User login
High early recurrence rates with Merkel cell carcinoma
, and more than half of all patients with stage IV disease will have a recurrence within 1 year of definitive therapy, results of a new study show.
A study of 618 patients with MCC who were enrolled in a Seattle-based data repository shows that among all patients the 5-year recurrence rate was 40%. The risk of recurrence within the first year was 11% for patients with pathologic stage I disease, 33% for those with stage IIA/IIB disease, 45% for those with stage IIIB disease, and 58% for patients with pathologic stage IV MCC.
Approximately 95% of all recurrences happened within 3 years of the initial diagnosis, report Aubriana McEvoy, MD, from the University of Washington in Seattle, and colleagues.
“This cohort study indicates that the highest yield (and likely most cost-effective) time period for detecting MCC recurrence is 1-3 years after diagnosis,” they write in a study published online in JAMA Dermatology.
The estimated annual incidence of MCC in the United States in 2018 was 2,000 according to the American Cancer Society. The annual incidence rate is rising rapidly, however, and is estimated to reach 3,284 by 2025, McEvoy and colleagues write.
Although MCC is known to have high recurrence rates and is associated with a higher mortality rate than malignant melanoma, recurrence rate data are not captured by either the Surveillance, Epidemiology, and End Results (SEER) database or by the National Cancer Database. As a result, estimates of recurrence rates with MCC have been all over the map, ranging from 27% to 77%, depending on the population studied.
But as senior author Paul Nghiem, MD, PhD, professor and chair of dermatology at the University of Washington, Seattle, told this news organization, recurrence rates over time in their study were remarkably consistent.
“The biggest surprise to me was that, when we broke our nearly 20-year cohort into three 5- or 6-year chunks, every one of the groups had a 40% recurrence rate, within 1%. So we feel really confident that’s the right number,” he said.
Dr. Nghiem and colleagues report that, in contrast to patients with MCC, approximately 19% of patients with melanoma will have a recurrence, as will an estimated 5%-9% of patients with squamous cell carcinoma and 1%-10% of patients with basal cell carcinoma.
The fact that recurrence rates of MCC have remained stable over time despite presumed improvements in definitive therapy is disappointing, Dr. Nghiem acknowledged. He noted that it’s still unclear whether immunotherapy will have the same dramatic effect on survival rates for patients with MCC as it has for patients with malignant melanoma.
The high recurrence rates following definitive therapy for patients with early-stage disease was a novel finding, commented Shawn Demehri, MD, PhD, director of the high-risk skin cancer clinic at Massachusetts General Hospital in Boston.
“When you’re looking at patients with stage I or stage II, and they have definitive surgery but still have recurrences at a higher rate than melanoma, it brings home the point that these are among the most aggressive tumors of the skin,” he said in an interview.
The high recurrence rates seen with MCC are attributable to a variety of factors.
“This is a rare cancer of mostly older individuals with a lot of comorbidities, and also a cancer that, even though it is a primary cancer, might be detected a little later than even a melanoma primary tumor, just because of the nature of the neuroendocrine tumor cells,” he said.
Dr. Demehri was not involved in the study.
Prospective cohort
The study cohort consisted of 618 patients with MCC. The median age of the patients was 69, and 227 (37%) were women. The patients were enrolled within 6 months of their diagnosis in the prospective data repository from 2003 through 2019. Of this group, 223 had a recurrence of MCC.
As noted, there was a high risk of recurrence within 1 year, ranging from 11% for patients with pathologic stage I tumors to 58% for those with stage IV disease, and 95% of all recurrences occurred within 3 years of definitive therapy.
To get a better picture of the natural history of MCC recurrence, the investigators studied a cohort of patients with pathologically confirmed MCC who were prospectively enrolled from January 2003 through April 2019 in a data repository maintained at the University of Washington.
In addition to disease stage, factors associated with increased recurrence risk in univariable analyses include immunosuppression (hazard ratio, 2.4; P < .001), male sex (HR, 1.9; P < .001), known primary lesion among patients with clinically detectable nodal disease (HR, 2.3; P = .001), and older age (HR, 1.1, P = .06 for each 10-year increase).
Of the 187 patients in the cohort who died during the study, 121 died from MCC. At 4 years after diagnosis, MCC-specific survival rates were 95% for patients with pathologic stage I, 84% with stage IIA/IIB, 80% with stage IIIA, 58% with stage IIIB, and 41% with stage IV.
Evidence supports close monitoring within the first 3 years for patients with stage I-II MCC. Local recurrence within or adjacent to the primary tumor scar was associated with a 5-year MCC-specific survival rate of 85%, compared with 88% of patients with stage I or II disease who did not have recurrences.
“Because more than 90% of MCC recurrences arise within 3 years, it is appropriate to adjust surveillance intensity accordingly. Stage- and time-specific recurrence data can assist in appropriately focusing surveillance resources on patients and time intervals in which recurrence risk is highest,” the authors wrote.
“If you’re a patient who has not had your cancer come back for 3, 4, or 5 years, you can really cut down on the intensity of your follow-up and scans,” Dr. Nghiem said.
“We do now have two excellent blood tests that are working very well, and we have really good ways to detect the cancer coming back early, and that’s important, because we have potentially curative therapies that tend to work better if you catch the cancer early,” he said.
The study was supported by the National Institutes of Health. Dr. Nghiem reported personal fees and institutional support outside the study from several companies and patents for Merkel cell therapies with the University of Washington and University of Denmark. Dr. Demehri has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, and more than half of all patients with stage IV disease will have a recurrence within 1 year of definitive therapy, results of a new study show.
A study of 618 patients with MCC who were enrolled in a Seattle-based data repository shows that among all patients the 5-year recurrence rate was 40%. The risk of recurrence within the first year was 11% for patients with pathologic stage I disease, 33% for those with stage IIA/IIB disease, 45% for those with stage IIIB disease, and 58% for patients with pathologic stage IV MCC.
Approximately 95% of all recurrences happened within 3 years of the initial diagnosis, report Aubriana McEvoy, MD, from the University of Washington in Seattle, and colleagues.
“This cohort study indicates that the highest yield (and likely most cost-effective) time period for detecting MCC recurrence is 1-3 years after diagnosis,” they write in a study published online in JAMA Dermatology.
The estimated annual incidence of MCC in the United States in 2018 was 2,000 according to the American Cancer Society. The annual incidence rate is rising rapidly, however, and is estimated to reach 3,284 by 2025, McEvoy and colleagues write.
Although MCC is known to have high recurrence rates and is associated with a higher mortality rate than malignant melanoma, recurrence rate data are not captured by either the Surveillance, Epidemiology, and End Results (SEER) database or by the National Cancer Database. As a result, estimates of recurrence rates with MCC have been all over the map, ranging from 27% to 77%, depending on the population studied.
But as senior author Paul Nghiem, MD, PhD, professor and chair of dermatology at the University of Washington, Seattle, told this news organization, recurrence rates over time in their study were remarkably consistent.
“The biggest surprise to me was that, when we broke our nearly 20-year cohort into three 5- or 6-year chunks, every one of the groups had a 40% recurrence rate, within 1%. So we feel really confident that’s the right number,” he said.
Dr. Nghiem and colleagues report that, in contrast to patients with MCC, approximately 19% of patients with melanoma will have a recurrence, as will an estimated 5%-9% of patients with squamous cell carcinoma and 1%-10% of patients with basal cell carcinoma.
The fact that recurrence rates of MCC have remained stable over time despite presumed improvements in definitive therapy is disappointing, Dr. Nghiem acknowledged. He noted that it’s still unclear whether immunotherapy will have the same dramatic effect on survival rates for patients with MCC as it has for patients with malignant melanoma.
The high recurrence rates following definitive therapy for patients with early-stage disease was a novel finding, commented Shawn Demehri, MD, PhD, director of the high-risk skin cancer clinic at Massachusetts General Hospital in Boston.
“When you’re looking at patients with stage I or stage II, and they have definitive surgery but still have recurrences at a higher rate than melanoma, it brings home the point that these are among the most aggressive tumors of the skin,” he said in an interview.
The high recurrence rates seen with MCC are attributable to a variety of factors.
“This is a rare cancer of mostly older individuals with a lot of comorbidities, and also a cancer that, even though it is a primary cancer, might be detected a little later than even a melanoma primary tumor, just because of the nature of the neuroendocrine tumor cells,” he said.
Dr. Demehri was not involved in the study.
Prospective cohort
The study cohort consisted of 618 patients with MCC. The median age of the patients was 69, and 227 (37%) were women. The patients were enrolled within 6 months of their diagnosis in the prospective data repository from 2003 through 2019. Of this group, 223 had a recurrence of MCC.
As noted, there was a high risk of recurrence within 1 year, ranging from 11% for patients with pathologic stage I tumors to 58% for those with stage IV disease, and 95% of all recurrences occurred within 3 years of definitive therapy.
To get a better picture of the natural history of MCC recurrence, the investigators studied a cohort of patients with pathologically confirmed MCC who were prospectively enrolled from January 2003 through April 2019 in a data repository maintained at the University of Washington.
In addition to disease stage, factors associated with increased recurrence risk in univariable analyses include immunosuppression (hazard ratio, 2.4; P < .001), male sex (HR, 1.9; P < .001), known primary lesion among patients with clinically detectable nodal disease (HR, 2.3; P = .001), and older age (HR, 1.1, P = .06 for each 10-year increase).
Of the 187 patients in the cohort who died during the study, 121 died from MCC. At 4 years after diagnosis, MCC-specific survival rates were 95% for patients with pathologic stage I, 84% with stage IIA/IIB, 80% with stage IIIA, 58% with stage IIIB, and 41% with stage IV.
Evidence supports close monitoring within the first 3 years for patients with stage I-II MCC. Local recurrence within or adjacent to the primary tumor scar was associated with a 5-year MCC-specific survival rate of 85%, compared with 88% of patients with stage I or II disease who did not have recurrences.
“Because more than 90% of MCC recurrences arise within 3 years, it is appropriate to adjust surveillance intensity accordingly. Stage- and time-specific recurrence data can assist in appropriately focusing surveillance resources on patients and time intervals in which recurrence risk is highest,” the authors wrote.
“If you’re a patient who has not had your cancer come back for 3, 4, or 5 years, you can really cut down on the intensity of your follow-up and scans,” Dr. Nghiem said.
“We do now have two excellent blood tests that are working very well, and we have really good ways to detect the cancer coming back early, and that’s important, because we have potentially curative therapies that tend to work better if you catch the cancer early,” he said.
The study was supported by the National Institutes of Health. Dr. Nghiem reported personal fees and institutional support outside the study from several companies and patents for Merkel cell therapies with the University of Washington and University of Denmark. Dr. Demehri has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, and more than half of all patients with stage IV disease will have a recurrence within 1 year of definitive therapy, results of a new study show.
A study of 618 patients with MCC who were enrolled in a Seattle-based data repository shows that among all patients the 5-year recurrence rate was 40%. The risk of recurrence within the first year was 11% for patients with pathologic stage I disease, 33% for those with stage IIA/IIB disease, 45% for those with stage IIIB disease, and 58% for patients with pathologic stage IV MCC.
Approximately 95% of all recurrences happened within 3 years of the initial diagnosis, report Aubriana McEvoy, MD, from the University of Washington in Seattle, and colleagues.
“This cohort study indicates that the highest yield (and likely most cost-effective) time period for detecting MCC recurrence is 1-3 years after diagnosis,” they write in a study published online in JAMA Dermatology.
The estimated annual incidence of MCC in the United States in 2018 was 2,000 according to the American Cancer Society. The annual incidence rate is rising rapidly, however, and is estimated to reach 3,284 by 2025, McEvoy and colleagues write.
Although MCC is known to have high recurrence rates and is associated with a higher mortality rate than malignant melanoma, recurrence rate data are not captured by either the Surveillance, Epidemiology, and End Results (SEER) database or by the National Cancer Database. As a result, estimates of recurrence rates with MCC have been all over the map, ranging from 27% to 77%, depending on the population studied.
But as senior author Paul Nghiem, MD, PhD, professor and chair of dermatology at the University of Washington, Seattle, told this news organization, recurrence rates over time in their study were remarkably consistent.
“The biggest surprise to me was that, when we broke our nearly 20-year cohort into three 5- or 6-year chunks, every one of the groups had a 40% recurrence rate, within 1%. So we feel really confident that’s the right number,” he said.
Dr. Nghiem and colleagues report that, in contrast to patients with MCC, approximately 19% of patients with melanoma will have a recurrence, as will an estimated 5%-9% of patients with squamous cell carcinoma and 1%-10% of patients with basal cell carcinoma.
The fact that recurrence rates of MCC have remained stable over time despite presumed improvements in definitive therapy is disappointing, Dr. Nghiem acknowledged. He noted that it’s still unclear whether immunotherapy will have the same dramatic effect on survival rates for patients with MCC as it has for patients with malignant melanoma.
The high recurrence rates following definitive therapy for patients with early-stage disease was a novel finding, commented Shawn Demehri, MD, PhD, director of the high-risk skin cancer clinic at Massachusetts General Hospital in Boston.
“When you’re looking at patients with stage I or stage II, and they have definitive surgery but still have recurrences at a higher rate than melanoma, it brings home the point that these are among the most aggressive tumors of the skin,” he said in an interview.
The high recurrence rates seen with MCC are attributable to a variety of factors.
“This is a rare cancer of mostly older individuals with a lot of comorbidities, and also a cancer that, even though it is a primary cancer, might be detected a little later than even a melanoma primary tumor, just because of the nature of the neuroendocrine tumor cells,” he said.
Dr. Demehri was not involved in the study.
Prospective cohort
The study cohort consisted of 618 patients with MCC. The median age of the patients was 69, and 227 (37%) were women. The patients were enrolled within 6 months of their diagnosis in the prospective data repository from 2003 through 2019. Of this group, 223 had a recurrence of MCC.
As noted, there was a high risk of recurrence within 1 year, ranging from 11% for patients with pathologic stage I tumors to 58% for those with stage IV disease, and 95% of all recurrences occurred within 3 years of definitive therapy.
To get a better picture of the natural history of MCC recurrence, the investigators studied a cohort of patients with pathologically confirmed MCC who were prospectively enrolled from January 2003 through April 2019 in a data repository maintained at the University of Washington.
In addition to disease stage, factors associated with increased recurrence risk in univariable analyses include immunosuppression (hazard ratio, 2.4; P < .001), male sex (HR, 1.9; P < .001), known primary lesion among patients with clinically detectable nodal disease (HR, 2.3; P = .001), and older age (HR, 1.1, P = .06 for each 10-year increase).
Of the 187 patients in the cohort who died during the study, 121 died from MCC. At 4 years after diagnosis, MCC-specific survival rates were 95% for patients with pathologic stage I, 84% with stage IIA/IIB, 80% with stage IIIA, 58% with stage IIIB, and 41% with stage IV.
Evidence supports close monitoring within the first 3 years for patients with stage I-II MCC. Local recurrence within or adjacent to the primary tumor scar was associated with a 5-year MCC-specific survival rate of 85%, compared with 88% of patients with stage I or II disease who did not have recurrences.
“Because more than 90% of MCC recurrences arise within 3 years, it is appropriate to adjust surveillance intensity accordingly. Stage- and time-specific recurrence data can assist in appropriately focusing surveillance resources on patients and time intervals in which recurrence risk is highest,” the authors wrote.
“If you’re a patient who has not had your cancer come back for 3, 4, or 5 years, you can really cut down on the intensity of your follow-up and scans,” Dr. Nghiem said.
“We do now have two excellent blood tests that are working very well, and we have really good ways to detect the cancer coming back early, and that’s important, because we have potentially curative therapies that tend to work better if you catch the cancer early,” he said.
The study was supported by the National Institutes of Health. Dr. Nghiem reported personal fees and institutional support outside the study from several companies and patents for Merkel cell therapies with the University of Washington and University of Denmark. Dr. Demehri has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Dermatologists driving use of vascular lasers in the Medicare population
In addition, as a proportion of Medicare charges submitted that were reimbursed, the highest reimbursements were for dermatologists and those in the Western geographic region.
Those are among the key findings from an analysis that aimed to characterize trends in use and reimbursement patterns of vascular lasers in the Medicare-insured population.
“There are several modalities for vascular laser treatment, including the pulse dye laser, the frequency doubled KTP laser, and others,” presenting author Partik Singh, MD, MBA, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “Laser treatment of vascular lesions may sometimes be covered by insurance, depending on the indication, but little is known about how and which clinicians are taking advantage of this covered treatment.”
Dr. Singh, a 2nd-year dermatology resident at the University of Rochester Medical Center, and coauthor Mara Weinstein Velez, MD, extracted data from the 2012-2018 Medicare Public Use File, which includes 100% fee-for-service, non–Medicare Advantage claims based on CPT codes, yet no information on patient data, clinical context, or indications. Outcomes of interest were total vascular laser claims per year, annual vascular laser claims per clinician, annual clinicians using vascular lasers, accepted reimbursements defined by the allowed charge or the submitted charge to Medicare, and clinical specialties and geographic location.
The researchers found that more than half of clinicians who used vascular lasers during the study period were dermatologists (55%), followed by general surgeons (6%), family practice/internal medicine physicians (5% each) and various others. Use of vascular lasers among all clinicians increased 10.5% annually during the study period, from 3,786 to 6,883, and was most pronounced among dermatologists, whose use increased 18.4% annually, from 1,878 to 5,182. “Nondermatologists did not have a big change in their overall utilization rate, but they did have a steady utilization of vascular lasers, roughly at almost 2,000 claims per year,” Dr. Singh said.
The researchers also observed that the use of vascular lasers on a per-clinician basis increased 7.4% annually among all clinicians during the study period, from 77.3 to 118.7. This was mostly driven by dermatologists, whose per-clinician use increased 10.4% annually, from 81.7 to 148.7. Use by nondermatologists remained about stable, with just a 0.1% increase annually, from 73.4 to 74. In addition, the number of clinicians who billed for vascular laser procedures increased 2.9% annually between 2012 and 2018, from 49 to 58. This growth was driven mostly by dermatologists, who increased their billing for vascular laser procedures by 7.2% annually, from 23 to 35 clinicians.
In other findings, dermatologists were reimbursed at 68.3% of submitted charges, compared with 59.3% of charges submitted by other clinicians (P = .0001), and reimbursement rates were greatest in the Western geographic region of the United States vs. the Northeast, Midwest, and Southern regions (73.1% vs. 50.2%, 65.4%, and 55.3%, respectively; P < .0001).
“Use of vascular lasers is increasing primarily among dermatologists, though there is steady use of these procedures by nondermatologists,” Dr. Singh concluded. “Medicare charges were more often fully reimbursed when billed by dermatologists and those in the Western U.S., perhaps suggesting a better familiarity with appropriate indications and better administrative resources for coverage of vascular laser procedures.”
After the meeting, Dr. Singh acknowledged certain limitations of the analysis, including the fact that it “was limited only to Medicare Part B fee-for-service claims, not including Medicare Advantage,” he told this news organization. “Our conclusions do not necessarily hold true for Medicaid or commercial insurers, for instance. Moreover, this dataset doesn’t provide patient-specific information, such as the indication for the procedure. Further studies are needed to characterize utilization of various lasers in not only Medicare beneficiaries, but also those with Medicaid, private insurance, and patients paying out-of-pocket. Additionally, study is also needed to explain why these differences in reimbursement hold true.”
The researchers reported having no relevant financial disclosures.
In addition, as a proportion of Medicare charges submitted that were reimbursed, the highest reimbursements were for dermatologists and those in the Western geographic region.
Those are among the key findings from an analysis that aimed to characterize trends in use and reimbursement patterns of vascular lasers in the Medicare-insured population.
“There are several modalities for vascular laser treatment, including the pulse dye laser, the frequency doubled KTP laser, and others,” presenting author Partik Singh, MD, MBA, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “Laser treatment of vascular lesions may sometimes be covered by insurance, depending on the indication, but little is known about how and which clinicians are taking advantage of this covered treatment.”
Dr. Singh, a 2nd-year dermatology resident at the University of Rochester Medical Center, and coauthor Mara Weinstein Velez, MD, extracted data from the 2012-2018 Medicare Public Use File, which includes 100% fee-for-service, non–Medicare Advantage claims based on CPT codes, yet no information on patient data, clinical context, or indications. Outcomes of interest were total vascular laser claims per year, annual vascular laser claims per clinician, annual clinicians using vascular lasers, accepted reimbursements defined by the allowed charge or the submitted charge to Medicare, and clinical specialties and geographic location.
The researchers found that more than half of clinicians who used vascular lasers during the study period were dermatologists (55%), followed by general surgeons (6%), family practice/internal medicine physicians (5% each) and various others. Use of vascular lasers among all clinicians increased 10.5% annually during the study period, from 3,786 to 6,883, and was most pronounced among dermatologists, whose use increased 18.4% annually, from 1,878 to 5,182. “Nondermatologists did not have a big change in their overall utilization rate, but they did have a steady utilization of vascular lasers, roughly at almost 2,000 claims per year,” Dr. Singh said.
The researchers also observed that the use of vascular lasers on a per-clinician basis increased 7.4% annually among all clinicians during the study period, from 77.3 to 118.7. This was mostly driven by dermatologists, whose per-clinician use increased 10.4% annually, from 81.7 to 148.7. Use by nondermatologists remained about stable, with just a 0.1% increase annually, from 73.4 to 74. In addition, the number of clinicians who billed for vascular laser procedures increased 2.9% annually between 2012 and 2018, from 49 to 58. This growth was driven mostly by dermatologists, who increased their billing for vascular laser procedures by 7.2% annually, from 23 to 35 clinicians.
In other findings, dermatologists were reimbursed at 68.3% of submitted charges, compared with 59.3% of charges submitted by other clinicians (P = .0001), and reimbursement rates were greatest in the Western geographic region of the United States vs. the Northeast, Midwest, and Southern regions (73.1% vs. 50.2%, 65.4%, and 55.3%, respectively; P < .0001).
“Use of vascular lasers is increasing primarily among dermatologists, though there is steady use of these procedures by nondermatologists,” Dr. Singh concluded. “Medicare charges were more often fully reimbursed when billed by dermatologists and those in the Western U.S., perhaps suggesting a better familiarity with appropriate indications and better administrative resources for coverage of vascular laser procedures.”
After the meeting, Dr. Singh acknowledged certain limitations of the analysis, including the fact that it “was limited only to Medicare Part B fee-for-service claims, not including Medicare Advantage,” he told this news organization. “Our conclusions do not necessarily hold true for Medicaid or commercial insurers, for instance. Moreover, this dataset doesn’t provide patient-specific information, such as the indication for the procedure. Further studies are needed to characterize utilization of various lasers in not only Medicare beneficiaries, but also those with Medicaid, private insurance, and patients paying out-of-pocket. Additionally, study is also needed to explain why these differences in reimbursement hold true.”
The researchers reported having no relevant financial disclosures.
In addition, as a proportion of Medicare charges submitted that were reimbursed, the highest reimbursements were for dermatologists and those in the Western geographic region.
Those are among the key findings from an analysis that aimed to characterize trends in use and reimbursement patterns of vascular lasers in the Medicare-insured population.
“There are several modalities for vascular laser treatment, including the pulse dye laser, the frequency doubled KTP laser, and others,” presenting author Partik Singh, MD, MBA, said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “Laser treatment of vascular lesions may sometimes be covered by insurance, depending on the indication, but little is known about how and which clinicians are taking advantage of this covered treatment.”
Dr. Singh, a 2nd-year dermatology resident at the University of Rochester Medical Center, and coauthor Mara Weinstein Velez, MD, extracted data from the 2012-2018 Medicare Public Use File, which includes 100% fee-for-service, non–Medicare Advantage claims based on CPT codes, yet no information on patient data, clinical context, or indications. Outcomes of interest were total vascular laser claims per year, annual vascular laser claims per clinician, annual clinicians using vascular lasers, accepted reimbursements defined by the allowed charge or the submitted charge to Medicare, and clinical specialties and geographic location.
The researchers found that more than half of clinicians who used vascular lasers during the study period were dermatologists (55%), followed by general surgeons (6%), family practice/internal medicine physicians (5% each) and various others. Use of vascular lasers among all clinicians increased 10.5% annually during the study period, from 3,786 to 6,883, and was most pronounced among dermatologists, whose use increased 18.4% annually, from 1,878 to 5,182. “Nondermatologists did not have a big change in their overall utilization rate, but they did have a steady utilization of vascular lasers, roughly at almost 2,000 claims per year,” Dr. Singh said.
The researchers also observed that the use of vascular lasers on a per-clinician basis increased 7.4% annually among all clinicians during the study period, from 77.3 to 118.7. This was mostly driven by dermatologists, whose per-clinician use increased 10.4% annually, from 81.7 to 148.7. Use by nondermatologists remained about stable, with just a 0.1% increase annually, from 73.4 to 74. In addition, the number of clinicians who billed for vascular laser procedures increased 2.9% annually between 2012 and 2018, from 49 to 58. This growth was driven mostly by dermatologists, who increased their billing for vascular laser procedures by 7.2% annually, from 23 to 35 clinicians.
In other findings, dermatologists were reimbursed at 68.3% of submitted charges, compared with 59.3% of charges submitted by other clinicians (P = .0001), and reimbursement rates were greatest in the Western geographic region of the United States vs. the Northeast, Midwest, and Southern regions (73.1% vs. 50.2%, 65.4%, and 55.3%, respectively; P < .0001).
“Use of vascular lasers is increasing primarily among dermatologists, though there is steady use of these procedures by nondermatologists,” Dr. Singh concluded. “Medicare charges were more often fully reimbursed when billed by dermatologists and those in the Western U.S., perhaps suggesting a better familiarity with appropriate indications and better administrative resources for coverage of vascular laser procedures.”
After the meeting, Dr. Singh acknowledged certain limitations of the analysis, including the fact that it “was limited only to Medicare Part B fee-for-service claims, not including Medicare Advantage,” he told this news organization. “Our conclusions do not necessarily hold true for Medicaid or commercial insurers, for instance. Moreover, this dataset doesn’t provide patient-specific information, such as the indication for the procedure. Further studies are needed to characterize utilization of various lasers in not only Medicare beneficiaries, but also those with Medicaid, private insurance, and patients paying out-of-pocket. Additionally, study is also needed to explain why these differences in reimbursement hold true.”
The researchers reported having no relevant financial disclosures.
FROM ASDS 2021
Elevated mortality seen in Merkel cell patients from rural areas
This paradox was discovered in an analysis of data from the Surveillance, Epidemiology, and End Results (SEER) Program that primary author Bryan T. Carroll, MD, PhD, and colleagues presented during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery.
“MCC is a rare and aggressive neoplasm of the skin with high mortality,” said coauthor Emma Larson, MD, a dermatology clinical research fellow at University Hospitals of Cleveland. “Previous studies have demonstrated that MCC survival is lower in low–dermatologist density areas. Associations are difficult to characterize without historical staging data aggregated from large registries. We hypothesized that decreased MCC survival is associated with rural counties.”
The researchers used 18 registries from the November 2019 SEER database to retrospectively evaluate adults who were diagnosed with MCC between 2004 and 2015 as confirmed by positive histology. Study endpoints were SEER historic stage at diagnosis and 5-year survival. MCC cases were stratified by 2013 USDA urban-rural continuum codes, which defines metropolitan counties as those with a population of 1 million or more, urban counties as those with a population of less than 1 million, and rural counties as nonmetropolitan counties not adjacent to a metropolitan area.
A total of 6,291 cases with a mean age of 75 years were included in the final analysis: 3,750 from metro areas, 2,235 from urban areas, and 306 from rural areas. A higher proportion of MCC patients from rural areas were male (69% vs. 62% from metro areas and 64% from urban areas) and white (97% vs. 95% and 96%, respectively). “This may contribute to differences in MCC care,” Dr. Larson said. “However, we also found that there is an increased incidence of locally staged disease in rural areas (51%) than in metro (44%) or urban (45%) areas (P = .02). In addition, fewer lymph node surgeries were performed in rural (50%) and urban (51%) areas than in metro areas (45%; P = .01).”
Overall survival was worse among patients in rural areas (a mean of 34 months), compared with those in urban (a mean of 41 months) and metro areas (a mean of 47 months; P = .02). “This may be due to the fact that rural counties have the higher risk factors for MCC incidence and death, but when we account for the confounders, including sex, age, race, and MCC stage, we still found a difference in overall survival in rural counties, compared to metro and urban counties,” Dr. Larson said.
Dr. Carroll, an associate professor of dermatology at University Hospitals of Cleveland, characterized the finding as “not what you’d expect with a higher incidence of local disease. Therefore, there is the potential for mis-staging in rural counties, where we did see that the interrogation of lymph nodes was done less frequently than in urban centers, which were more aligned with National Comprehensive Cancer Network guidelines during this time period. Still, after correction, rural location is still associated with a higher MCC mortality. There is a need for us to further interrogate what the causes are for this disparity in care between rural and urban centers.”
The other study authors were Dustin DeMeo and Christian Scheufele, MD. The researchers reported having no relevant financial disclosures.
This paradox was discovered in an analysis of data from the Surveillance, Epidemiology, and End Results (SEER) Program that primary author Bryan T. Carroll, MD, PhD, and colleagues presented during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery.
“MCC is a rare and aggressive neoplasm of the skin with high mortality,” said coauthor Emma Larson, MD, a dermatology clinical research fellow at University Hospitals of Cleveland. “Previous studies have demonstrated that MCC survival is lower in low–dermatologist density areas. Associations are difficult to characterize without historical staging data aggregated from large registries. We hypothesized that decreased MCC survival is associated with rural counties.”
The researchers used 18 registries from the November 2019 SEER database to retrospectively evaluate adults who were diagnosed with MCC between 2004 and 2015 as confirmed by positive histology. Study endpoints were SEER historic stage at diagnosis and 5-year survival. MCC cases were stratified by 2013 USDA urban-rural continuum codes, which defines metropolitan counties as those with a population of 1 million or more, urban counties as those with a population of less than 1 million, and rural counties as nonmetropolitan counties not adjacent to a metropolitan area.
A total of 6,291 cases with a mean age of 75 years were included in the final analysis: 3,750 from metro areas, 2,235 from urban areas, and 306 from rural areas. A higher proportion of MCC patients from rural areas were male (69% vs. 62% from metro areas and 64% from urban areas) and white (97% vs. 95% and 96%, respectively). “This may contribute to differences in MCC care,” Dr. Larson said. “However, we also found that there is an increased incidence of locally staged disease in rural areas (51%) than in metro (44%) or urban (45%) areas (P = .02). In addition, fewer lymph node surgeries were performed in rural (50%) and urban (51%) areas than in metro areas (45%; P = .01).”
Overall survival was worse among patients in rural areas (a mean of 34 months), compared with those in urban (a mean of 41 months) and metro areas (a mean of 47 months; P = .02). “This may be due to the fact that rural counties have the higher risk factors for MCC incidence and death, but when we account for the confounders, including sex, age, race, and MCC stage, we still found a difference in overall survival in rural counties, compared to metro and urban counties,” Dr. Larson said.
Dr. Carroll, an associate professor of dermatology at University Hospitals of Cleveland, characterized the finding as “not what you’d expect with a higher incidence of local disease. Therefore, there is the potential for mis-staging in rural counties, where we did see that the interrogation of lymph nodes was done less frequently than in urban centers, which were more aligned with National Comprehensive Cancer Network guidelines during this time period. Still, after correction, rural location is still associated with a higher MCC mortality. There is a need for us to further interrogate what the causes are for this disparity in care between rural and urban centers.”
The other study authors were Dustin DeMeo and Christian Scheufele, MD. The researchers reported having no relevant financial disclosures.
This paradox was discovered in an analysis of data from the Surveillance, Epidemiology, and End Results (SEER) Program that primary author Bryan T. Carroll, MD, PhD, and colleagues presented during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery.
“MCC is a rare and aggressive neoplasm of the skin with high mortality,” said coauthor Emma Larson, MD, a dermatology clinical research fellow at University Hospitals of Cleveland. “Previous studies have demonstrated that MCC survival is lower in low–dermatologist density areas. Associations are difficult to characterize without historical staging data aggregated from large registries. We hypothesized that decreased MCC survival is associated with rural counties.”
The researchers used 18 registries from the November 2019 SEER database to retrospectively evaluate adults who were diagnosed with MCC between 2004 and 2015 as confirmed by positive histology. Study endpoints were SEER historic stage at diagnosis and 5-year survival. MCC cases were stratified by 2013 USDA urban-rural continuum codes, which defines metropolitan counties as those with a population of 1 million or more, urban counties as those with a population of less than 1 million, and rural counties as nonmetropolitan counties not adjacent to a metropolitan area.
A total of 6,291 cases with a mean age of 75 years were included in the final analysis: 3,750 from metro areas, 2,235 from urban areas, and 306 from rural areas. A higher proportion of MCC patients from rural areas were male (69% vs. 62% from metro areas and 64% from urban areas) and white (97% vs. 95% and 96%, respectively). “This may contribute to differences in MCC care,” Dr. Larson said. “However, we also found that there is an increased incidence of locally staged disease in rural areas (51%) than in metro (44%) or urban (45%) areas (P = .02). In addition, fewer lymph node surgeries were performed in rural (50%) and urban (51%) areas than in metro areas (45%; P = .01).”
Overall survival was worse among patients in rural areas (a mean of 34 months), compared with those in urban (a mean of 41 months) and metro areas (a mean of 47 months; P = .02). “This may be due to the fact that rural counties have the higher risk factors for MCC incidence and death, but when we account for the confounders, including sex, age, race, and MCC stage, we still found a difference in overall survival in rural counties, compared to metro and urban counties,” Dr. Larson said.
Dr. Carroll, an associate professor of dermatology at University Hospitals of Cleveland, characterized the finding as “not what you’d expect with a higher incidence of local disease. Therefore, there is the potential for mis-staging in rural counties, where we did see that the interrogation of lymph nodes was done less frequently than in urban centers, which were more aligned with National Comprehensive Cancer Network guidelines during this time period. Still, after correction, rural location is still associated with a higher MCC mortality. There is a need for us to further interrogate what the causes are for this disparity in care between rural and urban centers.”
The other study authors were Dustin DeMeo and Christian Scheufele, MD. The researchers reported having no relevant financial disclosures.
FROM ASDS 2021
Filler complications involving vascular necrosis, vision changes on the rise
analysis showed.
“The ASDS estimates that 1.6 million soft tissue filler procedures were performed in 2019, a 78% increase from 2012,” presenting author Michelle Xiong, a 4th-year student at Brown University, Providence, R.I., said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “The popularity of dermal fillers continues to increase. With that, there is increasing concern of possible associated adverse events. Most concerning are those related to vascular occlusion.”
Under the supervision of senior author Kachiu C. Lee, MD, MPH, of Main Line Center for Laser Surgery in Ardmore, Pa., Ms. Xiong and colleagues analyzed the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database of medical device–related adverse event reports, to better understand and characterize dermal filler-related complications. They limited the analysis to adverse events involving injectable fillers from January 2014 to December 2020 and determined the number of complications by type per year and reviewed reports to identify injection site locations. Next, they used the binomial test to compare the proportion of complication categories from 2014 through 2016 and from 2017 through 2020.
In all, 5,994 reports were identified during the 7-year study period. To evaluate trends over time, the researchers estimated the rate of complications per 100 reports each year. While the absolute number of reports increased over time, the rate of adverse events per 100 reports decreased, suggesting an overall improvement in safety.
When the researchers focused on complications involving vascular occlusion, they found that vascular necrosis accounted for 3.5% of all complications, compared with vision changes (1.5% of all complications), and stroke (0.3% of all complications). When comparing the years 2014-2016 with 2017-2020, there was a significant increase in adverse events involving vascular necrosis (0.9%; P = .018) and vision changes (0.94%; P = .001), but no significant difference in the number of reports of stroke (-0.1%; P = .409). “This highlights that serious complications like necrosis and vision changes have increased over time,” Ms. Xiong said.
Overall, the three most common injection sites involving necrosis and vision changes were the cheek, the nose, and the nasolabial fold. The cheek was the most common site associated with stroke. “These findings are similar to those of previous studies, further emphasizing that the nose, nasolabial fold, and cheek are possibly challenging injection sites,” she said.
“In general, as the face is a highly vascular area with many anastomoses, it’s especially important to be aware of facial anatomy when injecting. In addition to awareness of anatomy, injection techniques can influence vascular complications. Unfortunately, the event narratives in the MAUDE database did not go into detail about the procedural technique.”
Ms. Xiong said that as the popularity of dermal fillers continues to grow, “it’s important for providers to understand the possible adverse events, both to better counsel patients and to improve safety management. The proportion of serious complications such as vascular necrosis and vision changes have increased from 2014 to 2020. This highlights an increased need for training to better understand facial anatomy and to emphasize practice techniques to minimize risk.”
Dr. Lee acknowledged certain limitations of the study, including that “submission of adverse events to the MAUDE database are not verified or standardized,” she told this news organization.
“With the ever-increasing popularity of fillers, it is not surprising that the absolute number of complications is rising, but it is also reassuring to see that the overall ratio of complications per hundred reports is down,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “I would be curious to know what proportion of filler complications are due to non–core practitioners compared to dermatologists and plastic surgeons.”
The researchers reported having no financial disclosures.
Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
analysis showed.
“The ASDS estimates that 1.6 million soft tissue filler procedures were performed in 2019, a 78% increase from 2012,” presenting author Michelle Xiong, a 4th-year student at Brown University, Providence, R.I., said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “The popularity of dermal fillers continues to increase. With that, there is increasing concern of possible associated adverse events. Most concerning are those related to vascular occlusion.”
Under the supervision of senior author Kachiu C. Lee, MD, MPH, of Main Line Center for Laser Surgery in Ardmore, Pa., Ms. Xiong and colleagues analyzed the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database of medical device–related adverse event reports, to better understand and characterize dermal filler-related complications. They limited the analysis to adverse events involving injectable fillers from January 2014 to December 2020 and determined the number of complications by type per year and reviewed reports to identify injection site locations. Next, they used the binomial test to compare the proportion of complication categories from 2014 through 2016 and from 2017 through 2020.
In all, 5,994 reports were identified during the 7-year study period. To evaluate trends over time, the researchers estimated the rate of complications per 100 reports each year. While the absolute number of reports increased over time, the rate of adverse events per 100 reports decreased, suggesting an overall improvement in safety.
When the researchers focused on complications involving vascular occlusion, they found that vascular necrosis accounted for 3.5% of all complications, compared with vision changes (1.5% of all complications), and stroke (0.3% of all complications). When comparing the years 2014-2016 with 2017-2020, there was a significant increase in adverse events involving vascular necrosis (0.9%; P = .018) and vision changes (0.94%; P = .001), but no significant difference in the number of reports of stroke (-0.1%; P = .409). “This highlights that serious complications like necrosis and vision changes have increased over time,” Ms. Xiong said.
Overall, the three most common injection sites involving necrosis and vision changes were the cheek, the nose, and the nasolabial fold. The cheek was the most common site associated with stroke. “These findings are similar to those of previous studies, further emphasizing that the nose, nasolabial fold, and cheek are possibly challenging injection sites,” she said.
“In general, as the face is a highly vascular area with many anastomoses, it’s especially important to be aware of facial anatomy when injecting. In addition to awareness of anatomy, injection techniques can influence vascular complications. Unfortunately, the event narratives in the MAUDE database did not go into detail about the procedural technique.”
Ms. Xiong said that as the popularity of dermal fillers continues to grow, “it’s important for providers to understand the possible adverse events, both to better counsel patients and to improve safety management. The proportion of serious complications such as vascular necrosis and vision changes have increased from 2014 to 2020. This highlights an increased need for training to better understand facial anatomy and to emphasize practice techniques to minimize risk.”
Dr. Lee acknowledged certain limitations of the study, including that “submission of adverse events to the MAUDE database are not verified or standardized,” she told this news organization.
“With the ever-increasing popularity of fillers, it is not surprising that the absolute number of complications is rising, but it is also reassuring to see that the overall ratio of complications per hundred reports is down,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “I would be curious to know what proportion of filler complications are due to non–core practitioners compared to dermatologists and plastic surgeons.”
The researchers reported having no financial disclosures.
Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
analysis showed.
“The ASDS estimates that 1.6 million soft tissue filler procedures were performed in 2019, a 78% increase from 2012,” presenting author Michelle Xiong, a 4th-year student at Brown University, Providence, R.I., said during a virtual abstract session at the annual meeting of the American Society for Dermatologic Surgery. “The popularity of dermal fillers continues to increase. With that, there is increasing concern of possible associated adverse events. Most concerning are those related to vascular occlusion.”
Under the supervision of senior author Kachiu C. Lee, MD, MPH, of Main Line Center for Laser Surgery in Ardmore, Pa., Ms. Xiong and colleagues analyzed the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database of medical device–related adverse event reports, to better understand and characterize dermal filler-related complications. They limited the analysis to adverse events involving injectable fillers from January 2014 to December 2020 and determined the number of complications by type per year and reviewed reports to identify injection site locations. Next, they used the binomial test to compare the proportion of complication categories from 2014 through 2016 and from 2017 through 2020.
In all, 5,994 reports were identified during the 7-year study period. To evaluate trends over time, the researchers estimated the rate of complications per 100 reports each year. While the absolute number of reports increased over time, the rate of adverse events per 100 reports decreased, suggesting an overall improvement in safety.
When the researchers focused on complications involving vascular occlusion, they found that vascular necrosis accounted for 3.5% of all complications, compared with vision changes (1.5% of all complications), and stroke (0.3% of all complications). When comparing the years 2014-2016 with 2017-2020, there was a significant increase in adverse events involving vascular necrosis (0.9%; P = .018) and vision changes (0.94%; P = .001), but no significant difference in the number of reports of stroke (-0.1%; P = .409). “This highlights that serious complications like necrosis and vision changes have increased over time,” Ms. Xiong said.
Overall, the three most common injection sites involving necrosis and vision changes were the cheek, the nose, and the nasolabial fold. The cheek was the most common site associated with stroke. “These findings are similar to those of previous studies, further emphasizing that the nose, nasolabial fold, and cheek are possibly challenging injection sites,” she said.
“In general, as the face is a highly vascular area with many anastomoses, it’s especially important to be aware of facial anatomy when injecting. In addition to awareness of anatomy, injection techniques can influence vascular complications. Unfortunately, the event narratives in the MAUDE database did not go into detail about the procedural technique.”
Ms. Xiong said that as the popularity of dermal fillers continues to grow, “it’s important for providers to understand the possible adverse events, both to better counsel patients and to improve safety management. The proportion of serious complications such as vascular necrosis and vision changes have increased from 2014 to 2020. This highlights an increased need for training to better understand facial anatomy and to emphasize practice techniques to minimize risk.”
Dr. Lee acknowledged certain limitations of the study, including that “submission of adverse events to the MAUDE database are not verified or standardized,” she told this news organization.
“With the ever-increasing popularity of fillers, it is not surprising that the absolute number of complications is rising, but it is also reassuring to see that the overall ratio of complications per hundred reports is down,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “I would be curious to know what proportion of filler complications are due to non–core practitioners compared to dermatologists and plastic surgeons.”
The researchers reported having no financial disclosures.
Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
FROM ASDS 2021
Pink or red actinic keratoses signal more inflammation
lesions.
Data suggest that up to 65% of squamous cell carcinomas (SCCs) were at some point diagnosed as AKs, wrote Jessica G. Labadie, MD, of the department of dermatology at Northwestern University, Chicago, and colleagues. Early identification of AKs is important to prevent progression to SCCs; previous studies have used histology or morphology, but not color, to characterize AK lesions, they said. In the study published in Dermatologic Surgery, the researchers analyzed images and histopathology slides to characterize AKs by color and to examine associations with inflammation and vasculature. They identified AKs from patients diagnosed between January 2018 and October 2019. The lesions were classified as white (4), brown (9), red (15), or pink (21).
Overall, white AKs had an absence of erythema and were significantly less likely to show inflammation on histopathology, compared with other colors. Brown AKs showed no significant increase in vascularity, but were significantly associated with pigment incontinence, basilar pigment presence, and absence of inflammation.
Notably, dermoscopy of red AKs revealed a distinctive polymorphous vessel pattern in most samples, as well as erythema in all. Similarly, all pink AKs showed erythema, and all showed inflammatory infiltrate on histology, although most did not show increased vascularity.
For all colors of AKs, there was a significant association between the presence of erythema on dermoscopy and the presence of inflammation on histology, while the absence of erythema on dermoscopy corresponded to a significant absence of inflammation on histology, the researchers noted.
“This report adds to the armamentarium of a dermatologist by proposing a novel way to characterize AK lesions,” the researchers wrote.
The study findings were limited by several factors including the inability to confirm which AKs would transform into SCCs based on color, and the inclusion of a study population with advanced AKs that may not generalize to typical AKs, the researchers noted. More research is needed to explore the impact of AK color on SCC development, they emphasized.
However, the results represent a novel way to characterize AK lesions, and triage them in a way that may spare some patients from unneeded biopsies, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
lesions.
Data suggest that up to 65% of squamous cell carcinomas (SCCs) were at some point diagnosed as AKs, wrote Jessica G. Labadie, MD, of the department of dermatology at Northwestern University, Chicago, and colleagues. Early identification of AKs is important to prevent progression to SCCs; previous studies have used histology or morphology, but not color, to characterize AK lesions, they said. In the study published in Dermatologic Surgery, the researchers analyzed images and histopathology slides to characterize AKs by color and to examine associations with inflammation and vasculature. They identified AKs from patients diagnosed between January 2018 and October 2019. The lesions were classified as white (4), brown (9), red (15), or pink (21).
Overall, white AKs had an absence of erythema and were significantly less likely to show inflammation on histopathology, compared with other colors. Brown AKs showed no significant increase in vascularity, but were significantly associated with pigment incontinence, basilar pigment presence, and absence of inflammation.
Notably, dermoscopy of red AKs revealed a distinctive polymorphous vessel pattern in most samples, as well as erythema in all. Similarly, all pink AKs showed erythema, and all showed inflammatory infiltrate on histology, although most did not show increased vascularity.
For all colors of AKs, there was a significant association between the presence of erythema on dermoscopy and the presence of inflammation on histology, while the absence of erythema on dermoscopy corresponded to a significant absence of inflammation on histology, the researchers noted.
“This report adds to the armamentarium of a dermatologist by proposing a novel way to characterize AK lesions,” the researchers wrote.
The study findings were limited by several factors including the inability to confirm which AKs would transform into SCCs based on color, and the inclusion of a study population with advanced AKs that may not generalize to typical AKs, the researchers noted. More research is needed to explore the impact of AK color on SCC development, they emphasized.
However, the results represent a novel way to characterize AK lesions, and triage them in a way that may spare some patients from unneeded biopsies, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
lesions.
Data suggest that up to 65% of squamous cell carcinomas (SCCs) were at some point diagnosed as AKs, wrote Jessica G. Labadie, MD, of the department of dermatology at Northwestern University, Chicago, and colleagues. Early identification of AKs is important to prevent progression to SCCs; previous studies have used histology or morphology, but not color, to characterize AK lesions, they said. In the study published in Dermatologic Surgery, the researchers analyzed images and histopathology slides to characterize AKs by color and to examine associations with inflammation and vasculature. They identified AKs from patients diagnosed between January 2018 and October 2019. The lesions were classified as white (4), brown (9), red (15), or pink (21).
Overall, white AKs had an absence of erythema and were significantly less likely to show inflammation on histopathology, compared with other colors. Brown AKs showed no significant increase in vascularity, but were significantly associated with pigment incontinence, basilar pigment presence, and absence of inflammation.
Notably, dermoscopy of red AKs revealed a distinctive polymorphous vessel pattern in most samples, as well as erythema in all. Similarly, all pink AKs showed erythema, and all showed inflammatory infiltrate on histology, although most did not show increased vascularity.
For all colors of AKs, there was a significant association between the presence of erythema on dermoscopy and the presence of inflammation on histology, while the absence of erythema on dermoscopy corresponded to a significant absence of inflammation on histology, the researchers noted.
“This report adds to the armamentarium of a dermatologist by proposing a novel way to characterize AK lesions,” the researchers wrote.
The study findings were limited by several factors including the inability to confirm which AKs would transform into SCCs based on color, and the inclusion of a study population with advanced AKs that may not generalize to typical AKs, the researchers noted. More research is needed to explore the impact of AK color on SCC development, they emphasized.
However, the results represent a novel way to characterize AK lesions, and triage them in a way that may spare some patients from unneeded biopsies, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM DERMATOLOGIC SURGERY
What are the legal risks of practicing laser cutaneous surgery?
The physician-patient relationship is a key factor in preventing litigation following cutaneous laser surgery, according to Mathew M. Avram, MD, JD.
“Numerous studies indicate that good communication and rapport are the most important means to avoid a lawsuit,” Dr. Avram, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “It is helpful to say that the outcome was not optimal or what you were anticipating. Communicate your plan [for the complication] clearly and honestly to your patient. The patient may not understand the severity of the complication. If they don’t, they will either leave it alone or they will go elsewhere and may receive poor care.” He added that in New England, “we have some stoic patients who may say ‘I don’t want to bother the doctor’ or ‘It’s my fault for having the procedure done.’ ”
Establishing effective communication with patients from the outset is good practice, he continued, because 75% of physicians in low-risk specialties will face a malpractice claim by age 65. Nearly a decade ago Dr. Avram, H. Ray Jalian, MD, and Chris Jalian, JD, published results from a national legal database analysis identifying common errors and risk factors for litigation in cutaneous surgery. Their search yielded 1,807 documents with 174 unique legal claims involving injury from a cutaneous laser treatment, from 1985 to 2012. The most common litigated procedures were laser hair removal, rejuvenation (mostly related to intense pulsed-light treatments), and laser treatment of leg veins, while the most common injuries sustained were burns, scars, and pigmentary changes. The most common causes of legal action were lack of informed consent and fraud.
Among the 120 cases with public decisions, cases favored the plaintiff 51% of the time. “That’s unusual,” said Dr. Avram, president of American Society for Dermatologic Surgery. “Usually, physicians do better, but I think the fact that they’re cosmetic cases probably shades things a little bit.” The median monetary award was $350,000 and ranged from $5,000 to $2,145,000. The two largest judgments were for improper use of topical anesthesia that led to deaths of patients in laser hair removal cases.
In a separate analysis, the same authors searched an online national database to identify the incidence of medical professional liability claims resulting from cutaneous laser surgery performed by nonphysician operators (NPOs) from 1999 to 2012. Among the 175 cases identified, 43% involved an NPO. “In fact, the cases involving NPOs exploded over a 4-year period; they grew from 36% in 2008 of cases to 78% in 2011,” Dr. Avram said. “This was even more true for laser hair removal.”
The practice setting turned out to be a factor. Only 23% of NPO litigation involving laser procedures arose in medical office settings, while 77% of cases involving NPOs were performed outside of traditional medical settings such as in salons and medical spas – mostly for laser hair removal. “We updated this information by examining the setting for nonphysician operator litigation between 2012 and 2017 and found that 66% of cases involving NPOs were performed outside of a traditional medical setting, while 34% of NPO litigation arose in medical office settings,” Dr. Avram said during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s close to a 2 to 1 ratio.”
In an analysis of medical professional liability claims involving Mohs surgery from 1989 to 2011, 26 of the 42 cases identified involved a primary defendant who was not a Mohs surgeon. In the 26 cases, the most common reasons for lawsuits were failure or delay of diagnosis of a skin cancer, cosmetic outcome issues, lack of informed consent, and delay or failure to refer to a Mohs surgeon. Of the cases that involved Mohs surgeons, the most common causes were lack of proper informed consent and cosmetic outcome issues, but “these cases were overwhelmingly decided in favor of the surgeons,” said Dr. Avram, one of the study authors.
On a related note, Dr. Avram underscored the importance of biopsy-site photography, “because patients and physicians misidentify biopsy sites too commonly,” he said. In a single-center study of 34 biopsy sites of cutaneous head and neck malignancies, patients misidentified the biopsy site 4-7 weeks out in 29% of the cases. Blinded dermatologists and the patient misidentified the biopsy site in 12% of the cases. “Good biopsy site photography should be mandatory in your practice,” he advised.
Clinicians can avoid cutaneous laser surgery complications only by not treating patients. “Complications and side effects are inevitable; you need to know your limits,” he said. “Even in skilled hands, if you treat enough patients, you will encounter challenging side effects. Do not perform a procedure that might produce a side effect that you cannot recognize and treat.”
The best way to avoid complications is to trust your eyes – not the laser – since the same device made by the same manufacturer may produce highly different outputs at the same setting (see J Am Acad Dermatol. 2016;74[5]:807-19).
“Moreover, lasers can produce much different energies after they have been serviced,” Dr. Avram said. “Do not memorize settings. Do not blindly replicate recommended settings from a colleague or a device manufacturer,” he advised. “Some devices are not externally calibrated. Therefore, the settings on one device may not translate the same way to yours. Often, device manufacturers underplay the settings. Safe and unsafe laser endpoints and close observation are the best means to avoiding clinical complications. That means you follow clinical endpoints, not fluences. The key clinical finding is the endpoint, not the energy setting.”
Temporary and expected side effects include erythema, edema, and purpura. “With these it’s just handholding and unlikely to lead to any legal consequences,” he continued. “With temporary hyperpigmentation that can occur with laser hair removal, time is one your side, because typically this will resolve before any litigation progresses. Permanent side effects from lasers and light sources and injectables are a different issue, things like permanent hypopigmentation, depigmentation, and scarring. These are most likely to produce liability.”
In Dr. Avram’s opinion, complications are best handled with widespread communication. “There is a temptation to avoid a patient with a poor outcome or side effect,” he said. “This is bad medicine and rightfully angers your patient and increases the risk of a lawsuit. [Resist] the temptation to avoid showing a poor outcome to a colleague. Many complications can be significantly improved or cleared with timely and appropriate interventions. You should always document your efforts.”
Dr. Avram disclosed that he has received consulting fees from Allergan and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
The physician-patient relationship is a key factor in preventing litigation following cutaneous laser surgery, according to Mathew M. Avram, MD, JD.
“Numerous studies indicate that good communication and rapport are the most important means to avoid a lawsuit,” Dr. Avram, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “It is helpful to say that the outcome was not optimal or what you were anticipating. Communicate your plan [for the complication] clearly and honestly to your patient. The patient may not understand the severity of the complication. If they don’t, they will either leave it alone or they will go elsewhere and may receive poor care.” He added that in New England, “we have some stoic patients who may say ‘I don’t want to bother the doctor’ or ‘It’s my fault for having the procedure done.’ ”
Establishing effective communication with patients from the outset is good practice, he continued, because 75% of physicians in low-risk specialties will face a malpractice claim by age 65. Nearly a decade ago Dr. Avram, H. Ray Jalian, MD, and Chris Jalian, JD, published results from a national legal database analysis identifying common errors and risk factors for litigation in cutaneous surgery. Their search yielded 1,807 documents with 174 unique legal claims involving injury from a cutaneous laser treatment, from 1985 to 2012. The most common litigated procedures were laser hair removal, rejuvenation (mostly related to intense pulsed-light treatments), and laser treatment of leg veins, while the most common injuries sustained were burns, scars, and pigmentary changes. The most common causes of legal action were lack of informed consent and fraud.
Among the 120 cases with public decisions, cases favored the plaintiff 51% of the time. “That’s unusual,” said Dr. Avram, president of American Society for Dermatologic Surgery. “Usually, physicians do better, but I think the fact that they’re cosmetic cases probably shades things a little bit.” The median monetary award was $350,000 and ranged from $5,000 to $2,145,000. The two largest judgments were for improper use of topical anesthesia that led to deaths of patients in laser hair removal cases.
In a separate analysis, the same authors searched an online national database to identify the incidence of medical professional liability claims resulting from cutaneous laser surgery performed by nonphysician operators (NPOs) from 1999 to 2012. Among the 175 cases identified, 43% involved an NPO. “In fact, the cases involving NPOs exploded over a 4-year period; they grew from 36% in 2008 of cases to 78% in 2011,” Dr. Avram said. “This was even more true for laser hair removal.”
The practice setting turned out to be a factor. Only 23% of NPO litigation involving laser procedures arose in medical office settings, while 77% of cases involving NPOs were performed outside of traditional medical settings such as in salons and medical spas – mostly for laser hair removal. “We updated this information by examining the setting for nonphysician operator litigation between 2012 and 2017 and found that 66% of cases involving NPOs were performed outside of a traditional medical setting, while 34% of NPO litigation arose in medical office settings,” Dr. Avram said during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s close to a 2 to 1 ratio.”
In an analysis of medical professional liability claims involving Mohs surgery from 1989 to 2011, 26 of the 42 cases identified involved a primary defendant who was not a Mohs surgeon. In the 26 cases, the most common reasons for lawsuits were failure or delay of diagnosis of a skin cancer, cosmetic outcome issues, lack of informed consent, and delay or failure to refer to a Mohs surgeon. Of the cases that involved Mohs surgeons, the most common causes were lack of proper informed consent and cosmetic outcome issues, but “these cases were overwhelmingly decided in favor of the surgeons,” said Dr. Avram, one of the study authors.
On a related note, Dr. Avram underscored the importance of biopsy-site photography, “because patients and physicians misidentify biopsy sites too commonly,” he said. In a single-center study of 34 biopsy sites of cutaneous head and neck malignancies, patients misidentified the biopsy site 4-7 weeks out in 29% of the cases. Blinded dermatologists and the patient misidentified the biopsy site in 12% of the cases. “Good biopsy site photography should be mandatory in your practice,” he advised.
Clinicians can avoid cutaneous laser surgery complications only by not treating patients. “Complications and side effects are inevitable; you need to know your limits,” he said. “Even in skilled hands, if you treat enough patients, you will encounter challenging side effects. Do not perform a procedure that might produce a side effect that you cannot recognize and treat.”
The best way to avoid complications is to trust your eyes – not the laser – since the same device made by the same manufacturer may produce highly different outputs at the same setting (see J Am Acad Dermatol. 2016;74[5]:807-19).
“Moreover, lasers can produce much different energies after they have been serviced,” Dr. Avram said. “Do not memorize settings. Do not blindly replicate recommended settings from a colleague or a device manufacturer,” he advised. “Some devices are not externally calibrated. Therefore, the settings on one device may not translate the same way to yours. Often, device manufacturers underplay the settings. Safe and unsafe laser endpoints and close observation are the best means to avoiding clinical complications. That means you follow clinical endpoints, not fluences. The key clinical finding is the endpoint, not the energy setting.”
Temporary and expected side effects include erythema, edema, and purpura. “With these it’s just handholding and unlikely to lead to any legal consequences,” he continued. “With temporary hyperpigmentation that can occur with laser hair removal, time is one your side, because typically this will resolve before any litigation progresses. Permanent side effects from lasers and light sources and injectables are a different issue, things like permanent hypopigmentation, depigmentation, and scarring. These are most likely to produce liability.”
In Dr. Avram’s opinion, complications are best handled with widespread communication. “There is a temptation to avoid a patient with a poor outcome or side effect,” he said. “This is bad medicine and rightfully angers your patient and increases the risk of a lawsuit. [Resist] the temptation to avoid showing a poor outcome to a colleague. Many complications can be significantly improved or cleared with timely and appropriate interventions. You should always document your efforts.”
Dr. Avram disclosed that he has received consulting fees from Allergan and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
The physician-patient relationship is a key factor in preventing litigation following cutaneous laser surgery, according to Mathew M. Avram, MD, JD.
“Numerous studies indicate that good communication and rapport are the most important means to avoid a lawsuit,” Dr. Avram, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “It is helpful to say that the outcome was not optimal or what you were anticipating. Communicate your plan [for the complication] clearly and honestly to your patient. The patient may not understand the severity of the complication. If they don’t, they will either leave it alone or they will go elsewhere and may receive poor care.” He added that in New England, “we have some stoic patients who may say ‘I don’t want to bother the doctor’ or ‘It’s my fault for having the procedure done.’ ”
Establishing effective communication with patients from the outset is good practice, he continued, because 75% of physicians in low-risk specialties will face a malpractice claim by age 65. Nearly a decade ago Dr. Avram, H. Ray Jalian, MD, and Chris Jalian, JD, published results from a national legal database analysis identifying common errors and risk factors for litigation in cutaneous surgery. Their search yielded 1,807 documents with 174 unique legal claims involving injury from a cutaneous laser treatment, from 1985 to 2012. The most common litigated procedures were laser hair removal, rejuvenation (mostly related to intense pulsed-light treatments), and laser treatment of leg veins, while the most common injuries sustained were burns, scars, and pigmentary changes. The most common causes of legal action were lack of informed consent and fraud.
Among the 120 cases with public decisions, cases favored the plaintiff 51% of the time. “That’s unusual,” said Dr. Avram, president of American Society for Dermatologic Surgery. “Usually, physicians do better, but I think the fact that they’re cosmetic cases probably shades things a little bit.” The median monetary award was $350,000 and ranged from $5,000 to $2,145,000. The two largest judgments were for improper use of topical anesthesia that led to deaths of patients in laser hair removal cases.
In a separate analysis, the same authors searched an online national database to identify the incidence of medical professional liability claims resulting from cutaneous laser surgery performed by nonphysician operators (NPOs) from 1999 to 2012. Among the 175 cases identified, 43% involved an NPO. “In fact, the cases involving NPOs exploded over a 4-year period; they grew from 36% in 2008 of cases to 78% in 2011,” Dr. Avram said. “This was even more true for laser hair removal.”
The practice setting turned out to be a factor. Only 23% of NPO litigation involving laser procedures arose in medical office settings, while 77% of cases involving NPOs were performed outside of traditional medical settings such as in salons and medical spas – mostly for laser hair removal. “We updated this information by examining the setting for nonphysician operator litigation between 2012 and 2017 and found that 66% of cases involving NPOs were performed outside of a traditional medical setting, while 34% of NPO litigation arose in medical office settings,” Dr. Avram said during the meeting, which was named What’s the Truth? and sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “That’s close to a 2 to 1 ratio.”
In an analysis of medical professional liability claims involving Mohs surgery from 1989 to 2011, 26 of the 42 cases identified involved a primary defendant who was not a Mohs surgeon. In the 26 cases, the most common reasons for lawsuits were failure or delay of diagnosis of a skin cancer, cosmetic outcome issues, lack of informed consent, and delay or failure to refer to a Mohs surgeon. Of the cases that involved Mohs surgeons, the most common causes were lack of proper informed consent and cosmetic outcome issues, but “these cases were overwhelmingly decided in favor of the surgeons,” said Dr. Avram, one of the study authors.
On a related note, Dr. Avram underscored the importance of biopsy-site photography, “because patients and physicians misidentify biopsy sites too commonly,” he said. In a single-center study of 34 biopsy sites of cutaneous head and neck malignancies, patients misidentified the biopsy site 4-7 weeks out in 29% of the cases. Blinded dermatologists and the patient misidentified the biopsy site in 12% of the cases. “Good biopsy site photography should be mandatory in your practice,” he advised.
Clinicians can avoid cutaneous laser surgery complications only by not treating patients. “Complications and side effects are inevitable; you need to know your limits,” he said. “Even in skilled hands, if you treat enough patients, you will encounter challenging side effects. Do not perform a procedure that might produce a side effect that you cannot recognize and treat.”
The best way to avoid complications is to trust your eyes – not the laser – since the same device made by the same manufacturer may produce highly different outputs at the same setting (see J Am Acad Dermatol. 2016;74[5]:807-19).
“Moreover, lasers can produce much different energies after they have been serviced,” Dr. Avram said. “Do not memorize settings. Do not blindly replicate recommended settings from a colleague or a device manufacturer,” he advised. “Some devices are not externally calibrated. Therefore, the settings on one device may not translate the same way to yours. Often, device manufacturers underplay the settings. Safe and unsafe laser endpoints and close observation are the best means to avoiding clinical complications. That means you follow clinical endpoints, not fluences. The key clinical finding is the endpoint, not the energy setting.”
Temporary and expected side effects include erythema, edema, and purpura. “With these it’s just handholding and unlikely to lead to any legal consequences,” he continued. “With temporary hyperpigmentation that can occur with laser hair removal, time is one your side, because typically this will resolve before any litigation progresses. Permanent side effects from lasers and light sources and injectables are a different issue, things like permanent hypopigmentation, depigmentation, and scarring. These are most likely to produce liability.”
In Dr. Avram’s opinion, complications are best handled with widespread communication. “There is a temptation to avoid a patient with a poor outcome or side effect,” he said. “This is bad medicine and rightfully angers your patient and increases the risk of a lawsuit. [Resist] the temptation to avoid showing a poor outcome to a colleague. Many complications can be significantly improved or cleared with timely and appropriate interventions. You should always document your efforts.”
Dr. Avram disclosed that he has received consulting fees from Allergan and Galderma. He is a member of the scientific advisory board for Allergan and Soliton, is an investigator for Endo, and holds stock options in La Jolla NanoMedical Inc.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
U.S. study finds racial, gender differences in surgical treatment of dermatofibrosarcoma protuberans
.
Current guidelines recommend Mohs micrographic surgery (MMS) as a first-line treatment for dermatofibrosarcoma protuberans, but the procedure may be inaccessible for certain populations and in some geographic areas, wrote Kevin J. Moore, MD, and Michael S. Chang, BA, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues. Wide local excision (WLE) is a less effective option; recurrence rates associated with this treatment are approximately 30% because of incomplete margin assessment, compared with about 3% with MMS, they noted.
In the study, published as a letter in the Journal of the American Academy of Dermatology, the investigators identified 2,370 cases of dermatofibrosarcoma protuberans using data from the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) Registry from 2000 to 2018. The mean age of the patients was 44 years; 55% were women. A total of 539 patients underwent MMS and 1,831 underwent WLE.
Overall, patients in the WLE group were more likely to be younger, male, Black, and single, the researchers noted. Those who had WLE, they added, were “more commonly deceased at study end date, recipients of adjuvant chemotherapy or radiation, and had truncal tumor locations.”
In a multivariate analysis, patients who were non-Hispanic, White, or other races (including American Indian, Alaskan Native, and Pacific Islander), were significantly more likely to undergo MMS compared with Black and Hispanic patients (adjusted odd ratio [aOR], 1.46, 1.66, and 2.42, respectively). Women were also significantly more likely than were men to undergo MMS (aOR, 1.24). Individuals living in the Western part of the United States were significantly more likely to undergo MMS.
The study findings were limited by several factors including the inability to control for insurance status, lack of data on re-excision, and the use of aggregate case data, the researchers noted. However, the results highlight the disparities in use of MMS for dermatofibrosarcoma protuberans, they said.
“Because MMS is associated with significantly improved outcomes, identifying at-risk patient populations and barriers to accessing MMS is essential,” the researchers noted. The results suggest that disparities persist in accessing MMS for many patients, notably Black and Hispanic males, they said. “Further work is necessary to identify mechanisms for increasing access to MMS,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
.
Current guidelines recommend Mohs micrographic surgery (MMS) as a first-line treatment for dermatofibrosarcoma protuberans, but the procedure may be inaccessible for certain populations and in some geographic areas, wrote Kevin J. Moore, MD, and Michael S. Chang, BA, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues. Wide local excision (WLE) is a less effective option; recurrence rates associated with this treatment are approximately 30% because of incomplete margin assessment, compared with about 3% with MMS, they noted.
In the study, published as a letter in the Journal of the American Academy of Dermatology, the investigators identified 2,370 cases of dermatofibrosarcoma protuberans using data from the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) Registry from 2000 to 2018. The mean age of the patients was 44 years; 55% were women. A total of 539 patients underwent MMS and 1,831 underwent WLE.
Overall, patients in the WLE group were more likely to be younger, male, Black, and single, the researchers noted. Those who had WLE, they added, were “more commonly deceased at study end date, recipients of adjuvant chemotherapy or radiation, and had truncal tumor locations.”
In a multivariate analysis, patients who were non-Hispanic, White, or other races (including American Indian, Alaskan Native, and Pacific Islander), were significantly more likely to undergo MMS compared with Black and Hispanic patients (adjusted odd ratio [aOR], 1.46, 1.66, and 2.42, respectively). Women were also significantly more likely than were men to undergo MMS (aOR, 1.24). Individuals living in the Western part of the United States were significantly more likely to undergo MMS.
The study findings were limited by several factors including the inability to control for insurance status, lack of data on re-excision, and the use of aggregate case data, the researchers noted. However, the results highlight the disparities in use of MMS for dermatofibrosarcoma protuberans, they said.
“Because MMS is associated with significantly improved outcomes, identifying at-risk patient populations and barriers to accessing MMS is essential,” the researchers noted. The results suggest that disparities persist in accessing MMS for many patients, notably Black and Hispanic males, they said. “Further work is necessary to identify mechanisms for increasing access to MMS,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
.
Current guidelines recommend Mohs micrographic surgery (MMS) as a first-line treatment for dermatofibrosarcoma protuberans, but the procedure may be inaccessible for certain populations and in some geographic areas, wrote Kevin J. Moore, MD, and Michael S. Chang, BA, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues. Wide local excision (WLE) is a less effective option; recurrence rates associated with this treatment are approximately 30% because of incomplete margin assessment, compared with about 3% with MMS, they noted.
In the study, published as a letter in the Journal of the American Academy of Dermatology, the investigators identified 2,370 cases of dermatofibrosarcoma protuberans using data from the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) Registry from 2000 to 2018. The mean age of the patients was 44 years; 55% were women. A total of 539 patients underwent MMS and 1,831 underwent WLE.
Overall, patients in the WLE group were more likely to be younger, male, Black, and single, the researchers noted. Those who had WLE, they added, were “more commonly deceased at study end date, recipients of adjuvant chemotherapy or radiation, and had truncal tumor locations.”
In a multivariate analysis, patients who were non-Hispanic, White, or other races (including American Indian, Alaskan Native, and Pacific Islander), were significantly more likely to undergo MMS compared with Black and Hispanic patients (adjusted odd ratio [aOR], 1.46, 1.66, and 2.42, respectively). Women were also significantly more likely than were men to undergo MMS (aOR, 1.24). Individuals living in the Western part of the United States were significantly more likely to undergo MMS.
The study findings were limited by several factors including the inability to control for insurance status, lack of data on re-excision, and the use of aggregate case data, the researchers noted. However, the results highlight the disparities in use of MMS for dermatofibrosarcoma protuberans, they said.
“Because MMS is associated with significantly improved outcomes, identifying at-risk patient populations and barriers to accessing MMS is essential,” the researchers noted. The results suggest that disparities persist in accessing MMS for many patients, notably Black and Hispanic males, they said. “Further work is necessary to identify mechanisms for increasing access to MMS,” they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM JAAD
Opioid prescriptions following Mohs surgery dropped over the last decade
by 26.3% between 2009 and 2020, according to a cross-sectional analysis of national insurance claims data.
The findings suggest that dermatologic surgeons generally understood opioid prescription risks and public health warnings about the opioid epidemic, corresponding study author Surya A. Veerabagu said in an interview.
“The frequency of opioid prescriptions after Mohs surgery went up a little bit from 2009 to 2011, but then it subsequently decreased,” said Ms. Veerabagu, a 4th-year student at Tulane University, New Orleans. “It very much correlates with the overarching opioid trends of the time. From 2010 to 2015, research questioning the safety of opioids increased and in 2012, national prescriptions claims for opioids began to decrease. More media outlets voiced concerns over the growing opioid epidemic, as well.”
As she and her associates noted in their study, published online Sept. 22 in JAMA Dermatology, sales of opioids skyrocketed, increasing by 400% from 1999 to 2011, while prescription opioid–related deaths exceeded deaths caused by heroin and cocaine combined.
“In 2016, the U.S. Department of Health and Human Services declared the opioid epidemic a public health emergency, and the Centers for Disease Control and Prevention released guidelines to curtail unnecessary opioid prescriptions,” they wrote. “Unfortunately, overdose deaths involving prescription opioids continued to increase even after these measures.”
The researchers drew from Optum Clinformatics Data Mart (Optum CDM), a nationally representative insurance claims database, and limited the analysis to 358,012 adults who underwent Mohs surgery and obtained an opioid prescription within 2 days of surgery in the United States from Jan. 1, 2009, to June 1, 2020. They found that 34.6% of patients underwent Mohs surgery with opioid claims in 2009. This rose to a peak of 39.6% in 2011, then decreased annually to a rate of 11.7% in 2020.
The four opioids obtained most during the study period were hydrocodone (55%), codeine (16.3%), oxycodone (12%), and tramadol (11.6%). However, over time, the proportion of patients who obtained hydrocodone fell 21.7% from a peak of 67.1% in 2011 to 45.4% in 2020, while the proportion of patients who obtained tramadol – generally recognized as a safer option – increased 26.3% from a low of 1.6% in 2009 to 27.9% in 2020.
“The switch from very addictive opioids like hydrocodone and oxycodone to weaker opioids like tramadol was fascinating to see,” said Ms. Veerabagu, who conducted the study during her research fellowship in the department of dermatology at the University of Pennsylvania, Philadelphia. “I remember at first thinking I had coded the data wrong. I reviewed the results with the team to ensure it was correct. We noticed that propoxyphene prescriptions suddenly dropped to 0% in 2011.” She found that the FDA warning in 2010 and recall regarding the use of propoxyphene because of cardiotoxicity correlated with her data, which, “in addition to the thorough review, convinced me that my coding was correct.” Prior to 2011, propoxyphene constituted 28% of prescriptions in 2009 and 24% of prescriptions in 2010.
In an interview, Maryam M. Asgari, MD, professor of dermatology at Harvard Medical School, Boston, said that the findings support recent opioid prescription recommendations following Mohs and other dermatologic procedures from professional societies including those from the American College of Mohs Surgery.
“More awareness has been raised in the past decade regarding the opioid epidemic and the rise of opioid abuse and deaths,” she said. “There has been increased scrutiny on procedures and prescribing of opioids post procedures.”
State-led efforts to lower the number of opioid prescriptions also play a role. For example, in 2016, Massachusetts launched the Massachusetts Prescription Awareness Tool (MassPAT), which imposes a 7-day limit on first-time prescriptions of opioids to patients and mandates that all prescribers check the prescription drug monitoring program before prescribing schedule II or III substances.
“The MassPAT system also gives you quarterly data on how your opioid prescriptions compare with those of your peers within your specialty and subspecialty,” Dr. Asgari said. “If you’re an outlier, I think that quickly leads you to change your prescribing patterns.”
Dr. Asgari noted that most opioids prescribed in the study by Ms. Veerabagu and colleagues were for cancers that arose on the head and neck. “There is still a perception among providers that cancers that arise in those anatomic sites can potentially cause more discomfort for the patient,” she said. “So, knowing more about the degree of pain among the head and neck cases would be an area of knowledge that would help provider behavior down the line.”
Ms. Veerabagu acknowledged certain limitations of the study, including the fact that unfilled prescriptions could not be accounted for, nor could opioids not taken or those obtained without a prescription. “We cannot survey patients in insurance claims database studies, so we have no way of knowing if everyone’s pain was adequately controlled from 2009 to 2020,” she said.
“The main takeaway message is to make sure doctors and patients share an open dialogue,” she added. “Informing patients of the major pros and cons of the appropriate postoperative pain management options available, including opioids’ addiction potential, is crucial. We hope our study adds to the larger continuing conversation of opioid usage within dermatology.”
The study’s senior author was Cerrene N. Giordano, MD, of the department of dermatology at the Hospital of the University of Pennsylvania, Philadelphia. Coauthor Jeremy R. Etzkorn, MD, is supported by a Dermatology Foundation Career Development Award in Dermatologic Surgery; coauthor Megan H. Noe, MD, MPH, reported receiving grants from Boehringer Ingelheim outside the submitted work. Another coauthor, Thuzar M. Shin, MD, PhD, reported receiving grants from Regeneron outside the submitted work. Dr. Asgari disclosed that she has received support from the Melanoma Research Alliance. She also contributes a chapter on skin cancer to UpToDate, for which she receives royalties.
by 26.3% between 2009 and 2020, according to a cross-sectional analysis of national insurance claims data.
The findings suggest that dermatologic surgeons generally understood opioid prescription risks and public health warnings about the opioid epidemic, corresponding study author Surya A. Veerabagu said in an interview.
“The frequency of opioid prescriptions after Mohs surgery went up a little bit from 2009 to 2011, but then it subsequently decreased,” said Ms. Veerabagu, a 4th-year student at Tulane University, New Orleans. “It very much correlates with the overarching opioid trends of the time. From 2010 to 2015, research questioning the safety of opioids increased and in 2012, national prescriptions claims for opioids began to decrease. More media outlets voiced concerns over the growing opioid epidemic, as well.”
As she and her associates noted in their study, published online Sept. 22 in JAMA Dermatology, sales of opioids skyrocketed, increasing by 400% from 1999 to 2011, while prescription opioid–related deaths exceeded deaths caused by heroin and cocaine combined.
“In 2016, the U.S. Department of Health and Human Services declared the opioid epidemic a public health emergency, and the Centers for Disease Control and Prevention released guidelines to curtail unnecessary opioid prescriptions,” they wrote. “Unfortunately, overdose deaths involving prescription opioids continued to increase even after these measures.”
The researchers drew from Optum Clinformatics Data Mart (Optum CDM), a nationally representative insurance claims database, and limited the analysis to 358,012 adults who underwent Mohs surgery and obtained an opioid prescription within 2 days of surgery in the United States from Jan. 1, 2009, to June 1, 2020. They found that 34.6% of patients underwent Mohs surgery with opioid claims in 2009. This rose to a peak of 39.6% in 2011, then decreased annually to a rate of 11.7% in 2020.
The four opioids obtained most during the study period were hydrocodone (55%), codeine (16.3%), oxycodone (12%), and tramadol (11.6%). However, over time, the proportion of patients who obtained hydrocodone fell 21.7% from a peak of 67.1% in 2011 to 45.4% in 2020, while the proportion of patients who obtained tramadol – generally recognized as a safer option – increased 26.3% from a low of 1.6% in 2009 to 27.9% in 2020.
“The switch from very addictive opioids like hydrocodone and oxycodone to weaker opioids like tramadol was fascinating to see,” said Ms. Veerabagu, who conducted the study during her research fellowship in the department of dermatology at the University of Pennsylvania, Philadelphia. “I remember at first thinking I had coded the data wrong. I reviewed the results with the team to ensure it was correct. We noticed that propoxyphene prescriptions suddenly dropped to 0% in 2011.” She found that the FDA warning in 2010 and recall regarding the use of propoxyphene because of cardiotoxicity correlated with her data, which, “in addition to the thorough review, convinced me that my coding was correct.” Prior to 2011, propoxyphene constituted 28% of prescriptions in 2009 and 24% of prescriptions in 2010.
In an interview, Maryam M. Asgari, MD, professor of dermatology at Harvard Medical School, Boston, said that the findings support recent opioid prescription recommendations following Mohs and other dermatologic procedures from professional societies including those from the American College of Mohs Surgery.
“More awareness has been raised in the past decade regarding the opioid epidemic and the rise of opioid abuse and deaths,” she said. “There has been increased scrutiny on procedures and prescribing of opioids post procedures.”
State-led efforts to lower the number of opioid prescriptions also play a role. For example, in 2016, Massachusetts launched the Massachusetts Prescription Awareness Tool (MassPAT), which imposes a 7-day limit on first-time prescriptions of opioids to patients and mandates that all prescribers check the prescription drug monitoring program before prescribing schedule II or III substances.
“The MassPAT system also gives you quarterly data on how your opioid prescriptions compare with those of your peers within your specialty and subspecialty,” Dr. Asgari said. “If you’re an outlier, I think that quickly leads you to change your prescribing patterns.”
Dr. Asgari noted that most opioids prescribed in the study by Ms. Veerabagu and colleagues were for cancers that arose on the head and neck. “There is still a perception among providers that cancers that arise in those anatomic sites can potentially cause more discomfort for the patient,” she said. “So, knowing more about the degree of pain among the head and neck cases would be an area of knowledge that would help provider behavior down the line.”
Ms. Veerabagu acknowledged certain limitations of the study, including the fact that unfilled prescriptions could not be accounted for, nor could opioids not taken or those obtained without a prescription. “We cannot survey patients in insurance claims database studies, so we have no way of knowing if everyone’s pain was adequately controlled from 2009 to 2020,” she said.
“The main takeaway message is to make sure doctors and patients share an open dialogue,” she added. “Informing patients of the major pros and cons of the appropriate postoperative pain management options available, including opioids’ addiction potential, is crucial. We hope our study adds to the larger continuing conversation of opioid usage within dermatology.”
The study’s senior author was Cerrene N. Giordano, MD, of the department of dermatology at the Hospital of the University of Pennsylvania, Philadelphia. Coauthor Jeremy R. Etzkorn, MD, is supported by a Dermatology Foundation Career Development Award in Dermatologic Surgery; coauthor Megan H. Noe, MD, MPH, reported receiving grants from Boehringer Ingelheim outside the submitted work. Another coauthor, Thuzar M. Shin, MD, PhD, reported receiving grants from Regeneron outside the submitted work. Dr. Asgari disclosed that she has received support from the Melanoma Research Alliance. She also contributes a chapter on skin cancer to UpToDate, for which she receives royalties.
by 26.3% between 2009 and 2020, according to a cross-sectional analysis of national insurance claims data.
The findings suggest that dermatologic surgeons generally understood opioid prescription risks and public health warnings about the opioid epidemic, corresponding study author Surya A. Veerabagu said in an interview.
“The frequency of opioid prescriptions after Mohs surgery went up a little bit from 2009 to 2011, but then it subsequently decreased,” said Ms. Veerabagu, a 4th-year student at Tulane University, New Orleans. “It very much correlates with the overarching opioid trends of the time. From 2010 to 2015, research questioning the safety of opioids increased and in 2012, national prescriptions claims for opioids began to decrease. More media outlets voiced concerns over the growing opioid epidemic, as well.”
As she and her associates noted in their study, published online Sept. 22 in JAMA Dermatology, sales of opioids skyrocketed, increasing by 400% from 1999 to 2011, while prescription opioid–related deaths exceeded deaths caused by heroin and cocaine combined.
“In 2016, the U.S. Department of Health and Human Services declared the opioid epidemic a public health emergency, and the Centers for Disease Control and Prevention released guidelines to curtail unnecessary opioid prescriptions,” they wrote. “Unfortunately, overdose deaths involving prescription opioids continued to increase even after these measures.”
The researchers drew from Optum Clinformatics Data Mart (Optum CDM), a nationally representative insurance claims database, and limited the analysis to 358,012 adults who underwent Mohs surgery and obtained an opioid prescription within 2 days of surgery in the United States from Jan. 1, 2009, to June 1, 2020. They found that 34.6% of patients underwent Mohs surgery with opioid claims in 2009. This rose to a peak of 39.6% in 2011, then decreased annually to a rate of 11.7% in 2020.
The four opioids obtained most during the study period were hydrocodone (55%), codeine (16.3%), oxycodone (12%), and tramadol (11.6%). However, over time, the proportion of patients who obtained hydrocodone fell 21.7% from a peak of 67.1% in 2011 to 45.4% in 2020, while the proportion of patients who obtained tramadol – generally recognized as a safer option – increased 26.3% from a low of 1.6% in 2009 to 27.9% in 2020.
“The switch from very addictive opioids like hydrocodone and oxycodone to weaker opioids like tramadol was fascinating to see,” said Ms. Veerabagu, who conducted the study during her research fellowship in the department of dermatology at the University of Pennsylvania, Philadelphia. “I remember at first thinking I had coded the data wrong. I reviewed the results with the team to ensure it was correct. We noticed that propoxyphene prescriptions suddenly dropped to 0% in 2011.” She found that the FDA warning in 2010 and recall regarding the use of propoxyphene because of cardiotoxicity correlated with her data, which, “in addition to the thorough review, convinced me that my coding was correct.” Prior to 2011, propoxyphene constituted 28% of prescriptions in 2009 and 24% of prescriptions in 2010.
In an interview, Maryam M. Asgari, MD, professor of dermatology at Harvard Medical School, Boston, said that the findings support recent opioid prescription recommendations following Mohs and other dermatologic procedures from professional societies including those from the American College of Mohs Surgery.
“More awareness has been raised in the past decade regarding the opioid epidemic and the rise of opioid abuse and deaths,” she said. “There has been increased scrutiny on procedures and prescribing of opioids post procedures.”
State-led efforts to lower the number of opioid prescriptions also play a role. For example, in 2016, Massachusetts launched the Massachusetts Prescription Awareness Tool (MassPAT), which imposes a 7-day limit on first-time prescriptions of opioids to patients and mandates that all prescribers check the prescription drug monitoring program before prescribing schedule II or III substances.
“The MassPAT system also gives you quarterly data on how your opioid prescriptions compare with those of your peers within your specialty and subspecialty,” Dr. Asgari said. “If you’re an outlier, I think that quickly leads you to change your prescribing patterns.”
Dr. Asgari noted that most opioids prescribed in the study by Ms. Veerabagu and colleagues were for cancers that arose on the head and neck. “There is still a perception among providers that cancers that arise in those anatomic sites can potentially cause more discomfort for the patient,” she said. “So, knowing more about the degree of pain among the head and neck cases would be an area of knowledge that would help provider behavior down the line.”
Ms. Veerabagu acknowledged certain limitations of the study, including the fact that unfilled prescriptions could not be accounted for, nor could opioids not taken or those obtained without a prescription. “We cannot survey patients in insurance claims database studies, so we have no way of knowing if everyone’s pain was adequately controlled from 2009 to 2020,” she said.
“The main takeaway message is to make sure doctors and patients share an open dialogue,” she added. “Informing patients of the major pros and cons of the appropriate postoperative pain management options available, including opioids’ addiction potential, is crucial. We hope our study adds to the larger continuing conversation of opioid usage within dermatology.”
The study’s senior author was Cerrene N. Giordano, MD, of the department of dermatology at the Hospital of the University of Pennsylvania, Philadelphia. Coauthor Jeremy R. Etzkorn, MD, is supported by a Dermatology Foundation Career Development Award in Dermatologic Surgery; coauthor Megan H. Noe, MD, MPH, reported receiving grants from Boehringer Ingelheim outside the submitted work. Another coauthor, Thuzar M. Shin, MD, PhD, reported receiving grants from Regeneron outside the submitted work. Dr. Asgari disclosed that she has received support from the Melanoma Research Alliance. She also contributes a chapter on skin cancer to UpToDate, for which she receives royalties.
FROM JAMA DERMATOLOGY
Medicare payments for most skin procedures dropped over last 15 years
according to a new analysis.
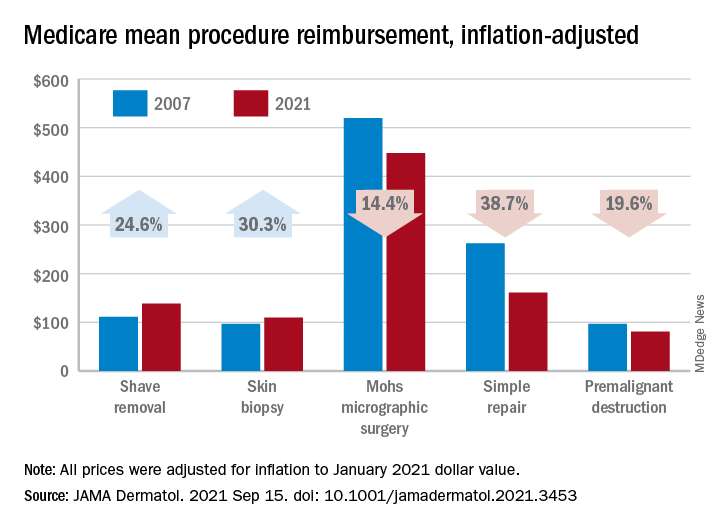
Large increases in mean reimbursement for skin biopsies (+30.3%) and shave removal (+24.6%) were not enough to offset lower rates for procedures such as simple repair (–38.7%), premalignant destruction (–19.6%), Mohs micrographic surgery (–14.4%), and flap repair (–14.1%), Rishabh S. Mazmudar, BS, of Case Western Reserve University, Cleveland, and associates said.
“Given Medicare’s contribution to a large proportion of health care expenditures, changes in Medicare reimbursement rates may result in parallel changes in private insurance reimbursement,” they wrote in JAMA Dermatology.
A recently published study showed that Medicare reimbursement for 20 dermatologic service codes had fallen by 10% between the two comparison years, 2000 and 2020. The current study expanded the number of procedures to 46 (divided into nine categories) and used historical Medicare fee schedules to examine annual trends over a 15-year period, Mr. Mazmudar and associates explained.
Other specialties have seen reimbursement fall by more than 4.8%, including emergency medicine (–21.2% from 2000 to 2020) and general surgery (–24.4% from 2000 to 2018), but “these comparisons are likely skewed by the disproportionate increase in reimbursement rates for biopsies and shave removals during this time period,” the investigators said.
If those two procedure categories were excluded from the analysis, the mean change in overall reimbursement for the remaining dermatologic procedures would be −9.6%, they noted.
Detailed payment information provided for 15 of the 46 procedures shows that only intermediate repair (+4.5%) and benign destruction (+2.3%) joined biopsies and shave excisions with increased reimbursement from 2007 to 2021. The smallest drop among the other procedures was –1.9% for malignant destruction, the research team reported.
The inflation-adjusted, year-by-year analysis showed that reimbursement for the nine procedure categories has gradually declined since peaking in 2011, with the most notable exceptions being biopsies and shave excisions. Both had been following the trend until 2013, when reimbursement for shave removals jumped by almost 30 percentage points, and 2019, when rates for biopsies soared by more than 30 percentage points, according to the investigators.
The increase for skin biopsies followed the split of the original CPT code into three categories, but “the jump in reimbursement for shave removals in 2013 requires further investigation,” Mr. Mazmudar and associates wrote.
The investigators did not disclose any conflicts of interest.
according to a new analysis.
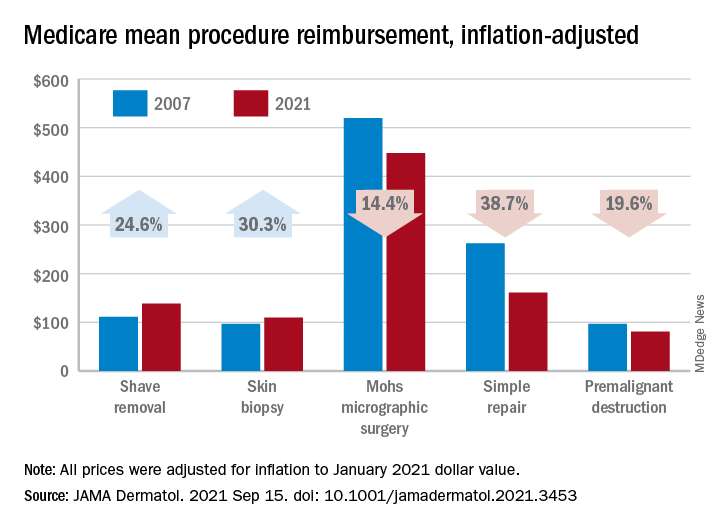
Large increases in mean reimbursement for skin biopsies (+30.3%) and shave removal (+24.6%) were not enough to offset lower rates for procedures such as simple repair (–38.7%), premalignant destruction (–19.6%), Mohs micrographic surgery (–14.4%), and flap repair (–14.1%), Rishabh S. Mazmudar, BS, of Case Western Reserve University, Cleveland, and associates said.
“Given Medicare’s contribution to a large proportion of health care expenditures, changes in Medicare reimbursement rates may result in parallel changes in private insurance reimbursement,” they wrote in JAMA Dermatology.
A recently published study showed that Medicare reimbursement for 20 dermatologic service codes had fallen by 10% between the two comparison years, 2000 and 2020. The current study expanded the number of procedures to 46 (divided into nine categories) and used historical Medicare fee schedules to examine annual trends over a 15-year period, Mr. Mazmudar and associates explained.
Other specialties have seen reimbursement fall by more than 4.8%, including emergency medicine (–21.2% from 2000 to 2020) and general surgery (–24.4% from 2000 to 2018), but “these comparisons are likely skewed by the disproportionate increase in reimbursement rates for biopsies and shave removals during this time period,” the investigators said.
If those two procedure categories were excluded from the analysis, the mean change in overall reimbursement for the remaining dermatologic procedures would be −9.6%, they noted.
Detailed payment information provided for 15 of the 46 procedures shows that only intermediate repair (+4.5%) and benign destruction (+2.3%) joined biopsies and shave excisions with increased reimbursement from 2007 to 2021. The smallest drop among the other procedures was –1.9% for malignant destruction, the research team reported.
The inflation-adjusted, year-by-year analysis showed that reimbursement for the nine procedure categories has gradually declined since peaking in 2011, with the most notable exceptions being biopsies and shave excisions. Both had been following the trend until 2013, when reimbursement for shave removals jumped by almost 30 percentage points, and 2019, when rates for biopsies soared by more than 30 percentage points, according to the investigators.
The increase for skin biopsies followed the split of the original CPT code into three categories, but “the jump in reimbursement for shave removals in 2013 requires further investigation,” Mr. Mazmudar and associates wrote.
The investigators did not disclose any conflicts of interest.
according to a new analysis.
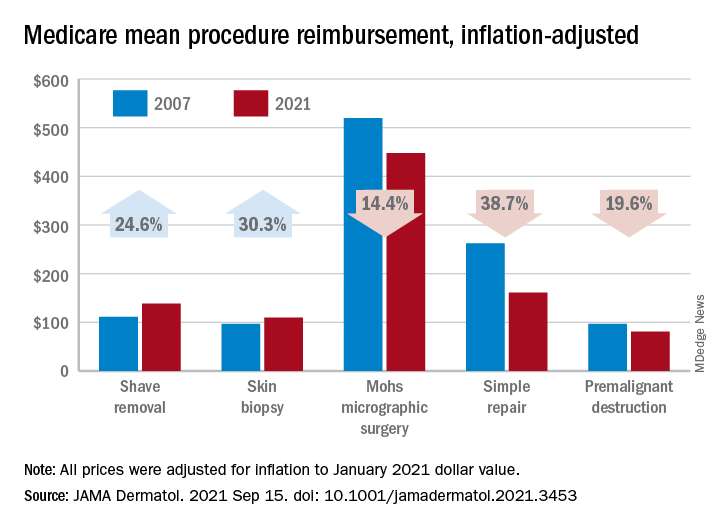
Large increases in mean reimbursement for skin biopsies (+30.3%) and shave removal (+24.6%) were not enough to offset lower rates for procedures such as simple repair (–38.7%), premalignant destruction (–19.6%), Mohs micrographic surgery (–14.4%), and flap repair (–14.1%), Rishabh S. Mazmudar, BS, of Case Western Reserve University, Cleveland, and associates said.
“Given Medicare’s contribution to a large proportion of health care expenditures, changes in Medicare reimbursement rates may result in parallel changes in private insurance reimbursement,” they wrote in JAMA Dermatology.
A recently published study showed that Medicare reimbursement for 20 dermatologic service codes had fallen by 10% between the two comparison years, 2000 and 2020. The current study expanded the number of procedures to 46 (divided into nine categories) and used historical Medicare fee schedules to examine annual trends over a 15-year period, Mr. Mazmudar and associates explained.
Other specialties have seen reimbursement fall by more than 4.8%, including emergency medicine (–21.2% from 2000 to 2020) and general surgery (–24.4% from 2000 to 2018), but “these comparisons are likely skewed by the disproportionate increase in reimbursement rates for biopsies and shave removals during this time period,” the investigators said.
If those two procedure categories were excluded from the analysis, the mean change in overall reimbursement for the remaining dermatologic procedures would be −9.6%, they noted.
Detailed payment information provided for 15 of the 46 procedures shows that only intermediate repair (+4.5%) and benign destruction (+2.3%) joined biopsies and shave excisions with increased reimbursement from 2007 to 2021. The smallest drop among the other procedures was –1.9% for malignant destruction, the research team reported.
The inflation-adjusted, year-by-year analysis showed that reimbursement for the nine procedure categories has gradually declined since peaking in 2011, with the most notable exceptions being biopsies and shave excisions. Both had been following the trend until 2013, when reimbursement for shave removals jumped by almost 30 percentage points, and 2019, when rates for biopsies soared by more than 30 percentage points, according to the investigators.
The increase for skin biopsies followed the split of the original CPT code into three categories, but “the jump in reimbursement for shave removals in 2013 requires further investigation,” Mr. Mazmudar and associates wrote.
The investigators did not disclose any conflicts of interest.
FROM JAMA DERMATOLOGY
Patient risk-benefit thresholds for antibiotic use in dermatologic surgery vary widely
(SSI) and had negligible side effects, in a prospective multicenter study.
In addition, a similar proportion of patients preferred to take an antibiotic if there was no SSI reduction and a high risk of adverse events.
Those are two key findings from the study aimed at understanding patient preferences for prophylactic oral antibiotic use following dermatologic surgery, which was published in Dermatologic Surgery.
“Patient risk-benefit thresholds for using antibiotics vary considerably,” the study’s corresponding author, Jeremy R. Etzkorn, MD, MS, of the department of dermatology at the Hospital of the University of Pennsylvania, Philadelphia, told this news organization. “Physicians should appreciate and consider the variation between patients before deciding to send in a prescription after skin surgery.”
To investigate patient preferences about taking antibiotics to prevent SSI relative to antibiotic efficacy and antibiotic-associated adverse drug reactions, Dr. Etzkorn and colleagues at six U.S. medical centers prospectively administered a web-based survey and discrete choice experiment to 388 adults including dermatologic surgery patients and their family members, as well as health care workers (defined as dermatologic surgery patients who work in health care, individuals who work in health care and are accompanying patients to their surgery, or staff in the dermatology clinic.) “A lot has been published about physician preferences and practice patterns with respect to antibiotic prescribing after dermatologic surgery,” Dr. Etzkorn noted. “This is the first study to evaluate patient preferences in a rigorous way.”
He and his coinvestigators used a technique from marketing and product research (conjoint analysis/discrete choice experiments) to quantify what patients think about using antibiotics and what trade-offs they are – or are not – willing to make to reduce their risk of infection.
Nearly half of the respondents (47%) were patients, 29% were family members of patients, 19% were health care workers, and the rest were described as patient caregivers or “other.” More than half (59%) were female, the mean age at surgery was 59 years, and 69% had college or postgraduate degrees.
More than half of respondents (55%) would choose to take an antibiotic if it reduced the SSI rate from 5% to 2.5% and if the risk of adverse drug reactions was low (defined as a 1% risk gastrointestinal upset, 0.5% risk itchy skin rash, and 0.01% risk ED visit). Even if an antibiotic could eliminate SSI risk entirely and had a low adverse drug reaction profile, 27% of respondents preferred not to take prophylactic oral antibiotics.
A subgroup analysis revealed that only 21% of health care workers would choose a moderate efficacy antibiotic (2.5% SSI risk) with a high adverse effect profile, compared with 41% of those who do not work in health care. Respondent age also drove treatment choice. For example, only 33% of respondents younger than age 65 would choose a moderate efficacy antibiotic (2.5% SSI risk) with a high adverse effect profile, compared with 45% of those aged 65 years and older.
“We knew patients would likely trade some antibiotic efficacy for some side effects, just as one would trade price for features when shopping for a car,” Dr. Etzkorn said. “We were shocked to see that over a quarter – 27% – of respondents preferred to not take antibiotics even if they were able to prevent all infections and had minimal side effects.”
“It’s interesting that between 27% [and] 55% of patients preferred no operative antibiotic prophylaxis despite a theoretical 100% cure rate for surgical-site infections,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study results.
“I think this mirrors dermatologist’s preferences, as a majority also prefer not to prescribe postoperative antibiotic therapy, unless operating in an area of or a patient with a high risk for infection. It would also be interesting to see if a less educated population would also have similar preferences.”
Dr. Etzkorn acknowledged certain limitations of the study, including that while it evaluated patient reported preferences, it did not include all possible risks and benefits, and “it does not measure actual patient behaviors.”
The researchers reported having no relevant financial disclosures. Dr. Etzkorn disclosed that he serves as a data safety monitoring board member for a clinical trial of Replimmune. Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
(SSI) and had negligible side effects, in a prospective multicenter study.
In addition, a similar proportion of patients preferred to take an antibiotic if there was no SSI reduction and a high risk of adverse events.
Those are two key findings from the study aimed at understanding patient preferences for prophylactic oral antibiotic use following dermatologic surgery, which was published in Dermatologic Surgery.
“Patient risk-benefit thresholds for using antibiotics vary considerably,” the study’s corresponding author, Jeremy R. Etzkorn, MD, MS, of the department of dermatology at the Hospital of the University of Pennsylvania, Philadelphia, told this news organization. “Physicians should appreciate and consider the variation between patients before deciding to send in a prescription after skin surgery.”
To investigate patient preferences about taking antibiotics to prevent SSI relative to antibiotic efficacy and antibiotic-associated adverse drug reactions, Dr. Etzkorn and colleagues at six U.S. medical centers prospectively administered a web-based survey and discrete choice experiment to 388 adults including dermatologic surgery patients and their family members, as well as health care workers (defined as dermatologic surgery patients who work in health care, individuals who work in health care and are accompanying patients to their surgery, or staff in the dermatology clinic.) “A lot has been published about physician preferences and practice patterns with respect to antibiotic prescribing after dermatologic surgery,” Dr. Etzkorn noted. “This is the first study to evaluate patient preferences in a rigorous way.”
He and his coinvestigators used a technique from marketing and product research (conjoint analysis/discrete choice experiments) to quantify what patients think about using antibiotics and what trade-offs they are – or are not – willing to make to reduce their risk of infection.
Nearly half of the respondents (47%) were patients, 29% were family members of patients, 19% were health care workers, and the rest were described as patient caregivers or “other.” More than half (59%) were female, the mean age at surgery was 59 years, and 69% had college or postgraduate degrees.
More than half of respondents (55%) would choose to take an antibiotic if it reduced the SSI rate from 5% to 2.5% and if the risk of adverse drug reactions was low (defined as a 1% risk gastrointestinal upset, 0.5% risk itchy skin rash, and 0.01% risk ED visit). Even if an antibiotic could eliminate SSI risk entirely and had a low adverse drug reaction profile, 27% of respondents preferred not to take prophylactic oral antibiotics.
A subgroup analysis revealed that only 21% of health care workers would choose a moderate efficacy antibiotic (2.5% SSI risk) with a high adverse effect profile, compared with 41% of those who do not work in health care. Respondent age also drove treatment choice. For example, only 33% of respondents younger than age 65 would choose a moderate efficacy antibiotic (2.5% SSI risk) with a high adverse effect profile, compared with 45% of those aged 65 years and older.
“We knew patients would likely trade some antibiotic efficacy for some side effects, just as one would trade price for features when shopping for a car,” Dr. Etzkorn said. “We were shocked to see that over a quarter – 27% – of respondents preferred to not take antibiotics even if they were able to prevent all infections and had minimal side effects.”
“It’s interesting that between 27% [and] 55% of patients preferred no operative antibiotic prophylaxis despite a theoretical 100% cure rate for surgical-site infections,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study results.
“I think this mirrors dermatologist’s preferences, as a majority also prefer not to prescribe postoperative antibiotic therapy, unless operating in an area of or a patient with a high risk for infection. It would also be interesting to see if a less educated population would also have similar preferences.”
Dr. Etzkorn acknowledged certain limitations of the study, including that while it evaluated patient reported preferences, it did not include all possible risks and benefits, and “it does not measure actual patient behaviors.”
The researchers reported having no relevant financial disclosures. Dr. Etzkorn disclosed that he serves as a data safety monitoring board member for a clinical trial of Replimmune. Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
(SSI) and had negligible side effects, in a prospective multicenter study.
In addition, a similar proportion of patients preferred to take an antibiotic if there was no SSI reduction and a high risk of adverse events.
Those are two key findings from the study aimed at understanding patient preferences for prophylactic oral antibiotic use following dermatologic surgery, which was published in Dermatologic Surgery.
“Patient risk-benefit thresholds for using antibiotics vary considerably,” the study’s corresponding author, Jeremy R. Etzkorn, MD, MS, of the department of dermatology at the Hospital of the University of Pennsylvania, Philadelphia, told this news organization. “Physicians should appreciate and consider the variation between patients before deciding to send in a prescription after skin surgery.”
To investigate patient preferences about taking antibiotics to prevent SSI relative to antibiotic efficacy and antibiotic-associated adverse drug reactions, Dr. Etzkorn and colleagues at six U.S. medical centers prospectively administered a web-based survey and discrete choice experiment to 388 adults including dermatologic surgery patients and their family members, as well as health care workers (defined as dermatologic surgery patients who work in health care, individuals who work in health care and are accompanying patients to their surgery, or staff in the dermatology clinic.) “A lot has been published about physician preferences and practice patterns with respect to antibiotic prescribing after dermatologic surgery,” Dr. Etzkorn noted. “This is the first study to evaluate patient preferences in a rigorous way.”
He and his coinvestigators used a technique from marketing and product research (conjoint analysis/discrete choice experiments) to quantify what patients think about using antibiotics and what trade-offs they are – or are not – willing to make to reduce their risk of infection.
Nearly half of the respondents (47%) were patients, 29% were family members of patients, 19% were health care workers, and the rest were described as patient caregivers or “other.” More than half (59%) were female, the mean age at surgery was 59 years, and 69% had college or postgraduate degrees.
More than half of respondents (55%) would choose to take an antibiotic if it reduced the SSI rate from 5% to 2.5% and if the risk of adverse drug reactions was low (defined as a 1% risk gastrointestinal upset, 0.5% risk itchy skin rash, and 0.01% risk ED visit). Even if an antibiotic could eliminate SSI risk entirely and had a low adverse drug reaction profile, 27% of respondents preferred not to take prophylactic oral antibiotics.
A subgroup analysis revealed that only 21% of health care workers would choose a moderate efficacy antibiotic (2.5% SSI risk) with a high adverse effect profile, compared with 41% of those who do not work in health care. Respondent age also drove treatment choice. For example, only 33% of respondents younger than age 65 would choose a moderate efficacy antibiotic (2.5% SSI risk) with a high adverse effect profile, compared with 45% of those aged 65 years and older.
“We knew patients would likely trade some antibiotic efficacy for some side effects, just as one would trade price for features when shopping for a car,” Dr. Etzkorn said. “We were shocked to see that over a quarter – 27% – of respondents preferred to not take antibiotics even if they were able to prevent all infections and had minimal side effects.”
“It’s interesting that between 27% [and] 55% of patients preferred no operative antibiotic prophylaxis despite a theoretical 100% cure rate for surgical-site infections,” said Lawrence J. Green, MD, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study results.
“I think this mirrors dermatologist’s preferences, as a majority also prefer not to prescribe postoperative antibiotic therapy, unless operating in an area of or a patient with a high risk for infection. It would also be interesting to see if a less educated population would also have similar preferences.”
Dr. Etzkorn acknowledged certain limitations of the study, including that while it evaluated patient reported preferences, it did not include all possible risks and benefits, and “it does not measure actual patient behaviors.”
The researchers reported having no relevant financial disclosures. Dr. Etzkorn disclosed that he serves as a data safety monitoring board member for a clinical trial of Replimmune. Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies.
FROM DERMATOLOGIC SURGERY