User login
Medical ‘myths’ persist despite evidence, says professor of medicine
These long-held pieces of dogma – or “medical myths” – were engraved during training or early in the careers of many physicians, and are difficult to overcome, noted Douglas Paauw, MD, professor of medicine at the University of Washington, Seattle.
“I think that myths persist because medical professionals get taught one way in training, given a ‘truth’ or ‘This is the way we do it,’ and then do not ever rethink, ‘Is it true?’ ” he said in an interview. “Studies pop up to question conventional wisdom, but unless the studies get highly publicized, they aren’t noticed.”
During his presentation, Dr. Paauw discussed three of what he considers to be some of the some of the medical myths that are in greatest need of being dispelled.
Shellfish allergy and radiocontrast
A myth persists that people with a shellfish allergy could have an allergic reaction when a contrast agent is used for a scan, he said.
This belief arose, because fish and shellfish contain iodine, and allergic reactions to seafood are fairly common, and contrast agents contain iodine, too, Dr. Paauw said.
The belief is widespread, with 65% of radiologists and 88.9% of interventional cardiologists saying they ask about seafood or shellfish allergies before administering contrast. And a third of radiologists and 50% of cardiologists said they would withhold contrast media or recommend a premedication for patients with such an allergy.
But the belief makes no sense, Dr. Pauuw said. Iodine is present in many other foods, including milk and bread, and allergies to shellfish are because of parvalbumin protein and tropomyosins, not iodine.
Colonoscopy dogma
It’s been long believed that people need to be on a clear, liquid diet for 1 or 2 days and need to drink a bowel-prep liquid before a colonoscopy, noted Dr. Paauw.
But the evidence shows this isn’t necessary, he said.
A 2020 study found that a low-residual diet, allowing foods such as meat, eggs, dairy, and bread, were comparable to the clear liquid diet in terms of bowel prep and detection of polyps during the exam. The patients on the low-residual diet had less nausea, less vomiting, and less hunger, and expressed more willingness to have a repeat colonoscopy.
“Let them eat,” Dr. Paauw said in his presentation.
Metronidazole and alcohol
There is a belief that patients shouldn’t drink alcohol if they are taking metronidazole, because of concerns about nausea, vomiting, flushing and other symptoms – also known as a disulfiramlike reaction, Dr. Paauw explained.
Case reports have been published, but the cases were presented as though a metronidazole-ethanol reaction was an established fact, and the authors didn’t provide evidence to justify this, Dr. Paauw said.
But it’s been shown in rat models that metronidazole can increase levels of acetaldehyde, the trigger of symptoms, in the colon, but not in the blood. And in a small placebo-controlled, randomized trial, six people were given metronidazole and ethanol and, after regular blood testing, no difference was seen in acetaldehyde blood levels, vital signs, or symptoms.
The Centers for Disease Control and Prevention has said that avoiding alcohol while taking metronidazole is unnecessary, said Dr. Paauw.
Sinus headaches
Contrary to common belief, headaches thought to be “sinus headaches” are usually migraine headaches, Dr. Paauw said.
In one study, 2,991 patients with six headaches in the previous 6 months were self-diagnosed or were physician-diagnosed with sinus headaches. But 88% of these headaches met the International Headache Society criteria for migraine headache.
Dr. Paauw said he hopes that clinicians reconsider the evidence regularly when deciding how to treat their patients, and not rely on bits of dogma.
“They stay with us,” he said, “and sometimes there are other ways to do it.”
Shien Tze, MD, an internist in Fargo, N,D,, said that patients sometimes also hold misconceptions, based on outdated dogma, that he needs to dispel.
“I try to convince them that this is a myth that is not based on evidence, not based on science,” he said. “I think it depends on the way you say it. If you say it in a calm, firm, not wishy-washy way, the patients believe you.”
Dr. Paauw reported no relevant financial disclosures. He serves on the editorial advisory board of Internal Medicine News, and he contributes “Myth of the Month” and “Pearl of the Month” columns to this publication.
These long-held pieces of dogma – or “medical myths” – were engraved during training or early in the careers of many physicians, and are difficult to overcome, noted Douglas Paauw, MD, professor of medicine at the University of Washington, Seattle.
“I think that myths persist because medical professionals get taught one way in training, given a ‘truth’ or ‘This is the way we do it,’ and then do not ever rethink, ‘Is it true?’ ” he said in an interview. “Studies pop up to question conventional wisdom, but unless the studies get highly publicized, they aren’t noticed.”
During his presentation, Dr. Paauw discussed three of what he considers to be some of the some of the medical myths that are in greatest need of being dispelled.
Shellfish allergy and radiocontrast
A myth persists that people with a shellfish allergy could have an allergic reaction when a contrast agent is used for a scan, he said.
This belief arose, because fish and shellfish contain iodine, and allergic reactions to seafood are fairly common, and contrast agents contain iodine, too, Dr. Paauw said.
The belief is widespread, with 65% of radiologists and 88.9% of interventional cardiologists saying they ask about seafood or shellfish allergies before administering contrast. And a third of radiologists and 50% of cardiologists said they would withhold contrast media or recommend a premedication for patients with such an allergy.
But the belief makes no sense, Dr. Pauuw said. Iodine is present in many other foods, including milk and bread, and allergies to shellfish are because of parvalbumin protein and tropomyosins, not iodine.
Colonoscopy dogma
It’s been long believed that people need to be on a clear, liquid diet for 1 or 2 days and need to drink a bowel-prep liquid before a colonoscopy, noted Dr. Paauw.
But the evidence shows this isn’t necessary, he said.
A 2020 study found that a low-residual diet, allowing foods such as meat, eggs, dairy, and bread, were comparable to the clear liquid diet in terms of bowel prep and detection of polyps during the exam. The patients on the low-residual diet had less nausea, less vomiting, and less hunger, and expressed more willingness to have a repeat colonoscopy.
“Let them eat,” Dr. Paauw said in his presentation.
Metronidazole and alcohol
There is a belief that patients shouldn’t drink alcohol if they are taking metronidazole, because of concerns about nausea, vomiting, flushing and other symptoms – also known as a disulfiramlike reaction, Dr. Paauw explained.
Case reports have been published, but the cases were presented as though a metronidazole-ethanol reaction was an established fact, and the authors didn’t provide evidence to justify this, Dr. Paauw said.
But it’s been shown in rat models that metronidazole can increase levels of acetaldehyde, the trigger of symptoms, in the colon, but not in the blood. And in a small placebo-controlled, randomized trial, six people were given metronidazole and ethanol and, after regular blood testing, no difference was seen in acetaldehyde blood levels, vital signs, or symptoms.
The Centers for Disease Control and Prevention has said that avoiding alcohol while taking metronidazole is unnecessary, said Dr. Paauw.
Sinus headaches
Contrary to common belief, headaches thought to be “sinus headaches” are usually migraine headaches, Dr. Paauw said.
In one study, 2,991 patients with six headaches in the previous 6 months were self-diagnosed or were physician-diagnosed with sinus headaches. But 88% of these headaches met the International Headache Society criteria for migraine headache.
Dr. Paauw said he hopes that clinicians reconsider the evidence regularly when deciding how to treat their patients, and not rely on bits of dogma.
“They stay with us,” he said, “and sometimes there are other ways to do it.”
Shien Tze, MD, an internist in Fargo, N,D,, said that patients sometimes also hold misconceptions, based on outdated dogma, that he needs to dispel.
“I try to convince them that this is a myth that is not based on evidence, not based on science,” he said. “I think it depends on the way you say it. If you say it in a calm, firm, not wishy-washy way, the patients believe you.”
Dr. Paauw reported no relevant financial disclosures. He serves on the editorial advisory board of Internal Medicine News, and he contributes “Myth of the Month” and “Pearl of the Month” columns to this publication.
These long-held pieces of dogma – or “medical myths” – were engraved during training or early in the careers of many physicians, and are difficult to overcome, noted Douglas Paauw, MD, professor of medicine at the University of Washington, Seattle.
“I think that myths persist because medical professionals get taught one way in training, given a ‘truth’ or ‘This is the way we do it,’ and then do not ever rethink, ‘Is it true?’ ” he said in an interview. “Studies pop up to question conventional wisdom, but unless the studies get highly publicized, they aren’t noticed.”
During his presentation, Dr. Paauw discussed three of what he considers to be some of the some of the medical myths that are in greatest need of being dispelled.
Shellfish allergy and radiocontrast
A myth persists that people with a shellfish allergy could have an allergic reaction when a contrast agent is used for a scan, he said.
This belief arose, because fish and shellfish contain iodine, and allergic reactions to seafood are fairly common, and contrast agents contain iodine, too, Dr. Paauw said.
The belief is widespread, with 65% of radiologists and 88.9% of interventional cardiologists saying they ask about seafood or shellfish allergies before administering contrast. And a third of radiologists and 50% of cardiologists said they would withhold contrast media or recommend a premedication for patients with such an allergy.
But the belief makes no sense, Dr. Pauuw said. Iodine is present in many other foods, including milk and bread, and allergies to shellfish are because of parvalbumin protein and tropomyosins, not iodine.
Colonoscopy dogma
It’s been long believed that people need to be on a clear, liquid diet for 1 or 2 days and need to drink a bowel-prep liquid before a colonoscopy, noted Dr. Paauw.
But the evidence shows this isn’t necessary, he said.
A 2020 study found that a low-residual diet, allowing foods such as meat, eggs, dairy, and bread, were comparable to the clear liquid diet in terms of bowel prep and detection of polyps during the exam. The patients on the low-residual diet had less nausea, less vomiting, and less hunger, and expressed more willingness to have a repeat colonoscopy.
“Let them eat,” Dr. Paauw said in his presentation.
Metronidazole and alcohol
There is a belief that patients shouldn’t drink alcohol if they are taking metronidazole, because of concerns about nausea, vomiting, flushing and other symptoms – also known as a disulfiramlike reaction, Dr. Paauw explained.
Case reports have been published, but the cases were presented as though a metronidazole-ethanol reaction was an established fact, and the authors didn’t provide evidence to justify this, Dr. Paauw said.
But it’s been shown in rat models that metronidazole can increase levels of acetaldehyde, the trigger of symptoms, in the colon, but not in the blood. And in a small placebo-controlled, randomized trial, six people were given metronidazole and ethanol and, after regular blood testing, no difference was seen in acetaldehyde blood levels, vital signs, or symptoms.
The Centers for Disease Control and Prevention has said that avoiding alcohol while taking metronidazole is unnecessary, said Dr. Paauw.
Sinus headaches
Contrary to common belief, headaches thought to be “sinus headaches” are usually migraine headaches, Dr. Paauw said.
In one study, 2,991 patients with six headaches in the previous 6 months were self-diagnosed or were physician-diagnosed with sinus headaches. But 88% of these headaches met the International Headache Society criteria for migraine headache.
Dr. Paauw said he hopes that clinicians reconsider the evidence regularly when deciding how to treat their patients, and not rely on bits of dogma.
“They stay with us,” he said, “and sometimes there are other ways to do it.”
Shien Tze, MD, an internist in Fargo, N,D,, said that patients sometimes also hold misconceptions, based on outdated dogma, that he needs to dispel.
“I try to convince them that this is a myth that is not based on evidence, not based on science,” he said. “I think it depends on the way you say it. If you say it in a calm, firm, not wishy-washy way, the patients believe you.”
Dr. Paauw reported no relevant financial disclosures. He serves on the editorial advisory board of Internal Medicine News, and he contributes “Myth of the Month” and “Pearl of the Month” columns to this publication.
AT INTERNAL MEDICINE 2022
Antibiotic treatment alone less effective in children with more appendicitis pain
Children who have greater acute appendicitis pain may be less likely to improve if they’re treated with antibiotics alone, according to a secondary analysis of a nonrandomized clinical trial.
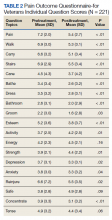
“While approximately 35% of families chose nonoperative management, a high pain score between 7-10 on a 10-point scale nearly doubled in-hospital treatment failure,” Rebecca M. Rentea, MD, a pediatric surgeon and the director of the Comprehensive Colorectal Center at Children’s Mercy Kansas City, Mo., told this news organization in an email.
“Even if nonoperative management of pediatric appendicitis did not work – resulting in the need to remove the appendix in 34% of cases – families were happy with their decisions 1 year later,” added Dr. Rentea, who coauthored an invited commentary about the study.
Lead study author Peter C. Minneci, MD, MHSc, a pediatric surgeon at Nationwide Children’s Hospital, Columbus, Ohio, and colleagues analyzed a subgroup of patients from a larger study in 10 tertiary children’s hospitals in the Midwest Pediatric Surgery Consortium.
As they reported in JAMA Network Open, the larger prospective, nonrandomized clinical trial enrolled 1,068 children between 2015 and 2018. The children ranged in age from 7 to 17 years, and they had imaging-confirmed appendicitis with an appendix diameter of 1.1 cm or less, no abscess, no appendicolith, and no phlegmon. White blood cell count was between 5,000 and 18,000 cells/μL, and abdominal pain began less than 48 hours before they received antibiotic therapy.
Caregivers chose either surgery or nonoperative antibiotic management. Patients who were treated first with antibiotics alone and who did not undergo appendectomy within 1 year were considered to have successfully completed nonoperative treatment.
The secondary analysis included the 370 children enrolled in the nonoperative group. Of these, 229 were boys, and the median age was 12.3 years. In this subgroup, the researchers compared outcomes after nonoperative, antibiotic management vs. surgery.
At 1 year, treatment failure had occurred in 125 patients, with 53 having undergone appendectomy during their first hospitalization, and 72 having experienced delayed treatment failure after being discharged.
- Higher patient-reported pain at presentation was linked to higher risk for in-hospital treatment failure (relative risk, 2.1; 95% confidence interval, 1.0-4.4) but not for delayed treatment failure (RR, 1.3; 95% CI, 0.7-2.3) or overall treatment failure at 1 year (RR, 1.5; 95% CI, 1.0-2.2).
- Pain lasting longer than 24 hours was linked to lower risk for delayed treatment failure (RR, 0.3; 95% CI, 0.1-1.0) but not for in-hospital treatment failure (RR, 1.2; 95% CI, 0.5-2.7) or treatment failure at 1 year (RR, 0.7; 95% CI, 0.4-1.2).
- Satisfaction with the decision was higher with successful nonoperative management at 30 days (28.0 vs. 27.0; difference, 1.0; 95% CI, 0.01-2.0) and at 1 year (28.1 vs 27.0; difference, 1.1; 95% CI, 0.2-2.0).
The researchers found no increased risk for treatment failure based on age, sex, race, ethnicity, white blood cell count, primary language, insurance status, transfer status, presentation symptoms, or imaging results.
Antibiotics-only is a safe option for children
“This study suggests that pediatric patients with uncomplicated acute appendicitis should be offered treatment options, including nonoperative management,” the authors write. “Treatment with antibiotics alone is a safe and equitable option for children, with no increased risk of treatment failure based on sociodemographic or objective clinical characteristics at presentation.”
But, the authors advise: “Families need to be made aware that treatment failure is not uncommon, and they should be provided with anticipatory guidance on how to proceed should symptoms recur.”
The investigators acknowledged limitations to the study, including the nonrandomized design that may have introduced bias, the loss to follow-up, and the study population being U.S. Midwest children, who may differ from children elsewhere in the country.
Shawn D. St Peter, MD, a pediatric surgeon, medical chair, and a senior vice president at Children’s Mercy Kansas City told this news organization in an email that having a nonoperative alternative to surgical appendectomy is important.
“Antibiotics are the initial treatment for appendicitis and can be the definitive treatment,” he said.
“Surprisingly, no sociodemographic or clinical characteristics were associated with an increased risk of nonoperative appendicitis treatment failure,” added Dr. St Peter, who coauthored the commentary with Dr. Rentea.
Howard C. Jen, MD, a pediatric surgeon at University of California, Los Angeles, Mattel Children’s Hospital, was not surprised by the findings.
“Nonoperative management for acute noncomplicated appendicitis in children continues to be safe and effective in highly selected patients,” he said in an email. “This alternative to surgery should be offered routinely to patients with early acute appendicitis.”
Dr. Jen, who was not involved with the current study, noted that it did not address the impact and costs to families of nonoperative management vs. surgery.
“For the most vulnerable children who had difficulties accessing medical care, what is the best treatment option? What factors are important to the families when making this decision?” he asked.
All study and editorial authors report no relevant financial relationships. The study was funded by the Patient-Centered Outcomes Research Institute and the National Center for Advancing Translational Sciences.
A version of this article first appeared on Medscape.com.
Children who have greater acute appendicitis pain may be less likely to improve if they’re treated with antibiotics alone, according to a secondary analysis of a nonrandomized clinical trial.
“While approximately 35% of families chose nonoperative management, a high pain score between 7-10 on a 10-point scale nearly doubled in-hospital treatment failure,” Rebecca M. Rentea, MD, a pediatric surgeon and the director of the Comprehensive Colorectal Center at Children’s Mercy Kansas City, Mo., told this news organization in an email.
“Even if nonoperative management of pediatric appendicitis did not work – resulting in the need to remove the appendix in 34% of cases – families were happy with their decisions 1 year later,” added Dr. Rentea, who coauthored an invited commentary about the study.
Lead study author Peter C. Minneci, MD, MHSc, a pediatric surgeon at Nationwide Children’s Hospital, Columbus, Ohio, and colleagues analyzed a subgroup of patients from a larger study in 10 tertiary children’s hospitals in the Midwest Pediatric Surgery Consortium.
As they reported in JAMA Network Open, the larger prospective, nonrandomized clinical trial enrolled 1,068 children between 2015 and 2018. The children ranged in age from 7 to 17 years, and they had imaging-confirmed appendicitis with an appendix diameter of 1.1 cm or less, no abscess, no appendicolith, and no phlegmon. White blood cell count was between 5,000 and 18,000 cells/μL, and abdominal pain began less than 48 hours before they received antibiotic therapy.
Caregivers chose either surgery or nonoperative antibiotic management. Patients who were treated first with antibiotics alone and who did not undergo appendectomy within 1 year were considered to have successfully completed nonoperative treatment.
The secondary analysis included the 370 children enrolled in the nonoperative group. Of these, 229 were boys, and the median age was 12.3 years. In this subgroup, the researchers compared outcomes after nonoperative, antibiotic management vs. surgery.
At 1 year, treatment failure had occurred in 125 patients, with 53 having undergone appendectomy during their first hospitalization, and 72 having experienced delayed treatment failure after being discharged.
- Higher patient-reported pain at presentation was linked to higher risk for in-hospital treatment failure (relative risk, 2.1; 95% confidence interval, 1.0-4.4) but not for delayed treatment failure (RR, 1.3; 95% CI, 0.7-2.3) or overall treatment failure at 1 year (RR, 1.5; 95% CI, 1.0-2.2).
- Pain lasting longer than 24 hours was linked to lower risk for delayed treatment failure (RR, 0.3; 95% CI, 0.1-1.0) but not for in-hospital treatment failure (RR, 1.2; 95% CI, 0.5-2.7) or treatment failure at 1 year (RR, 0.7; 95% CI, 0.4-1.2).
- Satisfaction with the decision was higher with successful nonoperative management at 30 days (28.0 vs. 27.0; difference, 1.0; 95% CI, 0.01-2.0) and at 1 year (28.1 vs 27.0; difference, 1.1; 95% CI, 0.2-2.0).
The researchers found no increased risk for treatment failure based on age, sex, race, ethnicity, white blood cell count, primary language, insurance status, transfer status, presentation symptoms, or imaging results.
Antibiotics-only is a safe option for children
“This study suggests that pediatric patients with uncomplicated acute appendicitis should be offered treatment options, including nonoperative management,” the authors write. “Treatment with antibiotics alone is a safe and equitable option for children, with no increased risk of treatment failure based on sociodemographic or objective clinical characteristics at presentation.”
But, the authors advise: “Families need to be made aware that treatment failure is not uncommon, and they should be provided with anticipatory guidance on how to proceed should symptoms recur.”
The investigators acknowledged limitations to the study, including the nonrandomized design that may have introduced bias, the loss to follow-up, and the study population being U.S. Midwest children, who may differ from children elsewhere in the country.
Shawn D. St Peter, MD, a pediatric surgeon, medical chair, and a senior vice president at Children’s Mercy Kansas City told this news organization in an email that having a nonoperative alternative to surgical appendectomy is important.
“Antibiotics are the initial treatment for appendicitis and can be the definitive treatment,” he said.
“Surprisingly, no sociodemographic or clinical characteristics were associated with an increased risk of nonoperative appendicitis treatment failure,” added Dr. St Peter, who coauthored the commentary with Dr. Rentea.
Howard C. Jen, MD, a pediatric surgeon at University of California, Los Angeles, Mattel Children’s Hospital, was not surprised by the findings.
“Nonoperative management for acute noncomplicated appendicitis in children continues to be safe and effective in highly selected patients,” he said in an email. “This alternative to surgery should be offered routinely to patients with early acute appendicitis.”
Dr. Jen, who was not involved with the current study, noted that it did not address the impact and costs to families of nonoperative management vs. surgery.
“For the most vulnerable children who had difficulties accessing medical care, what is the best treatment option? What factors are important to the families when making this decision?” he asked.
All study and editorial authors report no relevant financial relationships. The study was funded by the Patient-Centered Outcomes Research Institute and the National Center for Advancing Translational Sciences.
A version of this article first appeared on Medscape.com.
Children who have greater acute appendicitis pain may be less likely to improve if they’re treated with antibiotics alone, according to a secondary analysis of a nonrandomized clinical trial.
“While approximately 35% of families chose nonoperative management, a high pain score between 7-10 on a 10-point scale nearly doubled in-hospital treatment failure,” Rebecca M. Rentea, MD, a pediatric surgeon and the director of the Comprehensive Colorectal Center at Children’s Mercy Kansas City, Mo., told this news organization in an email.
“Even if nonoperative management of pediatric appendicitis did not work – resulting in the need to remove the appendix in 34% of cases – families were happy with their decisions 1 year later,” added Dr. Rentea, who coauthored an invited commentary about the study.
Lead study author Peter C. Minneci, MD, MHSc, a pediatric surgeon at Nationwide Children’s Hospital, Columbus, Ohio, and colleagues analyzed a subgroup of patients from a larger study in 10 tertiary children’s hospitals in the Midwest Pediatric Surgery Consortium.
As they reported in JAMA Network Open, the larger prospective, nonrandomized clinical trial enrolled 1,068 children between 2015 and 2018. The children ranged in age from 7 to 17 years, and they had imaging-confirmed appendicitis with an appendix diameter of 1.1 cm or less, no abscess, no appendicolith, and no phlegmon. White blood cell count was between 5,000 and 18,000 cells/μL, and abdominal pain began less than 48 hours before they received antibiotic therapy.
Caregivers chose either surgery or nonoperative antibiotic management. Patients who were treated first with antibiotics alone and who did not undergo appendectomy within 1 year were considered to have successfully completed nonoperative treatment.
The secondary analysis included the 370 children enrolled in the nonoperative group. Of these, 229 were boys, and the median age was 12.3 years. In this subgroup, the researchers compared outcomes after nonoperative, antibiotic management vs. surgery.
At 1 year, treatment failure had occurred in 125 patients, with 53 having undergone appendectomy during their first hospitalization, and 72 having experienced delayed treatment failure after being discharged.
- Higher patient-reported pain at presentation was linked to higher risk for in-hospital treatment failure (relative risk, 2.1; 95% confidence interval, 1.0-4.4) but not for delayed treatment failure (RR, 1.3; 95% CI, 0.7-2.3) or overall treatment failure at 1 year (RR, 1.5; 95% CI, 1.0-2.2).
- Pain lasting longer than 24 hours was linked to lower risk for delayed treatment failure (RR, 0.3; 95% CI, 0.1-1.0) but not for in-hospital treatment failure (RR, 1.2; 95% CI, 0.5-2.7) or treatment failure at 1 year (RR, 0.7; 95% CI, 0.4-1.2).
- Satisfaction with the decision was higher with successful nonoperative management at 30 days (28.0 vs. 27.0; difference, 1.0; 95% CI, 0.01-2.0) and at 1 year (28.1 vs 27.0; difference, 1.1; 95% CI, 0.2-2.0).
The researchers found no increased risk for treatment failure based on age, sex, race, ethnicity, white blood cell count, primary language, insurance status, transfer status, presentation symptoms, or imaging results.
Antibiotics-only is a safe option for children
“This study suggests that pediatric patients with uncomplicated acute appendicitis should be offered treatment options, including nonoperative management,” the authors write. “Treatment with antibiotics alone is a safe and equitable option for children, with no increased risk of treatment failure based on sociodemographic or objective clinical characteristics at presentation.”
But, the authors advise: “Families need to be made aware that treatment failure is not uncommon, and they should be provided with anticipatory guidance on how to proceed should symptoms recur.”
The investigators acknowledged limitations to the study, including the nonrandomized design that may have introduced bias, the loss to follow-up, and the study population being U.S. Midwest children, who may differ from children elsewhere in the country.
Shawn D. St Peter, MD, a pediatric surgeon, medical chair, and a senior vice president at Children’s Mercy Kansas City told this news organization in an email that having a nonoperative alternative to surgical appendectomy is important.
“Antibiotics are the initial treatment for appendicitis and can be the definitive treatment,” he said.
“Surprisingly, no sociodemographic or clinical characteristics were associated with an increased risk of nonoperative appendicitis treatment failure,” added Dr. St Peter, who coauthored the commentary with Dr. Rentea.
Howard C. Jen, MD, a pediatric surgeon at University of California, Los Angeles, Mattel Children’s Hospital, was not surprised by the findings.
“Nonoperative management for acute noncomplicated appendicitis in children continues to be safe and effective in highly selected patients,” he said in an email. “This alternative to surgery should be offered routinely to patients with early acute appendicitis.”
Dr. Jen, who was not involved with the current study, noted that it did not address the impact and costs to families of nonoperative management vs. surgery.
“For the most vulnerable children who had difficulties accessing medical care, what is the best treatment option? What factors are important to the families when making this decision?” he asked.
All study and editorial authors report no relevant financial relationships. The study was funded by the Patient-Centered Outcomes Research Institute and the National Center for Advancing Translational Sciences.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
CBT or hypnotherapy may help kids’ functional abdominal pain
Functional abdominal pain in childhood and adolescence is extremely stressful for patients and a therapeutic challenge for the physicians treating them. A meta-analysis of 33 randomized-controlled studies published in JAMA Pediatrics shows that cognitive-behavioral therapy or hypnotherapy promises the greatest therapy success.
“If children or adolescents complain about chronic abdominal pain and a detailed diagnostic does not reveal any somatic cause, this is referred to as functional abdominal pain,” Burkhard Rodeck, MD, general secretary of the German Society of Pediatrics and Adolescent Medicine in Berlin, told this news organization.
Signal perception disorder
“These patients are experiencing a signal perception disorder: normal body signals, such as a slight stomach rumble, are assigned to the pain category for them much more quickly than for other people,” said Dr. Rodeck. “The meta-analysis provides confirmation of this – functional abdominal pain is actually a biopsychosocial matter.”
In the standard therapy of functional abdominal pain, however, it is also possible to choose a medicinal approach. “Studies show that herbal preparations such as peppermint oil capsules have some efficacy, since they attenuate the strength of the signals being sent from the gastrointestinal tract to the brain, with the result that they are not perceived so quickly as pain. Probiotics can also potentially help,” added Dr. Rodeck.
“If this is unsuccessful, the child must be offered a psychologic/psychotherapeutic measure, usually cognitive-behavioral therapy.”
Comparison of psychosocial therapies
The meta-analysis was carried out by a research team at the University of Central Lancashire, Preston, United Kingdom. It included 2,657 children and adolescents between the ages of 7 and 17 years, of which two-thirds were girls.
Various psychosocial therapy approaches for functional abdominal pain, such as cognitive-behavioral therapy, educational assistance, hypnotherapy (directed at the digestive system), guided meditation with relaxation, yoga, or (visceral) osteopathy were investigated and compared in the studies – sometimes against each other and sometimes against no intervention.
Lead author Morris Gordon, MBChB, PhD, professor of evidence synthesis and systematic review at the University of Central Lancashire, and his colleagues reported that cognitive-behavioral therapy was 2.37-times more likely to result in therapy success than no intervention. To treat functional abdominal pain successfully in one child or adolescent, five children needed to be treated with cognitive-behavioral therapy.
Rarer, milder pain
The children and adolescents treated with cognitive-behavioral therapy also experienced less frequent and less severe abdominal pain than the children and adolescents who did not receive any intervention. The rate of side effect–related therapy discontinuations did not differ between the groups.
Hypnotherapy could also be associated with an improved outcome, compared with no intervention, added Dr. Gordon and his colleagues. Hypnotherapy was 2.86-times more likely to result in therapy success, and the number needed to treat was five.
The other therapeutic approaches investigated did not perform any better in the studies than no intervention. However, the authors noted that evidence of the effectiveness of cognitive-behavioral therapy and hypnotherapy is moderate or weak, especially owing to the high bias risk.
“The therapy for functional abdominal pain cannot be compared with the therapy for scarlet fever, for example, where penicillin is administered in the knowledge that recovery is guaranteed. There is evidence that cognitive-behavioral therapy and possibly also hypnotherapy may help, but this is not true for every patient,” said Dr. Rodeck.
Start with the pediatrician
Dr. Gordon and his co-authors suggested considering cognitive-behavioral therapy and hypnotherapy for the treatment of functional abdominal pain in children and adolescents. But they added that further randomized controlled studies are necessary to improve the quality of evidence and therefore the reliability of these results.
Children and adolescents with functional abdominal pain do not need to be sent directly to the psychologist for treatment, said Dr. Rodeck. The pediatric or adolescent medicine specialist can also administer the initial behavioral therapy measures. “Some patients manage with the behavioral therapy approaches we offer as pediatric and adolescent medicine specialists; others require professional support with psychologic expertise,” said Dr. Rodeck. Should outpatient treatment be unsuccessful, inpatient therapy in special psychosomatic clinics or wards remains an option.
Education offers relief
For many patients, being informed about the connections and mechanisms that play a role in functional abdominal pain can offer a lot of relief, said Dr. Rodeck. Offering coping strategies that can be used in the event of acute symptoms is also a part of this education.
“If patients have functional abdominal pain for which no organic cause can be found, this can lead to frustration, sadness, and despair. The problem can become even worse if they feel that they are not being taken seriously by the physician,” said Dr. Rodeck. These negative experiences can further exacerbate the pain perception disorder. The aim of behavioral therapy measures is therefore to interrupt and downregulate this vicious cycle.
“Constant investigations are not always helpful for patients with functional abdominal pain. Time must be taken with these patients to talk and explore the options. They have definite abdominal pain, they are not imagining it. They must be taken seriously,” he emphasized.
A version of this article first appeared on Medscape.com.
Functional abdominal pain in childhood and adolescence is extremely stressful for patients and a therapeutic challenge for the physicians treating them. A meta-analysis of 33 randomized-controlled studies published in JAMA Pediatrics shows that cognitive-behavioral therapy or hypnotherapy promises the greatest therapy success.
“If children or adolescents complain about chronic abdominal pain and a detailed diagnostic does not reveal any somatic cause, this is referred to as functional abdominal pain,” Burkhard Rodeck, MD, general secretary of the German Society of Pediatrics and Adolescent Medicine in Berlin, told this news organization.
Signal perception disorder
“These patients are experiencing a signal perception disorder: normal body signals, such as a slight stomach rumble, are assigned to the pain category for them much more quickly than for other people,” said Dr. Rodeck. “The meta-analysis provides confirmation of this – functional abdominal pain is actually a biopsychosocial matter.”
In the standard therapy of functional abdominal pain, however, it is also possible to choose a medicinal approach. “Studies show that herbal preparations such as peppermint oil capsules have some efficacy, since they attenuate the strength of the signals being sent from the gastrointestinal tract to the brain, with the result that they are not perceived so quickly as pain. Probiotics can also potentially help,” added Dr. Rodeck.
“If this is unsuccessful, the child must be offered a psychologic/psychotherapeutic measure, usually cognitive-behavioral therapy.”
Comparison of psychosocial therapies
The meta-analysis was carried out by a research team at the University of Central Lancashire, Preston, United Kingdom. It included 2,657 children and adolescents between the ages of 7 and 17 years, of which two-thirds were girls.
Various psychosocial therapy approaches for functional abdominal pain, such as cognitive-behavioral therapy, educational assistance, hypnotherapy (directed at the digestive system), guided meditation with relaxation, yoga, or (visceral) osteopathy were investigated and compared in the studies – sometimes against each other and sometimes against no intervention.
Lead author Morris Gordon, MBChB, PhD, professor of evidence synthesis and systematic review at the University of Central Lancashire, and his colleagues reported that cognitive-behavioral therapy was 2.37-times more likely to result in therapy success than no intervention. To treat functional abdominal pain successfully in one child or adolescent, five children needed to be treated with cognitive-behavioral therapy.
Rarer, milder pain
The children and adolescents treated with cognitive-behavioral therapy also experienced less frequent and less severe abdominal pain than the children and adolescents who did not receive any intervention. The rate of side effect–related therapy discontinuations did not differ between the groups.
Hypnotherapy could also be associated with an improved outcome, compared with no intervention, added Dr. Gordon and his colleagues. Hypnotherapy was 2.86-times more likely to result in therapy success, and the number needed to treat was five.
The other therapeutic approaches investigated did not perform any better in the studies than no intervention. However, the authors noted that evidence of the effectiveness of cognitive-behavioral therapy and hypnotherapy is moderate or weak, especially owing to the high bias risk.
“The therapy for functional abdominal pain cannot be compared with the therapy for scarlet fever, for example, where penicillin is administered in the knowledge that recovery is guaranteed. There is evidence that cognitive-behavioral therapy and possibly also hypnotherapy may help, but this is not true for every patient,” said Dr. Rodeck.
Start with the pediatrician
Dr. Gordon and his co-authors suggested considering cognitive-behavioral therapy and hypnotherapy for the treatment of functional abdominal pain in children and adolescents. But they added that further randomized controlled studies are necessary to improve the quality of evidence and therefore the reliability of these results.
Children and adolescents with functional abdominal pain do not need to be sent directly to the psychologist for treatment, said Dr. Rodeck. The pediatric or adolescent medicine specialist can also administer the initial behavioral therapy measures. “Some patients manage with the behavioral therapy approaches we offer as pediatric and adolescent medicine specialists; others require professional support with psychologic expertise,” said Dr. Rodeck. Should outpatient treatment be unsuccessful, inpatient therapy in special psychosomatic clinics or wards remains an option.
Education offers relief
For many patients, being informed about the connections and mechanisms that play a role in functional abdominal pain can offer a lot of relief, said Dr. Rodeck. Offering coping strategies that can be used in the event of acute symptoms is also a part of this education.
“If patients have functional abdominal pain for which no organic cause can be found, this can lead to frustration, sadness, and despair. The problem can become even worse if they feel that they are not being taken seriously by the physician,” said Dr. Rodeck. These negative experiences can further exacerbate the pain perception disorder. The aim of behavioral therapy measures is therefore to interrupt and downregulate this vicious cycle.
“Constant investigations are not always helpful for patients with functional abdominal pain. Time must be taken with these patients to talk and explore the options. They have definite abdominal pain, they are not imagining it. They must be taken seriously,” he emphasized.
A version of this article first appeared on Medscape.com.
Functional abdominal pain in childhood and adolescence is extremely stressful for patients and a therapeutic challenge for the physicians treating them. A meta-analysis of 33 randomized-controlled studies published in JAMA Pediatrics shows that cognitive-behavioral therapy or hypnotherapy promises the greatest therapy success.
“If children or adolescents complain about chronic abdominal pain and a detailed diagnostic does not reveal any somatic cause, this is referred to as functional abdominal pain,” Burkhard Rodeck, MD, general secretary of the German Society of Pediatrics and Adolescent Medicine in Berlin, told this news organization.
Signal perception disorder
“These patients are experiencing a signal perception disorder: normal body signals, such as a slight stomach rumble, are assigned to the pain category for them much more quickly than for other people,” said Dr. Rodeck. “The meta-analysis provides confirmation of this – functional abdominal pain is actually a biopsychosocial matter.”
In the standard therapy of functional abdominal pain, however, it is also possible to choose a medicinal approach. “Studies show that herbal preparations such as peppermint oil capsules have some efficacy, since they attenuate the strength of the signals being sent from the gastrointestinal tract to the brain, with the result that they are not perceived so quickly as pain. Probiotics can also potentially help,” added Dr. Rodeck.
“If this is unsuccessful, the child must be offered a psychologic/psychotherapeutic measure, usually cognitive-behavioral therapy.”
Comparison of psychosocial therapies
The meta-analysis was carried out by a research team at the University of Central Lancashire, Preston, United Kingdom. It included 2,657 children and adolescents between the ages of 7 and 17 years, of which two-thirds were girls.
Various psychosocial therapy approaches for functional abdominal pain, such as cognitive-behavioral therapy, educational assistance, hypnotherapy (directed at the digestive system), guided meditation with relaxation, yoga, or (visceral) osteopathy were investigated and compared in the studies – sometimes against each other and sometimes against no intervention.
Lead author Morris Gordon, MBChB, PhD, professor of evidence synthesis and systematic review at the University of Central Lancashire, and his colleagues reported that cognitive-behavioral therapy was 2.37-times more likely to result in therapy success than no intervention. To treat functional abdominal pain successfully in one child or adolescent, five children needed to be treated with cognitive-behavioral therapy.
Rarer, milder pain
The children and adolescents treated with cognitive-behavioral therapy also experienced less frequent and less severe abdominal pain than the children and adolescents who did not receive any intervention. The rate of side effect–related therapy discontinuations did not differ between the groups.
Hypnotherapy could also be associated with an improved outcome, compared with no intervention, added Dr. Gordon and his colleagues. Hypnotherapy was 2.86-times more likely to result in therapy success, and the number needed to treat was five.
The other therapeutic approaches investigated did not perform any better in the studies than no intervention. However, the authors noted that evidence of the effectiveness of cognitive-behavioral therapy and hypnotherapy is moderate or weak, especially owing to the high bias risk.
“The therapy for functional abdominal pain cannot be compared with the therapy for scarlet fever, for example, where penicillin is administered in the knowledge that recovery is guaranteed. There is evidence that cognitive-behavioral therapy and possibly also hypnotherapy may help, but this is not true for every patient,” said Dr. Rodeck.
Start with the pediatrician
Dr. Gordon and his co-authors suggested considering cognitive-behavioral therapy and hypnotherapy for the treatment of functional abdominal pain in children and adolescents. But they added that further randomized controlled studies are necessary to improve the quality of evidence and therefore the reliability of these results.
Children and adolescents with functional abdominal pain do not need to be sent directly to the psychologist for treatment, said Dr. Rodeck. The pediatric or adolescent medicine specialist can also administer the initial behavioral therapy measures. “Some patients manage with the behavioral therapy approaches we offer as pediatric and adolescent medicine specialists; others require professional support with psychologic expertise,” said Dr. Rodeck. Should outpatient treatment be unsuccessful, inpatient therapy in special psychosomatic clinics or wards remains an option.
Education offers relief
For many patients, being informed about the connections and mechanisms that play a role in functional abdominal pain can offer a lot of relief, said Dr. Rodeck. Offering coping strategies that can be used in the event of acute symptoms is also a part of this education.
“If patients have functional abdominal pain for which no organic cause can be found, this can lead to frustration, sadness, and despair. The problem can become even worse if they feel that they are not being taken seriously by the physician,” said Dr. Rodeck. These negative experiences can further exacerbate the pain perception disorder. The aim of behavioral therapy measures is therefore to interrupt and downregulate this vicious cycle.
“Constant investigations are not always helpful for patients with functional abdominal pain. Time must be taken with these patients to talk and explore the options. They have definite abdominal pain, they are not imagining it. They must be taken seriously,” he emphasized.
A version of this article first appeared on Medscape.com.
‘Where does it hurt?’: Primary care tips for common ortho problems
Knee and shoulder pain are common complaints for patients in the primary care office.
But identifying the source of the pain can be complicated,
and an accurate diagnosis of the underlying cause of discomfort is key to appropriate management – whether that involves simple home care options of ice and rest or a recommendation for a follow-up with a specialist.
Speaking at the annual meeting of the American College of Physicians, Greg Nakamoto, MD, department of orthopedics, Virginia Mason Medical Center, Seattle, discussed common knee and shoulder problems that patients often present with in the primary care setting, and offered tips on diagnosis and appropriate management.
The most common conditions causing knee pain are osteoarthritis and meniscal tears. “The differential for knee pain is broad,” Dr. Nakamoto said. “You have to have a way to divide it down, such as if it’s acute or chronic.”
The initial workup has several key components. The first steps: Determine the location of the pain – anterior, medial, lateral, posterior – and then whether it stems from an injury or is atraumatic.
“If you have to ask one question – ask where it hurts,” he said. “And is it from an injury or just wear and tear? That helps me when deciding if surgery is needed.”
Pain in the knee generally localizes well to the site of pathology, and knee pain of acute traumatic onset requires more scrutiny for problems best treated with early surgery. “This also helps establish whether radiographic findings are due to injury or degeneration,” Dr. Nakamoto said. “The presence of swelling guides the need for anti-inflammatories or cortisone.”
Palpating for tenderness along the joint line is important, as is palpating above and below the joint line, Dr. Nakamoto said.
“Tenderness limited to the joint line, combined with a meniscal exam maneuver that reproduces joint-line pain, is suggestive of pain from meniscal pathology,” he said.
Imaging is an important component of evaluating knee symptoms, and the question often arises as to when to order an MRI.
Dr. Nakamoto offered the following scenario: If significant osteoarthritis is evident on weight-bearing x-ray, treat the patient for the condition. However, if little or no osteoarthritis appears on x-ray, and if the onset of symptoms was traumatic and both patient history and physical examination suggest a meniscal tear, order an MRI.
An early MRI also is needed if the patient has had either atraumatic or traumatic onset of symptoms and their history and physical exams are suspicious for a mechanically locked or locking meniscus. For suspicion of a ruptured quadriceps or patellar tendon or a stress fracture, an MRI is needed urgently.
An MRI would be ordered later if the patient’s symptoms have not improved significantly after 3 months of conservative management.
Dr. Nakamoto stressed how common undiagnosed meniscus tears are in the general population. A third of men aged 50-59 years and nearly 20% of women in that age group have a tear, he said. “That number goes up to 56% and 51% in men and women aged 70-90 years, and 61% of these tears were in patients who were asymptomatic in the last month.”
In the setting of osteoarthritis, 76% of asymptomatic patients had a meniscus tear, and 91% of patients with symptomatic osteoarthritis had a meniscus tear, he added.
Treating knee pain
Treatment will vary depending on the underlying etiology of pain. For a possible meniscus tear, the recommendation is for a conservative intervention with ice, ibuprofen, knee immobilizer, and crutches, with a follow-up appointment in a week.
Three types of injections also can help:
- Cortisone for osteoarthritis or meniscus tears, swelling, and inflammation, and prophylaxis against inflammation.
- Viscosupplementation (intra‐articular hyaluronic acid) for chronic, baseline osteoarthritis symptoms.
- Regenerative therapies (platelet-rich plasma, stem cells, etc.) are used primarily for osteoarthritis (these do not regrow cartilage, but some patients report decreased pain).
The data on injections are mixed, Dr. Nakamoto said. For example, the results of a 2015 Cochrane review on cortisone injections for osteoarthritis reported that the benefits were small to moderate at 4‐6 weeks, and small to none at 13 weeks.
“There is a lot of controversy for viscosupplementation despite all of the data on it,” he said. “But the recommendations from professional organizations are mixed.”
He noted that he has been using viscosupplementation since the 1990s, and some patients do benefit from it.
Shoulder pain
The most common causes of shoulder pain are adhesive capsulitis, rotator cuff tears and tendinopathy, and impingement.
As with knee pain, the same assessment routine largely applies.
First, pinpoint the location: Is the trouble spot the lateral shoulder and upper arm, the trapezial ridge, or the shoulder blade?
Next, assess pain on movement: Does the patient experience discomfort reaching overhead or behind the back, or moving at the glenohumeral joint/capsule and engaging the rotator cuff? Check for stiffness, weakness, and decreased range of motion in the rotator cuff.
Determine if the cause of the pain is traumatic or atraumatic and stems from an acute injury versus degeneration or overuse.
As with the knee, imaging is a major component of the assessment and typically involves the use of x-ray. An MRI may be required for evaluating full- and partial-thickness tears and when contemplating surgery.
MRI also is necessary for evaluating cases of acute, traumatic shoulder injury, and patients exhibiting disability suggestive of a rotator cuff tear in an otherwise healthy tendon.
Some pain can be treated with cortisone injections or regenerative therapies, which generally are given at the acromioclavicular or glenohumeral joints or in the subacromial space. A 2005 meta-analysis found that subacromial injections of corticosteroids are effective for improvement for rotator cuff tendinitis up to a 9‐month period.
Surgery may be warranted in some cases, Dr. Nakamoto said. These include adhesive capsulitis, rotator cuff tear, acute traumatic injury in an otherwise healthy tendon, and chronic (or acute-on-chronic) tears in a degenerative tendon following a trial of conservative therapy.
A version of this article first appeared on Medscape.com.
Knee and shoulder pain are common complaints for patients in the primary care office.
But identifying the source of the pain can be complicated,
and an accurate diagnosis of the underlying cause of discomfort is key to appropriate management – whether that involves simple home care options of ice and rest or a recommendation for a follow-up with a specialist.
Speaking at the annual meeting of the American College of Physicians, Greg Nakamoto, MD, department of orthopedics, Virginia Mason Medical Center, Seattle, discussed common knee and shoulder problems that patients often present with in the primary care setting, and offered tips on diagnosis and appropriate management.
The most common conditions causing knee pain are osteoarthritis and meniscal tears. “The differential for knee pain is broad,” Dr. Nakamoto said. “You have to have a way to divide it down, such as if it’s acute or chronic.”
The initial workup has several key components. The first steps: Determine the location of the pain – anterior, medial, lateral, posterior – and then whether it stems from an injury or is atraumatic.
“If you have to ask one question – ask where it hurts,” he said. “And is it from an injury or just wear and tear? That helps me when deciding if surgery is needed.”
Pain in the knee generally localizes well to the site of pathology, and knee pain of acute traumatic onset requires more scrutiny for problems best treated with early surgery. “This also helps establish whether radiographic findings are due to injury or degeneration,” Dr. Nakamoto said. “The presence of swelling guides the need for anti-inflammatories or cortisone.”
Palpating for tenderness along the joint line is important, as is palpating above and below the joint line, Dr. Nakamoto said.
“Tenderness limited to the joint line, combined with a meniscal exam maneuver that reproduces joint-line pain, is suggestive of pain from meniscal pathology,” he said.
Imaging is an important component of evaluating knee symptoms, and the question often arises as to when to order an MRI.
Dr. Nakamoto offered the following scenario: If significant osteoarthritis is evident on weight-bearing x-ray, treat the patient for the condition. However, if little or no osteoarthritis appears on x-ray, and if the onset of symptoms was traumatic and both patient history and physical examination suggest a meniscal tear, order an MRI.
An early MRI also is needed if the patient has had either atraumatic or traumatic onset of symptoms and their history and physical exams are suspicious for a mechanically locked or locking meniscus. For suspicion of a ruptured quadriceps or patellar tendon or a stress fracture, an MRI is needed urgently.
An MRI would be ordered later if the patient’s symptoms have not improved significantly after 3 months of conservative management.
Dr. Nakamoto stressed how common undiagnosed meniscus tears are in the general population. A third of men aged 50-59 years and nearly 20% of women in that age group have a tear, he said. “That number goes up to 56% and 51% in men and women aged 70-90 years, and 61% of these tears were in patients who were asymptomatic in the last month.”
In the setting of osteoarthritis, 76% of asymptomatic patients had a meniscus tear, and 91% of patients with symptomatic osteoarthritis had a meniscus tear, he added.
Treating knee pain
Treatment will vary depending on the underlying etiology of pain. For a possible meniscus tear, the recommendation is for a conservative intervention with ice, ibuprofen, knee immobilizer, and crutches, with a follow-up appointment in a week.
Three types of injections also can help:
- Cortisone for osteoarthritis or meniscus tears, swelling, and inflammation, and prophylaxis against inflammation.
- Viscosupplementation (intra‐articular hyaluronic acid) for chronic, baseline osteoarthritis symptoms.
- Regenerative therapies (platelet-rich plasma, stem cells, etc.) are used primarily for osteoarthritis (these do not regrow cartilage, but some patients report decreased pain).
The data on injections are mixed, Dr. Nakamoto said. For example, the results of a 2015 Cochrane review on cortisone injections for osteoarthritis reported that the benefits were small to moderate at 4‐6 weeks, and small to none at 13 weeks.
“There is a lot of controversy for viscosupplementation despite all of the data on it,” he said. “But the recommendations from professional organizations are mixed.”
He noted that he has been using viscosupplementation since the 1990s, and some patients do benefit from it.
Shoulder pain
The most common causes of shoulder pain are adhesive capsulitis, rotator cuff tears and tendinopathy, and impingement.
As with knee pain, the same assessment routine largely applies.
First, pinpoint the location: Is the trouble spot the lateral shoulder and upper arm, the trapezial ridge, or the shoulder blade?
Next, assess pain on movement: Does the patient experience discomfort reaching overhead or behind the back, or moving at the glenohumeral joint/capsule and engaging the rotator cuff? Check for stiffness, weakness, and decreased range of motion in the rotator cuff.
Determine if the cause of the pain is traumatic or atraumatic and stems from an acute injury versus degeneration or overuse.
As with the knee, imaging is a major component of the assessment and typically involves the use of x-ray. An MRI may be required for evaluating full- and partial-thickness tears and when contemplating surgery.
MRI also is necessary for evaluating cases of acute, traumatic shoulder injury, and patients exhibiting disability suggestive of a rotator cuff tear in an otherwise healthy tendon.
Some pain can be treated with cortisone injections or regenerative therapies, which generally are given at the acromioclavicular or glenohumeral joints or in the subacromial space. A 2005 meta-analysis found that subacromial injections of corticosteroids are effective for improvement for rotator cuff tendinitis up to a 9‐month period.
Surgery may be warranted in some cases, Dr. Nakamoto said. These include adhesive capsulitis, rotator cuff tear, acute traumatic injury in an otherwise healthy tendon, and chronic (or acute-on-chronic) tears in a degenerative tendon following a trial of conservative therapy.
A version of this article first appeared on Medscape.com.
Knee and shoulder pain are common complaints for patients in the primary care office.
But identifying the source of the pain can be complicated,
and an accurate diagnosis of the underlying cause of discomfort is key to appropriate management – whether that involves simple home care options of ice and rest or a recommendation for a follow-up with a specialist.
Speaking at the annual meeting of the American College of Physicians, Greg Nakamoto, MD, department of orthopedics, Virginia Mason Medical Center, Seattle, discussed common knee and shoulder problems that patients often present with in the primary care setting, and offered tips on diagnosis and appropriate management.
The most common conditions causing knee pain are osteoarthritis and meniscal tears. “The differential for knee pain is broad,” Dr. Nakamoto said. “You have to have a way to divide it down, such as if it’s acute or chronic.”
The initial workup has several key components. The first steps: Determine the location of the pain – anterior, medial, lateral, posterior – and then whether it stems from an injury or is atraumatic.
“If you have to ask one question – ask where it hurts,” he said. “And is it from an injury or just wear and tear? That helps me when deciding if surgery is needed.”
Pain in the knee generally localizes well to the site of pathology, and knee pain of acute traumatic onset requires more scrutiny for problems best treated with early surgery. “This also helps establish whether radiographic findings are due to injury or degeneration,” Dr. Nakamoto said. “The presence of swelling guides the need for anti-inflammatories or cortisone.”
Palpating for tenderness along the joint line is important, as is palpating above and below the joint line, Dr. Nakamoto said.
“Tenderness limited to the joint line, combined with a meniscal exam maneuver that reproduces joint-line pain, is suggestive of pain from meniscal pathology,” he said.
Imaging is an important component of evaluating knee symptoms, and the question often arises as to when to order an MRI.
Dr. Nakamoto offered the following scenario: If significant osteoarthritis is evident on weight-bearing x-ray, treat the patient for the condition. However, if little or no osteoarthritis appears on x-ray, and if the onset of symptoms was traumatic and both patient history and physical examination suggest a meniscal tear, order an MRI.
An early MRI also is needed if the patient has had either atraumatic or traumatic onset of symptoms and their history and physical exams are suspicious for a mechanically locked or locking meniscus. For suspicion of a ruptured quadriceps or patellar tendon or a stress fracture, an MRI is needed urgently.
An MRI would be ordered later if the patient’s symptoms have not improved significantly after 3 months of conservative management.
Dr. Nakamoto stressed how common undiagnosed meniscus tears are in the general population. A third of men aged 50-59 years and nearly 20% of women in that age group have a tear, he said. “That number goes up to 56% and 51% in men and women aged 70-90 years, and 61% of these tears were in patients who were asymptomatic in the last month.”
In the setting of osteoarthritis, 76% of asymptomatic patients had a meniscus tear, and 91% of patients with symptomatic osteoarthritis had a meniscus tear, he added.
Treating knee pain
Treatment will vary depending on the underlying etiology of pain. For a possible meniscus tear, the recommendation is for a conservative intervention with ice, ibuprofen, knee immobilizer, and crutches, with a follow-up appointment in a week.
Three types of injections also can help:
- Cortisone for osteoarthritis or meniscus tears, swelling, and inflammation, and prophylaxis against inflammation.
- Viscosupplementation (intra‐articular hyaluronic acid) for chronic, baseline osteoarthritis symptoms.
- Regenerative therapies (platelet-rich plasma, stem cells, etc.) are used primarily for osteoarthritis (these do not regrow cartilage, but some patients report decreased pain).
The data on injections are mixed, Dr. Nakamoto said. For example, the results of a 2015 Cochrane review on cortisone injections for osteoarthritis reported that the benefits were small to moderate at 4‐6 weeks, and small to none at 13 weeks.
“There is a lot of controversy for viscosupplementation despite all of the data on it,” he said. “But the recommendations from professional organizations are mixed.”
He noted that he has been using viscosupplementation since the 1990s, and some patients do benefit from it.
Shoulder pain
The most common causes of shoulder pain are adhesive capsulitis, rotator cuff tears and tendinopathy, and impingement.
As with knee pain, the same assessment routine largely applies.
First, pinpoint the location: Is the trouble spot the lateral shoulder and upper arm, the trapezial ridge, or the shoulder blade?
Next, assess pain on movement: Does the patient experience discomfort reaching overhead or behind the back, or moving at the glenohumeral joint/capsule and engaging the rotator cuff? Check for stiffness, weakness, and decreased range of motion in the rotator cuff.
Determine if the cause of the pain is traumatic or atraumatic and stems from an acute injury versus degeneration or overuse.
As with the knee, imaging is a major component of the assessment and typically involves the use of x-ray. An MRI may be required for evaluating full- and partial-thickness tears and when contemplating surgery.
MRI also is necessary for evaluating cases of acute, traumatic shoulder injury, and patients exhibiting disability suggestive of a rotator cuff tear in an otherwise healthy tendon.
Some pain can be treated with cortisone injections or regenerative therapies, which generally are given at the acromioclavicular or glenohumeral joints or in the subacromial space. A 2005 meta-analysis found that subacromial injections of corticosteroids are effective for improvement for rotator cuff tendinitis up to a 9‐month period.
Surgery may be warranted in some cases, Dr. Nakamoto said. These include adhesive capsulitis, rotator cuff tear, acute traumatic injury in an otherwise healthy tendon, and chronic (or acute-on-chronic) tears in a degenerative tendon following a trial of conservative therapy.
A version of this article first appeared on Medscape.com.
FROM INTERNAL MEDICINE 2022
What’s the most likely cause of this man’s severe headaches?
He reports that these started 3 days ago. His headache is worse when he stands, and resolves when he lies down. Valsalva maneuver makes the headache much worse. The headaches are present in the occipital region. He also has noticed the onset of tinnitus. A physical exam reveals that his blood pressure is 110/70 mm Hg, his pulse is 60 beats per minute, and his temperature is 36.4° C. His standing BP is 105/60 mm Hg and standing pulse is 66 bpm. Both his neurologic exam and noncontrast head CT scan are normal.
Which of the following is the most likely diagnosis?
A) Subarachnoid hemorrhage
B) POTS (Postural orthostatic tachycardia syndrome)
C) Hypnic headache
D) Spontaneous intracranial hypotension (SIH)
E) Acoustic neuroma
The most likely cause for this patient’s headaches given his set of symptoms is spontaneous intracranial hypotension. Orthostatic headaches are common with POTS, but the absence of tachycardia with standing makes this diagnosis unlikely.
Spontaneous intracranial hypotension has symptoms that we are all familiar with in the post–lumbar puncture patient. In patients with post-LP headache, the positional nature makes it easy to diagnose. Patients who have had a lumbar puncture have a clear reason they have a cerebrospinal fluid (CSF) leak, leading to intracranial hypotension. Those with SIH do not.
Related research
Schievink summarized a lot of useful information in a review of patients with spontaneous intracranial hypotension.1 The incidence is about 5/100,000, with the most common age around 40 years old. The most common symptom is orthostatic headache. The headache usually occurs within 15 minutes upon standing, and many patients have the onset of headache rapidly upon standing.
Usually the headache improves with lying down, and it is often brought on with Valsalva maneuver. Many patients report headaches that are worse in the second half of the day.
Orthostatic headache occurs in almost all patients with spontaneous intracranial hypotension, but in one series it occurred only in 77% of patients with SIH.2 The patients who did not have typical headaches are more likely to have auditory symptoms such as tinnitus and muffled hearing.3
When you suspect SIH, appropriate workup is to start with brain MR imaging with contrast. Krantz and colleagues found dural enhancement was present in 83% of cases of SIH, venous distention sign in 75%, and brain sagging in 61%.4
About 10% of patients with SIH have normal brain imaging, so if the clinical features strongly suggest the diagnosis, moving on to spinal imaging with CT myelography or spinal MR are appropriate next steps.5
The causes of SIH are meningeal diverticula (usually in the thoracic or upper lumbar regions), ventral dural tears (usually from osteophytes), and cerebrospinal fluid–venous fistulas. Treatment of SIH has traditionally included a conservative approach of bed rest, oral hydration, and caffeine. The effectiveness of this is unknown, and, in one small series, 61% had headache symptoms at 6 months.6
Epidural blood patches are likely more rapidly effective than conservative therapy. In one study comparing the two treatments, Chung and colleagues found that 77% of the patients who received an epidural blood patch had complete headache relief at 4 weeks, compared with 40% of those who received conservative measures (P < .05).7
Clinical pearls
- Strongly consider SIH in patients with positional headache.
- Brain MR should be the first diagnostic test.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-96.
2. Mea E et al. Headache attributed to spontaneous intracranial hypotension. Neurol Sci. 2008;29:164-65.
3. Krantz PG et al. Spontaneous Intracranial Hypotension: 10 Myths and Misperceptions. Headache. 2018;58:948-59.
4. Krantz PG et. al. Imaging signs in spontaneous intracranial hypotension: prevalence and relationship to CSF pressure. AJNR Am J Neuroradiol. 2016;37:1374-8.
5. Krantz PG et al. Spontaneous intracranial hypotension: Pathogenesis, diagnosis, and treatment. Neuroimaging Clin N Am. 2019;29:581-94.
6. Kong D-S et. al. Clinical features and long-term results of spontaneous intracranial hypotension. Neurosurgery. 2005;57:91-6.
7. Chung SJ et al. Short- and long-term outcomes of spontaneous CSF hypovolemia. Eur Neurol. 2005;54:63-7.
He reports that these started 3 days ago. His headache is worse when he stands, and resolves when he lies down. Valsalva maneuver makes the headache much worse. The headaches are present in the occipital region. He also has noticed the onset of tinnitus. A physical exam reveals that his blood pressure is 110/70 mm Hg, his pulse is 60 beats per minute, and his temperature is 36.4° C. His standing BP is 105/60 mm Hg and standing pulse is 66 bpm. Both his neurologic exam and noncontrast head CT scan are normal.
Which of the following is the most likely diagnosis?
A) Subarachnoid hemorrhage
B) POTS (Postural orthostatic tachycardia syndrome)
C) Hypnic headache
D) Spontaneous intracranial hypotension (SIH)
E) Acoustic neuroma
The most likely cause for this patient’s headaches given his set of symptoms is spontaneous intracranial hypotension. Orthostatic headaches are common with POTS, but the absence of tachycardia with standing makes this diagnosis unlikely.
Spontaneous intracranial hypotension has symptoms that we are all familiar with in the post–lumbar puncture patient. In patients with post-LP headache, the positional nature makes it easy to diagnose. Patients who have had a lumbar puncture have a clear reason they have a cerebrospinal fluid (CSF) leak, leading to intracranial hypotension. Those with SIH do not.
Related research
Schievink summarized a lot of useful information in a review of patients with spontaneous intracranial hypotension.1 The incidence is about 5/100,000, with the most common age around 40 years old. The most common symptom is orthostatic headache. The headache usually occurs within 15 minutes upon standing, and many patients have the onset of headache rapidly upon standing.
Usually the headache improves with lying down, and it is often brought on with Valsalva maneuver. Many patients report headaches that are worse in the second half of the day.
Orthostatic headache occurs in almost all patients with spontaneous intracranial hypotension, but in one series it occurred only in 77% of patients with SIH.2 The patients who did not have typical headaches are more likely to have auditory symptoms such as tinnitus and muffled hearing.3
When you suspect SIH, appropriate workup is to start with brain MR imaging with contrast. Krantz and colleagues found dural enhancement was present in 83% of cases of SIH, venous distention sign in 75%, and brain sagging in 61%.4
About 10% of patients with SIH have normal brain imaging, so if the clinical features strongly suggest the diagnosis, moving on to spinal imaging with CT myelography or spinal MR are appropriate next steps.5
The causes of SIH are meningeal diverticula (usually in the thoracic or upper lumbar regions), ventral dural tears (usually from osteophytes), and cerebrospinal fluid–venous fistulas. Treatment of SIH has traditionally included a conservative approach of bed rest, oral hydration, and caffeine. The effectiveness of this is unknown, and, in one small series, 61% had headache symptoms at 6 months.6
Epidural blood patches are likely more rapidly effective than conservative therapy. In one study comparing the two treatments, Chung and colleagues found that 77% of the patients who received an epidural blood patch had complete headache relief at 4 weeks, compared with 40% of those who received conservative measures (P < .05).7
Clinical pearls
- Strongly consider SIH in patients with positional headache.
- Brain MR should be the first diagnostic test.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-96.
2. Mea E et al. Headache attributed to spontaneous intracranial hypotension. Neurol Sci. 2008;29:164-65.
3. Krantz PG et al. Spontaneous Intracranial Hypotension: 10 Myths and Misperceptions. Headache. 2018;58:948-59.
4. Krantz PG et. al. Imaging signs in spontaneous intracranial hypotension: prevalence and relationship to CSF pressure. AJNR Am J Neuroradiol. 2016;37:1374-8.
5. Krantz PG et al. Spontaneous intracranial hypotension: Pathogenesis, diagnosis, and treatment. Neuroimaging Clin N Am. 2019;29:581-94.
6. Kong D-S et. al. Clinical features and long-term results of spontaneous intracranial hypotension. Neurosurgery. 2005;57:91-6.
7. Chung SJ et al. Short- and long-term outcomes of spontaneous CSF hypovolemia. Eur Neurol. 2005;54:63-7.
He reports that these started 3 days ago. His headache is worse when he stands, and resolves when he lies down. Valsalva maneuver makes the headache much worse. The headaches are present in the occipital region. He also has noticed the onset of tinnitus. A physical exam reveals that his blood pressure is 110/70 mm Hg, his pulse is 60 beats per minute, and his temperature is 36.4° C. His standing BP is 105/60 mm Hg and standing pulse is 66 bpm. Both his neurologic exam and noncontrast head CT scan are normal.
Which of the following is the most likely diagnosis?
A) Subarachnoid hemorrhage
B) POTS (Postural orthostatic tachycardia syndrome)
C) Hypnic headache
D) Spontaneous intracranial hypotension (SIH)
E) Acoustic neuroma
The most likely cause for this patient’s headaches given his set of symptoms is spontaneous intracranial hypotension. Orthostatic headaches are common with POTS, but the absence of tachycardia with standing makes this diagnosis unlikely.
Spontaneous intracranial hypotension has symptoms that we are all familiar with in the post–lumbar puncture patient. In patients with post-LP headache, the positional nature makes it easy to diagnose. Patients who have had a lumbar puncture have a clear reason they have a cerebrospinal fluid (CSF) leak, leading to intracranial hypotension. Those with SIH do not.
Related research
Schievink summarized a lot of useful information in a review of patients with spontaneous intracranial hypotension.1 The incidence is about 5/100,000, with the most common age around 40 years old. The most common symptom is orthostatic headache. The headache usually occurs within 15 minutes upon standing, and many patients have the onset of headache rapidly upon standing.
Usually the headache improves with lying down, and it is often brought on with Valsalva maneuver. Many patients report headaches that are worse in the second half of the day.
Orthostatic headache occurs in almost all patients with spontaneous intracranial hypotension, but in one series it occurred only in 77% of patients with SIH.2 The patients who did not have typical headaches are more likely to have auditory symptoms such as tinnitus and muffled hearing.3
When you suspect SIH, appropriate workup is to start with brain MR imaging with contrast. Krantz and colleagues found dural enhancement was present in 83% of cases of SIH, venous distention sign in 75%, and brain sagging in 61%.4
About 10% of patients with SIH have normal brain imaging, so if the clinical features strongly suggest the diagnosis, moving on to spinal imaging with CT myelography or spinal MR are appropriate next steps.5
The causes of SIH are meningeal diverticula (usually in the thoracic or upper lumbar regions), ventral dural tears (usually from osteophytes), and cerebrospinal fluid–venous fistulas. Treatment of SIH has traditionally included a conservative approach of bed rest, oral hydration, and caffeine. The effectiveness of this is unknown, and, in one small series, 61% had headache symptoms at 6 months.6
Epidural blood patches are likely more rapidly effective than conservative therapy. In one study comparing the two treatments, Chung and colleagues found that 77% of the patients who received an epidural blood patch had complete headache relief at 4 weeks, compared with 40% of those who received conservative measures (P < .05).7
Clinical pearls
- Strongly consider SIH in patients with positional headache.
- Brain MR should be the first diagnostic test.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-96.
2. Mea E et al. Headache attributed to spontaneous intracranial hypotension. Neurol Sci. 2008;29:164-65.
3. Krantz PG et al. Spontaneous Intracranial Hypotension: 10 Myths and Misperceptions. Headache. 2018;58:948-59.
4. Krantz PG et. al. Imaging signs in spontaneous intracranial hypotension: prevalence and relationship to CSF pressure. AJNR Am J Neuroradiol. 2016;37:1374-8.
5. Krantz PG et al. Spontaneous intracranial hypotension: Pathogenesis, diagnosis, and treatment. Neuroimaging Clin N Am. 2019;29:581-94.
6. Kong D-S et. al. Clinical features and long-term results of spontaneous intracranial hypotension. Neurosurgery. 2005;57:91-6.
7. Chung SJ et al. Short- and long-term outcomes of spontaneous CSF hypovolemia. Eur Neurol. 2005;54:63-7.
Inadequate pain relief in OA, high opioid use before TKA
Inadequate pain relief was recorded in 68.8% of a sample of people with hip or knee OA who participated in the population-based EpiReumaPt study, researchers reported at the OARSI 2022 World Congress.
“This can be explained by a lack of effectiveness of current management strategies, low uptake of recommended interventions by health care professionals, and also by low adherence by patients to medication and lifestyle interventions,” said Daniela Sofia Albino Costa, MSc, a PhD student at NOVA University Lisbon.
In addition to looking at the prevalence of inadequate pain relief – defined as a score of 5 or higher on the Numeric Pain Rating Scale (NPRS) – the study she presented at the congress, which was sponsored by the Osteoarthritis Research Society International, looked at the predictors for inadequate pain control.
It was found that being female, obesity, and having multimorbidity doubled the risk of inadequate versus adequate pain control, with respective odds ratios of 2.32 (P < .001), 2.26 (P = .006), and 2.07 (P = .001). Overweight was also associated with an increased odds ratio for poor pain control (OR, 1.84; P = .0035).
“We found that patients with inadequate pain relief also have a low performance on activities of daily living and a low quality of life,” Ms. Costa said.
Nearly one-third (29%) of patients in the inadequate pain relief group (n = 765) took medication, versus 15% of patients in the adequate pain relief group (n = 270). This was mostly NSAIDs, but also included analgesics and antipyretics, and in a few cases (4.8% vs. 1.3%), simple opioids.
“We know that current care is not concordant with recommendations,” said Ms. Costa, noting that medication being used as first-line treatment and core nonpharmacologic interventions are being offered to less than half of patients who are eligible.
In addition, the rate for total joint replacement has increased globally, and pain is an important predictor for this.
“So, we need to evaluate pain control and current management offered to people with hip or knee arthritis to identify to identify areas for improvement,” Ms. Costa said.
High rates of prescription opioid use before TKA
In a separate study also presented at the congress, Daniel Rhon, DPT, DSc, director of musculoskeletal research in primary care at Brooke Army Medical Center in San Antonio, gave a worrying glimpse of high rates of opioid use in the 4 years before total knee arthroplasty (TKA).
Using data from the U.S. Military Health System, the records of all individuals who had a knee replacement procedure between January 2017 and December 2018 were studied, to identify and characterize the use of prescription opioids.
Of the 46,362 individuals, 52.9% had prior opioid use, despite the fact that “opioids are not recommended for the management of knee OA,” said Dr. Rhon.
He also reported that as many as 40% of those who had at least one prescription for opioids had received a high-potency drug, such as fentanyl or oxycodone. The mean age of participants overall was 65 years, with a higher mean for those receiving opioids than those who did not (68 vs. 61.5 years). Data on sex and ethnicity were not available in time for presentation at the congress.
“Most of these individuals are getting these opioid prescriptions probably within 6 months, which maybe aligns with escalation of pain and maybe the decision to have that knee replacement,” Dr. Rhon said. Individuals that used opioids filled their most recent prescription a median of 146 days before TKA to surgery, with a mean of 317 days.
“You can’t always link the reason for the opioid prescription, that’s not really clear in the database,” he admitted; however, an analysis was performed to check if other surgeries had been performed that may have warranted the opioid treatment. The results revealed that very few of the opioid users (4%-7%) had undergone another type of surgical procedure.
“So, we feel a little bit better, that these findings weren’t for other surgical procedures,” said Dr. Rhon. He added that future qualitative research was needed to understand why health care professionals were prescribing opioids, and why patients felt like they needed them.
“That’s bad,” Haxby Abbott, PhD, DPT, a research professor at the University of Otago, Dunedin, New Zealand, commented on Twitter.
Dr. Abbott, who was not involved in the study, added: “We’ve done a similar study of the whole NZ population [currently under review] – similar to Australia and not nearly as bad as you found. That needs urgent attention.”
Sharp rise in opioid use 2 years before TKA
Lower rates of opioid use before TKA were seen in two European cohorts, at 43% in England and 33% in Sweden, as reported by Clara Hellberg, PhD, MD, of Lund (Sweden) University. However, rates had increased over a 10-year study period from a respective 23% and 16%, with a sharp increase in use in the 2 years before knee replacement.
The analysis was based on 49,043 patients from the English national database Clinical Practice Research Datalink, and 5,955 patients from the Swedish Skåne Healthcare register who had undergone total knee replacement between 2015 and 2019 and were matched by age, sex and general practice to individuals not undergoing knee replacement.
The prevalence ratio for using opioids over a 10-year period increased from 1.6 to 2.7 in England, and from 1.6 to 2.6 in Sweden.
“While the overall prevalence of opioid use was higher in England, the majority of both cases and controls were using weak opioids,” Dr. Hellberg said.
“Codeine was classified as a weak opioid, whereas morphine was classified as a strong opioid,” she added.
In contrast, the proportion of people using strong opioids in Sweden was greater than in England, she said.
The high opioid use found in the study highlights “the need for better opioid stewardship, and the availability of acceptable, effective alternatives,” Dr. Hellberg and associates concluded in their abstract.
The study presented by Ms. Costa was funded by the Portuguese national funding agency for science, research and technology and by an independent research grant from Pfizer. Dr. Rhon acknowledged grant funding from the National Institutes of Health and the U.S. Department of Defense. Dr. Hellberg had no conflicts of interest to disclose.
Inadequate pain relief was recorded in 68.8% of a sample of people with hip or knee OA who participated in the population-based EpiReumaPt study, researchers reported at the OARSI 2022 World Congress.
“This can be explained by a lack of effectiveness of current management strategies, low uptake of recommended interventions by health care professionals, and also by low adherence by patients to medication and lifestyle interventions,” said Daniela Sofia Albino Costa, MSc, a PhD student at NOVA University Lisbon.
In addition to looking at the prevalence of inadequate pain relief – defined as a score of 5 or higher on the Numeric Pain Rating Scale (NPRS) – the study she presented at the congress, which was sponsored by the Osteoarthritis Research Society International, looked at the predictors for inadequate pain control.
It was found that being female, obesity, and having multimorbidity doubled the risk of inadequate versus adequate pain control, with respective odds ratios of 2.32 (P < .001), 2.26 (P = .006), and 2.07 (P = .001). Overweight was also associated with an increased odds ratio for poor pain control (OR, 1.84; P = .0035).
“We found that patients with inadequate pain relief also have a low performance on activities of daily living and a low quality of life,” Ms. Costa said.
Nearly one-third (29%) of patients in the inadequate pain relief group (n = 765) took medication, versus 15% of patients in the adequate pain relief group (n = 270). This was mostly NSAIDs, but also included analgesics and antipyretics, and in a few cases (4.8% vs. 1.3%), simple opioids.
“We know that current care is not concordant with recommendations,” said Ms. Costa, noting that medication being used as first-line treatment and core nonpharmacologic interventions are being offered to less than half of patients who are eligible.
In addition, the rate for total joint replacement has increased globally, and pain is an important predictor for this.
“So, we need to evaluate pain control and current management offered to people with hip or knee arthritis to identify to identify areas for improvement,” Ms. Costa said.
High rates of prescription opioid use before TKA
In a separate study also presented at the congress, Daniel Rhon, DPT, DSc, director of musculoskeletal research in primary care at Brooke Army Medical Center in San Antonio, gave a worrying glimpse of high rates of opioid use in the 4 years before total knee arthroplasty (TKA).
Using data from the U.S. Military Health System, the records of all individuals who had a knee replacement procedure between January 2017 and December 2018 were studied, to identify and characterize the use of prescription opioids.
Of the 46,362 individuals, 52.9% had prior opioid use, despite the fact that “opioids are not recommended for the management of knee OA,” said Dr. Rhon.
He also reported that as many as 40% of those who had at least one prescription for opioids had received a high-potency drug, such as fentanyl or oxycodone. The mean age of participants overall was 65 years, with a higher mean for those receiving opioids than those who did not (68 vs. 61.5 years). Data on sex and ethnicity were not available in time for presentation at the congress.
“Most of these individuals are getting these opioid prescriptions probably within 6 months, which maybe aligns with escalation of pain and maybe the decision to have that knee replacement,” Dr. Rhon said. Individuals that used opioids filled their most recent prescription a median of 146 days before TKA to surgery, with a mean of 317 days.
“You can’t always link the reason for the opioid prescription, that’s not really clear in the database,” he admitted; however, an analysis was performed to check if other surgeries had been performed that may have warranted the opioid treatment. The results revealed that very few of the opioid users (4%-7%) had undergone another type of surgical procedure.
“So, we feel a little bit better, that these findings weren’t for other surgical procedures,” said Dr. Rhon. He added that future qualitative research was needed to understand why health care professionals were prescribing opioids, and why patients felt like they needed them.
“That’s bad,” Haxby Abbott, PhD, DPT, a research professor at the University of Otago, Dunedin, New Zealand, commented on Twitter.
Dr. Abbott, who was not involved in the study, added: “We’ve done a similar study of the whole NZ population [currently under review] – similar to Australia and not nearly as bad as you found. That needs urgent attention.”
Sharp rise in opioid use 2 years before TKA
Lower rates of opioid use before TKA were seen in two European cohorts, at 43% in England and 33% in Sweden, as reported by Clara Hellberg, PhD, MD, of Lund (Sweden) University. However, rates had increased over a 10-year study period from a respective 23% and 16%, with a sharp increase in use in the 2 years before knee replacement.
The analysis was based on 49,043 patients from the English national database Clinical Practice Research Datalink, and 5,955 patients from the Swedish Skåne Healthcare register who had undergone total knee replacement between 2015 and 2019 and were matched by age, sex and general practice to individuals not undergoing knee replacement.
The prevalence ratio for using opioids over a 10-year period increased from 1.6 to 2.7 in England, and from 1.6 to 2.6 in Sweden.
“While the overall prevalence of opioid use was higher in England, the majority of both cases and controls were using weak opioids,” Dr. Hellberg said.
“Codeine was classified as a weak opioid, whereas morphine was classified as a strong opioid,” she added.
In contrast, the proportion of people using strong opioids in Sweden was greater than in England, she said.
The high opioid use found in the study highlights “the need for better opioid stewardship, and the availability of acceptable, effective alternatives,” Dr. Hellberg and associates concluded in their abstract.
The study presented by Ms. Costa was funded by the Portuguese national funding agency for science, research and technology and by an independent research grant from Pfizer. Dr. Rhon acknowledged grant funding from the National Institutes of Health and the U.S. Department of Defense. Dr. Hellberg had no conflicts of interest to disclose.
Inadequate pain relief was recorded in 68.8% of a sample of people with hip or knee OA who participated in the population-based EpiReumaPt study, researchers reported at the OARSI 2022 World Congress.
“This can be explained by a lack of effectiveness of current management strategies, low uptake of recommended interventions by health care professionals, and also by low adherence by patients to medication and lifestyle interventions,” said Daniela Sofia Albino Costa, MSc, a PhD student at NOVA University Lisbon.
In addition to looking at the prevalence of inadequate pain relief – defined as a score of 5 or higher on the Numeric Pain Rating Scale (NPRS) – the study she presented at the congress, which was sponsored by the Osteoarthritis Research Society International, looked at the predictors for inadequate pain control.
It was found that being female, obesity, and having multimorbidity doubled the risk of inadequate versus adequate pain control, with respective odds ratios of 2.32 (P < .001), 2.26 (P = .006), and 2.07 (P = .001). Overweight was also associated with an increased odds ratio for poor pain control (OR, 1.84; P = .0035).
“We found that patients with inadequate pain relief also have a low performance on activities of daily living and a low quality of life,” Ms. Costa said.
Nearly one-third (29%) of patients in the inadequate pain relief group (n = 765) took medication, versus 15% of patients in the adequate pain relief group (n = 270). This was mostly NSAIDs, but also included analgesics and antipyretics, and in a few cases (4.8% vs. 1.3%), simple opioids.
“We know that current care is not concordant with recommendations,” said Ms. Costa, noting that medication being used as first-line treatment and core nonpharmacologic interventions are being offered to less than half of patients who are eligible.
In addition, the rate for total joint replacement has increased globally, and pain is an important predictor for this.
“So, we need to evaluate pain control and current management offered to people with hip or knee arthritis to identify to identify areas for improvement,” Ms. Costa said.
High rates of prescription opioid use before TKA
In a separate study also presented at the congress, Daniel Rhon, DPT, DSc, director of musculoskeletal research in primary care at Brooke Army Medical Center in San Antonio, gave a worrying glimpse of high rates of opioid use in the 4 years before total knee arthroplasty (TKA).
Using data from the U.S. Military Health System, the records of all individuals who had a knee replacement procedure between January 2017 and December 2018 were studied, to identify and characterize the use of prescription opioids.
Of the 46,362 individuals, 52.9% had prior opioid use, despite the fact that “opioids are not recommended for the management of knee OA,” said Dr. Rhon.
He also reported that as many as 40% of those who had at least one prescription for opioids had received a high-potency drug, such as fentanyl or oxycodone. The mean age of participants overall was 65 years, with a higher mean for those receiving opioids than those who did not (68 vs. 61.5 years). Data on sex and ethnicity were not available in time for presentation at the congress.
“Most of these individuals are getting these opioid prescriptions probably within 6 months, which maybe aligns with escalation of pain and maybe the decision to have that knee replacement,” Dr. Rhon said. Individuals that used opioids filled their most recent prescription a median of 146 days before TKA to surgery, with a mean of 317 days.
“You can’t always link the reason for the opioid prescription, that’s not really clear in the database,” he admitted; however, an analysis was performed to check if other surgeries had been performed that may have warranted the opioid treatment. The results revealed that very few of the opioid users (4%-7%) had undergone another type of surgical procedure.
“So, we feel a little bit better, that these findings weren’t for other surgical procedures,” said Dr. Rhon. He added that future qualitative research was needed to understand why health care professionals were prescribing opioids, and why patients felt like they needed them.
“That’s bad,” Haxby Abbott, PhD, DPT, a research professor at the University of Otago, Dunedin, New Zealand, commented on Twitter.
Dr. Abbott, who was not involved in the study, added: “We’ve done a similar study of the whole NZ population [currently under review] – similar to Australia and not nearly as bad as you found. That needs urgent attention.”
Sharp rise in opioid use 2 years before TKA
Lower rates of opioid use before TKA were seen in two European cohorts, at 43% in England and 33% in Sweden, as reported by Clara Hellberg, PhD, MD, of Lund (Sweden) University. However, rates had increased over a 10-year study period from a respective 23% and 16%, with a sharp increase in use in the 2 years before knee replacement.
The analysis was based on 49,043 patients from the English national database Clinical Practice Research Datalink, and 5,955 patients from the Swedish Skåne Healthcare register who had undergone total knee replacement between 2015 and 2019 and were matched by age, sex and general practice to individuals not undergoing knee replacement.
The prevalence ratio for using opioids over a 10-year period increased from 1.6 to 2.7 in England, and from 1.6 to 2.6 in Sweden.
“While the overall prevalence of opioid use was higher in England, the majority of both cases and controls were using weak opioids,” Dr. Hellberg said.
“Codeine was classified as a weak opioid, whereas morphine was classified as a strong opioid,” she added.
In contrast, the proportion of people using strong opioids in Sweden was greater than in England, she said.
The high opioid use found in the study highlights “the need for better opioid stewardship, and the availability of acceptable, effective alternatives,” Dr. Hellberg and associates concluded in their abstract.
The study presented by Ms. Costa was funded by the Portuguese national funding agency for science, research and technology and by an independent research grant from Pfizer. Dr. Rhon acknowledged grant funding from the National Institutes of Health and the U.S. Department of Defense. Dr. Hellberg had no conflicts of interest to disclose.
FROM OARSI 2022
Somatic symptom disorder in primary care: A collaborative approach
THE CASE
James R* is a 30-year-old man who presented for a primary care walk-in visit due to dizziness, 2 days after he visited an emergency department (ED) for the same concern. He reported episodic symptoms lasting seconds to minutes, specifically when lying down. He said he had not fallen or experienced other physical trauma, did not have blurred vision or hearing loss, and was taking no medications. He also reported panic attacks, during which he experienced palpitations, trembling, paresthesia, and fear of dying. He stated that dizziness did not occur exclusively during panic episodes. His medical history was significant for hypertension; however, he reported significant anxiety related to medical visits. All home blood pressure readings he reported were within normal limits.
Upon examination, the patient had a blood pressure reading of 142/90 mm Hg and no evidence of nystagmus at rest. A neurologic exam was normal and a Dix-Hallpike maneuver reproduced subjective vertigo without nystagmus. Laboratory findings from the patient’s ED visit were negative for troponin and drug use, and blood oxygenation levels were within normal limits. At the time of this current visit, an electrocardiogram was unremarkable, with the exception of some tachycardia.
The presumptive diagnosis was benign paroxysmal positional vertigo (BPPV). An Epley maneuver was performed in the clinic and resulted in minimal symptom improvement. The physician taught Mr. R how to perform the Epley maneuver himself, prescribed a short course of meclizine, and referred him to the integrated mental health care service to address his panic attacks and anxiety.
Over the next few months, Mr. R continued to report significant distress about the dizzy spells, which persisted even after performing the Epley maneuver, and he reported that the meclizine was causing worsening vertigo. He received an ear-nose-and-throat consultation and cognitive behavioral therapy (CBT)–based consultation/interventions. He also reported avoiding multiple activities due to concerns about his dizziness.
●
*The patient’s name and other personally identifying information have been changed to protect his identity.
Somatic symptom disorder (SSD) is characterized by one or more physical symptoms associated with “excessive thoughts, feelings, or behaviors that result in distress and/or functional impairment.”1 Individuals with SSD are preoccupied with symptom-related severity, experience high symptom-related anxiety, or devote significant time and energy to the symptoms or heath concerns. With a diagnosis of SSD, physical symptoms experienced by the patient may or may not be medically explained. The same symptom need not be continuously present as long as the overall symptomatic presentation lasts 6 months or longer.
The specifier “with predominant pain” is used when pain dominates the presentation.1 Estimated prevalence of SSD in primary care ranges from 5% to 35%.2 The true scope of SSD is difficult to assess accurately since research tends to focus on medically unexplained symptoms, rather than excessive symptom-related concerns. Furthermore, terms such as “medically unexplained symptoms” and “functional syndromes” (including fibromyalgia and irritable bowel syndrome) are frequently used when describing SSD.3
One or more factors may contribute to unexplained symptoms: limitations of medical procedures and techniques, partial clinical information, patients’ inability to follow management recommendations, challenges in differential diagnostics, and access-to-care limitations preventing regular care and appropriate diagnostic work up.
What’s important to remember is that it’s the patient’s reaction to physical symptoms, rather than the presence of symptoms per se, that defines SSD.
Considerations in the differential diagnosis
When making a diagnosis of SSD, symptoms cannot:4
- be feigned or deliberately produced as in malingering or factitious disorder.
- result from physiologic effects of a substance (eg, intoxication, withdrawal, or adverse medication effects).
- constitute somatic delusions, as occur in psychotic disorders.
- constitute symptoms or deficits affecting voluntary motor or sensory function that are better explained by neurologic, medical, or psychiatric conditions (consider conversion disorder).
- be preoccupations with physical appearance flaws, as in body dysmorphic disorder.
- be accounted for by an anxiety disorder (eg, palpitations associated with panic attacks).
Continue to: Illness anxiety disorder...
Illness anxiety disorder is also characterized by significant health-related concerns; however, physical symptoms are either mild or absent.
Possible causes of SSD are varied and complex, including genetic and biological factors, family dynamics, behavioral modeling/learning, personality traits, difficulties with emotional regulation, and awareness.5 Patients may present with ongoing requests for symptom explanations, feelings of helplessness, fear of having concerns dismissed, and low motivation for change.3
Aids in supporting a diagnosis of SSD
It’s not appropriate to rely solely on questionnaires to make the diagnosis of SSD. However, brief screening tools are a time-efficient way to capture patients’ experiences and perceptions.6 Along with other components of clinical evaluation, brief symptom screens can both support the diagnosis and help in longitudinal symptom assessment.
Patient Health Questionnaire-15 (PHQ-15), developed for self-report screening in primary care, has desirable psychometric properties including appropriate internal reliability; convergent validity with measures of functional status, disability days, and symptom-related burden; and discriminant validity from measures of depressive symptoms.7 The PHQ-15 is an open access tool that is available in several languages. The respondent is asked to rate the extent of being bothered by a range of medical symptoms in the proceeding 4 weeks. Total scores range from 0 to 30, with higher scores indicating greater symptom aggravation. Cutoffs of 5, 10, and 15 correspond to mild, moderate, and severe symptom levels.8
Somatic Symptom Disorder - B Criteria Scale (SSD-12) aims to capture SSD symptoms in line with Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnostic criteria. It assesses cognitive, affective, and behavioral aspects of SSD.9 The SSD-12 is copyrighted and its use requires registration and purchase. Cutoffs by age and gender are available. SSD-12 has demonstrated appropriate reliability and validity.9
Continue to: Structured Clinical Interview for DSM Disorders
Structured Clinical Interview for DSM Disorders (SCID)10,11 is perhaps the most rigorous differential diagnostic tool. However, SCID administration requires training and skill; time for administration and cost of the materials may be prohibitive in primary care.
Finally, SSD symptoms are highly associated with depression and anxiety. Ongoing elevated screening scores for anxiety and depression refractory to interventions may indicate the possibility of overlooked SSD. Furthermore, use of SSD screening tools with anxiety and depression screening tools can provide a more comprehensive picture of impairment, as well as symptom progress.
Treatment: Avoid a split approach
Diagnosing and treating SSD can be challenging for physicians who focus on biomedically based approaches in patient care. Additional tests, studies, and prescriptions are likely to fuel (rather than pacify) patients’ concerns, as such steps divert attention from the underlying psychological needs and mechanisms which maintain SSD. Avoid using a split biopsychosocial approach—ie, beginning the inquiry and treatment planning from a biomedical perspective, and then falling back on psychosocial formulation when treatment efforts have been ineffective. Such an approach leads to understandable patient dissatisfaction and can be interpreted by them as the caregiver suggesting that physical symptoms are “all in [their] head.”12
These 4 tips can help
1. Use a biopsychosocial formulation when initiating treatment. Be familiar with biopsychosocial factors in SSD and develop a narrative for discussing this formulation with patients. For example: “Mr. R, we are going to use the following [medical tests/studies/medications] to understand the cause of your symptoms and better manage them. We also need to think about the role of stress and distress in your symptoms because these can also be at play with dizziness.” This may be particularly beneficial for a functional disorder, such as chronic pain. Incorporating patient education resources is an important step toward shared understanding (see Hunter Integrated Pain Service for chronic pain educational videos; www.tga.gov.au/chronic-pain-management-video-resource-brainman13).
2. Combine education about pathophysiology with patient-centered interviewing. Significant SSD symptom improvements were noted following a single 30-minute educational session, while motivational interviewing techniques were used to probe patients’ concerns.2
Continue to: Maintain professionalism and good clinical practice
3. Maintain professionalism and good clinical practice. Consider SSD a medical matter and address it accordingly: explore concerns fully, provide evidence-based responses, communicate empathy, and employ objective management strategies.14
4. Do not overlook the value of the relationship. A recent systematic review concluded that the relationship between the patient and care provider was central to the success of the interventions for symptom reduction.15
A controversial approach. Pharmacotherapy for SSD is controversial. While several trials of antidepressants and St. John’s wort have been positive and some authors have stated that all classes of antidepressants are effective for SSD, others maintain that questions regarding dosing, treatment duration, and sustainability of improvement have not been sufficiently addressed in research.16,17
Coordination of care issues
Primary care continues to be the de facto mental health system, and specialty services may be unavailable or declined by patients.18 CBT delivered in person or online is empirically supported as a treatment approach to medically unexplained symptoms and SSD.17,19-22
A recent meta-analysis of randomized controlled trials published by Jing and colleagues23 reported that CBT was effective for SSD symptom reduction, and that treatment gains were maintained 3 to 12 months post treatment. However, concerns about the practical implementation of CBT in primary care were raised because CBT was not shown to be effective in improving social functioning or reducing the number of medical visits. Symptom improvement was maximized with longer durations of treatment (> 10 sessions) and greater session lengths (> 50 minutes). Additionally, Abbass and colleagues24 brought up several methodologic (sampling and analysis) concerns related to Jing et al’s work.
Continue to: Overally, CBT's effect sizes...
Overall, CBT’s effect sizes are small, and patients who are open to biopsychosocial explanations for their symptoms and to receiving psychological services may differ from most patients seen in primary care practices.21 Furthermore, mental health providers may hesitate to diagnose SSD because they are concerned about missing a somatic illness.3 Therefore, when coordinating care with mental health providers, it may be beneficial to discuss the treatment approach, assess familiarity with the SSD diagnosis, and closely coordinate and collaborate on the treatment plan.
While physicians cannot be expected to function as psychotherapists, an understanding of CBT and techniques for SSD treatment can be beneficial. Integrated mental health services may hold promise in addressing SSD in primary care. Onsite availability of a behavioral health provider competent in providing evidence-based care can target SSD symptoms and support both patients and physicians.
THE CASE
Mr. R’s treatment course included multiple primary care appointments (scheduled and walk in), ED visits, and specialist visits (ENT/vestibular rehabilitation). He sought care as symptoms intensified, lasted longer, or occurred in new circumstances. He reported persistent fear of the symptoms and anxiety that serious medical causes had been overlooked. He also described distress associated with vertigo and his anxiety sensitivity (anxiety about being anxious).
The behavioral health consultant (BHC; psychologist) and physician talked to the patient about the biopsychosocial antecedents of his condition and the factors that perpetuate the anxiety and stress response. The BHC described the fight/flight/freeze response to the patient and explained its role in the physiologic stress response associated with somatic symptoms and panic. Educational materials (videos and handouts) were also provided to the patient to further illustrate these concepts. The BHC also discussed the role of interoceptive and situational avoidance and active coping (eg, engaging in safe activities); taught the patient relaxation and grounding techniques; and used cognitive disputation aimed at challenging catastrophic symptom interpretations.
The BHC and the patient’s physician established joint treatment goals that included improving functioning, promoting active coping, and decreasing distress associated with symptoms. After the initial medical and BHC visits, both vertigo and anxiety symptoms appeared to abate somewhat, but symptoms have been ongoing and distress and impairment have been variable. The patient’s family physician and BHC continue to work with him to optimize the care plan and treatment goals.
CORRESPONDENCE
Nataliya Pilipenko, PhD, ABPP, Center for Family and Community Medicine, Columbia University Vagelos College of Physicians and Surgeons, 630 West 168th Street, New York, NY 10032; [email protected]
ACKNOWLEDGEMENT
The author thanks Dr. Molly Warren for her collaboration and guidance.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition (DSM-5). American Psychiatric Publishing; 2013.
2. Johnson KK, Bennett C, Rochani H. Significant improvement of somatic symptom disorder with brief psychoeducational intervention by PMHNP in primary care. J Am Psychiatr Nurses Assoc. 2020;28:171-180. doi: 10.1177/1078390320960524
3. Weigel A, Maehder K, Witt M, et al. Psychotherapists’ perspective on the treatment of patients with somatic symptom disorders. J Psychosom Res. 2020;138:110228. doi: 10.1016/j.jpsychores.2020.110228
4. American Psychiatric Association. Handbook of Differential Diagnosis. American Psychiatric Publishing; 2014;234-235.
5. Mayo Clinic. Somatic symptom disorder. Accessed February 21, 2022. www.mayoclinic.org/diseases-conditions/somatic-symptom-disorder/symptoms-causes/syc-20377776?p=1
6. Toussaint A, Riedl B, Kehrer S, et al. Validity of the Somatic Symptom Disorder-B Criteria Scale (SSD-12) in primary care. Fam Pract. 2018;35:342-347. doi: 10.1093/fampra/cmx116
7. Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258-66. doi: 10.1097/00006842-200203000-00008
8. Kroenke K, Spitzer RL, Williams JB, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345-359. doi: 10.1016/j.genhosppsych.2010.03.006
9. Toussaint A, Löwe B, Brähler E, et al. The Somatic Symptom Disorder - B Criteria Scale (SSD-12): factorial structure, validity and population-based norms. J Psychosom Res. 2017;97:9-17. doi: 10.1016/j.jpsychores.2017.03.017
10. First MB, Williams JBW, Karg RS, Spitzer RL, eds. Structured Clinical Interview for DSM-5 Disorders, Research Version. American Psychiatric Association, 2015.
11. First MB, Williams JBW, Karg RS, Spitzer RL, eds. Structured Clinical Interview for DSM-5 Disorders, Clinician Version. American Psychiatric Publishing; 2016.
12. McDaniel SH, Hepworth J, Campbell TL, et al, eds. Family Oriented Primary Care. Springer Publishing Co; 2005:1-15.
13. Hunter Integrated Pain Service (2016). Brainman videos. Hunter New England Local Health District. New South Wales, Australia. Accessed February 21, 2022. www.tga.gov.au/chronic-pain-management-video-resource-brainman
14. Murray AM, Toussaint A, Althaus A, et al. The challenge of diagnosing non-specific, functional, and somatoform disorders: a systematic review of barriers to diagnosis in primary care. J Psychosom Res. 2016;80:1-10. doi: 10.1016/j.jpsychores.2015.11.002
15. Leaviss J, Davis S, Ren S, et al. Behavioral modification interventions for medically unexplained symptoms in primary care: systematic reviews and economic evaluation. Health Technol Assess. 2020;24:1-490. doi: 10.3310/hta24460
16. Kroenke K. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007;69:881-888. doi: 10.1097/PSY.0b013e31815b00c4
17. Steinbrecher N, Koerber S, Frieser D, et al. The prevalence of medically unexplained symptoms in primary care. Psychosomatics. 2011;52:263-271. doi: 10.1016/j.psym.2011.01.007
18. Kessler R, Stafford D. Primary care is the de facto mental health system. In Kessler R, Stafford D, eds. Collaborative Medicine Case Studies: Evidence in Practice. Springer Publishing Co, 2008; 9-21.
19. Barsky AJ, Ahern DK, Bauer MR, et al. A randomized trial of treatments for high-utilizing somatizing patients. J Gen Intern Med. 2013;28:1396-1404. doi: 10.1007/s11606-013-2392-6
20. Newby JM, Smith J, Uppal S, et al. Internet-based cognitive behavioral therapy versus psychoeducation control for illness anxiety disorder and somatic symptom disorder: A randomized controlled trial. J Consult Clin Psychol. 2018;86:89-98. doi: 10.1037/ccp0000248
21. van Dessel N, den Boeft M, van der Wouden JC, et al. Non-pharmacological interventions for somatoform disorders and medically unexplained physical symptoms (MUPS) in adults. Cochrane Database Syst Rev. 2014(11):CD011142. doi: 10.1002/14651858.CD011142.pub2
22. Verdurmen MJ, Videler AC, Kamperman AM, et al. Cognitive behavioral therapy for somatic symptom disorders in later life: a prospective comparative explorative pilot study in two clinical populations. Neuropsychiatr Dis Treat. 2017;13:2331-2339. doi: 10.2147/NDT.S141208
23. Liu J, Gill NS, Teodorczuk A, et al. The efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;245:98-112. doi: 10.1016/j.jad.2018.10.114
24. Abbass A, Leichsenring F, Steinert C. Re: Jing et al., the efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;255:S0165-0327(18)33197-5. doi: 10.1016/j.jad.2019.02.055
THE CASE
James R* is a 30-year-old man who presented for a primary care walk-in visit due to dizziness, 2 days after he visited an emergency department (ED) for the same concern. He reported episodic symptoms lasting seconds to minutes, specifically when lying down. He said he had not fallen or experienced other physical trauma, did not have blurred vision or hearing loss, and was taking no medications. He also reported panic attacks, during which he experienced palpitations, trembling, paresthesia, and fear of dying. He stated that dizziness did not occur exclusively during panic episodes. His medical history was significant for hypertension; however, he reported significant anxiety related to medical visits. All home blood pressure readings he reported were within normal limits.
Upon examination, the patient had a blood pressure reading of 142/90 mm Hg and no evidence of nystagmus at rest. A neurologic exam was normal and a Dix-Hallpike maneuver reproduced subjective vertigo without nystagmus. Laboratory findings from the patient’s ED visit were negative for troponin and drug use, and blood oxygenation levels were within normal limits. At the time of this current visit, an electrocardiogram was unremarkable, with the exception of some tachycardia.
The presumptive diagnosis was benign paroxysmal positional vertigo (BPPV). An Epley maneuver was performed in the clinic and resulted in minimal symptom improvement. The physician taught Mr. R how to perform the Epley maneuver himself, prescribed a short course of meclizine, and referred him to the integrated mental health care service to address his panic attacks and anxiety.
Over the next few months, Mr. R continued to report significant distress about the dizzy spells, which persisted even after performing the Epley maneuver, and he reported that the meclizine was causing worsening vertigo. He received an ear-nose-and-throat consultation and cognitive behavioral therapy (CBT)–based consultation/interventions. He also reported avoiding multiple activities due to concerns about his dizziness.
●
*The patient’s name and other personally identifying information have been changed to protect his identity.
Somatic symptom disorder (SSD) is characterized by one or more physical symptoms associated with “excessive thoughts, feelings, or behaviors that result in distress and/or functional impairment.”1 Individuals with SSD are preoccupied with symptom-related severity, experience high symptom-related anxiety, or devote significant time and energy to the symptoms or heath concerns. With a diagnosis of SSD, physical symptoms experienced by the patient may or may not be medically explained. The same symptom need not be continuously present as long as the overall symptomatic presentation lasts 6 months or longer.
The specifier “with predominant pain” is used when pain dominates the presentation.1 Estimated prevalence of SSD in primary care ranges from 5% to 35%.2 The true scope of SSD is difficult to assess accurately since research tends to focus on medically unexplained symptoms, rather than excessive symptom-related concerns. Furthermore, terms such as “medically unexplained symptoms” and “functional syndromes” (including fibromyalgia and irritable bowel syndrome) are frequently used when describing SSD.3
One or more factors may contribute to unexplained symptoms: limitations of medical procedures and techniques, partial clinical information, patients’ inability to follow management recommendations, challenges in differential diagnostics, and access-to-care limitations preventing regular care and appropriate diagnostic work up.
What’s important to remember is that it’s the patient’s reaction to physical symptoms, rather than the presence of symptoms per se, that defines SSD.
Considerations in the differential diagnosis
When making a diagnosis of SSD, symptoms cannot:4
- be feigned or deliberately produced as in malingering or factitious disorder.
- result from physiologic effects of a substance (eg, intoxication, withdrawal, or adverse medication effects).
- constitute somatic delusions, as occur in psychotic disorders.
- constitute symptoms or deficits affecting voluntary motor or sensory function that are better explained by neurologic, medical, or psychiatric conditions (consider conversion disorder).
- be preoccupations with physical appearance flaws, as in body dysmorphic disorder.
- be accounted for by an anxiety disorder (eg, palpitations associated with panic attacks).
Continue to: Illness anxiety disorder...
Illness anxiety disorder is also characterized by significant health-related concerns; however, physical symptoms are either mild or absent.
Possible causes of SSD are varied and complex, including genetic and biological factors, family dynamics, behavioral modeling/learning, personality traits, difficulties with emotional regulation, and awareness.5 Patients may present with ongoing requests for symptom explanations, feelings of helplessness, fear of having concerns dismissed, and low motivation for change.3
Aids in supporting a diagnosis of SSD
It’s not appropriate to rely solely on questionnaires to make the diagnosis of SSD. However, brief screening tools are a time-efficient way to capture patients’ experiences and perceptions.6 Along with other components of clinical evaluation, brief symptom screens can both support the diagnosis and help in longitudinal symptom assessment.
Patient Health Questionnaire-15 (PHQ-15), developed for self-report screening in primary care, has desirable psychometric properties including appropriate internal reliability; convergent validity with measures of functional status, disability days, and symptom-related burden; and discriminant validity from measures of depressive symptoms.7 The PHQ-15 is an open access tool that is available in several languages. The respondent is asked to rate the extent of being bothered by a range of medical symptoms in the proceeding 4 weeks. Total scores range from 0 to 30, with higher scores indicating greater symptom aggravation. Cutoffs of 5, 10, and 15 correspond to mild, moderate, and severe symptom levels.8
Somatic Symptom Disorder - B Criteria Scale (SSD-12) aims to capture SSD symptoms in line with Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnostic criteria. It assesses cognitive, affective, and behavioral aspects of SSD.9 The SSD-12 is copyrighted and its use requires registration and purchase. Cutoffs by age and gender are available. SSD-12 has demonstrated appropriate reliability and validity.9
Continue to: Structured Clinical Interview for DSM Disorders
Structured Clinical Interview for DSM Disorders (SCID)10,11 is perhaps the most rigorous differential diagnostic tool. However, SCID administration requires training and skill; time for administration and cost of the materials may be prohibitive in primary care.
Finally, SSD symptoms are highly associated with depression and anxiety. Ongoing elevated screening scores for anxiety and depression refractory to interventions may indicate the possibility of overlooked SSD. Furthermore, use of SSD screening tools with anxiety and depression screening tools can provide a more comprehensive picture of impairment, as well as symptom progress.
Treatment: Avoid a split approach
Diagnosing and treating SSD can be challenging for physicians who focus on biomedically based approaches in patient care. Additional tests, studies, and prescriptions are likely to fuel (rather than pacify) patients’ concerns, as such steps divert attention from the underlying psychological needs and mechanisms which maintain SSD. Avoid using a split biopsychosocial approach—ie, beginning the inquiry and treatment planning from a biomedical perspective, and then falling back on psychosocial formulation when treatment efforts have been ineffective. Such an approach leads to understandable patient dissatisfaction and can be interpreted by them as the caregiver suggesting that physical symptoms are “all in [their] head.”12
These 4 tips can help
1. Use a biopsychosocial formulation when initiating treatment. Be familiar with biopsychosocial factors in SSD and develop a narrative for discussing this formulation with patients. For example: “Mr. R, we are going to use the following [medical tests/studies/medications] to understand the cause of your symptoms and better manage them. We also need to think about the role of stress and distress in your symptoms because these can also be at play with dizziness.” This may be particularly beneficial for a functional disorder, such as chronic pain. Incorporating patient education resources is an important step toward shared understanding (see Hunter Integrated Pain Service for chronic pain educational videos; www.tga.gov.au/chronic-pain-management-video-resource-brainman13).
2. Combine education about pathophysiology with patient-centered interviewing. Significant SSD symptom improvements were noted following a single 30-minute educational session, while motivational interviewing techniques were used to probe patients’ concerns.2
Continue to: Maintain professionalism and good clinical practice
3. Maintain professionalism and good clinical practice. Consider SSD a medical matter and address it accordingly: explore concerns fully, provide evidence-based responses, communicate empathy, and employ objective management strategies.14
4. Do not overlook the value of the relationship. A recent systematic review concluded that the relationship between the patient and care provider was central to the success of the interventions for symptom reduction.15
A controversial approach. Pharmacotherapy for SSD is controversial. While several trials of antidepressants and St. John’s wort have been positive and some authors have stated that all classes of antidepressants are effective for SSD, others maintain that questions regarding dosing, treatment duration, and sustainability of improvement have not been sufficiently addressed in research.16,17
Coordination of care issues
Primary care continues to be the de facto mental health system, and specialty services may be unavailable or declined by patients.18 CBT delivered in person or online is empirically supported as a treatment approach to medically unexplained symptoms and SSD.17,19-22
A recent meta-analysis of randomized controlled trials published by Jing and colleagues23 reported that CBT was effective for SSD symptom reduction, and that treatment gains were maintained 3 to 12 months post treatment. However, concerns about the practical implementation of CBT in primary care were raised because CBT was not shown to be effective in improving social functioning or reducing the number of medical visits. Symptom improvement was maximized with longer durations of treatment (> 10 sessions) and greater session lengths (> 50 minutes). Additionally, Abbass and colleagues24 brought up several methodologic (sampling and analysis) concerns related to Jing et al’s work.
Continue to: Overally, CBT's effect sizes...
Overall, CBT’s effect sizes are small, and patients who are open to biopsychosocial explanations for their symptoms and to receiving psychological services may differ from most patients seen in primary care practices.21 Furthermore, mental health providers may hesitate to diagnose SSD because they are concerned about missing a somatic illness.3 Therefore, when coordinating care with mental health providers, it may be beneficial to discuss the treatment approach, assess familiarity with the SSD diagnosis, and closely coordinate and collaborate on the treatment plan.
While physicians cannot be expected to function as psychotherapists, an understanding of CBT and techniques for SSD treatment can be beneficial. Integrated mental health services may hold promise in addressing SSD in primary care. Onsite availability of a behavioral health provider competent in providing evidence-based care can target SSD symptoms and support both patients and physicians.
THE CASE
Mr. R’s treatment course included multiple primary care appointments (scheduled and walk in), ED visits, and specialist visits (ENT/vestibular rehabilitation). He sought care as symptoms intensified, lasted longer, or occurred in new circumstances. He reported persistent fear of the symptoms and anxiety that serious medical causes had been overlooked. He also described distress associated with vertigo and his anxiety sensitivity (anxiety about being anxious).
The behavioral health consultant (BHC; psychologist) and physician talked to the patient about the biopsychosocial antecedents of his condition and the factors that perpetuate the anxiety and stress response. The BHC described the fight/flight/freeze response to the patient and explained its role in the physiologic stress response associated with somatic symptoms and panic. Educational materials (videos and handouts) were also provided to the patient to further illustrate these concepts. The BHC also discussed the role of interoceptive and situational avoidance and active coping (eg, engaging in safe activities); taught the patient relaxation and grounding techniques; and used cognitive disputation aimed at challenging catastrophic symptom interpretations.
The BHC and the patient’s physician established joint treatment goals that included improving functioning, promoting active coping, and decreasing distress associated with symptoms. After the initial medical and BHC visits, both vertigo and anxiety symptoms appeared to abate somewhat, but symptoms have been ongoing and distress and impairment have been variable. The patient’s family physician and BHC continue to work with him to optimize the care plan and treatment goals.
CORRESPONDENCE
Nataliya Pilipenko, PhD, ABPP, Center for Family and Community Medicine, Columbia University Vagelos College of Physicians and Surgeons, 630 West 168th Street, New York, NY 10032; [email protected]
ACKNOWLEDGEMENT
The author thanks Dr. Molly Warren for her collaboration and guidance.
THE CASE
James R* is a 30-year-old man who presented for a primary care walk-in visit due to dizziness, 2 days after he visited an emergency department (ED) for the same concern. He reported episodic symptoms lasting seconds to minutes, specifically when lying down. He said he had not fallen or experienced other physical trauma, did not have blurred vision or hearing loss, and was taking no medications. He also reported panic attacks, during which he experienced palpitations, trembling, paresthesia, and fear of dying. He stated that dizziness did not occur exclusively during panic episodes. His medical history was significant for hypertension; however, he reported significant anxiety related to medical visits. All home blood pressure readings he reported were within normal limits.
Upon examination, the patient had a blood pressure reading of 142/90 mm Hg and no evidence of nystagmus at rest. A neurologic exam was normal and a Dix-Hallpike maneuver reproduced subjective vertigo without nystagmus. Laboratory findings from the patient’s ED visit were negative for troponin and drug use, and blood oxygenation levels were within normal limits. At the time of this current visit, an electrocardiogram was unremarkable, with the exception of some tachycardia.
The presumptive diagnosis was benign paroxysmal positional vertigo (BPPV). An Epley maneuver was performed in the clinic and resulted in minimal symptom improvement. The physician taught Mr. R how to perform the Epley maneuver himself, prescribed a short course of meclizine, and referred him to the integrated mental health care service to address his panic attacks and anxiety.
Over the next few months, Mr. R continued to report significant distress about the dizzy spells, which persisted even after performing the Epley maneuver, and he reported that the meclizine was causing worsening vertigo. He received an ear-nose-and-throat consultation and cognitive behavioral therapy (CBT)–based consultation/interventions. He also reported avoiding multiple activities due to concerns about his dizziness.
●
*The patient’s name and other personally identifying information have been changed to protect his identity.
Somatic symptom disorder (SSD) is characterized by one or more physical symptoms associated with “excessive thoughts, feelings, or behaviors that result in distress and/or functional impairment.”1 Individuals with SSD are preoccupied with symptom-related severity, experience high symptom-related anxiety, or devote significant time and energy to the symptoms or heath concerns. With a diagnosis of SSD, physical symptoms experienced by the patient may or may not be medically explained. The same symptom need not be continuously present as long as the overall symptomatic presentation lasts 6 months or longer.
The specifier “with predominant pain” is used when pain dominates the presentation.1 Estimated prevalence of SSD in primary care ranges from 5% to 35%.2 The true scope of SSD is difficult to assess accurately since research tends to focus on medically unexplained symptoms, rather than excessive symptom-related concerns. Furthermore, terms such as “medically unexplained symptoms” and “functional syndromes” (including fibromyalgia and irritable bowel syndrome) are frequently used when describing SSD.3
One or more factors may contribute to unexplained symptoms: limitations of medical procedures and techniques, partial clinical information, patients’ inability to follow management recommendations, challenges in differential diagnostics, and access-to-care limitations preventing regular care and appropriate diagnostic work up.
What’s important to remember is that it’s the patient’s reaction to physical symptoms, rather than the presence of symptoms per se, that defines SSD.
Considerations in the differential diagnosis
When making a diagnosis of SSD, symptoms cannot:4
- be feigned or deliberately produced as in malingering or factitious disorder.
- result from physiologic effects of a substance (eg, intoxication, withdrawal, or adverse medication effects).
- constitute somatic delusions, as occur in psychotic disorders.
- constitute symptoms or deficits affecting voluntary motor or sensory function that are better explained by neurologic, medical, or psychiatric conditions (consider conversion disorder).
- be preoccupations with physical appearance flaws, as in body dysmorphic disorder.
- be accounted for by an anxiety disorder (eg, palpitations associated with panic attacks).
Continue to: Illness anxiety disorder...
Illness anxiety disorder is also characterized by significant health-related concerns; however, physical symptoms are either mild or absent.
Possible causes of SSD are varied and complex, including genetic and biological factors, family dynamics, behavioral modeling/learning, personality traits, difficulties with emotional regulation, and awareness.5 Patients may present with ongoing requests for symptom explanations, feelings of helplessness, fear of having concerns dismissed, and low motivation for change.3
Aids in supporting a diagnosis of SSD
It’s not appropriate to rely solely on questionnaires to make the diagnosis of SSD. However, brief screening tools are a time-efficient way to capture patients’ experiences and perceptions.6 Along with other components of clinical evaluation, brief symptom screens can both support the diagnosis and help in longitudinal symptom assessment.
Patient Health Questionnaire-15 (PHQ-15), developed for self-report screening in primary care, has desirable psychometric properties including appropriate internal reliability; convergent validity with measures of functional status, disability days, and symptom-related burden; and discriminant validity from measures of depressive symptoms.7 The PHQ-15 is an open access tool that is available in several languages. The respondent is asked to rate the extent of being bothered by a range of medical symptoms in the proceeding 4 weeks. Total scores range from 0 to 30, with higher scores indicating greater symptom aggravation. Cutoffs of 5, 10, and 15 correspond to mild, moderate, and severe symptom levels.8
Somatic Symptom Disorder - B Criteria Scale (SSD-12) aims to capture SSD symptoms in line with Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnostic criteria. It assesses cognitive, affective, and behavioral aspects of SSD.9 The SSD-12 is copyrighted and its use requires registration and purchase. Cutoffs by age and gender are available. SSD-12 has demonstrated appropriate reliability and validity.9
Continue to: Structured Clinical Interview for DSM Disorders
Structured Clinical Interview for DSM Disorders (SCID)10,11 is perhaps the most rigorous differential diagnostic tool. However, SCID administration requires training and skill; time for administration and cost of the materials may be prohibitive in primary care.
Finally, SSD symptoms are highly associated with depression and anxiety. Ongoing elevated screening scores for anxiety and depression refractory to interventions may indicate the possibility of overlooked SSD. Furthermore, use of SSD screening tools with anxiety and depression screening tools can provide a more comprehensive picture of impairment, as well as symptom progress.
Treatment: Avoid a split approach
Diagnosing and treating SSD can be challenging for physicians who focus on biomedically based approaches in patient care. Additional tests, studies, and prescriptions are likely to fuel (rather than pacify) patients’ concerns, as such steps divert attention from the underlying psychological needs and mechanisms which maintain SSD. Avoid using a split biopsychosocial approach—ie, beginning the inquiry and treatment planning from a biomedical perspective, and then falling back on psychosocial formulation when treatment efforts have been ineffective. Such an approach leads to understandable patient dissatisfaction and can be interpreted by them as the caregiver suggesting that physical symptoms are “all in [their] head.”12
These 4 tips can help
1. Use a biopsychosocial formulation when initiating treatment. Be familiar with biopsychosocial factors in SSD and develop a narrative for discussing this formulation with patients. For example: “Mr. R, we are going to use the following [medical tests/studies/medications] to understand the cause of your symptoms and better manage them. We also need to think about the role of stress and distress in your symptoms because these can also be at play with dizziness.” This may be particularly beneficial for a functional disorder, such as chronic pain. Incorporating patient education resources is an important step toward shared understanding (see Hunter Integrated Pain Service for chronic pain educational videos; www.tga.gov.au/chronic-pain-management-video-resource-brainman13).
2. Combine education about pathophysiology with patient-centered interviewing. Significant SSD symptom improvements were noted following a single 30-minute educational session, while motivational interviewing techniques were used to probe patients’ concerns.2
Continue to: Maintain professionalism and good clinical practice
3. Maintain professionalism and good clinical practice. Consider SSD a medical matter and address it accordingly: explore concerns fully, provide evidence-based responses, communicate empathy, and employ objective management strategies.14
4. Do not overlook the value of the relationship. A recent systematic review concluded that the relationship between the patient and care provider was central to the success of the interventions for symptom reduction.15
A controversial approach. Pharmacotherapy for SSD is controversial. While several trials of antidepressants and St. John’s wort have been positive and some authors have stated that all classes of antidepressants are effective for SSD, others maintain that questions regarding dosing, treatment duration, and sustainability of improvement have not been sufficiently addressed in research.16,17
Coordination of care issues
Primary care continues to be the de facto mental health system, and specialty services may be unavailable or declined by patients.18 CBT delivered in person or online is empirically supported as a treatment approach to medically unexplained symptoms and SSD.17,19-22
A recent meta-analysis of randomized controlled trials published by Jing and colleagues23 reported that CBT was effective for SSD symptom reduction, and that treatment gains were maintained 3 to 12 months post treatment. However, concerns about the practical implementation of CBT in primary care were raised because CBT was not shown to be effective in improving social functioning or reducing the number of medical visits. Symptom improvement was maximized with longer durations of treatment (> 10 sessions) and greater session lengths (> 50 minutes). Additionally, Abbass and colleagues24 brought up several methodologic (sampling and analysis) concerns related to Jing et al’s work.
Continue to: Overally, CBT's effect sizes...
Overall, CBT’s effect sizes are small, and patients who are open to biopsychosocial explanations for their symptoms and to receiving psychological services may differ from most patients seen in primary care practices.21 Furthermore, mental health providers may hesitate to diagnose SSD because they are concerned about missing a somatic illness.3 Therefore, when coordinating care with mental health providers, it may be beneficial to discuss the treatment approach, assess familiarity with the SSD diagnosis, and closely coordinate and collaborate on the treatment plan.
While physicians cannot be expected to function as psychotherapists, an understanding of CBT and techniques for SSD treatment can be beneficial. Integrated mental health services may hold promise in addressing SSD in primary care. Onsite availability of a behavioral health provider competent in providing evidence-based care can target SSD symptoms and support both patients and physicians.
THE CASE
Mr. R’s treatment course included multiple primary care appointments (scheduled and walk in), ED visits, and specialist visits (ENT/vestibular rehabilitation). He sought care as symptoms intensified, lasted longer, or occurred in new circumstances. He reported persistent fear of the symptoms and anxiety that serious medical causes had been overlooked. He also described distress associated with vertigo and his anxiety sensitivity (anxiety about being anxious).
The behavioral health consultant (BHC; psychologist) and physician talked to the patient about the biopsychosocial antecedents of his condition and the factors that perpetuate the anxiety and stress response. The BHC described the fight/flight/freeze response to the patient and explained its role in the physiologic stress response associated with somatic symptoms and panic. Educational materials (videos and handouts) were also provided to the patient to further illustrate these concepts. The BHC also discussed the role of interoceptive and situational avoidance and active coping (eg, engaging in safe activities); taught the patient relaxation and grounding techniques; and used cognitive disputation aimed at challenging catastrophic symptom interpretations.
The BHC and the patient’s physician established joint treatment goals that included improving functioning, promoting active coping, and decreasing distress associated with symptoms. After the initial medical and BHC visits, both vertigo and anxiety symptoms appeared to abate somewhat, but symptoms have been ongoing and distress and impairment have been variable. The patient’s family physician and BHC continue to work with him to optimize the care plan and treatment goals.
CORRESPONDENCE
Nataliya Pilipenko, PhD, ABPP, Center for Family and Community Medicine, Columbia University Vagelos College of Physicians and Surgeons, 630 West 168th Street, New York, NY 10032; [email protected]
ACKNOWLEDGEMENT
The author thanks Dr. Molly Warren for her collaboration and guidance.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition (DSM-5). American Psychiatric Publishing; 2013.
2. Johnson KK, Bennett C, Rochani H. Significant improvement of somatic symptom disorder with brief psychoeducational intervention by PMHNP in primary care. J Am Psychiatr Nurses Assoc. 2020;28:171-180. doi: 10.1177/1078390320960524
3. Weigel A, Maehder K, Witt M, et al. Psychotherapists’ perspective on the treatment of patients with somatic symptom disorders. J Psychosom Res. 2020;138:110228. doi: 10.1016/j.jpsychores.2020.110228
4. American Psychiatric Association. Handbook of Differential Diagnosis. American Psychiatric Publishing; 2014;234-235.
5. Mayo Clinic. Somatic symptom disorder. Accessed February 21, 2022. www.mayoclinic.org/diseases-conditions/somatic-symptom-disorder/symptoms-causes/syc-20377776?p=1
6. Toussaint A, Riedl B, Kehrer S, et al. Validity of the Somatic Symptom Disorder-B Criteria Scale (SSD-12) in primary care. Fam Pract. 2018;35:342-347. doi: 10.1093/fampra/cmx116
7. Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258-66. doi: 10.1097/00006842-200203000-00008
8. Kroenke K, Spitzer RL, Williams JB, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345-359. doi: 10.1016/j.genhosppsych.2010.03.006
9. Toussaint A, Löwe B, Brähler E, et al. The Somatic Symptom Disorder - B Criteria Scale (SSD-12): factorial structure, validity and population-based norms. J Psychosom Res. 2017;97:9-17. doi: 10.1016/j.jpsychores.2017.03.017
10. First MB, Williams JBW, Karg RS, Spitzer RL, eds. Structured Clinical Interview for DSM-5 Disorders, Research Version. American Psychiatric Association, 2015.
11. First MB, Williams JBW, Karg RS, Spitzer RL, eds. Structured Clinical Interview for DSM-5 Disorders, Clinician Version. American Psychiatric Publishing; 2016.
12. McDaniel SH, Hepworth J, Campbell TL, et al, eds. Family Oriented Primary Care. Springer Publishing Co; 2005:1-15.
13. Hunter Integrated Pain Service (2016). Brainman videos. Hunter New England Local Health District. New South Wales, Australia. Accessed February 21, 2022. www.tga.gov.au/chronic-pain-management-video-resource-brainman
14. Murray AM, Toussaint A, Althaus A, et al. The challenge of diagnosing non-specific, functional, and somatoform disorders: a systematic review of barriers to diagnosis in primary care. J Psychosom Res. 2016;80:1-10. doi: 10.1016/j.jpsychores.2015.11.002
15. Leaviss J, Davis S, Ren S, et al. Behavioral modification interventions for medically unexplained symptoms in primary care: systematic reviews and economic evaluation. Health Technol Assess. 2020;24:1-490. doi: 10.3310/hta24460
16. Kroenke K. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007;69:881-888. doi: 10.1097/PSY.0b013e31815b00c4
17. Steinbrecher N, Koerber S, Frieser D, et al. The prevalence of medically unexplained symptoms in primary care. Psychosomatics. 2011;52:263-271. doi: 10.1016/j.psym.2011.01.007
18. Kessler R, Stafford D. Primary care is the de facto mental health system. In Kessler R, Stafford D, eds. Collaborative Medicine Case Studies: Evidence in Practice. Springer Publishing Co, 2008; 9-21.
19. Barsky AJ, Ahern DK, Bauer MR, et al. A randomized trial of treatments for high-utilizing somatizing patients. J Gen Intern Med. 2013;28:1396-1404. doi: 10.1007/s11606-013-2392-6
20. Newby JM, Smith J, Uppal S, et al. Internet-based cognitive behavioral therapy versus psychoeducation control for illness anxiety disorder and somatic symptom disorder: A randomized controlled trial. J Consult Clin Psychol. 2018;86:89-98. doi: 10.1037/ccp0000248
21. van Dessel N, den Boeft M, van der Wouden JC, et al. Non-pharmacological interventions for somatoform disorders and medically unexplained physical symptoms (MUPS) in adults. Cochrane Database Syst Rev. 2014(11):CD011142. doi: 10.1002/14651858.CD011142.pub2
22. Verdurmen MJ, Videler AC, Kamperman AM, et al. Cognitive behavioral therapy for somatic symptom disorders in later life: a prospective comparative explorative pilot study in two clinical populations. Neuropsychiatr Dis Treat. 2017;13:2331-2339. doi: 10.2147/NDT.S141208
23. Liu J, Gill NS, Teodorczuk A, et al. The efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;245:98-112. doi: 10.1016/j.jad.2018.10.114
24. Abbass A, Leichsenring F, Steinert C. Re: Jing et al., the efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;255:S0165-0327(18)33197-5. doi: 10.1016/j.jad.2019.02.055
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition (DSM-5). American Psychiatric Publishing; 2013.
2. Johnson KK, Bennett C, Rochani H. Significant improvement of somatic symptom disorder with brief psychoeducational intervention by PMHNP in primary care. J Am Psychiatr Nurses Assoc. 2020;28:171-180. doi: 10.1177/1078390320960524
3. Weigel A, Maehder K, Witt M, et al. Psychotherapists’ perspective on the treatment of patients with somatic symptom disorders. J Psychosom Res. 2020;138:110228. doi: 10.1016/j.jpsychores.2020.110228
4. American Psychiatric Association. Handbook of Differential Diagnosis. American Psychiatric Publishing; 2014;234-235.
5. Mayo Clinic. Somatic symptom disorder. Accessed February 21, 2022. www.mayoclinic.org/diseases-conditions/somatic-symptom-disorder/symptoms-causes/syc-20377776?p=1
6. Toussaint A, Riedl B, Kehrer S, et al. Validity of the Somatic Symptom Disorder-B Criteria Scale (SSD-12) in primary care. Fam Pract. 2018;35:342-347. doi: 10.1093/fampra/cmx116
7. Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258-66. doi: 10.1097/00006842-200203000-00008
8. Kroenke K, Spitzer RL, Williams JB, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345-359. doi: 10.1016/j.genhosppsych.2010.03.006
9. Toussaint A, Löwe B, Brähler E, et al. The Somatic Symptom Disorder - B Criteria Scale (SSD-12): factorial structure, validity and population-based norms. J Psychosom Res. 2017;97:9-17. doi: 10.1016/j.jpsychores.2017.03.017
10. First MB, Williams JBW, Karg RS, Spitzer RL, eds. Structured Clinical Interview for DSM-5 Disorders, Research Version. American Psychiatric Association, 2015.
11. First MB, Williams JBW, Karg RS, Spitzer RL, eds. Structured Clinical Interview for DSM-5 Disorders, Clinician Version. American Psychiatric Publishing; 2016.
12. McDaniel SH, Hepworth J, Campbell TL, et al, eds. Family Oriented Primary Care. Springer Publishing Co; 2005:1-15.
13. Hunter Integrated Pain Service (2016). Brainman videos. Hunter New England Local Health District. New South Wales, Australia. Accessed February 21, 2022. www.tga.gov.au/chronic-pain-management-video-resource-brainman
14. Murray AM, Toussaint A, Althaus A, et al. The challenge of diagnosing non-specific, functional, and somatoform disorders: a systematic review of barriers to diagnosis in primary care. J Psychosom Res. 2016;80:1-10. doi: 10.1016/j.jpsychores.2015.11.002
15. Leaviss J, Davis S, Ren S, et al. Behavioral modification interventions for medically unexplained symptoms in primary care: systematic reviews and economic evaluation. Health Technol Assess. 2020;24:1-490. doi: 10.3310/hta24460
16. Kroenke K. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007;69:881-888. doi: 10.1097/PSY.0b013e31815b00c4
17. Steinbrecher N, Koerber S, Frieser D, et al. The prevalence of medically unexplained symptoms in primary care. Psychosomatics. 2011;52:263-271. doi: 10.1016/j.psym.2011.01.007
18. Kessler R, Stafford D. Primary care is the de facto mental health system. In Kessler R, Stafford D, eds. Collaborative Medicine Case Studies: Evidence in Practice. Springer Publishing Co, 2008; 9-21.
19. Barsky AJ, Ahern DK, Bauer MR, et al. A randomized trial of treatments for high-utilizing somatizing patients. J Gen Intern Med. 2013;28:1396-1404. doi: 10.1007/s11606-013-2392-6
20. Newby JM, Smith J, Uppal S, et al. Internet-based cognitive behavioral therapy versus psychoeducation control for illness anxiety disorder and somatic symptom disorder: A randomized controlled trial. J Consult Clin Psychol. 2018;86:89-98. doi: 10.1037/ccp0000248
21. van Dessel N, den Boeft M, van der Wouden JC, et al. Non-pharmacological interventions for somatoform disorders and medically unexplained physical symptoms (MUPS) in adults. Cochrane Database Syst Rev. 2014(11):CD011142. doi: 10.1002/14651858.CD011142.pub2
22. Verdurmen MJ, Videler AC, Kamperman AM, et al. Cognitive behavioral therapy for somatic symptom disorders in later life: a prospective comparative explorative pilot study in two clinical populations. Neuropsychiatr Dis Treat. 2017;13:2331-2339. doi: 10.2147/NDT.S141208
23. Liu J, Gill NS, Teodorczuk A, et al. The efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;245:98-112. doi: 10.1016/j.jad.2018.10.114
24. Abbass A, Leichsenring F, Steinert C. Re: Jing et al., the efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;255:S0165-0327(18)33197-5. doi: 10.1016/j.jad.2019.02.055
Denosumab boosts bone strength in glucocorticoid users
Bone strength and microarchitecture remained stronger at 24 months after treatment with denosumab compared to risedronate, in a study of 110 adults using glucocorticoids.
Patients using glucocorticoids are at increased risk for vertebral and nonvertebral fractures at both the start of treatment or as treatment continues, wrote Piet Geusens, MD, of Maastricht University, the Netherlands, and colleagues.
Imaging data collected via high-resolution peripheral quantitative computed tomography (HR-pQCT) allow for the assessment of bone microarchitecture and strength, but specific data comparing the impact of bone treatment in patients using glucocorticoids are lacking, they said.
In a study published in the Journal of Bone and Mineral Research, the researchers identified a subset of 56 patients randomized to denosumab and 54 to risedronate patients out of a total of 590 patients who were enrolled in a phase 3 randomized, controlled trial of denosumab vs. risedronate for bone mineral density. The main results of the larger trial – presented at EULAR 2018 – showed greater increases in bone strength with denosumab over risedronate in patients receiving glucocorticoids.
In the current study, the researchers reviewed HR-pQCT scans of the distal radius and tibia at baseline, 12 months, and 24 months. Bone strength and microarchitecture were defined in terms of failure load (FL) as a primary outcome. Patients also were divided into subpopulations of those initiating glucocorticoid treatment (GC-I) and continuing treatment (GC-C).
Baseline characteristics were mainly balanced among the treatment groups within the GC-I and GC-C categories.
Among the GC-I patients, in the denosumab group, FL increased significantly from baseline to 12 months at the radius at tibia (1.8% and 1.7%, respectively) but did not change significantly in the risedronate group, which translated to a significant treatment difference between the drugs of 3.3% for radius and 2.5% for tibia.
At 24 months, the radius measure of FL was unchanged from baseline in denosumab patients but significantly decreased in risedronate patients, with a difference of –4.1%, which translated to a significant between-treatment difference at the radius of 5.6% (P < .001). Changes at the tibia were not significantly different between the groups at 24 months.
Among the GC-C patients, FL was unchanged from baseline to 12 months for both the denosumab and risedronate groups. However, FL significantly increased with denosumab (4.3%) and remained unchanged in the risedronate group.
The researchers also found significant differences between denosumab and risedronate in percentage changes in cortical bone mineral density, and less prominent changes and differences in trabecular bone mineral density.
The study findings were limited by several factors including the use of the HR-pQCT scanner, which limits the measurement of trabecular microarchitecture, and the use of only standard HR-pQCT parameters, which do not allow insight into endosteal changes, and the inability to correct for multiplicity of data, the researchers noted.
However, the results support the superiority of denosumab over risedronate for preventing FL and total bone mineral density loss at the radius and tibia in new glucocorticoid users, and for increasing FL and total bone mineral density at the radius in long-term glucocorticoid users, they said.
Denosumab therefore could be a useful therapeutic option and could inform decision-making in patients initiating GC-therapy or on long-term GC-therapy, they concluded.
The study was supported by Amgen. Dr. Geusens disclosed grants from Amgen, Celgene, Lilly, Merck, Pfizer, Roche, UCB, Fresenius, Mylan, and Sandoz, and grants and other funding from AbbVie, outside the current study.
Bone strength and microarchitecture remained stronger at 24 months after treatment with denosumab compared to risedronate, in a study of 110 adults using glucocorticoids.
Patients using glucocorticoids are at increased risk for vertebral and nonvertebral fractures at both the start of treatment or as treatment continues, wrote Piet Geusens, MD, of Maastricht University, the Netherlands, and colleagues.
Imaging data collected via high-resolution peripheral quantitative computed tomography (HR-pQCT) allow for the assessment of bone microarchitecture and strength, but specific data comparing the impact of bone treatment in patients using glucocorticoids are lacking, they said.
In a study published in the Journal of Bone and Mineral Research, the researchers identified a subset of 56 patients randomized to denosumab and 54 to risedronate patients out of a total of 590 patients who were enrolled in a phase 3 randomized, controlled trial of denosumab vs. risedronate for bone mineral density. The main results of the larger trial – presented at EULAR 2018 – showed greater increases in bone strength with denosumab over risedronate in patients receiving glucocorticoids.
In the current study, the researchers reviewed HR-pQCT scans of the distal radius and tibia at baseline, 12 months, and 24 months. Bone strength and microarchitecture were defined in terms of failure load (FL) as a primary outcome. Patients also were divided into subpopulations of those initiating glucocorticoid treatment (GC-I) and continuing treatment (GC-C).
Baseline characteristics were mainly balanced among the treatment groups within the GC-I and GC-C categories.
Among the GC-I patients, in the denosumab group, FL increased significantly from baseline to 12 months at the radius at tibia (1.8% and 1.7%, respectively) but did not change significantly in the risedronate group, which translated to a significant treatment difference between the drugs of 3.3% for radius and 2.5% for tibia.
At 24 months, the radius measure of FL was unchanged from baseline in denosumab patients but significantly decreased in risedronate patients, with a difference of –4.1%, which translated to a significant between-treatment difference at the radius of 5.6% (P < .001). Changes at the tibia were not significantly different between the groups at 24 months.
Among the GC-C patients, FL was unchanged from baseline to 12 months for both the denosumab and risedronate groups. However, FL significantly increased with denosumab (4.3%) and remained unchanged in the risedronate group.
The researchers also found significant differences between denosumab and risedronate in percentage changes in cortical bone mineral density, and less prominent changes and differences in trabecular bone mineral density.
The study findings were limited by several factors including the use of the HR-pQCT scanner, which limits the measurement of trabecular microarchitecture, and the use of only standard HR-pQCT parameters, which do not allow insight into endosteal changes, and the inability to correct for multiplicity of data, the researchers noted.
However, the results support the superiority of denosumab over risedronate for preventing FL and total bone mineral density loss at the radius and tibia in new glucocorticoid users, and for increasing FL and total bone mineral density at the radius in long-term glucocorticoid users, they said.
Denosumab therefore could be a useful therapeutic option and could inform decision-making in patients initiating GC-therapy or on long-term GC-therapy, they concluded.
The study was supported by Amgen. Dr. Geusens disclosed grants from Amgen, Celgene, Lilly, Merck, Pfizer, Roche, UCB, Fresenius, Mylan, and Sandoz, and grants and other funding from AbbVie, outside the current study.
Bone strength and microarchitecture remained stronger at 24 months after treatment with denosumab compared to risedronate, in a study of 110 adults using glucocorticoids.
Patients using glucocorticoids are at increased risk for vertebral and nonvertebral fractures at both the start of treatment or as treatment continues, wrote Piet Geusens, MD, of Maastricht University, the Netherlands, and colleagues.
Imaging data collected via high-resolution peripheral quantitative computed tomography (HR-pQCT) allow for the assessment of bone microarchitecture and strength, but specific data comparing the impact of bone treatment in patients using glucocorticoids are lacking, they said.
In a study published in the Journal of Bone and Mineral Research, the researchers identified a subset of 56 patients randomized to denosumab and 54 to risedronate patients out of a total of 590 patients who were enrolled in a phase 3 randomized, controlled trial of denosumab vs. risedronate for bone mineral density. The main results of the larger trial – presented at EULAR 2018 – showed greater increases in bone strength with denosumab over risedronate in patients receiving glucocorticoids.
In the current study, the researchers reviewed HR-pQCT scans of the distal radius and tibia at baseline, 12 months, and 24 months. Bone strength and microarchitecture were defined in terms of failure load (FL) as a primary outcome. Patients also were divided into subpopulations of those initiating glucocorticoid treatment (GC-I) and continuing treatment (GC-C).
Baseline characteristics were mainly balanced among the treatment groups within the GC-I and GC-C categories.
Among the GC-I patients, in the denosumab group, FL increased significantly from baseline to 12 months at the radius at tibia (1.8% and 1.7%, respectively) but did not change significantly in the risedronate group, which translated to a significant treatment difference between the drugs of 3.3% for radius and 2.5% for tibia.
At 24 months, the radius measure of FL was unchanged from baseline in denosumab patients but significantly decreased in risedronate patients, with a difference of –4.1%, which translated to a significant between-treatment difference at the radius of 5.6% (P < .001). Changes at the tibia were not significantly different between the groups at 24 months.
Among the GC-C patients, FL was unchanged from baseline to 12 months for both the denosumab and risedronate groups. However, FL significantly increased with denosumab (4.3%) and remained unchanged in the risedronate group.
The researchers also found significant differences between denosumab and risedronate in percentage changes in cortical bone mineral density, and less prominent changes and differences in trabecular bone mineral density.
The study findings were limited by several factors including the use of the HR-pQCT scanner, which limits the measurement of trabecular microarchitecture, and the use of only standard HR-pQCT parameters, which do not allow insight into endosteal changes, and the inability to correct for multiplicity of data, the researchers noted.
However, the results support the superiority of denosumab over risedronate for preventing FL and total bone mineral density loss at the radius and tibia in new glucocorticoid users, and for increasing FL and total bone mineral density at the radius in long-term glucocorticoid users, they said.
Denosumab therefore could be a useful therapeutic option and could inform decision-making in patients initiating GC-therapy or on long-term GC-therapy, they concluded.
The study was supported by Amgen. Dr. Geusens disclosed grants from Amgen, Celgene, Lilly, Merck, Pfizer, Roche, UCB, Fresenius, Mylan, and Sandoz, and grants and other funding from AbbVie, outside the current study.
FROM THE JOURNAL OF BONE AND MINERAL RESEARCH
Outcomes After Injection-Based Therapy: A Pain Outcomes Questionnaire for Veterans Univariate Analysis
Chronic pain is persistent or recurring pain lasting more than 3 months past normal healing time. Primary care professionals usually refer patients experiencing chronic pain to pain specialists to better identify, treat, and manage the pain. Chronic noncancer-related pain affects more Americans than diabetes mellitus, cardiac disease, and cancer combined.1 Veterans are no exception. The prevalence of severe pain was significantly higher in veterans compared with that of nonveterans who had back pain (21.6 vs 16.7%, respectively), jaw pain (37.5 vs 22.9%, respectively), severe headaches or migraine (26.4 vs 15.9%, respectively), and neck pain (27.7 vs 21.4%, respectively).2 At an individual level, those who experience chronic pain can expect impaired functional capacity, reduced ability to work, sleep disturbance, reduced social interactions, and considerable psychological distress. At a societal level, the cost of treating chronic pain is exorbitant, exceeding $600 billion annually, yet treatment outcomes remain variable at best.3 Greater efforts are needed to improve and standardize patient outcomes.
Interventional pain procedures performed under fluoroscopic or ultrasound guidance by specialist physicians have shown mixed responses in previous studies. Past systematic reviews demonstrate reductions in pain scores after lumbar or caudal epidural steroid injections (ESIs) and radiofrequency ablation of nerves supplying lumbar and thoracic facet joints.4-7 However, one review found insufficient evidence to support injection therapy for chronic low back pain.8 Unfortunately, the majority of the included studies evaluated outcomes using the visual analogue scale (VAS) or other limited factors, such as physical examination findings. Current biopsychosocial conceptualizations of chronic pain are beginning to recognize the complex nature of the experience of pain and highlighting the significance of multimodal management.9 It is vital that our assessment of chronic pain, like our treatment options, be multidimensional and reflect these underpinning principles.
The Pain Outcomes Questionnaire-For Veterans (POQ-VA) was developed within the Veterans Health Administration (VHA) by Clark and colleagues in 2003. It represents a brief but psychometrically sound pain outcomes instrument that assesses all key domains and meets accreditation body standards. The POQ-VA is valid and reliable for evaluating effectiveness of treatment of chronic noncancer pain in veterans in routine clinical practice.10 This review is the first study to use the POQ-VA to assess the impact of interventional pain procedures on veterans with chronic noncancer pain.
The aim of this study was to perform a retrospective review of POQ-VA scores before and after injection-based interventional treatment for chronic pain to determine whether the procedure affected patient outcomes. We hypothesized that POQ-VA scores would improve across multiple domains in the veteran population postprocedure. This study was approved by the Institutional Review Board (IRB-2018-053) at the Providence Veterans Affairs Medical Center (VAMC) in Rhode Island.
Methods
Using the Computerized Patient Record System, all adult veteran patients who had attended at least 2 appointments between April 1, 2009, and April 1, 2019 at the Providence VAMC interventional pain clinic were identified. POQ-VA reports were extracted provided the following criteria were met: (1) the veteran received an injection-based interventional treatment for chronic pain, including trigger point injections, ESIs, nerve blocks, and radiofrequency ablations; (2) the veteran completed POQ-VA both pre- and posttreatment; and (3) posttreatment POQ-VA reports were completed within 6 months of treatment. All patients who did not fit these criteria were excluded from the study.
After deidentification, 112 pre- and posttreatment POQ-VA reports were identified. All subsequent statistical analyses were conducted using Stata SE version 15. Descriptive statistics including mean, range, SD, and percent change were computed for POQ-VA domain—pain, mobility, activities of daily living (ADL), vitality, negative affect, fear, and total raw score—as well as for each POQ-VA question. Given that POQ-VA domain scores were found to be approximately normally distributed without outliers, domain scores were treated as continuous variables, and a paired samples t test was conducted to compare means among POQ-VA domains. Individual question responses were analyzed using nonparametric testing methods to account for the lack of normal distribution in each question, treating the range of 0 to 10 as an ordinal variable. A Wilcoxon matched-pairs signed-rank test was conducted to compare means among individual question responses before and after treatment.
Results
Of 112 included patients, 102 (91%) were male and 10 (9%) were female. The mean age was 62 years (range, 35-90). Diagnosis and procedures varied due to patient symptoms varying from muscle pain, nerve pain, degenerative disc disease, and osteoarthritis.
POQ-VA scores across all domains, including total raw score, showed statistically significant improvement after treatment (Table 1). Directionally, the POQ-VA scores for all 20 questions reflect a positive treatment response and 17 had statistically significant changes (P < .05) (Table 2). The changes in self-perceived energy level, safety, and feelings of tension were not statistically significant. Esteem had the greatest magnitude decrease, falling from 5.2 preprocedure to 3.8 postprocedure (P < .001). Other similarly significant magnitudes of improvement were seen from pre- to postprocedure in questions pertaining to grooming (2.2 to 1.6, P = .003) and the ability to use the bathroom (3.4 to 2.6, P < .001).
Discussion
The most important finding of this study was the ability of the POQ-VA to detect statistically significant positive responses to injection therapy across all domains. The largest improvements were in self-reported pain intensity, pain-related impairment in mobility and ADLs, and self-reported dysphoric effects. The single largest improvement posttreatment was a reduction in scores related to low self-esteem.
Chronic pain can be assessed in a variety of ways ranging from physical examination findings and subjective numerical ratings to extensive patient-reported questionnaires. The International Association for the Study of Pain acknowledges that pain is a complex experience and recommends assessment should be comprehensive.11 Many patient-reported questionnaires are available to clinicians, including some that address pain in a specific body part, such as the Oswestry Low Back Pain Disability Questionnaire, or those that focus on depression or quality-of-life measures, such as the SF-36.12,13
One major benefit of using the POQ-VA is its potential to demonstrate benefits across multiple domains, reflecting the complex nature of chronic pain. The POQ-VA also separates domain or scale scores, allowing clinicians to identify individuals with different patterns of dysfunction across domains.10 This separation also provides insight into which treatment options are best for chronic pain patients with predominant patterns or lower scores in certain domains. The use of a single summary score, as seen in other questionnaires such as the Roland-Morris Activity Scale, may conceal treatment-induced changes in specific outcome domains.14 Additionally, like many other similar instruments, the POQ-VA is easy to understand and use, requires no special training, takes little time to complete, and can be completed in person or over the phone.
As chronic pain has been studied further and its complexity recognized, more instruments have been developed and modified to reflect these new elements. There is no one scale applicable to all populations. A discussion about the strengths and weaknesses of each available assessment tool is outside the scope of this review. However, to date, the POQ-VA is the only instrument that has been validated to detect change following treatment of chronic pain in an exclusively veteran population.10 This validation emphasizes the importance of this study as it supports the use of this outcome measure to monitor treatment of pain in VA facilities.
One of the secondary findings indicated that injection therapy improved veterans’ physical activity levels and self-esteem and lowered pain scores as well as kinesiophobia and anxiety. The role of interventional procedures has been well established in the field of chronic pain, but their efficacy has been less clear. Injections are costly and not without risk, and these factors relegate them to fourth-line treatment options in most situations.15 Several meta-analyses have demonstrated small improvements in pain scores and patient-reported questionnaires after medial branch blocks, and lumbar or caudal ESIs for chronic back pain.5-7 However, an updated Cochrane Review concluded that there was insufficient evidence to support the use of injection therapy in subacute and chronic low back pain.8 The review acknowledged the limited methodologic quality of the trials and could not definitively report that injection therapy did not have benefits for certain subgroups of patients. The ability of researchers to detect benefit from an intervention is intrinsically linked to how outcomes are determined. The most interesting finding of our study was the patient-reported improved self-esteem scores. Many trials included in the systematic reviews discussed used outcome measures that did not have the multidimensional scope to demonstrate such a potential benefit.
Limitations
Our relatively small sample size represents the main shortcoming of this study. Because many posttreatment questionnaires were never collected, unfortunately, much potential data was lost. Most procedures performed were corticosteroid injections for the treatment of low back pain. This represented a combination of lumbar ESI, caudal ESI, medial branch blocks, and sacroiliac joint injections. The limited numbers meant that a further regression analysis of each injection type was not possible. Since few interventions treated pain in other areas of the body, it is difficult to determine whether procedures such as hip joint injections and ilioinguinal nerve blocks provided overall benefit. In the same vein, there is an inability to comment on which injection for chronic low back pain was the most efficacious.
The veteran population, while similar to the general population experiencing chronic pain, is more likely to experience PTSD and other mental health conditions.2 According to medical literature, no randomized controlled trials have been published examining pain interventions exclusively in veterans, so the applicability of these results needs further investigation. This study suggests there are potential benefits for the veteran population, not solely perhaps from receiving injection therapy, but to having access to an interventional pain clinic led by a pain physician within a network of other specialties. While limited by the inherent biases of a retrospective review, this study highlights the potential value in continuing to study this subgroup of patients, especially in the setting of an interdisciplinary approach.
Recent literature suggests interdisciplinary chronic pain management represents the best outcomes for patients’ physical, emotional, and social health, though these kinds of focused outpatient programs have not been studied on a large scale.16 The evolution of pain management in recent years to incorporating a biopsychosocial model has revolutionized how pain is treated and assessed, with multiple studies suggesting the greatest benefits lie in a multipronged approach.16,17 Past studies assessing individual interventions for chronic pain tend not to show strongly positive results, further reinforcing the idea that the answer does not lie in a specific treatment. Many veterans who were included in this study possibly had received or were receiving adjunct therapies such as physical therapy, cognitive behavioral therapy, and acupuncture for pain management, as well as oral and topical medications. Unfortunately, due to the selected methodology, it was not possible for us to gather those data. In turn, we were unable to determine how much these additional factors played a role in changing patient scores, alongside injection therapy. This inability to control variables in this type of research continues to present a challenge to data interpretation, even in the highest quality of research, as acknowledged by Staal and colleagues.8
Future research may be best focused by expanding our knowledge of outpatient interdisciplinary pain management programs. Some interventions may be more relevant for a particular group within a program, and this information can be useful to direct resources.18 Future prospects will require an appropriate multidimensional assessment tool, and the POQ-VA is an example of a valid and reliable option for monitoring progress in pain management in the veteran population.
Conclusions
The POQ-VA is the only instrument to date that has been validated to detect change following treatment of chronic pain in an exclusively veteran population. Our study is the first univariate analysis since the instrument’s validation in 2003. Our descriptive and inferential statistics suggest that the majority of veterans undergoing injection therapy for chronic pain had statistically significant improvements in POQ-VA measures within a 6-month period following treatment. In order to conduct more rigorous, multivariate studies, continued and more widespread use of the POQ-VA instrument is warranted.
1. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11(11):1230-1239. doi:10.1016/j.jpain.2010.07.002
2. Nahin RL. Severe Pain in Veterans: The effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254. doi:10.1016/j.jpain.2016.10.021
3. Witkin LR, Farrar JT, Ashburn MA. Can assessing chronic pain outcomes data improve outcomes?. Pain Med. 2013;14(6):779-791. doi:10.1111/pme.12075
4. Benyamin RM, Manchikanti L, Parr AT, et al. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012;15(4):E363-E404.
5. Zhai J, Zhang L, Li M, et al. Epidural injection with or without steroid in managing chronic low-back and lower extremity pain: a meta-analysis of 10 randomized controlled trials. Am J Ther. 2017;24(3):e259-e269. doi:10.1097/MJT.0000000000000265
6. Parr AT, Manchikanti L, Hameed H, et al. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Physician. 2012;15(3):E159-E198.
7. Lee CH, Chung CK, Kim CH. The efficacy of conventional radiofrequency denervation in patients with chronic low back pain originating from the facet joints: a meta-analysis of randomized controlled trials. Spine J. 2017;17(11):1770-1780. doi:10.1016/j.spinee.2017.05.006
8. Staal JB, de Bie R, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low-back pain. Cochrane Database Syst Rev. 2008;2008(3):CD001824. Published 2008 Jul 16. doi:10.1002/14651858.CD001824.pub3
9. Gironda RJ, Clark ME. Cluster analysis of the pain outcomes questionnaire. Pain Med. 2008;9(7):813-823. doi:10.1111/j.1526-4637.2007.00397.x
10. Clark ME, Gironda RJ, Young RW. Development and validation of the Pain Outcomes Questionnaire-VA. J Rehabil Res Dev. 2003;40(5):381-395. doi:10.1682/jrrd.2003.09.0381
11. Watt-Watson J, McGillion M, Lax L, et al. Evaluating an Innovative eLearning Pain Education Interprofessional Resource: A Pre-Post Study. Pain Med. 2019;20(1):37-49. doi:10.1093/pm/pny105
12. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271-273.
13. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473-483.
14. Jensen MP, Strom SE, Turner JA, Romano JM. Validity of the Sickness Impact Profile Roland scale as a measure of dysfunction in chronic pain patients. Pain. 1992;50(2):157-162. doi:10.1016/0304-3959(92)90156-6
15. Hylands-White N, Duarte RV, Raphael JH. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2017;37(1):29-42. doi:10.1007/s00296-016-3481-8
16. Bujak BK, Regan E, Beattie PF, Harrington S. The effectiveness of interdisciplinary intensive outpatient programs in a population with diverse chronic pain conditions: a systematic review and meta-analysis. Pain Manag. 2019;9(4):417-429. doi:10.2217/pmt-2018-0087
17. Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2002;(1):CD000963. doi:10.1002/14651858.CD000963
18. Wilson IR. Management of chronic pain through pain management programmes. Br Med Bull. 2017;124(1):55-64. doi:10.1093/bmb/ldx032
Chronic pain is persistent or recurring pain lasting more than 3 months past normal healing time. Primary care professionals usually refer patients experiencing chronic pain to pain specialists to better identify, treat, and manage the pain. Chronic noncancer-related pain affects more Americans than diabetes mellitus, cardiac disease, and cancer combined.1 Veterans are no exception. The prevalence of severe pain was significantly higher in veterans compared with that of nonveterans who had back pain (21.6 vs 16.7%, respectively), jaw pain (37.5 vs 22.9%, respectively), severe headaches or migraine (26.4 vs 15.9%, respectively), and neck pain (27.7 vs 21.4%, respectively).2 At an individual level, those who experience chronic pain can expect impaired functional capacity, reduced ability to work, sleep disturbance, reduced social interactions, and considerable psychological distress. At a societal level, the cost of treating chronic pain is exorbitant, exceeding $600 billion annually, yet treatment outcomes remain variable at best.3 Greater efforts are needed to improve and standardize patient outcomes.
Interventional pain procedures performed under fluoroscopic or ultrasound guidance by specialist physicians have shown mixed responses in previous studies. Past systematic reviews demonstrate reductions in pain scores after lumbar or caudal epidural steroid injections (ESIs) and radiofrequency ablation of nerves supplying lumbar and thoracic facet joints.4-7 However, one review found insufficient evidence to support injection therapy for chronic low back pain.8 Unfortunately, the majority of the included studies evaluated outcomes using the visual analogue scale (VAS) or other limited factors, such as physical examination findings. Current biopsychosocial conceptualizations of chronic pain are beginning to recognize the complex nature of the experience of pain and highlighting the significance of multimodal management.9 It is vital that our assessment of chronic pain, like our treatment options, be multidimensional and reflect these underpinning principles.
The Pain Outcomes Questionnaire-For Veterans (POQ-VA) was developed within the Veterans Health Administration (VHA) by Clark and colleagues in 2003. It represents a brief but psychometrically sound pain outcomes instrument that assesses all key domains and meets accreditation body standards. The POQ-VA is valid and reliable for evaluating effectiveness of treatment of chronic noncancer pain in veterans in routine clinical practice.10 This review is the first study to use the POQ-VA to assess the impact of interventional pain procedures on veterans with chronic noncancer pain.
The aim of this study was to perform a retrospective review of POQ-VA scores before and after injection-based interventional treatment for chronic pain to determine whether the procedure affected patient outcomes. We hypothesized that POQ-VA scores would improve across multiple domains in the veteran population postprocedure. This study was approved by the Institutional Review Board (IRB-2018-053) at the Providence Veterans Affairs Medical Center (VAMC) in Rhode Island.
Methods
Using the Computerized Patient Record System, all adult veteran patients who had attended at least 2 appointments between April 1, 2009, and April 1, 2019 at the Providence VAMC interventional pain clinic were identified. POQ-VA reports were extracted provided the following criteria were met: (1) the veteran received an injection-based interventional treatment for chronic pain, including trigger point injections, ESIs, nerve blocks, and radiofrequency ablations; (2) the veteran completed POQ-VA both pre- and posttreatment; and (3) posttreatment POQ-VA reports were completed within 6 months of treatment. All patients who did not fit these criteria were excluded from the study.
After deidentification, 112 pre- and posttreatment POQ-VA reports were identified. All subsequent statistical analyses were conducted using Stata SE version 15. Descriptive statistics including mean, range, SD, and percent change were computed for POQ-VA domain—pain, mobility, activities of daily living (ADL), vitality, negative affect, fear, and total raw score—as well as for each POQ-VA question. Given that POQ-VA domain scores were found to be approximately normally distributed without outliers, domain scores were treated as continuous variables, and a paired samples t test was conducted to compare means among POQ-VA domains. Individual question responses were analyzed using nonparametric testing methods to account for the lack of normal distribution in each question, treating the range of 0 to 10 as an ordinal variable. A Wilcoxon matched-pairs signed-rank test was conducted to compare means among individual question responses before and after treatment.
Results
Of 112 included patients, 102 (91%) were male and 10 (9%) were female. The mean age was 62 years (range, 35-90). Diagnosis and procedures varied due to patient symptoms varying from muscle pain, nerve pain, degenerative disc disease, and osteoarthritis.
POQ-VA scores across all domains, including total raw score, showed statistically significant improvement after treatment (Table 1). Directionally, the POQ-VA scores for all 20 questions reflect a positive treatment response and 17 had statistically significant changes (P < .05) (Table 2). The changes in self-perceived energy level, safety, and feelings of tension were not statistically significant. Esteem had the greatest magnitude decrease, falling from 5.2 preprocedure to 3.8 postprocedure (P < .001). Other similarly significant magnitudes of improvement were seen from pre- to postprocedure in questions pertaining to grooming (2.2 to 1.6, P = .003) and the ability to use the bathroom (3.4 to 2.6, P < .001).
Discussion
The most important finding of this study was the ability of the POQ-VA to detect statistically significant positive responses to injection therapy across all domains. The largest improvements were in self-reported pain intensity, pain-related impairment in mobility and ADLs, and self-reported dysphoric effects. The single largest improvement posttreatment was a reduction in scores related to low self-esteem.
Chronic pain can be assessed in a variety of ways ranging from physical examination findings and subjective numerical ratings to extensive patient-reported questionnaires. The International Association for the Study of Pain acknowledges that pain is a complex experience and recommends assessment should be comprehensive.11 Many patient-reported questionnaires are available to clinicians, including some that address pain in a specific body part, such as the Oswestry Low Back Pain Disability Questionnaire, or those that focus on depression or quality-of-life measures, such as the SF-36.12,13
One major benefit of using the POQ-VA is its potential to demonstrate benefits across multiple domains, reflecting the complex nature of chronic pain. The POQ-VA also separates domain or scale scores, allowing clinicians to identify individuals with different patterns of dysfunction across domains.10 This separation also provides insight into which treatment options are best for chronic pain patients with predominant patterns or lower scores in certain domains. The use of a single summary score, as seen in other questionnaires such as the Roland-Morris Activity Scale, may conceal treatment-induced changes in specific outcome domains.14 Additionally, like many other similar instruments, the POQ-VA is easy to understand and use, requires no special training, takes little time to complete, and can be completed in person or over the phone.
As chronic pain has been studied further and its complexity recognized, more instruments have been developed and modified to reflect these new elements. There is no one scale applicable to all populations. A discussion about the strengths and weaknesses of each available assessment tool is outside the scope of this review. However, to date, the POQ-VA is the only instrument that has been validated to detect change following treatment of chronic pain in an exclusively veteran population.10 This validation emphasizes the importance of this study as it supports the use of this outcome measure to monitor treatment of pain in VA facilities.
One of the secondary findings indicated that injection therapy improved veterans’ physical activity levels and self-esteem and lowered pain scores as well as kinesiophobia and anxiety. The role of interventional procedures has been well established in the field of chronic pain, but their efficacy has been less clear. Injections are costly and not without risk, and these factors relegate them to fourth-line treatment options in most situations.15 Several meta-analyses have demonstrated small improvements in pain scores and patient-reported questionnaires after medial branch blocks, and lumbar or caudal ESIs for chronic back pain.5-7 However, an updated Cochrane Review concluded that there was insufficient evidence to support the use of injection therapy in subacute and chronic low back pain.8 The review acknowledged the limited methodologic quality of the trials and could not definitively report that injection therapy did not have benefits for certain subgroups of patients. The ability of researchers to detect benefit from an intervention is intrinsically linked to how outcomes are determined. The most interesting finding of our study was the patient-reported improved self-esteem scores. Many trials included in the systematic reviews discussed used outcome measures that did not have the multidimensional scope to demonstrate such a potential benefit.
Limitations
Our relatively small sample size represents the main shortcoming of this study. Because many posttreatment questionnaires were never collected, unfortunately, much potential data was lost. Most procedures performed were corticosteroid injections for the treatment of low back pain. This represented a combination of lumbar ESI, caudal ESI, medial branch blocks, and sacroiliac joint injections. The limited numbers meant that a further regression analysis of each injection type was not possible. Since few interventions treated pain in other areas of the body, it is difficult to determine whether procedures such as hip joint injections and ilioinguinal nerve blocks provided overall benefit. In the same vein, there is an inability to comment on which injection for chronic low back pain was the most efficacious.
The veteran population, while similar to the general population experiencing chronic pain, is more likely to experience PTSD and other mental health conditions.2 According to medical literature, no randomized controlled trials have been published examining pain interventions exclusively in veterans, so the applicability of these results needs further investigation. This study suggests there are potential benefits for the veteran population, not solely perhaps from receiving injection therapy, but to having access to an interventional pain clinic led by a pain physician within a network of other specialties. While limited by the inherent biases of a retrospective review, this study highlights the potential value in continuing to study this subgroup of patients, especially in the setting of an interdisciplinary approach.
Recent literature suggests interdisciplinary chronic pain management represents the best outcomes for patients’ physical, emotional, and social health, though these kinds of focused outpatient programs have not been studied on a large scale.16 The evolution of pain management in recent years to incorporating a biopsychosocial model has revolutionized how pain is treated and assessed, with multiple studies suggesting the greatest benefits lie in a multipronged approach.16,17 Past studies assessing individual interventions for chronic pain tend not to show strongly positive results, further reinforcing the idea that the answer does not lie in a specific treatment. Many veterans who were included in this study possibly had received or were receiving adjunct therapies such as physical therapy, cognitive behavioral therapy, and acupuncture for pain management, as well as oral and topical medications. Unfortunately, due to the selected methodology, it was not possible for us to gather those data. In turn, we were unable to determine how much these additional factors played a role in changing patient scores, alongside injection therapy. This inability to control variables in this type of research continues to present a challenge to data interpretation, even in the highest quality of research, as acknowledged by Staal and colleagues.8
Future research may be best focused by expanding our knowledge of outpatient interdisciplinary pain management programs. Some interventions may be more relevant for a particular group within a program, and this information can be useful to direct resources.18 Future prospects will require an appropriate multidimensional assessment tool, and the POQ-VA is an example of a valid and reliable option for monitoring progress in pain management in the veteran population.
Conclusions
The POQ-VA is the only instrument to date that has been validated to detect change following treatment of chronic pain in an exclusively veteran population. Our study is the first univariate analysis since the instrument’s validation in 2003. Our descriptive and inferential statistics suggest that the majority of veterans undergoing injection therapy for chronic pain had statistically significant improvements in POQ-VA measures within a 6-month period following treatment. In order to conduct more rigorous, multivariate studies, continued and more widespread use of the POQ-VA instrument is warranted.
Chronic pain is persistent or recurring pain lasting more than 3 months past normal healing time. Primary care professionals usually refer patients experiencing chronic pain to pain specialists to better identify, treat, and manage the pain. Chronic noncancer-related pain affects more Americans than diabetes mellitus, cardiac disease, and cancer combined.1 Veterans are no exception. The prevalence of severe pain was significantly higher in veterans compared with that of nonveterans who had back pain (21.6 vs 16.7%, respectively), jaw pain (37.5 vs 22.9%, respectively), severe headaches or migraine (26.4 vs 15.9%, respectively), and neck pain (27.7 vs 21.4%, respectively).2 At an individual level, those who experience chronic pain can expect impaired functional capacity, reduced ability to work, sleep disturbance, reduced social interactions, and considerable psychological distress. At a societal level, the cost of treating chronic pain is exorbitant, exceeding $600 billion annually, yet treatment outcomes remain variable at best.3 Greater efforts are needed to improve and standardize patient outcomes.
Interventional pain procedures performed under fluoroscopic or ultrasound guidance by specialist physicians have shown mixed responses in previous studies. Past systematic reviews demonstrate reductions in pain scores after lumbar or caudal epidural steroid injections (ESIs) and radiofrequency ablation of nerves supplying lumbar and thoracic facet joints.4-7 However, one review found insufficient evidence to support injection therapy for chronic low back pain.8 Unfortunately, the majority of the included studies evaluated outcomes using the visual analogue scale (VAS) or other limited factors, such as physical examination findings. Current biopsychosocial conceptualizations of chronic pain are beginning to recognize the complex nature of the experience of pain and highlighting the significance of multimodal management.9 It is vital that our assessment of chronic pain, like our treatment options, be multidimensional and reflect these underpinning principles.
The Pain Outcomes Questionnaire-For Veterans (POQ-VA) was developed within the Veterans Health Administration (VHA) by Clark and colleagues in 2003. It represents a brief but psychometrically sound pain outcomes instrument that assesses all key domains and meets accreditation body standards. The POQ-VA is valid and reliable for evaluating effectiveness of treatment of chronic noncancer pain in veterans in routine clinical practice.10 This review is the first study to use the POQ-VA to assess the impact of interventional pain procedures on veterans with chronic noncancer pain.
The aim of this study was to perform a retrospective review of POQ-VA scores before and after injection-based interventional treatment for chronic pain to determine whether the procedure affected patient outcomes. We hypothesized that POQ-VA scores would improve across multiple domains in the veteran population postprocedure. This study was approved by the Institutional Review Board (IRB-2018-053) at the Providence Veterans Affairs Medical Center (VAMC) in Rhode Island.
Methods
Using the Computerized Patient Record System, all adult veteran patients who had attended at least 2 appointments between April 1, 2009, and April 1, 2019 at the Providence VAMC interventional pain clinic were identified. POQ-VA reports were extracted provided the following criteria were met: (1) the veteran received an injection-based interventional treatment for chronic pain, including trigger point injections, ESIs, nerve blocks, and radiofrequency ablations; (2) the veteran completed POQ-VA both pre- and posttreatment; and (3) posttreatment POQ-VA reports were completed within 6 months of treatment. All patients who did not fit these criteria were excluded from the study.
After deidentification, 112 pre- and posttreatment POQ-VA reports were identified. All subsequent statistical analyses were conducted using Stata SE version 15. Descriptive statistics including mean, range, SD, and percent change were computed for POQ-VA domain—pain, mobility, activities of daily living (ADL), vitality, negative affect, fear, and total raw score—as well as for each POQ-VA question. Given that POQ-VA domain scores were found to be approximately normally distributed without outliers, domain scores were treated as continuous variables, and a paired samples t test was conducted to compare means among POQ-VA domains. Individual question responses were analyzed using nonparametric testing methods to account for the lack of normal distribution in each question, treating the range of 0 to 10 as an ordinal variable. A Wilcoxon matched-pairs signed-rank test was conducted to compare means among individual question responses before and after treatment.
Results
Of 112 included patients, 102 (91%) were male and 10 (9%) were female. The mean age was 62 years (range, 35-90). Diagnosis and procedures varied due to patient symptoms varying from muscle pain, nerve pain, degenerative disc disease, and osteoarthritis.
POQ-VA scores across all domains, including total raw score, showed statistically significant improvement after treatment (Table 1). Directionally, the POQ-VA scores for all 20 questions reflect a positive treatment response and 17 had statistically significant changes (P < .05) (Table 2). The changes in self-perceived energy level, safety, and feelings of tension were not statistically significant. Esteem had the greatest magnitude decrease, falling from 5.2 preprocedure to 3.8 postprocedure (P < .001). Other similarly significant magnitudes of improvement were seen from pre- to postprocedure in questions pertaining to grooming (2.2 to 1.6, P = .003) and the ability to use the bathroom (3.4 to 2.6, P < .001).
Discussion
The most important finding of this study was the ability of the POQ-VA to detect statistically significant positive responses to injection therapy across all domains. The largest improvements were in self-reported pain intensity, pain-related impairment in mobility and ADLs, and self-reported dysphoric effects. The single largest improvement posttreatment was a reduction in scores related to low self-esteem.
Chronic pain can be assessed in a variety of ways ranging from physical examination findings and subjective numerical ratings to extensive patient-reported questionnaires. The International Association for the Study of Pain acknowledges that pain is a complex experience and recommends assessment should be comprehensive.11 Many patient-reported questionnaires are available to clinicians, including some that address pain in a specific body part, such as the Oswestry Low Back Pain Disability Questionnaire, or those that focus on depression or quality-of-life measures, such as the SF-36.12,13
One major benefit of using the POQ-VA is its potential to demonstrate benefits across multiple domains, reflecting the complex nature of chronic pain. The POQ-VA also separates domain or scale scores, allowing clinicians to identify individuals with different patterns of dysfunction across domains.10 This separation also provides insight into which treatment options are best for chronic pain patients with predominant patterns or lower scores in certain domains. The use of a single summary score, as seen in other questionnaires such as the Roland-Morris Activity Scale, may conceal treatment-induced changes in specific outcome domains.14 Additionally, like many other similar instruments, the POQ-VA is easy to understand and use, requires no special training, takes little time to complete, and can be completed in person or over the phone.
As chronic pain has been studied further and its complexity recognized, more instruments have been developed and modified to reflect these new elements. There is no one scale applicable to all populations. A discussion about the strengths and weaknesses of each available assessment tool is outside the scope of this review. However, to date, the POQ-VA is the only instrument that has been validated to detect change following treatment of chronic pain in an exclusively veteran population.10 This validation emphasizes the importance of this study as it supports the use of this outcome measure to monitor treatment of pain in VA facilities.
One of the secondary findings indicated that injection therapy improved veterans’ physical activity levels and self-esteem and lowered pain scores as well as kinesiophobia and anxiety. The role of interventional procedures has been well established in the field of chronic pain, but their efficacy has been less clear. Injections are costly and not without risk, and these factors relegate them to fourth-line treatment options in most situations.15 Several meta-analyses have demonstrated small improvements in pain scores and patient-reported questionnaires after medial branch blocks, and lumbar or caudal ESIs for chronic back pain.5-7 However, an updated Cochrane Review concluded that there was insufficient evidence to support the use of injection therapy in subacute and chronic low back pain.8 The review acknowledged the limited methodologic quality of the trials and could not definitively report that injection therapy did not have benefits for certain subgroups of patients. The ability of researchers to detect benefit from an intervention is intrinsically linked to how outcomes are determined. The most interesting finding of our study was the patient-reported improved self-esteem scores. Many trials included in the systematic reviews discussed used outcome measures that did not have the multidimensional scope to demonstrate such a potential benefit.
Limitations
Our relatively small sample size represents the main shortcoming of this study. Because many posttreatment questionnaires were never collected, unfortunately, much potential data was lost. Most procedures performed were corticosteroid injections for the treatment of low back pain. This represented a combination of lumbar ESI, caudal ESI, medial branch blocks, and sacroiliac joint injections. The limited numbers meant that a further regression analysis of each injection type was not possible. Since few interventions treated pain in other areas of the body, it is difficult to determine whether procedures such as hip joint injections and ilioinguinal nerve blocks provided overall benefit. In the same vein, there is an inability to comment on which injection for chronic low back pain was the most efficacious.
The veteran population, while similar to the general population experiencing chronic pain, is more likely to experience PTSD and other mental health conditions.2 According to medical literature, no randomized controlled trials have been published examining pain interventions exclusively in veterans, so the applicability of these results needs further investigation. This study suggests there are potential benefits for the veteran population, not solely perhaps from receiving injection therapy, but to having access to an interventional pain clinic led by a pain physician within a network of other specialties. While limited by the inherent biases of a retrospective review, this study highlights the potential value in continuing to study this subgroup of patients, especially in the setting of an interdisciplinary approach.
Recent literature suggests interdisciplinary chronic pain management represents the best outcomes for patients’ physical, emotional, and social health, though these kinds of focused outpatient programs have not been studied on a large scale.16 The evolution of pain management in recent years to incorporating a biopsychosocial model has revolutionized how pain is treated and assessed, with multiple studies suggesting the greatest benefits lie in a multipronged approach.16,17 Past studies assessing individual interventions for chronic pain tend not to show strongly positive results, further reinforcing the idea that the answer does not lie in a specific treatment. Many veterans who were included in this study possibly had received or were receiving adjunct therapies such as physical therapy, cognitive behavioral therapy, and acupuncture for pain management, as well as oral and topical medications. Unfortunately, due to the selected methodology, it was not possible for us to gather those data. In turn, we were unable to determine how much these additional factors played a role in changing patient scores, alongside injection therapy. This inability to control variables in this type of research continues to present a challenge to data interpretation, even in the highest quality of research, as acknowledged by Staal and colleagues.8
Future research may be best focused by expanding our knowledge of outpatient interdisciplinary pain management programs. Some interventions may be more relevant for a particular group within a program, and this information can be useful to direct resources.18 Future prospects will require an appropriate multidimensional assessment tool, and the POQ-VA is an example of a valid and reliable option for monitoring progress in pain management in the veteran population.
Conclusions
The POQ-VA is the only instrument to date that has been validated to detect change following treatment of chronic pain in an exclusively veteran population. Our study is the first univariate analysis since the instrument’s validation in 2003. Our descriptive and inferential statistics suggest that the majority of veterans undergoing injection therapy for chronic pain had statistically significant improvements in POQ-VA measures within a 6-month period following treatment. In order to conduct more rigorous, multivariate studies, continued and more widespread use of the POQ-VA instrument is warranted.
1. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11(11):1230-1239. doi:10.1016/j.jpain.2010.07.002
2. Nahin RL. Severe Pain in Veterans: The effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254. doi:10.1016/j.jpain.2016.10.021
3. Witkin LR, Farrar JT, Ashburn MA. Can assessing chronic pain outcomes data improve outcomes?. Pain Med. 2013;14(6):779-791. doi:10.1111/pme.12075
4. Benyamin RM, Manchikanti L, Parr AT, et al. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012;15(4):E363-E404.
5. Zhai J, Zhang L, Li M, et al. Epidural injection with or without steroid in managing chronic low-back and lower extremity pain: a meta-analysis of 10 randomized controlled trials. Am J Ther. 2017;24(3):e259-e269. doi:10.1097/MJT.0000000000000265
6. Parr AT, Manchikanti L, Hameed H, et al. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Physician. 2012;15(3):E159-E198.
7. Lee CH, Chung CK, Kim CH. The efficacy of conventional radiofrequency denervation in patients with chronic low back pain originating from the facet joints: a meta-analysis of randomized controlled trials. Spine J. 2017;17(11):1770-1780. doi:10.1016/j.spinee.2017.05.006
8. Staal JB, de Bie R, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low-back pain. Cochrane Database Syst Rev. 2008;2008(3):CD001824. Published 2008 Jul 16. doi:10.1002/14651858.CD001824.pub3
9. Gironda RJ, Clark ME. Cluster analysis of the pain outcomes questionnaire. Pain Med. 2008;9(7):813-823. doi:10.1111/j.1526-4637.2007.00397.x
10. Clark ME, Gironda RJ, Young RW. Development and validation of the Pain Outcomes Questionnaire-VA. J Rehabil Res Dev. 2003;40(5):381-395. doi:10.1682/jrrd.2003.09.0381
11. Watt-Watson J, McGillion M, Lax L, et al. Evaluating an Innovative eLearning Pain Education Interprofessional Resource: A Pre-Post Study. Pain Med. 2019;20(1):37-49. doi:10.1093/pm/pny105
12. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271-273.
13. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473-483.
14. Jensen MP, Strom SE, Turner JA, Romano JM. Validity of the Sickness Impact Profile Roland scale as a measure of dysfunction in chronic pain patients. Pain. 1992;50(2):157-162. doi:10.1016/0304-3959(92)90156-6
15. Hylands-White N, Duarte RV, Raphael JH. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2017;37(1):29-42. doi:10.1007/s00296-016-3481-8
16. Bujak BK, Regan E, Beattie PF, Harrington S. The effectiveness of interdisciplinary intensive outpatient programs in a population with diverse chronic pain conditions: a systematic review and meta-analysis. Pain Manag. 2019;9(4):417-429. doi:10.2217/pmt-2018-0087
17. Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2002;(1):CD000963. doi:10.1002/14651858.CD000963
18. Wilson IR. Management of chronic pain through pain management programmes. Br Med Bull. 2017;124(1):55-64. doi:10.1093/bmb/ldx032
1. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11(11):1230-1239. doi:10.1016/j.jpain.2010.07.002
2. Nahin RL. Severe Pain in Veterans: The effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254. doi:10.1016/j.jpain.2016.10.021
3. Witkin LR, Farrar JT, Ashburn MA. Can assessing chronic pain outcomes data improve outcomes?. Pain Med. 2013;14(6):779-791. doi:10.1111/pme.12075
4. Benyamin RM, Manchikanti L, Parr AT, et al. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012;15(4):E363-E404.
5. Zhai J, Zhang L, Li M, et al. Epidural injection with or without steroid in managing chronic low-back and lower extremity pain: a meta-analysis of 10 randomized controlled trials. Am J Ther. 2017;24(3):e259-e269. doi:10.1097/MJT.0000000000000265
6. Parr AT, Manchikanti L, Hameed H, et al. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Physician. 2012;15(3):E159-E198.
7. Lee CH, Chung CK, Kim CH. The efficacy of conventional radiofrequency denervation in patients with chronic low back pain originating from the facet joints: a meta-analysis of randomized controlled trials. Spine J. 2017;17(11):1770-1780. doi:10.1016/j.spinee.2017.05.006
8. Staal JB, de Bie R, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low-back pain. Cochrane Database Syst Rev. 2008;2008(3):CD001824. Published 2008 Jul 16. doi:10.1002/14651858.CD001824.pub3
9. Gironda RJ, Clark ME. Cluster analysis of the pain outcomes questionnaire. Pain Med. 2008;9(7):813-823. doi:10.1111/j.1526-4637.2007.00397.x
10. Clark ME, Gironda RJ, Young RW. Development and validation of the Pain Outcomes Questionnaire-VA. J Rehabil Res Dev. 2003;40(5):381-395. doi:10.1682/jrrd.2003.09.0381
11. Watt-Watson J, McGillion M, Lax L, et al. Evaluating an Innovative eLearning Pain Education Interprofessional Resource: A Pre-Post Study. Pain Med. 2019;20(1):37-49. doi:10.1093/pm/pny105
12. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271-273.
13. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473-483.
14. Jensen MP, Strom SE, Turner JA, Romano JM. Validity of the Sickness Impact Profile Roland scale as a measure of dysfunction in chronic pain patients. Pain. 1992;50(2):157-162. doi:10.1016/0304-3959(92)90156-6
15. Hylands-White N, Duarte RV, Raphael JH. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2017;37(1):29-42. doi:10.1007/s00296-016-3481-8
16. Bujak BK, Regan E, Beattie PF, Harrington S. The effectiveness of interdisciplinary intensive outpatient programs in a population with diverse chronic pain conditions: a systematic review and meta-analysis. Pain Manag. 2019;9(4):417-429. doi:10.2217/pmt-2018-0087
17. Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2002;(1):CD000963. doi:10.1002/14651858.CD000963
18. Wilson IR. Management of chronic pain through pain management programmes. Br Med Bull. 2017;124(1):55-64. doi:10.1093/bmb/ldx032
Medical cannabis may cut opioid use for back pain, OA
CHICAGO – Access to medical cannabis (MC) cut opioid prescriptions for patients with chronic noncancer back pain and patients with osteoarthritis, according to preliminary data presented at the annual meeting of the American Academy of Orthopaedic Surgeons.
For those with chronic back pain, the average morphine milligram equivalents (MME) per day dropped from 15.1 to 11.0 (n = 186; P < .01). More than one-third of the patients (38.7%) stopped taking morphine after they filled prescriptions for medical cannabis.
Opioid prescriptions were filled 6 months before access to MC and then were compared with 6 months after access to MC.
In analyzing subgroups, the researchers found that patients who started at less than 15 MME/day and more than 15 MME/day showed significant decreases after filling the MC prescription.
Almost half (48.5%) of the patients in the group that started at less than 15 MME daily dropped to 0 MME/day, and 13.5% of patients who were getting more than 15 MME/day stopped using opioids.
Data on filled opioid prescriptions were gathered from a Prescription Drug Monitoring Program (PDMP) system for patients diagnosed with chronic musculoskeletal noncancer back pain who were eligible for MC access between February 2018 and July 2019.
Medical cannabis has shown benefit in treating chronic pain, but evidence has been limited on whether it can reduce opioid use, which can lead to substance abuse, addiction, overdose, and death, the researchers noted.
Researchers found that using MC via multiple routes of administration seemed to be important.
Patients who used only a single administration route showed a statistically insignificant decrease in MME/day from 20.0 to 15.1 (n = 68; P = .054), whereas patients who used two or more routes showed a significant decrease from 13.2 to 9.5 (n = 76; P < .01).
“We have many patients who are benefiting from a single route of delivery for chronic orthopedic pain,” Ari Greis, DO, a physical medicine and rehabilitation specialist in Bryn Mawr, Pa., and a coauthor of the MC studies for both back pain and OA, said in an interview. “However, our data shows a greater reduction in opioid consumption in patients using more than one route of delivery.”
He said delivery modes in the studies included vaporized cannabis oil or flower; sublingual tinctures; capsules or tablets; and topical lotions, creams, and salves.
Dr. Greis is the director of the medical cannabis department at Rothman Orthopaedic Institute in Bryn Mawr, and is a senior fellow in the Institute of Emerging Health Professions and the Lambert Center for the Study of Medicinal Cannabis and Hemp, both in Philadelphia.
Medical cannabis also reduces opioids for OA
The same team of researchers, using the data from the PDMP system, showed that medical cannabis also helped reduce opioid use for osteoarthritis.
For patients using opioids for OA, there was a significant decrease in average MME/day of prescriptions filled by patients following MC access – from 18.2 to 9.8 (n = 40; P < .05). The average drop in MME/day was 46.3%. The percentage of patients who stopped using opioids was 37.5%. Pain score on a 0-10 visual analog scale decreased significantly from 6.6 (n = 36) to 5.0 (n = 26; P < .01) at 3 months and 5.4 (n = 16; P < .05) at 6 months.
Gary Stewart, MD, an orthopedic surgeon in Morrow, Ga., who was not part of the studies, told this news organization that the studies offer good preliminary data to offer help with the opioid issue.
“I sometimes feel that we, as orthopedic surgeons and physicians in general, are working with one hand behind our back. We’re taking something that is a heroin or morphine derivative and giving it to our patients when we know it has a high risk of building tolerance and addiction. But at the same time, we have no alternative,” he said.
He said it’s important to remember the results from the relatively small study are preliminary and observational. People used different forms and amounts of MC and the data show only that prescriptions were filled, but not whether the cannabis was used. Prospective, controlled studies where opioids go head-to-head with MC are needed, he said.
“Still, this can lead us to more studies to give us an option [apart from] an opioid that we know is highly addictive,” he said.
Dr. Stewart is a member of the AAOS Opioid Task Force. Dr. Greis and several coauthors have disclosed no relevant financial relationships, and other coauthors report financial ties to companies unrelated to the research presented.
A version of this article first appeared on Medscape.com.
CHICAGO – Access to medical cannabis (MC) cut opioid prescriptions for patients with chronic noncancer back pain and patients with osteoarthritis, according to preliminary data presented at the annual meeting of the American Academy of Orthopaedic Surgeons.
For those with chronic back pain, the average morphine milligram equivalents (MME) per day dropped from 15.1 to 11.0 (n = 186; P < .01). More than one-third of the patients (38.7%) stopped taking morphine after they filled prescriptions for medical cannabis.
Opioid prescriptions were filled 6 months before access to MC and then were compared with 6 months after access to MC.
In analyzing subgroups, the researchers found that patients who started at less than 15 MME/day and more than 15 MME/day showed significant decreases after filling the MC prescription.
Almost half (48.5%) of the patients in the group that started at less than 15 MME daily dropped to 0 MME/day, and 13.5% of patients who were getting more than 15 MME/day stopped using opioids.
Data on filled opioid prescriptions were gathered from a Prescription Drug Monitoring Program (PDMP) system for patients diagnosed with chronic musculoskeletal noncancer back pain who were eligible for MC access between February 2018 and July 2019.
Medical cannabis has shown benefit in treating chronic pain, but evidence has been limited on whether it can reduce opioid use, which can lead to substance abuse, addiction, overdose, and death, the researchers noted.
Researchers found that using MC via multiple routes of administration seemed to be important.
Patients who used only a single administration route showed a statistically insignificant decrease in MME/day from 20.0 to 15.1 (n = 68; P = .054), whereas patients who used two or more routes showed a significant decrease from 13.2 to 9.5 (n = 76; P < .01).
“We have many patients who are benefiting from a single route of delivery for chronic orthopedic pain,” Ari Greis, DO, a physical medicine and rehabilitation specialist in Bryn Mawr, Pa., and a coauthor of the MC studies for both back pain and OA, said in an interview. “However, our data shows a greater reduction in opioid consumption in patients using more than one route of delivery.”
He said delivery modes in the studies included vaporized cannabis oil or flower; sublingual tinctures; capsules or tablets; and topical lotions, creams, and salves.
Dr. Greis is the director of the medical cannabis department at Rothman Orthopaedic Institute in Bryn Mawr, and is a senior fellow in the Institute of Emerging Health Professions and the Lambert Center for the Study of Medicinal Cannabis and Hemp, both in Philadelphia.
Medical cannabis also reduces opioids for OA
The same team of researchers, using the data from the PDMP system, showed that medical cannabis also helped reduce opioid use for osteoarthritis.
For patients using opioids for OA, there was a significant decrease in average MME/day of prescriptions filled by patients following MC access – from 18.2 to 9.8 (n = 40; P < .05). The average drop in MME/day was 46.3%. The percentage of patients who stopped using opioids was 37.5%. Pain score on a 0-10 visual analog scale decreased significantly from 6.6 (n = 36) to 5.0 (n = 26; P < .01) at 3 months and 5.4 (n = 16; P < .05) at 6 months.
Gary Stewart, MD, an orthopedic surgeon in Morrow, Ga., who was not part of the studies, told this news organization that the studies offer good preliminary data to offer help with the opioid issue.
“I sometimes feel that we, as orthopedic surgeons and physicians in general, are working with one hand behind our back. We’re taking something that is a heroin or morphine derivative and giving it to our patients when we know it has a high risk of building tolerance and addiction. But at the same time, we have no alternative,” he said.
He said it’s important to remember the results from the relatively small study are preliminary and observational. People used different forms and amounts of MC and the data show only that prescriptions were filled, but not whether the cannabis was used. Prospective, controlled studies where opioids go head-to-head with MC are needed, he said.
“Still, this can lead us to more studies to give us an option [apart from] an opioid that we know is highly addictive,” he said.
Dr. Stewart is a member of the AAOS Opioid Task Force. Dr. Greis and several coauthors have disclosed no relevant financial relationships, and other coauthors report financial ties to companies unrelated to the research presented.
A version of this article first appeared on Medscape.com.
CHICAGO – Access to medical cannabis (MC) cut opioid prescriptions for patients with chronic noncancer back pain and patients with osteoarthritis, according to preliminary data presented at the annual meeting of the American Academy of Orthopaedic Surgeons.
For those with chronic back pain, the average morphine milligram equivalents (MME) per day dropped from 15.1 to 11.0 (n = 186; P < .01). More than one-third of the patients (38.7%) stopped taking morphine after they filled prescriptions for medical cannabis.
Opioid prescriptions were filled 6 months before access to MC and then were compared with 6 months after access to MC.
In analyzing subgroups, the researchers found that patients who started at less than 15 MME/day and more than 15 MME/day showed significant decreases after filling the MC prescription.
Almost half (48.5%) of the patients in the group that started at less than 15 MME daily dropped to 0 MME/day, and 13.5% of patients who were getting more than 15 MME/day stopped using opioids.
Data on filled opioid prescriptions were gathered from a Prescription Drug Monitoring Program (PDMP) system for patients diagnosed with chronic musculoskeletal noncancer back pain who were eligible for MC access between February 2018 and July 2019.
Medical cannabis has shown benefit in treating chronic pain, but evidence has been limited on whether it can reduce opioid use, which can lead to substance abuse, addiction, overdose, and death, the researchers noted.
Researchers found that using MC via multiple routes of administration seemed to be important.
Patients who used only a single administration route showed a statistically insignificant decrease in MME/day from 20.0 to 15.1 (n = 68; P = .054), whereas patients who used two or more routes showed a significant decrease from 13.2 to 9.5 (n = 76; P < .01).
“We have many patients who are benefiting from a single route of delivery for chronic orthopedic pain,” Ari Greis, DO, a physical medicine and rehabilitation specialist in Bryn Mawr, Pa., and a coauthor of the MC studies for both back pain and OA, said in an interview. “However, our data shows a greater reduction in opioid consumption in patients using more than one route of delivery.”
He said delivery modes in the studies included vaporized cannabis oil or flower; sublingual tinctures; capsules or tablets; and topical lotions, creams, and salves.
Dr. Greis is the director of the medical cannabis department at Rothman Orthopaedic Institute in Bryn Mawr, and is a senior fellow in the Institute of Emerging Health Professions and the Lambert Center for the Study of Medicinal Cannabis and Hemp, both in Philadelphia.
Medical cannabis also reduces opioids for OA
The same team of researchers, using the data from the PDMP system, showed that medical cannabis also helped reduce opioid use for osteoarthritis.
For patients using opioids for OA, there was a significant decrease in average MME/day of prescriptions filled by patients following MC access – from 18.2 to 9.8 (n = 40; P < .05). The average drop in MME/day was 46.3%. The percentage of patients who stopped using opioids was 37.5%. Pain score on a 0-10 visual analog scale decreased significantly from 6.6 (n = 36) to 5.0 (n = 26; P < .01) at 3 months and 5.4 (n = 16; P < .05) at 6 months.
Gary Stewart, MD, an orthopedic surgeon in Morrow, Ga., who was not part of the studies, told this news organization that the studies offer good preliminary data to offer help with the opioid issue.
“I sometimes feel that we, as orthopedic surgeons and physicians in general, are working with one hand behind our back. We’re taking something that is a heroin or morphine derivative and giving it to our patients when we know it has a high risk of building tolerance and addiction. But at the same time, we have no alternative,” he said.
He said it’s important to remember the results from the relatively small study are preliminary and observational. People used different forms and amounts of MC and the data show only that prescriptions were filled, but not whether the cannabis was used. Prospective, controlled studies where opioids go head-to-head with MC are needed, he said.
“Still, this can lead us to more studies to give us an option [apart from] an opioid that we know is highly addictive,” he said.
Dr. Stewart is a member of the AAOS Opioid Task Force. Dr. Greis and several coauthors have disclosed no relevant financial relationships, and other coauthors report financial ties to companies unrelated to the research presented.
A version of this article first appeared on Medscape.com.
AT AAOS 2022