User login
Cancer patient organizations critically affected by pandemic
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Analysis of early onset cancers suggests need for genetic testing
according to a presentation at the AACR virtual meeting II.
Investigators analyzed blood samples from 1,201 patients who were aged 18-39 years when diagnosed with a solid tumor malignancy.
In this group, there were 877 patients with early onset cancers, defined as cancers for which 39 years of age is greater than 1 standard deviation below the mean age of diagnosis for the cancer type.
The remaining 324 patients had young adult cancers, defined as cancers for which 39 years of age is less than 1 standard deviation below the mean age of diagnosis.
The most common early onset cancers were breast, colorectal, kidney, pancreas, and ovarian cancer.
The most common young adult cancers were sarcoma, brain cancer, and testicular cancer, as expected, said investigator Zsofia K. Stadler, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Stadler and colleagues performed next-generation sequencing of the patient samples using a panel of up to 88 genes previously implicated in cancer predisposition. This revealed a significantly higher prevalence of germline mutations in patients with early onset cancers than in those with young adult cancers – 21% and 13%, respectively (P = .002).
In patients with only high- and moderate-risk cancer susceptibility genes, the prevalence was 15% in the early onset group and 10% in the young adult group (P = .01). “Among the early onset cancer group, pancreas, breast, and kidney cancer patients harbored the highest rates of germline mutations,” Dr. Stadler said, noting that the spectrum of mutated genes differed in early onset and young adult cancer patients.
“In early onset patients, the most commonly mutated genes were BRCA1 and BRCA2 [4.9%], Lynch syndrome genes [2.2%], ATM [1.6%], and CHECK2 [1.7%],” Dr. Stadler said. “On the other hand, in young adults, TP53 mutations [2.2%], and SDHA and SDHB mutations dominated [1.9%], with the majority of mutations occurring in sarcoma patients.”
These findings suggest the prevalence of inherited cancer susceptibility syndromes in young adults with cancer is not uniform.
“We found a very high prevalence of germline mutations in young patients with cancer types that typically present at later ages,” Dr. Stadler said, referring to the early onset patients.
Conversely, the young adult cancer patients had a prevalence and spectrum of mutations more similar to what is seen in pediatric cancer populations, she noted.
The findings are surprising, according to AACR past president Elaine R. Mardis, PhD, of The Ohio State University in Columbus.
Dr. Mardis said the results show that, in young adults with early onset cancers, “the germline prevalence of these mutations is significantly higher than we had previously thought.”
“Although representing only about 4% of all cancers, young adults with cancer ... face unique challenges,” Dr. Stadler said. “Identifying whether a young patient’s cancer occurred in the setting of an inherited cancer predisposition syndrome is especially important in this patient population.”
Such knowledge “can significantly impact the risk of second primary cancers and the need for increased surveillance measures or even risk-reducing surgeries,” Dr. Stadler explained. She added that it can also have implications for identifying at-risk family members, such as younger siblings or children who should pursue genetic testing and appropriate prevention measures.
“Our results suggest that, among patients with early onset cancer, the increased prevalence of germline mutations supports a role for genetic testing, irrespective of tumor type,” Dr. Stadler said.
This study was partially funded by the Precision, Interception and Prevention Program, the Robert and Katie Niehaus Center for Inherited Cancer Genomics, the Marie-Josee and Henry R. Kravis Center for Molecular Oncology, and a National Cancer Institute Cancer Center Core Grant. Dr. Stadler reported that an immediate family member serves as a consultant in ophthalmology for Allergan, Adverum Biotechnologies, Alimera Sciences, BioMarin, Fortress Biotech, Genentech/Roche, Novartis, Optos, Regeneron, Regenxbio, and Spark Therapeutics. Dr. Mardis disclosed relationships with Qiagen NV, Pact Pharma LLC, Moderna Inc., and Interpreta LLC.
SOURCE: Stadler Z et al. AACR 2020, Abstract 1122.
according to a presentation at the AACR virtual meeting II.
Investigators analyzed blood samples from 1,201 patients who were aged 18-39 years when diagnosed with a solid tumor malignancy.
In this group, there were 877 patients with early onset cancers, defined as cancers for which 39 years of age is greater than 1 standard deviation below the mean age of diagnosis for the cancer type.
The remaining 324 patients had young adult cancers, defined as cancers for which 39 years of age is less than 1 standard deviation below the mean age of diagnosis.
The most common early onset cancers were breast, colorectal, kidney, pancreas, and ovarian cancer.
The most common young adult cancers were sarcoma, brain cancer, and testicular cancer, as expected, said investigator Zsofia K. Stadler, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Stadler and colleagues performed next-generation sequencing of the patient samples using a panel of up to 88 genes previously implicated in cancer predisposition. This revealed a significantly higher prevalence of germline mutations in patients with early onset cancers than in those with young adult cancers – 21% and 13%, respectively (P = .002).
In patients with only high- and moderate-risk cancer susceptibility genes, the prevalence was 15% in the early onset group and 10% in the young adult group (P = .01). “Among the early onset cancer group, pancreas, breast, and kidney cancer patients harbored the highest rates of germline mutations,” Dr. Stadler said, noting that the spectrum of mutated genes differed in early onset and young adult cancer patients.
“In early onset patients, the most commonly mutated genes were BRCA1 and BRCA2 [4.9%], Lynch syndrome genes [2.2%], ATM [1.6%], and CHECK2 [1.7%],” Dr. Stadler said. “On the other hand, in young adults, TP53 mutations [2.2%], and SDHA and SDHB mutations dominated [1.9%], with the majority of mutations occurring in sarcoma patients.”
These findings suggest the prevalence of inherited cancer susceptibility syndromes in young adults with cancer is not uniform.
“We found a very high prevalence of germline mutations in young patients with cancer types that typically present at later ages,” Dr. Stadler said, referring to the early onset patients.
Conversely, the young adult cancer patients had a prevalence and spectrum of mutations more similar to what is seen in pediatric cancer populations, she noted.
The findings are surprising, according to AACR past president Elaine R. Mardis, PhD, of The Ohio State University in Columbus.
Dr. Mardis said the results show that, in young adults with early onset cancers, “the germline prevalence of these mutations is significantly higher than we had previously thought.”
“Although representing only about 4% of all cancers, young adults with cancer ... face unique challenges,” Dr. Stadler said. “Identifying whether a young patient’s cancer occurred in the setting of an inherited cancer predisposition syndrome is especially important in this patient population.”
Such knowledge “can significantly impact the risk of second primary cancers and the need for increased surveillance measures or even risk-reducing surgeries,” Dr. Stadler explained. She added that it can also have implications for identifying at-risk family members, such as younger siblings or children who should pursue genetic testing and appropriate prevention measures.
“Our results suggest that, among patients with early onset cancer, the increased prevalence of germline mutations supports a role for genetic testing, irrespective of tumor type,” Dr. Stadler said.
This study was partially funded by the Precision, Interception and Prevention Program, the Robert and Katie Niehaus Center for Inherited Cancer Genomics, the Marie-Josee and Henry R. Kravis Center for Molecular Oncology, and a National Cancer Institute Cancer Center Core Grant. Dr. Stadler reported that an immediate family member serves as a consultant in ophthalmology for Allergan, Adverum Biotechnologies, Alimera Sciences, BioMarin, Fortress Biotech, Genentech/Roche, Novartis, Optos, Regeneron, Regenxbio, and Spark Therapeutics. Dr. Mardis disclosed relationships with Qiagen NV, Pact Pharma LLC, Moderna Inc., and Interpreta LLC.
SOURCE: Stadler Z et al. AACR 2020, Abstract 1122.
according to a presentation at the AACR virtual meeting II.
Investigators analyzed blood samples from 1,201 patients who were aged 18-39 years when diagnosed with a solid tumor malignancy.
In this group, there were 877 patients with early onset cancers, defined as cancers for which 39 years of age is greater than 1 standard deviation below the mean age of diagnosis for the cancer type.
The remaining 324 patients had young adult cancers, defined as cancers for which 39 years of age is less than 1 standard deviation below the mean age of diagnosis.
The most common early onset cancers were breast, colorectal, kidney, pancreas, and ovarian cancer.
The most common young adult cancers were sarcoma, brain cancer, and testicular cancer, as expected, said investigator Zsofia K. Stadler, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Stadler and colleagues performed next-generation sequencing of the patient samples using a panel of up to 88 genes previously implicated in cancer predisposition. This revealed a significantly higher prevalence of germline mutations in patients with early onset cancers than in those with young adult cancers – 21% and 13%, respectively (P = .002).
In patients with only high- and moderate-risk cancer susceptibility genes, the prevalence was 15% in the early onset group and 10% in the young adult group (P = .01). “Among the early onset cancer group, pancreas, breast, and kidney cancer patients harbored the highest rates of germline mutations,” Dr. Stadler said, noting that the spectrum of mutated genes differed in early onset and young adult cancer patients.
“In early onset patients, the most commonly mutated genes were BRCA1 and BRCA2 [4.9%], Lynch syndrome genes [2.2%], ATM [1.6%], and CHECK2 [1.7%],” Dr. Stadler said. “On the other hand, in young adults, TP53 mutations [2.2%], and SDHA and SDHB mutations dominated [1.9%], with the majority of mutations occurring in sarcoma patients.”
These findings suggest the prevalence of inherited cancer susceptibility syndromes in young adults with cancer is not uniform.
“We found a very high prevalence of germline mutations in young patients with cancer types that typically present at later ages,” Dr. Stadler said, referring to the early onset patients.
Conversely, the young adult cancer patients had a prevalence and spectrum of mutations more similar to what is seen in pediatric cancer populations, she noted.
The findings are surprising, according to AACR past president Elaine R. Mardis, PhD, of The Ohio State University in Columbus.
Dr. Mardis said the results show that, in young adults with early onset cancers, “the germline prevalence of these mutations is significantly higher than we had previously thought.”
“Although representing only about 4% of all cancers, young adults with cancer ... face unique challenges,” Dr. Stadler said. “Identifying whether a young patient’s cancer occurred in the setting of an inherited cancer predisposition syndrome is especially important in this patient population.”
Such knowledge “can significantly impact the risk of second primary cancers and the need for increased surveillance measures or even risk-reducing surgeries,” Dr. Stadler explained. She added that it can also have implications for identifying at-risk family members, such as younger siblings or children who should pursue genetic testing and appropriate prevention measures.
“Our results suggest that, among patients with early onset cancer, the increased prevalence of germline mutations supports a role for genetic testing, irrespective of tumor type,” Dr. Stadler said.
This study was partially funded by the Precision, Interception and Prevention Program, the Robert and Katie Niehaus Center for Inherited Cancer Genomics, the Marie-Josee and Henry R. Kravis Center for Molecular Oncology, and a National Cancer Institute Cancer Center Core Grant. Dr. Stadler reported that an immediate family member serves as a consultant in ophthalmology for Allergan, Adverum Biotechnologies, Alimera Sciences, BioMarin, Fortress Biotech, Genentech/Roche, Novartis, Optos, Regeneron, Regenxbio, and Spark Therapeutics. Dr. Mardis disclosed relationships with Qiagen NV, Pact Pharma LLC, Moderna Inc., and Interpreta LLC.
SOURCE: Stadler Z et al. AACR 2020, Abstract 1122.
FROM AACR 2020
Use of nonopioid pain meds is on the rise
Opioid and nonopioid prescription pain medications have taken different journeys since 2009, but they ended up in the same place in 2018, according to a recent report from the National Center for Health Statistics.
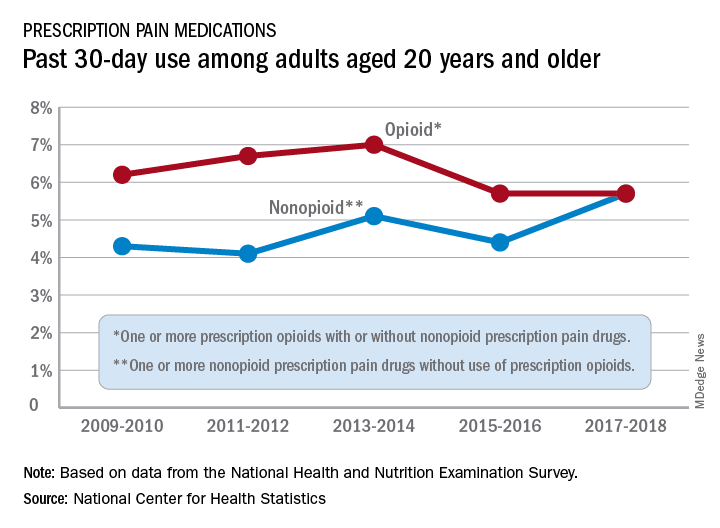
At least by one measure, anyway. Survey data from 2009 to 2010 show that 6.2% of adults aged 20 years and older had taken at least one prescription opioid in the last 30 days and 4.3% had used a prescription nonopioid without an opioid. By 2017-2018, past 30-day use of both drug groups was 5.7%, Craig M. Hales, MD, and associates said in an NCHS data brief.
“Opioids may be prescribed together with nonopioid pain medications, [but] nonpharmacologic and nonopioid-containing pharmacologic therapies are preferred for management of chronic pain,” the NCHS researchers noted.
as did the short-term increase in nonopioids from 2015-2016 to 2017-2018, but the 10-year trend for opioids was not significant, based on data from the National Health and Nutrition Examination Survey.
Much of the analysis focused on 2015-2018, when 30-day use of any prescription pain medication was reported by 10.7% of adults aged 20 years and older, with use of opioids at 5.7% and nonopioids at 5.0%. For women, use of any pain drug was 12.6% (6.4% opioid, 6.2% nonopioid) from 2015 to 2018, compared with 8.7% for men (4.9%, 3.8%), Dr. Hales and associates reported.
Past 30-day use of both opioids and nonopioids over those 4 years was highest for non-Hispanic whites and lowest, by a significant margin for both drug groups, among non-Hispanic Asian adults, a pattern that held for both men and women, they said.
Opioid and nonopioid prescription pain medications have taken different journeys since 2009, but they ended up in the same place in 2018, according to a recent report from the National Center for Health Statistics.
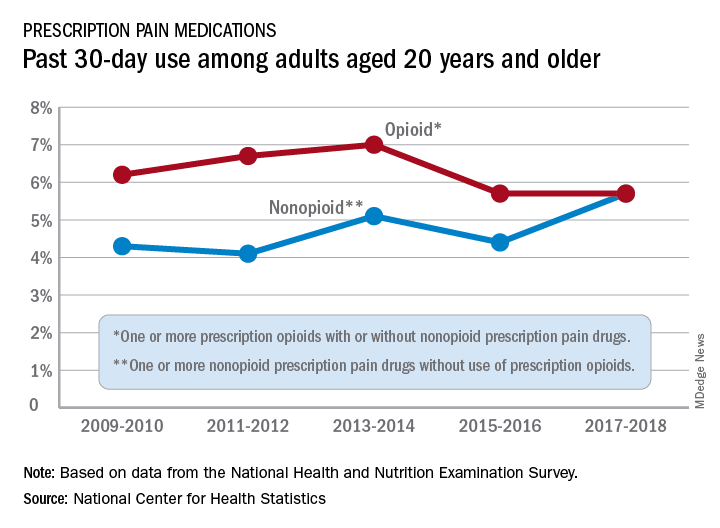
At least by one measure, anyway. Survey data from 2009 to 2010 show that 6.2% of adults aged 20 years and older had taken at least one prescription opioid in the last 30 days and 4.3% had used a prescription nonopioid without an opioid. By 2017-2018, past 30-day use of both drug groups was 5.7%, Craig M. Hales, MD, and associates said in an NCHS data brief.
“Opioids may be prescribed together with nonopioid pain medications, [but] nonpharmacologic and nonopioid-containing pharmacologic therapies are preferred for management of chronic pain,” the NCHS researchers noted.
as did the short-term increase in nonopioids from 2015-2016 to 2017-2018, but the 10-year trend for opioids was not significant, based on data from the National Health and Nutrition Examination Survey.
Much of the analysis focused on 2015-2018, when 30-day use of any prescription pain medication was reported by 10.7% of adults aged 20 years and older, with use of opioids at 5.7% and nonopioids at 5.0%. For women, use of any pain drug was 12.6% (6.4% opioid, 6.2% nonopioid) from 2015 to 2018, compared with 8.7% for men (4.9%, 3.8%), Dr. Hales and associates reported.
Past 30-day use of both opioids and nonopioids over those 4 years was highest for non-Hispanic whites and lowest, by a significant margin for both drug groups, among non-Hispanic Asian adults, a pattern that held for both men and women, they said.
Opioid and nonopioid prescription pain medications have taken different journeys since 2009, but they ended up in the same place in 2018, according to a recent report from the National Center for Health Statistics.
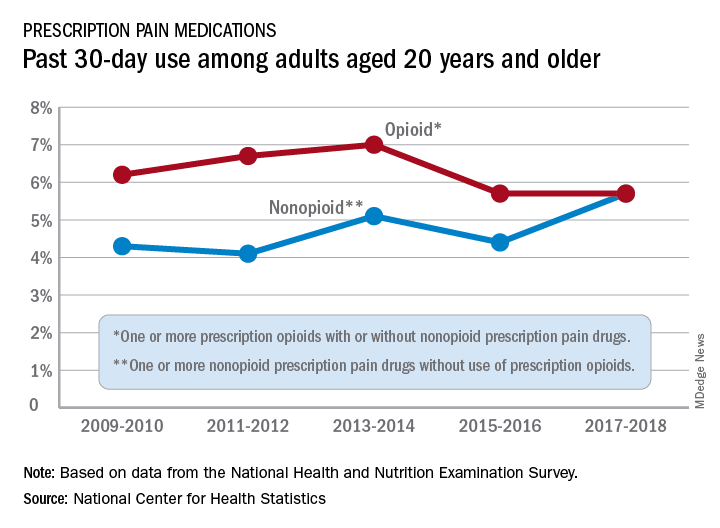
At least by one measure, anyway. Survey data from 2009 to 2010 show that 6.2% of adults aged 20 years and older had taken at least one prescription opioid in the last 30 days and 4.3% had used a prescription nonopioid without an opioid. By 2017-2018, past 30-day use of both drug groups was 5.7%, Craig M. Hales, MD, and associates said in an NCHS data brief.
“Opioids may be prescribed together with nonopioid pain medications, [but] nonpharmacologic and nonopioid-containing pharmacologic therapies are preferred for management of chronic pain,” the NCHS researchers noted.
as did the short-term increase in nonopioids from 2015-2016 to 2017-2018, but the 10-year trend for opioids was not significant, based on data from the National Health and Nutrition Examination Survey.
Much of the analysis focused on 2015-2018, when 30-day use of any prescription pain medication was reported by 10.7% of adults aged 20 years and older, with use of opioids at 5.7% and nonopioids at 5.0%. For women, use of any pain drug was 12.6% (6.4% opioid, 6.2% nonopioid) from 2015 to 2018, compared with 8.7% for men (4.9%, 3.8%), Dr. Hales and associates reported.
Past 30-day use of both opioids and nonopioids over those 4 years was highest for non-Hispanic whites and lowest, by a significant margin for both drug groups, among non-Hispanic Asian adults, a pattern that held for both men and women, they said.
FDA approves new indications for pembrolizumab
The Food and Drug Administration recently announced two new types of cancer that can be treated by the anti–PD-1 antibody pembrolizumab.
The new indications expand the use of pembrolizumab (Keytruda) to include treatment of patients with unresectable or metastatic tumor mutational burden–high (TMB-H) solid tumors as well as patients with cutaneous squamous cell carcinoma (cSCC). The FDA announced the new indications just 8 days apart, on June 16 and June 24.
In addition, on June 29, the FDA approved a third new indication for pembrolizumab, this time as first-line treatment for patients with unresectable or metastatic microsatellite instability–high or mismatch repair–deficient colorectal cancer.
The new approvals add to a wide range of oncology indications for which pembrolizumab can be used.
Accelerated approval to treat solid tumors
The FDA granted accelerated approval for pembrolizumab to treat children and adults with unresectable or metastatic TMB-H solid tumors that progressed after previous treatment or in instances where there are no satisfactory alternative treatment options.
The tumor mutational burden must be confirmed by an FDA-approved test. To that end, the FDA approved the FoundationOneCDx assay, which is designed to help physicians determine which patients meet the threshold for TMB-H malignancies (10 or more mutations per megabase).
The efficacy of pembrolizumab in TMB-H solid tumors was investigated in 10 cohorts from the multicenter, open-label KEYNOTE-158 trial. Participants received 200 mg of pembrolizumab intravenously every 3 weeks until their disease progressed or they experienced unacceptable toxicity.
Within this population, 102 patients had tumors that met the TMB-H definition. In this group, the overall response rate was 29%, including a 25% partial response rate and a 4% complete response rate.
The median duration of response was not reached, but 57% of participants experienced a response lasting 12 months or longer, and 50% had a response lasting 24 months or longer.
The most common adverse events associated with pembrolizumab in this trial were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain. Pembrolizumab is associated with immune-mediated side effects, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and skin adverse reactions, the FDA noted.
Safety and efficacy of pembrolizumab in pediatric patients with TMB-H central nervous system cancers have not been established.
New option for recurrent or metastatic cSCC
Physicians treating patients with cSCC that is not curable by surgery or radiation now have pembrolizumab to consider as another treatment option.
The cSCC approval is based on results of the multicenter, open-label KEYNOTE-629 trial. The dosage regimen was 200 mg of pembrolizumab intravenously every 3 weeks until cancer progressed, unacceptable toxicity arose, or 24 months of treatment were completed.
The objective response rate was 34%, and the median duration of response was not reached.
Adverse events were similar to those occurring in patients who received pembrolizumab as a single agent in other clinical trials, the FDA noted.
The Food and Drug Administration recently announced two new types of cancer that can be treated by the anti–PD-1 antibody pembrolizumab.
The new indications expand the use of pembrolizumab (Keytruda) to include treatment of patients with unresectable or metastatic tumor mutational burden–high (TMB-H) solid tumors as well as patients with cutaneous squamous cell carcinoma (cSCC). The FDA announced the new indications just 8 days apart, on June 16 and June 24.
In addition, on June 29, the FDA approved a third new indication for pembrolizumab, this time as first-line treatment for patients with unresectable or metastatic microsatellite instability–high or mismatch repair–deficient colorectal cancer.
The new approvals add to a wide range of oncology indications for which pembrolizumab can be used.
Accelerated approval to treat solid tumors
The FDA granted accelerated approval for pembrolizumab to treat children and adults with unresectable or metastatic TMB-H solid tumors that progressed after previous treatment or in instances where there are no satisfactory alternative treatment options.
The tumor mutational burden must be confirmed by an FDA-approved test. To that end, the FDA approved the FoundationOneCDx assay, which is designed to help physicians determine which patients meet the threshold for TMB-H malignancies (10 or more mutations per megabase).
The efficacy of pembrolizumab in TMB-H solid tumors was investigated in 10 cohorts from the multicenter, open-label KEYNOTE-158 trial. Participants received 200 mg of pembrolizumab intravenously every 3 weeks until their disease progressed or they experienced unacceptable toxicity.
Within this population, 102 patients had tumors that met the TMB-H definition. In this group, the overall response rate was 29%, including a 25% partial response rate and a 4% complete response rate.
The median duration of response was not reached, but 57% of participants experienced a response lasting 12 months or longer, and 50% had a response lasting 24 months or longer.
The most common adverse events associated with pembrolizumab in this trial were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain. Pembrolizumab is associated with immune-mediated side effects, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and skin adverse reactions, the FDA noted.
Safety and efficacy of pembrolizumab in pediatric patients with TMB-H central nervous system cancers have not been established.
New option for recurrent or metastatic cSCC
Physicians treating patients with cSCC that is not curable by surgery or radiation now have pembrolizumab to consider as another treatment option.
The cSCC approval is based on results of the multicenter, open-label KEYNOTE-629 trial. The dosage regimen was 200 mg of pembrolizumab intravenously every 3 weeks until cancer progressed, unacceptable toxicity arose, or 24 months of treatment were completed.
The objective response rate was 34%, and the median duration of response was not reached.
Adverse events were similar to those occurring in patients who received pembrolizumab as a single agent in other clinical trials, the FDA noted.
The Food and Drug Administration recently announced two new types of cancer that can be treated by the anti–PD-1 antibody pembrolizumab.
The new indications expand the use of pembrolizumab (Keytruda) to include treatment of patients with unresectable or metastatic tumor mutational burden–high (TMB-H) solid tumors as well as patients with cutaneous squamous cell carcinoma (cSCC). The FDA announced the new indications just 8 days apart, on June 16 and June 24.
In addition, on June 29, the FDA approved a third new indication for pembrolizumab, this time as first-line treatment for patients with unresectable or metastatic microsatellite instability–high or mismatch repair–deficient colorectal cancer.
The new approvals add to a wide range of oncology indications for which pembrolizumab can be used.
Accelerated approval to treat solid tumors
The FDA granted accelerated approval for pembrolizumab to treat children and adults with unresectable or metastatic TMB-H solid tumors that progressed after previous treatment or in instances where there are no satisfactory alternative treatment options.
The tumor mutational burden must be confirmed by an FDA-approved test. To that end, the FDA approved the FoundationOneCDx assay, which is designed to help physicians determine which patients meet the threshold for TMB-H malignancies (10 or more mutations per megabase).
The efficacy of pembrolizumab in TMB-H solid tumors was investigated in 10 cohorts from the multicenter, open-label KEYNOTE-158 trial. Participants received 200 mg of pembrolizumab intravenously every 3 weeks until their disease progressed or they experienced unacceptable toxicity.
Within this population, 102 patients had tumors that met the TMB-H definition. In this group, the overall response rate was 29%, including a 25% partial response rate and a 4% complete response rate.
The median duration of response was not reached, but 57% of participants experienced a response lasting 12 months or longer, and 50% had a response lasting 24 months or longer.
The most common adverse events associated with pembrolizumab in this trial were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain. Pembrolizumab is associated with immune-mediated side effects, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and skin adverse reactions, the FDA noted.
Safety and efficacy of pembrolizumab in pediatric patients with TMB-H central nervous system cancers have not been established.
New option for recurrent or metastatic cSCC
Physicians treating patients with cSCC that is not curable by surgery or radiation now have pembrolizumab to consider as another treatment option.
The cSCC approval is based on results of the multicenter, open-label KEYNOTE-629 trial. The dosage regimen was 200 mg of pembrolizumab intravenously every 3 weeks until cancer progressed, unacceptable toxicity arose, or 24 months of treatment were completed.
The objective response rate was 34%, and the median duration of response was not reached.
Adverse events were similar to those occurring in patients who received pembrolizumab as a single agent in other clinical trials, the FDA noted.
Personalized cancer vaccine may enhance checkpoint inhibitor activity
Combining a personalized cancer vaccine with an immune checkpoint inhibitor induced neoantigen-specific immune responses in most patients with advanced solid tumors in a phase 1b study.
Only two clinical responses were seen in this early investigation of the vaccine, RO7198457, combined with the PD-L1 inhibitor atezolizumab. However, T-cell responses were observed in about three-quarters of the patients evaluated, according to study investigator Juanita Lopez, MB BChir, PhD.
Those immune responses, coupled with preliminary evidence of infiltration of RO7198457-stimulated T cells into tumors, suggest the viability of this individualized anticancer strategy, according to Dr. Lopez, a consultant medical oncologist at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London.
“Failure of T-cell priming is a major cause of lack of response to immune checkpoint inhibitors,” Dr. Lopez said in an interview. “We hoped that, by eliciting a tumor-specific T-cell response, we would be able to overcome this.”
Preclinical data suggested the combination of vaccine and immune checkpoint inhibitors improved outcomes, which prompted the current study, added Dr. Lopez, who presented results from this study at the American Association for Cancer Research virtual meeting II.
Dr. Lopez noted that mutated neoantigens are recognized as foreign and have been shown to induce stronger T-cell responses, compared with shared antigens, likely because of a lack of central tolerance.
“Most of these mutated neoantigens are not shared between the patients, and therefore, targeted neoantigen-specific therapy requires an individualized approach,” she explained.
RO7198457 is manufactured on a per-patient basis and includes as many as 20 tumor-specific neoepitopes.
Study details
Dr. Lopez presented results from dose-escalation and expansion cohorts of the study, which included 142 patients with advanced solid tumors. The patients had colorectal, skin, kidney, lung, urothelial, breast, gynecologic, and head and neck cancers.
Most patients had low or no PD-L1 expression, and nearly 40% had received prior treatment with a checkpoint inhibitor.
Patients received nine doses of RO7198457 at 25-50 mcg during the 12-week induction stage. They then received RO7198457 every eight cycles until disease progression. Patients received atezolizumab at 1,200 mg on day 1 of each 21-day cycle.
Induction of proinflammatory cytokines was observed at each dose tested, and ex vivo T-cell responses were noted in 46 of 63 patients evaluated, or 73%.
T-cell receptors specific to RO7198457 were present posttreatment in a patient with rectal cancer, providing some preliminary evidence suggesting infiltration of RO7198457-stimulated T cells in the tumor, Dr. Lopez said.
There were two clinical responses. A patient with rectal cancer had a complete response, and a patient with triple-negative breast cancer had a partial response.
The combination of RO7198457 with atezolizumab was generally well tolerated, and the maximum tolerated dose was not reached, Dr. Lopez said. Most adverse events were grade 1/2, and immune-mediated adverse events were rare.
Implications and next steps
This study furthers earlier observations from neoantigen vaccine studies by linking dosing of the vaccine to dosing with immune checkpoint inhibitor, rather than giving the vaccine in the period leading up to immune checkpoint inhibitor administration, according to former AACR President Elaine R. Mardis, PhD, of Nationwide Children’s Hospital and The Ohio State University College of Medicine, both in Columbus.
That said, the implications for clinical practice remain unclear, according to Dr. Mardis.
“This combination did elicit an immune response that was highly specific for the neoantigen vaccine, but most patients did not receive a clinical benefit of disease response,” Dr. Mardis said in an interview. “This tells us the combination approach used was, overall, not quite right, and we need to continue to innovate in this area.”
The low clinical response rate in the study was likely caused in part by the fact that patients had very advanced disease and were heavily pretreated, according to Dr. Lopez
Randomized phase 2 studies of RO7198457 are now underway, Dr. Lopez said. One is a study of RO7198457 plus atezolizumab as adjuvant treatment for non–small cell lung cancer (NCT04267237). Another is testing RO7198457 in combination with pembrolizumab as first-line treatment for melanoma (NCT03815058).
The current study was funded by Genentech and BioNTech. Dr. Lopez reported disclosures related to Roche/Genentech, Basilea Pharmaceutica, and Genmab. Dr. Mardis reported disclosures related to Quiagen NV, PACT Pharma, Kiadis Pharma NV, and Interpreta.
SOURCE: Lopez J et al. AACR 2020, Abstract CT301.
Combining a personalized cancer vaccine with an immune checkpoint inhibitor induced neoantigen-specific immune responses in most patients with advanced solid tumors in a phase 1b study.
Only two clinical responses were seen in this early investigation of the vaccine, RO7198457, combined with the PD-L1 inhibitor atezolizumab. However, T-cell responses were observed in about three-quarters of the patients evaluated, according to study investigator Juanita Lopez, MB BChir, PhD.
Those immune responses, coupled with preliminary evidence of infiltration of RO7198457-stimulated T cells into tumors, suggest the viability of this individualized anticancer strategy, according to Dr. Lopez, a consultant medical oncologist at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London.
“Failure of T-cell priming is a major cause of lack of response to immune checkpoint inhibitors,” Dr. Lopez said in an interview. “We hoped that, by eliciting a tumor-specific T-cell response, we would be able to overcome this.”
Preclinical data suggested the combination of vaccine and immune checkpoint inhibitors improved outcomes, which prompted the current study, added Dr. Lopez, who presented results from this study at the American Association for Cancer Research virtual meeting II.
Dr. Lopez noted that mutated neoantigens are recognized as foreign and have been shown to induce stronger T-cell responses, compared with shared antigens, likely because of a lack of central tolerance.
“Most of these mutated neoantigens are not shared between the patients, and therefore, targeted neoantigen-specific therapy requires an individualized approach,” she explained.
RO7198457 is manufactured on a per-patient basis and includes as many as 20 tumor-specific neoepitopes.
Study details
Dr. Lopez presented results from dose-escalation and expansion cohorts of the study, which included 142 patients with advanced solid tumors. The patients had colorectal, skin, kidney, lung, urothelial, breast, gynecologic, and head and neck cancers.
Most patients had low or no PD-L1 expression, and nearly 40% had received prior treatment with a checkpoint inhibitor.
Patients received nine doses of RO7198457 at 25-50 mcg during the 12-week induction stage. They then received RO7198457 every eight cycles until disease progression. Patients received atezolizumab at 1,200 mg on day 1 of each 21-day cycle.
Induction of proinflammatory cytokines was observed at each dose tested, and ex vivo T-cell responses were noted in 46 of 63 patients evaluated, or 73%.
T-cell receptors specific to RO7198457 were present posttreatment in a patient with rectal cancer, providing some preliminary evidence suggesting infiltration of RO7198457-stimulated T cells in the tumor, Dr. Lopez said.
There were two clinical responses. A patient with rectal cancer had a complete response, and a patient with triple-negative breast cancer had a partial response.
The combination of RO7198457 with atezolizumab was generally well tolerated, and the maximum tolerated dose was not reached, Dr. Lopez said. Most adverse events were grade 1/2, and immune-mediated adverse events were rare.
Implications and next steps
This study furthers earlier observations from neoantigen vaccine studies by linking dosing of the vaccine to dosing with immune checkpoint inhibitor, rather than giving the vaccine in the period leading up to immune checkpoint inhibitor administration, according to former AACR President Elaine R. Mardis, PhD, of Nationwide Children’s Hospital and The Ohio State University College of Medicine, both in Columbus.
That said, the implications for clinical practice remain unclear, according to Dr. Mardis.
“This combination did elicit an immune response that was highly specific for the neoantigen vaccine, but most patients did not receive a clinical benefit of disease response,” Dr. Mardis said in an interview. “This tells us the combination approach used was, overall, not quite right, and we need to continue to innovate in this area.”
The low clinical response rate in the study was likely caused in part by the fact that patients had very advanced disease and were heavily pretreated, according to Dr. Lopez
Randomized phase 2 studies of RO7198457 are now underway, Dr. Lopez said. One is a study of RO7198457 plus atezolizumab as adjuvant treatment for non–small cell lung cancer (NCT04267237). Another is testing RO7198457 in combination with pembrolizumab as first-line treatment for melanoma (NCT03815058).
The current study was funded by Genentech and BioNTech. Dr. Lopez reported disclosures related to Roche/Genentech, Basilea Pharmaceutica, and Genmab. Dr. Mardis reported disclosures related to Quiagen NV, PACT Pharma, Kiadis Pharma NV, and Interpreta.
SOURCE: Lopez J et al. AACR 2020, Abstract CT301.
Combining a personalized cancer vaccine with an immune checkpoint inhibitor induced neoantigen-specific immune responses in most patients with advanced solid tumors in a phase 1b study.
Only two clinical responses were seen in this early investigation of the vaccine, RO7198457, combined with the PD-L1 inhibitor atezolizumab. However, T-cell responses were observed in about three-quarters of the patients evaluated, according to study investigator Juanita Lopez, MB BChir, PhD.
Those immune responses, coupled with preliminary evidence of infiltration of RO7198457-stimulated T cells into tumors, suggest the viability of this individualized anticancer strategy, according to Dr. Lopez, a consultant medical oncologist at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London.
“Failure of T-cell priming is a major cause of lack of response to immune checkpoint inhibitors,” Dr. Lopez said in an interview. “We hoped that, by eliciting a tumor-specific T-cell response, we would be able to overcome this.”
Preclinical data suggested the combination of vaccine and immune checkpoint inhibitors improved outcomes, which prompted the current study, added Dr. Lopez, who presented results from this study at the American Association for Cancer Research virtual meeting II.
Dr. Lopez noted that mutated neoantigens are recognized as foreign and have been shown to induce stronger T-cell responses, compared with shared antigens, likely because of a lack of central tolerance.
“Most of these mutated neoantigens are not shared between the patients, and therefore, targeted neoantigen-specific therapy requires an individualized approach,” she explained.
RO7198457 is manufactured on a per-patient basis and includes as many as 20 tumor-specific neoepitopes.
Study details
Dr. Lopez presented results from dose-escalation and expansion cohorts of the study, which included 142 patients with advanced solid tumors. The patients had colorectal, skin, kidney, lung, urothelial, breast, gynecologic, and head and neck cancers.
Most patients had low or no PD-L1 expression, and nearly 40% had received prior treatment with a checkpoint inhibitor.
Patients received nine doses of RO7198457 at 25-50 mcg during the 12-week induction stage. They then received RO7198457 every eight cycles until disease progression. Patients received atezolizumab at 1,200 mg on day 1 of each 21-day cycle.
Induction of proinflammatory cytokines was observed at each dose tested, and ex vivo T-cell responses were noted in 46 of 63 patients evaluated, or 73%.
T-cell receptors specific to RO7198457 were present posttreatment in a patient with rectal cancer, providing some preliminary evidence suggesting infiltration of RO7198457-stimulated T cells in the tumor, Dr. Lopez said.
There were two clinical responses. A patient with rectal cancer had a complete response, and a patient with triple-negative breast cancer had a partial response.
The combination of RO7198457 with atezolizumab was generally well tolerated, and the maximum tolerated dose was not reached, Dr. Lopez said. Most adverse events were grade 1/2, and immune-mediated adverse events were rare.
Implications and next steps
This study furthers earlier observations from neoantigen vaccine studies by linking dosing of the vaccine to dosing with immune checkpoint inhibitor, rather than giving the vaccine in the period leading up to immune checkpoint inhibitor administration, according to former AACR President Elaine R. Mardis, PhD, of Nationwide Children’s Hospital and The Ohio State University College of Medicine, both in Columbus.
That said, the implications for clinical practice remain unclear, according to Dr. Mardis.
“This combination did elicit an immune response that was highly specific for the neoantigen vaccine, but most patients did not receive a clinical benefit of disease response,” Dr. Mardis said in an interview. “This tells us the combination approach used was, overall, not quite right, and we need to continue to innovate in this area.”
The low clinical response rate in the study was likely caused in part by the fact that patients had very advanced disease and were heavily pretreated, according to Dr. Lopez
Randomized phase 2 studies of RO7198457 are now underway, Dr. Lopez said. One is a study of RO7198457 plus atezolizumab as adjuvant treatment for non–small cell lung cancer (NCT04267237). Another is testing RO7198457 in combination with pembrolizumab as first-line treatment for melanoma (NCT03815058).
The current study was funded by Genentech and BioNTech. Dr. Lopez reported disclosures related to Roche/Genentech, Basilea Pharmaceutica, and Genmab. Dr. Mardis reported disclosures related to Quiagen NV, PACT Pharma, Kiadis Pharma NV, and Interpreta.
SOURCE: Lopez J et al. AACR 2020, Abstract CT301.
FROM AACR 2020
More than 10,000 excess cancer deaths because of COVID-19 delays
A model created by the National Cancer Institute predicts that tens of thousands of excess cancer deaths will occur over the next decade as a result of missed screenings, delays in diagnosis, and reductions in oncology care caused by the COVID-19 pandemic.
“As director of NCI, I am deeply concerned about the potential impacts of delayed diagnoses and deferred or modified treatment plans on cancer incidence and mortality,” said Norman “Ned” Sharpless, MD.
“In the past 3 decades, we have seen steady and strong progress against death and suffering from cancer, thanks to improvements in prevention, screening, diagnosis, and treatment. I worry that the SARS-CoV-2 pandemic has put those decades of steady progress at risk and may precipitate reversals of these trends.”
In an editorial published June 19 in Science, Dr. Sharpless highlighted modeling performed by the NCI that predicts an excess of 10,000 deaths from breast and colorectal cancer over the next 10 years.
The number of excess deaths per year would peak in the next year or 2, likely sooner for colorectal than for breast cancer, but “for both cancer types, we believe the pandemic will influence cancer deaths for at least a decade.”
In an interview, Dr. Sharpless pointed out that this analysis is conservative because the researchers only evaluated two types of cancer. They chose breast and colorectal cancer because these are common cancers (accounting for about one-sixth of all cancers) with relatively high screening rates.
“We didn’t model other cancer types, but we have no reason to think that we’re not going to see the same thing with other types of malignancies,” he said. “That is a significant amount of excess mortality.”
Delayed diagnosis, modified therapy
One of the effects of the pandemic has been to cause delays in cancer diagnosis. “Routine screening has plummeted and is running at less than 90% in some systems,” Dr. Sharpless said.
“Most cancers are diagnosed when people experience symptoms and go see their doctors, and those symptomatic screening events are also not happening,” he continued. “Fear of contracting the coronavirus in health care settings has dissuaded people from visits.”
In some cases, a delay in diagnosis will allow the cancer to progress to a more advanced stage. “The earlier the diagnosis, the better, and if the stages are more advanced, patients will not do as well for virtually every kind of cancer,” he said.
In addition to delays in diagnosis, treatments are being postponed or modified for patients recently diagnosed with cancer. Because of delays and reductions in curative therapies, patients may be receiving less than optimal care.
“We are seeing a lot of nonstandard care,” said Dr. Sharpless. “All of these things add up to increased cancer morbidity and mortality.”
He also pointed out that the term “elective” is confusing and problematic. “It doesn’t mean that it’s not needed, just that it’s not an emergency and doesn’t need to be done today,” said Dr. Sharpless. “But if we’re talking about chemotherapy and surgery, we don’t think they can be delayed for too long – maybe a week, but not for several months.”
Dr. Sharpless feels that overall it is time for cancer care to resume as much as possible, because “ignoring cancer for too long is an untenable choice and may turn one public health crisis into another.”
“If we act now, we can make up for lost time,” he wrote in the editorial. “Clearly, postponing procedures and deferring care due to the pandemic was prudent at one time, but now that we have made it through the initial shock of the pandemic, I believe it is time to resume robust cancer care.”
Through their network of cancer centers, researchers with the NCI can develop innovative solutions that allow screening and treatment to move forward while maintaining safety. “We need to make patients feel safe, and we have to answer important questions quickly,” he said.
Impact of COVID-19 on cancer care
The COVID-19 pandemic has overwhelmed health care systems worldwide and has created major challenges for clinicians who are caring for patients with cancer.
As previously reported, hospitals reprioritized resources for an impending onslaught of COVID-19 patients. Services and procedures deemed to be nonessential were canceled or delayed, including surgeries and imaging.
In a survey conducted by the American Cancer Society Cancer Action Network, half of the 1219 respondents reported changes, delays, or disruptions to the care they were receiving. The services most frequently affected included in-person provider visits (50%), supportive services (20%), and imaging procedures to monitor tumor growth (20%).
In addition, 8% reported that their treatment, including chemotherapy and immunotherapy, had been affected by the COVID-19 pandemic.
In the United Kingdom, Cancer Research UK estimated that because of the disruption to cancer services, 2.4 million people did not undergo cancer screening or further testing or did not receive cancer treatment and that tens of thousands of cases have gone undiagnosed.
Similarly, a survey by Macmillan Cancer Support showed that almost half (45%) of cancer patients have experienced delays or cancellations of cancer treatments, or their treatments have been altered as a result of coronavirus, leaving many living in fear. Calling cancer “the forgotten C” of the pandemic, it warned of a potential cancer “time bomb” when, as the number of deaths from COVID-19 falls, cancer returns as the leading cause of death in the United Kingdom.
Last month, a report also predicted that there will be an excess of cancer deaths in both the United States and United Kingdom because of patients not accessing health care services.
The authors calculated that there will be 6270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients older than 40 years in the United States.
This article first appeared on Medscape.com.
A model created by the National Cancer Institute predicts that tens of thousands of excess cancer deaths will occur over the next decade as a result of missed screenings, delays in diagnosis, and reductions in oncology care caused by the COVID-19 pandemic.
“As director of NCI, I am deeply concerned about the potential impacts of delayed diagnoses and deferred or modified treatment plans on cancer incidence and mortality,” said Norman “Ned” Sharpless, MD.
“In the past 3 decades, we have seen steady and strong progress against death and suffering from cancer, thanks to improvements in prevention, screening, diagnosis, and treatment. I worry that the SARS-CoV-2 pandemic has put those decades of steady progress at risk and may precipitate reversals of these trends.”
In an editorial published June 19 in Science, Dr. Sharpless highlighted modeling performed by the NCI that predicts an excess of 10,000 deaths from breast and colorectal cancer over the next 10 years.
The number of excess deaths per year would peak in the next year or 2, likely sooner for colorectal than for breast cancer, but “for both cancer types, we believe the pandemic will influence cancer deaths for at least a decade.”
In an interview, Dr. Sharpless pointed out that this analysis is conservative because the researchers only evaluated two types of cancer. They chose breast and colorectal cancer because these are common cancers (accounting for about one-sixth of all cancers) with relatively high screening rates.
“We didn’t model other cancer types, but we have no reason to think that we’re not going to see the same thing with other types of malignancies,” he said. “That is a significant amount of excess mortality.”
Delayed diagnosis, modified therapy
One of the effects of the pandemic has been to cause delays in cancer diagnosis. “Routine screening has plummeted and is running at less than 90% in some systems,” Dr. Sharpless said.
“Most cancers are diagnosed when people experience symptoms and go see their doctors, and those symptomatic screening events are also not happening,” he continued. “Fear of contracting the coronavirus in health care settings has dissuaded people from visits.”
In some cases, a delay in diagnosis will allow the cancer to progress to a more advanced stage. “The earlier the diagnosis, the better, and if the stages are more advanced, patients will not do as well for virtually every kind of cancer,” he said.
In addition to delays in diagnosis, treatments are being postponed or modified for patients recently diagnosed with cancer. Because of delays and reductions in curative therapies, patients may be receiving less than optimal care.
“We are seeing a lot of nonstandard care,” said Dr. Sharpless. “All of these things add up to increased cancer morbidity and mortality.”
He also pointed out that the term “elective” is confusing and problematic. “It doesn’t mean that it’s not needed, just that it’s not an emergency and doesn’t need to be done today,” said Dr. Sharpless. “But if we’re talking about chemotherapy and surgery, we don’t think they can be delayed for too long – maybe a week, but not for several months.”
Dr. Sharpless feels that overall it is time for cancer care to resume as much as possible, because “ignoring cancer for too long is an untenable choice and may turn one public health crisis into another.”
“If we act now, we can make up for lost time,” he wrote in the editorial. “Clearly, postponing procedures and deferring care due to the pandemic was prudent at one time, but now that we have made it through the initial shock of the pandemic, I believe it is time to resume robust cancer care.”
Through their network of cancer centers, researchers with the NCI can develop innovative solutions that allow screening and treatment to move forward while maintaining safety. “We need to make patients feel safe, and we have to answer important questions quickly,” he said.
Impact of COVID-19 on cancer care
The COVID-19 pandemic has overwhelmed health care systems worldwide and has created major challenges for clinicians who are caring for patients with cancer.
As previously reported, hospitals reprioritized resources for an impending onslaught of COVID-19 patients. Services and procedures deemed to be nonessential were canceled or delayed, including surgeries and imaging.
In a survey conducted by the American Cancer Society Cancer Action Network, half of the 1219 respondents reported changes, delays, or disruptions to the care they were receiving. The services most frequently affected included in-person provider visits (50%), supportive services (20%), and imaging procedures to monitor tumor growth (20%).
In addition, 8% reported that their treatment, including chemotherapy and immunotherapy, had been affected by the COVID-19 pandemic.
In the United Kingdom, Cancer Research UK estimated that because of the disruption to cancer services, 2.4 million people did not undergo cancer screening or further testing or did not receive cancer treatment and that tens of thousands of cases have gone undiagnosed.
Similarly, a survey by Macmillan Cancer Support showed that almost half (45%) of cancer patients have experienced delays or cancellations of cancer treatments, or their treatments have been altered as a result of coronavirus, leaving many living in fear. Calling cancer “the forgotten C” of the pandemic, it warned of a potential cancer “time bomb” when, as the number of deaths from COVID-19 falls, cancer returns as the leading cause of death in the United Kingdom.
Last month, a report also predicted that there will be an excess of cancer deaths in both the United States and United Kingdom because of patients not accessing health care services.
The authors calculated that there will be 6270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients older than 40 years in the United States.
This article first appeared on Medscape.com.
A model created by the National Cancer Institute predicts that tens of thousands of excess cancer deaths will occur over the next decade as a result of missed screenings, delays in diagnosis, and reductions in oncology care caused by the COVID-19 pandemic.
“As director of NCI, I am deeply concerned about the potential impacts of delayed diagnoses and deferred or modified treatment plans on cancer incidence and mortality,” said Norman “Ned” Sharpless, MD.
“In the past 3 decades, we have seen steady and strong progress against death and suffering from cancer, thanks to improvements in prevention, screening, diagnosis, and treatment. I worry that the SARS-CoV-2 pandemic has put those decades of steady progress at risk and may precipitate reversals of these trends.”
In an editorial published June 19 in Science, Dr. Sharpless highlighted modeling performed by the NCI that predicts an excess of 10,000 deaths from breast and colorectal cancer over the next 10 years.
The number of excess deaths per year would peak in the next year or 2, likely sooner for colorectal than for breast cancer, but “for both cancer types, we believe the pandemic will influence cancer deaths for at least a decade.”
In an interview, Dr. Sharpless pointed out that this analysis is conservative because the researchers only evaluated two types of cancer. They chose breast and colorectal cancer because these are common cancers (accounting for about one-sixth of all cancers) with relatively high screening rates.
“We didn’t model other cancer types, but we have no reason to think that we’re not going to see the same thing with other types of malignancies,” he said. “That is a significant amount of excess mortality.”
Delayed diagnosis, modified therapy
One of the effects of the pandemic has been to cause delays in cancer diagnosis. “Routine screening has plummeted and is running at less than 90% in some systems,” Dr. Sharpless said.
“Most cancers are diagnosed when people experience symptoms and go see their doctors, and those symptomatic screening events are also not happening,” he continued. “Fear of contracting the coronavirus in health care settings has dissuaded people from visits.”
In some cases, a delay in diagnosis will allow the cancer to progress to a more advanced stage. “The earlier the diagnosis, the better, and if the stages are more advanced, patients will not do as well for virtually every kind of cancer,” he said.
In addition to delays in diagnosis, treatments are being postponed or modified for patients recently diagnosed with cancer. Because of delays and reductions in curative therapies, patients may be receiving less than optimal care.
“We are seeing a lot of nonstandard care,” said Dr. Sharpless. “All of these things add up to increased cancer morbidity and mortality.”
He also pointed out that the term “elective” is confusing and problematic. “It doesn’t mean that it’s not needed, just that it’s not an emergency and doesn’t need to be done today,” said Dr. Sharpless. “But if we’re talking about chemotherapy and surgery, we don’t think they can be delayed for too long – maybe a week, but not for several months.”
Dr. Sharpless feels that overall it is time for cancer care to resume as much as possible, because “ignoring cancer for too long is an untenable choice and may turn one public health crisis into another.”
“If we act now, we can make up for lost time,” he wrote in the editorial. “Clearly, postponing procedures and deferring care due to the pandemic was prudent at one time, but now that we have made it through the initial shock of the pandemic, I believe it is time to resume robust cancer care.”
Through their network of cancer centers, researchers with the NCI can develop innovative solutions that allow screening and treatment to move forward while maintaining safety. “We need to make patients feel safe, and we have to answer important questions quickly,” he said.
Impact of COVID-19 on cancer care
The COVID-19 pandemic has overwhelmed health care systems worldwide and has created major challenges for clinicians who are caring for patients with cancer.
As previously reported, hospitals reprioritized resources for an impending onslaught of COVID-19 patients. Services and procedures deemed to be nonessential were canceled or delayed, including surgeries and imaging.
In a survey conducted by the American Cancer Society Cancer Action Network, half of the 1219 respondents reported changes, delays, or disruptions to the care they were receiving. The services most frequently affected included in-person provider visits (50%), supportive services (20%), and imaging procedures to monitor tumor growth (20%).
In addition, 8% reported that their treatment, including chemotherapy and immunotherapy, had been affected by the COVID-19 pandemic.
In the United Kingdom, Cancer Research UK estimated that because of the disruption to cancer services, 2.4 million people did not undergo cancer screening or further testing or did not receive cancer treatment and that tens of thousands of cases have gone undiagnosed.
Similarly, a survey by Macmillan Cancer Support showed that almost half (45%) of cancer patients have experienced delays or cancellations of cancer treatments, or their treatments have been altered as a result of coronavirus, leaving many living in fear. Calling cancer “the forgotten C” of the pandemic, it warned of a potential cancer “time bomb” when, as the number of deaths from COVID-19 falls, cancer returns as the leading cause of death in the United Kingdom.
Last month, a report also predicted that there will be an excess of cancer deaths in both the United States and United Kingdom because of patients not accessing health care services.
The authors calculated that there will be 6270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients older than 40 years in the United States.
This article first appeared on Medscape.com.
‘Hospital at home’ cuts ED visits and costs for cancer patients
Visits to the emergency department (ED) and hospitalizations are often frequent occurrences for cancer patients, but what if the “hospital” could be brought into the home instead?
A new American cohort study provides evidence that this can be a workable option for cancer patients. The authors report improved patient outcomes, with 56% lower odds of unplanned hospitalizations (P = .001), 45% lower odds of ED visits (P = .037), and 50% lower cumulative charges (P = .001), as compared with patients who received usual care.
“The oncology hospital-at-home model of care that extends acute-level care to the patient at home offers promise in addressing a long-term gap in cancer care service delivery,” said lead author Kathi Mooney, PhD, RN, interim senior director of population sciences at the Huntsman Cancer Institute and distinguished professor of nursing at the University of Utah, Salt Lake City. “In light of the current global pandemic, we are compelled to consider new ways to provide cancer care, and the oncology hospital-at-home model is on point to address critical elements of an improved cancer care delivery system.”
Mooney presented the findings during the virtual scientific program of the American Society of Clinical Oncology 2020 annual meeting (abstract 7000).
The hospital-at-home model of care provides hospital-level care in the comfort of the patient’s home and is a component of many healthcare systems worldwide. Although it was introduced in the United States more than 2 decades ago, it has not been widely adopted or studied specifically in oncology.
Most cancer treatment is provided on an outpatient basis, which means that patients experience significant adverse events, toxicities, and disease progression while they are at home. Thus, Mooney noted, patients tend to rely heavily on the ED and sometimes experience unplanned hospitalizations and 30-day readmissions.
“These care patterns are distressing to the patients and their families and tax healthcare resources,” she said. “They are even more concerning and salient as we endeavor to protect cancer patients and provide cancer care during a pandemic.”
Currently, strategies to evaluate and support cancer patients and caregivers at home are limited. In 2018, the Huntsman Cancer Institute implemented Huntsman at Home, a demonstration project to evaluate the utility of an oncology hospital-at-home model.
Significantly Fewer Unplanned Hospitalizations
Huntsman at Home is run by nurse practitioner and registered nurse teams who deliver acute-level care at home. Physicians provide backup support for both medical oncology and palliative care. Nurse practitioners also work directly with the patient’s oncology team to coordinate care needs, including services such as social work and physical therapy.
To evaluate the hospital-at-home model, Mooney and colleagues compared patients who were enrolled in the program with those who received usual care. The usual-care comparison group was drawn from patients who lived in the Salt Lake City area. These patients would have qualified for enrollment in the Huntsman at Home program, but they lived outside the 20-mile service area.
The cohort included 367 patients (169 Huntsman at Home patients and 198 usual-care patients). Of those patients, 77% had stage IV cancer. A range of cancer types was represented; the most common were colon, gynecologic, prostate, and lung cancers. As compared to the usual-care group, those in the home model were more likely to be women (61% vs 43%).
During the first 30 days after admission, Huntsman at Home patients had significantly fewer unplanned hospitalizations (19.5% vs 35.4%) and a shorter length of stay (1.4 vs 2.6 days). Their care was also less expensive. The estimated charges for the hospital-at-home patients was $10,238, compared with $21,363 for the usual-care patients. There was no real difference in stays in the intensive care unit between the two groups.
Mooney noted that since there have been few studies of the hospital-at-home model for oncology patients, the investigators’ initial focus was on patients at hospital discharge who needed continued acute-level care and those who had acute problems identified through their oncology care clinic. Therefore, patients were not admitted to the program directly from emergency services, and chemotherapy infusions were not provided, although these are “other areas to consider in an oncology hospital-at-home model.”
Other limitations of the study were that it was not a randomized trial, and the evaluation was from a single program located at one comprehensive cancer center.
“These findings provide the oncology community with an opportunity to rethink cancer care as solely hospital- and clinic-based and instead reimagine care delivery that moves with the patient with key components provided at home,” said Mooney. “We plan to continue the development and evaluation of Huntsman at Home and extend care to admission from the emergency department.”
She added that, together with Flatiron Health, they are validating a tool to prospectively predict, on the basis of the likelihood of ED use, which patients may benefit from Huntsman at Home support. They also plan to extend care to patients who live at a distance from the cancer center and in rural communities, and may include chemotherapy infusion services.
Palliative Care Patients Prefer Home-Based Treatment
In a discussion of the paper, Lynne Wagner, PhD, a professor in the Department of Social Sciences and Health Policy with the Wake Forest School of Medicine, Winston-Salem, North Carolina, and a member of the Wake Forest Baptist Comprehensive Cancer Center, explained that some “aspects of healthcare are more translatable to a virtual or alternative delivery model than others. An area of cancer care greatly in need of innovation and quality improvement pertains to the management of oncologic emergencies.”
She pointed out that optimal care for oncologic emergencies requires the “intersection of oncology and emergency medicine specialists,” but there are often no well-defined processes for care coordination in place.
“Emergency department utilization could be reduced through greater precision with regard to risk stratification and early intervention and improved outpatient management, including improved symptom management,” said Wagner.
Wagner suggested that research should incorporate patient-reported outcomes so as to measure patient-centered benefits of home-based care. “Patients who are receiving palliative care services prefer home-based care, and it’s reasonable to anticipate this finding would extrapolate to the investigator’s target population,” she said. “However, there may also be unanticipated consequences, potentially including increased anxiety or increased burden on caretakers.”
In addition, the tangible and intangible costs associated with traveling to receive healthcare services and time away from work can be reduced with home-based care, and this should also be quantified. “The costs associated with COVID infection should be estimated to realize the full economic value of this care model, given significant reductions in cohort exposure afforded by home-based visits,” Wagner added.
The Huntsman at Home program is funded by the Huntsman Cancer Institute. The evaluation was funded by the Cambia Health Foundation. Mooney has a consulting or advisory role with Cognitive Medical System, Inc, and has patents, royalties, and other intellectual property for the development of Symptom Care at Home, a remote symptom-monitoring platform developed through research grants funded by the National Cancer Institute. No royalties have been received to date. Wagner has relationships with Celgene, Eli Lilly, Gilead Sciences, and Johnson & Johnson.
This article first appeared on Medscape.com.
Visits to the emergency department (ED) and hospitalizations are often frequent occurrences for cancer patients, but what if the “hospital” could be brought into the home instead?
A new American cohort study provides evidence that this can be a workable option for cancer patients. The authors report improved patient outcomes, with 56% lower odds of unplanned hospitalizations (P = .001), 45% lower odds of ED visits (P = .037), and 50% lower cumulative charges (P = .001), as compared with patients who received usual care.
“The oncology hospital-at-home model of care that extends acute-level care to the patient at home offers promise in addressing a long-term gap in cancer care service delivery,” said lead author Kathi Mooney, PhD, RN, interim senior director of population sciences at the Huntsman Cancer Institute and distinguished professor of nursing at the University of Utah, Salt Lake City. “In light of the current global pandemic, we are compelled to consider new ways to provide cancer care, and the oncology hospital-at-home model is on point to address critical elements of an improved cancer care delivery system.”
Mooney presented the findings during the virtual scientific program of the American Society of Clinical Oncology 2020 annual meeting (abstract 7000).
The hospital-at-home model of care provides hospital-level care in the comfort of the patient’s home and is a component of many healthcare systems worldwide. Although it was introduced in the United States more than 2 decades ago, it has not been widely adopted or studied specifically in oncology.
Most cancer treatment is provided on an outpatient basis, which means that patients experience significant adverse events, toxicities, and disease progression while they are at home. Thus, Mooney noted, patients tend to rely heavily on the ED and sometimes experience unplanned hospitalizations and 30-day readmissions.
“These care patterns are distressing to the patients and their families and tax healthcare resources,” she said. “They are even more concerning and salient as we endeavor to protect cancer patients and provide cancer care during a pandemic.”
Currently, strategies to evaluate and support cancer patients and caregivers at home are limited. In 2018, the Huntsman Cancer Institute implemented Huntsman at Home, a demonstration project to evaluate the utility of an oncology hospital-at-home model.
Significantly Fewer Unplanned Hospitalizations
Huntsman at Home is run by nurse practitioner and registered nurse teams who deliver acute-level care at home. Physicians provide backup support for both medical oncology and palliative care. Nurse practitioners also work directly with the patient’s oncology team to coordinate care needs, including services such as social work and physical therapy.
To evaluate the hospital-at-home model, Mooney and colleagues compared patients who were enrolled in the program with those who received usual care. The usual-care comparison group was drawn from patients who lived in the Salt Lake City area. These patients would have qualified for enrollment in the Huntsman at Home program, but they lived outside the 20-mile service area.
The cohort included 367 patients (169 Huntsman at Home patients and 198 usual-care patients). Of those patients, 77% had stage IV cancer. A range of cancer types was represented; the most common were colon, gynecologic, prostate, and lung cancers. As compared to the usual-care group, those in the home model were more likely to be women (61% vs 43%).
During the first 30 days after admission, Huntsman at Home patients had significantly fewer unplanned hospitalizations (19.5% vs 35.4%) and a shorter length of stay (1.4 vs 2.6 days). Their care was also less expensive. The estimated charges for the hospital-at-home patients was $10,238, compared with $21,363 for the usual-care patients. There was no real difference in stays in the intensive care unit between the two groups.
Mooney noted that since there have been few studies of the hospital-at-home model for oncology patients, the investigators’ initial focus was on patients at hospital discharge who needed continued acute-level care and those who had acute problems identified through their oncology care clinic. Therefore, patients were not admitted to the program directly from emergency services, and chemotherapy infusions were not provided, although these are “other areas to consider in an oncology hospital-at-home model.”
Other limitations of the study were that it was not a randomized trial, and the evaluation was from a single program located at one comprehensive cancer center.
“These findings provide the oncology community with an opportunity to rethink cancer care as solely hospital- and clinic-based and instead reimagine care delivery that moves with the patient with key components provided at home,” said Mooney. “We plan to continue the development and evaluation of Huntsman at Home and extend care to admission from the emergency department.”
She added that, together with Flatiron Health, they are validating a tool to prospectively predict, on the basis of the likelihood of ED use, which patients may benefit from Huntsman at Home support. They also plan to extend care to patients who live at a distance from the cancer center and in rural communities, and may include chemotherapy infusion services.
Palliative Care Patients Prefer Home-Based Treatment
In a discussion of the paper, Lynne Wagner, PhD, a professor in the Department of Social Sciences and Health Policy with the Wake Forest School of Medicine, Winston-Salem, North Carolina, and a member of the Wake Forest Baptist Comprehensive Cancer Center, explained that some “aspects of healthcare are more translatable to a virtual or alternative delivery model than others. An area of cancer care greatly in need of innovation and quality improvement pertains to the management of oncologic emergencies.”
She pointed out that optimal care for oncologic emergencies requires the “intersection of oncology and emergency medicine specialists,” but there are often no well-defined processes for care coordination in place.
“Emergency department utilization could be reduced through greater precision with regard to risk stratification and early intervention and improved outpatient management, including improved symptom management,” said Wagner.
Wagner suggested that research should incorporate patient-reported outcomes so as to measure patient-centered benefits of home-based care. “Patients who are receiving palliative care services prefer home-based care, and it’s reasonable to anticipate this finding would extrapolate to the investigator’s target population,” she said. “However, there may also be unanticipated consequences, potentially including increased anxiety or increased burden on caretakers.”
In addition, the tangible and intangible costs associated with traveling to receive healthcare services and time away from work can be reduced with home-based care, and this should also be quantified. “The costs associated with COVID infection should be estimated to realize the full economic value of this care model, given significant reductions in cohort exposure afforded by home-based visits,” Wagner added.
The Huntsman at Home program is funded by the Huntsman Cancer Institute. The evaluation was funded by the Cambia Health Foundation. Mooney has a consulting or advisory role with Cognitive Medical System, Inc, and has patents, royalties, and other intellectual property for the development of Symptom Care at Home, a remote symptom-monitoring platform developed through research grants funded by the National Cancer Institute. No royalties have been received to date. Wagner has relationships with Celgene, Eli Lilly, Gilead Sciences, and Johnson & Johnson.
This article first appeared on Medscape.com.
Visits to the emergency department (ED) and hospitalizations are often frequent occurrences for cancer patients, but what if the “hospital” could be brought into the home instead?
A new American cohort study provides evidence that this can be a workable option for cancer patients. The authors report improved patient outcomes, with 56% lower odds of unplanned hospitalizations (P = .001), 45% lower odds of ED visits (P = .037), and 50% lower cumulative charges (P = .001), as compared with patients who received usual care.
“The oncology hospital-at-home model of care that extends acute-level care to the patient at home offers promise in addressing a long-term gap in cancer care service delivery,” said lead author Kathi Mooney, PhD, RN, interim senior director of population sciences at the Huntsman Cancer Institute and distinguished professor of nursing at the University of Utah, Salt Lake City. “In light of the current global pandemic, we are compelled to consider new ways to provide cancer care, and the oncology hospital-at-home model is on point to address critical elements of an improved cancer care delivery system.”
Mooney presented the findings during the virtual scientific program of the American Society of Clinical Oncology 2020 annual meeting (abstract 7000).
The hospital-at-home model of care provides hospital-level care in the comfort of the patient’s home and is a component of many healthcare systems worldwide. Although it was introduced in the United States more than 2 decades ago, it has not been widely adopted or studied specifically in oncology.
Most cancer treatment is provided on an outpatient basis, which means that patients experience significant adverse events, toxicities, and disease progression while they are at home. Thus, Mooney noted, patients tend to rely heavily on the ED and sometimes experience unplanned hospitalizations and 30-day readmissions.
“These care patterns are distressing to the patients and their families and tax healthcare resources,” she said. “They are even more concerning and salient as we endeavor to protect cancer patients and provide cancer care during a pandemic.”
Currently, strategies to evaluate and support cancer patients and caregivers at home are limited. In 2018, the Huntsman Cancer Institute implemented Huntsman at Home, a demonstration project to evaluate the utility of an oncology hospital-at-home model.
Significantly Fewer Unplanned Hospitalizations
Huntsman at Home is run by nurse practitioner and registered nurse teams who deliver acute-level care at home. Physicians provide backup support for both medical oncology and palliative care. Nurse practitioners also work directly with the patient’s oncology team to coordinate care needs, including services such as social work and physical therapy.
To evaluate the hospital-at-home model, Mooney and colleagues compared patients who were enrolled in the program with those who received usual care. The usual-care comparison group was drawn from patients who lived in the Salt Lake City area. These patients would have qualified for enrollment in the Huntsman at Home program, but they lived outside the 20-mile service area.
The cohort included 367 patients (169 Huntsman at Home patients and 198 usual-care patients). Of those patients, 77% had stage IV cancer. A range of cancer types was represented; the most common were colon, gynecologic, prostate, and lung cancers. As compared to the usual-care group, those in the home model were more likely to be women (61% vs 43%).
During the first 30 days after admission, Huntsman at Home patients had significantly fewer unplanned hospitalizations (19.5% vs 35.4%) and a shorter length of stay (1.4 vs 2.6 days). Their care was also less expensive. The estimated charges for the hospital-at-home patients was $10,238, compared with $21,363 for the usual-care patients. There was no real difference in stays in the intensive care unit between the two groups.
Mooney noted that since there have been few studies of the hospital-at-home model for oncology patients, the investigators’ initial focus was on patients at hospital discharge who needed continued acute-level care and those who had acute problems identified through their oncology care clinic. Therefore, patients were not admitted to the program directly from emergency services, and chemotherapy infusions were not provided, although these are “other areas to consider in an oncology hospital-at-home model.”
Other limitations of the study were that it was not a randomized trial, and the evaluation was from a single program located at one comprehensive cancer center.
“These findings provide the oncology community with an opportunity to rethink cancer care as solely hospital- and clinic-based and instead reimagine care delivery that moves with the patient with key components provided at home,” said Mooney. “We plan to continue the development and evaluation of Huntsman at Home and extend care to admission from the emergency department.”
She added that, together with Flatiron Health, they are validating a tool to prospectively predict, on the basis of the likelihood of ED use, which patients may benefit from Huntsman at Home support. They also plan to extend care to patients who live at a distance from the cancer center and in rural communities, and may include chemotherapy infusion services.
Palliative Care Patients Prefer Home-Based Treatment
In a discussion of the paper, Lynne Wagner, PhD, a professor in the Department of Social Sciences and Health Policy with the Wake Forest School of Medicine, Winston-Salem, North Carolina, and a member of the Wake Forest Baptist Comprehensive Cancer Center, explained that some “aspects of healthcare are more translatable to a virtual or alternative delivery model than others. An area of cancer care greatly in need of innovation and quality improvement pertains to the management of oncologic emergencies.”
She pointed out that optimal care for oncologic emergencies requires the “intersection of oncology and emergency medicine specialists,” but there are often no well-defined processes for care coordination in place.
“Emergency department utilization could be reduced through greater precision with regard to risk stratification and early intervention and improved outpatient management, including improved symptom management,” said Wagner.
Wagner suggested that research should incorporate patient-reported outcomes so as to measure patient-centered benefits of home-based care. “Patients who are receiving palliative care services prefer home-based care, and it’s reasonable to anticipate this finding would extrapolate to the investigator’s target population,” she said. “However, there may also be unanticipated consequences, potentially including increased anxiety or increased burden on caretakers.”
In addition, the tangible and intangible costs associated with traveling to receive healthcare services and time away from work can be reduced with home-based care, and this should also be quantified. “The costs associated with COVID infection should be estimated to realize the full economic value of this care model, given significant reductions in cohort exposure afforded by home-based visits,” Wagner added.
The Huntsman at Home program is funded by the Huntsman Cancer Institute. The evaluation was funded by the Cambia Health Foundation. Mooney has a consulting or advisory role with Cognitive Medical System, Inc, and has patents, royalties, and other intellectual property for the development of Symptom Care at Home, a remote symptom-monitoring platform developed through research grants funded by the National Cancer Institute. No royalties have been received to date. Wagner has relationships with Celgene, Eli Lilly, Gilead Sciences, and Johnson & Johnson.
This article first appeared on Medscape.com.
FROM ASCO 2020
EBV may worsen immune checkpoint inhibitor–induced colitis
For patients with immune checkpoint inhibitor–induced colitis, Epstein-Barr virus (EBV) infection may increase risks of steroid-refractory disease and ulcers that contribute to colonic perforation, according to investigators.
Pending further research, routine monitoring of EBV status may be needed for patients undergoing checkpoint inhibitor therapy, reported lead author Matthew R. Pugh, FRCPath, of University Hospital of Wales, Cardiff, and colleagues.
“Few studies have investigated the role of viruses in the pathogenesis of immune-related colitis,” the investigators wrote. Their report is in Clinical Gastroenterology and Hepatology. While cytomegalovirus has been linked with worse disease, no studies to date have evaluated the role of EBV, they noted, despite theoretical concerns.
“A spectrum of EBV-positive lymphoproliferations shows a predilection for the GI tract, ranging from indolent lesions to aggressive lymphomas,” the investigators wrote. “One such proliferation, EBV-positive mucocutaneous ulcer (EBVMCU), is an indolent, ulcerating process associated with immunosuppression,” they added, referring to studies involving patients with inflammatory bowel disease.
To determine if EBV could be playing a similar role in cancer immunotherapy, the investigators retrospectively analyzed colon tissue samples from 16 patients who developed colitis after undergoing immune checkpoint inhibitor therapy between 2010 and 2018. Thirteen patients received an anti-CTLA-4 agent, three were treated with a PD-1 inhibitor, and four received both types of therapy. Most patients had advanced-stage melanoma (n = 14), while the remaining two patients had prostate and renal carcinoma, respectively. Ten samples were biopsies, whereas four specimens were collected from surgical repair of colon perforation.
EBV status was determined by chromogenic in situ hybridization for EBV-encoded small RNA, with positive samples further characterized by immunohistochemistry for CD3, CD15, CD20, CD30, CD138, MUM1, and PAX5. In addition, all samples were immunostained for cytomegalovirus, and PCR was used to assess B cell and T cell clonality.
The median time from induction of therapy to colitis onset was approximately 1 month (32.5 days), with symptoms typically lasting 3 weeks (22.5 days). Macroscopically, 10 patients had ulceration, and 6 displayed signs of hemorrhage.
EBVMCUs were found in four patients, of whom three had received anti-CTLA-4 therapy, one had received both anti-CTLA-4 and anti-PD-1 therapy, and all had undergone colonic resection. One case also tested positive for cytomegalovirus.
Immunostaining showed that EBVMCUs had underlying B cell and linear plasma cell infiltrates, with “a rim of small T lymphocytes at the base.” EBV-encoded small RNA expression was found in both plasma cells and small B cells.
The presence of EBVMCUs was significantly associated with more severe colitis.
All four EBV-positive patients had steroid-refractory colitis, compared with only two (12.5%) of the EBV-negative patients (P = .008), a difference that was echoed by the rate of colonic resection (100% vs. 12.5%; P .008). Furthermore, colon perforation occurred in all EBV-positive patients, versus none of the EBV-negative patients (P = .001).
For three EBV-positive patients, preresection biopsy samples were available, allowing for temporal analysis of EBV-encoded small RNA. Earlier samples had reduced or absent EBV-positive lymphoid cells, which offered some etiologic insight.
“The apparent absence or paucity of EBV-positive lymphoid cells in biopsies taken before resection suggests that EBVMCU is arising within preexisting immune-mediated inflammation rather than EBV driving the initial inflammatory insult,” the investigators wrote.
They suggested that EBVMCUs “likely contribute directly to colonic perforation,” since lesions are characterized by a form of localized tissue destruction that has been previously associated with colonic perforation in Crohn’s disease and intestinal perforation in rheumatoid arthritis.
Still, mechanisms of action remain unknown. “It is unclear why EBVMCUs should arise in the context of immune checkpoint regulator therapy, which, in contrast to conventional immunosuppressants, results in immune activation,” the investigators wrote. “It is possible that these patients may harbor residual immunosuppression resulting from their disease burden, advanced age, and prior immunosuppression.”
While more work is needed, Dr. Pugh and colleagues suggested that EBV testing may be valuable for some patients.
“The findings support the need for further studies investigating the role of EBV monitoring in immune checkpoint regulator therapy, which is not currently part of routine protocols.”
The study was funded by All Wales Lymphoma Panel. The investigators disclosed no conflicts of interest.
SOURCE: Pugh et al. Clin Gastroenterol Hepatol. 2019 Oct 11. doi: 10.1016/j.cgh.2019.09.031.
Immune checkpoint regulators (iCRs) have become common in the treatment for various cancers. Immune-related colitis (irColitis) is among the most common side effects of iCRs, as well as one of the most common etiologies of fatal toxicities from iCRs. However, much is still unknown on the pathophysiology behind irColitis or its complications. Pugh et al. performed detailed analyses of the potential role of Epstein-Barr virus (EBV) in irColitis. Rather than depend on serologies for EBV, the investigators utilized robust evaluation for colonic mucosal EBV with in situ hybridization, immunohistochemistry, and polymerase chain reaction. Interestingly, in the EBV-positive patients with endoscopic biopsies performed prior to perforation, EBV RNA were minimal or absent on endoscopic biopsies. This finding suggests EBV may be related to the immunosuppression used to treat the colitis rather than the primary driver of irColitis. This observation could have important clinical implications in using steroids for irColitis; we may be increasing the risk of perforation related to EBV by using steroids or other immunosuppression. While we need to interpret these findings with caution given the small sample size and comparisons between endoscopic biopsies and surgical specimens for EBV, this study highlights the potential role of EBV in steroid-refractory irColitis. An additional clinical implication from this study is that endoscopic biopsies did not identify patients who would eventually develop colonic perforation. We therefore cannot assume a patient with negative colonic biopsies for EBV is truly negative. Better means for assessing EBV status and predicting complications are still needed.
Jason K. Hou, MD, is assistant professor of medicine and gastroenterology; director of the GI and hepatology fellowship program; and director of research and IBD at Baylor College of Medicine, Houston. He is a staff physician in the department of gastroenterology, and medical director, IBD, at Michael E. DeBakey VA Medical Center, Houston. He has no conflicts of interest.
Immune checkpoint regulators (iCRs) have become common in the treatment for various cancers. Immune-related colitis (irColitis) is among the most common side effects of iCRs, as well as one of the most common etiologies of fatal toxicities from iCRs. However, much is still unknown on the pathophysiology behind irColitis or its complications. Pugh et al. performed detailed analyses of the potential role of Epstein-Barr virus (EBV) in irColitis. Rather than depend on serologies for EBV, the investigators utilized robust evaluation for colonic mucosal EBV with in situ hybridization, immunohistochemistry, and polymerase chain reaction. Interestingly, in the EBV-positive patients with endoscopic biopsies performed prior to perforation, EBV RNA were minimal or absent on endoscopic biopsies. This finding suggests EBV may be related to the immunosuppression used to treat the colitis rather than the primary driver of irColitis. This observation could have important clinical implications in using steroids for irColitis; we may be increasing the risk of perforation related to EBV by using steroids or other immunosuppression. While we need to interpret these findings with caution given the small sample size and comparisons between endoscopic biopsies and surgical specimens for EBV, this study highlights the potential role of EBV in steroid-refractory irColitis. An additional clinical implication from this study is that endoscopic biopsies did not identify patients who would eventually develop colonic perforation. We therefore cannot assume a patient with negative colonic biopsies for EBV is truly negative. Better means for assessing EBV status and predicting complications are still needed.
Jason K. Hou, MD, is assistant professor of medicine and gastroenterology; director of the GI and hepatology fellowship program; and director of research and IBD at Baylor College of Medicine, Houston. He is a staff physician in the department of gastroenterology, and medical director, IBD, at Michael E. DeBakey VA Medical Center, Houston. He has no conflicts of interest.
Immune checkpoint regulators (iCRs) have become common in the treatment for various cancers. Immune-related colitis (irColitis) is among the most common side effects of iCRs, as well as one of the most common etiologies of fatal toxicities from iCRs. However, much is still unknown on the pathophysiology behind irColitis or its complications. Pugh et al. performed detailed analyses of the potential role of Epstein-Barr virus (EBV) in irColitis. Rather than depend on serologies for EBV, the investigators utilized robust evaluation for colonic mucosal EBV with in situ hybridization, immunohistochemistry, and polymerase chain reaction. Interestingly, in the EBV-positive patients with endoscopic biopsies performed prior to perforation, EBV RNA were minimal or absent on endoscopic biopsies. This finding suggests EBV may be related to the immunosuppression used to treat the colitis rather than the primary driver of irColitis. This observation could have important clinical implications in using steroids for irColitis; we may be increasing the risk of perforation related to EBV by using steroids or other immunosuppression. While we need to interpret these findings with caution given the small sample size and comparisons between endoscopic biopsies and surgical specimens for EBV, this study highlights the potential role of EBV in steroid-refractory irColitis. An additional clinical implication from this study is that endoscopic biopsies did not identify patients who would eventually develop colonic perforation. We therefore cannot assume a patient with negative colonic biopsies for EBV is truly negative. Better means for assessing EBV status and predicting complications are still needed.
Jason K. Hou, MD, is assistant professor of medicine and gastroenterology; director of the GI and hepatology fellowship program; and director of research and IBD at Baylor College of Medicine, Houston. He is a staff physician in the department of gastroenterology, and medical director, IBD, at Michael E. DeBakey VA Medical Center, Houston. He has no conflicts of interest.
For patients with immune checkpoint inhibitor–induced colitis, Epstein-Barr virus (EBV) infection may increase risks of steroid-refractory disease and ulcers that contribute to colonic perforation, according to investigators.
Pending further research, routine monitoring of EBV status may be needed for patients undergoing checkpoint inhibitor therapy, reported lead author Matthew R. Pugh, FRCPath, of University Hospital of Wales, Cardiff, and colleagues.
“Few studies have investigated the role of viruses in the pathogenesis of immune-related colitis,” the investigators wrote. Their report is in Clinical Gastroenterology and Hepatology. While cytomegalovirus has been linked with worse disease, no studies to date have evaluated the role of EBV, they noted, despite theoretical concerns.
“A spectrum of EBV-positive lymphoproliferations shows a predilection for the GI tract, ranging from indolent lesions to aggressive lymphomas,” the investigators wrote. “One such proliferation, EBV-positive mucocutaneous ulcer (EBVMCU), is an indolent, ulcerating process associated with immunosuppression,” they added, referring to studies involving patients with inflammatory bowel disease.
To determine if EBV could be playing a similar role in cancer immunotherapy, the investigators retrospectively analyzed colon tissue samples from 16 patients who developed colitis after undergoing immune checkpoint inhibitor therapy between 2010 and 2018. Thirteen patients received an anti-CTLA-4 agent, three were treated with a PD-1 inhibitor, and four received both types of therapy. Most patients had advanced-stage melanoma (n = 14), while the remaining two patients had prostate and renal carcinoma, respectively. Ten samples were biopsies, whereas four specimens were collected from surgical repair of colon perforation.
EBV status was determined by chromogenic in situ hybridization for EBV-encoded small RNA, with positive samples further characterized by immunohistochemistry for CD3, CD15, CD20, CD30, CD138, MUM1, and PAX5. In addition, all samples were immunostained for cytomegalovirus, and PCR was used to assess B cell and T cell clonality.
The median time from induction of therapy to colitis onset was approximately 1 month (32.5 days), with symptoms typically lasting 3 weeks (22.5 days). Macroscopically, 10 patients had ulceration, and 6 displayed signs of hemorrhage.
EBVMCUs were found in four patients, of whom three had received anti-CTLA-4 therapy, one had received both anti-CTLA-4 and anti-PD-1 therapy, and all had undergone colonic resection. One case also tested positive for cytomegalovirus.
Immunostaining showed that EBVMCUs had underlying B cell and linear plasma cell infiltrates, with “a rim of small T lymphocytes at the base.” EBV-encoded small RNA expression was found in both plasma cells and small B cells.
The presence of EBVMCUs was significantly associated with more severe colitis.
All four EBV-positive patients had steroid-refractory colitis, compared with only two (12.5%) of the EBV-negative patients (P = .008), a difference that was echoed by the rate of colonic resection (100% vs. 12.5%; P .008). Furthermore, colon perforation occurred in all EBV-positive patients, versus none of the EBV-negative patients (P = .001).
For three EBV-positive patients, preresection biopsy samples were available, allowing for temporal analysis of EBV-encoded small RNA. Earlier samples had reduced or absent EBV-positive lymphoid cells, which offered some etiologic insight.
“The apparent absence or paucity of EBV-positive lymphoid cells in biopsies taken before resection suggests that EBVMCU is arising within preexisting immune-mediated inflammation rather than EBV driving the initial inflammatory insult,” the investigators wrote.
They suggested that EBVMCUs “likely contribute directly to colonic perforation,” since lesions are characterized by a form of localized tissue destruction that has been previously associated with colonic perforation in Crohn’s disease and intestinal perforation in rheumatoid arthritis.
Still, mechanisms of action remain unknown. “It is unclear why EBVMCUs should arise in the context of immune checkpoint regulator therapy, which, in contrast to conventional immunosuppressants, results in immune activation,” the investigators wrote. “It is possible that these patients may harbor residual immunosuppression resulting from their disease burden, advanced age, and prior immunosuppression.”
While more work is needed, Dr. Pugh and colleagues suggested that EBV testing may be valuable for some patients.
“The findings support the need for further studies investigating the role of EBV monitoring in immune checkpoint regulator therapy, which is not currently part of routine protocols.”
The study was funded by All Wales Lymphoma Panel. The investigators disclosed no conflicts of interest.
SOURCE: Pugh et al. Clin Gastroenterol Hepatol. 2019 Oct 11. doi: 10.1016/j.cgh.2019.09.031.
For patients with immune checkpoint inhibitor–induced colitis, Epstein-Barr virus (EBV) infection may increase risks of steroid-refractory disease and ulcers that contribute to colonic perforation, according to investigators.
Pending further research, routine monitoring of EBV status may be needed for patients undergoing checkpoint inhibitor therapy, reported lead author Matthew R. Pugh, FRCPath, of University Hospital of Wales, Cardiff, and colleagues.
“Few studies have investigated the role of viruses in the pathogenesis of immune-related colitis,” the investigators wrote. Their report is in Clinical Gastroenterology and Hepatology. While cytomegalovirus has been linked with worse disease, no studies to date have evaluated the role of EBV, they noted, despite theoretical concerns.
“A spectrum of EBV-positive lymphoproliferations shows a predilection for the GI tract, ranging from indolent lesions to aggressive lymphomas,” the investigators wrote. “One such proliferation, EBV-positive mucocutaneous ulcer (EBVMCU), is an indolent, ulcerating process associated with immunosuppression,” they added, referring to studies involving patients with inflammatory bowel disease.
To determine if EBV could be playing a similar role in cancer immunotherapy, the investigators retrospectively analyzed colon tissue samples from 16 patients who developed colitis after undergoing immune checkpoint inhibitor therapy between 2010 and 2018. Thirteen patients received an anti-CTLA-4 agent, three were treated with a PD-1 inhibitor, and four received both types of therapy. Most patients had advanced-stage melanoma (n = 14), while the remaining two patients had prostate and renal carcinoma, respectively. Ten samples were biopsies, whereas four specimens were collected from surgical repair of colon perforation.
EBV status was determined by chromogenic in situ hybridization for EBV-encoded small RNA, with positive samples further characterized by immunohistochemistry for CD3, CD15, CD20, CD30, CD138, MUM1, and PAX5. In addition, all samples were immunostained for cytomegalovirus, and PCR was used to assess B cell and T cell clonality.
The median time from induction of therapy to colitis onset was approximately 1 month (32.5 days), with symptoms typically lasting 3 weeks (22.5 days). Macroscopically, 10 patients had ulceration, and 6 displayed signs of hemorrhage.
EBVMCUs were found in four patients, of whom three had received anti-CTLA-4 therapy, one had received both anti-CTLA-4 and anti-PD-1 therapy, and all had undergone colonic resection. One case also tested positive for cytomegalovirus.
Immunostaining showed that EBVMCUs had underlying B cell and linear plasma cell infiltrates, with “a rim of small T lymphocytes at the base.” EBV-encoded small RNA expression was found in both plasma cells and small B cells.
The presence of EBVMCUs was significantly associated with more severe colitis.
All four EBV-positive patients had steroid-refractory colitis, compared with only two (12.5%) of the EBV-negative patients (P = .008), a difference that was echoed by the rate of colonic resection (100% vs. 12.5%; P .008). Furthermore, colon perforation occurred in all EBV-positive patients, versus none of the EBV-negative patients (P = .001).
For three EBV-positive patients, preresection biopsy samples were available, allowing for temporal analysis of EBV-encoded small RNA. Earlier samples had reduced or absent EBV-positive lymphoid cells, which offered some etiologic insight.
“The apparent absence or paucity of EBV-positive lymphoid cells in biopsies taken before resection suggests that EBVMCU is arising within preexisting immune-mediated inflammation rather than EBV driving the initial inflammatory insult,” the investigators wrote.
They suggested that EBVMCUs “likely contribute directly to colonic perforation,” since lesions are characterized by a form of localized tissue destruction that has been previously associated with colonic perforation in Crohn’s disease and intestinal perforation in rheumatoid arthritis.
Still, mechanisms of action remain unknown. “It is unclear why EBVMCUs should arise in the context of immune checkpoint regulator therapy, which, in contrast to conventional immunosuppressants, results in immune activation,” the investigators wrote. “It is possible that these patients may harbor residual immunosuppression resulting from their disease burden, advanced age, and prior immunosuppression.”
While more work is needed, Dr. Pugh and colleagues suggested that EBV testing may be valuable for some patients.
“The findings support the need for further studies investigating the role of EBV monitoring in immune checkpoint regulator therapy, which is not currently part of routine protocols.”
The study was funded by All Wales Lymphoma Panel. The investigators disclosed no conflicts of interest.
SOURCE: Pugh et al. Clin Gastroenterol Hepatol. 2019 Oct 11. doi: 10.1016/j.cgh.2019.09.031.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Can an app guide cancer treatment decisions during the pandemic?
Deciding which cancer patients need immediate treatment and who can safely wait is an uncomfortable assessment for cancer clinicians during the COVID-19 pandemic.
In early April, as the COVID-19 surge was bearing down on New York City, those treatment decisions were “a juggling act every single day,” Jonathan Yang, MD, PhD, a radiation oncologist from New York’s Memorial Sloan Kettering Cancer Center, told Medscape Medical News.
Eventually, a glut of guidelines, recommendations, and expert opinions aimed at helping oncologists emerged. The tools help navigate the complicated risk-benefit analysis of their patient’s risk of infection by SARS-CoV-2 and delaying therapy.
Now, a new tool, which appears to be the first of its kind, quantifies that risk-benefit analysis. But its presence immediately raises the question: can it help?
Three-Tier Systems Are Not Very Sophisticated
OncCOVID, a free tool that was launched May 26 by the University of Michigan, allows physicians to individualize risk estimates for delaying treatment of up to 25 early- to late-stage cancers. It includes more than 45 patient characteristics, such as age, location, cancer type, cancer stage, treatment plan, underlying medical conditions, and proposed length of delay in care.
Combining these personal details with data from the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) registry and the National Cancer Database, the Michigan app then estimates a patient’s 5- or 10-year survival with immediate vs delayed treatment and weighs that against their risk for COVID-19 using data from the Johns Hopkins Coronavirus Resource Center.
“We thought, isn’t it better to at least provide some evidence-based quantification, rather than a back-of-the-envelope three-tier system that is just sort of ‘made up’?“ explained one of the developers, Daniel Spratt, MD, associate professor of radiation oncology at Michigan Medicine.
Spratt explained that almost every organization, professional society, and government has created something like a three-tier system. Tier 1 represents urgent cases and patients who need immediate treatment. For tier 2, treatment can be delayed weeks or a month, and with tier 3, it can be delayed until the pandemic is over or it’s deemed safe.
“[This system] sounds good at first glance, but in cancer, we’re always talking about personalized medicine, and it’s mind-blowing that these tier systems are only based on urgency and prognosis,” he told Medscape Medical News.
Spratt offered an example. Consider a patient with a very aggressive brain tumor ― that patient is in tier 1 and should undergo treatment immediately. But will the treatment actually help? And how helpful would the procedure be if, say, the patient is 80 years old and, if infected, would have a 30% to 50% chance of dying from the coronavirus?
“If the model says this guy has a 5% harm and this one has 30% harm, you can use that to help prioritize,” summarized Spratt.
The app can generate risk estimates for patients living anywhere in the world and has already been accessed by people from 37 countries. However, Spratt cautions that it is primarily “designed and calibrated for the US.
“The estimates are based on very large US registries, and though it’s probably somewhat similar across much of the world, there’s probably certain cancer types that are more region specific ― especially something like stomach cancer or certain types of head and neck cancer in parts of Asia, for example,” he said.
Although the app’s COVID-19 data are specific to the county level in the United States, elsewhere in the world, it is only country specific.
“We’re using the best data we have for coronavirus, but everyone knows we still have large data gaps,” he acknowledged.
How Accurate?
Asked to comment on the app, Richard Bleicher, MD, leader of the Breast Cancer Program at Fox Chase Cancer Center, Philadelphia, praised the effort and the goal but had some concerns.
“Several questions arise, most important of which is, How accurate is this, and how has this been validated, if at all ― especially as it is too soon to see the outcomes of patients affected in this pandemic?” he told Medscape Medical News.
“We are imposing delays on a broad scale because of the coronavirus, and we are getting continuously changing data as we test more patients. But both situations are novel and may not be accurately represented by the data being pulled, because the datasets use patients from a few years ago, and confounders in these datasets may not apply to this situation,” Bleicher continued.
Although acknowledging the “value in delineating the risk of dying from cancer vs the risk of dying from the SARS-CoV-2 pandemic,” Bleicher urged caution in using the tool to make individual patient decisions.
“We need to remember that the best of modeling ... can be wildly inaccurate and needs to be validated using patients having the circumstances in question. ... This won’t be possible until long after the pandemic is completed, and so the model’s accuracy remains unknown.”
That sentiment was echoed by Giampaolo Bianchini, MD, head of the Breast Cancer Group, Department of Medical Oncology, Ospedale San Raffaele, in Milan, Italy.
“Arbitrarily postponing and modifying treatment strategies including surgery, radiation therapy, and medical therapy without properly balancing the risk/benefit ratio may lead to significantly worse cancer-related outcomes, which largely exceed the actual risks for COVID,” he wrote in an email.
“The OncCOVID app is a remarkable attempt to fill the gap between perception and estimation,” he said. The app provides side by side the COVID-19 risk estimation and the consequences of arbitrary deviation from the standard of care, observed Bianchini.
However, he pointed out weaknesses, including the fact that the “data generated in literature are not always of high quality and do not take into consideration relevant characteristics of the disease and treatment benefit. It should for sure be used, but then also interpreted with caution.”
Another Italian group responded more positively.
“In our opinion, it could be a useful tool for clinicians,” wrote colleagues Alessio Cortelinni and Giampiero Porzio, both medical oncologists at San Salvatore Hospital and the University of L’Aquila, in Italy. “This Web app might assist clinicians in balancing the risk/benefit ratio of being treated and/or access to the outpatient cancer center for each kind of patient (both early and advanced stages), in order to make a more tailored counseling,” they wrote in an email. “Importantly, the Web app might help those clinicians who work ‘alone,’ in peripheral centers, without resources, colleagues, and multidisciplinary tumor boards on whom they can rely.”
Bleicher, who was involved in the COVID-19 Breast Cancer Consortium’s recommendations for prioritizing breast cancer treatment, summarized that the app “may end up being close or accurate, but we won’t know except in hindsight.”
This article first appeared on Medscape.com.
Deciding which cancer patients need immediate treatment and who can safely wait is an uncomfortable assessment for cancer clinicians during the COVID-19 pandemic.
In early April, as the COVID-19 surge was bearing down on New York City, those treatment decisions were “a juggling act every single day,” Jonathan Yang, MD, PhD, a radiation oncologist from New York’s Memorial Sloan Kettering Cancer Center, told Medscape Medical News.
Eventually, a glut of guidelines, recommendations, and expert opinions aimed at helping oncologists emerged. The tools help navigate the complicated risk-benefit analysis of their patient’s risk of infection by SARS-CoV-2 and delaying therapy.
Now, a new tool, which appears to be the first of its kind, quantifies that risk-benefit analysis. But its presence immediately raises the question: can it help?
Three-Tier Systems Are Not Very Sophisticated
OncCOVID, a free tool that was launched May 26 by the University of Michigan, allows physicians to individualize risk estimates for delaying treatment of up to 25 early- to late-stage cancers. It includes more than 45 patient characteristics, such as age, location, cancer type, cancer stage, treatment plan, underlying medical conditions, and proposed length of delay in care.
Combining these personal details with data from the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) registry and the National Cancer Database, the Michigan app then estimates a patient’s 5- or 10-year survival with immediate vs delayed treatment and weighs that against their risk for COVID-19 using data from the Johns Hopkins Coronavirus Resource Center.
“We thought, isn’t it better to at least provide some evidence-based quantification, rather than a back-of-the-envelope three-tier system that is just sort of ‘made up’?“ explained one of the developers, Daniel Spratt, MD, associate professor of radiation oncology at Michigan Medicine.
Spratt explained that almost every organization, professional society, and government has created something like a three-tier system. Tier 1 represents urgent cases and patients who need immediate treatment. For tier 2, treatment can be delayed weeks or a month, and with tier 3, it can be delayed until the pandemic is over or it’s deemed safe.
“[This system] sounds good at first glance, but in cancer, we’re always talking about personalized medicine, and it’s mind-blowing that these tier systems are only based on urgency and prognosis,” he told Medscape Medical News.
Spratt offered an example. Consider a patient with a very aggressive brain tumor ― that patient is in tier 1 and should undergo treatment immediately. But will the treatment actually help? And how helpful would the procedure be if, say, the patient is 80 years old and, if infected, would have a 30% to 50% chance of dying from the coronavirus?
“If the model says this guy has a 5% harm and this one has 30% harm, you can use that to help prioritize,” summarized Spratt.
The app can generate risk estimates for patients living anywhere in the world and has already been accessed by people from 37 countries. However, Spratt cautions that it is primarily “designed and calibrated for the US.
“The estimates are based on very large US registries, and though it’s probably somewhat similar across much of the world, there’s probably certain cancer types that are more region specific ― especially something like stomach cancer or certain types of head and neck cancer in parts of Asia, for example,” he said.
Although the app’s COVID-19 data are specific to the county level in the United States, elsewhere in the world, it is only country specific.
“We’re using the best data we have for coronavirus, but everyone knows we still have large data gaps,” he acknowledged.
How Accurate?
Asked to comment on the app, Richard Bleicher, MD, leader of the Breast Cancer Program at Fox Chase Cancer Center, Philadelphia, praised the effort and the goal but had some concerns.
“Several questions arise, most important of which is, How accurate is this, and how has this been validated, if at all ― especially as it is too soon to see the outcomes of patients affected in this pandemic?” he told Medscape Medical News.
“We are imposing delays on a broad scale because of the coronavirus, and we are getting continuously changing data as we test more patients. But both situations are novel and may not be accurately represented by the data being pulled, because the datasets use patients from a few years ago, and confounders in these datasets may not apply to this situation,” Bleicher continued.
Although acknowledging the “value in delineating the risk of dying from cancer vs the risk of dying from the SARS-CoV-2 pandemic,” Bleicher urged caution in using the tool to make individual patient decisions.
“We need to remember that the best of modeling ... can be wildly inaccurate and needs to be validated using patients having the circumstances in question. ... This won’t be possible until long after the pandemic is completed, and so the model’s accuracy remains unknown.”
That sentiment was echoed by Giampaolo Bianchini, MD, head of the Breast Cancer Group, Department of Medical Oncology, Ospedale San Raffaele, in Milan, Italy.
“Arbitrarily postponing and modifying treatment strategies including surgery, radiation therapy, and medical therapy without properly balancing the risk/benefit ratio may lead to significantly worse cancer-related outcomes, which largely exceed the actual risks for COVID,” he wrote in an email.
“The OncCOVID app is a remarkable attempt to fill the gap between perception and estimation,” he said. The app provides side by side the COVID-19 risk estimation and the consequences of arbitrary deviation from the standard of care, observed Bianchini.
However, he pointed out weaknesses, including the fact that the “data generated in literature are not always of high quality and do not take into consideration relevant characteristics of the disease and treatment benefit. It should for sure be used, but then also interpreted with caution.”
Another Italian group responded more positively.
“In our opinion, it could be a useful tool for clinicians,” wrote colleagues Alessio Cortelinni and Giampiero Porzio, both medical oncologists at San Salvatore Hospital and the University of L’Aquila, in Italy. “This Web app might assist clinicians in balancing the risk/benefit ratio of being treated and/or access to the outpatient cancer center for each kind of patient (both early and advanced stages), in order to make a more tailored counseling,” they wrote in an email. “Importantly, the Web app might help those clinicians who work ‘alone,’ in peripheral centers, without resources, colleagues, and multidisciplinary tumor boards on whom they can rely.”
Bleicher, who was involved in the COVID-19 Breast Cancer Consortium’s recommendations for prioritizing breast cancer treatment, summarized that the app “may end up being close or accurate, but we won’t know except in hindsight.”
This article first appeared on Medscape.com.
Deciding which cancer patients need immediate treatment and who can safely wait is an uncomfortable assessment for cancer clinicians during the COVID-19 pandemic.
In early April, as the COVID-19 surge was bearing down on New York City, those treatment decisions were “a juggling act every single day,” Jonathan Yang, MD, PhD, a radiation oncologist from New York’s Memorial Sloan Kettering Cancer Center, told Medscape Medical News.
Eventually, a glut of guidelines, recommendations, and expert opinions aimed at helping oncologists emerged. The tools help navigate the complicated risk-benefit analysis of their patient’s risk of infection by SARS-CoV-2 and delaying therapy.
Now, a new tool, which appears to be the first of its kind, quantifies that risk-benefit analysis. But its presence immediately raises the question: can it help?
Three-Tier Systems Are Not Very Sophisticated
OncCOVID, a free tool that was launched May 26 by the University of Michigan, allows physicians to individualize risk estimates for delaying treatment of up to 25 early- to late-stage cancers. It includes more than 45 patient characteristics, such as age, location, cancer type, cancer stage, treatment plan, underlying medical conditions, and proposed length of delay in care.
Combining these personal details with data from the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) registry and the National Cancer Database, the Michigan app then estimates a patient’s 5- or 10-year survival with immediate vs delayed treatment and weighs that against their risk for COVID-19 using data from the Johns Hopkins Coronavirus Resource Center.
“We thought, isn’t it better to at least provide some evidence-based quantification, rather than a back-of-the-envelope three-tier system that is just sort of ‘made up’?“ explained one of the developers, Daniel Spratt, MD, associate professor of radiation oncology at Michigan Medicine.
Spratt explained that almost every organization, professional society, and government has created something like a three-tier system. Tier 1 represents urgent cases and patients who need immediate treatment. For tier 2, treatment can be delayed weeks or a month, and with tier 3, it can be delayed until the pandemic is over or it’s deemed safe.
“[This system] sounds good at first glance, but in cancer, we’re always talking about personalized medicine, and it’s mind-blowing that these tier systems are only based on urgency and prognosis,” he told Medscape Medical News.
Spratt offered an example. Consider a patient with a very aggressive brain tumor ― that patient is in tier 1 and should undergo treatment immediately. But will the treatment actually help? And how helpful would the procedure be if, say, the patient is 80 years old and, if infected, would have a 30% to 50% chance of dying from the coronavirus?
“If the model says this guy has a 5% harm and this one has 30% harm, you can use that to help prioritize,” summarized Spratt.
The app can generate risk estimates for patients living anywhere in the world and has already been accessed by people from 37 countries. However, Spratt cautions that it is primarily “designed and calibrated for the US.
“The estimates are based on very large US registries, and though it’s probably somewhat similar across much of the world, there’s probably certain cancer types that are more region specific ― especially something like stomach cancer or certain types of head and neck cancer in parts of Asia, for example,” he said.
Although the app’s COVID-19 data are specific to the county level in the United States, elsewhere in the world, it is only country specific.
“We’re using the best data we have for coronavirus, but everyone knows we still have large data gaps,” he acknowledged.
How Accurate?
Asked to comment on the app, Richard Bleicher, MD, leader of the Breast Cancer Program at Fox Chase Cancer Center, Philadelphia, praised the effort and the goal but had some concerns.
“Several questions arise, most important of which is, How accurate is this, and how has this been validated, if at all ― especially as it is too soon to see the outcomes of patients affected in this pandemic?” he told Medscape Medical News.
“We are imposing delays on a broad scale because of the coronavirus, and we are getting continuously changing data as we test more patients. But both situations are novel and may not be accurately represented by the data being pulled, because the datasets use patients from a few years ago, and confounders in these datasets may not apply to this situation,” Bleicher continued.
Although acknowledging the “value in delineating the risk of dying from cancer vs the risk of dying from the SARS-CoV-2 pandemic,” Bleicher urged caution in using the tool to make individual patient decisions.
“We need to remember that the best of modeling ... can be wildly inaccurate and needs to be validated using patients having the circumstances in question. ... This won’t be possible until long after the pandemic is completed, and so the model’s accuracy remains unknown.”
That sentiment was echoed by Giampaolo Bianchini, MD, head of the Breast Cancer Group, Department of Medical Oncology, Ospedale San Raffaele, in Milan, Italy.
“Arbitrarily postponing and modifying treatment strategies including surgery, radiation therapy, and medical therapy without properly balancing the risk/benefit ratio may lead to significantly worse cancer-related outcomes, which largely exceed the actual risks for COVID,” he wrote in an email.
“The OncCOVID app is a remarkable attempt to fill the gap between perception and estimation,” he said. The app provides side by side the COVID-19 risk estimation and the consequences of arbitrary deviation from the standard of care, observed Bianchini.
However, he pointed out weaknesses, including the fact that the “data generated in literature are not always of high quality and do not take into consideration relevant characteristics of the disease and treatment benefit. It should for sure be used, but then also interpreted with caution.”
Another Italian group responded more positively.
“In our opinion, it could be a useful tool for clinicians,” wrote colleagues Alessio Cortelinni and Giampiero Porzio, both medical oncologists at San Salvatore Hospital and the University of L’Aquila, in Italy. “This Web app might assist clinicians in balancing the risk/benefit ratio of being treated and/or access to the outpatient cancer center for each kind of patient (both early and advanced stages), in order to make a more tailored counseling,” they wrote in an email. “Importantly, the Web app might help those clinicians who work ‘alone,’ in peripheral centers, without resources, colleagues, and multidisciplinary tumor boards on whom they can rely.”
Bleicher, who was involved in the COVID-19 Breast Cancer Consortium’s recommendations for prioritizing breast cancer treatment, summarized that the app “may end up being close or accurate, but we won’t know except in hindsight.”
This article first appeared on Medscape.com.
‘A good and peaceful death’: Cancer hospice during the pandemic
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.

