User login
Clinical Guideline Highlights for the Hospitalist: Secondary Fracture Prevention for Hospitalized Patients
Osteoporosis is the most prevalent bone disease and a leading cause of morbidity and mortality in older people. According to the National Health and Nutrition Examination Survey, from 2005-2010, there were an estimated 10.2 million adults 50 years and older with osteoporosis and 43.4 million more with low bone mass in the United States.1 Osteoporotic fracture is a leading cause of hospitalization in the United States for women 55 years or older, ahead of heart attacks, stroke, and breast cancer.2 Despite elucidation of the pathogenesis of osteoporosis and the advent of effective and widely available therapies, a “treatment gap” separates the many patients who warrant therapy from the few who receive it. Systematic improvement strategies, such as coordinator-based fracture liaison services, have had a positive impact on addressing this treatment gap.3 There is an opportunity for hospitalists to further narrow this treatment gap.
The American Society of Bone and Mineral Research, in conjunction with the Center for Medical Technology Policy, developed consensus clinical recommendations to address secondary fracture prevention for people 65 years or older who have experienced a hip or vertebral fracture.4 We address six of the fundamental and two of the supplemental recommendations as they apply to the practice of hospital medicine.
KEY RECOMMENDATIONS FOR HOSPITALISTs
Recommendations 1 and 2
Communicate key information to the patient and their usual healthcare provider. Patients 65 years or older with a hip or vertebral fracture likely have osteoporosis and are at high risk for subsequent fractures, which can lead to a decline in function and an increase in mortality. Patients must be counseled regarding their diagnosis, their risks, and the actions they can take to manage their disease. Primary care providers must be notified of the occurrence of the fracture, the diagnosis of osteoporosis, and the plans for management.
We recommend hospitalists act as leading advocates for at-risk patients to ensure that this communication occurs during hospitalization. We encourage hospitals and institutions to adopt systematic interventions to facilitate postdischarge care for these patients. These may include implementing a fracture liaison service, with multidisciplinary secondary fracture–prevention strategies using physicians, pharmacists, nurses, social workers, and case managers for care coordination and treatment initiation.
Elderly patients with osteoporotic fragility fractures are at risk for further morbidity and mortality. Coordination of care between the inpatient care team and the primary care provider is necessary to reduce this risk. In addition to verbal communication and especially when verbal communication is not feasible, discharge documents provided to patients and outpatient providers should clearly identify the occurrence of a hip or vertebral fracture and a discharge diagnosis of osteoporosis if not previously documented, regardless of bone mineral density (BMD) results or lack of testing.
Recommendation 3
Regularly assess fall risk. Patients 65 years or older with a current or prior hip or vertebral fracture must be regularly assessed for risk of falls. Hospitalists can assess patients’ ongoing risk for falls at time of admission or during hospitalization. Risk factors include prior falls; advanced age; visual, auditory, or cognitive impairment; decreased muscle strength; gait and balance impairment; diabetes mellitus; use of multiple medications, and others.5 Specialist evaluation by a physical therapist or a physiatrist should be considered. Active medications should be reviewed for adverse effects and interactions. The use of diuretics, antipsychotics, antidepressants, benzodiazepines, antiepileptics, and opioids should be minimized.
Recommendations 4, 5, 6, and 11
Offer pharmacologic therapy and initiate calcium and vitamin D supplementation. Recommendations 4 through 6 and 11 advocate pharmacologic interventions including bisphosphonates, denosumab, vitamin D, and/or calcium to reduce the risk of future fractures. Bisphosphonates are the cornerstone of pharmacologic therapy for secondary fracture prevention. The efficacy of these agents for prevention of subsequent fractures outweighs the potential for interference in healing of surgically repaired bones.6 Oral bisphosphonate therapy should be initiated in the hospital or at discharge. Parenteral bisphosphonates and denosumab may be utilized in patients unable to tolerate or absorb oral bisphosphonates due to esophageal or other gastrointestinal disease. Initiation of these agents should be delayed until after vitamin D and calcium supplementation have been administered for 2 weeks after the fracture to reduce the risk of precipitating hypocalcemia, and they should not be used in patients with confirmed hypocalcemia until that is resolved. BMD measurement is not necessary prior to pharmacologic therapy initiation because the risk of fracture is elevated for these patients regardless of BMD. Patients without significant dental disease or planned oral or maxillofacial procedures may begin bisphosphonate therapy prior to a full dental assessment because risk of osteonecrosis of the jaw is low.
The guidelines recommend people 65 years or older with a hip or vertebral fracture receive daily supplementation of at least 800 IU vitamin D. Patients unable to achieve an intake of 1,200 mg/day of calcium from food sources should receive daily calcium supplementation. The effect of vitamin D monotherapy on fracture risk is not clear; however, strong evidence suggests that fracture risk is reduced when individuals at high risk of deficiency receive supplementation with vitamin D and calcium. Calcium supplementation alone has not demonstrated reduction in fracture risk. Total daily calcium intake above 1,500 mg has not been shown to provide additional benefit and is potentially harmful.
Recommendation 9
Counsel patients on lifestyle modifications and consider physical therapy. Tobacco has a deleterious effect on bone density and increases risk for osteoporotic fragility fracture.7 Hospitalists should obtain tobacco use history from all patients with an osteoporotic fracture and provide tobacco cessation counseling when appropriate. Excessive alcohol consumption increases the risk of fall injuries.8 Hospitalists should counsel patients to limit alcohol intake to a maximum of two drinks a day for men and one drink a day for women.
Weight-bearing and strength-training exercises, particularly those involving balance and trunk muscle strength, are associated with reduction in fall-risk. Exercise must be tailored to the patient’s physical capacity. Hospitalists may partner with physical therapists or physiatrists to facilitate development of an exercise plan to maximize benefit and minimize risk of injury.
CRITIQUE
We found this document to be highly informative and well cited, with ample evidence to support the recommendations.
Methods in Preparing Guidelines
The multistakeholder coalition did not employ a rigorous and standardized methodology for the guideline, such as GRADE (Grading of Recommendations Assessment, Development, and Evaluation); hence, no assessment of evidence quality, benefits and harms of an intervention, or resource use was provided.
Potential Conflicts for Guideline Authors
Eight guideline authors have pharmaceutical relationships with the manufacturer of one of the medications listed on the guidelines (Amgen-denosumab, Novartis-zoledronic acid). There are no disclosures reported from the multistakeholder coalition members who are not listed as guideline authors.
AREAS IN NEED OF FUTURE STUDY
We anticipate future studies may report outcomes focused on secondary prevention of fractures. Additionally, we would like to see new studies investigating patient-centered outcomes such as improvement in functional status and ambulatory independence based on improved postfracture medical therapies. We see an opportunity for studies assessing real-world outcomes to inform future recommendations, particularly after widespread implementation of secondary fracture prevention therapy either initiated during hospitalization or purposefully planned for after discharge.
We would like to see more trial data comparing the safety and cost-effectiveness of first-line therapy, namely oral bisphosphonates, to alternative treatments, particularly parenteral agents, which may improve treatment compliance because of the convenience in dosing frequency.
1. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520-2526. https://doi.org/10.1002/jbmr.2269
2. Singer A, Exuzides A, Spangler L, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90(1):53-62. https://doi.org/10.1016/j.mayocp.2014.09.011
3. McLellan AR, Gallacher SJ, Fraser M, McQuillian C. The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int. 2003;14(12):1028-1034. https://doi.org/10.1007/s00198-003-1507-z
4. Conley RB, Adib G, Adler RA, et al. Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition. J Bone Miner Res. 2020;35(1):36-52. https://doi.org/10.1002/jbmr.3877
5. Bueno-Cavanillas A, Padilla-Ruiz F, Jiménez-Moleón JJ, Peinado-Alonso CA, Gálvez-Vargas R. Risk factors in falls among the elderly according to extrinsic and intrinsic precipitating causes. Eur J Epidemiol. 2000;16(9):849-859. https://doi.org/10.1023/a:1007636531965
6. Vannucci L, Brandi ML. Healing of the bone with anti-fracture drugs. Expert Opin Pharmacother. 2016;17(17):2267-2272. https://doi.org/10.1080/14656566.2016.1241765
7. Law MR, Hackshaw AK. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ. 1997;315(7112):841-846. https://doi.org/10.1136/bmj.315.7112.841
8. Chen CM, Yoon YH. Usual alcohol consumption and risks for nonfatal fall injuries in the United States: results from the 2004-2013 National Health Interview Survey. Subst Use Misuse. 2017;52(9):1120-1132. https://doi.org/10.1080/10826084.2017.1293101
Osteoporosis is the most prevalent bone disease and a leading cause of morbidity and mortality in older people. According to the National Health and Nutrition Examination Survey, from 2005-2010, there were an estimated 10.2 million adults 50 years and older with osteoporosis and 43.4 million more with low bone mass in the United States.1 Osteoporotic fracture is a leading cause of hospitalization in the United States for women 55 years or older, ahead of heart attacks, stroke, and breast cancer.2 Despite elucidation of the pathogenesis of osteoporosis and the advent of effective and widely available therapies, a “treatment gap” separates the many patients who warrant therapy from the few who receive it. Systematic improvement strategies, such as coordinator-based fracture liaison services, have had a positive impact on addressing this treatment gap.3 There is an opportunity for hospitalists to further narrow this treatment gap.
The American Society of Bone and Mineral Research, in conjunction with the Center for Medical Technology Policy, developed consensus clinical recommendations to address secondary fracture prevention for people 65 years or older who have experienced a hip or vertebral fracture.4 We address six of the fundamental and two of the supplemental recommendations as they apply to the practice of hospital medicine.
KEY RECOMMENDATIONS FOR HOSPITALISTs
Recommendations 1 and 2
Communicate key information to the patient and their usual healthcare provider. Patients 65 years or older with a hip or vertebral fracture likely have osteoporosis and are at high risk for subsequent fractures, which can lead to a decline in function and an increase in mortality. Patients must be counseled regarding their diagnosis, their risks, and the actions they can take to manage their disease. Primary care providers must be notified of the occurrence of the fracture, the diagnosis of osteoporosis, and the plans for management.
We recommend hospitalists act as leading advocates for at-risk patients to ensure that this communication occurs during hospitalization. We encourage hospitals and institutions to adopt systematic interventions to facilitate postdischarge care for these patients. These may include implementing a fracture liaison service, with multidisciplinary secondary fracture–prevention strategies using physicians, pharmacists, nurses, social workers, and case managers for care coordination and treatment initiation.
Elderly patients with osteoporotic fragility fractures are at risk for further morbidity and mortality. Coordination of care between the inpatient care team and the primary care provider is necessary to reduce this risk. In addition to verbal communication and especially when verbal communication is not feasible, discharge documents provided to patients and outpatient providers should clearly identify the occurrence of a hip or vertebral fracture and a discharge diagnosis of osteoporosis if not previously documented, regardless of bone mineral density (BMD) results or lack of testing.
Recommendation 3
Regularly assess fall risk. Patients 65 years or older with a current or prior hip or vertebral fracture must be regularly assessed for risk of falls. Hospitalists can assess patients’ ongoing risk for falls at time of admission or during hospitalization. Risk factors include prior falls; advanced age; visual, auditory, or cognitive impairment; decreased muscle strength; gait and balance impairment; diabetes mellitus; use of multiple medications, and others.5 Specialist evaluation by a physical therapist or a physiatrist should be considered. Active medications should be reviewed for adverse effects and interactions. The use of diuretics, antipsychotics, antidepressants, benzodiazepines, antiepileptics, and opioids should be minimized.
Recommendations 4, 5, 6, and 11
Offer pharmacologic therapy and initiate calcium and vitamin D supplementation. Recommendations 4 through 6 and 11 advocate pharmacologic interventions including bisphosphonates, denosumab, vitamin D, and/or calcium to reduce the risk of future fractures. Bisphosphonates are the cornerstone of pharmacologic therapy for secondary fracture prevention. The efficacy of these agents for prevention of subsequent fractures outweighs the potential for interference in healing of surgically repaired bones.6 Oral bisphosphonate therapy should be initiated in the hospital or at discharge. Parenteral bisphosphonates and denosumab may be utilized in patients unable to tolerate or absorb oral bisphosphonates due to esophageal or other gastrointestinal disease. Initiation of these agents should be delayed until after vitamin D and calcium supplementation have been administered for 2 weeks after the fracture to reduce the risk of precipitating hypocalcemia, and they should not be used in patients with confirmed hypocalcemia until that is resolved. BMD measurement is not necessary prior to pharmacologic therapy initiation because the risk of fracture is elevated for these patients regardless of BMD. Patients without significant dental disease or planned oral or maxillofacial procedures may begin bisphosphonate therapy prior to a full dental assessment because risk of osteonecrosis of the jaw is low.
The guidelines recommend people 65 years or older with a hip or vertebral fracture receive daily supplementation of at least 800 IU vitamin D. Patients unable to achieve an intake of 1,200 mg/day of calcium from food sources should receive daily calcium supplementation. The effect of vitamin D monotherapy on fracture risk is not clear; however, strong evidence suggests that fracture risk is reduced when individuals at high risk of deficiency receive supplementation with vitamin D and calcium. Calcium supplementation alone has not demonstrated reduction in fracture risk. Total daily calcium intake above 1,500 mg has not been shown to provide additional benefit and is potentially harmful.
Recommendation 9
Counsel patients on lifestyle modifications and consider physical therapy. Tobacco has a deleterious effect on bone density and increases risk for osteoporotic fragility fracture.7 Hospitalists should obtain tobacco use history from all patients with an osteoporotic fracture and provide tobacco cessation counseling when appropriate. Excessive alcohol consumption increases the risk of fall injuries.8 Hospitalists should counsel patients to limit alcohol intake to a maximum of two drinks a day for men and one drink a day for women.
Weight-bearing and strength-training exercises, particularly those involving balance and trunk muscle strength, are associated with reduction in fall-risk. Exercise must be tailored to the patient’s physical capacity. Hospitalists may partner with physical therapists or physiatrists to facilitate development of an exercise plan to maximize benefit and minimize risk of injury.
CRITIQUE
We found this document to be highly informative and well cited, with ample evidence to support the recommendations.
Methods in Preparing Guidelines
The multistakeholder coalition did not employ a rigorous and standardized methodology for the guideline, such as GRADE (Grading of Recommendations Assessment, Development, and Evaluation); hence, no assessment of evidence quality, benefits and harms of an intervention, or resource use was provided.
Potential Conflicts for Guideline Authors
Eight guideline authors have pharmaceutical relationships with the manufacturer of one of the medications listed on the guidelines (Amgen-denosumab, Novartis-zoledronic acid). There are no disclosures reported from the multistakeholder coalition members who are not listed as guideline authors.
AREAS IN NEED OF FUTURE STUDY
We anticipate future studies may report outcomes focused on secondary prevention of fractures. Additionally, we would like to see new studies investigating patient-centered outcomes such as improvement in functional status and ambulatory independence based on improved postfracture medical therapies. We see an opportunity for studies assessing real-world outcomes to inform future recommendations, particularly after widespread implementation of secondary fracture prevention therapy either initiated during hospitalization or purposefully planned for after discharge.
We would like to see more trial data comparing the safety and cost-effectiveness of first-line therapy, namely oral bisphosphonates, to alternative treatments, particularly parenteral agents, which may improve treatment compliance because of the convenience in dosing frequency.
Osteoporosis is the most prevalent bone disease and a leading cause of morbidity and mortality in older people. According to the National Health and Nutrition Examination Survey, from 2005-2010, there were an estimated 10.2 million adults 50 years and older with osteoporosis and 43.4 million more with low bone mass in the United States.1 Osteoporotic fracture is a leading cause of hospitalization in the United States for women 55 years or older, ahead of heart attacks, stroke, and breast cancer.2 Despite elucidation of the pathogenesis of osteoporosis and the advent of effective and widely available therapies, a “treatment gap” separates the many patients who warrant therapy from the few who receive it. Systematic improvement strategies, such as coordinator-based fracture liaison services, have had a positive impact on addressing this treatment gap.3 There is an opportunity for hospitalists to further narrow this treatment gap.
The American Society of Bone and Mineral Research, in conjunction with the Center for Medical Technology Policy, developed consensus clinical recommendations to address secondary fracture prevention for people 65 years or older who have experienced a hip or vertebral fracture.4 We address six of the fundamental and two of the supplemental recommendations as they apply to the practice of hospital medicine.
KEY RECOMMENDATIONS FOR HOSPITALISTs
Recommendations 1 and 2
Communicate key information to the patient and their usual healthcare provider. Patients 65 years or older with a hip or vertebral fracture likely have osteoporosis and are at high risk for subsequent fractures, which can lead to a decline in function and an increase in mortality. Patients must be counseled regarding their diagnosis, their risks, and the actions they can take to manage their disease. Primary care providers must be notified of the occurrence of the fracture, the diagnosis of osteoporosis, and the plans for management.
We recommend hospitalists act as leading advocates for at-risk patients to ensure that this communication occurs during hospitalization. We encourage hospitals and institutions to adopt systematic interventions to facilitate postdischarge care for these patients. These may include implementing a fracture liaison service, with multidisciplinary secondary fracture–prevention strategies using physicians, pharmacists, nurses, social workers, and case managers for care coordination and treatment initiation.
Elderly patients with osteoporotic fragility fractures are at risk for further morbidity and mortality. Coordination of care between the inpatient care team and the primary care provider is necessary to reduce this risk. In addition to verbal communication and especially when verbal communication is not feasible, discharge documents provided to patients and outpatient providers should clearly identify the occurrence of a hip or vertebral fracture and a discharge diagnosis of osteoporosis if not previously documented, regardless of bone mineral density (BMD) results or lack of testing.
Recommendation 3
Regularly assess fall risk. Patients 65 years or older with a current or prior hip or vertebral fracture must be regularly assessed for risk of falls. Hospitalists can assess patients’ ongoing risk for falls at time of admission or during hospitalization. Risk factors include prior falls; advanced age; visual, auditory, or cognitive impairment; decreased muscle strength; gait and balance impairment; diabetes mellitus; use of multiple medications, and others.5 Specialist evaluation by a physical therapist or a physiatrist should be considered. Active medications should be reviewed for adverse effects and interactions. The use of diuretics, antipsychotics, antidepressants, benzodiazepines, antiepileptics, and opioids should be minimized.
Recommendations 4, 5, 6, and 11
Offer pharmacologic therapy and initiate calcium and vitamin D supplementation. Recommendations 4 through 6 and 11 advocate pharmacologic interventions including bisphosphonates, denosumab, vitamin D, and/or calcium to reduce the risk of future fractures. Bisphosphonates are the cornerstone of pharmacologic therapy for secondary fracture prevention. The efficacy of these agents for prevention of subsequent fractures outweighs the potential for interference in healing of surgically repaired bones.6 Oral bisphosphonate therapy should be initiated in the hospital or at discharge. Parenteral bisphosphonates and denosumab may be utilized in patients unable to tolerate or absorb oral bisphosphonates due to esophageal or other gastrointestinal disease. Initiation of these agents should be delayed until after vitamin D and calcium supplementation have been administered for 2 weeks after the fracture to reduce the risk of precipitating hypocalcemia, and they should not be used in patients with confirmed hypocalcemia until that is resolved. BMD measurement is not necessary prior to pharmacologic therapy initiation because the risk of fracture is elevated for these patients regardless of BMD. Patients without significant dental disease or planned oral or maxillofacial procedures may begin bisphosphonate therapy prior to a full dental assessment because risk of osteonecrosis of the jaw is low.
The guidelines recommend people 65 years or older with a hip or vertebral fracture receive daily supplementation of at least 800 IU vitamin D. Patients unable to achieve an intake of 1,200 mg/day of calcium from food sources should receive daily calcium supplementation. The effect of vitamin D monotherapy on fracture risk is not clear; however, strong evidence suggests that fracture risk is reduced when individuals at high risk of deficiency receive supplementation with vitamin D and calcium. Calcium supplementation alone has not demonstrated reduction in fracture risk. Total daily calcium intake above 1,500 mg has not been shown to provide additional benefit and is potentially harmful.
Recommendation 9
Counsel patients on lifestyle modifications and consider physical therapy. Tobacco has a deleterious effect on bone density and increases risk for osteoporotic fragility fracture.7 Hospitalists should obtain tobacco use history from all patients with an osteoporotic fracture and provide tobacco cessation counseling when appropriate. Excessive alcohol consumption increases the risk of fall injuries.8 Hospitalists should counsel patients to limit alcohol intake to a maximum of two drinks a day for men and one drink a day for women.
Weight-bearing and strength-training exercises, particularly those involving balance and trunk muscle strength, are associated with reduction in fall-risk. Exercise must be tailored to the patient’s physical capacity. Hospitalists may partner with physical therapists or physiatrists to facilitate development of an exercise plan to maximize benefit and minimize risk of injury.
CRITIQUE
We found this document to be highly informative and well cited, with ample evidence to support the recommendations.
Methods in Preparing Guidelines
The multistakeholder coalition did not employ a rigorous and standardized methodology for the guideline, such as GRADE (Grading of Recommendations Assessment, Development, and Evaluation); hence, no assessment of evidence quality, benefits and harms of an intervention, or resource use was provided.
Potential Conflicts for Guideline Authors
Eight guideline authors have pharmaceutical relationships with the manufacturer of one of the medications listed on the guidelines (Amgen-denosumab, Novartis-zoledronic acid). There are no disclosures reported from the multistakeholder coalition members who are not listed as guideline authors.
AREAS IN NEED OF FUTURE STUDY
We anticipate future studies may report outcomes focused on secondary prevention of fractures. Additionally, we would like to see new studies investigating patient-centered outcomes such as improvement in functional status and ambulatory independence based on improved postfracture medical therapies. We see an opportunity for studies assessing real-world outcomes to inform future recommendations, particularly after widespread implementation of secondary fracture prevention therapy either initiated during hospitalization or purposefully planned for after discharge.
We would like to see more trial data comparing the safety and cost-effectiveness of first-line therapy, namely oral bisphosphonates, to alternative treatments, particularly parenteral agents, which may improve treatment compliance because of the convenience in dosing frequency.
1. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520-2526. https://doi.org/10.1002/jbmr.2269
2. Singer A, Exuzides A, Spangler L, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90(1):53-62. https://doi.org/10.1016/j.mayocp.2014.09.011
3. McLellan AR, Gallacher SJ, Fraser M, McQuillian C. The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int. 2003;14(12):1028-1034. https://doi.org/10.1007/s00198-003-1507-z
4. Conley RB, Adib G, Adler RA, et al. Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition. J Bone Miner Res. 2020;35(1):36-52. https://doi.org/10.1002/jbmr.3877
5. Bueno-Cavanillas A, Padilla-Ruiz F, Jiménez-Moleón JJ, Peinado-Alonso CA, Gálvez-Vargas R. Risk factors in falls among the elderly according to extrinsic and intrinsic precipitating causes. Eur J Epidemiol. 2000;16(9):849-859. https://doi.org/10.1023/a:1007636531965
6. Vannucci L, Brandi ML. Healing of the bone with anti-fracture drugs. Expert Opin Pharmacother. 2016;17(17):2267-2272. https://doi.org/10.1080/14656566.2016.1241765
7. Law MR, Hackshaw AK. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ. 1997;315(7112):841-846. https://doi.org/10.1136/bmj.315.7112.841
8. Chen CM, Yoon YH. Usual alcohol consumption and risks for nonfatal fall injuries in the United States: results from the 2004-2013 National Health Interview Survey. Subst Use Misuse. 2017;52(9):1120-1132. https://doi.org/10.1080/10826084.2017.1293101
1. Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520-2526. https://doi.org/10.1002/jbmr.2269
2. Singer A, Exuzides A, Spangler L, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90(1):53-62. https://doi.org/10.1016/j.mayocp.2014.09.011
3. McLellan AR, Gallacher SJ, Fraser M, McQuillian C. The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int. 2003;14(12):1028-1034. https://doi.org/10.1007/s00198-003-1507-z
4. Conley RB, Adib G, Adler RA, et al. Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition. J Bone Miner Res. 2020;35(1):36-52. https://doi.org/10.1002/jbmr.3877
5. Bueno-Cavanillas A, Padilla-Ruiz F, Jiménez-Moleón JJ, Peinado-Alonso CA, Gálvez-Vargas R. Risk factors in falls among the elderly according to extrinsic and intrinsic precipitating causes. Eur J Epidemiol. 2000;16(9):849-859. https://doi.org/10.1023/a:1007636531965
6. Vannucci L, Brandi ML. Healing of the bone with anti-fracture drugs. Expert Opin Pharmacother. 2016;17(17):2267-2272. https://doi.org/10.1080/14656566.2016.1241765
7. Law MR, Hackshaw AK. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ. 1997;315(7112):841-846. https://doi.org/10.1136/bmj.315.7112.841
8. Chen CM, Yoon YH. Usual alcohol consumption and risks for nonfatal fall injuries in the United States: results from the 2004-2013 National Health Interview Survey. Subst Use Misuse. 2017;52(9):1120-1132. https://doi.org/10.1080/10826084.2017.1293101
© 2021 Society of Hospital Medicine
Protecting Children by Healing Their Caregivers
It was a busy night in the emergency department. EMS called to give a heads up—they were on their way with a girl who was “pretty banged up.” They warned us that the story seemed a little fishy. We thought we were ready. The trauma bay was organized; supplies were at the ready and everyone had a role. Within seconds of her arrival, it was clear that no one could ever have been truly prepared. She was unresponsive and unstable. Her injuries were widespread, brutal, and long term. My seasoned attendings would describe it as no less than horrific. There was no question—someone had done this to her.
After she was stabilized, her wounds were gently tended, her body was bathed, her hair was combed. She died several days later. While distressed, many members of her team took consolation in the idea that, after years of torture, she finally got to be loved.
It’s no wonder that every person involved with her care during her hospitalization was so deeply affected by her. How could anyone do this to another person? Or even worse, to an innocent child? “What a monster,” we said. “Only a monster could have done this.”
While anyone would agree that what this abuser—the girl’s mother—did was brutal and wrong, I would also argue that the underlying danger is much more systemic. We call her the “monster,” but I sense that the real monster is still lurking in the shadows, unnamed. I can’t help but try to understand this woman; it is unfair to condemn her without first learning her story. How were her actions guided by her own history of trauma, abuse, and violent discipline as a child? We preach to each other and to our learners that trauma-informed care is essential; you must not ask what’s wrong with you, but what happened to you. Founder and Director of the Equal Justice Initiative Bryan Stevenson has said that “each of us is more than the worst thing we’ve ever done.”1 It’s inhumane of us to dehumanize her for this atrocity, especially without pausing to ask how her environment, personal trauma, and understanding of child development set the risk.
It is important to understand the cycle of trauma and abuse. Traumatic experiences have been shown to alter neurodevelopment and the body’s stress response, particularly when experiences take place early in life, when they are repeated and long term, and when they are severe. We know that adverse childhood experiences are cumulative and result in adverse outcomes as adults, including increased likelihood of violent or criminal activity. We know that prior history of trauma, specifically child abuse, sexual abuse, or domestic violence, is associated with higher potential for child abuse later on.
The effect of experiencing trauma is such that only 22% of adults who experienced abuse or neglect as children will achieve resiliency.2 In a world in which social distancing and isolation have become the new normal, we must be even more aware of the effects of trauma on families. The COVID-19 pandemic has increased known risk factors for child abuse, including financial hardship, unemployment, increased anxiety, increased caregiver responsibilities, and decreased access to mental health services and community resources.3 Furthermore, virtual learning environments may have significant implications on the reporting of child abuse. Among cases of maltreatment of children that received an investigation or alternative response in 2018, 20.5% were reported by education personnel.4 While remote learning options may be necessary to minimize risk of viral spread, fewer interactions between children and mandatory reporters may result in child maltreatment going undetected. In the face of these challenges, I urge our healthcare system to use current constraints as fuel for creative interventions including the following:
- Applying advances in telemedicine to create a new opportunity to interface with families, provide mental health support, connect them with resources, and offer gentle guidance about safe parenting.
- Improving both screening methods for parental trauma and distress and referrals for support services.
- Advocating for adequate access to life-sustaining resources including shelter, food, and healthcare for all families. This is a necessary foundation for building resilience.
- Providing bias training for mandatory reporters to ensure that all children and their families are approached with respect and compassion.
- Prioritizing innovation that provides long-lasting, sustainable, and equitable access to support and healing.
To best protect our children, we must heal their adult caregivers; we must help them to conquer their monsters.
Our patient and her family have since visited me in my thoughts and dreams, less often now than before. While I never truly knew her, she has left an open void where there should have been the promise of a healthy, growing, and developing child. Within that void resides fear. I fear for other “hidden children” and the abuse they are at risk for experiencing. I fear that her siblings, now living without their mother, will become victims of the instability of being “in the system.” I fear that by turning to punishment as our only solution, we miss opportunities to prevent such tragedy. Despite the darkness, she also brings me hope. I hope that her siblings can rely on each other as a foundation for resilience. I hope that we as a healthcare system can continue to love our patients without question or condition. I hope that we as a society can invest in breaking the cycle of trauma and in supporting parents. I hope that we can create a system in which children can grow up free from abuse.
1. Stevenson B. Just Mercy: A Story of Justice and Redemption. Spiegel & Grau; 2015.
2. De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23(2):185-222. https://doi.org/10.1016/j.chc.2014.01.002
3. Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. 2017;72:71-81. https://doi.org/10.1016/j.childyouth.2016.10.016
4. Child Maltreatment 2018. Children’s Bureau, Youth and Families, Administration on Children, Administration for Children and Families, U.S. Department of Health & Human Services; January 15, 2020. Accessed May 10, 2020. https://www.acf.hhs.gov/cb/resource/child-maltreatment-2018
It was a busy night in the emergency department. EMS called to give a heads up—they were on their way with a girl who was “pretty banged up.” They warned us that the story seemed a little fishy. We thought we were ready. The trauma bay was organized; supplies were at the ready and everyone had a role. Within seconds of her arrival, it was clear that no one could ever have been truly prepared. She was unresponsive and unstable. Her injuries were widespread, brutal, and long term. My seasoned attendings would describe it as no less than horrific. There was no question—someone had done this to her.
After she was stabilized, her wounds were gently tended, her body was bathed, her hair was combed. She died several days later. While distressed, many members of her team took consolation in the idea that, after years of torture, she finally got to be loved.
It’s no wonder that every person involved with her care during her hospitalization was so deeply affected by her. How could anyone do this to another person? Or even worse, to an innocent child? “What a monster,” we said. “Only a monster could have done this.”
While anyone would agree that what this abuser—the girl’s mother—did was brutal and wrong, I would also argue that the underlying danger is much more systemic. We call her the “monster,” but I sense that the real monster is still lurking in the shadows, unnamed. I can’t help but try to understand this woman; it is unfair to condemn her without first learning her story. How were her actions guided by her own history of trauma, abuse, and violent discipline as a child? We preach to each other and to our learners that trauma-informed care is essential; you must not ask what’s wrong with you, but what happened to you. Founder and Director of the Equal Justice Initiative Bryan Stevenson has said that “each of us is more than the worst thing we’ve ever done.”1 It’s inhumane of us to dehumanize her for this atrocity, especially without pausing to ask how her environment, personal trauma, and understanding of child development set the risk.
It is important to understand the cycle of trauma and abuse. Traumatic experiences have been shown to alter neurodevelopment and the body’s stress response, particularly when experiences take place early in life, when they are repeated and long term, and when they are severe. We know that adverse childhood experiences are cumulative and result in adverse outcomes as adults, including increased likelihood of violent or criminal activity. We know that prior history of trauma, specifically child abuse, sexual abuse, or domestic violence, is associated with higher potential for child abuse later on.
The effect of experiencing trauma is such that only 22% of adults who experienced abuse or neglect as children will achieve resiliency.2 In a world in which social distancing and isolation have become the new normal, we must be even more aware of the effects of trauma on families. The COVID-19 pandemic has increased known risk factors for child abuse, including financial hardship, unemployment, increased anxiety, increased caregiver responsibilities, and decreased access to mental health services and community resources.3 Furthermore, virtual learning environments may have significant implications on the reporting of child abuse. Among cases of maltreatment of children that received an investigation or alternative response in 2018, 20.5% were reported by education personnel.4 While remote learning options may be necessary to minimize risk of viral spread, fewer interactions between children and mandatory reporters may result in child maltreatment going undetected. In the face of these challenges, I urge our healthcare system to use current constraints as fuel for creative interventions including the following:
- Applying advances in telemedicine to create a new opportunity to interface with families, provide mental health support, connect them with resources, and offer gentle guidance about safe parenting.
- Improving both screening methods for parental trauma and distress and referrals for support services.
- Advocating for adequate access to life-sustaining resources including shelter, food, and healthcare for all families. This is a necessary foundation for building resilience.
- Providing bias training for mandatory reporters to ensure that all children and their families are approached with respect and compassion.
- Prioritizing innovation that provides long-lasting, sustainable, and equitable access to support and healing.
To best protect our children, we must heal their adult caregivers; we must help them to conquer their monsters.
Our patient and her family have since visited me in my thoughts and dreams, less often now than before. While I never truly knew her, she has left an open void where there should have been the promise of a healthy, growing, and developing child. Within that void resides fear. I fear for other “hidden children” and the abuse they are at risk for experiencing. I fear that her siblings, now living without their mother, will become victims of the instability of being “in the system.” I fear that by turning to punishment as our only solution, we miss opportunities to prevent such tragedy. Despite the darkness, she also brings me hope. I hope that her siblings can rely on each other as a foundation for resilience. I hope that we as a healthcare system can continue to love our patients without question or condition. I hope that we as a society can invest in breaking the cycle of trauma and in supporting parents. I hope that we can create a system in which children can grow up free from abuse.
It was a busy night in the emergency department. EMS called to give a heads up—they were on their way with a girl who was “pretty banged up.” They warned us that the story seemed a little fishy. We thought we were ready. The trauma bay was organized; supplies were at the ready and everyone had a role. Within seconds of her arrival, it was clear that no one could ever have been truly prepared. She was unresponsive and unstable. Her injuries were widespread, brutal, and long term. My seasoned attendings would describe it as no less than horrific. There was no question—someone had done this to her.
After she was stabilized, her wounds were gently tended, her body was bathed, her hair was combed. She died several days later. While distressed, many members of her team took consolation in the idea that, after years of torture, she finally got to be loved.
It’s no wonder that every person involved with her care during her hospitalization was so deeply affected by her. How could anyone do this to another person? Or even worse, to an innocent child? “What a monster,” we said. “Only a monster could have done this.”
While anyone would agree that what this abuser—the girl’s mother—did was brutal and wrong, I would also argue that the underlying danger is much more systemic. We call her the “monster,” but I sense that the real monster is still lurking in the shadows, unnamed. I can’t help but try to understand this woman; it is unfair to condemn her without first learning her story. How were her actions guided by her own history of trauma, abuse, and violent discipline as a child? We preach to each other and to our learners that trauma-informed care is essential; you must not ask what’s wrong with you, but what happened to you. Founder and Director of the Equal Justice Initiative Bryan Stevenson has said that “each of us is more than the worst thing we’ve ever done.”1 It’s inhumane of us to dehumanize her for this atrocity, especially without pausing to ask how her environment, personal trauma, and understanding of child development set the risk.
It is important to understand the cycle of trauma and abuse. Traumatic experiences have been shown to alter neurodevelopment and the body’s stress response, particularly when experiences take place early in life, when they are repeated and long term, and when they are severe. We know that adverse childhood experiences are cumulative and result in adverse outcomes as adults, including increased likelihood of violent or criminal activity. We know that prior history of trauma, specifically child abuse, sexual abuse, or domestic violence, is associated with higher potential for child abuse later on.
The effect of experiencing trauma is such that only 22% of adults who experienced abuse or neglect as children will achieve resiliency.2 In a world in which social distancing and isolation have become the new normal, we must be even more aware of the effects of trauma on families. The COVID-19 pandemic has increased known risk factors for child abuse, including financial hardship, unemployment, increased anxiety, increased caregiver responsibilities, and decreased access to mental health services and community resources.3 Furthermore, virtual learning environments may have significant implications on the reporting of child abuse. Among cases of maltreatment of children that received an investigation or alternative response in 2018, 20.5% were reported by education personnel.4 While remote learning options may be necessary to minimize risk of viral spread, fewer interactions between children and mandatory reporters may result in child maltreatment going undetected. In the face of these challenges, I urge our healthcare system to use current constraints as fuel for creative interventions including the following:
- Applying advances in telemedicine to create a new opportunity to interface with families, provide mental health support, connect them with resources, and offer gentle guidance about safe parenting.
- Improving both screening methods for parental trauma and distress and referrals for support services.
- Advocating for adequate access to life-sustaining resources including shelter, food, and healthcare for all families. This is a necessary foundation for building resilience.
- Providing bias training for mandatory reporters to ensure that all children and their families are approached with respect and compassion.
- Prioritizing innovation that provides long-lasting, sustainable, and equitable access to support and healing.
To best protect our children, we must heal their adult caregivers; we must help them to conquer their monsters.
Our patient and her family have since visited me in my thoughts and dreams, less often now than before. While I never truly knew her, she has left an open void where there should have been the promise of a healthy, growing, and developing child. Within that void resides fear. I fear for other “hidden children” and the abuse they are at risk for experiencing. I fear that her siblings, now living without their mother, will become victims of the instability of being “in the system.” I fear that by turning to punishment as our only solution, we miss opportunities to prevent such tragedy. Despite the darkness, she also brings me hope. I hope that her siblings can rely on each other as a foundation for resilience. I hope that we as a healthcare system can continue to love our patients without question or condition. I hope that we as a society can invest in breaking the cycle of trauma and in supporting parents. I hope that we can create a system in which children can grow up free from abuse.
1. Stevenson B. Just Mercy: A Story of Justice and Redemption. Spiegel & Grau; 2015.
2. De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23(2):185-222. https://doi.org/10.1016/j.chc.2014.01.002
3. Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. 2017;72:71-81. https://doi.org/10.1016/j.childyouth.2016.10.016
4. Child Maltreatment 2018. Children’s Bureau, Youth and Families, Administration on Children, Administration for Children and Families, U.S. Department of Health & Human Services; January 15, 2020. Accessed May 10, 2020. https://www.acf.hhs.gov/cb/resource/child-maltreatment-2018
1. Stevenson B. Just Mercy: A Story of Justice and Redemption. Spiegel & Grau; 2015.
2. De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23(2):185-222. https://doi.org/10.1016/j.chc.2014.01.002
3. Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. 2017;72:71-81. https://doi.org/10.1016/j.childyouth.2016.10.016
4. Child Maltreatment 2018. Children’s Bureau, Youth and Families, Administration on Children, Administration for Children and Families, U.S. Department of Health & Human Services; January 15, 2020. Accessed May 10, 2020. https://www.acf.hhs.gov/cb/resource/child-maltreatment-2018
© 2021 Society of Hospital Medicine
Prioritizing High-Value, Equitable Care After the COVID-19 Shutdown: An Opportunity for a Healthcare Renaissance
The day after Memorial Day 2020 marked an important transition in the United States’ experience with coronavirus disease 2019 (COVID-19), with many states making initial plans to reopen.
This year’s widespread healthcare closures were necessary to reduce COVID-19 transmission and prepare for a future patient surge, but these closures had unintended consequences. Nearly half of adults polled said they or someone in their household had foregone or delayed care since the outbreak began.1 This was especially true for visits to emergency departments and doctors’ offices for strokes, heart attacks, and routine medical care.2 In a survey across 49 states, only 7% of primary care practices considered scheduling preventive visits as a high priority.3 Eleven percent of polled adults reported delaying care worsened their condition,1 and in hard-hit areas such as New York City, non-COVID mortality was 22% higher than expected.4
Avoidance of the medical system decreased not only use of necessary, high-value care but also use of low-value care. Low-value services are those in which the “potential for harms exceed the potential benefits,”5 such as unnecessary hospitalizations, avoidable emergency department or clinic visits, unwarranted or excessive diagnostic testing (eg, annual physicals), and certain procedures (eg, spinal fusion surgery for low-back pain).
KEEP PATIENTS CENTRAL IN REOPENING SERVICES TO DELIVER HIGH-VALUE CARE
Medical centers can better focus on high-value care by defining their high-risk patient populations; high-value treatments, procedures, and preventive care; and phases of reopening. During the first pandemic wave, medical centers tried to reassure patients about emergency care, such as coming in for chest pain or neurologic symptoms, through personal outreach and media campaigns. Outpatient virtual visits also continued, including primary care, specialty services, mental health treatment, and physical therapy. While reopening, some medical centers have assessed disparities by relying on their data analytics and, if available, embedded health services researchers to understand what care was stopped and what populations were most affected.
The University of California health systems, for example, had a learning collaborative focused on sharing methods to restore care delivery that prioritizes patient needs. Some campuses conducted analyses using both electronic health record data and input from patients and their care teams to identify clinical needs and determine patient outreach plans. Some approaches used machine learning models to identify patients at highest risk of hospitalization or emergency department visits over the next 12 months and to conduct additional outreach to schedule these patients in primary and specialty care if clinically appropriate. Similarly, surgical specialties identified the highest-priority nonemergent surgeries for scheduling, including cancer resection, radiation therapy, and pain-management procedures. Similar guidance toward the most meaningful care has been prioritized within the United States Department of Veterans Affairs.
The rapid deployment of telehealth and payment models that reimburse video and in-clinic visits equally created new opportunities for medical centers to expand high-value care in lower-cost home settings. Similarly, new infrastructure is being developed to help define smarter use of virtual visits and home-based lab collection and monitoring.
Medical centers also must pay careful attention to redeploying service capacity for underused, high-value services. The pandemic uncovered existing staff that could be redeployed to support these changes. For example, with an “all hands on deck” mentality during the pandemic, in some medical centers, analysts or care managers from less-prioritized or duplicative areas were reassigned to vital COVID-19 efforts. Medical centers may realize that this staff can provide more value in the future by supporting increased high-value, affordable healthcare.
DELIBERATELY AVOID LOW-VALUE CARE
During the intial wave of the pandemic, medical centers greatly reduced the care they provided, often focusing on delivering essential care. This preparation for a surge of COVID patients had the effect of halting many unnecessary services by moving care from the clinic to home under new reimbursement changes, such as those affecting telehealth payments. The experience of reducing low-value medical services and visits can be extended to limiting unnecessary diagnostic testing. Medical centers could, for example, focus only on tests that advance care plans; reduce unnecessary blood draws, procedures, and vital sign checks on stable patients; shift to medications with less-frequent dosing intervals; and consolidate visits by treatment teams.10,11
Medical centers, however, now face continued pressures to increase revenue because 75% report their organization’s top priority is focused on increasing patient volume.12
PROACTIVELY AVOID WORSENING HEALTHCARE DISPARITIES
As medical centers reboot, operational and clinical leaders must proactively view changes through an equity lens to avoid exacerbating health disparities among vulnerable populations. The pandemic has focused national attention on the severity and pervasiveness of disparities and created an imperative for substantive action to evaluate how every decision will affect health equity. For example, medical centers are expanding use of telehealth to improve patient outreach. However, in a survey of primary care physicians, 72% said they have patients who are unable to access telehealth because they do not have access to technology.3 Exclusion of these patients from programs risks worsening health disparities. In a recent survey, nearly 65% of medical centers report reexamining existing policies, protocols, and practices for patients at risk of disparities.12
REFORM TO SUPPORT HIGH-VALUE CARE DELIVERY
Medical centers nationwide will need payment reform that provides greater financial stability beyond the pandemic to support high-value care delivery. They also will need flexibility to invest in prevention and to deliver the appropriate intensity of care to meet patients’ and communities’ needs.15-17 Options to provide this support include prospective population-based payments that may create more resilience in protecting access to care when it is most needed. Models can include fully capitated payment for physician practices.19,20 For example, after Vermont entered a single accountable care organization (ACO) model with the Centers for Medicare & Medicaid Services (CMS) in 2018, they not only generated a $97 million Medicaid savings, but also had a financial cushion that was later used in their COVID-19 response.21,22 The advanced payments allowed primary care practices and community agencies to invest in a digital tool to support outreach to patient at high risk for virus complications.
Hospitals similarly can adapt global budgets that incentivize financial stewardship by encouraging clinicians to resume necessary services and not unnecessary ones.16 For example, CMS partnered with Pennsylvania’s Department of Health to provide prospective all-payer global budgets for rural hospitals and Maryland’s Health Services Cost Review Commission that negotiates a budget with each hospital. During the COVID-19 pandemic, hospitals in these programs have had more financial protection from fluctuating finances by allowing for easier shifts in service delivery location and adjustments in rates to compensate for declines in visits and procedures.23
Policy makers and payers also can hold medical centers accountable to evidence-based guidelines and appropriate use of care, especially when necessary but expensive (eg, percutaneous coronary interventions, spinal surgeries, or cancer care). Funding agencies, additionally, can support these efforts by focusing on research, dissemination, and reliable implementation of these practices.
CONCLUSION
The COVID-19 crisis presents a tremendous opportunity for each medical center to revitalize healthcare. This opportunity can be seized only with reform by policy makers, payers, and regulatory agencies who encourage restarting high-value care without low-value services. We must take deliberate action so the nation’s medical centers can better meet patients’ needs to make healthcare more resilient, efficient, and fair.
1. Hamel L, Kearney A, Kirzinger A, Lopes L, Muñana C, Brodie M. KFF Health Tracking Poll - May 2020: Impact of Coronavirus on Personal Health, Economic and Food Security, and Medicaid. Kaiser Family Foundation; May 27, 2020. Accessed August 9, 2020. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
2. McFarling UL. ‘Where are all our patients?’: Covid phobia is keeping people with serious heart symptoms away from ERs. STAT. April 23, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/
3. Primary Care & COVID-19: Week 4 Survey. Primary Care Collaborative; April 9, 2020. Accessed August 9, 2020. https://www.pcpcc.org/2020/04/08/primary-care-covid-19-week-4-survey
4. Olson DR, Huynh M, Fine A, et al. New York City Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team. Preliminary estimate of excess mortality during the COVID-19 outbreak — New York City, March 11–May 2, 2020. Morbidity and Mortality Weekly Report. May 11, 2020. Accessed August 9, 2020. https://stacks.cdc.gov/view/cdc/87858
5. Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000-1005. https://doi.org/10.1001/jama.280.11.1000
6. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501-1509. https://doi.org/10.1001/jama.2019.13978
7. Collins SR, Gunja MZ, Doty MM, Bhupal HK. Americans’ confidence in their ability to pay for health care is falling. To The Point blog. May 10, 2018. The Commonwealth Fund. Accessed August 9, 2020. https://www.commonwealthfund.org/blog/2018/americans-confidence-their-ability-pay-health-care-falling
8. Saad L. More Americans delaying medical treatment due to cost. Gallup News. December 9, 2019. Accessed August 9, 2020. https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx
9. Lee VS. Fee for service is a terrible way to pay for health care. Try a subscription model instead. STAT. June 12, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/06/12/fee-for-service-is-a-terrible-way-to-pay-for-health-care-try-a-subscription-model-instead/
10. Moriates C, Shah NT, Arora VM. A framework for the frontline: how hospitalists can improve healthcare value. J Hosp Med. 2016;11(4):297-302. https://doi.org/10.1002/jhm.2494
11. Seymann G, Komsoukaniants A, Bouland D, Jenkins I. The Silver Linings Playbook for Covid-19. KevinMD. June 12, 2020. Accessed August 9, 2020. https://www.kevinmd.com/blog/2020/06/the-silver-linings-playbook-for-covid-19.html
12. Advis In The News. Industry Professionals Weigh In: Future of Healthcare Survey. Advis. Accessed August 9, 2020. https://advis.com/advis-in-the-news/post-pandemic-survey-june2020/
13. APM Measurement Effort. Healthcare Learning Payment and Action Network; 2019. Accessed August 9, 2020. https://hcp-lan.org/workproducts/apm-infographic-2019.pdf
14. Mosley D, DeBehnke D. Rural hospital sustainability: new analysis shows worsening situation for rural hospitals, residents. Navigant; February 2019. Accessed August 9, 2020. https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospital-analysis-22019.pdf
15. Gondi S, Chokshi DA. Financial stability as a goal of payment reform—a lesson from COVID-19. JAMA Health Forum. August 6, 2020. Accessed August 9, 2020. https://jamanetwork.com/channels/health-forum/fullarticle/2769307
16. Murphy K, Koski-Vacirca R, Sharfstein J. Resilience in health care financing. JAMA. 2020;324(2):126-127. https://doi.org/10.1001/jama.2020.10417
17. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
18. Weiss AJ, Elixhauser A, Andrews RM. Statistical Brief #170: Characteristics of Operating Room Procedures in U.S. Hospitals, 2011. Healthcare Costs and Utilization Project, Agency for Healthcare Research and Quality; February 2014. Accessed August 9, 2020: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.pdf
19. Crook HL, Saunders RS, Bleser WK, Broome T, Muhlestein D, McLellan MB. Leveraging Payment Reforms For COVID-19 And Beyond: Recommendations For Medicare ACOs And CMS’s Interim Final Rule. Health Affairs Blog. May 29, 2020. Accessed August 9, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200528.402208/full/
20. Blue Cross NC Launches Comprehensive Program to Help Independent Primary Care Practices Stay in Business. Press release. BlueCross BlueShield of North Carolina; June 24, 2020. Accessed August 9, 2020. https://mediacenter.bcbsnc.com/news/blue-cross-nc-launches-comprehensive-program-to-help-independent-primary-care-practices-stay-in-business
21. RTI International. State Innovation Models (SIM) Initiative Evaluation: Model Test Year Five Annual Report. Centers for Medicaid & Medicare Services; December 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/cmmi/sim-rd1-mt-fifthannrpt.pdf
22. Wack A. A Message from OneCare CEO Vicki Loner: OneCare’s Response to the Pandemic. OneCare Vermont. May 1, 2020. Accessed August 9, 2020. https://www.onecarevt.org/20200501-covid19/
23. Haber S, Bell H, Morrison M, et al. Evaluation of the Maryland All-Payer Model: Vol 1: Final Report. Centers for Medicare & Medicaid Services; November 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/md-allpayer-finalevalrpt.pdf
The day after Memorial Day 2020 marked an important transition in the United States’ experience with coronavirus disease 2019 (COVID-19), with many states making initial plans to reopen.
This year’s widespread healthcare closures were necessary to reduce COVID-19 transmission and prepare for a future patient surge, but these closures had unintended consequences. Nearly half of adults polled said they or someone in their household had foregone or delayed care since the outbreak began.1 This was especially true for visits to emergency departments and doctors’ offices for strokes, heart attacks, and routine medical care.2 In a survey across 49 states, only 7% of primary care practices considered scheduling preventive visits as a high priority.3 Eleven percent of polled adults reported delaying care worsened their condition,1 and in hard-hit areas such as New York City, non-COVID mortality was 22% higher than expected.4
Avoidance of the medical system decreased not only use of necessary, high-value care but also use of low-value care. Low-value services are those in which the “potential for harms exceed the potential benefits,”5 such as unnecessary hospitalizations, avoidable emergency department or clinic visits, unwarranted or excessive diagnostic testing (eg, annual physicals), and certain procedures (eg, spinal fusion surgery for low-back pain).
KEEP PATIENTS CENTRAL IN REOPENING SERVICES TO DELIVER HIGH-VALUE CARE
Medical centers can better focus on high-value care by defining their high-risk patient populations; high-value treatments, procedures, and preventive care; and phases of reopening. During the first pandemic wave, medical centers tried to reassure patients about emergency care, such as coming in for chest pain or neurologic symptoms, through personal outreach and media campaigns. Outpatient virtual visits also continued, including primary care, specialty services, mental health treatment, and physical therapy. While reopening, some medical centers have assessed disparities by relying on their data analytics and, if available, embedded health services researchers to understand what care was stopped and what populations were most affected.
The University of California health systems, for example, had a learning collaborative focused on sharing methods to restore care delivery that prioritizes patient needs. Some campuses conducted analyses using both electronic health record data and input from patients and their care teams to identify clinical needs and determine patient outreach plans. Some approaches used machine learning models to identify patients at highest risk of hospitalization or emergency department visits over the next 12 months and to conduct additional outreach to schedule these patients in primary and specialty care if clinically appropriate. Similarly, surgical specialties identified the highest-priority nonemergent surgeries for scheduling, including cancer resection, radiation therapy, and pain-management procedures. Similar guidance toward the most meaningful care has been prioritized within the United States Department of Veterans Affairs.
The rapid deployment of telehealth and payment models that reimburse video and in-clinic visits equally created new opportunities for medical centers to expand high-value care in lower-cost home settings. Similarly, new infrastructure is being developed to help define smarter use of virtual visits and home-based lab collection and monitoring.
Medical centers also must pay careful attention to redeploying service capacity for underused, high-value services. The pandemic uncovered existing staff that could be redeployed to support these changes. For example, with an “all hands on deck” mentality during the pandemic, in some medical centers, analysts or care managers from less-prioritized or duplicative areas were reassigned to vital COVID-19 efforts. Medical centers may realize that this staff can provide more value in the future by supporting increased high-value, affordable healthcare.
DELIBERATELY AVOID LOW-VALUE CARE
During the intial wave of the pandemic, medical centers greatly reduced the care they provided, often focusing on delivering essential care. This preparation for a surge of COVID patients had the effect of halting many unnecessary services by moving care from the clinic to home under new reimbursement changes, such as those affecting telehealth payments. The experience of reducing low-value medical services and visits can be extended to limiting unnecessary diagnostic testing. Medical centers could, for example, focus only on tests that advance care plans; reduce unnecessary blood draws, procedures, and vital sign checks on stable patients; shift to medications with less-frequent dosing intervals; and consolidate visits by treatment teams.10,11
Medical centers, however, now face continued pressures to increase revenue because 75% report their organization’s top priority is focused on increasing patient volume.12
PROACTIVELY AVOID WORSENING HEALTHCARE DISPARITIES
As medical centers reboot, operational and clinical leaders must proactively view changes through an equity lens to avoid exacerbating health disparities among vulnerable populations. The pandemic has focused national attention on the severity and pervasiveness of disparities and created an imperative for substantive action to evaluate how every decision will affect health equity. For example, medical centers are expanding use of telehealth to improve patient outreach. However, in a survey of primary care physicians, 72% said they have patients who are unable to access telehealth because they do not have access to technology.3 Exclusion of these patients from programs risks worsening health disparities. In a recent survey, nearly 65% of medical centers report reexamining existing policies, protocols, and practices for patients at risk of disparities.12
REFORM TO SUPPORT HIGH-VALUE CARE DELIVERY
Medical centers nationwide will need payment reform that provides greater financial stability beyond the pandemic to support high-value care delivery. They also will need flexibility to invest in prevention and to deliver the appropriate intensity of care to meet patients’ and communities’ needs.15-17 Options to provide this support include prospective population-based payments that may create more resilience in protecting access to care when it is most needed. Models can include fully capitated payment for physician practices.19,20 For example, after Vermont entered a single accountable care organization (ACO) model with the Centers for Medicare & Medicaid Services (CMS) in 2018, they not only generated a $97 million Medicaid savings, but also had a financial cushion that was later used in their COVID-19 response.21,22 The advanced payments allowed primary care practices and community agencies to invest in a digital tool to support outreach to patient at high risk for virus complications.
Hospitals similarly can adapt global budgets that incentivize financial stewardship by encouraging clinicians to resume necessary services and not unnecessary ones.16 For example, CMS partnered with Pennsylvania’s Department of Health to provide prospective all-payer global budgets for rural hospitals and Maryland’s Health Services Cost Review Commission that negotiates a budget with each hospital. During the COVID-19 pandemic, hospitals in these programs have had more financial protection from fluctuating finances by allowing for easier shifts in service delivery location and adjustments in rates to compensate for declines in visits and procedures.23
Policy makers and payers also can hold medical centers accountable to evidence-based guidelines and appropriate use of care, especially when necessary but expensive (eg, percutaneous coronary interventions, spinal surgeries, or cancer care). Funding agencies, additionally, can support these efforts by focusing on research, dissemination, and reliable implementation of these practices.
CONCLUSION
The COVID-19 crisis presents a tremendous opportunity for each medical center to revitalize healthcare. This opportunity can be seized only with reform by policy makers, payers, and regulatory agencies who encourage restarting high-value care without low-value services. We must take deliberate action so the nation’s medical centers can better meet patients’ needs to make healthcare more resilient, efficient, and fair.
The day after Memorial Day 2020 marked an important transition in the United States’ experience with coronavirus disease 2019 (COVID-19), with many states making initial plans to reopen.
This year’s widespread healthcare closures were necessary to reduce COVID-19 transmission and prepare for a future patient surge, but these closures had unintended consequences. Nearly half of adults polled said they or someone in their household had foregone or delayed care since the outbreak began.1 This was especially true for visits to emergency departments and doctors’ offices for strokes, heart attacks, and routine medical care.2 In a survey across 49 states, only 7% of primary care practices considered scheduling preventive visits as a high priority.3 Eleven percent of polled adults reported delaying care worsened their condition,1 and in hard-hit areas such as New York City, non-COVID mortality was 22% higher than expected.4
Avoidance of the medical system decreased not only use of necessary, high-value care but also use of low-value care. Low-value services are those in which the “potential for harms exceed the potential benefits,”5 such as unnecessary hospitalizations, avoidable emergency department or clinic visits, unwarranted or excessive diagnostic testing (eg, annual physicals), and certain procedures (eg, spinal fusion surgery for low-back pain).
KEEP PATIENTS CENTRAL IN REOPENING SERVICES TO DELIVER HIGH-VALUE CARE
Medical centers can better focus on high-value care by defining their high-risk patient populations; high-value treatments, procedures, and preventive care; and phases of reopening. During the first pandemic wave, medical centers tried to reassure patients about emergency care, such as coming in for chest pain or neurologic symptoms, through personal outreach and media campaigns. Outpatient virtual visits also continued, including primary care, specialty services, mental health treatment, and physical therapy. While reopening, some medical centers have assessed disparities by relying on their data analytics and, if available, embedded health services researchers to understand what care was stopped and what populations were most affected.
The University of California health systems, for example, had a learning collaborative focused on sharing methods to restore care delivery that prioritizes patient needs. Some campuses conducted analyses using both electronic health record data and input from patients and their care teams to identify clinical needs and determine patient outreach plans. Some approaches used machine learning models to identify patients at highest risk of hospitalization or emergency department visits over the next 12 months and to conduct additional outreach to schedule these patients in primary and specialty care if clinically appropriate. Similarly, surgical specialties identified the highest-priority nonemergent surgeries for scheduling, including cancer resection, radiation therapy, and pain-management procedures. Similar guidance toward the most meaningful care has been prioritized within the United States Department of Veterans Affairs.
The rapid deployment of telehealth and payment models that reimburse video and in-clinic visits equally created new opportunities for medical centers to expand high-value care in lower-cost home settings. Similarly, new infrastructure is being developed to help define smarter use of virtual visits and home-based lab collection and monitoring.
Medical centers also must pay careful attention to redeploying service capacity for underused, high-value services. The pandemic uncovered existing staff that could be redeployed to support these changes. For example, with an “all hands on deck” mentality during the pandemic, in some medical centers, analysts or care managers from less-prioritized or duplicative areas were reassigned to vital COVID-19 efforts. Medical centers may realize that this staff can provide more value in the future by supporting increased high-value, affordable healthcare.
DELIBERATELY AVOID LOW-VALUE CARE
During the intial wave of the pandemic, medical centers greatly reduced the care they provided, often focusing on delivering essential care. This preparation for a surge of COVID patients had the effect of halting many unnecessary services by moving care from the clinic to home under new reimbursement changes, such as those affecting telehealth payments. The experience of reducing low-value medical services and visits can be extended to limiting unnecessary diagnostic testing. Medical centers could, for example, focus only on tests that advance care plans; reduce unnecessary blood draws, procedures, and vital sign checks on stable patients; shift to medications with less-frequent dosing intervals; and consolidate visits by treatment teams.10,11
Medical centers, however, now face continued pressures to increase revenue because 75% report their organization’s top priority is focused on increasing patient volume.12
PROACTIVELY AVOID WORSENING HEALTHCARE DISPARITIES
As medical centers reboot, operational and clinical leaders must proactively view changes through an equity lens to avoid exacerbating health disparities among vulnerable populations. The pandemic has focused national attention on the severity and pervasiveness of disparities and created an imperative for substantive action to evaluate how every decision will affect health equity. For example, medical centers are expanding use of telehealth to improve patient outreach. However, in a survey of primary care physicians, 72% said they have patients who are unable to access telehealth because they do not have access to technology.3 Exclusion of these patients from programs risks worsening health disparities. In a recent survey, nearly 65% of medical centers report reexamining existing policies, protocols, and practices for patients at risk of disparities.12
REFORM TO SUPPORT HIGH-VALUE CARE DELIVERY
Medical centers nationwide will need payment reform that provides greater financial stability beyond the pandemic to support high-value care delivery. They also will need flexibility to invest in prevention and to deliver the appropriate intensity of care to meet patients’ and communities’ needs.15-17 Options to provide this support include prospective population-based payments that may create more resilience in protecting access to care when it is most needed. Models can include fully capitated payment for physician practices.19,20 For example, after Vermont entered a single accountable care organization (ACO) model with the Centers for Medicare & Medicaid Services (CMS) in 2018, they not only generated a $97 million Medicaid savings, but also had a financial cushion that was later used in their COVID-19 response.21,22 The advanced payments allowed primary care practices and community agencies to invest in a digital tool to support outreach to patient at high risk for virus complications.
Hospitals similarly can adapt global budgets that incentivize financial stewardship by encouraging clinicians to resume necessary services and not unnecessary ones.16 For example, CMS partnered with Pennsylvania’s Department of Health to provide prospective all-payer global budgets for rural hospitals and Maryland’s Health Services Cost Review Commission that negotiates a budget with each hospital. During the COVID-19 pandemic, hospitals in these programs have had more financial protection from fluctuating finances by allowing for easier shifts in service delivery location and adjustments in rates to compensate for declines in visits and procedures.23
Policy makers and payers also can hold medical centers accountable to evidence-based guidelines and appropriate use of care, especially when necessary but expensive (eg, percutaneous coronary interventions, spinal surgeries, or cancer care). Funding agencies, additionally, can support these efforts by focusing on research, dissemination, and reliable implementation of these practices.
CONCLUSION
The COVID-19 crisis presents a tremendous opportunity for each medical center to revitalize healthcare. This opportunity can be seized only with reform by policy makers, payers, and regulatory agencies who encourage restarting high-value care without low-value services. We must take deliberate action so the nation’s medical centers can better meet patients’ needs to make healthcare more resilient, efficient, and fair.
1. Hamel L, Kearney A, Kirzinger A, Lopes L, Muñana C, Brodie M. KFF Health Tracking Poll - May 2020: Impact of Coronavirus on Personal Health, Economic and Food Security, and Medicaid. Kaiser Family Foundation; May 27, 2020. Accessed August 9, 2020. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
2. McFarling UL. ‘Where are all our patients?’: Covid phobia is keeping people with serious heart symptoms away from ERs. STAT. April 23, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/
3. Primary Care & COVID-19: Week 4 Survey. Primary Care Collaborative; April 9, 2020. Accessed August 9, 2020. https://www.pcpcc.org/2020/04/08/primary-care-covid-19-week-4-survey
4. Olson DR, Huynh M, Fine A, et al. New York City Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team. Preliminary estimate of excess mortality during the COVID-19 outbreak — New York City, March 11–May 2, 2020. Morbidity and Mortality Weekly Report. May 11, 2020. Accessed August 9, 2020. https://stacks.cdc.gov/view/cdc/87858
5. Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000-1005. https://doi.org/10.1001/jama.280.11.1000
6. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501-1509. https://doi.org/10.1001/jama.2019.13978
7. Collins SR, Gunja MZ, Doty MM, Bhupal HK. Americans’ confidence in their ability to pay for health care is falling. To The Point blog. May 10, 2018. The Commonwealth Fund. Accessed August 9, 2020. https://www.commonwealthfund.org/blog/2018/americans-confidence-their-ability-pay-health-care-falling
8. Saad L. More Americans delaying medical treatment due to cost. Gallup News. December 9, 2019. Accessed August 9, 2020. https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx
9. Lee VS. Fee for service is a terrible way to pay for health care. Try a subscription model instead. STAT. June 12, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/06/12/fee-for-service-is-a-terrible-way-to-pay-for-health-care-try-a-subscription-model-instead/
10. Moriates C, Shah NT, Arora VM. A framework for the frontline: how hospitalists can improve healthcare value. J Hosp Med. 2016;11(4):297-302. https://doi.org/10.1002/jhm.2494
11. Seymann G, Komsoukaniants A, Bouland D, Jenkins I. The Silver Linings Playbook for Covid-19. KevinMD. June 12, 2020. Accessed August 9, 2020. https://www.kevinmd.com/blog/2020/06/the-silver-linings-playbook-for-covid-19.html
12. Advis In The News. Industry Professionals Weigh In: Future of Healthcare Survey. Advis. Accessed August 9, 2020. https://advis.com/advis-in-the-news/post-pandemic-survey-june2020/
13. APM Measurement Effort. Healthcare Learning Payment and Action Network; 2019. Accessed August 9, 2020. https://hcp-lan.org/workproducts/apm-infographic-2019.pdf
14. Mosley D, DeBehnke D. Rural hospital sustainability: new analysis shows worsening situation for rural hospitals, residents. Navigant; February 2019. Accessed August 9, 2020. https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospital-analysis-22019.pdf
15. Gondi S, Chokshi DA. Financial stability as a goal of payment reform—a lesson from COVID-19. JAMA Health Forum. August 6, 2020. Accessed August 9, 2020. https://jamanetwork.com/channels/health-forum/fullarticle/2769307
16. Murphy K, Koski-Vacirca R, Sharfstein J. Resilience in health care financing. JAMA. 2020;324(2):126-127. https://doi.org/10.1001/jama.2020.10417
17. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
18. Weiss AJ, Elixhauser A, Andrews RM. Statistical Brief #170: Characteristics of Operating Room Procedures in U.S. Hospitals, 2011. Healthcare Costs and Utilization Project, Agency for Healthcare Research and Quality; February 2014. Accessed August 9, 2020: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.pdf
19. Crook HL, Saunders RS, Bleser WK, Broome T, Muhlestein D, McLellan MB. Leveraging Payment Reforms For COVID-19 And Beyond: Recommendations For Medicare ACOs And CMS’s Interim Final Rule. Health Affairs Blog. May 29, 2020. Accessed August 9, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200528.402208/full/
20. Blue Cross NC Launches Comprehensive Program to Help Independent Primary Care Practices Stay in Business. Press release. BlueCross BlueShield of North Carolina; June 24, 2020. Accessed August 9, 2020. https://mediacenter.bcbsnc.com/news/blue-cross-nc-launches-comprehensive-program-to-help-independent-primary-care-practices-stay-in-business
21. RTI International. State Innovation Models (SIM) Initiative Evaluation: Model Test Year Five Annual Report. Centers for Medicaid & Medicare Services; December 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/cmmi/sim-rd1-mt-fifthannrpt.pdf
22. Wack A. A Message from OneCare CEO Vicki Loner: OneCare’s Response to the Pandemic. OneCare Vermont. May 1, 2020. Accessed August 9, 2020. https://www.onecarevt.org/20200501-covid19/
23. Haber S, Bell H, Morrison M, et al. Evaluation of the Maryland All-Payer Model: Vol 1: Final Report. Centers for Medicare & Medicaid Services; November 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/md-allpayer-finalevalrpt.pdf
1. Hamel L, Kearney A, Kirzinger A, Lopes L, Muñana C, Brodie M. KFF Health Tracking Poll - May 2020: Impact of Coronavirus on Personal Health, Economic and Food Security, and Medicaid. Kaiser Family Foundation; May 27, 2020. Accessed August 9, 2020. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
2. McFarling UL. ‘Where are all our patients?’: Covid phobia is keeping people with serious heart symptoms away from ERs. STAT. April 23, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/
3. Primary Care & COVID-19: Week 4 Survey. Primary Care Collaborative; April 9, 2020. Accessed August 9, 2020. https://www.pcpcc.org/2020/04/08/primary-care-covid-19-week-4-survey
4. Olson DR, Huynh M, Fine A, et al. New York City Department of Health and Mental Hygiene (DOHMH) COVID-19 Response Team. Preliminary estimate of excess mortality during the COVID-19 outbreak — New York City, March 11–May 2, 2020. Morbidity and Mortality Weekly Report. May 11, 2020. Accessed August 9, 2020. https://stacks.cdc.gov/view/cdc/87858
5. Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000-1005. https://doi.org/10.1001/jama.280.11.1000
6. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501-1509. https://doi.org/10.1001/jama.2019.13978
7. Collins SR, Gunja MZ, Doty MM, Bhupal HK. Americans’ confidence in their ability to pay for health care is falling. To The Point blog. May 10, 2018. The Commonwealth Fund. Accessed August 9, 2020. https://www.commonwealthfund.org/blog/2018/americans-confidence-their-ability-pay-health-care-falling
8. Saad L. More Americans delaying medical treatment due to cost. Gallup News. December 9, 2019. Accessed August 9, 2020. https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx
9. Lee VS. Fee for service is a terrible way to pay for health care. Try a subscription model instead. STAT. June 12, 2020. Accessed August 9, 2020. https://www.statnews.com/2020/06/12/fee-for-service-is-a-terrible-way-to-pay-for-health-care-try-a-subscription-model-instead/
10. Moriates C, Shah NT, Arora VM. A framework for the frontline: how hospitalists can improve healthcare value. J Hosp Med. 2016;11(4):297-302. https://doi.org/10.1002/jhm.2494
11. Seymann G, Komsoukaniants A, Bouland D, Jenkins I. The Silver Linings Playbook for Covid-19. KevinMD. June 12, 2020. Accessed August 9, 2020. https://www.kevinmd.com/blog/2020/06/the-silver-linings-playbook-for-covid-19.html
12. Advis In The News. Industry Professionals Weigh In: Future of Healthcare Survey. Advis. Accessed August 9, 2020. https://advis.com/advis-in-the-news/post-pandemic-survey-june2020/
13. APM Measurement Effort. Healthcare Learning Payment and Action Network; 2019. Accessed August 9, 2020. https://hcp-lan.org/workproducts/apm-infographic-2019.pdf
14. Mosley D, DeBehnke D. Rural hospital sustainability: new analysis shows worsening situation for rural hospitals, residents. Navigant; February 2019. Accessed August 9, 2020. https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospital-analysis-22019.pdf
15. Gondi S, Chokshi DA. Financial stability as a goal of payment reform—a lesson from COVID-19. JAMA Health Forum. August 6, 2020. Accessed August 9, 2020. https://jamanetwork.com/channels/health-forum/fullarticle/2769307
16. Murphy K, Koski-Vacirca R, Sharfstein J. Resilience in health care financing. JAMA. 2020;324(2):126-127. https://doi.org/10.1001/jama.2020.10417
17. Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21):2127-2128. https://doi.org/10.1001/jama.2020.6269
18. Weiss AJ, Elixhauser A, Andrews RM. Statistical Brief #170: Characteristics of Operating Room Procedures in U.S. Hospitals, 2011. Healthcare Costs and Utilization Project, Agency for Healthcare Research and Quality; February 2014. Accessed August 9, 2020: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.pdf
19. Crook HL, Saunders RS, Bleser WK, Broome T, Muhlestein D, McLellan MB. Leveraging Payment Reforms For COVID-19 And Beyond: Recommendations For Medicare ACOs And CMS’s Interim Final Rule. Health Affairs Blog. May 29, 2020. Accessed August 9, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200528.402208/full/
20. Blue Cross NC Launches Comprehensive Program to Help Independent Primary Care Practices Stay in Business. Press release. BlueCross BlueShield of North Carolina; June 24, 2020. Accessed August 9, 2020. https://mediacenter.bcbsnc.com/news/blue-cross-nc-launches-comprehensive-program-to-help-independent-primary-care-practices-stay-in-business
21. RTI International. State Innovation Models (SIM) Initiative Evaluation: Model Test Year Five Annual Report. Centers for Medicaid & Medicare Services; December 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/cmmi/sim-rd1-mt-fifthannrpt.pdf
22. Wack A. A Message from OneCare CEO Vicki Loner: OneCare’s Response to the Pandemic. OneCare Vermont. May 1, 2020. Accessed August 9, 2020. https://www.onecarevt.org/20200501-covid19/
23. Haber S, Bell H, Morrison M, et al. Evaluation of the Maryland All-Payer Model: Vol 1: Final Report. Centers for Medicare & Medicaid Services; November 2019. Accessed August 9, 2020. https://downloads.cms.gov/files/md-allpayer-finalevalrpt.pdf
© 2021 Society of Hospital Medicine
Leveling the Playing Field: Accounting for Academic Productivity During the COVID-19 Pandemic
Professional upheavals caused by the coronavirus disease 2019 (COVID-19) pandemic have affected the academic productivity of many physicians. This is due in part to rapid changes in clinical care and medical education: physician-researchers have been redeployed to frontline clinical care; clinician-educators have been forced to rapidly transition in-person curricula to virtual platforms; and primary care physicians and subspecialists have been forced to transition to telehealth-based practices. In addition to these changes in clinical and educational responsibilities, the COVID-19 pandemic has substantially altered the personal lives of physicians. During the height of the pandemic, clinicians simultaneously wrestled with a lack of available childcare, unexpected home-schooling responsibilities, decreased income, and many other COVID-19-related stresses.1 Additionally, the ever-present “second pandemic” of structural racism, persistent health disparities, and racial inequity has further increased the personal and professional demands facing academic faculty.2
In particular, the pandemic has placed personal and professional pressure on female and minority faculty members. In spite of these pressures, however, the academic promotions process still requires rigid accounting of scholarly productivity. As the focus of academic practices has shifted to support clinical care during the pandemic, scholarly productivity has suffered for clinicians on the frontline. As a result, academic clinical faculty have expressed significant stress and concerns about failing to meet benchmarks for promotion (eg, publications, curricula development, national presentations). To counter these shifts (and the inherent inequity that they create for female clinicians and for men and women who are Black, Indigenous, and/or of color), academic institutions should not only recognize the effects the COVID-19 pandemic has had on faculty, but also adopt immediate solutions to more equitably account for such disruptions to academic portfolios. In this paper, we explore populations whose career trajectories are most at-risk and propose a framework to capture novel and nontraditional contributions while also acknowledging the rapid changes the COVID-19 pandemic has brought to academic medicine.
POPULATIONS AT RISK FOR CAREER DISRUPTION
Even before the COVID-19 pandemic, physician mothers, underrepresented racial/ethnic minority groups, and junior faculty were most at-risk for career disruptions. The closure of daycare facilities and schools and shift to online learning resulting from the pandemic, along with the common challenges of parenting, have taken a significant toll on the lives of working parents. Because women tend to carry a disproportionate share of childcare and household responsibilities, these changes have inequitably leveraged themselves as a “mommy tax” on working women.3,4
As underrepresented medicine faculty (particularly Black, Hispanic, Latino, and Native American clinicians) comprise only 8% of the academic medical workforce,they currently face a variety of personal and professional challenges.5 This is especially true for Black and Latinx physicians who have been experiencing an increased COVID-19 burden in their communities, while concurrently fighting entrenched structural racism and police violence. In academia, these challenges have worsened because of the “minority tax”—the toll of often uncompensated extra responsibilities (time or money) placed on minority faculty in the name of achieving diversity. The unintended consequences of these responsibilities result in having fewer mentors,6 caring for underserved populations,7 and performing more clinical care8 than non-underrepresented minority faculty. Because minority faculty are unlikely to be in leadership positions, it is reasonable to conclude they have been shouldering heavier clinical obligations and facing greater career disruption of scholarly work due to the COVID-19 pandemic.
Junior faculty (eg, instructors and assistant professors) also remain professionally vulnerable during the COVID-19 pandemic. Because junior faculty are often more clinically focused and less likely to hold leadership positions than senior faculty, they are more likely to have assumed frontline clinical positions, which come at the expense of academic work. Junior faculty are also at a critical building phase in their academic career—a time when they benefit from the opportunity to share their scholarly work and network at conferences. Unfortunately, many conferences have been canceled or moved to a virtual platform. Given that some institutions may be freezing academic funding for conferences due to budgetary shortfalls from the pandemic, junior faculty may be particularly at risk if they are not able to present their work. In addition, junior faculty often face disproportionate struggles at home, trying to balance demands of work and caring for young children. Considering the unique needs of each of these groups, it is especially important to consider intersectionality, or the compounded issues for individuals who exist in multiple disproportionately affected groups (eg, a Black female junior faculty member who is also a mother).
THE COVID-19-CURRICULUM VITAE MATRIX
The typical format of a professional curriculum vitae (CV) at most academic institutions does not allow one to document potential disruptions or novel contributions, including those that occurred during the COVID-19 pandemic. As a group of academic clinicians, educators, and researchers whose careers have been affected by the pandemic, we created a COVID-19 CV matrix, a potential framework to serve as a supplement for faculty. In this matrix, faculty members may document their contributions, disruptions that affected their work, and caregiving responsibilities during this time period, while also providing a rubric for promotions and tenure committees to equitably evaluate the pandemic period on an academic CV. Our COVID-19 CV matrix consists of six domains: (1) clinical care, (2) research, (3) education, (4) service, (5) advocacy/media, and (6) social media. These domains encompass traditional and nontraditional contributions made by healthcare professionals during the pandemic (Table). This matrix broadens the ability of both faculty and institutions to determine the actual impact of individuals during the pandemic.
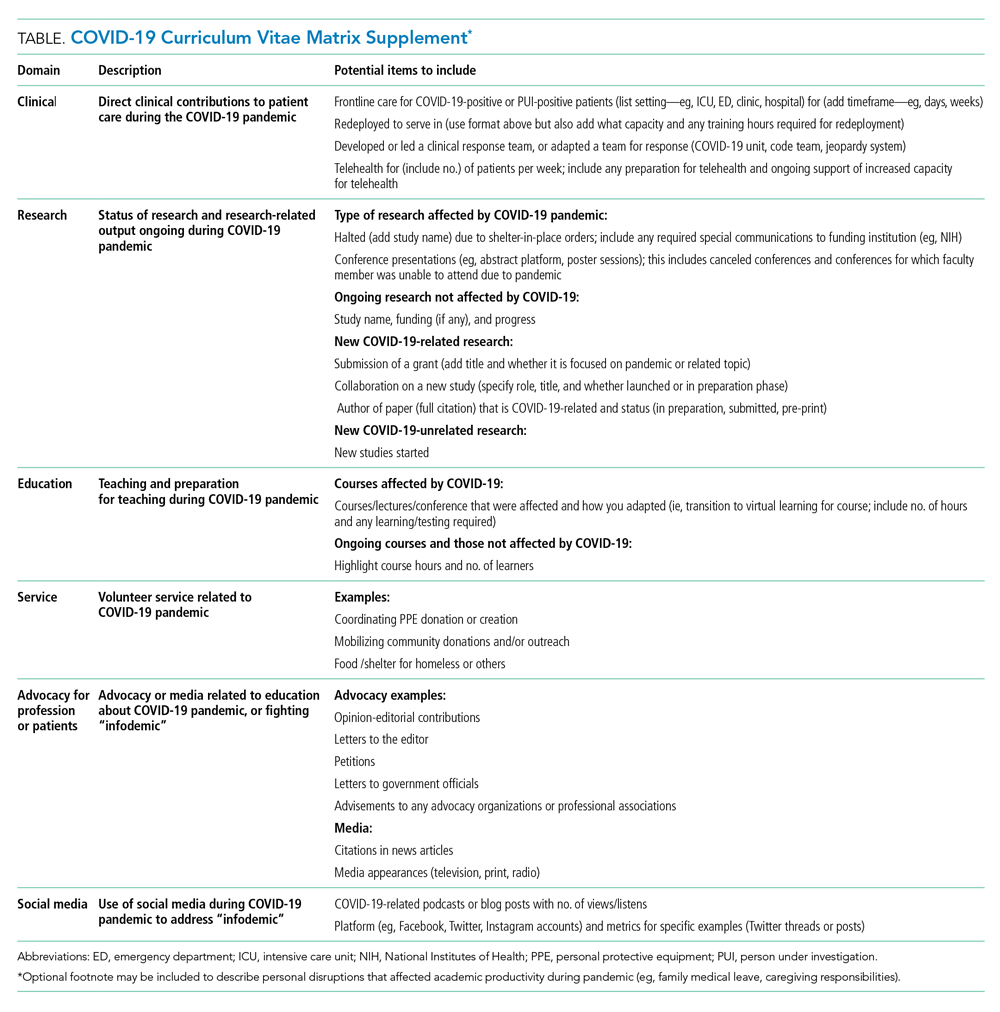
ACCOUNT FOR YOUR (NEW) IMPACT
Throughout the COVID-19 pandemic, academic faculty have been innovative, contributing in novel ways not routinely captured by promotions committees—eg, the digital health researcher who now directs the telemedicine response for their institution and the health disparities researcher who now leads daily webinar sessions on structural racism to medical students. Other novel contributions include advancing COVID-19 innovations and engaging in media and community advocacy (eg, organizing large-scale donations of equipment and funds to support organizations in need). While such nontraditional contributions may not have been readily captured or thought “CV worthy” in the past, faculty should now account for them. More importantly, promotions committees need to recognize that these pivots or alterations in career paths are not signals of professional failure, but rather evidence of a shifting landscape and the respective response of the individual. Furthermore, because these pivots often help fulfill an institutional mission, they are impactful.
ACKNOWLEDGE THE DISRUPTION
It is important for promotions and tenure committees to recognize the impact and disruption COVID-19 has had on traditional academic work, acknowledging the time and energy required for a faculty member to make needed work adjustments. This enables a leader to better assess how a faculty member’s academic portfolio has been affected. For example, researchers have had to halt studies, medical educators have had to redevelop and transition curricula to virtual platforms, and physicians have had to discontinue clinician quality improvement initiatives due to competing hospital priorities. Faculty members who document such unintentional alterations in their academic career path can explain to their institution how they have continued to positively influence their field and the community during the pandemic. This approach is analogous to the current model of accounting for clinical time when judging faculty members’ contributions in scholarly achievement.
The COVID-19 CV matrix has the potential to be annotated to explain the burden of one’s personal situation, which is often “invisible” in the professional environment. For example, many physicians have had to assume additional childcare responsibilities, tend to sick family members, friends, and even themselves. It is also possible that a faculty member has a partner who is also an essential worker, one who had to self-isolate due to COVID-19 exposure or illness, or who has been working overtime due to high patient volumes.
INSTITUTIONAL RESPONSE
How can institutions respond to the altered academic landscape caused by the COVID-19 pandemic? Promotions committees typically have two main tools at their disposal: adjusting the tenure clock or the benchmarks. Extending the period of time available to qualify for tenure is commonplace in the “publish-or-perish” academic tracks of university research professors. Clock adjustments are typically granted to faculty following the birth of a child or for other specific family- or health-related hardships, in accordance with the Family and Medical Leave Act. Unfortunately, tenure-clock extensions for female faculty members can exacerbate gender inequity: Data on tenure-clock extensions show a higher rate of tenure granted to male faculty compared to female faculty.9 For this reason, it is also important to explore adjustments or modifications to benchmark criteria. This could be accomplished by broadening the criteria for promotion, recognizing that impact occurs in many forms, thereby enabling meeting a benchmark. It can also occur by examining the trajectory of an individual within a promotion pathway before it was disrupted to determine impact. To avoid exacerbating social and gender inequities within academia, institutions should use these professional levers and create new ones to provide parity and equality across the promotional playing field. While the CV matrix openly acknowledges the disruptions and tangents the COVID-19 pandemic has had on academic careers, it remains important for academic institutions to recognize these disruptions and innovate the manner in which they acknowledge scholarly contributions.
Conclusion
While academic rigidity and known social taxes (minority and mommy taxes) are particularly problematic in the current climate, these issues have always been at play in evaluating academic success. Improved documentation of novel contributions, disruptions, caregiving, and other challenges can enable more holistic and timely professional advancement for all faculty, regardless of their sex, race, ethnicity, or social background. Ultimately, we hope this framework initiates further conversations among academic institutions on how to define productivity in an age where journal impact factor or number of publications is not the fullest measure of one’s impact in their field.
1. Jones Y, Durand V, Morton K, et al; ADVANCE PHM Steering Committee. Collateral damage: how covid-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
2. Manning KD. When grief and crises intersect: perspectives of a black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
3. Cohen P, Hsu T. Pandemic could scar a generation of working mothers. New York Times. Published June 3, 2020. Updated June 30, 2020. Accessed November 11, 2020. https://www.nytimes.com/2020/06/03/business/economy/coronavirus-working-women.html
4. Cain Miller C. Nearly half of men say they do most of the home schooling. 3 percent of women agree. Published May 6, 2020. Updated May 8, 2020. Accessed November 11, 2020. New York Times. https://www.nytimes.com/2020/05/06/upshot/pandemic-chores-homeschooling-gender.html
5. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. 2015;15:6. https://doi.org/10.1186/s12909-015-0290-9
6. Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: a new model for mentoring underrepresented minority faculty. Acad Med. 2006;81(3):275-279. https://doi.org/10.1097/00001888-200603000-00020
7. Pololi LH, Evans AT, Gibbs BK, Krupat E, Brennan RT, Civian JT. The experience of minority faculty who are underrepresented in medicine, at 26 representative U.S. medical schools. Acad Med. 2013;88(9):1308-1314. https://doi.org/10.1097/acm.0b013e31829eefff
8. Richert A, Campbell K, Rodríguez J, Borowsky IW, Parikh R, Colwell A. ACU workforce column: expanding and supporting the health care workforce. J Health Care Poor Underserved. 2013;24(4):1423-1431. https://doi.org/10.1353/hpu.2013.0162
9. Woitowich NC, Jain S, Arora VM, Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2020;29:10.1097/ACM.0000000000003782. https://doi.org/10.1097/acm.0000000000003782
Professional upheavals caused by the coronavirus disease 2019 (COVID-19) pandemic have affected the academic productivity of many physicians. This is due in part to rapid changes in clinical care and medical education: physician-researchers have been redeployed to frontline clinical care; clinician-educators have been forced to rapidly transition in-person curricula to virtual platforms; and primary care physicians and subspecialists have been forced to transition to telehealth-based practices. In addition to these changes in clinical and educational responsibilities, the COVID-19 pandemic has substantially altered the personal lives of physicians. During the height of the pandemic, clinicians simultaneously wrestled with a lack of available childcare, unexpected home-schooling responsibilities, decreased income, and many other COVID-19-related stresses.1 Additionally, the ever-present “second pandemic” of structural racism, persistent health disparities, and racial inequity has further increased the personal and professional demands facing academic faculty.2
In particular, the pandemic has placed personal and professional pressure on female and minority faculty members. In spite of these pressures, however, the academic promotions process still requires rigid accounting of scholarly productivity. As the focus of academic practices has shifted to support clinical care during the pandemic, scholarly productivity has suffered for clinicians on the frontline. As a result, academic clinical faculty have expressed significant stress and concerns about failing to meet benchmarks for promotion (eg, publications, curricula development, national presentations). To counter these shifts (and the inherent inequity that they create for female clinicians and for men and women who are Black, Indigenous, and/or of color), academic institutions should not only recognize the effects the COVID-19 pandemic has had on faculty, but also adopt immediate solutions to more equitably account for such disruptions to academic portfolios. In this paper, we explore populations whose career trajectories are most at-risk and propose a framework to capture novel and nontraditional contributions while also acknowledging the rapid changes the COVID-19 pandemic has brought to academic medicine.
POPULATIONS AT RISK FOR CAREER DISRUPTION
Even before the COVID-19 pandemic, physician mothers, underrepresented racial/ethnic minority groups, and junior faculty were most at-risk for career disruptions. The closure of daycare facilities and schools and shift to online learning resulting from the pandemic, along with the common challenges of parenting, have taken a significant toll on the lives of working parents. Because women tend to carry a disproportionate share of childcare and household responsibilities, these changes have inequitably leveraged themselves as a “mommy tax” on working women.3,4
As underrepresented medicine faculty (particularly Black, Hispanic, Latino, and Native American clinicians) comprise only 8% of the academic medical workforce,they currently face a variety of personal and professional challenges.5 This is especially true for Black and Latinx physicians who have been experiencing an increased COVID-19 burden in their communities, while concurrently fighting entrenched structural racism and police violence. In academia, these challenges have worsened because of the “minority tax”—the toll of often uncompensated extra responsibilities (time or money) placed on minority faculty in the name of achieving diversity. The unintended consequences of these responsibilities result in having fewer mentors,6 caring for underserved populations,7 and performing more clinical care8 than non-underrepresented minority faculty. Because minority faculty are unlikely to be in leadership positions, it is reasonable to conclude they have been shouldering heavier clinical obligations and facing greater career disruption of scholarly work due to the COVID-19 pandemic.
Junior faculty (eg, instructors and assistant professors) also remain professionally vulnerable during the COVID-19 pandemic. Because junior faculty are often more clinically focused and less likely to hold leadership positions than senior faculty, they are more likely to have assumed frontline clinical positions, which come at the expense of academic work. Junior faculty are also at a critical building phase in their academic career—a time when they benefit from the opportunity to share their scholarly work and network at conferences. Unfortunately, many conferences have been canceled or moved to a virtual platform. Given that some institutions may be freezing academic funding for conferences due to budgetary shortfalls from the pandemic, junior faculty may be particularly at risk if they are not able to present their work. In addition, junior faculty often face disproportionate struggles at home, trying to balance demands of work and caring for young children. Considering the unique needs of each of these groups, it is especially important to consider intersectionality, or the compounded issues for individuals who exist in multiple disproportionately affected groups (eg, a Black female junior faculty member who is also a mother).
THE COVID-19-CURRICULUM VITAE MATRIX
The typical format of a professional curriculum vitae (CV) at most academic institutions does not allow one to document potential disruptions or novel contributions, including those that occurred during the COVID-19 pandemic. As a group of academic clinicians, educators, and researchers whose careers have been affected by the pandemic, we created a COVID-19 CV matrix, a potential framework to serve as a supplement for faculty. In this matrix, faculty members may document their contributions, disruptions that affected their work, and caregiving responsibilities during this time period, while also providing a rubric for promotions and tenure committees to equitably evaluate the pandemic period on an academic CV. Our COVID-19 CV matrix consists of six domains: (1) clinical care, (2) research, (3) education, (4) service, (5) advocacy/media, and (6) social media. These domains encompass traditional and nontraditional contributions made by healthcare professionals during the pandemic (Table). This matrix broadens the ability of both faculty and institutions to determine the actual impact of individuals during the pandemic.
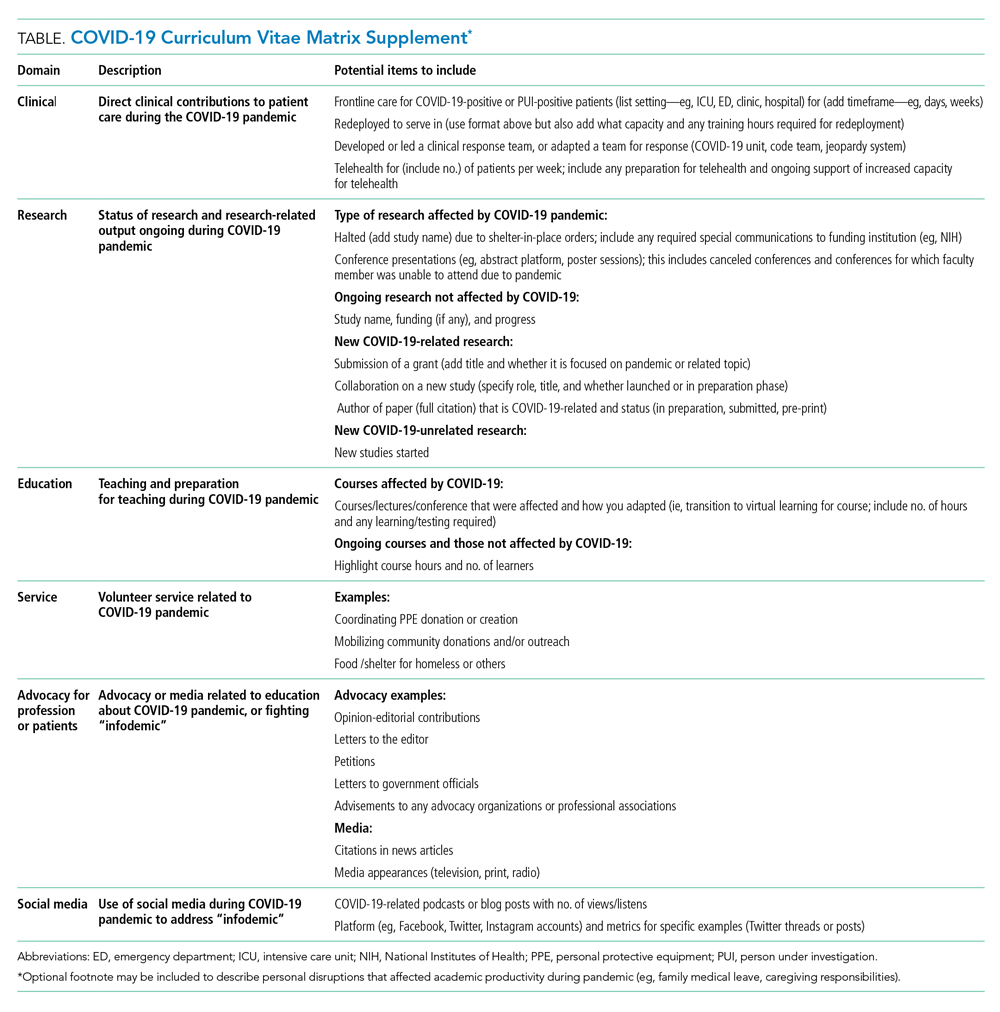
ACCOUNT FOR YOUR (NEW) IMPACT
Throughout the COVID-19 pandemic, academic faculty have been innovative, contributing in novel ways not routinely captured by promotions committees—eg, the digital health researcher who now directs the telemedicine response for their institution and the health disparities researcher who now leads daily webinar sessions on structural racism to medical students. Other novel contributions include advancing COVID-19 innovations and engaging in media and community advocacy (eg, organizing large-scale donations of equipment and funds to support organizations in need). While such nontraditional contributions may not have been readily captured or thought “CV worthy” in the past, faculty should now account for them. More importantly, promotions committees need to recognize that these pivots or alterations in career paths are not signals of professional failure, but rather evidence of a shifting landscape and the respective response of the individual. Furthermore, because these pivots often help fulfill an institutional mission, they are impactful.
ACKNOWLEDGE THE DISRUPTION
It is important for promotions and tenure committees to recognize the impact and disruption COVID-19 has had on traditional academic work, acknowledging the time and energy required for a faculty member to make needed work adjustments. This enables a leader to better assess how a faculty member’s academic portfolio has been affected. For example, researchers have had to halt studies, medical educators have had to redevelop and transition curricula to virtual platforms, and physicians have had to discontinue clinician quality improvement initiatives due to competing hospital priorities. Faculty members who document such unintentional alterations in their academic career path can explain to their institution how they have continued to positively influence their field and the community during the pandemic. This approach is analogous to the current model of accounting for clinical time when judging faculty members’ contributions in scholarly achievement.
The COVID-19 CV matrix has the potential to be annotated to explain the burden of one’s personal situation, which is often “invisible” in the professional environment. For example, many physicians have had to assume additional childcare responsibilities, tend to sick family members, friends, and even themselves. It is also possible that a faculty member has a partner who is also an essential worker, one who had to self-isolate due to COVID-19 exposure or illness, or who has been working overtime due to high patient volumes.
INSTITUTIONAL RESPONSE
How can institutions respond to the altered academic landscape caused by the COVID-19 pandemic? Promotions committees typically have two main tools at their disposal: adjusting the tenure clock or the benchmarks. Extending the period of time available to qualify for tenure is commonplace in the “publish-or-perish” academic tracks of university research professors. Clock adjustments are typically granted to faculty following the birth of a child or for other specific family- or health-related hardships, in accordance with the Family and Medical Leave Act. Unfortunately, tenure-clock extensions for female faculty members can exacerbate gender inequity: Data on tenure-clock extensions show a higher rate of tenure granted to male faculty compared to female faculty.9 For this reason, it is also important to explore adjustments or modifications to benchmark criteria. This could be accomplished by broadening the criteria for promotion, recognizing that impact occurs in many forms, thereby enabling meeting a benchmark. It can also occur by examining the trajectory of an individual within a promotion pathway before it was disrupted to determine impact. To avoid exacerbating social and gender inequities within academia, institutions should use these professional levers and create new ones to provide parity and equality across the promotional playing field. While the CV matrix openly acknowledges the disruptions and tangents the COVID-19 pandemic has had on academic careers, it remains important for academic institutions to recognize these disruptions and innovate the manner in which they acknowledge scholarly contributions.
Conclusion
While academic rigidity and known social taxes (minority and mommy taxes) are particularly problematic in the current climate, these issues have always been at play in evaluating academic success. Improved documentation of novel contributions, disruptions, caregiving, and other challenges can enable more holistic and timely professional advancement for all faculty, regardless of their sex, race, ethnicity, or social background. Ultimately, we hope this framework initiates further conversations among academic institutions on how to define productivity in an age where journal impact factor or number of publications is not the fullest measure of one’s impact in their field.
Professional upheavals caused by the coronavirus disease 2019 (COVID-19) pandemic have affected the academic productivity of many physicians. This is due in part to rapid changes in clinical care and medical education: physician-researchers have been redeployed to frontline clinical care; clinician-educators have been forced to rapidly transition in-person curricula to virtual platforms; and primary care physicians and subspecialists have been forced to transition to telehealth-based practices. In addition to these changes in clinical and educational responsibilities, the COVID-19 pandemic has substantially altered the personal lives of physicians. During the height of the pandemic, clinicians simultaneously wrestled with a lack of available childcare, unexpected home-schooling responsibilities, decreased income, and many other COVID-19-related stresses.1 Additionally, the ever-present “second pandemic” of structural racism, persistent health disparities, and racial inequity has further increased the personal and professional demands facing academic faculty.2
In particular, the pandemic has placed personal and professional pressure on female and minority faculty members. In spite of these pressures, however, the academic promotions process still requires rigid accounting of scholarly productivity. As the focus of academic practices has shifted to support clinical care during the pandemic, scholarly productivity has suffered for clinicians on the frontline. As a result, academic clinical faculty have expressed significant stress and concerns about failing to meet benchmarks for promotion (eg, publications, curricula development, national presentations). To counter these shifts (and the inherent inequity that they create for female clinicians and for men and women who are Black, Indigenous, and/or of color), academic institutions should not only recognize the effects the COVID-19 pandemic has had on faculty, but also adopt immediate solutions to more equitably account for such disruptions to academic portfolios. In this paper, we explore populations whose career trajectories are most at-risk and propose a framework to capture novel and nontraditional contributions while also acknowledging the rapid changes the COVID-19 pandemic has brought to academic medicine.
POPULATIONS AT RISK FOR CAREER DISRUPTION
Even before the COVID-19 pandemic, physician mothers, underrepresented racial/ethnic minority groups, and junior faculty were most at-risk for career disruptions. The closure of daycare facilities and schools and shift to online learning resulting from the pandemic, along with the common challenges of parenting, have taken a significant toll on the lives of working parents. Because women tend to carry a disproportionate share of childcare and household responsibilities, these changes have inequitably leveraged themselves as a “mommy tax” on working women.3,4
As underrepresented medicine faculty (particularly Black, Hispanic, Latino, and Native American clinicians) comprise only 8% of the academic medical workforce,they currently face a variety of personal and professional challenges.5 This is especially true for Black and Latinx physicians who have been experiencing an increased COVID-19 burden in their communities, while concurrently fighting entrenched structural racism and police violence. In academia, these challenges have worsened because of the “minority tax”—the toll of often uncompensated extra responsibilities (time or money) placed on minority faculty in the name of achieving diversity. The unintended consequences of these responsibilities result in having fewer mentors,6 caring for underserved populations,7 and performing more clinical care8 than non-underrepresented minority faculty. Because minority faculty are unlikely to be in leadership positions, it is reasonable to conclude they have been shouldering heavier clinical obligations and facing greater career disruption of scholarly work due to the COVID-19 pandemic.
Junior faculty (eg, instructors and assistant professors) also remain professionally vulnerable during the COVID-19 pandemic. Because junior faculty are often more clinically focused and less likely to hold leadership positions than senior faculty, they are more likely to have assumed frontline clinical positions, which come at the expense of academic work. Junior faculty are also at a critical building phase in their academic career—a time when they benefit from the opportunity to share their scholarly work and network at conferences. Unfortunately, many conferences have been canceled or moved to a virtual platform. Given that some institutions may be freezing academic funding for conferences due to budgetary shortfalls from the pandemic, junior faculty may be particularly at risk if they are not able to present their work. In addition, junior faculty often face disproportionate struggles at home, trying to balance demands of work and caring for young children. Considering the unique needs of each of these groups, it is especially important to consider intersectionality, or the compounded issues for individuals who exist in multiple disproportionately affected groups (eg, a Black female junior faculty member who is also a mother).
THE COVID-19-CURRICULUM VITAE MATRIX
The typical format of a professional curriculum vitae (CV) at most academic institutions does not allow one to document potential disruptions or novel contributions, including those that occurred during the COVID-19 pandemic. As a group of academic clinicians, educators, and researchers whose careers have been affected by the pandemic, we created a COVID-19 CV matrix, a potential framework to serve as a supplement for faculty. In this matrix, faculty members may document their contributions, disruptions that affected their work, and caregiving responsibilities during this time period, while also providing a rubric for promotions and tenure committees to equitably evaluate the pandemic period on an academic CV. Our COVID-19 CV matrix consists of six domains: (1) clinical care, (2) research, (3) education, (4) service, (5) advocacy/media, and (6) social media. These domains encompass traditional and nontraditional contributions made by healthcare professionals during the pandemic (Table). This matrix broadens the ability of both faculty and institutions to determine the actual impact of individuals during the pandemic.
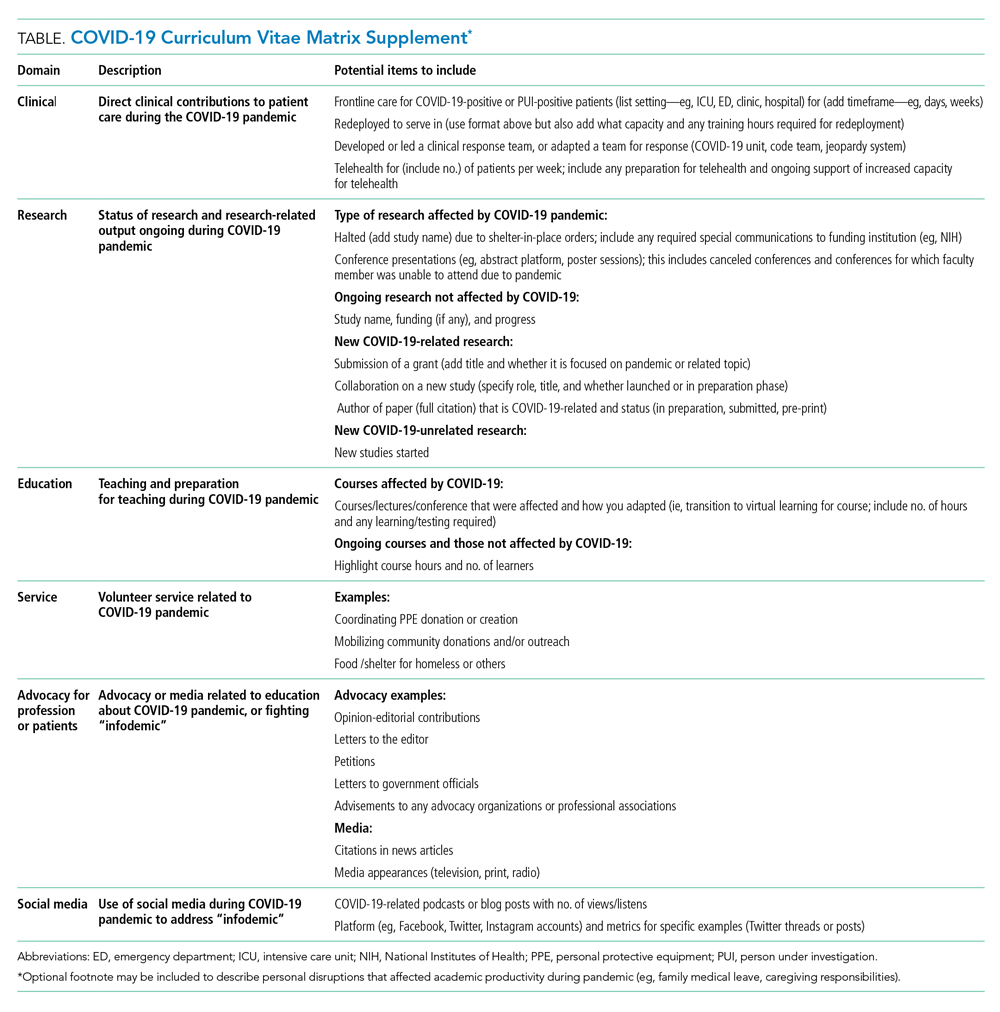
ACCOUNT FOR YOUR (NEW) IMPACT
Throughout the COVID-19 pandemic, academic faculty have been innovative, contributing in novel ways not routinely captured by promotions committees—eg, the digital health researcher who now directs the telemedicine response for their institution and the health disparities researcher who now leads daily webinar sessions on structural racism to medical students. Other novel contributions include advancing COVID-19 innovations and engaging in media and community advocacy (eg, organizing large-scale donations of equipment and funds to support organizations in need). While such nontraditional contributions may not have been readily captured or thought “CV worthy” in the past, faculty should now account for them. More importantly, promotions committees need to recognize that these pivots or alterations in career paths are not signals of professional failure, but rather evidence of a shifting landscape and the respective response of the individual. Furthermore, because these pivots often help fulfill an institutional mission, they are impactful.
ACKNOWLEDGE THE DISRUPTION
It is important for promotions and tenure committees to recognize the impact and disruption COVID-19 has had on traditional academic work, acknowledging the time and energy required for a faculty member to make needed work adjustments. This enables a leader to better assess how a faculty member’s academic portfolio has been affected. For example, researchers have had to halt studies, medical educators have had to redevelop and transition curricula to virtual platforms, and physicians have had to discontinue clinician quality improvement initiatives due to competing hospital priorities. Faculty members who document such unintentional alterations in their academic career path can explain to their institution how they have continued to positively influence their field and the community during the pandemic. This approach is analogous to the current model of accounting for clinical time when judging faculty members’ contributions in scholarly achievement.
The COVID-19 CV matrix has the potential to be annotated to explain the burden of one’s personal situation, which is often “invisible” in the professional environment. For example, many physicians have had to assume additional childcare responsibilities, tend to sick family members, friends, and even themselves. It is also possible that a faculty member has a partner who is also an essential worker, one who had to self-isolate due to COVID-19 exposure or illness, or who has been working overtime due to high patient volumes.
INSTITUTIONAL RESPONSE
How can institutions respond to the altered academic landscape caused by the COVID-19 pandemic? Promotions committees typically have two main tools at their disposal: adjusting the tenure clock or the benchmarks. Extending the period of time available to qualify for tenure is commonplace in the “publish-or-perish” academic tracks of university research professors. Clock adjustments are typically granted to faculty following the birth of a child or for other specific family- or health-related hardships, in accordance with the Family and Medical Leave Act. Unfortunately, tenure-clock extensions for female faculty members can exacerbate gender inequity: Data on tenure-clock extensions show a higher rate of tenure granted to male faculty compared to female faculty.9 For this reason, it is also important to explore adjustments or modifications to benchmark criteria. This could be accomplished by broadening the criteria for promotion, recognizing that impact occurs in many forms, thereby enabling meeting a benchmark. It can also occur by examining the trajectory of an individual within a promotion pathway before it was disrupted to determine impact. To avoid exacerbating social and gender inequities within academia, institutions should use these professional levers and create new ones to provide parity and equality across the promotional playing field. While the CV matrix openly acknowledges the disruptions and tangents the COVID-19 pandemic has had on academic careers, it remains important for academic institutions to recognize these disruptions and innovate the manner in which they acknowledge scholarly contributions.
Conclusion
While academic rigidity and known social taxes (minority and mommy taxes) are particularly problematic in the current climate, these issues have always been at play in evaluating academic success. Improved documentation of novel contributions, disruptions, caregiving, and other challenges can enable more holistic and timely professional advancement for all faculty, regardless of their sex, race, ethnicity, or social background. Ultimately, we hope this framework initiates further conversations among academic institutions on how to define productivity in an age where journal impact factor or number of publications is not the fullest measure of one’s impact in their field.
1. Jones Y, Durand V, Morton K, et al; ADVANCE PHM Steering Committee. Collateral damage: how covid-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
2. Manning KD. When grief and crises intersect: perspectives of a black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
3. Cohen P, Hsu T. Pandemic could scar a generation of working mothers. New York Times. Published June 3, 2020. Updated June 30, 2020. Accessed November 11, 2020. https://www.nytimes.com/2020/06/03/business/economy/coronavirus-working-women.html
4. Cain Miller C. Nearly half of men say they do most of the home schooling. 3 percent of women agree. Published May 6, 2020. Updated May 8, 2020. Accessed November 11, 2020. New York Times. https://www.nytimes.com/2020/05/06/upshot/pandemic-chores-homeschooling-gender.html
5. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. 2015;15:6. https://doi.org/10.1186/s12909-015-0290-9
6. Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: a new model for mentoring underrepresented minority faculty. Acad Med. 2006;81(3):275-279. https://doi.org/10.1097/00001888-200603000-00020
7. Pololi LH, Evans AT, Gibbs BK, Krupat E, Brennan RT, Civian JT. The experience of minority faculty who are underrepresented in medicine, at 26 representative U.S. medical schools. Acad Med. 2013;88(9):1308-1314. https://doi.org/10.1097/acm.0b013e31829eefff
8. Richert A, Campbell K, Rodríguez J, Borowsky IW, Parikh R, Colwell A. ACU workforce column: expanding and supporting the health care workforce. J Health Care Poor Underserved. 2013;24(4):1423-1431. https://doi.org/10.1353/hpu.2013.0162
9. Woitowich NC, Jain S, Arora VM, Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2020;29:10.1097/ACM.0000000000003782. https://doi.org/10.1097/acm.0000000000003782
1. Jones Y, Durand V, Morton K, et al; ADVANCE PHM Steering Committee. Collateral damage: how covid-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
2. Manning KD. When grief and crises intersect: perspectives of a black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
3. Cohen P, Hsu T. Pandemic could scar a generation of working mothers. New York Times. Published June 3, 2020. Updated June 30, 2020. Accessed November 11, 2020. https://www.nytimes.com/2020/06/03/business/economy/coronavirus-working-women.html
4. Cain Miller C. Nearly half of men say they do most of the home schooling. 3 percent of women agree. Published May 6, 2020. Updated May 8, 2020. Accessed November 11, 2020. New York Times. https://www.nytimes.com/2020/05/06/upshot/pandemic-chores-homeschooling-gender.html
5. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ. 2015;15:6. https://doi.org/10.1186/s12909-015-0290-9
6. Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: a new model for mentoring underrepresented minority faculty. Acad Med. 2006;81(3):275-279. https://doi.org/10.1097/00001888-200603000-00020
7. Pololi LH, Evans AT, Gibbs BK, Krupat E, Brennan RT, Civian JT. The experience of minority faculty who are underrepresented in medicine, at 26 representative U.S. medical schools. Acad Med. 2013;88(9):1308-1314. https://doi.org/10.1097/acm.0b013e31829eefff
8. Richert A, Campbell K, Rodríguez J, Borowsky IW, Parikh R, Colwell A. ACU workforce column: expanding and supporting the health care workforce. J Health Care Poor Underserved. 2013;24(4):1423-1431. https://doi.org/10.1353/hpu.2013.0162
9. Woitowich NC, Jain S, Arora VM, Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2020;29:10.1097/ACM.0000000000003782. https://doi.org/10.1097/acm.0000000000003782
© 2021 Society of Hospital Medicine
Analysis of Hospital Resource Availability and COVID-19 Mortality Across the United States
The COVID-19 pandemic is a crisis of mismatch between resources and infection burden. There is extraordinary heterogeneity across time and geography in the pandemic impact, with hospitals in New York City initially inundated while hospitals in major urban areas of California were comparatively quiet. Efforts to “flatten the curve” are intended to improve outcomes by reducing health system overload.1 In the case of hospital-based care, health systems’ primary resources include emergency and critical care bed and staff capacity.
Prior work has documented wide variability in intensive care capacity across the United States and hypothesized that even moderate disease outbreaks could overwhelm hospital referral regions (HRRs).2,3 Various simulations of outbreaks suggested that thousands of deaths are potentially preventable depending on the health system’s response,4 although the degree to which resource limitations have contributed to mortality during this COVID-19 pandemic has yet to be explored. The objective of this analysis was to examine the association between hospital resources and COVID-19 deaths amongst HRRs in the United States in the period from March 1 to July 26, 2020.
METHODS
Data
This was an analysis of the American Hospital Association Annual Survey Database from 2017 and 2018, including hospital resource variables such as total hospital beds, hospitalists, intensive care beds, intensivists, emergency physicians, and nurses.5 The analysis was limited to general medical and surgical hospitals capable of providing acute care services, defined as those reporting at least 500 emergency department visits in 2018. Where data were missing on analysis variables (26.0% missing overall), the data were drawn from the 2017 survey results (reduced to 23.8% missing) from the same site as available, and the remainder were imputed with multivariate imputation by chained equations. An identical analysis without imputation was performed as a sensitivity analysis that showed a similar pattern of results. Total resources were tabulated amongst HRRs, and the hospital resources per COVID-19 case calculated. HRRs are a geographic category devised to represent regional health care markets, and each includes hospital sites performing major procedures.3 These were the focus of the analysis because they may represent a meaningful geographic division of hospital-based resources. COVID-19 case and death counts (as of July 26, 2020) were drawn from publicly available county-level data curated by the New York Times from state and local governments as well as health departments nationwide,6 separated by month (ie, March, April, May, June, and July). Data on New York City were available in aggregate (rather than separated by borough). Cases and deaths were therefore apportioned to the three HRRs involving New York City in proportion to that area’s population. To adjust for the lag between COVID-19 cases and deaths,7,8 we offset deaths 2 weeks into the future so that the April COVID-19 death count for a given HRR included deaths that occurred for 1 month beginning 2 weeks after the start of April, and so on.
Analysis
We estimated Poisson distribution regressions for the outcome of COVID-19 death count in each HRR and month with one model for each of our six hospital-based resource variables. The offset (exposure) variable was COVID-19 case count. To adjust for the possibility of varying effects of hospital resources on deaths by month (ie, in anticipation that health systems might evolve in response to the pandemic over time), each model includes terms for the interaction between hospital-based resource and an indicator variable for month, as well as a fifth term for month. Standard errors were adjusted for clustering within HRR. We report resultant incident rate ratios (IRRs) with 95% CIs, and we report these as statistically significant at the 5% level only after adjustment for multiple comparisons across our six hospital-resource variables using the conservative Bonferroni adjustment. The pseudo-R2 for each of these six models is also reported to summarize the amount of variation in deaths explained. For our model with ICU beds per COVID-19 case, we perform postestimation prediction of number of deaths by HRR, assuming the counterfactual in which HRRs with fewer than average ICU beds per COVID-19 case instead had the average observed number of ICU beds per COVID-19 case by HRR in April, which functioned as a measure of early excess deaths potentially related to resource limitations. The study was classified as exempt by the Institutional Review Board at the Yale School of Medicine, New Haven, Connecticut. Analyses were conducted in Stata 15 (StataCorp LLC) and R.
RESULTS
A total of 4,453 hospitals across 306 HRRs were included and linked to 2,827 county-level COVID-19 case and death counts in each of 5 months (March through July 2020). The median HRR in our analysis included 14 hospitals, with a maximum of 76 hospitals (Los Angeles, California) and a minimum of 1 (Longview, Texas). Among HRRs, 206 (67.3%) had experienced caseloads exceeding 20 per 10,000 population, while 85 (27.8%) had experienced greater than 100 per 10,000 population in the peak month during the study period. The Table depicts results of each of six Poisson distribution regression models, with the finding that greater number of ICU beds (IRR, 0.194; 95% CI, 0.076-0.491), general medical/surgical beds (IRR, 0.800; 95% CI, 0.696-0.920), and nurses (IRR, 0.927; 95% CI, 0.888-0.967) per COVID-19 case in April were statistically significantly associated with reduced deaths.
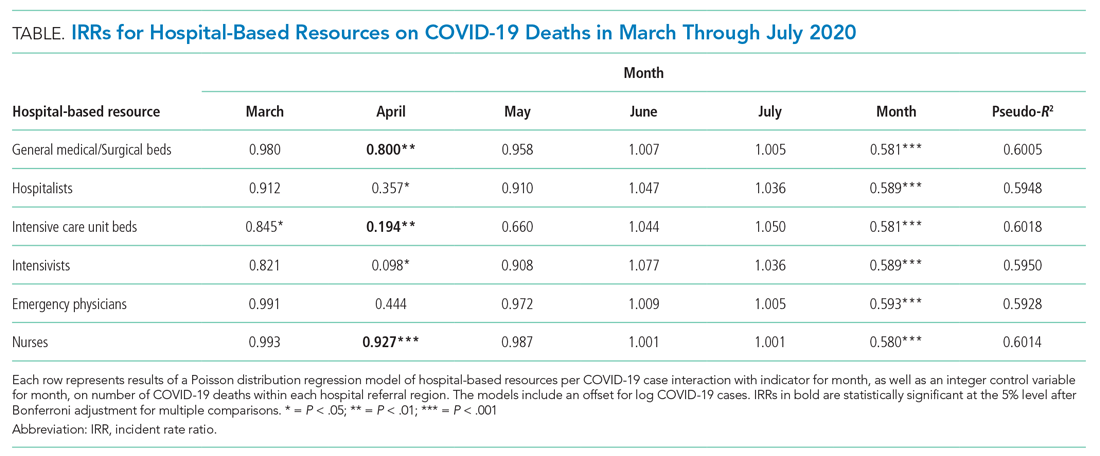
The model including ICU beds per COVID-19 case had the largest pseudo-R2 at 0.6018, which suggests that ICU bed availability explains the most variation in death count among hospital resource variables analyzed. The incident rate ratio in this model implies that, for an entire additional ICU bed for each COVID-19 case (a one-unit increase in that variable), there is an associated one-fifth decrease in incidence rate (IRR, 0.194) of death in April. The mean value among HRRs in April was 0.25 ICU beds per case (one ICU bed for every four COVID-19 cases), but it was as low as 0.01 to 0.005 in hard-hit areas (one ICU bed for every 100 to 200 COVID-19 cases). The early excess deaths observed in April were not observed in later months. The magnitude of this effect can be summarized as follows: If the 152 HRRs in April with fewer than the mean number of ICU beds per COVID-19 case were to instead have the mean number (one ICU bed for every four COVID-19 cases), our model estimates that there would have been 15,571 fewer deaths that month. The HRRs with the largest number of early excess deaths were Manhattan in New York City (1,466), Bronx in New York City (1,315), Boston, Massachusetts (1,293), Philadelphia, Pennsylvania (955), Hartford, Connecticut (682), Detroit, Michigan (499), and Camden, New Jersey (484). The Figure depicts HRRs in the United States with early excess deaths by this measure in April.
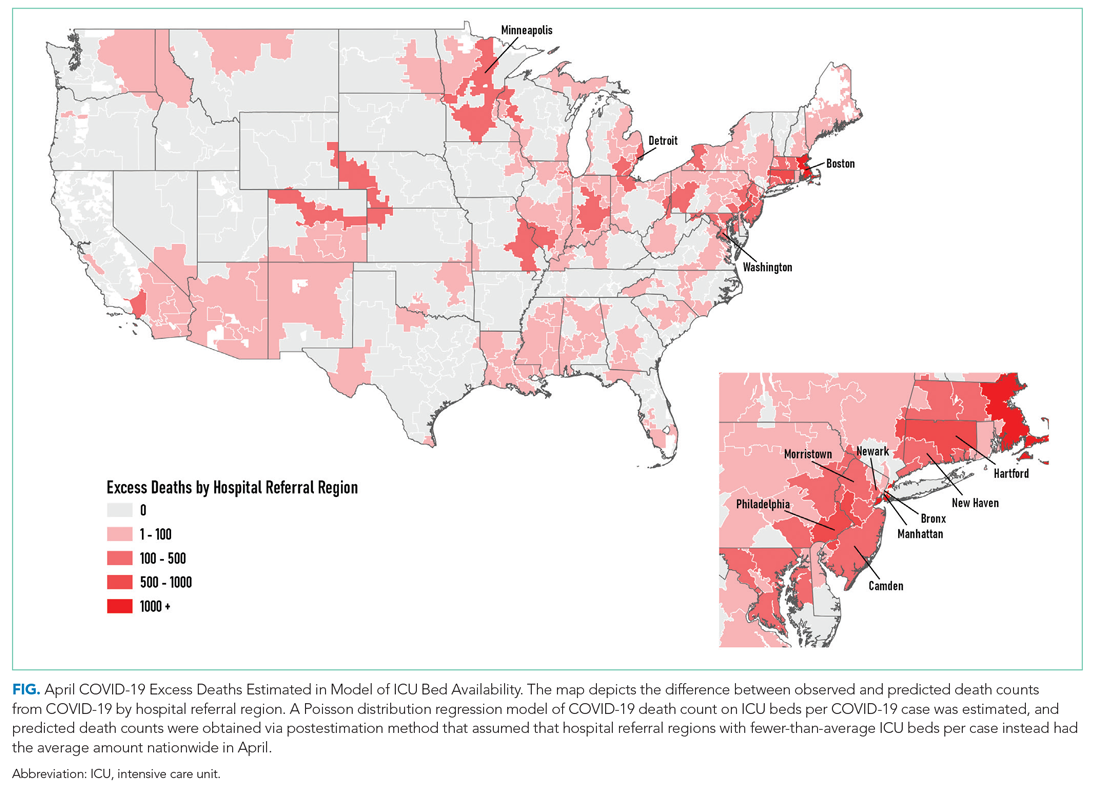
DISCUSSION
We found significant associations between availability of hospital-based resources and COVID-19 deaths in the month of April 2020. This observation was consistent across measures of both hospital bed and staff capacity but not statistically significant in all cases. This provides empiric evidence in support of a preprint simulation publication by Branas et al showing the potential for thousands of excess deaths related to lack of available resources.4 Interestingly, the relationship between hospital-based resources per COVID-19 case and death count is not seen in May, June, or July. This may be because hospitals and health systems were rapidly adapting to pandemic demands9 by shifting resources or reorganizing existing infrastructure to free up beds and personnel.
Our findings underscore the importance of analyses that address heterogeneity in health system response over time and across different geographic areas. That the relationship is not seen after the early pandemic period, when hospitals and health systems were most overwhelmed, suggests that health systems and communities were able to adapt. Importantly, this work does not address the likely complex relationships among hospital resources and outcomes (for example, the benefit of ICU bed availability is likely limited when there are insufficient intensivists and nurses). These complexities should be a focus of future work. Furthermore, hospital resource flexibility, community efforts to slow transmission, and improvements in testing availability and the management of COVID-19 among hospitalized patients may all play a role in attenuating the relationship between baseline resource limitations and outcomes for patients with COVID-19.
These results merit further granular studies to examine specific hospital resources and observed variation in outcomes. Prior literature has linked inpatient capacity—variously defined as high census, acuity, turnover, or delayed admission—to outcomes including mortality among patients with stroke, among those with acute coronary syndrome, and among those requiring intensive care.10 Literature from Italy’s experience shows there was large variation in the case fatality rate among regions of Northern Italy and argues this was partially due to hospital resource limitations.11 Future work can also address whether just-in-time resource mobilization, such as temporary ICU expansion, physician cross-staffing, telemedicine, and dedicated units for COVID-19 patients, attenuated the impact of potential hospital resource scarcity on outcomes.
The present analysis is limited by the quality of the data. There is likely variation of available COVID-19 testing by HRR. It may be that areas with larger outbreaks early on generally tested a smaller, sicker proportion of population-level cases than did those with smaller outbreaks. This effect may be reversed if larger HRRs in urban areas have health systems and public health departments more inclined toward or capable of doing more testing. Furthermore, deaths related to COVID-19 are likely related to community-based factors, including nonhealthcare resources and underlying population characteristics, that likely correlate with the availability of hospital-based resources within HRRs. Some have called into question whether, a priori, we should expect hospital-based capacity to be an important driver of mortality at all,12 arguing that, when critical care capacity is exceeded, resources may be efficiently reallocated away from patients who are least likely to benefit. Because we used the American Hospital Association data, this snapshot of hospital resources is not limited to critical care capacity because there could be alternative explanations for situations in which mortality for both COVID-19 and non–COVID-19 patients may be lower and hospital resources are better matched with demand. For example, patients may seek care earlier in their disease course (whether COVID-19 or otherwise)13 if their local emergency department is not thought to be overwhelmed with case volume.
CONCLUSION
We find that COVID-19 deaths vary among HRRs. The availability of several hospital-based resources is associated with death rates and supports early efforts across the United States to “flatten the curve” to prevent hospital overload. Continued surveillance of this relationship is essential to guide policymakers and hospitals seeking to balance the still limited supply of resources with the demands of caring for both infectious and noninfectious patients in the coming months of this outbreak and in future pandemics.
Acknowledgment
The authors gratefully acknowledge the help of Carolyn Lusch, AICP, in generating depictions of results in Geographic Information Systems.
1. Phua J, Weng L, Ling L, et al; Asian Critical Care Clinical Trials Group. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8(5):506-517. https://doi.org/10.1016/s2213-2600(20)30161-2
2. Carr BG, Addyson DK, Kahn JM. Variation in critical care beds per capita in the United States: implications for pandemic and disaster planning. JAMA. 2010;303(14):1371-1372. https://doi.org/10.1001/jama.2010.394
3. General FAQ. Dartmouth Atlas Project. 2020. Accessed July 8, 2020. https://www.dartmouthatlas.org/faq/
4. Branas CC, Rundle A, Pei S, et al. Flattening the curve before it flattens us: hospital critical care capacity limits and mortality from novel coronavirus (SARS-CoV2) cases in US counties. medRxiv. Preprint posted online April 6, 2020. https://doi.org/10.1101/2020.04.01.20049759
5. American Hospital Association Annual Survey Database. American Hospital Association. 2018. Accessed July 8, 2020. https://www.ahadata.com/aha-annual-survey-database
6. An Ongoing Repository of Data on Coronavirus Cases and Deaths in the U.S. New York Times. 2020. Accessed July 8, 2020. https://github.com/nytimes/covid-19-data
7. Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. 2020;20(7):773. https://doi.org/10.1016/s1473-3099(20)30195-x
8. Rosakis P, Marketou ME. Rethinking case fatality ratios for COVID-19 from a data-driven viewpoint. J Infect. 2020;81(2);e162-e164. https://doi.org/10.1016/j.jinf.2020.06.010
9. Auerbach A, O’Leary KJ, Greysen SR, et al; HOMERuN COVID-19 Collaborative Group. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15(8):483-488. https://doi.org/10.12788/jhm.3476
10. Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guide JM. The association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med. 2017;32(6):686-696. https://doi.org/10.1007/s11606-016-3936-3
11. Volpato S, Landi F, Incalzi RA. A frail health care system for an old population: lesson form [sic] the COVID-19 outbreak in Italy. J Gerontol Series A. 2020;75(9):e126-e127. https://doi.org/10.1093/gerona/glaa087
12. Wagner J, Gabler NB, Ratcliffe SJ, Brown SE, Strom BL, Halpern SD. Outcomes among patients discharged from busy intensive care units. Ann Intern Med. 2013;159(7):447-455. https://doi.org/10.7326/0003-4819-159-7-201310010-00004
13. Moroni F, Gramegna M, Agello S, et al. Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020;2(10):1620-1624. https://doi.org/10.1016/j.jaccas.2020.04.010
The COVID-19 pandemic is a crisis of mismatch between resources and infection burden. There is extraordinary heterogeneity across time and geography in the pandemic impact, with hospitals in New York City initially inundated while hospitals in major urban areas of California were comparatively quiet. Efforts to “flatten the curve” are intended to improve outcomes by reducing health system overload.1 In the case of hospital-based care, health systems’ primary resources include emergency and critical care bed and staff capacity.
Prior work has documented wide variability in intensive care capacity across the United States and hypothesized that even moderate disease outbreaks could overwhelm hospital referral regions (HRRs).2,3 Various simulations of outbreaks suggested that thousands of deaths are potentially preventable depending on the health system’s response,4 although the degree to which resource limitations have contributed to mortality during this COVID-19 pandemic has yet to be explored. The objective of this analysis was to examine the association between hospital resources and COVID-19 deaths amongst HRRs in the United States in the period from March 1 to July 26, 2020.
METHODS
Data
This was an analysis of the American Hospital Association Annual Survey Database from 2017 and 2018, including hospital resource variables such as total hospital beds, hospitalists, intensive care beds, intensivists, emergency physicians, and nurses.5 The analysis was limited to general medical and surgical hospitals capable of providing acute care services, defined as those reporting at least 500 emergency department visits in 2018. Where data were missing on analysis variables (26.0% missing overall), the data were drawn from the 2017 survey results (reduced to 23.8% missing) from the same site as available, and the remainder were imputed with multivariate imputation by chained equations. An identical analysis without imputation was performed as a sensitivity analysis that showed a similar pattern of results. Total resources were tabulated amongst HRRs, and the hospital resources per COVID-19 case calculated. HRRs are a geographic category devised to represent regional health care markets, and each includes hospital sites performing major procedures.3 These were the focus of the analysis because they may represent a meaningful geographic division of hospital-based resources. COVID-19 case and death counts (as of July 26, 2020) were drawn from publicly available county-level data curated by the New York Times from state and local governments as well as health departments nationwide,6 separated by month (ie, March, April, May, June, and July). Data on New York City were available in aggregate (rather than separated by borough). Cases and deaths were therefore apportioned to the three HRRs involving New York City in proportion to that area’s population. To adjust for the lag between COVID-19 cases and deaths,7,8 we offset deaths 2 weeks into the future so that the April COVID-19 death count for a given HRR included deaths that occurred for 1 month beginning 2 weeks after the start of April, and so on.
Analysis
We estimated Poisson distribution regressions for the outcome of COVID-19 death count in each HRR and month with one model for each of our six hospital-based resource variables. The offset (exposure) variable was COVID-19 case count. To adjust for the possibility of varying effects of hospital resources on deaths by month (ie, in anticipation that health systems might evolve in response to the pandemic over time), each model includes terms for the interaction between hospital-based resource and an indicator variable for month, as well as a fifth term for month. Standard errors were adjusted for clustering within HRR. We report resultant incident rate ratios (IRRs) with 95% CIs, and we report these as statistically significant at the 5% level only after adjustment for multiple comparisons across our six hospital-resource variables using the conservative Bonferroni adjustment. The pseudo-R2 for each of these six models is also reported to summarize the amount of variation in deaths explained. For our model with ICU beds per COVID-19 case, we perform postestimation prediction of number of deaths by HRR, assuming the counterfactual in which HRRs with fewer than average ICU beds per COVID-19 case instead had the average observed number of ICU beds per COVID-19 case by HRR in April, which functioned as a measure of early excess deaths potentially related to resource limitations. The study was classified as exempt by the Institutional Review Board at the Yale School of Medicine, New Haven, Connecticut. Analyses were conducted in Stata 15 (StataCorp LLC) and R.
RESULTS
A total of 4,453 hospitals across 306 HRRs were included and linked to 2,827 county-level COVID-19 case and death counts in each of 5 months (March through July 2020). The median HRR in our analysis included 14 hospitals, with a maximum of 76 hospitals (Los Angeles, California) and a minimum of 1 (Longview, Texas). Among HRRs, 206 (67.3%) had experienced caseloads exceeding 20 per 10,000 population, while 85 (27.8%) had experienced greater than 100 per 10,000 population in the peak month during the study period. The Table depicts results of each of six Poisson distribution regression models, with the finding that greater number of ICU beds (IRR, 0.194; 95% CI, 0.076-0.491), general medical/surgical beds (IRR, 0.800; 95% CI, 0.696-0.920), and nurses (IRR, 0.927; 95% CI, 0.888-0.967) per COVID-19 case in April were statistically significantly associated with reduced deaths.
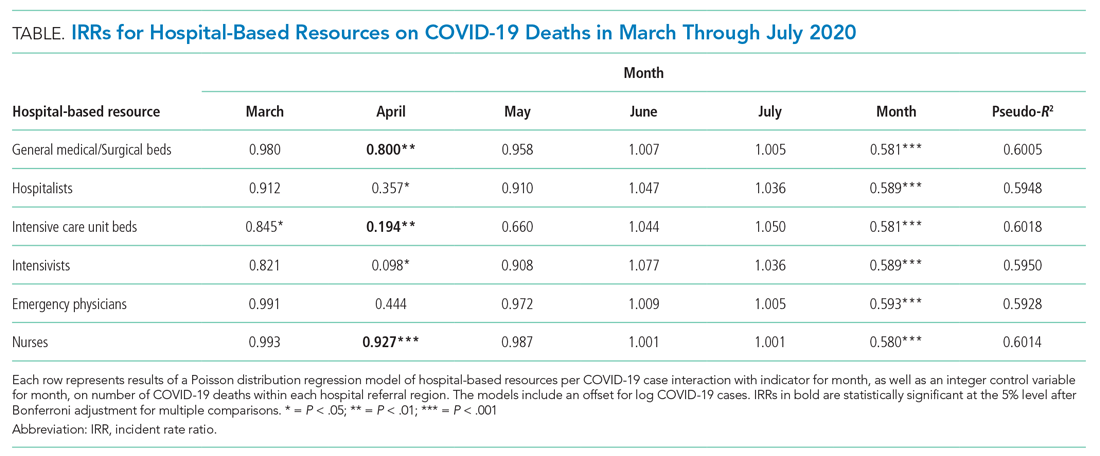
The model including ICU beds per COVID-19 case had the largest pseudo-R2 at 0.6018, which suggests that ICU bed availability explains the most variation in death count among hospital resource variables analyzed. The incident rate ratio in this model implies that, for an entire additional ICU bed for each COVID-19 case (a one-unit increase in that variable), there is an associated one-fifth decrease in incidence rate (IRR, 0.194) of death in April. The mean value among HRRs in April was 0.25 ICU beds per case (one ICU bed for every four COVID-19 cases), but it was as low as 0.01 to 0.005 in hard-hit areas (one ICU bed for every 100 to 200 COVID-19 cases). The early excess deaths observed in April were not observed in later months. The magnitude of this effect can be summarized as follows: If the 152 HRRs in April with fewer than the mean number of ICU beds per COVID-19 case were to instead have the mean number (one ICU bed for every four COVID-19 cases), our model estimates that there would have been 15,571 fewer deaths that month. The HRRs with the largest number of early excess deaths were Manhattan in New York City (1,466), Bronx in New York City (1,315), Boston, Massachusetts (1,293), Philadelphia, Pennsylvania (955), Hartford, Connecticut (682), Detroit, Michigan (499), and Camden, New Jersey (484). The Figure depicts HRRs in the United States with early excess deaths by this measure in April.
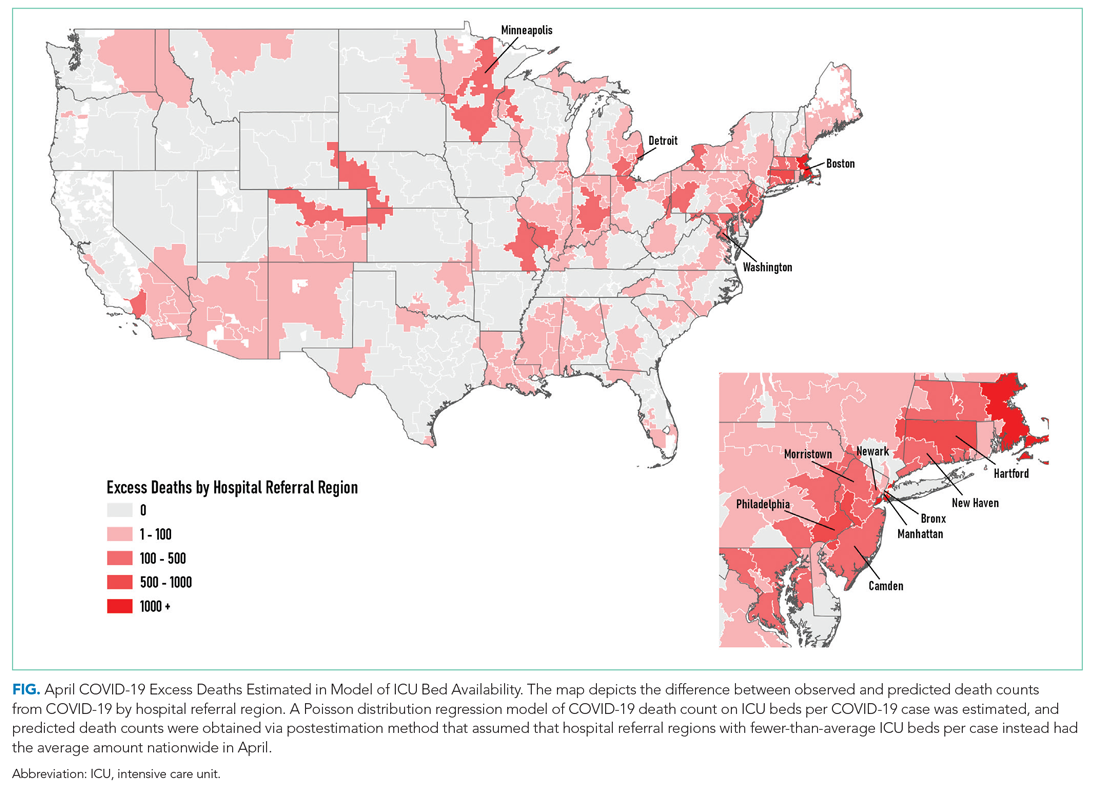
DISCUSSION
We found significant associations between availability of hospital-based resources and COVID-19 deaths in the month of April 2020. This observation was consistent across measures of both hospital bed and staff capacity but not statistically significant in all cases. This provides empiric evidence in support of a preprint simulation publication by Branas et al showing the potential for thousands of excess deaths related to lack of available resources.4 Interestingly, the relationship between hospital-based resources per COVID-19 case and death count is not seen in May, June, or July. This may be because hospitals and health systems were rapidly adapting to pandemic demands9 by shifting resources or reorganizing existing infrastructure to free up beds and personnel.
Our findings underscore the importance of analyses that address heterogeneity in health system response over time and across different geographic areas. That the relationship is not seen after the early pandemic period, when hospitals and health systems were most overwhelmed, suggests that health systems and communities were able to adapt. Importantly, this work does not address the likely complex relationships among hospital resources and outcomes (for example, the benefit of ICU bed availability is likely limited when there are insufficient intensivists and nurses). These complexities should be a focus of future work. Furthermore, hospital resource flexibility, community efforts to slow transmission, and improvements in testing availability and the management of COVID-19 among hospitalized patients may all play a role in attenuating the relationship between baseline resource limitations and outcomes for patients with COVID-19.
These results merit further granular studies to examine specific hospital resources and observed variation in outcomes. Prior literature has linked inpatient capacity—variously defined as high census, acuity, turnover, or delayed admission—to outcomes including mortality among patients with stroke, among those with acute coronary syndrome, and among those requiring intensive care.10 Literature from Italy’s experience shows there was large variation in the case fatality rate among regions of Northern Italy and argues this was partially due to hospital resource limitations.11 Future work can also address whether just-in-time resource mobilization, such as temporary ICU expansion, physician cross-staffing, telemedicine, and dedicated units for COVID-19 patients, attenuated the impact of potential hospital resource scarcity on outcomes.
The present analysis is limited by the quality of the data. There is likely variation of available COVID-19 testing by HRR. It may be that areas with larger outbreaks early on generally tested a smaller, sicker proportion of population-level cases than did those with smaller outbreaks. This effect may be reversed if larger HRRs in urban areas have health systems and public health departments more inclined toward or capable of doing more testing. Furthermore, deaths related to COVID-19 are likely related to community-based factors, including nonhealthcare resources and underlying population characteristics, that likely correlate with the availability of hospital-based resources within HRRs. Some have called into question whether, a priori, we should expect hospital-based capacity to be an important driver of mortality at all,12 arguing that, when critical care capacity is exceeded, resources may be efficiently reallocated away from patients who are least likely to benefit. Because we used the American Hospital Association data, this snapshot of hospital resources is not limited to critical care capacity because there could be alternative explanations for situations in which mortality for both COVID-19 and non–COVID-19 patients may be lower and hospital resources are better matched with demand. For example, patients may seek care earlier in their disease course (whether COVID-19 or otherwise)13 if their local emergency department is not thought to be overwhelmed with case volume.
CONCLUSION
We find that COVID-19 deaths vary among HRRs. The availability of several hospital-based resources is associated with death rates and supports early efforts across the United States to “flatten the curve” to prevent hospital overload. Continued surveillance of this relationship is essential to guide policymakers and hospitals seeking to balance the still limited supply of resources with the demands of caring for both infectious and noninfectious patients in the coming months of this outbreak and in future pandemics.
Acknowledgment
The authors gratefully acknowledge the help of Carolyn Lusch, AICP, in generating depictions of results in Geographic Information Systems.
The COVID-19 pandemic is a crisis of mismatch between resources and infection burden. There is extraordinary heterogeneity across time and geography in the pandemic impact, with hospitals in New York City initially inundated while hospitals in major urban areas of California were comparatively quiet. Efforts to “flatten the curve” are intended to improve outcomes by reducing health system overload.1 In the case of hospital-based care, health systems’ primary resources include emergency and critical care bed and staff capacity.
Prior work has documented wide variability in intensive care capacity across the United States and hypothesized that even moderate disease outbreaks could overwhelm hospital referral regions (HRRs).2,3 Various simulations of outbreaks suggested that thousands of deaths are potentially preventable depending on the health system’s response,4 although the degree to which resource limitations have contributed to mortality during this COVID-19 pandemic has yet to be explored. The objective of this analysis was to examine the association between hospital resources and COVID-19 deaths amongst HRRs in the United States in the period from March 1 to July 26, 2020.
METHODS
Data
This was an analysis of the American Hospital Association Annual Survey Database from 2017 and 2018, including hospital resource variables such as total hospital beds, hospitalists, intensive care beds, intensivists, emergency physicians, and nurses.5 The analysis was limited to general medical and surgical hospitals capable of providing acute care services, defined as those reporting at least 500 emergency department visits in 2018. Where data were missing on analysis variables (26.0% missing overall), the data were drawn from the 2017 survey results (reduced to 23.8% missing) from the same site as available, and the remainder were imputed with multivariate imputation by chained equations. An identical analysis without imputation was performed as a sensitivity analysis that showed a similar pattern of results. Total resources were tabulated amongst HRRs, and the hospital resources per COVID-19 case calculated. HRRs are a geographic category devised to represent regional health care markets, and each includes hospital sites performing major procedures.3 These were the focus of the analysis because they may represent a meaningful geographic division of hospital-based resources. COVID-19 case and death counts (as of July 26, 2020) were drawn from publicly available county-level data curated by the New York Times from state and local governments as well as health departments nationwide,6 separated by month (ie, March, April, May, June, and July). Data on New York City were available in aggregate (rather than separated by borough). Cases and deaths were therefore apportioned to the three HRRs involving New York City in proportion to that area’s population. To adjust for the lag between COVID-19 cases and deaths,7,8 we offset deaths 2 weeks into the future so that the April COVID-19 death count for a given HRR included deaths that occurred for 1 month beginning 2 weeks after the start of April, and so on.
Analysis
We estimated Poisson distribution regressions for the outcome of COVID-19 death count in each HRR and month with one model for each of our six hospital-based resource variables. The offset (exposure) variable was COVID-19 case count. To adjust for the possibility of varying effects of hospital resources on deaths by month (ie, in anticipation that health systems might evolve in response to the pandemic over time), each model includes terms for the interaction between hospital-based resource and an indicator variable for month, as well as a fifth term for month. Standard errors were adjusted for clustering within HRR. We report resultant incident rate ratios (IRRs) with 95% CIs, and we report these as statistically significant at the 5% level only after adjustment for multiple comparisons across our six hospital-resource variables using the conservative Bonferroni adjustment. The pseudo-R2 for each of these six models is also reported to summarize the amount of variation in deaths explained. For our model with ICU beds per COVID-19 case, we perform postestimation prediction of number of deaths by HRR, assuming the counterfactual in which HRRs with fewer than average ICU beds per COVID-19 case instead had the average observed number of ICU beds per COVID-19 case by HRR in April, which functioned as a measure of early excess deaths potentially related to resource limitations. The study was classified as exempt by the Institutional Review Board at the Yale School of Medicine, New Haven, Connecticut. Analyses were conducted in Stata 15 (StataCorp LLC) and R.
RESULTS
A total of 4,453 hospitals across 306 HRRs were included and linked to 2,827 county-level COVID-19 case and death counts in each of 5 months (March through July 2020). The median HRR in our analysis included 14 hospitals, with a maximum of 76 hospitals (Los Angeles, California) and a minimum of 1 (Longview, Texas). Among HRRs, 206 (67.3%) had experienced caseloads exceeding 20 per 10,000 population, while 85 (27.8%) had experienced greater than 100 per 10,000 population in the peak month during the study period. The Table depicts results of each of six Poisson distribution regression models, with the finding that greater number of ICU beds (IRR, 0.194; 95% CI, 0.076-0.491), general medical/surgical beds (IRR, 0.800; 95% CI, 0.696-0.920), and nurses (IRR, 0.927; 95% CI, 0.888-0.967) per COVID-19 case in April were statistically significantly associated with reduced deaths.
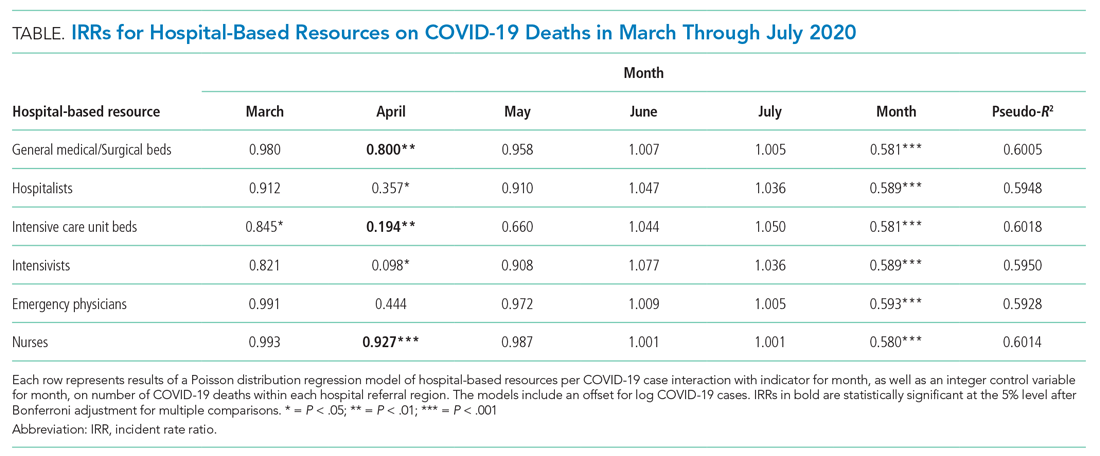
The model including ICU beds per COVID-19 case had the largest pseudo-R2 at 0.6018, which suggests that ICU bed availability explains the most variation in death count among hospital resource variables analyzed. The incident rate ratio in this model implies that, for an entire additional ICU bed for each COVID-19 case (a one-unit increase in that variable), there is an associated one-fifth decrease in incidence rate (IRR, 0.194) of death in April. The mean value among HRRs in April was 0.25 ICU beds per case (one ICU bed for every four COVID-19 cases), but it was as low as 0.01 to 0.005 in hard-hit areas (one ICU bed for every 100 to 200 COVID-19 cases). The early excess deaths observed in April were not observed in later months. The magnitude of this effect can be summarized as follows: If the 152 HRRs in April with fewer than the mean number of ICU beds per COVID-19 case were to instead have the mean number (one ICU bed for every four COVID-19 cases), our model estimates that there would have been 15,571 fewer deaths that month. The HRRs with the largest number of early excess deaths were Manhattan in New York City (1,466), Bronx in New York City (1,315), Boston, Massachusetts (1,293), Philadelphia, Pennsylvania (955), Hartford, Connecticut (682), Detroit, Michigan (499), and Camden, New Jersey (484). The Figure depicts HRRs in the United States with early excess deaths by this measure in April.
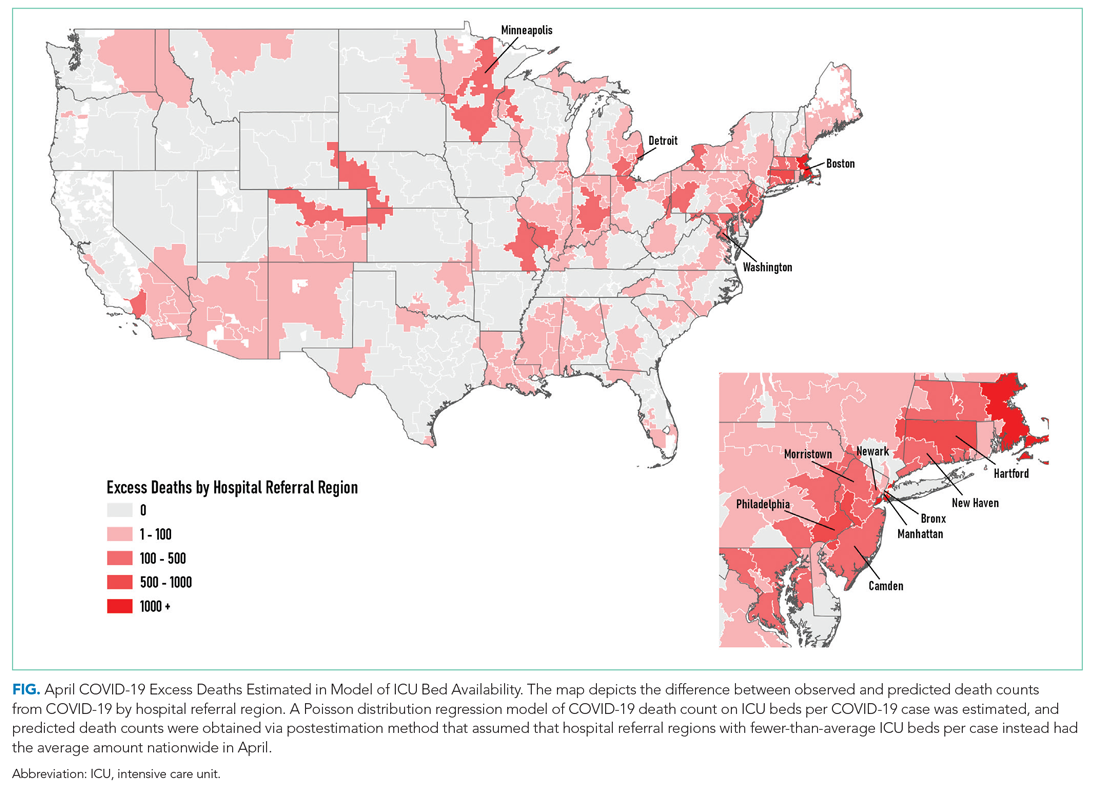
DISCUSSION
We found significant associations between availability of hospital-based resources and COVID-19 deaths in the month of April 2020. This observation was consistent across measures of both hospital bed and staff capacity but not statistically significant in all cases. This provides empiric evidence in support of a preprint simulation publication by Branas et al showing the potential for thousands of excess deaths related to lack of available resources.4 Interestingly, the relationship between hospital-based resources per COVID-19 case and death count is not seen in May, June, or July. This may be because hospitals and health systems were rapidly adapting to pandemic demands9 by shifting resources or reorganizing existing infrastructure to free up beds and personnel.
Our findings underscore the importance of analyses that address heterogeneity in health system response over time and across different geographic areas. That the relationship is not seen after the early pandemic period, when hospitals and health systems were most overwhelmed, suggests that health systems and communities were able to adapt. Importantly, this work does not address the likely complex relationships among hospital resources and outcomes (for example, the benefit of ICU bed availability is likely limited when there are insufficient intensivists and nurses). These complexities should be a focus of future work. Furthermore, hospital resource flexibility, community efforts to slow transmission, and improvements in testing availability and the management of COVID-19 among hospitalized patients may all play a role in attenuating the relationship between baseline resource limitations and outcomes for patients with COVID-19.
These results merit further granular studies to examine specific hospital resources and observed variation in outcomes. Prior literature has linked inpatient capacity—variously defined as high census, acuity, turnover, or delayed admission—to outcomes including mortality among patients with stroke, among those with acute coronary syndrome, and among those requiring intensive care.10 Literature from Italy’s experience shows there was large variation in the case fatality rate among regions of Northern Italy and argues this was partially due to hospital resource limitations.11 Future work can also address whether just-in-time resource mobilization, such as temporary ICU expansion, physician cross-staffing, telemedicine, and dedicated units for COVID-19 patients, attenuated the impact of potential hospital resource scarcity on outcomes.
The present analysis is limited by the quality of the data. There is likely variation of available COVID-19 testing by HRR. It may be that areas with larger outbreaks early on generally tested a smaller, sicker proportion of population-level cases than did those with smaller outbreaks. This effect may be reversed if larger HRRs in urban areas have health systems and public health departments more inclined toward or capable of doing more testing. Furthermore, deaths related to COVID-19 are likely related to community-based factors, including nonhealthcare resources and underlying population characteristics, that likely correlate with the availability of hospital-based resources within HRRs. Some have called into question whether, a priori, we should expect hospital-based capacity to be an important driver of mortality at all,12 arguing that, when critical care capacity is exceeded, resources may be efficiently reallocated away from patients who are least likely to benefit. Because we used the American Hospital Association data, this snapshot of hospital resources is not limited to critical care capacity because there could be alternative explanations for situations in which mortality for both COVID-19 and non–COVID-19 patients may be lower and hospital resources are better matched with demand. For example, patients may seek care earlier in their disease course (whether COVID-19 or otherwise)13 if their local emergency department is not thought to be overwhelmed with case volume.
CONCLUSION
We find that COVID-19 deaths vary among HRRs. The availability of several hospital-based resources is associated with death rates and supports early efforts across the United States to “flatten the curve” to prevent hospital overload. Continued surveillance of this relationship is essential to guide policymakers and hospitals seeking to balance the still limited supply of resources with the demands of caring for both infectious and noninfectious patients in the coming months of this outbreak and in future pandemics.
Acknowledgment
The authors gratefully acknowledge the help of Carolyn Lusch, AICP, in generating depictions of results in Geographic Information Systems.
1. Phua J, Weng L, Ling L, et al; Asian Critical Care Clinical Trials Group. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8(5):506-517. https://doi.org/10.1016/s2213-2600(20)30161-2
2. Carr BG, Addyson DK, Kahn JM. Variation in critical care beds per capita in the United States: implications for pandemic and disaster planning. JAMA. 2010;303(14):1371-1372. https://doi.org/10.1001/jama.2010.394
3. General FAQ. Dartmouth Atlas Project. 2020. Accessed July 8, 2020. https://www.dartmouthatlas.org/faq/
4. Branas CC, Rundle A, Pei S, et al. Flattening the curve before it flattens us: hospital critical care capacity limits and mortality from novel coronavirus (SARS-CoV2) cases in US counties. medRxiv. Preprint posted online April 6, 2020. https://doi.org/10.1101/2020.04.01.20049759
5. American Hospital Association Annual Survey Database. American Hospital Association. 2018. Accessed July 8, 2020. https://www.ahadata.com/aha-annual-survey-database
6. An Ongoing Repository of Data on Coronavirus Cases and Deaths in the U.S. New York Times. 2020. Accessed July 8, 2020. https://github.com/nytimes/covid-19-data
7. Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. 2020;20(7):773. https://doi.org/10.1016/s1473-3099(20)30195-x
8. Rosakis P, Marketou ME. Rethinking case fatality ratios for COVID-19 from a data-driven viewpoint. J Infect. 2020;81(2);e162-e164. https://doi.org/10.1016/j.jinf.2020.06.010
9. Auerbach A, O’Leary KJ, Greysen SR, et al; HOMERuN COVID-19 Collaborative Group. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15(8):483-488. https://doi.org/10.12788/jhm.3476
10. Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guide JM. The association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med. 2017;32(6):686-696. https://doi.org/10.1007/s11606-016-3936-3
11. Volpato S, Landi F, Incalzi RA. A frail health care system for an old population: lesson form [sic] the COVID-19 outbreak in Italy. J Gerontol Series A. 2020;75(9):e126-e127. https://doi.org/10.1093/gerona/glaa087
12. Wagner J, Gabler NB, Ratcliffe SJ, Brown SE, Strom BL, Halpern SD. Outcomes among patients discharged from busy intensive care units. Ann Intern Med. 2013;159(7):447-455. https://doi.org/10.7326/0003-4819-159-7-201310010-00004
13. Moroni F, Gramegna M, Agello S, et al. Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020;2(10):1620-1624. https://doi.org/10.1016/j.jaccas.2020.04.010
1. Phua J, Weng L, Ling L, et al; Asian Critical Care Clinical Trials Group. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8(5):506-517. https://doi.org/10.1016/s2213-2600(20)30161-2
2. Carr BG, Addyson DK, Kahn JM. Variation in critical care beds per capita in the United States: implications for pandemic and disaster planning. JAMA. 2010;303(14):1371-1372. https://doi.org/10.1001/jama.2010.394
3. General FAQ. Dartmouth Atlas Project. 2020. Accessed July 8, 2020. https://www.dartmouthatlas.org/faq/
4. Branas CC, Rundle A, Pei S, et al. Flattening the curve before it flattens us: hospital critical care capacity limits and mortality from novel coronavirus (SARS-CoV2) cases in US counties. medRxiv. Preprint posted online April 6, 2020. https://doi.org/10.1101/2020.04.01.20049759
5. American Hospital Association Annual Survey Database. American Hospital Association. 2018. Accessed July 8, 2020. https://www.ahadata.com/aha-annual-survey-database
6. An Ongoing Repository of Data on Coronavirus Cases and Deaths in the U.S. New York Times. 2020. Accessed July 8, 2020. https://github.com/nytimes/covid-19-data
7. Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. 2020;20(7):773. https://doi.org/10.1016/s1473-3099(20)30195-x
8. Rosakis P, Marketou ME. Rethinking case fatality ratios for COVID-19 from a data-driven viewpoint. J Infect. 2020;81(2);e162-e164. https://doi.org/10.1016/j.jinf.2020.06.010
9. Auerbach A, O’Leary KJ, Greysen SR, et al; HOMERuN COVID-19 Collaborative Group. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15(8):483-488. https://doi.org/10.12788/jhm.3476
10. Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guide JM. The association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med. 2017;32(6):686-696. https://doi.org/10.1007/s11606-016-3936-3
11. Volpato S, Landi F, Incalzi RA. A frail health care system for an old population: lesson form [sic] the COVID-19 outbreak in Italy. J Gerontol Series A. 2020;75(9):e126-e127. https://doi.org/10.1093/gerona/glaa087
12. Wagner J, Gabler NB, Ratcliffe SJ, Brown SE, Strom BL, Halpern SD. Outcomes among patients discharged from busy intensive care units. Ann Intern Med. 2013;159(7):447-455. https://doi.org/10.7326/0003-4819-159-7-201310010-00004
13. Moroni F, Gramegna M, Agello S, et al. Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020;2(10):1620-1624. https://doi.org/10.1016/j.jaccas.2020.04.010
© 2021 Society of Hospital Medicine
Examining the Interfacility Variation of Social Determinants of Health in the Veterans Health Administration
Social determinants of health (SDoH) are social, economic, environmental, and occupational factors that are known to influence an individual’s health care utilization and clinical outcomes.1,2 Because the Veterans Health Administration (VHA) is charged to address both the medical and nonmedical needs of the veteran population, it is increasingly interested in the impact SDoH have on veteran care.3,4 To combat the adverse impact of such factors, the VHA has implemented several large-scale programs across the US that focus on prevalent SDoH, such as homelessness, substance abuse, and alcohol use disorders.5,6 While such risk factors are generally universal in their distribution, variation across regions, between urban and rural spaces, and even within cities has been shown to exist in private settings.7 Understanding such variability potentially could be helpful to US Department of Veterans Affairs (VA) policymakers and leaders to better allocate funding and resources to address such issues.
Although previous work has highlighted regional and neighborhood-level variability of SDoH, no study has examined the facility-level variability of commonly encountered social risk factors within the VHA.4,8 The aim of this study was to describe the interfacility variation of 5 common SDoH known to influence health and health outcomes among a national cohort of veterans hospitalized for common medical issues by using administrative data.
Methods
We used a national cohort of veterans aged ≥ 65 years who were hospitalized at a VHA acute care facility with a primary discharge diagnosis of acute myocardial infarction (AMI), heart failure (HF), or pneumonia in 2012. These conditions were chosen because they are publicly reported and frequently used for interfacility comparison.
Using the International Classification of Diseases–9th Revision (ICD-9) and VHA clinical stop codes, we calculated the median documented proportion of patients with any of the following 5 SDoH: lived alone, marginal housing, alcohol use disorder, substance use disorder, and use of substance use services for patients presenting with HF, MI, and pneumonia (Table). These SDoH were chosen because they are intervenable risk factors for which the VHA has several programs (eg, homeless outreach, substance abuse, and tobacco cessation). To examine the variability of these SDoH across VHA facilities, we determined the number of hospitals that had a sufficient number of admissions (≥ 50) to be included in the analyses. We then examined the administratively documented, facility-level variation in the proportion of individuals with any of the 5 SDoH administrative codes and examined the distribution of their use across all qualifying facilities.
Because variability may be due to regional coding differences, we examined the difference in the estimated prevalence of the risk factor lives alone by using a previously developed natural language processing (NLP) program.9 The NLP program is a rule-based system designed to automatically extract information that requires inferencing from clinical notes (eg, discharge summaries and nursing, social work, emergency department physician, primary care, and hospital admission notes). For instance, the program identifies whether there was direct or indirect evidence that the patient did or did not live alone. In addition to extracting data on lives alone, the NLP program has the capacity to extract information on lack of social support and living alone—2 characteristics without VHA interventions, which were not examined here. The NLP program was developed and evaluated using at least 1 year of notes prior to index hospitalization. Because this program was developed and validated on a 2012 data set, we were limited to using a cohort from this year as well.
All analyses were conducted using SAS Version 9.4. The San Francisco VA Medical Center Institutional Review Board approved this study.
Results
In total, 21,991 patients with either HF (9,853), pneumonia (9,362), or AMI (2,776) were identified across 91 VHA facilities. The majority were male (98%) and had a median (SD) age of 77.0 (9.0) years. The median facility-level proportion of veterans who had any of the SDoH risk factors extracted through administrative codes was low across all conditions, ranging from 0.5 to 2.2%. The most prevalent factors among patients admitted for HF, AMI, and pneumonia were lives alone (2.0% [Interquartile range (IQR), 1.0-5.2], 1.4% [IQR, 0-3.4], and 1.9% [IQR, 0.7-5.4]), substance use disorder (1.2% [IQR, 0-2.2], 1.6% [IQR: 0-3.0], and 1.3% [IQR, 0-2.2] and use of substance use services (0.9% [IQR, 0-1.6%], 1.0% [IQR, 0-1.7%], and 1.6% [IQR, 0-2.2%], respectively [Table]).
When utilizing the NLP algorithm, the documented prevalence of lives alone in the free text of the medical record was higher than administrative coding across all conditions (12.3% vs. 2.2%; P < .01). Among each of the 3 assessed conditions, HF (14.4% vs 2.0%, P < .01) had higher levels of lives alone compared with pneumonia (11% vs 1.9%, P < .01), and AMI (10.2% vs 1.4%, P < .01) when using the NLP algorithm. When we examined the documented facility-level variation in the proportion of individuals with any of the 5 SDoH administrative codes or NLP, we found large variability across all facilities—regardless of extraction method (Figure).
Discussion
While SDoH are known to impact health outcomes, the presence of these risk factors in administrative data among individuals hospitalized for common medical issues is low and variable across VHA facilities. Understanding the documented, facility-level variability of these measures may assist the VHA in determining how it invests time and resources—as different facilities may disproportionately serve a higher number of vulnerable individuals. Beyond the VHA, these findings have generalizable lessons for the US health care system, which has come to recognize how these risk factors impact patients’ health.10
Although the proportion of individuals with any of the assessed SDoH identified by administrative data was low, our findings are in line with recent studies that showed other risk factors such as social isolation (0.65%), housing issues (0.19%), and financial strain (0.07%) had similarly low prevalence.8,11 Although the exact prevalence of such factors remains unclear, these findings highlight that SDoH do not appear to be well documented in administrative data. Low coding rates are likely due to the fact that SDoH administrative codes are not tied to financial reimbursement—thus not incentivizing their use by clinicians or hospital systems.
In 2014, an Institute of Medicine report suggested that collection of SDoH in electronic health data as a means to better empower clinicians and health care systems to address social disparities and further support research in SDoH.12 Since then, data collection using SDoH screening tools has become more common across settings, but is not consistently translated to standardized data due to lack of industry consensus and technical barriers.13 To improve this process, the Centers for Medicare and Medicaid Services created “z-codes” for the ICD-10 classification system—a subset of codes that are meant to better capture patients’ underlying social risk.14 It remains to be seen if such administrative codes have improved the documentation of SDoH.
As health care systems have grown to understand the impact of SDoH on health outcomes,other means of collecting these data have evolved.1,10 For example, NLP-based extraction methods and electronic screening tools have been proposed and utilized as alternative for obtaining this information. Our findings suggest that some of these measures (eg, lives alone) often may be documented as part of routine care in the electronic health record, thus highlighting NLP as a tool to obtain such data. However, other studies using NLP technology to extract SDoH have shown this technology is often complicated by quality issues (ie, missing data), complex methods, and poor integration with current information technology infrastructures—thus limiting its use in health care delivery.15-18
While variance among SDoH across a national health care system is natural, it remains an important systems-level characteristic that health care leaders and policymakers should appreciate. As health care systems disperse financial resources and initiate quality improvement initiatives to address SDoH, knowing that not all facilities are equally affected by SDoH should impact allocation of such resources and energies. Although previous work has highlighted regional and neighborhood levels of variation within the VHA and other health care systems, to our knowledge, this is the first study to examine variability at the facility-level within the VHA.2,4,13,19
Limitations
There are several limitations to this study. First, though our findings are in line with previous data in other health care systems, generalizability beyond the VA, which primarily cares for older, male patients, may be limited.8 Though, as the nation’s largest health care system, lessons from the VHA can still be useful for other health care systems as they consider SDoH variation. Second, among the many SDoH previously identified to impact health, our analysis only focused on 5 such variables. Administrative and medical record documentation of other SDoH may be more common and less variable across institutions. Third, while our data suggests facility-level variation in these measures, this may be in part related to variation in coding across facilities. However, the single SDoH variable extracted using NLP also varied at the facility-level, suggesting that coding may not entirely drive the variation observed.
Conclusions
As US health care systems continue to address SDoH, our findings highlight the various challenges in obtaining accurate data on a patient’s social risk. Moreover, these findings highlight the large variability that exists among institutions in a national integrated health care system. Future work should explore the prevalence and variance of other SDoH as a means to help guide resource allocation and prioritize spending to better address SDoH where it is most needed.
Acknowledgments
This work was supported by NHLBI R01 RO1 HL116522-01A1. Support for VA/CMS data is provided by the US Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (Project Numbers SDR 02-237 and 98-004).
1. Social determinants of health (SDOH). https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0312. Published December 1, 2017. Accessed December 8, 2020.
2. Hatef E, Searle KM, Predmore Z, et al. The Impact of Social Determinants of Health on hospitalization in the Veterans Health Administration. Am J Prev Med. 2019;56(6):811-818. doi:10.1016/j.amepre.2018.12.012
3. Lushniak BD, Alley DE, Ulin B, Graffunder C. The National Prevention Strategy: leveraging multiple sectors to improve population health. Am J Public Health. 2015;105(2):229-231. doi:10.2105/AJPH.2014.302257
4. Nelson K, Schwartz G, Hernandez S, Simonetti J, Curtis I, Fihn SD. The association between neighborhood environment and mortality: results from a national study of veterans. J Gen Intern Med. 2017;32(4):416-422. doi:10.1007/s11606-016-3905-x
5. Gundlapalli AV, Redd A, Bolton D, et al. Patient-aligned care team engagement to connect veterans experiencing homelessness with appropriate health care. Med Care. 2017;55 Suppl 9 Suppl 2:S104-S110. doi:10.1097/MLR.0000000000000770
6. Rash CJ, DePhilippis D. Considerations for implementing contingency management in substance abuse treatment clinics: the Veterans Affairs initiative as a model. Perspect Behav Sci. 2019;42(3):479-499. doi:10.1007/s40614-019-00204-3.
7. Ompad DC, Galea S, Caiaffa WT, Vlahov D. Social determinants of the health of urban populations: methodologic considerations. J Urban Health. 2007;84(3 Suppl):i42-i53. doi:10.1007/s11524-007-9168-4
8. Hatef E, Rouhizadeh M, Tia I, et al. Assessing the availability of data on social and behavioral determinants in structured and unstructured electronic health records: a retrospective analysis of a multilevel health care system. JMIR Med Inform. 2019;7(3):e13802. doi:10.2196/13802
9. Conway M, Keyhani S, Christensen L, et al. Moonstone: a novel natural language processing system for inferring social risk from clinical narratives. J Biomed Semantics. 2019;10(1):6. doi:10.1186/s13326-019-0198-0
10. Adler NE, Cutler DM, Fielding JE, et al. Addressing social determinants of health and health disparities: a vital direction for health and health care. Discussion Paper. NAM Perspectives. National Academy of Medicine, Washington, DC. doi:10.31478/201609t
11. Cottrell EK, Dambrun K, Cowburn S, et al. Variation in electronic health record documentation of social determinants of health across a national network of community health centers. Am J Prev Med. 2019;57(6):S65-S73. doi:10.1016/j.amepre.2019.07.014
12. Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records, Board on Population Health and Public Health Practice, Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. National Academies Press (US); 2015.
13. Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. Integrating Social And Medical Data To Improve Population Health: Opportunities And Barriers. Health Aff (Millwood). 2016;35(11):2116-2123. doi:10.1377/hlthaff.2016.0723
14. Centers for Medicare and Medicaid Service, Office of Minority Health. Z codes utilization among medicare fee-for-service (FFS) beneficiaries in 2017. Published January 2020. Accessed December 8, 2020. https://www.cms.gov/files/document/cms-omh-january2020-zcode-data-highlightpdf.pdf
15. Kharrazi H, Wang C, Scharfstein D. Prospective EHR-based clinical trials: the challenge of missing data. J Gen Intern Med. 2014;29(7):976-978. doi:10.1007/s11606-014-2883-0
16. Weiskopf NG, Weng C. Methods and dimensions of electronic health record data quality assessment: enabling reuse for clinical research. J Am Med Inform Assoc. 2013;20(1):144-151. doi:10.1136/amiajnl-2011-000681
17. Anzaldi LJ, Davison A, Boyd CM, Leff B, Kharrazi H. Comparing clinician descriptions of frailty and geriatric syndromes using electronic health records: a retrospective cohort study. BMC Geriatr. 2017;17(1):248. doi:10.1186/s12877-017-0645-7
18. Chen T, Dredze M, Weiner JP, Kharrazi H. Identifying vulnerable older adult populations by contextualizing geriatric syndrome information in clinical notes of electronic health records. J Am Med Inform Assoc. 2019;26(8-9):787-795. doi:10.1093/jamia/ocz093
19. Raphael E, Gaynes R, Hamad R. Cross-sectional analysis of place-based and racial disparities in hospitalisation rates by disease category in California in 2001 and 2011. BMJ Open. 2019;9(10):e031556. doi:10.1136/bmjopen-2019-031556
Social determinants of health (SDoH) are social, economic, environmental, and occupational factors that are known to influence an individual’s health care utilization and clinical outcomes.1,2 Because the Veterans Health Administration (VHA) is charged to address both the medical and nonmedical needs of the veteran population, it is increasingly interested in the impact SDoH have on veteran care.3,4 To combat the adverse impact of such factors, the VHA has implemented several large-scale programs across the US that focus on prevalent SDoH, such as homelessness, substance abuse, and alcohol use disorders.5,6 While such risk factors are generally universal in their distribution, variation across regions, between urban and rural spaces, and even within cities has been shown to exist in private settings.7 Understanding such variability potentially could be helpful to US Department of Veterans Affairs (VA) policymakers and leaders to better allocate funding and resources to address such issues.
Although previous work has highlighted regional and neighborhood-level variability of SDoH, no study has examined the facility-level variability of commonly encountered social risk factors within the VHA.4,8 The aim of this study was to describe the interfacility variation of 5 common SDoH known to influence health and health outcomes among a national cohort of veterans hospitalized for common medical issues by using administrative data.
Methods
We used a national cohort of veterans aged ≥ 65 years who were hospitalized at a VHA acute care facility with a primary discharge diagnosis of acute myocardial infarction (AMI), heart failure (HF), or pneumonia in 2012. These conditions were chosen because they are publicly reported and frequently used for interfacility comparison.
Using the International Classification of Diseases–9th Revision (ICD-9) and VHA clinical stop codes, we calculated the median documented proportion of patients with any of the following 5 SDoH: lived alone, marginal housing, alcohol use disorder, substance use disorder, and use of substance use services for patients presenting with HF, MI, and pneumonia (Table). These SDoH were chosen because they are intervenable risk factors for which the VHA has several programs (eg, homeless outreach, substance abuse, and tobacco cessation). To examine the variability of these SDoH across VHA facilities, we determined the number of hospitals that had a sufficient number of admissions (≥ 50) to be included in the analyses. We then examined the administratively documented, facility-level variation in the proportion of individuals with any of the 5 SDoH administrative codes and examined the distribution of their use across all qualifying facilities.
Because variability may be due to regional coding differences, we examined the difference in the estimated prevalence of the risk factor lives alone by using a previously developed natural language processing (NLP) program.9 The NLP program is a rule-based system designed to automatically extract information that requires inferencing from clinical notes (eg, discharge summaries and nursing, social work, emergency department physician, primary care, and hospital admission notes). For instance, the program identifies whether there was direct or indirect evidence that the patient did or did not live alone. In addition to extracting data on lives alone, the NLP program has the capacity to extract information on lack of social support and living alone—2 characteristics without VHA interventions, which were not examined here. The NLP program was developed and evaluated using at least 1 year of notes prior to index hospitalization. Because this program was developed and validated on a 2012 data set, we were limited to using a cohort from this year as well.
All analyses were conducted using SAS Version 9.4. The San Francisco VA Medical Center Institutional Review Board approved this study.
Results
In total, 21,991 patients with either HF (9,853), pneumonia (9,362), or AMI (2,776) were identified across 91 VHA facilities. The majority were male (98%) and had a median (SD) age of 77.0 (9.0) years. The median facility-level proportion of veterans who had any of the SDoH risk factors extracted through administrative codes was low across all conditions, ranging from 0.5 to 2.2%. The most prevalent factors among patients admitted for HF, AMI, and pneumonia were lives alone (2.0% [Interquartile range (IQR), 1.0-5.2], 1.4% [IQR, 0-3.4], and 1.9% [IQR, 0.7-5.4]), substance use disorder (1.2% [IQR, 0-2.2], 1.6% [IQR: 0-3.0], and 1.3% [IQR, 0-2.2] and use of substance use services (0.9% [IQR, 0-1.6%], 1.0% [IQR, 0-1.7%], and 1.6% [IQR, 0-2.2%], respectively [Table]).
When utilizing the NLP algorithm, the documented prevalence of lives alone in the free text of the medical record was higher than administrative coding across all conditions (12.3% vs. 2.2%; P < .01). Among each of the 3 assessed conditions, HF (14.4% vs 2.0%, P < .01) had higher levels of lives alone compared with pneumonia (11% vs 1.9%, P < .01), and AMI (10.2% vs 1.4%, P < .01) when using the NLP algorithm. When we examined the documented facility-level variation in the proportion of individuals with any of the 5 SDoH administrative codes or NLP, we found large variability across all facilities—regardless of extraction method (Figure).
Discussion
While SDoH are known to impact health outcomes, the presence of these risk factors in administrative data among individuals hospitalized for common medical issues is low and variable across VHA facilities. Understanding the documented, facility-level variability of these measures may assist the VHA in determining how it invests time and resources—as different facilities may disproportionately serve a higher number of vulnerable individuals. Beyond the VHA, these findings have generalizable lessons for the US health care system, which has come to recognize how these risk factors impact patients’ health.10
Although the proportion of individuals with any of the assessed SDoH identified by administrative data was low, our findings are in line with recent studies that showed other risk factors such as social isolation (0.65%), housing issues (0.19%), and financial strain (0.07%) had similarly low prevalence.8,11 Although the exact prevalence of such factors remains unclear, these findings highlight that SDoH do not appear to be well documented in administrative data. Low coding rates are likely due to the fact that SDoH administrative codes are not tied to financial reimbursement—thus not incentivizing their use by clinicians or hospital systems.
In 2014, an Institute of Medicine report suggested that collection of SDoH in electronic health data as a means to better empower clinicians and health care systems to address social disparities and further support research in SDoH.12 Since then, data collection using SDoH screening tools has become more common across settings, but is not consistently translated to standardized data due to lack of industry consensus and technical barriers.13 To improve this process, the Centers for Medicare and Medicaid Services created “z-codes” for the ICD-10 classification system—a subset of codes that are meant to better capture patients’ underlying social risk.14 It remains to be seen if such administrative codes have improved the documentation of SDoH.
As health care systems have grown to understand the impact of SDoH on health outcomes,other means of collecting these data have evolved.1,10 For example, NLP-based extraction methods and electronic screening tools have been proposed and utilized as alternative for obtaining this information. Our findings suggest that some of these measures (eg, lives alone) often may be documented as part of routine care in the electronic health record, thus highlighting NLP as a tool to obtain such data. However, other studies using NLP technology to extract SDoH have shown this technology is often complicated by quality issues (ie, missing data), complex methods, and poor integration with current information technology infrastructures—thus limiting its use in health care delivery.15-18
While variance among SDoH across a national health care system is natural, it remains an important systems-level characteristic that health care leaders and policymakers should appreciate. As health care systems disperse financial resources and initiate quality improvement initiatives to address SDoH, knowing that not all facilities are equally affected by SDoH should impact allocation of such resources and energies. Although previous work has highlighted regional and neighborhood levels of variation within the VHA and other health care systems, to our knowledge, this is the first study to examine variability at the facility-level within the VHA.2,4,13,19
Limitations
There are several limitations to this study. First, though our findings are in line with previous data in other health care systems, generalizability beyond the VA, which primarily cares for older, male patients, may be limited.8 Though, as the nation’s largest health care system, lessons from the VHA can still be useful for other health care systems as they consider SDoH variation. Second, among the many SDoH previously identified to impact health, our analysis only focused on 5 such variables. Administrative and medical record documentation of other SDoH may be more common and less variable across institutions. Third, while our data suggests facility-level variation in these measures, this may be in part related to variation in coding across facilities. However, the single SDoH variable extracted using NLP also varied at the facility-level, suggesting that coding may not entirely drive the variation observed.
Conclusions
As US health care systems continue to address SDoH, our findings highlight the various challenges in obtaining accurate data on a patient’s social risk. Moreover, these findings highlight the large variability that exists among institutions in a national integrated health care system. Future work should explore the prevalence and variance of other SDoH as a means to help guide resource allocation and prioritize spending to better address SDoH where it is most needed.
Acknowledgments
This work was supported by NHLBI R01 RO1 HL116522-01A1. Support for VA/CMS data is provided by the US Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (Project Numbers SDR 02-237 and 98-004).
Social determinants of health (SDoH) are social, economic, environmental, and occupational factors that are known to influence an individual’s health care utilization and clinical outcomes.1,2 Because the Veterans Health Administration (VHA) is charged to address both the medical and nonmedical needs of the veteran population, it is increasingly interested in the impact SDoH have on veteran care.3,4 To combat the adverse impact of such factors, the VHA has implemented several large-scale programs across the US that focus on prevalent SDoH, such as homelessness, substance abuse, and alcohol use disorders.5,6 While such risk factors are generally universal in their distribution, variation across regions, between urban and rural spaces, and even within cities has been shown to exist in private settings.7 Understanding such variability potentially could be helpful to US Department of Veterans Affairs (VA) policymakers and leaders to better allocate funding and resources to address such issues.
Although previous work has highlighted regional and neighborhood-level variability of SDoH, no study has examined the facility-level variability of commonly encountered social risk factors within the VHA.4,8 The aim of this study was to describe the interfacility variation of 5 common SDoH known to influence health and health outcomes among a national cohort of veterans hospitalized for common medical issues by using administrative data.
Methods
We used a national cohort of veterans aged ≥ 65 years who were hospitalized at a VHA acute care facility with a primary discharge diagnosis of acute myocardial infarction (AMI), heart failure (HF), or pneumonia in 2012. These conditions were chosen because they are publicly reported and frequently used for interfacility comparison.
Using the International Classification of Diseases–9th Revision (ICD-9) and VHA clinical stop codes, we calculated the median documented proportion of patients with any of the following 5 SDoH: lived alone, marginal housing, alcohol use disorder, substance use disorder, and use of substance use services for patients presenting with HF, MI, and pneumonia (Table). These SDoH were chosen because they are intervenable risk factors for which the VHA has several programs (eg, homeless outreach, substance abuse, and tobacco cessation). To examine the variability of these SDoH across VHA facilities, we determined the number of hospitals that had a sufficient number of admissions (≥ 50) to be included in the analyses. We then examined the administratively documented, facility-level variation in the proportion of individuals with any of the 5 SDoH administrative codes and examined the distribution of their use across all qualifying facilities.
Because variability may be due to regional coding differences, we examined the difference in the estimated prevalence of the risk factor lives alone by using a previously developed natural language processing (NLP) program.9 The NLP program is a rule-based system designed to automatically extract information that requires inferencing from clinical notes (eg, discharge summaries and nursing, social work, emergency department physician, primary care, and hospital admission notes). For instance, the program identifies whether there was direct or indirect evidence that the patient did or did not live alone. In addition to extracting data on lives alone, the NLP program has the capacity to extract information on lack of social support and living alone—2 characteristics without VHA interventions, which were not examined here. The NLP program was developed and evaluated using at least 1 year of notes prior to index hospitalization. Because this program was developed and validated on a 2012 data set, we were limited to using a cohort from this year as well.
All analyses were conducted using SAS Version 9.4. The San Francisco VA Medical Center Institutional Review Board approved this study.
Results
In total, 21,991 patients with either HF (9,853), pneumonia (9,362), or AMI (2,776) were identified across 91 VHA facilities. The majority were male (98%) and had a median (SD) age of 77.0 (9.0) years. The median facility-level proportion of veterans who had any of the SDoH risk factors extracted through administrative codes was low across all conditions, ranging from 0.5 to 2.2%. The most prevalent factors among patients admitted for HF, AMI, and pneumonia were lives alone (2.0% [Interquartile range (IQR), 1.0-5.2], 1.4% [IQR, 0-3.4], and 1.9% [IQR, 0.7-5.4]), substance use disorder (1.2% [IQR, 0-2.2], 1.6% [IQR: 0-3.0], and 1.3% [IQR, 0-2.2] and use of substance use services (0.9% [IQR, 0-1.6%], 1.0% [IQR, 0-1.7%], and 1.6% [IQR, 0-2.2%], respectively [Table]).
When utilizing the NLP algorithm, the documented prevalence of lives alone in the free text of the medical record was higher than administrative coding across all conditions (12.3% vs. 2.2%; P < .01). Among each of the 3 assessed conditions, HF (14.4% vs 2.0%, P < .01) had higher levels of lives alone compared with pneumonia (11% vs 1.9%, P < .01), and AMI (10.2% vs 1.4%, P < .01) when using the NLP algorithm. When we examined the documented facility-level variation in the proportion of individuals with any of the 5 SDoH administrative codes or NLP, we found large variability across all facilities—regardless of extraction method (Figure).
Discussion
While SDoH are known to impact health outcomes, the presence of these risk factors in administrative data among individuals hospitalized for common medical issues is low and variable across VHA facilities. Understanding the documented, facility-level variability of these measures may assist the VHA in determining how it invests time and resources—as different facilities may disproportionately serve a higher number of vulnerable individuals. Beyond the VHA, these findings have generalizable lessons for the US health care system, which has come to recognize how these risk factors impact patients’ health.10
Although the proportion of individuals with any of the assessed SDoH identified by administrative data was low, our findings are in line with recent studies that showed other risk factors such as social isolation (0.65%), housing issues (0.19%), and financial strain (0.07%) had similarly low prevalence.8,11 Although the exact prevalence of such factors remains unclear, these findings highlight that SDoH do not appear to be well documented in administrative data. Low coding rates are likely due to the fact that SDoH administrative codes are not tied to financial reimbursement—thus not incentivizing their use by clinicians or hospital systems.
In 2014, an Institute of Medicine report suggested that collection of SDoH in electronic health data as a means to better empower clinicians and health care systems to address social disparities and further support research in SDoH.12 Since then, data collection using SDoH screening tools has become more common across settings, but is not consistently translated to standardized data due to lack of industry consensus and technical barriers.13 To improve this process, the Centers for Medicare and Medicaid Services created “z-codes” for the ICD-10 classification system—a subset of codes that are meant to better capture patients’ underlying social risk.14 It remains to be seen if such administrative codes have improved the documentation of SDoH.
As health care systems have grown to understand the impact of SDoH on health outcomes,other means of collecting these data have evolved.1,10 For example, NLP-based extraction methods and electronic screening tools have been proposed and utilized as alternative for obtaining this information. Our findings suggest that some of these measures (eg, lives alone) often may be documented as part of routine care in the electronic health record, thus highlighting NLP as a tool to obtain such data. However, other studies using NLP technology to extract SDoH have shown this technology is often complicated by quality issues (ie, missing data), complex methods, and poor integration with current information technology infrastructures—thus limiting its use in health care delivery.15-18
While variance among SDoH across a national health care system is natural, it remains an important systems-level characteristic that health care leaders and policymakers should appreciate. As health care systems disperse financial resources and initiate quality improvement initiatives to address SDoH, knowing that not all facilities are equally affected by SDoH should impact allocation of such resources and energies. Although previous work has highlighted regional and neighborhood levels of variation within the VHA and other health care systems, to our knowledge, this is the first study to examine variability at the facility-level within the VHA.2,4,13,19
Limitations
There are several limitations to this study. First, though our findings are in line with previous data in other health care systems, generalizability beyond the VA, which primarily cares for older, male patients, may be limited.8 Though, as the nation’s largest health care system, lessons from the VHA can still be useful for other health care systems as they consider SDoH variation. Second, among the many SDoH previously identified to impact health, our analysis only focused on 5 such variables. Administrative and medical record documentation of other SDoH may be more common and less variable across institutions. Third, while our data suggests facility-level variation in these measures, this may be in part related to variation in coding across facilities. However, the single SDoH variable extracted using NLP also varied at the facility-level, suggesting that coding may not entirely drive the variation observed.
Conclusions
As US health care systems continue to address SDoH, our findings highlight the various challenges in obtaining accurate data on a patient’s social risk. Moreover, these findings highlight the large variability that exists among institutions in a national integrated health care system. Future work should explore the prevalence and variance of other SDoH as a means to help guide resource allocation and prioritize spending to better address SDoH where it is most needed.
Acknowledgments
This work was supported by NHLBI R01 RO1 HL116522-01A1. Support for VA/CMS data is provided by the US Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (Project Numbers SDR 02-237 and 98-004).
1. Social determinants of health (SDOH). https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0312. Published December 1, 2017. Accessed December 8, 2020.
2. Hatef E, Searle KM, Predmore Z, et al. The Impact of Social Determinants of Health on hospitalization in the Veterans Health Administration. Am J Prev Med. 2019;56(6):811-818. doi:10.1016/j.amepre.2018.12.012
3. Lushniak BD, Alley DE, Ulin B, Graffunder C. The National Prevention Strategy: leveraging multiple sectors to improve population health. Am J Public Health. 2015;105(2):229-231. doi:10.2105/AJPH.2014.302257
4. Nelson K, Schwartz G, Hernandez S, Simonetti J, Curtis I, Fihn SD. The association between neighborhood environment and mortality: results from a national study of veterans. J Gen Intern Med. 2017;32(4):416-422. doi:10.1007/s11606-016-3905-x
5. Gundlapalli AV, Redd A, Bolton D, et al. Patient-aligned care team engagement to connect veterans experiencing homelessness with appropriate health care. Med Care. 2017;55 Suppl 9 Suppl 2:S104-S110. doi:10.1097/MLR.0000000000000770
6. Rash CJ, DePhilippis D. Considerations for implementing contingency management in substance abuse treatment clinics: the Veterans Affairs initiative as a model. Perspect Behav Sci. 2019;42(3):479-499. doi:10.1007/s40614-019-00204-3.
7. Ompad DC, Galea S, Caiaffa WT, Vlahov D. Social determinants of the health of urban populations: methodologic considerations. J Urban Health. 2007;84(3 Suppl):i42-i53. doi:10.1007/s11524-007-9168-4
8. Hatef E, Rouhizadeh M, Tia I, et al. Assessing the availability of data on social and behavioral determinants in structured and unstructured electronic health records: a retrospective analysis of a multilevel health care system. JMIR Med Inform. 2019;7(3):e13802. doi:10.2196/13802
9. Conway M, Keyhani S, Christensen L, et al. Moonstone: a novel natural language processing system for inferring social risk from clinical narratives. J Biomed Semantics. 2019;10(1):6. doi:10.1186/s13326-019-0198-0
10. Adler NE, Cutler DM, Fielding JE, et al. Addressing social determinants of health and health disparities: a vital direction for health and health care. Discussion Paper. NAM Perspectives. National Academy of Medicine, Washington, DC. doi:10.31478/201609t
11. Cottrell EK, Dambrun K, Cowburn S, et al. Variation in electronic health record documentation of social determinants of health across a national network of community health centers. Am J Prev Med. 2019;57(6):S65-S73. doi:10.1016/j.amepre.2019.07.014
12. Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records, Board on Population Health and Public Health Practice, Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. National Academies Press (US); 2015.
13. Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. Integrating Social And Medical Data To Improve Population Health: Opportunities And Barriers. Health Aff (Millwood). 2016;35(11):2116-2123. doi:10.1377/hlthaff.2016.0723
14. Centers for Medicare and Medicaid Service, Office of Minority Health. Z codes utilization among medicare fee-for-service (FFS) beneficiaries in 2017. Published January 2020. Accessed December 8, 2020. https://www.cms.gov/files/document/cms-omh-january2020-zcode-data-highlightpdf.pdf
15. Kharrazi H, Wang C, Scharfstein D. Prospective EHR-based clinical trials: the challenge of missing data. J Gen Intern Med. 2014;29(7):976-978. doi:10.1007/s11606-014-2883-0
16. Weiskopf NG, Weng C. Methods and dimensions of electronic health record data quality assessment: enabling reuse for clinical research. J Am Med Inform Assoc. 2013;20(1):144-151. doi:10.1136/amiajnl-2011-000681
17. Anzaldi LJ, Davison A, Boyd CM, Leff B, Kharrazi H. Comparing clinician descriptions of frailty and geriatric syndromes using electronic health records: a retrospective cohort study. BMC Geriatr. 2017;17(1):248. doi:10.1186/s12877-017-0645-7
18. Chen T, Dredze M, Weiner JP, Kharrazi H. Identifying vulnerable older adult populations by contextualizing geriatric syndrome information in clinical notes of electronic health records. J Am Med Inform Assoc. 2019;26(8-9):787-795. doi:10.1093/jamia/ocz093
19. Raphael E, Gaynes R, Hamad R. Cross-sectional analysis of place-based and racial disparities in hospitalisation rates by disease category in California in 2001 and 2011. BMJ Open. 2019;9(10):e031556. doi:10.1136/bmjopen-2019-031556
1. Social determinants of health (SDOH). https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0312. Published December 1, 2017. Accessed December 8, 2020.
2. Hatef E, Searle KM, Predmore Z, et al. The Impact of Social Determinants of Health on hospitalization in the Veterans Health Administration. Am J Prev Med. 2019;56(6):811-818. doi:10.1016/j.amepre.2018.12.012
3. Lushniak BD, Alley DE, Ulin B, Graffunder C. The National Prevention Strategy: leveraging multiple sectors to improve population health. Am J Public Health. 2015;105(2):229-231. doi:10.2105/AJPH.2014.302257
4. Nelson K, Schwartz G, Hernandez S, Simonetti J, Curtis I, Fihn SD. The association between neighborhood environment and mortality: results from a national study of veterans. J Gen Intern Med. 2017;32(4):416-422. doi:10.1007/s11606-016-3905-x
5. Gundlapalli AV, Redd A, Bolton D, et al. Patient-aligned care team engagement to connect veterans experiencing homelessness with appropriate health care. Med Care. 2017;55 Suppl 9 Suppl 2:S104-S110. doi:10.1097/MLR.0000000000000770
6. Rash CJ, DePhilippis D. Considerations for implementing contingency management in substance abuse treatment clinics: the Veterans Affairs initiative as a model. Perspect Behav Sci. 2019;42(3):479-499. doi:10.1007/s40614-019-00204-3.
7. Ompad DC, Galea S, Caiaffa WT, Vlahov D. Social determinants of the health of urban populations: methodologic considerations. J Urban Health. 2007;84(3 Suppl):i42-i53. doi:10.1007/s11524-007-9168-4
8. Hatef E, Rouhizadeh M, Tia I, et al. Assessing the availability of data on social and behavioral determinants in structured and unstructured electronic health records: a retrospective analysis of a multilevel health care system. JMIR Med Inform. 2019;7(3):e13802. doi:10.2196/13802
9. Conway M, Keyhani S, Christensen L, et al. Moonstone: a novel natural language processing system for inferring social risk from clinical narratives. J Biomed Semantics. 2019;10(1):6. doi:10.1186/s13326-019-0198-0
10. Adler NE, Cutler DM, Fielding JE, et al. Addressing social determinants of health and health disparities: a vital direction for health and health care. Discussion Paper. NAM Perspectives. National Academy of Medicine, Washington, DC. doi:10.31478/201609t
11. Cottrell EK, Dambrun K, Cowburn S, et al. Variation in electronic health record documentation of social determinants of health across a national network of community health centers. Am J Prev Med. 2019;57(6):S65-S73. doi:10.1016/j.amepre.2019.07.014
12. Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records, Board on Population Health and Public Health Practice, Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. National Academies Press (US); 2015.
13. Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. Integrating Social And Medical Data To Improve Population Health: Opportunities And Barriers. Health Aff (Millwood). 2016;35(11):2116-2123. doi:10.1377/hlthaff.2016.0723
14. Centers for Medicare and Medicaid Service, Office of Minority Health. Z codes utilization among medicare fee-for-service (FFS) beneficiaries in 2017. Published January 2020. Accessed December 8, 2020. https://www.cms.gov/files/document/cms-omh-january2020-zcode-data-highlightpdf.pdf
15. Kharrazi H, Wang C, Scharfstein D. Prospective EHR-based clinical trials: the challenge of missing data. J Gen Intern Med. 2014;29(7):976-978. doi:10.1007/s11606-014-2883-0
16. Weiskopf NG, Weng C. Methods and dimensions of electronic health record data quality assessment: enabling reuse for clinical research. J Am Med Inform Assoc. 2013;20(1):144-151. doi:10.1136/amiajnl-2011-000681
17. Anzaldi LJ, Davison A, Boyd CM, Leff B, Kharrazi H. Comparing clinician descriptions of frailty and geriatric syndromes using electronic health records: a retrospective cohort study. BMC Geriatr. 2017;17(1):248. doi:10.1186/s12877-017-0645-7
18. Chen T, Dredze M, Weiner JP, Kharrazi H. Identifying vulnerable older adult populations by contextualizing geriatric syndrome information in clinical notes of electronic health records. J Am Med Inform Assoc. 2019;26(8-9):787-795. doi:10.1093/jamia/ocz093
19. Raphael E, Gaynes R, Hamad R. Cross-sectional analysis of place-based and racial disparities in hospitalisation rates by disease category in California in 2001 and 2011. BMJ Open. 2019;9(10):e031556. doi:10.1136/bmjopen-2019-031556
Caring for Patients at a COVID-19 Field Hospital
During the initial peak of coronavirus disease 2019 (COVID-19) cases, US models suggested hospital bed shortages, hinting at the dire possibility of an overwhelmed healthcare system.1,2 Such projections invoked widespread uncertainty and fear of massive loss of life secondary to an undersupply of treatment resources. This led many state governments to rush into a series of historically unprecedented interventions, including the rapid deployment of field hospitals. US state governments, in partnership with the Army Corps of Engineers, invested more than $660 million to transform convention halls, university campus buildings, and even abandoned industrial warehouses, into overflow hospitals for the care of COVID-19 patients.1 Such a national scale of field hospital construction is truly historic, never before having occurred at this speed and on this scale. The only other time field hospitals were deployed nearly as widely in the United States was during the Civil War.3
FIELD HOSPITALS DURING THE COVID-19 PANDEMIC
The use of COVID-19 field hospital resources has been variable, with patient volumes ranging from 0 at many to more than 1,000 at the Javits Center field hospital in New York City.1 In fact, most field hospitals did not treat any patients because early public health measures, such as stay-at-home orders, helped contain the virus in most states.1 As of this writing, the United States has seen a dramatic surge in COVID-19 transmission and hospitalizations. This has led many states to re-introduce field hospitals into their COVID emergency response.
Our site, the Baltimore Convention Center Field Hospital (BCCFH), is one of few sites that is still operational and, to our knowledge, is the longest-running US COVID-19 field hospital. We have cared for 543 patients since opening and have had no cardiac arrests or on-site deaths. To safely offload lower-acuity COVID-19 patients from Maryland hospitals, we designed admission criteria and care processes to provide medical care on site until patients are ready for discharge. However, we anticipated that some patients would decompensate and need to return to a higher level of care. Here, we share our experience with identifying, assessing, resuscitating, and transporting unstable patients. We believe that this process has allowed us to treat about 80% of our patients in place with successful discharge to outpatient care. We have safely transferred about 20% to a higher level of care, having learned from our early cases to refine and improve our rapid response process.
CASES
Case 1
A 39-year-old man was transferred to the BCCFH on his 9th day of symptoms following a 3-day hospital admission for COVID-19. On BCCFH day 1, he developed an oxygen requirement of 2 L/min and a fever of 39.9 oC. Testing revealed worsening hyponatremia and new proteinuria, and a chest radiograph showed increased bilateral interstitial infiltrates. Cefdinir and fluid restriction were initiated. On BCCFH day 2, the patient developed hypotension (88/55 mm Hg), tachycardia (180 bpm), an oxygen requirement of 3 L/min, and a brief syncopal episode while sitting in bed. The charge physician and nurse were directed to the bedside. They instructed staff to bring a stretcher and intravenous (IV) supplies. Unable to locate these supplies in the triage bay, the staff found them in various locations. An IV line was inserted, and fluids administered, after which vital signs improved. Emergency medical services (EMS), which were on standby outside the field hospital, were alerted via radio; they donned personal protective equipment (PPE) and arrived at the triage bay. They were redirected to patient bedside, whence they transported the patient to the hospital.
Case 2
A 64-year-old man with a history of homelessness, myocardial infarctions, cerebrovascular accident, and paroxysmal atrial fibrillation was transferred to the BCCFH on his 6th day of symptoms after a 2-day hospitalization with COVID-19 respiratory illness. On BCCFH day 1, he had a temperature of 39.3 oC and atypical chest pain. A laboratory workup was unrevealing. On BCCFH day 2, he had asymptomatic hypotension and a heart rate of 60-85 bpm while receiving his usual metoprolol dose. On BCCFH day 3, he reported dizziness and was found to be hypotensive (83/41 mm Hg) and febrile (38.6 oC). The rapid response team (RRT) was called over radio, and they quickly assessed the patient and transported him to the triage bay. EMS, signaled through the RRT radio announcement, arrived at the triage bay and transported the patient to a traditional hospital.
ABOUT THE BCCFH
The BCCFH, which opened in April 2020, is a 252-bed facility that’s spread over a single exhibit hall floor and cares for stable adult COVID-19 patients from any hospital or emergency department in Maryland (Appendix A). The site offers basic laboratory tests, radiography, a limited on-site pharmacy, and spot vital sign monitoring without telemetry. Both EMS and a certified registered nurse anesthetist are on standby in the nonclinical area and must don PPE before entering the patient care area when called. The appendices show the patient beds (Appendix B) and triage area (Appendix C) used for patient evaluation and resuscitation. Unlike conventional hospitals, the BCCFH has limited consultant access, and there are frequent changes in clinical teams. In addition to clinicians, our site has physical therapists, occupational therapists, and social work teams to assist in patient care and discharge planning. As of this writing, we have cared for 543 patients, sent to us from one-third of Maryland’s hospitals. Use during the first wave of COVID was variable, with some hospitals sending us just a few patients. One Baltimore hospital sent us 8% of its COVID-19 patients. Because the patients have an average 5-day stay, the BCCFH has offloaded 2,600 bed-days of care from acute hospitals.
ROLE OF THE RRT IN A FIELD HOSPITAL
COVID-19 field hospitals must be prepared to respond effectively to decompensating patients. In our experience, effective RRTs provide a standard and reproducible approach to patient emergencies. In the conventional hospital setting, these teams consist of clinicians who can be called on by any healthcare worker to quickly assess deteriorating patients and intervene with treatment. The purpose of an RRT is to provide immediate care to a patient before progression to respiratory or cardiac arrest. RRTs proliferated in US hospitals after 2004 when the Institute for Healthcare Improvement in Boston, Massachusetts, recommended such teams for improved quality of care. Though studies report conflicting findings on the impact of RRTs on mortality rates, these studies were performed in traditional hospitals with ample resources, consultants, and clinicians familiar with their patients rather than in resource-limited field hospitals.4-13 Our field hospital has found RRTs, and the principles behind them, useful in the identification and management of decompensating COVID-19 patients.
A FOUR-STEP RAPID RESPONSE FRAMEWORK: CASE CORRELATION
An approach to managing decompensating patients in a COVID-19 field hospital can be considered in four phases: identification, assessment, resuscitation, and transport. Referring to these phases, the first case shows opportunities for improvement in resuscitation and transport. Although decompensation was identified, the patient was not transported to the triage bay for resuscitation, and there was confusion when trying to obtain the proper equipment. Additionally, EMS awaited the patient in the triage bay, while he remained in his cubicle, which delayed transport to an acute care hospital. The second case shows opportunities for improvement in identification and assessment. The patient had signs of impending decompensation that were not immediately recognized and treated. However, once decompensation occurred, the RRT was called and the patient was transported quickly to the triage bay, and then to the hospital via EMS.
In our experience at the BCCFH, identification is a key phase in COVID-19 care at a field hospital. Identification involves recognizing impending deterioration, as well as understanding risk factors for decompensation. For COVID-19 specifically, this requires heightened awareness of patients who are in the 2nd to 3rd week of symptoms. Data from Wuhan, China, suggest that decompensation occurs predictably around symptom day 9.14,15 At the BCCFH, the median symptom duration for patients who decompensated and returned to a hospital was 13 days. In both introductory cases, patients were in the high-risk 2nd week of symptoms when decompensation occurred. Clinicians at the BCCFH now discuss patient symptom day during their handoffs, when rounding, and when making decisions regarding acute care transfer. Our team has also integrated clinical information from our electronic health record to create a dashboard describing those patients requiring acute care transfer to assist in identifying other trends or predictive factors (Appendix D).
LESSONS FROM THE FIELD HOSPITAL: IMPROVING CLINICAL PERFORMANCE
Although RRTs are designed to activate when an individual patient decompensates, they should fit within a larger operational framework for patient safety. Our experience with emergencies at the BCCFH has yielded four opportunities for learning relevant to COVID-19 care in nontraditional settings (Table). These lessons include how to update staff on clinical process changes, unify communication systems, create a clinical drilling culture, and review cases to improve performance. They illustrate the importance of standardizing emergency processes, conducting frequent updates and drills, and ensuring continuous improvement. We found that, while caring for patients with an unpredictable, novel disease in a nontraditional setting and while wearing PPE and working with new colleagues during every shift, the best approach to support patients and staff is to anticipate emergencies rather than relying on individual staff to develop on-the-spot solutions.
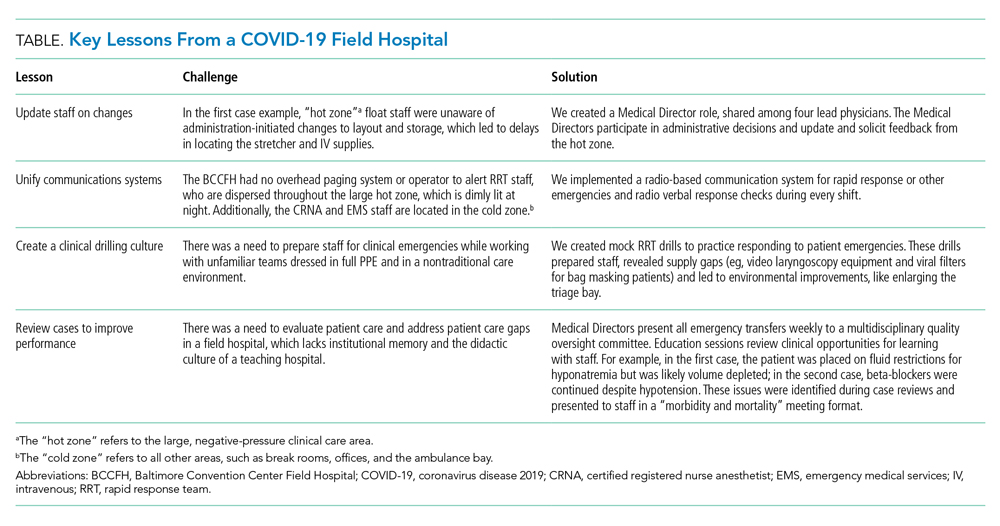
CONCLUSION
The COVID-19 era has seen the unprecedented construction and utilization of emergency field hospital facilities. Such facilities can serve to offload some COVID-19 patients from strained healthcare infrastructure and provide essential care to these patients. We share many of the unique physical and logistical considerations specific to a nontraditional site. We optimized our space, our equipment, and our communication system. We learned how to identify, assess, resuscitate, and transport decompensating COVID-19 patients. Ultimately, our field hospital has been well utilized and successful at caring for patients because of its adaptability, accessibility, and safety record. Of the 15% of patients we transferred to a hospital for care, 81% were successfully stabilized and were willing to return to the BCCFH to complete their care. Our design included supportive care such as social work, physical and occupational therapy, and treatment of comorbidities, such as diabetes and substance use disorder. Our model demonstrates an effective nonhospital option for the care of lower-acuity, medically complex COVID-19 patients. If such facilities are used in subsequent COVID-19 outbreaks, we advise structured planning for the care of decompensating patients that takes into account the need for effective communication, drilling, and ongoing process improvement.
1. Rose J. U.S. Field Hospitals Stand Down, Most Without Treating Any COVID-19 Patients. All Things Considered. NPR; May 7, 2020. Accessed July 21, 2020. https://www.npr.org/2020/05/07/851712311/u-s-field-hospitals-stand-down-most-without-treating-any-covid-19-patients
2. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305-1314. https://doi.org/10.1016/s0140-6736(20)30744-3
3. Reilly RF. Medical and surgical care during the American Civil War, 1861-1865. Proc (Bayl Univ Med Cent). 2016;29(2):138-142. https://doi.org/10.1080/08998280.2016.11929390
4. Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004;32(4):916-21. https://doi.org/10.1097/01.ccm.0000119428.02968.9e
5. Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003;179(6):283-287.
6. Bristow PJ, Hillman KM, Chey T, et al. Rates of in-hospital arrests, deaths and intensive care admissions: the effect of a medical emergency team. Med J Aust. 2000;173(5):236-240.
7. Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387-390. https://doi.org/10.1136/bmj.324.7334.387
8. DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL; Medical Emergency Response Improvement Team (MERIT). Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care. 2004;13(4):251-254. https://doi.org/10.1136/qhc.13.4.251
9. Goldhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A. The patient-at-risk team: identifying and managing seriously ill ward patients. Anaesthesia. 1999;54(9):853-860. https://doi.org/10.1046/j.1365-2044.1999.00996.x
10. Hillman K, Chen J, Cretikos M, et al; MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365(9477):2091-2097. https://doi.org/10.1016/s0140-6736(05)66733-5
11. Kenward G, Castle N, Hodgetts T, Shaikh L. Evaluation of a medical emergency team one year after implementation. Resuscitation. 2004;61(3):257-263. https://doi.org/10.1016/j.resuscitation.2004.01.021
12. Pittard AJ. Out of our reach? assessing the impact of introducing a critical care outreach service. Anaesthesia. 2003;58(9):882-885. https://doi.org/10.1046/j.1365-2044.2003.03331.x
13. Priestley G, Watson W, Rashidian A, et al. Introducing critical care outreach: a ward-randomised trial of phased introduction in a general hospital. Intensive Care Med. 2004;30(7):1398-1404. https://doi.org/10.1007/s00134-004-2268-7
14. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. https://doi.org/10.1016/s0140-6736(20)30566-3
15. Zhou Y, Li W, Wang D, et al. Clinical time course of COVID-19, its neurological manifestation and some thoughts on its management. Stroke Vasc Neurol. 2020;5(2):177-179. https://doi.org/10.1136/svn-2020-000398
During the initial peak of coronavirus disease 2019 (COVID-19) cases, US models suggested hospital bed shortages, hinting at the dire possibility of an overwhelmed healthcare system.1,2 Such projections invoked widespread uncertainty and fear of massive loss of life secondary to an undersupply of treatment resources. This led many state governments to rush into a series of historically unprecedented interventions, including the rapid deployment of field hospitals. US state governments, in partnership with the Army Corps of Engineers, invested more than $660 million to transform convention halls, university campus buildings, and even abandoned industrial warehouses, into overflow hospitals for the care of COVID-19 patients.1 Such a national scale of field hospital construction is truly historic, never before having occurred at this speed and on this scale. The only other time field hospitals were deployed nearly as widely in the United States was during the Civil War.3
FIELD HOSPITALS DURING THE COVID-19 PANDEMIC
The use of COVID-19 field hospital resources has been variable, with patient volumes ranging from 0 at many to more than 1,000 at the Javits Center field hospital in New York City.1 In fact, most field hospitals did not treat any patients because early public health measures, such as stay-at-home orders, helped contain the virus in most states.1 As of this writing, the United States has seen a dramatic surge in COVID-19 transmission and hospitalizations. This has led many states to re-introduce field hospitals into their COVID emergency response.
Our site, the Baltimore Convention Center Field Hospital (BCCFH), is one of few sites that is still operational and, to our knowledge, is the longest-running US COVID-19 field hospital. We have cared for 543 patients since opening and have had no cardiac arrests or on-site deaths. To safely offload lower-acuity COVID-19 patients from Maryland hospitals, we designed admission criteria and care processes to provide medical care on site until patients are ready for discharge. However, we anticipated that some patients would decompensate and need to return to a higher level of care. Here, we share our experience with identifying, assessing, resuscitating, and transporting unstable patients. We believe that this process has allowed us to treat about 80% of our patients in place with successful discharge to outpatient care. We have safely transferred about 20% to a higher level of care, having learned from our early cases to refine and improve our rapid response process.
CASES
Case 1
A 39-year-old man was transferred to the BCCFH on his 9th day of symptoms following a 3-day hospital admission for COVID-19. On BCCFH day 1, he developed an oxygen requirement of 2 L/min and a fever of 39.9 oC. Testing revealed worsening hyponatremia and new proteinuria, and a chest radiograph showed increased bilateral interstitial infiltrates. Cefdinir and fluid restriction were initiated. On BCCFH day 2, the patient developed hypotension (88/55 mm Hg), tachycardia (180 bpm), an oxygen requirement of 3 L/min, and a brief syncopal episode while sitting in bed. The charge physician and nurse were directed to the bedside. They instructed staff to bring a stretcher and intravenous (IV) supplies. Unable to locate these supplies in the triage bay, the staff found them in various locations. An IV line was inserted, and fluids administered, after which vital signs improved. Emergency medical services (EMS), which were on standby outside the field hospital, were alerted via radio; they donned personal protective equipment (PPE) and arrived at the triage bay. They were redirected to patient bedside, whence they transported the patient to the hospital.
Case 2
A 64-year-old man with a history of homelessness, myocardial infarctions, cerebrovascular accident, and paroxysmal atrial fibrillation was transferred to the BCCFH on his 6th day of symptoms after a 2-day hospitalization with COVID-19 respiratory illness. On BCCFH day 1, he had a temperature of 39.3 oC and atypical chest pain. A laboratory workup was unrevealing. On BCCFH day 2, he had asymptomatic hypotension and a heart rate of 60-85 bpm while receiving his usual metoprolol dose. On BCCFH day 3, he reported dizziness and was found to be hypotensive (83/41 mm Hg) and febrile (38.6 oC). The rapid response team (RRT) was called over radio, and they quickly assessed the patient and transported him to the triage bay. EMS, signaled through the RRT radio announcement, arrived at the triage bay and transported the patient to a traditional hospital.
ABOUT THE BCCFH
The BCCFH, which opened in April 2020, is a 252-bed facility that’s spread over a single exhibit hall floor and cares for stable adult COVID-19 patients from any hospital or emergency department in Maryland (Appendix A). The site offers basic laboratory tests, radiography, a limited on-site pharmacy, and spot vital sign monitoring without telemetry. Both EMS and a certified registered nurse anesthetist are on standby in the nonclinical area and must don PPE before entering the patient care area when called. The appendices show the patient beds (Appendix B) and triage area (Appendix C) used for patient evaluation and resuscitation. Unlike conventional hospitals, the BCCFH has limited consultant access, and there are frequent changes in clinical teams. In addition to clinicians, our site has physical therapists, occupational therapists, and social work teams to assist in patient care and discharge planning. As of this writing, we have cared for 543 patients, sent to us from one-third of Maryland’s hospitals. Use during the first wave of COVID was variable, with some hospitals sending us just a few patients. One Baltimore hospital sent us 8% of its COVID-19 patients. Because the patients have an average 5-day stay, the BCCFH has offloaded 2,600 bed-days of care from acute hospitals.
ROLE OF THE RRT IN A FIELD HOSPITAL
COVID-19 field hospitals must be prepared to respond effectively to decompensating patients. In our experience, effective RRTs provide a standard and reproducible approach to patient emergencies. In the conventional hospital setting, these teams consist of clinicians who can be called on by any healthcare worker to quickly assess deteriorating patients and intervene with treatment. The purpose of an RRT is to provide immediate care to a patient before progression to respiratory or cardiac arrest. RRTs proliferated in US hospitals after 2004 when the Institute for Healthcare Improvement in Boston, Massachusetts, recommended such teams for improved quality of care. Though studies report conflicting findings on the impact of RRTs on mortality rates, these studies were performed in traditional hospitals with ample resources, consultants, and clinicians familiar with their patients rather than in resource-limited field hospitals.4-13 Our field hospital has found RRTs, and the principles behind them, useful in the identification and management of decompensating COVID-19 patients.
A FOUR-STEP RAPID RESPONSE FRAMEWORK: CASE CORRELATION
An approach to managing decompensating patients in a COVID-19 field hospital can be considered in four phases: identification, assessment, resuscitation, and transport. Referring to these phases, the first case shows opportunities for improvement in resuscitation and transport. Although decompensation was identified, the patient was not transported to the triage bay for resuscitation, and there was confusion when trying to obtain the proper equipment. Additionally, EMS awaited the patient in the triage bay, while he remained in his cubicle, which delayed transport to an acute care hospital. The second case shows opportunities for improvement in identification and assessment. The patient had signs of impending decompensation that were not immediately recognized and treated. However, once decompensation occurred, the RRT was called and the patient was transported quickly to the triage bay, and then to the hospital via EMS.
In our experience at the BCCFH, identification is a key phase in COVID-19 care at a field hospital. Identification involves recognizing impending deterioration, as well as understanding risk factors for decompensation. For COVID-19 specifically, this requires heightened awareness of patients who are in the 2nd to 3rd week of symptoms. Data from Wuhan, China, suggest that decompensation occurs predictably around symptom day 9.14,15 At the BCCFH, the median symptom duration for patients who decompensated and returned to a hospital was 13 days. In both introductory cases, patients were in the high-risk 2nd week of symptoms when decompensation occurred. Clinicians at the BCCFH now discuss patient symptom day during their handoffs, when rounding, and when making decisions regarding acute care transfer. Our team has also integrated clinical information from our electronic health record to create a dashboard describing those patients requiring acute care transfer to assist in identifying other trends or predictive factors (Appendix D).
LESSONS FROM THE FIELD HOSPITAL: IMPROVING CLINICAL PERFORMANCE
Although RRTs are designed to activate when an individual patient decompensates, they should fit within a larger operational framework for patient safety. Our experience with emergencies at the BCCFH has yielded four opportunities for learning relevant to COVID-19 care in nontraditional settings (Table). These lessons include how to update staff on clinical process changes, unify communication systems, create a clinical drilling culture, and review cases to improve performance. They illustrate the importance of standardizing emergency processes, conducting frequent updates and drills, and ensuring continuous improvement. We found that, while caring for patients with an unpredictable, novel disease in a nontraditional setting and while wearing PPE and working with new colleagues during every shift, the best approach to support patients and staff is to anticipate emergencies rather than relying on individual staff to develop on-the-spot solutions.
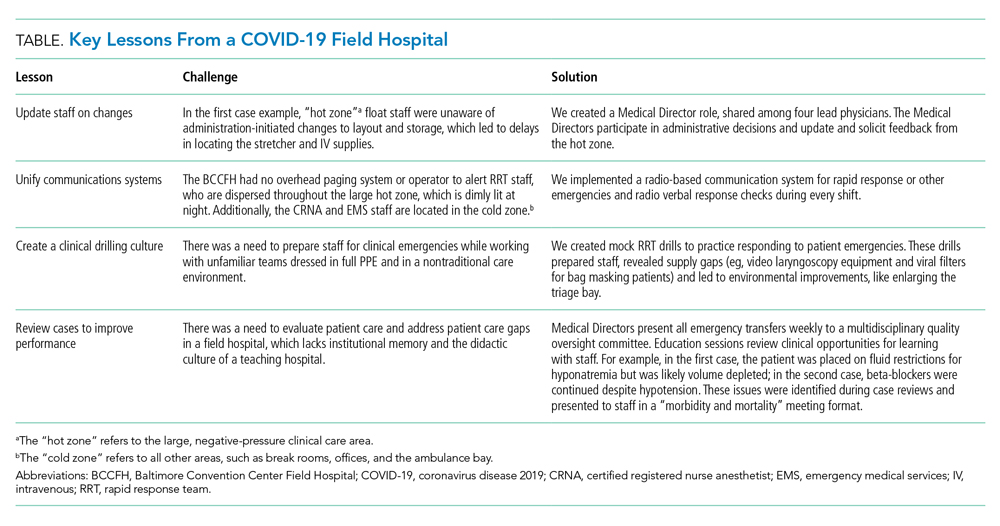
CONCLUSION
The COVID-19 era has seen the unprecedented construction and utilization of emergency field hospital facilities. Such facilities can serve to offload some COVID-19 patients from strained healthcare infrastructure and provide essential care to these patients. We share many of the unique physical and logistical considerations specific to a nontraditional site. We optimized our space, our equipment, and our communication system. We learned how to identify, assess, resuscitate, and transport decompensating COVID-19 patients. Ultimately, our field hospital has been well utilized and successful at caring for patients because of its adaptability, accessibility, and safety record. Of the 15% of patients we transferred to a hospital for care, 81% were successfully stabilized and were willing to return to the BCCFH to complete their care. Our design included supportive care such as social work, physical and occupational therapy, and treatment of comorbidities, such as diabetes and substance use disorder. Our model demonstrates an effective nonhospital option for the care of lower-acuity, medically complex COVID-19 patients. If such facilities are used in subsequent COVID-19 outbreaks, we advise structured planning for the care of decompensating patients that takes into account the need for effective communication, drilling, and ongoing process improvement.
During the initial peak of coronavirus disease 2019 (COVID-19) cases, US models suggested hospital bed shortages, hinting at the dire possibility of an overwhelmed healthcare system.1,2 Such projections invoked widespread uncertainty and fear of massive loss of life secondary to an undersupply of treatment resources. This led many state governments to rush into a series of historically unprecedented interventions, including the rapid deployment of field hospitals. US state governments, in partnership with the Army Corps of Engineers, invested more than $660 million to transform convention halls, university campus buildings, and even abandoned industrial warehouses, into overflow hospitals for the care of COVID-19 patients.1 Such a national scale of field hospital construction is truly historic, never before having occurred at this speed and on this scale. The only other time field hospitals were deployed nearly as widely in the United States was during the Civil War.3
FIELD HOSPITALS DURING THE COVID-19 PANDEMIC
The use of COVID-19 field hospital resources has been variable, with patient volumes ranging from 0 at many to more than 1,000 at the Javits Center field hospital in New York City.1 In fact, most field hospitals did not treat any patients because early public health measures, such as stay-at-home orders, helped contain the virus in most states.1 As of this writing, the United States has seen a dramatic surge in COVID-19 transmission and hospitalizations. This has led many states to re-introduce field hospitals into their COVID emergency response.
Our site, the Baltimore Convention Center Field Hospital (BCCFH), is one of few sites that is still operational and, to our knowledge, is the longest-running US COVID-19 field hospital. We have cared for 543 patients since opening and have had no cardiac arrests or on-site deaths. To safely offload lower-acuity COVID-19 patients from Maryland hospitals, we designed admission criteria and care processes to provide medical care on site until patients are ready for discharge. However, we anticipated that some patients would decompensate and need to return to a higher level of care. Here, we share our experience with identifying, assessing, resuscitating, and transporting unstable patients. We believe that this process has allowed us to treat about 80% of our patients in place with successful discharge to outpatient care. We have safely transferred about 20% to a higher level of care, having learned from our early cases to refine and improve our rapid response process.
CASES
Case 1
A 39-year-old man was transferred to the BCCFH on his 9th day of symptoms following a 3-day hospital admission for COVID-19. On BCCFH day 1, he developed an oxygen requirement of 2 L/min and a fever of 39.9 oC. Testing revealed worsening hyponatremia and new proteinuria, and a chest radiograph showed increased bilateral interstitial infiltrates. Cefdinir and fluid restriction were initiated. On BCCFH day 2, the patient developed hypotension (88/55 mm Hg), tachycardia (180 bpm), an oxygen requirement of 3 L/min, and a brief syncopal episode while sitting in bed. The charge physician and nurse were directed to the bedside. They instructed staff to bring a stretcher and intravenous (IV) supplies. Unable to locate these supplies in the triage bay, the staff found them in various locations. An IV line was inserted, and fluids administered, after which vital signs improved. Emergency medical services (EMS), which were on standby outside the field hospital, were alerted via radio; they donned personal protective equipment (PPE) and arrived at the triage bay. They were redirected to patient bedside, whence they transported the patient to the hospital.
Case 2
A 64-year-old man with a history of homelessness, myocardial infarctions, cerebrovascular accident, and paroxysmal atrial fibrillation was transferred to the BCCFH on his 6th day of symptoms after a 2-day hospitalization with COVID-19 respiratory illness. On BCCFH day 1, he had a temperature of 39.3 oC and atypical chest pain. A laboratory workup was unrevealing. On BCCFH day 2, he had asymptomatic hypotension and a heart rate of 60-85 bpm while receiving his usual metoprolol dose. On BCCFH day 3, he reported dizziness and was found to be hypotensive (83/41 mm Hg) and febrile (38.6 oC). The rapid response team (RRT) was called over radio, and they quickly assessed the patient and transported him to the triage bay. EMS, signaled through the RRT radio announcement, arrived at the triage bay and transported the patient to a traditional hospital.
ABOUT THE BCCFH
The BCCFH, which opened in April 2020, is a 252-bed facility that’s spread over a single exhibit hall floor and cares for stable adult COVID-19 patients from any hospital or emergency department in Maryland (Appendix A). The site offers basic laboratory tests, radiography, a limited on-site pharmacy, and spot vital sign monitoring without telemetry. Both EMS and a certified registered nurse anesthetist are on standby in the nonclinical area and must don PPE before entering the patient care area when called. The appendices show the patient beds (Appendix B) and triage area (Appendix C) used for patient evaluation and resuscitation. Unlike conventional hospitals, the BCCFH has limited consultant access, and there are frequent changes in clinical teams. In addition to clinicians, our site has physical therapists, occupational therapists, and social work teams to assist in patient care and discharge planning. As of this writing, we have cared for 543 patients, sent to us from one-third of Maryland’s hospitals. Use during the first wave of COVID was variable, with some hospitals sending us just a few patients. One Baltimore hospital sent us 8% of its COVID-19 patients. Because the patients have an average 5-day stay, the BCCFH has offloaded 2,600 bed-days of care from acute hospitals.
ROLE OF THE RRT IN A FIELD HOSPITAL
COVID-19 field hospitals must be prepared to respond effectively to decompensating patients. In our experience, effective RRTs provide a standard and reproducible approach to patient emergencies. In the conventional hospital setting, these teams consist of clinicians who can be called on by any healthcare worker to quickly assess deteriorating patients and intervene with treatment. The purpose of an RRT is to provide immediate care to a patient before progression to respiratory or cardiac arrest. RRTs proliferated in US hospitals after 2004 when the Institute for Healthcare Improvement in Boston, Massachusetts, recommended such teams for improved quality of care. Though studies report conflicting findings on the impact of RRTs on mortality rates, these studies were performed in traditional hospitals with ample resources, consultants, and clinicians familiar with their patients rather than in resource-limited field hospitals.4-13 Our field hospital has found RRTs, and the principles behind them, useful in the identification and management of decompensating COVID-19 patients.
A FOUR-STEP RAPID RESPONSE FRAMEWORK: CASE CORRELATION
An approach to managing decompensating patients in a COVID-19 field hospital can be considered in four phases: identification, assessment, resuscitation, and transport. Referring to these phases, the first case shows opportunities for improvement in resuscitation and transport. Although decompensation was identified, the patient was not transported to the triage bay for resuscitation, and there was confusion when trying to obtain the proper equipment. Additionally, EMS awaited the patient in the triage bay, while he remained in his cubicle, which delayed transport to an acute care hospital. The second case shows opportunities for improvement in identification and assessment. The patient had signs of impending decompensation that were not immediately recognized and treated. However, once decompensation occurred, the RRT was called and the patient was transported quickly to the triage bay, and then to the hospital via EMS.
In our experience at the BCCFH, identification is a key phase in COVID-19 care at a field hospital. Identification involves recognizing impending deterioration, as well as understanding risk factors for decompensation. For COVID-19 specifically, this requires heightened awareness of patients who are in the 2nd to 3rd week of symptoms. Data from Wuhan, China, suggest that decompensation occurs predictably around symptom day 9.14,15 At the BCCFH, the median symptom duration for patients who decompensated and returned to a hospital was 13 days. In both introductory cases, patients were in the high-risk 2nd week of symptoms when decompensation occurred. Clinicians at the BCCFH now discuss patient symptom day during their handoffs, when rounding, and when making decisions regarding acute care transfer. Our team has also integrated clinical information from our electronic health record to create a dashboard describing those patients requiring acute care transfer to assist in identifying other trends or predictive factors (Appendix D).
LESSONS FROM THE FIELD HOSPITAL: IMPROVING CLINICAL PERFORMANCE
Although RRTs are designed to activate when an individual patient decompensates, they should fit within a larger operational framework for patient safety. Our experience with emergencies at the BCCFH has yielded four opportunities for learning relevant to COVID-19 care in nontraditional settings (Table). These lessons include how to update staff on clinical process changes, unify communication systems, create a clinical drilling culture, and review cases to improve performance. They illustrate the importance of standardizing emergency processes, conducting frequent updates and drills, and ensuring continuous improvement. We found that, while caring for patients with an unpredictable, novel disease in a nontraditional setting and while wearing PPE and working with new colleagues during every shift, the best approach to support patients and staff is to anticipate emergencies rather than relying on individual staff to develop on-the-spot solutions.
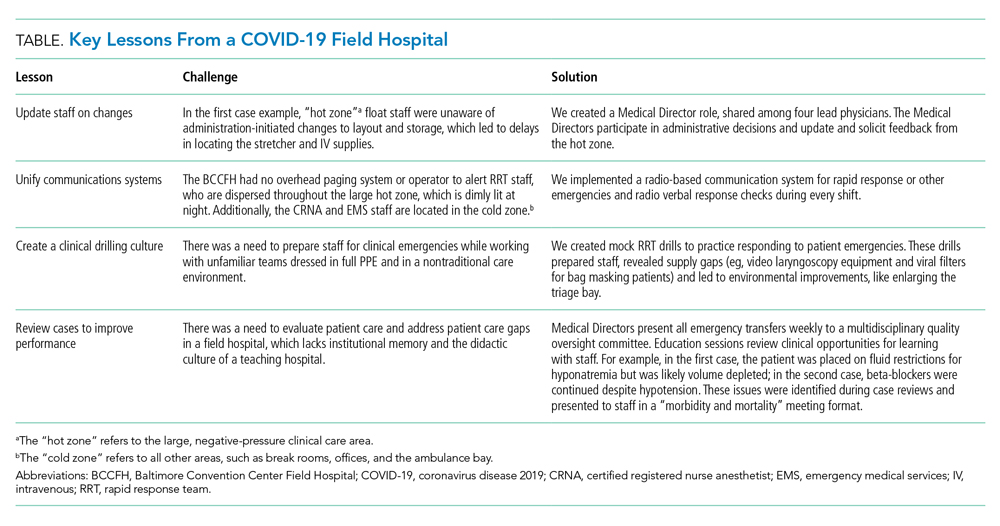
CONCLUSION
The COVID-19 era has seen the unprecedented construction and utilization of emergency field hospital facilities. Such facilities can serve to offload some COVID-19 patients from strained healthcare infrastructure and provide essential care to these patients. We share many of the unique physical and logistical considerations specific to a nontraditional site. We optimized our space, our equipment, and our communication system. We learned how to identify, assess, resuscitate, and transport decompensating COVID-19 patients. Ultimately, our field hospital has been well utilized and successful at caring for patients because of its adaptability, accessibility, and safety record. Of the 15% of patients we transferred to a hospital for care, 81% were successfully stabilized and were willing to return to the BCCFH to complete their care. Our design included supportive care such as social work, physical and occupational therapy, and treatment of comorbidities, such as diabetes and substance use disorder. Our model demonstrates an effective nonhospital option for the care of lower-acuity, medically complex COVID-19 patients. If such facilities are used in subsequent COVID-19 outbreaks, we advise structured planning for the care of decompensating patients that takes into account the need for effective communication, drilling, and ongoing process improvement.
1. Rose J. U.S. Field Hospitals Stand Down, Most Without Treating Any COVID-19 Patients. All Things Considered. NPR; May 7, 2020. Accessed July 21, 2020. https://www.npr.org/2020/05/07/851712311/u-s-field-hospitals-stand-down-most-without-treating-any-covid-19-patients
2. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305-1314. https://doi.org/10.1016/s0140-6736(20)30744-3
3. Reilly RF. Medical and surgical care during the American Civil War, 1861-1865. Proc (Bayl Univ Med Cent). 2016;29(2):138-142. https://doi.org/10.1080/08998280.2016.11929390
4. Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004;32(4):916-21. https://doi.org/10.1097/01.ccm.0000119428.02968.9e
5. Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003;179(6):283-287.
6. Bristow PJ, Hillman KM, Chey T, et al. Rates of in-hospital arrests, deaths and intensive care admissions: the effect of a medical emergency team. Med J Aust. 2000;173(5):236-240.
7. Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387-390. https://doi.org/10.1136/bmj.324.7334.387
8. DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL; Medical Emergency Response Improvement Team (MERIT). Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care. 2004;13(4):251-254. https://doi.org/10.1136/qhc.13.4.251
9. Goldhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A. The patient-at-risk team: identifying and managing seriously ill ward patients. Anaesthesia. 1999;54(9):853-860. https://doi.org/10.1046/j.1365-2044.1999.00996.x
10. Hillman K, Chen J, Cretikos M, et al; MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365(9477):2091-2097. https://doi.org/10.1016/s0140-6736(05)66733-5
11. Kenward G, Castle N, Hodgetts T, Shaikh L. Evaluation of a medical emergency team one year after implementation. Resuscitation. 2004;61(3):257-263. https://doi.org/10.1016/j.resuscitation.2004.01.021
12. Pittard AJ. Out of our reach? assessing the impact of introducing a critical care outreach service. Anaesthesia. 2003;58(9):882-885. https://doi.org/10.1046/j.1365-2044.2003.03331.x
13. Priestley G, Watson W, Rashidian A, et al. Introducing critical care outreach: a ward-randomised trial of phased introduction in a general hospital. Intensive Care Med. 2004;30(7):1398-1404. https://doi.org/10.1007/s00134-004-2268-7
14. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. https://doi.org/10.1016/s0140-6736(20)30566-3
15. Zhou Y, Li W, Wang D, et al. Clinical time course of COVID-19, its neurological manifestation and some thoughts on its management. Stroke Vasc Neurol. 2020;5(2):177-179. https://doi.org/10.1136/svn-2020-000398
1. Rose J. U.S. Field Hospitals Stand Down, Most Without Treating Any COVID-19 Patients. All Things Considered. NPR; May 7, 2020. Accessed July 21, 2020. https://www.npr.org/2020/05/07/851712311/u-s-field-hospitals-stand-down-most-without-treating-any-covid-19-patients
2. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305-1314. https://doi.org/10.1016/s0140-6736(20)30744-3
3. Reilly RF. Medical and surgical care during the American Civil War, 1861-1865. Proc (Bayl Univ Med Cent). 2016;29(2):138-142. https://doi.org/10.1080/08998280.2016.11929390
4. Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004;32(4):916-21. https://doi.org/10.1097/01.ccm.0000119428.02968.9e
5. Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003;179(6):283-287.
6. Bristow PJ, Hillman KM, Chey T, et al. Rates of in-hospital arrests, deaths and intensive care admissions: the effect of a medical emergency team. Med J Aust. 2000;173(5):236-240.
7. Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387-390. https://doi.org/10.1136/bmj.324.7334.387
8. DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL; Medical Emergency Response Improvement Team (MERIT). Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care. 2004;13(4):251-254. https://doi.org/10.1136/qhc.13.4.251
9. Goldhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A. The patient-at-risk team: identifying and managing seriously ill ward patients. Anaesthesia. 1999;54(9):853-860. https://doi.org/10.1046/j.1365-2044.1999.00996.x
10. Hillman K, Chen J, Cretikos M, et al; MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365(9477):2091-2097. https://doi.org/10.1016/s0140-6736(05)66733-5
11. Kenward G, Castle N, Hodgetts T, Shaikh L. Evaluation of a medical emergency team one year after implementation. Resuscitation. 2004;61(3):257-263. https://doi.org/10.1016/j.resuscitation.2004.01.021
12. Pittard AJ. Out of our reach? assessing the impact of introducing a critical care outreach service. Anaesthesia. 2003;58(9):882-885. https://doi.org/10.1046/j.1365-2044.2003.03331.x
13. Priestley G, Watson W, Rashidian A, et al. Introducing critical care outreach: a ward-randomised trial of phased introduction in a general hospital. Intensive Care Med. 2004;30(7):1398-1404. https://doi.org/10.1007/s00134-004-2268-7
14. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. https://doi.org/10.1016/s0140-6736(20)30566-3
15. Zhou Y, Li W, Wang D, et al. Clinical time course of COVID-19, its neurological manifestation and some thoughts on its management. Stroke Vasc Neurol. 2020;5(2):177-179. https://doi.org/10.1136/svn-2020-000398
© 2021 Society of Hospital Medicine
Building a New Framework for Equity: Pediatric Hospital Medicine Must Lead the Way
Pediatric Hospital Medicine (PHM) only recently became a recognized pediatric subspecialty with the first certification exam taking place in 2019. As a new field composed largely of women, it has a unique opportunity to set the example of how to operationalize gender equity in leadership by tracking metrics, creating intentional processes for hiring and promotion, and implementing policies in a transparent way.
In this issue of the Journal of Hospital Medicine, Allan et al1 report that women, who comprise 70% of the field, appear proportionally represented in associate/assistant but not senior leadership roles when compared to the PHM field at large. Eighty-one percent of associate division directors but only 55% of division directors were women, and 82% of assistant fellowship directors but only 66% of fellowship directors were women. These downward trends in the proportion of women in leadership roles as the roles become more senior is not an unfamiliar pattern. This echoes academic pediatric positions more broadly: women’s representation slides from 63% of active physicians to approximately 57% active faculty and then to 26% as department chairs.2 The same story holds true for deans’ offices in US medical schools, where 34% of associate deans are women and yet only 18% of deans are women. The number of women deans has only increased by about one each year, on average, since 2009.3 C-suite leadership roles in healthcare mimic this same downward trajectory.4 Burden et al found that while there was equal gender representation of hospitalists and general internists who worked in university hospitals, women led only a minority of (adult) hospital medicine (16%) or general internal medicine (35%) sections or divisions at university hospitals.5 Women with intersectionality, such as Black women and other women of color, are even more grossly underrepresented in leadership roles.
How can we change this pattern to ensure that leadership in PHM, and in medicine in general, represents diverse voices and reflects the community it serves? Allan et al have established an important baseline for tracking gender equity in PHM. Institutions, organizations, and societies must now prioritize, value and promote a culture of diversity, inclusivity, sponsorship, and allyship. For example, institutions can create and enforce policies in which compensation and promotion are tied to a leader’s achievement of transparent gender equity and diversity targets to ensure accountability. Institutions should commit dedicated and substantive funding to diversity, equity, and inclusion efforts and provide a regular diversity report that tracks gender distribution, hiring and attrition, and representation in leadership. Institutions should implement “best search practices” for all leadership positions. Additionally, all faculty should receive regular and ongoing professional development planning to enhance academic productivity and professional satisfaction and improve retention.
Women in medicine disproportionately experience many issues, including harassment, bias, and childcare and household responsibilities, that adversely affect their career trajectory. PHM is in a unique position to trailblaze a new framework for ensuring gender equity in its field. Let’s not lose this opportunity to set a new course that other specialties can follow.
1. Allan JM, Kim JL, Ralston SL, et al. Gender distribution in pediatric hospital medicine leadership. J Hosp Med. 2021;16:31-33. https://doi.org/10.12788/jhm.3555
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144 (5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Lautenberger DM, Dandar VM. The State of Women in Academic Medicine 2018-2019. Association of American Medical Colleges; 2020.
4. Berlin G, Darino L, Groh R, Kumar P. Women in Healthcare: Moving From the Front Lines to the Top Rung. McKinsey & Company; August 15, 2020.
5. Burden M, Frank MG, Keniston A, et al. Gender disparities for academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
Pediatric Hospital Medicine (PHM) only recently became a recognized pediatric subspecialty with the first certification exam taking place in 2019. As a new field composed largely of women, it has a unique opportunity to set the example of how to operationalize gender equity in leadership by tracking metrics, creating intentional processes for hiring and promotion, and implementing policies in a transparent way.
In this issue of the Journal of Hospital Medicine, Allan et al1 report that women, who comprise 70% of the field, appear proportionally represented in associate/assistant but not senior leadership roles when compared to the PHM field at large. Eighty-one percent of associate division directors but only 55% of division directors were women, and 82% of assistant fellowship directors but only 66% of fellowship directors were women. These downward trends in the proportion of women in leadership roles as the roles become more senior is not an unfamiliar pattern. This echoes academic pediatric positions more broadly: women’s representation slides from 63% of active physicians to approximately 57% active faculty and then to 26% as department chairs.2 The same story holds true for deans’ offices in US medical schools, where 34% of associate deans are women and yet only 18% of deans are women. The number of women deans has only increased by about one each year, on average, since 2009.3 C-suite leadership roles in healthcare mimic this same downward trajectory.4 Burden et al found that while there was equal gender representation of hospitalists and general internists who worked in university hospitals, women led only a minority of (adult) hospital medicine (16%) or general internal medicine (35%) sections or divisions at university hospitals.5 Women with intersectionality, such as Black women and other women of color, are even more grossly underrepresented in leadership roles.
How can we change this pattern to ensure that leadership in PHM, and in medicine in general, represents diverse voices and reflects the community it serves? Allan et al have established an important baseline for tracking gender equity in PHM. Institutions, organizations, and societies must now prioritize, value and promote a culture of diversity, inclusivity, sponsorship, and allyship. For example, institutions can create and enforce policies in which compensation and promotion are tied to a leader’s achievement of transparent gender equity and diversity targets to ensure accountability. Institutions should commit dedicated and substantive funding to diversity, equity, and inclusion efforts and provide a regular diversity report that tracks gender distribution, hiring and attrition, and representation in leadership. Institutions should implement “best search practices” for all leadership positions. Additionally, all faculty should receive regular and ongoing professional development planning to enhance academic productivity and professional satisfaction and improve retention.
Women in medicine disproportionately experience many issues, including harassment, bias, and childcare and household responsibilities, that adversely affect their career trajectory. PHM is in a unique position to trailblaze a new framework for ensuring gender equity in its field. Let’s not lose this opportunity to set a new course that other specialties can follow.
Pediatric Hospital Medicine (PHM) only recently became a recognized pediatric subspecialty with the first certification exam taking place in 2019. As a new field composed largely of women, it has a unique opportunity to set the example of how to operationalize gender equity in leadership by tracking metrics, creating intentional processes for hiring and promotion, and implementing policies in a transparent way.
In this issue of the Journal of Hospital Medicine, Allan et al1 report that women, who comprise 70% of the field, appear proportionally represented in associate/assistant but not senior leadership roles when compared to the PHM field at large. Eighty-one percent of associate division directors but only 55% of division directors were women, and 82% of assistant fellowship directors but only 66% of fellowship directors were women. These downward trends in the proportion of women in leadership roles as the roles become more senior is not an unfamiliar pattern. This echoes academic pediatric positions more broadly: women’s representation slides from 63% of active physicians to approximately 57% active faculty and then to 26% as department chairs.2 The same story holds true for deans’ offices in US medical schools, where 34% of associate deans are women and yet only 18% of deans are women. The number of women deans has only increased by about one each year, on average, since 2009.3 C-suite leadership roles in healthcare mimic this same downward trajectory.4 Burden et al found that while there was equal gender representation of hospitalists and general internists who worked in university hospitals, women led only a minority of (adult) hospital medicine (16%) or general internal medicine (35%) sections or divisions at university hospitals.5 Women with intersectionality, such as Black women and other women of color, are even more grossly underrepresented in leadership roles.
How can we change this pattern to ensure that leadership in PHM, and in medicine in general, represents diverse voices and reflects the community it serves? Allan et al have established an important baseline for tracking gender equity in PHM. Institutions, organizations, and societies must now prioritize, value and promote a culture of diversity, inclusivity, sponsorship, and allyship. For example, institutions can create and enforce policies in which compensation and promotion are tied to a leader’s achievement of transparent gender equity and diversity targets to ensure accountability. Institutions should commit dedicated and substantive funding to diversity, equity, and inclusion efforts and provide a regular diversity report that tracks gender distribution, hiring and attrition, and representation in leadership. Institutions should implement “best search practices” for all leadership positions. Additionally, all faculty should receive regular and ongoing professional development planning to enhance academic productivity and professional satisfaction and improve retention.
Women in medicine disproportionately experience many issues, including harassment, bias, and childcare and household responsibilities, that adversely affect their career trajectory. PHM is in a unique position to trailblaze a new framework for ensuring gender equity in its field. Let’s not lose this opportunity to set a new course that other specialties can follow.
1. Allan JM, Kim JL, Ralston SL, et al. Gender distribution in pediatric hospital medicine leadership. J Hosp Med. 2021;16:31-33. https://doi.org/10.12788/jhm.3555
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144 (5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Lautenberger DM, Dandar VM. The State of Women in Academic Medicine 2018-2019. Association of American Medical Colleges; 2020.
4. Berlin G, Darino L, Groh R, Kumar P. Women in Healthcare: Moving From the Front Lines to the Top Rung. McKinsey & Company; August 15, 2020.
5. Burden M, Frank MG, Keniston A, et al. Gender disparities for academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
1. Allan JM, Kim JL, Ralston SL, et al. Gender distribution in pediatric hospital medicine leadership. J Hosp Med. 2021;16:31-33. https://doi.org/10.12788/jhm.3555
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144 (5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Lautenberger DM, Dandar VM. The State of Women in Academic Medicine 2018-2019. Association of American Medical Colleges; 2020.
4. Berlin G, Darino L, Groh R, Kumar P. Women in Healthcare: Moving From the Front Lines to the Top Rung. McKinsey & Company; August 15, 2020.
5. Burden M, Frank MG, Keniston A, et al. Gender disparities for academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
© 2021 Society of Hospital Medicine
Email: [email protected]; Telephone: 215-991-8240; Twitter: @ELAMProgram; @NancyDSpector.
Deimplementation: Discontinuing Low-Value, Potentially Harmful Hospital Care
Nearly 30% of healthcare spending may relate to overuse of unnecessary medical interventions.1 Deimplementation of such practices can reduce negative outcomes and unnecessary costs.2 Nonetheless, changing practice is difficult. Why is it so hard to stop doing things that don’t work? A variety of factors influences deimplementation, and research aiming to identify and understand these factors can promote the delivery of more appropriate care.2
In this issue, Wolk et al describe barriers and facilitators in deimplementing non-guideline adherent use of continuous pulse oximetry (CPO) in pediatric patients with bronchiolitis not requiring supplemental oxygen.3 Unnecessary CPO use for these patients is associated with increased hospitalization rates, length of stay, alarm fatigue, and costs, without evidence of improved clinical outcomes. Despite these data, many hospitals participating in the multicenter Eliminating Monitor Overuse study struggled to decrease CPO usage. The authors conducted semistructured interviews with a broad range of stakeholders from 12 hospitals, representing a variety of institutions with low and high CPO utilization rates.
Specific barriers to deimplementation included institutional factors, eg, unclear or missing guidelines, a culture of high utilization, and challenges educating medical staff. Perceived parental discomfort with stopping CPO was also observed. Four key facilitators were noted: strong institutional leadership, evidence-based guidelines, electronic health record order sets or reminders, and clear institutional policy. These results are similar to other deimplementation studies.
A commonality to deimplementation studies is the difficulty of changing practice. Much like implementation, deimplementation requires multipronged approaches that are sensitive to contextual factors. Interventions must account for local conditions, such as resource availability, practice norms, current workflows and processes of care, relationships among clinicians, and leadership, to create feasible and sustainable change.
Deimplementation may be even more challenging than implementation of new practices, however, because of loss aversion—the tendency to prefer avoiding losses to acquiring equivalent gains. “Taking away” something that clinicians are used to, even when proven to not be helpful, can feel uncomfortable, hindering adoption. Rather than simply discontinuing a practice, replacing it with a better option may help to overcome behavioral inertia and motivate change.
Underscoring the importance of local influences, clinicians often respond more to their close colleagues’ practices than to knowledge of national guidelines. Leveraging existing peer networks can facilitate collaboration, learning, and behavior change.4 Nudge strategies, in which local contexts are primed to promote desired behaviors, are also increasingly used.4 Priming has been effective in deimplementation efforts in medication prescribing and diagnostic testing.4
Including patients’ and families’ perspectives in deimplementation research is critical to practice change. Because diagnostic and treatment plans occur in the context of collaborative decision-making with patients, caregivers, and families, these groups are critical to engage in deimplementation efforts.
Hospitalists’ efforts at the front line of improvement require us to become more proficient in not only adopting evidence-based practices, but also in discontinuing ineffective ones. Identifying what we should stop doing is only the first step. Deimplementation is critical to this effort. Wolk et al provide insights into factors that influence deimplementation success. However, more work is needed, particularly regarding adapting approaches to local contexts, minimizing perceived loss, leveraging local conditions to shape behavior, and partnering with patients and families to achieve higher-value care.
1. Brownlee S, Chalkidou K, Doust J, at al. Evidence for overuse of medical services around the world. Lancet. 2017;390(10090):156-168. https://doi.org/10.1016/S0140-6736(16)32585-5
2. Norton WE, Chambers DA. Unpacking the complexities of de-implementing inappropriate health interventions. Implement Sci. 2020;15(1):2. https://doi.org/10.1186/s13012-019-0960-9
3. Wolk CB, Schondelmeyer AC, Barg FK, et al. Barriers and facilitators to guideline-adherent pulse oximetry use in bronchiolitis. J Hosp Med. 2021;16:23-30. https://doi.org/10.12788/jhm.3535
4 Yoong SL, Hall A, Stacey F, et al. Nudge strategies to improve healthcare providers’ implementation of evidence-based guidelines, policies and practices: a systematic review of trials included within Cochrane systematic reviews. Implement Sci. 2020;15(1):50. https://doi.org/10.1186/s13012-020-01011-0
Nearly 30% of healthcare spending may relate to overuse of unnecessary medical interventions.1 Deimplementation of such practices can reduce negative outcomes and unnecessary costs.2 Nonetheless, changing practice is difficult. Why is it so hard to stop doing things that don’t work? A variety of factors influences deimplementation, and research aiming to identify and understand these factors can promote the delivery of more appropriate care.2
In this issue, Wolk et al describe barriers and facilitators in deimplementing non-guideline adherent use of continuous pulse oximetry (CPO) in pediatric patients with bronchiolitis not requiring supplemental oxygen.3 Unnecessary CPO use for these patients is associated with increased hospitalization rates, length of stay, alarm fatigue, and costs, without evidence of improved clinical outcomes. Despite these data, many hospitals participating in the multicenter Eliminating Monitor Overuse study struggled to decrease CPO usage. The authors conducted semistructured interviews with a broad range of stakeholders from 12 hospitals, representing a variety of institutions with low and high CPO utilization rates.
Specific barriers to deimplementation included institutional factors, eg, unclear or missing guidelines, a culture of high utilization, and challenges educating medical staff. Perceived parental discomfort with stopping CPO was also observed. Four key facilitators were noted: strong institutional leadership, evidence-based guidelines, electronic health record order sets or reminders, and clear institutional policy. These results are similar to other deimplementation studies.
A commonality to deimplementation studies is the difficulty of changing practice. Much like implementation, deimplementation requires multipronged approaches that are sensitive to contextual factors. Interventions must account for local conditions, such as resource availability, practice norms, current workflows and processes of care, relationships among clinicians, and leadership, to create feasible and sustainable change.
Deimplementation may be even more challenging than implementation of new practices, however, because of loss aversion—the tendency to prefer avoiding losses to acquiring equivalent gains. “Taking away” something that clinicians are used to, even when proven to not be helpful, can feel uncomfortable, hindering adoption. Rather than simply discontinuing a practice, replacing it with a better option may help to overcome behavioral inertia and motivate change.
Underscoring the importance of local influences, clinicians often respond more to their close colleagues’ practices than to knowledge of national guidelines. Leveraging existing peer networks can facilitate collaboration, learning, and behavior change.4 Nudge strategies, in which local contexts are primed to promote desired behaviors, are also increasingly used.4 Priming has been effective in deimplementation efforts in medication prescribing and diagnostic testing.4
Including patients’ and families’ perspectives in deimplementation research is critical to practice change. Because diagnostic and treatment plans occur in the context of collaborative decision-making with patients, caregivers, and families, these groups are critical to engage in deimplementation efforts.
Hospitalists’ efforts at the front line of improvement require us to become more proficient in not only adopting evidence-based practices, but also in discontinuing ineffective ones. Identifying what we should stop doing is only the first step. Deimplementation is critical to this effort. Wolk et al provide insights into factors that influence deimplementation success. However, more work is needed, particularly regarding adapting approaches to local contexts, minimizing perceived loss, leveraging local conditions to shape behavior, and partnering with patients and families to achieve higher-value care.
Nearly 30% of healthcare spending may relate to overuse of unnecessary medical interventions.1 Deimplementation of such practices can reduce negative outcomes and unnecessary costs.2 Nonetheless, changing practice is difficult. Why is it so hard to stop doing things that don’t work? A variety of factors influences deimplementation, and research aiming to identify and understand these factors can promote the delivery of more appropriate care.2
In this issue, Wolk et al describe barriers and facilitators in deimplementing non-guideline adherent use of continuous pulse oximetry (CPO) in pediatric patients with bronchiolitis not requiring supplemental oxygen.3 Unnecessary CPO use for these patients is associated with increased hospitalization rates, length of stay, alarm fatigue, and costs, without evidence of improved clinical outcomes. Despite these data, many hospitals participating in the multicenter Eliminating Monitor Overuse study struggled to decrease CPO usage. The authors conducted semistructured interviews with a broad range of stakeholders from 12 hospitals, representing a variety of institutions with low and high CPO utilization rates.
Specific barriers to deimplementation included institutional factors, eg, unclear or missing guidelines, a culture of high utilization, and challenges educating medical staff. Perceived parental discomfort with stopping CPO was also observed. Four key facilitators were noted: strong institutional leadership, evidence-based guidelines, electronic health record order sets or reminders, and clear institutional policy. These results are similar to other deimplementation studies.
A commonality to deimplementation studies is the difficulty of changing practice. Much like implementation, deimplementation requires multipronged approaches that are sensitive to contextual factors. Interventions must account for local conditions, such as resource availability, practice norms, current workflows and processes of care, relationships among clinicians, and leadership, to create feasible and sustainable change.
Deimplementation may be even more challenging than implementation of new practices, however, because of loss aversion—the tendency to prefer avoiding losses to acquiring equivalent gains. “Taking away” something that clinicians are used to, even when proven to not be helpful, can feel uncomfortable, hindering adoption. Rather than simply discontinuing a practice, replacing it with a better option may help to overcome behavioral inertia and motivate change.
Underscoring the importance of local influences, clinicians often respond more to their close colleagues’ practices than to knowledge of national guidelines. Leveraging existing peer networks can facilitate collaboration, learning, and behavior change.4 Nudge strategies, in which local contexts are primed to promote desired behaviors, are also increasingly used.4 Priming has been effective in deimplementation efforts in medication prescribing and diagnostic testing.4
Including patients’ and families’ perspectives in deimplementation research is critical to practice change. Because diagnostic and treatment plans occur in the context of collaborative decision-making with patients, caregivers, and families, these groups are critical to engage in deimplementation efforts.
Hospitalists’ efforts at the front line of improvement require us to become more proficient in not only adopting evidence-based practices, but also in discontinuing ineffective ones. Identifying what we should stop doing is only the first step. Deimplementation is critical to this effort. Wolk et al provide insights into factors that influence deimplementation success. However, more work is needed, particularly regarding adapting approaches to local contexts, minimizing perceived loss, leveraging local conditions to shape behavior, and partnering with patients and families to achieve higher-value care.
1. Brownlee S, Chalkidou K, Doust J, at al. Evidence for overuse of medical services around the world. Lancet. 2017;390(10090):156-168. https://doi.org/10.1016/S0140-6736(16)32585-5
2. Norton WE, Chambers DA. Unpacking the complexities of de-implementing inappropriate health interventions. Implement Sci. 2020;15(1):2. https://doi.org/10.1186/s13012-019-0960-9
3. Wolk CB, Schondelmeyer AC, Barg FK, et al. Barriers and facilitators to guideline-adherent pulse oximetry use in bronchiolitis. J Hosp Med. 2021;16:23-30. https://doi.org/10.12788/jhm.3535
4 Yoong SL, Hall A, Stacey F, et al. Nudge strategies to improve healthcare providers’ implementation of evidence-based guidelines, policies and practices: a systematic review of trials included within Cochrane systematic reviews. Implement Sci. 2020;15(1):50. https://doi.org/10.1186/s13012-020-01011-0
1. Brownlee S, Chalkidou K, Doust J, at al. Evidence for overuse of medical services around the world. Lancet. 2017;390(10090):156-168. https://doi.org/10.1016/S0140-6736(16)32585-5
2. Norton WE, Chambers DA. Unpacking the complexities of de-implementing inappropriate health interventions. Implement Sci. 2020;15(1):2. https://doi.org/10.1186/s13012-019-0960-9
3. Wolk CB, Schondelmeyer AC, Barg FK, et al. Barriers and facilitators to guideline-adherent pulse oximetry use in bronchiolitis. J Hosp Med. 2021;16:23-30. https://doi.org/10.12788/jhm.3535
4 Yoong SL, Hall A, Stacey F, et al. Nudge strategies to improve healthcare providers’ implementation of evidence-based guidelines, policies and practices: a systematic review of trials included within Cochrane systematic reviews. Implement Sci. 2020;15(1):50. https://doi.org/10.1186/s13012-020-01011-0
© 2021 Society of Hospital Medicine
Email: [email protected];Telephone: 415-476-1742; Twitter: @shradhakulk.
Care Transitions: A Complex Problem That Requires a Complexity Mindset
In recent years, there has been increased scrutiny of transitions of care in medicine, particularly at hospital discharge. Much focus has been on preventing readmissions, motivated at least in part by the Affordable Care Act’s Hospital Readmissions Reduction Program, which financially penalizes hospitals for higher-than-expected readmission rates.1 However, the problem of transition from hospital to home is not just a readmissions issue—it is a quality and patient safety issue.2 Therefore, measuring readmissions alone is inadequate. More effective systems for transition from hospital to home are needed in order to deliver high-quality care that actually restores patient well-being after hospitalization.
In this month’s issue of Journal of Hospital Medicine, Schnipper and Samal, et al report the results of a stepped-wedge randomized trial examining the effect of a multifaceted intervention on postdischarge patient-centered outcomes when compared with usual care.3 At 30 days after discharge, adverse events were reduced from 23 per 100 patients in the usual care group to 18 per 100 patients in the intervention group, with an incidence rate ratio of 0.55 (95% CI, 0.35-0.84) after adjustment for study month and baseline characteristics. Interestingly, there was no statistically significant difference in nonelective readmissions, and penetrance was notably poor: The majority of components of the intervention were received by fewer than half of intended patients, and 13% failed to receive any component at all.
With such incomplete implementation, what explains the reduction in adverse events? To best answer this, it is helpful to recognize the transition from hospital to home as a complex problem rather than a complicated one.4 The difference is key. Complicated problems follow a predictable set of rules that can be thought of and planned for, and when the plan is methodically followed, complicated problems can be solved. Complex problems, on the other hand, have a more unpredictable interplay between multiple nonindependent and sometimes unknown factors. Complex problems cannot be solved by merely following a well-designed plan; rather, they require tremendous preparation, adaptability, and active management as the problem plays itself out.
Fortunately, Schnipper and Samal, et al properly identified the problem of transition from hospital to home as complex and approached it from a complexity mindset. In their design of a multifaceted intervention, they aimed high and cast a wide net. Understanding that different practices have different cultures and resources, they standardized the function of the intervention components rather than the exact form. As the trial progressed, they allowed for modification of the intervention, incorporating input from multiple stakeholders and feedback from early failures. Thus, by recognizing and embracing the complexity of the problem, the authors set themselves and their patients up for success. The most likely explanation for the observed effect of the intervention on this complex problem is therefore quite simple: The study design allowed for the components most likely to work to be most readily implemented on a patient-by-patient and practice-by-practice basis.
While the trial aims to imitate the “real world,” it does not leave clear-cut answers for real healthcare professionals. Without knowing if any individual component of the intervention was effective on its own, it may be difficult for institutions to justify the cost of implementation. And while there should be adequate incentive to action for any intervention that improves how patients function or feel, without a reduction in readmissions, the financial downside may in some instances be prohibitive.
Despite these limitations, the path forward is clear. Institutions looking to implement a similar program now should approach the problem with a complexity mindset, even if their downstream interventions may differ. Researchers looking to design similar trials should focus on narrowing the scope of the intervention while maintaining a complexity mindset, which might help lead to more widespread implementation of evidence-based interventions in the future. In teaching us more about the approach to finding a solution than the solution itself, the present study marks an important next step in hospital to home transitions of care and transitions-of-care research.
1. McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131(20):1796-1803. https://doi.org/10.1161/circulationaha.114.010270
2. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345-349.
3. Schnipper JL, Samal L, Nolido N, et al. The effects of a multifaceted intervention to improve care transitions within an accountable care organization: results of a stepped-wedge cluster-randomized trial. J Hosp Med. 2020:16:15-22. https://doi.org/10.12788/jhm.3513
4. Kinni T. “The critical difference between complex and complicated: featured excerpt from It’s Not Complicated: The Art and Science of Complexity for Business.” MIT Sloan Management Review. June 21, 2017. Accessed August 12, 2020. https://sloanreview.mit.edu/article/the-critical-difference-between-comp...
In recent years, there has been increased scrutiny of transitions of care in medicine, particularly at hospital discharge. Much focus has been on preventing readmissions, motivated at least in part by the Affordable Care Act’s Hospital Readmissions Reduction Program, which financially penalizes hospitals for higher-than-expected readmission rates.1 However, the problem of transition from hospital to home is not just a readmissions issue—it is a quality and patient safety issue.2 Therefore, measuring readmissions alone is inadequate. More effective systems for transition from hospital to home are needed in order to deliver high-quality care that actually restores patient well-being after hospitalization.
In this month’s issue of Journal of Hospital Medicine, Schnipper and Samal, et al report the results of a stepped-wedge randomized trial examining the effect of a multifaceted intervention on postdischarge patient-centered outcomes when compared with usual care.3 At 30 days after discharge, adverse events were reduced from 23 per 100 patients in the usual care group to 18 per 100 patients in the intervention group, with an incidence rate ratio of 0.55 (95% CI, 0.35-0.84) after adjustment for study month and baseline characteristics. Interestingly, there was no statistically significant difference in nonelective readmissions, and penetrance was notably poor: The majority of components of the intervention were received by fewer than half of intended patients, and 13% failed to receive any component at all.
With such incomplete implementation, what explains the reduction in adverse events? To best answer this, it is helpful to recognize the transition from hospital to home as a complex problem rather than a complicated one.4 The difference is key. Complicated problems follow a predictable set of rules that can be thought of and planned for, and when the plan is methodically followed, complicated problems can be solved. Complex problems, on the other hand, have a more unpredictable interplay between multiple nonindependent and sometimes unknown factors. Complex problems cannot be solved by merely following a well-designed plan; rather, they require tremendous preparation, adaptability, and active management as the problem plays itself out.
Fortunately, Schnipper and Samal, et al properly identified the problem of transition from hospital to home as complex and approached it from a complexity mindset. In their design of a multifaceted intervention, they aimed high and cast a wide net. Understanding that different practices have different cultures and resources, they standardized the function of the intervention components rather than the exact form. As the trial progressed, they allowed for modification of the intervention, incorporating input from multiple stakeholders and feedback from early failures. Thus, by recognizing and embracing the complexity of the problem, the authors set themselves and their patients up for success. The most likely explanation for the observed effect of the intervention on this complex problem is therefore quite simple: The study design allowed for the components most likely to work to be most readily implemented on a patient-by-patient and practice-by-practice basis.
While the trial aims to imitate the “real world,” it does not leave clear-cut answers for real healthcare professionals. Without knowing if any individual component of the intervention was effective on its own, it may be difficult for institutions to justify the cost of implementation. And while there should be adequate incentive to action for any intervention that improves how patients function or feel, without a reduction in readmissions, the financial downside may in some instances be prohibitive.
Despite these limitations, the path forward is clear. Institutions looking to implement a similar program now should approach the problem with a complexity mindset, even if their downstream interventions may differ. Researchers looking to design similar trials should focus on narrowing the scope of the intervention while maintaining a complexity mindset, which might help lead to more widespread implementation of evidence-based interventions in the future. In teaching us more about the approach to finding a solution than the solution itself, the present study marks an important next step in hospital to home transitions of care and transitions-of-care research.
In recent years, there has been increased scrutiny of transitions of care in medicine, particularly at hospital discharge. Much focus has been on preventing readmissions, motivated at least in part by the Affordable Care Act’s Hospital Readmissions Reduction Program, which financially penalizes hospitals for higher-than-expected readmission rates.1 However, the problem of transition from hospital to home is not just a readmissions issue—it is a quality and patient safety issue.2 Therefore, measuring readmissions alone is inadequate. More effective systems for transition from hospital to home are needed in order to deliver high-quality care that actually restores patient well-being after hospitalization.
In this month’s issue of Journal of Hospital Medicine, Schnipper and Samal, et al report the results of a stepped-wedge randomized trial examining the effect of a multifaceted intervention on postdischarge patient-centered outcomes when compared with usual care.3 At 30 days after discharge, adverse events were reduced from 23 per 100 patients in the usual care group to 18 per 100 patients in the intervention group, with an incidence rate ratio of 0.55 (95% CI, 0.35-0.84) after adjustment for study month and baseline characteristics. Interestingly, there was no statistically significant difference in nonelective readmissions, and penetrance was notably poor: The majority of components of the intervention were received by fewer than half of intended patients, and 13% failed to receive any component at all.
With such incomplete implementation, what explains the reduction in adverse events? To best answer this, it is helpful to recognize the transition from hospital to home as a complex problem rather than a complicated one.4 The difference is key. Complicated problems follow a predictable set of rules that can be thought of and planned for, and when the plan is methodically followed, complicated problems can be solved. Complex problems, on the other hand, have a more unpredictable interplay between multiple nonindependent and sometimes unknown factors. Complex problems cannot be solved by merely following a well-designed plan; rather, they require tremendous preparation, adaptability, and active management as the problem plays itself out.
Fortunately, Schnipper and Samal, et al properly identified the problem of transition from hospital to home as complex and approached it from a complexity mindset. In their design of a multifaceted intervention, they aimed high and cast a wide net. Understanding that different practices have different cultures and resources, they standardized the function of the intervention components rather than the exact form. As the trial progressed, they allowed for modification of the intervention, incorporating input from multiple stakeholders and feedback from early failures. Thus, by recognizing and embracing the complexity of the problem, the authors set themselves and their patients up for success. The most likely explanation for the observed effect of the intervention on this complex problem is therefore quite simple: The study design allowed for the components most likely to work to be most readily implemented on a patient-by-patient and practice-by-practice basis.
While the trial aims to imitate the “real world,” it does not leave clear-cut answers for real healthcare professionals. Without knowing if any individual component of the intervention was effective on its own, it may be difficult for institutions to justify the cost of implementation. And while there should be adequate incentive to action for any intervention that improves how patients function or feel, without a reduction in readmissions, the financial downside may in some instances be prohibitive.
Despite these limitations, the path forward is clear. Institutions looking to implement a similar program now should approach the problem with a complexity mindset, even if their downstream interventions may differ. Researchers looking to design similar trials should focus on narrowing the scope of the intervention while maintaining a complexity mindset, which might help lead to more widespread implementation of evidence-based interventions in the future. In teaching us more about the approach to finding a solution than the solution itself, the present study marks an important next step in hospital to home transitions of care and transitions-of-care research.
1. McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131(20):1796-1803. https://doi.org/10.1161/circulationaha.114.010270
2. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345-349.
3. Schnipper JL, Samal L, Nolido N, et al. The effects of a multifaceted intervention to improve care transitions within an accountable care organization: results of a stepped-wedge cluster-randomized trial. J Hosp Med. 2020:16:15-22. https://doi.org/10.12788/jhm.3513
4. Kinni T. “The critical difference between complex and complicated: featured excerpt from It’s Not Complicated: The Art and Science of Complexity for Business.” MIT Sloan Management Review. June 21, 2017. Accessed August 12, 2020. https://sloanreview.mit.edu/article/the-critical-difference-between-comp...
1. McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131(20):1796-1803. https://doi.org/10.1161/circulationaha.114.010270
2. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345-349.
3. Schnipper JL, Samal L, Nolido N, et al. The effects of a multifaceted intervention to improve care transitions within an accountable care organization: results of a stepped-wedge cluster-randomized trial. J Hosp Med. 2020:16:15-22. https://doi.org/10.12788/jhm.3513
4. Kinni T. “The critical difference between complex and complicated: featured excerpt from It’s Not Complicated: The Art and Science of Complexity for Business.” MIT Sloan Management Review. June 21, 2017. Accessed August 12, 2020. https://sloanreview.mit.edu/article/the-critical-difference-between-comp...
© 2021 Society of Hospital Medicine
Email: [email protected]; Telephone: 212-746-4071.