User login
FDA expands Essure’s postmarketing surveillance study
The study, ordered in 2016, will now run 5 years instead of 3, and the cohort will be enlarged to add any women who elect implantation while the device is still on the market, FDA Commissioner Scott Gottlieb, MD, announced in a press statement. The agency also added a key biological measure: All patients with Essure will undergo regular blood work to evaluate proinflammatory markers that could be device related.
“We’re requiring additional blood testing of patients enrolled in follow-up visits during the study to learn more about patients’ levels of certain inflammatory markers that can be indicators of increased inflammation,” Dr. Gottlieb said. “This could help us better evaluate potential immune reactions to the device and whether these findings are associated with symptoms that patients have reported related to Essure.”
The device has been associated with severe problems in some patients, he noted.
“I personally had the opportunity to meet with women who have been adversely affected by Essure to listen and learn about their concerns. Some of the women I spoke with developed significant medical problems that they ascribe to their use of the product. We remain committed to these women and to improving how we monitor the safety of medical devices, including those related to women’s health.”
The study expansion comes as Bayer is facing more than 16,000 lawsuits over adverse events associated with Essure implantation.
Since its approval, Essure is estimated to have been used by more than 750,000 patients worldwide. Bayer claims the device is 99% effective in preventing pregnancy, but it’s also been associated with some serious risks, including persistent pain, perforation of the uterus and fallopian tubes, and migration of the coils into the pelvis or abdomen. In view of these – and more than 15,000 adverse events reported to the FDA – the agency announced new restrictions on Essure earlier this year. Those restrictions, plus a prior boxed warning on the label, contributed to about a 70% decline in U.S. sales, which Bayer says prompted the discontinuation.
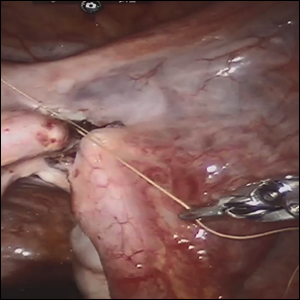
The open-label prospective observational study will compare women who have the Essure device to a matched cohort that underwent laparoscopic tubal ligation. The main safety endpoints are chronic pelvic pain and abnormal uterine bleeding, as well as the new measure of inflammatory markers. As of Dec. 3, 791 patients have been enrolled (293 in the Essure arm and 498 in the laparoscopic tubal ligation arm).
Women who have the implant now and remain free of any adverse events should probably keep the device, Dr. Gottlieb advised.
“We believe women who’ve been using Essure successfully to prevent pregnancy can and should continue to do so. Women who suspect the device may be related to symptoms they are experiencing, such as persistent pain, should talk to their doctor on what steps may be appropriate. Device removal has its own risks. Patients should discuss the benefits and risks of any procedure with their health care providers before deciding on the best option for them.”
The study, ordered in 2016, will now run 5 years instead of 3, and the cohort will be enlarged to add any women who elect implantation while the device is still on the market, FDA Commissioner Scott Gottlieb, MD, announced in a press statement. The agency also added a key biological measure: All patients with Essure will undergo regular blood work to evaluate proinflammatory markers that could be device related.
“We’re requiring additional blood testing of patients enrolled in follow-up visits during the study to learn more about patients’ levels of certain inflammatory markers that can be indicators of increased inflammation,” Dr. Gottlieb said. “This could help us better evaluate potential immune reactions to the device and whether these findings are associated with symptoms that patients have reported related to Essure.”
The device has been associated with severe problems in some patients, he noted.
“I personally had the opportunity to meet with women who have been adversely affected by Essure to listen and learn about their concerns. Some of the women I spoke with developed significant medical problems that they ascribe to their use of the product. We remain committed to these women and to improving how we monitor the safety of medical devices, including those related to women’s health.”
The study expansion comes as Bayer is facing more than 16,000 lawsuits over adverse events associated with Essure implantation.
Since its approval, Essure is estimated to have been used by more than 750,000 patients worldwide. Bayer claims the device is 99% effective in preventing pregnancy, but it’s also been associated with some serious risks, including persistent pain, perforation of the uterus and fallopian tubes, and migration of the coils into the pelvis or abdomen. In view of these – and more than 15,000 adverse events reported to the FDA – the agency announced new restrictions on Essure earlier this year. Those restrictions, plus a prior boxed warning on the label, contributed to about a 70% decline in U.S. sales, which Bayer says prompted the discontinuation.
The open-label prospective observational study will compare women who have the Essure device to a matched cohort that underwent laparoscopic tubal ligation. The main safety endpoints are chronic pelvic pain and abnormal uterine bleeding, as well as the new measure of inflammatory markers. As of Dec. 3, 791 patients have been enrolled (293 in the Essure arm and 498 in the laparoscopic tubal ligation arm).
Women who have the implant now and remain free of any adverse events should probably keep the device, Dr. Gottlieb advised.
“We believe women who’ve been using Essure successfully to prevent pregnancy can and should continue to do so. Women who suspect the device may be related to symptoms they are experiencing, such as persistent pain, should talk to their doctor on what steps may be appropriate. Device removal has its own risks. Patients should discuss the benefits and risks of any procedure with their health care providers before deciding on the best option for them.”
The study, ordered in 2016, will now run 5 years instead of 3, and the cohort will be enlarged to add any women who elect implantation while the device is still on the market, FDA Commissioner Scott Gottlieb, MD, announced in a press statement. The agency also added a key biological measure: All patients with Essure will undergo regular blood work to evaluate proinflammatory markers that could be device related.
“We’re requiring additional blood testing of patients enrolled in follow-up visits during the study to learn more about patients’ levels of certain inflammatory markers that can be indicators of increased inflammation,” Dr. Gottlieb said. “This could help us better evaluate potential immune reactions to the device and whether these findings are associated with symptoms that patients have reported related to Essure.”
The device has been associated with severe problems in some patients, he noted.
“I personally had the opportunity to meet with women who have been adversely affected by Essure to listen and learn about their concerns. Some of the women I spoke with developed significant medical problems that they ascribe to their use of the product. We remain committed to these women and to improving how we monitor the safety of medical devices, including those related to women’s health.”
The study expansion comes as Bayer is facing more than 16,000 lawsuits over adverse events associated with Essure implantation.
Since its approval, Essure is estimated to have been used by more than 750,000 patients worldwide. Bayer claims the device is 99% effective in preventing pregnancy, but it’s also been associated with some serious risks, including persistent pain, perforation of the uterus and fallopian tubes, and migration of the coils into the pelvis or abdomen. In view of these – and more than 15,000 adverse events reported to the FDA – the agency announced new restrictions on Essure earlier this year. Those restrictions, plus a prior boxed warning on the label, contributed to about a 70% decline in U.S. sales, which Bayer says prompted the discontinuation.
The open-label prospective observational study will compare women who have the Essure device to a matched cohort that underwent laparoscopic tubal ligation. The main safety endpoints are chronic pelvic pain and abnormal uterine bleeding, as well as the new measure of inflammatory markers. As of Dec. 3, 791 patients have been enrolled (293 in the Essure arm and 498 in the laparoscopic tubal ligation arm).
Women who have the implant now and remain free of any adverse events should probably keep the device, Dr. Gottlieb advised.
“We believe women who’ve been using Essure successfully to prevent pregnancy can and should continue to do so. Women who suspect the device may be related to symptoms they are experiencing, such as persistent pain, should talk to their doctor on what steps may be appropriate. Device removal has its own risks. Patients should discuss the benefits and risks of any procedure with their health care providers before deciding on the best option for them.”
Infertility appears to be increased among women with epilepsy
NEW ORLEANS – based on a retrospective study presented at the annual meeting of the American Epilepsy Society.
Data recorded in the 2010-2014 Epilepsy Birth Control Registry indicates a 9.2% infertility rate and a 22.5% impaired fecundity rate among American women with epilepsy. Both rates are higher than the general population infertility rate of 6.0% and the 12.1% rate of impaired fecundity cited by the Centers for Disease Control and Prevention.
However, differences between the study of women with epilepsy and the study of the general population may limit the validity of this comparison, said Devon B. MacEachern, clinical and research coordinator at Neuroendocrine Associates in Wellesley Hills, Mass.
It is likewise uncertain whether use of antiepileptic drugs (AEDs) affects women’s fertility or fecundity.
The Epilepsy Birth Control Registry collected data from an Internet-based survey of 1,144 community-dwelling women with epilepsy aged 18-47 years. Participants provided information about demographics, epilepsy, AEDs, reproduction, and contraception.
The researchers focused on rates of infertility, impaired fecundity, and live birth or unaborted pregnancy among 978 American women, and additionally examined whether these outcomes were related to AED use.
Infertility was defined as the percentage of participants who had unprotected sex but did not become pregnant by 1 year. Impaired fecundity was the percentage of participants who were infertile or did not carry a pregnancy to live birth. The study excluded from the impaired fecundity analysis the 41 respondents whose only outcomes were induced abortions. The 18% of pregnancies that terminated as induced abortions were excluded from the live birth rate analysis.
In all, 373 registry participants had 724 pregnancies and 422 births between 1981 and 2013. The women had an average of 2.15 pregnancies at a mean age of 24.9 years (range, 13-44 years). In addition, 38 women (9.2%) tried to conceive, but were infertile. Of 306 women with a first pregnancy, 222 (72.5%) had a live birth. Among 292 women with two pregnancies, 260 (89.0%) had at least one live birth, and 180 (61.6%) had two live births.
Of the 373 women, 84 (22.5%) with pregnancies had impaired fecundity. The risk of impaired fecundity tended to be higher among women on AED polytherapy than among women on no AED (risk ratio, 1.74).
The ratio of live births to pregnancy (71.0%) was similar among women on no AEDs (71.3%), those on AED monotherapy (71.8%), and those on polytherapy (69.7%). The live birth rate was 67.5% for women taking enzyme-inducing AEDs, 89.1% for women taking glucuronidated AEDs, 72.8% for women taking nonenzyme-inducing AEDs, 63.3% for women taking enzyme-inhibiting AEDs, and 69.7% for women on polytherapy. Lamotrigine use was associated with the highest ratio of live births to pregnancies at 89.1%; valproate use was associated with the lowest ratio of live births to pregnancies at 63.3%.
The investigation was funded by the Epilepsy Foundation and Lundbeck.
SOURCE: MacEachern DB et al. AES 2018, Abstract 1.426.
NEW ORLEANS – based on a retrospective study presented at the annual meeting of the American Epilepsy Society.
Data recorded in the 2010-2014 Epilepsy Birth Control Registry indicates a 9.2% infertility rate and a 22.5% impaired fecundity rate among American women with epilepsy. Both rates are higher than the general population infertility rate of 6.0% and the 12.1% rate of impaired fecundity cited by the Centers for Disease Control and Prevention.
However, differences between the study of women with epilepsy and the study of the general population may limit the validity of this comparison, said Devon B. MacEachern, clinical and research coordinator at Neuroendocrine Associates in Wellesley Hills, Mass.
It is likewise uncertain whether use of antiepileptic drugs (AEDs) affects women’s fertility or fecundity.
The Epilepsy Birth Control Registry collected data from an Internet-based survey of 1,144 community-dwelling women with epilepsy aged 18-47 years. Participants provided information about demographics, epilepsy, AEDs, reproduction, and contraception.
The researchers focused on rates of infertility, impaired fecundity, and live birth or unaborted pregnancy among 978 American women, and additionally examined whether these outcomes were related to AED use.
Infertility was defined as the percentage of participants who had unprotected sex but did not become pregnant by 1 year. Impaired fecundity was the percentage of participants who were infertile or did not carry a pregnancy to live birth. The study excluded from the impaired fecundity analysis the 41 respondents whose only outcomes were induced abortions. The 18% of pregnancies that terminated as induced abortions were excluded from the live birth rate analysis.
In all, 373 registry participants had 724 pregnancies and 422 births between 1981 and 2013. The women had an average of 2.15 pregnancies at a mean age of 24.9 years (range, 13-44 years). In addition, 38 women (9.2%) tried to conceive, but were infertile. Of 306 women with a first pregnancy, 222 (72.5%) had a live birth. Among 292 women with two pregnancies, 260 (89.0%) had at least one live birth, and 180 (61.6%) had two live births.
Of the 373 women, 84 (22.5%) with pregnancies had impaired fecundity. The risk of impaired fecundity tended to be higher among women on AED polytherapy than among women on no AED (risk ratio, 1.74).
The ratio of live births to pregnancy (71.0%) was similar among women on no AEDs (71.3%), those on AED monotherapy (71.8%), and those on polytherapy (69.7%). The live birth rate was 67.5% for women taking enzyme-inducing AEDs, 89.1% for women taking glucuronidated AEDs, 72.8% for women taking nonenzyme-inducing AEDs, 63.3% for women taking enzyme-inhibiting AEDs, and 69.7% for women on polytherapy. Lamotrigine use was associated with the highest ratio of live births to pregnancies at 89.1%; valproate use was associated with the lowest ratio of live births to pregnancies at 63.3%.
The investigation was funded by the Epilepsy Foundation and Lundbeck.
SOURCE: MacEachern DB et al. AES 2018, Abstract 1.426.
NEW ORLEANS – based on a retrospective study presented at the annual meeting of the American Epilepsy Society.
Data recorded in the 2010-2014 Epilepsy Birth Control Registry indicates a 9.2% infertility rate and a 22.5% impaired fecundity rate among American women with epilepsy. Both rates are higher than the general population infertility rate of 6.0% and the 12.1% rate of impaired fecundity cited by the Centers for Disease Control and Prevention.
However, differences between the study of women with epilepsy and the study of the general population may limit the validity of this comparison, said Devon B. MacEachern, clinical and research coordinator at Neuroendocrine Associates in Wellesley Hills, Mass.
It is likewise uncertain whether use of antiepileptic drugs (AEDs) affects women’s fertility or fecundity.
The Epilepsy Birth Control Registry collected data from an Internet-based survey of 1,144 community-dwelling women with epilepsy aged 18-47 years. Participants provided information about demographics, epilepsy, AEDs, reproduction, and contraception.
The researchers focused on rates of infertility, impaired fecundity, and live birth or unaborted pregnancy among 978 American women, and additionally examined whether these outcomes were related to AED use.
Infertility was defined as the percentage of participants who had unprotected sex but did not become pregnant by 1 year. Impaired fecundity was the percentage of participants who were infertile or did not carry a pregnancy to live birth. The study excluded from the impaired fecundity analysis the 41 respondents whose only outcomes were induced abortions. The 18% of pregnancies that terminated as induced abortions were excluded from the live birth rate analysis.
In all, 373 registry participants had 724 pregnancies and 422 births between 1981 and 2013. The women had an average of 2.15 pregnancies at a mean age of 24.9 years (range, 13-44 years). In addition, 38 women (9.2%) tried to conceive, but were infertile. Of 306 women with a first pregnancy, 222 (72.5%) had a live birth. Among 292 women with two pregnancies, 260 (89.0%) had at least one live birth, and 180 (61.6%) had two live births.
Of the 373 women, 84 (22.5%) with pregnancies had impaired fecundity. The risk of impaired fecundity tended to be higher among women on AED polytherapy than among women on no AED (risk ratio, 1.74).
The ratio of live births to pregnancy (71.0%) was similar among women on no AEDs (71.3%), those on AED monotherapy (71.8%), and those on polytherapy (69.7%). The live birth rate was 67.5% for women taking enzyme-inducing AEDs, 89.1% for women taking glucuronidated AEDs, 72.8% for women taking nonenzyme-inducing AEDs, 63.3% for women taking enzyme-inhibiting AEDs, and 69.7% for women on polytherapy. Lamotrigine use was associated with the highest ratio of live births to pregnancies at 89.1%; valproate use was associated with the lowest ratio of live births to pregnancies at 63.3%.
The investigation was funded by the Epilepsy Foundation and Lundbeck.
SOURCE: MacEachern DB et al. AES 2018, Abstract 1.426.
REPORTING FROM AES 2018
Key clinical point: Women with epilepsy may have more difficulty conceiving or carrying a pregnancy to term than women without epilepsy.
Major finding: The rate of infertility is 9.2% and the rate of impaired fecundity is 22.5% among women with epilepsy.
Study details: A retrospective analysis of 373 participants in the Epilepsy Birth Control Registry.
Disclosures: The investigation was funded by the Epilepsy Foundation and Lundbeck.
Source: MacEachern DB et al. AES 2018, Abstract 1.426.
PCOS linked to increased cancer risk in premenopausal women
based on an analysis of nearly 3.5 million women in a large Swedish database.
Women with PCOS had a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and more than a doubling in the risk of ovarian and pancreatic cancers. Once women reached menopausal status, however, their cancer risk was comparable to that of women without a history of PCOS.
“Several carcinogenic processes are associated with PCOS, including dyslipidemia, hyperinsulinemia, and chronic inflammation,” wrote Weimin Ye, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues. “Our study indicates that cancer may need to be added to the spectrum of long-term health consequences of PCOS and warrants increased surveillance among those patients.”
The research letter was published online in JAMA Oncology.
The team examined the relationship between PCOS and primary cancers in about 3.5 million women over a span of up to 24 years (1985-2009), although the mean follow-up time was not mentioned. To examine the potential impact of menopause, they conducted separate multivariate logistic regression analyses for those younger than 51 years, and those aged 51 years or older. The analyses controlled for use of some medications (metformin, oral contraceptives, and hormone therapy); as well as educational level (a proxy for socioeconomic status); smoking; parity (a proxy for fertility); parental cancers; and diabetes.
Overall, 14,764 women had been diagnosed with PCOS; they were a mean of 28 years at baseline and 182 developed a primary cancer 1 year or more after PCOS diagnosis.
These women had a 15% overall increased risk of cancer, compared with women without PCOS.
The risks for specific cancers also were increased, compared with women without PCOS, including endometrial (hazard ratio, 2.62), ovarian (HR, 2.16), endocrine (HR, 1.92), pancreatic (HR, 3.4), kidney (HR, 3.0), and skeletal and hematopoietic (HR, 1.69) cancers.
The risks were associated with younger age, however. In the group under age 51 years, the overall risk was 22% higher. The increased risk of specific cancers were endometrial (HR, 6.45), ovarian (HR, 2.55), pancreatic (HR, 6.68), kidney (HR, 4.57), and endocrine (not thyroid) gland (HR, 2.9) cancers.
The authors had no relevant financial disclosures.
SOURCE: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
based on an analysis of nearly 3.5 million women in a large Swedish database.
Women with PCOS had a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and more than a doubling in the risk of ovarian and pancreatic cancers. Once women reached menopausal status, however, their cancer risk was comparable to that of women without a history of PCOS.
“Several carcinogenic processes are associated with PCOS, including dyslipidemia, hyperinsulinemia, and chronic inflammation,” wrote Weimin Ye, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues. “Our study indicates that cancer may need to be added to the spectrum of long-term health consequences of PCOS and warrants increased surveillance among those patients.”
The research letter was published online in JAMA Oncology.
The team examined the relationship between PCOS and primary cancers in about 3.5 million women over a span of up to 24 years (1985-2009), although the mean follow-up time was not mentioned. To examine the potential impact of menopause, they conducted separate multivariate logistic regression analyses for those younger than 51 years, and those aged 51 years or older. The analyses controlled for use of some medications (metformin, oral contraceptives, and hormone therapy); as well as educational level (a proxy for socioeconomic status); smoking; parity (a proxy for fertility); parental cancers; and diabetes.
Overall, 14,764 women had been diagnosed with PCOS; they were a mean of 28 years at baseline and 182 developed a primary cancer 1 year or more after PCOS diagnosis.
These women had a 15% overall increased risk of cancer, compared with women without PCOS.
The risks for specific cancers also were increased, compared with women without PCOS, including endometrial (hazard ratio, 2.62), ovarian (HR, 2.16), endocrine (HR, 1.92), pancreatic (HR, 3.4), kidney (HR, 3.0), and skeletal and hematopoietic (HR, 1.69) cancers.
The risks were associated with younger age, however. In the group under age 51 years, the overall risk was 22% higher. The increased risk of specific cancers were endometrial (HR, 6.45), ovarian (HR, 2.55), pancreatic (HR, 6.68), kidney (HR, 4.57), and endocrine (not thyroid) gland (HR, 2.9) cancers.
The authors had no relevant financial disclosures.
SOURCE: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
based on an analysis of nearly 3.5 million women in a large Swedish database.
Women with PCOS had a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and more than a doubling in the risk of ovarian and pancreatic cancers. Once women reached menopausal status, however, their cancer risk was comparable to that of women without a history of PCOS.
“Several carcinogenic processes are associated with PCOS, including dyslipidemia, hyperinsulinemia, and chronic inflammation,” wrote Weimin Ye, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues. “Our study indicates that cancer may need to be added to the spectrum of long-term health consequences of PCOS and warrants increased surveillance among those patients.”
The research letter was published online in JAMA Oncology.
The team examined the relationship between PCOS and primary cancers in about 3.5 million women over a span of up to 24 years (1985-2009), although the mean follow-up time was not mentioned. To examine the potential impact of menopause, they conducted separate multivariate logistic regression analyses for those younger than 51 years, and those aged 51 years or older. The analyses controlled for use of some medications (metformin, oral contraceptives, and hormone therapy); as well as educational level (a proxy for socioeconomic status); smoking; parity (a proxy for fertility); parental cancers; and diabetes.
Overall, 14,764 women had been diagnosed with PCOS; they were a mean of 28 years at baseline and 182 developed a primary cancer 1 year or more after PCOS diagnosis.
These women had a 15% overall increased risk of cancer, compared with women without PCOS.
The risks for specific cancers also were increased, compared with women without PCOS, including endometrial (hazard ratio, 2.62), ovarian (HR, 2.16), endocrine (HR, 1.92), pancreatic (HR, 3.4), kidney (HR, 3.0), and skeletal and hematopoietic (HR, 1.69) cancers.
The risks were associated with younger age, however. In the group under age 51 years, the overall risk was 22% higher. The increased risk of specific cancers were endometrial (HR, 6.45), ovarian (HR, 2.55), pancreatic (HR, 6.68), kidney (HR, 4.57), and endocrine (not thyroid) gland (HR, 2.9) cancers.
The authors had no relevant financial disclosures.
SOURCE: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
FROM JAMA ONCOLOGY
Key clinical point: Polycystic ovarian syndrome may be associated with increased cancer risks among younger women.
Major finding: Among premenopausal women, there was a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and a more than doubling in the risk of ovarian and pancreatic cancers
Study details: The study examined risks in 3.5 million women with up to 24 years of follow-up.
Disclosures: The study authors had no financial disclosures.
Source: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
NIH director expresses concern over CRISPR-cas9 baby claim
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
The National Institutes of Health is deeply concerned about the work just presented at the Second International Summit on Human Genome Editing in Hong Kong by Dr. He Jiankui, who described his effort using CRISPR-Cas9 on human embryos to disable the CCR5 gene. He claims that the two embryos were subsequently implanted, and infant twins have been born.
This work represents a deeply disturbing willingness by Dr. He and his team to flout international ethical norms. The project was largely carried out in secret, the medical necessity for inactivation of CCR5 in these infants is utterly unconvincing, the informed consent process appears highly questionable, and the possibility of damaging off-target effects has not been satisfactorily explored. It is profoundly unfortunate that the first apparent application of this powerful technique to the human germline has been carried out so irresponsibly.
The need for development of binding international consensus on setting limits for this kind of research, now being debated in Hong Kong, has never been more apparent. Without such limits, the world will face the serious risk of a deluge of similarly ill-considered and unethical projects.
Should such epic scientific misadventures proceed, a technology with enormous promise for prevention and treatment of disease will be overshadowed by justifiable public outrage, fear, and disgust.
Lest there be any doubt, and as we have stated previously, NIH does not support the use of gene-editing technologies in human embryos.
Francis S. Collins, M.D., Ph.D. is director of the National Institutes of Health. His comments were made in a statement Nov. 28.
Levonorgestrel implant right after delivery does not affect breastfeeding, infant growth
Researchers found no significant differences in infant growth, changes in breastfeeding initiation or breastfeeding continuation at 3-month and 6-month follow-up among women who received a levonorgestrel contraception implant very soon after delivery, compared with women who waited to receive the implant.
“These findings are consistent with the preponderance of literature supporting the hypothesis that progestin-containing contraceptives do not compromise a woman’s ability to initiate or sustain breastfeeding and do not adversely affect infant growth,” Sarah Averbach, MD, of the University of California, San Francisco, and her colleagues wrote in their study published in Contraception.
Dr. Averbach and her colleagues randomized 96 women to receive a two-rod levonorgestrel (LNG)–releasing subdermal contraceptive implant within 5 days of delivery (mean time, 36 hours post delivery) and 87 women to delay the implant to between 6 and 8 weeks at a postpartum follow-up visit (mean time, 68 days). The women were a minimum of 18 years old with a recent vaginal or cesarean section delivery at a Ugandan hospital; 55% of the women had at least three children, and 73% said they had prior experience breastfeeding. The researchers then examined infant weight change and infant head circumference change at 6 months from birth, time to lactogenesis, and whether mothers continued to breastfeed at 3 months and 6 months after birth.
Infant weight was similar in the immediate-implant group (4,632 g), compared with the delayed-implant group (4,407 g; P = .26); infant head circumference was similar between both groups (9.3 cm vs. 9.5 cm; P = .70) at 6 months as well. The time to lactogenesis was not significantly different in the immediate-implant (65 hours) and delayed-implant (63 hours; P = .84) groups. At 3 months, 74% of immediate-implant participants and 71% of delayed-implant participants said they were breastfeeding exclusively (P = .74); at 6 months, 48% of immediate implant participants and 52% of delayed implant participants reported exclusive breastfeeding (P equals .58).
Limitations of the study included follow-up to only 6 months and selection of participants with previous breastfeeding experience. Researchers also noted better measurements of infant and maternal breast milk intake also could be used and limit generalization of the results.
This study was funded by the Society of Family Planning Research Fund. Dr. Averbach is supported by an award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The other authors had no relevant financial disclosures.
SOURCE: Averbach S et al. Contraception. 2018. doi: 10.1016/j.contraception.2018.10.008.
Researchers found no significant differences in infant growth, changes in breastfeeding initiation or breastfeeding continuation at 3-month and 6-month follow-up among women who received a levonorgestrel contraception implant very soon after delivery, compared with women who waited to receive the implant.
“These findings are consistent with the preponderance of literature supporting the hypothesis that progestin-containing contraceptives do not compromise a woman’s ability to initiate or sustain breastfeeding and do not adversely affect infant growth,” Sarah Averbach, MD, of the University of California, San Francisco, and her colleagues wrote in their study published in Contraception.
Dr. Averbach and her colleagues randomized 96 women to receive a two-rod levonorgestrel (LNG)–releasing subdermal contraceptive implant within 5 days of delivery (mean time, 36 hours post delivery) and 87 women to delay the implant to between 6 and 8 weeks at a postpartum follow-up visit (mean time, 68 days). The women were a minimum of 18 years old with a recent vaginal or cesarean section delivery at a Ugandan hospital; 55% of the women had at least three children, and 73% said they had prior experience breastfeeding. The researchers then examined infant weight change and infant head circumference change at 6 months from birth, time to lactogenesis, and whether mothers continued to breastfeed at 3 months and 6 months after birth.
Infant weight was similar in the immediate-implant group (4,632 g), compared with the delayed-implant group (4,407 g; P = .26); infant head circumference was similar between both groups (9.3 cm vs. 9.5 cm; P = .70) at 6 months as well. The time to lactogenesis was not significantly different in the immediate-implant (65 hours) and delayed-implant (63 hours; P = .84) groups. At 3 months, 74% of immediate-implant participants and 71% of delayed-implant participants said they were breastfeeding exclusively (P = .74); at 6 months, 48% of immediate implant participants and 52% of delayed implant participants reported exclusive breastfeeding (P equals .58).
Limitations of the study included follow-up to only 6 months and selection of participants with previous breastfeeding experience. Researchers also noted better measurements of infant and maternal breast milk intake also could be used and limit generalization of the results.
This study was funded by the Society of Family Planning Research Fund. Dr. Averbach is supported by an award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The other authors had no relevant financial disclosures.
SOURCE: Averbach S et al. Contraception. 2018. doi: 10.1016/j.contraception.2018.10.008.
Researchers found no significant differences in infant growth, changes in breastfeeding initiation or breastfeeding continuation at 3-month and 6-month follow-up among women who received a levonorgestrel contraception implant very soon after delivery, compared with women who waited to receive the implant.
“These findings are consistent with the preponderance of literature supporting the hypothesis that progestin-containing contraceptives do not compromise a woman’s ability to initiate or sustain breastfeeding and do not adversely affect infant growth,” Sarah Averbach, MD, of the University of California, San Francisco, and her colleagues wrote in their study published in Contraception.
Dr. Averbach and her colleagues randomized 96 women to receive a two-rod levonorgestrel (LNG)–releasing subdermal contraceptive implant within 5 days of delivery (mean time, 36 hours post delivery) and 87 women to delay the implant to between 6 and 8 weeks at a postpartum follow-up visit (mean time, 68 days). The women were a minimum of 18 years old with a recent vaginal or cesarean section delivery at a Ugandan hospital; 55% of the women had at least three children, and 73% said they had prior experience breastfeeding. The researchers then examined infant weight change and infant head circumference change at 6 months from birth, time to lactogenesis, and whether mothers continued to breastfeed at 3 months and 6 months after birth.
Infant weight was similar in the immediate-implant group (4,632 g), compared with the delayed-implant group (4,407 g; P = .26); infant head circumference was similar between both groups (9.3 cm vs. 9.5 cm; P = .70) at 6 months as well. The time to lactogenesis was not significantly different in the immediate-implant (65 hours) and delayed-implant (63 hours; P = .84) groups. At 3 months, 74% of immediate-implant participants and 71% of delayed-implant participants said they were breastfeeding exclusively (P = .74); at 6 months, 48% of immediate implant participants and 52% of delayed implant participants reported exclusive breastfeeding (P equals .58).
Limitations of the study included follow-up to only 6 months and selection of participants with previous breastfeeding experience. Researchers also noted better measurements of infant and maternal breast milk intake also could be used and limit generalization of the results.
This study was funded by the Society of Family Planning Research Fund. Dr. Averbach is supported by an award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The other authors had no relevant financial disclosures.
SOURCE: Averbach S et al. Contraception. 2018. doi: 10.1016/j.contraception.2018.10.008.
FROM CONTRACEPTION
Key clinical point:
Major finding: Infant weight was similar in the immediate-implant group (4,632 g), compared with the delayed-implant group (4,407 g; P = .26); infant head circumference was similar between both groups (9.3 cm vs. 9.5 cm; P = .70) at 6 months as well.
Study details: A randomized trial of 96 women in Uganda who received a contraceptive implant less than 5 days after delivery and 86 women who received the implant between 6 and 8 weeks post partum.
Disclosures: This study was funded by the Society of Family Planning Research Fund. Dr. Averbach is supported by an award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The other authors had no relevant financial disclosures.
Source: Averbach S et al. Contraception. 2018. doi: 10.1016/j.contraception.2018.10.008.
Frozen embryo transfer benefits limited to subgroups
Elective frozen embryo transfer for fertility treatment is only associated with an higher live birth rate among individuals with polycystic ovarian syndrome or hyper-responders, or those who underwent preimplantation genetic testing for aneuploidy, research suggests.
Use of frozen embryo transfer also appeared to lower the risk of moderate to severe ovarian hyperstimulation syndrome, although there may be an increased risk of preeclampsia, compared with use of fresh embryos.
A systematic review and meta-analysis, published in Human Reproduction Update, looked at 11 randomized, controlled trials (RCTs) involving 5,379 patients comparing the reproductive, obstetric, and perinatal outcomes of fresh versus frozen embryo transfer for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
Matheus Roque, MD, from the ORIGEN–Center for Reproductive Medicine in Rio de Janiero, and his coauthors found that, overall, elective frozen embryo transfer was associated with a 12% higher chance of live birth than fresh (P = .04), although the quality of evidence was low.
When the researchers looked at the effects in different subgroups, they found hyper-responders and individuals with polycystic ovary syndrome had a 16% higher chance of live birth with frozen rather than fresh transfer (P = .004). But among individuals who were normal responders or without polycystic ovary syndrome, there was no significant improvement in live birth rate in the frozen embryo group, compared with the fresh embryo group.
There also was a significant 33% higher live birth rate with frozen embryos, compared with fresh when blastocysts were transferred, although this was deemed very low quality evidence.
In patients who underwent preimplantation genetic testing for aneuploidy, the use of frozen embryos was associated with a 55% higher chance of live birth, compared with the use of fresh embryos (P = .005), but no difference was seen in patients who didn’t have preimplantation genetic testing.
Another subanalysis examined the effects of different routes of progesterone administration and found patients who received intramuscular injections as luteal phase support had a 20% higher chance of live birth with frozen rather than fresh embryos. But no differences were seen for vaginal or oral progesterone.
Researchers also found that the method of embryo cryopreservation, whether slow freezing or vitrification, did not have any impact on live birth rates.
However, patients who underwent frozen embryo transfer showed a 58% lower risk of moderate to severe ovarian hyperstimulation syndrome, compared with those who had fresh embryo transfer. At the same time, the risk of preeclampsia was 79% higher with frozen, compared with fresh transfer.
“There are currently no clinical data supporting the indiscriminate use of eFET [elective frozen embryo transfer] for all patients submitted to IVF/ICSI,” Dr. Roque and his coauthors wrote. “Based on the available RCTs, it seems appropriate to implement this strategy in patients at risk of OHSS [ovarian hyperstimulation syndrome], in hyper-responders, and in those undergoing PGT-A [preimplantation genetic testing for aneuploidy] at the blastocyst stage.”
No funding or conflicts of interest were reported.
SOURCE: Roque M et al. Hum Reprod Update. 2018 Nov 2. doi: 10.1093/humupd/dmy033.
Elective frozen embryo transfer for fertility treatment is only associated with an higher live birth rate among individuals with polycystic ovarian syndrome or hyper-responders, or those who underwent preimplantation genetic testing for aneuploidy, research suggests.
Use of frozen embryo transfer also appeared to lower the risk of moderate to severe ovarian hyperstimulation syndrome, although there may be an increased risk of preeclampsia, compared with use of fresh embryos.
A systematic review and meta-analysis, published in Human Reproduction Update, looked at 11 randomized, controlled trials (RCTs) involving 5,379 patients comparing the reproductive, obstetric, and perinatal outcomes of fresh versus frozen embryo transfer for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
Matheus Roque, MD, from the ORIGEN–Center for Reproductive Medicine in Rio de Janiero, and his coauthors found that, overall, elective frozen embryo transfer was associated with a 12% higher chance of live birth than fresh (P = .04), although the quality of evidence was low.
When the researchers looked at the effects in different subgroups, they found hyper-responders and individuals with polycystic ovary syndrome had a 16% higher chance of live birth with frozen rather than fresh transfer (P = .004). But among individuals who were normal responders or without polycystic ovary syndrome, there was no significant improvement in live birth rate in the frozen embryo group, compared with the fresh embryo group.
There also was a significant 33% higher live birth rate with frozen embryos, compared with fresh when blastocysts were transferred, although this was deemed very low quality evidence.
In patients who underwent preimplantation genetic testing for aneuploidy, the use of frozen embryos was associated with a 55% higher chance of live birth, compared with the use of fresh embryos (P = .005), but no difference was seen in patients who didn’t have preimplantation genetic testing.
Another subanalysis examined the effects of different routes of progesterone administration and found patients who received intramuscular injections as luteal phase support had a 20% higher chance of live birth with frozen rather than fresh embryos. But no differences were seen for vaginal or oral progesterone.
Researchers also found that the method of embryo cryopreservation, whether slow freezing or vitrification, did not have any impact on live birth rates.
However, patients who underwent frozen embryo transfer showed a 58% lower risk of moderate to severe ovarian hyperstimulation syndrome, compared with those who had fresh embryo transfer. At the same time, the risk of preeclampsia was 79% higher with frozen, compared with fresh transfer.
“There are currently no clinical data supporting the indiscriminate use of eFET [elective frozen embryo transfer] for all patients submitted to IVF/ICSI,” Dr. Roque and his coauthors wrote. “Based on the available RCTs, it seems appropriate to implement this strategy in patients at risk of OHSS [ovarian hyperstimulation syndrome], in hyper-responders, and in those undergoing PGT-A [preimplantation genetic testing for aneuploidy] at the blastocyst stage.”
No funding or conflicts of interest were reported.
SOURCE: Roque M et al. Hum Reprod Update. 2018 Nov 2. doi: 10.1093/humupd/dmy033.
Elective frozen embryo transfer for fertility treatment is only associated with an higher live birth rate among individuals with polycystic ovarian syndrome or hyper-responders, or those who underwent preimplantation genetic testing for aneuploidy, research suggests.
Use of frozen embryo transfer also appeared to lower the risk of moderate to severe ovarian hyperstimulation syndrome, although there may be an increased risk of preeclampsia, compared with use of fresh embryos.
A systematic review and meta-analysis, published in Human Reproduction Update, looked at 11 randomized, controlled trials (RCTs) involving 5,379 patients comparing the reproductive, obstetric, and perinatal outcomes of fresh versus frozen embryo transfer for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
Matheus Roque, MD, from the ORIGEN–Center for Reproductive Medicine in Rio de Janiero, and his coauthors found that, overall, elective frozen embryo transfer was associated with a 12% higher chance of live birth than fresh (P = .04), although the quality of evidence was low.
When the researchers looked at the effects in different subgroups, they found hyper-responders and individuals with polycystic ovary syndrome had a 16% higher chance of live birth with frozen rather than fresh transfer (P = .004). But among individuals who were normal responders or without polycystic ovary syndrome, there was no significant improvement in live birth rate in the frozen embryo group, compared with the fresh embryo group.
There also was a significant 33% higher live birth rate with frozen embryos, compared with fresh when blastocysts were transferred, although this was deemed very low quality evidence.
In patients who underwent preimplantation genetic testing for aneuploidy, the use of frozen embryos was associated with a 55% higher chance of live birth, compared with the use of fresh embryos (P = .005), but no difference was seen in patients who didn’t have preimplantation genetic testing.
Another subanalysis examined the effects of different routes of progesterone administration and found patients who received intramuscular injections as luteal phase support had a 20% higher chance of live birth with frozen rather than fresh embryos. But no differences were seen for vaginal or oral progesterone.
Researchers also found that the method of embryo cryopreservation, whether slow freezing or vitrification, did not have any impact on live birth rates.
However, patients who underwent frozen embryo transfer showed a 58% lower risk of moderate to severe ovarian hyperstimulation syndrome, compared with those who had fresh embryo transfer. At the same time, the risk of preeclampsia was 79% higher with frozen, compared with fresh transfer.
“There are currently no clinical data supporting the indiscriminate use of eFET [elective frozen embryo transfer] for all patients submitted to IVF/ICSI,” Dr. Roque and his coauthors wrote. “Based on the available RCTs, it seems appropriate to implement this strategy in patients at risk of OHSS [ovarian hyperstimulation syndrome], in hyper-responders, and in those undergoing PGT-A [preimplantation genetic testing for aneuploidy] at the blastocyst stage.”
No funding or conflicts of interest were reported.
SOURCE: Roque M et al. Hum Reprod Update. 2018 Nov 2. doi: 10.1093/humupd/dmy033.
BY BIANCA NOGRADY FROM HUMAN REPRODUCTION UPDATE
Key clinical point: Certain subgroups of women may benefit from frozen versus fresh embryo transfer for in vitro fertilization/intracytoplasmic sperm injection.
Major finding:
Study details: A systematic review and meta-analysis of 11 randomized, controlled trials involving 5,379 patients.
Disclosures: No funding or conflicts of interest were reported.
Source: Roque M et al. Hum Reprod Update. 2018 Nov 2. doi: 10.1093/humupd/dmy033.
CKD, and even dialysis, may not be barriers to pregnancy
SAN DIEGO – Nephrologists are often uncomfortable with the idea of advising women with chronic kidney disease (CKD) about pregnancy, a physician told colleagues. They must do better, she said, with sensitivity and insight into once-extreme possibilities like pregnancy during dialysis.
“For many women, having a child is a life goal, and our women with chronic kidney disease are not different,” said Michelle Hladunewich, MD, of Toronto’s Sunnybrook Health Sciences Center. “When we don’t know what we should do, we tend to over-aggressively counsel our women, and that can traumatize them. It’s our role as nephrologists to help them find the safest window to have their pregnancy,” she said at the meeting sponsored by the American Society of Nephrology.
According to Dr. Hladunewich, there are tens of thousands of women of child-bearing age in the United States who have CKD, end-stage renal disease (ESRD), and kidney transplants. However, she said, research presented at Kidney Week 2018 suggested that many nephrologists do not feel confident about counseling patients regarding issues such as pregnancy outcomes in CKD. “We are not that comfortable with it, but we have to become more comfortable,” she said. “We need to be prepared to talk about contraception if they don’t want to have a child or the plan about how to have a child if they do.”
It’s especially important to understand that while women can fear birth defects and the exacerbation of their disease, they may also feel “they’re not fulfilling a societal norm to have a child like everyone else,” she said.
The risks of pregnancy in CKD can affect the mother (via worse kidney function) and/or the fetus (preeclampsia, poor fetal growth, preterm delivery).
In a 2015 study, Italian researchers compared 504 pregnancies in women with CKD to 836 low-risk pregnancies in women without CKD. They found that the risks of adverse outcomes increased in women at higher stages of CKD, compared with those at lower stages: “Renal function matters, and a stepwise increase in the risk of adverse maternal-fetal outcomes is observed from stage 1 to stages 4-5.”
In addition, the researchers noted that their research suggests “the presence of a baseline risk linked to CKD per se” (J Am Soc Nephrol. 2015 Aug; 26[8]:2011-22).
Dr. Hladunewich recommended focusing on “the safest window of opportunity.” Some patients will progress to end-stage renal disease, and an earlier pregnancy during CKD is a better option, she said. As a result, encouraging an earlier pregnancy can be a wise idea.
In some cases, though, a patient may be far into the stages of CKD. Dr. Hladunewich spoke about the case of a 31-year-old patient with a 29-year history of type 1 diabetes mellitus. She’d had one miscarriage, one preterm birth, and one twin pregnancy that was terminated because of safety concerns including rapid loss of kidney function.
The patient saw Dr. Hladunewich when she had a glomerular filtration rate of 25 mL/min, 3.5 g per 24 hour of proteinuria, and hypertension. The patient had a question: “Dr. Michelle, when can I try again?”
Dr. Hladunewich joked that “I had a small stroke.” But then, she said, “I got to the business of pregnancy counseling.”
She told the woman that her progression to end-stage renal disease was likely inevitable, and “adverse pregnancy outcomes were almost guaranteed.”
The woman responded: “Not now? When?” That, Dr. Hladunewich said, “was when I had my second stroke.”
But there is a possible solution: Pregnancy during dialysis. “Historically, we’ve said absolutely no pregnancy on dialysis,” she said, “but times are changing. We believe aggressive dialysis improves fetal maternal and fetal outcomes.”
Indeed, Dr. Hladunewich led a 2014 study that linked extensive dialysis during pregnancy (compared with less dialysis) to a better likelihood of outcomes such as live birth rate and normal birth weight (JASN May 2014;25[5]:1103-9).
As she noted, “we do offer it as a reproductive option” to patients like the one she mentioned – those who are in ESRD, approaching it, or are nearing the end of their child-bearing years with no transplant in sight. In transplant cases, she said, adequate graft function is linked to good pregnancy outcomes.
Dr. Hladunewich added that it’s important to monitor and adjust treatment of patients during the postpartum period. She said it’s especially important to understand the risks of drugs during breastfeeding. Both dialysis and transplant patients can breastfeed, she said.
Dr. Hladunewich reports no disclosures.
SOURCE: Kidney Week 2018, Abstract FR-OR078.
SAN DIEGO – Nephrologists are often uncomfortable with the idea of advising women with chronic kidney disease (CKD) about pregnancy, a physician told colleagues. They must do better, she said, with sensitivity and insight into once-extreme possibilities like pregnancy during dialysis.
“For many women, having a child is a life goal, and our women with chronic kidney disease are not different,” said Michelle Hladunewich, MD, of Toronto’s Sunnybrook Health Sciences Center. “When we don’t know what we should do, we tend to over-aggressively counsel our women, and that can traumatize them. It’s our role as nephrologists to help them find the safest window to have their pregnancy,” she said at the meeting sponsored by the American Society of Nephrology.
According to Dr. Hladunewich, there are tens of thousands of women of child-bearing age in the United States who have CKD, end-stage renal disease (ESRD), and kidney transplants. However, she said, research presented at Kidney Week 2018 suggested that many nephrologists do not feel confident about counseling patients regarding issues such as pregnancy outcomes in CKD. “We are not that comfortable with it, but we have to become more comfortable,” she said. “We need to be prepared to talk about contraception if they don’t want to have a child or the plan about how to have a child if they do.”
It’s especially important to understand that while women can fear birth defects and the exacerbation of their disease, they may also feel “they’re not fulfilling a societal norm to have a child like everyone else,” she said.
The risks of pregnancy in CKD can affect the mother (via worse kidney function) and/or the fetus (preeclampsia, poor fetal growth, preterm delivery).
In a 2015 study, Italian researchers compared 504 pregnancies in women with CKD to 836 low-risk pregnancies in women without CKD. They found that the risks of adverse outcomes increased in women at higher stages of CKD, compared with those at lower stages: “Renal function matters, and a stepwise increase in the risk of adverse maternal-fetal outcomes is observed from stage 1 to stages 4-5.”
In addition, the researchers noted that their research suggests “the presence of a baseline risk linked to CKD per se” (J Am Soc Nephrol. 2015 Aug; 26[8]:2011-22).
Dr. Hladunewich recommended focusing on “the safest window of opportunity.” Some patients will progress to end-stage renal disease, and an earlier pregnancy during CKD is a better option, she said. As a result, encouraging an earlier pregnancy can be a wise idea.
In some cases, though, a patient may be far into the stages of CKD. Dr. Hladunewich spoke about the case of a 31-year-old patient with a 29-year history of type 1 diabetes mellitus. She’d had one miscarriage, one preterm birth, and one twin pregnancy that was terminated because of safety concerns including rapid loss of kidney function.
The patient saw Dr. Hladunewich when she had a glomerular filtration rate of 25 mL/min, 3.5 g per 24 hour of proteinuria, and hypertension. The patient had a question: “Dr. Michelle, when can I try again?”
Dr. Hladunewich joked that “I had a small stroke.” But then, she said, “I got to the business of pregnancy counseling.”
She told the woman that her progression to end-stage renal disease was likely inevitable, and “adverse pregnancy outcomes were almost guaranteed.”
The woman responded: “Not now? When?” That, Dr. Hladunewich said, “was when I had my second stroke.”
But there is a possible solution: Pregnancy during dialysis. “Historically, we’ve said absolutely no pregnancy on dialysis,” she said, “but times are changing. We believe aggressive dialysis improves fetal maternal and fetal outcomes.”
Indeed, Dr. Hladunewich led a 2014 study that linked extensive dialysis during pregnancy (compared with less dialysis) to a better likelihood of outcomes such as live birth rate and normal birth weight (JASN May 2014;25[5]:1103-9).
As she noted, “we do offer it as a reproductive option” to patients like the one she mentioned – those who are in ESRD, approaching it, or are nearing the end of their child-bearing years with no transplant in sight. In transplant cases, she said, adequate graft function is linked to good pregnancy outcomes.
Dr. Hladunewich added that it’s important to monitor and adjust treatment of patients during the postpartum period. She said it’s especially important to understand the risks of drugs during breastfeeding. Both dialysis and transplant patients can breastfeed, she said.
Dr. Hladunewich reports no disclosures.
SOURCE: Kidney Week 2018, Abstract FR-OR078.
SAN DIEGO – Nephrologists are often uncomfortable with the idea of advising women with chronic kidney disease (CKD) about pregnancy, a physician told colleagues. They must do better, she said, with sensitivity and insight into once-extreme possibilities like pregnancy during dialysis.
“For many women, having a child is a life goal, and our women with chronic kidney disease are not different,” said Michelle Hladunewich, MD, of Toronto’s Sunnybrook Health Sciences Center. “When we don’t know what we should do, we tend to over-aggressively counsel our women, and that can traumatize them. It’s our role as nephrologists to help them find the safest window to have their pregnancy,” she said at the meeting sponsored by the American Society of Nephrology.
According to Dr. Hladunewich, there are tens of thousands of women of child-bearing age in the United States who have CKD, end-stage renal disease (ESRD), and kidney transplants. However, she said, research presented at Kidney Week 2018 suggested that many nephrologists do not feel confident about counseling patients regarding issues such as pregnancy outcomes in CKD. “We are not that comfortable with it, but we have to become more comfortable,” she said. “We need to be prepared to talk about contraception if they don’t want to have a child or the plan about how to have a child if they do.”
It’s especially important to understand that while women can fear birth defects and the exacerbation of their disease, they may also feel “they’re not fulfilling a societal norm to have a child like everyone else,” she said.
The risks of pregnancy in CKD can affect the mother (via worse kidney function) and/or the fetus (preeclampsia, poor fetal growth, preterm delivery).
In a 2015 study, Italian researchers compared 504 pregnancies in women with CKD to 836 low-risk pregnancies in women without CKD. They found that the risks of adverse outcomes increased in women at higher stages of CKD, compared with those at lower stages: “Renal function matters, and a stepwise increase in the risk of adverse maternal-fetal outcomes is observed from stage 1 to stages 4-5.”
In addition, the researchers noted that their research suggests “the presence of a baseline risk linked to CKD per se” (J Am Soc Nephrol. 2015 Aug; 26[8]:2011-22).
Dr. Hladunewich recommended focusing on “the safest window of opportunity.” Some patients will progress to end-stage renal disease, and an earlier pregnancy during CKD is a better option, she said. As a result, encouraging an earlier pregnancy can be a wise idea.
In some cases, though, a patient may be far into the stages of CKD. Dr. Hladunewich spoke about the case of a 31-year-old patient with a 29-year history of type 1 diabetes mellitus. She’d had one miscarriage, one preterm birth, and one twin pregnancy that was terminated because of safety concerns including rapid loss of kidney function.
The patient saw Dr. Hladunewich when she had a glomerular filtration rate of 25 mL/min, 3.5 g per 24 hour of proteinuria, and hypertension. The patient had a question: “Dr. Michelle, when can I try again?”
Dr. Hladunewich joked that “I had a small stroke.” But then, she said, “I got to the business of pregnancy counseling.”
She told the woman that her progression to end-stage renal disease was likely inevitable, and “adverse pregnancy outcomes were almost guaranteed.”
The woman responded: “Not now? When?” That, Dr. Hladunewich said, “was when I had my second stroke.”
But there is a possible solution: Pregnancy during dialysis. “Historically, we’ve said absolutely no pregnancy on dialysis,” she said, “but times are changing. We believe aggressive dialysis improves fetal maternal and fetal outcomes.”
Indeed, Dr. Hladunewich led a 2014 study that linked extensive dialysis during pregnancy (compared with less dialysis) to a better likelihood of outcomes such as live birth rate and normal birth weight (JASN May 2014;25[5]:1103-9).
As she noted, “we do offer it as a reproductive option” to patients like the one she mentioned – those who are in ESRD, approaching it, or are nearing the end of their child-bearing years with no transplant in sight. In transplant cases, she said, adequate graft function is linked to good pregnancy outcomes.
Dr. Hladunewich added that it’s important to monitor and adjust treatment of patients during the postpartum period. She said it’s especially important to understand the risks of drugs during breastfeeding. Both dialysis and transplant patients can breastfeed, she said.
Dr. Hladunewich reports no disclosures.
SOURCE: Kidney Week 2018, Abstract FR-OR078.
REPORTING FROM KIDNEY WEEK 2018
Concerns over discretion, efficacy lead teen females to use emergency contraception
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
FROM THE JOURNAL OF PEDIATRIC AND ADOLESCENT GYNECOLOGY
Key clinical point: 65% of adolescent females who were interviewed incorrectly believed that emergency contraception is 90%-99% effective.
Major finding: Adolescents who use emergency contraception prefer it over nonemergent contraception because it is perceived as easy to use and a more private alternative.
Study details: A study of 28 interviews of adolescent females who self-reported emergency contraception use.
Disclosures: The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
Source: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
Ob.Gyn. News welcomes Dr. Trolice to the board
Dr. Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando, responsible for the medical education of ob.gyn. residents and medical students, as well as medical endocrinology fellows. He is past president of the Florida Society of Reproductive Endocrinology & Infertility (REI) and past division director of REI at Winnie Palmer Hospital, part of Orlando Health.
He is double board-certified in REI and ob.gyn., maintains annual recertification, and has been awarded the American Medical Association’s “Physicians’ Recognition Award” annually. He holds the unique distinction of being a fellow in all three American colleges: ob.gyn., surgeons, and endocrinology. His colleagues select him as a “Top Doctor in America” annually, one among the top 5% of doctors in the United States. In 2018, he was awarded the “Social Responsibility Award” by the National Polycystic Ovary Syndrome Association. For 10 years, his foundation, Fertile Dreams, organized seminars to increase fertility awareness and granted national scholarships for those unable to afford in vitro fertilization (IVF) treatment.
Dr. Trolice serves on committees for the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. He has conducted scientific studies with resultant numerous publications and been appointed a reviewer in many leading medical journals and textbooks. He has lectured at numerous physician and patient seminars around the country. In addition, he is interviewed regularly on TV news/talk shows, radio, podcasts, print/online magazines, and newspapers on reproductive health topics. In the fall of 2018, he launched a podcast entitled “Fertility Health” featuring discussions with national experts on pertinent infertility and reproductive medicine topics. His current book is on the infertility journey, to be published by Harvard Common Press in mid 2019.
Dr. Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando, responsible for the medical education of ob.gyn. residents and medical students, as well as medical endocrinology fellows. He is past president of the Florida Society of Reproductive Endocrinology & Infertility (REI) and past division director of REI at Winnie Palmer Hospital, part of Orlando Health.
He is double board-certified in REI and ob.gyn., maintains annual recertification, and has been awarded the American Medical Association’s “Physicians’ Recognition Award” annually. He holds the unique distinction of being a fellow in all three American colleges: ob.gyn., surgeons, and endocrinology. His colleagues select him as a “Top Doctor in America” annually, one among the top 5% of doctors in the United States. In 2018, he was awarded the “Social Responsibility Award” by the National Polycystic Ovary Syndrome Association. For 10 years, his foundation, Fertile Dreams, organized seminars to increase fertility awareness and granted national scholarships for those unable to afford in vitro fertilization (IVF) treatment.
Dr. Trolice serves on committees for the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. He has conducted scientific studies with resultant numerous publications and been appointed a reviewer in many leading medical journals and textbooks. He has lectured at numerous physician and patient seminars around the country. In addition, he is interviewed regularly on TV news/talk shows, radio, podcasts, print/online magazines, and newspapers on reproductive health topics. In the fall of 2018, he launched a podcast entitled “Fertility Health” featuring discussions with national experts on pertinent infertility and reproductive medicine topics. His current book is on the infertility journey, to be published by Harvard Common Press in mid 2019.
Dr. Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando, responsible for the medical education of ob.gyn. residents and medical students, as well as medical endocrinology fellows. He is past president of the Florida Society of Reproductive Endocrinology & Infertility (REI) and past division director of REI at Winnie Palmer Hospital, part of Orlando Health.
He is double board-certified in REI and ob.gyn., maintains annual recertification, and has been awarded the American Medical Association’s “Physicians’ Recognition Award” annually. He holds the unique distinction of being a fellow in all three American colleges: ob.gyn., surgeons, and endocrinology. His colleagues select him as a “Top Doctor in America” annually, one among the top 5% of doctors in the United States. In 2018, he was awarded the “Social Responsibility Award” by the National Polycystic Ovary Syndrome Association. For 10 years, his foundation, Fertile Dreams, organized seminars to increase fertility awareness and granted national scholarships for those unable to afford in vitro fertilization (IVF) treatment.
Dr. Trolice serves on committees for the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. He has conducted scientific studies with resultant numerous publications and been appointed a reviewer in many leading medical journals and textbooks. He has lectured at numerous physician and patient seminars around the country. In addition, he is interviewed regularly on TV news/talk shows, radio, podcasts, print/online magazines, and newspapers on reproductive health topics. In the fall of 2018, he launched a podcast entitled “Fertility Health” featuring discussions with national experts on pertinent infertility and reproductive medicine topics. His current book is on the infertility journey, to be published by Harvard Common Press in mid 2019.
Robot-assisted laparoscopic tubal anastomosis following sterilization

Female sterilization is the most common method of contraception worldwide, and the second most common contraceptive method used in the United States. Approximately 643,000 sterilization procedures are performed annually.1 Approximately 1% to 3% of women who undergo sterilization will subsequently undergo a sterilization reversal.2 Although multiple variables have been identified, change in marital status is the most commonly cited reason for desiring a tubal reversal.3,4 Tubal anastomosis can be a technically challenging surgical procedure when done by laparoscopy, especially given the microsurgical elements that are required. Several modifications, including limiting the number of sutures, have evolved as a result of its tedious nature.5 By leveraging 3D magnification, articulating instruments, and tremor filtration, it is only natural that robotic surgery has been applied to tubal anastomosis.
In this video, we review some background information surrounding a tubal reversal, followed by demonstration of a robotic interpretation of a 2-stitch anastomosis technique in a patient who successfully conceived and delivered.6 Overall robot-assisted laparoscopic tubal anastomosis is a feasible and safe option for women who desire reversal of surgical sterilization, with pregnancy and live-birth rates comparable to those observed when an open technique is utilized.7 I hope that you will find this video beneficial to your clinical practice.
- Chan LM, Westhoff CL. Tubal sterilization trends in the United States. Fertil Steril. 2010;94:1-6.
- Moss CC. Sterilization: a review and update. Obstet Gynecol Clin North Am. 2015-12-01;42:713-724.
- Gordts S, Campo R, Puttemans P, Gordts S. Clinical factors determining pregnancy outcome after microsurgical tubal anastomosis. Fertil Steril. 2009;92:1198-1202.
- Chi I-C, Jones DB. Incidence, risk factors, and prevention of poststerilization regret in women. Obstet Gynecol Surv. 1994;49:722-732.
- Dubuisson JB, Swolin K. Laparoscopic tubal anastomosis (the one stitch technique): preliminary results. Human Reprod. 1995;10:2044-2046.
- Bissonnette FCA, Lapensee L, Bouzayen R. Outpatient laparoscopic tubal anastomosis and subsequent fertility. Fertil Steril. 1999;72:549-552.
- Caillet M, Vandromme J, Rozenberg S, Paesmans M, Germay O, Degueldre M. Robotically assisted laparoscopic microsurgical tubal anastomosis: a retrospective study. Fertil Steril. 2010;94:1844-1847.

Female sterilization is the most common method of contraception worldwide, and the second most common contraceptive method used in the United States. Approximately 643,000 sterilization procedures are performed annually.1 Approximately 1% to 3% of women who undergo sterilization will subsequently undergo a sterilization reversal.2 Although multiple variables have been identified, change in marital status is the most commonly cited reason for desiring a tubal reversal.3,4 Tubal anastomosis can be a technically challenging surgical procedure when done by laparoscopy, especially given the microsurgical elements that are required. Several modifications, including limiting the number of sutures, have evolved as a result of its tedious nature.5 By leveraging 3D magnification, articulating instruments, and tremor filtration, it is only natural that robotic surgery has been applied to tubal anastomosis.
In this video, we review some background information surrounding a tubal reversal, followed by demonstration of a robotic interpretation of a 2-stitch anastomosis technique in a patient who successfully conceived and delivered.6 Overall robot-assisted laparoscopic tubal anastomosis is a feasible and safe option for women who desire reversal of surgical sterilization, with pregnancy and live-birth rates comparable to those observed when an open technique is utilized.7 I hope that you will find this video beneficial to your clinical practice.

Female sterilization is the most common method of contraception worldwide, and the second most common contraceptive method used in the United States. Approximately 643,000 sterilization procedures are performed annually.1 Approximately 1% to 3% of women who undergo sterilization will subsequently undergo a sterilization reversal.2 Although multiple variables have been identified, change in marital status is the most commonly cited reason for desiring a tubal reversal.3,4 Tubal anastomosis can be a technically challenging surgical procedure when done by laparoscopy, especially given the microsurgical elements that are required. Several modifications, including limiting the number of sutures, have evolved as a result of its tedious nature.5 By leveraging 3D magnification, articulating instruments, and tremor filtration, it is only natural that robotic surgery has been applied to tubal anastomosis.
In this video, we review some background information surrounding a tubal reversal, followed by demonstration of a robotic interpretation of a 2-stitch anastomosis technique in a patient who successfully conceived and delivered.6 Overall robot-assisted laparoscopic tubal anastomosis is a feasible and safe option for women who desire reversal of surgical sterilization, with pregnancy and live-birth rates comparable to those observed when an open technique is utilized.7 I hope that you will find this video beneficial to your clinical practice.
- Chan LM, Westhoff CL. Tubal sterilization trends in the United States. Fertil Steril. 2010;94:1-6.
- Moss CC. Sterilization: a review and update. Obstet Gynecol Clin North Am. 2015-12-01;42:713-724.
- Gordts S, Campo R, Puttemans P, Gordts S. Clinical factors determining pregnancy outcome after microsurgical tubal anastomosis. Fertil Steril. 2009;92:1198-1202.
- Chi I-C, Jones DB. Incidence, risk factors, and prevention of poststerilization regret in women. Obstet Gynecol Surv. 1994;49:722-732.
- Dubuisson JB, Swolin K. Laparoscopic tubal anastomosis (the one stitch technique): preliminary results. Human Reprod. 1995;10:2044-2046.
- Bissonnette FCA, Lapensee L, Bouzayen R. Outpatient laparoscopic tubal anastomosis and subsequent fertility. Fertil Steril. 1999;72:549-552.
- Caillet M, Vandromme J, Rozenberg S, Paesmans M, Germay O, Degueldre M. Robotically assisted laparoscopic microsurgical tubal anastomosis: a retrospective study. Fertil Steril. 2010;94:1844-1847.
- Chan LM, Westhoff CL. Tubal sterilization trends in the United States. Fertil Steril. 2010;94:1-6.
- Moss CC. Sterilization: a review and update. Obstet Gynecol Clin North Am. 2015-12-01;42:713-724.
- Gordts S, Campo R, Puttemans P, Gordts S. Clinical factors determining pregnancy outcome after microsurgical tubal anastomosis. Fertil Steril. 2009;92:1198-1202.
- Chi I-C, Jones DB. Incidence, risk factors, and prevention of poststerilization regret in women. Obstet Gynecol Surv. 1994;49:722-732.
- Dubuisson JB, Swolin K. Laparoscopic tubal anastomosis (the one stitch technique): preliminary results. Human Reprod. 1995;10:2044-2046.
- Bissonnette FCA, Lapensee L, Bouzayen R. Outpatient laparoscopic tubal anastomosis and subsequent fertility. Fertil Steril. 1999;72:549-552.
- Caillet M, Vandromme J, Rozenberg S, Paesmans M, Germay O, Degueldre M. Robotically assisted laparoscopic microsurgical tubal anastomosis: a retrospective study. Fertil Steril. 2010;94:1844-1847.