User login
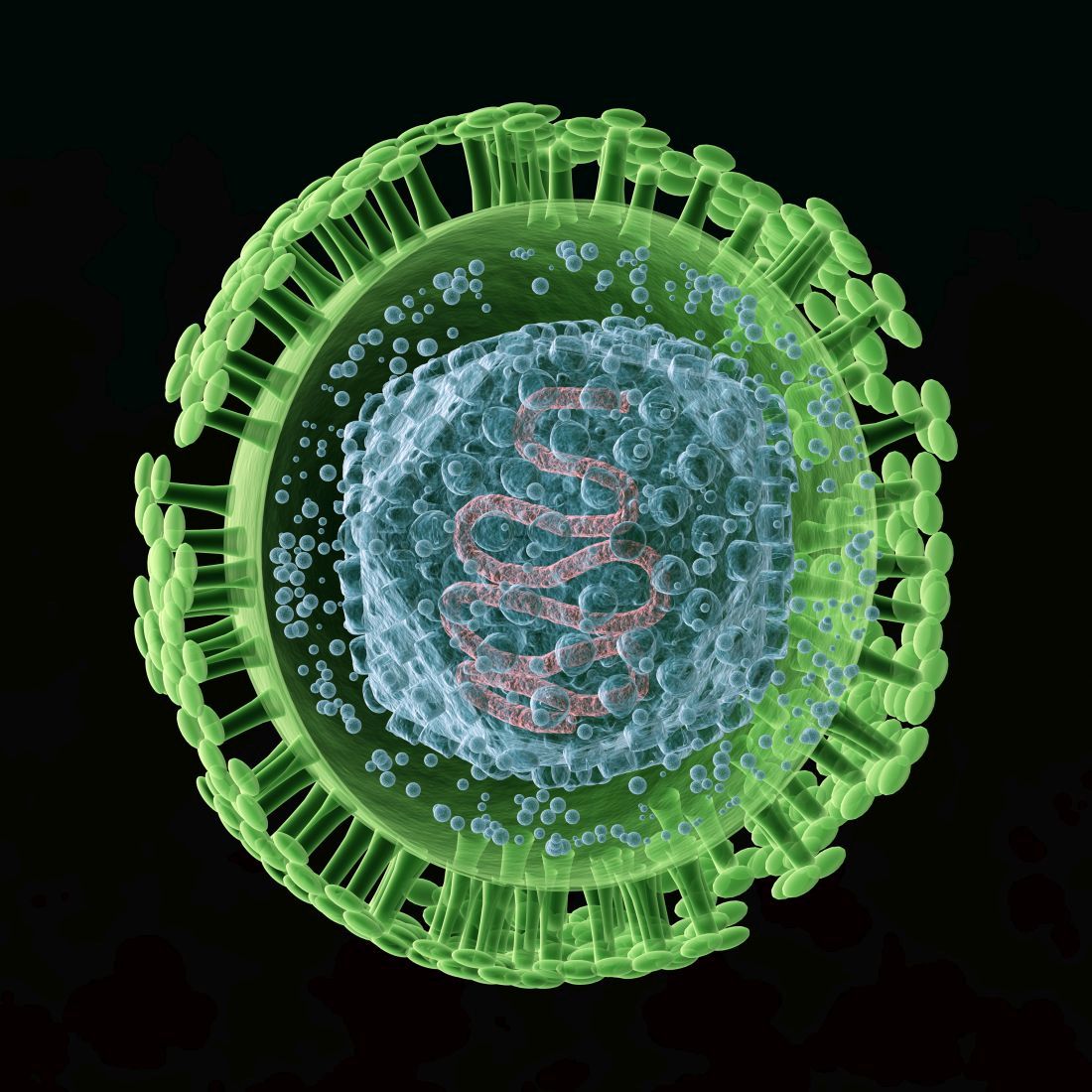
Meet our newest genetically engineered frenemy, herpes
Herpes to the rescue
Let’s face it: When people hear the word “herpes,” their first thoughts are not positive. But what if herpes could be a hero?
Scientists have found a way to make a strain of herpes that kills cancer because, hey, it’s 2022, and anything is possible. Trials have been going well and this seems like a safe and effective way to fight cancer.
Viruses may be one of our oldest enemies, but it’s also been said that the enemy of my enemy is my friend. So why not make herpes the enemy of cancer, thereby turning it into our friend? The genetically modified herpes virus is injected directly into tumors, where it destroys cancer cells from within. But wait, there’s more! The patient’s immune system also senses the virus and springs into action against it and the cancer in which it is residing.
During the phase 1 trial, three of the nine patients saw tumor reduction and the therapy proved safe as well. Future trials will be able to more specifically target various cancer types and make the treatment better. For once, we are rooting for you, herpes.
A breath of not-so-fresh air
There’s nothing quite like that first real warm day of spring. You can finally open the windows and clear out the old stuffy air that’s been hanging around all winter long. It’s a ritual that’s now backed up with some science in the form of a new study. Turns out that there’s actually a fair amount of smog in the average home. That’s right, smog’s not just for the big city anymore.
As part of the HOMEChem project, a whole host of scientists gathered together under one roof in a typical suburban house and immediately started doing chores. Cooking, cleaning, the works. No, it wasn’t because they had trashed the place the night before. They had set up instrumentation all around the house to measure the chemical makeup of the air inside. A scientist’s idea of a wild party.
The results are perhaps not all that surprising, but interesting nonetheless. Your homemade smog certainly won’t kill you, but there’s both an increased amount and higher concentration of airborne toxins in indoor air, compared with outdoors. Benzene and formaldehyde were common, as were acrolein (a pulmonary toxicant emitted by lumber and burning fats) and isocyanic acid (which can react with proteins in the human body). The researchers noted that most of these chemicals can be removed with proper ventilation.
Although cleaning is certainly responsible for a fair share of the chemicals, cooking generally produced more toxic compounds, similar to what’s found in wildfire smoke. One of the researchers said this makes sense, since a wildfire can be considered an “extreme form of cooking.” Scientists may not know how to party, but their idea of a barbecue sounds … interesting. We’re looking forward to an upcoming study out of California: Can a 1-million acre wildfire adequately cook a ribeye steak?
We’re dying to try composting ... with humans, that is
We here at LOTME are not really fans of politicians, except as objects of ridicule. That is kind of fun. Whether we’re watching Fox News, listening to NPR, or reading Vladimir Putin’s fashion blog, one thing remains clear: If you want actual information, don’t ask a politician.
There are, of course, always exceptions, and we just found one: California state representative Cristina Garcia. Rep. Garcia sponsored a bill just signed into law by Gov. Gavin Newsom that legalizes the practice of human composting, the reduction of remains by “placing bodies in individual vessels and fostering gentle transformation into a nutrient-dense soil.”
Since we’ve written about this sort of thing before – Washington was the first state to legalize the process back in 2019 – we’re more interested now in what Rep. Garcia told NBC News while describing her motivation: “I’ve always wanted to be a tree. The idea of having my family sitting under my shade one day – that brings a lot of joy.” How great is that? Tree-hugging is just not enough. Be the tree.
California is the fifth state to provide its residents with the human composting option, the other three being Colorado, Oregon, and Vermont. The process “typically involves putting a body into a steel vessel, then covering it with organic materials like straw, wood chips and alfalfa. Microbes break down the corpse and the plant matter, transforming the various components into nutrient-rich soil in roughly 30 days,” Smithsonian Magazine explained.
We just happen to have some good news for Rep. Garcia about that wanting-to-be-a-tree business. She’s already pretty close. For more on that, we go to our correspondent from beyond the grave, Carl Sagan, who shares a thought about trees. And no, we couldn’t just write out his quote here. You have to hear it in Dr. Sagan’s own voice.
That’ll be one pandemic with extra distress. Hold the goals
When the COVID-19 pandemic first hit it put a lot of stuff on hold for everyone. Couldn’t eat inside at your favorite restaurant, attend that long-awaited concert, or travel out of the country. Those were all pretty bad, but it was the disruption of pursuing long-term goals that seemed to have the most effect on people’s mental health.
Investigators from the University of Waterloo (Ont.) looked at how putting such goals on hold affected people’s mental well-being. The study’s 226 participants were asked about their “COVID-frozen” goals and the degree to which they were able to actively pursue each goal and how committed they were to achieving it.
What they found was that the participants’ COVID-frozen goals were associated with feelings of psychological distress, such as anxiety, depressive symptoms, stress, and lowered life satisfaction. It was only when participants were able to disengage from goal rumination that well-being was impacted positively.
“Goal rumination is compulsive and can aggravate worries and frustrations while also taking away mental resources from other goals,” Candice Hubley, lead author and a PhD candidate in psychology, said in a written statement. So in short, you’re only stressing yourself out more about something that is far off in the distance when you could be focusing more on short-term, tangible goals instead.
Now, no one is saying to give up on your goals. Just take them one at a time. You’ll have better life satisfaction and your COVID-frozen goals will thaw out before you know it.
Herpes to the rescue
Let’s face it: When people hear the word “herpes,” their first thoughts are not positive. But what if herpes could be a hero?
Scientists have found a way to make a strain of herpes that kills cancer because, hey, it’s 2022, and anything is possible. Trials have been going well and this seems like a safe and effective way to fight cancer.
Viruses may be one of our oldest enemies, but it’s also been said that the enemy of my enemy is my friend. So why not make herpes the enemy of cancer, thereby turning it into our friend? The genetically modified herpes virus is injected directly into tumors, where it destroys cancer cells from within. But wait, there’s more! The patient’s immune system also senses the virus and springs into action against it and the cancer in which it is residing.
During the phase 1 trial, three of the nine patients saw tumor reduction and the therapy proved safe as well. Future trials will be able to more specifically target various cancer types and make the treatment better. For once, we are rooting for you, herpes.
A breath of not-so-fresh air
There’s nothing quite like that first real warm day of spring. You can finally open the windows and clear out the old stuffy air that’s been hanging around all winter long. It’s a ritual that’s now backed up with some science in the form of a new study. Turns out that there’s actually a fair amount of smog in the average home. That’s right, smog’s not just for the big city anymore.
As part of the HOMEChem project, a whole host of scientists gathered together under one roof in a typical suburban house and immediately started doing chores. Cooking, cleaning, the works. No, it wasn’t because they had trashed the place the night before. They had set up instrumentation all around the house to measure the chemical makeup of the air inside. A scientist’s idea of a wild party.
The results are perhaps not all that surprising, but interesting nonetheless. Your homemade smog certainly won’t kill you, but there’s both an increased amount and higher concentration of airborne toxins in indoor air, compared with outdoors. Benzene and formaldehyde were common, as were acrolein (a pulmonary toxicant emitted by lumber and burning fats) and isocyanic acid (which can react with proteins in the human body). The researchers noted that most of these chemicals can be removed with proper ventilation.
Although cleaning is certainly responsible for a fair share of the chemicals, cooking generally produced more toxic compounds, similar to what’s found in wildfire smoke. One of the researchers said this makes sense, since a wildfire can be considered an “extreme form of cooking.” Scientists may not know how to party, but their idea of a barbecue sounds … interesting. We’re looking forward to an upcoming study out of California: Can a 1-million acre wildfire adequately cook a ribeye steak?
We’re dying to try composting ... with humans, that is
We here at LOTME are not really fans of politicians, except as objects of ridicule. That is kind of fun. Whether we’re watching Fox News, listening to NPR, or reading Vladimir Putin’s fashion blog, one thing remains clear: If you want actual information, don’t ask a politician.
There are, of course, always exceptions, and we just found one: California state representative Cristina Garcia. Rep. Garcia sponsored a bill just signed into law by Gov. Gavin Newsom that legalizes the practice of human composting, the reduction of remains by “placing bodies in individual vessels and fostering gentle transformation into a nutrient-dense soil.”
Since we’ve written about this sort of thing before – Washington was the first state to legalize the process back in 2019 – we’re more interested now in what Rep. Garcia told NBC News while describing her motivation: “I’ve always wanted to be a tree. The idea of having my family sitting under my shade one day – that brings a lot of joy.” How great is that? Tree-hugging is just not enough. Be the tree.
California is the fifth state to provide its residents with the human composting option, the other three being Colorado, Oregon, and Vermont. The process “typically involves putting a body into a steel vessel, then covering it with organic materials like straw, wood chips and alfalfa. Microbes break down the corpse and the plant matter, transforming the various components into nutrient-rich soil in roughly 30 days,” Smithsonian Magazine explained.
We just happen to have some good news for Rep. Garcia about that wanting-to-be-a-tree business. She’s already pretty close. For more on that, we go to our correspondent from beyond the grave, Carl Sagan, who shares a thought about trees. And no, we couldn’t just write out his quote here. You have to hear it in Dr. Sagan’s own voice.
That’ll be one pandemic with extra distress. Hold the goals
When the COVID-19 pandemic first hit it put a lot of stuff on hold for everyone. Couldn’t eat inside at your favorite restaurant, attend that long-awaited concert, or travel out of the country. Those were all pretty bad, but it was the disruption of pursuing long-term goals that seemed to have the most effect on people’s mental health.
Investigators from the University of Waterloo (Ont.) looked at how putting such goals on hold affected people’s mental well-being. The study’s 226 participants were asked about their “COVID-frozen” goals and the degree to which they were able to actively pursue each goal and how committed they were to achieving it.
What they found was that the participants’ COVID-frozen goals were associated with feelings of psychological distress, such as anxiety, depressive symptoms, stress, and lowered life satisfaction. It was only when participants were able to disengage from goal rumination that well-being was impacted positively.
“Goal rumination is compulsive and can aggravate worries and frustrations while also taking away mental resources from other goals,” Candice Hubley, lead author and a PhD candidate in psychology, said in a written statement. So in short, you’re only stressing yourself out more about something that is far off in the distance when you could be focusing more on short-term, tangible goals instead.
Now, no one is saying to give up on your goals. Just take them one at a time. You’ll have better life satisfaction and your COVID-frozen goals will thaw out before you know it.
Herpes to the rescue
Let’s face it: When people hear the word “herpes,” their first thoughts are not positive. But what if herpes could be a hero?
Scientists have found a way to make a strain of herpes that kills cancer because, hey, it’s 2022, and anything is possible. Trials have been going well and this seems like a safe and effective way to fight cancer.
Viruses may be one of our oldest enemies, but it’s also been said that the enemy of my enemy is my friend. So why not make herpes the enemy of cancer, thereby turning it into our friend? The genetically modified herpes virus is injected directly into tumors, where it destroys cancer cells from within. But wait, there’s more! The patient’s immune system also senses the virus and springs into action against it and the cancer in which it is residing.
During the phase 1 trial, three of the nine patients saw tumor reduction and the therapy proved safe as well. Future trials will be able to more specifically target various cancer types and make the treatment better. For once, we are rooting for you, herpes.
A breath of not-so-fresh air
There’s nothing quite like that first real warm day of spring. You can finally open the windows and clear out the old stuffy air that’s been hanging around all winter long. It’s a ritual that’s now backed up with some science in the form of a new study. Turns out that there’s actually a fair amount of smog in the average home. That’s right, smog’s not just for the big city anymore.
As part of the HOMEChem project, a whole host of scientists gathered together under one roof in a typical suburban house and immediately started doing chores. Cooking, cleaning, the works. No, it wasn’t because they had trashed the place the night before. They had set up instrumentation all around the house to measure the chemical makeup of the air inside. A scientist’s idea of a wild party.
The results are perhaps not all that surprising, but interesting nonetheless. Your homemade smog certainly won’t kill you, but there’s both an increased amount and higher concentration of airborne toxins in indoor air, compared with outdoors. Benzene and formaldehyde were common, as were acrolein (a pulmonary toxicant emitted by lumber and burning fats) and isocyanic acid (which can react with proteins in the human body). The researchers noted that most of these chemicals can be removed with proper ventilation.
Although cleaning is certainly responsible for a fair share of the chemicals, cooking generally produced more toxic compounds, similar to what’s found in wildfire smoke. One of the researchers said this makes sense, since a wildfire can be considered an “extreme form of cooking.” Scientists may not know how to party, but their idea of a barbecue sounds … interesting. We’re looking forward to an upcoming study out of California: Can a 1-million acre wildfire adequately cook a ribeye steak?
We’re dying to try composting ... with humans, that is
We here at LOTME are not really fans of politicians, except as objects of ridicule. That is kind of fun. Whether we’re watching Fox News, listening to NPR, or reading Vladimir Putin’s fashion blog, one thing remains clear: If you want actual information, don’t ask a politician.
There are, of course, always exceptions, and we just found one: California state representative Cristina Garcia. Rep. Garcia sponsored a bill just signed into law by Gov. Gavin Newsom that legalizes the practice of human composting, the reduction of remains by “placing bodies in individual vessels and fostering gentle transformation into a nutrient-dense soil.”
Since we’ve written about this sort of thing before – Washington was the first state to legalize the process back in 2019 – we’re more interested now in what Rep. Garcia told NBC News while describing her motivation: “I’ve always wanted to be a tree. The idea of having my family sitting under my shade one day – that brings a lot of joy.” How great is that? Tree-hugging is just not enough. Be the tree.
California is the fifth state to provide its residents with the human composting option, the other three being Colorado, Oregon, and Vermont. The process “typically involves putting a body into a steel vessel, then covering it with organic materials like straw, wood chips and alfalfa. Microbes break down the corpse and the plant matter, transforming the various components into nutrient-rich soil in roughly 30 days,” Smithsonian Magazine explained.
We just happen to have some good news for Rep. Garcia about that wanting-to-be-a-tree business. She’s already pretty close. For more on that, we go to our correspondent from beyond the grave, Carl Sagan, who shares a thought about trees. And no, we couldn’t just write out his quote here. You have to hear it in Dr. Sagan’s own voice.
That’ll be one pandemic with extra distress. Hold the goals
When the COVID-19 pandemic first hit it put a lot of stuff on hold for everyone. Couldn’t eat inside at your favorite restaurant, attend that long-awaited concert, or travel out of the country. Those were all pretty bad, but it was the disruption of pursuing long-term goals that seemed to have the most effect on people’s mental health.
Investigators from the University of Waterloo (Ont.) looked at how putting such goals on hold affected people’s mental well-being. The study’s 226 participants were asked about their “COVID-frozen” goals and the degree to which they were able to actively pursue each goal and how committed they were to achieving it.
What they found was that the participants’ COVID-frozen goals were associated with feelings of psychological distress, such as anxiety, depressive symptoms, stress, and lowered life satisfaction. It was only when participants were able to disengage from goal rumination that well-being was impacted positively.
“Goal rumination is compulsive and can aggravate worries and frustrations while also taking away mental resources from other goals,” Candice Hubley, lead author and a PhD candidate in psychology, said in a written statement. So in short, you’re only stressing yourself out more about something that is far off in the distance when you could be focusing more on short-term, tangible goals instead.
Now, no one is saying to give up on your goals. Just take them one at a time. You’ll have better life satisfaction and your COVID-frozen goals will thaw out before you know it.
Safer opioid supply program in Canada helps those who face overdose risks
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANADIAN MEDICAL ASSOCIATION JOURNAL
Could a vaccine (and more) fix the fentanyl crisis?
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
Unconventional wisdom: Major depression tied to childhood trauma is treatable
Despite a higher symptom burden, patients with major depressive disorder (MDD) and a history of childhood trauma (CT) can achieve significant recovery following treatment with a combination of pharmacotherapy and psychotherapy, new research suggests.
Results from a meta-analysis of 29 studies from 1966 to 2019, which included almost 7,000 adults with MDD, showed that more than 60% reported a history of CT. But despite having more severe depression at baseline, those with CT benefited from active treatment. Effect sizes were comparable, and dropout rates were similar to those of their counterparts without CT.
“Evidence-based psychotherapy and pharmacotherapy should be offered to depressed patients, regardless of their childhood trauma status,” lead author Erika Kuzminskaite, MSc, a PhD candidate at Amsterdam UMC department of psychiatry, the Netherlands, told this news organization.
“Screening for childhood trauma is important to identify individuals at risk for more severe course of the disorder and post-treatment residual symptoms,” she added.
The study was published online in the Lancet Psychiatry.
Common and potent risk factor
The researchers note that CT is common and is a potent risk factor for depression. Previous studies have “consistently indicated significantly higher severity and persistence of depressive symptoms in adult patients with depression and a history of childhood trauma.”
Previous individual and meta-analytic studies “indicated poorer response to first-line depression treatments in patients with childhood trauma, compared to those without trauma, suggesting the need for new personalized treatments for depressed patients with childhood trauma history,” Ms. Kuzminskaite said.
“However, the evidence on poorer treatment outcomes has not been definitive, and a comprehensive meta-analysis of available findings has been lacking,” she added.
The previous meta-analyses showed high between-study heterogeneity, and some primary studies reported similar or even superior improvement for patients with CT, compared with those without such history, following treatment with evidence-based psychotherapy or pharmacotherapy.
Previous studies also did not investigate the “relative contribution of different childhood trauma types.”
To address this gap, investigators in the Childhood Trauma Meta-Analysis Study Group conducted the “largest and most comprehensive study of available evidence examining the effects of childhood trauma on the efficacy and effectiveness of first-line treatments for adults with MDD.”
To be included, a study had to focus on adults over 18 years old who had received a primary diagnosis of depression. The study had to have included an available assessment of childhood trauma, and patients were required to have undergone psychotherapy and/or pharmacotherapy for depression alone or in combination with other guideline-recommended treatments. Studies were also required to have a comparator group, when applicable, and to have reported depression severity before and after the acute treatment phase.
Of 10,505 publications, 54 trials met inclusion criteria; of these, 29 (20 randomized controlled trials and 9 open trials), encompassing 6,830 participants aged 18-85 years, included data that had been made available by authors of the various studies and were included in the current analysis.
Most studies focused on MDD; 11 trials focused on patients with chronic or treatment-resistant depression.
The primary outcome was “depression severity change from baseline to the end of the acute treatment phase” (expressed as standardized effect size – Hedges’ g).
Greater treatment motivation?
Of the included patients, 62% reported a history of CT. They were found to have more severe depression at baseline, compared with those without CT (g = .202; 95% confidence interval, 0.145-0.258; I² = 0%).
The benefits from active treatment obtained by these patients with CT were similar to the benefits obtained by their counterparts without CT (between-group treatment effect difference: g = .016; 95% CI, –0.094-0.125; I² = 44.3%).
No significant difference in active treatment effects (in comparison with control condition) was found between individuals with and those without CT (g = .605; 95% CI, 0.294-0.916; I² = 58.0%; and g = .178; 95% CI, –0.195-0.552; I² = 67.5%, respectively; between-group difference P = .051).
Dropout rates were similar for the participants with and those without CT (risk ratio, 1.063; 95% CI, 0.945-1.195; I² = 0%).
“Findings did not significantly differ by childhood trauma type, study design, depression diagnosis, assessment method of childhood trauma, study quality, year, or treatment type or length,” the authors report.
The findings did, however, differ by country, with North American studies showing larger treatment effects for patients with CT, compared with studies conducted in Asian-Pacific countries (g = 0.150; 95% CI, 0.030-0.269; vs. g = 0.255; 95% CI, –0.508- –0.002, respectively; corrected false discovery rate, 0.0080). “However, because of limited power, these findings should be interpreted with caution,” the authors warn.
“It could be a chance finding and is certainly not causal,” Ms. Kuzminskaite suggested.
Most studies (21 of the 29) had a “moderate to high risk of bias.” But when the researchers conducted a sensitivity analysis in the low-bias studies, they found that results were similar to those of the primary analysis that included all the studies.
“Treatments were similarly effective for patients with and without childhood trauma, with slightly larger active treatment (vs. control condition – placebo, wait list, care-as-usual) effects for patients with childhood trauma history,” Ms. Kuzminskaite said.
“Some evidence suggests that patients with childhood trauma are characterized by greater treatment motivation,” she noted. Moreover, “they are also more severely depressed prior to treatment [and] thus have more room for improvement.”
‘Hopeful message’
Commenting for this news organization, Yvette Sheline, MD, McLure professor of psychiatry, radiology, and neurology and director of the center for neuromodulation in depression and Stress, University of Pennsylvania, Philadelphia, called it a “well-executed” and “straightforward” study “with clear-cut findings.”
Dr. Sheline, the director of the section on mood, anxiety, and trauma, who was not involved with the study, agrees with the authors’ conclusions – “to use evidence-based treatments for depression in all patients,” with or without a history of CT.
In an accompanying editorial, Antoine Yrondi, MD, PhD, of Université de Toulouse (France), called the findings “important and encouraging” but cautioned that CT could be associated with conditions other than depression, which could make MDD “more difficult to treat.”
Nevertheless, the meta-analysis “delivers a hopeful message to patients with childhood trauma that evidence-based psychotherapy and pharmacotherapy could improve depressive symptoms,” Dr. Yrondi said.
Dr. Yrondi encouraged physicians not to neglect CT in patients with MDD. “For this, it is important that physicians are trained to evaluate childhood trauma and to take it into account in their daily practice.”
No source of funding for the study was listed. The authors and Dr. Sheline have disclosed no relevant financial relationships. Dr. Yrondi has received speaker’s honoraria from AstraZeneca, Janssen, Lundbeck, Otsuka, and Jazz and has carried out clinical studies in relation to the development of a medicine for Janssen and Lundbeck that are unrelated to this work.
A version of this article first appeared on Medscape.com.
Despite a higher symptom burden, patients with major depressive disorder (MDD) and a history of childhood trauma (CT) can achieve significant recovery following treatment with a combination of pharmacotherapy and psychotherapy, new research suggests.
Results from a meta-analysis of 29 studies from 1966 to 2019, which included almost 7,000 adults with MDD, showed that more than 60% reported a history of CT. But despite having more severe depression at baseline, those with CT benefited from active treatment. Effect sizes were comparable, and dropout rates were similar to those of their counterparts without CT.
“Evidence-based psychotherapy and pharmacotherapy should be offered to depressed patients, regardless of their childhood trauma status,” lead author Erika Kuzminskaite, MSc, a PhD candidate at Amsterdam UMC department of psychiatry, the Netherlands, told this news organization.
“Screening for childhood trauma is important to identify individuals at risk for more severe course of the disorder and post-treatment residual symptoms,” she added.
The study was published online in the Lancet Psychiatry.
Common and potent risk factor
The researchers note that CT is common and is a potent risk factor for depression. Previous studies have “consistently indicated significantly higher severity and persistence of depressive symptoms in adult patients with depression and a history of childhood trauma.”
Previous individual and meta-analytic studies “indicated poorer response to first-line depression treatments in patients with childhood trauma, compared to those without trauma, suggesting the need for new personalized treatments for depressed patients with childhood trauma history,” Ms. Kuzminskaite said.
“However, the evidence on poorer treatment outcomes has not been definitive, and a comprehensive meta-analysis of available findings has been lacking,” she added.
The previous meta-analyses showed high between-study heterogeneity, and some primary studies reported similar or even superior improvement for patients with CT, compared with those without such history, following treatment with evidence-based psychotherapy or pharmacotherapy.
Previous studies also did not investigate the “relative contribution of different childhood trauma types.”
To address this gap, investigators in the Childhood Trauma Meta-Analysis Study Group conducted the “largest and most comprehensive study of available evidence examining the effects of childhood trauma on the efficacy and effectiveness of first-line treatments for adults with MDD.”
To be included, a study had to focus on adults over 18 years old who had received a primary diagnosis of depression. The study had to have included an available assessment of childhood trauma, and patients were required to have undergone psychotherapy and/or pharmacotherapy for depression alone or in combination with other guideline-recommended treatments. Studies were also required to have a comparator group, when applicable, and to have reported depression severity before and after the acute treatment phase.
Of 10,505 publications, 54 trials met inclusion criteria; of these, 29 (20 randomized controlled trials and 9 open trials), encompassing 6,830 participants aged 18-85 years, included data that had been made available by authors of the various studies and were included in the current analysis.
Most studies focused on MDD; 11 trials focused on patients with chronic or treatment-resistant depression.
The primary outcome was “depression severity change from baseline to the end of the acute treatment phase” (expressed as standardized effect size – Hedges’ g).
Greater treatment motivation?
Of the included patients, 62% reported a history of CT. They were found to have more severe depression at baseline, compared with those without CT (g = .202; 95% confidence interval, 0.145-0.258; I² = 0%).
The benefits from active treatment obtained by these patients with CT were similar to the benefits obtained by their counterparts without CT (between-group treatment effect difference: g = .016; 95% CI, –0.094-0.125; I² = 44.3%).
No significant difference in active treatment effects (in comparison with control condition) was found between individuals with and those without CT (g = .605; 95% CI, 0.294-0.916; I² = 58.0%; and g = .178; 95% CI, –0.195-0.552; I² = 67.5%, respectively; between-group difference P = .051).
Dropout rates were similar for the participants with and those without CT (risk ratio, 1.063; 95% CI, 0.945-1.195; I² = 0%).
“Findings did not significantly differ by childhood trauma type, study design, depression diagnosis, assessment method of childhood trauma, study quality, year, or treatment type or length,” the authors report.
The findings did, however, differ by country, with North American studies showing larger treatment effects for patients with CT, compared with studies conducted in Asian-Pacific countries (g = 0.150; 95% CI, 0.030-0.269; vs. g = 0.255; 95% CI, –0.508- –0.002, respectively; corrected false discovery rate, 0.0080). “However, because of limited power, these findings should be interpreted with caution,” the authors warn.
“It could be a chance finding and is certainly not causal,” Ms. Kuzminskaite suggested.
Most studies (21 of the 29) had a “moderate to high risk of bias.” But when the researchers conducted a sensitivity analysis in the low-bias studies, they found that results were similar to those of the primary analysis that included all the studies.
“Treatments were similarly effective for patients with and without childhood trauma, with slightly larger active treatment (vs. control condition – placebo, wait list, care-as-usual) effects for patients with childhood trauma history,” Ms. Kuzminskaite said.
“Some evidence suggests that patients with childhood trauma are characterized by greater treatment motivation,” she noted. Moreover, “they are also more severely depressed prior to treatment [and] thus have more room for improvement.”
‘Hopeful message’
Commenting for this news organization, Yvette Sheline, MD, McLure professor of psychiatry, radiology, and neurology and director of the center for neuromodulation in depression and Stress, University of Pennsylvania, Philadelphia, called it a “well-executed” and “straightforward” study “with clear-cut findings.”
Dr. Sheline, the director of the section on mood, anxiety, and trauma, who was not involved with the study, agrees with the authors’ conclusions – “to use evidence-based treatments for depression in all patients,” with or without a history of CT.
In an accompanying editorial, Antoine Yrondi, MD, PhD, of Université de Toulouse (France), called the findings “important and encouraging” but cautioned that CT could be associated with conditions other than depression, which could make MDD “more difficult to treat.”
Nevertheless, the meta-analysis “delivers a hopeful message to patients with childhood trauma that evidence-based psychotherapy and pharmacotherapy could improve depressive symptoms,” Dr. Yrondi said.
Dr. Yrondi encouraged physicians not to neglect CT in patients with MDD. “For this, it is important that physicians are trained to evaluate childhood trauma and to take it into account in their daily practice.”
No source of funding for the study was listed. The authors and Dr. Sheline have disclosed no relevant financial relationships. Dr. Yrondi has received speaker’s honoraria from AstraZeneca, Janssen, Lundbeck, Otsuka, and Jazz and has carried out clinical studies in relation to the development of a medicine for Janssen and Lundbeck that are unrelated to this work.
A version of this article first appeared on Medscape.com.
Despite a higher symptom burden, patients with major depressive disorder (MDD) and a history of childhood trauma (CT) can achieve significant recovery following treatment with a combination of pharmacotherapy and psychotherapy, new research suggests.
Results from a meta-analysis of 29 studies from 1966 to 2019, which included almost 7,000 adults with MDD, showed that more than 60% reported a history of CT. But despite having more severe depression at baseline, those with CT benefited from active treatment. Effect sizes were comparable, and dropout rates were similar to those of their counterparts without CT.
“Evidence-based psychotherapy and pharmacotherapy should be offered to depressed patients, regardless of their childhood trauma status,” lead author Erika Kuzminskaite, MSc, a PhD candidate at Amsterdam UMC department of psychiatry, the Netherlands, told this news organization.
“Screening for childhood trauma is important to identify individuals at risk for more severe course of the disorder and post-treatment residual symptoms,” she added.
The study was published online in the Lancet Psychiatry.
Common and potent risk factor
The researchers note that CT is common and is a potent risk factor for depression. Previous studies have “consistently indicated significantly higher severity and persistence of depressive symptoms in adult patients with depression and a history of childhood trauma.”
Previous individual and meta-analytic studies “indicated poorer response to first-line depression treatments in patients with childhood trauma, compared to those without trauma, suggesting the need for new personalized treatments for depressed patients with childhood trauma history,” Ms. Kuzminskaite said.
“However, the evidence on poorer treatment outcomes has not been definitive, and a comprehensive meta-analysis of available findings has been lacking,” she added.
The previous meta-analyses showed high between-study heterogeneity, and some primary studies reported similar or even superior improvement for patients with CT, compared with those without such history, following treatment with evidence-based psychotherapy or pharmacotherapy.
Previous studies also did not investigate the “relative contribution of different childhood trauma types.”
To address this gap, investigators in the Childhood Trauma Meta-Analysis Study Group conducted the “largest and most comprehensive study of available evidence examining the effects of childhood trauma on the efficacy and effectiveness of first-line treatments for adults with MDD.”
To be included, a study had to focus on adults over 18 years old who had received a primary diagnosis of depression. The study had to have included an available assessment of childhood trauma, and patients were required to have undergone psychotherapy and/or pharmacotherapy for depression alone or in combination with other guideline-recommended treatments. Studies were also required to have a comparator group, when applicable, and to have reported depression severity before and after the acute treatment phase.
Of 10,505 publications, 54 trials met inclusion criteria; of these, 29 (20 randomized controlled trials and 9 open trials), encompassing 6,830 participants aged 18-85 years, included data that had been made available by authors of the various studies and were included in the current analysis.
Most studies focused on MDD; 11 trials focused on patients with chronic or treatment-resistant depression.
The primary outcome was “depression severity change from baseline to the end of the acute treatment phase” (expressed as standardized effect size – Hedges’ g).
Greater treatment motivation?
Of the included patients, 62% reported a history of CT. They were found to have more severe depression at baseline, compared with those without CT (g = .202; 95% confidence interval, 0.145-0.258; I² = 0%).
The benefits from active treatment obtained by these patients with CT were similar to the benefits obtained by their counterparts without CT (between-group treatment effect difference: g = .016; 95% CI, –0.094-0.125; I² = 44.3%).
No significant difference in active treatment effects (in comparison with control condition) was found between individuals with and those without CT (g = .605; 95% CI, 0.294-0.916; I² = 58.0%; and g = .178; 95% CI, –0.195-0.552; I² = 67.5%, respectively; between-group difference P = .051).
Dropout rates were similar for the participants with and those without CT (risk ratio, 1.063; 95% CI, 0.945-1.195; I² = 0%).
“Findings did not significantly differ by childhood trauma type, study design, depression diagnosis, assessment method of childhood trauma, study quality, year, or treatment type or length,” the authors report.
The findings did, however, differ by country, with North American studies showing larger treatment effects for patients with CT, compared with studies conducted in Asian-Pacific countries (g = 0.150; 95% CI, 0.030-0.269; vs. g = 0.255; 95% CI, –0.508- –0.002, respectively; corrected false discovery rate, 0.0080). “However, because of limited power, these findings should be interpreted with caution,” the authors warn.
“It could be a chance finding and is certainly not causal,” Ms. Kuzminskaite suggested.
Most studies (21 of the 29) had a “moderate to high risk of bias.” But when the researchers conducted a sensitivity analysis in the low-bias studies, they found that results were similar to those of the primary analysis that included all the studies.
“Treatments were similarly effective for patients with and without childhood trauma, with slightly larger active treatment (vs. control condition – placebo, wait list, care-as-usual) effects for patients with childhood trauma history,” Ms. Kuzminskaite said.
“Some evidence suggests that patients with childhood trauma are characterized by greater treatment motivation,” she noted. Moreover, “they are also more severely depressed prior to treatment [and] thus have more room for improvement.”
‘Hopeful message’
Commenting for this news organization, Yvette Sheline, MD, McLure professor of psychiatry, radiology, and neurology and director of the center for neuromodulation in depression and Stress, University of Pennsylvania, Philadelphia, called it a “well-executed” and “straightforward” study “with clear-cut findings.”
Dr. Sheline, the director of the section on mood, anxiety, and trauma, who was not involved with the study, agrees with the authors’ conclusions – “to use evidence-based treatments for depression in all patients,” with or without a history of CT.
In an accompanying editorial, Antoine Yrondi, MD, PhD, of Université de Toulouse (France), called the findings “important and encouraging” but cautioned that CT could be associated with conditions other than depression, which could make MDD “more difficult to treat.”
Nevertheless, the meta-analysis “delivers a hopeful message to patients with childhood trauma that evidence-based psychotherapy and pharmacotherapy could improve depressive symptoms,” Dr. Yrondi said.
Dr. Yrondi encouraged physicians not to neglect CT in patients with MDD. “For this, it is important that physicians are trained to evaluate childhood trauma and to take it into account in their daily practice.”
No source of funding for the study was listed. The authors and Dr. Sheline have disclosed no relevant financial relationships. Dr. Yrondi has received speaker’s honoraria from AstraZeneca, Janssen, Lundbeck, Otsuka, and Jazz and has carried out clinical studies in relation to the development of a medicine for Janssen and Lundbeck that are unrelated to this work.
A version of this article first appeared on Medscape.com.
FROM LANCET PSYCHIATRY
Not just a bad dream: Nightmares may predict dementia
Results from a large cohort study showed that healthy middle-aged adults who had bad dreams at least once a week were four times more likely to experience cognitive decline over the following decade, and older adults were twice as likely to be diagnosed with dementia, compared with peers who never had bad dreams.
Frequent nightmares may “identify people who are at high risk of developing dementia in the future, several years or decades before the characteristic memory and thinking problems emerge,” study investigator Abidemi Otaiku, BMBS, University of Birmingham, England, said in an interview.
“This would be the optimum time for doctors to intervene to try and slow down or prevent dementia from developing,” Dr. Otaiku said.
The findings were published online in The Lancet journal eClinicalMedicine).
Distressing dreams
Distressing dreams have been previously associated with faster cognitive decline and increased dementia risk in patients with Parkinson’s disease (PD), but whether the same holds for individuals from the general population without PD is unknown.
To investigate, Dr. Otaiku examined data from three community-based cohorts in the United States. This included 605 middle-aged adults (aged 35-64 years) who were followed for up to 13 years and 2,600 adults aged 79 and older who were followed for up to 7 years. All were considered cognitively normal at baseline.
The prevalence of frequent distressing dreams, defined as occurring “once a week or more,” was higher in the older cohort compared with the middle-aged cohort (6.9% vs. 6.0%, respectively).
This is in line with other research that showed distressing dreams remain relatively stable throughout early adulthood and then progressively increase in prevalence from middle to older adulthood.
After adjustment for all covariates, a higher frequency of distressing dreams was linearly and statistically significantly associated with a higher risk for cognitive decline in middle-aged adults (P = .016) and a higher risk for dementia in older adults (P = .001).
In the fully adjusted model, compared with middle-aged adults who never had bad dreams, those who reported having one or more bad dreams weekly had a fourfold risk for cognitive decline (adjusted odds ratio [aOR], 3.99; 95% confidence interval [CI], 1.07-14.85).
Older adults who had one or more bad dreams weekly had a greater than twofold increased risk for developing dementia (aOR, 2.21; 95% CI, 1.35-3.62).
Early days
In sex-stratified analyses, distressing dreams were strongly and statistically significantly associated with cognitive decline and dementia in men, but were only weakly and nonsignificantly associated with cognitive decline and dementia in women.
Dr. Otaiku said he suspects some individuals in the preclinical phase of dementia have “subtle neurodegeneration occurring over time in the right frontal lobe: the area of the brain that helps to downregulate negative emotions whilst we are awake, and also whilst we are dreaming.”
This could result in “depression and anxiety in the day, and nightmares and bad dreams during the night,” he said.
It is possible that treatment for frequent nightmares may help to slow cognitive decline and delay or prevent dementia, Dr. Otaiku added.
He noted that prazosin is used to treat nightmares and has been shown to prevent memory decline and reduce amyloid B generation in preclinical studies of Alzheimer’s disease.
“This is an exciting prospect [but] it is still early days and we will need research to see whether treating nightmares might help to reduce dementia risk down the line,” Dr. Otaiku said.
Credible research
In an interview regarding these findings, Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association, said: “This is credible research consistent with the idea that sleep disturbances may be a risk factor or warning sign of cognitive decline.”
She added that “what’s novel here” is the researchers examined distressing dreams – not more physical sleep disturbances and disorders such as insomnia or apnea.
“However, nightmares can disturb sleep in the same way these disorders do by waking people up in the middle of the night,” said Dr. Carrillo, who was not involved with the study.
“Previous research has pointed to nightmares being indicative of potential changes in the brain that can precede other dementias like Parkinson’s disease. More research is needed to tease out what exactly is happening in the brain during nightmares that may be contributing to this increased risk,” she said.
Dr. Carrillo noted that “getting good sleep” is important for overall health, which includes brain health.
“The good news is there are treatments – both drug and nondrug – that can help address sleep disturbances,” she added.
This study received no external funding. Dr. Otaiku and Dr. Carrillo have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a large cohort study showed that healthy middle-aged adults who had bad dreams at least once a week were four times more likely to experience cognitive decline over the following decade, and older adults were twice as likely to be diagnosed with dementia, compared with peers who never had bad dreams.
Frequent nightmares may “identify people who are at high risk of developing dementia in the future, several years or decades before the characteristic memory and thinking problems emerge,” study investigator Abidemi Otaiku, BMBS, University of Birmingham, England, said in an interview.
“This would be the optimum time for doctors to intervene to try and slow down or prevent dementia from developing,” Dr. Otaiku said.
The findings were published online in The Lancet journal eClinicalMedicine).
Distressing dreams
Distressing dreams have been previously associated with faster cognitive decline and increased dementia risk in patients with Parkinson’s disease (PD), but whether the same holds for individuals from the general population without PD is unknown.
To investigate, Dr. Otaiku examined data from three community-based cohorts in the United States. This included 605 middle-aged adults (aged 35-64 years) who were followed for up to 13 years and 2,600 adults aged 79 and older who were followed for up to 7 years. All were considered cognitively normal at baseline.
The prevalence of frequent distressing dreams, defined as occurring “once a week or more,” was higher in the older cohort compared with the middle-aged cohort (6.9% vs. 6.0%, respectively).
This is in line with other research that showed distressing dreams remain relatively stable throughout early adulthood and then progressively increase in prevalence from middle to older adulthood.
After adjustment for all covariates, a higher frequency of distressing dreams was linearly and statistically significantly associated with a higher risk for cognitive decline in middle-aged adults (P = .016) and a higher risk for dementia in older adults (P = .001).
In the fully adjusted model, compared with middle-aged adults who never had bad dreams, those who reported having one or more bad dreams weekly had a fourfold risk for cognitive decline (adjusted odds ratio [aOR], 3.99; 95% confidence interval [CI], 1.07-14.85).
Older adults who had one or more bad dreams weekly had a greater than twofold increased risk for developing dementia (aOR, 2.21; 95% CI, 1.35-3.62).
Early days
In sex-stratified analyses, distressing dreams were strongly and statistically significantly associated with cognitive decline and dementia in men, but were only weakly and nonsignificantly associated with cognitive decline and dementia in women.
Dr. Otaiku said he suspects some individuals in the preclinical phase of dementia have “subtle neurodegeneration occurring over time in the right frontal lobe: the area of the brain that helps to downregulate negative emotions whilst we are awake, and also whilst we are dreaming.”
This could result in “depression and anxiety in the day, and nightmares and bad dreams during the night,” he said.
It is possible that treatment for frequent nightmares may help to slow cognitive decline and delay or prevent dementia, Dr. Otaiku added.
He noted that prazosin is used to treat nightmares and has been shown to prevent memory decline and reduce amyloid B generation in preclinical studies of Alzheimer’s disease.
“This is an exciting prospect [but] it is still early days and we will need research to see whether treating nightmares might help to reduce dementia risk down the line,” Dr. Otaiku said.
Credible research
In an interview regarding these findings, Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association, said: “This is credible research consistent with the idea that sleep disturbances may be a risk factor or warning sign of cognitive decline.”
She added that “what’s novel here” is the researchers examined distressing dreams – not more physical sleep disturbances and disorders such as insomnia or apnea.
“However, nightmares can disturb sleep in the same way these disorders do by waking people up in the middle of the night,” said Dr. Carrillo, who was not involved with the study.
“Previous research has pointed to nightmares being indicative of potential changes in the brain that can precede other dementias like Parkinson’s disease. More research is needed to tease out what exactly is happening in the brain during nightmares that may be contributing to this increased risk,” she said.
Dr. Carrillo noted that “getting good sleep” is important for overall health, which includes brain health.
“The good news is there are treatments – both drug and nondrug – that can help address sleep disturbances,” she added.
This study received no external funding. Dr. Otaiku and Dr. Carrillo have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a large cohort study showed that healthy middle-aged adults who had bad dreams at least once a week were four times more likely to experience cognitive decline over the following decade, and older adults were twice as likely to be diagnosed with dementia, compared with peers who never had bad dreams.
Frequent nightmares may “identify people who are at high risk of developing dementia in the future, several years or decades before the characteristic memory and thinking problems emerge,” study investigator Abidemi Otaiku, BMBS, University of Birmingham, England, said in an interview.
“This would be the optimum time for doctors to intervene to try and slow down or prevent dementia from developing,” Dr. Otaiku said.
The findings were published online in The Lancet journal eClinicalMedicine).
Distressing dreams
Distressing dreams have been previously associated with faster cognitive decline and increased dementia risk in patients with Parkinson’s disease (PD), but whether the same holds for individuals from the general population without PD is unknown.
To investigate, Dr. Otaiku examined data from three community-based cohorts in the United States. This included 605 middle-aged adults (aged 35-64 years) who were followed for up to 13 years and 2,600 adults aged 79 and older who were followed for up to 7 years. All were considered cognitively normal at baseline.
The prevalence of frequent distressing dreams, defined as occurring “once a week or more,” was higher in the older cohort compared with the middle-aged cohort (6.9% vs. 6.0%, respectively).
This is in line with other research that showed distressing dreams remain relatively stable throughout early adulthood and then progressively increase in prevalence from middle to older adulthood.
After adjustment for all covariates, a higher frequency of distressing dreams was linearly and statistically significantly associated with a higher risk for cognitive decline in middle-aged adults (P = .016) and a higher risk for dementia in older adults (P = .001).
In the fully adjusted model, compared with middle-aged adults who never had bad dreams, those who reported having one or more bad dreams weekly had a fourfold risk for cognitive decline (adjusted odds ratio [aOR], 3.99; 95% confidence interval [CI], 1.07-14.85).
Older adults who had one or more bad dreams weekly had a greater than twofold increased risk for developing dementia (aOR, 2.21; 95% CI, 1.35-3.62).
Early days
In sex-stratified analyses, distressing dreams were strongly and statistically significantly associated with cognitive decline and dementia in men, but were only weakly and nonsignificantly associated with cognitive decline and dementia in women.
Dr. Otaiku said he suspects some individuals in the preclinical phase of dementia have “subtle neurodegeneration occurring over time in the right frontal lobe: the area of the brain that helps to downregulate negative emotions whilst we are awake, and also whilst we are dreaming.”
This could result in “depression and anxiety in the day, and nightmares and bad dreams during the night,” he said.
It is possible that treatment for frequent nightmares may help to slow cognitive decline and delay or prevent dementia, Dr. Otaiku added.
He noted that prazosin is used to treat nightmares and has been shown to prevent memory decline and reduce amyloid B generation in preclinical studies of Alzheimer’s disease.
“This is an exciting prospect [but] it is still early days and we will need research to see whether treating nightmares might help to reduce dementia risk down the line,” Dr. Otaiku said.
Credible research
In an interview regarding these findings, Maria C. Carrillo, PhD, chief science officer for the Alzheimer’s Association, said: “This is credible research consistent with the idea that sleep disturbances may be a risk factor or warning sign of cognitive decline.”
She added that “what’s novel here” is the researchers examined distressing dreams – not more physical sleep disturbances and disorders such as insomnia or apnea.
“However, nightmares can disturb sleep in the same way these disorders do by waking people up in the middle of the night,” said Dr. Carrillo, who was not involved with the study.
“Previous research has pointed to nightmares being indicative of potential changes in the brain that can precede other dementias like Parkinson’s disease. More research is needed to tease out what exactly is happening in the brain during nightmares that may be contributing to this increased risk,” she said.
Dr. Carrillo noted that “getting good sleep” is important for overall health, which includes brain health.
“The good news is there are treatments – both drug and nondrug – that can help address sleep disturbances,” she added.
This study received no external funding. Dr. Otaiku and Dr. Carrillo have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ECLINICALMEDICINE
Gender-affirming mastectomy boosts image and quality of life in gender-diverse youth
Adolescents and young adults who undergo “top surgery” for gender dysphoria overwhelmingly report being satisfied with the procedure in the near-term, new research shows.
The results of the prospective cohort study, reported recently in JAMA Pediatrics, suggest that the surgery can help facilitate gender congruence and comfort with body image for transmasculine and nonbinary youth. The authors, from Northwestern University, Chicago, said the findings may “help dispel misconceptions that gender-affirming treatment is experimental and support evidence-based practices of top surgery.”
Sumanas Jordan, MD, PhD, assistant professor of plastic surgery at Northwestern University, Chicago, and a coauthor of the study, said the study was the first prospective, matched cohort analysis showing that chest surgery improves outcomes in this age group.
“We focused our study on chest dysphoria, the distress due to the presence of breasts, and gender congruence, the feeling of alignment between identity and physical characteristics,” Dr. Jordan said. “We will continue to study the effect of surgery in other areas of health, such as physical functioning and quality of life, and follow our patients longer term.”
As many as 9% of adolescents and young adults identify as transgender or nonbinary - a group underrepresented in the pediatric literature, Dr. Jordan’s group said. Chest dysphoria often is associated with psychosocial issues such as depression and anxiety.
“Dysphoria can lead to a range of negative physical and emotional consequences, such as avoidance of exercise and sports, harmful chest-binding practices, functional limitations, and suicidal ideation, said M. Brett Cooper, MD, MEd, assistant professor of pediatrics, and adolescent and young adult medicine, at UT Southwestern Medical Center/Children’s Health, Dallas. “These young people often bind for several hours a day to reduce the presence of their chest.”
The study
The Northwestern team recruited 81 patients with a mean age of 18.6 years whose sex at birth was assigned female. Patients were overwhelmingly White (89%), and the majority (59%) were transgender male, the remaining patients nonbinary.
The population sample included patients aged 13-24 who underwent top surgery from December 2019 to April 2021 and a matched control group of those who did not have surgery.
Outcomes measures were assessed preoperatively and 3 months after surgery.
Thirty-six surgical patients and 34 of those in the control arm completed the outcomes measures. Surgical complications were minimal. Propensity analyses suggested an association between surgery and substantial improvements in scores on the following study endpoints:
- Chest dysphoria measure (–25.58 points, 95% confidence interval [CI], –29.18 to –21.98).
- Transgender congruence scale (7.78 points, 95%: CI, 6.06-9.50)
- Body image scale (–7.20 points, 95% CI, –11.68 to –2.72).
The patients who underwent top surgery reported significant improvements in scores of chest dysphoria, transgender congruence, and body image. The results for patients younger than age 18 paralleled those for older participants in the study.
While the results corroborate other studies showing that gender-affirming therapy improves mental health and quality of life among these young people, the researchers cautioned that some insurers require testosterone therapy for 1 year before their plans will cover the costs of gender-affirming surgery.
This may negatively affect those nonbinary patients who do not undergo hormone therapy,” the researchers wrote. They are currently collecting 1-year follow-up data to determine the long-term effects of top surgery on chest dysphoria, gender congruence, and body image.
As surgical patients progress through adult life, does the risk of regret increase? “We did not address regret in this short-term study,” Dr. Jordan said. “However, previous studies have shown very low levels of regret.”
An accompanying editorial concurred that top surgery is effective and medically necessary in this population of young people.
Calling the study “an important milestone in gender affirmation research,” Kishan M. Thadikonda, MD, and Katherine M. Gast, MD, MS, of the school of medicine and public health at the University of Wisconsin in Madison, said it will be important to follow this young cohort to prove these benefits will endure as patients age.
They cautioned, however, that nonbinary patients represented just 13% of the patient total and only 8% of the surgical cohort. Nonbinary patients are not well understood as a patient population when it comes to gender-affirmation surgery and are often included in studies with transgender patients despite clear differences, they noted.
Current setbacks
According to Dr. Cooper, politics is already affecting care in Texas. “Due to the sociopolitical climate in my state in regard to gender-affirming care, I have also seen a few young people have their surgeries either canceled or postponed by their parents,” he said. “This has led to a worsening of mental health in these patients.”
Dr. Cooper stressed the need for more research on the perspective of non-White and socioeconomically disadvantaged youth.
“This study also highlights the disparity between patients who have commercial insurance versus those who are on Medicaid,” he said. “Medicaid plans often do not cover this, so those patients usually have to continue to suffer or pay for this surgery out of their own pocket.”
This study was supported by the Northwestern University Clinical and Translational Sciences Institute, funded in part by the National Institutes of Health. Funding also came from the Plastic Surgery Foundation and American Association of Pediatric Plastic Surgery. Dr. Jordan received grants from the Plastic Surgery Foundation during the study. One coauthor reported consultant fees from CVS Caremark for consulting outside the submitted work, and another reported grants from the National Institutes of Health outside the submitted work. Dr. Cooper disclosed no competing interests relevant to his comments. The editorial commentators disclosed no conflicts of interest.
Adolescents and young adults who undergo “top surgery” for gender dysphoria overwhelmingly report being satisfied with the procedure in the near-term, new research shows.
The results of the prospective cohort study, reported recently in JAMA Pediatrics, suggest that the surgery can help facilitate gender congruence and comfort with body image for transmasculine and nonbinary youth. The authors, from Northwestern University, Chicago, said the findings may “help dispel misconceptions that gender-affirming treatment is experimental and support evidence-based practices of top surgery.”
Sumanas Jordan, MD, PhD, assistant professor of plastic surgery at Northwestern University, Chicago, and a coauthor of the study, said the study was the first prospective, matched cohort analysis showing that chest surgery improves outcomes in this age group.
“We focused our study on chest dysphoria, the distress due to the presence of breasts, and gender congruence, the feeling of alignment between identity and physical characteristics,” Dr. Jordan said. “We will continue to study the effect of surgery in other areas of health, such as physical functioning and quality of life, and follow our patients longer term.”
As many as 9% of adolescents and young adults identify as transgender or nonbinary - a group underrepresented in the pediatric literature, Dr. Jordan’s group said. Chest dysphoria often is associated with psychosocial issues such as depression and anxiety.
“Dysphoria can lead to a range of negative physical and emotional consequences, such as avoidance of exercise and sports, harmful chest-binding practices, functional limitations, and suicidal ideation, said M. Brett Cooper, MD, MEd, assistant professor of pediatrics, and adolescent and young adult medicine, at UT Southwestern Medical Center/Children’s Health, Dallas. “These young people often bind for several hours a day to reduce the presence of their chest.”
The study
The Northwestern team recruited 81 patients with a mean age of 18.6 years whose sex at birth was assigned female. Patients were overwhelmingly White (89%), and the majority (59%) were transgender male, the remaining patients nonbinary.
The population sample included patients aged 13-24 who underwent top surgery from December 2019 to April 2021 and a matched control group of those who did not have surgery.
Outcomes measures were assessed preoperatively and 3 months after surgery.
Thirty-six surgical patients and 34 of those in the control arm completed the outcomes measures. Surgical complications were minimal. Propensity analyses suggested an association between surgery and substantial improvements in scores on the following study endpoints:
- Chest dysphoria measure (–25.58 points, 95% confidence interval [CI], –29.18 to –21.98).
- Transgender congruence scale (7.78 points, 95%: CI, 6.06-9.50)
- Body image scale (–7.20 points, 95% CI, –11.68 to –2.72).
The patients who underwent top surgery reported significant improvements in scores of chest dysphoria, transgender congruence, and body image. The results for patients younger than age 18 paralleled those for older participants in the study.
While the results corroborate other studies showing that gender-affirming therapy improves mental health and quality of life among these young people, the researchers cautioned that some insurers require testosterone therapy for 1 year before their plans will cover the costs of gender-affirming surgery.
This may negatively affect those nonbinary patients who do not undergo hormone therapy,” the researchers wrote. They are currently collecting 1-year follow-up data to determine the long-term effects of top surgery on chest dysphoria, gender congruence, and body image.
As surgical patients progress through adult life, does the risk of regret increase? “We did not address regret in this short-term study,” Dr. Jordan said. “However, previous studies have shown very low levels of regret.”
An accompanying editorial concurred that top surgery is effective and medically necessary in this population of young people.
Calling the study “an important milestone in gender affirmation research,” Kishan M. Thadikonda, MD, and Katherine M. Gast, MD, MS, of the school of medicine and public health at the University of Wisconsin in Madison, said it will be important to follow this young cohort to prove these benefits will endure as patients age.
They cautioned, however, that nonbinary patients represented just 13% of the patient total and only 8% of the surgical cohort. Nonbinary patients are not well understood as a patient population when it comes to gender-affirmation surgery and are often included in studies with transgender patients despite clear differences, they noted.
Current setbacks
According to Dr. Cooper, politics is already affecting care in Texas. “Due to the sociopolitical climate in my state in regard to gender-affirming care, I have also seen a few young people have their surgeries either canceled or postponed by their parents,” he said. “This has led to a worsening of mental health in these patients.”
Dr. Cooper stressed the need for more research on the perspective of non-White and socioeconomically disadvantaged youth.
“This study also highlights the disparity between patients who have commercial insurance versus those who are on Medicaid,” he said. “Medicaid plans often do not cover this, so those patients usually have to continue to suffer or pay for this surgery out of their own pocket.”
This study was supported by the Northwestern University Clinical and Translational Sciences Institute, funded in part by the National Institutes of Health. Funding also came from the Plastic Surgery Foundation and American Association of Pediatric Plastic Surgery. Dr. Jordan received grants from the Plastic Surgery Foundation during the study. One coauthor reported consultant fees from CVS Caremark for consulting outside the submitted work, and another reported grants from the National Institutes of Health outside the submitted work. Dr. Cooper disclosed no competing interests relevant to his comments. The editorial commentators disclosed no conflicts of interest.
Adolescents and young adults who undergo “top surgery” for gender dysphoria overwhelmingly report being satisfied with the procedure in the near-term, new research shows.
The results of the prospective cohort study, reported recently in JAMA Pediatrics, suggest that the surgery can help facilitate gender congruence and comfort with body image for transmasculine and nonbinary youth. The authors, from Northwestern University, Chicago, said the findings may “help dispel misconceptions that gender-affirming treatment is experimental and support evidence-based practices of top surgery.”
Sumanas Jordan, MD, PhD, assistant professor of plastic surgery at Northwestern University, Chicago, and a coauthor of the study, said the study was the first prospective, matched cohort analysis showing that chest surgery improves outcomes in this age group.
“We focused our study on chest dysphoria, the distress due to the presence of breasts, and gender congruence, the feeling of alignment between identity and physical characteristics,” Dr. Jordan said. “We will continue to study the effect of surgery in other areas of health, such as physical functioning and quality of life, and follow our patients longer term.”
As many as 9% of adolescents and young adults identify as transgender or nonbinary - a group underrepresented in the pediatric literature, Dr. Jordan’s group said. Chest dysphoria often is associated with psychosocial issues such as depression and anxiety.
“Dysphoria can lead to a range of negative physical and emotional consequences, such as avoidance of exercise and sports, harmful chest-binding practices, functional limitations, and suicidal ideation, said M. Brett Cooper, MD, MEd, assistant professor of pediatrics, and adolescent and young adult medicine, at UT Southwestern Medical Center/Children’s Health, Dallas. “These young people often bind for several hours a day to reduce the presence of their chest.”
The study
The Northwestern team recruited 81 patients with a mean age of 18.6 years whose sex at birth was assigned female. Patients were overwhelmingly White (89%), and the majority (59%) were transgender male, the remaining patients nonbinary.
The population sample included patients aged 13-24 who underwent top surgery from December 2019 to April 2021 and a matched control group of those who did not have surgery.
Outcomes measures were assessed preoperatively and 3 months after surgery.
Thirty-six surgical patients and 34 of those in the control arm completed the outcomes measures. Surgical complications were minimal. Propensity analyses suggested an association between surgery and substantial improvements in scores on the following study endpoints:
- Chest dysphoria measure (–25.58 points, 95% confidence interval [CI], –29.18 to –21.98).
- Transgender congruence scale (7.78 points, 95%: CI, 6.06-9.50)
- Body image scale (–7.20 points, 95% CI, –11.68 to –2.72).
The patients who underwent top surgery reported significant improvements in scores of chest dysphoria, transgender congruence, and body image. The results for patients younger than age 18 paralleled those for older participants in the study.
While the results corroborate other studies showing that gender-affirming therapy improves mental health and quality of life among these young people, the researchers cautioned that some insurers require testosterone therapy for 1 year before their plans will cover the costs of gender-affirming surgery.
This may negatively affect those nonbinary patients who do not undergo hormone therapy,” the researchers wrote. They are currently collecting 1-year follow-up data to determine the long-term effects of top surgery on chest dysphoria, gender congruence, and body image.
As surgical patients progress through adult life, does the risk of regret increase? “We did not address regret in this short-term study,” Dr. Jordan said. “However, previous studies have shown very low levels of regret.”
An accompanying editorial concurred that top surgery is effective and medically necessary in this population of young people.
Calling the study “an important milestone in gender affirmation research,” Kishan M. Thadikonda, MD, and Katherine M. Gast, MD, MS, of the school of medicine and public health at the University of Wisconsin in Madison, said it will be important to follow this young cohort to prove these benefits will endure as patients age.
They cautioned, however, that nonbinary patients represented just 13% of the patient total and only 8% of the surgical cohort. Nonbinary patients are not well understood as a patient population when it comes to gender-affirmation surgery and are often included in studies with transgender patients despite clear differences, they noted.
Current setbacks
According to Dr. Cooper, politics is already affecting care in Texas. “Due to the sociopolitical climate in my state in regard to gender-affirming care, I have also seen a few young people have their surgeries either canceled or postponed by their parents,” he said. “This has led to a worsening of mental health in these patients.”
Dr. Cooper stressed the need for more research on the perspective of non-White and socioeconomically disadvantaged youth.
“This study also highlights the disparity between patients who have commercial insurance versus those who are on Medicaid,” he said. “Medicaid plans often do not cover this, so those patients usually have to continue to suffer or pay for this surgery out of their own pocket.”
This study was supported by the Northwestern University Clinical and Translational Sciences Institute, funded in part by the National Institutes of Health. Funding also came from the Plastic Surgery Foundation and American Association of Pediatric Plastic Surgery. Dr. Jordan received grants from the Plastic Surgery Foundation during the study. One coauthor reported consultant fees from CVS Caremark for consulting outside the submitted work, and another reported grants from the National Institutes of Health outside the submitted work. Dr. Cooper disclosed no competing interests relevant to his comments. The editorial commentators disclosed no conflicts of interest.
FROM JAMA PEDIATRICS
Timing of food intake a novel strategy for treating mood disorders?
new research suggests.
Investigators at Brigham and Women’s Hospital, Boston, created a simulated nightwork schedule for 19 individuals in a laboratory setting. Participants then engaged in two different meal timing models – daytime-only meals (DMI), and meals taken during both daytime and nighttime (DNMC).
Depression- and anxiety-like mood levels increased by 26% and 16%, respectively, among the daytime and nighttime eaters, but there was no such increase in daytime-only eaters.
“Our findings provide evidence for the timing of food intake as a novel strategy to potentially minimize mood vulnerability in individuals experiencing circadian misalignment, such as people engaged in shift work, experiencing jet lag, or suffering from circadian rhythm disorders,” co–corresponding author Frank A.J.L. Scheer, PhD, director of the medical chronobiology program, Brigham and Women’s Hospital, Boston, said in a news release.
The study was published online in the Proceedings of the National Academy of Sciences.
Misaligned circadian clock
“Shift workers often experience a misalignment between their central circadian clock in the brain and daily behaviors, such as sleep/wake and fasting/eating cycles,” senior author Sarah Chellappa, MD, PhD, currently the Alexander Von Humboldt Experienced Fellow in the department of nuclear medicine, University of Cologne (Germany). Dr. Chellappa was a postdoctoral fellow at Brigham and Women’s Hospital when the study was conducted.
“They also have a 25%-40% higher risk of depression and anxiety,” she continued. “Since meal timing is important for physical health and diet is important for mood, we sought to find out whether meal timing can benefit mental health as well.”
Given that impaired glycemic control is a “risk factor for mood disruption,” the researchers tested the prediction that daytime eating “would prevent mood vulnerability, despite simulated night work.”
To investigate the question, they conducted a parallel-design, randomized clinical trial that included a 14-day circadian laboratory protocol with 19 healthy adults (12 men, 7 women; mean age, 26.5 ± 4.1 years) who underwent a forced desynchrony (FD) in dim light for 4 “days,” each of which consisted of 28 hours. Each 28-hour “day” resulted in an additional 4-hour misalignment between the central circadian clock and external behavioral/environmental cycles.
By the fourth day, the participants were misaligned by 12 hours, compared to baseline (that is, the first day). They were then randomly assigned to two groups.
The DNMC group – the control group – had a “typical 28-hour FD protocol,” with behavioral and environmental cycles (sleep/wake, rest/activity, supine/upright posture, dark during scheduled sleep/dim light during wakefulness) scheduled on a 28-hour cycle. Thus, they took their meals during both “daytime” and “nighttime,” which is the typical way that night workers eat.
The DMI group underwent a modified 28-hour FD protocol, with all cycles scheduled on a 28-hour basis, except for the fasting/eating cycle, which was scheduled on a 24-hour basis, resulting in meals consumed only during the “daytime.”
Depression- and anxiety-like mood (which “correspond to an amalgam of mood states typically observed in depression and anxiety) were assessed every hour during the 4 FD days, using computerized visual analogue scales.
Nutritional psychiatry
Participants in the DNMC group experienced an increase from baseline in depression- and anxiety-like mood levels of 26.2% (95% confidence interval, 21-31.5; P = .001; P value using false discovery rate, .01; effect-size r, 0.78) and 16.1% (95% CI, 8.5-23.6; P = .005; PFDR, .001; effect-size r, 0.47), respectively.
By contrast, a similar increase did not take place in the DMI group for either depression- or anxiety-like mood levels (95% CI, –5.7% to 7.4%, P not significant and 95% CI, –3.1% to 9.9%, P not significant, respectively).
The researchers tested “whether increase mood vulnerability during simulated night work was associated with the degree of internal circadian misalignment” — defined as “change in the phase difference between the acrophase of circadian glucose rhythms and the bathyphase of circadian body temperature rhythms.”
They found that a larger degree of internal circadian misalignment was “robustly associated” with more depression-like (r, 0.77; P = .001) and anxiety-like (r, 0.67; P = .002) mood levels during simulated night work.
The findings imply that meal timing had “moderate to large effects in depression-like and anxiety-like mood levels during night work, and that such effects were associated with the degree of internal circadian misalignment,” the authors wrote.
The laboratory protocol of both groups was identical except for the timing of meals. The authors noted that the “relevance of diet on sleep, circadian rhythms, and mental health is receiving growing awareness with the emergence of a new field, nutritional psychiatry.”
People who experience depression “often report poor-quality diets with high carbohydrate intake,” and there is evidence that adherence to the Mediterranean diet is associated “with lower odds of depression, anxiety, and psychological distress.”
They cautioned that although these emerging studies suggest an association between dietary factors and mental health, “experimental studies in individuals with depression and/or anxiety/anxiety-related disorders are required to determine causality and direction of effects.”
They described meal timing as “an emerging aspect of nutrition, with increasing research interest because of its influence on physical health.” However, they noted, “the causal role of the timing of food intake on mental health remains to be tested.”
Novel findings
Commenting for this article, Kathleen Merikangas, PhD, distinguished investigator and chief, genetic epidemiology research branch, intramural research program, National Institute of Mental Health, Bethesda, Md., described the research as important with novel findings.
The research “employs the elegant, carefully controlled laboratory procedures that have unraveled the influence of light and other environmental cues on sleep and circadian rhythms over the past 2 decades,” said Dr. Merikangas, who was not involved with the study.
“One of the most significant contributions of this work is its demonstration of the importance of investigating circadian rhythms of multiple systems rather than solely focusing on sleep, eating, or emotional states that have often been studied in isolation,” she pointed out.
“Growing evidence from basic research highlights the interdependence of multiple human systems that should be built into interventions that tend to focus on one or two domains.”
She recommended that this work be replicated “in more diverse samples ... in both controlled and naturalistic settings...to test both the generalizability and mechanism of these intriguing findings.”
The study was funded by the National Institutes of Health. Individual investigators were funded by the Alexander Von Humboldt Foundation and the American Diabetes Association. Dr. Chellappa disclosed no relevant financial relationships. Dr. Merikangas disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators at Brigham and Women’s Hospital, Boston, created a simulated nightwork schedule for 19 individuals in a laboratory setting. Participants then engaged in two different meal timing models – daytime-only meals (DMI), and meals taken during both daytime and nighttime (DNMC).
Depression- and anxiety-like mood levels increased by 26% and 16%, respectively, among the daytime and nighttime eaters, but there was no such increase in daytime-only eaters.
“Our findings provide evidence for the timing of food intake as a novel strategy to potentially minimize mood vulnerability in individuals experiencing circadian misalignment, such as people engaged in shift work, experiencing jet lag, or suffering from circadian rhythm disorders,” co–corresponding author Frank A.J.L. Scheer, PhD, director of the medical chronobiology program, Brigham and Women’s Hospital, Boston, said in a news release.
The study was published online in the Proceedings of the National Academy of Sciences.
Misaligned circadian clock
“Shift workers often experience a misalignment between their central circadian clock in the brain and daily behaviors, such as sleep/wake and fasting/eating cycles,” senior author Sarah Chellappa, MD, PhD, currently the Alexander Von Humboldt Experienced Fellow in the department of nuclear medicine, University of Cologne (Germany). Dr. Chellappa was a postdoctoral fellow at Brigham and Women’s Hospital when the study was conducted.
“They also have a 25%-40% higher risk of depression and anxiety,” she continued. “Since meal timing is important for physical health and diet is important for mood, we sought to find out whether meal timing can benefit mental health as well.”
Given that impaired glycemic control is a “risk factor for mood disruption,” the researchers tested the prediction that daytime eating “would prevent mood vulnerability, despite simulated night work.”
To investigate the question, they conducted a parallel-design, randomized clinical trial that included a 14-day circadian laboratory protocol with 19 healthy adults (12 men, 7 women; mean age, 26.5 ± 4.1 years) who underwent a forced desynchrony (FD) in dim light for 4 “days,” each of which consisted of 28 hours. Each 28-hour “day” resulted in an additional 4-hour misalignment between the central circadian clock and external behavioral/environmental cycles.
By the fourth day, the participants were misaligned by 12 hours, compared to baseline (that is, the first day). They were then randomly assigned to two groups.
The DNMC group – the control group – had a “typical 28-hour FD protocol,” with behavioral and environmental cycles (sleep/wake, rest/activity, supine/upright posture, dark during scheduled sleep/dim light during wakefulness) scheduled on a 28-hour cycle. Thus, they took their meals during both “daytime” and “nighttime,” which is the typical way that night workers eat.
The DMI group underwent a modified 28-hour FD protocol, with all cycles scheduled on a 28-hour basis, except for the fasting/eating cycle, which was scheduled on a 24-hour basis, resulting in meals consumed only during the “daytime.”
Depression- and anxiety-like mood (which “correspond to an amalgam of mood states typically observed in depression and anxiety) were assessed every hour during the 4 FD days, using computerized visual analogue scales.
Nutritional psychiatry
Participants in the DNMC group experienced an increase from baseline in depression- and anxiety-like mood levels of 26.2% (95% confidence interval, 21-31.5; P = .001; P value using false discovery rate, .01; effect-size r, 0.78) and 16.1% (95% CI, 8.5-23.6; P = .005; PFDR, .001; effect-size r, 0.47), respectively.
By contrast, a similar increase did not take place in the DMI group for either depression- or anxiety-like mood levels (95% CI, –5.7% to 7.4%, P not significant and 95% CI, –3.1% to 9.9%, P not significant, respectively).
The researchers tested “whether increase mood vulnerability during simulated night work was associated with the degree of internal circadian misalignment” — defined as “change in the phase difference between the acrophase of circadian glucose rhythms and the bathyphase of circadian body temperature rhythms.”
They found that a larger degree of internal circadian misalignment was “robustly associated” with more depression-like (r, 0.77; P = .001) and anxiety-like (r, 0.67; P = .002) mood levels during simulated night work.
The findings imply that meal timing had “moderate to large effects in depression-like and anxiety-like mood levels during night work, and that such effects were associated with the degree of internal circadian misalignment,” the authors wrote.
The laboratory protocol of both groups was identical except for the timing of meals. The authors noted that the “relevance of diet on sleep, circadian rhythms, and mental health is receiving growing awareness with the emergence of a new field, nutritional psychiatry.”
People who experience depression “often report poor-quality diets with high carbohydrate intake,” and there is evidence that adherence to the Mediterranean diet is associated “with lower odds of depression, anxiety, and psychological distress.”
They cautioned that although these emerging studies suggest an association between dietary factors and mental health, “experimental studies in individuals with depression and/or anxiety/anxiety-related disorders are required to determine causality and direction of effects.”
They described meal timing as “an emerging aspect of nutrition, with increasing research interest because of its influence on physical health.” However, they noted, “the causal role of the timing of food intake on mental health remains to be tested.”
Novel findings
Commenting for this article, Kathleen Merikangas, PhD, distinguished investigator and chief, genetic epidemiology research branch, intramural research program, National Institute of Mental Health, Bethesda, Md., described the research as important with novel findings.
The research “employs the elegant, carefully controlled laboratory procedures that have unraveled the influence of light and other environmental cues on sleep and circadian rhythms over the past 2 decades,” said Dr. Merikangas, who was not involved with the study.
“One of the most significant contributions of this work is its demonstration of the importance of investigating circadian rhythms of multiple systems rather than solely focusing on sleep, eating, or emotional states that have often been studied in isolation,” she pointed out.
“Growing evidence from basic research highlights the interdependence of multiple human systems that should be built into interventions that tend to focus on one or two domains.”
She recommended that this work be replicated “in more diverse samples ... in both controlled and naturalistic settings...to test both the generalizability and mechanism of these intriguing findings.”
The study was funded by the National Institutes of Health. Individual investigators were funded by the Alexander Von Humboldt Foundation and the American Diabetes Association. Dr. Chellappa disclosed no relevant financial relationships. Dr. Merikangas disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators at Brigham and Women’s Hospital, Boston, created a simulated nightwork schedule for 19 individuals in a laboratory setting. Participants then engaged in two different meal timing models – daytime-only meals (DMI), and meals taken during both daytime and nighttime (DNMC).
Depression- and anxiety-like mood levels increased by 26% and 16%, respectively, among the daytime and nighttime eaters, but there was no such increase in daytime-only eaters.
“Our findings provide evidence for the timing of food intake as a novel strategy to potentially minimize mood vulnerability in individuals experiencing circadian misalignment, such as people engaged in shift work, experiencing jet lag, or suffering from circadian rhythm disorders,” co–corresponding author Frank A.J.L. Scheer, PhD, director of the medical chronobiology program, Brigham and Women’s Hospital, Boston, said in a news release.
The study was published online in the Proceedings of the National Academy of Sciences.
Misaligned circadian clock
“Shift workers often experience a misalignment between their central circadian clock in the brain and daily behaviors, such as sleep/wake and fasting/eating cycles,” senior author Sarah Chellappa, MD, PhD, currently the Alexander Von Humboldt Experienced Fellow in the department of nuclear medicine, University of Cologne (Germany). Dr. Chellappa was a postdoctoral fellow at Brigham and Women’s Hospital when the study was conducted.
“They also have a 25%-40% higher risk of depression and anxiety,” she continued. “Since meal timing is important for physical health and diet is important for mood, we sought to find out whether meal timing can benefit mental health as well.”
Given that impaired glycemic control is a “risk factor for mood disruption,” the researchers tested the prediction that daytime eating “would prevent mood vulnerability, despite simulated night work.”
To investigate the question, they conducted a parallel-design, randomized clinical trial that included a 14-day circadian laboratory protocol with 19 healthy adults (12 men, 7 women; mean age, 26.5 ± 4.1 years) who underwent a forced desynchrony (FD) in dim light for 4 “days,” each of which consisted of 28 hours. Each 28-hour “day” resulted in an additional 4-hour misalignment between the central circadian clock and external behavioral/environmental cycles.
By the fourth day, the participants were misaligned by 12 hours, compared to baseline (that is, the first day). They were then randomly assigned to two groups.
The DNMC group – the control group – had a “typical 28-hour FD protocol,” with behavioral and environmental cycles (sleep/wake, rest/activity, supine/upright posture, dark during scheduled sleep/dim light during wakefulness) scheduled on a 28-hour cycle. Thus, they took their meals during both “daytime” and “nighttime,” which is the typical way that night workers eat.
The DMI group underwent a modified 28-hour FD protocol, with all cycles scheduled on a 28-hour basis, except for the fasting/eating cycle, which was scheduled on a 24-hour basis, resulting in meals consumed only during the “daytime.”
Depression- and anxiety-like mood (which “correspond to an amalgam of mood states typically observed in depression and anxiety) were assessed every hour during the 4 FD days, using computerized visual analogue scales.
Nutritional psychiatry
Participants in the DNMC group experienced an increase from baseline in depression- and anxiety-like mood levels of 26.2% (95% confidence interval, 21-31.5; P = .001; P value using false discovery rate, .01; effect-size r, 0.78) and 16.1% (95% CI, 8.5-23.6; P = .005; PFDR, .001; effect-size r, 0.47), respectively.
By contrast, a similar increase did not take place in the DMI group for either depression- or anxiety-like mood levels (95% CI, –5.7% to 7.4%, P not significant and 95% CI, –3.1% to 9.9%, P not significant, respectively).
The researchers tested “whether increase mood vulnerability during simulated night work was associated with the degree of internal circadian misalignment” — defined as “change in the phase difference between the acrophase of circadian glucose rhythms and the bathyphase of circadian body temperature rhythms.”
They found that a larger degree of internal circadian misalignment was “robustly associated” with more depression-like (r, 0.77; P = .001) and anxiety-like (r, 0.67; P = .002) mood levels during simulated night work.
The findings imply that meal timing had “moderate to large effects in depression-like and anxiety-like mood levels during night work, and that such effects were associated with the degree of internal circadian misalignment,” the authors wrote.
The laboratory protocol of both groups was identical except for the timing of meals. The authors noted that the “relevance of diet on sleep, circadian rhythms, and mental health is receiving growing awareness with the emergence of a new field, nutritional psychiatry.”
People who experience depression “often report poor-quality diets with high carbohydrate intake,” and there is evidence that adherence to the Mediterranean diet is associated “with lower odds of depression, anxiety, and psychological distress.”
They cautioned that although these emerging studies suggest an association between dietary factors and mental health, “experimental studies in individuals with depression and/or anxiety/anxiety-related disorders are required to determine causality and direction of effects.”
They described meal timing as “an emerging aspect of nutrition, with increasing research interest because of its influence on physical health.” However, they noted, “the causal role of the timing of food intake on mental health remains to be tested.”
Novel findings
Commenting for this article, Kathleen Merikangas, PhD, distinguished investigator and chief, genetic epidemiology research branch, intramural research program, National Institute of Mental Health, Bethesda, Md., described the research as important with novel findings.
The research “employs the elegant, carefully controlled laboratory procedures that have unraveled the influence of light and other environmental cues on sleep and circadian rhythms over the past 2 decades,” said Dr. Merikangas, who was not involved with the study.
“One of the most significant contributions of this work is its demonstration of the importance of investigating circadian rhythms of multiple systems rather than solely focusing on sleep, eating, or emotional states that have often been studied in isolation,” she pointed out.
“Growing evidence from basic research highlights the interdependence of multiple human systems that should be built into interventions that tend to focus on one or two domains.”
She recommended that this work be replicated “in more diverse samples ... in both controlled and naturalistic settings...to test both the generalizability and mechanism of these intriguing findings.”
The study was funded by the National Institutes of Health. Individual investigators were funded by the Alexander Von Humboldt Foundation and the American Diabetes Association. Dr. Chellappa disclosed no relevant financial relationships. Dr. Merikangas disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCE
Minorities hit especially hard by overdose deaths during COVID
The results underscore the “urgency of expanding prevention, treatment, and harm reduction interventions tailored to specific populations, especially American Indian or Alaska Native and Black populations, given long-standing structural racism and inequities in accessing these services,” the researchers note.
The study was published online in JAMA Network Open.
‘Urgent need’ for education
From February 2020 to August 2021, drug overdose deaths in the United States rose 37%, and these deaths were largely due to synthetic opioids other than methadone – primarily fentanyl or analogs – and methamphetamine.
Yet, data are lacking regarding racial and ethnic disparities in overdose death rates.
To investigate, Beth Han, MD, PhD, with the National Institute on Drug Abuse, and colleagues analyzed federal drug overdose death data for individuals aged 15-34 and 35-64 from March 2018 to August 2021.
Among individuals aged 15-34, from March 2018 to August 2021, overdose death rates involving any drug, fentanyl, and methamphetamine with or without fentanyl, increased overall.
For the 6 months from March to August 2021, non-Hispanic Native American or Alaska Native men had the highest rates overall involving any drug, fentanyl, and methamphetamine without fentanyl, with rates of 42.0, 30.2, and 6.0 per 100,000, respectively.
The highest rates (per 100,000) of drug overdose deaths involving methamphetamine with fentanyl were for Native American or Alaska Native men (9.2) and women (8.0) and non-Hispanic White men (6.7).
Among people aged 35-64, from March to August 2021, overall drug overdose rates (per 100,000) were highest among non-Hispanic Black men (61.2) and Native American or Alaska Native men (60.0), and fentanyl-involved death rates were highest among Black men (43.3).
Rates involving methamphetamine with fentanyl were highest among Native American or Alaska Native men (12.6) and women (9.4) and White men (9.5).
Rates involving methamphetamine without fentanyl were highest among Native American or Alaska Native men (22.9).
The researchers note the findings highlight the “urgent need” for education on dangers of methamphetamine and fentanyl.
Expanding access to naloxone, fentanyl test strips, and treatments for substance use disorders to disproportionately affected populations is also critical to help curb disparities in drug overdose deaths, they add.
Limitations of the study are that overdose deaths may be underestimated because of the use of 2021 provisional data and that racial or ethnic identification may be misclassified, especially for Native American or Alaska Native people.
This study was sponsored by the National Institute on Drug Abuse of the National Institutes of Health and the Centers for Disease Control and Prevention. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
The results underscore the “urgency of expanding prevention, treatment, and harm reduction interventions tailored to specific populations, especially American Indian or Alaska Native and Black populations, given long-standing structural racism and inequities in accessing these services,” the researchers note.
The study was published online in JAMA Network Open.
‘Urgent need’ for education
From February 2020 to August 2021, drug overdose deaths in the United States rose 37%, and these deaths were largely due to synthetic opioids other than methadone – primarily fentanyl or analogs – and methamphetamine.
Yet, data are lacking regarding racial and ethnic disparities in overdose death rates.
To investigate, Beth Han, MD, PhD, with the National Institute on Drug Abuse, and colleagues analyzed federal drug overdose death data for individuals aged 15-34 and 35-64 from March 2018 to August 2021.
Among individuals aged 15-34, from March 2018 to August 2021, overdose death rates involving any drug, fentanyl, and methamphetamine with or without fentanyl, increased overall.
For the 6 months from March to August 2021, non-Hispanic Native American or Alaska Native men had the highest rates overall involving any drug, fentanyl, and methamphetamine without fentanyl, with rates of 42.0, 30.2, and 6.0 per 100,000, respectively.
The highest rates (per 100,000) of drug overdose deaths involving methamphetamine with fentanyl were for Native American or Alaska Native men (9.2) and women (8.0) and non-Hispanic White men (6.7).
Among people aged 35-64, from March to August 2021, overall drug overdose rates (per 100,000) were highest among non-Hispanic Black men (61.2) and Native American or Alaska Native men (60.0), and fentanyl-involved death rates were highest among Black men (43.3).
Rates involving methamphetamine with fentanyl were highest among Native American or Alaska Native men (12.6) and women (9.4) and White men (9.5).
Rates involving methamphetamine without fentanyl were highest among Native American or Alaska Native men (22.9).
The researchers note the findings highlight the “urgent need” for education on dangers of methamphetamine and fentanyl.
Expanding access to naloxone, fentanyl test strips, and treatments for substance use disorders to disproportionately affected populations is also critical to help curb disparities in drug overdose deaths, they add.
Limitations of the study are that overdose deaths may be underestimated because of the use of 2021 provisional data and that racial or ethnic identification may be misclassified, especially for Native American or Alaska Native people.
This study was sponsored by the National Institute on Drug Abuse of the National Institutes of Health and the Centers for Disease Control and Prevention. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
The results underscore the “urgency of expanding prevention, treatment, and harm reduction interventions tailored to specific populations, especially American Indian or Alaska Native and Black populations, given long-standing structural racism and inequities in accessing these services,” the researchers note.
The study was published online in JAMA Network Open.
‘Urgent need’ for education
From February 2020 to August 2021, drug overdose deaths in the United States rose 37%, and these deaths were largely due to synthetic opioids other than methadone – primarily fentanyl or analogs – and methamphetamine.
Yet, data are lacking regarding racial and ethnic disparities in overdose death rates.
To investigate, Beth Han, MD, PhD, with the National Institute on Drug Abuse, and colleagues analyzed federal drug overdose death data for individuals aged 15-34 and 35-64 from March 2018 to August 2021.
Among individuals aged 15-34, from March 2018 to August 2021, overdose death rates involving any drug, fentanyl, and methamphetamine with or without fentanyl, increased overall.
For the 6 months from March to August 2021, non-Hispanic Native American or Alaska Native men had the highest rates overall involving any drug, fentanyl, and methamphetamine without fentanyl, with rates of 42.0, 30.2, and 6.0 per 100,000, respectively.
The highest rates (per 100,000) of drug overdose deaths involving methamphetamine with fentanyl were for Native American or Alaska Native men (9.2) and women (8.0) and non-Hispanic White men (6.7).
Among people aged 35-64, from March to August 2021, overall drug overdose rates (per 100,000) were highest among non-Hispanic Black men (61.2) and Native American or Alaska Native men (60.0), and fentanyl-involved death rates were highest among Black men (43.3).
Rates involving methamphetamine with fentanyl were highest among Native American or Alaska Native men (12.6) and women (9.4) and White men (9.5).
Rates involving methamphetamine without fentanyl were highest among Native American or Alaska Native men (22.9).
The researchers note the findings highlight the “urgent need” for education on dangers of methamphetamine and fentanyl.
Expanding access to naloxone, fentanyl test strips, and treatments for substance use disorders to disproportionately affected populations is also critical to help curb disparities in drug overdose deaths, they add.
Limitations of the study are that overdose deaths may be underestimated because of the use of 2021 provisional data and that racial or ethnic identification may be misclassified, especially for Native American or Alaska Native people.
This study was sponsored by the National Institute on Drug Abuse of the National Institutes of Health and the Centers for Disease Control and Prevention. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
‘Concerning’ rate of benzo/Z-drug use in IBD
Patients with inflammatory bowel disease (IBD) are 70% more likely to use benzodiazepines and “Z-drugs” than are the general population, a large study from Canada suggests.
Mood/anxiety disorders and sleep disorders are common in patients with IBD, but few studies have looked at use of benzodiazepines and Z-drugs (such as zolpidem, zaleplon, and eszopiclone) in this patient population.
The results are “concerning, and especially as the IBD population ages, these drugs are associated with health risks, including something as simple as falls,” first author Charles Bernstein, MD, of the IBD clinical and research centre, University of Manitoba, Winnipeg, told this news organization.
“Clinicians need to find better strategies to deal with anxiety disorders and sleep disorders in the IBD population,” Dr. Bernstein said.
The study was published online in the American Journal of Gastroenterology.
High burden of use
Using administrative data from Manitoba, Dr. Bernstein and colleagues identified 5,741 patients with IBD (2,381 with Crohn’s disease and 3,360 with ulcerative colitis) and matched them (1:5) to 28,661 population controls without IBD.
Over a 20-year period (1997-2017), there was a “high burden” of benzodiazepine and Z-drug use in the IBD population. In 2017, roughly 20% of Manitobans with IBD were using benzodiazepines, and 20% were using Z-drugs, the study team reports.
The benzodiazepine use rate (per 1,000) was 28.06 in the IBD cohort vs. 16.83 in the non-IBD population (adjusted rate ratio, 1.67). The use rate for Z-drugs was 21.07 in the IBD cohort vs. 11.26 in the non-IBD population (adjusted RR, 1.87).
Benzodiazepine use declined from 1997 to 2016, but it remained at least 50% higher in patients with IBD than in the general population over this period, the researchers found. The rate of Z-drug use also was higher in the IBD population than in the general population but remained stable over the 20-year study period.
Regardless of age, men and women had similarly high use rates for benzodiazepines, Z-drugs, and joint use of benzodiazepines and Z-drugs. The highest incidence rates for joint benzodiazepine and Z-drug use were in young adults (age 18-44 years), and these rates were similar among men and women.
Patients with IBD and a mood/anxiety disorder also were more likely to use benzodiazepines and Z-drugs and to be continuous users than were those without a mood/anxiety disorder.
Mental health and IBD go hand in hand
“The results are not very surprising, but they highlight the importance of mental health and mood disturbances in patients with IBD,” Ashwin Ananthakrishnan, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who wasn’t involved in the study, told this news organization.
“It is important for treating physicians to be aware of the important mental health implications of IBD diagnosis and disease activity, to screen patients for these disturbances, and to institute early effective interventions,” Dr. Ananthakrishnan said.
Also offering perspective, Laurie Keefer, PhD, academic health psychologist and director of psychobehavioral research within the division of gastroenterology, Mount Sinai Health System, New York, said that she is “concerned but not surprised” by the results of this study.
“One in three patients with IBD meets criteria for an anxiety disorder,” Dr. Keefer told this news organization.
And with the ongoing mental health crisis and shortage of mental health providers, “gastroenterologists are, unfortunately, in the position where they may have to manage these issues,” she said.
Dr. Keefer noted that when patients are first diagnosed with IBD, they will likely be on prednisone, and “an antidote” for the side effects of prednisone are benzodiazepines and sleeping medications because prednisone itself causes insomnia. “However, that’s really just a band-aid,” she said.
A major concern, said Dr. Keefer, is that young men and women who are diagnosed with IBD in their 20s may start using these drugs and become reliant on them.
“People do build up a tolerance to these drugs, so they need more and more to receive the same effect,” she said.
A better approach is to figure out why patients are so anxious and teach them skills to manage their anxiety and sleep problems so that they’re not dependent on these drugs, Dr. Keefer said.
“There are behavioral strategies that can help. These are harder to do, and they’re not a quick fix. However, they are skills you can learn in your 20s and so when you have an IBD flare at 50, you have the skills to deal with it,” she said.
“We just have to be a little more proactive in really encouraging patients to learn disease management skills,” Dr. Keefer added.
The study was funded by the Canadian Institutes of Health Research and Crohn’s and Colitis Canada. Dr. Bernstein has disclosed relationships with AbbVie Canada, Amgen Canada, Bristol-Myers Squibb Canada, Roche Canada, Janssen Canada, Sandoz Canada, Takeda and Takeda Canada, Pfizer Canada, Mylan Pharmaceuticals, and Medtronic Canada. Dr. Ananthakrishnan and Dr. Keefer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with inflammatory bowel disease (IBD) are 70% more likely to use benzodiazepines and “Z-drugs” than are the general population, a large study from Canada suggests.
Mood/anxiety disorders and sleep disorders are common in patients with IBD, but few studies have looked at use of benzodiazepines and Z-drugs (such as zolpidem, zaleplon, and eszopiclone) in this patient population.
The results are “concerning, and especially as the IBD population ages, these drugs are associated with health risks, including something as simple as falls,” first author Charles Bernstein, MD, of the IBD clinical and research centre, University of Manitoba, Winnipeg, told this news organization.
“Clinicians need to find better strategies to deal with anxiety disorders and sleep disorders in the IBD population,” Dr. Bernstein said.
The study was published online in the American Journal of Gastroenterology.
High burden of use
Using administrative data from Manitoba, Dr. Bernstein and colleagues identified 5,741 patients with IBD (2,381 with Crohn’s disease and 3,360 with ulcerative colitis) and matched them (1:5) to 28,661 population controls without IBD.
Over a 20-year period (1997-2017), there was a “high burden” of benzodiazepine and Z-drug use in the IBD population. In 2017, roughly 20% of Manitobans with IBD were using benzodiazepines, and 20% were using Z-drugs, the study team reports.
The benzodiazepine use rate (per 1,000) was 28.06 in the IBD cohort vs. 16.83 in the non-IBD population (adjusted rate ratio, 1.67). The use rate for Z-drugs was 21.07 in the IBD cohort vs. 11.26 in the non-IBD population (adjusted RR, 1.87).
Benzodiazepine use declined from 1997 to 2016, but it remained at least 50% higher in patients with IBD than in the general population over this period, the researchers found. The rate of Z-drug use also was higher in the IBD population than in the general population but remained stable over the 20-year study period.
Regardless of age, men and women had similarly high use rates for benzodiazepines, Z-drugs, and joint use of benzodiazepines and Z-drugs. The highest incidence rates for joint benzodiazepine and Z-drug use were in young adults (age 18-44 years), and these rates were similar among men and women.
Patients with IBD and a mood/anxiety disorder also were more likely to use benzodiazepines and Z-drugs and to be continuous users than were those without a mood/anxiety disorder.
Mental health and IBD go hand in hand
“The results are not very surprising, but they highlight the importance of mental health and mood disturbances in patients with IBD,” Ashwin Ananthakrishnan, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who wasn’t involved in the study, told this news organization.
“It is important for treating physicians to be aware of the important mental health implications of IBD diagnosis and disease activity, to screen patients for these disturbances, and to institute early effective interventions,” Dr. Ananthakrishnan said.
Also offering perspective, Laurie Keefer, PhD, academic health psychologist and director of psychobehavioral research within the division of gastroenterology, Mount Sinai Health System, New York, said that she is “concerned but not surprised” by the results of this study.
“One in three patients with IBD meets criteria for an anxiety disorder,” Dr. Keefer told this news organization.
And with the ongoing mental health crisis and shortage of mental health providers, “gastroenterologists are, unfortunately, in the position where they may have to manage these issues,” she said.
Dr. Keefer noted that when patients are first diagnosed with IBD, they will likely be on prednisone, and “an antidote” for the side effects of prednisone are benzodiazepines and sleeping medications because prednisone itself causes insomnia. “However, that’s really just a band-aid,” she said.
A major concern, said Dr. Keefer, is that young men and women who are diagnosed with IBD in their 20s may start using these drugs and become reliant on them.
“People do build up a tolerance to these drugs, so they need more and more to receive the same effect,” she said.
A better approach is to figure out why patients are so anxious and teach them skills to manage their anxiety and sleep problems so that they’re not dependent on these drugs, Dr. Keefer said.
“There are behavioral strategies that can help. These are harder to do, and they’re not a quick fix. However, they are skills you can learn in your 20s and so when you have an IBD flare at 50, you have the skills to deal with it,” she said.
“We just have to be a little more proactive in really encouraging patients to learn disease management skills,” Dr. Keefer added.
The study was funded by the Canadian Institutes of Health Research and Crohn’s and Colitis Canada. Dr. Bernstein has disclosed relationships with AbbVie Canada, Amgen Canada, Bristol-Myers Squibb Canada, Roche Canada, Janssen Canada, Sandoz Canada, Takeda and Takeda Canada, Pfizer Canada, Mylan Pharmaceuticals, and Medtronic Canada. Dr. Ananthakrishnan and Dr. Keefer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with inflammatory bowel disease (IBD) are 70% more likely to use benzodiazepines and “Z-drugs” than are the general population, a large study from Canada suggests.
Mood/anxiety disorders and sleep disorders are common in patients with IBD, but few studies have looked at use of benzodiazepines and Z-drugs (such as zolpidem, zaleplon, and eszopiclone) in this patient population.
The results are “concerning, and especially as the IBD population ages, these drugs are associated with health risks, including something as simple as falls,” first author Charles Bernstein, MD, of the IBD clinical and research centre, University of Manitoba, Winnipeg, told this news organization.
“Clinicians need to find better strategies to deal with anxiety disorders and sleep disorders in the IBD population,” Dr. Bernstein said.
The study was published online in the American Journal of Gastroenterology.
High burden of use
Using administrative data from Manitoba, Dr. Bernstein and colleagues identified 5,741 patients with IBD (2,381 with Crohn’s disease and 3,360 with ulcerative colitis) and matched them (1:5) to 28,661 population controls without IBD.
Over a 20-year period (1997-2017), there was a “high burden” of benzodiazepine and Z-drug use in the IBD population. In 2017, roughly 20% of Manitobans with IBD were using benzodiazepines, and 20% were using Z-drugs, the study team reports.
The benzodiazepine use rate (per 1,000) was 28.06 in the IBD cohort vs. 16.83 in the non-IBD population (adjusted rate ratio, 1.67). The use rate for Z-drugs was 21.07 in the IBD cohort vs. 11.26 in the non-IBD population (adjusted RR, 1.87).
Benzodiazepine use declined from 1997 to 2016, but it remained at least 50% higher in patients with IBD than in the general population over this period, the researchers found. The rate of Z-drug use also was higher in the IBD population than in the general population but remained stable over the 20-year study period.
Regardless of age, men and women had similarly high use rates for benzodiazepines, Z-drugs, and joint use of benzodiazepines and Z-drugs. The highest incidence rates for joint benzodiazepine and Z-drug use were in young adults (age 18-44 years), and these rates were similar among men and women.
Patients with IBD and a mood/anxiety disorder also were more likely to use benzodiazepines and Z-drugs and to be continuous users than were those without a mood/anxiety disorder.
Mental health and IBD go hand in hand
“The results are not very surprising, but they highlight the importance of mental health and mood disturbances in patients with IBD,” Ashwin Ananthakrishnan, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who wasn’t involved in the study, told this news organization.
“It is important for treating physicians to be aware of the important mental health implications of IBD diagnosis and disease activity, to screen patients for these disturbances, and to institute early effective interventions,” Dr. Ananthakrishnan said.
Also offering perspective, Laurie Keefer, PhD, academic health psychologist and director of psychobehavioral research within the division of gastroenterology, Mount Sinai Health System, New York, said that she is “concerned but not surprised” by the results of this study.
“One in three patients with IBD meets criteria for an anxiety disorder,” Dr. Keefer told this news organization.
And with the ongoing mental health crisis and shortage of mental health providers, “gastroenterologists are, unfortunately, in the position where they may have to manage these issues,” she said.
Dr. Keefer noted that when patients are first diagnosed with IBD, they will likely be on prednisone, and “an antidote” for the side effects of prednisone are benzodiazepines and sleeping medications because prednisone itself causes insomnia. “However, that’s really just a band-aid,” she said.
A major concern, said Dr. Keefer, is that young men and women who are diagnosed with IBD in their 20s may start using these drugs and become reliant on them.
“People do build up a tolerance to these drugs, so they need more and more to receive the same effect,” she said.
A better approach is to figure out why patients are so anxious and teach them skills to manage their anxiety and sleep problems so that they’re not dependent on these drugs, Dr. Keefer said.
“There are behavioral strategies that can help. These are harder to do, and they’re not a quick fix. However, they are skills you can learn in your 20s and so when you have an IBD flare at 50, you have the skills to deal with it,” she said.
“We just have to be a little more proactive in really encouraging patients to learn disease management skills,” Dr. Keefer added.
The study was funded by the Canadian Institutes of Health Research and Crohn’s and Colitis Canada. Dr. Bernstein has disclosed relationships with AbbVie Canada, Amgen Canada, Bristol-Myers Squibb Canada, Roche Canada, Janssen Canada, Sandoz Canada, Takeda and Takeda Canada, Pfizer Canada, Mylan Pharmaceuticals, and Medtronic Canada. Dr. Ananthakrishnan and Dr. Keefer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF GASTROENTEROLOGY
Toward a new open-door model for psychiatric wards
If isolated, patients with mental disorders may end up having higher levels of social impairment. This has led several hospitals in Spain to set up open-door departments that are more accessible.
The purpose of the open-door model is to help remove the stigma from individuals who need to be admitted to a psychiatric ward because they have a mental disorder.
Traditional locked wards
According to the World Health Organization (WHO), in 2019, one in every eight people were living with a mental disorder. Having the least restrictive type of mental health care is one of the 10 basic principles listed in a 1996 reference document from the WHO.
Among people suffering from severe psychiatric disorders, there is a high probability of being involuntarily admitted to a psychiatry ward with locked doors (PWLD). Admission to a PWLD involves the application of a set of measures that restrict the individual’s freedom.
The main argument for keeping the doors locked is that it prevents suicides and self-harm behavior, as well as abscondment. But in recent years, efforts have been made to apply a model called open-door policy psychiatry wards (ODPWs).
Open wards model
Experiments were undertaken in various countries, including the United Kingdom, Australia, Switzerland, and Germany. Investigators found that the new forms of hospitalization led to a reduction in conflictive events; self-harm behavior; restrictive measures, such as seclusion, mechanical restraints, and chemical restraints; as well as forced medication. On the basis of these findings, ODPWs were launched.
According to Ignacio García Cabeza, MD, psychiatrist and coordinator of the department of psychiatry at Gregorio Marañón General University Hospital in Madrid, “The open wards model is founded on the idea of respecting the patient and their autonomy. In addition, it advocates a reduction in coercive measures.
“We wanted our department to be the same as the other departments in the hospital, with patients going in and out, receiving treatment, and being able to have family visits,” he explained. “A patient’s diagnosis should not factor into these things. People with schizophrenia, people with any type of mental disorder, should be able to enjoy this minimally restrictive environment.”
This model also implies fundamental changes in the interaction between health care professionals and patients. The implementation of new nursing care models, among which the Safewards model stands out, is a key element for the success of the project.
Based on a set of tools for preventing and managing conflict, the Safewards model seeks to modify the factors that regulate the relationship between staff and patients. Use of this model brought about a 15% reduction in the rate of conflictive events and a 23% reduction in the rate of coercive interventions, in comparison with a control group.
One of the major debates is about whether every patient should be able to choose this open-door system. For Dr. García Cabeza, the answer is yes, but with one caveat. “There’s a certain group of patients who perhaps need to be in locked wards, who perhaps require greater means of control – patients whose conditions put them at a high risk of suicide or of self-harm behavior or of absconding.”
He had no hesitation in saying that an open-door ward increases the patient’s self-esteem. It helps promote autonomy and a sense of control and of normalcy with respect to a community. “The idea is to get to the point where we’ve got an atmosphere, a climate, that serves to benefit the therapeutic actions that are going to continue to influence the patient’s future progress and their treatment.”
That’s why it’s important to bring about the kind of health care activities that can prevent the patient from experiencing some of the negative psychological effects, such as distrust and feeling removed from normalcy. “In traditional locked wards, the patient feels incapable of making decisions. They feel that they have very little to do with [and have] no say in the decisions made, and a lot of times, this leads to a situation where, after discharge, the patient ends up giving up on the treatments. If we can manage to break this perception held by the patient,” Dr. García Cabeza suggested, “it’s quite likely that we’ll manage to improve the course of their disorder in general.”
What the literature says
The effect of ODPW has been investigated through comparative studies with PWLD and research of the transition from PWLD to ODPW, both from a therapeutic and safety a point of view.
A 15-year observational study published in The Lancet Psychiatry found that, with respect to abscondment, suicide attempts, and suicide, there were no significant differences between hospitals with open-door policies and those without.
A subsequent study that was published in 2017 found that on open wards, any aggressive behavior and restraint or seclusion were less likely than on closed wards.
The Spanish situation
This system is already at work in some Spanish hospitals, among them Inca Comarcal Hospital (Palma de Mallorca), Elda General University Hospital (Alicante), Germans Trias i Pujol Hospital in Badalona, and Gregorio Marañón General University Hospital in Madrid.
“At Gregorio Marañón, we started the experiment just before the pandemic hit. We’re up and running now, but still with some limitations; the patient can go in and out, but not with the flexibility we’d like,” explained Dr. García Cabeza. “An open ward plays a clinical, patient-care role and a symbolic one as well. Locking the doors has a lot to do with the fear felt toward these patients. It’s a stigma that they’ve had to deal with and that they continue to have to deal with. In terms of the symbolic role, there’s also the fear that comes with giving these patients some rights.”
While the experiment at Gregorio Marañón’s psychiatric ward “is still very much in the early stages,” there have been no recorded incidents related to its open-door policy. Dr. García Cabeza is aware of the challenges of such a policy, “starting with assistance when conflictive events arise. Challenges faced by the staff – especially the nursing staff, as they’re the ones who are with the patients 24 hours day – and challenges faced by those in charge of providing care. In all of this, there are new things to learn and be aware of, new ways of understanding and looking at the patient-physician relationship. The fears are still there – they haven’t been done away with. But the way we conduct ourselves should be adjusted, matching how we act toward other patients. Although the differences have to be taken into account, we have to try to normalize, as much as possible, the environment where patients with mental disorders receive treatment.”
Dr. García Cabeza has no doubts. “The most sensible and reasonable decisions need to be made at these sites so as to allow the broadest applicability to cases. Anyone who needs psychiatric hospitalization and who is competent to consent to admission and who voluntarily agrees to be admitted – they can and must be placed in an open ward.”
The hope is that in the future, the number of open wards will increase and the number of locked wards – which have more stigma attached to them – will go down. The involvement of the staff and appropriate institutional support are essential to making this a reality.
This article was translated from Univadis Spain.
If isolated, patients with mental disorders may end up having higher levels of social impairment. This has led several hospitals in Spain to set up open-door departments that are more accessible.
The purpose of the open-door model is to help remove the stigma from individuals who need to be admitted to a psychiatric ward because they have a mental disorder.
Traditional locked wards
According to the World Health Organization (WHO), in 2019, one in every eight people were living with a mental disorder. Having the least restrictive type of mental health care is one of the 10 basic principles listed in a 1996 reference document from the WHO.
Among people suffering from severe psychiatric disorders, there is a high probability of being involuntarily admitted to a psychiatry ward with locked doors (PWLD). Admission to a PWLD involves the application of a set of measures that restrict the individual’s freedom.
The main argument for keeping the doors locked is that it prevents suicides and self-harm behavior, as well as abscondment. But in recent years, efforts have been made to apply a model called open-door policy psychiatry wards (ODPWs).
Open wards model
Experiments were undertaken in various countries, including the United Kingdom, Australia, Switzerland, and Germany. Investigators found that the new forms of hospitalization led to a reduction in conflictive events; self-harm behavior; restrictive measures, such as seclusion, mechanical restraints, and chemical restraints; as well as forced medication. On the basis of these findings, ODPWs were launched.
According to Ignacio García Cabeza, MD, psychiatrist and coordinator of the department of psychiatry at Gregorio Marañón General University Hospital in Madrid, “The open wards model is founded on the idea of respecting the patient and their autonomy. In addition, it advocates a reduction in coercive measures.
“We wanted our department to be the same as the other departments in the hospital, with patients going in and out, receiving treatment, and being able to have family visits,” he explained. “A patient’s diagnosis should not factor into these things. People with schizophrenia, people with any type of mental disorder, should be able to enjoy this minimally restrictive environment.”
This model also implies fundamental changes in the interaction between health care professionals and patients. The implementation of new nursing care models, among which the Safewards model stands out, is a key element for the success of the project.
Based on a set of tools for preventing and managing conflict, the Safewards model seeks to modify the factors that regulate the relationship between staff and patients. Use of this model brought about a 15% reduction in the rate of conflictive events and a 23% reduction in the rate of coercive interventions, in comparison with a control group.
One of the major debates is about whether every patient should be able to choose this open-door system. For Dr. García Cabeza, the answer is yes, but with one caveat. “There’s a certain group of patients who perhaps need to be in locked wards, who perhaps require greater means of control – patients whose conditions put them at a high risk of suicide or of self-harm behavior or of absconding.”
He had no hesitation in saying that an open-door ward increases the patient’s self-esteem. It helps promote autonomy and a sense of control and of normalcy with respect to a community. “The idea is to get to the point where we’ve got an atmosphere, a climate, that serves to benefit the therapeutic actions that are going to continue to influence the patient’s future progress and their treatment.”
That’s why it’s important to bring about the kind of health care activities that can prevent the patient from experiencing some of the negative psychological effects, such as distrust and feeling removed from normalcy. “In traditional locked wards, the patient feels incapable of making decisions. They feel that they have very little to do with [and have] no say in the decisions made, and a lot of times, this leads to a situation where, after discharge, the patient ends up giving up on the treatments. If we can manage to break this perception held by the patient,” Dr. García Cabeza suggested, “it’s quite likely that we’ll manage to improve the course of their disorder in general.”
What the literature says
The effect of ODPW has been investigated through comparative studies with PWLD and research of the transition from PWLD to ODPW, both from a therapeutic and safety a point of view.
A 15-year observational study published in The Lancet Psychiatry found that, with respect to abscondment, suicide attempts, and suicide, there were no significant differences between hospitals with open-door policies and those without.
A subsequent study that was published in 2017 found that on open wards, any aggressive behavior and restraint or seclusion were less likely than on closed wards.
The Spanish situation
This system is already at work in some Spanish hospitals, among them Inca Comarcal Hospital (Palma de Mallorca), Elda General University Hospital (Alicante), Germans Trias i Pujol Hospital in Badalona, and Gregorio Marañón General University Hospital in Madrid.
“At Gregorio Marañón, we started the experiment just before the pandemic hit. We’re up and running now, but still with some limitations; the patient can go in and out, but not with the flexibility we’d like,” explained Dr. García Cabeza. “An open ward plays a clinical, patient-care role and a symbolic one as well. Locking the doors has a lot to do with the fear felt toward these patients. It’s a stigma that they’ve had to deal with and that they continue to have to deal with. In terms of the symbolic role, there’s also the fear that comes with giving these patients some rights.”
While the experiment at Gregorio Marañón’s psychiatric ward “is still very much in the early stages,” there have been no recorded incidents related to its open-door policy. Dr. García Cabeza is aware of the challenges of such a policy, “starting with assistance when conflictive events arise. Challenges faced by the staff – especially the nursing staff, as they’re the ones who are with the patients 24 hours day – and challenges faced by those in charge of providing care. In all of this, there are new things to learn and be aware of, new ways of understanding and looking at the patient-physician relationship. The fears are still there – they haven’t been done away with. But the way we conduct ourselves should be adjusted, matching how we act toward other patients. Although the differences have to be taken into account, we have to try to normalize, as much as possible, the environment where patients with mental disorders receive treatment.”
Dr. García Cabeza has no doubts. “The most sensible and reasonable decisions need to be made at these sites so as to allow the broadest applicability to cases. Anyone who needs psychiatric hospitalization and who is competent to consent to admission and who voluntarily agrees to be admitted – they can and must be placed in an open ward.”
The hope is that in the future, the number of open wards will increase and the number of locked wards – which have more stigma attached to them – will go down. The involvement of the staff and appropriate institutional support are essential to making this a reality.
This article was translated from Univadis Spain.
If isolated, patients with mental disorders may end up having higher levels of social impairment. This has led several hospitals in Spain to set up open-door departments that are more accessible.
The purpose of the open-door model is to help remove the stigma from individuals who need to be admitted to a psychiatric ward because they have a mental disorder.
Traditional locked wards
According to the World Health Organization (WHO), in 2019, one in every eight people were living with a mental disorder. Having the least restrictive type of mental health care is one of the 10 basic principles listed in a 1996 reference document from the WHO.
Among people suffering from severe psychiatric disorders, there is a high probability of being involuntarily admitted to a psychiatry ward with locked doors (PWLD). Admission to a PWLD involves the application of a set of measures that restrict the individual’s freedom.
The main argument for keeping the doors locked is that it prevents suicides and self-harm behavior, as well as abscondment. But in recent years, efforts have been made to apply a model called open-door policy psychiatry wards (ODPWs).
Open wards model
Experiments were undertaken in various countries, including the United Kingdom, Australia, Switzerland, and Germany. Investigators found that the new forms of hospitalization led to a reduction in conflictive events; self-harm behavior; restrictive measures, such as seclusion, mechanical restraints, and chemical restraints; as well as forced medication. On the basis of these findings, ODPWs were launched.
According to Ignacio García Cabeza, MD, psychiatrist and coordinator of the department of psychiatry at Gregorio Marañón General University Hospital in Madrid, “The open wards model is founded on the idea of respecting the patient and their autonomy. In addition, it advocates a reduction in coercive measures.
“We wanted our department to be the same as the other departments in the hospital, with patients going in and out, receiving treatment, and being able to have family visits,” he explained. “A patient’s diagnosis should not factor into these things. People with schizophrenia, people with any type of mental disorder, should be able to enjoy this minimally restrictive environment.”
This model also implies fundamental changes in the interaction between health care professionals and patients. The implementation of new nursing care models, among which the Safewards model stands out, is a key element for the success of the project.
Based on a set of tools for preventing and managing conflict, the Safewards model seeks to modify the factors that regulate the relationship between staff and patients. Use of this model brought about a 15% reduction in the rate of conflictive events and a 23% reduction in the rate of coercive interventions, in comparison with a control group.
One of the major debates is about whether every patient should be able to choose this open-door system. For Dr. García Cabeza, the answer is yes, but with one caveat. “There’s a certain group of patients who perhaps need to be in locked wards, who perhaps require greater means of control – patients whose conditions put them at a high risk of suicide or of self-harm behavior or of absconding.”
He had no hesitation in saying that an open-door ward increases the patient’s self-esteem. It helps promote autonomy and a sense of control and of normalcy with respect to a community. “The idea is to get to the point where we’ve got an atmosphere, a climate, that serves to benefit the therapeutic actions that are going to continue to influence the patient’s future progress and their treatment.”
That’s why it’s important to bring about the kind of health care activities that can prevent the patient from experiencing some of the negative psychological effects, such as distrust and feeling removed from normalcy. “In traditional locked wards, the patient feels incapable of making decisions. They feel that they have very little to do with [and have] no say in the decisions made, and a lot of times, this leads to a situation where, after discharge, the patient ends up giving up on the treatments. If we can manage to break this perception held by the patient,” Dr. García Cabeza suggested, “it’s quite likely that we’ll manage to improve the course of their disorder in general.”
What the literature says
The effect of ODPW has been investigated through comparative studies with PWLD and research of the transition from PWLD to ODPW, both from a therapeutic and safety a point of view.
A 15-year observational study published in The Lancet Psychiatry found that, with respect to abscondment, suicide attempts, and suicide, there were no significant differences between hospitals with open-door policies and those without.
A subsequent study that was published in 2017 found that on open wards, any aggressive behavior and restraint or seclusion were less likely than on closed wards.
The Spanish situation
This system is already at work in some Spanish hospitals, among them Inca Comarcal Hospital (Palma de Mallorca), Elda General University Hospital (Alicante), Germans Trias i Pujol Hospital in Badalona, and Gregorio Marañón General University Hospital in Madrid.
“At Gregorio Marañón, we started the experiment just before the pandemic hit. We’re up and running now, but still with some limitations; the patient can go in and out, but not with the flexibility we’d like,” explained Dr. García Cabeza. “An open ward plays a clinical, patient-care role and a symbolic one as well. Locking the doors has a lot to do with the fear felt toward these patients. It’s a stigma that they’ve had to deal with and that they continue to have to deal with. In terms of the symbolic role, there’s also the fear that comes with giving these patients some rights.”
While the experiment at Gregorio Marañón’s psychiatric ward “is still very much in the early stages,” there have been no recorded incidents related to its open-door policy. Dr. García Cabeza is aware of the challenges of such a policy, “starting with assistance when conflictive events arise. Challenges faced by the staff – especially the nursing staff, as they’re the ones who are with the patients 24 hours day – and challenges faced by those in charge of providing care. In all of this, there are new things to learn and be aware of, new ways of understanding and looking at the patient-physician relationship. The fears are still there – they haven’t been done away with. But the way we conduct ourselves should be adjusted, matching how we act toward other patients. Although the differences have to be taken into account, we have to try to normalize, as much as possible, the environment where patients with mental disorders receive treatment.”
Dr. García Cabeza has no doubts. “The most sensible and reasonable decisions need to be made at these sites so as to allow the broadest applicability to cases. Anyone who needs psychiatric hospitalization and who is competent to consent to admission and who voluntarily agrees to be admitted – they can and must be placed in an open ward.”
The hope is that in the future, the number of open wards will increase and the number of locked wards – which have more stigma attached to them – will go down. The involvement of the staff and appropriate institutional support are essential to making this a reality.
This article was translated from Univadis Spain.