User login
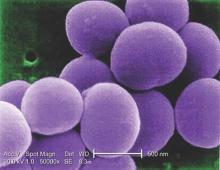
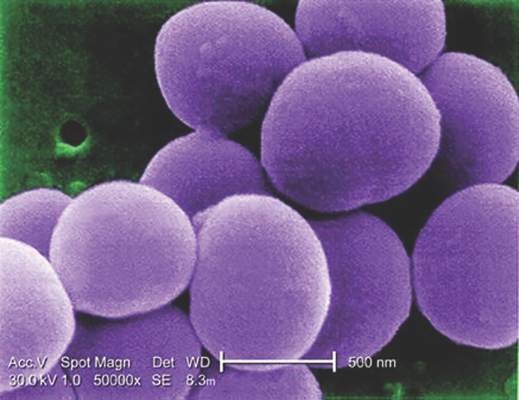
Glucocorticoids increase risk of S. aureus bacteremia
Use of systemic glucocorticoids significantly increased risk for community-acquired Staphylococcus aureus bacteremia (CA-SAB) in a dose-dependent fashion, based on data from a large Danish registry.
On average, current users of systemic glucocorticoids had an adjusted 2.5-fold increased risk of CA-SAB, compared with nonusers. The risk was most pronounced in long-term users of glucocorticoids, including patients with connective tissue disease and patients with chronic pulmonary disease. Among new users of glucocorticoids, the risk of CA-SAB was highest for patients with cancer, in the retrospective, case-control study published by Mayo Clinic Proceedings.
Dr. Jesper Smit of Aalborg (Denmark) University and his colleagues, looked at all 2,638 patients admitted with first-time CA-SAB and 26,379 matched population controls in Northern Denmark medical databases between January 1, 2000, and December 31, 2011.
New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Risk of CA-SAB rose in a dose-dependent fashion as 90-day cumulative doses increased. For subjects taking a cumulative dose of 150 mg or less, the adjusted OR for CA-SAB was 1.3. At a cumulative dose of 500-1000 mg, OR rose to 2.4. At a cumulative dose greater than 1000 mg, OR was 6.2.
Risk did not differ based on individuals’ sex, age group, or the severity of any comorbidity.
“This is the first study to specifically investigate whether the use of glucocorticoids is associated with increased risk of CA-SAB,” the authors concluded, adding that “these results extend the current knowledge of risk factors for CA-SAB and may serve as a reminder for clinicians to carefully weigh the elevated risk against the potential beneficial effect of glucocorticoid therapy, particularly in patients with concomitant CA-SAB risk factors.”
This study was supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
Use of systemic glucocorticoids significantly increased risk for community-acquired Staphylococcus aureus bacteremia (CA-SAB) in a dose-dependent fashion, based on data from a large Danish registry.
On average, current users of systemic glucocorticoids had an adjusted 2.5-fold increased risk of CA-SAB, compared with nonusers. The risk was most pronounced in long-term users of glucocorticoids, including patients with connective tissue disease and patients with chronic pulmonary disease. Among new users of glucocorticoids, the risk of CA-SAB was highest for patients with cancer, in the retrospective, case-control study published by Mayo Clinic Proceedings.
Dr. Jesper Smit of Aalborg (Denmark) University and his colleagues, looked at all 2,638 patients admitted with first-time CA-SAB and 26,379 matched population controls in Northern Denmark medical databases between January 1, 2000, and December 31, 2011.
New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Risk of CA-SAB rose in a dose-dependent fashion as 90-day cumulative doses increased. For subjects taking a cumulative dose of 150 mg or less, the adjusted OR for CA-SAB was 1.3. At a cumulative dose of 500-1000 mg, OR rose to 2.4. At a cumulative dose greater than 1000 mg, OR was 6.2.
Risk did not differ based on individuals’ sex, age group, or the severity of any comorbidity.
“This is the first study to specifically investigate whether the use of glucocorticoids is associated with increased risk of CA-SAB,” the authors concluded, adding that “these results extend the current knowledge of risk factors for CA-SAB and may serve as a reminder for clinicians to carefully weigh the elevated risk against the potential beneficial effect of glucocorticoid therapy, particularly in patients with concomitant CA-SAB risk factors.”
This study was supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
Use of systemic glucocorticoids significantly increased risk for community-acquired Staphylococcus aureus bacteremia (CA-SAB) in a dose-dependent fashion, based on data from a large Danish registry.
On average, current users of systemic glucocorticoids had an adjusted 2.5-fold increased risk of CA-SAB, compared with nonusers. The risk was most pronounced in long-term users of glucocorticoids, including patients with connective tissue disease and patients with chronic pulmonary disease. Among new users of glucocorticoids, the risk of CA-SAB was highest for patients with cancer, in the retrospective, case-control study published by Mayo Clinic Proceedings.
Dr. Jesper Smit of Aalborg (Denmark) University and his colleagues, looked at all 2,638 patients admitted with first-time CA-SAB and 26,379 matched population controls in Northern Denmark medical databases between January 1, 2000, and December 31, 2011.
New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Risk of CA-SAB rose in a dose-dependent fashion as 90-day cumulative doses increased. For subjects taking a cumulative dose of 150 mg or less, the adjusted OR for CA-SAB was 1.3. At a cumulative dose of 500-1000 mg, OR rose to 2.4. At a cumulative dose greater than 1000 mg, OR was 6.2.
Risk did not differ based on individuals’ sex, age group, or the severity of any comorbidity.
“This is the first study to specifically investigate whether the use of glucocorticoids is associated with increased risk of CA-SAB,” the authors concluded, adding that “these results extend the current knowledge of risk factors for CA-SAB and may serve as a reminder for clinicians to carefully weigh the elevated risk against the potential beneficial effect of glucocorticoid therapy, particularly in patients with concomitant CA-SAB risk factors.”
This study was supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
FROM MAYO CLINIC PROCEEDINGS
Key clinical point: Taking glucocorticoids can significantly increase the risk of contracting community-acquired Staphylococcus aureus bacteremia (CA-SAB).
Major finding: New glucocorticoid users had an odds ratio for CA-SAB of 2.7, slightly higher than the OR of 2.3 for long-term users. Former glucocorticoid users had a considerably lower OR for CA-SAB of 1.3.
Data source: Retrospective, case-control study of all adults with first-time CA-SAB in Northern Denmark medical registries between 2000 and 2011.
Disclosures: Study supported by grants from Heinrich Kopp, Hertha Christensen, and North Denmark Health Sciences Research foundation. The authors did not report any relevant financial disclosures.
Statins improve ovarian cancer survival
SAN DIEGO – Statin therapy was independently associated with a substantial survival benefit in women with ovarian cancer in an analysis of the linked Surveillance, Epidemiology and End Results and Medicare databases.
“This is the largest series ever reported supporting the anticancer effect of statin therapy on epithelial ovarian cancer with a concomitant improvement in overall survival. A prospective study in ovarian cancer patients is warranted. Identification of biomarkers that may predict response to statins would help further select patient populations and guide therapy,” Dr. Tilley Jenkins Vogel said in presenting the study results at the annual meeting of the Society of Gynecologic Oncology.
She and her coinvestigators at Cedars-Sinai Medical Center in Los Angeles identified 1,510 women in the SEER registry who were diagnosed with epithelial ovarian cancer during 2007-2009, underwent primary surgical resection, and survived for at least 60 days post surgery. Forty-nine percent were stage III, 25% stage IV. Forty-two percent of the women were on a statin.
Mean overall survival in the statin users was 32.2 months compared to 28.7 months in nonusers. In the stage III cohort, mean overall survival in statin users versus nonusers was 31.7 and 25.9 months.
In a multivariate analysis adjusted for potential confounders of age, race, heart disease and other comorbid conditions prior to cancer diagnosis, and the use of platinum-based chemotherapy, statin therapy was independently associated with a 34% reduction in the risk of mortality. In women whose ovarian cancer histology was serous, statin use was associated with a 31% reduction in death; in those with a nonserous histology, it was a 48% reduction, Dr. Vogel continued.
Diving deeper into the dataset, she found that the overall survival benefit was present only in the 89% of statin users who were on lipophilic statins, such as atorvastatin or simvastatin. This is consistent with other investigators’ reports that the noncardiovascular benefits of statin therapy are largely restricted to the lipophilic class of the LDL-lowering agents.
An anti–ovarian cancer benefit for statin therapy appears to have biologic plausibility, according to Dr. Vogel. She and her coworkers have previously shown synergistic cytotoxicity in vitro when statins are administered concurrently with platinum chemotherapy.
“This effect is believed to be mediated by greater inhibition of cell proliferation, increased apoptosis, and modification of proteins in the RAS pathway,” she said.
Rapidly growing cells, such as cancer cells, require cholesterol to synthesize cell membrane. It’s hypothesized that one mechanism for statins’ anticancer effect is that by reducing intracellular cholesterol levels the drugs interfere with this process, Dr. Vogel noted.
She reported having no financial conflicts regarding this study, conducted without commercial support.
SAN DIEGO – Statin therapy was independently associated with a substantial survival benefit in women with ovarian cancer in an analysis of the linked Surveillance, Epidemiology and End Results and Medicare databases.
“This is the largest series ever reported supporting the anticancer effect of statin therapy on epithelial ovarian cancer with a concomitant improvement in overall survival. A prospective study in ovarian cancer patients is warranted. Identification of biomarkers that may predict response to statins would help further select patient populations and guide therapy,” Dr. Tilley Jenkins Vogel said in presenting the study results at the annual meeting of the Society of Gynecologic Oncology.
She and her coinvestigators at Cedars-Sinai Medical Center in Los Angeles identified 1,510 women in the SEER registry who were diagnosed with epithelial ovarian cancer during 2007-2009, underwent primary surgical resection, and survived for at least 60 days post surgery. Forty-nine percent were stage III, 25% stage IV. Forty-two percent of the women were on a statin.
Mean overall survival in the statin users was 32.2 months compared to 28.7 months in nonusers. In the stage III cohort, mean overall survival in statin users versus nonusers was 31.7 and 25.9 months.
In a multivariate analysis adjusted for potential confounders of age, race, heart disease and other comorbid conditions prior to cancer diagnosis, and the use of platinum-based chemotherapy, statin therapy was independently associated with a 34% reduction in the risk of mortality. In women whose ovarian cancer histology was serous, statin use was associated with a 31% reduction in death; in those with a nonserous histology, it was a 48% reduction, Dr. Vogel continued.
Diving deeper into the dataset, she found that the overall survival benefit was present only in the 89% of statin users who were on lipophilic statins, such as atorvastatin or simvastatin. This is consistent with other investigators’ reports that the noncardiovascular benefits of statin therapy are largely restricted to the lipophilic class of the LDL-lowering agents.
An anti–ovarian cancer benefit for statin therapy appears to have biologic plausibility, according to Dr. Vogel. She and her coworkers have previously shown synergistic cytotoxicity in vitro when statins are administered concurrently with platinum chemotherapy.
“This effect is believed to be mediated by greater inhibition of cell proliferation, increased apoptosis, and modification of proteins in the RAS pathway,” she said.
Rapidly growing cells, such as cancer cells, require cholesterol to synthesize cell membrane. It’s hypothesized that one mechanism for statins’ anticancer effect is that by reducing intracellular cholesterol levels the drugs interfere with this process, Dr. Vogel noted.
She reported having no financial conflicts regarding this study, conducted without commercial support.
SAN DIEGO – Statin therapy was independently associated with a substantial survival benefit in women with ovarian cancer in an analysis of the linked Surveillance, Epidemiology and End Results and Medicare databases.
“This is the largest series ever reported supporting the anticancer effect of statin therapy on epithelial ovarian cancer with a concomitant improvement in overall survival. A prospective study in ovarian cancer patients is warranted. Identification of biomarkers that may predict response to statins would help further select patient populations and guide therapy,” Dr. Tilley Jenkins Vogel said in presenting the study results at the annual meeting of the Society of Gynecologic Oncology.
She and her coinvestigators at Cedars-Sinai Medical Center in Los Angeles identified 1,510 women in the SEER registry who were diagnosed with epithelial ovarian cancer during 2007-2009, underwent primary surgical resection, and survived for at least 60 days post surgery. Forty-nine percent were stage III, 25% stage IV. Forty-two percent of the women were on a statin.
Mean overall survival in the statin users was 32.2 months compared to 28.7 months in nonusers. In the stage III cohort, mean overall survival in statin users versus nonusers was 31.7 and 25.9 months.
In a multivariate analysis adjusted for potential confounders of age, race, heart disease and other comorbid conditions prior to cancer diagnosis, and the use of platinum-based chemotherapy, statin therapy was independently associated with a 34% reduction in the risk of mortality. In women whose ovarian cancer histology was serous, statin use was associated with a 31% reduction in death; in those with a nonserous histology, it was a 48% reduction, Dr. Vogel continued.
Diving deeper into the dataset, she found that the overall survival benefit was present only in the 89% of statin users who were on lipophilic statins, such as atorvastatin or simvastatin. This is consistent with other investigators’ reports that the noncardiovascular benefits of statin therapy are largely restricted to the lipophilic class of the LDL-lowering agents.
An anti–ovarian cancer benefit for statin therapy appears to have biologic plausibility, according to Dr. Vogel. She and her coworkers have previously shown synergistic cytotoxicity in vitro when statins are administered concurrently with platinum chemotherapy.
“This effect is believed to be mediated by greater inhibition of cell proliferation, increased apoptosis, and modification of proteins in the RAS pathway,” she said.
Rapidly growing cells, such as cancer cells, require cholesterol to synthesize cell membrane. It’s hypothesized that one mechanism for statins’ anticancer effect is that by reducing intracellular cholesterol levels the drugs interfere with this process, Dr. Vogel noted.
She reported having no financial conflicts regarding this study, conducted without commercial support.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
Adjuvant AI therapy for breast cancer: 10 years is superior to 5 years
CHICAGO – Extending adjuvant aromatase inhibitor (AI) therapy from 5 years to 10 years further reduces the risk of recurrence and new breast cancer in postmenopausal women treated for early disease, according to findings of the MA17.R trial.
In the phase III trial conducted by the Canadian Cancer Trials Group and the North American Breast Cancer Group, 1,918 postmenopausal women who had completed about 5 years of AI therapy (preceded by tamoxifen in the majority of cases) were randomized to take the AI letrozole or to stop therapy by taking placebo for an additional 5 years.
Compared with peers who stopped, women who continued AI therapy for 5 more years had a 34% lower risk of recurrence or contralateral breast cancer, investigators reported in sessions and a press briefing at the annual meeting of the American Society of Clinical Oncology. The trade-off was a small increase in the rates of skeletal adverse events such as fractures; quality of life was essentially unaffected.
“MA17.R is the first study to show the benefit of extending an adjuvant aromatase inhibitor beyond 5 years,” commented lead investigator Paul E. Goss, M.D., director of the Breast Cancer Research Program at the Massachusetts General Hospital and a professor of medicine at Harvard Medical School, both in Boston. “Unlike many anticancer therapies, aromatase inhibitors are readily accessible around the world, and therefore, our results will further improve the outcome of many women with breast cancer.”
The disease-free survival curves will likely separate further, given a “legacy effect” of endocrine therapy that persists after it ends, he predicted. “And I think overall survival will eventually become positive in MA.17R. … The Food and Drug Administration has taken the opinion that overall survival follows disease-free survival like night follows day for endocrine therapies, and I think they are correct, I think that’s what we see in all the trials.”
Implications
It remains unclear how patients should be managed after 10 years of an AI, according to Dr. Goss. “That’s uncharted waters,” he elaborated. “We know from the curve of the natural history of this disease that it chronically relapses, and we continue to see patients 25 years after their primary diagnosis with a recurrence.” Some data in mice suggest there may be benefit from continuing the AI until recurrence. “I don’t think that would be entered into in clinical practice as a rule, because there is no clinical trial of that,” he said. “But this data will now take the aromatase inhibitors out to 10 years.”
The MA.17R trial’s findings show that extended duration of AI therapy is “clinically valuable,” according to ASCO expert Harold J. Burstein, M.D., Ph.D., a senior physician at the Dana-Farber Cancer Institute and an associate professor of medicine at the Harvard Medical School in Boston. He predicted the findings will have at least two consequences.
“One is tremendous interest in longer durations of therapy with the AI, but also some tailoring of treatment based on how the patient has fared with their therapy and on their baseline risk of recurrence. So women who have less risky cancer will probably be less inclined to pursue these longer durations, and women who have higher-risk cancers will be more inclined,” he explained.
Also, “women who have finished 5 years of an AI without any prior tamoxifen I think are going to be very compelled by these data, whereas women who have had 5 years of tamoxifen, 5 years of an AI, and are already 10 years out probably get less benefit numerically from yet longer duration of therapy,” he added. “And we are certainly not at the point of saying that women should be on these drugs for the rest of their lives.”
MA.17R design
Postmenopausal women were eligible for MA.17R if they had undergone resection of hormone receptor–positive early breast cancer and had already completed about 5 years of therapy with any of the three AIs currently on the market. In the large majority of cases, they also had previously received tamoxifen.
Many of the women came from the parent MA.17 trial, which tested an initial 5 years of letrozole (brand name Femara) against placebo after tamoxifen therapy. Longer-term results of that trial, previously reported (J Clin Oncol. 2012;30:718-21), showed that this duration of letrozole had a significant disease-free survival benefit (hazard ratio, .52) and overall survival benefit (HR, .61).
In the MA.17R trial, the women were randomized to letrozole or a placebo for an additional 5 years, with a primary endpoint of disease-free survival and secondary endpoints including safety and quality of life.
Efficacy and safety
After a median follow-up of 6.3 years, the 5-year rate of disease-free survival was 95% with letrozole and 91% with placebo, according to results reported by Dr. Goss in a plenary session at the meeting and simultaneously published (N Engl J Med. 2016. June 5 doi: 10.1056/NEJMoa1604700).
The difference translated to a more than one-third reduction in the risk of disease recurrence or the occurrence of contralateral breast cancer (HR, .66; P = .01). Roughly three-fourths of recurrences were distant.
The groups did not differ significantly with respect to the rate of overall survival, which was 93% with letrozole and 94% with placebo.
The annual incidence of contralateral breast cancer was sharply lower in the letrozole group, at 0.21%, than in the placebo group, at 0.49%, translating to a more than one-half reduction in this risk of this outcome (HR, .42; P = .007).
No new toxicities or emergent symptoms were noted from extending AI therapy, according to Dr. Goss. However, the letrozole group significantly more commonly experienced bone pain (18% vs. 14%), bone fractures (14% vs. 9%), and new-onset osteoporosis (11% vs. 6%). Therefore, “bone health remains important for risk-benefit consideration,” he said.
Patient-reported outcomes
In a separate session and the press briefing, Dr. Julie Lemieux, a researcher at the Centre Hospitalier affilié Universitaire de Québec, reported the trial’s patient-reported outcomes, ascertained from questionnaires completed at baseline and annually out to 5 years.
In general, both the letrozole and placebo groups had small deteriorations over time in global quality of life as assessed from summary scores on the mental and physical scales of the 36-item Short Form Health Survey (SF-36). But both also had small improvements over time in scores on the Menopause-Specific Quality of Life (MENQOL) scale.
When compared, the two groups were statistically indistinguishable on most of these measures. The only significant difference was greater worsening in the letrozole group on the role function-physical subscale of the SF-36, which pertains to difficulty performing work or physical activity due to physical health. However, the difference averaged just 3.2 points, which fell short of the 5 points that the investigators considered clinically important.
“The limitation of this analysis was that it was a highly selected population. All of these women had already tolerated 5 years of an aromatase inhibitor, and about 70% had received 5 years of tamoxifen before,” Dr. Lemieux commented. “Also, they were clinical trial participants.”
Nonetheless, these findings “are very reassuring for those women who want a longer duration of adjuvant endocrine therapy that they can expect a preserved quality of life,” she concluded.
Dr. Goss disclosed that he had no relevant conflicts of interest. Dr. Lemieux disclosed that she had no relevant conflicts of interest. The trial received support from Novartis.
CHICAGO – Extending adjuvant aromatase inhibitor (AI) therapy from 5 years to 10 years further reduces the risk of recurrence and new breast cancer in postmenopausal women treated for early disease, according to findings of the MA17.R trial.
In the phase III trial conducted by the Canadian Cancer Trials Group and the North American Breast Cancer Group, 1,918 postmenopausal women who had completed about 5 years of AI therapy (preceded by tamoxifen in the majority of cases) were randomized to take the AI letrozole or to stop therapy by taking placebo for an additional 5 years.
Compared with peers who stopped, women who continued AI therapy for 5 more years had a 34% lower risk of recurrence or contralateral breast cancer, investigators reported in sessions and a press briefing at the annual meeting of the American Society of Clinical Oncology. The trade-off was a small increase in the rates of skeletal adverse events such as fractures; quality of life was essentially unaffected.
“MA17.R is the first study to show the benefit of extending an adjuvant aromatase inhibitor beyond 5 years,” commented lead investigator Paul E. Goss, M.D., director of the Breast Cancer Research Program at the Massachusetts General Hospital and a professor of medicine at Harvard Medical School, both in Boston. “Unlike many anticancer therapies, aromatase inhibitors are readily accessible around the world, and therefore, our results will further improve the outcome of many women with breast cancer.”
The disease-free survival curves will likely separate further, given a “legacy effect” of endocrine therapy that persists after it ends, he predicted. “And I think overall survival will eventually become positive in MA.17R. … The Food and Drug Administration has taken the opinion that overall survival follows disease-free survival like night follows day for endocrine therapies, and I think they are correct, I think that’s what we see in all the trials.”
Implications
It remains unclear how patients should be managed after 10 years of an AI, according to Dr. Goss. “That’s uncharted waters,” he elaborated. “We know from the curve of the natural history of this disease that it chronically relapses, and we continue to see patients 25 years after their primary diagnosis with a recurrence.” Some data in mice suggest there may be benefit from continuing the AI until recurrence. “I don’t think that would be entered into in clinical practice as a rule, because there is no clinical trial of that,” he said. “But this data will now take the aromatase inhibitors out to 10 years.”
The MA.17R trial’s findings show that extended duration of AI therapy is “clinically valuable,” according to ASCO expert Harold J. Burstein, M.D., Ph.D., a senior physician at the Dana-Farber Cancer Institute and an associate professor of medicine at the Harvard Medical School in Boston. He predicted the findings will have at least two consequences.
“One is tremendous interest in longer durations of therapy with the AI, but also some tailoring of treatment based on how the patient has fared with their therapy and on their baseline risk of recurrence. So women who have less risky cancer will probably be less inclined to pursue these longer durations, and women who have higher-risk cancers will be more inclined,” he explained.
Also, “women who have finished 5 years of an AI without any prior tamoxifen I think are going to be very compelled by these data, whereas women who have had 5 years of tamoxifen, 5 years of an AI, and are already 10 years out probably get less benefit numerically from yet longer duration of therapy,” he added. “And we are certainly not at the point of saying that women should be on these drugs for the rest of their lives.”
MA.17R design
Postmenopausal women were eligible for MA.17R if they had undergone resection of hormone receptor–positive early breast cancer and had already completed about 5 years of therapy with any of the three AIs currently on the market. In the large majority of cases, they also had previously received tamoxifen.
Many of the women came from the parent MA.17 trial, which tested an initial 5 years of letrozole (brand name Femara) against placebo after tamoxifen therapy. Longer-term results of that trial, previously reported (J Clin Oncol. 2012;30:718-21), showed that this duration of letrozole had a significant disease-free survival benefit (hazard ratio, .52) and overall survival benefit (HR, .61).
In the MA.17R trial, the women were randomized to letrozole or a placebo for an additional 5 years, with a primary endpoint of disease-free survival and secondary endpoints including safety and quality of life.
Efficacy and safety
After a median follow-up of 6.3 years, the 5-year rate of disease-free survival was 95% with letrozole and 91% with placebo, according to results reported by Dr. Goss in a plenary session at the meeting and simultaneously published (N Engl J Med. 2016. June 5 doi: 10.1056/NEJMoa1604700).
The difference translated to a more than one-third reduction in the risk of disease recurrence or the occurrence of contralateral breast cancer (HR, .66; P = .01). Roughly three-fourths of recurrences were distant.
The groups did not differ significantly with respect to the rate of overall survival, which was 93% with letrozole and 94% with placebo.
The annual incidence of contralateral breast cancer was sharply lower in the letrozole group, at 0.21%, than in the placebo group, at 0.49%, translating to a more than one-half reduction in this risk of this outcome (HR, .42; P = .007).
No new toxicities or emergent symptoms were noted from extending AI therapy, according to Dr. Goss. However, the letrozole group significantly more commonly experienced bone pain (18% vs. 14%), bone fractures (14% vs. 9%), and new-onset osteoporosis (11% vs. 6%). Therefore, “bone health remains important for risk-benefit consideration,” he said.
Patient-reported outcomes
In a separate session and the press briefing, Dr. Julie Lemieux, a researcher at the Centre Hospitalier affilié Universitaire de Québec, reported the trial’s patient-reported outcomes, ascertained from questionnaires completed at baseline and annually out to 5 years.
In general, both the letrozole and placebo groups had small deteriorations over time in global quality of life as assessed from summary scores on the mental and physical scales of the 36-item Short Form Health Survey (SF-36). But both also had small improvements over time in scores on the Menopause-Specific Quality of Life (MENQOL) scale.
When compared, the two groups were statistically indistinguishable on most of these measures. The only significant difference was greater worsening in the letrozole group on the role function-physical subscale of the SF-36, which pertains to difficulty performing work or physical activity due to physical health. However, the difference averaged just 3.2 points, which fell short of the 5 points that the investigators considered clinically important.
“The limitation of this analysis was that it was a highly selected population. All of these women had already tolerated 5 years of an aromatase inhibitor, and about 70% had received 5 years of tamoxifen before,” Dr. Lemieux commented. “Also, they were clinical trial participants.”
Nonetheless, these findings “are very reassuring for those women who want a longer duration of adjuvant endocrine therapy that they can expect a preserved quality of life,” she concluded.
Dr. Goss disclosed that he had no relevant conflicts of interest. Dr. Lemieux disclosed that she had no relevant conflicts of interest. The trial received support from Novartis.
CHICAGO – Extending adjuvant aromatase inhibitor (AI) therapy from 5 years to 10 years further reduces the risk of recurrence and new breast cancer in postmenopausal women treated for early disease, according to findings of the MA17.R trial.
In the phase III trial conducted by the Canadian Cancer Trials Group and the North American Breast Cancer Group, 1,918 postmenopausal women who had completed about 5 years of AI therapy (preceded by tamoxifen in the majority of cases) were randomized to take the AI letrozole or to stop therapy by taking placebo for an additional 5 years.
Compared with peers who stopped, women who continued AI therapy for 5 more years had a 34% lower risk of recurrence or contralateral breast cancer, investigators reported in sessions and a press briefing at the annual meeting of the American Society of Clinical Oncology. The trade-off was a small increase in the rates of skeletal adverse events such as fractures; quality of life was essentially unaffected.
“MA17.R is the first study to show the benefit of extending an adjuvant aromatase inhibitor beyond 5 years,” commented lead investigator Paul E. Goss, M.D., director of the Breast Cancer Research Program at the Massachusetts General Hospital and a professor of medicine at Harvard Medical School, both in Boston. “Unlike many anticancer therapies, aromatase inhibitors are readily accessible around the world, and therefore, our results will further improve the outcome of many women with breast cancer.”
The disease-free survival curves will likely separate further, given a “legacy effect” of endocrine therapy that persists after it ends, he predicted. “And I think overall survival will eventually become positive in MA.17R. … The Food and Drug Administration has taken the opinion that overall survival follows disease-free survival like night follows day for endocrine therapies, and I think they are correct, I think that’s what we see in all the trials.”
Implications
It remains unclear how patients should be managed after 10 years of an AI, according to Dr. Goss. “That’s uncharted waters,” he elaborated. “We know from the curve of the natural history of this disease that it chronically relapses, and we continue to see patients 25 years after their primary diagnosis with a recurrence.” Some data in mice suggest there may be benefit from continuing the AI until recurrence. “I don’t think that would be entered into in clinical practice as a rule, because there is no clinical trial of that,” he said. “But this data will now take the aromatase inhibitors out to 10 years.”
The MA.17R trial’s findings show that extended duration of AI therapy is “clinically valuable,” according to ASCO expert Harold J. Burstein, M.D., Ph.D., a senior physician at the Dana-Farber Cancer Institute and an associate professor of medicine at the Harvard Medical School in Boston. He predicted the findings will have at least two consequences.
“One is tremendous interest in longer durations of therapy with the AI, but also some tailoring of treatment based on how the patient has fared with their therapy and on their baseline risk of recurrence. So women who have less risky cancer will probably be less inclined to pursue these longer durations, and women who have higher-risk cancers will be more inclined,” he explained.
Also, “women who have finished 5 years of an AI without any prior tamoxifen I think are going to be very compelled by these data, whereas women who have had 5 years of tamoxifen, 5 years of an AI, and are already 10 years out probably get less benefit numerically from yet longer duration of therapy,” he added. “And we are certainly not at the point of saying that women should be on these drugs for the rest of their lives.”
MA.17R design
Postmenopausal women were eligible for MA.17R if they had undergone resection of hormone receptor–positive early breast cancer and had already completed about 5 years of therapy with any of the three AIs currently on the market. In the large majority of cases, they also had previously received tamoxifen.
Many of the women came from the parent MA.17 trial, which tested an initial 5 years of letrozole (brand name Femara) against placebo after tamoxifen therapy. Longer-term results of that trial, previously reported (J Clin Oncol. 2012;30:718-21), showed that this duration of letrozole had a significant disease-free survival benefit (hazard ratio, .52) and overall survival benefit (HR, .61).
In the MA.17R trial, the women were randomized to letrozole or a placebo for an additional 5 years, with a primary endpoint of disease-free survival and secondary endpoints including safety and quality of life.
Efficacy and safety
After a median follow-up of 6.3 years, the 5-year rate of disease-free survival was 95% with letrozole and 91% with placebo, according to results reported by Dr. Goss in a plenary session at the meeting and simultaneously published (N Engl J Med. 2016. June 5 doi: 10.1056/NEJMoa1604700).
The difference translated to a more than one-third reduction in the risk of disease recurrence or the occurrence of contralateral breast cancer (HR, .66; P = .01). Roughly three-fourths of recurrences were distant.
The groups did not differ significantly with respect to the rate of overall survival, which was 93% with letrozole and 94% with placebo.
The annual incidence of contralateral breast cancer was sharply lower in the letrozole group, at 0.21%, than in the placebo group, at 0.49%, translating to a more than one-half reduction in this risk of this outcome (HR, .42; P = .007).
No new toxicities or emergent symptoms were noted from extending AI therapy, according to Dr. Goss. However, the letrozole group significantly more commonly experienced bone pain (18% vs. 14%), bone fractures (14% vs. 9%), and new-onset osteoporosis (11% vs. 6%). Therefore, “bone health remains important for risk-benefit consideration,” he said.
Patient-reported outcomes
In a separate session and the press briefing, Dr. Julie Lemieux, a researcher at the Centre Hospitalier affilié Universitaire de Québec, reported the trial’s patient-reported outcomes, ascertained from questionnaires completed at baseline and annually out to 5 years.
In general, both the letrozole and placebo groups had small deteriorations over time in global quality of life as assessed from summary scores on the mental and physical scales of the 36-item Short Form Health Survey (SF-36). But both also had small improvements over time in scores on the Menopause-Specific Quality of Life (MENQOL) scale.
When compared, the two groups were statistically indistinguishable on most of these measures. The only significant difference was greater worsening in the letrozole group on the role function-physical subscale of the SF-36, which pertains to difficulty performing work or physical activity due to physical health. However, the difference averaged just 3.2 points, which fell short of the 5 points that the investigators considered clinically important.
“The limitation of this analysis was that it was a highly selected population. All of these women had already tolerated 5 years of an aromatase inhibitor, and about 70% had received 5 years of tamoxifen before,” Dr. Lemieux commented. “Also, they were clinical trial participants.”
Nonetheless, these findings “are very reassuring for those women who want a longer duration of adjuvant endocrine therapy that they can expect a preserved quality of life,” she concluded.
Dr. Goss disclosed that he had no relevant conflicts of interest. Dr. Lemieux disclosed that she had no relevant conflicts of interest. The trial received support from Novartis.
AT ASCO 2016
Key clinical point: Extending adjuvant AI therapy out to 10 years improves disease-free survival and is generally safe and well tolerated.
Major finding: Patients who continued taking an AI out to 10 years had a 34% lower risk of recurrence or contralateral breast cancer than peers who stopped after 5 years.
Data source: A randomized placebo-controlled phase III trial among 1,918 postmenopausal women who had already completed 5 years of AI therapy (MA17.R trial).
Disclosures: Dr. Goss disclosed that he had no relevant conflicts of interest. Dr. Lemieux disclosed that she had no relevant conflicts of interest. The trial received support from Novartis.
Web app boosts lung cancer survival
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: A Web-based app improves survival for advanced lung cancer patients.
Major finding: Survival improved by 26% for web-app patients vs. controls.
Data source: Multicenter, prospective, phase III, randomized trial of 121 patients.
Disclosures: Dr. Denis has received honoraria and expenses from several pharmaceutical companies and has received institutional research funding from Sivan. Dr. Patricia Ganz reported stock and other ownership interest in Abbott Laboratories, GlaxoSmithKline, Johnson & Johnson, Merck, Novartis, Pfizer, and Teva.
End-of-life aggressive cancer care continues despite recommendations
CHICAGO – Aggressive care for most patients with incurable solid tumors continued in the final 30 days of life, and one-third died in the hospital, a recent, large retrospective study of health claims data on more than 28,000 patients shows, and there was no decrease in this practice over a recent 7-year period, despite recommendations to the contrary.
“Aggressive medical care for patients with incurable cancers at the end of life is widely recognized to be harmful to patients and their families,” Dr. Ronald Chen of the University of North Carolina at Chapel Hill said at the annual meeting of the American Society of Clinical Oncology.
As part of the Choosing Wisely campaign in 2012, the American Society of Clinical Oncology’s first recommendation was not to use cancer-directed therapy for patients with solid tumors when there is no strong evidence supporting the clinical value of further anticancer treatment. It also recommended more use of palliative and supportive care. However, the impact of these recommendations on clinical care in younger cancer populations was unknown.
In a study of patients younger than 65 years with solid tumors who died in 2007-2014, Dr. Chen and his associates studied the use of several items that could be considered to be aggressive therapy. They included chemotherapy, radiotherapy, invasive procedures, emergency room visits, hospitalization, intensive care use, and in-hospital death. Patients had any of five common metastatic diseases: breast, lung, prostate, colorectal, or pancreatic cancers (n = 5,855; 12,764; 1,508; 5,207; 3,397, respectively).
The source material for the study was large commercial insurance claims data on patients across 14 states. Investigators evaluated the proportion of patients who received forms of aggressive care in the final 30 days of life.
“Overall, the findings are remarkably consistent across the five diseases. And overall, about three-quarters of patients received at least one form of aggressive care in the last 30 days of life,” Dr. Chen said (range, 71.2%-75.9% of patients). Almost two-thirds of patients (61.6%-65.1%) were admitted to the hospital or went to the emergency department, about 20% of patients (15.9%-20.6%) received intensive care, and one-third of patients (30.3%-35.4%) died in the hospital instead of at home. About 25%-30% of patients received chemotherapy or an invasive procedure, such as a biopsy or a form of surgery. Radiation therapy was used the least and was administered to about 5%-20% of patients.
Looking at the overall use of aggressive care for each of the cancers studied, the researchers found virtually no trend over time, that is, from the second quarter of 2012, when ASCO issued its Choosing Wisely guidelines, through the fourth quarter of 2014. For each of the cancers, aggressive care was delivered to just about 75% of patients across all quarters. Looking further back, the investigators found the same proportions of patients receiving aggressive care in the last 30 days of life during the years 2007-2011.
They also looked specifically at the use of chemotherapy and did not find a change after the Choosing Wisely recommendations, “nor did we find a significant increase in the use of hospice from before 2012 to afterward,” Dr. Chen said. “Additional efforts are critically needed to improve end-of-life care for patients with terminal cancers to ensure that the care provided meets the goals and preferences of patients and their families.” Fewer than one-fifth of patients used hospice care.
Press conference moderator Dr. Patricia Ganz, director of cancer prevention and control research at the Jonsson Comprehensive Cancer Center of the University of California, Los Angeles, called the study “interesting and important for several reasons.” First, there have been very few studies on the topic on the younger (up to age 65) cancer population although the SEER-Medicare database has been used as a source of claims data for older cancer patients. One may like to know if the younger population is being treated more aggressively than the older population is, as well as other patterns of care.
“Giving chemotherapy in the last 30 days of life has been a coping measure for a very long time,” she said. “It’s been nationally looked at as one of our failures in giving good end-of-life care, and so the fact that there wasn’t any dramatic change at 2012 doesn’t bother me in the sense that we’ve been talking about this for a very long time, and we haven’t seen any movement.” She said there is a lot left to do in delivering high quality end-of-life care.
Dr. Chen said more education of both patients and physicians is needed to improve conversations about goals and expectations, as well as palliative care and hospice. These types of care need to be made more accessible, he said.
Limitations of the study include a lack of information on the cause of death (whether related to the cancer, the treatment received, or other), and researchers did not review the medical records to investigate the medical reasons for the use of aggressive care near the end of life.
CHICAGO – Aggressive care for most patients with incurable solid tumors continued in the final 30 days of life, and one-third died in the hospital, a recent, large retrospective study of health claims data on more than 28,000 patients shows, and there was no decrease in this practice over a recent 7-year period, despite recommendations to the contrary.
“Aggressive medical care for patients with incurable cancers at the end of life is widely recognized to be harmful to patients and their families,” Dr. Ronald Chen of the University of North Carolina at Chapel Hill said at the annual meeting of the American Society of Clinical Oncology.
As part of the Choosing Wisely campaign in 2012, the American Society of Clinical Oncology’s first recommendation was not to use cancer-directed therapy for patients with solid tumors when there is no strong evidence supporting the clinical value of further anticancer treatment. It also recommended more use of palliative and supportive care. However, the impact of these recommendations on clinical care in younger cancer populations was unknown.
In a study of patients younger than 65 years with solid tumors who died in 2007-2014, Dr. Chen and his associates studied the use of several items that could be considered to be aggressive therapy. They included chemotherapy, radiotherapy, invasive procedures, emergency room visits, hospitalization, intensive care use, and in-hospital death. Patients had any of five common metastatic diseases: breast, lung, prostate, colorectal, or pancreatic cancers (n = 5,855; 12,764; 1,508; 5,207; 3,397, respectively).
The source material for the study was large commercial insurance claims data on patients across 14 states. Investigators evaluated the proportion of patients who received forms of aggressive care in the final 30 days of life.
“Overall, the findings are remarkably consistent across the five diseases. And overall, about three-quarters of patients received at least one form of aggressive care in the last 30 days of life,” Dr. Chen said (range, 71.2%-75.9% of patients). Almost two-thirds of patients (61.6%-65.1%) were admitted to the hospital or went to the emergency department, about 20% of patients (15.9%-20.6%) received intensive care, and one-third of patients (30.3%-35.4%) died in the hospital instead of at home. About 25%-30% of patients received chemotherapy or an invasive procedure, such as a biopsy or a form of surgery. Radiation therapy was used the least and was administered to about 5%-20% of patients.
Looking at the overall use of aggressive care for each of the cancers studied, the researchers found virtually no trend over time, that is, from the second quarter of 2012, when ASCO issued its Choosing Wisely guidelines, through the fourth quarter of 2014. For each of the cancers, aggressive care was delivered to just about 75% of patients across all quarters. Looking further back, the investigators found the same proportions of patients receiving aggressive care in the last 30 days of life during the years 2007-2011.
They also looked specifically at the use of chemotherapy and did not find a change after the Choosing Wisely recommendations, “nor did we find a significant increase in the use of hospice from before 2012 to afterward,” Dr. Chen said. “Additional efforts are critically needed to improve end-of-life care for patients with terminal cancers to ensure that the care provided meets the goals and preferences of patients and their families.” Fewer than one-fifth of patients used hospice care.
Press conference moderator Dr. Patricia Ganz, director of cancer prevention and control research at the Jonsson Comprehensive Cancer Center of the University of California, Los Angeles, called the study “interesting and important for several reasons.” First, there have been very few studies on the topic on the younger (up to age 65) cancer population although the SEER-Medicare database has been used as a source of claims data for older cancer patients. One may like to know if the younger population is being treated more aggressively than the older population is, as well as other patterns of care.
“Giving chemotherapy in the last 30 days of life has been a coping measure for a very long time,” she said. “It’s been nationally looked at as one of our failures in giving good end-of-life care, and so the fact that there wasn’t any dramatic change at 2012 doesn’t bother me in the sense that we’ve been talking about this for a very long time, and we haven’t seen any movement.” She said there is a lot left to do in delivering high quality end-of-life care.
Dr. Chen said more education of both patients and physicians is needed to improve conversations about goals and expectations, as well as palliative care and hospice. These types of care need to be made more accessible, he said.
Limitations of the study include a lack of information on the cause of death (whether related to the cancer, the treatment received, or other), and researchers did not review the medical records to investigate the medical reasons for the use of aggressive care near the end of life.
CHICAGO – Aggressive care for most patients with incurable solid tumors continued in the final 30 days of life, and one-third died in the hospital, a recent, large retrospective study of health claims data on more than 28,000 patients shows, and there was no decrease in this practice over a recent 7-year period, despite recommendations to the contrary.
“Aggressive medical care for patients with incurable cancers at the end of life is widely recognized to be harmful to patients and their families,” Dr. Ronald Chen of the University of North Carolina at Chapel Hill said at the annual meeting of the American Society of Clinical Oncology.
As part of the Choosing Wisely campaign in 2012, the American Society of Clinical Oncology’s first recommendation was not to use cancer-directed therapy for patients with solid tumors when there is no strong evidence supporting the clinical value of further anticancer treatment. It also recommended more use of palliative and supportive care. However, the impact of these recommendations on clinical care in younger cancer populations was unknown.
In a study of patients younger than 65 years with solid tumors who died in 2007-2014, Dr. Chen and his associates studied the use of several items that could be considered to be aggressive therapy. They included chemotherapy, radiotherapy, invasive procedures, emergency room visits, hospitalization, intensive care use, and in-hospital death. Patients had any of five common metastatic diseases: breast, lung, prostate, colorectal, or pancreatic cancers (n = 5,855; 12,764; 1,508; 5,207; 3,397, respectively).
The source material for the study was large commercial insurance claims data on patients across 14 states. Investigators evaluated the proportion of patients who received forms of aggressive care in the final 30 days of life.
“Overall, the findings are remarkably consistent across the five diseases. And overall, about three-quarters of patients received at least one form of aggressive care in the last 30 days of life,” Dr. Chen said (range, 71.2%-75.9% of patients). Almost two-thirds of patients (61.6%-65.1%) were admitted to the hospital or went to the emergency department, about 20% of patients (15.9%-20.6%) received intensive care, and one-third of patients (30.3%-35.4%) died in the hospital instead of at home. About 25%-30% of patients received chemotherapy or an invasive procedure, such as a biopsy or a form of surgery. Radiation therapy was used the least and was administered to about 5%-20% of patients.
Looking at the overall use of aggressive care for each of the cancers studied, the researchers found virtually no trend over time, that is, from the second quarter of 2012, when ASCO issued its Choosing Wisely guidelines, through the fourth quarter of 2014. For each of the cancers, aggressive care was delivered to just about 75% of patients across all quarters. Looking further back, the investigators found the same proportions of patients receiving aggressive care in the last 30 days of life during the years 2007-2011.
They also looked specifically at the use of chemotherapy and did not find a change after the Choosing Wisely recommendations, “nor did we find a significant increase in the use of hospice from before 2012 to afterward,” Dr. Chen said. “Additional efforts are critically needed to improve end-of-life care for patients with terminal cancers to ensure that the care provided meets the goals and preferences of patients and their families.” Fewer than one-fifth of patients used hospice care.
Press conference moderator Dr. Patricia Ganz, director of cancer prevention and control research at the Jonsson Comprehensive Cancer Center of the University of California, Los Angeles, called the study “interesting and important for several reasons.” First, there have been very few studies on the topic on the younger (up to age 65) cancer population although the SEER-Medicare database has been used as a source of claims data for older cancer patients. One may like to know if the younger population is being treated more aggressively than the older population is, as well as other patterns of care.
“Giving chemotherapy in the last 30 days of life has been a coping measure for a very long time,” she said. “It’s been nationally looked at as one of our failures in giving good end-of-life care, and so the fact that there wasn’t any dramatic change at 2012 doesn’t bother me in the sense that we’ve been talking about this for a very long time, and we haven’t seen any movement.” She said there is a lot left to do in delivering high quality end-of-life care.
Dr. Chen said more education of both patients and physicians is needed to improve conversations about goals and expectations, as well as palliative care and hospice. These types of care need to be made more accessible, he said.
Limitations of the study include a lack of information on the cause of death (whether related to the cancer, the treatment received, or other), and researchers did not review the medical records to investigate the medical reasons for the use of aggressive care near the end of life.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: End-of-life aggressive cancer care continues unabated despite Choosing Wisely recommendations.
Major finding: Three-quarters of cancer patients received aggressive therapies at end of life.
Data source: Retrospective study of health claims data on 28,731 patients younger than 65 years with incurable cancers.
Disclosures: The study received funding from the North Carolina Translational and Clinical Sciences Institute. Dr. Chen reported consulting or advisory roles with Medivation/Astellas and research funding from Accuray. Dr. Patricia Ganz reported stock and other ownership interest in Abbott Laboratories, GlaxoSmithKline, Johnson & Johnson, Merck, Novartis, Pfizer, and Teva.
Cancer drugs most affordable in Australia, least in India and China
CHICAGO – Cancer drugs are most expensive in the United States and least expensive in India and South Africa, but when taking into account a nation’s wealth and cost of living, the treatments are most affordable in Australia, and least affordable in India and China. The United States is somewhat in between, according to an analysis presented at the annual meeting of the American Society of Clinical Oncology.
“Value has become a major buzzword in cancer care. In addition to existing methods of cost effectiveness, new frameworks have been developed by ASCO, [the National Comprehensive Cancer Network], [the European Society for Medical Oncology], and [the American Board of Internal Medicine]. However, ultimately value boils down to a simple equation,” said Dr. Daniel A. Goldstein of Rabin Medical Center, Petah Tikva, Israel.
“Value is benefit divided by cost. In this study, we interrogated the denominator in this equation. Cost. And we did this on a global perspective.”
Dr. Goldstein and his associates collected drug prices of 15 generic and 8 patented drugs and calculated retail prices in seven countries (Australia, India, China, South Africa, Israel, the United Kingdom, and the United States) for 1 month of therapy using a standardized body surface area to determine dosage. The United States had the highest median monthly retail prices at just under $9,000 for patented drugs. China, Israel, the U.K., and Australia had similar median monthly retail prices that were just under $3,000. India and South Africa had the lowest median monthly retail prices for patented drugs.
Median monthly generic retail prices were fairly similar across the seven countries.
“It is currently unclear how the difference in prices relates to ability to pay for payers in different countries,” Dr. Goldstein said. To assess affordability, the investigators calculated the monthly drug price as a percentage of gross domestic product per capita at purchasing power parity (GDPcap), a measurement that takes into account a nation’s wealth and cost of living.
Cancer drugs were the most affordable in Australia. Monthly drug prices were 3% of GDPcap for generics and 71% for patented drugs. In the United States, the cost of generics was 14% of GDPcap while patented drugs were 192% of GDPcap. Cancer drugs were least affordable in India and China. Monthly drug prices were 48% of GDPcap for generic drugs in China, 288% for patented drugs, 33% for generic drugs in India, and 313% for patented drugs.
“Despite lower drug prices in India and China, these drugs appear to be less affordable than in other countries. In the USA despite having the highest GDP per capita, given the higher drug prices, the drugs appear to be less affordable than in other developed countries. And we see a similar pattern for generic drugs but with a lower magnitude. And this is mostly driven by differences in GDP per capita rather than differences in drug prices,” Dr. Rabin said.
“This is a very interesting international comparative study, and I think the concept of affordability is a novel one because we tend to just look at the cost and say it is so much less expensive in other parts of the world but looking at affordability adds another dimension to the many nuanced issues [of cost],” commented moderator Dr. Patricia Ganz of the University of California, Los Angeles.
A major limitation of this study was the inability to implicate the role of health insurance, drug discounts, rebates, and medical assistance programs into affordability. In response to a question from a reporter, Dr. Goldstein said that wealth disparities within countries would also be an important factor to more thoroughly understand the ability of patients to pay for cancer treatments.
Dr. Goldstein added that a better understanding of a drug’s benefit (improvements on life expectancy, toxicity, duration of therapy, and so on) is also important to truly understand the value of drugs on a global level.
“There are several questions this study does not answer,” Dr. Goldstein said. “Should drugs be priced the same globally? Is there an ethical duty to price drugs relative to an individual or population’s level of wealth? And is there a difference between drugs used in curative and metastatic setting[s]? Should governments or insurance companies provide all drugs with proven efficacy?”
This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.
CHICAGO – Cancer drugs are most expensive in the United States and least expensive in India and South Africa, but when taking into account a nation’s wealth and cost of living, the treatments are most affordable in Australia, and least affordable in India and China. The United States is somewhat in between, according to an analysis presented at the annual meeting of the American Society of Clinical Oncology.
“Value has become a major buzzword in cancer care. In addition to existing methods of cost effectiveness, new frameworks have been developed by ASCO, [the National Comprehensive Cancer Network], [the European Society for Medical Oncology], and [the American Board of Internal Medicine]. However, ultimately value boils down to a simple equation,” said Dr. Daniel A. Goldstein of Rabin Medical Center, Petah Tikva, Israel.
“Value is benefit divided by cost. In this study, we interrogated the denominator in this equation. Cost. And we did this on a global perspective.”
Dr. Goldstein and his associates collected drug prices of 15 generic and 8 patented drugs and calculated retail prices in seven countries (Australia, India, China, South Africa, Israel, the United Kingdom, and the United States) for 1 month of therapy using a standardized body surface area to determine dosage. The United States had the highest median monthly retail prices at just under $9,000 for patented drugs. China, Israel, the U.K., and Australia had similar median monthly retail prices that were just under $3,000. India and South Africa had the lowest median monthly retail prices for patented drugs.
Median monthly generic retail prices were fairly similar across the seven countries.
“It is currently unclear how the difference in prices relates to ability to pay for payers in different countries,” Dr. Goldstein said. To assess affordability, the investigators calculated the monthly drug price as a percentage of gross domestic product per capita at purchasing power parity (GDPcap), a measurement that takes into account a nation’s wealth and cost of living.
Cancer drugs were the most affordable in Australia. Monthly drug prices were 3% of GDPcap for generics and 71% for patented drugs. In the United States, the cost of generics was 14% of GDPcap while patented drugs were 192% of GDPcap. Cancer drugs were least affordable in India and China. Monthly drug prices were 48% of GDPcap for generic drugs in China, 288% for patented drugs, 33% for generic drugs in India, and 313% for patented drugs.
“Despite lower drug prices in India and China, these drugs appear to be less affordable than in other countries. In the USA despite having the highest GDP per capita, given the higher drug prices, the drugs appear to be less affordable than in other developed countries. And we see a similar pattern for generic drugs but with a lower magnitude. And this is mostly driven by differences in GDP per capita rather than differences in drug prices,” Dr. Rabin said.
“This is a very interesting international comparative study, and I think the concept of affordability is a novel one because we tend to just look at the cost and say it is so much less expensive in other parts of the world but looking at affordability adds another dimension to the many nuanced issues [of cost],” commented moderator Dr. Patricia Ganz of the University of California, Los Angeles.
A major limitation of this study was the inability to implicate the role of health insurance, drug discounts, rebates, and medical assistance programs into affordability. In response to a question from a reporter, Dr. Goldstein said that wealth disparities within countries would also be an important factor to more thoroughly understand the ability of patients to pay for cancer treatments.
Dr. Goldstein added that a better understanding of a drug’s benefit (improvements on life expectancy, toxicity, duration of therapy, and so on) is also important to truly understand the value of drugs on a global level.
“There are several questions this study does not answer,” Dr. Goldstein said. “Should drugs be priced the same globally? Is there an ethical duty to price drugs relative to an individual or population’s level of wealth? And is there a difference between drugs used in curative and metastatic setting[s]? Should governments or insurance companies provide all drugs with proven efficacy?”
This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.
CHICAGO – Cancer drugs are most expensive in the United States and least expensive in India and South Africa, but when taking into account a nation’s wealth and cost of living, the treatments are most affordable in Australia, and least affordable in India and China. The United States is somewhat in between, according to an analysis presented at the annual meeting of the American Society of Clinical Oncology.
“Value has become a major buzzword in cancer care. In addition to existing methods of cost effectiveness, new frameworks have been developed by ASCO, [the National Comprehensive Cancer Network], [the European Society for Medical Oncology], and [the American Board of Internal Medicine]. However, ultimately value boils down to a simple equation,” said Dr. Daniel A. Goldstein of Rabin Medical Center, Petah Tikva, Israel.
“Value is benefit divided by cost. In this study, we interrogated the denominator in this equation. Cost. And we did this on a global perspective.”
Dr. Goldstein and his associates collected drug prices of 15 generic and 8 patented drugs and calculated retail prices in seven countries (Australia, India, China, South Africa, Israel, the United Kingdom, and the United States) for 1 month of therapy using a standardized body surface area to determine dosage. The United States had the highest median monthly retail prices at just under $9,000 for patented drugs. China, Israel, the U.K., and Australia had similar median monthly retail prices that were just under $3,000. India and South Africa had the lowest median monthly retail prices for patented drugs.
Median monthly generic retail prices were fairly similar across the seven countries.
“It is currently unclear how the difference in prices relates to ability to pay for payers in different countries,” Dr. Goldstein said. To assess affordability, the investigators calculated the monthly drug price as a percentage of gross domestic product per capita at purchasing power parity (GDPcap), a measurement that takes into account a nation’s wealth and cost of living.
Cancer drugs were the most affordable in Australia. Monthly drug prices were 3% of GDPcap for generics and 71% for patented drugs. In the United States, the cost of generics was 14% of GDPcap while patented drugs were 192% of GDPcap. Cancer drugs were least affordable in India and China. Monthly drug prices were 48% of GDPcap for generic drugs in China, 288% for patented drugs, 33% for generic drugs in India, and 313% for patented drugs.
“Despite lower drug prices in India and China, these drugs appear to be less affordable than in other countries. In the USA despite having the highest GDP per capita, given the higher drug prices, the drugs appear to be less affordable than in other developed countries. And we see a similar pattern for generic drugs but with a lower magnitude. And this is mostly driven by differences in GDP per capita rather than differences in drug prices,” Dr. Rabin said.
“This is a very interesting international comparative study, and I think the concept of affordability is a novel one because we tend to just look at the cost and say it is so much less expensive in other parts of the world but looking at affordability adds another dimension to the many nuanced issues [of cost],” commented moderator Dr. Patricia Ganz of the University of California, Los Angeles.
A major limitation of this study was the inability to implicate the role of health insurance, drug discounts, rebates, and medical assistance programs into affordability. In response to a question from a reporter, Dr. Goldstein said that wealth disparities within countries would also be an important factor to more thoroughly understand the ability of patients to pay for cancer treatments.
Dr. Goldstein added that a better understanding of a drug’s benefit (improvements on life expectancy, toxicity, duration of therapy, and so on) is also important to truly understand the value of drugs on a global level.
“There are several questions this study does not answer,” Dr. Goldstein said. “Should drugs be priced the same globally? Is there an ethical duty to price drugs relative to an individual or population’s level of wealth? And is there a difference between drugs used in curative and metastatic setting[s]? Should governments or insurance companies provide all drugs with proven efficacy?”
This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Taking into account a country’s wealth and cost of living, cancer drugs are most affordable in Australia, least affordable in India and China.
Major finding: In Australia, monthly drug prices were 3% of gross domestic product per capita at purchasing power parity (GDPcap) for generics and 71% for patented drugs. Monthly drug prices in China were 48% of GDPcap for generic drugs and 288% for patented drugs, while in India prices were 33% of GDPcap for generic drugs and 313% for patented drugs.
Data source: A multinational study of cancer drug prices, wealth, and cost of living.
Disclosures: This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.
A new sort of consultant: Advising doctors, patients on California’s aid-in-dying law
BERKELEY, Calif. – Few people have the unusual set of professional experiences that Dr. Lonny Shavelson does. He worked as an emergency room physician in Berkeley for years – while also working as a journalist. He has written several books and takes hauntingly beautiful photographs.
Now, just as California’s aid-in-dying law takes effect June 9, Dr. Shavelson has added another specialty: A consultant to physicians and terminally ill patients who have questions about how it works.
“Can I just sit back and watch?” Dr. Shavelson asked from his cottage office. “This is really an amazing opportunity to be part of establishing policy and initiating something in medicine. This is a major change … [that] very, very few people know anything about and how to do it.”
Dr. Shavelson is the author of the 1995 book, “A Chosen Death,” which followed five terminally ill people over 2 years as they determined whether to amass drugs on their own and end their lives at a time of their choosing. He was present at the death of all of them.
He followed the issue closely for several years, but ultimately moved on to other projects – among them a book about addiction and a documentary about people who identify as neither male nor female.
Then last fall came the surprising passage of California’s End of Life Option Act, giving terminally ill adults with 6 months to live the right to request lethal medication to end their lives. The law takes effect June 9.
Dr. Shavelson decided he had to act, adding that he feels “quite guilty” about having been away from the issue while others pushed it forward.
His website, Bay Area End of Life Options, went up in April, and he’s outlined the law at “grand rounds” at several Bay Area hospitals this spring. His practice will be focused on consulting not only with physicians whose patients request aid-in-dying, but also with patients themselves. As he indicates on his site, he will offer care to patients who choose him as their “attending End-of-Life physician.”
Dr. Shavelson is adamant that this is “something that has to be done right.” To him, that means starting every patient encounter with a one-word question: “Why?”
“In fact, it’s the only initial approach that I think is acceptable. If somebody calls me and says, ‘I want to take the medication, my first question is, ‘Why? Let me talk to you about all the various alternatives and all the ways that we can think about this.’ ”
Dr. Shavelson worries that patients may seek aid-in-dying because they are in pain. So first, he would like all his patients to be enrolled in hospice care.
“This can only work when you’re sure that the patients have been given the best end-of-life care, which to me is most guaranteed by being a part of hospice or at least having a good palliative care physician. Then this is a rational decision. If you’re doing it otherwise, it’s because of lack of good care.”
California is the fifth state to legalize aid-in-dying, joining Oregon, Washington, Vermont, and Montana. The option is very rarely used. For example, in 2014 in Oregon, just 155 lethal prescriptions were written under the state’s law, and 105 people ultimately took the medicine and died.
Under the California law, two doctors must agree that a patient has 6 months or less to live. The patient must be mentally competent. At least one of the meetings between the patient and his or her doctor must be private, with no one else present, to ensure the patient is acting independently.
Patients must be able to swallow the medication themselves and must affirm in writing, within the 48 hours before taking the medication, that they will do so.
Dr. Shavelson says he has been surprised by the poor understanding of the law among some health care providers. One insisted the law was not taking effect this year; another asked how the law would benefit his patients with Alzheimer’s disease. (Patients with dementia don’t qualify under the law because they are not mentally competent.)
The law does not require that health care providers participate in ending terminally ill patients’ lives. Many physicians are “queasy” about the law, Dr. Shavelson said, and are unwilling to prescribe to patients who request the lethal medication – even when they think having such a law in place is the right thing to do.
“My response to that is as health care providers, you might have been uncomfortable the first time you drew blood. You might have been uncomfortable the first time you took out somebody’s gall bladder,” he said. “If it’s a medical procedure you believe in and you believe it’s the patient’s right, then it’s your obligation to learn how to do it – and do it correctly.”
Dr. Shavelson predicts that many physicians who are initially reluctant to provide this option to their patients may become more comfortable after the law goes into effect and they see how it works.
Dr. Burt Presberg, an East Bay psychiatrist who works with cancer patients and their families, attended a talk by Dr. Shavelson, and it led to some soul searching.
He wrestles with his own comfort level in handling patient requests. When he talks, he often pivots from his initial point to “on the other hand.”
Dr. Presberg says he is concerned that patients suffer from clinical depression at the end of life. Sometimes they feel they are a burden to family members who could “really push for the end of life to happen a little sooner than the patient themselves.”
His experience is that terminally ill patients with clinical depression can be successfully treated. He said he believes Dr. Shavelson will be aware of the need to treat depression,”but I do have concerns about other physicians.”
“On the other hand,” he added, “I think it’s really good that this is an option.”
Dr. Shavelson says he’s already received a handful of calls from patients, but mostly he’s spent his time before the law takes effect talking to other physicians. He needs a consulting physician and a pharmacist who will accept prescriptions for a lethal dose of medicine.
Then his mind returns to the patient. “It’s important … that we’re moving forward,” he said. “It’s crucial that we do that because this is part of the rights of patient care to have a certain level of autonomy in how they die.”
To him, this type of care “isn’t so tangibly different” from other kinds of questions doctors address.
“I’m just one of those docs who sees dying as a process, and [the] method of death is less important than making sure it’s a good death.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation. This story is part of a partnership that includes KQED, NPR, and Kaiser Health News.
BERKELEY, Calif. – Few people have the unusual set of professional experiences that Dr. Lonny Shavelson does. He worked as an emergency room physician in Berkeley for years – while also working as a journalist. He has written several books and takes hauntingly beautiful photographs.
Now, just as California’s aid-in-dying law takes effect June 9, Dr. Shavelson has added another specialty: A consultant to physicians and terminally ill patients who have questions about how it works.
“Can I just sit back and watch?” Dr. Shavelson asked from his cottage office. “This is really an amazing opportunity to be part of establishing policy and initiating something in medicine. This is a major change … [that] very, very few people know anything about and how to do it.”
Dr. Shavelson is the author of the 1995 book, “A Chosen Death,” which followed five terminally ill people over 2 years as they determined whether to amass drugs on their own and end their lives at a time of their choosing. He was present at the death of all of them.
He followed the issue closely for several years, but ultimately moved on to other projects – among them a book about addiction and a documentary about people who identify as neither male nor female.
Then last fall came the surprising passage of California’s End of Life Option Act, giving terminally ill adults with 6 months to live the right to request lethal medication to end their lives. The law takes effect June 9.
Dr. Shavelson decided he had to act, adding that he feels “quite guilty” about having been away from the issue while others pushed it forward.
His website, Bay Area End of Life Options, went up in April, and he’s outlined the law at “grand rounds” at several Bay Area hospitals this spring. His practice will be focused on consulting not only with physicians whose patients request aid-in-dying, but also with patients themselves. As he indicates on his site, he will offer care to patients who choose him as their “attending End-of-Life physician.”
Dr. Shavelson is adamant that this is “something that has to be done right.” To him, that means starting every patient encounter with a one-word question: “Why?”
“In fact, it’s the only initial approach that I think is acceptable. If somebody calls me and says, ‘I want to take the medication, my first question is, ‘Why? Let me talk to you about all the various alternatives and all the ways that we can think about this.’ ”
Dr. Shavelson worries that patients may seek aid-in-dying because they are in pain. So first, he would like all his patients to be enrolled in hospice care.
“This can only work when you’re sure that the patients have been given the best end-of-life care, which to me is most guaranteed by being a part of hospice or at least having a good palliative care physician. Then this is a rational decision. If you’re doing it otherwise, it’s because of lack of good care.”
California is the fifth state to legalize aid-in-dying, joining Oregon, Washington, Vermont, and Montana. The option is very rarely used. For example, in 2014 in Oregon, just 155 lethal prescriptions were written under the state’s law, and 105 people ultimately took the medicine and died.
Under the California law, two doctors must agree that a patient has 6 months or less to live. The patient must be mentally competent. At least one of the meetings between the patient and his or her doctor must be private, with no one else present, to ensure the patient is acting independently.
Patients must be able to swallow the medication themselves and must affirm in writing, within the 48 hours before taking the medication, that they will do so.
Dr. Shavelson says he has been surprised by the poor understanding of the law among some health care providers. One insisted the law was not taking effect this year; another asked how the law would benefit his patients with Alzheimer’s disease. (Patients with dementia don’t qualify under the law because they are not mentally competent.)
The law does not require that health care providers participate in ending terminally ill patients’ lives. Many physicians are “queasy” about the law, Dr. Shavelson said, and are unwilling to prescribe to patients who request the lethal medication – even when they think having such a law in place is the right thing to do.
“My response to that is as health care providers, you might have been uncomfortable the first time you drew blood. You might have been uncomfortable the first time you took out somebody’s gall bladder,” he said. “If it’s a medical procedure you believe in and you believe it’s the patient’s right, then it’s your obligation to learn how to do it – and do it correctly.”
Dr. Shavelson predicts that many physicians who are initially reluctant to provide this option to their patients may become more comfortable after the law goes into effect and they see how it works.
Dr. Burt Presberg, an East Bay psychiatrist who works with cancer patients and their families, attended a talk by Dr. Shavelson, and it led to some soul searching.
He wrestles with his own comfort level in handling patient requests. When he talks, he often pivots from his initial point to “on the other hand.”
Dr. Presberg says he is concerned that patients suffer from clinical depression at the end of life. Sometimes they feel they are a burden to family members who could “really push for the end of life to happen a little sooner than the patient themselves.”
His experience is that terminally ill patients with clinical depression can be successfully treated. He said he believes Dr. Shavelson will be aware of the need to treat depression,”but I do have concerns about other physicians.”
“On the other hand,” he added, “I think it’s really good that this is an option.”
Dr. Shavelson says he’s already received a handful of calls from patients, but mostly he’s spent his time before the law takes effect talking to other physicians. He needs a consulting physician and a pharmacist who will accept prescriptions for a lethal dose of medicine.
Then his mind returns to the patient. “It’s important … that we’re moving forward,” he said. “It’s crucial that we do that because this is part of the rights of patient care to have a certain level of autonomy in how they die.”
To him, this type of care “isn’t so tangibly different” from other kinds of questions doctors address.
“I’m just one of those docs who sees dying as a process, and [the] method of death is less important than making sure it’s a good death.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation. This story is part of a partnership that includes KQED, NPR, and Kaiser Health News.
BERKELEY, Calif. – Few people have the unusual set of professional experiences that Dr. Lonny Shavelson does. He worked as an emergency room physician in Berkeley for years – while also working as a journalist. He has written several books and takes hauntingly beautiful photographs.
Now, just as California’s aid-in-dying law takes effect June 9, Dr. Shavelson has added another specialty: A consultant to physicians and terminally ill patients who have questions about how it works.
“Can I just sit back and watch?” Dr. Shavelson asked from his cottage office. “This is really an amazing opportunity to be part of establishing policy and initiating something in medicine. This is a major change … [that] very, very few people know anything about and how to do it.”
Dr. Shavelson is the author of the 1995 book, “A Chosen Death,” which followed five terminally ill people over 2 years as they determined whether to amass drugs on their own and end their lives at a time of their choosing. He was present at the death of all of them.
He followed the issue closely for several years, but ultimately moved on to other projects – among them a book about addiction and a documentary about people who identify as neither male nor female.
Then last fall came the surprising passage of California’s End of Life Option Act, giving terminally ill adults with 6 months to live the right to request lethal medication to end their lives. The law takes effect June 9.
Dr. Shavelson decided he had to act, adding that he feels “quite guilty” about having been away from the issue while others pushed it forward.
His website, Bay Area End of Life Options, went up in April, and he’s outlined the law at “grand rounds” at several Bay Area hospitals this spring. His practice will be focused on consulting not only with physicians whose patients request aid-in-dying, but also with patients themselves. As he indicates on his site, he will offer care to patients who choose him as their “attending End-of-Life physician.”
Dr. Shavelson is adamant that this is “something that has to be done right.” To him, that means starting every patient encounter with a one-word question: “Why?”
“In fact, it’s the only initial approach that I think is acceptable. If somebody calls me and says, ‘I want to take the medication, my first question is, ‘Why? Let me talk to you about all the various alternatives and all the ways that we can think about this.’ ”
Dr. Shavelson worries that patients may seek aid-in-dying because they are in pain. So first, he would like all his patients to be enrolled in hospice care.
“This can only work when you’re sure that the patients have been given the best end-of-life care, which to me is most guaranteed by being a part of hospice or at least having a good palliative care physician. Then this is a rational decision. If you’re doing it otherwise, it’s because of lack of good care.”
California is the fifth state to legalize aid-in-dying, joining Oregon, Washington, Vermont, and Montana. The option is very rarely used. For example, in 2014 in Oregon, just 155 lethal prescriptions were written under the state’s law, and 105 people ultimately took the medicine and died.
Under the California law, two doctors must agree that a patient has 6 months or less to live. The patient must be mentally competent. At least one of the meetings between the patient and his or her doctor must be private, with no one else present, to ensure the patient is acting independently.
Patients must be able to swallow the medication themselves and must affirm in writing, within the 48 hours before taking the medication, that they will do so.
Dr. Shavelson says he has been surprised by the poor understanding of the law among some health care providers. One insisted the law was not taking effect this year; another asked how the law would benefit his patients with Alzheimer’s disease. (Patients with dementia don’t qualify under the law because they are not mentally competent.)
The law does not require that health care providers participate in ending terminally ill patients’ lives. Many physicians are “queasy” about the law, Dr. Shavelson said, and are unwilling to prescribe to patients who request the lethal medication – even when they think having such a law in place is the right thing to do.
“My response to that is as health care providers, you might have been uncomfortable the first time you drew blood. You might have been uncomfortable the first time you took out somebody’s gall bladder,” he said. “If it’s a medical procedure you believe in and you believe it’s the patient’s right, then it’s your obligation to learn how to do it – and do it correctly.”
Dr. Shavelson predicts that many physicians who are initially reluctant to provide this option to their patients may become more comfortable after the law goes into effect and they see how it works.
Dr. Burt Presberg, an East Bay psychiatrist who works with cancer patients and their families, attended a talk by Dr. Shavelson, and it led to some soul searching.
He wrestles with his own comfort level in handling patient requests. When he talks, he often pivots from his initial point to “on the other hand.”
Dr. Presberg says he is concerned that patients suffer from clinical depression at the end of life. Sometimes they feel they are a burden to family members who could “really push for the end of life to happen a little sooner than the patient themselves.”
His experience is that terminally ill patients with clinical depression can be successfully treated. He said he believes Dr. Shavelson will be aware of the need to treat depression,”but I do have concerns about other physicians.”
“On the other hand,” he added, “I think it’s really good that this is an option.”
Dr. Shavelson says he’s already received a handful of calls from patients, but mostly he’s spent his time before the law takes effect talking to other physicians. He needs a consulting physician and a pharmacist who will accept prescriptions for a lethal dose of medicine.
Then his mind returns to the patient. “It’s important … that we’re moving forward,” he said. “It’s crucial that we do that because this is part of the rights of patient care to have a certain level of autonomy in how they die.”
To him, this type of care “isn’t so tangibly different” from other kinds of questions doctors address.
“I’m just one of those docs who sees dying as a process, and [the] method of death is less important than making sure it’s a good death.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation. This story is part of a partnership that includes KQED, NPR, and Kaiser Health News.
Targeting vagal activity could improve breast cancer survival
ATLANTA – Vagal activity predicts survival in patients with metastatic or recurrent breast cancer, a study showed.
The findings are intriguing, given that vagal activity is modifiable, according to Dr. David Spiegel, Willson Professor of Psychiatry and Behavioral Sciences and director of the center on stress and health at Stanford (Calif.) University.
The study, conducted by Dr. Spiegel and his colleagues, is one of several that together are beginning to elucidate the connections among sleep, stress, and vagal tone, and the effects these factors have on cancer outcomes. For example, in one earlier study of metastatic breast cancer patients, the group demonstrated that good sleep efficiency predicted longer survival (Sleep. 2014 May 1;37[5]:837-42).
“There’s something about sleep that we think has an effect on disease progression,” Dr. Spiegel said at the annual meeting of the American Psychiatric Association.
In another study, the team showed that breast cancer patients who slept better at night had better vagal tone the following morning.
“We all kind of know that a problem that has been keeping you from getting to sleep or worrying you a lot the night before suddenly seems more soluble in the morning after you’ve had a good night’s sleep. You’re better able to self-soothe in the morning,” he said, noting the importance of this evidence that “sleep improves vagal tone.”
Heart rate variability is a good measure of vagal tone, vagal activity, and the ability to self-soothe, he explained, noting that heart rate variability also predicts longer survival with cardiac disease; it seems to reduce the risk of fatal arrhythmias, and also predicts recovery from myocardial infarction.
Others have suggested that it might have an effect on cancer, and there seems to be a link between vagal activity and inflammatory processes, Dr. Spiegel said.
“There is reason to think that poor heart rate variability might be associated with cancer progression as well, and that’s what we wanted to study in a group of metastatic cancer patients,” he said.
Dr. Spiegel and his colleagues measured high-frequency heart rate variability (HF-HRV), which appears to be the best measure of parasympathetic tone, has been associated with longer survival in humans and animals, and is related to immune system functioning.
“We hypothesized that higher heart rate variability would predict longer survival in patients with MRBC [metastatic or recurrent breast cancer],” he said.
In 87 patients with metastases to bone, skin, or viscera who underwent a variety of stress measures, including a 5-minute resting baseline electrocardiogram, 43 had higher HF-HRV, and 44 had lower HF-HRV. Higher baseline HF-HRV did, indeed, predict significantly longer survival (hazard ratio, 0.75).
“The main hypothesis was confirmed – that patients with better vagal tone, higher high-frequency heart rate variability had significantly longer survival over the ensuing 7 years, compared with the patients who had poorer heart rate variability, poorer vagal tone,” he said (Psychosom Med. 2015;77[4]:346-55).
Visceral metastasis status and baseline heart rate both were related to HF-HRV and survival, and the combination of HF-HRV and heart rate further improved survival prediction (HR, 0.64), he noted.
“This is basically coactivation of higher parasympathetic and lower sympathetic activity related to longer survival,” he explained.
Reconstructive surgery, the presence of visceral metastases, and sleep efficiency each were found to be associated with heart rate variability; thus several analyses were conducted “to try to disentangle these relationships and determine what the major variables were that predicted survival,” Dr. Spiegel said.
“It turns out that heart rate variability and visceral metastases were significantly related, and heart rate variability did not predict survival,” he said, explaining that those with visceral metastases (and therefore, cancer with a much poorer prognosis) died sooner, but heart rate variability didn’t make much of a difference. “Where we saw the heart rate variability effect was among those with better prognosis.”
A combination measure of high heart rate variability (“a pretty pure measure of vagal activity, not sympathetic activity”) and low heart rate (“more driven by the sympathetic adrenal-medullary system”) is an even stronger predictor of overall survival, he said.
This suggests that autonomic nervous system variables play a strong role in predicting overall cancer survival, Dr. Spiegel said, noting that depression was not a confounder.
“This is important, because we have, in other studies, found that depression is associated with lower heart rate variability, as you might expect,” he said. In fact, depression has been found to predict shorter survival in cancer patients over a period of 10 years. In an earlier study, cancer patients with worsening depression in the first year died sooner than those with depression that improved during the first year (J Clin Oncol. 2011;29[4]:413-20).
“The median survival difference was about 2 years, so this is not a trivial difference in overall survival,” he said, stressing that the finding is based on more chronic and severe depression.
Other studies have demonstrated relationships between circadian rhythm disruption and cancer survival. In one such study involving patients with metastatic colorectal cancer, circadian rhythm/rest activity cycle (more activity during the day, more rest at night) was associated with better quality of life and predicted survival.
“This has been shown now in several cancers, and it’s clear that a combination of higher activity and better sleep predict longer survival with different kinds of cancers,” Dr. Spiegel said, explaining that a hallmark of a healthy hypothalamic-pituitary-adrenal axis is good diurnal variation of cortisol with high levels in the morning and declining levels throughout the day.
Women with metastatic breast cancer and poorer survival tended to have flat or increasing levels of cortisol throughout the day, he said, adding that the same was true in a study of patients with lung cancer, and that there is evidence that those among them with flatter, more abnormal cortisol patterns throughout the day also have shorter survival.
Animal studies suggest that cortisol might directly suppress the activity of tumor suppressor genes, he explained, noting that there is also increasing evidence of autonomic dysregulation effects on inflammatory processes associated with tumor growth.
“Some basic research on this in animal models shows that if you block adrenergic arousal, you can block the growth of blood vessels from tumors. This has led some people to look at the use of antiadrenergic drugs like the beta-blocker propranolol, and it turned out – to everyone’s surprise – that breast cancer patients who happened to be on beta-blockers for hypertension actually lived longer than those who didn’t,” he said.
This adds to the growing evidence that dysregulation in the sympathetic and parasympathetic systems have effects on survival, he said.
A look at another factor related to sleep disruption – bedtime misalignment – showed that patients who adhere to their preferred sleep pattern, and who are therefore sleeping better, had a difference in disease-free interval; those whose bedtime was misaligned had a shorter time between diagnosis and disease recurrence (Chronobiol Int. 2014 Mar 31[2]214-21).
“Disease-free interval is a very strong predictor of ultimate overall survival, so there seems to be another relationship here between circadian disruption and disease progression in breast cancer,” Dr. Spiegel said.
Taken together, these findings demonstrate a strong association between vagal activity and survival in patients with metastatic or recurrent breast cancer, extending the known predictive window of HF-HRV beyond palliative care to cancer, Dr. Spiegel said.
“Vagal activity can be altered through behavioral, pharmacological, and surgical interventions and thus may be a promising target for increasing survival in patients with metastatic cancer,” he said.
Dr. Spiegel’s studies were funded by the National Cancer Institute and the National Institute on Aging.
ATLANTA – Vagal activity predicts survival in patients with metastatic or recurrent breast cancer, a study showed.
The findings are intriguing, given that vagal activity is modifiable, according to Dr. David Spiegel, Willson Professor of Psychiatry and Behavioral Sciences and director of the center on stress and health at Stanford (Calif.) University.
The study, conducted by Dr. Spiegel and his colleagues, is one of several that together are beginning to elucidate the connections among sleep, stress, and vagal tone, and the effects these factors have on cancer outcomes. For example, in one earlier study of metastatic breast cancer patients, the group demonstrated that good sleep efficiency predicted longer survival (Sleep. 2014 May 1;37[5]:837-42).
“There’s something about sleep that we think has an effect on disease progression,” Dr. Spiegel said at the annual meeting of the American Psychiatric Association.
In another study, the team showed that breast cancer patients who slept better at night had better vagal tone the following morning.
“We all kind of know that a problem that has been keeping you from getting to sleep or worrying you a lot the night before suddenly seems more soluble in the morning after you’ve had a good night’s sleep. You’re better able to self-soothe in the morning,” he said, noting the importance of this evidence that “sleep improves vagal tone.”
Heart rate variability is a good measure of vagal tone, vagal activity, and the ability to self-soothe, he explained, noting that heart rate variability also predicts longer survival with cardiac disease; it seems to reduce the risk of fatal arrhythmias, and also predicts recovery from myocardial infarction.
Others have suggested that it might have an effect on cancer, and there seems to be a link between vagal activity and inflammatory processes, Dr. Spiegel said.
“There is reason to think that poor heart rate variability might be associated with cancer progression as well, and that’s what we wanted to study in a group of metastatic cancer patients,” he said.
Dr. Spiegel and his colleagues measured high-frequency heart rate variability (HF-HRV), which appears to be the best measure of parasympathetic tone, has been associated with longer survival in humans and animals, and is related to immune system functioning.
“We hypothesized that higher heart rate variability would predict longer survival in patients with MRBC [metastatic or recurrent breast cancer],” he said.
In 87 patients with metastases to bone, skin, or viscera who underwent a variety of stress measures, including a 5-minute resting baseline electrocardiogram, 43 had higher HF-HRV, and 44 had lower HF-HRV. Higher baseline HF-HRV did, indeed, predict significantly longer survival (hazard ratio, 0.75).
“The main hypothesis was confirmed – that patients with better vagal tone, higher high-frequency heart rate variability had significantly longer survival over the ensuing 7 years, compared with the patients who had poorer heart rate variability, poorer vagal tone,” he said (Psychosom Med. 2015;77[4]:346-55).
Visceral metastasis status and baseline heart rate both were related to HF-HRV and survival, and the combination of HF-HRV and heart rate further improved survival prediction (HR, 0.64), he noted.
“This is basically coactivation of higher parasympathetic and lower sympathetic activity related to longer survival,” he explained.
Reconstructive surgery, the presence of visceral metastases, and sleep efficiency each were found to be associated with heart rate variability; thus several analyses were conducted “to try to disentangle these relationships and determine what the major variables were that predicted survival,” Dr. Spiegel said.
“It turns out that heart rate variability and visceral metastases were significantly related, and heart rate variability did not predict survival,” he said, explaining that those with visceral metastases (and therefore, cancer with a much poorer prognosis) died sooner, but heart rate variability didn’t make much of a difference. “Where we saw the heart rate variability effect was among those with better prognosis.”
A combination measure of high heart rate variability (“a pretty pure measure of vagal activity, not sympathetic activity”) and low heart rate (“more driven by the sympathetic adrenal-medullary system”) is an even stronger predictor of overall survival, he said.
This suggests that autonomic nervous system variables play a strong role in predicting overall cancer survival, Dr. Spiegel said, noting that depression was not a confounder.
“This is important, because we have, in other studies, found that depression is associated with lower heart rate variability, as you might expect,” he said. In fact, depression has been found to predict shorter survival in cancer patients over a period of 10 years. In an earlier study, cancer patients with worsening depression in the first year died sooner than those with depression that improved during the first year (J Clin Oncol. 2011;29[4]:413-20).
“The median survival difference was about 2 years, so this is not a trivial difference in overall survival,” he said, stressing that the finding is based on more chronic and severe depression.
Other studies have demonstrated relationships between circadian rhythm disruption and cancer survival. In one such study involving patients with metastatic colorectal cancer, circadian rhythm/rest activity cycle (more activity during the day, more rest at night) was associated with better quality of life and predicted survival.
“This has been shown now in several cancers, and it’s clear that a combination of higher activity and better sleep predict longer survival with different kinds of cancers,” Dr. Spiegel said, explaining that a hallmark of a healthy hypothalamic-pituitary-adrenal axis is good diurnal variation of cortisol with high levels in the morning and declining levels throughout the day.
Women with metastatic breast cancer and poorer survival tended to have flat or increasing levels of cortisol throughout the day, he said, adding that the same was true in a study of patients with lung cancer, and that there is evidence that those among them with flatter, more abnormal cortisol patterns throughout the day also have shorter survival.
Animal studies suggest that cortisol might directly suppress the activity of tumor suppressor genes, he explained, noting that there is also increasing evidence of autonomic dysregulation effects on inflammatory processes associated with tumor growth.
“Some basic research on this in animal models shows that if you block adrenergic arousal, you can block the growth of blood vessels from tumors. This has led some people to look at the use of antiadrenergic drugs like the beta-blocker propranolol, and it turned out – to everyone’s surprise – that breast cancer patients who happened to be on beta-blockers for hypertension actually lived longer than those who didn’t,” he said.
This adds to the growing evidence that dysregulation in the sympathetic and parasympathetic systems have effects on survival, he said.
A look at another factor related to sleep disruption – bedtime misalignment – showed that patients who adhere to their preferred sleep pattern, and who are therefore sleeping better, had a difference in disease-free interval; those whose bedtime was misaligned had a shorter time between diagnosis and disease recurrence (Chronobiol Int. 2014 Mar 31[2]214-21).
“Disease-free interval is a very strong predictor of ultimate overall survival, so there seems to be another relationship here between circadian disruption and disease progression in breast cancer,” Dr. Spiegel said.
Taken together, these findings demonstrate a strong association between vagal activity and survival in patients with metastatic or recurrent breast cancer, extending the known predictive window of HF-HRV beyond palliative care to cancer, Dr. Spiegel said.
“Vagal activity can be altered through behavioral, pharmacological, and surgical interventions and thus may be a promising target for increasing survival in patients with metastatic cancer,” he said.
Dr. Spiegel’s studies were funded by the National Cancer Institute and the National Institute on Aging.
ATLANTA – Vagal activity predicts survival in patients with metastatic or recurrent breast cancer, a study showed.
The findings are intriguing, given that vagal activity is modifiable, according to Dr. David Spiegel, Willson Professor of Psychiatry and Behavioral Sciences and director of the center on stress and health at Stanford (Calif.) University.
The study, conducted by Dr. Spiegel and his colleagues, is one of several that together are beginning to elucidate the connections among sleep, stress, and vagal tone, and the effects these factors have on cancer outcomes. For example, in one earlier study of metastatic breast cancer patients, the group demonstrated that good sleep efficiency predicted longer survival (Sleep. 2014 May 1;37[5]:837-42).
“There’s something about sleep that we think has an effect on disease progression,” Dr. Spiegel said at the annual meeting of the American Psychiatric Association.
In another study, the team showed that breast cancer patients who slept better at night had better vagal tone the following morning.
“We all kind of know that a problem that has been keeping you from getting to sleep or worrying you a lot the night before suddenly seems more soluble in the morning after you’ve had a good night’s sleep. You’re better able to self-soothe in the morning,” he said, noting the importance of this evidence that “sleep improves vagal tone.”
Heart rate variability is a good measure of vagal tone, vagal activity, and the ability to self-soothe, he explained, noting that heart rate variability also predicts longer survival with cardiac disease; it seems to reduce the risk of fatal arrhythmias, and also predicts recovery from myocardial infarction.
Others have suggested that it might have an effect on cancer, and there seems to be a link between vagal activity and inflammatory processes, Dr. Spiegel said.
“There is reason to think that poor heart rate variability might be associated with cancer progression as well, and that’s what we wanted to study in a group of metastatic cancer patients,” he said.
Dr. Spiegel and his colleagues measured high-frequency heart rate variability (HF-HRV), which appears to be the best measure of parasympathetic tone, has been associated with longer survival in humans and animals, and is related to immune system functioning.
“We hypothesized that higher heart rate variability would predict longer survival in patients with MRBC [metastatic or recurrent breast cancer],” he said.
In 87 patients with metastases to bone, skin, or viscera who underwent a variety of stress measures, including a 5-minute resting baseline electrocardiogram, 43 had higher HF-HRV, and 44 had lower HF-HRV. Higher baseline HF-HRV did, indeed, predict significantly longer survival (hazard ratio, 0.75).
“The main hypothesis was confirmed – that patients with better vagal tone, higher high-frequency heart rate variability had significantly longer survival over the ensuing 7 years, compared with the patients who had poorer heart rate variability, poorer vagal tone,” he said (Psychosom Med. 2015;77[4]:346-55).
Visceral metastasis status and baseline heart rate both were related to HF-HRV and survival, and the combination of HF-HRV and heart rate further improved survival prediction (HR, 0.64), he noted.
“This is basically coactivation of higher parasympathetic and lower sympathetic activity related to longer survival,” he explained.
Reconstructive surgery, the presence of visceral metastases, and sleep efficiency each were found to be associated with heart rate variability; thus several analyses were conducted “to try to disentangle these relationships and determine what the major variables were that predicted survival,” Dr. Spiegel said.
“It turns out that heart rate variability and visceral metastases were significantly related, and heart rate variability did not predict survival,” he said, explaining that those with visceral metastases (and therefore, cancer with a much poorer prognosis) died sooner, but heart rate variability didn’t make much of a difference. “Where we saw the heart rate variability effect was among those with better prognosis.”
A combination measure of high heart rate variability (“a pretty pure measure of vagal activity, not sympathetic activity”) and low heart rate (“more driven by the sympathetic adrenal-medullary system”) is an even stronger predictor of overall survival, he said.
This suggests that autonomic nervous system variables play a strong role in predicting overall cancer survival, Dr. Spiegel said, noting that depression was not a confounder.
“This is important, because we have, in other studies, found that depression is associated with lower heart rate variability, as you might expect,” he said. In fact, depression has been found to predict shorter survival in cancer patients over a period of 10 years. In an earlier study, cancer patients with worsening depression in the first year died sooner than those with depression that improved during the first year (J Clin Oncol. 2011;29[4]:413-20).
“The median survival difference was about 2 years, so this is not a trivial difference in overall survival,” he said, stressing that the finding is based on more chronic and severe depression.
Other studies have demonstrated relationships between circadian rhythm disruption and cancer survival. In one such study involving patients with metastatic colorectal cancer, circadian rhythm/rest activity cycle (more activity during the day, more rest at night) was associated with better quality of life and predicted survival.
“This has been shown now in several cancers, and it’s clear that a combination of higher activity and better sleep predict longer survival with different kinds of cancers,” Dr. Spiegel said, explaining that a hallmark of a healthy hypothalamic-pituitary-adrenal axis is good diurnal variation of cortisol with high levels in the morning and declining levels throughout the day.
Women with metastatic breast cancer and poorer survival tended to have flat or increasing levels of cortisol throughout the day, he said, adding that the same was true in a study of patients with lung cancer, and that there is evidence that those among them with flatter, more abnormal cortisol patterns throughout the day also have shorter survival.
Animal studies suggest that cortisol might directly suppress the activity of tumor suppressor genes, he explained, noting that there is also increasing evidence of autonomic dysregulation effects on inflammatory processes associated with tumor growth.
“Some basic research on this in animal models shows that if you block adrenergic arousal, you can block the growth of blood vessels from tumors. This has led some people to look at the use of antiadrenergic drugs like the beta-blocker propranolol, and it turned out – to everyone’s surprise – that breast cancer patients who happened to be on beta-blockers for hypertension actually lived longer than those who didn’t,” he said.
This adds to the growing evidence that dysregulation in the sympathetic and parasympathetic systems have effects on survival, he said.
A look at another factor related to sleep disruption – bedtime misalignment – showed that patients who adhere to their preferred sleep pattern, and who are therefore sleeping better, had a difference in disease-free interval; those whose bedtime was misaligned had a shorter time between diagnosis and disease recurrence (Chronobiol Int. 2014 Mar 31[2]214-21).
“Disease-free interval is a very strong predictor of ultimate overall survival, so there seems to be another relationship here between circadian disruption and disease progression in breast cancer,” Dr. Spiegel said.
Taken together, these findings demonstrate a strong association between vagal activity and survival in patients with metastatic or recurrent breast cancer, extending the known predictive window of HF-HRV beyond palliative care to cancer, Dr. Spiegel said.
“Vagal activity can be altered through behavioral, pharmacological, and surgical interventions and thus may be a promising target for increasing survival in patients with metastatic cancer,” he said.
Dr. Spiegel’s studies were funded by the National Cancer Institute and the National Institute on Aging.
AT THE APA ANNUAL MEETING
Key clinical point: Vagal activity predicted survival in patients with metastatic or recurrent breast cancer.
Major finding: Higher baseline HF-HRV predicted significantly longer survival (hazard ratio, 0.75).
Data source: A study of 87 patients with metastatic or recurrent breast cancer.
Disclosures: Dr. Spiegel’s studies were funded by the National Cancer Institute and the National Institute on Aging.
Advances in the management of multiple myeloma
Multiple myeloma (MM) is a bone marrow- based malignancy of plasma cells that is diagnosed in over 30,000 patients annually in the United States. Despite the many recent advances in the treatment of MM, it remains an incurable disease. Thus, the need for the development of new effective therapies remains critical for these patients.
Smoldering MM
In general, it has not been shown that patients with smoldering MM (SMM) benefit from early treatment, but recent studies have identified a subset of patients who are at high-risk and may require therapy more quickly. Recent guidelines from the International Myeloma Working Group recommend immediate treatment of this subgroup of SMM.1 However, although findings in a Spanish study suggested that early treatment of high-risk SMM patients with the immunomodulatory agent (IMiD) lenalidomide and dexamethasone improves overall survival (OS),2 the design of that study limits its clinical applicability, and no other randomized trials have been completed to show the advantage of early therapy for these patients.
Specific drugs
The development of novel agents such as proteasome inhibitors (PIs), IMiDs, histone deacetylase inhibitors (HDACIs), and monoclonal antibodies (mAbs) in recent years has vastly changed the approach to the treatment of MM patients.
PIs that are cytotoxic to MM cells, such as bortezomib, have become a foundation for MM treatment over the past decade. However, patients develop drug resistance to bortezomib by acquiring gene mutations and through other mechanisms. In recent years, newer forms of PIs such as carfilzomib and the oral formulations ixazomib and oprozomib have been and are currently being developed.3 Preclinical studies have shown that resistance to one PI can be overcome with treatment with another PI.4
Click on the PDF icon at the top of this introduction to read the full article.
Multiple myeloma (MM) is a bone marrow- based malignancy of plasma cells that is diagnosed in over 30,000 patients annually in the United States. Despite the many recent advances in the treatment of MM, it remains an incurable disease. Thus, the need for the development of new effective therapies remains critical for these patients.
Smoldering MM
In general, it has not been shown that patients with smoldering MM (SMM) benefit from early treatment, but recent studies have identified a subset of patients who are at high-risk and may require therapy more quickly. Recent guidelines from the International Myeloma Working Group recommend immediate treatment of this subgroup of SMM.1 However, although findings in a Spanish study suggested that early treatment of high-risk SMM patients with the immunomodulatory agent (IMiD) lenalidomide and dexamethasone improves overall survival (OS),2 the design of that study limits its clinical applicability, and no other randomized trials have been completed to show the advantage of early therapy for these patients.
Specific drugs
The development of novel agents such as proteasome inhibitors (PIs), IMiDs, histone deacetylase inhibitors (HDACIs), and monoclonal antibodies (mAbs) in recent years has vastly changed the approach to the treatment of MM patients.
PIs that are cytotoxic to MM cells, such as bortezomib, have become a foundation for MM treatment over the past decade. However, patients develop drug resistance to bortezomib by acquiring gene mutations and through other mechanisms. In recent years, newer forms of PIs such as carfilzomib and the oral formulations ixazomib and oprozomib have been and are currently being developed.3 Preclinical studies have shown that resistance to one PI can be overcome with treatment with another PI.4
Click on the PDF icon at the top of this introduction to read the full article.
Multiple myeloma (MM) is a bone marrow- based malignancy of plasma cells that is diagnosed in over 30,000 patients annually in the United States. Despite the many recent advances in the treatment of MM, it remains an incurable disease. Thus, the need for the development of new effective therapies remains critical for these patients.
Smoldering MM
In general, it has not been shown that patients with smoldering MM (SMM) benefit from early treatment, but recent studies have identified a subset of patients who are at high-risk and may require therapy more quickly. Recent guidelines from the International Myeloma Working Group recommend immediate treatment of this subgroup of SMM.1 However, although findings in a Spanish study suggested that early treatment of high-risk SMM patients with the immunomodulatory agent (IMiD) lenalidomide and dexamethasone improves overall survival (OS),2 the design of that study limits its clinical applicability, and no other randomized trials have been completed to show the advantage of early therapy for these patients.
Specific drugs
The development of novel agents such as proteasome inhibitors (PIs), IMiDs, histone deacetylase inhibitors (HDACIs), and monoclonal antibodies (mAbs) in recent years has vastly changed the approach to the treatment of MM patients.
PIs that are cytotoxic to MM cells, such as bortezomib, have become a foundation for MM treatment over the past decade. However, patients develop drug resistance to bortezomib by acquiring gene mutations and through other mechanisms. In recent years, newer forms of PIs such as carfilzomib and the oral formulations ixazomib and oprozomib have been and are currently being developed.3 Preclinical studies have shown that resistance to one PI can be overcome with treatment with another PI.4
Click on the PDF icon at the top of this introduction to read the full article.