User login
Early pregnancy loss and abortion: Medical management is safe, effective
NASHVILLE, TENN. – Medical management of abortion and early pregnancy loss is best achieved with both mifepristone and misoprostol, according to Sarah W. Prager, MD.
First-trimester procedures account for about 90% of elective abortions, with about two-thirds of those occurring before 8 weeks of gestation and 80% occurring in the first 10 weeks – and therefore considered eligible for medical management, Dr. Prager, director of the Family Planning Division and Family Planning Fellowship at the University of Washington, Seattle, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“We estimate that it’s approximately 31% of all abortions that are done using medication, but it’s about 45% of those eligible by gestational age,” she noted.
The alternative is uterine aspiration, and in the absence of a clear contraindication, patient preference should determine management choice, she said.
The same is true for early pregnancy loss (spontaneous abortion), which is the most common complication of early pregnancy, occurring in about 20% of clinically recognized pregnancies.
“That means that there are about 1 million spontaneous abortions happening annually in the United States, and about 80% of those are in the first trimester,” Dr. Prager said.
Expectant management is an additional option for managing early pregnancy loss, she noted.
Candidates
Medical management is appropriate for patients who are undergoing elective abortion at up to about 70 days of gestation or with pregnancy loss in the first trimester.
“They should have stable vital signs, no evidence of infection, no allergies to the medications being used, no serious social or medical problems,” Dr. Prager said, explaining that “a shared decision making process” is important for patients with extreme anxiety or homelessness/lack of stable housing, for example, in order to make sure that medical management is a good option.
“While she definitely gets to have the final say, unless there is a real medical contraindication, it definitely should be part of that decision making,” Dr. Prager said, adding that adequate counseling and acceptance by the patient of the risks and side effects also are imperative.
Protocol
The most effective evidence-based treatment protocol for elective abortion through day 70 of gestation includes a 200-mg oral dose of mifepristone, followed 24-72 hours later with at-home buccal or vaginal administration of an 800-mcg dose of misoprostol, with follow up within 1-2 weeks, Dr. Prager said, citing a 2010 Cochrane review.
The Food and Drug Administration–approved protocol, which was updated in April 2016, adheres closely to those findings, except that it calls for misoprostol within 48 hours of mifepristone dosing. Optional repeat dosing of misoprostol is allowed, as well, she noted.
Buccal or vaginal administration of misoprostol is preferable to oral and sublingual administration because while the latter approaches provide more rapid onset, the former approaches provide significantly better sustained action over a 5-hour period of time.
“And by not having that big peak at the beginning, it actually decreases the side effects that women experience with the misoprostol medication,” she said.
Misoprostol can also be given alone for early pregnancy loss management – also at a dose of 800 mcg buccally or vaginally – with repeat dosing at 12-24 hours for incomplete abortion. However, new data suggest that, before about 63 days of gestation, giving two doses 3 hours apart is slightly more effective. That approach can also be repeated if necessary, Dr. Prager said.
Pain management is an important part of treatment, as both miscarriage and medication abortion can range from uncomfortable to extremely painful, depending on the patient, her prior obstetric experience, and her life experiences.
“I recommend talking to all your patients about pain management. For most people, just using some type of NSAID is probably going to be sufficient,” she said, noting that some women will require a narcotic.
Antiemetic medication may also be necessary, as some women will experience nausea and vomiting.
Complications and intervention
Major complications are rare with medical management of first-trimester abortion and early pregnancy loss, but can include ongoing pregnancy, which is infrequent but possible; incomplete abortion, which is easily managed; and allergic reactions, which are “extremely rare,” Dr. Prager said.
Hemorrhage can occur, but isn’t common and usually is at a level that doesn’t require blood transfusion. “But it does require somebody to come in, potentially needing uterine aspiration or sometimes just a second dose of misoprostol,” she said.
Serious infections are “extraordinarily uncommon,” with an actual risk of infectious death of 0.5 per 100,000, and therefore antibiotic prophylaxis is not recommended.
“This is not to say that there can’t be serious infectious problems with medication abortion, and actually also with spontaneous abortion ... but it’s extremely rare,” Dr. Prager said, adding that “there are also consequences to giving everybody antibiotics if they are not necessary. I, personally, am way more afraid of antibiotic resistance these days than I am about preventing an infection from an medication abortion.”
Intervention is necessary in certain situations, including when the gestational sac remains and when the patient continues to have clinical symptoms or has developed clinical symptoms, she said.
“Does she now show signs of infection? Is she bleeding very heavily or [is she] extremely uncomfortable with cramping? Those are all really great reasons to intervene,” she said.
Sometimes patients just prefer to switch to an alternative method of management, particularly in cases of early pregnancy loss when medical management has “not been successful after some period of time,” Dr. Prager added.
Outcomes
Studies have shown that the success rates with a single dose of 400-800 mcg of misoprostol range from 25% to 88%, and with repeat dosing for incomplete abortion at 24 hours, the success rate improves to between 80% and 88%. The success rate with placebo is 16%-60%; this indicates that “some miscarriages just happen expectantly,” Dr. Prager explained.
“We already knew that ... and that’s why expectant management is an option with early pregnancy loss,” she said, adding that expectant management works about 50% of the time – “if you wait long enough.”
However, success rates with medical management depend on the type of miscarriage; the rate is close to 100% with incomplete abortion, but for other types, such as anembryonic pregnancy or fetal demise, it is slightly less effective at about 87%, Dr. Prager noted.
When mifepristone and misoprostol are both used, success rates for early pregnancy loss range from 52% to 84% in observational trials and using nonstandard doses, and between 90% and 93% with standard dosing.
Other recent data, which led to a 2016 “reaffirmation” of an ACOG practice bulletin on medical management of first-trimester abortion, show an 83% success rate with the combination therapy in anembryonic pregnancies, and a 25% reduction in the need for further intervention (N Engl J Med. 2018;378:2161-70).
“So it really was significantly more effective to be using that addition of the mifepristone,” she said. “My take-home message about this is that, if mifepristone is something that you have easily available to you at your clinical site, absolutely use it, because it creates better outcomes for your patients. However, if it’s not available to you ... it is still perfectly reasonable for patients to choose medication management of their early pregnancy loss and use misoprostol only.
“It is effective enough, and that is just part of your informed consent.”
Postabortion care
Postmiscarriage care is important and involves several components, Dr. Prager said.
- RhoGAM treatment. The use of RhoGAM to prevent Rh immunization has been routine, but data increasingly suggest this is not necessary, and in some countries it is not given at all, particularly at 8 or fewer weeks of gestation and sometimes even during the whole first trimester for early pregnancy loss. “That is not common practice yet in the United States; I’m not recommending at this time that everybody change their practice ... but I will say that there are some really interesting studies going on right now in the United States that are looking specifically at this, and I think we may, within the next 10 years or so, change this practice of giving RhoGAM at all gestational ages,” she said.
- Counseling about bleeding. Light to moderate bleeding after abortion is common for about 2 weeks after abortion, with normal menses returning between 4 and 8 weeks, and typically around 6 weeks. “I usually ask patients to come back and see me if they have not had what seems to be a normal period to them 8 weeks following their completed process,” Dr. Prager said.
- Counseling about human chorionic gonadotropin levels. It is also helpful to inform patients that human chorionic gonadotropin may remain present for about 2-4 weeks after completed abortion, resulting in a positive pregnancy test during that time. A positive test at 4 weeks may still be normal, but warrants evaluation to determine why the patient is testing positive.
- Counseling about conception timing. Data do not support delaying repeat pregnancy after abortion. Studies show no difference in the ability to conceive or in pregnancy outcomes among women who conceive without delay after early pregnancy loss and in those who wait at least 3 months. “So what I now tell women is ‘when you’re emotionally ready to start trying to get pregnant again, it’s perfectly medically acceptable to do so. There’s no biologic reason why you have to wait,’ ” she said.
- Contraception initiation. Contraception, including IUDs, can be initiated right away after elective or spontaneous abortion. However, for IUD insertion after medical abortion, it is important to first use ultrasound to confirm complete abortion, Dr. Prager said.
- Grief counseling. This may be appropriate in cases of early pregnancy loss and for elective abortions. “Both groups of people may need some counseling, may be experiencing grief around this process – and they may not be,” she said. “I think we just need to be sensitive about asking our patients what their needs might be around this.”
Future directions
The future of medical management for first trimester abortion may involve “demedicalization,” Dr. Prager said.
“There are many papers coming out now about clinic versus home use of mifepristone,” she said, explaining that home use would require removing the FDA’s Risk Evaluation and Mitigation Strategy restriction that requires that the drug be dispensed in a clinic by a physician or physician extender.
Studies are also looking at prescriptions, pharmacist provision of mifepristone, and mailing of medications to women in rural areas.
Another area of research beyond these “really creative ways of using these medications” is whether medical management is effective beyond 10 weeks. A study that will soon be published is looking at mifepristone and two doses of misoprostol at 11 weeks, she noted.
“I think from pregnancy diagnosis through at least week 10 – soon we will see potentially week 11 – medical abortion techniques are safe, they’re effective, and they’re extremely well accepted by patients,” she said. “Also ... a diverse group of clinicians can be trained to offer medical abortion and provide back-up so that access can be improved.”
Dr. Prager reported having no financial disclosures.
NASHVILLE, TENN. – Medical management of abortion and early pregnancy loss is best achieved with both mifepristone and misoprostol, according to Sarah W. Prager, MD.
First-trimester procedures account for about 90% of elective abortions, with about two-thirds of those occurring before 8 weeks of gestation and 80% occurring in the first 10 weeks – and therefore considered eligible for medical management, Dr. Prager, director of the Family Planning Division and Family Planning Fellowship at the University of Washington, Seattle, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“We estimate that it’s approximately 31% of all abortions that are done using medication, but it’s about 45% of those eligible by gestational age,” she noted.
The alternative is uterine aspiration, and in the absence of a clear contraindication, patient preference should determine management choice, she said.
The same is true for early pregnancy loss (spontaneous abortion), which is the most common complication of early pregnancy, occurring in about 20% of clinically recognized pregnancies.
“That means that there are about 1 million spontaneous abortions happening annually in the United States, and about 80% of those are in the first trimester,” Dr. Prager said.
Expectant management is an additional option for managing early pregnancy loss, she noted.
Candidates
Medical management is appropriate for patients who are undergoing elective abortion at up to about 70 days of gestation or with pregnancy loss in the first trimester.
“They should have stable vital signs, no evidence of infection, no allergies to the medications being used, no serious social or medical problems,” Dr. Prager said, explaining that “a shared decision making process” is important for patients with extreme anxiety or homelessness/lack of stable housing, for example, in order to make sure that medical management is a good option.
“While she definitely gets to have the final say, unless there is a real medical contraindication, it definitely should be part of that decision making,” Dr. Prager said, adding that adequate counseling and acceptance by the patient of the risks and side effects also are imperative.
Protocol
The most effective evidence-based treatment protocol for elective abortion through day 70 of gestation includes a 200-mg oral dose of mifepristone, followed 24-72 hours later with at-home buccal or vaginal administration of an 800-mcg dose of misoprostol, with follow up within 1-2 weeks, Dr. Prager said, citing a 2010 Cochrane review.
The Food and Drug Administration–approved protocol, which was updated in April 2016, adheres closely to those findings, except that it calls for misoprostol within 48 hours of mifepristone dosing. Optional repeat dosing of misoprostol is allowed, as well, she noted.
Buccal or vaginal administration of misoprostol is preferable to oral and sublingual administration because while the latter approaches provide more rapid onset, the former approaches provide significantly better sustained action over a 5-hour period of time.
“And by not having that big peak at the beginning, it actually decreases the side effects that women experience with the misoprostol medication,” she said.
Misoprostol can also be given alone for early pregnancy loss management – also at a dose of 800 mcg buccally or vaginally – with repeat dosing at 12-24 hours for incomplete abortion. However, new data suggest that, before about 63 days of gestation, giving two doses 3 hours apart is slightly more effective. That approach can also be repeated if necessary, Dr. Prager said.
Pain management is an important part of treatment, as both miscarriage and medication abortion can range from uncomfortable to extremely painful, depending on the patient, her prior obstetric experience, and her life experiences.
“I recommend talking to all your patients about pain management. For most people, just using some type of NSAID is probably going to be sufficient,” she said, noting that some women will require a narcotic.
Antiemetic medication may also be necessary, as some women will experience nausea and vomiting.
Complications and intervention
Major complications are rare with medical management of first-trimester abortion and early pregnancy loss, but can include ongoing pregnancy, which is infrequent but possible; incomplete abortion, which is easily managed; and allergic reactions, which are “extremely rare,” Dr. Prager said.
Hemorrhage can occur, but isn’t common and usually is at a level that doesn’t require blood transfusion. “But it does require somebody to come in, potentially needing uterine aspiration or sometimes just a second dose of misoprostol,” she said.
Serious infections are “extraordinarily uncommon,” with an actual risk of infectious death of 0.5 per 100,000, and therefore antibiotic prophylaxis is not recommended.
“This is not to say that there can’t be serious infectious problems with medication abortion, and actually also with spontaneous abortion ... but it’s extremely rare,” Dr. Prager said, adding that “there are also consequences to giving everybody antibiotics if they are not necessary. I, personally, am way more afraid of antibiotic resistance these days than I am about preventing an infection from an medication abortion.”
Intervention is necessary in certain situations, including when the gestational sac remains and when the patient continues to have clinical symptoms or has developed clinical symptoms, she said.
“Does she now show signs of infection? Is she bleeding very heavily or [is she] extremely uncomfortable with cramping? Those are all really great reasons to intervene,” she said.
Sometimes patients just prefer to switch to an alternative method of management, particularly in cases of early pregnancy loss when medical management has “not been successful after some period of time,” Dr. Prager added.
Outcomes
Studies have shown that the success rates with a single dose of 400-800 mcg of misoprostol range from 25% to 88%, and with repeat dosing for incomplete abortion at 24 hours, the success rate improves to between 80% and 88%. The success rate with placebo is 16%-60%; this indicates that “some miscarriages just happen expectantly,” Dr. Prager explained.
“We already knew that ... and that’s why expectant management is an option with early pregnancy loss,” she said, adding that expectant management works about 50% of the time – “if you wait long enough.”
However, success rates with medical management depend on the type of miscarriage; the rate is close to 100% with incomplete abortion, but for other types, such as anembryonic pregnancy or fetal demise, it is slightly less effective at about 87%, Dr. Prager noted.
When mifepristone and misoprostol are both used, success rates for early pregnancy loss range from 52% to 84% in observational trials and using nonstandard doses, and between 90% and 93% with standard dosing.
Other recent data, which led to a 2016 “reaffirmation” of an ACOG practice bulletin on medical management of first-trimester abortion, show an 83% success rate with the combination therapy in anembryonic pregnancies, and a 25% reduction in the need for further intervention (N Engl J Med. 2018;378:2161-70).
“So it really was significantly more effective to be using that addition of the mifepristone,” she said. “My take-home message about this is that, if mifepristone is something that you have easily available to you at your clinical site, absolutely use it, because it creates better outcomes for your patients. However, if it’s not available to you ... it is still perfectly reasonable for patients to choose medication management of their early pregnancy loss and use misoprostol only.
“It is effective enough, and that is just part of your informed consent.”
Postabortion care
Postmiscarriage care is important and involves several components, Dr. Prager said.
- RhoGAM treatment. The use of RhoGAM to prevent Rh immunization has been routine, but data increasingly suggest this is not necessary, and in some countries it is not given at all, particularly at 8 or fewer weeks of gestation and sometimes even during the whole first trimester for early pregnancy loss. “That is not common practice yet in the United States; I’m not recommending at this time that everybody change their practice ... but I will say that there are some really interesting studies going on right now in the United States that are looking specifically at this, and I think we may, within the next 10 years or so, change this practice of giving RhoGAM at all gestational ages,” she said.
- Counseling about bleeding. Light to moderate bleeding after abortion is common for about 2 weeks after abortion, with normal menses returning between 4 and 8 weeks, and typically around 6 weeks. “I usually ask patients to come back and see me if they have not had what seems to be a normal period to them 8 weeks following their completed process,” Dr. Prager said.
- Counseling about human chorionic gonadotropin levels. It is also helpful to inform patients that human chorionic gonadotropin may remain present for about 2-4 weeks after completed abortion, resulting in a positive pregnancy test during that time. A positive test at 4 weeks may still be normal, but warrants evaluation to determine why the patient is testing positive.
- Counseling about conception timing. Data do not support delaying repeat pregnancy after abortion. Studies show no difference in the ability to conceive or in pregnancy outcomes among women who conceive without delay after early pregnancy loss and in those who wait at least 3 months. “So what I now tell women is ‘when you’re emotionally ready to start trying to get pregnant again, it’s perfectly medically acceptable to do so. There’s no biologic reason why you have to wait,’ ” she said.
- Contraception initiation. Contraception, including IUDs, can be initiated right away after elective or spontaneous abortion. However, for IUD insertion after medical abortion, it is important to first use ultrasound to confirm complete abortion, Dr. Prager said.
- Grief counseling. This may be appropriate in cases of early pregnancy loss and for elective abortions. “Both groups of people may need some counseling, may be experiencing grief around this process – and they may not be,” she said. “I think we just need to be sensitive about asking our patients what their needs might be around this.”
Future directions
The future of medical management for first trimester abortion may involve “demedicalization,” Dr. Prager said.
“There are many papers coming out now about clinic versus home use of mifepristone,” she said, explaining that home use would require removing the FDA’s Risk Evaluation and Mitigation Strategy restriction that requires that the drug be dispensed in a clinic by a physician or physician extender.
Studies are also looking at prescriptions, pharmacist provision of mifepristone, and mailing of medications to women in rural areas.
Another area of research beyond these “really creative ways of using these medications” is whether medical management is effective beyond 10 weeks. A study that will soon be published is looking at mifepristone and two doses of misoprostol at 11 weeks, she noted.
“I think from pregnancy diagnosis through at least week 10 – soon we will see potentially week 11 – medical abortion techniques are safe, they’re effective, and they’re extremely well accepted by patients,” she said. “Also ... a diverse group of clinicians can be trained to offer medical abortion and provide back-up so that access can be improved.”
Dr. Prager reported having no financial disclosures.
NASHVILLE, TENN. – Medical management of abortion and early pregnancy loss is best achieved with both mifepristone and misoprostol, according to Sarah W. Prager, MD.
First-trimester procedures account for about 90% of elective abortions, with about two-thirds of those occurring before 8 weeks of gestation and 80% occurring in the first 10 weeks – and therefore considered eligible for medical management, Dr. Prager, director of the Family Planning Division and Family Planning Fellowship at the University of Washington, Seattle, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“We estimate that it’s approximately 31% of all abortions that are done using medication, but it’s about 45% of those eligible by gestational age,” she noted.
The alternative is uterine aspiration, and in the absence of a clear contraindication, patient preference should determine management choice, she said.
The same is true for early pregnancy loss (spontaneous abortion), which is the most common complication of early pregnancy, occurring in about 20% of clinically recognized pregnancies.
“That means that there are about 1 million spontaneous abortions happening annually in the United States, and about 80% of those are in the first trimester,” Dr. Prager said.
Expectant management is an additional option for managing early pregnancy loss, she noted.
Candidates
Medical management is appropriate for patients who are undergoing elective abortion at up to about 70 days of gestation or with pregnancy loss in the first trimester.
“They should have stable vital signs, no evidence of infection, no allergies to the medications being used, no serious social or medical problems,” Dr. Prager said, explaining that “a shared decision making process” is important for patients with extreme anxiety or homelessness/lack of stable housing, for example, in order to make sure that medical management is a good option.
“While she definitely gets to have the final say, unless there is a real medical contraindication, it definitely should be part of that decision making,” Dr. Prager said, adding that adequate counseling and acceptance by the patient of the risks and side effects also are imperative.
Protocol
The most effective evidence-based treatment protocol for elective abortion through day 70 of gestation includes a 200-mg oral dose of mifepristone, followed 24-72 hours later with at-home buccal or vaginal administration of an 800-mcg dose of misoprostol, with follow up within 1-2 weeks, Dr. Prager said, citing a 2010 Cochrane review.
The Food and Drug Administration–approved protocol, which was updated in April 2016, adheres closely to those findings, except that it calls for misoprostol within 48 hours of mifepristone dosing. Optional repeat dosing of misoprostol is allowed, as well, she noted.
Buccal or vaginal administration of misoprostol is preferable to oral and sublingual administration because while the latter approaches provide more rapid onset, the former approaches provide significantly better sustained action over a 5-hour period of time.
“And by not having that big peak at the beginning, it actually decreases the side effects that women experience with the misoprostol medication,” she said.
Misoprostol can also be given alone for early pregnancy loss management – also at a dose of 800 mcg buccally or vaginally – with repeat dosing at 12-24 hours for incomplete abortion. However, new data suggest that, before about 63 days of gestation, giving two doses 3 hours apart is slightly more effective. That approach can also be repeated if necessary, Dr. Prager said.
Pain management is an important part of treatment, as both miscarriage and medication abortion can range from uncomfortable to extremely painful, depending on the patient, her prior obstetric experience, and her life experiences.
“I recommend talking to all your patients about pain management. For most people, just using some type of NSAID is probably going to be sufficient,” she said, noting that some women will require a narcotic.
Antiemetic medication may also be necessary, as some women will experience nausea and vomiting.
Complications and intervention
Major complications are rare with medical management of first-trimester abortion and early pregnancy loss, but can include ongoing pregnancy, which is infrequent but possible; incomplete abortion, which is easily managed; and allergic reactions, which are “extremely rare,” Dr. Prager said.
Hemorrhage can occur, but isn’t common and usually is at a level that doesn’t require blood transfusion. “But it does require somebody to come in, potentially needing uterine aspiration or sometimes just a second dose of misoprostol,” she said.
Serious infections are “extraordinarily uncommon,” with an actual risk of infectious death of 0.5 per 100,000, and therefore antibiotic prophylaxis is not recommended.
“This is not to say that there can’t be serious infectious problems with medication abortion, and actually also with spontaneous abortion ... but it’s extremely rare,” Dr. Prager said, adding that “there are also consequences to giving everybody antibiotics if they are not necessary. I, personally, am way more afraid of antibiotic resistance these days than I am about preventing an infection from an medication abortion.”
Intervention is necessary in certain situations, including when the gestational sac remains and when the patient continues to have clinical symptoms or has developed clinical symptoms, she said.
“Does she now show signs of infection? Is she bleeding very heavily or [is she] extremely uncomfortable with cramping? Those are all really great reasons to intervene,” she said.
Sometimes patients just prefer to switch to an alternative method of management, particularly in cases of early pregnancy loss when medical management has “not been successful after some period of time,” Dr. Prager added.
Outcomes
Studies have shown that the success rates with a single dose of 400-800 mcg of misoprostol range from 25% to 88%, and with repeat dosing for incomplete abortion at 24 hours, the success rate improves to between 80% and 88%. The success rate with placebo is 16%-60%; this indicates that “some miscarriages just happen expectantly,” Dr. Prager explained.
“We already knew that ... and that’s why expectant management is an option with early pregnancy loss,” she said, adding that expectant management works about 50% of the time – “if you wait long enough.”
However, success rates with medical management depend on the type of miscarriage; the rate is close to 100% with incomplete abortion, but for other types, such as anembryonic pregnancy or fetal demise, it is slightly less effective at about 87%, Dr. Prager noted.
When mifepristone and misoprostol are both used, success rates for early pregnancy loss range from 52% to 84% in observational trials and using nonstandard doses, and between 90% and 93% with standard dosing.
Other recent data, which led to a 2016 “reaffirmation” of an ACOG practice bulletin on medical management of first-trimester abortion, show an 83% success rate with the combination therapy in anembryonic pregnancies, and a 25% reduction in the need for further intervention (N Engl J Med. 2018;378:2161-70).
“So it really was significantly more effective to be using that addition of the mifepristone,” she said. “My take-home message about this is that, if mifepristone is something that you have easily available to you at your clinical site, absolutely use it, because it creates better outcomes for your patients. However, if it’s not available to you ... it is still perfectly reasonable for patients to choose medication management of their early pregnancy loss and use misoprostol only.
“It is effective enough, and that is just part of your informed consent.”
Postabortion care
Postmiscarriage care is important and involves several components, Dr. Prager said.
- RhoGAM treatment. The use of RhoGAM to prevent Rh immunization has been routine, but data increasingly suggest this is not necessary, and in some countries it is not given at all, particularly at 8 or fewer weeks of gestation and sometimes even during the whole first trimester for early pregnancy loss. “That is not common practice yet in the United States; I’m not recommending at this time that everybody change their practice ... but I will say that there are some really interesting studies going on right now in the United States that are looking specifically at this, and I think we may, within the next 10 years or so, change this practice of giving RhoGAM at all gestational ages,” she said.
- Counseling about bleeding. Light to moderate bleeding after abortion is common for about 2 weeks after abortion, with normal menses returning between 4 and 8 weeks, and typically around 6 weeks. “I usually ask patients to come back and see me if they have not had what seems to be a normal period to them 8 weeks following their completed process,” Dr. Prager said.
- Counseling about human chorionic gonadotropin levels. It is also helpful to inform patients that human chorionic gonadotropin may remain present for about 2-4 weeks after completed abortion, resulting in a positive pregnancy test during that time. A positive test at 4 weeks may still be normal, but warrants evaluation to determine why the patient is testing positive.
- Counseling about conception timing. Data do not support delaying repeat pregnancy after abortion. Studies show no difference in the ability to conceive or in pregnancy outcomes among women who conceive without delay after early pregnancy loss and in those who wait at least 3 months. “So what I now tell women is ‘when you’re emotionally ready to start trying to get pregnant again, it’s perfectly medically acceptable to do so. There’s no biologic reason why you have to wait,’ ” she said.
- Contraception initiation. Contraception, including IUDs, can be initiated right away after elective or spontaneous abortion. However, for IUD insertion after medical abortion, it is important to first use ultrasound to confirm complete abortion, Dr. Prager said.
- Grief counseling. This may be appropriate in cases of early pregnancy loss and for elective abortions. “Both groups of people may need some counseling, may be experiencing grief around this process – and they may not be,” she said. “I think we just need to be sensitive about asking our patients what their needs might be around this.”
Future directions
The future of medical management for first trimester abortion may involve “demedicalization,” Dr. Prager said.
“There are many papers coming out now about clinic versus home use of mifepristone,” she said, explaining that home use would require removing the FDA’s Risk Evaluation and Mitigation Strategy restriction that requires that the drug be dispensed in a clinic by a physician or physician extender.
Studies are also looking at prescriptions, pharmacist provision of mifepristone, and mailing of medications to women in rural areas.
Another area of research beyond these “really creative ways of using these medications” is whether medical management is effective beyond 10 weeks. A study that will soon be published is looking at mifepristone and two doses of misoprostol at 11 weeks, she noted.
“I think from pregnancy diagnosis through at least week 10 – soon we will see potentially week 11 – medical abortion techniques are safe, they’re effective, and they’re extremely well accepted by patients,” she said. “Also ... a diverse group of clinicians can be trained to offer medical abortion and provide back-up so that access can be improved.”
Dr. Prager reported having no financial disclosures.
EXPERT ANALYSIS FROM ACOG 2019
How do new BP guidelines affect identifying risk for hypertensive disorders of pregnancy?
Hauspurg A, Parry S, Mercer BM, et al. Blood pressure trajectory and category and risk of hypertensive disorders of pregnancy in nulliparous women. Am J Obstet Gynecol. 2019. pii: S0002-9378(19)30807-5. doi: 10.1016/j.ajog.2019.06.031.
EXPERT COMMENTARY
Hauspurg and colleagues set out to determine whether redefined BP category (normal, < 120/80 mm Hg) and trajectory (a difference of ≥ 5 mm Hg systolic, diastolic, or mean arterial pressure between the first and second prenatal visit) helps to identify women at increased risk for developing hypertensive disorders of pregnancy or preeclampsia.
With respect to the former variable, such an association was demonstrated in the first National Institutes of Health–funded preeclampsia prevention trial published in 1993, which used low-dose aspirin.1 In that trial, low-dose aspirin was not found to be effective in preventing preeclampsia in young, healthy nulliparous women. Interestingly, the 2 factors most associated with developing preeclampsia were an initial systolic BP of 120 to 134 mm Hg and an initial weight of >60 kg. For most clinicians, these findings would not be helpful in trying to better identify a high-risk group.
Details of the study
The idea of BP “trajectory” is interesting in the Hauspurg and colleagues’ study. The authors analyzed data from the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b), a prospective cohort study, and included a very large population of almost 9,000 women in the analysis. Participants were classified according to their BP measurement at the first study visit, with BP categories based on updated American College of Cardiology/American Heart Association guidelines. The primary outcome was the risk of hypertensive disorders of pregnancy, including gestational hypertension and preeclampsia.
The data analysis found that elevated BP was associated with an adjusted risk ratio (aRR) of 1.54 (95% confidence interval [CI], 1.18–2.02). Stage 1 hypertension was associated with an aRR of 2.16 (95% CI, 1.31–3.57). Compared with women whose BP had a downward systolic trajectory, women with normal BP and an upward systolic trajectory had a 41% increased risk of any hypertensive disorder of pregnancy (aRR, 1.41; 95% CI, 1.20–1.65).
Study strengths and limitations
While the large study population is a strength of this study, there are a number of limitations, such as the use of BP measurements during pregnancy only, without having pre-pregnancy measurements available. Further, a single BP measurement during each visit is also a drawback, although the standardized measurement by study staff is a strength.
Anticlimactic conclusions. The conclusions of the study, however, are either not surprising, not clinically meaningful, or of little value to clinicians at present, at least with respect to patient management.
Continue to: Conclusions that were not surprising included...
Conclusions that were not surprising included a statistically lower chance of indicated preterm delivery in the normal BP group than in the elevated BP or stage 1 hypertension groups. Conclusions that were not meaningful included a statistically significant lower birthweight in the elevated BP group (3,269 g) and in the stage 1 hypertension group (3,258 g) compared with the normal BP group (3,279 g), but the clinical significance of these differences is arguable.
Lastly is the issue of what these data mean for clinical practice. The idea of identifying high-risk groups is attractive, provided that there are effective intervention strategies available. If one follows the United States Preventive Services Task Force (USPSTF) recommendations for preeclampsia prevention,2 then virtually every nulliparous woman is a candidate for low-dose aspirin for preeclampsia prophylaxis. Beyond that, the current data do not support any change in the standard clinical practice of managing these “now identified” high-risk women. Increasing prenatal visits, using biomarkers to further delineate risk, and using uterine artery Doppler studies are all strategies that have been or are being investigated, but as yet they are not supported by conclusive data documenting improved outcomes—a sentiment supported by both the USPSTF3 and the authors of the study.
Until further data are available, my advice to clinicians is to pay close attention to all risk factors for any of the hypertensive disorders of pregnancy. Initial BP and BP trajectory are important but probably something that sound clinical judgment would identify anyway. My recommendation is to continue to use those methods of prophylaxis, fetal surveillance, and indications for delivery that are supported by current data and await the additional investigations that Hauspurg and colleagues suggest need to be done before altering your management of women at increased risk for any of the hypertensive disorders of pregnancy.
JOHN T. REPKE, MD
- Sibai BM, Caritis SN, Thom E, et al; National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine. Prevention of preeclampsia with low-dose aspirin in healthy nulliparous pregnant women. N Engl J Med. 1993;329:1213-1218.
- United States Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: preventive medication. September 2014. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/low-dose-aspirin-use-for-the-prevention-of-morbidity-and-mortality-from-preeclampsia-preventive-medication. Accessed July 30, 2019.
- United States Preventive Service Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for preeclampsia: US Preventive Services Task Force recommendation statement. JAMA. 2017;387:1661-1667.
Hauspurg A, Parry S, Mercer BM, et al. Blood pressure trajectory and category and risk of hypertensive disorders of pregnancy in nulliparous women. Am J Obstet Gynecol. 2019. pii: S0002-9378(19)30807-5. doi: 10.1016/j.ajog.2019.06.031.
EXPERT COMMENTARY
Hauspurg and colleagues set out to determine whether redefined BP category (normal, < 120/80 mm Hg) and trajectory (a difference of ≥ 5 mm Hg systolic, diastolic, or mean arterial pressure between the first and second prenatal visit) helps to identify women at increased risk for developing hypertensive disorders of pregnancy or preeclampsia.
With respect to the former variable, such an association was demonstrated in the first National Institutes of Health–funded preeclampsia prevention trial published in 1993, which used low-dose aspirin.1 In that trial, low-dose aspirin was not found to be effective in preventing preeclampsia in young, healthy nulliparous women. Interestingly, the 2 factors most associated with developing preeclampsia were an initial systolic BP of 120 to 134 mm Hg and an initial weight of >60 kg. For most clinicians, these findings would not be helpful in trying to better identify a high-risk group.
Details of the study
The idea of BP “trajectory” is interesting in the Hauspurg and colleagues’ study. The authors analyzed data from the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b), a prospective cohort study, and included a very large population of almost 9,000 women in the analysis. Participants were classified according to their BP measurement at the first study visit, with BP categories based on updated American College of Cardiology/American Heart Association guidelines. The primary outcome was the risk of hypertensive disorders of pregnancy, including gestational hypertension and preeclampsia.
The data analysis found that elevated BP was associated with an adjusted risk ratio (aRR) of 1.54 (95% confidence interval [CI], 1.18–2.02). Stage 1 hypertension was associated with an aRR of 2.16 (95% CI, 1.31–3.57). Compared with women whose BP had a downward systolic trajectory, women with normal BP and an upward systolic trajectory had a 41% increased risk of any hypertensive disorder of pregnancy (aRR, 1.41; 95% CI, 1.20–1.65).
Study strengths and limitations
While the large study population is a strength of this study, there are a number of limitations, such as the use of BP measurements during pregnancy only, without having pre-pregnancy measurements available. Further, a single BP measurement during each visit is also a drawback, although the standardized measurement by study staff is a strength.
Anticlimactic conclusions. The conclusions of the study, however, are either not surprising, not clinically meaningful, or of little value to clinicians at present, at least with respect to patient management.
Continue to: Conclusions that were not surprising included...
Conclusions that were not surprising included a statistically lower chance of indicated preterm delivery in the normal BP group than in the elevated BP or stage 1 hypertension groups. Conclusions that were not meaningful included a statistically significant lower birthweight in the elevated BP group (3,269 g) and in the stage 1 hypertension group (3,258 g) compared with the normal BP group (3,279 g), but the clinical significance of these differences is arguable.
Lastly is the issue of what these data mean for clinical practice. The idea of identifying high-risk groups is attractive, provided that there are effective intervention strategies available. If one follows the United States Preventive Services Task Force (USPSTF) recommendations for preeclampsia prevention,2 then virtually every nulliparous woman is a candidate for low-dose aspirin for preeclampsia prophylaxis. Beyond that, the current data do not support any change in the standard clinical practice of managing these “now identified” high-risk women. Increasing prenatal visits, using biomarkers to further delineate risk, and using uterine artery Doppler studies are all strategies that have been or are being investigated, but as yet they are not supported by conclusive data documenting improved outcomes—a sentiment supported by both the USPSTF3 and the authors of the study.
Until further data are available, my advice to clinicians is to pay close attention to all risk factors for any of the hypertensive disorders of pregnancy. Initial BP and BP trajectory are important but probably something that sound clinical judgment would identify anyway. My recommendation is to continue to use those methods of prophylaxis, fetal surveillance, and indications for delivery that are supported by current data and await the additional investigations that Hauspurg and colleagues suggest need to be done before altering your management of women at increased risk for any of the hypertensive disorders of pregnancy.
JOHN T. REPKE, MD
Hauspurg A, Parry S, Mercer BM, et al. Blood pressure trajectory and category and risk of hypertensive disorders of pregnancy in nulliparous women. Am J Obstet Gynecol. 2019. pii: S0002-9378(19)30807-5. doi: 10.1016/j.ajog.2019.06.031.
EXPERT COMMENTARY
Hauspurg and colleagues set out to determine whether redefined BP category (normal, < 120/80 mm Hg) and trajectory (a difference of ≥ 5 mm Hg systolic, diastolic, or mean arterial pressure between the first and second prenatal visit) helps to identify women at increased risk for developing hypertensive disorders of pregnancy or preeclampsia.
With respect to the former variable, such an association was demonstrated in the first National Institutes of Health–funded preeclampsia prevention trial published in 1993, which used low-dose aspirin.1 In that trial, low-dose aspirin was not found to be effective in preventing preeclampsia in young, healthy nulliparous women. Interestingly, the 2 factors most associated with developing preeclampsia were an initial systolic BP of 120 to 134 mm Hg and an initial weight of >60 kg. For most clinicians, these findings would not be helpful in trying to better identify a high-risk group.
Details of the study
The idea of BP “trajectory” is interesting in the Hauspurg and colleagues’ study. The authors analyzed data from the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b), a prospective cohort study, and included a very large population of almost 9,000 women in the analysis. Participants were classified according to their BP measurement at the first study visit, with BP categories based on updated American College of Cardiology/American Heart Association guidelines. The primary outcome was the risk of hypertensive disorders of pregnancy, including gestational hypertension and preeclampsia.
The data analysis found that elevated BP was associated with an adjusted risk ratio (aRR) of 1.54 (95% confidence interval [CI], 1.18–2.02). Stage 1 hypertension was associated with an aRR of 2.16 (95% CI, 1.31–3.57). Compared with women whose BP had a downward systolic trajectory, women with normal BP and an upward systolic trajectory had a 41% increased risk of any hypertensive disorder of pregnancy (aRR, 1.41; 95% CI, 1.20–1.65).
Study strengths and limitations
While the large study population is a strength of this study, there are a number of limitations, such as the use of BP measurements during pregnancy only, without having pre-pregnancy measurements available. Further, a single BP measurement during each visit is also a drawback, although the standardized measurement by study staff is a strength.
Anticlimactic conclusions. The conclusions of the study, however, are either not surprising, not clinically meaningful, or of little value to clinicians at present, at least with respect to patient management.
Continue to: Conclusions that were not surprising included...
Conclusions that were not surprising included a statistically lower chance of indicated preterm delivery in the normal BP group than in the elevated BP or stage 1 hypertension groups. Conclusions that were not meaningful included a statistically significant lower birthweight in the elevated BP group (3,269 g) and in the stage 1 hypertension group (3,258 g) compared with the normal BP group (3,279 g), but the clinical significance of these differences is arguable.
Lastly is the issue of what these data mean for clinical practice. The idea of identifying high-risk groups is attractive, provided that there are effective intervention strategies available. If one follows the United States Preventive Services Task Force (USPSTF) recommendations for preeclampsia prevention,2 then virtually every nulliparous woman is a candidate for low-dose aspirin for preeclampsia prophylaxis. Beyond that, the current data do not support any change in the standard clinical practice of managing these “now identified” high-risk women. Increasing prenatal visits, using biomarkers to further delineate risk, and using uterine artery Doppler studies are all strategies that have been or are being investigated, but as yet they are not supported by conclusive data documenting improved outcomes—a sentiment supported by both the USPSTF3 and the authors of the study.
Until further data are available, my advice to clinicians is to pay close attention to all risk factors for any of the hypertensive disorders of pregnancy. Initial BP and BP trajectory are important but probably something that sound clinical judgment would identify anyway. My recommendation is to continue to use those methods of prophylaxis, fetal surveillance, and indications for delivery that are supported by current data and await the additional investigations that Hauspurg and colleagues suggest need to be done before altering your management of women at increased risk for any of the hypertensive disorders of pregnancy.
JOHN T. REPKE, MD
- Sibai BM, Caritis SN, Thom E, et al; National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine. Prevention of preeclampsia with low-dose aspirin in healthy nulliparous pregnant women. N Engl J Med. 1993;329:1213-1218.
- United States Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: preventive medication. September 2014. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/low-dose-aspirin-use-for-the-prevention-of-morbidity-and-mortality-from-preeclampsia-preventive-medication. Accessed July 30, 2019.
- United States Preventive Service Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for preeclampsia: US Preventive Services Task Force recommendation statement. JAMA. 2017;387:1661-1667.
- Sibai BM, Caritis SN, Thom E, et al; National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine. Prevention of preeclampsia with low-dose aspirin in healthy nulliparous pregnant women. N Engl J Med. 1993;329:1213-1218.
- United States Preventive Services Task Force. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: preventive medication. September 2014. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/low-dose-aspirin-use-for-the-prevention-of-morbidity-and-mortality-from-preeclampsia-preventive-medication. Accessed July 30, 2019.
- United States Preventive Service Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for preeclampsia: US Preventive Services Task Force recommendation statement. JAMA. 2017;387:1661-1667.
Click for Credit: Predicting preeclampsia; MI & stroke post-cancer Dx; more
Here are 5 articles from the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Smoking cessation could delay or prevent rheumatoid arthritis
To take the posttest, go to: https://bit.ly/2YguN2r
Expires February 22, 2020
2. No increased pregnancy loss risk for women conceiving soon after stillbirth
To take the posttest, go to: https://bit.ly/2ZnMaLc
Expires March 4, 2020
3. Total plasma tau correlates with dementia onset, Alzheimer’s disease
To take the posttest, go to: https://bit.ly/2YeglYV
Expires March 9, 2020
4. MI, strokes spike during 30 days after cancer diagnosis
To take the posttest, go to: https://bit.ly/2GCKZAv
Expires March 12, 2020
5. Combination model predicts imminent preeclampsia
To take the posttest, go to: https://bit.ly/2LTohrO
Expires February 21, 2020
Here are 5 articles from the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Smoking cessation could delay or prevent rheumatoid arthritis
To take the posttest, go to: https://bit.ly/2YguN2r
Expires February 22, 2020
2. No increased pregnancy loss risk for women conceiving soon after stillbirth
To take the posttest, go to: https://bit.ly/2ZnMaLc
Expires March 4, 2020
3. Total plasma tau correlates with dementia onset, Alzheimer’s disease
To take the posttest, go to: https://bit.ly/2YeglYV
Expires March 9, 2020
4. MI, strokes spike during 30 days after cancer diagnosis
To take the posttest, go to: https://bit.ly/2GCKZAv
Expires March 12, 2020
5. Combination model predicts imminent preeclampsia
To take the posttest, go to: https://bit.ly/2LTohrO
Expires February 21, 2020
Here are 5 articles from the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Smoking cessation could delay or prevent rheumatoid arthritis
To take the posttest, go to: https://bit.ly/2YguN2r
Expires February 22, 2020
2. No increased pregnancy loss risk for women conceiving soon after stillbirth
To take the posttest, go to: https://bit.ly/2ZnMaLc
Expires March 4, 2020
3. Total plasma tau correlates with dementia onset, Alzheimer’s disease
To take the posttest, go to: https://bit.ly/2YeglYV
Expires March 9, 2020
4. MI, strokes spike during 30 days after cancer diagnosis
To take the posttest, go to: https://bit.ly/2GCKZAv
Expires March 12, 2020
5. Combination model predicts imminent preeclampsia
To take the posttest, go to: https://bit.ly/2LTohrO
Expires February 21, 2020
Preeclampsia doubles risk of postpartum transfusion reactions
Women with preeclampsia were found to be at the highest risk for transfusion reactions when receiving a blood transfusion post partum, according to results from a retrospective study.
Additionally, all women who received a transfusion postpartum were twice as likely to experience a procedure-related complication, compared with nonpregnant controls who received identical care.
“The objective of our study was to assess the incidence and risk factors for postpartum [transfusion reactions] in women transfused with red blood cells, plasma, or platelets post partum,” wrote Lars Thurn, PhD, of the Karolinska Institute in Stockholm and colleagues. The findings were reported in Blood Advances.
The researchers conducted a population-based cohort study that included a total of 517,854 women who gave birth in Stockholm County over a period of 21 years. Of those included, 12,183 (2.4%) received a blood transfusion postpartum.
Data was obtained from the Swedish National Birth Registry and was linked to the Stockholm Transfusion Database in order to evaluate the risk of transfusion reactions in pregnant women versus nonpregnant controls.
The researchers identified a total of 96 transfusion reactions postpartum for a prevalence of 79 per 10,000, compared with 40 per 10,000 among nonpregnant controls (odds ratio, 2.0; 95% confidence interval, 1.6-2.5).
The risk of transfusion-related reactions was more than double in pregnant women with preeclampsia versus pregnant women without the condition (OR, 2.1; 95% CI, 1.7-2.6).
“Preeclampsia, induced labor, and preterm delivery were significant risk factors for [transfusion reactions], but we found no differences due to parity, donor gender, or blood group,” the researchers wrote.
The large sample size was a major strength of the study, while a key limitation was the retrospective design.
“Our findings suggest heightened attention be paid when patients with preeclampsia are being evaluated for blood transfusions post partum,” the researchers concluded.
The study was partially funded by Södra Sjukvårdsregionen. The researchers reported having no conflicts of interest.
SOURCE: Thurn L et al. Blood Adv. 2019 Jul 31. doi: 10.1182/bloodadvances.2019000074.
Women with preeclampsia were found to be at the highest risk for transfusion reactions when receiving a blood transfusion post partum, according to results from a retrospective study.
Additionally, all women who received a transfusion postpartum were twice as likely to experience a procedure-related complication, compared with nonpregnant controls who received identical care.
“The objective of our study was to assess the incidence and risk factors for postpartum [transfusion reactions] in women transfused with red blood cells, plasma, or platelets post partum,” wrote Lars Thurn, PhD, of the Karolinska Institute in Stockholm and colleagues. The findings were reported in Blood Advances.
The researchers conducted a population-based cohort study that included a total of 517,854 women who gave birth in Stockholm County over a period of 21 years. Of those included, 12,183 (2.4%) received a blood transfusion postpartum.
Data was obtained from the Swedish National Birth Registry and was linked to the Stockholm Transfusion Database in order to evaluate the risk of transfusion reactions in pregnant women versus nonpregnant controls.
The researchers identified a total of 96 transfusion reactions postpartum for a prevalence of 79 per 10,000, compared with 40 per 10,000 among nonpregnant controls (odds ratio, 2.0; 95% confidence interval, 1.6-2.5).
The risk of transfusion-related reactions was more than double in pregnant women with preeclampsia versus pregnant women without the condition (OR, 2.1; 95% CI, 1.7-2.6).
“Preeclampsia, induced labor, and preterm delivery were significant risk factors for [transfusion reactions], but we found no differences due to parity, donor gender, or blood group,” the researchers wrote.
The large sample size was a major strength of the study, while a key limitation was the retrospective design.
“Our findings suggest heightened attention be paid when patients with preeclampsia are being evaluated for blood transfusions post partum,” the researchers concluded.
The study was partially funded by Södra Sjukvårdsregionen. The researchers reported having no conflicts of interest.
SOURCE: Thurn L et al. Blood Adv. 2019 Jul 31. doi: 10.1182/bloodadvances.2019000074.
Women with preeclampsia were found to be at the highest risk for transfusion reactions when receiving a blood transfusion post partum, according to results from a retrospective study.
Additionally, all women who received a transfusion postpartum were twice as likely to experience a procedure-related complication, compared with nonpregnant controls who received identical care.
“The objective of our study was to assess the incidence and risk factors for postpartum [transfusion reactions] in women transfused with red blood cells, plasma, or platelets post partum,” wrote Lars Thurn, PhD, of the Karolinska Institute in Stockholm and colleagues. The findings were reported in Blood Advances.
The researchers conducted a population-based cohort study that included a total of 517,854 women who gave birth in Stockholm County over a period of 21 years. Of those included, 12,183 (2.4%) received a blood transfusion postpartum.
Data was obtained from the Swedish National Birth Registry and was linked to the Stockholm Transfusion Database in order to evaluate the risk of transfusion reactions in pregnant women versus nonpregnant controls.
The researchers identified a total of 96 transfusion reactions postpartum for a prevalence of 79 per 10,000, compared with 40 per 10,000 among nonpregnant controls (odds ratio, 2.0; 95% confidence interval, 1.6-2.5).
The risk of transfusion-related reactions was more than double in pregnant women with preeclampsia versus pregnant women without the condition (OR, 2.1; 95% CI, 1.7-2.6).
“Preeclampsia, induced labor, and preterm delivery were significant risk factors for [transfusion reactions], but we found no differences due to parity, donor gender, or blood group,” the researchers wrote.
The large sample size was a major strength of the study, while a key limitation was the retrospective design.
“Our findings suggest heightened attention be paid when patients with preeclampsia are being evaluated for blood transfusions post partum,” the researchers concluded.
The study was partially funded by Södra Sjukvårdsregionen. The researchers reported having no conflicts of interest.
SOURCE: Thurn L et al. Blood Adv. 2019 Jul 31. doi: 10.1182/bloodadvances.2019000074.
FROM BLOOD ADVANCES
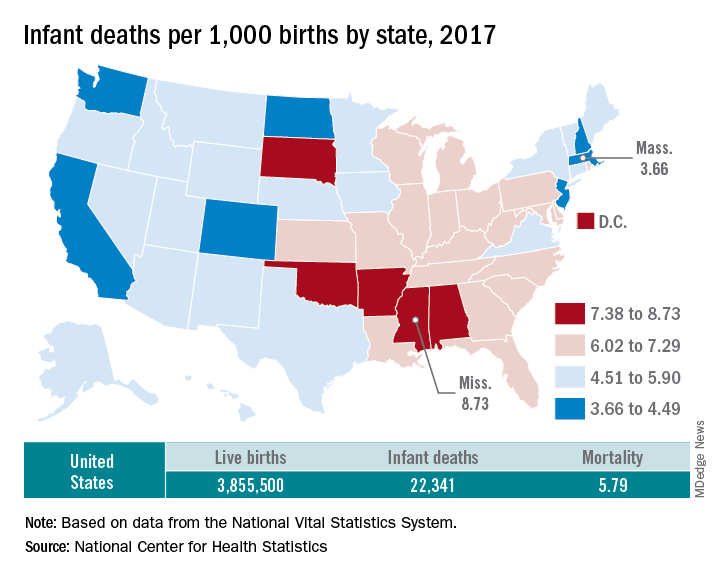
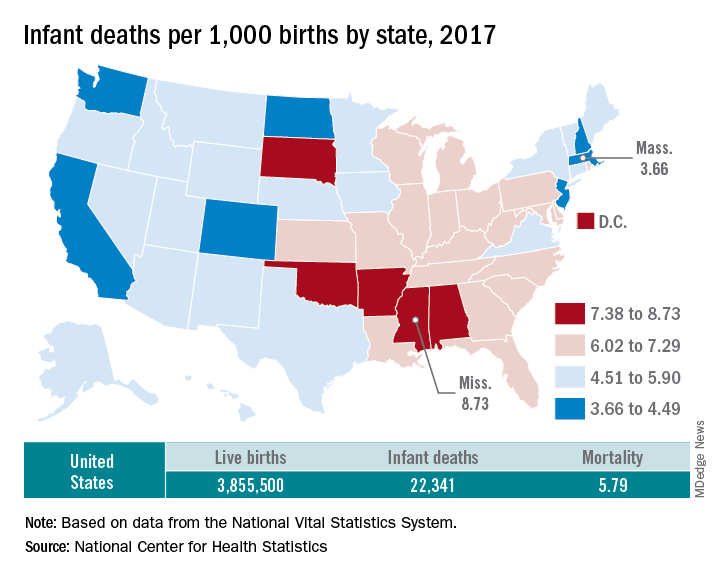
U.S. infant mortality continued slow decline in 2017
according to data released Aug. 1 by the National Center for Health Statistics, based on data from the National Vital Statistics System.
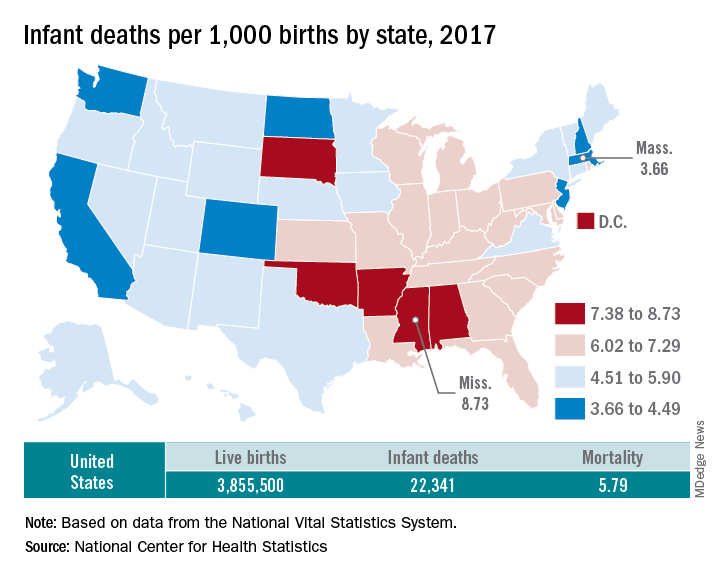
The rate for 2017 was 5.79 deaths per 1,000 live births, which was not statistically different from the rate of 5.87 in 2016, the National Center for Health Statistics said in a new report. Neonatal and postneonatal mortality – 3.85 and 1.94 per 1,000, respectively – both showed the same nonsignificant drop from 2016 to 2017.
About two-thirds of the infants who died in 2017 were children born preterm (less than 37 weeks’ gestation), the NCHS said, and “the mortality rate for infants born before 28 weeks of gestation [389.4 per 1,000] was 183 times the rate for term infants” born at 37-41 weeks.
Rates at the state level in 2017 ranged from a low of 3.66 deaths/1,000 live births in Massachusetts to a high of 8.73/1,000 in Mississippi. Washington (3.88) was the only other state with a rate below 4.0, while Arkansas (8.10) was the only other state above 8.0 (The District of Columbia had a rate of 8.16.). Infant mortality was significantly lower than the national rate in 11 states and significantly higher in 15 states and D.C., according to the report.
Overall, in 2017, 3,855,500 live births occurred, with 22,341 infants having died before the age of 1 year, data from the National Vital Statistics System’s linked birth/infant death file show. In 1995, the first year that the linked file was available, the corresponding numbers were 3,899,589 births and 29,505 deaths, for a rate of 7.57 deaths/1,000 live births.
according to data released Aug. 1 by the National Center for Health Statistics, based on data from the National Vital Statistics System.
The rate for 2017 was 5.79 deaths per 1,000 live births, which was not statistically different from the rate of 5.87 in 2016, the National Center for Health Statistics said in a new report. Neonatal and postneonatal mortality – 3.85 and 1.94 per 1,000, respectively – both showed the same nonsignificant drop from 2016 to 2017.
About two-thirds of the infants who died in 2017 were children born preterm (less than 37 weeks’ gestation), the NCHS said, and “the mortality rate for infants born before 28 weeks of gestation [389.4 per 1,000] was 183 times the rate for term infants” born at 37-41 weeks.
Rates at the state level in 2017 ranged from a low of 3.66 deaths/1,000 live births in Massachusetts to a high of 8.73/1,000 in Mississippi. Washington (3.88) was the only other state with a rate below 4.0, while Arkansas (8.10) was the only other state above 8.0 (The District of Columbia had a rate of 8.16.). Infant mortality was significantly lower than the national rate in 11 states and significantly higher in 15 states and D.C., according to the report.
Overall, in 2017, 3,855,500 live births occurred, with 22,341 infants having died before the age of 1 year, data from the National Vital Statistics System’s linked birth/infant death file show. In 1995, the first year that the linked file was available, the corresponding numbers were 3,899,589 births and 29,505 deaths, for a rate of 7.57 deaths/1,000 live births.
according to data released Aug. 1 by the National Center for Health Statistics, based on data from the National Vital Statistics System.
The rate for 2017 was 5.79 deaths per 1,000 live births, which was not statistically different from the rate of 5.87 in 2016, the National Center for Health Statistics said in a new report. Neonatal and postneonatal mortality – 3.85 and 1.94 per 1,000, respectively – both showed the same nonsignificant drop from 2016 to 2017.
About two-thirds of the infants who died in 2017 were children born preterm (less than 37 weeks’ gestation), the NCHS said, and “the mortality rate for infants born before 28 weeks of gestation [389.4 per 1,000] was 183 times the rate for term infants” born at 37-41 weeks.
Rates at the state level in 2017 ranged from a low of 3.66 deaths/1,000 live births in Massachusetts to a high of 8.73/1,000 in Mississippi. Washington (3.88) was the only other state with a rate below 4.0, while Arkansas (8.10) was the only other state above 8.0 (The District of Columbia had a rate of 8.16.). Infant mortality was significantly lower than the national rate in 11 states and significantly higher in 15 states and D.C., according to the report.
Overall, in 2017, 3,855,500 live births occurred, with 22,341 infants having died before the age of 1 year, data from the National Vital Statistics System’s linked birth/infant death file show. In 1995, the first year that the linked file was available, the corresponding numbers were 3,899,589 births and 29,505 deaths, for a rate of 7.57 deaths/1,000 live births.
Placental bacteria not linked to adverse pregnancy outcomes
such as preeclampsia or spontaneous preterm birth, a study has found.
Dr. Marcus C. de Goffau, of Wellcome Sanger Institute, Cambridge, England, and coauthors wrote that placental dysfunction is linked to a number of common adverse pregnancy outcomes, but in many cases the cause of that dysfunction is unknown.
“Several studies have used sequencing-based methods for bacterial detection (metagenomics and 16S rRNA gene amplicon sequencing), and have concluded that the placenta is physiologically colonized by a diverse population of bacteria (the ‘placental microbiome’) and that the nature of this colonization may differ between healthy and complicated pregnancies,” they wrote.
In a paper published in the July 31 edition of Nature (doi: 10.1038/s41586-019-1451-5), researchers reported the outcomes of a study involving two cohorts. The first included 80 babies delivered by prelabor caesarean section, of whom 20 were small for gestational age, 20 were delivered to mothers with preeclampsia, and 40 were matched controls. The second cohort comprised 100 patients with preeclampsia, 100 small-for-gestational-age infants, 100 preterm births, and 198 matched controls, with two controls having been used twice.
The bacterial content of the placentas was analyzed via deep metagenomic sequencing of total DNA and 16S rRNA gene amplicon sequencing in cohort 1, and 16S rRNA gene amplicon from two different kits for cohort 2’s samples. In the first cohort, samples were also spiked with Salmonella bongori as a positive control.
For cohort 1, researchers were able to detect the S. bongori in all samples, but all other bacterial signals showed clear links to different batches, which the authors said showed they were the result of contamination. This was further supported by the discovery that the Escherichia coli signal seen in a number of batches was all from the same bacterial strain.
In the second cohort, researchers found Bradyrhizobium in nearly all samples, and Burkholderia – which has been thought to play a role in preterm birth – in some samples.
However in the case of the Burkholderia, significant variation between different runs of tests was found, and both Bradyrhizobium and Burkholderia were also found in negative controls.
Researchers also saw a high prevalence of four “ecologically unexpected” bacterial groups but were able to show that these were likely contaminants from a reagent used to wash the placental samples.
The study found that vaginal organisms such as lactobacilli and vaginosis-associated bacteria were more abundant in the second cohort, where babies were delivered by a mix of vaginal, intrapartum and prelabor caesarean section, compared with the first cohort, who were all prelabor caesarean section deliveries.
The only organism that met all the criteria for a genuine placenta-associated bacterial signal was Streptococcus agalactiae, but the authors found no association between it and pregnancy outcomes.
However, they did sound a warning that the perinatal transmission of S. agalactiae from the mother’s genital tract to the neonate could be a cause of fatal sepsis in the infant.
“Further studies will be required to determine the association between the presence of the organism in the placenta and fetal or neonatal disease,” they wrote.
The researchers also found significant associations between the delivery-associated vaginal bacteria Lactobacillus iners and preeclampsia, and between Streptococcus anginosus and the Ureaplasma genus – both of which are associated with vaginosis – and preterm birth.
“We conclude that bacterial placental infection is not a major cause of placentally related complications of human pregnancy and that the human placenta does not have a resident microbiome,” the authors wrote. “Although we see no evidence of a placental microbiome, the frequency of detection of vaginal bacteria in the placenta increased after intrapartum [cesarean] section, suggesting ascending or haematogenous spread.”
The Medical Research Council and the National Institute for Health Research Cambridge Biomedical Research Centre supported the study. Five authors declared grants and support from private industry outside the submitted work.
SOURCE: de Goffau M et al. Nature. 2019 Jul 31. doi: 10.1038/s41586-019-1451-5.
such as preeclampsia or spontaneous preterm birth, a study has found.
Dr. Marcus C. de Goffau, of Wellcome Sanger Institute, Cambridge, England, and coauthors wrote that placental dysfunction is linked to a number of common adverse pregnancy outcomes, but in many cases the cause of that dysfunction is unknown.
“Several studies have used sequencing-based methods for bacterial detection (metagenomics and 16S rRNA gene amplicon sequencing), and have concluded that the placenta is physiologically colonized by a diverse population of bacteria (the ‘placental microbiome’) and that the nature of this colonization may differ between healthy and complicated pregnancies,” they wrote.
In a paper published in the July 31 edition of Nature (doi: 10.1038/s41586-019-1451-5), researchers reported the outcomes of a study involving two cohorts. The first included 80 babies delivered by prelabor caesarean section, of whom 20 were small for gestational age, 20 were delivered to mothers with preeclampsia, and 40 were matched controls. The second cohort comprised 100 patients with preeclampsia, 100 small-for-gestational-age infants, 100 preterm births, and 198 matched controls, with two controls having been used twice.
The bacterial content of the placentas was analyzed via deep metagenomic sequencing of total DNA and 16S rRNA gene amplicon sequencing in cohort 1, and 16S rRNA gene amplicon from two different kits for cohort 2’s samples. In the first cohort, samples were also spiked with Salmonella bongori as a positive control.
For cohort 1, researchers were able to detect the S. bongori in all samples, but all other bacterial signals showed clear links to different batches, which the authors said showed they were the result of contamination. This was further supported by the discovery that the Escherichia coli signal seen in a number of batches was all from the same bacterial strain.
In the second cohort, researchers found Bradyrhizobium in nearly all samples, and Burkholderia – which has been thought to play a role in preterm birth – in some samples.
However in the case of the Burkholderia, significant variation between different runs of tests was found, and both Bradyrhizobium and Burkholderia were also found in negative controls.
Researchers also saw a high prevalence of four “ecologically unexpected” bacterial groups but were able to show that these were likely contaminants from a reagent used to wash the placental samples.
The study found that vaginal organisms such as lactobacilli and vaginosis-associated bacteria were more abundant in the second cohort, where babies were delivered by a mix of vaginal, intrapartum and prelabor caesarean section, compared with the first cohort, who were all prelabor caesarean section deliveries.
The only organism that met all the criteria for a genuine placenta-associated bacterial signal was Streptococcus agalactiae, but the authors found no association between it and pregnancy outcomes.
However, they did sound a warning that the perinatal transmission of S. agalactiae from the mother’s genital tract to the neonate could be a cause of fatal sepsis in the infant.
“Further studies will be required to determine the association between the presence of the organism in the placenta and fetal or neonatal disease,” they wrote.
The researchers also found significant associations between the delivery-associated vaginal bacteria Lactobacillus iners and preeclampsia, and between Streptococcus anginosus and the Ureaplasma genus – both of which are associated with vaginosis – and preterm birth.
“We conclude that bacterial placental infection is not a major cause of placentally related complications of human pregnancy and that the human placenta does not have a resident microbiome,” the authors wrote. “Although we see no evidence of a placental microbiome, the frequency of detection of vaginal bacteria in the placenta increased after intrapartum [cesarean] section, suggesting ascending or haematogenous spread.”
The Medical Research Council and the National Institute for Health Research Cambridge Biomedical Research Centre supported the study. Five authors declared grants and support from private industry outside the submitted work.
SOURCE: de Goffau M et al. Nature. 2019 Jul 31. doi: 10.1038/s41586-019-1451-5.
such as preeclampsia or spontaneous preterm birth, a study has found.
Dr. Marcus C. de Goffau, of Wellcome Sanger Institute, Cambridge, England, and coauthors wrote that placental dysfunction is linked to a number of common adverse pregnancy outcomes, but in many cases the cause of that dysfunction is unknown.
“Several studies have used sequencing-based methods for bacterial detection (metagenomics and 16S rRNA gene amplicon sequencing), and have concluded that the placenta is physiologically colonized by a diverse population of bacteria (the ‘placental microbiome’) and that the nature of this colonization may differ between healthy and complicated pregnancies,” they wrote.
In a paper published in the July 31 edition of Nature (doi: 10.1038/s41586-019-1451-5), researchers reported the outcomes of a study involving two cohorts. The first included 80 babies delivered by prelabor caesarean section, of whom 20 were small for gestational age, 20 were delivered to mothers with preeclampsia, and 40 were matched controls. The second cohort comprised 100 patients with preeclampsia, 100 small-for-gestational-age infants, 100 preterm births, and 198 matched controls, with two controls having been used twice.
The bacterial content of the placentas was analyzed via deep metagenomic sequencing of total DNA and 16S rRNA gene amplicon sequencing in cohort 1, and 16S rRNA gene amplicon from two different kits for cohort 2’s samples. In the first cohort, samples were also spiked with Salmonella bongori as a positive control.
For cohort 1, researchers were able to detect the S. bongori in all samples, but all other bacterial signals showed clear links to different batches, which the authors said showed they were the result of contamination. This was further supported by the discovery that the Escherichia coli signal seen in a number of batches was all from the same bacterial strain.
In the second cohort, researchers found Bradyrhizobium in nearly all samples, and Burkholderia – which has been thought to play a role in preterm birth – in some samples.
However in the case of the Burkholderia, significant variation between different runs of tests was found, and both Bradyrhizobium and Burkholderia were also found in negative controls.
Researchers also saw a high prevalence of four “ecologically unexpected” bacterial groups but were able to show that these were likely contaminants from a reagent used to wash the placental samples.
The study found that vaginal organisms such as lactobacilli and vaginosis-associated bacteria were more abundant in the second cohort, where babies were delivered by a mix of vaginal, intrapartum and prelabor caesarean section, compared with the first cohort, who were all prelabor caesarean section deliveries.
The only organism that met all the criteria for a genuine placenta-associated bacterial signal was Streptococcus agalactiae, but the authors found no association between it and pregnancy outcomes.
However, they did sound a warning that the perinatal transmission of S. agalactiae from the mother’s genital tract to the neonate could be a cause of fatal sepsis in the infant.
“Further studies will be required to determine the association between the presence of the organism in the placenta and fetal or neonatal disease,” they wrote.
The researchers also found significant associations between the delivery-associated vaginal bacteria Lactobacillus iners and preeclampsia, and between Streptococcus anginosus and the Ureaplasma genus – both of which are associated with vaginosis – and preterm birth.
“We conclude that bacterial placental infection is not a major cause of placentally related complications of human pregnancy and that the human placenta does not have a resident microbiome,” the authors wrote. “Although we see no evidence of a placental microbiome, the frequency of detection of vaginal bacteria in the placenta increased after intrapartum [cesarean] section, suggesting ascending or haematogenous spread.”
The Medical Research Council and the National Institute for Health Research Cambridge Biomedical Research Centre supported the study. Five authors declared grants and support from private industry outside the submitted work.
SOURCE: de Goffau M et al. Nature. 2019 Jul 31. doi: 10.1038/s41586-019-1451-5.
FROM NATURE
Key clinical point: Researchers found no evidence of a placental biome or a link between placental bacterial contamination and adverse pregnancy outcomes.
Major finding: No bacterial contamination of the placenta was associated with adverse pregnancy outcomes such as preeclampsia.
Study details: Cohort study of more than 500 placental samples.
Disclosures: The Medical Research Council and the National Institute for Health Research Cambridge Biomedical Research Centre supported the study. Five authors declared grants and support from private industry outside the submitted work.
Source: de Goffau M et al. Nature. 2019 Jul 31. doi: 10.1038/s41586-019-1451-5.
Don’t Mix Off-label Use With Off-the-rack Pills
A pregnant woman in Wisconsin received prenatal care from a family practitioner. The patient had hypertension, so at about 38 weeks’ gestation, the decision was made to induce labor.
On May 15, 2012, the family practitioner used misoprostol to induce labor. The patient received 100 mcg vaginally at 12:24
At 1:28
Variable late decelerations occurred at 11:36
Although the family practitioner was present at the bedside at 12:40
The on-call physician accomplished a vacuum delivery at 1:30
The child now has severe cerebral palsy, with gross motor involvement in the arms and legs. He can communicate through augmentative communication devices but cannot actually speak. He will require full-time care for the rest of his life.
Continue to: The defense took the position...
The defense took the position that while the dosage of misoprostol was excessive, the drug was no longer active in the mother’s body, based on its half-life, when the fetal distress occurred.
VERDICT
Four days before trial, the case was settled for $9 million.
COMMENTARY
I suspect many of you have made a pot roast—and at least some of you have used the simple, tried-and-true method of putting the meat into the slow cooker with a packet of onion soup mix. It makes a tasty dinner with minimal effort. But onion soup packets are for making onion soup—not seasoning pot roast. Guess what? You just used that soup mix off-label!
As clinicians, we all use medications for clinical indications that haven’t been specifically authorized by the FDA—and we shouldn’t stop. Off-label prescribing is legal, common, and often supported by the standard of care.
But there is a risk: The pill or tablet prepared by the manufacturer is generally aimed at the intended on-label use, not off-label uses. In this case, misoprostol (brand name, Cytotec) is approved by the FDA for prevention and treatment of gastrointestinal ulcers and peptic ulcer disease. The package insert describes dosing as follows:
The recommended adult oral dose of Cytotec for reducing the risk of NSAID-induced gastric ulcers is 200 mcg four times daily with food. If this dose cannot be tolerated, a dose of 100 mcg can be used.1
Continue to: We should not be shocked...
We should not be shocked, then, that Cytotec is supplied as 100- and 200-mcg round white tablets. However, it is frequently used off label for cervical ripening during labor at a dose of “25 mcg inserted into the posterior vaginal fornix.”2
This brings us to the malpractice trap. While off-label use may be appropriate, off-label uses may not neatly “fit” with the substance prepared by the manufacturer. To be properly administered for cervical ripening, the available tablet of misoprostol must be cut with a pill cutter or razor prior to administration.3 Furthermore, dosage is more accurate if the tablet fragments are individually weighed after cutting.3
In this case, the discrepancy between the pill prepared by the manufacturer (100 mcg) and the dosage needed (25 mcg) appears to have caught the defendant family practitioner off guard. So the take-home message is: Use medications as supported by the standard of care—but when using a drug off label, do not assume the product supplied by the manufacturer is appropriate for use as is.
Another interesting aspect of this case is the defense strategy. Most clinicians are aware that the tort of negligence involves (1) duty, (2) breach, (3) causation, and (4) harm. However, it is more logically consistent to think of the elements in this way: (1) duty, (2) breach, (3) harm, and if harm has occurred, (4) examine causation (ie, the logical connection between breach and harm).
In malpractice cases, attorneys frequently focus on one of these specific elements. In this case, the physician’s duty of care and the harm stemming from cerebral palsy are clearly established. Thus, breach and causation take center stage.
Continue to: The defense lawyers...
The defense lawyers acknowledged there was a breach, noting the dosage was “excessive.” However, they argued that this error didn’t matter because the drug was no longer active in the patient’s body. In other words, there was no causal connection between the inappropriately high dose and the resultant uterine tachysystole and fetal distress. This is a difficult road for several reasons.
First, the chief danger of using misoprostol is uterine hyperstimulation and fetal distress. The defense would have to argue the hyperstimulation and fetal distress were coincidental and unrelated to the misoprostol—which carries a black box warning for these very adverse effects. The plaintiff’s attorney is sure to make a big deal out of the black box warning in front of the jury—noting any reasonable clinician practicing obstetrics should be aware of the risks that come with misoprostol’s use. You can almost hear the argument in summation: “It is so important, they drew a warning box around it.”
Furthermore, making the argument that the misoprostol was not in the mother’s system at the time the fetal distress started would entail dueling expert testimony about pharmacokinetics and bioavailability—concepts that are difficult for lay jurors to understand. Misoprostol has a half-life of about 20 to 40 min when administered orally and about 60 min when administered vaginally.4 We know the mother received the overdose of misoprostol at 12:24
The plaintiff’s team might counter with an expert’s explanation that misoprostol’s bioavailability is increased 2- to 3-fold with vaginal versus oral administration. It would also be observed that compared with oral administration, vaginal administration of misoprostol is associated with a slower increase in plasma concentrations but longer elevations (peaking about 1-2 hours after vaginal administration).5
At best, the defense expert would be able to argue that the serum level likely peaked 1 to 2 hours after administration (1:24-2:24
Continue to: Most jurors would...
Most jurors would take a skeptical view of the defendant’s argument that the negative outcome in this case was coincidental. Some might even be angered by it. This realization likely prompted the defense to settle this case for $9 million.
IN SUMMARY
Onion soup mix makes great soup, but it’s an even better seasoning for pot roast. Similarly, there are pharmacologic agents that are effective for conditions for which they are not formally indicated. Do not withhold judicious off-label use of medications when appropriate. However, be aware that off-label uses may require extra attention, and dosing and administration may not be consistent with the product you have on hand. Don’t hesitate to seek guidance from pharmacy colleagues when you have questions—they are an underutilized resource and are generally happy to share their expertise.
1. Cytotec [package insert]. New York, NY: Pfizer Inc; 2009.
2. Misoprostol: dosing considerations. PDR: Prescribers’ Digital Reference. www.pdr.net/drug-summary/Cytotec-misoprostol-1044#8. Accessed July 29, 2019.
3. Williams MC, Tsibris JC, Davis G, et al. Dose variation that is associated with approximated one-quarter tablet doses of misoprostol. Am J Obstet Gynecol. 2002;187(3):615-619.
4. Yount SM, Lassiter N. The pharmacology of prostaglandins for induction of labor. J Midwifery Womens Health. 2013;58(2):133-144; quiz 238-239.
5. Danielsson KG, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93(2):275-280.
A pregnant woman in Wisconsin received prenatal care from a family practitioner. The patient had hypertension, so at about 38 weeks’ gestation, the decision was made to induce labor.
On May 15, 2012, the family practitioner used misoprostol to induce labor. The patient received 100 mcg vaginally at 12:24
At 1:28
Variable late decelerations occurred at 11:36
Although the family practitioner was present at the bedside at 12:40
The on-call physician accomplished a vacuum delivery at 1:30
The child now has severe cerebral palsy, with gross motor involvement in the arms and legs. He can communicate through augmentative communication devices but cannot actually speak. He will require full-time care for the rest of his life.
Continue to: The defense took the position...
The defense took the position that while the dosage of misoprostol was excessive, the drug was no longer active in the mother’s body, based on its half-life, when the fetal distress occurred.
VERDICT
Four days before trial, the case was settled for $9 million.
COMMENTARY
I suspect many of you have made a pot roast—and at least some of you have used the simple, tried-and-true method of putting the meat into the slow cooker with a packet of onion soup mix. It makes a tasty dinner with minimal effort. But onion soup packets are for making onion soup—not seasoning pot roast. Guess what? You just used that soup mix off-label!
As clinicians, we all use medications for clinical indications that haven’t been specifically authorized by the FDA—and we shouldn’t stop. Off-label prescribing is legal, common, and often supported by the standard of care.
But there is a risk: The pill or tablet prepared by the manufacturer is generally aimed at the intended on-label use, not off-label uses. In this case, misoprostol (brand name, Cytotec) is approved by the FDA for prevention and treatment of gastrointestinal ulcers and peptic ulcer disease. The package insert describes dosing as follows:
The recommended adult oral dose of Cytotec for reducing the risk of NSAID-induced gastric ulcers is 200 mcg four times daily with food. If this dose cannot be tolerated, a dose of 100 mcg can be used.1
Continue to: We should not be shocked...
We should not be shocked, then, that Cytotec is supplied as 100- and 200-mcg round white tablets. However, it is frequently used off label for cervical ripening during labor at a dose of “25 mcg inserted into the posterior vaginal fornix.”2
This brings us to the malpractice trap. While off-label use may be appropriate, off-label uses may not neatly “fit” with the substance prepared by the manufacturer. To be properly administered for cervical ripening, the available tablet of misoprostol must be cut with a pill cutter or razor prior to administration.3 Furthermore, dosage is more accurate if the tablet fragments are individually weighed after cutting.3
In this case, the discrepancy between the pill prepared by the manufacturer (100 mcg) and the dosage needed (25 mcg) appears to have caught the defendant family practitioner off guard. So the take-home message is: Use medications as supported by the standard of care—but when using a drug off label, do not assume the product supplied by the manufacturer is appropriate for use as is.
Another interesting aspect of this case is the defense strategy. Most clinicians are aware that the tort of negligence involves (1) duty, (2) breach, (3) causation, and (4) harm. However, it is more logically consistent to think of the elements in this way: (1) duty, (2) breach, (3) harm, and if harm has occurred, (4) examine causation (ie, the logical connection between breach and harm).
In malpractice cases, attorneys frequently focus on one of these specific elements. In this case, the physician’s duty of care and the harm stemming from cerebral palsy are clearly established. Thus, breach and causation take center stage.
Continue to: The defense lawyers...
The defense lawyers acknowledged there was a breach, noting the dosage was “excessive.” However, they argued that this error didn’t matter because the drug was no longer active in the patient’s body. In other words, there was no causal connection between the inappropriately high dose and the resultant uterine tachysystole and fetal distress. This is a difficult road for several reasons.
First, the chief danger of using misoprostol is uterine hyperstimulation and fetal distress. The defense would have to argue the hyperstimulation and fetal distress were coincidental and unrelated to the misoprostol—which carries a black box warning for these very adverse effects. The plaintiff’s attorney is sure to make a big deal out of the black box warning in front of the jury—noting any reasonable clinician practicing obstetrics should be aware of the risks that come with misoprostol’s use. You can almost hear the argument in summation: “It is so important, they drew a warning box around it.”
Furthermore, making the argument that the misoprostol was not in the mother’s system at the time the fetal distress started would entail dueling expert testimony about pharmacokinetics and bioavailability—concepts that are difficult for lay jurors to understand. Misoprostol has a half-life of about 20 to 40 min when administered orally and about 60 min when administered vaginally.4 We know the mother received the overdose of misoprostol at 12:24
The plaintiff’s team might counter with an expert’s explanation that misoprostol’s bioavailability is increased 2- to 3-fold with vaginal versus oral administration. It would also be observed that compared with oral administration, vaginal administration of misoprostol is associated with a slower increase in plasma concentrations but longer elevations (peaking about 1-2 hours after vaginal administration).5
At best, the defense expert would be able to argue that the serum level likely peaked 1 to 2 hours after administration (1:24-2:24
Continue to: Most jurors would...
Most jurors would take a skeptical view of the defendant’s argument that the negative outcome in this case was coincidental. Some might even be angered by it. This realization likely prompted the defense to settle this case for $9 million.
IN SUMMARY
Onion soup mix makes great soup, but it’s an even better seasoning for pot roast. Similarly, there are pharmacologic agents that are effective for conditions for which they are not formally indicated. Do not withhold judicious off-label use of medications when appropriate. However, be aware that off-label uses may require extra attention, and dosing and administration may not be consistent with the product you have on hand. Don’t hesitate to seek guidance from pharmacy colleagues when you have questions—they are an underutilized resource and are generally happy to share their expertise.
A pregnant woman in Wisconsin received prenatal care from a family practitioner. The patient had hypertension, so at about 38 weeks’ gestation, the decision was made to induce labor.
On May 15, 2012, the family practitioner used misoprostol to induce labor. The patient received 100 mcg vaginally at 12:24
At 1:28
Variable late decelerations occurred at 11:36
Although the family practitioner was present at the bedside at 12:40
The on-call physician accomplished a vacuum delivery at 1:30
The child now has severe cerebral palsy, with gross motor involvement in the arms and legs. He can communicate through augmentative communication devices but cannot actually speak. He will require full-time care for the rest of his life.
Continue to: The defense took the position...
The defense took the position that while the dosage of misoprostol was excessive, the drug was no longer active in the mother’s body, based on its half-life, when the fetal distress occurred.
VERDICT
Four days before trial, the case was settled for $9 million.
COMMENTARY
I suspect many of you have made a pot roast—and at least some of you have used the simple, tried-and-true method of putting the meat into the slow cooker with a packet of onion soup mix. It makes a tasty dinner with minimal effort. But onion soup packets are for making onion soup—not seasoning pot roast. Guess what? You just used that soup mix off-label!
As clinicians, we all use medications for clinical indications that haven’t been specifically authorized by the FDA—and we shouldn’t stop. Off-label prescribing is legal, common, and often supported by the standard of care.
But there is a risk: The pill or tablet prepared by the manufacturer is generally aimed at the intended on-label use, not off-label uses. In this case, misoprostol (brand name, Cytotec) is approved by the FDA for prevention and treatment of gastrointestinal ulcers and peptic ulcer disease. The package insert describes dosing as follows:
The recommended adult oral dose of Cytotec for reducing the risk of NSAID-induced gastric ulcers is 200 mcg four times daily with food. If this dose cannot be tolerated, a dose of 100 mcg can be used.1
Continue to: We should not be shocked...
We should not be shocked, then, that Cytotec is supplied as 100- and 200-mcg round white tablets. However, it is frequently used off label for cervical ripening during labor at a dose of “25 mcg inserted into the posterior vaginal fornix.”2
This brings us to the malpractice trap. While off-label use may be appropriate, off-label uses may not neatly “fit” with the substance prepared by the manufacturer. To be properly administered for cervical ripening, the available tablet of misoprostol must be cut with a pill cutter or razor prior to administration.3 Furthermore, dosage is more accurate if the tablet fragments are individually weighed after cutting.3
In this case, the discrepancy between the pill prepared by the manufacturer (100 mcg) and the dosage needed (25 mcg) appears to have caught the defendant family practitioner off guard. So the take-home message is: Use medications as supported by the standard of care—but when using a drug off label, do not assume the product supplied by the manufacturer is appropriate for use as is.
Another interesting aspect of this case is the defense strategy. Most clinicians are aware that the tort of negligence involves (1) duty, (2) breach, (3) causation, and (4) harm. However, it is more logically consistent to think of the elements in this way: (1) duty, (2) breach, (3) harm, and if harm has occurred, (4) examine causation (ie, the logical connection between breach and harm).
In malpractice cases, attorneys frequently focus on one of these specific elements. In this case, the physician’s duty of care and the harm stemming from cerebral palsy are clearly established. Thus, breach and causation take center stage.
Continue to: The defense lawyers...
The defense lawyers acknowledged there was a breach, noting the dosage was “excessive.” However, they argued that this error didn’t matter because the drug was no longer active in the patient’s body. In other words, there was no causal connection between the inappropriately high dose and the resultant uterine tachysystole and fetal distress. This is a difficult road for several reasons.
First, the chief danger of using misoprostol is uterine hyperstimulation and fetal distress. The defense would have to argue the hyperstimulation and fetal distress were coincidental and unrelated to the misoprostol—which carries a black box warning for these very adverse effects. The plaintiff’s attorney is sure to make a big deal out of the black box warning in front of the jury—noting any reasonable clinician practicing obstetrics should be aware of the risks that come with misoprostol’s use. You can almost hear the argument in summation: “It is so important, they drew a warning box around it.”
Furthermore, making the argument that the misoprostol was not in the mother’s system at the time the fetal distress started would entail dueling expert testimony about pharmacokinetics and bioavailability—concepts that are difficult for lay jurors to understand. Misoprostol has a half-life of about 20 to 40 min when administered orally and about 60 min when administered vaginally.4 We know the mother received the overdose of misoprostol at 12:24
The plaintiff’s team might counter with an expert’s explanation that misoprostol’s bioavailability is increased 2- to 3-fold with vaginal versus oral administration. It would also be observed that compared with oral administration, vaginal administration of misoprostol is associated with a slower increase in plasma concentrations but longer elevations (peaking about 1-2 hours after vaginal administration).5
At best, the defense expert would be able to argue that the serum level likely peaked 1 to 2 hours after administration (1:24-2:24
Continue to: Most jurors would...
Most jurors would take a skeptical view of the defendant’s argument that the negative outcome in this case was coincidental. Some might even be angered by it. This realization likely prompted the defense to settle this case for $9 million.
IN SUMMARY
Onion soup mix makes great soup, but it’s an even better seasoning for pot roast. Similarly, there are pharmacologic agents that are effective for conditions for which they are not formally indicated. Do not withhold judicious off-label use of medications when appropriate. However, be aware that off-label uses may require extra attention, and dosing and administration may not be consistent with the product you have on hand. Don’t hesitate to seek guidance from pharmacy colleagues when you have questions—they are an underutilized resource and are generally happy to share their expertise.
1. Cytotec [package insert]. New York, NY: Pfizer Inc; 2009.
2. Misoprostol: dosing considerations. PDR: Prescribers’ Digital Reference. www.pdr.net/drug-summary/Cytotec-misoprostol-1044#8. Accessed July 29, 2019.
3. Williams MC, Tsibris JC, Davis G, et al. Dose variation that is associated with approximated one-quarter tablet doses of misoprostol. Am J Obstet Gynecol. 2002;187(3):615-619.
4. Yount SM, Lassiter N. The pharmacology of prostaglandins for induction of labor. J Midwifery Womens Health. 2013;58(2):133-144; quiz 238-239.
5. Danielsson KG, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93(2):275-280.
1. Cytotec [package insert]. New York, NY: Pfizer Inc; 2009.
2. Misoprostol: dosing considerations. PDR: Prescribers’ Digital Reference. www.pdr.net/drug-summary/Cytotec-misoprostol-1044#8. Accessed July 29, 2019.
3. Williams MC, Tsibris JC, Davis G, et al. Dose variation that is associated with approximated one-quarter tablet doses of misoprostol. Am J Obstet Gynecol. 2002;187(3):615-619.
4. Yount SM, Lassiter N. The pharmacology of prostaglandins for induction of labor. J Midwifery Womens Health. 2013;58(2):133-144; quiz 238-239.
5. Danielsson KG, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93(2):275-280.
Second trimester fetal loss: Shared decision-making, patient preference are key
NASHVILLE, TENN. – , according to Sarah W. Prager, MD.
Therefore, in the absence of clear contraindications in settings where both options are available, patient preference should prevail, Dr. Prager, director of the family planning division and family planning fellowship at the University of Washington, Seattle, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
However, shared decision-making is imperative, she said.
Shared decision-making “can be extremely important for satisfaction with this process,” she said, explaining that provider-driven decisions can be paternalistic and often are based on what the provider might do in the same situation.
“But that may not be what the patient wants,” she added.
Conversely, patient-led decision-making can lead to information overload.
“She’s coming to you because you’re the expert. She wants your opinion on this,” Dr. Prager said, noting that sharing the process through “information transfer” allows for the “best, most appropriate decision” to be made.
“Patient engagement is the practice of actively involving and supporting the patient in health care and treatment decision-making activities, and this is really what I’m talking about,” she said, adding that patient engagement is “critically important in many situations, and especially in the setting of pregnancy loss.”
That’s because patients feel powerless in this situation, she explained. Engaging them in the decision-making process can “give them a little bit of that power back” by respecting autonomy, enhancing agency, improving health status, reducing decisional conflict, and limiting test use, thereby improving overall satisfaction.
Two randomized control trials, each designed to compare surgical management and medical management for terminations at up to 20 weeks of gestation, highlight the role and importance of patient preference, Dr. Prager said.
The first – a 2004 study – was stopped early because of slow enrollment, with 29 of 47 eligible subjects declining randomization. Among 93% of those who declined, there was a preference for surgical management. The second, a 2010 study, enrolled 122 patients after 107 of 229 eligible subjects (47%) declined randomization, again because most (67%) preferred surgery (BJOG. 2004;111[2]:148-53; BJOG. 2010;117[12]:1512-20).
Reasons given for preferring surgical management included less psychological trauma and deeper anesthesia, whereas reasons given for induction preference included less wait time and a desire to avoid general anesthesia.
Helping patients make the best decision requires a discussion about potential complications for each approach, Dr. Prager said.
Surgical management, which involves dilation and evacuation (D&E), is used for about 95% of second-trimester abortions overall, but medical management may be underreported, particularly for management of pregnancy loss, Dr. Prager said. “We don’t have clear statistics” in that setting.
The overall rate of complications is low for surgical management, with data suggesting a rate of up to 4%. Uterine perforation occurs in 0.2%-0.3% of procedures, cervical laceration occurs in up to 1%, and retained placenta occurs in less than 1%, she said.
The complication rate for medical management – induction with either misoprostol or mifepristone + misoprostol (the latter is the recommended approach) – is much higher at up to 29%, but that includes retained placenta, which happens in up to 10% of procedures. Uterine rupture occurs in 0.04%-0.28% of procedures, she said.
“With either surgical management or medication management of pregnancy loss, we need to keep in mind the possibility of disseminated intravascular coagulation, which is rare, but certainly possible,” she said.
Other factors that may be important to patients deciding between surgical and medical management for second-trimester fetal loss include:
- Anesthesia, which is local plus intravenous sedation for surgery, compared with IV narcotics and potentially an epidural or other type of regional anesthesia for medical management.
- Duration, which is 5-20 minutes for surgery, compared with 6-11 hours with mifepristone + misoprostol, and up to 20 hours with misoprostol alone.
- Location, which is done on an outpatient basis for surgery, compared with inpatient care for medical management.
- Cost, which is $1,000-$5,000 for surgery vs. $3,000-$9,000 for medical management.
- Contact with the fetus, which typically involves the possibility of partial viewing and an opportunity to obtain footprints as a memento if an intact procedure is attempted during surgery vs. full viewing and possibly holding the baby after delivery following medical management. This is often the key deciding factor for patients.
- Provider factors, in terms of training and skills. Surgery involves a need for specialized training, whereas medical management requires no extra training, she said, adding that “not all ob.gyns. across the country are competent or comfortable providing a D&E, particularly in the later second-trimester time period.” However, the availability of family planing fellowships will increase the number of centers across the country where both options will be available, she noted.
- The possibility of fetal autopsy, which surgery often (but not always) allows, but medical management always allows.
- Involvement level, which is provider heavy for surgery vs. patient heavy for medical management.
“Moving toward an evidence-based, patient-centered care model requires a lot of us, as providers, to really work at dropping our assumptions. We often have strong opinions about what we think we would do in that setting, and it can be tricky for us to set that aside and allow patients to really ask questions and discuss their values so that we can then advocate best for our patients after they know exactly what their options are,” she said.
Dr. Prager reported having no relevant disclosures.
NASHVILLE, TENN. – , according to Sarah W. Prager, MD.
Therefore, in the absence of clear contraindications in settings where both options are available, patient preference should prevail, Dr. Prager, director of the family planning division and family planning fellowship at the University of Washington, Seattle, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
However, shared decision-making is imperative, she said.
Shared decision-making “can be extremely important for satisfaction with this process,” she said, explaining that provider-driven decisions can be paternalistic and often are based on what the provider might do in the same situation.
“But that may not be what the patient wants,” she added.
Conversely, patient-led decision-making can lead to information overload.
“She’s coming to you because you’re the expert. She wants your opinion on this,” Dr. Prager said, noting that sharing the process through “information transfer” allows for the “best, most appropriate decision” to be made.
“Patient engagement is the practice of actively involving and supporting the patient in health care and treatment decision-making activities, and this is really what I’m talking about,” she said, adding that patient engagement is “critically important in many situations, and especially in the setting of pregnancy loss.”
That’s because patients feel powerless in this situation, she explained. Engaging them in the decision-making process can “give them a little bit of that power back” by respecting autonomy, enhancing agency, improving health status, reducing decisional conflict, and limiting test use, thereby improving overall satisfaction.
Two randomized control trials, each designed to compare surgical management and medical management for terminations at up to 20 weeks of gestation, highlight the role and importance of patient preference, Dr. Prager said.
The first – a 2004 study – was stopped early because of slow enrollment, with 29 of 47 eligible subjects declining randomization. Among 93% of those who declined, there was a preference for surgical management. The second, a 2010 study, enrolled 122 patients after 107 of 229 eligible subjects (47%) declined randomization, again because most (67%) preferred surgery (BJOG. 2004;111[2]:148-53; BJOG. 2010;117[12]:1512-20).
Reasons given for preferring surgical management included less psychological trauma and deeper anesthesia, whereas reasons given for induction preference included less wait time and a desire to avoid general anesthesia.
Helping patients make the best decision requires a discussion about potential complications for each approach, Dr. Prager said.
Surgical management, which involves dilation and evacuation (D&E), is used for about 95% of second-trimester abortions overall, but medical management may be underreported, particularly for management of pregnancy loss, Dr. Prager said. “We don’t have clear statistics” in that setting.
The overall rate of complications is low for surgical management, with data suggesting a rate of up to 4%. Uterine perforation occurs in 0.2%-0.3% of procedures, cervical laceration occurs in up to 1%, and retained placenta occurs in less than 1%, she said.
The complication rate for medical management – induction with either misoprostol or mifepristone + misoprostol (the latter is the recommended approach) – is much higher at up to 29%, but that includes retained placenta, which happens in up to 10% of procedures. Uterine rupture occurs in 0.04%-0.28% of procedures, she said.
“With either surgical management or medication management of pregnancy loss, we need to keep in mind the possibility of disseminated intravascular coagulation, which is rare, but certainly possible,” she said.
Other factors that may be important to patients deciding between surgical and medical management for second-trimester fetal loss include:
- Anesthesia, which is local plus intravenous sedation for surgery, compared with IV narcotics and potentially an epidural or other type of regional anesthesia for medical management.
- Duration, which is 5-20 minutes for surgery, compared with 6-11 hours with mifepristone + misoprostol, and up to 20 hours with misoprostol alone.
- Location, which is done on an outpatient basis for surgery, compared with inpatient care for medical management.
- Cost, which is $1,000-$5,000 for surgery vs. $3,000-$9,000 for medical management.
- Contact with the fetus, which typically involves the possibility of partial viewing and an opportunity to obtain footprints as a memento if an intact procedure is attempted during surgery vs. full viewing and possibly holding the baby after delivery following medical management. This is often the key deciding factor for patients.
- Provider factors, in terms of training and skills. Surgery involves a need for specialized training, whereas medical management requires no extra training, she said, adding that “not all ob.gyns. across the country are competent or comfortable providing a D&E, particularly in the later second-trimester time period.” However, the availability of family planing fellowships will increase the number of centers across the country where both options will be available, she noted.
- The possibility of fetal autopsy, which surgery often (but not always) allows, but medical management always allows.
- Involvement level, which is provider heavy for surgery vs. patient heavy for medical management.
“Moving toward an evidence-based, patient-centered care model requires a lot of us, as providers, to really work at dropping our assumptions. We often have strong opinions about what we think we would do in that setting, and it can be tricky for us to set that aside and allow patients to really ask questions and discuss their values so that we can then advocate best for our patients after they know exactly what their options are,” she said.
Dr. Prager reported having no relevant disclosures.
NASHVILLE, TENN. – , according to Sarah W. Prager, MD.
Therefore, in the absence of clear contraindications in settings where both options are available, patient preference should prevail, Dr. Prager, director of the family planning division and family planning fellowship at the University of Washington, Seattle, said at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
However, shared decision-making is imperative, she said.
Shared decision-making “can be extremely important for satisfaction with this process,” she said, explaining that provider-driven decisions can be paternalistic and often are based on what the provider might do in the same situation.
“But that may not be what the patient wants,” she added.
Conversely, patient-led decision-making can lead to information overload.
“She’s coming to you because you’re the expert. She wants your opinion on this,” Dr. Prager said, noting that sharing the process through “information transfer” allows for the “best, most appropriate decision” to be made.
“Patient engagement is the practice of actively involving and supporting the patient in health care and treatment decision-making activities, and this is really what I’m talking about,” she said, adding that patient engagement is “critically important in many situations, and especially in the setting of pregnancy loss.”
That’s because patients feel powerless in this situation, she explained. Engaging them in the decision-making process can “give them a little bit of that power back” by respecting autonomy, enhancing agency, improving health status, reducing decisional conflict, and limiting test use, thereby improving overall satisfaction.
Two randomized control trials, each designed to compare surgical management and medical management for terminations at up to 20 weeks of gestation, highlight the role and importance of patient preference, Dr. Prager said.
The first – a 2004 study – was stopped early because of slow enrollment, with 29 of 47 eligible subjects declining randomization. Among 93% of those who declined, there was a preference for surgical management. The second, a 2010 study, enrolled 122 patients after 107 of 229 eligible subjects (47%) declined randomization, again because most (67%) preferred surgery (BJOG. 2004;111[2]:148-53; BJOG. 2010;117[12]:1512-20).
Reasons given for preferring surgical management included less psychological trauma and deeper anesthesia, whereas reasons given for induction preference included less wait time and a desire to avoid general anesthesia.
Helping patients make the best decision requires a discussion about potential complications for each approach, Dr. Prager said.
Surgical management, which involves dilation and evacuation (D&E), is used for about 95% of second-trimester abortions overall, but medical management may be underreported, particularly for management of pregnancy loss, Dr. Prager said. “We don’t have clear statistics” in that setting.
The overall rate of complications is low for surgical management, with data suggesting a rate of up to 4%. Uterine perforation occurs in 0.2%-0.3% of procedures, cervical laceration occurs in up to 1%, and retained placenta occurs in less than 1%, she said.
The complication rate for medical management – induction with either misoprostol or mifepristone + misoprostol (the latter is the recommended approach) – is much higher at up to 29%, but that includes retained placenta, which happens in up to 10% of procedures. Uterine rupture occurs in 0.04%-0.28% of procedures, she said.
“With either surgical management or medication management of pregnancy loss, we need to keep in mind the possibility of disseminated intravascular coagulation, which is rare, but certainly possible,” she said.
Other factors that may be important to patients deciding between surgical and medical management for second-trimester fetal loss include:
- Anesthesia, which is local plus intravenous sedation for surgery, compared with IV narcotics and potentially an epidural or other type of regional anesthesia for medical management.
- Duration, which is 5-20 minutes for surgery, compared with 6-11 hours with mifepristone + misoprostol, and up to 20 hours with misoprostol alone.
- Location, which is done on an outpatient basis for surgery, compared with inpatient care for medical management.
- Cost, which is $1,000-$5,000 for surgery vs. $3,000-$9,000 for medical management.
- Contact with the fetus, which typically involves the possibility of partial viewing and an opportunity to obtain footprints as a memento if an intact procedure is attempted during surgery vs. full viewing and possibly holding the baby after delivery following medical management. This is often the key deciding factor for patients.
- Provider factors, in terms of training and skills. Surgery involves a need for specialized training, whereas medical management requires no extra training, she said, adding that “not all ob.gyns. across the country are competent or comfortable providing a D&E, particularly in the later second-trimester time period.” However, the availability of family planing fellowships will increase the number of centers across the country where both options will be available, she noted.
- The possibility of fetal autopsy, which surgery often (but not always) allows, but medical management always allows.
- Involvement level, which is provider heavy for surgery vs. patient heavy for medical management.
“Moving toward an evidence-based, patient-centered care model requires a lot of us, as providers, to really work at dropping our assumptions. We often have strong opinions about what we think we would do in that setting, and it can be tricky for us to set that aside and allow patients to really ask questions and discuss their values so that we can then advocate best for our patients after they know exactly what their options are,” she said.
Dr. Prager reported having no relevant disclosures.
EXPERT ANALYSIS FROM ACOG 2019
Fetal alcohol exposure overlooked again?
New study on large youth sample is well done – with a glaring exception
In 2016, two researchers published a meta-analysis on gray matter abnormalities in youth who had conduct problems.
The study by Jack C. Rogers, PhD, and Stephane A. De Brito, PhD, found 13 well-done studies that included 394 youth with conduct problems and 390 typically developing youth. Compared with the typically developing youth, the conduct-disordered youth had decreased gray matter volume (JAMA Psychiatry. 2016 Jan;73[1]:64-72).
As I knew one of the researchers in one of the studies that made the cut, I called him up and asked whether their research had controlled for fetal alcohol exposure. They had not. I found this very curious because my experience is that youth who have been labeled with conduct disorder often have histories of prenatal fetal alcohol exposure. In addition, my understanding is that youth who have been exposed to prenatal alcohol often have symptoms of conduct disorder. Furthermore, research has shown that such youth have smaller brains (Dev Med Child Neurol. 2001 Mar;43[3]:148-54). I wondered whether the youth studied in that trial had been exposed to alcohol prenatally.
More recently, this problem has resurfaced. An article by Antonia N. Kaczkurkin, PhD, and associates about a large sample of youth was nicely done. But again, the variable of fetal alcohol exposure was not considered. The study was an elegant one that provides a strong rationale for consideration of a “psychopathology factor” in human life (Am J Psychiatry. 2019 Jun 24. doi: 10.1176/appi.ajp.2019.1807035). It shored up that argument by doing neuroimaging studies on a reasonably large sample of youth and showed that reduced cortical thickness (gray matter volume) was associated with overall psychopathology. With the exception of failing to consider the variable of fetal alcohol exposure, the study is a valuable addition to our understanding of what might be going on with psychiatric disorders.
Unfortunately – while hating to sound like a broken record – I noticed that there was no consideration of fetal alcohol exposure as a cause for the findings of the study. It does not seem like a large leap to hypothesize some of these brain imaging studies that find smaller brain components associated with psychopathology and conduct disorder to be a dynamic of fetal alcohol exposure.
It seems to me that we made a huge mistake in public health in asking women only whether they were drinking while they were pregnant because it was the wrong question. The right question is – “When did you realize you were pregnant, and were you doing any social drinking before you knew you were pregnant?”
The former editor of the American Journal of Psychiatry – Robert A. Freedman, MD – suggests that by giving phosphatidyl choline to pregnant women, such problems could be prevented.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago. In 2019, he was awarded the Adolph Meyer Award by the American Psychiatric Association for lifetime achievement in psychiatric research.
New study on large youth sample is well done – with a glaring exception
New study on large youth sample is well done – with a glaring exception
In 2016, two researchers published a meta-analysis on gray matter abnormalities in youth who had conduct problems.
The study by Jack C. Rogers, PhD, and Stephane A. De Brito, PhD, found 13 well-done studies that included 394 youth with conduct problems and 390 typically developing youth. Compared with the typically developing youth, the conduct-disordered youth had decreased gray matter volume (JAMA Psychiatry. 2016 Jan;73[1]:64-72).
As I knew one of the researchers in one of the studies that made the cut, I called him up and asked whether their research had controlled for fetal alcohol exposure. They had not. I found this very curious because my experience is that youth who have been labeled with conduct disorder often have histories of prenatal fetal alcohol exposure. In addition, my understanding is that youth who have been exposed to prenatal alcohol often have symptoms of conduct disorder. Furthermore, research has shown that such youth have smaller brains (Dev Med Child Neurol. 2001 Mar;43[3]:148-54). I wondered whether the youth studied in that trial had been exposed to alcohol prenatally.
More recently, this problem has resurfaced. An article by Antonia N. Kaczkurkin, PhD, and associates about a large sample of youth was nicely done. But again, the variable of fetal alcohol exposure was not considered. The study was an elegant one that provides a strong rationale for consideration of a “psychopathology factor” in human life (Am J Psychiatry. 2019 Jun 24. doi: 10.1176/appi.ajp.2019.1807035). It shored up that argument by doing neuroimaging studies on a reasonably large sample of youth and showed that reduced cortical thickness (gray matter volume) was associated with overall psychopathology. With the exception of failing to consider the variable of fetal alcohol exposure, the study is a valuable addition to our understanding of what might be going on with psychiatric disorders.
Unfortunately – while hating to sound like a broken record – I noticed that there was no consideration of fetal alcohol exposure as a cause for the findings of the study. It does not seem like a large leap to hypothesize some of these brain imaging studies that find smaller brain components associated with psychopathology and conduct disorder to be a dynamic of fetal alcohol exposure.
It seems to me that we made a huge mistake in public health in asking women only whether they were drinking while they were pregnant because it was the wrong question. The right question is – “When did you realize you were pregnant, and were you doing any social drinking before you knew you were pregnant?”
The former editor of the American Journal of Psychiatry – Robert A. Freedman, MD – suggests that by giving phosphatidyl choline to pregnant women, such problems could be prevented.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago. In 2019, he was awarded the Adolph Meyer Award by the American Psychiatric Association for lifetime achievement in psychiatric research.
In 2016, two researchers published a meta-analysis on gray matter abnormalities in youth who had conduct problems.
The study by Jack C. Rogers, PhD, and Stephane A. De Brito, PhD, found 13 well-done studies that included 394 youth with conduct problems and 390 typically developing youth. Compared with the typically developing youth, the conduct-disordered youth had decreased gray matter volume (JAMA Psychiatry. 2016 Jan;73[1]:64-72).
As I knew one of the researchers in one of the studies that made the cut, I called him up and asked whether their research had controlled for fetal alcohol exposure. They had not. I found this very curious because my experience is that youth who have been labeled with conduct disorder often have histories of prenatal fetal alcohol exposure. In addition, my understanding is that youth who have been exposed to prenatal alcohol often have symptoms of conduct disorder. Furthermore, research has shown that such youth have smaller brains (Dev Med Child Neurol. 2001 Mar;43[3]:148-54). I wondered whether the youth studied in that trial had been exposed to alcohol prenatally.
More recently, this problem has resurfaced. An article by Antonia N. Kaczkurkin, PhD, and associates about a large sample of youth was nicely done. But again, the variable of fetal alcohol exposure was not considered. The study was an elegant one that provides a strong rationale for consideration of a “psychopathology factor” in human life (Am J Psychiatry. 2019 Jun 24. doi: 10.1176/appi.ajp.2019.1807035). It shored up that argument by doing neuroimaging studies on a reasonably large sample of youth and showed that reduced cortical thickness (gray matter volume) was associated with overall psychopathology. With the exception of failing to consider the variable of fetal alcohol exposure, the study is a valuable addition to our understanding of what might be going on with psychiatric disorders.
Unfortunately – while hating to sound like a broken record – I noticed that there was no consideration of fetal alcohol exposure as a cause for the findings of the study. It does not seem like a large leap to hypothesize some of these brain imaging studies that find smaller brain components associated with psychopathology and conduct disorder to be a dynamic of fetal alcohol exposure.
It seems to me that we made a huge mistake in public health in asking women only whether they were drinking while they were pregnant because it was the wrong question. The right question is – “When did you realize you were pregnant, and were you doing any social drinking before you knew you were pregnant?”
The former editor of the American Journal of Psychiatry – Robert A. Freedman, MD – suggests that by giving phosphatidyl choline to pregnant women, such problems could be prevented.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago. In 2019, he was awarded the Adolph Meyer Award by the American Psychiatric Association for lifetime achievement in psychiatric research.
U.S. fertility rate, teen births are on the decline
The general fertility rate in the United States decreased 2% between 2017 and 2018, according to a report from the Centers for Disease Control and Prevention.
Fertility rates, defined as births per 1,000 women aged 15-44 years, declined for all racial/ethnic groups studied.
Teen birth rates, or births among girls aged 15-19 years, declined from 2017 to 2018 as well.
These data come from the National Vital Statistics System’s Natality Data File, which includes information from birth certificates for all births in the United States.
The data show a decline in the general fertility rate from 60.3 per 1,000 women in 2017 to 59.1 per 1,000 women in 2018, a significant decrease (P less than .05).
Fertility rates declined across the three largest racial/ethnic groups studied, decreasing:
- 3% in Hispanic women, from 67.6 to 65.9 per 1,000.
- 2% in non-Hispanic black women, from 63.1 to 62.0 per 1,000.
- 2% in non-Hispanic white women, from 57.2 to 56.3 per 1,000.
Similarly, teen birth rates declined 7% from 2017 to 2018, decreasing from 18.8 to 17.4 births per 1,000 girls aged 15-19 years (P less than .05). Rates decreased:
- 8% in Hispanic teens, from 28.9 to 26.7 per 1,000.
- 4% in non-Hispanic black teens, from 27.5 to 26.3 per 1,000.
- 8% in non-Hispanic white teens, from 13.2 to 12.1 per 1,000.
The data also show an increase in the rate of vaginal births after previous cesarean (VBAC) delivery. The percentage of VBAC deliveries increased from 12.8% in 2017 to 13.3% in 2018 (P less than .05).
VBAC delivery rates increased across all racial/ethnic groups studied, although the increase among non-Hispanic back women was not significant.
Finally, the report shows an increase in preterm and early term births from 2017 to 2018. Preterm deliveries (less than 37 weeks of gestation) increased from 9.93% to 10.02%, and early term deliveries (37-38 weeks) increased from 26.00% to 26.53% (P less than .05).
At the same time, full-term births (39-40 weeks) decreased from 57.49% to 57.24%, and late- and post-term births (41 weeks or more) decreased from 6.58 % to 6.20% (P less than .05). These findings were consistent across the racial/ethnic groups studied.
SOURCE: Martin JA et al. NCHS Data Brief. 2019 July; no 346.
The general fertility rate in the United States decreased 2% between 2017 and 2018, according to a report from the Centers for Disease Control and Prevention.
Fertility rates, defined as births per 1,000 women aged 15-44 years, declined for all racial/ethnic groups studied.
Teen birth rates, or births among girls aged 15-19 years, declined from 2017 to 2018 as well.
These data come from the National Vital Statistics System’s Natality Data File, which includes information from birth certificates for all births in the United States.
The data show a decline in the general fertility rate from 60.3 per 1,000 women in 2017 to 59.1 per 1,000 women in 2018, a significant decrease (P less than .05).
Fertility rates declined across the three largest racial/ethnic groups studied, decreasing:
- 3% in Hispanic women, from 67.6 to 65.9 per 1,000.
- 2% in non-Hispanic black women, from 63.1 to 62.0 per 1,000.
- 2% in non-Hispanic white women, from 57.2 to 56.3 per 1,000.
Similarly, teen birth rates declined 7% from 2017 to 2018, decreasing from 18.8 to 17.4 births per 1,000 girls aged 15-19 years (P less than .05). Rates decreased:
- 8% in Hispanic teens, from 28.9 to 26.7 per 1,000.
- 4% in non-Hispanic black teens, from 27.5 to 26.3 per 1,000.
- 8% in non-Hispanic white teens, from 13.2 to 12.1 per 1,000.
The data also show an increase in the rate of vaginal births after previous cesarean (VBAC) delivery. The percentage of VBAC deliveries increased from 12.8% in 2017 to 13.3% in 2018 (P less than .05).
VBAC delivery rates increased across all racial/ethnic groups studied, although the increase among non-Hispanic back women was not significant.
Finally, the report shows an increase in preterm and early term births from 2017 to 2018. Preterm deliveries (less than 37 weeks of gestation) increased from 9.93% to 10.02%, and early term deliveries (37-38 weeks) increased from 26.00% to 26.53% (P less than .05).
At the same time, full-term births (39-40 weeks) decreased from 57.49% to 57.24%, and late- and post-term births (41 weeks or more) decreased from 6.58 % to 6.20% (P less than .05). These findings were consistent across the racial/ethnic groups studied.
SOURCE: Martin JA et al. NCHS Data Brief. 2019 July; no 346.
The general fertility rate in the United States decreased 2% between 2017 and 2018, according to a report from the Centers for Disease Control and Prevention.
Fertility rates, defined as births per 1,000 women aged 15-44 years, declined for all racial/ethnic groups studied.
Teen birth rates, or births among girls aged 15-19 years, declined from 2017 to 2018 as well.
These data come from the National Vital Statistics System’s Natality Data File, which includes information from birth certificates for all births in the United States.
The data show a decline in the general fertility rate from 60.3 per 1,000 women in 2017 to 59.1 per 1,000 women in 2018, a significant decrease (P less than .05).
Fertility rates declined across the three largest racial/ethnic groups studied, decreasing:
- 3% in Hispanic women, from 67.6 to 65.9 per 1,000.
- 2% in non-Hispanic black women, from 63.1 to 62.0 per 1,000.
- 2% in non-Hispanic white women, from 57.2 to 56.3 per 1,000.
Similarly, teen birth rates declined 7% from 2017 to 2018, decreasing from 18.8 to 17.4 births per 1,000 girls aged 15-19 years (P less than .05). Rates decreased:
- 8% in Hispanic teens, from 28.9 to 26.7 per 1,000.
- 4% in non-Hispanic black teens, from 27.5 to 26.3 per 1,000.
- 8% in non-Hispanic white teens, from 13.2 to 12.1 per 1,000.
The data also show an increase in the rate of vaginal births after previous cesarean (VBAC) delivery. The percentage of VBAC deliveries increased from 12.8% in 2017 to 13.3% in 2018 (P less than .05).
VBAC delivery rates increased across all racial/ethnic groups studied, although the increase among non-Hispanic back women was not significant.
Finally, the report shows an increase in preterm and early term births from 2017 to 2018. Preterm deliveries (less than 37 weeks of gestation) increased from 9.93% to 10.02%, and early term deliveries (37-38 weeks) increased from 26.00% to 26.53% (P less than .05).
At the same time, full-term births (39-40 weeks) decreased from 57.49% to 57.24%, and late- and post-term births (41 weeks or more) decreased from 6.58 % to 6.20% (P less than .05). These findings were consistent across the racial/ethnic groups studied.
SOURCE: Martin JA et al. NCHS Data Brief. 2019 July; no 346.














