User login
Self-directed digital exercise plan improves knee OA
Adults with knee osteoarthritis (OA) who participated in a self-directed, web-based exercise program with automated text-message reminders and encouragement for 6 months showed significant improvement in overall knee pain and physical function, compared with patients who received web-based OA information alone, in a randomized trial of 180 individuals.
The results support a role for web-based exercise intervention to improve knee OA patients’ access to recommended exercises and to assist clinicians in managing patients on a population level, according to the first author of the study, Rachel Kate Nelligan, of the University of Melbourne, and colleagues. Their report is in JAMA Internal Medicine.
“Our free-to-access, unsupervised program could serve as an entry-level intervention, with participants who do not experience clinical benefits progressing to subsequent steps for more intensive, personalized management,” they said. “Such an approach has the potential to better distribute limited health care resources and reduce demand for contact with health professionals, thus improving access for those requiring it.”
Only two other randomized, clinical trials have evaluated web-based interventions for OA without contact from health professionals, according to the authors. While one of those did not find any differences in outcomes at 4 months when comparing a self-directed progressive lower-limb strength, flexibility, and walking program to being on a wait list, a separate trial evaluating a 9-module physical activity program in adults with knee and/or hip OA vs. a wait-list control group found evidence for efficacy for physical function at 3 months, but not quality of life or function in sport and recreation.
For the current study, researchers recruited 206 adults in Australia with clinically diagnosed knee OA via online advertisements and a volunteer database. Participants were aged 45 years or older, and reported activity-related knee pain and morning knee stiffness lasting at least 30 minutes; knee pain on most days for at least 3 months; and average knee pain severity of 4 or higher on an 11-point numeric rating scale in the previous week. In addition, participants were required to own a cell phone with text messaging, have Internet access, and be able to complete assessments.
Patients randomized to the intervention of the My Knee Exercise website received web-based information about OA and the value of exercise, with a 24-week self-directed program of strengthening exercises plus automated text messages to motivate behavior changes and encourage adherence to the exercise program. Controls received access to web-based information about OA and the value of exercise, but without the prescribed exercises or texts. Patients in the intervention group received an average of 60 text messages during the study period, and the average reply rate was 73%.
The primary study outcomes were changes in overall knee pain based on a numeric 0-10 rating scale and changes in physical function based on the Western Ontario and McMaster Universities Osteoarthritis Index 0-68 scale. A total of 180 participants completed both primary outcome measures at 24 weeks. The average age of the participants was 60 years, and 61% were women.
After 24 weeks, the intervention group averaged significantly greater improvement of 1.6 units for overall knee pain (P < .001) and 5.2 units for physical function (P = .002), compared with controls.
In addition, the proportion of patients who exceeded the minimal clinically important difference in pain improvement of at least 1.8 units was significantly higher in the intervention group, compared with controls (72.1% vs. 42.0%; P < .001). Similarly, more intervention-group patients achieved the minimal clinically important difference in WOMAC physical function of improvement of at least 6 units (68.0% vs. 40.8%; P < .001).
Secondary outcomes included additional measures of knee pain, knee function for sport and recreation, quality of life, physical activity, self-efficacy, overall improvement, and treatment satisfaction. Between-group differences favored the intervention on most measures, including Knee Injury and Osteoarthritis Outcome Score subscales for pain, sports/recreation, and quality of life; health-related quality of life; Arthritis Self-Efficacy Scale (ASES) pain subscale, individual change since baseline, and overall patient satisfaction. “Changes in PASE [Physical Activity Scale for the Elderly], ASES function, and SEE [Self Efficacy Exercise] were similar in both groups,” the researchers said.
No serious adverse events were reported by any study participants. Eight patients in the intervention group reported knee pain during the study, compared with one of the controls, and use of pain medications was similar between the groups, except that more control participants used massage, heat or cold, and topical anti-inflammatories.
The results suggest that a majority of participants in the intervention group improved pain and function without the need for in-person contact with a health professional, the researchers noted. However, more intensive management may be needed to support the 30% who did not benefit from the unsupervised approach, they said.
The study findings were limited by several factors, including the potential bias of a volunteer study population, possible lack of generalizability to individuals with lower levels of education or self-efficacy, and lack of direct comparison between web-based intervention and clinician-delivered intervention, the researchers noted.
The study was funded by the National Health and Medical Research Council, whose fellowships supported two of the authors. Lead author Ms. Nelligan disclosed a PhD scholarship from the Australian Government Research Training Program and personal fees from the University of Melbourne unrelated to the current study.
Adults with knee osteoarthritis (OA) who participated in a self-directed, web-based exercise program with automated text-message reminders and encouragement for 6 months showed significant improvement in overall knee pain and physical function, compared with patients who received web-based OA information alone, in a randomized trial of 180 individuals.
The results support a role for web-based exercise intervention to improve knee OA patients’ access to recommended exercises and to assist clinicians in managing patients on a population level, according to the first author of the study, Rachel Kate Nelligan, of the University of Melbourne, and colleagues. Their report is in JAMA Internal Medicine.
“Our free-to-access, unsupervised program could serve as an entry-level intervention, with participants who do not experience clinical benefits progressing to subsequent steps for more intensive, personalized management,” they said. “Such an approach has the potential to better distribute limited health care resources and reduce demand for contact with health professionals, thus improving access for those requiring it.”
Only two other randomized, clinical trials have evaluated web-based interventions for OA without contact from health professionals, according to the authors. While one of those did not find any differences in outcomes at 4 months when comparing a self-directed progressive lower-limb strength, flexibility, and walking program to being on a wait list, a separate trial evaluating a 9-module physical activity program in adults with knee and/or hip OA vs. a wait-list control group found evidence for efficacy for physical function at 3 months, but not quality of life or function in sport and recreation.
For the current study, researchers recruited 206 adults in Australia with clinically diagnosed knee OA via online advertisements and a volunteer database. Participants were aged 45 years or older, and reported activity-related knee pain and morning knee stiffness lasting at least 30 minutes; knee pain on most days for at least 3 months; and average knee pain severity of 4 or higher on an 11-point numeric rating scale in the previous week. In addition, participants were required to own a cell phone with text messaging, have Internet access, and be able to complete assessments.
Patients randomized to the intervention of the My Knee Exercise website received web-based information about OA and the value of exercise, with a 24-week self-directed program of strengthening exercises plus automated text messages to motivate behavior changes and encourage adherence to the exercise program. Controls received access to web-based information about OA and the value of exercise, but without the prescribed exercises or texts. Patients in the intervention group received an average of 60 text messages during the study period, and the average reply rate was 73%.
The primary study outcomes were changes in overall knee pain based on a numeric 0-10 rating scale and changes in physical function based on the Western Ontario and McMaster Universities Osteoarthritis Index 0-68 scale. A total of 180 participants completed both primary outcome measures at 24 weeks. The average age of the participants was 60 years, and 61% were women.
After 24 weeks, the intervention group averaged significantly greater improvement of 1.6 units for overall knee pain (P < .001) and 5.2 units for physical function (P = .002), compared with controls.
In addition, the proportion of patients who exceeded the minimal clinically important difference in pain improvement of at least 1.8 units was significantly higher in the intervention group, compared with controls (72.1% vs. 42.0%; P < .001). Similarly, more intervention-group patients achieved the minimal clinically important difference in WOMAC physical function of improvement of at least 6 units (68.0% vs. 40.8%; P < .001).
Secondary outcomes included additional measures of knee pain, knee function for sport and recreation, quality of life, physical activity, self-efficacy, overall improvement, and treatment satisfaction. Between-group differences favored the intervention on most measures, including Knee Injury and Osteoarthritis Outcome Score subscales for pain, sports/recreation, and quality of life; health-related quality of life; Arthritis Self-Efficacy Scale (ASES) pain subscale, individual change since baseline, and overall patient satisfaction. “Changes in PASE [Physical Activity Scale for the Elderly], ASES function, and SEE [Self Efficacy Exercise] were similar in both groups,” the researchers said.
No serious adverse events were reported by any study participants. Eight patients in the intervention group reported knee pain during the study, compared with one of the controls, and use of pain medications was similar between the groups, except that more control participants used massage, heat or cold, and topical anti-inflammatories.
The results suggest that a majority of participants in the intervention group improved pain and function without the need for in-person contact with a health professional, the researchers noted. However, more intensive management may be needed to support the 30% who did not benefit from the unsupervised approach, they said.
The study findings were limited by several factors, including the potential bias of a volunteer study population, possible lack of generalizability to individuals with lower levels of education or self-efficacy, and lack of direct comparison between web-based intervention and clinician-delivered intervention, the researchers noted.
The study was funded by the National Health and Medical Research Council, whose fellowships supported two of the authors. Lead author Ms. Nelligan disclosed a PhD scholarship from the Australian Government Research Training Program and personal fees from the University of Melbourne unrelated to the current study.
Adults with knee osteoarthritis (OA) who participated in a self-directed, web-based exercise program with automated text-message reminders and encouragement for 6 months showed significant improvement in overall knee pain and physical function, compared with patients who received web-based OA information alone, in a randomized trial of 180 individuals.
The results support a role for web-based exercise intervention to improve knee OA patients’ access to recommended exercises and to assist clinicians in managing patients on a population level, according to the first author of the study, Rachel Kate Nelligan, of the University of Melbourne, and colleagues. Their report is in JAMA Internal Medicine.
“Our free-to-access, unsupervised program could serve as an entry-level intervention, with participants who do not experience clinical benefits progressing to subsequent steps for more intensive, personalized management,” they said. “Such an approach has the potential to better distribute limited health care resources and reduce demand for contact with health professionals, thus improving access for those requiring it.”
Only two other randomized, clinical trials have evaluated web-based interventions for OA without contact from health professionals, according to the authors. While one of those did not find any differences in outcomes at 4 months when comparing a self-directed progressive lower-limb strength, flexibility, and walking program to being on a wait list, a separate trial evaluating a 9-module physical activity program in adults with knee and/or hip OA vs. a wait-list control group found evidence for efficacy for physical function at 3 months, but not quality of life or function in sport and recreation.
For the current study, researchers recruited 206 adults in Australia with clinically diagnosed knee OA via online advertisements and a volunteer database. Participants were aged 45 years or older, and reported activity-related knee pain and morning knee stiffness lasting at least 30 minutes; knee pain on most days for at least 3 months; and average knee pain severity of 4 or higher on an 11-point numeric rating scale in the previous week. In addition, participants were required to own a cell phone with text messaging, have Internet access, and be able to complete assessments.
Patients randomized to the intervention of the My Knee Exercise website received web-based information about OA and the value of exercise, with a 24-week self-directed program of strengthening exercises plus automated text messages to motivate behavior changes and encourage adherence to the exercise program. Controls received access to web-based information about OA and the value of exercise, but without the prescribed exercises or texts. Patients in the intervention group received an average of 60 text messages during the study period, and the average reply rate was 73%.
The primary study outcomes were changes in overall knee pain based on a numeric 0-10 rating scale and changes in physical function based on the Western Ontario and McMaster Universities Osteoarthritis Index 0-68 scale. A total of 180 participants completed both primary outcome measures at 24 weeks. The average age of the participants was 60 years, and 61% were women.
After 24 weeks, the intervention group averaged significantly greater improvement of 1.6 units for overall knee pain (P < .001) and 5.2 units for physical function (P = .002), compared with controls.
In addition, the proportion of patients who exceeded the minimal clinically important difference in pain improvement of at least 1.8 units was significantly higher in the intervention group, compared with controls (72.1% vs. 42.0%; P < .001). Similarly, more intervention-group patients achieved the minimal clinically important difference in WOMAC physical function of improvement of at least 6 units (68.0% vs. 40.8%; P < .001).
Secondary outcomes included additional measures of knee pain, knee function for sport and recreation, quality of life, physical activity, self-efficacy, overall improvement, and treatment satisfaction. Between-group differences favored the intervention on most measures, including Knee Injury and Osteoarthritis Outcome Score subscales for pain, sports/recreation, and quality of life; health-related quality of life; Arthritis Self-Efficacy Scale (ASES) pain subscale, individual change since baseline, and overall patient satisfaction. “Changes in PASE [Physical Activity Scale for the Elderly], ASES function, and SEE [Self Efficacy Exercise] were similar in both groups,” the researchers said.
No serious adverse events were reported by any study participants. Eight patients in the intervention group reported knee pain during the study, compared with one of the controls, and use of pain medications was similar between the groups, except that more control participants used massage, heat or cold, and topical anti-inflammatories.
The results suggest that a majority of participants in the intervention group improved pain and function without the need for in-person contact with a health professional, the researchers noted. However, more intensive management may be needed to support the 30% who did not benefit from the unsupervised approach, they said.
The study findings were limited by several factors, including the potential bias of a volunteer study population, possible lack of generalizability to individuals with lower levels of education or self-efficacy, and lack of direct comparison between web-based intervention and clinician-delivered intervention, the researchers noted.
The study was funded by the National Health and Medical Research Council, whose fellowships supported two of the authors. Lead author Ms. Nelligan disclosed a PhD scholarship from the Australian Government Research Training Program and personal fees from the University of Melbourne unrelated to the current study.
FROM JAMA INTERNAL MEDICINE
Rheumatology clinics find success with smoking cessation referral program
A new protocol designed to help patients in rheumatology clinics quit smoking proved both efficient and effective in referring willing participants to free tobacco quit lines.
“Rheumatology visits provide a unique opportunity to address smoking as a chronic modifiable risk factor in populations at high risk for cardiovascular disease, pulmonary disease, and rheumatic disease progression,” wrote Christie M. Bartels, MD, chief of the division of rheumatology at the University of Wisconsin, Madison, and colleagues. The study was published in Arthritis Care & Research.
To assess the effectiveness of implementing a smoking cessation protocol for patients with rheumatic diseases, the researchers launched a quasi-experimental cohort study in which their Quit Connect protocol was tested at three rheumatology clinics. Adapting the Ask, Advise, Connect primary care protocol to a new setting, nurses and medical assistants were trained to use electronic health record (EHR) prompts that would check if patients who smoked were ready to quit within 30 days, advise them to do so, and then use electronic referrals to connect them to state-run tobacco quit lines. An extended baseline period – October 2012 to March 2016 – was compared to a 6-month intervention period from April to October 2016.
Across 54,090 pre- and postimplementation rheumatology clinic visits, 4,601 were with current smokers. Demographics were similar across both periods: The mean age of the patients was 51 years, about two-thirds were female, and 85% were White.
Clinicians’ assessment of tobacco use before and after implementation of the program stayed steady at 96% of patient visits, but the percentage of tobacco users’ visits that included checking for readiness to quit within the next 30 days rose from 3% (135 of 4,078) to 80% (421 of 523).
Before the implementation of the program, 0.6% of eligible visits with current smokers included a quit-line referral offer. After implementation, 93 (18%) of the 523 smokers who visited – 122 of whom said they were ready to quit – were offered referrals, a 26-fold increase. Of the 93 offered referrals, 66 (71%) accepted and 16 set a quit date or reported having quit; 11 accepted counseling services and nicotine replacement.
Although clinic staff reported encountering several obstacles, such as the need to craft nonthreatening language for challenging patients, they also contributed their own talking points that were included in the EHR tools and desktop brochures. On average, the protocol took less than 90 seconds to perform.
Rheumatologists can make headway on patients quitting smoking
“While smoking cessation programs require time and resources to implement, this study suggests a role for evidence-based protocols within rheumatology centers,” Medha Barbhaiya, MD, a rheumatologist at the Hospital for Special Surgery in New York, said in an interview. “Given that current smokers are at an increased risk of developing more severe rheumatic disease and cardiovascular disease, and patients often visit their rheumatologist multiple times yearly, rheumatologists may be well-positioned to address smoking cessation with patients.”
In regard to next steps, she noted that “while future large studies in diverse cohorts are needed to confirm these findings, implementing a formal smoking cessation protocol within rheumatology centers may provide a unique opportunity for rheumatologists to directly help patients modify their disease risk, leading to improved health outcomes.”
The authors acknowledged their study’s limitations, including the fact that it was a prepost design and not a randomized trial. They also recognized that many tobacco users require 8-10 attempts before permanently quitting, likely lessening the lasting impact of the short-term study. They did cite expert analysis, however, that says “connecting patients to evidence-based resources makes them more likely to permanently quit.”
The study was supported in part by Pfizer’s office of Independent Grants for Learning and Change and by a grant collaboration from the University of Wisconsin Clinical and Translational Science Award and the University of Wisconsin School of Medicine and Public Health’s Wisconsin Partnership Program, through the NIH National Center for Advancing Translational Sciences.
A new protocol designed to help patients in rheumatology clinics quit smoking proved both efficient and effective in referring willing participants to free tobacco quit lines.
“Rheumatology visits provide a unique opportunity to address smoking as a chronic modifiable risk factor in populations at high risk for cardiovascular disease, pulmonary disease, and rheumatic disease progression,” wrote Christie M. Bartels, MD, chief of the division of rheumatology at the University of Wisconsin, Madison, and colleagues. The study was published in Arthritis Care & Research.
To assess the effectiveness of implementing a smoking cessation protocol for patients with rheumatic diseases, the researchers launched a quasi-experimental cohort study in which their Quit Connect protocol was tested at three rheumatology clinics. Adapting the Ask, Advise, Connect primary care protocol to a new setting, nurses and medical assistants were trained to use electronic health record (EHR) prompts that would check if patients who smoked were ready to quit within 30 days, advise them to do so, and then use electronic referrals to connect them to state-run tobacco quit lines. An extended baseline period – October 2012 to March 2016 – was compared to a 6-month intervention period from April to October 2016.
Across 54,090 pre- and postimplementation rheumatology clinic visits, 4,601 were with current smokers. Demographics were similar across both periods: The mean age of the patients was 51 years, about two-thirds were female, and 85% were White.
Clinicians’ assessment of tobacco use before and after implementation of the program stayed steady at 96% of patient visits, but the percentage of tobacco users’ visits that included checking for readiness to quit within the next 30 days rose from 3% (135 of 4,078) to 80% (421 of 523).
Before the implementation of the program, 0.6% of eligible visits with current smokers included a quit-line referral offer. After implementation, 93 (18%) of the 523 smokers who visited – 122 of whom said they were ready to quit – were offered referrals, a 26-fold increase. Of the 93 offered referrals, 66 (71%) accepted and 16 set a quit date or reported having quit; 11 accepted counseling services and nicotine replacement.
Although clinic staff reported encountering several obstacles, such as the need to craft nonthreatening language for challenging patients, they also contributed their own talking points that were included in the EHR tools and desktop brochures. On average, the protocol took less than 90 seconds to perform.
Rheumatologists can make headway on patients quitting smoking
“While smoking cessation programs require time and resources to implement, this study suggests a role for evidence-based protocols within rheumatology centers,” Medha Barbhaiya, MD, a rheumatologist at the Hospital for Special Surgery in New York, said in an interview. “Given that current smokers are at an increased risk of developing more severe rheumatic disease and cardiovascular disease, and patients often visit their rheumatologist multiple times yearly, rheumatologists may be well-positioned to address smoking cessation with patients.”
In regard to next steps, she noted that “while future large studies in diverse cohorts are needed to confirm these findings, implementing a formal smoking cessation protocol within rheumatology centers may provide a unique opportunity for rheumatologists to directly help patients modify their disease risk, leading to improved health outcomes.”
The authors acknowledged their study’s limitations, including the fact that it was a prepost design and not a randomized trial. They also recognized that many tobacco users require 8-10 attempts before permanently quitting, likely lessening the lasting impact of the short-term study. They did cite expert analysis, however, that says “connecting patients to evidence-based resources makes them more likely to permanently quit.”
The study was supported in part by Pfizer’s office of Independent Grants for Learning and Change and by a grant collaboration from the University of Wisconsin Clinical and Translational Science Award and the University of Wisconsin School of Medicine and Public Health’s Wisconsin Partnership Program, through the NIH National Center for Advancing Translational Sciences.
A new protocol designed to help patients in rheumatology clinics quit smoking proved both efficient and effective in referring willing participants to free tobacco quit lines.
“Rheumatology visits provide a unique opportunity to address smoking as a chronic modifiable risk factor in populations at high risk for cardiovascular disease, pulmonary disease, and rheumatic disease progression,” wrote Christie M. Bartels, MD, chief of the division of rheumatology at the University of Wisconsin, Madison, and colleagues. The study was published in Arthritis Care & Research.
To assess the effectiveness of implementing a smoking cessation protocol for patients with rheumatic diseases, the researchers launched a quasi-experimental cohort study in which their Quit Connect protocol was tested at three rheumatology clinics. Adapting the Ask, Advise, Connect primary care protocol to a new setting, nurses and medical assistants were trained to use electronic health record (EHR) prompts that would check if patients who smoked were ready to quit within 30 days, advise them to do so, and then use electronic referrals to connect them to state-run tobacco quit lines. An extended baseline period – October 2012 to March 2016 – was compared to a 6-month intervention period from April to October 2016.
Across 54,090 pre- and postimplementation rheumatology clinic visits, 4,601 were with current smokers. Demographics were similar across both periods: The mean age of the patients was 51 years, about two-thirds were female, and 85% were White.
Clinicians’ assessment of tobacco use before and after implementation of the program stayed steady at 96% of patient visits, but the percentage of tobacco users’ visits that included checking for readiness to quit within the next 30 days rose from 3% (135 of 4,078) to 80% (421 of 523).
Before the implementation of the program, 0.6% of eligible visits with current smokers included a quit-line referral offer. After implementation, 93 (18%) of the 523 smokers who visited – 122 of whom said they were ready to quit – were offered referrals, a 26-fold increase. Of the 93 offered referrals, 66 (71%) accepted and 16 set a quit date or reported having quit; 11 accepted counseling services and nicotine replacement.
Although clinic staff reported encountering several obstacles, such as the need to craft nonthreatening language for challenging patients, they also contributed their own talking points that were included in the EHR tools and desktop brochures. On average, the protocol took less than 90 seconds to perform.
Rheumatologists can make headway on patients quitting smoking
“While smoking cessation programs require time and resources to implement, this study suggests a role for evidence-based protocols within rheumatology centers,” Medha Barbhaiya, MD, a rheumatologist at the Hospital for Special Surgery in New York, said in an interview. “Given that current smokers are at an increased risk of developing more severe rheumatic disease and cardiovascular disease, and patients often visit their rheumatologist multiple times yearly, rheumatologists may be well-positioned to address smoking cessation with patients.”
In regard to next steps, she noted that “while future large studies in diverse cohorts are needed to confirm these findings, implementing a formal smoking cessation protocol within rheumatology centers may provide a unique opportunity for rheumatologists to directly help patients modify their disease risk, leading to improved health outcomes.”
The authors acknowledged their study’s limitations, including the fact that it was a prepost design and not a randomized trial. They also recognized that many tobacco users require 8-10 attempts before permanently quitting, likely lessening the lasting impact of the short-term study. They did cite expert analysis, however, that says “connecting patients to evidence-based resources makes them more likely to permanently quit.”
The study was supported in part by Pfizer’s office of Independent Grants for Learning and Change and by a grant collaboration from the University of Wisconsin Clinical and Translational Science Award and the University of Wisconsin School of Medicine and Public Health’s Wisconsin Partnership Program, through the NIH National Center for Advancing Translational Sciences.
FROM ARTHRITIS CARE & RESEARCH
VEXAS: A novel rheumatologic, hematologic syndrome that’s making waves
Older men with a novel adult-onset, severe autoinflammatory syndrome known by the acronym VEXAS are likely hiding in plain sight in many adult rheumatology, hematology, and dermatology practices. New clinical features are being described to fill out the clinical profile of such patients who may be currently misdiagnosed with other conditions, according to researchers who first described the syndrome in the last quarter of 2020.

VEXAS is often misdiagnosed as treatment-refractory relapsing polychondritis, polyarteritis nodosa, Sweet syndrome, or giant cell arteritis. These seemingly unrelated disorders are actually tied together by a single thread recently unraveled by David B. Beck, MD, PhD, a clinical fellow at the National Human Genome Research Institute, and colleagues, including rheumatologist Marcela Ferrada, MD, and others at institutes of the National Institutes of Health, Bethesda, Md. The connection between these disparate clinical presentations lies in somatic mutations in UBA1, a gene that initiates cytoplasmic ubiquitylation, a process by which misfolded proteins are tagged for degradation. VEXAS appears primarily limited to men because the UBA1 gene lies on the X chromosome, although it may be possible for women to have it because of an acquired loss of X chromosome.
VEXAS is an acronym for:
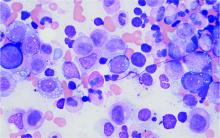
- Vacuoles in bone marrow cells
- E-1 activating enzyme, which is what UBA1 encodes for
- X-linked
- Autoinflammatory
- Somatic mutation featuring hematologic mosaicism
Dr. Beck said that VEXAS is “probably affecting thousands of Americans,” but it is tough to say this early in the understanding of the disease. He estimated that the prevalence of VEXAS could be 1 per 20,000-30,000 individuals.
A new way of looking for disease
VEXAS has caused a major stir among geneticists because of the novel manner in which Dr. Beck and his coinvestigators made their discovery. Instead of starting out in the traditional path to discovery of a new genetic disease – that is, by looking for clinical similarities among patients with undiagnosed diseases and then conducting a search for a gene or genes that might explain the shared patient symptoms – the investigators took a genotype-first approach. They scanned the mapped genomic sequences of patients in the National Institutes of Health Undiagnosed Diseases Network, which led them to zero in on mutations in UBA1 as their top candidate.
“We targeted the ubiquitin-proteasome pathway, because it has been implicated in many autoinflammatory diseases – for example, HA20 [A20 haploinsufficiency] and CANDLE syndrome [Chronic Atypical Neutrophilic Dermatosis with Lipodystrophy and Elevated temperature]. Many of these recurrent inflammatory diseases are caused by mutations within this pathway,” Dr. Beck said in an interview.
Next, they analyzed the genomes of patients in other NIH databases and patients from other study populations at the University College London and Leeds Teaching Hospitals NHS Trust in the United Kingdom in a search for UBA1 somatic mutations, eventually identifying 25 men with the shared features they called VEXAS. These 25 formed the basis for their initial report on the syndrome in the New England Journal of Medicine.
Most autoinflammatory diseases appear in childhood because they stem from germline mutations. VEXAS syndrome, because of somatic mutations with mosaicism, appears to manifest later in life: The median age of the initial 25-man cohort was 64 years, ranging from 45 to 80 years. It’s a severe disorder. By the time the investigators were preparing their paper for publication, 10 of the 25 patients, or 40%, had died.
“I think that somatic mutations may account for a significant percentage of severe. adult-onset rheumatologic diseases, and it may change the way we think about treating them based on having a genetic diagnosis,” Dr. Beck said.
“This approach could be expanded to look at other pathways we know are important in inflammation, or alternatively, it could be completely unbiased and look for any shared variation that occurs across undiagnosed patients with inflammatory diseases. I think that one thing that’s important about our study is that previously we had been looking for mutations that really in most cases were the same sort of germline mutations present in [pediatric] patients who have disease at early onset, but now we’re thinking about things differently. There may be a different type of genetics that drives adult-onset rheumatologic disease, and this would be somatic mutations which are not present in every cell of the body, just in the blood, and that’s why there’s just this blood-based disease.”
When to suspect VEXAS syndrome
Consider the possibility of VEXAS in middle-aged or older men in a rheumatology clinic with characteristics suggestive of treatment-refractory relapsing polychondritis, giant cell arteritis, polyarteritis nodosa, or Sweet syndrome. In the original series of 25 men, 15 were diagnosed with relapsing polychondritis, 8 with Sweet syndrome, 3 with polyarteritis nodosa, and 1 with giant cell arteritis.
Men with VEXAS often have periodic fevers, pulmonary infiltrates, a history of unprovoked venous thromboembolic events, neutrophilic dermatoses, and/or hematologic abnormalities such as myelodysplastic syndrome, multiple myeloma, or monoclonal gammopathy of unknown origin.
Bone marrow biopsy will show vacuoles in myeloid and erythroid precursor cells. Inflammatory marker levels are very high: In the NIH series, the median C-reactive protein was 73 mg/L and median erythrocyte sedimentation rate was 97 mm/hr. The diagnosis of VEXAS can be confirmed by genetic testing performed by Dr. Beck and his NIH coworkers ([email protected]).
In interviews, Dr. Beck and Dr. Ferrada emphasized that management of VEXAS requires a multidisciplinary team of clinicians including rheumatologists, hematologists, and dermatologists.
Dr. Ferrada said that rheumatologists could suspect VEXAS in patients who have very high inflammatory markers and do not have a clear diagnosis or do not meet all criteria for other rheumatologic diseases, particularly in older men, but it’s possible in younger men as well. Hematologists could also consider VEXAS in patients with macrocytic anemia or macrocytosis without an explanation and inflammatory features, she said.
Dr. Ferrada, Dr. Beck, and colleagues also published a study in Arthritis & Rheumatology that presents a useful clinical algorithm for deciding whether to order genetic screening for VEXAS in patients with relapsing polychondritis.
First off, Dr. Ferrada and colleagues performed whole-exome sequencing and testing for UBA1 variants in an observational cohort of 92 relapsing polychondritis patients to determine the prevalence of VEXAS, which turned out to be 8%. They added an additional 6 patients with relapsing polychondritis and VEXAS from other cohorts, for a total of 13. The investigators determined that patients with VEXAS were older at disease onset, and more likely to have fever, ear chondritis, DVT, pulmonary infiltrates, skin involvement, and periorbital edema. In contrast, the RP cohort had a significantly higher prevalence of airway chondritis, joint involvement, and vestibular symptoms.
Dr. Ferrada’s algorithm for picking out VEXAS in patients who meet diagnostic criteria for relapsing polychondritis is based upon a few simple factors readily apparent in screening patient charts: male sex; age at onset older than 50 years; macrocytic anemia; and thrombocytopenia. Those four variables, when present, identify VEXAS within an RP cohort with 100% sensitivity and 96% specificity. “As we learn more about [VEXAS] and how it presents earlier, I think we are going to be able to find different manifestations or laboratory data that are going to allow us to diagnose these patients earlier,” she said. “The whole role of that algorithm was to guide clinicians who see patients with relapsing polychondritis to test these patients for the mutation, but I think over time that is going to evolve.”
Researchers are taking similar approaches for other clinical diagnoses to see which should be referred for UBA1 testing, Dr. Beck said.
Myelodysplastic syndrome and hematologic abnormalities
While patients with both myelodysplastic syndrome and relapsing polychondritis have been known in the literature for many years, it’s not until now that researchers are seeing a connection between the two, Dr. Ferrada said.
A majority of the VEXAS patients in the NEJM study had a workup for myelodysplastic syndrome, but only 24% met criteria. However, many were within the spectrum of myelodysplastic disease and some did not meet criteria because their anemia was attributed to a rheumatologic diagnosis and they did not have a known genetic driver of myelodysplastic syndrome, Dr. Beck said. It also fits with this new evidence that UBA1 is probably a driver of myelodysplastic syndrome in and of itself, and that anemia and hematologic involvement are not secondary to the rheumatologic disease; they are linked to the same disease process.
Dr. Beck said that there may be a subset of patients who present with primarily hematologic manifestations, noting the NEJM study could have ascertainment bias because the researchers analyzed mainly patients presenting to their clinic with relapsing polychondritis and severe inflammation. NIH researchers also are still looking in their cohort for any association with hematologic malignancies that preceded clinical manifestations, he said.
More cases reported
As of early April, another 27 cases had been reported in the literature as more researchers have begun to look for patients with UBA1 mutations, some with additional presenting clinical features associated with VEXAS, including chronic progressive inflammatory arthritis, Kikuchi-Fujimoto disease, spondyloarthritis, and bacterial pneumonia.
“Many times with rare diseases, we can’t get enough patients to understand the full spectrum of the disease, but this disease seems to be far more common than we would have expected. We’re actually getting many referrals,” Dr. Beck said.
It appears so far that the range of somatic UBA1 mutations that have been discovered in VEXAS patients does make a difference in the severity of clinical presentation and could potentially be useful in prognosis, Dr. Beck said.
Right now, NIH researchers are asking patients about their natural clinical course, assessing disease activity, and determining which treatments get a response, with the ultimate goal of a treatment trial at the NIH.
Treatment
Developing better treatments for VEXAS syndrome is a priority. In the initial report on VEXAS, the researchers found that the only reliably effective therapy is high-dose corticosteroids. Dr. Ferrada said that NIH investigators have begun thinking about agents that target both the hematologic and inflammatory features of VEXAS. “Most patients get exposed to treatments that are targeted to decrease the inflammatory process, and some of these treatments help partially but not completely to decrease the amount of steroids that patients are taking. For example, one of the medications is tocilizumab. [It was used in] patients who had previous diagnosis of relapsing polychondritis, but they still had to take steroids and their hematologic manifestations keep progressing. We’re in the process of figuring out medications that may help in treating both.” Dr. Ferrada added that because the source of the mutation is in the bone marrow, transplantation may be an effective option.
Laboratory work to identify potential treatments for VEXAS in studies of model organisms could identify treatments outside of the classic anti-inflammatory agents, such as targeting certain cell types in the bone marrow or the ubiquitin-proteasome pathway, Dr. Beck said. “We think that however UBA1 works to initiate inflammation may be important not just in VEXAS but in other diseases. Rare diseases may be informing the mechanisms in common diseases.”
The VEXAS NEJM study was sponsored by the NIH Intramural Research Programs and by an EU Horizon 2020 Research and Innovation Program grant. Dr. Beck reported a patent pending on “Diagnosis and Treatment of VEXAS with Mosaic Missense Mutations in UBA1.”
Older men with a novel adult-onset, severe autoinflammatory syndrome known by the acronym VEXAS are likely hiding in plain sight in many adult rheumatology, hematology, and dermatology practices. New clinical features are being described to fill out the clinical profile of such patients who may be currently misdiagnosed with other conditions, according to researchers who first described the syndrome in the last quarter of 2020.

VEXAS is often misdiagnosed as treatment-refractory relapsing polychondritis, polyarteritis nodosa, Sweet syndrome, or giant cell arteritis. These seemingly unrelated disorders are actually tied together by a single thread recently unraveled by David B. Beck, MD, PhD, a clinical fellow at the National Human Genome Research Institute, and colleagues, including rheumatologist Marcela Ferrada, MD, and others at institutes of the National Institutes of Health, Bethesda, Md. The connection between these disparate clinical presentations lies in somatic mutations in UBA1, a gene that initiates cytoplasmic ubiquitylation, a process by which misfolded proteins are tagged for degradation. VEXAS appears primarily limited to men because the UBA1 gene lies on the X chromosome, although it may be possible for women to have it because of an acquired loss of X chromosome.
VEXAS is an acronym for:
- Vacuoles in bone marrow cells
- E-1 activating enzyme, which is what UBA1 encodes for
- X-linked
- Autoinflammatory
- Somatic mutation featuring hematologic mosaicism
Dr. Beck said that VEXAS is “probably affecting thousands of Americans,” but it is tough to say this early in the understanding of the disease. He estimated that the prevalence of VEXAS could be 1 per 20,000-30,000 individuals.
A new way of looking for disease
VEXAS has caused a major stir among geneticists because of the novel manner in which Dr. Beck and his coinvestigators made their discovery. Instead of starting out in the traditional path to discovery of a new genetic disease – that is, by looking for clinical similarities among patients with undiagnosed diseases and then conducting a search for a gene or genes that might explain the shared patient symptoms – the investigators took a genotype-first approach. They scanned the mapped genomic sequences of patients in the National Institutes of Health Undiagnosed Diseases Network, which led them to zero in on mutations in UBA1 as their top candidate.
“We targeted the ubiquitin-proteasome pathway, because it has been implicated in many autoinflammatory diseases – for example, HA20 [A20 haploinsufficiency] and CANDLE syndrome [Chronic Atypical Neutrophilic Dermatosis with Lipodystrophy and Elevated temperature]. Many of these recurrent inflammatory diseases are caused by mutations within this pathway,” Dr. Beck said in an interview.
Next, they analyzed the genomes of patients in other NIH databases and patients from other study populations at the University College London and Leeds Teaching Hospitals NHS Trust in the United Kingdom in a search for UBA1 somatic mutations, eventually identifying 25 men with the shared features they called VEXAS. These 25 formed the basis for their initial report on the syndrome in the New England Journal of Medicine.
Most autoinflammatory diseases appear in childhood because they stem from germline mutations. VEXAS syndrome, because of somatic mutations with mosaicism, appears to manifest later in life: The median age of the initial 25-man cohort was 64 years, ranging from 45 to 80 years. It’s a severe disorder. By the time the investigators were preparing their paper for publication, 10 of the 25 patients, or 40%, had died.
“I think that somatic mutations may account for a significant percentage of severe. adult-onset rheumatologic diseases, and it may change the way we think about treating them based on having a genetic diagnosis,” Dr. Beck said.
“This approach could be expanded to look at other pathways we know are important in inflammation, or alternatively, it could be completely unbiased and look for any shared variation that occurs across undiagnosed patients with inflammatory diseases. I think that one thing that’s important about our study is that previously we had been looking for mutations that really in most cases were the same sort of germline mutations present in [pediatric] patients who have disease at early onset, but now we’re thinking about things differently. There may be a different type of genetics that drives adult-onset rheumatologic disease, and this would be somatic mutations which are not present in every cell of the body, just in the blood, and that’s why there’s just this blood-based disease.”
When to suspect VEXAS syndrome
Consider the possibility of VEXAS in middle-aged or older men in a rheumatology clinic with characteristics suggestive of treatment-refractory relapsing polychondritis, giant cell arteritis, polyarteritis nodosa, or Sweet syndrome. In the original series of 25 men, 15 were diagnosed with relapsing polychondritis, 8 with Sweet syndrome, 3 with polyarteritis nodosa, and 1 with giant cell arteritis.
Men with VEXAS often have periodic fevers, pulmonary infiltrates, a history of unprovoked venous thromboembolic events, neutrophilic dermatoses, and/or hematologic abnormalities such as myelodysplastic syndrome, multiple myeloma, or monoclonal gammopathy of unknown origin.
Bone marrow biopsy will show vacuoles in myeloid and erythroid precursor cells. Inflammatory marker levels are very high: In the NIH series, the median C-reactive protein was 73 mg/L and median erythrocyte sedimentation rate was 97 mm/hr. The diagnosis of VEXAS can be confirmed by genetic testing performed by Dr. Beck and his NIH coworkers ([email protected]).
In interviews, Dr. Beck and Dr. Ferrada emphasized that management of VEXAS requires a multidisciplinary team of clinicians including rheumatologists, hematologists, and dermatologists.
Dr. Ferrada said that rheumatologists could suspect VEXAS in patients who have very high inflammatory markers and do not have a clear diagnosis or do not meet all criteria for other rheumatologic diseases, particularly in older men, but it’s possible in younger men as well. Hematologists could also consider VEXAS in patients with macrocytic anemia or macrocytosis without an explanation and inflammatory features, she said.
Dr. Ferrada, Dr. Beck, and colleagues also published a study in Arthritis & Rheumatology that presents a useful clinical algorithm for deciding whether to order genetic screening for VEXAS in patients with relapsing polychondritis.
First off, Dr. Ferrada and colleagues performed whole-exome sequencing and testing for UBA1 variants in an observational cohort of 92 relapsing polychondritis patients to determine the prevalence of VEXAS, which turned out to be 8%. They added an additional 6 patients with relapsing polychondritis and VEXAS from other cohorts, for a total of 13. The investigators determined that patients with VEXAS were older at disease onset, and more likely to have fever, ear chondritis, DVT, pulmonary infiltrates, skin involvement, and periorbital edema. In contrast, the RP cohort had a significantly higher prevalence of airway chondritis, joint involvement, and vestibular symptoms.
Dr. Ferrada’s algorithm for picking out VEXAS in patients who meet diagnostic criteria for relapsing polychondritis is based upon a few simple factors readily apparent in screening patient charts: male sex; age at onset older than 50 years; macrocytic anemia; and thrombocytopenia. Those four variables, when present, identify VEXAS within an RP cohort with 100% sensitivity and 96% specificity. “As we learn more about [VEXAS] and how it presents earlier, I think we are going to be able to find different manifestations or laboratory data that are going to allow us to diagnose these patients earlier,” she said. “The whole role of that algorithm was to guide clinicians who see patients with relapsing polychondritis to test these patients for the mutation, but I think over time that is going to evolve.”
Researchers are taking similar approaches for other clinical diagnoses to see which should be referred for UBA1 testing, Dr. Beck said.
Myelodysplastic syndrome and hematologic abnormalities
While patients with both myelodysplastic syndrome and relapsing polychondritis have been known in the literature for many years, it’s not until now that researchers are seeing a connection between the two, Dr. Ferrada said.
A majority of the VEXAS patients in the NEJM study had a workup for myelodysplastic syndrome, but only 24% met criteria. However, many were within the spectrum of myelodysplastic disease and some did not meet criteria because their anemia was attributed to a rheumatologic diagnosis and they did not have a known genetic driver of myelodysplastic syndrome, Dr. Beck said. It also fits with this new evidence that UBA1 is probably a driver of myelodysplastic syndrome in and of itself, and that anemia and hematologic involvement are not secondary to the rheumatologic disease; they are linked to the same disease process.
Dr. Beck said that there may be a subset of patients who present with primarily hematologic manifestations, noting the NEJM study could have ascertainment bias because the researchers analyzed mainly patients presenting to their clinic with relapsing polychondritis and severe inflammation. NIH researchers also are still looking in their cohort for any association with hematologic malignancies that preceded clinical manifestations, he said.
More cases reported
As of early April, another 27 cases had been reported in the literature as more researchers have begun to look for patients with UBA1 mutations, some with additional presenting clinical features associated with VEXAS, including chronic progressive inflammatory arthritis, Kikuchi-Fujimoto disease, spondyloarthritis, and bacterial pneumonia.
“Many times with rare diseases, we can’t get enough patients to understand the full spectrum of the disease, but this disease seems to be far more common than we would have expected. We’re actually getting many referrals,” Dr. Beck said.
It appears so far that the range of somatic UBA1 mutations that have been discovered in VEXAS patients does make a difference in the severity of clinical presentation and could potentially be useful in prognosis, Dr. Beck said.
Right now, NIH researchers are asking patients about their natural clinical course, assessing disease activity, and determining which treatments get a response, with the ultimate goal of a treatment trial at the NIH.
Treatment
Developing better treatments for VEXAS syndrome is a priority. In the initial report on VEXAS, the researchers found that the only reliably effective therapy is high-dose corticosteroids. Dr. Ferrada said that NIH investigators have begun thinking about agents that target both the hematologic and inflammatory features of VEXAS. “Most patients get exposed to treatments that are targeted to decrease the inflammatory process, and some of these treatments help partially but not completely to decrease the amount of steroids that patients are taking. For example, one of the medications is tocilizumab. [It was used in] patients who had previous diagnosis of relapsing polychondritis, but they still had to take steroids and their hematologic manifestations keep progressing. We’re in the process of figuring out medications that may help in treating both.” Dr. Ferrada added that because the source of the mutation is in the bone marrow, transplantation may be an effective option.
Laboratory work to identify potential treatments for VEXAS in studies of model organisms could identify treatments outside of the classic anti-inflammatory agents, such as targeting certain cell types in the bone marrow or the ubiquitin-proteasome pathway, Dr. Beck said. “We think that however UBA1 works to initiate inflammation may be important not just in VEXAS but in other diseases. Rare diseases may be informing the mechanisms in common diseases.”
The VEXAS NEJM study was sponsored by the NIH Intramural Research Programs and by an EU Horizon 2020 Research and Innovation Program grant. Dr. Beck reported a patent pending on “Diagnosis and Treatment of VEXAS with Mosaic Missense Mutations in UBA1.”
Older men with a novel adult-onset, severe autoinflammatory syndrome known by the acronym VEXAS are likely hiding in plain sight in many adult rheumatology, hematology, and dermatology practices. New clinical features are being described to fill out the clinical profile of such patients who may be currently misdiagnosed with other conditions, according to researchers who first described the syndrome in the last quarter of 2020.

VEXAS is often misdiagnosed as treatment-refractory relapsing polychondritis, polyarteritis nodosa, Sweet syndrome, or giant cell arteritis. These seemingly unrelated disorders are actually tied together by a single thread recently unraveled by David B. Beck, MD, PhD, a clinical fellow at the National Human Genome Research Institute, and colleagues, including rheumatologist Marcela Ferrada, MD, and others at institutes of the National Institutes of Health, Bethesda, Md. The connection between these disparate clinical presentations lies in somatic mutations in UBA1, a gene that initiates cytoplasmic ubiquitylation, a process by which misfolded proteins are tagged for degradation. VEXAS appears primarily limited to men because the UBA1 gene lies on the X chromosome, although it may be possible for women to have it because of an acquired loss of X chromosome.
VEXAS is an acronym for:
- Vacuoles in bone marrow cells
- E-1 activating enzyme, which is what UBA1 encodes for
- X-linked
- Autoinflammatory
- Somatic mutation featuring hematologic mosaicism
Dr. Beck said that VEXAS is “probably affecting thousands of Americans,” but it is tough to say this early in the understanding of the disease. He estimated that the prevalence of VEXAS could be 1 per 20,000-30,000 individuals.
A new way of looking for disease
VEXAS has caused a major stir among geneticists because of the novel manner in which Dr. Beck and his coinvestigators made their discovery. Instead of starting out in the traditional path to discovery of a new genetic disease – that is, by looking for clinical similarities among patients with undiagnosed diseases and then conducting a search for a gene or genes that might explain the shared patient symptoms – the investigators took a genotype-first approach. They scanned the mapped genomic sequences of patients in the National Institutes of Health Undiagnosed Diseases Network, which led them to zero in on mutations in UBA1 as their top candidate.
“We targeted the ubiquitin-proteasome pathway, because it has been implicated in many autoinflammatory diseases – for example, HA20 [A20 haploinsufficiency] and CANDLE syndrome [Chronic Atypical Neutrophilic Dermatosis with Lipodystrophy and Elevated temperature]. Many of these recurrent inflammatory diseases are caused by mutations within this pathway,” Dr. Beck said in an interview.
Next, they analyzed the genomes of patients in other NIH databases and patients from other study populations at the University College London and Leeds Teaching Hospitals NHS Trust in the United Kingdom in a search for UBA1 somatic mutations, eventually identifying 25 men with the shared features they called VEXAS. These 25 formed the basis for their initial report on the syndrome in the New England Journal of Medicine.
Most autoinflammatory diseases appear in childhood because they stem from germline mutations. VEXAS syndrome, because of somatic mutations with mosaicism, appears to manifest later in life: The median age of the initial 25-man cohort was 64 years, ranging from 45 to 80 years. It’s a severe disorder. By the time the investigators were preparing their paper for publication, 10 of the 25 patients, or 40%, had died.
“I think that somatic mutations may account for a significant percentage of severe. adult-onset rheumatologic diseases, and it may change the way we think about treating them based on having a genetic diagnosis,” Dr. Beck said.
“This approach could be expanded to look at other pathways we know are important in inflammation, or alternatively, it could be completely unbiased and look for any shared variation that occurs across undiagnosed patients with inflammatory diseases. I think that one thing that’s important about our study is that previously we had been looking for mutations that really in most cases were the same sort of germline mutations present in [pediatric] patients who have disease at early onset, but now we’re thinking about things differently. There may be a different type of genetics that drives adult-onset rheumatologic disease, and this would be somatic mutations which are not present in every cell of the body, just in the blood, and that’s why there’s just this blood-based disease.”
When to suspect VEXAS syndrome
Consider the possibility of VEXAS in middle-aged or older men in a rheumatology clinic with characteristics suggestive of treatment-refractory relapsing polychondritis, giant cell arteritis, polyarteritis nodosa, or Sweet syndrome. In the original series of 25 men, 15 were diagnosed with relapsing polychondritis, 8 with Sweet syndrome, 3 with polyarteritis nodosa, and 1 with giant cell arteritis.
Men with VEXAS often have periodic fevers, pulmonary infiltrates, a history of unprovoked venous thromboembolic events, neutrophilic dermatoses, and/or hematologic abnormalities such as myelodysplastic syndrome, multiple myeloma, or monoclonal gammopathy of unknown origin.
Bone marrow biopsy will show vacuoles in myeloid and erythroid precursor cells. Inflammatory marker levels are very high: In the NIH series, the median C-reactive protein was 73 mg/L and median erythrocyte sedimentation rate was 97 mm/hr. The diagnosis of VEXAS can be confirmed by genetic testing performed by Dr. Beck and his NIH coworkers ([email protected]).
In interviews, Dr. Beck and Dr. Ferrada emphasized that management of VEXAS requires a multidisciplinary team of clinicians including rheumatologists, hematologists, and dermatologists.
Dr. Ferrada said that rheumatologists could suspect VEXAS in patients who have very high inflammatory markers and do not have a clear diagnosis or do not meet all criteria for other rheumatologic diseases, particularly in older men, but it’s possible in younger men as well. Hematologists could also consider VEXAS in patients with macrocytic anemia or macrocytosis without an explanation and inflammatory features, she said.
Dr. Ferrada, Dr. Beck, and colleagues also published a study in Arthritis & Rheumatology that presents a useful clinical algorithm for deciding whether to order genetic screening for VEXAS in patients with relapsing polychondritis.
First off, Dr. Ferrada and colleagues performed whole-exome sequencing and testing for UBA1 variants in an observational cohort of 92 relapsing polychondritis patients to determine the prevalence of VEXAS, which turned out to be 8%. They added an additional 6 patients with relapsing polychondritis and VEXAS from other cohorts, for a total of 13. The investigators determined that patients with VEXAS were older at disease onset, and more likely to have fever, ear chondritis, DVT, pulmonary infiltrates, skin involvement, and periorbital edema. In contrast, the RP cohort had a significantly higher prevalence of airway chondritis, joint involvement, and vestibular symptoms.
Dr. Ferrada’s algorithm for picking out VEXAS in patients who meet diagnostic criteria for relapsing polychondritis is based upon a few simple factors readily apparent in screening patient charts: male sex; age at onset older than 50 years; macrocytic anemia; and thrombocytopenia. Those four variables, when present, identify VEXAS within an RP cohort with 100% sensitivity and 96% specificity. “As we learn more about [VEXAS] and how it presents earlier, I think we are going to be able to find different manifestations or laboratory data that are going to allow us to diagnose these patients earlier,” she said. “The whole role of that algorithm was to guide clinicians who see patients with relapsing polychondritis to test these patients for the mutation, but I think over time that is going to evolve.”
Researchers are taking similar approaches for other clinical diagnoses to see which should be referred for UBA1 testing, Dr. Beck said.
Myelodysplastic syndrome and hematologic abnormalities
While patients with both myelodysplastic syndrome and relapsing polychondritis have been known in the literature for many years, it’s not until now that researchers are seeing a connection between the two, Dr. Ferrada said.
A majority of the VEXAS patients in the NEJM study had a workup for myelodysplastic syndrome, but only 24% met criteria. However, many were within the spectrum of myelodysplastic disease and some did not meet criteria because their anemia was attributed to a rheumatologic diagnosis and they did not have a known genetic driver of myelodysplastic syndrome, Dr. Beck said. It also fits with this new evidence that UBA1 is probably a driver of myelodysplastic syndrome in and of itself, and that anemia and hematologic involvement are not secondary to the rheumatologic disease; they are linked to the same disease process.
Dr. Beck said that there may be a subset of patients who present with primarily hematologic manifestations, noting the NEJM study could have ascertainment bias because the researchers analyzed mainly patients presenting to their clinic with relapsing polychondritis and severe inflammation. NIH researchers also are still looking in their cohort for any association with hematologic malignancies that preceded clinical manifestations, he said.
More cases reported
As of early April, another 27 cases had been reported in the literature as more researchers have begun to look for patients with UBA1 mutations, some with additional presenting clinical features associated with VEXAS, including chronic progressive inflammatory arthritis, Kikuchi-Fujimoto disease, spondyloarthritis, and bacterial pneumonia.
“Many times with rare diseases, we can’t get enough patients to understand the full spectrum of the disease, but this disease seems to be far more common than we would have expected. We’re actually getting many referrals,” Dr. Beck said.
It appears so far that the range of somatic UBA1 mutations that have been discovered in VEXAS patients does make a difference in the severity of clinical presentation and could potentially be useful in prognosis, Dr. Beck said.
Right now, NIH researchers are asking patients about their natural clinical course, assessing disease activity, and determining which treatments get a response, with the ultimate goal of a treatment trial at the NIH.
Treatment
Developing better treatments for VEXAS syndrome is a priority. In the initial report on VEXAS, the researchers found that the only reliably effective therapy is high-dose corticosteroids. Dr. Ferrada said that NIH investigators have begun thinking about agents that target both the hematologic and inflammatory features of VEXAS. “Most patients get exposed to treatments that are targeted to decrease the inflammatory process, and some of these treatments help partially but not completely to decrease the amount of steroids that patients are taking. For example, one of the medications is tocilizumab. [It was used in] patients who had previous diagnosis of relapsing polychondritis, but they still had to take steroids and their hematologic manifestations keep progressing. We’re in the process of figuring out medications that may help in treating both.” Dr. Ferrada added that because the source of the mutation is in the bone marrow, transplantation may be an effective option.
Laboratory work to identify potential treatments for VEXAS in studies of model organisms could identify treatments outside of the classic anti-inflammatory agents, such as targeting certain cell types in the bone marrow or the ubiquitin-proteasome pathway, Dr. Beck said. “We think that however UBA1 works to initiate inflammation may be important not just in VEXAS but in other diseases. Rare diseases may be informing the mechanisms in common diseases.”
The VEXAS NEJM study was sponsored by the NIH Intramural Research Programs and by an EU Horizon 2020 Research and Innovation Program grant. Dr. Beck reported a patent pending on “Diagnosis and Treatment of VEXAS with Mosaic Missense Mutations in UBA1.”
Researchers stress importance of second COVID-19 vaccine dose for infliximab users
Patients being treated with infliximab had weakened immune responses to the first dose of the ChAdOx1 nCoV-19 (Oxford/AstraZeneca) and BNT162b2 (Pfizer/BioNTech) vaccines, compared with patients on vedolizumab (Entyvio), although a very significant number of patients from both groups seroconverted after their second dose, according to a new U.K. study of patients with inflammatory bowel disease (IBD).
“Antibody testing and adapted vaccine schedules should be considered to protect these at-risk patients,” Nicholas A. Kennedy, PhD, MBBS, of the University of Exeter (England) and colleagues wrote in a preprint published March 29 on MedRxiv.
Infliximab is an anti–tumor necrosis factor (anti-TNF) monoclonal antibody that’s approved to treat adult and pediatric Crohn’s disease and ulcerative colitis, as well as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and plaque psoriasis, whereas vedolizumab, a gut selective anti-integrin alpha4beta7 monoclonal antibody that is not associated with impaired systemic immune responses, is approved to treat Crohn’s disease and ulcerative colitis in adults.
A previous study from Kennedy and colleagues revealed that IBD patients on infliximab showed a weakened COVID-19 antibody response compared with patients on vedolizumab. To determine if treatment with anti-TNF drugs impacted the efficacy of the first shot of these two-dose COVID-19 vaccines, the researchers used data from the CLARITY IBD study to assess 865 infliximab- and 428 vedolizumab-treated participants without evidence of prior SARS-CoV-2 infection who had received uninterrupted biologic therapy since being recruited between Sept. 22 and Dec. 23, 2020.
In the 3-10 weeks after initial vaccination, geometric mean concentrations for SARS-CoV-2 anti-spike protein receptor-binding protein antibodies were lower in patients on infliximab, compared with patients on vedolizumab for both the Pfizer (6.0 U/mL [5.9] versus 28.8 U/mL [5.4], P < .0001) and AstraZeneca (4.7 U/mL [4.9] versus 13.8 U/mL [5.9]; P < .0001) vaccines. The researchers’ multivariable models reinforced those findings, with antibody concentrations lower in infliximab-treated patients for both the Pfizer (fold change, 0.29; 95% confidence interval, 0.21-0.40; P < .0001) and AstraZeneca (FC, 0.39; 95% CI, 0.30-0.51; P < .0001) vaccines.
After second doses of the two-dose Pfizer vaccine, 85% of patients on infliximab and 86% of patients on vedolizumab seroconverted (P = .68); similarly high seroconversion rates were seen in patients who had been infected with SARS-CoV-2 prior to receiving either vaccine. Several patient characteristics were associated with lower antibody concentrations regardless of vaccine type: being 60 years or older, use of immunomodulators, having Crohn’s disease, and being a smoker. Alternatively, non-White ethnicity was associated with higher antibody concentrations.
Evidence has ‘unclear clinical significance’
“These data, which require peer review, do not change my opinion on the safety and efficacy of COVID-19 vaccines in patients taking TNF inhibitors such as infliximab as monotherapy for the treatment of psoriatic disease,” Joel M. Gelfand MD, director of the psoriasis and phototherapy treatment center at the University of Pennsylvania, Philadelphia, said in an interview.
“First, two peer-reviewed studies found good antibody response in patients on TNF inhibitors receiving COVID-19 vaccines (doi: 10.1136/annrheumdis-2021-220289; 10.1136/annrheumdis-2021-220272). Second, antibody responses were robust in the small cohort that received the second dose of a COVID-19 vaccine. We already know that, for the two messenger RNA-based vaccines available under emergency use authorization in the U.S., a second dose is required for optimal efficacy. Thus, evidence of a reduced antibody response after just one dose is of unclear clinical significance. Third, antibody responses are only a surrogate marker, and a low antibody response doesn’t necessarily mean the patient will not be protected by the vaccine.”
Focus on the second dose of a two-dose regimen
“Tell me about the response in people who got both doses of a vaccine that you’re supposed to get both doses of,” Jeffrey Curtis, MD, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham, said in an interview. “The number of patients in that subset was small [n = 27] but in my opinion that’s the most clinically relevant analysis and the one that patients and clinicians want answered.”
He also emphasized the uncertainty around what ‘protection’ means in these early days of studying COVID-19 vaccine responses. “You can define seroprotection or seroconversion as some absolute level of an antibody response, but if you want to say ‘Mrs. Smith, your antibody level was X,’ on whatever arbitrary scale with whoever’s arbitrary lab test, nobody actually knows that Mrs. Smith is now protected from SARS-CoV-2, or how protected,” he said.
“What is not terribly controversial is: If you can’t detect antibodies, the vaccine didn’t ‘take,’ if you will. But if I tell you that the mean antibody level was X with one drug and then 2X with another drug, does that mean that you’re twice as protected? We don’t know that. I’m fearful that people are looking at these studies and thinking that more is better. It might be, but we don’t know that to be true.”
Debating the cause of weakened immune responses
“The biological plausibility of being on an anti-TNF affecting your immune reaction to a messenger RNA or even a replication-deficient viral vector vaccine doesn’t make sense,” David T. Rubin, MD, professor of medicine at the University of Chicago and chair of the National Scientific Advisory Committee of the Crohn’s and Colitis Foundation, said in an interview.
“I’m sure immunologists may differ with me on this, but given what we have come to appreciate about these vaccine mechanisms, this finding doesn’t make intuitive sense. So we need to make sure that, when this happens, we look to the next studies and try to understand, was there any other confounder that may have resulted in these findings that was not adequately adjusted for or addressed in some other way?
“When you have a study of this size, you argue, ‘Because it’s so large, any effect that was seen must be real,’ ” he added. “Alternatively, to have a study of this size, by its very nature you are limited in being able to control for certain other factors or differences between the groups.”
That said, he commended the authors for their study and acknowledged the potential questions it raises about the single-shot Johnson & Johnson vaccine. “If you only get one and you’re on infliximab, this study implies that maybe that’s not enough,” he said. “Despite the fact that Johnson & Johnson was approved as a single dose, it may be necessary to think about it as the first of two, or maybe it’s not the preferred vaccine in this group of patients.”
The study was supported by the Royal Devon and Exeter and Hull University Hospital Foundation NHS Trusts and unrestricted educational grants from Biogen (Switzerland), Celltrion Healthcare (South Korea), Galapagos NV (Belgium), and F. Hoffmann-La Roche (Switzerland). The authors acknowledged numerous potential conflicts of interest, including receiving grants, personal fees, and nonfinancial support from various pharmaceutical companies.
Patients being treated with infliximab had weakened immune responses to the first dose of the ChAdOx1 nCoV-19 (Oxford/AstraZeneca) and BNT162b2 (Pfizer/BioNTech) vaccines, compared with patients on vedolizumab (Entyvio), although a very significant number of patients from both groups seroconverted after their second dose, according to a new U.K. study of patients with inflammatory bowel disease (IBD).
“Antibody testing and adapted vaccine schedules should be considered to protect these at-risk patients,” Nicholas A. Kennedy, PhD, MBBS, of the University of Exeter (England) and colleagues wrote in a preprint published March 29 on MedRxiv.
Infliximab is an anti–tumor necrosis factor (anti-TNF) monoclonal antibody that’s approved to treat adult and pediatric Crohn’s disease and ulcerative colitis, as well as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and plaque psoriasis, whereas vedolizumab, a gut selective anti-integrin alpha4beta7 monoclonal antibody that is not associated with impaired systemic immune responses, is approved to treat Crohn’s disease and ulcerative colitis in adults.
A previous study from Kennedy and colleagues revealed that IBD patients on infliximab showed a weakened COVID-19 antibody response compared with patients on vedolizumab. To determine if treatment with anti-TNF drugs impacted the efficacy of the first shot of these two-dose COVID-19 vaccines, the researchers used data from the CLARITY IBD study to assess 865 infliximab- and 428 vedolizumab-treated participants without evidence of prior SARS-CoV-2 infection who had received uninterrupted biologic therapy since being recruited between Sept. 22 and Dec. 23, 2020.
In the 3-10 weeks after initial vaccination, geometric mean concentrations for SARS-CoV-2 anti-spike protein receptor-binding protein antibodies were lower in patients on infliximab, compared with patients on vedolizumab for both the Pfizer (6.0 U/mL [5.9] versus 28.8 U/mL [5.4], P < .0001) and AstraZeneca (4.7 U/mL [4.9] versus 13.8 U/mL [5.9]; P < .0001) vaccines. The researchers’ multivariable models reinforced those findings, with antibody concentrations lower in infliximab-treated patients for both the Pfizer (fold change, 0.29; 95% confidence interval, 0.21-0.40; P < .0001) and AstraZeneca (FC, 0.39; 95% CI, 0.30-0.51; P < .0001) vaccines.
After second doses of the two-dose Pfizer vaccine, 85% of patients on infliximab and 86% of patients on vedolizumab seroconverted (P = .68); similarly high seroconversion rates were seen in patients who had been infected with SARS-CoV-2 prior to receiving either vaccine. Several patient characteristics were associated with lower antibody concentrations regardless of vaccine type: being 60 years or older, use of immunomodulators, having Crohn’s disease, and being a smoker. Alternatively, non-White ethnicity was associated with higher antibody concentrations.
Evidence has ‘unclear clinical significance’
“These data, which require peer review, do not change my opinion on the safety and efficacy of COVID-19 vaccines in patients taking TNF inhibitors such as infliximab as monotherapy for the treatment of psoriatic disease,” Joel M. Gelfand MD, director of the psoriasis and phototherapy treatment center at the University of Pennsylvania, Philadelphia, said in an interview.
“First, two peer-reviewed studies found good antibody response in patients on TNF inhibitors receiving COVID-19 vaccines (doi: 10.1136/annrheumdis-2021-220289; 10.1136/annrheumdis-2021-220272). Second, antibody responses were robust in the small cohort that received the second dose of a COVID-19 vaccine. We already know that, for the two messenger RNA-based vaccines available under emergency use authorization in the U.S., a second dose is required for optimal efficacy. Thus, evidence of a reduced antibody response after just one dose is of unclear clinical significance. Third, antibody responses are only a surrogate marker, and a low antibody response doesn’t necessarily mean the patient will not be protected by the vaccine.”
Focus on the second dose of a two-dose regimen
“Tell me about the response in people who got both doses of a vaccine that you’re supposed to get both doses of,” Jeffrey Curtis, MD, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham, said in an interview. “The number of patients in that subset was small [n = 27] but in my opinion that’s the most clinically relevant analysis and the one that patients and clinicians want answered.”
He also emphasized the uncertainty around what ‘protection’ means in these early days of studying COVID-19 vaccine responses. “You can define seroprotection or seroconversion as some absolute level of an antibody response, but if you want to say ‘Mrs. Smith, your antibody level was X,’ on whatever arbitrary scale with whoever’s arbitrary lab test, nobody actually knows that Mrs. Smith is now protected from SARS-CoV-2, or how protected,” he said.
“What is not terribly controversial is: If you can’t detect antibodies, the vaccine didn’t ‘take,’ if you will. But if I tell you that the mean antibody level was X with one drug and then 2X with another drug, does that mean that you’re twice as protected? We don’t know that. I’m fearful that people are looking at these studies and thinking that more is better. It might be, but we don’t know that to be true.”
Debating the cause of weakened immune responses
“The biological plausibility of being on an anti-TNF affecting your immune reaction to a messenger RNA or even a replication-deficient viral vector vaccine doesn’t make sense,” David T. Rubin, MD, professor of medicine at the University of Chicago and chair of the National Scientific Advisory Committee of the Crohn’s and Colitis Foundation, said in an interview.
“I’m sure immunologists may differ with me on this, but given what we have come to appreciate about these vaccine mechanisms, this finding doesn’t make intuitive sense. So we need to make sure that, when this happens, we look to the next studies and try to understand, was there any other confounder that may have resulted in these findings that was not adequately adjusted for or addressed in some other way?
“When you have a study of this size, you argue, ‘Because it’s so large, any effect that was seen must be real,’ ” he added. “Alternatively, to have a study of this size, by its very nature you are limited in being able to control for certain other factors or differences between the groups.”
That said, he commended the authors for their study and acknowledged the potential questions it raises about the single-shot Johnson & Johnson vaccine. “If you only get one and you’re on infliximab, this study implies that maybe that’s not enough,” he said. “Despite the fact that Johnson & Johnson was approved as a single dose, it may be necessary to think about it as the first of two, or maybe it’s not the preferred vaccine in this group of patients.”
The study was supported by the Royal Devon and Exeter and Hull University Hospital Foundation NHS Trusts and unrestricted educational grants from Biogen (Switzerland), Celltrion Healthcare (South Korea), Galapagos NV (Belgium), and F. Hoffmann-La Roche (Switzerland). The authors acknowledged numerous potential conflicts of interest, including receiving grants, personal fees, and nonfinancial support from various pharmaceutical companies.
Patients being treated with infliximab had weakened immune responses to the first dose of the ChAdOx1 nCoV-19 (Oxford/AstraZeneca) and BNT162b2 (Pfizer/BioNTech) vaccines, compared with patients on vedolizumab (Entyvio), although a very significant number of patients from both groups seroconverted after their second dose, according to a new U.K. study of patients with inflammatory bowel disease (IBD).
“Antibody testing and adapted vaccine schedules should be considered to protect these at-risk patients,” Nicholas A. Kennedy, PhD, MBBS, of the University of Exeter (England) and colleagues wrote in a preprint published March 29 on MedRxiv.
Infliximab is an anti–tumor necrosis factor (anti-TNF) monoclonal antibody that’s approved to treat adult and pediatric Crohn’s disease and ulcerative colitis, as well as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and plaque psoriasis, whereas vedolizumab, a gut selective anti-integrin alpha4beta7 monoclonal antibody that is not associated with impaired systemic immune responses, is approved to treat Crohn’s disease and ulcerative colitis in adults.
A previous study from Kennedy and colleagues revealed that IBD patients on infliximab showed a weakened COVID-19 antibody response compared with patients on vedolizumab. To determine if treatment with anti-TNF drugs impacted the efficacy of the first shot of these two-dose COVID-19 vaccines, the researchers used data from the CLARITY IBD study to assess 865 infliximab- and 428 vedolizumab-treated participants without evidence of prior SARS-CoV-2 infection who had received uninterrupted biologic therapy since being recruited between Sept. 22 and Dec. 23, 2020.
In the 3-10 weeks after initial vaccination, geometric mean concentrations for SARS-CoV-2 anti-spike protein receptor-binding protein antibodies were lower in patients on infliximab, compared with patients on vedolizumab for both the Pfizer (6.0 U/mL [5.9] versus 28.8 U/mL [5.4], P < .0001) and AstraZeneca (4.7 U/mL [4.9] versus 13.8 U/mL [5.9]; P < .0001) vaccines. The researchers’ multivariable models reinforced those findings, with antibody concentrations lower in infliximab-treated patients for both the Pfizer (fold change, 0.29; 95% confidence interval, 0.21-0.40; P < .0001) and AstraZeneca (FC, 0.39; 95% CI, 0.30-0.51; P < .0001) vaccines.
After second doses of the two-dose Pfizer vaccine, 85% of patients on infliximab and 86% of patients on vedolizumab seroconverted (P = .68); similarly high seroconversion rates were seen in patients who had been infected with SARS-CoV-2 prior to receiving either vaccine. Several patient characteristics were associated with lower antibody concentrations regardless of vaccine type: being 60 years or older, use of immunomodulators, having Crohn’s disease, and being a smoker. Alternatively, non-White ethnicity was associated with higher antibody concentrations.
Evidence has ‘unclear clinical significance’
“These data, which require peer review, do not change my opinion on the safety and efficacy of COVID-19 vaccines in patients taking TNF inhibitors such as infliximab as monotherapy for the treatment of psoriatic disease,” Joel M. Gelfand MD, director of the psoriasis and phototherapy treatment center at the University of Pennsylvania, Philadelphia, said in an interview.
“First, two peer-reviewed studies found good antibody response in patients on TNF inhibitors receiving COVID-19 vaccines (doi: 10.1136/annrheumdis-2021-220289; 10.1136/annrheumdis-2021-220272). Second, antibody responses were robust in the small cohort that received the second dose of a COVID-19 vaccine. We already know that, for the two messenger RNA-based vaccines available under emergency use authorization in the U.S., a second dose is required for optimal efficacy. Thus, evidence of a reduced antibody response after just one dose is of unclear clinical significance. Third, antibody responses are only a surrogate marker, and a low antibody response doesn’t necessarily mean the patient will not be protected by the vaccine.”
Focus on the second dose of a two-dose regimen
“Tell me about the response in people who got both doses of a vaccine that you’re supposed to get both doses of,” Jeffrey Curtis, MD, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham, said in an interview. “The number of patients in that subset was small [n = 27] but in my opinion that’s the most clinically relevant analysis and the one that patients and clinicians want answered.”
He also emphasized the uncertainty around what ‘protection’ means in these early days of studying COVID-19 vaccine responses. “You can define seroprotection or seroconversion as some absolute level of an antibody response, but if you want to say ‘Mrs. Smith, your antibody level was X,’ on whatever arbitrary scale with whoever’s arbitrary lab test, nobody actually knows that Mrs. Smith is now protected from SARS-CoV-2, or how protected,” he said.
“What is not terribly controversial is: If you can’t detect antibodies, the vaccine didn’t ‘take,’ if you will. But if I tell you that the mean antibody level was X with one drug and then 2X with another drug, does that mean that you’re twice as protected? We don’t know that. I’m fearful that people are looking at these studies and thinking that more is better. It might be, but we don’t know that to be true.”
Debating the cause of weakened immune responses
“The biological plausibility of being on an anti-TNF affecting your immune reaction to a messenger RNA or even a replication-deficient viral vector vaccine doesn’t make sense,” David T. Rubin, MD, professor of medicine at the University of Chicago and chair of the National Scientific Advisory Committee of the Crohn’s and Colitis Foundation, said in an interview.
“I’m sure immunologists may differ with me on this, but given what we have come to appreciate about these vaccine mechanisms, this finding doesn’t make intuitive sense. So we need to make sure that, when this happens, we look to the next studies and try to understand, was there any other confounder that may have resulted in these findings that was not adequately adjusted for or addressed in some other way?
“When you have a study of this size, you argue, ‘Because it’s so large, any effect that was seen must be real,’ ” he added. “Alternatively, to have a study of this size, by its very nature you are limited in being able to control for certain other factors or differences between the groups.”
That said, he commended the authors for their study and acknowledged the potential questions it raises about the single-shot Johnson & Johnson vaccine. “If you only get one and you’re on infliximab, this study implies that maybe that’s not enough,” he said. “Despite the fact that Johnson & Johnson was approved as a single dose, it may be necessary to think about it as the first of two, or maybe it’s not the preferred vaccine in this group of patients.”
The study was supported by the Royal Devon and Exeter and Hull University Hospital Foundation NHS Trusts and unrestricted educational grants from Biogen (Switzerland), Celltrion Healthcare (South Korea), Galapagos NV (Belgium), and F. Hoffmann-La Roche (Switzerland). The authors acknowledged numerous potential conflicts of interest, including receiving grants, personal fees, and nonfinancial support from various pharmaceutical companies.
FROM MEDRXIV
Febuxostat, allopurinol real-world cardiovascular risk appears equal
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
Febuxostat (Uloric) was not associated with increased cardiovascular risk in patients with gout when compared to those who used allopurinol, in an analysis of new users of the drugs in Medicare fee-for-service claims data from the period of 2008-2016.
The findings, published March 25 in the Journal of the American Heart Association, update and echo the results from a similar previous study by the same Brigham and Women’s Hospital research group that covered 2008-2013 Medicare claims data. That original claims data study from 2018 sought to confirm the findings of the postmarketing surveillance CARES (Cardiovascular Safety of Febuxostat and Allopurinol in Patients With Gout and Cardiovascular Morbidities) trial that led to a boxed warning for increased risk of cardiovascular and all-cause mortality vs. allopurinol. The trial, however, did not show a higher rate of major adverse cardiovascular events (MACE) overall with febuxostat.
The recency of the new data with more febuxostat-exposed patients overall provides greater reassurance on the safety of the drug, corresponding author Seoyoung C. Kim, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview. “We also were able to get data on cause of death, which we did not have before when we conducted our first paper.”
Dr. Kim said she was not surprised by any of the findings, which were consistent with the results of her earlier work. “Our result on CV death also was consistent and reassuring,” she noted.
The newest Medicare claims study also corroborates results from FAST (Febuxostat Versus Allopurinol Streamlined Trial), a separate postmarketing surveillance study that was ordered by the European Medicines Agency after febuxostat’s approval in 2009. It showed that the two drugs were noninferior to each other for the risk of all-cause mortality or a composite cardiovascular outcome (hospitalization for nonfatal myocardial infarction, biomarker-positive acute coronary syndrome, nonfatal stroke, or cardiovascular death).
“While CARES showed higher CV death and all-cause death rates in febuxostat compared to allopurinol, FAST did not,” Dr. Kim noted. “Our study of more than 111,000 older gout patients treated with either febuxostat or allopurinol in real-world settings also did not find a difference in the risk of MACE, CV mortality, or all-cause mortality,” she added. “Taking these data all together, I think we can be more certain about the CV safety of febuxostat when its use is clinically indicated or needed,” she said.
Study details
Dr. Kim, first author Ajinkya Pawar, PhD, of Brigham and Women’s, and colleagues identified 467,461 people with gout aged 65 years and older who had been enrolled in Medicare for at least a year. They then used propensity-score matching to compare 27,881 first-time users of febuxostat with 83,643 first-time users of allopurinol on the primary outcome of the incidence of major adverse cardiovascular events (MACE), defined as the first occurrence of myocardial infarction, stroke, or cardiovascular mortality.
In the updated study, the mean follow‐up periods for febuxostat and allopurinol were 284 days and 339 days, respectively. Overall, febuxostat was noninferior to allopurinol with regard to MACE (hazard ratio, 0.99; 95% confidence interval, 0.93-1.05), and the results were consistent among patients with baseline CVD (HR, 0.94). In addition, rates of secondary outcomes of MI, stroke, and cardiovascular mortality were not significantly different between febuxostat and allopurinol patients, except for all-cause mortality (HR, 0.92; 95% CI, 0.87-0.98).
The study findings were limited mainly by the potential bias caused by nonadherence to medications, and potential for residual confounding and misclassification bias, the researchers noted.
However, the study was strengthened by its incident new-user design that allowed only patients with no use of either medication for a year before the first dispensing and its active comparator design, and the data are generalizable to the greater population of older gout patients, they said.
Consequently, the data from this large, real-world study support the safety of febuxostat with regard to cardiovascular risk in gout patients, including those with baseline cardiovascular disease, they concluded.
The study was supported by the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital. Dr. Kim disclosed research grants to Brigham and Women’s Hospital from Roche, Pfizer, AbbVie, and Bristol‐Myers Squibb for unrelated studies. Another author reported serving as the principal investigator with research grants from Vertex, Bayer, and Novartis to Brigham and Women’s Hospital for unrelated projects.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Experts highlight recent breakthroughs in psoriatic arthritis
Apremilast (Otezla) monotherapy may be an effective option in oligoarticular psoriatic arthritis, Alexis R. Ogdie, MD, reported at the 2021 Rheumatology Winter Clinical Symposium.
Her analysis of apremilast data from the CORRONA Registry was among several recent highlights in psoriatic arthritis (PsA) cited by speakers at the meeting. Other significant developments included a large pan-Scandinavian study that reassuringly found no increased risk of solid cancers in tumor necrosis factor (TNF) inhibitor–treated patients with PsA, and evidence to suggest a sex difference in the efficacy of both secukinumab (Cosentyx) and adalimumab (Humira), with men responding better than women to two biologics with differing mechanisms of action.
A role for apremilast in oligoarticular disease?
Dr. Ogdie presented an analysis of 150 patients in the U.S. observational CORRONA Registry who initiated monotherapy for oligoarticular PsA and were followed for 6 months. Thirty-four started on apremilast, 15 on methotrexate, and 101 on a biologic. Even though the apremilast group had higher baseline disease activity than did those who started on methotrexate, at 6 months a swollen joint count of 1 or 0 was present in 41% of the apremilast-treated patients, compared with none on methotrexate and 15% on a biologic agent.
A tender joint count of 0-1 was documented at 6 months in 24% of patients on apremilast, 13% with methotrexate, and 21% on a biologic agent. Apremilast’s numeric superiority in outcomes compared to methotrexate in this exploratory study wasn’t subjected to statistical analysis because of the small sample size. However, the ongoing phase 4, double-blind, placebo-controlled, multicenter FOREMOST trial in 330 patients with early oligoarticular PsA should provide more definitive efficacy data, noted Dr. Ogdie, a rheumatologist and epidemiologist at the University of Pennsylvania, Philadelphia.
RWCS program director Arthur Kavanaugh, MD, said, “The most recent EULAR [European Alliance of Associations for Rheumatology] PsA guidelines totally discount apremilast, and I think mostly on the basis of cost, but then they also say that in groups of people it’s not as effective as methotrexate.”
“This study shows to me that, even though it’s a registry, with all the caveats about getting data from registries, apremilast certainly can be an effective drug,” said Dr. Kavanaugh, a rheumatologist and professor of medicine at the University of California, San Diego.
Another valuable piece of information from the CORRONA analysis is that it zeros in on patients with oligoarticular PsA.
“Almost all of our PsA studies are focused on people with polyarticular disease. What about those who have lesser involvement? That, of course, is important in the clinic,” he noted.
Dr. Ogdie concurred.
“If we study only polyarticular disease and we make all of our assumptions based on polyarticular disease, we might be leaving out at least half of the patients with PsA. And those patients may not need a bigger gun. Apremilast and methotrexate are kind of in the same group for that mild oligoarticular disease, and they probably work just fine,” she said.
A final point: “We really don’t have good outcome measures to study oligoarticular disease well. The ACR20 is not good because a 20% improvement in three joints is not readily measurable. That’s why trialists enroll patients with high joint count numbers,” according to the rheumatologist.
No increased risk of solid cancers in PsA patients treated with TNF inhibitors
A new analysis of clinical rheumatology registries in five Nordic countries finally puts to rest any concerns that treatment of PsA with TNF inhibitors is associated with increased risk of solid cancers. The same group previously reported no link between TNF inhibitors and lymphoma in PsA.
The solid cancers study included 9,655 PsA patients who started a first TNF inhibitor during 2001-2017, 14,809 others not treated with biologics, and 31,350 matched general population controls. Linkage to Swedish, Norwegian, Danish, Icelandic, and Finnish national cancer registries showed that the adjusted risk for solid cancer in TNF inhibitor–treated, compared with biologic-naive PsA patients, was 1.0. Similarly, the pooled standardized incidence ratio of solid cancer in TNF inhibitor–treated PsA patients compared to the general population was 1.0. There was no signal of a differential risk for incident cancer for any of the eight malignancies studied: lung, colorectal, breast, prostate, uterine, brain, liver, and pancreatic cancer.
“I like this study a lot because it’s specific to PsA rather than extrapolating from rheumatoid arthritis data, where we have a bunch more information for a much longer period of time, but it’s a different population,” Dr. Kavanaugh said.
Dr. Ogdie said, “I talk to my patients about this particular study or the same group’s earlier lymphoma study all the time.”
“I have to say, these are important data for the dermatology world because there are dermatologists who are still not convinced that TNF inhibitors don’t have an increased risk of malignancy. This kind of information is going to be helpful,” observed Eric M. Ruderman, MD, professor of medicine (rheumatology) at Northwestern University, Chicago.
Greater efficacy for biologics in males than females with PsA?
A secondary analysis of the phase 3b EXCEED trial raised the intriguing possibility that both secukinumab, an interleukin-17A inhibitor, and adalimumab, a TNF inhibitor, have greater efficacy in men than in women with PsA. In this randomized trial of 853 biologic-naive patients with PsA, the ACR20 response rate to secukinumab at week 52 was 61% in females versus 74% in males, with ACR50 rates of 43% in females and 55.3% in males. The ACR20 rate with adalimumab was 51.5% in females and 70.2% in males. Similarly, the corresponding ACR50s were 32.6% and 55.3%, respectively. Minimal disease activity was achieved in 36.2% of women and 51% of men on secukinumab, and in 24.2% of women and 49.8% of men on adalimumab.
“These are randomized patients, so you really shouldn’t see these big differences in minimal disease activity,” Dr. Ogdie noted. “The question is why do men seem to respond better to therapy than women? I don’t think it’s the fibromyalgia-ness. There’s probably some biologic rationale for this that we just don’t understand yet. Maybe hormonal interactions.”
This gender difference in response is an important issue because it can potentially distort outcomes in head-to-head drug trials, Dr. Ruderman added.
“That gender difference is not likely to be huge if you’re looking at a placebo-controlled trial because the difference between the active drug and placebo is going to outweigh it. But when you have two active drugs, if there’s an imbalance in terms of how many men or women there are on each of the two drugs, you may end up with an efficacy difference that’s not real but is based on gender and not response to the drug,” he explained.
Roy M. Fleischmann, MD, a rheumatologist and clinical trialist at the University of Texas, Dallas, rose from the audience to pronounce the EXCEED male-versus-female analysis “very interesting.”
“We should go back and look at other trials and see if that occurred, and if it did, then we have to think about that going forward,” he proposed.
Dr. Ogdie, Dr. Kavanaugh, and Dr. Ruderman reported having financial relationships with numerous pharmaceutical companies.
Apremilast (Otezla) monotherapy may be an effective option in oligoarticular psoriatic arthritis, Alexis R. Ogdie, MD, reported at the 2021 Rheumatology Winter Clinical Symposium.
Her analysis of apremilast data from the CORRONA Registry was among several recent highlights in psoriatic arthritis (PsA) cited by speakers at the meeting. Other significant developments included a large pan-Scandinavian study that reassuringly found no increased risk of solid cancers in tumor necrosis factor (TNF) inhibitor–treated patients with PsA, and evidence to suggest a sex difference in the efficacy of both secukinumab (Cosentyx) and adalimumab (Humira), with men responding better than women to two biologics with differing mechanisms of action.
A role for apremilast in oligoarticular disease?
Dr. Ogdie presented an analysis of 150 patients in the U.S. observational CORRONA Registry who initiated monotherapy for oligoarticular PsA and were followed for 6 months. Thirty-four started on apremilast, 15 on methotrexate, and 101 on a biologic. Even though the apremilast group had higher baseline disease activity than did those who started on methotrexate, at 6 months a swollen joint count of 1 or 0 was present in 41% of the apremilast-treated patients, compared with none on methotrexate and 15% on a biologic agent.
A tender joint count of 0-1 was documented at 6 months in 24% of patients on apremilast, 13% with methotrexate, and 21% on a biologic agent. Apremilast’s numeric superiority in outcomes compared to methotrexate in this exploratory study wasn’t subjected to statistical analysis because of the small sample size. However, the ongoing phase 4, double-blind, placebo-controlled, multicenter FOREMOST trial in 330 patients with early oligoarticular PsA should provide more definitive efficacy data, noted Dr. Ogdie, a rheumatologist and epidemiologist at the University of Pennsylvania, Philadelphia.
RWCS program director Arthur Kavanaugh, MD, said, “The most recent EULAR [European Alliance of Associations for Rheumatology] PsA guidelines totally discount apremilast, and I think mostly on the basis of cost, but then they also say that in groups of people it’s not as effective as methotrexate.”
“This study shows to me that, even though it’s a registry, with all the caveats about getting data from registries, apremilast certainly can be an effective drug,” said Dr. Kavanaugh, a rheumatologist and professor of medicine at the University of California, San Diego.
Another valuable piece of information from the CORRONA analysis is that it zeros in on patients with oligoarticular PsA.
“Almost all of our PsA studies are focused on people with polyarticular disease. What about those who have lesser involvement? That, of course, is important in the clinic,” he noted.
Dr. Ogdie concurred.
“If we study only polyarticular disease and we make all of our assumptions based on polyarticular disease, we might be leaving out at least half of the patients with PsA. And those patients may not need a bigger gun. Apremilast and methotrexate are kind of in the same group for that mild oligoarticular disease, and they probably work just fine,” she said.
A final point: “We really don’t have good outcome measures to study oligoarticular disease well. The ACR20 is not good because a 20% improvement in three joints is not readily measurable. That’s why trialists enroll patients with high joint count numbers,” according to the rheumatologist.
No increased risk of solid cancers in PsA patients treated with TNF inhibitors
A new analysis of clinical rheumatology registries in five Nordic countries finally puts to rest any concerns that treatment of PsA with TNF inhibitors is associated with increased risk of solid cancers. The same group previously reported no link between TNF inhibitors and lymphoma in PsA.
The solid cancers study included 9,655 PsA patients who started a first TNF inhibitor during 2001-2017, 14,809 others not treated with biologics, and 31,350 matched general population controls. Linkage to Swedish, Norwegian, Danish, Icelandic, and Finnish national cancer registries showed that the adjusted risk for solid cancer in TNF inhibitor–treated, compared with biologic-naive PsA patients, was 1.0. Similarly, the pooled standardized incidence ratio of solid cancer in TNF inhibitor–treated PsA patients compared to the general population was 1.0. There was no signal of a differential risk for incident cancer for any of the eight malignancies studied: lung, colorectal, breast, prostate, uterine, brain, liver, and pancreatic cancer.
“I like this study a lot because it’s specific to PsA rather than extrapolating from rheumatoid arthritis data, where we have a bunch more information for a much longer period of time, but it’s a different population,” Dr. Kavanaugh said.
Dr. Ogdie said, “I talk to my patients about this particular study or the same group’s earlier lymphoma study all the time.”
“I have to say, these are important data for the dermatology world because there are dermatologists who are still not convinced that TNF inhibitors don’t have an increased risk of malignancy. This kind of information is going to be helpful,” observed Eric M. Ruderman, MD, professor of medicine (rheumatology) at Northwestern University, Chicago.
Greater efficacy for biologics in males than females with PsA?
A secondary analysis of the phase 3b EXCEED trial raised the intriguing possibility that both secukinumab, an interleukin-17A inhibitor, and adalimumab, a TNF inhibitor, have greater efficacy in men than in women with PsA. In this randomized trial of 853 biologic-naive patients with PsA, the ACR20 response rate to secukinumab at week 52 was 61% in females versus 74% in males, with ACR50 rates of 43% in females and 55.3% in males. The ACR20 rate with adalimumab was 51.5% in females and 70.2% in males. Similarly, the corresponding ACR50s were 32.6% and 55.3%, respectively. Minimal disease activity was achieved in 36.2% of women and 51% of men on secukinumab, and in 24.2% of women and 49.8% of men on adalimumab.
“These are randomized patients, so you really shouldn’t see these big differences in minimal disease activity,” Dr. Ogdie noted. “The question is why do men seem to respond better to therapy than women? I don’t think it’s the fibromyalgia-ness. There’s probably some biologic rationale for this that we just don’t understand yet. Maybe hormonal interactions.”
This gender difference in response is an important issue because it can potentially distort outcomes in head-to-head drug trials, Dr. Ruderman added.
“That gender difference is not likely to be huge if you’re looking at a placebo-controlled trial because the difference between the active drug and placebo is going to outweigh it. But when you have two active drugs, if there’s an imbalance in terms of how many men or women there are on each of the two drugs, you may end up with an efficacy difference that’s not real but is based on gender and not response to the drug,” he explained.
Roy M. Fleischmann, MD, a rheumatologist and clinical trialist at the University of Texas, Dallas, rose from the audience to pronounce the EXCEED male-versus-female analysis “very interesting.”
“We should go back and look at other trials and see if that occurred, and if it did, then we have to think about that going forward,” he proposed.
Dr. Ogdie, Dr. Kavanaugh, and Dr. Ruderman reported having financial relationships with numerous pharmaceutical companies.
Apremilast (Otezla) monotherapy may be an effective option in oligoarticular psoriatic arthritis, Alexis R. Ogdie, MD, reported at the 2021 Rheumatology Winter Clinical Symposium.
Her analysis of apremilast data from the CORRONA Registry was among several recent highlights in psoriatic arthritis (PsA) cited by speakers at the meeting. Other significant developments included a large pan-Scandinavian study that reassuringly found no increased risk of solid cancers in tumor necrosis factor (TNF) inhibitor–treated patients with PsA, and evidence to suggest a sex difference in the efficacy of both secukinumab (Cosentyx) and adalimumab (Humira), with men responding better than women to two biologics with differing mechanisms of action.
A role for apremilast in oligoarticular disease?
Dr. Ogdie presented an analysis of 150 patients in the U.S. observational CORRONA Registry who initiated monotherapy for oligoarticular PsA and were followed for 6 months. Thirty-four started on apremilast, 15 on methotrexate, and 101 on a biologic. Even though the apremilast group had higher baseline disease activity than did those who started on methotrexate, at 6 months a swollen joint count of 1 or 0 was present in 41% of the apremilast-treated patients, compared with none on methotrexate and 15% on a biologic agent.
A tender joint count of 0-1 was documented at 6 months in 24% of patients on apremilast, 13% with methotrexate, and 21% on a biologic agent. Apremilast’s numeric superiority in outcomes compared to methotrexate in this exploratory study wasn’t subjected to statistical analysis because of the small sample size. However, the ongoing phase 4, double-blind, placebo-controlled, multicenter FOREMOST trial in 330 patients with early oligoarticular PsA should provide more definitive efficacy data, noted Dr. Ogdie, a rheumatologist and epidemiologist at the University of Pennsylvania, Philadelphia.
RWCS program director Arthur Kavanaugh, MD, said, “The most recent EULAR [European Alliance of Associations for Rheumatology] PsA guidelines totally discount apremilast, and I think mostly on the basis of cost, but then they also say that in groups of people it’s not as effective as methotrexate.”
“This study shows to me that, even though it’s a registry, with all the caveats about getting data from registries, apremilast certainly can be an effective drug,” said Dr. Kavanaugh, a rheumatologist and professor of medicine at the University of California, San Diego.
Another valuable piece of information from the CORRONA analysis is that it zeros in on patients with oligoarticular PsA.
“Almost all of our PsA studies are focused on people with polyarticular disease. What about those who have lesser involvement? That, of course, is important in the clinic,” he noted.
Dr. Ogdie concurred.
“If we study only polyarticular disease and we make all of our assumptions based on polyarticular disease, we might be leaving out at least half of the patients with PsA. And those patients may not need a bigger gun. Apremilast and methotrexate are kind of in the same group for that mild oligoarticular disease, and they probably work just fine,” she said.
A final point: “We really don’t have good outcome measures to study oligoarticular disease well. The ACR20 is not good because a 20% improvement in three joints is not readily measurable. That’s why trialists enroll patients with high joint count numbers,” according to the rheumatologist.
No increased risk of solid cancers in PsA patients treated with TNF inhibitors
A new analysis of clinical rheumatology registries in five Nordic countries finally puts to rest any concerns that treatment of PsA with TNF inhibitors is associated with increased risk of solid cancers. The same group previously reported no link between TNF inhibitors and lymphoma in PsA.
The solid cancers study included 9,655 PsA patients who started a first TNF inhibitor during 2001-2017, 14,809 others not treated with biologics, and 31,350 matched general population controls. Linkage to Swedish, Norwegian, Danish, Icelandic, and Finnish national cancer registries showed that the adjusted risk for solid cancer in TNF inhibitor–treated, compared with biologic-naive PsA patients, was 1.0. Similarly, the pooled standardized incidence ratio of solid cancer in TNF inhibitor–treated PsA patients compared to the general population was 1.0. There was no signal of a differential risk for incident cancer for any of the eight malignancies studied: lung, colorectal, breast, prostate, uterine, brain, liver, and pancreatic cancer.
“I like this study a lot because it’s specific to PsA rather than extrapolating from rheumatoid arthritis data, where we have a bunch more information for a much longer period of time, but it’s a different population,” Dr. Kavanaugh said.
Dr. Ogdie said, “I talk to my patients about this particular study or the same group’s earlier lymphoma study all the time.”
“I have to say, these are important data for the dermatology world because there are dermatologists who are still not convinced that TNF inhibitors don’t have an increased risk of malignancy. This kind of information is going to be helpful,” observed Eric M. Ruderman, MD, professor of medicine (rheumatology) at Northwestern University, Chicago.
Greater efficacy for biologics in males than females with PsA?
A secondary analysis of the phase 3b EXCEED trial raised the intriguing possibility that both secukinumab, an interleukin-17A inhibitor, and adalimumab, a TNF inhibitor, have greater efficacy in men than in women with PsA. In this randomized trial of 853 biologic-naive patients with PsA, the ACR20 response rate to secukinumab at week 52 was 61% in females versus 74% in males, with ACR50 rates of 43% in females and 55.3% in males. The ACR20 rate with adalimumab was 51.5% in females and 70.2% in males. Similarly, the corresponding ACR50s were 32.6% and 55.3%, respectively. Minimal disease activity was achieved in 36.2% of women and 51% of men on secukinumab, and in 24.2% of women and 49.8% of men on adalimumab.
“These are randomized patients, so you really shouldn’t see these big differences in minimal disease activity,” Dr. Ogdie noted. “The question is why do men seem to respond better to therapy than women? I don’t think it’s the fibromyalgia-ness. There’s probably some biologic rationale for this that we just don’t understand yet. Maybe hormonal interactions.”
This gender difference in response is an important issue because it can potentially distort outcomes in head-to-head drug trials, Dr. Ruderman added.
“That gender difference is not likely to be huge if you’re looking at a placebo-controlled trial because the difference between the active drug and placebo is going to outweigh it. But when you have two active drugs, if there’s an imbalance in terms of how many men or women there are on each of the two drugs, you may end up with an efficacy difference that’s not real but is based on gender and not response to the drug,” he explained.
Roy M. Fleischmann, MD, a rheumatologist and clinical trialist at the University of Texas, Dallas, rose from the audience to pronounce the EXCEED male-versus-female analysis “very interesting.”
“We should go back and look at other trials and see if that occurred, and if it did, then we have to think about that going forward,” he proposed.
Dr. Ogdie, Dr. Kavanaugh, and Dr. Ruderman reported having financial relationships with numerous pharmaceutical companies.
FROM RWCS 2021
COVID-19 vaccination in RMD patients: Safety data “reassuring”
Two reports support the safety and immunogenicity of SARS-CoV-2 mRNA vaccines in patients with rheumatic and musculoskeletal diseases (RMDs) and represent the first available data on such patients.
In an observational cohort study published in Annals of the Rheumatic Diseases, Caoilfhionn M. Connolly, MD, of Johns Hopkins University, Baltimore, and colleagues reviewed data from 325 adults with RMDs who received the first dose of SARS-CoV-2 mRNA vaccine during the period of Dec. 17, 2020, to Feb. 11, 2021. Of these, 51% received the Pfizer/BioNTech vaccine and 49% received the Moderna vaccine.
The patients, who were invited to participate on social media, were aged 34-54 years, 96% were women, and 89% were White. Inflammatory arthritis was the most common RMD condition (38%), followed by systemic lupus erythematosus (28%) and overlap connective tissue disease (19%). The patients were using a range of immunomodulatory treatment regimens, including nonbiologic disease modifying antirheumatic drugs (DMARDs) in 44%, biologics in 19%, and combination therapy in 37%.
Overall, 89% of patients reported localized symptoms of pain, swelling, and erythema, and 69% reported systemic symptoms. Fatigue was the most common systemic symptom, and 7.4% reported severe fatigue.
None of the patients experienced allergic reactions requiring epinephrine, and 3% reported new infections that required treatment.
“These early, reassuring results may ameliorate concern among patients and provide guidance for rheumatology providers in critical discussions regarding vaccine hesitancy or refusal,” they concluded.
Antibody responses
In another study published in Annals of the Rheumatic Diseases by the same group of researchers, antibody responses against the receptor binding domain of the SARS-CoV-2 spike protein were seen in 74% of 123 adults with an RMD at 18-26 days after receiving a first dose of SARS-CoV-2 mRNA vaccine (52% Pfizer vaccine and 48% Moderna) between Jan. 8, 2021, and Feb. 12, 2021.
The most common diagnoses in these patients were inflammatory arthritis (28%), systemic lupus erythematosus (20%), and Sjögren’s syndrome (13%). A total of 28% of participants reported taking no immunomodulatory agents, 19% reported nonbiologic DMARDs, 14% reported biologic DMARDs, and 19% reported combination therapy.
Although no differences appeared based on disease groups or overall categories of immunomodulatory therapies, patients whose treatment included mycophenolate or rituximab were significantly less likely to develop antibody responses than were patients not taking these medications (P = .001 and P = .04, respectively). Although rituximab and methotrexate have been associated with reduced responses to vaccines such as the flu vaccine, methotrexate was not associated with reduced vaccine response in this study. A total of 94% of patients taking a tumor necrosis factor inhibitor had detectable antibodies.
The studies’ findings were limited by several factors including a lack of longer-term safety data; the small, nonrandomized sample of mainly white women; limited information on immunomodulatory drug dosage and timing; lack of serial antibody measurements; use of an enzyme immunoassay designed to detect antibody response after natural infection; and the inclusion of data only on the first dose of a two-dose vaccine series, the researchers noted. However, the data should provide additional reassurance to RMD patients and their health care teams about vaccination against COVID-19, they said.
Both studies were supported by the Ben-Dov family. In addition, the studies were supported by grants to various study authors from the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Allergy and Infectious Diseases, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the Transplantation and Immunology Research Network of the American Society of Transplantation. One author disclosed financial relationships with Sanofi, Novartis, CSL Behring, Jazz Pharmaceuticals, Veloxis, Mallinckrodt, and Thermo Fisher Scientific. The other researchers had no financial conflicts to disclose.
Two reports support the safety and immunogenicity of SARS-CoV-2 mRNA vaccines in patients with rheumatic and musculoskeletal diseases (RMDs) and represent the first available data on such patients.
In an observational cohort study published in Annals of the Rheumatic Diseases, Caoilfhionn M. Connolly, MD, of Johns Hopkins University, Baltimore, and colleagues reviewed data from 325 adults with RMDs who received the first dose of SARS-CoV-2 mRNA vaccine during the period of Dec. 17, 2020, to Feb. 11, 2021. Of these, 51% received the Pfizer/BioNTech vaccine and 49% received the Moderna vaccine.
The patients, who were invited to participate on social media, were aged 34-54 years, 96% were women, and 89% were White. Inflammatory arthritis was the most common RMD condition (38%), followed by systemic lupus erythematosus (28%) and overlap connective tissue disease (19%). The patients were using a range of immunomodulatory treatment regimens, including nonbiologic disease modifying antirheumatic drugs (DMARDs) in 44%, biologics in 19%, and combination therapy in 37%.
Overall, 89% of patients reported localized symptoms of pain, swelling, and erythema, and 69% reported systemic symptoms. Fatigue was the most common systemic symptom, and 7.4% reported severe fatigue.
None of the patients experienced allergic reactions requiring epinephrine, and 3% reported new infections that required treatment.
“These early, reassuring results may ameliorate concern among patients and provide guidance for rheumatology providers in critical discussions regarding vaccine hesitancy or refusal,” they concluded.
Antibody responses
In another study published in Annals of the Rheumatic Diseases by the same group of researchers, antibody responses against the receptor binding domain of the SARS-CoV-2 spike protein were seen in 74% of 123 adults with an RMD at 18-26 days after receiving a first dose of SARS-CoV-2 mRNA vaccine (52% Pfizer vaccine and 48% Moderna) between Jan. 8, 2021, and Feb. 12, 2021.
The most common diagnoses in these patients were inflammatory arthritis (28%), systemic lupus erythematosus (20%), and Sjögren’s syndrome (13%). A total of 28% of participants reported taking no immunomodulatory agents, 19% reported nonbiologic DMARDs, 14% reported biologic DMARDs, and 19% reported combination therapy.
Although no differences appeared based on disease groups or overall categories of immunomodulatory therapies, patients whose treatment included mycophenolate or rituximab were significantly less likely to develop antibody responses than were patients not taking these medications (P = .001 and P = .04, respectively). Although rituximab and methotrexate have been associated with reduced responses to vaccines such as the flu vaccine, methotrexate was not associated with reduced vaccine response in this study. A total of 94% of patients taking a tumor necrosis factor inhibitor had detectable antibodies.
The studies’ findings were limited by several factors including a lack of longer-term safety data; the small, nonrandomized sample of mainly white women; limited information on immunomodulatory drug dosage and timing; lack of serial antibody measurements; use of an enzyme immunoassay designed to detect antibody response after natural infection; and the inclusion of data only on the first dose of a two-dose vaccine series, the researchers noted. However, the data should provide additional reassurance to RMD patients and their health care teams about vaccination against COVID-19, they said.
Both studies were supported by the Ben-Dov family. In addition, the studies were supported by grants to various study authors from the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Allergy and Infectious Diseases, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the Transplantation and Immunology Research Network of the American Society of Transplantation. One author disclosed financial relationships with Sanofi, Novartis, CSL Behring, Jazz Pharmaceuticals, Veloxis, Mallinckrodt, and Thermo Fisher Scientific. The other researchers had no financial conflicts to disclose.
Two reports support the safety and immunogenicity of SARS-CoV-2 mRNA vaccines in patients with rheumatic and musculoskeletal diseases (RMDs) and represent the first available data on such patients.
In an observational cohort study published in Annals of the Rheumatic Diseases, Caoilfhionn M. Connolly, MD, of Johns Hopkins University, Baltimore, and colleagues reviewed data from 325 adults with RMDs who received the first dose of SARS-CoV-2 mRNA vaccine during the period of Dec. 17, 2020, to Feb. 11, 2021. Of these, 51% received the Pfizer/BioNTech vaccine and 49% received the Moderna vaccine.
The patients, who were invited to participate on social media, were aged 34-54 years, 96% were women, and 89% were White. Inflammatory arthritis was the most common RMD condition (38%), followed by systemic lupus erythematosus (28%) and overlap connective tissue disease (19%). The patients were using a range of immunomodulatory treatment regimens, including nonbiologic disease modifying antirheumatic drugs (DMARDs) in 44%, biologics in 19%, and combination therapy in 37%.
Overall, 89% of patients reported localized symptoms of pain, swelling, and erythema, and 69% reported systemic symptoms. Fatigue was the most common systemic symptom, and 7.4% reported severe fatigue.
None of the patients experienced allergic reactions requiring epinephrine, and 3% reported new infections that required treatment.
“These early, reassuring results may ameliorate concern among patients and provide guidance for rheumatology providers in critical discussions regarding vaccine hesitancy or refusal,” they concluded.
Antibody responses
In another study published in Annals of the Rheumatic Diseases by the same group of researchers, antibody responses against the receptor binding domain of the SARS-CoV-2 spike protein were seen in 74% of 123 adults with an RMD at 18-26 days after receiving a first dose of SARS-CoV-2 mRNA vaccine (52% Pfizer vaccine and 48% Moderna) between Jan. 8, 2021, and Feb. 12, 2021.
The most common diagnoses in these patients were inflammatory arthritis (28%), systemic lupus erythematosus (20%), and Sjögren’s syndrome (13%). A total of 28% of participants reported taking no immunomodulatory agents, 19% reported nonbiologic DMARDs, 14% reported biologic DMARDs, and 19% reported combination therapy.
Although no differences appeared based on disease groups or overall categories of immunomodulatory therapies, patients whose treatment included mycophenolate or rituximab were significantly less likely to develop antibody responses than were patients not taking these medications (P = .001 and P = .04, respectively). Although rituximab and methotrexate have been associated with reduced responses to vaccines such as the flu vaccine, methotrexate was not associated with reduced vaccine response in this study. A total of 94% of patients taking a tumor necrosis factor inhibitor had detectable antibodies.
The studies’ findings were limited by several factors including a lack of longer-term safety data; the small, nonrandomized sample of mainly white women; limited information on immunomodulatory drug dosage and timing; lack of serial antibody measurements; use of an enzyme immunoassay designed to detect antibody response after natural infection; and the inclusion of data only on the first dose of a two-dose vaccine series, the researchers noted. However, the data should provide additional reassurance to RMD patients and their health care teams about vaccination against COVID-19, they said.
Both studies were supported by the Ben-Dov family. In addition, the studies were supported by grants to various study authors from the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Allergy and Infectious Diseases, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the Transplantation and Immunology Research Network of the American Society of Transplantation. One author disclosed financial relationships with Sanofi, Novartis, CSL Behring, Jazz Pharmaceuticals, Veloxis, Mallinckrodt, and Thermo Fisher Scientific. The other researchers had no financial conflicts to disclose.
FROM ANNALS OF THE RHEUMATIC DISEASES
FDA warning letters target OTC cannabidiol product claims for pain relief
The Food and Drug Administration has warned two manufacturers about illegal marketing of drugs containing cannabidiol (CBD) for over-the-counter use without an approved new drug application, for using substandard manufacturing processes, and for failure to comply with current good manufacturing practices. These warnings add to 51 previous warning letters issued by the FDA since 2015 to other manufacturers of products containing CBD who were violating the Federal Food, Drug, and Cosmetic Act.
In a news release, the agency explained that its two most recent letters, sent to Honest Globe Inc. on March 15 and BioLyte Laboratories LLC on March 18, were issued because CBD has “known pharmacologic effects on humans, with demonstrated risks, it cannot be legally marketed as an inactive ingredient in OTC drug products that are not reviewed and approved by the FDA.” They also describe the companies’ failures to comply with current good manufacturing practices.
“The FDA continues to alert the public to potential safety and efficacy concerns with unapproved CBD products sold online and in stores across the country,” FDA Principal Deputy Commissioner Amy P. Abernethy, MD, PhD, said in the release. “It’s important that consumers understand that the FDA has only approved one drug containing CBD as an ingredient [Epidiolex]. These other, unapproved, CBD products may have dangerous health impacts and side effects. We remain focused on exploring potential pathways for CBD products to be lawfully marketed while also educating the public about these outstanding questions of CBD’s safety. Meanwhile, we will continue to monitor and take action, as needed, against companies that unlawfully market their products – prioritizing those that pose a risk to public health.”
The specific products from Santa Ana, Calif.–based Honest Globe that the FDA called unapproved new drugs and misbranded under the Federal Food, Drug, and Cosmetic Act included Elixicure Original Pain Relief and Elixicure Lavender Pain Relief, both of which were described as containing CBD. Products from Grand Rapids, Mich.–based BioLyte Laboratories LLC that the FDA similarly cited for violations included Silver Gel, Silver Gel with Aloe, Silver Liquid Supplement, Therapeutic Pain Gel, Pain Relief Cream, and Magnesium Oil Spray.
The agency has asked the two companies to respond to its letters within 15 working days, “stating how they will address these violations or providing their reasoning and supporting information as to why they believe these products are not in violation of the law. Failure to adequately address the violations promptly may result in legal action, including product seizure and/or injunction.”
The Food and Drug Administration has warned two manufacturers about illegal marketing of drugs containing cannabidiol (CBD) for over-the-counter use without an approved new drug application, for using substandard manufacturing processes, and for failure to comply with current good manufacturing practices. These warnings add to 51 previous warning letters issued by the FDA since 2015 to other manufacturers of products containing CBD who were violating the Federal Food, Drug, and Cosmetic Act.
In a news release, the agency explained that its two most recent letters, sent to Honest Globe Inc. on March 15 and BioLyte Laboratories LLC on March 18, were issued because CBD has “known pharmacologic effects on humans, with demonstrated risks, it cannot be legally marketed as an inactive ingredient in OTC drug products that are not reviewed and approved by the FDA.” They also describe the companies’ failures to comply with current good manufacturing practices.
“The FDA continues to alert the public to potential safety and efficacy concerns with unapproved CBD products sold online and in stores across the country,” FDA Principal Deputy Commissioner Amy P. Abernethy, MD, PhD, said in the release. “It’s important that consumers understand that the FDA has only approved one drug containing CBD as an ingredient [Epidiolex]. These other, unapproved, CBD products may have dangerous health impacts and side effects. We remain focused on exploring potential pathways for CBD products to be lawfully marketed while also educating the public about these outstanding questions of CBD’s safety. Meanwhile, we will continue to monitor and take action, as needed, against companies that unlawfully market their products – prioritizing those that pose a risk to public health.”
The specific products from Santa Ana, Calif.–based Honest Globe that the FDA called unapproved new drugs and misbranded under the Federal Food, Drug, and Cosmetic Act included Elixicure Original Pain Relief and Elixicure Lavender Pain Relief, both of which were described as containing CBD. Products from Grand Rapids, Mich.–based BioLyte Laboratories LLC that the FDA similarly cited for violations included Silver Gel, Silver Gel with Aloe, Silver Liquid Supplement, Therapeutic Pain Gel, Pain Relief Cream, and Magnesium Oil Spray.
The agency has asked the two companies to respond to its letters within 15 working days, “stating how they will address these violations or providing their reasoning and supporting information as to why they believe these products are not in violation of the law. Failure to adequately address the violations promptly may result in legal action, including product seizure and/or injunction.”
The Food and Drug Administration has warned two manufacturers about illegal marketing of drugs containing cannabidiol (CBD) for over-the-counter use without an approved new drug application, for using substandard manufacturing processes, and for failure to comply with current good manufacturing practices. These warnings add to 51 previous warning letters issued by the FDA since 2015 to other manufacturers of products containing CBD who were violating the Federal Food, Drug, and Cosmetic Act.
In a news release, the agency explained that its two most recent letters, sent to Honest Globe Inc. on March 15 and BioLyte Laboratories LLC on March 18, were issued because CBD has “known pharmacologic effects on humans, with demonstrated risks, it cannot be legally marketed as an inactive ingredient in OTC drug products that are not reviewed and approved by the FDA.” They also describe the companies’ failures to comply with current good manufacturing practices.
“The FDA continues to alert the public to potential safety and efficacy concerns with unapproved CBD products sold online and in stores across the country,” FDA Principal Deputy Commissioner Amy P. Abernethy, MD, PhD, said in the release. “It’s important that consumers understand that the FDA has only approved one drug containing CBD as an ingredient [Epidiolex]. These other, unapproved, CBD products may have dangerous health impacts and side effects. We remain focused on exploring potential pathways for CBD products to be lawfully marketed while also educating the public about these outstanding questions of CBD’s safety. Meanwhile, we will continue to monitor and take action, as needed, against companies that unlawfully market their products – prioritizing those that pose a risk to public health.”
The specific products from Santa Ana, Calif.–based Honest Globe that the FDA called unapproved new drugs and misbranded under the Federal Food, Drug, and Cosmetic Act included Elixicure Original Pain Relief and Elixicure Lavender Pain Relief, both of which were described as containing CBD. Products from Grand Rapids, Mich.–based BioLyte Laboratories LLC that the FDA similarly cited for violations included Silver Gel, Silver Gel with Aloe, Silver Liquid Supplement, Therapeutic Pain Gel, Pain Relief Cream, and Magnesium Oil Spray.
The agency has asked the two companies to respond to its letters within 15 working days, “stating how they will address these violations or providing their reasoning and supporting information as to why they believe these products are not in violation of the law. Failure to adequately address the violations promptly may result in legal action, including product seizure and/or injunction.”
COVID-19’s impact on lupus inpatients examined in study
Severe COVID-19 infection was more likely in hospitalized patients with systemic lupus erythematosus (SLE) who had comorbidities and risk factors associated with severe infection in the general population, notably older age, male gender, and hypertension, based on data from a nationwide epidemiologic study of inpatients in France.
“Recently, anti-interferon antibodies have been implicated in severe SARS-CoV-2 infection while it has been known for decades that patients with SLE may produce such autoantibodies,” but large-scale data on the risk of severe COVID-19 infection in SLE patients are limited, Arthur Mageau, MD, of Bichat–Claude Bernard Hospital in Paris, and colleagues wrote.
In a research letter published in Annals of the Rheumatic Diseases, the researchers used the French health care database Programme de Médicalisation des Systèmes d’Information to identify 11,055 adult SLE patients who had at least one hospital stay between March 1, 2020, and Oct.31, 2020. Of these, 1,411 (12.8%) also were diagnosed with COVID-19, and these patients had a total of 1,721 hospital stays.
Overall, in-hospital mortality was approximately four times higher among SLE patients with COVID-19 infection, compared with SLE patients without COVID-19 infection (9.5% vs. 2.4%, P < .001), and 293 (17%) of the COVID-19 hospital stays involved an intensive care unit. In the ICU, 78 (26.7%) of the COVID-19 patients required invasive ventilation, and 71 (24.7%) required noninvasive mechanical ventilation.
The SLE patients with COVID-19 who died were significantly more likely than the SLE patients with COVID-19 who recovered to be older and male, and to have conditions including chronic kidney disease, high blood pressure, chronic pulmonary disease, and a history of cardiovascular events or lupus nephritis. The study findings were limited by the focus on hospitalized patients only, so the results cannot be generalized to all lupus patients, the researchers said.
“Interestingly, while the overall mortality rate was lower in SLE/COVID-19–positive inpatients as compared with the total population admitted for SARS-CoV-2 infection in France during the same period (9.5% vs 15.7%, P < .0001), the mortality rate at a younger age tended to be higher in patients with SLE,” the researchers wrote, but the difference for these younger patients was not statistically significant. This disparity may be caused by the reduced need for immunosuppressive drugs in SLE patients as they age, and the observed increased mortality in younger SLE patients, compared with the general population, suggests that SLE may promote poor outcomes from COVID-19 infection.
Dr. Mageau received PhD fellowship support from the Agence Nationale pour la recherche. He and the other researchers had no financial conflicts to disclose. The study received no outside funding.
Severe COVID-19 infection was more likely in hospitalized patients with systemic lupus erythematosus (SLE) who had comorbidities and risk factors associated with severe infection in the general population, notably older age, male gender, and hypertension, based on data from a nationwide epidemiologic study of inpatients in France.
“Recently, anti-interferon antibodies have been implicated in severe SARS-CoV-2 infection while it has been known for decades that patients with SLE may produce such autoantibodies,” but large-scale data on the risk of severe COVID-19 infection in SLE patients are limited, Arthur Mageau, MD, of Bichat–Claude Bernard Hospital in Paris, and colleagues wrote.
In a research letter published in Annals of the Rheumatic Diseases, the researchers used the French health care database Programme de Médicalisation des Systèmes d’Information to identify 11,055 adult SLE patients who had at least one hospital stay between March 1, 2020, and Oct.31, 2020. Of these, 1,411 (12.8%) also were diagnosed with COVID-19, and these patients had a total of 1,721 hospital stays.
Overall, in-hospital mortality was approximately four times higher among SLE patients with COVID-19 infection, compared with SLE patients without COVID-19 infection (9.5% vs. 2.4%, P < .001), and 293 (17%) of the COVID-19 hospital stays involved an intensive care unit. In the ICU, 78 (26.7%) of the COVID-19 patients required invasive ventilation, and 71 (24.7%) required noninvasive mechanical ventilation.
The SLE patients with COVID-19 who died were significantly more likely than the SLE patients with COVID-19 who recovered to be older and male, and to have conditions including chronic kidney disease, high blood pressure, chronic pulmonary disease, and a history of cardiovascular events or lupus nephritis. The study findings were limited by the focus on hospitalized patients only, so the results cannot be generalized to all lupus patients, the researchers said.
“Interestingly, while the overall mortality rate was lower in SLE/COVID-19–positive inpatients as compared with the total population admitted for SARS-CoV-2 infection in France during the same period (9.5% vs 15.7%, P < .0001), the mortality rate at a younger age tended to be higher in patients with SLE,” the researchers wrote, but the difference for these younger patients was not statistically significant. This disparity may be caused by the reduced need for immunosuppressive drugs in SLE patients as they age, and the observed increased mortality in younger SLE patients, compared with the general population, suggests that SLE may promote poor outcomes from COVID-19 infection.
Dr. Mageau received PhD fellowship support from the Agence Nationale pour la recherche. He and the other researchers had no financial conflicts to disclose. The study received no outside funding.
Severe COVID-19 infection was more likely in hospitalized patients with systemic lupus erythematosus (SLE) who had comorbidities and risk factors associated with severe infection in the general population, notably older age, male gender, and hypertension, based on data from a nationwide epidemiologic study of inpatients in France.
“Recently, anti-interferon antibodies have been implicated in severe SARS-CoV-2 infection while it has been known for decades that patients with SLE may produce such autoantibodies,” but large-scale data on the risk of severe COVID-19 infection in SLE patients are limited, Arthur Mageau, MD, of Bichat–Claude Bernard Hospital in Paris, and colleagues wrote.
In a research letter published in Annals of the Rheumatic Diseases, the researchers used the French health care database Programme de Médicalisation des Systèmes d’Information to identify 11,055 adult SLE patients who had at least one hospital stay between March 1, 2020, and Oct.31, 2020. Of these, 1,411 (12.8%) also were diagnosed with COVID-19, and these patients had a total of 1,721 hospital stays.
Overall, in-hospital mortality was approximately four times higher among SLE patients with COVID-19 infection, compared with SLE patients without COVID-19 infection (9.5% vs. 2.4%, P < .001), and 293 (17%) of the COVID-19 hospital stays involved an intensive care unit. In the ICU, 78 (26.7%) of the COVID-19 patients required invasive ventilation, and 71 (24.7%) required noninvasive mechanical ventilation.
The SLE patients with COVID-19 who died were significantly more likely than the SLE patients with COVID-19 who recovered to be older and male, and to have conditions including chronic kidney disease, high blood pressure, chronic pulmonary disease, and a history of cardiovascular events or lupus nephritis. The study findings were limited by the focus on hospitalized patients only, so the results cannot be generalized to all lupus patients, the researchers said.
“Interestingly, while the overall mortality rate was lower in SLE/COVID-19–positive inpatients as compared with the total population admitted for SARS-CoV-2 infection in France during the same period (9.5% vs 15.7%, P < .0001), the mortality rate at a younger age tended to be higher in patients with SLE,” the researchers wrote, but the difference for these younger patients was not statistically significant. This disparity may be caused by the reduced need for immunosuppressive drugs in SLE patients as they age, and the observed increased mortality in younger SLE patients, compared with the general population, suggests that SLE may promote poor outcomes from COVID-19 infection.
Dr. Mageau received PhD fellowship support from the Agence Nationale pour la recherche. He and the other researchers had no financial conflicts to disclose. The study received no outside funding.
FROM ANNALS OF THE RHEUMATIC DISEASES
Abdominal aortic calcification may further raise known fracture risk
A new study has found that older men with high levels of abdominal aortic calcification (AAC) and a prevalent vertebral fracture – both of which can be assessed via lateral spine radiographs – are at increased risk of hip, clinical vertebral, and major osteoporotic fractures.
“The results of this study and others suggest that it may be appropriate to expand lateral spine imaging to include those with a significant pre-test probability of higher AAC being present,” wrote John T. Schousboe, MD, of the Park Nicollet Clinic and HealthPartners Institute in Bloomington, Minn. The study was published in the Journal of Bone and Mineral Research.
To determine the impact of prevalent vertebral fractures and AAC on fracture risk, the researchers assessed the lateral spine radiographs of 5,365 men who were enrolled in the Osteoporotic Fractures in Men (MrOS) study. All participants were 65 years or older, community dwelling, able to walk without assistance, and without bilateral hip arthroplasties. They split patients’ 24-point AAC (ACC-24) scores at the baseline visit into four levels: 0-1, 2-4, 5-8, and greater than 9. Self-reports of fractures were solicited from the cohort every 4 months.
Of all participants, 7.6% (n = 407) had a prevalent vertebral fracture at baseline. They were, on average, 1.5 years older than participants without a fracture; they were also more likely to be white and to have a prior nonspine fracture, along with having a lower femoral neck BMD (0.718 g/cm2, compared with 0.787 g/cm2; P < .001). In addition, significantly more men with a prevalent vertebral fracture had an AAC score greater than 9 (27% vs. 21.2%).
After an average follow-up period of 12.4 years (standard deviation, 5.2), 634 men had a major osteoporotic fracture, 283 had a hip fracture, 206 had a clinical vertebral fracture, and 2,626 died without having any of the three. After adjustment for risk factors such as age, prior nonspine fracture, and prevalent vertebral fracture, men with higher AAC-24 scores had a higher risk of major osteoporotic fracture, compared with men who had scores of 0-1: a hazard ratio of 1.38 (95% confidence interval, 1.10-1.73; P < .001) for scores 2-4, a HR of 1.45 (95% CI, 1.14-1.84; P < .001) for scores 5-8, and a HR of 1.65 (95% CI, 1.29-2.10; P < .001) for scores greater than 9.
Similar findings were reported regarding risk of hip fractures: a HR of 1.54 (95% CI, 1.07-2.20; P < .001) for men with AAC-24 scores 2-4, a HR of 1.40 (95% CI, 0.96-2.06; P < .001) for scores 5-8, and a HR of 2.17 (95% CI, 1.50-3.13; P < .001) for scores greater than 9. AAC-24 score severity was not associated with a higher risk of clinical vertebral fractures.
After adjustment for risk factors and AAC-24 score, men with prevalent vertebral fractures had an increased risk of all three fracture outcomes, compared with men without any fractures at baseline: a HR of 1.56 (95% CI, 1.12-2.16; P < .001) for hip fracture, a HR of 1.85 (95% CI, 1.48-2.31; P < .001) for major osteoporotic fracture, and a HR of 2.76 (95% CI, 1.94-3.91; P < .001) for clinical vertebral fracture.
Adjusting for competing mortality produced similar results: men with higher levels of AAC had increased risk of major osteoporotic fracture and hip fracture, although AAC-24 score was not associated with higher risk of clinical vertebral fractures. Prevalent vertebral fractures were also still associated with higher risk of hip (subdistribution HR, 1.42; 95% CI, 1.01-2.00; P = .004), major osteoporotic fracture (SHR, 1.71; 95% CI, 1.36-2.14; P < .001), and clinical vertebral fracture (SHR, 2.46; 95% CI, 1.72-3.52; P < .001).
Fracture risk assessment proves to be “a nice proof of concept”
“It’s well known that prevalent fractures predict future fractures,” said Thomas M. Link, MD, PhD, chief of the musculoskeletal imaging section in the department of radiology and biomedical imaging at the University of California, San Francisco, in an interview. “The new finding is that aortic calcifications combined with prevalent fractures perform better in predicting major osteoporotic fractures. Traditionally on radiographs, we note that patients who have more calcifications in vessels have less density or calcium in the bone, so this is a nice proof of concept.”
“While the study shows excellent reproducibility, it is not clear how the AAC-24 score was validated,” he added. “Theoretically, abdominal CT could be used for this.”
Along with validation of the AAC-24 score on lateral spine radiographs, he expressed a desire that future research would be “clearer regarding how this would potentially impact patient management. Prevalent fractures already are an indication to treat patients with osteoporosis-specific drugs. How would the results of this study impact management beyond that?”
The authors acknowledged their study’s other potential limitations, including limits in their ability to estimate absolute and relative hip fracture risk in men with low AAC scores but a prevalent vertebral fracture. In addition, they noted that their cohort was “mostly white, healthy, community-dwelling older men” and therefore may not be generalizable to other populations.
The study was supported by the National Institutes of Health, including grants from the National Institute on Aging, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Center for Advancing Translational Sciences, and the NIH Roadmap for Medical Research. One author reported being supported by a National Heart Foundation of Australia Future Leader Fellowship. The others disclosed no potential conflicts of interest.
A new study has found that older men with high levels of abdominal aortic calcification (AAC) and a prevalent vertebral fracture – both of which can be assessed via lateral spine radiographs – are at increased risk of hip, clinical vertebral, and major osteoporotic fractures.
“The results of this study and others suggest that it may be appropriate to expand lateral spine imaging to include those with a significant pre-test probability of higher AAC being present,” wrote John T. Schousboe, MD, of the Park Nicollet Clinic and HealthPartners Institute in Bloomington, Minn. The study was published in the Journal of Bone and Mineral Research.
To determine the impact of prevalent vertebral fractures and AAC on fracture risk, the researchers assessed the lateral spine radiographs of 5,365 men who were enrolled in the Osteoporotic Fractures in Men (MrOS) study. All participants were 65 years or older, community dwelling, able to walk without assistance, and without bilateral hip arthroplasties. They split patients’ 24-point AAC (ACC-24) scores at the baseline visit into four levels: 0-1, 2-4, 5-8, and greater than 9. Self-reports of fractures were solicited from the cohort every 4 months.
Of all participants, 7.6% (n = 407) had a prevalent vertebral fracture at baseline. They were, on average, 1.5 years older than participants without a fracture; they were also more likely to be white and to have a prior nonspine fracture, along with having a lower femoral neck BMD (0.718 g/cm2, compared with 0.787 g/cm2; P < .001). In addition, significantly more men with a prevalent vertebral fracture had an AAC score greater than 9 (27% vs. 21.2%).
After an average follow-up period of 12.4 years (standard deviation, 5.2), 634 men had a major osteoporotic fracture, 283 had a hip fracture, 206 had a clinical vertebral fracture, and 2,626 died without having any of the three. After adjustment for risk factors such as age, prior nonspine fracture, and prevalent vertebral fracture, men with higher AAC-24 scores had a higher risk of major osteoporotic fracture, compared with men who had scores of 0-1: a hazard ratio of 1.38 (95% confidence interval, 1.10-1.73; P < .001) for scores 2-4, a HR of 1.45 (95% CI, 1.14-1.84; P < .001) for scores 5-8, and a HR of 1.65 (95% CI, 1.29-2.10; P < .001) for scores greater than 9.
Similar findings were reported regarding risk of hip fractures: a HR of 1.54 (95% CI, 1.07-2.20; P < .001) for men with AAC-24 scores 2-4, a HR of 1.40 (95% CI, 0.96-2.06; P < .001) for scores 5-8, and a HR of 2.17 (95% CI, 1.50-3.13; P < .001) for scores greater than 9. AAC-24 score severity was not associated with a higher risk of clinical vertebral fractures.
After adjustment for risk factors and AAC-24 score, men with prevalent vertebral fractures had an increased risk of all three fracture outcomes, compared with men without any fractures at baseline: a HR of 1.56 (95% CI, 1.12-2.16; P < .001) for hip fracture, a HR of 1.85 (95% CI, 1.48-2.31; P < .001) for major osteoporotic fracture, and a HR of 2.76 (95% CI, 1.94-3.91; P < .001) for clinical vertebral fracture.
Adjusting for competing mortality produced similar results: men with higher levels of AAC had increased risk of major osteoporotic fracture and hip fracture, although AAC-24 score was not associated with higher risk of clinical vertebral fractures. Prevalent vertebral fractures were also still associated with higher risk of hip (subdistribution HR, 1.42; 95% CI, 1.01-2.00; P = .004), major osteoporotic fracture (SHR, 1.71; 95% CI, 1.36-2.14; P < .001), and clinical vertebral fracture (SHR, 2.46; 95% CI, 1.72-3.52; P < .001).
Fracture risk assessment proves to be “a nice proof of concept”
“It’s well known that prevalent fractures predict future fractures,” said Thomas M. Link, MD, PhD, chief of the musculoskeletal imaging section in the department of radiology and biomedical imaging at the University of California, San Francisco, in an interview. “The new finding is that aortic calcifications combined with prevalent fractures perform better in predicting major osteoporotic fractures. Traditionally on radiographs, we note that patients who have more calcifications in vessels have less density or calcium in the bone, so this is a nice proof of concept.”
“While the study shows excellent reproducibility, it is not clear how the AAC-24 score was validated,” he added. “Theoretically, abdominal CT could be used for this.”
Along with validation of the AAC-24 score on lateral spine radiographs, he expressed a desire that future research would be “clearer regarding how this would potentially impact patient management. Prevalent fractures already are an indication to treat patients with osteoporosis-specific drugs. How would the results of this study impact management beyond that?”
The authors acknowledged their study’s other potential limitations, including limits in their ability to estimate absolute and relative hip fracture risk in men with low AAC scores but a prevalent vertebral fracture. In addition, they noted that their cohort was “mostly white, healthy, community-dwelling older men” and therefore may not be generalizable to other populations.
The study was supported by the National Institutes of Health, including grants from the National Institute on Aging, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Center for Advancing Translational Sciences, and the NIH Roadmap for Medical Research. One author reported being supported by a National Heart Foundation of Australia Future Leader Fellowship. The others disclosed no potential conflicts of interest.
A new study has found that older men with high levels of abdominal aortic calcification (AAC) and a prevalent vertebral fracture – both of which can be assessed via lateral spine radiographs – are at increased risk of hip, clinical vertebral, and major osteoporotic fractures.
“The results of this study and others suggest that it may be appropriate to expand lateral spine imaging to include those with a significant pre-test probability of higher AAC being present,” wrote John T. Schousboe, MD, of the Park Nicollet Clinic and HealthPartners Institute in Bloomington, Minn. The study was published in the Journal of Bone and Mineral Research.
To determine the impact of prevalent vertebral fractures and AAC on fracture risk, the researchers assessed the lateral spine radiographs of 5,365 men who were enrolled in the Osteoporotic Fractures in Men (MrOS) study. All participants were 65 years or older, community dwelling, able to walk without assistance, and without bilateral hip arthroplasties. They split patients’ 24-point AAC (ACC-24) scores at the baseline visit into four levels: 0-1, 2-4, 5-8, and greater than 9. Self-reports of fractures were solicited from the cohort every 4 months.
Of all participants, 7.6% (n = 407) had a prevalent vertebral fracture at baseline. They were, on average, 1.5 years older than participants without a fracture; they were also more likely to be white and to have a prior nonspine fracture, along with having a lower femoral neck BMD (0.718 g/cm2, compared with 0.787 g/cm2; P < .001). In addition, significantly more men with a prevalent vertebral fracture had an AAC score greater than 9 (27% vs. 21.2%).
After an average follow-up period of 12.4 years (standard deviation, 5.2), 634 men had a major osteoporotic fracture, 283 had a hip fracture, 206 had a clinical vertebral fracture, and 2,626 died without having any of the three. After adjustment for risk factors such as age, prior nonspine fracture, and prevalent vertebral fracture, men with higher AAC-24 scores had a higher risk of major osteoporotic fracture, compared with men who had scores of 0-1: a hazard ratio of 1.38 (95% confidence interval, 1.10-1.73; P < .001) for scores 2-4, a HR of 1.45 (95% CI, 1.14-1.84; P < .001) for scores 5-8, and a HR of 1.65 (95% CI, 1.29-2.10; P < .001) for scores greater than 9.
Similar findings were reported regarding risk of hip fractures: a HR of 1.54 (95% CI, 1.07-2.20; P < .001) for men with AAC-24 scores 2-4, a HR of 1.40 (95% CI, 0.96-2.06; P < .001) for scores 5-8, and a HR of 2.17 (95% CI, 1.50-3.13; P < .001) for scores greater than 9. AAC-24 score severity was not associated with a higher risk of clinical vertebral fractures.
After adjustment for risk factors and AAC-24 score, men with prevalent vertebral fractures had an increased risk of all three fracture outcomes, compared with men without any fractures at baseline: a HR of 1.56 (95% CI, 1.12-2.16; P < .001) for hip fracture, a HR of 1.85 (95% CI, 1.48-2.31; P < .001) for major osteoporotic fracture, and a HR of 2.76 (95% CI, 1.94-3.91; P < .001) for clinical vertebral fracture.
Adjusting for competing mortality produced similar results: men with higher levels of AAC had increased risk of major osteoporotic fracture and hip fracture, although AAC-24 score was not associated with higher risk of clinical vertebral fractures. Prevalent vertebral fractures were also still associated with higher risk of hip (subdistribution HR, 1.42; 95% CI, 1.01-2.00; P = .004), major osteoporotic fracture (SHR, 1.71; 95% CI, 1.36-2.14; P < .001), and clinical vertebral fracture (SHR, 2.46; 95% CI, 1.72-3.52; P < .001).
Fracture risk assessment proves to be “a nice proof of concept”
“It’s well known that prevalent fractures predict future fractures,” said Thomas M. Link, MD, PhD, chief of the musculoskeletal imaging section in the department of radiology and biomedical imaging at the University of California, San Francisco, in an interview. “The new finding is that aortic calcifications combined with prevalent fractures perform better in predicting major osteoporotic fractures. Traditionally on radiographs, we note that patients who have more calcifications in vessels have less density or calcium in the bone, so this is a nice proof of concept.”
“While the study shows excellent reproducibility, it is not clear how the AAC-24 score was validated,” he added. “Theoretically, abdominal CT could be used for this.”
Along with validation of the AAC-24 score on lateral spine radiographs, he expressed a desire that future research would be “clearer regarding how this would potentially impact patient management. Prevalent fractures already are an indication to treat patients with osteoporosis-specific drugs. How would the results of this study impact management beyond that?”
The authors acknowledged their study’s other potential limitations, including limits in their ability to estimate absolute and relative hip fracture risk in men with low AAC scores but a prevalent vertebral fracture. In addition, they noted that their cohort was “mostly white, healthy, community-dwelling older men” and therefore may not be generalizable to other populations.
The study was supported by the National Institutes of Health, including grants from the National Institute on Aging, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the National Center for Advancing Translational Sciences, and the NIH Roadmap for Medical Research. One author reported being supported by a National Heart Foundation of Australia Future Leader Fellowship. The others disclosed no potential conflicts of interest.
FROM THE JOURNAL OF BONE AND MINERAL RESEARCH