User login
‘Deaths of despair’ rising, but only in the U.S.
In the United States,
This is not the case in 16 other industrialized nations, however, including Canada, Australia, and Japan, where mortality rates are actually decreasing.
One likely reason is that other countries take better care of their citizens from cradle to grave, authors Peter Sterling, PhD, and Michael Platt, PhD, of the University of Pennsylvania, Philadelphia, wrote in a special communication in JAMA Psychiatry published online Feb. 2.
In the United States, individuals and families often struggle in isolation to navigate the life cycle, whereas other countries offer communal assistance to every life stage, and this support protects individuals and families in the long term, they noted.
The United States could solve this “health crisis” by adopting the best practices of these other nations, they wrote.
U.S. is an outlier
From an anthropological perspective, Dr. Sterling and Dr. Platt point out that “hunter-gatherers” prioritized food, comfort, and companionship. When one of these needs is unexpectedly met, the surprise triggers a pulse of the feel-good hormone dopamine.
However, much of modern life offers few opportunities for surprise and dopamine pulses.
“It is the difference between a day’s hard walk to finally encounter and kill a wild pig to feed the family and community versus a quick trip to aisle 7 to select a pork roast in plastic wrap,” Dr. Sterling and Dr. Platt noted.
The hunter-gatherers were far more physically active, and cardiovascular disease, diabetes, obesity, and hypertension were virtually unknown.
The small-scale societies of hunters and gatherers depended on strong family bonds and cooperation with community members.
Modern life is more isolating, often with hours spent alone in front of a computer screen.
Yet the lack of natural dopamine producers in modern society and the increased social isolation is not unique to the United States but holds across the board for industrialized nations.
So why has the United States suffered more deaths of despair?
Dr. Sterling and Dr. Platt assert that it comes down to public support other countries provide their citizens across the life span, from prenatal care and quality preschool and elementary school to affordable (or free) education beyond high school.
This support did not require “bloody revolutions, just simple agreements to prepay basic human needs from public funds collected as taxes,” Dr. Sterling and Dr. Platt noted.
By adopting some of the best practices pioneered by other wealthy nations, the United States could reduce despair and restore to many the will to live, they added.
However, they caution against the “medicalization” of every identified cause of rising death rates.
“Every symptom of despair has been defined as a disorder or dysregulation within the individual. This incorrectly frames the problem, forcing individuals to grapple on their own,” they wrote.
“It also emphasizes treatment by pharmacology, providing innumerable drugs for anxiety, depression, anger, psychosis, and obesity, plus new drugs to treat addictions to the old drugs. We cannot defeat despair solely with pills – to the contrary, pills will only deepen it,” they added.
Dr. Platt reported receiving grant support from the National Institutes of Health, the National Science Foundation, and the Charles E. Kaufman Foundation. He is cofounder of Cogwear and a scientific adviser to Neuroflow, Amplio, Blue Horizon International, and Progenity. Dr. Sterling has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the United States,
This is not the case in 16 other industrialized nations, however, including Canada, Australia, and Japan, where mortality rates are actually decreasing.
One likely reason is that other countries take better care of their citizens from cradle to grave, authors Peter Sterling, PhD, and Michael Platt, PhD, of the University of Pennsylvania, Philadelphia, wrote in a special communication in JAMA Psychiatry published online Feb. 2.
In the United States, individuals and families often struggle in isolation to navigate the life cycle, whereas other countries offer communal assistance to every life stage, and this support protects individuals and families in the long term, they noted.
The United States could solve this “health crisis” by adopting the best practices of these other nations, they wrote.
U.S. is an outlier
From an anthropological perspective, Dr. Sterling and Dr. Platt point out that “hunter-gatherers” prioritized food, comfort, and companionship. When one of these needs is unexpectedly met, the surprise triggers a pulse of the feel-good hormone dopamine.
However, much of modern life offers few opportunities for surprise and dopamine pulses.
“It is the difference between a day’s hard walk to finally encounter and kill a wild pig to feed the family and community versus a quick trip to aisle 7 to select a pork roast in plastic wrap,” Dr. Sterling and Dr. Platt noted.
The hunter-gatherers were far more physically active, and cardiovascular disease, diabetes, obesity, and hypertension were virtually unknown.
The small-scale societies of hunters and gatherers depended on strong family bonds and cooperation with community members.
Modern life is more isolating, often with hours spent alone in front of a computer screen.
Yet the lack of natural dopamine producers in modern society and the increased social isolation is not unique to the United States but holds across the board for industrialized nations.
So why has the United States suffered more deaths of despair?
Dr. Sterling and Dr. Platt assert that it comes down to public support other countries provide their citizens across the life span, from prenatal care and quality preschool and elementary school to affordable (or free) education beyond high school.
This support did not require “bloody revolutions, just simple agreements to prepay basic human needs from public funds collected as taxes,” Dr. Sterling and Dr. Platt noted.
By adopting some of the best practices pioneered by other wealthy nations, the United States could reduce despair and restore to many the will to live, they added.
However, they caution against the “medicalization” of every identified cause of rising death rates.
“Every symptom of despair has been defined as a disorder or dysregulation within the individual. This incorrectly frames the problem, forcing individuals to grapple on their own,” they wrote.
“It also emphasizes treatment by pharmacology, providing innumerable drugs for anxiety, depression, anger, psychosis, and obesity, plus new drugs to treat addictions to the old drugs. We cannot defeat despair solely with pills – to the contrary, pills will only deepen it,” they added.
Dr. Platt reported receiving grant support from the National Institutes of Health, the National Science Foundation, and the Charles E. Kaufman Foundation. He is cofounder of Cogwear and a scientific adviser to Neuroflow, Amplio, Blue Horizon International, and Progenity. Dr. Sterling has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the United States,
This is not the case in 16 other industrialized nations, however, including Canada, Australia, and Japan, where mortality rates are actually decreasing.
One likely reason is that other countries take better care of their citizens from cradle to grave, authors Peter Sterling, PhD, and Michael Platt, PhD, of the University of Pennsylvania, Philadelphia, wrote in a special communication in JAMA Psychiatry published online Feb. 2.
In the United States, individuals and families often struggle in isolation to navigate the life cycle, whereas other countries offer communal assistance to every life stage, and this support protects individuals and families in the long term, they noted.
The United States could solve this “health crisis” by adopting the best practices of these other nations, they wrote.
U.S. is an outlier
From an anthropological perspective, Dr. Sterling and Dr. Platt point out that “hunter-gatherers” prioritized food, comfort, and companionship. When one of these needs is unexpectedly met, the surprise triggers a pulse of the feel-good hormone dopamine.
However, much of modern life offers few opportunities for surprise and dopamine pulses.
“It is the difference between a day’s hard walk to finally encounter and kill a wild pig to feed the family and community versus a quick trip to aisle 7 to select a pork roast in plastic wrap,” Dr. Sterling and Dr. Platt noted.
The hunter-gatherers were far more physically active, and cardiovascular disease, diabetes, obesity, and hypertension were virtually unknown.
The small-scale societies of hunters and gatherers depended on strong family bonds and cooperation with community members.
Modern life is more isolating, often with hours spent alone in front of a computer screen.
Yet the lack of natural dopamine producers in modern society and the increased social isolation is not unique to the United States but holds across the board for industrialized nations.
So why has the United States suffered more deaths of despair?
Dr. Sterling and Dr. Platt assert that it comes down to public support other countries provide their citizens across the life span, from prenatal care and quality preschool and elementary school to affordable (or free) education beyond high school.
This support did not require “bloody revolutions, just simple agreements to prepay basic human needs from public funds collected as taxes,” Dr. Sterling and Dr. Platt noted.
By adopting some of the best practices pioneered by other wealthy nations, the United States could reduce despair and restore to many the will to live, they added.
However, they caution against the “medicalization” of every identified cause of rising death rates.
“Every symptom of despair has been defined as a disorder or dysregulation within the individual. This incorrectly frames the problem, forcing individuals to grapple on their own,” they wrote.
“It also emphasizes treatment by pharmacology, providing innumerable drugs for anxiety, depression, anger, psychosis, and obesity, plus new drugs to treat addictions to the old drugs. We cannot defeat despair solely with pills – to the contrary, pills will only deepen it,” they added.
Dr. Platt reported receiving grant support from the National Institutes of Health, the National Science Foundation, and the Charles E. Kaufman Foundation. He is cofounder of Cogwear and a scientific adviser to Neuroflow, Amplio, Blue Horizon International, and Progenity. Dr. Sterling has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Case report: Male with acute new-onset suicidal ideation tied to SARS-CoV-2
An otherwise healthy 55-year-old male, with no previous psychiatric or medical history, sought care with a family medicine physician for the first time in decades.
Medical symptoms began Oct. 9, 2021, with “some leg weakness and mild sniffles.” Since he was going to be at a public event, he decided to take a PCR test for the SARS-CoV-2 virus on Oct. 13. The patient tested positive.
His symptoms continued to worsen, and he experienced severe body fatigue, sleep disturbance, and lethargy. “A few days after my positive test, the cognitive and physical symptoms dramatically ramped up,” the patient recalled.
Because of those worsening symptoms, on Oct. 20, the patient obtained a new patient appointment with a family medicine physician. After a telemedicine evaluation, the family medicine physician began a multifaceted early outpatient COVID-19 treatment protocol,1 as I (C.M.W.) and colleagues wrote about late last year. However, this treatment began late in the course because of the patient’s initial resistance to seek care.
This early outpatient treatment protocol for COVID-19 included vitamin D3 125 mcg (5,000 ICU), N-acetylcysteine (NAC) 600 mg every day x 30 days; acetylsalicylic acid 325 mg every day x 30 days; azithromycin 250 mg b.i.d. before every meal x 10 days; hydroxychloroquine sulfate 200 mg b.i.d. x 10 days; ivermectin 3 mg, 5 pills daily x 10 days; zinc sulfate 220 mg (50 mg elemental) every day x 30 days; and a prednisone taper (30 mg daily x 3 days, tapering down 5 mg every 3 days). Hydroxyzine 50 mg at bedtime as needed was added for sleep. The patient did not comment to the family physician on any of the psychological or psychiatric symptoms and responded appropriately to questions during the Oct. 20 initial evaluation.
However, he later described that around the time the PCR was positive, For example, he was watching a simple YouTube video for work and “everything was confusing me ... it rattled me, and I couldn’t understand it.” He described his COVID-19 mind as: “The words in my head would come out in a jumbled order, like the message from the words in my brain to my mouth would get crossed. I had trouble spelling and texting. Total cognitive breakdown. I couldn’t do simple mathematics.”
Despite his physical exhaustion, he endured a 3-day period of sleep deprivation. During this time, he recalled looking up at the roof and thinking, “I need to jump off the roof” or thinking, “I might want to throw myself under a bus.” He did not initially reveal his suicidal thoughts to his family medicine physician. After beginning COVID-19 treatment, the patient had two nights of sleep and felt notably improved, and his physical symptoms began to remit. However, the sleeplessness quickly returned “with a vengeance” along with “silly suicidal thoughts.” The thoughts took on a more obsessional quality. For example, he repeatedly thought of jumping out of his second-story bedroom to the living room below and was preoccupied by continually looking at people’s roofs and thinking about jumping. Those thoughts intensified and culminated in his “going missing,” leading his wife to call the police. It was discovered that he had driven to a local bridge and was contemplating jumping off.
After that “going missing” incident, the patient and his wife reached out to their family medicine physician. He reevaluated the patient and, given the new information about the psychiatric symptoms, strongly recommended stat crisis and psychiatric consultation. After discussing the case on the same day, both the family medicine physician and the psychiatrist recommended stat hospital emergency department (ED) assessment on Oct. 29. In the ED, a head CT without contrast at the recommendation of both psychiatrist and family physician, routine electrolytes, CBC with differential, and EKG all were within normal limits. The ED initially discharged him home after crisis evaluation, deciding he was not an imminent risk to himself or others.
The next day, the psychiatrist spoke on the phone with the patient, family medicine physician, and the patient’s wife to arrange an initial assessment. At that time, it remained unclear to all whether the obsessional thoughts had resolved to such a degree that the patient could resist acting upon them. Further, the patient’s sleep architecture had not returned to normal. All agreed another emergency ED assessment was indicated. Ultimately, after voluntary re-evaluation and a difficult hold in the crisis unit, the patient was admitted for psychiatric hospitalization on Oct. 29 and discharged on Nov. 4.
In the psychiatric hospital, venlafaxine XR was started and titrated to 75 mg. The patient was discovered to be hypertensive, and hydrochlorothiazide was started. The discharge diagnosis was major depressive disorder, single episode, severe, without psychotic features.
Posthospitalization course
He was seen for his initial psychiatric outpatient assessment postpsychiatric hospitalization on Nov. 9, as he had not yet been formally evaluated by the psychiatrist because of the emergency situation.
Gabapentin 300 mg by mouth at bedtime was started, and his sleep architecture was restored. The initial plan to titrate venlafaxine XR into dual selective norepinephrine reuptake inhibitor dose range was terminated, and his psychiatrist considered tapering and discontinuing the venlafaxine XR. A clinical examination, additional history, and collateral data no longer necessarily pointed to an active major depressive disorder or even unspecified depressive disorder, though to be sure, the patient was taking 75 mg of venlafaxine XR. While there were seasonal stressors, historically, nothing had risen to the level of MDD.
The obsessions driving his thoughts to jump off buildings and bridges had completely remitted. His cognitive ability returned to baseline with an ability to focus and perform the complicated tasks of his high-intensity work by the Dec. 8 psychiatric examination, where he was accompanied by his wife. He described feeling like, “I snapped back to like I was before this crazy stuff happened.” His mood was reported as, “Very good; like my old self” and this was confirmed by his wife. His affect was calmer and less tense. He was now using gabapentin sparingly for sleep. We continued to entertain discontinuing the venlafaxine XR, considering this recent severe episode likely driven by the COVID-19 virus. The decision was made to continue venlafaxine XR through the winter rather than discontinuing, remaining on the conservative side of treatment. The patient’s diagnosis was changed from “MDD, single episode,” to “mood disorder due to known physiologic condition (COVID-19) (F06.31) with depressive features; resolving.” At the patient’s follow-up examination on Jan. 5, 2022, he was continuing to do well, stating, “The whole series of crazy events happened to someone else.” The hydrochlorothiazide had been discontinued, and the patient’s blood pressure and pulse were normal at 119/81 and 69, respectively. He had made strategic changes at work to lessen stressors during the typically difficult months.
Discussion
Literature has discussed neuropsychiatric sequelae of COVID-19.2 The cited example questions whether psychiatric symptoms are tied directly to the viral infection or to the “host’s immune response.” We believe our case represents a direct neurocognitive/neuropsychiatric insult due to the COVID-19 infection.
This case presents a 55-year-old male with no previous psychiatric or medical history with new onset significant and debilitating cognitive impairment and obsessive thoughts of throwing himself from his bedroom balcony ending up at a bridge struggling with an irrational thought of jumping; ultimately requiring psychiatric hospitalization for acute suicidal thoughts. The patient’s psychiatric symptoms arose prior to any and all medication treatment. The obsessive thoughts correlated both with the onset of SARS-CoV-2 infection and a period of sleep deprivation subsequent to the infection. A course of steroid treatment and taper were started after the onset of neurocognitive-psychiatric symptoms, though there is close timing. We submit that the patient experienced, as part of the initial neurocognitive psychiatric initiating cascade, a COVID-19–induced sleep deprivation that was not etiologic but part of the process; since, even when sleep returned to normal, it was still several weeks before full cognitive function returned to baseline.
An argument could be made for possible MDD or unspecified depressive disorder, as historically there had been work-related stressors for the patient at this time of year because of the chronological nature of his work; though previously nothing presented with obsessional suicidal thinking and nothing with any cognitive impairment – let alone to this incapacitating degree.
The patient describes his seasonal work much like an accountant’s work at the beginning of each year. In the patient’s case, the months of September and October are historically “nonstop, working days,” which then slow down in the winter months for a period of recuperation. In gathering his past history of symptoms, he denied neurovegetative symptoms to meet full diagnostic criteria for MDD or unspecified depressive disorder, absent this episode in the presence of SARS-CoV-2 infection.
We could also consider a contributory negative “organic push” by the viral load and prednisone helping to express an underlying unspecified depression or MDD, but for the profound and unusual presentation. There was little prodrome of depressive symptoms (again, he reported his “typical” extraordinary work burden for this time of year, which is common in his industry).
In this patient, the symptoms have remitted completely. However, the patient is currently taking venlafaxine XR 75 mg. We have considered tapering and discontinuing the venlafaxine – since it is not entirely clear that he needs to be on this medication – so this question remains an open one. We did decide, however, to continue the venlafaxine until after the winter months and to reassess at that time.
Conclusion
The patient presented with new onset psychological and psychiatric symptoms in addition to physiologic symptoms; the former symptoms were not revealed prior to initial family medicine evaluation. As the symptoms worsened, he and his wife sought additional consultation with family physician, psychiatrists, and ED. Steroid treatment may have played a part in exacerbation of symptoms, but the neuropsychiatric cognitive symptoms were present prior to initiation of all pharmacologic and medical treatment. The successful outcome of this case was based upon quick action and collaboration between the family medicine physician, the psychiatrist, and the ED physician. The value of communication, assessment, and action via phone call and text cannot be overstated. Future considerations include further large-scale evaluation of multifaceted early treatment of patients with COVID-19 within the first 72 hours of symptoms to prevent not only hospitalization, morbidity, and mortality, but newly recognized psychological and psychiatric syndromes.3,4
Lastly, fluvoxamine might have been a better choice for adjunctive early treatment of COVID-19.5 As a matter of distinction, if a lingering mood disorder or obsessive-compulsive disorder remain a result of SARS-CoV-2 or if one were to start an antidepressant during the course of illness, it would be reasonable to consider fluvoxamine as a potential first-line agent.
Dr. Kohanski is a fellowship trained forensic psychiatrist and a diplomate of the American Board of Psychiatry & Neurology. She maintains a private practice in Somerset, N.J., and is a frequent media commentator and medical podcaster. Dr. Kohanski has no conflicts of interest. Dr. Wax is a residency-trained osteopathic family medicine physician in independent private practice in Mullica Hill, N.J. He has authored multiple papers over 2 decades on topics such as SARS-CoV-2 and COVID-19 early treatment. He has been a speaker and media host over 2 decades and served on the National Physicians Council on Healthcare Policy’s congressional subcommittee. Dr. Wax has no conflicts of interest.
References
1. Rev Cardiovasc Med. 2020 Dec 30;21(4):517-30.
2. Brain Behav Immun. 2020 Jul;87:34-9.
3. Trav Med Infect Dis. 2020 May-Jun 35;10738.
4. Kirsch S. “Early treatment for COVID is key to better outcomes.” Times of India. 2021 May 21.
5. Lancet. 2022 Jan 1;10(1):E42-E51.
An otherwise healthy 55-year-old male, with no previous psychiatric or medical history, sought care with a family medicine physician for the first time in decades.
Medical symptoms began Oct. 9, 2021, with “some leg weakness and mild sniffles.” Since he was going to be at a public event, he decided to take a PCR test for the SARS-CoV-2 virus on Oct. 13. The patient tested positive.
His symptoms continued to worsen, and he experienced severe body fatigue, sleep disturbance, and lethargy. “A few days after my positive test, the cognitive and physical symptoms dramatically ramped up,” the patient recalled.
Because of those worsening symptoms, on Oct. 20, the patient obtained a new patient appointment with a family medicine physician. After a telemedicine evaluation, the family medicine physician began a multifaceted early outpatient COVID-19 treatment protocol,1 as I (C.M.W.) and colleagues wrote about late last year. However, this treatment began late in the course because of the patient’s initial resistance to seek care.
This early outpatient treatment protocol for COVID-19 included vitamin D3 125 mcg (5,000 ICU), N-acetylcysteine (NAC) 600 mg every day x 30 days; acetylsalicylic acid 325 mg every day x 30 days; azithromycin 250 mg b.i.d. before every meal x 10 days; hydroxychloroquine sulfate 200 mg b.i.d. x 10 days; ivermectin 3 mg, 5 pills daily x 10 days; zinc sulfate 220 mg (50 mg elemental) every day x 30 days; and a prednisone taper (30 mg daily x 3 days, tapering down 5 mg every 3 days). Hydroxyzine 50 mg at bedtime as needed was added for sleep. The patient did not comment to the family physician on any of the psychological or psychiatric symptoms and responded appropriately to questions during the Oct. 20 initial evaluation.
However, he later described that around the time the PCR was positive, For example, he was watching a simple YouTube video for work and “everything was confusing me ... it rattled me, and I couldn’t understand it.” He described his COVID-19 mind as: “The words in my head would come out in a jumbled order, like the message from the words in my brain to my mouth would get crossed. I had trouble spelling and texting. Total cognitive breakdown. I couldn’t do simple mathematics.”
Despite his physical exhaustion, he endured a 3-day period of sleep deprivation. During this time, he recalled looking up at the roof and thinking, “I need to jump off the roof” or thinking, “I might want to throw myself under a bus.” He did not initially reveal his suicidal thoughts to his family medicine physician. After beginning COVID-19 treatment, the patient had two nights of sleep and felt notably improved, and his physical symptoms began to remit. However, the sleeplessness quickly returned “with a vengeance” along with “silly suicidal thoughts.” The thoughts took on a more obsessional quality. For example, he repeatedly thought of jumping out of his second-story bedroom to the living room below and was preoccupied by continually looking at people’s roofs and thinking about jumping. Those thoughts intensified and culminated in his “going missing,” leading his wife to call the police. It was discovered that he had driven to a local bridge and was contemplating jumping off.
After that “going missing” incident, the patient and his wife reached out to their family medicine physician. He reevaluated the patient and, given the new information about the psychiatric symptoms, strongly recommended stat crisis and psychiatric consultation. After discussing the case on the same day, both the family medicine physician and the psychiatrist recommended stat hospital emergency department (ED) assessment on Oct. 29. In the ED, a head CT without contrast at the recommendation of both psychiatrist and family physician, routine electrolytes, CBC with differential, and EKG all were within normal limits. The ED initially discharged him home after crisis evaluation, deciding he was not an imminent risk to himself or others.
The next day, the psychiatrist spoke on the phone with the patient, family medicine physician, and the patient’s wife to arrange an initial assessment. At that time, it remained unclear to all whether the obsessional thoughts had resolved to such a degree that the patient could resist acting upon them. Further, the patient’s sleep architecture had not returned to normal. All agreed another emergency ED assessment was indicated. Ultimately, after voluntary re-evaluation and a difficult hold in the crisis unit, the patient was admitted for psychiatric hospitalization on Oct. 29 and discharged on Nov. 4.
In the psychiatric hospital, venlafaxine XR was started and titrated to 75 mg. The patient was discovered to be hypertensive, and hydrochlorothiazide was started. The discharge diagnosis was major depressive disorder, single episode, severe, without psychotic features.
Posthospitalization course
He was seen for his initial psychiatric outpatient assessment postpsychiatric hospitalization on Nov. 9, as he had not yet been formally evaluated by the psychiatrist because of the emergency situation.
Gabapentin 300 mg by mouth at bedtime was started, and his sleep architecture was restored. The initial plan to titrate venlafaxine XR into dual selective norepinephrine reuptake inhibitor dose range was terminated, and his psychiatrist considered tapering and discontinuing the venlafaxine XR. A clinical examination, additional history, and collateral data no longer necessarily pointed to an active major depressive disorder or even unspecified depressive disorder, though to be sure, the patient was taking 75 mg of venlafaxine XR. While there were seasonal stressors, historically, nothing had risen to the level of MDD.
The obsessions driving his thoughts to jump off buildings and bridges had completely remitted. His cognitive ability returned to baseline with an ability to focus and perform the complicated tasks of his high-intensity work by the Dec. 8 psychiatric examination, where he was accompanied by his wife. He described feeling like, “I snapped back to like I was before this crazy stuff happened.” His mood was reported as, “Very good; like my old self” and this was confirmed by his wife. His affect was calmer and less tense. He was now using gabapentin sparingly for sleep. We continued to entertain discontinuing the venlafaxine XR, considering this recent severe episode likely driven by the COVID-19 virus. The decision was made to continue venlafaxine XR through the winter rather than discontinuing, remaining on the conservative side of treatment. The patient’s diagnosis was changed from “MDD, single episode,” to “mood disorder due to known physiologic condition (COVID-19) (F06.31) with depressive features; resolving.” At the patient’s follow-up examination on Jan. 5, 2022, he was continuing to do well, stating, “The whole series of crazy events happened to someone else.” The hydrochlorothiazide had been discontinued, and the patient’s blood pressure and pulse were normal at 119/81 and 69, respectively. He had made strategic changes at work to lessen stressors during the typically difficult months.
Discussion
Literature has discussed neuropsychiatric sequelae of COVID-19.2 The cited example questions whether psychiatric symptoms are tied directly to the viral infection or to the “host’s immune response.” We believe our case represents a direct neurocognitive/neuropsychiatric insult due to the COVID-19 infection.
This case presents a 55-year-old male with no previous psychiatric or medical history with new onset significant and debilitating cognitive impairment and obsessive thoughts of throwing himself from his bedroom balcony ending up at a bridge struggling with an irrational thought of jumping; ultimately requiring psychiatric hospitalization for acute suicidal thoughts. The patient’s psychiatric symptoms arose prior to any and all medication treatment. The obsessive thoughts correlated both with the onset of SARS-CoV-2 infection and a period of sleep deprivation subsequent to the infection. A course of steroid treatment and taper were started after the onset of neurocognitive-psychiatric symptoms, though there is close timing. We submit that the patient experienced, as part of the initial neurocognitive psychiatric initiating cascade, a COVID-19–induced sleep deprivation that was not etiologic but part of the process; since, even when sleep returned to normal, it was still several weeks before full cognitive function returned to baseline.
An argument could be made for possible MDD or unspecified depressive disorder, as historically there had been work-related stressors for the patient at this time of year because of the chronological nature of his work; though previously nothing presented with obsessional suicidal thinking and nothing with any cognitive impairment – let alone to this incapacitating degree.
The patient describes his seasonal work much like an accountant’s work at the beginning of each year. In the patient’s case, the months of September and October are historically “nonstop, working days,” which then slow down in the winter months for a period of recuperation. In gathering his past history of symptoms, he denied neurovegetative symptoms to meet full diagnostic criteria for MDD or unspecified depressive disorder, absent this episode in the presence of SARS-CoV-2 infection.
We could also consider a contributory negative “organic push” by the viral load and prednisone helping to express an underlying unspecified depression or MDD, but for the profound and unusual presentation. There was little prodrome of depressive symptoms (again, he reported his “typical” extraordinary work burden for this time of year, which is common in his industry).
In this patient, the symptoms have remitted completely. However, the patient is currently taking venlafaxine XR 75 mg. We have considered tapering and discontinuing the venlafaxine – since it is not entirely clear that he needs to be on this medication – so this question remains an open one. We did decide, however, to continue the venlafaxine until after the winter months and to reassess at that time.
Conclusion
The patient presented with new onset psychological and psychiatric symptoms in addition to physiologic symptoms; the former symptoms were not revealed prior to initial family medicine evaluation. As the symptoms worsened, he and his wife sought additional consultation with family physician, psychiatrists, and ED. Steroid treatment may have played a part in exacerbation of symptoms, but the neuropsychiatric cognitive symptoms were present prior to initiation of all pharmacologic and medical treatment. The successful outcome of this case was based upon quick action and collaboration between the family medicine physician, the psychiatrist, and the ED physician. The value of communication, assessment, and action via phone call and text cannot be overstated. Future considerations include further large-scale evaluation of multifaceted early treatment of patients with COVID-19 within the first 72 hours of symptoms to prevent not only hospitalization, morbidity, and mortality, but newly recognized psychological and psychiatric syndromes.3,4
Lastly, fluvoxamine might have been a better choice for adjunctive early treatment of COVID-19.5 As a matter of distinction, if a lingering mood disorder or obsessive-compulsive disorder remain a result of SARS-CoV-2 or if one were to start an antidepressant during the course of illness, it would be reasonable to consider fluvoxamine as a potential first-line agent.
Dr. Kohanski is a fellowship trained forensic psychiatrist and a diplomate of the American Board of Psychiatry & Neurology. She maintains a private practice in Somerset, N.J., and is a frequent media commentator and medical podcaster. Dr. Kohanski has no conflicts of interest. Dr. Wax is a residency-trained osteopathic family medicine physician in independent private practice in Mullica Hill, N.J. He has authored multiple papers over 2 decades on topics such as SARS-CoV-2 and COVID-19 early treatment. He has been a speaker and media host over 2 decades and served on the National Physicians Council on Healthcare Policy’s congressional subcommittee. Dr. Wax has no conflicts of interest.
References
1. Rev Cardiovasc Med. 2020 Dec 30;21(4):517-30.
2. Brain Behav Immun. 2020 Jul;87:34-9.
3. Trav Med Infect Dis. 2020 May-Jun 35;10738.
4. Kirsch S. “Early treatment for COVID is key to better outcomes.” Times of India. 2021 May 21.
5. Lancet. 2022 Jan 1;10(1):E42-E51.
An otherwise healthy 55-year-old male, with no previous psychiatric or medical history, sought care with a family medicine physician for the first time in decades.
Medical symptoms began Oct. 9, 2021, with “some leg weakness and mild sniffles.” Since he was going to be at a public event, he decided to take a PCR test for the SARS-CoV-2 virus on Oct. 13. The patient tested positive.
His symptoms continued to worsen, and he experienced severe body fatigue, sleep disturbance, and lethargy. “A few days after my positive test, the cognitive and physical symptoms dramatically ramped up,” the patient recalled.
Because of those worsening symptoms, on Oct. 20, the patient obtained a new patient appointment with a family medicine physician. After a telemedicine evaluation, the family medicine physician began a multifaceted early outpatient COVID-19 treatment protocol,1 as I (C.M.W.) and colleagues wrote about late last year. However, this treatment began late in the course because of the patient’s initial resistance to seek care.
This early outpatient treatment protocol for COVID-19 included vitamin D3 125 mcg (5,000 ICU), N-acetylcysteine (NAC) 600 mg every day x 30 days; acetylsalicylic acid 325 mg every day x 30 days; azithromycin 250 mg b.i.d. before every meal x 10 days; hydroxychloroquine sulfate 200 mg b.i.d. x 10 days; ivermectin 3 mg, 5 pills daily x 10 days; zinc sulfate 220 mg (50 mg elemental) every day x 30 days; and a prednisone taper (30 mg daily x 3 days, tapering down 5 mg every 3 days). Hydroxyzine 50 mg at bedtime as needed was added for sleep. The patient did not comment to the family physician on any of the psychological or psychiatric symptoms and responded appropriately to questions during the Oct. 20 initial evaluation.
However, he later described that around the time the PCR was positive, For example, he was watching a simple YouTube video for work and “everything was confusing me ... it rattled me, and I couldn’t understand it.” He described his COVID-19 mind as: “The words in my head would come out in a jumbled order, like the message from the words in my brain to my mouth would get crossed. I had trouble spelling and texting. Total cognitive breakdown. I couldn’t do simple mathematics.”
Despite his physical exhaustion, he endured a 3-day period of sleep deprivation. During this time, he recalled looking up at the roof and thinking, “I need to jump off the roof” or thinking, “I might want to throw myself under a bus.” He did not initially reveal his suicidal thoughts to his family medicine physician. After beginning COVID-19 treatment, the patient had two nights of sleep and felt notably improved, and his physical symptoms began to remit. However, the sleeplessness quickly returned “with a vengeance” along with “silly suicidal thoughts.” The thoughts took on a more obsessional quality. For example, he repeatedly thought of jumping out of his second-story bedroom to the living room below and was preoccupied by continually looking at people’s roofs and thinking about jumping. Those thoughts intensified and culminated in his “going missing,” leading his wife to call the police. It was discovered that he had driven to a local bridge and was contemplating jumping off.
After that “going missing” incident, the patient and his wife reached out to their family medicine physician. He reevaluated the patient and, given the new information about the psychiatric symptoms, strongly recommended stat crisis and psychiatric consultation. After discussing the case on the same day, both the family medicine physician and the psychiatrist recommended stat hospital emergency department (ED) assessment on Oct. 29. In the ED, a head CT without contrast at the recommendation of both psychiatrist and family physician, routine electrolytes, CBC with differential, and EKG all were within normal limits. The ED initially discharged him home after crisis evaluation, deciding he was not an imminent risk to himself or others.
The next day, the psychiatrist spoke on the phone with the patient, family medicine physician, and the patient’s wife to arrange an initial assessment. At that time, it remained unclear to all whether the obsessional thoughts had resolved to such a degree that the patient could resist acting upon them. Further, the patient’s sleep architecture had not returned to normal. All agreed another emergency ED assessment was indicated. Ultimately, after voluntary re-evaluation and a difficult hold in the crisis unit, the patient was admitted for psychiatric hospitalization on Oct. 29 and discharged on Nov. 4.
In the psychiatric hospital, venlafaxine XR was started and titrated to 75 mg. The patient was discovered to be hypertensive, and hydrochlorothiazide was started. The discharge diagnosis was major depressive disorder, single episode, severe, without psychotic features.
Posthospitalization course
He was seen for his initial psychiatric outpatient assessment postpsychiatric hospitalization on Nov. 9, as he had not yet been formally evaluated by the psychiatrist because of the emergency situation.
Gabapentin 300 mg by mouth at bedtime was started, and his sleep architecture was restored. The initial plan to titrate venlafaxine XR into dual selective norepinephrine reuptake inhibitor dose range was terminated, and his psychiatrist considered tapering and discontinuing the venlafaxine XR. A clinical examination, additional history, and collateral data no longer necessarily pointed to an active major depressive disorder or even unspecified depressive disorder, though to be sure, the patient was taking 75 mg of venlafaxine XR. While there were seasonal stressors, historically, nothing had risen to the level of MDD.
The obsessions driving his thoughts to jump off buildings and bridges had completely remitted. His cognitive ability returned to baseline with an ability to focus and perform the complicated tasks of his high-intensity work by the Dec. 8 psychiatric examination, where he was accompanied by his wife. He described feeling like, “I snapped back to like I was before this crazy stuff happened.” His mood was reported as, “Very good; like my old self” and this was confirmed by his wife. His affect was calmer and less tense. He was now using gabapentin sparingly for sleep. We continued to entertain discontinuing the venlafaxine XR, considering this recent severe episode likely driven by the COVID-19 virus. The decision was made to continue venlafaxine XR through the winter rather than discontinuing, remaining on the conservative side of treatment. The patient’s diagnosis was changed from “MDD, single episode,” to “mood disorder due to known physiologic condition (COVID-19) (F06.31) with depressive features; resolving.” At the patient’s follow-up examination on Jan. 5, 2022, he was continuing to do well, stating, “The whole series of crazy events happened to someone else.” The hydrochlorothiazide had been discontinued, and the patient’s blood pressure and pulse were normal at 119/81 and 69, respectively. He had made strategic changes at work to lessen stressors during the typically difficult months.
Discussion
Literature has discussed neuropsychiatric sequelae of COVID-19.2 The cited example questions whether psychiatric symptoms are tied directly to the viral infection or to the “host’s immune response.” We believe our case represents a direct neurocognitive/neuropsychiatric insult due to the COVID-19 infection.
This case presents a 55-year-old male with no previous psychiatric or medical history with new onset significant and debilitating cognitive impairment and obsessive thoughts of throwing himself from his bedroom balcony ending up at a bridge struggling with an irrational thought of jumping; ultimately requiring psychiatric hospitalization for acute suicidal thoughts. The patient’s psychiatric symptoms arose prior to any and all medication treatment. The obsessive thoughts correlated both with the onset of SARS-CoV-2 infection and a period of sleep deprivation subsequent to the infection. A course of steroid treatment and taper were started after the onset of neurocognitive-psychiatric symptoms, though there is close timing. We submit that the patient experienced, as part of the initial neurocognitive psychiatric initiating cascade, a COVID-19–induced sleep deprivation that was not etiologic but part of the process; since, even when sleep returned to normal, it was still several weeks before full cognitive function returned to baseline.
An argument could be made for possible MDD or unspecified depressive disorder, as historically there had been work-related stressors for the patient at this time of year because of the chronological nature of his work; though previously nothing presented with obsessional suicidal thinking and nothing with any cognitive impairment – let alone to this incapacitating degree.
The patient describes his seasonal work much like an accountant’s work at the beginning of each year. In the patient’s case, the months of September and October are historically “nonstop, working days,” which then slow down in the winter months for a period of recuperation. In gathering his past history of symptoms, he denied neurovegetative symptoms to meet full diagnostic criteria for MDD or unspecified depressive disorder, absent this episode in the presence of SARS-CoV-2 infection.
We could also consider a contributory negative “organic push” by the viral load and prednisone helping to express an underlying unspecified depression or MDD, but for the profound and unusual presentation. There was little prodrome of depressive symptoms (again, he reported his “typical” extraordinary work burden for this time of year, which is common in his industry).
In this patient, the symptoms have remitted completely. However, the patient is currently taking venlafaxine XR 75 mg. We have considered tapering and discontinuing the venlafaxine – since it is not entirely clear that he needs to be on this medication – so this question remains an open one. We did decide, however, to continue the venlafaxine until after the winter months and to reassess at that time.
Conclusion
The patient presented with new onset psychological and psychiatric symptoms in addition to physiologic symptoms; the former symptoms were not revealed prior to initial family medicine evaluation. As the symptoms worsened, he and his wife sought additional consultation with family physician, psychiatrists, and ED. Steroid treatment may have played a part in exacerbation of symptoms, but the neuropsychiatric cognitive symptoms were present prior to initiation of all pharmacologic and medical treatment. The successful outcome of this case was based upon quick action and collaboration between the family medicine physician, the psychiatrist, and the ED physician. The value of communication, assessment, and action via phone call and text cannot be overstated. Future considerations include further large-scale evaluation of multifaceted early treatment of patients with COVID-19 within the first 72 hours of symptoms to prevent not only hospitalization, morbidity, and mortality, but newly recognized psychological and psychiatric syndromes.3,4
Lastly, fluvoxamine might have been a better choice for adjunctive early treatment of COVID-19.5 As a matter of distinction, if a lingering mood disorder or obsessive-compulsive disorder remain a result of SARS-CoV-2 or if one were to start an antidepressant during the course of illness, it would be reasonable to consider fluvoxamine as a potential first-line agent.
Dr. Kohanski is a fellowship trained forensic psychiatrist and a diplomate of the American Board of Psychiatry & Neurology. She maintains a private practice in Somerset, N.J., and is a frequent media commentator and medical podcaster. Dr. Kohanski has no conflicts of interest. Dr. Wax is a residency-trained osteopathic family medicine physician in independent private practice in Mullica Hill, N.J. He has authored multiple papers over 2 decades on topics such as SARS-CoV-2 and COVID-19 early treatment. He has been a speaker and media host over 2 decades and served on the National Physicians Council on Healthcare Policy’s congressional subcommittee. Dr. Wax has no conflicts of interest.
References
1. Rev Cardiovasc Med. 2020 Dec 30;21(4):517-30.
2. Brain Behav Immun. 2020 Jul;87:34-9.
3. Trav Med Infect Dis. 2020 May-Jun 35;10738.
4. Kirsch S. “Early treatment for COVID is key to better outcomes.” Times of India. 2021 May 21.
5. Lancet. 2022 Jan 1;10(1):E42-E51.
HIV stigma persists globally, according to Harris poll
Four decades into the AIDS epidemic and for some, it’s as if gains in awareness, advances in prevention and treatment, and the concept of undetected equals untransmissable (U=U) never happened. In its place,
Accordingly, findings from a Harris poll conducted Oct. 13-18, 2021, among 5,047 adults (18 and older) residing in Australia, Portugal, the United Kingdom, and the United States, reveal that 88% of those surveyed believe that negative perceptions toward people living with HIV persist even though HIV infection can be effectively managed with antiretroviral therapy (ART). Conversely, three-quarters (76%) are unaware of U=U, and the fact that someone with HIV who is taking effective treatment cannot pass it on to their partner. Two-thirds incorrectly believe that a person living with HIV can pass it onto their baby, even when they are ART adherent.
“The survey made me think of people who work in HIV clinics, and how much of a bubble I think that we in the HIV field live in,” Nneka Nwokolo, MBBS, senior global medical director at ViiV Healthcare, London, and practicing consultant in sexual health and HIV medicine, told this news organization. “I think that we generally feel that everyone knows as much as we do or feels the way that we do.”
Misconceptions abound across the globe
The online survey, which was commissioned by ViiV Healthcare, also highlights that one in five adults do not know that anyone can acquire HIV regardless of lifestyle, thereby perpetuating the stereotype that HIV is a disease that only affects certain populations, such as men who have sex with men (MSM) or transgender women (TGW).
Pervasive stereotypes and stigmatization only serve to magnify preexisting social inequities that affect access to appropriate care. A recent editorial published in the journal AIDS and Behavior underscores that stigma experienced by marginalized populations in particular (for example, Black MSM, TGW) is directly linked to decreased access to and use of effective HIV prevention and treatment services. Additionally, once stigma becomes internalized, it might further affect overall well-being, mental health, and social support.
“One of the most significant consequences of the ongoing stigma is that people are scared to test and then they end up coming to services late [when] they’re really ill,” explained Dr. Nwokolo. “It goes back to the early days when HIV was a death sentence ... it’s still there. I have one patient who to this day hates the fact that he has HIV, that he has to come to the clinic – it’s a reminder of why he hates himself.”
Great strides in testing and advances in treatment might be helping to reframe HIV as a chronic but treatable and preventable disease. Nevertheless, survey findings also revealed that nearly three out of five adults incorrectly believe that a person living with HIV will have a shorter lifespan than someone who is HIV negative, even if they are on effective treatment.
These beliefs are especially true among Dr. Nwokolo’s patient base, most of whom are Africans who’ve immigrated to the United Kingdom from countries that have been devastated by the HIV epidemic. “Those who’ve never tested are reluctant to do so because they are afraid that they will have the same outcome as the people that they know that they’ve left behind,” she said.
HIV stigma in the era of 90-90-90
While there has been progress toward achieving UN AID’s 90-90-90 targets (that is, 90% living with HIV know their status, 90% who know their status are on ART, and 90% of people on ART are virally suppressed), exclusion and isolation – the key hallmarks of stigma – may ultimately be the most important barriers preventing a lofty goal to end the AIDS epidemic by the year 2030.
“Here we are, 40 years in and we are still facing such ignorance, some stigma,” Carl Schmid, MBA, former cochair of the Presidential Advisory Council on HIV/AIDS, and executive director of HIV+Policy Institute, told this news organization. “It’s gotten better, but it is really putting a damper on people being tested, getting treated, getting access to PrEP.” Mr. Schmid was not involved in the Harris Poll.
Mr. Schmid also said that, in addition to broader outreach and education as well as dissemination of information about HIV and AIDS from the White House and other government leaders, physician involvement is essential.
“They’re the ones that need to step up. They have to talk about sex with their patients, [but] they don’t do that, especially in the South among certain populations,” he noted.
Data support the unique challenges faced by at-risk individuals living in the southern United States. Not only do Southern states account for roughly half of all new HIV cases annually, but Black MSM and Black women account for the majority of new diagnoses, according to the Centers for Disease Control and Prevention. Data have also demonstrated discrimination and prejudice toward people with HIV persist among many medical professionals in the South (especially those working in rural areas).
But this is not only a Southern problem; a 2018 review of studies in clinicians across the United States published in AIDS Patient Care and STDs linked provider fear of acquiring HIV through occupational exposure to reduced quality of care, refusal of care, and anxiety, especially among providers with limited awareness of PrEP. Discordant attitudes around making a priority to address HIV-related stigma versus other health care needs also reduced overall care delivery and patient experience.
“I think that the first thing that we as HIV clinicians can and should do – and is definitely within our power to do – is to educate our peers about HIV,” Dr. Nwokolo said, “HIV has gone off the radar, but it’s still out there.”
The study was commissioned by Viiv Healthcare. Dr. Nwokolo is an employee of ViiV Healthcare. Mr. Schmid disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Four decades into the AIDS epidemic and for some, it’s as if gains in awareness, advances in prevention and treatment, and the concept of undetected equals untransmissable (U=U) never happened. In its place,
Accordingly, findings from a Harris poll conducted Oct. 13-18, 2021, among 5,047 adults (18 and older) residing in Australia, Portugal, the United Kingdom, and the United States, reveal that 88% of those surveyed believe that negative perceptions toward people living with HIV persist even though HIV infection can be effectively managed with antiretroviral therapy (ART). Conversely, three-quarters (76%) are unaware of U=U, and the fact that someone with HIV who is taking effective treatment cannot pass it on to their partner. Two-thirds incorrectly believe that a person living with HIV can pass it onto their baby, even when they are ART adherent.
“The survey made me think of people who work in HIV clinics, and how much of a bubble I think that we in the HIV field live in,” Nneka Nwokolo, MBBS, senior global medical director at ViiV Healthcare, London, and practicing consultant in sexual health and HIV medicine, told this news organization. “I think that we generally feel that everyone knows as much as we do or feels the way that we do.”
Misconceptions abound across the globe
The online survey, which was commissioned by ViiV Healthcare, also highlights that one in five adults do not know that anyone can acquire HIV regardless of lifestyle, thereby perpetuating the stereotype that HIV is a disease that only affects certain populations, such as men who have sex with men (MSM) or transgender women (TGW).
Pervasive stereotypes and stigmatization only serve to magnify preexisting social inequities that affect access to appropriate care. A recent editorial published in the journal AIDS and Behavior underscores that stigma experienced by marginalized populations in particular (for example, Black MSM, TGW) is directly linked to decreased access to and use of effective HIV prevention and treatment services. Additionally, once stigma becomes internalized, it might further affect overall well-being, mental health, and social support.
“One of the most significant consequences of the ongoing stigma is that people are scared to test and then they end up coming to services late [when] they’re really ill,” explained Dr. Nwokolo. “It goes back to the early days when HIV was a death sentence ... it’s still there. I have one patient who to this day hates the fact that he has HIV, that he has to come to the clinic – it’s a reminder of why he hates himself.”
Great strides in testing and advances in treatment might be helping to reframe HIV as a chronic but treatable and preventable disease. Nevertheless, survey findings also revealed that nearly three out of five adults incorrectly believe that a person living with HIV will have a shorter lifespan than someone who is HIV negative, even if they are on effective treatment.
These beliefs are especially true among Dr. Nwokolo’s patient base, most of whom are Africans who’ve immigrated to the United Kingdom from countries that have been devastated by the HIV epidemic. “Those who’ve never tested are reluctant to do so because they are afraid that they will have the same outcome as the people that they know that they’ve left behind,” she said.
HIV stigma in the era of 90-90-90
While there has been progress toward achieving UN AID’s 90-90-90 targets (that is, 90% living with HIV know their status, 90% who know their status are on ART, and 90% of people on ART are virally suppressed), exclusion and isolation – the key hallmarks of stigma – may ultimately be the most important barriers preventing a lofty goal to end the AIDS epidemic by the year 2030.
“Here we are, 40 years in and we are still facing such ignorance, some stigma,” Carl Schmid, MBA, former cochair of the Presidential Advisory Council on HIV/AIDS, and executive director of HIV+Policy Institute, told this news organization. “It’s gotten better, but it is really putting a damper on people being tested, getting treated, getting access to PrEP.” Mr. Schmid was not involved in the Harris Poll.
Mr. Schmid also said that, in addition to broader outreach and education as well as dissemination of information about HIV and AIDS from the White House and other government leaders, physician involvement is essential.
“They’re the ones that need to step up. They have to talk about sex with their patients, [but] they don’t do that, especially in the South among certain populations,” he noted.
Data support the unique challenges faced by at-risk individuals living in the southern United States. Not only do Southern states account for roughly half of all new HIV cases annually, but Black MSM and Black women account for the majority of new diagnoses, according to the Centers for Disease Control and Prevention. Data have also demonstrated discrimination and prejudice toward people with HIV persist among many medical professionals in the South (especially those working in rural areas).
But this is not only a Southern problem; a 2018 review of studies in clinicians across the United States published in AIDS Patient Care and STDs linked provider fear of acquiring HIV through occupational exposure to reduced quality of care, refusal of care, and anxiety, especially among providers with limited awareness of PrEP. Discordant attitudes around making a priority to address HIV-related stigma versus other health care needs also reduced overall care delivery and patient experience.
“I think that the first thing that we as HIV clinicians can and should do – and is definitely within our power to do – is to educate our peers about HIV,” Dr. Nwokolo said, “HIV has gone off the radar, but it’s still out there.”
The study was commissioned by Viiv Healthcare. Dr. Nwokolo is an employee of ViiV Healthcare. Mr. Schmid disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Four decades into the AIDS epidemic and for some, it’s as if gains in awareness, advances in prevention and treatment, and the concept of undetected equals untransmissable (U=U) never happened. In its place,
Accordingly, findings from a Harris poll conducted Oct. 13-18, 2021, among 5,047 adults (18 and older) residing in Australia, Portugal, the United Kingdom, and the United States, reveal that 88% of those surveyed believe that negative perceptions toward people living with HIV persist even though HIV infection can be effectively managed with antiretroviral therapy (ART). Conversely, three-quarters (76%) are unaware of U=U, and the fact that someone with HIV who is taking effective treatment cannot pass it on to their partner. Two-thirds incorrectly believe that a person living with HIV can pass it onto their baby, even when they are ART adherent.
“The survey made me think of people who work in HIV clinics, and how much of a bubble I think that we in the HIV field live in,” Nneka Nwokolo, MBBS, senior global medical director at ViiV Healthcare, London, and practicing consultant in sexual health and HIV medicine, told this news organization. “I think that we generally feel that everyone knows as much as we do or feels the way that we do.”
Misconceptions abound across the globe
The online survey, which was commissioned by ViiV Healthcare, also highlights that one in five adults do not know that anyone can acquire HIV regardless of lifestyle, thereby perpetuating the stereotype that HIV is a disease that only affects certain populations, such as men who have sex with men (MSM) or transgender women (TGW).
Pervasive stereotypes and stigmatization only serve to magnify preexisting social inequities that affect access to appropriate care. A recent editorial published in the journal AIDS and Behavior underscores that stigma experienced by marginalized populations in particular (for example, Black MSM, TGW) is directly linked to decreased access to and use of effective HIV prevention and treatment services. Additionally, once stigma becomes internalized, it might further affect overall well-being, mental health, and social support.
“One of the most significant consequences of the ongoing stigma is that people are scared to test and then they end up coming to services late [when] they’re really ill,” explained Dr. Nwokolo. “It goes back to the early days when HIV was a death sentence ... it’s still there. I have one patient who to this day hates the fact that he has HIV, that he has to come to the clinic – it’s a reminder of why he hates himself.”
Great strides in testing and advances in treatment might be helping to reframe HIV as a chronic but treatable and preventable disease. Nevertheless, survey findings also revealed that nearly three out of five adults incorrectly believe that a person living with HIV will have a shorter lifespan than someone who is HIV negative, even if they are on effective treatment.
These beliefs are especially true among Dr. Nwokolo’s patient base, most of whom are Africans who’ve immigrated to the United Kingdom from countries that have been devastated by the HIV epidemic. “Those who’ve never tested are reluctant to do so because they are afraid that they will have the same outcome as the people that they know that they’ve left behind,” she said.
HIV stigma in the era of 90-90-90
While there has been progress toward achieving UN AID’s 90-90-90 targets (that is, 90% living with HIV know their status, 90% who know their status are on ART, and 90% of people on ART are virally suppressed), exclusion and isolation – the key hallmarks of stigma – may ultimately be the most important barriers preventing a lofty goal to end the AIDS epidemic by the year 2030.
“Here we are, 40 years in and we are still facing such ignorance, some stigma,” Carl Schmid, MBA, former cochair of the Presidential Advisory Council on HIV/AIDS, and executive director of HIV+Policy Institute, told this news organization. “It’s gotten better, but it is really putting a damper on people being tested, getting treated, getting access to PrEP.” Mr. Schmid was not involved in the Harris Poll.
Mr. Schmid also said that, in addition to broader outreach and education as well as dissemination of information about HIV and AIDS from the White House and other government leaders, physician involvement is essential.
“They’re the ones that need to step up. They have to talk about sex with their patients, [but] they don’t do that, especially in the South among certain populations,” he noted.
Data support the unique challenges faced by at-risk individuals living in the southern United States. Not only do Southern states account for roughly half of all new HIV cases annually, but Black MSM and Black women account for the majority of new diagnoses, according to the Centers for Disease Control and Prevention. Data have also demonstrated discrimination and prejudice toward people with HIV persist among many medical professionals in the South (especially those working in rural areas).
But this is not only a Southern problem; a 2018 review of studies in clinicians across the United States published in AIDS Patient Care and STDs linked provider fear of acquiring HIV through occupational exposure to reduced quality of care, refusal of care, and anxiety, especially among providers with limited awareness of PrEP. Discordant attitudes around making a priority to address HIV-related stigma versus other health care needs also reduced overall care delivery and patient experience.
“I think that the first thing that we as HIV clinicians can and should do – and is definitely within our power to do – is to educate our peers about HIV,” Dr. Nwokolo said, “HIV has gone off the radar, but it’s still out there.”
The study was commissioned by Viiv Healthcare. Dr. Nwokolo is an employee of ViiV Healthcare. Mr. Schmid disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychedelic therapy and suicide: A myth busted?
A commonly held belief that classic psychedelic therapy can trigger suicidal thoughts, actions, or other types of self-harm is not supported by research, and, in fact, the opposite may be true.
Results from a meta-analysis of individual patient data showed that psychedelic therapy was associated with large, acute, and sustained decreases in suicidality across a range of clinical patient populations.
“ It gives us a better understanding of the effects of psychedelics on suicidality in the context of clinical trials,” study investigator Cory Weissman, MD, department of psychiatry, University of Toronto, told this news organization.
The evidence suggests psychedelic therapy “may reduce suicidal ideation when administered in the appropriate setting and offered to carefully screened patients,” Dr. Weissman said.
The findings were published online Jan. 18 in The Journal of Clinical Psychiatry.
More research needed
The analysis included seven psychedelic therapy clinical trials that had data on suicidality. Five of the trials used psilocybin plus psychotherapy and two used ayahuasca plus psychotherapy. All seven trials had a “low” risk of bias.
Patients included in the trials had treatment-resistant major depressive disorder (MDD), recurrent MDD, AIDS-related demoralization, and distress related to life-threatening cancer.
The meta-analytic results showed significant decreases in suicidality at all acute time points (80 to 240 minutes post administration) and at most post-acute time points (1 day to 4 months post administration).
Effect sizes for reductions in suicidality were “large” at all acute time points, with standardized mean differences (SMD) ranging from -1.48 to -1.72, and remained large from 1 day to 3-4 months after therapy (SMD range, -1.50 to -2.36).
At 6 months, the effect size for reductions in suicidality with psychedelic therapy was “medium” (SMD, -0.65).
Large effect sizes for reductions in suicidality occurred across the different patient populations represented in the trial, the investigators note.
No study reported any suicide-related adverse events because of administration of a psychedelic. There were also “very few” acute (6.5%) or postacute (3.0%) elevations in suicidality, “providing support for the safety of psychedelic therapy within controlled contexts,” the researchers write.
They caution, however, that large controlled trials that specifically evaluate the effect of psychedelic therapy on suicidality are needed.
Promising avenue
In an accompanying editorial, Daniel Grossman, BS, and Peter Hendricks, PhD, department of health behavior, University of Alabama at Birmingham, note that results of this review warrant “optimism” for use of psychedelics for treatment of suicidality.
Based on this study and others, classic psychedelic therapy for suicidality appears to be a “promising avenue” for further investigation, they write.
However, research and anecdotes about increased suicidality and other self-harm attributed to psychedelic therapy, “though evidently rare, remain a critical concern” for further research to address, Dr. Grossman and Dr. Hendricks add.
The hope is that future research “clarifies who is most subject to these risks, what factors best identify them, and how best to navigate their treatment safely,” they write.
The meta-analysis had no funding. Dr. Weissman receives funding from the Brain and Behavior Research Foundation and serves on the advisory board of GoodCap Pharmaceuticals. Dr. Hendricks is on the scientific advisory board of Bright Minds Biosciences, Eleusis Benefit Corporation, and Rest Pharmaceuticals.
A version of this article first appeared on Medscape.com.
A commonly held belief that classic psychedelic therapy can trigger suicidal thoughts, actions, or other types of self-harm is not supported by research, and, in fact, the opposite may be true.
Results from a meta-analysis of individual patient data showed that psychedelic therapy was associated with large, acute, and sustained decreases in suicidality across a range of clinical patient populations.
“ It gives us a better understanding of the effects of psychedelics on suicidality in the context of clinical trials,” study investigator Cory Weissman, MD, department of psychiatry, University of Toronto, told this news organization.
The evidence suggests psychedelic therapy “may reduce suicidal ideation when administered in the appropriate setting and offered to carefully screened patients,” Dr. Weissman said.
The findings were published online Jan. 18 in The Journal of Clinical Psychiatry.
More research needed
The analysis included seven psychedelic therapy clinical trials that had data on suicidality. Five of the trials used psilocybin plus psychotherapy and two used ayahuasca plus psychotherapy. All seven trials had a “low” risk of bias.
Patients included in the trials had treatment-resistant major depressive disorder (MDD), recurrent MDD, AIDS-related demoralization, and distress related to life-threatening cancer.
The meta-analytic results showed significant decreases in suicidality at all acute time points (80 to 240 minutes post administration) and at most post-acute time points (1 day to 4 months post administration).
Effect sizes for reductions in suicidality were “large” at all acute time points, with standardized mean differences (SMD) ranging from -1.48 to -1.72, and remained large from 1 day to 3-4 months after therapy (SMD range, -1.50 to -2.36).
At 6 months, the effect size for reductions in suicidality with psychedelic therapy was “medium” (SMD, -0.65).
Large effect sizes for reductions in suicidality occurred across the different patient populations represented in the trial, the investigators note.
No study reported any suicide-related adverse events because of administration of a psychedelic. There were also “very few” acute (6.5%) or postacute (3.0%) elevations in suicidality, “providing support for the safety of psychedelic therapy within controlled contexts,” the researchers write.
They caution, however, that large controlled trials that specifically evaluate the effect of psychedelic therapy on suicidality are needed.
Promising avenue
In an accompanying editorial, Daniel Grossman, BS, and Peter Hendricks, PhD, department of health behavior, University of Alabama at Birmingham, note that results of this review warrant “optimism” for use of psychedelics for treatment of suicidality.
Based on this study and others, classic psychedelic therapy for suicidality appears to be a “promising avenue” for further investigation, they write.
However, research and anecdotes about increased suicidality and other self-harm attributed to psychedelic therapy, “though evidently rare, remain a critical concern” for further research to address, Dr. Grossman and Dr. Hendricks add.
The hope is that future research “clarifies who is most subject to these risks, what factors best identify them, and how best to navigate their treatment safely,” they write.
The meta-analysis had no funding. Dr. Weissman receives funding from the Brain and Behavior Research Foundation and serves on the advisory board of GoodCap Pharmaceuticals. Dr. Hendricks is on the scientific advisory board of Bright Minds Biosciences, Eleusis Benefit Corporation, and Rest Pharmaceuticals.
A version of this article first appeared on Medscape.com.
A commonly held belief that classic psychedelic therapy can trigger suicidal thoughts, actions, or other types of self-harm is not supported by research, and, in fact, the opposite may be true.
Results from a meta-analysis of individual patient data showed that psychedelic therapy was associated with large, acute, and sustained decreases in suicidality across a range of clinical patient populations.
“ It gives us a better understanding of the effects of psychedelics on suicidality in the context of clinical trials,” study investigator Cory Weissman, MD, department of psychiatry, University of Toronto, told this news organization.
The evidence suggests psychedelic therapy “may reduce suicidal ideation when administered in the appropriate setting and offered to carefully screened patients,” Dr. Weissman said.
The findings were published online Jan. 18 in The Journal of Clinical Psychiatry.
More research needed
The analysis included seven psychedelic therapy clinical trials that had data on suicidality. Five of the trials used psilocybin plus psychotherapy and two used ayahuasca plus psychotherapy. All seven trials had a “low” risk of bias.
Patients included in the trials had treatment-resistant major depressive disorder (MDD), recurrent MDD, AIDS-related demoralization, and distress related to life-threatening cancer.
The meta-analytic results showed significant decreases in suicidality at all acute time points (80 to 240 minutes post administration) and at most post-acute time points (1 day to 4 months post administration).
Effect sizes for reductions in suicidality were “large” at all acute time points, with standardized mean differences (SMD) ranging from -1.48 to -1.72, and remained large from 1 day to 3-4 months after therapy (SMD range, -1.50 to -2.36).
At 6 months, the effect size for reductions in suicidality with psychedelic therapy was “medium” (SMD, -0.65).
Large effect sizes for reductions in suicidality occurred across the different patient populations represented in the trial, the investigators note.
No study reported any suicide-related adverse events because of administration of a psychedelic. There were also “very few” acute (6.5%) or postacute (3.0%) elevations in suicidality, “providing support for the safety of psychedelic therapy within controlled contexts,” the researchers write.
They caution, however, that large controlled trials that specifically evaluate the effect of psychedelic therapy on suicidality are needed.
Promising avenue
In an accompanying editorial, Daniel Grossman, BS, and Peter Hendricks, PhD, department of health behavior, University of Alabama at Birmingham, note that results of this review warrant “optimism” for use of psychedelics for treatment of suicidality.
Based on this study and others, classic psychedelic therapy for suicidality appears to be a “promising avenue” for further investigation, they write.
However, research and anecdotes about increased suicidality and other self-harm attributed to psychedelic therapy, “though evidently rare, remain a critical concern” for further research to address, Dr. Grossman and Dr. Hendricks add.
The hope is that future research “clarifies who is most subject to these risks, what factors best identify them, and how best to navigate their treatment safely,” they write.
The meta-analysis had no funding. Dr. Weissman receives funding from the Brain and Behavior Research Foundation and serves on the advisory board of GoodCap Pharmaceuticals. Dr. Hendricks is on the scientific advisory board of Bright Minds Biosciences, Eleusis Benefit Corporation, and Rest Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Assessing imminent suicide risk: What about future planning?
A patient who has the ability to plan for their future can be reassuring for a clinician who is conducting an imminent suicide risk evaluation. However, that patient may report future plans even as they are contemplating suicide. Therefore, this variable should not be simplified categorically to the mere presence or absence of future plans. Such plans, and the process by which they are produced, should be examined more closely. In this article, we explore the relationship between a patient’s intent to die by suicide in the near future and their ability to maintain future planning. We also use case examples to highlight certain characteristics that may allow future planning to be integrated more reliably into the assessment of imminent risk of suicide.
An inherent challenge
Suicide risk assessment can be challenging due to the numerous factors that can contribute to a patient’s suicidal intent.1 Some individuals don’t seek help when they develop suicidal thoughts, and even among those who do, recognizing who may be at greater risk is not an easy task. Sometimes, this leads to inadequate interventions and a subsequent failure to ensure safety, or to an overreaction and unnecessary hospitalization.
A common difficulty is a patient’s unwillingness to cooperate with the examination.2 Some patients do not present voluntarily, while others may seek help but then conceal suicidal intent. In a sample of 66 psychotherapy patients who reported concealing suicidal ideation from their therapist and provided short essay responses explaining their motives for doing so, approximately 70% said fear of involuntary hospitalization was their motive to hide those thoughts from their doctor.3 Other reasons for concealment are shame, stigma, embarrassment, fear of rejection, and loss of autonomy.3-5 Moreover, higher levels of suicidal ideation are associated with treatment avoidance.6 Therefore, it is important to improve suicide predictability independent of the patient report. In a survey of 1,150 emergency physicians in Australasia, Canada, the United Kingdom, and the United States, the need for evidence-based guidelines on when to hospitalize a patient at risk for suicide was ranked as the 7th-highest priority.7 There are limitations to using suicide risk assessment scales,8,9 because scales designed to have high sensitivity are less specific, and those with high specificity fail to identify individuals at high risk.9,10 Most of the research conducted in this area has focused on the risk of suicide in 2 to 6 months, and not on imminent risk.11
What is ‘imminent’ risk?
There is no specific time definition for “imminent risk,” but the Lifeline Standards, Trainings, and Practices Subcommittee, a group of national and international experts in suicide prevention, defines imminent risk of suicide as the belief that there is a “close temporal connection between the person’s current risk status and actions that could lead to his/her suicide.”12 Practically, suicide could be considered imminent when it occurs within a few days of the evaluation. However, suicide may take place within a few days of an evaluation due to new life events or impulsive actions, which may explain why imminent risk of suicide can be difficult to define and predict. In clinical practice, there is little evidence-based knowledge about estimating imminent risk. Recent studies have explored certain aspects of a patient’s history in the attempt to improve imminent risk predictability.13 In light of the complexity of this matter and the lack of widely validated tools, clinicians are encouraged to share their experience with other clinicians while the efforts to advance evidence-based knowledge and tools continue.
The function of future planning
Future planning is a mental process embedded in several crucial executive functions. It operates on a daily basis to organize, prioritize, and carry out tasks to achieve day-to-day and more distant future goals. Some research has found that a decreased ability to generate positive future thoughts is linked to increased suicide risk in the long term.14-17 Positive future planning can be affected by even minor fluctuations in mood because the additional processing capacity needed during these mood changes may limit one’s ability to generate positive future thoughts.18 Patients experiencing mood episodes are known to experience cognitive dysfunctions.19-21 However, additional measurable cognitive changes have been detected in patients who are suicidal. For example, in a small study (N = 33) of patients with depression, those who were experiencing suicidal thoughts underperformed on several measures of executive functioning compared to patients with no suicidal ideation.22
However, when addressing imminent rather than future suicide risk, even neutral future plans—such as day-to-day plans or those addressing barriers to treatment—can be a meaningful indicator of the investment in one’s future beyond a potential near-term suicide, and therefore can be explored to further inform the risk evaluation. Significant mental resources can be consumed due to the level of distress associated with contemplating suicide, and therefore patients may have a reduced capacity for day-to-day planning. Thus, serious suicide contemplation is less likely in the presence of typical future planning.
Continue to: Characteristics of future planning...
Characteristics of future planning
Some patients may pretend to engage in future planning to indicate the absence of suicidal intent. This necessitates a more nuanced assessment of future plans beyond whether they exist or not by examining the genuineness of such plans, and the authenticity of the process by which they are produced. The Table lists 3 characteristics of future plans/future planning that, based on our clinical experience, can be helpful to evaluate during an imminent suicide risk evaluation. These are described in the following case examples.
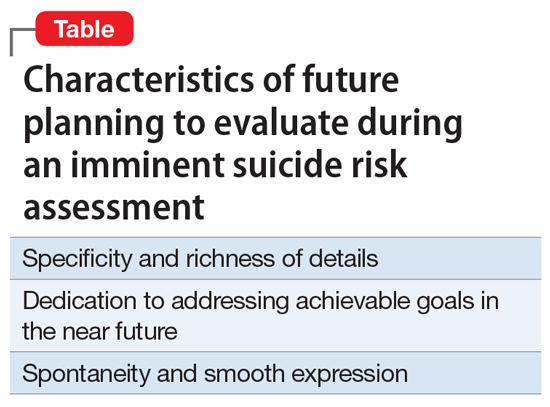
Specificity and richness of details
CASE 1
Mr. A, a college student, presents to the emergency department (ED) complaining of depression and suicidal thoughts that he is able to dismiss. He would like to avoid starting a medication because he has finals in 2 weeks and is worried about adverse effects. He learned about cognitive-behavioral therapy and is interested in getting a referral to a specific office because it is located within a walking distance from campus and easy for him to access because he does not own a car.
The volume of details expressed in a patient’s future plans is important. The more detailed these plans are, the more likely the patient is invested in them. Attendance to the details, especially when addressing expected barriers to treatment, such as transportation, can be evidence of genuine future planning and subsequently of low imminent suicide risk. Spreng et al23 found that autobiographic plans that are more specific and richer in detail recruit additional brain regions that are not recruited in plans that are sparsely detailed or constructed from more generalized representations.
CASE 2
An ambulance transports Ms. B, age 42, from a primary care clinic to the ED because she has been having suicidal thoughts, with a plan to hang herself, for the past 2 days. During the evaluation, Ms. B denies having further suicidal thoughts and declines inpatient admission. She claims that she cannot be away from her children because she is their primary caretaker. Collateral information reveals that Ms. B’s mother has been caring for her children for the last 2 weeks because Ms. B has been too depressed to do so. She continues to refuse admission and is in tears while trying to explain how her absence due to inpatient treatment will be detrimental to her children. Eventually, she angrily accuses the clinician of abusing her children by forcing her to be hospitalized.
In an effort to conceal suicidal intent, patients may present obligations or excuses that would be an obstacle to psychiatric hospitalization. This might give a false perception of intact future planning. However, in these cases, patients often fail to volunteer details about their future plans or show evidence for actual attendance to their obligations. Due to the lack of tangible details to explain the negative effects of inpatient treatment, patients may compensate by using an exaggerated emotional response, with a strong emotional attachment to the obligation and severe distress over their potential inability to fulfill it due to a psychiatric hospitalization. This may contribute to concealing suicidal intent in a different way. A patient may be distressed by the prospect of losing their autonomy or ability to attempt suicide if hospitalized, and they may employ a false excuse as a substitute for the actual reason underlying their distress. A clinician may be falsely reassured if they do not accurately perceive the true cause of the emotional distress. Upon deeper exploration, the expressed emotional attachment is often found to be superficial and has little substantive support.
Continue to: Dedication to addressing acheivable goals in the near future...
Dedication to addressing achievable goals in the near future
CASE 3
Ms. C, age 15, survived a suicide attempt via a medication overdose. She says that she regrets what she did and is not planning to attempt suicide again. Ms. C says she no longer wants to die because in the future she wants to help people by becoming a nurse. She adds that there is a lot waiting for her because she wants to travel all over the world.
Ms. D, age 15, also survived a suicide attempt via a medication overdose. She also says that she regrets what she did and is not planning to attempt suicide again. Ms. D asks whether the physician would be willing to contact the school on her behalf to explain why she had to miss class and to ask for accommodations at school to assist with her panic attacks.
Future planning that involves a patient generating new plans to address current circumstances or the near future may be more reliable than future planning in which a patient repeats their previously constructed plans for the distant future. Eliciting more distant plans, such as a career or family-oriented decisions, indicates the ability to access these “memorized” plans rather than the ability to generate future plans.
Plans that address the distant future, such as those expressed by Ms. C, may have stronger neurologic imprints as a result of repeated memorization and modifications over the years, which may allow a patient to access these plans even while under the stress associated with suicidal thinking. On the other hand, plans that address the near future, such as those expressed by Ms. D, are likely generated in response to current circumstances, which indicates the presence of adequate mental capacity to attend to the current situation, and hence, less preoccupation with suicidal thinking. There might be a neurologic basis for this: some evidence suggests that executive frontoparietal control is recruited in achievable, near-future planning, whereas abstract, difficult-to-achieve, more distant planning fails to engage these additional brain regions.23,24
Spontaneity and smooth expression
CASE 4
Mr. E, age 48, reassures his psychiatrist that he has no intent to act on his suicidal thoughts. When he is offered treatment options, he explains that he would like to start pharmacologic treatment because he only has a few weeks left before he relocates for a new job. The clinician discusses starting a specific medication, and Mr. E expresses interest unless the medication will interfere with his future position as a machine operator. Later, he declines social work assistance to establish care in his new location, preferring to first get the new health care insurance.
A smooth and noncalculated flow of future plans in a patient’s speech allows their plans to be more believable. Plans that naturally flow in response to a verbal exchange and without direct inquiry from the clinician are less likely to be confabulated. This leaves clinicians with the burden of improving the skill of subtly eliciting a patient’s future plans while avoiding directly asking about them. Directly inquiring about such plans may easily tip off the patient that their future planning is under investigation, which may result in misleading responses.
Although future plans that are expressed abruptly, without introductory verbal exchange, or are explicitly linked to why the patient doesn’t intend to kill themselves, can be genuine, the clinician may need to be skeptical about their significance during the risk evaluation. While facing such challenges, clinicians could attempt to shift the patient’s attention away from a safety and disposition-focused conversation toward a less goal-directed verbal exchange during which other opportunities for smooth expression of future plans may emerge. For example, if a patient suddenly discusses how much they care about X in attempt to emphasize why they are not contemplating suicide, the clinician may respond by gently asking the patient to talk more about X.
Continue to: Adopt a more nuanced approach...
Adopt a more nuanced approach
Assessment of the imminent risk of suicide is complicated and not well researched. A patient’s future planning can be used to better inform the evaluation. A patient may have a limited ability to generate future plans while contemplating suicide. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans. The process of future planning may indicate low imminent suicide risk when it leads the patient to generate new plans to address current circumstances or the near future. When evaluating a patient’s imminent suicide risk, clinicians should consider abandoning a binary “is there future planning or not” approach and adopting a more complex, nuanced understanding to appropriately utilize this important factor in the risk assessment.
Bottom Line
A patient’s ability to plan for the future should be explored during an assessment of imminent suicide risk. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans.
1. Gilbert AM, Garno JL, Braga RJ, et al. Clinical and cognitive correlates of suicide attempts in bipolar disorder: is suicide predictable? J Clin Psychiatry. 2011;72(8):1027-1033.
2. Obegi JH. Your patient refuses a suicide risk assessment. Now what? Current Psychiatry. 2021;20(4):45.
3. Blanchard M, Farber BA. “It is never okay to talk about suicide”: Patients’ reasons for concealing suicidal ideation in psychotherapy. Psychother Res. 2020;30(1):124-136.
4. Richards JE, Whiteside U, Ludman EJ, et al. Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: a qualitative study. Psychiatr Serv. 2019;70(1):40-45.
5. Fulginiti A, Frey LM. Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death Stud. 2019;43(9):562-569.
6. Wilson CJ, Deane FP, Marshall KL, et al. Adolescents’ suicidal thinking and reluctance to consult general medical practitioners. J Youth Adolesc. 2010;39(4):343-356.
7. Eagles D, Stiell IG, Clement CM, et al. International survey of emergency physicians’ priorities for clinical decision rules. Acad Emerg Med. 2008;15(2):177-182.
8. Swedish Council on Health Technology Assessment (SBU): SBU Systematic Review Summaries. Instruments for Suicide Risk Assessment. Summary and Conclusions. SBU Yellow Report No. 242. 2015. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK350492/
9. Runeson B, Odeberg J, Pettersson A, et al. Instruments for the assessment of suicide risk: a systematic review evaluating the certainty of the evidence. PLoS One. 2017;12(7):e0180292. doi:10.1371/journal.pone.0180292
10. Steeg S, Quinlivan L, Nowland R, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry. 2018;18(1):113.
11. Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. J Consult Clin Psychol. 2007;75(5):707-715.
12. Draper J, Murphy G, Vega E, et al. Helping callers to the National Suicide Prevention Lifeline who are at imminent risk of suicide: the importance of active engagement, active rescue, and collaboration between crisis and emergency services. Suicide Life Threat Behav. 2015;45(3):261-270.
13. Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S176-S180.
14. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
15. MacLeod AK, Tata P, Evans K, et al. Recovery of positive future thinking within a high-risk parasuicide group: results from a pilot randomized controlled trial. Br J Clin Psychol. 1998;37(4):371-379.
16. MacLeod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2005;44(Pt 4):495-504.
17. O’Connor RC, Smyth R, Williams JM. Intrapersonal positive future thinking predicts repeat suicide attempts in hospital-treated suicide attempters. J Consult Clin Psychol. 2015;83(1):169-176.
18. O’Connor RC, Williams JMG. The relationship between positive future thinking, brooding, defeat and entrapment. Personality and Individual Differences. 2014;70:29-34.
19. Castaneda AE, Tuulio-Henriksson A, Marttunen M, et al. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008;106(1-2):1-27.
20. Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200-206.
21. Buoli M, Caldiroli A, Caletti E, et al. The impact of mood episodes and duration of illness on cognition in bipolar disorder. Compr Psychiatry. 2014;55(7):1561-1566.
22. Marzuk PM, Hartwell N, Leon AC, et al. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand. 2005;112(4):294-301.
23. Spreng RN, Gerlach KD, Turner GR, et al. Autobiographical planning and the brain: activation and its modulation by qualitative features. J Cogn Neurosci. 2015;27(11):2147-2157.
24. Spreng RN, Sepulcre J, Turner GR, et al. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci. 2013;25(1):74-86.
A patient who has the ability to plan for their future can be reassuring for a clinician who is conducting an imminent suicide risk evaluation. However, that patient may report future plans even as they are contemplating suicide. Therefore, this variable should not be simplified categorically to the mere presence or absence of future plans. Such plans, and the process by which they are produced, should be examined more closely. In this article, we explore the relationship between a patient’s intent to die by suicide in the near future and their ability to maintain future planning. We also use case examples to highlight certain characteristics that may allow future planning to be integrated more reliably into the assessment of imminent risk of suicide.
An inherent challenge
Suicide risk assessment can be challenging due to the numerous factors that can contribute to a patient’s suicidal intent.1 Some individuals don’t seek help when they develop suicidal thoughts, and even among those who do, recognizing who may be at greater risk is not an easy task. Sometimes, this leads to inadequate interventions and a subsequent failure to ensure safety, or to an overreaction and unnecessary hospitalization.
A common difficulty is a patient’s unwillingness to cooperate with the examination.2 Some patients do not present voluntarily, while others may seek help but then conceal suicidal intent. In a sample of 66 psychotherapy patients who reported concealing suicidal ideation from their therapist and provided short essay responses explaining their motives for doing so, approximately 70% said fear of involuntary hospitalization was their motive to hide those thoughts from their doctor.3 Other reasons for concealment are shame, stigma, embarrassment, fear of rejection, and loss of autonomy.3-5 Moreover, higher levels of suicidal ideation are associated with treatment avoidance.6 Therefore, it is important to improve suicide predictability independent of the patient report. In a survey of 1,150 emergency physicians in Australasia, Canada, the United Kingdom, and the United States, the need for evidence-based guidelines on when to hospitalize a patient at risk for suicide was ranked as the 7th-highest priority.7 There are limitations to using suicide risk assessment scales,8,9 because scales designed to have high sensitivity are less specific, and those with high specificity fail to identify individuals at high risk.9,10 Most of the research conducted in this area has focused on the risk of suicide in 2 to 6 months, and not on imminent risk.11
What is ‘imminent’ risk?
There is no specific time definition for “imminent risk,” but the Lifeline Standards, Trainings, and Practices Subcommittee, a group of national and international experts in suicide prevention, defines imminent risk of suicide as the belief that there is a “close temporal connection between the person’s current risk status and actions that could lead to his/her suicide.”12 Practically, suicide could be considered imminent when it occurs within a few days of the evaluation. However, suicide may take place within a few days of an evaluation due to new life events or impulsive actions, which may explain why imminent risk of suicide can be difficult to define and predict. In clinical practice, there is little evidence-based knowledge about estimating imminent risk. Recent studies have explored certain aspects of a patient’s history in the attempt to improve imminent risk predictability.13 In light of the complexity of this matter and the lack of widely validated tools, clinicians are encouraged to share their experience with other clinicians while the efforts to advance evidence-based knowledge and tools continue.
The function of future planning
Future planning is a mental process embedded in several crucial executive functions. It operates on a daily basis to organize, prioritize, and carry out tasks to achieve day-to-day and more distant future goals. Some research has found that a decreased ability to generate positive future thoughts is linked to increased suicide risk in the long term.14-17 Positive future planning can be affected by even minor fluctuations in mood because the additional processing capacity needed during these mood changes may limit one’s ability to generate positive future thoughts.18 Patients experiencing mood episodes are known to experience cognitive dysfunctions.19-21 However, additional measurable cognitive changes have been detected in patients who are suicidal. For example, in a small study (N = 33) of patients with depression, those who were experiencing suicidal thoughts underperformed on several measures of executive functioning compared to patients with no suicidal ideation.22
However, when addressing imminent rather than future suicide risk, even neutral future plans—such as day-to-day plans or those addressing barriers to treatment—can be a meaningful indicator of the investment in one’s future beyond a potential near-term suicide, and therefore can be explored to further inform the risk evaluation. Significant mental resources can be consumed due to the level of distress associated with contemplating suicide, and therefore patients may have a reduced capacity for day-to-day planning. Thus, serious suicide contemplation is less likely in the presence of typical future planning.
Continue to: Characteristics of future planning...
Characteristics of future planning
Some patients may pretend to engage in future planning to indicate the absence of suicidal intent. This necessitates a more nuanced assessment of future plans beyond whether they exist or not by examining the genuineness of such plans, and the authenticity of the process by which they are produced. The Table lists 3 characteristics of future plans/future planning that, based on our clinical experience, can be helpful to evaluate during an imminent suicide risk evaluation. These are described in the following case examples.
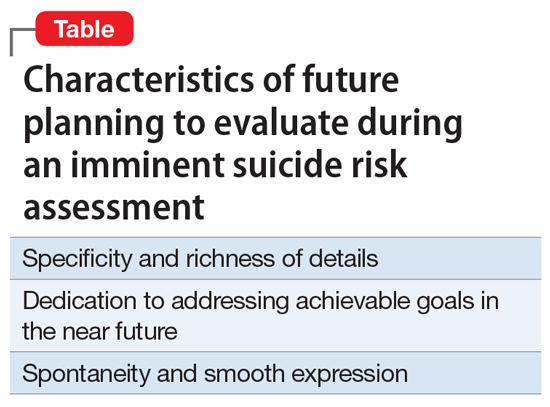
Specificity and richness of details
CASE 1
Mr. A, a college student, presents to the emergency department (ED) complaining of depression and suicidal thoughts that he is able to dismiss. He would like to avoid starting a medication because he has finals in 2 weeks and is worried about adverse effects. He learned about cognitive-behavioral therapy and is interested in getting a referral to a specific office because it is located within a walking distance from campus and easy for him to access because he does not own a car.
The volume of details expressed in a patient’s future plans is important. The more detailed these plans are, the more likely the patient is invested in them. Attendance to the details, especially when addressing expected barriers to treatment, such as transportation, can be evidence of genuine future planning and subsequently of low imminent suicide risk. Spreng et al23 found that autobiographic plans that are more specific and richer in detail recruit additional brain regions that are not recruited in plans that are sparsely detailed or constructed from more generalized representations.
CASE 2
An ambulance transports Ms. B, age 42, from a primary care clinic to the ED because she has been having suicidal thoughts, with a plan to hang herself, for the past 2 days. During the evaluation, Ms. B denies having further suicidal thoughts and declines inpatient admission. She claims that she cannot be away from her children because she is their primary caretaker. Collateral information reveals that Ms. B’s mother has been caring for her children for the last 2 weeks because Ms. B has been too depressed to do so. She continues to refuse admission and is in tears while trying to explain how her absence due to inpatient treatment will be detrimental to her children. Eventually, she angrily accuses the clinician of abusing her children by forcing her to be hospitalized.
In an effort to conceal suicidal intent, patients may present obligations or excuses that would be an obstacle to psychiatric hospitalization. This might give a false perception of intact future planning. However, in these cases, patients often fail to volunteer details about their future plans or show evidence for actual attendance to their obligations. Due to the lack of tangible details to explain the negative effects of inpatient treatment, patients may compensate by using an exaggerated emotional response, with a strong emotional attachment to the obligation and severe distress over their potential inability to fulfill it due to a psychiatric hospitalization. This may contribute to concealing suicidal intent in a different way. A patient may be distressed by the prospect of losing their autonomy or ability to attempt suicide if hospitalized, and they may employ a false excuse as a substitute for the actual reason underlying their distress. A clinician may be falsely reassured if they do not accurately perceive the true cause of the emotional distress. Upon deeper exploration, the expressed emotional attachment is often found to be superficial and has little substantive support.
Continue to: Dedication to addressing acheivable goals in the near future...
Dedication to addressing achievable goals in the near future
CASE 3
Ms. C, age 15, survived a suicide attempt via a medication overdose. She says that she regrets what she did and is not planning to attempt suicide again. Ms. C says she no longer wants to die because in the future she wants to help people by becoming a nurse. She adds that there is a lot waiting for her because she wants to travel all over the world.
Ms. D, age 15, also survived a suicide attempt via a medication overdose. She also says that she regrets what she did and is not planning to attempt suicide again. Ms. D asks whether the physician would be willing to contact the school on her behalf to explain why she had to miss class and to ask for accommodations at school to assist with her panic attacks.
Future planning that involves a patient generating new plans to address current circumstances or the near future may be more reliable than future planning in which a patient repeats their previously constructed plans for the distant future. Eliciting more distant plans, such as a career or family-oriented decisions, indicates the ability to access these “memorized” plans rather than the ability to generate future plans.
Plans that address the distant future, such as those expressed by Ms. C, may have stronger neurologic imprints as a result of repeated memorization and modifications over the years, which may allow a patient to access these plans even while under the stress associated with suicidal thinking. On the other hand, plans that address the near future, such as those expressed by Ms. D, are likely generated in response to current circumstances, which indicates the presence of adequate mental capacity to attend to the current situation, and hence, less preoccupation with suicidal thinking. There might be a neurologic basis for this: some evidence suggests that executive frontoparietal control is recruited in achievable, near-future planning, whereas abstract, difficult-to-achieve, more distant planning fails to engage these additional brain regions.23,24
Spontaneity and smooth expression
CASE 4
Mr. E, age 48, reassures his psychiatrist that he has no intent to act on his suicidal thoughts. When he is offered treatment options, he explains that he would like to start pharmacologic treatment because he only has a few weeks left before he relocates for a new job. The clinician discusses starting a specific medication, and Mr. E expresses interest unless the medication will interfere with his future position as a machine operator. Later, he declines social work assistance to establish care in his new location, preferring to first get the new health care insurance.
A smooth and noncalculated flow of future plans in a patient’s speech allows their plans to be more believable. Plans that naturally flow in response to a verbal exchange and without direct inquiry from the clinician are less likely to be confabulated. This leaves clinicians with the burden of improving the skill of subtly eliciting a patient’s future plans while avoiding directly asking about them. Directly inquiring about such plans may easily tip off the patient that their future planning is under investigation, which may result in misleading responses.
Although future plans that are expressed abruptly, without introductory verbal exchange, or are explicitly linked to why the patient doesn’t intend to kill themselves, can be genuine, the clinician may need to be skeptical about their significance during the risk evaluation. While facing such challenges, clinicians could attempt to shift the patient’s attention away from a safety and disposition-focused conversation toward a less goal-directed verbal exchange during which other opportunities for smooth expression of future plans may emerge. For example, if a patient suddenly discusses how much they care about X in attempt to emphasize why they are not contemplating suicide, the clinician may respond by gently asking the patient to talk more about X.
Continue to: Adopt a more nuanced approach...
Adopt a more nuanced approach
Assessment of the imminent risk of suicide is complicated and not well researched. A patient’s future planning can be used to better inform the evaluation. A patient may have a limited ability to generate future plans while contemplating suicide. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans. The process of future planning may indicate low imminent suicide risk when it leads the patient to generate new plans to address current circumstances or the near future. When evaluating a patient’s imminent suicide risk, clinicians should consider abandoning a binary “is there future planning or not” approach and adopting a more complex, nuanced understanding to appropriately utilize this important factor in the risk assessment.
Bottom Line
A patient’s ability to plan for the future should be explored during an assessment of imminent suicide risk. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans.
A patient who has the ability to plan for their future can be reassuring for a clinician who is conducting an imminent suicide risk evaluation. However, that patient may report future plans even as they are contemplating suicide. Therefore, this variable should not be simplified categorically to the mere presence or absence of future plans. Such plans, and the process by which they are produced, should be examined more closely. In this article, we explore the relationship between a patient’s intent to die by suicide in the near future and their ability to maintain future planning. We also use case examples to highlight certain characteristics that may allow future planning to be integrated more reliably into the assessment of imminent risk of suicide.
An inherent challenge
Suicide risk assessment can be challenging due to the numerous factors that can contribute to a patient’s suicidal intent.1 Some individuals don’t seek help when they develop suicidal thoughts, and even among those who do, recognizing who may be at greater risk is not an easy task. Sometimes, this leads to inadequate interventions and a subsequent failure to ensure safety, or to an overreaction and unnecessary hospitalization.
A common difficulty is a patient’s unwillingness to cooperate with the examination.2 Some patients do not present voluntarily, while others may seek help but then conceal suicidal intent. In a sample of 66 psychotherapy patients who reported concealing suicidal ideation from their therapist and provided short essay responses explaining their motives for doing so, approximately 70% said fear of involuntary hospitalization was their motive to hide those thoughts from their doctor.3 Other reasons for concealment are shame, stigma, embarrassment, fear of rejection, and loss of autonomy.3-5 Moreover, higher levels of suicidal ideation are associated with treatment avoidance.6 Therefore, it is important to improve suicide predictability independent of the patient report. In a survey of 1,150 emergency physicians in Australasia, Canada, the United Kingdom, and the United States, the need for evidence-based guidelines on when to hospitalize a patient at risk for suicide was ranked as the 7th-highest priority.7 There are limitations to using suicide risk assessment scales,8,9 because scales designed to have high sensitivity are less specific, and those with high specificity fail to identify individuals at high risk.9,10 Most of the research conducted in this area has focused on the risk of suicide in 2 to 6 months, and not on imminent risk.11
What is ‘imminent’ risk?
There is no specific time definition for “imminent risk,” but the Lifeline Standards, Trainings, and Practices Subcommittee, a group of national and international experts in suicide prevention, defines imminent risk of suicide as the belief that there is a “close temporal connection between the person’s current risk status and actions that could lead to his/her suicide.”12 Practically, suicide could be considered imminent when it occurs within a few days of the evaluation. However, suicide may take place within a few days of an evaluation due to new life events or impulsive actions, which may explain why imminent risk of suicide can be difficult to define and predict. In clinical practice, there is little evidence-based knowledge about estimating imminent risk. Recent studies have explored certain aspects of a patient’s history in the attempt to improve imminent risk predictability.13 In light of the complexity of this matter and the lack of widely validated tools, clinicians are encouraged to share their experience with other clinicians while the efforts to advance evidence-based knowledge and tools continue.
The function of future planning
Future planning is a mental process embedded in several crucial executive functions. It operates on a daily basis to organize, prioritize, and carry out tasks to achieve day-to-day and more distant future goals. Some research has found that a decreased ability to generate positive future thoughts is linked to increased suicide risk in the long term.14-17 Positive future planning can be affected by even minor fluctuations in mood because the additional processing capacity needed during these mood changes may limit one’s ability to generate positive future thoughts.18 Patients experiencing mood episodes are known to experience cognitive dysfunctions.19-21 However, additional measurable cognitive changes have been detected in patients who are suicidal. For example, in a small study (N = 33) of patients with depression, those who were experiencing suicidal thoughts underperformed on several measures of executive functioning compared to patients with no suicidal ideation.22
However, when addressing imminent rather than future suicide risk, even neutral future plans—such as day-to-day plans or those addressing barriers to treatment—can be a meaningful indicator of the investment in one’s future beyond a potential near-term suicide, and therefore can be explored to further inform the risk evaluation. Significant mental resources can be consumed due to the level of distress associated with contemplating suicide, and therefore patients may have a reduced capacity for day-to-day planning. Thus, serious suicide contemplation is less likely in the presence of typical future planning.
Continue to: Characteristics of future planning...
Characteristics of future planning
Some patients may pretend to engage in future planning to indicate the absence of suicidal intent. This necessitates a more nuanced assessment of future plans beyond whether they exist or not by examining the genuineness of such plans, and the authenticity of the process by which they are produced. The Table lists 3 characteristics of future plans/future planning that, based on our clinical experience, can be helpful to evaluate during an imminent suicide risk evaluation. These are described in the following case examples.
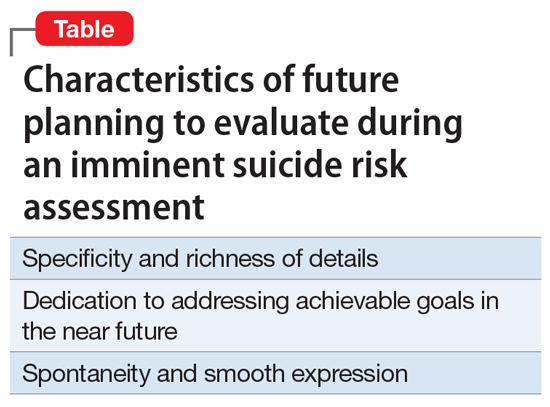
Specificity and richness of details
CASE 1
Mr. A, a college student, presents to the emergency department (ED) complaining of depression and suicidal thoughts that he is able to dismiss. He would like to avoid starting a medication because he has finals in 2 weeks and is worried about adverse effects. He learned about cognitive-behavioral therapy and is interested in getting a referral to a specific office because it is located within a walking distance from campus and easy for him to access because he does not own a car.
The volume of details expressed in a patient’s future plans is important. The more detailed these plans are, the more likely the patient is invested in them. Attendance to the details, especially when addressing expected barriers to treatment, such as transportation, can be evidence of genuine future planning and subsequently of low imminent suicide risk. Spreng et al23 found that autobiographic plans that are more specific and richer in detail recruit additional brain regions that are not recruited in plans that are sparsely detailed or constructed from more generalized representations.
CASE 2
An ambulance transports Ms. B, age 42, from a primary care clinic to the ED because she has been having suicidal thoughts, with a plan to hang herself, for the past 2 days. During the evaluation, Ms. B denies having further suicidal thoughts and declines inpatient admission. She claims that she cannot be away from her children because she is their primary caretaker. Collateral information reveals that Ms. B’s mother has been caring for her children for the last 2 weeks because Ms. B has been too depressed to do so. She continues to refuse admission and is in tears while trying to explain how her absence due to inpatient treatment will be detrimental to her children. Eventually, she angrily accuses the clinician of abusing her children by forcing her to be hospitalized.
In an effort to conceal suicidal intent, patients may present obligations or excuses that would be an obstacle to psychiatric hospitalization. This might give a false perception of intact future planning. However, in these cases, patients often fail to volunteer details about their future plans or show evidence for actual attendance to their obligations. Due to the lack of tangible details to explain the negative effects of inpatient treatment, patients may compensate by using an exaggerated emotional response, with a strong emotional attachment to the obligation and severe distress over their potential inability to fulfill it due to a psychiatric hospitalization. This may contribute to concealing suicidal intent in a different way. A patient may be distressed by the prospect of losing their autonomy or ability to attempt suicide if hospitalized, and they may employ a false excuse as a substitute for the actual reason underlying their distress. A clinician may be falsely reassured if they do not accurately perceive the true cause of the emotional distress. Upon deeper exploration, the expressed emotional attachment is often found to be superficial and has little substantive support.
Continue to: Dedication to addressing acheivable goals in the near future...
Dedication to addressing achievable goals in the near future
CASE 3
Ms. C, age 15, survived a suicide attempt via a medication overdose. She says that she regrets what she did and is not planning to attempt suicide again. Ms. C says she no longer wants to die because in the future she wants to help people by becoming a nurse. She adds that there is a lot waiting for her because she wants to travel all over the world.
Ms. D, age 15, also survived a suicide attempt via a medication overdose. She also says that she regrets what she did and is not planning to attempt suicide again. Ms. D asks whether the physician would be willing to contact the school on her behalf to explain why she had to miss class and to ask for accommodations at school to assist with her panic attacks.
Future planning that involves a patient generating new plans to address current circumstances or the near future may be more reliable than future planning in which a patient repeats their previously constructed plans for the distant future. Eliciting more distant plans, such as a career or family-oriented decisions, indicates the ability to access these “memorized” plans rather than the ability to generate future plans.
Plans that address the distant future, such as those expressed by Ms. C, may have stronger neurologic imprints as a result of repeated memorization and modifications over the years, which may allow a patient to access these plans even while under the stress associated with suicidal thinking. On the other hand, plans that address the near future, such as those expressed by Ms. D, are likely generated in response to current circumstances, which indicates the presence of adequate mental capacity to attend to the current situation, and hence, less preoccupation with suicidal thinking. There might be a neurologic basis for this: some evidence suggests that executive frontoparietal control is recruited in achievable, near-future planning, whereas abstract, difficult-to-achieve, more distant planning fails to engage these additional brain regions.23,24
Spontaneity and smooth expression
CASE 4
Mr. E, age 48, reassures his psychiatrist that he has no intent to act on his suicidal thoughts. When he is offered treatment options, he explains that he would like to start pharmacologic treatment because he only has a few weeks left before he relocates for a new job. The clinician discusses starting a specific medication, and Mr. E expresses interest unless the medication will interfere with his future position as a machine operator. Later, he declines social work assistance to establish care in his new location, preferring to first get the new health care insurance.
A smooth and noncalculated flow of future plans in a patient’s speech allows their plans to be more believable. Plans that naturally flow in response to a verbal exchange and without direct inquiry from the clinician are less likely to be confabulated. This leaves clinicians with the burden of improving the skill of subtly eliciting a patient’s future plans while avoiding directly asking about them. Directly inquiring about such plans may easily tip off the patient that their future planning is under investigation, which may result in misleading responses.
Although future plans that are expressed abruptly, without introductory verbal exchange, or are explicitly linked to why the patient doesn’t intend to kill themselves, can be genuine, the clinician may need to be skeptical about their significance during the risk evaluation. While facing such challenges, clinicians could attempt to shift the patient’s attention away from a safety and disposition-focused conversation toward a less goal-directed verbal exchange during which other opportunities for smooth expression of future plans may emerge. For example, if a patient suddenly discusses how much they care about X in attempt to emphasize why they are not contemplating suicide, the clinician may respond by gently asking the patient to talk more about X.
Continue to: Adopt a more nuanced approach...
Adopt a more nuanced approach
Assessment of the imminent risk of suicide is complicated and not well researched. A patient’s future planning can be used to better inform the evaluation. A patient may have a limited ability to generate future plans while contemplating suicide. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans. The process of future planning may indicate low imminent suicide risk when it leads the patient to generate new plans to address current circumstances or the near future. When evaluating a patient’s imminent suicide risk, clinicians should consider abandoning a binary “is there future planning or not” approach and adopting a more complex, nuanced understanding to appropriately utilize this important factor in the risk assessment.
Bottom Line
A patient’s ability to plan for the future should be explored during an assessment of imminent suicide risk. Future plans that are specific, rich in details, achievable, dedicated to addressing the near future, and expressed smoothly and in a noncalculated fashion may be more reliable than other types of plans.
1. Gilbert AM, Garno JL, Braga RJ, et al. Clinical and cognitive correlates of suicide attempts in bipolar disorder: is suicide predictable? J Clin Psychiatry. 2011;72(8):1027-1033.
2. Obegi JH. Your patient refuses a suicide risk assessment. Now what? Current Psychiatry. 2021;20(4):45.
3. Blanchard M, Farber BA. “It is never okay to talk about suicide”: Patients’ reasons for concealing suicidal ideation in psychotherapy. Psychother Res. 2020;30(1):124-136.
4. Richards JE, Whiteside U, Ludman EJ, et al. Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: a qualitative study. Psychiatr Serv. 2019;70(1):40-45.
5. Fulginiti A, Frey LM. Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death Stud. 2019;43(9):562-569.
6. Wilson CJ, Deane FP, Marshall KL, et al. Adolescents’ suicidal thinking and reluctance to consult general medical practitioners. J Youth Adolesc. 2010;39(4):343-356.
7. Eagles D, Stiell IG, Clement CM, et al. International survey of emergency physicians’ priorities for clinical decision rules. Acad Emerg Med. 2008;15(2):177-182.
8. Swedish Council on Health Technology Assessment (SBU): SBU Systematic Review Summaries. Instruments for Suicide Risk Assessment. Summary and Conclusions. SBU Yellow Report No. 242. 2015. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK350492/
9. Runeson B, Odeberg J, Pettersson A, et al. Instruments for the assessment of suicide risk: a systematic review evaluating the certainty of the evidence. PLoS One. 2017;12(7):e0180292. doi:10.1371/journal.pone.0180292
10. Steeg S, Quinlivan L, Nowland R, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry. 2018;18(1):113.
11. Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. J Consult Clin Psychol. 2007;75(5):707-715.
12. Draper J, Murphy G, Vega E, et al. Helping callers to the National Suicide Prevention Lifeline who are at imminent risk of suicide: the importance of active engagement, active rescue, and collaboration between crisis and emergency services. Suicide Life Threat Behav. 2015;45(3):261-270.
13. Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S176-S180.
14. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
15. MacLeod AK, Tata P, Evans K, et al. Recovery of positive future thinking within a high-risk parasuicide group: results from a pilot randomized controlled trial. Br J Clin Psychol. 1998;37(4):371-379.
16. MacLeod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2005;44(Pt 4):495-504.
17. O’Connor RC, Smyth R, Williams JM. Intrapersonal positive future thinking predicts repeat suicide attempts in hospital-treated suicide attempters. J Consult Clin Psychol. 2015;83(1):169-176.
18. O’Connor RC, Williams JMG. The relationship between positive future thinking, brooding, defeat and entrapment. Personality and Individual Differences. 2014;70:29-34.
19. Castaneda AE, Tuulio-Henriksson A, Marttunen M, et al. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008;106(1-2):1-27.
20. Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200-206.
21. Buoli M, Caldiroli A, Caletti E, et al. The impact of mood episodes and duration of illness on cognition in bipolar disorder. Compr Psychiatry. 2014;55(7):1561-1566.
22. Marzuk PM, Hartwell N, Leon AC, et al. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand. 2005;112(4):294-301.
23. Spreng RN, Gerlach KD, Turner GR, et al. Autobiographical planning and the brain: activation and its modulation by qualitative features. J Cogn Neurosci. 2015;27(11):2147-2157.
24. Spreng RN, Sepulcre J, Turner GR, et al. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci. 2013;25(1):74-86.
1. Gilbert AM, Garno JL, Braga RJ, et al. Clinical and cognitive correlates of suicide attempts in bipolar disorder: is suicide predictable? J Clin Psychiatry. 2011;72(8):1027-1033.
2. Obegi JH. Your patient refuses a suicide risk assessment. Now what? Current Psychiatry. 2021;20(4):45.
3. Blanchard M, Farber BA. “It is never okay to talk about suicide”: Patients’ reasons for concealing suicidal ideation in psychotherapy. Psychother Res. 2020;30(1):124-136.
4. Richards JE, Whiteside U, Ludman EJ, et al. Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: a qualitative study. Psychiatr Serv. 2019;70(1):40-45.
5. Fulginiti A, Frey LM. Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death Stud. 2019;43(9):562-569.
6. Wilson CJ, Deane FP, Marshall KL, et al. Adolescents’ suicidal thinking and reluctance to consult general medical practitioners. J Youth Adolesc. 2010;39(4):343-356.
7. Eagles D, Stiell IG, Clement CM, et al. International survey of emergency physicians’ priorities for clinical decision rules. Acad Emerg Med. 2008;15(2):177-182.
8. Swedish Council on Health Technology Assessment (SBU): SBU Systematic Review Summaries. Instruments for Suicide Risk Assessment. Summary and Conclusions. SBU Yellow Report No. 242. 2015. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK350492/
9. Runeson B, Odeberg J, Pettersson A, et al. Instruments for the assessment of suicide risk: a systematic review evaluating the certainty of the evidence. PLoS One. 2017;12(7):e0180292. doi:10.1371/journal.pone.0180292
10. Steeg S, Quinlivan L, Nowland R, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry. 2018;18(1):113.
11. Nock MK, Banaji MR. Prediction of suicide ideation and attempts among adolescents using a brief performance-based test. J Consult Clin Psychol. 2007;75(5):707-715.
12. Draper J, Murphy G, Vega E, et al. Helping callers to the National Suicide Prevention Lifeline who are at imminent risk of suicide: the importance of active engagement, active rescue, and collaboration between crisis and emergency services. Suicide Life Threat Behav. 2015;45(3):261-270.
13. Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S176-S180.
14. MacLeod AK, Pankhania B, Lee M, et al. Parasuicide, depression and the anticipation of positive and negative future experiences. Psychol Med. 1997;27(4):973-977.
15. MacLeod AK, Tata P, Evans K, et al. Recovery of positive future thinking within a high-risk parasuicide group: results from a pilot randomized controlled trial. Br J Clin Psychol. 1998;37(4):371-379.
16. MacLeod AK, Tata P, Tyrer P, et al. Hopelessness and positive and negative future thinking in parasuicide. Br J Clin Psychol. 2005;44(Pt 4):495-504.
17. O’Connor RC, Smyth R, Williams JM. Intrapersonal positive future thinking predicts repeat suicide attempts in hospital-treated suicide attempters. J Consult Clin Psychol. 2015;83(1):169-176.
18. O’Connor RC, Williams JMG. The relationship between positive future thinking, brooding, defeat and entrapment. Personality and Individual Differences. 2014;70:29-34.
19. Castaneda AE, Tuulio-Henriksson A, Marttunen M, et al. A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord. 2008;106(1-2):1-27.
20. Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200-206.
21. Buoli M, Caldiroli A, Caletti E, et al. The impact of mood episodes and duration of illness on cognition in bipolar disorder. Compr Psychiatry. 2014;55(7):1561-1566.
22. Marzuk PM, Hartwell N, Leon AC, et al. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand. 2005;112(4):294-301.
23. Spreng RN, Gerlach KD, Turner GR, et al. Autobiographical planning and the brain: activation and its modulation by qualitative features. J Cogn Neurosci. 2015;27(11):2147-2157.
24. Spreng RN, Sepulcre J, Turner GR, et al. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci. 2013;25(1):74-86.
Depressed and awkward: Is it more than that?
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
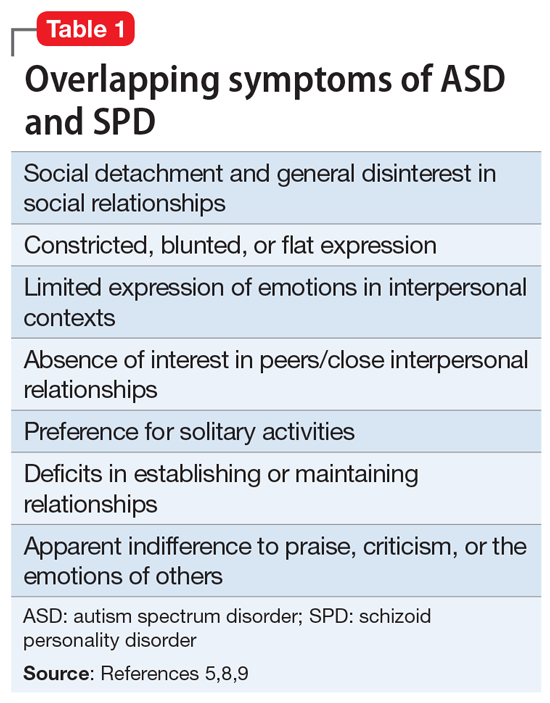
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
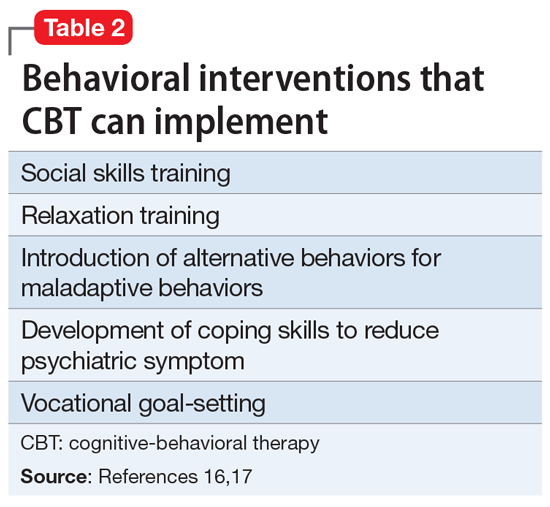
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
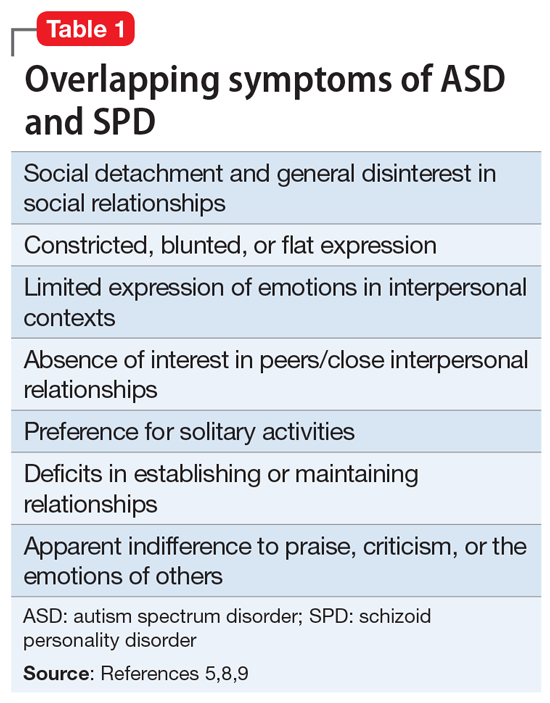
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
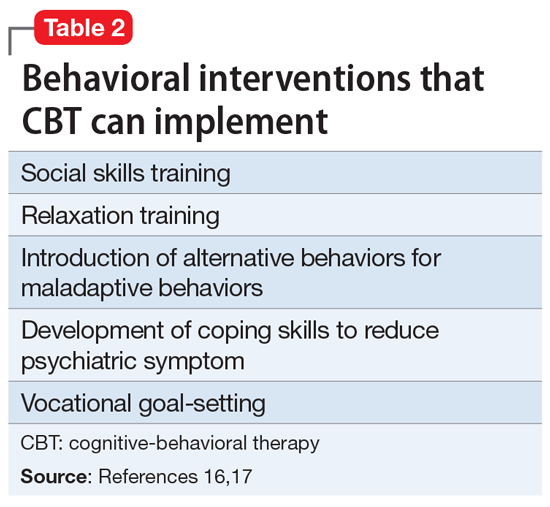
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
CASE Treatment-resistant MDD
Ms. P, age 21, presents to the outpatient clinic. She has diagnoses of treatment-resistant major depressive disorder (MDD) and schizoid personality disorder (SPD). Ms. P was diagnosed with MDD 3 years ago after reporting symptoms of prevailing sadness for approximately 8 years, described as feelings of worthlessness, anhedonia, social withdrawal, and decreased hygiene and self-care behaviors, as well as suicidal ideation and self-harm. SPD was diagnosed 1 year earlier based on her “odd” behaviors and disheveled appearance following observation and in collateral with her family. Her odd behaviors are described as spending most of her time alone, preferring solitary activities, and having little contact with people other than her parents.
Ms. P reports that she was previously treated with citalopram, 20 mg/d, bupropion, 150 mg/d, aripiprazole, 3.75 mg/d, topiramate, 100 mg twice daily, and melatonin, 9 mg/d at bedtime, but discontinued follow-up appointments and medications after no significant improvement in symptoms.
[polldaddy:11027942]
The authors’ observations
The term “schizoid” first made its debut in the medical community to describe the prodromal social withdrawal and isolation observed in schizophrenia.1 The use of schizoid to describe a personality type first occurred in DSM-III in 1980.2 SPD is a Cluster A personality disorder that groups personalities characterized by common traits that are “odd” or “eccentric” and may resemble the positive and/or negative symptoms of schizophrenia.3,4 Relatively uncommon in clinical settings, SPD includes individuals who do not desire or enjoy close relationships. Those afflicted with SPD will be described as isolated, aloof, and detached from social relationships with others, even immediate family members. Individuals with SPD may appear indifferent to criticism and praise, and may take pleasure in only a few activities. They may exhibit a general absence of affective range, which contributes to their characterization as flat, blunted, or emotionally vacant. SPD is more commonly diagnosed in males and may be present in childhood and adolescence. These children are typified by solitariness, poor peer relationships, and underachievement in school. SPD impacts 3.1% to 4.9% of the United States population and approximately 1% of community populations.5,6
EVALUATION Persistent depressive symptoms
Ms. P is accompanied by her parents for the examination. She reports a chronic, persistent sad mood, hopelessness, anergia, insomnia, anhedonia, and decreased concentration and appetite. She says she experiences episodes of intense worry, along with tension, restlessness, feelings of being on the edge, irritability, and difficulty relaxing. Socially, she is withdrawn, preferring to stay alone in her room most of the day watching YouTube or trying to write stories. She has 2 friends with whom she does not interact with in person, but rather through digital means. Ms. P has never enjoyed attending school and feels “nervous” when she is around people. She has difficulty expressing her thoughts and often looks to her parents for help. Her parents add that getting Ms. P to attend school was a struggle, which resulted in periods of home schooling throughout high school.
The treating team prescribes citalopram, 10 mg/d, and aripiprazole, 2 mg/d. On subsequent follow-up visits, Ms. P’s depression improves with an increase in citalopram to 40 mg/d. Psychotherapy is added to her treatment plan to help address the persistent social deficits, odd behavior, and anxieties.
Continue to: Evaluation Psychological assessment...
EVALUATION Psychological assessment
At her psychotherapy intake appointment with the clinical neuropsychologist, Ms. P is dressed in purple from head to toe and sits clutching her purse and looking at the ground. She is overweight with clean, fitting clothing. Ms. P takes a secondary role during most of the interview, allowing her parents to answer most questions. When asked why she is starting therapy, Ms. P replies, “Well, I’ve been using the bathroom a lot.” She describes a feeling of comfort and calmness while in the restroom. Suddenly, she asks her parents to exit the exam room for a moment. Once they leave, she leans in and whispers, “Have you ever heard of self-sabotage? I think that’s what I’m doing.”
Her mood is euthymic, with a blunted affect. She scores 2 on the Patient Health Questionnaire-9 (PHQ-9) and 10 on the Generalized Anxiety Disorder 7-item scale (GAD-7), which indicates the positive impact of medication on her depressive symptoms but continuing moderate anxious distress. She endorses fear of the night, insomnia, and suicidal ideation. She reports an unusual “constant itching sensation,” resulting in hours of repetitive excoriation. Physical examination reveals several significant scars and scabs covering her bilateral upper and lower extremities. Her vocational history is brief; she had held 2 entry-level customer service positions that lasted <1 year. She was fired due to excessive bathroom use.
As the interview progresses, the intake clinician’s background in neuropsychological assessment facilitates screening for possible developmental disorders. Given the nature of the referral and psychotherapy intake, a full neuropsychological assessment is not conducted. The clinician emphasizes verbal abstraction and theory of mind. Ms. P’s IQ was estimated to be average by Wide Range Achievement Test 4 word reading and interview questions about her academic history. Questions are abstracted from the Autism Diagnostic Observation Schedule, Module 4, to assess for conversation ability, emotional insight, awareness and expression, relationships, and areas of functioning in daily living. Developmental history questions, such as those found on the Adaptive Behavior Assessment System, 3rd edition, help guide developmental information provided by parents in the areas of communication, emotion and eye-gaze, gestures, sensory function, language, social functioning, hygiene behavior, and specific interests.
Ms. P’s mother describes a normal pregnancy and delivery; however, she states that Ms. P was “born with problems,” including difficulty with rooting and sucking, and required gastrointestinal intubation until age 3. Cyclical vomiting followed normal food consumption. Ambulation, language acquisition, toilet training, and hygiene behavior were delayed. Ms. P experienced improvements with early intervention in intensive physical and occupational therapy.
Ms. P’s hygiene is well below average, and she requires cueing from her parents. She attended general education until she reached high school, when she began special education. She was sensitive to sensory stimulation from infancy, with sensory sensitivity to textures. Ms. P continues to report sensory sensitivity and lapses in hygiene.
She has difficulty establishing and maintaining relationships with her peers, and prefers solitary activities. Ms. P has no history of romantic relationships, although she does desire one. When asked about her understanding of various relationships, Ms. P’s responses are stereotyped, such as “I know someone is my friend because they are nice to me” and “People get married because they love each other.” She struggles to offer greater insight into the nuances that form lasting relationships and bonds. Ms. P struggles to imitate and describe the physical and internal cues of several basic emotions (eg, fear, joy, anger).
Her conversational and social skills are assessed by asking her to engage in a conversation with the examiner as if meeting for the first time. Her speech is reciprocal, aprosodic, and delayed. The conversation is one-sided, and the examiner fills in several awkward pauses. Ms. P’s gaze at times is intense and prolonged, especially when responding to questions. She tends to use descriptive statements (eg, “I like your purple pen, I like your shirt”) to engage in conversation, rather than gathering more information through reflective statements, questions, or expressing a shared interest.
Ms. P’s verbal abstraction is screened using questions from the Wechsler Adult Intelligence Scale, 4th edition Similarities subtest, to which she provides several responses within normal limits. Her understanding of colloquial speech is assessed by asking her the meaning of common phrases (eg, “Get knocked down 9 times, get up 10,” “Jack and Jill are 2 peas in a pod”). On many occasions, she is able to limit her response to 1 word, (eg, “resiliency”), demonstrating intact ability to decipher idioms.
[polldaddy:11027971]
The authors’ observations
Upon reflection of Ms. P’s clinical presentation and history of developmental delays, social deficits, sensory sensitivity since infancy, and repetitive behaviors (all which continue to impact her), the clinical team concluded that the diagnosis of autism spectrum disorder (ASD) helps explain the patient’s “odd” behaviors, more so than SPD.
ASD is a heterogenous, complex neuropsychiatric disorder characterized by a persistent deficit in social reciprocity, verbal, and nonverbal communication, and includes a pattern of restricted, repetitive and/or stereotyped behaviors and/or interests.5 The term “autismus” is Greek meaning “self,” and was first used to classify the qualities of “morbid self-admiration” observed in prodromal schizophrenia.7
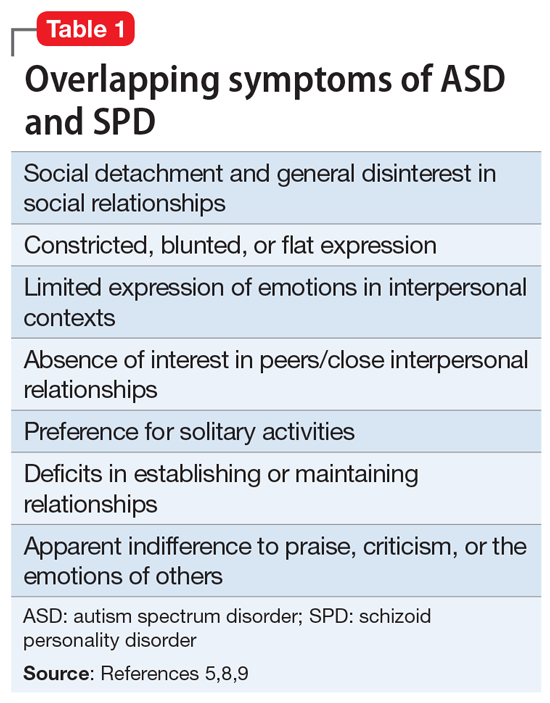
To properly distinguish these disorders, keep in mind that patients with ASD have repetitive and restricted patterns of behaviors or interests that are not found in SPD, and experience deficits in forming, maintaining, and understanding relationships since they lack those skills, while patients with SPD are more prone to desire solitary activities and limited relationships.5,9
There has been an increased interest in determining why for some patients the diagnosis of ASD is delayed until they reach adulthood. Limited or no access to the patient’s childhood caregiver to obtain a developmental history, as well as generational differences on what constitutes typical childhood behavior, could contribute to a delayed diagnosis of ASD until adulthood. Some patients develop camouflaging strategies that allow them to navigate social expectations to a limited degree, such as learning stock phrases, imitating gestures, and telling anecdotes. Another factor to consider is that co-occurring psychiatric disorders may take center stage when patients present for mental health services.10 Fusar-Poli et al11 investigated the characteristics of patients who received a diagnosis of ASD in adulthood. They found that the median time from the initial clinical evaluation to diagnosis of ASD in adulthood was 11 years. In adults identified with ASD, their cognitive abilities ranged from average to above average, and they required less support. Additionally, they also had higher rates of being previously diagnosed with psychotic disorders and personality disorders.11
It is important to keep in mind that the wide spectrum of autism as currently defined by DSM-5 and its overlap of symptoms with other psychiatric disorders can make the diagnosis challenging for both child and adolescent psychiatrists and adult psychiatrists and might help explain why severe cases of ASD are more readily identified earlier than milder cases of ASD.10
Ms. P’s case is also an example of how women are more likely than men to be overlooked when evaluated for ASD. According to DSM-5, the estimated gender ratio for ASD is believed to be 4:1 (male:female).5 However, upon systematic review and meta-analysis, Loomes et al12 found that the gender ratio may be closer to 3:1 (male:female). These authors suggested that diagnostic bias and a failure of passive case ascertainment to estimate gender ratios as stated by DSM-5 in identifying ASD might explain the lower gender ratio.12 A growing body of evidence suggests that ASD is different in males and females. A 2019 qualitative study by Milner et al13 found that female participants reported using masking and camouflaging strategies to appear neurotypical. Compensatory behaviors were found to be linked to a delay in diagnosis and support for ASD.13
Cognitive ability as measured by IQ has also been found to be a factor in receiving a diagnosis of ASD. In a 2010 secondary analysis of a population-based study of the prevalence of ASD, Giarelli et al14found that girls with cognitive impairments as measured by IQ were less likely to be diagnosed with ASD than boys with cognitive impairment, despite meeting the criteria for ASD. Females tend to exhibit fewer repetitive behaviors than males, and tend to be more likely to show accompanying intellectual disability, which suggests that females with ASD may go unrecognized when they exhibit average intelligence with less impairment of behavior and subtler manifestation of social and communication deficits.15 Consequently, females tend to receive this diagnosis later than males.
Continue to: Treatment...
TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score
[polldaddy:11027990]
The authors’ observations
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.
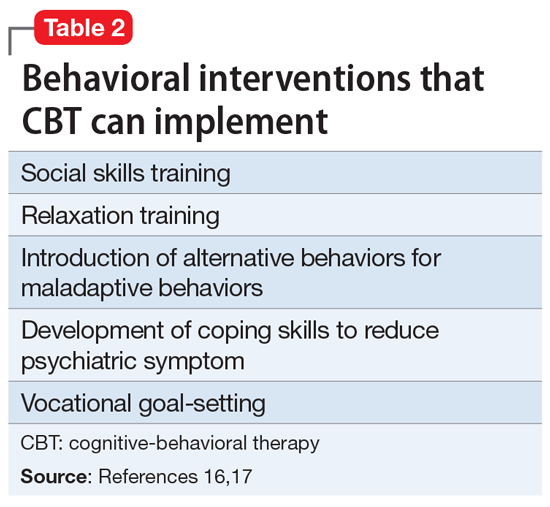
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
1. Fariba K, Gupta V. Schizoid personality disorder. StatPearls Publishing. Updated June 9, 2021. Accessed January 6, 2021. https://www.ncbi.nlm.nih.gov/books/NBK559234/
2. Diagnostic and Statistical Manual of Mental Disorders: DSM-III. 3rd ed rev. American Psychiatric Association; 1987.
3. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32(4):515-528. doi:10.1007/s10862-010-9183-8
4. Kalus O, Bernstein DP, Siever LJ. Schizoid personality disorder: a review of current status and implications for DSM-IV. Journal of Personality Disorders. 1993;7(1), 43-52.
5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
6. Eaton NR, Greene AL. Personality disorders: community prevalence and socio-demographic correlates. Curr Opin Psychol. 2018;21:28-32. doi:10.1016/j.copsyc.2017.09.001
7. Vatano
8. Ritsner MS. Handbook of Schizophrenia Spectrum Disorders, Volume I: Conceptual Issues and Neurobiological Advances. Springer; 2011.
9. Cook ML, Zhang Y, Constantino JN. On the continuity between autistic and schizoid personality disorder trait burden: a prospective study in adolescence. J Nerv Ment Dis. 2020;208(2):94-100. doi:10.1097/NMD.0000000000001105
10. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013-1027. doi:10.1016/S2215-0366(15)00277-1
11. Fusar-Poli L, Brondino N, Politi P, et al. Missed diagnoses and misdiagnoses of adults with autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2020;10.1007/s00406-020-01189-2. doi:10.1007/s00406-020-01189-w
12. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474. doi:10.1016/j.jaac.2017.03.013
13. Milner V, McIntosh H, Colvert E, et al. A qualitative exploration of the female experience of autism spectrum disorder (ASD). J Autism Dev Disord. 2019;49(6):2389-2402. doi:10.1007/s10803-019-03906-4
14. Giarelli E, Wiggins LD, Rice CE, et al. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disabil Health J. 2010;3(2):107-116. doi:10.1016/j.dhjo.2009.07.001
15. Frazier TW, Georgiades S, Bishop SL, et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry. 2014;53(3):329-40.e403. doi:10.1016/j.jaac.2013.12.004
16. Julius RJ, Novitsky MA Jr, et al. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34-44. doi:10.1097/01.pra.0000344917.43780.77
17. Spain D, Sin J, Chalder T, et al. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Research in Autism Spectrum Disorders. 2015;9, 151-162. https://doi.org/10.1016/j.rasd.2014.10.019
18. Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687-694. doi:10.1007/s10803-012-1615-8
Ketamine versus ECT for depression: First head-to-head results
Intravenous ketamine is effective for treating depression but is inferior to electroconvulsive therapy (ECT), new research suggests.
In the first head-to-head trial, ECT was more effective than intravenous ketamine in hospitalized patients with severe depression, with higher remission rates and a greater reduction in symptoms.
However, ketamine led to remission in nearly half of participants and is a “valuable” option for treating severe depression, particularly in younger patients, the investigators noted.
The high rate of remission for ketamine infusion “indicates that it definitely can be used in a clinical setting, but it is more probable that a patient will achieve remission with ECT compared to ketamine,” principal investigator Pouya Movahed Rad, MD, PhD (pharmacology), senior consultant and researcher in psychiatry, Lund (Sweden) University, said in an interview.
Results of the KetECT study were recently published online in the International Journal of Neuropsychopharmacology.
Primary focus on remission
The parallel, open-label, noninferiority study included 186 patients aged 18-85 years who were hospitalized with severe unipolar depression and had a score of at least 20 on the Montgomery-Åsberg Depression Rating Scale (MADRS).
Participants were randomly allocated (1:1) to thrice-weekly infusions of racemic ketamine (0.5 mg/kg over 40 minutes) or ECT. All patients continued to take their antidepressant medication during the study. The primary outcome was remission, defined as a MADRS score of 10 or less.
Results showed the remission rate was significantly higher in the ECT group than in the ketamine group (63% vs. 46%, respectively; P = .026). The 95% confidence interval of the difference in remission rates was estimated between 2% and 30%.
Both ketamine and ECT required a median of six treatment sessions to induce remission.
Post-hoc analysis indicated that age was a factor in the findings. In the ECT group, remission was significantly more likely in older patients (51-85 years), compared with younger patients (18-50 years), with remission rates of 77% and 50%, respectively.
But the opposite was true in the ketamine group, with significantly higher remission rates in younger versus older patients (61% vs. 37%).
The study results also support the safety and efficacy of ketamine in patients with psychotic depression, which was present in 15% of patients in the ECT group and 18% of those in the ketamine group.
In this subgroup, half of patients with psychotic depression remitted after ketamine, with no indications of adverse reactions particular for these patients. The remission rate with ECT was 79%.
During the 12-month follow-up period, rate of relapse among remitters was similar at 64% in the ECT group and 70% in the ketamine group (log rank P = .44).
Let the patient decide
As expected, ECT and ketamine had distinct side effect profiles. Subjectively reported prolonged amnesia was more common with ECT and reports of dissociative side effects, anxiety, blurred vision, euphoria, vertigo, and diplopia (double vision) were more common with ketamine.
“Dissociative symptoms were, as expected, observed during treatment with ketamine, but they were brief and in the majority of cases mild and tolerable,” Dr. Movahed Rad said.
The investigators noted that participating study sites all had long-time experience with ECT but no experience administering ketamine.
“Staffs, and some patients, were familiar with side effects common to ECT but were less prepared for the adverse psychological effects of ketamine. This, and knowing ECT was available after the study, probably contributed to the higher dropout rate in the ketamine group,” they wrote.
If both ECT and ketamine are available, “the patient’s preference should, of course, be taken in account when choosing treatment,” said Dr. Movahed Rad.
“ or other somatic risk factor. Patients who have not responded to ECT or have had unacceptable side effects should be offered ketamine infusion and vice versa,” he added.
A good alternative
Commenting on the findings, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, said the data confirm ECT is highly effective for treatment-resistant depression and show that “newcomer” intravenous ketamine also performs “exceptionally well.”
“This is an extremely important study that really establishes the efficacy of ketamine in a very difficult to treat population,” added Dr. McIntyre, who was not involved in the research.
He added that this “rigorous, well-designed study addresses a critical question” about the comparative efficacy of ECT and intravenous ketamine. It also makes “quite a strong statement about the efficacy of ketamine in younger people.”
He cautioned, however, that this study represents the “first data point and, of course, is not the final word on the topic. There are other studies currently still ongoing that are also comparing ECT to IV ketamine and we’ll look forward to seeing the results.”
The fact that 15%-20% of the study patients had psychotic depression is also noteworthy, said Dr. McIntyre.
“We’ve been hesitant to use ketamine in these patients, I think for obvious reasons, but we recently published a paper showing that it is safe and very effective in these patients,” he said.
Having ketamine as a treatment option is important because the majority of patients who could benefit from ECT decline it, often because of the stigma associated with the procedure, which is often portrayed negatively in films and other media.
“I have been recommending ECT almost every day of my professional life and 98 times out of 100 people say: ‘Thanks but no thanks.’ That’s a problem because ECT is so effective,” Dr. McIntyre said.
The study was funded by the Swedish Research Council, Crafoord Foundation, Skåne Regional Council, Königska Foundation, Lions Forskningsfond Skåne, and the OM Perssons donation foundation. Dr. Movahed Rad has received lecturer honoraria from Lundbeck. Dr. McIntyre has received research grant support from the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation and speaker/consultation fees from Lundbeck, Janssen, and other companies. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
Intravenous ketamine is effective for treating depression but is inferior to electroconvulsive therapy (ECT), new research suggests.
In the first head-to-head trial, ECT was more effective than intravenous ketamine in hospitalized patients with severe depression, with higher remission rates and a greater reduction in symptoms.
However, ketamine led to remission in nearly half of participants and is a “valuable” option for treating severe depression, particularly in younger patients, the investigators noted.
The high rate of remission for ketamine infusion “indicates that it definitely can be used in a clinical setting, but it is more probable that a patient will achieve remission with ECT compared to ketamine,” principal investigator Pouya Movahed Rad, MD, PhD (pharmacology), senior consultant and researcher in psychiatry, Lund (Sweden) University, said in an interview.
Results of the KetECT study were recently published online in the International Journal of Neuropsychopharmacology.
Primary focus on remission
The parallel, open-label, noninferiority study included 186 patients aged 18-85 years who were hospitalized with severe unipolar depression and had a score of at least 20 on the Montgomery-Åsberg Depression Rating Scale (MADRS).
Participants were randomly allocated (1:1) to thrice-weekly infusions of racemic ketamine (0.5 mg/kg over 40 minutes) or ECT. All patients continued to take their antidepressant medication during the study. The primary outcome was remission, defined as a MADRS score of 10 or less.
Results showed the remission rate was significantly higher in the ECT group than in the ketamine group (63% vs. 46%, respectively; P = .026). The 95% confidence interval of the difference in remission rates was estimated between 2% and 30%.
Both ketamine and ECT required a median of six treatment sessions to induce remission.
Post-hoc analysis indicated that age was a factor in the findings. In the ECT group, remission was significantly more likely in older patients (51-85 years), compared with younger patients (18-50 years), with remission rates of 77% and 50%, respectively.
But the opposite was true in the ketamine group, with significantly higher remission rates in younger versus older patients (61% vs. 37%).
The study results also support the safety and efficacy of ketamine in patients with psychotic depression, which was present in 15% of patients in the ECT group and 18% of those in the ketamine group.
In this subgroup, half of patients with psychotic depression remitted after ketamine, with no indications of adverse reactions particular for these patients. The remission rate with ECT was 79%.
During the 12-month follow-up period, rate of relapse among remitters was similar at 64% in the ECT group and 70% in the ketamine group (log rank P = .44).
Let the patient decide
As expected, ECT and ketamine had distinct side effect profiles. Subjectively reported prolonged amnesia was more common with ECT and reports of dissociative side effects, anxiety, blurred vision, euphoria, vertigo, and diplopia (double vision) were more common with ketamine.
“Dissociative symptoms were, as expected, observed during treatment with ketamine, but they were brief and in the majority of cases mild and tolerable,” Dr. Movahed Rad said.
The investigators noted that participating study sites all had long-time experience with ECT but no experience administering ketamine.
“Staffs, and some patients, were familiar with side effects common to ECT but were less prepared for the adverse psychological effects of ketamine. This, and knowing ECT was available after the study, probably contributed to the higher dropout rate in the ketamine group,” they wrote.
If both ECT and ketamine are available, “the patient’s preference should, of course, be taken in account when choosing treatment,” said Dr. Movahed Rad.
“ or other somatic risk factor. Patients who have not responded to ECT or have had unacceptable side effects should be offered ketamine infusion and vice versa,” he added.
A good alternative
Commenting on the findings, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, said the data confirm ECT is highly effective for treatment-resistant depression and show that “newcomer” intravenous ketamine also performs “exceptionally well.”
“This is an extremely important study that really establishes the efficacy of ketamine in a very difficult to treat population,” added Dr. McIntyre, who was not involved in the research.
He added that this “rigorous, well-designed study addresses a critical question” about the comparative efficacy of ECT and intravenous ketamine. It also makes “quite a strong statement about the efficacy of ketamine in younger people.”
He cautioned, however, that this study represents the “first data point and, of course, is not the final word on the topic. There are other studies currently still ongoing that are also comparing ECT to IV ketamine and we’ll look forward to seeing the results.”
The fact that 15%-20% of the study patients had psychotic depression is also noteworthy, said Dr. McIntyre.
“We’ve been hesitant to use ketamine in these patients, I think for obvious reasons, but we recently published a paper showing that it is safe and very effective in these patients,” he said.
Having ketamine as a treatment option is important because the majority of patients who could benefit from ECT decline it, often because of the stigma associated with the procedure, which is often portrayed negatively in films and other media.
“I have been recommending ECT almost every day of my professional life and 98 times out of 100 people say: ‘Thanks but no thanks.’ That’s a problem because ECT is so effective,” Dr. McIntyre said.
The study was funded by the Swedish Research Council, Crafoord Foundation, Skåne Regional Council, Königska Foundation, Lions Forskningsfond Skåne, and the OM Perssons donation foundation. Dr. Movahed Rad has received lecturer honoraria from Lundbeck. Dr. McIntyre has received research grant support from the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation and speaker/consultation fees from Lundbeck, Janssen, and other companies. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
Intravenous ketamine is effective for treating depression but is inferior to electroconvulsive therapy (ECT), new research suggests.
In the first head-to-head trial, ECT was more effective than intravenous ketamine in hospitalized patients with severe depression, with higher remission rates and a greater reduction in symptoms.
However, ketamine led to remission in nearly half of participants and is a “valuable” option for treating severe depression, particularly in younger patients, the investigators noted.
The high rate of remission for ketamine infusion “indicates that it definitely can be used in a clinical setting, but it is more probable that a patient will achieve remission with ECT compared to ketamine,” principal investigator Pouya Movahed Rad, MD, PhD (pharmacology), senior consultant and researcher in psychiatry, Lund (Sweden) University, said in an interview.
Results of the KetECT study were recently published online in the International Journal of Neuropsychopharmacology.
Primary focus on remission
The parallel, open-label, noninferiority study included 186 patients aged 18-85 years who were hospitalized with severe unipolar depression and had a score of at least 20 on the Montgomery-Åsberg Depression Rating Scale (MADRS).
Participants were randomly allocated (1:1) to thrice-weekly infusions of racemic ketamine (0.5 mg/kg over 40 minutes) or ECT. All patients continued to take their antidepressant medication during the study. The primary outcome was remission, defined as a MADRS score of 10 or less.
Results showed the remission rate was significantly higher in the ECT group than in the ketamine group (63% vs. 46%, respectively; P = .026). The 95% confidence interval of the difference in remission rates was estimated between 2% and 30%.
Both ketamine and ECT required a median of six treatment sessions to induce remission.
Post-hoc analysis indicated that age was a factor in the findings. In the ECT group, remission was significantly more likely in older patients (51-85 years), compared with younger patients (18-50 years), with remission rates of 77% and 50%, respectively.
But the opposite was true in the ketamine group, with significantly higher remission rates in younger versus older patients (61% vs. 37%).
The study results also support the safety and efficacy of ketamine in patients with psychotic depression, which was present in 15% of patients in the ECT group and 18% of those in the ketamine group.
In this subgroup, half of patients with psychotic depression remitted after ketamine, with no indications of adverse reactions particular for these patients. The remission rate with ECT was 79%.
During the 12-month follow-up period, rate of relapse among remitters was similar at 64% in the ECT group and 70% in the ketamine group (log rank P = .44).
Let the patient decide
As expected, ECT and ketamine had distinct side effect profiles. Subjectively reported prolonged amnesia was more common with ECT and reports of dissociative side effects, anxiety, blurred vision, euphoria, vertigo, and diplopia (double vision) were more common with ketamine.
“Dissociative symptoms were, as expected, observed during treatment with ketamine, but they were brief and in the majority of cases mild and tolerable,” Dr. Movahed Rad said.
The investigators noted that participating study sites all had long-time experience with ECT but no experience administering ketamine.
“Staffs, and some patients, were familiar with side effects common to ECT but were less prepared for the adverse psychological effects of ketamine. This, and knowing ECT was available after the study, probably contributed to the higher dropout rate in the ketamine group,” they wrote.
If both ECT and ketamine are available, “the patient’s preference should, of course, be taken in account when choosing treatment,” said Dr. Movahed Rad.
“ or other somatic risk factor. Patients who have not responded to ECT or have had unacceptable side effects should be offered ketamine infusion and vice versa,” he added.
A good alternative
Commenting on the findings, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, said the data confirm ECT is highly effective for treatment-resistant depression and show that “newcomer” intravenous ketamine also performs “exceptionally well.”
“This is an extremely important study that really establishes the efficacy of ketamine in a very difficult to treat population,” added Dr. McIntyre, who was not involved in the research.
He added that this “rigorous, well-designed study addresses a critical question” about the comparative efficacy of ECT and intravenous ketamine. It also makes “quite a strong statement about the efficacy of ketamine in younger people.”
He cautioned, however, that this study represents the “first data point and, of course, is not the final word on the topic. There are other studies currently still ongoing that are also comparing ECT to IV ketamine and we’ll look forward to seeing the results.”
The fact that 15%-20% of the study patients had psychotic depression is also noteworthy, said Dr. McIntyre.
“We’ve been hesitant to use ketamine in these patients, I think for obvious reasons, but we recently published a paper showing that it is safe and very effective in these patients,” he said.
Having ketamine as a treatment option is important because the majority of patients who could benefit from ECT decline it, often because of the stigma associated with the procedure, which is often portrayed negatively in films and other media.
“I have been recommending ECT almost every day of my professional life and 98 times out of 100 people say: ‘Thanks but no thanks.’ That’s a problem because ECT is so effective,” Dr. McIntyre said.
The study was funded by the Swedish Research Council, Crafoord Foundation, Skåne Regional Council, Königska Foundation, Lions Forskningsfond Skåne, and the OM Perssons donation foundation. Dr. Movahed Rad has received lecturer honoraria from Lundbeck. Dr. McIntyre has received research grant support from the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation and speaker/consultation fees from Lundbeck, Janssen, and other companies. McIntyre is also CEO of AltMed.
A version of this article first appeared on Medscape.com.
FROM THE INTERNATIONAL JOURNAL OF NEUROPSYCHOPHARMACOLOGY
New AAD guidelines eye comorbidities in adults with atopic dermatitis
While it’s well established that atopic dermatitis (AD) in adults is associated with asthma, allergic rhinitis, and other atopic conditions, the links between AD and other comorbidities are coming into clearer focus.
, published evidence supports an association between AD and comorbidities that may not be on the radar of clinicians and patients, including substance use, attention-deficit/hyperactivity disorder (ADHD), elements of metabolic syndrome, and various cardiovascular conditions.
“There are more comorbidities with AD than we anticipated, that are supported by data in the literature,” Dawn M.R. Davis, MD, cochair and an author of the guidelines, told this news organization. “We are learning more about the interconnectivity of various medical conditions,” she continued. “Many skin diseases over time have been noted to be impactful to the whole person and not only the skin. A classic example of that is psoriasis. We now understand that psoriasis is a multisystem inflammatory disorder.”
As for AD, “we’ve always appreciated that AD patients tend to be at higher risk for other atopic diseases such as asthma, allergic rhinoconjunctivitis, and food allergies,” said Dr. Davis, of the departments of dermatology and pediatrics at the Mayo Clinic, Rochester, Minn. “With further research, we are now able to delineate those associations more intimately and have data to support our suspicions. Additionally, we’re now understanding that these inflammatory conditions can impact more than the end organ involved, such as the skin and AD. We wanted to look at how AD can affect the whole patient.”
For the guidelines, which are the first of their kind and were published online in the Journal of the American Academy of Dermatology, Dr. Davis and project cochair Robert Sidbury, MD, MPH, chief of dermatology at Seattle Children’s Hospital, led a multidisciplinary group of 12 experts to review the association between AD and selected comorbidities. They applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) for prognosis approach for assessing the certainty of the evidence and provided statements of association based on the available evidence.
With respect to highlights for atopic and allergic conditions, the guideline authors found high-quality evidence that AD in adults is associated with food allergies, moderate-quality evidence that AD is associated with asthma, and low-quality evidence that AD in adults may be associated with eosinophilic esophagitis.
In the realm of mental health and substance use, ample evidence exists to support an association between AD and mental health conditions such as depression and anxiety, the guidelines state. “For many patients, low mood may be driven by the symptoms of AD, including chronic itch and poor sleep,” Dr. Davis and her coauthors wrote. “Successfully treating AD may alleviate depressive symptoms for some patients; for others, assessment and treatment specific to their mental health may be needed.”
The guidelines also state that low-quality evidence exists to suggest that AD in adults may be associated with alcohol abuse disorders and cigarette smoking.
The authors noted “limited but consistent evidence” supporting a link between AD and adverse bone health, including osteoporosis and fractures, while associations between AD and cardiovascular risk factors and comorbidities, including hypertension, myocardial infarction, and stroke, are more controversial.
“I have published on bone health and AD so that was not as surprising to me,” Dr. Davis said in the interview. “I found a lot of the evidence in the guidelines to be validating of patterns that we see in our patients. The most significant learning point for me was [the link to] cardiovascular disease and the link to specific mental health and substance use disorders. It validates how impactful AD is to the individual.”
According to the guidelines, moderate-quality evidence exists linking AD in adults to both alopecia areata and urticaria. “Because we are dermatologists and take care of both of those diseases, be mindful of that in your daily practice,” Dr. Davis advised. “I would also encourage our colleagues to remember to educate patients on the comorbidities of AD so that they are empowered, and to screen for those comorbidities in your office based on the patient and their history and physical exam, to the level that you think is appropriate for that person’s individual’s care.”
Christine Ko, MD, who was asked to comment on the guidelines, characterized some of the reported comorbidity associations as predictable, such as asthma, food allergy, allergic rhinitis, and skin infections. “As the authors comment, ‘associations between AD and other atopic and allergic conditions have been recognized for decades and even contribute to diagnostic criteria for AD,’ ” said Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn, who was not involved with the guidelines. “I was a bit surprised to see that atopic dermatitis in adults is associated with osteoporosis and fractures. As the authors suggest, this could be secondary to treatment with oral prednisone, and it is possible that use of dupilumab and JAK inhibitors may lessen this association.”
Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore, who was not involved with the guidelines, and was also asked to comment, said that the guidelines underscore the importance of informing adults with AD “of the risks of unchecked inflammation and the potential for multiple disease comorbidities.” Dr. Kwatra, who has AD, added that “these results make me want to be more proactive in treating my eczema to reduce the potential for development of these comorbidities.”
He pointed out that the guidelines did not address racial and ethnic differences in the observed comorbidities. “Unfortunately, minority populations have a greater comorbidity burden in many inflammatory skin diseases so this will be another area needing further investigation,” he said. “As an example, our group found from multicenter data that black patients with atopic dermatitis have higher levels of C-reactive protein, blood eosinophils, and other inflammatory biomarkers.”
The AAD guidelines are the first in a four-part series on AD expected to be published over the next 1-2 years, Dr. Davis said. The subsequent guidelines will address topicals, phototherapy/systemics, and pediatrics.
The study was funded by internal funds from the AAD. Dr. Davis reported having no financial disclosures. Dr. Sidbury disclosed that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, and an investigator for Brickell Biotech and Galderma. He is also a consultant for Galderma Global and Microes. Dr. Ko reported having no financial disclosures. Dr. Kwatra is a member of the board of directors of the Skin of Color Society. He is also an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron Pharmaceuticals, and Sanofi, and has served as an investigator for Galderma, Pfizer, and Sanofi.
While it’s well established that atopic dermatitis (AD) in adults is associated with asthma, allergic rhinitis, and other atopic conditions, the links between AD and other comorbidities are coming into clearer focus.
, published evidence supports an association between AD and comorbidities that may not be on the radar of clinicians and patients, including substance use, attention-deficit/hyperactivity disorder (ADHD), elements of metabolic syndrome, and various cardiovascular conditions.
“There are more comorbidities with AD than we anticipated, that are supported by data in the literature,” Dawn M.R. Davis, MD, cochair and an author of the guidelines, told this news organization. “We are learning more about the interconnectivity of various medical conditions,” she continued. “Many skin diseases over time have been noted to be impactful to the whole person and not only the skin. A classic example of that is psoriasis. We now understand that psoriasis is a multisystem inflammatory disorder.”
As for AD, “we’ve always appreciated that AD patients tend to be at higher risk for other atopic diseases such as asthma, allergic rhinoconjunctivitis, and food allergies,” said Dr. Davis, of the departments of dermatology and pediatrics at the Mayo Clinic, Rochester, Minn. “With further research, we are now able to delineate those associations more intimately and have data to support our suspicions. Additionally, we’re now understanding that these inflammatory conditions can impact more than the end organ involved, such as the skin and AD. We wanted to look at how AD can affect the whole patient.”
For the guidelines, which are the first of their kind and were published online in the Journal of the American Academy of Dermatology, Dr. Davis and project cochair Robert Sidbury, MD, MPH, chief of dermatology at Seattle Children’s Hospital, led a multidisciplinary group of 12 experts to review the association between AD and selected comorbidities. They applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) for prognosis approach for assessing the certainty of the evidence and provided statements of association based on the available evidence.
With respect to highlights for atopic and allergic conditions, the guideline authors found high-quality evidence that AD in adults is associated with food allergies, moderate-quality evidence that AD is associated with asthma, and low-quality evidence that AD in adults may be associated with eosinophilic esophagitis.
In the realm of mental health and substance use, ample evidence exists to support an association between AD and mental health conditions such as depression and anxiety, the guidelines state. “For many patients, low mood may be driven by the symptoms of AD, including chronic itch and poor sleep,” Dr. Davis and her coauthors wrote. “Successfully treating AD may alleviate depressive symptoms for some patients; for others, assessment and treatment specific to their mental health may be needed.”
The guidelines also state that low-quality evidence exists to suggest that AD in adults may be associated with alcohol abuse disorders and cigarette smoking.
The authors noted “limited but consistent evidence” supporting a link between AD and adverse bone health, including osteoporosis and fractures, while associations between AD and cardiovascular risk factors and comorbidities, including hypertension, myocardial infarction, and stroke, are more controversial.
“I have published on bone health and AD so that was not as surprising to me,” Dr. Davis said in the interview. “I found a lot of the evidence in the guidelines to be validating of patterns that we see in our patients. The most significant learning point for me was [the link to] cardiovascular disease and the link to specific mental health and substance use disorders. It validates how impactful AD is to the individual.”
According to the guidelines, moderate-quality evidence exists linking AD in adults to both alopecia areata and urticaria. “Because we are dermatologists and take care of both of those diseases, be mindful of that in your daily practice,” Dr. Davis advised. “I would also encourage our colleagues to remember to educate patients on the comorbidities of AD so that they are empowered, and to screen for those comorbidities in your office based on the patient and their history and physical exam, to the level that you think is appropriate for that person’s individual’s care.”
Christine Ko, MD, who was asked to comment on the guidelines, characterized some of the reported comorbidity associations as predictable, such as asthma, food allergy, allergic rhinitis, and skin infections. “As the authors comment, ‘associations between AD and other atopic and allergic conditions have been recognized for decades and even contribute to diagnostic criteria for AD,’ ” said Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn, who was not involved with the guidelines. “I was a bit surprised to see that atopic dermatitis in adults is associated with osteoporosis and fractures. As the authors suggest, this could be secondary to treatment with oral prednisone, and it is possible that use of dupilumab and JAK inhibitors may lessen this association.”
Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore, who was not involved with the guidelines, and was also asked to comment, said that the guidelines underscore the importance of informing adults with AD “of the risks of unchecked inflammation and the potential for multiple disease comorbidities.” Dr. Kwatra, who has AD, added that “these results make me want to be more proactive in treating my eczema to reduce the potential for development of these comorbidities.”
He pointed out that the guidelines did not address racial and ethnic differences in the observed comorbidities. “Unfortunately, minority populations have a greater comorbidity burden in many inflammatory skin diseases so this will be another area needing further investigation,” he said. “As an example, our group found from multicenter data that black patients with atopic dermatitis have higher levels of C-reactive protein, blood eosinophils, and other inflammatory biomarkers.”
The AAD guidelines are the first in a four-part series on AD expected to be published over the next 1-2 years, Dr. Davis said. The subsequent guidelines will address topicals, phototherapy/systemics, and pediatrics.
The study was funded by internal funds from the AAD. Dr. Davis reported having no financial disclosures. Dr. Sidbury disclosed that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, and an investigator for Brickell Biotech and Galderma. He is also a consultant for Galderma Global and Microes. Dr. Ko reported having no financial disclosures. Dr. Kwatra is a member of the board of directors of the Skin of Color Society. He is also an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron Pharmaceuticals, and Sanofi, and has served as an investigator for Galderma, Pfizer, and Sanofi.
While it’s well established that atopic dermatitis (AD) in adults is associated with asthma, allergic rhinitis, and other atopic conditions, the links between AD and other comorbidities are coming into clearer focus.
, published evidence supports an association between AD and comorbidities that may not be on the radar of clinicians and patients, including substance use, attention-deficit/hyperactivity disorder (ADHD), elements of metabolic syndrome, and various cardiovascular conditions.
“There are more comorbidities with AD than we anticipated, that are supported by data in the literature,” Dawn M.R. Davis, MD, cochair and an author of the guidelines, told this news organization. “We are learning more about the interconnectivity of various medical conditions,” she continued. “Many skin diseases over time have been noted to be impactful to the whole person and not only the skin. A classic example of that is psoriasis. We now understand that psoriasis is a multisystem inflammatory disorder.”
As for AD, “we’ve always appreciated that AD patients tend to be at higher risk for other atopic diseases such as asthma, allergic rhinoconjunctivitis, and food allergies,” said Dr. Davis, of the departments of dermatology and pediatrics at the Mayo Clinic, Rochester, Minn. “With further research, we are now able to delineate those associations more intimately and have data to support our suspicions. Additionally, we’re now understanding that these inflammatory conditions can impact more than the end organ involved, such as the skin and AD. We wanted to look at how AD can affect the whole patient.”
For the guidelines, which are the first of their kind and were published online in the Journal of the American Academy of Dermatology, Dr. Davis and project cochair Robert Sidbury, MD, MPH, chief of dermatology at Seattle Children’s Hospital, led a multidisciplinary group of 12 experts to review the association between AD and selected comorbidities. They applied the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) for prognosis approach for assessing the certainty of the evidence and provided statements of association based on the available evidence.
With respect to highlights for atopic and allergic conditions, the guideline authors found high-quality evidence that AD in adults is associated with food allergies, moderate-quality evidence that AD is associated with asthma, and low-quality evidence that AD in adults may be associated with eosinophilic esophagitis.
In the realm of mental health and substance use, ample evidence exists to support an association between AD and mental health conditions such as depression and anxiety, the guidelines state. “For many patients, low mood may be driven by the symptoms of AD, including chronic itch and poor sleep,” Dr. Davis and her coauthors wrote. “Successfully treating AD may alleviate depressive symptoms for some patients; for others, assessment and treatment specific to their mental health may be needed.”
The guidelines also state that low-quality evidence exists to suggest that AD in adults may be associated with alcohol abuse disorders and cigarette smoking.
The authors noted “limited but consistent evidence” supporting a link between AD and adverse bone health, including osteoporosis and fractures, while associations between AD and cardiovascular risk factors and comorbidities, including hypertension, myocardial infarction, and stroke, are more controversial.
“I have published on bone health and AD so that was not as surprising to me,” Dr. Davis said in the interview. “I found a lot of the evidence in the guidelines to be validating of patterns that we see in our patients. The most significant learning point for me was [the link to] cardiovascular disease and the link to specific mental health and substance use disorders. It validates how impactful AD is to the individual.”
According to the guidelines, moderate-quality evidence exists linking AD in adults to both alopecia areata and urticaria. “Because we are dermatologists and take care of both of those diseases, be mindful of that in your daily practice,” Dr. Davis advised. “I would also encourage our colleagues to remember to educate patients on the comorbidities of AD so that they are empowered, and to screen for those comorbidities in your office based on the patient and their history and physical exam, to the level that you think is appropriate for that person’s individual’s care.”
Christine Ko, MD, who was asked to comment on the guidelines, characterized some of the reported comorbidity associations as predictable, such as asthma, food allergy, allergic rhinitis, and skin infections. “As the authors comment, ‘associations between AD and other atopic and allergic conditions have been recognized for decades and even contribute to diagnostic criteria for AD,’ ” said Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn, who was not involved with the guidelines. “I was a bit surprised to see that atopic dermatitis in adults is associated with osteoporosis and fractures. As the authors suggest, this could be secondary to treatment with oral prednisone, and it is possible that use of dupilumab and JAK inhibitors may lessen this association.”
Shawn G. Kwatra, MD, of the department of dermatology at Johns Hopkins University, Baltimore, who was not involved with the guidelines, and was also asked to comment, said that the guidelines underscore the importance of informing adults with AD “of the risks of unchecked inflammation and the potential for multiple disease comorbidities.” Dr. Kwatra, who has AD, added that “these results make me want to be more proactive in treating my eczema to reduce the potential for development of these comorbidities.”
He pointed out that the guidelines did not address racial and ethnic differences in the observed comorbidities. “Unfortunately, minority populations have a greater comorbidity burden in many inflammatory skin diseases so this will be another area needing further investigation,” he said. “As an example, our group found from multicenter data that black patients with atopic dermatitis have higher levels of C-reactive protein, blood eosinophils, and other inflammatory biomarkers.”
The AAD guidelines are the first in a four-part series on AD expected to be published over the next 1-2 years, Dr. Davis said. The subsequent guidelines will address topicals, phototherapy/systemics, and pediatrics.
The study was funded by internal funds from the AAD. Dr. Davis reported having no financial disclosures. Dr. Sidbury disclosed that he serves as an advisory board member for Pfizer, a principal investigator for Regeneron, and an investigator for Brickell Biotech and Galderma. He is also a consultant for Galderma Global and Microes. Dr. Ko reported having no financial disclosures. Dr. Kwatra is a member of the board of directors of the Skin of Color Society. He is also an advisory board member/consultant for AbbVie, Galderma, Incyte, Pfizer, Regeneron Pharmaceuticals, and Sanofi, and has served as an investigator for Galderma, Pfizer, and Sanofi.
FROM JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Brain stimulation for improved memory?
Electrical brain stimulation may have the potential to improve verbal memory, results of a small study of patients with epilepsy suggest.
Investigators observed improvements in patients implanted with a responsive neurostimulation system (RNS) to control seizures, in that the patients had improved word recall when the system was activated.
Beyond epilepsy, “we suspect that our results would be broadly applicable regardless of the underlying condition, for example, memory loss with Alzheimer’s disease or traumatic brain injury,” Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, said in an interview.
“Mental health conditions such as depression or psychosis could also benefit from targeted electrical stimulation. While we focused on enhancing a preferred brain function [such as memory], parallel areas of research may target enhancing function [such as weakness following stroke] or suppressing function [to manage conditions such as chronic pain,]” Dr. Haneef added.
The study was published online Jan. 17, 2022, in Neurosurgery.
As reported by this news organization, Following implantation of the system, patients attend the clinic for adjustments about every 8-12 weeks.
The investigators studied 17 patients with epilepsy and RNS implants who attended the clinic for routine appointments. A clinical neuropsychologist administered the Hopkins Verbal Learning Test–Revised (HVLT-R), a well-validated list-learning measure of memory and verbal learning.
Patients were read a list of 12 semantically related words and asked to recall the list after three different learning trials. Active or sham stimulation was performed for every third word presented for immediate recall.
The investigators found that the HVLT-R delayed recall raw score was higher for the stimulation condition, compared with the nonstimulation condition (paired t-test, P = .04; effect size, d = 0.627).
“The patients were not aware of when the RNS system was being activated. We alternated when patients were undergoing stimulation versus no stimulation, and still found that when patients’ RNS systems were activated, their memory recall score was greater than when there was no stimulation,” Dr. Haneef said in a release.
This suggests the “human memory can be potentially improved by direct electrical brain stimulation at extremely low currents,” Dr. Haneef said in an interview.
Most patients in the study had stimulation of the hippocampus, the brain’s memory center.
“Moving forward we would want to look at how different patterns or standardized stimulation patterns affect memory. Ultimately, the underlying brain rhythms responsible for these changes in brain function need to be understood so that a more targeted and precise application of electrical stimulation can be achieved,” Dr. Haneef said.
The researchers also caution that, for this preliminary study, no follow-up testing was conducted to determine whether the memory improvement was transient and settled back to baseline after a specified period.
However, they note, this study lays the groundwork for larger-scale and extensive studies examining the nuanced effects of brain stimulation on human cognition and memory.
The study was funded by the Mike Hogg Foundation. Dr. Haneef and two coauthors received coverage for travel expenses but no honorarium for a NeuroPace advisory meeting.
A version of this article first appeared on Medscape.com.
Electrical brain stimulation may have the potential to improve verbal memory, results of a small study of patients with epilepsy suggest.
Investigators observed improvements in patients implanted with a responsive neurostimulation system (RNS) to control seizures, in that the patients had improved word recall when the system was activated.
Beyond epilepsy, “we suspect that our results would be broadly applicable regardless of the underlying condition, for example, memory loss with Alzheimer’s disease or traumatic brain injury,” Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, said in an interview.
“Mental health conditions such as depression or psychosis could also benefit from targeted electrical stimulation. While we focused on enhancing a preferred brain function [such as memory], parallel areas of research may target enhancing function [such as weakness following stroke] or suppressing function [to manage conditions such as chronic pain,]” Dr. Haneef added.
The study was published online Jan. 17, 2022, in Neurosurgery.
As reported by this news organization, Following implantation of the system, patients attend the clinic for adjustments about every 8-12 weeks.
The investigators studied 17 patients with epilepsy and RNS implants who attended the clinic for routine appointments. A clinical neuropsychologist administered the Hopkins Verbal Learning Test–Revised (HVLT-R), a well-validated list-learning measure of memory and verbal learning.
Patients were read a list of 12 semantically related words and asked to recall the list after three different learning trials. Active or sham stimulation was performed for every third word presented for immediate recall.
The investigators found that the HVLT-R delayed recall raw score was higher for the stimulation condition, compared with the nonstimulation condition (paired t-test, P = .04; effect size, d = 0.627).
“The patients were not aware of when the RNS system was being activated. We alternated when patients were undergoing stimulation versus no stimulation, and still found that when patients’ RNS systems were activated, their memory recall score was greater than when there was no stimulation,” Dr. Haneef said in a release.
This suggests the “human memory can be potentially improved by direct electrical brain stimulation at extremely low currents,” Dr. Haneef said in an interview.
Most patients in the study had stimulation of the hippocampus, the brain’s memory center.
“Moving forward we would want to look at how different patterns or standardized stimulation patterns affect memory. Ultimately, the underlying brain rhythms responsible for these changes in brain function need to be understood so that a more targeted and precise application of electrical stimulation can be achieved,” Dr. Haneef said.
The researchers also caution that, for this preliminary study, no follow-up testing was conducted to determine whether the memory improvement was transient and settled back to baseline after a specified period.
However, they note, this study lays the groundwork for larger-scale and extensive studies examining the nuanced effects of brain stimulation on human cognition and memory.
The study was funded by the Mike Hogg Foundation. Dr. Haneef and two coauthors received coverage for travel expenses but no honorarium for a NeuroPace advisory meeting.
A version of this article first appeared on Medscape.com.
Electrical brain stimulation may have the potential to improve verbal memory, results of a small study of patients with epilepsy suggest.
Investigators observed improvements in patients implanted with a responsive neurostimulation system (RNS) to control seizures, in that the patients had improved word recall when the system was activated.
Beyond epilepsy, “we suspect that our results would be broadly applicable regardless of the underlying condition, for example, memory loss with Alzheimer’s disease or traumatic brain injury,” Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, said in an interview.
“Mental health conditions such as depression or psychosis could also benefit from targeted electrical stimulation. While we focused on enhancing a preferred brain function [such as memory], parallel areas of research may target enhancing function [such as weakness following stroke] or suppressing function [to manage conditions such as chronic pain,]” Dr. Haneef added.
The study was published online Jan. 17, 2022, in Neurosurgery.
As reported by this news organization, Following implantation of the system, patients attend the clinic for adjustments about every 8-12 weeks.
The investigators studied 17 patients with epilepsy and RNS implants who attended the clinic for routine appointments. A clinical neuropsychologist administered the Hopkins Verbal Learning Test–Revised (HVLT-R), a well-validated list-learning measure of memory and verbal learning.
Patients were read a list of 12 semantically related words and asked to recall the list after three different learning trials. Active or sham stimulation was performed for every third word presented for immediate recall.
The investigators found that the HVLT-R delayed recall raw score was higher for the stimulation condition, compared with the nonstimulation condition (paired t-test, P = .04; effect size, d = 0.627).
“The patients were not aware of when the RNS system was being activated. We alternated when patients were undergoing stimulation versus no stimulation, and still found that when patients’ RNS systems were activated, their memory recall score was greater than when there was no stimulation,” Dr. Haneef said in a release.
This suggests the “human memory can be potentially improved by direct electrical brain stimulation at extremely low currents,” Dr. Haneef said in an interview.
Most patients in the study had stimulation of the hippocampus, the brain’s memory center.
“Moving forward we would want to look at how different patterns or standardized stimulation patterns affect memory. Ultimately, the underlying brain rhythms responsible for these changes in brain function need to be understood so that a more targeted and precise application of electrical stimulation can be achieved,” Dr. Haneef said.
The researchers also caution that, for this preliminary study, no follow-up testing was conducted to determine whether the memory improvement was transient and settled back to baseline after a specified period.
However, they note, this study lays the groundwork for larger-scale and extensive studies examining the nuanced effects of brain stimulation on human cognition and memory.
The study was funded by the Mike Hogg Foundation. Dr. Haneef and two coauthors received coverage for travel expenses but no honorarium for a NeuroPace advisory meeting.
A version of this article first appeared on Medscape.com.
FROM NEUROSURGERY
Ketamine an ‘intriguing new therapy’ for alcoholism
Three weekly infusions of the dissociative anesthetic ketamine coupled with mindfulness-based relapse prevention therapy may help adults with alcohol use disorder (AUD) maintain abstinence, new research suggests.
Preliminary results from a phase 2, double-blind, placebo-controlled trial show ketamine was well tolerated and, compared with placebo, associated with more days of abstinence from alcohol at 6 months.
The results suggest ketamine plus psychological therapy may be a “new, relatively brief treatment that has long lasting effects in AUD,” Celia Morgan, PhD, professor of psychopharmacology, University of Exeter, United Kingdom, told this news organization.
The study was published online Jan. 11 in the American Journal of Psychiatry.
Target depression
Depressive symptoms are common in patients under treatment for AUD and increase relapse risk.
“Ketamine may support alcohol abstinence by temporarily alleviating depressive symptoms during the high-risk relapse period in the weeks after detoxification,” the investigators note.
Ketamine may also provide a “temporary boost to synaptogenesis and neurogenesis, which may allow psychological therapies and new strategies for managing addiction to embed more readily,” they add.
To test these theories, the researchers recruited 96 adults (mean age, 44 years, 35 women) with severe AUD to participate in the trial.
All participants had to abstain from alcohol for at least 24 hours before the trial started and have a reading of 0.0 on a breath alcohol test at the baseline visit.
Participants were randomly allocated to one of four groups:
1. three weekly ketamine infusions of 0.8 mg/kg IV over 40 minutes plus psychological therapy
2. three saline infusions plus psychological therapy
3. three ketamine infusions plus alcohol education
4. three saline infusions plus alcohol education
The primary outcome was self-reported percentage of days abstinent, as well as confirmed alcohol relapse at 6-month follow-up.
(mean difference, 10.1%; 95% confidence interval, 1.1-19.0), “although confidence intervals were wide, consistent with a proof-of-concept study,” the authors note.
The greatest reduction in total days off alcohol occurred in the ketamine plus relapse-prevention therapy group compared with the saline plus alcohol education group (mean difference, 15.9%; 95% CI, 3.8-28.1).
There was no significant difference in relapse rate between the ketamine and placebo groups. No serious adverse effects were reported in any participant.
Growing evidence
These findings support some other studies that have also suggested a benefit of ketamine in AUD.
As reported by this news organization, one recent study found a single infusion of ketamine combined with counseling may help alcohol-dependent patients curb their drinking.
A separate study showed that a single dose of ketamine plus therapy that focused on reactivating drinking-related “maladaptive reward memories” reduced drinking urges and alcohol intake more than just ketamine or a placebo infusion alone.
“That ketamine can reduce both alcohol use and depression in AUD is encouraging therapeutically,” the researchers write.
“While a clear link between depression and AUD is acknowledged, alcohol and mental health services still struggle to meet the needs of dual-diagnosis patients, so ketamine may represent a solution to this long-standing comorbidity,” they add.
Dr. Morgan said in an interview that adjunctive ketamine with relapse-prevention therapy is “currently being delivered in Awakn Clinics in the U.K. and Norway, but we need to conduct the phase 3 trial in order to make the treatment more widely accessible.”
An ‘Intriguing new therapy’
Reached for comment, Timothy Brennan, MD, MPH, chief of clinical services, Addiction Institute of Mount Sinai, New York, said ketamine “continues to be an intriguing new therapy for a variety of mental health conditions.”
“Unfortunately, the study did not show any difference in rates of relapse to alcohol, though an improvement in days of abstinence is certainly noteworthy,” Dr. Brennan said in an interview.
“Because this was just a proof-of-concept study and did not compare ketamine to any FDA-approved pharmacotherapy for alcohol, it remains too early to recommend ketamine infusions to those suffering from alcohol use disorder,” he cautioned.
The study was supported by the Medical Research Council. Dr. Morgan has received royalties for KARE (Ketamine for Reduction of Alcoholic Relapse) therapy license distribution. KARE therapy is licensed from University of Exeter to Awakn Life Sciences. Dr. Morgan has received research funding from Awakn Life Sciences and has served as a consultant for Janssen Pharmaceuticals. Other coauthors have disclosed relationships with industry; the full list can be found with the original article. Dr. Brennan has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Three weekly infusions of the dissociative anesthetic ketamine coupled with mindfulness-based relapse prevention therapy may help adults with alcohol use disorder (AUD) maintain abstinence, new research suggests.
Preliminary results from a phase 2, double-blind, placebo-controlled trial show ketamine was well tolerated and, compared with placebo, associated with more days of abstinence from alcohol at 6 months.
The results suggest ketamine plus psychological therapy may be a “new, relatively brief treatment that has long lasting effects in AUD,” Celia Morgan, PhD, professor of psychopharmacology, University of Exeter, United Kingdom, told this news organization.
The study was published online Jan. 11 in the American Journal of Psychiatry.
Target depression
Depressive symptoms are common in patients under treatment for AUD and increase relapse risk.
“Ketamine may support alcohol abstinence by temporarily alleviating depressive symptoms during the high-risk relapse period in the weeks after detoxification,” the investigators note.
Ketamine may also provide a “temporary boost to synaptogenesis and neurogenesis, which may allow psychological therapies and new strategies for managing addiction to embed more readily,” they add.
To test these theories, the researchers recruited 96 adults (mean age, 44 years, 35 women) with severe AUD to participate in the trial.
All participants had to abstain from alcohol for at least 24 hours before the trial started and have a reading of 0.0 on a breath alcohol test at the baseline visit.
Participants were randomly allocated to one of four groups:
1. three weekly ketamine infusions of 0.8 mg/kg IV over 40 minutes plus psychological therapy
2. three saline infusions plus psychological therapy
3. three ketamine infusions plus alcohol education
4. three saline infusions plus alcohol education
The primary outcome was self-reported percentage of days abstinent, as well as confirmed alcohol relapse at 6-month follow-up.
(mean difference, 10.1%; 95% confidence interval, 1.1-19.0), “although confidence intervals were wide, consistent with a proof-of-concept study,” the authors note.
The greatest reduction in total days off alcohol occurred in the ketamine plus relapse-prevention therapy group compared with the saline plus alcohol education group (mean difference, 15.9%; 95% CI, 3.8-28.1).
There was no significant difference in relapse rate between the ketamine and placebo groups. No serious adverse effects were reported in any participant.
Growing evidence
These findings support some other studies that have also suggested a benefit of ketamine in AUD.
As reported by this news organization, one recent study found a single infusion of ketamine combined with counseling may help alcohol-dependent patients curb their drinking.
A separate study showed that a single dose of ketamine plus therapy that focused on reactivating drinking-related “maladaptive reward memories” reduced drinking urges and alcohol intake more than just ketamine or a placebo infusion alone.
“That ketamine can reduce both alcohol use and depression in AUD is encouraging therapeutically,” the researchers write.
“While a clear link between depression and AUD is acknowledged, alcohol and mental health services still struggle to meet the needs of dual-diagnosis patients, so ketamine may represent a solution to this long-standing comorbidity,” they add.
Dr. Morgan said in an interview that adjunctive ketamine with relapse-prevention therapy is “currently being delivered in Awakn Clinics in the U.K. and Norway, but we need to conduct the phase 3 trial in order to make the treatment more widely accessible.”
An ‘Intriguing new therapy’
Reached for comment, Timothy Brennan, MD, MPH, chief of clinical services, Addiction Institute of Mount Sinai, New York, said ketamine “continues to be an intriguing new therapy for a variety of mental health conditions.”
“Unfortunately, the study did not show any difference in rates of relapse to alcohol, though an improvement in days of abstinence is certainly noteworthy,” Dr. Brennan said in an interview.
“Because this was just a proof-of-concept study and did not compare ketamine to any FDA-approved pharmacotherapy for alcohol, it remains too early to recommend ketamine infusions to those suffering from alcohol use disorder,” he cautioned.
The study was supported by the Medical Research Council. Dr. Morgan has received royalties for KARE (Ketamine for Reduction of Alcoholic Relapse) therapy license distribution. KARE therapy is licensed from University of Exeter to Awakn Life Sciences. Dr. Morgan has received research funding from Awakn Life Sciences and has served as a consultant for Janssen Pharmaceuticals. Other coauthors have disclosed relationships with industry; the full list can be found with the original article. Dr. Brennan has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Three weekly infusions of the dissociative anesthetic ketamine coupled with mindfulness-based relapse prevention therapy may help adults with alcohol use disorder (AUD) maintain abstinence, new research suggests.
Preliminary results from a phase 2, double-blind, placebo-controlled trial show ketamine was well tolerated and, compared with placebo, associated with more days of abstinence from alcohol at 6 months.
The results suggest ketamine plus psychological therapy may be a “new, relatively brief treatment that has long lasting effects in AUD,” Celia Morgan, PhD, professor of psychopharmacology, University of Exeter, United Kingdom, told this news organization.
The study was published online Jan. 11 in the American Journal of Psychiatry.
Target depression
Depressive symptoms are common in patients under treatment for AUD and increase relapse risk.
“Ketamine may support alcohol abstinence by temporarily alleviating depressive symptoms during the high-risk relapse period in the weeks after detoxification,” the investigators note.
Ketamine may also provide a “temporary boost to synaptogenesis and neurogenesis, which may allow psychological therapies and new strategies for managing addiction to embed more readily,” they add.
To test these theories, the researchers recruited 96 adults (mean age, 44 years, 35 women) with severe AUD to participate in the trial.
All participants had to abstain from alcohol for at least 24 hours before the trial started and have a reading of 0.0 on a breath alcohol test at the baseline visit.
Participants were randomly allocated to one of four groups:
1. three weekly ketamine infusions of 0.8 mg/kg IV over 40 minutes plus psychological therapy
2. three saline infusions plus psychological therapy
3. three ketamine infusions plus alcohol education
4. three saline infusions plus alcohol education
The primary outcome was self-reported percentage of days abstinent, as well as confirmed alcohol relapse at 6-month follow-up.
(mean difference, 10.1%; 95% confidence interval, 1.1-19.0), “although confidence intervals were wide, consistent with a proof-of-concept study,” the authors note.
The greatest reduction in total days off alcohol occurred in the ketamine plus relapse-prevention therapy group compared with the saline plus alcohol education group (mean difference, 15.9%; 95% CI, 3.8-28.1).
There was no significant difference in relapse rate between the ketamine and placebo groups. No serious adverse effects were reported in any participant.
Growing evidence
These findings support some other studies that have also suggested a benefit of ketamine in AUD.
As reported by this news organization, one recent study found a single infusion of ketamine combined with counseling may help alcohol-dependent patients curb their drinking.
A separate study showed that a single dose of ketamine plus therapy that focused on reactivating drinking-related “maladaptive reward memories” reduced drinking urges and alcohol intake more than just ketamine or a placebo infusion alone.
“That ketamine can reduce both alcohol use and depression in AUD is encouraging therapeutically,” the researchers write.
“While a clear link between depression and AUD is acknowledged, alcohol and mental health services still struggle to meet the needs of dual-diagnosis patients, so ketamine may represent a solution to this long-standing comorbidity,” they add.
Dr. Morgan said in an interview that adjunctive ketamine with relapse-prevention therapy is “currently being delivered in Awakn Clinics in the U.K. and Norway, but we need to conduct the phase 3 trial in order to make the treatment more widely accessible.”
An ‘Intriguing new therapy’
Reached for comment, Timothy Brennan, MD, MPH, chief of clinical services, Addiction Institute of Mount Sinai, New York, said ketamine “continues to be an intriguing new therapy for a variety of mental health conditions.”
“Unfortunately, the study did not show any difference in rates of relapse to alcohol, though an improvement in days of abstinence is certainly noteworthy,” Dr. Brennan said in an interview.
“Because this was just a proof-of-concept study and did not compare ketamine to any FDA-approved pharmacotherapy for alcohol, it remains too early to recommend ketamine infusions to those suffering from alcohol use disorder,” he cautioned.
The study was supported by the Medical Research Council. Dr. Morgan has received royalties for KARE (Ketamine for Reduction of Alcoholic Relapse) therapy license distribution. KARE therapy is licensed from University of Exeter to Awakn Life Sciences. Dr. Morgan has received research funding from Awakn Life Sciences and has served as a consultant for Janssen Pharmaceuticals. Other coauthors have disclosed relationships with industry; the full list can be found with the original article. Dr. Brennan has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.