User login
New guideline offers recommendations for reproductive health in patients with rheumatic diseases
A new guideline from the American College of Rheumatology offers the organization’s first clinical recommendations on how to manage reproductive health issues in patients with rheumatic and musculoskeletal diseases (RMDs).
“With the development of this guideline, the ACR recognizes the key role of clinical rheumatologists not only in managing disease activity but also in understanding the interactions of RMDs and their therapies in the context of reproductive health,” wrote Lisa R. Sammaritano, MD, of Weill Cornell Medicine and the Hospital for Special Surgery in New York, and coauthors. The guideline was published in Arthritis & Rheumatology.
To develop an evidence-based guideline on reproductive health in RMD patients, the researchers embarked on a systematic review of studies in areas like contraception, pregnancy and lactation, assisted reproductive technology (ART), fertility preservation, and hormone therapy. The guideline contains 12 ungraded good practice statements and 131 graded recommendations, all developed through the Grading of Recommendations Assessment, Development, and Evaluation methodology.
In counseling patients about these areas of care, the guideline says that rheumatologists and other clinicians “must collaborate with specialists in the fields of obstetrics-gynecology, maternal-fetal medicine, and reproductive endocrinology and infertility.”
“One thing this guideline does well is highlight the importance of involving maternal-fetal medicine colleagues,” Alison Cahill, MD, a professor in the department of women’s health at the University of Texas at Austin and a maternal-fetal medicine specialist within UT Health Austin’s Women’s Health Institute, said when asked for comment on the guideline. “We’re always very happy to see patients ahead of time who are planning pregnancy to be able to discuss what the care plan would look like. And specifically, to address medications, if required, for their rheumatologic care.
“As we learn more and more,” she added, “we’ve come to understand that most treatments and medications are actually safe or relatively safe to take in pregnancy. Certainly, the benefit of taking them outweighs any small or theoretic risks. On the flip side, the guideline does a nice job of highlighting the importance of good disease control, both at the time of conception and during pregnancy.”
Contraception
In regard to contraception, the guideline strongly recommends the use of effective contraceptives – with a conditional recommendation of IUDs or a subdermal progestin implant – in fertile women with a RMD who have neither systemic lupus erythematosus (SLE) nor positive antiphospholipid antibody (aPL). They also strongly recommend discussing the use of emergency contraception with all RMD patients.
For SLE patients, the guideline strongly recommends the use of effective contraceptives in those with stable or low disease activity who are not positive for aPL. They also strongly recommend progestin‐only or IUD contraceptives over combined estrogen‐progestin contraception. For aPL-positive patients, the guideline strongly recommends against combined estrogen‐progestin contraceptives and for levonorgestrel or copper IUDs or the progestin‐only pill.
Assisted reproductive technology
In regard to ART, the guideline strongly recommends proceeding as needed in aPL-negative women with uncomplicated, stable RMD who are on pregnancy‐compatible medications. They also strongly recommend deferring ART in any RMD patients with moderately or severely active disease.
For aPL-positive patients undergoing ART procedures, they strongly recommend prophylactic anticoagulation with heparin or low-molecular-weight heparin (LMWH) in women with obstetric antiphospholipid syndrome (APS) and therapeutic anticoagulation in women with thrombotic APS. In patients undergoing embryo and oocyte cryopreservation, they strongly recommend continuing immunosuppressive and biologic therapies – the exception being cyclophosphamide (CYC) – for anyone in stable condition.
Fertility preservation
In regard to fertility preservation in patients taking CYC, the guideline strongly suggests sperm cryopreservation as good practice prior to treatment. They also conditionally recommend monthly gonadotropin‐releasing hormone agonist cotherapy in premenopausal women with RMD.
Hormone therapy
In regard to menopause and hormone therapy, the guideline strongly suggests hormone therapy as good practice in postmenopausal women with RMD, without SLE or positive aPL, and who have severe vasomotor symptoms. Hormone therapy is conditionally recommended in patients with SLE, without positive aPL, and with no contraindications. For aPL-positive patients, they strongly recommend against hormone therapy in women with obstetric and/or thrombotic APS.
Pregnancy assessment and management
Among the many recommendations regarding pregnancy assessment and management, the guideline strongly suggests counseling women with RMD who are considering pregnancy to take into account the improved outcomes for pregnant women with low disease activity. They strongly recommend that women considering pregnancy should switch to pregnancy‐compatible medication and pause to assess its efficacy and tolerability before moving forward, along with strongly recommending that pregnant women with active disease initiate or continue a pregnancy‐compatible steroid‐sparing medication. They also recommend testing for anti‐Ro/SS-A and anti‐La/SS-B in women with SLE, Sjögren’s syndrome, systemic sclerosis, or rheumatoid arthritis, but only once and only before or early in the pregnancy.
For women with systemic sclerosis who develop scleroderma renal crisis during pregnancy, the authors strongly advise using ACE inhibitors or angiotensin receptor blockers “because the risk of maternal or fetal death with untreated disease is higher than the risk associated with use of these medications during pregnancy.”
Among women with SLE, the recommendations strongly call for testing either before or early in pregnancy for anticardiolipin antibody, anti–beta2-glycoprotein I, or positive lupus anticoagulant, as well as initiating or continuing hydroxychloroquine (HCQ) if possible. Starting in the first trimester, the authors also conditionally recommend that SLE patients take low-dose aspirin daily
For pregnant women who test positive for aPL but do not meet criteria for obstetric or thrombotic APS, the guideline conditionally recommends prophylactic treatment with low-dose aspirin daily to protect against preeclampsia. When obstetric APS criteria are met, the guideline strongly advises combined treatment with daily low-dose aspirin and prophylactic-dose heparin (or LMWH), as well as prophylactic-dose anticoagulation for 6-12 weeks post partum. When patients have thrombotic APS, this combination treatment should contain heparin dose at a therapeutic level throughout pregnancy and postpartum. However, the authors conditionally recommend against giving low-dose aspirin plus prophylactic-dose heparin to women without obstetric APS. For refractory obstetric APS, the guideline also contains recommendations that are conditionally against treatment with intravenous immunoglobulin or an increased LMWH dose and strongly against adding prednisone to prophylactic-dose heparin or LMWH and low-dose aspirin. In pregnant patients with primary APS, the authors conditionally advise adding HCQ to prophylactic-dose heparin or LMWH and low-dose aspirin therapy. However, women with aPL who do not meet APS criteria or have another indication for HCQ are conditionally advised against prophylactic treatment with the antimalarial.
For women with Anti-Ro/SS-A and/or anti-La/SS-B antibodies in pregnancy, there is conditional advice to use HCQ. When there is no history of an infant with complete heart block or neonatal lupus erythematosus among women with these antibodies, the guideline conditionally advises serial fetal echocardiography (less often than weekly) starting between 16 and 18 weeks and continuing through 26 weeks, but this should be weekly when there is a prior history. Treatment with oral dexamethasone 4 mg daily is conditionally advised when there is echocardiographic evidence of fetal first- or second-degree heart block, but dexamethasone is not recommended when complete heart block is present.
Finally, in regard to medication use, the authors strongly recommend that men who are planning to be fathers continue on HCQ, azathioprine, 6‐mercaptopurine, colchicine, or tumor necrosis factor inhibitors. Conditional treatment recommendations for men planning for pregnancy include methotrexate, mycophenolate mofetil/mycophenolic acid (MMF), leflunomide, sulfasalazine, calcineurin inhibitors, and NSAIDs. They also strongly recommend that this group of men discontinue CYC and thalidomide.
Pregnant women are strongly recommended to discontinue methotrexate, leflunomide (with cholestyramine washout if there are detectable serum levels of its metabolite prior to pregnancy or as soon as it is confirmed), MMF, CYC, and thalidomide within 3 months prior to conception, and they strongly recommend HCQ (in women with SLE), azathioprine/6‐mercaptopurine, colchicine, or sulfasalazine for use throughout pregnancy. They strongly recommend a combination of low‐dose aspirin and prophylactic‐dose heparin for pregnant women with obstetric APS, along with low‐dose aspirin and therapeutic‐dose heparin for women with thrombotic APS throughout pregnancy and postpartum. However, for women with SLE and those who test positive for aPL but do not meet criteria for obstetric or thrombotic APS, the authors conditionally recommend low-dose aspirin starting in the first trimester.
The guideline suggests that women with RMD should be encouraged to breastfeed if they are willing and able; they also suggest that disease control be maintained through lactation‐compatible medications and that the risks and benefits be reviewed on a patient-by-patient basis. Treatment with HCQ, colchicine, sulfasalazine, rituximab, and all tumor necrosis factor inhibitors are strongly recommended as being compatible with breastfeeding, and they strongly recommend against using CYC, leflunomide, MMF, and thalidomide while breastfeeding.
The authors acknowledged the limitations of their guideline, including the literature review being conducted on studies involving adults and an “inability to include recommendations for uncommon but important clinical situations,” including those involving transgender patients and hormonal therapies.
The authors reported numerous potential conflicts of interest, including receiving research support, consulting fees, speaking fees, and honoraria from various pharmaceutical companies.
SOURCE: Sammaritano LR et al. Arthritis Rheumatol. 2020 Feb 23. doi: 10.1002/art.41191.
A new guideline from the American College of Rheumatology offers the organization’s first clinical recommendations on how to manage reproductive health issues in patients with rheumatic and musculoskeletal diseases (RMDs).
“With the development of this guideline, the ACR recognizes the key role of clinical rheumatologists not only in managing disease activity but also in understanding the interactions of RMDs and their therapies in the context of reproductive health,” wrote Lisa R. Sammaritano, MD, of Weill Cornell Medicine and the Hospital for Special Surgery in New York, and coauthors. The guideline was published in Arthritis & Rheumatology.
To develop an evidence-based guideline on reproductive health in RMD patients, the researchers embarked on a systematic review of studies in areas like contraception, pregnancy and lactation, assisted reproductive technology (ART), fertility preservation, and hormone therapy. The guideline contains 12 ungraded good practice statements and 131 graded recommendations, all developed through the Grading of Recommendations Assessment, Development, and Evaluation methodology.
In counseling patients about these areas of care, the guideline says that rheumatologists and other clinicians “must collaborate with specialists in the fields of obstetrics-gynecology, maternal-fetal medicine, and reproductive endocrinology and infertility.”
“One thing this guideline does well is highlight the importance of involving maternal-fetal medicine colleagues,” Alison Cahill, MD, a professor in the department of women’s health at the University of Texas at Austin and a maternal-fetal medicine specialist within UT Health Austin’s Women’s Health Institute, said when asked for comment on the guideline. “We’re always very happy to see patients ahead of time who are planning pregnancy to be able to discuss what the care plan would look like. And specifically, to address medications, if required, for their rheumatologic care.
“As we learn more and more,” she added, “we’ve come to understand that most treatments and medications are actually safe or relatively safe to take in pregnancy. Certainly, the benefit of taking them outweighs any small or theoretic risks. On the flip side, the guideline does a nice job of highlighting the importance of good disease control, both at the time of conception and during pregnancy.”
Contraception
In regard to contraception, the guideline strongly recommends the use of effective contraceptives – with a conditional recommendation of IUDs or a subdermal progestin implant – in fertile women with a RMD who have neither systemic lupus erythematosus (SLE) nor positive antiphospholipid antibody (aPL). They also strongly recommend discussing the use of emergency contraception with all RMD patients.
For SLE patients, the guideline strongly recommends the use of effective contraceptives in those with stable or low disease activity who are not positive for aPL. They also strongly recommend progestin‐only or IUD contraceptives over combined estrogen‐progestin contraception. For aPL-positive patients, the guideline strongly recommends against combined estrogen‐progestin contraceptives and for levonorgestrel or copper IUDs or the progestin‐only pill.
Assisted reproductive technology
In regard to ART, the guideline strongly recommends proceeding as needed in aPL-negative women with uncomplicated, stable RMD who are on pregnancy‐compatible medications. They also strongly recommend deferring ART in any RMD patients with moderately or severely active disease.
For aPL-positive patients undergoing ART procedures, they strongly recommend prophylactic anticoagulation with heparin or low-molecular-weight heparin (LMWH) in women with obstetric antiphospholipid syndrome (APS) and therapeutic anticoagulation in women with thrombotic APS. In patients undergoing embryo and oocyte cryopreservation, they strongly recommend continuing immunosuppressive and biologic therapies – the exception being cyclophosphamide (CYC) – for anyone in stable condition.
Fertility preservation
In regard to fertility preservation in patients taking CYC, the guideline strongly suggests sperm cryopreservation as good practice prior to treatment. They also conditionally recommend monthly gonadotropin‐releasing hormone agonist cotherapy in premenopausal women with RMD.
Hormone therapy
In regard to menopause and hormone therapy, the guideline strongly suggests hormone therapy as good practice in postmenopausal women with RMD, without SLE or positive aPL, and who have severe vasomotor symptoms. Hormone therapy is conditionally recommended in patients with SLE, without positive aPL, and with no contraindications. For aPL-positive patients, they strongly recommend against hormone therapy in women with obstetric and/or thrombotic APS.
Pregnancy assessment and management
Among the many recommendations regarding pregnancy assessment and management, the guideline strongly suggests counseling women with RMD who are considering pregnancy to take into account the improved outcomes for pregnant women with low disease activity. They strongly recommend that women considering pregnancy should switch to pregnancy‐compatible medication and pause to assess its efficacy and tolerability before moving forward, along with strongly recommending that pregnant women with active disease initiate or continue a pregnancy‐compatible steroid‐sparing medication. They also recommend testing for anti‐Ro/SS-A and anti‐La/SS-B in women with SLE, Sjögren’s syndrome, systemic sclerosis, or rheumatoid arthritis, but only once and only before or early in the pregnancy.
For women with systemic sclerosis who develop scleroderma renal crisis during pregnancy, the authors strongly advise using ACE inhibitors or angiotensin receptor blockers “because the risk of maternal or fetal death with untreated disease is higher than the risk associated with use of these medications during pregnancy.”
Among women with SLE, the recommendations strongly call for testing either before or early in pregnancy for anticardiolipin antibody, anti–beta2-glycoprotein I, or positive lupus anticoagulant, as well as initiating or continuing hydroxychloroquine (HCQ) if possible. Starting in the first trimester, the authors also conditionally recommend that SLE patients take low-dose aspirin daily
For pregnant women who test positive for aPL but do not meet criteria for obstetric or thrombotic APS, the guideline conditionally recommends prophylactic treatment with low-dose aspirin daily to protect against preeclampsia. When obstetric APS criteria are met, the guideline strongly advises combined treatment with daily low-dose aspirin and prophylactic-dose heparin (or LMWH), as well as prophylactic-dose anticoagulation for 6-12 weeks post partum. When patients have thrombotic APS, this combination treatment should contain heparin dose at a therapeutic level throughout pregnancy and postpartum. However, the authors conditionally recommend against giving low-dose aspirin plus prophylactic-dose heparin to women without obstetric APS. For refractory obstetric APS, the guideline also contains recommendations that are conditionally against treatment with intravenous immunoglobulin or an increased LMWH dose and strongly against adding prednisone to prophylactic-dose heparin or LMWH and low-dose aspirin. In pregnant patients with primary APS, the authors conditionally advise adding HCQ to prophylactic-dose heparin or LMWH and low-dose aspirin therapy. However, women with aPL who do not meet APS criteria or have another indication for HCQ are conditionally advised against prophylactic treatment with the antimalarial.
For women with Anti-Ro/SS-A and/or anti-La/SS-B antibodies in pregnancy, there is conditional advice to use HCQ. When there is no history of an infant with complete heart block or neonatal lupus erythematosus among women with these antibodies, the guideline conditionally advises serial fetal echocardiography (less often than weekly) starting between 16 and 18 weeks and continuing through 26 weeks, but this should be weekly when there is a prior history. Treatment with oral dexamethasone 4 mg daily is conditionally advised when there is echocardiographic evidence of fetal first- or second-degree heart block, but dexamethasone is not recommended when complete heart block is present.
Finally, in regard to medication use, the authors strongly recommend that men who are planning to be fathers continue on HCQ, azathioprine, 6‐mercaptopurine, colchicine, or tumor necrosis factor inhibitors. Conditional treatment recommendations for men planning for pregnancy include methotrexate, mycophenolate mofetil/mycophenolic acid (MMF), leflunomide, sulfasalazine, calcineurin inhibitors, and NSAIDs. They also strongly recommend that this group of men discontinue CYC and thalidomide.
Pregnant women are strongly recommended to discontinue methotrexate, leflunomide (with cholestyramine washout if there are detectable serum levels of its metabolite prior to pregnancy or as soon as it is confirmed), MMF, CYC, and thalidomide within 3 months prior to conception, and they strongly recommend HCQ (in women with SLE), azathioprine/6‐mercaptopurine, colchicine, or sulfasalazine for use throughout pregnancy. They strongly recommend a combination of low‐dose aspirin and prophylactic‐dose heparin for pregnant women with obstetric APS, along with low‐dose aspirin and therapeutic‐dose heparin for women with thrombotic APS throughout pregnancy and postpartum. However, for women with SLE and those who test positive for aPL but do not meet criteria for obstetric or thrombotic APS, the authors conditionally recommend low-dose aspirin starting in the first trimester.
The guideline suggests that women with RMD should be encouraged to breastfeed if they are willing and able; they also suggest that disease control be maintained through lactation‐compatible medications and that the risks and benefits be reviewed on a patient-by-patient basis. Treatment with HCQ, colchicine, sulfasalazine, rituximab, and all tumor necrosis factor inhibitors are strongly recommended as being compatible with breastfeeding, and they strongly recommend against using CYC, leflunomide, MMF, and thalidomide while breastfeeding.
The authors acknowledged the limitations of their guideline, including the literature review being conducted on studies involving adults and an “inability to include recommendations for uncommon but important clinical situations,” including those involving transgender patients and hormonal therapies.
The authors reported numerous potential conflicts of interest, including receiving research support, consulting fees, speaking fees, and honoraria from various pharmaceutical companies.
SOURCE: Sammaritano LR et al. Arthritis Rheumatol. 2020 Feb 23. doi: 10.1002/art.41191.
A new guideline from the American College of Rheumatology offers the organization’s first clinical recommendations on how to manage reproductive health issues in patients with rheumatic and musculoskeletal diseases (RMDs).
“With the development of this guideline, the ACR recognizes the key role of clinical rheumatologists not only in managing disease activity but also in understanding the interactions of RMDs and their therapies in the context of reproductive health,” wrote Lisa R. Sammaritano, MD, of Weill Cornell Medicine and the Hospital for Special Surgery in New York, and coauthors. The guideline was published in Arthritis & Rheumatology.
To develop an evidence-based guideline on reproductive health in RMD patients, the researchers embarked on a systematic review of studies in areas like contraception, pregnancy and lactation, assisted reproductive technology (ART), fertility preservation, and hormone therapy. The guideline contains 12 ungraded good practice statements and 131 graded recommendations, all developed through the Grading of Recommendations Assessment, Development, and Evaluation methodology.
In counseling patients about these areas of care, the guideline says that rheumatologists and other clinicians “must collaborate with specialists in the fields of obstetrics-gynecology, maternal-fetal medicine, and reproductive endocrinology and infertility.”
“One thing this guideline does well is highlight the importance of involving maternal-fetal medicine colleagues,” Alison Cahill, MD, a professor in the department of women’s health at the University of Texas at Austin and a maternal-fetal medicine specialist within UT Health Austin’s Women’s Health Institute, said when asked for comment on the guideline. “We’re always very happy to see patients ahead of time who are planning pregnancy to be able to discuss what the care plan would look like. And specifically, to address medications, if required, for their rheumatologic care.
“As we learn more and more,” she added, “we’ve come to understand that most treatments and medications are actually safe or relatively safe to take in pregnancy. Certainly, the benefit of taking them outweighs any small or theoretic risks. On the flip side, the guideline does a nice job of highlighting the importance of good disease control, both at the time of conception and during pregnancy.”
Contraception
In regard to contraception, the guideline strongly recommends the use of effective contraceptives – with a conditional recommendation of IUDs or a subdermal progestin implant – in fertile women with a RMD who have neither systemic lupus erythematosus (SLE) nor positive antiphospholipid antibody (aPL). They also strongly recommend discussing the use of emergency contraception with all RMD patients.
For SLE patients, the guideline strongly recommends the use of effective contraceptives in those with stable or low disease activity who are not positive for aPL. They also strongly recommend progestin‐only or IUD contraceptives over combined estrogen‐progestin contraception. For aPL-positive patients, the guideline strongly recommends against combined estrogen‐progestin contraceptives and for levonorgestrel or copper IUDs or the progestin‐only pill.
Assisted reproductive technology
In regard to ART, the guideline strongly recommends proceeding as needed in aPL-negative women with uncomplicated, stable RMD who are on pregnancy‐compatible medications. They also strongly recommend deferring ART in any RMD patients with moderately or severely active disease.
For aPL-positive patients undergoing ART procedures, they strongly recommend prophylactic anticoagulation with heparin or low-molecular-weight heparin (LMWH) in women with obstetric antiphospholipid syndrome (APS) and therapeutic anticoagulation in women with thrombotic APS. In patients undergoing embryo and oocyte cryopreservation, they strongly recommend continuing immunosuppressive and biologic therapies – the exception being cyclophosphamide (CYC) – for anyone in stable condition.
Fertility preservation
In regard to fertility preservation in patients taking CYC, the guideline strongly suggests sperm cryopreservation as good practice prior to treatment. They also conditionally recommend monthly gonadotropin‐releasing hormone agonist cotherapy in premenopausal women with RMD.
Hormone therapy
In regard to menopause and hormone therapy, the guideline strongly suggests hormone therapy as good practice in postmenopausal women with RMD, without SLE or positive aPL, and who have severe vasomotor symptoms. Hormone therapy is conditionally recommended in patients with SLE, without positive aPL, and with no contraindications. For aPL-positive patients, they strongly recommend against hormone therapy in women with obstetric and/or thrombotic APS.
Pregnancy assessment and management
Among the many recommendations regarding pregnancy assessment and management, the guideline strongly suggests counseling women with RMD who are considering pregnancy to take into account the improved outcomes for pregnant women with low disease activity. They strongly recommend that women considering pregnancy should switch to pregnancy‐compatible medication and pause to assess its efficacy and tolerability before moving forward, along with strongly recommending that pregnant women with active disease initiate or continue a pregnancy‐compatible steroid‐sparing medication. They also recommend testing for anti‐Ro/SS-A and anti‐La/SS-B in women with SLE, Sjögren’s syndrome, systemic sclerosis, or rheumatoid arthritis, but only once and only before or early in the pregnancy.
For women with systemic sclerosis who develop scleroderma renal crisis during pregnancy, the authors strongly advise using ACE inhibitors or angiotensin receptor blockers “because the risk of maternal or fetal death with untreated disease is higher than the risk associated with use of these medications during pregnancy.”
Among women with SLE, the recommendations strongly call for testing either before or early in pregnancy for anticardiolipin antibody, anti–beta2-glycoprotein I, or positive lupus anticoagulant, as well as initiating or continuing hydroxychloroquine (HCQ) if possible. Starting in the first trimester, the authors also conditionally recommend that SLE patients take low-dose aspirin daily
For pregnant women who test positive for aPL but do not meet criteria for obstetric or thrombotic APS, the guideline conditionally recommends prophylactic treatment with low-dose aspirin daily to protect against preeclampsia. When obstetric APS criteria are met, the guideline strongly advises combined treatment with daily low-dose aspirin and prophylactic-dose heparin (or LMWH), as well as prophylactic-dose anticoagulation for 6-12 weeks post partum. When patients have thrombotic APS, this combination treatment should contain heparin dose at a therapeutic level throughout pregnancy and postpartum. However, the authors conditionally recommend against giving low-dose aspirin plus prophylactic-dose heparin to women without obstetric APS. For refractory obstetric APS, the guideline also contains recommendations that are conditionally against treatment with intravenous immunoglobulin or an increased LMWH dose and strongly against adding prednisone to prophylactic-dose heparin or LMWH and low-dose aspirin. In pregnant patients with primary APS, the authors conditionally advise adding HCQ to prophylactic-dose heparin or LMWH and low-dose aspirin therapy. However, women with aPL who do not meet APS criteria or have another indication for HCQ are conditionally advised against prophylactic treatment with the antimalarial.
For women with Anti-Ro/SS-A and/or anti-La/SS-B antibodies in pregnancy, there is conditional advice to use HCQ. When there is no history of an infant with complete heart block or neonatal lupus erythematosus among women with these antibodies, the guideline conditionally advises serial fetal echocardiography (less often than weekly) starting between 16 and 18 weeks and continuing through 26 weeks, but this should be weekly when there is a prior history. Treatment with oral dexamethasone 4 mg daily is conditionally advised when there is echocardiographic evidence of fetal first- or second-degree heart block, but dexamethasone is not recommended when complete heart block is present.
Finally, in regard to medication use, the authors strongly recommend that men who are planning to be fathers continue on HCQ, azathioprine, 6‐mercaptopurine, colchicine, or tumor necrosis factor inhibitors. Conditional treatment recommendations for men planning for pregnancy include methotrexate, mycophenolate mofetil/mycophenolic acid (MMF), leflunomide, sulfasalazine, calcineurin inhibitors, and NSAIDs. They also strongly recommend that this group of men discontinue CYC and thalidomide.
Pregnant women are strongly recommended to discontinue methotrexate, leflunomide (with cholestyramine washout if there are detectable serum levels of its metabolite prior to pregnancy or as soon as it is confirmed), MMF, CYC, and thalidomide within 3 months prior to conception, and they strongly recommend HCQ (in women with SLE), azathioprine/6‐mercaptopurine, colchicine, or sulfasalazine for use throughout pregnancy. They strongly recommend a combination of low‐dose aspirin and prophylactic‐dose heparin for pregnant women with obstetric APS, along with low‐dose aspirin and therapeutic‐dose heparin for women with thrombotic APS throughout pregnancy and postpartum. However, for women with SLE and those who test positive for aPL but do not meet criteria for obstetric or thrombotic APS, the authors conditionally recommend low-dose aspirin starting in the first trimester.
The guideline suggests that women with RMD should be encouraged to breastfeed if they are willing and able; they also suggest that disease control be maintained through lactation‐compatible medications and that the risks and benefits be reviewed on a patient-by-patient basis. Treatment with HCQ, colchicine, sulfasalazine, rituximab, and all tumor necrosis factor inhibitors are strongly recommended as being compatible with breastfeeding, and they strongly recommend against using CYC, leflunomide, MMF, and thalidomide while breastfeeding.
The authors acknowledged the limitations of their guideline, including the literature review being conducted on studies involving adults and an “inability to include recommendations for uncommon but important clinical situations,” including those involving transgender patients and hormonal therapies.
The authors reported numerous potential conflicts of interest, including receiving research support, consulting fees, speaking fees, and honoraria from various pharmaceutical companies.
SOURCE: Sammaritano LR et al. Arthritis Rheumatol. 2020 Feb 23. doi: 10.1002/art.41191.
FROM ARTHRITIS & RHEUMATOLOGY
Community-wide initiative ups teen LARC adoption sixfold
In Rochester, N.Y., a comprehensive community initiative that raised awareness about and delivered training in the use of long-acting reversible contraceptives (LARCs) significantly upped LARC adoption among sexually active female high schoolers.
Over the course of the 3-year project, LARC use rose from about 4% to 24% in this group, a statistically significant increase (P less than .0001). During the same time period, LARC use increased nationally, as well, but at a lower rate, rising from 2% to 5% for the same population, while New York state saw LARC use rise from 2% to 5%.
In New York City, where an unrelated LARC awareness campaign was conducted, LARC use went from 3% to 5% over the study period for sexually active female high school students. Comparing the trend in LARC use in Rochester to the secular trend in these control groups showed significantly higher uptake over time in Rochester (P less than .0001).
Through a series of lunch-and-learn talks given to adults who work with adolescents in community-based settings and in medical settings, the Greater Rochester LARC Initiative reached more than 1,300 individuals during July 2014-June 2017, C. Andrew Aligne, MD, MPH, of the University of Rochester (N.Y.), and coauthors reported in the American Journal of Obstetrics and Gynecology.
Of the 81 total talks delivered, 50 were in medical settings, reaching 703 attendees ranging from front-office personnel to primary care physicians, advanced practice clinicians, and nurses; the talks in community-based settings reached 662 attendees.
“We use the term ‘community detailing’ to describe the design of the intervention because it was an innovative hybrid of academic detailing and community health education,” explained Dr. Aligne and colleagues. This approach is a unique, feasible, and effective approach to unintended adolescent pregnancy programs. “The community detailing approach could be a useful complement to programs for preventing unintended adolescent pregnancy.”
The study’s primary outcome measure was LARC use among sexually active female high school students as identified by responses on the U.S. Centers for Disease Control and Statistics’ Youth Risk Behavior Survey (YRBS).
YRBS data were examined for the years 2013, 2015, and 2017, spanning the period before and after the LARC initiative was begun. A separate question about LARC use wasn’t included in the 2013 YRBS survey, so the investigators used a generous estimate that two-thirds of respondents who reported using the “other” contraceptive category for that year were using LARCs. That category was chosen by a total of 6% of respondents, and encompassed LARC use along with use of the patch, ring, diaphragm, and fertility awareness, explained Dr. Aligne and collaborators.
Addressing the problem of failure to use a condom with LARC use, Dr. Aligne and collaborators found overall low rates of dual-method use, but higher rates in Rochester than in the comparison groups. In Rochester, 78% of respondents reported that they also did not use condoms. This figure was lower than the 91% reported for the United States as a whole, and also was lower than the 93% reported in New York City and the 85% reported in New York state. No increase in sexually transmitted infections was seen in Rochester’s sexually active high school females during the study period.
“Our main finding of increased LARC use is consistent with the literature demonstrating that many sexually active young women, including adolescents, will choose LARC if they are given access not only to birth control itself, but also to accurate information about various contraceptive methods,” concluded Dr. Aligne and his associates.
A practical strength of the Greater Rochester LARC initiative was that it capitalized on existing resources, such as New York state’s preexisting program for free access to contraception and similar provisions in the Affordable Care Act. Also, local Title X clinics that were enrolled in New York’s free contraception initiative already had practitioners who were trained and able to provide same-day LARC insertion.
Pediatricians engaged in the initiative were able to receive free training from LARC manufacturers, as mandated by the Food and Drug Administration. Through collaboration with implant manufacturers, Rochester LARC Initiative staff were able to piggyback on training sessions to add education about contraception counseling and the importance of offering access to all contraception methods.
Taken as a whole, the LARC Initiative could be scaled up, wrote Dr. Aligne and his coauthors, a potential boon in the 21 states where qualifying individuals younger than 19 years of age are eligible for Medicaid reimbursement for family planning services. “Even though easy LARC access is far from universal, there are vast areas of the nation where cost need not be seen as an insurmountable barrier.” Dr. Aligne and coauthors also addressed the fraught history of reproductive justice in the United States, cautioning that universal LARC adoption was not – and should not be – the goal of such initiatives. “There is a history of reproductive coercion in the U.S. including forced sterilization of women of color; therefore, it is critical that LARC methods not be imposed on any particular group. On the other hand, LARC should not be withheld deliberately from adolescents who want it, as this is another form of injustice,” they wrote. “The goal should be to empower individuals to decide what is right for them in a context of social and reproductive justice.”
Using the nationally administered YRBS was a significant strength of the study, commented Dr. Aligne and his collaborators. “This allowed us to employ the study design of pre-post with a nonrandomized control group,” the investigators noted, adding that the “relatively rigorous” methodology reduced the risk of problems with internal validity, and also allowed comparisons between changes in Rochester and those at the state and national level.
However, the researchers acknowledged that the study was not a randomized trial, and there’s always the possibility of unknown confounders contributing to LARC uptake during the study period. Also, the YRBS is a self-report instrument and only includes those enrolled in school.
Dr. Aligne reported that his spouse received compensation for providing contraceptive implant insertion training, as did two coauthors. The LARC initiative was supported by a grant from the Greater Rochester Health Foundation.
SOURCE: Aligne CA et al. Am J Obstet Gynecol. 2020 Jan 22. doi: 10.1016/j.ajog.2020.01.029.
In Rochester, N.Y., a comprehensive community initiative that raised awareness about and delivered training in the use of long-acting reversible contraceptives (LARCs) significantly upped LARC adoption among sexually active female high schoolers.
Over the course of the 3-year project, LARC use rose from about 4% to 24% in this group, a statistically significant increase (P less than .0001). During the same time period, LARC use increased nationally, as well, but at a lower rate, rising from 2% to 5% for the same population, while New York state saw LARC use rise from 2% to 5%.
In New York City, where an unrelated LARC awareness campaign was conducted, LARC use went from 3% to 5% over the study period for sexually active female high school students. Comparing the trend in LARC use in Rochester to the secular trend in these control groups showed significantly higher uptake over time in Rochester (P less than .0001).
Through a series of lunch-and-learn talks given to adults who work with adolescents in community-based settings and in medical settings, the Greater Rochester LARC Initiative reached more than 1,300 individuals during July 2014-June 2017, C. Andrew Aligne, MD, MPH, of the University of Rochester (N.Y.), and coauthors reported in the American Journal of Obstetrics and Gynecology.
Of the 81 total talks delivered, 50 were in medical settings, reaching 703 attendees ranging from front-office personnel to primary care physicians, advanced practice clinicians, and nurses; the talks in community-based settings reached 662 attendees.
“We use the term ‘community detailing’ to describe the design of the intervention because it was an innovative hybrid of academic detailing and community health education,” explained Dr. Aligne and colleagues. This approach is a unique, feasible, and effective approach to unintended adolescent pregnancy programs. “The community detailing approach could be a useful complement to programs for preventing unintended adolescent pregnancy.”
The study’s primary outcome measure was LARC use among sexually active female high school students as identified by responses on the U.S. Centers for Disease Control and Statistics’ Youth Risk Behavior Survey (YRBS).
YRBS data were examined for the years 2013, 2015, and 2017, spanning the period before and after the LARC initiative was begun. A separate question about LARC use wasn’t included in the 2013 YRBS survey, so the investigators used a generous estimate that two-thirds of respondents who reported using the “other” contraceptive category for that year were using LARCs. That category was chosen by a total of 6% of respondents, and encompassed LARC use along with use of the patch, ring, diaphragm, and fertility awareness, explained Dr. Aligne and collaborators.
Addressing the problem of failure to use a condom with LARC use, Dr. Aligne and collaborators found overall low rates of dual-method use, but higher rates in Rochester than in the comparison groups. In Rochester, 78% of respondents reported that they also did not use condoms. This figure was lower than the 91% reported for the United States as a whole, and also was lower than the 93% reported in New York City and the 85% reported in New York state. No increase in sexually transmitted infections was seen in Rochester’s sexually active high school females during the study period.
“Our main finding of increased LARC use is consistent with the literature demonstrating that many sexually active young women, including adolescents, will choose LARC if they are given access not only to birth control itself, but also to accurate information about various contraceptive methods,” concluded Dr. Aligne and his associates.
A practical strength of the Greater Rochester LARC initiative was that it capitalized on existing resources, such as New York state’s preexisting program for free access to contraception and similar provisions in the Affordable Care Act. Also, local Title X clinics that were enrolled in New York’s free contraception initiative already had practitioners who were trained and able to provide same-day LARC insertion.
Pediatricians engaged in the initiative were able to receive free training from LARC manufacturers, as mandated by the Food and Drug Administration. Through collaboration with implant manufacturers, Rochester LARC Initiative staff were able to piggyback on training sessions to add education about contraception counseling and the importance of offering access to all contraception methods.
Taken as a whole, the LARC Initiative could be scaled up, wrote Dr. Aligne and his coauthors, a potential boon in the 21 states where qualifying individuals younger than 19 years of age are eligible for Medicaid reimbursement for family planning services. “Even though easy LARC access is far from universal, there are vast areas of the nation where cost need not be seen as an insurmountable barrier.” Dr. Aligne and coauthors also addressed the fraught history of reproductive justice in the United States, cautioning that universal LARC adoption was not – and should not be – the goal of such initiatives. “There is a history of reproductive coercion in the U.S. including forced sterilization of women of color; therefore, it is critical that LARC methods not be imposed on any particular group. On the other hand, LARC should not be withheld deliberately from adolescents who want it, as this is another form of injustice,” they wrote. “The goal should be to empower individuals to decide what is right for them in a context of social and reproductive justice.”
Using the nationally administered YRBS was a significant strength of the study, commented Dr. Aligne and his collaborators. “This allowed us to employ the study design of pre-post with a nonrandomized control group,” the investigators noted, adding that the “relatively rigorous” methodology reduced the risk of problems with internal validity, and also allowed comparisons between changes in Rochester and those at the state and national level.
However, the researchers acknowledged that the study was not a randomized trial, and there’s always the possibility of unknown confounders contributing to LARC uptake during the study period. Also, the YRBS is a self-report instrument and only includes those enrolled in school.
Dr. Aligne reported that his spouse received compensation for providing contraceptive implant insertion training, as did two coauthors. The LARC initiative was supported by a grant from the Greater Rochester Health Foundation.
SOURCE: Aligne CA et al. Am J Obstet Gynecol. 2020 Jan 22. doi: 10.1016/j.ajog.2020.01.029.
In Rochester, N.Y., a comprehensive community initiative that raised awareness about and delivered training in the use of long-acting reversible contraceptives (LARCs) significantly upped LARC adoption among sexually active female high schoolers.
Over the course of the 3-year project, LARC use rose from about 4% to 24% in this group, a statistically significant increase (P less than .0001). During the same time period, LARC use increased nationally, as well, but at a lower rate, rising from 2% to 5% for the same population, while New York state saw LARC use rise from 2% to 5%.
In New York City, where an unrelated LARC awareness campaign was conducted, LARC use went from 3% to 5% over the study period for sexually active female high school students. Comparing the trend in LARC use in Rochester to the secular trend in these control groups showed significantly higher uptake over time in Rochester (P less than .0001).
Through a series of lunch-and-learn talks given to adults who work with adolescents in community-based settings and in medical settings, the Greater Rochester LARC Initiative reached more than 1,300 individuals during July 2014-June 2017, C. Andrew Aligne, MD, MPH, of the University of Rochester (N.Y.), and coauthors reported in the American Journal of Obstetrics and Gynecology.
Of the 81 total talks delivered, 50 were in medical settings, reaching 703 attendees ranging from front-office personnel to primary care physicians, advanced practice clinicians, and nurses; the talks in community-based settings reached 662 attendees.
“We use the term ‘community detailing’ to describe the design of the intervention because it was an innovative hybrid of academic detailing and community health education,” explained Dr. Aligne and colleagues. This approach is a unique, feasible, and effective approach to unintended adolescent pregnancy programs. “The community detailing approach could be a useful complement to programs for preventing unintended adolescent pregnancy.”
The study’s primary outcome measure was LARC use among sexually active female high school students as identified by responses on the U.S. Centers for Disease Control and Statistics’ Youth Risk Behavior Survey (YRBS).
YRBS data were examined for the years 2013, 2015, and 2017, spanning the period before and after the LARC initiative was begun. A separate question about LARC use wasn’t included in the 2013 YRBS survey, so the investigators used a generous estimate that two-thirds of respondents who reported using the “other” contraceptive category for that year were using LARCs. That category was chosen by a total of 6% of respondents, and encompassed LARC use along with use of the patch, ring, diaphragm, and fertility awareness, explained Dr. Aligne and collaborators.
Addressing the problem of failure to use a condom with LARC use, Dr. Aligne and collaborators found overall low rates of dual-method use, but higher rates in Rochester than in the comparison groups. In Rochester, 78% of respondents reported that they also did not use condoms. This figure was lower than the 91% reported for the United States as a whole, and also was lower than the 93% reported in New York City and the 85% reported in New York state. No increase in sexually transmitted infections was seen in Rochester’s sexually active high school females during the study period.
“Our main finding of increased LARC use is consistent with the literature demonstrating that many sexually active young women, including adolescents, will choose LARC if they are given access not only to birth control itself, but also to accurate information about various contraceptive methods,” concluded Dr. Aligne and his associates.
A practical strength of the Greater Rochester LARC initiative was that it capitalized on existing resources, such as New York state’s preexisting program for free access to contraception and similar provisions in the Affordable Care Act. Also, local Title X clinics that were enrolled in New York’s free contraception initiative already had practitioners who were trained and able to provide same-day LARC insertion.
Pediatricians engaged in the initiative were able to receive free training from LARC manufacturers, as mandated by the Food and Drug Administration. Through collaboration with implant manufacturers, Rochester LARC Initiative staff were able to piggyback on training sessions to add education about contraception counseling and the importance of offering access to all contraception methods.
Taken as a whole, the LARC Initiative could be scaled up, wrote Dr. Aligne and his coauthors, a potential boon in the 21 states where qualifying individuals younger than 19 years of age are eligible for Medicaid reimbursement for family planning services. “Even though easy LARC access is far from universal, there are vast areas of the nation where cost need not be seen as an insurmountable barrier.” Dr. Aligne and coauthors also addressed the fraught history of reproductive justice in the United States, cautioning that universal LARC adoption was not – and should not be – the goal of such initiatives. “There is a history of reproductive coercion in the U.S. including forced sterilization of women of color; therefore, it is critical that LARC methods not be imposed on any particular group. On the other hand, LARC should not be withheld deliberately from adolescents who want it, as this is another form of injustice,” they wrote. “The goal should be to empower individuals to decide what is right for them in a context of social and reproductive justice.”
Using the nationally administered YRBS was a significant strength of the study, commented Dr. Aligne and his collaborators. “This allowed us to employ the study design of pre-post with a nonrandomized control group,” the investigators noted, adding that the “relatively rigorous” methodology reduced the risk of problems with internal validity, and also allowed comparisons between changes in Rochester and those at the state and national level.
However, the researchers acknowledged that the study was not a randomized trial, and there’s always the possibility of unknown confounders contributing to LARC uptake during the study period. Also, the YRBS is a self-report instrument and only includes those enrolled in school.
Dr. Aligne reported that his spouse received compensation for providing contraceptive implant insertion training, as did two coauthors. The LARC initiative was supported by a grant from the Greater Rochester Health Foundation.
SOURCE: Aligne CA et al. Am J Obstet Gynecol. 2020 Jan 22. doi: 10.1016/j.ajog.2020.01.029.
FROM AJOG
FDA approves weekly contraceptive patch Twirla
in women whose body mass index is less than 30 kg/m2 and for whom a combined hormonal contraceptive is appropriate.
Applied weekly to the abdomen, buttock, or upper torso (excluding the breasts), Twirla delivers a 30-mcg daily dose of ethinyl estradiol and 120-mcg daily dose of levonorgestrel.
“Twirla is an important addition to available hormonal contraceptive methods, allowing prescribers to now offer appropriate U.S. women a weekly transdermal option that delivers estrogen levels in line with labeled doses of many commonly prescribed oral contraceptives, David Portman, MD, an obstetrician/gynecologist in Columbus, Ohio, and a primary investigator of the SECURE trial, said in a news release issued by the company.
Twirla was evaluated in “a diverse population providing important data to prescribers and to women seeking contraception. It is vital to expand the full range of contraceptive methods and inform the choices that fit an individual’s family planning needs and lifestyle,” Dr. Portman added.
As part of approval, the FDA will require Agile Therapeutics to conduct a long-term, prospective, observational postmarketing study to assess risks for venous thromboembolism and arterial thromboembolism in new users of Twirla, compared with new users of other combined hormonal contraceptives.
Twirla is contraindicated in women at high risk for arterial or venous thrombotic disease, including women with a BMI equal to or greater than 30 kg/m2; women who have headaches with focal neurologic symptoms or migraine with aura; and women older than 35 years who have any migraine headache.
Twirla also should be avoided in women who have liver tumors, acute viral hepatitis, decompensated cirrhosis, liver disease, or undiagnosed abnormal uterine bleeding. It also should be avoided during pregnancy; in women who currently have or who have history of breast cancer or other estrogen- or progestin-sensitive cancer; in women who are hypersensitivity to any components of Twirla; and in women who use hepatitis C drug combinations containing ombitasvir/paraparesis/ritonavir, with or without dasabuvir.
Because cigarette smoking increases the risk for serious cardiovascular events from combined hormonal contraceptive use, Twirla also is contraindicated in women older than 35 who smoke.
Twirla will contain a boxed warning that will include these risks about cigarette smoking and the serious cardiovascular events, and it will stipulate that Twirla is contraindicated in women with a BMI greater than 30 kg/m2.
This article first appeared on Medscape.com.
in women whose body mass index is less than 30 kg/m2 and for whom a combined hormonal contraceptive is appropriate.
Applied weekly to the abdomen, buttock, or upper torso (excluding the breasts), Twirla delivers a 30-mcg daily dose of ethinyl estradiol and 120-mcg daily dose of levonorgestrel.
“Twirla is an important addition to available hormonal contraceptive methods, allowing prescribers to now offer appropriate U.S. women a weekly transdermal option that delivers estrogen levels in line with labeled doses of many commonly prescribed oral contraceptives, David Portman, MD, an obstetrician/gynecologist in Columbus, Ohio, and a primary investigator of the SECURE trial, said in a news release issued by the company.
Twirla was evaluated in “a diverse population providing important data to prescribers and to women seeking contraception. It is vital to expand the full range of contraceptive methods and inform the choices that fit an individual’s family planning needs and lifestyle,” Dr. Portman added.
As part of approval, the FDA will require Agile Therapeutics to conduct a long-term, prospective, observational postmarketing study to assess risks for venous thromboembolism and arterial thromboembolism in new users of Twirla, compared with new users of other combined hormonal contraceptives.
Twirla is contraindicated in women at high risk for arterial or venous thrombotic disease, including women with a BMI equal to or greater than 30 kg/m2; women who have headaches with focal neurologic symptoms or migraine with aura; and women older than 35 years who have any migraine headache.
Twirla also should be avoided in women who have liver tumors, acute viral hepatitis, decompensated cirrhosis, liver disease, or undiagnosed abnormal uterine bleeding. It also should be avoided during pregnancy; in women who currently have or who have history of breast cancer or other estrogen- or progestin-sensitive cancer; in women who are hypersensitivity to any components of Twirla; and in women who use hepatitis C drug combinations containing ombitasvir/paraparesis/ritonavir, with or without dasabuvir.
Because cigarette smoking increases the risk for serious cardiovascular events from combined hormonal contraceptive use, Twirla also is contraindicated in women older than 35 who smoke.
Twirla will contain a boxed warning that will include these risks about cigarette smoking and the serious cardiovascular events, and it will stipulate that Twirla is contraindicated in women with a BMI greater than 30 kg/m2.
This article first appeared on Medscape.com.
in women whose body mass index is less than 30 kg/m2 and for whom a combined hormonal contraceptive is appropriate.
Applied weekly to the abdomen, buttock, or upper torso (excluding the breasts), Twirla delivers a 30-mcg daily dose of ethinyl estradiol and 120-mcg daily dose of levonorgestrel.
“Twirla is an important addition to available hormonal contraceptive methods, allowing prescribers to now offer appropriate U.S. women a weekly transdermal option that delivers estrogen levels in line with labeled doses of many commonly prescribed oral contraceptives, David Portman, MD, an obstetrician/gynecologist in Columbus, Ohio, and a primary investigator of the SECURE trial, said in a news release issued by the company.
Twirla was evaluated in “a diverse population providing important data to prescribers and to women seeking contraception. It is vital to expand the full range of contraceptive methods and inform the choices that fit an individual’s family planning needs and lifestyle,” Dr. Portman added.
As part of approval, the FDA will require Agile Therapeutics to conduct a long-term, prospective, observational postmarketing study to assess risks for venous thromboembolism and arterial thromboembolism in new users of Twirla, compared with new users of other combined hormonal contraceptives.
Twirla is contraindicated in women at high risk for arterial or venous thrombotic disease, including women with a BMI equal to or greater than 30 kg/m2; women who have headaches with focal neurologic symptoms or migraine with aura; and women older than 35 years who have any migraine headache.
Twirla also should be avoided in women who have liver tumors, acute viral hepatitis, decompensated cirrhosis, liver disease, or undiagnosed abnormal uterine bleeding. It also should be avoided during pregnancy; in women who currently have or who have history of breast cancer or other estrogen- or progestin-sensitive cancer; in women who are hypersensitivity to any components of Twirla; and in women who use hepatitis C drug combinations containing ombitasvir/paraparesis/ritonavir, with or without dasabuvir.
Because cigarette smoking increases the risk for serious cardiovascular events from combined hormonal contraceptive use, Twirla also is contraindicated in women older than 35 who smoke.
Twirla will contain a boxed warning that will include these risks about cigarette smoking and the serious cardiovascular events, and it will stipulate that Twirla is contraindicated in women with a BMI greater than 30 kg/m2.
This article first appeared on Medscape.com.
What is optimal hormonal treatment for women with polycystic ovary syndrome?
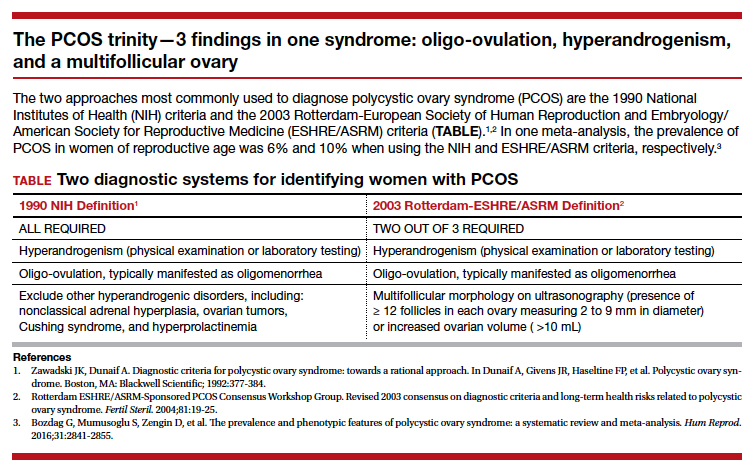
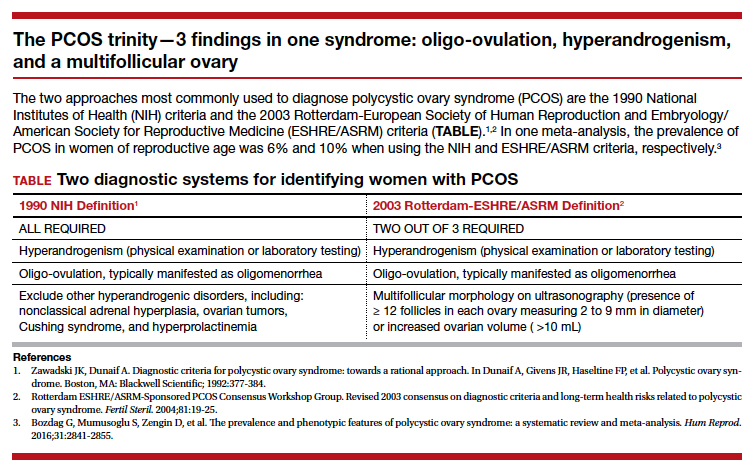
Polycystic ovary syndrome (PCOS) is the triad of oligo-ovulation resulting in oligomenorrhea, hyperandrogenism and, often, an excess number of small antral follicles on high-resolution pelvic ultrasound. One meta-analysis reported that, in women of reproductive age, the prevalence of PCOS was 10% using the Rotterdam-European Society of Human Reproduction and Embryology/American Society for Reproductive Medicine (ESHRE/ASRM) criteria1 and 6% using the National Institutes of Health 1990 diagnostic criteria.2 (See “The PCOS trinity—3 findings in one syndrome: oligo-ovulation, hyperandrogenism, and a multifollicular ovary.”3)
PCOS is caused by abnormalities in 3 systems: reproductive, metabolic, and dermatologic. Reproductive abnormalities commonly observed in women with PCOS include4:
- an increase in pituitary secretion of luteinizing hormone (LH), resulting from both an increase in LH pulse amplitude and LH pulse frequency, suggesting a primary hypothalamic disorder
- an increase in ovarian secretion of androstenedione and testosterone due to stimulation by LH and possibly insulin
- oligo-ovulation with chronically low levels of progesterone that can result in endometrial hyperplasia
- ovulatory infertility.
Metabolic abnormalities commonly observed in women with PCOS include5,6:
- insulin resistance and hyperinsulinemia
- excess adipose tissue in the liver
- excess visceral fat
- elevated adipokines
- obesity
- an increased prevalence of glucose intolerance and frank diabetes.
Dermatologic abnormalities commonly observed in women with PCOS include7:
- facial hirsutism
- acne
- androgenetic alopecia.
Given that PCOS is caused by abnormalities in the reproductive, metabolic, and dermatologic systems, it is appropriate to consider multimodal hormonal therapy that addresses all 3 problems. In my practice, I believe that the best approach to the long-term hormonal treatment of PCOS for many women is to prescribe a combination of 3 medicines: a combination estrogen-progestin oral contraceptive (COC), an insulin sensitizer, and an antiandrogen.
The COC reduces pituitary secretion of LH, decreases ovarian androgen production, and prevents the development of endometrial hyperplasia. When taken cyclically, the COC treatment also restores regular withdrawal uterine bleeding.
An insulin sensitizer, such as metformin or pioglitazone, helps to reduce insulin resistance, glucose intolerance, and hepatic adipose content, rebalancing central metabolism. It is important to include diet and exercise in the long-term treatment of PCOS, and I always encourage these lifestyle changes. However, my patients usually report that they have tried multiple times to restrict dietary caloric intake and increase exercise and have been unable to rebalance their metabolism with these interventions alone. Of note, in the women with PCOS and a body mass index >35 kg/m2, bariatric surgery, such as a sleeve gastrectomy, often results in marked improvement of their PCOS.8
The antiandrogen spironolactone provides effective treatment for the dermatologic problems of facial hirsutism and acne. Some COCs containing the progestins drospirenone, norgestimate, and norethindrone acetate are approved by the US Food and Drug Administration for the treatment of acne. A common approach I use in practice is to prescribe a COC, plus spironolactone 100 mg daily plus metformin extended-release 750 mg to 1,500 mg daily.
Continue to: Which COCs have low androgenicity?...
Which COCs have low androgenicity?
I believe that every COC is an effective treatment for PCOS, regardless of the androgenicity of the progestin in the contraceptive. However, some dermatologists believe that combination contraceptives containing progestins with low androgenicity, such as drospirenone, norgestimate, and desogestrel, are more likely to improve acne than contraceptives with an androgenic progestin such as levonorgestrel. In one study in which 2,147 women with acne were treated by one dermatologic practice, the percentage of women reporting that a birth control pill helped to improve their acne was 66% for pills containing drospirenone, 53% for pills containing norgestimate, 44% for pills containing desogestrel, 30% for pills containing norethindrone, and 25% for pills containing levonorgestrel. In the same study, the percent of women reporting that a birth control pill made their acne worse was 3% for pills containing drospirenone, 6% for pills containing norgestimate, 2% for pills containing desogestrel, 8% for pills containing norethindrone, and 10% for pills containing levonorgestrel.9 Given these findings, when treating a woman with PCOS, I generally prescribe a contraceptive that does not contain levonorgestrel.

Why is a spironolactone dose of 100 mg a good choice for PCOS treatment?
Spironolactone, an antiandrogen and inhibitor of 5-alpha-reductase, is commonly prescribed for the treatment of hirsutism and acne at doses ranging from 50 mg to 200 mg daily.10,11 In my clinical experience, spironolactone at a dose of 200 mg daily commonly causes irregular and bothersome uterine bleeding while spironolactone at a dose of 100 mg daily is seldom associated with irregular bleeding. I believe that spironolactone at a dose of 100 mg daily results in superior clinical efficacy than a 50-mg daily dose, although studies report that both doses are effective in the treatment of acne and hirsutism. Spironolactone should not be prescribed to women with renal failure because it can result in severe hyperkalemia. In a study of spironolactone safety in the treatment of acne, no adverse effects on the kidney, liver, or adrenal glands were reported over 8 years of use.12
What insulin sensitizers are useful in rebalancing the metabolic abnormalities observed with PCOS?
Diet and exercise are superb approaches to rebalancing metabolic abnormalities, but for many of my patients they are insufficient and treatment with an insulin sensitizer is warranted. The most commonly utilized insulin sensitizer for the treatment of PCOS is metformin because it is very inexpensive and has a low risk of serious adverse effects such as lactic acidosis. Metformin increases peripheral glucose uptake and reduces gastrointestinal glucose absorption. Insulin sensitizers also decrease visceral fat, a major source of adipokines. One major disadvantage of metformin is that at doses in the range of 1,500 mg to 2,250 mg it often causes gastrointestinal adverse effects such as borborygmi, nausea, abdominal discomfort, and loose stools.
Thiazolidinediones, including pioglitazone, have been reported to be effective in rebalancing central metabolism in women with PCOS. Pioglitazone carries a black box warning of an increased risk of congestive heart failure and nonfatal myocardial infarction. Pioglitazone is also associated with a risk of hepatotoxicity. However, at the pioglitazone dose commonly used in the treatment of PCOS (7.5 mg daily), these serious adverse effects are rare. In practice, I initiate metformin at a dose of 750 mg daily using the extended-release formulation. I increase the metformin dose to 1,500 mg daily if the patient has no bothersome gastrointestinal symptoms on the lower dose. If the patient cannot tolerate metformin treatment because of adverse effects, I will use pioglitazone 7.5 mg daily.
Continue to: Treatment of PCOS in women who are carriers of the Factor V Leiden mutation...
Treatment of PCOS in women who are carriers of the Factor V Leiden mutation
The Factor V Leiden allele is associated with an increased risk of venous thromboembolism. Estrogen-progestin contraception is contraindicated in women with the Factor V Leiden mutation. The prevalence of this mutation varies by race and ethnicity. It is present in about 5% of white, 2% of Hispanic, 1% of black, 1% of Native American, and 0.5% of Asian women. In women with PCOS who are known to be carriers of the mutation, dual therapy with metformin and spironolactone is highly effective.13-15 For these women I also offer a levonorgestrel IUD to provide contraception and reduce the risk of endometrial hyperplasia.
Combination triple medication treatment of PCOS
Optimal treatment of the reproductive, metabolic, and dermatologic problems associated with PCOS requires multimodal medications including an estrogen-progestin contraceptive, an antiandrogen, and an insulin sensitizer. In my practice, I initiate treatment of PCOS by offering patients 3 medications: a COC, spironolactone 100 mg daily, and metformin extended-release formulation 750 mg daily. Some patients elect dual medication therapy (COC plus spironolactone or COC plus metformin), but many patients select treatment with all 3 medications. Although triple medication treatment of PCOS has not been tested in large randomized clinical trials, small trials report that triple medication treatment produces optimal improvement in the reproductive, metabolic, and dermatologic problems associated with PCOS.16-18
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19-25.
- Zawadski JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In Dunaif A, Givens JR, Haseltine FP, et al. Polycystic ovary syndrome. Boston, MA: Blackwell Scientific; 1992:377-384.
- Bozdag G, Mumusoglu S, Zengin D, et al. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2016;31:2841-2855.
- Baskind NE, Balen AH. Hypothalamic-pituitary, ovarian and adrenal contributions to polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2016;37:80-97.
- Gilbert EW, Tay CT, Hiam DS, et al. Comorbidities and complications of polycystic ovary syndrome: an overview of systematic reviews. Clin Endocrinol (Oxf). 2018;89:683-699.
- Harsha Varma S, Tirupati S, Pradeep TV, et al. Insulin resistance and hyperandrogenemia independently predict nonalcoholic fatty liver disease in women with polycystic ovary syndrome. Diabetes Metab Syndr. 2019;13:1065-1069.
- Housman E, Reynolds RV. Polycystic ovary syndrome: a review for dermatologists: Part I. Diagnosis and manifestations. J Am Acad Dermatol. 2014;71:847.e1-e10.
- Dilday J, Derickson M, Kuckelman J, et al. Sleeve gastrectomy for obesity in polycystic ovarian syndrome: a pilot study evaluating weight loss and fertility outcomes. Obes Surg. 2019;29:93-98.
- Lortscher D, Admani S, Satur N, et al. Hormonal contraceptives and acne: a retrospective analysis of 2147 patients. J Drugs Dermatol. 2016;15:670-674.
- Brown J, Farquhar C, Lee O, et al. Spironolactone versus placebo or in combination with steroids for hirsutism and/or acne. Cochrane Database Syst Rev. 2009;CD000194.
- Shaw JC. Low-dose adjunctive spironolactone in the treatment of acne in women: a retrospective analysis of 85 consecutively treated patients. J Am Acad Dermatol. 2000;43:498-502.
- Shaw JC, White LE. Long-term safety of spironolactone in acne: results of an 8-year follow-up study. J Cutan Med Surg. 2002;6:541-545.
- Ganie MA, Khurana ML, Nisar S, et al. Improved efficacy of low-dose spironolactone and metformin combination than either drug alone in the management of women with polycystic ovary syndrome (PCOS): a six-month, open-label randomized study. J Clin Endocrinol Metab. 2013;98:3599-3607.
- Mazza A, Fruci B, Guzzi P, et al. In PCOS patients the addition of low-dose spironolactone induces a more marked reduction of clinical and biochemical hyperandrogenism than metformin alone. Nutr Metab Cardiovascular Dis. 2014;24:132-139.
- Ganie MA, Khurana ML, Eunice M, et al. Comparison of efficacy of spironolactone with metformin in the management of polycystic ovary syndrome: an open-labeled study. J Clin Endocrinol Metab. 2004;89:2756-2762.
- Ibanez L, de Zegher F. Low-dose combination flutamide, metformin and an oral contraceptive for non-obese, young women with polycystic ovary syndrome. Hum Reprod. 2003;18:57-60.
- Ibanez L, de Zegher F. Flutamide-metformin plus an oral contraceptive (OC) for young women with polycystic ovary syndrome: switch from third- to fourth-generation OC reduces body adiposity. Hum Reprod. 2004;19:1725-1727.
Polycystic ovary syndrome (PCOS) is the triad of oligo-ovulation resulting in oligomenorrhea, hyperandrogenism and, often, an excess number of small antral follicles on high-resolution pelvic ultrasound. One meta-analysis reported that, in women of reproductive age, the prevalence of PCOS was 10% using the Rotterdam-European Society of Human Reproduction and Embryology/American Society for Reproductive Medicine (ESHRE/ASRM) criteria1 and 6% using the National Institutes of Health 1990 diagnostic criteria.2 (See “The PCOS trinity—3 findings in one syndrome: oligo-ovulation, hyperandrogenism, and a multifollicular ovary.”3)
PCOS is caused by abnormalities in 3 systems: reproductive, metabolic, and dermatologic. Reproductive abnormalities commonly observed in women with PCOS include4:
- an increase in pituitary secretion of luteinizing hormone (LH), resulting from both an increase in LH pulse amplitude and LH pulse frequency, suggesting a primary hypothalamic disorder
- an increase in ovarian secretion of androstenedione and testosterone due to stimulation by LH and possibly insulin
- oligo-ovulation with chronically low levels of progesterone that can result in endometrial hyperplasia
- ovulatory infertility.
Metabolic abnormalities commonly observed in women with PCOS include5,6:
- insulin resistance and hyperinsulinemia
- excess adipose tissue in the liver
- excess visceral fat
- elevated adipokines
- obesity
- an increased prevalence of glucose intolerance and frank diabetes.
Dermatologic abnormalities commonly observed in women with PCOS include7:
- facial hirsutism
- acne
- androgenetic alopecia.
Given that PCOS is caused by abnormalities in the reproductive, metabolic, and dermatologic systems, it is appropriate to consider multimodal hormonal therapy that addresses all 3 problems. In my practice, I believe that the best approach to the long-term hormonal treatment of PCOS for many women is to prescribe a combination of 3 medicines: a combination estrogen-progestin oral contraceptive (COC), an insulin sensitizer, and an antiandrogen.
The COC reduces pituitary secretion of LH, decreases ovarian androgen production, and prevents the development of endometrial hyperplasia. When taken cyclically, the COC treatment also restores regular withdrawal uterine bleeding.
An insulin sensitizer, such as metformin or pioglitazone, helps to reduce insulin resistance, glucose intolerance, and hepatic adipose content, rebalancing central metabolism. It is important to include diet and exercise in the long-term treatment of PCOS, and I always encourage these lifestyle changes. However, my patients usually report that they have tried multiple times to restrict dietary caloric intake and increase exercise and have been unable to rebalance their metabolism with these interventions alone. Of note, in the women with PCOS and a body mass index >35 kg/m2, bariatric surgery, such as a sleeve gastrectomy, often results in marked improvement of their PCOS.8
The antiandrogen spironolactone provides effective treatment for the dermatologic problems of facial hirsutism and acne. Some COCs containing the progestins drospirenone, norgestimate, and norethindrone acetate are approved by the US Food and Drug Administration for the treatment of acne. A common approach I use in practice is to prescribe a COC, plus spironolactone 100 mg daily plus metformin extended-release 750 mg to 1,500 mg daily.
Continue to: Which COCs have low androgenicity?...
Which COCs have low androgenicity?
I believe that every COC is an effective treatment for PCOS, regardless of the androgenicity of the progestin in the contraceptive. However, some dermatologists believe that combination contraceptives containing progestins with low androgenicity, such as drospirenone, norgestimate, and desogestrel, are more likely to improve acne than contraceptives with an androgenic progestin such as levonorgestrel. In one study in which 2,147 women with acne were treated by one dermatologic practice, the percentage of women reporting that a birth control pill helped to improve their acne was 66% for pills containing drospirenone, 53% for pills containing norgestimate, 44% for pills containing desogestrel, 30% for pills containing norethindrone, and 25% for pills containing levonorgestrel. In the same study, the percent of women reporting that a birth control pill made their acne worse was 3% for pills containing drospirenone, 6% for pills containing norgestimate, 2% for pills containing desogestrel, 8% for pills containing norethindrone, and 10% for pills containing levonorgestrel.9 Given these findings, when treating a woman with PCOS, I generally prescribe a contraceptive that does not contain levonorgestrel.

Why is a spironolactone dose of 100 mg a good choice for PCOS treatment?
Spironolactone, an antiandrogen and inhibitor of 5-alpha-reductase, is commonly prescribed for the treatment of hirsutism and acne at doses ranging from 50 mg to 200 mg daily.10,11 In my clinical experience, spironolactone at a dose of 200 mg daily commonly causes irregular and bothersome uterine bleeding while spironolactone at a dose of 100 mg daily is seldom associated with irregular bleeding. I believe that spironolactone at a dose of 100 mg daily results in superior clinical efficacy than a 50-mg daily dose, although studies report that both doses are effective in the treatment of acne and hirsutism. Spironolactone should not be prescribed to women with renal failure because it can result in severe hyperkalemia. In a study of spironolactone safety in the treatment of acne, no adverse effects on the kidney, liver, or adrenal glands were reported over 8 years of use.12
What insulin sensitizers are useful in rebalancing the metabolic abnormalities observed with PCOS?
Diet and exercise are superb approaches to rebalancing metabolic abnormalities, but for many of my patients they are insufficient and treatment with an insulin sensitizer is warranted. The most commonly utilized insulin sensitizer for the treatment of PCOS is metformin because it is very inexpensive and has a low risk of serious adverse effects such as lactic acidosis. Metformin increases peripheral glucose uptake and reduces gastrointestinal glucose absorption. Insulin sensitizers also decrease visceral fat, a major source of adipokines. One major disadvantage of metformin is that at doses in the range of 1,500 mg to 2,250 mg it often causes gastrointestinal adverse effects such as borborygmi, nausea, abdominal discomfort, and loose stools.
Thiazolidinediones, including pioglitazone, have been reported to be effective in rebalancing central metabolism in women with PCOS. Pioglitazone carries a black box warning of an increased risk of congestive heart failure and nonfatal myocardial infarction. Pioglitazone is also associated with a risk of hepatotoxicity. However, at the pioglitazone dose commonly used in the treatment of PCOS (7.5 mg daily), these serious adverse effects are rare. In practice, I initiate metformin at a dose of 750 mg daily using the extended-release formulation. I increase the metformin dose to 1,500 mg daily if the patient has no bothersome gastrointestinal symptoms on the lower dose. If the patient cannot tolerate metformin treatment because of adverse effects, I will use pioglitazone 7.5 mg daily.
Continue to: Treatment of PCOS in women who are carriers of the Factor V Leiden mutation...
Treatment of PCOS in women who are carriers of the Factor V Leiden mutation
The Factor V Leiden allele is associated with an increased risk of venous thromboembolism. Estrogen-progestin contraception is contraindicated in women with the Factor V Leiden mutation. The prevalence of this mutation varies by race and ethnicity. It is present in about 5% of white, 2% of Hispanic, 1% of black, 1% of Native American, and 0.5% of Asian women. In women with PCOS who are known to be carriers of the mutation, dual therapy with metformin and spironolactone is highly effective.13-15 For these women I also offer a levonorgestrel IUD to provide contraception and reduce the risk of endometrial hyperplasia.
Combination triple medication treatment of PCOS
Optimal treatment of the reproductive, metabolic, and dermatologic problems associated with PCOS requires multimodal medications including an estrogen-progestin contraceptive, an antiandrogen, and an insulin sensitizer. In my practice, I initiate treatment of PCOS by offering patients 3 medications: a COC, spironolactone 100 mg daily, and metformin extended-release formulation 750 mg daily. Some patients elect dual medication therapy (COC plus spironolactone or COC plus metformin), but many patients select treatment with all 3 medications. Although triple medication treatment of PCOS has not been tested in large randomized clinical trials, small trials report that triple medication treatment produces optimal improvement in the reproductive, metabolic, and dermatologic problems associated with PCOS.16-18
Polycystic ovary syndrome (PCOS) is the triad of oligo-ovulation resulting in oligomenorrhea, hyperandrogenism and, often, an excess number of small antral follicles on high-resolution pelvic ultrasound. One meta-analysis reported that, in women of reproductive age, the prevalence of PCOS was 10% using the Rotterdam-European Society of Human Reproduction and Embryology/American Society for Reproductive Medicine (ESHRE/ASRM) criteria1 and 6% using the National Institutes of Health 1990 diagnostic criteria.2 (See “The PCOS trinity—3 findings in one syndrome: oligo-ovulation, hyperandrogenism, and a multifollicular ovary.”3)
PCOS is caused by abnormalities in 3 systems: reproductive, metabolic, and dermatologic. Reproductive abnormalities commonly observed in women with PCOS include4:
- an increase in pituitary secretion of luteinizing hormone (LH), resulting from both an increase in LH pulse amplitude and LH pulse frequency, suggesting a primary hypothalamic disorder
- an increase in ovarian secretion of androstenedione and testosterone due to stimulation by LH and possibly insulin
- oligo-ovulation with chronically low levels of progesterone that can result in endometrial hyperplasia
- ovulatory infertility.
Metabolic abnormalities commonly observed in women with PCOS include5,6:
- insulin resistance and hyperinsulinemia
- excess adipose tissue in the liver
- excess visceral fat
- elevated adipokines
- obesity
- an increased prevalence of glucose intolerance and frank diabetes.
Dermatologic abnormalities commonly observed in women with PCOS include7:
- facial hirsutism
- acne
- androgenetic alopecia.
Given that PCOS is caused by abnormalities in the reproductive, metabolic, and dermatologic systems, it is appropriate to consider multimodal hormonal therapy that addresses all 3 problems. In my practice, I believe that the best approach to the long-term hormonal treatment of PCOS for many women is to prescribe a combination of 3 medicines: a combination estrogen-progestin oral contraceptive (COC), an insulin sensitizer, and an antiandrogen.
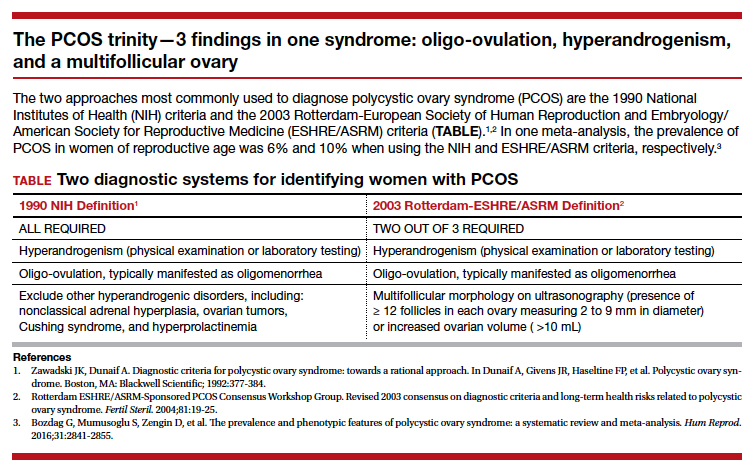
The COC reduces pituitary secretion of LH, decreases ovarian androgen production, and prevents the development of endometrial hyperplasia. When taken cyclically, the COC treatment also restores regular withdrawal uterine bleeding.
An insulin sensitizer, such as metformin or pioglitazone, helps to reduce insulin resistance, glucose intolerance, and hepatic adipose content, rebalancing central metabolism. It is important to include diet and exercise in the long-term treatment of PCOS, and I always encourage these lifestyle changes. However, my patients usually report that they have tried multiple times to restrict dietary caloric intake and increase exercise and have been unable to rebalance their metabolism with these interventions alone. Of note, in the women with PCOS and a body mass index >35 kg/m2, bariatric surgery, such as a sleeve gastrectomy, often results in marked improvement of their PCOS.8
The antiandrogen spironolactone provides effective treatment for the dermatologic problems of facial hirsutism and acne. Some COCs containing the progestins drospirenone, norgestimate, and norethindrone acetate are approved by the US Food and Drug Administration for the treatment of acne. A common approach I use in practice is to prescribe a COC, plus spironolactone 100 mg daily plus metformin extended-release 750 mg to 1,500 mg daily.
Continue to: Which COCs have low androgenicity?...
Which COCs have low androgenicity?
I believe that every COC is an effective treatment for PCOS, regardless of the androgenicity of the progestin in the contraceptive. However, some dermatologists believe that combination contraceptives containing progestins with low androgenicity, such as drospirenone, norgestimate, and desogestrel, are more likely to improve acne than contraceptives with an androgenic progestin such as levonorgestrel. In one study in which 2,147 women with acne were treated by one dermatologic practice, the percentage of women reporting that a birth control pill helped to improve their acne was 66% for pills containing drospirenone, 53% for pills containing norgestimate, 44% for pills containing desogestrel, 30% for pills containing norethindrone, and 25% for pills containing levonorgestrel. In the same study, the percent of women reporting that a birth control pill made their acne worse was 3% for pills containing drospirenone, 6% for pills containing norgestimate, 2% for pills containing desogestrel, 8% for pills containing norethindrone, and 10% for pills containing levonorgestrel.9 Given these findings, when treating a woman with PCOS, I generally prescribe a contraceptive that does not contain levonorgestrel.

Why is a spironolactone dose of 100 mg a good choice for PCOS treatment?
Spironolactone, an antiandrogen and inhibitor of 5-alpha-reductase, is commonly prescribed for the treatment of hirsutism and acne at doses ranging from 50 mg to 200 mg daily.10,11 In my clinical experience, spironolactone at a dose of 200 mg daily commonly causes irregular and bothersome uterine bleeding while spironolactone at a dose of 100 mg daily is seldom associated with irregular bleeding. I believe that spironolactone at a dose of 100 mg daily results in superior clinical efficacy than a 50-mg daily dose, although studies report that both doses are effective in the treatment of acne and hirsutism. Spironolactone should not be prescribed to women with renal failure because it can result in severe hyperkalemia. In a study of spironolactone safety in the treatment of acne, no adverse effects on the kidney, liver, or adrenal glands were reported over 8 years of use.12
What insulin sensitizers are useful in rebalancing the metabolic abnormalities observed with PCOS?
Diet and exercise are superb approaches to rebalancing metabolic abnormalities, but for many of my patients they are insufficient and treatment with an insulin sensitizer is warranted. The most commonly utilized insulin sensitizer for the treatment of PCOS is metformin because it is very inexpensive and has a low risk of serious adverse effects such as lactic acidosis. Metformin increases peripheral glucose uptake and reduces gastrointestinal glucose absorption. Insulin sensitizers also decrease visceral fat, a major source of adipokines. One major disadvantage of metformin is that at doses in the range of 1,500 mg to 2,250 mg it often causes gastrointestinal adverse effects such as borborygmi, nausea, abdominal discomfort, and loose stools.
Thiazolidinediones, including pioglitazone, have been reported to be effective in rebalancing central metabolism in women with PCOS. Pioglitazone carries a black box warning of an increased risk of congestive heart failure and nonfatal myocardial infarction. Pioglitazone is also associated with a risk of hepatotoxicity. However, at the pioglitazone dose commonly used in the treatment of PCOS (7.5 mg daily), these serious adverse effects are rare. In practice, I initiate metformin at a dose of 750 mg daily using the extended-release formulation. I increase the metformin dose to 1,500 mg daily if the patient has no bothersome gastrointestinal symptoms on the lower dose. If the patient cannot tolerate metformin treatment because of adverse effects, I will use pioglitazone 7.5 mg daily.
Continue to: Treatment of PCOS in women who are carriers of the Factor V Leiden mutation...
Treatment of PCOS in women who are carriers of the Factor V Leiden mutation
The Factor V Leiden allele is associated with an increased risk of venous thromboembolism. Estrogen-progestin contraception is contraindicated in women with the Factor V Leiden mutation. The prevalence of this mutation varies by race and ethnicity. It is present in about 5% of white, 2% of Hispanic, 1% of black, 1% of Native American, and 0.5% of Asian women. In women with PCOS who are known to be carriers of the mutation, dual therapy with metformin and spironolactone is highly effective.13-15 For these women I also offer a levonorgestrel IUD to provide contraception and reduce the risk of endometrial hyperplasia.
Combination triple medication treatment of PCOS
Optimal treatment of the reproductive, metabolic, and dermatologic problems associated with PCOS requires multimodal medications including an estrogen-progestin contraceptive, an antiandrogen, and an insulin sensitizer. In my practice, I initiate treatment of PCOS by offering patients 3 medications: a COC, spironolactone 100 mg daily, and metformin extended-release formulation 750 mg daily. Some patients elect dual medication therapy (COC plus spironolactone or COC plus metformin), but many patients select treatment with all 3 medications. Although triple medication treatment of PCOS has not been tested in large randomized clinical trials, small trials report that triple medication treatment produces optimal improvement in the reproductive, metabolic, and dermatologic problems associated with PCOS.16-18
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19-25.
- Zawadski JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In Dunaif A, Givens JR, Haseltine FP, et al. Polycystic ovary syndrome. Boston, MA: Blackwell Scientific; 1992:377-384.
- Bozdag G, Mumusoglu S, Zengin D, et al. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2016;31:2841-2855.
- Baskind NE, Balen AH. Hypothalamic-pituitary, ovarian and adrenal contributions to polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2016;37:80-97.
- Gilbert EW, Tay CT, Hiam DS, et al. Comorbidities and complications of polycystic ovary syndrome: an overview of systematic reviews. Clin Endocrinol (Oxf). 2018;89:683-699.
- Harsha Varma S, Tirupati S, Pradeep TV, et al. Insulin resistance and hyperandrogenemia independently predict nonalcoholic fatty liver disease in women with polycystic ovary syndrome. Diabetes Metab Syndr. 2019;13:1065-1069.
- Housman E, Reynolds RV. Polycystic ovary syndrome: a review for dermatologists: Part I. Diagnosis and manifestations. J Am Acad Dermatol. 2014;71:847.e1-e10.
- Dilday J, Derickson M, Kuckelman J, et al. Sleeve gastrectomy for obesity in polycystic ovarian syndrome: a pilot study evaluating weight loss and fertility outcomes. Obes Surg. 2019;29:93-98.
- Lortscher D, Admani S, Satur N, et al. Hormonal contraceptives and acne: a retrospective analysis of 2147 patients. J Drugs Dermatol. 2016;15:670-674.
- Brown J, Farquhar C, Lee O, et al. Spironolactone versus placebo or in combination with steroids for hirsutism and/or acne. Cochrane Database Syst Rev. 2009;CD000194.
- Shaw JC. Low-dose adjunctive spironolactone in the treatment of acne in women: a retrospective analysis of 85 consecutively treated patients. J Am Acad Dermatol. 2000;43:498-502.
- Shaw JC, White LE. Long-term safety of spironolactone in acne: results of an 8-year follow-up study. J Cutan Med Surg. 2002;6:541-545.
- Ganie MA, Khurana ML, Nisar S, et al. Improved efficacy of low-dose spironolactone and metformin combination than either drug alone in the management of women with polycystic ovary syndrome (PCOS): a six-month, open-label randomized study. J Clin Endocrinol Metab. 2013;98:3599-3607.
- Mazza A, Fruci B, Guzzi P, et al. In PCOS patients the addition of low-dose spironolactone induces a more marked reduction of clinical and biochemical hyperandrogenism than metformin alone. Nutr Metab Cardiovascular Dis. 2014;24:132-139.
- Ganie MA, Khurana ML, Eunice M, et al. Comparison of efficacy of spironolactone with metformin in the management of polycystic ovary syndrome: an open-labeled study. J Clin Endocrinol Metab. 2004;89:2756-2762.
- Ibanez L, de Zegher F. Low-dose combination flutamide, metformin and an oral contraceptive for non-obese, young women with polycystic ovary syndrome. Hum Reprod. 2003;18:57-60.
- Ibanez L, de Zegher F. Flutamide-metformin plus an oral contraceptive (OC) for young women with polycystic ovary syndrome: switch from third- to fourth-generation OC reduces body adiposity. Hum Reprod. 2004;19:1725-1727.
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19-25.
- Zawadski JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In Dunaif A, Givens JR, Haseltine FP, et al. Polycystic ovary syndrome. Boston, MA: Blackwell Scientific; 1992:377-384.
- Bozdag G, Mumusoglu S, Zengin D, et al. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2016;31:2841-2855.
- Baskind NE, Balen AH. Hypothalamic-pituitary, ovarian and adrenal contributions to polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2016;37:80-97.
- Gilbert EW, Tay CT, Hiam DS, et al. Comorbidities and complications of polycystic ovary syndrome: an overview of systematic reviews. Clin Endocrinol (Oxf). 2018;89:683-699.
- Harsha Varma S, Tirupati S, Pradeep TV, et al. Insulin resistance and hyperandrogenemia independently predict nonalcoholic fatty liver disease in women with polycystic ovary syndrome. Diabetes Metab Syndr. 2019;13:1065-1069.
- Housman E, Reynolds RV. Polycystic ovary syndrome: a review for dermatologists: Part I. Diagnosis and manifestations. J Am Acad Dermatol. 2014;71:847.e1-e10.
- Dilday J, Derickson M, Kuckelman J, et al. Sleeve gastrectomy for obesity in polycystic ovarian syndrome: a pilot study evaluating weight loss and fertility outcomes. Obes Surg. 2019;29:93-98.
- Lortscher D, Admani S, Satur N, et al. Hormonal contraceptives and acne: a retrospective analysis of 2147 patients. J Drugs Dermatol. 2016;15:670-674.
- Brown J, Farquhar C, Lee O, et al. Spironolactone versus placebo or in combination with steroids for hirsutism and/or acne. Cochrane Database Syst Rev. 2009;CD000194.
- Shaw JC. Low-dose adjunctive spironolactone in the treatment of acne in women: a retrospective analysis of 85 consecutively treated patients. J Am Acad Dermatol. 2000;43:498-502.
- Shaw JC, White LE. Long-term safety of spironolactone in acne: results of an 8-year follow-up study. J Cutan Med Surg. 2002;6:541-545.
- Ganie MA, Khurana ML, Nisar S, et al. Improved efficacy of low-dose spironolactone and metformin combination than either drug alone in the management of women with polycystic ovary syndrome (PCOS): a six-month, open-label randomized study. J Clin Endocrinol Metab. 2013;98:3599-3607.
- Mazza A, Fruci B, Guzzi P, et al. In PCOS patients the addition of low-dose spironolactone induces a more marked reduction of clinical and biochemical hyperandrogenism than metformin alone. Nutr Metab Cardiovascular Dis. 2014;24:132-139.
- Ganie MA, Khurana ML, Eunice M, et al. Comparison of efficacy of spironolactone with metformin in the management of polycystic ovary syndrome: an open-labeled study. J Clin Endocrinol Metab. 2004;89:2756-2762.
- Ibanez L, de Zegher F. Low-dose combination flutamide, metformin and an oral contraceptive for non-obese, young women with polycystic ovary syndrome. Hum Reprod. 2003;18:57-60.
- Ibanez L, de Zegher F. Flutamide-metformin plus an oral contraceptive (OC) for young women with polycystic ovary syndrome: switch from third- to fourth-generation OC reduces body adiposity. Hum Reprod. 2004;19:1725-1727.
High-dose progesterone to reverse mifepristone held still 'experimental'
A study of high-dose progesterone as a mifepristone antagonist to reverse medical abortion has been stopped early because of safety concerns, but the authors say mifepristone antagonization should not be considered impossible.
In Obstetrics & Gynecology, Mitchell D. Creinin, MD, of the University of California, Davis, and coauthors reported the outcomes of a double-blind, placebo-controlled trial investigating the efficacy and safety of high-dose oral progesterone as a mifepristone antagonist. The study intended to enroll more women at 44–63 days of gestation who were planning surgical abortion, but stopped enrolling after 12 patients because of hemorrhage concerns.
Women were given a 200-mg dose of oral mifepristone, then randomized to either 200 mg oral progesterone or placebo 24 hours later, taken twice daily for 3 days then once daily until their planned surgical abortion 14-16 days after enrollment.
The approved method of medical abortion in the United States involves a combination of mifepristone followed by the prostaglandin analogue misoprostol 24-48 hours later, a combination designed to improve efficacy of the treatment.
There have been reports of some patients changing their minds in between taking the mifepristone and the misoprostol. The fact that mifepristone binds strongly to the progesterone receptor has led to the idea that its action could be reversed with high-dose progesterone as an antagonist.
In this study, three women – two in the placebo group and one in the progesterone group – experienced severe bleeding requiring ambulance transport to the emergency department 2-3 days after taking the mifepristone.
The study found that four of the six patients in the progesterone group, and two of the six patients in the placebo group had continuing pregnancies at 2 weeks.
There were two patients – one in each group – who did not complete the study. One in the placebo group left after taking the mifepristone because of anxiety about bleeding, and had a suction aspiration. The second women completed two of the four doses of progesterone, then requested a suction aspiration.
Dr. Creinin and coauthors wrote that while the study ended early, they found that there were no significant differences in the side effects experienced by patients treated with progesterone, compared with those on placebo – apart from a worsening of some pregnancy symptoms such as vomiting and tiredness.
However, patients should be told of the risk of using mifepristone for medical abortion without using misoprostol, they said, as this was associated with severe hemorrhage even with progesterone treatment.
“Because of the potential dangers for patients who opt not to use misoprostol after mifepristone ingestion, any mifepristone antagonization treatment must be considered experimental,” Dr. Creinin and associates wrote.
The Society of Family Planning Research Fund supported the study. One author declared a consultancy with a laboratory providing medical consultation for clinicians regarding mifepristone, and a second author was an employee of Planned Parenthood. No other conflicts of interest were declared.
SOURCE: Creinin M et al. Obstet Gynecol 2019 Dec 5. doi: 10.1097/AOG.0000000000003620.
I think that this study highlights the importance of scientific rigor approved by an institutional review board when we counsel and care for our patients. As ob.gyns., we have to remember the privilege that women entrust us with their health and well being. To a certain extent, we also care for their families within our scope of reproductive health. We practice based on the best evidence available and consider referral to another trusted provider when we feel that we cannot provide unbiased care. I also feel obligated to share my opinion that legislators should trust the scientific and clinical community to not only prioritize women and their health, but also avoid introducing legislation that infringes on medicine.
Catherine Cansino, MD, MPH, is associate clinical professor of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the Creinin et al. article. Dr. Cansino is on the Ob.Gyn. News editorial advisory board.
I think that this study highlights the importance of scientific rigor approved by an institutional review board when we counsel and care for our patients. As ob.gyns., we have to remember the privilege that women entrust us with their health and well being. To a certain extent, we also care for their families within our scope of reproductive health. We practice based on the best evidence available and consider referral to another trusted provider when we feel that we cannot provide unbiased care. I also feel obligated to share my opinion that legislators should trust the scientific and clinical community to not only prioritize women and their health, but also avoid introducing legislation that infringes on medicine.
Catherine Cansino, MD, MPH, is associate clinical professor of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the Creinin et al. article. Dr. Cansino is on the Ob.Gyn. News editorial advisory board.
I think that this study highlights the importance of scientific rigor approved by an institutional review board when we counsel and care for our patients. As ob.gyns., we have to remember the privilege that women entrust us with their health and well being. To a certain extent, we also care for their families within our scope of reproductive health. We practice based on the best evidence available and consider referral to another trusted provider when we feel that we cannot provide unbiased care. I also feel obligated to share my opinion that legislators should trust the scientific and clinical community to not only prioritize women and their health, but also avoid introducing legislation that infringes on medicine.
Catherine Cansino, MD, MPH, is associate clinical professor of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the Creinin et al. article. Dr. Cansino is on the Ob.Gyn. News editorial advisory board.
A study of high-dose progesterone as a mifepristone antagonist to reverse medical abortion has been stopped early because of safety concerns, but the authors say mifepristone antagonization should not be considered impossible.
In Obstetrics & Gynecology, Mitchell D. Creinin, MD, of the University of California, Davis, and coauthors reported the outcomes of a double-blind, placebo-controlled trial investigating the efficacy and safety of high-dose oral progesterone as a mifepristone antagonist. The study intended to enroll more women at 44–63 days of gestation who were planning surgical abortion, but stopped enrolling after 12 patients because of hemorrhage concerns.
Women were given a 200-mg dose of oral mifepristone, then randomized to either 200 mg oral progesterone or placebo 24 hours later, taken twice daily for 3 days then once daily until their planned surgical abortion 14-16 days after enrollment.
The approved method of medical abortion in the United States involves a combination of mifepristone followed by the prostaglandin analogue misoprostol 24-48 hours later, a combination designed to improve efficacy of the treatment.
There have been reports of some patients changing their minds in between taking the mifepristone and the misoprostol. The fact that mifepristone binds strongly to the progesterone receptor has led to the idea that its action could be reversed with high-dose progesterone as an antagonist.
In this study, three women – two in the placebo group and one in the progesterone group – experienced severe bleeding requiring ambulance transport to the emergency department 2-3 days after taking the mifepristone.
The study found that four of the six patients in the progesterone group, and two of the six patients in the placebo group had continuing pregnancies at 2 weeks.
There were two patients – one in each group – who did not complete the study. One in the placebo group left after taking the mifepristone because of anxiety about bleeding, and had a suction aspiration. The second women completed two of the four doses of progesterone, then requested a suction aspiration.
Dr. Creinin and coauthors wrote that while the study ended early, they found that there were no significant differences in the side effects experienced by patients treated with progesterone, compared with those on placebo – apart from a worsening of some pregnancy symptoms such as vomiting and tiredness.
However, patients should be told of the risk of using mifepristone for medical abortion without using misoprostol, they said, as this was associated with severe hemorrhage even with progesterone treatment.
“Because of the potential dangers for patients who opt not to use misoprostol after mifepristone ingestion, any mifepristone antagonization treatment must be considered experimental,” Dr. Creinin and associates wrote.
The Society of Family Planning Research Fund supported the study. One author declared a consultancy with a laboratory providing medical consultation for clinicians regarding mifepristone, and a second author was an employee of Planned Parenthood. No other conflicts of interest were declared.
SOURCE: Creinin M et al. Obstet Gynecol 2019 Dec 5. doi: 10.1097/AOG.0000000000003620.
A study of high-dose progesterone as a mifepristone antagonist to reverse medical abortion has been stopped early because of safety concerns, but the authors say mifepristone antagonization should not be considered impossible.
In Obstetrics & Gynecology, Mitchell D. Creinin, MD, of the University of California, Davis, and coauthors reported the outcomes of a double-blind, placebo-controlled trial investigating the efficacy and safety of high-dose oral progesterone as a mifepristone antagonist. The study intended to enroll more women at 44–63 days of gestation who were planning surgical abortion, but stopped enrolling after 12 patients because of hemorrhage concerns.
Women were given a 200-mg dose of oral mifepristone, then randomized to either 200 mg oral progesterone or placebo 24 hours later, taken twice daily for 3 days then once daily until their planned surgical abortion 14-16 days after enrollment.
The approved method of medical abortion in the United States involves a combination of mifepristone followed by the prostaglandin analogue misoprostol 24-48 hours later, a combination designed to improve efficacy of the treatment.
There have been reports of some patients changing their minds in between taking the mifepristone and the misoprostol. The fact that mifepristone binds strongly to the progesterone receptor has led to the idea that its action could be reversed with high-dose progesterone as an antagonist.
In this study, three women – two in the placebo group and one in the progesterone group – experienced severe bleeding requiring ambulance transport to the emergency department 2-3 days after taking the mifepristone.
The study found that four of the six patients in the progesterone group, and two of the six patients in the placebo group had continuing pregnancies at 2 weeks.
There were two patients – one in each group – who did not complete the study. One in the placebo group left after taking the mifepristone because of anxiety about bleeding, and had a suction aspiration. The second women completed two of the four doses of progesterone, then requested a suction aspiration.
Dr. Creinin and coauthors wrote that while the study ended early, they found that there were no significant differences in the side effects experienced by patients treated with progesterone, compared with those on placebo – apart from a worsening of some pregnancy symptoms such as vomiting and tiredness.
However, patients should be told of the risk of using mifepristone for medical abortion without using misoprostol, they said, as this was associated with severe hemorrhage even with progesterone treatment.
“Because of the potential dangers for patients who opt not to use misoprostol after mifepristone ingestion, any mifepristone antagonization treatment must be considered experimental,” Dr. Creinin and associates wrote.
The Society of Family Planning Research Fund supported the study. One author declared a consultancy with a laboratory providing medical consultation for clinicians regarding mifepristone, and a second author was an employee of Planned Parenthood. No other conflicts of interest were declared.
SOURCE: Creinin M et al. Obstet Gynecol 2019 Dec 5. doi: 10.1097/AOG.0000000000003620.
FROM OBSTETRICS & GYNECOLOGY
iPLEDGE vexes dermatologists treating transgender patients
Physicians treating transgender patients – in particular, transgender men who were born female – are faced with a confusing process when prescribing isotretinoin for severe acne.
A research letter published in the Journal of the American Academy of Dermatology reports that established to prevent female patients from starting isotretinoin therapy while pregnant or from becoming pregnant while exposed to the teratogenic medication.
Nearly 90% of respondents favored changing the current gender-specific categories in iPLEDGE to gender-neutral ones, classifying patients only by whether or not they have the ability to become pregnant.
For their research, Courtney Ensslin, MD, of the department of dermatology at Johns Hopkins University, Baltimore, and colleagues, distributed an 18-point questionnaire to 385 members of the Association of Professors of Dermatology that included questions assessing clinicians’ knowledge about the reproductive potential of transgender men and women. The recipients were asked to distribute it to faculty members and residents. The survey also described three clinical scenarios in which the physician needed to decide how to register a patient in iPLEDGE. The clinicians largely opted to class transgender men as women with childbearing potential, even if the category conflicted with the patient’s self-identified and legally recognized male gender.
Of the 136 clinicians who responded, 60% were women, almost half were aged 25-34 years. About 12% of respondents said the complexities of prescribing isotretinoin to a transgender patient led them to choose alternative therapies. And the survey revealed some gaps on providers’ general literacy on transgender patients and their reproductive potential. For example, fewer than a third of respondents answered correctly as to whether testosterone treatment decreases the quality and development of an immature ovum.
The researchers wrote that the survey results, while limited by a small sample of respondents that skewed toward younger women providers, suggest that “continued education on fertility in transgender patients is needed because prescribers must fully understand each patient’s reproductive potential to safely prescribe teratogenic medications.” Additionally, they pointed out, the results support ongoing efforts to reform iPLEDGE, as the current categories “do not offer an inclusive approach to care for transgender patients.”
Earlier this year the American Academy of Dermatology issued a position statement that described a number of ongoing initiatives aimed at improving treatment for patients who are members of gender and sexual minorities. These included the “revision of the AAD position statement on isotretinoin to support a gender-neutral categorization model for [iPLEDGE] … based on child-bearing potential rather than on gender identity,” the statement said.
Dr. Ensslin and colleagues reported conflicts of interest related to their research. The study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health.
SOURCE: Ensslin C et al. J Am Acad Dermatol. 2019 Dec;81(6):1426-9.
Physicians treating transgender patients – in particular, transgender men who were born female – are faced with a confusing process when prescribing isotretinoin for severe acne.
A research letter published in the Journal of the American Academy of Dermatology reports that established to prevent female patients from starting isotretinoin therapy while pregnant or from becoming pregnant while exposed to the teratogenic medication.
Nearly 90% of respondents favored changing the current gender-specific categories in iPLEDGE to gender-neutral ones, classifying patients only by whether or not they have the ability to become pregnant.
For their research, Courtney Ensslin, MD, of the department of dermatology at Johns Hopkins University, Baltimore, and colleagues, distributed an 18-point questionnaire to 385 members of the Association of Professors of Dermatology that included questions assessing clinicians’ knowledge about the reproductive potential of transgender men and women. The recipients were asked to distribute it to faculty members and residents. The survey also described three clinical scenarios in which the physician needed to decide how to register a patient in iPLEDGE. The clinicians largely opted to class transgender men as women with childbearing potential, even if the category conflicted with the patient’s self-identified and legally recognized male gender.
Of the 136 clinicians who responded, 60% were women, almost half were aged 25-34 years. About 12% of respondents said the complexities of prescribing isotretinoin to a transgender patient led them to choose alternative therapies. And the survey revealed some gaps on providers’ general literacy on transgender patients and their reproductive potential. For example, fewer than a third of respondents answered correctly as to whether testosterone treatment decreases the quality and development of an immature ovum.
The researchers wrote that the survey results, while limited by a small sample of respondents that skewed toward younger women providers, suggest that “continued education on fertility in transgender patients is needed because prescribers must fully understand each patient’s reproductive potential to safely prescribe teratogenic medications.” Additionally, they pointed out, the results support ongoing efforts to reform iPLEDGE, as the current categories “do not offer an inclusive approach to care for transgender patients.”
Earlier this year the American Academy of Dermatology issued a position statement that described a number of ongoing initiatives aimed at improving treatment for patients who are members of gender and sexual minorities. These included the “revision of the AAD position statement on isotretinoin to support a gender-neutral categorization model for [iPLEDGE] … based on child-bearing potential rather than on gender identity,” the statement said.
Dr. Ensslin and colleagues reported conflicts of interest related to their research. The study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health.
SOURCE: Ensslin C et al. J Am Acad Dermatol. 2019 Dec;81(6):1426-9.
Physicians treating transgender patients – in particular, transgender men who were born female – are faced with a confusing process when prescribing isotretinoin for severe acne.
A research letter published in the Journal of the American Academy of Dermatology reports that established to prevent female patients from starting isotretinoin therapy while pregnant or from becoming pregnant while exposed to the teratogenic medication.
Nearly 90% of respondents favored changing the current gender-specific categories in iPLEDGE to gender-neutral ones, classifying patients only by whether or not they have the ability to become pregnant.
For their research, Courtney Ensslin, MD, of the department of dermatology at Johns Hopkins University, Baltimore, and colleagues, distributed an 18-point questionnaire to 385 members of the Association of Professors of Dermatology that included questions assessing clinicians’ knowledge about the reproductive potential of transgender men and women. The recipients were asked to distribute it to faculty members and residents. The survey also described three clinical scenarios in which the physician needed to decide how to register a patient in iPLEDGE. The clinicians largely opted to class transgender men as women with childbearing potential, even if the category conflicted with the patient’s self-identified and legally recognized male gender.
Of the 136 clinicians who responded, 60% were women, almost half were aged 25-34 years. About 12% of respondents said the complexities of prescribing isotretinoin to a transgender patient led them to choose alternative therapies. And the survey revealed some gaps on providers’ general literacy on transgender patients and their reproductive potential. For example, fewer than a third of respondents answered correctly as to whether testosterone treatment decreases the quality and development of an immature ovum.
The researchers wrote that the survey results, while limited by a small sample of respondents that skewed toward younger women providers, suggest that “continued education on fertility in transgender patients is needed because prescribers must fully understand each patient’s reproductive potential to safely prescribe teratogenic medications.” Additionally, they pointed out, the results support ongoing efforts to reform iPLEDGE, as the current categories “do not offer an inclusive approach to care for transgender patients.”
Earlier this year the American Academy of Dermatology issued a position statement that described a number of ongoing initiatives aimed at improving treatment for patients who are members of gender and sexual minorities. These included the “revision of the AAD position statement on isotretinoin to support a gender-neutral categorization model for [iPLEDGE] … based on child-bearing potential rather than on gender identity,” the statement said.
Dr. Ensslin and colleagues reported conflicts of interest related to their research. The study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health.
SOURCE: Ensslin C et al. J Am Acad Dermatol. 2019 Dec;81(6):1426-9.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Poll: Do you agree that hormonal contraception (OCPs, progesterone-only pills, the patch, vaginal rings, and DMPA) should be offered OTC?
[polldaddy:10476065]
[polldaddy:10476065]
[polldaddy:10476065]
Oral contraceptive use associated with smaller hypothalamic and pituitary volumes
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
REPORTING FROM RSNA 2019
Learning about and prescribing emergency contraception
As health care providers to children, we always are learning. And with new knowledge we sometimes can be taken out of our comfort zone. One of those areas are teenagers, contraception, safe-sex counseling, and now emergency contraception (EC). In residency you have your 1-month adolescent medicine rotation to try and absorb every bit of information like a sponge, but there also will be a level of discomfort and uncertainty. However, as medical providers we cannot let the above prevent us from giving well-rounded and informed care.
When our teens disclose the most private moment of their life, we have to be armed and ready to not only comfort them, but advise and guide them to making a decision so that they can ensure their safety. The answers regarding sexual activity are becoming more and more alarming, especially in our younger patients. Therefore, this is an important discussion to have at every visit (not just well-child checks), so that education opportunities are not missed and our patients feel a sense of normalcy about discussing reproductive health with their health care provider and or parents.
We all have our personal beliefs, but we cannot let that guide our decision on what care or education we give our patients. Unfortunately, I have heard many health care providers judge our patients for their promiscuity, when we need to educate them – not be their judge and jury. Our teens go through different stages of growth and development, and with these stages come experimentation and risk taking. So as their health care providers, we need to be up to date on the information out there.
With regards with EC, some of our patients think that they can get it only after having unprotected sex. However, they should know that the oral ECs can be given to them at any time, so should they be in the situation above, they have an immediate remedy. With the different options come different counseling and different instructions on administration and follow-up. In residency, we might not have learned the skill of inserting an IUD, which is another form of EC; that is why there are many resources available. These resources include hands-on workshops, videos on counseling, and your friendly neighborhood adolescent medicine physician or ob.gyn.
EC can give our patients that sense of relief, especially when they have unprotected sex. However, they also need to have a sense of responsibility for their actions because you do not want them to engage in high-risk behaviors. Just as we are responsible to provide up-to-date care, our patients must take ownership of their health and well-being. Also If they are engaging in unprotected sex, they are just as responsible; therefore, they should know everything about contraception as well as EC. They should feel comfortable talking to their partners about contraception. Health care providers should make them feel comfortable receiving EC that they can give to their female partner.
We need to become knowledgeable and comfortable prescribing EC, as well as incorporating it in our routine care. This is a policy that I strongly believe should be part of every pediatrician’s and family physician’s office, especially when there is a lack of resources. Of the different options that are available, the oral forms of EC – especially Ella or Plan B step 1 (levonorgestrel) – would be the easiest to prescribe and counsel on. I would not recommend the options where multiple pills need to be taken more than once a day, because compliance becomes a factor. Also knowing that these options are available over the counter also is helpful because our community pharmacist also can help with medication administration and counseling.
In summary, I strongly recommend the discussion of EC in the office, especially the general pediatrician’s office. I recommend that, for those physicians’ who may be uncomfortable, that they should start with the “easier” options of oral progestins (Ella or Plan B step 1). As you become more comfortable with the information and counseling, you can learn skills such as IUD insertions, so you then can offer more options.
As health care providers to children, we always are learning. And with new knowledge we sometimes can be taken out of our comfort zone. One of those areas are teenagers, contraception, safe-sex counseling, and now emergency contraception (EC). In residency you have your 1-month adolescent medicine rotation to try and absorb every bit of information like a sponge, but there also will be a level of discomfort and uncertainty. However, as medical providers we cannot let the above prevent us from giving well-rounded and informed care.
When our teens disclose the most private moment of their life, we have to be armed and ready to not only comfort them, but advise and guide them to making a decision so that they can ensure their safety. The answers regarding sexual activity are becoming more and more alarming, especially in our younger patients. Therefore, this is an important discussion to have at every visit (not just well-child checks), so that education opportunities are not missed and our patients feel a sense of normalcy about discussing reproductive health with their health care provider and or parents.
We all have our personal beliefs, but we cannot let that guide our decision on what care or education we give our patients. Unfortunately, I have heard many health care providers judge our patients for their promiscuity, when we need to educate them – not be their judge and jury. Our teens go through different stages of growth and development, and with these stages come experimentation and risk taking. So as their health care providers, we need to be up to date on the information out there.
With regards with EC, some of our patients think that they can get it only after having unprotected sex. However, they should know that the oral ECs can be given to them at any time, so should they be in the situation above, they have an immediate remedy. With the different options come different counseling and different instructions on administration and follow-up. In residency, we might not have learned the skill of inserting an IUD, which is another form of EC; that is why there are many resources available. These resources include hands-on workshops, videos on counseling, and your friendly neighborhood adolescent medicine physician or ob.gyn.
EC can give our patients that sense of relief, especially when they have unprotected sex. However, they also need to have a sense of responsibility for their actions because you do not want them to engage in high-risk behaviors. Just as we are responsible to provide up-to-date care, our patients must take ownership of their health and well-being. Also If they are engaging in unprotected sex, they are just as responsible; therefore, they should know everything about contraception as well as EC. They should feel comfortable talking to their partners about contraception. Health care providers should make them feel comfortable receiving EC that they can give to their female partner.
We need to become knowledgeable and comfortable prescribing EC, as well as incorporating it in our routine care. This is a policy that I strongly believe should be part of every pediatrician’s and family physician’s office, especially when there is a lack of resources. Of the different options that are available, the oral forms of EC – especially Ella or Plan B step 1 (levonorgestrel) – would be the easiest to prescribe and counsel on. I would not recommend the options where multiple pills need to be taken more than once a day, because compliance becomes a factor. Also knowing that these options are available over the counter also is helpful because our community pharmacist also can help with medication administration and counseling.
In summary, I strongly recommend the discussion of EC in the office, especially the general pediatrician’s office. I recommend that, for those physicians’ who may be uncomfortable, that they should start with the “easier” options of oral progestins (Ella or Plan B step 1). As you become more comfortable with the information and counseling, you can learn skills such as IUD insertions, so you then can offer more options.
As health care providers to children, we always are learning. And with new knowledge we sometimes can be taken out of our comfort zone. One of those areas are teenagers, contraception, safe-sex counseling, and now emergency contraception (EC). In residency you have your 1-month adolescent medicine rotation to try and absorb every bit of information like a sponge, but there also will be a level of discomfort and uncertainty. However, as medical providers we cannot let the above prevent us from giving well-rounded and informed care.
When our teens disclose the most private moment of their life, we have to be armed and ready to not only comfort them, but advise and guide them to making a decision so that they can ensure their safety. The answers regarding sexual activity are becoming more and more alarming, especially in our younger patients. Therefore, this is an important discussion to have at every visit (not just well-child checks), so that education opportunities are not missed and our patients feel a sense of normalcy about discussing reproductive health with their health care provider and or parents.
We all have our personal beliefs, but we cannot let that guide our decision on what care or education we give our patients. Unfortunately, I have heard many health care providers judge our patients for their promiscuity, when we need to educate them – not be their judge and jury. Our teens go through different stages of growth and development, and with these stages come experimentation and risk taking. So as their health care providers, we need to be up to date on the information out there.
With regards with EC, some of our patients think that they can get it only after having unprotected sex. However, they should know that the oral ECs can be given to them at any time, so should they be in the situation above, they have an immediate remedy. With the different options come different counseling and different instructions on administration and follow-up. In residency, we might not have learned the skill of inserting an IUD, which is another form of EC; that is why there are many resources available. These resources include hands-on workshops, videos on counseling, and your friendly neighborhood adolescent medicine physician or ob.gyn.
EC can give our patients that sense of relief, especially when they have unprotected sex. However, they also need to have a sense of responsibility for their actions because you do not want them to engage in high-risk behaviors. Just as we are responsible to provide up-to-date care, our patients must take ownership of their health and well-being. Also If they are engaging in unprotected sex, they are just as responsible; therefore, they should know everything about contraception as well as EC. They should feel comfortable talking to their partners about contraception. Health care providers should make them feel comfortable receiving EC that they can give to their female partner.
We need to become knowledgeable and comfortable prescribing EC, as well as incorporating it in our routine care. This is a policy that I strongly believe should be part of every pediatrician’s and family physician’s office, especially when there is a lack of resources. Of the different options that are available, the oral forms of EC – especially Ella or Plan B step 1 (levonorgestrel) – would be the easiest to prescribe and counsel on. I would not recommend the options where multiple pills need to be taken more than once a day, because compliance becomes a factor. Also knowing that these options are available over the counter also is helpful because our community pharmacist also can help with medication administration and counseling.
In summary, I strongly recommend the discussion of EC in the office, especially the general pediatrician’s office. I recommend that, for those physicians’ who may be uncomfortable, that they should start with the “easier” options of oral progestins (Ella or Plan B step 1). As you become more comfortable with the information and counseling, you can learn skills such as IUD insertions, so you then can offer more options.
OTC hormonal contraception: An important goal in the fight for reproductive justice
A new American College of Obstetricians and Gynecologists (ACOG) committee opinion addresses how contraception access can be improved through over-the-counter (OTC) hormonal contraception for people of all ages—including oral contraceptive pills (OCPs), progesterone-only pills, the patch, vaginal rings, and depot medroxyprogesterone acetate (DMPA). Although ACOG endorses OTC contraception, some health care providers may be hesitant to support the increase in accessibility for a variety of reasons. We are hopeful that we address these concerns and that all clinicians can move to support ACOG’s position.
Easing access to hormonal contraception is a first step
OCPs are the most widely used contraception among teens and women of reproductive age in the United States.1 Although the Affordable Care Act (ACA) mandated health insurance coverage for contraception, many barriers continue to exist, including obtaining a prescription. Only 13 states have made it legal to obtain hormonal contraception through a pharmacist.2 There also has been an increase in the number of telemedicine and online services that deliver contraceptives to individuals’ homes. While these efforts have helped to decrease barriers to hormonal contraception access for some patients, they only reach a small segment of the population. As clinicians, we should strive to make contraception universally accessible and affordable to everyone who desires to use it. OTC provision can bring us closer to this goal.
Addressing the misconceptions about contraception
Adverse events with hormonal contraception are rarer than one may think. There are few risks associated with hormonal contraception. Venous thromboembolus (VTE) is a serious, although rare, adverse effect (AE) of hormonal contraception. The rate of VTE with combined oral contraception is estimated at 3 to 8 events per 10,000 patient-years, and VTE is even less common with progestin-only contraception (1 to 5 per 10,000 patient-years). For both types of hormonal contraception, the risk of VTE is smaller than with pregnancy, which is 5 to 20 per 10,000 patient-years.3 There are comorbidities that increase the risk of VTE and other AEs of hormonal contraception. In the setting of OTC hormonal contraception, individuals would self-screen for contraindications in order to reduce these complications.
Patients have the aptitude to self-screen for contraindications. Studies looking at the ability of patients over the age of 18 to self-screen for contraindications to hormonal contraception have found that patients do appropriately screen themselves. In fact, they are often more conservative than a physician in avoiding hormonal contraceptive methods.4 Patients younger than age 18 rarely have contraindications to hormonal contraception, but limited studies have shown that they too are able to successfully self-screen.5 ACOG recommends self-screening tools be provided with all OTC combined hormonal contraceptive methods to aid an individual’s contraceptive choice.
Most patients continue their well person care. Some opponents to ACOG’s position also have expressed concern that people who access their contraception OTC will forego their annual exam with their provider. However, studies have shown that the majority of people will continue to make their preventative health care visits.6,7
We need to invest in preventing unplanned pregnancy
Currently, hormonal contraception is covered by health insurance under the ACA, with some caveats. Without a prescription, patients may have to pay full price for their contraception. However, one can find generic OCPs for less than $10 per pack out of pocket. Any cost can be prohibitive to many patients; thus, transition to OTC access to contraception also should ensure limiting the cost to the patient. One possible solution to mitigate costs is to require insurance companies to cover the cost of OTC hormonal contraceptives. (See action item below.)
Reduction in unplanned pregnancies improves public health and public expense, and broadening access to effective forms of contraception is imperative in reducing unplanned pregnancies. Every $1 invested in contraception access realizes $7.09 in savings.8 By making hormonal contraception widely available OTC, access could be improved dramatically—although pharmacist provision of hormonal contraception may be a necessary intermediate step. ACOG’s most recent committee opinion encourages all reproductive health care providers to be strong advocates for this improvement in access. As women’s health providers, we should work to decrease access barriers for our patients; working toward OTC contraception is a critical step in equal access to birth control methods for all of our patients.
Action items
Remember, before a pill can move to OTC access, the manufacturing (pharmaceutical) company must submit an application to the US Food and Drug Administration to obtain this status. Once submitted, the process may take 3 to 4 years to be completed. Currently, no company has submitted an OTC application and no hormonal birth control is available OTC. Find resources for OTC birth control access here: http://ocsotc.org/ and www.freethepill.org.
- Talk to your state representatives about why both OTC birth control access and direct pharmacy availability are important to increasing access and decreasing disparities in reproductive health care. Find your local and federal representatives here and check the status of OCP access in your state here.
- Representative Ayanna Pressley (D-MA) and Senator Patty Murray (D-WA) both have introduced legislation—the Affordability is Access Act (HR 3296/S1847)—to ensure insurance coverage for OTC contraception. Call your representative and ask them to cosponsor this legislation.
- Be mindful of legislation that promotes OTC OCPs but limits access to some populations (minors) and increases cost sharing to the patient. This type of legislation can create harmful barriers to access for some of our patients
- Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Rep. 2012;(60):1-25.
- Free the pill. What’s the law in your state? Ibis Reproductive Health website. http://freethepill.org/statepolicies. Accessed November 15, 2019.
- U.S. Food and Drug Administration. FDA Drug Safety Communication: updated information about the risk of blood clots in women taking birth control pills containing drospirenone. https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed November 15, 2019.
- Grossman D, Fernandez L, Hopkins K, et al. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstet Gynecol. 2008;112:572e8.
- Williams R, Hensel D, Lehmann A, et al. Adolescent self-screening for contraindications to combined oral contraceptive pills [abstract]. Contraception. 2015;92:380.
- Hopkins K, Grossman D, White K, et al. Reproductive health preventive screening among clinic vs. over-the-counter oral contraceptive users. Contraception. 2012;86:376-382.
- Grindlay K, Grossman D. Interest in over-the-counter access to a progestin-only pill among women in the United States. Womens Health Issues. 2018;28:144-151.
- Frost JJ, Sonfield A, Zolna MR, et al. Return on investment: a fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92:696-749.
A new American College of Obstetricians and Gynecologists (ACOG) committee opinion addresses how contraception access can be improved through over-the-counter (OTC) hormonal contraception for people of all ages—including oral contraceptive pills (OCPs), progesterone-only pills, the patch, vaginal rings, and depot medroxyprogesterone acetate (DMPA). Although ACOG endorses OTC contraception, some health care providers may be hesitant to support the increase in accessibility for a variety of reasons. We are hopeful that we address these concerns and that all clinicians can move to support ACOG’s position.
Easing access to hormonal contraception is a first step
OCPs are the most widely used contraception among teens and women of reproductive age in the United States.1 Although the Affordable Care Act (ACA) mandated health insurance coverage for contraception, many barriers continue to exist, including obtaining a prescription. Only 13 states have made it legal to obtain hormonal contraception through a pharmacist.2 There also has been an increase in the number of telemedicine and online services that deliver contraceptives to individuals’ homes. While these efforts have helped to decrease barriers to hormonal contraception access for some patients, they only reach a small segment of the population. As clinicians, we should strive to make contraception universally accessible and affordable to everyone who desires to use it. OTC provision can bring us closer to this goal.
Addressing the misconceptions about contraception
Adverse events with hormonal contraception are rarer than one may think. There are few risks associated with hormonal contraception. Venous thromboembolus (VTE) is a serious, although rare, adverse effect (AE) of hormonal contraception. The rate of VTE with combined oral contraception is estimated at 3 to 8 events per 10,000 patient-years, and VTE is even less common with progestin-only contraception (1 to 5 per 10,000 patient-years). For both types of hormonal contraception, the risk of VTE is smaller than with pregnancy, which is 5 to 20 per 10,000 patient-years.3 There are comorbidities that increase the risk of VTE and other AEs of hormonal contraception. In the setting of OTC hormonal contraception, individuals would self-screen for contraindications in order to reduce these complications.
Patients have the aptitude to self-screen for contraindications. Studies looking at the ability of patients over the age of 18 to self-screen for contraindications to hormonal contraception have found that patients do appropriately screen themselves. In fact, they are often more conservative than a physician in avoiding hormonal contraceptive methods.4 Patients younger than age 18 rarely have contraindications to hormonal contraception, but limited studies have shown that they too are able to successfully self-screen.5 ACOG recommends self-screening tools be provided with all OTC combined hormonal contraceptive methods to aid an individual’s contraceptive choice.
Most patients continue their well person care. Some opponents to ACOG’s position also have expressed concern that people who access their contraception OTC will forego their annual exam with their provider. However, studies have shown that the majority of people will continue to make their preventative health care visits.6,7
We need to invest in preventing unplanned pregnancy
Currently, hormonal contraception is covered by health insurance under the ACA, with some caveats. Without a prescription, patients may have to pay full price for their contraception. However, one can find generic OCPs for less than $10 per pack out of pocket. Any cost can be prohibitive to many patients; thus, transition to OTC access to contraception also should ensure limiting the cost to the patient. One possible solution to mitigate costs is to require insurance companies to cover the cost of OTC hormonal contraceptives. (See action item below.)
Reduction in unplanned pregnancies improves public health and public expense, and broadening access to effective forms of contraception is imperative in reducing unplanned pregnancies. Every $1 invested in contraception access realizes $7.09 in savings.8 By making hormonal contraception widely available OTC, access could be improved dramatically—although pharmacist provision of hormonal contraception may be a necessary intermediate step. ACOG’s most recent committee opinion encourages all reproductive health care providers to be strong advocates for this improvement in access. As women’s health providers, we should work to decrease access barriers for our patients; working toward OTC contraception is a critical step in equal access to birth control methods for all of our patients.
Action items
Remember, before a pill can move to OTC access, the manufacturing (pharmaceutical) company must submit an application to the US Food and Drug Administration to obtain this status. Once submitted, the process may take 3 to 4 years to be completed. Currently, no company has submitted an OTC application and no hormonal birth control is available OTC. Find resources for OTC birth control access here: http://ocsotc.org/ and www.freethepill.org.
- Talk to your state representatives about why both OTC birth control access and direct pharmacy availability are important to increasing access and decreasing disparities in reproductive health care. Find your local and federal representatives here and check the status of OCP access in your state here.
- Representative Ayanna Pressley (D-MA) and Senator Patty Murray (D-WA) both have introduced legislation—the Affordability is Access Act (HR 3296/S1847)—to ensure insurance coverage for OTC contraception. Call your representative and ask them to cosponsor this legislation.
- Be mindful of legislation that promotes OTC OCPs but limits access to some populations (minors) and increases cost sharing to the patient. This type of legislation can create harmful barriers to access for some of our patients
A new American College of Obstetricians and Gynecologists (ACOG) committee opinion addresses how contraception access can be improved through over-the-counter (OTC) hormonal contraception for people of all ages—including oral contraceptive pills (OCPs), progesterone-only pills, the patch, vaginal rings, and depot medroxyprogesterone acetate (DMPA). Although ACOG endorses OTC contraception, some health care providers may be hesitant to support the increase in accessibility for a variety of reasons. We are hopeful that we address these concerns and that all clinicians can move to support ACOG’s position.
Easing access to hormonal contraception is a first step
OCPs are the most widely used contraception among teens and women of reproductive age in the United States.1 Although the Affordable Care Act (ACA) mandated health insurance coverage for contraception, many barriers continue to exist, including obtaining a prescription. Only 13 states have made it legal to obtain hormonal contraception through a pharmacist.2 There also has been an increase in the number of telemedicine and online services that deliver contraceptives to individuals’ homes. While these efforts have helped to decrease barriers to hormonal contraception access for some patients, they only reach a small segment of the population. As clinicians, we should strive to make contraception universally accessible and affordable to everyone who desires to use it. OTC provision can bring us closer to this goal.
Addressing the misconceptions about contraception
Adverse events with hormonal contraception are rarer than one may think. There are few risks associated with hormonal contraception. Venous thromboembolus (VTE) is a serious, although rare, adverse effect (AE) of hormonal contraception. The rate of VTE with combined oral contraception is estimated at 3 to 8 events per 10,000 patient-years, and VTE is even less common with progestin-only contraception (1 to 5 per 10,000 patient-years). For both types of hormonal contraception, the risk of VTE is smaller than with pregnancy, which is 5 to 20 per 10,000 patient-years.3 There are comorbidities that increase the risk of VTE and other AEs of hormonal contraception. In the setting of OTC hormonal contraception, individuals would self-screen for contraindications in order to reduce these complications.
Patients have the aptitude to self-screen for contraindications. Studies looking at the ability of patients over the age of 18 to self-screen for contraindications to hormonal contraception have found that patients do appropriately screen themselves. In fact, they are often more conservative than a physician in avoiding hormonal contraceptive methods.4 Patients younger than age 18 rarely have contraindications to hormonal contraception, but limited studies have shown that they too are able to successfully self-screen.5 ACOG recommends self-screening tools be provided with all OTC combined hormonal contraceptive methods to aid an individual’s contraceptive choice.
Most patients continue their well person care. Some opponents to ACOG’s position also have expressed concern that people who access their contraception OTC will forego their annual exam with their provider. However, studies have shown that the majority of people will continue to make their preventative health care visits.6,7
We need to invest in preventing unplanned pregnancy
Currently, hormonal contraception is covered by health insurance under the ACA, with some caveats. Without a prescription, patients may have to pay full price for their contraception. However, one can find generic OCPs for less than $10 per pack out of pocket. Any cost can be prohibitive to many patients; thus, transition to OTC access to contraception also should ensure limiting the cost to the patient. One possible solution to mitigate costs is to require insurance companies to cover the cost of OTC hormonal contraceptives. (See action item below.)
Reduction in unplanned pregnancies improves public health and public expense, and broadening access to effective forms of contraception is imperative in reducing unplanned pregnancies. Every $1 invested in contraception access realizes $7.09 in savings.8 By making hormonal contraception widely available OTC, access could be improved dramatically—although pharmacist provision of hormonal contraception may be a necessary intermediate step. ACOG’s most recent committee opinion encourages all reproductive health care providers to be strong advocates for this improvement in access. As women’s health providers, we should work to decrease access barriers for our patients; working toward OTC contraception is a critical step in equal access to birth control methods for all of our patients.
Action items
Remember, before a pill can move to OTC access, the manufacturing (pharmaceutical) company must submit an application to the US Food and Drug Administration to obtain this status. Once submitted, the process may take 3 to 4 years to be completed. Currently, no company has submitted an OTC application and no hormonal birth control is available OTC. Find resources for OTC birth control access here: http://ocsotc.org/ and www.freethepill.org.
- Talk to your state representatives about why both OTC birth control access and direct pharmacy availability are important to increasing access and decreasing disparities in reproductive health care. Find your local and federal representatives here and check the status of OCP access in your state here.
- Representative Ayanna Pressley (D-MA) and Senator Patty Murray (D-WA) both have introduced legislation—the Affordability is Access Act (HR 3296/S1847)—to ensure insurance coverage for OTC contraception. Call your representative and ask them to cosponsor this legislation.
- Be mindful of legislation that promotes OTC OCPs but limits access to some populations (minors) and increases cost sharing to the patient. This type of legislation can create harmful barriers to access for some of our patients
- Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Rep. 2012;(60):1-25.
- Free the pill. What’s the law in your state? Ibis Reproductive Health website. http://freethepill.org/statepolicies. Accessed November 15, 2019.
- U.S. Food and Drug Administration. FDA Drug Safety Communication: updated information about the risk of blood clots in women taking birth control pills containing drospirenone. https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed November 15, 2019.
- Grossman D, Fernandez L, Hopkins K, et al. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstet Gynecol. 2008;112:572e8.
- Williams R, Hensel D, Lehmann A, et al. Adolescent self-screening for contraindications to combined oral contraceptive pills [abstract]. Contraception. 2015;92:380.
- Hopkins K, Grossman D, White K, et al. Reproductive health preventive screening among clinic vs. over-the-counter oral contraceptive users. Contraception. 2012;86:376-382.
- Grindlay K, Grossman D. Interest in over-the-counter access to a progestin-only pill among women in the United States. Womens Health Issues. 2018;28:144-151.
- Frost JJ, Sonfield A, Zolna MR, et al. Return on investment: a fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92:696-749.
- Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Rep. 2012;(60):1-25.
- Free the pill. What’s the law in your state? Ibis Reproductive Health website. http://freethepill.org/statepolicies. Accessed November 15, 2019.
- U.S. Food and Drug Administration. FDA Drug Safety Communication: updated information about the risk of blood clots in women taking birth control pills containing drospirenone. https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed November 15, 2019.
- Grossman D, Fernandez L, Hopkins K, et al. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstet Gynecol. 2008;112:572e8.
- Williams R, Hensel D, Lehmann A, et al. Adolescent self-screening for contraindications to combined oral contraceptive pills [abstract]. Contraception. 2015;92:380.
- Hopkins K, Grossman D, White K, et al. Reproductive health preventive screening among clinic vs. over-the-counter oral contraceptive users. Contraception. 2012;86:376-382.
- Grindlay K, Grossman D. Interest in over-the-counter access to a progestin-only pill among women in the United States. Womens Health Issues. 2018;28:144-151.
- Frost JJ, Sonfield A, Zolna MR, et al. Return on investment: a fuller assessment of the benefits and cost savings of the US publicly funded family planning program. Milbank Q. 2014;92:696-749.