer more value in identifying responders to PPI than individual metrics, but the combination also offer greater value in “subsequently predicting response to escalation of antireflux management,” study authors C. Prakash Gyawali, MD, of Washington University, St. Louis, and colleagues wrote in Gastroenterology.
Currently in question is the applicability of thresholds for metrics from pH impedance monitoring for studies performed on PPI. According to Dr. Gyawali and colleagues, thresholds from the Lyon Consensus may be too high and likewise lack optimal sensitivity for detecting refractory acid burden in patients on PPI, while thresholds based on pH-metry alone, as reported in other publications, may also lack specificity.
To determine which metrics from “on PPI” pH impedance studies predict escalation therapy needs, the researchers analyzed deidentified pH impedance studies performed in healthy volunteers (n=66; median age, 37.5 years) and patients with GERD (n = 43; median age, 57.0 years); both groups were on twice-daily PPI. The investigators compared median values for pH impedance metrics between healthy volunteers and patients with proven GERD using validated measures.
Data were included from a total of three groups: tracings from European and North American healthy volunteers who received twice-daily PPI for 5-7 days; tracings from European patients with heartburn-predominant proven GERD with prior abnormal reflux monitoring off PPI who subsequently received twice-daily PPI; and tracings from a cohort of patients with regurgitation-predominant, proven GERD and prior abnormal reflux monitoring off PPI who subsequently received twice-daily PPI.
A improvement in heartburn of at least 50%, as recorded on 4-point Likert-type scales, defined PPI responders and improvements following antireflux surgery in the European comparison group. Additionally, an improvement of at least 50% on the GERD Health-Related Quality of Life scale also characterized PPI responders and improvements following magnetic sphincter augmentation in the North American comparison group.
There was no significant difference between PPI responders and nonresponders in terms of individual conventional and novel reflux metrics. The combinations of metrics associated with abnormal reflux burden and abnormal mucosal integrity (acid exposure time >4%, >80 reflux episodes, and MNBI <1,500 ohms) were observed in 32.6% of patients with heartburn and 40.5% of patients with regurgitation-predominant GERD, but no healthy volunteers. The combinations were also observed in 57.1% and 82.4% of nonresponders, respectively.
The authors defined a borderline category (acid exposure time, >0.5% but <4%; >40 but <80 reflux episodes), which accounted for 32.6% of patients with heartburn-predominant GERD and 50% of those regurgitation-predominant GERD. Nonresponse among these borderline cases was identified in 28.6% and 81%, respectively.
“Performance characteristics of the presence of abnormal reflux burden and/or abnormal mucosal integrity in predicting PPI nonresponse consisted of sensitivity, 0.50; specificity, 0.71; and AUC, 0.59 (P = .15),” the authors explained. “Performance characteristics of abnormal and borderline reflux burden categories together in predicting PPI nonresponse consisted of sensitivity, 0.86; specificity, 0.36; and AUC, 0.62 (P = .07).”
Limitations of this study included its retrospective nature, small sample sizes for the healthy volunteer and GERD populations, and the lack of data on relevant clinical information, including body mass index, dietary patterns, and PPI types and doses. Additionally, the findings may lack generalizability because of the inclusion of only patients with GERD who underwent surgical management.
Despite these limitations, the researchers wrote that the findings and identified “thresholds will be useful in planning prospective outcome studies to conclusively determine when to escalate antireflux therapy when GERD symptoms persist despite bid PPI therapy.”
The study researchers reported conflicts of interest with several pharmaceutical companies. No funding was reported for the study.
FROM GASTROENTEROLOGY
Rivaroxaban’s single daily dose may lead to higher bleeding risk than other DOACs
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
FROM ANNALS OF INTERNAL MEDICINE
Extraesophageal symptoms of GERD
Patients often present with symptoms that are not classic for reflux such as chronic cough, worsening asthma, sore throat, or globus.
In the upper GI section of the postgraduate course program, Rena Yadlapati, MD, and C. Prakash Gyawali, MD, MRCP, educated us about optimal strategies for diagnosis and treatment of this difficult group of patients. Dr. Gyawali reminded us of risk stratification of patients into those with high or low likelihood of reflux as contributing etiology for patients with suspected extraesophageal reflux. Dr. Yadlapti reviewed the utility of the HASBEER score in stratifying patients into these two risk categories. Patients with known reflux at baseline and/or if they have classic symptoms of reflux in addition to extraesophageal symptoms may be at higher likelihood of having abnormal esophageal acid exposure than those without classic heartburn and/or regurgitation. The low-risk group may then benefit from diagnostic testing off PPI therapy (either impedance/pH monitoring or wireless pH testing), whereas those in the high-risk group for reflux may undergo impedance pH testing on PPI therapy to ensure control of reflux while on therapy.
Dr. Yadlapati also updated the audience about lack of robust data to suggest clinical utility for oropharyngeal pH test or salivary pepsin assay testing. It was generally agreed on that the majority of patients who do not respond to aggressive acid suppressive therapy likely do not have reflux related extraesophageal symptoms and alternative etiologies may be at play.
Finally, both investigators outlined the importance of neuromodulation in those whose symptoms may be due to “irritable larynx.” They emphasized the role of tricyclics as well as gabapentin as off label uses for patients who have normal reflux testing and continue to have chronic cough or globus sensation.
Michael F. Vaezi, MD, PhD, MSc, is an associate chief and a clinical director of the division of gastroenterology, hepatology, and nutrition and director of the Clinical Research and Center for Esophageal Disorders at Vanderbilt University, Nashville, Tenn. He reports consulting for Phathom, Ironwood, Diversatek, Isothrive, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
Patients often present with symptoms that are not classic for reflux such as chronic cough, worsening asthma, sore throat, or globus.
In the upper GI section of the postgraduate course program, Rena Yadlapati, MD, and C. Prakash Gyawali, MD, MRCP, educated us about optimal strategies for diagnosis and treatment of this difficult group of patients. Dr. Gyawali reminded us of risk stratification of patients into those with high or low likelihood of reflux as contributing etiology for patients with suspected extraesophageal reflux. Dr. Yadlapti reviewed the utility of the HASBEER score in stratifying patients into these two risk categories. Patients with known reflux at baseline and/or if they have classic symptoms of reflux in addition to extraesophageal symptoms may be at higher likelihood of having abnormal esophageal acid exposure than those without classic heartburn and/or regurgitation. The low-risk group may then benefit from diagnostic testing off PPI therapy (either impedance/pH monitoring or wireless pH testing), whereas those in the high-risk group for reflux may undergo impedance pH testing on PPI therapy to ensure control of reflux while on therapy.
Dr. Yadlapati also updated the audience about lack of robust data to suggest clinical utility for oropharyngeal pH test or salivary pepsin assay testing. It was generally agreed on that the majority of patients who do not respond to aggressive acid suppressive therapy likely do not have reflux related extraesophageal symptoms and alternative etiologies may be at play.
Finally, both investigators outlined the importance of neuromodulation in those whose symptoms may be due to “irritable larynx.” They emphasized the role of tricyclics as well as gabapentin as off label uses for patients who have normal reflux testing and continue to have chronic cough or globus sensation.
Michael F. Vaezi, MD, PhD, MSc, is an associate chief and a clinical director of the division of gastroenterology, hepatology, and nutrition and director of the Clinical Research and Center for Esophageal Disorders at Vanderbilt University, Nashville, Tenn. He reports consulting for Phathom, Ironwood, Diversatek, Isothrive, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
Patients often present with symptoms that are not classic for reflux such as chronic cough, worsening asthma, sore throat, or globus.
In the upper GI section of the postgraduate course program, Rena Yadlapati, MD, and C. Prakash Gyawali, MD, MRCP, educated us about optimal strategies for diagnosis and treatment of this difficult group of patients. Dr. Gyawali reminded us of risk stratification of patients into those with high or low likelihood of reflux as contributing etiology for patients with suspected extraesophageal reflux. Dr. Yadlapti reviewed the utility of the HASBEER score in stratifying patients into these two risk categories. Patients with known reflux at baseline and/or if they have classic symptoms of reflux in addition to extraesophageal symptoms may be at higher likelihood of having abnormal esophageal acid exposure than those without classic heartburn and/or regurgitation. The low-risk group may then benefit from diagnostic testing off PPI therapy (either impedance/pH monitoring or wireless pH testing), whereas those in the high-risk group for reflux may undergo impedance pH testing on PPI therapy to ensure control of reflux while on therapy.
Dr. Yadlapati also updated the audience about lack of robust data to suggest clinical utility for oropharyngeal pH test or salivary pepsin assay testing. It was generally agreed on that the majority of patients who do not respond to aggressive acid suppressive therapy likely do not have reflux related extraesophageal symptoms and alternative etiologies may be at play.
Finally, both investigators outlined the importance of neuromodulation in those whose symptoms may be due to “irritable larynx.” They emphasized the role of tricyclics as well as gabapentin as off label uses for patients who have normal reflux testing and continue to have chronic cough or globus sensation.
Michael F. Vaezi, MD, PhD, MSc, is an associate chief and a clinical director of the division of gastroenterology, hepatology, and nutrition and director of the Clinical Research and Center for Esophageal Disorders at Vanderbilt University, Nashville, Tenn. He reports consulting for Phathom, Ironwood, Diversatek, Isothrive, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
Gastric cancer: Family history–based H. pylori strategy would be cost effective
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
FROM GASTROENTEROLOGY
Is Nissen fundoplication the best we can do?
As an esophagologist that does not perform fundoplication, LINX, or TIF, I find it difficult to debate the merits of one procedure over another based on my experience. In fact, I have always stated that it is difficult to assess a procedure or test that one has not used. That being said, maybe the fact that I have not performed these procedures makes me more objective and I can only use my experience with patients and the data to make the case that we need options beyond Nissen fundoplication.
The recent VA Randomized trial in refractory GERD published by Spechler and colleagues once again highlighted the fact that there are some patients that require a mechanical solution to reflux disease.1 In this study, the authors carefully defined a patient population with refractory GERD and showed that Nissen fundoplication was superior to medical management in patients who did not respond to proton pump inhibitors. However, of the 27 patients who underwent fundoplication, one patient had major complications which required a repeat operation and prolonged hospital stay. These findings highlight the main problem with Nissen fundoplication. Dr. Watson elegantly argued in his assertion during our debate that Nissen and fundoplication are not the same. In this position, he was noting the side effects associated with Nissen fundoplication,2 and he focused his argument on the comparison between a partial wrap versus LINX and TIF to level the playing field. On that note, I agree with Dr. Watson that a well-done partial fundoplication is a great option for patients with a mechanical problem.
Nonetheless, Redo operations have an escalating risk of severe debilitating consequences and we should do everything possible to reduce that risk.3 The LINX and the TIF procedure have data to support their effectiveness, and the initial studies a more favorable side effect profile.4,5 The ability to perform these procedures in patients with hiatal hernia and the fact that these approaches do not exclude the possibility of fundoplication in the future make them an attractive alternative.
In the end, more rigorous comparative studies should be performed to truly determine which approach is better. Although we have good surgical and medical options, we all recognize that they are not perfect and we should not settle on the current state of GERD management.
John E. Pandolfino, MD, MSCI, is the Hans Popper Professor of Medicine and Division Chief, Gastroenterology and Hepatology at Northwestern University, Chicago. He disclosed relationships with Ethicon/Johnson & Johnson, Endogastric Solutions, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
References
1. Spechler SJ et al. N Engl J Med. 2019 Oct 17;381[16]:1513-23.
2. Yadlapati R et al. Am J Gastroenterol. 2018 Aug;113[8]:1137-47.
3. Singhal S et al. J Gastrointest Surg. 2018 Feb;22[2]:177-86.
4. Ganz RA et al. Clin Gastroenterol Hepatol. 2016 May;14(5):671-7.
Endosc Int Open. 2019 May;7(5):E647-E654
As an esophagologist that does not perform fundoplication, LINX, or TIF, I find it difficult to debate the merits of one procedure over another based on my experience. In fact, I have always stated that it is difficult to assess a procedure or test that one has not used. That being said, maybe the fact that I have not performed these procedures makes me more objective and I can only use my experience with patients and the data to make the case that we need options beyond Nissen fundoplication.
The recent VA Randomized trial in refractory GERD published by Spechler and colleagues once again highlighted the fact that there are some patients that require a mechanical solution to reflux disease.1 In this study, the authors carefully defined a patient population with refractory GERD and showed that Nissen fundoplication was superior to medical management in patients who did not respond to proton pump inhibitors. However, of the 27 patients who underwent fundoplication, one patient had major complications which required a repeat operation and prolonged hospital stay. These findings highlight the main problem with Nissen fundoplication. Dr. Watson elegantly argued in his assertion during our debate that Nissen and fundoplication are not the same. In this position, he was noting the side effects associated with Nissen fundoplication,2 and he focused his argument on the comparison between a partial wrap versus LINX and TIF to level the playing field. On that note, I agree with Dr. Watson that a well-done partial fundoplication is a great option for patients with a mechanical problem.
Nonetheless, Redo operations have an escalating risk of severe debilitating consequences and we should do everything possible to reduce that risk.3 The LINX and the TIF procedure have data to support their effectiveness, and the initial studies a more favorable side effect profile.4,5 The ability to perform these procedures in patients with hiatal hernia and the fact that these approaches do not exclude the possibility of fundoplication in the future make them an attractive alternative.
In the end, more rigorous comparative studies should be performed to truly determine which approach is better. Although we have good surgical and medical options, we all recognize that they are not perfect and we should not settle on the current state of GERD management.
John E. Pandolfino, MD, MSCI, is the Hans Popper Professor of Medicine and Division Chief, Gastroenterology and Hepatology at Northwestern University, Chicago. He disclosed relationships with Ethicon/Johnson & Johnson, Endogastric Solutions, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
References
1. Spechler SJ et al. N Engl J Med. 2019 Oct 17;381[16]:1513-23.
2. Yadlapati R et al. Am J Gastroenterol. 2018 Aug;113[8]:1137-47.
3. Singhal S et al. J Gastrointest Surg. 2018 Feb;22[2]:177-86.
4. Ganz RA et al. Clin Gastroenterol Hepatol. 2016 May;14(5):671-7.
Endosc Int Open. 2019 May;7(5):E647-E654
As an esophagologist that does not perform fundoplication, LINX, or TIF, I find it difficult to debate the merits of one procedure over another based on my experience. In fact, I have always stated that it is difficult to assess a procedure or test that one has not used. That being said, maybe the fact that I have not performed these procedures makes me more objective and I can only use my experience with patients and the data to make the case that we need options beyond Nissen fundoplication.
The recent VA Randomized trial in refractory GERD published by Spechler and colleagues once again highlighted the fact that there are some patients that require a mechanical solution to reflux disease.1 In this study, the authors carefully defined a patient population with refractory GERD and showed that Nissen fundoplication was superior to medical management in patients who did not respond to proton pump inhibitors. However, of the 27 patients who underwent fundoplication, one patient had major complications which required a repeat operation and prolonged hospital stay. These findings highlight the main problem with Nissen fundoplication. Dr. Watson elegantly argued in his assertion during our debate that Nissen and fundoplication are not the same. In this position, he was noting the side effects associated with Nissen fundoplication,2 and he focused his argument on the comparison between a partial wrap versus LINX and TIF to level the playing field. On that note, I agree with Dr. Watson that a well-done partial fundoplication is a great option for patients with a mechanical problem.
Nonetheless, Redo operations have an escalating risk of severe debilitating consequences and we should do everything possible to reduce that risk.3 The LINX and the TIF procedure have data to support their effectiveness, and the initial studies a more favorable side effect profile.4,5 The ability to perform these procedures in patients with hiatal hernia and the fact that these approaches do not exclude the possibility of fundoplication in the future make them an attractive alternative.
In the end, more rigorous comparative studies should be performed to truly determine which approach is better. Although we have good surgical and medical options, we all recognize that they are not perfect and we should not settle on the current state of GERD management.
John E. Pandolfino, MD, MSCI, is the Hans Popper Professor of Medicine and Division Chief, Gastroenterology and Hepatology at Northwestern University, Chicago. He disclosed relationships with Ethicon/Johnson & Johnson, Endogastric Solutions, and Medtronic. These remarks were made during one of the AGA Postgraduate Course sessions held at DDW 2021.
References
1. Spechler SJ et al. N Engl J Med. 2019 Oct 17;381[16]:1513-23.
2. Yadlapati R et al. Am J Gastroenterol. 2018 Aug;113[8]:1137-47.
3. Singhal S et al. J Gastrointest Surg. 2018 Feb;22[2]:177-86.
4. Ganz RA et al. Clin Gastroenterol Hepatol. 2016 May;14(5):671-7.
Endosc Int Open. 2019 May;7(5):E647-E654
Most stent misdeployments in EUS-GE are manageable
Most instances of stent misdeployment in cases of endoscopic ultrasound–guided gastroenterostomy (EUS-GE) can be managed endoscopically, based on data from 16 tertiary care centers in the United States and Europe.
EUS-GE provides a viable alternative to traditional surgical gastroenterostomy and stent placement for patients with gastric outlet obstruction (GOO), but the potential for stent misdeployment has limited adoption of the procedure because it remains the most common cause of technical failures and adverse events, Bachir Ghandour, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
However, data on outcomes and management of stent misdeployment during EUS-GE are limited, and the researchers hypothesized that most stent misdeployments could be managed endoscopically.
In a retrospective study published in Gastrointestinal Endoscopy, the researchers reviewed data from 467 EUS-GE procedures performed for gastric outlet obstruction between March 2015 and December 2020 at eight centers in the United States and eight in Europe. The primary outcome was the rate and severity of stent misdeployment.
Stent misdeployment occurred in 46 patients (9.9%). Of these, 73.2% occurred during the operators’ first 13 cases.
The researchers created a classification system of stent misdeployment according to type, depending on which flange was misdeployed.
Type I was the most common, and occurred in 29 patients; this type was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach without evidence of a resulting enterotomy”; type II (14 patients) was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach despite an enterotomy (i.e., visual confirmation of stent having penetrated targeted small bowel, under EUS or fluoroscopy, but migrated out on deployment)”; type III (1 patient) was defined as “the deployment of the distal flange in the small bowel and proximal flange in the peritoneum”; and type IV (2 patients) was defined as “the deployment of the distal flange in the colon and proximal flange in the stomach resulting in a gastrocolic anastomosis,” the researchers wrote.
The researchers also classified the stent misdeployment in terms of severity as mild (28 patients), moderate (11 patients), severe (6 cases) or fatal (1 case) based on the American Society for Gastrointestinal Endoscopy lexicon.
Overall, type I was significantly more likely to be mild in severity, compared with type II (75.9% vs. 42.9%; P = .04), although the rate of surgical repair was similar between these two types (10.3% vs. 7.1%). Rates of ICU admission were approximately 7% in patients with type I and type II stent misdeployments, and the median postprocedural stay was 4 days for these two groups.
Same-session salvage management of GOO was achieved by EUS/endoscopic-GE in 24 patients, duodenal stent placement in 6 patients, duodenal dilation in 1 patient, and gastroenterostomy with natural orifice transluminal endoscopic surgery in 3 patients. Of the remaining 12 patients, GOO was managed with subsequent EUS-GE in 6 patients and surgical GI in 6 patients.
The study findings were limited by several factors including the retrospective design and inclusion of a time period that encompassed changes and improvements in the EUS-GE, the researchers noted. The small sample size of type III and IV stent misdeployments prohibited comparison with other types.
However, the cohort size was relatively large, compared with previous studies, and included a range of centers and countries with different strategies for managing stent misdeployments. Given the steep learning curve for EUS-GE, the study findings may help endoscopists better understand the implications and potential consequences of stent misdeployment by classifying the misdeployments into types. “We believe that such a classification or categorization of the different types is important because patient outcomes vary depending on the specific [stent misdeployment] subtype and site of injury. Such a classification will also be very helpful for future research by standardizing the terminology,” the researchers said.
“Although [stent misdeployment] is not infrequent during EUS-GE, with a rate of approximately 10%, the majority of cases are mild in severity and can be managed or repaired endoscopically without ill consequences,” they concluded. “Surgical intervention is required in less than 11% of the cases.”
Data support safe stent use in GI disease
“The lines continue to be blurred between surgical and endoscopic management of gastrointestinal disease, especially with a rise in therapeutic EUS,” Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Stent misdeployment has been commonly reported during EUS-GE and may limit uptake of this more technically challenging procedure,” Dr. Ketwaroo said. “A comprehensive assessment of stent misdeployment, with suggestions for management and a classification system that predicts outcomes, can help practitioners to more confidently perform this procedure.”
Risks associated with misdeployed stents include “inability to perform the endoscopic management of gastric outlet obstruction, as well as adverse events such as peritonitis,” said Dr. Ketwaroo. He noted that, in most cases, the defect was closed and same-session salvage was performed, primarily by repeat EUS-GE.
Dr. Ketwaroo highlighted one challenge to endoscopic management of stent misdeployment. “If the proximal flange is deployed/slips into peritoneum (type III by currently proposed classification system), it can be more difficult to retrieve the stent,” but “this complication was treated with surgery, and it was very rare – only one case of this in the study,” he explained. “This is a large retrospective multicenter study, which adds validity to the generalizability of the study.” However, prospective studies will be needed as EUS-GE is more widely adopted, he added.
The study received no outside funding. Lead author Dr. Ghandour had no financial conflicts to disclose. Other authors disclosed industry relationships, such as consulting for Boston Scientific, Apollo, Olympus America, Medtronic, and GI Supply. Dr. Ketwaroo had no financial conflicts to disclose, but serves as a member of the GI & Hepatology News editorial advisory board.
Most instances of stent misdeployment in cases of endoscopic ultrasound–guided gastroenterostomy (EUS-GE) can be managed endoscopically, based on data from 16 tertiary care centers in the United States and Europe.
EUS-GE provides a viable alternative to traditional surgical gastroenterostomy and stent placement for patients with gastric outlet obstruction (GOO), but the potential for stent misdeployment has limited adoption of the procedure because it remains the most common cause of technical failures and adverse events, Bachir Ghandour, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
However, data on outcomes and management of stent misdeployment during EUS-GE are limited, and the researchers hypothesized that most stent misdeployments could be managed endoscopically.
In a retrospective study published in Gastrointestinal Endoscopy, the researchers reviewed data from 467 EUS-GE procedures performed for gastric outlet obstruction between March 2015 and December 2020 at eight centers in the United States and eight in Europe. The primary outcome was the rate and severity of stent misdeployment.
Stent misdeployment occurred in 46 patients (9.9%). Of these, 73.2% occurred during the operators’ first 13 cases.
The researchers created a classification system of stent misdeployment according to type, depending on which flange was misdeployed.
Type I was the most common, and occurred in 29 patients; this type was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach without evidence of a resulting enterotomy”; type II (14 patients) was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach despite an enterotomy (i.e., visual confirmation of stent having penetrated targeted small bowel, under EUS or fluoroscopy, but migrated out on deployment)”; type III (1 patient) was defined as “the deployment of the distal flange in the small bowel and proximal flange in the peritoneum”; and type IV (2 patients) was defined as “the deployment of the distal flange in the colon and proximal flange in the stomach resulting in a gastrocolic anastomosis,” the researchers wrote.
The researchers also classified the stent misdeployment in terms of severity as mild (28 patients), moderate (11 patients), severe (6 cases) or fatal (1 case) based on the American Society for Gastrointestinal Endoscopy lexicon.
Overall, type I was significantly more likely to be mild in severity, compared with type II (75.9% vs. 42.9%; P = .04), although the rate of surgical repair was similar between these two types (10.3% vs. 7.1%). Rates of ICU admission were approximately 7% in patients with type I and type II stent misdeployments, and the median postprocedural stay was 4 days for these two groups.
Same-session salvage management of GOO was achieved by EUS/endoscopic-GE in 24 patients, duodenal stent placement in 6 patients, duodenal dilation in 1 patient, and gastroenterostomy with natural orifice transluminal endoscopic surgery in 3 patients. Of the remaining 12 patients, GOO was managed with subsequent EUS-GE in 6 patients and surgical GI in 6 patients.
The study findings were limited by several factors including the retrospective design and inclusion of a time period that encompassed changes and improvements in the EUS-GE, the researchers noted. The small sample size of type III and IV stent misdeployments prohibited comparison with other types.
However, the cohort size was relatively large, compared with previous studies, and included a range of centers and countries with different strategies for managing stent misdeployments. Given the steep learning curve for EUS-GE, the study findings may help endoscopists better understand the implications and potential consequences of stent misdeployment by classifying the misdeployments into types. “We believe that such a classification or categorization of the different types is important because patient outcomes vary depending on the specific [stent misdeployment] subtype and site of injury. Such a classification will also be very helpful for future research by standardizing the terminology,” the researchers said.
“Although [stent misdeployment] is not infrequent during EUS-GE, with a rate of approximately 10%, the majority of cases are mild in severity and can be managed or repaired endoscopically without ill consequences,” they concluded. “Surgical intervention is required in less than 11% of the cases.”
Data support safe stent use in GI disease
“The lines continue to be blurred between surgical and endoscopic management of gastrointestinal disease, especially with a rise in therapeutic EUS,” Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Stent misdeployment has been commonly reported during EUS-GE and may limit uptake of this more technically challenging procedure,” Dr. Ketwaroo said. “A comprehensive assessment of stent misdeployment, with suggestions for management and a classification system that predicts outcomes, can help practitioners to more confidently perform this procedure.”
Risks associated with misdeployed stents include “inability to perform the endoscopic management of gastric outlet obstruction, as well as adverse events such as peritonitis,” said Dr. Ketwaroo. He noted that, in most cases, the defect was closed and same-session salvage was performed, primarily by repeat EUS-GE.
Dr. Ketwaroo highlighted one challenge to endoscopic management of stent misdeployment. “If the proximal flange is deployed/slips into peritoneum (type III by currently proposed classification system), it can be more difficult to retrieve the stent,” but “this complication was treated with surgery, and it was very rare – only one case of this in the study,” he explained. “This is a large retrospective multicenter study, which adds validity to the generalizability of the study.” However, prospective studies will be needed as EUS-GE is more widely adopted, he added.
The study received no outside funding. Lead author Dr. Ghandour had no financial conflicts to disclose. Other authors disclosed industry relationships, such as consulting for Boston Scientific, Apollo, Olympus America, Medtronic, and GI Supply. Dr. Ketwaroo had no financial conflicts to disclose, but serves as a member of the GI & Hepatology News editorial advisory board.
Most instances of stent misdeployment in cases of endoscopic ultrasound–guided gastroenterostomy (EUS-GE) can be managed endoscopically, based on data from 16 tertiary care centers in the United States and Europe.
EUS-GE provides a viable alternative to traditional surgical gastroenterostomy and stent placement for patients with gastric outlet obstruction (GOO), but the potential for stent misdeployment has limited adoption of the procedure because it remains the most common cause of technical failures and adverse events, Bachir Ghandour, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
However, data on outcomes and management of stent misdeployment during EUS-GE are limited, and the researchers hypothesized that most stent misdeployments could be managed endoscopically.
In a retrospective study published in Gastrointestinal Endoscopy, the researchers reviewed data from 467 EUS-GE procedures performed for gastric outlet obstruction between March 2015 and December 2020 at eight centers in the United States and eight in Europe. The primary outcome was the rate and severity of stent misdeployment.
Stent misdeployment occurred in 46 patients (9.9%). Of these, 73.2% occurred during the operators’ first 13 cases.
The researchers created a classification system of stent misdeployment according to type, depending on which flange was misdeployed.
Type I was the most common, and occurred in 29 patients; this type was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach without evidence of a resulting enterotomy”; type II (14 patients) was defined as “the deployment of the distal flange in the peritoneum and proximal flange in the stomach despite an enterotomy (i.e., visual confirmation of stent having penetrated targeted small bowel, under EUS or fluoroscopy, but migrated out on deployment)”; type III (1 patient) was defined as “the deployment of the distal flange in the small bowel and proximal flange in the peritoneum”; and type IV (2 patients) was defined as “the deployment of the distal flange in the colon and proximal flange in the stomach resulting in a gastrocolic anastomosis,” the researchers wrote.
The researchers also classified the stent misdeployment in terms of severity as mild (28 patients), moderate (11 patients), severe (6 cases) or fatal (1 case) based on the American Society for Gastrointestinal Endoscopy lexicon.
Overall, type I was significantly more likely to be mild in severity, compared with type II (75.9% vs. 42.9%; P = .04), although the rate of surgical repair was similar between these two types (10.3% vs. 7.1%). Rates of ICU admission were approximately 7% in patients with type I and type II stent misdeployments, and the median postprocedural stay was 4 days for these two groups.
Same-session salvage management of GOO was achieved by EUS/endoscopic-GE in 24 patients, duodenal stent placement in 6 patients, duodenal dilation in 1 patient, and gastroenterostomy with natural orifice transluminal endoscopic surgery in 3 patients. Of the remaining 12 patients, GOO was managed with subsequent EUS-GE in 6 patients and surgical GI in 6 patients.
The study findings were limited by several factors including the retrospective design and inclusion of a time period that encompassed changes and improvements in the EUS-GE, the researchers noted. The small sample size of type III and IV stent misdeployments prohibited comparison with other types.
However, the cohort size was relatively large, compared with previous studies, and included a range of centers and countries with different strategies for managing stent misdeployments. Given the steep learning curve for EUS-GE, the study findings may help endoscopists better understand the implications and potential consequences of stent misdeployment by classifying the misdeployments into types. “We believe that such a classification or categorization of the different types is important because patient outcomes vary depending on the specific [stent misdeployment] subtype and site of injury. Such a classification will also be very helpful for future research by standardizing the terminology,” the researchers said.
“Although [stent misdeployment] is not infrequent during EUS-GE, with a rate of approximately 10%, the majority of cases are mild in severity and can be managed or repaired endoscopically without ill consequences,” they concluded. “Surgical intervention is required in less than 11% of the cases.”
Data support safe stent use in GI disease
“The lines continue to be blurred between surgical and endoscopic management of gastrointestinal disease, especially with a rise in therapeutic EUS,” Gyanprakash A. Ketwaroo, MD, of Baylor College of Medicine, Houston, said in an interview.
“Stent misdeployment has been commonly reported during EUS-GE and may limit uptake of this more technically challenging procedure,” Dr. Ketwaroo said. “A comprehensive assessment of stent misdeployment, with suggestions for management and a classification system that predicts outcomes, can help practitioners to more confidently perform this procedure.”
Risks associated with misdeployed stents include “inability to perform the endoscopic management of gastric outlet obstruction, as well as adverse events such as peritonitis,” said Dr. Ketwaroo. He noted that, in most cases, the defect was closed and same-session salvage was performed, primarily by repeat EUS-GE.
Dr. Ketwaroo highlighted one challenge to endoscopic management of stent misdeployment. “If the proximal flange is deployed/slips into peritoneum (type III by currently proposed classification system), it can be more difficult to retrieve the stent,” but “this complication was treated with surgery, and it was very rare – only one case of this in the study,” he explained. “This is a large retrospective multicenter study, which adds validity to the generalizability of the study.” However, prospective studies will be needed as EUS-GE is more widely adopted, he added.
The study received no outside funding. Lead author Dr. Ghandour had no financial conflicts to disclose. Other authors disclosed industry relationships, such as consulting for Boston Scientific, Apollo, Olympus America, Medtronic, and GI Supply. Dr. Ketwaroo had no financial conflicts to disclose, but serves as a member of the GI & Hepatology News editorial advisory board.
FROM GASTROINTESTINAL ENDOSCOPY
Prebiotic in development shows promise for reducing GERD symptoms
A prebiotic therapy in development significantly reduced the number of days per month that people with gastroesophageal reflux disease (GERD) experienced heartburn.
The prebiotic treatment, maltosyl-isomalto-oligosaccharides (MIMO, ISOT-101), under development by ISOThrive, was also associated with reduced symptom severity and improved quality of life, John Selling, MD, chief medical officer at ISOThrive, said during the presentation of his study at the virtual Digestive Disease Week (DDW) 2021.
ISOT-101 is a nondigestible, nonabsorbable prebiotic carbohydrate produced by bacterial fermentation of sucrose and maltose. It was “possibly a staple of the bacterial diet that was present in the human diet during the past 10,000 years,” Dr. Selling said. He is a clinical associate professor of medicine and gastroenterology at Stanford (Calif.) University.
The prebiotic, however, “has been absent in our diet for about 50 to 100 years, driven by changes in agriculture, food production, food preservation, and dietary preferences,” he added.
Acid suppression treatments, such as proton pump inhibitors (PPIs), have long been a staple of treating GERD. However, about 40% of people taking PPIs still have symptoms, Dr. Selling said. He noted that there are concerns about the health risks associated with long-term PPI use.
A prebiotic could work because the distal esophageal microbiome in people with GERD “differs greatly” from that of healthy persons, Dr. Selling said. The prebiotic could help reduce an abnormal increase in gram-negative bacteria in these patients, for example. These bacterial strains express lipopolysaccharides on their outer cell membranes, which, in turn, alter cytokine signaling. This mechanism could lead to the hyperinflammatory state associated with GERD.
Dr. Selling and colleagues hypothesized that this treatment could help resolve GERD symptoms in two ways. The prebiotic could selectively feed the beneficial gram-positive bacteria in the distal esophagus, thereby helping to restore a healthy balance of bacteria. ISOT-101 could also produce bacteriocins that help kill the harmful gram-negative bacteria and control inflammation.
To assess the efficacy and tolerability of ISOT-101, Dr. Selling and colleagues plan to evaluate use of the agent in 110 people with GERD. The data presented at this year’s DDW are based on the first 44 participants to complete the study protocol.
Participants had to have active symptoms four or more days a week. They verbally reported symptoms to investigators and completed a daily ReQuest validated GERD symptom questionnaire.
After a week of baseline screening, participants consumed about a quarter teaspoon of ISOT-101 as the last substance swallowed before bed every night. The investigators asked participants to rate their GI symptoms, general well-being including any sleep disturbances, and quality of life on the Short Form 36 (SF-36) health survey. Participants also recorded use of any other medications during the 4-week study.
“I thought this was a very interesting study, as it proposes an alternative approach to manage patients with GERD,” Richa Shukla, MD, who was not affiliated with the research, said in an interview when asked to comment. “We see many patients with typical GERD symptoms who do not respond to PPI therapy, and perhaps considering an alternative cause and treatment may help with these patients.”
Dr. Shukla shared a couple of caveats. “This is a relatively small study, and it has not yet completed its enrollment target, so it will be helpful to see what the results are with the full study.” Also, it would be useful to know how many participants also took a PPI during the study, she said.
“Essentially, a lot remains unknown, but the study holds promise for patients,” added Dr. Shukla, assistant professor in the section of gastroenterology and hepatology at Baylor College of Medicine, Houston. “I think there is a lot of interest in the microbiome and how modulating it can impact inflammatory conditions.”
Key findings
The increase in heartburn-free days translated to more than eight additional days a month in which patients had no complaints of acid or heartburn. The difference from baseline was statistically significant (P < .001).
About two-thirds (66%) of participants were classified as “strong responders” to treatment, meaning they experienced an improvement of >50% in their ReQuest symptom scores over the 4 weeks. Again, the difference compared to baseline was statistically significant (P < .001).
The researchers also reported statistically significant improvements in quality-of-life indicators, such as well-being and sleep (P < .001).
The primary endpoint of the study was tolerability. The prebiotic was defined as tolerable if the ReQuest symptom scores and SF-36 scores remained constant or improved by the fourth week. ReQuest symptom scores improved for 89% of participants.
Two participants experienced nausea. No other adverse events related to ISOT-101 were reported. For five participants, ReQuest GI subscores worsened over time. For four participants, ReQuest total symptom scores worsened over time; that score represents a sum of GI and general well-being scores.
Unanswered questions
Inflammation in GERD is likely due to bacterial dysbiosis and acid-induced injury, Dr. Selling said.
If development of the prebiotic continues successfully, it could represent a paradigm shift in this clinical area, he said. “It suggests moving from acid reduction to also reducing dysbiosis as a treatment modality.”
But it remains unclear whether ISOT-101 would be indicated as monotherapy or for use in combination with other therapies for GERD.
Another unanswered question is whether the agent could be used to treat progressive disease. “This type of bacterial dysbiosis remains throughout the disease progression, from GERD to Barrett’s esophagus to esophageal adenocarcinoma,” Dr. Selling said.
The investigators reported that further controlled studies are forthcoming.
Dr. Selling is a co-founder and chief medical officer at ISOThrive. Dr. Shukla has disclosed no relevant financial relationships. David Johnson, MD, one of the authors of the abstract, is an advisor and contributor to Medscape.
A version of this article first appeared on Medscape.com.
A prebiotic therapy in development significantly reduced the number of days per month that people with gastroesophageal reflux disease (GERD) experienced heartburn.
The prebiotic treatment, maltosyl-isomalto-oligosaccharides (MIMO, ISOT-101), under development by ISOThrive, was also associated with reduced symptom severity and improved quality of life, John Selling, MD, chief medical officer at ISOThrive, said during the presentation of his study at the virtual Digestive Disease Week (DDW) 2021.
ISOT-101 is a nondigestible, nonabsorbable prebiotic carbohydrate produced by bacterial fermentation of sucrose and maltose. It was “possibly a staple of the bacterial diet that was present in the human diet during the past 10,000 years,” Dr. Selling said. He is a clinical associate professor of medicine and gastroenterology at Stanford (Calif.) University.
The prebiotic, however, “has been absent in our diet for about 50 to 100 years, driven by changes in agriculture, food production, food preservation, and dietary preferences,” he added.
Acid suppression treatments, such as proton pump inhibitors (PPIs), have long been a staple of treating GERD. However, about 40% of people taking PPIs still have symptoms, Dr. Selling said. He noted that there are concerns about the health risks associated with long-term PPI use.
A prebiotic could work because the distal esophageal microbiome in people with GERD “differs greatly” from that of healthy persons, Dr. Selling said. The prebiotic could help reduce an abnormal increase in gram-negative bacteria in these patients, for example. These bacterial strains express lipopolysaccharides on their outer cell membranes, which, in turn, alter cytokine signaling. This mechanism could lead to the hyperinflammatory state associated with GERD.
Dr. Selling and colleagues hypothesized that this treatment could help resolve GERD symptoms in two ways. The prebiotic could selectively feed the beneficial gram-positive bacteria in the distal esophagus, thereby helping to restore a healthy balance of bacteria. ISOT-101 could also produce bacteriocins that help kill the harmful gram-negative bacteria and control inflammation.
To assess the efficacy and tolerability of ISOT-101, Dr. Selling and colleagues plan to evaluate use of the agent in 110 people with GERD. The data presented at this year’s DDW are based on the first 44 participants to complete the study protocol.
Participants had to have active symptoms four or more days a week. They verbally reported symptoms to investigators and completed a daily ReQuest validated GERD symptom questionnaire.
After a week of baseline screening, participants consumed about a quarter teaspoon of ISOT-101 as the last substance swallowed before bed every night. The investigators asked participants to rate their GI symptoms, general well-being including any sleep disturbances, and quality of life on the Short Form 36 (SF-36) health survey. Participants also recorded use of any other medications during the 4-week study.
“I thought this was a very interesting study, as it proposes an alternative approach to manage patients with GERD,” Richa Shukla, MD, who was not affiliated with the research, said in an interview when asked to comment. “We see many patients with typical GERD symptoms who do not respond to PPI therapy, and perhaps considering an alternative cause and treatment may help with these patients.”
Dr. Shukla shared a couple of caveats. “This is a relatively small study, and it has not yet completed its enrollment target, so it will be helpful to see what the results are with the full study.” Also, it would be useful to know how many participants also took a PPI during the study, she said.
“Essentially, a lot remains unknown, but the study holds promise for patients,” added Dr. Shukla, assistant professor in the section of gastroenterology and hepatology at Baylor College of Medicine, Houston. “I think there is a lot of interest in the microbiome and how modulating it can impact inflammatory conditions.”
Key findings
The increase in heartburn-free days translated to more than eight additional days a month in which patients had no complaints of acid or heartburn. The difference from baseline was statistically significant (P < .001).
About two-thirds (66%) of participants were classified as “strong responders” to treatment, meaning they experienced an improvement of >50% in their ReQuest symptom scores over the 4 weeks. Again, the difference compared to baseline was statistically significant (P < .001).
The researchers also reported statistically significant improvements in quality-of-life indicators, such as well-being and sleep (P < .001).
The primary endpoint of the study was tolerability. The prebiotic was defined as tolerable if the ReQuest symptom scores and SF-36 scores remained constant or improved by the fourth week. ReQuest symptom scores improved for 89% of participants.
Two participants experienced nausea. No other adverse events related to ISOT-101 were reported. For five participants, ReQuest GI subscores worsened over time. For four participants, ReQuest total symptom scores worsened over time; that score represents a sum of GI and general well-being scores.
Unanswered questions
Inflammation in GERD is likely due to bacterial dysbiosis and acid-induced injury, Dr. Selling said.
If development of the prebiotic continues successfully, it could represent a paradigm shift in this clinical area, he said. “It suggests moving from acid reduction to also reducing dysbiosis as a treatment modality.”
But it remains unclear whether ISOT-101 would be indicated as monotherapy or for use in combination with other therapies for GERD.
Another unanswered question is whether the agent could be used to treat progressive disease. “This type of bacterial dysbiosis remains throughout the disease progression, from GERD to Barrett’s esophagus to esophageal adenocarcinoma,” Dr. Selling said.
The investigators reported that further controlled studies are forthcoming.
Dr. Selling is a co-founder and chief medical officer at ISOThrive. Dr. Shukla has disclosed no relevant financial relationships. David Johnson, MD, one of the authors of the abstract, is an advisor and contributor to Medscape.
A version of this article first appeared on Medscape.com.
A prebiotic therapy in development significantly reduced the number of days per month that people with gastroesophageal reflux disease (GERD) experienced heartburn.
The prebiotic treatment, maltosyl-isomalto-oligosaccharides (MIMO, ISOT-101), under development by ISOThrive, was also associated with reduced symptom severity and improved quality of life, John Selling, MD, chief medical officer at ISOThrive, said during the presentation of his study at the virtual Digestive Disease Week (DDW) 2021.
ISOT-101 is a nondigestible, nonabsorbable prebiotic carbohydrate produced by bacterial fermentation of sucrose and maltose. It was “possibly a staple of the bacterial diet that was present in the human diet during the past 10,000 years,” Dr. Selling said. He is a clinical associate professor of medicine and gastroenterology at Stanford (Calif.) University.
The prebiotic, however, “has been absent in our diet for about 50 to 100 years, driven by changes in agriculture, food production, food preservation, and dietary preferences,” he added.
Acid suppression treatments, such as proton pump inhibitors (PPIs), have long been a staple of treating GERD. However, about 40% of people taking PPIs still have symptoms, Dr. Selling said. He noted that there are concerns about the health risks associated with long-term PPI use.
A prebiotic could work because the distal esophageal microbiome in people with GERD “differs greatly” from that of healthy persons, Dr. Selling said. The prebiotic could help reduce an abnormal increase in gram-negative bacteria in these patients, for example. These bacterial strains express lipopolysaccharides on their outer cell membranes, which, in turn, alter cytokine signaling. This mechanism could lead to the hyperinflammatory state associated with GERD.
Dr. Selling and colleagues hypothesized that this treatment could help resolve GERD symptoms in two ways. The prebiotic could selectively feed the beneficial gram-positive bacteria in the distal esophagus, thereby helping to restore a healthy balance of bacteria. ISOT-101 could also produce bacteriocins that help kill the harmful gram-negative bacteria and control inflammation.
To assess the efficacy and tolerability of ISOT-101, Dr. Selling and colleagues plan to evaluate use of the agent in 110 people with GERD. The data presented at this year’s DDW are based on the first 44 participants to complete the study protocol.
Participants had to have active symptoms four or more days a week. They verbally reported symptoms to investigators and completed a daily ReQuest validated GERD symptom questionnaire.
After a week of baseline screening, participants consumed about a quarter teaspoon of ISOT-101 as the last substance swallowed before bed every night. The investigators asked participants to rate their GI symptoms, general well-being including any sleep disturbances, and quality of life on the Short Form 36 (SF-36) health survey. Participants also recorded use of any other medications during the 4-week study.
“I thought this was a very interesting study, as it proposes an alternative approach to manage patients with GERD,” Richa Shukla, MD, who was not affiliated with the research, said in an interview when asked to comment. “We see many patients with typical GERD symptoms who do not respond to PPI therapy, and perhaps considering an alternative cause and treatment may help with these patients.”
Dr. Shukla shared a couple of caveats. “This is a relatively small study, and it has not yet completed its enrollment target, so it will be helpful to see what the results are with the full study.” Also, it would be useful to know how many participants also took a PPI during the study, she said.
“Essentially, a lot remains unknown, but the study holds promise for patients,” added Dr. Shukla, assistant professor in the section of gastroenterology and hepatology at Baylor College of Medicine, Houston. “I think there is a lot of interest in the microbiome and how modulating it can impact inflammatory conditions.”
Key findings
The increase in heartburn-free days translated to more than eight additional days a month in which patients had no complaints of acid or heartburn. The difference from baseline was statistically significant (P < .001).
About two-thirds (66%) of participants were classified as “strong responders” to treatment, meaning they experienced an improvement of >50% in their ReQuest symptom scores over the 4 weeks. Again, the difference compared to baseline was statistically significant (P < .001).
The researchers also reported statistically significant improvements in quality-of-life indicators, such as well-being and sleep (P < .001).
The primary endpoint of the study was tolerability. The prebiotic was defined as tolerable if the ReQuest symptom scores and SF-36 scores remained constant or improved by the fourth week. ReQuest symptom scores improved for 89% of participants.
Two participants experienced nausea. No other adverse events related to ISOT-101 were reported. For five participants, ReQuest GI subscores worsened over time. For four participants, ReQuest total symptom scores worsened over time; that score represents a sum of GI and general well-being scores.
Unanswered questions
Inflammation in GERD is likely due to bacterial dysbiosis and acid-induced injury, Dr. Selling said.
If development of the prebiotic continues successfully, it could represent a paradigm shift in this clinical area, he said. “It suggests moving from acid reduction to also reducing dysbiosis as a treatment modality.”
But it remains unclear whether ISOT-101 would be indicated as monotherapy or for use in combination with other therapies for GERD.
Another unanswered question is whether the agent could be used to treat progressive disease. “This type of bacterial dysbiosis remains throughout the disease progression, from GERD to Barrett’s esophagus to esophageal adenocarcinoma,” Dr. Selling said.
The investigators reported that further controlled studies are forthcoming.
Dr. Selling is a co-founder and chief medical officer at ISOThrive. Dr. Shukla has disclosed no relevant financial relationships. David Johnson, MD, one of the authors of the abstract, is an advisor and contributor to Medscape.
A version of this article first appeared on Medscape.com.