User login
Link between pediatric hepatitis and adenovirus 41 still unclear
While two new studies reiterate a possible relationship between adenovirus 41 and acute hepatitis of unknown cause in children, whether these infections are significant or merely bystanders remains unclear.
In both studies – one conducted in Alabama and the other conducted in the United Kingdom – researchers found that 90% of children with acute hepatitis of unknown cause tested positive for adenovirus 41. The virus subtype is not an uncommon infection, but it usually causes gastroenteritis in children.
“Across the world, adenovirus continues to be a common signal” in these pediatric hepatitis cases, said Helena Gutierrez, MD, the medical director of the Pediatric Liver Transplant Program at the University of Alabama at Birmingham, in an interview. She led one of the studies. More data are necessary to understand what role this virus may play in these cases, she said.
In November, the Alabama Department of Public Health and the U.S. Centers for Disease Control and Prevention began investigating a cluster of severe pediatric hepatitis cases at the Children’s of Alabama hospital in Birmingham. These children also tested positive for adenovirus. In April, the United Kingdom announced they were investigating similar cases, and the CDC expanded their search nationally. As of July 8, 1,010 cases in 35 countries have been reported to the World Health Organization. There are 263 confirmed cases in the United Kingdom and 332 cases under investigation by the CDC in the United States, according to the most recent counts.
The two studies, both published in the New England Journal of Medicine, provide additional clinical data on a number of these mysterious hepatitis cases. Dr. Gutierrez’s study looked at nine children admitted for hepatitis of unknown origin between October 1 and February 28. Patients had a median age of 2 years 11 months and two required liver transplants, and there were no deaths.
Eight out of nine patients (89%) tested positive for adenovirus, and all five of the samples that were of sufficient quality for gene sequencing tested positive for adenovirus 41. None of the six liver biopsies performed found signs of adenovirus infection, but the liver tissue samples of three patients tested positive for adenovirus via PCR.
The second study involved 44 children referred to a liver transplantation center in the United Kingdom between January 1 and April 11, 2022. The median age for patients was 4 years. Six children required liver transplants, and there were no deaths. Of the 30 patients who underwent molecular adenovirus testing, 27 (90%) were positive for adenovirus 41. Liver samples of nine children (3 from biopsies and 6 from explanted livers) all tested negative for adenovirus antibodies.
In both studies, however, the median adenovirus viral load of patients needing a transplant was much higher than the viral loads in children who did not require liver transplants.
Although most of the clinical features and test results of these cases suggest that adenovirus may be involved, the negative results in histology are “intriguing,” Chayarani Kelgeri, MD, a consultant pediatric hepatologist at the Birmingham Women’s and Children’s Hospital, U.K., said in an email. She is the lead author of the U.K. study. “Whether this is because the liver injury we see is an aftermath of the viral infection, the mechanism of injury is immune mediated, and if other cofactors are involved is being explored,” she added. “Further investigations being undertaken by UK Health Security Agency will add to our understanding of this illness.”
Although there is a high adenovirus positivity rate amongst these cases, there is not enough evidence yet to say adenovirus 41 is a new cause of pediatric hepatitis in previously healthy children, said Saul Karpen, MD, PhD, the division chief of pediatric gastroenterology, hepatology, and nutrition at Emory University School of Medicine, Atlanta. He wrote an editorial accompanying the two NEJM studies.
The CDC has not yet found an increase in pediatric hepatitis cases, according to a recent analysis, though the United Kingdom has found an uptick in cases this year, he told this news organization. Also, the cases highlighted in both articles showed no histological evidence of adenovirus in liver biopsies. “That’s completely opposite of what we generally see in adenoviral hepatitis that can be quite severe,” he said, adding that in general, there are detectable viral particles and antigens in affected livers.
“These two important reports indicate to those inside and outside the field of pediatric hepatology that registries and clinical studies of acute hepatitis in children are sorely needed,” Dr. Karpen writes in the editorial; “It is likely that with greater attention to collecting data on cases and biospecimens from children with acute hepatitis, we will be able to determine whether this one virus, human adenovirus 41, is of relevance to this important and serious condition in children.”
Dr. Gutierrez, Dr. Kelgeri, and Dr. Karpen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
While two new studies reiterate a possible relationship between adenovirus 41 and acute hepatitis of unknown cause in children, whether these infections are significant or merely bystanders remains unclear.
In both studies – one conducted in Alabama and the other conducted in the United Kingdom – researchers found that 90% of children with acute hepatitis of unknown cause tested positive for adenovirus 41. The virus subtype is not an uncommon infection, but it usually causes gastroenteritis in children.
“Across the world, adenovirus continues to be a common signal” in these pediatric hepatitis cases, said Helena Gutierrez, MD, the medical director of the Pediatric Liver Transplant Program at the University of Alabama at Birmingham, in an interview. She led one of the studies. More data are necessary to understand what role this virus may play in these cases, she said.
In November, the Alabama Department of Public Health and the U.S. Centers for Disease Control and Prevention began investigating a cluster of severe pediatric hepatitis cases at the Children’s of Alabama hospital in Birmingham. These children also tested positive for adenovirus. In April, the United Kingdom announced they were investigating similar cases, and the CDC expanded their search nationally. As of July 8, 1,010 cases in 35 countries have been reported to the World Health Organization. There are 263 confirmed cases in the United Kingdom and 332 cases under investigation by the CDC in the United States, according to the most recent counts.
The two studies, both published in the New England Journal of Medicine, provide additional clinical data on a number of these mysterious hepatitis cases. Dr. Gutierrez’s study looked at nine children admitted for hepatitis of unknown origin between October 1 and February 28. Patients had a median age of 2 years 11 months and two required liver transplants, and there were no deaths.
Eight out of nine patients (89%) tested positive for adenovirus, and all five of the samples that were of sufficient quality for gene sequencing tested positive for adenovirus 41. None of the six liver biopsies performed found signs of adenovirus infection, but the liver tissue samples of three patients tested positive for adenovirus via PCR.
The second study involved 44 children referred to a liver transplantation center in the United Kingdom between January 1 and April 11, 2022. The median age for patients was 4 years. Six children required liver transplants, and there were no deaths. Of the 30 patients who underwent molecular adenovirus testing, 27 (90%) were positive for adenovirus 41. Liver samples of nine children (3 from biopsies and 6 from explanted livers) all tested negative for adenovirus antibodies.
In both studies, however, the median adenovirus viral load of patients needing a transplant was much higher than the viral loads in children who did not require liver transplants.
Although most of the clinical features and test results of these cases suggest that adenovirus may be involved, the negative results in histology are “intriguing,” Chayarani Kelgeri, MD, a consultant pediatric hepatologist at the Birmingham Women’s and Children’s Hospital, U.K., said in an email. She is the lead author of the U.K. study. “Whether this is because the liver injury we see is an aftermath of the viral infection, the mechanism of injury is immune mediated, and if other cofactors are involved is being explored,” she added. “Further investigations being undertaken by UK Health Security Agency will add to our understanding of this illness.”
Although there is a high adenovirus positivity rate amongst these cases, there is not enough evidence yet to say adenovirus 41 is a new cause of pediatric hepatitis in previously healthy children, said Saul Karpen, MD, PhD, the division chief of pediatric gastroenterology, hepatology, and nutrition at Emory University School of Medicine, Atlanta. He wrote an editorial accompanying the two NEJM studies.
The CDC has not yet found an increase in pediatric hepatitis cases, according to a recent analysis, though the United Kingdom has found an uptick in cases this year, he told this news organization. Also, the cases highlighted in both articles showed no histological evidence of adenovirus in liver biopsies. “That’s completely opposite of what we generally see in adenoviral hepatitis that can be quite severe,” he said, adding that in general, there are detectable viral particles and antigens in affected livers.
“These two important reports indicate to those inside and outside the field of pediatric hepatology that registries and clinical studies of acute hepatitis in children are sorely needed,” Dr. Karpen writes in the editorial; “It is likely that with greater attention to collecting data on cases and biospecimens from children with acute hepatitis, we will be able to determine whether this one virus, human adenovirus 41, is of relevance to this important and serious condition in children.”
Dr. Gutierrez, Dr. Kelgeri, and Dr. Karpen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
While two new studies reiterate a possible relationship between adenovirus 41 and acute hepatitis of unknown cause in children, whether these infections are significant or merely bystanders remains unclear.
In both studies – one conducted in Alabama and the other conducted in the United Kingdom – researchers found that 90% of children with acute hepatitis of unknown cause tested positive for adenovirus 41. The virus subtype is not an uncommon infection, but it usually causes gastroenteritis in children.
“Across the world, adenovirus continues to be a common signal” in these pediatric hepatitis cases, said Helena Gutierrez, MD, the medical director of the Pediatric Liver Transplant Program at the University of Alabama at Birmingham, in an interview. She led one of the studies. More data are necessary to understand what role this virus may play in these cases, she said.
In November, the Alabama Department of Public Health and the U.S. Centers for Disease Control and Prevention began investigating a cluster of severe pediatric hepatitis cases at the Children’s of Alabama hospital in Birmingham. These children also tested positive for adenovirus. In April, the United Kingdom announced they were investigating similar cases, and the CDC expanded their search nationally. As of July 8, 1,010 cases in 35 countries have been reported to the World Health Organization. There are 263 confirmed cases in the United Kingdom and 332 cases under investigation by the CDC in the United States, according to the most recent counts.
The two studies, both published in the New England Journal of Medicine, provide additional clinical data on a number of these mysterious hepatitis cases. Dr. Gutierrez’s study looked at nine children admitted for hepatitis of unknown origin between October 1 and February 28. Patients had a median age of 2 years 11 months and two required liver transplants, and there were no deaths.
Eight out of nine patients (89%) tested positive for adenovirus, and all five of the samples that were of sufficient quality for gene sequencing tested positive for adenovirus 41. None of the six liver biopsies performed found signs of adenovirus infection, but the liver tissue samples of three patients tested positive for adenovirus via PCR.
The second study involved 44 children referred to a liver transplantation center in the United Kingdom between January 1 and April 11, 2022. The median age for patients was 4 years. Six children required liver transplants, and there were no deaths. Of the 30 patients who underwent molecular adenovirus testing, 27 (90%) were positive for adenovirus 41. Liver samples of nine children (3 from biopsies and 6 from explanted livers) all tested negative for adenovirus antibodies.
In both studies, however, the median adenovirus viral load of patients needing a transplant was much higher than the viral loads in children who did not require liver transplants.
Although most of the clinical features and test results of these cases suggest that adenovirus may be involved, the negative results in histology are “intriguing,” Chayarani Kelgeri, MD, a consultant pediatric hepatologist at the Birmingham Women’s and Children’s Hospital, U.K., said in an email. She is the lead author of the U.K. study. “Whether this is because the liver injury we see is an aftermath of the viral infection, the mechanism of injury is immune mediated, and if other cofactors are involved is being explored,” she added. “Further investigations being undertaken by UK Health Security Agency will add to our understanding of this illness.”
Although there is a high adenovirus positivity rate amongst these cases, there is not enough evidence yet to say adenovirus 41 is a new cause of pediatric hepatitis in previously healthy children, said Saul Karpen, MD, PhD, the division chief of pediatric gastroenterology, hepatology, and nutrition at Emory University School of Medicine, Atlanta. He wrote an editorial accompanying the two NEJM studies.
The CDC has not yet found an increase in pediatric hepatitis cases, according to a recent analysis, though the United Kingdom has found an uptick in cases this year, he told this news organization. Also, the cases highlighted in both articles showed no histological evidence of adenovirus in liver biopsies. “That’s completely opposite of what we generally see in adenoviral hepatitis that can be quite severe,” he said, adding that in general, there are detectable viral particles and antigens in affected livers.
“These two important reports indicate to those inside and outside the field of pediatric hepatology that registries and clinical studies of acute hepatitis in children are sorely needed,” Dr. Karpen writes in the editorial; “It is likely that with greater attention to collecting data on cases and biospecimens from children with acute hepatitis, we will be able to determine whether this one virus, human adenovirus 41, is of relevance to this important and serious condition in children.”
Dr. Gutierrez, Dr. Kelgeri, and Dr. Karpen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New insights into worldwide biliary tract cancer incidence, mortality
Incidence and mortality for biliary tract cancer (BTC) are both on the rise worldwide, according to a new analysis of data from the International Agency for Research on Cancer and the World Health Organization.
This diverse group of hepatic and perihepatic cancers include gallbladder cancer (GBC), intrahepatic and extrahepatic cholangiocarcinoma (ICC and ECC), and ampulla of Vater cancer. Although BTC is considered rare, incidence of its subtypes can vary significantly by geographic region. Because BTC is typically asymptomatic in its early stage, diagnosis is often made after tumors have spread, when there are few therapeutic options available. In the United States and Europe, 5-year survival is less than 20%.
Although previous studies have examined worldwide BTC incidence, few looked at multiple global regions or at all subtypes. Instead, subtypes may be grouped together and reported as composites, or BTC is lumped together with primary liver cancer. “To our knowledge, this is the first report combining data on worldwide incidence and mortality of all BTC subtypes per the International Classification of Diseases, Tenth Revision,” the authors wrote in the study, published online in Gastro Hep Advances.
The researchers pointed out that classification coding systems have improved at defining BTC subtypes, so that studies using older coding subtypes could cause misinterpretation of incidence rates.
BTC subtypes also have unique sets of risk factors and different prognoses and treatment outcomes. “Thus, there is a need to define accurate epidemiologic trends that will allow specific risk factors to be identified, guiding experts in implementing policies to improve diagnosis and survival,” the authors wrote.
The study included data from 22 countries. BTC incidence ranged from 1.12 cases per 100,000 person-years in Vietnam to 12.42 in Chile. As expected, incidence rates were higher in the Asia-Pacific region (1.12-9.00) and South America (2.73-12.42), compared with Europe (2.00-3.59) and North America (2.33-2.35). Within the United States, Asian Americans had a higher BTC incidence than the general population (2.99 vs. 2.33).
In most countries, new cases were dominated by GBC, while ICC was the most common cause of death.
In each country, older patients were 5-10 times more likely to die than BTC patients generally. The sixth and seventh decades of life are the most common time of diagnosis, and treatment options may be limited in older patients.
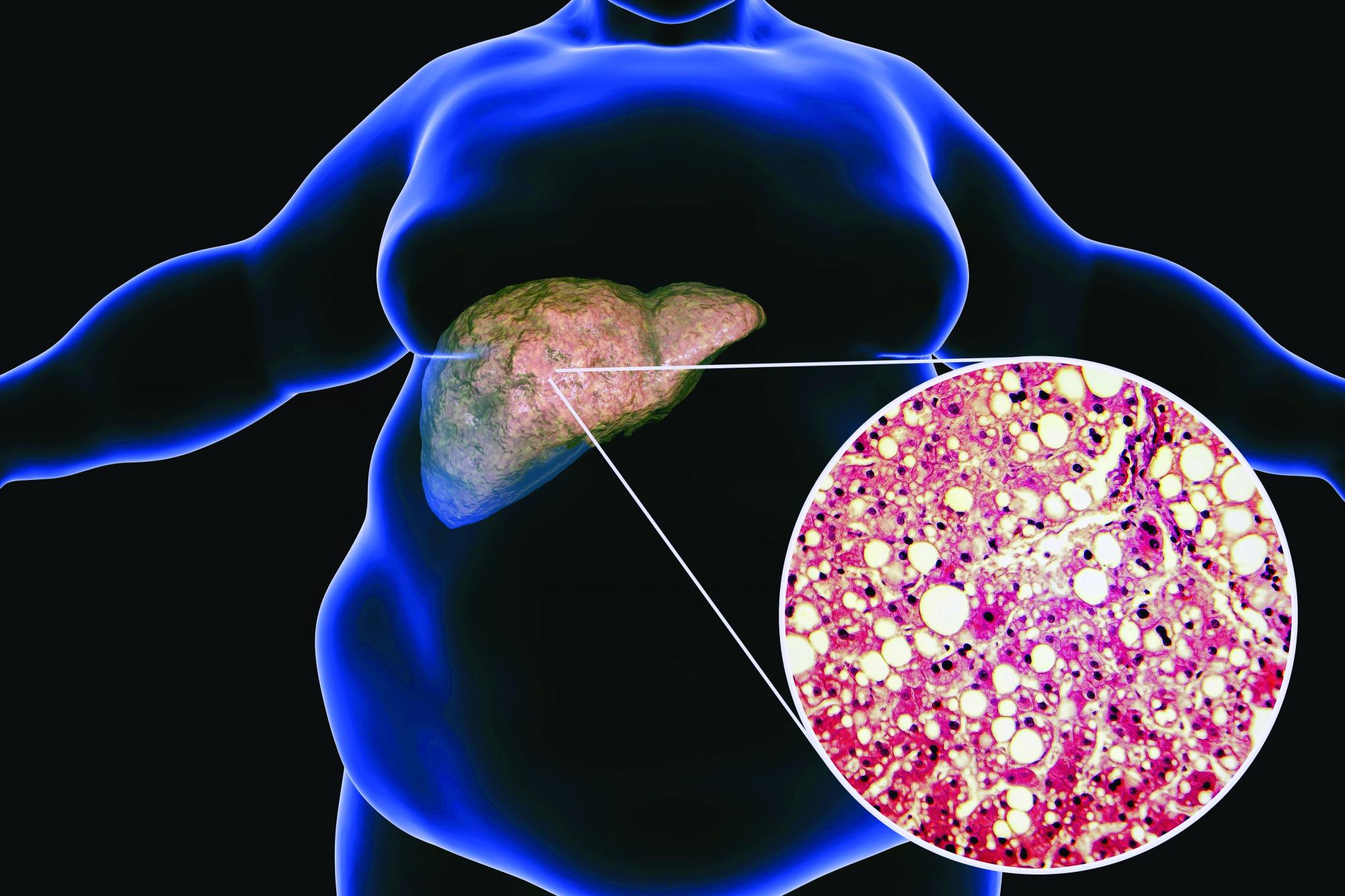
Risk factors for BTC may include common comorbidities like obesity, nonalcoholic fatty liver disease, and diabetes. Each is increasing individually, which may in turn contribute to rising BTC incidence. Observational analyses suggest that obesity may contribute to risk of ECC and gallbladder cancer, while diabetes and obesity may raise the risk of ICC. Smoking is associated with increased risk of all BTC subtypes except GBC, and alcohol consumption is associated with ICC.
“This study highlights how each subtype may be vulnerable to specific risk factors and emphasizes the value of separating epidemiologic data by subtype in order to better understand disease etiology,” the researchers wrote.
Risk factors associated with incidence and mortality from BTC aren’t limited to clinical characteristics. Genetic susceptibility may also play a role in incidence and mortality of different subtypes. There is also a relationship between gallstones and BTC risk. In Chile, about 50% of women have gallstones versus 17% of women in the United States. The cancer incidence is 27 per 100,000 person-years in Chile and 2 per 100,000 person-years in the United States. BTC is also the leading cause of cancer death among women in Chile.
The authors also highlighted the high rates of gallbladder cancer in India, despite a low prevalence of gallstones. Incidences can vary with geography along the flow of the Ganges River, which might reflect varying risks from contamination caused by agricultural runoff or industrial or human waste.
Worldwide BTC incidence and mortality was generally higher among women than men, with the exception of ampulla of Vater cancer, which was more common in men.
The study is limited by quality of data, which varied significantly between countries. Mortality data was missing from some countries know to have high BTC incidence. The databases had little survival data, which could have provided insights into treatment efficacy.
The study was funded by AstraZeneca. The authors have extensive financial relationships with pharmaceutical companies.
Biliary tract cancers (BTCs) are understudied malignancies with poor prognoses. A major impediment to a deeper understanding of BTC epidemiology is that the term BTC encompasses a heterogeneous group of cancers including cholangiocarcinoma (both intrahepatic and extrahepatic), as well as ampullary and gallbladder cancer. Studies have often lumped all BTC subgroups together despite differences in their geographic distribution, risk factors, and underlying pathogenesis. Furthermore, epidemiological reporting has often grouped “intrahepatic liver and bile duct cancers” which include hepatocellular carcinoma, a biologically different entity requiring a separate management strategy.
The study highlights the importance of future policy work to address the risk factors for BTCs that vary by region and that will likely evolve over time. It also stresses the urgent need for both early diagnostic strategies and improved biomarker-driven medical therapy, areas of ongoing research requiring accelerated development.
Irun Bhan, MD, is a transplant hepatologist at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. He has no relevant conflicts.
Biliary tract cancers (BTCs) are understudied malignancies with poor prognoses. A major impediment to a deeper understanding of BTC epidemiology is that the term BTC encompasses a heterogeneous group of cancers including cholangiocarcinoma (both intrahepatic and extrahepatic), as well as ampullary and gallbladder cancer. Studies have often lumped all BTC subgroups together despite differences in their geographic distribution, risk factors, and underlying pathogenesis. Furthermore, epidemiological reporting has often grouped “intrahepatic liver and bile duct cancers” which include hepatocellular carcinoma, a biologically different entity requiring a separate management strategy.
The study highlights the importance of future policy work to address the risk factors for BTCs that vary by region and that will likely evolve over time. It also stresses the urgent need for both early diagnostic strategies and improved biomarker-driven medical therapy, areas of ongoing research requiring accelerated development.
Irun Bhan, MD, is a transplant hepatologist at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. He has no relevant conflicts.
Biliary tract cancers (BTCs) are understudied malignancies with poor prognoses. A major impediment to a deeper understanding of BTC epidemiology is that the term BTC encompasses a heterogeneous group of cancers including cholangiocarcinoma (both intrahepatic and extrahepatic), as well as ampullary and gallbladder cancer. Studies have often lumped all BTC subgroups together despite differences in their geographic distribution, risk factors, and underlying pathogenesis. Furthermore, epidemiological reporting has often grouped “intrahepatic liver and bile duct cancers” which include hepatocellular carcinoma, a biologically different entity requiring a separate management strategy.
The study highlights the importance of future policy work to address the risk factors for BTCs that vary by region and that will likely evolve over time. It also stresses the urgent need for both early diagnostic strategies and improved biomarker-driven medical therapy, areas of ongoing research requiring accelerated development.
Irun Bhan, MD, is a transplant hepatologist at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. He has no relevant conflicts.
Incidence and mortality for biliary tract cancer (BTC) are both on the rise worldwide, according to a new analysis of data from the International Agency for Research on Cancer and the World Health Organization.
This diverse group of hepatic and perihepatic cancers include gallbladder cancer (GBC), intrahepatic and extrahepatic cholangiocarcinoma (ICC and ECC), and ampulla of Vater cancer. Although BTC is considered rare, incidence of its subtypes can vary significantly by geographic region. Because BTC is typically asymptomatic in its early stage, diagnosis is often made after tumors have spread, when there are few therapeutic options available. In the United States and Europe, 5-year survival is less than 20%.
Although previous studies have examined worldwide BTC incidence, few looked at multiple global regions or at all subtypes. Instead, subtypes may be grouped together and reported as composites, or BTC is lumped together with primary liver cancer. “To our knowledge, this is the first report combining data on worldwide incidence and mortality of all BTC subtypes per the International Classification of Diseases, Tenth Revision,” the authors wrote in the study, published online in Gastro Hep Advances.
The researchers pointed out that classification coding systems have improved at defining BTC subtypes, so that studies using older coding subtypes could cause misinterpretation of incidence rates.
BTC subtypes also have unique sets of risk factors and different prognoses and treatment outcomes. “Thus, there is a need to define accurate epidemiologic trends that will allow specific risk factors to be identified, guiding experts in implementing policies to improve diagnosis and survival,” the authors wrote.
The study included data from 22 countries. BTC incidence ranged from 1.12 cases per 100,000 person-years in Vietnam to 12.42 in Chile. As expected, incidence rates were higher in the Asia-Pacific region (1.12-9.00) and South America (2.73-12.42), compared with Europe (2.00-3.59) and North America (2.33-2.35). Within the United States, Asian Americans had a higher BTC incidence than the general population (2.99 vs. 2.33).
In most countries, new cases were dominated by GBC, while ICC was the most common cause of death.
In each country, older patients were 5-10 times more likely to die than BTC patients generally. The sixth and seventh decades of life are the most common time of diagnosis, and treatment options may be limited in older patients.
Risk factors for BTC may include common comorbidities like obesity, nonalcoholic fatty liver disease, and diabetes. Each is increasing individually, which may in turn contribute to rising BTC incidence. Observational analyses suggest that obesity may contribute to risk of ECC and gallbladder cancer, while diabetes and obesity may raise the risk of ICC. Smoking is associated with increased risk of all BTC subtypes except GBC, and alcohol consumption is associated with ICC.
“This study highlights how each subtype may be vulnerable to specific risk factors and emphasizes the value of separating epidemiologic data by subtype in order to better understand disease etiology,” the researchers wrote.
Risk factors associated with incidence and mortality from BTC aren’t limited to clinical characteristics. Genetic susceptibility may also play a role in incidence and mortality of different subtypes. There is also a relationship between gallstones and BTC risk. In Chile, about 50% of women have gallstones versus 17% of women in the United States. The cancer incidence is 27 per 100,000 person-years in Chile and 2 per 100,000 person-years in the United States. BTC is also the leading cause of cancer death among women in Chile.
The authors also highlighted the high rates of gallbladder cancer in India, despite a low prevalence of gallstones. Incidences can vary with geography along the flow of the Ganges River, which might reflect varying risks from contamination caused by agricultural runoff or industrial or human waste.
Worldwide BTC incidence and mortality was generally higher among women than men, with the exception of ampulla of Vater cancer, which was more common in men.
The study is limited by quality of data, which varied significantly between countries. Mortality data was missing from some countries know to have high BTC incidence. The databases had little survival data, which could have provided insights into treatment efficacy.
The study was funded by AstraZeneca. The authors have extensive financial relationships with pharmaceutical companies.
Incidence and mortality for biliary tract cancer (BTC) are both on the rise worldwide, according to a new analysis of data from the International Agency for Research on Cancer and the World Health Organization.
This diverse group of hepatic and perihepatic cancers include gallbladder cancer (GBC), intrahepatic and extrahepatic cholangiocarcinoma (ICC and ECC), and ampulla of Vater cancer. Although BTC is considered rare, incidence of its subtypes can vary significantly by geographic region. Because BTC is typically asymptomatic in its early stage, diagnosis is often made after tumors have spread, when there are few therapeutic options available. In the United States and Europe, 5-year survival is less than 20%.
Although previous studies have examined worldwide BTC incidence, few looked at multiple global regions or at all subtypes. Instead, subtypes may be grouped together and reported as composites, or BTC is lumped together with primary liver cancer. “To our knowledge, this is the first report combining data on worldwide incidence and mortality of all BTC subtypes per the International Classification of Diseases, Tenth Revision,” the authors wrote in the study, published online in Gastro Hep Advances.
The researchers pointed out that classification coding systems have improved at defining BTC subtypes, so that studies using older coding subtypes could cause misinterpretation of incidence rates.
BTC subtypes also have unique sets of risk factors and different prognoses and treatment outcomes. “Thus, there is a need to define accurate epidemiologic trends that will allow specific risk factors to be identified, guiding experts in implementing policies to improve diagnosis and survival,” the authors wrote.
The study included data from 22 countries. BTC incidence ranged from 1.12 cases per 100,000 person-years in Vietnam to 12.42 in Chile. As expected, incidence rates were higher in the Asia-Pacific region (1.12-9.00) and South America (2.73-12.42), compared with Europe (2.00-3.59) and North America (2.33-2.35). Within the United States, Asian Americans had a higher BTC incidence than the general population (2.99 vs. 2.33).
In most countries, new cases were dominated by GBC, while ICC was the most common cause of death.
In each country, older patients were 5-10 times more likely to die than BTC patients generally. The sixth and seventh decades of life are the most common time of diagnosis, and treatment options may be limited in older patients.
Risk factors for BTC may include common comorbidities like obesity, nonalcoholic fatty liver disease, and diabetes. Each is increasing individually, which may in turn contribute to rising BTC incidence. Observational analyses suggest that obesity may contribute to risk of ECC and gallbladder cancer, while diabetes and obesity may raise the risk of ICC. Smoking is associated with increased risk of all BTC subtypes except GBC, and alcohol consumption is associated with ICC.
“This study highlights how each subtype may be vulnerable to specific risk factors and emphasizes the value of separating epidemiologic data by subtype in order to better understand disease etiology,” the researchers wrote.
Risk factors associated with incidence and mortality from BTC aren’t limited to clinical characteristics. Genetic susceptibility may also play a role in incidence and mortality of different subtypes. There is also a relationship between gallstones and BTC risk. In Chile, about 50% of women have gallstones versus 17% of women in the United States. The cancer incidence is 27 per 100,000 person-years in Chile and 2 per 100,000 person-years in the United States. BTC is also the leading cause of cancer death among women in Chile.
The authors also highlighted the high rates of gallbladder cancer in India, despite a low prevalence of gallstones. Incidences can vary with geography along the flow of the Ganges River, which might reflect varying risks from contamination caused by agricultural runoff or industrial or human waste.
Worldwide BTC incidence and mortality was generally higher among women than men, with the exception of ampulla of Vater cancer, which was more common in men.
The study is limited by quality of data, which varied significantly between countries. Mortality data was missing from some countries know to have high BTC incidence. The databases had little survival data, which could have provided insights into treatment efficacy.
The study was funded by AstraZeneca. The authors have extensive financial relationships with pharmaceutical companies.
FROM GASTRO HEP ADVANCES
Bulevirtide reduces hepatitis D viral load in difficult-to-treat patients
Bulevirtide (Hepcludex) monotherapy significantly reduces the load of hepatitis delta virus (HDV) and is safe in difficult-to-treat patients with compensated cirrhosis and clinically significant portal hypertension, according to the results of an ongoing 1-year study.
In presenting a poster with these findings at the annual International Liver Congress, sponsored by the European Association for the Study of the Liver, lead author Elisabetta Degasperi, MD, from the Grand Hospital Maggiore Policlinico in Milan, said that they were important “because they confirm the safety of this drug in real life.”
Dr. Degasperi and colleagues showed that bulevirtide leads to a significant viral response in 78% of patients by week 48, which was measured using the outcome of greater than 2 log decline in HDV RNA from baseline.
Dr. Degasperi added that the research still needed to assess the longer-term benefits, but
Addressing an immense, unmet therapeutic need
HDV requires the presence of hepatitis B virus to replicate. Bulevirtide blocks the entry of HDV and hepatitis B virus into hepatocytes.
In July 2020, it was conditionally approved in the European Economic Area for use to treat chronic HDV infection in adults with compensated liver disease upon confirmation of HDV RNA in the blood. It currently remains an investigational agent in the United States, as well as outside of the EEA.
The ongoing trial led by Dr. Degasperi is specifically conducted in patients with compensated cirrhosis who also have clinically significant portal hypertension, where safety and efficacy are unknown.
Dr. Degasperi said in an interview that, although HDV was rare, there is nonetheless an “immense” need for effective therapies against it, especially in young patients with advanced liver disease.
“We have a lot of patients with hepatitis D who have not responded to other antiviral treatment. Right now, the only other available treatment is pegylated interferon,” she said. “Unfortunately, rates of sustained viral response to pegylated interferon are extremely low at around 30% of patients.”
Chronic HDV is the most severe form of viral hepatitis and can have mortality rates as high as 50% within 5 years in patients with cirrhosis.
The management of hepatitis D is also complicated by the fact that patients with advanced cirrhosis and clinically significant portal hypertension cannot be treated with pegylated interferon owing to lack of efficacy and safety reasons, including a high risk for decompensation and liver-related complications. Pegylated interferon is contraindicated in these patients.
Bulevirtide at 48 weeks: A closer look at the findings
Eighteen patients with HDV, compensated cirrhosis, and clinically significant portal hypertension were consecutively enrolled in this single-center, longitudinal study.
All received bulevirtide monotherapy at 2 mg/day and underwent monitoring every 2 months. They were also treated with nucleotide analogs for their hepatitis B virus, which was suppressed when they began bulevirtide.
Clinical and virologic characteristics were collected at baseline, at weeks 4 and 8, and then every 8 weeks thereafter.
Bulevirtide led to a significant viral response such that by week 48, HDV RNA declined by 3.1 log IU/mL (range, 0.2-4.6 log IU/mL), was undetectable in six patients (33%), and was less than 100 IU/L in 50% of patients. Two patients were nonresponders. In addition, 78% of patients achieved at least an HDV RNA 2 log decline from baseline.
There was also a normalization of biochemical response in the majority of patients.
Alanine aminotransferase normalization was seen in 89% of patients and declined by a median of 34 U/L (range, 15-76 U/L) over 48 weeks. Aspartate aminotransferase declined to 39 U/L (range, 21-92 U/L). A combined response was seen in 72% of patients, reported Dr. Degasperi.
“Previously, we only had results from a phase 2 study, so we had no idea of the results over such a long treatment period,” said Dr. Degasperi. “It is also the first time we have been able to treat these patients with such advanced disease that is so difficult to manage.”
“Real-world results are typically inferior to those from clinical trials, but the viral decline is comparable to phase 2 trials, and the first report of the phase 3 trial,” said Dr. Degasperi.
Gamma-glutamyltransferase, alpha-fetoprotein, immunoglobulin G, and gamma-globulin levels also improved, whereas hepatitis B surface antigen, hepatitis B virus RNA, hepatitis B core-related antigen, platelet, and bilirubin values did not significantly change.
“All patients were Child-Pugh score A, so well-compensated [disease]. However, they increased a little bit in liver function by week 48,” Dr. Degasperi said. “This was important for this very advanced disease population.”
She added that the safety profile was very favorable, with no adverse events, including no injection-site reactions.
There was an asymptomatic increase in serum bile acids. “No patients complained about itching or pruritus,” Dr. Degasperi said.
What’s ahead for bulevirtide?
In a comment, Marc Bourlière, MD, from Saint Joseph Hospital in Marseilles, France, welcomed the decrease in viral load.
“This is known to be beneficial in terms of reducing morbidity and mortality in hepatitis D,” he said. “Remember that this disease is very difficult to treat, and until now, we have had no drug available. Pegylated interferon achieves cure in only 30% of patients, and half of these relapse, so actually only 15% have a meaningful response from pegylated interferon.”
“The main issue is its use as a daily subcutaneous injection. In clinical practice, it is a little bit complicated to set up, but once done, it is quite well accepted,” he said.
“I’m impressed with these results to date because there are no other compounds that have, as yet, achieved such results. This is impressive,” he added. “But whether it translates into a long-term response we don’t yet know.”
Dr. Bourlière also noted the meaningful 2-point log decline, noting that “HDV RNA negativity where treatment can be stopped would be really meaningful, but this endpoint is hard to obtain.”
Dr. Bourlière is awaiting results of the current ongoing phase 2/3 study, which would help determine a possible final treatment duration. He is also curious to settle the ongoing debate about whether bulevirtide should be used alone or in combination.
“We need to combine bulevirtide with pegylated interferon in less-advanced patients, because we know it is more potent and active against the HDV RNA,” he said.
Dr. Degasperi has previously declared she was on the advisory board for AbbVie and has spoken and taught for Gilead, MSD, and AbbVie. Dr. Bourlière declared interests with all companies involved in the R&D of liver therapies.
A version of this article first appeared on Medscape.com.
Bulevirtide (Hepcludex) monotherapy significantly reduces the load of hepatitis delta virus (HDV) and is safe in difficult-to-treat patients with compensated cirrhosis and clinically significant portal hypertension, according to the results of an ongoing 1-year study.
In presenting a poster with these findings at the annual International Liver Congress, sponsored by the European Association for the Study of the Liver, lead author Elisabetta Degasperi, MD, from the Grand Hospital Maggiore Policlinico in Milan, said that they were important “because they confirm the safety of this drug in real life.”
Dr. Degasperi and colleagues showed that bulevirtide leads to a significant viral response in 78% of patients by week 48, which was measured using the outcome of greater than 2 log decline in HDV RNA from baseline.
Dr. Degasperi added that the research still needed to assess the longer-term benefits, but
Addressing an immense, unmet therapeutic need
HDV requires the presence of hepatitis B virus to replicate. Bulevirtide blocks the entry of HDV and hepatitis B virus into hepatocytes.
In July 2020, it was conditionally approved in the European Economic Area for use to treat chronic HDV infection in adults with compensated liver disease upon confirmation of HDV RNA in the blood. It currently remains an investigational agent in the United States, as well as outside of the EEA.
The ongoing trial led by Dr. Degasperi is specifically conducted in patients with compensated cirrhosis who also have clinically significant portal hypertension, where safety and efficacy are unknown.
Dr. Degasperi said in an interview that, although HDV was rare, there is nonetheless an “immense” need for effective therapies against it, especially in young patients with advanced liver disease.
“We have a lot of patients with hepatitis D who have not responded to other antiviral treatment. Right now, the only other available treatment is pegylated interferon,” she said. “Unfortunately, rates of sustained viral response to pegylated interferon are extremely low at around 30% of patients.”
Chronic HDV is the most severe form of viral hepatitis and can have mortality rates as high as 50% within 5 years in patients with cirrhosis.
The management of hepatitis D is also complicated by the fact that patients with advanced cirrhosis and clinically significant portal hypertension cannot be treated with pegylated interferon owing to lack of efficacy and safety reasons, including a high risk for decompensation and liver-related complications. Pegylated interferon is contraindicated in these patients.
Bulevirtide at 48 weeks: A closer look at the findings
Eighteen patients with HDV, compensated cirrhosis, and clinically significant portal hypertension were consecutively enrolled in this single-center, longitudinal study.
All received bulevirtide monotherapy at 2 mg/day and underwent monitoring every 2 months. They were also treated with nucleotide analogs for their hepatitis B virus, which was suppressed when they began bulevirtide.
Clinical and virologic characteristics were collected at baseline, at weeks 4 and 8, and then every 8 weeks thereafter.
Bulevirtide led to a significant viral response such that by week 48, HDV RNA declined by 3.1 log IU/mL (range, 0.2-4.6 log IU/mL), was undetectable in six patients (33%), and was less than 100 IU/L in 50% of patients. Two patients were nonresponders. In addition, 78% of patients achieved at least an HDV RNA 2 log decline from baseline.
There was also a normalization of biochemical response in the majority of patients.
Alanine aminotransferase normalization was seen in 89% of patients and declined by a median of 34 U/L (range, 15-76 U/L) over 48 weeks. Aspartate aminotransferase declined to 39 U/L (range, 21-92 U/L). A combined response was seen in 72% of patients, reported Dr. Degasperi.
“Previously, we only had results from a phase 2 study, so we had no idea of the results over such a long treatment period,” said Dr. Degasperi. “It is also the first time we have been able to treat these patients with such advanced disease that is so difficult to manage.”
“Real-world results are typically inferior to those from clinical trials, but the viral decline is comparable to phase 2 trials, and the first report of the phase 3 trial,” said Dr. Degasperi.
Gamma-glutamyltransferase, alpha-fetoprotein, immunoglobulin G, and gamma-globulin levels also improved, whereas hepatitis B surface antigen, hepatitis B virus RNA, hepatitis B core-related antigen, platelet, and bilirubin values did not significantly change.
“All patients were Child-Pugh score A, so well-compensated [disease]. However, they increased a little bit in liver function by week 48,” Dr. Degasperi said. “This was important for this very advanced disease population.”
She added that the safety profile was very favorable, with no adverse events, including no injection-site reactions.
There was an asymptomatic increase in serum bile acids. “No patients complained about itching or pruritus,” Dr. Degasperi said.
What’s ahead for bulevirtide?
In a comment, Marc Bourlière, MD, from Saint Joseph Hospital in Marseilles, France, welcomed the decrease in viral load.
“This is known to be beneficial in terms of reducing morbidity and mortality in hepatitis D,” he said. “Remember that this disease is very difficult to treat, and until now, we have had no drug available. Pegylated interferon achieves cure in only 30% of patients, and half of these relapse, so actually only 15% have a meaningful response from pegylated interferon.”
“The main issue is its use as a daily subcutaneous injection. In clinical practice, it is a little bit complicated to set up, but once done, it is quite well accepted,” he said.
“I’m impressed with these results to date because there are no other compounds that have, as yet, achieved such results. This is impressive,” he added. “But whether it translates into a long-term response we don’t yet know.”
Dr. Bourlière also noted the meaningful 2-point log decline, noting that “HDV RNA negativity where treatment can be stopped would be really meaningful, but this endpoint is hard to obtain.”
Dr. Bourlière is awaiting results of the current ongoing phase 2/3 study, which would help determine a possible final treatment duration. He is also curious to settle the ongoing debate about whether bulevirtide should be used alone or in combination.
“We need to combine bulevirtide with pegylated interferon in less-advanced patients, because we know it is more potent and active against the HDV RNA,” he said.
Dr. Degasperi has previously declared she was on the advisory board for AbbVie and has spoken and taught for Gilead, MSD, and AbbVie. Dr. Bourlière declared interests with all companies involved in the R&D of liver therapies.
A version of this article first appeared on Medscape.com.
Bulevirtide (Hepcludex) monotherapy significantly reduces the load of hepatitis delta virus (HDV) and is safe in difficult-to-treat patients with compensated cirrhosis and clinically significant portal hypertension, according to the results of an ongoing 1-year study.
In presenting a poster with these findings at the annual International Liver Congress, sponsored by the European Association for the Study of the Liver, lead author Elisabetta Degasperi, MD, from the Grand Hospital Maggiore Policlinico in Milan, said that they were important “because they confirm the safety of this drug in real life.”
Dr. Degasperi and colleagues showed that bulevirtide leads to a significant viral response in 78% of patients by week 48, which was measured using the outcome of greater than 2 log decline in HDV RNA from baseline.
Dr. Degasperi added that the research still needed to assess the longer-term benefits, but
Addressing an immense, unmet therapeutic need
HDV requires the presence of hepatitis B virus to replicate. Bulevirtide blocks the entry of HDV and hepatitis B virus into hepatocytes.
In July 2020, it was conditionally approved in the European Economic Area for use to treat chronic HDV infection in adults with compensated liver disease upon confirmation of HDV RNA in the blood. It currently remains an investigational agent in the United States, as well as outside of the EEA.
The ongoing trial led by Dr. Degasperi is specifically conducted in patients with compensated cirrhosis who also have clinically significant portal hypertension, where safety and efficacy are unknown.
Dr. Degasperi said in an interview that, although HDV was rare, there is nonetheless an “immense” need for effective therapies against it, especially in young patients with advanced liver disease.
“We have a lot of patients with hepatitis D who have not responded to other antiviral treatment. Right now, the only other available treatment is pegylated interferon,” she said. “Unfortunately, rates of sustained viral response to pegylated interferon are extremely low at around 30% of patients.”
Chronic HDV is the most severe form of viral hepatitis and can have mortality rates as high as 50% within 5 years in patients with cirrhosis.
The management of hepatitis D is also complicated by the fact that patients with advanced cirrhosis and clinically significant portal hypertension cannot be treated with pegylated interferon owing to lack of efficacy and safety reasons, including a high risk for decompensation and liver-related complications. Pegylated interferon is contraindicated in these patients.
Bulevirtide at 48 weeks: A closer look at the findings
Eighteen patients with HDV, compensated cirrhosis, and clinically significant portal hypertension were consecutively enrolled in this single-center, longitudinal study.
All received bulevirtide monotherapy at 2 mg/day and underwent monitoring every 2 months. They were also treated with nucleotide analogs for their hepatitis B virus, which was suppressed when they began bulevirtide.
Clinical and virologic characteristics were collected at baseline, at weeks 4 and 8, and then every 8 weeks thereafter.
Bulevirtide led to a significant viral response such that by week 48, HDV RNA declined by 3.1 log IU/mL (range, 0.2-4.6 log IU/mL), was undetectable in six patients (33%), and was less than 100 IU/L in 50% of patients. Two patients were nonresponders. In addition, 78% of patients achieved at least an HDV RNA 2 log decline from baseline.
There was also a normalization of biochemical response in the majority of patients.
Alanine aminotransferase normalization was seen in 89% of patients and declined by a median of 34 U/L (range, 15-76 U/L) over 48 weeks. Aspartate aminotransferase declined to 39 U/L (range, 21-92 U/L). A combined response was seen in 72% of patients, reported Dr. Degasperi.
“Previously, we only had results from a phase 2 study, so we had no idea of the results over such a long treatment period,” said Dr. Degasperi. “It is also the first time we have been able to treat these patients with such advanced disease that is so difficult to manage.”
“Real-world results are typically inferior to those from clinical trials, but the viral decline is comparable to phase 2 trials, and the first report of the phase 3 trial,” said Dr. Degasperi.
Gamma-glutamyltransferase, alpha-fetoprotein, immunoglobulin G, and gamma-globulin levels also improved, whereas hepatitis B surface antigen, hepatitis B virus RNA, hepatitis B core-related antigen, platelet, and bilirubin values did not significantly change.
“All patients were Child-Pugh score A, so well-compensated [disease]. However, they increased a little bit in liver function by week 48,” Dr. Degasperi said. “This was important for this very advanced disease population.”
She added that the safety profile was very favorable, with no adverse events, including no injection-site reactions.
There was an asymptomatic increase in serum bile acids. “No patients complained about itching or pruritus,” Dr. Degasperi said.
What’s ahead for bulevirtide?
In a comment, Marc Bourlière, MD, from Saint Joseph Hospital in Marseilles, France, welcomed the decrease in viral load.
“This is known to be beneficial in terms of reducing morbidity and mortality in hepatitis D,” he said. “Remember that this disease is very difficult to treat, and until now, we have had no drug available. Pegylated interferon achieves cure in only 30% of patients, and half of these relapse, so actually only 15% have a meaningful response from pegylated interferon.”
“The main issue is its use as a daily subcutaneous injection. In clinical practice, it is a little bit complicated to set up, but once done, it is quite well accepted,” he said.
“I’m impressed with these results to date because there are no other compounds that have, as yet, achieved such results. This is impressive,” he added. “But whether it translates into a long-term response we don’t yet know.”
Dr. Bourlière also noted the meaningful 2-point log decline, noting that “HDV RNA negativity where treatment can be stopped would be really meaningful, but this endpoint is hard to obtain.”
Dr. Bourlière is awaiting results of the current ongoing phase 2/3 study, which would help determine a possible final treatment duration. He is also curious to settle the ongoing debate about whether bulevirtide should be used alone or in combination.
“We need to combine bulevirtide with pegylated interferon in less-advanced patients, because we know it is more potent and active against the HDV RNA,” he said.
Dr. Degasperi has previously declared she was on the advisory board for AbbVie and has spoken and taught for Gilead, MSD, and AbbVie. Dr. Bourlière declared interests with all companies involved in the R&D of liver therapies.
A version of this article first appeared on Medscape.com.
FROM ILC 2022
Finding HBV ‘cure’ may mean going ‘back to the drawing board’
LONDON – Achieving a functional cure for hepatitis B virus (HBV) is not going to be easily achieved with the drugs that are currently in development, according to a presentation at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
“Intriguing results have been presented at ILC 2022 that must be carefully interpreted,” said Jean-Michel Pawlotsky, MD, PhD, of Henri Mondor Hospital in Créteil, France, during the viral hepatitis highlights session on the closing day of the meeting.
“New HBV drug development looks more complicated than initially expected and its goals and strategies need to be redefined and refocused,” he added
“This is really something that came from the discussions we had during the sessions but also in the corridors,” Dr. Pawlotsky added. “We know it’s going to be difficult; we have to reset, restart – not from zero, but from not much – and revise our strategy,” he suggested.
There are many new drugs under investigation for HBV, Dr. Pawlotsky said, noting that the number of studies being presented at the meeting was reminiscent of the flurry of activity before a functional cure for hepatitis C had been found. “It’s good to see that this is happening again for HBV,” he said.
Indeed, there are many new direct-acting antiviral agents, immunomodulatory, or other approaches being tested, and some of the more advanced studies are “teaching us a few things and probably raising more questions than getting answers,” Dr. Pawlotsky said.
The B-CLEAR study
One these studies is the phase 2b B-CLEAR study presented during the late-breaker session. This study involved bepirovirsen, an antisense oligonucleotide, and tested its efficacy and safety in patients with chronic hepatitis B virus infection who were either on or off stable nucleos(t)ide analogue (NA/NUC) therapy.
A similar proportion (28% and 29%, respectively) of patients achieved an hepatitis B surface antigen (HBsAg) level below the lower limit of quantification at the end of 24 weeks treatment. However, the effect on HBsAg varied according to the treatment arm, with changes to the dosing or switching to placebo indicating that the effect might wane when the treatment is stopped or if the dose is reduced.
“Interestingly, ALT elevations were observed in association with most HBsAg declines,” Dr. Pawlotsky pointed out. “I think we still have to determine whether this is good flare/bad flare, good sign/bad sign, of what is going to happen afterward.”
The REEF studies
Another approach highlighted was the combination of the silencing or small interfering RNA (siRNA) JNJ-3989 with the capsid assembly modulator (CAM) JNJ-6379 in the phase 2 REEF-1 and REEF-2 studies.
REEF-1, conducted in patients who were either hepatitis B e antigen (HBeAg) positive or negative who were not treated with NA/NUC or were NA/NUC suppressed, showed a dose-dependent, but variable effect among individual patients as might be expected at the end of 48 weeks’ treatment. This was sustained at week 72, which was 24 weeks’ follow-up after stopping treatment.
However, pointed out Dr. Pawlotsky “I think the most important part of this is that if you add a CAM on top of the siRNA, you do not improve the effect on HBsAg levels.”
Then there is the REEF-2 study, testing the same combination but in only patients who were NA suppressed or HBeAg negative alongside standard NA/NUC therapy. As well as being the first novel combination treatment trial to report, this was essentially a stopping trial, Kosh Agarwal, BMedSci (Hons), MBBS, MD, one of the study’s investigators explained separately at a media briefing.
Patients (n = 130) were treated for 48 weeks, then all treatment – including NA/NUC – was discontinued, with 48 weeks of follow-up after discontinuation, said Dr. Agarwal, who is a consultant hepatologist based at the Institute of Liver Studies at King’s College Hospital, London. He presented data from the first 24 week period after treatment had ended.
At the end of treatment, the combination had resulted in a mean reduction in HBsAg of 1.89 log10 IU/mL versus a reduction of 0.06 for the NA/NUC-only group, which acted as the control group in this trial. But “no patient in this study lost their surface antigen, i.e., were cured of their hepatitis B in the active arm or in the control arm,” Dr. Agarwal said.
“We didn’t achieve a cure, but a significant proportion were in a ‘controlled’ viral stage,” said Dr. Agarwal. Indeed, during his presentation of the findings, he showed that HBsAg inhibition was maintained in the majority (72%) of patients after stopping the combination.
While the trial’s primary endpoint wasn’t met, “it’s a really important study,” said Dr. Agarwal. “This [study] was fulfilled and delivered in the COVID era, so a lot of patients were looked after very carefully by sites in Europe,” he observed.
Further follow-up from the trial is expected, and Dr. Agarwal said that the subsequent discussion will “take us back to the drawing board to think about whether we need better antiviral treatments or whether we need to think about different combinations, and whether actually stopping treatment with every treatment is the right strategy to take.”
Both Dr. Agarwal and Dr. Pawlotsky flagged up the case of one patient in the trial who had been in the control arm and had experienced severe HBV reactivation that required a liver transplant.
“This patient is a warning signal,” Dr. Pawlotsky suggested in his talk. “When we think about NUC stopping, we have to think about the potential benefit in terms of HbsAg loss but also the potential risks.”
While Dr. Agarwal had noted that it highlights that “careful design of retreatment criteria is important in studies assessing the NA/NUC-stopping concept”.
Monoclonal antibody shows promise
Other combinations could involve an siRNA and an immunomodulatory agent and, during the poster sessions at the meeting, Dr. Agarwal also presented data from an ongoing phase 1 study with a novel, neutralizing monoclonal antibody called VIR-3434.
This monoclonal antibody is novel because it is thought to have several modes of action, first by binding to HBV and affecting its entry into liver cells, then by presenting the virus to T cells and stimulating a ‘vaccinal’ or immune effect, and then by helping the with the clearance of HBsAg and delivery of the virus to dendritic cells.
In the study, single doses of VIR-3434 were found to be well tolerated and to produce rapid reductions in HBsAg, with the highest dose used (300 mg) producing the greatest and most durable effect up to week 8.
VIR-3434 is also being tested in combination with other drugs in the phase 2 MARCH trial. One of these combinations is VIR-3434 together with an investigational siRNA dubbed VIR-2218. Preclinical work presented at ILC 2022 suggests that this combination appears to be capable of reducing HBsAg to a greater extent than using either agent alone.
Rethinking the strategy to get to a cure
Of course, VIR-3434 is one of several immunomodulatory compounds in development. There are therapeutic vaccines, drugs targeting the innate immune response, other monoclonal antibodies, T-cell receptors, checkpoint inhibitors and PD-L1 inhibitors. Then there are other compounds such as entry inhibitors, apoptosis inducers, and farnesoid X receptor agonists.
“I finish this meeting with more questions than answers,” Dr. Pawlotsky said. “What is the right target to enhance specific anti-HBV immunity? Does in vivo induction of immune responses translate into any beneficial effect on HBV infection? Will therapeutic vaccines every work in a viral infection?”
Moreover, he asked, “how can we avoid the side effect of enhancing multiple and complex nonspecific immune responses? Are treatment-induced flares good flares or bad flares? All of these are questions that are really unanswered and that we’ll have to get answers to in the near future.”
The B-CLEAR study was sponsored by GlaxoSmithKline. The REEF-2 study was sponsored by Janssen Research & Development. The VIR-3434 studies were funded by Vir Biotechnology. Dr. Pawlotsky has received grant and research support, acted as a consultant, adviser, or speaker, and participated in advisory boards for multiple pharmaceutical and biotechnology companies. This news organization was unable to verify Dr. Agarwal’s ties to Vir Biotechnology, but he presented one of the posters on VIR-3434 at the meeting and has been involved in the phase 1 study that was reported.
LONDON – Achieving a functional cure for hepatitis B virus (HBV) is not going to be easily achieved with the drugs that are currently in development, according to a presentation at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
“Intriguing results have been presented at ILC 2022 that must be carefully interpreted,” said Jean-Michel Pawlotsky, MD, PhD, of Henri Mondor Hospital in Créteil, France, during the viral hepatitis highlights session on the closing day of the meeting.
“New HBV drug development looks more complicated than initially expected and its goals and strategies need to be redefined and refocused,” he added
“This is really something that came from the discussions we had during the sessions but also in the corridors,” Dr. Pawlotsky added. “We know it’s going to be difficult; we have to reset, restart – not from zero, but from not much – and revise our strategy,” he suggested.
There are many new drugs under investigation for HBV, Dr. Pawlotsky said, noting that the number of studies being presented at the meeting was reminiscent of the flurry of activity before a functional cure for hepatitis C had been found. “It’s good to see that this is happening again for HBV,” he said.
Indeed, there are many new direct-acting antiviral agents, immunomodulatory, or other approaches being tested, and some of the more advanced studies are “teaching us a few things and probably raising more questions than getting answers,” Dr. Pawlotsky said.
The B-CLEAR study
One these studies is the phase 2b B-CLEAR study presented during the late-breaker session. This study involved bepirovirsen, an antisense oligonucleotide, and tested its efficacy and safety in patients with chronic hepatitis B virus infection who were either on or off stable nucleos(t)ide analogue (NA/NUC) therapy.
A similar proportion (28% and 29%, respectively) of patients achieved an hepatitis B surface antigen (HBsAg) level below the lower limit of quantification at the end of 24 weeks treatment. However, the effect on HBsAg varied according to the treatment arm, with changes to the dosing or switching to placebo indicating that the effect might wane when the treatment is stopped or if the dose is reduced.
“Interestingly, ALT elevations were observed in association with most HBsAg declines,” Dr. Pawlotsky pointed out. “I think we still have to determine whether this is good flare/bad flare, good sign/bad sign, of what is going to happen afterward.”
The REEF studies
Another approach highlighted was the combination of the silencing or small interfering RNA (siRNA) JNJ-3989 with the capsid assembly modulator (CAM) JNJ-6379 in the phase 2 REEF-1 and REEF-2 studies.
REEF-1, conducted in patients who were either hepatitis B e antigen (HBeAg) positive or negative who were not treated with NA/NUC or were NA/NUC suppressed, showed a dose-dependent, but variable effect among individual patients as might be expected at the end of 48 weeks’ treatment. This was sustained at week 72, which was 24 weeks’ follow-up after stopping treatment.
However, pointed out Dr. Pawlotsky “I think the most important part of this is that if you add a CAM on top of the siRNA, you do not improve the effect on HBsAg levels.”
Then there is the REEF-2 study, testing the same combination but in only patients who were NA suppressed or HBeAg negative alongside standard NA/NUC therapy. As well as being the first novel combination treatment trial to report, this was essentially a stopping trial, Kosh Agarwal, BMedSci (Hons), MBBS, MD, one of the study’s investigators explained separately at a media briefing.
Patients (n = 130) were treated for 48 weeks, then all treatment – including NA/NUC – was discontinued, with 48 weeks of follow-up after discontinuation, said Dr. Agarwal, who is a consultant hepatologist based at the Institute of Liver Studies at King’s College Hospital, London. He presented data from the first 24 week period after treatment had ended.
At the end of treatment, the combination had resulted in a mean reduction in HBsAg of 1.89 log10 IU/mL versus a reduction of 0.06 for the NA/NUC-only group, which acted as the control group in this trial. But “no patient in this study lost their surface antigen, i.e., were cured of their hepatitis B in the active arm or in the control arm,” Dr. Agarwal said.
“We didn’t achieve a cure, but a significant proportion were in a ‘controlled’ viral stage,” said Dr. Agarwal. Indeed, during his presentation of the findings, he showed that HBsAg inhibition was maintained in the majority (72%) of patients after stopping the combination.
While the trial’s primary endpoint wasn’t met, “it’s a really important study,” said Dr. Agarwal. “This [study] was fulfilled and delivered in the COVID era, so a lot of patients were looked after very carefully by sites in Europe,” he observed.
Further follow-up from the trial is expected, and Dr. Agarwal said that the subsequent discussion will “take us back to the drawing board to think about whether we need better antiviral treatments or whether we need to think about different combinations, and whether actually stopping treatment with every treatment is the right strategy to take.”
Both Dr. Agarwal and Dr. Pawlotsky flagged up the case of one patient in the trial who had been in the control arm and had experienced severe HBV reactivation that required a liver transplant.
“This patient is a warning signal,” Dr. Pawlotsky suggested in his talk. “When we think about NUC stopping, we have to think about the potential benefit in terms of HbsAg loss but also the potential risks.”
While Dr. Agarwal had noted that it highlights that “careful design of retreatment criteria is important in studies assessing the NA/NUC-stopping concept”.
Monoclonal antibody shows promise
Other combinations could involve an siRNA and an immunomodulatory agent and, during the poster sessions at the meeting, Dr. Agarwal also presented data from an ongoing phase 1 study with a novel, neutralizing monoclonal antibody called VIR-3434.
This monoclonal antibody is novel because it is thought to have several modes of action, first by binding to HBV and affecting its entry into liver cells, then by presenting the virus to T cells and stimulating a ‘vaccinal’ or immune effect, and then by helping the with the clearance of HBsAg and delivery of the virus to dendritic cells.
In the study, single doses of VIR-3434 were found to be well tolerated and to produce rapid reductions in HBsAg, with the highest dose used (300 mg) producing the greatest and most durable effect up to week 8.
VIR-3434 is also being tested in combination with other drugs in the phase 2 MARCH trial. One of these combinations is VIR-3434 together with an investigational siRNA dubbed VIR-2218. Preclinical work presented at ILC 2022 suggests that this combination appears to be capable of reducing HBsAg to a greater extent than using either agent alone.
Rethinking the strategy to get to a cure
Of course, VIR-3434 is one of several immunomodulatory compounds in development. There are therapeutic vaccines, drugs targeting the innate immune response, other monoclonal antibodies, T-cell receptors, checkpoint inhibitors and PD-L1 inhibitors. Then there are other compounds such as entry inhibitors, apoptosis inducers, and farnesoid X receptor agonists.
“I finish this meeting with more questions than answers,” Dr. Pawlotsky said. “What is the right target to enhance specific anti-HBV immunity? Does in vivo induction of immune responses translate into any beneficial effect on HBV infection? Will therapeutic vaccines every work in a viral infection?”
Moreover, he asked, “how can we avoid the side effect of enhancing multiple and complex nonspecific immune responses? Are treatment-induced flares good flares or bad flares? All of these are questions that are really unanswered and that we’ll have to get answers to in the near future.”
The B-CLEAR study was sponsored by GlaxoSmithKline. The REEF-2 study was sponsored by Janssen Research & Development. The VIR-3434 studies were funded by Vir Biotechnology. Dr. Pawlotsky has received grant and research support, acted as a consultant, adviser, or speaker, and participated in advisory boards for multiple pharmaceutical and biotechnology companies. This news organization was unable to verify Dr. Agarwal’s ties to Vir Biotechnology, but he presented one of the posters on VIR-3434 at the meeting and has been involved in the phase 1 study that was reported.
LONDON – Achieving a functional cure for hepatitis B virus (HBV) is not going to be easily achieved with the drugs that are currently in development, according to a presentation at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
“Intriguing results have been presented at ILC 2022 that must be carefully interpreted,” said Jean-Michel Pawlotsky, MD, PhD, of Henri Mondor Hospital in Créteil, France, during the viral hepatitis highlights session on the closing day of the meeting.
“New HBV drug development looks more complicated than initially expected and its goals and strategies need to be redefined and refocused,” he added
“This is really something that came from the discussions we had during the sessions but also in the corridors,” Dr. Pawlotsky added. “We know it’s going to be difficult; we have to reset, restart – not from zero, but from not much – and revise our strategy,” he suggested.
There are many new drugs under investigation for HBV, Dr. Pawlotsky said, noting that the number of studies being presented at the meeting was reminiscent of the flurry of activity before a functional cure for hepatitis C had been found. “It’s good to see that this is happening again for HBV,” he said.
Indeed, there are many new direct-acting antiviral agents, immunomodulatory, or other approaches being tested, and some of the more advanced studies are “teaching us a few things and probably raising more questions than getting answers,” Dr. Pawlotsky said.
The B-CLEAR study
One these studies is the phase 2b B-CLEAR study presented during the late-breaker session. This study involved bepirovirsen, an antisense oligonucleotide, and tested its efficacy and safety in patients with chronic hepatitis B virus infection who were either on or off stable nucleos(t)ide analogue (NA/NUC) therapy.
A similar proportion (28% and 29%, respectively) of patients achieved an hepatitis B surface antigen (HBsAg) level below the lower limit of quantification at the end of 24 weeks treatment. However, the effect on HBsAg varied according to the treatment arm, with changes to the dosing or switching to placebo indicating that the effect might wane when the treatment is stopped or if the dose is reduced.
“Interestingly, ALT elevations were observed in association with most HBsAg declines,” Dr. Pawlotsky pointed out. “I think we still have to determine whether this is good flare/bad flare, good sign/bad sign, of what is going to happen afterward.”
The REEF studies
Another approach highlighted was the combination of the silencing or small interfering RNA (siRNA) JNJ-3989 with the capsid assembly modulator (CAM) JNJ-6379 in the phase 2 REEF-1 and REEF-2 studies.
REEF-1, conducted in patients who were either hepatitis B e antigen (HBeAg) positive or negative who were not treated with NA/NUC or were NA/NUC suppressed, showed a dose-dependent, but variable effect among individual patients as might be expected at the end of 48 weeks’ treatment. This was sustained at week 72, which was 24 weeks’ follow-up after stopping treatment.
However, pointed out Dr. Pawlotsky “I think the most important part of this is that if you add a CAM on top of the siRNA, you do not improve the effect on HBsAg levels.”
Then there is the REEF-2 study, testing the same combination but in only patients who were NA suppressed or HBeAg negative alongside standard NA/NUC therapy. As well as being the first novel combination treatment trial to report, this was essentially a stopping trial, Kosh Agarwal, BMedSci (Hons), MBBS, MD, one of the study’s investigators explained separately at a media briefing.
Patients (n = 130) were treated for 48 weeks, then all treatment – including NA/NUC – was discontinued, with 48 weeks of follow-up after discontinuation, said Dr. Agarwal, who is a consultant hepatologist based at the Institute of Liver Studies at King’s College Hospital, London. He presented data from the first 24 week period after treatment had ended.
At the end of treatment, the combination had resulted in a mean reduction in HBsAg of 1.89 log10 IU/mL versus a reduction of 0.06 for the NA/NUC-only group, which acted as the control group in this trial. But “no patient in this study lost their surface antigen, i.e., were cured of their hepatitis B in the active arm or in the control arm,” Dr. Agarwal said.
“We didn’t achieve a cure, but a significant proportion were in a ‘controlled’ viral stage,” said Dr. Agarwal. Indeed, during his presentation of the findings, he showed that HBsAg inhibition was maintained in the majority (72%) of patients after stopping the combination.
While the trial’s primary endpoint wasn’t met, “it’s a really important study,” said Dr. Agarwal. “This [study] was fulfilled and delivered in the COVID era, so a lot of patients were looked after very carefully by sites in Europe,” he observed.
Further follow-up from the trial is expected, and Dr. Agarwal said that the subsequent discussion will “take us back to the drawing board to think about whether we need better antiviral treatments or whether we need to think about different combinations, and whether actually stopping treatment with every treatment is the right strategy to take.”
Both Dr. Agarwal and Dr. Pawlotsky flagged up the case of one patient in the trial who had been in the control arm and had experienced severe HBV reactivation that required a liver transplant.
“This patient is a warning signal,” Dr. Pawlotsky suggested in his talk. “When we think about NUC stopping, we have to think about the potential benefit in terms of HbsAg loss but also the potential risks.”
While Dr. Agarwal had noted that it highlights that “careful design of retreatment criteria is important in studies assessing the NA/NUC-stopping concept”.
Monoclonal antibody shows promise
Other combinations could involve an siRNA and an immunomodulatory agent and, during the poster sessions at the meeting, Dr. Agarwal also presented data from an ongoing phase 1 study with a novel, neutralizing monoclonal antibody called VIR-3434.
This monoclonal antibody is novel because it is thought to have several modes of action, first by binding to HBV and affecting its entry into liver cells, then by presenting the virus to T cells and stimulating a ‘vaccinal’ or immune effect, and then by helping the with the clearance of HBsAg and delivery of the virus to dendritic cells.
In the study, single doses of VIR-3434 were found to be well tolerated and to produce rapid reductions in HBsAg, with the highest dose used (300 mg) producing the greatest and most durable effect up to week 8.
VIR-3434 is also being tested in combination with other drugs in the phase 2 MARCH trial. One of these combinations is VIR-3434 together with an investigational siRNA dubbed VIR-2218. Preclinical work presented at ILC 2022 suggests that this combination appears to be capable of reducing HBsAg to a greater extent than using either agent alone.
Rethinking the strategy to get to a cure
Of course, VIR-3434 is one of several immunomodulatory compounds in development. There are therapeutic vaccines, drugs targeting the innate immune response, other monoclonal antibodies, T-cell receptors, checkpoint inhibitors and PD-L1 inhibitors. Then there are other compounds such as entry inhibitors, apoptosis inducers, and farnesoid X receptor agonists.
“I finish this meeting with more questions than answers,” Dr. Pawlotsky said. “What is the right target to enhance specific anti-HBV immunity? Does in vivo induction of immune responses translate into any beneficial effect on HBV infection? Will therapeutic vaccines every work in a viral infection?”
Moreover, he asked, “how can we avoid the side effect of enhancing multiple and complex nonspecific immune responses? Are treatment-induced flares good flares or bad flares? All of these are questions that are really unanswered and that we’ll have to get answers to in the near future.”
The B-CLEAR study was sponsored by GlaxoSmithKline. The REEF-2 study was sponsored by Janssen Research & Development. The VIR-3434 studies were funded by Vir Biotechnology. Dr. Pawlotsky has received grant and research support, acted as a consultant, adviser, or speaker, and participated in advisory boards for multiple pharmaceutical and biotechnology companies. This news organization was unable to verify Dr. Agarwal’s ties to Vir Biotechnology, but he presented one of the posters on VIR-3434 at the meeting and has been involved in the phase 1 study that was reported.
AT ILC 2022
Statins in NAFLD: Taking a closer look at benefits
LONDON – Substantial reductions in liver fat and fibrosis can be achieved with statin therapy, according to research presented at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
Statins are thought to have multiple beneficial actions in people with fatty liver disease, but there has been little insight into how they may be exerting such effects.
Now, data from the Rotterdam Study and others suggest that statins may be reducing the formation of lipid droplets as well as influencing the expression of important inflammatory genes.
The results “require further confirmation,” the team behind the work said, which was done at Erasmus Medical Center in Rotterdam, the Netherlands, in collaboration with researchers at The First Affiliated Hospital of Wenzhou (China) Medical University.
“Statins are inversely associated with multiple components of the NAFLD [nonalcoholic fatty liver disease] spectrum,” said Ibrahim Ayada, a PhD student in the department of gastroenterology and hepatology at Erasmus MC.
“Statins can inhibit lipid synthesis in organoids and statins also exhibit healthy inflammatory effects, which might contribute to the hepatoprotective effects that we observe in our population studies,” Mr. Ayada said.
A rising problem that needs addressing
Together NAFLD and NASH constitute a significant and increasing health burden, Mr. Ayada observed, noting that there were an estimated 64 million people in the United States and 52 million people in Europe, at least, with the rise mirroring the obesity pandemic.
“The number of patients visiting outpatient clinics has nearly doubled within a study period of 5 years,” he said.
“There is no pharmacologic therapy,” he reminded his audience, observing that fatty liver disease was a major indication for liver transplantation.
Statins are a long-standing staple of cardiovascular disease management and are known to have pleiotropic effects, Mr. Ayada explained. Their use in NAFLD and non-alcoholic steatohepatitis (NASH) has been purported but is supported by inconclusive evidence.
Indeed, a prior Cochrane review performed in 2013 found only two studies that were eligible for analysis and had “high risk of bias and a small numbers of participants,” according to the review’s authors.
Examining the connection
To look at the possible benefits of statins in people with NASH and examine how these effects might be occurring, Mr. Ayada and collaborators first took data from the Rotterdam Study, a large population-based prospective cohort that has been collecting data on its participants since the early 90s.
Data on over 4,500 participants were examined and of these, just over 1,000 had NAFLD. Statin versus no statin use was found to be associated with around a 30% reduction in fatty liver disease, with an odds ratio or 0.72 for NAFLD.
Then, looking only at a subset of patients with biopsy-proven NAFLD, statin use was associated with a 45% reduction in NASH (OR, 0.55) and a 24% reduction in fibrosis, although only the NASH reduction was significant (P = .031). The purpose of this cohort is to look at potential biomarkers and all participants had donated blood, urine, and stool samples; all were of Chinese descent, Mr. Ayada said.
“We then pooled our results with existing evidence in a meta-analysis,” said Mr. Ayada, including 16 studies. While results showed an overall inverse association, only the findings for a reduction in NAFLD and fibrosis were significant; the relationship between statins and NASH was not significant.
Investigating mechanistic effects
Then, for the second part of their work, Mr. Ayada and associates looked at potential mechanistic effects of statins.
“We did part two because we knew part one was going to be cross-sectional and we could only show the association and not causality, so we tried to shed some light on possible pathways,” he said.
To do this they used a novel model of liver organoids developed to study fatty liver disease and test potential therapeutics. In this model human liver organoids are exposed to sodium lactate, sodium pyruvate, and octanoic acid, which induce the formation of lipid droplets. Exposing the organoids to statins – simvastatin and lovastatin were used in the experiments – resulted in a reduced number of the induced lipid droplets.
“Although all concentrations of statins significantly inhibited the lipid size versus the control, the major effect was quite modest,” observed Mr. Ayada. The effect was most noticeable at the highest dose used (10 micromolar), and what they think might be happening is that the statins are clearing the smaller droplets first, leaving the larger ones behind.
Next, they looked at the effect of statin treatment on inflammatory gene expression in liver-derived monocytes. These will turn into macrophages and play a key role in chronic inflammation, Mr. Ayada explained. Initial results suggest that several proinflammatory cytokines such as interleukin-1 beta, IL-6, and IL-8 may be downplayed by statin therapy.
An anti-inflammatory effect of statins was also reported in unrelated poster presentations at the congress. While researchers Seul Ki Han and associated from South Korea showed an anti-inflammatory effect of a combination of simvastatin and ezetimibe (SAT083), a Dutch team found that atorvastatin reduced the infiltration of hepatic macrophages, neutrophils, and monocytes, as well as lowering levels of proinflammatory cytokines (SAT033).
Statins for NASH – a missed opportunity?
“As far as I am aware there is no robust evidence from large, randomized trials to suggest statins lessen chances of NAFLD, or improve its surrogate markers such as ALT or GGT [gamma-glutamyltransferase] levels,” Naveed Sattar, PhD, FRCP, FRCPath, FRSE, FMedSci, commented in an interview.
“The Rotterdam study is merely cross-sectional and cannot answer the question of causality,” added Dr. Sattar, who is professor of metabolic medicine and Honorary Consultant in Cardiovascular & Medical Science at the University of Glasgow. “It may be people who have less NAFLD are more likely to be prescribed statins, perhaps because doctors are wary of prescribing statins to those with slightly deranged liver tests,” he qualified.
Moreover, said Dr. Sattar, “prior evidence shows statins are underused in people with heart disease but who have NAFLD, which represents a missed opportunity to prevent heart disease.
“If statins had positive effects for preventing conversion of NAFLD to NASH or lessening fibrosis, I believe we would have known that by now.”
As for use of statins in future treatments of fatty liver disease, Dr. Sattar said: “I would not pin my hopes on statins to improve liver health, but doctors need to remember statins are safe in people with NAFLD or NASH and they should not be withheld in those who have existing cardiovascular disease or at elevated risk.”
The study received no commercial funding. Mr. Ayada and Dr. Sattar had no relevant conflicts of interest.
LONDON – Substantial reductions in liver fat and fibrosis can be achieved with statin therapy, according to research presented at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
Statins are thought to have multiple beneficial actions in people with fatty liver disease, but there has been little insight into how they may be exerting such effects.
Now, data from the Rotterdam Study and others suggest that statins may be reducing the formation of lipid droplets as well as influencing the expression of important inflammatory genes.
The results “require further confirmation,” the team behind the work said, which was done at Erasmus Medical Center in Rotterdam, the Netherlands, in collaboration with researchers at The First Affiliated Hospital of Wenzhou (China) Medical University.
“Statins are inversely associated with multiple components of the NAFLD [nonalcoholic fatty liver disease] spectrum,” said Ibrahim Ayada, a PhD student in the department of gastroenterology and hepatology at Erasmus MC.
“Statins can inhibit lipid synthesis in organoids and statins also exhibit healthy inflammatory effects, which might contribute to the hepatoprotective effects that we observe in our population studies,” Mr. Ayada said.
A rising problem that needs addressing
Together NAFLD and NASH constitute a significant and increasing health burden, Mr. Ayada observed, noting that there were an estimated 64 million people in the United States and 52 million people in Europe, at least, with the rise mirroring the obesity pandemic.
“The number of patients visiting outpatient clinics has nearly doubled within a study period of 5 years,” he said.
“There is no pharmacologic therapy,” he reminded his audience, observing that fatty liver disease was a major indication for liver transplantation.
Statins are a long-standing staple of cardiovascular disease management and are known to have pleiotropic effects, Mr. Ayada explained. Their use in NAFLD and non-alcoholic steatohepatitis (NASH) has been purported but is supported by inconclusive evidence.
Indeed, a prior Cochrane review performed in 2013 found only two studies that were eligible for analysis and had “high risk of bias and a small numbers of participants,” according to the review’s authors.
Examining the connection
To look at the possible benefits of statins in people with NASH and examine how these effects might be occurring, Mr. Ayada and collaborators first took data from the Rotterdam Study, a large population-based prospective cohort that has been collecting data on its participants since the early 90s.
Data on over 4,500 participants were examined and of these, just over 1,000 had NAFLD. Statin versus no statin use was found to be associated with around a 30% reduction in fatty liver disease, with an odds ratio or 0.72 for NAFLD.
Then, looking only at a subset of patients with biopsy-proven NAFLD, statin use was associated with a 45% reduction in NASH (OR, 0.55) and a 24% reduction in fibrosis, although only the NASH reduction was significant (P = .031). The purpose of this cohort is to look at potential biomarkers and all participants had donated blood, urine, and stool samples; all were of Chinese descent, Mr. Ayada said.
“We then pooled our results with existing evidence in a meta-analysis,” said Mr. Ayada, including 16 studies. While results showed an overall inverse association, only the findings for a reduction in NAFLD and fibrosis were significant; the relationship between statins and NASH was not significant.
Investigating mechanistic effects
Then, for the second part of their work, Mr. Ayada and associates looked at potential mechanistic effects of statins.
“We did part two because we knew part one was going to be cross-sectional and we could only show the association and not causality, so we tried to shed some light on possible pathways,” he said.
To do this they used a novel model of liver organoids developed to study fatty liver disease and test potential therapeutics. In this model human liver organoids are exposed to sodium lactate, sodium pyruvate, and octanoic acid, which induce the formation of lipid droplets. Exposing the organoids to statins – simvastatin and lovastatin were used in the experiments – resulted in a reduced number of the induced lipid droplets.
“Although all concentrations of statins significantly inhibited the lipid size versus the control, the major effect was quite modest,” observed Mr. Ayada. The effect was most noticeable at the highest dose used (10 micromolar), and what they think might be happening is that the statins are clearing the smaller droplets first, leaving the larger ones behind.
Next, they looked at the effect of statin treatment on inflammatory gene expression in liver-derived monocytes. These will turn into macrophages and play a key role in chronic inflammation, Mr. Ayada explained. Initial results suggest that several proinflammatory cytokines such as interleukin-1 beta, IL-6, and IL-8 may be downplayed by statin therapy.
An anti-inflammatory effect of statins was also reported in unrelated poster presentations at the congress. While researchers Seul Ki Han and associated from South Korea showed an anti-inflammatory effect of a combination of simvastatin and ezetimibe (SAT083), a Dutch team found that atorvastatin reduced the infiltration of hepatic macrophages, neutrophils, and monocytes, as well as lowering levels of proinflammatory cytokines (SAT033).
Statins for NASH – a missed opportunity?
“As far as I am aware there is no robust evidence from large, randomized trials to suggest statins lessen chances of NAFLD, or improve its surrogate markers such as ALT or GGT [gamma-glutamyltransferase] levels,” Naveed Sattar, PhD, FRCP, FRCPath, FRSE, FMedSci, commented in an interview.
“The Rotterdam study is merely cross-sectional and cannot answer the question of causality,” added Dr. Sattar, who is professor of metabolic medicine and Honorary Consultant in Cardiovascular & Medical Science at the University of Glasgow. “It may be people who have less NAFLD are more likely to be prescribed statins, perhaps because doctors are wary of prescribing statins to those with slightly deranged liver tests,” he qualified.
Moreover, said Dr. Sattar, “prior evidence shows statins are underused in people with heart disease but who have NAFLD, which represents a missed opportunity to prevent heart disease.
“If statins had positive effects for preventing conversion of NAFLD to NASH or lessening fibrosis, I believe we would have known that by now.”
As for use of statins in future treatments of fatty liver disease, Dr. Sattar said: “I would not pin my hopes on statins to improve liver health, but doctors need to remember statins are safe in people with NAFLD or NASH and they should not be withheld in those who have existing cardiovascular disease or at elevated risk.”
The study received no commercial funding. Mr. Ayada and Dr. Sattar had no relevant conflicts of interest.
LONDON – Substantial reductions in liver fat and fibrosis can be achieved with statin therapy, according to research presented at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
Statins are thought to have multiple beneficial actions in people with fatty liver disease, but there has been little insight into how they may be exerting such effects.
Now, data from the Rotterdam Study and others suggest that statins may be reducing the formation of lipid droplets as well as influencing the expression of important inflammatory genes.
The results “require further confirmation,” the team behind the work said, which was done at Erasmus Medical Center in Rotterdam, the Netherlands, in collaboration with researchers at The First Affiliated Hospital of Wenzhou (China) Medical University.
“Statins are inversely associated with multiple components of the NAFLD [nonalcoholic fatty liver disease] spectrum,” said Ibrahim Ayada, a PhD student in the department of gastroenterology and hepatology at Erasmus MC.
“Statins can inhibit lipid synthesis in organoids and statins also exhibit healthy inflammatory effects, which might contribute to the hepatoprotective effects that we observe in our population studies,” Mr. Ayada said.
A rising problem that needs addressing
Together NAFLD and NASH constitute a significant and increasing health burden, Mr. Ayada observed, noting that there were an estimated 64 million people in the United States and 52 million people in Europe, at least, with the rise mirroring the obesity pandemic.
“The number of patients visiting outpatient clinics has nearly doubled within a study period of 5 years,” he said.
“There is no pharmacologic therapy,” he reminded his audience, observing that fatty liver disease was a major indication for liver transplantation.
Statins are a long-standing staple of cardiovascular disease management and are known to have pleiotropic effects, Mr. Ayada explained. Their use in NAFLD and non-alcoholic steatohepatitis (NASH) has been purported but is supported by inconclusive evidence.
Indeed, a prior Cochrane review performed in 2013 found only two studies that were eligible for analysis and had “high risk of bias and a small numbers of participants,” according to the review’s authors.
Examining the connection
To look at the possible benefits of statins in people with NASH and examine how these effects might be occurring, Mr. Ayada and collaborators first took data from the Rotterdam Study, a large population-based prospective cohort that has been collecting data on its participants since the early 90s.
Data on over 4,500 participants were examined and of these, just over 1,000 had NAFLD. Statin versus no statin use was found to be associated with around a 30% reduction in fatty liver disease, with an odds ratio or 0.72 for NAFLD.
Then, looking only at a subset of patients with biopsy-proven NAFLD, statin use was associated with a 45% reduction in NASH (OR, 0.55) and a 24% reduction in fibrosis, although only the NASH reduction was significant (P = .031). The purpose of this cohort is to look at potential biomarkers and all participants had donated blood, urine, and stool samples; all were of Chinese descent, Mr. Ayada said.
“We then pooled our results with existing evidence in a meta-analysis,” said Mr. Ayada, including 16 studies. While results showed an overall inverse association, only the findings for a reduction in NAFLD and fibrosis were significant; the relationship between statins and NASH was not significant.
Investigating mechanistic effects
Then, for the second part of their work, Mr. Ayada and associates looked at potential mechanistic effects of statins.
“We did part two because we knew part one was going to be cross-sectional and we could only show the association and not causality, so we tried to shed some light on possible pathways,” he said.
To do this they used a novel model of liver organoids developed to study fatty liver disease and test potential therapeutics. In this model human liver organoids are exposed to sodium lactate, sodium pyruvate, and octanoic acid, which induce the formation of lipid droplets. Exposing the organoids to statins – simvastatin and lovastatin were used in the experiments – resulted in a reduced number of the induced lipid droplets.
“Although all concentrations of statins significantly inhibited the lipid size versus the control, the major effect was quite modest,” observed Mr. Ayada. The effect was most noticeable at the highest dose used (10 micromolar), and what they think might be happening is that the statins are clearing the smaller droplets first, leaving the larger ones behind.
Next, they looked at the effect of statin treatment on inflammatory gene expression in liver-derived monocytes. These will turn into macrophages and play a key role in chronic inflammation, Mr. Ayada explained. Initial results suggest that several proinflammatory cytokines such as interleukin-1 beta, IL-6, and IL-8 may be downplayed by statin therapy.
An anti-inflammatory effect of statins was also reported in unrelated poster presentations at the congress. While researchers Seul Ki Han and associated from South Korea showed an anti-inflammatory effect of a combination of simvastatin and ezetimibe (SAT083), a Dutch team found that atorvastatin reduced the infiltration of hepatic macrophages, neutrophils, and monocytes, as well as lowering levels of proinflammatory cytokines (SAT033).
Statins for NASH – a missed opportunity?
“As far as I am aware there is no robust evidence from large, randomized trials to suggest statins lessen chances of NAFLD, or improve its surrogate markers such as ALT or GGT [gamma-glutamyltransferase] levels,” Naveed Sattar, PhD, FRCP, FRCPath, FRSE, FMedSci, commented in an interview.
“The Rotterdam study is merely cross-sectional and cannot answer the question of causality,” added Dr. Sattar, who is professor of metabolic medicine and Honorary Consultant in Cardiovascular & Medical Science at the University of Glasgow. “It may be people who have less NAFLD are more likely to be prescribed statins, perhaps because doctors are wary of prescribing statins to those with slightly deranged liver tests,” he qualified.
Moreover, said Dr. Sattar, “prior evidence shows statins are underused in people with heart disease but who have NAFLD, which represents a missed opportunity to prevent heart disease.
“If statins had positive effects for preventing conversion of NAFLD to NASH or lessening fibrosis, I believe we would have known that by now.”
As for use of statins in future treatments of fatty liver disease, Dr. Sattar said: “I would not pin my hopes on statins to improve liver health, but doctors need to remember statins are safe in people with NAFLD or NASH and they should not be withheld in those who have existing cardiovascular disease or at elevated risk.”
The study received no commercial funding. Mr. Ayada and Dr. Sattar had no relevant conflicts of interest.
AT ILC 2022
Phase 3 data shows bulevirtide benefit in hepatitis D
LONDON – Bulevirtide may not just treat but perhaps be a potential cure for hepatitis D in some patients, as was suggested at the annual International Liver Congress.
Data from an ongoing phase 3 trial showed that, after 48 weeks of treatment, almost half of those treated with bulevirtide achieved the combined primary endpoint of reduced or undetectable hepatitis delta virus (HDV) RNA levels and normalized ALT levels.
“The good message for our patients is that the initial data of the smaller phase 2 trials will really be confirmed, so the drug works,” Heiner Wedemeyer, MD, said at a media briefing ahead of his presentation at the meeting sponsored by the European Association for the Study of the Liver .
“It induces a decline in viral load and, very importantly for us as hepatologists, liver enzymes normalize, this is really good news” added Dr. Wedemeyer, who is the clinic director of the department of gastroenterology, hepatology, and endocrinology at Hannover (Germany) Medical School.
“This is really an almost historic moment for hepatology,” he said. “It’s the first time that these patients have an antiviral treatment; they are afraid of dying and now they have a hope.”
Giving his thoughts, Thomas Berg, MD, Secretary General of EASL, said: “We are entering into a golden age of hepatology science when it comes to viral hepatitis.
Dr. Berg, also of University Clinic Leipzig (Germany), added: “We have several million people worldwide living with viral hepatitis; we have a cure for hepatitis C but there’s no cure for hepatitis B or hepatitis D, so these data give me great hope that we have scientific momentum with us.”
Pivotal phase 3 study
The MYR301 trial is an important and pivotal study for bulevirtide, which is a first-in-class HDV entry inhibitor. While it was approved for use Europe in 2020 under the brand name Hepcludex, the drug remains investigational in the United States.
“We were really surprised that EMA [European Medicines Agency] went forward, granting approval because there was no alternative available at that time,” Dr. Wedemeyer said. That approval is conditional, however, and was based on the results of phase 2 studies with the proviso that further data needed would need to be provided. Hopefully, the phase 3 findings will mean that the drug will receive full official approval, he said.
Overall, 150 patients with chronic hepatitis D were recruited into the phase 3 study and randomized to receive one of two doses of bulevirtide (2 mg or 10 mg) for 144 weeks or delayed treatment for 48 weeks followed by the higher dose of the drug until the remainder of the treatment period. Bulevirtide was given as once-daily subcutaneous injection.
The mean age of participants was 41 years, the majority (82.7%) were White, and just under half already had liver cirrhosis. For inclusion, Dr. Wedemeyer said that they had to have compensated cirrhosis.
Just over half had received prior interferon therapy and almost two-thirds were receiving concomitant nucleos(t)ide (NUC) treatment.
Key results
The primary endpoint was defined as a combination of decreased HDV RNA (defined as undetectable or a 2 log or greater decrease) and normalized ALT (defined as 3.1 U/L or less in women and 4.1 U/L or less in men). This was assessed after 48 weeks’ treatment and was achieved by 45% of participants given the 2-mg dose of bulevirtide, 48% of those given the 10-mg dose, and by 2% of those who had delayed treatment (P < .0001 for both doses, compared with delayed treatment).
The treatment benefit was consistent across all subgroups of patients, including those with cirrhosis, Dr. Wedemeyer reported.
Looking at some of the secondary endpoints, he reported that, when considering only decreased HDV RNA, the rate of response was over 70% with both dose of bulevirtide at week 48, compared with just 4% for delayed treatment (P < .0001), although there was no significant difference in rates of undetectable HDV RNA between the two doses. ALT normalization rates were 51%-56% versus 12% for delayed treatment (P < .0001).
A further benefit was seen in liver stiffness, with values reduced by at least three points at week 48 with either dose of bulevirtide, compared with an increase of almost 1 point for delayed treatment.
As for side effects, one of the concerns for bulevirtide is an increase in serum bile acids, but when this occurred, it occurred early and remained steady over the course of treatment, with a less pronounced effect in the 2 mg–dosed group than the 10 mg–dosed group. There were no serious adverse reactions related to bulevirtide or any adverse event that led to stopping the drug.
“There are always questions that need to be answered,” Dr. Wedemeyer acknowledged. Indeed, it’s unclear for how long patients need to be treated and if treatment with interferon is needed. In the phase 2 studies (MYR202 and MYR203), bulevirtide was given at the same time as pegylated interferon alpha (peg-IFNa) or tenofovir, whereas in the phase 3 MYR301 trial, it was given as monotherapy.
Real-world experience
“We have already some real-world data in parallel to this phase 3 trial,” Dr. Wedemeyer said. “So, for us in the hepatitis D field, it is a really exciting time; [it’s] completely novel data and game-changing for patients.”
“The results are similar to our real life study, but in our real-life study, we have some patients treated with interferon and some not treated with interferon,” Hélène Fontaine, MD, of Hôpital Cochin in Paris, observed in an interview.
She reported preliminary results from the prospective BuleDelta cohort, which showed a virologic response rate of 58% and ALT normalization in 46% of patients.
“Virologic response was achieved in more patients receiving bulevirtide in combination with interferon,” she said. Indeed, 84% of patient who received peg-IFNa versus 39% of those who did not achieved a virologic response. However, rates of ALT normalization were more frequent in those received bulevirtide monotherapy than in combination with peg-IFN1 (54% vs. 35%).
A greater benefit of combining bulevirtide with interferon therapy was also seen in another real-world study presented by Victor de Lédinghen, MD, PhD, of Bordeaux (France) University Hospital. After 18 months of treatment, bulevirtide plus peg-IFNa was associated with undetectable HDV RNA in 57% of patients versus 33% of those given the drug as monotherapy.
“Of course, if you add interferon, it’s better than without but you cannot use interferon in all patients,” he observed in an interview.
Results are good but could be better, he suggested, noting that the results are dependent on patients injecting themselves correctly on a daily basis.
At the media briefing Dr. Wedemeyer also commented on how bulevirtide must be delivered.
“The only, let’s say, disadvantage is that it has to be injected because it’s a peptide, which requires daily injections, but patients managed very well,” Dr. Wedemeyer said.
“There is some evidence from single cases that we may stop treatment and that the virus does not come back,” he said, but stressed that patients should not stop treatment on their own as the risk is not known.
“For patients with advanced disease I consider this as a maintenance treatment,” Dr. Wedemeyer said, at least for the time being.
The MYR3201 study was funded by Gilead Sciences. The BuleDelta cohort is sponsored by the ANRS Maladies Infectieuses Emergencies. Dr. Wedemeyer acknowledged research funding, acting as a consultant to, and giving paid lectures on behalf of Gilead Sciences and MYR as well as having ties to multiple pharmaceutical and biotechnology companies. Dr. Berg, Dr. Fontaine, and Dr. de Lédinghen had no conflicts of interest to report.
LONDON – Bulevirtide may not just treat but perhaps be a potential cure for hepatitis D in some patients, as was suggested at the annual International Liver Congress.
Data from an ongoing phase 3 trial showed that, after 48 weeks of treatment, almost half of those treated with bulevirtide achieved the combined primary endpoint of reduced or undetectable hepatitis delta virus (HDV) RNA levels and normalized ALT levels.
“The good message for our patients is that the initial data of the smaller phase 2 trials will really be confirmed, so the drug works,” Heiner Wedemeyer, MD, said at a media briefing ahead of his presentation at the meeting sponsored by the European Association for the Study of the Liver .
“It induces a decline in viral load and, very importantly for us as hepatologists, liver enzymes normalize, this is really good news” added Dr. Wedemeyer, who is the clinic director of the department of gastroenterology, hepatology, and endocrinology at Hannover (Germany) Medical School.
“This is really an almost historic moment for hepatology,” he said. “It’s the first time that these patients have an antiviral treatment; they are afraid of dying and now they have a hope.”
Giving his thoughts, Thomas Berg, MD, Secretary General of EASL, said: “We are entering into a golden age of hepatology science when it comes to viral hepatitis.
Dr. Berg, also of University Clinic Leipzig (Germany), added: “We have several million people worldwide living with viral hepatitis; we have a cure for hepatitis C but there’s no cure for hepatitis B or hepatitis D, so these data give me great hope that we have scientific momentum with us.”
Pivotal phase 3 study
The MYR301 trial is an important and pivotal study for bulevirtide, which is a first-in-class HDV entry inhibitor. While it was approved for use Europe in 2020 under the brand name Hepcludex, the drug remains investigational in the United States.
“We were really surprised that EMA [European Medicines Agency] went forward, granting approval because there was no alternative available at that time,” Dr. Wedemeyer said. That approval is conditional, however, and was based on the results of phase 2 studies with the proviso that further data needed would need to be provided. Hopefully, the phase 3 findings will mean that the drug will receive full official approval, he said.
Overall, 150 patients with chronic hepatitis D were recruited into the phase 3 study and randomized to receive one of two doses of bulevirtide (2 mg or 10 mg) for 144 weeks or delayed treatment for 48 weeks followed by the higher dose of the drug until the remainder of the treatment period. Bulevirtide was given as once-daily subcutaneous injection.
The mean age of participants was 41 years, the majority (82.7%) were White, and just under half already had liver cirrhosis. For inclusion, Dr. Wedemeyer said that they had to have compensated cirrhosis.
Just over half had received prior interferon therapy and almost two-thirds were receiving concomitant nucleos(t)ide (NUC) treatment.
Key results
The primary endpoint was defined as a combination of decreased HDV RNA (defined as undetectable or a 2 log or greater decrease) and normalized ALT (defined as 3.1 U/L or less in women and 4.1 U/L or less in men). This was assessed after 48 weeks’ treatment and was achieved by 45% of participants given the 2-mg dose of bulevirtide, 48% of those given the 10-mg dose, and by 2% of those who had delayed treatment (P < .0001 for both doses, compared with delayed treatment).
The treatment benefit was consistent across all subgroups of patients, including those with cirrhosis, Dr. Wedemeyer reported.
Looking at some of the secondary endpoints, he reported that, when considering only decreased HDV RNA, the rate of response was over 70% with both dose of bulevirtide at week 48, compared with just 4% for delayed treatment (P < .0001), although there was no significant difference in rates of undetectable HDV RNA between the two doses. ALT normalization rates were 51%-56% versus 12% for delayed treatment (P < .0001).
A further benefit was seen in liver stiffness, with values reduced by at least three points at week 48 with either dose of bulevirtide, compared with an increase of almost 1 point for delayed treatment.
As for side effects, one of the concerns for bulevirtide is an increase in serum bile acids, but when this occurred, it occurred early and remained steady over the course of treatment, with a less pronounced effect in the 2 mg–dosed group than the 10 mg–dosed group. There were no serious adverse reactions related to bulevirtide or any adverse event that led to stopping the drug.
“There are always questions that need to be answered,” Dr. Wedemeyer acknowledged. Indeed, it’s unclear for how long patients need to be treated and if treatment with interferon is needed. In the phase 2 studies (MYR202 and MYR203), bulevirtide was given at the same time as pegylated interferon alpha (peg-IFNa) or tenofovir, whereas in the phase 3 MYR301 trial, it was given as monotherapy.
Real-world experience
“We have already some real-world data in parallel to this phase 3 trial,” Dr. Wedemeyer said. “So, for us in the hepatitis D field, it is a really exciting time; [it’s] completely novel data and game-changing for patients.”
“The results are similar to our real life study, but in our real-life study, we have some patients treated with interferon and some not treated with interferon,” Hélène Fontaine, MD, of Hôpital Cochin in Paris, observed in an interview.
She reported preliminary results from the prospective BuleDelta cohort, which showed a virologic response rate of 58% and ALT normalization in 46% of patients.
“Virologic response was achieved in more patients receiving bulevirtide in combination with interferon,” she said. Indeed, 84% of patient who received peg-IFNa versus 39% of those who did not achieved a virologic response. However, rates of ALT normalization were more frequent in those received bulevirtide monotherapy than in combination with peg-IFN1 (54% vs. 35%).
A greater benefit of combining bulevirtide with interferon therapy was also seen in another real-world study presented by Victor de Lédinghen, MD, PhD, of Bordeaux (France) University Hospital. After 18 months of treatment, bulevirtide plus peg-IFNa was associated with undetectable HDV RNA in 57% of patients versus 33% of those given the drug as monotherapy.
“Of course, if you add interferon, it’s better than without but you cannot use interferon in all patients,” he observed in an interview.
Results are good but could be better, he suggested, noting that the results are dependent on patients injecting themselves correctly on a daily basis.
At the media briefing Dr. Wedemeyer also commented on how bulevirtide must be delivered.
“The only, let’s say, disadvantage is that it has to be injected because it’s a peptide, which requires daily injections, but patients managed very well,” Dr. Wedemeyer said.
“There is some evidence from single cases that we may stop treatment and that the virus does not come back,” he said, but stressed that patients should not stop treatment on their own as the risk is not known.
“For patients with advanced disease I consider this as a maintenance treatment,” Dr. Wedemeyer said, at least for the time being.
The MYR3201 study was funded by Gilead Sciences. The BuleDelta cohort is sponsored by the ANRS Maladies Infectieuses Emergencies. Dr. Wedemeyer acknowledged research funding, acting as a consultant to, and giving paid lectures on behalf of Gilead Sciences and MYR as well as having ties to multiple pharmaceutical and biotechnology companies. Dr. Berg, Dr. Fontaine, and Dr. de Lédinghen had no conflicts of interest to report.
LONDON – Bulevirtide may not just treat but perhaps be a potential cure for hepatitis D in some patients, as was suggested at the annual International Liver Congress.
Data from an ongoing phase 3 trial showed that, after 48 weeks of treatment, almost half of those treated with bulevirtide achieved the combined primary endpoint of reduced or undetectable hepatitis delta virus (HDV) RNA levels and normalized ALT levels.
“The good message for our patients is that the initial data of the smaller phase 2 trials will really be confirmed, so the drug works,” Heiner Wedemeyer, MD, said at a media briefing ahead of his presentation at the meeting sponsored by the European Association for the Study of the Liver .
“It induces a decline in viral load and, very importantly for us as hepatologists, liver enzymes normalize, this is really good news” added Dr. Wedemeyer, who is the clinic director of the department of gastroenterology, hepatology, and endocrinology at Hannover (Germany) Medical School.
“This is really an almost historic moment for hepatology,” he said. “It’s the first time that these patients have an antiviral treatment; they are afraid of dying and now they have a hope.”
Giving his thoughts, Thomas Berg, MD, Secretary General of EASL, said: “We are entering into a golden age of hepatology science when it comes to viral hepatitis.
Dr. Berg, also of University Clinic Leipzig (Germany), added: “We have several million people worldwide living with viral hepatitis; we have a cure for hepatitis C but there’s no cure for hepatitis B or hepatitis D, so these data give me great hope that we have scientific momentum with us.”
Pivotal phase 3 study
The MYR301 trial is an important and pivotal study for bulevirtide, which is a first-in-class HDV entry inhibitor. While it was approved for use Europe in 2020 under the brand name Hepcludex, the drug remains investigational in the United States.
“We were really surprised that EMA [European Medicines Agency] went forward, granting approval because there was no alternative available at that time,” Dr. Wedemeyer said. That approval is conditional, however, and was based on the results of phase 2 studies with the proviso that further data needed would need to be provided. Hopefully, the phase 3 findings will mean that the drug will receive full official approval, he said.
Overall, 150 patients with chronic hepatitis D were recruited into the phase 3 study and randomized to receive one of two doses of bulevirtide (2 mg or 10 mg) for 144 weeks or delayed treatment for 48 weeks followed by the higher dose of the drug until the remainder of the treatment period. Bulevirtide was given as once-daily subcutaneous injection.
The mean age of participants was 41 years, the majority (82.7%) were White, and just under half already had liver cirrhosis. For inclusion, Dr. Wedemeyer said that they had to have compensated cirrhosis.
Just over half had received prior interferon therapy and almost two-thirds were receiving concomitant nucleos(t)ide (NUC) treatment.
Key results
The primary endpoint was defined as a combination of decreased HDV RNA (defined as undetectable or a 2 log or greater decrease) and normalized ALT (defined as 3.1 U/L or less in women and 4.1 U/L or less in men). This was assessed after 48 weeks’ treatment and was achieved by 45% of participants given the 2-mg dose of bulevirtide, 48% of those given the 10-mg dose, and by 2% of those who had delayed treatment (P < .0001 for both doses, compared with delayed treatment).
The treatment benefit was consistent across all subgroups of patients, including those with cirrhosis, Dr. Wedemeyer reported.
Looking at some of the secondary endpoints, he reported that, when considering only decreased HDV RNA, the rate of response was over 70% with both dose of bulevirtide at week 48, compared with just 4% for delayed treatment (P < .0001), although there was no significant difference in rates of undetectable HDV RNA between the two doses. ALT normalization rates were 51%-56% versus 12% for delayed treatment (P < .0001).
A further benefit was seen in liver stiffness, with values reduced by at least three points at week 48 with either dose of bulevirtide, compared with an increase of almost 1 point for delayed treatment.
As for side effects, one of the concerns for bulevirtide is an increase in serum bile acids, but when this occurred, it occurred early and remained steady over the course of treatment, with a less pronounced effect in the 2 mg–dosed group than the 10 mg–dosed group. There were no serious adverse reactions related to bulevirtide or any adverse event that led to stopping the drug.
“There are always questions that need to be answered,” Dr. Wedemeyer acknowledged. Indeed, it’s unclear for how long patients need to be treated and if treatment with interferon is needed. In the phase 2 studies (MYR202 and MYR203), bulevirtide was given at the same time as pegylated interferon alpha (peg-IFNa) or tenofovir, whereas in the phase 3 MYR301 trial, it was given as monotherapy.
Real-world experience
“We have already some real-world data in parallel to this phase 3 trial,” Dr. Wedemeyer said. “So, for us in the hepatitis D field, it is a really exciting time; [it’s] completely novel data and game-changing for patients.”
“The results are similar to our real life study, but in our real-life study, we have some patients treated with interferon and some not treated with interferon,” Hélène Fontaine, MD, of Hôpital Cochin in Paris, observed in an interview.
She reported preliminary results from the prospective BuleDelta cohort, which showed a virologic response rate of 58% and ALT normalization in 46% of patients.
“Virologic response was achieved in more patients receiving bulevirtide in combination with interferon,” she said. Indeed, 84% of patient who received peg-IFNa versus 39% of those who did not achieved a virologic response. However, rates of ALT normalization were more frequent in those received bulevirtide monotherapy than in combination with peg-IFN1 (54% vs. 35%).
A greater benefit of combining bulevirtide with interferon therapy was also seen in another real-world study presented by Victor de Lédinghen, MD, PhD, of Bordeaux (France) University Hospital. After 18 months of treatment, bulevirtide plus peg-IFNa was associated with undetectable HDV RNA in 57% of patients versus 33% of those given the drug as monotherapy.
“Of course, if you add interferon, it’s better than without but you cannot use interferon in all patients,” he observed in an interview.
Results are good but could be better, he suggested, noting that the results are dependent on patients injecting themselves correctly on a daily basis.
At the media briefing Dr. Wedemeyer also commented on how bulevirtide must be delivered.
“The only, let’s say, disadvantage is that it has to be injected because it’s a peptide, which requires daily injections, but patients managed very well,” Dr. Wedemeyer said.
“There is some evidence from single cases that we may stop treatment and that the virus does not come back,” he said, but stressed that patients should not stop treatment on their own as the risk is not known.
“For patients with advanced disease I consider this as a maintenance treatment,” Dr. Wedemeyer said, at least for the time being.
The MYR3201 study was funded by Gilead Sciences. The BuleDelta cohort is sponsored by the ANRS Maladies Infectieuses Emergencies. Dr. Wedemeyer acknowledged research funding, acting as a consultant to, and giving paid lectures on behalf of Gilead Sciences and MYR as well as having ties to multiple pharmaceutical and biotechnology companies. Dr. Berg, Dr. Fontaine, and Dr. de Lédinghen had no conflicts of interest to report.
AT ILC 2022
Low-carb, high-fat diet improves A1c, reduces liver fat
LONDON – A low-carbohydrate, high-fat (LCHF) diet reduced the progression of nonalcoholic fatty liver disease (NAFLD), and despite no calorie restriction, participants with both NAFLD and type 2 diabetes lost 5.8% of their body weight, according to a randomized controlled study.
“Based on these results, the LCHF diet may be recommended to people with NAFLD and type 2 diabetes,” said Camilla Dalby Hansen, MD, department of gastroenterology and hepatology, Odense University Hospital, Denmark, who presented the data at the International Liver Congress (ILC) 2022.
“Basically, if you have fat in your liver, you will benefit from eating fat,” she said.
The LCHF diet was compared with a low-fat, high-carbohydrate diet more typically followed for these conditions. The low-fat diet was also found to reduce the progression of NAFLD, but to a lesser extent than the LCHF diet.
Dr. Dalby Hansen called their study one of the most extensive investigations of the LCHF diet in patients with type 2 diabetes and fatty liver disease.
“Combining this [reduction in NAFLD score] with the huge weight loss, the lower HbA1c [blood sugar], the lowering of blood pressure in women, the rise in HDL levels, and reduction in triglycerides – all in all, this diet is very promising,” she said.
Stephen Harrison, MD, visiting professor, University of Oxford, United Kingdom, medical director of Pinnacle Clinical Research and president of Summit Clinical Research, San Antonio, commended Dr. Dalby Hansen on her methodology, which included before-and-after liver biopsies. “It’s a heinous effort to do paired liver biopsies in a lifestyle modification trial. That’s huge.”
“This study tells me that the way we manage patients doesn’t change – it is still lifestyle modification,” said Dr. Harrison, who was not involved with the study. “It’s eat less [rather] than more. It’s exercise and try to lose weight. In the long term, we give patients benefit, and we show that the disease has improved, and we offer something that means they can maintain a healthy life.”
He added that the relatively small and short trial was informative.
“They improved the NAFLD activity score [NAS],” he said. “I don’t know by how much. There was no change in fibrosis, but we wouldn’t expect this at 6 months.”
“It’s provocative work, and it gives us healthy information about how we can help manage our patients from a lifestyle perspective,” he concluded.
‘Do not lose weight. Eat until you are full’
In the study, 110 participants with type 2 diabetes and NAFLD, aged 18-78 years, were allocated to the LCHF diet, and 55 were allocated to the low-fat diet for 6 months.
The researchers performed liver biopsies at baseline and 6 months, which were blinded for scoring.
Participants had ongoing dietitian consultations, with follow-up visits at 3 and 6 months. Compliance was reported continuously through an online food diary platform.
The primary endpoint was change in glycemic control as measured by A1c level over 6 months. The secondary endpoints comprised the proportion of participants with changes in the NAS of at least 2 points over 6 months. Both these measures were compared between the two dietary groups.
The two groups were matched at baseline, with a mean age of 55-57 years, 58% were women, 89% with metabolic syndrome, and a mean BMI 34 kg/m2.
In baseline liver disease, F1 level fibrosis was the most common (58%), followed by hepatic steatosis (S1, 47%; S2, 32%), with a median NAS of 3, and 19% had nonalcoholic steatohepatitis.
The special thing about these diets was that participants were told to “not lose weight, but eat until you are full,” remarked Dr. Dalby Hansen.
Those on the LCHF diet consumed an average of 61% energy from fat, 13% from carbohydrates, and 23% from protein, compared with the low-fat diet, which comprised an average of 29% energy from fat, 46% from carbohydrates, and 21% from protein.
“It’s a lot of fat and corresponds to a quarter of a liter of olive oil per day,” said Dr. Dalby Hansen. “They really had to change their mindset a lot, because it was difficult for them to start eating all these fats, especially since we’ve all been told for decades that it isn’t good. But we supported them, and they got into it.”
The LCHF diet was primarily comprised of unsaturated fats – for example, avocado, oil, nuts, and seeds – but also included saturated fats, such as cheese, cream, and high-fat dairy products. Participants were free to eat unsaturated and saturated fats, but Dr. Dalby Hansen and her team advised participants that “good” unsaturated fats were preferable.
“Also, this diet contained vegetables but no bread, no potatoes, no rice, and no pasta. It was low in carbohydrates, below 20%,” she added.
Improved glycemic control, reduced liver fat
“We found that the LCHF diet improved diabetes control, it reduced the fat in the liver, and, even though they’re eating as many calories as they were used to until they were full, they lost 5.8% of body weight,” said Dr. Dalby Hansen in reporting the results. Participants in the low-fat group lost only 1.8% of body weight.
However, mean calorie intake dropped in both groups, by –2.2% in the LCHF group and –8.7% in the low-fat group.
“The LCHF diet improved the primary outcome of A1c by 9.5 mmol/mol, which is similar to some anti-diabetic medications, such as DPP-4 inhibitors and SGLT2 inhibitors,” she said.
The low-fat group reduced A1c by 3.4 mmol/mol, resulting in a between-group difference of 6.1 mmol/mol.
“Upon follow-up of 3 months, after stopping the diets, on average the participants in both groups returned their HbA1c levels to nearly baseline values,” she said. Results were adjusted for weight loss and baseline values.
Both diets also improved the NAS. The proportion of participants who improved their NAS score by 2 or more points was 22% in the LCHF group versus 17% in the low-fat group (P = 0.58). Additionally, in the LCHF group, 70% of participants improved their score by 1 or more points, compared with 49% in the low-fat group and fewer in the LCHF group experienced a worsening of their score (1% vs. 23%, respectively).
One participant on LCHF had high triglycerides of 12 mmol/L after 3 months. Overall, the low-density lipoprotein increased marginally by 0.2 mmol per liter in the high-fat group, said Dr. Dalby Hansen.
Dr. Dalby Hansen noted some limitations. The findings might not be applicable in more severe NAFLD, dietary assessment relied on self-reporting, no food was provided, and participants had to cook themselves. It was also an open-label study because of the nature of the intervention.
Some hope for more sustainable dieting
Many diets are difficult to adhere to, remarked Dr. Dalby Hansen. “We thought this [diet] might be easier to comply with in the longer term, and we hope that these results might provide patients with more options.”
She added that most people who started the diet adapted and complied with it. “However, it might not be for everyone, but I think we can say that if people try, and it fits into their lives, then they go for it.”
However, “it is not about going out and eating whatever fat and how much of it you want. It’s important that you cut the carbohydrates too,” she said. “With this approach, we really saw amazing results.”
Dr. Dalby Hansen added that having various diets available, including the LCHF one, meant that as clinicians they could empower patients to take control of their metabolic health.
“We can ask them directly, ‘What would fit into their life?’” she said. “We know that one size does not fit at all, and I believe that if we could engage patients more, then they can take control of their own situation.”
Asked whether these findings were enough to change guidelines, Zobair Younossi, MD, professor and chairman, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., remarked that it was the sugar at work here.
“Dietary fat – it’s not the same as fat in the liver, and this diet has more to do with the sugar levels,” he said.
“I’m always reluctant to take results from a short-term study without long-term follow-up,” Dr. Younossi said. “I want to know will patients live longer, and long-term data are needed for this. Until I have that strong evidence that outcomes are going to change, or at least some sign that the outcome is going to change, it is too early to change any guidelines.”
Dr. Dalby Hansen reports no relevant financial relationships. Dr. Harrison reported financial relationships with numerous pharmaceutical companies. Dr. Younossi reports the following financial relationships: research funds and/or consultant to Abbott, Allergan, Bristol Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
LONDON – A low-carbohydrate, high-fat (LCHF) diet reduced the progression of nonalcoholic fatty liver disease (NAFLD), and despite no calorie restriction, participants with both NAFLD and type 2 diabetes lost 5.8% of their body weight, according to a randomized controlled study.
“Based on these results, the LCHF diet may be recommended to people with NAFLD and type 2 diabetes,” said Camilla Dalby Hansen, MD, department of gastroenterology and hepatology, Odense University Hospital, Denmark, who presented the data at the International Liver Congress (ILC) 2022.
“Basically, if you have fat in your liver, you will benefit from eating fat,” she said.
The LCHF diet was compared with a low-fat, high-carbohydrate diet more typically followed for these conditions. The low-fat diet was also found to reduce the progression of NAFLD, but to a lesser extent than the LCHF diet.
Dr. Dalby Hansen called their study one of the most extensive investigations of the LCHF diet in patients with type 2 diabetes and fatty liver disease.
“Combining this [reduction in NAFLD score] with the huge weight loss, the lower HbA1c [blood sugar], the lowering of blood pressure in women, the rise in HDL levels, and reduction in triglycerides – all in all, this diet is very promising,” she said.
Stephen Harrison, MD, visiting professor, University of Oxford, United Kingdom, medical director of Pinnacle Clinical Research and president of Summit Clinical Research, San Antonio, commended Dr. Dalby Hansen on her methodology, which included before-and-after liver biopsies. “It’s a heinous effort to do paired liver biopsies in a lifestyle modification trial. That’s huge.”
“This study tells me that the way we manage patients doesn’t change – it is still lifestyle modification,” said Dr. Harrison, who was not involved with the study. “It’s eat less [rather] than more. It’s exercise and try to lose weight. In the long term, we give patients benefit, and we show that the disease has improved, and we offer something that means they can maintain a healthy life.”
He added that the relatively small and short trial was informative.
“They improved the NAFLD activity score [NAS],” he said. “I don’t know by how much. There was no change in fibrosis, but we wouldn’t expect this at 6 months.”
“It’s provocative work, and it gives us healthy information about how we can help manage our patients from a lifestyle perspective,” he concluded.
‘Do not lose weight. Eat until you are full’
In the study, 110 participants with type 2 diabetes and NAFLD, aged 18-78 years, were allocated to the LCHF diet, and 55 were allocated to the low-fat diet for 6 months.
The researchers performed liver biopsies at baseline and 6 months, which were blinded for scoring.
Participants had ongoing dietitian consultations, with follow-up visits at 3 and 6 months. Compliance was reported continuously through an online food diary platform.
The primary endpoint was change in glycemic control as measured by A1c level over 6 months. The secondary endpoints comprised the proportion of participants with changes in the NAS of at least 2 points over 6 months. Both these measures were compared between the two dietary groups.
The two groups were matched at baseline, with a mean age of 55-57 years, 58% were women, 89% with metabolic syndrome, and a mean BMI 34 kg/m2.
In baseline liver disease, F1 level fibrosis was the most common (58%), followed by hepatic steatosis (S1, 47%; S2, 32%), with a median NAS of 3, and 19% had nonalcoholic steatohepatitis.
The special thing about these diets was that participants were told to “not lose weight, but eat until you are full,” remarked Dr. Dalby Hansen.
Those on the LCHF diet consumed an average of 61% energy from fat, 13% from carbohydrates, and 23% from protein, compared with the low-fat diet, which comprised an average of 29% energy from fat, 46% from carbohydrates, and 21% from protein.
“It’s a lot of fat and corresponds to a quarter of a liter of olive oil per day,” said Dr. Dalby Hansen. “They really had to change their mindset a lot, because it was difficult for them to start eating all these fats, especially since we’ve all been told for decades that it isn’t good. But we supported them, and they got into it.”
The LCHF diet was primarily comprised of unsaturated fats – for example, avocado, oil, nuts, and seeds – but also included saturated fats, such as cheese, cream, and high-fat dairy products. Participants were free to eat unsaturated and saturated fats, but Dr. Dalby Hansen and her team advised participants that “good” unsaturated fats were preferable.
“Also, this diet contained vegetables but no bread, no potatoes, no rice, and no pasta. It was low in carbohydrates, below 20%,” she added.
Improved glycemic control, reduced liver fat
“We found that the LCHF diet improved diabetes control, it reduced the fat in the liver, and, even though they’re eating as many calories as they were used to until they were full, they lost 5.8% of body weight,” said Dr. Dalby Hansen in reporting the results. Participants in the low-fat group lost only 1.8% of body weight.
However, mean calorie intake dropped in both groups, by –2.2% in the LCHF group and –8.7% in the low-fat group.
“The LCHF diet improved the primary outcome of A1c by 9.5 mmol/mol, which is similar to some anti-diabetic medications, such as DPP-4 inhibitors and SGLT2 inhibitors,” she said.
The low-fat group reduced A1c by 3.4 mmol/mol, resulting in a between-group difference of 6.1 mmol/mol.
“Upon follow-up of 3 months, after stopping the diets, on average the participants in both groups returned their HbA1c levels to nearly baseline values,” she said. Results were adjusted for weight loss and baseline values.
Both diets also improved the NAS. The proportion of participants who improved their NAS score by 2 or more points was 22% in the LCHF group versus 17% in the low-fat group (P = 0.58). Additionally, in the LCHF group, 70% of participants improved their score by 1 or more points, compared with 49% in the low-fat group and fewer in the LCHF group experienced a worsening of their score (1% vs. 23%, respectively).
One participant on LCHF had high triglycerides of 12 mmol/L after 3 months. Overall, the low-density lipoprotein increased marginally by 0.2 mmol per liter in the high-fat group, said Dr. Dalby Hansen.
Dr. Dalby Hansen noted some limitations. The findings might not be applicable in more severe NAFLD, dietary assessment relied on self-reporting, no food was provided, and participants had to cook themselves. It was also an open-label study because of the nature of the intervention.
Some hope for more sustainable dieting
Many diets are difficult to adhere to, remarked Dr. Dalby Hansen. “We thought this [diet] might be easier to comply with in the longer term, and we hope that these results might provide patients with more options.”
She added that most people who started the diet adapted and complied with it. “However, it might not be for everyone, but I think we can say that if people try, and it fits into their lives, then they go for it.”
However, “it is not about going out and eating whatever fat and how much of it you want. It’s important that you cut the carbohydrates too,” she said. “With this approach, we really saw amazing results.”
Dr. Dalby Hansen added that having various diets available, including the LCHF one, meant that as clinicians they could empower patients to take control of their metabolic health.
“We can ask them directly, ‘What would fit into their life?’” she said. “We know that one size does not fit at all, and I believe that if we could engage patients more, then they can take control of their own situation.”
Asked whether these findings were enough to change guidelines, Zobair Younossi, MD, professor and chairman, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., remarked that it was the sugar at work here.
“Dietary fat – it’s not the same as fat in the liver, and this diet has more to do with the sugar levels,” he said.
“I’m always reluctant to take results from a short-term study without long-term follow-up,” Dr. Younossi said. “I want to know will patients live longer, and long-term data are needed for this. Until I have that strong evidence that outcomes are going to change, or at least some sign that the outcome is going to change, it is too early to change any guidelines.”
Dr. Dalby Hansen reports no relevant financial relationships. Dr. Harrison reported financial relationships with numerous pharmaceutical companies. Dr. Younossi reports the following financial relationships: research funds and/or consultant to Abbott, Allergan, Bristol Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
LONDON – A low-carbohydrate, high-fat (LCHF) diet reduced the progression of nonalcoholic fatty liver disease (NAFLD), and despite no calorie restriction, participants with both NAFLD and type 2 diabetes lost 5.8% of their body weight, according to a randomized controlled study.
“Based on these results, the LCHF diet may be recommended to people with NAFLD and type 2 diabetes,” said Camilla Dalby Hansen, MD, department of gastroenterology and hepatology, Odense University Hospital, Denmark, who presented the data at the International Liver Congress (ILC) 2022.
“Basically, if you have fat in your liver, you will benefit from eating fat,” she said.
The LCHF diet was compared with a low-fat, high-carbohydrate diet more typically followed for these conditions. The low-fat diet was also found to reduce the progression of NAFLD, but to a lesser extent than the LCHF diet.
Dr. Dalby Hansen called their study one of the most extensive investigations of the LCHF diet in patients with type 2 diabetes and fatty liver disease.
“Combining this [reduction in NAFLD score] with the huge weight loss, the lower HbA1c [blood sugar], the lowering of blood pressure in women, the rise in HDL levels, and reduction in triglycerides – all in all, this diet is very promising,” she said.
Stephen Harrison, MD, visiting professor, University of Oxford, United Kingdom, medical director of Pinnacle Clinical Research and president of Summit Clinical Research, San Antonio, commended Dr. Dalby Hansen on her methodology, which included before-and-after liver biopsies. “It’s a heinous effort to do paired liver biopsies in a lifestyle modification trial. That’s huge.”
“This study tells me that the way we manage patients doesn’t change – it is still lifestyle modification,” said Dr. Harrison, who was not involved with the study. “It’s eat less [rather] than more. It’s exercise and try to lose weight. In the long term, we give patients benefit, and we show that the disease has improved, and we offer something that means they can maintain a healthy life.”
He added that the relatively small and short trial was informative.
“They improved the NAFLD activity score [NAS],” he said. “I don’t know by how much. There was no change in fibrosis, but we wouldn’t expect this at 6 months.”
“It’s provocative work, and it gives us healthy information about how we can help manage our patients from a lifestyle perspective,” he concluded.
‘Do not lose weight. Eat until you are full’
In the study, 110 participants with type 2 diabetes and NAFLD, aged 18-78 years, were allocated to the LCHF diet, and 55 were allocated to the low-fat diet for 6 months.
The researchers performed liver biopsies at baseline and 6 months, which were blinded for scoring.
Participants had ongoing dietitian consultations, with follow-up visits at 3 and 6 months. Compliance was reported continuously through an online food diary platform.
The primary endpoint was change in glycemic control as measured by A1c level over 6 months. The secondary endpoints comprised the proportion of participants with changes in the NAS of at least 2 points over 6 months. Both these measures were compared between the two dietary groups.
The two groups were matched at baseline, with a mean age of 55-57 years, 58% were women, 89% with metabolic syndrome, and a mean BMI 34 kg/m2.
In baseline liver disease, F1 level fibrosis was the most common (58%), followed by hepatic steatosis (S1, 47%; S2, 32%), with a median NAS of 3, and 19% had nonalcoholic steatohepatitis.
The special thing about these diets was that participants were told to “not lose weight, but eat until you are full,” remarked Dr. Dalby Hansen.
Those on the LCHF diet consumed an average of 61% energy from fat, 13% from carbohydrates, and 23% from protein, compared with the low-fat diet, which comprised an average of 29% energy from fat, 46% from carbohydrates, and 21% from protein.
“It’s a lot of fat and corresponds to a quarter of a liter of olive oil per day,” said Dr. Dalby Hansen. “They really had to change their mindset a lot, because it was difficult for them to start eating all these fats, especially since we’ve all been told for decades that it isn’t good. But we supported them, and they got into it.”
The LCHF diet was primarily comprised of unsaturated fats – for example, avocado, oil, nuts, and seeds – but also included saturated fats, such as cheese, cream, and high-fat dairy products. Participants were free to eat unsaturated and saturated fats, but Dr. Dalby Hansen and her team advised participants that “good” unsaturated fats were preferable.
“Also, this diet contained vegetables but no bread, no potatoes, no rice, and no pasta. It was low in carbohydrates, below 20%,” she added.
Improved glycemic control, reduced liver fat
“We found that the LCHF diet improved diabetes control, it reduced the fat in the liver, and, even though they’re eating as many calories as they were used to until they were full, they lost 5.8% of body weight,” said Dr. Dalby Hansen in reporting the results. Participants in the low-fat group lost only 1.8% of body weight.
However, mean calorie intake dropped in both groups, by –2.2% in the LCHF group and –8.7% in the low-fat group.
“The LCHF diet improved the primary outcome of A1c by 9.5 mmol/mol, which is similar to some anti-diabetic medications, such as DPP-4 inhibitors and SGLT2 inhibitors,” she said.
The low-fat group reduced A1c by 3.4 mmol/mol, resulting in a between-group difference of 6.1 mmol/mol.
“Upon follow-up of 3 months, after stopping the diets, on average the participants in both groups returned their HbA1c levels to nearly baseline values,” she said. Results were adjusted for weight loss and baseline values.
Both diets also improved the NAS. The proportion of participants who improved their NAS score by 2 or more points was 22% in the LCHF group versus 17% in the low-fat group (P = 0.58). Additionally, in the LCHF group, 70% of participants improved their score by 1 or more points, compared with 49% in the low-fat group and fewer in the LCHF group experienced a worsening of their score (1% vs. 23%, respectively).
One participant on LCHF had high triglycerides of 12 mmol/L after 3 months. Overall, the low-density lipoprotein increased marginally by 0.2 mmol per liter in the high-fat group, said Dr. Dalby Hansen.
Dr. Dalby Hansen noted some limitations. The findings might not be applicable in more severe NAFLD, dietary assessment relied on self-reporting, no food was provided, and participants had to cook themselves. It was also an open-label study because of the nature of the intervention.
Some hope for more sustainable dieting
Many diets are difficult to adhere to, remarked Dr. Dalby Hansen. “We thought this [diet] might be easier to comply with in the longer term, and we hope that these results might provide patients with more options.”
She added that most people who started the diet adapted and complied with it. “However, it might not be for everyone, but I think we can say that if people try, and it fits into their lives, then they go for it.”
However, “it is not about going out and eating whatever fat and how much of it you want. It’s important that you cut the carbohydrates too,” she said. “With this approach, we really saw amazing results.”
Dr. Dalby Hansen added that having various diets available, including the LCHF one, meant that as clinicians they could empower patients to take control of their metabolic health.
“We can ask them directly, ‘What would fit into their life?’” she said. “We know that one size does not fit at all, and I believe that if we could engage patients more, then they can take control of their own situation.”
Asked whether these findings were enough to change guidelines, Zobair Younossi, MD, professor and chairman, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., remarked that it was the sugar at work here.
“Dietary fat – it’s not the same as fat in the liver, and this diet has more to do with the sugar levels,” he said.
“I’m always reluctant to take results from a short-term study without long-term follow-up,” Dr. Younossi said. “I want to know will patients live longer, and long-term data are needed for this. Until I have that strong evidence that outcomes are going to change, or at least some sign that the outcome is going to change, it is too early to change any guidelines.”
Dr. Dalby Hansen reports no relevant financial relationships. Dr. Harrison reported financial relationships with numerous pharmaceutical companies. Dr. Younossi reports the following financial relationships: research funds and/or consultant to Abbott, Allergan, Bristol Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
AT ILC 2022
Acute hepatitis cases in children show declining trend; adenovirus, COVID-19 remain key leads
LONDON – Case numbers of acute hepatitis in children show “a declining trajectory,” and COVID-19 and adenovirus remain the most likely, but as yet unproven, causative agents, said experts in an update at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
Philippa Easterbrook, MD, medical expert at the World Health Organization Global HIV, Hepatitis, and STI Programme, shared the latest case numbers and working hypotheses of possible causative agents in the outbreak of acute hepatitis among children in Europe and beyond.
Global data across the five WHO regions show there were 244 cases in the past month, bringing the total to 894 probable cases reported since October 2021 from 33 countries.
“It’s important to remember that this includes new cases, as well as retrospectively identified cases,” Dr.Easterbrook said. “Over half (52%) are from the European region, while 262 cases (30% of the global total) are from the United Kingdom.”
Data from Europe and the United States show a declining trajectory of reports of new cases. “This is a positive development,” she said.
The second highest reporting region is the Americas, she said, with 368 cases total, 290 cases of which come from the United States, accounting for 35% of the global total.
“Together the United Kingdom and the United States make up 65% of the global total,” she said.
Dr. Easterbrook added that 17 of the 33 reporting countries had more than five cases. Most cases (75%) are in young children under 5 years of age.
Serious cases are relatively few, but 44 (5%) children have required liver transplantation. Data from the European region show that 30% have required intensive care at some point during their hospitalization. There have been 18 (2%) reported deaths.
Possible post-COVID phenomenon, adenovirus most commonly reported
Dr. Easterbrook acknowledged the emerging hypothesis of a post-COVID phenomenon.
“Is this a variant of the rare but recognized multisystem inflammatory syndrome condition in children that’s been reported, often 1-2 months after COVID, causing widespread organ damage?” But she pointed out that the reported COVID cases with hepatitis “don’t seem to fit these features.”
Adenovirus remains the most commonly detected virus in acute hepatitis in children, found in 53% of cases overall, she said. The adenovirus detection rate is higher in the United Kingdom, at 68%.
“There are quite high rates of detection, but they’re not in all cases. There does seem to be a high rate of detection in the younger age groups and in those who are developing severe disease, so perhaps there is some link to severity,” Dr. Easterbrook said.
The working hypotheses continue to favor adenovirus together with past or current SARS-CoV-2 infection, as proposed early in the outbreak, she said. “These either work independently or work together as cofactors in some way to result in hepatitis. And there has been some clear progress on this. WHO is bringing together the data from different countries on some of these working hypotheses.”
Dr. Easterbrook highlighted the importance of procuring global data, especially given that two countries are reporting the majority of cases and in high numbers. “It’s a mixed picture with different rates of adenovirus detection and of COVID,” she said. “We need good-quality data collected in a standardized way.” WHO is requesting that countries provide these data.
She also highlighted the need for good in-depth studies, citing the UK Health Security Agency as an example of this. “There’s only a few countries that have the capacity or the patient numbers to look at this in detail, for example, the U.K. and the UKHSA.”
She noted that the UKHSA had laid out a comprehensive, systematic set of further investigations. For example, a case-control study is trying to establish whether there is a difference in the rate of adenovirus detection in children with hepatitis compared with other hospitalized children at the same time. “This aims to really tease out whether adenovirus is a cause or just a bystander,” she said.
She added that there were also genetic studies investigating whether genes were predisposing some children to develop a more severe form of disease. Other studies are evaluating the immune response of the patients.
Dr. Easterbrook added that the WHO will soon launch a global survey asking whether the reports of acute hepatitis are greater than the expected background rate for cases of hepatitis of unknown etiology.
Acute hepatitis is not new, but high caseload is
Also speaking at the ILC special briefing was Maria Buti, MD, PhD, policy and public health chair for the European Association for the Study of the Liver, and chief of the internal medicine and hepatology department at Hospital General Universitari Valle Hebron in Barcelona.
Dr. Buti drew attention to the fact that severe acute hepatitis of unknown etiology in children is not new.
“We have cases of acute hepatitis that even needed liver transplantation some years ago, and every year in our clinics we see these type of patients,” Dr. Buti remarked. What is really new, she added, is the amount of cases, particularly in the United Kingdom.
Dr. Easterbrook and Dr. Buti have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LONDON – Case numbers of acute hepatitis in children show “a declining trajectory,” and COVID-19 and adenovirus remain the most likely, but as yet unproven, causative agents, said experts in an update at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
Philippa Easterbrook, MD, medical expert at the World Health Organization Global HIV, Hepatitis, and STI Programme, shared the latest case numbers and working hypotheses of possible causative agents in the outbreak of acute hepatitis among children in Europe and beyond.
Global data across the five WHO regions show there were 244 cases in the past month, bringing the total to 894 probable cases reported since October 2021 from 33 countries.
“It’s important to remember that this includes new cases, as well as retrospectively identified cases,” Dr.Easterbrook said. “Over half (52%) are from the European region, while 262 cases (30% of the global total) are from the United Kingdom.”
Data from Europe and the United States show a declining trajectory of reports of new cases. “This is a positive development,” she said.
The second highest reporting region is the Americas, she said, with 368 cases total, 290 cases of which come from the United States, accounting for 35% of the global total.
“Together the United Kingdom and the United States make up 65% of the global total,” she said.
Dr. Easterbrook added that 17 of the 33 reporting countries had more than five cases. Most cases (75%) are in young children under 5 years of age.
Serious cases are relatively few, but 44 (5%) children have required liver transplantation. Data from the European region show that 30% have required intensive care at some point during their hospitalization. There have been 18 (2%) reported deaths.
Possible post-COVID phenomenon, adenovirus most commonly reported
Dr. Easterbrook acknowledged the emerging hypothesis of a post-COVID phenomenon.
“Is this a variant of the rare but recognized multisystem inflammatory syndrome condition in children that’s been reported, often 1-2 months after COVID, causing widespread organ damage?” But she pointed out that the reported COVID cases with hepatitis “don’t seem to fit these features.”
Adenovirus remains the most commonly detected virus in acute hepatitis in children, found in 53% of cases overall, she said. The adenovirus detection rate is higher in the United Kingdom, at 68%.
“There are quite high rates of detection, but they’re not in all cases. There does seem to be a high rate of detection in the younger age groups and in those who are developing severe disease, so perhaps there is some link to severity,” Dr. Easterbrook said.
The working hypotheses continue to favor adenovirus together with past or current SARS-CoV-2 infection, as proposed early in the outbreak, she said. “These either work independently or work together as cofactors in some way to result in hepatitis. And there has been some clear progress on this. WHO is bringing together the data from different countries on some of these working hypotheses.”
Dr. Easterbrook highlighted the importance of procuring global data, especially given that two countries are reporting the majority of cases and in high numbers. “It’s a mixed picture with different rates of adenovirus detection and of COVID,” she said. “We need good-quality data collected in a standardized way.” WHO is requesting that countries provide these data.
She also highlighted the need for good in-depth studies, citing the UK Health Security Agency as an example of this. “There’s only a few countries that have the capacity or the patient numbers to look at this in detail, for example, the U.K. and the UKHSA.”
She noted that the UKHSA had laid out a comprehensive, systematic set of further investigations. For example, a case-control study is trying to establish whether there is a difference in the rate of adenovirus detection in children with hepatitis compared with other hospitalized children at the same time. “This aims to really tease out whether adenovirus is a cause or just a bystander,” she said.
She added that there were also genetic studies investigating whether genes were predisposing some children to develop a more severe form of disease. Other studies are evaluating the immune response of the patients.
Dr. Easterbrook added that the WHO will soon launch a global survey asking whether the reports of acute hepatitis are greater than the expected background rate for cases of hepatitis of unknown etiology.
Acute hepatitis is not new, but high caseload is
Also speaking at the ILC special briefing was Maria Buti, MD, PhD, policy and public health chair for the European Association for the Study of the Liver, and chief of the internal medicine and hepatology department at Hospital General Universitari Valle Hebron in Barcelona.
Dr. Buti drew attention to the fact that severe acute hepatitis of unknown etiology in children is not new.
“We have cases of acute hepatitis that even needed liver transplantation some years ago, and every year in our clinics we see these type of patients,” Dr. Buti remarked. What is really new, she added, is the amount of cases, particularly in the United Kingdom.
Dr. Easterbrook and Dr. Buti have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LONDON – Case numbers of acute hepatitis in children show “a declining trajectory,” and COVID-19 and adenovirus remain the most likely, but as yet unproven, causative agents, said experts in an update at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
Philippa Easterbrook, MD, medical expert at the World Health Organization Global HIV, Hepatitis, and STI Programme, shared the latest case numbers and working hypotheses of possible causative agents in the outbreak of acute hepatitis among children in Europe and beyond.
Global data across the five WHO regions show there were 244 cases in the past month, bringing the total to 894 probable cases reported since October 2021 from 33 countries.
“It’s important to remember that this includes new cases, as well as retrospectively identified cases,” Dr.Easterbrook said. “Over half (52%) are from the European region, while 262 cases (30% of the global total) are from the United Kingdom.”
Data from Europe and the United States show a declining trajectory of reports of new cases. “This is a positive development,” she said.
The second highest reporting region is the Americas, she said, with 368 cases total, 290 cases of which come from the United States, accounting for 35% of the global total.
“Together the United Kingdom and the United States make up 65% of the global total,” she said.
Dr. Easterbrook added that 17 of the 33 reporting countries had more than five cases. Most cases (75%) are in young children under 5 years of age.
Serious cases are relatively few, but 44 (5%) children have required liver transplantation. Data from the European region show that 30% have required intensive care at some point during their hospitalization. There have been 18 (2%) reported deaths.
Possible post-COVID phenomenon, adenovirus most commonly reported
Dr. Easterbrook acknowledged the emerging hypothesis of a post-COVID phenomenon.
“Is this a variant of the rare but recognized multisystem inflammatory syndrome condition in children that’s been reported, often 1-2 months after COVID, causing widespread organ damage?” But she pointed out that the reported COVID cases with hepatitis “don’t seem to fit these features.”
Adenovirus remains the most commonly detected virus in acute hepatitis in children, found in 53% of cases overall, she said. The adenovirus detection rate is higher in the United Kingdom, at 68%.
“There are quite high rates of detection, but they’re not in all cases. There does seem to be a high rate of detection in the younger age groups and in those who are developing severe disease, so perhaps there is some link to severity,” Dr. Easterbrook said.
The working hypotheses continue to favor adenovirus together with past or current SARS-CoV-2 infection, as proposed early in the outbreak, she said. “These either work independently or work together as cofactors in some way to result in hepatitis. And there has been some clear progress on this. WHO is bringing together the data from different countries on some of these working hypotheses.”
Dr. Easterbrook highlighted the importance of procuring global data, especially given that two countries are reporting the majority of cases and in high numbers. “It’s a mixed picture with different rates of adenovirus detection and of COVID,” she said. “We need good-quality data collected in a standardized way.” WHO is requesting that countries provide these data.
She also highlighted the need for good in-depth studies, citing the UK Health Security Agency as an example of this. “There’s only a few countries that have the capacity or the patient numbers to look at this in detail, for example, the U.K. and the UKHSA.”
She noted that the UKHSA had laid out a comprehensive, systematic set of further investigations. For example, a case-control study is trying to establish whether there is a difference in the rate of adenovirus detection in children with hepatitis compared with other hospitalized children at the same time. “This aims to really tease out whether adenovirus is a cause or just a bystander,” she said.
She added that there were also genetic studies investigating whether genes were predisposing some children to develop a more severe form of disease. Other studies are evaluating the immune response of the patients.
Dr. Easterbrook added that the WHO will soon launch a global survey asking whether the reports of acute hepatitis are greater than the expected background rate for cases of hepatitis of unknown etiology.
Acute hepatitis is not new, but high caseload is
Also speaking at the ILC special briefing was Maria Buti, MD, PhD, policy and public health chair for the European Association for the Study of the Liver, and chief of the internal medicine and hepatology department at Hospital General Universitari Valle Hebron in Barcelona.
Dr. Buti drew attention to the fact that severe acute hepatitis of unknown etiology in children is not new.
“We have cases of acute hepatitis that even needed liver transplantation some years ago, and every year in our clinics we see these type of patients,” Dr. Buti remarked. What is really new, she added, is the amount of cases, particularly in the United Kingdom.
Dr. Easterbrook and Dr. Buti have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ILC 2022
Pemvidutide promising for fatty liver disease
LONDON – Weight loss, lipid reductions, and “robust improvements” in lipid species associated with nonalcoholic fatty liver disease were achieved in patients who were treated with pemvidutide in a first-in-human, phase 1 clinical trial reported at the annual International Liver Congress, sponsored by the European Association for the Study of the Liver.
The presenting study investigator, Stephen A. Harrison, MD, said that pemvidutide, which is also being developed for the treatment of obesity, appeared to be well tolerated. There were no serious or severe adverse events, and no patient had to discontinue treatment because of side effects.
Overall, “pemvidutide represents a promising new agent,” said Dr. Harrison, medical director of Pinnacle Research in San Antonio, Texas.
Dual incretin effect
Pemvidutide is a “balanced” dual agonist of glucagon-like peptide 1 (GLP-1) and glucagon, Dr. Harrison explained in his oral abstract.
“With glucagon, we are working to drive energy expenditure up, and with GLP-1, we’re decreasing food intake,” Dr. Harrison said.
What might set pemvidutide apart from other incretins lies within its structure, Dr. Harrison suggested. The structure has two main regions – one with greater GLP-1 specificity and the other with greater glucagon specificity, and these two areas are linked by a propriety technology called a EuPort™ domain. This is an area which allows the drug to bind to albumin, which increases its serum half-life and enables weekly dosing while slowing its entry into the bloodstream.
“Ultimately, we think that this has impacts, hypothetically, on tolerability and potentially mitigating the need for dose escalation,” said Dr. Harrison.
Weight loss results
The phase 1 study Dr. Harrison presented had a randomized, double-blind, placebo-controlled design with single and multiple ascending doses (SAD/MAD) of pemvidutide being tested. He presented data on the MAD phase only, noting that the SAD phase had been used to determine what doses to use in the latter.
Seventy individuals with a body mass index of between 25 and 40 kg/m2 were recruited and 34 of these were enrolled in the MAD phase of the study. Three doses of pemvidutide were used, given subcutaneously once a week for 12 weeks: Seven participants received 1.2 mg, 9 were given 1.8 mg, 11 had 2.4 mg, and 7 subjects were treated with placebo. Dr. Harrison noted that there were no caloric restrictions in the trial and no lifestyle modifications or interventions.
The average age of study participants ranged from 27 to 35 years and the mean BMI was 30-31 kg/m2 across each group, with their lipid parameters in the upper range of normal.
Clear weight loss reductions were seen across all the pemvidutide groups versus placebo, with the greatest percentage changes in weight loss seen with the two higher doses used. At week 12, there was a 4.9%, 10.3% and 9.0% weight loss in the 1.2-mg, 1.8-mg and 2.4-mg pemvidutide groups compared to 1.6% in placebo-treated individuals.
All patients in the 1.8-mg group achieved a 5% or greater weight loss, Dr. Harrison observed, but there “was a plateauing” effect with the 2.4-mg dose with 89% of patients achieving this target. In comparison, a third of patients on the lowest dose and 20% of those on placebo achieved this target.
The trajectory of weight loss seen in the trial suggests that “the rate of weight loss would continue beyond 12 weeks if we were to continue the therapy” Dr. Harrison said.
Lipid changes and liver fat reductions
Levels of serum lipids from baseline to week 12 fell to a greater extent with pemvidutide treatment than with placebo, in the range of –27% for total cholesterol in the two highest dose groups, –25% for LDL-cholesterol for those groups, –37% for triglycerides for the 1.2- and 1.8-mg groups, and reductions in apolipoprotein B were seen.
“We saw an initial decline in HDL [high-density lipoprotein],” Dr. Harrison said, noting that “this is consistent with prior studies looking at rapid weight loss, and over time, this mitigates as you continue to treat at least based on other mechanisms of action or other drugs with similar mechanisms.”
Pemvidutide treatment was also associated with increased lipid oxidation and decreased lipid synthesis, and “there was a robust decrease in lipids implicated in NASH inflammation,” Dr. Harrison pointed out.
Importantly, in five of eight participants who had high levels of liver fat at baseline – defined as a 5% or greater magnetic resonance imaging–derived proton-density-fat-fraction (MRI-PDFF) – showed a decrease to undetectable limits (1.5% or less). This was a greater than 90% reduction in liver fat, Dr. Harrison said. All five patients were in the 1.8-mg and 2.4-mg groups.
As for side effects, these were “predominantly upper GI, with nausea and vomiting.” These were mild in most cases, but he pointed out that five patients treated with the 1.8-mg dose experienced moderate nausea and three experienced moderate vomiting. Mild diarrhea and constipation were also seen in two of patients given this dose but was not reported in any of the other groups.
During the discussion following the presentation, it was pointed out that there was no clear dose-dependent effect considering the 1.8-mg dose seemed to have a stronger effect in some areas than the 2.4-mg dose. That’s a fair point, Dr. Harrison responded, reiterating it was a small study with a short treatment duration, but that there did look like a plateauing effect, “at least in patients with a mean BMI of between 30 and 31.”
Dr. Harrison was asked about potential effects on insulin levels and if that was a worry because, if glucagon is stimulated, it could increase insulin. That in turn might encourage insulin resistance and promote worse outcomes.
“If you look outside of just this program, glucagon agonism has been dosed in a lot of patients over time, and we haven’t seen that,” Dr. Harrison replied. Pemvidutide is an agonist rather than antagonist, so perhaps the [nonalcoholic steatohepatitis]–inducing effects seen before with glucagon antagonism won’t occur, he suggested.
Dr. Harrison disclosed ties to Altimmune (the study sponsor), Akero, Axcella, Bristol Myers Squibb, Cirius, CiVi Biopharma, Conatus, Corcept, CymaBay, Enyo, Galectin, Genentech, Genfit, Gilead, Hepion, Hightide, HistoIndex, Intercept, Madrigal, Metacrine, NGM Bio, Novartis, Novo Nordisk, NorthSea, Pfizer, Sagimet, Viking, and 89Bio.
LONDON – Weight loss, lipid reductions, and “robust improvements” in lipid species associated with nonalcoholic fatty liver disease were achieved in patients who were treated with pemvidutide in a first-in-human, phase 1 clinical trial reported at the annual International Liver Congress, sponsored by the European Association for the Study of the Liver.
The presenting study investigator, Stephen A. Harrison, MD, said that pemvidutide, which is also being developed for the treatment of obesity, appeared to be well tolerated. There were no serious or severe adverse events, and no patient had to discontinue treatment because of side effects.
Overall, “pemvidutide represents a promising new agent,” said Dr. Harrison, medical director of Pinnacle Research in San Antonio, Texas.
Dual incretin effect
Pemvidutide is a “balanced” dual agonist of glucagon-like peptide 1 (GLP-1) and glucagon, Dr. Harrison explained in his oral abstract.
“With glucagon, we are working to drive energy expenditure up, and with GLP-1, we’re decreasing food intake,” Dr. Harrison said.
What might set pemvidutide apart from other incretins lies within its structure, Dr. Harrison suggested. The structure has two main regions – one with greater GLP-1 specificity and the other with greater glucagon specificity, and these two areas are linked by a propriety technology called a EuPort™ domain. This is an area which allows the drug to bind to albumin, which increases its serum half-life and enables weekly dosing while slowing its entry into the bloodstream.
“Ultimately, we think that this has impacts, hypothetically, on tolerability and potentially mitigating the need for dose escalation,” said Dr. Harrison.
Weight loss results
The phase 1 study Dr. Harrison presented had a randomized, double-blind, placebo-controlled design with single and multiple ascending doses (SAD/MAD) of pemvidutide being tested. He presented data on the MAD phase only, noting that the SAD phase had been used to determine what doses to use in the latter.
Seventy individuals with a body mass index of between 25 and 40 kg/m2 were recruited and 34 of these were enrolled in the MAD phase of the study. Three doses of pemvidutide were used, given subcutaneously once a week for 12 weeks: Seven participants received 1.2 mg, 9 were given 1.8 mg, 11 had 2.4 mg, and 7 subjects were treated with placebo. Dr. Harrison noted that there were no caloric restrictions in the trial and no lifestyle modifications or interventions.
The average age of study participants ranged from 27 to 35 years and the mean BMI was 30-31 kg/m2 across each group, with their lipid parameters in the upper range of normal.
Clear weight loss reductions were seen across all the pemvidutide groups versus placebo, with the greatest percentage changes in weight loss seen with the two higher doses used. At week 12, there was a 4.9%, 10.3% and 9.0% weight loss in the 1.2-mg, 1.8-mg and 2.4-mg pemvidutide groups compared to 1.6% in placebo-treated individuals.
All patients in the 1.8-mg group achieved a 5% or greater weight loss, Dr. Harrison observed, but there “was a plateauing” effect with the 2.4-mg dose with 89% of patients achieving this target. In comparison, a third of patients on the lowest dose and 20% of those on placebo achieved this target.
The trajectory of weight loss seen in the trial suggests that “the rate of weight loss would continue beyond 12 weeks if we were to continue the therapy” Dr. Harrison said.
Lipid changes and liver fat reductions
Levels of serum lipids from baseline to week 12 fell to a greater extent with pemvidutide treatment than with placebo, in the range of –27% for total cholesterol in the two highest dose groups, –25% for LDL-cholesterol for those groups, –37% for triglycerides for the 1.2- and 1.8-mg groups, and reductions in apolipoprotein B were seen.
“We saw an initial decline in HDL [high-density lipoprotein],” Dr. Harrison said, noting that “this is consistent with prior studies looking at rapid weight loss, and over time, this mitigates as you continue to treat at least based on other mechanisms of action or other drugs with similar mechanisms.”
Pemvidutide treatment was also associated with increased lipid oxidation and decreased lipid synthesis, and “there was a robust decrease in lipids implicated in NASH inflammation,” Dr. Harrison pointed out.
Importantly, in five of eight participants who had high levels of liver fat at baseline – defined as a 5% or greater magnetic resonance imaging–derived proton-density-fat-fraction (MRI-PDFF) – showed a decrease to undetectable limits (1.5% or less). This was a greater than 90% reduction in liver fat, Dr. Harrison said. All five patients were in the 1.8-mg and 2.4-mg groups.
As for side effects, these were “predominantly upper GI, with nausea and vomiting.” These were mild in most cases, but he pointed out that five patients treated with the 1.8-mg dose experienced moderate nausea and three experienced moderate vomiting. Mild diarrhea and constipation were also seen in two of patients given this dose but was not reported in any of the other groups.
During the discussion following the presentation, it was pointed out that there was no clear dose-dependent effect considering the 1.8-mg dose seemed to have a stronger effect in some areas than the 2.4-mg dose. That’s a fair point, Dr. Harrison responded, reiterating it was a small study with a short treatment duration, but that there did look like a plateauing effect, “at least in patients with a mean BMI of between 30 and 31.”
Dr. Harrison was asked about potential effects on insulin levels and if that was a worry because, if glucagon is stimulated, it could increase insulin. That in turn might encourage insulin resistance and promote worse outcomes.
“If you look outside of just this program, glucagon agonism has been dosed in a lot of patients over time, and we haven’t seen that,” Dr. Harrison replied. Pemvidutide is an agonist rather than antagonist, so perhaps the [nonalcoholic steatohepatitis]–inducing effects seen before with glucagon antagonism won’t occur, he suggested.
Dr. Harrison disclosed ties to Altimmune (the study sponsor), Akero, Axcella, Bristol Myers Squibb, Cirius, CiVi Biopharma, Conatus, Corcept, CymaBay, Enyo, Galectin, Genentech, Genfit, Gilead, Hepion, Hightide, HistoIndex, Intercept, Madrigal, Metacrine, NGM Bio, Novartis, Novo Nordisk, NorthSea, Pfizer, Sagimet, Viking, and 89Bio.
LONDON – Weight loss, lipid reductions, and “robust improvements” in lipid species associated with nonalcoholic fatty liver disease were achieved in patients who were treated with pemvidutide in a first-in-human, phase 1 clinical trial reported at the annual International Liver Congress, sponsored by the European Association for the Study of the Liver.
The presenting study investigator, Stephen A. Harrison, MD, said that pemvidutide, which is also being developed for the treatment of obesity, appeared to be well tolerated. There were no serious or severe adverse events, and no patient had to discontinue treatment because of side effects.
Overall, “pemvidutide represents a promising new agent,” said Dr. Harrison, medical director of Pinnacle Research in San Antonio, Texas.
Dual incretin effect
Pemvidutide is a “balanced” dual agonist of glucagon-like peptide 1 (GLP-1) and glucagon, Dr. Harrison explained in his oral abstract.
“With glucagon, we are working to drive energy expenditure up, and with GLP-1, we’re decreasing food intake,” Dr. Harrison said.
What might set pemvidutide apart from other incretins lies within its structure, Dr. Harrison suggested. The structure has two main regions – one with greater GLP-1 specificity and the other with greater glucagon specificity, and these two areas are linked by a propriety technology called a EuPort™ domain. This is an area which allows the drug to bind to albumin, which increases its serum half-life and enables weekly dosing while slowing its entry into the bloodstream.
“Ultimately, we think that this has impacts, hypothetically, on tolerability and potentially mitigating the need for dose escalation,” said Dr. Harrison.
Weight loss results
The phase 1 study Dr. Harrison presented had a randomized, double-blind, placebo-controlled design with single and multiple ascending doses (SAD/MAD) of pemvidutide being tested. He presented data on the MAD phase only, noting that the SAD phase had been used to determine what doses to use in the latter.
Seventy individuals with a body mass index of between 25 and 40 kg/m2 were recruited and 34 of these were enrolled in the MAD phase of the study. Three doses of pemvidutide were used, given subcutaneously once a week for 12 weeks: Seven participants received 1.2 mg, 9 were given 1.8 mg, 11 had 2.4 mg, and 7 subjects were treated with placebo. Dr. Harrison noted that there were no caloric restrictions in the trial and no lifestyle modifications or interventions.
The average age of study participants ranged from 27 to 35 years and the mean BMI was 30-31 kg/m2 across each group, with their lipid parameters in the upper range of normal.
Clear weight loss reductions were seen across all the pemvidutide groups versus placebo, with the greatest percentage changes in weight loss seen with the two higher doses used. At week 12, there was a 4.9%, 10.3% and 9.0% weight loss in the 1.2-mg, 1.8-mg and 2.4-mg pemvidutide groups compared to 1.6% in placebo-treated individuals.
All patients in the 1.8-mg group achieved a 5% or greater weight loss, Dr. Harrison observed, but there “was a plateauing” effect with the 2.4-mg dose with 89% of patients achieving this target. In comparison, a third of patients on the lowest dose and 20% of those on placebo achieved this target.
The trajectory of weight loss seen in the trial suggests that “the rate of weight loss would continue beyond 12 weeks if we were to continue the therapy” Dr. Harrison said.
Lipid changes and liver fat reductions
Levels of serum lipids from baseline to week 12 fell to a greater extent with pemvidutide treatment than with placebo, in the range of –27% for total cholesterol in the two highest dose groups, –25% for LDL-cholesterol for those groups, –37% for triglycerides for the 1.2- and 1.8-mg groups, and reductions in apolipoprotein B were seen.
“We saw an initial decline in HDL [high-density lipoprotein],” Dr. Harrison said, noting that “this is consistent with prior studies looking at rapid weight loss, and over time, this mitigates as you continue to treat at least based on other mechanisms of action or other drugs with similar mechanisms.”
Pemvidutide treatment was also associated with increased lipid oxidation and decreased lipid synthesis, and “there was a robust decrease in lipids implicated in NASH inflammation,” Dr. Harrison pointed out.
Importantly, in five of eight participants who had high levels of liver fat at baseline – defined as a 5% or greater magnetic resonance imaging–derived proton-density-fat-fraction (MRI-PDFF) – showed a decrease to undetectable limits (1.5% or less). This was a greater than 90% reduction in liver fat, Dr. Harrison said. All five patients were in the 1.8-mg and 2.4-mg groups.
As for side effects, these were “predominantly upper GI, with nausea and vomiting.” These were mild in most cases, but he pointed out that five patients treated with the 1.8-mg dose experienced moderate nausea and three experienced moderate vomiting. Mild diarrhea and constipation were also seen in two of patients given this dose but was not reported in any of the other groups.
During the discussion following the presentation, it was pointed out that there was no clear dose-dependent effect considering the 1.8-mg dose seemed to have a stronger effect in some areas than the 2.4-mg dose. That’s a fair point, Dr. Harrison responded, reiterating it was a small study with a short treatment duration, but that there did look like a plateauing effect, “at least in patients with a mean BMI of between 30 and 31.”
Dr. Harrison was asked about potential effects on insulin levels and if that was a worry because, if glucagon is stimulated, it could increase insulin. That in turn might encourage insulin resistance and promote worse outcomes.
“If you look outside of just this program, glucagon agonism has been dosed in a lot of patients over time, and we haven’t seen that,” Dr. Harrison replied. Pemvidutide is an agonist rather than antagonist, so perhaps the [nonalcoholic steatohepatitis]–inducing effects seen before with glucagon antagonism won’t occur, he suggested.
Dr. Harrison disclosed ties to Altimmune (the study sponsor), Akero, Axcella, Bristol Myers Squibb, Cirius, CiVi Biopharma, Conatus, Corcept, CymaBay, Enyo, Galectin, Genentech, Genfit, Gilead, Hepion, Hightide, HistoIndex, Intercept, Madrigal, Metacrine, NGM Bio, Novartis, Novo Nordisk, NorthSea, Pfizer, Sagimet, Viking, and 89Bio.
AT ILC 2022
Fatty liver disease drives rise in liver cancer deaths
LONDON – Around the world, nonalcoholic fatty liver disease (NAFLD) has driven an increase in deaths from liver cancer over the past decade, overtaking alcoholic liver disease, hepatitis B, and hepatitis C, according to an analysis of the Global Burden of Disease Study 2019.
A global rise in liver cancer deaths and chronic liver disease reflects changes in underlying health patterns, said Zobair Younossi, MD, MPH, professor and chair, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., who presented the analysis at the International Liver Congress (ILC) 2022.
“NAFLD and NASH [nonalcoholic steatohepatitis] are rapidly becoming the main causes of cirrhosis and liver cancer in the world,” Dr. Younossi told this news organization. “We have known about the increasing prevalence for some time, but now the outcomes in terms of mortality are catching up,” he said.
“The bottom line of this study is that the burden of this disease [NAFLD] is going up, and it will be the most important disease of the next decade or so,” he said, adding that “the largest annual percentage increase in rates of mortality from liver cancer or chronic liver disease cirrhosis is related to NAFLD.”
Specifically, during the decade of 2009-2019, the annual percent change (APC) of +1.33% in the global liver cancer death rate was driven by the fact that the APC for NAFLD was +2.47%. By comparison, the APC for alcoholic liver disease was +1.91%; for hepatitis B, the APC was +0.21%; and for hepatitis C, the APC was +1.12%.
Aleksander Krag, MD, PhD, professor and senior consultant of hepatology and director of Odense Liver Research Centre at SDU and Odense University Hospital, Denmark, who chaired the session in which this presentation was a part, acknowledged the importance of recognizing the contribution of NAFLD to liver cancer mortality.
“Liver diseases are on the rise. They are the fastest rising cause of death in the United Kingdom, faster than heart disease and other cancers. NAFLD in particular is the fastest growing cause of liver cancer, and the leading cause in France and the United States,” he remarked.
Dr. Krag also highlighted the costs of disease management.
“Managing fatty liver disease in Europe is estimated at €35 billion in direct health care, so we need to do something now,” he stressed.
“The global burden of NAFLD is so high that we need both prevention and treatment tools,” Dr. Krag said. “Change to lifestyle is a ‘no-brainer’ and costs governments very little. For the sake of our young people, we need to take this very seriously. At a political level, we can easily implement this, for example, by banning junk food advertisements, but also educating young people and their families. Good drugs will also help.”
NAFLD: The liver manifestation of type 2 diabetes
About 25%-30% of the global population have NAFLD, and 3%-5% have NASH. Dr. Younossi highlighted that the U.S. transplant database shows that NAFLD was the second indication for all liver transplants in the country. NAFLD also was a leading cause of liver transplants for patients with hepatocellular carcinoma.
There are around two billion cases of chronic liver disease globally, he said. He noted that over time, there has been an increase in all kinds of liver diseases, as reflected in the annual percent change.
“The global epidemic of obesity and type 2 diabetes is driving the rise in NAFLD, but even among lean people, the prevalence of NAFLD is around 9%,” Dr. Younossi said. “Alongside the eye and kidney complications of diabetes, this is the liver manifestation of type 2 diabetes.”
To assess global liver disease and death, Dr. Younossi and his colleagues turned to the Global Burden of Disease Study, which gathered data from around 7,000 investigators located across 22 different regions of the world, comprising 156 countries.
They calculated the incidence, prevalence, mortality, and disability-adjusted life-years (DALYs) in relation to liver cancer and chronic liver disease, including the APC. They linked the data to changes in four liver diseases: NAFLD, alcoholic liver disease, hepatitis B infection, and hepatitis C infection.
The cases of NAFLD reported in the study had been diagnosed by ultrasound or other imaging. Importantly, the prevalence of NAFLD was adjusted for alcohol use in the various national populations, explained Dr. Younossi.
In 2019, they reported that globally, the overall prevalence of liver disease reached 1.69 billion (liver cancer, 0.04%; chronic liver disease, 99.96%), with an incidence of 2.59 million (liver cancer, 20.7%; chronic liver disease, 79.3%), mortality of 1.95 million (liver cancer, 24.8%; chronic liver disease, 75.3%), and DALYs of 58.7 million (liver cancer, 21.3%; chronic liver disease, 78.7%).
Between 2009 and 2019, deaths from liver cancer rose by 27.2%, and deaths from chronic liver disease rose by 10.6%. DALYs from liver cancer rose by 21.9%, and DALYs from chronic liver disease were up by 5.1%.
In contrast to the increase in liver cancer deaths, deaths from chronic liver disease decreased (APC, –0.18%). The decrease was driven by a decrease in hepatitis B (APC, –1.83%). APCs for hepatitis C (+0.37%), alcoholic liver disease (+0.45%), and NAFLD (+1.33%) increased.
“The burden of hepatitis B–related mortality has decreased because we have been so good at vaccinating people,” Dr. Younossi remarked.
NAFLD ‘exploding’ in Middle East, North Africa, and East Asia
The increase in NAFLD has been seen in all regions of the world, but a breakdown by region shows that NAFLD is primarily “exploding” with highest prevalence and mortality in the Middle East (mostly Egypt, Iran, and Turkey), North Africa, and East Asia, said Dr. Younossi. In addition, there are large increases in the West and South America.
“We knew that the prevalence was high in the Middle East, but we now know that mortality is also high, so we are connecting these data,” said Dr. Younossi.
Awareness lacking
Dr. Younossi pressed the fact that awareness among the general population, primary care providers, and policymakers is very low. “From my perspective, raising awareness of NAFLD is the number one priority, and that is the value of this study.”
He added that more people will become aware as testing becomes more manageable.
“There are some noninvasive tests being developed, so in the future, we won’t have to do liver biopsies to diagnose these patients,” he said. “Currently, there are some excellent treatments being developed.”
“The WHO [World Health Organization] does not mention NAFLD as an important noncommunicable disease, and this too has to change,” Dr. Younossi added.
Dr. Younossi has received research funds and/or has consulted for Abbott, Allergan, Bristol-Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk. Dr. Krag has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LONDON – Around the world, nonalcoholic fatty liver disease (NAFLD) has driven an increase in deaths from liver cancer over the past decade, overtaking alcoholic liver disease, hepatitis B, and hepatitis C, according to an analysis of the Global Burden of Disease Study 2019.
A global rise in liver cancer deaths and chronic liver disease reflects changes in underlying health patterns, said Zobair Younossi, MD, MPH, professor and chair, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., who presented the analysis at the International Liver Congress (ILC) 2022.
“NAFLD and NASH [nonalcoholic steatohepatitis] are rapidly becoming the main causes of cirrhosis and liver cancer in the world,” Dr. Younossi told this news organization. “We have known about the increasing prevalence for some time, but now the outcomes in terms of mortality are catching up,” he said.
“The bottom line of this study is that the burden of this disease [NAFLD] is going up, and it will be the most important disease of the next decade or so,” he said, adding that “the largest annual percentage increase in rates of mortality from liver cancer or chronic liver disease cirrhosis is related to NAFLD.”
Specifically, during the decade of 2009-2019, the annual percent change (APC) of +1.33% in the global liver cancer death rate was driven by the fact that the APC for NAFLD was +2.47%. By comparison, the APC for alcoholic liver disease was +1.91%; for hepatitis B, the APC was +0.21%; and for hepatitis C, the APC was +1.12%.
Aleksander Krag, MD, PhD, professor and senior consultant of hepatology and director of Odense Liver Research Centre at SDU and Odense University Hospital, Denmark, who chaired the session in which this presentation was a part, acknowledged the importance of recognizing the contribution of NAFLD to liver cancer mortality.
“Liver diseases are on the rise. They are the fastest rising cause of death in the United Kingdom, faster than heart disease and other cancers. NAFLD in particular is the fastest growing cause of liver cancer, and the leading cause in France and the United States,” he remarked.
Dr. Krag also highlighted the costs of disease management.
“Managing fatty liver disease in Europe is estimated at €35 billion in direct health care, so we need to do something now,” he stressed.
“The global burden of NAFLD is so high that we need both prevention and treatment tools,” Dr. Krag said. “Change to lifestyle is a ‘no-brainer’ and costs governments very little. For the sake of our young people, we need to take this very seriously. At a political level, we can easily implement this, for example, by banning junk food advertisements, but also educating young people and their families. Good drugs will also help.”
NAFLD: The liver manifestation of type 2 diabetes
About 25%-30% of the global population have NAFLD, and 3%-5% have NASH. Dr. Younossi highlighted that the U.S. transplant database shows that NAFLD was the second indication for all liver transplants in the country. NAFLD also was a leading cause of liver transplants for patients with hepatocellular carcinoma.
There are around two billion cases of chronic liver disease globally, he said. He noted that over time, there has been an increase in all kinds of liver diseases, as reflected in the annual percent change.
“The global epidemic of obesity and type 2 diabetes is driving the rise in NAFLD, but even among lean people, the prevalence of NAFLD is around 9%,” Dr. Younossi said. “Alongside the eye and kidney complications of diabetes, this is the liver manifestation of type 2 diabetes.”
To assess global liver disease and death, Dr. Younossi and his colleagues turned to the Global Burden of Disease Study, which gathered data from around 7,000 investigators located across 22 different regions of the world, comprising 156 countries.
They calculated the incidence, prevalence, mortality, and disability-adjusted life-years (DALYs) in relation to liver cancer and chronic liver disease, including the APC. They linked the data to changes in four liver diseases: NAFLD, alcoholic liver disease, hepatitis B infection, and hepatitis C infection.
The cases of NAFLD reported in the study had been diagnosed by ultrasound or other imaging. Importantly, the prevalence of NAFLD was adjusted for alcohol use in the various national populations, explained Dr. Younossi.
In 2019, they reported that globally, the overall prevalence of liver disease reached 1.69 billion (liver cancer, 0.04%; chronic liver disease, 99.96%), with an incidence of 2.59 million (liver cancer, 20.7%; chronic liver disease, 79.3%), mortality of 1.95 million (liver cancer, 24.8%; chronic liver disease, 75.3%), and DALYs of 58.7 million (liver cancer, 21.3%; chronic liver disease, 78.7%).
Between 2009 and 2019, deaths from liver cancer rose by 27.2%, and deaths from chronic liver disease rose by 10.6%. DALYs from liver cancer rose by 21.9%, and DALYs from chronic liver disease were up by 5.1%.
In contrast to the increase in liver cancer deaths, deaths from chronic liver disease decreased (APC, –0.18%). The decrease was driven by a decrease in hepatitis B (APC, –1.83%). APCs for hepatitis C (+0.37%), alcoholic liver disease (+0.45%), and NAFLD (+1.33%) increased.
“The burden of hepatitis B–related mortality has decreased because we have been so good at vaccinating people,” Dr. Younossi remarked.
NAFLD ‘exploding’ in Middle East, North Africa, and East Asia
The increase in NAFLD has been seen in all regions of the world, but a breakdown by region shows that NAFLD is primarily “exploding” with highest prevalence and mortality in the Middle East (mostly Egypt, Iran, and Turkey), North Africa, and East Asia, said Dr. Younossi. In addition, there are large increases in the West and South America.
“We knew that the prevalence was high in the Middle East, but we now know that mortality is also high, so we are connecting these data,” said Dr. Younossi.
Awareness lacking
Dr. Younossi pressed the fact that awareness among the general population, primary care providers, and policymakers is very low. “From my perspective, raising awareness of NAFLD is the number one priority, and that is the value of this study.”
He added that more people will become aware as testing becomes more manageable.
“There are some noninvasive tests being developed, so in the future, we won’t have to do liver biopsies to diagnose these patients,” he said. “Currently, there are some excellent treatments being developed.”
“The WHO [World Health Organization] does not mention NAFLD as an important noncommunicable disease, and this too has to change,” Dr. Younossi added.
Dr. Younossi has received research funds and/or has consulted for Abbott, Allergan, Bristol-Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk. Dr. Krag has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LONDON – Around the world, nonalcoholic fatty liver disease (NAFLD) has driven an increase in deaths from liver cancer over the past decade, overtaking alcoholic liver disease, hepatitis B, and hepatitis C, according to an analysis of the Global Burden of Disease Study 2019.
A global rise in liver cancer deaths and chronic liver disease reflects changes in underlying health patterns, said Zobair Younossi, MD, MPH, professor and chair, department of medicine, Inova Fairfax Medical Campus, Falls Church, Va., who presented the analysis at the International Liver Congress (ILC) 2022.
“NAFLD and NASH [nonalcoholic steatohepatitis] are rapidly becoming the main causes of cirrhosis and liver cancer in the world,” Dr. Younossi told this news organization. “We have known about the increasing prevalence for some time, but now the outcomes in terms of mortality are catching up,” he said.
“The bottom line of this study is that the burden of this disease [NAFLD] is going up, and it will be the most important disease of the next decade or so,” he said, adding that “the largest annual percentage increase in rates of mortality from liver cancer or chronic liver disease cirrhosis is related to NAFLD.”
Specifically, during the decade of 2009-2019, the annual percent change (APC) of +1.33% in the global liver cancer death rate was driven by the fact that the APC for NAFLD was +2.47%. By comparison, the APC for alcoholic liver disease was +1.91%; for hepatitis B, the APC was +0.21%; and for hepatitis C, the APC was +1.12%.
Aleksander Krag, MD, PhD, professor and senior consultant of hepatology and director of Odense Liver Research Centre at SDU and Odense University Hospital, Denmark, who chaired the session in which this presentation was a part, acknowledged the importance of recognizing the contribution of NAFLD to liver cancer mortality.
“Liver diseases are on the rise. They are the fastest rising cause of death in the United Kingdom, faster than heart disease and other cancers. NAFLD in particular is the fastest growing cause of liver cancer, and the leading cause in France and the United States,” he remarked.
Dr. Krag also highlighted the costs of disease management.
“Managing fatty liver disease in Europe is estimated at €35 billion in direct health care, so we need to do something now,” he stressed.
“The global burden of NAFLD is so high that we need both prevention and treatment tools,” Dr. Krag said. “Change to lifestyle is a ‘no-brainer’ and costs governments very little. For the sake of our young people, we need to take this very seriously. At a political level, we can easily implement this, for example, by banning junk food advertisements, but also educating young people and their families. Good drugs will also help.”
NAFLD: The liver manifestation of type 2 diabetes
About 25%-30% of the global population have NAFLD, and 3%-5% have NASH. Dr. Younossi highlighted that the U.S. transplant database shows that NAFLD was the second indication for all liver transplants in the country. NAFLD also was a leading cause of liver transplants for patients with hepatocellular carcinoma.
There are around two billion cases of chronic liver disease globally, he said. He noted that over time, there has been an increase in all kinds of liver diseases, as reflected in the annual percent change.
“The global epidemic of obesity and type 2 diabetes is driving the rise in NAFLD, but even among lean people, the prevalence of NAFLD is around 9%,” Dr. Younossi said. “Alongside the eye and kidney complications of diabetes, this is the liver manifestation of type 2 diabetes.”
To assess global liver disease and death, Dr. Younossi and his colleagues turned to the Global Burden of Disease Study, which gathered data from around 7,000 investigators located across 22 different regions of the world, comprising 156 countries.
They calculated the incidence, prevalence, mortality, and disability-adjusted life-years (DALYs) in relation to liver cancer and chronic liver disease, including the APC. They linked the data to changes in four liver diseases: NAFLD, alcoholic liver disease, hepatitis B infection, and hepatitis C infection.
The cases of NAFLD reported in the study had been diagnosed by ultrasound or other imaging. Importantly, the prevalence of NAFLD was adjusted for alcohol use in the various national populations, explained Dr. Younossi.
In 2019, they reported that globally, the overall prevalence of liver disease reached 1.69 billion (liver cancer, 0.04%; chronic liver disease, 99.96%), with an incidence of 2.59 million (liver cancer, 20.7%; chronic liver disease, 79.3%), mortality of 1.95 million (liver cancer, 24.8%; chronic liver disease, 75.3%), and DALYs of 58.7 million (liver cancer, 21.3%; chronic liver disease, 78.7%).
Between 2009 and 2019, deaths from liver cancer rose by 27.2%, and deaths from chronic liver disease rose by 10.6%. DALYs from liver cancer rose by 21.9%, and DALYs from chronic liver disease were up by 5.1%.
In contrast to the increase in liver cancer deaths, deaths from chronic liver disease decreased (APC, –0.18%). The decrease was driven by a decrease in hepatitis B (APC, –1.83%). APCs for hepatitis C (+0.37%), alcoholic liver disease (+0.45%), and NAFLD (+1.33%) increased.
“The burden of hepatitis B–related mortality has decreased because we have been so good at vaccinating people,” Dr. Younossi remarked.
NAFLD ‘exploding’ in Middle East, North Africa, and East Asia
The increase in NAFLD has been seen in all regions of the world, but a breakdown by region shows that NAFLD is primarily “exploding” with highest prevalence and mortality in the Middle East (mostly Egypt, Iran, and Turkey), North Africa, and East Asia, said Dr. Younossi. In addition, there are large increases in the West and South America.
“We knew that the prevalence was high in the Middle East, but we now know that mortality is also high, so we are connecting these data,” said Dr. Younossi.
Awareness lacking
Dr. Younossi pressed the fact that awareness among the general population, primary care providers, and policymakers is very low. “From my perspective, raising awareness of NAFLD is the number one priority, and that is the value of this study.”
He added that more people will become aware as testing becomes more manageable.
“There are some noninvasive tests being developed, so in the future, we won’t have to do liver biopsies to diagnose these patients,” he said. “Currently, there are some excellent treatments being developed.”
“The WHO [World Health Organization] does not mention NAFLD as an important noncommunicable disease, and this too has to change,” Dr. Younossi added.
Dr. Younossi has received research funds and/or has consulted for Abbott, Allergan, Bristol-Myers Squibb, Echosens, Genfit, Gilead Sciences, Intercept, Madrigal, Merck, and Novo Nordisk. Dr. Krag has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ILC 2022