User login
Silent ischemia isn’t what it used to be
SNOWMASS, COLO. – The concept that silent myocardial ischemia is clinically detrimental has fallen by the wayside, and routine screening for this phenomenon can no longer be recommended, Patrick T. O’Gara, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
What a difference a decade or 2 can make.
“Think about where we were 25 years ago, when we worried about people who had transient ST-segment depression without angina on Holter monitoring. We would wig out, chase them down the street, try to tackle them and load them up with medications and think about balloon [percutaneous transluminal coronary angioplasty]. And now we’re at the point where it doesn’t seem to help with respect to quality of life, let alone death or myocardial infarction,” observed Dr. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
The end of the line for the now-discredited notion that silent ischemia carries clinical significance approaching that of ischemia plus angina pectoris was the landmark ISCHEMIA trial, reported in November 2019 at the annual scientific sessions of the American Heart Association. This randomized trial asked the question: Is there any high-risk subgroup of patients with stable ischemic heart disease not involving the left main coronary artery for whom a strategy of routine revascularization improves hard outcomes in the current era of highly effective, guideline-directed medical therapy?
The answer turned out to be no. At 5 years of follow-up of 5,179 randomized patients with baseline stable coronary artery disease (CAD) and rigorously determined baseline moderate or severe ischemia affecting more than 10% of the myocardium, there was no difference between patients randomized to routine revascularization plus optimal medical therapy versus those on optimal medical therapy alone in the primary combined outcome of cardiovascular death, MI, heart failure, cardiac arrest, or hospitalization for unstable angina.
Of note, 35% of participants in the ISCHEMIA trial had moderate or severe silent ischemia. Like those who had angina, they achieved no additional benefit from a strategy of routine revascularization in terms of the primary outcome. ISCHEMIA participants with angina did show significant and durable improvements in quality of life and angina control with routine revascularization; however, those with silent ischemia showed little or no such improvement with an invasive strategy.
That being said, Dr. O’Gara added that he supports the ISCHEMIA investigators’ efforts to obtain funding from the National Institutes of Health for another 5 years or so of follow-up in order to determine whether revascularization actually does lead to improvement in the hard outcomes.
“Remember, in the STICH trial it took 10 years to show superiority of CABG [coronary artery bypass surgery] versus medical therapy to treat ischemic cardiomyopathy [N Engl J Med 2016; 374:1511-20]. My own view is that it’s too premature to throw the baby out with the bathwater. I think shared decision making is still very important, and I think, for many of our patients, relief of angina and improved quality of life are legitimate reasons in a low-risk situation with a good interventionalist to proceed,” he said.
Dr. O’Gara traced the history of medical thinking about silent ischemia. The notion that silent ischemia carried a clinical significance comparable with ischemia with angina gained wide credence more than 30 years ago, when investigators from the National Institutes of Health–sponsored Coronary Artery Surgery Study registry reported: “Patients with either silent or symptomatic ischemia during exercise testing have a similar risk of developing an acute myocardial infarction or sudden death – except in the three-vessel CAD subgroup, where the risk is greater in silent ischemia” (Am J Cardiol. 1988 Dec 1;62[17]:1155-8).
“This was a very important observation and led to many, many recommendations about screening and making sure that you took the expression of ST-segment depression on exercise treadmill testing pretty seriously, even if your patient did not have angina,” Dr. O’Gara recalled.
The prevailing wisdom that silent ischemia was detrimental took a hit in the Detection of Ischemia in Asymptomatic Diabetics (DIAC) trial. DIAC was conducted at a time when it had become clear that type 2 diabetes was a condition associated with increased cardiovascular risk, and that various methods of imaging were more accurate than treadmill exercise testing for the detection of underlying CAD. But when 1,123 DIAC participants with type 2 diabetes were randomized to screening with adenosine-stress radionuclide myocardial perfusion imaging or not and prospectively followed for roughly 5 years, it turned out there was no between-group difference in cardiac death or MI (JAMA. 2009 Apr 15;301[15]:1547-55).
“This pretty much put the lid on going out of one’s way to do routine screening of this nature in persons with diabetes who were considered to be at higher than average risk for the development of coronary disease,” the cardiologist commented.
Another fissure in the idea that silent ischemia was worth searching for and treating came from CLARIFY, an observational international registry of more than 20,000 individuals with stable CAD, roughly 12% of whom had silent ischemia, a figure in line with the prevalence reported in other studies. The 2-year rate of cardiovascular death or MI in the group with silent ischemia didn’t differ from the rate in patients with neither angina nor provocable ischemia. In contrast, rates of cardiovascular death or MI were significantly higher in the groups with angina but no ischemia or angina with ischemia (JAMA Intern Med. 2014 Oct;174[10]:1651-9).
“There’s something about the expression of angina that’s a very key clinical marker,” Dr. O’Gara observed.
He noted that just a few months before the ISCHEMIA trial results were released, a report from the far-smaller, randomized second Medicine, Angioplasty, or Surgery Study “threw cold water” on the notion that stress-induced ischemia in patients with multivessel CAD is a bad thing. Over 10 years of follow-up, the risk of major adverse cardiovascular events or deterioration in left ventricular function was identical in patients with or without baseline ischemia on stress testing performed after percutaneous coronary intervention, CABG surgery, or initiation of medical therapy (JAMA Intern Med. 2019 Jul 22. doi: 10.1001/jamainternmed.2019.2227).
What the guidelines say
The 6-year-old U.S. guidelines on the diagnosis and management of patients with stable ischemic heart disease are clearly out of date on the topic of silent ischemia (Circulation. 2014 Nov 4;130[19]:1749-67). The recommendations are based on expert opinion formed prior to the massive amount of new evidence that has since become available. For example, the current guidelines state as a class IIa, level of evidence C recommendation that exercise or pharmacologic stress can be useful for follow-up assessment at 2-year or greater intervals in patients with stable ischemic heart disease with prior evidence of silent ischemia.
“This is a very weak recommendation. The class of recommendation says it would be reasonable, but in the absence of an evidence base and in light of newer information, I’m not sure that it approaches even a class IIa level of recommendation,” according to Dr. O’Gara.
The 2019 European Society of Cardiology guidelines on chronic coronary syndromes are similarly weak on silent ischemia. The European guidelines state that patients with diabetes or chronic kidney disease may have a higher burden of silent ischemia, might be at higher risk for atherosclerotic cardiovascular disease events, and that periodic ECGs and functional testing every 3-5 years might be considered.
“Obviously there’s a lot of leeway there in how you wish to interpret that,” Dr. O’Gara said. “And this did not rise to the level where they’d put it in the table of recommendations, but it’s simply included as part of the explanatory text.”
What’s coming next in stable ischemic heart disease
“Nowadays all the rage has to do with coronary microvascular dysfunction,” according to Dr. O’Gara. “I think all of the research interest currently is focused on the coronary microcirculation as perhaps the next frontier in our understanding of why it is that ischemia can occur in the absence of epicardial coronary disease.”
He highly recommended a review article entitled: “Reappraisal of Ischemic Heart Disease,” in which an international trio of prominent cardiologists asserted that coronary microvascular dysfunction not only plays a pivotal pathogenic role in angina pectoris, but also in a phenomenon known as microvascular angina – that is, angina in the absence of obstructive CAD. Microvascular angina may explain the roughly one-third of patients who experience acute coronary syndrome without epicardial coronary artery stenosis or thrombosis. The authors delved into the structural and functional mechanisms underlying coronary microvascular dysfunction, while noting that effective treatment of this common phenomenon remains a major unmet need (Circulation. 2018 Oct 2;138[14]:1463-80).
Dr. O’Gara reported receiving funding from the National Heart, Lung, and Blood Institute; from Medtronic in conjunction with the ongoing pivotal APOLLO transcatheter mitral valve replacement trial; from Edwards Lifesciences for the ongoing EARLY TAVR trial; and from Medtrace Pharma, a Danish company developing an innovative form of PET diagnostic imaging.
SNOWMASS, COLO. – The concept that silent myocardial ischemia is clinically detrimental has fallen by the wayside, and routine screening for this phenomenon can no longer be recommended, Patrick T. O’Gara, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
What a difference a decade or 2 can make.
“Think about where we were 25 years ago, when we worried about people who had transient ST-segment depression without angina on Holter monitoring. We would wig out, chase them down the street, try to tackle them and load them up with medications and think about balloon [percutaneous transluminal coronary angioplasty]. And now we’re at the point where it doesn’t seem to help with respect to quality of life, let alone death or myocardial infarction,” observed Dr. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
The end of the line for the now-discredited notion that silent ischemia carries clinical significance approaching that of ischemia plus angina pectoris was the landmark ISCHEMIA trial, reported in November 2019 at the annual scientific sessions of the American Heart Association. This randomized trial asked the question: Is there any high-risk subgroup of patients with stable ischemic heart disease not involving the left main coronary artery for whom a strategy of routine revascularization improves hard outcomes in the current era of highly effective, guideline-directed medical therapy?
The answer turned out to be no. At 5 years of follow-up of 5,179 randomized patients with baseline stable coronary artery disease (CAD) and rigorously determined baseline moderate or severe ischemia affecting more than 10% of the myocardium, there was no difference between patients randomized to routine revascularization plus optimal medical therapy versus those on optimal medical therapy alone in the primary combined outcome of cardiovascular death, MI, heart failure, cardiac arrest, or hospitalization for unstable angina.
Of note, 35% of participants in the ISCHEMIA trial had moderate or severe silent ischemia. Like those who had angina, they achieved no additional benefit from a strategy of routine revascularization in terms of the primary outcome. ISCHEMIA participants with angina did show significant and durable improvements in quality of life and angina control with routine revascularization; however, those with silent ischemia showed little or no such improvement with an invasive strategy.
That being said, Dr. O’Gara added that he supports the ISCHEMIA investigators’ efforts to obtain funding from the National Institutes of Health for another 5 years or so of follow-up in order to determine whether revascularization actually does lead to improvement in the hard outcomes.
“Remember, in the STICH trial it took 10 years to show superiority of CABG [coronary artery bypass surgery] versus medical therapy to treat ischemic cardiomyopathy [N Engl J Med 2016; 374:1511-20]. My own view is that it’s too premature to throw the baby out with the bathwater. I think shared decision making is still very important, and I think, for many of our patients, relief of angina and improved quality of life are legitimate reasons in a low-risk situation with a good interventionalist to proceed,” he said.
Dr. O’Gara traced the history of medical thinking about silent ischemia. The notion that silent ischemia carried a clinical significance comparable with ischemia with angina gained wide credence more than 30 years ago, when investigators from the National Institutes of Health–sponsored Coronary Artery Surgery Study registry reported: “Patients with either silent or symptomatic ischemia during exercise testing have a similar risk of developing an acute myocardial infarction or sudden death – except in the three-vessel CAD subgroup, where the risk is greater in silent ischemia” (Am J Cardiol. 1988 Dec 1;62[17]:1155-8).
“This was a very important observation and led to many, many recommendations about screening and making sure that you took the expression of ST-segment depression on exercise treadmill testing pretty seriously, even if your patient did not have angina,” Dr. O’Gara recalled.
The prevailing wisdom that silent ischemia was detrimental took a hit in the Detection of Ischemia in Asymptomatic Diabetics (DIAC) trial. DIAC was conducted at a time when it had become clear that type 2 diabetes was a condition associated with increased cardiovascular risk, and that various methods of imaging were more accurate than treadmill exercise testing for the detection of underlying CAD. But when 1,123 DIAC participants with type 2 diabetes were randomized to screening with adenosine-stress radionuclide myocardial perfusion imaging or not and prospectively followed for roughly 5 years, it turned out there was no between-group difference in cardiac death or MI (JAMA. 2009 Apr 15;301[15]:1547-55).
“This pretty much put the lid on going out of one’s way to do routine screening of this nature in persons with diabetes who were considered to be at higher than average risk for the development of coronary disease,” the cardiologist commented.
Another fissure in the idea that silent ischemia was worth searching for and treating came from CLARIFY, an observational international registry of more than 20,000 individuals with stable CAD, roughly 12% of whom had silent ischemia, a figure in line with the prevalence reported in other studies. The 2-year rate of cardiovascular death or MI in the group with silent ischemia didn’t differ from the rate in patients with neither angina nor provocable ischemia. In contrast, rates of cardiovascular death or MI were significantly higher in the groups with angina but no ischemia or angina with ischemia (JAMA Intern Med. 2014 Oct;174[10]:1651-9).
“There’s something about the expression of angina that’s a very key clinical marker,” Dr. O’Gara observed.
He noted that just a few months before the ISCHEMIA trial results were released, a report from the far-smaller, randomized second Medicine, Angioplasty, or Surgery Study “threw cold water” on the notion that stress-induced ischemia in patients with multivessel CAD is a bad thing. Over 10 years of follow-up, the risk of major adverse cardiovascular events or deterioration in left ventricular function was identical in patients with or without baseline ischemia on stress testing performed after percutaneous coronary intervention, CABG surgery, or initiation of medical therapy (JAMA Intern Med. 2019 Jul 22. doi: 10.1001/jamainternmed.2019.2227).
What the guidelines say
The 6-year-old U.S. guidelines on the diagnosis and management of patients with stable ischemic heart disease are clearly out of date on the topic of silent ischemia (Circulation. 2014 Nov 4;130[19]:1749-67). The recommendations are based on expert opinion formed prior to the massive amount of new evidence that has since become available. For example, the current guidelines state as a class IIa, level of evidence C recommendation that exercise or pharmacologic stress can be useful for follow-up assessment at 2-year or greater intervals in patients with stable ischemic heart disease with prior evidence of silent ischemia.
“This is a very weak recommendation. The class of recommendation says it would be reasonable, but in the absence of an evidence base and in light of newer information, I’m not sure that it approaches even a class IIa level of recommendation,” according to Dr. O’Gara.
The 2019 European Society of Cardiology guidelines on chronic coronary syndromes are similarly weak on silent ischemia. The European guidelines state that patients with diabetes or chronic kidney disease may have a higher burden of silent ischemia, might be at higher risk for atherosclerotic cardiovascular disease events, and that periodic ECGs and functional testing every 3-5 years might be considered.
“Obviously there’s a lot of leeway there in how you wish to interpret that,” Dr. O’Gara said. “And this did not rise to the level where they’d put it in the table of recommendations, but it’s simply included as part of the explanatory text.”
What’s coming next in stable ischemic heart disease
“Nowadays all the rage has to do with coronary microvascular dysfunction,” according to Dr. O’Gara. “I think all of the research interest currently is focused on the coronary microcirculation as perhaps the next frontier in our understanding of why it is that ischemia can occur in the absence of epicardial coronary disease.”
He highly recommended a review article entitled: “Reappraisal of Ischemic Heart Disease,” in which an international trio of prominent cardiologists asserted that coronary microvascular dysfunction not only plays a pivotal pathogenic role in angina pectoris, but also in a phenomenon known as microvascular angina – that is, angina in the absence of obstructive CAD. Microvascular angina may explain the roughly one-third of patients who experience acute coronary syndrome without epicardial coronary artery stenosis or thrombosis. The authors delved into the structural and functional mechanisms underlying coronary microvascular dysfunction, while noting that effective treatment of this common phenomenon remains a major unmet need (Circulation. 2018 Oct 2;138[14]:1463-80).
Dr. O’Gara reported receiving funding from the National Heart, Lung, and Blood Institute; from Medtronic in conjunction with the ongoing pivotal APOLLO transcatheter mitral valve replacement trial; from Edwards Lifesciences for the ongoing EARLY TAVR trial; and from Medtrace Pharma, a Danish company developing an innovative form of PET diagnostic imaging.
SNOWMASS, COLO. – The concept that silent myocardial ischemia is clinically detrimental has fallen by the wayside, and routine screening for this phenomenon can no longer be recommended, Patrick T. O’Gara, MD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
What a difference a decade or 2 can make.
“Think about where we were 25 years ago, when we worried about people who had transient ST-segment depression without angina on Holter monitoring. We would wig out, chase them down the street, try to tackle them and load them up with medications and think about balloon [percutaneous transluminal coronary angioplasty]. And now we’re at the point where it doesn’t seem to help with respect to quality of life, let alone death or myocardial infarction,” observed Dr. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
The end of the line for the now-discredited notion that silent ischemia carries clinical significance approaching that of ischemia plus angina pectoris was the landmark ISCHEMIA trial, reported in November 2019 at the annual scientific sessions of the American Heart Association. This randomized trial asked the question: Is there any high-risk subgroup of patients with stable ischemic heart disease not involving the left main coronary artery for whom a strategy of routine revascularization improves hard outcomes in the current era of highly effective, guideline-directed medical therapy?
The answer turned out to be no. At 5 years of follow-up of 5,179 randomized patients with baseline stable coronary artery disease (CAD) and rigorously determined baseline moderate or severe ischemia affecting more than 10% of the myocardium, there was no difference between patients randomized to routine revascularization plus optimal medical therapy versus those on optimal medical therapy alone in the primary combined outcome of cardiovascular death, MI, heart failure, cardiac arrest, or hospitalization for unstable angina.
Of note, 35% of participants in the ISCHEMIA trial had moderate or severe silent ischemia. Like those who had angina, they achieved no additional benefit from a strategy of routine revascularization in terms of the primary outcome. ISCHEMIA participants with angina did show significant and durable improvements in quality of life and angina control with routine revascularization; however, those with silent ischemia showed little or no such improvement with an invasive strategy.
That being said, Dr. O’Gara added that he supports the ISCHEMIA investigators’ efforts to obtain funding from the National Institutes of Health for another 5 years or so of follow-up in order to determine whether revascularization actually does lead to improvement in the hard outcomes.
“Remember, in the STICH trial it took 10 years to show superiority of CABG [coronary artery bypass surgery] versus medical therapy to treat ischemic cardiomyopathy [N Engl J Med 2016; 374:1511-20]. My own view is that it’s too premature to throw the baby out with the bathwater. I think shared decision making is still very important, and I think, for many of our patients, relief of angina and improved quality of life are legitimate reasons in a low-risk situation with a good interventionalist to proceed,” he said.
Dr. O’Gara traced the history of medical thinking about silent ischemia. The notion that silent ischemia carried a clinical significance comparable with ischemia with angina gained wide credence more than 30 years ago, when investigators from the National Institutes of Health–sponsored Coronary Artery Surgery Study registry reported: “Patients with either silent or symptomatic ischemia during exercise testing have a similar risk of developing an acute myocardial infarction or sudden death – except in the three-vessel CAD subgroup, where the risk is greater in silent ischemia” (Am J Cardiol. 1988 Dec 1;62[17]:1155-8).
“This was a very important observation and led to many, many recommendations about screening and making sure that you took the expression of ST-segment depression on exercise treadmill testing pretty seriously, even if your patient did not have angina,” Dr. O’Gara recalled.
The prevailing wisdom that silent ischemia was detrimental took a hit in the Detection of Ischemia in Asymptomatic Diabetics (DIAC) trial. DIAC was conducted at a time when it had become clear that type 2 diabetes was a condition associated with increased cardiovascular risk, and that various methods of imaging were more accurate than treadmill exercise testing for the detection of underlying CAD. But when 1,123 DIAC participants with type 2 diabetes were randomized to screening with adenosine-stress radionuclide myocardial perfusion imaging or not and prospectively followed for roughly 5 years, it turned out there was no between-group difference in cardiac death or MI (JAMA. 2009 Apr 15;301[15]:1547-55).
“This pretty much put the lid on going out of one’s way to do routine screening of this nature in persons with diabetes who were considered to be at higher than average risk for the development of coronary disease,” the cardiologist commented.
Another fissure in the idea that silent ischemia was worth searching for and treating came from CLARIFY, an observational international registry of more than 20,000 individuals with stable CAD, roughly 12% of whom had silent ischemia, a figure in line with the prevalence reported in other studies. The 2-year rate of cardiovascular death or MI in the group with silent ischemia didn’t differ from the rate in patients with neither angina nor provocable ischemia. In contrast, rates of cardiovascular death or MI were significantly higher in the groups with angina but no ischemia or angina with ischemia (JAMA Intern Med. 2014 Oct;174[10]:1651-9).
“There’s something about the expression of angina that’s a very key clinical marker,” Dr. O’Gara observed.
He noted that just a few months before the ISCHEMIA trial results were released, a report from the far-smaller, randomized second Medicine, Angioplasty, or Surgery Study “threw cold water” on the notion that stress-induced ischemia in patients with multivessel CAD is a bad thing. Over 10 years of follow-up, the risk of major adverse cardiovascular events or deterioration in left ventricular function was identical in patients with or without baseline ischemia on stress testing performed after percutaneous coronary intervention, CABG surgery, or initiation of medical therapy (JAMA Intern Med. 2019 Jul 22. doi: 10.1001/jamainternmed.2019.2227).
What the guidelines say
The 6-year-old U.S. guidelines on the diagnosis and management of patients with stable ischemic heart disease are clearly out of date on the topic of silent ischemia (Circulation. 2014 Nov 4;130[19]:1749-67). The recommendations are based on expert opinion formed prior to the massive amount of new evidence that has since become available. For example, the current guidelines state as a class IIa, level of evidence C recommendation that exercise or pharmacologic stress can be useful for follow-up assessment at 2-year or greater intervals in patients with stable ischemic heart disease with prior evidence of silent ischemia.
“This is a very weak recommendation. The class of recommendation says it would be reasonable, but in the absence of an evidence base and in light of newer information, I’m not sure that it approaches even a class IIa level of recommendation,” according to Dr. O’Gara.
The 2019 European Society of Cardiology guidelines on chronic coronary syndromes are similarly weak on silent ischemia. The European guidelines state that patients with diabetes or chronic kidney disease may have a higher burden of silent ischemia, might be at higher risk for atherosclerotic cardiovascular disease events, and that periodic ECGs and functional testing every 3-5 years might be considered.
“Obviously there’s a lot of leeway there in how you wish to interpret that,” Dr. O’Gara said. “And this did not rise to the level where they’d put it in the table of recommendations, but it’s simply included as part of the explanatory text.”
What’s coming next in stable ischemic heart disease
“Nowadays all the rage has to do with coronary microvascular dysfunction,” according to Dr. O’Gara. “I think all of the research interest currently is focused on the coronary microcirculation as perhaps the next frontier in our understanding of why it is that ischemia can occur in the absence of epicardial coronary disease.”
He highly recommended a review article entitled: “Reappraisal of Ischemic Heart Disease,” in which an international trio of prominent cardiologists asserted that coronary microvascular dysfunction not only plays a pivotal pathogenic role in angina pectoris, but also in a phenomenon known as microvascular angina – that is, angina in the absence of obstructive CAD. Microvascular angina may explain the roughly one-third of patients who experience acute coronary syndrome without epicardial coronary artery stenosis or thrombosis. The authors delved into the structural and functional mechanisms underlying coronary microvascular dysfunction, while noting that effective treatment of this common phenomenon remains a major unmet need (Circulation. 2018 Oct 2;138[14]:1463-80).
Dr. O’Gara reported receiving funding from the National Heart, Lung, and Blood Institute; from Medtronic in conjunction with the ongoing pivotal APOLLO transcatheter mitral valve replacement trial; from Edwards Lifesciences for the ongoing EARLY TAVR trial; and from Medtrace Pharma, a Danish company developing an innovative form of PET diagnostic imaging.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
What 2019’s top five CAD trials tell us
SNOWMASS, COLO. – A repeated theme threading through much of one prominent interventional cardiologist’s personal list of the top five coronary artery disease (CAD) trials of the past year is that aspirin is very often more trouble than it’s worth.
“For some years I’ve been concerned that the only thing that aspirin does [in patients after percutaneous coronary intervention] is increase your risk of bleeding. It doesn’t really provide any additional ischemic protection,” Malcolm R. Bell, MBBS, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’ll remind you that, when we go back to the early stent days, observed Dr. Bell, professor of medicine and vice chair of the department of cardiovascular medicine at the Mayo Clinic in Rochester, Minn.
Here are the key takeaway messages from his five most important randomized trials in CAD during the last year.
AUGUSTUS
For years, cardiologists have grappled with how to best manage high-cardiovascular-risk patients with atrial fibrillation who seem like they might benefit from triple-antithrombotic therapy. AUGUSTUS supplied the answer: Don’t do it. Skip the aspirin and turn instead to a P2Y12 inhibitor plus a non–vitamin K antagonist oral anticoagulant (NOAC), rather than warfarin.
“I would like you to think of triple therapy as a triple threat. That’s really what triple therapy is all about”– a three-pronged threat to patient safety, Dr. Bell commented.
In AUGUSTUS, 4,614 patients with atrial fibrillation and CAD with an acute coronary syndrome (ACS) and/or percutaneous coronary intervention (PCI) in 33 countries were placed on a P2Y12 inhibitor – most often clopidogrel – and randomized double blind to either apixaban (Eliquis) or warfarin, and further to aspirin or placebo, for 6 months of antithrombotic therapy. The strategy of a P2Y12 inhibitor and apixaban without aspirin was the clear winner, resulting in significantly less major bleeding, mortality, and hospitalizations than treatment with a P2Y12 inhibitor and warfarin, with or without aspirin. Most importantly, ischemic event rates didn’t differ between the apixaban and warfarin groups. And patients randomized to aspirin had rates of ischemic events and death or hospitalization similar to placebo-treated controls, meaning aspirin accomplished nothing (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
Dr. Bell noted that a meta-analysis of AUGUSTUS and three smaller randomized trials including more than 10,000 AUGUSTUS-type patients with atrial fibrillation concluded that a treatment strategy utilizing a NOAC and a P2Y12 inhibitor resulted in less bleeding than warfarin plus DAPT, and at no cost in terms of excess ischemic events. Moreover, regimens without aspirin resulted in less intracranial and other major bleeding without any difference in major adverse cardiovascular events (JAMA Cardiol. 2019 Jun 19. doi: 10.1001/jamacardio.2019.1880).
A key message of these four trials is that a NOAC is preferable to warfarin, so much so that, in high-risk patients who are already on warfarin, it’s worth considering a switch to a NOAC.
“And we should really be avoiding DAPT,” Dr. Bell added.
How soon after an ACS and/or PCI should patients with atrial fibrillation stop taking aspirin?
“In AUGUSTUS, randomization occurred at a median of 6 days, so we know that half the patients stopped their aspirin by then. In our own practice, we’re just dropping the aspirin for the most part before the patient leaves the hospital. I think if you leave them with instructions to stop the aspirin in a week’s time or a month’s time it just leads to confusion. And we should also remember that half of the major bleeding after PCI or ACS happens in the first 30 days, so it doesn’t make a lot of sense to say that we should continue it for a month and then drop it,” according to the cardiologist.
SMART-CHOICE and STOPDAPT-2
These two large multicenter studies demonstrate that DAPT can safely be stopped early if needed. SMART-CHOICE from South Korea and STOPDAPT-2 from Japan each randomized roughly 3,000 patients undergoing PCI to 12 months of DAPT or to DAPT for only 3 months or 1 month, respectively, at which point the aspirin was dropped and patients in the abbreviated DAPT arm continued on P2Y12 inhibitor monotherapy, mostly clopidogrel, for the remainder of the 12 months. In the Japanese STOPDAPT-2 trial, 1 month of DAPT proved superior to 12 months of DAPT for the primary composite endpoint of cardiovascular death, MI, stroke, definite stent thrombosis, or major or minor bleeding at 12 months (JAMA. 2019 Jun 25;321[24]:2414-27). In the South Korean SMART-CHOICE trial, 3 months of DAPT was noninferior to 12 months for major adverse cardiac and cerebrovascular events, and superior in terms of bleeding risk (JAMA. 2019 Jun 25;321[24]:2428-37). Of note, roughly half of patients in the two trials were lower-risk individuals undergoing PCI for stable angina.
Dr. Bell noted that, while the TWILIGHT trial (Ticagrelor With or Without Aspirin in High-Risk Patients After PCI) didn’t make his top-five list, it certainly fits well with the two East Asian studies. The TWILIGHT investigators randomized more than 7,000 patients to 12 months of DAPT or discontinuation of aspirin after 3 months. The result: a lower incidence of clinically relevant bleeding with ticagrelor monotherapy, and with no increased risk of death, MI, or stroke, compared with 12 months of DAPT (N Engl J Med. 2019 Nov 21;381[21]:2032-42).
“Again, I would just question what the added value of aspirin is here,” Dr. Bell commented. “Many interventional cardiologists are absolutely terrified of their patients having stent thrombosis, but with second-generation drug-eluting stents – the stents we’re putting in day in and day out – the risk of stent thrombosis is less than 1%. And in these two trials it was less than 0.5%. There’s more risk of having major bleeding events than there is of ischemia, so I think the balance is in favor of preventing bleeding. We know that major bleeding predicts short- and long-term mortality.”
COLCOT
This double-blind trial randomized 4,745 patients within 30 days post MI to low-dose colchicine or placebo on top of excellent rates of background guideline-directed medical therapy. The goal was to see if this anti-inflammatory agent could reduce cardiovascular events independent of any lipid-lowering effect, as was earlier seen with canakinumab in the CANTOS trial. It did so to a statistically significant but relatively modest degree, with a 5.5% rate of the composite cardiovascular events endpoint in the colchicine group and 7.1% in placebo-treated controls (N Engl J Med. 2019 Dec 26;381[26]:2497-505). But Dr. Bell was unimpressed.
“All-cause mortality was identical at 1.8% in both groups. So colchicine is not saving lives. In fact, the only real differences were in stroke – but the study wasn’t powered to look at stroke – and in urgent hospitalization for angina leading to revascularization, which is a soft endpoint,” he observed.
Plus, 2.5% of patients were lost to follow-up, which Dr. Bell considers “a little concerning” in a trial conducted in the current era.
“In my opinion, the evidence that colchicine is effective is weak, and I don’t think really supports the drug’s routine use post MI. We already send these patients out on numerous medications. We have to think about cost/benefit, and if a patient asks me: ‘Is this going to prevent another heart attack or make me live longer?’ I think the unequivocal answer is no,” he said.
These days colchicine is no longer an inexpensive drug, either, at an average cost of $300-$400 per month, the cardiologist added.
COMPLETE
This study randomized more than 4,000 patients with ST-segment elevation MI (STEMI) and multivessel disease to primary PCI of the culprit lesion only or to staged complete revascularization via PCI of all angiographically significant nonculprit lesions. Complete revascularization proved to be the superior strategy, with a 26% reduction in the risk of the composite of cardiovascular death or MI at a median of 3 years (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
The optimal timing of the staged procedure remains unclear, since the study didn’t specify a protocol.
“I’m still a bit uncomfortable doing multivessel PCI at 2 o’clock in the morning in the setting of STEMI in someone I’ve never met before. I don’t think there’s a rush to do anything then. Often in this middle-of-the-night stuff, we miss things or we overinterpret things. I think it’s better to let the patient cool down, get to know them,” according to Dr. Bell.
EXCEL
Publication of the 5-year outcomes of the largest-ever randomized trial of PCI versus coronary artery bypass grafting (CABG) for left main coronary disease has led to furious controversy, with a few of the surgeons involved in the study opting to publically broadcast allegations of misbehavior on the part of the interventional cardiologist study leadership, charges that have been strongly denied.
The actual results are in line with findings reported from smaller randomized trials. At 5 years in EXCEL, there was no significant difference between the PCI and CABG groups in the primary composite endpoint of death, cerebrovascular accident, or MI (N Engl J Med. 2019 Nov 7;381[19]:1820-30). The all-cause mortality rate was 13% in the PCI arm and 9.9% with CABG, but this finding comes with a caveat.
“I’ll emphasize this trial was never powered to look at mortality. Neither were any of the other randomized trials. On the other hand, I don’t think you can necessarily ignore the finding of an absolute 3.1% difference,” Dr. Bell said.
PCI and CABG are both very good, mature therapies for left main disease, in his view. In the setting of more-complex coronary disease in younger patients, he often views the complete revascularization offered by surgery as the preferred option. On the other hand, in an 80-year-old with severe comorbidities, clearly PCI is attractive.
He considers the highly public nature of this interspecialty spat a regrettable black eye for the entire field of cardiovascular medicine. And he predicted that an ongoing outside neutral-party review of the study data and procedures will conclude, as he has, “there was no malfeasance at all in the trial.”
Dr. Bell reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – A repeated theme threading through much of one prominent interventional cardiologist’s personal list of the top five coronary artery disease (CAD) trials of the past year is that aspirin is very often more trouble than it’s worth.
“For some years I’ve been concerned that the only thing that aspirin does [in patients after percutaneous coronary intervention] is increase your risk of bleeding. It doesn’t really provide any additional ischemic protection,” Malcolm R. Bell, MBBS, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’ll remind you that, when we go back to the early stent days, observed Dr. Bell, professor of medicine and vice chair of the department of cardiovascular medicine at the Mayo Clinic in Rochester, Minn.
Here are the key takeaway messages from his five most important randomized trials in CAD during the last year.
AUGUSTUS
For years, cardiologists have grappled with how to best manage high-cardiovascular-risk patients with atrial fibrillation who seem like they might benefit from triple-antithrombotic therapy. AUGUSTUS supplied the answer: Don’t do it. Skip the aspirin and turn instead to a P2Y12 inhibitor plus a non–vitamin K antagonist oral anticoagulant (NOAC), rather than warfarin.
“I would like you to think of triple therapy as a triple threat. That’s really what triple therapy is all about”– a three-pronged threat to patient safety, Dr. Bell commented.
In AUGUSTUS, 4,614 patients with atrial fibrillation and CAD with an acute coronary syndrome (ACS) and/or percutaneous coronary intervention (PCI) in 33 countries were placed on a P2Y12 inhibitor – most often clopidogrel – and randomized double blind to either apixaban (Eliquis) or warfarin, and further to aspirin or placebo, for 6 months of antithrombotic therapy. The strategy of a P2Y12 inhibitor and apixaban without aspirin was the clear winner, resulting in significantly less major bleeding, mortality, and hospitalizations than treatment with a P2Y12 inhibitor and warfarin, with or without aspirin. Most importantly, ischemic event rates didn’t differ between the apixaban and warfarin groups. And patients randomized to aspirin had rates of ischemic events and death or hospitalization similar to placebo-treated controls, meaning aspirin accomplished nothing (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
Dr. Bell noted that a meta-analysis of AUGUSTUS and three smaller randomized trials including more than 10,000 AUGUSTUS-type patients with atrial fibrillation concluded that a treatment strategy utilizing a NOAC and a P2Y12 inhibitor resulted in less bleeding than warfarin plus DAPT, and at no cost in terms of excess ischemic events. Moreover, regimens without aspirin resulted in less intracranial and other major bleeding without any difference in major adverse cardiovascular events (JAMA Cardiol. 2019 Jun 19. doi: 10.1001/jamacardio.2019.1880).
A key message of these four trials is that a NOAC is preferable to warfarin, so much so that, in high-risk patients who are already on warfarin, it’s worth considering a switch to a NOAC.
“And we should really be avoiding DAPT,” Dr. Bell added.
How soon after an ACS and/or PCI should patients with atrial fibrillation stop taking aspirin?
“In AUGUSTUS, randomization occurred at a median of 6 days, so we know that half the patients stopped their aspirin by then. In our own practice, we’re just dropping the aspirin for the most part before the patient leaves the hospital. I think if you leave them with instructions to stop the aspirin in a week’s time or a month’s time it just leads to confusion. And we should also remember that half of the major bleeding after PCI or ACS happens in the first 30 days, so it doesn’t make a lot of sense to say that we should continue it for a month and then drop it,” according to the cardiologist.
SMART-CHOICE and STOPDAPT-2
These two large multicenter studies demonstrate that DAPT can safely be stopped early if needed. SMART-CHOICE from South Korea and STOPDAPT-2 from Japan each randomized roughly 3,000 patients undergoing PCI to 12 months of DAPT or to DAPT for only 3 months or 1 month, respectively, at which point the aspirin was dropped and patients in the abbreviated DAPT arm continued on P2Y12 inhibitor monotherapy, mostly clopidogrel, for the remainder of the 12 months. In the Japanese STOPDAPT-2 trial, 1 month of DAPT proved superior to 12 months of DAPT for the primary composite endpoint of cardiovascular death, MI, stroke, definite stent thrombosis, or major or minor bleeding at 12 months (JAMA. 2019 Jun 25;321[24]:2414-27). In the South Korean SMART-CHOICE trial, 3 months of DAPT was noninferior to 12 months for major adverse cardiac and cerebrovascular events, and superior in terms of bleeding risk (JAMA. 2019 Jun 25;321[24]:2428-37). Of note, roughly half of patients in the two trials were lower-risk individuals undergoing PCI for stable angina.
Dr. Bell noted that, while the TWILIGHT trial (Ticagrelor With or Without Aspirin in High-Risk Patients After PCI) didn’t make his top-five list, it certainly fits well with the two East Asian studies. The TWILIGHT investigators randomized more than 7,000 patients to 12 months of DAPT or discontinuation of aspirin after 3 months. The result: a lower incidence of clinically relevant bleeding with ticagrelor monotherapy, and with no increased risk of death, MI, or stroke, compared with 12 months of DAPT (N Engl J Med. 2019 Nov 21;381[21]:2032-42).
“Again, I would just question what the added value of aspirin is here,” Dr. Bell commented. “Many interventional cardiologists are absolutely terrified of their patients having stent thrombosis, but with second-generation drug-eluting stents – the stents we’re putting in day in and day out – the risk of stent thrombosis is less than 1%. And in these two trials it was less than 0.5%. There’s more risk of having major bleeding events than there is of ischemia, so I think the balance is in favor of preventing bleeding. We know that major bleeding predicts short- and long-term mortality.”
COLCOT
This double-blind trial randomized 4,745 patients within 30 days post MI to low-dose colchicine or placebo on top of excellent rates of background guideline-directed medical therapy. The goal was to see if this anti-inflammatory agent could reduce cardiovascular events independent of any lipid-lowering effect, as was earlier seen with canakinumab in the CANTOS trial. It did so to a statistically significant but relatively modest degree, with a 5.5% rate of the composite cardiovascular events endpoint in the colchicine group and 7.1% in placebo-treated controls (N Engl J Med. 2019 Dec 26;381[26]:2497-505). But Dr. Bell was unimpressed.
“All-cause mortality was identical at 1.8% in both groups. So colchicine is not saving lives. In fact, the only real differences were in stroke – but the study wasn’t powered to look at stroke – and in urgent hospitalization for angina leading to revascularization, which is a soft endpoint,” he observed.
Plus, 2.5% of patients were lost to follow-up, which Dr. Bell considers “a little concerning” in a trial conducted in the current era.
“In my opinion, the evidence that colchicine is effective is weak, and I don’t think really supports the drug’s routine use post MI. We already send these patients out on numerous medications. We have to think about cost/benefit, and if a patient asks me: ‘Is this going to prevent another heart attack or make me live longer?’ I think the unequivocal answer is no,” he said.
These days colchicine is no longer an inexpensive drug, either, at an average cost of $300-$400 per month, the cardiologist added.
COMPLETE
This study randomized more than 4,000 patients with ST-segment elevation MI (STEMI) and multivessel disease to primary PCI of the culprit lesion only or to staged complete revascularization via PCI of all angiographically significant nonculprit lesions. Complete revascularization proved to be the superior strategy, with a 26% reduction in the risk of the composite of cardiovascular death or MI at a median of 3 years (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
The optimal timing of the staged procedure remains unclear, since the study didn’t specify a protocol.
“I’m still a bit uncomfortable doing multivessel PCI at 2 o’clock in the morning in the setting of STEMI in someone I’ve never met before. I don’t think there’s a rush to do anything then. Often in this middle-of-the-night stuff, we miss things or we overinterpret things. I think it’s better to let the patient cool down, get to know them,” according to Dr. Bell.
EXCEL
Publication of the 5-year outcomes of the largest-ever randomized trial of PCI versus coronary artery bypass grafting (CABG) for left main coronary disease has led to furious controversy, with a few of the surgeons involved in the study opting to publically broadcast allegations of misbehavior on the part of the interventional cardiologist study leadership, charges that have been strongly denied.
The actual results are in line with findings reported from smaller randomized trials. At 5 years in EXCEL, there was no significant difference between the PCI and CABG groups in the primary composite endpoint of death, cerebrovascular accident, or MI (N Engl J Med. 2019 Nov 7;381[19]:1820-30). The all-cause mortality rate was 13% in the PCI arm and 9.9% with CABG, but this finding comes with a caveat.
“I’ll emphasize this trial was never powered to look at mortality. Neither were any of the other randomized trials. On the other hand, I don’t think you can necessarily ignore the finding of an absolute 3.1% difference,” Dr. Bell said.
PCI and CABG are both very good, mature therapies for left main disease, in his view. In the setting of more-complex coronary disease in younger patients, he often views the complete revascularization offered by surgery as the preferred option. On the other hand, in an 80-year-old with severe comorbidities, clearly PCI is attractive.
He considers the highly public nature of this interspecialty spat a regrettable black eye for the entire field of cardiovascular medicine. And he predicted that an ongoing outside neutral-party review of the study data and procedures will conclude, as he has, “there was no malfeasance at all in the trial.”
Dr. Bell reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – A repeated theme threading through much of one prominent interventional cardiologist’s personal list of the top five coronary artery disease (CAD) trials of the past year is that aspirin is very often more trouble than it’s worth.
“For some years I’ve been concerned that the only thing that aspirin does [in patients after percutaneous coronary intervention] is increase your risk of bleeding. It doesn’t really provide any additional ischemic protection,” Malcolm R. Bell, MBBS, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’ll remind you that, when we go back to the early stent days, observed Dr. Bell, professor of medicine and vice chair of the department of cardiovascular medicine at the Mayo Clinic in Rochester, Minn.
Here are the key takeaway messages from his five most important randomized trials in CAD during the last year.
AUGUSTUS
For years, cardiologists have grappled with how to best manage high-cardiovascular-risk patients with atrial fibrillation who seem like they might benefit from triple-antithrombotic therapy. AUGUSTUS supplied the answer: Don’t do it. Skip the aspirin and turn instead to a P2Y12 inhibitor plus a non–vitamin K antagonist oral anticoagulant (NOAC), rather than warfarin.
“I would like you to think of triple therapy as a triple threat. That’s really what triple therapy is all about”– a three-pronged threat to patient safety, Dr. Bell commented.
In AUGUSTUS, 4,614 patients with atrial fibrillation and CAD with an acute coronary syndrome (ACS) and/or percutaneous coronary intervention (PCI) in 33 countries were placed on a P2Y12 inhibitor – most often clopidogrel – and randomized double blind to either apixaban (Eliquis) or warfarin, and further to aspirin or placebo, for 6 months of antithrombotic therapy. The strategy of a P2Y12 inhibitor and apixaban without aspirin was the clear winner, resulting in significantly less major bleeding, mortality, and hospitalizations than treatment with a P2Y12 inhibitor and warfarin, with or without aspirin. Most importantly, ischemic event rates didn’t differ between the apixaban and warfarin groups. And patients randomized to aspirin had rates of ischemic events and death or hospitalization similar to placebo-treated controls, meaning aspirin accomplished nothing (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
Dr. Bell noted that a meta-analysis of AUGUSTUS and three smaller randomized trials including more than 10,000 AUGUSTUS-type patients with atrial fibrillation concluded that a treatment strategy utilizing a NOAC and a P2Y12 inhibitor resulted in less bleeding than warfarin plus DAPT, and at no cost in terms of excess ischemic events. Moreover, regimens without aspirin resulted in less intracranial and other major bleeding without any difference in major adverse cardiovascular events (JAMA Cardiol. 2019 Jun 19. doi: 10.1001/jamacardio.2019.1880).
A key message of these four trials is that a NOAC is preferable to warfarin, so much so that, in high-risk patients who are already on warfarin, it’s worth considering a switch to a NOAC.
“And we should really be avoiding DAPT,” Dr. Bell added.
How soon after an ACS and/or PCI should patients with atrial fibrillation stop taking aspirin?
“In AUGUSTUS, randomization occurred at a median of 6 days, so we know that half the patients stopped their aspirin by then. In our own practice, we’re just dropping the aspirin for the most part before the patient leaves the hospital. I think if you leave them with instructions to stop the aspirin in a week’s time or a month’s time it just leads to confusion. And we should also remember that half of the major bleeding after PCI or ACS happens in the first 30 days, so it doesn’t make a lot of sense to say that we should continue it for a month and then drop it,” according to the cardiologist.
SMART-CHOICE and STOPDAPT-2
These two large multicenter studies demonstrate that DAPT can safely be stopped early if needed. SMART-CHOICE from South Korea and STOPDAPT-2 from Japan each randomized roughly 3,000 patients undergoing PCI to 12 months of DAPT or to DAPT for only 3 months or 1 month, respectively, at which point the aspirin was dropped and patients in the abbreviated DAPT arm continued on P2Y12 inhibitor monotherapy, mostly clopidogrel, for the remainder of the 12 months. In the Japanese STOPDAPT-2 trial, 1 month of DAPT proved superior to 12 months of DAPT for the primary composite endpoint of cardiovascular death, MI, stroke, definite stent thrombosis, or major or minor bleeding at 12 months (JAMA. 2019 Jun 25;321[24]:2414-27). In the South Korean SMART-CHOICE trial, 3 months of DAPT was noninferior to 12 months for major adverse cardiac and cerebrovascular events, and superior in terms of bleeding risk (JAMA. 2019 Jun 25;321[24]:2428-37). Of note, roughly half of patients in the two trials were lower-risk individuals undergoing PCI for stable angina.
Dr. Bell noted that, while the TWILIGHT trial (Ticagrelor With or Without Aspirin in High-Risk Patients After PCI) didn’t make his top-five list, it certainly fits well with the two East Asian studies. The TWILIGHT investigators randomized more than 7,000 patients to 12 months of DAPT or discontinuation of aspirin after 3 months. The result: a lower incidence of clinically relevant bleeding with ticagrelor monotherapy, and with no increased risk of death, MI, or stroke, compared with 12 months of DAPT (N Engl J Med. 2019 Nov 21;381[21]:2032-42).
“Again, I would just question what the added value of aspirin is here,” Dr. Bell commented. “Many interventional cardiologists are absolutely terrified of their patients having stent thrombosis, but with second-generation drug-eluting stents – the stents we’re putting in day in and day out – the risk of stent thrombosis is less than 1%. And in these two trials it was less than 0.5%. There’s more risk of having major bleeding events than there is of ischemia, so I think the balance is in favor of preventing bleeding. We know that major bleeding predicts short- and long-term mortality.”
COLCOT
This double-blind trial randomized 4,745 patients within 30 days post MI to low-dose colchicine or placebo on top of excellent rates of background guideline-directed medical therapy. The goal was to see if this anti-inflammatory agent could reduce cardiovascular events independent of any lipid-lowering effect, as was earlier seen with canakinumab in the CANTOS trial. It did so to a statistically significant but relatively modest degree, with a 5.5% rate of the composite cardiovascular events endpoint in the colchicine group and 7.1% in placebo-treated controls (N Engl J Med. 2019 Dec 26;381[26]:2497-505). But Dr. Bell was unimpressed.
“All-cause mortality was identical at 1.8% in both groups. So colchicine is not saving lives. In fact, the only real differences were in stroke – but the study wasn’t powered to look at stroke – and in urgent hospitalization for angina leading to revascularization, which is a soft endpoint,” he observed.
Plus, 2.5% of patients were lost to follow-up, which Dr. Bell considers “a little concerning” in a trial conducted in the current era.
“In my opinion, the evidence that colchicine is effective is weak, and I don’t think really supports the drug’s routine use post MI. We already send these patients out on numerous medications. We have to think about cost/benefit, and if a patient asks me: ‘Is this going to prevent another heart attack or make me live longer?’ I think the unequivocal answer is no,” he said.
These days colchicine is no longer an inexpensive drug, either, at an average cost of $300-$400 per month, the cardiologist added.
COMPLETE
This study randomized more than 4,000 patients with ST-segment elevation MI (STEMI) and multivessel disease to primary PCI of the culprit lesion only or to staged complete revascularization via PCI of all angiographically significant nonculprit lesions. Complete revascularization proved to be the superior strategy, with a 26% reduction in the risk of the composite of cardiovascular death or MI at a median of 3 years (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
The optimal timing of the staged procedure remains unclear, since the study didn’t specify a protocol.
“I’m still a bit uncomfortable doing multivessel PCI at 2 o’clock in the morning in the setting of STEMI in someone I’ve never met before. I don’t think there’s a rush to do anything then. Often in this middle-of-the-night stuff, we miss things or we overinterpret things. I think it’s better to let the patient cool down, get to know them,” according to Dr. Bell.
EXCEL
Publication of the 5-year outcomes of the largest-ever randomized trial of PCI versus coronary artery bypass grafting (CABG) for left main coronary disease has led to furious controversy, with a few of the surgeons involved in the study opting to publically broadcast allegations of misbehavior on the part of the interventional cardiologist study leadership, charges that have been strongly denied.
The actual results are in line with findings reported from smaller randomized trials. At 5 years in EXCEL, there was no significant difference between the PCI and CABG groups in the primary composite endpoint of death, cerebrovascular accident, or MI (N Engl J Med. 2019 Nov 7;381[19]:1820-30). The all-cause mortality rate was 13% in the PCI arm and 9.9% with CABG, but this finding comes with a caveat.
“I’ll emphasize this trial was never powered to look at mortality. Neither were any of the other randomized trials. On the other hand, I don’t think you can necessarily ignore the finding of an absolute 3.1% difference,” Dr. Bell said.
PCI and CABG are both very good, mature therapies for left main disease, in his view. In the setting of more-complex coronary disease in younger patients, he often views the complete revascularization offered by surgery as the preferred option. On the other hand, in an 80-year-old with severe comorbidities, clearly PCI is attractive.
He considers the highly public nature of this interspecialty spat a regrettable black eye for the entire field of cardiovascular medicine. And he predicted that an ongoing outside neutral-party review of the study data and procedures will conclude, as he has, “there was no malfeasance at all in the trial.”
Dr. Bell reported having no financial conflicts regarding his presentation.
REPORTING FROM ACC SNOWMASS 2020
BP levels during endovascular stroke therapy affect neurologic outcomes
For patients with acute ischemic stroke, prolonged durations of blood pressure above or below certain thresholds during endovascular therapy may be linked to poor functional outcome, results of a retrospective study suggest.
Mean arterial blood pressure (MABP) lower than 70 mm Hg for 10 minutes or more, or higher than 90 mm Hg for 45 minutes or more, represented “critical thresholds” associated with worse neurologic outcomes, the study authors wrote in JAMA Neurology.
“These results suggest MABP may be a modifiable therapeutic target to prevent or reduce poor functional outcome in patients undergoing endovascular therapy for acute ischemic stroke, and that MABP should possibly be maintained within such narrow limits, wrote the authors, led by Mads Rasmussen, MD, PhD, of the department of anesthesia at Aarhus (Denmark) University Hospital.
The findings come from an analysis of BP data from 365 patients with acute ischemic stroke enrolled in three randomized trials evaluating different strategies for anesthesia. Among those patients, the mean age was approximately 71 years, and about 45% were women.
The investigators looked at a variety of BP-related variables during endovascular therapy to assess their impact on functional outcome, based on modified Rankin Scale (mRS) scores at 90 days.
Having an MABP below 70 mm Hg for a cumulative time of at least 10 minutes substantially increased odds of higher 90-day mRS scores (odds ratio, 1.51; 95% confidence interval, 1.02-2.22), according to Dr. Rasmussen and colleagues. The number needed to harm (NNH) at this threshold was 10; in other words, to harm 1 patient, 10 patients are needed with procedural MABP below 70 mm Hg for at least 10 minutes.
Likewise, having an MABP above 90 mm Hg for a cumulated time of at least 45 minutes significantly increased odds of higher 90-day mRS scores, with an OR of 1.49 (95% CI, 1.11-2.02) and a number needed to harm of 10.
Odds of shifting toward a worse neurologic outcome increased by 62% for every continuous 10 minutes of MABP below 70 mm Hg, and by 8% for every continuous 10 minutes above 90 mm Hg.
The maximum MABP during the procedure was significantly associated with neurologic outcomes in the study, while by contrast, maximum procedural systolic BP was not, according to the investigators.
In general, the study findings suggest that MABP is “more sensitive” than systolic BP when assessing hypotension and hypertension in these patients. However, these findings are subject to a number of limitations, the investigators wrote, including the retrospective nature of the analysis and the selected group of patients enrolled in studies designed to evaluate anesthesia strategies, not hemodynamic management.
“Randomized studies are needed to determine the optimal blood pressure management strategy during endovascular therapy,” the investigators wrote.
Dr. Rasmussen reported grant support from the Health Research Foundation of Central Denmark Region and the National Helicopter Emergency Medical Service Foundation. Coauthors reported receiving grant support from the Novo Nordisk Foundation; a research award from the Patient-Centered Outcomes Research Institute; and personal fees from Abbott Medical Sweden, I4L Innovation for Life, Boehringer Ingelheim, Medtronic, and Zoll.
SOURCE: Rasmussen M et al. JAMA Neurol. 2020 Jan 27. doi: 10.1001/jamaneurol.2019.4838.
For patients with acute ischemic stroke, prolonged durations of blood pressure above or below certain thresholds during endovascular therapy may be linked to poor functional outcome, results of a retrospective study suggest.
Mean arterial blood pressure (MABP) lower than 70 mm Hg for 10 minutes or more, or higher than 90 mm Hg for 45 minutes or more, represented “critical thresholds” associated with worse neurologic outcomes, the study authors wrote in JAMA Neurology.
“These results suggest MABP may be a modifiable therapeutic target to prevent or reduce poor functional outcome in patients undergoing endovascular therapy for acute ischemic stroke, and that MABP should possibly be maintained within such narrow limits, wrote the authors, led by Mads Rasmussen, MD, PhD, of the department of anesthesia at Aarhus (Denmark) University Hospital.
The findings come from an analysis of BP data from 365 patients with acute ischemic stroke enrolled in three randomized trials evaluating different strategies for anesthesia. Among those patients, the mean age was approximately 71 years, and about 45% were women.
The investigators looked at a variety of BP-related variables during endovascular therapy to assess their impact on functional outcome, based on modified Rankin Scale (mRS) scores at 90 days.
Having an MABP below 70 mm Hg for a cumulative time of at least 10 minutes substantially increased odds of higher 90-day mRS scores (odds ratio, 1.51; 95% confidence interval, 1.02-2.22), according to Dr. Rasmussen and colleagues. The number needed to harm (NNH) at this threshold was 10; in other words, to harm 1 patient, 10 patients are needed with procedural MABP below 70 mm Hg for at least 10 minutes.
Likewise, having an MABP above 90 mm Hg for a cumulated time of at least 45 minutes significantly increased odds of higher 90-day mRS scores, with an OR of 1.49 (95% CI, 1.11-2.02) and a number needed to harm of 10.
Odds of shifting toward a worse neurologic outcome increased by 62% for every continuous 10 minutes of MABP below 70 mm Hg, and by 8% for every continuous 10 minutes above 90 mm Hg.
The maximum MABP during the procedure was significantly associated with neurologic outcomes in the study, while by contrast, maximum procedural systolic BP was not, according to the investigators.
In general, the study findings suggest that MABP is “more sensitive” than systolic BP when assessing hypotension and hypertension in these patients. However, these findings are subject to a number of limitations, the investigators wrote, including the retrospective nature of the analysis and the selected group of patients enrolled in studies designed to evaluate anesthesia strategies, not hemodynamic management.
“Randomized studies are needed to determine the optimal blood pressure management strategy during endovascular therapy,” the investigators wrote.
Dr. Rasmussen reported grant support from the Health Research Foundation of Central Denmark Region and the National Helicopter Emergency Medical Service Foundation. Coauthors reported receiving grant support from the Novo Nordisk Foundation; a research award from the Patient-Centered Outcomes Research Institute; and personal fees from Abbott Medical Sweden, I4L Innovation for Life, Boehringer Ingelheim, Medtronic, and Zoll.
SOURCE: Rasmussen M et al. JAMA Neurol. 2020 Jan 27. doi: 10.1001/jamaneurol.2019.4838.
For patients with acute ischemic stroke, prolonged durations of blood pressure above or below certain thresholds during endovascular therapy may be linked to poor functional outcome, results of a retrospective study suggest.
Mean arterial blood pressure (MABP) lower than 70 mm Hg for 10 minutes or more, or higher than 90 mm Hg for 45 minutes or more, represented “critical thresholds” associated with worse neurologic outcomes, the study authors wrote in JAMA Neurology.
“These results suggest MABP may be a modifiable therapeutic target to prevent or reduce poor functional outcome in patients undergoing endovascular therapy for acute ischemic stroke, and that MABP should possibly be maintained within such narrow limits, wrote the authors, led by Mads Rasmussen, MD, PhD, of the department of anesthesia at Aarhus (Denmark) University Hospital.
The findings come from an analysis of BP data from 365 patients with acute ischemic stroke enrolled in three randomized trials evaluating different strategies for anesthesia. Among those patients, the mean age was approximately 71 years, and about 45% were women.
The investigators looked at a variety of BP-related variables during endovascular therapy to assess their impact on functional outcome, based on modified Rankin Scale (mRS) scores at 90 days.
Having an MABP below 70 mm Hg for a cumulative time of at least 10 minutes substantially increased odds of higher 90-day mRS scores (odds ratio, 1.51; 95% confidence interval, 1.02-2.22), according to Dr. Rasmussen and colleagues. The number needed to harm (NNH) at this threshold was 10; in other words, to harm 1 patient, 10 patients are needed with procedural MABP below 70 mm Hg for at least 10 minutes.
Likewise, having an MABP above 90 mm Hg for a cumulated time of at least 45 minutes significantly increased odds of higher 90-day mRS scores, with an OR of 1.49 (95% CI, 1.11-2.02) and a number needed to harm of 10.
Odds of shifting toward a worse neurologic outcome increased by 62% for every continuous 10 minutes of MABP below 70 mm Hg, and by 8% for every continuous 10 minutes above 90 mm Hg.
The maximum MABP during the procedure was significantly associated with neurologic outcomes in the study, while by contrast, maximum procedural systolic BP was not, according to the investigators.
In general, the study findings suggest that MABP is “more sensitive” than systolic BP when assessing hypotension and hypertension in these patients. However, these findings are subject to a number of limitations, the investigators wrote, including the retrospective nature of the analysis and the selected group of patients enrolled in studies designed to evaluate anesthesia strategies, not hemodynamic management.
“Randomized studies are needed to determine the optimal blood pressure management strategy during endovascular therapy,” the investigators wrote.
Dr. Rasmussen reported grant support from the Health Research Foundation of Central Denmark Region and the National Helicopter Emergency Medical Service Foundation. Coauthors reported receiving grant support from the Novo Nordisk Foundation; a research award from the Patient-Centered Outcomes Research Institute; and personal fees from Abbott Medical Sweden, I4L Innovation for Life, Boehringer Ingelheim, Medtronic, and Zoll.
SOURCE: Rasmussen M et al. JAMA Neurol. 2020 Jan 27. doi: 10.1001/jamaneurol.2019.4838.
FROM JAMA NEUROLOGY
FFR use nearly halved 1-year mortality risk in ischemic heart disease
Use of fractional flow reserve significantly improved 1-year mortality rates in adults with stable ischemic heart disease, according to a review of 17,989 patients.
Although fractional flow reserve (FFR) has demonstrated value in guiding coronary revascularization, its impact on outcomes in patients with stable ischemic heart disease has not been well studied in a large population, wrote Rushi V. Parikh, MD, of the University of California, Los Angeles, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers analyzed data from the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program for adults who underwent coronary angiography between January 2009 and September 2017. The study included patients with angiographically intermediate disease, defined as 40%-69% diameter stenosis on visual inspection.
The rate of FFR use increased from 14.8% to 18.5% during the study period for all patients with intermediate lesions, and from 44% to 75% for those who had percutaneous coronary intervention, the researchers wrote.
Overall, based on hazard models, 1-year mortality was significantly lower in patients who underwent FFR, compared with those who had angiography only (2.8% vs. 5.9%; P less than 0.001). In addition, FFR use in revascularization was associated with a 43% reduced 1-year mortality risk, compared with angiography only.
The findings were limited by several factors, including the observational nature of the study, inability to distinguish between cardiovascular and noncardiovascular mortality, lack of data on the technical performance of the FFR, and a relatively short follow-up period, the researchers noted.
However, the results were strengthened by the large sample size, and support the use of FFR-guided revascularization in patients with angiographically intermediate stenosis, they wrote.
“Future registry-based studies accounting for all physiologic modalities are warranted to accurately quantify the landscape of coronary physiology-guided revascularization,” they added.
The study was supported in part by the Rocky Mountain Regional VA Medical Center in Aurora, Colo. Lead author Dr. Parikh had no financial conflicts to disclose.
SOURCE: Parikh RV et al. J Am Coll Cardiol. 2020 Feb 4;75:409-19.
Although the study suggests that the use of fractional flow reserve (FFR) has increased, it remains underused despite evidence and recommendations, wrote Julien Adjedj, MD, and Benoit Guillon, MD, in an accompanying editorial (J Am Coll Cardiol. 2020 Feb 4;75:420-1).
“Of course, time, cost, and need for hyperemia are often perceived as stumbling blocks. Yet, the real question is whether the cardiology community – not only interventional cardiologists – has truly adopted FFR (i.e., using it routinely and treating according to the results),” they wrote.
The editorialists noted that, in this study, typical predictors of FFR included younger age, multivessel or left main disease, previous history of percutaneous coronary intervention, no heart failure, and higher left ventricular ejection fraction.
“However, neither the absence of documented ischemia nor the presence of symptoms influenced the use of FFR. Significant site-level variation in FFR was observed,” they wrote. “This important finding suggests that the main reason for FFR underutilization in the contemporary era is operator belief regarding the utility of coronary physiology, and that revised reimbursement policies and additional education/training may not have a meaningful impact on FFR adoption.”
The editorialists emphasized that, although FFR use has increased, the findings of a significant decrease in mortality support additional use of FFR “and good reasons to do so.”
Dr. Adjedj is affiliated with the Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland, and had no financial conflicts to disclose. Dr. Guillon is affiliated with the University Hospital Jean Minjoz in Besançon, France, and disclosed a grant from Sanofi and participation in a conference for Abbott.
Although the study suggests that the use of fractional flow reserve (FFR) has increased, it remains underused despite evidence and recommendations, wrote Julien Adjedj, MD, and Benoit Guillon, MD, in an accompanying editorial (J Am Coll Cardiol. 2020 Feb 4;75:420-1).
“Of course, time, cost, and need for hyperemia are often perceived as stumbling blocks. Yet, the real question is whether the cardiology community – not only interventional cardiologists – has truly adopted FFR (i.e., using it routinely and treating according to the results),” they wrote.
The editorialists noted that, in this study, typical predictors of FFR included younger age, multivessel or left main disease, previous history of percutaneous coronary intervention, no heart failure, and higher left ventricular ejection fraction.
“However, neither the absence of documented ischemia nor the presence of symptoms influenced the use of FFR. Significant site-level variation in FFR was observed,” they wrote. “This important finding suggests that the main reason for FFR underutilization in the contemporary era is operator belief regarding the utility of coronary physiology, and that revised reimbursement policies and additional education/training may not have a meaningful impact on FFR adoption.”
The editorialists emphasized that, although FFR use has increased, the findings of a significant decrease in mortality support additional use of FFR “and good reasons to do so.”
Dr. Adjedj is affiliated with the Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland, and had no financial conflicts to disclose. Dr. Guillon is affiliated with the University Hospital Jean Minjoz in Besançon, France, and disclosed a grant from Sanofi and participation in a conference for Abbott.
Although the study suggests that the use of fractional flow reserve (FFR) has increased, it remains underused despite evidence and recommendations, wrote Julien Adjedj, MD, and Benoit Guillon, MD, in an accompanying editorial (J Am Coll Cardiol. 2020 Feb 4;75:420-1).
“Of course, time, cost, and need for hyperemia are often perceived as stumbling blocks. Yet, the real question is whether the cardiology community – not only interventional cardiologists – has truly adopted FFR (i.e., using it routinely and treating according to the results),” they wrote.
The editorialists noted that, in this study, typical predictors of FFR included younger age, multivessel or left main disease, previous history of percutaneous coronary intervention, no heart failure, and higher left ventricular ejection fraction.
“However, neither the absence of documented ischemia nor the presence of symptoms influenced the use of FFR. Significant site-level variation in FFR was observed,” they wrote. “This important finding suggests that the main reason for FFR underutilization in the contemporary era is operator belief regarding the utility of coronary physiology, and that revised reimbursement policies and additional education/training may not have a meaningful impact on FFR adoption.”
The editorialists emphasized that, although FFR use has increased, the findings of a significant decrease in mortality support additional use of FFR “and good reasons to do so.”
Dr. Adjedj is affiliated with the Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland, and had no financial conflicts to disclose. Dr. Guillon is affiliated with the University Hospital Jean Minjoz in Besançon, France, and disclosed a grant from Sanofi and participation in a conference for Abbott.
Use of fractional flow reserve significantly improved 1-year mortality rates in adults with stable ischemic heart disease, according to a review of 17,989 patients.
Although fractional flow reserve (FFR) has demonstrated value in guiding coronary revascularization, its impact on outcomes in patients with stable ischemic heart disease has not been well studied in a large population, wrote Rushi V. Parikh, MD, of the University of California, Los Angeles, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers analyzed data from the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program for adults who underwent coronary angiography between January 2009 and September 2017. The study included patients with angiographically intermediate disease, defined as 40%-69% diameter stenosis on visual inspection.
The rate of FFR use increased from 14.8% to 18.5% during the study period for all patients with intermediate lesions, and from 44% to 75% for those who had percutaneous coronary intervention, the researchers wrote.
Overall, based on hazard models, 1-year mortality was significantly lower in patients who underwent FFR, compared with those who had angiography only (2.8% vs. 5.9%; P less than 0.001). In addition, FFR use in revascularization was associated with a 43% reduced 1-year mortality risk, compared with angiography only.
The findings were limited by several factors, including the observational nature of the study, inability to distinguish between cardiovascular and noncardiovascular mortality, lack of data on the technical performance of the FFR, and a relatively short follow-up period, the researchers noted.
However, the results were strengthened by the large sample size, and support the use of FFR-guided revascularization in patients with angiographically intermediate stenosis, they wrote.
“Future registry-based studies accounting for all physiologic modalities are warranted to accurately quantify the landscape of coronary physiology-guided revascularization,” they added.
The study was supported in part by the Rocky Mountain Regional VA Medical Center in Aurora, Colo. Lead author Dr. Parikh had no financial conflicts to disclose.
SOURCE: Parikh RV et al. J Am Coll Cardiol. 2020 Feb 4;75:409-19.
Use of fractional flow reserve significantly improved 1-year mortality rates in adults with stable ischemic heart disease, according to a review of 17,989 patients.
Although fractional flow reserve (FFR) has demonstrated value in guiding coronary revascularization, its impact on outcomes in patients with stable ischemic heart disease has not been well studied in a large population, wrote Rushi V. Parikh, MD, of the University of California, Los Angeles, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers analyzed data from the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program for adults who underwent coronary angiography between January 2009 and September 2017. The study included patients with angiographically intermediate disease, defined as 40%-69% diameter stenosis on visual inspection.
The rate of FFR use increased from 14.8% to 18.5% during the study period for all patients with intermediate lesions, and from 44% to 75% for those who had percutaneous coronary intervention, the researchers wrote.
Overall, based on hazard models, 1-year mortality was significantly lower in patients who underwent FFR, compared with those who had angiography only (2.8% vs. 5.9%; P less than 0.001). In addition, FFR use in revascularization was associated with a 43% reduced 1-year mortality risk, compared with angiography only.
The findings were limited by several factors, including the observational nature of the study, inability to distinguish between cardiovascular and noncardiovascular mortality, lack of data on the technical performance of the FFR, and a relatively short follow-up period, the researchers noted.
However, the results were strengthened by the large sample size, and support the use of FFR-guided revascularization in patients with angiographically intermediate stenosis, they wrote.
“Future registry-based studies accounting for all physiologic modalities are warranted to accurately quantify the landscape of coronary physiology-guided revascularization,” they added.
The study was supported in part by the Rocky Mountain Regional VA Medical Center in Aurora, Colo. Lead author Dr. Parikh had no financial conflicts to disclose.
SOURCE: Parikh RV et al. J Am Coll Cardiol. 2020 Feb 4;75:409-19.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Use of fractional flow reserve to assist in revascularization significantly reduced the 1-year mortality risk in patients with stable ischemic heart disease.
Major finding:
Study details: The data come from a review of 17,989 patients who underwent coronary angiography during 2009-2017.
Disclosures: The study was supported in part by the Rocky Mountain Regional Veterans Affairs Medical Center in Aurora, Colo. Lead author Dr. Parikh had no financial conflicts to disclose.
Source: Parikh RV et al. J Am Coll Cardiol. 2020 Feb 4;75:409-19.
Catheter cryoablation effective for persistent AFib in pivotal trial
NATIONAL HARBOR, MD. – , setting the stage for the device to become the first to receive U.S. labeling for catheter ablation in this atrial fibrillation population.
The Arctic Front Advance cryoballoon, used on 165 patients with persistent atrial fibrillation (AFib) enrolled in the trial, produced a 55% rate of treatment success, including freedom from recurrent AFib during 12 months of follow-up, and produced one prespecified serious adverse event in the primary safety endpoint.
Both results easily surpassed the prespecified performance goals set by negotiation with the FDA, Hugh Calkins, MD, said at the annual International AF Symposium. The trial design included no control group and instead assessed safety and efficacy against prespecified standards set by the regulatory agency.
The cryoballoon “showed excellent performance. I don’t see how this could possibly be turned down by the FDA,” said Dr. Calkins, professor of medicine and director of the cardiac arrhythmia service at Johns Hopkins Medicine in Baltimore.
Cardiac electrophysiologists have for years routinely performed catheter ablation procedures on patients with persistent AFib even though the devices, based on ablation by radiofrequency or by chilling, have been labeled for use only in treating patients with paroxysmal AFib. Although this off-label use has not resulted in any problems with health insurance coverage, Dr. Calkins said, it has kept manufacturers from marketing their ablation devices for use in persistent AFib patients.
If the reported data result in labeling for the tested cryoballoon for persistant AFib patients, “it will have a big impact,” he predicted. “People have used cryoballoons for ablating persistent AFib for years, but this would put more fuel in the fire, both the [very positive] safety and efficacy data, and getting an FDA label, which is worth a lot,” he said in an interview.
But Dr. Calkins stopped short of anticipating that the results would convince operators experienced and focused on performing radiofrequency ablation to switch to cryo devices for treating persistent AFib patients. “People are pretty stuck in their ways,” he noted, and reports are expected soon from pivotal trials that are now testing various radiofrequency devices, as well as other types of cryo devices, in persistent AFib patients, so the range of device options labeled for this population may soon grow even more.
The STOP Persistent AF trial ran at 25 sites in the United States, Canada, and Japan during March 2017-August 2019, and included 165 adults with symptomatic, persistent AFib who had not responded to at least one antiarrhythmic drug and had a history of AFib episodes lasting at least 7 days but with no episodes persisting for 6 months or longer. The study excluded patients with prior ablation or left atrial surgery, a recent cerebrovascular event, substantially reduced left ventricular function, or substantial left atrial enlargement.
The enrolled patients were an average 65 years of age and 70% were men. Patients had been diagnosed with paroxysmal AFib an average of 5 years before study entry and with persistent AFib a little over 6 months before entry. The most recent AFib episode of enrolled patients averaged about 60 days, on average they had been unsuccessfully treated with just over one antiarrhythmic drug, and on average they had previously undergone about two cardioversions, after which their arrhythmia recurred.
The primary efficacy endpoint – a 55% rate of acute procedural success plus freedom from AFib recurrence during the 9 months following a 90-day blanking period immediately after ablation plus no added or increased antiarrhythmic drugs – significantly exceeded the prespecified performance goal of a 40% rate, Dr. Calkins reported. The study used the standard measure of recurrence as any 30-second or longer AFib episode detected during a weekly ECG telemonitoring session or during 48-hour ambulatory ECG monitoring at 6- and 12-month follow-ups or during in-office 12-lead ECG assessment at 3-, 6-, and 12-month follow-up. Twelve-month follow-up occurred for 145 of the enrolled patients.
The only prespecified primary safety event was one episode of cardiac perforation, which occurred during a repeat procedure. This rate of one safety event among 165 patients (0.6%) fell well within the prespecified safety performance goal of no more than 13%. In addition to this perforation, five additional serious adverse events (3%) occurred that were attributable to the cryoballoon treatment, including two cases of vascular pseudoaneurysm, one puncture-site hematoma, one case of pericarditis, and one episode of atrial tachycardia. Four additional serious adverse events occurred that were attributable to the ablation procedure (one acute cardiac failure, one postprocedure ileus, one respiratory failure, and one urinary tract infection), for an overall serious event rate of 5%.
During follow-up, 13% of patients had a repeat ablation procedure, following an initial ablation limited to pulmonary-vein isolation (PVI). The overall rate of 1-year efficacy, including the relatively low rate of need for redo ablation, “are an impressive endorsement of a PVI-only strategy” for initial ablation, Dr. Calkins said. “I’m a strong believer in PVI only for the first ablation for both paroxysmal and persistent AFib.”
He also noted that the 30-second threshold for scoring recurrent arrhythmia episodes following the 90-day blanking period after ablation was a very conservative measure of treatment failure, but it continues to define recurrence in this and many other current AFib ablation studies because it is the historical criteria for measuring ablation success or failure. It is especially important to maintain this criteria in a study that relied on prespecified performance criteria rather than a control arm for judging efficacy, Dr. Calkins said.
The study also included three quality-of-life measures. Patient scores on the Atrial Fibrillation Effect on Quality-of-Life (AFEQT) questionnaire rose by an average of nearly 26 points from baseline to 12 months, a statistically significant and clinically meaningful increase. Scores on both the physical and mental domains of the Short Form-12 (SF-12) improved from baseline by an average of about five points on each subscale, also statistically significant and clinically meaningful changes. Patients also reported statistically significant and in some cases substantial reductions in the prevalence rates of each of five different AFib symptoms: dizziness, dyspnea, fatigue, palpitations, and rapid heartbeat.
The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
NATIONAL HARBOR, MD. – , setting the stage for the device to become the first to receive U.S. labeling for catheter ablation in this atrial fibrillation population.
The Arctic Front Advance cryoballoon, used on 165 patients with persistent atrial fibrillation (AFib) enrolled in the trial, produced a 55% rate of treatment success, including freedom from recurrent AFib during 12 months of follow-up, and produced one prespecified serious adverse event in the primary safety endpoint.
Both results easily surpassed the prespecified performance goals set by negotiation with the FDA, Hugh Calkins, MD, said at the annual International AF Symposium. The trial design included no control group and instead assessed safety and efficacy against prespecified standards set by the regulatory agency.
The cryoballoon “showed excellent performance. I don’t see how this could possibly be turned down by the FDA,” said Dr. Calkins, professor of medicine and director of the cardiac arrhythmia service at Johns Hopkins Medicine in Baltimore.
Cardiac electrophysiologists have for years routinely performed catheter ablation procedures on patients with persistent AFib even though the devices, based on ablation by radiofrequency or by chilling, have been labeled for use only in treating patients with paroxysmal AFib. Although this off-label use has not resulted in any problems with health insurance coverage, Dr. Calkins said, it has kept manufacturers from marketing their ablation devices for use in persistent AFib patients.
If the reported data result in labeling for the tested cryoballoon for persistant AFib patients, “it will have a big impact,” he predicted. “People have used cryoballoons for ablating persistent AFib for years, but this would put more fuel in the fire, both the [very positive] safety and efficacy data, and getting an FDA label, which is worth a lot,” he said in an interview.
But Dr. Calkins stopped short of anticipating that the results would convince operators experienced and focused on performing radiofrequency ablation to switch to cryo devices for treating persistent AFib patients. “People are pretty stuck in their ways,” he noted, and reports are expected soon from pivotal trials that are now testing various radiofrequency devices, as well as other types of cryo devices, in persistent AFib patients, so the range of device options labeled for this population may soon grow even more.
The STOP Persistent AF trial ran at 25 sites in the United States, Canada, and Japan during March 2017-August 2019, and included 165 adults with symptomatic, persistent AFib who had not responded to at least one antiarrhythmic drug and had a history of AFib episodes lasting at least 7 days but with no episodes persisting for 6 months or longer. The study excluded patients with prior ablation or left atrial surgery, a recent cerebrovascular event, substantially reduced left ventricular function, or substantial left atrial enlargement.
The enrolled patients were an average 65 years of age and 70% were men. Patients had been diagnosed with paroxysmal AFib an average of 5 years before study entry and with persistent AFib a little over 6 months before entry. The most recent AFib episode of enrolled patients averaged about 60 days, on average they had been unsuccessfully treated with just over one antiarrhythmic drug, and on average they had previously undergone about two cardioversions, after which their arrhythmia recurred.
The primary efficacy endpoint – a 55% rate of acute procedural success plus freedom from AFib recurrence during the 9 months following a 90-day blanking period immediately after ablation plus no added or increased antiarrhythmic drugs – significantly exceeded the prespecified performance goal of a 40% rate, Dr. Calkins reported. The study used the standard measure of recurrence as any 30-second or longer AFib episode detected during a weekly ECG telemonitoring session or during 48-hour ambulatory ECG monitoring at 6- and 12-month follow-ups or during in-office 12-lead ECG assessment at 3-, 6-, and 12-month follow-up. Twelve-month follow-up occurred for 145 of the enrolled patients.
The only prespecified primary safety event was one episode of cardiac perforation, which occurred during a repeat procedure. This rate of one safety event among 165 patients (0.6%) fell well within the prespecified safety performance goal of no more than 13%. In addition to this perforation, five additional serious adverse events (3%) occurred that were attributable to the cryoballoon treatment, including two cases of vascular pseudoaneurysm, one puncture-site hematoma, one case of pericarditis, and one episode of atrial tachycardia. Four additional serious adverse events occurred that were attributable to the ablation procedure (one acute cardiac failure, one postprocedure ileus, one respiratory failure, and one urinary tract infection), for an overall serious event rate of 5%.
During follow-up, 13% of patients had a repeat ablation procedure, following an initial ablation limited to pulmonary-vein isolation (PVI). The overall rate of 1-year efficacy, including the relatively low rate of need for redo ablation, “are an impressive endorsement of a PVI-only strategy” for initial ablation, Dr. Calkins said. “I’m a strong believer in PVI only for the first ablation for both paroxysmal and persistent AFib.”
He also noted that the 30-second threshold for scoring recurrent arrhythmia episodes following the 90-day blanking period after ablation was a very conservative measure of treatment failure, but it continues to define recurrence in this and many other current AFib ablation studies because it is the historical criteria for measuring ablation success or failure. It is especially important to maintain this criteria in a study that relied on prespecified performance criteria rather than a control arm for judging efficacy, Dr. Calkins said.
The study also included three quality-of-life measures. Patient scores on the Atrial Fibrillation Effect on Quality-of-Life (AFEQT) questionnaire rose by an average of nearly 26 points from baseline to 12 months, a statistically significant and clinically meaningful increase. Scores on both the physical and mental domains of the Short Form-12 (SF-12) improved from baseline by an average of about five points on each subscale, also statistically significant and clinically meaningful changes. Patients also reported statistically significant and in some cases substantial reductions in the prevalence rates of each of five different AFib symptoms: dizziness, dyspnea, fatigue, palpitations, and rapid heartbeat.
The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
NATIONAL HARBOR, MD. – , setting the stage for the device to become the first to receive U.S. labeling for catheter ablation in this atrial fibrillation population.
The Arctic Front Advance cryoballoon, used on 165 patients with persistent atrial fibrillation (AFib) enrolled in the trial, produced a 55% rate of treatment success, including freedom from recurrent AFib during 12 months of follow-up, and produced one prespecified serious adverse event in the primary safety endpoint.
Both results easily surpassed the prespecified performance goals set by negotiation with the FDA, Hugh Calkins, MD, said at the annual International AF Symposium. The trial design included no control group and instead assessed safety and efficacy against prespecified standards set by the regulatory agency.
The cryoballoon “showed excellent performance. I don’t see how this could possibly be turned down by the FDA,” said Dr. Calkins, professor of medicine and director of the cardiac arrhythmia service at Johns Hopkins Medicine in Baltimore.
Cardiac electrophysiologists have for years routinely performed catheter ablation procedures on patients with persistent AFib even though the devices, based on ablation by radiofrequency or by chilling, have been labeled for use only in treating patients with paroxysmal AFib. Although this off-label use has not resulted in any problems with health insurance coverage, Dr. Calkins said, it has kept manufacturers from marketing their ablation devices for use in persistent AFib patients.
If the reported data result in labeling for the tested cryoballoon for persistant AFib patients, “it will have a big impact,” he predicted. “People have used cryoballoons for ablating persistent AFib for years, but this would put more fuel in the fire, both the [very positive] safety and efficacy data, and getting an FDA label, which is worth a lot,” he said in an interview.
But Dr. Calkins stopped short of anticipating that the results would convince operators experienced and focused on performing radiofrequency ablation to switch to cryo devices for treating persistent AFib patients. “People are pretty stuck in their ways,” he noted, and reports are expected soon from pivotal trials that are now testing various radiofrequency devices, as well as other types of cryo devices, in persistent AFib patients, so the range of device options labeled for this population may soon grow even more.
The STOP Persistent AF trial ran at 25 sites in the United States, Canada, and Japan during March 2017-August 2019, and included 165 adults with symptomatic, persistent AFib who had not responded to at least one antiarrhythmic drug and had a history of AFib episodes lasting at least 7 days but with no episodes persisting for 6 months or longer. The study excluded patients with prior ablation or left atrial surgery, a recent cerebrovascular event, substantially reduced left ventricular function, or substantial left atrial enlargement.
The enrolled patients were an average 65 years of age and 70% were men. Patients had been diagnosed with paroxysmal AFib an average of 5 years before study entry and with persistent AFib a little over 6 months before entry. The most recent AFib episode of enrolled patients averaged about 60 days, on average they had been unsuccessfully treated with just over one antiarrhythmic drug, and on average they had previously undergone about two cardioversions, after which their arrhythmia recurred.
The primary efficacy endpoint – a 55% rate of acute procedural success plus freedom from AFib recurrence during the 9 months following a 90-day blanking period immediately after ablation plus no added or increased antiarrhythmic drugs – significantly exceeded the prespecified performance goal of a 40% rate, Dr. Calkins reported. The study used the standard measure of recurrence as any 30-second or longer AFib episode detected during a weekly ECG telemonitoring session or during 48-hour ambulatory ECG monitoring at 6- and 12-month follow-ups or during in-office 12-lead ECG assessment at 3-, 6-, and 12-month follow-up. Twelve-month follow-up occurred for 145 of the enrolled patients.
The only prespecified primary safety event was one episode of cardiac perforation, which occurred during a repeat procedure. This rate of one safety event among 165 patients (0.6%) fell well within the prespecified safety performance goal of no more than 13%. In addition to this perforation, five additional serious adverse events (3%) occurred that were attributable to the cryoballoon treatment, including two cases of vascular pseudoaneurysm, one puncture-site hematoma, one case of pericarditis, and one episode of atrial tachycardia. Four additional serious adverse events occurred that were attributable to the ablation procedure (one acute cardiac failure, one postprocedure ileus, one respiratory failure, and one urinary tract infection), for an overall serious event rate of 5%.
During follow-up, 13% of patients had a repeat ablation procedure, following an initial ablation limited to pulmonary-vein isolation (PVI). The overall rate of 1-year efficacy, including the relatively low rate of need for redo ablation, “are an impressive endorsement of a PVI-only strategy” for initial ablation, Dr. Calkins said. “I’m a strong believer in PVI only for the first ablation for both paroxysmal and persistent AFib.”
He also noted that the 30-second threshold for scoring recurrent arrhythmia episodes following the 90-day blanking period after ablation was a very conservative measure of treatment failure, but it continues to define recurrence in this and many other current AFib ablation studies because it is the historical criteria for measuring ablation success or failure. It is especially important to maintain this criteria in a study that relied on prespecified performance criteria rather than a control arm for judging efficacy, Dr. Calkins said.
The study also included three quality-of-life measures. Patient scores on the Atrial Fibrillation Effect on Quality-of-Life (AFEQT) questionnaire rose by an average of nearly 26 points from baseline to 12 months, a statistically significant and clinically meaningful increase. Scores on both the physical and mental domains of the Short Form-12 (SF-12) improved from baseline by an average of about five points on each subscale, also statistically significant and clinically meaningful changes. Patients also reported statistically significant and in some cases substantial reductions in the prevalence rates of each of five different AFib symptoms: dizziness, dyspnea, fatigue, palpitations, and rapid heartbeat.
The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
REPORTING FROM THE AF SYMPOSIUM 2020
Key clinical point: Catheter ablation using a cryoballoon was safe and effective for patients with persistent atrial fibrillation in a pivotal trial.
Major finding: The rate of freedom from treatment failure after 12 months was 55%, significantly exceeding the prespecified performance goal of 40%.
Study details: A multicenter, international study with 165 enrolled patients.
Disclosures: The study was funded by Medtronic, the company that markets the tested cryoballoon (Arctic Front Advance). Dr. Calkins has been a consultant to and has received honoraria from Medtronic, as well as from Abbott, AtriCure, Boehringer Ingelheim, Boston Scientific, and Johnson & Johnson.
Redo PCI or CABG, left main patients pay a price: EXCEL
Repeat revascularization was more frequent after left main percutaneous coronary intervention than after coronary artery bypass surgery, but raised the mortality risk after both procedures in a secondary EXCEL analysis.
The 3-year rate of any repeat revascularization was 12.9% after PCI and 7.6% after CABG (hazard ratio, 1.73; 95% confidence interval, 1.28-2.33).
“It’s a real difference and shouldn’t be minimized. About 1 in 20 patients will need an additional repeat revascularization after PCI, compared with surgery,” study author Gregg Stone, MD, Icahn School of Medicine at Mount Sinai in New York, said in an interview. “Surgery is a more durable procedure in that regard, and patients need to be informed of that by heart team discussions.”
That said, Dr. Stone highlighted other differences between the two strategies, including more bleeding and atrial fibrillation after surgery and better early quality of life after PCI. There’s also an early myocardial infarction (MI) benefit with PCI but a late MI benefit with surgery, which “is probably a more important difference between the two, as opposed to the difference in repeat revascularization,” he added.
Although the increased need to perform repeat vascularization after PCI is not unexpected, the analysis of 346 repeat revascularizations in 185 patients provides more details on the timing and prognosis of these procedures in left main disease.
The need for repeat revascularization was independently associated with 3-year all-cause mortality (adjusted HR, 2.05; 95% CI, 1.13-3.70) and cardiovascular mortality (adjusted HR, 4.22; 95% CI, 2.10-8.48) for both PCI and CABG (P for interaction = .85 for both outcomes).
The increase in mortality risk, however, was smaller than that for MI (adjusted HR, 4.03; 95% CI, 2.43-6.67) or stroke (adjusted HR, 16.62; 95% CI, 9.97-27.69).
The risk for death peaked in the 30 days after redo revascularization and then declined during follow-up. Most of the deaths were cardiovascular (74/128).
The incidence of repeat left main PCI was only 17.5%, whereas the left main was the most common site for redo revascularization in the CABG group.
Repeat revascularization of the index target vessel and target lesion – but not of other lesions – were both strongly associated with increased all-cause and cardiovascular mortality, the authors reported January 15 in JACC: Cardiovascular Interventions.
“It just continues to show that, no matter what intervention we use, we haven’t achieved perfection yet and the opportunities for improvement and decision making between a PCI and a CABG is still up in the air,” Richard J. Shemin, MD, chief of cardiac surgery, UCLA Medical Center, Los Angeles, said in an interview. “And there’s some evidence to suggest coronary bypass might be better in terms of mortality and the need for repeat revascularization.”
Enhancing durability
“Measures to reduce the need for repeat revascularization including improved stent platforms and implantation technique, use of pan-arterial bypass grafting, and aggressive risk factor control with guideline-directed medical therapy may improve prognosis after both PCI and CABG,” the authors concluded.
In a linked editorial, David O. Williams, MD, and Pinak B. Shah, MD, both with Brigham and Women’s Hospital and Harvard Medical School, Boston, say intravascular imaging should be “mandatory for all complex PCI,” but that intravascular ultrasound was used in only 77.2% of cases in EXCEL.
“There are also data suggesting careful image guidance during complex PCI is associated with a mortality benefit,” they wrote. “In a similar fashion, arterial revascularization (especially with a mammary artery graft to the [left anterior descending]) and complete revascularization during CABG needs to be achieved.”
“Surgeons need to be intellectually challenged to not take the easy way out and just do a saphenous vein graft,” Dr. Shemin agreed. “And because we are dealing with an underlying progressive disease, continued medical and preventive measures to prevent atherosclerosis are key.”
Higher body mass index, insulin-treated diabetes, and hemodynamic support during the procedure were associated with a higher risk for repeat revascularization after PCI, whereas statin use at discharge was protective.
Younger age, female sex, and peripheral vascular disease were independent predictors of repeat revascularization after CABG.
Most redo procedures were performed by PCI in both groups. However, repeat revascularization by CABG was more common during follow-up in patients randomized to initial PCI vs. CABG (3.3% vs .0.8%; P = .0002) and was significantly associated with increased all-cause mortality.
“This observation suggests that CABG should be reserved for repeat revascularization procedures that are not amenable to repeat PCI, irrespective of the initial revascularization approach,” the authors wrote.
The editorialists point out that more than half of EXCEL patients with one repeat revascularization went on to have another. Overall, 55.1% of patients underwent one repeat revascularization, 22.2% underwent two redos, and 22.7% underwent more than two redos.
Although enhancing the durability of the initial revascularization is an important goal, “one might also conclude that a safer and potentially more durable treatment specifically developed for recurrent lesions is as equally an important objective,” they opined.
5-year kerfuffle
As previously reported, the EXCEL trial’s 5-year analysis showed no significant difference between PCI and CABG for the primary endpoint of all-cause death, MI, or stroke.
However, recent allegations that key MI data were withheld have called into question the final conclusion of relative parity and led the European Association for Cardio-Thoracic Surgery (EACTS) to withdraw support for the left main portion of the 2018 EACTS-European Society of Cardiology (ESC) clinical guidelines based on 3-year EXCEL outcomes.
On January 14, the Society of Thoracic Surgeons (STS) joined EACTS and the American Association for Thoracic Surgery in calling for independent reanalysis of the EXCEL data.
“Any final conclusions drawn from the EXCEL trial will not only affect the actions of physicians, surgeons, regulatory agencies, and third-party payers but, more importantly, they will seriously impact the health and wellbeing of our patients and their families for years to come,” the statement says.
“Given such potentially profound consequences, the Society believes that the final interpretation regarding the outcomes of the EXCEL study should wait until an independent analysis of all aspects of the EXCEL study has been performed.”
EXCEL was sponsored by Abbott Vascular. Dr. Stone reported speaker honoraria from Terumo and Amaranth and serving as a consultant to Reva. Coauthor conflict of interest disclosures are listed in the paper. Dr. Shemin reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
Repeat revascularization was more frequent after left main percutaneous coronary intervention than after coronary artery bypass surgery, but raised the mortality risk after both procedures in a secondary EXCEL analysis.
The 3-year rate of any repeat revascularization was 12.9% after PCI and 7.6% after CABG (hazard ratio, 1.73; 95% confidence interval, 1.28-2.33).
“It’s a real difference and shouldn’t be minimized. About 1 in 20 patients will need an additional repeat revascularization after PCI, compared with surgery,” study author Gregg Stone, MD, Icahn School of Medicine at Mount Sinai in New York, said in an interview. “Surgery is a more durable procedure in that regard, and patients need to be informed of that by heart team discussions.”
That said, Dr. Stone highlighted other differences between the two strategies, including more bleeding and atrial fibrillation after surgery and better early quality of life after PCI. There’s also an early myocardial infarction (MI) benefit with PCI but a late MI benefit with surgery, which “is probably a more important difference between the two, as opposed to the difference in repeat revascularization,” he added.
Although the increased need to perform repeat vascularization after PCI is not unexpected, the analysis of 346 repeat revascularizations in 185 patients provides more details on the timing and prognosis of these procedures in left main disease.
The need for repeat revascularization was independently associated with 3-year all-cause mortality (adjusted HR, 2.05; 95% CI, 1.13-3.70) and cardiovascular mortality (adjusted HR, 4.22; 95% CI, 2.10-8.48) for both PCI and CABG (P for interaction = .85 for both outcomes).
The increase in mortality risk, however, was smaller than that for MI (adjusted HR, 4.03; 95% CI, 2.43-6.67) or stroke (adjusted HR, 16.62; 95% CI, 9.97-27.69).
The risk for death peaked in the 30 days after redo revascularization and then declined during follow-up. Most of the deaths were cardiovascular (74/128).
The incidence of repeat left main PCI was only 17.5%, whereas the left main was the most common site for redo revascularization in the CABG group.
Repeat revascularization of the index target vessel and target lesion – but not of other lesions – were both strongly associated with increased all-cause and cardiovascular mortality, the authors reported January 15 in JACC: Cardiovascular Interventions.
“It just continues to show that, no matter what intervention we use, we haven’t achieved perfection yet and the opportunities for improvement and decision making between a PCI and a CABG is still up in the air,” Richard J. Shemin, MD, chief of cardiac surgery, UCLA Medical Center, Los Angeles, said in an interview. “And there’s some evidence to suggest coronary bypass might be better in terms of mortality and the need for repeat revascularization.”
Enhancing durability
“Measures to reduce the need for repeat revascularization including improved stent platforms and implantation technique, use of pan-arterial bypass grafting, and aggressive risk factor control with guideline-directed medical therapy may improve prognosis after both PCI and CABG,” the authors concluded.
In a linked editorial, David O. Williams, MD, and Pinak B. Shah, MD, both with Brigham and Women’s Hospital and Harvard Medical School, Boston, say intravascular imaging should be “mandatory for all complex PCI,” but that intravascular ultrasound was used in only 77.2% of cases in EXCEL.
“There are also data suggesting careful image guidance during complex PCI is associated with a mortality benefit,” they wrote. “In a similar fashion, arterial revascularization (especially with a mammary artery graft to the [left anterior descending]) and complete revascularization during CABG needs to be achieved.”
“Surgeons need to be intellectually challenged to not take the easy way out and just do a saphenous vein graft,” Dr. Shemin agreed. “And because we are dealing with an underlying progressive disease, continued medical and preventive measures to prevent atherosclerosis are key.”
Higher body mass index, insulin-treated diabetes, and hemodynamic support during the procedure were associated with a higher risk for repeat revascularization after PCI, whereas statin use at discharge was protective.
Younger age, female sex, and peripheral vascular disease were independent predictors of repeat revascularization after CABG.
Most redo procedures were performed by PCI in both groups. However, repeat revascularization by CABG was more common during follow-up in patients randomized to initial PCI vs. CABG (3.3% vs .0.8%; P = .0002) and was significantly associated with increased all-cause mortality.
“This observation suggests that CABG should be reserved for repeat revascularization procedures that are not amenable to repeat PCI, irrespective of the initial revascularization approach,” the authors wrote.
The editorialists point out that more than half of EXCEL patients with one repeat revascularization went on to have another. Overall, 55.1% of patients underwent one repeat revascularization, 22.2% underwent two redos, and 22.7% underwent more than two redos.
Although enhancing the durability of the initial revascularization is an important goal, “one might also conclude that a safer and potentially more durable treatment specifically developed for recurrent lesions is as equally an important objective,” they opined.
5-year kerfuffle
As previously reported, the EXCEL trial’s 5-year analysis showed no significant difference between PCI and CABG for the primary endpoint of all-cause death, MI, or stroke.
However, recent allegations that key MI data were withheld have called into question the final conclusion of relative parity and led the European Association for Cardio-Thoracic Surgery (EACTS) to withdraw support for the left main portion of the 2018 EACTS-European Society of Cardiology (ESC) clinical guidelines based on 3-year EXCEL outcomes.
On January 14, the Society of Thoracic Surgeons (STS) joined EACTS and the American Association for Thoracic Surgery in calling for independent reanalysis of the EXCEL data.
“Any final conclusions drawn from the EXCEL trial will not only affect the actions of physicians, surgeons, regulatory agencies, and third-party payers but, more importantly, they will seriously impact the health and wellbeing of our patients and their families for years to come,” the statement says.
“Given such potentially profound consequences, the Society believes that the final interpretation regarding the outcomes of the EXCEL study should wait until an independent analysis of all aspects of the EXCEL study has been performed.”
EXCEL was sponsored by Abbott Vascular. Dr. Stone reported speaker honoraria from Terumo and Amaranth and serving as a consultant to Reva. Coauthor conflict of interest disclosures are listed in the paper. Dr. Shemin reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
Repeat revascularization was more frequent after left main percutaneous coronary intervention than after coronary artery bypass surgery, but raised the mortality risk after both procedures in a secondary EXCEL analysis.
The 3-year rate of any repeat revascularization was 12.9% after PCI and 7.6% after CABG (hazard ratio, 1.73; 95% confidence interval, 1.28-2.33).
“It’s a real difference and shouldn’t be minimized. About 1 in 20 patients will need an additional repeat revascularization after PCI, compared with surgery,” study author Gregg Stone, MD, Icahn School of Medicine at Mount Sinai in New York, said in an interview. “Surgery is a more durable procedure in that regard, and patients need to be informed of that by heart team discussions.”
That said, Dr. Stone highlighted other differences between the two strategies, including more bleeding and atrial fibrillation after surgery and better early quality of life after PCI. There’s also an early myocardial infarction (MI) benefit with PCI but a late MI benefit with surgery, which “is probably a more important difference between the two, as opposed to the difference in repeat revascularization,” he added.
Although the increased need to perform repeat vascularization after PCI is not unexpected, the analysis of 346 repeat revascularizations in 185 patients provides more details on the timing and prognosis of these procedures in left main disease.
The need for repeat revascularization was independently associated with 3-year all-cause mortality (adjusted HR, 2.05; 95% CI, 1.13-3.70) and cardiovascular mortality (adjusted HR, 4.22; 95% CI, 2.10-8.48) for both PCI and CABG (P for interaction = .85 for both outcomes).
The increase in mortality risk, however, was smaller than that for MI (adjusted HR, 4.03; 95% CI, 2.43-6.67) or stroke (adjusted HR, 16.62; 95% CI, 9.97-27.69).
The risk for death peaked in the 30 days after redo revascularization and then declined during follow-up. Most of the deaths were cardiovascular (74/128).
The incidence of repeat left main PCI was only 17.5%, whereas the left main was the most common site for redo revascularization in the CABG group.
Repeat revascularization of the index target vessel and target lesion – but not of other lesions – were both strongly associated with increased all-cause and cardiovascular mortality, the authors reported January 15 in JACC: Cardiovascular Interventions.
“It just continues to show that, no matter what intervention we use, we haven’t achieved perfection yet and the opportunities for improvement and decision making between a PCI and a CABG is still up in the air,” Richard J. Shemin, MD, chief of cardiac surgery, UCLA Medical Center, Los Angeles, said in an interview. “And there’s some evidence to suggest coronary bypass might be better in terms of mortality and the need for repeat revascularization.”
Enhancing durability
“Measures to reduce the need for repeat revascularization including improved stent platforms and implantation technique, use of pan-arterial bypass grafting, and aggressive risk factor control with guideline-directed medical therapy may improve prognosis after both PCI and CABG,” the authors concluded.
In a linked editorial, David O. Williams, MD, and Pinak B. Shah, MD, both with Brigham and Women’s Hospital and Harvard Medical School, Boston, say intravascular imaging should be “mandatory for all complex PCI,” but that intravascular ultrasound was used in only 77.2% of cases in EXCEL.
“There are also data suggesting careful image guidance during complex PCI is associated with a mortality benefit,” they wrote. “In a similar fashion, arterial revascularization (especially with a mammary artery graft to the [left anterior descending]) and complete revascularization during CABG needs to be achieved.”
“Surgeons need to be intellectually challenged to not take the easy way out and just do a saphenous vein graft,” Dr. Shemin agreed. “And because we are dealing with an underlying progressive disease, continued medical and preventive measures to prevent atherosclerosis are key.”
Higher body mass index, insulin-treated diabetes, and hemodynamic support during the procedure were associated with a higher risk for repeat revascularization after PCI, whereas statin use at discharge was protective.
Younger age, female sex, and peripheral vascular disease were independent predictors of repeat revascularization after CABG.
Most redo procedures were performed by PCI in both groups. However, repeat revascularization by CABG was more common during follow-up in patients randomized to initial PCI vs. CABG (3.3% vs .0.8%; P = .0002) and was significantly associated with increased all-cause mortality.
“This observation suggests that CABG should be reserved for repeat revascularization procedures that are not amenable to repeat PCI, irrespective of the initial revascularization approach,” the authors wrote.
The editorialists point out that more than half of EXCEL patients with one repeat revascularization went on to have another. Overall, 55.1% of patients underwent one repeat revascularization, 22.2% underwent two redos, and 22.7% underwent more than two redos.
Although enhancing the durability of the initial revascularization is an important goal, “one might also conclude that a safer and potentially more durable treatment specifically developed for recurrent lesions is as equally an important objective,” they opined.
5-year kerfuffle
As previously reported, the EXCEL trial’s 5-year analysis showed no significant difference between PCI and CABG for the primary endpoint of all-cause death, MI, or stroke.
However, recent allegations that key MI data were withheld have called into question the final conclusion of relative parity and led the European Association for Cardio-Thoracic Surgery (EACTS) to withdraw support for the left main portion of the 2018 EACTS-European Society of Cardiology (ESC) clinical guidelines based on 3-year EXCEL outcomes.
On January 14, the Society of Thoracic Surgeons (STS) joined EACTS and the American Association for Thoracic Surgery in calling for independent reanalysis of the EXCEL data.
“Any final conclusions drawn from the EXCEL trial will not only affect the actions of physicians, surgeons, regulatory agencies, and third-party payers but, more importantly, they will seriously impact the health and wellbeing of our patients and their families for years to come,” the statement says.
“Given such potentially profound consequences, the Society believes that the final interpretation regarding the outcomes of the EXCEL study should wait until an independent analysis of all aspects of the EXCEL study has been performed.”
EXCEL was sponsored by Abbott Vascular. Dr. Stone reported speaker honoraria from Terumo and Amaranth and serving as a consultant to Reva. Coauthor conflict of interest disclosures are listed in the paper. Dr. Shemin reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
Why STEMI patients benefit from PCI of nonculprit lesions
PHILADELPHIA – Nearly half of patients with ST-elevation MI and multivessel coronary artery disease in the landmark COMPLETE trial had an obstructive coronary lesion with vulnerable plaque morphology in a segment far from the culprit lesion, Natalia Pinilla-Echeverri, MD, reported at the American Heart Association scientific sessions.
This novel finding from an optical coherence tomography (OCT) substudy of COMPLETE provides a likely mechanistic explanation for the major clinical benefits documented in the full COMPLETE trial, noted Dr. Pinilla-Echeverri, a cardiologist at the Population Health Research Institute at McMaster University, Hamilton, Ont.
COMPLETE was a multinational trial which randomized 4,041 ST-elevation MI (STEMI) patients with multivessel disease to culprit lesion–only percutaneous coronary intervention (PCI) or additional routine angiography–guided staged PCI of nonculprit obstructive lesions with at least 70% stenosis. As previously reported, the risk of the coprimary composite endpoint comprising cardiovascular death, new MI, or ischemia-driven revascularization was reduced by 49% over 3 years of follow-up in the group with staged PCI of nonculprit lesions, with an impressive number needed to treat of just 13 (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
Dr. Pinella-Echeverri reported on the 93 patients who participated in the OCT substudy, the purpose of which was to determine the prevalence of high-risk, vulnerable plaque in obstructive and nonobstructive nonculprit lesions. For this purpose, vulnerable plaque was defined as thin-cap fibroatheroma (TCFA), a coronary lesion known to pose high risk of worsening stenosis, plaque rupture, and cardiovascular events.
Of note, these 93 patients had a total of 425 diseased segments: 150 obstructive and 275 nonobstructive.
“This is reassuring that the concept of acute coronary syndrome implies a diffuse pathophysiology of affecting not only the culprit segment but the coronary vasculature as a whole,” Dr. Pinella-Echeverri observed.
The main study finding, however, was that TCFA was significantly more prevalent in obstructive, compared with nonobstructive, nonculprit lesions by a margin of 35% to 23%. The obstructive and nonobstructive TCFA lesions had a similar lipid-rich composition; however, the obstructive ones were significantly longer and had a smaller mean lumen area.
When breaking down the prevalence of TCFA per patient, 47% of patients had a nonculprit obstructive lesion with vulnerable plaque morphology. Another 20% had nonobstructive TCFA lesions. And only 32% of the STEMI patients had no TCFA in their obstructive or nonobstructive segments.
Discussant Frans Van de Werf, MD, PhD, commented: “This [OCT substudy result] immediately explains the clinical benefit observed with preventive PCI in STEMI patients with obstructive multivessel disease.”
The finding that 20% of the STEMI patients had nonobstructive lesions with vulnerable plaque morphology by OCT provides powerful support for the current guideline-recommended strategy of immediately starting STEMI patients on intensive lipid-lowering therapy, added Dr. Van de Werf, professor of medicine at the Catholic University of Leuven (Belgium).
He argued that the decision to revascularize nonculprit lesions by means of PCI versus the more complete revascularization achieved via coronary artery bypass graft surgery shouldn’t be made during the initial primary PCI, citing evidence that when the decision gets made at that time, coronary artery bypass grafting (CABG) is less likely to be chosen.
“I believe that OCT and [fractional flow reserve] should not be performed during the index primary PCI, not only for the comfort of the patient, but also for the better selection of complete revascularization. Interventional cardiologists should not forget that CABG might be a better revascularization treatment in some cases, such as left main disease and diabetes mellitus,” the cardiologist cautioned.
The COMPLETE OCT Substudy was supported by Abbott Vascular, the Population Health Research Institute, Hamilton Health Sciences, and the Canadian Institutes of Health Research.
PHILADELPHIA – Nearly half of patients with ST-elevation MI and multivessel coronary artery disease in the landmark COMPLETE trial had an obstructive coronary lesion with vulnerable plaque morphology in a segment far from the culprit lesion, Natalia Pinilla-Echeverri, MD, reported at the American Heart Association scientific sessions.
This novel finding from an optical coherence tomography (OCT) substudy of COMPLETE provides a likely mechanistic explanation for the major clinical benefits documented in the full COMPLETE trial, noted Dr. Pinilla-Echeverri, a cardiologist at the Population Health Research Institute at McMaster University, Hamilton, Ont.
COMPLETE was a multinational trial which randomized 4,041 ST-elevation MI (STEMI) patients with multivessel disease to culprit lesion–only percutaneous coronary intervention (PCI) or additional routine angiography–guided staged PCI of nonculprit obstructive lesions with at least 70% stenosis. As previously reported, the risk of the coprimary composite endpoint comprising cardiovascular death, new MI, or ischemia-driven revascularization was reduced by 49% over 3 years of follow-up in the group with staged PCI of nonculprit lesions, with an impressive number needed to treat of just 13 (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
Dr. Pinella-Echeverri reported on the 93 patients who participated in the OCT substudy, the purpose of which was to determine the prevalence of high-risk, vulnerable plaque in obstructive and nonobstructive nonculprit lesions. For this purpose, vulnerable plaque was defined as thin-cap fibroatheroma (TCFA), a coronary lesion known to pose high risk of worsening stenosis, plaque rupture, and cardiovascular events.
Of note, these 93 patients had a total of 425 diseased segments: 150 obstructive and 275 nonobstructive.
“This is reassuring that the concept of acute coronary syndrome implies a diffuse pathophysiology of affecting not only the culprit segment but the coronary vasculature as a whole,” Dr. Pinella-Echeverri observed.
The main study finding, however, was that TCFA was significantly more prevalent in obstructive, compared with nonobstructive, nonculprit lesions by a margin of 35% to 23%. The obstructive and nonobstructive TCFA lesions had a similar lipid-rich composition; however, the obstructive ones were significantly longer and had a smaller mean lumen area.
When breaking down the prevalence of TCFA per patient, 47% of patients had a nonculprit obstructive lesion with vulnerable plaque morphology. Another 20% had nonobstructive TCFA lesions. And only 32% of the STEMI patients had no TCFA in their obstructive or nonobstructive segments.
Discussant Frans Van de Werf, MD, PhD, commented: “This [OCT substudy result] immediately explains the clinical benefit observed with preventive PCI in STEMI patients with obstructive multivessel disease.”
The finding that 20% of the STEMI patients had nonobstructive lesions with vulnerable plaque morphology by OCT provides powerful support for the current guideline-recommended strategy of immediately starting STEMI patients on intensive lipid-lowering therapy, added Dr. Van de Werf, professor of medicine at the Catholic University of Leuven (Belgium).
He argued that the decision to revascularize nonculprit lesions by means of PCI versus the more complete revascularization achieved via coronary artery bypass graft surgery shouldn’t be made during the initial primary PCI, citing evidence that when the decision gets made at that time, coronary artery bypass grafting (CABG) is less likely to be chosen.
“I believe that OCT and [fractional flow reserve] should not be performed during the index primary PCI, not only for the comfort of the patient, but also for the better selection of complete revascularization. Interventional cardiologists should not forget that CABG might be a better revascularization treatment in some cases, such as left main disease and diabetes mellitus,” the cardiologist cautioned.
The COMPLETE OCT Substudy was supported by Abbott Vascular, the Population Health Research Institute, Hamilton Health Sciences, and the Canadian Institutes of Health Research.
PHILADELPHIA – Nearly half of patients with ST-elevation MI and multivessel coronary artery disease in the landmark COMPLETE trial had an obstructive coronary lesion with vulnerable plaque morphology in a segment far from the culprit lesion, Natalia Pinilla-Echeverri, MD, reported at the American Heart Association scientific sessions.
This novel finding from an optical coherence tomography (OCT) substudy of COMPLETE provides a likely mechanistic explanation for the major clinical benefits documented in the full COMPLETE trial, noted Dr. Pinilla-Echeverri, a cardiologist at the Population Health Research Institute at McMaster University, Hamilton, Ont.
COMPLETE was a multinational trial which randomized 4,041 ST-elevation MI (STEMI) patients with multivessel disease to culprit lesion–only percutaneous coronary intervention (PCI) or additional routine angiography–guided staged PCI of nonculprit obstructive lesions with at least 70% stenosis. As previously reported, the risk of the coprimary composite endpoint comprising cardiovascular death, new MI, or ischemia-driven revascularization was reduced by 49% over 3 years of follow-up in the group with staged PCI of nonculprit lesions, with an impressive number needed to treat of just 13 (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
Dr. Pinella-Echeverri reported on the 93 patients who participated in the OCT substudy, the purpose of which was to determine the prevalence of high-risk, vulnerable plaque in obstructive and nonobstructive nonculprit lesions. For this purpose, vulnerable plaque was defined as thin-cap fibroatheroma (TCFA), a coronary lesion known to pose high risk of worsening stenosis, plaque rupture, and cardiovascular events.
Of note, these 93 patients had a total of 425 diseased segments: 150 obstructive and 275 nonobstructive.
“This is reassuring that the concept of acute coronary syndrome implies a diffuse pathophysiology of affecting not only the culprit segment but the coronary vasculature as a whole,” Dr. Pinella-Echeverri observed.
The main study finding, however, was that TCFA was significantly more prevalent in obstructive, compared with nonobstructive, nonculprit lesions by a margin of 35% to 23%. The obstructive and nonobstructive TCFA lesions had a similar lipid-rich composition; however, the obstructive ones were significantly longer and had a smaller mean lumen area.
When breaking down the prevalence of TCFA per patient, 47% of patients had a nonculprit obstructive lesion with vulnerable plaque morphology. Another 20% had nonobstructive TCFA lesions. And only 32% of the STEMI patients had no TCFA in their obstructive or nonobstructive segments.
Discussant Frans Van de Werf, MD, PhD, commented: “This [OCT substudy result] immediately explains the clinical benefit observed with preventive PCI in STEMI patients with obstructive multivessel disease.”
The finding that 20% of the STEMI patients had nonobstructive lesions with vulnerable plaque morphology by OCT provides powerful support for the current guideline-recommended strategy of immediately starting STEMI patients on intensive lipid-lowering therapy, added Dr. Van de Werf, professor of medicine at the Catholic University of Leuven (Belgium).
He argued that the decision to revascularize nonculprit lesions by means of PCI versus the more complete revascularization achieved via coronary artery bypass graft surgery shouldn’t be made during the initial primary PCI, citing evidence that when the decision gets made at that time, coronary artery bypass grafting (CABG) is less likely to be chosen.
“I believe that OCT and [fractional flow reserve] should not be performed during the index primary PCI, not only for the comfort of the patient, but also for the better selection of complete revascularization. Interventional cardiologists should not forget that CABG might be a better revascularization treatment in some cases, such as left main disease and diabetes mellitus,” the cardiologist cautioned.
The COMPLETE OCT Substudy was supported by Abbott Vascular, the Population Health Research Institute, Hamilton Health Sciences, and the Canadian Institutes of Health Research.
REPORTING FROM AHA 2019
Cardiovascular risks associated with cannabis use
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
RECOVERY: Early SAVR benefits asymptomatic severe AS patients
PHILADELPHIA – Early aortic valve replacement surgery for patients with asymptomatic, severe aortic stenosis has been a controversial strategy, but the first randomized trial comparing early surgery with conservative management found that early-surgery patients had a 17-fold improved survival at 8 years, according to trial results reported at the American Heart Association scientific sessions.
Albeit small – 145 patients randomized to early surgery or conservative therapy – the RECOVERY trial results provide important evidence to support early preemptive aortic valve replacement for patients with asymptomatic but severe aortic stenosis, said Duk-Hyun Kang, MD, of the division of cardiology, Asan Medical Center in Seoul, South Korea.
The trial randomized 73 patients to early surgical aortic valve replacement (SAVR) and 72 to conventional treatment. Baseline characteristics were similar between the two groups, with a mean EuroSCORE II of 0.9, peak aortic-valve jet velocity (Vmax) of 5.1 m/sec, and mean aortic-valve area of 0.63 cm2. Fifty-three conventional treatment patients went on to have SAVR when symptoms developed during follow-up. There were no operation-related deaths in either group, although one early surgery patient had a stroke and one conventional treatment patients had an MI during the operative period.
At a median follow-up of 6.2 years, 1 early-surgery patient (1.4%) and 11 conventional-therapy patients (15.3%) died from operative or cardiovascular death, Dr. Kang said (P = 0.003). “The number needed to treat to prevent one cardiovascular death within 4 years was 20 patients,” Dr. Kang said. At 4 and 8 years, the cumulative incidences of operative CV or death were 1.4% for both in the early-surgery group and 5.7% and 25.5% in the conventional-treatment group, Dr. Kang said (P = 0.003).
Rates of all-cause mortality were 6.8% and 20.8% (P = 0.030) in the respective groups. “The number needed to treat to save one life in 4 years was 16 patients,” Dr. Kang said. At 4 and 8 years, the cumulative incidence of any-cause death was 4.1% and 10.2% in the early-surgery patients and 9.7% and 31.8% in the conventional group (P = 0.018).
Among the trial limitations Dr. Kang acknowledged were that the population had severe AS with aortic velocity of 4.5 m/sec or greater. “The benefit of early surgery may be relatively smaller in asymptomatic patients with less severe aortic stenosis,” he said.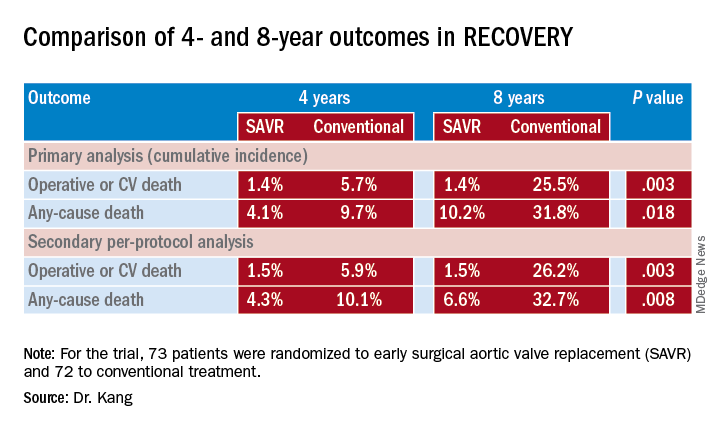
Not all patients had an exercise test to confirm their asymptomatic status, but as discussant Robert Bonow, MD, of Northwestern University in Chicago pointed out, “this is what we’re dealing with clinically.” Also the mean age of the patient population – 64.9 years – is relatively young, and they had a high incidence of bicuspid aortic valve, few comorbidities, and low operative risk, Dr. Kang said. “Thus, our study population is quite different from the populations enrolled in the TAVR [transcatheter AVR] trials, and the results of our study cannot be directly applied to early TAVR for asymptomatic severe aortic stenosis,” he said.
The mean age in both the PARTNER 3 (N Engl J Med. 2019;380:1695-705) and EVOLUT (N Engl J Med. 2019;380:1706-15) trials comparing TAVR and SAVR in low-risk patients was 73.6 years, and they had higher rates of comorbidities than did the RECOVERY patients.
Dr. Bonow said the RECOVERY findings add to the PARTNER 3 and EVOLUT findings and raise the question about rethinking guideline indications for AVR in asymptomatic severe AS patients. “Should we be talking about moving our Vmax threshold down to 4.5 m/sec, or maybe increasing the Class IIa indications to Class I?” he said. “I think we need to wait to see more data to support these excellent results.”
However, most of these asymptomatic patients do eventually have surgery “in a very short period of time,” Dr. Bonow said. “So from a clinical management point of view, I think we already have the data suggesting that we could move the ball forward, and now we have these excellent outcome data from Korea as well.”
Results were published simultaneously in the New England Journal of Medicine (2019 Nov 16. doi: 10.1056/NEJMoa1912846).
Dr. Kang and Dr. Bonow had no financial relationships to disclose.
PHILADELPHIA – Early aortic valve replacement surgery for patients with asymptomatic, severe aortic stenosis has been a controversial strategy, but the first randomized trial comparing early surgery with conservative management found that early-surgery patients had a 17-fold improved survival at 8 years, according to trial results reported at the American Heart Association scientific sessions.
Albeit small – 145 patients randomized to early surgery or conservative therapy – the RECOVERY trial results provide important evidence to support early preemptive aortic valve replacement for patients with asymptomatic but severe aortic stenosis, said Duk-Hyun Kang, MD, of the division of cardiology, Asan Medical Center in Seoul, South Korea.
The trial randomized 73 patients to early surgical aortic valve replacement (SAVR) and 72 to conventional treatment. Baseline characteristics were similar between the two groups, with a mean EuroSCORE II of 0.9, peak aortic-valve jet velocity (Vmax) of 5.1 m/sec, and mean aortic-valve area of 0.63 cm2. Fifty-three conventional treatment patients went on to have SAVR when symptoms developed during follow-up. There were no operation-related deaths in either group, although one early surgery patient had a stroke and one conventional treatment patients had an MI during the operative period.
At a median follow-up of 6.2 years, 1 early-surgery patient (1.4%) and 11 conventional-therapy patients (15.3%) died from operative or cardiovascular death, Dr. Kang said (P = 0.003). “The number needed to treat to prevent one cardiovascular death within 4 years was 20 patients,” Dr. Kang said. At 4 and 8 years, the cumulative incidences of operative CV or death were 1.4% for both in the early-surgery group and 5.7% and 25.5% in the conventional-treatment group, Dr. Kang said (P = 0.003).
Rates of all-cause mortality were 6.8% and 20.8% (P = 0.030) in the respective groups. “The number needed to treat to save one life in 4 years was 16 patients,” Dr. Kang said. At 4 and 8 years, the cumulative incidence of any-cause death was 4.1% and 10.2% in the early-surgery patients and 9.7% and 31.8% in the conventional group (P = 0.018).
Among the trial limitations Dr. Kang acknowledged were that the population had severe AS with aortic velocity of 4.5 m/sec or greater. “The benefit of early surgery may be relatively smaller in asymptomatic patients with less severe aortic stenosis,” he said.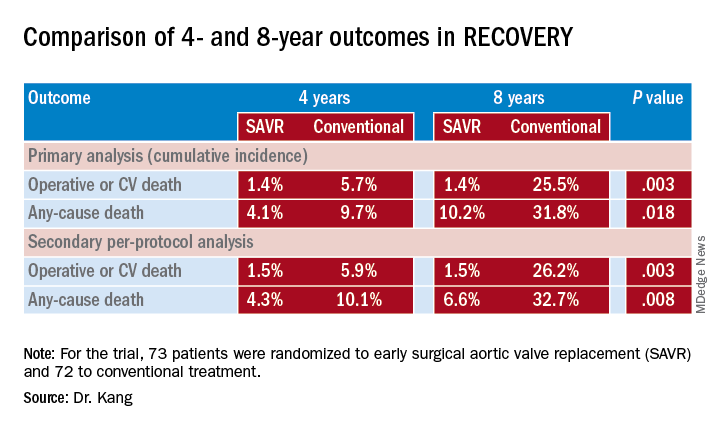
Not all patients had an exercise test to confirm their asymptomatic status, but as discussant Robert Bonow, MD, of Northwestern University in Chicago pointed out, “this is what we’re dealing with clinically.” Also the mean age of the patient population – 64.9 years – is relatively young, and they had a high incidence of bicuspid aortic valve, few comorbidities, and low operative risk, Dr. Kang said. “Thus, our study population is quite different from the populations enrolled in the TAVR [transcatheter AVR] trials, and the results of our study cannot be directly applied to early TAVR for asymptomatic severe aortic stenosis,” he said.
The mean age in both the PARTNER 3 (N Engl J Med. 2019;380:1695-705) and EVOLUT (N Engl J Med. 2019;380:1706-15) trials comparing TAVR and SAVR in low-risk patients was 73.6 years, and they had higher rates of comorbidities than did the RECOVERY patients.
Dr. Bonow said the RECOVERY findings add to the PARTNER 3 and EVOLUT findings and raise the question about rethinking guideline indications for AVR in asymptomatic severe AS patients. “Should we be talking about moving our Vmax threshold down to 4.5 m/sec, or maybe increasing the Class IIa indications to Class I?” he said. “I think we need to wait to see more data to support these excellent results.”
However, most of these asymptomatic patients do eventually have surgery “in a very short period of time,” Dr. Bonow said. “So from a clinical management point of view, I think we already have the data suggesting that we could move the ball forward, and now we have these excellent outcome data from Korea as well.”
Results were published simultaneously in the New England Journal of Medicine (2019 Nov 16. doi: 10.1056/NEJMoa1912846).
Dr. Kang and Dr. Bonow had no financial relationships to disclose.
PHILADELPHIA – Early aortic valve replacement surgery for patients with asymptomatic, severe aortic stenosis has been a controversial strategy, but the first randomized trial comparing early surgery with conservative management found that early-surgery patients had a 17-fold improved survival at 8 years, according to trial results reported at the American Heart Association scientific sessions.
Albeit small – 145 patients randomized to early surgery or conservative therapy – the RECOVERY trial results provide important evidence to support early preemptive aortic valve replacement for patients with asymptomatic but severe aortic stenosis, said Duk-Hyun Kang, MD, of the division of cardiology, Asan Medical Center in Seoul, South Korea.
The trial randomized 73 patients to early surgical aortic valve replacement (SAVR) and 72 to conventional treatment. Baseline characteristics were similar between the two groups, with a mean EuroSCORE II of 0.9, peak aortic-valve jet velocity (Vmax) of 5.1 m/sec, and mean aortic-valve area of 0.63 cm2. Fifty-three conventional treatment patients went on to have SAVR when symptoms developed during follow-up. There were no operation-related deaths in either group, although one early surgery patient had a stroke and one conventional treatment patients had an MI during the operative period.
At a median follow-up of 6.2 years, 1 early-surgery patient (1.4%) and 11 conventional-therapy patients (15.3%) died from operative or cardiovascular death, Dr. Kang said (P = 0.003). “The number needed to treat to prevent one cardiovascular death within 4 years was 20 patients,” Dr. Kang said. At 4 and 8 years, the cumulative incidences of operative CV or death were 1.4% for both in the early-surgery group and 5.7% and 25.5% in the conventional-treatment group, Dr. Kang said (P = 0.003).
Rates of all-cause mortality were 6.8% and 20.8% (P = 0.030) in the respective groups. “The number needed to treat to save one life in 4 years was 16 patients,” Dr. Kang said. At 4 and 8 years, the cumulative incidence of any-cause death was 4.1% and 10.2% in the early-surgery patients and 9.7% and 31.8% in the conventional group (P = 0.018).
Among the trial limitations Dr. Kang acknowledged were that the population had severe AS with aortic velocity of 4.5 m/sec or greater. “The benefit of early surgery may be relatively smaller in asymptomatic patients with less severe aortic stenosis,” he said.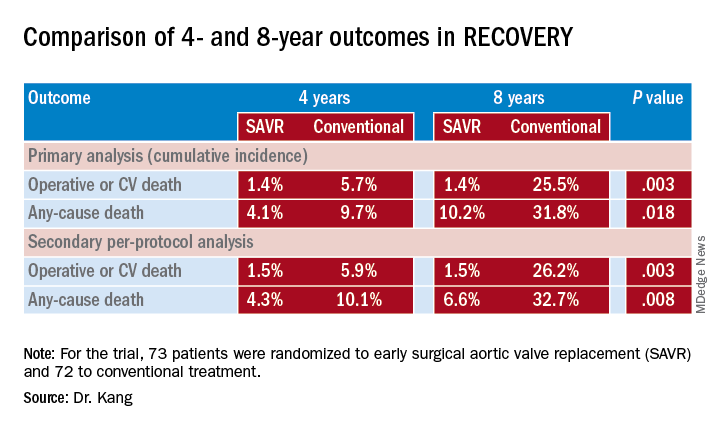
Not all patients had an exercise test to confirm their asymptomatic status, but as discussant Robert Bonow, MD, of Northwestern University in Chicago pointed out, “this is what we’re dealing with clinically.” Also the mean age of the patient population – 64.9 years – is relatively young, and they had a high incidence of bicuspid aortic valve, few comorbidities, and low operative risk, Dr. Kang said. “Thus, our study population is quite different from the populations enrolled in the TAVR [transcatheter AVR] trials, and the results of our study cannot be directly applied to early TAVR for asymptomatic severe aortic stenosis,” he said.
The mean age in both the PARTNER 3 (N Engl J Med. 2019;380:1695-705) and EVOLUT (N Engl J Med. 2019;380:1706-15) trials comparing TAVR and SAVR in low-risk patients was 73.6 years, and they had higher rates of comorbidities than did the RECOVERY patients.
Dr. Bonow said the RECOVERY findings add to the PARTNER 3 and EVOLUT findings and raise the question about rethinking guideline indications for AVR in asymptomatic severe AS patients. “Should we be talking about moving our Vmax threshold down to 4.5 m/sec, or maybe increasing the Class IIa indications to Class I?” he said. “I think we need to wait to see more data to support these excellent results.”
However, most of these asymptomatic patients do eventually have surgery “in a very short period of time,” Dr. Bonow said. “So from a clinical management point of view, I think we already have the data suggesting that we could move the ball forward, and now we have these excellent outcome data from Korea as well.”
Results were published simultaneously in the New England Journal of Medicine (2019 Nov 16. doi: 10.1056/NEJMoa1912846).
Dr. Kang and Dr. Bonow had no financial relationships to disclose.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Coronary function testing during angiography boosts 1-year angina outcomes
PHILADELPHIA – Longer and more extensive follow-up of the positive CorMicA trial confirmed that clinicians who receive added information on the presence or absence of microvascular coronary disease or coronary vasospasm in patients with chronic, stable angina but without detectable coronary obstruction adjust patient treatment in ways that produce better outcomes.
For example, expanded 1-year follow-up of the 151-patient, multicenter, CorMicA randomized study showed that stable angina patients without coronary obstruction treated by clinicians aware of microvascular or vasospastic coronary disease had blood pressures that averaged about 12/5 mm Hg lower than those of patients in the control arm, in which this information was kept blinded.
Clinicians in the study who received information about diagnoses of microvascular angina, vasospastic angina, both, or neither, generally better tailored the treatments they gave these patients, were more likely to prescribe cardiac rehabilitation to these patients, and successfully capped increases in blood pressure that occurred in the control patients, Colin Berry, MD, said at the American Heart Association scientific sessions. The investigators made the diagnoses of microvascular and vasospastic angina using an “invasive diagnostic procedure” that involved placing a wire with pressure and temperature sensors in a selected coronary artery and measuring flow patterns that resulted from a systemic infusion of adenosine and from incremental, intracoronary infusions of acetylcholine.
The CorMicA results “tell us that, if we use existing drugs and nonpharmacologic treatments, we can improve patients’ quality of life,” said Dr. Berry, co-lead investigator of the study and professor of cardiology and imaging at the University of Glasgow. “There were probably two drivers of change in treatment” between the intervention arm where clinicians learned whether their patients had microvascular angina or vasospasm, and the control arm where this information was kept blinded. Some patients reclassified as having microvascular disease or vasospasm were restarted on standard agents for treatment of coronary artery disease such as statins and ACE inhibitors that had previously been stopped, noted Dr. Berry. The identification of a specific type of vascular disorder also helped guide treatment. For example, patients identified as having vasospasm were taken off of beta-blockers, which are contraindicated in these patients, and instead began treatment with a calcium channel antagonist, he said.
“CorMicA was a landmark trial. The interventional cardiologists at my center believe that the testing [for microvascular and vasospastic angina] should be used routinely, based on the reported data,” said Harmony R. Reynolds, MD, a cardiologist at NYU Langone Health in New York.
The CorMicA (Coronary Microvascular Angina) trial enrolled 391 patients at either of two hospitals in Scotland during November 2016–November 2017. All patients were scheduled for clinically indicated, elective diagnostic angiography for suspected stable angina. Clinicians identified a coronary obstruction in 206 patients that excluded them from the main CorMicA analysis. They focused on the 181 without coronary obstruction visible by angiography, and specifically the 151 of these patients who underwent the invasive diagnostic procedure, with 76 randomized to have their diagnostic-procedure results relayed to their treating physicians and 75 patients whose diagnostic results remained blinded. The study’s primary endpoint was the mean difference in angina severity at 6 months after treatment assessed by the Seattle Angina Questionnaire (SAQ) summary score. After 6 months, the between-group difference in average SAQ summary scores was 11.7 units, a statistically significant as well as clinically meaningful benefit that linked with knowledge of the coronary function of patients based on invasive testing (J Am Coll Cardiol. 2018 Dec 11;72[23 Part A]:2841-55).
The prespecified 1-year follow-up with another SAQ took place for 142 of the 151 randomized patients, and showed ongoing separation of SAQ scores between the intervention and control patients, reaching a statistically significant mean difference of 13.6 units, Dr. Berry reported. Other benefits that linked with dissemination of results from the invasive diagnostic procedure included maintenance of the quality-of-life benefit seen after 6 months, an incremental further reduction in illness perception from 6 to 12 months, and a substantial further improvement in global treatment satisfaction, which grew from a 30% higher level in the intervention group compared with controls at 6 months to a 44% between-group difference after 12 months. Concurrently with Dr. Berry’s report, the results appeared online (JACC: Cardiovasc Interv. 2020 Jan 13;13[1] 33-45).
Additional findings for various clinical measures that were not part of the 6-month findings provided further insight into the impact that clinician knowledge about microvascular disease or vasospasm had on patients. These metrics suggested that the benefits in the intervention patients may have largely resulted from their avoiding elevations in risk markers that occurred among controls who received routine care.
For example, after 12 months, average 12/5 mm Hg differences in systolic and diastolic blood pressures between the two arms was nearly all because of pressure increases from baseline in the control patients with only very small drops in pressure from baseline among the intervention patients. Weight measurements after 1 year showed that the control patients were on average 1.3 kg heavier than the intervention patients, again mostly because of weight increases among the controls. Enrollment in a cardiac rehabilitation program at 12 months had occurred for 40% of the intervention patients and 16% of the controls, a 73% relative increase in the intervention arm, Dr. Berry reported.
The invasive, coronary, physiological assessments used in CorMicA led to stratified medical therapy and created an opportunity for better long-term angina treatment in patients without obstructive coronary disease, Dr. Berry concluded. He stressed the need to further test this hypothesis in larger, prospective studies, and to assess its cost effectiveness. But the proof-of-concept demonstrated by the CorMicA results indicate a role for more thorough investigation of coronary dysfunction when obstructive disease is absent, with the opportunity to use this information to better tailor treatment. The findings also highlight the potential for new drug development that can address nonobstructive microvascular or vasospastic coronary disease, he said.
Dr. Berry has been a speaker on behalf of Abbott Vascular, and he has received research funding from AstraZeneca, GlaxoSmithKline, HeartFlow, Novartis, and Siemens Healthcare. Dr. Reynolds had no disclosures.
SOURCE: Ford TJ. AHA 2019, session FS.AOS.03 abstract.
PHILADELPHIA – Longer and more extensive follow-up of the positive CorMicA trial confirmed that clinicians who receive added information on the presence or absence of microvascular coronary disease or coronary vasospasm in patients with chronic, stable angina but without detectable coronary obstruction adjust patient treatment in ways that produce better outcomes.
For example, expanded 1-year follow-up of the 151-patient, multicenter, CorMicA randomized study showed that stable angina patients without coronary obstruction treated by clinicians aware of microvascular or vasospastic coronary disease had blood pressures that averaged about 12/5 mm Hg lower than those of patients in the control arm, in which this information was kept blinded.
Clinicians in the study who received information about diagnoses of microvascular angina, vasospastic angina, both, or neither, generally better tailored the treatments they gave these patients, were more likely to prescribe cardiac rehabilitation to these patients, and successfully capped increases in blood pressure that occurred in the control patients, Colin Berry, MD, said at the American Heart Association scientific sessions. The investigators made the diagnoses of microvascular and vasospastic angina using an “invasive diagnostic procedure” that involved placing a wire with pressure and temperature sensors in a selected coronary artery and measuring flow patterns that resulted from a systemic infusion of adenosine and from incremental, intracoronary infusions of acetylcholine.
The CorMicA results “tell us that, if we use existing drugs and nonpharmacologic treatments, we can improve patients’ quality of life,” said Dr. Berry, co-lead investigator of the study and professor of cardiology and imaging at the University of Glasgow. “There were probably two drivers of change in treatment” between the intervention arm where clinicians learned whether their patients had microvascular angina or vasospasm, and the control arm where this information was kept blinded. Some patients reclassified as having microvascular disease or vasospasm were restarted on standard agents for treatment of coronary artery disease such as statins and ACE inhibitors that had previously been stopped, noted Dr. Berry. The identification of a specific type of vascular disorder also helped guide treatment. For example, patients identified as having vasospasm were taken off of beta-blockers, which are contraindicated in these patients, and instead began treatment with a calcium channel antagonist, he said.
“CorMicA was a landmark trial. The interventional cardiologists at my center believe that the testing [for microvascular and vasospastic angina] should be used routinely, based on the reported data,” said Harmony R. Reynolds, MD, a cardiologist at NYU Langone Health in New York.
The CorMicA (Coronary Microvascular Angina) trial enrolled 391 patients at either of two hospitals in Scotland during November 2016–November 2017. All patients were scheduled for clinically indicated, elective diagnostic angiography for suspected stable angina. Clinicians identified a coronary obstruction in 206 patients that excluded them from the main CorMicA analysis. They focused on the 181 without coronary obstruction visible by angiography, and specifically the 151 of these patients who underwent the invasive diagnostic procedure, with 76 randomized to have their diagnostic-procedure results relayed to their treating physicians and 75 patients whose diagnostic results remained blinded. The study’s primary endpoint was the mean difference in angina severity at 6 months after treatment assessed by the Seattle Angina Questionnaire (SAQ) summary score. After 6 months, the between-group difference in average SAQ summary scores was 11.7 units, a statistically significant as well as clinically meaningful benefit that linked with knowledge of the coronary function of patients based on invasive testing (J Am Coll Cardiol. 2018 Dec 11;72[23 Part A]:2841-55).
The prespecified 1-year follow-up with another SAQ took place for 142 of the 151 randomized patients, and showed ongoing separation of SAQ scores between the intervention and control patients, reaching a statistically significant mean difference of 13.6 units, Dr. Berry reported. Other benefits that linked with dissemination of results from the invasive diagnostic procedure included maintenance of the quality-of-life benefit seen after 6 months, an incremental further reduction in illness perception from 6 to 12 months, and a substantial further improvement in global treatment satisfaction, which grew from a 30% higher level in the intervention group compared with controls at 6 months to a 44% between-group difference after 12 months. Concurrently with Dr. Berry’s report, the results appeared online (JACC: Cardiovasc Interv. 2020 Jan 13;13[1] 33-45).
Additional findings for various clinical measures that were not part of the 6-month findings provided further insight into the impact that clinician knowledge about microvascular disease or vasospasm had on patients. These metrics suggested that the benefits in the intervention patients may have largely resulted from their avoiding elevations in risk markers that occurred among controls who received routine care.
For example, after 12 months, average 12/5 mm Hg differences in systolic and diastolic blood pressures between the two arms was nearly all because of pressure increases from baseline in the control patients with only very small drops in pressure from baseline among the intervention patients. Weight measurements after 1 year showed that the control patients were on average 1.3 kg heavier than the intervention patients, again mostly because of weight increases among the controls. Enrollment in a cardiac rehabilitation program at 12 months had occurred for 40% of the intervention patients and 16% of the controls, a 73% relative increase in the intervention arm, Dr. Berry reported.
The invasive, coronary, physiological assessments used in CorMicA led to stratified medical therapy and created an opportunity for better long-term angina treatment in patients without obstructive coronary disease, Dr. Berry concluded. He stressed the need to further test this hypothesis in larger, prospective studies, and to assess its cost effectiveness. But the proof-of-concept demonstrated by the CorMicA results indicate a role for more thorough investigation of coronary dysfunction when obstructive disease is absent, with the opportunity to use this information to better tailor treatment. The findings also highlight the potential for new drug development that can address nonobstructive microvascular or vasospastic coronary disease, he said.
Dr. Berry has been a speaker on behalf of Abbott Vascular, and he has received research funding from AstraZeneca, GlaxoSmithKline, HeartFlow, Novartis, and Siemens Healthcare. Dr. Reynolds had no disclosures.
SOURCE: Ford TJ. AHA 2019, session FS.AOS.03 abstract.
PHILADELPHIA – Longer and more extensive follow-up of the positive CorMicA trial confirmed that clinicians who receive added information on the presence or absence of microvascular coronary disease or coronary vasospasm in patients with chronic, stable angina but without detectable coronary obstruction adjust patient treatment in ways that produce better outcomes.
For example, expanded 1-year follow-up of the 151-patient, multicenter, CorMicA randomized study showed that stable angina patients without coronary obstruction treated by clinicians aware of microvascular or vasospastic coronary disease had blood pressures that averaged about 12/5 mm Hg lower than those of patients in the control arm, in which this information was kept blinded.
Clinicians in the study who received information about diagnoses of microvascular angina, vasospastic angina, both, or neither, generally better tailored the treatments they gave these patients, were more likely to prescribe cardiac rehabilitation to these patients, and successfully capped increases in blood pressure that occurred in the control patients, Colin Berry, MD, said at the American Heart Association scientific sessions. The investigators made the diagnoses of microvascular and vasospastic angina using an “invasive diagnostic procedure” that involved placing a wire with pressure and temperature sensors in a selected coronary artery and measuring flow patterns that resulted from a systemic infusion of adenosine and from incremental, intracoronary infusions of acetylcholine.
The CorMicA results “tell us that, if we use existing drugs and nonpharmacologic treatments, we can improve patients’ quality of life,” said Dr. Berry, co-lead investigator of the study and professor of cardiology and imaging at the University of Glasgow. “There were probably two drivers of change in treatment” between the intervention arm where clinicians learned whether their patients had microvascular angina or vasospasm, and the control arm where this information was kept blinded. Some patients reclassified as having microvascular disease or vasospasm were restarted on standard agents for treatment of coronary artery disease such as statins and ACE inhibitors that had previously been stopped, noted Dr. Berry. The identification of a specific type of vascular disorder also helped guide treatment. For example, patients identified as having vasospasm were taken off of beta-blockers, which are contraindicated in these patients, and instead began treatment with a calcium channel antagonist, he said.
“CorMicA was a landmark trial. The interventional cardiologists at my center believe that the testing [for microvascular and vasospastic angina] should be used routinely, based on the reported data,” said Harmony R. Reynolds, MD, a cardiologist at NYU Langone Health in New York.
The CorMicA (Coronary Microvascular Angina) trial enrolled 391 patients at either of two hospitals in Scotland during November 2016–November 2017. All patients were scheduled for clinically indicated, elective diagnostic angiography for suspected stable angina. Clinicians identified a coronary obstruction in 206 patients that excluded them from the main CorMicA analysis. They focused on the 181 without coronary obstruction visible by angiography, and specifically the 151 of these patients who underwent the invasive diagnostic procedure, with 76 randomized to have their diagnostic-procedure results relayed to their treating physicians and 75 patients whose diagnostic results remained blinded. The study’s primary endpoint was the mean difference in angina severity at 6 months after treatment assessed by the Seattle Angina Questionnaire (SAQ) summary score. After 6 months, the between-group difference in average SAQ summary scores was 11.7 units, a statistically significant as well as clinically meaningful benefit that linked with knowledge of the coronary function of patients based on invasive testing (J Am Coll Cardiol. 2018 Dec 11;72[23 Part A]:2841-55).
The prespecified 1-year follow-up with another SAQ took place for 142 of the 151 randomized patients, and showed ongoing separation of SAQ scores between the intervention and control patients, reaching a statistically significant mean difference of 13.6 units, Dr. Berry reported. Other benefits that linked with dissemination of results from the invasive diagnostic procedure included maintenance of the quality-of-life benefit seen after 6 months, an incremental further reduction in illness perception from 6 to 12 months, and a substantial further improvement in global treatment satisfaction, which grew from a 30% higher level in the intervention group compared with controls at 6 months to a 44% between-group difference after 12 months. Concurrently with Dr. Berry’s report, the results appeared online (JACC: Cardiovasc Interv. 2020 Jan 13;13[1] 33-45).
Additional findings for various clinical measures that were not part of the 6-month findings provided further insight into the impact that clinician knowledge about microvascular disease or vasospasm had on patients. These metrics suggested that the benefits in the intervention patients may have largely resulted from their avoiding elevations in risk markers that occurred among controls who received routine care.
For example, after 12 months, average 12/5 mm Hg differences in systolic and diastolic blood pressures between the two arms was nearly all because of pressure increases from baseline in the control patients with only very small drops in pressure from baseline among the intervention patients. Weight measurements after 1 year showed that the control patients were on average 1.3 kg heavier than the intervention patients, again mostly because of weight increases among the controls. Enrollment in a cardiac rehabilitation program at 12 months had occurred for 40% of the intervention patients and 16% of the controls, a 73% relative increase in the intervention arm, Dr. Berry reported.
The invasive, coronary, physiological assessments used in CorMicA led to stratified medical therapy and created an opportunity for better long-term angina treatment in patients without obstructive coronary disease, Dr. Berry concluded. He stressed the need to further test this hypothesis in larger, prospective studies, and to assess its cost effectiveness. But the proof-of-concept demonstrated by the CorMicA results indicate a role for more thorough investigation of coronary dysfunction when obstructive disease is absent, with the opportunity to use this information to better tailor treatment. The findings also highlight the potential for new drug development that can address nonobstructive microvascular or vasospastic coronary disease, he said.
Dr. Berry has been a speaker on behalf of Abbott Vascular, and he has received research funding from AstraZeneca, GlaxoSmithKline, HeartFlow, Novartis, and Siemens Healthcare. Dr. Reynolds had no disclosures.
SOURCE: Ford TJ. AHA 2019, session FS.AOS.03 abstract.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS