User login
For MD-IQ on Family Practice News, but a regular topic for Rheumatology News
ACR 2016 continues big buffet of basic and clinical science sessions
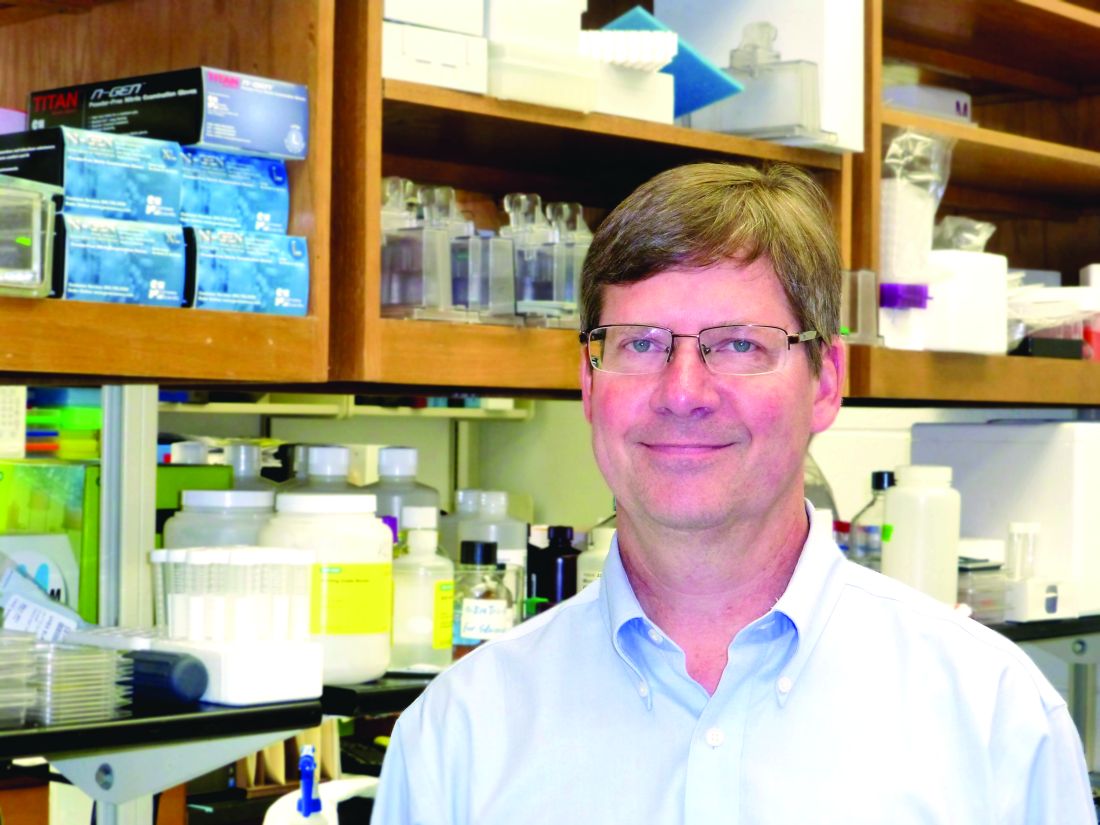
This year’s annual meeting of the American College of Rheumatology will feature cutting-edge research and results of studies that directly affect how attendees will manage patients once they are back in the clinical setting, according to both Richard Loeser, MD, program chair of the Annual Meeting Planning Committee (AMPC), and Gregory Gardner, MD, clinical subchair of the AMPC, who suggested special sessions of interest culled from the more than 450 sessions to be presented.
“It is an exciting time in rheumatology. Basic research is being translated into new therapies before our very eyes. Areas on the program this year that have translational potential include immunometabolism, blocking interleukin-1 (IL-1), T-cell receptor signaling, and meta-analysis of gene expression data. The meeting will also feature trials that refine and advance the management of rheumatologic diseases, including results on studies of new biologics,” Dr. Loeser said.
Hot sessions
Luke O’Neill, MD, will talk about immunometabolism Monday at 7:30 a.m. This session will explore a newly described connection between energy metabolism and the immune system and the link with inflammation.
Charles Dinarello, MD, will give the Philip Hensch Memorial Lecture Sunday at 8:30 a.m. on blocking IL-1 in inflammatory diseases. He will cover a host of diseases from gout to cancer, Dr. Loeser noted.
Another hot topic, T-cell receptor signaling in autoimmune diseases and the development of new therapies, will be discussed by Arthur Weiss, MD, Tuesday morning at 7:30 a.m.
Tuesday at 11:00 a.m., Peter Lipsky, MD, will tackle big data mining, presenting a meta-analysis of gene expression datasets to identify novel pathways and targets in systemic lupus erythematosus (SLE).
“SLE lags behind rheumatoid arthritis in therapeutic advances. A number of trials of biologics have failed in SLE, whereas they have been found effective in rheumatoid arthritis,” Dr. Loeser explained.
Clinical slant
Sunday’s Plenary session at 11:00 a.m. will feature several top-rated abstracts, among them results of a phase III study on tocilizumab in giant cell arteritis to be presented by John Stone, MD. “Tocilizumab is a major breakthrough as a steroid-sparing treatment for the most common form of vasculitis that affects older adults,” Dr. Loeser said.
At 2:30 p.m. on Sunday at The Great Debate, Paul Emery, MD, and Arthur Kavanaugh, MD, will tackle the very important clinical topic of “To Taper or Not to Taper? – Biologic DMARDs in Low Rheumatoid Arthritis Disease Activity.”
“People aren’t sure what to do. The fear with tapering is rebound, with the disease coming back even more forcefully. There is new evidence to suggest that tapering may be safe under certain circumstances. This session should inform attendees on how to make the decision to taper and on the best way to do it,” Dr. Loeser commented.
The Late-Breaking Abstract session on Tuesday at 4:30 p.m. will feature six clinical trials. Dr. Loeser singled out a study to be presented by Elaine Husni, MD, on “Vascular Safety of Celecoxib versus Ibuprofen or Naproxen” in more than 20,000 patients with osteoarthritis or rheumatoid arthritis.
“The fear is that COX-2 inhibitors have increased cardiovascular risk. The data from this study that will be presented at the meeting should answer the question of whether or not this is true in patients with arthritis,” Dr. Loeser explained.
Wednesday at 7:30 a.m. Candida Fratazzi, MD, will talk about “Emerging Biosimilars in Therapeutic Management,” a subject of great interest since they have the potential to be equally effective and less expensive than current biologics.
Two “bookends” of the meeting will frame the opening and closing. Sunday at 7:30 a.m., the “Year in Review” session will feature the best published studies on rheumatologic diseases from the past year, based on the judgment of two experts. Ingrid Lundberg, MD, will present the best clinical studies and Bruce Cronstein, MD, will present the best basic science studies. Wednesday at 7:30 a.m., John Cush, MD, and Dr. Kavanaugh will present the “Rheumatology Roundup” of the best abstracts and put them into context. “This session is usually quite entertaining,” Dr. Loeser said.
More sessions of clinical import
“In keeping with our meeting theme of fine-tuning our care of patients with rheumatic disease, I want to point out several sessions,” Dr. Gardner said.
Attendees interested in sessions on clinical applicability will have to choose between two different sessions Monday at 4:30 p.m.: one on dermatomyositis, a relatively rare but difficult-to-treat entity, and the other about treatment of the patient with rheumatoid arthritis when the patient is not well and suffering from comorbidities.
Monday at 8:30 a.m., an “Osteoporosis Update” will give listeners perspective on current and future therapies.
Sunday at 2:30 p.m., new guidelines for steroid-induced osteoporosis will be presented.
“Four or five sessions on the Tech Track will show rheumatologists how they can improve their practice by using technology,” Dr. Gardner said. “Several high-quality sessions are important to educators, including ‘Flipped Classroom, Technology, and Reflection’ [Monday at 12:30 p.m.] and ‘Year in Review’ [Sunday at 1:00 p.m.].”
Monday at 11:00 a.m., the Plenary session will feature Workforce Study results on how many rheumatologists will be needed in the year 2030, and in which geographic locations. This session will also include a discussion of the impact of part-time rheumatologists.
“Two sessions I am excited about are ‘Treat to Target in 2016,’ Tuesday at 4:30 p.m., and ‘Rheumatic Diseases in Native Americans,’ Sunday at 11:00 a.m.,” Dr. Gardner noted. “Concurrent abstract sessions throughout the meeting will feature discussions on new biologics, small molecules, and gene therapy.”
This year’s annual meeting of the American College of Rheumatology will feature cutting-edge research and results of studies that directly affect how attendees will manage patients once they are back in the clinical setting, according to both Richard Loeser, MD, program chair of the Annual Meeting Planning Committee (AMPC), and Gregory Gardner, MD, clinical subchair of the AMPC, who suggested special sessions of interest culled from the more than 450 sessions to be presented.
“It is an exciting time in rheumatology. Basic research is being translated into new therapies before our very eyes. Areas on the program this year that have translational potential include immunometabolism, blocking interleukin-1 (IL-1), T-cell receptor signaling, and meta-analysis of gene expression data. The meeting will also feature trials that refine and advance the management of rheumatologic diseases, including results on studies of new biologics,” Dr. Loeser said.
Hot sessions
Luke O’Neill, MD, will talk about immunometabolism Monday at 7:30 a.m. This session will explore a newly described connection between energy metabolism and the immune system and the link with inflammation.
Charles Dinarello, MD, will give the Philip Hensch Memorial Lecture Sunday at 8:30 a.m. on blocking IL-1 in inflammatory diseases. He will cover a host of diseases from gout to cancer, Dr. Loeser noted.
Another hot topic, T-cell receptor signaling in autoimmune diseases and the development of new therapies, will be discussed by Arthur Weiss, MD, Tuesday morning at 7:30 a.m.
Tuesday at 11:00 a.m., Peter Lipsky, MD, will tackle big data mining, presenting a meta-analysis of gene expression datasets to identify novel pathways and targets in systemic lupus erythematosus (SLE).
“SLE lags behind rheumatoid arthritis in therapeutic advances. A number of trials of biologics have failed in SLE, whereas they have been found effective in rheumatoid arthritis,” Dr. Loeser explained.
Clinical slant
Sunday’s Plenary session at 11:00 a.m. will feature several top-rated abstracts, among them results of a phase III study on tocilizumab in giant cell arteritis to be presented by John Stone, MD. “Tocilizumab is a major breakthrough as a steroid-sparing treatment for the most common form of vasculitis that affects older adults,” Dr. Loeser said.
At 2:30 p.m. on Sunday at The Great Debate, Paul Emery, MD, and Arthur Kavanaugh, MD, will tackle the very important clinical topic of “To Taper or Not to Taper? – Biologic DMARDs in Low Rheumatoid Arthritis Disease Activity.”
“People aren’t sure what to do. The fear with tapering is rebound, with the disease coming back even more forcefully. There is new evidence to suggest that tapering may be safe under certain circumstances. This session should inform attendees on how to make the decision to taper and on the best way to do it,” Dr. Loeser commented.
The Late-Breaking Abstract session on Tuesday at 4:30 p.m. will feature six clinical trials. Dr. Loeser singled out a study to be presented by Elaine Husni, MD, on “Vascular Safety of Celecoxib versus Ibuprofen or Naproxen” in more than 20,000 patients with osteoarthritis or rheumatoid arthritis.
“The fear is that COX-2 inhibitors have increased cardiovascular risk. The data from this study that will be presented at the meeting should answer the question of whether or not this is true in patients with arthritis,” Dr. Loeser explained.
Wednesday at 7:30 a.m. Candida Fratazzi, MD, will talk about “Emerging Biosimilars in Therapeutic Management,” a subject of great interest since they have the potential to be equally effective and less expensive than current biologics.
Two “bookends” of the meeting will frame the opening and closing. Sunday at 7:30 a.m., the “Year in Review” session will feature the best published studies on rheumatologic diseases from the past year, based on the judgment of two experts. Ingrid Lundberg, MD, will present the best clinical studies and Bruce Cronstein, MD, will present the best basic science studies. Wednesday at 7:30 a.m., John Cush, MD, and Dr. Kavanaugh will present the “Rheumatology Roundup” of the best abstracts and put them into context. “This session is usually quite entertaining,” Dr. Loeser said.
More sessions of clinical import
“In keeping with our meeting theme of fine-tuning our care of patients with rheumatic disease, I want to point out several sessions,” Dr. Gardner said.
Attendees interested in sessions on clinical applicability will have to choose between two different sessions Monday at 4:30 p.m.: one on dermatomyositis, a relatively rare but difficult-to-treat entity, and the other about treatment of the patient with rheumatoid arthritis when the patient is not well and suffering from comorbidities.
Monday at 8:30 a.m., an “Osteoporosis Update” will give listeners perspective on current and future therapies.
Sunday at 2:30 p.m., new guidelines for steroid-induced osteoporosis will be presented.
“Four or five sessions on the Tech Track will show rheumatologists how they can improve their practice by using technology,” Dr. Gardner said. “Several high-quality sessions are important to educators, including ‘Flipped Classroom, Technology, and Reflection’ [Monday at 12:30 p.m.] and ‘Year in Review’ [Sunday at 1:00 p.m.].”
Monday at 11:00 a.m., the Plenary session will feature Workforce Study results on how many rheumatologists will be needed in the year 2030, and in which geographic locations. This session will also include a discussion of the impact of part-time rheumatologists.
“Two sessions I am excited about are ‘Treat to Target in 2016,’ Tuesday at 4:30 p.m., and ‘Rheumatic Diseases in Native Americans,’ Sunday at 11:00 a.m.,” Dr. Gardner noted. “Concurrent abstract sessions throughout the meeting will feature discussions on new biologics, small molecules, and gene therapy.”
This year’s annual meeting of the American College of Rheumatology will feature cutting-edge research and results of studies that directly affect how attendees will manage patients once they are back in the clinical setting, according to both Richard Loeser, MD, program chair of the Annual Meeting Planning Committee (AMPC), and Gregory Gardner, MD, clinical subchair of the AMPC, who suggested special sessions of interest culled from the more than 450 sessions to be presented.
“It is an exciting time in rheumatology. Basic research is being translated into new therapies before our very eyes. Areas on the program this year that have translational potential include immunometabolism, blocking interleukin-1 (IL-1), T-cell receptor signaling, and meta-analysis of gene expression data. The meeting will also feature trials that refine and advance the management of rheumatologic diseases, including results on studies of new biologics,” Dr. Loeser said.
Hot sessions
Luke O’Neill, MD, will talk about immunometabolism Monday at 7:30 a.m. This session will explore a newly described connection between energy metabolism and the immune system and the link with inflammation.
Charles Dinarello, MD, will give the Philip Hensch Memorial Lecture Sunday at 8:30 a.m. on blocking IL-1 in inflammatory diseases. He will cover a host of diseases from gout to cancer, Dr. Loeser noted.
Another hot topic, T-cell receptor signaling in autoimmune diseases and the development of new therapies, will be discussed by Arthur Weiss, MD, Tuesday morning at 7:30 a.m.
Tuesday at 11:00 a.m., Peter Lipsky, MD, will tackle big data mining, presenting a meta-analysis of gene expression datasets to identify novel pathways and targets in systemic lupus erythematosus (SLE).
“SLE lags behind rheumatoid arthritis in therapeutic advances. A number of trials of biologics have failed in SLE, whereas they have been found effective in rheumatoid arthritis,” Dr. Loeser explained.
Clinical slant
Sunday’s Plenary session at 11:00 a.m. will feature several top-rated abstracts, among them results of a phase III study on tocilizumab in giant cell arteritis to be presented by John Stone, MD. “Tocilizumab is a major breakthrough as a steroid-sparing treatment for the most common form of vasculitis that affects older adults,” Dr. Loeser said.
At 2:30 p.m. on Sunday at The Great Debate, Paul Emery, MD, and Arthur Kavanaugh, MD, will tackle the very important clinical topic of “To Taper or Not to Taper? – Biologic DMARDs in Low Rheumatoid Arthritis Disease Activity.”
“People aren’t sure what to do. The fear with tapering is rebound, with the disease coming back even more forcefully. There is new evidence to suggest that tapering may be safe under certain circumstances. This session should inform attendees on how to make the decision to taper and on the best way to do it,” Dr. Loeser commented.
The Late-Breaking Abstract session on Tuesday at 4:30 p.m. will feature six clinical trials. Dr. Loeser singled out a study to be presented by Elaine Husni, MD, on “Vascular Safety of Celecoxib versus Ibuprofen or Naproxen” in more than 20,000 patients with osteoarthritis or rheumatoid arthritis.
“The fear is that COX-2 inhibitors have increased cardiovascular risk. The data from this study that will be presented at the meeting should answer the question of whether or not this is true in patients with arthritis,” Dr. Loeser explained.
Wednesday at 7:30 a.m. Candida Fratazzi, MD, will talk about “Emerging Biosimilars in Therapeutic Management,” a subject of great interest since they have the potential to be equally effective and less expensive than current biologics.
Two “bookends” of the meeting will frame the opening and closing. Sunday at 7:30 a.m., the “Year in Review” session will feature the best published studies on rheumatologic diseases from the past year, based on the judgment of two experts. Ingrid Lundberg, MD, will present the best clinical studies and Bruce Cronstein, MD, will present the best basic science studies. Wednesday at 7:30 a.m., John Cush, MD, and Dr. Kavanaugh will present the “Rheumatology Roundup” of the best abstracts and put them into context. “This session is usually quite entertaining,” Dr. Loeser said.
More sessions of clinical import
“In keeping with our meeting theme of fine-tuning our care of patients with rheumatic disease, I want to point out several sessions,” Dr. Gardner said.
Attendees interested in sessions on clinical applicability will have to choose between two different sessions Monday at 4:30 p.m.: one on dermatomyositis, a relatively rare but difficult-to-treat entity, and the other about treatment of the patient with rheumatoid arthritis when the patient is not well and suffering from comorbidities.
Monday at 8:30 a.m., an “Osteoporosis Update” will give listeners perspective on current and future therapies.
Sunday at 2:30 p.m., new guidelines for steroid-induced osteoporosis will be presented.
“Four or five sessions on the Tech Track will show rheumatologists how they can improve their practice by using technology,” Dr. Gardner said. “Several high-quality sessions are important to educators, including ‘Flipped Classroom, Technology, and Reflection’ [Monday at 12:30 p.m.] and ‘Year in Review’ [Sunday at 1:00 p.m.].”
Monday at 11:00 a.m., the Plenary session will feature Workforce Study results on how many rheumatologists will be needed in the year 2030, and in which geographic locations. This session will also include a discussion of the impact of part-time rheumatologists.
“Two sessions I am excited about are ‘Treat to Target in 2016,’ Tuesday at 4:30 p.m., and ‘Rheumatic Diseases in Native Americans,’ Sunday at 11:00 a.m.,” Dr. Gardner noted. “Concurrent abstract sessions throughout the meeting will feature discussions on new biologics, small molecules, and gene therapy.”
FROM THE ACR ANNUAL MEETING
Anti–nerve growth factor drug has long-term OA pain benefit, but unclear safety
Treatment for a year with the human anti–nerve growth factor monoclonal antibody fulranumab provided pain relief and functional benefits to patients with moderate to severe chronic osteoarthritis knee or hip pain but continued to show signs that the biologic may contribute to rapid progression of disease in a proportion of patients who came to need joint replacement, especially when used concurrently with nonsteroidal anti-inflammatory drugs.
The findings come from the double-blind extension phase of a 12-week, phase II, placebo-controlled, double-blind, randomized study that found significant reduction in the average pain intensity score (P less than or equal to .030) for patients who took fulranumab (Pain. 2013 Oct;154[10]:1910-9). The investigators wanted to determine the long-term safety of the biologic in light of the Food and Drug Administration’s 2010 “clinical hold” on studies of anti–nerve growth factor (anti-NGF) drugs such as fulranumab after concerns emerged that the class of anti-NGF antibodies may be associated with potential treatment-emergent adverse events (TEAEs) leading to joint destruction.
The long-term safety and efficacy results in the extension phase of the study when fulranumab was given as an adjunctive therapy to standard pain therapy revealed higher rates of serious TEAEs, including joint replacement, that were associated with fulranumab. While most of those TEAEs were independently adjudicated to stem from normal progression of OA, one-fifth of the patients on fulranumab who needed joint replacement had rapid progression of OA (RPOA).
Investigators led by Panna Sanga, MD, director of clinical research at Janssen, sought to determine the effects of the anti-NGF biologic as an adjunctive therapy to standard pain therapy over a 92-week period in 401 patients who had completed the 12-week efficacy study, as well as over a 26-week posttreatment follow-up. In the current extension phase of the trial, patients continued on their randomized dose in the original trial of placebo or subcutaneous fulranumab 1 mg or 3 mg every 4 weeks or fulranumab 3 mg, 6 mg, or 10 mg every 8 weeks, but they were permitted to change their concurrent pain medications as clinically needed.
Although the study intended for patients to receive 2 years of treatment (104 weeks), the FDA’s clinical hold meant that the median duration of exposure to fulranumab in the extension study was only 365-393 days across the dosing regimens, the authors explained (Arthritis Rheumatol. 2016 Oct 16 doi: 10.1002/art.39943).
Overall, 421 (90%) of 466 intent-to-treat patients experienced at least one TEAE during both study phases, with similar incidence between those randomized to placebo (n = 69, 88%) and the fulranumab groups (n = 352, 91%).
TEAEs that occurred with a frequency of 10% or more among all fulranumab-treated patients were arthralgia (21%), OA (18%), paresthesia, and upper respiratory tract infection (13% each), while these were arthralgia (15%), OA (14%), and sinusitis (12%) among patients randomized to placebo.
A total of 109 patients (23%) reported serious TEAEs, including 13 (17%) taking placebo and 96 (25%) taking fulranumab. Serious TEAEs that were reported in 5% or more of patients in the fulranumab groups were knee arthroplasty (n = 38, 10%) and hip arthroplasty (n = 26, 7%). Overall, 81 joint replacements occurred in 71 patients (placebo: n = , 11%; fulranumab: n = 63, 89%).
An independent adjudication committee that the study sponsor, Janssen, established after the study was put on hold ruled that the majority of these joint replacements resulted from the normal progression of OA (n = 56, 79%). However, the adjudication committee determined that 15 (21%) patients in the fulranumab treatment groups had RPOA.
The study authors pointed out that the patients with RPOA regularly used NSAIDs and had a prior history of OA in the affected joint. Nevertheless, because of the small number of RPOA cases per treatment group, a drug or dose effect for RPOA could not be evaluated, they said.
“Future studies are warranted to demonstrate whether limiting the use of concomitant chronic NSAIDs and using only lower doses of fulranumab may reduce the risk of RPOA,” they wrote.
The extension study also looked at the longer-term efficacy of fulranumab. Efficacy endpoints on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales and the Patient Global Assessment (PGA) scores that looked at changes from baseline showed that in comparison with placebo, dosing regimens of fulranumab 3 mg every 4 weeks and 10 mg every 8 weeks gave “continued effective relief of the pain associated with knee and hip OA as early as week 4 and was maintained up to week 53,” the researchers reported.
These results were further corroborated by improvements in physical function on the WOMAC physical function subscale and PGA scale scores, which suggested “sustained efficacy of long-term fulranumab treatment,” they said.
All authors except one were employees of Janssen.
Treatment for a year with the human anti–nerve growth factor monoclonal antibody fulranumab provided pain relief and functional benefits to patients with moderate to severe chronic osteoarthritis knee or hip pain but continued to show signs that the biologic may contribute to rapid progression of disease in a proportion of patients who came to need joint replacement, especially when used concurrently with nonsteroidal anti-inflammatory drugs.
The findings come from the double-blind extension phase of a 12-week, phase II, placebo-controlled, double-blind, randomized study that found significant reduction in the average pain intensity score (P less than or equal to .030) for patients who took fulranumab (Pain. 2013 Oct;154[10]:1910-9). The investigators wanted to determine the long-term safety of the biologic in light of the Food and Drug Administration’s 2010 “clinical hold” on studies of anti–nerve growth factor (anti-NGF) drugs such as fulranumab after concerns emerged that the class of anti-NGF antibodies may be associated with potential treatment-emergent adverse events (TEAEs) leading to joint destruction.
The long-term safety and efficacy results in the extension phase of the study when fulranumab was given as an adjunctive therapy to standard pain therapy revealed higher rates of serious TEAEs, including joint replacement, that were associated with fulranumab. While most of those TEAEs were independently adjudicated to stem from normal progression of OA, one-fifth of the patients on fulranumab who needed joint replacement had rapid progression of OA (RPOA).
Investigators led by Panna Sanga, MD, director of clinical research at Janssen, sought to determine the effects of the anti-NGF biologic as an adjunctive therapy to standard pain therapy over a 92-week period in 401 patients who had completed the 12-week efficacy study, as well as over a 26-week posttreatment follow-up. In the current extension phase of the trial, patients continued on their randomized dose in the original trial of placebo or subcutaneous fulranumab 1 mg or 3 mg every 4 weeks or fulranumab 3 mg, 6 mg, or 10 mg every 8 weeks, but they were permitted to change their concurrent pain medications as clinically needed.
Although the study intended for patients to receive 2 years of treatment (104 weeks), the FDA’s clinical hold meant that the median duration of exposure to fulranumab in the extension study was only 365-393 days across the dosing regimens, the authors explained (Arthritis Rheumatol. 2016 Oct 16 doi: 10.1002/art.39943).
Overall, 421 (90%) of 466 intent-to-treat patients experienced at least one TEAE during both study phases, with similar incidence between those randomized to placebo (n = 69, 88%) and the fulranumab groups (n = 352, 91%).
TEAEs that occurred with a frequency of 10% or more among all fulranumab-treated patients were arthralgia (21%), OA (18%), paresthesia, and upper respiratory tract infection (13% each), while these were arthralgia (15%), OA (14%), and sinusitis (12%) among patients randomized to placebo.
A total of 109 patients (23%) reported serious TEAEs, including 13 (17%) taking placebo and 96 (25%) taking fulranumab. Serious TEAEs that were reported in 5% or more of patients in the fulranumab groups were knee arthroplasty (n = 38, 10%) and hip arthroplasty (n = 26, 7%). Overall, 81 joint replacements occurred in 71 patients (placebo: n = , 11%; fulranumab: n = 63, 89%).
An independent adjudication committee that the study sponsor, Janssen, established after the study was put on hold ruled that the majority of these joint replacements resulted from the normal progression of OA (n = 56, 79%). However, the adjudication committee determined that 15 (21%) patients in the fulranumab treatment groups had RPOA.
The study authors pointed out that the patients with RPOA regularly used NSAIDs and had a prior history of OA in the affected joint. Nevertheless, because of the small number of RPOA cases per treatment group, a drug or dose effect for RPOA could not be evaluated, they said.
“Future studies are warranted to demonstrate whether limiting the use of concomitant chronic NSAIDs and using only lower doses of fulranumab may reduce the risk of RPOA,” they wrote.
The extension study also looked at the longer-term efficacy of fulranumab. Efficacy endpoints on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales and the Patient Global Assessment (PGA) scores that looked at changes from baseline showed that in comparison with placebo, dosing regimens of fulranumab 3 mg every 4 weeks and 10 mg every 8 weeks gave “continued effective relief of the pain associated with knee and hip OA as early as week 4 and was maintained up to week 53,” the researchers reported.
These results were further corroborated by improvements in physical function on the WOMAC physical function subscale and PGA scale scores, which suggested “sustained efficacy of long-term fulranumab treatment,” they said.
All authors except one were employees of Janssen.
Treatment for a year with the human anti–nerve growth factor monoclonal antibody fulranumab provided pain relief and functional benefits to patients with moderate to severe chronic osteoarthritis knee or hip pain but continued to show signs that the biologic may contribute to rapid progression of disease in a proportion of patients who came to need joint replacement, especially when used concurrently with nonsteroidal anti-inflammatory drugs.
The findings come from the double-blind extension phase of a 12-week, phase II, placebo-controlled, double-blind, randomized study that found significant reduction in the average pain intensity score (P less than or equal to .030) for patients who took fulranumab (Pain. 2013 Oct;154[10]:1910-9). The investigators wanted to determine the long-term safety of the biologic in light of the Food and Drug Administration’s 2010 “clinical hold” on studies of anti–nerve growth factor (anti-NGF) drugs such as fulranumab after concerns emerged that the class of anti-NGF antibodies may be associated with potential treatment-emergent adverse events (TEAEs) leading to joint destruction.
The long-term safety and efficacy results in the extension phase of the study when fulranumab was given as an adjunctive therapy to standard pain therapy revealed higher rates of serious TEAEs, including joint replacement, that were associated with fulranumab. While most of those TEAEs were independently adjudicated to stem from normal progression of OA, one-fifth of the patients on fulranumab who needed joint replacement had rapid progression of OA (RPOA).
Investigators led by Panna Sanga, MD, director of clinical research at Janssen, sought to determine the effects of the anti-NGF biologic as an adjunctive therapy to standard pain therapy over a 92-week period in 401 patients who had completed the 12-week efficacy study, as well as over a 26-week posttreatment follow-up. In the current extension phase of the trial, patients continued on their randomized dose in the original trial of placebo or subcutaneous fulranumab 1 mg or 3 mg every 4 weeks or fulranumab 3 mg, 6 mg, or 10 mg every 8 weeks, but they were permitted to change their concurrent pain medications as clinically needed.
Although the study intended for patients to receive 2 years of treatment (104 weeks), the FDA’s clinical hold meant that the median duration of exposure to fulranumab in the extension study was only 365-393 days across the dosing regimens, the authors explained (Arthritis Rheumatol. 2016 Oct 16 doi: 10.1002/art.39943).
Overall, 421 (90%) of 466 intent-to-treat patients experienced at least one TEAE during both study phases, with similar incidence between those randomized to placebo (n = 69, 88%) and the fulranumab groups (n = 352, 91%).
TEAEs that occurred with a frequency of 10% or more among all fulranumab-treated patients were arthralgia (21%), OA (18%), paresthesia, and upper respiratory tract infection (13% each), while these were arthralgia (15%), OA (14%), and sinusitis (12%) among patients randomized to placebo.
A total of 109 patients (23%) reported serious TEAEs, including 13 (17%) taking placebo and 96 (25%) taking fulranumab. Serious TEAEs that were reported in 5% or more of patients in the fulranumab groups were knee arthroplasty (n = 38, 10%) and hip arthroplasty (n = 26, 7%). Overall, 81 joint replacements occurred in 71 patients (placebo: n = , 11%; fulranumab: n = 63, 89%).
An independent adjudication committee that the study sponsor, Janssen, established after the study was put on hold ruled that the majority of these joint replacements resulted from the normal progression of OA (n = 56, 79%). However, the adjudication committee determined that 15 (21%) patients in the fulranumab treatment groups had RPOA.
The study authors pointed out that the patients with RPOA regularly used NSAIDs and had a prior history of OA in the affected joint. Nevertheless, because of the small number of RPOA cases per treatment group, a drug or dose effect for RPOA could not be evaluated, they said.
“Future studies are warranted to demonstrate whether limiting the use of concomitant chronic NSAIDs and using only lower doses of fulranumab may reduce the risk of RPOA,” they wrote.
The extension study also looked at the longer-term efficacy of fulranumab. Efficacy endpoints on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales and the Patient Global Assessment (PGA) scores that looked at changes from baseline showed that in comparison with placebo, dosing regimens of fulranumab 3 mg every 4 weeks and 10 mg every 8 weeks gave “continued effective relief of the pain associated with knee and hip OA as early as week 4 and was maintained up to week 53,” the researchers reported.
These results were further corroborated by improvements in physical function on the WOMAC physical function subscale and PGA scale scores, which suggested “sustained efficacy of long-term fulranumab treatment,” they said.
All authors except one were employees of Janssen.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:
Major finding: A total of 81 joint replacements occurred in 71 patients (placebo: n = 8, 11%; fulranumab: n = 63, 89%).
Data source: Phase II randomized double-blind extension study of 401 patients with moderate to severe chronic OA knee or hip pain.
Disclosures: All authors except one were employees of Janssen, which funded the study.
Beta-blockers reduce pain, opioid use in osteoarthritis
Beta-blockers were associated with less pain and lower opioid consumption in a case-control study of nearly 900 patients with osteoarthritis, Ana Valdes, PhD, and her colleagues reported in Arthritis Care & Research.
There is some mechanistic support for the association, which has been observed in other pain disorders, noted Dr. Valdes of the University of Nottingham (England) and her coauthors (Arthritis Care Res. 2016 Oct 1. doi: 10.1002/acr.23091).
The cohort was drawn from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. Dr. Valdes and her associates examined the effect of beta-blocker use on pain as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain score in 873 patients with knee and/or hip osteoarthritis. All were already taking at least one antihypertensive drug. The presence of “joint pain” was defined as a WOMAC score of less than 75. The multivariate analysis adjusted for age, gender, body mass index, knee or hip OA, history of other joint replacement, anxiety, and depression. Patients were a mean of about 69 years old; 347 were taking a beta-blocker.
After adjusting for the confounders, those taking the drugs were 32% less likely to report joint pain (odds ratio, 0.68). The effect seemed time bound: For every year on a beta-blocker, patients had a 4% decline in the risk of joint pain. The benefit was of similar magnitude regardless of whether patients had joint replacement. Beta-blockers also reduced the rate of opioid prescription by 27% (OR, 0.73), the authors noted.
They also found a similar benefit to the use of adrenergic blockers in general, but not with alpha-blockers. No other class of antihypertensive drugs showed any association with joint pain or with prescription of analgesics.
“These results might raise some future research questions for the treatment of hypertension in individuals with joint pain. Current guidance [in both the United Kingdom and United States] state that beta-blockers should no longer be preferred as an initial therapy for routine hypertension and should be used only when there is a compelling indication other than blood pressure control (for example, angina or chronic heart failure). If confirmed in randomized controlled trials, the data presented here could suggest that, in people with chronic joint pain beta-blockers may be considered as part of their antihypertensive regimen.”
The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
Beta-blockers were associated with less pain and lower opioid consumption in a case-control study of nearly 900 patients with osteoarthritis, Ana Valdes, PhD, and her colleagues reported in Arthritis Care & Research.
There is some mechanistic support for the association, which has been observed in other pain disorders, noted Dr. Valdes of the University of Nottingham (England) and her coauthors (Arthritis Care Res. 2016 Oct 1. doi: 10.1002/acr.23091).
The cohort was drawn from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. Dr. Valdes and her associates examined the effect of beta-blocker use on pain as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain score in 873 patients with knee and/or hip osteoarthritis. All were already taking at least one antihypertensive drug. The presence of “joint pain” was defined as a WOMAC score of less than 75. The multivariate analysis adjusted for age, gender, body mass index, knee or hip OA, history of other joint replacement, anxiety, and depression. Patients were a mean of about 69 years old; 347 were taking a beta-blocker.
After adjusting for the confounders, those taking the drugs were 32% less likely to report joint pain (odds ratio, 0.68). The effect seemed time bound: For every year on a beta-blocker, patients had a 4% decline in the risk of joint pain. The benefit was of similar magnitude regardless of whether patients had joint replacement. Beta-blockers also reduced the rate of opioid prescription by 27% (OR, 0.73), the authors noted.
They also found a similar benefit to the use of adrenergic blockers in general, but not with alpha-blockers. No other class of antihypertensive drugs showed any association with joint pain or with prescription of analgesics.
“These results might raise some future research questions for the treatment of hypertension in individuals with joint pain. Current guidance [in both the United Kingdom and United States] state that beta-blockers should no longer be preferred as an initial therapy for routine hypertension and should be used only when there is a compelling indication other than blood pressure control (for example, angina or chronic heart failure). If confirmed in randomized controlled trials, the data presented here could suggest that, in people with chronic joint pain beta-blockers may be considered as part of their antihypertensive regimen.”
The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
Beta-blockers were associated with less pain and lower opioid consumption in a case-control study of nearly 900 patients with osteoarthritis, Ana Valdes, PhD, and her colleagues reported in Arthritis Care & Research.
There is some mechanistic support for the association, which has been observed in other pain disorders, noted Dr. Valdes of the University of Nottingham (England) and her coauthors (Arthritis Care Res. 2016 Oct 1. doi: 10.1002/acr.23091).
The cohort was drawn from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. Dr. Valdes and her associates examined the effect of beta-blocker use on pain as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain score in 873 patients with knee and/or hip osteoarthritis. All were already taking at least one antihypertensive drug. The presence of “joint pain” was defined as a WOMAC score of less than 75. The multivariate analysis adjusted for age, gender, body mass index, knee or hip OA, history of other joint replacement, anxiety, and depression. Patients were a mean of about 69 years old; 347 were taking a beta-blocker.
After adjusting for the confounders, those taking the drugs were 32% less likely to report joint pain (odds ratio, 0.68). The effect seemed time bound: For every year on a beta-blocker, patients had a 4% decline in the risk of joint pain. The benefit was of similar magnitude regardless of whether patients had joint replacement. Beta-blockers also reduced the rate of opioid prescription by 27% (OR, 0.73), the authors noted.
They also found a similar benefit to the use of adrenergic blockers in general, but not with alpha-blockers. No other class of antihypertensive drugs showed any association with joint pain or with prescription of analgesics.
“These results might raise some future research questions for the treatment of hypertension in individuals with joint pain. Current guidance [in both the United Kingdom and United States] state that beta-blockers should no longer be preferred as an initial therapy for routine hypertension and should be used only when there is a compelling indication other than blood pressure control (for example, angina or chronic heart failure). If confirmed in randomized controlled trials, the data presented here could suggest that, in people with chronic joint pain beta-blockers may be considered as part of their antihypertensive regimen.”
The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: The likelihood of joint pain was 32% and opioid use 27% lower in patients taking beta-blockers, compared with those not taking them.
Data source: The case-control study comprised 873 patients.
Disclosures: The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
Severe joint pain in adults with arthritis continues to rise
The prevalence of severe joint pain among adults with diagnosed arthritis continues to increase, researchers from the Centers for Disease Control and Prevention reported in the Oct. 7 Morbidity and Mortality Weekly Report.
In 2014, more than one-fourth of adults with arthritis had severe joint pain. That is about 14.6 million Americans with severe joint pain, a significant increase from 2002 when there were an estimated 10.5 million adults with severe joint pain, according to Kamil E. Barbour, PhD, and his associates from the National Center for Chronic Disease Prevention and Health Promotion (MMWR. 2016 Oct 7;65[39]:1052-6).
Severe joint pain was also more prevalent among patients with overall fair or poor health who were obese or had heart disease, diabetes, or serious psychological distress, the investigators reported.
The investigators defined people with arthritis as those who had “been told by a doctor or other health professional” that they have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia. Severe joint pain was defined as a response of 7 or higher on a scale of 0-10 for rating joint pain on average over the past 30 days.
Recently, the U.S. Department of Health & Human Services released its National Pain Strategy, the nation’s first broad, federal effort aimed at developing strategies to reduce the burden of pain among Americans. The initiatives major objectives are to take steps to reduce barriers to pain care, and to increase patient knowledge of treatment options and risks, Dr. Barbour and his associates wrote.
“Health care providers and public health practitioners can begin to implement the recommendations [from the National Pain Strategy] and improve pain care among adults with arthritis and [severe joint pain] by prioritizing self-management education and appropriate physical activity interventions as effective nonpharmacologic ways to reduce pain and improve health outcomes,” the researchers added.
[email protected]
On Twitter @jessnicolecraig
The prevalence of severe joint pain among adults with diagnosed arthritis continues to increase, researchers from the Centers for Disease Control and Prevention reported in the Oct. 7 Morbidity and Mortality Weekly Report.
In 2014, more than one-fourth of adults with arthritis had severe joint pain. That is about 14.6 million Americans with severe joint pain, a significant increase from 2002 when there were an estimated 10.5 million adults with severe joint pain, according to Kamil E. Barbour, PhD, and his associates from the National Center for Chronic Disease Prevention and Health Promotion (MMWR. 2016 Oct 7;65[39]:1052-6).
Severe joint pain was also more prevalent among patients with overall fair or poor health who were obese or had heart disease, diabetes, or serious psychological distress, the investigators reported.
The investigators defined people with arthritis as those who had “been told by a doctor or other health professional” that they have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia. Severe joint pain was defined as a response of 7 or higher on a scale of 0-10 for rating joint pain on average over the past 30 days.
Recently, the U.S. Department of Health & Human Services released its National Pain Strategy, the nation’s first broad, federal effort aimed at developing strategies to reduce the burden of pain among Americans. The initiatives major objectives are to take steps to reduce barriers to pain care, and to increase patient knowledge of treatment options and risks, Dr. Barbour and his associates wrote.
“Health care providers and public health practitioners can begin to implement the recommendations [from the National Pain Strategy] and improve pain care among adults with arthritis and [severe joint pain] by prioritizing self-management education and appropriate physical activity interventions as effective nonpharmacologic ways to reduce pain and improve health outcomes,” the researchers added.
[email protected]
On Twitter @jessnicolecraig
The prevalence of severe joint pain among adults with diagnosed arthritis continues to increase, researchers from the Centers for Disease Control and Prevention reported in the Oct. 7 Morbidity and Mortality Weekly Report.
In 2014, more than one-fourth of adults with arthritis had severe joint pain. That is about 14.6 million Americans with severe joint pain, a significant increase from 2002 when there were an estimated 10.5 million adults with severe joint pain, according to Kamil E. Barbour, PhD, and his associates from the National Center for Chronic Disease Prevention and Health Promotion (MMWR. 2016 Oct 7;65[39]:1052-6).
Severe joint pain was also more prevalent among patients with overall fair or poor health who were obese or had heart disease, diabetes, or serious psychological distress, the investigators reported.
The investigators defined people with arthritis as those who had “been told by a doctor or other health professional” that they have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia. Severe joint pain was defined as a response of 7 or higher on a scale of 0-10 for rating joint pain on average over the past 30 days.
Recently, the U.S. Department of Health & Human Services released its National Pain Strategy, the nation’s first broad, federal effort aimed at developing strategies to reduce the burden of pain among Americans. The initiatives major objectives are to take steps to reduce barriers to pain care, and to increase patient knowledge of treatment options and risks, Dr. Barbour and his associates wrote.
“Health care providers and public health practitioners can begin to implement the recommendations [from the National Pain Strategy] and improve pain care among adults with arthritis and [severe joint pain] by prioritizing self-management education and appropriate physical activity interventions as effective nonpharmacologic ways to reduce pain and improve health outcomes,” the researchers added.
[email protected]
On Twitter @jessnicolecraig
FROM MMWR
Key clinical point:
Major finding: The estimated number of U.S. adults with severe joint pain rose from 10.5 million in 2002 to 14.6 million in 2014.
Data source: Analysis of data from the National Health Interview Survey in 2002, 2003, 2006, 2009, and 2014.
Disclosures: The authors are federal government employees and have no financial disclosures.
Pain starting in knee later arises in other joints
People who develop knee pain associated with osteoarthritis often subsequently develop pain in other joints, according to a study of two observational, community-based cohorts that could not discern any pattern of new pain sites.
In the “first investigation of the association of knee pain with pain in multiple other sites,” David T. Felson, MD, of Boston University and his colleagues reported that the regions where pain developed after first appearing in the knee varied from person to person and occurred in both upper and lower extremities, which goes against the hypothesis that adjacent joints are most often affected by knee pain.
The study involved patients from the MOST (Multicenter Osteoarthritis Study) trial, including 281 with knee pain at the index visit (168 unilaterally) and 852 without, as well as patients from OAI (the Osteoarthritis Initiative), including 412 with knee pain at the index visit (241 unilaterally), and 1,941 without. The investigators assessed the patients’ data for 14 total joints outside of the knees: 2 each of feet, ankles, hips, hands, wrists, elbows, and shoulders (Arthritis Rheumatol. 2016 Sep 2. doi: 10.1002/art.39848).
Patients with new-onset knee pain at the index visit reported a mean of 2.3 painful joints outside the knee, compared with a significantly lower number of 1.3 reported by those without knee pain. The mean number of nonknee joints with pain was higher among patients with bilateral knee pain, compared with unilateral knee pain. The percentage of patients who reported pain outside the knee rose with the number of painful knees: 80% for two, 64% for one, and 50% for none.
The patients who developed new unilateral knee pain at the index visit also experienced an increase in prevalent joint pain in multiple joints in upper- and lower-extremity sites. In particular, the investigators noted that ipsilateral prevalent hip joint pain, which they characterized as pain in the groin or front of the thigh, was more than twice as likely to occur among those with new unilateral knee pain at the index visit, but the odds for contralateral hip joint pain did not reach statistical significance. The comparisons were adjusted for age, sex, body mass index, depression at the index visit, study (MOST or OAI), and count of painful upper and lower limb joints at the index visit (excluding knees).
When examining only patients with new-onset joint pain outside of the knee, the odds of patients with new knee pain to later develop new-onset joint pain outside the knee were 30% higher than for those without knee pain. Patients with new knee pain had a mean 2.6 new painful joints out of 12.1 eligible joints, compared with 2.0 new painful joints in those without knee pain out of 12.7 eligible joints. (Joint regions with prevalent symptoms at the index visit were excluded as incident painful sites.) Patients with knee pain also had a consistently higher rate of new-onset pain in nonknee joints when compared with patients without knee pain in at least half of the follow-up visits over the course of the MOST and OAI studies. Sensitivity analyses indicated that the association between knee pain and subsequent pain in other joints was not driven by the inclusion of patients with widespread pain.
“There was no clear-cut predilection for pain in any specific lower-extremity joint region,” the investigators wrote.
The investigators noted that other researchers have suggested that patients with knee pain may be at higher risk for lower-extremity joint pain because of changes to their gait that gradually cause damage to other joints, but evidence in this study doesn’t “necessarily support the argument that in persons with knee pain, aberrant loading by altered movement patterns induces pain in only nearby joints. Our findings suggest that the sites affected are more than just hip and ankle and that there is no special predilection for pain in these locations.”
While the investigators cannot differentiate underlying mechanisms for their study’s finding of multiple co-occurring sites of joint pain in people with new-onset knee pain, they suggested that it “supports either a predilection for osteoarthritic changes at multiple joint sites and/or raises the possibility that nervous system–driven pain sensitization increases the risk not only of widespread pain but even of regional pain. Since symptomatic OA is unusual in some of these painful sites (e.g., elbow, shoulder, ankle), pain sensitization would seem a more likely explanation.”
Some of the study’s limitations described by the investigators included the uncertainty surrounding whether new-onset knee pain was truly new onset or whether it was a reoccurrence, and also the fact that most of the people in the two cohorts had multiple sites of joint pain at both the baseline and the index visit and there were too few people with no sites of pain outside the knee to carry out subanalyses in that group, which “speaks to the high prevalence of multiple joint pains in older adult cohorts.”
The research was supported by grants from the National Institutes of Health. The authors had no disclosures to report.
People who develop knee pain associated with osteoarthritis often subsequently develop pain in other joints, according to a study of two observational, community-based cohorts that could not discern any pattern of new pain sites.
In the “first investigation of the association of knee pain with pain in multiple other sites,” David T. Felson, MD, of Boston University and his colleagues reported that the regions where pain developed after first appearing in the knee varied from person to person and occurred in both upper and lower extremities, which goes against the hypothesis that adjacent joints are most often affected by knee pain.
The study involved patients from the MOST (Multicenter Osteoarthritis Study) trial, including 281 with knee pain at the index visit (168 unilaterally) and 852 without, as well as patients from OAI (the Osteoarthritis Initiative), including 412 with knee pain at the index visit (241 unilaterally), and 1,941 without. The investigators assessed the patients’ data for 14 total joints outside of the knees: 2 each of feet, ankles, hips, hands, wrists, elbows, and shoulders (Arthritis Rheumatol. 2016 Sep 2. doi: 10.1002/art.39848).
Patients with new-onset knee pain at the index visit reported a mean of 2.3 painful joints outside the knee, compared with a significantly lower number of 1.3 reported by those without knee pain. The mean number of nonknee joints with pain was higher among patients with bilateral knee pain, compared with unilateral knee pain. The percentage of patients who reported pain outside the knee rose with the number of painful knees: 80% for two, 64% for one, and 50% for none.
The patients who developed new unilateral knee pain at the index visit also experienced an increase in prevalent joint pain in multiple joints in upper- and lower-extremity sites. In particular, the investigators noted that ipsilateral prevalent hip joint pain, which they characterized as pain in the groin or front of the thigh, was more than twice as likely to occur among those with new unilateral knee pain at the index visit, but the odds for contralateral hip joint pain did not reach statistical significance. The comparisons were adjusted for age, sex, body mass index, depression at the index visit, study (MOST or OAI), and count of painful upper and lower limb joints at the index visit (excluding knees).
When examining only patients with new-onset joint pain outside of the knee, the odds of patients with new knee pain to later develop new-onset joint pain outside the knee were 30% higher than for those without knee pain. Patients with new knee pain had a mean 2.6 new painful joints out of 12.1 eligible joints, compared with 2.0 new painful joints in those without knee pain out of 12.7 eligible joints. (Joint regions with prevalent symptoms at the index visit were excluded as incident painful sites.) Patients with knee pain also had a consistently higher rate of new-onset pain in nonknee joints when compared with patients without knee pain in at least half of the follow-up visits over the course of the MOST and OAI studies. Sensitivity analyses indicated that the association between knee pain and subsequent pain in other joints was not driven by the inclusion of patients with widespread pain.
“There was no clear-cut predilection for pain in any specific lower-extremity joint region,” the investigators wrote.
The investigators noted that other researchers have suggested that patients with knee pain may be at higher risk for lower-extremity joint pain because of changes to their gait that gradually cause damage to other joints, but evidence in this study doesn’t “necessarily support the argument that in persons with knee pain, aberrant loading by altered movement patterns induces pain in only nearby joints. Our findings suggest that the sites affected are more than just hip and ankle and that there is no special predilection for pain in these locations.”
While the investigators cannot differentiate underlying mechanisms for their study’s finding of multiple co-occurring sites of joint pain in people with new-onset knee pain, they suggested that it “supports either a predilection for osteoarthritic changes at multiple joint sites and/or raises the possibility that nervous system–driven pain sensitization increases the risk not only of widespread pain but even of regional pain. Since symptomatic OA is unusual in some of these painful sites (e.g., elbow, shoulder, ankle), pain sensitization would seem a more likely explanation.”
Some of the study’s limitations described by the investigators included the uncertainty surrounding whether new-onset knee pain was truly new onset or whether it was a reoccurrence, and also the fact that most of the people in the two cohorts had multiple sites of joint pain at both the baseline and the index visit and there were too few people with no sites of pain outside the knee to carry out subanalyses in that group, which “speaks to the high prevalence of multiple joint pains in older adult cohorts.”
The research was supported by grants from the National Institutes of Health. The authors had no disclosures to report.
People who develop knee pain associated with osteoarthritis often subsequently develop pain in other joints, according to a study of two observational, community-based cohorts that could not discern any pattern of new pain sites.
In the “first investigation of the association of knee pain with pain in multiple other sites,” David T. Felson, MD, of Boston University and his colleagues reported that the regions where pain developed after first appearing in the knee varied from person to person and occurred in both upper and lower extremities, which goes against the hypothesis that adjacent joints are most often affected by knee pain.
The study involved patients from the MOST (Multicenter Osteoarthritis Study) trial, including 281 with knee pain at the index visit (168 unilaterally) and 852 without, as well as patients from OAI (the Osteoarthritis Initiative), including 412 with knee pain at the index visit (241 unilaterally), and 1,941 without. The investigators assessed the patients’ data for 14 total joints outside of the knees: 2 each of feet, ankles, hips, hands, wrists, elbows, and shoulders (Arthritis Rheumatol. 2016 Sep 2. doi: 10.1002/art.39848).
Patients with new-onset knee pain at the index visit reported a mean of 2.3 painful joints outside the knee, compared with a significantly lower number of 1.3 reported by those without knee pain. The mean number of nonknee joints with pain was higher among patients with bilateral knee pain, compared with unilateral knee pain. The percentage of patients who reported pain outside the knee rose with the number of painful knees: 80% for two, 64% for one, and 50% for none.
The patients who developed new unilateral knee pain at the index visit also experienced an increase in prevalent joint pain in multiple joints in upper- and lower-extremity sites. In particular, the investigators noted that ipsilateral prevalent hip joint pain, which they characterized as pain in the groin or front of the thigh, was more than twice as likely to occur among those with new unilateral knee pain at the index visit, but the odds for contralateral hip joint pain did not reach statistical significance. The comparisons were adjusted for age, sex, body mass index, depression at the index visit, study (MOST or OAI), and count of painful upper and lower limb joints at the index visit (excluding knees).
When examining only patients with new-onset joint pain outside of the knee, the odds of patients with new knee pain to later develop new-onset joint pain outside the knee were 30% higher than for those without knee pain. Patients with new knee pain had a mean 2.6 new painful joints out of 12.1 eligible joints, compared with 2.0 new painful joints in those without knee pain out of 12.7 eligible joints. (Joint regions with prevalent symptoms at the index visit were excluded as incident painful sites.) Patients with knee pain also had a consistently higher rate of new-onset pain in nonknee joints when compared with patients without knee pain in at least half of the follow-up visits over the course of the MOST and OAI studies. Sensitivity analyses indicated that the association between knee pain and subsequent pain in other joints was not driven by the inclusion of patients with widespread pain.
“There was no clear-cut predilection for pain in any specific lower-extremity joint region,” the investigators wrote.
The investigators noted that other researchers have suggested that patients with knee pain may be at higher risk for lower-extremity joint pain because of changes to their gait that gradually cause damage to other joints, but evidence in this study doesn’t “necessarily support the argument that in persons with knee pain, aberrant loading by altered movement patterns induces pain in only nearby joints. Our findings suggest that the sites affected are more than just hip and ankle and that there is no special predilection for pain in these locations.”
While the investigators cannot differentiate underlying mechanisms for their study’s finding of multiple co-occurring sites of joint pain in people with new-onset knee pain, they suggested that it “supports either a predilection for osteoarthritic changes at multiple joint sites and/or raises the possibility that nervous system–driven pain sensitization increases the risk not only of widespread pain but even of regional pain. Since symptomatic OA is unusual in some of these painful sites (e.g., elbow, shoulder, ankle), pain sensitization would seem a more likely explanation.”
Some of the study’s limitations described by the investigators included the uncertainty surrounding whether new-onset knee pain was truly new onset or whether it was a reoccurrence, and also the fact that most of the people in the two cohorts had multiple sites of joint pain at both the baseline and the index visit and there were too few people with no sites of pain outside the knee to carry out subanalyses in that group, which “speaks to the high prevalence of multiple joint pains in older adult cohorts.”
The research was supported by grants from the National Institutes of Health. The authors had no disclosures to report.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point:People with frequently painful knees often develop pain in joints outside the knee, and the sites vary from person to person.
Major finding: The odds of patients with new knee pain to later develop joint pain outside the knee were 30% higher than for those without knee pain.
Data source: A study of 693 persons with index visit knee pain and 2,793 without it from two community-based cohorts.
Disclosures: The research was supported by grants from the National Institutes of Health. The authors had no disclosures to report.
Tailored exercise boosts physical function for knee OA patients with comorbidities
Adults with knee osteoarthritis and at least one comorbid condition significantly improved their physical function after a comorbidity-targeted 20-week exercise program in a randomized, controlled trial of 126 patients.
“Guidelines on knee osteoarthritis do not provide guidance on tailoring exercise therapy to the presence of comorbidity,” wrote Mariëtte de Rooij of the Amsterdam Rehabilitation Research Center and her colleagues. “In clinical practice, comorbidity is a frequent reason to exclude patients from exercise therapy,” they noted.
The researchers randomized 126 adults with knee osteoarthritis and at least one of the following comorbidities: coronary disease, heart failure, type 2 diabetes, chronic obstructive pulmonary disease, or obesity (body mass index 30 kg/m2 or higher). The treatment group participated in a 20-week exercise program adapted to their comorbidities and physical limitations. Each program included aerobic exercise and strength training in two 30- to 60-minute sessions per week, supervised by a physical therapist. The control group received their current medical care for knee osteoarthritis and were placed on a waiting list for exercise therapy. Baseline characteristics and demographics were similar between the two groups, with mean ages of about 63 years, 81% with bilateral knee osteoarthritis, and a mean duration of symptoms of about 9 years. Patients with absolute contraindications for exercise therapy (such as myocardial infarction within the past 3 months) were excluded (Arthritis Care Res. 2016 Aug 26. doi: 10.1002/acr.23013).
In a follow-up visit 3 months after the end of the exercise program, patients in the treatment group averaged an 11.6-point (33%) improvement on the Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale and a 59-meter (15%) improvement on the 6-minute walk test, compared with controls.
In addition, patients in the treatment group reported a 1.7-point (27%) improvement on the Numeric Rating Scale for knee pain severity. No serious adverse events related to the exercise therapy were reported.
The exercise programs were adapted to the patients by adjusting the frequency, intensity, timing, and type (FITT) of exercises, educating patients about the impact of exercise on their comorbidities, and by coaching patients to ease fears of exertion or to encourage weight loss.
“This is the first study showing that tailored exercise therapy is efficacious in improving physical functioning and is safe in patients with knee osteoarthritis and severe comorbidities,” the researchers said. The findings were limited by several factors including a small sample size that made it impossible to analyze the impact of exercise on any specific comorbidity, and the lack of cost-effectiveness data. However, “the results should encourage clinicians to consider exercise therapy as a treatment option for patients with knee osteoarthritis, even in the presence of severe comorbidity,” the researchers added.
The trial was supported by the Royal Dutch Society for Physical Therapy and Merck Sharp & Dohme. The researchers had no financial conflicts to disclose.
Adults with knee osteoarthritis and at least one comorbid condition significantly improved their physical function after a comorbidity-targeted 20-week exercise program in a randomized, controlled trial of 126 patients.
“Guidelines on knee osteoarthritis do not provide guidance on tailoring exercise therapy to the presence of comorbidity,” wrote Mariëtte de Rooij of the Amsterdam Rehabilitation Research Center and her colleagues. “In clinical practice, comorbidity is a frequent reason to exclude patients from exercise therapy,” they noted.
The researchers randomized 126 adults with knee osteoarthritis and at least one of the following comorbidities: coronary disease, heart failure, type 2 diabetes, chronic obstructive pulmonary disease, or obesity (body mass index 30 kg/m2 or higher). The treatment group participated in a 20-week exercise program adapted to their comorbidities and physical limitations. Each program included aerobic exercise and strength training in two 30- to 60-minute sessions per week, supervised by a physical therapist. The control group received their current medical care for knee osteoarthritis and were placed on a waiting list for exercise therapy. Baseline characteristics and demographics were similar between the two groups, with mean ages of about 63 years, 81% with bilateral knee osteoarthritis, and a mean duration of symptoms of about 9 years. Patients with absolute contraindications for exercise therapy (such as myocardial infarction within the past 3 months) were excluded (Arthritis Care Res. 2016 Aug 26. doi: 10.1002/acr.23013).
In a follow-up visit 3 months after the end of the exercise program, patients in the treatment group averaged an 11.6-point (33%) improvement on the Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale and a 59-meter (15%) improvement on the 6-minute walk test, compared with controls.
In addition, patients in the treatment group reported a 1.7-point (27%) improvement on the Numeric Rating Scale for knee pain severity. No serious adverse events related to the exercise therapy were reported.
The exercise programs were adapted to the patients by adjusting the frequency, intensity, timing, and type (FITT) of exercises, educating patients about the impact of exercise on their comorbidities, and by coaching patients to ease fears of exertion or to encourage weight loss.
“This is the first study showing that tailored exercise therapy is efficacious in improving physical functioning and is safe in patients with knee osteoarthritis and severe comorbidities,” the researchers said. The findings were limited by several factors including a small sample size that made it impossible to analyze the impact of exercise on any specific comorbidity, and the lack of cost-effectiveness data. However, “the results should encourage clinicians to consider exercise therapy as a treatment option for patients with knee osteoarthritis, even in the presence of severe comorbidity,” the researchers added.
The trial was supported by the Royal Dutch Society for Physical Therapy and Merck Sharp & Dohme. The researchers had no financial conflicts to disclose.
Adults with knee osteoarthritis and at least one comorbid condition significantly improved their physical function after a comorbidity-targeted 20-week exercise program in a randomized, controlled trial of 126 patients.
“Guidelines on knee osteoarthritis do not provide guidance on tailoring exercise therapy to the presence of comorbidity,” wrote Mariëtte de Rooij of the Amsterdam Rehabilitation Research Center and her colleagues. “In clinical practice, comorbidity is a frequent reason to exclude patients from exercise therapy,” they noted.
The researchers randomized 126 adults with knee osteoarthritis and at least one of the following comorbidities: coronary disease, heart failure, type 2 diabetes, chronic obstructive pulmonary disease, or obesity (body mass index 30 kg/m2 or higher). The treatment group participated in a 20-week exercise program adapted to their comorbidities and physical limitations. Each program included aerobic exercise and strength training in two 30- to 60-minute sessions per week, supervised by a physical therapist. The control group received their current medical care for knee osteoarthritis and were placed on a waiting list for exercise therapy. Baseline characteristics and demographics were similar between the two groups, with mean ages of about 63 years, 81% with bilateral knee osteoarthritis, and a mean duration of symptoms of about 9 years. Patients with absolute contraindications for exercise therapy (such as myocardial infarction within the past 3 months) were excluded (Arthritis Care Res. 2016 Aug 26. doi: 10.1002/acr.23013).
In a follow-up visit 3 months after the end of the exercise program, patients in the treatment group averaged an 11.6-point (33%) improvement on the Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale and a 59-meter (15%) improvement on the 6-minute walk test, compared with controls.
In addition, patients in the treatment group reported a 1.7-point (27%) improvement on the Numeric Rating Scale for knee pain severity. No serious adverse events related to the exercise therapy were reported.
The exercise programs were adapted to the patients by adjusting the frequency, intensity, timing, and type (FITT) of exercises, educating patients about the impact of exercise on their comorbidities, and by coaching patients to ease fears of exertion or to encourage weight loss.
“This is the first study showing that tailored exercise therapy is efficacious in improving physical functioning and is safe in patients with knee osteoarthritis and severe comorbidities,” the researchers said. The findings were limited by several factors including a small sample size that made it impossible to analyze the impact of exercise on any specific comorbidity, and the lack of cost-effectiveness data. However, “the results should encourage clinicians to consider exercise therapy as a treatment option for patients with knee osteoarthritis, even in the presence of severe comorbidity,” the researchers added.
The trial was supported by the Royal Dutch Society for Physical Therapy and Merck Sharp & Dohme. The researchers had no financial conflicts to disclose.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: Adults with knee osteoarthritis and at least one comorbid condition had significant improvement in physical function after a 20-week targeted exercise program.
Major finding: After a 20-week exercise program tailored to their comorbid conditions, knee OA patients improved by an average of 33% on a physical function scale, compared with controls.
Data source: A randomized, controlled trial of 126 adults with knee osteoarthritis and at least one comorbid condition.
Disclosures: The trial was supported by the Royal Dutch Society for Physical Therapy and Merck Sharp & Dohme. The researchers had no financial conflicts to disclose.
FDA: New labeling warns against combining opioids, benzodiazepines
Labeling for prescription opioid pain or cough medicines and benzodiazepines will now carry the strongest available warning regarding serious side effects and death associated with their combined use, according to the Food and Drug Administration.
The new boxed warnings urge health care professionals to limit prescribing opioid pain medicines with benzodiazepines or other central nervous system depressants only to patients for whom alternative treatment options are inadequate, and to limit dosages and treatment duration to the minimum possible while achieving the desired clinical effect.
“First, the FDA is requiring companies to update their product labeling for ... benzodiazepines and opioids to include possible harms when they are used together. Second, we are requiring new or updated medication guides for these drugs reflecting those same warnings,” said Doug Throckmorton, MD, deputy director of the FDA’s Center for Drug Evaluation and Research, during a telebriefing.
Opioids will include a warning regarding prescribing with benzodiazepines and other central nervous system depressants, including alcohol. Benzodiazepines will include a warning regarding prescribing with opioids.
In addition, the FDA has issued a safety communication to “warn the public about the serious risk of taking these products together to help make doctors more cautious and patients better informed,” Dr. Throckmorton said.
The action comes amid ongoing efforts to address an epidemic of opioid addiction across the United States, and in response to a first-of-its-kind “citizen petition” calling for the boxed warnings.
A coalition of health officials from multiple cities, states, and U.S. territories initiated that petition in February, and thousands of concerned community members started an additional online petition. Those petitions were in response to both the increasing combined use of opioids and benzodiazepines and a concomitant increase in the risk of serious side effects and deaths associated with their combined use, according to Baltimore City Health Commissioner Leana Wen, MD.
As an emergency physician, Dr. Wen said that she has seen firsthand the alarming trends; one in three unintentional overdose deaths from prescribed opioids also involve benzodiazepines, she noted.
“In my state of Maryland in 2014, benzodiazepines were associated with 19% of prescription opioid deaths, and 59% of benzodiazepine-associated deaths involved prescription opioids. We also noted the growing biological evidence that combining these medications caused sleepiness and slowed breathing, increasing the likelihood of a fatal overdose,” she said.
Dr. Throckmorton further noted that emergency department visits and deaths involving patients prescribed both opioids and benzodiazepines have increased significantly over time. From 2004 to 2011, the rate of nonmedical use–related emergency department visits increased significantly each year, and overdose deaths involving both drug classes during that period nearly tripled on an annual basis.
“Communities have been seeing this trend for some time, but ultimately we needed data in order to act today,” FDA Commissioner Robert Califf, MD, said during the telebriefing.
The current action is just “one part of a larger effort to address this epidemic.
“We remain focused and deeply committed to contributing to the comprehensive effort to address the opioid epidemic,” Dr. Califf said. The FDA “will continue to monitor these products carefully and take additional actions as needed, and will share updates with the public as necessary as we work to address this public health crisis.”
Dr. Califf noted that the current action is part of the FDA’s Opioids Action Plan, which is “importantly not meant just to cover illicit or abusive use of opioids.”
“So, you’ll be hearing a lot more from us, because this is a national crisis that is not going away. We’re making progress on the prescribing, and we’re seeing a reduction in the use of opioids now,” he noted. “But we’re still seeing many overdoses.
“This is a continuum, and we’ll continue to try to do everything we can to address the epidemic,” Dr. Califf concluded.
Labeling for prescription opioid pain or cough medicines and benzodiazepines will now carry the strongest available warning regarding serious side effects and death associated with their combined use, according to the Food and Drug Administration.
The new boxed warnings urge health care professionals to limit prescribing opioid pain medicines with benzodiazepines or other central nervous system depressants only to patients for whom alternative treatment options are inadequate, and to limit dosages and treatment duration to the minimum possible while achieving the desired clinical effect.
“First, the FDA is requiring companies to update their product labeling for ... benzodiazepines and opioids to include possible harms when they are used together. Second, we are requiring new or updated medication guides for these drugs reflecting those same warnings,” said Doug Throckmorton, MD, deputy director of the FDA’s Center for Drug Evaluation and Research, during a telebriefing.
Opioids will include a warning regarding prescribing with benzodiazepines and other central nervous system depressants, including alcohol. Benzodiazepines will include a warning regarding prescribing with opioids.
In addition, the FDA has issued a safety communication to “warn the public about the serious risk of taking these products together to help make doctors more cautious and patients better informed,” Dr. Throckmorton said.
The action comes amid ongoing efforts to address an epidemic of opioid addiction across the United States, and in response to a first-of-its-kind “citizen petition” calling for the boxed warnings.
A coalition of health officials from multiple cities, states, and U.S. territories initiated that petition in February, and thousands of concerned community members started an additional online petition. Those petitions were in response to both the increasing combined use of opioids and benzodiazepines and a concomitant increase in the risk of serious side effects and deaths associated with their combined use, according to Baltimore City Health Commissioner Leana Wen, MD.
As an emergency physician, Dr. Wen said that she has seen firsthand the alarming trends; one in three unintentional overdose deaths from prescribed opioids also involve benzodiazepines, she noted.
“In my state of Maryland in 2014, benzodiazepines were associated with 19% of prescription opioid deaths, and 59% of benzodiazepine-associated deaths involved prescription opioids. We also noted the growing biological evidence that combining these medications caused sleepiness and slowed breathing, increasing the likelihood of a fatal overdose,” she said.
Dr. Throckmorton further noted that emergency department visits and deaths involving patients prescribed both opioids and benzodiazepines have increased significantly over time. From 2004 to 2011, the rate of nonmedical use–related emergency department visits increased significantly each year, and overdose deaths involving both drug classes during that period nearly tripled on an annual basis.
“Communities have been seeing this trend for some time, but ultimately we needed data in order to act today,” FDA Commissioner Robert Califf, MD, said during the telebriefing.
The current action is just “one part of a larger effort to address this epidemic.
“We remain focused and deeply committed to contributing to the comprehensive effort to address the opioid epidemic,” Dr. Califf said. The FDA “will continue to monitor these products carefully and take additional actions as needed, and will share updates with the public as necessary as we work to address this public health crisis.”
Dr. Califf noted that the current action is part of the FDA’s Opioids Action Plan, which is “importantly not meant just to cover illicit or abusive use of opioids.”
“So, you’ll be hearing a lot more from us, because this is a national crisis that is not going away. We’re making progress on the prescribing, and we’re seeing a reduction in the use of opioids now,” he noted. “But we’re still seeing many overdoses.
“This is a continuum, and we’ll continue to try to do everything we can to address the epidemic,” Dr. Califf concluded.
Labeling for prescription opioid pain or cough medicines and benzodiazepines will now carry the strongest available warning regarding serious side effects and death associated with their combined use, according to the Food and Drug Administration.
The new boxed warnings urge health care professionals to limit prescribing opioid pain medicines with benzodiazepines or other central nervous system depressants only to patients for whom alternative treatment options are inadequate, and to limit dosages and treatment duration to the minimum possible while achieving the desired clinical effect.
“First, the FDA is requiring companies to update their product labeling for ... benzodiazepines and opioids to include possible harms when they are used together. Second, we are requiring new or updated medication guides for these drugs reflecting those same warnings,” said Doug Throckmorton, MD, deputy director of the FDA’s Center for Drug Evaluation and Research, during a telebriefing.
Opioids will include a warning regarding prescribing with benzodiazepines and other central nervous system depressants, including alcohol. Benzodiazepines will include a warning regarding prescribing with opioids.
In addition, the FDA has issued a safety communication to “warn the public about the serious risk of taking these products together to help make doctors more cautious and patients better informed,” Dr. Throckmorton said.
The action comes amid ongoing efforts to address an epidemic of opioid addiction across the United States, and in response to a first-of-its-kind “citizen petition” calling for the boxed warnings.
A coalition of health officials from multiple cities, states, and U.S. territories initiated that petition in February, and thousands of concerned community members started an additional online petition. Those petitions were in response to both the increasing combined use of opioids and benzodiazepines and a concomitant increase in the risk of serious side effects and deaths associated with their combined use, according to Baltimore City Health Commissioner Leana Wen, MD.
As an emergency physician, Dr. Wen said that she has seen firsthand the alarming trends; one in three unintentional overdose deaths from prescribed opioids also involve benzodiazepines, she noted.
“In my state of Maryland in 2014, benzodiazepines were associated with 19% of prescription opioid deaths, and 59% of benzodiazepine-associated deaths involved prescription opioids. We also noted the growing biological evidence that combining these medications caused sleepiness and slowed breathing, increasing the likelihood of a fatal overdose,” she said.
Dr. Throckmorton further noted that emergency department visits and deaths involving patients prescribed both opioids and benzodiazepines have increased significantly over time. From 2004 to 2011, the rate of nonmedical use–related emergency department visits increased significantly each year, and overdose deaths involving both drug classes during that period nearly tripled on an annual basis.
“Communities have been seeing this trend for some time, but ultimately we needed data in order to act today,” FDA Commissioner Robert Califf, MD, said during the telebriefing.
The current action is just “one part of a larger effort to address this epidemic.
“We remain focused and deeply committed to contributing to the comprehensive effort to address the opioid epidemic,” Dr. Califf said. The FDA “will continue to monitor these products carefully and take additional actions as needed, and will share updates with the public as necessary as we work to address this public health crisis.”
Dr. Califf noted that the current action is part of the FDA’s Opioids Action Plan, which is “importantly not meant just to cover illicit or abusive use of opioids.”
“So, you’ll be hearing a lot more from us, because this is a national crisis that is not going away. We’re making progress on the prescribing, and we’re seeing a reduction in the use of opioids now,” he noted. “But we’re still seeing many overdoses.
“This is a continuum, and we’ll continue to try to do everything we can to address the epidemic,” Dr. Califf concluded.
Small study: Placebo bests chondroitin, glucosamine combo for knee osteoarthritis
Combination therapy involving chondroitin sulfate and glucosamine sulfate proved no better than placebo for the management of pain and functional impairment brought on by knee osteoarthritis, in a double-blind, randomized trial.
“This is the first RCT sponsored by a pharmaceutical company to evaluate the efficacy of a combination of CS [chondroitin sulfate] plus GS [glucosamine sulfate] and including a [Data and Safety Monitoring Board] composed of independent experts charged with ensuring participant safety and accurate, bias-free data,” wrote the authors, led by Jorge A. Roman-Blas, MD, of Fundación Jiménez Díaz in Madrid (Arthritis Rheumatol. 2016 Jul 31. doi: 10.1002/art.39819).
Dr. Roman-Blas and his coinvestigators recruited patients with Kellgren-Lawrence stages II-III knee osteoarthritis from one orthopedic surgery and nine rheumatology centers across Spain. The study was split into two parts; the first part would have half of the patients complete the study in 6 months, followed by an interim analysis and evaluation of the data. If deemed okay by the Data and Safety Monitoring Board, the second part of the study would proceed, in which half of the patients would again complete the study in 6 months.
Ultimately, the study comprised 164 patients. They were randomized in a 1:1 ratio into cohorts receiving either a placebo or a regimen of 1,200 mg CS derived from bovine tracheal cartilage plus 1,500 mg of crystalline GS derived from crustaceans. The primary endpoint was reduction in pain from baseline evaluation, which was based on the visual analog scale (VAS) of 1-100 mm.
Patients in the combination therapy cohort had a lower average reduction in pain at 6 months than did those taking the placebo. In the modified intention-to-treat population, those taking CS+GS therapy had an average reduction of 11.8 ± 2.4 mm, or 19%, compared with baseline. On the other hand, those in the placebo cohort recorded a 20.5 ± 2.4 mm, or 33%, reduction in pain (P = .029). Based on this analysis, the trial was stopped early at 6 months to prevent “overexposure of additional patients to placebo treatment,” the investigators said.
However, pain measured by VAS did not differ between the groups in a per-protocol analysis. Furthermore, when taking Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores into account, there was no significant difference in improvement between CS+GS therapy and placebo in pain and function, for both intention-to-treat and per-protocol subjects.
Although placebo was more effective in pain reduction in the modified intent-to-treat analysis than was CS plus GS combination treatment, the effect size of placebo was small and the effect size of CS plus GS in this study was smaller than in previous studies, the investigators noted. “These findings may be related to the fact that GS may interfere with the absorption of CS and therefore reduce its local effect. Eventually, our patients may have had less severe pain than those in other studies, which would justify a lesser effect after the pharmacological intervention,” the authors wrote. “Furthermore, when the main outcome studied is particularly subjective, the placebo effect can overcome the effect of the active drug.”
Tedec Meiji Farma SA of Madrid funded the study. Dr. Roman-Blas and his coauthors did not report any relevant financial disclosures.
Combination therapy involving chondroitin sulfate and glucosamine sulfate proved no better than placebo for the management of pain and functional impairment brought on by knee osteoarthritis, in a double-blind, randomized trial.
“This is the first RCT sponsored by a pharmaceutical company to evaluate the efficacy of a combination of CS [chondroitin sulfate] plus GS [glucosamine sulfate] and including a [Data and Safety Monitoring Board] composed of independent experts charged with ensuring participant safety and accurate, bias-free data,” wrote the authors, led by Jorge A. Roman-Blas, MD, of Fundación Jiménez Díaz in Madrid (Arthritis Rheumatol. 2016 Jul 31. doi: 10.1002/art.39819).
Dr. Roman-Blas and his coinvestigators recruited patients with Kellgren-Lawrence stages II-III knee osteoarthritis from one orthopedic surgery and nine rheumatology centers across Spain. The study was split into two parts; the first part would have half of the patients complete the study in 6 months, followed by an interim analysis and evaluation of the data. If deemed okay by the Data and Safety Monitoring Board, the second part of the study would proceed, in which half of the patients would again complete the study in 6 months.
Ultimately, the study comprised 164 patients. They were randomized in a 1:1 ratio into cohorts receiving either a placebo or a regimen of 1,200 mg CS derived from bovine tracheal cartilage plus 1,500 mg of crystalline GS derived from crustaceans. The primary endpoint was reduction in pain from baseline evaluation, which was based on the visual analog scale (VAS) of 1-100 mm.
Patients in the combination therapy cohort had a lower average reduction in pain at 6 months than did those taking the placebo. In the modified intention-to-treat population, those taking CS+GS therapy had an average reduction of 11.8 ± 2.4 mm, or 19%, compared with baseline. On the other hand, those in the placebo cohort recorded a 20.5 ± 2.4 mm, or 33%, reduction in pain (P = .029). Based on this analysis, the trial was stopped early at 6 months to prevent “overexposure of additional patients to placebo treatment,” the investigators said.
However, pain measured by VAS did not differ between the groups in a per-protocol analysis. Furthermore, when taking Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores into account, there was no significant difference in improvement between CS+GS therapy and placebo in pain and function, for both intention-to-treat and per-protocol subjects.
Although placebo was more effective in pain reduction in the modified intent-to-treat analysis than was CS plus GS combination treatment, the effect size of placebo was small and the effect size of CS plus GS in this study was smaller than in previous studies, the investigators noted. “These findings may be related to the fact that GS may interfere with the absorption of CS and therefore reduce its local effect. Eventually, our patients may have had less severe pain than those in other studies, which would justify a lesser effect after the pharmacological intervention,” the authors wrote. “Furthermore, when the main outcome studied is particularly subjective, the placebo effect can overcome the effect of the active drug.”
Tedec Meiji Farma SA of Madrid funded the study. Dr. Roman-Blas and his coauthors did not report any relevant financial disclosures.
Combination therapy involving chondroitin sulfate and glucosamine sulfate proved no better than placebo for the management of pain and functional impairment brought on by knee osteoarthritis, in a double-blind, randomized trial.
“This is the first RCT sponsored by a pharmaceutical company to evaluate the efficacy of a combination of CS [chondroitin sulfate] plus GS [glucosamine sulfate] and including a [Data and Safety Monitoring Board] composed of independent experts charged with ensuring participant safety and accurate, bias-free data,” wrote the authors, led by Jorge A. Roman-Blas, MD, of Fundación Jiménez Díaz in Madrid (Arthritis Rheumatol. 2016 Jul 31. doi: 10.1002/art.39819).
Dr. Roman-Blas and his coinvestigators recruited patients with Kellgren-Lawrence stages II-III knee osteoarthritis from one orthopedic surgery and nine rheumatology centers across Spain. The study was split into two parts; the first part would have half of the patients complete the study in 6 months, followed by an interim analysis and evaluation of the data. If deemed okay by the Data and Safety Monitoring Board, the second part of the study would proceed, in which half of the patients would again complete the study in 6 months.
Ultimately, the study comprised 164 patients. They were randomized in a 1:1 ratio into cohorts receiving either a placebo or a regimen of 1,200 mg CS derived from bovine tracheal cartilage plus 1,500 mg of crystalline GS derived from crustaceans. The primary endpoint was reduction in pain from baseline evaluation, which was based on the visual analog scale (VAS) of 1-100 mm.
Patients in the combination therapy cohort had a lower average reduction in pain at 6 months than did those taking the placebo. In the modified intention-to-treat population, those taking CS+GS therapy had an average reduction of 11.8 ± 2.4 mm, or 19%, compared with baseline. On the other hand, those in the placebo cohort recorded a 20.5 ± 2.4 mm, or 33%, reduction in pain (P = .029). Based on this analysis, the trial was stopped early at 6 months to prevent “overexposure of additional patients to placebo treatment,” the investigators said.
However, pain measured by VAS did not differ between the groups in a per-protocol analysis. Furthermore, when taking Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores into account, there was no significant difference in improvement between CS+GS therapy and placebo in pain and function, for both intention-to-treat and per-protocol subjects.
Although placebo was more effective in pain reduction in the modified intent-to-treat analysis than was CS plus GS combination treatment, the effect size of placebo was small and the effect size of CS plus GS in this study was smaller than in previous studies, the investigators noted. “These findings may be related to the fact that GS may interfere with the absorption of CS and therefore reduce its local effect. Eventually, our patients may have had less severe pain than those in other studies, which would justify a lesser effect after the pharmacological intervention,” the authors wrote. “Furthermore, when the main outcome studied is particularly subjective, the placebo effect can overcome the effect of the active drug.”
Tedec Meiji Farma SA of Madrid funded the study. Dr. Roman-Blas and his coauthors did not report any relevant financial disclosures.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Chondroitin sulfate plus glucosamine sulfate is ineffective at reducing pain and functional impairment in patients with knee osteoarthritis.
Major finding: CS plus GS treatment registered a 19% reduction in joint pain in the modified intention-to-treat population, versus the 33% reduction brought on by the placebo (P = .029).
Data source: A multicenter, randomized, double-blind, placebo-controlled study of 164 patients with Kellgren-Lawrence stages II-III knee osteoarthritis.
Disclosures: Tedec Meiji Farma SA of Madrid funded the study. The authors reported no relevant financial disclosures.
FDA accepting comments on draft guidelines on compounding law
The Food and Drug Administration is currently accepting public comments on the agency’s proposed plans to implement a law that will restrict compounding of human drug products.
A statement issued by the FDA provides links to two draft guidances that describe how the agency “would implement provisions of federal law that restrict compounding human drug products that are essentially copies of commercially available or approved drug products.” One draft guidance and the legal restrictions referenced therein are relevant to physicians and pharmacists, as well as state-licensed pharmacies or federal facilities that compound drugs, according to the FDA. The other guidance applies to outsourcing facilities.
Although compounded drug products, such as a medication made without a dye for a patient allergic to that dye, or a medication made into liquid form for a patient who cannot swallow a pill, “may benefit certain patients whose medical needs cannot be met by a commercially available or an FDA-approved drug product,” the FDA statement said. “Taking compounded drug products that are essentially copies of a commercially available or approved drug needlessly exposes patients to drug products that FDA has not evaluated for safety, effectiveness, and quality. In addition, the compounded drugs may not have been produced according to appropriate quality standards. Such compounding would also undermine the new drug approval and over-the-counter drug monograph systems in the United States.”
The statement refers to serious adverse events, including infections and deaths that have resulted from “poor-quality” compounded drugs.
Written or electronic comments can be submitted until Oct. 11, and information on submitting comments is available at regulations.gov.
The Food and Drug Administration is currently accepting public comments on the agency’s proposed plans to implement a law that will restrict compounding of human drug products.
A statement issued by the FDA provides links to two draft guidances that describe how the agency “would implement provisions of federal law that restrict compounding human drug products that are essentially copies of commercially available or approved drug products.” One draft guidance and the legal restrictions referenced therein are relevant to physicians and pharmacists, as well as state-licensed pharmacies or federal facilities that compound drugs, according to the FDA. The other guidance applies to outsourcing facilities.
Although compounded drug products, such as a medication made without a dye for a patient allergic to that dye, or a medication made into liquid form for a patient who cannot swallow a pill, “may benefit certain patients whose medical needs cannot be met by a commercially available or an FDA-approved drug product,” the FDA statement said. “Taking compounded drug products that are essentially copies of a commercially available or approved drug needlessly exposes patients to drug products that FDA has not evaluated for safety, effectiveness, and quality. In addition, the compounded drugs may not have been produced according to appropriate quality standards. Such compounding would also undermine the new drug approval and over-the-counter drug monograph systems in the United States.”
The statement refers to serious adverse events, including infections and deaths that have resulted from “poor-quality” compounded drugs.
Written or electronic comments can be submitted until Oct. 11, and information on submitting comments is available at regulations.gov.
The Food and Drug Administration is currently accepting public comments on the agency’s proposed plans to implement a law that will restrict compounding of human drug products.
A statement issued by the FDA provides links to two draft guidances that describe how the agency “would implement provisions of federal law that restrict compounding human drug products that are essentially copies of commercially available or approved drug products.” One draft guidance and the legal restrictions referenced therein are relevant to physicians and pharmacists, as well as state-licensed pharmacies or federal facilities that compound drugs, according to the FDA. The other guidance applies to outsourcing facilities.
Although compounded drug products, such as a medication made without a dye for a patient allergic to that dye, or a medication made into liquid form for a patient who cannot swallow a pill, “may benefit certain patients whose medical needs cannot be met by a commercially available or an FDA-approved drug product,” the FDA statement said. “Taking compounded drug products that are essentially copies of a commercially available or approved drug needlessly exposes patients to drug products that FDA has not evaluated for safety, effectiveness, and quality. In addition, the compounded drugs may not have been produced according to appropriate quality standards. Such compounding would also undermine the new drug approval and over-the-counter drug monograph systems in the United States.”
The statement refers to serious adverse events, including infections and deaths that have resulted from “poor-quality” compounded drugs.
Written or electronic comments can be submitted until Oct. 11, and information on submitting comments is available at regulations.gov.
Study identifies distinct OA fatigue trajectories
A new study has identified three distinct trajectories of fatigue levels in patients with early symptomatic osteoarthritis (OA) in the knee and hip, report Jadran Botterman, MSc, and coauthors from the department of psychology, health, and technology at the University of Twente (the Netherlands).
Six years of data were collected from the CHECK (Cohort Hip and Cohort Knee) participants and then separated into distinct trajectories using growth mixture modeling. Three distinct fatigue trajectories were found: low fatigue, low to high fatigue, and high fatigue.
The authors found a significant association between trajectory and patient characteristics. Women, patients with comorbid disease, and patients using medications were more likely to have a high fatigue trajectory, Dr. Botterman and his colleagues reported.
“Identification of these trajectories with differing patient characteristics may warrant tailored psychosocial interventions for patients with elevated levels of fatigue,” the authors concluded.
Read the full article in the Journal of Rheumatology.
A new study has identified three distinct trajectories of fatigue levels in patients with early symptomatic osteoarthritis (OA) in the knee and hip, report Jadran Botterman, MSc, and coauthors from the department of psychology, health, and technology at the University of Twente (the Netherlands).
Six years of data were collected from the CHECK (Cohort Hip and Cohort Knee) participants and then separated into distinct trajectories using growth mixture modeling. Three distinct fatigue trajectories were found: low fatigue, low to high fatigue, and high fatigue.
The authors found a significant association between trajectory and patient characteristics. Women, patients with comorbid disease, and patients using medications were more likely to have a high fatigue trajectory, Dr. Botterman and his colleagues reported.
“Identification of these trajectories with differing patient characteristics may warrant tailored psychosocial interventions for patients with elevated levels of fatigue,” the authors concluded.
Read the full article in the Journal of Rheumatology.
A new study has identified three distinct trajectories of fatigue levels in patients with early symptomatic osteoarthritis (OA) in the knee and hip, report Jadran Botterman, MSc, and coauthors from the department of psychology, health, and technology at the University of Twente (the Netherlands).
Six years of data were collected from the CHECK (Cohort Hip and Cohort Knee) participants and then separated into distinct trajectories using growth mixture modeling. Three distinct fatigue trajectories were found: low fatigue, low to high fatigue, and high fatigue.
The authors found a significant association between trajectory and patient characteristics. Women, patients with comorbid disease, and patients using medications were more likely to have a high fatigue trajectory, Dr. Botterman and his colleagues reported.
“Identification of these trajectories with differing patient characteristics may warrant tailored psychosocial interventions for patients with elevated levels of fatigue,” the authors concluded.
Read the full article in the Journal of Rheumatology.
FROM THE JOURNAL OF RHEUMATOLOGY