User login
For MD-IQ use only
Education and networking are driving forces behind Converge platform
As Jade Myers set out to help create the virtual platform for SHM Converge, she was aware, through surveys and other communication, that the top wish of members of the Society of Hospital Medicine was an extensive and interactive educational experience.
“People really wanted to get back to the in-person conference,” said Ms. Myers, SHM’s director of meetings. “While we couldn’t do that, we can provide the same caliber and as robust an experience from an educational perspective as we would for an in-person activity.”
That has required significant revamping of the virtual platform compared to the platform for last year’s annual conference. In 2020, there was only one session running live at a time. This year, there will be 12 sessions running at the same time. There will also be more opportunities for networking, as well as other features for enjoyment and a sense of calm.
Here are some features of the SHM Converge platform:
- A host segment to kick-start each day, with an introduction of the day’s sessions and events.
- Nine didactic educational sessions at any given time. These sessions will include a live chat for peer-to-peer engagement, as well as questions and answers throughout the session to continue the discussion between speakers and participants.
- Three workshops at any given time. These sessions – on topics such as communication, gender equity, and clinical guidelines – will provide an opportunity for dynamic small-group discussion.
- A scientific abstract poster competition and reception, with an e-gallery of about 700 posters, providing a networking opportunity and highlighting emerging scientific and clinical cases.
- Special Interest Forums, in the form of live, interactive Zoom conferences. There will be 25 forums, which are designed to build community and facilitate collaboration.
- A variety of games, including trivia and a word scramble.
- Personalized profiles with information such as “Hospitalist in Training,” or “Committee Member.” These will be visible to other attendees to make it easier for people to connect when they have something in common.
- Early- and Mid-Career Speed Mentorship, in which a mentor and mentee can interact one-on-one, with each mentee able to meet with two mentors, with pairings designed for the best mentorship experience.
- Sessions on wellness and resilience.
“People are kind of Zoom fatigued,” Ms. Myers said, “so we’re trying to meet their needs while also offering an opportunity for respite, because our attendees are on the front lines right now, and they’re dealing with all types of fatigue and challenging times.”
The annual conference was on target for a banner year in 2020 before the COVID-19 pandemic forced the cancellation of the in-person conference in San Diego, and SHM Converge is a product of planning that began then, as organizers started considering a virtual event.
“In 2020, we were slated to have the largest conference in person that we have ever had,” said Hayleigh Scott, SHM’s meeting projects manager. “San Diego was going to be our really big year.”
But attendance at last year’s virtual conference was a fraction of what was expected at the in-person conference. This year, that seems poised to improve. There will be many more offerings, with more than 125 AMA PRA Category 1 Credits™ and 45 Maintenance of Certification points possible, Ms. Myers said. Because attendees won’t have to worry about being in two places at once, it will be possible to secure more CME credits at SHM Converge than at any previous SHM annual conference, she said.
The volume of content will be a heavy load on SHM personnel. Last year, three society staff members were on hand at each session to make sure it ran smoothly and to answer questions. With 12 sessions running simultaneously this year, many more staff members will need to be involved. But that is not unfamiliar for the society during meeting week, Ms. Myers said.
“We’re going to need to pull from pretty much our entire staff in order to make this conference happen, which is exciting and daunting,” she said. “It’s always been an all-hands-on-deck program and this is going to be more similar to an in-person conference in that way.”
As Jade Myers set out to help create the virtual platform for SHM Converge, she was aware, through surveys and other communication, that the top wish of members of the Society of Hospital Medicine was an extensive and interactive educational experience.
“People really wanted to get back to the in-person conference,” said Ms. Myers, SHM’s director of meetings. “While we couldn’t do that, we can provide the same caliber and as robust an experience from an educational perspective as we would for an in-person activity.”
That has required significant revamping of the virtual platform compared to the platform for last year’s annual conference. In 2020, there was only one session running live at a time. This year, there will be 12 sessions running at the same time. There will also be more opportunities for networking, as well as other features for enjoyment and a sense of calm.
Here are some features of the SHM Converge platform:
- A host segment to kick-start each day, with an introduction of the day’s sessions and events.
- Nine didactic educational sessions at any given time. These sessions will include a live chat for peer-to-peer engagement, as well as questions and answers throughout the session to continue the discussion between speakers and participants.
- Three workshops at any given time. These sessions – on topics such as communication, gender equity, and clinical guidelines – will provide an opportunity for dynamic small-group discussion.
- A scientific abstract poster competition and reception, with an e-gallery of about 700 posters, providing a networking opportunity and highlighting emerging scientific and clinical cases.
- Special Interest Forums, in the form of live, interactive Zoom conferences. There will be 25 forums, which are designed to build community and facilitate collaboration.
- A variety of games, including trivia and a word scramble.
- Personalized profiles with information such as “Hospitalist in Training,” or “Committee Member.” These will be visible to other attendees to make it easier for people to connect when they have something in common.
- Early- and Mid-Career Speed Mentorship, in which a mentor and mentee can interact one-on-one, with each mentee able to meet with two mentors, with pairings designed for the best mentorship experience.
- Sessions on wellness and resilience.
“People are kind of Zoom fatigued,” Ms. Myers said, “so we’re trying to meet their needs while also offering an opportunity for respite, because our attendees are on the front lines right now, and they’re dealing with all types of fatigue and challenging times.”
The annual conference was on target for a banner year in 2020 before the COVID-19 pandemic forced the cancellation of the in-person conference in San Diego, and SHM Converge is a product of planning that began then, as organizers started considering a virtual event.
“In 2020, we were slated to have the largest conference in person that we have ever had,” said Hayleigh Scott, SHM’s meeting projects manager. “San Diego was going to be our really big year.”
But attendance at last year’s virtual conference was a fraction of what was expected at the in-person conference. This year, that seems poised to improve. There will be many more offerings, with more than 125 AMA PRA Category 1 Credits™ and 45 Maintenance of Certification points possible, Ms. Myers said. Because attendees won’t have to worry about being in two places at once, it will be possible to secure more CME credits at SHM Converge than at any previous SHM annual conference, she said.
The volume of content will be a heavy load on SHM personnel. Last year, three society staff members were on hand at each session to make sure it ran smoothly and to answer questions. With 12 sessions running simultaneously this year, many more staff members will need to be involved. But that is not unfamiliar for the society during meeting week, Ms. Myers said.
“We’re going to need to pull from pretty much our entire staff in order to make this conference happen, which is exciting and daunting,” she said. “It’s always been an all-hands-on-deck program and this is going to be more similar to an in-person conference in that way.”
As Jade Myers set out to help create the virtual platform for SHM Converge, she was aware, through surveys and other communication, that the top wish of members of the Society of Hospital Medicine was an extensive and interactive educational experience.
“People really wanted to get back to the in-person conference,” said Ms. Myers, SHM’s director of meetings. “While we couldn’t do that, we can provide the same caliber and as robust an experience from an educational perspective as we would for an in-person activity.”
That has required significant revamping of the virtual platform compared to the platform for last year’s annual conference. In 2020, there was only one session running live at a time. This year, there will be 12 sessions running at the same time. There will also be more opportunities for networking, as well as other features for enjoyment and a sense of calm.
Here are some features of the SHM Converge platform:
- A host segment to kick-start each day, with an introduction of the day’s sessions and events.
- Nine didactic educational sessions at any given time. These sessions will include a live chat for peer-to-peer engagement, as well as questions and answers throughout the session to continue the discussion between speakers and participants.
- Three workshops at any given time. These sessions – on topics such as communication, gender equity, and clinical guidelines – will provide an opportunity for dynamic small-group discussion.
- A scientific abstract poster competition and reception, with an e-gallery of about 700 posters, providing a networking opportunity and highlighting emerging scientific and clinical cases.
- Special Interest Forums, in the form of live, interactive Zoom conferences. There will be 25 forums, which are designed to build community and facilitate collaboration.
- A variety of games, including trivia and a word scramble.
- Personalized profiles with information such as “Hospitalist in Training,” or “Committee Member.” These will be visible to other attendees to make it easier for people to connect when they have something in common.
- Early- and Mid-Career Speed Mentorship, in which a mentor and mentee can interact one-on-one, with each mentee able to meet with two mentors, with pairings designed for the best mentorship experience.
- Sessions on wellness and resilience.
“People are kind of Zoom fatigued,” Ms. Myers said, “so we’re trying to meet their needs while also offering an opportunity for respite, because our attendees are on the front lines right now, and they’re dealing with all types of fatigue and challenging times.”
The annual conference was on target for a banner year in 2020 before the COVID-19 pandemic forced the cancellation of the in-person conference in San Diego, and SHM Converge is a product of planning that began then, as organizers started considering a virtual event.
“In 2020, we were slated to have the largest conference in person that we have ever had,” said Hayleigh Scott, SHM’s meeting projects manager. “San Diego was going to be our really big year.”
But attendance at last year’s virtual conference was a fraction of what was expected at the in-person conference. This year, that seems poised to improve. There will be many more offerings, with more than 125 AMA PRA Category 1 Credits™ and 45 Maintenance of Certification points possible, Ms. Myers said. Because attendees won’t have to worry about being in two places at once, it will be possible to secure more CME credits at SHM Converge than at any previous SHM annual conference, she said.
The volume of content will be a heavy load on SHM personnel. Last year, three society staff members were on hand at each session to make sure it ran smoothly and to answer questions. With 12 sessions running simultaneously this year, many more staff members will need to be involved. But that is not unfamiliar for the society during meeting week, Ms. Myers said.
“We’re going to need to pull from pretty much our entire staff in order to make this conference happen, which is exciting and daunting,” she said. “It’s always been an all-hands-on-deck program and this is going to be more similar to an in-person conference in that way.”
Hospitalist advisory board picks ‘must-see’ Converge sessions
With dozens and dozens of sessions on the SHM Converge program, picking what to go to can feel virtually impossible.
The editorial board of The Hospitalist is here to help. With knowledge in an array of subspecialties – and experience in attending many SHM annual conferences, they have pointed out sessions they consider “must see,” whether based on the importance of the topic, the entertainment aspect, or the dynamic qualities of the speakers.
Here are their selections:
Ilaria Gadalla, DMSc, PA-C, physician assistant department chair, South University, West Palm Beach, Fla.
What You Say, What They Hear: Conversations with Your Hospital C-suite (Tuesday, May 4, 1:40 p.m. to 2:40 p.m.)
“As a department leader, developing my communication skills is always an area I seek to improve,” Dr. Gadalla said. “Tips to help with interpreting the audience and tailoring presentations for receptive feedback are invaluable tools.”
Hiring the Right Hospitalist: The Other Kind of Choosing Wisely (Wednesday, May 5, 2 p.m. to 3 p.m.)
“[This] is also an interesting session – selection criteria in the age of virtual interviewing is challenging,” she said. “I look forward to benefiting from my colleagues’ experience to enhance my leadership style.”
Shyam Odeti, MD, SFHM, FAAFP, MBA, hospitalist at Ballad Health, Johnson City, Tenn.
Understanding High-Value Care: Cost, Rationing, Overuse, and Underuse: Workshop (Tuesday May 4, 1:40 p.m. to 2:40 p.m.)
“Health care in the U.S. is expensive, and we have to pay utmost attention to the cost while providing the highest-quality medical care and service to sustain the health care,” Dr. Odeti said. “I am excited about this workshop organized by Dr. Justin Glasgow, Dr. Sarah Baron, Dr. Mona Krouss, and Dr. Harry Cho. I have known these leaders in the health care quality and patient safety arena over several years and their immense contributions to their organizations and the quality improvement special interest group of SHM. This workshop will help us understand how to define value in health care, implement high-value care, and eliminate low-value care.”
Hospitalists Piloting the Twin Engines of the Mid-Revenue Cycle Ship: A Primer on Utilization Management and Clinical Documentation Improvement (Thursday, May 6, 2:30 p.m. to 3:30 p.m.)
“The business of running hospitals carries with it many financial challenges,” Dr. Odeti said. “The intersection of tremendous fixed overhead and the vagaries of payer behavior is the cause. The COVID-19 pandemic and its devastating impact have compounded the problem. Hospitalists are natural institution leaders who are fundamental in overcoming this impasse through taking command and piloting the twin-engine ship of utilization management and clinical documentation improvement. These two domains working in synergy with experienced pilots are critical to attaining both high-quality care and the long-term viability of our health care systems. Dr. Aziz Ansari has been an expert in this domain and a highly sought-after speaker at SHM annual conferences. His sessions are incredibly captivating and educational.”
Harry Cho, MD, FACP, SFHM, chief value officer at NYC Health+ Hospitals
Medical Jeopardy (Thursday, May 6, 2:30 p.m. to 3:10 p.m.)
“[I am] always looking forward to a fun-filled session for medical learning with this fantastic group of facilitators,” Dr. Cho said.
Back to the Future - Things I Wish I Knew Earlier in my Career (Wednesday, May 5, 3:50 p.m. to 4:30 p.m.)
“Listening to Brad Sharpe brings me back to the days in training, eagerly absorbing every pearl of wisdom from mentors,” he said.
Marina Farah, MD, MHA, performance improvement consultant, FarahMD Consulting, Corvallis, Ore.
“I am excited to learn more about best practices and lessons learned from adopting telehealth in the hospital setting,” Dr. Farah said.
The Biden Administration, the 117th Congress, and What We Might See in Healthcare (Friday, May 7, 3:30 p.m. to 4:10 p.m.)
“I am looking forward to learning more about upcoming legislation and policy changes that impact U.S. health care delivery and provider reimbursement,” she said.
James Kim, MD, associate professor of medicine, Emory University, Atlanta
Health Equity and Disparities in Hospitalized Patients (Tuesday, May 4, 3:30 p.m. to 4:10 p.m. )
“[Kimberly Manning, MD] is an amazing speaker, and I know that this is a topic that she can speak about both eloquently and passionately,” Dr. Kim said. “She has been advocating for her patients at Grady for years and so this is something that she has first-hand experience about.”
Top 5 Clinical Practice Guidelines Every Hospitalist Needs to Know: Workshop (Wednesday, May 5, 3:50 p.m. to 4:50 p.m. )
“This sounds like a high-yield session,” he said. “For busy clinicians, being able to know what guidelines should affect your daily practice is extremely important.”
Lonika Sood, MD, MHPE, FACP, FHM, clinical education director of internal medicine, Washington State University, Spokane
“This is an important conversation that has surfaced with the pandemic, and likely has caused a lot of confusion amongst frontline clinicians and patients,” Dr. Sood said. “I look forward to hearing about some strategies from the presenters.”
Behind the Curtain: How a Journal Works (Friday, May 7, 3:30 p.m. to 4:30 p.m.)
“The Journal of Hospital Medicine is on the forefront of providing high-quality scientific information relevant to hospital medicine, and it would be helpful to hear of the presenters’ successes and challenges.”
Anika Kumar, MD, FAAP, FHM, assistant professor of pediatrics, Cleveland Clinic Lerner College of Medicine
Fireside Chat: Story-telling and the Nocturnist in Pediatrics (Tuesday, May 4, 3:30 p.m. to 4:50 p.m.)
“I look forward to their discussion about storytelling and the role narrative medicine plays in patient care, especially pediatrics,” Dr. Kumar said.
Febrile Infant Update (Thursday, May 6, 3:10 p.m. to 3:50 p.m.)
“This clinical update session with Dr. Russell McCulloh will be exciting, as caring for febrile infants is bread-and-butter pediatric hospital medicine,” she said. “And this update will help review new research in this diagnosis.”
Kranthi Sitammagari, MD, FACP, CHCQM-PHYADV, director of clinical operations, quality, and patient experience, Atrium Health Hospitalist Group, Monroe, N.C.
Any session in the “Clinical Updates” and “Quality” tracks
“I would recommend ‘Clinical Updates’ and ‘Quality’ sessions, as they are so close to my practice and I look forward to those sessions,” Dr. Sitammagari said. “Clinical Updates provide the latest updates in clinical practice which is very useful for everyday patient management for hospitalists. Quality sessions discuss innovative ways to improve the quality of hospitalist practice.”
Raman Palabindala, MD, SFHM, medical director of utilization management, University of Mississippi Medical Center, Jackson
Medical Jeopardy (Thursday, May 6, 2:30 p.m. to 3:10 p.m.)
“I will always promote my fun event, Medical Jeopardy (Dr. Palabindala is a moderator). It is going to be a challenge between three great attendings from three great organizations across the country to win the national Jeopardy competition. Not only will you learn a lot, but you also will have a lot of fun. I am sure it is going to be more entertaining this time, given virtual play.”
LAMA’s DRAMA: Left AMA – Documentation & Rules of AMA (Friday, May 7, 3:30 p.m. to 4:30 p.m.)
“I also recommend the talk by Dr. Medarametla not just for the title LAMA DRAMA (for ‘left against medical advice’),” he said. “We all need to learn this one to the core and I am sure he will deliver the most engaging presentation.”
With dozens and dozens of sessions on the SHM Converge program, picking what to go to can feel virtually impossible.
The editorial board of The Hospitalist is here to help. With knowledge in an array of subspecialties – and experience in attending many SHM annual conferences, they have pointed out sessions they consider “must see,” whether based on the importance of the topic, the entertainment aspect, or the dynamic qualities of the speakers.
Here are their selections:
Ilaria Gadalla, DMSc, PA-C, physician assistant department chair, South University, West Palm Beach, Fla.
What You Say, What They Hear: Conversations with Your Hospital C-suite (Tuesday, May 4, 1:40 p.m. to 2:40 p.m.)
“As a department leader, developing my communication skills is always an area I seek to improve,” Dr. Gadalla said. “Tips to help with interpreting the audience and tailoring presentations for receptive feedback are invaluable tools.”
Hiring the Right Hospitalist: The Other Kind of Choosing Wisely (Wednesday, May 5, 2 p.m. to 3 p.m.)
“[This] is also an interesting session – selection criteria in the age of virtual interviewing is challenging,” she said. “I look forward to benefiting from my colleagues’ experience to enhance my leadership style.”
Shyam Odeti, MD, SFHM, FAAFP, MBA, hospitalist at Ballad Health, Johnson City, Tenn.
Understanding High-Value Care: Cost, Rationing, Overuse, and Underuse: Workshop (Tuesday May 4, 1:40 p.m. to 2:40 p.m.)
“Health care in the U.S. is expensive, and we have to pay utmost attention to the cost while providing the highest-quality medical care and service to sustain the health care,” Dr. Odeti said. “I am excited about this workshop organized by Dr. Justin Glasgow, Dr. Sarah Baron, Dr. Mona Krouss, and Dr. Harry Cho. I have known these leaders in the health care quality and patient safety arena over several years and their immense contributions to their organizations and the quality improvement special interest group of SHM. This workshop will help us understand how to define value in health care, implement high-value care, and eliminate low-value care.”
Hospitalists Piloting the Twin Engines of the Mid-Revenue Cycle Ship: A Primer on Utilization Management and Clinical Documentation Improvement (Thursday, May 6, 2:30 p.m. to 3:30 p.m.)
“The business of running hospitals carries with it many financial challenges,” Dr. Odeti said. “The intersection of tremendous fixed overhead and the vagaries of payer behavior is the cause. The COVID-19 pandemic and its devastating impact have compounded the problem. Hospitalists are natural institution leaders who are fundamental in overcoming this impasse through taking command and piloting the twin-engine ship of utilization management and clinical documentation improvement. These two domains working in synergy with experienced pilots are critical to attaining both high-quality care and the long-term viability of our health care systems. Dr. Aziz Ansari has been an expert in this domain and a highly sought-after speaker at SHM annual conferences. His sessions are incredibly captivating and educational.”
Harry Cho, MD, FACP, SFHM, chief value officer at NYC Health+ Hospitals
Medical Jeopardy (Thursday, May 6, 2:30 p.m. to 3:10 p.m.)
“[I am] always looking forward to a fun-filled session for medical learning with this fantastic group of facilitators,” Dr. Cho said.
Back to the Future - Things I Wish I Knew Earlier in my Career (Wednesday, May 5, 3:50 p.m. to 4:30 p.m.)
“Listening to Brad Sharpe brings me back to the days in training, eagerly absorbing every pearl of wisdom from mentors,” he said.
Marina Farah, MD, MHA, performance improvement consultant, FarahMD Consulting, Corvallis, Ore.
“I am excited to learn more about best practices and lessons learned from adopting telehealth in the hospital setting,” Dr. Farah said.
The Biden Administration, the 117th Congress, and What We Might See in Healthcare (Friday, May 7, 3:30 p.m. to 4:10 p.m.)
“I am looking forward to learning more about upcoming legislation and policy changes that impact U.S. health care delivery and provider reimbursement,” she said.
James Kim, MD, associate professor of medicine, Emory University, Atlanta
Health Equity and Disparities in Hospitalized Patients (Tuesday, May 4, 3:30 p.m. to 4:10 p.m. )
“[Kimberly Manning, MD] is an amazing speaker, and I know that this is a topic that she can speak about both eloquently and passionately,” Dr. Kim said. “She has been advocating for her patients at Grady for years and so this is something that she has first-hand experience about.”
Top 5 Clinical Practice Guidelines Every Hospitalist Needs to Know: Workshop (Wednesday, May 5, 3:50 p.m. to 4:50 p.m. )
“This sounds like a high-yield session,” he said. “For busy clinicians, being able to know what guidelines should affect your daily practice is extremely important.”
Lonika Sood, MD, MHPE, FACP, FHM, clinical education director of internal medicine, Washington State University, Spokane
“This is an important conversation that has surfaced with the pandemic, and likely has caused a lot of confusion amongst frontline clinicians and patients,” Dr. Sood said. “I look forward to hearing about some strategies from the presenters.”
Behind the Curtain: How a Journal Works (Friday, May 7, 3:30 p.m. to 4:30 p.m.)
“The Journal of Hospital Medicine is on the forefront of providing high-quality scientific information relevant to hospital medicine, and it would be helpful to hear of the presenters’ successes and challenges.”
Anika Kumar, MD, FAAP, FHM, assistant professor of pediatrics, Cleveland Clinic Lerner College of Medicine
Fireside Chat: Story-telling and the Nocturnist in Pediatrics (Tuesday, May 4, 3:30 p.m. to 4:50 p.m.)
“I look forward to their discussion about storytelling and the role narrative medicine plays in patient care, especially pediatrics,” Dr. Kumar said.
Febrile Infant Update (Thursday, May 6, 3:10 p.m. to 3:50 p.m.)
“This clinical update session with Dr. Russell McCulloh will be exciting, as caring for febrile infants is bread-and-butter pediatric hospital medicine,” she said. “And this update will help review new research in this diagnosis.”
Kranthi Sitammagari, MD, FACP, CHCQM-PHYADV, director of clinical operations, quality, and patient experience, Atrium Health Hospitalist Group, Monroe, N.C.
Any session in the “Clinical Updates” and “Quality” tracks
“I would recommend ‘Clinical Updates’ and ‘Quality’ sessions, as they are so close to my practice and I look forward to those sessions,” Dr. Sitammagari said. “Clinical Updates provide the latest updates in clinical practice which is very useful for everyday patient management for hospitalists. Quality sessions discuss innovative ways to improve the quality of hospitalist practice.”
Raman Palabindala, MD, SFHM, medical director of utilization management, University of Mississippi Medical Center, Jackson
Medical Jeopardy (Thursday, May 6, 2:30 p.m. to 3:10 p.m.)
“I will always promote my fun event, Medical Jeopardy (Dr. Palabindala is a moderator). It is going to be a challenge between three great attendings from three great organizations across the country to win the national Jeopardy competition. Not only will you learn a lot, but you also will have a lot of fun. I am sure it is going to be more entertaining this time, given virtual play.”
LAMA’s DRAMA: Left AMA – Documentation & Rules of AMA (Friday, May 7, 3:30 p.m. to 4:30 p.m.)
“I also recommend the talk by Dr. Medarametla not just for the title LAMA DRAMA (for ‘left against medical advice’),” he said. “We all need to learn this one to the core and I am sure he will deliver the most engaging presentation.”
With dozens and dozens of sessions on the SHM Converge program, picking what to go to can feel virtually impossible.
The editorial board of The Hospitalist is here to help. With knowledge in an array of subspecialties – and experience in attending many SHM annual conferences, they have pointed out sessions they consider “must see,” whether based on the importance of the topic, the entertainment aspect, or the dynamic qualities of the speakers.
Here are their selections:
Ilaria Gadalla, DMSc, PA-C, physician assistant department chair, South University, West Palm Beach, Fla.
What You Say, What They Hear: Conversations with Your Hospital C-suite (Tuesday, May 4, 1:40 p.m. to 2:40 p.m.)
“As a department leader, developing my communication skills is always an area I seek to improve,” Dr. Gadalla said. “Tips to help with interpreting the audience and tailoring presentations for receptive feedback are invaluable tools.”
Hiring the Right Hospitalist: The Other Kind of Choosing Wisely (Wednesday, May 5, 2 p.m. to 3 p.m.)
“[This] is also an interesting session – selection criteria in the age of virtual interviewing is challenging,” she said. “I look forward to benefiting from my colleagues’ experience to enhance my leadership style.”
Shyam Odeti, MD, SFHM, FAAFP, MBA, hospitalist at Ballad Health, Johnson City, Tenn.
Understanding High-Value Care: Cost, Rationing, Overuse, and Underuse: Workshop (Tuesday May 4, 1:40 p.m. to 2:40 p.m.)
“Health care in the U.S. is expensive, and we have to pay utmost attention to the cost while providing the highest-quality medical care and service to sustain the health care,” Dr. Odeti said. “I am excited about this workshop organized by Dr. Justin Glasgow, Dr. Sarah Baron, Dr. Mona Krouss, and Dr. Harry Cho. I have known these leaders in the health care quality and patient safety arena over several years and their immense contributions to their organizations and the quality improvement special interest group of SHM. This workshop will help us understand how to define value in health care, implement high-value care, and eliminate low-value care.”
Hospitalists Piloting the Twin Engines of the Mid-Revenue Cycle Ship: A Primer on Utilization Management and Clinical Documentation Improvement (Thursday, May 6, 2:30 p.m. to 3:30 p.m.)
“The business of running hospitals carries with it many financial challenges,” Dr. Odeti said. “The intersection of tremendous fixed overhead and the vagaries of payer behavior is the cause. The COVID-19 pandemic and its devastating impact have compounded the problem. Hospitalists are natural institution leaders who are fundamental in overcoming this impasse through taking command and piloting the twin-engine ship of utilization management and clinical documentation improvement. These two domains working in synergy with experienced pilots are critical to attaining both high-quality care and the long-term viability of our health care systems. Dr. Aziz Ansari has been an expert in this domain and a highly sought-after speaker at SHM annual conferences. His sessions are incredibly captivating and educational.”
Harry Cho, MD, FACP, SFHM, chief value officer at NYC Health+ Hospitals
Medical Jeopardy (Thursday, May 6, 2:30 p.m. to 3:10 p.m.)
“[I am] always looking forward to a fun-filled session for medical learning with this fantastic group of facilitators,” Dr. Cho said.
Back to the Future - Things I Wish I Knew Earlier in my Career (Wednesday, May 5, 3:50 p.m. to 4:30 p.m.)
“Listening to Brad Sharpe brings me back to the days in training, eagerly absorbing every pearl of wisdom from mentors,” he said.
Marina Farah, MD, MHA, performance improvement consultant, FarahMD Consulting, Corvallis, Ore.
“I am excited to learn more about best practices and lessons learned from adopting telehealth in the hospital setting,” Dr. Farah said.
The Biden Administration, the 117th Congress, and What We Might See in Healthcare (Friday, May 7, 3:30 p.m. to 4:10 p.m.)
“I am looking forward to learning more about upcoming legislation and policy changes that impact U.S. health care delivery and provider reimbursement,” she said.
James Kim, MD, associate professor of medicine, Emory University, Atlanta
Health Equity and Disparities in Hospitalized Patients (Tuesday, May 4, 3:30 p.m. to 4:10 p.m. )
“[Kimberly Manning, MD] is an amazing speaker, and I know that this is a topic that she can speak about both eloquently and passionately,” Dr. Kim said. “She has been advocating for her patients at Grady for years and so this is something that she has first-hand experience about.”
Top 5 Clinical Practice Guidelines Every Hospitalist Needs to Know: Workshop (Wednesday, May 5, 3:50 p.m. to 4:50 p.m. )
“This sounds like a high-yield session,” he said. “For busy clinicians, being able to know what guidelines should affect your daily practice is extremely important.”
Lonika Sood, MD, MHPE, FACP, FHM, clinical education director of internal medicine, Washington State University, Spokane
“This is an important conversation that has surfaced with the pandemic, and likely has caused a lot of confusion amongst frontline clinicians and patients,” Dr. Sood said. “I look forward to hearing about some strategies from the presenters.”
Behind the Curtain: How a Journal Works (Friday, May 7, 3:30 p.m. to 4:30 p.m.)
“The Journal of Hospital Medicine is on the forefront of providing high-quality scientific information relevant to hospital medicine, and it would be helpful to hear of the presenters’ successes and challenges.”
Anika Kumar, MD, FAAP, FHM, assistant professor of pediatrics, Cleveland Clinic Lerner College of Medicine
Fireside Chat: Story-telling and the Nocturnist in Pediatrics (Tuesday, May 4, 3:30 p.m. to 4:50 p.m.)
“I look forward to their discussion about storytelling and the role narrative medicine plays in patient care, especially pediatrics,” Dr. Kumar said.
Febrile Infant Update (Thursday, May 6, 3:10 p.m. to 3:50 p.m.)
“This clinical update session with Dr. Russell McCulloh will be exciting, as caring for febrile infants is bread-and-butter pediatric hospital medicine,” she said. “And this update will help review new research in this diagnosis.”
Kranthi Sitammagari, MD, FACP, CHCQM-PHYADV, director of clinical operations, quality, and patient experience, Atrium Health Hospitalist Group, Monroe, N.C.
Any session in the “Clinical Updates” and “Quality” tracks
“I would recommend ‘Clinical Updates’ and ‘Quality’ sessions, as they are so close to my practice and I look forward to those sessions,” Dr. Sitammagari said. “Clinical Updates provide the latest updates in clinical practice which is very useful for everyday patient management for hospitalists. Quality sessions discuss innovative ways to improve the quality of hospitalist practice.”
Raman Palabindala, MD, SFHM, medical director of utilization management, University of Mississippi Medical Center, Jackson
Medical Jeopardy (Thursday, May 6, 2:30 p.m. to 3:10 p.m.)
“I will always promote my fun event, Medical Jeopardy (Dr. Palabindala is a moderator). It is going to be a challenge between three great attendings from three great organizations across the country to win the national Jeopardy competition. Not only will you learn a lot, but you also will have a lot of fun. I am sure it is going to be more entertaining this time, given virtual play.”
LAMA’s DRAMA: Left AMA – Documentation & Rules of AMA (Friday, May 7, 3:30 p.m. to 4:30 p.m.)
“I also recommend the talk by Dr. Medarametla not just for the title LAMA DRAMA (for ‘left against medical advice’),” he said. “We all need to learn this one to the core and I am sure he will deliver the most engaging presentation.”
Immigrant hospitalists to share diverse experiences
Ingrid Pinzon, MD, FACP, was working as a medical assistant to a physician a decade ago when she heard the doctor prescribe ibuprofen to a woman who was in the latter stages of pregnancy. Dr. Pinzon was a doctor, having received her education and training in Colombia, but because she had emigrated to the United States and hadn’t yet completed her certification and training here, she was not recognized yet as an American physician.
But she knew that ibuprofen was not recommended during late-term pregnancy, and she was alarmed. She informed the physician of the mistake. The doctor headed to Google, Dr. Pinzon said, and called the patient to rescind the ibuprofen prescription. But she soon fired Dr. Pinzon, seemingly for having had the courage to speak up.
Dr. Pinzon, now medical director of care coordination at Emory Johns Creek Hospital in Atlanta, will describe her experience as an immigrant physician in the Society of Hospital Medicine Converge session: “A Walk in Our Shoes: Immigrant Physicians Sharing Their Stories.” She will be joined by Patricia O’Brien, MD, PhD, FAAP, a pediatric hospitalist in Tampa; Manpreet Malik, MD, a hospitalist at Emory University; and Benji Mathews, MD, SFHM, FACP, chief of hospital medicine at HealthPartners and associate professor at the University of Minnesota.
They will describe their struggles to find their way in the United States, along with the satisfaction of having hard work pay off with better lives for themselves and their families. And together, they’ll provide a variety of narratives that will show, contrary to how many Americans view immigrants, how the experiences of immigrants don’t follow the same path, but each one carves out a path of his or her own.
“The thrust of this is really storytelling, along with putting into context what we can do to help our hospitalist brothers and sisters who are immigrants, and shining the light on it,” Dr. O’Brien said.
Dr. Pinzon was working as a doctor for the Colombian government when she began receiving threats from soldiers in a guerrilla army, which didn’t agree with her alignment with the government. One day, a guerrilla soldier threatened her and her two daughters – aged 5 and 11 at the time – and accurately described her daughters’ whereabouts.
Less than a week later, she and her daughters flew from Bogota to the United States, never to return to Colombia.
“I dropped everything I had when I came here,” she said. An immigration attorney initially recommended that she marry an American man in order to stay in the United States. When Dr. Pinzon declined, they pursued political asylum, and she received it less than a year later.
For 3 years, she worked jobs as assistants in medical offices and in other jobs, well below her education level, as she guided her daughters through school and went through the U.S. medical certification process. She was besieged by doubt constantly, she said.
“I cried for 3 years in a row,” she said. “I wanted to go back to my country. I didn’t want to stay here.”
Finally, she did her medical residency between 2011 and 2014, and got a job with Emory. Her daughters are grown, and one is a doctor in general surgery residency. Dr. Pinzon said she is happy to care for patients, particularly those who are Spanish-speaking and struggle as she did. But she often encounters patients who don’t hide that they dislike her accent.
“I will mute the TV and I will say: ‘I have a strong accent and so I want to make sure communication is clear,’ ” she said. “We have to prove ourselves all of the time. I feel like I have to prove myself to my patients that I’m a good doctor all of the time.” American-born doctors, she added, “shouldn’t take for granted what they already have.”
Dr. O’Brien grew up in Ireland, but in the late 1980s, the country was in a serious recession, with unemployment close to 20%, and her father applied for residency in Canada and the United States. They were accepted in Canada first, and moved there in 1988. A few years later, her parents moved them to Florida.
“They knew in order for us to do well, we had to go abroad,” she said. Dr. O’Brien went to college, medical school and graduate school in Florida, and completed residency in Cincinnati. Feeling the tug of her birthplace, she moved back to Ireland and worked there for a couple years.
“I never really wanted to leave because it was my home,” she said. While there, she came to a new-found appreciation for the U.S. health care system. It’s true that, in Ireland, everyone is insured, but there long wait times – for example, up to 2 years for a sedated nonurgent MRI for a child. She once had to send a patient to Dublin in a taxi with a nurse because an ambulance was unavailable.
“After going back to Ireland, where – I honestly thought I was going to go back and settle there – I realized how visionary my parents were in moving us,” Dr. O’Brien said. “This system in the U.S., there are lot of things broken about it, but we have all the resources.”
She moved back to the United States in August 2016, during a period of anti-immigrant rhetoric.
Nonetheless, Dr. O’Brien said she is happy to be here despite the lack of tolerance she sees in a minority of the U.S. population.
“Have a bit of sensitivity toward your provider. Maybe they speak with an accent. Maybe they don’t speak English perfectly. Maybe they have a different skin color. But their intention is good and it’s to help you and improve your health,” she said.
Ingrid Pinzon, MD, FACP, was working as a medical assistant to a physician a decade ago when she heard the doctor prescribe ibuprofen to a woman who was in the latter stages of pregnancy. Dr. Pinzon was a doctor, having received her education and training in Colombia, but because she had emigrated to the United States and hadn’t yet completed her certification and training here, she was not recognized yet as an American physician.
But she knew that ibuprofen was not recommended during late-term pregnancy, and she was alarmed. She informed the physician of the mistake. The doctor headed to Google, Dr. Pinzon said, and called the patient to rescind the ibuprofen prescription. But she soon fired Dr. Pinzon, seemingly for having had the courage to speak up.
Dr. Pinzon, now medical director of care coordination at Emory Johns Creek Hospital in Atlanta, will describe her experience as an immigrant physician in the Society of Hospital Medicine Converge session: “A Walk in Our Shoes: Immigrant Physicians Sharing Their Stories.” She will be joined by Patricia O’Brien, MD, PhD, FAAP, a pediatric hospitalist in Tampa; Manpreet Malik, MD, a hospitalist at Emory University; and Benji Mathews, MD, SFHM, FACP, chief of hospital medicine at HealthPartners and associate professor at the University of Minnesota.
They will describe their struggles to find their way in the United States, along with the satisfaction of having hard work pay off with better lives for themselves and their families. And together, they’ll provide a variety of narratives that will show, contrary to how many Americans view immigrants, how the experiences of immigrants don’t follow the same path, but each one carves out a path of his or her own.
“The thrust of this is really storytelling, along with putting into context what we can do to help our hospitalist brothers and sisters who are immigrants, and shining the light on it,” Dr. O’Brien said.
Dr. Pinzon was working as a doctor for the Colombian government when she began receiving threats from soldiers in a guerrilla army, which didn’t agree with her alignment with the government. One day, a guerrilla soldier threatened her and her two daughters – aged 5 and 11 at the time – and accurately described her daughters’ whereabouts.
Less than a week later, she and her daughters flew from Bogota to the United States, never to return to Colombia.
“I dropped everything I had when I came here,” she said. An immigration attorney initially recommended that she marry an American man in order to stay in the United States. When Dr. Pinzon declined, they pursued political asylum, and she received it less than a year later.
For 3 years, she worked jobs as assistants in medical offices and in other jobs, well below her education level, as she guided her daughters through school and went through the U.S. medical certification process. She was besieged by doubt constantly, she said.
“I cried for 3 years in a row,” she said. “I wanted to go back to my country. I didn’t want to stay here.”
Finally, she did her medical residency between 2011 and 2014, and got a job with Emory. Her daughters are grown, and one is a doctor in general surgery residency. Dr. Pinzon said she is happy to care for patients, particularly those who are Spanish-speaking and struggle as she did. But she often encounters patients who don’t hide that they dislike her accent.
“I will mute the TV and I will say: ‘I have a strong accent and so I want to make sure communication is clear,’ ” she said. “We have to prove ourselves all of the time. I feel like I have to prove myself to my patients that I’m a good doctor all of the time.” American-born doctors, she added, “shouldn’t take for granted what they already have.”
Dr. O’Brien grew up in Ireland, but in the late 1980s, the country was in a serious recession, with unemployment close to 20%, and her father applied for residency in Canada and the United States. They were accepted in Canada first, and moved there in 1988. A few years later, her parents moved them to Florida.
“They knew in order for us to do well, we had to go abroad,” she said. Dr. O’Brien went to college, medical school and graduate school in Florida, and completed residency in Cincinnati. Feeling the tug of her birthplace, she moved back to Ireland and worked there for a couple years.
“I never really wanted to leave because it was my home,” she said. While there, she came to a new-found appreciation for the U.S. health care system. It’s true that, in Ireland, everyone is insured, but there long wait times – for example, up to 2 years for a sedated nonurgent MRI for a child. She once had to send a patient to Dublin in a taxi with a nurse because an ambulance was unavailable.
“After going back to Ireland, where – I honestly thought I was going to go back and settle there – I realized how visionary my parents were in moving us,” Dr. O’Brien said. “This system in the U.S., there are lot of things broken about it, but we have all the resources.”
She moved back to the United States in August 2016, during a period of anti-immigrant rhetoric.
Nonetheless, Dr. O’Brien said she is happy to be here despite the lack of tolerance she sees in a minority of the U.S. population.
“Have a bit of sensitivity toward your provider. Maybe they speak with an accent. Maybe they don’t speak English perfectly. Maybe they have a different skin color. But their intention is good and it’s to help you and improve your health,” she said.
Ingrid Pinzon, MD, FACP, was working as a medical assistant to a physician a decade ago when she heard the doctor prescribe ibuprofen to a woman who was in the latter stages of pregnancy. Dr. Pinzon was a doctor, having received her education and training in Colombia, but because she had emigrated to the United States and hadn’t yet completed her certification and training here, she was not recognized yet as an American physician.
But she knew that ibuprofen was not recommended during late-term pregnancy, and she was alarmed. She informed the physician of the mistake. The doctor headed to Google, Dr. Pinzon said, and called the patient to rescind the ibuprofen prescription. But she soon fired Dr. Pinzon, seemingly for having had the courage to speak up.
Dr. Pinzon, now medical director of care coordination at Emory Johns Creek Hospital in Atlanta, will describe her experience as an immigrant physician in the Society of Hospital Medicine Converge session: “A Walk in Our Shoes: Immigrant Physicians Sharing Their Stories.” She will be joined by Patricia O’Brien, MD, PhD, FAAP, a pediatric hospitalist in Tampa; Manpreet Malik, MD, a hospitalist at Emory University; and Benji Mathews, MD, SFHM, FACP, chief of hospital medicine at HealthPartners and associate professor at the University of Minnesota.
They will describe their struggles to find their way in the United States, along with the satisfaction of having hard work pay off with better lives for themselves and their families. And together, they’ll provide a variety of narratives that will show, contrary to how many Americans view immigrants, how the experiences of immigrants don’t follow the same path, but each one carves out a path of his or her own.
“The thrust of this is really storytelling, along with putting into context what we can do to help our hospitalist brothers and sisters who are immigrants, and shining the light on it,” Dr. O’Brien said.
Dr. Pinzon was working as a doctor for the Colombian government when she began receiving threats from soldiers in a guerrilla army, which didn’t agree with her alignment with the government. One day, a guerrilla soldier threatened her and her two daughters – aged 5 and 11 at the time – and accurately described her daughters’ whereabouts.
Less than a week later, she and her daughters flew from Bogota to the United States, never to return to Colombia.
“I dropped everything I had when I came here,” she said. An immigration attorney initially recommended that she marry an American man in order to stay in the United States. When Dr. Pinzon declined, they pursued political asylum, and she received it less than a year later.
For 3 years, she worked jobs as assistants in medical offices and in other jobs, well below her education level, as she guided her daughters through school and went through the U.S. medical certification process. She was besieged by doubt constantly, she said.
“I cried for 3 years in a row,” she said. “I wanted to go back to my country. I didn’t want to stay here.”
Finally, she did her medical residency between 2011 and 2014, and got a job with Emory. Her daughters are grown, and one is a doctor in general surgery residency. Dr. Pinzon said she is happy to care for patients, particularly those who are Spanish-speaking and struggle as she did. But she often encounters patients who don’t hide that they dislike her accent.
“I will mute the TV and I will say: ‘I have a strong accent and so I want to make sure communication is clear,’ ” she said. “We have to prove ourselves all of the time. I feel like I have to prove myself to my patients that I’m a good doctor all of the time.” American-born doctors, she added, “shouldn’t take for granted what they already have.”
Dr. O’Brien grew up in Ireland, but in the late 1980s, the country was in a serious recession, with unemployment close to 20%, and her father applied for residency in Canada and the United States. They were accepted in Canada first, and moved there in 1988. A few years later, her parents moved them to Florida.
“They knew in order for us to do well, we had to go abroad,” she said. Dr. O’Brien went to college, medical school and graduate school in Florida, and completed residency in Cincinnati. Feeling the tug of her birthplace, she moved back to Ireland and worked there for a couple years.
“I never really wanted to leave because it was my home,” she said. While there, she came to a new-found appreciation for the U.S. health care system. It’s true that, in Ireland, everyone is insured, but there long wait times – for example, up to 2 years for a sedated nonurgent MRI for a child. She once had to send a patient to Dublin in a taxi with a nurse because an ambulance was unavailable.
“After going back to Ireland, where – I honestly thought I was going to go back and settle there – I realized how visionary my parents were in moving us,” Dr. O’Brien said. “This system in the U.S., there are lot of things broken about it, but we have all the resources.”
She moved back to the United States in August 2016, during a period of anti-immigrant rhetoric.
Nonetheless, Dr. O’Brien said she is happy to be here despite the lack of tolerance she sees in a minority of the U.S. population.
“Have a bit of sensitivity toward your provider. Maybe they speak with an accent. Maybe they don’t speak English perfectly. Maybe they have a different skin color. But their intention is good and it’s to help you and improve your health,” she said.
SHM Converge to be an ‘intellectual feast’
Course director Dr. Daniel Steinberg highlights top content
The weeks leading up to our Annual Conference always trigger certain rituals for me.
Deciding which sessions to attend feels like planning an intellectual feast mixed with an exercise in compromise, as I realize there is just no way to attend every session that I want to. Scheduling all my plans to connect over dinner and drinks with current and former colleagues is a logistical challenge I undertake with anticipation and some stress, especially when I’m the one tasked with making restaurant reservations. Thinking about how to pay for it all means digging out the rules around my CME faculty allowance, after first figuring out if I still even have a CME allowance, of course.
In the years that I am presenting, there are the last-minute emails with my co-presenters to arrange a time to run through our slides together on site. The prospect of seeing cherished colleagues and friends from SHM mixes with the fact that I know I will miss my wife and young son while I am away. Overall though, I am filled with a tremendous sense of excitement, a feeling that I enjoy in a sustained way for weeks before the meeting.
My excitement for SHM Converge is just as strong, but different in some great and important ways. The availability of on-demand content means I won’t have to choose one session over another this year – I can have my cake and eat it, too. Without the need to travel, expenses will be considerably less, and I won’t need to be away from my family.
But what I am most thrilled about when I think about SHM Converge is the content. A year of planning by our outstanding SHM staff, leadership, and Annual Conference Committee has produced a lineup of world-class speakers. Our virtual platform will offer a rich interactive and networking experience. Perennial favorite sessions, such as the Great Debate, Rapid Fire, and Update sessions will provide attendees the chance to update their core clinical knowledge across the breadth of hospital medicine.
Many aspects of health equity will be explored. Over 15 sessions and four special-interest forums covering topics such as racial and gender inequities, implicit bias, vulnerable populations, and ethics will help attendees not only understand the issues but also will show them how they can take action to make a difference.
Clinical and operational aspects of COVID-19 will also be covered at SHM Converge as speakers share the tremendous innovation, triumphs, and challenges that have taken place over the past year. Wellness and resilience are, of course, as relevant as ever, and sessions on balancing parenthood and work, learning from personal failures, and how to handle uncertainty and be resilient are among the topics that will be covered.
The essence of what we will do at SHM Converge in May is captured in our new meeting logo, an animation of nodes connecting with each other through lines that travel short and long, and intersect along the way. It’s a great representation of the togetherness, community, and mutual support that is at the core of who we are as SHM – now, more than ever. Thank you for joining us!
Dr. Steinberg is chief patient safety officer at Mount Sinai Downtown, and associate dean for quality/patient safety in GME, Mount Sinai Health System, New York. He is professor of medicine and medical education at the Icahn School of Medicine at Mount Sinai, and course director of SHM Converge.
Course director Dr. Daniel Steinberg highlights top content
Course director Dr. Daniel Steinberg highlights top content
The weeks leading up to our Annual Conference always trigger certain rituals for me.
Deciding which sessions to attend feels like planning an intellectual feast mixed with an exercise in compromise, as I realize there is just no way to attend every session that I want to. Scheduling all my plans to connect over dinner and drinks with current and former colleagues is a logistical challenge I undertake with anticipation and some stress, especially when I’m the one tasked with making restaurant reservations. Thinking about how to pay for it all means digging out the rules around my CME faculty allowance, after first figuring out if I still even have a CME allowance, of course.
In the years that I am presenting, there are the last-minute emails with my co-presenters to arrange a time to run through our slides together on site. The prospect of seeing cherished colleagues and friends from SHM mixes with the fact that I know I will miss my wife and young son while I am away. Overall though, I am filled with a tremendous sense of excitement, a feeling that I enjoy in a sustained way for weeks before the meeting.
My excitement for SHM Converge is just as strong, but different in some great and important ways. The availability of on-demand content means I won’t have to choose one session over another this year – I can have my cake and eat it, too. Without the need to travel, expenses will be considerably less, and I won’t need to be away from my family.
But what I am most thrilled about when I think about SHM Converge is the content. A year of planning by our outstanding SHM staff, leadership, and Annual Conference Committee has produced a lineup of world-class speakers. Our virtual platform will offer a rich interactive and networking experience. Perennial favorite sessions, such as the Great Debate, Rapid Fire, and Update sessions will provide attendees the chance to update their core clinical knowledge across the breadth of hospital medicine.
Many aspects of health equity will be explored. Over 15 sessions and four special-interest forums covering topics such as racial and gender inequities, implicit bias, vulnerable populations, and ethics will help attendees not only understand the issues but also will show them how they can take action to make a difference.
Clinical and operational aspects of COVID-19 will also be covered at SHM Converge as speakers share the tremendous innovation, triumphs, and challenges that have taken place over the past year. Wellness and resilience are, of course, as relevant as ever, and sessions on balancing parenthood and work, learning from personal failures, and how to handle uncertainty and be resilient are among the topics that will be covered.
The essence of what we will do at SHM Converge in May is captured in our new meeting logo, an animation of nodes connecting with each other through lines that travel short and long, and intersect along the way. It’s a great representation of the togetherness, community, and mutual support that is at the core of who we are as SHM – now, more than ever. Thank you for joining us!
Dr. Steinberg is chief patient safety officer at Mount Sinai Downtown, and associate dean for quality/patient safety in GME, Mount Sinai Health System, New York. He is professor of medicine and medical education at the Icahn School of Medicine at Mount Sinai, and course director of SHM Converge.
The weeks leading up to our Annual Conference always trigger certain rituals for me.
Deciding which sessions to attend feels like planning an intellectual feast mixed with an exercise in compromise, as I realize there is just no way to attend every session that I want to. Scheduling all my plans to connect over dinner and drinks with current and former colleagues is a logistical challenge I undertake with anticipation and some stress, especially when I’m the one tasked with making restaurant reservations. Thinking about how to pay for it all means digging out the rules around my CME faculty allowance, after first figuring out if I still even have a CME allowance, of course.
In the years that I am presenting, there are the last-minute emails with my co-presenters to arrange a time to run through our slides together on site. The prospect of seeing cherished colleagues and friends from SHM mixes with the fact that I know I will miss my wife and young son while I am away. Overall though, I am filled with a tremendous sense of excitement, a feeling that I enjoy in a sustained way for weeks before the meeting.
My excitement for SHM Converge is just as strong, but different in some great and important ways. The availability of on-demand content means I won’t have to choose one session over another this year – I can have my cake and eat it, too. Without the need to travel, expenses will be considerably less, and I won’t need to be away from my family.
But what I am most thrilled about when I think about SHM Converge is the content. A year of planning by our outstanding SHM staff, leadership, and Annual Conference Committee has produced a lineup of world-class speakers. Our virtual platform will offer a rich interactive and networking experience. Perennial favorite sessions, such as the Great Debate, Rapid Fire, and Update sessions will provide attendees the chance to update their core clinical knowledge across the breadth of hospital medicine.
Many aspects of health equity will be explored. Over 15 sessions and four special-interest forums covering topics such as racial and gender inequities, implicit bias, vulnerable populations, and ethics will help attendees not only understand the issues but also will show them how they can take action to make a difference.
Clinical and operational aspects of COVID-19 will also be covered at SHM Converge as speakers share the tremendous innovation, triumphs, and challenges that have taken place over the past year. Wellness and resilience are, of course, as relevant as ever, and sessions on balancing parenthood and work, learning from personal failures, and how to handle uncertainty and be resilient are among the topics that will be covered.
The essence of what we will do at SHM Converge in May is captured in our new meeting logo, an animation of nodes connecting with each other through lines that travel short and long, and intersect along the way. It’s a great representation of the togetherness, community, and mutual support that is at the core of who we are as SHM – now, more than ever. Thank you for joining us!
Dr. Steinberg is chief patient safety officer at Mount Sinai Downtown, and associate dean for quality/patient safety in GME, Mount Sinai Health System, New York. He is professor of medicine and medical education at the Icahn School of Medicine at Mount Sinai, and course director of SHM Converge.
COVID concerns, private equities, and virtual realities
I am hopeful that we are beginning to see a sustained decline in COVID-19 cases and hospitalizations. Although, total COVID-19 cases and deaths continue to rise (more than 460,000 deaths in the United States), vaccinations and treatment options have reduced the prevalence of severe disease, hospitalizations, and mortality rates. Worries about variants continue, but we now will enter a prolonged phase before we finally subdue COVID-19 and fully open our economies.
Health systems and practices are looking ahead and beginning to focus on how practice will look after COVID-19. From a business standpoint, we are seeing an accelerating consolidation of community practices. We anticipate the first resale of a private equity (PE)–acquired GI practice: Gastro Health was the first practice to join with a PE firm in 2016. Published rumors suggest a sale of the (now larger, multistate) practice at 15-times-plus EBITDA (earnings before interest, taxes, depreciation, and amortization) could begin as early as this quarter. It would not be a surprise to see 40% of independent gastroenterologists employed in a PE-backed model within a few years. Health systems and payers (especially United Health Group) continue to scoop up practices as well.
Clinical care has been changed forever. I expect fully 30% of visits will remain virtual, and innovative health systems will capitalize on that fact to right-size their brick-and-mortar facilities. Start-up companies will virtualize care and develop new models that allow board-certified gastroenterologist to focus on care they only can provide, resulting in substantial cost savings and (hopefully) similar or better outcomes. Remote patient monitoring (both reactive and predictive) is now firmly entrenched in our care armamentarium.
As you will see in this issue, we must create more effective interventions for NAFLD. Obesity will play an increasingly important role in the development of digestive and liver disease, so gastroenterologists must develop better tools and processes to combat root causes.
Begin thinking about DDW. While it again will be a virtual meeting, the content will be rich. Virtual meetings open up additional possibilities to gain new knowledge, although those personal connections over cocktails will be sorely missed.
John I. Allen, MD, MBA, AGAF
Editor in Chief
I am hopeful that we are beginning to see a sustained decline in COVID-19 cases and hospitalizations. Although, total COVID-19 cases and deaths continue to rise (more than 460,000 deaths in the United States), vaccinations and treatment options have reduced the prevalence of severe disease, hospitalizations, and mortality rates. Worries about variants continue, but we now will enter a prolonged phase before we finally subdue COVID-19 and fully open our economies.
Health systems and practices are looking ahead and beginning to focus on how practice will look after COVID-19. From a business standpoint, we are seeing an accelerating consolidation of community practices. We anticipate the first resale of a private equity (PE)–acquired GI practice: Gastro Health was the first practice to join with a PE firm in 2016. Published rumors suggest a sale of the (now larger, multistate) practice at 15-times-plus EBITDA (earnings before interest, taxes, depreciation, and amortization) could begin as early as this quarter. It would not be a surprise to see 40% of independent gastroenterologists employed in a PE-backed model within a few years. Health systems and payers (especially United Health Group) continue to scoop up practices as well.
Clinical care has been changed forever. I expect fully 30% of visits will remain virtual, and innovative health systems will capitalize on that fact to right-size their brick-and-mortar facilities. Start-up companies will virtualize care and develop new models that allow board-certified gastroenterologist to focus on care they only can provide, resulting in substantial cost savings and (hopefully) similar or better outcomes. Remote patient monitoring (both reactive and predictive) is now firmly entrenched in our care armamentarium.
As you will see in this issue, we must create more effective interventions for NAFLD. Obesity will play an increasingly important role in the development of digestive and liver disease, so gastroenterologists must develop better tools and processes to combat root causes.
Begin thinking about DDW. While it again will be a virtual meeting, the content will be rich. Virtual meetings open up additional possibilities to gain new knowledge, although those personal connections over cocktails will be sorely missed.
John I. Allen, MD, MBA, AGAF
Editor in Chief
I am hopeful that we are beginning to see a sustained decline in COVID-19 cases and hospitalizations. Although, total COVID-19 cases and deaths continue to rise (more than 460,000 deaths in the United States), vaccinations and treatment options have reduced the prevalence of severe disease, hospitalizations, and mortality rates. Worries about variants continue, but we now will enter a prolonged phase before we finally subdue COVID-19 and fully open our economies.
Health systems and practices are looking ahead and beginning to focus on how practice will look after COVID-19. From a business standpoint, we are seeing an accelerating consolidation of community practices. We anticipate the first resale of a private equity (PE)–acquired GI practice: Gastro Health was the first practice to join with a PE firm in 2016. Published rumors suggest a sale of the (now larger, multistate) practice at 15-times-plus EBITDA (earnings before interest, taxes, depreciation, and amortization) could begin as early as this quarter. It would not be a surprise to see 40% of independent gastroenterologists employed in a PE-backed model within a few years. Health systems and payers (especially United Health Group) continue to scoop up practices as well.
Clinical care has been changed forever. I expect fully 30% of visits will remain virtual, and innovative health systems will capitalize on that fact to right-size their brick-and-mortar facilities. Start-up companies will virtualize care and develop new models that allow board-certified gastroenterologist to focus on care they only can provide, resulting in substantial cost savings and (hopefully) similar or better outcomes. Remote patient monitoring (both reactive and predictive) is now firmly entrenched in our care armamentarium.
As you will see in this issue, we must create more effective interventions for NAFLD. Obesity will play an increasingly important role in the development of digestive and liver disease, so gastroenterologists must develop better tools and processes to combat root causes.
Begin thinking about DDW. While it again will be a virtual meeting, the content will be rich. Virtual meetings open up additional possibilities to gain new knowledge, although those personal connections over cocktails will be sorely missed.
John I. Allen, MD, MBA, AGAF
Editor in Chief
March 2021 - What's your diagnosis?
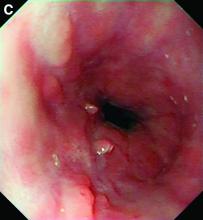
Answer: esophageal Crohn’s disease.
The esophageal biopsies demonstrate severe chronic inflammation of the subepithelial tissue with marked lymphocytic infiltration and the presence of granulomas containing multinucleate giant cells (Figure B, arrow). Given his immunosuppression with azathioprine, stains for cytomegalovirus, herpes simplex virus, and mycobacterial and fungal organisms were performed and returned negative.
A diagnosis of esophageal Crohn’s disease was made, and adalimumab was recommenced. A rapid and dramatic clinical improvement was observed, with complete resolution of his symptoms. Adalimumab trough levels were checked and found to be therapeutic (9 mcg/mL). Repeat esophagogastroduodenoscopy at 6 months showed healing of the esophageal ulceration, with residual scarring and the presence of two postinflammatory polyps (Figure C). The histopathology was consistent with quiescent Crohn’s disease.
Recognition of this very rare manifestation of Crohn’s is challenging but important so that appropriate treatment is not delayed. It is both unexplained and unusual for Crohn’s disease to flare in a new gastrointestinal location. Moreover, although accurate adult prevalence data for esophageal Crohn’s are scarce, retrospective data suggest it is present in just 0.2% of Crohn’s disease patients.1 By contrast, gastroesophageal reflux disease prevalence is between 18% and 28% of the total population in North America. Esophageal Crohn’s commonly leads to nonspecific symptoms that resemble gastroesophageal reflux disease, and as for acid reflux, the mid and distal esophagus are the most common sites of involvement. In keeping with the behavior of luminal Crohn’s disease, progression from inflammation to stenosis (causing marked dysphagia) or perforation (leading to fistula formation) may occur.2 Histopathology typically demonstrates chronic inflammation, although noncaseating granulomas are seen in the minority (7%-39%) of patients.3 Multiple deep biopsies are recommended to improve diagnostic yield,3 and our case demonstrates the value of repeat endoscopic evaluation.
Unsurprisingly given its rarity, there are no systematic data on optimal treatment. Acid suppression therapy may provide symptomatic benefit but does not treat the underlying inflammatory process. Oral prednisolone, topical budesonide, and immunomodulators including thiopurines have been used in case series, but biological therapy (typically anti–tumor necrosis factor therapy) is likely to be required for severe disease.2,3 There are no data on the use of more novel biologics. Critically, almost all reported cases of esophageal Crohn’s disease have concomitant intestinal disease, and the presence of upper gastrointestinal Crohn’s predicts a more severe disease phenotype, supporting the use of more aggressive medical therapy in this instance.3
References
1. Decker GA et al. Inflamm Bowel Dis. 2001 May;7(2):113-9.
2. De Felice KM et al. Inflamm Bowel Dis. 2015 Sep;21(9):2106-13.
3. Laube R et al. J Gastroenterol Hepatol. 2018 Feb;33(2):355-64.
Answer: esophageal Crohn’s disease.
The esophageal biopsies demonstrate severe chronic inflammation of the subepithelial tissue with marked lymphocytic infiltration and the presence of granulomas containing multinucleate giant cells (Figure B, arrow). Given his immunosuppression with azathioprine, stains for cytomegalovirus, herpes simplex virus, and mycobacterial and fungal organisms were performed and returned negative.
A diagnosis of esophageal Crohn’s disease was made, and adalimumab was recommenced. A rapid and dramatic clinical improvement was observed, with complete resolution of his symptoms. Adalimumab trough levels were checked and found to be therapeutic (9 mcg/mL). Repeat esophagogastroduodenoscopy at 6 months showed healing of the esophageal ulceration, with residual scarring and the presence of two postinflammatory polyps (Figure C). The histopathology was consistent with quiescent Crohn’s disease.
Recognition of this very rare manifestation of Crohn’s is challenging but important so that appropriate treatment is not delayed. It is both unexplained and unusual for Crohn’s disease to flare in a new gastrointestinal location. Moreover, although accurate adult prevalence data for esophageal Crohn’s are scarce, retrospective data suggest it is present in just 0.2% of Crohn’s disease patients.1 By contrast, gastroesophageal reflux disease prevalence is between 18% and 28% of the total population in North America. Esophageal Crohn’s commonly leads to nonspecific symptoms that resemble gastroesophageal reflux disease, and as for acid reflux, the mid and distal esophagus are the most common sites of involvement. In keeping with the behavior of luminal Crohn’s disease, progression from inflammation to stenosis (causing marked dysphagia) or perforation (leading to fistula formation) may occur.2 Histopathology typically demonstrates chronic inflammation, although noncaseating granulomas are seen in the minority (7%-39%) of patients.3 Multiple deep biopsies are recommended to improve diagnostic yield,3 and our case demonstrates the value of repeat endoscopic evaluation.
Unsurprisingly given its rarity, there are no systematic data on optimal treatment. Acid suppression therapy may provide symptomatic benefit but does not treat the underlying inflammatory process. Oral prednisolone, topical budesonide, and immunomodulators including thiopurines have been used in case series, but biological therapy (typically anti–tumor necrosis factor therapy) is likely to be required for severe disease.2,3 There are no data on the use of more novel biologics. Critically, almost all reported cases of esophageal Crohn’s disease have concomitant intestinal disease, and the presence of upper gastrointestinal Crohn’s predicts a more severe disease phenotype, supporting the use of more aggressive medical therapy in this instance.3
References
1. Decker GA et al. Inflamm Bowel Dis. 2001 May;7(2):113-9.
2. De Felice KM et al. Inflamm Bowel Dis. 2015 Sep;21(9):2106-13.
3. Laube R et al. J Gastroenterol Hepatol. 2018 Feb;33(2):355-64.
Answer: esophageal Crohn’s disease.
The esophageal biopsies demonstrate severe chronic inflammation of the subepithelial tissue with marked lymphocytic infiltration and the presence of granulomas containing multinucleate giant cells (Figure B, arrow). Given his immunosuppression with azathioprine, stains for cytomegalovirus, herpes simplex virus, and mycobacterial and fungal organisms were performed and returned negative.
A diagnosis of esophageal Crohn’s disease was made, and adalimumab was recommenced. A rapid and dramatic clinical improvement was observed, with complete resolution of his symptoms. Adalimumab trough levels were checked and found to be therapeutic (9 mcg/mL). Repeat esophagogastroduodenoscopy at 6 months showed healing of the esophageal ulceration, with residual scarring and the presence of two postinflammatory polyps (Figure C). The histopathology was consistent with quiescent Crohn’s disease.
Recognition of this very rare manifestation of Crohn’s is challenging but important so that appropriate treatment is not delayed. It is both unexplained and unusual for Crohn’s disease to flare in a new gastrointestinal location. Moreover, although accurate adult prevalence data for esophageal Crohn’s are scarce, retrospective data suggest it is present in just 0.2% of Crohn’s disease patients.1 By contrast, gastroesophageal reflux disease prevalence is between 18% and 28% of the total population in North America. Esophageal Crohn’s commonly leads to nonspecific symptoms that resemble gastroesophageal reflux disease, and as for acid reflux, the mid and distal esophagus are the most common sites of involvement. In keeping with the behavior of luminal Crohn’s disease, progression from inflammation to stenosis (causing marked dysphagia) or perforation (leading to fistula formation) may occur.2 Histopathology typically demonstrates chronic inflammation, although noncaseating granulomas are seen in the minority (7%-39%) of patients.3 Multiple deep biopsies are recommended to improve diagnostic yield,3 and our case demonstrates the value of repeat endoscopic evaluation.
Unsurprisingly given its rarity, there are no systematic data on optimal treatment. Acid suppression therapy may provide symptomatic benefit but does not treat the underlying inflammatory process. Oral prednisolone, topical budesonide, and immunomodulators including thiopurines have been used in case series, but biological therapy (typically anti–tumor necrosis factor therapy) is likely to be required for severe disease.2,3 There are no data on the use of more novel biologics. Critically, almost all reported cases of esophageal Crohn’s disease have concomitant intestinal disease, and the presence of upper gastrointestinal Crohn’s predicts a more severe disease phenotype, supporting the use of more aggressive medical therapy in this instance.3
References
1. Decker GA et al. Inflamm Bowel Dis. 2001 May;7(2):113-9.
2. De Felice KM et al. Inflamm Bowel Dis. 2015 Sep;21(9):2106-13.
3. Laube R et al. J Gastroenterol Hepatol. 2018 Feb;33(2):355-64.
A 49-year-old man presented with symptoms of retrosternal discomfort and mild dysphagia to solids. He had a 30-year history of ileocolonic Crohn's disease requiring previous resections of the ileum and sigmoid colon. Clinical remission had been achieved with adalimumab and azathioprine combination therapy, with the subsequent decision to de-escalate to maintenance with azathioprine monotherapy after consideration of the risks and benefits of dual immunosuppression. After 5 years of azathioprine monotherapy, complete endoscopic remission was reconfirmed at a recent ileocolonoscopy.
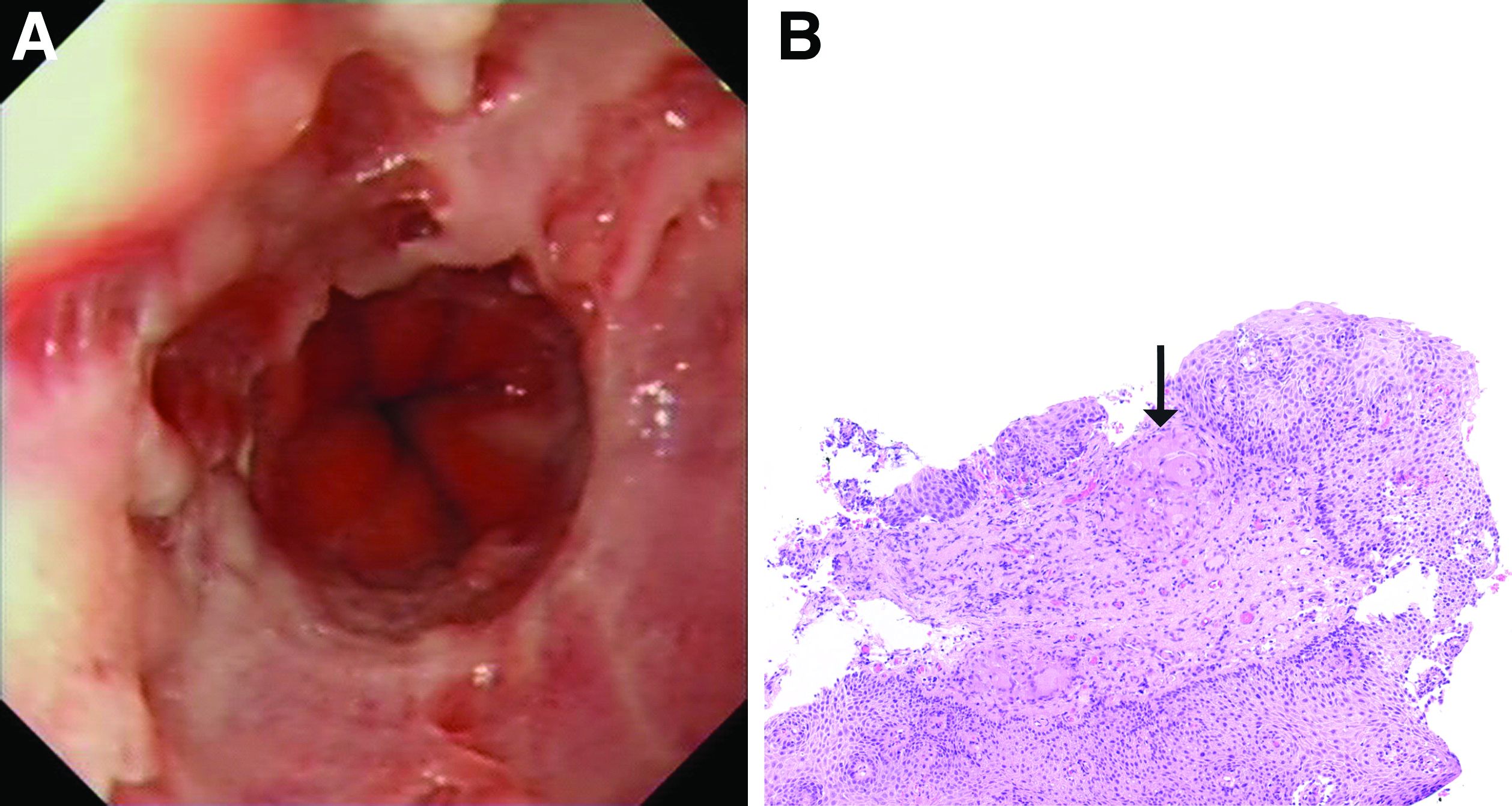
To investigate his upper gastrointestinal symptoms he underwent esophagogastroduodenoscopy that demonstrated severe esophagitis (Los Angeles grade D) of the lower esophagus with biopsies confirming apparent reflux esophagitis. However, his symptoms worsened despite a course of high dose proton pump inhibitor, and a repeat esophagogastroduodenoscopy was performed. This demonstrated deep longitudinal ulcers and inflammation of the lower two-thirds of the esophagus (Figure A). Biopsies were sent for histopathologic analysis (Figure B).
Innovation requires experimentation
A call for more health care trials
Successful innovation requires experimentation, according to a recent editorial in BMJ Quality & Safety – that’s why health systems should engage in more experimenting, more systematically, to improve health care.
“Most health systems implement interventions without testing them against other designs,” said co-author Mitesh S. Patel, MD, MBA, MS, of the University of Pennsylvania, Philadelphia. “This means that good ideas are often not spread (because we don’t know how impactful they are) and bad ones persist (because we don’t realize they don’t work).”
Dr. Patel, who is director of the Penn Medicine Nudge Unit at the Perelman Center for Advanced Medicine, encourages health systems and clinicians to implement new interventions in testable ways such as through a randomized trial, so that we can learn what works and why. A more systematic approach could help to expand programs that work and improve workflow and patient care.
“First, we must embed research teams within health systems in order to create the capacity for this kind of work. Expertise is required to identify a promising intervention, design the conceptual approach, conduct the technical implementation and rigorously evaluate the trial. These teams are also able to design interventions within the context of existing workflows in order to ensure that successful projects can be quickly scaled and that ineffective initiatives can be seamlessly terminated.” the authors wrote.
“Second, we must take advantage of existing data systems. The field of health care is ripe with detailed and reliable administrative data and electronic medical record data. These data offer the potential to do high-quality, low-cost, rapid trials. Third, we must measure a wide range of meaningful outcomes. We should examine the effect of interventions on health care costs, health care utilization and health outcomes.”
Next steps could be focused on thinking about the key priority areas and how can experiments be used to generate new knowledge on what works and what does not. “Luckily, the complex world of health care provides endless opportunities for rapid-cycle, randomized trials that target health care costs and outcomes,” Dr. Patel said.
Reference
1. Oakes AH, Patel MS. A nudge towards increased experimentation to more rapidly improve healthcare. BMJ Qual Saf. 2020;29:179-181. doi: 10.1136/bmjqs-2019-009948. Accessed Dec 3, 2019.
A call for more health care trials
A call for more health care trials
Successful innovation requires experimentation, according to a recent editorial in BMJ Quality & Safety – that’s why health systems should engage in more experimenting, more systematically, to improve health care.
“Most health systems implement interventions without testing them against other designs,” said co-author Mitesh S. Patel, MD, MBA, MS, of the University of Pennsylvania, Philadelphia. “This means that good ideas are often not spread (because we don’t know how impactful they are) and bad ones persist (because we don’t realize they don’t work).”
Dr. Patel, who is director of the Penn Medicine Nudge Unit at the Perelman Center for Advanced Medicine, encourages health systems and clinicians to implement new interventions in testable ways such as through a randomized trial, so that we can learn what works and why. A more systematic approach could help to expand programs that work and improve workflow and patient care.
“First, we must embed research teams within health systems in order to create the capacity for this kind of work. Expertise is required to identify a promising intervention, design the conceptual approach, conduct the technical implementation and rigorously evaluate the trial. These teams are also able to design interventions within the context of existing workflows in order to ensure that successful projects can be quickly scaled and that ineffective initiatives can be seamlessly terminated.” the authors wrote.
“Second, we must take advantage of existing data systems. The field of health care is ripe with detailed and reliable administrative data and electronic medical record data. These data offer the potential to do high-quality, low-cost, rapid trials. Third, we must measure a wide range of meaningful outcomes. We should examine the effect of interventions on health care costs, health care utilization and health outcomes.”
Next steps could be focused on thinking about the key priority areas and how can experiments be used to generate new knowledge on what works and what does not. “Luckily, the complex world of health care provides endless opportunities for rapid-cycle, randomized trials that target health care costs and outcomes,” Dr. Patel said.
Reference
1. Oakes AH, Patel MS. A nudge towards increased experimentation to more rapidly improve healthcare. BMJ Qual Saf. 2020;29:179-181. doi: 10.1136/bmjqs-2019-009948. Accessed Dec 3, 2019.
Successful innovation requires experimentation, according to a recent editorial in BMJ Quality & Safety – that’s why health systems should engage in more experimenting, more systematically, to improve health care.
“Most health systems implement interventions without testing them against other designs,” said co-author Mitesh S. Patel, MD, MBA, MS, of the University of Pennsylvania, Philadelphia. “This means that good ideas are often not spread (because we don’t know how impactful they are) and bad ones persist (because we don’t realize they don’t work).”
Dr. Patel, who is director of the Penn Medicine Nudge Unit at the Perelman Center for Advanced Medicine, encourages health systems and clinicians to implement new interventions in testable ways such as through a randomized trial, so that we can learn what works and why. A more systematic approach could help to expand programs that work and improve workflow and patient care.
“First, we must embed research teams within health systems in order to create the capacity for this kind of work. Expertise is required to identify a promising intervention, design the conceptual approach, conduct the technical implementation and rigorously evaluate the trial. These teams are also able to design interventions within the context of existing workflows in order to ensure that successful projects can be quickly scaled and that ineffective initiatives can be seamlessly terminated.” the authors wrote.
“Second, we must take advantage of existing data systems. The field of health care is ripe with detailed and reliable administrative data and electronic medical record data. These data offer the potential to do high-quality, low-cost, rapid trials. Third, we must measure a wide range of meaningful outcomes. We should examine the effect of interventions on health care costs, health care utilization and health outcomes.”
Next steps could be focused on thinking about the key priority areas and how can experiments be used to generate new knowledge on what works and what does not. “Luckily, the complex world of health care provides endless opportunities for rapid-cycle, randomized trials that target health care costs and outcomes,” Dr. Patel said.
Reference
1. Oakes AH, Patel MS. A nudge towards increased experimentation to more rapidly improve healthcare. BMJ Qual Saf. 2020;29:179-181. doi: 10.1136/bmjqs-2019-009948. Accessed Dec 3, 2019.
SHM Converge: New format, fresh content
While we all long for a traditional in-person meeting “like the good old days”, there are some significant advantages to a virtual meeting like Converge.
The most significant advantage is the ability to review more content than ever before, as we offer a combination of live and recorded “on-demand” sessions. This allows for incredible flexibility in garnering “top-shelf” content from hospital medicine experts around the country, without having to choose from competing sessions. We are especially looking forward to new sessions this year focused on COVID-19; diversity, equity, and inclusion; and resilience.
The Converge conference will still be offering networking sessions throughout – even in the virtual conference environment. We consider networking a vital and endearing part of the value equation for SHM members. For example, we now can participate in several Special Interest Forums, since many of us have several niche interests and want to take advantage of more than one of these networking opportunities. We also carefully preserved the signature “Update in Hospital Medicine” session, as well as the scientific abstract poster reception and the Best of Research and Innovation sessions. These are long-term favorites at the annual conference and lend themselves well to virtual transformation. Some of the workshops and special sessions have exclusive audience engagement and are not offered on demand, so signing up early for these sessions is highly recommended.
SHM remains the professional home for hospitalists, and we rely on the annual conference to keep us all informed on current and forward-thinking clinical practice, practice management, leadership, academics, research, and other topics. This is one of many examples of how SHM has been able to pivot to meet the needs of hospitalists throughout the pandemic. Not only have we successfully converted “traditional” meetings into virtual meetings, but we have been able to curate and deliver content faster and more seamlessly than ever before.
Whether via The Hospitalist, the Journal of Hospital Medicine, the SHM website, or our other educational platforms, SHM has remained committed to being the single “source of truth” for all things hospital medicine. Within the tumultuous political landscape of the past year, the SHM advocacy team has been more active and engaged than ever, in advocating for a myriad of hospitalist-related legislative changes. These are just a few of the ways SHM continues to add value to hospitalist members every day.
Although we will certainly miss seeing each other in person, we are confident that the SHM team will meet and exceed expectations on content delivery and will take advantage of the virtual format to improve content access. We look forward to “seeing” you at SHM Converge this year and hope you take advantage of the enhanced delivery and access to an array of amazing content!
Dr. Scheurer is president of the Society of Hospital Medicine. She is a hospitalist and chief quality officer, MUSC Health System, Medical University of South Carolina, Charleston.
While we all long for a traditional in-person meeting “like the good old days”, there are some significant advantages to a virtual meeting like Converge.
The most significant advantage is the ability to review more content than ever before, as we offer a combination of live and recorded “on-demand” sessions. This allows for incredible flexibility in garnering “top-shelf” content from hospital medicine experts around the country, without having to choose from competing sessions. We are especially looking forward to new sessions this year focused on COVID-19; diversity, equity, and inclusion; and resilience.
The Converge conference will still be offering networking sessions throughout – even in the virtual conference environment. We consider networking a vital and endearing part of the value equation for SHM members. For example, we now can participate in several Special Interest Forums, since many of us have several niche interests and want to take advantage of more than one of these networking opportunities. We also carefully preserved the signature “Update in Hospital Medicine” session, as well as the scientific abstract poster reception and the Best of Research and Innovation sessions. These are long-term favorites at the annual conference and lend themselves well to virtual transformation. Some of the workshops and special sessions have exclusive audience engagement and are not offered on demand, so signing up early for these sessions is highly recommended.
SHM remains the professional home for hospitalists, and we rely on the annual conference to keep us all informed on current and forward-thinking clinical practice, practice management, leadership, academics, research, and other topics. This is one of many examples of how SHM has been able to pivot to meet the needs of hospitalists throughout the pandemic. Not only have we successfully converted “traditional” meetings into virtual meetings, but we have been able to curate and deliver content faster and more seamlessly than ever before.
Whether via The Hospitalist, the Journal of Hospital Medicine, the SHM website, or our other educational platforms, SHM has remained committed to being the single “source of truth” for all things hospital medicine. Within the tumultuous political landscape of the past year, the SHM advocacy team has been more active and engaged than ever, in advocating for a myriad of hospitalist-related legislative changes. These are just a few of the ways SHM continues to add value to hospitalist members every day.
Although we will certainly miss seeing each other in person, we are confident that the SHM team will meet and exceed expectations on content delivery and will take advantage of the virtual format to improve content access. We look forward to “seeing” you at SHM Converge this year and hope you take advantage of the enhanced delivery and access to an array of amazing content!
Dr. Scheurer is president of the Society of Hospital Medicine. She is a hospitalist and chief quality officer, MUSC Health System, Medical University of South Carolina, Charleston.
While we all long for a traditional in-person meeting “like the good old days”, there are some significant advantages to a virtual meeting like Converge.
The most significant advantage is the ability to review more content than ever before, as we offer a combination of live and recorded “on-demand” sessions. This allows for incredible flexibility in garnering “top-shelf” content from hospital medicine experts around the country, without having to choose from competing sessions. We are especially looking forward to new sessions this year focused on COVID-19; diversity, equity, and inclusion; and resilience.
The Converge conference will still be offering networking sessions throughout – even in the virtual conference environment. We consider networking a vital and endearing part of the value equation for SHM members. For example, we now can participate in several Special Interest Forums, since many of us have several niche interests and want to take advantage of more than one of these networking opportunities. We also carefully preserved the signature “Update in Hospital Medicine” session, as well as the scientific abstract poster reception and the Best of Research and Innovation sessions. These are long-term favorites at the annual conference and lend themselves well to virtual transformation. Some of the workshops and special sessions have exclusive audience engagement and are not offered on demand, so signing up early for these sessions is highly recommended.
SHM remains the professional home for hospitalists, and we rely on the annual conference to keep us all informed on current and forward-thinking clinical practice, practice management, leadership, academics, research, and other topics. This is one of many examples of how SHM has been able to pivot to meet the needs of hospitalists throughout the pandemic. Not only have we successfully converted “traditional” meetings into virtual meetings, but we have been able to curate and deliver content faster and more seamlessly than ever before.
Whether via The Hospitalist, the Journal of Hospital Medicine, the SHM website, or our other educational platforms, SHM has remained committed to being the single “source of truth” for all things hospital medicine. Within the tumultuous political landscape of the past year, the SHM advocacy team has been more active and engaged than ever, in advocating for a myriad of hospitalist-related legislative changes. These are just a few of the ways SHM continues to add value to hospitalist members every day.
Although we will certainly miss seeing each other in person, we are confident that the SHM team will meet and exceed expectations on content delivery and will take advantage of the virtual format to improve content access. We look forward to “seeing” you at SHM Converge this year and hope you take advantage of the enhanced delivery and access to an array of amazing content!
Dr. Scheurer is president of the Society of Hospital Medicine. She is a hospitalist and chief quality officer, MUSC Health System, Medical University of South Carolina, Charleston.
Accessing data during EHR downtime
Reducing loss of efficiency
Electronic health record (EHR) implementations involve long downtimes, which are an under-recognized patient safety risk, as clinicians are forced to switch to completely manual, paper-based, and important unfamiliar workflows to care for their acutely ill patients, said Subha Airan-Javia, MD, FAMIA, a hospitalist at the University of Pennsylvania, Philadelphia.
“In this setting, we discovered an unanticipated benefit of our tool [Carelign, initially built to digitize the handoff process] as a clinical resource during EHR downtime, giving clinicians access to critical data as well as an electronic platform to collaborate as a team around the care of their patients,” she said.
There are two important takeaways from their study on this issue. “The first is that Carelign was able to give clinicians access to clinical data that would otherwise have been unavailable, including vitals, labs, medications, care plans and care team assignments,” Dr. Airan-Javia said. “This undoubtedly mitigated patient safety risks during the EHR downtime.”
The second: “As many clinicians know, any change in workflow, even for a few hours, can make providing a high level of patient care very difficult,” she added. “During a downtime without a tool like Carelign, clinicians have to rely on paper and bedside charts, writing notes on paper and then re-typing them into the EHR when it is back up. This adds to the already excessive amount of administrative work that is burning clinicians out.” Using a tool like Carelign means no such loss in efficiency.
“A tool like Carelign, particularly because it is something that can be used without having to integrate it with the EHR, can put some control back into a hospitalist’s hands, to have a say in their workflow,” Dr. Airan-Javia said. “In a world where EHRs are designed to optimize billing, it can be game-changer to have a tool like Carelign that was created by a practicing clinician, for clinicians. Anyone interested in this area is welcome to reach out to me at [email protected] for collaboration or more information.”
Reference
1. Airan-Javia SL, et al. Mind the gap: Revolutionizing the EHR downtime experience with an interoperable workflow tool. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract 380. https://www.shmabstracts.com/abstract/mind-the-gap-revolutionizing-the-ehr-downtime-experience-with-an-interoperable-workflow-tool/. Accessed Dec 11, 2019.
Reducing loss of efficiency
Reducing loss of efficiency
Electronic health record (EHR) implementations involve long downtimes, which are an under-recognized patient safety risk, as clinicians are forced to switch to completely manual, paper-based, and important unfamiliar workflows to care for their acutely ill patients, said Subha Airan-Javia, MD, FAMIA, a hospitalist at the University of Pennsylvania, Philadelphia.
“In this setting, we discovered an unanticipated benefit of our tool [Carelign, initially built to digitize the handoff process] as a clinical resource during EHR downtime, giving clinicians access to critical data as well as an electronic platform to collaborate as a team around the care of their patients,” she said.
There are two important takeaways from their study on this issue. “The first is that Carelign was able to give clinicians access to clinical data that would otherwise have been unavailable, including vitals, labs, medications, care plans and care team assignments,” Dr. Airan-Javia said. “This undoubtedly mitigated patient safety risks during the EHR downtime.”
The second: “As many clinicians know, any change in workflow, even for a few hours, can make providing a high level of patient care very difficult,” she added. “During a downtime without a tool like Carelign, clinicians have to rely on paper and bedside charts, writing notes on paper and then re-typing them into the EHR when it is back up. This adds to the already excessive amount of administrative work that is burning clinicians out.” Using a tool like Carelign means no such loss in efficiency.
“A tool like Carelign, particularly because it is something that can be used without having to integrate it with the EHR, can put some control back into a hospitalist’s hands, to have a say in their workflow,” Dr. Airan-Javia said. “In a world where EHRs are designed to optimize billing, it can be game-changer to have a tool like Carelign that was created by a practicing clinician, for clinicians. Anyone interested in this area is welcome to reach out to me at [email protected] for collaboration or more information.”
Reference
1. Airan-Javia SL, et al. Mind the gap: Revolutionizing the EHR downtime experience with an interoperable workflow tool. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract 380. https://www.shmabstracts.com/abstract/mind-the-gap-revolutionizing-the-ehr-downtime-experience-with-an-interoperable-workflow-tool/. Accessed Dec 11, 2019.
Electronic health record (EHR) implementations involve long downtimes, which are an under-recognized patient safety risk, as clinicians are forced to switch to completely manual, paper-based, and important unfamiliar workflows to care for their acutely ill patients, said Subha Airan-Javia, MD, FAMIA, a hospitalist at the University of Pennsylvania, Philadelphia.
“In this setting, we discovered an unanticipated benefit of our tool [Carelign, initially built to digitize the handoff process] as a clinical resource during EHR downtime, giving clinicians access to critical data as well as an electronic platform to collaborate as a team around the care of their patients,” she said.
There are two important takeaways from their study on this issue. “The first is that Carelign was able to give clinicians access to clinical data that would otherwise have been unavailable, including vitals, labs, medications, care plans and care team assignments,” Dr. Airan-Javia said. “This undoubtedly mitigated patient safety risks during the EHR downtime.”
The second: “As many clinicians know, any change in workflow, even for a few hours, can make providing a high level of patient care very difficult,” she added. “During a downtime without a tool like Carelign, clinicians have to rely on paper and bedside charts, writing notes on paper and then re-typing them into the EHR when it is back up. This adds to the already excessive amount of administrative work that is burning clinicians out.” Using a tool like Carelign means no such loss in efficiency.
“A tool like Carelign, particularly because it is something that can be used without having to integrate it with the EHR, can put some control back into a hospitalist’s hands, to have a say in their workflow,” Dr. Airan-Javia said. “In a world where EHRs are designed to optimize billing, it can be game-changer to have a tool like Carelign that was created by a practicing clinician, for clinicians. Anyone interested in this area is welcome to reach out to me at [email protected] for collaboration or more information.”
Reference
1. Airan-Javia SL, et al. Mind the gap: Revolutionizing the EHR downtime experience with an interoperable workflow tool. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract 380. https://www.shmabstracts.com/abstract/mind-the-gap-revolutionizing-the-ehr-downtime-experience-with-an-interoperable-workflow-tool/. Accessed Dec 11, 2019.
How do you run a hospital with no running water?
It’s bad enough that this month’s historic snowstorm left ordinary Texans scrambling for heat and resorting to melted snow for drinking, washing, and flushing. But what about hospitals, where sanitation is paramount and ample water is a sine qua non?
As pipes burst, pumps froze, and water pressure plummeted, patient care was affected as well as maintenance, food preparation, laundry, and heat. To counter the problems, several Texas hospitals stepped up to the plate with inventive responses.
“At the worst point, two of our hospitals, Houston Methodist West and Houston Methodist Baytown, had no city water supply, one for over 48 hours and the other for 72 hours,” said Marc L. Boom, MD, MBA, Houston Methodist’s president and CEO.
Although the main hospital had a reserve supply of potable water, a supply of water for laundry, cooking, and cleaning was another matter. “We introduced significant water restrictions and had to have 6,000-gallon tankers bring in extra water,” Dr. Boom said.
One hospital in the network got creative. When it rained the day after the ice storm, the staff rigged up a rain collection system using the huge bins that move linens around the hospital to collect nonpotable water for cleaning and flushing toilets, Dr. Boom said. Another hospital was able to provide showers for staff by bringing in bathroom trailers with self-contained water supplies of the kind used at some sporting events.
And at some facilities, patients were discharged into the lobby as they could not return home with transportation, electricity, and water systems crippled. With widespread challenges continuing, even as temperatures warmed, President Biden signed a major disaster declaration Feb. 20 that will provide emergency assistance to residents and businesses in more than a third of Texas counties, including those surrounding Houston, Dallas, and Austin.
Although conditions forced the rescheduling of some nonemergent surgeries, the water shortage had no impact on COVID-19 care, except for the unavailability of showers in the case of mobile patients. “At the worst, they just had to use bucket flushing for the toilets,” Dr. Boom said.
And in an unexpected win, when a Harris County freezer for COVID-19 vaccine storage failed and threatened to spoil 8,400 precious doses, Dr. Boom’s center was able to take delivery on 1,000 doses and administer them in 3 hours at a hastily set up ad hoc immunization center.
In all this, the lessons of the pandemic had a positive preparatory role. “2020 taught us to be agile as things change and to align our goals across different medical teams,” said Ben Saldana, MD, medical director of Houston Methodist’s emergency care centers. “And we were prepared for hurricanes, but not for snow.”
Increased pressure on emergency departments
As the outages continued and stress levels in the community rose, the network started seeing exacerbations of chronic conditions after the power shut-down incapacitated electrical devices running machines for heart assistance, oxygen delivery, and sleep apnea. “We started seeing food-borne illness and carbon monoxide poisoning, as well as more heart attacks, strokes, and sepsis,” Dr. Saldana said.
One serious strain on the network’s main hospital was the sudden need to accommodate large numbers of patients on dialysis, a procedure that uses a lot of water and is typically performed in small, vulnerable community facilities with limited infrastructure and no generators. “The hospitals are their backup and act as a safety net for them,” Boom said. Some hospital areas generally used for other types of conditions had to be marshaled for renal care.
Emergency rooms became pop-up dialysis centers, Dr. Saldana said. “And if the water pressure dropped, we had to cut dialysis time from the standard 4 hours to 2. That’s like putting a band-aid on patients.”
Fortunately, municipal water pressure in the Houston area has steadily risen and is almost back to normal. And according to Dr. Boom, the brutal storm may yet have a silver lining: a decline in county coronavirus cases as the storm and icy road conditions forced people to stay sequestered at home.
Further north in Austin, a number of hospitals lost municipal water pressure, creating a series of problems. Among them was St. David’s South Austin Medical Center, at which, according to reports in the Austin American-Statesman, staff members were at one point asked to use trash bags to remove waste from toilets, to refrain from showering, and to clean their hands only with sanitizer.
A statement issued by David Huffstutler, CEO of St. David’s HealthCare, acknowledged that the heating system is based on a water-fed boiler. When the building lost heat owing to lack of water, some patients had to be transferred elsewhere or discharged. The hospital distributed jugs and bottles of water for handwashing and drinking, and was working with city officials to obtain portable toilets.
Meanwhile, officials at Austin’s Dell Children’s Medical Center acknowledged in a memo that its toilets no longer had “flushing capabilities.” Other area hospitals in the Ascension Seton network were also suffering from compromised water supplies last week, according to local news reports.
Washroom facilities were affected elsewhere as well. A post on a medical association Facebook page referred to a memo ordering staff to use a single toilet in an outpatient area for bowel movements and warned them to limit their time there. No paper or other products were to be used in other toilets designated for urination.
‘The pandemic was the prelude to the ice storm’
Some hospitals fared better. Along the Coastal Bend, Corpus Christi Medical Center managed to maintain its electricity and water supply to ensure continuity of hospital services after the storm, according to a statement.
But back in Houston, Liz Youngblood, MBA, RN, president of Baylor St. Luke’s Medical Center, said a number of hospitals in her network experienced low water pressure after the storm.
“Fortunately, we had water conservation measures and low-water alerts in place for such emergencies,” she said. “And we rely on water tankers to help maintain enough pressure for the basics.”
Some of the challenges posed by the storm are quite similar to what St. Luke’s faced after Hurricane Harvey in 2017. “We had already made plans to address them and so we felt prepared,” Ms. Youngblood said.
And thanks to COVID-19, Texas hospitals have been operating in crisis mode for the past year. “The pandemic was the prelude to the ice storm,” said Gina Blocker, MD, a St. Luke’s ED physician, “so we had measures and teams in place. We did have some reduction in water pressure, though the pressure was still good.”
But the hospital was inundated with patients looking for shelter. “Some were just scared about what might happen to them if their heat didn’t come back on and they wanted to be where they could get care,” Dr. Blocker said. Others came in with expected storm-related injuries such as hypothermia and carbon monoxide poisoning.
According to Ms. Youngblood, little compromise in patient care was necessary except for the cancellation of some operations and vaccinations owing to the treacherous travel conditions. “But one of the biggest remaining issues is that we need plenty of blood, so we’re encouraging people to donate at their local centers.”
A version of this article first appeared on Medscape.com
It’s bad enough that this month’s historic snowstorm left ordinary Texans scrambling for heat and resorting to melted snow for drinking, washing, and flushing. But what about hospitals, where sanitation is paramount and ample water is a sine qua non?
As pipes burst, pumps froze, and water pressure plummeted, patient care was affected as well as maintenance, food preparation, laundry, and heat. To counter the problems, several Texas hospitals stepped up to the plate with inventive responses.
“At the worst point, two of our hospitals, Houston Methodist West and Houston Methodist Baytown, had no city water supply, one for over 48 hours and the other for 72 hours,” said Marc L. Boom, MD, MBA, Houston Methodist’s president and CEO.
Although the main hospital had a reserve supply of potable water, a supply of water for laundry, cooking, and cleaning was another matter. “We introduced significant water restrictions and had to have 6,000-gallon tankers bring in extra water,” Dr. Boom said.
One hospital in the network got creative. When it rained the day after the ice storm, the staff rigged up a rain collection system using the huge bins that move linens around the hospital to collect nonpotable water for cleaning and flushing toilets, Dr. Boom said. Another hospital was able to provide showers for staff by bringing in bathroom trailers with self-contained water supplies of the kind used at some sporting events.
And at some facilities, patients were discharged into the lobby as they could not return home with transportation, electricity, and water systems crippled. With widespread challenges continuing, even as temperatures warmed, President Biden signed a major disaster declaration Feb. 20 that will provide emergency assistance to residents and businesses in more than a third of Texas counties, including those surrounding Houston, Dallas, and Austin.
Although conditions forced the rescheduling of some nonemergent surgeries, the water shortage had no impact on COVID-19 care, except for the unavailability of showers in the case of mobile patients. “At the worst, they just had to use bucket flushing for the toilets,” Dr. Boom said.
And in an unexpected win, when a Harris County freezer for COVID-19 vaccine storage failed and threatened to spoil 8,400 precious doses, Dr. Boom’s center was able to take delivery on 1,000 doses and administer them in 3 hours at a hastily set up ad hoc immunization center.
In all this, the lessons of the pandemic had a positive preparatory role. “2020 taught us to be agile as things change and to align our goals across different medical teams,” said Ben Saldana, MD, medical director of Houston Methodist’s emergency care centers. “And we were prepared for hurricanes, but not for snow.”
Increased pressure on emergency departments
As the outages continued and stress levels in the community rose, the network started seeing exacerbations of chronic conditions after the power shut-down incapacitated electrical devices running machines for heart assistance, oxygen delivery, and sleep apnea. “We started seeing food-borne illness and carbon monoxide poisoning, as well as more heart attacks, strokes, and sepsis,” Dr. Saldana said.
One serious strain on the network’s main hospital was the sudden need to accommodate large numbers of patients on dialysis, a procedure that uses a lot of water and is typically performed in small, vulnerable community facilities with limited infrastructure and no generators. “The hospitals are their backup and act as a safety net for them,” Boom said. Some hospital areas generally used for other types of conditions had to be marshaled for renal care.
Emergency rooms became pop-up dialysis centers, Dr. Saldana said. “And if the water pressure dropped, we had to cut dialysis time from the standard 4 hours to 2. That’s like putting a band-aid on patients.”
Fortunately, municipal water pressure in the Houston area has steadily risen and is almost back to normal. And according to Dr. Boom, the brutal storm may yet have a silver lining: a decline in county coronavirus cases as the storm and icy road conditions forced people to stay sequestered at home.
Further north in Austin, a number of hospitals lost municipal water pressure, creating a series of problems. Among them was St. David’s South Austin Medical Center, at which, according to reports in the Austin American-Statesman, staff members were at one point asked to use trash bags to remove waste from toilets, to refrain from showering, and to clean their hands only with sanitizer.
A statement issued by David Huffstutler, CEO of St. David’s HealthCare, acknowledged that the heating system is based on a water-fed boiler. When the building lost heat owing to lack of water, some patients had to be transferred elsewhere or discharged. The hospital distributed jugs and bottles of water for handwashing and drinking, and was working with city officials to obtain portable toilets.
Meanwhile, officials at Austin’s Dell Children’s Medical Center acknowledged in a memo that its toilets no longer had “flushing capabilities.” Other area hospitals in the Ascension Seton network were also suffering from compromised water supplies last week, according to local news reports.
Washroom facilities were affected elsewhere as well. A post on a medical association Facebook page referred to a memo ordering staff to use a single toilet in an outpatient area for bowel movements and warned them to limit their time there. No paper or other products were to be used in other toilets designated for urination.
‘The pandemic was the prelude to the ice storm’
Some hospitals fared better. Along the Coastal Bend, Corpus Christi Medical Center managed to maintain its electricity and water supply to ensure continuity of hospital services after the storm, according to a statement.
But back in Houston, Liz Youngblood, MBA, RN, president of Baylor St. Luke’s Medical Center, said a number of hospitals in her network experienced low water pressure after the storm.
“Fortunately, we had water conservation measures and low-water alerts in place for such emergencies,” she said. “And we rely on water tankers to help maintain enough pressure for the basics.”
Some of the challenges posed by the storm are quite similar to what St. Luke’s faced after Hurricane Harvey in 2017. “We had already made plans to address them and so we felt prepared,” Ms. Youngblood said.
And thanks to COVID-19, Texas hospitals have been operating in crisis mode for the past year. “The pandemic was the prelude to the ice storm,” said Gina Blocker, MD, a St. Luke’s ED physician, “so we had measures and teams in place. We did have some reduction in water pressure, though the pressure was still good.”
But the hospital was inundated with patients looking for shelter. “Some were just scared about what might happen to them if their heat didn’t come back on and they wanted to be where they could get care,” Dr. Blocker said. Others came in with expected storm-related injuries such as hypothermia and carbon monoxide poisoning.
According to Ms. Youngblood, little compromise in patient care was necessary except for the cancellation of some operations and vaccinations owing to the treacherous travel conditions. “But one of the biggest remaining issues is that we need plenty of blood, so we’re encouraging people to donate at their local centers.”
A version of this article first appeared on Medscape.com
It’s bad enough that this month’s historic snowstorm left ordinary Texans scrambling for heat and resorting to melted snow for drinking, washing, and flushing. But what about hospitals, where sanitation is paramount and ample water is a sine qua non?
As pipes burst, pumps froze, and water pressure plummeted, patient care was affected as well as maintenance, food preparation, laundry, and heat. To counter the problems, several Texas hospitals stepped up to the plate with inventive responses.
“At the worst point, two of our hospitals, Houston Methodist West and Houston Methodist Baytown, had no city water supply, one for over 48 hours and the other for 72 hours,” said Marc L. Boom, MD, MBA, Houston Methodist’s president and CEO.
Although the main hospital had a reserve supply of potable water, a supply of water for laundry, cooking, and cleaning was another matter. “We introduced significant water restrictions and had to have 6,000-gallon tankers bring in extra water,” Dr. Boom said.
One hospital in the network got creative. When it rained the day after the ice storm, the staff rigged up a rain collection system using the huge bins that move linens around the hospital to collect nonpotable water for cleaning and flushing toilets, Dr. Boom said. Another hospital was able to provide showers for staff by bringing in bathroom trailers with self-contained water supplies of the kind used at some sporting events.
And at some facilities, patients were discharged into the lobby as they could not return home with transportation, electricity, and water systems crippled. With widespread challenges continuing, even as temperatures warmed, President Biden signed a major disaster declaration Feb. 20 that will provide emergency assistance to residents and businesses in more than a third of Texas counties, including those surrounding Houston, Dallas, and Austin.
Although conditions forced the rescheduling of some nonemergent surgeries, the water shortage had no impact on COVID-19 care, except for the unavailability of showers in the case of mobile patients. “At the worst, they just had to use bucket flushing for the toilets,” Dr. Boom said.
And in an unexpected win, when a Harris County freezer for COVID-19 vaccine storage failed and threatened to spoil 8,400 precious doses, Dr. Boom’s center was able to take delivery on 1,000 doses and administer them in 3 hours at a hastily set up ad hoc immunization center.
In all this, the lessons of the pandemic had a positive preparatory role. “2020 taught us to be agile as things change and to align our goals across different medical teams,” said Ben Saldana, MD, medical director of Houston Methodist’s emergency care centers. “And we were prepared for hurricanes, but not for snow.”
Increased pressure on emergency departments
As the outages continued and stress levels in the community rose, the network started seeing exacerbations of chronic conditions after the power shut-down incapacitated electrical devices running machines for heart assistance, oxygen delivery, and sleep apnea. “We started seeing food-borne illness and carbon monoxide poisoning, as well as more heart attacks, strokes, and sepsis,” Dr. Saldana said.
One serious strain on the network’s main hospital was the sudden need to accommodate large numbers of patients on dialysis, a procedure that uses a lot of water and is typically performed in small, vulnerable community facilities with limited infrastructure and no generators. “The hospitals are their backup and act as a safety net for them,” Boom said. Some hospital areas generally used for other types of conditions had to be marshaled for renal care.
Emergency rooms became pop-up dialysis centers, Dr. Saldana said. “And if the water pressure dropped, we had to cut dialysis time from the standard 4 hours to 2. That’s like putting a band-aid on patients.”
Fortunately, municipal water pressure in the Houston area has steadily risen and is almost back to normal. And according to Dr. Boom, the brutal storm may yet have a silver lining: a decline in county coronavirus cases as the storm and icy road conditions forced people to stay sequestered at home.
Further north in Austin, a number of hospitals lost municipal water pressure, creating a series of problems. Among them was St. David’s South Austin Medical Center, at which, according to reports in the Austin American-Statesman, staff members were at one point asked to use trash bags to remove waste from toilets, to refrain from showering, and to clean their hands only with sanitizer.
A statement issued by David Huffstutler, CEO of St. David’s HealthCare, acknowledged that the heating system is based on a water-fed boiler. When the building lost heat owing to lack of water, some patients had to be transferred elsewhere or discharged. The hospital distributed jugs and bottles of water for handwashing and drinking, and was working with city officials to obtain portable toilets.
Meanwhile, officials at Austin’s Dell Children’s Medical Center acknowledged in a memo that its toilets no longer had “flushing capabilities.” Other area hospitals in the Ascension Seton network were also suffering from compromised water supplies last week, according to local news reports.
Washroom facilities were affected elsewhere as well. A post on a medical association Facebook page referred to a memo ordering staff to use a single toilet in an outpatient area for bowel movements and warned them to limit their time there. No paper or other products were to be used in other toilets designated for urination.
‘The pandemic was the prelude to the ice storm’
Some hospitals fared better. Along the Coastal Bend, Corpus Christi Medical Center managed to maintain its electricity and water supply to ensure continuity of hospital services after the storm, according to a statement.
But back in Houston, Liz Youngblood, MBA, RN, president of Baylor St. Luke’s Medical Center, said a number of hospitals in her network experienced low water pressure after the storm.
“Fortunately, we had water conservation measures and low-water alerts in place for such emergencies,” she said. “And we rely on water tankers to help maintain enough pressure for the basics.”
Some of the challenges posed by the storm are quite similar to what St. Luke’s faced after Hurricane Harvey in 2017. “We had already made plans to address them and so we felt prepared,” Ms. Youngblood said.
And thanks to COVID-19, Texas hospitals have been operating in crisis mode for the past year. “The pandemic was the prelude to the ice storm,” said Gina Blocker, MD, a St. Luke’s ED physician, “so we had measures and teams in place. We did have some reduction in water pressure, though the pressure was still good.”
But the hospital was inundated with patients looking for shelter. “Some were just scared about what might happen to them if their heat didn’t come back on and they wanted to be where they could get care,” Dr. Blocker said. Others came in with expected storm-related injuries such as hypothermia and carbon monoxide poisoning.
According to Ms. Youngblood, little compromise in patient care was necessary except for the cancellation of some operations and vaccinations owing to the treacherous travel conditions. “But one of the biggest remaining issues is that we need plenty of blood, so we’re encouraging people to donate at their local centers.”
A version of this article first appeared on Medscape.com