User login
Would routine use of tranexamic acid for PPH be cost-effective in the United States?
Sudhof LS, Shainker SA, Einerson BD. Tranexamic acid in the routine treatment of postpartum hemorrhage in the United States: a cost-effectiveness analysis. Am J Obstet Gynecol. Published online June 18, 2019. doi.org/10.1016/j.ajog.2019.06.030.
EXPERT COMMENTARY
Postpartum hemorrhage is a leading cause of morbidity and mortality in the United States. The World Maternal Antifibrinolytic (WOMAN) trial showed that the use of TXA, an antifibrinolytic agent, for PPH decreases hemorrhage-related mortality and laparotomy. Routine use of TXA for PPH has demonstrated cost-effectiveness in low-resource countries, where hemorrhage-related mortality rates are higher than in the United States. This study aimed to determine if routine use of TXA for PPH in the United States also is cost-effective.
Details of the study
Sudhof and colleagues conducted a decision-tree analysis to compare the cost-effectiveness of 3 strategies regarding routine use of TXA for PPH in the United States: no TXA, TXA given at any time, and TXA given within 3 hours of delivery.
Health care system perspective. In the primary analysis, the 3 strategies were evaluated from the perspective of the health care system. Outcomes included cost, number of laparotomies, and maternal deaths from delivery until 6 weeks postpartum. Rates of hemorrhage and related complications, as well as cost assumptions, were derived from multiple US-based studies. The relative risk reduction in death and laparotomy with TXA in the United States was assumed to be similar to that found in the WOMAN trial (19% and 36%, respectively).
Societal perspective. In the secondary analysis, the 3 TXA strategies were evaluated from the societal perspective, comparing quality-adjusted life-years (QALYs) and cost per QALY. For both the primary and secondary analyses, sensitivity analyses were performed across a range of values for each input.
Main findings. Tranexamic acid use would be cost saving if the relative risk reduction for maternal death with TXA was greater than approximately 5%, which is significantly lower than that seen in the WOMAN trial (19%). The primary analysis demonstrated that—assuming a 3% rate of PPH—giving TXA to women with PPH would save $11.3 million, prevent 334 laparotomies, and avert 9 maternal deaths annually in the United States. This cost saving nearly tripled if TXA was administered within 3 hours of delivery, with 5 additional maternal deaths prevented.
Secondary analysis incorporating QALYs also showed TXA use to be cost-effective. These findings held through various sensitivity analyses.
Continue to: Study strengths and limitations...
Study strengths and limitations
This study is novel in its critical objective to determine the cost-effectiveness of routine use of TXA for PPH in the United States. Robust modeling using Monte Carlo estimation and a variety of sensitivity analyses add reliability to the authors’ findings.
This work is limited, however, by the assumptions put into the authors’ models. For example, outcome data regarding effectiveness of TXA was taken from the WOMAN trial, which was not performed within the United States. In addition, it is difficult to quantify in dollars an event as profound as a maternal death. The authors recognize that they likely underestimate the “cost” of a maternal death, but that this underestimation would only increase the cost-effectiveness of TXA.
Finally, it is important to take into account that such economic analyses are helpful to inform institutional guidelines and hemorrhage protocols, but that patient-specific decision-making should be individualized based on the clinical scenario at hand.
Routine use of TXA for PPH, particularly within 3 hours of delivery, is likely cost-effective in the United States. Consideration should be given to including TXA in institutional hemorrhage protocols.
REBECCA F. HAMM, MD, and ADI HIRSHBERG, MD
Sudhof LS, Shainker SA, Einerson BD. Tranexamic acid in the routine treatment of postpartum hemorrhage in the United States: a cost-effectiveness analysis. Am J Obstet Gynecol. Published online June 18, 2019. doi.org/10.1016/j.ajog.2019.06.030.
EXPERT COMMENTARY
Postpartum hemorrhage is a leading cause of morbidity and mortality in the United States. The World Maternal Antifibrinolytic (WOMAN) trial showed that the use of TXA, an antifibrinolytic agent, for PPH decreases hemorrhage-related mortality and laparotomy. Routine use of TXA for PPH has demonstrated cost-effectiveness in low-resource countries, where hemorrhage-related mortality rates are higher than in the United States. This study aimed to determine if routine use of TXA for PPH in the United States also is cost-effective.
Details of the study
Sudhof and colleagues conducted a decision-tree analysis to compare the cost-effectiveness of 3 strategies regarding routine use of TXA for PPH in the United States: no TXA, TXA given at any time, and TXA given within 3 hours of delivery.
Health care system perspective. In the primary analysis, the 3 strategies were evaluated from the perspective of the health care system. Outcomes included cost, number of laparotomies, and maternal deaths from delivery until 6 weeks postpartum. Rates of hemorrhage and related complications, as well as cost assumptions, were derived from multiple US-based studies. The relative risk reduction in death and laparotomy with TXA in the United States was assumed to be similar to that found in the WOMAN trial (19% and 36%, respectively).
Societal perspective. In the secondary analysis, the 3 TXA strategies were evaluated from the societal perspective, comparing quality-adjusted life-years (QALYs) and cost per QALY. For both the primary and secondary analyses, sensitivity analyses were performed across a range of values for each input.
Main findings. Tranexamic acid use would be cost saving if the relative risk reduction for maternal death with TXA was greater than approximately 5%, which is significantly lower than that seen in the WOMAN trial (19%). The primary analysis demonstrated that—assuming a 3% rate of PPH—giving TXA to women with PPH would save $11.3 million, prevent 334 laparotomies, and avert 9 maternal deaths annually in the United States. This cost saving nearly tripled if TXA was administered within 3 hours of delivery, with 5 additional maternal deaths prevented.
Secondary analysis incorporating QALYs also showed TXA use to be cost-effective. These findings held through various sensitivity analyses.
Continue to: Study strengths and limitations...
Study strengths and limitations
This study is novel in its critical objective to determine the cost-effectiveness of routine use of TXA for PPH in the United States. Robust modeling using Monte Carlo estimation and a variety of sensitivity analyses add reliability to the authors’ findings.
This work is limited, however, by the assumptions put into the authors’ models. For example, outcome data regarding effectiveness of TXA was taken from the WOMAN trial, which was not performed within the United States. In addition, it is difficult to quantify in dollars an event as profound as a maternal death. The authors recognize that they likely underestimate the “cost” of a maternal death, but that this underestimation would only increase the cost-effectiveness of TXA.
Finally, it is important to take into account that such economic analyses are helpful to inform institutional guidelines and hemorrhage protocols, but that patient-specific decision-making should be individualized based on the clinical scenario at hand.
Routine use of TXA for PPH, particularly within 3 hours of delivery, is likely cost-effective in the United States. Consideration should be given to including TXA in institutional hemorrhage protocols.
REBECCA F. HAMM, MD, and ADI HIRSHBERG, MD
Sudhof LS, Shainker SA, Einerson BD. Tranexamic acid in the routine treatment of postpartum hemorrhage in the United States: a cost-effectiveness analysis. Am J Obstet Gynecol. Published online June 18, 2019. doi.org/10.1016/j.ajog.2019.06.030.
EXPERT COMMENTARY
Postpartum hemorrhage is a leading cause of morbidity and mortality in the United States. The World Maternal Antifibrinolytic (WOMAN) trial showed that the use of TXA, an antifibrinolytic agent, for PPH decreases hemorrhage-related mortality and laparotomy. Routine use of TXA for PPH has demonstrated cost-effectiveness in low-resource countries, where hemorrhage-related mortality rates are higher than in the United States. This study aimed to determine if routine use of TXA for PPH in the United States also is cost-effective.
Details of the study
Sudhof and colleagues conducted a decision-tree analysis to compare the cost-effectiveness of 3 strategies regarding routine use of TXA for PPH in the United States: no TXA, TXA given at any time, and TXA given within 3 hours of delivery.
Health care system perspective. In the primary analysis, the 3 strategies were evaluated from the perspective of the health care system. Outcomes included cost, number of laparotomies, and maternal deaths from delivery until 6 weeks postpartum. Rates of hemorrhage and related complications, as well as cost assumptions, were derived from multiple US-based studies. The relative risk reduction in death and laparotomy with TXA in the United States was assumed to be similar to that found in the WOMAN trial (19% and 36%, respectively).
Societal perspective. In the secondary analysis, the 3 TXA strategies were evaluated from the societal perspective, comparing quality-adjusted life-years (QALYs) and cost per QALY. For both the primary and secondary analyses, sensitivity analyses were performed across a range of values for each input.
Main findings. Tranexamic acid use would be cost saving if the relative risk reduction for maternal death with TXA was greater than approximately 5%, which is significantly lower than that seen in the WOMAN trial (19%). The primary analysis demonstrated that—assuming a 3% rate of PPH—giving TXA to women with PPH would save $11.3 million, prevent 334 laparotomies, and avert 9 maternal deaths annually in the United States. This cost saving nearly tripled if TXA was administered within 3 hours of delivery, with 5 additional maternal deaths prevented.
Secondary analysis incorporating QALYs also showed TXA use to be cost-effective. These findings held through various sensitivity analyses.
Continue to: Study strengths and limitations...
Study strengths and limitations
This study is novel in its critical objective to determine the cost-effectiveness of routine use of TXA for PPH in the United States. Robust modeling using Monte Carlo estimation and a variety of sensitivity analyses add reliability to the authors’ findings.
This work is limited, however, by the assumptions put into the authors’ models. For example, outcome data regarding effectiveness of TXA was taken from the WOMAN trial, which was not performed within the United States. In addition, it is difficult to quantify in dollars an event as profound as a maternal death. The authors recognize that they likely underestimate the “cost” of a maternal death, but that this underestimation would only increase the cost-effectiveness of TXA.
Finally, it is important to take into account that such economic analyses are helpful to inform institutional guidelines and hemorrhage protocols, but that patient-specific decision-making should be individualized based on the clinical scenario at hand.
Routine use of TXA for PPH, particularly within 3 hours of delivery, is likely cost-effective in the United States. Consideration should be given to including TXA in institutional hemorrhage protocols.
REBECCA F. HAMM, MD, and ADI HIRSHBERG, MD
The case for outpatient cervical ripening for IOL at term for low-risk pregnancies
Case 1 Induction at 39 weeks in a healthy nulliparous woman
A healthy 35-year-old woman (G1P0) at 39 weeks 0 days and with an uncomplicated pregnancy presents to your office for a routine prenatal visit. She inquires about scheduling an induction of labor, noting that she read a news story about induction at 39 weeks and that it might lower her chance of having a cesarean delivery (CD).
You perform a cervical exam—she is 1 cm dilated, 3 cm long, -2 station, posterior, and firm. You sweep her membranes after obtaining verbal consent. After describing the induction process, you explain that she might be hospitalized for several days before the birth given the need for cervical ripening. “You mean I need to stay in the hospital for the entire process?” she asks incredulously.
Over the past 20 years, the percentage of patients undergoing induction of labor (IOL) has increased from 10% to 25%.1 This percentage likely will rise over time, particularly in the wake of a recent randomized controlled trial suggesting potential maternal benefits, such as reduced CD rate, for nulliparas induced at 39 weeks compared with expectant management.2 Although there have not been any changes to guidelines for timing of IOL from such professional societies such as the American College of Obstetricians and Gynecologists (ACOG) or the Society for Maternal-Fetal Medicine, key considerations of rising IOL volume include patient experience, labor and delivery (L&D) units’ capacity and resources, and associated health care costs.
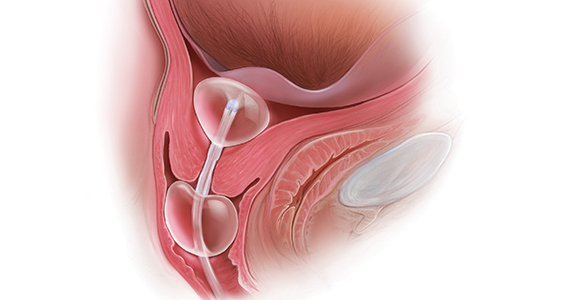
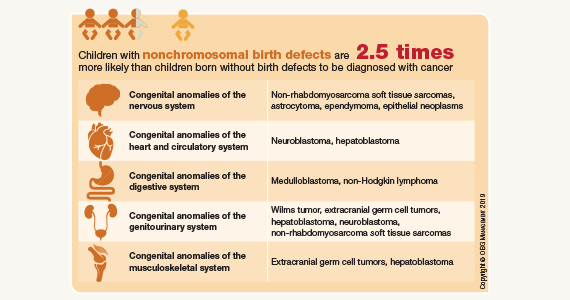
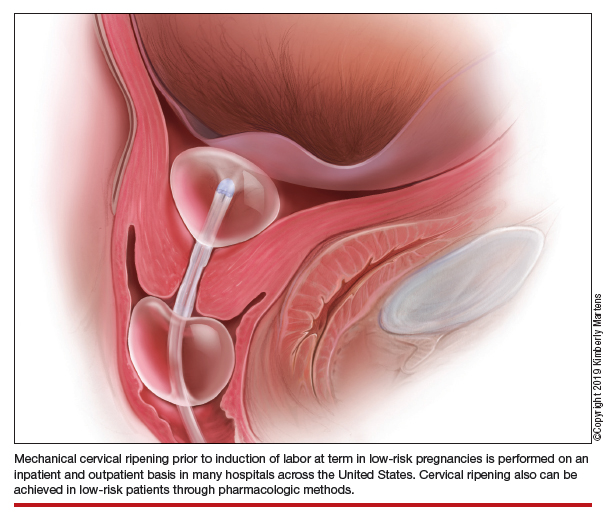
An essential part of successful induction involves patience. Induction can be a lengthy process, particularly for nulliparas with unripe cervices. Cervical ripening is a necessary component of successful labor induction, whether achieved mechanically or pharmacologically with synthetic prostaglandins, and it has been shown to lower the chance of CD.3,4 However, achieving a ripe cervix is often the lengthiest part of an induction, and not uncommonly consumes 12 to 24 hours or more of inpatient time. Investigators have sought ways to make this process more expeditious. For example, the FOR-MOMI trial demonstrated that the induction-to-delivery time was several hours shorter when cervical ripening combined mechanical and pharmacologic approaches (Foley balloon plus misoprostol), compared with either method alone, without any increase in maternal or fetal complication rates.5
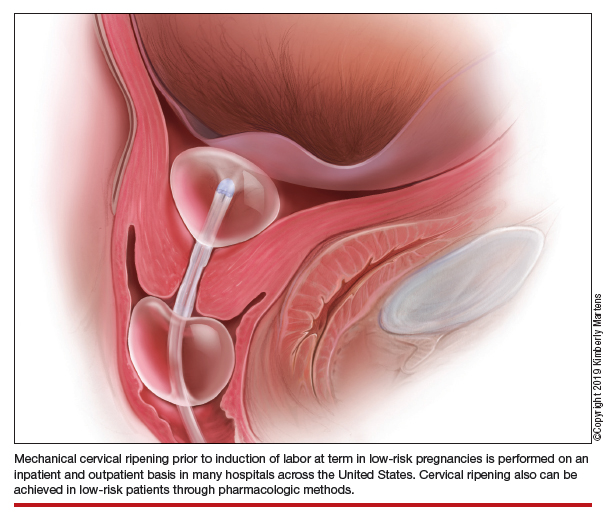
Better yet, what if admission to the L&D unit for IOL at term could be deferred until the cervix is ripe? A number of hospitals in the United States have successfully introduced outpatient cervical ripening, and several small observational and randomized controlled trials have reported good results in terms of safety, efficacy and time saved, and patient experience. Here, we will make the case that outpatient cervical ripening should be the standard of care for low-risk pregnancies.
Mechanical cervical ripening
Safety
Although data are limited on the safety, the authors of an ACOG Practice Bulletin suggest that, based on the available evidence of mechanical ripening in an inpatient setting, it is also appropriate in the outpatient setting.6 Unlike cervical ripening using prostaglandins, mechanical ripening is not associated with tachysystole, fetal intolerance of labor, or meconium staining.3 A cohort study of nearly 2,000 low-risk patients who underwent Foley catheter placement for cervical ripening using an outpatient protocol but monitored overnight as inpatients and evaluated for adverse outcomes found no CD for fetal distress, vaginal bleeding, placental abruption, or intrapartum stillbirth.7 The authors posited that, given this safety profile in the inpatient setting, that mechanical cervical ripening with a Foley catheter would be appropriate for outpatient use in low-risk populations. Other systematic reviews have been reassuring as well, with exceedingly low complication rates during inpatient mechanical cervical ripening.8 These data advocate for the evaluation of cervical ripening in the outpatient setting.
The evidence for outpatient mechanical ripening, although again limited, also has demonstrated safety. There does not appear to be an increased rate of maternal or neonatal complications, including infectious morbidity, postpartum hemorrhage, CD, operative vaginal delivery, or fetal distress.9-12
Continue to: Efficacy and length-of-stay...
Efficacy and length-of-stay
Efficacy also generally has been shown to be similar when mechanical methods are used in the inpatient and outpatient settings. Small randomized trials of outpatient versus inpatient Foley catheter ripening have shown decreased length of stay (by 10 to 13 hours) and similar or less oxytocin use in the outpatient groups, as well as similar Bishop scores after cervical ripening and no difference in maternal or fetal outcomes.9,11,13,14
One major concern with increasing IOL prevalence is the availability of hospital resources and the associated health care costs, given the known increased length of inpatient stay due to cervical ripening time. Admission to an L&D unit is resource intensive; the costs are similar to admission to an intensive care unit in many hospitals given its level of acuity and high nurse/patient ratio. However, given the safety of outpatient mechanical cervical ripening described above, we argue that routinely admitting low-risk patients for mechanical ripening constitutes a suboptimal use of costly resources.
Indeed, data suggest significant inpatient time savings if cervical ripening can be accomplished prior to admission. A cost-effectiveness analysis in the Netherlands demonstrated a nearly 1,000-euro decrease in cost per induction when Foley catheter induction was done on an outpatient basis.15 Interestingly, a recent trial confined to multiparas found no differences in hospital time when comparing outpatient ripening with Foley balloon alone with inpatient ripening with Foley balloon plus simultaneous oxytocin.10 This certainly merits further study, but it may be that the largest time- and cost-savings are among nulliparas.
Patient preferences
Relatively few studies specifically have addressed patient experiences with outpatient versus inpatient mechanical cervical ripening. Outpatient cervical ripening may provide patients with the benefits of being in the comfort of their own homes with their preferred support persons, increased mobility, more bodily autonomy, and satisfaction with their birthing process.
In a pilot trial involving 48 women, inpatient was compared with outpatient cervical ripening using a Foley balloon. Those in the outpatient group reported getting more rest, feeling less isolated, and having enough privacy. However, participants in both groups were equally satisfied and equally likely to recommend their method of induction to others.11 Another study comparing outpatient versus inpatient Foley balloon cervical ripening found that 85% of patients who underwent outpatient ripening were satisfied with the induction method; however, no query or comparison was done with the inpatient group.12 A trial comparing outpatient mechanical cervical ripening with inpatient misoprostol found that outpatient participants reported several hours more sleep and less pain.16 And in a discrete choice experiment of British gravidas, participants favored the option of outpatient cervical ripening, even if it meant an extra 1.4 trips to the hospital and over an hour of extra travel time.17
While these preliminary findings provide some insight that patients may prefer an outpatient approach to cervical ripening, more studies are needed to fully evaluate patient desires.
Continue to: Our approach to mechanical cervical ripening...
Our approach to mechanical cervical ripening
Most patients undergoing scheduled IOL are reasonable candidates for outpatient cervical ripening based on safety and efficacy. By definition, scheduling in advance implies that the provider has determined that outpatient management is reasonable until that date, and the plan for outpatient ripening need not prolong this period.
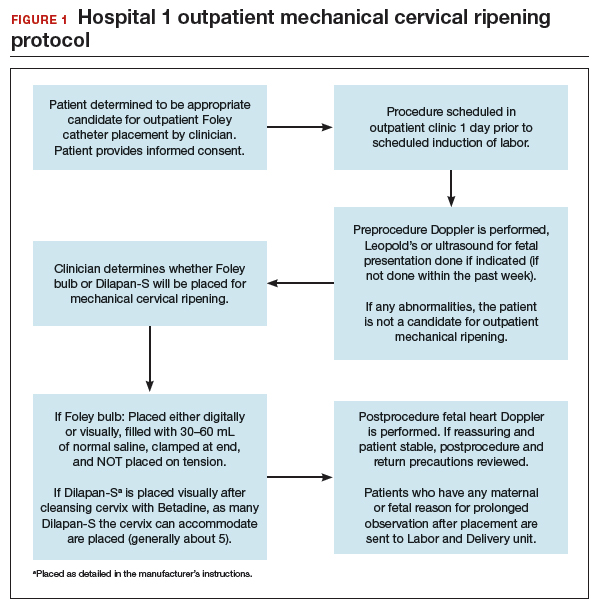
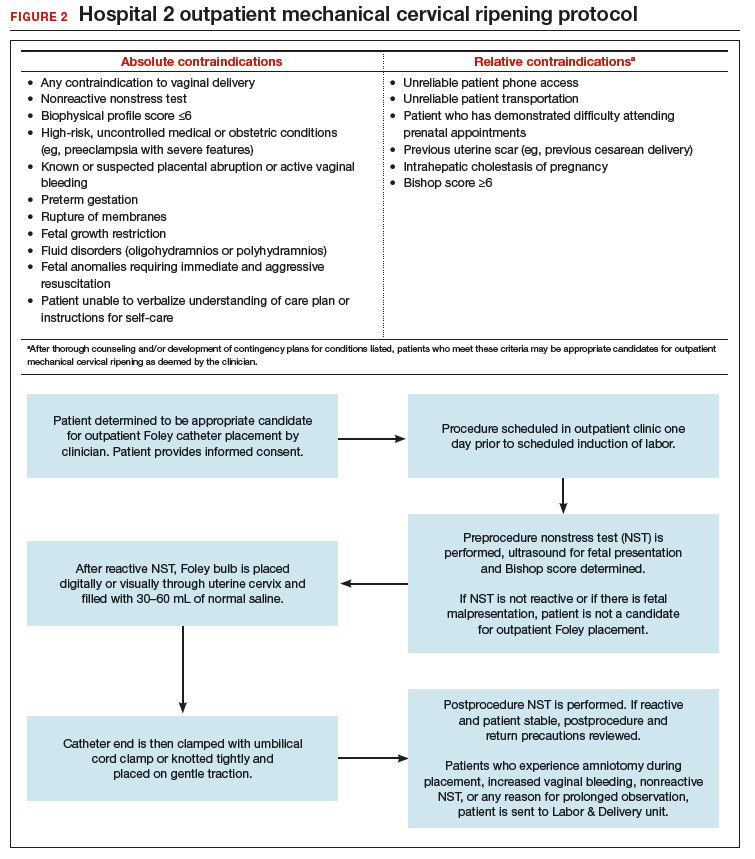
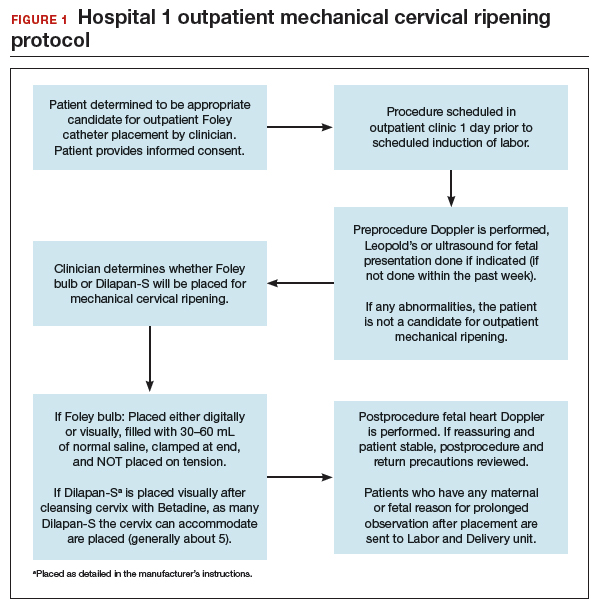
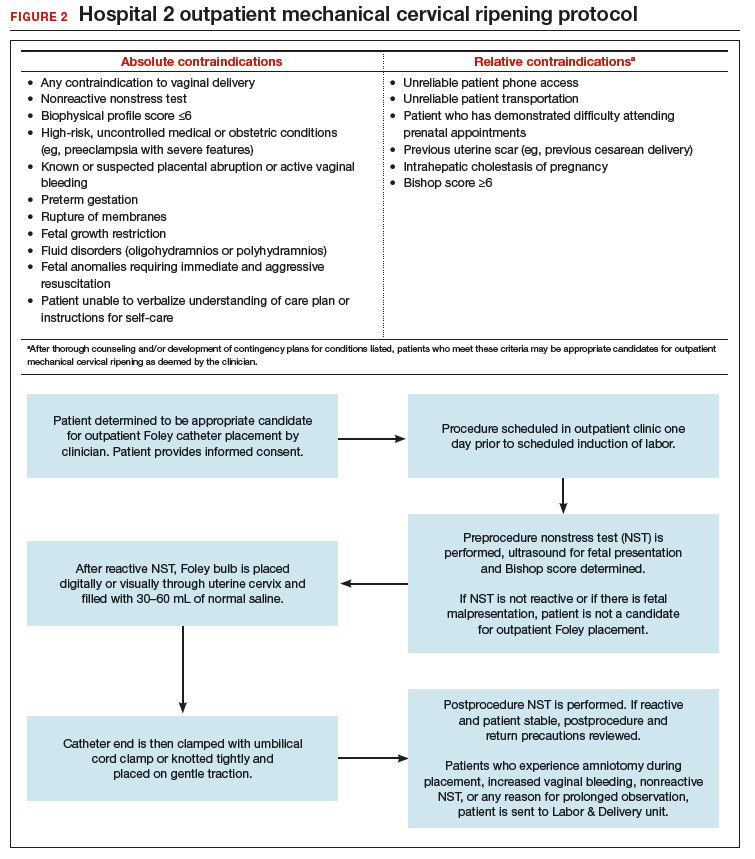
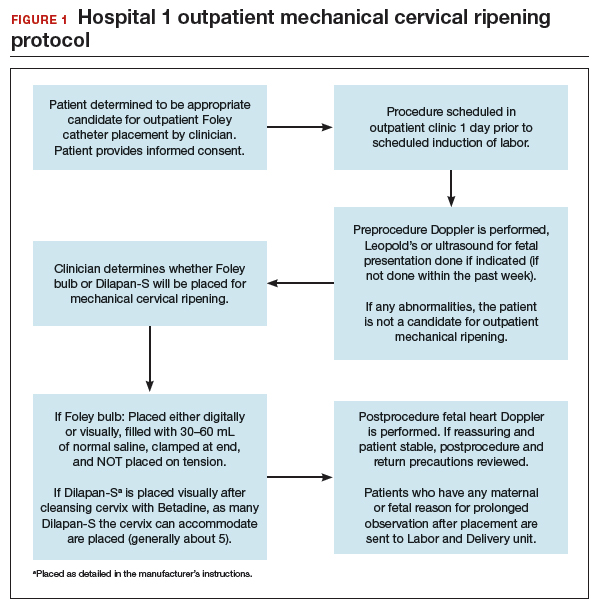
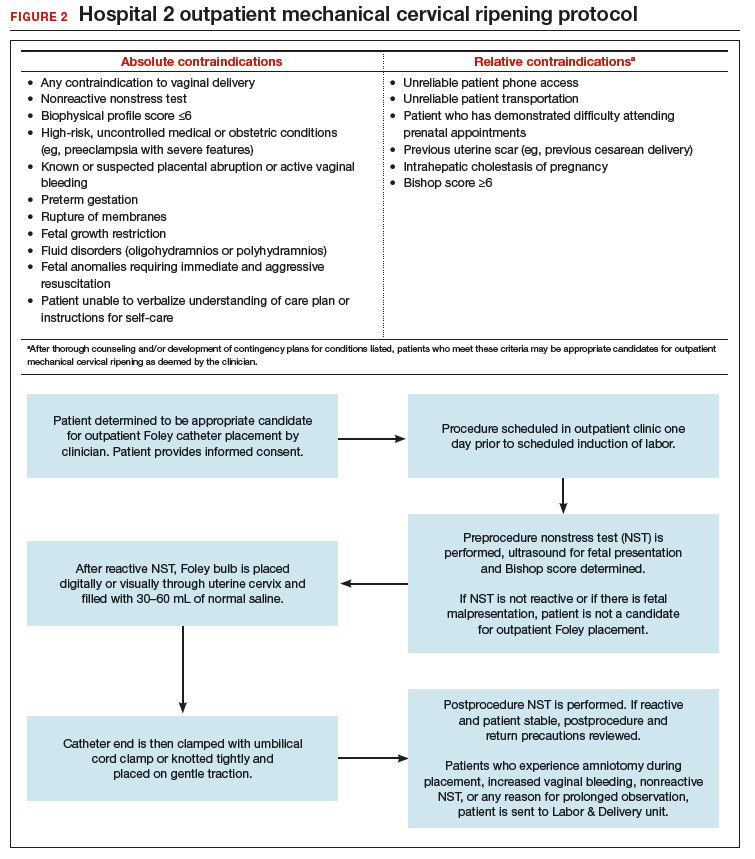
FIGURES 1 and 2 show protocols for our 2 hospital centers, which regularly allow for outpatient mechanical cervical ripening. In the process of protocol development, we identified absolute and relative contraindications to determine appropriate candidates. We exclude women who require inpatient management of medical or obstetric conditions (for example, women with severe preeclampsia or any condition requiring continuous fetal monitoring). We also do not routinely recommend outpatient cervical ripening to patients who do not have the necessary social conditions to make this process as safe as possible (including stable housing, reliable transportation, and a support person), although this occurs with some exceptions depending on individual patient situations.
Some examples of ideal candidates for outpatient mechanical cervical ripening include those undergoing elective or routine prolonged gestation inductions, or inductions for well-controlled, stable conditions (chronic hypertension and gestational diabetes). At one center, after thorough counseling and assessment, outpatient cervical ripening is also offered to patients with mild risk factors, including twins, prior low transverse CD, stable preeclampsia without severe features, isolated oligohydramnios with otherwise reassuring fetal status, and other similar conditions.
After mechanical cervical ripening placement (either Foley catheter or mechanical dilators), the clinician completes a postprocedure safety checklist and detailed procedure documentation, including number and type of foreign bodies placed. If there are any concerns regarding maternal or fetal well-being, the patient is sent to L&D for evaluation. If the procedure was tolerated well, the patient is discharged home, after a reactive postprocedure nonstress test is done, with detailed instructions for self-care, as well as with a list of symptoms that warrant prompt evaluation prior to scheduled induction time. In a large California hospital group following a similar protocol, only about 5% of women presented in labor before their scheduled induction.18
Case 2 Cervical ripening for labor preparation in low-risk pregnancy
A 32-year-old woman (G1P0) with an uncomplicated pregnancy at 40 weeks and 3 days presents to your office for a routine prenatal visit. Her vital signs are normal, and her fetus is vertex with an estimated fetal weight of 7.5 lb by Leopald’s maneuvers. You perform a cervical exam and find that her cervix is closed, long, and posterior.
You discuss with her your recommendation for induction of labor by 41 weeks, and she agrees. You also discuss the need for cervical ripening and recommend misoprostol given her closed cervix. You explain that several doses may be needed to get her cervix ready for labor, and she asks, “Do I have to stay in the hospital that whole time?”
Pharmacologic cervical ripening
Efficacy
There are multiple pharmacologic agents that can be used for ripening an unfavorable cervix. The main agents used in the United States are prostaglandins, either PGE1 (oral or vaginal misoprostol) or PGE2 in a gel or sustained-release vaginal insert (dinoprostone).
Outpatient misoprostol to avoid labor induction. Many studies have looked at outpatient misoprostol use as a “prophylactic measure” (to prevent the need for labor induction). For example, Gaffaney and colleagues showed that administering outpatient oral misoprostol (100 µg every 24 hours for up to 3 doses) after 40 weeks’ gestation to women with an unfavorable cervix significantly decreased the time to delivery by a day and a half.19 Similarly, PonMalar and colleagues demonstrated that administering 25 µg of vaginal misoprostol in a single dose as an outpatient after stripping the membranes significantly reduced time to delivery by 2 days.20 And Stitely and colleagues found a significant reduction in the need for labor induction with the use of outpatient vaginal misoprostol. They administered up to 2 doses of misoprostol 25 µg vaginally every 24 hours for the 48 hours prior to a scheduled postdates induction and found a large reduction in the need for labor induction (11% vs 85%; P<.01).21
Continue to: Multiple protocols and regimens...
Multiple protocols and regimens have been studied but, overall, the findings suggest that administering outpatient misoprostol may shorten the time interval to spontaneous labor and decrease the need for a formal labor induction.19-23
Inpatient compared with outpatient prostaglandin use. These trials of “prophylactic” misoprostol generally have compared outpatient administration of misoprostol with placebo. Prostaglandins are one of the most common methods of inpatient cervical ripening, so what about comparisons of inpatient cervical ripening with outpatient prostaglandin administration? There are a handful of studies that make this comparison.
Chang and colleagues looked retrospectively at inpatient and outpatient misoprostol and found that outpatient administration saved 3 to 5 hours on labor and delivery.24 Biem and colleagues randomly assigned women to either inpatient cervical ripening with PGE2 intravaginal inserts or 1 hour of inpatient monitoring after PGE2 administration and then outpatient discharge until the onset of labor or for a nonstress test at 12 hours. They found that those who underwent outpatient ripening spent 8 hours less on labor and delivery and were more highly satisfied with the initial 12 hours of labor induction experience (56% vs 39%; P<.01).25
The largest randomized controlled trial conducted to study outpatient prostaglandin use was the OPRA study (involving 827 women). Investigators compared inpatient to outpatient PGE2 intravaginal gel.26 The primary outcome was total oxytocin administration, which was not different between groups. The study was underpowered, however, as 50% of women labored spontaneously postrandomization. But in the outpatient arm, less than half of the women required additional inpatient ripening, and nearly 40% returned in spontaneous labor, suggesting that outpatient prostaglandin administration may indeed save women a significant amount of time on labor and delivery.
Safety
The safety of outpatient administration of prostaglandins is the biggest concern, especially since, when prostaglandins are compared to outpatient Foley catheter use, Foleys are overall associated with less tachysystole, fetal intolerance, and meconium-stained fluid.3 Foley catheter use for cervical ripening may not be an appropriate choice for all patients, however. For instance, our case patient has a closed cervix, which could make Foley insertion uncomfortable or even impossible. Misoprostol use also offers the potential for flexibility in cervical ripening protocols as patients need not return for Foley balloon removal and indeed labor induction need not take place immediately after administration of misoprostol.
Patients also may prefer outpatient cervical ripening with misoprostol over a Foley. There are some data to suggest that women, overall, have a preference toward prostaglandins; in the PROBAAT-II trial, which compared inpatient oral misoprostol to Foley catheter for cervical ripening, 12% of women in the Foley arm would have preferred another method of induction (vs 6% in the misoprostol arm; P = .02).27 This preference may be magnified in an outpatient setting.
But, again, is outpatient administration of prostaglandins safe? The published trials thus far have not reported an increase in out-of-hospital deliveries or adverse fetal outcomes. However, studies have been of limited size to see more rare outcomes. Unfortunately, an adequately powered study to demonstrate safety is likely never to be accomplished, given that if used responsibly (in low-risk patients with adequate monitoring after administration) the incidence of adverse fetal outcomes during the at-home portion of cervical ripening is likely to be very low. With responsible use, outpatient administration of prostaglandins should be safe. Women are monitored after misoprostol administration and are not sent home if there are any concerns for fetal distress or if frequent contractions continue. Misoprostol reaches maximum blood concentration 30 minutes after oral administration and 70 to 80 minutes after vaginal administration.28 After this time, if contractions start to intensify it is likely that misoprostol has triggered spontaneous labor. In this setting, women are routinely allowed to spontaneously labor at home. One may even argue that outpatient misoprostol could lead to improved safety, as women essentially have a contraction stress test prior to spontaneous labor, and misoprostol administration as an outpatient, as opposed to as an inpatient, may allow for longer time intervals between doses, which could prevent dose stacking.
Continue to: Our approach to pharmacologic cervical ripening...
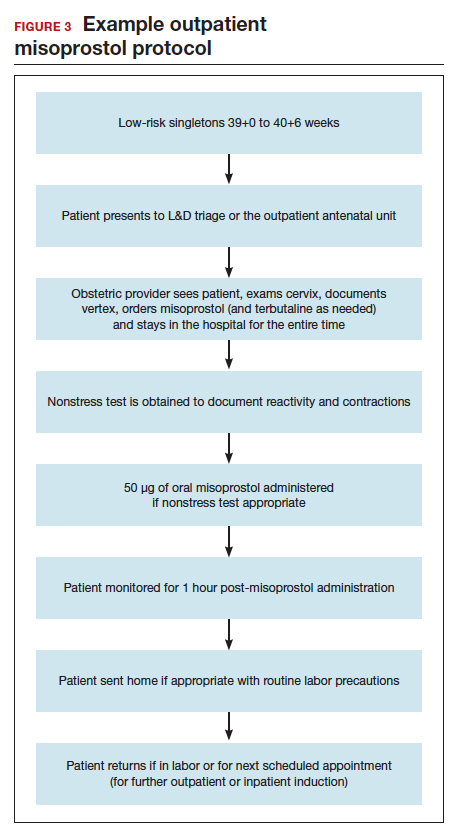
Our approach to pharmacologic cervical ripening
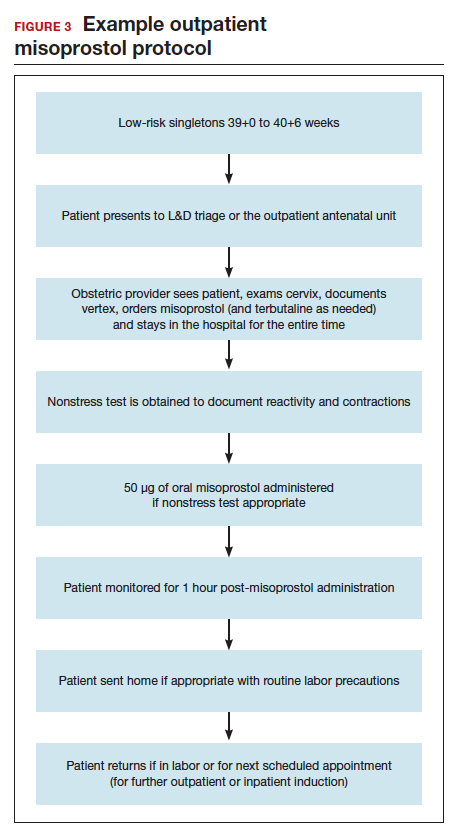
Our hospital has been conducting outpatient cervical ripening using vaginal misoprostol for more th
Conclusion
While the data continue to be limited, we strongly believe there is sufficient quality evidence from a safety and efficacy perspective to support implementation and evaluation of outpatient cervical ripening protocols for low-risk pregnancies. In the setting of renewed commitments to reducing suboptimal health care costs and utilization as well as increasing patient satisfaction and control in their birthing experiences, we posit it is the responsibility of obstetricians, L&D leadership, and health care institutions to explore the implementation of outpatient cervical ripening for appropriate candidates in their settings.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2015. Natl Vital Stat Rep. 2017;66:1.
- Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- Jozwiak M, Bloemenkamp KW, Kelly AJ, et al. Mechanical methods for induction of labor. Cochrane Database Syst Rev. 2012;(3):CD001233.
- Alfirevic Z, Kelly AJ, Dowswell T. Intravenous oxytocin alone for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2009;(4):CD003246.
- Levine LD, Downes KL, Elovitz MA, et al. Mechanical and pharmacologic methods of labor induction: a randomized controlled trial. Obstet Gynecol. 2016;128:1357-1364.
- ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin no. 107: induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397. Reaffirmed 2019.
- Sciscione AC, Bedder CL, Hoffman MK, et al. The timing of adverse events with Foley catheter preinduction cervical ripening; implications for outpatient use. Am J Perinatol. 2014;31:781-786.
- Diederen M, Gommers J, Wilkinson C, et al. Safety of the balloon catheter for cervical ripening in outpatient care: complications during the period from insertion to expulsion of a balloon catheter in the process of labour induction: a systematic review. BJOG. 2018;125:1086-1095.
- McKenna DS, Duke JM. Effectiveness and infectious morbidity of outpatient cervical ripening with a Foley catheter. J Reprod Med. 2004;49:28-32.
- Kuper SG, Jauk VC, George DM, et al. Outpatient Foley catheter for induction of labor in parous women: a randomized controlled trial. Obstet Gynecol. 2018;132:94-101.
- Wilkinson C, Adelson P, Turnbull D. A comparison of inpatient with outpatient balloon catheter cervical ripening: a pilot randomized controlled trial. BMC Pregnancy Childbirth. 2015;15:126.
- Kruit H, Heikinheimo O, Ulander VM, et al. Foley catheter induction of labor as an outpatient procedure. J Perinatol. 2016;36:618-622.
- Sciscione AC, Muench M, Pollock M, et al. Transcervical Foley catheter for preinduction cervical ripening in an outpatient versus inpatient setting. Obstet Gynecol. 2001;98(5 pt 1):751-756.
- Policiano C, Pimenta M, Martins D, et al. Outpatient versus inpatient cervix priming with Foley catheter: a randomized trial. Eur J Obstet Gynecol Reprod Biol. 2017;210:1-6.
- Ten Eikelder M, van Baaren GJ, Oude Rengerink K, et al. Comparing induction of labour with oral misoprostol or Foley catheter at term: cost effectiveness analysis of a randomised controlled multi-centre non-inferiority trial. BJOG. 2018;125:375-383.
- Henry A, Madan A, Reid R, et al. Outpatient Foley catheter versus inpatient prostaglandin E2 gel for induction of labour: a randomised trial. BMC Pregnancy Childbirth. 2013;13:25.
- Howard K, Gerard K, Adelson P, et al. Women’s preferences for inpatient and outpatient priming for labour induction: a discrete choice experiment. BMC Health Serv Res. 2014;14:330.
- Main E, LaGrew D; California Maternal Quality Care Collaborative. Induction of labor risks, benefits, and techniques for increasing success. June 14, 2017. https://www .cmqcc.org/resource/induction-labor-risk-benefits-and-techniques-increasing -success. Accessed August 21, 2019.
- Gaffaney CA, Saul LL, Rumney PJ, et al. Outpatient oral misoprostol for prolonged pregnancies: a pilot investigation. Am J Perinatol. 2009;26:673-677.
- PonMalar J, Benjamin SJ, Abraham A, et al. Randomized double-blind placebo controlled study of preinduction cervical priming with 25 µg of misoprostol in the outpatient setting to prevent formal induction of labour. Arch Gynecol Obstet. 2017;295:33-38.
- Stitely ML, Browning J, Fowler M, et al. Outpatient cervical ripening with intravaginal misoprostol. Obstet Gynecol. 2000;96(5 pt 1):684-688.
- McKenna DS, Ester JB, Proffitt M, et al. Misoprostol outpatient cervical ripening without subsequent induction of labor: a randomized trial. Obstet Gynecol. 2004;104:579-584.
- Oboro VO, Tabowei TO. Outpatient misoprostol cervical ripening withoutsubsequent induction of labor to prevent post-term pregnancy. Acta Obstet Gynecol Scand. 2005;84:628-631.
- Chang DW, Velazquez MD, Colyer M, et al. Vaginal misoprostol for cervical ripening at term: comparison of outpatient vs. inpatient administration. J Reprod Med. 2005;50:735-739.
- Biem SR, Turnell RW, Olatunbosun O, et al. A randomized controlled trial of outpatient versus inpatient labour induction with vaginal controlled-release prostaglandin-E2: effectiveness and satisfaction. J Obstet Gynaecol Can. 2003;25:23-31.
- Wilkinson C, Bryce R, Adelson P, et al. A randomised controlled trial of outpatient compared with inpatient cervical ripening with prostaglandin E₂ (OPRA study). BJOG. 2015;122:94-104.
- Ten Eikelder ML, van de Meent MM, Mast K, et al. Women’s experiences with and preference for induction of labor with oral misoprostol or Foley catheter at term. Am J Perinatol. 2017;34:138-146.
- Tang OS, Gemzell-Danielsson K, Ho PC. Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet. 2007;99 (suppl 2):S160-S167.
Case 1 Induction at 39 weeks in a healthy nulliparous woman
A healthy 35-year-old woman (G1P0) at 39 weeks 0 days and with an uncomplicated pregnancy presents to your office for a routine prenatal visit. She inquires about scheduling an induction of labor, noting that she read a news story about induction at 39 weeks and that it might lower her chance of having a cesarean delivery (CD).
You perform a cervical exam—she is 1 cm dilated, 3 cm long, -2 station, posterior, and firm. You sweep her membranes after obtaining verbal consent. After describing the induction process, you explain that she might be hospitalized for several days before the birth given the need for cervical ripening. “You mean I need to stay in the hospital for the entire process?” she asks incredulously.
Over the past 20 years, the percentage of patients undergoing induction of labor (IOL) has increased from 10% to 25%.1 This percentage likely will rise over time, particularly in the wake of a recent randomized controlled trial suggesting potential maternal benefits, such as reduced CD rate, for nulliparas induced at 39 weeks compared with expectant management.2 Although there have not been any changes to guidelines for timing of IOL from such professional societies such as the American College of Obstetricians and Gynecologists (ACOG) or the Society for Maternal-Fetal Medicine, key considerations of rising IOL volume include patient experience, labor and delivery (L&D) units’ capacity and resources, and associated health care costs.
An essential part of successful induction involves patience. Induction can be a lengthy process, particularly for nulliparas with unripe cervices. Cervical ripening is a necessary component of successful labor induction, whether achieved mechanically or pharmacologically with synthetic prostaglandins, and it has been shown to lower the chance of CD.3,4 However, achieving a ripe cervix is often the lengthiest part of an induction, and not uncommonly consumes 12 to 24 hours or more of inpatient time. Investigators have sought ways to make this process more expeditious. For example, the FOR-MOMI trial demonstrated that the induction-to-delivery time was several hours shorter when cervical ripening combined mechanical and pharmacologic approaches (Foley balloon plus misoprostol), compared with either method alone, without any increase in maternal or fetal complication rates.5
Better yet, what if admission to the L&D unit for IOL at term could be deferred until the cervix is ripe? A number of hospitals in the United States have successfully introduced outpatient cervical ripening, and several small observational and randomized controlled trials have reported good results in terms of safety, efficacy and time saved, and patient experience. Here, we will make the case that outpatient cervical ripening should be the standard of care for low-risk pregnancies.
Mechanical cervical ripening
Safety
Although data are limited on the safety, the authors of an ACOG Practice Bulletin suggest that, based on the available evidence of mechanical ripening in an inpatient setting, it is also appropriate in the outpatient setting.6 Unlike cervical ripening using prostaglandins, mechanical ripening is not associated with tachysystole, fetal intolerance of labor, or meconium staining.3 A cohort study of nearly 2,000 low-risk patients who underwent Foley catheter placement for cervical ripening using an outpatient protocol but monitored overnight as inpatients and evaluated for adverse outcomes found no CD for fetal distress, vaginal bleeding, placental abruption, or intrapartum stillbirth.7 The authors posited that, given this safety profile in the inpatient setting, that mechanical cervical ripening with a Foley catheter would be appropriate for outpatient use in low-risk populations. Other systematic reviews have been reassuring as well, with exceedingly low complication rates during inpatient mechanical cervical ripening.8 These data advocate for the evaluation of cervical ripening in the outpatient setting.
The evidence for outpatient mechanical ripening, although again limited, also has demonstrated safety. There does not appear to be an increased rate of maternal or neonatal complications, including infectious morbidity, postpartum hemorrhage, CD, operative vaginal delivery, or fetal distress.9-12
Continue to: Efficacy and length-of-stay...
Efficacy and length-of-stay
Efficacy also generally has been shown to be similar when mechanical methods are used in the inpatient and outpatient settings. Small randomized trials of outpatient versus inpatient Foley catheter ripening have shown decreased length of stay (by 10 to 13 hours) and similar or less oxytocin use in the outpatient groups, as well as similar Bishop scores after cervical ripening and no difference in maternal or fetal outcomes.9,11,13,14
One major concern with increasing IOL prevalence is the availability of hospital resources and the associated health care costs, given the known increased length of inpatient stay due to cervical ripening time. Admission to an L&D unit is resource intensive; the costs are similar to admission to an intensive care unit in many hospitals given its level of acuity and high nurse/patient ratio. However, given the safety of outpatient mechanical cervical ripening described above, we argue that routinely admitting low-risk patients for mechanical ripening constitutes a suboptimal use of costly resources.
Indeed, data suggest significant inpatient time savings if cervical ripening can be accomplished prior to admission. A cost-effectiveness analysis in the Netherlands demonstrated a nearly 1,000-euro decrease in cost per induction when Foley catheter induction was done on an outpatient basis.15 Interestingly, a recent trial confined to multiparas found no differences in hospital time when comparing outpatient ripening with Foley balloon alone with inpatient ripening with Foley balloon plus simultaneous oxytocin.10 This certainly merits further study, but it may be that the largest time- and cost-savings are among nulliparas.
Patient preferences
Relatively few studies specifically have addressed patient experiences with outpatient versus inpatient mechanical cervical ripening. Outpatient cervical ripening may provide patients with the benefits of being in the comfort of their own homes with their preferred support persons, increased mobility, more bodily autonomy, and satisfaction with their birthing process.
In a pilot trial involving 48 women, inpatient was compared with outpatient cervical ripening using a Foley balloon. Those in the outpatient group reported getting more rest, feeling less isolated, and having enough privacy. However, participants in both groups were equally satisfied and equally likely to recommend their method of induction to others.11 Another study comparing outpatient versus inpatient Foley balloon cervical ripening found that 85% of patients who underwent outpatient ripening were satisfied with the induction method; however, no query or comparison was done with the inpatient group.12 A trial comparing outpatient mechanical cervical ripening with inpatient misoprostol found that outpatient participants reported several hours more sleep and less pain.16 And in a discrete choice experiment of British gravidas, participants favored the option of outpatient cervical ripening, even if it meant an extra 1.4 trips to the hospital and over an hour of extra travel time.17
While these preliminary findings provide some insight that patients may prefer an outpatient approach to cervical ripening, more studies are needed to fully evaluate patient desires.
Continue to: Our approach to mechanical cervical ripening...
Our approach to mechanical cervical ripening
Most patients undergoing scheduled IOL are reasonable candidates for outpatient cervical ripening based on safety and efficacy. By definition, scheduling in advance implies that the provider has determined that outpatient management is reasonable until that date, and the plan for outpatient ripening need not prolong this period.
FIGURES 1 and 2 show protocols for our 2 hospital centers, which regularly allow for outpatient mechanical cervical ripening. In the process of protocol development, we identified absolute and relative contraindications to determine appropriate candidates. We exclude women who require inpatient management of medical or obstetric conditions (for example, women with severe preeclampsia or any condition requiring continuous fetal monitoring). We also do not routinely recommend outpatient cervical ripening to patients who do not have the necessary social conditions to make this process as safe as possible (including stable housing, reliable transportation, and a support person), although this occurs with some exceptions depending on individual patient situations.
Some examples of ideal candidates for outpatient mechanical cervical ripening include those undergoing elective or routine prolonged gestation inductions, or inductions for well-controlled, stable conditions (chronic hypertension and gestational diabetes). At one center, after thorough counseling and assessment, outpatient cervical ripening is also offered to patients with mild risk factors, including twins, prior low transverse CD, stable preeclampsia without severe features, isolated oligohydramnios with otherwise reassuring fetal status, and other similar conditions.
After mechanical cervical ripening placement (either Foley catheter or mechanical dilators), the clinician completes a postprocedure safety checklist and detailed procedure documentation, including number and type of foreign bodies placed. If there are any concerns regarding maternal or fetal well-being, the patient is sent to L&D for evaluation. If the procedure was tolerated well, the patient is discharged home, after a reactive postprocedure nonstress test is done, with detailed instructions for self-care, as well as with a list of symptoms that warrant prompt evaluation prior to scheduled induction time. In a large California hospital group following a similar protocol, only about 5% of women presented in labor before their scheduled induction.18
Case 2 Cervical ripening for labor preparation in low-risk pregnancy
A 32-year-old woman (G1P0) with an uncomplicated pregnancy at 40 weeks and 3 days presents to your office for a routine prenatal visit. Her vital signs are normal, and her fetus is vertex with an estimated fetal weight of 7.5 lb by Leopald’s maneuvers. You perform a cervical exam and find that her cervix is closed, long, and posterior.
You discuss with her your recommendation for induction of labor by 41 weeks, and she agrees. You also discuss the need for cervical ripening and recommend misoprostol given her closed cervix. You explain that several doses may be needed to get her cervix ready for labor, and she asks, “Do I have to stay in the hospital that whole time?”
Pharmacologic cervical ripening
Efficacy
There are multiple pharmacologic agents that can be used for ripening an unfavorable cervix. The main agents used in the United States are prostaglandins, either PGE1 (oral or vaginal misoprostol) or PGE2 in a gel or sustained-release vaginal insert (dinoprostone).
Outpatient misoprostol to avoid labor induction. Many studies have looked at outpatient misoprostol use as a “prophylactic measure” (to prevent the need for labor induction). For example, Gaffaney and colleagues showed that administering outpatient oral misoprostol (100 µg every 24 hours for up to 3 doses) after 40 weeks’ gestation to women with an unfavorable cervix significantly decreased the time to delivery by a day and a half.19 Similarly, PonMalar and colleagues demonstrated that administering 25 µg of vaginal misoprostol in a single dose as an outpatient after stripping the membranes significantly reduced time to delivery by 2 days.20 And Stitely and colleagues found a significant reduction in the need for labor induction with the use of outpatient vaginal misoprostol. They administered up to 2 doses of misoprostol 25 µg vaginally every 24 hours for the 48 hours prior to a scheduled postdates induction and found a large reduction in the need for labor induction (11% vs 85%; P<.01).21
Continue to: Multiple protocols and regimens...
Multiple protocols and regimens have been studied but, overall, the findings suggest that administering outpatient misoprostol may shorten the time interval to spontaneous labor and decrease the need for a formal labor induction.19-23
Inpatient compared with outpatient prostaglandin use. These trials of “prophylactic” misoprostol generally have compared outpatient administration of misoprostol with placebo. Prostaglandins are one of the most common methods of inpatient cervical ripening, so what about comparisons of inpatient cervical ripening with outpatient prostaglandin administration? There are a handful of studies that make this comparison.
Chang and colleagues looked retrospectively at inpatient and outpatient misoprostol and found that outpatient administration saved 3 to 5 hours on labor and delivery.24 Biem and colleagues randomly assigned women to either inpatient cervical ripening with PGE2 intravaginal inserts or 1 hour of inpatient monitoring after PGE2 administration and then outpatient discharge until the onset of labor or for a nonstress test at 12 hours. They found that those who underwent outpatient ripening spent 8 hours less on labor and delivery and were more highly satisfied with the initial 12 hours of labor induction experience (56% vs 39%; P<.01).25
The largest randomized controlled trial conducted to study outpatient prostaglandin use was the OPRA study (involving 827 women). Investigators compared inpatient to outpatient PGE2 intravaginal gel.26 The primary outcome was total oxytocin administration, which was not different between groups. The study was underpowered, however, as 50% of women labored spontaneously postrandomization. But in the outpatient arm, less than half of the women required additional inpatient ripening, and nearly 40% returned in spontaneous labor, suggesting that outpatient prostaglandin administration may indeed save women a significant amount of time on labor and delivery.
Safety
The safety of outpatient administration of prostaglandins is the biggest concern, especially since, when prostaglandins are compared to outpatient Foley catheter use, Foleys are overall associated with less tachysystole, fetal intolerance, and meconium-stained fluid.3 Foley catheter use for cervical ripening may not be an appropriate choice for all patients, however. For instance, our case patient has a closed cervix, which could make Foley insertion uncomfortable or even impossible. Misoprostol use also offers the potential for flexibility in cervical ripening protocols as patients need not return for Foley balloon removal and indeed labor induction need not take place immediately after administration of misoprostol.
Patients also may prefer outpatient cervical ripening with misoprostol over a Foley. There are some data to suggest that women, overall, have a preference toward prostaglandins; in the PROBAAT-II trial, which compared inpatient oral misoprostol to Foley catheter for cervical ripening, 12% of women in the Foley arm would have preferred another method of induction (vs 6% in the misoprostol arm; P = .02).27 This preference may be magnified in an outpatient setting.
But, again, is outpatient administration of prostaglandins safe? The published trials thus far have not reported an increase in out-of-hospital deliveries or adverse fetal outcomes. However, studies have been of limited size to see more rare outcomes. Unfortunately, an adequately powered study to demonstrate safety is likely never to be accomplished, given that if used responsibly (in low-risk patients with adequate monitoring after administration) the incidence of adverse fetal outcomes during the at-home portion of cervical ripening is likely to be very low. With responsible use, outpatient administration of prostaglandins should be safe. Women are monitored after misoprostol administration and are not sent home if there are any concerns for fetal distress or if frequent contractions continue. Misoprostol reaches maximum blood concentration 30 minutes after oral administration and 70 to 80 minutes after vaginal administration.28 After this time, if contractions start to intensify it is likely that misoprostol has triggered spontaneous labor. In this setting, women are routinely allowed to spontaneously labor at home. One may even argue that outpatient misoprostol could lead to improved safety, as women essentially have a contraction stress test prior to spontaneous labor, and misoprostol administration as an outpatient, as opposed to as an inpatient, may allow for longer time intervals between doses, which could prevent dose stacking.
Continue to: Our approach to pharmacologic cervical ripening...
Our approach to pharmacologic cervical ripening
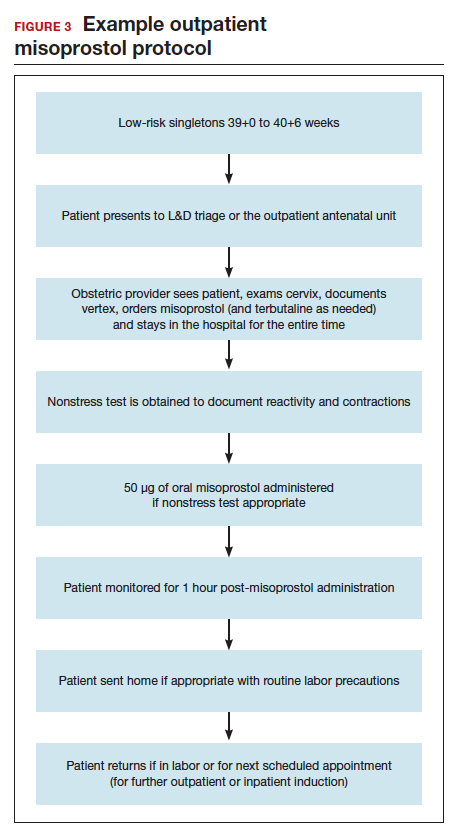
Our hospital has been conducting outpatient cervical ripening using vaginal misoprostol for more th
Conclusion
While the data continue to be limited, we strongly believe there is sufficient quality evidence from a safety and efficacy perspective to support implementation and evaluation of outpatient cervical ripening protocols for low-risk pregnancies. In the setting of renewed commitments to reducing suboptimal health care costs and utilization as well as increasing patient satisfaction and control in their birthing experiences, we posit it is the responsibility of obstetricians, L&D leadership, and health care institutions to explore the implementation of outpatient cervical ripening for appropriate candidates in their settings.
Case 1 Induction at 39 weeks in a healthy nulliparous woman
A healthy 35-year-old woman (G1P0) at 39 weeks 0 days and with an uncomplicated pregnancy presents to your office for a routine prenatal visit. She inquires about scheduling an induction of labor, noting that she read a news story about induction at 39 weeks and that it might lower her chance of having a cesarean delivery (CD).
You perform a cervical exam—she is 1 cm dilated, 3 cm long, -2 station, posterior, and firm. You sweep her membranes after obtaining verbal consent. After describing the induction process, you explain that she might be hospitalized for several days before the birth given the need for cervical ripening. “You mean I need to stay in the hospital for the entire process?” she asks incredulously.
Over the past 20 years, the percentage of patients undergoing induction of labor (IOL) has increased from 10% to 25%.1 This percentage likely will rise over time, particularly in the wake of a recent randomized controlled trial suggesting potential maternal benefits, such as reduced CD rate, for nulliparas induced at 39 weeks compared with expectant management.2 Although there have not been any changes to guidelines for timing of IOL from such professional societies such as the American College of Obstetricians and Gynecologists (ACOG) or the Society for Maternal-Fetal Medicine, key considerations of rising IOL volume include patient experience, labor and delivery (L&D) units’ capacity and resources, and associated health care costs.
An essential part of successful induction involves patience. Induction can be a lengthy process, particularly for nulliparas with unripe cervices. Cervical ripening is a necessary component of successful labor induction, whether achieved mechanically or pharmacologically with synthetic prostaglandins, and it has been shown to lower the chance of CD.3,4 However, achieving a ripe cervix is often the lengthiest part of an induction, and not uncommonly consumes 12 to 24 hours or more of inpatient time. Investigators have sought ways to make this process more expeditious. For example, the FOR-MOMI trial demonstrated that the induction-to-delivery time was several hours shorter when cervical ripening combined mechanical and pharmacologic approaches (Foley balloon plus misoprostol), compared with either method alone, without any increase in maternal or fetal complication rates.5
Better yet, what if admission to the L&D unit for IOL at term could be deferred until the cervix is ripe? A number of hospitals in the United States have successfully introduced outpatient cervical ripening, and several small observational and randomized controlled trials have reported good results in terms of safety, efficacy and time saved, and patient experience. Here, we will make the case that outpatient cervical ripening should be the standard of care for low-risk pregnancies.
Mechanical cervical ripening
Safety
Although data are limited on the safety, the authors of an ACOG Practice Bulletin suggest that, based on the available evidence of mechanical ripening in an inpatient setting, it is also appropriate in the outpatient setting.6 Unlike cervical ripening using prostaglandins, mechanical ripening is not associated with tachysystole, fetal intolerance of labor, or meconium staining.3 A cohort study of nearly 2,000 low-risk patients who underwent Foley catheter placement for cervical ripening using an outpatient protocol but monitored overnight as inpatients and evaluated for adverse outcomes found no CD for fetal distress, vaginal bleeding, placental abruption, or intrapartum stillbirth.7 The authors posited that, given this safety profile in the inpatient setting, that mechanical cervical ripening with a Foley catheter would be appropriate for outpatient use in low-risk populations. Other systematic reviews have been reassuring as well, with exceedingly low complication rates during inpatient mechanical cervical ripening.8 These data advocate for the evaluation of cervical ripening in the outpatient setting.
The evidence for outpatient mechanical ripening, although again limited, also has demonstrated safety. There does not appear to be an increased rate of maternal or neonatal complications, including infectious morbidity, postpartum hemorrhage, CD, operative vaginal delivery, or fetal distress.9-12
Continue to: Efficacy and length-of-stay...
Efficacy and length-of-stay
Efficacy also generally has been shown to be similar when mechanical methods are used in the inpatient and outpatient settings. Small randomized trials of outpatient versus inpatient Foley catheter ripening have shown decreased length of stay (by 10 to 13 hours) and similar or less oxytocin use in the outpatient groups, as well as similar Bishop scores after cervical ripening and no difference in maternal or fetal outcomes.9,11,13,14
One major concern with increasing IOL prevalence is the availability of hospital resources and the associated health care costs, given the known increased length of inpatient stay due to cervical ripening time. Admission to an L&D unit is resource intensive; the costs are similar to admission to an intensive care unit in many hospitals given its level of acuity and high nurse/patient ratio. However, given the safety of outpatient mechanical cervical ripening described above, we argue that routinely admitting low-risk patients for mechanical ripening constitutes a suboptimal use of costly resources.
Indeed, data suggest significant inpatient time savings if cervical ripening can be accomplished prior to admission. A cost-effectiveness analysis in the Netherlands demonstrated a nearly 1,000-euro decrease in cost per induction when Foley catheter induction was done on an outpatient basis.15 Interestingly, a recent trial confined to multiparas found no differences in hospital time when comparing outpatient ripening with Foley balloon alone with inpatient ripening with Foley balloon plus simultaneous oxytocin.10 This certainly merits further study, but it may be that the largest time- and cost-savings are among nulliparas.
Patient preferences
Relatively few studies specifically have addressed patient experiences with outpatient versus inpatient mechanical cervical ripening. Outpatient cervical ripening may provide patients with the benefits of being in the comfort of their own homes with their preferred support persons, increased mobility, more bodily autonomy, and satisfaction with their birthing process.
In a pilot trial involving 48 women, inpatient was compared with outpatient cervical ripening using a Foley balloon. Those in the outpatient group reported getting more rest, feeling less isolated, and having enough privacy. However, participants in both groups were equally satisfied and equally likely to recommend their method of induction to others.11 Another study comparing outpatient versus inpatient Foley balloon cervical ripening found that 85% of patients who underwent outpatient ripening were satisfied with the induction method; however, no query or comparison was done with the inpatient group.12 A trial comparing outpatient mechanical cervical ripening with inpatient misoprostol found that outpatient participants reported several hours more sleep and less pain.16 And in a discrete choice experiment of British gravidas, participants favored the option of outpatient cervical ripening, even if it meant an extra 1.4 trips to the hospital and over an hour of extra travel time.17
While these preliminary findings provide some insight that patients may prefer an outpatient approach to cervical ripening, more studies are needed to fully evaluate patient desires.
Continue to: Our approach to mechanical cervical ripening...
Our approach to mechanical cervical ripening
Most patients undergoing scheduled IOL are reasonable candidates for outpatient cervical ripening based on safety and efficacy. By definition, scheduling in advance implies that the provider has determined that outpatient management is reasonable until that date, and the plan for outpatient ripening need not prolong this period.
FIGURES 1 and 2 show protocols for our 2 hospital centers, which regularly allow for outpatient mechanical cervical ripening. In the process of protocol development, we identified absolute and relative contraindications to determine appropriate candidates. We exclude women who require inpatient management of medical or obstetric conditions (for example, women with severe preeclampsia or any condition requiring continuous fetal monitoring). We also do not routinely recommend outpatient cervical ripening to patients who do not have the necessary social conditions to make this process as safe as possible (including stable housing, reliable transportation, and a support person), although this occurs with some exceptions depending on individual patient situations.
Some examples of ideal candidates for outpatient mechanical cervical ripening include those undergoing elective or routine prolonged gestation inductions, or inductions for well-controlled, stable conditions (chronic hypertension and gestational diabetes). At one center, after thorough counseling and assessment, outpatient cervical ripening is also offered to patients with mild risk factors, including twins, prior low transverse CD, stable preeclampsia without severe features, isolated oligohydramnios with otherwise reassuring fetal status, and other similar conditions.
After mechanical cervical ripening placement (either Foley catheter or mechanical dilators), the clinician completes a postprocedure safety checklist and detailed procedure documentation, including number and type of foreign bodies placed. If there are any concerns regarding maternal or fetal well-being, the patient is sent to L&D for evaluation. If the procedure was tolerated well, the patient is discharged home, after a reactive postprocedure nonstress test is done, with detailed instructions for self-care, as well as with a list of symptoms that warrant prompt evaluation prior to scheduled induction time. In a large California hospital group following a similar protocol, only about 5% of women presented in labor before their scheduled induction.18
Case 2 Cervical ripening for labor preparation in low-risk pregnancy
A 32-year-old woman (G1P0) with an uncomplicated pregnancy at 40 weeks and 3 days presents to your office for a routine prenatal visit. Her vital signs are normal, and her fetus is vertex with an estimated fetal weight of 7.5 lb by Leopald’s maneuvers. You perform a cervical exam and find that her cervix is closed, long, and posterior.
You discuss with her your recommendation for induction of labor by 41 weeks, and she agrees. You also discuss the need for cervical ripening and recommend misoprostol given her closed cervix. You explain that several doses may be needed to get her cervix ready for labor, and she asks, “Do I have to stay in the hospital that whole time?”
Pharmacologic cervical ripening
Efficacy
There are multiple pharmacologic agents that can be used for ripening an unfavorable cervix. The main agents used in the United States are prostaglandins, either PGE1 (oral or vaginal misoprostol) or PGE2 in a gel or sustained-release vaginal insert (dinoprostone).
Outpatient misoprostol to avoid labor induction. Many studies have looked at outpatient misoprostol use as a “prophylactic measure” (to prevent the need for labor induction). For example, Gaffaney and colleagues showed that administering outpatient oral misoprostol (100 µg every 24 hours for up to 3 doses) after 40 weeks’ gestation to women with an unfavorable cervix significantly decreased the time to delivery by a day and a half.19 Similarly, PonMalar and colleagues demonstrated that administering 25 µg of vaginal misoprostol in a single dose as an outpatient after stripping the membranes significantly reduced time to delivery by 2 days.20 And Stitely and colleagues found a significant reduction in the need for labor induction with the use of outpatient vaginal misoprostol. They administered up to 2 doses of misoprostol 25 µg vaginally every 24 hours for the 48 hours prior to a scheduled postdates induction and found a large reduction in the need for labor induction (11% vs 85%; P<.01).21
Continue to: Multiple protocols and regimens...
Multiple protocols and regimens have been studied but, overall, the findings suggest that administering outpatient misoprostol may shorten the time interval to spontaneous labor and decrease the need for a formal labor induction.19-23
Inpatient compared with outpatient prostaglandin use. These trials of “prophylactic” misoprostol generally have compared outpatient administration of misoprostol with placebo. Prostaglandins are one of the most common methods of inpatient cervical ripening, so what about comparisons of inpatient cervical ripening with outpatient prostaglandin administration? There are a handful of studies that make this comparison.
Chang and colleagues looked retrospectively at inpatient and outpatient misoprostol and found that outpatient administration saved 3 to 5 hours on labor and delivery.24 Biem and colleagues randomly assigned women to either inpatient cervical ripening with PGE2 intravaginal inserts or 1 hour of inpatient monitoring after PGE2 administration and then outpatient discharge until the onset of labor or for a nonstress test at 12 hours. They found that those who underwent outpatient ripening spent 8 hours less on labor and delivery and were more highly satisfied with the initial 12 hours of labor induction experience (56% vs 39%; P<.01).25
The largest randomized controlled trial conducted to study outpatient prostaglandin use was the OPRA study (involving 827 women). Investigators compared inpatient to outpatient PGE2 intravaginal gel.26 The primary outcome was total oxytocin administration, which was not different between groups. The study was underpowered, however, as 50% of women labored spontaneously postrandomization. But in the outpatient arm, less than half of the women required additional inpatient ripening, and nearly 40% returned in spontaneous labor, suggesting that outpatient prostaglandin administration may indeed save women a significant amount of time on labor and delivery.
Safety
The safety of outpatient administration of prostaglandins is the biggest concern, especially since, when prostaglandins are compared to outpatient Foley catheter use, Foleys are overall associated with less tachysystole, fetal intolerance, and meconium-stained fluid.3 Foley catheter use for cervical ripening may not be an appropriate choice for all patients, however. For instance, our case patient has a closed cervix, which could make Foley insertion uncomfortable or even impossible. Misoprostol use also offers the potential for flexibility in cervical ripening protocols as patients need not return for Foley balloon removal and indeed labor induction need not take place immediately after administration of misoprostol.
Patients also may prefer outpatient cervical ripening with misoprostol over a Foley. There are some data to suggest that women, overall, have a preference toward prostaglandins; in the PROBAAT-II trial, which compared inpatient oral misoprostol to Foley catheter for cervical ripening, 12% of women in the Foley arm would have preferred another method of induction (vs 6% in the misoprostol arm; P = .02).27 This preference may be magnified in an outpatient setting.
But, again, is outpatient administration of prostaglandins safe? The published trials thus far have not reported an increase in out-of-hospital deliveries or adverse fetal outcomes. However, studies have been of limited size to see more rare outcomes. Unfortunately, an adequately powered study to demonstrate safety is likely never to be accomplished, given that if used responsibly (in low-risk patients with adequate monitoring after administration) the incidence of adverse fetal outcomes during the at-home portion of cervical ripening is likely to be very low. With responsible use, outpatient administration of prostaglandins should be safe. Women are monitored after misoprostol administration and are not sent home if there are any concerns for fetal distress or if frequent contractions continue. Misoprostol reaches maximum blood concentration 30 minutes after oral administration and 70 to 80 minutes after vaginal administration.28 After this time, if contractions start to intensify it is likely that misoprostol has triggered spontaneous labor. In this setting, women are routinely allowed to spontaneously labor at home. One may even argue that outpatient misoprostol could lead to improved safety, as women essentially have a contraction stress test prior to spontaneous labor, and misoprostol administration as an outpatient, as opposed to as an inpatient, may allow for longer time intervals between doses, which could prevent dose stacking.
Continue to: Our approach to pharmacologic cervical ripening...
Our approach to pharmacologic cervical ripening
Our hospital has been conducting outpatient cervical ripening using vaginal misoprostol for more th
Conclusion
While the data continue to be limited, we strongly believe there is sufficient quality evidence from a safety and efficacy perspective to support implementation and evaluation of outpatient cervical ripening protocols for low-risk pregnancies. In the setting of renewed commitments to reducing suboptimal health care costs and utilization as well as increasing patient satisfaction and control in their birthing experiences, we posit it is the responsibility of obstetricians, L&D leadership, and health care institutions to explore the implementation of outpatient cervical ripening for appropriate candidates in their settings.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2015. Natl Vital Stat Rep. 2017;66:1.
- Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- Jozwiak M, Bloemenkamp KW, Kelly AJ, et al. Mechanical methods for induction of labor. Cochrane Database Syst Rev. 2012;(3):CD001233.
- Alfirevic Z, Kelly AJ, Dowswell T. Intravenous oxytocin alone for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2009;(4):CD003246.
- Levine LD, Downes KL, Elovitz MA, et al. Mechanical and pharmacologic methods of labor induction: a randomized controlled trial. Obstet Gynecol. 2016;128:1357-1364.
- ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin no. 107: induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397. Reaffirmed 2019.
- Sciscione AC, Bedder CL, Hoffman MK, et al. The timing of adverse events with Foley catheter preinduction cervical ripening; implications for outpatient use. Am J Perinatol. 2014;31:781-786.
- Diederen M, Gommers J, Wilkinson C, et al. Safety of the balloon catheter for cervical ripening in outpatient care: complications during the period from insertion to expulsion of a balloon catheter in the process of labour induction: a systematic review. BJOG. 2018;125:1086-1095.
- McKenna DS, Duke JM. Effectiveness and infectious morbidity of outpatient cervical ripening with a Foley catheter. J Reprod Med. 2004;49:28-32.
- Kuper SG, Jauk VC, George DM, et al. Outpatient Foley catheter for induction of labor in parous women: a randomized controlled trial. Obstet Gynecol. 2018;132:94-101.
- Wilkinson C, Adelson P, Turnbull D. A comparison of inpatient with outpatient balloon catheter cervical ripening: a pilot randomized controlled trial. BMC Pregnancy Childbirth. 2015;15:126.
- Kruit H, Heikinheimo O, Ulander VM, et al. Foley catheter induction of labor as an outpatient procedure. J Perinatol. 2016;36:618-622.
- Sciscione AC, Muench M, Pollock M, et al. Transcervical Foley catheter for preinduction cervical ripening in an outpatient versus inpatient setting. Obstet Gynecol. 2001;98(5 pt 1):751-756.
- Policiano C, Pimenta M, Martins D, et al. Outpatient versus inpatient cervix priming with Foley catheter: a randomized trial. Eur J Obstet Gynecol Reprod Biol. 2017;210:1-6.
- Ten Eikelder M, van Baaren GJ, Oude Rengerink K, et al. Comparing induction of labour with oral misoprostol or Foley catheter at term: cost effectiveness analysis of a randomised controlled multi-centre non-inferiority trial. BJOG. 2018;125:375-383.
- Henry A, Madan A, Reid R, et al. Outpatient Foley catheter versus inpatient prostaglandin E2 gel for induction of labour: a randomised trial. BMC Pregnancy Childbirth. 2013;13:25.
- Howard K, Gerard K, Adelson P, et al. Women’s preferences for inpatient and outpatient priming for labour induction: a discrete choice experiment. BMC Health Serv Res. 2014;14:330.
- Main E, LaGrew D; California Maternal Quality Care Collaborative. Induction of labor risks, benefits, and techniques for increasing success. June 14, 2017. https://www .cmqcc.org/resource/induction-labor-risk-benefits-and-techniques-increasing -success. Accessed August 21, 2019.
- Gaffaney CA, Saul LL, Rumney PJ, et al. Outpatient oral misoprostol for prolonged pregnancies: a pilot investigation. Am J Perinatol. 2009;26:673-677.
- PonMalar J, Benjamin SJ, Abraham A, et al. Randomized double-blind placebo controlled study of preinduction cervical priming with 25 µg of misoprostol in the outpatient setting to prevent formal induction of labour. Arch Gynecol Obstet. 2017;295:33-38.
- Stitely ML, Browning J, Fowler M, et al. Outpatient cervical ripening with intravaginal misoprostol. Obstet Gynecol. 2000;96(5 pt 1):684-688.
- McKenna DS, Ester JB, Proffitt M, et al. Misoprostol outpatient cervical ripening without subsequent induction of labor: a randomized trial. Obstet Gynecol. 2004;104:579-584.
- Oboro VO, Tabowei TO. Outpatient misoprostol cervical ripening withoutsubsequent induction of labor to prevent post-term pregnancy. Acta Obstet Gynecol Scand. 2005;84:628-631.
- Chang DW, Velazquez MD, Colyer M, et al. Vaginal misoprostol for cervical ripening at term: comparison of outpatient vs. inpatient administration. J Reprod Med. 2005;50:735-739.
- Biem SR, Turnell RW, Olatunbosun O, et al. A randomized controlled trial of outpatient versus inpatient labour induction with vaginal controlled-release prostaglandin-E2: effectiveness and satisfaction. J Obstet Gynaecol Can. 2003;25:23-31.
- Wilkinson C, Bryce R, Adelson P, et al. A randomised controlled trial of outpatient compared with inpatient cervical ripening with prostaglandin E₂ (OPRA study). BJOG. 2015;122:94-104.
- Ten Eikelder ML, van de Meent MM, Mast K, et al. Women’s experiences with and preference for induction of labor with oral misoprostol or Foley catheter at term. Am J Perinatol. 2017;34:138-146.
- Tang OS, Gemzell-Danielsson K, Ho PC. Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet. 2007;99 (suppl 2):S160-S167.
- Martin JA, Hamilton BE, Osterman MJ, et al. Births: final data for 2015. Natl Vital Stat Rep. 2017;66:1.
- Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- Jozwiak M, Bloemenkamp KW, Kelly AJ, et al. Mechanical methods for induction of labor. Cochrane Database Syst Rev. 2012;(3):CD001233.
- Alfirevic Z, Kelly AJ, Dowswell T. Intravenous oxytocin alone for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2009;(4):CD003246.
- Levine LD, Downes KL, Elovitz MA, et al. Mechanical and pharmacologic methods of labor induction: a randomized controlled trial. Obstet Gynecol. 2016;128:1357-1364.
- ACOG Committee on Practice Bulletins—Obstetrics. ACOG practice bulletin no. 107: induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397. Reaffirmed 2019.
- Sciscione AC, Bedder CL, Hoffman MK, et al. The timing of adverse events with Foley catheter preinduction cervical ripening; implications for outpatient use. Am J Perinatol. 2014;31:781-786.
- Diederen M, Gommers J, Wilkinson C, et al. Safety of the balloon catheter for cervical ripening in outpatient care: complications during the period from insertion to expulsion of a balloon catheter in the process of labour induction: a systematic review. BJOG. 2018;125:1086-1095.
- McKenna DS, Duke JM. Effectiveness and infectious morbidity of outpatient cervical ripening with a Foley catheter. J Reprod Med. 2004;49:28-32.
- Kuper SG, Jauk VC, George DM, et al. Outpatient Foley catheter for induction of labor in parous women: a randomized controlled trial. Obstet Gynecol. 2018;132:94-101.
- Wilkinson C, Adelson P, Turnbull D. A comparison of inpatient with outpatient balloon catheter cervical ripening: a pilot randomized controlled trial. BMC Pregnancy Childbirth. 2015;15:126.
- Kruit H, Heikinheimo O, Ulander VM, et al. Foley catheter induction of labor as an outpatient procedure. J Perinatol. 2016;36:618-622.
- Sciscione AC, Muench M, Pollock M, et al. Transcervical Foley catheter for preinduction cervical ripening in an outpatient versus inpatient setting. Obstet Gynecol. 2001;98(5 pt 1):751-756.
- Policiano C, Pimenta M, Martins D, et al. Outpatient versus inpatient cervix priming with Foley catheter: a randomized trial. Eur J Obstet Gynecol Reprod Biol. 2017;210:1-6.
- Ten Eikelder M, van Baaren GJ, Oude Rengerink K, et al. Comparing induction of labour with oral misoprostol or Foley catheter at term: cost effectiveness analysis of a randomised controlled multi-centre non-inferiority trial. BJOG. 2018;125:375-383.
- Henry A, Madan A, Reid R, et al. Outpatient Foley catheter versus inpatient prostaglandin E2 gel for induction of labour: a randomised trial. BMC Pregnancy Childbirth. 2013;13:25.
- Howard K, Gerard K, Adelson P, et al. Women’s preferences for inpatient and outpatient priming for labour induction: a discrete choice experiment. BMC Health Serv Res. 2014;14:330.
- Main E, LaGrew D; California Maternal Quality Care Collaborative. Induction of labor risks, benefits, and techniques for increasing success. June 14, 2017. https://www .cmqcc.org/resource/induction-labor-risk-benefits-and-techniques-increasing -success. Accessed August 21, 2019.
- Gaffaney CA, Saul LL, Rumney PJ, et al. Outpatient oral misoprostol for prolonged pregnancies: a pilot investigation. Am J Perinatol. 2009;26:673-677.
- PonMalar J, Benjamin SJ, Abraham A, et al. Randomized double-blind placebo controlled study of preinduction cervical priming with 25 µg of misoprostol in the outpatient setting to prevent formal induction of labour. Arch Gynecol Obstet. 2017;295:33-38.
- Stitely ML, Browning J, Fowler M, et al. Outpatient cervical ripening with intravaginal misoprostol. Obstet Gynecol. 2000;96(5 pt 1):684-688.
- McKenna DS, Ester JB, Proffitt M, et al. Misoprostol outpatient cervical ripening without subsequent induction of labor: a randomized trial. Obstet Gynecol. 2004;104:579-584.
- Oboro VO, Tabowei TO. Outpatient misoprostol cervical ripening withoutsubsequent induction of labor to prevent post-term pregnancy. Acta Obstet Gynecol Scand. 2005;84:628-631.
- Chang DW, Velazquez MD, Colyer M, et al. Vaginal misoprostol for cervical ripening at term: comparison of outpatient vs. inpatient administration. J Reprod Med. 2005;50:735-739.
- Biem SR, Turnell RW, Olatunbosun O, et al. A randomized controlled trial of outpatient versus inpatient labour induction with vaginal controlled-release prostaglandin-E2: effectiveness and satisfaction. J Obstet Gynaecol Can. 2003;25:23-31.
- Wilkinson C, Bryce R, Adelson P, et al. A randomised controlled trial of outpatient compared with inpatient cervical ripening with prostaglandin E₂ (OPRA study). BJOG. 2015;122:94-104.
- Ten Eikelder ML, van de Meent MM, Mast K, et al. Women’s experiences with and preference for induction of labor with oral misoprostol or Foley catheter at term. Am J Perinatol. 2017;34:138-146.
- Tang OS, Gemzell-Danielsson K, Ho PC. Misoprostol: pharmacokinetic profiles, effects on the uterus and side-effects. Int J Gynaecol Obstet. 2007;99 (suppl 2):S160-S167.
Click for Credit: Fasting rules for surgery; Biomarkers for PSA vs OA; more
Here are 5 articles from the September issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. No birth rate gains from levothyroxine in pregnancy
To take the posttest, go to: https://bit.ly/2ZoXzK8
Expires March 23, 2020
2. Simple screening for risk of falling in elderly can guide prevention
To take the posttest, go to: https://bit.ly/2NKXxu3
Expires March 24, 2020
3. Time to revisit fasting rules for surgery patients
To take the posttest, go to: https://bit.ly/2HHwHiD
Expires March 26, 2020
4. Four biomarkers could distinguish psoriatic arthritis from osteoarthritis
To take the posttest, go to: https://bit.ly/344WPNS
Expires March 28, 2020
5. More chest compression–only CPR leads to increased survival rates
To take the posttest, go to: https://bit.ly/30CahGF
Expires April 1, 2020
Here are 5 articles from the September issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. No birth rate gains from levothyroxine in pregnancy
To take the posttest, go to: https://bit.ly/2ZoXzK8
Expires March 23, 2020
2. Simple screening for risk of falling in elderly can guide prevention
To take the posttest, go to: https://bit.ly/2NKXxu3
Expires March 24, 2020
3. Time to revisit fasting rules for surgery patients
To take the posttest, go to: https://bit.ly/2HHwHiD
Expires March 26, 2020
4. Four biomarkers could distinguish psoriatic arthritis from osteoarthritis
To take the posttest, go to: https://bit.ly/344WPNS
Expires March 28, 2020
5. More chest compression–only CPR leads to increased survival rates
To take the posttest, go to: https://bit.ly/30CahGF
Expires April 1, 2020
Here are 5 articles from the September issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. No birth rate gains from levothyroxine in pregnancy
To take the posttest, go to: https://bit.ly/2ZoXzK8
Expires March 23, 2020
2. Simple screening for risk of falling in elderly can guide prevention
To take the posttest, go to: https://bit.ly/2NKXxu3
Expires March 24, 2020
3. Time to revisit fasting rules for surgery patients
To take the posttest, go to: https://bit.ly/2HHwHiD
Expires March 26, 2020
4. Four biomarkers could distinguish psoriatic arthritis from osteoarthritis
To take the posttest, go to: https://bit.ly/344WPNS
Expires March 28, 2020
5. More chest compression–only CPR leads to increased survival rates
To take the posttest, go to: https://bit.ly/30CahGF
Expires April 1, 2020
Predictive model estimates likelihood of failing induction of labor in obese patients
reported researchers from the University of Cincinnati and Cincinnati Children’s Hospital Medical Center.
The ten variables included in the model were prior vaginal delivery; prior cesarean delivery; maternal height, age, and weight at delivery; parity; gestational weight gain; Medicaid insurance; pregestational diabetes; and chronic hypertension, said Robert M. Rossi, MD, of the university and associates, who developed the model.
“Our hope is that this model may be useful as a tool to estimate an individualized risk based on commonly available prenatal factors that may assist in delivery planning and allocation of appropriate resources,” the investigators said in a study summarizing their findings, published in Obstetrics & Gynecology.
The researchers conducted a population-based, retrospective cohort study of delivery records from 1,098,981 obese women in a National Center for Health Statistics birth-death cohort database who underwent induction of labor between 2012 and 2016. Of these women, 825,797 (75%) women succeeded in delivering after induction, while 273,184 (25%) women failed to deliver after induction of labor and instead underwent cesarean section. The women included in the study had a body mass index of 30 or higher and underwent induction between 37 weeks and 44 weeks of gestation.
The class of obesity prior to pregnancy impacted the rate of induction failure, as patients with class I obesity had a rate of cesarean section of 21.6% (95% confidence interval, 21.4%-21.7%), while women with class II obesity had a rate of 25% (95% CI, 24.8%-25.2%) and women with class III obesity had a rate of 31% (95% CI, 30.8%-31.3%). Women also were more likely to fail induction if they had received fertility treatment, if they were older than 35 years, if they were of non-Hispanic black race, if they had gestational weight gain or maternal weight gain, if they had pregestational diabetes or gestational diabetes, or if they had gestational hypertension or preeclampsia (all P less than .001). Factors that made a woman less likely to undergo cesarean delivery were Medicaid insurance status or receiving Special Supplemental Nutrition Program for Women, Infant and Children (SNAP WIC) support.
Under the predictive model, the receiver operator characteristic curve (ROC) had an area under the curve (AUC) of 0.79 (95% CI, 0.78-0.79), and subsequent validation of the model using a different external U.S. birth cohort dataset showed an AUC of 0.77 (95% CI, 0.76-0.77). In both datasets, the model was calibrated to predict failure of induction of labor up to 75%, at which point the model overestimated the risk in patients, Dr. Rossi and associates said.
“Although we do not stipulate that an elective cesarean delivery should be offered for ‘high risk’ obese women, this tool may allow the provider to have a heightened awareness and prepare accordingly with timing of delivery, increased staffing, and anesthesia presence, particularly given the higher rates of maternal and neonatal adverse outcomes after a failed induction of labor,” said Dr. Rossi and colleagues.
Martina Louise Badell, MD, commented in an interview, “This is well-designed, large, population-based cohort study of more than 1 million obese women with a singleton pregnancy who underwent induction of labor. To determine the chance of successful induction of labor, a 10-variable model was created. This model achieved an AUC of 0.79, which is fairly good accuracy.
“They created an easy-to-use risk calculator as a tool to help identify chance of successful induction of labor in obese women. Similar to the VBAC [vaginal birth after cesarean] calculator, this calculator may help clinicians with patient-specific counseling, risk stratifying, and delivery planning,” said Dr. Badell, a maternal-fetal medicine specialist who is director of the Emory Perinatal Center at Emory University, Atlanta. Dr. Badell, who was not a coauthor of this study, was asked to comment on the study’s merit.
The authors reported no relevant financial disclosures. Dr. Badell had no relevant financial disclosures. There was no external funding.
SOURCE: Rossi R et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003377.
reported researchers from the University of Cincinnati and Cincinnati Children’s Hospital Medical Center.
The ten variables included in the model were prior vaginal delivery; prior cesarean delivery; maternal height, age, and weight at delivery; parity; gestational weight gain; Medicaid insurance; pregestational diabetes; and chronic hypertension, said Robert M. Rossi, MD, of the university and associates, who developed the model.
“Our hope is that this model may be useful as a tool to estimate an individualized risk based on commonly available prenatal factors that may assist in delivery planning and allocation of appropriate resources,” the investigators said in a study summarizing their findings, published in Obstetrics & Gynecology.
The researchers conducted a population-based, retrospective cohort study of delivery records from 1,098,981 obese women in a National Center for Health Statistics birth-death cohort database who underwent induction of labor between 2012 and 2016. Of these women, 825,797 (75%) women succeeded in delivering after induction, while 273,184 (25%) women failed to deliver after induction of labor and instead underwent cesarean section. The women included in the study had a body mass index of 30 or higher and underwent induction between 37 weeks and 44 weeks of gestation.
The class of obesity prior to pregnancy impacted the rate of induction failure, as patients with class I obesity had a rate of cesarean section of 21.6% (95% confidence interval, 21.4%-21.7%), while women with class II obesity had a rate of 25% (95% CI, 24.8%-25.2%) and women with class III obesity had a rate of 31% (95% CI, 30.8%-31.3%). Women also were more likely to fail induction if they had received fertility treatment, if they were older than 35 years, if they were of non-Hispanic black race, if they had gestational weight gain or maternal weight gain, if they had pregestational diabetes or gestational diabetes, or if they had gestational hypertension or preeclampsia (all P less than .001). Factors that made a woman less likely to undergo cesarean delivery were Medicaid insurance status or receiving Special Supplemental Nutrition Program for Women, Infant and Children (SNAP WIC) support.
Under the predictive model, the receiver operator characteristic curve (ROC) had an area under the curve (AUC) of 0.79 (95% CI, 0.78-0.79), and subsequent validation of the model using a different external U.S. birth cohort dataset showed an AUC of 0.77 (95% CI, 0.76-0.77). In both datasets, the model was calibrated to predict failure of induction of labor up to 75%, at which point the model overestimated the risk in patients, Dr. Rossi and associates said.
“Although we do not stipulate that an elective cesarean delivery should be offered for ‘high risk’ obese women, this tool may allow the provider to have a heightened awareness and prepare accordingly with timing of delivery, increased staffing, and anesthesia presence, particularly given the higher rates of maternal and neonatal adverse outcomes after a failed induction of labor,” said Dr. Rossi and colleagues.
Martina Louise Badell, MD, commented in an interview, “This is well-designed, large, population-based cohort study of more than 1 million obese women with a singleton pregnancy who underwent induction of labor. To determine the chance of successful induction of labor, a 10-variable model was created. This model achieved an AUC of 0.79, which is fairly good accuracy.
“They created an easy-to-use risk calculator as a tool to help identify chance of successful induction of labor in obese women. Similar to the VBAC [vaginal birth after cesarean] calculator, this calculator may help clinicians with patient-specific counseling, risk stratifying, and delivery planning,” said Dr. Badell, a maternal-fetal medicine specialist who is director of the Emory Perinatal Center at Emory University, Atlanta. Dr. Badell, who was not a coauthor of this study, was asked to comment on the study’s merit.
The authors reported no relevant financial disclosures. Dr. Badell had no relevant financial disclosures. There was no external funding.
SOURCE: Rossi R et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003377.
reported researchers from the University of Cincinnati and Cincinnati Children’s Hospital Medical Center.
The ten variables included in the model were prior vaginal delivery; prior cesarean delivery; maternal height, age, and weight at delivery; parity; gestational weight gain; Medicaid insurance; pregestational diabetes; and chronic hypertension, said Robert M. Rossi, MD, of the university and associates, who developed the model.
“Our hope is that this model may be useful as a tool to estimate an individualized risk based on commonly available prenatal factors that may assist in delivery planning and allocation of appropriate resources,” the investigators said in a study summarizing their findings, published in Obstetrics & Gynecology.
The researchers conducted a population-based, retrospective cohort study of delivery records from 1,098,981 obese women in a National Center for Health Statistics birth-death cohort database who underwent induction of labor between 2012 and 2016. Of these women, 825,797 (75%) women succeeded in delivering after induction, while 273,184 (25%) women failed to deliver after induction of labor and instead underwent cesarean section. The women included in the study had a body mass index of 30 or higher and underwent induction between 37 weeks and 44 weeks of gestation.
The class of obesity prior to pregnancy impacted the rate of induction failure, as patients with class I obesity had a rate of cesarean section of 21.6% (95% confidence interval, 21.4%-21.7%), while women with class II obesity had a rate of 25% (95% CI, 24.8%-25.2%) and women with class III obesity had a rate of 31% (95% CI, 30.8%-31.3%). Women also were more likely to fail induction if they had received fertility treatment, if they were older than 35 years, if they were of non-Hispanic black race, if they had gestational weight gain or maternal weight gain, if they had pregestational diabetes or gestational diabetes, or if they had gestational hypertension or preeclampsia (all P less than .001). Factors that made a woman less likely to undergo cesarean delivery were Medicaid insurance status or receiving Special Supplemental Nutrition Program for Women, Infant and Children (SNAP WIC) support.
Under the predictive model, the receiver operator characteristic curve (ROC) had an area under the curve (AUC) of 0.79 (95% CI, 0.78-0.79), and subsequent validation of the model using a different external U.S. birth cohort dataset showed an AUC of 0.77 (95% CI, 0.76-0.77). In both datasets, the model was calibrated to predict failure of induction of labor up to 75%, at which point the model overestimated the risk in patients, Dr. Rossi and associates said.
“Although we do not stipulate that an elective cesarean delivery should be offered for ‘high risk’ obese women, this tool may allow the provider to have a heightened awareness and prepare accordingly with timing of delivery, increased staffing, and anesthesia presence, particularly given the higher rates of maternal and neonatal adverse outcomes after a failed induction of labor,” said Dr. Rossi and colleagues.
Martina Louise Badell, MD, commented in an interview, “This is well-designed, large, population-based cohort study of more than 1 million obese women with a singleton pregnancy who underwent induction of labor. To determine the chance of successful induction of labor, a 10-variable model was created. This model achieved an AUC of 0.79, which is fairly good accuracy.
“They created an easy-to-use risk calculator as a tool to help identify chance of successful induction of labor in obese women. Similar to the VBAC [vaginal birth after cesarean] calculator, this calculator may help clinicians with patient-specific counseling, risk stratifying, and delivery planning,” said Dr. Badell, a maternal-fetal medicine specialist who is director of the Emory Perinatal Center at Emory University, Atlanta. Dr. Badell, who was not a coauthor of this study, was asked to comment on the study’s merit.
The authors reported no relevant financial disclosures. Dr. Badell had no relevant financial disclosures. There was no external funding.
SOURCE: Rossi R et al. Obstet Gynecol. 2019. doi: 10.1097/AOG.0000000000003377.
FROM OBSTETRICS & GYNECOLOGY
Endometriosis is linked to adverse pregnancy outcomes
a large study has found.
Leslie V. Farland, ScD, of the University of Arizona, Tucson, and coauthors reported their analysis of data from 196,722 pregnancies in 116,429 women aged 25-42 years enrolled in the Nurses Health Study II cohort in Obstetrics & Gynecology.
Among the women with eligible pregnancies, 4.5% had laparoscopically confirmed endometriosis. These women were found to have a 40% higher risk of spontaneous abortion than were women without endometriosis (19.3% vs. 12.3%) and a 46% higher risk of ectopic pregnancy (1.8% vs. 0.8%). The risk of ectopic pregnancy was even more pronounced in women without a history of infertility.
Researchers also saw a 16% higher risk of preterm birth in women with endometriosis (12% in women with endometriosis vs. 8.1% in women without endometriosis), and a 16% greater risk of low-birth-weight babies (5.6% in women with endometriosis vs. 3.6% in women without endometriosis).
There also was the suggestion of an increased risk of stillbirth, although the researchers said this finding should be interpreted with caution because of the small sample size.
Women with endometriosis also had a 35% greater risk of gestational diabetes than did women without endometriosis. This association was stronger in women younger than age 35 years, in women without a history of infertility, and in women undergoing their second or later pregnancy. Endometriosis also was associated with a 30% greater risk of hypertensive disorders of pregnancy, particularly in second or later pregnancies.
Dr. Farland and associates wrote that recent research on the relationship between endometriosis and pregnancy outcomes had yielded “mixed results.”
“For example, much of the research to date has been conducted among women attending infertility clinics, which may conflate the influence of advanced maternal age, fertility treatment, and infertility itself with endometriosis, given the known elevated risk of adverse pregnancy outcomes in this population,” they wrote.
They suggested that one possible mechanism for the association between endometriosis and adverse pregnancy outcomes was progesterone resistance, which was hypothesized to affect genes important for embryo implantation and therefore contribute to pregnancy loss. Another mechanism could be increased inflammation, which may increase the risk of preterm birth and abnormal placentation.
“Elucidating mechanisms of association and possible pathways for intervention or screening procedures will be critical to improve the health of women with endometriosis and their children,” they wrote.
Katrina Mark, MD, commented in an interview, “This study, which identifies an increased risk of adverse pregnancy outcomes in women with endometriosis, is an important step in improving reproductive success.
“Although some explanations for these findings were postulated by the researchers, the next step will be to study the underlying physiology that leads to these complications so that interventions can be offered to improve outcomes,” said Dr. Mark, who is an associate professor of obstetrics, gynecology & reproductive sciences at the University of Maryland School of Medicine. Dr. Mark, who is not a coauthor of the study, was asked to comment on the study’s merit.
The study was supported by grants from the National Institutes of Health. Daniela A. Carusi, MD, received funding from UpToDate; Andrew W. Horne, MB, ChB, PhD, declared European government grants funding and consultancies with the pharmaceutical sector unrelated to the present study; Jorge E. Chavarro, MD, and Stacey A. Missmer, ScD, declared institutional funding from the NIH, and Dr. Missmer also received institutional funding from other funding bodies, as well as consulting fees. Dr. Farland and the remaining coauthors had no relevant financial disclosures. Dr. Mark has no relevant financial disclosures.
SOURCE: Farland LV et al. Obstetr Gynecol. 2019. doi: 10.1097/AOG.0000000000003410.
a large study has found.
Leslie V. Farland, ScD, of the University of Arizona, Tucson, and coauthors reported their analysis of data from 196,722 pregnancies in 116,429 women aged 25-42 years enrolled in the Nurses Health Study II cohort in Obstetrics & Gynecology.
Among the women with eligible pregnancies, 4.5% had laparoscopically confirmed endometriosis. These women were found to have a 40% higher risk of spontaneous abortion than were women without endometriosis (19.3% vs. 12.3%) and a 46% higher risk of ectopic pregnancy (1.8% vs. 0.8%). The risk of ectopic pregnancy was even more pronounced in women without a history of infertility.
Researchers also saw a 16% higher risk of preterm birth in women with endometriosis (12% in women with endometriosis vs. 8.1% in women without endometriosis), and a 16% greater risk of low-birth-weight babies (5.6% in women with endometriosis vs. 3.6% in women without endometriosis).
There also was the suggestion of an increased risk of stillbirth, although the researchers said this finding should be interpreted with caution because of the small sample size.
Women with endometriosis also had a 35% greater risk of gestational diabetes than did women without endometriosis. This association was stronger in women younger than age 35 years, in women without a history of infertility, and in women undergoing their second or later pregnancy. Endometriosis also was associated with a 30% greater risk of hypertensive disorders of pregnancy, particularly in second or later pregnancies.
Dr. Farland and associates wrote that recent research on the relationship between endometriosis and pregnancy outcomes had yielded “mixed results.”
“For example, much of the research to date has been conducted among women attending infertility clinics, which may conflate the influence of advanced maternal age, fertility treatment, and infertility itself with endometriosis, given the known elevated risk of adverse pregnancy outcomes in this population,” they wrote.
They suggested that one possible mechanism for the association between endometriosis and adverse pregnancy outcomes was progesterone resistance, which was hypothesized to affect genes important for embryo implantation and therefore contribute to pregnancy loss. Another mechanism could be increased inflammation, which may increase the risk of preterm birth and abnormal placentation.
“Elucidating mechanisms of association and possible pathways for intervention or screening procedures will be critical to improve the health of women with endometriosis and their children,” they wrote.
Katrina Mark, MD, commented in an interview, “This study, which identifies an increased risk of adverse pregnancy outcomes in women with endometriosis, is an important step in improving reproductive success.
“Although some explanations for these findings were postulated by the researchers, the next step will be to study the underlying physiology that leads to these complications so that interventions can be offered to improve outcomes,” said Dr. Mark, who is an associate professor of obstetrics, gynecology & reproductive sciences at the University of Maryland School of Medicine. Dr. Mark, who is not a coauthor of the study, was asked to comment on the study’s merit.
The study was supported by grants from the National Institutes of Health. Daniela A. Carusi, MD, received funding from UpToDate; Andrew W. Horne, MB, ChB, PhD, declared European government grants funding and consultancies with the pharmaceutical sector unrelated to the present study; Jorge E. Chavarro, MD, and Stacey A. Missmer, ScD, declared institutional funding from the NIH, and Dr. Missmer also received institutional funding from other funding bodies, as well as consulting fees. Dr. Farland and the remaining coauthors had no relevant financial disclosures. Dr. Mark has no relevant financial disclosures.
SOURCE: Farland LV et al. Obstetr Gynecol. 2019. doi: 10.1097/AOG.0000000000003410.
a large study has found.
Leslie V. Farland, ScD, of the University of Arizona, Tucson, and coauthors reported their analysis of data from 196,722 pregnancies in 116,429 women aged 25-42 years enrolled in the Nurses Health Study II cohort in Obstetrics & Gynecology.
Among the women with eligible pregnancies, 4.5% had laparoscopically confirmed endometriosis. These women were found to have a 40% higher risk of spontaneous abortion than were women without endometriosis (19.3% vs. 12.3%) and a 46% higher risk of ectopic pregnancy (1.8% vs. 0.8%). The risk of ectopic pregnancy was even more pronounced in women without a history of infertility.
Researchers also saw a 16% higher risk of preterm birth in women with endometriosis (12% in women with endometriosis vs. 8.1% in women without endometriosis), and a 16% greater risk of low-birth-weight babies (5.6% in women with endometriosis vs. 3.6% in women without endometriosis).
There also was the suggestion of an increased risk of stillbirth, although the researchers said this finding should be interpreted with caution because of the small sample size.
Women with endometriosis also had a 35% greater risk of gestational diabetes than did women without endometriosis. This association was stronger in women younger than age 35 years, in women without a history of infertility, and in women undergoing their second or later pregnancy. Endometriosis also was associated with a 30% greater risk of hypertensive disorders of pregnancy, particularly in second or later pregnancies.
Dr. Farland and associates wrote that recent research on the relationship between endometriosis and pregnancy outcomes had yielded “mixed results.”
“For example, much of the research to date has been conducted among women attending infertility clinics, which may conflate the influence of advanced maternal age, fertility treatment, and infertility itself with endometriosis, given the known elevated risk of adverse pregnancy outcomes in this population,” they wrote.
They suggested that one possible mechanism for the association between endometriosis and adverse pregnancy outcomes was progesterone resistance, which was hypothesized to affect genes important for embryo implantation and therefore contribute to pregnancy loss. Another mechanism could be increased inflammation, which may increase the risk of preterm birth and abnormal placentation.
“Elucidating mechanisms of association and possible pathways for intervention or screening procedures will be critical to improve the health of women with endometriosis and their children,” they wrote.
Katrina Mark, MD, commented in an interview, “This study, which identifies an increased risk of adverse pregnancy outcomes in women with endometriosis, is an important step in improving reproductive success.
“Although some explanations for these findings were postulated by the researchers, the next step will be to study the underlying physiology that leads to these complications so that interventions can be offered to improve outcomes,” said Dr. Mark, who is an associate professor of obstetrics, gynecology & reproductive sciences at the University of Maryland School of Medicine. Dr. Mark, who is not a coauthor of the study, was asked to comment on the study’s merit.
The study was supported by grants from the National Institutes of Health. Daniela A. Carusi, MD, received funding from UpToDate; Andrew W. Horne, MB, ChB, PhD, declared European government grants funding and consultancies with the pharmaceutical sector unrelated to the present study; Jorge E. Chavarro, MD, and Stacey A. Missmer, ScD, declared institutional funding from the NIH, and Dr. Missmer also received institutional funding from other funding bodies, as well as consulting fees. Dr. Farland and the remaining coauthors had no relevant financial disclosures. Dr. Mark has no relevant financial disclosures.
SOURCE: Farland LV et al. Obstetr Gynecol. 2019. doi: 10.1097/AOG.0000000000003410.
FROM OBSTETRICS & GYNECOLOGY
Poll: Reduce number of prenatal care visits?
[polldaddy:10359495]
[polldaddy:10359495]
[polldaddy:10359495]
Fluoride exposure during pregnancy tied to lower IQ score in children
with boys having a lower mean score than girls, according to a recent prospective, multicenter birth cohort study.
“These findings were observed at fluoride levels typically found in white North American women,” wrote Rivka Green, York University, Toronto, and colleagues. “This indicates the possible need to reduce fluoride intake during pregnancy.”
This study confirms findings in a 2017 study suggesting a relationship between maternal fluoride levels and children’s later cognitive scores.
Ms. Green and colleagues evaluated 512 mother-child pairs in the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort from six Canadian cities. The children were born between 2008 and 2012, underwent neurodevelopmental testing between 3 and 4 years, and were assessed using the Wechsler Preschool and Primary Scale of Intelligence, Third Edition. Full Scale IQ (FSIQ) test.
Of these, 400 mother-child pairs had data on fluoride intake, IQ, and complete covariate data; 141 of these mothers lived in areas with fluoridated tap water, while 228 mothers lived in areas without fluoridated tap water. Maternal urinary fluoride adjusted for specific gravity (MUFSG) was averaged across three trimesters of data, and the estimated fluoride level was obtained through self-reported exposure by women included in the study.
The researchers found mothers living in areas with fluoridated water had significantly higher MUFSG levels (0.69 mg/L), compared with women in areas without fluoridated water (0.40 mg/L; P equals .001). The median estimated fluoride intake was significantly higher among women living in areas with fluoridated water (0.93 mg per day) than in women who did not live in areas with fluoridated water (0.30 mg per day; P less than .001).
Overall, children scored a mean 107.16 (range, 52-143) on the IQ test, and girls had significantly higher mean IQ scores than did boys (109.56 vs. 104.61; P = .001). After adjusting for covariates of maternal age, race, parity, smoking, and alcohol status during pregnancy, child gender, gestational age, and birth weight, the researchers found a significant interaction between MUFSG and the child’s gender (P = .02), and a 1-mg/L MUFSG increase was associated with a decrease in 4.49 IQ points in boys (95% confidence interval, −8.38 to −0.60) but not girls. There also was an association between 1-mg higher daily intake of maternal fluoride intake and decreased IQ score in both boys and girls (−3.66; 95% CI, −7.16 to −0.15 ; P = .04).
Ms. Green and her colleagues acknowledged several limitations with the study, such as the short half-life of urinary fluoride and the potential inaccuracy of maternal urinary samples at predicting fetal exposure to fluoride, the self-reported nature of estimated fluoride consumption, lack of availability of maternal IQ data, and not including postnatal exposure and consumption of fluoride.
In a related editorial, David C. Bellinger, PhD, MSc, referred to a previous prospective study in Mexico City by Bashash et al. that found a maternal fluoride level of 0.9 mg/L was associated with a decrease in cognitive scores in children at 4 years and between 6 years and 12 years (Environ Health Perspect. 2017;125(9):097017. doi: 10.1289/EHP655), and noted the effect sizes seen in the Mexico City study were similar to those reported by Green et al. “If the effect sizes reported by Green et al. and others are valid, the total cognitive loss at the population level that might be associated with children’s prenatal exposure to fluoride could be substantial,” he said.
The study raises many questions, including whether there is a concentration where neurotoxicity risk is negligible, if gender plays a role (there was no gender risk difference in Bashash et al.), whether other developmental domains are affected apart from IQ, and if postnatal exposure carries a risk, Dr. Bellinger said. “The findings of Green et al. and others indicate that a dispassionate and tempered discussion of fluoride’s potential neurotoxicity is warranted, including consideration of what additional research is needed to reach more definitive conclusions about the implications, if any, for public health,” he said.
Dimitri A. Christakis, MD, MPH, editor of JAMA Pediatrics and director of the Center for Child Health, Behavior, and Development at Seattle Children’s Research Institute, said in an editor’s note that it was not an easy decision to publish the article because of the potential implications of the findings.
“The mission of the journal is to ensure that child health is optimized by bringing the best available evidence to the fore,” he said. “Publishing it serves as testament to the fact that JAMA Pediatrics is committed to disseminating the best science based entirely on the rigor of the methods and the soundness of the hypotheses tested, regardless of how contentious the results may be.”
However, “scientific inquiry is an iterative process,” Dr. Christakis said, and rarely does a single study provide “definitive evidence.
“We hope that purveyors and consumers of these findings are mindful of that as the implications of this study are debated in the public arena.”
This study was funded in a grant from the National Institute of Environmental Health Science, and the MIREC Study was funded by Chemicals Management Plan at Health Canada, the Ontario Ministry of the Environment, and the Canadian Institutes for Health Research. Dr. Bruce Lanphear reported being an unpaid expert witness for an upcoming case involving the U.S. Environmental Protection Agency and water fluoridation. Dr. Richard Hornung reported receiving personal fees from York University. Dr. E. Angeles Martinez-Mier reported receiving grants from the National Institutes of Health. The other authors report no relevant conflicts of interest. Dr. Bellinger reported no relevant conflicts of interest with regard to his editorial.
SOURCEs: Green R et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2019.1729; Bellinger. JAMA Pediatr. 2019. doi: 10.1001/ jamapediatrics.2019.1728.
with boys having a lower mean score than girls, according to a recent prospective, multicenter birth cohort study.
“These findings were observed at fluoride levels typically found in white North American women,” wrote Rivka Green, York University, Toronto, and colleagues. “This indicates the possible need to reduce fluoride intake during pregnancy.”
This study confirms findings in a 2017 study suggesting a relationship between maternal fluoride levels and children’s later cognitive scores.
Ms. Green and colleagues evaluated 512 mother-child pairs in the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort from six Canadian cities. The children were born between 2008 and 2012, underwent neurodevelopmental testing between 3 and 4 years, and were assessed using the Wechsler Preschool and Primary Scale of Intelligence, Third Edition. Full Scale IQ (FSIQ) test.
Of these, 400 mother-child pairs had data on fluoride intake, IQ, and complete covariate data; 141 of these mothers lived in areas with fluoridated tap water, while 228 mothers lived in areas without fluoridated tap water. Maternal urinary fluoride adjusted for specific gravity (MUFSG) was averaged across three trimesters of data, and the estimated fluoride level was obtained through self-reported exposure by women included in the study.
The researchers found mothers living in areas with fluoridated water had significantly higher MUFSG levels (0.69 mg/L), compared with women in areas without fluoridated water (0.40 mg/L; P equals .001). The median estimated fluoride intake was significantly higher among women living in areas with fluoridated water (0.93 mg per day) than in women who did not live in areas with fluoridated water (0.30 mg per day; P less than .001).
Overall, children scored a mean 107.16 (range, 52-143) on the IQ test, and girls had significantly higher mean IQ scores than did boys (109.56 vs. 104.61; P = .001). After adjusting for covariates of maternal age, race, parity, smoking, and alcohol status during pregnancy, child gender, gestational age, and birth weight, the researchers found a significant interaction between MUFSG and the child’s gender (P = .02), and a 1-mg/L MUFSG increase was associated with a decrease in 4.49 IQ points in boys (95% confidence interval, −8.38 to −0.60) but not girls. There also was an association between 1-mg higher daily intake of maternal fluoride intake and decreased IQ score in both boys and girls (−3.66; 95% CI, −7.16 to −0.15 ; P = .04).
Ms. Green and her colleagues acknowledged several limitations with the study, such as the short half-life of urinary fluoride and the potential inaccuracy of maternal urinary samples at predicting fetal exposure to fluoride, the self-reported nature of estimated fluoride consumption, lack of availability of maternal IQ data, and not including postnatal exposure and consumption of fluoride.
In a related editorial, David C. Bellinger, PhD, MSc, referred to a previous prospective study in Mexico City by Bashash et al. that found a maternal fluoride level of 0.9 mg/L was associated with a decrease in cognitive scores in children at 4 years and between 6 years and 12 years (Environ Health Perspect. 2017;125(9):097017. doi: 10.1289/EHP655), and noted the effect sizes seen in the Mexico City study were similar to those reported by Green et al. “If the effect sizes reported by Green et al. and others are valid, the total cognitive loss at the population level that might be associated with children’s prenatal exposure to fluoride could be substantial,” he said.
The study raises many questions, including whether there is a concentration where neurotoxicity risk is negligible, if gender plays a role (there was no gender risk difference in Bashash et al.), whether other developmental domains are affected apart from IQ, and if postnatal exposure carries a risk, Dr. Bellinger said. “The findings of Green et al. and others indicate that a dispassionate and tempered discussion of fluoride’s potential neurotoxicity is warranted, including consideration of what additional research is needed to reach more definitive conclusions about the implications, if any, for public health,” he said.
Dimitri A. Christakis, MD, MPH, editor of JAMA Pediatrics and director of the Center for Child Health, Behavior, and Development at Seattle Children’s Research Institute, said in an editor’s note that it was not an easy decision to publish the article because of the potential implications of the findings.
“The mission of the journal is to ensure that child health is optimized by bringing the best available evidence to the fore,” he said. “Publishing it serves as testament to the fact that JAMA Pediatrics is committed to disseminating the best science based entirely on the rigor of the methods and the soundness of the hypotheses tested, regardless of how contentious the results may be.”
However, “scientific inquiry is an iterative process,” Dr. Christakis said, and rarely does a single study provide “definitive evidence.
“We hope that purveyors and consumers of these findings are mindful of that as the implications of this study are debated in the public arena.”
This study was funded in a grant from the National Institute of Environmental Health Science, and the MIREC Study was funded by Chemicals Management Plan at Health Canada, the Ontario Ministry of the Environment, and the Canadian Institutes for Health Research. Dr. Bruce Lanphear reported being an unpaid expert witness for an upcoming case involving the U.S. Environmental Protection Agency and water fluoridation. Dr. Richard Hornung reported receiving personal fees from York University. Dr. E. Angeles Martinez-Mier reported receiving grants from the National Institutes of Health. The other authors report no relevant conflicts of interest. Dr. Bellinger reported no relevant conflicts of interest with regard to his editorial.
SOURCEs: Green R et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2019.1729; Bellinger. JAMA Pediatr. 2019. doi: 10.1001/ jamapediatrics.2019.1728.
with boys having a lower mean score than girls, according to a recent prospective, multicenter birth cohort study.
“These findings were observed at fluoride levels typically found in white North American women,” wrote Rivka Green, York University, Toronto, and colleagues. “This indicates the possible need to reduce fluoride intake during pregnancy.”
This study confirms findings in a 2017 study suggesting a relationship between maternal fluoride levels and children’s later cognitive scores.
Ms. Green and colleagues evaluated 512 mother-child pairs in the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort from six Canadian cities. The children were born between 2008 and 2012, underwent neurodevelopmental testing between 3 and 4 years, and were assessed using the Wechsler Preschool and Primary Scale of Intelligence, Third Edition. Full Scale IQ (FSIQ) test.
Of these, 400 mother-child pairs had data on fluoride intake, IQ, and complete covariate data; 141 of these mothers lived in areas with fluoridated tap water, while 228 mothers lived in areas without fluoridated tap water. Maternal urinary fluoride adjusted for specific gravity (MUFSG) was averaged across three trimesters of data, and the estimated fluoride level was obtained through self-reported exposure by women included in the study.
The researchers found mothers living in areas with fluoridated water had significantly higher MUFSG levels (0.69 mg/L), compared with women in areas without fluoridated water (0.40 mg/L; P equals .001). The median estimated fluoride intake was significantly higher among women living in areas with fluoridated water (0.93 mg per day) than in women who did not live in areas with fluoridated water (0.30 mg per day; P less than .001).
Overall, children scored a mean 107.16 (range, 52-143) on the IQ test, and girls had significantly higher mean IQ scores than did boys (109.56 vs. 104.61; P = .001). After adjusting for covariates of maternal age, race, parity, smoking, and alcohol status during pregnancy, child gender, gestational age, and birth weight, the researchers found a significant interaction between MUFSG and the child’s gender (P = .02), and a 1-mg/L MUFSG increase was associated with a decrease in 4.49 IQ points in boys (95% confidence interval, −8.38 to −0.60) but not girls. There also was an association between 1-mg higher daily intake of maternal fluoride intake and decreased IQ score in both boys and girls (−3.66; 95% CI, −7.16 to −0.15 ; P = .04).
Ms. Green and her colleagues acknowledged several limitations with the study, such as the short half-life of urinary fluoride and the potential inaccuracy of maternal urinary samples at predicting fetal exposure to fluoride, the self-reported nature of estimated fluoride consumption, lack of availability of maternal IQ data, and not including postnatal exposure and consumption of fluoride.
In a related editorial, David C. Bellinger, PhD, MSc, referred to a previous prospective study in Mexico City by Bashash et al. that found a maternal fluoride level of 0.9 mg/L was associated with a decrease in cognitive scores in children at 4 years and between 6 years and 12 years (Environ Health Perspect. 2017;125(9):097017. doi: 10.1289/EHP655), and noted the effect sizes seen in the Mexico City study were similar to those reported by Green et al. “If the effect sizes reported by Green et al. and others are valid, the total cognitive loss at the population level that might be associated with children’s prenatal exposure to fluoride could be substantial,” he said.
The study raises many questions, including whether there is a concentration where neurotoxicity risk is negligible, if gender plays a role (there was no gender risk difference in Bashash et al.), whether other developmental domains are affected apart from IQ, and if postnatal exposure carries a risk, Dr. Bellinger said. “The findings of Green et al. and others indicate that a dispassionate and tempered discussion of fluoride’s potential neurotoxicity is warranted, including consideration of what additional research is needed to reach more definitive conclusions about the implications, if any, for public health,” he said.
Dimitri A. Christakis, MD, MPH, editor of JAMA Pediatrics and director of the Center for Child Health, Behavior, and Development at Seattle Children’s Research Institute, said in an editor’s note that it was not an easy decision to publish the article because of the potential implications of the findings.
“The mission of the journal is to ensure that child health is optimized by bringing the best available evidence to the fore,” he said. “Publishing it serves as testament to the fact that JAMA Pediatrics is committed to disseminating the best science based entirely on the rigor of the methods and the soundness of the hypotheses tested, regardless of how contentious the results may be.”
However, “scientific inquiry is an iterative process,” Dr. Christakis said, and rarely does a single study provide “definitive evidence.
“We hope that purveyors and consumers of these findings are mindful of that as the implications of this study are debated in the public arena.”
This study was funded in a grant from the National Institute of Environmental Health Science, and the MIREC Study was funded by Chemicals Management Plan at Health Canada, the Ontario Ministry of the Environment, and the Canadian Institutes for Health Research. Dr. Bruce Lanphear reported being an unpaid expert witness for an upcoming case involving the U.S. Environmental Protection Agency and water fluoridation. Dr. Richard Hornung reported receiving personal fees from York University. Dr. E. Angeles Martinez-Mier reported receiving grants from the National Institutes of Health. The other authors report no relevant conflicts of interest. Dr. Bellinger reported no relevant conflicts of interest with regard to his editorial.
SOURCEs: Green R et al. JAMA Pediatr. 2019. doi: 10.1001/jamapediatrics.2019.1729; Bellinger. JAMA Pediatr. 2019. doi: 10.1001/ jamapediatrics.2019.1728.
FROM JAMA PEDIATRICS
Safety of ondansetron for nausea and vomiting of pregnancy
Nausea and vomiting of pregnancy (NVP) affects up to 80% of pregnant women, most commonly between 5 and 18 weeks of gestation. In addition, its extreme form, hyperemesis gravidarum, affects less than 3% of pregnancies.1 Certainly with hyperemesis gravidarum, and oftentimes with less severe NVP, pharmacologic treatment is desired or required. One of the choices for such treatment has been ondansetron, a 5-HT3 receptor antagonist, which has been used off label for NVP and is now available in generic form. However, there have been concerns raised regarding the fetal safety of this medication, last reviewed in Ob.Gyn. News by Gideon Koren, MD, in a commentary published in 2013.
Since then, the escalating use of ondansetron in the United States has been described using a large dataset covering 2.3 million, predominantly commercially insured, pregnancies that resulted in live births from 2001 to 2015.1 Over that period of time, any outpatient pharmacy dispensing of an antiemetic in pregnancy increased from 17.0% in 2001 to 27.2% in 2014. That increase was entirely accounted for by a dramatic rise in oral ondansetron use beginning in 2006. By 2014, 22.4% of pregnancies in the database had received a prescription for ondansetron.
There have been two studies that have suggested an increased risk in specific major birth defects with first-trimester ondansetron use. The first, published in 2012, used data from the National Birth Defects Prevention case control study from 1997 to 2004 to examine risks with NVP and its treatments for the most common noncardiac defects in the dataset. These included cleft lip with or without cleft palate, cleft palate alone, neural tube defects, and hypospadias. NVP itself was not associated with any increased risks for the selected defects. In contrast, ondansetron was associated with an increased risk for cleft palate alone based on seven exposed cases (adjusted odds ratio, 2.37; 95% confidence interval, 1.18-4.76).2
A second study published in 2014 used data from the Swedish Medical Birth Register from 1998 to 2012 to identify 1,349 infants whose mothers reported taking ondansetron in early pregnancy. While no overall increased risk of major birth defects was found with early pregnancy ondansetron use, compared with no such use, there was a significant increased risk noted for cardiovascular defects, particularly cardiac septum defects (any cardiac defect OR, 1.62; 95% CI, 1.04-2.14; cardiac septum defects risk ratio, 2.05; 95% CI, 1.19-3.28).3 No cases of cleft palate were reported among exposed cases in that study.
In contrast, in another study, Danish National Birth Cohort data on 608,385 pregnancies from 2004 to 2011 were used to compare major birth defect outcomes among 1,233 women exposed to ondansetron in the first trimester with those of 4,392 unexposed women.4 The birth prevalence of any major birth defect was identical (2.9%) in both exposed and unexposed groups (adjusted prevalence OR, 1.12; 95% CI, 0.69-1.82). No cases of cleft palate were reported among exposed cases and the crude OR for any cardiac defect approximated the null (1.04; 95% CI, 0.52-1.95). Two other smaller or less well-designed studies did not support an increased risk for major birth defects overall (Fejzo et al. 2016 Jul;62:87-91; Einarson et al. 2004Aug 23. doi: 10.1111/j.1471-0528.2004.00236.x).
To date, although the data are conflicting, they are consistent with either a small increased risk for selected cardiac defects and perhaps cleft palate, or no increased risk at all. However, with recent data indicating that nearly one-quarter of insured pregnant women in the United States have been prescribed ondansetron in early pregnancy, there is an urgency to conduct additional rigorous studies of sufficient sample size to determine on balance if there is a small individual increased risk associated with this treatment that translates to a larger public health problem.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no conflicts of interest to disclose related to this column.
References:
1. Taylor LG et al. Antiemetic use among pregnant women in the United States: the escalating use of ondansetron. Pharmacoepidemiol Drug Saf. 2017 May;26(5):592-6.
2. Anderka M et al. Medications used to treat nausea and vomiting of pregnancy and the risk of selected birth defects. Birth Defects Res A Clin Mol Teratol. 2012 Jan;94(1):22-30.
3. Danielsson B et al. Use of ondansetron during pregnancy and congenital malformations in the infant. Reprod Toxicol. 2014 Dec;50:134-7.
4. Pasternak B et al. Ondansetron in pregnancy and risk of adverse fetal outcomes. N Engl J Med. 2013 Feb 28;368(9):814-23.
Nausea and vomiting of pregnancy (NVP) affects up to 80% of pregnant women, most commonly between 5 and 18 weeks of gestation. In addition, its extreme form, hyperemesis gravidarum, affects less than 3% of pregnancies.1 Certainly with hyperemesis gravidarum, and oftentimes with less severe NVP, pharmacologic treatment is desired or required. One of the choices for such treatment has been ondansetron, a 5-HT3 receptor antagonist, which has been used off label for NVP and is now available in generic form. However, there have been concerns raised regarding the fetal safety of this medication, last reviewed in Ob.Gyn. News by Gideon Koren, MD, in a commentary published in 2013.
Since then, the escalating use of ondansetron in the United States has been described using a large dataset covering 2.3 million, predominantly commercially insured, pregnancies that resulted in live births from 2001 to 2015.1 Over that period of time, any outpatient pharmacy dispensing of an antiemetic in pregnancy increased from 17.0% in 2001 to 27.2% in 2014. That increase was entirely accounted for by a dramatic rise in oral ondansetron use beginning in 2006. By 2014, 22.4% of pregnancies in the database had received a prescription for ondansetron.
There have been two studies that have suggested an increased risk in specific major birth defects with first-trimester ondansetron use. The first, published in 2012, used data from the National Birth Defects Prevention case control study from 1997 to 2004 to examine risks with NVP and its treatments for the most common noncardiac defects in the dataset. These included cleft lip with or without cleft palate, cleft palate alone, neural tube defects, and hypospadias. NVP itself was not associated with any increased risks for the selected defects. In contrast, ondansetron was associated with an increased risk for cleft palate alone based on seven exposed cases (adjusted odds ratio, 2.37; 95% confidence interval, 1.18-4.76).2
A second study published in 2014 used data from the Swedish Medical Birth Register from 1998 to 2012 to identify 1,349 infants whose mothers reported taking ondansetron in early pregnancy. While no overall increased risk of major birth defects was found with early pregnancy ondansetron use, compared with no such use, there was a significant increased risk noted for cardiovascular defects, particularly cardiac septum defects (any cardiac defect OR, 1.62; 95% CI, 1.04-2.14; cardiac septum defects risk ratio, 2.05; 95% CI, 1.19-3.28).3 No cases of cleft palate were reported among exposed cases in that study.
In contrast, in another study, Danish National Birth Cohort data on 608,385 pregnancies from 2004 to 2011 were used to compare major birth defect outcomes among 1,233 women exposed to ondansetron in the first trimester with those of 4,392 unexposed women.4 The birth prevalence of any major birth defect was identical (2.9%) in both exposed and unexposed groups (adjusted prevalence OR, 1.12; 95% CI, 0.69-1.82). No cases of cleft palate were reported among exposed cases and the crude OR for any cardiac defect approximated the null (1.04; 95% CI, 0.52-1.95). Two other smaller or less well-designed studies did not support an increased risk for major birth defects overall (Fejzo et al. 2016 Jul;62:87-91; Einarson et al. 2004Aug 23. doi: 10.1111/j.1471-0528.2004.00236.x).
To date, although the data are conflicting, they are consistent with either a small increased risk for selected cardiac defects and perhaps cleft palate, or no increased risk at all. However, with recent data indicating that nearly one-quarter of insured pregnant women in the United States have been prescribed ondansetron in early pregnancy, there is an urgency to conduct additional rigorous studies of sufficient sample size to determine on balance if there is a small individual increased risk associated with this treatment that translates to a larger public health problem.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no conflicts of interest to disclose related to this column.
References:
1. Taylor LG et al. Antiemetic use among pregnant women in the United States: the escalating use of ondansetron. Pharmacoepidemiol Drug Saf. 2017 May;26(5):592-6.
2. Anderka M et al. Medications used to treat nausea and vomiting of pregnancy and the risk of selected birth defects. Birth Defects Res A Clin Mol Teratol. 2012 Jan;94(1):22-30.
3. Danielsson B et al. Use of ondansetron during pregnancy and congenital malformations in the infant. Reprod Toxicol. 2014 Dec;50:134-7.
4. Pasternak B et al. Ondansetron in pregnancy and risk of adverse fetal outcomes. N Engl J Med. 2013 Feb 28;368(9):814-23.
Nausea and vomiting of pregnancy (NVP) affects up to 80% of pregnant women, most commonly between 5 and 18 weeks of gestation. In addition, its extreme form, hyperemesis gravidarum, affects less than 3% of pregnancies.1 Certainly with hyperemesis gravidarum, and oftentimes with less severe NVP, pharmacologic treatment is desired or required. One of the choices for such treatment has been ondansetron, a 5-HT3 receptor antagonist, which has been used off label for NVP and is now available in generic form. However, there have been concerns raised regarding the fetal safety of this medication, last reviewed in Ob.Gyn. News by Gideon Koren, MD, in a commentary published in 2013.
Since then, the escalating use of ondansetron in the United States has been described using a large dataset covering 2.3 million, predominantly commercially insured, pregnancies that resulted in live births from 2001 to 2015.1 Over that period of time, any outpatient pharmacy dispensing of an antiemetic in pregnancy increased from 17.0% in 2001 to 27.2% in 2014. That increase was entirely accounted for by a dramatic rise in oral ondansetron use beginning in 2006. By 2014, 22.4% of pregnancies in the database had received a prescription for ondansetron.
There have been two studies that have suggested an increased risk in specific major birth defects with first-trimester ondansetron use. The first, published in 2012, used data from the National Birth Defects Prevention case control study from 1997 to 2004 to examine risks with NVP and its treatments for the most common noncardiac defects in the dataset. These included cleft lip with or without cleft palate, cleft palate alone, neural tube defects, and hypospadias. NVP itself was not associated with any increased risks for the selected defects. In contrast, ondansetron was associated with an increased risk for cleft palate alone based on seven exposed cases (adjusted odds ratio, 2.37; 95% confidence interval, 1.18-4.76).2
A second study published in 2014 used data from the Swedish Medical Birth Register from 1998 to 2012 to identify 1,349 infants whose mothers reported taking ondansetron in early pregnancy. While no overall increased risk of major birth defects was found with early pregnancy ondansetron use, compared with no such use, there was a significant increased risk noted for cardiovascular defects, particularly cardiac septum defects (any cardiac defect OR, 1.62; 95% CI, 1.04-2.14; cardiac septum defects risk ratio, 2.05; 95% CI, 1.19-3.28).3 No cases of cleft palate were reported among exposed cases in that study.
In contrast, in another study, Danish National Birth Cohort data on 608,385 pregnancies from 2004 to 2011 were used to compare major birth defect outcomes among 1,233 women exposed to ondansetron in the first trimester with those of 4,392 unexposed women.4 The birth prevalence of any major birth defect was identical (2.9%) in both exposed and unexposed groups (adjusted prevalence OR, 1.12; 95% CI, 0.69-1.82). No cases of cleft palate were reported among exposed cases and the crude OR for any cardiac defect approximated the null (1.04; 95% CI, 0.52-1.95). Two other smaller or less well-designed studies did not support an increased risk for major birth defects overall (Fejzo et al. 2016 Jul;62:87-91; Einarson et al. 2004Aug 23. doi: 10.1111/j.1471-0528.2004.00236.x).
To date, although the data are conflicting, they are consistent with either a small increased risk for selected cardiac defects and perhaps cleft palate, or no increased risk at all. However, with recent data indicating that nearly one-quarter of insured pregnant women in the United States have been prescribed ondansetron in early pregnancy, there is an urgency to conduct additional rigorous studies of sufficient sample size to determine on balance if there is a small individual increased risk associated with this treatment that translates to a larger public health problem.
Dr. Chambers is professor of pediatrics and director of clinical research at Rady Children’s Hospital and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is also director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no conflicts of interest to disclose related to this column.
References:
1. Taylor LG et al. Antiemetic use among pregnant women in the United States: the escalating use of ondansetron. Pharmacoepidemiol Drug Saf. 2017 May;26(5):592-6.
2. Anderka M et al. Medications used to treat nausea and vomiting of pregnancy and the risk of selected birth defects. Birth Defects Res A Clin Mol Teratol. 2012 Jan;94(1):22-30.
3. Danielsson B et al. Use of ondansetron during pregnancy and congenital malformations in the infant. Reprod Toxicol. 2014 Dec;50:134-7.
4. Pasternak B et al. Ondansetron in pregnancy and risk of adverse fetal outcomes. N Engl J Med. 2013 Feb 28;368(9):814-23.
Product Update: Osphena’s NDA, new hysteroscope, TempSure RF technology, Resilient stirrup covers
OSPHENA HAS NEW INDICATION
FOR MORE INFORMATION, VISIT: https://www.osphena.com/.
NEW 3-IN-1 HYSTEROSCOPE
FOR MORE INFORMATION, VISIT: https://gynsurgicalsolutions.com/product/omni-hysteroscope/.
SURGICAL RF TECHNOLOGY
FOR MORE INFORMATION, VISIT: https://www.cynosure.com/tempsure-platform.
PROFESSIONAL FOOT SUPPORTS
FOR MORE INFORMATION, VISIT: https://www.comenitymed.com.
OSPHENA HAS NEW INDICATION
FOR MORE INFORMATION, VISIT: https://www.osphena.com/.
NEW 3-IN-1 HYSTEROSCOPE
FOR MORE INFORMATION, VISIT: https://gynsurgicalsolutions.com/product/omni-hysteroscope/.
SURGICAL RF TECHNOLOGY
FOR MORE INFORMATION, VISIT: https://www.cynosure.com/tempsure-platform.
PROFESSIONAL FOOT SUPPORTS
FOR MORE INFORMATION, VISIT: https://www.comenitymed.com.
OSPHENA HAS NEW INDICATION
FOR MORE INFORMATION, VISIT: https://www.osphena.com/.
NEW 3-IN-1 HYSTEROSCOPE
FOR MORE INFORMATION, VISIT: https://gynsurgicalsolutions.com/product/omni-hysteroscope/.
SURGICAL RF TECHNOLOGY
FOR MORE INFORMATION, VISIT: https://www.cynosure.com/tempsure-platform.
PROFESSIONAL FOOT SUPPORTS
FOR MORE INFORMATION, VISIT: https://www.comenitymed.com.
Which birth defects are associated with childhood cancer risk?