User login
Drug-induced immune hemolytic anemia associated with albumin-bound paclitaxel
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Click on the PDF icon at the top of this introduction to read the full article.
Life-threatening hypoglycemia resulting from a nonislet cell tumor
Nonislet cell tumor-induced hypoglycemia (NICTH), also known as Doege-Potter syndrome, is a rare paraneoplastic syndrome seen in association with various nonpancreatic tumors, benign and malignant, and comprising mesenchymal, vascular, or epithelial cell types. We report a case of recurrent life-threatening hypoglycemia from a large pelvic solitary fibrous tumor.
Click on the PDF icon at the top of this introduction to read the full article.
Nonislet cell tumor-induced hypoglycemia (NICTH), also known as Doege-Potter syndrome, is a rare paraneoplastic syndrome seen in association with various nonpancreatic tumors, benign and malignant, and comprising mesenchymal, vascular, or epithelial cell types. We report a case of recurrent life-threatening hypoglycemia from a large pelvic solitary fibrous tumor.
Click on the PDF icon at the top of this introduction to read the full article.
Nonislet cell tumor-induced hypoglycemia (NICTH), also known as Doege-Potter syndrome, is a rare paraneoplastic syndrome seen in association with various nonpancreatic tumors, benign and malignant, and comprising mesenchymal, vascular, or epithelial cell types. We report a case of recurrent life-threatening hypoglycemia from a large pelvic solitary fibrous tumor.
Click on the PDF icon at the top of this introduction to read the full article.
Lung cancer in HIV-infected patients and the role of targeted therapy
Lung cancer is one of the most common malignancies in HIV-infected patients. Prevalence and mortality outcomes are higher in HIV-infected populations than in noninfected patients. There are several oral agents available for patients who harbor specific mutations, but little is known about mutations and affected pathways in HIV-infected patients with lung cancer. Recent trials have facilitated the inclusion of HIV-infected patients in clinical trials, but the population is remains underrepresented in oncology trials. Here, we review the literature on lung cancer in HIV-infected patients, and discuss common mutations in lung cancer and HIV-infected patients, the role of mutational analysis, and the potential role of targeted therapy in the treatment of lung cancer in HIV-infected populations.
Click on the PDF icon at the top of this introduction to read the full article.
Lung cancer is one of the most common malignancies in HIV-infected patients. Prevalence and mortality outcomes are higher in HIV-infected populations than in noninfected patients. There are several oral agents available for patients who harbor specific mutations, but little is known about mutations and affected pathways in HIV-infected patients with lung cancer. Recent trials have facilitated the inclusion of HIV-infected patients in clinical trials, but the population is remains underrepresented in oncology trials. Here, we review the literature on lung cancer in HIV-infected patients, and discuss common mutations in lung cancer and HIV-infected patients, the role of mutational analysis, and the potential role of targeted therapy in the treatment of lung cancer in HIV-infected populations.
Click on the PDF icon at the top of this introduction to read the full article.
Lung cancer is one of the most common malignancies in HIV-infected patients. Prevalence and mortality outcomes are higher in HIV-infected populations than in noninfected patients. There are several oral agents available for patients who harbor specific mutations, but little is known about mutations and affected pathways in HIV-infected patients with lung cancer. Recent trials have facilitated the inclusion of HIV-infected patients in clinical trials, but the population is remains underrepresented in oncology trials. Here, we review the literature on lung cancer in HIV-infected patients, and discuss common mutations in lung cancer and HIV-infected patients, the role of mutational analysis, and the potential role of targeted therapy in the treatment of lung cancer in HIV-infected populations.
Click on the PDF icon at the top of this introduction to read the full article.
Re-personalizing precision medicine: is there a role for patient-reported outcomes?
In the opinion of most, precision medicine is the future of cancer therapeutics. By producing response rates well into double digits, and substantially extending progression-free and overall survival, the molecular testing of tumors to select optimal treatment may be a way to justify the high cost of new and emerging therapeutics. The road to this future will likely be long and winding, however, with a string of incremental successes amid inevitable disappointments. Our patients will walk this road with us, agreeing to testing and treatment when those tests come back positive for an eligible mutation.
Click on the PDF icon at the top of this introduction to read the full article.
In the opinion of most, precision medicine is the future of cancer therapeutics. By producing response rates well into double digits, and substantially extending progression-free and overall survival, the molecular testing of tumors to select optimal treatment may be a way to justify the high cost of new and emerging therapeutics. The road to this future will likely be long and winding, however, with a string of incremental successes amid inevitable disappointments. Our patients will walk this road with us, agreeing to testing and treatment when those tests come back positive for an eligible mutation.
Click on the PDF icon at the top of this introduction to read the full article.
In the opinion of most, precision medicine is the future of cancer therapeutics. By producing response rates well into double digits, and substantially extending progression-free and overall survival, the molecular testing of tumors to select optimal treatment may be a way to justify the high cost of new and emerging therapeutics. The road to this future will likely be long and winding, however, with a string of incremental successes amid inevitable disappointments. Our patients will walk this road with us, agreeing to testing and treatment when those tests come back positive for an eligible mutation.
Click on the PDF icon at the top of this introduction to read the full article.
Mixed results for cancer survivorship care plan
A cancer survivorship care plan increased the information patients received yet failed to increase patient satisfaction with cancer care. Moreover, patients who received care plans experienced more symptoms, were more concerned about their illness, and were more affected emotionally than were those who did not, according to a study published online Aug. 24 in Journal of Clinical Oncology.
The Institute of Medicine and other groups recommend survivorship care plans (SCPs) for all cancer survivors to help them deal with the challenges they face after diagnosis. Yet few studies have examined SCPs’ effectiveness. To do so, researchers performed what they described as the first pragmatic, cluster-randomized longitudinal trial comparing an automatically generated SCP against usual care in routine clinical practice.
The study involved 221 women with newly diagnosed endometrial cancer treated at 12 medical centers in the Netherlands. Six of the hospitals were randomly assigned to provide usual care (102 patients) and six to provide SCPs (119 patients) immediately after initial surgery, with updated SCPs offered 6 and 12 months later, said Kim A. H. Nicolaije of Tilburg University and the Comprehensive Cancer Center the Netherlands, Eindhoven, and her associates.
Usual care included verbal and written information about diagnosis and treatment, the recovery period, signs of recurrence, and hospital contacts; no additional information was given during follow-up, except for referrals when indicated.
The SCP entailed a treatment summary tailored to each patient’s diagnostic test results, tumor stage and grade, comorbidities, and evolving complications. It addressed possible short- and long-term effects of the cancer and its treatments on physical, social, and sexual life; signs of recurrence and secondary tumors; services such as rehabilitation, psychosocial support, and supportive care; and contact information for hospital personnel and outside specialists.
At follow-up, participants in the SCP group said they’d received more information about their disease, its treatments, other services available to them, different places where they could seek care, and ways they could help themselves get well, compared with the usual-care group. Yet there were no significant differences between the two study groups in several measures of satisfaction with the information provided or with the care itself. Furthermore, patients in the SCP group said they experienced more symptoms, were more concerned about their illness, and were more affected emotionally than were those in the usual-care group.
The SCPs called for including patients’ primary care physicians in the plans while usual care did not, and patients in the SCP group reported having more cancer-related contact with their primary-care physicians than those in the usual-care group. Yet this increased contact did not lead to better patient satisfaction, Ms. Nicolaije and her associates said (J Clin Oncol 2015 Aug 24. doi:10.1200/JCO.2014.60.3399).
It is unclear whether these effects are harmful or beneficial for patients. “One could argue that receiving an SCP raises patients’ awareness of cancer-related symptoms and empowers them to find the necessary support,” even if they don’t recognize this as a benefit, the investigators added.
The Dutch Cancer Society supported the study. Ms. Nicolaije reported having no conflicts of interest; a coauthor reported receiving research funding and reimbursement for expenses from Janssen Pharmaceuticals.
Survivorship care plans have been recommended for the past decade, but their implementation has been slow, low, and sporadic. And we still don’t have a clear answer as to their effectiveness.
The medical community should recognize that null or negative results on SCP effectiveness, such as those reported by Nicolaije et al., may not reflect some inherent defect of SCPs but rather the poor or inconsistent implementation of an SCP. Fully 26% of the patients in the SCP group in this trial reported that they had never in fact received an SCP.
In addition, being better informed about late or long-term effects of cancer or its treatment may well give rise to “increased concerns” and feeling “more emotionally affected” in the year following diagnosis, but may also yield great benefits later on – a possibility that wasn’t addressed in this trial.
Deborah K. Mayer, Ph.D., is at the University of North Carolina School of Nursing and Lineberger Comprehensive Cancer Center, both in Chapel Hill. She reported having no conflicts of interest; one of her associates reported serving as a consultant to Medivation/Astellas Pharma and receiving research funding from Accuray. Dr. Mayer and her associates made these remarks in an editorial accompanying Ms. Nicolaije’s report (J Clin Oncol 2015 Aug 24. doi:10.1200/JCO.2015.62.6937).
Survivorship care plans have been recommended for the past decade, but their implementation has been slow, low, and sporadic. And we still don’t have a clear answer as to their effectiveness.
The medical community should recognize that null or negative results on SCP effectiveness, such as those reported by Nicolaije et al., may not reflect some inherent defect of SCPs but rather the poor or inconsistent implementation of an SCP. Fully 26% of the patients in the SCP group in this trial reported that they had never in fact received an SCP.
In addition, being better informed about late or long-term effects of cancer or its treatment may well give rise to “increased concerns” and feeling “more emotionally affected” in the year following diagnosis, but may also yield great benefits later on – a possibility that wasn’t addressed in this trial.
Deborah K. Mayer, Ph.D., is at the University of North Carolina School of Nursing and Lineberger Comprehensive Cancer Center, both in Chapel Hill. She reported having no conflicts of interest; one of her associates reported serving as a consultant to Medivation/Astellas Pharma and receiving research funding from Accuray. Dr. Mayer and her associates made these remarks in an editorial accompanying Ms. Nicolaije’s report (J Clin Oncol 2015 Aug 24. doi:10.1200/JCO.2015.62.6937).
Survivorship care plans have been recommended for the past decade, but their implementation has been slow, low, and sporadic. And we still don’t have a clear answer as to their effectiveness.
The medical community should recognize that null or negative results on SCP effectiveness, such as those reported by Nicolaije et al., may not reflect some inherent defect of SCPs but rather the poor or inconsistent implementation of an SCP. Fully 26% of the patients in the SCP group in this trial reported that they had never in fact received an SCP.
In addition, being better informed about late or long-term effects of cancer or its treatment may well give rise to “increased concerns” and feeling “more emotionally affected” in the year following diagnosis, but may also yield great benefits later on – a possibility that wasn’t addressed in this trial.
Deborah K. Mayer, Ph.D., is at the University of North Carolina School of Nursing and Lineberger Comprehensive Cancer Center, both in Chapel Hill. She reported having no conflicts of interest; one of her associates reported serving as a consultant to Medivation/Astellas Pharma and receiving research funding from Accuray. Dr. Mayer and her associates made these remarks in an editorial accompanying Ms. Nicolaije’s report (J Clin Oncol 2015 Aug 24. doi:10.1200/JCO.2015.62.6937).
A cancer survivorship care plan increased the information patients received yet failed to increase patient satisfaction with cancer care. Moreover, patients who received care plans experienced more symptoms, were more concerned about their illness, and were more affected emotionally than were those who did not, according to a study published online Aug. 24 in Journal of Clinical Oncology.
The Institute of Medicine and other groups recommend survivorship care plans (SCPs) for all cancer survivors to help them deal with the challenges they face after diagnosis. Yet few studies have examined SCPs’ effectiveness. To do so, researchers performed what they described as the first pragmatic, cluster-randomized longitudinal trial comparing an automatically generated SCP against usual care in routine clinical practice.
The study involved 221 women with newly diagnosed endometrial cancer treated at 12 medical centers in the Netherlands. Six of the hospitals were randomly assigned to provide usual care (102 patients) and six to provide SCPs (119 patients) immediately after initial surgery, with updated SCPs offered 6 and 12 months later, said Kim A. H. Nicolaije of Tilburg University and the Comprehensive Cancer Center the Netherlands, Eindhoven, and her associates.
Usual care included verbal and written information about diagnosis and treatment, the recovery period, signs of recurrence, and hospital contacts; no additional information was given during follow-up, except for referrals when indicated.
The SCP entailed a treatment summary tailored to each patient’s diagnostic test results, tumor stage and grade, comorbidities, and evolving complications. It addressed possible short- and long-term effects of the cancer and its treatments on physical, social, and sexual life; signs of recurrence and secondary tumors; services such as rehabilitation, psychosocial support, and supportive care; and contact information for hospital personnel and outside specialists.
At follow-up, participants in the SCP group said they’d received more information about their disease, its treatments, other services available to them, different places where they could seek care, and ways they could help themselves get well, compared with the usual-care group. Yet there were no significant differences between the two study groups in several measures of satisfaction with the information provided or with the care itself. Furthermore, patients in the SCP group said they experienced more symptoms, were more concerned about their illness, and were more affected emotionally than were those in the usual-care group.
The SCPs called for including patients’ primary care physicians in the plans while usual care did not, and patients in the SCP group reported having more cancer-related contact with their primary-care physicians than those in the usual-care group. Yet this increased contact did not lead to better patient satisfaction, Ms. Nicolaije and her associates said (J Clin Oncol 2015 Aug 24. doi:10.1200/JCO.2014.60.3399).
It is unclear whether these effects are harmful or beneficial for patients. “One could argue that receiving an SCP raises patients’ awareness of cancer-related symptoms and empowers them to find the necessary support,” even if they don’t recognize this as a benefit, the investigators added.
The Dutch Cancer Society supported the study. Ms. Nicolaije reported having no conflicts of interest; a coauthor reported receiving research funding and reimbursement for expenses from Janssen Pharmaceuticals.
A cancer survivorship care plan increased the information patients received yet failed to increase patient satisfaction with cancer care. Moreover, patients who received care plans experienced more symptoms, were more concerned about their illness, and were more affected emotionally than were those who did not, according to a study published online Aug. 24 in Journal of Clinical Oncology.
The Institute of Medicine and other groups recommend survivorship care plans (SCPs) for all cancer survivors to help them deal with the challenges they face after diagnosis. Yet few studies have examined SCPs’ effectiveness. To do so, researchers performed what they described as the first pragmatic, cluster-randomized longitudinal trial comparing an automatically generated SCP against usual care in routine clinical practice.
The study involved 221 women with newly diagnosed endometrial cancer treated at 12 medical centers in the Netherlands. Six of the hospitals were randomly assigned to provide usual care (102 patients) and six to provide SCPs (119 patients) immediately after initial surgery, with updated SCPs offered 6 and 12 months later, said Kim A. H. Nicolaije of Tilburg University and the Comprehensive Cancer Center the Netherlands, Eindhoven, and her associates.
Usual care included verbal and written information about diagnosis and treatment, the recovery period, signs of recurrence, and hospital contacts; no additional information was given during follow-up, except for referrals when indicated.
The SCP entailed a treatment summary tailored to each patient’s diagnostic test results, tumor stage and grade, comorbidities, and evolving complications. It addressed possible short- and long-term effects of the cancer and its treatments on physical, social, and sexual life; signs of recurrence and secondary tumors; services such as rehabilitation, psychosocial support, and supportive care; and contact information for hospital personnel and outside specialists.
At follow-up, participants in the SCP group said they’d received more information about their disease, its treatments, other services available to them, different places where they could seek care, and ways they could help themselves get well, compared with the usual-care group. Yet there were no significant differences between the two study groups in several measures of satisfaction with the information provided or with the care itself. Furthermore, patients in the SCP group said they experienced more symptoms, were more concerned about their illness, and were more affected emotionally than were those in the usual-care group.
The SCPs called for including patients’ primary care physicians in the plans while usual care did not, and patients in the SCP group reported having more cancer-related contact with their primary-care physicians than those in the usual-care group. Yet this increased contact did not lead to better patient satisfaction, Ms. Nicolaije and her associates said (J Clin Oncol 2015 Aug 24. doi:10.1200/JCO.2014.60.3399).
It is unclear whether these effects are harmful or beneficial for patients. “One could argue that receiving an SCP raises patients’ awareness of cancer-related symptoms and empowers them to find the necessary support,” even if they don’t recognize this as a benefit, the investigators added.
The Dutch Cancer Society supported the study. Ms. Nicolaije reported having no conflicts of interest; a coauthor reported receiving research funding and reimbursement for expenses from Janssen Pharmaceuticals.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: A cancer survivorship care plan did not improve endometrial cancer patients’ satisfaction with information provision or with health care.
Major finding: Participants in the SCP group said they had received more information about their disease, its treatments, other services available to them, and ways they could help themselves get well, compared with the usual-care group, but they did not report more satisfaction with the information or with their cancer care.
Data source: A longitudinal, cluster-randomized trial of 221 women with newly diagnosed endometrial cancer treated at 12 hospitals in the Netherlands and followed for 1 year.
Disclosures: The Dutch Cancer Society supported the study. Ms. Nicolaije reported having no conflicts of interest; a coauthor reported receiving research funding and reimbursement for expenses from Janssen Pharmaceuticals.
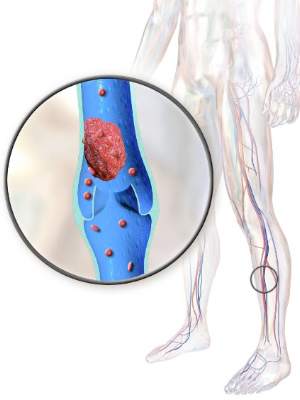
Warfarin as effective as LMWH to prevent recurrent VTEs in cancer patients
In cancer patients with acute, symptomatic venous thromboembolisms, daily tinzaparin does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding compared with warfarin, but does reduce clinically-relevant nonmajor bleeding, according to a 900-patient randomized trial published in JAMA.
Tinzaparin (Innohep) is a low-molecular-weight heparin (LMWH) marketed outside the United States. LMWHs are generally recommended over warfarin to treat acute venous thromboembolism (VTE) in cancer patients, but the recommendation is based mostly on a single trial over a decade old; that might explain why, worldwide, vitamin K antagonists are still heavily used in patients with cancer-associated thrombosis, said the authors, led by Dr. Agnes Lee, of the University of British Columbia (Vancouver).
To revisit the issue in the modern treatment era, Dr. Lee and her colleagues randomized 449 adults with active cancer and documented deep vein thrombosis or pulmonary embolism to tinzaparin (175 IU/kg) once daily for 6 months, and 451 others to 6 months of conventional therapy with tinzaparin (175 IU/kg) once daily for 5-10 days followed by warfarin dose adjusted to maintain therapeutic range (JAMA. 2015;314[7]:677-86).
The subjects were recruited from 164 centers in Asia, Africa, Europe, Canada, and Central and South America; all had a life expectancy greater than 6 months. The mean age in the study was 59 years, and 60% of the subjects were women. Gynecologic and colorectal cancers were the most common in the study.
Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (hazard ratio [HR] 0.65; 95% CI 0.41-1.03; P = .07).
There was major bleeding in 12 (2.7%) tinzaparin patients and 11 (2.4%) warfarin patients, an insignificant difference (HR 0.89; 95% CI 0.40-1.99; P = .77); 150 tinzaparin patients (33.4%) and 138 warfarin patients (30.6%) died in the trial, also an insignificant difference (HR, 1.08; 95% CI 0.85-1.36; P = .54).
There were 49 (10.9%) clinically relevant but nonmajor bleeds in the tinzaparin group versus 69 (15.3%) among warfarin patients, a difference that was significant (HR 0.58; 95% CI 0.40-0.84; P = .004). Clinically relevant nonmajor bleeding meant nonfatal bleeding outside of a critical area or organ that still required intervention but did not cause a fall in hemoglobin greater than 2 g/dL.
There were fewer than anticipated thrombotic events in the warfarin group. “We had expected a recurrence rate of 12.6% with warfarin; the observed rate was only 10.5%. This potentially affected the power of the trial to detect a benefit associated with tinzaparin.” Also, “a significant reduction in recurrent [VTEs] might be observed with tinzaparin” among patients at higher risk for them than were in the study, the investigators said.
Even so, the trial did demonstrate “that tinzaparin, even when given at a full therapeutic dose for up to 6 months, is safe in a broad oncology population,” they said.
LEO Pharma, makers of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. Dr. Lee reported honoraria, consulting fees, and research funding from the company. Other authors reported payments from LEO for those or other reasons.
In cancer patients with acute, symptomatic venous thromboembolisms, daily tinzaparin does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding compared with warfarin, but does reduce clinically-relevant nonmajor bleeding, according to a 900-patient randomized trial published in JAMA.
Tinzaparin (Innohep) is a low-molecular-weight heparin (LMWH) marketed outside the United States. LMWHs are generally recommended over warfarin to treat acute venous thromboembolism (VTE) in cancer patients, but the recommendation is based mostly on a single trial over a decade old; that might explain why, worldwide, vitamin K antagonists are still heavily used in patients with cancer-associated thrombosis, said the authors, led by Dr. Agnes Lee, of the University of British Columbia (Vancouver).
To revisit the issue in the modern treatment era, Dr. Lee and her colleagues randomized 449 adults with active cancer and documented deep vein thrombosis or pulmonary embolism to tinzaparin (175 IU/kg) once daily for 6 months, and 451 others to 6 months of conventional therapy with tinzaparin (175 IU/kg) once daily for 5-10 days followed by warfarin dose adjusted to maintain therapeutic range (JAMA. 2015;314[7]:677-86).
The subjects were recruited from 164 centers in Asia, Africa, Europe, Canada, and Central and South America; all had a life expectancy greater than 6 months. The mean age in the study was 59 years, and 60% of the subjects were women. Gynecologic and colorectal cancers were the most common in the study.
Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (hazard ratio [HR] 0.65; 95% CI 0.41-1.03; P = .07).
There was major bleeding in 12 (2.7%) tinzaparin patients and 11 (2.4%) warfarin patients, an insignificant difference (HR 0.89; 95% CI 0.40-1.99; P = .77); 150 tinzaparin patients (33.4%) and 138 warfarin patients (30.6%) died in the trial, also an insignificant difference (HR, 1.08; 95% CI 0.85-1.36; P = .54).
There were 49 (10.9%) clinically relevant but nonmajor bleeds in the tinzaparin group versus 69 (15.3%) among warfarin patients, a difference that was significant (HR 0.58; 95% CI 0.40-0.84; P = .004). Clinically relevant nonmajor bleeding meant nonfatal bleeding outside of a critical area or organ that still required intervention but did not cause a fall in hemoglobin greater than 2 g/dL.
There were fewer than anticipated thrombotic events in the warfarin group. “We had expected a recurrence rate of 12.6% with warfarin; the observed rate was only 10.5%. This potentially affected the power of the trial to detect a benefit associated with tinzaparin.” Also, “a significant reduction in recurrent [VTEs] might be observed with tinzaparin” among patients at higher risk for them than were in the study, the investigators said.
Even so, the trial did demonstrate “that tinzaparin, even when given at a full therapeutic dose for up to 6 months, is safe in a broad oncology population,” they said.
LEO Pharma, makers of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. Dr. Lee reported honoraria, consulting fees, and research funding from the company. Other authors reported payments from LEO for those or other reasons.
In cancer patients with acute, symptomatic venous thromboembolisms, daily tinzaparin does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding compared with warfarin, but does reduce clinically-relevant nonmajor bleeding, according to a 900-patient randomized trial published in JAMA.
Tinzaparin (Innohep) is a low-molecular-weight heparin (LMWH) marketed outside the United States. LMWHs are generally recommended over warfarin to treat acute venous thromboembolism (VTE) in cancer patients, but the recommendation is based mostly on a single trial over a decade old; that might explain why, worldwide, vitamin K antagonists are still heavily used in patients with cancer-associated thrombosis, said the authors, led by Dr. Agnes Lee, of the University of British Columbia (Vancouver).
To revisit the issue in the modern treatment era, Dr. Lee and her colleagues randomized 449 adults with active cancer and documented deep vein thrombosis or pulmonary embolism to tinzaparin (175 IU/kg) once daily for 6 months, and 451 others to 6 months of conventional therapy with tinzaparin (175 IU/kg) once daily for 5-10 days followed by warfarin dose adjusted to maintain therapeutic range (JAMA. 2015;314[7]:677-86).
The subjects were recruited from 164 centers in Asia, Africa, Europe, Canada, and Central and South America; all had a life expectancy greater than 6 months. The mean age in the study was 59 years, and 60% of the subjects were women. Gynecologic and colorectal cancers were the most common in the study.
Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (hazard ratio [HR] 0.65; 95% CI 0.41-1.03; P = .07).
There was major bleeding in 12 (2.7%) tinzaparin patients and 11 (2.4%) warfarin patients, an insignificant difference (HR 0.89; 95% CI 0.40-1.99; P = .77); 150 tinzaparin patients (33.4%) and 138 warfarin patients (30.6%) died in the trial, also an insignificant difference (HR, 1.08; 95% CI 0.85-1.36; P = .54).
There were 49 (10.9%) clinically relevant but nonmajor bleeds in the tinzaparin group versus 69 (15.3%) among warfarin patients, a difference that was significant (HR 0.58; 95% CI 0.40-0.84; P = .004). Clinically relevant nonmajor bleeding meant nonfatal bleeding outside of a critical area or organ that still required intervention but did not cause a fall in hemoglobin greater than 2 g/dL.
There were fewer than anticipated thrombotic events in the warfarin group. “We had expected a recurrence rate of 12.6% with warfarin; the observed rate was only 10.5%. This potentially affected the power of the trial to detect a benefit associated with tinzaparin.” Also, “a significant reduction in recurrent [VTEs] might be observed with tinzaparin” among patients at higher risk for them than were in the study, the investigators said.
Even so, the trial did demonstrate “that tinzaparin, even when given at a full therapeutic dose for up to 6 months, is safe in a broad oncology population,” they said.
LEO Pharma, makers of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. Dr. Lee reported honoraria, consulting fees, and research funding from the company. Other authors reported payments from LEO for those or other reasons.
FROM JAMA
Key clinical point: In cancer patients, tinzaparin (Innohep) does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding when compared to warfarin.
Major finding: Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (HR 0.65; 95% CI 0.41-1.03; P = .07).
Data source: Randomized trial with 900 subjects.
Disclosures: LEO Pharma, maker of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. The investigators reported honoraria, consulting fees, and other payments from the company.
Immune-related patterns of response present challenges
With the race to develop cancer immunotherapies escalating and new agents appearing in the clinic, oncologists’ decision-making toolbox will need to evolve.
“As immunotherapeutics become increasingly available to patients, clinicians face a major challenge in the evaluation of these novel drugs – the accurate determination of clinical efficacy,” physician-scientists recently wrote in a commentary published online in the Journal of Clinical Oncology.
Response evaluation criteria in solid tumors (RECIST) have typically driven oncologists’ decision making. Patients undergo scans and radiographic measurements to determine the extent of change in tumor size. Scan, treat, repeat is a mantra for advanced cancer patients, so much so some patients have sought to trademark the phrase for T-shirts. And significant tumor growth has traditionally signaled treatment failure.
But although some patients have responded to immune-targeted treatment with tumor shrinkage or stable disease that would be consistent with existing RECIST criteria, distinct immune-related patterns of response are also emerging, including pseudoprogression, said Dr. Victoria L. Chiou and Dr. Mauricio Burotto, both medical oncology fellows at the National Cancer Institute, in their commentary (Jour Clin Onc. 2015 Aug 10. doi: 10.1200/JCO.2015.61.6870).
Investigators first addressed this issue by proposing immune response criteria in 2009, based on data from ipilimumab phase II trials in patients with advanced melanoma. Dr. Jedd D. Wolchok of Memorial Sloan Kettering Cancer Center, New York, and his associates expanded on RECIST by adding two additional patterns of response: response after an increase in total tumor burden and response in the presence of new lesions. All patterns of response were associated with favorable survival, Dr. Wolchok and associates said (Clin Cancer Res 2009 Dec 1. doi: 10.1158/1078-0432.CCR-09-1624).
Subsequent trials in patients with advanced melanoma have confirmed that a subset of patients who are responders using immune response criteria would have been misclassified using RECIST alone.
In a study of patients with metastatic melanoma treated with nivolumab, 10% experienced distinct immune-related responses, according to Dr. Chiou and Dr. Burotto. In another study of patients with advanced melanoma, this one evaluating anti–PD-1 monoclonal antibody pembrolizumab, 6.7% of patients of the patients experienced pseudoprogression, and overall, 12% of patients were classified as responders or as having stable disease by immune response criteria but would have been classified as having progressive disease by RECIST.
It is time to expand on those first immune response criteria, Dr. Chiou and Dr. Burotto conclude. “Five years after the introduction of the immune response criteria, it is necessary to fully characterize the patterns of immune-related phenomena, to understand these patterns across multiple solid tumor types, and to evaluate how these guidelines are used in current clinical practice,” they wrote.
The Food and Drug Administration agrees. Though guidelines for industry were published in 2011 regarding cancer vaccines, there is no specific guidance on approval criteria for other cancer immunotherapies such as checkpoint inhibitors, Dr. Gideon Blumenthal, team leader in the FDA’s Office of Hematology and Oncology Products, Center for Drug Evaluation and Research, said in an interview.
“However, the FDA is actively looking at other metrics of response beyond conventional RECIST criteria, both to help industry in early ‘go/no-go’ decision making, as well as for helping in the design of later stages of trial design and to help inform approval decisions,” he said.
The FDA is interested in investigating internal data sets of immunotherapy trials, and in collaborating with external stakeholders to determine what the optimal endpoints for cancer immunotherapies will be. Median PFS and PFS hazard ratios do not appear to capture the overall survival benefit that patients derive from immunotherapies, particularly in early lung cancer trials with which he is most familiar, Dr. Blumenthal said.
“Overall survival remains the gold standard endpoint in oncology as it is a direct measure of clinical benefit and less subject to bias, but as more effective therapies come on line and patients live longer, overall survival will become more challenging to detect,” he said.
On Twitter @NikolaidesLaura
With the race to develop cancer immunotherapies escalating and new agents appearing in the clinic, oncologists’ decision-making toolbox will need to evolve.
“As immunotherapeutics become increasingly available to patients, clinicians face a major challenge in the evaluation of these novel drugs – the accurate determination of clinical efficacy,” physician-scientists recently wrote in a commentary published online in the Journal of Clinical Oncology.
Response evaluation criteria in solid tumors (RECIST) have typically driven oncologists’ decision making. Patients undergo scans and radiographic measurements to determine the extent of change in tumor size. Scan, treat, repeat is a mantra for advanced cancer patients, so much so some patients have sought to trademark the phrase for T-shirts. And significant tumor growth has traditionally signaled treatment failure.
But although some patients have responded to immune-targeted treatment with tumor shrinkage or stable disease that would be consistent with existing RECIST criteria, distinct immune-related patterns of response are also emerging, including pseudoprogression, said Dr. Victoria L. Chiou and Dr. Mauricio Burotto, both medical oncology fellows at the National Cancer Institute, in their commentary (Jour Clin Onc. 2015 Aug 10. doi: 10.1200/JCO.2015.61.6870).
Investigators first addressed this issue by proposing immune response criteria in 2009, based on data from ipilimumab phase II trials in patients with advanced melanoma. Dr. Jedd D. Wolchok of Memorial Sloan Kettering Cancer Center, New York, and his associates expanded on RECIST by adding two additional patterns of response: response after an increase in total tumor burden and response in the presence of new lesions. All patterns of response were associated with favorable survival, Dr. Wolchok and associates said (Clin Cancer Res 2009 Dec 1. doi: 10.1158/1078-0432.CCR-09-1624).
Subsequent trials in patients with advanced melanoma have confirmed that a subset of patients who are responders using immune response criteria would have been misclassified using RECIST alone.
In a study of patients with metastatic melanoma treated with nivolumab, 10% experienced distinct immune-related responses, according to Dr. Chiou and Dr. Burotto. In another study of patients with advanced melanoma, this one evaluating anti–PD-1 monoclonal antibody pembrolizumab, 6.7% of patients of the patients experienced pseudoprogression, and overall, 12% of patients were classified as responders or as having stable disease by immune response criteria but would have been classified as having progressive disease by RECIST.
It is time to expand on those first immune response criteria, Dr. Chiou and Dr. Burotto conclude. “Five years after the introduction of the immune response criteria, it is necessary to fully characterize the patterns of immune-related phenomena, to understand these patterns across multiple solid tumor types, and to evaluate how these guidelines are used in current clinical practice,” they wrote.
The Food and Drug Administration agrees. Though guidelines for industry were published in 2011 regarding cancer vaccines, there is no specific guidance on approval criteria for other cancer immunotherapies such as checkpoint inhibitors, Dr. Gideon Blumenthal, team leader in the FDA’s Office of Hematology and Oncology Products, Center for Drug Evaluation and Research, said in an interview.
“However, the FDA is actively looking at other metrics of response beyond conventional RECIST criteria, both to help industry in early ‘go/no-go’ decision making, as well as for helping in the design of later stages of trial design and to help inform approval decisions,” he said.
The FDA is interested in investigating internal data sets of immunotherapy trials, and in collaborating with external stakeholders to determine what the optimal endpoints for cancer immunotherapies will be. Median PFS and PFS hazard ratios do not appear to capture the overall survival benefit that patients derive from immunotherapies, particularly in early lung cancer trials with which he is most familiar, Dr. Blumenthal said.
“Overall survival remains the gold standard endpoint in oncology as it is a direct measure of clinical benefit and less subject to bias, but as more effective therapies come on line and patients live longer, overall survival will become more challenging to detect,” he said.
On Twitter @NikolaidesLaura
With the race to develop cancer immunotherapies escalating and new agents appearing in the clinic, oncologists’ decision-making toolbox will need to evolve.
“As immunotherapeutics become increasingly available to patients, clinicians face a major challenge in the evaluation of these novel drugs – the accurate determination of clinical efficacy,” physician-scientists recently wrote in a commentary published online in the Journal of Clinical Oncology.
Response evaluation criteria in solid tumors (RECIST) have typically driven oncologists’ decision making. Patients undergo scans and radiographic measurements to determine the extent of change in tumor size. Scan, treat, repeat is a mantra for advanced cancer patients, so much so some patients have sought to trademark the phrase for T-shirts. And significant tumor growth has traditionally signaled treatment failure.
But although some patients have responded to immune-targeted treatment with tumor shrinkage or stable disease that would be consistent with existing RECIST criteria, distinct immune-related patterns of response are also emerging, including pseudoprogression, said Dr. Victoria L. Chiou and Dr. Mauricio Burotto, both medical oncology fellows at the National Cancer Institute, in their commentary (Jour Clin Onc. 2015 Aug 10. doi: 10.1200/JCO.2015.61.6870).
Investigators first addressed this issue by proposing immune response criteria in 2009, based on data from ipilimumab phase II trials in patients with advanced melanoma. Dr. Jedd D. Wolchok of Memorial Sloan Kettering Cancer Center, New York, and his associates expanded on RECIST by adding two additional patterns of response: response after an increase in total tumor burden and response in the presence of new lesions. All patterns of response were associated with favorable survival, Dr. Wolchok and associates said (Clin Cancer Res 2009 Dec 1. doi: 10.1158/1078-0432.CCR-09-1624).
Subsequent trials in patients with advanced melanoma have confirmed that a subset of patients who are responders using immune response criteria would have been misclassified using RECIST alone.
In a study of patients with metastatic melanoma treated with nivolumab, 10% experienced distinct immune-related responses, according to Dr. Chiou and Dr. Burotto. In another study of patients with advanced melanoma, this one evaluating anti–PD-1 monoclonal antibody pembrolizumab, 6.7% of patients of the patients experienced pseudoprogression, and overall, 12% of patients were classified as responders or as having stable disease by immune response criteria but would have been classified as having progressive disease by RECIST.
It is time to expand on those first immune response criteria, Dr. Chiou and Dr. Burotto conclude. “Five years after the introduction of the immune response criteria, it is necessary to fully characterize the patterns of immune-related phenomena, to understand these patterns across multiple solid tumor types, and to evaluate how these guidelines are used in current clinical practice,” they wrote.
The Food and Drug Administration agrees. Though guidelines for industry were published in 2011 regarding cancer vaccines, there is no specific guidance on approval criteria for other cancer immunotherapies such as checkpoint inhibitors, Dr. Gideon Blumenthal, team leader in the FDA’s Office of Hematology and Oncology Products, Center for Drug Evaluation and Research, said in an interview.
“However, the FDA is actively looking at other metrics of response beyond conventional RECIST criteria, both to help industry in early ‘go/no-go’ decision making, as well as for helping in the design of later stages of trial design and to help inform approval decisions,” he said.
The FDA is interested in investigating internal data sets of immunotherapy trials, and in collaborating with external stakeholders to determine what the optimal endpoints for cancer immunotherapies will be. Median PFS and PFS hazard ratios do not appear to capture the overall survival benefit that patients derive from immunotherapies, particularly in early lung cancer trials with which he is most familiar, Dr. Blumenthal said.
“Overall survival remains the gold standard endpoint in oncology as it is a direct measure of clinical benefit and less subject to bias, but as more effective therapies come on line and patients live longer, overall survival will become more challenging to detect,” he said.
On Twitter @NikolaidesLaura
Antidepressant, anxiolytic use higher among cancer survivors
WASHINGTON – Cancer survivors are almost twice as likely to be taking medication for anxiety, depression, or both, compared with people who have never had cancer, according to investigators from the Centers for Disease Control and Prevention.
Data from a national survey of more than 48,000 adults show that 15.1% of cancer survivors reported taking drugs for anxiety, and 14% reported taking depression medications, compared with 8.7% and 7.9%, respectively, of adults who never had a cancer diagnosis, reported Nikki A. Hawkins, Ph.D., a behavioral scientist in the CDC’s division of cancer prevention and control.
“We do know that there is a large population of cancer survivors in the U.S. taking these medications for anxiety and depression, which likely reflects the elevated emotional burden on this population,” she said at the joint congress of the International Psycho-Oncology Society and the American Psychosocial Oncology Society.
Dr. Hawkins and her colleagues examined data from the National Health Interview Survey, a nationwide sample of approximately 35,000 U.S. households containing information on about 87,500 people.
The survey asks whether adult participants ever had cancer, the type, and their age at diagnosis, and includes questions about health behaviors such as smoking, as well as access to health care and utilization of preventive and screening services such as human-papillomavirus vaccination and Pap smear for cervical cancer prevention/detection, mammography for breast cancer screening, and fecal occult blood testing, sigmoidoscopy, or colonoscopy for colorectal cancer screening.
Since 2010, a subset of survey participants has been asked questions about functioning and disability, including physical domains (vision, hearing, mobility, etc.), and affect, including whether they take medications for depression and/or “for feeling worried, nervous, or anxious.”
The investigators included those who took part in the survey from 2010 through 2013, including 3,184 cancer survivors and 44,997 controls (no cancer diagnosis).
Sites of most recent cancer diagnoses include breast (in women), prostate, skin (melanoma), cervix, colorectal, hematologic, ovary/uterus, and other.
In all, 15% of patients had been diagnosed within the past 2 years, 29% from 2 to 5 years, 21% from 6 to 10 years, and 36% 11 or more years (numbers exceed 100% because of rounding).
Nearly twice as many cancer survivors reported taking medication for depression or anxiety, compared with the controls: 18% of survivors reported taking either of the medications, compared with 10.4% of controls. This translates into an estimate for the overall U.S. population of 2,383,954 cancer survivors taking medication for either anxiety or depression, Dr. Hawkins said.
Factors predictive of depression or anxiety medication use among cancer survivors included being female, white, non-Hispanic, age younger than 65 years, having never been married, lower levels of education, having a usual place for medical care, and a having a higher number of chronic health conditions.
With the exception of levels of education, the same factors were also predictive of anxiety and/or medication use among controls, the investigators found.
The study was limited by the use of self-reported survey data, and lack of information on the onset or duration of medication use, specific medications taken, or use of other nonpharmacologic therapies for anxiety or depression, Dr. Hawkins acknowledged.
Nonetheless, “these estimates can serve as a benchmark for medication use among the U.S. cancer survivor population, and moving forward, it will be important to look at the duration and onset of use to see exactly when the increase in medication happens and why it happens at that time,” she said.
WASHINGTON – Cancer survivors are almost twice as likely to be taking medication for anxiety, depression, or both, compared with people who have never had cancer, according to investigators from the Centers for Disease Control and Prevention.
Data from a national survey of more than 48,000 adults show that 15.1% of cancer survivors reported taking drugs for anxiety, and 14% reported taking depression medications, compared with 8.7% and 7.9%, respectively, of adults who never had a cancer diagnosis, reported Nikki A. Hawkins, Ph.D., a behavioral scientist in the CDC’s division of cancer prevention and control.
“We do know that there is a large population of cancer survivors in the U.S. taking these medications for anxiety and depression, which likely reflects the elevated emotional burden on this population,” she said at the joint congress of the International Psycho-Oncology Society and the American Psychosocial Oncology Society.
Dr. Hawkins and her colleagues examined data from the National Health Interview Survey, a nationwide sample of approximately 35,000 U.S. households containing information on about 87,500 people.
The survey asks whether adult participants ever had cancer, the type, and their age at diagnosis, and includes questions about health behaviors such as smoking, as well as access to health care and utilization of preventive and screening services such as human-papillomavirus vaccination and Pap smear for cervical cancer prevention/detection, mammography for breast cancer screening, and fecal occult blood testing, sigmoidoscopy, or colonoscopy for colorectal cancer screening.
Since 2010, a subset of survey participants has been asked questions about functioning and disability, including physical domains (vision, hearing, mobility, etc.), and affect, including whether they take medications for depression and/or “for feeling worried, nervous, or anxious.”
The investigators included those who took part in the survey from 2010 through 2013, including 3,184 cancer survivors and 44,997 controls (no cancer diagnosis).
Sites of most recent cancer diagnoses include breast (in women), prostate, skin (melanoma), cervix, colorectal, hematologic, ovary/uterus, and other.
In all, 15% of patients had been diagnosed within the past 2 years, 29% from 2 to 5 years, 21% from 6 to 10 years, and 36% 11 or more years (numbers exceed 100% because of rounding).
Nearly twice as many cancer survivors reported taking medication for depression or anxiety, compared with the controls: 18% of survivors reported taking either of the medications, compared with 10.4% of controls. This translates into an estimate for the overall U.S. population of 2,383,954 cancer survivors taking medication for either anxiety or depression, Dr. Hawkins said.
Factors predictive of depression or anxiety medication use among cancer survivors included being female, white, non-Hispanic, age younger than 65 years, having never been married, lower levels of education, having a usual place for medical care, and a having a higher number of chronic health conditions.
With the exception of levels of education, the same factors were also predictive of anxiety and/or medication use among controls, the investigators found.
The study was limited by the use of self-reported survey data, and lack of information on the onset or duration of medication use, specific medications taken, or use of other nonpharmacologic therapies for anxiety or depression, Dr. Hawkins acknowledged.
Nonetheless, “these estimates can serve as a benchmark for medication use among the U.S. cancer survivor population, and moving forward, it will be important to look at the duration and onset of use to see exactly when the increase in medication happens and why it happens at that time,” she said.
WASHINGTON – Cancer survivors are almost twice as likely to be taking medication for anxiety, depression, or both, compared with people who have never had cancer, according to investigators from the Centers for Disease Control and Prevention.
Data from a national survey of more than 48,000 adults show that 15.1% of cancer survivors reported taking drugs for anxiety, and 14% reported taking depression medications, compared with 8.7% and 7.9%, respectively, of adults who never had a cancer diagnosis, reported Nikki A. Hawkins, Ph.D., a behavioral scientist in the CDC’s division of cancer prevention and control.
“We do know that there is a large population of cancer survivors in the U.S. taking these medications for anxiety and depression, which likely reflects the elevated emotional burden on this population,” she said at the joint congress of the International Psycho-Oncology Society and the American Psychosocial Oncology Society.
Dr. Hawkins and her colleagues examined data from the National Health Interview Survey, a nationwide sample of approximately 35,000 U.S. households containing information on about 87,500 people.
The survey asks whether adult participants ever had cancer, the type, and their age at diagnosis, and includes questions about health behaviors such as smoking, as well as access to health care and utilization of preventive and screening services such as human-papillomavirus vaccination and Pap smear for cervical cancer prevention/detection, mammography for breast cancer screening, and fecal occult blood testing, sigmoidoscopy, or colonoscopy for colorectal cancer screening.
Since 2010, a subset of survey participants has been asked questions about functioning and disability, including physical domains (vision, hearing, mobility, etc.), and affect, including whether they take medications for depression and/or “for feeling worried, nervous, or anxious.”
The investigators included those who took part in the survey from 2010 through 2013, including 3,184 cancer survivors and 44,997 controls (no cancer diagnosis).
Sites of most recent cancer diagnoses include breast (in women), prostate, skin (melanoma), cervix, colorectal, hematologic, ovary/uterus, and other.
In all, 15% of patients had been diagnosed within the past 2 years, 29% from 2 to 5 years, 21% from 6 to 10 years, and 36% 11 or more years (numbers exceed 100% because of rounding).
Nearly twice as many cancer survivors reported taking medication for depression or anxiety, compared with the controls: 18% of survivors reported taking either of the medications, compared with 10.4% of controls. This translates into an estimate for the overall U.S. population of 2,383,954 cancer survivors taking medication for either anxiety or depression, Dr. Hawkins said.
Factors predictive of depression or anxiety medication use among cancer survivors included being female, white, non-Hispanic, age younger than 65 years, having never been married, lower levels of education, having a usual place for medical care, and a having a higher number of chronic health conditions.
With the exception of levels of education, the same factors were also predictive of anxiety and/or medication use among controls, the investigators found.
The study was limited by the use of self-reported survey data, and lack of information on the onset or duration of medication use, specific medications taken, or use of other nonpharmacologic therapies for anxiety or depression, Dr. Hawkins acknowledged.
Nonetheless, “these estimates can serve as a benchmark for medication use among the U.S. cancer survivor population, and moving forward, it will be important to look at the duration and onset of use to see exactly when the increase in medication happens and why it happens at that time,” she said.
AT THE WORLD CONGRESS OF PSYCHO-ONCOLOGY
Key clinical point: Adult cancer survivors are nearly twice as likely to be taking drugs for anxiety or depression, compared with adults who never had cancer.
Major finding: A total of 18% of cancer survivors reported taking medication for either anxiety or depression, compared with 10.4% of controls.
Data source: National Health Interview Survey data on 3,184 cancer survivors and 44,997 controls.
Disclosures: The study was supported by the CDC. Dr. Hawkins is a CDC employee but reported no other conflicts of interest.
Ipilimumab’s immune-related adverse effects greater in ‘real-world patients’
Patients treated with ipilimumab for metastatic melanoma should be prepared for immune-related adverse effects, and physicians should expect to treat them early and aggressively, according to a report published online Aug. 17 in Journal of Clinical Oncology.
Severe immune-related adverse effects such as diarrhea, hepatitis, and hypophysitis were common in a retrospective analysis of the medical records of 298 patients treated during a 27-month period at Memorial Sloan Kettering Cancer Center, New York. Corticosteroids were not adequate to control symptoms in a substantial number of cases, and additional systemic immunosuppressive therapy was required, said Dr. Troy Z. Horvat of Memorial Sloan Kettering and his associates.
From their institutional experience, the investigators suspected that the incidence of clinically significant adverse effects of ipilimumab was higher than has been previously reported and higher than would be expected just by counting the number of events qualifying as grade 3 or higher by National Cancer Institute criteria. They also suspected that the need for immunosuppressive therapy was greater than generally expected. Previous studies showed adverse event rates ranging from 6% to 19%, and did not give any information regarding corticosteroid use.
Their analysis confirmed these suspicions, showing that 31% of patients developed grade 3, 4, or 5 adverse effects and 35% required corticosteroid therapy. This is more than twice the rate of grade 3 or higher toxicity reported in clinical trials of ipilimumab. Adverse effects included diarrhea (50 patients), which led to bowel perforation in 3 patients; hepatitis (22 patients); dermatitis (21 patients); endocrinopathies (14); hypophysitis (6); uveitis (2); pneumonitis (1); seizure (1); arthritis (1); and hearing loss (1). These effects were severe enough to cause 19% of patients to discontinue ipilimumab.
About one-third of the patients who received systemic corticosteroids – 10% of the total study population – required additional immunotherapy, including infliximab, mycophenolate, or adalimumab, Dr. Horvat and his associates said (J Clin Oncol 2015 Aug 17 [doi:10.1200/JCO.2015.60.8448]).
This study’s higher rates of adverse events, of corticosteroid therapy, and of further immunosuppressive therapy are likely attributable to the treatment team’s considerable experience with ipilimumab in real-world patients. As clinicians gain such experience, they become more familiar with associated adverse events, allowing earlier identification and intervention, the investigators said.
“In our experience, if improvement in ipilimumab-related adverse effects is not evident early in the treatment with high-dose systemic corticosteroids, more prolonged treatment rarely leads to benefit, and patients usually end up requiring infliximab anyway. ... We believe the overall risk-to-benefit ratio favors the early use of infliximab rather than prolonged treatment with corticosteroids,” they noted.
The median overall survival and median time to treatment failure were not affected by either the occurrence of adverse events or the use of corticosteroids. Overall, 12% of these patients achieved long-term disease control and didn’t require further melanoma treatment. Based on their findings and those of another research group, “we believe that patients and physicians should not be concerned that ipilimumab-related adverse events requiring systemic immunosuppression will compromise the therapeutic benefit,” Dr. Horvat and his associates said.
Patients treated with ipilimumab for metastatic melanoma should be prepared for immune-related adverse effects, and physicians should expect to treat them early and aggressively, according to a report published online Aug. 17 in Journal of Clinical Oncology.
Severe immune-related adverse effects such as diarrhea, hepatitis, and hypophysitis were common in a retrospective analysis of the medical records of 298 patients treated during a 27-month period at Memorial Sloan Kettering Cancer Center, New York. Corticosteroids were not adequate to control symptoms in a substantial number of cases, and additional systemic immunosuppressive therapy was required, said Dr. Troy Z. Horvat of Memorial Sloan Kettering and his associates.
From their institutional experience, the investigators suspected that the incidence of clinically significant adverse effects of ipilimumab was higher than has been previously reported and higher than would be expected just by counting the number of events qualifying as grade 3 or higher by National Cancer Institute criteria. They also suspected that the need for immunosuppressive therapy was greater than generally expected. Previous studies showed adverse event rates ranging from 6% to 19%, and did not give any information regarding corticosteroid use.
Their analysis confirmed these suspicions, showing that 31% of patients developed grade 3, 4, or 5 adverse effects and 35% required corticosteroid therapy. This is more than twice the rate of grade 3 or higher toxicity reported in clinical trials of ipilimumab. Adverse effects included diarrhea (50 patients), which led to bowel perforation in 3 patients; hepatitis (22 patients); dermatitis (21 patients); endocrinopathies (14); hypophysitis (6); uveitis (2); pneumonitis (1); seizure (1); arthritis (1); and hearing loss (1). These effects were severe enough to cause 19% of patients to discontinue ipilimumab.
About one-third of the patients who received systemic corticosteroids – 10% of the total study population – required additional immunotherapy, including infliximab, mycophenolate, or adalimumab, Dr. Horvat and his associates said (J Clin Oncol 2015 Aug 17 [doi:10.1200/JCO.2015.60.8448]).
This study’s higher rates of adverse events, of corticosteroid therapy, and of further immunosuppressive therapy are likely attributable to the treatment team’s considerable experience with ipilimumab in real-world patients. As clinicians gain such experience, they become more familiar with associated adverse events, allowing earlier identification and intervention, the investigators said.
“In our experience, if improvement in ipilimumab-related adverse effects is not evident early in the treatment with high-dose systemic corticosteroids, more prolonged treatment rarely leads to benefit, and patients usually end up requiring infliximab anyway. ... We believe the overall risk-to-benefit ratio favors the early use of infliximab rather than prolonged treatment with corticosteroids,” they noted.
The median overall survival and median time to treatment failure were not affected by either the occurrence of adverse events or the use of corticosteroids. Overall, 12% of these patients achieved long-term disease control and didn’t require further melanoma treatment. Based on their findings and those of another research group, “we believe that patients and physicians should not be concerned that ipilimumab-related adverse events requiring systemic immunosuppression will compromise the therapeutic benefit,” Dr. Horvat and his associates said.
Patients treated with ipilimumab for metastatic melanoma should be prepared for immune-related adverse effects, and physicians should expect to treat them early and aggressively, according to a report published online Aug. 17 in Journal of Clinical Oncology.
Severe immune-related adverse effects such as diarrhea, hepatitis, and hypophysitis were common in a retrospective analysis of the medical records of 298 patients treated during a 27-month period at Memorial Sloan Kettering Cancer Center, New York. Corticosteroids were not adequate to control symptoms in a substantial number of cases, and additional systemic immunosuppressive therapy was required, said Dr. Troy Z. Horvat of Memorial Sloan Kettering and his associates.
From their institutional experience, the investigators suspected that the incidence of clinically significant adverse effects of ipilimumab was higher than has been previously reported and higher than would be expected just by counting the number of events qualifying as grade 3 or higher by National Cancer Institute criteria. They also suspected that the need for immunosuppressive therapy was greater than generally expected. Previous studies showed adverse event rates ranging from 6% to 19%, and did not give any information regarding corticosteroid use.
Their analysis confirmed these suspicions, showing that 31% of patients developed grade 3, 4, or 5 adverse effects and 35% required corticosteroid therapy. This is more than twice the rate of grade 3 or higher toxicity reported in clinical trials of ipilimumab. Adverse effects included diarrhea (50 patients), which led to bowel perforation in 3 patients; hepatitis (22 patients); dermatitis (21 patients); endocrinopathies (14); hypophysitis (6); uveitis (2); pneumonitis (1); seizure (1); arthritis (1); and hearing loss (1). These effects were severe enough to cause 19% of patients to discontinue ipilimumab.
About one-third of the patients who received systemic corticosteroids – 10% of the total study population – required additional immunotherapy, including infliximab, mycophenolate, or adalimumab, Dr. Horvat and his associates said (J Clin Oncol 2015 Aug 17 [doi:10.1200/JCO.2015.60.8448]).
This study’s higher rates of adverse events, of corticosteroid therapy, and of further immunosuppressive therapy are likely attributable to the treatment team’s considerable experience with ipilimumab in real-world patients. As clinicians gain such experience, they become more familiar with associated adverse events, allowing earlier identification and intervention, the investigators said.
“In our experience, if improvement in ipilimumab-related adverse effects is not evident early in the treatment with high-dose systemic corticosteroids, more prolonged treatment rarely leads to benefit, and patients usually end up requiring infliximab anyway. ... We believe the overall risk-to-benefit ratio favors the early use of infliximab rather than prolonged treatment with corticosteroids,” they noted.
The median overall survival and median time to treatment failure were not affected by either the occurrence of adverse events or the use of corticosteroids. Overall, 12% of these patients achieved long-term disease control and didn’t require further melanoma treatment. Based on their findings and those of another research group, “we believe that patients and physicians should not be concerned that ipilimumab-related adverse events requiring systemic immunosuppression will compromise the therapeutic benefit,” Dr. Horvat and his associates said.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Physicians and patients should be prepared for immune-related adverse effects from ipilimumab for treatment of metastatic melanoma.
Major finding: Just under one-third of patients developed grade 3, 4, or 5 adverse effects and 35% of patients required corticosteroid therapy, more than twice the rate of grade 3 or higher toxicity reported in clinical trials of ipilimumab.
Data source: A single-center retrospective analysis of adverse effects from ipilimumab therapy in 298 patients treated during a 27-month period.
Disclosures: This study was supported in part by the John K. Figge Fund. Dr. Horvat reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
Weight program effective for breast cancer survivors
A group-based behavioral weight loss program supplemented with personal contact and support was effective in helping overweight or obese breast cancer survivors lose a clinically meaningful amount of weight, investigators reported online Aug. 17 in the Journal of Clinical Oncology.
“Women who have been diagnosed and treated for breast cancer often have special issues and problems, such as treatment-related adverse effects, fatigue, and depression, that can complicate weight management efforts,” wrote Cheryl L. Rock, Ph.D., of the University of California, San Diego, Moores Cancer Center in La Jolla, and her colleagues.
The results from this trial demonstrate that weight loss, even though it was modest, and increased physical activity can be achieved in this population and suggest that these issues can be overcome, the authors noted.
The multicenter trial included 692 overweight or obese breast cancer survivors who were randomly assigned to either the intervention group – which included a cognitive-behavioral weight loss program with telephone counseling and tailored newsletters to support initial weight loss and subsequent maintenance – or a control group with a less intensive intervention (J Clin Oncol. 2015 Aug. 17 doi: 10.1200/JCO.2015.61.1095).
At 6 months, the mean weight loss in the intervention group was 5.9%; at 12 months, the weight loss held steady and was maintained at 6%. In the control group, weight loss was 1.3% at 6 months and 1.5% at 12 months.
At 18 months, the women in the intervention group were 4.7% below their baseline weight, and at 24 months they weighed 3.7% less than at entry into the study. Those in the control group were 1.3% below baseline weight at 18 months and 1.1% below at 24 months.
The weight loss intervention was more effective among women older than 55 years than in younger women, who may need counseling and resources beyond that offered in this study, to achieve sufficient weight loss, Dr. Rock and her associates added.
The study was supported by the National Cancer Institute and by a grant from the National Center for Research Resources, a component of the NIH, and NIH Roadmap for Medical Research. Dr. Rock reported research funding from Jenny Craig and Nestle USA, and several of the coauthors reported financial relationships with various corporations.
A group-based behavioral weight loss program supplemented with personal contact and support was effective in helping overweight or obese breast cancer survivors lose a clinically meaningful amount of weight, investigators reported online Aug. 17 in the Journal of Clinical Oncology.
“Women who have been diagnosed and treated for breast cancer often have special issues and problems, such as treatment-related adverse effects, fatigue, and depression, that can complicate weight management efforts,” wrote Cheryl L. Rock, Ph.D., of the University of California, San Diego, Moores Cancer Center in La Jolla, and her colleagues.
The results from this trial demonstrate that weight loss, even though it was modest, and increased physical activity can be achieved in this population and suggest that these issues can be overcome, the authors noted.
The multicenter trial included 692 overweight or obese breast cancer survivors who were randomly assigned to either the intervention group – which included a cognitive-behavioral weight loss program with telephone counseling and tailored newsletters to support initial weight loss and subsequent maintenance – or a control group with a less intensive intervention (J Clin Oncol. 2015 Aug. 17 doi: 10.1200/JCO.2015.61.1095).
At 6 months, the mean weight loss in the intervention group was 5.9%; at 12 months, the weight loss held steady and was maintained at 6%. In the control group, weight loss was 1.3% at 6 months and 1.5% at 12 months.
At 18 months, the women in the intervention group were 4.7% below their baseline weight, and at 24 months they weighed 3.7% less than at entry into the study. Those in the control group were 1.3% below baseline weight at 18 months and 1.1% below at 24 months.
The weight loss intervention was more effective among women older than 55 years than in younger women, who may need counseling and resources beyond that offered in this study, to achieve sufficient weight loss, Dr. Rock and her associates added.
The study was supported by the National Cancer Institute and by a grant from the National Center for Research Resources, a component of the NIH, and NIH Roadmap for Medical Research. Dr. Rock reported research funding from Jenny Craig and Nestle USA, and several of the coauthors reported financial relationships with various corporations.
A group-based behavioral weight loss program supplemented with personal contact and support was effective in helping overweight or obese breast cancer survivors lose a clinically meaningful amount of weight, investigators reported online Aug. 17 in the Journal of Clinical Oncology.
“Women who have been diagnosed and treated for breast cancer often have special issues and problems, such as treatment-related adverse effects, fatigue, and depression, that can complicate weight management efforts,” wrote Cheryl L. Rock, Ph.D., of the University of California, San Diego, Moores Cancer Center in La Jolla, and her colleagues.
The results from this trial demonstrate that weight loss, even though it was modest, and increased physical activity can be achieved in this population and suggest that these issues can be overcome, the authors noted.
The multicenter trial included 692 overweight or obese breast cancer survivors who were randomly assigned to either the intervention group – which included a cognitive-behavioral weight loss program with telephone counseling and tailored newsletters to support initial weight loss and subsequent maintenance – or a control group with a less intensive intervention (J Clin Oncol. 2015 Aug. 17 doi: 10.1200/JCO.2015.61.1095).
At 6 months, the mean weight loss in the intervention group was 5.9%; at 12 months, the weight loss held steady and was maintained at 6%. In the control group, weight loss was 1.3% at 6 months and 1.5% at 12 months.
At 18 months, the women in the intervention group were 4.7% below their baseline weight, and at 24 months they weighed 3.7% less than at entry into the study. Those in the control group were 1.3% below baseline weight at 18 months and 1.1% below at 24 months.
The weight loss intervention was more effective among women older than 55 years than in younger women, who may need counseling and resources beyond that offered in this study, to achieve sufficient weight loss, Dr. Rock and her associates added.
The study was supported by the National Cancer Institute and by a grant from the National Center for Research Resources, a component of the NIH, and NIH Roadmap for Medical Research. Dr. Rock reported research funding from Jenny Craig and Nestle USA, and several of the coauthors reported financial relationships with various corporations.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: A group-based behavioral weight loss intervention can lead to clinically meaningful weight loss in overweight/obese breast cancer survivors
Major finding: At 24 months, mean weight loss was more than double in the intervention group, compared with controls (3.7% vs 1.3%).
Data source: Multicenter randomized trial involving 692 overweight/obese women who were about 2 years post treatment for early-stage breast cancer.
Disclosures: The study was supported by the National Cancer Institute and by a grant from the National Center for Research Resources, a component of the NIH, and NIH Roadmap for Medical Research. Dr. Rock reported research funding from Jenny Craig and Nestle USA, and several of the coauthors reported financial relationships with various corporations.