User login
BCMA-targeted platforms could alter MM therapy
New York—Three novel treatment strategies that target B-cell maturation antigen (BCMA) are showing promise in recent multiple myeloma (MM) clinical trials, according to Shaji K. Kumar, MD, of Mayo Clinic Cancer Center in Rochester, Minnesota.
The strategies include B-cell maturation antigen (BCMA) antibody-drug conjugate, BCMA-specific chimeric antigen receptor (CAR) T-cell therapies, and bispecific T-cell engagers (BiTEs).
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these 3 platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar told attendees at the NCCN 13th Annual Congress: Hematologic Malignancies.
BCMA is required for plasma cell survival and is broadly expressed on malignant plasma cells.
BCMA antibody-drug conjugate
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent. It produced an overall response rate of 67% at the 2 highest dose levels in 9 MM patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, he said, including in an upcoming phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone or bortezomib plus dexamethasone in patients with relapsed or refractory disease.
BCMA-specific CAR T-cell therapy
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma, according to Dr. Kumar, involves bb2121. bb2121 showed durable clinical responses in heavily pretreated patients, according to an ASH 2017 presentation.
“The overall response rate is quite significant,” Dr. Kumar said. He related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the responses were lasting, he said, with 5 patients in ongoing response for more than a year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar added.
Another novel CAR T-cell product, LCAR-B38M, has demonstrated promising results. LCAR-B38M principally targets BCMA and has led to a significant number of patients achieving stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and different costimulatory molecules are currently in clinical trials, Dr. Kumar said.
BiTEs
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short timeframe, so having an approach that is off-the-shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies to watch that are under investigation include AMG 420 and PF-06863135, he said.
New York—Three novel treatment strategies that target B-cell maturation antigen (BCMA) are showing promise in recent multiple myeloma (MM) clinical trials, according to Shaji K. Kumar, MD, of Mayo Clinic Cancer Center in Rochester, Minnesota.
The strategies include B-cell maturation antigen (BCMA) antibody-drug conjugate, BCMA-specific chimeric antigen receptor (CAR) T-cell therapies, and bispecific T-cell engagers (BiTEs).
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these 3 platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar told attendees at the NCCN 13th Annual Congress: Hematologic Malignancies.
BCMA is required for plasma cell survival and is broadly expressed on malignant plasma cells.
BCMA antibody-drug conjugate
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent. It produced an overall response rate of 67% at the 2 highest dose levels in 9 MM patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, he said, including in an upcoming phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone or bortezomib plus dexamethasone in patients with relapsed or refractory disease.
BCMA-specific CAR T-cell therapy
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma, according to Dr. Kumar, involves bb2121. bb2121 showed durable clinical responses in heavily pretreated patients, according to an ASH 2017 presentation.
“The overall response rate is quite significant,” Dr. Kumar said. He related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the responses were lasting, he said, with 5 patients in ongoing response for more than a year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar added.
Another novel CAR T-cell product, LCAR-B38M, has demonstrated promising results. LCAR-B38M principally targets BCMA and has led to a significant number of patients achieving stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and different costimulatory molecules are currently in clinical trials, Dr. Kumar said.
BiTEs
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short timeframe, so having an approach that is off-the-shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies to watch that are under investigation include AMG 420 and PF-06863135, he said.
New York—Three novel treatment strategies that target B-cell maturation antigen (BCMA) are showing promise in recent multiple myeloma (MM) clinical trials, according to Shaji K. Kumar, MD, of Mayo Clinic Cancer Center in Rochester, Minnesota.
The strategies include B-cell maturation antigen (BCMA) antibody-drug conjugate, BCMA-specific chimeric antigen receptor (CAR) T-cell therapies, and bispecific T-cell engagers (BiTEs).
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these 3 platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar told attendees at the NCCN 13th Annual Congress: Hematologic Malignancies.
BCMA is required for plasma cell survival and is broadly expressed on malignant plasma cells.
BCMA antibody-drug conjugate
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent. It produced an overall response rate of 67% at the 2 highest dose levels in 9 MM patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, he said, including in an upcoming phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone or bortezomib plus dexamethasone in patients with relapsed or refractory disease.
BCMA-specific CAR T-cell therapy
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma, according to Dr. Kumar, involves bb2121. bb2121 showed durable clinical responses in heavily pretreated patients, according to an ASH 2017 presentation.
“The overall response rate is quite significant,” Dr. Kumar said. He related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the responses were lasting, he said, with 5 patients in ongoing response for more than a year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar added.
Another novel CAR T-cell product, LCAR-B38M, has demonstrated promising results. LCAR-B38M principally targets BCMA and has led to a significant number of patients achieving stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and different costimulatory molecules are currently in clinical trials, Dr. Kumar said.
BiTEs
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short timeframe, so having an approach that is off-the-shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies to watch that are under investigation include AMG 420 and PF-06863135, he said.
FDA authorizes ClonoSEQ to detect MRD in ALL, myeloma
, the U.S. Food and Drug Administration announced. Marketing authorization of the ClonoSEQ assay was granted to Adaptive Biotechnologies.
The ClonoSEQ assay is an in vitro diagnostic test that uses multiplex polymerase chain reaction and next-generation sequencing to identify and quantify certain gene sequences in DNA extracted from the bone marrow from patients with ALL or multiple myeloma. This is a single-site assay collected by the patient’s provider and sent to Adaptive Biotechnologies for evaluation.
The ClonoSEQ assay is capable of detecting minimal residual disease at levels below 1 in 1 million cells. Currently, providers test for MRD using flow cytometry assays or polymerase chain reaction–based assays. Those methods are usually capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
“Determining whether a patient has residual cancer cells remaining after treatment provides information on how well a patient has responded to therapy and how long remission may last. Having a highly sensitive test available to measure minimal residual disease in ALL or multiple myeloma patients can help providers manage their patients’ care,” FDA Commissioner Scott Gottlieb, MD, said in a press release.
Along with this authorization, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the accuracy, reliability, and effectiveness of tests intended to be used as an aid to measure MRD to assess the change in burden of disease during and after treatment. These special controls, when met along with general controls, provide a reasonable assurance of safety and effectiveness for these tests, the agency said in the release. This action also creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through the FDA’s 510(k) process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a previously approved device.
“The FDA is applying novel regulatory approaches to make sure that these rapidly evolving [next-generation sequencing] tests are accurate and reliable. At the same time, we’re seeing more and more laboratory-developed tests seek marketing authorization from the FDA,” he said, adding that the agency has put forward a plan to modernize the regulatory framework for all in vitro clinical tests.
The FDA evaluated data to demonstrate clinical validity from a retrospective analysis of samples obtained from three previously conducted clinical studies including 273 patients with ALL, an ongoing study of 323 patients with multiple myeloma, and a study of 706 patients with multiple myeloma, according to the FDA release.
For patients with ALL, the ClonoSEQ assay was used to assess MRD at various disease burden thresholds to show that the MRD level correlated with event-free survival – the length of time, after treatment, that the patient remains free of certain complications or events. Patients whose ClonoSEQ assay result was MRD negative had longer event-free survival, while patients with higher MRD assay results had lower event-free survival. Similar patterns of results were seen for progression-free and disease-free survival in patients with multiple myeloma.
, the U.S. Food and Drug Administration announced. Marketing authorization of the ClonoSEQ assay was granted to Adaptive Biotechnologies.
The ClonoSEQ assay is an in vitro diagnostic test that uses multiplex polymerase chain reaction and next-generation sequencing to identify and quantify certain gene sequences in DNA extracted from the bone marrow from patients with ALL or multiple myeloma. This is a single-site assay collected by the patient’s provider and sent to Adaptive Biotechnologies for evaluation.
The ClonoSEQ assay is capable of detecting minimal residual disease at levels below 1 in 1 million cells. Currently, providers test for MRD using flow cytometry assays or polymerase chain reaction–based assays. Those methods are usually capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
“Determining whether a patient has residual cancer cells remaining after treatment provides information on how well a patient has responded to therapy and how long remission may last. Having a highly sensitive test available to measure minimal residual disease in ALL or multiple myeloma patients can help providers manage their patients’ care,” FDA Commissioner Scott Gottlieb, MD, said in a press release.
Along with this authorization, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the accuracy, reliability, and effectiveness of tests intended to be used as an aid to measure MRD to assess the change in burden of disease during and after treatment. These special controls, when met along with general controls, provide a reasonable assurance of safety and effectiveness for these tests, the agency said in the release. This action also creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through the FDA’s 510(k) process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a previously approved device.
“The FDA is applying novel regulatory approaches to make sure that these rapidly evolving [next-generation sequencing] tests are accurate and reliable. At the same time, we’re seeing more and more laboratory-developed tests seek marketing authorization from the FDA,” he said, adding that the agency has put forward a plan to modernize the regulatory framework for all in vitro clinical tests.
The FDA evaluated data to demonstrate clinical validity from a retrospective analysis of samples obtained from three previously conducted clinical studies including 273 patients with ALL, an ongoing study of 323 patients with multiple myeloma, and a study of 706 patients with multiple myeloma, according to the FDA release.
For patients with ALL, the ClonoSEQ assay was used to assess MRD at various disease burden thresholds to show that the MRD level correlated with event-free survival – the length of time, after treatment, that the patient remains free of certain complications or events. Patients whose ClonoSEQ assay result was MRD negative had longer event-free survival, while patients with higher MRD assay results had lower event-free survival. Similar patterns of results were seen for progression-free and disease-free survival in patients with multiple myeloma.
, the U.S. Food and Drug Administration announced. Marketing authorization of the ClonoSEQ assay was granted to Adaptive Biotechnologies.
The ClonoSEQ assay is an in vitro diagnostic test that uses multiplex polymerase chain reaction and next-generation sequencing to identify and quantify certain gene sequences in DNA extracted from the bone marrow from patients with ALL or multiple myeloma. This is a single-site assay collected by the patient’s provider and sent to Adaptive Biotechnologies for evaluation.
The ClonoSEQ assay is capable of detecting minimal residual disease at levels below 1 in 1 million cells. Currently, providers test for MRD using flow cytometry assays or polymerase chain reaction–based assays. Those methods are usually capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
“Determining whether a patient has residual cancer cells remaining after treatment provides information on how well a patient has responded to therapy and how long remission may last. Having a highly sensitive test available to measure minimal residual disease in ALL or multiple myeloma patients can help providers manage their patients’ care,” FDA Commissioner Scott Gottlieb, MD, said in a press release.
Along with this authorization, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the accuracy, reliability, and effectiveness of tests intended to be used as an aid to measure MRD to assess the change in burden of disease during and after treatment. These special controls, when met along with general controls, provide a reasonable assurance of safety and effectiveness for these tests, the agency said in the release. This action also creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through the FDA’s 510(k) process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a previously approved device.
“The FDA is applying novel regulatory approaches to make sure that these rapidly evolving [next-generation sequencing] tests are accurate and reliable. At the same time, we’re seeing more and more laboratory-developed tests seek marketing authorization from the FDA,” he said, adding that the agency has put forward a plan to modernize the regulatory framework for all in vitro clinical tests.
The FDA evaluated data to demonstrate clinical validity from a retrospective analysis of samples obtained from three previously conducted clinical studies including 273 patients with ALL, an ongoing study of 323 patients with multiple myeloma, and a study of 706 patients with multiple myeloma, according to the FDA release.
For patients with ALL, the ClonoSEQ assay was used to assess MRD at various disease burden thresholds to show that the MRD level correlated with event-free survival – the length of time, after treatment, that the patient remains free of certain complications or events. Patients whose ClonoSEQ assay result was MRD negative had longer event-free survival, while patients with higher MRD assay results had lower event-free survival. Similar patterns of results were seen for progression-free and disease-free survival in patients with multiple myeloma.
First NGS assay approved for MRD detection in ALL or MM
The U.S. Food and Drug Administration has authorized the first next-generation sequencing (NGS)-based assay to be marketed for minimal residual disease (MRD) testing in patients with acute lymphoblastic leukemia (ALL) or multiple myeloma (MM).
The assay, called clonoSEQ®, uses both polymerase chain reaction (PCR) and NGS to identify and quantify gene sequences in DNA from patients’ bone marrow.
ClonoSEQ Assay can detect MRD levels below 1 in 1 million cells. By comparison flow cytometry assays or PCR-based assays are capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
The clonoSEQ Assay is marketed by Adaptive Biotechnologies.
The FDA based its authorization on data from three clinical studies, one with 273 ALL patients, an ongoing study of 323 MM patients, and another MM trial with 706 patients.
Validation in ALL
As described in the clonoSEQ Assay Technical Information, a subset of 273 patients originally enrolled in the Children’s Oncology Group AALL0232 (NCT00075725) and AALL0331 (NCT00103285) studies had left-over bone marrow specimens to evaluate the performance of the clonoSEQ Assay.
MRD as determined by MRD negativity at less than 10-4 predicted improved event-free survival (EFS) irrespective of age. MRD-positive patients had a 2.74 higher event risk compared to MRD-negative patients.
Similar findings between MRD negativity and EFS in pediatric ALL using an earlier version of the assay were published in Blood.
Validation in MM
The ongoing phase 3 DFCI Study 10-106 (NCT01208662) is comparing conventional treatment with lenalidomide, bortezomib and dexamethasone to high-dose treatment with stem cell transplant as initial management of MM patients less than 65 years.
According to clonoSEQ’s technical information, bone marrow samples from 323 of the 720 patients originally enrolled were available and evaluable for MRD assessment.
ClonoSEQ measurements demonstrated that MRD status at a threshold of 10-5 significantly predicts progression-free survival (PFS) in all patients (P=0.027).
And samples from 75 patients who had achieved complete remission (CR) showed a modest association with disease-free survival (DFS) and lower MRD levels (P=0.064).
In the phase 3 ALCYONE trial, investigators randomly assigned 706 treatment-naïve MM patients ineligible for hematopoietic stem cell transplant to bortezomib, melphalan, and prednisone with or without daratumumab.
MRD assessments were made using the clonoSEQ Assay at screening, at confirmation of CR or stringent CR, and at intervals after patients achieved a CR.
Patients who did not achieve CR were considered MRD positive. The threshold for the MRD analysis was 10-5.
Investigators found that patients who were MRD negative by the clonoSEQ Assay had longer PFS compared to MRD-positive patients, regardless of treatment group.
For additional information on the clonoSEQ Assay consult the Technical Information available online.
The U.S. Food and Drug Administration has authorized the first next-generation sequencing (NGS)-based assay to be marketed for minimal residual disease (MRD) testing in patients with acute lymphoblastic leukemia (ALL) or multiple myeloma (MM).
The assay, called clonoSEQ®, uses both polymerase chain reaction (PCR) and NGS to identify and quantify gene sequences in DNA from patients’ bone marrow.
ClonoSEQ Assay can detect MRD levels below 1 in 1 million cells. By comparison flow cytometry assays or PCR-based assays are capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
The clonoSEQ Assay is marketed by Adaptive Biotechnologies.
The FDA based its authorization on data from three clinical studies, one with 273 ALL patients, an ongoing study of 323 MM patients, and another MM trial with 706 patients.
Validation in ALL
As described in the clonoSEQ Assay Technical Information, a subset of 273 patients originally enrolled in the Children’s Oncology Group AALL0232 (NCT00075725) and AALL0331 (NCT00103285) studies had left-over bone marrow specimens to evaluate the performance of the clonoSEQ Assay.
MRD as determined by MRD negativity at less than 10-4 predicted improved event-free survival (EFS) irrespective of age. MRD-positive patients had a 2.74 higher event risk compared to MRD-negative patients.
Similar findings between MRD negativity and EFS in pediatric ALL using an earlier version of the assay were published in Blood.
Validation in MM
The ongoing phase 3 DFCI Study 10-106 (NCT01208662) is comparing conventional treatment with lenalidomide, bortezomib and dexamethasone to high-dose treatment with stem cell transplant as initial management of MM patients less than 65 years.
According to clonoSEQ’s technical information, bone marrow samples from 323 of the 720 patients originally enrolled were available and evaluable for MRD assessment.
ClonoSEQ measurements demonstrated that MRD status at a threshold of 10-5 significantly predicts progression-free survival (PFS) in all patients (P=0.027).
And samples from 75 patients who had achieved complete remission (CR) showed a modest association with disease-free survival (DFS) and lower MRD levels (P=0.064).
In the phase 3 ALCYONE trial, investigators randomly assigned 706 treatment-naïve MM patients ineligible for hematopoietic stem cell transplant to bortezomib, melphalan, and prednisone with or without daratumumab.
MRD assessments were made using the clonoSEQ Assay at screening, at confirmation of CR or stringent CR, and at intervals after patients achieved a CR.
Patients who did not achieve CR were considered MRD positive. The threshold for the MRD analysis was 10-5.
Investigators found that patients who were MRD negative by the clonoSEQ Assay had longer PFS compared to MRD-positive patients, regardless of treatment group.
For additional information on the clonoSEQ Assay consult the Technical Information available online.
The U.S. Food and Drug Administration has authorized the first next-generation sequencing (NGS)-based assay to be marketed for minimal residual disease (MRD) testing in patients with acute lymphoblastic leukemia (ALL) or multiple myeloma (MM).
The assay, called clonoSEQ®, uses both polymerase chain reaction (PCR) and NGS to identify and quantify gene sequences in DNA from patients’ bone marrow.
ClonoSEQ Assay can detect MRD levels below 1 in 1 million cells. By comparison flow cytometry assays or PCR-based assays are capable of measuring MRD down to 1 in 10,000 or 1 in 100,000 cells.
The clonoSEQ Assay is marketed by Adaptive Biotechnologies.
The FDA based its authorization on data from three clinical studies, one with 273 ALL patients, an ongoing study of 323 MM patients, and another MM trial with 706 patients.
Validation in ALL
As described in the clonoSEQ Assay Technical Information, a subset of 273 patients originally enrolled in the Children’s Oncology Group AALL0232 (NCT00075725) and AALL0331 (NCT00103285) studies had left-over bone marrow specimens to evaluate the performance of the clonoSEQ Assay.
MRD as determined by MRD negativity at less than 10-4 predicted improved event-free survival (EFS) irrespective of age. MRD-positive patients had a 2.74 higher event risk compared to MRD-negative patients.
Similar findings between MRD negativity and EFS in pediatric ALL using an earlier version of the assay were published in Blood.
Validation in MM
The ongoing phase 3 DFCI Study 10-106 (NCT01208662) is comparing conventional treatment with lenalidomide, bortezomib and dexamethasone to high-dose treatment with stem cell transplant as initial management of MM patients less than 65 years.
According to clonoSEQ’s technical information, bone marrow samples from 323 of the 720 patients originally enrolled were available and evaluable for MRD assessment.
ClonoSEQ measurements demonstrated that MRD status at a threshold of 10-5 significantly predicts progression-free survival (PFS) in all patients (P=0.027).
And samples from 75 patients who had achieved complete remission (CR) showed a modest association with disease-free survival (DFS) and lower MRD levels (P=0.064).
In the phase 3 ALCYONE trial, investigators randomly assigned 706 treatment-naïve MM patients ineligible for hematopoietic stem cell transplant to bortezomib, melphalan, and prednisone with or without daratumumab.
MRD assessments were made using the clonoSEQ Assay at screening, at confirmation of CR or stringent CR, and at intervals after patients achieved a CR.
Patients who did not achieve CR were considered MRD positive. The threshold for the MRD analysis was 10-5.
Investigators found that patients who were MRD negative by the clonoSEQ Assay had longer PFS compared to MRD-positive patients, regardless of treatment group.
For additional information on the clonoSEQ Assay consult the Technical Information available online.
CHMP backs proposed biosimilars of pegfilgrastim
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for three proposed biosimilars of pegfilgrastim—Ziextenzo, Pelmeg, and Fulphila.
If approved by the European Commission (EC), these products would be used for the same indication as the reference medicine, Neulasta (pegfilgrastim).
Neulasta has been EC-approved since 2002 to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults who receive cytotoxic chemotherapy to treat malignancies except chronic myeloid leukemia and myelodysplastic syndromes.
According to the CHMP, data suggest that Ziextenzo, Pelmeg, and Fulphila all have quality, efficacy, and safety profiles comparable to Neulasta.
The EC is expected to make a decision on the approval of Ziextenzo, Pelmeg, and Fulphila within 67 days of the CHMP’s opinion.
The EC’s decision will apply to the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions based on the EC’s judgement.
Ziextenzo is being developed by Sandoz GmbH, Pelmeg is being developed by Cinfa Biotech S.L., and Fulphila is being developed by MYLAN S.A.S.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for three proposed biosimilars of pegfilgrastim—Ziextenzo, Pelmeg, and Fulphila.
If approved by the European Commission (EC), these products would be used for the same indication as the reference medicine, Neulasta (pegfilgrastim).
Neulasta has been EC-approved since 2002 to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults who receive cytotoxic chemotherapy to treat malignancies except chronic myeloid leukemia and myelodysplastic syndromes.
According to the CHMP, data suggest that Ziextenzo, Pelmeg, and Fulphila all have quality, efficacy, and safety profiles comparable to Neulasta.
The EC is expected to make a decision on the approval of Ziextenzo, Pelmeg, and Fulphila within 67 days of the CHMP’s opinion.
The EC’s decision will apply to the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions based on the EC’s judgement.
Ziextenzo is being developed by Sandoz GmbH, Pelmeg is being developed by Cinfa Biotech S.L., and Fulphila is being developed by MYLAN S.A.S.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for three proposed biosimilars of pegfilgrastim—Ziextenzo, Pelmeg, and Fulphila.
If approved by the European Commission (EC), these products would be used for the same indication as the reference medicine, Neulasta (pegfilgrastim).
Neulasta has been EC-approved since 2002 to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults who receive cytotoxic chemotherapy to treat malignancies except chronic myeloid leukemia and myelodysplastic syndromes.
According to the CHMP, data suggest that Ziextenzo, Pelmeg, and Fulphila all have quality, efficacy, and safety profiles comparable to Neulasta.
The EC is expected to make a decision on the approval of Ziextenzo, Pelmeg, and Fulphila within 67 days of the CHMP’s opinion.
The EC’s decision will apply to the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions based on the EC’s judgement.
Ziextenzo is being developed by Sandoz GmbH, Pelmeg is being developed by Cinfa Biotech S.L., and Fulphila is being developed by MYLAN S.A.S.
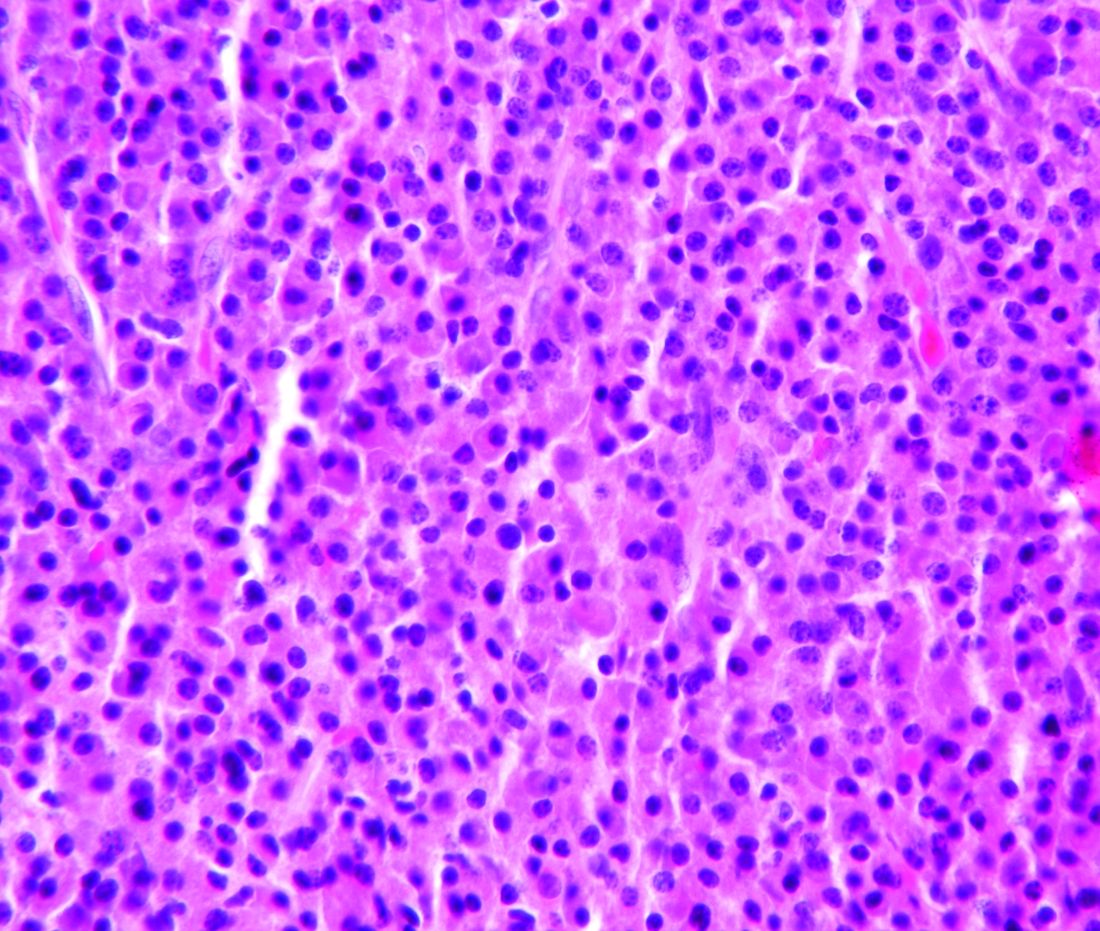
AKT inhibitor exhibits activity against MM
Preclinical research suggests an AKT inhibitor could be effective against multiple myeloma (MM).
The inhibitor, HS1793, is a derivative of the antioxidant compound resveratrol.
Investigators found that HS1793 decreased AKT signaling to induce mitochondria-mediated cell death in MM cells.
HS1793 was cytotoxic to MM cells in a mouse model of human metastatic myeloma and in human MM cells in vitro.
Jin Han, MD, PhD, of Inje University in Busan, South Korea, and colleagues reported these results in Cancer Letters.
“AKT is frequently activated in MM cells, and the incidence of AKT activation correlates positively with disease activity,” the authors noted.
They had screened 400 compounds and identified HS1793 as the most promising AKT inhibitor. Experiments suggested that HS1793 inhibits AKT activation by interfering with the interaction between AKT and its promoter, HSP90.
HS1793 exhibited antimyeloma activity in human MM cell lines. The investigators said this appeared to be from a dose-dependent effect that allowed for mitochondria-mediated programmed cell death.
In additional experiments, the team found that HS1793’s inhibition of AKT/HSP90 interaction results in cell death by suppressing NF-κB signaling. HS1793-induced cell death was caused by the direct inhibition of AKT that, in turn, suppressed NF-κB activation.
The investigators found that HS1793 “dramatically decreased” lytic skull and femur lesions in a mouse model of MM metastatic to bone. And mice that received HS1793 had superior survival, when compared to mice that received vehicle control.
The investigators also showed that HS1793 was cytotoxic to MM cells but not normal plasma cells isolated from patients with MM.
“Given that HS1793 treatment specifically induced the death of primary and relapsed MM cells, HS1793 offers excellent translational potential as a novel MM therapy,” the authors wrote.
This research was supported by grants from the Korean government. The investigators reported no potential conflicts of interest.
Preclinical research suggests an AKT inhibitor could be effective against multiple myeloma (MM).
The inhibitor, HS1793, is a derivative of the antioxidant compound resveratrol.
Investigators found that HS1793 decreased AKT signaling to induce mitochondria-mediated cell death in MM cells.
HS1793 was cytotoxic to MM cells in a mouse model of human metastatic myeloma and in human MM cells in vitro.
Jin Han, MD, PhD, of Inje University in Busan, South Korea, and colleagues reported these results in Cancer Letters.
“AKT is frequently activated in MM cells, and the incidence of AKT activation correlates positively with disease activity,” the authors noted.
They had screened 400 compounds and identified HS1793 as the most promising AKT inhibitor. Experiments suggested that HS1793 inhibits AKT activation by interfering with the interaction between AKT and its promoter, HSP90.
HS1793 exhibited antimyeloma activity in human MM cell lines. The investigators said this appeared to be from a dose-dependent effect that allowed for mitochondria-mediated programmed cell death.
In additional experiments, the team found that HS1793’s inhibition of AKT/HSP90 interaction results in cell death by suppressing NF-κB signaling. HS1793-induced cell death was caused by the direct inhibition of AKT that, in turn, suppressed NF-κB activation.
The investigators found that HS1793 “dramatically decreased” lytic skull and femur lesions in a mouse model of MM metastatic to bone. And mice that received HS1793 had superior survival, when compared to mice that received vehicle control.
The investigators also showed that HS1793 was cytotoxic to MM cells but not normal plasma cells isolated from patients with MM.
“Given that HS1793 treatment specifically induced the death of primary and relapsed MM cells, HS1793 offers excellent translational potential as a novel MM therapy,” the authors wrote.
This research was supported by grants from the Korean government. The investigators reported no potential conflicts of interest.
Preclinical research suggests an AKT inhibitor could be effective against multiple myeloma (MM).
The inhibitor, HS1793, is a derivative of the antioxidant compound resveratrol.
Investigators found that HS1793 decreased AKT signaling to induce mitochondria-mediated cell death in MM cells.
HS1793 was cytotoxic to MM cells in a mouse model of human metastatic myeloma and in human MM cells in vitro.
Jin Han, MD, PhD, of Inje University in Busan, South Korea, and colleagues reported these results in Cancer Letters.
“AKT is frequently activated in MM cells, and the incidence of AKT activation correlates positively with disease activity,” the authors noted.
They had screened 400 compounds and identified HS1793 as the most promising AKT inhibitor. Experiments suggested that HS1793 inhibits AKT activation by interfering with the interaction between AKT and its promoter, HSP90.
HS1793 exhibited antimyeloma activity in human MM cell lines. The investigators said this appeared to be from a dose-dependent effect that allowed for mitochondria-mediated programmed cell death.
In additional experiments, the team found that HS1793’s inhibition of AKT/HSP90 interaction results in cell death by suppressing NF-κB signaling. HS1793-induced cell death was caused by the direct inhibition of AKT that, in turn, suppressed NF-κB activation.
The investigators found that HS1793 “dramatically decreased” lytic skull and femur lesions in a mouse model of MM metastatic to bone. And mice that received HS1793 had superior survival, when compared to mice that received vehicle control.
The investigators also showed that HS1793 was cytotoxic to MM cells but not normal plasma cells isolated from patients with MM.
“Given that HS1793 treatment specifically induced the death of primary and relapsed MM cells, HS1793 offers excellent translational potential as a novel MM therapy,” the authors wrote.
This research was supported by grants from the Korean government. The investigators reported no potential conflicts of interest.
ASCO addresses financial barriers to cancer clinical trials
The American Society of Clinical Oncology (ASCO) has issued a policy statement addressing financial barriers to patient participation in cancer clinical trials.
ASCO’s policy statement outlines a series of recommendations designed to address multiple financial barriers that impede access to clinical trials, including patient costs that aren’t covered consistently by health insurance; a lack of information provided to patients about clinical trial costs; and limited available research data on financial hardships related to participation in clinical trials.
“Clinical trials are essential for evaluating the safety and efficacy of new cancer treatments, but cancer researchers have seen consistently low patient participation levels—especially among underserved patient populations—in part, due to the financial burdens facing many patients with cancer,” said ASCO President Monica M. Bertagnolli, MD.
“Addressing financial barriers will help improve the enrollment rate and the efficiency, quality, and applicability of cancer research. By including more—and more diverse—participants in our research studies, we expand our ability to care for all patients.”
The recommendations in ASCO’s policy statement include:
- Improve payer clinical trial coverage policies. Payment policies should be revised to be made consistent, streamlined, and transparent to all stakeholders.
- Payers should have clear definitions of “routine costs.”
- Payers should streamline prior authorization processes and facilitate trial enrollment through provider reimbursement of clinical trial-related services.
- State Medicaid programs should universally guarantee coverage of routine care costs of clinical trials for their beneficiaries.
- The U.S. Centers for Medicare & Medicaid Services (CMS) should revise current policy that requires Medicare Advantage beneficiaries to revert to fee-for-service coverage during clinical trials.
- CMS’s Innovation Center should explore the effectiveness of alternative payment models in support of clinical trial accrual.
- During the clinical trials development and enrollment process, provide patients with clear, transparent information about potential trial-related out-of-pocket costs and include mechanisms to support patient financial/health literacy.
- Clinical trial sponsors should perform—and make available to enrolling institutions—comprehensive, prospective coverage analyses.
- Research sites should consider offering in-house financial navigation/counseling to patients or consider partnering with organizations that provide such services.
- Design clinical trials to minimize incremental costs, consistent with scientific objectives and participant safety.
- Remove impediments to ethically appropriate financial compensation for trial-related out-of-pocket costs. Provision of such financial support should not be considered undue inducement.
- Office for Human Research Protections should develop guidance on targeted financial support.
- Incentivize research that will better characterize patient costs incurred for participating in cancer clinical trials and support the longer-term development of tools to identify and mitigate the risk of trial-associated financial hardship.
“Continued progress against cancer depends on improving patient access to participation in clinical research,” Dr. Bertagnolli said.
“The recommendations in ASCO’s statement aim to ensure that no patient is denied access to a clinical trial for financial reasons and that patients are not harmed financially because of their contributions to advancing science. Ultimately, this is about strengthening the nation’s cancer research enterprise as a whole.”
The American Society of Clinical Oncology (ASCO) has issued a policy statement addressing financial barriers to patient participation in cancer clinical trials.
ASCO’s policy statement outlines a series of recommendations designed to address multiple financial barriers that impede access to clinical trials, including patient costs that aren’t covered consistently by health insurance; a lack of information provided to patients about clinical trial costs; and limited available research data on financial hardships related to participation in clinical trials.
“Clinical trials are essential for evaluating the safety and efficacy of new cancer treatments, but cancer researchers have seen consistently low patient participation levels—especially among underserved patient populations—in part, due to the financial burdens facing many patients with cancer,” said ASCO President Monica M. Bertagnolli, MD.
“Addressing financial barriers will help improve the enrollment rate and the efficiency, quality, and applicability of cancer research. By including more—and more diverse—participants in our research studies, we expand our ability to care for all patients.”
The recommendations in ASCO’s policy statement include:
- Improve payer clinical trial coverage policies. Payment policies should be revised to be made consistent, streamlined, and transparent to all stakeholders.
- Payers should have clear definitions of “routine costs.”
- Payers should streamline prior authorization processes and facilitate trial enrollment through provider reimbursement of clinical trial-related services.
- State Medicaid programs should universally guarantee coverage of routine care costs of clinical trials for their beneficiaries.
- The U.S. Centers for Medicare & Medicaid Services (CMS) should revise current policy that requires Medicare Advantage beneficiaries to revert to fee-for-service coverage during clinical trials.
- CMS’s Innovation Center should explore the effectiveness of alternative payment models in support of clinical trial accrual.
- During the clinical trials development and enrollment process, provide patients with clear, transparent information about potential trial-related out-of-pocket costs and include mechanisms to support patient financial/health literacy.
- Clinical trial sponsors should perform—and make available to enrolling institutions—comprehensive, prospective coverage analyses.
- Research sites should consider offering in-house financial navigation/counseling to patients or consider partnering with organizations that provide such services.
- Design clinical trials to minimize incremental costs, consistent with scientific objectives and participant safety.
- Remove impediments to ethically appropriate financial compensation for trial-related out-of-pocket costs. Provision of such financial support should not be considered undue inducement.
- Office for Human Research Protections should develop guidance on targeted financial support.
- Incentivize research that will better characterize patient costs incurred for participating in cancer clinical trials and support the longer-term development of tools to identify and mitigate the risk of trial-associated financial hardship.
“Continued progress against cancer depends on improving patient access to participation in clinical research,” Dr. Bertagnolli said.
“The recommendations in ASCO’s statement aim to ensure that no patient is denied access to a clinical trial for financial reasons and that patients are not harmed financially because of their contributions to advancing science. Ultimately, this is about strengthening the nation’s cancer research enterprise as a whole.”
The American Society of Clinical Oncology (ASCO) has issued a policy statement addressing financial barriers to patient participation in cancer clinical trials.
ASCO’s policy statement outlines a series of recommendations designed to address multiple financial barriers that impede access to clinical trials, including patient costs that aren’t covered consistently by health insurance; a lack of information provided to patients about clinical trial costs; and limited available research data on financial hardships related to participation in clinical trials.
“Clinical trials are essential for evaluating the safety and efficacy of new cancer treatments, but cancer researchers have seen consistently low patient participation levels—especially among underserved patient populations—in part, due to the financial burdens facing many patients with cancer,” said ASCO President Monica M. Bertagnolli, MD.
“Addressing financial barriers will help improve the enrollment rate and the efficiency, quality, and applicability of cancer research. By including more—and more diverse—participants in our research studies, we expand our ability to care for all patients.”
The recommendations in ASCO’s policy statement include:
- Improve payer clinical trial coverage policies. Payment policies should be revised to be made consistent, streamlined, and transparent to all stakeholders.
- Payers should have clear definitions of “routine costs.”
- Payers should streamline prior authorization processes and facilitate trial enrollment through provider reimbursement of clinical trial-related services.
- State Medicaid programs should universally guarantee coverage of routine care costs of clinical trials for their beneficiaries.
- The U.S. Centers for Medicare & Medicaid Services (CMS) should revise current policy that requires Medicare Advantage beneficiaries to revert to fee-for-service coverage during clinical trials.
- CMS’s Innovation Center should explore the effectiveness of alternative payment models in support of clinical trial accrual.
- During the clinical trials development and enrollment process, provide patients with clear, transparent information about potential trial-related out-of-pocket costs and include mechanisms to support patient financial/health literacy.
- Clinical trial sponsors should perform—and make available to enrolling institutions—comprehensive, prospective coverage analyses.
- Research sites should consider offering in-house financial navigation/counseling to patients or consider partnering with organizations that provide such services.
- Design clinical trials to minimize incremental costs, consistent with scientific objectives and participant safety.
- Remove impediments to ethically appropriate financial compensation for trial-related out-of-pocket costs. Provision of such financial support should not be considered undue inducement.
- Office for Human Research Protections should develop guidance on targeted financial support.
- Incentivize research that will better characterize patient costs incurred for participating in cancer clinical trials and support the longer-term development of tools to identify and mitigate the risk of trial-associated financial hardship.
“Continued progress against cancer depends on improving patient access to participation in clinical research,” Dr. Bertagnolli said.
“The recommendations in ASCO’s statement aim to ensure that no patient is denied access to a clinical trial for financial reasons and that patients are not harmed financially because of their contributions to advancing science. Ultimately, this is about strengthening the nation’s cancer research enterprise as a whole.”
Early CAR T data on P-BCMA-101 in refractory myeloma
Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma.
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome (CRS), but the condition resolved without use of tocilizumab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated multiple myeloma. They had a median of six prior therapies. The median age was 60 years, and most of the patients were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51 x 106 (n = 3), 152 x 106 (n = 7), and 430 x 106 (n = 1).
As of Aug. 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and five had thrombocytopenia.
Researchers suspected CRS in one patient, but the condition resolved without tocilizumab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was evaluable only by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma.
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome (CRS), but the condition resolved without use of tocilizumab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated multiple myeloma. They had a median of six prior therapies. The median age was 60 years, and most of the patients were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51 x 106 (n = 3), 152 x 106 (n = 7), and 430 x 106 (n = 1).
As of Aug. 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and five had thrombocytopenia.
Researchers suspected CRS in one patient, but the condition resolved without tocilizumab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was evaluable only by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma.
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome (CRS), but the condition resolved without use of tocilizumab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated multiple myeloma. They had a median of six prior therapies. The median age was 60 years, and most of the patients were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51 x 106 (n = 3), 152 x 106 (n = 7), and 430 x 106 (n = 1).
As of Aug. 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and five had thrombocytopenia.
Researchers suspected CRS in one patient, but the condition resolved without tocilizumab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was evaluable only by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
FROM THE 2018 CAR-TCR SUMMIT
Key clinical point: The chimeric antigen receptor .
Major finding: All 11 patients have shown signs of response, and 8 patients achieved a partial response or better.
Study details: Eleven patients have been treated thus far in this phase 1 trial.
Disclosures: This trial is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
Doc reports ‘very encouraging’ results in penta-refractory MM
HOUSTON—Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma (MM), according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Mount Sinai School of Medicine in New York, N.Y., presented these results at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting as abstract MM-255.*
“The additional phase 2b clinical results ... are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said.
“Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM study.”
The study (NCT02336815) included 122 patients with penta-refractory MM. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of 7 (range, 3-18) prior treatment regimens. Their median age was 65 (range, 40-86), 58% were male, and 53% had high-risk cytogenetics.
Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Response and survival
Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10-6 and one at 1 x 10-4.
Six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses (PRs), 16 (13.1%) had minimal responses (MRs), and 48 (39.3%) had stable disease (SD).
Sixteen patients (13.1%) had progressive disease (PD), and 10 (8.2%) were not evaluable for response.
The overall response rate (PR or better) was 26.2% (n=32), the clinical benefit rate (MR or better) was 39.3% (n=48), and the disease control rate (SD or better) was 78.7% (n=98).
The median duration of response was 4.4 months (range, <1 to 12.2 months).
The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had PD or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. It was 15.6 months in patients with an MR or better and 1.7 months in patients who had PD or were not evaluable (P<0.0001).
Safety
The most common non-hematologic treatment-related adverse events (AEs) were fatigue/asthenia (69.9%), nausea (69.1%), anorexia (52.0%), weight loss (47.2%), vomiting (35.0%), diarrhea (33.3%), and hyponatremia (30.9%).
Hematologic treatment-related AEs included thrombocytopenia (67.5%), anemia (48.0%), neutropenia (35.8%), leukopenia (29.3%), and lymphopenia (13.8%).
The “most important” grade 3/4 AEs, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%).
Twenty-three patients (19.5%) discontinued treatment due to a related AE.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GSK.
*Information in the abstract differs from the presentation.
HOUSTON—Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma (MM), according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Mount Sinai School of Medicine in New York, N.Y., presented these results at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting as abstract MM-255.*
“The additional phase 2b clinical results ... are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said.
“Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM study.”
The study (NCT02336815) included 122 patients with penta-refractory MM. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of 7 (range, 3-18) prior treatment regimens. Their median age was 65 (range, 40-86), 58% were male, and 53% had high-risk cytogenetics.
Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Response and survival
Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10-6 and one at 1 x 10-4.
Six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses (PRs), 16 (13.1%) had minimal responses (MRs), and 48 (39.3%) had stable disease (SD).
Sixteen patients (13.1%) had progressive disease (PD), and 10 (8.2%) were not evaluable for response.
The overall response rate (PR or better) was 26.2% (n=32), the clinical benefit rate (MR or better) was 39.3% (n=48), and the disease control rate (SD or better) was 78.7% (n=98).
The median duration of response was 4.4 months (range, <1 to 12.2 months).
The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had PD or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. It was 15.6 months in patients with an MR or better and 1.7 months in patients who had PD or were not evaluable (P<0.0001).
Safety
The most common non-hematologic treatment-related adverse events (AEs) were fatigue/asthenia (69.9%), nausea (69.1%), anorexia (52.0%), weight loss (47.2%), vomiting (35.0%), diarrhea (33.3%), and hyponatremia (30.9%).
Hematologic treatment-related AEs included thrombocytopenia (67.5%), anemia (48.0%), neutropenia (35.8%), leukopenia (29.3%), and lymphopenia (13.8%).
The “most important” grade 3/4 AEs, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%).
Twenty-three patients (19.5%) discontinued treatment due to a related AE.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GSK.
*Information in the abstract differs from the presentation.
HOUSTON—Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma (MM), according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Mount Sinai School of Medicine in New York, N.Y., presented these results at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting as abstract MM-255.*
“The additional phase 2b clinical results ... are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said.
“Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM study.”
The study (NCT02336815) included 122 patients with penta-refractory MM. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of 7 (range, 3-18) prior treatment regimens. Their median age was 65 (range, 40-86), 58% were male, and 53% had high-risk cytogenetics.
Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Response and survival
Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10-6 and one at 1 x 10-4.
Six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses (PRs), 16 (13.1%) had minimal responses (MRs), and 48 (39.3%) had stable disease (SD).
Sixteen patients (13.1%) had progressive disease (PD), and 10 (8.2%) were not evaluable for response.
The overall response rate (PR or better) was 26.2% (n=32), the clinical benefit rate (MR or better) was 39.3% (n=48), and the disease control rate (SD or better) was 78.7% (n=98).
The median duration of response was 4.4 months (range, <1 to 12.2 months).
The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had PD or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. It was 15.6 months in patients with an MR or better and 1.7 months in patients who had PD or were not evaluable (P<0.0001).
Safety
The most common non-hematologic treatment-related adverse events (AEs) were fatigue/asthenia (69.9%), nausea (69.1%), anorexia (52.0%), weight loss (47.2%), vomiting (35.0%), diarrhea (33.3%), and hyponatremia (30.9%).
Hematologic treatment-related AEs included thrombocytopenia (67.5%), anemia (48.0%), neutropenia (35.8%), leukopenia (29.3%), and lymphopenia (13.8%).
The “most important” grade 3/4 AEs, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%).
Twenty-three patients (19.5%) discontinued treatment due to a related AE.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GSK.
*Information in the abstract differs from the presentation.
STORM trial shows response in penta-refractory myeloma
Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma, according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%. The median progression-free survival was 3.7 months and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Icahn School of Medicine at Mount Sinai, New York, presented these results at the annual meeting of the Society of Hematologic Oncology.
“The additional phase 2b clinical results… are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said in a statement. “Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM [Selinexor Treatment of Refractory Myeloma] study.”
STORM (NCT02336815) included 122 patients with penta-refractory multiple myeloma. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of seven prior treatment regimens. Their median age was 65 years, a little more than half were men, and more than half had high-risk cytogenetics. Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10–6 and one at 1 x 10–4.
Very good partial responses were seen in 4.9% of patients, 19.7% had partial responses, 13.1% had minimal responses (MRs), and 39.3% had stable disease. Progressive disease occurred in 13.1% of patients; 8.2% were not evaluable for response.
The overall response rate (partial response or better) was 26.2%, the clinical benefit rate (MR or better) was 39.3%, and the disease control rate (stable disease or better) was 78.7%.
The median duration of response was 4.4 months. The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had progressive disease or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. Overall survival was 15.6 months in patients with an MR or better and 1.7 months in patients who had progressive disease or were not evaluable (P less than .0001).
The “most important” grade 3/4 adverse events, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%). A total of 23 patients (19.5%) discontinued treatment because of a related adverse.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GlaxoSmithKline.
SOURCE: Jagannath S et al. SOHO 2018, Abstract MM-255
Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma, according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%. The median progression-free survival was 3.7 months and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Icahn School of Medicine at Mount Sinai, New York, presented these results at the annual meeting of the Society of Hematologic Oncology.
“The additional phase 2b clinical results… are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said in a statement. “Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM [Selinexor Treatment of Refractory Myeloma] study.”
STORM (NCT02336815) included 122 patients with penta-refractory multiple myeloma. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of seven prior treatment regimens. Their median age was 65 years, a little more than half were men, and more than half had high-risk cytogenetics. Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10–6 and one at 1 x 10–4.
Very good partial responses were seen in 4.9% of patients, 19.7% had partial responses, 13.1% had minimal responses (MRs), and 39.3% had stable disease. Progressive disease occurred in 13.1% of patients; 8.2% were not evaluable for response.
The overall response rate (partial response or better) was 26.2%, the clinical benefit rate (MR or better) was 39.3%, and the disease control rate (stable disease or better) was 78.7%.
The median duration of response was 4.4 months. The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had progressive disease or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. Overall survival was 15.6 months in patients with an MR or better and 1.7 months in patients who had progressive disease or were not evaluable (P less than .0001).
The “most important” grade 3/4 adverse events, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%). A total of 23 patients (19.5%) discontinued treatment because of a related adverse.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GlaxoSmithKline.
SOURCE: Jagannath S et al. SOHO 2018, Abstract MM-255
Treatment with selinexor and low-dose dexamethasone can provide a “meaningful clinical benefit” in patients with penta-refractory multiple myeloma, according to the principal investigator of the STORM trial.
Updated results from this phase 2 trial showed that selinexor and low-dose dexamethasone produced an overall response rate of 26.2% and a clinical benefit rate of 39.3%. The median progression-free survival was 3.7 months and the median overall survival was 8.6 months.
The trial’s principal investigator, Sundar Jagannath, MBBS, of the Icahn School of Medicine at Mount Sinai, New York, presented these results at the annual meeting of the Society of Hematologic Oncology.
“The additional phase 2b clinical results… are very encouraging for the patients suffering from penta-refractory multiple myeloma and their families,” Dr. Jagannath said in a statement. “Of particular significance, for the nearly 40% of patients who had a minimal response or better, the median survival was 15.6 months, which provided the opportunity for a meaningful clinical benefit for patients on the STORM [Selinexor Treatment of Refractory Myeloma] study.”
STORM (NCT02336815) included 122 patients with penta-refractory multiple myeloma. They had previously received bortezomib, carfilzomib, lenalidomide, pomalidomide, daratumumab, alkylating agents, and glucocorticoids. Their disease was refractory to glucocorticoids, at least one proteasome inhibitor, at least one immunomodulatory drug, daratumumab, and their most recent therapy.
The patients had received a median of seven prior treatment regimens. Their median age was 65 years, a little more than half were men, and more than half had high-risk cytogenetics. Patients received oral selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.Two patients (1.6%) achieved stringent complete responses. They also had minimal residual disease negativity, one at the level of 1 x 10–6 and one at 1 x 10–4.
Very good partial responses were seen in 4.9% of patients, 19.7% had partial responses, 13.1% had minimal responses (MRs), and 39.3% had stable disease. Progressive disease occurred in 13.1% of patients; 8.2% were not evaluable for response.
The overall response rate (partial response or better) was 26.2%, the clinical benefit rate (MR or better) was 39.3%, and the disease control rate (stable disease or better) was 78.7%.
The median duration of response was 4.4 months. The median progression-free survival was 3.7 months overall, 4.6 months in patients with an MR or better, and 1.1 months in patients who had progressive disease or were not evaluable.
The median overall survival was 8.6 months for the entire cohort. Overall survival was 15.6 months in patients with an MR or better and 1.7 months in patients who had progressive disease or were not evaluable (P less than .0001).
The “most important” grade 3/4 adverse events, according to Dr. Jagannath, were thrombocytopenia (53.7%), anemia (29.3%), fatigue (22.8%), hyponatremia (16.3%), nausea (9.8%), diarrhea (6.5%), anorexia (3.3%), and emesis (3.3%). A total of 23 patients (19.5%) discontinued treatment because of a related adverse.
This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GlaxoSmithKline.
SOURCE: Jagannath S et al. SOHO 2018, Abstract MM-255
FROM SOHO 2018
Key clinical point:
Major finding: The overall response rate was 26.2% and the clinical benefit rate was 39.3%.
Study details: A phase 2 trial of 122 patients with penta-refractory multiple myeloma.
Disclosures: This study was sponsored by Karyopharm Therapeutics. Dr. Jagannath reported relationships with Karyopharm, Janssen, Celgene, Amgen, and GlaxoSmithKline.
Source: Jagannath S et al. SOHO 2018, Abstract MM-255.
CAR T-cell therapy elicits responses in MM
BOSTON—Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma (MM).
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome, but the condition resolved without use of tociluzimab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated MM. They had a median of six prior therapies. Their median age was 60, and 73% were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51×106 (n=3), 152×106 (n=7), and 430×106 (n=1).
As of August 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and 5 had thrombocytopenia.
Researchers suspected cytokine release syndrome in one patient, but the condition resolved without tociluzimab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was only evaluable by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
“We believe our advantages of a purified product, where all cells express the CAR molecule, and a product with high levels of stem cell memory T cells, producing a more gradual and prolonged immune response against tumor cells, provide a significantly better therapeutic index when compared with other CAR-T therapeutics. We are also encouraged that P-BCMA-101 is demonstrating significant efficacy even at doses that have been ineffective for other anti-BCMA CAR-T therapies and that our response rates continue to improve as the dose increases.”
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
BOSTON—Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma (MM).
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome, but the condition resolved without use of tociluzimab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated MM. They had a median of six prior therapies. Their median age was 60, and 73% were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51×106 (n=3), 152×106 (n=7), and 430×106 (n=1).
As of August 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and 5 had thrombocytopenia.
Researchers suspected cytokine release syndrome in one patient, but the condition resolved without tociluzimab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was only evaluable by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
“We believe our advantages of a purified product, where all cells express the CAR molecule, and a product with high levels of stem cell memory T cells, producing a more gradual and prolonged immune response against tumor cells, provide a significantly better therapeutic index when compared with other CAR-T therapeutics. We are also encouraged that P-BCMA-101 is demonstrating significant efficacy even at doses that have been ineffective for other anti-BCMA CAR-T therapies and that our response rates continue to improve as the dose increases.”
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
BOSTON—Early results from a phase 1 trial suggest the chimeric antigen receptor (CAR) T-cell therapy P-BCMA-101 can produce responses in patients with relapsed/refractory multiple myeloma (MM).
All 11 patients treated have experienced some clinical response, with 8 patients achieving a partial response (PR) or better.
The most common adverse events were neutropenia and thrombocytopenia. One patient was suspected to have cytokine release syndrome, but the condition resolved without use of tociluzimab or steroids.
These results were presented at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
Dr. Ostertag presented data on 11 patients with heavily pretreated MM. They had a median of six prior therapies. Their median age was 60, and 73% were considered high risk.
Prior to receiving P-BCMA-101, patients received conditioning with fludarabine (30 mg/m2) and cyclophosphamide (300 mg/m2) for 3 days.
Patients were then treated across three dose groups with average CAR T-cell doses of 51×106 (n=3), 152×106 (n=7), and 430×106 (n=1).
As of August 10, 2018, all 11 patients were still on study.
There were no dose-limiting toxicities. Eight patients developed neutropenia, and 5 had thrombocytopenia.
Researchers suspected cytokine release syndrome in one patient, but the condition resolved without tociluzimab or steroid treatment. There was no neurotoxicity reported, and none of the patients required admission to an intensive care unit.
All patients showed improvement in biomarkers following treatment.
Ten patients were evaluable for response by International Myeloma Working Group criteria. Seven of these patients achieved at least a PR, including very good partial responses (VGPRs) and stringent complete response (CR).
The eleventh patient also responded to treatment, but this patient has oligosecretory disease and was only evaluable by PET. The patient had a near-CR by PET.
Poseida Therapeutics would not disclose additional details regarding how many patients achieved a PR, VGPR, or CR, but the company plans to release more information on response at an upcoming meeting.
“The latest data results show that P-BCMA-101 induces deep responses in a heavily pretreated population with relapsed/refractory multiple myeloma, with some patients reaching VGPR and even stringent CR at early efficacy assessments,” Dr. Ostertag said.
“We believe our advantages of a purified product, where all cells express the CAR molecule, and a product with high levels of stem cell memory T cells, producing a more gradual and prolonged immune response against tumor cells, provide a significantly better therapeutic index when compared with other CAR-T therapeutics. We are also encouraged that P-BCMA-101 is demonstrating significant efficacy even at doses that have been ineffective for other anti-BCMA CAR-T therapies and that our response rates continue to improve as the dose increases.”
This study (NCT03288493) is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.