User login
Britney Spears – Reflections on conservatorship
If you are a psychiatrist who has done a public lecture in the past year, you likely encountered the question, “What about Britney’s conservatorship?” Many psychiatrists are far removed from conservatorship evaluations, doing the different yet still important work of alleviating mental suffering without paddling in the controversial waters of involuntary treatment. Others judiciously hide behind the veil of the prudent Goldwater Rule in avoiding such discussions altogether. Regardless of whether psychiatry attempts to stay out of such affairs publicly, our field remains intimately involved in the process itself. This can lead to negative views of psychiatry among the public – that of a medical specialty with ulterior motives operating at the behest of the state.
Some psychiatrists simplistically advocate against any form of involuntary treatment.1 In many ways, this may appear noble. However, the reality of mental illness, with its potential harm to self and others, introduces the potential for dire consequences of such a position. If society is unwilling to accept behavior that may lead to harm, but psychiatry is unwilling to intervene, then other avenues of restricting such behavior will emerge. Those avenues traditionally have included conscription of law enforcement and the incarceration of patients with mental illness.
Yet, therein lies the conundrum of Ms. Spears and other celebrities on conservatorship. At face value, they do not appear to require conservatorship. We do not think it violates the Goldwater Rule to render this observation. In fact, it may reassure the public if the American Psychiatric Association, as well as individual psychiatrists, were more open about the goal, intent, and limitations of conservatorships.
The process of establishing conservatorships is not driven solely by mental health professionals. Rather, conservatorship laws permit society to enact, through psychiatrists, its desire to alleviate behaviors considered unacceptable in the context of mental illness.
In California, it has resulted in our famous or infamous “5150,” which asks psychiatrists to comment on the danger to self, danger to others, and grave disability of our patients. It can be helpful to frame these criteria regarding the relationship between society and our patients. The criteria of danger to self represents society’s wish to intervene in cases of patients with imminent intent of self-harm, operating under the presumption that a suicide can be prevented. Danger to others represents the societal angst, at times exaggerated,2 about people with mental illness perpetuating homicides, especially when off their medication. Grave disability represents public shame at the thought of persons so lost to mental illness they are unable to provide for themselves or even accept food, clothing, and shelter.
While an involuntary hold is necessary at times, working against our patients engenders revolting feelings. We often rationalize involuntary holds as illustrative of sincere compassion for our patients’ suffering and an attempt to lift them out of such tragic conditions. Our patients regularly do not feel our compassion when we are making an argument in a hearing for the restriction of their rights. They see our efforts as an attempt to lock them away “for their own good” because of society’s discomfort with homelessness. As such, we wonder whether our role becomes one of doctors for society, prescribing a treatment for the emotional distress of the community, and at times for ourselves, rather than that of the patient.
One may be perplexed as to how a celebrity could be considered gravely disabled. Celebrities generally have enough income to afford food, clothing, and shelter. One could justifiably ask why an individual with no history of violence would be considered a danger to others. Similarly, one may wonder how, in the absence of any reported attempts to engage in self-harm, with no visible marks of self-harm, someone is determined to be a danger to himself or herself. The bafflement on the part of one on the outside of these determinations can be sharply contrasted by the desperation felt by family members whose loved ones with mental illness appear to meet those criteria yet are consistently turned away by mental health programs and hospitals.
Not uncommonly, it is families advocating for involuntary hospitalization – while lamenting our strict criteria – that prevent doctors from intervening until some tragic fate befalls their loved ones. They criticize what they consider to be too-stringent mental health laws and are infuriated by seemingly obtuse insurance policies limiting care to patients. Most of our colleagues working with those who have severe mental illness share the frustration of these families over the scarcity of psychiatry beds. Therefore, it is particularly shocking when the most mediatized story about conservatorship is not about how hard it is to obtain. The story is about a singer who was seemingly safe, caring for herself, and yet still ended up on a conservatorship.
We wonder whether there is a question of magnitude. Are homeless patients more difficult to place on conservatorship because society sees a lesser stake? One could argue that Ms. Spears and other celebrities would have so much to lose in a single episode of mental illness. A week with mania or psychosis could cause irreparable damage to their persona, opportunity for employment, and their fortune. On the contrary, many of our patients on conservatorship have little to their names, and no one keeping up on their reputation. Triers of facts should ask themselves about the nature of their motivations. Envy, a desire to live vicariously through celebrities, or even less ethical motivations – such as a desire to control and exert authority over those individuals – can influence our decisions.
Throughout the past year, when asked about Ms. Spears, we have pointed out the obvious – she seemingly has a life incompatible with meeting criteria for a psychiatric conservatorship. We have outlined the role, history, and limitations of psychiatric conservatorship. We have shared how such cases are often approached, when required for our own patients or when asked by the court to do so. We have discussed the significant oversight of the system, including the public conservator’s office, which frequently refuses petitions outright. There are hearing officers, who, in the early stages of this process, weigh our case against that of the patients, aided by passionately driven patient advocates. There is the public defender’s office, which, at least in San Diego, vigorously defends the rights of those with mental illness. Most importantly, there are judges who adjudicate those cases with diligence and humility.
As the story has continued to be in the news, we have had numerous conversations about Ms. Spears’ conservatorship with colleagues sharing strong opinions on her case. Many of these colleagues do not have forensic practices and we inevitably find ourselves responding along the lines of, “It is easy to say this, but quite a different thing to prove it in court.” It is hard not to imagine testifying in such a high-profile conservatorship case; testifying, in front of jurors, about a celebrity who may have engaged in what some considered to be unusual behavior.
Conservatorship laws are not about the minutia or criteria of a specific mental health disorder. Patients do not meet criteria for conservatorship by having a certain number of delusional thoughts or a specific type of hallucination. Patients meet criteria for conservatorship because of state-enacted laws based on social factors – such as danger and self-care – the population wishes to treat, even if against the will of those treated. Under this light, one must recognize that a conservatorship trial is not just about mental illness but about how society wants to care for human beings. Psychiatric illness itself is not grounds for conservatorship. Oftentimes, severely ill patients win a hearing for grave disability by simply accepting a referral for housing, showing up to court clothed, and eating the meals provided at the hospital.
With understanding that these laws pertain specifically to behaviors resulting from mental illness that society finds unacceptable, the narrative of a celebrity conservatorship can be considered differently. The stories of celebrities being used and abused by deleterious beings and deleterious conditions have become a genre. Paul Prenter’s treatment of Freddie Mercury documented in the 2018 movie “Bohemian Rhapsody” and John Reid’s alleged betrayal of Elton John, who was suffering from a substance use disorder, documented in the 2019 movie “Rocketman,” are recent examples, among many.
Imagine yourself, as a juror, deciding on the fate of a celebrity. Would you require them to have lost all property, including the clothing on their backs, before intervening? Consider the next time you hear of a celebrity swindled from his or her fortune in a time of crisis and whether it would have been righteous to prevent it. We personally have, at times, argued for restraint in psychiatry’s desire to have more power. This concern extends not only to our ability to control people, but also our ability to force them into being subjected to psychotropic medications with well-known side effects.
At the same time, we remain cognizant of the magnified impact of adverse outcomes on public figures. John Hinckley Jr. did not attempt to murder a bystander; he attempted to kill the president of the United States when he shot at President Ronald Reagan in 1981. That incident led to considerable changes in our laws about insanity. More recently, society was particularly affected by Tom Hanks’ COVID-19 diagnosis. Mr. Hanks’ illness led to scientifically measurable changes in the public’s beliefs regarding the pandemic.3
On the other hand, and of equal importance to the desire to protect public figures from adverse events, is the risk that those same laws intended to protect will harm. From unsanitary asylums to disproportionate placements of minorities on psychiatric holds, we are concerned with unbridled control in the hands of those meant to cure and care. Sadly, there is also a cinematic genre of unprincipled and detrimental mental health treatment, from Brian Wilson’s treatment by his psychologist documented in “Love & Mercy,” to the upcoming “The Shrink Next Door,” featuring a psychiatrist swindling his patient.
With this additional understanding and analysis, we now ask our colleagues what it would take for them to intervene. Would a celebrity losing $100,000,000 because of mental illness constitute a form of grave disability despite remaining dressed? Would a celebrity engaging in significant drug use constitute a form of self-harm despite still recording albums? Would a celebrity failing to fulfill a social commitment to others, including children, constitute a form of harm to others? Those are not trivial questions to answer, and we are glad the Goldwater Rule reminds us of the limitations of speculating on people we do not know.
Nonetheless, the question of conservatorship is more complex than simply saying: “They make money; they have clothes on; this is absurd.” While this may be a catchy, compelling, and relevant argument, when confronted with a more complete narrative, triers of facts may feel compelled to intervene because, in the end, conservatorship laws are about what society is willing to accept rather than an enumeration of psychiatric symptoms.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1. Badre N et al. “Coercion and the critical psychiatrist.” In Critical Psychiatry. Springer, Cham, 2019. doi: 10.1007/97-3-030-02732-2_7.
2. Barnes SS and Badre N. Psychiatr Serv. 2016 Jul 1;67(7)784-6.
3. Myrick JG and Willoughby JF. Health Commun. 2021 Jan 14;1-9.
If you are a psychiatrist who has done a public lecture in the past year, you likely encountered the question, “What about Britney’s conservatorship?” Many psychiatrists are far removed from conservatorship evaluations, doing the different yet still important work of alleviating mental suffering without paddling in the controversial waters of involuntary treatment. Others judiciously hide behind the veil of the prudent Goldwater Rule in avoiding such discussions altogether. Regardless of whether psychiatry attempts to stay out of such affairs publicly, our field remains intimately involved in the process itself. This can lead to negative views of psychiatry among the public – that of a medical specialty with ulterior motives operating at the behest of the state.
Some psychiatrists simplistically advocate against any form of involuntary treatment.1 In many ways, this may appear noble. However, the reality of mental illness, with its potential harm to self and others, introduces the potential for dire consequences of such a position. If society is unwilling to accept behavior that may lead to harm, but psychiatry is unwilling to intervene, then other avenues of restricting such behavior will emerge. Those avenues traditionally have included conscription of law enforcement and the incarceration of patients with mental illness.
Yet, therein lies the conundrum of Ms. Spears and other celebrities on conservatorship. At face value, they do not appear to require conservatorship. We do not think it violates the Goldwater Rule to render this observation. In fact, it may reassure the public if the American Psychiatric Association, as well as individual psychiatrists, were more open about the goal, intent, and limitations of conservatorships.
The process of establishing conservatorships is not driven solely by mental health professionals. Rather, conservatorship laws permit society to enact, through psychiatrists, its desire to alleviate behaviors considered unacceptable in the context of mental illness.
In California, it has resulted in our famous or infamous “5150,” which asks psychiatrists to comment on the danger to self, danger to others, and grave disability of our patients. It can be helpful to frame these criteria regarding the relationship between society and our patients. The criteria of danger to self represents society’s wish to intervene in cases of patients with imminent intent of self-harm, operating under the presumption that a suicide can be prevented. Danger to others represents the societal angst, at times exaggerated,2 about people with mental illness perpetuating homicides, especially when off their medication. Grave disability represents public shame at the thought of persons so lost to mental illness they are unable to provide for themselves or even accept food, clothing, and shelter.
While an involuntary hold is necessary at times, working against our patients engenders revolting feelings. We often rationalize involuntary holds as illustrative of sincere compassion for our patients’ suffering and an attempt to lift them out of such tragic conditions. Our patients regularly do not feel our compassion when we are making an argument in a hearing for the restriction of their rights. They see our efforts as an attempt to lock them away “for their own good” because of society’s discomfort with homelessness. As such, we wonder whether our role becomes one of doctors for society, prescribing a treatment for the emotional distress of the community, and at times for ourselves, rather than that of the patient.
One may be perplexed as to how a celebrity could be considered gravely disabled. Celebrities generally have enough income to afford food, clothing, and shelter. One could justifiably ask why an individual with no history of violence would be considered a danger to others. Similarly, one may wonder how, in the absence of any reported attempts to engage in self-harm, with no visible marks of self-harm, someone is determined to be a danger to himself or herself. The bafflement on the part of one on the outside of these determinations can be sharply contrasted by the desperation felt by family members whose loved ones with mental illness appear to meet those criteria yet are consistently turned away by mental health programs and hospitals.
Not uncommonly, it is families advocating for involuntary hospitalization – while lamenting our strict criteria – that prevent doctors from intervening until some tragic fate befalls their loved ones. They criticize what they consider to be too-stringent mental health laws and are infuriated by seemingly obtuse insurance policies limiting care to patients. Most of our colleagues working with those who have severe mental illness share the frustration of these families over the scarcity of psychiatry beds. Therefore, it is particularly shocking when the most mediatized story about conservatorship is not about how hard it is to obtain. The story is about a singer who was seemingly safe, caring for herself, and yet still ended up on a conservatorship.
We wonder whether there is a question of magnitude. Are homeless patients more difficult to place on conservatorship because society sees a lesser stake? One could argue that Ms. Spears and other celebrities would have so much to lose in a single episode of mental illness. A week with mania or psychosis could cause irreparable damage to their persona, opportunity for employment, and their fortune. On the contrary, many of our patients on conservatorship have little to their names, and no one keeping up on their reputation. Triers of facts should ask themselves about the nature of their motivations. Envy, a desire to live vicariously through celebrities, or even less ethical motivations – such as a desire to control and exert authority over those individuals – can influence our decisions.
Throughout the past year, when asked about Ms. Spears, we have pointed out the obvious – she seemingly has a life incompatible with meeting criteria for a psychiatric conservatorship. We have outlined the role, history, and limitations of psychiatric conservatorship. We have shared how such cases are often approached, when required for our own patients or when asked by the court to do so. We have discussed the significant oversight of the system, including the public conservator’s office, which frequently refuses petitions outright. There are hearing officers, who, in the early stages of this process, weigh our case against that of the patients, aided by passionately driven patient advocates. There is the public defender’s office, which, at least in San Diego, vigorously defends the rights of those with mental illness. Most importantly, there are judges who adjudicate those cases with diligence and humility.
As the story has continued to be in the news, we have had numerous conversations about Ms. Spears’ conservatorship with colleagues sharing strong opinions on her case. Many of these colleagues do not have forensic practices and we inevitably find ourselves responding along the lines of, “It is easy to say this, but quite a different thing to prove it in court.” It is hard not to imagine testifying in such a high-profile conservatorship case; testifying, in front of jurors, about a celebrity who may have engaged in what some considered to be unusual behavior.
Conservatorship laws are not about the minutia or criteria of a specific mental health disorder. Patients do not meet criteria for conservatorship by having a certain number of delusional thoughts or a specific type of hallucination. Patients meet criteria for conservatorship because of state-enacted laws based on social factors – such as danger and self-care – the population wishes to treat, even if against the will of those treated. Under this light, one must recognize that a conservatorship trial is not just about mental illness but about how society wants to care for human beings. Psychiatric illness itself is not grounds for conservatorship. Oftentimes, severely ill patients win a hearing for grave disability by simply accepting a referral for housing, showing up to court clothed, and eating the meals provided at the hospital.
With understanding that these laws pertain specifically to behaviors resulting from mental illness that society finds unacceptable, the narrative of a celebrity conservatorship can be considered differently. The stories of celebrities being used and abused by deleterious beings and deleterious conditions have become a genre. Paul Prenter’s treatment of Freddie Mercury documented in the 2018 movie “Bohemian Rhapsody” and John Reid’s alleged betrayal of Elton John, who was suffering from a substance use disorder, documented in the 2019 movie “Rocketman,” are recent examples, among many.
Imagine yourself, as a juror, deciding on the fate of a celebrity. Would you require them to have lost all property, including the clothing on their backs, before intervening? Consider the next time you hear of a celebrity swindled from his or her fortune in a time of crisis and whether it would have been righteous to prevent it. We personally have, at times, argued for restraint in psychiatry’s desire to have more power. This concern extends not only to our ability to control people, but also our ability to force them into being subjected to psychotropic medications with well-known side effects.
At the same time, we remain cognizant of the magnified impact of adverse outcomes on public figures. John Hinckley Jr. did not attempt to murder a bystander; he attempted to kill the president of the United States when he shot at President Ronald Reagan in 1981. That incident led to considerable changes in our laws about insanity. More recently, society was particularly affected by Tom Hanks’ COVID-19 diagnosis. Mr. Hanks’ illness led to scientifically measurable changes in the public’s beliefs regarding the pandemic.3
On the other hand, and of equal importance to the desire to protect public figures from adverse events, is the risk that those same laws intended to protect will harm. From unsanitary asylums to disproportionate placements of minorities on psychiatric holds, we are concerned with unbridled control in the hands of those meant to cure and care. Sadly, there is also a cinematic genre of unprincipled and detrimental mental health treatment, from Brian Wilson’s treatment by his psychologist documented in “Love & Mercy,” to the upcoming “The Shrink Next Door,” featuring a psychiatrist swindling his patient.
With this additional understanding and analysis, we now ask our colleagues what it would take for them to intervene. Would a celebrity losing $100,000,000 because of mental illness constitute a form of grave disability despite remaining dressed? Would a celebrity engaging in significant drug use constitute a form of self-harm despite still recording albums? Would a celebrity failing to fulfill a social commitment to others, including children, constitute a form of harm to others? Those are not trivial questions to answer, and we are glad the Goldwater Rule reminds us of the limitations of speculating on people we do not know.
Nonetheless, the question of conservatorship is more complex than simply saying: “They make money; they have clothes on; this is absurd.” While this may be a catchy, compelling, and relevant argument, when confronted with a more complete narrative, triers of facts may feel compelled to intervene because, in the end, conservatorship laws are about what society is willing to accept rather than an enumeration of psychiatric symptoms.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1. Badre N et al. “Coercion and the critical psychiatrist.” In Critical Psychiatry. Springer, Cham, 2019. doi: 10.1007/97-3-030-02732-2_7.
2. Barnes SS and Badre N. Psychiatr Serv. 2016 Jul 1;67(7)784-6.
3. Myrick JG and Willoughby JF. Health Commun. 2021 Jan 14;1-9.
If you are a psychiatrist who has done a public lecture in the past year, you likely encountered the question, “What about Britney’s conservatorship?” Many psychiatrists are far removed from conservatorship evaluations, doing the different yet still important work of alleviating mental suffering without paddling in the controversial waters of involuntary treatment. Others judiciously hide behind the veil of the prudent Goldwater Rule in avoiding such discussions altogether. Regardless of whether psychiatry attempts to stay out of such affairs publicly, our field remains intimately involved in the process itself. This can lead to negative views of psychiatry among the public – that of a medical specialty with ulterior motives operating at the behest of the state.
Some psychiatrists simplistically advocate against any form of involuntary treatment.1 In many ways, this may appear noble. However, the reality of mental illness, with its potential harm to self and others, introduces the potential for dire consequences of such a position. If society is unwilling to accept behavior that may lead to harm, but psychiatry is unwilling to intervene, then other avenues of restricting such behavior will emerge. Those avenues traditionally have included conscription of law enforcement and the incarceration of patients with mental illness.
Yet, therein lies the conundrum of Ms. Spears and other celebrities on conservatorship. At face value, they do not appear to require conservatorship. We do not think it violates the Goldwater Rule to render this observation. In fact, it may reassure the public if the American Psychiatric Association, as well as individual psychiatrists, were more open about the goal, intent, and limitations of conservatorships.
The process of establishing conservatorships is not driven solely by mental health professionals. Rather, conservatorship laws permit society to enact, through psychiatrists, its desire to alleviate behaviors considered unacceptable in the context of mental illness.
In California, it has resulted in our famous or infamous “5150,” which asks psychiatrists to comment on the danger to self, danger to others, and grave disability of our patients. It can be helpful to frame these criteria regarding the relationship between society and our patients. The criteria of danger to self represents society’s wish to intervene in cases of patients with imminent intent of self-harm, operating under the presumption that a suicide can be prevented. Danger to others represents the societal angst, at times exaggerated,2 about people with mental illness perpetuating homicides, especially when off their medication. Grave disability represents public shame at the thought of persons so lost to mental illness they are unable to provide for themselves or even accept food, clothing, and shelter.
While an involuntary hold is necessary at times, working against our patients engenders revolting feelings. We often rationalize involuntary holds as illustrative of sincere compassion for our patients’ suffering and an attempt to lift them out of such tragic conditions. Our patients regularly do not feel our compassion when we are making an argument in a hearing for the restriction of their rights. They see our efforts as an attempt to lock them away “for their own good” because of society’s discomfort with homelessness. As such, we wonder whether our role becomes one of doctors for society, prescribing a treatment for the emotional distress of the community, and at times for ourselves, rather than that of the patient.
One may be perplexed as to how a celebrity could be considered gravely disabled. Celebrities generally have enough income to afford food, clothing, and shelter. One could justifiably ask why an individual with no history of violence would be considered a danger to others. Similarly, one may wonder how, in the absence of any reported attempts to engage in self-harm, with no visible marks of self-harm, someone is determined to be a danger to himself or herself. The bafflement on the part of one on the outside of these determinations can be sharply contrasted by the desperation felt by family members whose loved ones with mental illness appear to meet those criteria yet are consistently turned away by mental health programs and hospitals.
Not uncommonly, it is families advocating for involuntary hospitalization – while lamenting our strict criteria – that prevent doctors from intervening until some tragic fate befalls their loved ones. They criticize what they consider to be too-stringent mental health laws and are infuriated by seemingly obtuse insurance policies limiting care to patients. Most of our colleagues working with those who have severe mental illness share the frustration of these families over the scarcity of psychiatry beds. Therefore, it is particularly shocking when the most mediatized story about conservatorship is not about how hard it is to obtain. The story is about a singer who was seemingly safe, caring for herself, and yet still ended up on a conservatorship.
We wonder whether there is a question of magnitude. Are homeless patients more difficult to place on conservatorship because society sees a lesser stake? One could argue that Ms. Spears and other celebrities would have so much to lose in a single episode of mental illness. A week with mania or psychosis could cause irreparable damage to their persona, opportunity for employment, and their fortune. On the contrary, many of our patients on conservatorship have little to their names, and no one keeping up on their reputation. Triers of facts should ask themselves about the nature of their motivations. Envy, a desire to live vicariously through celebrities, or even less ethical motivations – such as a desire to control and exert authority over those individuals – can influence our decisions.
Throughout the past year, when asked about Ms. Spears, we have pointed out the obvious – she seemingly has a life incompatible with meeting criteria for a psychiatric conservatorship. We have outlined the role, history, and limitations of psychiatric conservatorship. We have shared how such cases are often approached, when required for our own patients or when asked by the court to do so. We have discussed the significant oversight of the system, including the public conservator’s office, which frequently refuses petitions outright. There are hearing officers, who, in the early stages of this process, weigh our case against that of the patients, aided by passionately driven patient advocates. There is the public defender’s office, which, at least in San Diego, vigorously defends the rights of those with mental illness. Most importantly, there are judges who adjudicate those cases with diligence and humility.
As the story has continued to be in the news, we have had numerous conversations about Ms. Spears’ conservatorship with colleagues sharing strong opinions on her case. Many of these colleagues do not have forensic practices and we inevitably find ourselves responding along the lines of, “It is easy to say this, but quite a different thing to prove it in court.” It is hard not to imagine testifying in such a high-profile conservatorship case; testifying, in front of jurors, about a celebrity who may have engaged in what some considered to be unusual behavior.
Conservatorship laws are not about the minutia or criteria of a specific mental health disorder. Patients do not meet criteria for conservatorship by having a certain number of delusional thoughts or a specific type of hallucination. Patients meet criteria for conservatorship because of state-enacted laws based on social factors – such as danger and self-care – the population wishes to treat, even if against the will of those treated. Under this light, one must recognize that a conservatorship trial is not just about mental illness but about how society wants to care for human beings. Psychiatric illness itself is not grounds for conservatorship. Oftentimes, severely ill patients win a hearing for grave disability by simply accepting a referral for housing, showing up to court clothed, and eating the meals provided at the hospital.
With understanding that these laws pertain specifically to behaviors resulting from mental illness that society finds unacceptable, the narrative of a celebrity conservatorship can be considered differently. The stories of celebrities being used and abused by deleterious beings and deleterious conditions have become a genre. Paul Prenter’s treatment of Freddie Mercury documented in the 2018 movie “Bohemian Rhapsody” and John Reid’s alleged betrayal of Elton John, who was suffering from a substance use disorder, documented in the 2019 movie “Rocketman,” are recent examples, among many.
Imagine yourself, as a juror, deciding on the fate of a celebrity. Would you require them to have lost all property, including the clothing on their backs, before intervening? Consider the next time you hear of a celebrity swindled from his or her fortune in a time of crisis and whether it would have been righteous to prevent it. We personally have, at times, argued for restraint in psychiatry’s desire to have more power. This concern extends not only to our ability to control people, but also our ability to force them into being subjected to psychotropic medications with well-known side effects.
At the same time, we remain cognizant of the magnified impact of adverse outcomes on public figures. John Hinckley Jr. did not attempt to murder a bystander; he attempted to kill the president of the United States when he shot at President Ronald Reagan in 1981. That incident led to considerable changes in our laws about insanity. More recently, society was particularly affected by Tom Hanks’ COVID-19 diagnosis. Mr. Hanks’ illness led to scientifically measurable changes in the public’s beliefs regarding the pandemic.3
On the other hand, and of equal importance to the desire to protect public figures from adverse events, is the risk that those same laws intended to protect will harm. From unsanitary asylums to disproportionate placements of minorities on psychiatric holds, we are concerned with unbridled control in the hands of those meant to cure and care. Sadly, there is also a cinematic genre of unprincipled and detrimental mental health treatment, from Brian Wilson’s treatment by his psychologist documented in “Love & Mercy,” to the upcoming “The Shrink Next Door,” featuring a psychiatrist swindling his patient.
With this additional understanding and analysis, we now ask our colleagues what it would take for them to intervene. Would a celebrity losing $100,000,000 because of mental illness constitute a form of grave disability despite remaining dressed? Would a celebrity engaging in significant drug use constitute a form of self-harm despite still recording albums? Would a celebrity failing to fulfill a social commitment to others, including children, constitute a form of harm to others? Those are not trivial questions to answer, and we are glad the Goldwater Rule reminds us of the limitations of speculating on people we do not know.
Nonetheless, the question of conservatorship is more complex than simply saying: “They make money; they have clothes on; this is absurd.” While this may be a catchy, compelling, and relevant argument, when confronted with a more complete narrative, triers of facts may feel compelled to intervene because, in the end, conservatorship laws are about what society is willing to accept rather than an enumeration of psychiatric symptoms.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1. Badre N et al. “Coercion and the critical psychiatrist.” In Critical Psychiatry. Springer, Cham, 2019. doi: 10.1007/97-3-030-02732-2_7.
2. Barnes SS and Badre N. Psychiatr Serv. 2016 Jul 1;67(7)784-6.
3. Myrick JG and Willoughby JF. Health Commun. 2021 Jan 14;1-9.
FDA stands firm on deadline for clozapine REMS recertification
Despite objections from the American Psychiatric Association and other national groups, federal regulators are sticking to the Nov. 15 deadline for the modified clozapine risk evaluation and mitigation strategy (REMS) program.
The modifications will require all those who prescribe and dispense clozapine to be recertified. Prescribers and pharmacies who fail to be certified by this date will no longer be able to prescribe/dispense the drug.
Clozapine is used to treat schizophrenia that is not well controlled with standard antipsychotics. It is also prescribed to patients with recurrent suicidal behavior associated with schizophrenia or schizoaffective disorder.
Although it is highly effective in some patients, it also carries serious risks. Specifically, it can decrease the neutrophil count, which can lead to severe neutropenia, serious infections, and death. As a result, those taking the drug must undergo regular absolute neutrophil count (ANC) monitoring. Clozapine REMS is intended to maximize the benefits of the drug and minimize risk.
The U.S. Food and Drug Administration first announced modifications to the program in July. Under the new rules, pharmacies will no longer be permitted to use telecommunication verification, also known as the switch system, to verify safe use conditions. Instead, the authorization to dispense will be obtained either through the contact center or online via the REMS website.
Furthermore, a new patient status form (PFS) will be used to document absolute ANC monitoring for all outpatients and the form must be submitted monthly.
In addition to the APA, opponents of the new recertification rules include the College of Psychiatric and Neurologic Pharmacists, the National Council for Mental Wellbeing, the National Association of State Mental Health Program Directors, the National Alliance on Mental Illness, the American Psychiatric Nurses Association, and the American Pharmacists Association.
No more access to patient data
Among other concerns, the coalition argues the new requirements will make it more difficult for clinicians to access data on patients’ previous clozapine history. Many clinicians depend on these data, which were maintained in the earlier REMS and in previous manufacturer-maintained clozapine monitoring systems.
The FDA told this news organization in a statement that the Clozapine Products Manufacturers’ Group “was not able to incorporate this data into the modified REMS database because of technical reasons. The new REMS contact center will have access to the historical data should a health care provider need the information,” the FDA said.
The FDA could not immediately provide this news organization with more detail on the nature of the “technical reasons” cited as a cause for the new hurdle that prevents clinicians from accessing these previously available data.
In a September letter to the FDA, the coalition pushed back, writing that it is “unreasonable to deny prescribers of this data that they entered. Furthermore, the lack of historical data could result in harm to patients in some circumstances.”
The coalition asked the FDA to intervene and ask the drug’s manufacturers to reinstate prescriber access to the information.
In a response to questions on this issue from this news organization, the FDA said in a written response the historical data had not been lost, but would be maintained “for record-keeping purposes.”
The FDA also said agency officials met on Oct. 10 with members of the professional organizations who authored the letter to hear their concerns about the clozapine REMS program. The CPMG, which has the responsibility for implementing the REMS, was also represented at the meeting, the FDA said.
“Based on concerns raised by stakeholders, the CPMG has recently begun to address some of the concerns raised in the letter including updating the prescriber/prescriber designee relationship and enrollment process to allow for a designee to be affiliated with multiple prescribers,” the FDA told this news organization.
“The recent updates also enable prescriber designees to self-enroll/create credentials, send affiliation requests to prescribers, and attest/perform functions on behalf of prescribers. It is our understanding that the CPMG is disseminating this information to stakeholders,” the agency added.
Bigger burden, bad timing
In an interview, Robert Cotes, MD, who serves as a member of the clinical expert team for Serious Mental Illness Adviser, a joint initiative of the APA and the Substance Abuse and Mental Health Services Administration, said the changes to the clozapine REMS will likely increase the administrative burden on clinicians.
In the letter to the FDA, the APA and other groups in the coalition expressed concern about patient status forms, which are five pages long. The coalition has requested that the FDA develop a form where clinicians can submit monitoring results on multiple patients at one time, with PDF forms presented in a fillable format.
“The concern is that if the workflows become more laborious for people, it could result in treatment interruptions for individuals on clozapine or potentially it may steer prescribers away from using clozapine for people who may need it,” said Dr. Cotes.
Also commenting for this news organization, Raymond C. Love, PharmD, professor and vice chair at the University of Maryland School of Pharmacy, Baltimore, emphasized the poor timing of the switch to a new clozapine REMS.
“Pharmacies are overloaded right now due to COVID tests and influenza and COVID boosters and COVID vaccinations for kids,” making it a tough time to manage the demands of the clozapine REMS re-enrollment, he said.
A version of this article first appeared on Medscape.com.
Despite objections from the American Psychiatric Association and other national groups, federal regulators are sticking to the Nov. 15 deadline for the modified clozapine risk evaluation and mitigation strategy (REMS) program.
The modifications will require all those who prescribe and dispense clozapine to be recertified. Prescribers and pharmacies who fail to be certified by this date will no longer be able to prescribe/dispense the drug.
Clozapine is used to treat schizophrenia that is not well controlled with standard antipsychotics. It is also prescribed to patients with recurrent suicidal behavior associated with schizophrenia or schizoaffective disorder.
Although it is highly effective in some patients, it also carries serious risks. Specifically, it can decrease the neutrophil count, which can lead to severe neutropenia, serious infections, and death. As a result, those taking the drug must undergo regular absolute neutrophil count (ANC) monitoring. Clozapine REMS is intended to maximize the benefits of the drug and minimize risk.
The U.S. Food and Drug Administration first announced modifications to the program in July. Under the new rules, pharmacies will no longer be permitted to use telecommunication verification, also known as the switch system, to verify safe use conditions. Instead, the authorization to dispense will be obtained either through the contact center or online via the REMS website.
Furthermore, a new patient status form (PFS) will be used to document absolute ANC monitoring for all outpatients and the form must be submitted monthly.
In addition to the APA, opponents of the new recertification rules include the College of Psychiatric and Neurologic Pharmacists, the National Council for Mental Wellbeing, the National Association of State Mental Health Program Directors, the National Alliance on Mental Illness, the American Psychiatric Nurses Association, and the American Pharmacists Association.
No more access to patient data
Among other concerns, the coalition argues the new requirements will make it more difficult for clinicians to access data on patients’ previous clozapine history. Many clinicians depend on these data, which were maintained in the earlier REMS and in previous manufacturer-maintained clozapine monitoring systems.
The FDA told this news organization in a statement that the Clozapine Products Manufacturers’ Group “was not able to incorporate this data into the modified REMS database because of technical reasons. The new REMS contact center will have access to the historical data should a health care provider need the information,” the FDA said.
The FDA could not immediately provide this news organization with more detail on the nature of the “technical reasons” cited as a cause for the new hurdle that prevents clinicians from accessing these previously available data.
In a September letter to the FDA, the coalition pushed back, writing that it is “unreasonable to deny prescribers of this data that they entered. Furthermore, the lack of historical data could result in harm to patients in some circumstances.”
The coalition asked the FDA to intervene and ask the drug’s manufacturers to reinstate prescriber access to the information.
In a response to questions on this issue from this news organization, the FDA said in a written response the historical data had not been lost, but would be maintained “for record-keeping purposes.”
The FDA also said agency officials met on Oct. 10 with members of the professional organizations who authored the letter to hear their concerns about the clozapine REMS program. The CPMG, which has the responsibility for implementing the REMS, was also represented at the meeting, the FDA said.
“Based on concerns raised by stakeholders, the CPMG has recently begun to address some of the concerns raised in the letter including updating the prescriber/prescriber designee relationship and enrollment process to allow for a designee to be affiliated with multiple prescribers,” the FDA told this news organization.
“The recent updates also enable prescriber designees to self-enroll/create credentials, send affiliation requests to prescribers, and attest/perform functions on behalf of prescribers. It is our understanding that the CPMG is disseminating this information to stakeholders,” the agency added.
Bigger burden, bad timing
In an interview, Robert Cotes, MD, who serves as a member of the clinical expert team for Serious Mental Illness Adviser, a joint initiative of the APA and the Substance Abuse and Mental Health Services Administration, said the changes to the clozapine REMS will likely increase the administrative burden on clinicians.
In the letter to the FDA, the APA and other groups in the coalition expressed concern about patient status forms, which are five pages long. The coalition has requested that the FDA develop a form where clinicians can submit monitoring results on multiple patients at one time, with PDF forms presented in a fillable format.
“The concern is that if the workflows become more laborious for people, it could result in treatment interruptions for individuals on clozapine or potentially it may steer prescribers away from using clozapine for people who may need it,” said Dr. Cotes.
Also commenting for this news organization, Raymond C. Love, PharmD, professor and vice chair at the University of Maryland School of Pharmacy, Baltimore, emphasized the poor timing of the switch to a new clozapine REMS.
“Pharmacies are overloaded right now due to COVID tests and influenza and COVID boosters and COVID vaccinations for kids,” making it a tough time to manage the demands of the clozapine REMS re-enrollment, he said.
A version of this article first appeared on Medscape.com.
Despite objections from the American Psychiatric Association and other national groups, federal regulators are sticking to the Nov. 15 deadline for the modified clozapine risk evaluation and mitigation strategy (REMS) program.
The modifications will require all those who prescribe and dispense clozapine to be recertified. Prescribers and pharmacies who fail to be certified by this date will no longer be able to prescribe/dispense the drug.
Clozapine is used to treat schizophrenia that is not well controlled with standard antipsychotics. It is also prescribed to patients with recurrent suicidal behavior associated with schizophrenia or schizoaffective disorder.
Although it is highly effective in some patients, it also carries serious risks. Specifically, it can decrease the neutrophil count, which can lead to severe neutropenia, serious infections, and death. As a result, those taking the drug must undergo regular absolute neutrophil count (ANC) monitoring. Clozapine REMS is intended to maximize the benefits of the drug and minimize risk.
The U.S. Food and Drug Administration first announced modifications to the program in July. Under the new rules, pharmacies will no longer be permitted to use telecommunication verification, also known as the switch system, to verify safe use conditions. Instead, the authorization to dispense will be obtained either through the contact center or online via the REMS website.
Furthermore, a new patient status form (PFS) will be used to document absolute ANC monitoring for all outpatients and the form must be submitted monthly.
In addition to the APA, opponents of the new recertification rules include the College of Psychiatric and Neurologic Pharmacists, the National Council for Mental Wellbeing, the National Association of State Mental Health Program Directors, the National Alliance on Mental Illness, the American Psychiatric Nurses Association, and the American Pharmacists Association.
No more access to patient data
Among other concerns, the coalition argues the new requirements will make it more difficult for clinicians to access data on patients’ previous clozapine history. Many clinicians depend on these data, which were maintained in the earlier REMS and in previous manufacturer-maintained clozapine monitoring systems.
The FDA told this news organization in a statement that the Clozapine Products Manufacturers’ Group “was not able to incorporate this data into the modified REMS database because of technical reasons. The new REMS contact center will have access to the historical data should a health care provider need the information,” the FDA said.
The FDA could not immediately provide this news organization with more detail on the nature of the “technical reasons” cited as a cause for the new hurdle that prevents clinicians from accessing these previously available data.
In a September letter to the FDA, the coalition pushed back, writing that it is “unreasonable to deny prescribers of this data that they entered. Furthermore, the lack of historical data could result in harm to patients in some circumstances.”
The coalition asked the FDA to intervene and ask the drug’s manufacturers to reinstate prescriber access to the information.
In a response to questions on this issue from this news organization, the FDA said in a written response the historical data had not been lost, but would be maintained “for record-keeping purposes.”
The FDA also said agency officials met on Oct. 10 with members of the professional organizations who authored the letter to hear their concerns about the clozapine REMS program. The CPMG, which has the responsibility for implementing the REMS, was also represented at the meeting, the FDA said.
“Based on concerns raised by stakeholders, the CPMG has recently begun to address some of the concerns raised in the letter including updating the prescriber/prescriber designee relationship and enrollment process to allow for a designee to be affiliated with multiple prescribers,” the FDA told this news organization.
“The recent updates also enable prescriber designees to self-enroll/create credentials, send affiliation requests to prescribers, and attest/perform functions on behalf of prescribers. It is our understanding that the CPMG is disseminating this information to stakeholders,” the agency added.
Bigger burden, bad timing
In an interview, Robert Cotes, MD, who serves as a member of the clinical expert team for Serious Mental Illness Adviser, a joint initiative of the APA and the Substance Abuse and Mental Health Services Administration, said the changes to the clozapine REMS will likely increase the administrative burden on clinicians.
In the letter to the FDA, the APA and other groups in the coalition expressed concern about patient status forms, which are five pages long. The coalition has requested that the FDA develop a form where clinicians can submit monitoring results on multiple patients at one time, with PDF forms presented in a fillable format.
“The concern is that if the workflows become more laborious for people, it could result in treatment interruptions for individuals on clozapine or potentially it may steer prescribers away from using clozapine for people who may need it,” said Dr. Cotes.
Also commenting for this news organization, Raymond C. Love, PharmD, professor and vice chair at the University of Maryland School of Pharmacy, Baltimore, emphasized the poor timing of the switch to a new clozapine REMS.
“Pharmacies are overloaded right now due to COVID tests and influenza and COVID boosters and COVID vaccinations for kids,” making it a tough time to manage the demands of the clozapine REMS re-enrollment, he said.
A version of this article first appeared on Medscape.com.
Aaron Beck: An appreciation
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
City or country life? Genetic risk for mental illness may decide
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
FDA not recognizing efficacy of psychopharmacologic therapies
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
Open notes: Big benefits, few harms in psychiatry, experts say
There are multiple benefits and few harms from sharing clinical notes in patients with mental illness, results of a poll of international experts show.
As of April 5, 2021, new federal rules in the United States mandate that all patients are offered online access to their electronic health record.
“Given that sharing notes in psychiatry is likely to be more complicated than in some other specialties, we were unsure whether experts would consider the practice more harmful than beneficial,” Charlotte Blease, PhD, of Beth Israel Deaconess Medical Center in Boston, told this news organization.
“However, the results of our poll suggest clinicians’ anxieties about sharing mental health notes with patients may be misplaced. We found clear consensus among experts that the benefits of online access to clinical notes could outweigh the risks,” Dr. Blease said in a news release.
The study was published online in PLOS ONE.
Empowering patients
Investigators used an online Delphi poll, an established methodology used to investigate emerging health care policy – including in psychiatry – to solicit the views of an international panel of experts on the mental health effects of sharing clinical notes.
The panel included clinicians, chief medical information officers, patient advocates, and informatics experts with extensive experience and research knowledge about patient access to mental health notes.
There was consensus among the panel that offering online access to mental health notes could enhance patients’ understanding about their diagnosis, care plan, and rationale for treatments.
There was also consensus that access to clinical notes could enhance patient recall about what was communicated and improve mental health patients’ sense of control over their health care.
The panel also agreed that blocking mental health notes could lead to greater harms including increased feelings of stigmatization.
Confirmatory findings
The poll results support an earlier study by Dr. Blease and colleagues that evaluated the experiences of patients in accessing their online clinical notes.
Among these patients with major depressive disorder, schizophrenia, schizoaffective disorder, or bipolar-related disorder, “access helped to clarify why medications had been prescribed, improved understanding about side effects, and 20% of patients reported doing a better job taking their meds as prescribed,” said Dr. Blease.
However, the expert panel in the Delphi poll predicted that with “open notes” some patients might demand changes to their clinical notes, and that mental health clinicians might be less detailed/accurate in documenting negative aspects of the patient relationship, details about patients’ personalities, or symptoms of paranoia in patients.
“If some patients feel more judged or offended by what they read, this may undermine the therapeutic relationship. ,” she added.
“In some clinical cases where there is more focus on emergency care than in forming a therapeutic relationship, for example emergency department visits, we know almost nothing about the risks and benefits associated with OpenNotes,” senior author John Torous, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, said in an interview.
“One thing is clear,” Dr. Blease said. “Patient access to their online medical records is now mainstream, and we need more clinician education on how to write notes that patients will read, and more guidance among patients on the benefits and risks of accessing their notes.”
Support for this research was provided by a J. F. Keane Scholar Award and a Swedish Research Council on Health, Working Life, and Welfare grant. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There are multiple benefits and few harms from sharing clinical notes in patients with mental illness, results of a poll of international experts show.
As of April 5, 2021, new federal rules in the United States mandate that all patients are offered online access to their electronic health record.
“Given that sharing notes in psychiatry is likely to be more complicated than in some other specialties, we were unsure whether experts would consider the practice more harmful than beneficial,” Charlotte Blease, PhD, of Beth Israel Deaconess Medical Center in Boston, told this news organization.
“However, the results of our poll suggest clinicians’ anxieties about sharing mental health notes with patients may be misplaced. We found clear consensus among experts that the benefits of online access to clinical notes could outweigh the risks,” Dr. Blease said in a news release.
The study was published online in PLOS ONE.
Empowering patients
Investigators used an online Delphi poll, an established methodology used to investigate emerging health care policy – including in psychiatry – to solicit the views of an international panel of experts on the mental health effects of sharing clinical notes.
The panel included clinicians, chief medical information officers, patient advocates, and informatics experts with extensive experience and research knowledge about patient access to mental health notes.
There was consensus among the panel that offering online access to mental health notes could enhance patients’ understanding about their diagnosis, care plan, and rationale for treatments.
There was also consensus that access to clinical notes could enhance patient recall about what was communicated and improve mental health patients’ sense of control over their health care.
The panel also agreed that blocking mental health notes could lead to greater harms including increased feelings of stigmatization.
Confirmatory findings
The poll results support an earlier study by Dr. Blease and colleagues that evaluated the experiences of patients in accessing their online clinical notes.
Among these patients with major depressive disorder, schizophrenia, schizoaffective disorder, or bipolar-related disorder, “access helped to clarify why medications had been prescribed, improved understanding about side effects, and 20% of patients reported doing a better job taking their meds as prescribed,” said Dr. Blease.
However, the expert panel in the Delphi poll predicted that with “open notes” some patients might demand changes to their clinical notes, and that mental health clinicians might be less detailed/accurate in documenting negative aspects of the patient relationship, details about patients’ personalities, or symptoms of paranoia in patients.
“If some patients feel more judged or offended by what they read, this may undermine the therapeutic relationship. ,” she added.
“In some clinical cases where there is more focus on emergency care than in forming a therapeutic relationship, for example emergency department visits, we know almost nothing about the risks and benefits associated with OpenNotes,” senior author John Torous, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, said in an interview.
“One thing is clear,” Dr. Blease said. “Patient access to their online medical records is now mainstream, and we need more clinician education on how to write notes that patients will read, and more guidance among patients on the benefits and risks of accessing their notes.”
Support for this research was provided by a J. F. Keane Scholar Award and a Swedish Research Council on Health, Working Life, and Welfare grant. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There are multiple benefits and few harms from sharing clinical notes in patients with mental illness, results of a poll of international experts show.
As of April 5, 2021, new federal rules in the United States mandate that all patients are offered online access to their electronic health record.
“Given that sharing notes in psychiatry is likely to be more complicated than in some other specialties, we were unsure whether experts would consider the practice more harmful than beneficial,” Charlotte Blease, PhD, of Beth Israel Deaconess Medical Center in Boston, told this news organization.
“However, the results of our poll suggest clinicians’ anxieties about sharing mental health notes with patients may be misplaced. We found clear consensus among experts that the benefits of online access to clinical notes could outweigh the risks,” Dr. Blease said in a news release.
The study was published online in PLOS ONE.
Empowering patients
Investigators used an online Delphi poll, an established methodology used to investigate emerging health care policy – including in psychiatry – to solicit the views of an international panel of experts on the mental health effects of sharing clinical notes.
The panel included clinicians, chief medical information officers, patient advocates, and informatics experts with extensive experience and research knowledge about patient access to mental health notes.
There was consensus among the panel that offering online access to mental health notes could enhance patients’ understanding about their diagnosis, care plan, and rationale for treatments.
There was also consensus that access to clinical notes could enhance patient recall about what was communicated and improve mental health patients’ sense of control over their health care.
The panel also agreed that blocking mental health notes could lead to greater harms including increased feelings of stigmatization.
Confirmatory findings
The poll results support an earlier study by Dr. Blease and colleagues that evaluated the experiences of patients in accessing their online clinical notes.
Among these patients with major depressive disorder, schizophrenia, schizoaffective disorder, or bipolar-related disorder, “access helped to clarify why medications had been prescribed, improved understanding about side effects, and 20% of patients reported doing a better job taking their meds as prescribed,” said Dr. Blease.
However, the expert panel in the Delphi poll predicted that with “open notes” some patients might demand changes to their clinical notes, and that mental health clinicians might be less detailed/accurate in documenting negative aspects of the patient relationship, details about patients’ personalities, or symptoms of paranoia in patients.
“If some patients feel more judged or offended by what they read, this may undermine the therapeutic relationship. ,” she added.
“In some clinical cases where there is more focus on emergency care than in forming a therapeutic relationship, for example emergency department visits, we know almost nothing about the risks and benefits associated with OpenNotes,” senior author John Torous, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, said in an interview.
“One thing is clear,” Dr. Blease said. “Patient access to their online medical records is now mainstream, and we need more clinician education on how to write notes that patients will read, and more guidance among patients on the benefits and risks of accessing their notes.”
Support for this research was provided by a J. F. Keane Scholar Award and a Swedish Research Council on Health, Working Life, and Welfare grant. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Calcineurin inhibitor–induced psychosis
Mrs. C, age 68, is experiencing worsening paranoid delusions. She believes that because she lied about her income when she was younger, the FBI is tracking her and wants to poison her food and spray dangerous fumes in her house. Her paranoia has made it hard for her to sleep, eat, or feel safe in her home.
Mrs. C’s daughter reports that her mother’s delusions started 3 years ago and have worsened in recent months. Mrs. C has no psychiatric history. Her medical history is significant for renal transplant in 2015, type 2 diabetes, hyperlipidemia, hypertension, and hypothyroidism. She is currently normotensive. Mrs. C’s home medications include cyclosporine, which is a calcineurin inhibitor, 125 mg twice daily (trough level = 138 mcg/L); mycophenolate mofetil, 500 mg twice daily; cinacalcet, 30 mg 3 times a week; metformin, 500 mg twice daily; amlodipine, 5 mg twice daily; levothyroxine, 112 mcg/d; and atorvastatin, 40 mg at bedtime.
As you review her medications, you wonder if the cyclosporine she began receiving after her kidney transplant could be causing or contributing to her worsening paranoid delusions.
Kidney transplantation has become an ideal treatment for patients with end-stage renal disease. In 2020, 22,817 kidney transplants were performed in the United States.1 Compared with dialysis, kidney transplant allows patients the chance to return to a satisfactory quality of life.2 However, to ensure a successful and long-lasting transplant, patients must be started and maintained on lifelong immunosuppressant agents that have potential adverse effects, including nephrotoxicity and hypertension. Further, immunosuppressant agents—particularly calcineurin inhibitors—are associated with potential adverse effects on mental health. The most commonly documented mental health-related adverse effects include insomnia, anxiety, depression, and confusion.3 In this article, we discuss the risk of severe psychosis associated with the use of calcineurin inhibitors.
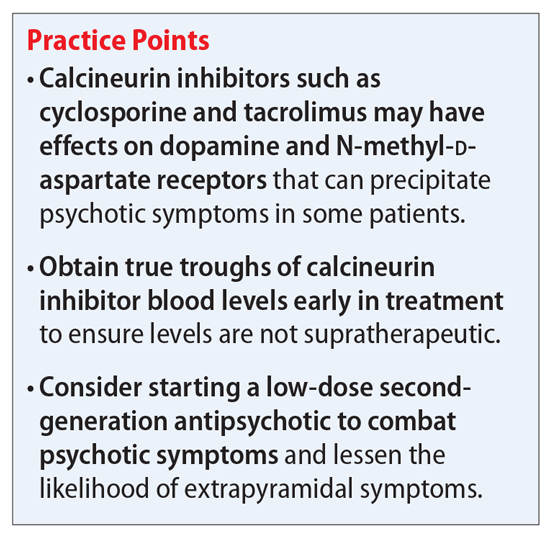
Calcineurin inhibitors and psychiatric symptoms
Cyclosporine and tacrolimus are calcineurin inhibitors that are commonly used as immunosuppressant agents after kidney transplantation. They primarily work by specifically and competitively binding to and inhibiting the calcineurin protein to reduce the transcriptional activation of cytokine genes for interleukin-2, tumor necrosis factor-alpha, interleukin-3, interleukin-4, CD40L (CD40 ligand), granulocyte-macrophage colony-stimulating factor, and interferon-gamma.4,5 The ultimate downstream effect is reduced proliferation of T lymphocytes and thereby an immunosuppressed state that will protect against organ rejection. However, this is not the only downstream effect that can occur from inhibiting calcineurin. Cyclosporine and tacrolimus may modulate the activity of dopamine and N-methyl-
An increased effect of dopamine in the mesocortical dopaminergic pathway has long been a suspected cause for psychotic symptoms. A study conducted in rodents suggested that tacrolimus selectively modifies the responsivity and sensitivity of postsynaptic dopamine-2 (D2) and dopamine-3 (D3) receptors.9 These receptors are important when discussing psychosis because antipsychotic medications work primarily by blocking dopamine D2, while many also block the D3 receptor. We hypothesize that modifying the responsivity and sensitivity of these 2 receptors could increase the risk of a person developing psychosis. It may also provide insight into how to best treat a psychotic episode.
Tacrolimus has been shown to elicit inhibition of NMDA-induced neurotransmitter release and augmentation of depolarization-induced neurotransmitter release.10 In theory, this potential inhibition at the NMDA receptors may lead to a compensatory and excessive release of glutamate. Elevated glutamate levels in the brain could lead to psychiatric symptoms, including psychosis. This is supported by the psychosis caused by many NMDA receptor antagonists, such as phencyclidine (PCP) and ketamine. Furthermore, a study examining calcineurin in knockout mice showed that the spectrum of behavioral abnormalities was strikingly similar to those in schizophrenia models.11 These mice displayed impaired working memory, impaired attentional function, social withdrawal, and psychomotor agitation. This further supports the idea that calcineurin inhibition can play a significant role in causing psychiatric symptoms by affecting both dopamine and NMDA receptors.
Continue to: How to address calcineurin inhibitor–induced psychosis...
How to address calcineurin inhibitor–induced psychosis
Here we outline a potential treatment strategy to combat psychosis secondary to calcineurin inhibitors. First, evaluate the patient’s calcineurin inhibitor level (either cyclosporine or tacrolimus). Levels should be drawn as a true trough and doses adjusted if necessary via appropriate consultation with a transplant specialist. Because many of the adverse effects associated with these agents are dose-dependent, we suspect that the risk of psychosis and other mental health–related adverse effects may also follow this trend.
Assuming that the calcineurin inhibitor cannot be stopped, changed to a different agent, or subject to a dose decrease, we recommend initiating an antipsychotic medication to control psychotic symptoms. Given the potential effect of calcineurin inhibitors on dopamine, we suggest trialing a second-generation antipsychotic with relatively high affinity for dopamine D2 receptors, such as risperidone or paliperidone. However, compared with patients with schizophrenia, patients receiving a calcineurin inhibitor may be more likely to develop extrapyramidal symptoms (EPS). Therefore, to avoid potential adverse effects, consider using a lower starting dose or an antipsychotic medication with less dopamine D2 affinity, such as quetiapine, olanzapine, or aripiprazole. Furthermore, because post-transplant patients may be at a higher risk for depression, which may be secondary to medication adverse effects, we suggest avoiding first-generation antipsychotics (FGAs) such as haloperidol because FGAs may worsen depressive symptoms.
We recommend initiating risperidone, 1 mg twice a day, for patients with psychosis secondary to a calcineurin inhibitor. If the patient develops EPS, consider switching to an antipsychotic medication with a less potent dopamine D2 blockade, such as quetiapine, olanzapine, or aripiprazole. We recommend an antipsychotic switch rather than adding benztropine or diphenhydramine to the regimen because many transplant recipients may be older patients, and adding anticholinergic medications can be problematic for this population. However, if the patient is younger or has responded particularly well to risperidone, the benefit of adding an anticholinergic medication may outweigh the risks. This decision should be made on an individual basis and may include other options, such as a switch to quetiapine, olanzapine, or aripiprazole. While these agents may not block the D2 receptor as strongly as risperidone, they all are effective and approved for adjunct therapy in major depressive disorder. We recommend quetiapine and olanzapine as second-line agents because of their potential for sedation and significant weight gain. While aripiprazole has a great metabolic adverse effect profile, its mechanism of action as a partial D2 agonist may make it difficult to control psychotic symptoms in this patient population compared with true D2 antagonists.
Continue to: CASE CONTINUED...
CASE CONTINUED
Mrs. C is admitted to the inpatient psychiatric unit and started on risperidone, 1 mg twice daily. Initially, she complains of lightheadedness at night due to the risperidone, so her dose is changed to 2 mg at bedtime. Gradually, she begins to show mild improvement. Previously, she reported feeling frightened of staff members, but after a few days she reports that she feels safe at the hospital. However, her delusions of being monitored by the FBI persist.
After 9 days of hospitalization, Mrs. C is discharged home to the care of her daughter. At first, she does well, but unfortunately she begins to refuse to take her medication and returns to her baseline.
Related Resources
- Gok F, Eroglu MZ. Acute psychotic disorder associated with immunosuppressive agent use after renal transplantation: a case report. Psychiatry and Clinical Psychopharmacology. 2017;3:314-316.
- Bersani G, Marino P, Valerani G, et al. Manic-like psychosis associated with elevated trough tacrolimus blood concentrations 17 years after kidney transplant. Case Rep Psychiatry. 2013;2013:926395. doi: 10.1155/2013/926395
Drug Brand Names
Amlodipine • Norvasc
Aripiprazole • Abilify
Atorvastatin • Lipitor
Benztropine • Cogentin
Cinacalcet • Sensipar
Cyclosporine • Gengraf
Haloperidol • Haldol
Ketamine • Ketalar
Levothyroxine • Synthroid
Metformin • Glucophage
Mycophenolate mofetil • CellCept
Olanzapine • Zyprexa
Quetiapine • Seroquel
Paliperidone • Invega
Risperidone • Risperdal
Tacrolimus • Prograf
1. Health Resources & Services Administration. US Government Information on Organ Donor Transplantation. Organ Donation Statistics. Updated October 1, 2020. Accessed October 8, 2021. https://www.organdonor.gov/learn/organ-donation-statistics/detailed-description#fig1
2. De Pasquale C, Veroux M, Indelicato L, et al. Psychopathological aspects of kidney transplantation: efficacy of a multidisciplinary team. World J Transplant. 2014;4(4):267-275.
3. Gengraf capsules [package insert]. North Chicago, IL: AbbVie Inc; 2017.
4. Wiederrecht G, Lam E, Hung S, et al. The mechanism of action of FK-506 and cyclosporin A. Ann N Y Acad Sci. 1993;696:9-19.
5. Schreiber SL, Crabtree GR. The mechanism of action of cyclosporin A and FK506. Immunol Today. 1992;13(4):136-142.
6. Scherrer U, Vissing SF, Morgan BJ, et al. Cyclosporine-induced sympathetic activation and hypertension after heart transplantation. N Engl J Med. 1990;323(11):693-699.
7. Fulya G, Meliha ZE. Acute psychotic disorder associated with immunosuppressive agent use after renal transplantation: a case report. Psychiatry and Clinical Psychopharmacology. 2017;27(3):314-316.
8. Tan TC, Robinson PJ. Mechanisms of calcineurin inhibitor-induced neurotoxicity. Transplant Rev. 2006;20(1):49-60.
9. Masatsuna S, Norio M, Nori Takei, et al. Tacrolimus, a specific inhibitor of calcineurin, modifies the locomotor activity of quinpirole, but not that of SKF82958, in male rats. Eur J Pharmacol. 2002;438(1-2):93-97.
10. Gold BG. FK506 and the role of immunophilins in nerve regeneration. Mol Neurobiol. 1997;15(3):285-306.
11. Miyakawa T, Leiter LM, Gerber DJ. Conditional calcineurin knockout mice exhibit multiple abnormal behaviors related to schizophrenia. Proc Natl Acad Sci U S A. 2003;100(15): 8987-8992.
Mrs. C, age 68, is experiencing worsening paranoid delusions. She believes that because she lied about her income when she was younger, the FBI is tracking her and wants to poison her food and spray dangerous fumes in her house. Her paranoia has made it hard for her to sleep, eat, or feel safe in her home.
Mrs. C’s daughter reports that her mother’s delusions started 3 years ago and have worsened in recent months. Mrs. C has no psychiatric history. Her medical history is significant for renal transplant in 2015, type 2 diabetes, hyperlipidemia, hypertension, and hypothyroidism. She is currently normotensive. Mrs. C’s home medications include cyclosporine, which is a calcineurin inhibitor, 125 mg twice daily (trough level = 138 mcg/L); mycophenolate mofetil, 500 mg twice daily; cinacalcet, 30 mg 3 times a week; metformin, 500 mg twice daily; amlodipine, 5 mg twice daily; levothyroxine, 112 mcg/d; and atorvastatin, 40 mg at bedtime.
As you review her medications, you wonder if the cyclosporine she began receiving after her kidney transplant could be causing or contributing to her worsening paranoid delusions.
Kidney transplantation has become an ideal treatment for patients with end-stage renal disease. In 2020, 22,817 kidney transplants were performed in the United States.1 Compared with dialysis, kidney transplant allows patients the chance to return to a satisfactory quality of life.2 However, to ensure a successful and long-lasting transplant, patients must be started and maintained on lifelong immunosuppressant agents that have potential adverse effects, including nephrotoxicity and hypertension. Further, immunosuppressant agents—particularly calcineurin inhibitors—are associated with potential adverse effects on mental health. The most commonly documented mental health-related adverse effects include insomnia, anxiety, depression, and confusion.3 In this article, we discuss the risk of severe psychosis associated with the use of calcineurin inhibitors.
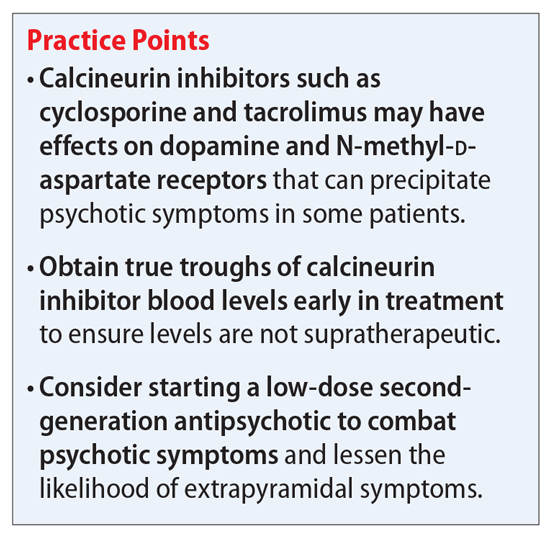
Calcineurin inhibitors and psychiatric symptoms
Cyclosporine and tacrolimus are calcineurin inhibitors that are commonly used as immunosuppressant agents after kidney transplantation. They primarily work by specifically and competitively binding to and inhibiting the calcineurin protein to reduce the transcriptional activation of cytokine genes for interleukin-2, tumor necrosis factor-alpha, interleukin-3, interleukin-4, CD40L (CD40 ligand), granulocyte-macrophage colony-stimulating factor, and interferon-gamma.4,5 The ultimate downstream effect is reduced proliferation of T lymphocytes and thereby an immunosuppressed state that will protect against organ rejection. However, this is not the only downstream effect that can occur from inhibiting calcineurin. Cyclosporine and tacrolimus may modulate the activity of dopamine and N-methyl-
An increased effect of dopamine in the mesocortical dopaminergic pathway has long been a suspected cause for psychotic symptoms. A study conducted in rodents suggested that tacrolimus selectively modifies the responsivity and sensitivity of postsynaptic dopamine-2 (D2) and dopamine-3 (D3) receptors.9 These receptors are important when discussing psychosis because antipsychotic medications work primarily by blocking dopamine D2, while many also block the D3 receptor. We hypothesize that modifying the responsivity and sensitivity of these 2 receptors could increase the risk of a person developing psychosis. It may also provide insight into how to best treat a psychotic episode.
Tacrolimus has been shown to elicit inhibition of NMDA-induced neurotransmitter release and augmentation of depolarization-induced neurotransmitter release.10 In theory, this potential inhibition at the NMDA receptors may lead to a compensatory and excessive release of glutamate. Elevated glutamate levels in the brain could lead to psychiatric symptoms, including psychosis. This is supported by the psychosis caused by many NMDA receptor antagonists, such as phencyclidine (PCP) and ketamine. Furthermore, a study examining calcineurin in knockout mice showed that the spectrum of behavioral abnormalities was strikingly similar to those in schizophrenia models.11 These mice displayed impaired working memory, impaired attentional function, social withdrawal, and psychomotor agitation. This further supports the idea that calcineurin inhibition can play a significant role in causing psychiatric symptoms by affecting both dopamine and NMDA receptors.
Continue to: How to address calcineurin inhibitor–induced psychosis...
How to address calcineurin inhibitor–induced psychosis
Here we outline a potential treatment strategy to combat psychosis secondary to calcineurin inhibitors. First, evaluate the patient’s calcineurin inhibitor level (either cyclosporine or tacrolimus). Levels should be drawn as a true trough and doses adjusted if necessary via appropriate consultation with a transplant specialist. Because many of the adverse effects associated with these agents are dose-dependent, we suspect that the risk of psychosis and other mental health–related adverse effects may also follow this trend.
Assuming that the calcineurin inhibitor cannot be stopped, changed to a different agent, or subject to a dose decrease, we recommend initiating an antipsychotic medication to control psychotic symptoms. Given the potential effect of calcineurin inhibitors on dopamine, we suggest trialing a second-generation antipsychotic with relatively high affinity for dopamine D2 receptors, such as risperidone or paliperidone. However, compared with patients with schizophrenia, patients receiving a calcineurin inhibitor may be more likely to develop extrapyramidal symptoms (EPS). Therefore, to avoid potential adverse effects, consider using a lower starting dose or an antipsychotic medication with less dopamine D2 affinity, such as quetiapine, olanzapine, or aripiprazole. Furthermore, because post-transplant patients may be at a higher risk for depression, which may be secondary to medication adverse effects, we suggest avoiding first-generation antipsychotics (FGAs) such as haloperidol because FGAs may worsen depressive symptoms.
We recommend initiating risperidone, 1 mg twice a day, for patients with psychosis secondary to a calcineurin inhibitor. If the patient develops EPS, consider switching to an antipsychotic medication with a less potent dopamine D2 blockade, such as quetiapine, olanzapine, or aripiprazole. We recommend an antipsychotic switch rather than adding benztropine or diphenhydramine to the regimen because many transplant recipients may be older patients, and adding anticholinergic medications can be problematic for this population. However, if the patient is younger or has responded particularly well to risperidone, the benefit of adding an anticholinergic medication may outweigh the risks. This decision should be made on an individual basis and may include other options, such as a switch to quetiapine, olanzapine, or aripiprazole. While these agents may not block the D2 receptor as strongly as risperidone, they all are effective and approved for adjunct therapy in major depressive disorder. We recommend quetiapine and olanzapine as second-line agents because of their potential for sedation and significant weight gain. While aripiprazole has a great metabolic adverse effect profile, its mechanism of action as a partial D2 agonist may make it difficult to control psychotic symptoms in this patient population compared with true D2 antagonists.
Continue to: CASE CONTINUED...
CASE CONTINUED
Mrs. C is admitted to the inpatient psychiatric unit and started on risperidone, 1 mg twice daily. Initially, she complains of lightheadedness at night due to the risperidone, so her dose is changed to 2 mg at bedtime. Gradually, she begins to show mild improvement. Previously, she reported feeling frightened of staff members, but after a few days she reports that she feels safe at the hospital. However, her delusions of being monitored by the FBI persist.
After 9 days of hospitalization, Mrs. C is discharged home to the care of her daughter. At first, she does well, but unfortunately she begins to refuse to take her medication and returns to her baseline.
Related Resources
- Gok F, Eroglu MZ. Acute psychotic disorder associated with immunosuppressive agent use after renal transplantation: a case report. Psychiatry and Clinical Psychopharmacology. 2017;3:314-316.
- Bersani G, Marino P, Valerani G, et al. Manic-like psychosis associated with elevated trough tacrolimus blood concentrations 17 years after kidney transplant. Case Rep Psychiatry. 2013;2013:926395. doi: 10.1155/2013/926395
Drug Brand Names
Amlodipine • Norvasc
Aripiprazole • Abilify
Atorvastatin • Lipitor
Benztropine • Cogentin
Cinacalcet • Sensipar
Cyclosporine • Gengraf
Haloperidol • Haldol
Ketamine • Ketalar
Levothyroxine • Synthroid
Metformin • Glucophage
Mycophenolate mofetil • CellCept
Olanzapine • Zyprexa
Quetiapine • Seroquel
Paliperidone • Invega
Risperidone • Risperdal
Tacrolimus • Prograf
Mrs. C, age 68, is experiencing worsening paranoid delusions. She believes that because she lied about her income when she was younger, the FBI is tracking her and wants to poison her food and spray dangerous fumes in her house. Her paranoia has made it hard for her to sleep, eat, or feel safe in her home.
Mrs. C’s daughter reports that her mother’s delusions started 3 years ago and have worsened in recent months. Mrs. C has no psychiatric history. Her medical history is significant for renal transplant in 2015, type 2 diabetes, hyperlipidemia, hypertension, and hypothyroidism. She is currently normotensive. Mrs. C’s home medications include cyclosporine, which is a calcineurin inhibitor, 125 mg twice daily (trough level = 138 mcg/L); mycophenolate mofetil, 500 mg twice daily; cinacalcet, 30 mg 3 times a week; metformin, 500 mg twice daily; amlodipine, 5 mg twice daily; levothyroxine, 112 mcg/d; and atorvastatin, 40 mg at bedtime.
As you review her medications, you wonder if the cyclosporine she began receiving after her kidney transplant could be causing or contributing to her worsening paranoid delusions.
Kidney transplantation has become an ideal treatment for patients with end-stage renal disease. In 2020, 22,817 kidney transplants were performed in the United States.1 Compared with dialysis, kidney transplant allows patients the chance to return to a satisfactory quality of life.2 However, to ensure a successful and long-lasting transplant, patients must be started and maintained on lifelong immunosuppressant agents that have potential adverse effects, including nephrotoxicity and hypertension. Further, immunosuppressant agents—particularly calcineurin inhibitors—are associated with potential adverse effects on mental health. The most commonly documented mental health-related adverse effects include insomnia, anxiety, depression, and confusion.3 In this article, we discuss the risk of severe psychosis associated with the use of calcineurin inhibitors.
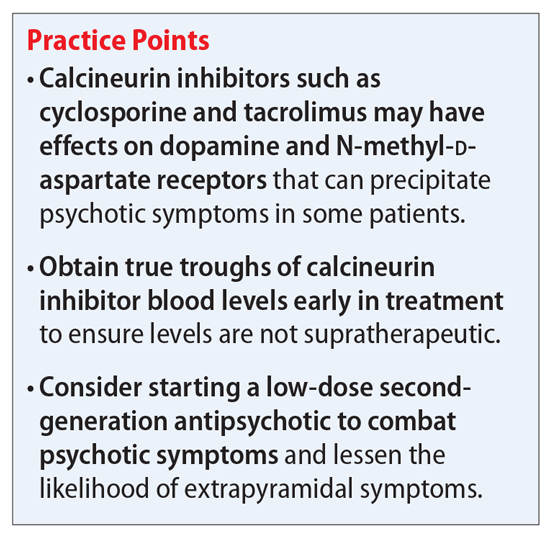
Calcineurin inhibitors and psychiatric symptoms
Cyclosporine and tacrolimus are calcineurin inhibitors that are commonly used as immunosuppressant agents after kidney transplantation. They primarily work by specifically and competitively binding to and inhibiting the calcineurin protein to reduce the transcriptional activation of cytokine genes for interleukin-2, tumor necrosis factor-alpha, interleukin-3, interleukin-4, CD40L (CD40 ligand), granulocyte-macrophage colony-stimulating factor, and interferon-gamma.4,5 The ultimate downstream effect is reduced proliferation of T lymphocytes and thereby an immunosuppressed state that will protect against organ rejection. However, this is not the only downstream effect that can occur from inhibiting calcineurin. Cyclosporine and tacrolimus may modulate the activity of dopamine and N-methyl-
An increased effect of dopamine in the mesocortical dopaminergic pathway has long been a suspected cause for psychotic symptoms. A study conducted in rodents suggested that tacrolimus selectively modifies the responsivity and sensitivity of postsynaptic dopamine-2 (D2) and dopamine-3 (D3) receptors.9 These receptors are important when discussing psychosis because antipsychotic medications work primarily by blocking dopamine D2, while many also block the D3 receptor. We hypothesize that modifying the responsivity and sensitivity of these 2 receptors could increase the risk of a person developing psychosis. It may also provide insight into how to best treat a psychotic episode.
Tacrolimus has been shown to elicit inhibition of NMDA-induced neurotransmitter release and augmentation of depolarization-induced neurotransmitter release.10 In theory, this potential inhibition at the NMDA receptors may lead to a compensatory and excessive release of glutamate. Elevated glutamate levels in the brain could lead to psychiatric symptoms, including psychosis. This is supported by the psychosis caused by many NMDA receptor antagonists, such as phencyclidine (PCP) and ketamine. Furthermore, a study examining calcineurin in knockout mice showed that the spectrum of behavioral abnormalities was strikingly similar to those in schizophrenia models.11 These mice displayed impaired working memory, impaired attentional function, social withdrawal, and psychomotor agitation. This further supports the idea that calcineurin inhibition can play a significant role in causing psychiatric symptoms by affecting both dopamine and NMDA receptors.
Continue to: How to address calcineurin inhibitor–induced psychosis...
How to address calcineurin inhibitor–induced psychosis
Here we outline a potential treatment strategy to combat psychosis secondary to calcineurin inhibitors. First, evaluate the patient’s calcineurin inhibitor level (either cyclosporine or tacrolimus). Levels should be drawn as a true trough and doses adjusted if necessary via appropriate consultation with a transplant specialist. Because many of the adverse effects associated with these agents are dose-dependent, we suspect that the risk of psychosis and other mental health–related adverse effects may also follow this trend.
Assuming that the calcineurin inhibitor cannot be stopped, changed to a different agent, or subject to a dose decrease, we recommend initiating an antipsychotic medication to control psychotic symptoms. Given the potential effect of calcineurin inhibitors on dopamine, we suggest trialing a second-generation antipsychotic with relatively high affinity for dopamine D2 receptors, such as risperidone or paliperidone. However, compared with patients with schizophrenia, patients receiving a calcineurin inhibitor may be more likely to develop extrapyramidal symptoms (EPS). Therefore, to avoid potential adverse effects, consider using a lower starting dose or an antipsychotic medication with less dopamine D2 affinity, such as quetiapine, olanzapine, or aripiprazole. Furthermore, because post-transplant patients may be at a higher risk for depression, which may be secondary to medication adverse effects, we suggest avoiding first-generation antipsychotics (FGAs) such as haloperidol because FGAs may worsen depressive symptoms.
We recommend initiating risperidone, 1 mg twice a day, for patients with psychosis secondary to a calcineurin inhibitor. If the patient develops EPS, consider switching to an antipsychotic medication with a less potent dopamine D2 blockade, such as quetiapine, olanzapine, or aripiprazole. We recommend an antipsychotic switch rather than adding benztropine or diphenhydramine to the regimen because many transplant recipients may be older patients, and adding anticholinergic medications can be problematic for this population. However, if the patient is younger or has responded particularly well to risperidone, the benefit of adding an anticholinergic medication may outweigh the risks. This decision should be made on an individual basis and may include other options, such as a switch to quetiapine, olanzapine, or aripiprazole. While these agents may not block the D2 receptor as strongly as risperidone, they all are effective and approved for adjunct therapy in major depressive disorder. We recommend quetiapine and olanzapine as second-line agents because of their potential for sedation and significant weight gain. While aripiprazole has a great metabolic adverse effect profile, its mechanism of action as a partial D2 agonist may make it difficult to control psychotic symptoms in this patient population compared with true D2 antagonists.
Continue to: CASE CONTINUED...
CASE CONTINUED
Mrs. C is admitted to the inpatient psychiatric unit and started on risperidone, 1 mg twice daily. Initially, she complains of lightheadedness at night due to the risperidone, so her dose is changed to 2 mg at bedtime. Gradually, she begins to show mild improvement. Previously, she reported feeling frightened of staff members, but after a few days she reports that she feels safe at the hospital. However, her delusions of being monitored by the FBI persist.
After 9 days of hospitalization, Mrs. C is discharged home to the care of her daughter. At first, she does well, but unfortunately she begins to refuse to take her medication and returns to her baseline.
Related Resources
- Gok F, Eroglu MZ. Acute psychotic disorder associated with immunosuppressive agent use after renal transplantation: a case report. Psychiatry and Clinical Psychopharmacology. 2017;3:314-316.
- Bersani G, Marino P, Valerani G, et al. Manic-like psychosis associated with elevated trough tacrolimus blood concentrations 17 years after kidney transplant. Case Rep Psychiatry. 2013;2013:926395. doi: 10.1155/2013/926395
Drug Brand Names
Amlodipine • Norvasc
Aripiprazole • Abilify
Atorvastatin • Lipitor
Benztropine • Cogentin
Cinacalcet • Sensipar
Cyclosporine • Gengraf
Haloperidol • Haldol
Ketamine • Ketalar
Levothyroxine • Synthroid
Metformin • Glucophage
Mycophenolate mofetil • CellCept
Olanzapine • Zyprexa
Quetiapine • Seroquel
Paliperidone • Invega
Risperidone • Risperdal
Tacrolimus • Prograf
1. Health Resources & Services Administration. US Government Information on Organ Donor Transplantation. Organ Donation Statistics. Updated October 1, 2020. Accessed October 8, 2021. https://www.organdonor.gov/learn/organ-donation-statistics/detailed-description#fig1
2. De Pasquale C, Veroux M, Indelicato L, et al. Psychopathological aspects of kidney transplantation: efficacy of a multidisciplinary team. World J Transplant. 2014;4(4):267-275.
3. Gengraf capsules [package insert]. North Chicago, IL: AbbVie Inc; 2017.
4. Wiederrecht G, Lam E, Hung S, et al. The mechanism of action of FK-506 and cyclosporin A. Ann N Y Acad Sci. 1993;696:9-19.
5. Schreiber SL, Crabtree GR. The mechanism of action of cyclosporin A and FK506. Immunol Today. 1992;13(4):136-142.
6. Scherrer U, Vissing SF, Morgan BJ, et al. Cyclosporine-induced sympathetic activation and hypertension after heart transplantation. N Engl J Med. 1990;323(11):693-699.
7. Fulya G, Meliha ZE. Acute psychotic disorder associated with immunosuppressive agent use after renal transplantation: a case report. Psychiatry and Clinical Psychopharmacology. 2017;27(3):314-316.
8. Tan TC, Robinson PJ. Mechanisms of calcineurin inhibitor-induced neurotoxicity. Transplant Rev. 2006;20(1):49-60.
9. Masatsuna S, Norio M, Nori Takei, et al. Tacrolimus, a specific inhibitor of calcineurin, modifies the locomotor activity of quinpirole, but not that of SKF82958, in male rats. Eur J Pharmacol. 2002;438(1-2):93-97.
10. Gold BG. FK506 and the role of immunophilins in nerve regeneration. Mol Neurobiol. 1997;15(3):285-306.
11. Miyakawa T, Leiter LM, Gerber DJ. Conditional calcineurin knockout mice exhibit multiple abnormal behaviors related to schizophrenia. Proc Natl Acad Sci U S A. 2003;100(15): 8987-8992.
1. Health Resources & Services Administration. US Government Information on Organ Donor Transplantation. Organ Donation Statistics. Updated October 1, 2020. Accessed October 8, 2021. https://www.organdonor.gov/learn/organ-donation-statistics/detailed-description#fig1
2. De Pasquale C, Veroux M, Indelicato L, et al. Psychopathological aspects of kidney transplantation: efficacy of a multidisciplinary team. World J Transplant. 2014;4(4):267-275.
3. Gengraf capsules [package insert]. North Chicago, IL: AbbVie Inc; 2017.
4. Wiederrecht G, Lam E, Hung S, et al. The mechanism of action of FK-506 and cyclosporin A. Ann N Y Acad Sci. 1993;696:9-19.
5. Schreiber SL, Crabtree GR. The mechanism of action of cyclosporin A and FK506. Immunol Today. 1992;13(4):136-142.
6. Scherrer U, Vissing SF, Morgan BJ, et al. Cyclosporine-induced sympathetic activation and hypertension after heart transplantation. N Engl J Med. 1990;323(11):693-699.
7. Fulya G, Meliha ZE. Acute psychotic disorder associated with immunosuppressive agent use after renal transplantation: a case report. Psychiatry and Clinical Psychopharmacology. 2017;27(3):314-316.
8. Tan TC, Robinson PJ. Mechanisms of calcineurin inhibitor-induced neurotoxicity. Transplant Rev. 2006;20(1):49-60.
9. Masatsuna S, Norio M, Nori Takei, et al. Tacrolimus, a specific inhibitor of calcineurin, modifies the locomotor activity of quinpirole, but not that of SKF82958, in male rats. Eur J Pharmacol. 2002;438(1-2):93-97.
10. Gold BG. FK506 and the role of immunophilins in nerve regeneration. Mol Neurobiol. 1997;15(3):285-306.
11. Miyakawa T, Leiter LM, Gerber DJ. Conditional calcineurin knockout mice exhibit multiple abnormal behaviors related to schizophrenia. Proc Natl Acad Sci U S A. 2003;100(15): 8987-8992.
Sleep problems in mental illness highly pervasive
An inpatient psychiatric diagnosis at some point over a lifetime is significantly associated with a range of sleep problems, results from the largest study of its kind show.
A prior diagnosis of major depression, schizophrenia, anxiety, or bipolar disorder was associated with a later bedtime, earlier waking time, and significantly poorer sleep quality that included frequent awakenings during the night and shorter sleep bouts.
“We were struck by the pervasiveness of sleep problems across all the diagnoses of mental illness and sleep parameters we looked at,” study investigator Michael Wainberg, PhD, a postdoctoral fellow at the Krembil Centre for Neuroinformatics at the Center for Addiction and Mental Health (CAMH), Toronto, told this news organization. “This suggests there may need to be even more of an emphasis on sleep in these patients than there already is.”
The study, which includes data from nearly 90,000 adults in the United Kingdom, was published online October 12 in PLoS Medicine.
Trove of data
Data for the analysis comes from the UK Biobank, a large-scale biomedical database launched in 2006 that has collected biological and medical data on more than 500,000 individuals who consented to provide blood, urine, and saliva samples and detailed lifestyle information that is matched to their medical records.
Between 2013 and 2015, more than 103,000 of these participants agreed to wear accelerometers on their wrists for 24 hours a day for 7 days, collecting a trove of data for researchers to mine.
“This allows us to get at objectively derived sleep measures and to measure them in greater numbers of people who have experienced mental illness,” said senior author Shreejoy Tripathy, PhD, assistant professor at the University of Toronto and independent scientist for CAMH. “You can study multiple disorders at once and the influence of other variables that might not be possible in the context of other studies.”
The research is the first known large-scale transdiagnostic study of objectively measured sleep and mental health. Insomnia and other sleep disorders are common among people with mental illness, as shown in prior research, including at least one study that used the same dataset the team employed for this project.
The new findings add to that body of work, Dr. Wainberg said, and look beyond just how long a person sleeps to the quality of the sleep they get.
“We found that the metrics of sleep quality seem to be affected more than mere sleep duration,” he said.
Unexpected finding
After excluding participants with faulty accelerometers and those who didn’t wear them for the entire 7-day study period, data from 89,205 participants (aged 43-79, 56% female, 97% self-reported White) was included. Lifetime inpatient psychiatric diagnoses were reported in 2.5% of the entire cohort.
Researchers looked at 10 sleep measures: bedtime, wake-up time, sleep duration, wake after sleep onset, sleep efficiency, number of awakenings, duration of longest sleep bout, number of naps, and variability in bedtime and sleep duration.
Although the effect sizes were small, having any psychiatric diagnosis was associated with significantly lower scores on every sleep measure except sleep duration.
Compared with those with no inpatient psychiatric diagnosis, those with any psychiatric diagnosis were significantly more likely to:
- have a later bedtime (beta = 0.07; 95% confidence interval, 0.06-0.09)
- have later wake-up time (beta = 0.10; 95% CI, 0.09-0.11)
- wake after sleep onset (beta = 0.10; 95% CI, 0.09-0.12)
- have poorer sleep efficiency (beta = –0.12; 95% CI, −0.14 to −0.11)
- have more awakenings (beta = 0.10; 95% CI, 0.09-0.11)
- have shorter duration of their longest sleep bout (beta = –0.09; 95% CI, −0.11 to −0.08)
- take more naps (beta = 0.11; 95% CI, 0.09-0.12)
- have greater variability in their bedtime (beta = 0.08; 95% CI, 0.06-0.09)
- have greater variability in their sleep duration (beta = 0.10; 95% CI, 0.09-0.12)
The only significant differences in sleep duration were found in those with lifetime major depressive disorder, who slept significantly less (beta = −0.02; P = .003), and in those with lifetime schizophrenia, who slept significantly longer (beta = 0.02; P = .0008).
Researchers found similar results when they examined patient-reported sleep measures collected when participants enrolled in the biobank, long before they agreed to wear an accelerometer.
“Everyone with a lifetime mental illness diagnosis trended toward worse sleep quality, regardless of their diagnosis,” Dr. Tripathy said. “We didn’t expect to see that.”
Limitations of the biobank data prohibited analysis by age and past or current use of psychiatric medications. In addition, investigators were unable to determine whether mental illness was active or controlled at the time of the study. Information on these, and other factors, is needed to truly begin to understand the real-world status of sleep patterns in people with mental illness, the researchers note.
However, the biobank data demonstrates how this type of information can be collected, helping Dr. Tripathy and others to design a new study that will launch next year with patients at CAMH. This effort is part of the BrainHealth Databank, a project that aims to develop a patient data bank similar to the one in the UK that was used for this study.
“We’ve shown that you can use wearable devices to measure correlates of sleep and derive insights about the objective measurements of sleep and associate them with mental illness diagnosis,” Dr. Tripathy said.
The study received no outside funding. Dr. Wainberg and Dr. Tripathy report receiving funding from Kavli Foundation, Krembil Foundation, CAMH Discovery Fund, the McLaughlin Foundation, NSERC, and CIHR. Disclosures for other authors are fully listed in the original article.
A version of this article first appeared on Medscape.com.
An inpatient psychiatric diagnosis at some point over a lifetime is significantly associated with a range of sleep problems, results from the largest study of its kind show.
A prior diagnosis of major depression, schizophrenia, anxiety, or bipolar disorder was associated with a later bedtime, earlier waking time, and significantly poorer sleep quality that included frequent awakenings during the night and shorter sleep bouts.
“We were struck by the pervasiveness of sleep problems across all the diagnoses of mental illness and sleep parameters we looked at,” study investigator Michael Wainberg, PhD, a postdoctoral fellow at the Krembil Centre for Neuroinformatics at the Center for Addiction and Mental Health (CAMH), Toronto, told this news organization. “This suggests there may need to be even more of an emphasis on sleep in these patients than there already is.”
The study, which includes data from nearly 90,000 adults in the United Kingdom, was published online October 12 in PLoS Medicine.
Trove of data
Data for the analysis comes from the UK Biobank, a large-scale biomedical database launched in 2006 that has collected biological and medical data on more than 500,000 individuals who consented to provide blood, urine, and saliva samples and detailed lifestyle information that is matched to their medical records.
Between 2013 and 2015, more than 103,000 of these participants agreed to wear accelerometers on their wrists for 24 hours a day for 7 days, collecting a trove of data for researchers to mine.
“This allows us to get at objectively derived sleep measures and to measure them in greater numbers of people who have experienced mental illness,” said senior author Shreejoy Tripathy, PhD, assistant professor at the University of Toronto and independent scientist for CAMH. “You can study multiple disorders at once and the influence of other variables that might not be possible in the context of other studies.”
The research is the first known large-scale transdiagnostic study of objectively measured sleep and mental health. Insomnia and other sleep disorders are common among people with mental illness, as shown in prior research, including at least one study that used the same dataset the team employed for this project.
The new findings add to that body of work, Dr. Wainberg said, and look beyond just how long a person sleeps to the quality of the sleep they get.
“We found that the metrics of sleep quality seem to be affected more than mere sleep duration,” he said.
Unexpected finding
After excluding participants with faulty accelerometers and those who didn’t wear them for the entire 7-day study period, data from 89,205 participants (aged 43-79, 56% female, 97% self-reported White) was included. Lifetime inpatient psychiatric diagnoses were reported in 2.5% of the entire cohort.
Researchers looked at 10 sleep measures: bedtime, wake-up time, sleep duration, wake after sleep onset, sleep efficiency, number of awakenings, duration of longest sleep bout, number of naps, and variability in bedtime and sleep duration.
Although the effect sizes were small, having any psychiatric diagnosis was associated with significantly lower scores on every sleep measure except sleep duration.
Compared with those with no inpatient psychiatric diagnosis, those with any psychiatric diagnosis were significantly more likely to:
- have a later bedtime (beta = 0.07; 95% confidence interval, 0.06-0.09)
- have later wake-up time (beta = 0.10; 95% CI, 0.09-0.11)
- wake after sleep onset (beta = 0.10; 95% CI, 0.09-0.12)
- have poorer sleep efficiency (beta = –0.12; 95% CI, −0.14 to −0.11)
- have more awakenings (beta = 0.10; 95% CI, 0.09-0.11)
- have shorter duration of their longest sleep bout (beta = –0.09; 95% CI, −0.11 to −0.08)
- take more naps (beta = 0.11; 95% CI, 0.09-0.12)
- have greater variability in their bedtime (beta = 0.08; 95% CI, 0.06-0.09)
- have greater variability in their sleep duration (beta = 0.10; 95% CI, 0.09-0.12)
The only significant differences in sleep duration were found in those with lifetime major depressive disorder, who slept significantly less (beta = −0.02; P = .003), and in those with lifetime schizophrenia, who slept significantly longer (beta = 0.02; P = .0008).
Researchers found similar results when they examined patient-reported sleep measures collected when participants enrolled in the biobank, long before they agreed to wear an accelerometer.
“Everyone with a lifetime mental illness diagnosis trended toward worse sleep quality, regardless of their diagnosis,” Dr. Tripathy said. “We didn’t expect to see that.”
Limitations of the biobank data prohibited analysis by age and past or current use of psychiatric medications. In addition, investigators were unable to determine whether mental illness was active or controlled at the time of the study. Information on these, and other factors, is needed to truly begin to understand the real-world status of sleep patterns in people with mental illness, the researchers note.
However, the biobank data demonstrates how this type of information can be collected, helping Dr. Tripathy and others to design a new study that will launch next year with patients at CAMH. This effort is part of the BrainHealth Databank, a project that aims to develop a patient data bank similar to the one in the UK that was used for this study.
“We’ve shown that you can use wearable devices to measure correlates of sleep and derive insights about the objective measurements of sleep and associate them with mental illness diagnosis,” Dr. Tripathy said.
The study received no outside funding. Dr. Wainberg and Dr. Tripathy report receiving funding from Kavli Foundation, Krembil Foundation, CAMH Discovery Fund, the McLaughlin Foundation, NSERC, and CIHR. Disclosures for other authors are fully listed in the original article.
A version of this article first appeared on Medscape.com.
An inpatient psychiatric diagnosis at some point over a lifetime is significantly associated with a range of sleep problems, results from the largest study of its kind show.
A prior diagnosis of major depression, schizophrenia, anxiety, or bipolar disorder was associated with a later bedtime, earlier waking time, and significantly poorer sleep quality that included frequent awakenings during the night and shorter sleep bouts.
“We were struck by the pervasiveness of sleep problems across all the diagnoses of mental illness and sleep parameters we looked at,” study investigator Michael Wainberg, PhD, a postdoctoral fellow at the Krembil Centre for Neuroinformatics at the Center for Addiction and Mental Health (CAMH), Toronto, told this news organization. “This suggests there may need to be even more of an emphasis on sleep in these patients than there already is.”
The study, which includes data from nearly 90,000 adults in the United Kingdom, was published online October 12 in PLoS Medicine.
Trove of data
Data for the analysis comes from the UK Biobank, a large-scale biomedical database launched in 2006 that has collected biological and medical data on more than 500,000 individuals who consented to provide blood, urine, and saliva samples and detailed lifestyle information that is matched to their medical records.
Between 2013 and 2015, more than 103,000 of these participants agreed to wear accelerometers on their wrists for 24 hours a day for 7 days, collecting a trove of data for researchers to mine.
“This allows us to get at objectively derived sleep measures and to measure them in greater numbers of people who have experienced mental illness,” said senior author Shreejoy Tripathy, PhD, assistant professor at the University of Toronto and independent scientist for CAMH. “You can study multiple disorders at once and the influence of other variables that might not be possible in the context of other studies.”
The research is the first known large-scale transdiagnostic study of objectively measured sleep and mental health. Insomnia and other sleep disorders are common among people with mental illness, as shown in prior research, including at least one study that used the same dataset the team employed for this project.
The new findings add to that body of work, Dr. Wainberg said, and look beyond just how long a person sleeps to the quality of the sleep they get.
“We found that the metrics of sleep quality seem to be affected more than mere sleep duration,” he said.
Unexpected finding
After excluding participants with faulty accelerometers and those who didn’t wear them for the entire 7-day study period, data from 89,205 participants (aged 43-79, 56% female, 97% self-reported White) was included. Lifetime inpatient psychiatric diagnoses were reported in 2.5% of the entire cohort.
Researchers looked at 10 sleep measures: bedtime, wake-up time, sleep duration, wake after sleep onset, sleep efficiency, number of awakenings, duration of longest sleep bout, number of naps, and variability in bedtime and sleep duration.
Although the effect sizes were small, having any psychiatric diagnosis was associated with significantly lower scores on every sleep measure except sleep duration.
Compared with those with no inpatient psychiatric diagnosis, those with any psychiatric diagnosis were significantly more likely to:
- have a later bedtime (beta = 0.07; 95% confidence interval, 0.06-0.09)
- have later wake-up time (beta = 0.10; 95% CI, 0.09-0.11)
- wake after sleep onset (beta = 0.10; 95% CI, 0.09-0.12)
- have poorer sleep efficiency (beta = –0.12; 95% CI, −0.14 to −0.11)
- have more awakenings (beta = 0.10; 95% CI, 0.09-0.11)
- have shorter duration of their longest sleep bout (beta = –0.09; 95% CI, −0.11 to −0.08)
- take more naps (beta = 0.11; 95% CI, 0.09-0.12)
- have greater variability in their bedtime (beta = 0.08; 95% CI, 0.06-0.09)
- have greater variability in their sleep duration (beta = 0.10; 95% CI, 0.09-0.12)
The only significant differences in sleep duration were found in those with lifetime major depressive disorder, who slept significantly less (beta = −0.02; P = .003), and in those with lifetime schizophrenia, who slept significantly longer (beta = 0.02; P = .0008).
Researchers found similar results when they examined patient-reported sleep measures collected when participants enrolled in the biobank, long before they agreed to wear an accelerometer.
“Everyone with a lifetime mental illness diagnosis trended toward worse sleep quality, regardless of their diagnosis,” Dr. Tripathy said. “We didn’t expect to see that.”
Limitations of the biobank data prohibited analysis by age and past or current use of psychiatric medications. In addition, investigators were unable to determine whether mental illness was active or controlled at the time of the study. Information on these, and other factors, is needed to truly begin to understand the real-world status of sleep patterns in people with mental illness, the researchers note.
However, the biobank data demonstrates how this type of information can be collected, helping Dr. Tripathy and others to design a new study that will launch next year with patients at CAMH. This effort is part of the BrainHealth Databank, a project that aims to develop a patient data bank similar to the one in the UK that was used for this study.
“We’ve shown that you can use wearable devices to measure correlates of sleep and derive insights about the objective measurements of sleep and associate them with mental illness diagnosis,” Dr. Tripathy said.
The study received no outside funding. Dr. Wainberg and Dr. Tripathy report receiving funding from Kavli Foundation, Krembil Foundation, CAMH Discovery Fund, the McLaughlin Foundation, NSERC, and CIHR. Disclosures for other authors are fully listed in the original article.
A version of this article first appeared on Medscape.com.
Substance use or substance use disorder: A question of judgment
Substance use disorders can be a thorny topic in residency because of our role as gatekeepers of mental hospitals during our training. Intoxicated patients often get dismissed as a burden and distraction, malingering their way into a comfortable place to regain sobriety. This is extremely prevalent, often constituting the majority of patients seen during an emergency department call.
A typical interview may elicit any or all symptoms in the DSM yet be best explained by substance use intoxication or withdrawal. Alcohol and other CNS depressants commonly cause feelings of sadness and/or suicidality. Methamphetamine and other CNS stimulants commonly cause symptoms of psychosis or mania, followed by feelings of sadness and/or suicidality.
Different EDs have different degrees of patience for individuals in the process of becoming sober. Some departments will pressure clinicians into quickly discarding those patients and often frown upon any attempt at providing solace by raising the concern of reinforcing maladaptive behavior. A mystery-meat sandwich of admirable blandness may be the extent of help offered. Some more fortunate patients also receive a juice box or even a taxi voucher in an especially generous ED. This is always against our better judgment, of course, as we are told those gestures encourage abuse.
Other EDs will permit patients to remain until sober, allowing for another evaluation without the influence of controlled substances. We are reminded of many conversations with patients with substance use disorders, where topics discussed included: 1. Recommendation to seek substance use services, which are often nonexistent or with wait lists spanning months; 2. Education on the role of mental health hospitals and how patients’ despair in the context of intoxication does not meet some scriptural criteria; 3. Pep talks aided by such previously described sandwiches and juice boxes to encourage a sobering patient to leave the facility of their own will.
Methamphetamine, heroin, and alcohol are rarely one-and-done endeavors. We sparingly see our patients for their very first ED visit while intoxicated or crashing. They know how the system runs and which ED will more readily allow them an overnight stay. The number of times they have been recommended for substance use treatment is beyond counting – they may have been on a wait list a handful of times. They are aware of our reluctance to provide inpatient psychiatric treatment for substance use, but it is worth a shot trying, anyway – sometimes they get lucky. Usually it is the pep talk, relief from hunger pangs, and daylight that get them out the doors – until next time.
It is under this context that many trainees become psychiatrists, a process that solidifies the separation between drug use and mental illness. Many graduate from residency practically equating substance use disorder with malingering or futility. This can take on a surreal quality as many localities have recently adopted particular forms or requirements like the dispensation of naloxone syringes to all patients with substance use disorders. While the desire and effort are noble, it may suggest to a patient presenting for help that society’s main interest is to avoid seeing them die rather than help with available resources for maintaining sobriety.
Therein lies the conundrum, a conundrum that spans psychiatry to society. The conundrum is our ambivalence between punishing the choice of drug use or healing the substance use disorder. Should we discharge the intoxicated patient as soon as they are safe to walk out, or should we make every effort possible to find long-term solutions?
The calculation becomes more complex
A defining moment appears to have been society’s reconsideration of its stance on substance use disorders when affluent White teenagers started dying in the suburbs from pain pills overdoses. Suddenly, those children needed and deserved treatment, not punishment. We find ourselves far away from a time when the loudest societal commentary on substance use entailed mothers advocating for harsher sentences against drunk drivers.
More recently, as psychiatry and large contingents of society have decided to take up the mantle of equity and social justice, we have begun to make progress in decriminalizing substance use in an effort to reverse systemic discrimination toward minority groups. This has taken many shapes, including drug legalization, criminal justice reform, and even the provision of clean substance use paraphernalia for safer use of IV drugs. Police reform has led to reluctance to arrest or press charges for nonviolent crimes and reduced police presence in minority neighborhoods. The “rich White teenager” approach is now recommended in all neighborhoods.
Society’s attempt at decriminalizing drug use has run parallel with psychiatry’s recent attempts at reduced pathologizing of behaviors more prevalent in underprivileged groups and cultures. This runs the gamut, from avoiding the use of the term “agitated” because of its racial connotations, to advocating for reduced rates of schizophrenia diagnoses in Black males.1 A diagnosis of substance use disorder carries with it similar troublesome societal implications. Decriminalization, legalization, provision of substances to the population, normalization, and other societal reforms will likely have an impact on the prevalence of substance use disorder diagnoses, which involve many criteria dependent on societal context.
It would be expected that criteria such as hazardous use, social problems, and attempts to quit will decrease as social acceptance increases. How might this affect access to substance use treatment, an already extremely limited resource?
Now, as forensic psychiatrists, we find ourselves adjudicating on the role of drugs at a time when society is wrestling with its attitude on the breadth of responsibility possessed by people who use drugs. In California, as in many other states, insanity laws exclude those who were insane as a result of drug use, as a testament to or possibly a remnant of how society feels about the role of choice and responsibility in the use of drugs. Yet another defendant who admits to drug use may on the contrary receive a much more lenient plea deal if willing to commit to sobriety. But in a never-ending maze of differing judgments and opinions, a less understanding district attorney may argue that the additional risk posed by the use of drugs and resulting impulsivity may actually warrant a heavier sentence.
In a recent attempt at atonement for our past punitive stance on drug users, we have found a desire to protect those who use drugs by punishing those who sell, at times forgetting that these populations are deeply intertwined. A recent law permits the federal charge of distribution of fentanyl resulting in death, which carries the mandatory minimum of 20 years in prison. Yet, if the user whom we are trying to protect by this law is also the one selling, what are we left with?
Fentanyl has been a particularly tragic development in the history of mankind and drug use. Substance use has rarely been so easily linked to accidental death. While many physicians can easily explain the safety of fentanyl when used as prescribed and in controlled settings, this is certainly not the case in the community. Measuring micrograms of fentanyl is outside the knowledge and capabilities of most drug dealers, who are not equipped with pharmacy-grade scales. Yet, as a result, they sell and customers buy quantities of fentanyl that range from homeopathically low to lethally high because of a mixture of negligence and deliberate indifference.
Another effort at atonement has been attempts at decriminalizing drug use and releasing many nonviolent offenders. This can, however, encourage bystanders to report more acts as crime rather than public intoxication, to ensure a police response when confronted by intoxicated people. Whereas previously an inebriated person who is homeless may have been called for and asked to seek shelter, they now get called on, and subsequently charged for, allegedly mumbling a threat by a frustrated bystander.
The release of offenders has its limits. Many placements on probation require sobriety and result in longer sentences for the use of substances that are otherwise decriminalized. The decriminalization and reexamination of substance use by society should widen the scope from simply considering crime to examining the use of drugs throughout the legal system and even beyond.
The DSM and psychiatry are not intended or equipped to adjudicate disputes on where the lines should be drawn between determinism and free will. We are knowledgeable of patients with substance use disorders, the effect of intoxicating substances, and the capacity of patients with substance use disorders to act in law-abiding ways. Our field can inform without simply advocating whether our patients should be punished. While society is currently struggling with how to apportion blame, psychiatry should resist the urge to impose medical solutions to social problems. Our solutions would almost certainly be grossly limited as we are still struggling to repent for lobotomizing “uppity” young women2 and using electroshock therapy to disrupt perverse impulses in homosexual males.3 Social norms and political zeitgeists change over time while the psychological and physiological principles underlying our understanding of mental illness should, in theory, stay relatively constant. Psychiatry’s answers for societal ills do not usually improve with time but rather have a tendency to be humbling.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1.Medlock MM et al., eds. “Racism and Psychiatry: Contemporary Issues and Interventions” (New York: Springer, 2018).
2. Tone A and Koziol M. CMAJ. 2018:190(20):e624-5.
3. McGuire RJ and Vallance M. BMJ. 1964;1(5376):151-3.
Substance use disorders can be a thorny topic in residency because of our role as gatekeepers of mental hospitals during our training. Intoxicated patients often get dismissed as a burden and distraction, malingering their way into a comfortable place to regain sobriety. This is extremely prevalent, often constituting the majority of patients seen during an emergency department call.
A typical interview may elicit any or all symptoms in the DSM yet be best explained by substance use intoxication or withdrawal. Alcohol and other CNS depressants commonly cause feelings of sadness and/or suicidality. Methamphetamine and other CNS stimulants commonly cause symptoms of psychosis or mania, followed by feelings of sadness and/or suicidality.
Different EDs have different degrees of patience for individuals in the process of becoming sober. Some departments will pressure clinicians into quickly discarding those patients and often frown upon any attempt at providing solace by raising the concern of reinforcing maladaptive behavior. A mystery-meat sandwich of admirable blandness may be the extent of help offered. Some more fortunate patients also receive a juice box or even a taxi voucher in an especially generous ED. This is always against our better judgment, of course, as we are told those gestures encourage abuse.
Other EDs will permit patients to remain until sober, allowing for another evaluation without the influence of controlled substances. We are reminded of many conversations with patients with substance use disorders, where topics discussed included: 1. Recommendation to seek substance use services, which are often nonexistent or with wait lists spanning months; 2. Education on the role of mental health hospitals and how patients’ despair in the context of intoxication does not meet some scriptural criteria; 3. Pep talks aided by such previously described sandwiches and juice boxes to encourage a sobering patient to leave the facility of their own will.
Methamphetamine, heroin, and alcohol are rarely one-and-done endeavors. We sparingly see our patients for their very first ED visit while intoxicated or crashing. They know how the system runs and which ED will more readily allow them an overnight stay. The number of times they have been recommended for substance use treatment is beyond counting – they may have been on a wait list a handful of times. They are aware of our reluctance to provide inpatient psychiatric treatment for substance use, but it is worth a shot trying, anyway – sometimes they get lucky. Usually it is the pep talk, relief from hunger pangs, and daylight that get them out the doors – until next time.
It is under this context that many trainees become psychiatrists, a process that solidifies the separation between drug use and mental illness. Many graduate from residency practically equating substance use disorder with malingering or futility. This can take on a surreal quality as many localities have recently adopted particular forms or requirements like the dispensation of naloxone syringes to all patients with substance use disorders. While the desire and effort are noble, it may suggest to a patient presenting for help that society’s main interest is to avoid seeing them die rather than help with available resources for maintaining sobriety.
Therein lies the conundrum, a conundrum that spans psychiatry to society. The conundrum is our ambivalence between punishing the choice of drug use or healing the substance use disorder. Should we discharge the intoxicated patient as soon as they are safe to walk out, or should we make every effort possible to find long-term solutions?
The calculation becomes more complex
A defining moment appears to have been society’s reconsideration of its stance on substance use disorders when affluent White teenagers started dying in the suburbs from pain pills overdoses. Suddenly, those children needed and deserved treatment, not punishment. We find ourselves far away from a time when the loudest societal commentary on substance use entailed mothers advocating for harsher sentences against drunk drivers.
More recently, as psychiatry and large contingents of society have decided to take up the mantle of equity and social justice, we have begun to make progress in decriminalizing substance use in an effort to reverse systemic discrimination toward minority groups. This has taken many shapes, including drug legalization, criminal justice reform, and even the provision of clean substance use paraphernalia for safer use of IV drugs. Police reform has led to reluctance to arrest or press charges for nonviolent crimes and reduced police presence in minority neighborhoods. The “rich White teenager” approach is now recommended in all neighborhoods.
Society’s attempt at decriminalizing drug use has run parallel with psychiatry’s recent attempts at reduced pathologizing of behaviors more prevalent in underprivileged groups and cultures. This runs the gamut, from avoiding the use of the term “agitated” because of its racial connotations, to advocating for reduced rates of schizophrenia diagnoses in Black males.1 A diagnosis of substance use disorder carries with it similar troublesome societal implications. Decriminalization, legalization, provision of substances to the population, normalization, and other societal reforms will likely have an impact on the prevalence of substance use disorder diagnoses, which involve many criteria dependent on societal context.
It would be expected that criteria such as hazardous use, social problems, and attempts to quit will decrease as social acceptance increases. How might this affect access to substance use treatment, an already extremely limited resource?
Now, as forensic psychiatrists, we find ourselves adjudicating on the role of drugs at a time when society is wrestling with its attitude on the breadth of responsibility possessed by people who use drugs. In California, as in many other states, insanity laws exclude those who were insane as a result of drug use, as a testament to or possibly a remnant of how society feels about the role of choice and responsibility in the use of drugs. Yet another defendant who admits to drug use may on the contrary receive a much more lenient plea deal if willing to commit to sobriety. But in a never-ending maze of differing judgments and opinions, a less understanding district attorney may argue that the additional risk posed by the use of drugs and resulting impulsivity may actually warrant a heavier sentence.
In a recent attempt at atonement for our past punitive stance on drug users, we have found a desire to protect those who use drugs by punishing those who sell, at times forgetting that these populations are deeply intertwined. A recent law permits the federal charge of distribution of fentanyl resulting in death, which carries the mandatory minimum of 20 years in prison. Yet, if the user whom we are trying to protect by this law is also the one selling, what are we left with?
Fentanyl has been a particularly tragic development in the history of mankind and drug use. Substance use has rarely been so easily linked to accidental death. While many physicians can easily explain the safety of fentanyl when used as prescribed and in controlled settings, this is certainly not the case in the community. Measuring micrograms of fentanyl is outside the knowledge and capabilities of most drug dealers, who are not equipped with pharmacy-grade scales. Yet, as a result, they sell and customers buy quantities of fentanyl that range from homeopathically low to lethally high because of a mixture of negligence and deliberate indifference.
Another effort at atonement has been attempts at decriminalizing drug use and releasing many nonviolent offenders. This can, however, encourage bystanders to report more acts as crime rather than public intoxication, to ensure a police response when confronted by intoxicated people. Whereas previously an inebriated person who is homeless may have been called for and asked to seek shelter, they now get called on, and subsequently charged for, allegedly mumbling a threat by a frustrated bystander.
The release of offenders has its limits. Many placements on probation require sobriety and result in longer sentences for the use of substances that are otherwise decriminalized. The decriminalization and reexamination of substance use by society should widen the scope from simply considering crime to examining the use of drugs throughout the legal system and even beyond.
The DSM and psychiatry are not intended or equipped to adjudicate disputes on where the lines should be drawn between determinism and free will. We are knowledgeable of patients with substance use disorders, the effect of intoxicating substances, and the capacity of patients with substance use disorders to act in law-abiding ways. Our field can inform without simply advocating whether our patients should be punished. While society is currently struggling with how to apportion blame, psychiatry should resist the urge to impose medical solutions to social problems. Our solutions would almost certainly be grossly limited as we are still struggling to repent for lobotomizing “uppity” young women2 and using electroshock therapy to disrupt perverse impulses in homosexual males.3 Social norms and political zeitgeists change over time while the psychological and physiological principles underlying our understanding of mental illness should, in theory, stay relatively constant. Psychiatry’s answers for societal ills do not usually improve with time but rather have a tendency to be humbling.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1.Medlock MM et al., eds. “Racism and Psychiatry: Contemporary Issues and Interventions” (New York: Springer, 2018).
2. Tone A and Koziol M. CMAJ. 2018:190(20):e624-5.
3. McGuire RJ and Vallance M. BMJ. 1964;1(5376):151-3.
Substance use disorders can be a thorny topic in residency because of our role as gatekeepers of mental hospitals during our training. Intoxicated patients often get dismissed as a burden and distraction, malingering their way into a comfortable place to regain sobriety. This is extremely prevalent, often constituting the majority of patients seen during an emergency department call.
A typical interview may elicit any or all symptoms in the DSM yet be best explained by substance use intoxication or withdrawal. Alcohol and other CNS depressants commonly cause feelings of sadness and/or suicidality. Methamphetamine and other CNS stimulants commonly cause symptoms of psychosis or mania, followed by feelings of sadness and/or suicidality.
Different EDs have different degrees of patience for individuals in the process of becoming sober. Some departments will pressure clinicians into quickly discarding those patients and often frown upon any attempt at providing solace by raising the concern of reinforcing maladaptive behavior. A mystery-meat sandwich of admirable blandness may be the extent of help offered. Some more fortunate patients also receive a juice box or even a taxi voucher in an especially generous ED. This is always against our better judgment, of course, as we are told those gestures encourage abuse.
Other EDs will permit patients to remain until sober, allowing for another evaluation without the influence of controlled substances. We are reminded of many conversations with patients with substance use disorders, where topics discussed included: 1. Recommendation to seek substance use services, which are often nonexistent or with wait lists spanning months; 2. Education on the role of mental health hospitals and how patients’ despair in the context of intoxication does not meet some scriptural criteria; 3. Pep talks aided by such previously described sandwiches and juice boxes to encourage a sobering patient to leave the facility of their own will.
Methamphetamine, heroin, and alcohol are rarely one-and-done endeavors. We sparingly see our patients for their very first ED visit while intoxicated or crashing. They know how the system runs and which ED will more readily allow them an overnight stay. The number of times they have been recommended for substance use treatment is beyond counting – they may have been on a wait list a handful of times. They are aware of our reluctance to provide inpatient psychiatric treatment for substance use, but it is worth a shot trying, anyway – sometimes they get lucky. Usually it is the pep talk, relief from hunger pangs, and daylight that get them out the doors – until next time.
It is under this context that many trainees become psychiatrists, a process that solidifies the separation between drug use and mental illness. Many graduate from residency practically equating substance use disorder with malingering or futility. This can take on a surreal quality as many localities have recently adopted particular forms or requirements like the dispensation of naloxone syringes to all patients with substance use disorders. While the desire and effort are noble, it may suggest to a patient presenting for help that society’s main interest is to avoid seeing them die rather than help with available resources for maintaining sobriety.
Therein lies the conundrum, a conundrum that spans psychiatry to society. The conundrum is our ambivalence between punishing the choice of drug use or healing the substance use disorder. Should we discharge the intoxicated patient as soon as they are safe to walk out, or should we make every effort possible to find long-term solutions?
The calculation becomes more complex
A defining moment appears to have been society’s reconsideration of its stance on substance use disorders when affluent White teenagers started dying in the suburbs from pain pills overdoses. Suddenly, those children needed and deserved treatment, not punishment. We find ourselves far away from a time when the loudest societal commentary on substance use entailed mothers advocating for harsher sentences against drunk drivers.
More recently, as psychiatry and large contingents of society have decided to take up the mantle of equity and social justice, we have begun to make progress in decriminalizing substance use in an effort to reverse systemic discrimination toward minority groups. This has taken many shapes, including drug legalization, criminal justice reform, and even the provision of clean substance use paraphernalia for safer use of IV drugs. Police reform has led to reluctance to arrest or press charges for nonviolent crimes and reduced police presence in minority neighborhoods. The “rich White teenager” approach is now recommended in all neighborhoods.
Society’s attempt at decriminalizing drug use has run parallel with psychiatry’s recent attempts at reduced pathologizing of behaviors more prevalent in underprivileged groups and cultures. This runs the gamut, from avoiding the use of the term “agitated” because of its racial connotations, to advocating for reduced rates of schizophrenia diagnoses in Black males.1 A diagnosis of substance use disorder carries with it similar troublesome societal implications. Decriminalization, legalization, provision of substances to the population, normalization, and other societal reforms will likely have an impact on the prevalence of substance use disorder diagnoses, which involve many criteria dependent on societal context.
It would be expected that criteria such as hazardous use, social problems, and attempts to quit will decrease as social acceptance increases. How might this affect access to substance use treatment, an already extremely limited resource?
Now, as forensic psychiatrists, we find ourselves adjudicating on the role of drugs at a time when society is wrestling with its attitude on the breadth of responsibility possessed by people who use drugs. In California, as in many other states, insanity laws exclude those who were insane as a result of drug use, as a testament to or possibly a remnant of how society feels about the role of choice and responsibility in the use of drugs. Yet another defendant who admits to drug use may on the contrary receive a much more lenient plea deal if willing to commit to sobriety. But in a never-ending maze of differing judgments and opinions, a less understanding district attorney may argue that the additional risk posed by the use of drugs and resulting impulsivity may actually warrant a heavier sentence.
In a recent attempt at atonement for our past punitive stance on drug users, we have found a desire to protect those who use drugs by punishing those who sell, at times forgetting that these populations are deeply intertwined. A recent law permits the federal charge of distribution of fentanyl resulting in death, which carries the mandatory minimum of 20 years in prison. Yet, if the user whom we are trying to protect by this law is also the one selling, what are we left with?
Fentanyl has been a particularly tragic development in the history of mankind and drug use. Substance use has rarely been so easily linked to accidental death. While many physicians can easily explain the safety of fentanyl when used as prescribed and in controlled settings, this is certainly not the case in the community. Measuring micrograms of fentanyl is outside the knowledge and capabilities of most drug dealers, who are not equipped with pharmacy-grade scales. Yet, as a result, they sell and customers buy quantities of fentanyl that range from homeopathically low to lethally high because of a mixture of negligence and deliberate indifference.
Another effort at atonement has been attempts at decriminalizing drug use and releasing many nonviolent offenders. This can, however, encourage bystanders to report more acts as crime rather than public intoxication, to ensure a police response when confronted by intoxicated people. Whereas previously an inebriated person who is homeless may have been called for and asked to seek shelter, they now get called on, and subsequently charged for, allegedly mumbling a threat by a frustrated bystander.
The release of offenders has its limits. Many placements on probation require sobriety and result in longer sentences for the use of substances that are otherwise decriminalized. The decriminalization and reexamination of substance use by society should widen the scope from simply considering crime to examining the use of drugs throughout the legal system and even beyond.
The DSM and psychiatry are not intended or equipped to adjudicate disputes on where the lines should be drawn between determinism and free will. We are knowledgeable of patients with substance use disorders, the effect of intoxicating substances, and the capacity of patients with substance use disorders to act in law-abiding ways. Our field can inform without simply advocating whether our patients should be punished. While society is currently struggling with how to apportion blame, psychiatry should resist the urge to impose medical solutions to social problems. Our solutions would almost certainly be grossly limited as we are still struggling to repent for lobotomizing “uppity” young women2 and using electroshock therapy to disrupt perverse impulses in homosexual males.3 Social norms and political zeitgeists change over time while the psychological and physiological principles underlying our understanding of mental illness should, in theory, stay relatively constant. Psychiatry’s answers for societal ills do not usually improve with time but rather have a tendency to be humbling.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research.
References
1.Medlock MM et al., eds. “Racism and Psychiatry: Contemporary Issues and Interventions” (New York: Springer, 2018).
2. Tone A and Koziol M. CMAJ. 2018:190(20):e624-5.
3. McGuire RJ and Vallance M. BMJ. 1964;1(5376):151-3.
Alleged on-the-job violence, racism, prompts psych workers to head to D.C.
A dozen workers from a psychiatric hospital near Seattle flew to Washington, D.C. to picket the National Association for Behavioral Healthcare’s annual meeting in an effort to get their employer to meet demands for a safer work environment, better staffing, and the hiring of security professionals.
They are also demanding that their employer, Cascade Behavioral Health Hospital, a private psychiatric facility owned by Acadia Healthcare and located in Tukwila, Washington, address what they call “racist harassment” by managers who have allegedly told many workers, who are primarily people of color, that they are going to be “filtered out,” Alazar Yirgu, a mental health technician at the facility, told this news organization.
The workers have been conducting a “safety strike” to protest working conditions at Cascade since early August. The protest in Tukwila began after a dozen or more workers were hurt in an August 1 incident during which they had attempted to restrain a violent patient.
“We’ve been out there for 2 months, and we will continue until our voice is heard,” said Mr. Yirgu, who was hospitalized as a result of the August patient outburst that he said has left him unable to work since the incident.
On Oct. 7, Mr. Yirgu and coworkers brought the protest to Washington, D.C., in a continued effort to voice their need for adequate personal protective equipment, increased staffing, and the hiring of security personnel.
“Any health care professional should not be fearful to do their job, because once they are in that state of mind, once they are fearful for themselves, then they are not doing their jobs; they are preoccupied with their fears,” said Mr. Yirgu, who has worked as a technician for 6 years.
Unsafe patient load
The workers reacted quickly after the August 1 patient outburst because there have been multiple previous incidents, Mr. Yirgu said.
In a 2019 news story by the Seattle Times, the newspaper reported there had been 65 assaults on patients or staff at Cascade from 2016 to 2018, resulting in concussions and broken bones in some instances.
Mr. Yirgu said that more recently, a patient broke a second story window, jumped to the ground, and ran off.
At the facility, workers are often assigned to as many as a dozen or more patients, he said, noting that at other psychiatric institutions, he’s cared for a maximum of five patients at once.
The Tukwila police have pushed back against the workers’ description of the incident in which Mr. Yirgu was injured, and Cascade Behavioral Health has aggressively defended its facility.
According to Mr. Yirgu, the expletive-spewing patient was clearly a danger to himself and others – especially after he stole a key card that would give him access to the entire facility, including the kitchen where knives were stored.
When more than a dozen staff answered the unit’s “Code Gray,” they were unable to subdue or restrain him. Mr. Yirgu ended up on the floor underneath the patient after the patient had jumped off a table.
As the incident unfolded, several workers called the police, who initially refused to go to the facility, saying that a new law prevented them from assisting with the restraint if there was no assault.
The Tukwila Police Department report shows that officers finally did go to the facility and determined that “a crime had not been committed based on the information presented to them, that there was no imminent threat of bodily harm, and that there was no legal grounds or authority for them to assist medical staff with physically restraining a patient.”
Cascade pushes back
A Service Employees International Union (SEIU) report shows about 70 workers refused to come in to work after the incident and began picketing outside the facility.
Cascade called it an illegal strike because the protesters had not given 10-days’ notice, as required by federal law, and moved to terminate those who participated. The local SEIU chapter, 1199NW, suggested the workers call their walkout a “safety strike,” because it was organized primarily to protest working conditions.
Meanwhile Cascade, which has erected a large fence so that no one in the facility can see the protesters, has said the strike is primarily about ongoing contract negotiations with the facility’s nurses and its union.
“The Union has been trying to apply unfair – and in some cases we believe unlawful – external pressures to this process, including picketing, work stoppages, smear campaigns, and false accusations,” Cascade CEO Christopher West wrote on the company’s website in mid-August.
He said the facility had “ample personal protective equipment” and that the “well-being and safety of our patients and staff always have been and will be our key priorities.”
In response to a request for comment, Cascade said in an emailed statement that physical confrontations had decreased by almost 50% and elopements (unauthorized leaving of the facility) by 80% from 2018 to 2021.
Cascade spokesperson Gretchen Hommrich said in the statement that the workers it has terminated “were let go for cause in violation to their employment agreement” and said the company still aimed to negotiate a new agreement with the union.
The “efforts outside of the bargaining process serve no productive purpose and have only brought harm to the residents they claim to serve,” said Ms. Hommrich.
‘Safety is the sole purpose’
Mr. Yirgu said it was outrageous to suggest workers were picketing over contract negotiations. “Safety is the sole purpose of this strike,” he said.
He noted that his patient care goal is to have a lot of one-on-one time with his patients, helping them navigate back to the outside world. The facility is supposed to be a safe place, Mr. Yirgu added. Violence inside the facility traumatizes the patients and may worsen their condition and delay their progress, he said.
“If I can’t keep them safe, there’s no way I’m going to be able to see them eye-to-eye when I told them I’d keep them safe and then they’re not anymore,” said Mr. Yirgu.
So far, 22 workers have been “terminated,” meaning they received a termination notice, have been taken off the work schedule by the employer, or otherwise been informed that the employer has deemed them to be separated, the SEIU reports. The organization has filed unfair labor practice (ULPs) for all 22.
A version of this article first appeared on Medscape.com.
A dozen workers from a psychiatric hospital near Seattle flew to Washington, D.C. to picket the National Association for Behavioral Healthcare’s annual meeting in an effort to get their employer to meet demands for a safer work environment, better staffing, and the hiring of security professionals.
They are also demanding that their employer, Cascade Behavioral Health Hospital, a private psychiatric facility owned by Acadia Healthcare and located in Tukwila, Washington, address what they call “racist harassment” by managers who have allegedly told many workers, who are primarily people of color, that they are going to be “filtered out,” Alazar Yirgu, a mental health technician at the facility, told this news organization.
The workers have been conducting a “safety strike” to protest working conditions at Cascade since early August. The protest in Tukwila began after a dozen or more workers were hurt in an August 1 incident during which they had attempted to restrain a violent patient.
“We’ve been out there for 2 months, and we will continue until our voice is heard,” said Mr. Yirgu, who was hospitalized as a result of the August patient outburst that he said has left him unable to work since the incident.
On Oct. 7, Mr. Yirgu and coworkers brought the protest to Washington, D.C., in a continued effort to voice their need for adequate personal protective equipment, increased staffing, and the hiring of security personnel.
“Any health care professional should not be fearful to do their job, because once they are in that state of mind, once they are fearful for themselves, then they are not doing their jobs; they are preoccupied with their fears,” said Mr. Yirgu, who has worked as a technician for 6 years.
Unsafe patient load
The workers reacted quickly after the August 1 patient outburst because there have been multiple previous incidents, Mr. Yirgu said.
In a 2019 news story by the Seattle Times, the newspaper reported there had been 65 assaults on patients or staff at Cascade from 2016 to 2018, resulting in concussions and broken bones in some instances.
Mr. Yirgu said that more recently, a patient broke a second story window, jumped to the ground, and ran off.
At the facility, workers are often assigned to as many as a dozen or more patients, he said, noting that at other psychiatric institutions, he’s cared for a maximum of five patients at once.
The Tukwila police have pushed back against the workers’ description of the incident in which Mr. Yirgu was injured, and Cascade Behavioral Health has aggressively defended its facility.
According to Mr. Yirgu, the expletive-spewing patient was clearly a danger to himself and others – especially after he stole a key card that would give him access to the entire facility, including the kitchen where knives were stored.
When more than a dozen staff answered the unit’s “Code Gray,” they were unable to subdue or restrain him. Mr. Yirgu ended up on the floor underneath the patient after the patient had jumped off a table.
As the incident unfolded, several workers called the police, who initially refused to go to the facility, saying that a new law prevented them from assisting with the restraint if there was no assault.
The Tukwila Police Department report shows that officers finally did go to the facility and determined that “a crime had not been committed based on the information presented to them, that there was no imminent threat of bodily harm, and that there was no legal grounds or authority for them to assist medical staff with physically restraining a patient.”
Cascade pushes back
A Service Employees International Union (SEIU) report shows about 70 workers refused to come in to work after the incident and began picketing outside the facility.
Cascade called it an illegal strike because the protesters had not given 10-days’ notice, as required by federal law, and moved to terminate those who participated. The local SEIU chapter, 1199NW, suggested the workers call their walkout a “safety strike,” because it was organized primarily to protest working conditions.
Meanwhile Cascade, which has erected a large fence so that no one in the facility can see the protesters, has said the strike is primarily about ongoing contract negotiations with the facility’s nurses and its union.
“The Union has been trying to apply unfair – and in some cases we believe unlawful – external pressures to this process, including picketing, work stoppages, smear campaigns, and false accusations,” Cascade CEO Christopher West wrote on the company’s website in mid-August.
He said the facility had “ample personal protective equipment” and that the “well-being and safety of our patients and staff always have been and will be our key priorities.”
In response to a request for comment, Cascade said in an emailed statement that physical confrontations had decreased by almost 50% and elopements (unauthorized leaving of the facility) by 80% from 2018 to 2021.
Cascade spokesperson Gretchen Hommrich said in the statement that the workers it has terminated “were let go for cause in violation to their employment agreement” and said the company still aimed to negotiate a new agreement with the union.
The “efforts outside of the bargaining process serve no productive purpose and have only brought harm to the residents they claim to serve,” said Ms. Hommrich.
‘Safety is the sole purpose’
Mr. Yirgu said it was outrageous to suggest workers were picketing over contract negotiations. “Safety is the sole purpose of this strike,” he said.
He noted that his patient care goal is to have a lot of one-on-one time with his patients, helping them navigate back to the outside world. The facility is supposed to be a safe place, Mr. Yirgu added. Violence inside the facility traumatizes the patients and may worsen their condition and delay their progress, he said.
“If I can’t keep them safe, there’s no way I’m going to be able to see them eye-to-eye when I told them I’d keep them safe and then they’re not anymore,” said Mr. Yirgu.
So far, 22 workers have been “terminated,” meaning they received a termination notice, have been taken off the work schedule by the employer, or otherwise been informed that the employer has deemed them to be separated, the SEIU reports. The organization has filed unfair labor practice (ULPs) for all 22.
A version of this article first appeared on Medscape.com.
A dozen workers from a psychiatric hospital near Seattle flew to Washington, D.C. to picket the National Association for Behavioral Healthcare’s annual meeting in an effort to get their employer to meet demands for a safer work environment, better staffing, and the hiring of security professionals.
They are also demanding that their employer, Cascade Behavioral Health Hospital, a private psychiatric facility owned by Acadia Healthcare and located in Tukwila, Washington, address what they call “racist harassment” by managers who have allegedly told many workers, who are primarily people of color, that they are going to be “filtered out,” Alazar Yirgu, a mental health technician at the facility, told this news organization.
The workers have been conducting a “safety strike” to protest working conditions at Cascade since early August. The protest in Tukwila began after a dozen or more workers were hurt in an August 1 incident during which they had attempted to restrain a violent patient.
“We’ve been out there for 2 months, and we will continue until our voice is heard,” said Mr. Yirgu, who was hospitalized as a result of the August patient outburst that he said has left him unable to work since the incident.
On Oct. 7, Mr. Yirgu and coworkers brought the protest to Washington, D.C., in a continued effort to voice their need for adequate personal protective equipment, increased staffing, and the hiring of security personnel.
“Any health care professional should not be fearful to do their job, because once they are in that state of mind, once they are fearful for themselves, then they are not doing their jobs; they are preoccupied with their fears,” said Mr. Yirgu, who has worked as a technician for 6 years.
Unsafe patient load
The workers reacted quickly after the August 1 patient outburst because there have been multiple previous incidents, Mr. Yirgu said.
In a 2019 news story by the Seattle Times, the newspaper reported there had been 65 assaults on patients or staff at Cascade from 2016 to 2018, resulting in concussions and broken bones in some instances.
Mr. Yirgu said that more recently, a patient broke a second story window, jumped to the ground, and ran off.
At the facility, workers are often assigned to as many as a dozen or more patients, he said, noting that at other psychiatric institutions, he’s cared for a maximum of five patients at once.
The Tukwila police have pushed back against the workers’ description of the incident in which Mr. Yirgu was injured, and Cascade Behavioral Health has aggressively defended its facility.
According to Mr. Yirgu, the expletive-spewing patient was clearly a danger to himself and others – especially after he stole a key card that would give him access to the entire facility, including the kitchen where knives were stored.
When more than a dozen staff answered the unit’s “Code Gray,” they were unable to subdue or restrain him. Mr. Yirgu ended up on the floor underneath the patient after the patient had jumped off a table.
As the incident unfolded, several workers called the police, who initially refused to go to the facility, saying that a new law prevented them from assisting with the restraint if there was no assault.
The Tukwila Police Department report shows that officers finally did go to the facility and determined that “a crime had not been committed based on the information presented to them, that there was no imminent threat of bodily harm, and that there was no legal grounds or authority for them to assist medical staff with physically restraining a patient.”
Cascade pushes back
A Service Employees International Union (SEIU) report shows about 70 workers refused to come in to work after the incident and began picketing outside the facility.
Cascade called it an illegal strike because the protesters had not given 10-days’ notice, as required by federal law, and moved to terminate those who participated. The local SEIU chapter, 1199NW, suggested the workers call their walkout a “safety strike,” because it was organized primarily to protest working conditions.
Meanwhile Cascade, which has erected a large fence so that no one in the facility can see the protesters, has said the strike is primarily about ongoing contract negotiations with the facility’s nurses and its union.
“The Union has been trying to apply unfair – and in some cases we believe unlawful – external pressures to this process, including picketing, work stoppages, smear campaigns, and false accusations,” Cascade CEO Christopher West wrote on the company’s website in mid-August.
He said the facility had “ample personal protective equipment” and that the “well-being and safety of our patients and staff always have been and will be our key priorities.”
In response to a request for comment, Cascade said in an emailed statement that physical confrontations had decreased by almost 50% and elopements (unauthorized leaving of the facility) by 80% from 2018 to 2021.
Cascade spokesperson Gretchen Hommrich said in the statement that the workers it has terminated “were let go for cause in violation to their employment agreement” and said the company still aimed to negotiate a new agreement with the union.
The “efforts outside of the bargaining process serve no productive purpose and have only brought harm to the residents they claim to serve,” said Ms. Hommrich.
‘Safety is the sole purpose’
Mr. Yirgu said it was outrageous to suggest workers were picketing over contract negotiations. “Safety is the sole purpose of this strike,” he said.
He noted that his patient care goal is to have a lot of one-on-one time with his patients, helping them navigate back to the outside world. The facility is supposed to be a safe place, Mr. Yirgu added. Violence inside the facility traumatizes the patients and may worsen their condition and delay their progress, he said.
“If I can’t keep them safe, there’s no way I’m going to be able to see them eye-to-eye when I told them I’d keep them safe and then they’re not anymore,” said Mr. Yirgu.
So far, 22 workers have been “terminated,” meaning they received a termination notice, have been taken off the work schedule by the employer, or otherwise been informed that the employer has deemed them to be separated, the SEIU reports. The organization has filed unfair labor practice (ULPs) for all 22.
A version of this article first appeared on Medscape.com.