User login
Better PFS may not mean better HRQOL
Cancer treatments that prolong progression-free survival (PFS) may not improve health-related quality of life (HRQOL), researchers reported in JAMA Internal Medicine.
The researchers failed to find a significant association between PFS and HRQOL in an analysis of cancer clinical trials.
“There are only two reasons to use progression-free survival as a valid endpoint in oncology,” said study author Feng Xie, PhD, of McMaster University in Hamilton, Ontario, Canada.
“One is that it is a valid surrogate marker for overall survival. The second is the assumption that patients who live longer without disease progression will have better health-related quality of life, even without longer survival.”
“Given the increased use of progression-free survival as the primary outcome in new oncology drug trials, and uncertainty of overall survival, it remains possible that patients are receiving toxic and/or expensive treatments without experiencing important benefit.”
With this in mind, Dr. Xie and his colleagues conducted a review and meta-analysis of 52 articles reporting on 38 randomized clinical trials. The trials included 13,979 patients with 12 types of cancer, including 1 trial of patients with multiple myeloma.
The median follow-up in these trials ranged from 10.5 months to 66.0 months.
The median PFS of patients who received the trial interventions ranged from 1.8 months to 33.7 months.
For 28 of the trials (74%), patients who received the trial intervention had better PFS than patients who received the comparator. Overall, the mean difference in median PFS between the intervention and comparator arms was 1.91 months.
HRQOL was measured with 6 different instruments* across the trials, and the types of HRQOL measured varied. Thirty trials included global HRQOL, 20 included physical, and 13 included emotional HRQOL. The duration of reported or measured HRQOL ranged from 1 month to 34 months.
Improved global HRQOL was reported in 53% of trials (16/30), improved physical HRQOL was reported in 55% (11/20), and improved emotional HRQOL was reported in 62% (8/13). The mean difference in change of HRQOL adjusted to per-month values was −0.39 for global, 0.26 for physical, and 1.08 for emotional HRQOL.
The slope of the association between the difference in median PFS and the difference in HRQOL change was:
- 0.12 (95% confidence interval [CI], −0.27 to 0.52) for global HRQOL
- −0.20 (95% CI,−0.62 to 0.23) for physical HRQOL
- 0.78 (95% CI, −0.05 to 1.60) for emotional HRQOL.
Dr. Xie and his colleagues said these results suggest there is no significant association between PFS and HRQOL, so interventions prolonging PFS may not improve HRQOL.
“Therefore, to ensure patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure health-related quality of life directly and accurately, ensuring adequate duration and follow-up, and publish it,” Dr. Xie said.
He also argued for the need to “revisit this issue of using surrogate outcomes to measure the safety and efficacy of new oncology drugs.”
Dr. Xie and his colleagues did not report any conflicts of interest. One study author (Marcin Waligora, PhD) reported funding from the National Science Centre in Poland.
*EORTC-QLQ-C30, FACT-G19, Lung Cancer Symptom Scale, EQ-5D, 8-item linear analog self-assessment (LASA) questionnaire, and clinician-reported Karnofsky score
Cancer treatments that prolong progression-free survival (PFS) may not improve health-related quality of life (HRQOL), researchers reported in JAMA Internal Medicine.
The researchers failed to find a significant association between PFS and HRQOL in an analysis of cancer clinical trials.
“There are only two reasons to use progression-free survival as a valid endpoint in oncology,” said study author Feng Xie, PhD, of McMaster University in Hamilton, Ontario, Canada.
“One is that it is a valid surrogate marker for overall survival. The second is the assumption that patients who live longer without disease progression will have better health-related quality of life, even without longer survival.”
“Given the increased use of progression-free survival as the primary outcome in new oncology drug trials, and uncertainty of overall survival, it remains possible that patients are receiving toxic and/or expensive treatments without experiencing important benefit.”
With this in mind, Dr. Xie and his colleagues conducted a review and meta-analysis of 52 articles reporting on 38 randomized clinical trials. The trials included 13,979 patients with 12 types of cancer, including 1 trial of patients with multiple myeloma.
The median follow-up in these trials ranged from 10.5 months to 66.0 months.
The median PFS of patients who received the trial interventions ranged from 1.8 months to 33.7 months.
For 28 of the trials (74%), patients who received the trial intervention had better PFS than patients who received the comparator. Overall, the mean difference in median PFS between the intervention and comparator arms was 1.91 months.
HRQOL was measured with 6 different instruments* across the trials, and the types of HRQOL measured varied. Thirty trials included global HRQOL, 20 included physical, and 13 included emotional HRQOL. The duration of reported or measured HRQOL ranged from 1 month to 34 months.
Improved global HRQOL was reported in 53% of trials (16/30), improved physical HRQOL was reported in 55% (11/20), and improved emotional HRQOL was reported in 62% (8/13). The mean difference in change of HRQOL adjusted to per-month values was −0.39 for global, 0.26 for physical, and 1.08 for emotional HRQOL.
The slope of the association between the difference in median PFS and the difference in HRQOL change was:
- 0.12 (95% confidence interval [CI], −0.27 to 0.52) for global HRQOL
- −0.20 (95% CI,−0.62 to 0.23) for physical HRQOL
- 0.78 (95% CI, −0.05 to 1.60) for emotional HRQOL.
Dr. Xie and his colleagues said these results suggest there is no significant association between PFS and HRQOL, so interventions prolonging PFS may not improve HRQOL.
“Therefore, to ensure patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure health-related quality of life directly and accurately, ensuring adequate duration and follow-up, and publish it,” Dr. Xie said.
He also argued for the need to “revisit this issue of using surrogate outcomes to measure the safety and efficacy of new oncology drugs.”
Dr. Xie and his colleagues did not report any conflicts of interest. One study author (Marcin Waligora, PhD) reported funding from the National Science Centre in Poland.
*EORTC-QLQ-C30, FACT-G19, Lung Cancer Symptom Scale, EQ-5D, 8-item linear analog self-assessment (LASA) questionnaire, and clinician-reported Karnofsky score
Cancer treatments that prolong progression-free survival (PFS) may not improve health-related quality of life (HRQOL), researchers reported in JAMA Internal Medicine.
The researchers failed to find a significant association between PFS and HRQOL in an analysis of cancer clinical trials.
“There are only two reasons to use progression-free survival as a valid endpoint in oncology,” said study author Feng Xie, PhD, of McMaster University in Hamilton, Ontario, Canada.
“One is that it is a valid surrogate marker for overall survival. The second is the assumption that patients who live longer without disease progression will have better health-related quality of life, even without longer survival.”
“Given the increased use of progression-free survival as the primary outcome in new oncology drug trials, and uncertainty of overall survival, it remains possible that patients are receiving toxic and/or expensive treatments without experiencing important benefit.”
With this in mind, Dr. Xie and his colleagues conducted a review and meta-analysis of 52 articles reporting on 38 randomized clinical trials. The trials included 13,979 patients with 12 types of cancer, including 1 trial of patients with multiple myeloma.
The median follow-up in these trials ranged from 10.5 months to 66.0 months.
The median PFS of patients who received the trial interventions ranged from 1.8 months to 33.7 months.
For 28 of the trials (74%), patients who received the trial intervention had better PFS than patients who received the comparator. Overall, the mean difference in median PFS between the intervention and comparator arms was 1.91 months.
HRQOL was measured with 6 different instruments* across the trials, and the types of HRQOL measured varied. Thirty trials included global HRQOL, 20 included physical, and 13 included emotional HRQOL. The duration of reported or measured HRQOL ranged from 1 month to 34 months.
Improved global HRQOL was reported in 53% of trials (16/30), improved physical HRQOL was reported in 55% (11/20), and improved emotional HRQOL was reported in 62% (8/13). The mean difference in change of HRQOL adjusted to per-month values was −0.39 for global, 0.26 for physical, and 1.08 for emotional HRQOL.
The slope of the association between the difference in median PFS and the difference in HRQOL change was:
- 0.12 (95% confidence interval [CI], −0.27 to 0.52) for global HRQOL
- −0.20 (95% CI,−0.62 to 0.23) for physical HRQOL
- 0.78 (95% CI, −0.05 to 1.60) for emotional HRQOL.
Dr. Xie and his colleagues said these results suggest there is no significant association between PFS and HRQOL, so interventions prolonging PFS may not improve HRQOL.
“Therefore, to ensure patients are truly obtaining important benefit from cancer therapies, clinical trial investigators should measure health-related quality of life directly and accurately, ensuring adequate duration and follow-up, and publish it,” Dr. Xie said.
He also argued for the need to “revisit this issue of using surrogate outcomes to measure the safety and efficacy of new oncology drugs.”
Dr. Xie and his colleagues did not report any conflicts of interest. One study author (Marcin Waligora, PhD) reported funding from the National Science Centre in Poland.
*EORTC-QLQ-C30, FACT-G19, Lung Cancer Symptom Scale, EQ-5D, 8-item linear analog self-assessment (LASA) questionnaire, and clinician-reported Karnofsky score
FDA offers guidance on MRD assessment in blood cancer trials
The of patients with hematologic malignancies.
The FDA said it developed the document to assist drug sponsors who are planning to use minimal residual disease (MRD) as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” FDA Commissioner Scott Gottlieb, MD, said in a statement.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
MRD could potentially be used as a biomarker in clinical trials – specifically as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker, according to the draft guidance. Additionally, MRD could be used as a surrogate endpoint or “to select patients at high risk or to enrich the trial population.”
The draft guidance also provides specific considerations for MRD assessment in individual hematologic malignancies, including acute lymphoblastic leukemia, acute myeloid leukemia, acute promyelocytic leukemia, chronic lymphocytic leukemia, chronic myeloid leukemia, and multiple myeloma.
The full document is available on the FDA website.
The of patients with hematologic malignancies.
The FDA said it developed the document to assist drug sponsors who are planning to use minimal residual disease (MRD) as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” FDA Commissioner Scott Gottlieb, MD, said in a statement.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
MRD could potentially be used as a biomarker in clinical trials – specifically as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker, according to the draft guidance. Additionally, MRD could be used as a surrogate endpoint or “to select patients at high risk or to enrich the trial population.”
The draft guidance also provides specific considerations for MRD assessment in individual hematologic malignancies, including acute lymphoblastic leukemia, acute myeloid leukemia, acute promyelocytic leukemia, chronic lymphocytic leukemia, chronic myeloid leukemia, and multiple myeloma.
The full document is available on the FDA website.
The of patients with hematologic malignancies.
The FDA said it developed the document to assist drug sponsors who are planning to use minimal residual disease (MRD) as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” FDA Commissioner Scott Gottlieb, MD, said in a statement.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
MRD could potentially be used as a biomarker in clinical trials – specifically as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker, according to the draft guidance. Additionally, MRD could be used as a surrogate endpoint or “to select patients at high risk or to enrich the trial population.”
The draft guidance also provides specific considerations for MRD assessment in individual hematologic malignancies, including acute lymphoblastic leukemia, acute myeloid leukemia, acute promyelocytic leukemia, chronic lymphocytic leukemia, chronic myeloid leukemia, and multiple myeloma.
The full document is available on the FDA website.
FDA issues draft guidance on MRD
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
Questions surround MRD assessment in MM
DUBROVNIK, CROATIA—Clinical trials are needed to answer the many questions related to minimal residual disease (MRD) assessment in multiple myeloma (MM), according to a speaker at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
MM patients are increasingly assessed for MRD, which is a strong prognostic factor and surrogate for overall survival, according to Toni Valković, MD, PhD, of University Hospital Center Rijeka in Croatia.
However, Dr. Valković said MRD assessment has not become a part of routine clinical practice, perhaps because we haven’t determined the best way to utilize MRD assessment in MM patients.
The optimal sensitivity threshold, technique, and timing of MRD assessment are not known, and it isn’t clear how MRD should be used to guide treatment.
What we know
Dr. Valković cited studies showing that MRD negativity is associated with superior survival in MM1, and, when MRD negativity is achieved, high-risk cytogenetics, age, and previous treatment regimens appear to have no further impact on prognosis.2
Dr. Valković went on to explain the benefits and detriments of multiparametric flow cytometry (MFC) and next-generation sequencing (NGS) for MRD assessment.3
NGS requires a baseline patient sample, but MFC does not. More cells are required with MFC than with NGS (>5 million vs. <1 million).
With MFC, samples must be processed within 24 to 48 hours, whereas, with NGS, fresh or stored samples can be used. MFC can be done in a few hours, while NGS can take several days.
Despite these differences, both methods provide similar levels of sensitivity for detecting MRD (≥1 in 105).
Dr. Valković also noted that MRD should be evaluated outside the bone marrow as well, which can be done with positron emission tomography-computed tomography (PET-CT).
Research has shown that patients who are MRD-negative according to both MFC and PET-CT have better outcomes than patients who are MRD-positive by MFC, PET-CT, or both.4
What we don’t know
Though he compared MFC and NGS, Dr. Valković said we don’t know the optimal technique for assessing MRD in the bone marrow.
Another uncertainty is the optimal sensitivity threshold. In the POLLUX study5, researchers found that a threshold of 10-4 resulted in lots of patients with MRD negativity, but some of these were false-negatives.
So although 10-4 proved inaccurate, it isn’t clear if the optimal threshold is 10-5 or 10-6, Dr. Valković said.
Likewise, it isn’t clear if PET-CT is the optimal method for evaluating MRD outside the bone marrow.
In a study published in 2017, PET produced false-negatives in MM patients.6 In 11% of patients (26/227), there was evidence of disease with diffusion-weighted magnetic resonance imaging with background signal suppression, but there was no apparent disease with PET. The researchers said low expression of hexokinase-2 was associated with a false-negative PET result.
Finally, Dr. Valković said we don’t know how best to use MRD to tailor therapy in MM patients. He posed the following questions:
- If patients don’t achieve MRD negativity, should they continue on the therapy?
- If MRD-negative patients become MRD-positive, should they begin therapy immediately, or should treatment be put off until a biochemical or clinical relapse?
- Should MRD status be used to determine the number of treatment cycles a patient receives, the timing of transplant, or when to begin and end maintenance therapy?
“There are a lot of issues and unanswered questions related to the optimal techniques for the evaluation of MRD and their sensitivity, the timing for MRD assessment during and after therapy, and its role in the treatment decisions, which should be answered in future clinical studies,” Dr. Valković concluded.
He did not declare any conflicts of interest.
1. Munshi NC et al. JAMA Oncol. 2017;3(1):28-35. doi:10.1001/jamaoncol.2016.3160
2. Paiva B et al. Blood. 2016 Jun 23;127(25):3165-74. doi: 10.1182/blood-2016-03-705319
3. Kumar S et al. Lancet Oncol. 2016; 17 (8):e328-46 doi: https://doi.org/10.1016/S1470-2045(16)30206-6
4. Fernandez RA et al. Blood. 2017; 130:3098
5. Dimopoulos MA et al. Haematologica. 2018 Sep 20. pii: haematol.2018.194282. doi: 10.3324/haematol.2018.194282
6. Rasche L et al. Blood. 2017 Jul 6;130(1):30-34. doi: 10.1182/blood-2017-03-774422
DUBROVNIK, CROATIA—Clinical trials are needed to answer the many questions related to minimal residual disease (MRD) assessment in multiple myeloma (MM), according to a speaker at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
MM patients are increasingly assessed for MRD, which is a strong prognostic factor and surrogate for overall survival, according to Toni Valković, MD, PhD, of University Hospital Center Rijeka in Croatia.
However, Dr. Valković said MRD assessment has not become a part of routine clinical practice, perhaps because we haven’t determined the best way to utilize MRD assessment in MM patients.
The optimal sensitivity threshold, technique, and timing of MRD assessment are not known, and it isn’t clear how MRD should be used to guide treatment.
What we know
Dr. Valković cited studies showing that MRD negativity is associated with superior survival in MM1, and, when MRD negativity is achieved, high-risk cytogenetics, age, and previous treatment regimens appear to have no further impact on prognosis.2
Dr. Valković went on to explain the benefits and detriments of multiparametric flow cytometry (MFC) and next-generation sequencing (NGS) for MRD assessment.3
NGS requires a baseline patient sample, but MFC does not. More cells are required with MFC than with NGS (>5 million vs. <1 million).
With MFC, samples must be processed within 24 to 48 hours, whereas, with NGS, fresh or stored samples can be used. MFC can be done in a few hours, while NGS can take several days.
Despite these differences, both methods provide similar levels of sensitivity for detecting MRD (≥1 in 105).
Dr. Valković also noted that MRD should be evaluated outside the bone marrow as well, which can be done with positron emission tomography-computed tomography (PET-CT).
Research has shown that patients who are MRD-negative according to both MFC and PET-CT have better outcomes than patients who are MRD-positive by MFC, PET-CT, or both.4
What we don’t know
Though he compared MFC and NGS, Dr. Valković said we don’t know the optimal technique for assessing MRD in the bone marrow.
Another uncertainty is the optimal sensitivity threshold. In the POLLUX study5, researchers found that a threshold of 10-4 resulted in lots of patients with MRD negativity, but some of these were false-negatives.
So although 10-4 proved inaccurate, it isn’t clear if the optimal threshold is 10-5 or 10-6, Dr. Valković said.
Likewise, it isn’t clear if PET-CT is the optimal method for evaluating MRD outside the bone marrow.
In a study published in 2017, PET produced false-negatives in MM patients.6 In 11% of patients (26/227), there was evidence of disease with diffusion-weighted magnetic resonance imaging with background signal suppression, but there was no apparent disease with PET. The researchers said low expression of hexokinase-2 was associated with a false-negative PET result.
Finally, Dr. Valković said we don’t know how best to use MRD to tailor therapy in MM patients. He posed the following questions:
- If patients don’t achieve MRD negativity, should they continue on the therapy?
- If MRD-negative patients become MRD-positive, should they begin therapy immediately, or should treatment be put off until a biochemical or clinical relapse?
- Should MRD status be used to determine the number of treatment cycles a patient receives, the timing of transplant, or when to begin and end maintenance therapy?
“There are a lot of issues and unanswered questions related to the optimal techniques for the evaluation of MRD and their sensitivity, the timing for MRD assessment during and after therapy, and its role in the treatment decisions, which should be answered in future clinical studies,” Dr. Valković concluded.
He did not declare any conflicts of interest.
1. Munshi NC et al. JAMA Oncol. 2017;3(1):28-35. doi:10.1001/jamaoncol.2016.3160
2. Paiva B et al. Blood. 2016 Jun 23;127(25):3165-74. doi: 10.1182/blood-2016-03-705319
3. Kumar S et al. Lancet Oncol. 2016; 17 (8):e328-46 doi: https://doi.org/10.1016/S1470-2045(16)30206-6
4. Fernandez RA et al. Blood. 2017; 130:3098
5. Dimopoulos MA et al. Haematologica. 2018 Sep 20. pii: haematol.2018.194282. doi: 10.3324/haematol.2018.194282
6. Rasche L et al. Blood. 2017 Jul 6;130(1):30-34. doi: 10.1182/blood-2017-03-774422
DUBROVNIK, CROATIA—Clinical trials are needed to answer the many questions related to minimal residual disease (MRD) assessment in multiple myeloma (MM), according to a speaker at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
MM patients are increasingly assessed for MRD, which is a strong prognostic factor and surrogate for overall survival, according to Toni Valković, MD, PhD, of University Hospital Center Rijeka in Croatia.
However, Dr. Valković said MRD assessment has not become a part of routine clinical practice, perhaps because we haven’t determined the best way to utilize MRD assessment in MM patients.
The optimal sensitivity threshold, technique, and timing of MRD assessment are not known, and it isn’t clear how MRD should be used to guide treatment.
What we know
Dr. Valković cited studies showing that MRD negativity is associated with superior survival in MM1, and, when MRD negativity is achieved, high-risk cytogenetics, age, and previous treatment regimens appear to have no further impact on prognosis.2
Dr. Valković went on to explain the benefits and detriments of multiparametric flow cytometry (MFC) and next-generation sequencing (NGS) for MRD assessment.3
NGS requires a baseline patient sample, but MFC does not. More cells are required with MFC than with NGS (>5 million vs. <1 million).
With MFC, samples must be processed within 24 to 48 hours, whereas, with NGS, fresh or stored samples can be used. MFC can be done in a few hours, while NGS can take several days.
Despite these differences, both methods provide similar levels of sensitivity for detecting MRD (≥1 in 105).
Dr. Valković also noted that MRD should be evaluated outside the bone marrow as well, which can be done with positron emission tomography-computed tomography (PET-CT).
Research has shown that patients who are MRD-negative according to both MFC and PET-CT have better outcomes than patients who are MRD-positive by MFC, PET-CT, or both.4
What we don’t know
Though he compared MFC and NGS, Dr. Valković said we don’t know the optimal technique for assessing MRD in the bone marrow.
Another uncertainty is the optimal sensitivity threshold. In the POLLUX study5, researchers found that a threshold of 10-4 resulted in lots of patients with MRD negativity, but some of these were false-negatives.
So although 10-4 proved inaccurate, it isn’t clear if the optimal threshold is 10-5 or 10-6, Dr. Valković said.
Likewise, it isn’t clear if PET-CT is the optimal method for evaluating MRD outside the bone marrow.
In a study published in 2017, PET produced false-negatives in MM patients.6 In 11% of patients (26/227), there was evidence of disease with diffusion-weighted magnetic resonance imaging with background signal suppression, but there was no apparent disease with PET. The researchers said low expression of hexokinase-2 was associated with a false-negative PET result.
Finally, Dr. Valković said we don’t know how best to use MRD to tailor therapy in MM patients. He posed the following questions:
- If patients don’t achieve MRD negativity, should they continue on the therapy?
- If MRD-negative patients become MRD-positive, should they begin therapy immediately, or should treatment be put off until a biochemical or clinical relapse?
- Should MRD status be used to determine the number of treatment cycles a patient receives, the timing of transplant, or when to begin and end maintenance therapy?
“There are a lot of issues and unanswered questions related to the optimal techniques for the evaluation of MRD and their sensitivity, the timing for MRD assessment during and after therapy, and its role in the treatment decisions, which should be answered in future clinical studies,” Dr. Valković concluded.
He did not declare any conflicts of interest.
1. Munshi NC et al. JAMA Oncol. 2017;3(1):28-35. doi:10.1001/jamaoncol.2016.3160
2. Paiva B et al. Blood. 2016 Jun 23;127(25):3165-74. doi: 10.1182/blood-2016-03-705319
3. Kumar S et al. Lancet Oncol. 2016; 17 (8):e328-46 doi: https://doi.org/10.1016/S1470-2045(16)30206-6
4. Fernandez RA et al. Blood. 2017; 130:3098
5. Dimopoulos MA et al. Haematologica. 2018 Sep 20. pii: haematol.2018.194282. doi: 10.3324/haematol.2018.194282
6. Rasche L et al. Blood. 2017 Jul 6;130(1):30-34. doi: 10.1182/blood-2017-03-774422
STRO-001 receives orphan designation for MM
The U.S. Food and Drug Administration (FDA) has granted orphan designation to STRO-001 for the treatment of multiple myeloma (MM).
STRO-001 is an antibody-drug conjugate targeting CD74, a protein highly expressed in MM and other B-cell malignancies.
Sutro Biopharma, Inc., is currently studying STRO-001 in a phase 1 trial enrolling separate dose-escalation cohorts for MM and B-cell lymphoma.
Preclinical research of STRO-001 in MM was presented at the 2017 ASH Annual Meeting.
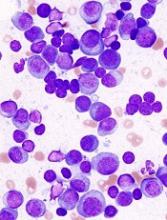
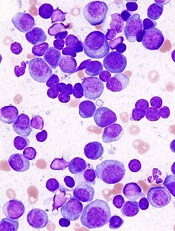
Researchers examined bone marrow samples from MM patients and detected CD74 expression in 35 of the 36 samples, including specimens from patients who were treatment-naïve and patients who had been heavily pretreated with chemotherapy and stem cell transplant.
The researchers then found that STRO-001 demonstrated cytotoxicity in MM cell lines.
STRO-001 also reduced tumor burden in two disseminated xenograft models (ARP-1 and MM.1S) and prolonged survival in one of them (MM.1S).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan designation to STRO-001 for the treatment of multiple myeloma (MM).
STRO-001 is an antibody-drug conjugate targeting CD74, a protein highly expressed in MM and other B-cell malignancies.
Sutro Biopharma, Inc., is currently studying STRO-001 in a phase 1 trial enrolling separate dose-escalation cohorts for MM and B-cell lymphoma.
Preclinical research of STRO-001 in MM was presented at the 2017 ASH Annual Meeting.
Researchers examined bone marrow samples from MM patients and detected CD74 expression in 35 of the 36 samples, including specimens from patients who were treatment-naïve and patients who had been heavily pretreated with chemotherapy and stem cell transplant.
The researchers then found that STRO-001 demonstrated cytotoxicity in MM cell lines.
STRO-001 also reduced tumor burden in two disseminated xenograft models (ARP-1 and MM.1S) and prolonged survival in one of them (MM.1S).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan designation to STRO-001 for the treatment of multiple myeloma (MM).
STRO-001 is an antibody-drug conjugate targeting CD74, a protein highly expressed in MM and other B-cell malignancies.
Sutro Biopharma, Inc., is currently studying STRO-001 in a phase 1 trial enrolling separate dose-escalation cohorts for MM and B-cell lymphoma.
Preclinical research of STRO-001 in MM was presented at the 2017 ASH Annual Meeting.
Researchers examined bone marrow samples from MM patients and detected CD74 expression in 35 of the 36 samples, including specimens from patients who were treatment-naïve and patients who had been heavily pretreated with chemotherapy and stem cell transplant.
The researchers then found that STRO-001 demonstrated cytotoxicity in MM cell lines.
STRO-001 also reduced tumor burden in two disseminated xenograft models (ARP-1 and MM.1S) and prolonged survival in one of them (MM.1S).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
Selinexor receives priority review for penta-refractory MM
The U.S. Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for selinexor.
With this NDA, Karyopharm Therapeutics Inc., is seeking accelerated approval for selinexor, an oral selective inhibitor of nuclear export compound, as a treatment for penta-refractory multiple myeloma (MM).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA plans to make a decision on the NDA for selinexor by April 6, 2019.
Selinexor also has orphan drug and fast track designations from the FDA for the treatment of penta-refractory MM.
Selinexor has demonstrated a clinical benefit in penta-refractory MM patients in the phase 2 STORM trial, according to researchers.
Results from this trial were recently presented at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting.
STORM included 122 patients with penta-refractory MM. They received selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Two patients (1.6%) achieved stringent complete responses (with minimal residual disease negativity), six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses, and 16 (13.1%) had minimal responses.
Forty-eight patients (39.3%) had stable disease, 16 (13.1%) had progressive disease, and 10 (8.2%) were not evaluable for response.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
Common treatment-related adverse events included fatigue/asthenia (69.9%), nausea (69.1%), thrombocytopenia (67.5%), anorexia (52.0%), anemia (48.0%), weight loss (47.2%), neutropenia (35.8%), vomiting (35.0%), diarrhea (33.3%), hyponatremia (30.9%), leukopenia (29.3%), and lymphopenia (13.8%).
Trials of selinexor were placed on partial clinical hold in March 2017 due to a lack of information about serious adverse events. However, the hold was lifted for trials of patients with hematologic malignancies at the end of that same month.
The U.S. Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for selinexor.
With this NDA, Karyopharm Therapeutics Inc., is seeking accelerated approval for selinexor, an oral selective inhibitor of nuclear export compound, as a treatment for penta-refractory multiple myeloma (MM).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA plans to make a decision on the NDA for selinexor by April 6, 2019.
Selinexor also has orphan drug and fast track designations from the FDA for the treatment of penta-refractory MM.
Selinexor has demonstrated a clinical benefit in penta-refractory MM patients in the phase 2 STORM trial, according to researchers.
Results from this trial were recently presented at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting.
STORM included 122 patients with penta-refractory MM. They received selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Two patients (1.6%) achieved stringent complete responses (with minimal residual disease negativity), six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses, and 16 (13.1%) had minimal responses.
Forty-eight patients (39.3%) had stable disease, 16 (13.1%) had progressive disease, and 10 (8.2%) were not evaluable for response.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
Common treatment-related adverse events included fatigue/asthenia (69.9%), nausea (69.1%), thrombocytopenia (67.5%), anorexia (52.0%), anemia (48.0%), weight loss (47.2%), neutropenia (35.8%), vomiting (35.0%), diarrhea (33.3%), hyponatremia (30.9%), leukopenia (29.3%), and lymphopenia (13.8%).
Trials of selinexor were placed on partial clinical hold in March 2017 due to a lack of information about serious adverse events. However, the hold was lifted for trials of patients with hematologic malignancies at the end of that same month.
The U.S. Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for selinexor.
With this NDA, Karyopharm Therapeutics Inc., is seeking accelerated approval for selinexor, an oral selective inhibitor of nuclear export compound, as a treatment for penta-refractory multiple myeloma (MM).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA plans to make a decision on the NDA for selinexor by April 6, 2019.
Selinexor also has orphan drug and fast track designations from the FDA for the treatment of penta-refractory MM.
Selinexor has demonstrated a clinical benefit in penta-refractory MM patients in the phase 2 STORM trial, according to researchers.
Results from this trial were recently presented at the Society of Hematologic Oncology (SOHO) 2018 Annual Meeting.
STORM included 122 patients with penta-refractory MM. They received selinexor at 80 mg twice weekly plus dexamethasone at 20 mg twice weekly until disease progression.
Two patients (1.6%) achieved stringent complete responses (with minimal residual disease negativity), six patients (4.9%) had very good partial responses, 24 (19.7%) had partial responses, and 16 (13.1%) had minimal responses.
Forty-eight patients (39.3%) had stable disease, 16 (13.1%) had progressive disease, and 10 (8.2%) were not evaluable for response.
The median progression-free survival was 3.7 months, and the median overall survival was 8.6 months.
Common treatment-related adverse events included fatigue/asthenia (69.9%), nausea (69.1%), thrombocytopenia (67.5%), anorexia (52.0%), anemia (48.0%), weight loss (47.2%), neutropenia (35.8%), vomiting (35.0%), diarrhea (33.3%), hyponatremia (30.9%), leukopenia (29.3%), and lymphopenia (13.8%).
Trials of selinexor were placed on partial clinical hold in March 2017 due to a lack of information about serious adverse events. However, the hold was lifted for trials of patients with hematologic malignancies at the end of that same month.
Quadruplet therapy could be the future in MM
New York—Four-drug combinations are holding promise for the treatment of multiple myeloma (MM), although data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center.
The efficacy of multiple triplet regimens has been well documented, and data are now emerging on the potential of 4-drug combinations.
“Triplet therapy is the standard,” she said during a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies, “and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, she said, is SWOG 0777, an open label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable. The trial was recently reported in The Lancet.
The median progression free survival (PFS) was 43 months for the triplet, versus 30 months for the two-drug regimen (P=0.0018).
Likewise, median overall survival (OS) was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P=0.025).
“Very convincingly, just receiving that short exposure to bortezomib,” she said, “ended up causing a substantial increase of progression-free and overall survival.”
Effective triplet regimens include the combination of carfilzomib, lenalidomide, and dexamethasone (KRd), cyclophosphamide, bortezomib, and dexamethasone (CyBorD), and more recently, ixazomib, lenalidomide, and dexamethasone (IRd).
These regimens have “excellent” response rates and survival data, Dr. Callander noted.
Quadruplet data
The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at ASCO 2017 (abstract 8002).
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data also presented at ASCO 2017 (abstract 8000), with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr Callander conjectured.
Four versus three drug strategies are being evaluated in ongoing randomized clinical trials including patients with previously untreated myeloma, she said.
These studies include Cassiopeia (NCT02541383), which is evaluating bortezomib, thalidomide, and dexamethasone with or without daratumumab, and GRIFFIN (NCT02874742), which is looking at VRd with or without daratumumab.
Daratumumab received an additional indication in myeloma, this time as part of a 4-drug regimen, several months ago, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The U.S. Food and Drug Administration (FDA) approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE (MMY3007) study, published in The New England Journal of Medicine, showing an 18-month PFS of 71.6% for the 4-drug combination versus 50.2% for VMP alone (P<0.001).
New York—Four-drug combinations are holding promise for the treatment of multiple myeloma (MM), although data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center.
The efficacy of multiple triplet regimens has been well documented, and data are now emerging on the potential of 4-drug combinations.
“Triplet therapy is the standard,” she said during a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies, “and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, she said, is SWOG 0777, an open label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable. The trial was recently reported in The Lancet.
The median progression free survival (PFS) was 43 months for the triplet, versus 30 months for the two-drug regimen (P=0.0018).
Likewise, median overall survival (OS) was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P=0.025).
“Very convincingly, just receiving that short exposure to bortezomib,” she said, “ended up causing a substantial increase of progression-free and overall survival.”
Effective triplet regimens include the combination of carfilzomib, lenalidomide, and dexamethasone (KRd), cyclophosphamide, bortezomib, and dexamethasone (CyBorD), and more recently, ixazomib, lenalidomide, and dexamethasone (IRd).
These regimens have “excellent” response rates and survival data, Dr. Callander noted.
Quadruplet data
The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at ASCO 2017 (abstract 8002).
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data also presented at ASCO 2017 (abstract 8000), with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr Callander conjectured.
Four versus three drug strategies are being evaluated in ongoing randomized clinical trials including patients with previously untreated myeloma, she said.
These studies include Cassiopeia (NCT02541383), which is evaluating bortezomib, thalidomide, and dexamethasone with or without daratumumab, and GRIFFIN (NCT02874742), which is looking at VRd with or without daratumumab.
Daratumumab received an additional indication in myeloma, this time as part of a 4-drug regimen, several months ago, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The U.S. Food and Drug Administration (FDA) approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE (MMY3007) study, published in The New England Journal of Medicine, showing an 18-month PFS of 71.6% for the 4-drug combination versus 50.2% for VMP alone (P<0.001).
New York—Four-drug combinations are holding promise for the treatment of multiple myeloma (MM), although data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center.
The efficacy of multiple triplet regimens has been well documented, and data are now emerging on the potential of 4-drug combinations.
“Triplet therapy is the standard,” she said during a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies, “and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, she said, is SWOG 0777, an open label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable. The trial was recently reported in The Lancet.
The median progression free survival (PFS) was 43 months for the triplet, versus 30 months for the two-drug regimen (P=0.0018).
Likewise, median overall survival (OS) was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P=0.025).
“Very convincingly, just receiving that short exposure to bortezomib,” she said, “ended up causing a substantial increase of progression-free and overall survival.”
Effective triplet regimens include the combination of carfilzomib, lenalidomide, and dexamethasone (KRd), cyclophosphamide, bortezomib, and dexamethasone (CyBorD), and more recently, ixazomib, lenalidomide, and dexamethasone (IRd).
These regimens have “excellent” response rates and survival data, Dr. Callander noted.
Quadruplet data
The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at ASCO 2017 (abstract 8002).
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data also presented at ASCO 2017 (abstract 8000), with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr Callander conjectured.
Four versus three drug strategies are being evaluated in ongoing randomized clinical trials including patients with previously untreated myeloma, she said.
These studies include Cassiopeia (NCT02541383), which is evaluating bortezomib, thalidomide, and dexamethasone with or without daratumumab, and GRIFFIN (NCT02874742), which is looking at VRd with or without daratumumab.
Daratumumab received an additional indication in myeloma, this time as part of a 4-drug regimen, several months ago, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The U.S. Food and Drug Administration (FDA) approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE (MMY3007) study, published in The New England Journal of Medicine, showing an 18-month PFS of 71.6% for the 4-drug combination versus 50.2% for VMP alone (P<0.001).
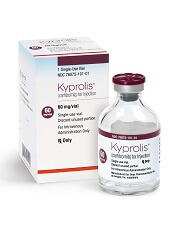
Carfilzomib receives approval for once-weekly dosing
The U.S. Food and Drug Administration (FDA) has approved carfilzomib (Kyprolis) for a once-weekly dosing option in combination with dexamethasone for patients with relapsed or refractory multiple myeloma (MM).
Carfilzomib administered once-weekly at 70 mg/m2 with dexamethasone achieved a superior progression-free survival (PFS) and overall response rates (ORR) compared to twice-weekly carfilzomib at doses of 27 mg/m2.
Carfilzomib is not, however, approved for the twice-weekly 27 mg/m2 dose with dexamethasone alone, but with dexamethasone and lenalidomide.
The FDA based its approval on data from the phase 3 ARROW trial.
The FDA reviewed and approved the supplemental New Drug Application under its Oncology Center of Excellence Real-Time Oncology Review and Assessment Aid pilot program. The program is exploring a more efficient review process to ensure that safe and effective treatments are available to patients as soon as possible.
The FDA approved the carfilzomib application in just over a month.
ARROW
The ARROW study, reported at the 2018 ASCO annual meeting and published in The Lancet, evaluated 478 patients with relapsed or refractory MM who had received at least two but no more than three prior therapies. Prior therapies could include bortezomib and an immunomodulatory drug.
Patients randomized to the investigational arm receive a 30-minute infusion of once-weekly carfilzomib (20 mg/m2 on day 1 of cycle 1; 70 mg/m2 on days 8 and 15 of cycle 1; and 70 mg/m2 on days 1, 8 and 15 of subsequent cycles) with 40 mg of dexamethasone.
Patients randomized to the comparator arm received a 10-minute infusion of twice-weekly carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1; 27 mg/m2 on days 8, 9, 15 and 16 of cycle 1; and 27 mg/m2 on days 1, 2, 8, 9, 15 and 16 of subsequent cycles) with 40 mg of dexamethasone.
Patients in the once-weekly arm achieved a statistically significant 3.7-month improvement in PFS compared to the twice-weekly regimen. Median PFS was 11.2 months for the once-weekly patients and 7.6 months for the twice-weekly group (P=0.0014).
Patients in the once-weekly group had a 62.9% ORR compared to 40.8% for those treated twice weekly (P<0.0001).
More patients (7.1%) in the once-weekly group had complete responses or better than those in the twice-weekly arm (1.7%).
The safety profile of the two arms were comparable, with no new safety risks identified in the once-weekly arm.
Treatment-emergent adverse events occurring in 20% or more patients in either arm included anemia, diarrhea, fatigue, hypertension, insomnia, and pyrexia.
First approved in 2012, carfilzomib has indications for the following in the U.S.:
- Treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy in combination with dexamethasone or with lenalidomide plus dexamethasone.
- As a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy.
Amgen manufactures carfilzomib for Onyx Pharmaceuticals, Inc.
Prescribing information for carfilzomib is available online.
The U.S. Food and Drug Administration (FDA) has approved carfilzomib (Kyprolis) for a once-weekly dosing option in combination with dexamethasone for patients with relapsed or refractory multiple myeloma (MM).
Carfilzomib administered once-weekly at 70 mg/m2 with dexamethasone achieved a superior progression-free survival (PFS) and overall response rates (ORR) compared to twice-weekly carfilzomib at doses of 27 mg/m2.
Carfilzomib is not, however, approved for the twice-weekly 27 mg/m2 dose with dexamethasone alone, but with dexamethasone and lenalidomide.
The FDA based its approval on data from the phase 3 ARROW trial.
The FDA reviewed and approved the supplemental New Drug Application under its Oncology Center of Excellence Real-Time Oncology Review and Assessment Aid pilot program. The program is exploring a more efficient review process to ensure that safe and effective treatments are available to patients as soon as possible.
The FDA approved the carfilzomib application in just over a month.
ARROW
The ARROW study, reported at the 2018 ASCO annual meeting and published in The Lancet, evaluated 478 patients with relapsed or refractory MM who had received at least two but no more than three prior therapies. Prior therapies could include bortezomib and an immunomodulatory drug.
Patients randomized to the investigational arm receive a 30-minute infusion of once-weekly carfilzomib (20 mg/m2 on day 1 of cycle 1; 70 mg/m2 on days 8 and 15 of cycle 1; and 70 mg/m2 on days 1, 8 and 15 of subsequent cycles) with 40 mg of dexamethasone.
Patients randomized to the comparator arm received a 10-minute infusion of twice-weekly carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1; 27 mg/m2 on days 8, 9, 15 and 16 of cycle 1; and 27 mg/m2 on days 1, 2, 8, 9, 15 and 16 of subsequent cycles) with 40 mg of dexamethasone.
Patients in the once-weekly arm achieved a statistically significant 3.7-month improvement in PFS compared to the twice-weekly regimen. Median PFS was 11.2 months for the once-weekly patients and 7.6 months for the twice-weekly group (P=0.0014).
Patients in the once-weekly group had a 62.9% ORR compared to 40.8% for those treated twice weekly (P<0.0001).
More patients (7.1%) in the once-weekly group had complete responses or better than those in the twice-weekly arm (1.7%).
The safety profile of the two arms were comparable, with no new safety risks identified in the once-weekly arm.
Treatment-emergent adverse events occurring in 20% or more patients in either arm included anemia, diarrhea, fatigue, hypertension, insomnia, and pyrexia.
First approved in 2012, carfilzomib has indications for the following in the U.S.:
- Treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy in combination with dexamethasone or with lenalidomide plus dexamethasone.
- As a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy.
Amgen manufactures carfilzomib for Onyx Pharmaceuticals, Inc.
Prescribing information for carfilzomib is available online.
The U.S. Food and Drug Administration (FDA) has approved carfilzomib (Kyprolis) for a once-weekly dosing option in combination with dexamethasone for patients with relapsed or refractory multiple myeloma (MM).
Carfilzomib administered once-weekly at 70 mg/m2 with dexamethasone achieved a superior progression-free survival (PFS) and overall response rates (ORR) compared to twice-weekly carfilzomib at doses of 27 mg/m2.
Carfilzomib is not, however, approved for the twice-weekly 27 mg/m2 dose with dexamethasone alone, but with dexamethasone and lenalidomide.
The FDA based its approval on data from the phase 3 ARROW trial.
The FDA reviewed and approved the supplemental New Drug Application under its Oncology Center of Excellence Real-Time Oncology Review and Assessment Aid pilot program. The program is exploring a more efficient review process to ensure that safe and effective treatments are available to patients as soon as possible.
The FDA approved the carfilzomib application in just over a month.
ARROW
The ARROW study, reported at the 2018 ASCO annual meeting and published in The Lancet, evaluated 478 patients with relapsed or refractory MM who had received at least two but no more than three prior therapies. Prior therapies could include bortezomib and an immunomodulatory drug.
Patients randomized to the investigational arm receive a 30-minute infusion of once-weekly carfilzomib (20 mg/m2 on day 1 of cycle 1; 70 mg/m2 on days 8 and 15 of cycle 1; and 70 mg/m2 on days 1, 8 and 15 of subsequent cycles) with 40 mg of dexamethasone.
Patients randomized to the comparator arm received a 10-minute infusion of twice-weekly carfilzomib (20 mg/m2 on days 1 and 2 of cycle 1; 27 mg/m2 on days 8, 9, 15 and 16 of cycle 1; and 27 mg/m2 on days 1, 2, 8, 9, 15 and 16 of subsequent cycles) with 40 mg of dexamethasone.
Patients in the once-weekly arm achieved a statistically significant 3.7-month improvement in PFS compared to the twice-weekly regimen. Median PFS was 11.2 months for the once-weekly patients and 7.6 months for the twice-weekly group (P=0.0014).
Patients in the once-weekly group had a 62.9% ORR compared to 40.8% for those treated twice weekly (P<0.0001).
More patients (7.1%) in the once-weekly group had complete responses or better than those in the twice-weekly arm (1.7%).
The safety profile of the two arms were comparable, with no new safety risks identified in the once-weekly arm.
Treatment-emergent adverse events occurring in 20% or more patients in either arm included anemia, diarrhea, fatigue, hypertension, insomnia, and pyrexia.
First approved in 2012, carfilzomib has indications for the following in the U.S.:
- Treatment of patients with relapsed or refractory multiple myeloma who have received one to three lines of therapy in combination with dexamethasone or with lenalidomide plus dexamethasone.
- As a single agent for the treatment of patients with relapsed or refractory multiple myeloma who have received one or more lines of therapy.
Amgen manufactures carfilzomib for Onyx Pharmaceuticals, Inc.
Prescribing information for carfilzomib is available online.
Will quad therapy become the new standard in myeloma?
NEW YORK – , though data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center, Madison.
“The outlook for myeloma patients is quite good,” Dr. Callander said at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
“Triplet therapy is the standard, and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, according to Dr. Callander, is SWOG 0777, an open-label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable (Lancet. 2017 Feb 4;389[10068]:519-27).
The median progression-free survival was 43 months for the triplet, versus 30 months for the two-drug regimen (P = .0018); likewise, median overall survival was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P = .025).
“Very convincingly, just receiving that short exposure to bortezomib ended up causing a substantial increase of progression-free and overall survival,” Dr. Callander said.
The efficacy of multiple triplet regimens has been documented, including the combination of carfilzomib, lenalidomide, and dexamethasone (KRd); cyclophosphamide, bortezomib, and dexamethasone (CyBorD); and more recently, ixazomib, lenalidomide, and dexamethasone (IRd). These regimens have “excellent” response rates and survival data, Dr. Callander said.
Data is now emerging on the potential role of four-drug combinations, she added. The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at the 2017 annual meeting of the American Society of Clinical Oncology.
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data presented at ASCO in 2017, with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr. Callander told the NCCN attendees.
Four- versus three-drug strategies are being evaluated in ongoing randomized clinical trials, including patients with previously untreated myeloma, she said. Those studies include Cassiopeia, which is evaluating bortezomib, thalidomide, and dexamethasone (with or without daratumumab), and GRIFFIN, which is looking at VRd (with or without daratumumab).
Daratumumab recently received an additional indication in the treatment of myeloma, this time as part of a four-drug regimen, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The Food and Drug Administration approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE study, showing an 18-month progression-free survival rate of 71.6% for the four-drug combination versus 50.2% for VMP alone (N Engl J Med. 2018;378:518-28).
Dr. Callander reported having no relevant financial disclosures.
NEW YORK – , though data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center, Madison.
“The outlook for myeloma patients is quite good,” Dr. Callander said at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
“Triplet therapy is the standard, and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, according to Dr. Callander, is SWOG 0777, an open-label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable (Lancet. 2017 Feb 4;389[10068]:519-27).
The median progression-free survival was 43 months for the triplet, versus 30 months for the two-drug regimen (P = .0018); likewise, median overall survival was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P = .025).
“Very convincingly, just receiving that short exposure to bortezomib ended up causing a substantial increase of progression-free and overall survival,” Dr. Callander said.
The efficacy of multiple triplet regimens has been documented, including the combination of carfilzomib, lenalidomide, and dexamethasone (KRd); cyclophosphamide, bortezomib, and dexamethasone (CyBorD); and more recently, ixazomib, lenalidomide, and dexamethasone (IRd). These regimens have “excellent” response rates and survival data, Dr. Callander said.
Data is now emerging on the potential role of four-drug combinations, she added. The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at the 2017 annual meeting of the American Society of Clinical Oncology.
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data presented at ASCO in 2017, with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr. Callander told the NCCN attendees.
Four- versus three-drug strategies are being evaluated in ongoing randomized clinical trials, including patients with previously untreated myeloma, she said. Those studies include Cassiopeia, which is evaluating bortezomib, thalidomide, and dexamethasone (with or without daratumumab), and GRIFFIN, which is looking at VRd (with or without daratumumab).
Daratumumab recently received an additional indication in the treatment of myeloma, this time as part of a four-drug regimen, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The Food and Drug Administration approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE study, showing an 18-month progression-free survival rate of 71.6% for the four-drug combination versus 50.2% for VMP alone (N Engl J Med. 2018;378:518-28).
Dr. Callander reported having no relevant financial disclosures.
NEW YORK – , though data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center, Madison.
“The outlook for myeloma patients is quite good,” Dr. Callander said at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
“Triplet therapy is the standard, and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, according to Dr. Callander, is SWOG 0777, an open-label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable (Lancet. 2017 Feb 4;389[10068]:519-27).
The median progression-free survival was 43 months for the triplet, versus 30 months for the two-drug regimen (P = .0018); likewise, median overall survival was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P = .025).
“Very convincingly, just receiving that short exposure to bortezomib ended up causing a substantial increase of progression-free and overall survival,” Dr. Callander said.
The efficacy of multiple triplet regimens has been documented, including the combination of carfilzomib, lenalidomide, and dexamethasone (KRd); cyclophosphamide, bortezomib, and dexamethasone (CyBorD); and more recently, ixazomib, lenalidomide, and dexamethasone (IRd). These regimens have “excellent” response rates and survival data, Dr. Callander said.
Data is now emerging on the potential role of four-drug combinations, she added. The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at the 2017 annual meeting of the American Society of Clinical Oncology.
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data presented at ASCO in 2017, with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr. Callander told the NCCN attendees.
Four- versus three-drug strategies are being evaluated in ongoing randomized clinical trials, including patients with previously untreated myeloma, she said. Those studies include Cassiopeia, which is evaluating bortezomib, thalidomide, and dexamethasone (with or without daratumumab), and GRIFFIN, which is looking at VRd (with or without daratumumab).
Daratumumab recently received an additional indication in the treatment of myeloma, this time as part of a four-drug regimen, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The Food and Drug Administration approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE study, showing an 18-month progression-free survival rate of 71.6% for the four-drug combination versus 50.2% for VMP alone (N Engl J Med. 2018;378:518-28).
Dr. Callander reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM NCCN HEMATOLOGIC MALIGNANCIES
B-cell maturation antigen targeted in myeloma trials
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
EXPERT ANALYSIS FROM THE NCCN HEMATOLOGIC MALIGNANCIES CONGRESS