User login
Strengthening faith during coronavirus: An Islamic perspective
"Ramadan will be depressing this year,” a patient told me as I entered the room for an evaluation. This is one of many similar reactions my patients expressed in March, when mosques began to close and social distancing parameters were put in place to limit the spread of coronavirus disease 2019 (COVID-19). Muslims began to adjust to new social norms, such as replacing warm hugs with waving hands from 6 feet away. They were suddenly advised to avoid century-long cultural practices, such as spending time with extended family, visiting the sick and the elderly, and meeting for Jummah (Friday) prayer at mosque. With increasing anxiety and uncertainty in the air, I began thinking about how the pandemic would psychologically affect Islamic spirituality, especially during Ramadan (the Islamic month of fasting) this year.
As a Muslim psychiatry resident working on an inpatient psychiatric unit and in a psychiatry consultation service during the COVID-19 pandemic, I often explore spirituality and faith with my patients as a way of providing supportive therapy for anxiety. Many of my Christian patients endorsed anxiety about how Easter would be “terrible” this year because they could not attend church. Upon hearing this, I realized that I could not picture a Ramadan during which I was not permitted to go to mosque. How was I supposed to provide supportive therapy for my patients when I also felt so uncertain? These concerns led me to take a step back and remind myself of what I frequently tell my patients when they feel hopeless: “With every difficulty, there comes an opportunity to gain a new perspective.”
A time for spirituality
When Ramadan began in April, many people who are Muslim and were working from home told me that it felt strange to have so much time during the day to pray, reflect, and read the Quran. Others mentioned that they enjoyed the peace of Iftar (breaking fast) at home, because they could avoid the hustle and bustle of this at mosque. Halfway through Ramadan, a Muslim patient I was treating reported that her “coronavirus anxiety” had improved as she began focusing her energy on Allah, rather than spending hours watching the news and obsessing over death tolls.
Due to the pandemic, many more opportunities for donating to those in need arose, which led my religious community to perform Zakat (providing charity) and send supplies to food banks in our area. Because of social distancing, Muslim families were able to spend more time preparing meals, learning together, and supporting each other. Although mosques were closed due to the pandemic, it seemed as though each home became its own gathering place for spirituality, gratitude, and self-reflection. By the end of Ramadan, the values of self-discipline, empathy, and patience became self-evident.
Increased attention to mental health among Muslims
Psychologically, I believe resilience has grown stronger among Muslims worldwide during this pandemic. Along with adopting a positive mindset, Muslims have committed to creating their own routines to combat anxiety during this stressful time. The Salat (praying 5 times a day) and Taharat (cleanliness) that Islam emphasizes have been helpful in creating structure to offset the uncertainty and fear that is associated with COVID-19.
The discussion of mental illness, which previously has been regarded as a culturally stigmatized topic, has been gaining significant recognition within Islamic communities. Depression, anxiety, and self-care are now emphasized during virtual sermons, and contact information for mental health hotlines and professionals are being rapidly disseminated. There is now a greater sense of encouragement for people of Islamic faith to seek psychiatric help when needed.
Although COVID-19 has limited some social and physical religious practices, this pandemic has helped to strengthen faith and spirituality not only among Muslims, but also people of other faiths. During periods of stress, change, and uncertainty, it is important to remember that “With every difficulty, there comes an opportunity to gain a new perspective.” Although mosques and churches continue to stay closed and anxiety persists, I can now confidently reassure my patients that through this experience we are becoming resilient and learning to value patience, gratitude, and empathy more than ever.
"Ramadan will be depressing this year,” a patient told me as I entered the room for an evaluation. This is one of many similar reactions my patients expressed in March, when mosques began to close and social distancing parameters were put in place to limit the spread of coronavirus disease 2019 (COVID-19). Muslims began to adjust to new social norms, such as replacing warm hugs with waving hands from 6 feet away. They were suddenly advised to avoid century-long cultural practices, such as spending time with extended family, visiting the sick and the elderly, and meeting for Jummah (Friday) prayer at mosque. With increasing anxiety and uncertainty in the air, I began thinking about how the pandemic would psychologically affect Islamic spirituality, especially during Ramadan (the Islamic month of fasting) this year.
As a Muslim psychiatry resident working on an inpatient psychiatric unit and in a psychiatry consultation service during the COVID-19 pandemic, I often explore spirituality and faith with my patients as a way of providing supportive therapy for anxiety. Many of my Christian patients endorsed anxiety about how Easter would be “terrible” this year because they could not attend church. Upon hearing this, I realized that I could not picture a Ramadan during which I was not permitted to go to mosque. How was I supposed to provide supportive therapy for my patients when I also felt so uncertain? These concerns led me to take a step back and remind myself of what I frequently tell my patients when they feel hopeless: “With every difficulty, there comes an opportunity to gain a new perspective.”
A time for spirituality
When Ramadan began in April, many people who are Muslim and were working from home told me that it felt strange to have so much time during the day to pray, reflect, and read the Quran. Others mentioned that they enjoyed the peace of Iftar (breaking fast) at home, because they could avoid the hustle and bustle of this at mosque. Halfway through Ramadan, a Muslim patient I was treating reported that her “coronavirus anxiety” had improved as she began focusing her energy on Allah, rather than spending hours watching the news and obsessing over death tolls.
Due to the pandemic, many more opportunities for donating to those in need arose, which led my religious community to perform Zakat (providing charity) and send supplies to food banks in our area. Because of social distancing, Muslim families were able to spend more time preparing meals, learning together, and supporting each other. Although mosques were closed due to the pandemic, it seemed as though each home became its own gathering place for spirituality, gratitude, and self-reflection. By the end of Ramadan, the values of self-discipline, empathy, and patience became self-evident.
Increased attention to mental health among Muslims
Psychologically, I believe resilience has grown stronger among Muslims worldwide during this pandemic. Along with adopting a positive mindset, Muslims have committed to creating their own routines to combat anxiety during this stressful time. The Salat (praying 5 times a day) and Taharat (cleanliness) that Islam emphasizes have been helpful in creating structure to offset the uncertainty and fear that is associated with COVID-19.
The discussion of mental illness, which previously has been regarded as a culturally stigmatized topic, has been gaining significant recognition within Islamic communities. Depression, anxiety, and self-care are now emphasized during virtual sermons, and contact information for mental health hotlines and professionals are being rapidly disseminated. There is now a greater sense of encouragement for people of Islamic faith to seek psychiatric help when needed.
Although COVID-19 has limited some social and physical religious practices, this pandemic has helped to strengthen faith and spirituality not only among Muslims, but also people of other faiths. During periods of stress, change, and uncertainty, it is important to remember that “With every difficulty, there comes an opportunity to gain a new perspective.” Although mosques and churches continue to stay closed and anxiety persists, I can now confidently reassure my patients that through this experience we are becoming resilient and learning to value patience, gratitude, and empathy more than ever.
"Ramadan will be depressing this year,” a patient told me as I entered the room for an evaluation. This is one of many similar reactions my patients expressed in March, when mosques began to close and social distancing parameters were put in place to limit the spread of coronavirus disease 2019 (COVID-19). Muslims began to adjust to new social norms, such as replacing warm hugs with waving hands from 6 feet away. They were suddenly advised to avoid century-long cultural practices, such as spending time with extended family, visiting the sick and the elderly, and meeting for Jummah (Friday) prayer at mosque. With increasing anxiety and uncertainty in the air, I began thinking about how the pandemic would psychologically affect Islamic spirituality, especially during Ramadan (the Islamic month of fasting) this year.
As a Muslim psychiatry resident working on an inpatient psychiatric unit and in a psychiatry consultation service during the COVID-19 pandemic, I often explore spirituality and faith with my patients as a way of providing supportive therapy for anxiety. Many of my Christian patients endorsed anxiety about how Easter would be “terrible” this year because they could not attend church. Upon hearing this, I realized that I could not picture a Ramadan during which I was not permitted to go to mosque. How was I supposed to provide supportive therapy for my patients when I also felt so uncertain? These concerns led me to take a step back and remind myself of what I frequently tell my patients when they feel hopeless: “With every difficulty, there comes an opportunity to gain a new perspective.”
A time for spirituality
When Ramadan began in April, many people who are Muslim and were working from home told me that it felt strange to have so much time during the day to pray, reflect, and read the Quran. Others mentioned that they enjoyed the peace of Iftar (breaking fast) at home, because they could avoid the hustle and bustle of this at mosque. Halfway through Ramadan, a Muslim patient I was treating reported that her “coronavirus anxiety” had improved as she began focusing her energy on Allah, rather than spending hours watching the news and obsessing over death tolls.
Due to the pandemic, many more opportunities for donating to those in need arose, which led my religious community to perform Zakat (providing charity) and send supplies to food banks in our area. Because of social distancing, Muslim families were able to spend more time preparing meals, learning together, and supporting each other. Although mosques were closed due to the pandemic, it seemed as though each home became its own gathering place for spirituality, gratitude, and self-reflection. By the end of Ramadan, the values of self-discipline, empathy, and patience became self-evident.
Increased attention to mental health among Muslims
Psychologically, I believe resilience has grown stronger among Muslims worldwide during this pandemic. Along with adopting a positive mindset, Muslims have committed to creating their own routines to combat anxiety during this stressful time. The Salat (praying 5 times a day) and Taharat (cleanliness) that Islam emphasizes have been helpful in creating structure to offset the uncertainty and fear that is associated with COVID-19.
The discussion of mental illness, which previously has been regarded as a culturally stigmatized topic, has been gaining significant recognition within Islamic communities. Depression, anxiety, and self-care are now emphasized during virtual sermons, and contact information for mental health hotlines and professionals are being rapidly disseminated. There is now a greater sense of encouragement for people of Islamic faith to seek psychiatric help when needed.
Although COVID-19 has limited some social and physical religious practices, this pandemic has helped to strengthen faith and spirituality not only among Muslims, but also people of other faiths. During periods of stress, change, and uncertainty, it is important to remember that “With every difficulty, there comes an opportunity to gain a new perspective.” Although mosques and churches continue to stay closed and anxiety persists, I can now confidently reassure my patients that through this experience we are becoming resilient and learning to value patience, gratitude, and empathy more than ever.
Gender gaps persist in academic rheumatology
They’re less likely to hold a higher-level professorship position, feature as a senior author on a paper, or receive a federal grant. Two recent studies underscore progress for and barriers to career advancement.
One cross-sectional analysis of practicing U.S. rheumatologists found that fewer women are professors compared with men (12.6% vs. 36.8%) or associate professors (17.5% vs. 28%). A larger proportion of women serve as assistant professors (55.5% vs. 31.5%). From a leadership perspective, women are making progress. Their odds are similar to men as far as holding a fellowship or division director position in a rheumatology division.
For this study, published in Arthritis & Rheumatology on Aug. 16, April Jorge, MD, and her colleagues at Massachusetts General Hospital and Harvard Medical School, both in Boston, identified 6,125 rheumatologists from a database of all licensed physicians and used multivariate logistic regression to assess gender differences in academic advancement. They arrived at their results after accounting for variables such as age, research and academic appointments, publications, achievements, and years since residency graduation.
Women rheumatologists are younger, completing their residency more recently than their male colleagues. Their numbers in academic rheumatology have gradually increased over the last few decades, recently outpacing men. In 2015, the American College of Rheumatology reported that women made up 41% of the workforce and 66% of rheumatology fellows. Dr. Jorge and associates stressed the importance of fostering women in leadership positions and ensuring gender equity in academic career advancement.
Women also had fewer publications and grants from the National Institutes of Health. Several factors could account for this, such as time spent in the workforce or on parental leave, work-life balance, and mentorship. “However, gender differences in academic promotion remained after adjusting for each of these typical promotion criteria, indicating that other unidentified factors also contribute to the gap in promotion for women academic rheumatologists,” the investigators noted.
The authors weren’t able to assess how parental leave and work effort affected results or why pay differences existed between men and women. They also weren’t able to determine how many physicians left academic practice. “If greater numbers of women than men left the academic rheumatology workforce – for one of many reasons, including that they were not promoted – our findings could underestimate sex differences in academic rank,” they acknowledged.
Lower authorship rate examined
Fewer women in full or associate professor positions might explain why female authorship on research papers is underrepresented, according to another study published Aug. 18 in Arthritis & Rheumatology. Ekta Bagga and colleagues at the University of Auckland (New Zealand) examined 7,651 original research articles from high-impact rheumatology and general medical journals published during 2015-2019 and reported that women were much less likely to achieve first or senior author positions in reports of randomized, controlled trials. This was especially true for studies initiated and funded by industry, compared with other research designs.
More gender parity existed for first authorship than senior authorship – women first authors and senior authors appeared in 51.5% and 35.3% of the papers, respectively. For all geographical regions, the proportion of women senior authors fell below 40%. Representation was especially low in regions other than Europe and North America. These observations likely reflect gender disparities in the medical workforce, Nicola Dalbeth, MD, the study’s senior author, said in an interview.
“We know that, although women make up almost half the rheumatology workforce in many countries around the world, we are less likely to be in positions of senior academic leadership,” added Dr. Dalbeth, a rheumatologist and professor at the University of Auckland’s Bone and Joint Research Group. Institutions and industry should take steps to ensure that women rheumatologists get equal representation, particularly in clinical trial development, she added.
The study had its limitations, one of which was that the researchers didn’t analyze individual author names. This means that one person may have authored multiple articles. “Given the relatively low number of women in academic rheumatology leadership positions, our method of analysis may have overrepresented the number of women authors of rheumatology publications, particularly in senior positions,” stated Dr. Dalbeth and colleagues.
Implicit bias in academia
The articles by Jorge et al. and Bagga et al. suggest that implicit bias is as prevalent in medicine as it is in general society, Jason Kolfenbach, MD, said in an interview. Dr. Kolfenbach is an associate professor of medicine and rheumatology and director of the rheumatology fellowship program at University of Colorado at Denver, Aurora.
“The study by Jorge et al. is eye opening because it demonstrates that academic promotion is lower among women even after adjustment for some of these measures of academic productivity,” Dr. Kolfenbach said. It’s likely that bias plays some role “since there is a human element behind promotions committees, as well as committees selecting faculty for the creation of guidelines and speaker panels at national conferences.”
The study by Bagga et al. “matches my personal perception of industry-sponsored studies and pharmaceutical-sponsored speakers bureaus, namely that they are overrepresented by male faculty,” Dr. Kolfenbach continued.
Prior to COVID-19, the department of medicine at the University of Colorado had begun participating in a formal program called the Bias Reduction in Internal Medicine Initiative, a National Institutes of Health–sponsored study. “I’m hopeful programs such as this can lead to a more equitable situation than described by the findings in these two studies,” he added.
Article type, country of origin play a role
Other research corroborates the findings in these two papers. Giovanni Adami, MD, and coauthors examined 366 rheumatology guidelines and recommendations and determined that only 32% featured a female first author. However, authorship did increase for women over time, achieving parity in 2017.
There are several points to consider when exploring gender disparity, Dr. Adami said in an interview. “Original articles, industry-sponsored articles, and recommendation articles explore different disparities,” he offered. Recommendations and industry-sponsored articles are usually authored by international experts such as division directors or full professors. Original articles, in comparison, aren’t as affected by the “opinion leader” effect, he added.
Country of origin is also a crucial aspect, Dr. Adami said. In his own search of guidelines and articles published by Japanese or Chinese researchers, he noticed that males made up the vast majority of authors. “The cultural aspects of the country where research develops is a vital thing to consider when analyzing gender disparity.”
Dr. Adami’s homeland of Italy is a case in point: most of the division chiefs and professors are male. “Here in Italy, there’s a common belief that a woman cannot pursue an academic career or aim for a leadership position,” he noted.
Italy’s public university system has seen some improvements in gender parity, he continued. “For example, in 2009 there were 61,000 new medical students in Italy, and the majority [57%] were female. Nonetheless, we still have more male professors of medicine and more male PhD candidates.”
Gender gap narrows for conference speakers
In another study, rheumatologists Jean Liew, MD, of the University of Washington, Seattle, and Kanika Monga, MD, of the University of Texas Health Science Center at Houston, found notable gender gaps in speakers at ACR conferences. Women represented under 50% of speakers at these meetings over a 2-year period. “Although the gender gap at recent ACR meetings was narrower as compared with other conferences, we must remain cognizant of its presence and continue to work towards equal representation,” the authors wrote in a correspondence letter in Annals of the Rheumatic Diseases.
Dr. Monga said she was excited to see so many studies on the topic of gender disparities in rheumatology. The Jorge et al. and Bagga et al. papers “delve deeper into quantifying the gender gap in rheumatology. These studies allow us to better identify where the discrepancies may be,” she said in an interview.
“I found it very interesting that women were less likely to be promoted in academic rank but as likely as men to hold leadership positions,” Dr. Monga said. She agreed with the authors that criteria for academic promotion should be reassessed to ensure that it values the diversity of scholarly work that rheumatologists pursue.
Men may still outnumber women speakers at ACR meetings, but the Liew and Monga study did report a 4.2% increase in female speaker representation from 2017 to 2018. “We were happy to note that that continued to be the case at The American College of Rheumatology’s Annual Meeting in 2019. I hope that this reflects a positive change in our specialty,” she said.
Dr. Dalbeth’s study received support from a University of Auckland Summer Studentship Award. She has received consulting fees, speaker fees, or grants from AstraZeneca, Horizon, Amgen, Janssen, and other companies outside of the submitted work. The other authors declared no competing interests.
Dr. Jorge receives funds from the Rheumatology Research Foundation. The senior author on her study receives funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
They’re less likely to hold a higher-level professorship position, feature as a senior author on a paper, or receive a federal grant. Two recent studies underscore progress for and barriers to career advancement.
One cross-sectional analysis of practicing U.S. rheumatologists found that fewer women are professors compared with men (12.6% vs. 36.8%) or associate professors (17.5% vs. 28%). A larger proportion of women serve as assistant professors (55.5% vs. 31.5%). From a leadership perspective, women are making progress. Their odds are similar to men as far as holding a fellowship or division director position in a rheumatology division.
For this study, published in Arthritis & Rheumatology on Aug. 16, April Jorge, MD, and her colleagues at Massachusetts General Hospital and Harvard Medical School, both in Boston, identified 6,125 rheumatologists from a database of all licensed physicians and used multivariate logistic regression to assess gender differences in academic advancement. They arrived at their results after accounting for variables such as age, research and academic appointments, publications, achievements, and years since residency graduation.
Women rheumatologists are younger, completing their residency more recently than their male colleagues. Their numbers in academic rheumatology have gradually increased over the last few decades, recently outpacing men. In 2015, the American College of Rheumatology reported that women made up 41% of the workforce and 66% of rheumatology fellows. Dr. Jorge and associates stressed the importance of fostering women in leadership positions and ensuring gender equity in academic career advancement.
Women also had fewer publications and grants from the National Institutes of Health. Several factors could account for this, such as time spent in the workforce or on parental leave, work-life balance, and mentorship. “However, gender differences in academic promotion remained after adjusting for each of these typical promotion criteria, indicating that other unidentified factors also contribute to the gap in promotion for women academic rheumatologists,” the investigators noted.
The authors weren’t able to assess how parental leave and work effort affected results or why pay differences existed between men and women. They also weren’t able to determine how many physicians left academic practice. “If greater numbers of women than men left the academic rheumatology workforce – for one of many reasons, including that they were not promoted – our findings could underestimate sex differences in academic rank,” they acknowledged.
Lower authorship rate examined
Fewer women in full or associate professor positions might explain why female authorship on research papers is underrepresented, according to another study published Aug. 18 in Arthritis & Rheumatology. Ekta Bagga and colleagues at the University of Auckland (New Zealand) examined 7,651 original research articles from high-impact rheumatology and general medical journals published during 2015-2019 and reported that women were much less likely to achieve first or senior author positions in reports of randomized, controlled trials. This was especially true for studies initiated and funded by industry, compared with other research designs.
More gender parity existed for first authorship than senior authorship – women first authors and senior authors appeared in 51.5% and 35.3% of the papers, respectively. For all geographical regions, the proportion of women senior authors fell below 40%. Representation was especially low in regions other than Europe and North America. These observations likely reflect gender disparities in the medical workforce, Nicola Dalbeth, MD, the study’s senior author, said in an interview.
“We know that, although women make up almost half the rheumatology workforce in many countries around the world, we are less likely to be in positions of senior academic leadership,” added Dr. Dalbeth, a rheumatologist and professor at the University of Auckland’s Bone and Joint Research Group. Institutions and industry should take steps to ensure that women rheumatologists get equal representation, particularly in clinical trial development, she added.
The study had its limitations, one of which was that the researchers didn’t analyze individual author names. This means that one person may have authored multiple articles. “Given the relatively low number of women in academic rheumatology leadership positions, our method of analysis may have overrepresented the number of women authors of rheumatology publications, particularly in senior positions,” stated Dr. Dalbeth and colleagues.
Implicit bias in academia
The articles by Jorge et al. and Bagga et al. suggest that implicit bias is as prevalent in medicine as it is in general society, Jason Kolfenbach, MD, said in an interview. Dr. Kolfenbach is an associate professor of medicine and rheumatology and director of the rheumatology fellowship program at University of Colorado at Denver, Aurora.
“The study by Jorge et al. is eye opening because it demonstrates that academic promotion is lower among women even after adjustment for some of these measures of academic productivity,” Dr. Kolfenbach said. It’s likely that bias plays some role “since there is a human element behind promotions committees, as well as committees selecting faculty for the creation of guidelines and speaker panels at national conferences.”
The study by Bagga et al. “matches my personal perception of industry-sponsored studies and pharmaceutical-sponsored speakers bureaus, namely that they are overrepresented by male faculty,” Dr. Kolfenbach continued.
Prior to COVID-19, the department of medicine at the University of Colorado had begun participating in a formal program called the Bias Reduction in Internal Medicine Initiative, a National Institutes of Health–sponsored study. “I’m hopeful programs such as this can lead to a more equitable situation than described by the findings in these two studies,” he added.
Article type, country of origin play a role
Other research corroborates the findings in these two papers. Giovanni Adami, MD, and coauthors examined 366 rheumatology guidelines and recommendations and determined that only 32% featured a female first author. However, authorship did increase for women over time, achieving parity in 2017.
There are several points to consider when exploring gender disparity, Dr. Adami said in an interview. “Original articles, industry-sponsored articles, and recommendation articles explore different disparities,” he offered. Recommendations and industry-sponsored articles are usually authored by international experts such as division directors or full professors. Original articles, in comparison, aren’t as affected by the “opinion leader” effect, he added.
Country of origin is also a crucial aspect, Dr. Adami said. In his own search of guidelines and articles published by Japanese or Chinese researchers, he noticed that males made up the vast majority of authors. “The cultural aspects of the country where research develops is a vital thing to consider when analyzing gender disparity.”
Dr. Adami’s homeland of Italy is a case in point: most of the division chiefs and professors are male. “Here in Italy, there’s a common belief that a woman cannot pursue an academic career or aim for a leadership position,” he noted.
Italy’s public university system has seen some improvements in gender parity, he continued. “For example, in 2009 there were 61,000 new medical students in Italy, and the majority [57%] were female. Nonetheless, we still have more male professors of medicine and more male PhD candidates.”
Gender gap narrows for conference speakers
In another study, rheumatologists Jean Liew, MD, of the University of Washington, Seattle, and Kanika Monga, MD, of the University of Texas Health Science Center at Houston, found notable gender gaps in speakers at ACR conferences. Women represented under 50% of speakers at these meetings over a 2-year period. “Although the gender gap at recent ACR meetings was narrower as compared with other conferences, we must remain cognizant of its presence and continue to work towards equal representation,” the authors wrote in a correspondence letter in Annals of the Rheumatic Diseases.
Dr. Monga said she was excited to see so many studies on the topic of gender disparities in rheumatology. The Jorge et al. and Bagga et al. papers “delve deeper into quantifying the gender gap in rheumatology. These studies allow us to better identify where the discrepancies may be,” she said in an interview.
“I found it very interesting that women were less likely to be promoted in academic rank but as likely as men to hold leadership positions,” Dr. Monga said. She agreed with the authors that criteria for academic promotion should be reassessed to ensure that it values the diversity of scholarly work that rheumatologists pursue.
Men may still outnumber women speakers at ACR meetings, but the Liew and Monga study did report a 4.2% increase in female speaker representation from 2017 to 2018. “We were happy to note that that continued to be the case at The American College of Rheumatology’s Annual Meeting in 2019. I hope that this reflects a positive change in our specialty,” she said.
Dr. Dalbeth’s study received support from a University of Auckland Summer Studentship Award. She has received consulting fees, speaker fees, or grants from AstraZeneca, Horizon, Amgen, Janssen, and other companies outside of the submitted work. The other authors declared no competing interests.
Dr. Jorge receives funds from the Rheumatology Research Foundation. The senior author on her study receives funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
They’re less likely to hold a higher-level professorship position, feature as a senior author on a paper, or receive a federal grant. Two recent studies underscore progress for and barriers to career advancement.
One cross-sectional analysis of practicing U.S. rheumatologists found that fewer women are professors compared with men (12.6% vs. 36.8%) or associate professors (17.5% vs. 28%). A larger proportion of women serve as assistant professors (55.5% vs. 31.5%). From a leadership perspective, women are making progress. Their odds are similar to men as far as holding a fellowship or division director position in a rheumatology division.
For this study, published in Arthritis & Rheumatology on Aug. 16, April Jorge, MD, and her colleagues at Massachusetts General Hospital and Harvard Medical School, both in Boston, identified 6,125 rheumatologists from a database of all licensed physicians and used multivariate logistic regression to assess gender differences in academic advancement. They arrived at their results after accounting for variables such as age, research and academic appointments, publications, achievements, and years since residency graduation.
Women rheumatologists are younger, completing their residency more recently than their male colleagues. Their numbers in academic rheumatology have gradually increased over the last few decades, recently outpacing men. In 2015, the American College of Rheumatology reported that women made up 41% of the workforce and 66% of rheumatology fellows. Dr. Jorge and associates stressed the importance of fostering women in leadership positions and ensuring gender equity in academic career advancement.
Women also had fewer publications and grants from the National Institutes of Health. Several factors could account for this, such as time spent in the workforce or on parental leave, work-life balance, and mentorship. “However, gender differences in academic promotion remained after adjusting for each of these typical promotion criteria, indicating that other unidentified factors also contribute to the gap in promotion for women academic rheumatologists,” the investigators noted.
The authors weren’t able to assess how parental leave and work effort affected results or why pay differences existed between men and women. They also weren’t able to determine how many physicians left academic practice. “If greater numbers of women than men left the academic rheumatology workforce – for one of many reasons, including that they were not promoted – our findings could underestimate sex differences in academic rank,” they acknowledged.
Lower authorship rate examined
Fewer women in full or associate professor positions might explain why female authorship on research papers is underrepresented, according to another study published Aug. 18 in Arthritis & Rheumatology. Ekta Bagga and colleagues at the University of Auckland (New Zealand) examined 7,651 original research articles from high-impact rheumatology and general medical journals published during 2015-2019 and reported that women were much less likely to achieve first or senior author positions in reports of randomized, controlled trials. This was especially true for studies initiated and funded by industry, compared with other research designs.
More gender parity existed for first authorship than senior authorship – women first authors and senior authors appeared in 51.5% and 35.3% of the papers, respectively. For all geographical regions, the proportion of women senior authors fell below 40%. Representation was especially low in regions other than Europe and North America. These observations likely reflect gender disparities in the medical workforce, Nicola Dalbeth, MD, the study’s senior author, said in an interview.
“We know that, although women make up almost half the rheumatology workforce in many countries around the world, we are less likely to be in positions of senior academic leadership,” added Dr. Dalbeth, a rheumatologist and professor at the University of Auckland’s Bone and Joint Research Group. Institutions and industry should take steps to ensure that women rheumatologists get equal representation, particularly in clinical trial development, she added.
The study had its limitations, one of which was that the researchers didn’t analyze individual author names. This means that one person may have authored multiple articles. “Given the relatively low number of women in academic rheumatology leadership positions, our method of analysis may have overrepresented the number of women authors of rheumatology publications, particularly in senior positions,” stated Dr. Dalbeth and colleagues.
Implicit bias in academia
The articles by Jorge et al. and Bagga et al. suggest that implicit bias is as prevalent in medicine as it is in general society, Jason Kolfenbach, MD, said in an interview. Dr. Kolfenbach is an associate professor of medicine and rheumatology and director of the rheumatology fellowship program at University of Colorado at Denver, Aurora.
“The study by Jorge et al. is eye opening because it demonstrates that academic promotion is lower among women even after adjustment for some of these measures of academic productivity,” Dr. Kolfenbach said. It’s likely that bias plays some role “since there is a human element behind promotions committees, as well as committees selecting faculty for the creation of guidelines and speaker panels at national conferences.”
The study by Bagga et al. “matches my personal perception of industry-sponsored studies and pharmaceutical-sponsored speakers bureaus, namely that they are overrepresented by male faculty,” Dr. Kolfenbach continued.
Prior to COVID-19, the department of medicine at the University of Colorado had begun participating in a formal program called the Bias Reduction in Internal Medicine Initiative, a National Institutes of Health–sponsored study. “I’m hopeful programs such as this can lead to a more equitable situation than described by the findings in these two studies,” he added.
Article type, country of origin play a role
Other research corroborates the findings in these two papers. Giovanni Adami, MD, and coauthors examined 366 rheumatology guidelines and recommendations and determined that only 32% featured a female first author. However, authorship did increase for women over time, achieving parity in 2017.
There are several points to consider when exploring gender disparity, Dr. Adami said in an interview. “Original articles, industry-sponsored articles, and recommendation articles explore different disparities,” he offered. Recommendations and industry-sponsored articles are usually authored by international experts such as division directors or full professors. Original articles, in comparison, aren’t as affected by the “opinion leader” effect, he added.
Country of origin is also a crucial aspect, Dr. Adami said. In his own search of guidelines and articles published by Japanese or Chinese researchers, he noticed that males made up the vast majority of authors. “The cultural aspects of the country where research develops is a vital thing to consider when analyzing gender disparity.”
Dr. Adami’s homeland of Italy is a case in point: most of the division chiefs and professors are male. “Here in Italy, there’s a common belief that a woman cannot pursue an academic career or aim for a leadership position,” he noted.
Italy’s public university system has seen some improvements in gender parity, he continued. “For example, in 2009 there were 61,000 new medical students in Italy, and the majority [57%] were female. Nonetheless, we still have more male professors of medicine and more male PhD candidates.”
Gender gap narrows for conference speakers
In another study, rheumatologists Jean Liew, MD, of the University of Washington, Seattle, and Kanika Monga, MD, of the University of Texas Health Science Center at Houston, found notable gender gaps in speakers at ACR conferences. Women represented under 50% of speakers at these meetings over a 2-year period. “Although the gender gap at recent ACR meetings was narrower as compared with other conferences, we must remain cognizant of its presence and continue to work towards equal representation,” the authors wrote in a correspondence letter in Annals of the Rheumatic Diseases.
Dr. Monga said she was excited to see so many studies on the topic of gender disparities in rheumatology. The Jorge et al. and Bagga et al. papers “delve deeper into quantifying the gender gap in rheumatology. These studies allow us to better identify where the discrepancies may be,” she said in an interview.
“I found it very interesting that women were less likely to be promoted in academic rank but as likely as men to hold leadership positions,” Dr. Monga said. She agreed with the authors that criteria for academic promotion should be reassessed to ensure that it values the diversity of scholarly work that rheumatologists pursue.
Men may still outnumber women speakers at ACR meetings, but the Liew and Monga study did report a 4.2% increase in female speaker representation from 2017 to 2018. “We were happy to note that that continued to be the case at The American College of Rheumatology’s Annual Meeting in 2019. I hope that this reflects a positive change in our specialty,” she said.
Dr. Dalbeth’s study received support from a University of Auckland Summer Studentship Award. She has received consulting fees, speaker fees, or grants from AstraZeneca, Horizon, Amgen, Janssen, and other companies outside of the submitted work. The other authors declared no competing interests.
Dr. Jorge receives funds from the Rheumatology Research Foundation. The senior author on her study receives funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Coping with COVID-19, racism, and other stressors
The start of a new school year is usually a time of excitement and return to routine, structure, and consistency for children, teenagers, and families. With the current COVID-19 pandemic, this year is anything but typical. Face masks, hand washing, physical distancing, remote learning, and restrictions on extracurricular activities are just a few of the changes experienced by children in schools. At home, the disruptions and uncertainty for families are equally dramatic with loss of employment, limited child care, risk of eviction and foreclosure, food insecurity, and growing numbers of families directly impacted by loss of health and life due to the coronavirus.
While every family is impacted by the current global pandemic, the realities of the pandemic have thrown increasing light on the racial, social, and structural injustices in our system. People of color are much more likely to be infected, have more severe disease, and die from COVID-19; they are more likely to experience the socioeconomic impacts.1 Centuries of racial injustice and inequity have been highlighted not just by this pandemic but by ongoing differential treatment of people of color in our education, health, justice, economic, and housing systems. The murders of George Floyd, Breonna Taylor, Ahmaud Arbery, and too many others are just one source of the constant stress facing children and families of color.
While each family and individual currently faces a distinct combination of stressors and adversity, no one has been spared from these disruptions. International, national, and local communities all need to continue efforts to overcome the current pandemic and systemic racism. As providers, we have a profound opportunity and responsibility to engage both in advocacy for our communities and the individual care of children and families. We are aware of the negative impacts of acute and chronic stress on long-term health outcomes but are equally familiar with the power of resilience.
Resilience has broadly been defined as the “process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress.”2 Some have argued that resilience should be further defined to include an individual making a “conscious effort to move forward” after or during adversity.3 Another definition with particular utility in considering how to develop and promote resilience describes it as “a process to harness resources to sustain well-being.”3 This definition not only discusses the end result, but the need to reach beyond the current capacity of an individual by harnessing both internal and external resources. These resources may be as tangible as money, food, infrastructure, or treatment, but also can include relationships, social capital, and the lived experience of others. Social supports, mature mentors, and solid bonds with parents/caregivers are critical resources for the development of child and adolescent resilience.4,5
by both being a resource and helping them harness other resources that can lead to physical, emotional, and relationship well-being. To do this, consider incorporating the following into your practice:
Help children and adolescents identify and reach out to positive supports
Research has shown the importance of a stable adult figure in the development of resilience in children.4,5 Ideally, parents will be a major positive support to their children in times of crisis. When parents are not appropriate supports, teachers, coaches, mentors, grandparents, or other extended family members can provide the needed support for children to be resilient across educational, emotional, and relationship domains.4 To find out who your patients have as a stable adult figure, ask the following or a related question: “Who do you have in your life who you can talk to or get support from on a regular basis?”
Screen for substance use and mental health challenges
Do this for children, adolescents, AND adults. Then treat and refer to appropriate treatment as indicated. Rates of depression, anxiety, suicide, substance use, and overdose all have increased with recent events.6 Treating parents with mental health and substance use disorders will not only facilitate their ability to be a positive support and role model for their children and promote resilience, but it has been shown to decrease child psychopathology.7 Providing parents with referrals for substance use and mental health services as well as educating them on the importance of self-care is vital for helping the development of children.
Provide parents with resources on how to cope with ongoing stressors
These stressors may be related to the COVID-19 pandemic, racism, or both. By providing resources to parents, they can better help their children overcome stressors. Multiple organizations have free online collections to support parents and families including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and many others (See below for a list of resources).
Encourage families to find and develop purpose and meaning during this time. Children and families have devoted their time to many activities, some more adaptive and health promoting than others. If we think of resilience as the process of “moving forward” then developing goals and plans to be productive can be helpful and “meaning-making.”3 Spending time together as families, developing skills, accomplishing goals, becoming involved in important social movements, or volunteering all can be ways that individuals and families can develop feelings of self-worth, purpose, and accomplishment.2
Dr. Heward is a child and adolescent psychiatrist at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email him at [email protected].
Resources: Coping with COVID-19
1. American Academy of Pediatrics HealthyChildren.org page on COVID-19.
2. American Academy of Child and Adolescent Psychiatry COVID-19 Resources for Families.
3. American Psychiatric Association COVID-19 Resources for Families.
4. American Psychological Association COVID-19 Information and Resources.
Resources: Racism and discrimination
1. American Academy of Pediatrics Talking to Children About Racial Bias.
2. American Academy of Child and Adolescent Psychiatry Racism Resource Library.
3. American Psychological Association Bias, Discrimination, and Equity Resources.
References
1. “Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the U.S.” Substance Abuse and Mental Health Services Administration. (Submitted by Office of Behavioral Health Equity).
2. “Building your resilience.” American Psychological Association.
3. Eur J Psychotraumatol. 2014 Oct 1. doi: 10.3402/ejpt.v5.25338.
4. Psychological and biological factors associated with resilience to stress and trauma, in “The Unbroken Soul: Tragedy, Trauma, and Human Resilience” (Lanham, Md.: Jason Aronson, 2008, pp.129-51).
5. Biol Psychiatry. 2019 Sep 15. doi: 10.1016/j.biopsych.2019.07.012.
6. MMWR Morb Mortal Wkly Rep. 2020;69:1049-57.
7. J Am Acad Child Adolesc Psychiatry. 2008 Apr;47(4):379-89.
The start of a new school year is usually a time of excitement and return to routine, structure, and consistency for children, teenagers, and families. With the current COVID-19 pandemic, this year is anything but typical. Face masks, hand washing, physical distancing, remote learning, and restrictions on extracurricular activities are just a few of the changes experienced by children in schools. At home, the disruptions and uncertainty for families are equally dramatic with loss of employment, limited child care, risk of eviction and foreclosure, food insecurity, and growing numbers of families directly impacted by loss of health and life due to the coronavirus.
While every family is impacted by the current global pandemic, the realities of the pandemic have thrown increasing light on the racial, social, and structural injustices in our system. People of color are much more likely to be infected, have more severe disease, and die from COVID-19; they are more likely to experience the socioeconomic impacts.1 Centuries of racial injustice and inequity have been highlighted not just by this pandemic but by ongoing differential treatment of people of color in our education, health, justice, economic, and housing systems. The murders of George Floyd, Breonna Taylor, Ahmaud Arbery, and too many others are just one source of the constant stress facing children and families of color.
While each family and individual currently faces a distinct combination of stressors and adversity, no one has been spared from these disruptions. International, national, and local communities all need to continue efforts to overcome the current pandemic and systemic racism. As providers, we have a profound opportunity and responsibility to engage both in advocacy for our communities and the individual care of children and families. We are aware of the negative impacts of acute and chronic stress on long-term health outcomes but are equally familiar with the power of resilience.
Resilience has broadly been defined as the “process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress.”2 Some have argued that resilience should be further defined to include an individual making a “conscious effort to move forward” after or during adversity.3 Another definition with particular utility in considering how to develop and promote resilience describes it as “a process to harness resources to sustain well-being.”3 This definition not only discusses the end result, but the need to reach beyond the current capacity of an individual by harnessing both internal and external resources. These resources may be as tangible as money, food, infrastructure, or treatment, but also can include relationships, social capital, and the lived experience of others. Social supports, mature mentors, and solid bonds with parents/caregivers are critical resources for the development of child and adolescent resilience.4,5
by both being a resource and helping them harness other resources that can lead to physical, emotional, and relationship well-being. To do this, consider incorporating the following into your practice:
Help children and adolescents identify and reach out to positive supports
Research has shown the importance of a stable adult figure in the development of resilience in children.4,5 Ideally, parents will be a major positive support to their children in times of crisis. When parents are not appropriate supports, teachers, coaches, mentors, grandparents, or other extended family members can provide the needed support for children to be resilient across educational, emotional, and relationship domains.4 To find out who your patients have as a stable adult figure, ask the following or a related question: “Who do you have in your life who you can talk to or get support from on a regular basis?”
Screen for substance use and mental health challenges
Do this for children, adolescents, AND adults. Then treat and refer to appropriate treatment as indicated. Rates of depression, anxiety, suicide, substance use, and overdose all have increased with recent events.6 Treating parents with mental health and substance use disorders will not only facilitate their ability to be a positive support and role model for their children and promote resilience, but it has been shown to decrease child psychopathology.7 Providing parents with referrals for substance use and mental health services as well as educating them on the importance of self-care is vital for helping the development of children.
Provide parents with resources on how to cope with ongoing stressors
These stressors may be related to the COVID-19 pandemic, racism, or both. By providing resources to parents, they can better help their children overcome stressors. Multiple organizations have free online collections to support parents and families including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and many others (See below for a list of resources).
Encourage families to find and develop purpose and meaning during this time. Children and families have devoted their time to many activities, some more adaptive and health promoting than others. If we think of resilience as the process of “moving forward” then developing goals and plans to be productive can be helpful and “meaning-making.”3 Spending time together as families, developing skills, accomplishing goals, becoming involved in important social movements, or volunteering all can be ways that individuals and families can develop feelings of self-worth, purpose, and accomplishment.2
Dr. Heward is a child and adolescent psychiatrist at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email him at [email protected].
Resources: Coping with COVID-19
1. American Academy of Pediatrics HealthyChildren.org page on COVID-19.
2. American Academy of Child and Adolescent Psychiatry COVID-19 Resources for Families.
3. American Psychiatric Association COVID-19 Resources for Families.
4. American Psychological Association COVID-19 Information and Resources.
Resources: Racism and discrimination
1. American Academy of Pediatrics Talking to Children About Racial Bias.
2. American Academy of Child and Adolescent Psychiatry Racism Resource Library.
3. American Psychological Association Bias, Discrimination, and Equity Resources.
References
1. “Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the U.S.” Substance Abuse and Mental Health Services Administration. (Submitted by Office of Behavioral Health Equity).
2. “Building your resilience.” American Psychological Association.
3. Eur J Psychotraumatol. 2014 Oct 1. doi: 10.3402/ejpt.v5.25338.
4. Psychological and biological factors associated with resilience to stress and trauma, in “The Unbroken Soul: Tragedy, Trauma, and Human Resilience” (Lanham, Md.: Jason Aronson, 2008, pp.129-51).
5. Biol Psychiatry. 2019 Sep 15. doi: 10.1016/j.biopsych.2019.07.012.
6. MMWR Morb Mortal Wkly Rep. 2020;69:1049-57.
7. J Am Acad Child Adolesc Psychiatry. 2008 Apr;47(4):379-89.
The start of a new school year is usually a time of excitement and return to routine, structure, and consistency for children, teenagers, and families. With the current COVID-19 pandemic, this year is anything but typical. Face masks, hand washing, physical distancing, remote learning, and restrictions on extracurricular activities are just a few of the changes experienced by children in schools. At home, the disruptions and uncertainty for families are equally dramatic with loss of employment, limited child care, risk of eviction and foreclosure, food insecurity, and growing numbers of families directly impacted by loss of health and life due to the coronavirus.
While every family is impacted by the current global pandemic, the realities of the pandemic have thrown increasing light on the racial, social, and structural injustices in our system. People of color are much more likely to be infected, have more severe disease, and die from COVID-19; they are more likely to experience the socioeconomic impacts.1 Centuries of racial injustice and inequity have been highlighted not just by this pandemic but by ongoing differential treatment of people of color in our education, health, justice, economic, and housing systems. The murders of George Floyd, Breonna Taylor, Ahmaud Arbery, and too many others are just one source of the constant stress facing children and families of color.
While each family and individual currently faces a distinct combination of stressors and adversity, no one has been spared from these disruptions. International, national, and local communities all need to continue efforts to overcome the current pandemic and systemic racism. As providers, we have a profound opportunity and responsibility to engage both in advocacy for our communities and the individual care of children and families. We are aware of the negative impacts of acute and chronic stress on long-term health outcomes but are equally familiar with the power of resilience.
Resilience has broadly been defined as the “process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress.”2 Some have argued that resilience should be further defined to include an individual making a “conscious effort to move forward” after or during adversity.3 Another definition with particular utility in considering how to develop and promote resilience describes it as “a process to harness resources to sustain well-being.”3 This definition not only discusses the end result, but the need to reach beyond the current capacity of an individual by harnessing both internal and external resources. These resources may be as tangible as money, food, infrastructure, or treatment, but also can include relationships, social capital, and the lived experience of others. Social supports, mature mentors, and solid bonds with parents/caregivers are critical resources for the development of child and adolescent resilience.4,5
by both being a resource and helping them harness other resources that can lead to physical, emotional, and relationship well-being. To do this, consider incorporating the following into your practice:
Help children and adolescents identify and reach out to positive supports
Research has shown the importance of a stable adult figure in the development of resilience in children.4,5 Ideally, parents will be a major positive support to their children in times of crisis. When parents are not appropriate supports, teachers, coaches, mentors, grandparents, or other extended family members can provide the needed support for children to be resilient across educational, emotional, and relationship domains.4 To find out who your patients have as a stable adult figure, ask the following or a related question: “Who do you have in your life who you can talk to or get support from on a regular basis?”
Screen for substance use and mental health challenges
Do this for children, adolescents, AND adults. Then treat and refer to appropriate treatment as indicated. Rates of depression, anxiety, suicide, substance use, and overdose all have increased with recent events.6 Treating parents with mental health and substance use disorders will not only facilitate their ability to be a positive support and role model for their children and promote resilience, but it has been shown to decrease child psychopathology.7 Providing parents with referrals for substance use and mental health services as well as educating them on the importance of self-care is vital for helping the development of children.
Provide parents with resources on how to cope with ongoing stressors
These stressors may be related to the COVID-19 pandemic, racism, or both. By providing resources to parents, they can better help their children overcome stressors. Multiple organizations have free online collections to support parents and families including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and many others (See below for a list of resources).
Encourage families to find and develop purpose and meaning during this time. Children and families have devoted their time to many activities, some more adaptive and health promoting than others. If we think of resilience as the process of “moving forward” then developing goals and plans to be productive can be helpful and “meaning-making.”3 Spending time together as families, developing skills, accomplishing goals, becoming involved in important social movements, or volunteering all can be ways that individuals and families can develop feelings of self-worth, purpose, and accomplishment.2
Dr. Heward is a child and adolescent psychiatrist at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email him at [email protected].
Resources: Coping with COVID-19
1. American Academy of Pediatrics HealthyChildren.org page on COVID-19.
2. American Academy of Child and Adolescent Psychiatry COVID-19 Resources for Families.
3. American Psychiatric Association COVID-19 Resources for Families.
4. American Psychological Association COVID-19 Information and Resources.
Resources: Racism and discrimination
1. American Academy of Pediatrics Talking to Children About Racial Bias.
2. American Academy of Child and Adolescent Psychiatry Racism Resource Library.
3. American Psychological Association Bias, Discrimination, and Equity Resources.
References
1. “Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the U.S.” Substance Abuse and Mental Health Services Administration. (Submitted by Office of Behavioral Health Equity).
2. “Building your resilience.” American Psychological Association.
3. Eur J Psychotraumatol. 2014 Oct 1. doi: 10.3402/ejpt.v5.25338.
4. Psychological and biological factors associated with resilience to stress and trauma, in “The Unbroken Soul: Tragedy, Trauma, and Human Resilience” (Lanham, Md.: Jason Aronson, 2008, pp.129-51).
5. Biol Psychiatry. 2019 Sep 15. doi: 10.1016/j.biopsych.2019.07.012.
6. MMWR Morb Mortal Wkly Rep. 2020;69:1049-57.
7. J Am Acad Child Adolesc Psychiatry. 2008 Apr;47(4):379-89.
Dear 2020, where do we go from here?
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
Psoriasis in Patients of Color: Differences in Morphology, Clinical Presentation, and Treatment
Psoriasis is a chronic inflammatory skin disease that affects 2% to 3% of individuals worldwide.1 Despite extensive research, the majority of clinical data are in white patients with limited data in patients of color, yet a number of differences are known. The prevalence of psoriasis differs among racial and ethnic groups, with lower prevalence in racial minorities.2 A cross-sectional American study using data from 2009 through 2010 showed the prevalence for psoriasis was 3.6% in white patients, 1.9% in black patients, 1.6% in Hispanic patients, and 1.4% in other racial groups.3 Psoriasis presents differently in patients of color, both in morphology and severity. Cultural differences and stigma may contribute to the differences seen in severity but also to the psychological impact and treatment choices in patients of color compared to white patients.4 It has even been theorized that treatment efficacy could differ because of potential genetic differences.5 Psoriasis in patients of color is an emerging clinical issue that requires further attention so that dermatologists can learn about, diagnose, and treat them.
We report 3 cases of patients of color with psoriasis who presented to an urban and racially diverse dermatology clinic affiliated with Scarborough General Hospital in Toronto, Ontario, Canada. A retrospective chart review was performed on these high-yield representative cases to demonstrate differences in color and morphology, disease severity, and treatment in patients of various races seen at our clinic. After informed consent was obtained, photographs were taken of patient cutaneous findings to illustrate these differences. Discussion with these selected patients yielded supplementary qualitative data, highlighting individual perspectives of their disease.
Case Series
Patient 1
A 53-year-old black man from Grenada presented to our clinic with a history of psoriasis for a number of years that presented as violaceous plaques throughout large portions of the body (Figure 1). He previously had achieved inadequate results while using topical therapies, methotrexate, acitretin, apremilast, ustekinumab, ixekizumab, and guselkumab at adequate or even maximum doses. His disease affected 30% of the body surface area, with a psoriasis area and severity index score of 27 and a dermatology life quality index score of 23. The patient’s life was quite affected by psoriasis, with emphasis on choice of clothing worn and effect on body image. He also discussed the stigma psoriasis may have in black patients, stating that he has been told multiple times that “black people do not get psoriasis.”
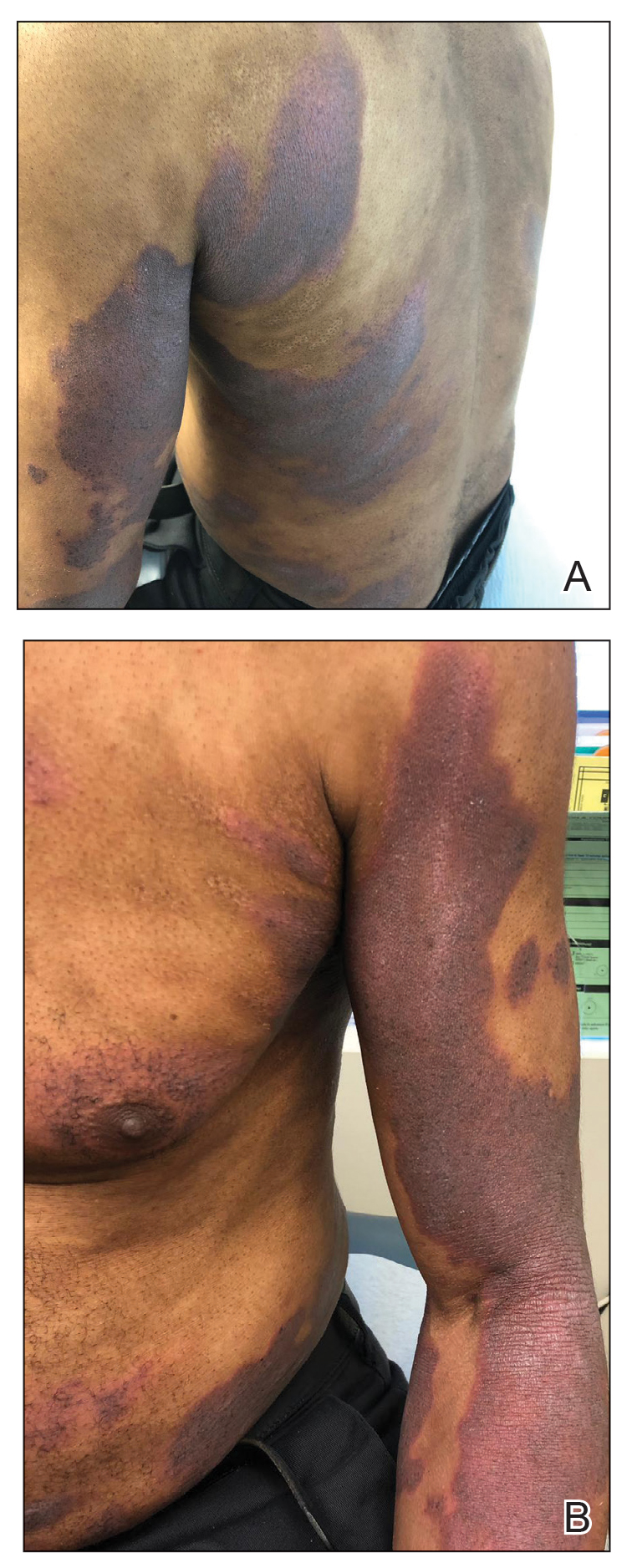
Patient 2
A 27-year-old man from India presented with guttate psoriasis (Figure 2). He was treated with methotrexate 2 years prior and currently is on maintenance therapy with topical treatments alone. His main concerns pertained to the persistent dyschromia that occurred secondary to the psoriatic lesions. Through discussion, the patient stated that he “would do anything to get rid of it.”
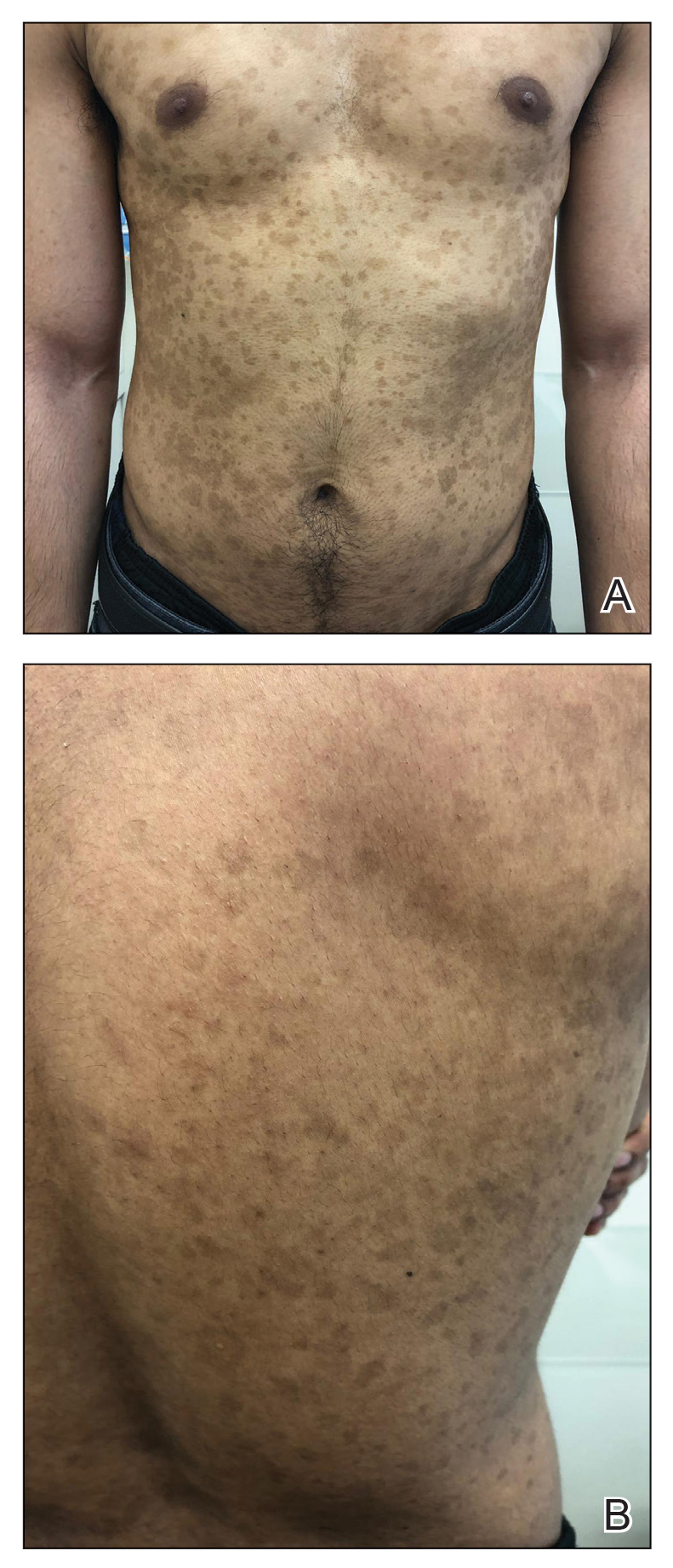
Patient 3
A 49-year-old man from the Philippines presented to our clinic with plaque psoriasis that predominantly affected the trunk and scalp (Figure 3). He had been treated with methotrexate and phototherapy with suboptimal efficacy and was planning for biologic therapy. Although he had active plaques on the trunk, the patient stated, “I am most bothered by my scalp,” particularly referring to the itch and scale and their effects on hair and hairstyling.
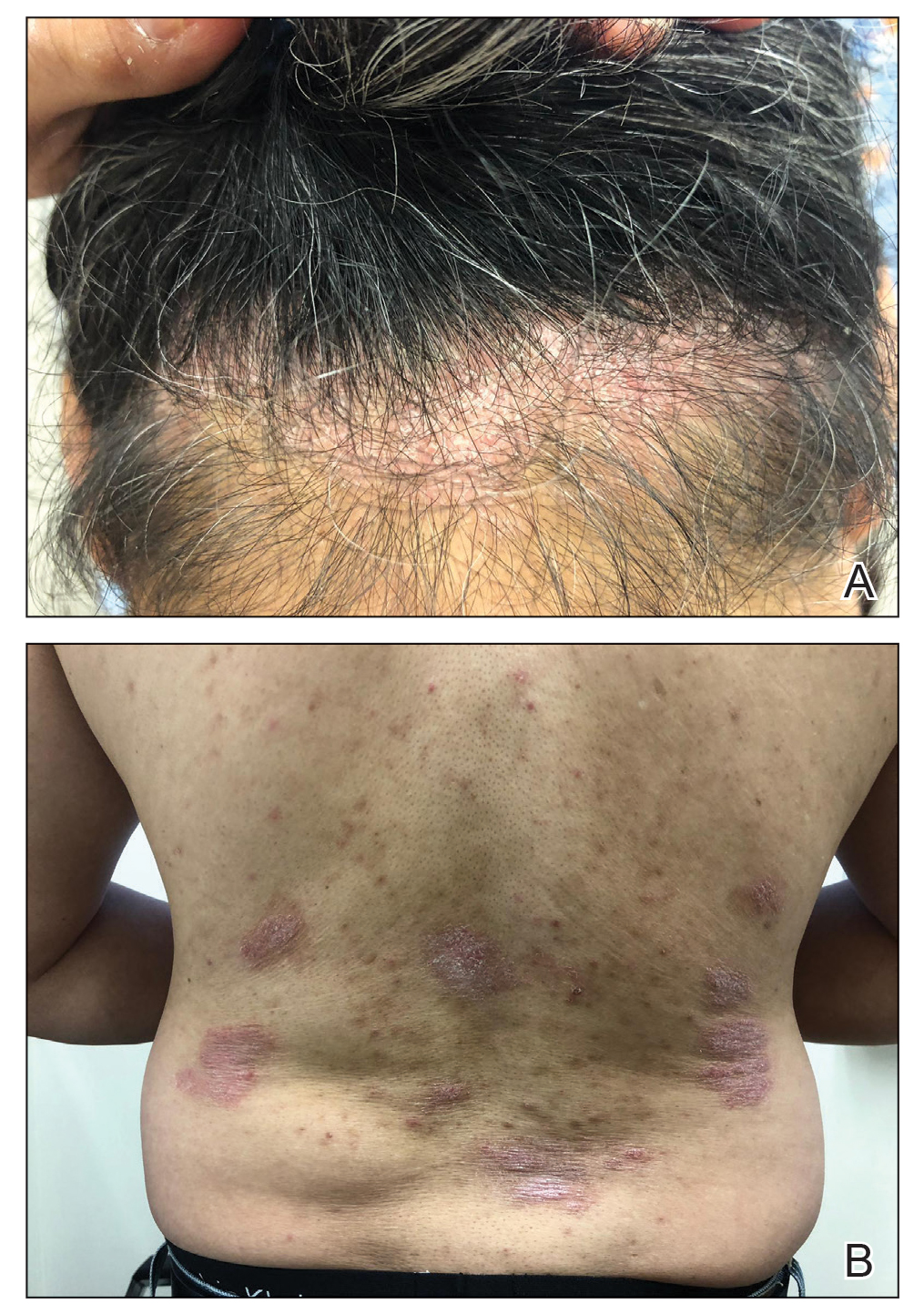
Comment
Clinical differences in patients of color with psoriasis affect the management of the disease. Special consideration should be given to variances in morphology, presentation, treatment, and psychosocial factors in the management of psoriasis for these patient populations, as summarized in the eTable.
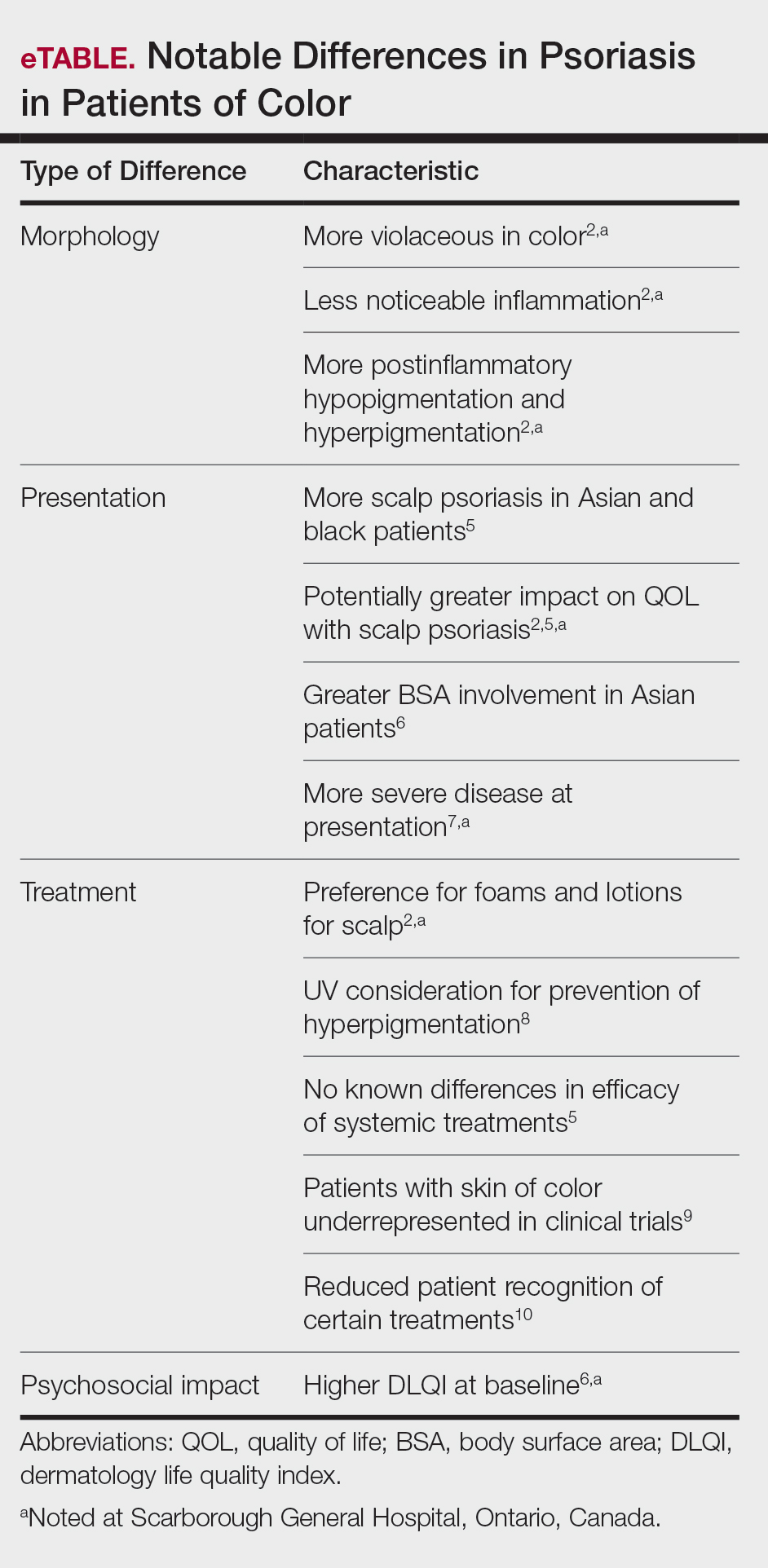
Morphology
At our clinic, patients of color have been found to have differences in morphology, including lesions that are more violaceous in color, as seen in patient 1; less noticeable inflammation; and more postinflammatory hypopigmentation and hyperpigmentation changes, as seen in patient 2. These changes are supported by the literature and differ from typical psoriasis plaques, which are pink-red and have more overlying scale. The varied morphology also may affect the differential, and other mimickers may be considered, such as lichen planus, cutaneous lupus erythematosus, and sarcoidosis.2
Presentation
There are differences in presentation among patients of color, particularly in distribution, type of psoriasis, and severity. As seen in patient 3, Asian and black patients are more likely to present with scalp psoriasis.2,5 Hairstyling and hair care practices can differ considerably between racial groups. Given the differences in hairstyling, scalp psoriasis also may have a greater impact on patient quality of life (QOL).
Racial differences affect the type of psoriasis seen. Asian patients are more likely to present with pustular and erythrodermic psoriasis and less likely to present with inverse psoriasis compared to white patients. Hispanic patients are more likely to present with pustular psoriasis.11 Black patients have been reported to have lower frequencies of psoriatic arthritis compared to white patients.12 Recognition of these differences may help guide initial choice for therapeutics.
Notably, patients of color may present with much more severe psoriasis, particularly Asian and Hispanic patients.7 One retrospective study looking at patients with psoriasis treated with etanercept found that Asian patients were more likely to have greater baseline body surface area involvement.6 An American cross-sectional study reported higher psoriasis area and severity index scores in black patients compared to white patients,12 possibly because patients of color do not normalize the experience of having psoriasis and feel stigmatized, which can cause delays in seeking medical attention and worsen disease burden. For patient 1, the stigma of black patients having psoriasis affected his body image and may have led to a delay in seeking medical attention due to him not believing it was possible for people of his skin color to have psoriasis. Increased disease severity may contribute to treatment resistance or numerous trials of topicals or biologics before the disease improves. Patient education in the community as well as patient support groups are paramount, and increased awareness of psoriasis can help improve disease management.
Treatment
Topical therapies are the first-line treatment of psoriasis. Although there is no evidence showing differences in topical treatment efficacy, patient preference for different topical treatments may vary based on race. For example, patients with Afro-textured hair may prefer foams and lotions and would avoid shampoo therapies, as frequent hair washing may not be feasible with certain hairstyles and may cause hair breakage or dryness.2
UV therapy can be an effective treatment modality for patients with psoriasis. The strength of therapy tends to be dictated by the Fitzpatrick skin phototype rather than race. Darker-skinned individuals may have an increased risk for hyperpigmentation, so caution should be taken to prevent burning during therapy. Suberythemogenic dosing—70% of minimal erythema dose—of narrowband UVB treatments has shown the same efficacy as using minimal erythema dose in patients with darker skin types in addition to fair-skinned patients.8
Although we found poor efficacy of systemic treatments in patient 1, to our knowledge, studies examining the efficacy of systemic therapeutic options have not shown differences in patients of color.6,13 Studies show similar efficacy in treatments among races, particularly biologic therapies.5 However, patients with skin of color historically have been underrepresented in clinical trials,9 which may contribute to these patients, particularly black patients, being less familiar with biologics as a treatment option for psoriasis, as reported by Takeshita et al.10 Therefore, patient-centered discussions regarding treatment choices are important to ensure patients understand all options available to manage their disease.
Psychosocial Impact
Because of its chronic remitting course, psoriasis has a notable psychosocial impact on the lives of all patients, though the literature suggests there may be more of an impact on QOL in patients of color. Higher baseline dermatology life quality index scores have been reported in patients of color compared to white patients.6 Kerr et al12 reported significantly greater psoriasis area and severity index scores (P=.06) and greater psychological impact in black patients compared to white patients. Stress also was more likely to be reported as a trigger for psoriasis in patients of Hispanic background compared to white patients.14 Many patients report body image issues with large physical lesions; however, the difference may lie in personal and cultural views about psoriasis, as one of our patients stated, “black people do not get psoriasis.” In addition to the cosmetic challenges that patients face with active lesions, postinflammatory pigmentary changes can be equally as burdensome to patients, as one of our patients stated he “would do anything to get rid of it.” Increased rates of depression and anxiety in patients of color can worsen their outlook on the condition.15,16 The increased stigma and burden of psoriasis in patients of color calls for clinicians to counsel and address psoriasis in a holistic way and refer patients to psoriasis support groups when appropriate. Although the burden of psoriasis is clear, more studies can be carried out to investigate the impact on QOL in different ethnic populations.
Dermatology Education
Although differences have been found in patients of color with psoriasis, dissemination of this knowledge continues to be a challenge. In dermatology residency programs, the majority of teaching is provided with examples of skin diseases in white patients, which can complicate pattern recognition and diagnostic ability for trainees. Although dermatologists recognize that ethnic skin has unique dermatologic considerations, there is a persistent need for increasing skin of color education within dermatology residency programs.17,18 Implementing more educational programs on skin of color has been proposed, and these programs will continue to be in demand as our population increasingly diversifies.19
Conclusion
Psoriasis in patients of color carries unique challenges when compared to psoriasis in white patients. Differences in morphology and presentation can make the disease difficult to accurately diagnose. These differences in addition to cultural differences may contribute to a greater impact on QOL and psychological health. Although treatment preferences and recognition may differ, treatment efficacy has so far been similar, albeit with a low proportion of patients with skin of color included in clinical trials.
Further focus should now lie within knowledge translation of these differences, which would normalize the condition for patients, support them seeking medical attention sooner, and inform them of all treatment options possible. For clinicians, more attention on the differences would help make earlier diagnoses, personalize physician-patient conversations, and advocate for further education on this issue in residency training programs.
- National Psoriasis Foundation. Statistics. https://www.psoriasis.org/content/statistics. Accessed July 14, 2020.
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7:16-24.
- Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70:512-516.
- Goff KL, Karimkhani C, Boyers LN, et al. The global burden of psoriatic skin disease. Br J Dermatol. 2015;172:1665-1668.
- Kaufman BP, Alexis AF. Psoriasis in skin of color: insights into the epidemiology, clinical presentation, genetics, quality-of-life impact, and treatment of psoriasis in non-white racial/ethnic groups. Am J Clin Dermatol. 2018;19:405-423.
- Shah SK, Arthur A, Yang YC, et al. A retrospective study to investigate racial and ethnic variations in the treatment of psoriasis with etanercept. J Drugs Dermatol. 2011;10:866-872.
- Abrouk M, Lee K, Brodsky M, et al. Ethnicity affects the presenting severity of psoriasis. J Am Acad Dermatol. 2017;77:180-182.
- Youssef RM, Mahgoub D, Mashaly HM, et al. Different narrowband UVB dosage regimens in dark skinned psoriatics: a preliminary study. Photodermatol Photoimmunol Photomed. 2008;24:256-259.
- Charrow A, Xia F Di, Joyce C, et al. Diversity in dermatology clinical trials: a systematic review. JAMA Dermatol. 2017;153:193-198.
- Takeshita J, Eriksen WT, Raziano VT, et al. Racial differences in perceptions of psoriasis therapies: implications for racial disparities in psoriasis treatment. J Invest Dermatol. 2019;139:1672-1679.
- Yan D, Afifi L, Jeon C, et al. A cross-sectional study of the distribution of psoriasis subtypes in different ethno-racial groups. Dermatol Online J. 2018;24. pii:13030/qt5z21q4k2.
- Kerr GS, Qaiyumi S, Richards J, et al. Psoriasis and psoriatic arthritis in African-American patients—the need to measure disease burden. Clin Rheumatol. 2015;34:1753-1759.
- Edson-Heredia E, Sterling KL, Alatorre CI, et al. Heterogeneity of response to biologic treatment: perspective for psoriasis. J Invest Dermatol. 2014;134:18-23.
- Yan D, Afifi L, Jeon C, et al. A cross-sectional study of psoriasis triggers among different ethno-racial groups. J Am Acad Dermatol. 2017;77:756-758.
- Bailey RK, Mokonogho J, Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat. 2019;15:603-609.
- Jackson C, Maibach H. Ethnic and socioeconomic disparities in dermatology. J Dermatolog Treat. 2016;27:290-291.
- Salam A, Dadzie OE. Dermatology training in the U.K.: does it reflect the changing demographics of our population? Br J Dermatol. 2013;169:1360-1362.
- Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol. 2008;59:615-618.
- Ogunyemi B, Miller-Monthrope Y. The state of ethnic dermatology in Canada. J Cutan Med Surg. 2017;21:464-466.
Psoriasis is a chronic inflammatory skin disease that affects 2% to 3% of individuals worldwide.1 Despite extensive research, the majority of clinical data are in white patients with limited data in patients of color, yet a number of differences are known. The prevalence of psoriasis differs among racial and ethnic groups, with lower prevalence in racial minorities.2 A cross-sectional American study using data from 2009 through 2010 showed the prevalence for psoriasis was 3.6% in white patients, 1.9% in black patients, 1.6% in Hispanic patients, and 1.4% in other racial groups.3 Psoriasis presents differently in patients of color, both in morphology and severity. Cultural differences and stigma may contribute to the differences seen in severity but also to the psychological impact and treatment choices in patients of color compared to white patients.4 It has even been theorized that treatment efficacy could differ because of potential genetic differences.5 Psoriasis in patients of color is an emerging clinical issue that requires further attention so that dermatologists can learn about, diagnose, and treat them.
We report 3 cases of patients of color with psoriasis who presented to an urban and racially diverse dermatology clinic affiliated with Scarborough General Hospital in Toronto, Ontario, Canada. A retrospective chart review was performed on these high-yield representative cases to demonstrate differences in color and morphology, disease severity, and treatment in patients of various races seen at our clinic. After informed consent was obtained, photographs were taken of patient cutaneous findings to illustrate these differences. Discussion with these selected patients yielded supplementary qualitative data, highlighting individual perspectives of their disease.
Case Series
Patient 1
A 53-year-old black man from Grenada presented to our clinic with a history of psoriasis for a number of years that presented as violaceous plaques throughout large portions of the body (Figure 1). He previously had achieved inadequate results while using topical therapies, methotrexate, acitretin, apremilast, ustekinumab, ixekizumab, and guselkumab at adequate or even maximum doses. His disease affected 30% of the body surface area, with a psoriasis area and severity index score of 27 and a dermatology life quality index score of 23. The patient’s life was quite affected by psoriasis, with emphasis on choice of clothing worn and effect on body image. He also discussed the stigma psoriasis may have in black patients, stating that he has been told multiple times that “black people do not get psoriasis.”
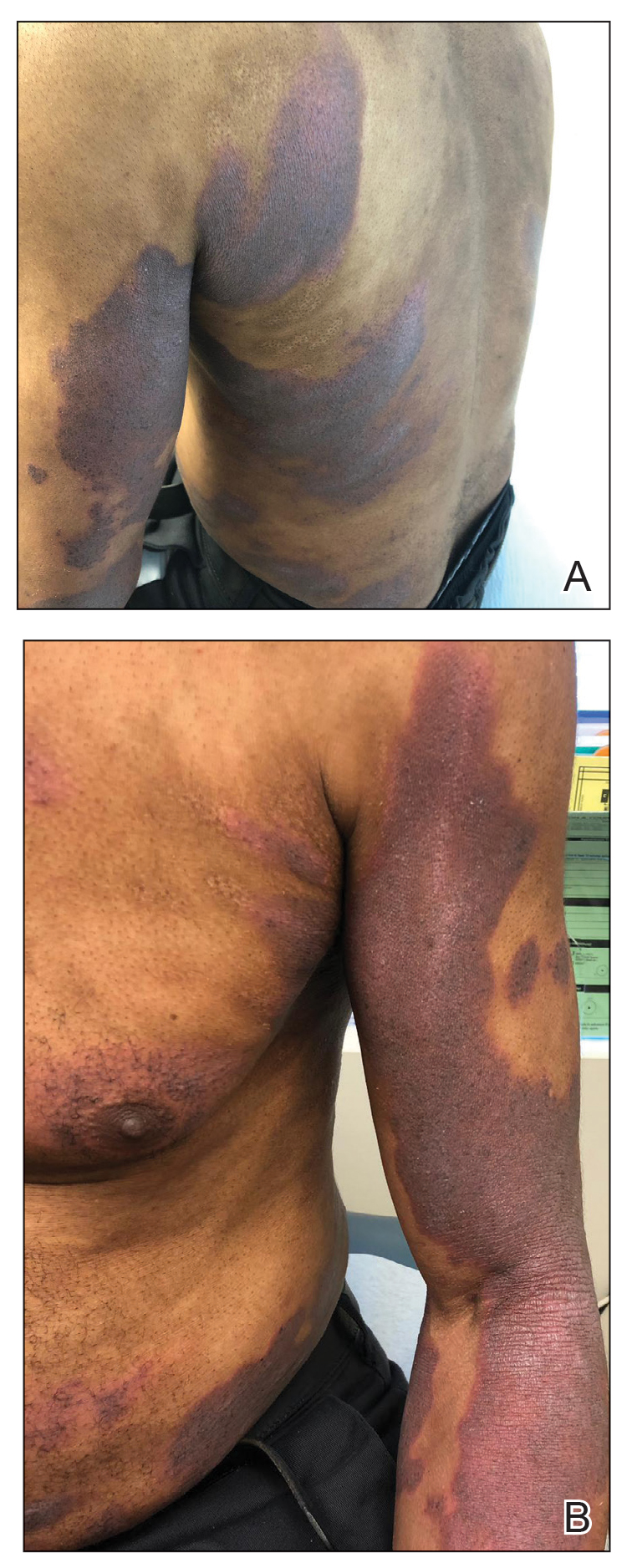
Patient 2
A 27-year-old man from India presented with guttate psoriasis (Figure 2). He was treated with methotrexate 2 years prior and currently is on maintenance therapy with topical treatments alone. His main concerns pertained to the persistent dyschromia that occurred secondary to the psoriatic lesions. Through discussion, the patient stated that he “would do anything to get rid of it.”
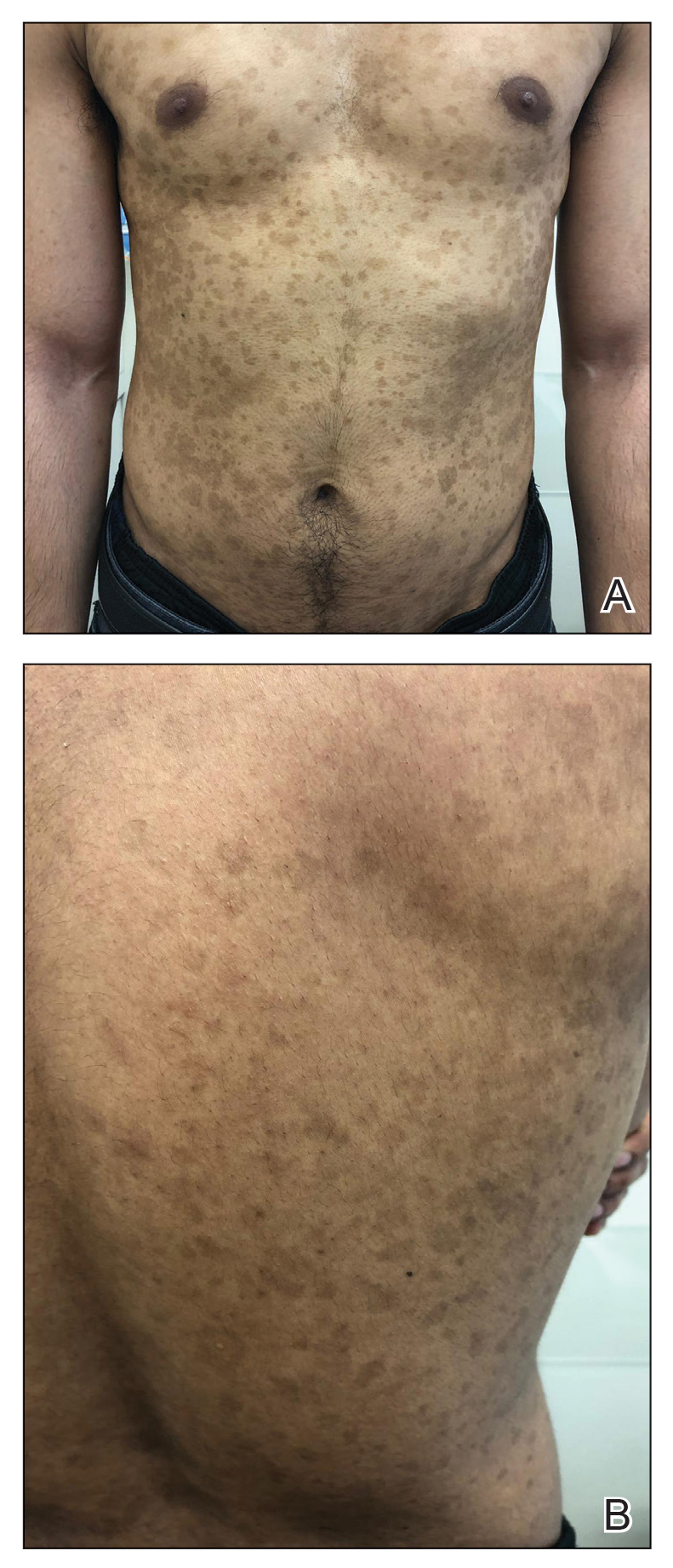
Patient 3
A 49-year-old man from the Philippines presented to our clinic with plaque psoriasis that predominantly affected the trunk and scalp (Figure 3). He had been treated with methotrexate and phototherapy with suboptimal efficacy and was planning for biologic therapy. Although he had active plaques on the trunk, the patient stated, “I am most bothered by my scalp,” particularly referring to the itch and scale and their effects on hair and hairstyling.
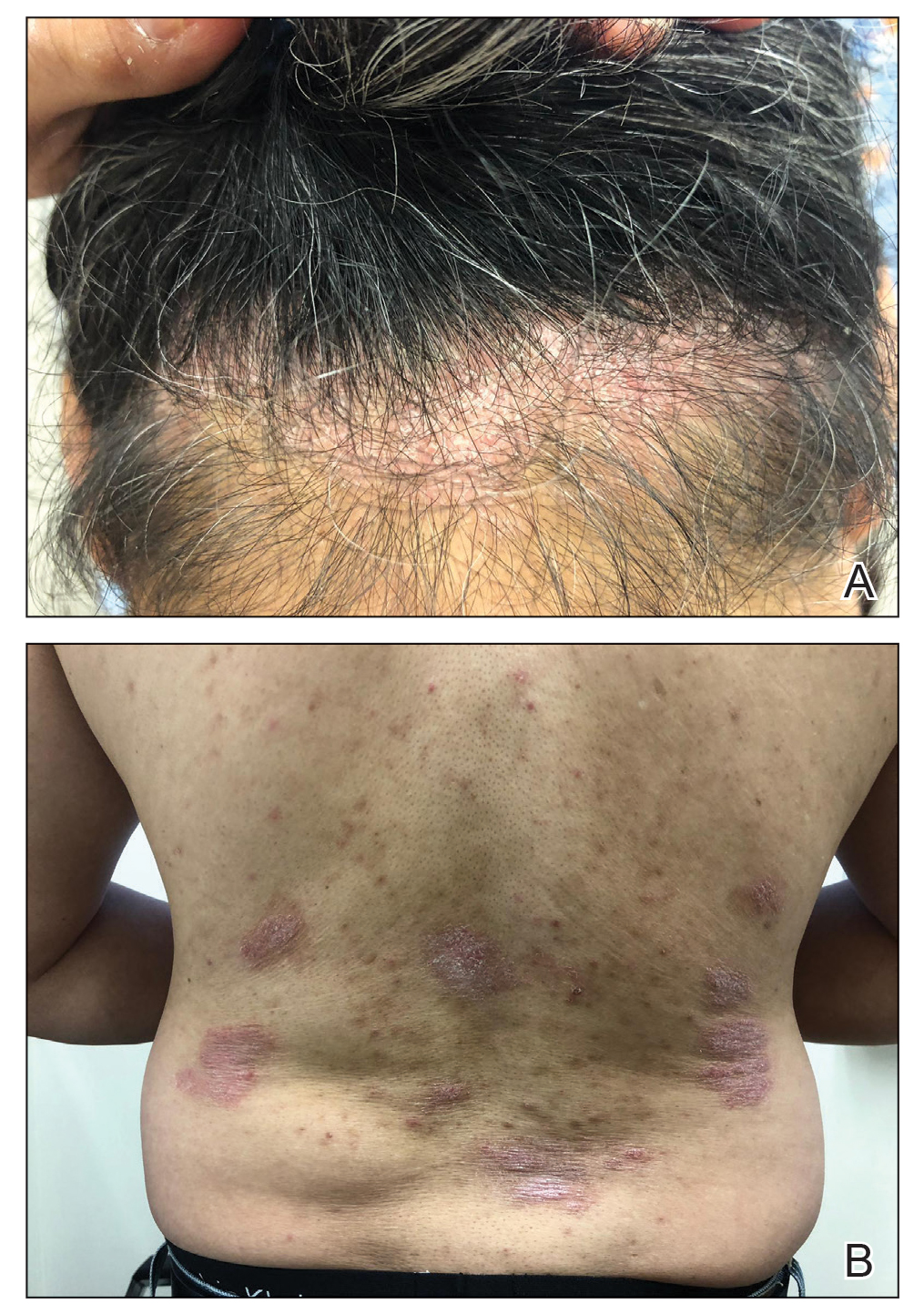
Comment
Clinical differences in patients of color with psoriasis affect the management of the disease. Special consideration should be given to variances in morphology, presentation, treatment, and psychosocial factors in the management of psoriasis for these patient populations, as summarized in the eTable.
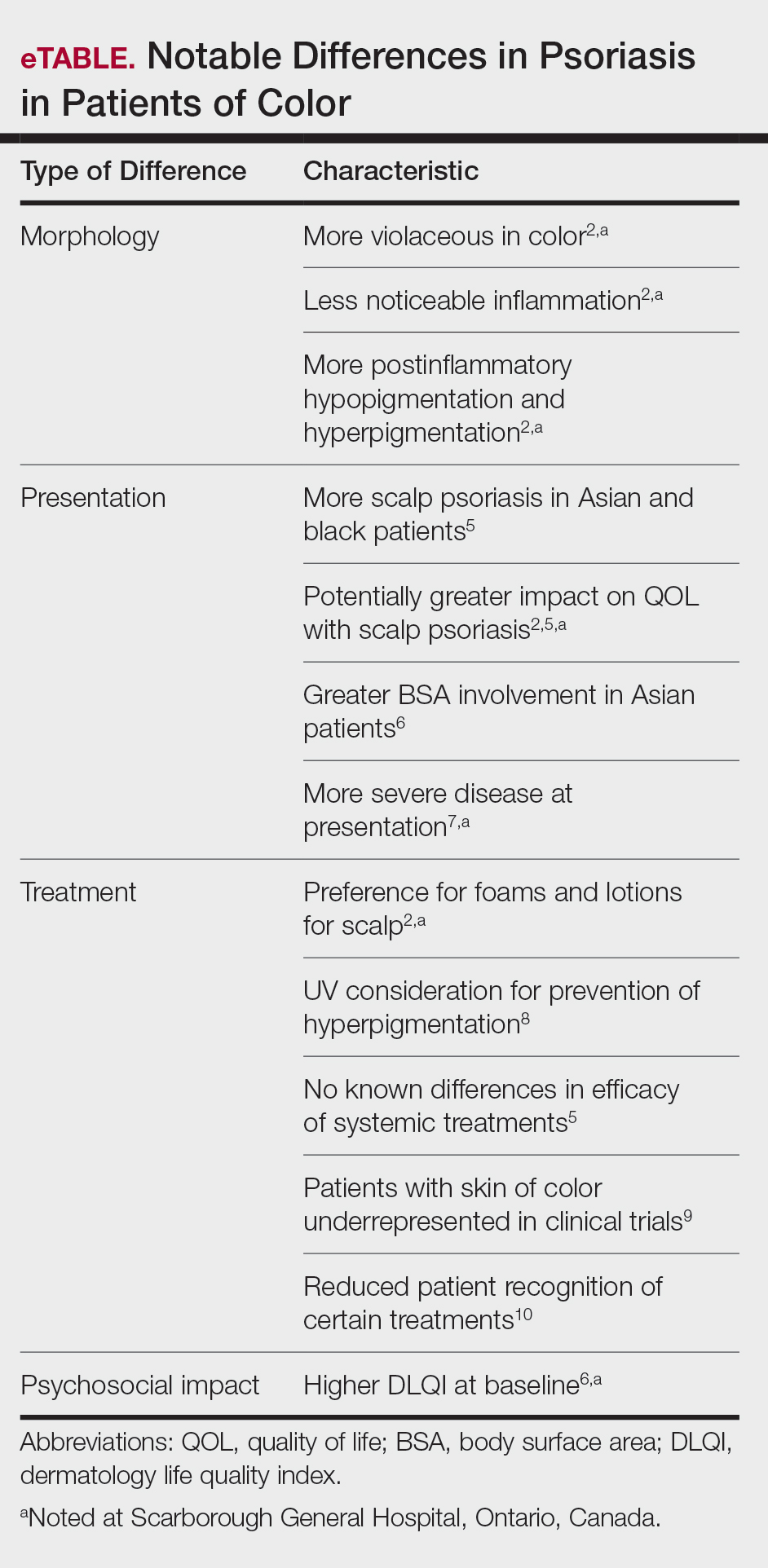
Morphology
At our clinic, patients of color have been found to have differences in morphology, including lesions that are more violaceous in color, as seen in patient 1; less noticeable inflammation; and more postinflammatory hypopigmentation and hyperpigmentation changes, as seen in patient 2. These changes are supported by the literature and differ from typical psoriasis plaques, which are pink-red and have more overlying scale. The varied morphology also may affect the differential, and other mimickers may be considered, such as lichen planus, cutaneous lupus erythematosus, and sarcoidosis.2
Presentation
There are differences in presentation among patients of color, particularly in distribution, type of psoriasis, and severity. As seen in patient 3, Asian and black patients are more likely to present with scalp psoriasis.2,5 Hairstyling and hair care practices can differ considerably between racial groups. Given the differences in hairstyling, scalp psoriasis also may have a greater impact on patient quality of life (QOL).
Racial differences affect the type of psoriasis seen. Asian patients are more likely to present with pustular and erythrodermic psoriasis and less likely to present with inverse psoriasis compared to white patients. Hispanic patients are more likely to present with pustular psoriasis.11 Black patients have been reported to have lower frequencies of psoriatic arthritis compared to white patients.12 Recognition of these differences may help guide initial choice for therapeutics.
Notably, patients of color may present with much more severe psoriasis, particularly Asian and Hispanic patients.7 One retrospective study looking at patients with psoriasis treated with etanercept found that Asian patients were more likely to have greater baseline body surface area involvement.6 An American cross-sectional study reported higher psoriasis area and severity index scores in black patients compared to white patients,12 possibly because patients of color do not normalize the experience of having psoriasis and feel stigmatized, which can cause delays in seeking medical attention and worsen disease burden. For patient 1, the stigma of black patients having psoriasis affected his body image and may have led to a delay in seeking medical attention due to him not believing it was possible for people of his skin color to have psoriasis. Increased disease severity may contribute to treatment resistance or numerous trials of topicals or biologics before the disease improves. Patient education in the community as well as patient support groups are paramount, and increased awareness of psoriasis can help improve disease management.
Treatment
Topical therapies are the first-line treatment of psoriasis. Although there is no evidence showing differences in topical treatment efficacy, patient preference for different topical treatments may vary based on race. For example, patients with Afro-textured hair may prefer foams and lotions and would avoid shampoo therapies, as frequent hair washing may not be feasible with certain hairstyles and may cause hair breakage or dryness.2
UV therapy can be an effective treatment modality for patients with psoriasis. The strength of therapy tends to be dictated by the Fitzpatrick skin phototype rather than race. Darker-skinned individuals may have an increased risk for hyperpigmentation, so caution should be taken to prevent burning during therapy. Suberythemogenic dosing—70% of minimal erythema dose—of narrowband UVB treatments has shown the same efficacy as using minimal erythema dose in patients with darker skin types in addition to fair-skinned patients.8
Although we found poor efficacy of systemic treatments in patient 1, to our knowledge, studies examining the efficacy of systemic therapeutic options have not shown differences in patients of color.6,13 Studies show similar efficacy in treatments among races, particularly biologic therapies.5 However, patients with skin of color historically have been underrepresented in clinical trials,9 which may contribute to these patients, particularly black patients, being less familiar with biologics as a treatment option for psoriasis, as reported by Takeshita et al.10 Therefore, patient-centered discussions regarding treatment choices are important to ensure patients understand all options available to manage their disease.
Psychosocial Impact
Because of its chronic remitting course, psoriasis has a notable psychosocial impact on the lives of all patients, though the literature suggests there may be more of an impact on QOL in patients of color. Higher baseline dermatology life quality index scores have been reported in patients of color compared to white patients.6 Kerr et al12 reported significantly greater psoriasis area and severity index scores (P=.06) and greater psychological impact in black patients compared to white patients. Stress also was more likely to be reported as a trigger for psoriasis in patients of Hispanic background compared to white patients.14 Many patients report body image issues with large physical lesions; however, the difference may lie in personal and cultural views about psoriasis, as one of our patients stated, “black people do not get psoriasis.” In addition to the cosmetic challenges that patients face with active lesions, postinflammatory pigmentary changes can be equally as burdensome to patients, as one of our patients stated he “would do anything to get rid of it.” Increased rates of depression and anxiety in patients of color can worsen their outlook on the condition.15,16 The increased stigma and burden of psoriasis in patients of color calls for clinicians to counsel and address psoriasis in a holistic way and refer patients to psoriasis support groups when appropriate. Although the burden of psoriasis is clear, more studies can be carried out to investigate the impact on QOL in different ethnic populations.
Dermatology Education
Although differences have been found in patients of color with psoriasis, dissemination of this knowledge continues to be a challenge. In dermatology residency programs, the majority of teaching is provided with examples of skin diseases in white patients, which can complicate pattern recognition and diagnostic ability for trainees. Although dermatologists recognize that ethnic skin has unique dermatologic considerations, there is a persistent need for increasing skin of color education within dermatology residency programs.17,18 Implementing more educational programs on skin of color has been proposed, and these programs will continue to be in demand as our population increasingly diversifies.19
Conclusion
Psoriasis in patients of color carries unique challenges when compared to psoriasis in white patients. Differences in morphology and presentation can make the disease difficult to accurately diagnose. These differences in addition to cultural differences may contribute to a greater impact on QOL and psychological health. Although treatment preferences and recognition may differ, treatment efficacy has so far been similar, albeit with a low proportion of patients with skin of color included in clinical trials.
Further focus should now lie within knowledge translation of these differences, which would normalize the condition for patients, support them seeking medical attention sooner, and inform them of all treatment options possible. For clinicians, more attention on the differences would help make earlier diagnoses, personalize physician-patient conversations, and advocate for further education on this issue in residency training programs.
Psoriasis is a chronic inflammatory skin disease that affects 2% to 3% of individuals worldwide.1 Despite extensive research, the majority of clinical data are in white patients with limited data in patients of color, yet a number of differences are known. The prevalence of psoriasis differs among racial and ethnic groups, with lower prevalence in racial minorities.2 A cross-sectional American study using data from 2009 through 2010 showed the prevalence for psoriasis was 3.6% in white patients, 1.9% in black patients, 1.6% in Hispanic patients, and 1.4% in other racial groups.3 Psoriasis presents differently in patients of color, both in morphology and severity. Cultural differences and stigma may contribute to the differences seen in severity but also to the psychological impact and treatment choices in patients of color compared to white patients.4 It has even been theorized that treatment efficacy could differ because of potential genetic differences.5 Psoriasis in patients of color is an emerging clinical issue that requires further attention so that dermatologists can learn about, diagnose, and treat them.
We report 3 cases of patients of color with psoriasis who presented to an urban and racially diverse dermatology clinic affiliated with Scarborough General Hospital in Toronto, Ontario, Canada. A retrospective chart review was performed on these high-yield representative cases to demonstrate differences in color and morphology, disease severity, and treatment in patients of various races seen at our clinic. After informed consent was obtained, photographs were taken of patient cutaneous findings to illustrate these differences. Discussion with these selected patients yielded supplementary qualitative data, highlighting individual perspectives of their disease.
Case Series
Patient 1
A 53-year-old black man from Grenada presented to our clinic with a history of psoriasis for a number of years that presented as violaceous plaques throughout large portions of the body (Figure 1). He previously had achieved inadequate results while using topical therapies, methotrexate, acitretin, apremilast, ustekinumab, ixekizumab, and guselkumab at adequate or even maximum doses. His disease affected 30% of the body surface area, with a psoriasis area and severity index score of 27 and a dermatology life quality index score of 23. The patient’s life was quite affected by psoriasis, with emphasis on choice of clothing worn and effect on body image. He also discussed the stigma psoriasis may have in black patients, stating that he has been told multiple times that “black people do not get psoriasis.”
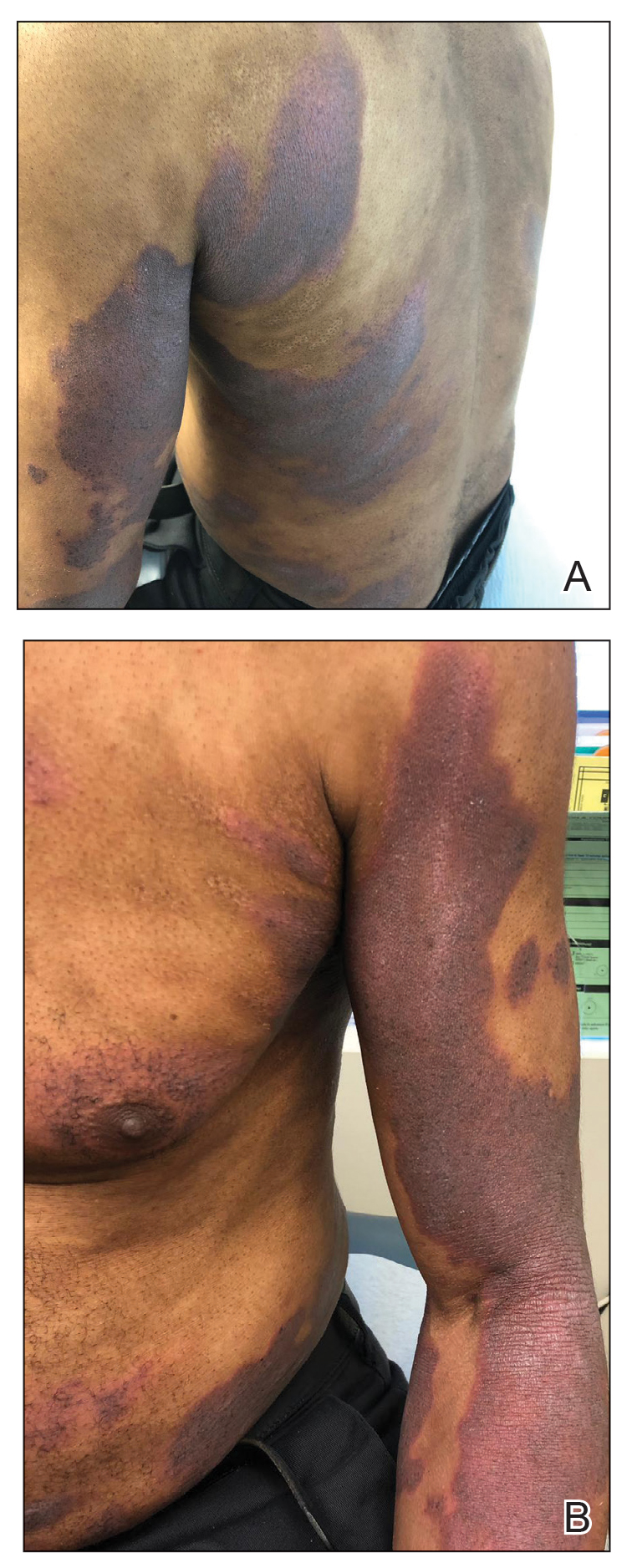
Patient 2
A 27-year-old man from India presented with guttate psoriasis (Figure 2). He was treated with methotrexate 2 years prior and currently is on maintenance therapy with topical treatments alone. His main concerns pertained to the persistent dyschromia that occurred secondary to the psoriatic lesions. Through discussion, the patient stated that he “would do anything to get rid of it.”
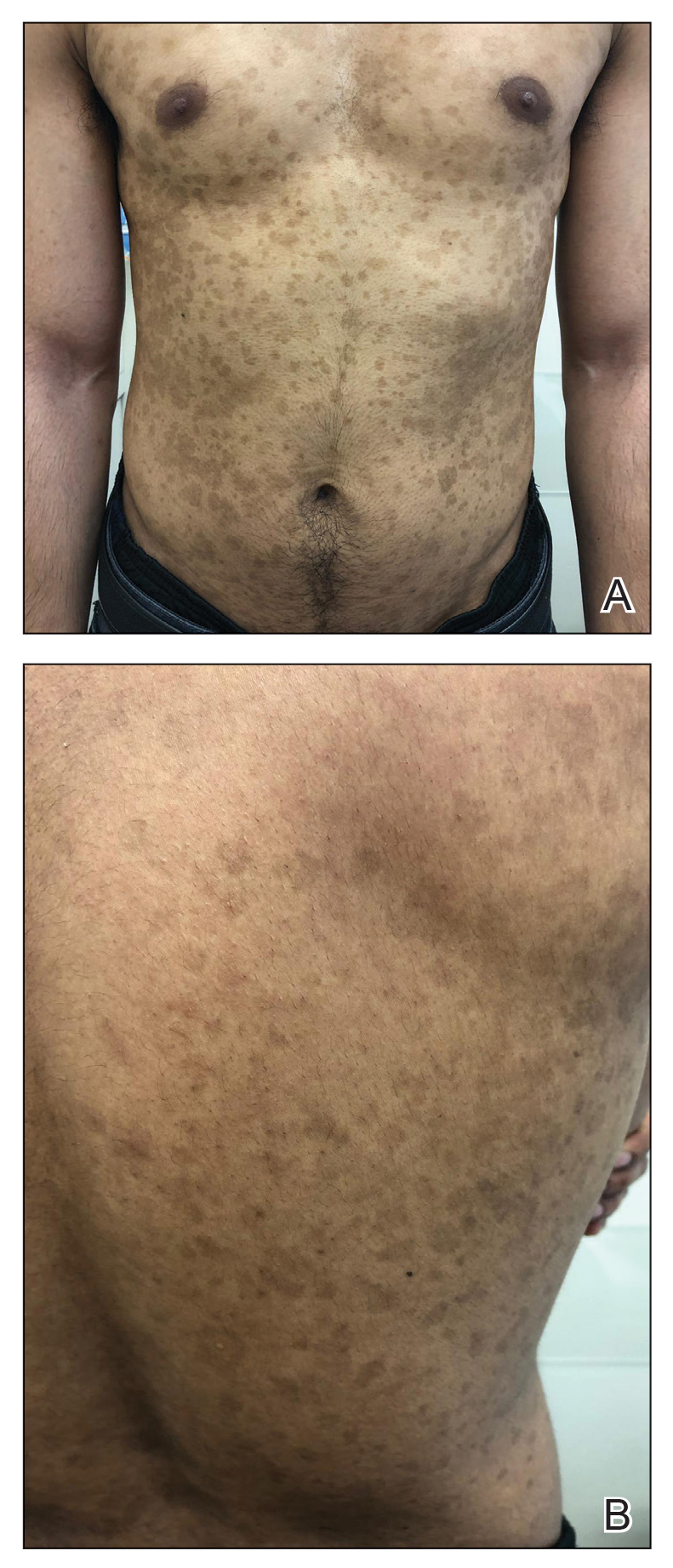
Patient 3
A 49-year-old man from the Philippines presented to our clinic with plaque psoriasis that predominantly affected the trunk and scalp (Figure 3). He had been treated with methotrexate and phototherapy with suboptimal efficacy and was planning for biologic therapy. Although he had active plaques on the trunk, the patient stated, “I am most bothered by my scalp,” particularly referring to the itch and scale and their effects on hair and hairstyling.
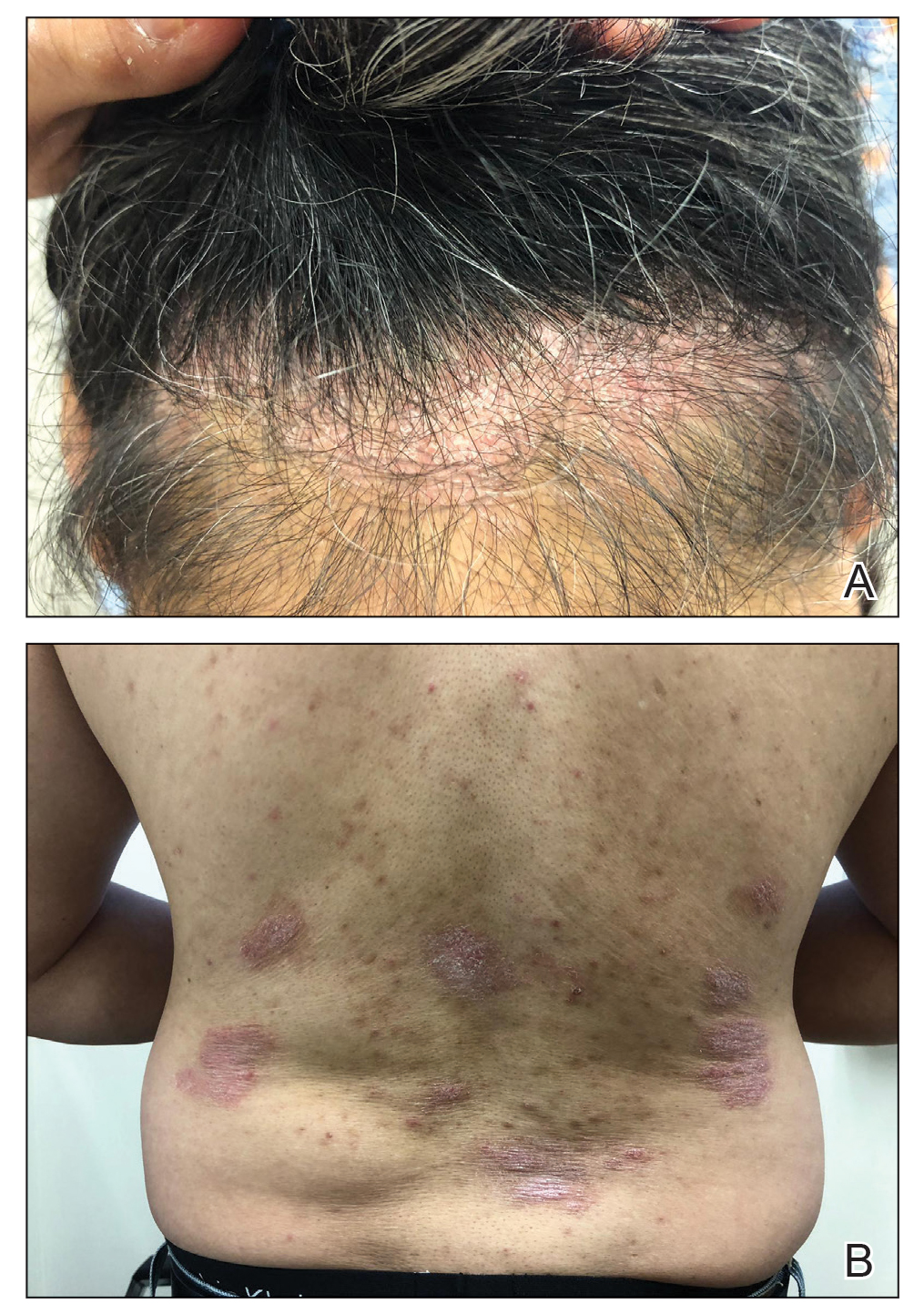
Comment
Clinical differences in patients of color with psoriasis affect the management of the disease. Special consideration should be given to variances in morphology, presentation, treatment, and psychosocial factors in the management of psoriasis for these patient populations, as summarized in the eTable.
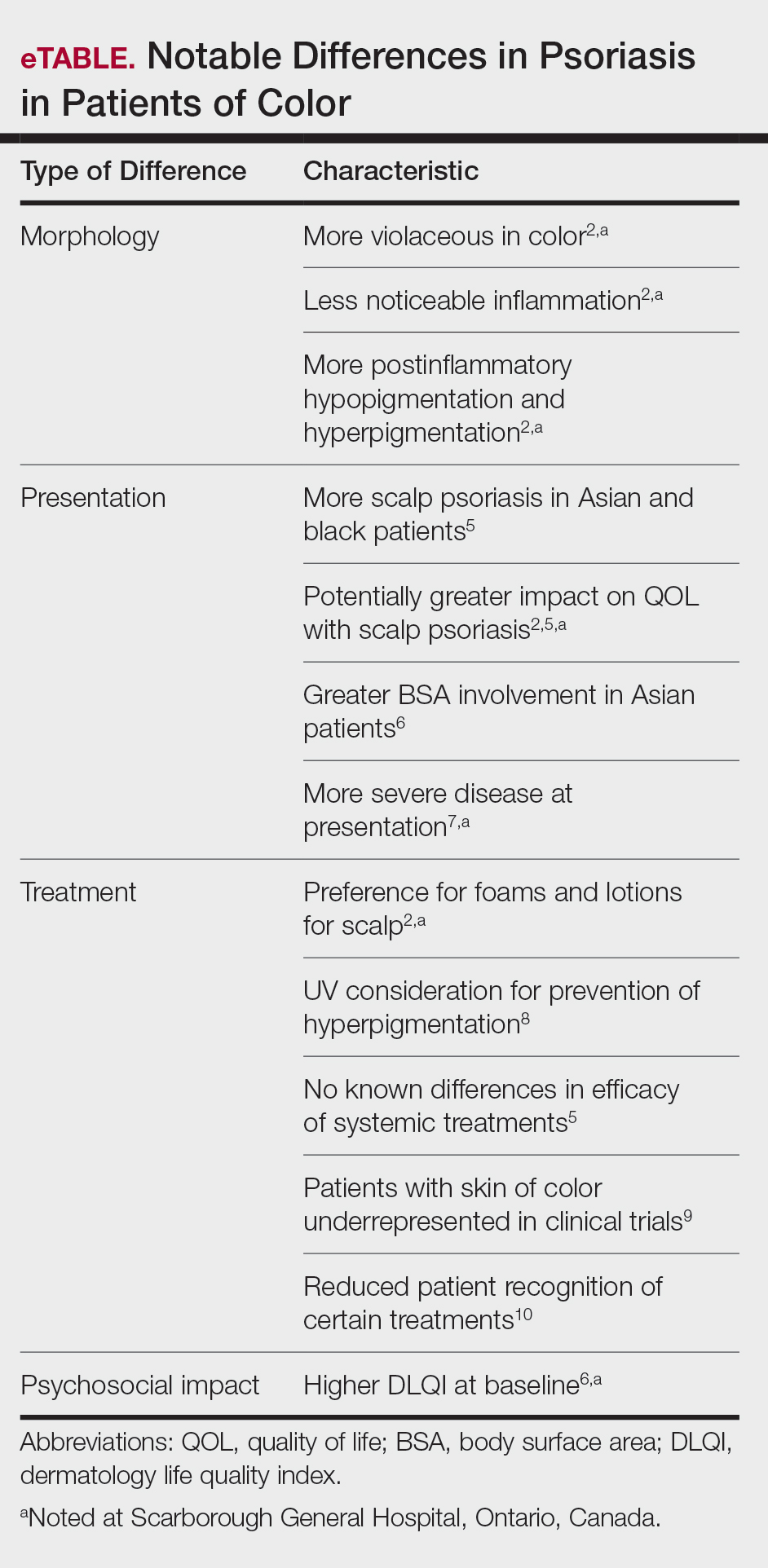
Morphology
At our clinic, patients of color have been found to have differences in morphology, including lesions that are more violaceous in color, as seen in patient 1; less noticeable inflammation; and more postinflammatory hypopigmentation and hyperpigmentation changes, as seen in patient 2. These changes are supported by the literature and differ from typical psoriasis plaques, which are pink-red and have more overlying scale. The varied morphology also may affect the differential, and other mimickers may be considered, such as lichen planus, cutaneous lupus erythematosus, and sarcoidosis.2
Presentation
There are differences in presentation among patients of color, particularly in distribution, type of psoriasis, and severity. As seen in patient 3, Asian and black patients are more likely to present with scalp psoriasis.2,5 Hairstyling and hair care practices can differ considerably between racial groups. Given the differences in hairstyling, scalp psoriasis also may have a greater impact on patient quality of life (QOL).
Racial differences affect the type of psoriasis seen. Asian patients are more likely to present with pustular and erythrodermic psoriasis and less likely to present with inverse psoriasis compared to white patients. Hispanic patients are more likely to present with pustular psoriasis.11 Black patients have been reported to have lower frequencies of psoriatic arthritis compared to white patients.12 Recognition of these differences may help guide initial choice for therapeutics.
Notably, patients of color may present with much more severe psoriasis, particularly Asian and Hispanic patients.7 One retrospective study looking at patients with psoriasis treated with etanercept found that Asian patients were more likely to have greater baseline body surface area involvement.6 An American cross-sectional study reported higher psoriasis area and severity index scores in black patients compared to white patients,12 possibly because patients of color do not normalize the experience of having psoriasis and feel stigmatized, which can cause delays in seeking medical attention and worsen disease burden. For patient 1, the stigma of black patients having psoriasis affected his body image and may have led to a delay in seeking medical attention due to him not believing it was possible for people of his skin color to have psoriasis. Increased disease severity may contribute to treatment resistance or numerous trials of topicals or biologics before the disease improves. Patient education in the community as well as patient support groups are paramount, and increased awareness of psoriasis can help improve disease management.
Treatment
Topical therapies are the first-line treatment of psoriasis. Although there is no evidence showing differences in topical treatment efficacy, patient preference for different topical treatments may vary based on race. For example, patients with Afro-textured hair may prefer foams and lotions and would avoid shampoo therapies, as frequent hair washing may not be feasible with certain hairstyles and may cause hair breakage or dryness.2
UV therapy can be an effective treatment modality for patients with psoriasis. The strength of therapy tends to be dictated by the Fitzpatrick skin phototype rather than race. Darker-skinned individuals may have an increased risk for hyperpigmentation, so caution should be taken to prevent burning during therapy. Suberythemogenic dosing—70% of minimal erythema dose—of narrowband UVB treatments has shown the same efficacy as using minimal erythema dose in patients with darker skin types in addition to fair-skinned patients.8
Although we found poor efficacy of systemic treatments in patient 1, to our knowledge, studies examining the efficacy of systemic therapeutic options have not shown differences in patients of color.6,13 Studies show similar efficacy in treatments among races, particularly biologic therapies.5 However, patients with skin of color historically have been underrepresented in clinical trials,9 which may contribute to these patients, particularly black patients, being less familiar with biologics as a treatment option for psoriasis, as reported by Takeshita et al.10 Therefore, patient-centered discussions regarding treatment choices are important to ensure patients understand all options available to manage their disease.
Psychosocial Impact
Because of its chronic remitting course, psoriasis has a notable psychosocial impact on the lives of all patients, though the literature suggests there may be more of an impact on QOL in patients of color. Higher baseline dermatology life quality index scores have been reported in patients of color compared to white patients.6 Kerr et al12 reported significantly greater psoriasis area and severity index scores (P=.06) and greater psychological impact in black patients compared to white patients. Stress also was more likely to be reported as a trigger for psoriasis in patients of Hispanic background compared to white patients.14 Many patients report body image issues with large physical lesions; however, the difference may lie in personal and cultural views about psoriasis, as one of our patients stated, “black people do not get psoriasis.” In addition to the cosmetic challenges that patients face with active lesions, postinflammatory pigmentary changes can be equally as burdensome to patients, as one of our patients stated he “would do anything to get rid of it.” Increased rates of depression and anxiety in patients of color can worsen their outlook on the condition.15,16 The increased stigma and burden of psoriasis in patients of color calls for clinicians to counsel and address psoriasis in a holistic way and refer patients to psoriasis support groups when appropriate. Although the burden of psoriasis is clear, more studies can be carried out to investigate the impact on QOL in different ethnic populations.
Dermatology Education
Although differences have been found in patients of color with psoriasis, dissemination of this knowledge continues to be a challenge. In dermatology residency programs, the majority of teaching is provided with examples of skin diseases in white patients, which can complicate pattern recognition and diagnostic ability for trainees. Although dermatologists recognize that ethnic skin has unique dermatologic considerations, there is a persistent need for increasing skin of color education within dermatology residency programs.17,18 Implementing more educational programs on skin of color has been proposed, and these programs will continue to be in demand as our population increasingly diversifies.19
Conclusion
Psoriasis in patients of color carries unique challenges when compared to psoriasis in white patients. Differences in morphology and presentation can make the disease difficult to accurately diagnose. These differences in addition to cultural differences may contribute to a greater impact on QOL and psychological health. Although treatment preferences and recognition may differ, treatment efficacy has so far been similar, albeit with a low proportion of patients with skin of color included in clinical trials.
Further focus should now lie within knowledge translation of these differences, which would normalize the condition for patients, support them seeking medical attention sooner, and inform them of all treatment options possible. For clinicians, more attention on the differences would help make earlier diagnoses, personalize physician-patient conversations, and advocate for further education on this issue in residency training programs.
- National Psoriasis Foundation. Statistics. https://www.psoriasis.org/content/statistics. Accessed July 14, 2020.
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7:16-24.
- Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70:512-516.
- Goff KL, Karimkhani C, Boyers LN, et al. The global burden of psoriatic skin disease. Br J Dermatol. 2015;172:1665-1668.
- Kaufman BP, Alexis AF. Psoriasis in skin of color: insights into the epidemiology, clinical presentation, genetics, quality-of-life impact, and treatment of psoriasis in non-white racial/ethnic groups. Am J Clin Dermatol. 2018;19:405-423.
- Shah SK, Arthur A, Yang YC, et al. A retrospective study to investigate racial and ethnic variations in the treatment of psoriasis with etanercept. J Drugs Dermatol. 2011;10:866-872.
- Abrouk M, Lee K, Brodsky M, et al. Ethnicity affects the presenting severity of psoriasis. J Am Acad Dermatol. 2017;77:180-182.
- Youssef RM, Mahgoub D, Mashaly HM, et al. Different narrowband UVB dosage regimens in dark skinned psoriatics: a preliminary study. Photodermatol Photoimmunol Photomed. 2008;24:256-259.
- Charrow A, Xia F Di, Joyce C, et al. Diversity in dermatology clinical trials: a systematic review. JAMA Dermatol. 2017;153:193-198.
- Takeshita J, Eriksen WT, Raziano VT, et al. Racial differences in perceptions of psoriasis therapies: implications for racial disparities in psoriasis treatment. J Invest Dermatol. 2019;139:1672-1679.
- Yan D, Afifi L, Jeon C, et al. A cross-sectional study of the distribution of psoriasis subtypes in different ethno-racial groups. Dermatol Online J. 2018;24. pii:13030/qt5z21q4k2.
- Kerr GS, Qaiyumi S, Richards J, et al. Psoriasis and psoriatic arthritis in African-American patients—the need to measure disease burden. Clin Rheumatol. 2015;34:1753-1759.
- Edson-Heredia E, Sterling KL, Alatorre CI, et al. Heterogeneity of response to biologic treatment: perspective for psoriasis. J Invest Dermatol. 2014;134:18-23.
- Yan D, Afifi L, Jeon C, et al. A cross-sectional study of psoriasis triggers among different ethno-racial groups. J Am Acad Dermatol. 2017;77:756-758.
- Bailey RK, Mokonogho J, Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat. 2019;15:603-609.
- Jackson C, Maibach H. Ethnic and socioeconomic disparities in dermatology. J Dermatolog Treat. 2016;27:290-291.
- Salam A, Dadzie OE. Dermatology training in the U.K.: does it reflect the changing demographics of our population? Br J Dermatol. 2013;169:1360-1362.
- Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol. 2008;59:615-618.
- Ogunyemi B, Miller-Monthrope Y. The state of ethnic dermatology in Canada. J Cutan Med Surg. 2017;21:464-466.
- National Psoriasis Foundation. Statistics. https://www.psoriasis.org/content/statistics. Accessed July 14, 2020.
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7:16-24.
- Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70:512-516.
- Goff KL, Karimkhani C, Boyers LN, et al. The global burden of psoriatic skin disease. Br J Dermatol. 2015;172:1665-1668.
- Kaufman BP, Alexis AF. Psoriasis in skin of color: insights into the epidemiology, clinical presentation, genetics, quality-of-life impact, and treatment of psoriasis in non-white racial/ethnic groups. Am J Clin Dermatol. 2018;19:405-423.
- Shah SK, Arthur A, Yang YC, et al. A retrospective study to investigate racial and ethnic variations in the treatment of psoriasis with etanercept. J Drugs Dermatol. 2011;10:866-872.
- Abrouk M, Lee K, Brodsky M, et al. Ethnicity affects the presenting severity of psoriasis. J Am Acad Dermatol. 2017;77:180-182.
- Youssef RM, Mahgoub D, Mashaly HM, et al. Different narrowband UVB dosage regimens in dark skinned psoriatics: a preliminary study. Photodermatol Photoimmunol Photomed. 2008;24:256-259.
- Charrow A, Xia F Di, Joyce C, et al. Diversity in dermatology clinical trials: a systematic review. JAMA Dermatol. 2017;153:193-198.
- Takeshita J, Eriksen WT, Raziano VT, et al. Racial differences in perceptions of psoriasis therapies: implications for racial disparities in psoriasis treatment. J Invest Dermatol. 2019;139:1672-1679.
- Yan D, Afifi L, Jeon C, et al. A cross-sectional study of the distribution of psoriasis subtypes in different ethno-racial groups. Dermatol Online J. 2018;24. pii:13030/qt5z21q4k2.
- Kerr GS, Qaiyumi S, Richards J, et al. Psoriasis and psoriatic arthritis in African-American patients—the need to measure disease burden. Clin Rheumatol. 2015;34:1753-1759.
- Edson-Heredia E, Sterling KL, Alatorre CI, et al. Heterogeneity of response to biologic treatment: perspective for psoriasis. J Invest Dermatol. 2014;134:18-23.
- Yan D, Afifi L, Jeon C, et al. A cross-sectional study of psoriasis triggers among different ethno-racial groups. J Am Acad Dermatol. 2017;77:756-758.
- Bailey RK, Mokonogho J, Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat. 2019;15:603-609.
- Jackson C, Maibach H. Ethnic and socioeconomic disparities in dermatology. J Dermatolog Treat. 2016;27:290-291.
- Salam A, Dadzie OE. Dermatology training in the U.K.: does it reflect the changing demographics of our population? Br J Dermatol. 2013;169:1360-1362.
- Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol. 2008;59:615-618.
- Ogunyemi B, Miller-Monthrope Y. The state of ethnic dermatology in Canada. J Cutan Med Surg. 2017;21:464-466.
Practice Points
- There are key differences in psoriasis in patients with skin of color, including the morphology, clinical presentation, treatment, and psychosocial impact.
- Recognition and awareness of these differences may normalize the condition for patients, support them seeking medical attention sooner, and better inform them of all possible treatment options.
- Advocating further education on these differences in residency training and continuing medical education programs may help physicians make earlier diagnoses and personalize physician-patient conversations.
APA tackles structural racism in psychiatry, itself
Amanda Calhoun, MD, recalls noticing a distinct empathy gap while she trained at a youth psychiatric unit.
A White male patient hurled the N-word at a Black patient, and the majority White staff did nothing. “And then [they] told me the White patient was struggling and that’s why they allowed it, even though he was aggressive,” said Dr. Calhoun, psychiatry resident at Yale University in New Haven, Conn. But Dr. Calhoun noticed less restraint on the part of her colleagues while she was treating an angry female Black Latinx patient.
“I remember staff saying she was a nightmare; they called her the B-word; she was ‘a terror.’ How is that this patient isn’t viewed as struggling, where the other patient is? I don’t understand the difference here.”
And, Dr. Calhoun said, “when a patient can complain that they feel they were treated differently based on skin color, [the White majority staff] would just say they have borderline personality disorder or they’re depressed.
“When the staff is not diverse, I really see differential treatment in who gets the benefit of the doubt and their empathy.”
Psychiatrists such as Dr. Calhoun can list countless other examples of institutional racism, interpersonal racism, and prejudice in psychiatry. They see signs of institutional racism in clinical care, academia, and in research. Some are questioning the American Psychiatric Association decision to put on hiatus the Institute on Psychiatric Services, its fall annual meeting that has traditionally served as a vehicle for examining the treatment of underserved communities.
Against that backdrop – and after the killing of George Floyd and amid the disproportionate impact of COVID-19 on communities of color – the APA launched an effort the group says is aimed at reforming itself and psychiatry as a whole. In June, the APA announced the formation of the Presidential Task Force to Address Structural Racism Throughout Psychiatry, and the panel – focused on anti-Black racism – has begun its yearlong work.
A specialty with inherent contradictions
Jeffrey Geller, MD, MPH, the APA’s president, acknowledged in an interview that racism in psychiatry is older than the APA – which celebrated its 175th anniversary as an association last year.
As Dr. Geller pointed out recently, Benjamin Rush, MD, a founding father of the United States and the father of American psychiatry, was an abolitionist who owned one enslaved man – and thought the intelligence and morality of Black people were equal to that of their White counterparts.1 Dr. Rush also thought the skin color of Black people was a manifestation of a type of leprosy that he called “Negritude.”2 “Rush was a remarkable mix of contradictions,” Dr. Geller wrote.
Altha J. Stewart, MD, the first and only Black president of the APA, declined to be interviewed for this article.
But as Dr. Stewart was wrapping up her term as president, she reportedly3 said that a 1970 paper titled “Dimensions of Institutional Racism in Psychiatry” by the late Melvin Sabshin, MD, and associates was essentially a blueprint for moving the specialty forward.
That paper, published in the American Journal of Psychiatry, took psychiatry to task on many levels. One of the barriers that Black psychiatric patients must overcome, according to Dr. Sabshin and associates, is the “biases of the White therapist, who must overcome his cultural blind spots, reactive guilt, and unconscious prejudice.” They called community psychiatry paternalistic. Furthermore, Dr. Sabshin, who would later serve as medical director of the APA for almost 25 years, criticized White mental health professionals for viewing Black communities as “seething cauldrons of psychopathology”:
“They create stereotypes of absent fathers, primitive rage, psychopathy, self-depreciation, promiscuity, deficits in intellectual capacity, and lack of psychological sensitivity,” Dr. Sabshin and his associates wrote. “Gross pathological caricaturization ignores the enormous variation of behavior in black communities. ... The obsession with black psychopathology has been so great that it has retarded serious consideration of racism as it pertains to white psychopathology.”4
In other words, White American psychiatrists adopted the prevailing views of society at large toward Black people. More recently, “there was a period in this country where Black people were thought to be at higher risk of developing issues like schizophrenia5 instead of depression,” said Gregory Scott Brown, MD, of the Center for Green Psychiatry and the University of Texas in Austin.
“Pharmaceutical companies developed ads for antipsychotic medications that portrayed angry Black men or women. This got into the heads of who may have been conditioned without knowing it,” he said.
In addition, psychiatry has failed to diversify its ranks. To this day, Dr. Geller said, “Black psychiatrists are underrepresented in academic settings, leadership positions, hospitals, and clinics. Black patients are suffering because of inequities in access to care in treatment, and even those who receive treatment are often misdiagnosed since we don’t account for the extended community’s trauma.” About 2% of U.S. psychiatrists are Black, and Black people make up 13% of the U.S. population.6
The low percentage of Black psychiatrists hurts the field for many reasons, said task force member Steven Starks, MD, clinical assistant professor of psychiatry at the University of Houston, and not solely because the gap forces many Black patients to be treated by non-Black psychiatrists. “The association has a large, broad impact on our field and profession through the DSM, and work in areas like government relations and access to care and insurance,” Dr. Starks said.
Task force gets mixed reviews
After the announcement, Dr. Geller named the psychiatrists who will serve, and the task force, chaired by Cheryl D. Wills, MD, assistant professor of psychiatry at Case Western Reserve University in Cleveland, got to work quickly.
The task force has conducted an online town hall and will conduct another one on Aug. 24. It also released the results of a survey of nearly 500 members about the top three areas that the task force should address.
“Access to Healthcare/Mental Healthcare” received the most votes (97) as the recommended top priority, followed by “Socio-Economic Conditions and Factors” (49). These two areas also received the most first-, second- and third-priority votes overall (173 and 166, respectively).
The other areas with high numbers of first priority votes were “Lack of Minority Psychiatrists, Faculty and Leaders” and “Education for Psychiatrists,” both tied at 46. Those areas received 142 and 122 total votes supporting them as first, second, and third priorities.
Thirty-seven members said “Racism within the APA/APA Actions” should be the top priority. A small number of respondents appeared to doubt the need for such a task force: Nineteen thought the top priority should be “Questioning the Concept of Structural Racism/Task Force.”
Meanwhile, some psychiatrists are raising questions about the task force’s makeup.
Ruth S. Shim, MD, MPH, the Luke & Grace Kim Professor of Cultural Psychiatry at the University of California, Davis, said that she was disappointed by the task force’s membership. Specifically, Dr. Shim said, the task force does not include enough APA members she sees as qualified to address structural racism.
“While many of the Black psychiatrists who are members of the task force are experts in issues of diversity, inclusion, and equity, other members of the board of trustees who were appointed to this task force do not have any expertise in this area,” said Dr. Shim, who wrote a scathing commentary7 in July about the APA’s failures regarding structural racism. “I believe the selection of members could have been more thoughtful and more inclusive of diverse perspectives and voices.”
Dr. Geller countered that the task force includes a mix of APA board members and non–board members with various types of expertise. “Certain board members were chosen because their colleagues on the board “were already involved in task forces and other projects,” he said.
How the task force is envisioned
Dr. Geller’s goals for the task force, which will operate at least through his 1-year term as president, are ambitious.
“I hope the task force will identify structural racism wherever it’s taking place – where psychiatrists practice, within the APA itself,” Dr. Geller said. “It will be an educational process so we can inform members and ourselves about clear and subtle structural racism. Then we’re going to proffer solutions in several areas that can rectify some of what we’ve been doing and the negative outcomes that have resulted in areas of leadership such as access to care, treatment, hospital and clinic administration, health insurance, and academia. It’s clear that this is a massive undertaking.”
For her part, Dr. Shim thinks the task force might chip around the edges of the structural problems in the specialty – rather than focusing on the roots. “The task force is set up to fail,” she said. “To truly dismantle structural racism in the APA, the leadership of the organization – the CEO, the executive committee, and the board of trustees – must do the hard work of deep self-reflection and self-study to recognize the role that they have played in perpetuating and upholding White supremacy in the organization.
“I do not believe the task force will be capable of doing this, as this is not what they have been tasked to do,” Dr. Shim said.
Task force member Dr. Starks said he believes there is potential for progress within the APA. While Black members have been frustrated by an APA power structure that seems both harmful and unchangeable, he said, “this is an opportunity for us to re-root and achieve equity in mental health.”
He added that the priorities of the task force are not set in stone. “Those things that are listed on the website may change and evolve over time as we report back to the board and develop our functions internally,” said Dr. Starks, who praised Dr. Shim’s commentary as “courageous.”
The website lists these initial charges for the task force:
- Providing education and resources on APA’s and psychiatry’s history regarding structural racism.
- Explaining the current impact of structural racism on the mental health of our patients and colleagues.
- Developing achievable and actionable recommendations for change to eliminate structural racism in the APA and psychiatry now and in the future.
- Providing reports with specific recommendations for achievable actions to the APA board of trustees at each of its meetings through May 2021.
- Monitoring the implementation of tasks.
Meanwhile, the task force is reporting to the APA board of directors each month. The entity is tied to the 1-year presidential term of Dr. Geller, which ends in spring 2021, but Dr. Starks said he hopes it will continue in another form – such as a formal committee.
Importance of cultural competence
Dr. Brown highlighted the importance of cultural competence – “making sure that we are looking at patients in the context of their cultural background, their religion, their race, so we can make informed decisions without jumping to conclusions too soon.”
For example, if an African American man or woman talks about hearing God’s voice, “we shouldn’t necessarily brush it off or diminish it as psychiatric illness if it’s in the context of that person’s religious background,” Dr. Brown said.
Francis G. Lu, MD, agreed. He said the task force should explore cultural competency on both clinical and systems levels.
“An antidote to structural racism would be systems cultural competence involving organizations, clinics, and teams looking beyond patient care issues,” said Dr. Lu, the Luke & Grace Kim Professor in Cultural Psychiatry Emeritus at the University of California, Davis. A good starting point, he said, is the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care, also known as the National CLAS Standards.
Looking forward, Olusola Ajilore, MD, PhD, called for a focus on targeted efforts aimed at encouraging more minority medical students to become psychiatrists.
“We have a field with a lot of crucial questions that have yet to be answered,” said Dr. Ajilore, associate director of residency training and education at the University of Illinois at Chicago. “With more Black psychiatrists, we might be more aware of some of the research questions that affect our community, such as the mental health consequences of exposure to racism and prejudice.”
However, the role of White psychiatrists cannot be overemphasized, said Constance E. Dunlap, MD, clinical professor of psychiatry and behavioral sciences at George Washington University in Washington.
“Whites can make a difference by acknowledging the racial hierarchy that ‘unfairly disadvantages some ... and unfairly advantages others’ – to use the language8 offered by Dr. Camara Phyllis Jones, said Dr. Dunlap.
“As psychiatrists – as physicians – we are obligated to help patients see themselves and the world more clearly. This starts with our own self-appraisal and extends to our work, whether it is in a psychodynamic space or a community psychiatry setting,” Dr. Dunlap said. “Bottom line, instead of focusing on guilt, I tell my White colleagues and patients: You have privilege, use it constructively to benefit the world.”
Dr. Calhoun said she hopes to see mandated integration of training about racism into psychiatric education. “Rather than a special racism lecture, I’d like to see instruction implemented throughout. It should be essential for psychiatrists to learn about the historical racism of psychiatry and the current racial inequities that exist among psychiatric patients.”
The practice of community psychiatry,9 almost by definition, is uniquely positioned to break through some of those structural issues. “The community psychiatry approach to treatment is not specific to any race or cultural group – because each person is treated as an individual,” said Stephanie Le Melle, MD, MS, director of public psychiatry education at Columbia University and the New York Psychiatric Institute. “The social determinants of health, culture, and social justice experience of each person is taken into consideration,” said Dr. Le Melle.
“Community psychiatry steps outside of the traditional medical model of symptoms and illness, and focuses on understanding the person’s strengths and goals – and helps them to live their best lives.”
Dr. Le Melle also views diversifying the psychiatric workforce as imperative.
“For many African American, Latinx, and other marginalized populations that have had to deal with systemic and structural racism, discrimination, and historical abuse at the hands of psychiatry, it can be difficult to establish trust,” said Dr. Le Melle. “Therefore, diversity of our workforce and cultural humility are also crucial for engagement.”
The APA’s decision to not go forward with this year’s Institute on Psychiatric Services: The Mental Health Services Conference undermines the group’s credibility on these issues, according to some psychiatrists.
The IPS meeting, founded in 1948, is “where we traditionally teach and present about the social determinants of health and racism,” said Dr. Le Melle. “If the APA is serious about addressing the social determinants of health, bias, and discrimination against marginalized people and cultural humility, it needs to embrace and grow community psychiatry, not cut it.”
When asked about the IPS conference, Dr. Geller said that it has been scheduled for October 2021 in New York City. He also said the decision to skip the 2020 conference was made 2 years ago. The conference’s organizing committee decided to cancel the event when hotel space in the preferred city could not be arranged, Dr. Geller said.
Meanwhile, in a widely circulated letter that was sent to the APA board of trustees on Aug. 7, numerous leaders in psychiatry from across the country are citing steps they say the APA must take from “continuing impacts of structural racism that will greatly harm underserved patients, [minority and underrepresented] (M/UR) psychiatrists, and the APA as a whole.”
One step the leaders asked the APA to take was to hire an independent entity to investigate the organization’s “workplace culture, staff morale, and experiences of staff members and M/UR psychiatrists who support and/or work at the organization or have previously been dismissed or departed.”
Dr. Calhoun said she agrees that an internal examination would be productive.
“I’d like to see multiple people in positions of power (in the APA) in order to forward agendas,” Dr. Calhoun said. “Unless we do, we’ll have no way to achieve the goal of getting rid of structural racism.”
Dr. Calhoun, Dr. Geller, Dr. Brown, Dr. Starks, Dr. Lu, Dr. Ajilore, Dr. Dunlap, and Dr. Le Melle reported no relevant disclosures. Dr. Shim disclosed receiving royalties from American Psychiatric Association Publishing. Dr. Stewart is a coeditor of “Black Mental Health: Patients, Providers, and Systems” (American Psychiatric Association Publishing, 2018).
References
1. Geller J. Psychiatric News. 2020 Jun 23.
2. Washington HA. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans From Colonial Times to the Present. (New York: Doubleday), 2006.
3. ”Stewart brings a robust and eventful presidential year to a close.” Psychiatric News Daily. 2019 May 18.
4. Sabshin M et al. Am J Psychiatry. 1970 Dec;127:6.
5. Metzl JM. The Protest Psychosis: How Schizophrenia Became a Black Disease. (Boston: Beacon Press), 2009.
6. U.S. Census Bureau. Population estimates. 2019 Jul 1.
7. Shim RS. “Structural racism is why I’m leaving organized psychiatry. statnews.com. 2020 Jul 1.
8. Jones CP. Ethn Dis;28(Suppl):231-4.
9. Ewalt JR and Ewalt PA. Am J Psychiatry. 2006 Apr 1. doi: 10.1176/ajp.126.1.43.
Amanda Calhoun, MD, recalls noticing a distinct empathy gap while she trained at a youth psychiatric unit.
A White male patient hurled the N-word at a Black patient, and the majority White staff did nothing. “And then [they] told me the White patient was struggling and that’s why they allowed it, even though he was aggressive,” said Dr. Calhoun, psychiatry resident at Yale University in New Haven, Conn. But Dr. Calhoun noticed less restraint on the part of her colleagues while she was treating an angry female Black Latinx patient.
“I remember staff saying she was a nightmare; they called her the B-word; she was ‘a terror.’ How is that this patient isn’t viewed as struggling, where the other patient is? I don’t understand the difference here.”
And, Dr. Calhoun said, “when a patient can complain that they feel they were treated differently based on skin color, [the White majority staff] would just say they have borderline personality disorder or they’re depressed.
“When the staff is not diverse, I really see differential treatment in who gets the benefit of the doubt and their empathy.”
Psychiatrists such as Dr. Calhoun can list countless other examples of institutional racism, interpersonal racism, and prejudice in psychiatry. They see signs of institutional racism in clinical care, academia, and in research. Some are questioning the American Psychiatric Association decision to put on hiatus the Institute on Psychiatric Services, its fall annual meeting that has traditionally served as a vehicle for examining the treatment of underserved communities.
Against that backdrop – and after the killing of George Floyd and amid the disproportionate impact of COVID-19 on communities of color – the APA launched an effort the group says is aimed at reforming itself and psychiatry as a whole. In June, the APA announced the formation of the Presidential Task Force to Address Structural Racism Throughout Psychiatry, and the panel – focused on anti-Black racism – has begun its yearlong work.
A specialty with inherent contradictions
Jeffrey Geller, MD, MPH, the APA’s president, acknowledged in an interview that racism in psychiatry is older than the APA – which celebrated its 175th anniversary as an association last year.
As Dr. Geller pointed out recently, Benjamin Rush, MD, a founding father of the United States and the father of American psychiatry, was an abolitionist who owned one enslaved man – and thought the intelligence and morality of Black people were equal to that of their White counterparts.1 Dr. Rush also thought the skin color of Black people was a manifestation of a type of leprosy that he called “Negritude.”2 “Rush was a remarkable mix of contradictions,” Dr. Geller wrote.
Altha J. Stewart, MD, the first and only Black president of the APA, declined to be interviewed for this article.
But as Dr. Stewart was wrapping up her term as president, she reportedly3 said that a 1970 paper titled “Dimensions of Institutional Racism in Psychiatry” by the late Melvin Sabshin, MD, and associates was essentially a blueprint for moving the specialty forward.
That paper, published in the American Journal of Psychiatry, took psychiatry to task on many levels. One of the barriers that Black psychiatric patients must overcome, according to Dr. Sabshin and associates, is the “biases of the White therapist, who must overcome his cultural blind spots, reactive guilt, and unconscious prejudice.” They called community psychiatry paternalistic. Furthermore, Dr. Sabshin, who would later serve as medical director of the APA for almost 25 years, criticized White mental health professionals for viewing Black communities as “seething cauldrons of psychopathology”:
“They create stereotypes of absent fathers, primitive rage, psychopathy, self-depreciation, promiscuity, deficits in intellectual capacity, and lack of psychological sensitivity,” Dr. Sabshin and his associates wrote. “Gross pathological caricaturization ignores the enormous variation of behavior in black communities. ... The obsession with black psychopathology has been so great that it has retarded serious consideration of racism as it pertains to white psychopathology.”4
In other words, White American psychiatrists adopted the prevailing views of society at large toward Black people. More recently, “there was a period in this country where Black people were thought to be at higher risk of developing issues like schizophrenia5 instead of depression,” said Gregory Scott Brown, MD, of the Center for Green Psychiatry and the University of Texas in Austin.
“Pharmaceutical companies developed ads for antipsychotic medications that portrayed angry Black men or women. This got into the heads of who may have been conditioned without knowing it,” he said.
In addition, psychiatry has failed to diversify its ranks. To this day, Dr. Geller said, “Black psychiatrists are underrepresented in academic settings, leadership positions, hospitals, and clinics. Black patients are suffering because of inequities in access to care in treatment, and even those who receive treatment are often misdiagnosed since we don’t account for the extended community’s trauma.” About 2% of U.S. psychiatrists are Black, and Black people make up 13% of the U.S. population.6
The low percentage of Black psychiatrists hurts the field for many reasons, said task force member Steven Starks, MD, clinical assistant professor of psychiatry at the University of Houston, and not solely because the gap forces many Black patients to be treated by non-Black psychiatrists. “The association has a large, broad impact on our field and profession through the DSM, and work in areas like government relations and access to care and insurance,” Dr. Starks said.
Task force gets mixed reviews
After the announcement, Dr. Geller named the psychiatrists who will serve, and the task force, chaired by Cheryl D. Wills, MD, assistant professor of psychiatry at Case Western Reserve University in Cleveland, got to work quickly.
The task force has conducted an online town hall and will conduct another one on Aug. 24. It also released the results of a survey of nearly 500 members about the top three areas that the task force should address.
“Access to Healthcare/Mental Healthcare” received the most votes (97) as the recommended top priority, followed by “Socio-Economic Conditions and Factors” (49). These two areas also received the most first-, second- and third-priority votes overall (173 and 166, respectively).
The other areas with high numbers of first priority votes were “Lack of Minority Psychiatrists, Faculty and Leaders” and “Education for Psychiatrists,” both tied at 46. Those areas received 142 and 122 total votes supporting them as first, second, and third priorities.
Thirty-seven members said “Racism within the APA/APA Actions” should be the top priority. A small number of respondents appeared to doubt the need for such a task force: Nineteen thought the top priority should be “Questioning the Concept of Structural Racism/Task Force.”
Meanwhile, some psychiatrists are raising questions about the task force’s makeup.
Ruth S. Shim, MD, MPH, the Luke & Grace Kim Professor of Cultural Psychiatry at the University of California, Davis, said that she was disappointed by the task force’s membership. Specifically, Dr. Shim said, the task force does not include enough APA members she sees as qualified to address structural racism.
“While many of the Black psychiatrists who are members of the task force are experts in issues of diversity, inclusion, and equity, other members of the board of trustees who were appointed to this task force do not have any expertise in this area,” said Dr. Shim, who wrote a scathing commentary7 in July about the APA’s failures regarding structural racism. “I believe the selection of members could have been more thoughtful and more inclusive of diverse perspectives and voices.”
Dr. Geller countered that the task force includes a mix of APA board members and non–board members with various types of expertise. “Certain board members were chosen because their colleagues on the board “were already involved in task forces and other projects,” he said.
How the task force is envisioned
Dr. Geller’s goals for the task force, which will operate at least through his 1-year term as president, are ambitious.
“I hope the task force will identify structural racism wherever it’s taking place – where psychiatrists practice, within the APA itself,” Dr. Geller said. “It will be an educational process so we can inform members and ourselves about clear and subtle structural racism. Then we’re going to proffer solutions in several areas that can rectify some of what we’ve been doing and the negative outcomes that have resulted in areas of leadership such as access to care, treatment, hospital and clinic administration, health insurance, and academia. It’s clear that this is a massive undertaking.”
For her part, Dr. Shim thinks the task force might chip around the edges of the structural problems in the specialty – rather than focusing on the roots. “The task force is set up to fail,” she said. “To truly dismantle structural racism in the APA, the leadership of the organization – the CEO, the executive committee, and the board of trustees – must do the hard work of deep self-reflection and self-study to recognize the role that they have played in perpetuating and upholding White supremacy in the organization.
“I do not believe the task force will be capable of doing this, as this is not what they have been tasked to do,” Dr. Shim said.
Task force member Dr. Starks said he believes there is potential for progress within the APA. While Black members have been frustrated by an APA power structure that seems both harmful and unchangeable, he said, “this is an opportunity for us to re-root and achieve equity in mental health.”
He added that the priorities of the task force are not set in stone. “Those things that are listed on the website may change and evolve over time as we report back to the board and develop our functions internally,” said Dr. Starks, who praised Dr. Shim’s commentary as “courageous.”
The website lists these initial charges for the task force:
- Providing education and resources on APA’s and psychiatry’s history regarding structural racism.
- Explaining the current impact of structural racism on the mental health of our patients and colleagues.
- Developing achievable and actionable recommendations for change to eliminate structural racism in the APA and psychiatry now and in the future.
- Providing reports with specific recommendations for achievable actions to the APA board of trustees at each of its meetings through May 2021.
- Monitoring the implementation of tasks.
Meanwhile, the task force is reporting to the APA board of directors each month. The entity is tied to the 1-year presidential term of Dr. Geller, which ends in spring 2021, but Dr. Starks said he hopes it will continue in another form – such as a formal committee.
Importance of cultural competence
Dr. Brown highlighted the importance of cultural competence – “making sure that we are looking at patients in the context of their cultural background, their religion, their race, so we can make informed decisions without jumping to conclusions too soon.”
For example, if an African American man or woman talks about hearing God’s voice, “we shouldn’t necessarily brush it off or diminish it as psychiatric illness if it’s in the context of that person’s religious background,” Dr. Brown said.
Francis G. Lu, MD, agreed. He said the task force should explore cultural competency on both clinical and systems levels.
“An antidote to structural racism would be systems cultural competence involving organizations, clinics, and teams looking beyond patient care issues,” said Dr. Lu, the Luke & Grace Kim Professor in Cultural Psychiatry Emeritus at the University of California, Davis. A good starting point, he said, is the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care, also known as the National CLAS Standards.
Looking forward, Olusola Ajilore, MD, PhD, called for a focus on targeted efforts aimed at encouraging more minority medical students to become psychiatrists.
“We have a field with a lot of crucial questions that have yet to be answered,” said Dr. Ajilore, associate director of residency training and education at the University of Illinois at Chicago. “With more Black psychiatrists, we might be more aware of some of the research questions that affect our community, such as the mental health consequences of exposure to racism and prejudice.”
However, the role of White psychiatrists cannot be overemphasized, said Constance E. Dunlap, MD, clinical professor of psychiatry and behavioral sciences at George Washington University in Washington.
“Whites can make a difference by acknowledging the racial hierarchy that ‘unfairly disadvantages some ... and unfairly advantages others’ – to use the language8 offered by Dr. Camara Phyllis Jones, said Dr. Dunlap.
“As psychiatrists – as physicians – we are obligated to help patients see themselves and the world more clearly. This starts with our own self-appraisal and extends to our work, whether it is in a psychodynamic space or a community psychiatry setting,” Dr. Dunlap said. “Bottom line, instead of focusing on guilt, I tell my White colleagues and patients: You have privilege, use it constructively to benefit the world.”
Dr. Calhoun said she hopes to see mandated integration of training about racism into psychiatric education. “Rather than a special racism lecture, I’d like to see instruction implemented throughout. It should be essential for psychiatrists to learn about the historical racism of psychiatry and the current racial inequities that exist among psychiatric patients.”
The practice of community psychiatry,9 almost by definition, is uniquely positioned to break through some of those structural issues. “The community psychiatry approach to treatment is not specific to any race or cultural group – because each person is treated as an individual,” said Stephanie Le Melle, MD, MS, director of public psychiatry education at Columbia University and the New York Psychiatric Institute. “The social determinants of health, culture, and social justice experience of each person is taken into consideration,” said Dr. Le Melle.
“Community psychiatry steps outside of the traditional medical model of symptoms and illness, and focuses on understanding the person’s strengths and goals – and helps them to live their best lives.”
Dr. Le Melle also views diversifying the psychiatric workforce as imperative.
“For many African American, Latinx, and other marginalized populations that have had to deal with systemic and structural racism, discrimination, and historical abuse at the hands of psychiatry, it can be difficult to establish trust,” said Dr. Le Melle. “Therefore, diversity of our workforce and cultural humility are also crucial for engagement.”
The APA’s decision to not go forward with this year’s Institute on Psychiatric Services: The Mental Health Services Conference undermines the group’s credibility on these issues, according to some psychiatrists.
The IPS meeting, founded in 1948, is “where we traditionally teach and present about the social determinants of health and racism,” said Dr. Le Melle. “If the APA is serious about addressing the social determinants of health, bias, and discrimination against marginalized people and cultural humility, it needs to embrace and grow community psychiatry, not cut it.”
When asked about the IPS conference, Dr. Geller said that it has been scheduled for October 2021 in New York City. He also said the decision to skip the 2020 conference was made 2 years ago. The conference’s organizing committee decided to cancel the event when hotel space in the preferred city could not be arranged, Dr. Geller said.
Meanwhile, in a widely circulated letter that was sent to the APA board of trustees on Aug. 7, numerous leaders in psychiatry from across the country are citing steps they say the APA must take from “continuing impacts of structural racism that will greatly harm underserved patients, [minority and underrepresented] (M/UR) psychiatrists, and the APA as a whole.”
One step the leaders asked the APA to take was to hire an independent entity to investigate the organization’s “workplace culture, staff morale, and experiences of staff members and M/UR psychiatrists who support and/or work at the organization or have previously been dismissed or departed.”
Dr. Calhoun said she agrees that an internal examination would be productive.
“I’d like to see multiple people in positions of power (in the APA) in order to forward agendas,” Dr. Calhoun said. “Unless we do, we’ll have no way to achieve the goal of getting rid of structural racism.”
Dr. Calhoun, Dr. Geller, Dr. Brown, Dr. Starks, Dr. Lu, Dr. Ajilore, Dr. Dunlap, and Dr. Le Melle reported no relevant disclosures. Dr. Shim disclosed receiving royalties from American Psychiatric Association Publishing. Dr. Stewart is a coeditor of “Black Mental Health: Patients, Providers, and Systems” (American Psychiatric Association Publishing, 2018).
References
1. Geller J. Psychiatric News. 2020 Jun 23.
2. Washington HA. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans From Colonial Times to the Present. (New York: Doubleday), 2006.
3. ”Stewart brings a robust and eventful presidential year to a close.” Psychiatric News Daily. 2019 May 18.
4. Sabshin M et al. Am J Psychiatry. 1970 Dec;127:6.
5. Metzl JM. The Protest Psychosis: How Schizophrenia Became a Black Disease. (Boston: Beacon Press), 2009.
6. U.S. Census Bureau. Population estimates. 2019 Jul 1.
7. Shim RS. “Structural racism is why I’m leaving organized psychiatry. statnews.com. 2020 Jul 1.
8. Jones CP. Ethn Dis;28(Suppl):231-4.
9. Ewalt JR and Ewalt PA. Am J Psychiatry. 2006 Apr 1. doi: 10.1176/ajp.126.1.43.
Amanda Calhoun, MD, recalls noticing a distinct empathy gap while she trained at a youth psychiatric unit.
A White male patient hurled the N-word at a Black patient, and the majority White staff did nothing. “And then [they] told me the White patient was struggling and that’s why they allowed it, even though he was aggressive,” said Dr. Calhoun, psychiatry resident at Yale University in New Haven, Conn. But Dr. Calhoun noticed less restraint on the part of her colleagues while she was treating an angry female Black Latinx patient.
“I remember staff saying she was a nightmare; they called her the B-word; she was ‘a terror.’ How is that this patient isn’t viewed as struggling, where the other patient is? I don’t understand the difference here.”
And, Dr. Calhoun said, “when a patient can complain that they feel they were treated differently based on skin color, [the White majority staff] would just say they have borderline personality disorder or they’re depressed.
“When the staff is not diverse, I really see differential treatment in who gets the benefit of the doubt and their empathy.”
Psychiatrists such as Dr. Calhoun can list countless other examples of institutional racism, interpersonal racism, and prejudice in psychiatry. They see signs of institutional racism in clinical care, academia, and in research. Some are questioning the American Psychiatric Association decision to put on hiatus the Institute on Psychiatric Services, its fall annual meeting that has traditionally served as a vehicle for examining the treatment of underserved communities.
Against that backdrop – and after the killing of George Floyd and amid the disproportionate impact of COVID-19 on communities of color – the APA launched an effort the group says is aimed at reforming itself and psychiatry as a whole. In June, the APA announced the formation of the Presidential Task Force to Address Structural Racism Throughout Psychiatry, and the panel – focused on anti-Black racism – has begun its yearlong work.
A specialty with inherent contradictions
Jeffrey Geller, MD, MPH, the APA’s president, acknowledged in an interview that racism in psychiatry is older than the APA – which celebrated its 175th anniversary as an association last year.
As Dr. Geller pointed out recently, Benjamin Rush, MD, a founding father of the United States and the father of American psychiatry, was an abolitionist who owned one enslaved man – and thought the intelligence and morality of Black people were equal to that of their White counterparts.1 Dr. Rush also thought the skin color of Black people was a manifestation of a type of leprosy that he called “Negritude.”2 “Rush was a remarkable mix of contradictions,” Dr. Geller wrote.
Altha J. Stewart, MD, the first and only Black president of the APA, declined to be interviewed for this article.
But as Dr. Stewart was wrapping up her term as president, she reportedly3 said that a 1970 paper titled “Dimensions of Institutional Racism in Psychiatry” by the late Melvin Sabshin, MD, and associates was essentially a blueprint for moving the specialty forward.
That paper, published in the American Journal of Psychiatry, took psychiatry to task on many levels. One of the barriers that Black psychiatric patients must overcome, according to Dr. Sabshin and associates, is the “biases of the White therapist, who must overcome his cultural blind spots, reactive guilt, and unconscious prejudice.” They called community psychiatry paternalistic. Furthermore, Dr. Sabshin, who would later serve as medical director of the APA for almost 25 years, criticized White mental health professionals for viewing Black communities as “seething cauldrons of psychopathology”:
“They create stereotypes of absent fathers, primitive rage, psychopathy, self-depreciation, promiscuity, deficits in intellectual capacity, and lack of psychological sensitivity,” Dr. Sabshin and his associates wrote. “Gross pathological caricaturization ignores the enormous variation of behavior in black communities. ... The obsession with black psychopathology has been so great that it has retarded serious consideration of racism as it pertains to white psychopathology.”4
In other words, White American psychiatrists adopted the prevailing views of society at large toward Black people. More recently, “there was a period in this country where Black people were thought to be at higher risk of developing issues like schizophrenia5 instead of depression,” said Gregory Scott Brown, MD, of the Center for Green Psychiatry and the University of Texas in Austin.
“Pharmaceutical companies developed ads for antipsychotic medications that portrayed angry Black men or women. This got into the heads of who may have been conditioned without knowing it,” he said.
In addition, psychiatry has failed to diversify its ranks. To this day, Dr. Geller said, “Black psychiatrists are underrepresented in academic settings, leadership positions, hospitals, and clinics. Black patients are suffering because of inequities in access to care in treatment, and even those who receive treatment are often misdiagnosed since we don’t account for the extended community’s trauma.” About 2% of U.S. psychiatrists are Black, and Black people make up 13% of the U.S. population.6
The low percentage of Black psychiatrists hurts the field for many reasons, said task force member Steven Starks, MD, clinical assistant professor of psychiatry at the University of Houston, and not solely because the gap forces many Black patients to be treated by non-Black psychiatrists. “The association has a large, broad impact on our field and profession through the DSM, and work in areas like government relations and access to care and insurance,” Dr. Starks said.
Task force gets mixed reviews
After the announcement, Dr. Geller named the psychiatrists who will serve, and the task force, chaired by Cheryl D. Wills, MD, assistant professor of psychiatry at Case Western Reserve University in Cleveland, got to work quickly.
The task force has conducted an online town hall and will conduct another one on Aug. 24. It also released the results of a survey of nearly 500 members about the top three areas that the task force should address.
“Access to Healthcare/Mental Healthcare” received the most votes (97) as the recommended top priority, followed by “Socio-Economic Conditions and Factors” (49). These two areas also received the most first-, second- and third-priority votes overall (173 and 166, respectively).
The other areas with high numbers of first priority votes were “Lack of Minority Psychiatrists, Faculty and Leaders” and “Education for Psychiatrists,” both tied at 46. Those areas received 142 and 122 total votes supporting them as first, second, and third priorities.
Thirty-seven members said “Racism within the APA/APA Actions” should be the top priority. A small number of respondents appeared to doubt the need for such a task force: Nineteen thought the top priority should be “Questioning the Concept of Structural Racism/Task Force.”
Meanwhile, some psychiatrists are raising questions about the task force’s makeup.
Ruth S. Shim, MD, MPH, the Luke & Grace Kim Professor of Cultural Psychiatry at the University of California, Davis, said that she was disappointed by the task force’s membership. Specifically, Dr. Shim said, the task force does not include enough APA members she sees as qualified to address structural racism.
“While many of the Black psychiatrists who are members of the task force are experts in issues of diversity, inclusion, and equity, other members of the board of trustees who were appointed to this task force do not have any expertise in this area,” said Dr. Shim, who wrote a scathing commentary7 in July about the APA’s failures regarding structural racism. “I believe the selection of members could have been more thoughtful and more inclusive of diverse perspectives and voices.”
Dr. Geller countered that the task force includes a mix of APA board members and non–board members with various types of expertise. “Certain board members were chosen because their colleagues on the board “were already involved in task forces and other projects,” he said.
How the task force is envisioned
Dr. Geller’s goals for the task force, which will operate at least through his 1-year term as president, are ambitious.
“I hope the task force will identify structural racism wherever it’s taking place – where psychiatrists practice, within the APA itself,” Dr. Geller said. “It will be an educational process so we can inform members and ourselves about clear and subtle structural racism. Then we’re going to proffer solutions in several areas that can rectify some of what we’ve been doing and the negative outcomes that have resulted in areas of leadership such as access to care, treatment, hospital and clinic administration, health insurance, and academia. It’s clear that this is a massive undertaking.”
For her part, Dr. Shim thinks the task force might chip around the edges of the structural problems in the specialty – rather than focusing on the roots. “The task force is set up to fail,” she said. “To truly dismantle structural racism in the APA, the leadership of the organization – the CEO, the executive committee, and the board of trustees – must do the hard work of deep self-reflection and self-study to recognize the role that they have played in perpetuating and upholding White supremacy in the organization.
“I do not believe the task force will be capable of doing this, as this is not what they have been tasked to do,” Dr. Shim said.
Task force member Dr. Starks said he believes there is potential for progress within the APA. While Black members have been frustrated by an APA power structure that seems both harmful and unchangeable, he said, “this is an opportunity for us to re-root and achieve equity in mental health.”
He added that the priorities of the task force are not set in stone. “Those things that are listed on the website may change and evolve over time as we report back to the board and develop our functions internally,” said Dr. Starks, who praised Dr. Shim’s commentary as “courageous.”
The website lists these initial charges for the task force:
- Providing education and resources on APA’s and psychiatry’s history regarding structural racism.
- Explaining the current impact of structural racism on the mental health of our patients and colleagues.
- Developing achievable and actionable recommendations for change to eliminate structural racism in the APA and psychiatry now and in the future.
- Providing reports with specific recommendations for achievable actions to the APA board of trustees at each of its meetings through May 2021.
- Monitoring the implementation of tasks.
Meanwhile, the task force is reporting to the APA board of directors each month. The entity is tied to the 1-year presidential term of Dr. Geller, which ends in spring 2021, but Dr. Starks said he hopes it will continue in another form – such as a formal committee.
Importance of cultural competence
Dr. Brown highlighted the importance of cultural competence – “making sure that we are looking at patients in the context of their cultural background, their religion, their race, so we can make informed decisions without jumping to conclusions too soon.”
For example, if an African American man or woman talks about hearing God’s voice, “we shouldn’t necessarily brush it off or diminish it as psychiatric illness if it’s in the context of that person’s religious background,” Dr. Brown said.
Francis G. Lu, MD, agreed. He said the task force should explore cultural competency on both clinical and systems levels.
“An antidote to structural racism would be systems cultural competence involving organizations, clinics, and teams looking beyond patient care issues,” said Dr. Lu, the Luke & Grace Kim Professor in Cultural Psychiatry Emeritus at the University of California, Davis. A good starting point, he said, is the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care, also known as the National CLAS Standards.
Looking forward, Olusola Ajilore, MD, PhD, called for a focus on targeted efforts aimed at encouraging more minority medical students to become psychiatrists.
“We have a field with a lot of crucial questions that have yet to be answered,” said Dr. Ajilore, associate director of residency training and education at the University of Illinois at Chicago. “With more Black psychiatrists, we might be more aware of some of the research questions that affect our community, such as the mental health consequences of exposure to racism and prejudice.”
However, the role of White psychiatrists cannot be overemphasized, said Constance E. Dunlap, MD, clinical professor of psychiatry and behavioral sciences at George Washington University in Washington.
“Whites can make a difference by acknowledging the racial hierarchy that ‘unfairly disadvantages some ... and unfairly advantages others’ – to use the language8 offered by Dr. Camara Phyllis Jones, said Dr. Dunlap.
“As psychiatrists – as physicians – we are obligated to help patients see themselves and the world more clearly. This starts with our own self-appraisal and extends to our work, whether it is in a psychodynamic space or a community psychiatry setting,” Dr. Dunlap said. “Bottom line, instead of focusing on guilt, I tell my White colleagues and patients: You have privilege, use it constructively to benefit the world.”
Dr. Calhoun said she hopes to see mandated integration of training about racism into psychiatric education. “Rather than a special racism lecture, I’d like to see instruction implemented throughout. It should be essential for psychiatrists to learn about the historical racism of psychiatry and the current racial inequities that exist among psychiatric patients.”
The practice of community psychiatry,9 almost by definition, is uniquely positioned to break through some of those structural issues. “The community psychiatry approach to treatment is not specific to any race or cultural group – because each person is treated as an individual,” said Stephanie Le Melle, MD, MS, director of public psychiatry education at Columbia University and the New York Psychiatric Institute. “The social determinants of health, culture, and social justice experience of each person is taken into consideration,” said Dr. Le Melle.
“Community psychiatry steps outside of the traditional medical model of symptoms and illness, and focuses on understanding the person’s strengths and goals – and helps them to live their best lives.”
Dr. Le Melle also views diversifying the psychiatric workforce as imperative.
“For many African American, Latinx, and other marginalized populations that have had to deal with systemic and structural racism, discrimination, and historical abuse at the hands of psychiatry, it can be difficult to establish trust,” said Dr. Le Melle. “Therefore, diversity of our workforce and cultural humility are also crucial for engagement.”
The APA’s decision to not go forward with this year’s Institute on Psychiatric Services: The Mental Health Services Conference undermines the group’s credibility on these issues, according to some psychiatrists.
The IPS meeting, founded in 1948, is “where we traditionally teach and present about the social determinants of health and racism,” said Dr. Le Melle. “If the APA is serious about addressing the social determinants of health, bias, and discrimination against marginalized people and cultural humility, it needs to embrace and grow community psychiatry, not cut it.”
When asked about the IPS conference, Dr. Geller said that it has been scheduled for October 2021 in New York City. He also said the decision to skip the 2020 conference was made 2 years ago. The conference’s organizing committee decided to cancel the event when hotel space in the preferred city could not be arranged, Dr. Geller said.
Meanwhile, in a widely circulated letter that was sent to the APA board of trustees on Aug. 7, numerous leaders in psychiatry from across the country are citing steps they say the APA must take from “continuing impacts of structural racism that will greatly harm underserved patients, [minority and underrepresented] (M/UR) psychiatrists, and the APA as a whole.”
One step the leaders asked the APA to take was to hire an independent entity to investigate the organization’s “workplace culture, staff morale, and experiences of staff members and M/UR psychiatrists who support and/or work at the organization or have previously been dismissed or departed.”
Dr. Calhoun said she agrees that an internal examination would be productive.
“I’d like to see multiple people in positions of power (in the APA) in order to forward agendas,” Dr. Calhoun said. “Unless we do, we’ll have no way to achieve the goal of getting rid of structural racism.”
Dr. Calhoun, Dr. Geller, Dr. Brown, Dr. Starks, Dr. Lu, Dr. Ajilore, Dr. Dunlap, and Dr. Le Melle reported no relevant disclosures. Dr. Shim disclosed receiving royalties from American Psychiatric Association Publishing. Dr. Stewart is a coeditor of “Black Mental Health: Patients, Providers, and Systems” (American Psychiatric Association Publishing, 2018).
References
1. Geller J. Psychiatric News. 2020 Jun 23.
2. Washington HA. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans From Colonial Times to the Present. (New York: Doubleday), 2006.
3. ”Stewart brings a robust and eventful presidential year to a close.” Psychiatric News Daily. 2019 May 18.
4. Sabshin M et al. Am J Psychiatry. 1970 Dec;127:6.
5. Metzl JM. The Protest Psychosis: How Schizophrenia Became a Black Disease. (Boston: Beacon Press), 2009.
6. U.S. Census Bureau. Population estimates. 2019 Jul 1.
7. Shim RS. “Structural racism is why I’m leaving organized psychiatry. statnews.com. 2020 Jul 1.
8. Jones CP. Ethn Dis;28(Suppl):231-4.
9. Ewalt JR and Ewalt PA. Am J Psychiatry. 2006 Apr 1. doi: 10.1176/ajp.126.1.43.
Health disparities training falls short for internal medicine residents
Less than half of internal medicine residency program directors report formal curricula on the topic of health disparities, according to findings of a survey of medical directors and residents across the United States.
Despite recommendations from the Institute of Medicine going back to 2002 calling for increased education on the topic for health care providers, data from a 2012 survey showed that only 17% of internal medicine programs had a health disparities curriculum, wrote Denise M. Dupras, MD, of the Mayo Medical School, Rochester, Minn., and colleagues.
To describe internal medicine residency training programs’ curricula and educational experiences on health disparities and to determine residents’ perceptions of training, the researchers designed a cross-sectional survey study including 227 program directors and 22,723 internal medicine residents. The survey was conducted from August to November 2015.
Overall, 91 program directors (40%) reported a curriculum in health disparities, but only 16 of them described the quality of their education as very good or excellent. In 56% of the programs, outcomes of the curriculum were not measured.
A majority (90%) of the programs included racial/ethnic diversity and socioeconomic status in their curricula, 58% included information about limited English proficiency, and 53% included information about gender identity and sexual orientation.
Reported barriers to curriculum development in 132 programs that did not have a health disparities curriculum included lack of time in the current curriculum, insufficient faculty skill to teach the topic, lack of institutional support, and lack of faculty interest, the researchers noted.
A total of 13,251 residents (70%) reported receiving some training in caring for patients at risk for health disparities over 3 years of training, and 10,494 (80%) of these rated the quality as very good or excellent. “Residents who cared for a larger proportion of underserved patients perceived that they received health disparities training at a higher rate,” the researchers wrote. However, increased care of at-risk populations does not necessarily translate into increased knowledge and skills. “Our finding that residents’ rating of the quality of their training was not associated with the presence of a curriculum in health disparities in their program also raises a concern that perceptions may overestimate the acquisition of needed skills,” they added.
The major limitation of the study was “that residents were not asked directly if they were exposed to a curriculum in health disparities but rather if they received training in the care of patients who would be at risk, which raises the concern that we cannot distinguish between their recognition of a formal and informal curriculum,” the researchers noted. In addition, the survey could not confirm that program directors were aware of all training. “Furthermore, because the survey items were embedded in larger program director survey, we were limited in the ability to ask them to define more specifically the components of their health disparities curricula,” they wrote.
However, the results were strengthened by the large and comprehensive study population, and highlight not only the need for standardized health disparities curricula, but also the need for research to determine the most effective domains for such curricula in graduate medical education, they emphasized.
“There are opportunities to explore partnerships among residencies, institutional clinical practices, and communities for productive collaborations around disparities-related quality improvement projects to address gaps in health care that are specific to the populations they serve,” they concluded.
The surveys were conducted in 2015 and the comparative work in 2018, prior to the COVID-19 pandemic and the subsequent increased concerns about disparities in health care, Dr. Dupras said in an interview.
“We conducted the survey because we recognized that health disparities were still prevalent in our society despite calls to improve the education of our learners to address them. We wanted to determine what our programs were providing for educational curriculum and what our learners were experiencing,” she said.
“We did not know what the surveys would show, so I cannot say that we were surprised by the findings,” said Dr. Dupras. “One of the challenges in interpreting our results is inherent in studies that rely on surveys. We cannot know how those filling out the surveys interpret the questions.” The study results yield several messages.
“First, residency training programs have opportunities to do a better job in developing educational opportunities related to health disparities; second, residents learn in the context of care and we must optimize education around these experiences; third, every patient is different. It is time to move towards cultural humility, since the risk for disparities is not associated with one patient characteristic, but composed of multiple factors,” she said.
“Given that 5 years has passed since our original survey, it would be important to repeat the survey and consider expanding it to include other training programs that provide frontline care, such as family medicine and pediatrics,” Dr. Dupras noted.
Dr. Dupras and colleagues had no financial conflicts to disclose.
SOURCE: Dupras DM et al. JAMA Netw Open. 2020 Aug 10. doi: 10.1001/jamanetworkopen.2020.12757.
Less than half of internal medicine residency program directors report formal curricula on the topic of health disparities, according to findings of a survey of medical directors and residents across the United States.
Despite recommendations from the Institute of Medicine going back to 2002 calling for increased education on the topic for health care providers, data from a 2012 survey showed that only 17% of internal medicine programs had a health disparities curriculum, wrote Denise M. Dupras, MD, of the Mayo Medical School, Rochester, Minn., and colleagues.
To describe internal medicine residency training programs’ curricula and educational experiences on health disparities and to determine residents’ perceptions of training, the researchers designed a cross-sectional survey study including 227 program directors and 22,723 internal medicine residents. The survey was conducted from August to November 2015.
Overall, 91 program directors (40%) reported a curriculum in health disparities, but only 16 of them described the quality of their education as very good or excellent. In 56% of the programs, outcomes of the curriculum were not measured.
A majority (90%) of the programs included racial/ethnic diversity and socioeconomic status in their curricula, 58% included information about limited English proficiency, and 53% included information about gender identity and sexual orientation.
Reported barriers to curriculum development in 132 programs that did not have a health disparities curriculum included lack of time in the current curriculum, insufficient faculty skill to teach the topic, lack of institutional support, and lack of faculty interest, the researchers noted.
A total of 13,251 residents (70%) reported receiving some training in caring for patients at risk for health disparities over 3 years of training, and 10,494 (80%) of these rated the quality as very good or excellent. “Residents who cared for a larger proportion of underserved patients perceived that they received health disparities training at a higher rate,” the researchers wrote. However, increased care of at-risk populations does not necessarily translate into increased knowledge and skills. “Our finding that residents’ rating of the quality of their training was not associated with the presence of a curriculum in health disparities in their program also raises a concern that perceptions may overestimate the acquisition of needed skills,” they added.
The major limitation of the study was “that residents were not asked directly if they were exposed to a curriculum in health disparities but rather if they received training in the care of patients who would be at risk, which raises the concern that we cannot distinguish between their recognition of a formal and informal curriculum,” the researchers noted. In addition, the survey could not confirm that program directors were aware of all training. “Furthermore, because the survey items were embedded in larger program director survey, we were limited in the ability to ask them to define more specifically the components of their health disparities curricula,” they wrote.
However, the results were strengthened by the large and comprehensive study population, and highlight not only the need for standardized health disparities curricula, but also the need for research to determine the most effective domains for such curricula in graduate medical education, they emphasized.
“There are opportunities to explore partnerships among residencies, institutional clinical practices, and communities for productive collaborations around disparities-related quality improvement projects to address gaps in health care that are specific to the populations they serve,” they concluded.
The surveys were conducted in 2015 and the comparative work in 2018, prior to the COVID-19 pandemic and the subsequent increased concerns about disparities in health care, Dr. Dupras said in an interview.
“We conducted the survey because we recognized that health disparities were still prevalent in our society despite calls to improve the education of our learners to address them. We wanted to determine what our programs were providing for educational curriculum and what our learners were experiencing,” she said.
“We did not know what the surveys would show, so I cannot say that we were surprised by the findings,” said Dr. Dupras. “One of the challenges in interpreting our results is inherent in studies that rely on surveys. We cannot know how those filling out the surveys interpret the questions.” The study results yield several messages.
“First, residency training programs have opportunities to do a better job in developing educational opportunities related to health disparities; second, residents learn in the context of care and we must optimize education around these experiences; third, every patient is different. It is time to move towards cultural humility, since the risk for disparities is not associated with one patient characteristic, but composed of multiple factors,” she said.
“Given that 5 years has passed since our original survey, it would be important to repeat the survey and consider expanding it to include other training programs that provide frontline care, such as family medicine and pediatrics,” Dr. Dupras noted.
Dr. Dupras and colleagues had no financial conflicts to disclose.
SOURCE: Dupras DM et al. JAMA Netw Open. 2020 Aug 10. doi: 10.1001/jamanetworkopen.2020.12757.
Less than half of internal medicine residency program directors report formal curricula on the topic of health disparities, according to findings of a survey of medical directors and residents across the United States.
Despite recommendations from the Institute of Medicine going back to 2002 calling for increased education on the topic for health care providers, data from a 2012 survey showed that only 17% of internal medicine programs had a health disparities curriculum, wrote Denise M. Dupras, MD, of the Mayo Medical School, Rochester, Minn., and colleagues.
To describe internal medicine residency training programs’ curricula and educational experiences on health disparities and to determine residents’ perceptions of training, the researchers designed a cross-sectional survey study including 227 program directors and 22,723 internal medicine residents. The survey was conducted from August to November 2015.
Overall, 91 program directors (40%) reported a curriculum in health disparities, but only 16 of them described the quality of their education as very good or excellent. In 56% of the programs, outcomes of the curriculum were not measured.
A majority (90%) of the programs included racial/ethnic diversity and socioeconomic status in their curricula, 58% included information about limited English proficiency, and 53% included information about gender identity and sexual orientation.
Reported barriers to curriculum development in 132 programs that did not have a health disparities curriculum included lack of time in the current curriculum, insufficient faculty skill to teach the topic, lack of institutional support, and lack of faculty interest, the researchers noted.
A total of 13,251 residents (70%) reported receiving some training in caring for patients at risk for health disparities over 3 years of training, and 10,494 (80%) of these rated the quality as very good or excellent. “Residents who cared for a larger proportion of underserved patients perceived that they received health disparities training at a higher rate,” the researchers wrote. However, increased care of at-risk populations does not necessarily translate into increased knowledge and skills. “Our finding that residents’ rating of the quality of their training was not associated with the presence of a curriculum in health disparities in their program also raises a concern that perceptions may overestimate the acquisition of needed skills,” they added.
The major limitation of the study was “that residents were not asked directly if they were exposed to a curriculum in health disparities but rather if they received training in the care of patients who would be at risk, which raises the concern that we cannot distinguish between their recognition of a formal and informal curriculum,” the researchers noted. In addition, the survey could not confirm that program directors were aware of all training. “Furthermore, because the survey items were embedded in larger program director survey, we were limited in the ability to ask them to define more specifically the components of their health disparities curricula,” they wrote.
However, the results were strengthened by the large and comprehensive study population, and highlight not only the need for standardized health disparities curricula, but also the need for research to determine the most effective domains for such curricula in graduate medical education, they emphasized.
“There are opportunities to explore partnerships among residencies, institutional clinical practices, and communities for productive collaborations around disparities-related quality improvement projects to address gaps in health care that are specific to the populations they serve,” they concluded.
The surveys were conducted in 2015 and the comparative work in 2018, prior to the COVID-19 pandemic and the subsequent increased concerns about disparities in health care, Dr. Dupras said in an interview.
“We conducted the survey because we recognized that health disparities were still prevalent in our society despite calls to improve the education of our learners to address them. We wanted to determine what our programs were providing for educational curriculum and what our learners were experiencing,” she said.
“We did not know what the surveys would show, so I cannot say that we were surprised by the findings,” said Dr. Dupras. “One of the challenges in interpreting our results is inherent in studies that rely on surveys. We cannot know how those filling out the surveys interpret the questions.” The study results yield several messages.
“First, residency training programs have opportunities to do a better job in developing educational opportunities related to health disparities; second, residents learn in the context of care and we must optimize education around these experiences; third, every patient is different. It is time to move towards cultural humility, since the risk for disparities is not associated with one patient characteristic, but composed of multiple factors,” she said.
“Given that 5 years has passed since our original survey, it would be important to repeat the survey and consider expanding it to include other training programs that provide frontline care, such as family medicine and pediatrics,” Dr. Dupras noted.
Dr. Dupras and colleagues had no financial conflicts to disclose.
SOURCE: Dupras DM et al. JAMA Netw Open. 2020 Aug 10. doi: 10.1001/jamanetworkopen.2020.12757.
FROM JAMA NETWORK OPEN
Antiaffirmative action paper blasted on Twitter now retracted
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
An article published in March in the Journal of the American Heart Association that raised a ruckus on #medtwitter this week has now been retracted.
It’s unclear what prompted the public explosion of anger, sadness, and recrimination that ultimately led to the retraction of this article – which flew almost completely under the radar when it first appeared online and in print – but it’s crystal clear why it might offend.
To many readers, the paper, written by Norman C. Wang, MD, MSc, an electrophysiologist at the University of Pittsburgh Medical Center, is a “racist” rant that relies on half-truths (J Am Heart Assoc. 2020 Mar 24. doi: 10.1161/JAHA.120.015959).
Officially, the article, “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity Considerations for the Cardiology Workforce in the United States of America From 1969 to 2019,” was retracted after the American Heart Association “became aware of serious concerns after publication. The author’s institution, the University of Pittsburgh Medical Center, has notified the Editor‐in‐Chief that the article contains many misconceptions and misquotes and that together those inaccuracies, misstatements, and selective misreading of source materials strip the paper of its scientific validity,” the retraction reads (J Am Heart Assoc. 2020 Aug 6. doi: 10.1161/JAHA.119.014602).
The journal will be publishing a detailed rebuttal, the notice adds: “This retraction notice will be updated with a link to the rebuttal when it publishes.”
“The Editor‐in‐Chief deeply regrets publishing the article and offers his apologies,” it further reads. “The American Heart Association and the Editor‐in‐Chief have determined that the best interest of the public and the research community will be served by issuing this notice of retraction. The author does not agree to the retraction.”
In the paper, Dr. Wang argues that affirmative action policies designed to increase minority representation in medical schools and cardiovascular training programs result in unqualified applicants being admitted, where they will struggle to succeed.
The article itself is a dense review of the topic of diversity, inclusion, and equity, aiming to “critically assess current paradigms, and to consider potential solutions to anticipated challenges,” according to its author. Supported by 108 references, Dr. Wang concludes with a lengthy quote from tennis great Arthur Ashe, an opponent of affirmative action who died in 1993.
Affirmative action, said Mr. Ashe, is “an insult to the people it intended to help.” Dr. Wang suggests that “racial and ethnic preferences for undergraduate and medical school admissions should be gradually rolled back with a target end year of 2028.”
He cites the $16 billion in federal funding that cardiovascular disease training programs receive every year to support graduate medical education in support of this contention.
#Medtwitter explodes
“My entire lived experience contradicts everything in that racist @JAHA_AHA article, as does the experience of so many others. So, I know it’s just a bad opinion piece passed off as ‘research’ that shouldn’t have been published. Still the damage has been done. We MUST do better,” tweeted Bryan A. Smith, MD, University of Chicago Medicine.
According to its Altmetric score, the article received very little attention back in March and April. There were three tweets referencing it, including one from JAHA announcing its publication. Since Aug. 2, an additional 390-odd Tweets from 347 Twitter users have been registered. None appear to be complimentary. Several days into the Twitter storm, the article was officially retracted.
“This article is shocking and makes me sad,” Martha Gulati, MD, University of Arizona, Phoenix, said in an interview. “We are all working so hard to make cardiology more inclusive and diverse, and this takes us like 1,000 steps backwards.”
For her part, Dr. Gulati would have liked a retraction earlier in the week. “The analysis was selective and incorrect, and the statements made intimate that minority trainees were selected based on affirmative action rather than their merits,” she said. It also suggested that their presence was representative of a decline in standards in cardiology programs that take underrepresented minorities (URMs).
Standard arguments against affirmative action
According to Dr. Wang, who did not respond to a request to comment for this article, allowing minority students into medical school with academic records that are weaker than their classmates sets them up for failure.
“Many do not complete their intended programs or do not attain academic success to be attractive candidates for subsequent educational programs or employment,” he wrote.
This is a standard argument of opponents to affirmative action, said Quinn Capers IV, MD. Dr. Capers, a longtime advocate for diversity in medicine, acknowledges that, “on average,” test scores for Blacks, Hispanics, and Native Americans tend to be lower than for White applicants for a wide range of reasons, many of which are related to systemic racism.
“This is the strongest weapon opponents to affirmative action have, and they keep coming back to it, but it’s out of step with how many in academic medicine feel,” said Dr. Capers, who is an interventional cardiologist and the vice dean for faculty affairs at Ohio State University, Columbus.
This is why, he added, most medical schools have embraced the Association of American Medical Colleges’ concept of “holistic review,” which judges potential physicians on their academic records, their personal experiences, and their individual attributes.
“Standardized tests and academic records are important, but so are the experiences one has gone through and the individual attributes they may have. How resilient are you? How compassionate? Our embrace of this more holistic approach, I believe, is helping many medical schools move toward having a more diverse class that is closer to reflecting the needs of our multicultural and multiracial society,” Dr. Capers said.
To be clear, Dr. Capers is not afraid of having a discussion on this topic and denies that the uproar against this article represents “cancel culture.”
“Hey, I love to debate and I’m not against hearing divisive voices, but then let’s have a debate and hear both sides. But there are several problems with the way they did this. No. 1, they called it a ‘white paper,’ which to most people means it reflects the views of the organization, not a specific individual, and, secondly, it’s more than an opinion piece in that he manipulates facts to make his points, with no chance for rebuttal.”
Several have also questioned how this paper, which is written by a nonexpert in the field, passed peer review.
The article contains some accurate historical references, said Dr. Capers, but intertwined with this history the author editorializes in a fashion that is “charged with racism.” In other places, Dr. Wang is just outright wrong, he added.
“I can also tell you that, in one place where he quotes me specifically, what he says is quite damaging and completely wrong. He quotes something we wrote but cuts off the final sentence, making it seem as though we acknowledged that we had to artificially rank minority applicants high, just so we could say we have a diverse fellowship program.
“It’s frankly very hard to believe that was an accident,” Dr. Capers added.
AHA backs away, promises investigation
The article has been disowned by all levels of the AHA leadership – past, present, and future.
In an Editor’s Note, Barry London, MD, PhD, the Editor in chief of the Journal of the American Heart Association, apologized for his role and the role of his staff in publishing the article.
“JAHA will support all efforts to correct this error, including but not limited to the publication of alternate viewpoints, which we solicited at the time of publication but have not yet been submitted to the journal. In addition, we will work to improve our peer review system to prevent future missteps of this type,” Dr. London wrote. “I can only hope that igniting a discussion around diversity in cardiology will ultimately fuel new ideas and lead to real advances.”
“I want to emphasize in the strongest possible terms that this paper does not represent the views of the AHA as an organization or its leadership. This paper should never have been published. A thorough investigation is rightly being conducted,” tweeted Mitchell S.V. Elkind, MD, MPhil, who took over the AHA presidency last month.
“Author’s views are racist and not consistent with my values nor AHA,” tweeted Robert Harrington, MD, immediate past president of the AHA. ‘Investigation is underway into how it made it through the editorial process. Like you, I want to know what happened. I am angry, frustrated and disappointed that this piece was published; expect review soon.’
“Agree with @HeartBobH. It is impossible not to hear and feel the hurt and pain out there on a very personal level, especially among our young colleagues. You are valued, and worthy. Please stay tuned and then help all of us work to be better,” tweeted Donald Lloyd-Jones, MD, president-elect of AHA.
A version of this article originally appeared on Medscape.com.
COVID-19–related skin changes: The hidden racism in documentation
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Marked improvements seen for women in dermatology since the 1970s
Wilma F. Bergfeld, MD, one of only five women in her medical school class of 1964 and the third female in her dermatology residency program, had recently been appointed as a junior clinical dermatologist and head of dermatopathology at the Cleveland Clinic when she was told by a superior that she would not be promoted or invited to serve on any committee or decision-making group.
“I was told I should go home at night and take care of my husband and two children,” she recalled of that moment in the 1970s. The comment made her feel “outraged,” and it drove her, calmly and steadily, to work harder and to “challenge the system.”
Dr. Bergfeld not only was elected to the Cleveland Clinic’s board of governors and board of trustees and served as president of the Clinic’s staff in 1990, she also became the first woman president of the American Academy of Dermatology (1992) and led numerous other dermatologic organizations. Much earlier on, in 1973, to help fulfill her vision of “women helping women,” she had also founded the Women’s Dermatologic Society (WDS). Three years earlier, in 1970, 6.9% of the approximately 4,000 dermatologists in the United States were women, according to the American Medical Association.
Today, when she goes to work as the long-time director of the Clinic’s dermatopathology fellowship and professor of dermatology and pathology at the Cleveland Clinic Educational Foundation, she sees a transformed staff and, more broadly, a national physician workforce in which women made up almost 50% of active dermatologists in 2017 and almost 60% of dermatology residents in 2018, according to data from the American Association of Medical Colleges.
It’s a different and better world, she and other women dermatologists said, but one in which women must continue to mentor other women and continue to challenge the system. Achieving work-life balance, fairer compensation, and a greater proportion of women in the higher ranks of academia are all on their work list.
Women’s impact on the specialty
Dr. Bergfeld and Molly Hinshaw, MD, the current president of the WDS, said they believe women are drawn to dermatology for its visual nature, the growth in diagnostic tests and therapies, and the opportunity to diagnose early and prevent progression of disease in patients of all ages. “It’s a small but mighty specialty,” said Dr. Hinshaw, associate professor of dermatology and section chief of dermatopathology at the University of Wisconsin–Madison.
It’s also a versatile specialty with a variety of subspecialties and niches to pursue – and women have been stepping in to fill unmet needs, Dr. Hinshaw said. “Women dermatologists are directing vulvar specialty clinics across the country, for example. There aren’t that many, but they’re filling an important niche. We have one at [our university] and it is packed.”
Women have also been drawn to the in-demand subspecialty of pediatric dermatology, she noted. They now make up more than two-thirds of all pediatric dermatologists, and many in practice have trained the old-fashioned way, completing two residencies. “That’s [involved] self-selection into an additional year of years training and a commitment to caring for special populations that, quite honestly, takes more time,” said Dr. Hinshaw, who, as part of her dermatology practice, runs a nail clinic at UW Health in Madison.
Amy S. Paller, MD, who chairs the department of dermatology at Northwestern University, Chicago, where she is professor of dermatology and pediatrics and directs the Skin Biology & Diseases Resource-Based Center, is one of these women. She took a long and determined journey into the subspecialty, encountering bias and discouragement while actively seeking out mentors who helped her advance.
While in medical school at Stanford (Calif.) University in the late 1970s in a class “very progressively” made up of about one-third women, Dr. Paller met Alvin Jacobs, MD, who, in 1975, had founded the Society for Pediatric Dermatology. “There wasn’t much pediatric dermatology in the world at the time, and it was Al who helped [me realize] that it combined my love of genetic research with my [desire] to work with children,” she recalled.
Per Dr. Jacob’s advice, she went to Northwestern to train in both pediatrics and dermatology under Nancy Esterly, MD, who “is considered by many to be the mother of pediatric dermatology.” And knowing that she wanted to do research, Dr. Paller also worked with Ruth Freinkel, MD, who “was the strongest bench researcher” at Northwestern. (Dr. Freinkel had been one of the first female dermatology residents at Harvard and was the first full-time faculty member in dermatology at Northwestern).
After completing postdoctoral research at the University of North Carolina at Chapel Hill, Dr. Paller returned to Chicago and assumed Dr. Esterly’s position as chief of dermatology at the Children’s National Hospital of Chicago. It was there that “someone in a leadership position questioned me about how I could possibly be a scientist, a strong clinician, and a good mother to my three children – and suggested that I drop research,” Dr. Paller recalled.
“I think this person was trying to be helpful to me, but I was shocked,” she said. Just as Dr. Bergfeld had done, Dr. Paller channeled her frustration into new pursuits.
“It made me go home and think, how could I strengthen myself? What else could I do?” she said. “Soon after, with a highly supportive husband, I did a ‘pseudosabbatical,’ basically spending every ounce of spare time I had working with one of the premier female scientists in the country, Elaine Fuchs, and learning molecular biology” in her lab at the University of Chicago.
“I think we’ve all had discrimination along the way. Sometimes there’s implicit bias and sometimes there’s overt bias,” said Dr. Paller, who in 2004 led the society which her mentor Dr. Jacobs had founded several decades earlier. “I just jumped right in, and that’s enabled me to find good role models.”
Across dermatology broadly, the often holistic nature of the specialty – of the ability to peer into the body and its internal health – is another quality that women have been drawn to and advanced, Dr. Hinshaw said. “One of the reasons why I chose dermatology is because it’s a window to total patient health. Patients often see their dermatologists as physicians who help them identify next steps in their health care, who can help them address issues related to their overall health and well-being, including their mental health.”
In a WDS membership survey conducted in 2018, most respondents reported that they frequently or occasionally detect and diagnose systemic/internal diseases and conditions in their female patients, and that they consult and collaborate with different kinds of physicians (Int J Womens Dermatol. 2018 Nov 15;4[4]:189-92).
And in a March 2019 “Dialogues in Dermatology” podcast episode on the history and advancement of women in dermatology produced by the American Academy of Dermatology, Pearl Grimes, MD, a clinical professor of dermatology of the University of California, Los Angeles, and then-president of the WDS, described why “total women’s health” had become an additional focus for the society.
“We’re already gatekeepers” in many respects, Dr. Grimes said. “In addition to my addressing specific skin issues, my patients query me on hormone issues, on nutrition, on stress-related issues….and on [what other physicians they should see].”
Phoebe Rich, MD, who owns a small all-woman practice and a research center in Portland, Oregon, said that, in general, many women also communicate and practice in a way that facilitates holistic care. “These qualities aren’t exclusive to women, but women are very caring. We take time and are interested in [patients’] lives in general, not just their disease.”
Disparities in academia
Dermatology departments in academic medicine have burgeoned in size in the past 50 years, and women are well represented overall. In 2018, women comprised 51.2% of dermatology department faculty – up from 10.8% in 1970 – a current proportion that ranks fifth among specialties for the proportion of female faculty, according to a cross-sectional study of faculty diversity trends using data from the AAMC faculty roster (JAMA Dermatol. 2020 Jan 8;156[3]:280-7).
The AAMC data show the share of women dermatology faculty declining at each subsequent rank, however – a finding that suggests that women are not promoted as quickly or to the same levels of leadership as men, the report’s authors noted. (Dermatology isn’t alone: The AAMC issued a call to action on gender equity in medicine this year, citing this inverse association.)
Another recently published study of gender trends in academic dermatology – this one looking at a smaller sample of data from 15 institutions – similarly found that women dermatologists made up a majority of faculty (53.6%) and were well represented as assistant professors (60.7%) but underrepresented as full professors (17%).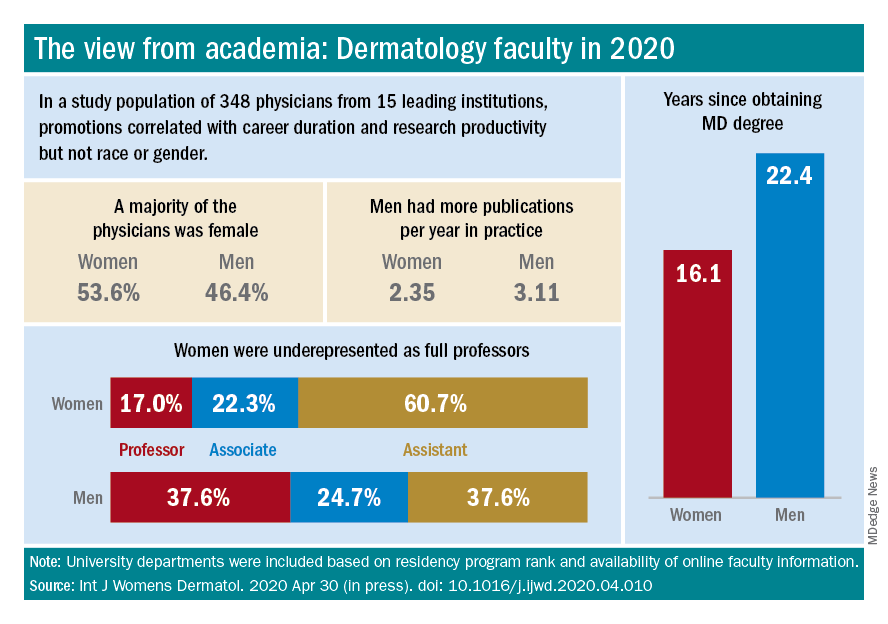
This study differed from the larger AAMC study, however, in that it controlled for “achievement indicators” – career duration, publications per year, and National Institutes of Health research funding – and found that gender alone was not associated with higher rank. Instead, promotions were correlated most significantly with NIH research funding and also with career duration and publications per year.
“If research achievement is to be used as a benchmark for academic promotion, increased efforts are needed to support the research activities of women,” the authors wrote, adding that recognition should be given to other factors as well.
Dr. Paller and Dr. Hinshaw both described the situation as complex and multifaceted. Some research on promotion in academia in general – but not all – has suggested that women do need to publish more than men in order to be promoted. But “the promotion process also has within it the ability to use judgment [about] the impact and merits of work,” said Dr. Hinshaw. “Not all publications [and levels of authorship] may be considered equal, for instance.”
Dr. Hinshaw said she is also concerned by data showing that women still perform the majority of household duties, “even in households in which both partners work outside the home equivalently.” As long as this is the case, women may be “inherently disadvantaged” in their ability to have adequate research time and to advance.
From where she sits, Dr. Paller sees several factors at play: “The pipeline, achievement during the pipeline, and decision-making about advancement” on the part of women themselves. Having served on search committees for top leadership in specialties in which women are well represented, she said, “I’ve seen fewer women who’ve come forward and been interested in rising into a chair or a dean position.”
And “having talked to so many women,” Dr. Paller added, “I think there’s a phenomenon where it’s harder for women to accept positions [that require] a significant change.”
Women “are nurturers, which makes them extremely good [leaders] and chairs, but it also makes it harder to make life changes that affect the people they love,” she said, noting that becoming a department chair or a dean often involves moving. “I also think that women in general are happier and committed to what they’re [currently] doing.”
Dr. Paller is optimistic that, with the support of department chairs and continued attention to role modeling and mentoring, the portrait of women in academic dermatology will continue to improve. Currently, 34 chairs of dermatology departments are female, she noted. “That number was 11 less 15 years ago.”
In the meantime, researchers are increasingly documenting trends in women’s editorships of journals as well as leadership and speaking opportunities at professional conferences.
The authors of one study published this year, for instance, reviewed the editorial boards of dermatology journals and found that women occupied 18% of editor in chief roles, 36% of deputy editor positions, and 22% of overall editorial board roles (Int J Womens Dermatol. 2019 Sep 12;6[1]:20-4). Other research shows women comprising 43% of all authorships across 23 dermatologic journals from 2008 to May 2017, 50.2% of first authorships, and 33.1% of last authorships (BMJ Open. 2018 Apr 13;8[4]:e020089).
Both in academic medicine and in practice, a gender pay gap still affects women physicians across the board. Medscape’s 2020 dermatologist compensation report shows male dermatologists earning about 12% more than their female peers (average, $435,000 vs. $387,000, respectively), while the average number of hours per week spent seeing patients is similar (36.2 vs. 35.6 hours, respectively).
And in its 2020 statement on gender equity, the AAMC said that women in academic medicine are offered less in starting salary, negotiated pay, and other forms of compensation than men “despite equal effort, rank, training, and experience.”
It’s complicated to tease apart all the factors that may be involved – but important to keep challenging the system, said Dr. Bergfeld, who was a long-time board adviser for Dermatology News. “I was underpaid,” she noted, and “this was only rectified in the last 10 years.”
Work-life balance
In the AAD podcast on women in dermatology, Dr. Grimes said that achieving a healthy and balanced work life remains one of the greatest challenges for women dermatologists – and it may be even greater than in the past given the growing numbers of group practices. “When women enter the realm of group practice, they have less flexibility in controlling their time and their own schedules.”
If Anna Hare, MD, is any indication, younger dermatologists may buck this trend. The daughter of Dr. Rich in Portland, Dr. Hare joined her mother’s dermatology practice and research center knowing that she’d have “the respect and flexibility for deciding how I want to practice.”
Younger dermatologists, she said, place “more of an emphasis on work-life balance and quality of life.”
Fortunately, said Dr. Bergfeld, women have advanced enough in the ranks of dermatology that, in networking, in mentorship, and in workplace settings, attention can be paid more fully to discussions about work-life management – “how to manage your life when you’re working with family and kids and parents.”
In the 1970s, at the Cleveland Clinic, “there were only five women on staff and we were fighting for [basic] rights,” she said. “We wanted equality – we were [perceived as] little worker bees….We needed to climb as the men did to positions of leadership and address the problems of women.”
In pursuing their goals and making further progress, women dermatologists today should be “steady and calm,” she advised. Formally acquiring leadership skills and communication skills is a timeless need. And when there are biases or conflicts, “you cannot have righteous indignation, you cannot have revenge. You have to calm yourself and move forward.”
Wilma F. Bergfeld, MD, one of only five women in her medical school class of 1964 and the third female in her dermatology residency program, had recently been appointed as a junior clinical dermatologist and head of dermatopathology at the Cleveland Clinic when she was told by a superior that she would not be promoted or invited to serve on any committee or decision-making group.
“I was told I should go home at night and take care of my husband and two children,” she recalled of that moment in the 1970s. The comment made her feel “outraged,” and it drove her, calmly and steadily, to work harder and to “challenge the system.”
Dr. Bergfeld not only was elected to the Cleveland Clinic’s board of governors and board of trustees and served as president of the Clinic’s staff in 1990, she also became the first woman president of the American Academy of Dermatology (1992) and led numerous other dermatologic organizations. Much earlier on, in 1973, to help fulfill her vision of “women helping women,” she had also founded the Women’s Dermatologic Society (WDS). Three years earlier, in 1970, 6.9% of the approximately 4,000 dermatologists in the United States were women, according to the American Medical Association.
Today, when she goes to work as the long-time director of the Clinic’s dermatopathology fellowship and professor of dermatology and pathology at the Cleveland Clinic Educational Foundation, she sees a transformed staff and, more broadly, a national physician workforce in which women made up almost 50% of active dermatologists in 2017 and almost 60% of dermatology residents in 2018, according to data from the American Association of Medical Colleges.
It’s a different and better world, she and other women dermatologists said, but one in which women must continue to mentor other women and continue to challenge the system. Achieving work-life balance, fairer compensation, and a greater proportion of women in the higher ranks of academia are all on their work list.
Women’s impact on the specialty
Dr. Bergfeld and Molly Hinshaw, MD, the current president of the WDS, said they believe women are drawn to dermatology for its visual nature, the growth in diagnostic tests and therapies, and the opportunity to diagnose early and prevent progression of disease in patients of all ages. “It’s a small but mighty specialty,” said Dr. Hinshaw, associate professor of dermatology and section chief of dermatopathology at the University of Wisconsin–Madison.
It’s also a versatile specialty with a variety of subspecialties and niches to pursue – and women have been stepping in to fill unmet needs, Dr. Hinshaw said. “Women dermatologists are directing vulvar specialty clinics across the country, for example. There aren’t that many, but they’re filling an important niche. We have one at [our university] and it is packed.”
Women have also been drawn to the in-demand subspecialty of pediatric dermatology, she noted. They now make up more than two-thirds of all pediatric dermatologists, and many in practice have trained the old-fashioned way, completing two residencies. “That’s [involved] self-selection into an additional year of years training and a commitment to caring for special populations that, quite honestly, takes more time,” said Dr. Hinshaw, who, as part of her dermatology practice, runs a nail clinic at UW Health in Madison.
Amy S. Paller, MD, who chairs the department of dermatology at Northwestern University, Chicago, where she is professor of dermatology and pediatrics and directs the Skin Biology & Diseases Resource-Based Center, is one of these women. She took a long and determined journey into the subspecialty, encountering bias and discouragement while actively seeking out mentors who helped her advance.
While in medical school at Stanford (Calif.) University in the late 1970s in a class “very progressively” made up of about one-third women, Dr. Paller met Alvin Jacobs, MD, who, in 1975, had founded the Society for Pediatric Dermatology. “There wasn’t much pediatric dermatology in the world at the time, and it was Al who helped [me realize] that it combined my love of genetic research with my [desire] to work with children,” she recalled.
Per Dr. Jacob’s advice, she went to Northwestern to train in both pediatrics and dermatology under Nancy Esterly, MD, who “is considered by many to be the mother of pediatric dermatology.” And knowing that she wanted to do research, Dr. Paller also worked with Ruth Freinkel, MD, who “was the strongest bench researcher” at Northwestern. (Dr. Freinkel had been one of the first female dermatology residents at Harvard and was the first full-time faculty member in dermatology at Northwestern).
After completing postdoctoral research at the University of North Carolina at Chapel Hill, Dr. Paller returned to Chicago and assumed Dr. Esterly’s position as chief of dermatology at the Children’s National Hospital of Chicago. It was there that “someone in a leadership position questioned me about how I could possibly be a scientist, a strong clinician, and a good mother to my three children – and suggested that I drop research,” Dr. Paller recalled.
“I think this person was trying to be helpful to me, but I was shocked,” she said. Just as Dr. Bergfeld had done, Dr. Paller channeled her frustration into new pursuits.
“It made me go home and think, how could I strengthen myself? What else could I do?” she said. “Soon after, with a highly supportive husband, I did a ‘pseudosabbatical,’ basically spending every ounce of spare time I had working with one of the premier female scientists in the country, Elaine Fuchs, and learning molecular biology” in her lab at the University of Chicago.
“I think we’ve all had discrimination along the way. Sometimes there’s implicit bias and sometimes there’s overt bias,” said Dr. Paller, who in 2004 led the society which her mentor Dr. Jacobs had founded several decades earlier. “I just jumped right in, and that’s enabled me to find good role models.”
Across dermatology broadly, the often holistic nature of the specialty – of the ability to peer into the body and its internal health – is another quality that women have been drawn to and advanced, Dr. Hinshaw said. “One of the reasons why I chose dermatology is because it’s a window to total patient health. Patients often see their dermatologists as physicians who help them identify next steps in their health care, who can help them address issues related to their overall health and well-being, including their mental health.”
In a WDS membership survey conducted in 2018, most respondents reported that they frequently or occasionally detect and diagnose systemic/internal diseases and conditions in their female patients, and that they consult and collaborate with different kinds of physicians (Int J Womens Dermatol. 2018 Nov 15;4[4]:189-92).
And in a March 2019 “Dialogues in Dermatology” podcast episode on the history and advancement of women in dermatology produced by the American Academy of Dermatology, Pearl Grimes, MD, a clinical professor of dermatology of the University of California, Los Angeles, and then-president of the WDS, described why “total women’s health” had become an additional focus for the society.
“We’re already gatekeepers” in many respects, Dr. Grimes said. “In addition to my addressing specific skin issues, my patients query me on hormone issues, on nutrition, on stress-related issues….and on [what other physicians they should see].”
Phoebe Rich, MD, who owns a small all-woman practice and a research center in Portland, Oregon, said that, in general, many women also communicate and practice in a way that facilitates holistic care. “These qualities aren’t exclusive to women, but women are very caring. We take time and are interested in [patients’] lives in general, not just their disease.”
Disparities in academia
Dermatology departments in academic medicine have burgeoned in size in the past 50 years, and women are well represented overall. In 2018, women comprised 51.2% of dermatology department faculty – up from 10.8% in 1970 – a current proportion that ranks fifth among specialties for the proportion of female faculty, according to a cross-sectional study of faculty diversity trends using data from the AAMC faculty roster (JAMA Dermatol. 2020 Jan 8;156[3]:280-7).
The AAMC data show the share of women dermatology faculty declining at each subsequent rank, however – a finding that suggests that women are not promoted as quickly or to the same levels of leadership as men, the report’s authors noted. (Dermatology isn’t alone: The AAMC issued a call to action on gender equity in medicine this year, citing this inverse association.)
Another recently published study of gender trends in academic dermatology – this one looking at a smaller sample of data from 15 institutions – similarly found that women dermatologists made up a majority of faculty (53.6%) and were well represented as assistant professors (60.7%) but underrepresented as full professors (17%).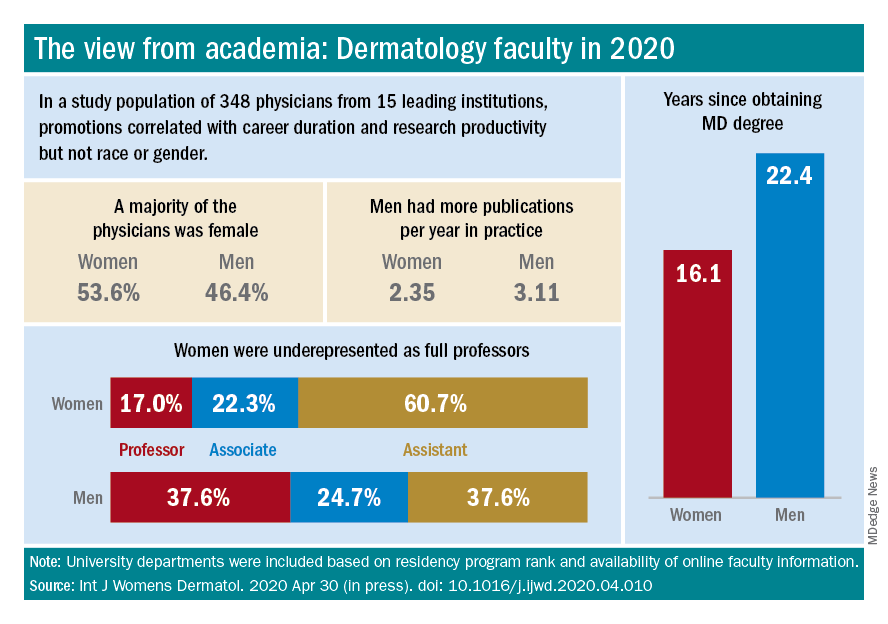
This study differed from the larger AAMC study, however, in that it controlled for “achievement indicators” – career duration, publications per year, and National Institutes of Health research funding – and found that gender alone was not associated with higher rank. Instead, promotions were correlated most significantly with NIH research funding and also with career duration and publications per year.
“If research achievement is to be used as a benchmark for academic promotion, increased efforts are needed to support the research activities of women,” the authors wrote, adding that recognition should be given to other factors as well.
Dr. Paller and Dr. Hinshaw both described the situation as complex and multifaceted. Some research on promotion in academia in general – but not all – has suggested that women do need to publish more than men in order to be promoted. But “the promotion process also has within it the ability to use judgment [about] the impact and merits of work,” said Dr. Hinshaw. “Not all publications [and levels of authorship] may be considered equal, for instance.”
Dr. Hinshaw said she is also concerned by data showing that women still perform the majority of household duties, “even in households in which both partners work outside the home equivalently.” As long as this is the case, women may be “inherently disadvantaged” in their ability to have adequate research time and to advance.
From where she sits, Dr. Paller sees several factors at play: “The pipeline, achievement during the pipeline, and decision-making about advancement” on the part of women themselves. Having served on search committees for top leadership in specialties in which women are well represented, she said, “I’ve seen fewer women who’ve come forward and been interested in rising into a chair or a dean position.”
And “having talked to so many women,” Dr. Paller added, “I think there’s a phenomenon where it’s harder for women to accept positions [that require] a significant change.”
Women “are nurturers, which makes them extremely good [leaders] and chairs, but it also makes it harder to make life changes that affect the people they love,” she said, noting that becoming a department chair or a dean often involves moving. “I also think that women in general are happier and committed to what they’re [currently] doing.”
Dr. Paller is optimistic that, with the support of department chairs and continued attention to role modeling and mentoring, the portrait of women in academic dermatology will continue to improve. Currently, 34 chairs of dermatology departments are female, she noted. “That number was 11 less 15 years ago.”
In the meantime, researchers are increasingly documenting trends in women’s editorships of journals as well as leadership and speaking opportunities at professional conferences.
The authors of one study published this year, for instance, reviewed the editorial boards of dermatology journals and found that women occupied 18% of editor in chief roles, 36% of deputy editor positions, and 22% of overall editorial board roles (Int J Womens Dermatol. 2019 Sep 12;6[1]:20-4). Other research shows women comprising 43% of all authorships across 23 dermatologic journals from 2008 to May 2017, 50.2% of first authorships, and 33.1% of last authorships (BMJ Open. 2018 Apr 13;8[4]:e020089).
Both in academic medicine and in practice, a gender pay gap still affects women physicians across the board. Medscape’s 2020 dermatologist compensation report shows male dermatologists earning about 12% more than their female peers (average, $435,000 vs. $387,000, respectively), while the average number of hours per week spent seeing patients is similar (36.2 vs. 35.6 hours, respectively).
And in its 2020 statement on gender equity, the AAMC said that women in academic medicine are offered less in starting salary, negotiated pay, and other forms of compensation than men “despite equal effort, rank, training, and experience.”
It’s complicated to tease apart all the factors that may be involved – but important to keep challenging the system, said Dr. Bergfeld, who was a long-time board adviser for Dermatology News. “I was underpaid,” she noted, and “this was only rectified in the last 10 years.”
Work-life balance
In the AAD podcast on women in dermatology, Dr. Grimes said that achieving a healthy and balanced work life remains one of the greatest challenges for women dermatologists – and it may be even greater than in the past given the growing numbers of group practices. “When women enter the realm of group practice, they have less flexibility in controlling their time and their own schedules.”
If Anna Hare, MD, is any indication, younger dermatologists may buck this trend. The daughter of Dr. Rich in Portland, Dr. Hare joined her mother’s dermatology practice and research center knowing that she’d have “the respect and flexibility for deciding how I want to practice.”
Younger dermatologists, she said, place “more of an emphasis on work-life balance and quality of life.”
Fortunately, said Dr. Bergfeld, women have advanced enough in the ranks of dermatology that, in networking, in mentorship, and in workplace settings, attention can be paid more fully to discussions about work-life management – “how to manage your life when you’re working with family and kids and parents.”
In the 1970s, at the Cleveland Clinic, “there were only five women on staff and we were fighting for [basic] rights,” she said. “We wanted equality – we were [perceived as] little worker bees….We needed to climb as the men did to positions of leadership and address the problems of women.”
In pursuing their goals and making further progress, women dermatologists today should be “steady and calm,” she advised. Formally acquiring leadership skills and communication skills is a timeless need. And when there are biases or conflicts, “you cannot have righteous indignation, you cannot have revenge. You have to calm yourself and move forward.”
Wilma F. Bergfeld, MD, one of only five women in her medical school class of 1964 and the third female in her dermatology residency program, had recently been appointed as a junior clinical dermatologist and head of dermatopathology at the Cleveland Clinic when she was told by a superior that she would not be promoted or invited to serve on any committee or decision-making group.
“I was told I should go home at night and take care of my husband and two children,” she recalled of that moment in the 1970s. The comment made her feel “outraged,” and it drove her, calmly and steadily, to work harder and to “challenge the system.”
Dr. Bergfeld not only was elected to the Cleveland Clinic’s board of governors and board of trustees and served as president of the Clinic’s staff in 1990, she also became the first woman president of the American Academy of Dermatology (1992) and led numerous other dermatologic organizations. Much earlier on, in 1973, to help fulfill her vision of “women helping women,” she had also founded the Women’s Dermatologic Society (WDS). Three years earlier, in 1970, 6.9% of the approximately 4,000 dermatologists in the United States were women, according to the American Medical Association.
Today, when she goes to work as the long-time director of the Clinic’s dermatopathology fellowship and professor of dermatology and pathology at the Cleveland Clinic Educational Foundation, she sees a transformed staff and, more broadly, a national physician workforce in which women made up almost 50% of active dermatologists in 2017 and almost 60% of dermatology residents in 2018, according to data from the American Association of Medical Colleges.
It’s a different and better world, she and other women dermatologists said, but one in which women must continue to mentor other women and continue to challenge the system. Achieving work-life balance, fairer compensation, and a greater proportion of women in the higher ranks of academia are all on their work list.
Women’s impact on the specialty
Dr. Bergfeld and Molly Hinshaw, MD, the current president of the WDS, said they believe women are drawn to dermatology for its visual nature, the growth in diagnostic tests and therapies, and the opportunity to diagnose early and prevent progression of disease in patients of all ages. “It’s a small but mighty specialty,” said Dr. Hinshaw, associate professor of dermatology and section chief of dermatopathology at the University of Wisconsin–Madison.
It’s also a versatile specialty with a variety of subspecialties and niches to pursue – and women have been stepping in to fill unmet needs, Dr. Hinshaw said. “Women dermatologists are directing vulvar specialty clinics across the country, for example. There aren’t that many, but they’re filling an important niche. We have one at [our university] and it is packed.”
Women have also been drawn to the in-demand subspecialty of pediatric dermatology, she noted. They now make up more than two-thirds of all pediatric dermatologists, and many in practice have trained the old-fashioned way, completing two residencies. “That’s [involved] self-selection into an additional year of years training and a commitment to caring for special populations that, quite honestly, takes more time,” said Dr. Hinshaw, who, as part of her dermatology practice, runs a nail clinic at UW Health in Madison.
Amy S. Paller, MD, who chairs the department of dermatology at Northwestern University, Chicago, where she is professor of dermatology and pediatrics and directs the Skin Biology & Diseases Resource-Based Center, is one of these women. She took a long and determined journey into the subspecialty, encountering bias and discouragement while actively seeking out mentors who helped her advance.
While in medical school at Stanford (Calif.) University in the late 1970s in a class “very progressively” made up of about one-third women, Dr. Paller met Alvin Jacobs, MD, who, in 1975, had founded the Society for Pediatric Dermatology. “There wasn’t much pediatric dermatology in the world at the time, and it was Al who helped [me realize] that it combined my love of genetic research with my [desire] to work with children,” she recalled.
Per Dr. Jacob’s advice, she went to Northwestern to train in both pediatrics and dermatology under Nancy Esterly, MD, who “is considered by many to be the mother of pediatric dermatology.” And knowing that she wanted to do research, Dr. Paller also worked with Ruth Freinkel, MD, who “was the strongest bench researcher” at Northwestern. (Dr. Freinkel had been one of the first female dermatology residents at Harvard and was the first full-time faculty member in dermatology at Northwestern).
After completing postdoctoral research at the University of North Carolina at Chapel Hill, Dr. Paller returned to Chicago and assumed Dr. Esterly’s position as chief of dermatology at the Children’s National Hospital of Chicago. It was there that “someone in a leadership position questioned me about how I could possibly be a scientist, a strong clinician, and a good mother to my three children – and suggested that I drop research,” Dr. Paller recalled.
“I think this person was trying to be helpful to me, but I was shocked,” she said. Just as Dr. Bergfeld had done, Dr. Paller channeled her frustration into new pursuits.
“It made me go home and think, how could I strengthen myself? What else could I do?” she said. “Soon after, with a highly supportive husband, I did a ‘pseudosabbatical,’ basically spending every ounce of spare time I had working with one of the premier female scientists in the country, Elaine Fuchs, and learning molecular biology” in her lab at the University of Chicago.
“I think we’ve all had discrimination along the way. Sometimes there’s implicit bias and sometimes there’s overt bias,” said Dr. Paller, who in 2004 led the society which her mentor Dr. Jacobs had founded several decades earlier. “I just jumped right in, and that’s enabled me to find good role models.”
Across dermatology broadly, the often holistic nature of the specialty – of the ability to peer into the body and its internal health – is another quality that women have been drawn to and advanced, Dr. Hinshaw said. “One of the reasons why I chose dermatology is because it’s a window to total patient health. Patients often see their dermatologists as physicians who help them identify next steps in their health care, who can help them address issues related to their overall health and well-being, including their mental health.”
In a WDS membership survey conducted in 2018, most respondents reported that they frequently or occasionally detect and diagnose systemic/internal diseases and conditions in their female patients, and that they consult and collaborate with different kinds of physicians (Int J Womens Dermatol. 2018 Nov 15;4[4]:189-92).
And in a March 2019 “Dialogues in Dermatology” podcast episode on the history and advancement of women in dermatology produced by the American Academy of Dermatology, Pearl Grimes, MD, a clinical professor of dermatology of the University of California, Los Angeles, and then-president of the WDS, described why “total women’s health” had become an additional focus for the society.
“We’re already gatekeepers” in many respects, Dr. Grimes said. “In addition to my addressing specific skin issues, my patients query me on hormone issues, on nutrition, on stress-related issues….and on [what other physicians they should see].”
Phoebe Rich, MD, who owns a small all-woman practice and a research center in Portland, Oregon, said that, in general, many women also communicate and practice in a way that facilitates holistic care. “These qualities aren’t exclusive to women, but women are very caring. We take time and are interested in [patients’] lives in general, not just their disease.”
Disparities in academia
Dermatology departments in academic medicine have burgeoned in size in the past 50 years, and women are well represented overall. In 2018, women comprised 51.2% of dermatology department faculty – up from 10.8% in 1970 – a current proportion that ranks fifth among specialties for the proportion of female faculty, according to a cross-sectional study of faculty diversity trends using data from the AAMC faculty roster (JAMA Dermatol. 2020 Jan 8;156[3]:280-7).
The AAMC data show the share of women dermatology faculty declining at each subsequent rank, however – a finding that suggests that women are not promoted as quickly or to the same levels of leadership as men, the report’s authors noted. (Dermatology isn’t alone: The AAMC issued a call to action on gender equity in medicine this year, citing this inverse association.)
Another recently published study of gender trends in academic dermatology – this one looking at a smaller sample of data from 15 institutions – similarly found that women dermatologists made up a majority of faculty (53.6%) and were well represented as assistant professors (60.7%) but underrepresented as full professors (17%).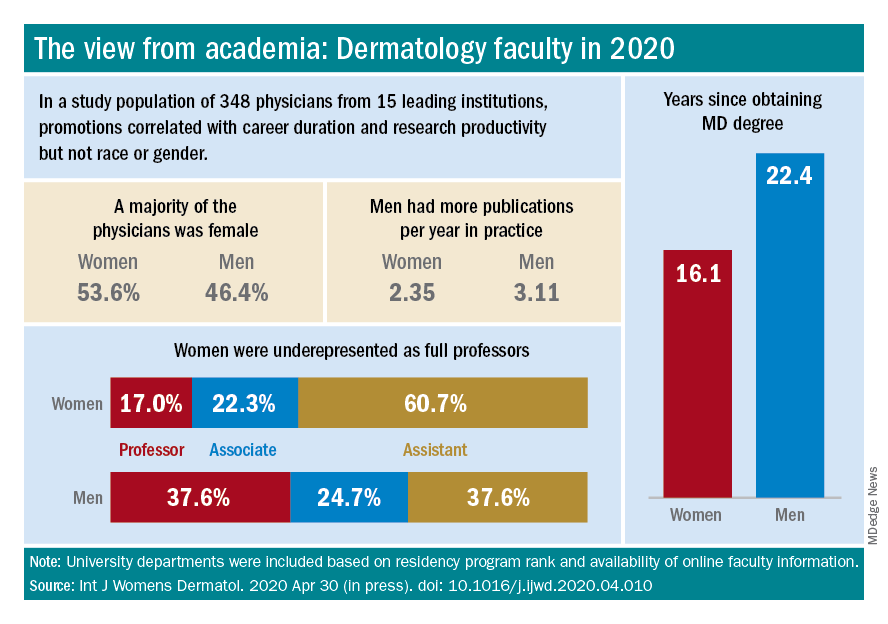
This study differed from the larger AAMC study, however, in that it controlled for “achievement indicators” – career duration, publications per year, and National Institutes of Health research funding – and found that gender alone was not associated with higher rank. Instead, promotions were correlated most significantly with NIH research funding and also with career duration and publications per year.
“If research achievement is to be used as a benchmark for academic promotion, increased efforts are needed to support the research activities of women,” the authors wrote, adding that recognition should be given to other factors as well.
Dr. Paller and Dr. Hinshaw both described the situation as complex and multifaceted. Some research on promotion in academia in general – but not all – has suggested that women do need to publish more than men in order to be promoted. But “the promotion process also has within it the ability to use judgment [about] the impact and merits of work,” said Dr. Hinshaw. “Not all publications [and levels of authorship] may be considered equal, for instance.”
Dr. Hinshaw said she is also concerned by data showing that women still perform the majority of household duties, “even in households in which both partners work outside the home equivalently.” As long as this is the case, women may be “inherently disadvantaged” in their ability to have adequate research time and to advance.
From where she sits, Dr. Paller sees several factors at play: “The pipeline, achievement during the pipeline, and decision-making about advancement” on the part of women themselves. Having served on search committees for top leadership in specialties in which women are well represented, she said, “I’ve seen fewer women who’ve come forward and been interested in rising into a chair or a dean position.”
And “having talked to so many women,” Dr. Paller added, “I think there’s a phenomenon where it’s harder for women to accept positions [that require] a significant change.”
Women “are nurturers, which makes them extremely good [leaders] and chairs, but it also makes it harder to make life changes that affect the people they love,” she said, noting that becoming a department chair or a dean often involves moving. “I also think that women in general are happier and committed to what they’re [currently] doing.”
Dr. Paller is optimistic that, with the support of department chairs and continued attention to role modeling and mentoring, the portrait of women in academic dermatology will continue to improve. Currently, 34 chairs of dermatology departments are female, she noted. “That number was 11 less 15 years ago.”
In the meantime, researchers are increasingly documenting trends in women’s editorships of journals as well as leadership and speaking opportunities at professional conferences.
The authors of one study published this year, for instance, reviewed the editorial boards of dermatology journals and found that women occupied 18% of editor in chief roles, 36% of deputy editor positions, and 22% of overall editorial board roles (Int J Womens Dermatol. 2019 Sep 12;6[1]:20-4). Other research shows women comprising 43% of all authorships across 23 dermatologic journals from 2008 to May 2017, 50.2% of first authorships, and 33.1% of last authorships (BMJ Open. 2018 Apr 13;8[4]:e020089).
Both in academic medicine and in practice, a gender pay gap still affects women physicians across the board. Medscape’s 2020 dermatologist compensation report shows male dermatologists earning about 12% more than their female peers (average, $435,000 vs. $387,000, respectively), while the average number of hours per week spent seeing patients is similar (36.2 vs. 35.6 hours, respectively).
And in its 2020 statement on gender equity, the AAMC said that women in academic medicine are offered less in starting salary, negotiated pay, and other forms of compensation than men “despite equal effort, rank, training, and experience.”
It’s complicated to tease apart all the factors that may be involved – but important to keep challenging the system, said Dr. Bergfeld, who was a long-time board adviser for Dermatology News. “I was underpaid,” she noted, and “this was only rectified in the last 10 years.”
Work-life balance
In the AAD podcast on women in dermatology, Dr. Grimes said that achieving a healthy and balanced work life remains one of the greatest challenges for women dermatologists – and it may be even greater than in the past given the growing numbers of group practices. “When women enter the realm of group practice, they have less flexibility in controlling their time and their own schedules.”
If Anna Hare, MD, is any indication, younger dermatologists may buck this trend. The daughter of Dr. Rich in Portland, Dr. Hare joined her mother’s dermatology practice and research center knowing that she’d have “the respect and flexibility for deciding how I want to practice.”
Younger dermatologists, she said, place “more of an emphasis on work-life balance and quality of life.”
Fortunately, said Dr. Bergfeld, women have advanced enough in the ranks of dermatology that, in networking, in mentorship, and in workplace settings, attention can be paid more fully to discussions about work-life management – “how to manage your life when you’re working with family and kids and parents.”
In the 1970s, at the Cleveland Clinic, “there were only five women on staff and we were fighting for [basic] rights,” she said. “We wanted equality – we were [perceived as] little worker bees….We needed to climb as the men did to positions of leadership and address the problems of women.”
In pursuing their goals and making further progress, women dermatologists today should be “steady and calm,” she advised. Formally acquiring leadership skills and communication skills is a timeless need. And when there are biases or conflicts, “you cannot have righteous indignation, you cannot have revenge. You have to calm yourself and move forward.”






















