User login
Atypical Cardiac Metastasis From a Typical Rectal Cancer
BACKGROUND: The heart is an unusual site of metastasis from any malignancy. The pericardium is the most frequently involved site of cardiac metastasis. Myocardial metastasis is rare and metastasis only to heart without evidence of spread anywhere else is extremely rare. Here we present a case of rectal cancer with metastasis only to heart.
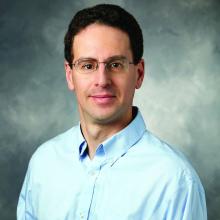
CASE REPORT: A 64-year-old man was found to have a large ulcerated mass in the upper rectum, 15cm above the anal verge during colonoscopy. Biopsy of the mass revealed poorly differentiated invasive adenocarcinoma. After 5 weeks of neo adjuvant capecitabine with concurrent radiation, he underwent robotic low anterior resection (LAR) with coloanal anastomosis with loop ileostomy. Pathology revealed 5cm poorly differentiated adenocarcinoma of rectum invading through muscularis propria with 7/17 lymph nodes and margins involved with adenocarcinoma. He was staged as ypT3pN2bM0 (Stage IIIC, AJCC 8th edition, 2017). Adjuvant therapy was delayed until 12 weeks from surgery due to wound dehiscence/infection. After 5 cycles of adjuvant capecitabine and oxaliplatin, a follow up contrast CT chest/abdomen/pelvis revealed 2.3cm mass extending from pericardium to myocardium. Transesophageal echocardiogram(TEE) and cardiac MRI revealed 2 separate masses(1cm and 2cm) in the right ventricle (RV) free wall projecting into RV cavity concerning for free wall metastases. After 3 weeks, he presented to ED with shortness of breath. Transthoracic echocardiogram(TTE) showed large pericardial effusion with cardiac tamponade. 1250ml of pericardial fluid was removed by pericardiocentesis and cytology revealed metastatic colorectal adenocarcinoma. CT chest/abdomen/pelvis with IV contrast did not show any other site of metastasis. He was started on systemic chemotherapy with Fluorouracil and Irinotecan (FOLFIRI). He has tolerated FOLFIRI for a year without recurrence of pericardial effusion.
CONCLUSION: Most cardiac metastases are associated with widely metastatic disease, but this case is unique in having only cardiac metastasis from a previously resected rectal adenocarcinoma. Although often clinically silent, cardiac metastases should be considered in any patient with cancer and new cardiac symptoms. TTE is the initial imaging test but TEE, Cardiac CT and Cardiac MRI may help further characterize and delineate the extent of cardiac disease. A multidisciplinary team to evaluate and manage the patient with cardiac metastasis is recommended.
BACKGROUND: The heart is an unusual site of metastasis from any malignancy. The pericardium is the most frequently involved site of cardiac metastasis. Myocardial metastasis is rare and metastasis only to heart without evidence of spread anywhere else is extremely rare. Here we present a case of rectal cancer with metastasis only to heart.
CASE REPORT: A 64-year-old man was found to have a large ulcerated mass in the upper rectum, 15cm above the anal verge during colonoscopy. Biopsy of the mass revealed poorly differentiated invasive adenocarcinoma. After 5 weeks of neo adjuvant capecitabine with concurrent radiation, he underwent robotic low anterior resection (LAR) with coloanal anastomosis with loop ileostomy. Pathology revealed 5cm poorly differentiated adenocarcinoma of rectum invading through muscularis propria with 7/17 lymph nodes and margins involved with adenocarcinoma. He was staged as ypT3pN2bM0 (Stage IIIC, AJCC 8th edition, 2017). Adjuvant therapy was delayed until 12 weeks from surgery due to wound dehiscence/infection. After 5 cycles of adjuvant capecitabine and oxaliplatin, a follow up contrast CT chest/abdomen/pelvis revealed 2.3cm mass extending from pericardium to myocardium. Transesophageal echocardiogram(TEE) and cardiac MRI revealed 2 separate masses(1cm and 2cm) in the right ventricle (RV) free wall projecting into RV cavity concerning for free wall metastases. After 3 weeks, he presented to ED with shortness of breath. Transthoracic echocardiogram(TTE) showed large pericardial effusion with cardiac tamponade. 1250ml of pericardial fluid was removed by pericardiocentesis and cytology revealed metastatic colorectal adenocarcinoma. CT chest/abdomen/pelvis with IV contrast did not show any other site of metastasis. He was started on systemic chemotherapy with Fluorouracil and Irinotecan (FOLFIRI). He has tolerated FOLFIRI for a year without recurrence of pericardial effusion.
CONCLUSION: Most cardiac metastases are associated with widely metastatic disease, but this case is unique in having only cardiac metastasis from a previously resected rectal adenocarcinoma. Although often clinically silent, cardiac metastases should be considered in any patient with cancer and new cardiac symptoms. TTE is the initial imaging test but TEE, Cardiac CT and Cardiac MRI may help further characterize and delineate the extent of cardiac disease. A multidisciplinary team to evaluate and manage the patient with cardiac metastasis is recommended.
BACKGROUND: The heart is an unusual site of metastasis from any malignancy. The pericardium is the most frequently involved site of cardiac metastasis. Myocardial metastasis is rare and metastasis only to heart without evidence of spread anywhere else is extremely rare. Here we present a case of rectal cancer with metastasis only to heart.
CASE REPORT: A 64-year-old man was found to have a large ulcerated mass in the upper rectum, 15cm above the anal verge during colonoscopy. Biopsy of the mass revealed poorly differentiated invasive adenocarcinoma. After 5 weeks of neo adjuvant capecitabine with concurrent radiation, he underwent robotic low anterior resection (LAR) with coloanal anastomosis with loop ileostomy. Pathology revealed 5cm poorly differentiated adenocarcinoma of rectum invading through muscularis propria with 7/17 lymph nodes and margins involved with adenocarcinoma. He was staged as ypT3pN2bM0 (Stage IIIC, AJCC 8th edition, 2017). Adjuvant therapy was delayed until 12 weeks from surgery due to wound dehiscence/infection. After 5 cycles of adjuvant capecitabine and oxaliplatin, a follow up contrast CT chest/abdomen/pelvis revealed 2.3cm mass extending from pericardium to myocardium. Transesophageal echocardiogram(TEE) and cardiac MRI revealed 2 separate masses(1cm and 2cm) in the right ventricle (RV) free wall projecting into RV cavity concerning for free wall metastases. After 3 weeks, he presented to ED with shortness of breath. Transthoracic echocardiogram(TTE) showed large pericardial effusion with cardiac tamponade. 1250ml of pericardial fluid was removed by pericardiocentesis and cytology revealed metastatic colorectal adenocarcinoma. CT chest/abdomen/pelvis with IV contrast did not show any other site of metastasis. He was started on systemic chemotherapy with Fluorouracil and Irinotecan (FOLFIRI). He has tolerated FOLFIRI for a year without recurrence of pericardial effusion.
CONCLUSION: Most cardiac metastases are associated with widely metastatic disease, but this case is unique in having only cardiac metastasis from a previously resected rectal adenocarcinoma. Although often clinically silent, cardiac metastases should be considered in any patient with cancer and new cardiac symptoms. TTE is the initial imaging test but TEE, Cardiac CT and Cardiac MRI may help further characterize and delineate the extent of cardiac disease. A multidisciplinary team to evaluate and manage the patient with cardiac metastasis is recommended.
Antihypertensives linked to reduced risk of colorectal cancer
Treating hypertension with angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) was associated with a reduced risk for colorectal cancer, according to findings from a large retrospective study.
However, another study reported just over a year ago suggested that ACE inhibitors, but not ARBs, are associated with an increased risk for lung cancer. An expert approached for comment emphasized that both studies are observational, and, as such, they only show an association, not causation.
In this latest study, published online July 6 in the journal Hypertension, the use of ACE inhibitors/ARBs was associated with a 22% lower risk for colorectal cancer developing within 3 years after a negative baseline colonoscopy.
This is the largest study to date, with a cohort of more than 185,000 patients, to suggest a significant protective effect for these two common antihypertensive medications, the authors note. The risk of developing colorectal cancer decreased with longer duration of ACE inhibitor/ARB use, with a 5% reduction in adjusted hazard ratio risk for each year of use. However, this effect was limited to patients who had negative colonoscopies within a 3-year period and did not extend beyond that point.
Lead author Wai K. Leung, MD, clinical professor of medicine at the University of Hong Kong, explained that they are not advising patients to take ACE inhibitors simply to prevent cancer. “Unlike aspirin and statins, the potential chemopreventive role of ACE inhibitors on cancer has never been established,” he said in an interview. “The study findings may favor the use of ACE inhibitors in the treatment of hypertension, over many other antihypertensives, in some patients for preventing colorectal cancer.”
Increased or reduced risk?
There has been considerable debate about the potential carcinogenic effects of ACE inhibitors and ARBs, and the relationship with “various solid organ cancer risks have been unsettled,” the authors note. Studies have produced conflicting results – showing no overall cancer risk and a modestly increased overall cancer risk – associated with these agents.
A recent study reported that ACE inhibitors, as compared with ARBs, increased risk for lung cancer by 14%. The risk for lung cancer increased by 22% among those using ACE inhibitors for 5 years, and the risk peaked at 31% for patients who took ACE inhibitors for 10 years or longer.
The lead author of that lung cancer study, Laurent Azoulay, PhD, of McGill University in Montreal, offered some thoughts on the seemingly conflicting data now being reported showing a reduction in the risk of colorectal cancer.
“In a nutshell, this study has important methodologic issues that can explain the observed findings,” he said in an interview.
Dr. Azoulay pointed out that, in the univariate model, the use of ACE inhibitors/ARBs was associated with a 26% increased risk of colorectal cancer. “It is only after propensity score adjustment that the effect estimate reversed in the protective direction,” he pointed out. “However, the variables included in the propensity score model were measured in the same time window as the exposure, which can lead to an overadjustment bias and generate spurious findings.”
Another issue is that the study period did not begin at the time of the exposure, but rather at a distant point after treatment initiation – in this case, colorectal cancer screening. “As such, the authors excluded patients who were previously diagnosed with colorectal cancer prior to that point, which likely included patients exposed to ACE inhibitors/ARBs,” he said. “This approach can lead to the inclusion of the ‘survivors’ for whom the risk of developing colorectal cancer is lower.
“But certainly,” Dr. Azoulay added, “this possible association should be investigated using methodologically sound approaches.”
Take-home message for physicians
Another expert emphasized the observational nature of both studies. Raymond Townsend, MD, director of the Hypertension Program and a professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia, said: “First and foremost, these are observational studies and cannot make inference about causality; they can only show associations.”
He pointed out that, sometimes, associations are truly present, whereas at other times, there is bias or confounding that cannot be controlled for statistically because it is “unknown.” That said, the size of this latest study is a plus, and there is a reasonable follow-up period.
“The take-home [message] for practitioners is that there may be a benefit in keeping older people on ACE inhibitors on the likelihood of developing colorectal cancer if your last colonoscopy was negative,” Dr. Townsend, who was not involved in the study, said in an interview.
But there are some questions that remain unanswered regarding characteristics of the cohort, Dr. Townsend noted. “Who were the people having the colonoscopy in the first place? Were they a group at higher risk? Why were some on an ACE inhibitors/ARBs and many others not?”
There are other conclusions that clinicians can glean from this. “Make a choice of treatment for a patient based on your best estimate of what will lower their blood pressure and prevent hypertension-mediated organ damage,” said Dr. Townsend, who is also an American Heart Association volunteer expert. “Keep in mind that patients hear about these studies and read unreviewed blogs on the web and so have questions.”
He emphasized that it always comes back to two things. “One is that every treatment decision is inherently a risk-benefit scenario,” he said. “And second is that most of our patients are adults, and if they choose to not be treated for their hypertension despite our best advice and reasoning with them, relinquish control and let them proceed as they wish, offering to renegotiate in the future when and if they reconsider.”
Study details
In the latest study, Dr. Leung and colleagues conducted a retrospective cohort study and used data from an electronic health care database of the Hong Kong Hospital Authority. A total of 187,897 individuals aged 40 years and older had undergone colonoscopy between 2005 and 2013 with a negative result and were included in the analysis.
The study’s primary outcome was colorectal cancer that was diagnosed between 6 and 36 months after undergoing colonoscopy, and the median age at colonoscopy was 60.6 years. Within this population, 30,856 patients (16.4%) used ACE inhibitors/ARBs.
Between 6 months and 3 years after undergoing colonoscopy, 854 cases of colorectal cancer were diagnosed, with an incidence rate of 15.2 per 10,000 person-years. The median time between colonoscopy and diagnosis was 1.2 years.
ACE inhibitor/ARB users had a median duration of 3.3 years of use within the 5-year period before their colonoscopy. Within this group, there were 169 (0.55%) cases of colorectal cancer. On univariate analysis, the crude hazard ratio (HR) of colorectal cancer and ACE inhibitor/ARB use was 1.26 (P = .008), but on propensity score regression adjustment, the adjusted HR became 0.78.
The propensity score absolute reduction in risk for users was 3.2 per 10,000 person-years versus nonusers, and stratification by subsite showed an HR of 0.77 for distal cancers and 0.83 for proximal cancers.
In a subgroup analysis, the benefits of ACE inhibitors and ARBs were seen in patients aged 55 years or older (adjusted HR, 0.79) and in those with a history of colonic polyps (adjusted HR, 0.71).
The authors also assessed if there was an association between these medications and other types of cancer. On univariate analysis, usage was associated with an increased risk of lung and prostate cancer but lower risk of breast cancer. But after propensity score regression adjustment, the associations were no longer there.
The study was funded by the Health and Medical Research Fund of the Hong Kong SAR Government. Dr. Leung has received honorarium for attending advisory board meetings of AbbVie, Takeda, and Abbott Laboratories; coauthor Esther W. Chan has received funding support from Pfizer, Bristol-Myers Squibb, Bayer, Takeda, Janssen (a division of Johnson & Johnson); Research Grants Council of Hong Kong; Narcotics Division, Security Bureau; and the National Natural Science Foundation of China, all for work unrelated to the current study. None of the other authors have disclosed relevant financial relationships. Dr. Azoulay has disclosed no relevant financial relationships. Dr. Townsend is employed by Penn Medicine.
A version of this article originally appeared on Medscape.com.
Treating hypertension with angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) was associated with a reduced risk for colorectal cancer, according to findings from a large retrospective study.
However, another study reported just over a year ago suggested that ACE inhibitors, but not ARBs, are associated with an increased risk for lung cancer. An expert approached for comment emphasized that both studies are observational, and, as such, they only show an association, not causation.
In this latest study, published online July 6 in the journal Hypertension, the use of ACE inhibitors/ARBs was associated with a 22% lower risk for colorectal cancer developing within 3 years after a negative baseline colonoscopy.
This is the largest study to date, with a cohort of more than 185,000 patients, to suggest a significant protective effect for these two common antihypertensive medications, the authors note. The risk of developing colorectal cancer decreased with longer duration of ACE inhibitor/ARB use, with a 5% reduction in adjusted hazard ratio risk for each year of use. However, this effect was limited to patients who had negative colonoscopies within a 3-year period and did not extend beyond that point.
Lead author Wai K. Leung, MD, clinical professor of medicine at the University of Hong Kong, explained that they are not advising patients to take ACE inhibitors simply to prevent cancer. “Unlike aspirin and statins, the potential chemopreventive role of ACE inhibitors on cancer has never been established,” he said in an interview. “The study findings may favor the use of ACE inhibitors in the treatment of hypertension, over many other antihypertensives, in some patients for preventing colorectal cancer.”
Increased or reduced risk?
There has been considerable debate about the potential carcinogenic effects of ACE inhibitors and ARBs, and the relationship with “various solid organ cancer risks have been unsettled,” the authors note. Studies have produced conflicting results – showing no overall cancer risk and a modestly increased overall cancer risk – associated with these agents.
A recent study reported that ACE inhibitors, as compared with ARBs, increased risk for lung cancer by 14%. The risk for lung cancer increased by 22% among those using ACE inhibitors for 5 years, and the risk peaked at 31% for patients who took ACE inhibitors for 10 years or longer.
The lead author of that lung cancer study, Laurent Azoulay, PhD, of McGill University in Montreal, offered some thoughts on the seemingly conflicting data now being reported showing a reduction in the risk of colorectal cancer.
“In a nutshell, this study has important methodologic issues that can explain the observed findings,” he said in an interview.
Dr. Azoulay pointed out that, in the univariate model, the use of ACE inhibitors/ARBs was associated with a 26% increased risk of colorectal cancer. “It is only after propensity score adjustment that the effect estimate reversed in the protective direction,” he pointed out. “However, the variables included in the propensity score model were measured in the same time window as the exposure, which can lead to an overadjustment bias and generate spurious findings.”
Another issue is that the study period did not begin at the time of the exposure, but rather at a distant point after treatment initiation – in this case, colorectal cancer screening. “As such, the authors excluded patients who were previously diagnosed with colorectal cancer prior to that point, which likely included patients exposed to ACE inhibitors/ARBs,” he said. “This approach can lead to the inclusion of the ‘survivors’ for whom the risk of developing colorectal cancer is lower.
“But certainly,” Dr. Azoulay added, “this possible association should be investigated using methodologically sound approaches.”
Take-home message for physicians
Another expert emphasized the observational nature of both studies. Raymond Townsend, MD, director of the Hypertension Program and a professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia, said: “First and foremost, these are observational studies and cannot make inference about causality; they can only show associations.”
He pointed out that, sometimes, associations are truly present, whereas at other times, there is bias or confounding that cannot be controlled for statistically because it is “unknown.” That said, the size of this latest study is a plus, and there is a reasonable follow-up period.
“The take-home [message] for practitioners is that there may be a benefit in keeping older people on ACE inhibitors on the likelihood of developing colorectal cancer if your last colonoscopy was negative,” Dr. Townsend, who was not involved in the study, said in an interview.
But there are some questions that remain unanswered regarding characteristics of the cohort, Dr. Townsend noted. “Who were the people having the colonoscopy in the first place? Were they a group at higher risk? Why were some on an ACE inhibitors/ARBs and many others not?”
There are other conclusions that clinicians can glean from this. “Make a choice of treatment for a patient based on your best estimate of what will lower their blood pressure and prevent hypertension-mediated organ damage,” said Dr. Townsend, who is also an American Heart Association volunteer expert. “Keep in mind that patients hear about these studies and read unreviewed blogs on the web and so have questions.”
He emphasized that it always comes back to two things. “One is that every treatment decision is inherently a risk-benefit scenario,” he said. “And second is that most of our patients are adults, and if they choose to not be treated for their hypertension despite our best advice and reasoning with them, relinquish control and let them proceed as they wish, offering to renegotiate in the future when and if they reconsider.”
Study details
In the latest study, Dr. Leung and colleagues conducted a retrospective cohort study and used data from an electronic health care database of the Hong Kong Hospital Authority. A total of 187,897 individuals aged 40 years and older had undergone colonoscopy between 2005 and 2013 with a negative result and were included in the analysis.
The study’s primary outcome was colorectal cancer that was diagnosed between 6 and 36 months after undergoing colonoscopy, and the median age at colonoscopy was 60.6 years. Within this population, 30,856 patients (16.4%) used ACE inhibitors/ARBs.
Between 6 months and 3 years after undergoing colonoscopy, 854 cases of colorectal cancer were diagnosed, with an incidence rate of 15.2 per 10,000 person-years. The median time between colonoscopy and diagnosis was 1.2 years.
ACE inhibitor/ARB users had a median duration of 3.3 years of use within the 5-year period before their colonoscopy. Within this group, there were 169 (0.55%) cases of colorectal cancer. On univariate analysis, the crude hazard ratio (HR) of colorectal cancer and ACE inhibitor/ARB use was 1.26 (P = .008), but on propensity score regression adjustment, the adjusted HR became 0.78.
The propensity score absolute reduction in risk for users was 3.2 per 10,000 person-years versus nonusers, and stratification by subsite showed an HR of 0.77 for distal cancers and 0.83 for proximal cancers.
In a subgroup analysis, the benefits of ACE inhibitors and ARBs were seen in patients aged 55 years or older (adjusted HR, 0.79) and in those with a history of colonic polyps (adjusted HR, 0.71).
The authors also assessed if there was an association between these medications and other types of cancer. On univariate analysis, usage was associated with an increased risk of lung and prostate cancer but lower risk of breast cancer. But after propensity score regression adjustment, the associations were no longer there.
The study was funded by the Health and Medical Research Fund of the Hong Kong SAR Government. Dr. Leung has received honorarium for attending advisory board meetings of AbbVie, Takeda, and Abbott Laboratories; coauthor Esther W. Chan has received funding support from Pfizer, Bristol-Myers Squibb, Bayer, Takeda, Janssen (a division of Johnson & Johnson); Research Grants Council of Hong Kong; Narcotics Division, Security Bureau; and the National Natural Science Foundation of China, all for work unrelated to the current study. None of the other authors have disclosed relevant financial relationships. Dr. Azoulay has disclosed no relevant financial relationships. Dr. Townsend is employed by Penn Medicine.
A version of this article originally appeared on Medscape.com.
Treating hypertension with angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) was associated with a reduced risk for colorectal cancer, according to findings from a large retrospective study.
However, another study reported just over a year ago suggested that ACE inhibitors, but not ARBs, are associated with an increased risk for lung cancer. An expert approached for comment emphasized that both studies are observational, and, as such, they only show an association, not causation.
In this latest study, published online July 6 in the journal Hypertension, the use of ACE inhibitors/ARBs was associated with a 22% lower risk for colorectal cancer developing within 3 years after a negative baseline colonoscopy.
This is the largest study to date, with a cohort of more than 185,000 patients, to suggest a significant protective effect for these two common antihypertensive medications, the authors note. The risk of developing colorectal cancer decreased with longer duration of ACE inhibitor/ARB use, with a 5% reduction in adjusted hazard ratio risk for each year of use. However, this effect was limited to patients who had negative colonoscopies within a 3-year period and did not extend beyond that point.
Lead author Wai K. Leung, MD, clinical professor of medicine at the University of Hong Kong, explained that they are not advising patients to take ACE inhibitors simply to prevent cancer. “Unlike aspirin and statins, the potential chemopreventive role of ACE inhibitors on cancer has never been established,” he said in an interview. “The study findings may favor the use of ACE inhibitors in the treatment of hypertension, over many other antihypertensives, in some patients for preventing colorectal cancer.”
Increased or reduced risk?
There has been considerable debate about the potential carcinogenic effects of ACE inhibitors and ARBs, and the relationship with “various solid organ cancer risks have been unsettled,” the authors note. Studies have produced conflicting results – showing no overall cancer risk and a modestly increased overall cancer risk – associated with these agents.
A recent study reported that ACE inhibitors, as compared with ARBs, increased risk for lung cancer by 14%. The risk for lung cancer increased by 22% among those using ACE inhibitors for 5 years, and the risk peaked at 31% for patients who took ACE inhibitors for 10 years or longer.
The lead author of that lung cancer study, Laurent Azoulay, PhD, of McGill University in Montreal, offered some thoughts on the seemingly conflicting data now being reported showing a reduction in the risk of colorectal cancer.
“In a nutshell, this study has important methodologic issues that can explain the observed findings,” he said in an interview.
Dr. Azoulay pointed out that, in the univariate model, the use of ACE inhibitors/ARBs was associated with a 26% increased risk of colorectal cancer. “It is only after propensity score adjustment that the effect estimate reversed in the protective direction,” he pointed out. “However, the variables included in the propensity score model were measured in the same time window as the exposure, which can lead to an overadjustment bias and generate spurious findings.”
Another issue is that the study period did not begin at the time of the exposure, but rather at a distant point after treatment initiation – in this case, colorectal cancer screening. “As such, the authors excluded patients who were previously diagnosed with colorectal cancer prior to that point, which likely included patients exposed to ACE inhibitors/ARBs,” he said. “This approach can lead to the inclusion of the ‘survivors’ for whom the risk of developing colorectal cancer is lower.
“But certainly,” Dr. Azoulay added, “this possible association should be investigated using methodologically sound approaches.”
Take-home message for physicians
Another expert emphasized the observational nature of both studies. Raymond Townsend, MD, director of the Hypertension Program and a professor of medicine at the Hospital of the University of Pennsylvania, Philadelphia, said: “First and foremost, these are observational studies and cannot make inference about causality; they can only show associations.”
He pointed out that, sometimes, associations are truly present, whereas at other times, there is bias or confounding that cannot be controlled for statistically because it is “unknown.” That said, the size of this latest study is a plus, and there is a reasonable follow-up period.
“The take-home [message] for practitioners is that there may be a benefit in keeping older people on ACE inhibitors on the likelihood of developing colorectal cancer if your last colonoscopy was negative,” Dr. Townsend, who was not involved in the study, said in an interview.
But there are some questions that remain unanswered regarding characteristics of the cohort, Dr. Townsend noted. “Who were the people having the colonoscopy in the first place? Were they a group at higher risk? Why were some on an ACE inhibitors/ARBs and many others not?”
There are other conclusions that clinicians can glean from this. “Make a choice of treatment for a patient based on your best estimate of what will lower their blood pressure and prevent hypertension-mediated organ damage,” said Dr. Townsend, who is also an American Heart Association volunteer expert. “Keep in mind that patients hear about these studies and read unreviewed blogs on the web and so have questions.”
He emphasized that it always comes back to two things. “One is that every treatment decision is inherently a risk-benefit scenario,” he said. “And second is that most of our patients are adults, and if they choose to not be treated for their hypertension despite our best advice and reasoning with them, relinquish control and let them proceed as they wish, offering to renegotiate in the future when and if they reconsider.”
Study details
In the latest study, Dr. Leung and colleagues conducted a retrospective cohort study and used data from an electronic health care database of the Hong Kong Hospital Authority. A total of 187,897 individuals aged 40 years and older had undergone colonoscopy between 2005 and 2013 with a negative result and were included in the analysis.
The study’s primary outcome was colorectal cancer that was diagnosed between 6 and 36 months after undergoing colonoscopy, and the median age at colonoscopy was 60.6 years. Within this population, 30,856 patients (16.4%) used ACE inhibitors/ARBs.
Between 6 months and 3 years after undergoing colonoscopy, 854 cases of colorectal cancer were diagnosed, with an incidence rate of 15.2 per 10,000 person-years. The median time between colonoscopy and diagnosis was 1.2 years.
ACE inhibitor/ARB users had a median duration of 3.3 years of use within the 5-year period before their colonoscopy. Within this group, there were 169 (0.55%) cases of colorectal cancer. On univariate analysis, the crude hazard ratio (HR) of colorectal cancer and ACE inhibitor/ARB use was 1.26 (P = .008), but on propensity score regression adjustment, the adjusted HR became 0.78.
The propensity score absolute reduction in risk for users was 3.2 per 10,000 person-years versus nonusers, and stratification by subsite showed an HR of 0.77 for distal cancers and 0.83 for proximal cancers.
In a subgroup analysis, the benefits of ACE inhibitors and ARBs were seen in patients aged 55 years or older (adjusted HR, 0.79) and in those with a history of colonic polyps (adjusted HR, 0.71).
The authors also assessed if there was an association between these medications and other types of cancer. On univariate analysis, usage was associated with an increased risk of lung and prostate cancer but lower risk of breast cancer. But after propensity score regression adjustment, the associations were no longer there.
The study was funded by the Health and Medical Research Fund of the Hong Kong SAR Government. Dr. Leung has received honorarium for attending advisory board meetings of AbbVie, Takeda, and Abbott Laboratories; coauthor Esther W. Chan has received funding support from Pfizer, Bristol-Myers Squibb, Bayer, Takeda, Janssen (a division of Johnson & Johnson); Research Grants Council of Hong Kong; Narcotics Division, Security Bureau; and the National Natural Science Foundation of China, all for work unrelated to the current study. None of the other authors have disclosed relevant financial relationships. Dr. Azoulay has disclosed no relevant financial relationships. Dr. Townsend is employed by Penn Medicine.
A version of this article originally appeared on Medscape.com.
Endoscopic full-thickness resection of colorectal lesions appears safe and effective
Endoscopic full-thickness resection (eFTR) of complex colorectal lesions appears safe and effective, based on prospective data from 20 Dutch hospitals.
Macroscopic complete en bloc resection was achieved in 83.9% of procedures with an adverse event rate of 9.3%, reported lead author Liselotte W. Zwager, a PhD candidate at the University of Amsterdam, and colleagues.
“With the advantage of enabling a transmural resection, eFTR offers an alternative to radical surgery in lesions considered incurable with current resection techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD),” the investigators wrote in Endoscopy.
But more data are needed for widespread adoption, they noted. “Several studies have reported encouraging results on the short-term safety and efficacy of eFTR for numerous indications. However, firm conclusions on clinical results will require analysis of large prospective series of patients in everyday clinical practice.”
The present study provided data from 362 patients who underwent 367 procedures at 5 academic and 15 nonacademic centers in the Netherlands.
Patients were eligible for eFTR if polyps were nonlifting or in difficult-to-reach locations, or if T1 colorectal cancer (CRC) was suspected. In addition, eFTR was performed for subepithelial tumors, and as secondary completion treatment after incomplete endoscopic resection of T1 CRC with a positive or nonassessable resection margin. Lesions greater than 30 mm were excluded because of device diameter constraints.
The primary outcome was macroscopic complete en bloc resection. Secondary outcomes included adverse events, full-thickness resection rate, and clinical success, the latter of which was defined by tumor-free resection margins (R0).
Out of 367 procedures, eFTR was most frequently conducted because of incomplete resection of T1 CRC (41%), followed by nonlifting or difficult-to-reach polyps (36%), suspected T1 CRC (19%), and least often, subepithelial tumors (4%).
Complete en bloc resection was achieved in 83.9% of procedures. Excluding 21 procedures in which eFTR was not performed because of inaccessibility of the lesion (n = 7) or immobility of tissue prohibiting retraction of the lesion into the cap (n = 14), R0 was achieved in 82.4% of cases. Among the same group, full-thickness resection rate was comparable, at 83.2%.
Adverse events occurred in 34 patients (9.3%), among whom 10 (2.7%) underwent emergency surgery for perforations or appendicitis.
“In conclusion,” the investigators wrote, “eFTR is an exciting, innovative resection technique that is clinically feasible and safe for complex colorectal lesions, with the potential to obviate the need for surgical resection. Further efficacy studies on eFTR as a primary and secondary treatment option for T1 CRC are needed, focusing on both the short- and long-term oncologic results.”
Peter V. Draganov, MD, of the University of Florida, Gainesville, called the R0 resection rate “respectable,” and suggested that the study “reconfirms on a larger scale that eFTR with the full-thickness resection device is successful in the majority of cases.”
“The full-thickness resection device expands our armamentarium to remove difficult polyps and early CRC,” he said.
Still, Dr. Draganov, who has previously advised careful patient selection for eFTR, noted certain drawbacks of the technique. “The presented data highlight some of the limitations of the full-thickness resection device, including the relatively small size of the lesion [median diameter, 23 mm] that can be resected, and challenges related to accessing and capturing the lesion due to the limited visibility and maneuverability of the device.”
Ultimately, Dr. Draganov supported the investigators’ call for more data. “Before eFTR becomes a primary modality for management of T1 CRC, we do need follow-up data on long-term cancer-related outcomes,” he said.
The study was supported by Ovesco Endoscopy. The investigators disclosed additional relationships with Cook, Ethicon, Olympus, and others.
SOURCE: Zwager LW et al. Endoscopy. 2020 Jun 4. doi: 10.1055/a-1176-1107.
Endoscopic full-thickness resection (eFTR) of complex colorectal lesions appears safe and effective, based on prospective data from 20 Dutch hospitals.
Macroscopic complete en bloc resection was achieved in 83.9% of procedures with an adverse event rate of 9.3%, reported lead author Liselotte W. Zwager, a PhD candidate at the University of Amsterdam, and colleagues.
“With the advantage of enabling a transmural resection, eFTR offers an alternative to radical surgery in lesions considered incurable with current resection techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD),” the investigators wrote in Endoscopy.
But more data are needed for widespread adoption, they noted. “Several studies have reported encouraging results on the short-term safety and efficacy of eFTR for numerous indications. However, firm conclusions on clinical results will require analysis of large prospective series of patients in everyday clinical practice.”
The present study provided data from 362 patients who underwent 367 procedures at 5 academic and 15 nonacademic centers in the Netherlands.
Patients were eligible for eFTR if polyps were nonlifting or in difficult-to-reach locations, or if T1 colorectal cancer (CRC) was suspected. In addition, eFTR was performed for subepithelial tumors, and as secondary completion treatment after incomplete endoscopic resection of T1 CRC with a positive or nonassessable resection margin. Lesions greater than 30 mm were excluded because of device diameter constraints.
The primary outcome was macroscopic complete en bloc resection. Secondary outcomes included adverse events, full-thickness resection rate, and clinical success, the latter of which was defined by tumor-free resection margins (R0).
Out of 367 procedures, eFTR was most frequently conducted because of incomplete resection of T1 CRC (41%), followed by nonlifting or difficult-to-reach polyps (36%), suspected T1 CRC (19%), and least often, subepithelial tumors (4%).
Complete en bloc resection was achieved in 83.9% of procedures. Excluding 21 procedures in which eFTR was not performed because of inaccessibility of the lesion (n = 7) or immobility of tissue prohibiting retraction of the lesion into the cap (n = 14), R0 was achieved in 82.4% of cases. Among the same group, full-thickness resection rate was comparable, at 83.2%.
Adverse events occurred in 34 patients (9.3%), among whom 10 (2.7%) underwent emergency surgery for perforations or appendicitis.
“In conclusion,” the investigators wrote, “eFTR is an exciting, innovative resection technique that is clinically feasible and safe for complex colorectal lesions, with the potential to obviate the need for surgical resection. Further efficacy studies on eFTR as a primary and secondary treatment option for T1 CRC are needed, focusing on both the short- and long-term oncologic results.”
Peter V. Draganov, MD, of the University of Florida, Gainesville, called the R0 resection rate “respectable,” and suggested that the study “reconfirms on a larger scale that eFTR with the full-thickness resection device is successful in the majority of cases.”
“The full-thickness resection device expands our armamentarium to remove difficult polyps and early CRC,” he said.
Still, Dr. Draganov, who has previously advised careful patient selection for eFTR, noted certain drawbacks of the technique. “The presented data highlight some of the limitations of the full-thickness resection device, including the relatively small size of the lesion [median diameter, 23 mm] that can be resected, and challenges related to accessing and capturing the lesion due to the limited visibility and maneuverability of the device.”
Ultimately, Dr. Draganov supported the investigators’ call for more data. “Before eFTR becomes a primary modality for management of T1 CRC, we do need follow-up data on long-term cancer-related outcomes,” he said.
The study was supported by Ovesco Endoscopy. The investigators disclosed additional relationships with Cook, Ethicon, Olympus, and others.
SOURCE: Zwager LW et al. Endoscopy. 2020 Jun 4. doi: 10.1055/a-1176-1107.
Endoscopic full-thickness resection (eFTR) of complex colorectal lesions appears safe and effective, based on prospective data from 20 Dutch hospitals.
Macroscopic complete en bloc resection was achieved in 83.9% of procedures with an adverse event rate of 9.3%, reported lead author Liselotte W. Zwager, a PhD candidate at the University of Amsterdam, and colleagues.
“With the advantage of enabling a transmural resection, eFTR offers an alternative to radical surgery in lesions considered incurable with current resection techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD),” the investigators wrote in Endoscopy.
But more data are needed for widespread adoption, they noted. “Several studies have reported encouraging results on the short-term safety and efficacy of eFTR for numerous indications. However, firm conclusions on clinical results will require analysis of large prospective series of patients in everyday clinical practice.”
The present study provided data from 362 patients who underwent 367 procedures at 5 academic and 15 nonacademic centers in the Netherlands.
Patients were eligible for eFTR if polyps were nonlifting or in difficult-to-reach locations, or if T1 colorectal cancer (CRC) was suspected. In addition, eFTR was performed for subepithelial tumors, and as secondary completion treatment after incomplete endoscopic resection of T1 CRC with a positive or nonassessable resection margin. Lesions greater than 30 mm were excluded because of device diameter constraints.
The primary outcome was macroscopic complete en bloc resection. Secondary outcomes included adverse events, full-thickness resection rate, and clinical success, the latter of which was defined by tumor-free resection margins (R0).
Out of 367 procedures, eFTR was most frequently conducted because of incomplete resection of T1 CRC (41%), followed by nonlifting or difficult-to-reach polyps (36%), suspected T1 CRC (19%), and least often, subepithelial tumors (4%).
Complete en bloc resection was achieved in 83.9% of procedures. Excluding 21 procedures in which eFTR was not performed because of inaccessibility of the lesion (n = 7) or immobility of tissue prohibiting retraction of the lesion into the cap (n = 14), R0 was achieved in 82.4% of cases. Among the same group, full-thickness resection rate was comparable, at 83.2%.
Adverse events occurred in 34 patients (9.3%), among whom 10 (2.7%) underwent emergency surgery for perforations or appendicitis.
“In conclusion,” the investigators wrote, “eFTR is an exciting, innovative resection technique that is clinically feasible and safe for complex colorectal lesions, with the potential to obviate the need for surgical resection. Further efficacy studies on eFTR as a primary and secondary treatment option for T1 CRC are needed, focusing on both the short- and long-term oncologic results.”
Peter V. Draganov, MD, of the University of Florida, Gainesville, called the R0 resection rate “respectable,” and suggested that the study “reconfirms on a larger scale that eFTR with the full-thickness resection device is successful in the majority of cases.”
“The full-thickness resection device expands our armamentarium to remove difficult polyps and early CRC,” he said.
Still, Dr. Draganov, who has previously advised careful patient selection for eFTR, noted certain drawbacks of the technique. “The presented data highlight some of the limitations of the full-thickness resection device, including the relatively small size of the lesion [median diameter, 23 mm] that can be resected, and challenges related to accessing and capturing the lesion due to the limited visibility and maneuverability of the device.”
Ultimately, Dr. Draganov supported the investigators’ call for more data. “Before eFTR becomes a primary modality for management of T1 CRC, we do need follow-up data on long-term cancer-related outcomes,” he said.
The study was supported by Ovesco Endoscopy. The investigators disclosed additional relationships with Cook, Ethicon, Olympus, and others.
SOURCE: Zwager LW et al. Endoscopy. 2020 Jun 4. doi: 10.1055/a-1176-1107.
FROM ENDOSCOPY
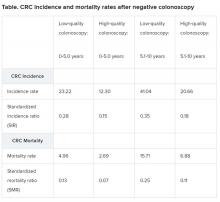
Single negative colonoscopy predicts low colorectal cancer risk
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
a new study concludes.
The population-based study showed a durable reduction in CRC risk over 17.4 years of follow-up.
“Our findings confirm that a 10-year interval between high-quality screening colonoscopies [as is currently recommended] is safe and that there is no benefit from more frequent screening,” lead author Nastazja Pilonis, MD, from the Maria Sklodowska-Curie National Research Institute of Oncology in Warsaw, Poland, told Medscape Medical News.
“Furthermore, our findings suggest that this interval could even be prolonged, provided the baseline colonoscopy is of high quality,” she added.
However, she emphasized that “only high-quality colonoscopy provided a durable reduction in mortality risk,” and noted that “low-quality colonoscopy was associated with a significantly increased risk of CRC death after the first 5 years following the examination.”
The study was published online May 25 in the Annals of Internal Medicine.
Polish Colonoscopy Screening Program
The study included 165,887 average-risk patients enrolled in the Polish Colonoscopy Screening Program who had a single negative screening colonoscopy between October 2000 and December 2011.
Negative colonoscopy was defined as an examination where no evidence of any neoplastic lesion was found.
A high-quality screening colonoscopy was defined by three key properties: cecal intubation, adequate bowel preparation, and an endoscopist’s adenoma detection rate (ADR) of 20% or greater calculated on a yearly basis.
A total of 505 different endoscopists performed the colonoscopies over a median follow-up of 10.1 years.
Compared with the general population, among individuals with a negative colonoscopy, the incidence of CRC was 72% lower and CRC mortality was 81% lower over a period of 5.1 to 10 years, Pilonis and colleagues report.
“This was mainly driven by long-lasting reductions in CRC incidence and mortality (by 84% and 90%, respectively) after high-quality screening colonoscopies,” the investigators emphasize.
Beyond 10 years of follow-up, reductions in CRC incidence and mortality were similar to those observed for the earlier period of 5.1 to 10 years but only for participants who had had a high-quality screening colonoscopy, they emphasize.
Subgroup analyses
In addition, subgroup analyses showed that high-quality colonoscopy – although not those of low-quality – effectively reduced the incidence of, and mortality from, CRC in women and in the proximal colon.
As Pilonis pointed out, previous studies have suggested that women may not benefit from screening colonoscopy to the same extent as men. Plus previous research suggests a reduced CRC risk in the proximal colon relative to that in the distal colon.
Overall, standardized incidence ratios (SIRs) and standardized mortality ratios (SMRs) significantly differed between men and women in the current study, but this difference was not observed after high-quality examinations, the investigators report.
“This is an extremely important finding because, for the first time, we showed that when you have high-quality colonoscopy, women benefit from screening colonoscopy as much as men,” Pilonis emphasized.
Similarly, high-quality screening colonoscopy was associated with a 50% reduction in mortality in the proximal colon throughout the 17.4-year follow-up, whereas there was no decrease in mortality from CRC in the proximal colon with low-quality colonoscopies.
As Pilonis noted, lesions in the proximal colon are more subtle and are harder to detect.”It’s also easier to achieve good bowel preparation in the distal colon than in the proximal colon,” she added.
Women are also more prone to develop lesions in the right (proximal) side of the colon and appear to have more pain with colonoscopy than men, all of which could have contributed to previous reports of colonoscopy not being very effective in women or for the detection of lesions in the proximal colon, as Pilonis suggested.
As the authors explain, current guidelines recommend a 10-year screening interval for the average-risk patient when colonoscopy results are negative.
This interval was partially based on the estimated time it was thought to take an adenoma to progress to a carcinoma and partially on the estimated sensitivity of screening colonoscopy.
“We showed that high-quality is a prerequisite for safe intervals between colonoscopies, Pilonis said. “So I would say that if, at a certain age, a patient has a negative colonoscopy of high-quality, a negative colonoscopy is highly predictive of a very low future risk of CRC,” she added.
The study was funded by the Polish Ministry of Health.
This article first appeared on Medscape.com.
Blood test detects colon cancer in single-center study
Blood assay studied for colorectal cancer screening.
A blood test detected 11 of 11 cases of colorectal cancer in a study involving 354 patients, and also spotted a majority of cases – 40 out of 53 – in which participants had advanced adenomas, an investigator said.
Results from a single-center study of CellMax Life’s FirstSight blood test were released as a poster as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
For a study conducted at one site, the Veterans Affairs Palo Alto (Calif.) Healthcare System, Shai Friedland, MD, and colleagues recruited 354 patients between ages 45 and 80 who were scheduled for elective colonoscopy. The researchers excluded people with a personal history of cancer or inflammatory bowel disease. They used CellMax’s FirstSight test on blood samples from the study participants.
The FirstSight test result was positive for colorectal cancer in all 11 patients in the study who were found by colonoscopy to have this condition, said Dr. Friedland, who is a professor of medicine at Stanford (Calif.) University and chief of gastroenterology at the VA Palo Alto Healthcare System. Thus, the test showed a sensitivity of 100% in this instance.
Among the 53 study participants found by colonoscopy to have advanced adenoma, 40 were positive on FirstSight; thus, so the test has a sensitivity of 75.5% for this result.
Among 79 patients who had negative colonoscopy results, meaning they were judged free of cancer or polyps, the test showed 8 as having signs of disease or growths.
“If you had a large adenoma that was removed years ago and now you have a negative colonoscopy, your score might still be high,” Dr. Friedland said in a recorded presentation for DDW. “In other words, the changes that are detectable in your blood might persist even after the polypectomy.”
He said there are plans to soon start a large-scale multicenter study of the CellMax assay.
“The blood test has the potential to fill an unmet need by giving patients a highly sensitive convenient option for colorectal cancer screening,” he said.
CellMax already is seeking to position its test as a more convenient alternative to either colonoscopy or the Cologuard screening test. Many patients put off cancer screening because of the need to take time off from work and the invasive nature of colonoscopy. Exact Sciences has used direct-to-consumer advertising to promote its Cologuard home-based test as a more convenient alternative to colonoscopy, but its product requires patients to collect their own stool samples and mail them to a lab, a process many people find off-putting.
Public health advocates, including the U.S. Preventive Services Task Force (USPSTF), have for years been pressing for wider screening of American adults for colon cancer. USPSTF is in the midst of updating its recommendations on colon cancer. In announcing its latest update of these recommendations in 2016, USPSTF said “the best screening test is the one that gets done” (JAMA. 2016;315[23]:2564-75).
USPSTF pressed for maximizing the total proportion of the eligible population, a point Dr. Friedland echoed in a CellMax press release.
“For colon cancer screening to be most effective, it is essential to detect precancerous polyps and then perform a colonoscopy to remove the polyps,” said Dr. Friedland in the CellMax press release. “Giving patients the option of getting a blood test for screening would undoubtedly increase compliance and thereby reduce mortality from colorectal cancer.”
In the DDW presentation, Dr. Friedland and colleagues also said the CellMax test showed greater sensitivity (100%) for colorectal cancer and advanced precancerous lesions (75.5%) than did Cologuard (92.3% for colorectal cancer and 42.4% for advanced precancerous lesions).
Cara Connelly, Director of Public Relations and Corporate Communications for Exact Sciences said that the company “is dedicated to getting more people screened for colorectal cancer and applaud the researchers for their efforts. We look forward to hearing more about the performance of this test in a prospective multisite study with nonsymptomatic patients.”
Naresh T. Gunaratnam, MD, a gastroenterologist and research director at Huron Gastro in Ypsilanti, Mich., said he is concerned that aggressive promotion of alternative tests may obscure the benefits of colonoscopy. Dr. Gunaratnam, a 2019 winner of the American Gastroenterological Association (AGA) Distinguished Clinician Award, has been a public critic of the marketing of colon cancer tests, which emphasize the convenience of these products. When asked by MDedge to comment on the CellMax-funded study, Dr. Gunaratnam said alternative tests do have a place for the care of patients who cannot or will not have a colonoscopy.
“But if you convince a patient who would be willing to have a colonoscopy not to, that’s a disservice,” he said.
“If you want the best test, the one that is best at finding cancers and finding polyps and the only one that can remove the polyp, that’s colonoscopy,” Dr. Gunaratnam added. “One day there may be a pill you can swallow that blows up the polyps, but we’re not there yet. We have to mechanically remove them.”
SOURCE: Friedland S et al. DDW 2020, eposter 575.
Blood assay studied for colorectal cancer screening.
Blood assay studied for colorectal cancer screening.
A blood test detected 11 of 11 cases of colorectal cancer in a study involving 354 patients, and also spotted a majority of cases – 40 out of 53 – in which participants had advanced adenomas, an investigator said.
Results from a single-center study of CellMax Life’s FirstSight blood test were released as a poster as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
For a study conducted at one site, the Veterans Affairs Palo Alto (Calif.) Healthcare System, Shai Friedland, MD, and colleagues recruited 354 patients between ages 45 and 80 who were scheduled for elective colonoscopy. The researchers excluded people with a personal history of cancer or inflammatory bowel disease. They used CellMax’s FirstSight test on blood samples from the study participants.
The FirstSight test result was positive for colorectal cancer in all 11 patients in the study who were found by colonoscopy to have this condition, said Dr. Friedland, who is a professor of medicine at Stanford (Calif.) University and chief of gastroenterology at the VA Palo Alto Healthcare System. Thus, the test showed a sensitivity of 100% in this instance.
Among the 53 study participants found by colonoscopy to have advanced adenoma, 40 were positive on FirstSight; thus, so the test has a sensitivity of 75.5% for this result.
Among 79 patients who had negative colonoscopy results, meaning they were judged free of cancer or polyps, the test showed 8 as having signs of disease or growths.
“If you had a large adenoma that was removed years ago and now you have a negative colonoscopy, your score might still be high,” Dr. Friedland said in a recorded presentation for DDW. “In other words, the changes that are detectable in your blood might persist even after the polypectomy.”
He said there are plans to soon start a large-scale multicenter study of the CellMax assay.
“The blood test has the potential to fill an unmet need by giving patients a highly sensitive convenient option for colorectal cancer screening,” he said.
CellMax already is seeking to position its test as a more convenient alternative to either colonoscopy or the Cologuard screening test. Many patients put off cancer screening because of the need to take time off from work and the invasive nature of colonoscopy. Exact Sciences has used direct-to-consumer advertising to promote its Cologuard home-based test as a more convenient alternative to colonoscopy, but its product requires patients to collect their own stool samples and mail them to a lab, a process many people find off-putting.
Public health advocates, including the U.S. Preventive Services Task Force (USPSTF), have for years been pressing for wider screening of American adults for colon cancer. USPSTF is in the midst of updating its recommendations on colon cancer. In announcing its latest update of these recommendations in 2016, USPSTF said “the best screening test is the one that gets done” (JAMA. 2016;315[23]:2564-75).
USPSTF pressed for maximizing the total proportion of the eligible population, a point Dr. Friedland echoed in a CellMax press release.
“For colon cancer screening to be most effective, it is essential to detect precancerous polyps and then perform a colonoscopy to remove the polyps,” said Dr. Friedland in the CellMax press release. “Giving patients the option of getting a blood test for screening would undoubtedly increase compliance and thereby reduce mortality from colorectal cancer.”
In the DDW presentation, Dr. Friedland and colleagues also said the CellMax test showed greater sensitivity (100%) for colorectal cancer and advanced precancerous lesions (75.5%) than did Cologuard (92.3% for colorectal cancer and 42.4% for advanced precancerous lesions).
Cara Connelly, Director of Public Relations and Corporate Communications for Exact Sciences said that the company “is dedicated to getting more people screened for colorectal cancer and applaud the researchers for their efforts. We look forward to hearing more about the performance of this test in a prospective multisite study with nonsymptomatic patients.”
Naresh T. Gunaratnam, MD, a gastroenterologist and research director at Huron Gastro in Ypsilanti, Mich., said he is concerned that aggressive promotion of alternative tests may obscure the benefits of colonoscopy. Dr. Gunaratnam, a 2019 winner of the American Gastroenterological Association (AGA) Distinguished Clinician Award, has been a public critic of the marketing of colon cancer tests, which emphasize the convenience of these products. When asked by MDedge to comment on the CellMax-funded study, Dr. Gunaratnam said alternative tests do have a place for the care of patients who cannot or will not have a colonoscopy.
“But if you convince a patient who would be willing to have a colonoscopy not to, that’s a disservice,” he said.
“If you want the best test, the one that is best at finding cancers and finding polyps and the only one that can remove the polyp, that’s colonoscopy,” Dr. Gunaratnam added. “One day there may be a pill you can swallow that blows up the polyps, but we’re not there yet. We have to mechanically remove them.”
SOURCE: Friedland S et al. DDW 2020, eposter 575.
A blood test detected 11 of 11 cases of colorectal cancer in a study involving 354 patients, and also spotted a majority of cases – 40 out of 53 – in which participants had advanced adenomas, an investigator said.
Results from a single-center study of CellMax Life’s FirstSight blood test were released as a poster as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
For a study conducted at one site, the Veterans Affairs Palo Alto (Calif.) Healthcare System, Shai Friedland, MD, and colleagues recruited 354 patients between ages 45 and 80 who were scheduled for elective colonoscopy. The researchers excluded people with a personal history of cancer or inflammatory bowel disease. They used CellMax’s FirstSight test on blood samples from the study participants.
The FirstSight test result was positive for colorectal cancer in all 11 patients in the study who were found by colonoscopy to have this condition, said Dr. Friedland, who is a professor of medicine at Stanford (Calif.) University and chief of gastroenterology at the VA Palo Alto Healthcare System. Thus, the test showed a sensitivity of 100% in this instance.
Among the 53 study participants found by colonoscopy to have advanced adenoma, 40 were positive on FirstSight; thus, so the test has a sensitivity of 75.5% for this result.
Among 79 patients who had negative colonoscopy results, meaning they were judged free of cancer or polyps, the test showed 8 as having signs of disease or growths.
“If you had a large adenoma that was removed years ago and now you have a negative colonoscopy, your score might still be high,” Dr. Friedland said in a recorded presentation for DDW. “In other words, the changes that are detectable in your blood might persist even after the polypectomy.”
He said there are plans to soon start a large-scale multicenter study of the CellMax assay.
“The blood test has the potential to fill an unmet need by giving patients a highly sensitive convenient option for colorectal cancer screening,” he said.
CellMax already is seeking to position its test as a more convenient alternative to either colonoscopy or the Cologuard screening test. Many patients put off cancer screening because of the need to take time off from work and the invasive nature of colonoscopy. Exact Sciences has used direct-to-consumer advertising to promote its Cologuard home-based test as a more convenient alternative to colonoscopy, but its product requires patients to collect their own stool samples and mail them to a lab, a process many people find off-putting.
Public health advocates, including the U.S. Preventive Services Task Force (USPSTF), have for years been pressing for wider screening of American adults for colon cancer. USPSTF is in the midst of updating its recommendations on colon cancer. In announcing its latest update of these recommendations in 2016, USPSTF said “the best screening test is the one that gets done” (JAMA. 2016;315[23]:2564-75).
USPSTF pressed for maximizing the total proportion of the eligible population, a point Dr. Friedland echoed in a CellMax press release.
“For colon cancer screening to be most effective, it is essential to detect precancerous polyps and then perform a colonoscopy to remove the polyps,” said Dr. Friedland in the CellMax press release. “Giving patients the option of getting a blood test for screening would undoubtedly increase compliance and thereby reduce mortality from colorectal cancer.”
In the DDW presentation, Dr. Friedland and colleagues also said the CellMax test showed greater sensitivity (100%) for colorectal cancer and advanced precancerous lesions (75.5%) than did Cologuard (92.3% for colorectal cancer and 42.4% for advanced precancerous lesions).
Cara Connelly, Director of Public Relations and Corporate Communications for Exact Sciences said that the company “is dedicated to getting more people screened for colorectal cancer and applaud the researchers for their efforts. We look forward to hearing more about the performance of this test in a prospective multisite study with nonsymptomatic patients.”
Naresh T. Gunaratnam, MD, a gastroenterologist and research director at Huron Gastro in Ypsilanti, Mich., said he is concerned that aggressive promotion of alternative tests may obscure the benefits of colonoscopy. Dr. Gunaratnam, a 2019 winner of the American Gastroenterological Association (AGA) Distinguished Clinician Award, has been a public critic of the marketing of colon cancer tests, which emphasize the convenience of these products. When asked by MDedge to comment on the CellMax-funded study, Dr. Gunaratnam said alternative tests do have a place for the care of patients who cannot or will not have a colonoscopy.
“But if you convince a patient who would be willing to have a colonoscopy not to, that’s a disservice,” he said.
“If you want the best test, the one that is best at finding cancers and finding polyps and the only one that can remove the polyp, that’s colonoscopy,” Dr. Gunaratnam added. “One day there may be a pill you can swallow that blows up the polyps, but we’re not there yet. We have to mechanically remove them.”
SOURCE: Friedland S et al. DDW 2020, eposter 575.
FROM DDW 2020
Performance of the Veterans Choice Program for Improving Access to Colonoscopy at a Tertiary VA Facility
In April 2014, amid concerns for long wait times for care within the US Department of Veterans Affairs (VA) Veterans Health Administration (VHA), the Veterans Access, Choice, and Accountability Act was signed into law. This included the Veterans Choice Program (VCP), which included a provision for veterans to be referred outside of the VA to the community for care if their nearest VHA facility could not provide the requested care within 30 days of the clinically indicated date.1 Since implementation of the VCP, both media outlets and policy researchers have raised concerns about both the timeliness and quality of care provided through this program.2-4
Specifically for colonoscopy, referral outside of the VA in the pre-VCP era resulted in lower adenoma detection rate (ADR) and decreased adherence to surveillance guidelines when compared with matched VA control colonoscopies, raising concerns about quality assurance.5 Colorectal cancer (CRC) screening and timely colonoscopy is a VA priority; however, the performance of the VCP for colonoscopy timelines and quality has not been examined in detail.
Methods
We identified 3,855 veterans at the VA Pittsburgh Healthcare System (VAPHS) who were referred for colonoscopy in the community by using VCP from June 2015 through May 2017, using a query for colonoscopy procedure orders within the VA Corporate Data Warehouse. A total of 190 patients had a colonoscopy completed in the community by utilizing the VCP during this time frame.
At VAPHS, veterans who are referred for colonoscopy are contacted by a scheduler. The scheduler contacts the patient and offers the first available colonoscopy date at VAPHS and schedules the procedure for this date. However, if this date is > 30 days from the procedure order date, the scheduler gives the veteran the option of being contacted by VCP to schedule a colonoscopy within the community (Figure 1). We measured the time interval from the date of the initially scheduled first available colonoscopy at VAPHS to the date the colonoscopy was actually performed through VCP.
Quality assurance also was assessed by checking for the availability of records of colonoscopies performed through the VCP in the VA electronic health record (EHR) system. Colonoscopy procedure reports also were reviewed to assess for documentation of established colonoscopy quality metrics for examinations performed through the VCP. Additionally, we reviewed records scanned into the VA EHR pertaining to the VCP colonoscopy, including pathology information and pre- or postvisit records if available.
Data extraction was initiated in November 2017 to allow for at least 6 months of lead time for outside health records from the community to be received and scanned into the EHR for the veteran at VAPHS. For colonoscopy quality metrics, we chose 3 metrics that are universally documented for all colonoscopy procedures performed at VAPHS: quality of bowel preparation, cecal withdrawal time, and performance of retroflexion in the rectum. Documentation of these quality metrics is recommended in gastroenterology practice guidelinesand/or required by VA national policy.6,7
We separately reviewed a sample of 350 of the 3,855 patients referred for colonoscopy through VCP at VAPHS during the same time period to investigate overall VCP utilization. This sample was representative at a 95% CI with 5% margin of error of the total and sampled from 2 high-volume referral months (October and November 2015) and 3 low-volume months (January, February, and March 2017). Detailed data were collected regarding the colonoscopy scheduling and VCP referral process, including dates of colonoscopy procedure request; scheduling within the VAPHS; scheduling through the VCP; and ultimately if, when, and where (VAPHS vs community) a veteran had a colonoscopy performed. Wait times for colonoscopy procedures performed at the VAPHS and those performed through the VCP were compared.
The institutional review board at VAPHS reviewed and approved this quality improvement study.
Statistical Analysis
For the 190 veterans who had a colonoscopy performed through VCP, a 1-sample Wilcoxon signed rank test was used with a null hypothesis that the median difference in days between first available VAPHS colonoscopy and community colonoscopy dates was 0. For the utilization sample of 350 veterans, an independent samples median test was used to compare the median wait times for colonoscopy procedures performed at the VA and those performed through VCP. IBM SPSS Version 25 was used for all statistical analysis.
Results
Of the 190 identified colonoscopies completed in the community utilizing VCP, scanned records could not be found for 29 procedures (15.3%) (Table). VCP procedures were performed a median 2 days earlier than the first available VAPHS procedure, but this difference was not statistically significant (P = .62) (Figure 2). Although 52% of colonoscopies occurred sooner through VCP than the initially scheduled VAPHS date, 44% were performed later, and there was wide variability in the difference between these dates, ranging from 49 days sooner to 165 days later.
Pathology results from VCP procedures for which tissue samples were obtained were absent in 11.9% (14 of 118) of procedures. There were no clear follow-up recommendations to referring VA health care providers in the 18% (29 of 161) of available procedure reports. In VCP procedures, documentation of selected quality metrics: bowel preparation, cecal withdrawal time, and rectal retroflexion, were deficient in 27.3%, 70.2%, and 32.9%, respectively (Figure 3).
The utilization dataset sample included 350 veterans who were offered a VCP colonoscopy because the first available VAPHS procedure could not be scheduled for > 30 days. Of these patients, 231 (66%) ultimately had their colonoscopy performed at VAPHS. An additional 26.6% of the patients in the utilization sample were lost in the scheduling process (ie, could not be contacted, cancelled and could not be rescheduled, or were a “no show” their scheduled VAPHS procedure). An unknown number of these patients may have had a procedure outside of the VA, but there are no records to confirm or exclude this possibility. Ultimately, there were only 26 (7.4%) confirmed VCP colonoscopy procedures within the utilization sample (Figure 4). The median actual wait time for colonoscopy was 61 days for VA procedures and 66 days for procedures referred through the VCP, which was not statistically significant (P = .15).
Discussion
This is the first study to evaluate the performance of the VCP for colonoscopy referrals. Consistent with recently reported data in other specialties, colonoscopy referrals through VCP did not lead to more timely procedures overall, although there was wide variation.8 The use of VCP for veteran referral to the community for colonoscopy led to fragmentation of care—with 15% of records for VCP colonoscopies unavailable in the VA EHR 6 months after the procedure. In addition, there were 45 pre- or postprocedure visits in the community, which is not standard practice at VAPHS, and therefore may add to the cost of care for veterans.
Documentation of selected colonoscopy quality metrics were deficient in 27.3% to 70.2% of available VCP procedure reports. Although many veterans were eligible for VCP referral for colonoscopy, only 7.4% had a documented procedure through VCP, and two-thirds of veterans eligible for VCP participation had their colonoscopy performed at the VAPHS, reflecting overall low utilization of the program.
The national average wait time for VCP referrals for multiple specialties was estimated to be 51 days in a 2018 Government Accountability Office (GAO) report, which is similar to our findings.9 The GAO report also concluded that the VCP does not have timeliness standards and notes missed opportunities to develop a mechanism for record transfer between the community and the VA. Our finding of missing colonoscopy procedure and pathology reports within the VA EHR is consistent with this claim. Our analysis revealed that widely accepted quality standards for colonoscopy, those that are required at the VA and monitored for quality assurance at the VAPHS, are not being consistently reported for veterans who undergo procedures in the community. Last, the overall low utilization rate, combined with overall similar wait times for colonoscopies referred through the VCP vs those done at the VA, should lead to reconsideration of offering community care referral to all veterans based solely on static wait time cutoffs.
Limitations
There are several limitations to our analysis. First, all data were extracted via chart review by one author; therefore, some scanned procedure or pathology reports or pre- and postprocedure records may have been missed. Second, these data are representative of a single VA medical center and may not reflect trends nationwide. Third, there are many factors that can influence veteran decision making regarding when and where colonoscopy procedures are performed, which could be related to the VCP community care referral process or independent of this. Finally, colonoscopies performed through the VCP are grouped and may not reflect variability in the performance of community practices that veterans were referred to though the VCP.
Adenoma detection rates (ADR) were not included in the assessment for 2 reasons. First, there was an insufficient number of screening colonoscopies to use for the ADR calculation. Second, a composite non-VA ADR of multiple community endoscopists in different practices would likely be inaccurate and not clinically meaningful. Of note, the VAPHS does calculate and maintain ADR information as a practice for its endoscopists.
Conclusions
Our findings are particularly important as the VA expands access to care in the community through the VA Mission Act, which replaces the VCP but continues to include a static wait time threshold of 28 days for referral to community-based care.10 Especially for colonoscopies with the indication of screening or surveillance, wait times > 28 days are likely not clinically significant. Additionally, this study demonstrates that there also are delays in access to colonoscopy by community-based care providers, and potentially reflects widespread colonoscopy access issues that are not unique to the VA.
Our findings are similar to other published results and reports and raise similar concerns about the pitfalls of veteran referral into the community, including (1) similar wait times for the community and the VA; (2) the risk of fragmented care; (3) unevenquality of care; and (4) low overall utilization of VCP for colonoscopy.11 We agree with the GAO’s recommendations, which include establishing clinically meaningful wait time thresholds, systemic monitoring of the timeliness of care, and additional mechanisms for seamless transfer of complete records of care into the VA system. If a referral is placed for community-based care, this should come with an expectation that the care will be offered and can be delivered sooner than would be possible at the VA. We additionally recommend that standards for reporting quality metrics, including ADR, also be required of community colonoscopy providers contracted to provide care for veterans through the VA Mission Act. Importantly, we recommend that data for comparative wait times and quality metrics for VA and the community should be publicly available for veterans so that they may make more informed choices about where they receive health care.
Acknowledgments
The authors thank Kaneen Allen, PhD, for her administrative assistance and guidance.
1. Veterans Access, Choice, and Accountability Act of 2014. 42 USC §1395 (2014).
2. Farmer CM, Hosek SD. Did we improve veterans health care? It’s unclear. https://www.rand.org/blog/2016/05/did-we-improve-veterans-health-care-its-unclear.html. Published May 24, 2016. Accessed April 20, 2020.
3. Farmer CM, Hosek SD, Adamson DM. balancing demand and supply for veterans’ health care: a summary of three RAND assessments conducted under the Veterans Choice Act. Rand Health Q. 2016;6(1):12.
4. Mattocks KM, Mengeling M, Sadler A, Baldor R, Bastian L. The Veterans Choice Act: a qualitative examination of rapid policy implementation in the Department of Veterans Affairs. Med Care. 2017;55(suppl 7)(suppl 1):S71-S75.
5. Bartel MJ, Robertson DJ, Pohl H. Colonoscopy practice for veterans within and outside the Veterans Affairs setting: a matched cohort study. Gastrointest Endosc. 2016;84(2):272-278.
6. Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Am J Gastroenterol. 2015;110(1):72-90.
7. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1015, colorectal cancer screening. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3068.Published December 30, 2014. Accessed April 12, 2020.
8. Penn M, Bhatnagar S, Kuy S, et al. Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs medical centers. JAMA Netw Open. 2019;2(1):e187096.
9. US Government Accountability Office. Veterans Choice Program: improvements needed to address access-related challenges as VA plans consolidation of its community care programs. https://www.gao.gov/assets/700/692271.pdf. Published June 4, 2018. Accessed April 12, 2020.
10. VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018. 38 USC §1703 (2018).
11. Barnett PG, Hong JS, Carey E, Grunwald GK, Joynt Maddox K, Maddox TM. Comparison of accessibility, cost, and quality of elective coronary revascularization between Veterans Affairs and community care hospitals. JAMA Cardiol. 2018;3(2):133-141.
In April 2014, amid concerns for long wait times for care within the US Department of Veterans Affairs (VA) Veterans Health Administration (VHA), the Veterans Access, Choice, and Accountability Act was signed into law. This included the Veterans Choice Program (VCP), which included a provision for veterans to be referred outside of the VA to the community for care if their nearest VHA facility could not provide the requested care within 30 days of the clinically indicated date.1 Since implementation of the VCP, both media outlets and policy researchers have raised concerns about both the timeliness and quality of care provided through this program.2-4
Specifically for colonoscopy, referral outside of the VA in the pre-VCP era resulted in lower adenoma detection rate (ADR) and decreased adherence to surveillance guidelines when compared with matched VA control colonoscopies, raising concerns about quality assurance.5 Colorectal cancer (CRC) screening and timely colonoscopy is a VA priority; however, the performance of the VCP for colonoscopy timelines and quality has not been examined in detail.
Methods
We identified 3,855 veterans at the VA Pittsburgh Healthcare System (VAPHS) who were referred for colonoscopy in the community by using VCP from June 2015 through May 2017, using a query for colonoscopy procedure orders within the VA Corporate Data Warehouse. A total of 190 patients had a colonoscopy completed in the community by utilizing the VCP during this time frame.
At VAPHS, veterans who are referred for colonoscopy are contacted by a scheduler. The scheduler contacts the patient and offers the first available colonoscopy date at VAPHS and schedules the procedure for this date. However, if this date is > 30 days from the procedure order date, the scheduler gives the veteran the option of being contacted by VCP to schedule a colonoscopy within the community (Figure 1). We measured the time interval from the date of the initially scheduled first available colonoscopy at VAPHS to the date the colonoscopy was actually performed through VCP.
Quality assurance also was assessed by checking for the availability of records of colonoscopies performed through the VCP in the VA electronic health record (EHR) system. Colonoscopy procedure reports also were reviewed to assess for documentation of established colonoscopy quality metrics for examinations performed through the VCP. Additionally, we reviewed records scanned into the VA EHR pertaining to the VCP colonoscopy, including pathology information and pre- or postvisit records if available.
Data extraction was initiated in November 2017 to allow for at least 6 months of lead time for outside health records from the community to be received and scanned into the EHR for the veteran at VAPHS. For colonoscopy quality metrics, we chose 3 metrics that are universally documented for all colonoscopy procedures performed at VAPHS: quality of bowel preparation, cecal withdrawal time, and performance of retroflexion in the rectum. Documentation of these quality metrics is recommended in gastroenterology practice guidelinesand/or required by VA national policy.6,7
We separately reviewed a sample of 350 of the 3,855 patients referred for colonoscopy through VCP at VAPHS during the same time period to investigate overall VCP utilization. This sample was representative at a 95% CI with 5% margin of error of the total and sampled from 2 high-volume referral months (October and November 2015) and 3 low-volume months (January, February, and March 2017). Detailed data were collected regarding the colonoscopy scheduling and VCP referral process, including dates of colonoscopy procedure request; scheduling within the VAPHS; scheduling through the VCP; and ultimately if, when, and where (VAPHS vs community) a veteran had a colonoscopy performed. Wait times for colonoscopy procedures performed at the VAPHS and those performed through the VCP were compared.
The institutional review board at VAPHS reviewed and approved this quality improvement study.
Statistical Analysis
For the 190 veterans who had a colonoscopy performed through VCP, a 1-sample Wilcoxon signed rank test was used with a null hypothesis that the median difference in days between first available VAPHS colonoscopy and community colonoscopy dates was 0. For the utilization sample of 350 veterans, an independent samples median test was used to compare the median wait times for colonoscopy procedures performed at the VA and those performed through VCP. IBM SPSS Version 25 was used for all statistical analysis.
Results
Of the 190 identified colonoscopies completed in the community utilizing VCP, scanned records could not be found for 29 procedures (15.3%) (Table). VCP procedures were performed a median 2 days earlier than the first available VAPHS procedure, but this difference was not statistically significant (P = .62) (Figure 2). Although 52% of colonoscopies occurred sooner through VCP than the initially scheduled VAPHS date, 44% were performed later, and there was wide variability in the difference between these dates, ranging from 49 days sooner to 165 days later.
Pathology results from VCP procedures for which tissue samples were obtained were absent in 11.9% (14 of 118) of procedures. There were no clear follow-up recommendations to referring VA health care providers in the 18% (29 of 161) of available procedure reports. In VCP procedures, documentation of selected quality metrics: bowel preparation, cecal withdrawal time, and rectal retroflexion, were deficient in 27.3%, 70.2%, and 32.9%, respectively (Figure 3).
The utilization dataset sample included 350 veterans who were offered a VCP colonoscopy because the first available VAPHS procedure could not be scheduled for > 30 days. Of these patients, 231 (66%) ultimately had their colonoscopy performed at VAPHS. An additional 26.6% of the patients in the utilization sample were lost in the scheduling process (ie, could not be contacted, cancelled and could not be rescheduled, or were a “no show” their scheduled VAPHS procedure). An unknown number of these patients may have had a procedure outside of the VA, but there are no records to confirm or exclude this possibility. Ultimately, there were only 26 (7.4%) confirmed VCP colonoscopy procedures within the utilization sample (Figure 4). The median actual wait time for colonoscopy was 61 days for VA procedures and 66 days for procedures referred through the VCP, which was not statistically significant (P = .15).
Discussion
This is the first study to evaluate the performance of the VCP for colonoscopy referrals. Consistent with recently reported data in other specialties, colonoscopy referrals through VCP did not lead to more timely procedures overall, although there was wide variation.8 The use of VCP for veteran referral to the community for colonoscopy led to fragmentation of care—with 15% of records for VCP colonoscopies unavailable in the VA EHR 6 months after the procedure. In addition, there were 45 pre- or postprocedure visits in the community, which is not standard practice at VAPHS, and therefore may add to the cost of care for veterans.
Documentation of selected colonoscopy quality metrics were deficient in 27.3% to 70.2% of available VCP procedure reports. Although many veterans were eligible for VCP referral for colonoscopy, only 7.4% had a documented procedure through VCP, and two-thirds of veterans eligible for VCP participation had their colonoscopy performed at the VAPHS, reflecting overall low utilization of the program.
The national average wait time for VCP referrals for multiple specialties was estimated to be 51 days in a 2018 Government Accountability Office (GAO) report, which is similar to our findings.9 The GAO report also concluded that the VCP does not have timeliness standards and notes missed opportunities to develop a mechanism for record transfer between the community and the VA. Our finding of missing colonoscopy procedure and pathology reports within the VA EHR is consistent with this claim. Our analysis revealed that widely accepted quality standards for colonoscopy, those that are required at the VA and monitored for quality assurance at the VAPHS, are not being consistently reported for veterans who undergo procedures in the community. Last, the overall low utilization rate, combined with overall similar wait times for colonoscopies referred through the VCP vs those done at the VA, should lead to reconsideration of offering community care referral to all veterans based solely on static wait time cutoffs.
Limitations
There are several limitations to our analysis. First, all data were extracted via chart review by one author; therefore, some scanned procedure or pathology reports or pre- and postprocedure records may have been missed. Second, these data are representative of a single VA medical center and may not reflect trends nationwide. Third, there are many factors that can influence veteran decision making regarding when and where colonoscopy procedures are performed, which could be related to the VCP community care referral process or independent of this. Finally, colonoscopies performed through the VCP are grouped and may not reflect variability in the performance of community practices that veterans were referred to though the VCP.
Adenoma detection rates (ADR) were not included in the assessment for 2 reasons. First, there was an insufficient number of screening colonoscopies to use for the ADR calculation. Second, a composite non-VA ADR of multiple community endoscopists in different practices would likely be inaccurate and not clinically meaningful. Of note, the VAPHS does calculate and maintain ADR information as a practice for its endoscopists.
Conclusions
Our findings are particularly important as the VA expands access to care in the community through the VA Mission Act, which replaces the VCP but continues to include a static wait time threshold of 28 days for referral to community-based care.10 Especially for colonoscopies with the indication of screening or surveillance, wait times > 28 days are likely not clinically significant. Additionally, this study demonstrates that there also are delays in access to colonoscopy by community-based care providers, and potentially reflects widespread colonoscopy access issues that are not unique to the VA.
Our findings are similar to other published results and reports and raise similar concerns about the pitfalls of veteran referral into the community, including (1) similar wait times for the community and the VA; (2) the risk of fragmented care; (3) unevenquality of care; and (4) low overall utilization of VCP for colonoscopy.11 We agree with the GAO’s recommendations, which include establishing clinically meaningful wait time thresholds, systemic monitoring of the timeliness of care, and additional mechanisms for seamless transfer of complete records of care into the VA system. If a referral is placed for community-based care, this should come with an expectation that the care will be offered and can be delivered sooner than would be possible at the VA. We additionally recommend that standards for reporting quality metrics, including ADR, also be required of community colonoscopy providers contracted to provide care for veterans through the VA Mission Act. Importantly, we recommend that data for comparative wait times and quality metrics for VA and the community should be publicly available for veterans so that they may make more informed choices about where they receive health care.
Acknowledgments
The authors thank Kaneen Allen, PhD, for her administrative assistance and guidance.
In April 2014, amid concerns for long wait times for care within the US Department of Veterans Affairs (VA) Veterans Health Administration (VHA), the Veterans Access, Choice, and Accountability Act was signed into law. This included the Veterans Choice Program (VCP), which included a provision for veterans to be referred outside of the VA to the community for care if their nearest VHA facility could not provide the requested care within 30 days of the clinically indicated date.1 Since implementation of the VCP, both media outlets and policy researchers have raised concerns about both the timeliness and quality of care provided through this program.2-4
Specifically for colonoscopy, referral outside of the VA in the pre-VCP era resulted in lower adenoma detection rate (ADR) and decreased adherence to surveillance guidelines when compared with matched VA control colonoscopies, raising concerns about quality assurance.5 Colorectal cancer (CRC) screening and timely colonoscopy is a VA priority; however, the performance of the VCP for colonoscopy timelines and quality has not been examined in detail.
Methods
We identified 3,855 veterans at the VA Pittsburgh Healthcare System (VAPHS) who were referred for colonoscopy in the community by using VCP from June 2015 through May 2017, using a query for colonoscopy procedure orders within the VA Corporate Data Warehouse. A total of 190 patients had a colonoscopy completed in the community by utilizing the VCP during this time frame.
At VAPHS, veterans who are referred for colonoscopy are contacted by a scheduler. The scheduler contacts the patient and offers the first available colonoscopy date at VAPHS and schedules the procedure for this date. However, if this date is > 30 days from the procedure order date, the scheduler gives the veteran the option of being contacted by VCP to schedule a colonoscopy within the community (Figure 1). We measured the time interval from the date of the initially scheduled first available colonoscopy at VAPHS to the date the colonoscopy was actually performed through VCP.
Quality assurance also was assessed by checking for the availability of records of colonoscopies performed through the VCP in the VA electronic health record (EHR) system. Colonoscopy procedure reports also were reviewed to assess for documentation of established colonoscopy quality metrics for examinations performed through the VCP. Additionally, we reviewed records scanned into the VA EHR pertaining to the VCP colonoscopy, including pathology information and pre- or postvisit records if available.
Data extraction was initiated in November 2017 to allow for at least 6 months of lead time for outside health records from the community to be received and scanned into the EHR for the veteran at VAPHS. For colonoscopy quality metrics, we chose 3 metrics that are universally documented for all colonoscopy procedures performed at VAPHS: quality of bowel preparation, cecal withdrawal time, and performance of retroflexion in the rectum. Documentation of these quality metrics is recommended in gastroenterology practice guidelinesand/or required by VA national policy.6,7
We separately reviewed a sample of 350 of the 3,855 patients referred for colonoscopy through VCP at VAPHS during the same time period to investigate overall VCP utilization. This sample was representative at a 95% CI with 5% margin of error of the total and sampled from 2 high-volume referral months (October and November 2015) and 3 low-volume months (January, February, and March 2017). Detailed data were collected regarding the colonoscopy scheduling and VCP referral process, including dates of colonoscopy procedure request; scheduling within the VAPHS; scheduling through the VCP; and ultimately if, when, and where (VAPHS vs community) a veteran had a colonoscopy performed. Wait times for colonoscopy procedures performed at the VAPHS and those performed through the VCP were compared.
The institutional review board at VAPHS reviewed and approved this quality improvement study.
Statistical Analysis
For the 190 veterans who had a colonoscopy performed through VCP, a 1-sample Wilcoxon signed rank test was used with a null hypothesis that the median difference in days between first available VAPHS colonoscopy and community colonoscopy dates was 0. For the utilization sample of 350 veterans, an independent samples median test was used to compare the median wait times for colonoscopy procedures performed at the VA and those performed through VCP. IBM SPSS Version 25 was used for all statistical analysis.
Results
Of the 190 identified colonoscopies completed in the community utilizing VCP, scanned records could not be found for 29 procedures (15.3%) (Table). VCP procedures were performed a median 2 days earlier than the first available VAPHS procedure, but this difference was not statistically significant (P = .62) (Figure 2). Although 52% of colonoscopies occurred sooner through VCP than the initially scheduled VAPHS date, 44% were performed later, and there was wide variability in the difference between these dates, ranging from 49 days sooner to 165 days later.
Pathology results from VCP procedures for which tissue samples were obtained were absent in 11.9% (14 of 118) of procedures. There were no clear follow-up recommendations to referring VA health care providers in the 18% (29 of 161) of available procedure reports. In VCP procedures, documentation of selected quality metrics: bowel preparation, cecal withdrawal time, and rectal retroflexion, were deficient in 27.3%, 70.2%, and 32.9%, respectively (Figure 3).
The utilization dataset sample included 350 veterans who were offered a VCP colonoscopy because the first available VAPHS procedure could not be scheduled for > 30 days. Of these patients, 231 (66%) ultimately had their colonoscopy performed at VAPHS. An additional 26.6% of the patients in the utilization sample were lost in the scheduling process (ie, could not be contacted, cancelled and could not be rescheduled, or were a “no show” their scheduled VAPHS procedure). An unknown number of these patients may have had a procedure outside of the VA, but there are no records to confirm or exclude this possibility. Ultimately, there were only 26 (7.4%) confirmed VCP colonoscopy procedures within the utilization sample (Figure 4). The median actual wait time for colonoscopy was 61 days for VA procedures and 66 days for procedures referred through the VCP, which was not statistically significant (P = .15).
Discussion
This is the first study to evaluate the performance of the VCP for colonoscopy referrals. Consistent with recently reported data in other specialties, colonoscopy referrals through VCP did not lead to more timely procedures overall, although there was wide variation.8 The use of VCP for veteran referral to the community for colonoscopy led to fragmentation of care—with 15% of records for VCP colonoscopies unavailable in the VA EHR 6 months after the procedure. In addition, there were 45 pre- or postprocedure visits in the community, which is not standard practice at VAPHS, and therefore may add to the cost of care for veterans.
Documentation of selected colonoscopy quality metrics were deficient in 27.3% to 70.2% of available VCP procedure reports. Although many veterans were eligible for VCP referral for colonoscopy, only 7.4% had a documented procedure through VCP, and two-thirds of veterans eligible for VCP participation had their colonoscopy performed at the VAPHS, reflecting overall low utilization of the program.
The national average wait time for VCP referrals for multiple specialties was estimated to be 51 days in a 2018 Government Accountability Office (GAO) report, which is similar to our findings.9 The GAO report also concluded that the VCP does not have timeliness standards and notes missed opportunities to develop a mechanism for record transfer between the community and the VA. Our finding of missing colonoscopy procedure and pathology reports within the VA EHR is consistent with this claim. Our analysis revealed that widely accepted quality standards for colonoscopy, those that are required at the VA and monitored for quality assurance at the VAPHS, are not being consistently reported for veterans who undergo procedures in the community. Last, the overall low utilization rate, combined with overall similar wait times for colonoscopies referred through the VCP vs those done at the VA, should lead to reconsideration of offering community care referral to all veterans based solely on static wait time cutoffs.
Limitations
There are several limitations to our analysis. First, all data were extracted via chart review by one author; therefore, some scanned procedure or pathology reports or pre- and postprocedure records may have been missed. Second, these data are representative of a single VA medical center and may not reflect trends nationwide. Third, there are many factors that can influence veteran decision making regarding when and where colonoscopy procedures are performed, which could be related to the VCP community care referral process or independent of this. Finally, colonoscopies performed through the VCP are grouped and may not reflect variability in the performance of community practices that veterans were referred to though the VCP.
Adenoma detection rates (ADR) were not included in the assessment for 2 reasons. First, there was an insufficient number of screening colonoscopies to use for the ADR calculation. Second, a composite non-VA ADR of multiple community endoscopists in different practices would likely be inaccurate and not clinically meaningful. Of note, the VAPHS does calculate and maintain ADR information as a practice for its endoscopists.
Conclusions
Our findings are particularly important as the VA expands access to care in the community through the VA Mission Act, which replaces the VCP but continues to include a static wait time threshold of 28 days for referral to community-based care.10 Especially for colonoscopies with the indication of screening or surveillance, wait times > 28 days are likely not clinically significant. Additionally, this study demonstrates that there also are delays in access to colonoscopy by community-based care providers, and potentially reflects widespread colonoscopy access issues that are not unique to the VA.
Our findings are similar to other published results and reports and raise similar concerns about the pitfalls of veteran referral into the community, including (1) similar wait times for the community and the VA; (2) the risk of fragmented care; (3) unevenquality of care; and (4) low overall utilization of VCP for colonoscopy.11 We agree with the GAO’s recommendations, which include establishing clinically meaningful wait time thresholds, systemic monitoring of the timeliness of care, and additional mechanisms for seamless transfer of complete records of care into the VA system. If a referral is placed for community-based care, this should come with an expectation that the care will be offered and can be delivered sooner than would be possible at the VA. We additionally recommend that standards for reporting quality metrics, including ADR, also be required of community colonoscopy providers contracted to provide care for veterans through the VA Mission Act. Importantly, we recommend that data for comparative wait times and quality metrics for VA and the community should be publicly available for veterans so that they may make more informed choices about where they receive health care.
Acknowledgments
The authors thank Kaneen Allen, PhD, for her administrative assistance and guidance.
1. Veterans Access, Choice, and Accountability Act of 2014. 42 USC §1395 (2014).
2. Farmer CM, Hosek SD. Did we improve veterans health care? It’s unclear. https://www.rand.org/blog/2016/05/did-we-improve-veterans-health-care-its-unclear.html. Published May 24, 2016. Accessed April 20, 2020.
3. Farmer CM, Hosek SD, Adamson DM. balancing demand and supply for veterans’ health care: a summary of three RAND assessments conducted under the Veterans Choice Act. Rand Health Q. 2016;6(1):12.
4. Mattocks KM, Mengeling M, Sadler A, Baldor R, Bastian L. The Veterans Choice Act: a qualitative examination of rapid policy implementation in the Department of Veterans Affairs. Med Care. 2017;55(suppl 7)(suppl 1):S71-S75.
5. Bartel MJ, Robertson DJ, Pohl H. Colonoscopy practice for veterans within and outside the Veterans Affairs setting: a matched cohort study. Gastrointest Endosc. 2016;84(2):272-278.
6. Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Am J Gastroenterol. 2015;110(1):72-90.
7. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1015, colorectal cancer screening. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3068.Published December 30, 2014. Accessed April 12, 2020.
8. Penn M, Bhatnagar S, Kuy S, et al. Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs medical centers. JAMA Netw Open. 2019;2(1):e187096.
9. US Government Accountability Office. Veterans Choice Program: improvements needed to address access-related challenges as VA plans consolidation of its community care programs. https://www.gao.gov/assets/700/692271.pdf. Published June 4, 2018. Accessed April 12, 2020.
10. VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018. 38 USC §1703 (2018).
11. Barnett PG, Hong JS, Carey E, Grunwald GK, Joynt Maddox K, Maddox TM. Comparison of accessibility, cost, and quality of elective coronary revascularization between Veterans Affairs and community care hospitals. JAMA Cardiol. 2018;3(2):133-141.
1. Veterans Access, Choice, and Accountability Act of 2014. 42 USC §1395 (2014).
2. Farmer CM, Hosek SD. Did we improve veterans health care? It’s unclear. https://www.rand.org/blog/2016/05/did-we-improve-veterans-health-care-its-unclear.html. Published May 24, 2016. Accessed April 20, 2020.
3. Farmer CM, Hosek SD, Adamson DM. balancing demand and supply for veterans’ health care: a summary of three RAND assessments conducted under the Veterans Choice Act. Rand Health Q. 2016;6(1):12.
4. Mattocks KM, Mengeling M, Sadler A, Baldor R, Bastian L. The Veterans Choice Act: a qualitative examination of rapid policy implementation in the Department of Veterans Affairs. Med Care. 2017;55(suppl 7)(suppl 1):S71-S75.
5. Bartel MJ, Robertson DJ, Pohl H. Colonoscopy practice for veterans within and outside the Veterans Affairs setting: a matched cohort study. Gastrointest Endosc. 2016;84(2):272-278.
6. Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Am J Gastroenterol. 2015;110(1):72-90.
7. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1015, colorectal cancer screening. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3068.Published December 30, 2014. Accessed April 12, 2020.
8. Penn M, Bhatnagar S, Kuy S, et al. Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs medical centers. JAMA Netw Open. 2019;2(1):e187096.
9. US Government Accountability Office. Veterans Choice Program: improvements needed to address access-related challenges as VA plans consolidation of its community care programs. https://www.gao.gov/assets/700/692271.pdf. Published June 4, 2018. Accessed April 12, 2020.
10. VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018. 38 USC §1703 (2018).
11. Barnett PG, Hong JS, Carey E, Grunwald GK, Joynt Maddox K, Maddox TM. Comparison of accessibility, cost, and quality of elective coronary revascularization between Veterans Affairs and community care hospitals. JAMA Cardiol. 2018;3(2):133-141.
Testicular Swelling as an Initial Presentation of a Patient With Metastatic Gastric Cancer (FULL)
Gastric cancer is one of the most common cancers and the second most common cause of cancer-related death worldwide.1 Patients with an early-stage gastric cancer are often asymptomatic, and about 30% to 40% of patients present with distant metastases.2 The most common sites of metastasis are the liver, peritoneum, and the lymph nodes. In more advanced stages, gastric cancers spread to the lungs, brain, bones, soft tissues, and other sites. Krukenberg tumors are classic but rare occurrences of gastric cancer metastasis to ovaries in females. In men, it is rare for gastric cancer to metastasize to the testes. Only a few cases of testicular metastasis from gastric cancer have been reported in the literature.3-5
Primary testicular neoplasms typically present with unilateral testicular swelling. In rare instances, testicular swelling can be an initial presentation of a metastatic cancer. In this article, we report a man who initially presented with right testicular swelling and was eventually diagnosed with a secondary testicular cancer from an aggressive metastatic gastric adenocarcinoma.
Case Presentation
A 43-year-old male presented to his primary care physician with a 6-month history of right testicular swelling and unintentional weight loss of 33 pounds. An ultrasound of the scrotum and the testes showed a 4.5-cm hypoechoic and predominantly cystic mass in the right testis. Serum levels of β-human chorionic gonadotropin, α-feto protein and lactate dehydrogenase were within normal limits.
A primary testicular neoplasm was suspected. The patient underwent a right-sided inguinal orchiectomy. The pathology of the resected testis revealed an intestinal type adenocarcinoma with mucinous and signet-ring cell features (Figure).
A staging Fluorine-18 fluorodeoxyglucose positron emission tomography scan revealed extensive hypermetabolic peritoneal nodules consistent with peritoneal carcinomatosis. The patient started palliative chemotherapy with 5-fluorouracil and oxaliplatin but rapidly declined with progressive abdominal symptoms after completion of 2 cycles. He discontinued chemotherapy and eventually opted for supportive care focusing on comfort.
Discussion
Testicular neoplasm is the most common solid tumor in men aged 20 to 34 years in the US.6 More than 90% of testicular neoplasms are germ-cell tumors and originate from the testes.6 Secondary neoplasms of the testes from solid tumors are rare. In an autopsy series, secondary neoplasms from solid tumors represented 4.6% of all testicular neoplasms.7 The reported frequencies of primary sites of origin vary based on the report. In a relatively large series, the most common solid tumors of origin were the prostate (35%) and lungs (20%).8 Among hematologic malignancies, lymphomas may originate from or secondarily involve the testes. Primary testicular lymphomas account for approximately 5% of testicular neoplasms and commonly occur in men aged > 60 years.9 Testicular involvement of acute myeloid or lymphoid leukemia may happen at diagnosis, but relapses of acute leukemia in a testicular site are more common and well recognized.10,11
Our report shows a rare occurrence of a testicular swelling as an initial presentation of an aggressive metastatic gastric adenocarcinoma. When a patient presents with a testicular swelling, a testicular neoplasm is suspected based on the clinical examination, serum tumor markers, and ultrasonographic examination of the testes. Inguinal orchiectomy is the initial standard of care, and pathologic examination of a resected testis renders the confirmatory diagnosis. The overwhelming majority of these patients have primary testicular neoplasms, predominantly testicular germ-cell tumors. A small group may have atypical and rare tumors requiring additional workup to establish a diagnosis.
Metastatic spread of a solid tumor to a testicular site is rare. A testis is somewhat protected by the distinct anatomy that is offered by the blood-testis barrier. The tunica vaginalis, an external fibrous covering sheath of the testis, separates the testis from the peritoneal cavity and provides additional protection. Nevertheless, possible routes of secondary metastatic spread may include hematogenous and lymphovascular spread, cavitary dissemination and peritoneal seeding. Among gastric cancers, diffuse gastric cancer subtype is commonly associated with signet-ring cells. These cells lack adhesion and invade as single cells or small groups, leading to scattered tumor cells and a higher probability of seeding.
Our patient exhibited extensive peritoneal carcinomatosis, so peritoneal seeding likely played a dominant role in disseminating the cancer to the testis. It should be noted that possible primary sites of signet-ring cell metastatic adenocarcinomas are broad and may include the stomach and other GI and pancreaticobiliary sites, as well as the lung, bladder, breast, and gynecologic tract. Immunohistochemistry is often of limited value in establishing the primary site. Diagnosis is best established on clinical grounds, as was done in our patient.
When signet-ring cells are encountered in an orchiectomy specimen and a primary extratesticular site of origin cannot be identified, it is important to consider rare variants of primary testicular tumors in the differential diagnosis. A number of primary testicular tumors have signetring morphology. These include primary signetring cell stromal tumor of the testis (PSRST),12 seminoma with signet-ring cell predominance,13 and a primary signet-ring cell germ-cell carcinoma of the testes (PSRGCT).14
Seminoma and PSRST variants generally are differentiated from adenocarcinoma by a lack of mucin production and the absence of keratin expression. PSRGCT is considered a
malignant somatic-type transformation of a testicular germ-cell tumor and germ-cell clonality is established by abnormal 12p chromosome through fluorescent in situ hybridization testing.13 PSRST is a benign tumor with excellent prognosis. Seminoma variants with signet-ring cell predominance and PSRGCT are managed as germ-cell tumors and are also considered to have good outcome. In contrast, testicular involvements from metastatic adenocarcinomas, including gastric cancers, are managed with multidisciplinary approach, including systemic chemotherapy. Despite this, patients have a poor outcome with a median survival of about 1 year.2
Conclusion
Advanced gastric adenocarcinoma can metastasize to the testes, and patients may present with a testicular swelling as an initial presentation. It is important to differentiate secondary testicular cancers from rare variants of primary testicular tumors because the prognosis and management vary substantially.
1. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Dicker D, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1(4):505-527.
2. Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet. 2016;388(10060):2654-2664.
3. Qazi HA, Manikandan R, Foster CS, Fordham MV. Testicular metastasis from gastric carcinoma. Urology. 2006;68(4):890.e7-e8.
4. Civelek B, Aksoy S, Kos T, et al. Isolated testicular metastasis of gastric cancer. J Gastrointest Canc. 2012;43(suppl 1):S64-S66.
5. Li B, Cai H, Kang ZC, et al. Testicular metastasis from gastric carcinoma: a case report. World J of Gastroenterol. 2015;21(21):6764-6768.
6. National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer stat facts: testicular cancer. https://seer.cancer.gov/statfacts/html/testis.html. Updated September 10, 2018. Accessed April 10, 2019.
7. Dutt N, Bates AW, Baithun SI. Secondary neoplasms of the male genital tract with different patterns of involvement in adults and children. Histopathology. 2000;37(4):323-331.
8. Haupt HM, Mann RB, Trump DL, Abeloff MD. Metastatic carcinoma involving the testis. Clinical and pathologic distinction from primary testicular neoplasms. Cancer.1984;54 (4):709-714.
9. Cheah CY, Wirth A, Seymour JF. Primary testicular lymphoma. Blood. 2014;123(4):486-493.
10. Kawamoto K, Miyoshi H, Yoshida N, Takizawa J, Sone H, Ohshima K. Clinicopathological, cytogenetic, and prognostic analysis of 131 myeloid sarcoma patients. Am J Surg Pathol. 2016;40(11):1473-1483.
11. Kulkarni KP, Marwaha RK, Trehan A, Bansal D. Testicular relapse in childhood acute lymphoblastic leukemia: the challenges and lessons. Indian J Cancer. 2010;47(2):134-138.
12. Kuo CY, Wen MC, Wang J, Jan YJ. Signet-ring stromal tumor of the testis: a case report and literature review. Hum Pathol. 2009;40(4):584-587.
13. Ulbright TM, Young RH. Seminoma with conspicuous signet ring cells: a rare, previously uncharacterized morphologic variant. Am J Surg Pathol. 2008;32(8):1175-1181.
14. Williamson SR, Kum JB, Shah SR, et al. Signet ring cell carcinoma of the testis: clinicopathologic and molecular evidence for germ cell tumor origin—a case report. Am J
Surg Pathol. 2012;36(2):311-315.
Gastric cancer is one of the most common cancers and the second most common cause of cancer-related death worldwide.1 Patients with an early-stage gastric cancer are often asymptomatic, and about 30% to 40% of patients present with distant metastases.2 The most common sites of metastasis are the liver, peritoneum, and the lymph nodes. In more advanced stages, gastric cancers spread to the lungs, brain, bones, soft tissues, and other sites. Krukenberg tumors are classic but rare occurrences of gastric cancer metastasis to ovaries in females. In men, it is rare for gastric cancer to metastasize to the testes. Only a few cases of testicular metastasis from gastric cancer have been reported in the literature.3-5
Primary testicular neoplasms typically present with unilateral testicular swelling. In rare instances, testicular swelling can be an initial presentation of a metastatic cancer. In this article, we report a man who initially presented with right testicular swelling and was eventually diagnosed with a secondary testicular cancer from an aggressive metastatic gastric adenocarcinoma.
Case Presentation
A 43-year-old male presented to his primary care physician with a 6-month history of right testicular swelling and unintentional weight loss of 33 pounds. An ultrasound of the scrotum and the testes showed a 4.5-cm hypoechoic and predominantly cystic mass in the right testis. Serum levels of β-human chorionic gonadotropin, α-feto protein and lactate dehydrogenase were within normal limits.
A primary testicular neoplasm was suspected. The patient underwent a right-sided inguinal orchiectomy. The pathology of the resected testis revealed an intestinal type adenocarcinoma with mucinous and signet-ring cell features (Figure).
A staging Fluorine-18 fluorodeoxyglucose positron emission tomography scan revealed extensive hypermetabolic peritoneal nodules consistent with peritoneal carcinomatosis. The patient started palliative chemotherapy with 5-fluorouracil and oxaliplatin but rapidly declined with progressive abdominal symptoms after completion of 2 cycles. He discontinued chemotherapy and eventually opted for supportive care focusing on comfort.
Discussion
Testicular neoplasm is the most common solid tumor in men aged 20 to 34 years in the US.6 More than 90% of testicular neoplasms are germ-cell tumors and originate from the testes.6 Secondary neoplasms of the testes from solid tumors are rare. In an autopsy series, secondary neoplasms from solid tumors represented 4.6% of all testicular neoplasms.7 The reported frequencies of primary sites of origin vary based on the report. In a relatively large series, the most common solid tumors of origin were the prostate (35%) and lungs (20%).8 Among hematologic malignancies, lymphomas may originate from or secondarily involve the testes. Primary testicular lymphomas account for approximately 5% of testicular neoplasms and commonly occur in men aged > 60 years.9 Testicular involvement of acute myeloid or lymphoid leukemia may happen at diagnosis, but relapses of acute leukemia in a testicular site are more common and well recognized.10,11
Our report shows a rare occurrence of a testicular swelling as an initial presentation of an aggressive metastatic gastric adenocarcinoma. When a patient presents with a testicular swelling, a testicular neoplasm is suspected based on the clinical examination, serum tumor markers, and ultrasonographic examination of the testes. Inguinal orchiectomy is the initial standard of care, and pathologic examination of a resected testis renders the confirmatory diagnosis. The overwhelming majority of these patients have primary testicular neoplasms, predominantly testicular germ-cell tumors. A small group may have atypical and rare tumors requiring additional workup to establish a diagnosis.
Metastatic spread of a solid tumor to a testicular site is rare. A testis is somewhat protected by the distinct anatomy that is offered by the blood-testis barrier. The tunica vaginalis, an external fibrous covering sheath of the testis, separates the testis from the peritoneal cavity and provides additional protection. Nevertheless, possible routes of secondary metastatic spread may include hematogenous and lymphovascular spread, cavitary dissemination and peritoneal seeding. Among gastric cancers, diffuse gastric cancer subtype is commonly associated with signet-ring cells. These cells lack adhesion and invade as single cells or small groups, leading to scattered tumor cells and a higher probability of seeding.
Our patient exhibited extensive peritoneal carcinomatosis, so peritoneal seeding likely played a dominant role in disseminating the cancer to the testis. It should be noted that possible primary sites of signet-ring cell metastatic adenocarcinomas are broad and may include the stomach and other GI and pancreaticobiliary sites, as well as the lung, bladder, breast, and gynecologic tract. Immunohistochemistry is often of limited value in establishing the primary site. Diagnosis is best established on clinical grounds, as was done in our patient.
When signet-ring cells are encountered in an orchiectomy specimen and a primary extratesticular site of origin cannot be identified, it is important to consider rare variants of primary testicular tumors in the differential diagnosis. A number of primary testicular tumors have signetring morphology. These include primary signetring cell stromal tumor of the testis (PSRST),12 seminoma with signet-ring cell predominance,13 and a primary signet-ring cell germ-cell carcinoma of the testes (PSRGCT).14
Seminoma and PSRST variants generally are differentiated from adenocarcinoma by a lack of mucin production and the absence of keratin expression. PSRGCT is considered a
malignant somatic-type transformation of a testicular germ-cell tumor and germ-cell clonality is established by abnormal 12p chromosome through fluorescent in situ hybridization testing.13 PSRST is a benign tumor with excellent prognosis. Seminoma variants with signet-ring cell predominance and PSRGCT are managed as germ-cell tumors and are also considered to have good outcome. In contrast, testicular involvements from metastatic adenocarcinomas, including gastric cancers, are managed with multidisciplinary approach, including systemic chemotherapy. Despite this, patients have a poor outcome with a median survival of about 1 year.2
Conclusion
Advanced gastric adenocarcinoma can metastasize to the testes, and patients may present with a testicular swelling as an initial presentation. It is important to differentiate secondary testicular cancers from rare variants of primary testicular tumors because the prognosis and management vary substantially.
Gastric cancer is one of the most common cancers and the second most common cause of cancer-related death worldwide.1 Patients with an early-stage gastric cancer are often asymptomatic, and about 30% to 40% of patients present with distant metastases.2 The most common sites of metastasis are the liver, peritoneum, and the lymph nodes. In more advanced stages, gastric cancers spread to the lungs, brain, bones, soft tissues, and other sites. Krukenberg tumors are classic but rare occurrences of gastric cancer metastasis to ovaries in females. In men, it is rare for gastric cancer to metastasize to the testes. Only a few cases of testicular metastasis from gastric cancer have been reported in the literature.3-5
Primary testicular neoplasms typically present with unilateral testicular swelling. In rare instances, testicular swelling can be an initial presentation of a metastatic cancer. In this article, we report a man who initially presented with right testicular swelling and was eventually diagnosed with a secondary testicular cancer from an aggressive metastatic gastric adenocarcinoma.
Case Presentation
A 43-year-old male presented to his primary care physician with a 6-month history of right testicular swelling and unintentional weight loss of 33 pounds. An ultrasound of the scrotum and the testes showed a 4.5-cm hypoechoic and predominantly cystic mass in the right testis. Serum levels of β-human chorionic gonadotropin, α-feto protein and lactate dehydrogenase were within normal limits.
A primary testicular neoplasm was suspected. The patient underwent a right-sided inguinal orchiectomy. The pathology of the resected testis revealed an intestinal type adenocarcinoma with mucinous and signet-ring cell features (Figure).
A staging Fluorine-18 fluorodeoxyglucose positron emission tomography scan revealed extensive hypermetabolic peritoneal nodules consistent with peritoneal carcinomatosis. The patient started palliative chemotherapy with 5-fluorouracil and oxaliplatin but rapidly declined with progressive abdominal symptoms after completion of 2 cycles. He discontinued chemotherapy and eventually opted for supportive care focusing on comfort.
Discussion
Testicular neoplasm is the most common solid tumor in men aged 20 to 34 years in the US.6 More than 90% of testicular neoplasms are germ-cell tumors and originate from the testes.6 Secondary neoplasms of the testes from solid tumors are rare. In an autopsy series, secondary neoplasms from solid tumors represented 4.6% of all testicular neoplasms.7 The reported frequencies of primary sites of origin vary based on the report. In a relatively large series, the most common solid tumors of origin were the prostate (35%) and lungs (20%).8 Among hematologic malignancies, lymphomas may originate from or secondarily involve the testes. Primary testicular lymphomas account for approximately 5% of testicular neoplasms and commonly occur in men aged > 60 years.9 Testicular involvement of acute myeloid or lymphoid leukemia may happen at diagnosis, but relapses of acute leukemia in a testicular site are more common and well recognized.10,11
Our report shows a rare occurrence of a testicular swelling as an initial presentation of an aggressive metastatic gastric adenocarcinoma. When a patient presents with a testicular swelling, a testicular neoplasm is suspected based on the clinical examination, serum tumor markers, and ultrasonographic examination of the testes. Inguinal orchiectomy is the initial standard of care, and pathologic examination of a resected testis renders the confirmatory diagnosis. The overwhelming majority of these patients have primary testicular neoplasms, predominantly testicular germ-cell tumors. A small group may have atypical and rare tumors requiring additional workup to establish a diagnosis.
Metastatic spread of a solid tumor to a testicular site is rare. A testis is somewhat protected by the distinct anatomy that is offered by the blood-testis barrier. The tunica vaginalis, an external fibrous covering sheath of the testis, separates the testis from the peritoneal cavity and provides additional protection. Nevertheless, possible routes of secondary metastatic spread may include hematogenous and lymphovascular spread, cavitary dissemination and peritoneal seeding. Among gastric cancers, diffuse gastric cancer subtype is commonly associated with signet-ring cells. These cells lack adhesion and invade as single cells or small groups, leading to scattered tumor cells and a higher probability of seeding.
Our patient exhibited extensive peritoneal carcinomatosis, so peritoneal seeding likely played a dominant role in disseminating the cancer to the testis. It should be noted that possible primary sites of signet-ring cell metastatic adenocarcinomas are broad and may include the stomach and other GI and pancreaticobiliary sites, as well as the lung, bladder, breast, and gynecologic tract. Immunohistochemistry is often of limited value in establishing the primary site. Diagnosis is best established on clinical grounds, as was done in our patient.
When signet-ring cells are encountered in an orchiectomy specimen and a primary extratesticular site of origin cannot be identified, it is important to consider rare variants of primary testicular tumors in the differential diagnosis. A number of primary testicular tumors have signetring morphology. These include primary signetring cell stromal tumor of the testis (PSRST),12 seminoma with signet-ring cell predominance,13 and a primary signet-ring cell germ-cell carcinoma of the testes (PSRGCT).14
Seminoma and PSRST variants generally are differentiated from adenocarcinoma by a lack of mucin production and the absence of keratin expression. PSRGCT is considered a
malignant somatic-type transformation of a testicular germ-cell tumor and germ-cell clonality is established by abnormal 12p chromosome through fluorescent in situ hybridization testing.13 PSRST is a benign tumor with excellent prognosis. Seminoma variants with signet-ring cell predominance and PSRGCT are managed as germ-cell tumors and are also considered to have good outcome. In contrast, testicular involvements from metastatic adenocarcinomas, including gastric cancers, are managed with multidisciplinary approach, including systemic chemotherapy. Despite this, patients have a poor outcome with a median survival of about 1 year.2
Conclusion
Advanced gastric adenocarcinoma can metastasize to the testes, and patients may present with a testicular swelling as an initial presentation. It is important to differentiate secondary testicular cancers from rare variants of primary testicular tumors because the prognosis and management vary substantially.
1. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Dicker D, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1(4):505-527.
2. Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet. 2016;388(10060):2654-2664.
3. Qazi HA, Manikandan R, Foster CS, Fordham MV. Testicular metastasis from gastric carcinoma. Urology. 2006;68(4):890.e7-e8.
4. Civelek B, Aksoy S, Kos T, et al. Isolated testicular metastasis of gastric cancer. J Gastrointest Canc. 2012;43(suppl 1):S64-S66.
5. Li B, Cai H, Kang ZC, et al. Testicular metastasis from gastric carcinoma: a case report. World J of Gastroenterol. 2015;21(21):6764-6768.
6. National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer stat facts: testicular cancer. https://seer.cancer.gov/statfacts/html/testis.html. Updated September 10, 2018. Accessed April 10, 2019.
7. Dutt N, Bates AW, Baithun SI. Secondary neoplasms of the male genital tract with different patterns of involvement in adults and children. Histopathology. 2000;37(4):323-331.
8. Haupt HM, Mann RB, Trump DL, Abeloff MD. Metastatic carcinoma involving the testis. Clinical and pathologic distinction from primary testicular neoplasms. Cancer.1984;54 (4):709-714.
9. Cheah CY, Wirth A, Seymour JF. Primary testicular lymphoma. Blood. 2014;123(4):486-493.
10. Kawamoto K, Miyoshi H, Yoshida N, Takizawa J, Sone H, Ohshima K. Clinicopathological, cytogenetic, and prognostic analysis of 131 myeloid sarcoma patients. Am J Surg Pathol. 2016;40(11):1473-1483.
11. Kulkarni KP, Marwaha RK, Trehan A, Bansal D. Testicular relapse in childhood acute lymphoblastic leukemia: the challenges and lessons. Indian J Cancer. 2010;47(2):134-138.
12. Kuo CY, Wen MC, Wang J, Jan YJ. Signet-ring stromal tumor of the testis: a case report and literature review. Hum Pathol. 2009;40(4):584-587.
13. Ulbright TM, Young RH. Seminoma with conspicuous signet ring cells: a rare, previously uncharacterized morphologic variant. Am J Surg Pathol. 2008;32(8):1175-1181.
14. Williamson SR, Kum JB, Shah SR, et al. Signet ring cell carcinoma of the testis: clinicopathologic and molecular evidence for germ cell tumor origin—a case report. Am J
Surg Pathol. 2012;36(2):311-315.
1. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Dicker D, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1(4):505-527.
2. Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet. 2016;388(10060):2654-2664.
3. Qazi HA, Manikandan R, Foster CS, Fordham MV. Testicular metastasis from gastric carcinoma. Urology. 2006;68(4):890.e7-e8.
4. Civelek B, Aksoy S, Kos T, et al. Isolated testicular metastasis of gastric cancer. J Gastrointest Canc. 2012;43(suppl 1):S64-S66.
5. Li B, Cai H, Kang ZC, et al. Testicular metastasis from gastric carcinoma: a case report. World J of Gastroenterol. 2015;21(21):6764-6768.
6. National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer stat facts: testicular cancer. https://seer.cancer.gov/statfacts/html/testis.html. Updated September 10, 2018. Accessed April 10, 2019.
7. Dutt N, Bates AW, Baithun SI. Secondary neoplasms of the male genital tract with different patterns of involvement in adults and children. Histopathology. 2000;37(4):323-331.
8. Haupt HM, Mann RB, Trump DL, Abeloff MD. Metastatic carcinoma involving the testis. Clinical and pathologic distinction from primary testicular neoplasms. Cancer.1984;54 (4):709-714.
9. Cheah CY, Wirth A, Seymour JF. Primary testicular lymphoma. Blood. 2014;123(4):486-493.
10. Kawamoto K, Miyoshi H, Yoshida N, Takizawa J, Sone H, Ohshima K. Clinicopathological, cytogenetic, and prognostic analysis of 131 myeloid sarcoma patients. Am J Surg Pathol. 2016;40(11):1473-1483.
11. Kulkarni KP, Marwaha RK, Trehan A, Bansal D. Testicular relapse in childhood acute lymphoblastic leukemia: the challenges and lessons. Indian J Cancer. 2010;47(2):134-138.
12. Kuo CY, Wen MC, Wang J, Jan YJ. Signet-ring stromal tumor of the testis: a case report and literature review. Hum Pathol. 2009;40(4):584-587.
13. Ulbright TM, Young RH. Seminoma with conspicuous signet ring cells: a rare, previously uncharacterized morphologic variant. Am J Surg Pathol. 2008;32(8):1175-1181.
14. Williamson SR, Kum JB, Shah SR, et al. Signet ring cell carcinoma of the testis: clinicopathologic and molecular evidence for germ cell tumor origin—a case report. Am J
Surg Pathol. 2012;36(2):311-315.
Cardiovascular Effects of Tyrosine Kinase Inhibitors in Patients With Advanced Renal Cell Carcinoma at the VA San Diego Healthcare System (FULL)
Patients who have or are at high risk for developing cardiovascular disease and who are taking tyrosine kinase inhibitors for renal cell carcinoma should receive routine cardiovascular event monitoring during the first 4 months of therapy.
Targeted therapies have transformed the treatment of many malignant diseases by inhibiting molecular pathways involved in tumor growth and oncogenesis. Although these therapies can prevent disease progression, toxicities often result. Renal cell carcinoma (RCC) is one of many cancers that responds well to these therapies.
RCC accounts for 2% to 3% of all malignancies in adults worldwide. About 30% of patients with RCC present with metastatic or advanced disease.1 Cytokine therapy was the standard of care until multitargeted tyrosine kinase inhibitors (TKIs) were developed. Over the past 12 years, the US Food and Drug Administration (FDA) has approved 6 TKIs for the treatment of RCC: axitinib, cabozantinib, lenvatinib, pazopanib, sorafenib, and sunitinib. Vascular endothelial growth factor receptor (VEGFR) is one of many tyrosine kinase receptors targeted by these medications. This mechanism prevents angiogenesis and consequently increases the risk for hypertension, bleeding, and clot formation.
Given these risks, many patients were excluded from the initial clinical trials of these medications if they had a history of uncontrolled hypertension, advanced heart failure (HF), or a significant cardiovascular (CV) event within 6 months prior to study enrollment. Many of these studies did not report the incidence of CV events (other than hypertension) that occurred during the early trials.2 The recommended monitoring for TKI therapies is focused mainly on blood pressure. For patients on pazopanib and sunitinib therapy, baseline and periodic electrocardiograms (ECGs) are recommended; echocardiograms are recommended only for patients with a history of cardiac disease.3,4 In patients on sorafenib therapy, ECG is recommended for those at risk for corrected QT (QTc) intervalprolongation.5
According to a meta-analysis of the literature published between 1966 and 2013,many studies reported a CV toxicity risk associated with the TKIs used in RCC treatment.6 However, some studies have found modest, not clinically significant changes in cardiac function in patients with advanced disease. In 2013, Hall and colleagues found 73% of patients they studied experienced some type of CV toxicity, whereas only 33% of patients had CV toxicity when hypertension was excluded.7 Interestingly, Rini and colleagues found that RCC patients receiving sunitinib had better response rates and progression-free survival when they developed hypertension compared with those who did not develop hypertension.8
A review of several studies revealed similar numbers in patients on TKI therapy presenting with symptomatic HF, but Hall and colleagues found that 27% of patients developed asymptomatic left ventricular dysfunction.7,9,10 These results suggest routine monitoring may allow for appropriate preventive interventions. In patients receiving TKI therapy, CV events, including QTc prolongation, left ventricular HF, myocardial infarction (MI), hypertension, pulmonary hypertension, and stroke, were commonly reported by investigators.7,9,10 Currently, there are no studies of the incidence of CV events for the 5 TKIs (axitinib, cabozantinib, pazopanib, sorafenib, sunitinib) in this patient population.
TKI therapy may require cardiac monitoring of all patients, as studies have associated TKIs with CV toxicity in varying degrees. Therefore, the authors set out to determine the incidence of CV events as well as time to first CV event in patients with and without a history of CV disease (CVD) who received a TKI for advanced RCC. More frequent monitoring for CV toxicity may present opportunities for clinical interventions for all patients on TKI therapy—especially for those with HF or other diseases in which the goal of therapy is to prevent disease progression. As TKIs have emerged as the standard treatment option for advanced RCC, many patients will continue therapy until disease progression or intolerable toxicity. Identifying and using appropriate monitoring parameters can lead to preventive interventions that allow patients to benefit from TKI therapy longer. At the US Department of Veterans Affairs (VA) San Diego Healthcare System (VASDHS), patients undergo routine cardiac monitoring at the discretion of the provider.
In this retrospective study, the authors wanted to determine the incidence of CV events in patients with and without a history of CVD who were receiving TKIs for advanced RCC. The authors also wanted to evaluate time to CV event from start of therapy in order to determine how often monitoring may be needed. The outcomes of this study may lead to a change in practice and development of monitoring parameters to ensure appropriate and adequate management of TKI therapy in RCC.
Methods
Each year, the VASDHS oncology team diagnose 5 to 10 patients with RCC who begin TKI therapy. When sorafenib was approved by the FDA in 2005, VASDHS estimated that about 100 of its patients had an RCC diagnosis and would be treated with a TKI between December 2005 and July 2017.
The authors identified VASDHS patients with a diagnosis of advanced RCC who received axitinib, cabozantinib, pazopanib, sorafenib, or sunitinib between December 1, 2005 and July 31, 2017. Patients were included if they had been on therapy for at least 30 days. The VASDHS pharmacy informatics team assisted in extracting a list of patients with an ICD-9 or ICD-10 diagnosis of RCC and using prescription fills for any of the 5 TKIs previously noted. Medical records were reviewed for frequency of prescription fills, age, sex, Eastern Cooperative Oncology Group (ECOG) performance status, TKI treatment duration, previous history of CVD, ethnicity, and smoking status. If documented, the incidence of CV events was reviewed for each patient at 0, 1, 3, 6, and 12 months. Patients who received medications (Appendix) for their CVD were assessed for adherence based on history of prescription refills from their medical records. Adherence was evaluated for the duration that patients were concurrently taking an oral TKI. The institutional review board at VASDHS approved the study design.
All patients included in this study started TKI therapy since the December 2005 FDA approval of sorafenib, the first oral TKI for treatment of RCC. Each new start was recorded as a separate event, regardless of previous oral TKI therapy. Albiges and colleagues found that the approximate median time from starting TKI therapy to complete response was 12.6 months, and the median duration of TKI therapy after complete response was 10.3 months.11 Based on these results, the follow-up period for patients in this study was 2 years after the start of each TKI therapy. For data analysis, patients were stratified by CVD history (yes or no). In addition, composite outcomes were evaluated to identify a potential cumulative increased risk for CV events for patients who had been on multiple TKI therapies.
For this study, CV toxicities were characterized using Common Terminology Criteria for Adverse Events (CTCAE) version 4.03; severity of adverse events (AEs) was graded 1 to 5. CTCAE commonly has been used to assess AEs in oncology clinical trials. The CV AEs selected for this study included QTc prolongation, hypertension, left ventricular dysfunction, stroke, myocardial infarction (MI), and pulmonary arterial hypertension.
Primary outcomes included incidence of CV events and time to first CV event after initiation of TKI therapy. Secondary outcomes included changes in ECG or echocardiogram results at 0, 1, 3, 6, and 12 months. Secondary outcomes at scheduled time points were not readily available for every patient, but any available time points were gathered to aid in identifying an optimal period for cardiac monitoring. In addition, patients with a history of CVD were evaluated for adherence to common first-line therapies for each disease.
A Fischer exact test was used to compare the incidence of CV events in patients with and without a history of CVD (significance level, α = 0.05). A subgroup analysis was used to compare the incidence of CV events in patients who experienced a CV event (significance level, α = 0.05). A Kaplan-Meier survival curve was used to determine time to first CV event. A log-rank test with significance level set at α = 0.05 also was used.
Results
An initial database search identified 134 patients who received TKI therapy at VASDHS between December 1, 2005 and July 31, 2017. According to retrospective chart review, 54 patients met the inclusion criteria for the study (Table 1).
Patients without a history of CVD (17%) did not experience any CV events while on TKI therapy. Of the patients with a history of CVD, 9 (20%) experienced ≥ 1 CV event. Fifty-five percent of the events experienced were hypertension. One patient experienced QTc prolongation, and 2 patients experienced MI. As already noted, each new start of TKI was recorded as a separate event, regardless of previous TKI therapy. Among patients with a history of CVD, 2 experienced 2 CV events. Overall, 11 CV events occurred among patients who received ≥ 1 TKI, corresponding to an overall incidence of 24% (Table 2). 
Of the 13 patients who were exposed to ≥ 2 TKI therapies, 2 experienced a CV event. Both patients were started on sunitinib and were switched to sorafenib. One of these used sunitinib for 7 months, experienced a partial response and was switched to sorafenib (with a 3-month break between therapies). The second patient was on sunitinib for 24 months, with multiple doses held because of low blood counts and diarrhea. While on sunitinib, this patient experienced a HF exacerbation, determined to be caused by the underlying disease. This event occurred 17 months after sunitinib was started, and therapy was continued for another 7 months. The patient was switched to sorafenib because of poor tolerability and disease progression. While on sorafenib, this patient experienced grade 1 QTc prolongation.
Discussion
Of the available oral TKI therapies for RCC, sunitinib and sorafenib have the most data associated with nonhypertensive CV toxicity.2,7-10,12 Instudies, the percentage of patients who experienced CV toxicity while on sunitinib or sorafenib has ranged widely, from 2.7% to 33.8%; the variance may be attributable to differences in how institutions report CV toxicities.7-9
According to the prescribing information for TKIs, hypertension is frequently reported as an AE for all 5 TKIs, and BP monitoring is recommended.3,4 However, the development of hypertension with these TKIs has been associated with response to therapy.7 With pazopanib, sorafenib, and sunitinib, there is a higher incidence of other AEs: edema, HF, MI, and QTc prolongation. Baseline ECG is recommended for all patients started on pazopanib and sunitinib and for patients with a history of CVD who are started on sorafenib. An ECG is recommended for patients with a history of CVD who are started on pazopanib and sunitinib.
Even with the medication prescribing information recommendations, it is unclear how frequently patients should be monitored. At VASDHS, CV monitoring for any patient started on a TKI remains at the discretion of the oncologist. There are concerns that ordering cardiac monitoring tests, which might be unnecessary, will change or guide therapy. In this study, data evaluation revealed 1 patient who experienced a CV event had a CVD history that was not documented in the patient’s medical history. It is important that providers obtain a detailed clinical assessment of patients CV history during each visit to determine whether CV monitoring should be considered. Patients also may benefit from additional counseling to emphasize the importance of adherence to CV medication therapy to reduce the incidence of these events.
Data from this study indicate that routine CV monitoring should be considered in patients with CVD, in keeping with current medication prescribing information recommendations. Of the patients who had a CV event, 54% experienced hypertension, 18% MI, and 28% stroke, QTc prolongation, or congestive HF.
Limitations
This retrospective study had several limitations. Many patients did not have a baseline cardiac monitoring test or any monitoring during therapy. Often, a cardiac test was performed only when the patient was symptomatic or experiencing a CV event. In addition, because of intolerance or nonadherence to therapy, many patients discontinued treatment early, before completing 30 days. That axitinib and cabozantinib are newer therapies and not first-line at VASDHS during the data collection period accounts for the small number of patients on these therapies. Therapy was shorter for patients started on pazopanib, axitinib, and cabozantinib than it was for patients on sunitinib and sorafenib. Duration of therapy may affect treatment-related events, but the majority of patients in this study experienced an event within 4 months of therapy. About half of the patients who experienced an event were nonadherent to their CV medication regimen. Another potential limitation is that this study was conducted at VASDHS, where most patients are male (RCC incidence is 2:1 male:female).
Conclusion
In this study, CV events occurred in 24% of patients with a history of CVD; 11% of these events were nonhypertensive. Baseline cardiac monitoring was not performed for most patients started on TKI therapy, but tests were performed once patients became symptomatic. The study results suggest that high-risk patients should undergo routine cardiac monitoring during the first 4 months of TKI therapy, in keeping with medication package insert monitoring recommendations. Cardiac monitoring of high-risk patients will allow for earlier identification of cardiac decline and offer opportunities for interventions, such as pharmacist-driven protocols to start CV medications. Implementation of this study’s recommendations should be evaluated to determine whether outcomes improve with routine cardiac monitoring in these high-risk patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, FrontlineMedical Communications Inc., the US Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects— before administering pharmacologic therapy to patients.
1. Rini, BI, Escudier B, Tomczak P, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2011;378(9807):1931-1939.
2. Tolcher AW, Appleman LJ, Shapiro GI, et al. A phase I open-label study evaluating the cardiovascular safety of sorafenib in patients with advanced cancer. Cancer Chemother Pharmacol. 2011;67(4):751-764.
3. Votrient [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2017.
4. Sutent [package insert]. New York, NY: Pfizer Labs; 2018.
5. Nexavar [package insert]. Wayne, NJ; Bayer HealthCare Pharmaceuticals Inc; 2018.
6. Ghatalia P, Morgan CJ, Je Y, et al. Congestive heart failure with vascular endothelial growth factor receptor tyrosine kinase inhibitors. Crit Rev Oncol Hematol 2015;94:228–237.
7. Hall PS, Harshman LC, Srinivas S, Witteles RM. The frequency and severity of cardiovascular toxicity from targeted therapy in advanced renal cell carcinoma patients. JACC Heart Fail. 2013;1(1):72-78.
8. Rini BI, Cohen DP, Lu DR, et al. Hypertension as a biomarker of efficacy in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst. 2011;103(9):763-773.
9. Richards CJ, Je Y, Schutz FA, et al. Incidence and risk of congestive heart failure in patients with renal and nonrenal cell carcinoma treated with sunitinib. J Clin Oncol. 2011;29(25):3450-3456.
10. Schmidinger M, Zielinski CC, Vogl UM, et al. Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2008;26(32):5204-5212.
11. Albiges L, Oudard S, Negrier S, et al. Complete remission with tyrosine kinase inhibitors in renal cell carcinoma. J Clin Oncol. 2012;30(5):482-487.
12. Jang S, Zheng C, Tsai HT, et al. Cardiovascular toxicity after antiangiogenic therapy in persons older than 65 years with advanced renal cell carcinoma. Cancer. 2016;122(1):124-130
13. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
14. Yancy CW, Jessup M, Bozkurt B, et al. ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. JACC. 2017;70(6):776-803.
15. Kernan WN, Ovbiagele B, Black HR, et al; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160-2236.
16. O’Gara PT, Kushner FG, Ascheim DD, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. JACC. 2013;61(4):e78-e140.
17. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228.
18. Galiè N, Humbert M, Vachiery JL, et al; ESC Scientific Document Group. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119.
Patients who have or are at high risk for developing cardiovascular disease and who are taking tyrosine kinase inhibitors for renal cell carcinoma should receive routine cardiovascular event monitoring during the first 4 months of therapy.
Patients who have or are at high risk for developing cardiovascular disease and who are taking tyrosine kinase inhibitors for renal cell carcinoma should receive routine cardiovascular event monitoring during the first 4 months of therapy.
Targeted therapies have transformed the treatment of many malignant diseases by inhibiting molecular pathways involved in tumor growth and oncogenesis. Although these therapies can prevent disease progression, toxicities often result. Renal cell carcinoma (RCC) is one of many cancers that responds well to these therapies.
RCC accounts for 2% to 3% of all malignancies in adults worldwide. About 30% of patients with RCC present with metastatic or advanced disease.1 Cytokine therapy was the standard of care until multitargeted tyrosine kinase inhibitors (TKIs) were developed. Over the past 12 years, the US Food and Drug Administration (FDA) has approved 6 TKIs for the treatment of RCC: axitinib, cabozantinib, lenvatinib, pazopanib, sorafenib, and sunitinib. Vascular endothelial growth factor receptor (VEGFR) is one of many tyrosine kinase receptors targeted by these medications. This mechanism prevents angiogenesis and consequently increases the risk for hypertension, bleeding, and clot formation.
Given these risks, many patients were excluded from the initial clinical trials of these medications if they had a history of uncontrolled hypertension, advanced heart failure (HF), or a significant cardiovascular (CV) event within 6 months prior to study enrollment. Many of these studies did not report the incidence of CV events (other than hypertension) that occurred during the early trials.2 The recommended monitoring for TKI therapies is focused mainly on blood pressure. For patients on pazopanib and sunitinib therapy, baseline and periodic electrocardiograms (ECGs) are recommended; echocardiograms are recommended only for patients with a history of cardiac disease.3,4 In patients on sorafenib therapy, ECG is recommended for those at risk for corrected QT (QTc) intervalprolongation.5
According to a meta-analysis of the literature published between 1966 and 2013,many studies reported a CV toxicity risk associated with the TKIs used in RCC treatment.6 However, some studies have found modest, not clinically significant changes in cardiac function in patients with advanced disease. In 2013, Hall and colleagues found 73% of patients they studied experienced some type of CV toxicity, whereas only 33% of patients had CV toxicity when hypertension was excluded.7 Interestingly, Rini and colleagues found that RCC patients receiving sunitinib had better response rates and progression-free survival when they developed hypertension compared with those who did not develop hypertension.8
A review of several studies revealed similar numbers in patients on TKI therapy presenting with symptomatic HF, but Hall and colleagues found that 27% of patients developed asymptomatic left ventricular dysfunction.7,9,10 These results suggest routine monitoring may allow for appropriate preventive interventions. In patients receiving TKI therapy, CV events, including QTc prolongation, left ventricular HF, myocardial infarction (MI), hypertension, pulmonary hypertension, and stroke, were commonly reported by investigators.7,9,10 Currently, there are no studies of the incidence of CV events for the 5 TKIs (axitinib, cabozantinib, pazopanib, sorafenib, sunitinib) in this patient population.
TKI therapy may require cardiac monitoring of all patients, as studies have associated TKIs with CV toxicity in varying degrees. Therefore, the authors set out to determine the incidence of CV events as well as time to first CV event in patients with and without a history of CV disease (CVD) who received a TKI for advanced RCC. More frequent monitoring for CV toxicity may present opportunities for clinical interventions for all patients on TKI therapy—especially for those with HF or other diseases in which the goal of therapy is to prevent disease progression. As TKIs have emerged as the standard treatment option for advanced RCC, many patients will continue therapy until disease progression or intolerable toxicity. Identifying and using appropriate monitoring parameters can lead to preventive interventions that allow patients to benefit from TKI therapy longer. At the US Department of Veterans Affairs (VA) San Diego Healthcare System (VASDHS), patients undergo routine cardiac monitoring at the discretion of the provider.
In this retrospective study, the authors wanted to determine the incidence of CV events in patients with and without a history of CVD who were receiving TKIs for advanced RCC. The authors also wanted to evaluate time to CV event from start of therapy in order to determine how often monitoring may be needed. The outcomes of this study may lead to a change in practice and development of monitoring parameters to ensure appropriate and adequate management of TKI therapy in RCC.
Methods
Each year, the VASDHS oncology team diagnose 5 to 10 patients with RCC who begin TKI therapy. When sorafenib was approved by the FDA in 2005, VASDHS estimated that about 100 of its patients had an RCC diagnosis and would be treated with a TKI between December 2005 and July 2017.
The authors identified VASDHS patients with a diagnosis of advanced RCC who received axitinib, cabozantinib, pazopanib, sorafenib, or sunitinib between December 1, 2005 and July 31, 2017. Patients were included if they had been on therapy for at least 30 days. The VASDHS pharmacy informatics team assisted in extracting a list of patients with an ICD-9 or ICD-10 diagnosis of RCC and using prescription fills for any of the 5 TKIs previously noted. Medical records were reviewed for frequency of prescription fills, age, sex, Eastern Cooperative Oncology Group (ECOG) performance status, TKI treatment duration, previous history of CVD, ethnicity, and smoking status. If documented, the incidence of CV events was reviewed for each patient at 0, 1, 3, 6, and 12 months. Patients who received medications (Appendix) for their CVD were assessed for adherence based on history of prescription refills from their medical records. Adherence was evaluated for the duration that patients were concurrently taking an oral TKI. The institutional review board at VASDHS approved the study design.
All patients included in this study started TKI therapy since the December 2005 FDA approval of sorafenib, the first oral TKI for treatment of RCC. Each new start was recorded as a separate event, regardless of previous oral TKI therapy. Albiges and colleagues found that the approximate median time from starting TKI therapy to complete response was 12.6 months, and the median duration of TKI therapy after complete response was 10.3 months.11 Based on these results, the follow-up period for patients in this study was 2 years after the start of each TKI therapy. For data analysis, patients were stratified by CVD history (yes or no). In addition, composite outcomes were evaluated to identify a potential cumulative increased risk for CV events for patients who had been on multiple TKI therapies.
For this study, CV toxicities were characterized using Common Terminology Criteria for Adverse Events (CTCAE) version 4.03; severity of adverse events (AEs) was graded 1 to 5. CTCAE commonly has been used to assess AEs in oncology clinical trials. The CV AEs selected for this study included QTc prolongation, hypertension, left ventricular dysfunction, stroke, myocardial infarction (MI), and pulmonary arterial hypertension.
Primary outcomes included incidence of CV events and time to first CV event after initiation of TKI therapy. Secondary outcomes included changes in ECG or echocardiogram results at 0, 1, 3, 6, and 12 months. Secondary outcomes at scheduled time points were not readily available for every patient, but any available time points were gathered to aid in identifying an optimal period for cardiac monitoring. In addition, patients with a history of CVD were evaluated for adherence to common first-line therapies for each disease.
A Fischer exact test was used to compare the incidence of CV events in patients with and without a history of CVD (significance level, α = 0.05). A subgroup analysis was used to compare the incidence of CV events in patients who experienced a CV event (significance level, α = 0.05). A Kaplan-Meier survival curve was used to determine time to first CV event. A log-rank test with significance level set at α = 0.05 also was used.
Results
An initial database search identified 134 patients who received TKI therapy at VASDHS between December 1, 2005 and July 31, 2017. According to retrospective chart review, 54 patients met the inclusion criteria for the study (Table 1).
Patients without a history of CVD (17%) did not experience any CV events while on TKI therapy. Of the patients with a history of CVD, 9 (20%) experienced ≥ 1 CV event. Fifty-five percent of the events experienced were hypertension. One patient experienced QTc prolongation, and 2 patients experienced MI. As already noted, each new start of TKI was recorded as a separate event, regardless of previous TKI therapy. Among patients with a history of CVD, 2 experienced 2 CV events. Overall, 11 CV events occurred among patients who received ≥ 1 TKI, corresponding to an overall incidence of 24% (Table 2). 
Of the 13 patients who were exposed to ≥ 2 TKI therapies, 2 experienced a CV event. Both patients were started on sunitinib and were switched to sorafenib. One of these used sunitinib for 7 months, experienced a partial response and was switched to sorafenib (with a 3-month break between therapies). The second patient was on sunitinib for 24 months, with multiple doses held because of low blood counts and diarrhea. While on sunitinib, this patient experienced a HF exacerbation, determined to be caused by the underlying disease. This event occurred 17 months after sunitinib was started, and therapy was continued for another 7 months. The patient was switched to sorafenib because of poor tolerability and disease progression. While on sorafenib, this patient experienced grade 1 QTc prolongation.
Discussion
Of the available oral TKI therapies for RCC, sunitinib and sorafenib have the most data associated with nonhypertensive CV toxicity.2,7-10,12 Instudies, the percentage of patients who experienced CV toxicity while on sunitinib or sorafenib has ranged widely, from 2.7% to 33.8%; the variance may be attributable to differences in how institutions report CV toxicities.7-9
According to the prescribing information for TKIs, hypertension is frequently reported as an AE for all 5 TKIs, and BP monitoring is recommended.3,4 However, the development of hypertension with these TKIs has been associated with response to therapy.7 With pazopanib, sorafenib, and sunitinib, there is a higher incidence of other AEs: edema, HF, MI, and QTc prolongation. Baseline ECG is recommended for all patients started on pazopanib and sunitinib and for patients with a history of CVD who are started on sorafenib. An ECG is recommended for patients with a history of CVD who are started on pazopanib and sunitinib.
Even with the medication prescribing information recommendations, it is unclear how frequently patients should be monitored. At VASDHS, CV monitoring for any patient started on a TKI remains at the discretion of the oncologist. There are concerns that ordering cardiac monitoring tests, which might be unnecessary, will change or guide therapy. In this study, data evaluation revealed 1 patient who experienced a CV event had a CVD history that was not documented in the patient’s medical history. It is important that providers obtain a detailed clinical assessment of patients CV history during each visit to determine whether CV monitoring should be considered. Patients also may benefit from additional counseling to emphasize the importance of adherence to CV medication therapy to reduce the incidence of these events.
Data from this study indicate that routine CV monitoring should be considered in patients with CVD, in keeping with current medication prescribing information recommendations. Of the patients who had a CV event, 54% experienced hypertension, 18% MI, and 28% stroke, QTc prolongation, or congestive HF.
Limitations
This retrospective study had several limitations. Many patients did not have a baseline cardiac monitoring test or any monitoring during therapy. Often, a cardiac test was performed only when the patient was symptomatic or experiencing a CV event. In addition, because of intolerance or nonadherence to therapy, many patients discontinued treatment early, before completing 30 days. That axitinib and cabozantinib are newer therapies and not first-line at VASDHS during the data collection period accounts for the small number of patients on these therapies. Therapy was shorter for patients started on pazopanib, axitinib, and cabozantinib than it was for patients on sunitinib and sorafenib. Duration of therapy may affect treatment-related events, but the majority of patients in this study experienced an event within 4 months of therapy. About half of the patients who experienced an event were nonadherent to their CV medication regimen. Another potential limitation is that this study was conducted at VASDHS, where most patients are male (RCC incidence is 2:1 male:female).
Conclusion
In this study, CV events occurred in 24% of patients with a history of CVD; 11% of these events were nonhypertensive. Baseline cardiac monitoring was not performed for most patients started on TKI therapy, but tests were performed once patients became symptomatic. The study results suggest that high-risk patients should undergo routine cardiac monitoring during the first 4 months of TKI therapy, in keeping with medication package insert monitoring recommendations. Cardiac monitoring of high-risk patients will allow for earlier identification of cardiac decline and offer opportunities for interventions, such as pharmacist-driven protocols to start CV medications. Implementation of this study’s recommendations should be evaluated to determine whether outcomes improve with routine cardiac monitoring in these high-risk patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, FrontlineMedical Communications Inc., the US Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects— before administering pharmacologic therapy to patients.
Targeted therapies have transformed the treatment of many malignant diseases by inhibiting molecular pathways involved in tumor growth and oncogenesis. Although these therapies can prevent disease progression, toxicities often result. Renal cell carcinoma (RCC) is one of many cancers that responds well to these therapies.
RCC accounts for 2% to 3% of all malignancies in adults worldwide. About 30% of patients with RCC present with metastatic or advanced disease.1 Cytokine therapy was the standard of care until multitargeted tyrosine kinase inhibitors (TKIs) were developed. Over the past 12 years, the US Food and Drug Administration (FDA) has approved 6 TKIs for the treatment of RCC: axitinib, cabozantinib, lenvatinib, pazopanib, sorafenib, and sunitinib. Vascular endothelial growth factor receptor (VEGFR) is one of many tyrosine kinase receptors targeted by these medications. This mechanism prevents angiogenesis and consequently increases the risk for hypertension, bleeding, and clot formation.
Given these risks, many patients were excluded from the initial clinical trials of these medications if they had a history of uncontrolled hypertension, advanced heart failure (HF), or a significant cardiovascular (CV) event within 6 months prior to study enrollment. Many of these studies did not report the incidence of CV events (other than hypertension) that occurred during the early trials.2 The recommended monitoring for TKI therapies is focused mainly on blood pressure. For patients on pazopanib and sunitinib therapy, baseline and periodic electrocardiograms (ECGs) are recommended; echocardiograms are recommended only for patients with a history of cardiac disease.3,4 In patients on sorafenib therapy, ECG is recommended for those at risk for corrected QT (QTc) intervalprolongation.5
According to a meta-analysis of the literature published between 1966 and 2013,many studies reported a CV toxicity risk associated with the TKIs used in RCC treatment.6 However, some studies have found modest, not clinically significant changes in cardiac function in patients with advanced disease. In 2013, Hall and colleagues found 73% of patients they studied experienced some type of CV toxicity, whereas only 33% of patients had CV toxicity when hypertension was excluded.7 Interestingly, Rini and colleagues found that RCC patients receiving sunitinib had better response rates and progression-free survival when they developed hypertension compared with those who did not develop hypertension.8
A review of several studies revealed similar numbers in patients on TKI therapy presenting with symptomatic HF, but Hall and colleagues found that 27% of patients developed asymptomatic left ventricular dysfunction.7,9,10 These results suggest routine monitoring may allow for appropriate preventive interventions. In patients receiving TKI therapy, CV events, including QTc prolongation, left ventricular HF, myocardial infarction (MI), hypertension, pulmonary hypertension, and stroke, were commonly reported by investigators.7,9,10 Currently, there are no studies of the incidence of CV events for the 5 TKIs (axitinib, cabozantinib, pazopanib, sorafenib, sunitinib) in this patient population.
TKI therapy may require cardiac monitoring of all patients, as studies have associated TKIs with CV toxicity in varying degrees. Therefore, the authors set out to determine the incidence of CV events as well as time to first CV event in patients with and without a history of CV disease (CVD) who received a TKI for advanced RCC. More frequent monitoring for CV toxicity may present opportunities for clinical interventions for all patients on TKI therapy—especially for those with HF or other diseases in which the goal of therapy is to prevent disease progression. As TKIs have emerged as the standard treatment option for advanced RCC, many patients will continue therapy until disease progression or intolerable toxicity. Identifying and using appropriate monitoring parameters can lead to preventive interventions that allow patients to benefit from TKI therapy longer. At the US Department of Veterans Affairs (VA) San Diego Healthcare System (VASDHS), patients undergo routine cardiac monitoring at the discretion of the provider.
In this retrospective study, the authors wanted to determine the incidence of CV events in patients with and without a history of CVD who were receiving TKIs for advanced RCC. The authors also wanted to evaluate time to CV event from start of therapy in order to determine how often monitoring may be needed. The outcomes of this study may lead to a change in practice and development of monitoring parameters to ensure appropriate and adequate management of TKI therapy in RCC.
Methods
Each year, the VASDHS oncology team diagnose 5 to 10 patients with RCC who begin TKI therapy. When sorafenib was approved by the FDA in 2005, VASDHS estimated that about 100 of its patients had an RCC diagnosis and would be treated with a TKI between December 2005 and July 2017.
The authors identified VASDHS patients with a diagnosis of advanced RCC who received axitinib, cabozantinib, pazopanib, sorafenib, or sunitinib between December 1, 2005 and July 31, 2017. Patients were included if they had been on therapy for at least 30 days. The VASDHS pharmacy informatics team assisted in extracting a list of patients with an ICD-9 or ICD-10 diagnosis of RCC and using prescription fills for any of the 5 TKIs previously noted. Medical records were reviewed for frequency of prescription fills, age, sex, Eastern Cooperative Oncology Group (ECOG) performance status, TKI treatment duration, previous history of CVD, ethnicity, and smoking status. If documented, the incidence of CV events was reviewed for each patient at 0, 1, 3, 6, and 12 months. Patients who received medications (Appendix) for their CVD were assessed for adherence based on history of prescription refills from their medical records. Adherence was evaluated for the duration that patients were concurrently taking an oral TKI. The institutional review board at VASDHS approved the study design.
All patients included in this study started TKI therapy since the December 2005 FDA approval of sorafenib, the first oral TKI for treatment of RCC. Each new start was recorded as a separate event, regardless of previous oral TKI therapy. Albiges and colleagues found that the approximate median time from starting TKI therapy to complete response was 12.6 months, and the median duration of TKI therapy after complete response was 10.3 months.11 Based on these results, the follow-up period for patients in this study was 2 years after the start of each TKI therapy. For data analysis, patients were stratified by CVD history (yes or no). In addition, composite outcomes were evaluated to identify a potential cumulative increased risk for CV events for patients who had been on multiple TKI therapies.
For this study, CV toxicities were characterized using Common Terminology Criteria for Adverse Events (CTCAE) version 4.03; severity of adverse events (AEs) was graded 1 to 5. CTCAE commonly has been used to assess AEs in oncology clinical trials. The CV AEs selected for this study included QTc prolongation, hypertension, left ventricular dysfunction, stroke, myocardial infarction (MI), and pulmonary arterial hypertension.
Primary outcomes included incidence of CV events and time to first CV event after initiation of TKI therapy. Secondary outcomes included changes in ECG or echocardiogram results at 0, 1, 3, 6, and 12 months. Secondary outcomes at scheduled time points were not readily available for every patient, but any available time points were gathered to aid in identifying an optimal period for cardiac monitoring. In addition, patients with a history of CVD were evaluated for adherence to common first-line therapies for each disease.
A Fischer exact test was used to compare the incidence of CV events in patients with and without a history of CVD (significance level, α = 0.05). A subgroup analysis was used to compare the incidence of CV events in patients who experienced a CV event (significance level, α = 0.05). A Kaplan-Meier survival curve was used to determine time to first CV event. A log-rank test with significance level set at α = 0.05 also was used.
Results
An initial database search identified 134 patients who received TKI therapy at VASDHS between December 1, 2005 and July 31, 2017. According to retrospective chart review, 54 patients met the inclusion criteria for the study (Table 1).
Patients without a history of CVD (17%) did not experience any CV events while on TKI therapy. Of the patients with a history of CVD, 9 (20%) experienced ≥ 1 CV event. Fifty-five percent of the events experienced were hypertension. One patient experienced QTc prolongation, and 2 patients experienced MI. As already noted, each new start of TKI was recorded as a separate event, regardless of previous TKI therapy. Among patients with a history of CVD, 2 experienced 2 CV events. Overall, 11 CV events occurred among patients who received ≥ 1 TKI, corresponding to an overall incidence of 24% (Table 2). 
Of the 13 patients who were exposed to ≥ 2 TKI therapies, 2 experienced a CV event. Both patients were started on sunitinib and were switched to sorafenib. One of these used sunitinib for 7 months, experienced a partial response and was switched to sorafenib (with a 3-month break between therapies). The second patient was on sunitinib for 24 months, with multiple doses held because of low blood counts and diarrhea. While on sunitinib, this patient experienced a HF exacerbation, determined to be caused by the underlying disease. This event occurred 17 months after sunitinib was started, and therapy was continued for another 7 months. The patient was switched to sorafenib because of poor tolerability and disease progression. While on sorafenib, this patient experienced grade 1 QTc prolongation.
Discussion
Of the available oral TKI therapies for RCC, sunitinib and sorafenib have the most data associated with nonhypertensive CV toxicity.2,7-10,12 Instudies, the percentage of patients who experienced CV toxicity while on sunitinib or sorafenib has ranged widely, from 2.7% to 33.8%; the variance may be attributable to differences in how institutions report CV toxicities.7-9
According to the prescribing information for TKIs, hypertension is frequently reported as an AE for all 5 TKIs, and BP monitoring is recommended.3,4 However, the development of hypertension with these TKIs has been associated with response to therapy.7 With pazopanib, sorafenib, and sunitinib, there is a higher incidence of other AEs: edema, HF, MI, and QTc prolongation. Baseline ECG is recommended for all patients started on pazopanib and sunitinib and for patients with a history of CVD who are started on sorafenib. An ECG is recommended for patients with a history of CVD who are started on pazopanib and sunitinib.
Even with the medication prescribing information recommendations, it is unclear how frequently patients should be monitored. At VASDHS, CV monitoring for any patient started on a TKI remains at the discretion of the oncologist. There are concerns that ordering cardiac monitoring tests, which might be unnecessary, will change or guide therapy. In this study, data evaluation revealed 1 patient who experienced a CV event had a CVD history that was not documented in the patient’s medical history. It is important that providers obtain a detailed clinical assessment of patients CV history during each visit to determine whether CV monitoring should be considered. Patients also may benefit from additional counseling to emphasize the importance of adherence to CV medication therapy to reduce the incidence of these events.
Data from this study indicate that routine CV monitoring should be considered in patients with CVD, in keeping with current medication prescribing information recommendations. Of the patients who had a CV event, 54% experienced hypertension, 18% MI, and 28% stroke, QTc prolongation, or congestive HF.
Limitations
This retrospective study had several limitations. Many patients did not have a baseline cardiac monitoring test or any monitoring during therapy. Often, a cardiac test was performed only when the patient was symptomatic or experiencing a CV event. In addition, because of intolerance or nonadherence to therapy, many patients discontinued treatment early, before completing 30 days. That axitinib and cabozantinib are newer therapies and not first-line at VASDHS during the data collection period accounts for the small number of patients on these therapies. Therapy was shorter for patients started on pazopanib, axitinib, and cabozantinib than it was for patients on sunitinib and sorafenib. Duration of therapy may affect treatment-related events, but the majority of patients in this study experienced an event within 4 months of therapy. About half of the patients who experienced an event were nonadherent to their CV medication regimen. Another potential limitation is that this study was conducted at VASDHS, where most patients are male (RCC incidence is 2:1 male:female).
Conclusion
In this study, CV events occurred in 24% of patients with a history of CVD; 11% of these events were nonhypertensive. Baseline cardiac monitoring was not performed for most patients started on TKI therapy, but tests were performed once patients became symptomatic. The study results suggest that high-risk patients should undergo routine cardiac monitoring during the first 4 months of TKI therapy, in keeping with medication package insert monitoring recommendations. Cardiac monitoring of high-risk patients will allow for earlier identification of cardiac decline and offer opportunities for interventions, such as pharmacist-driven protocols to start CV medications. Implementation of this study’s recommendations should be evaluated to determine whether outcomes improve with routine cardiac monitoring in these high-risk patients.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, FrontlineMedical Communications Inc., the US Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects— before administering pharmacologic therapy to patients.
1. Rini, BI, Escudier B, Tomczak P, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2011;378(9807):1931-1939.
2. Tolcher AW, Appleman LJ, Shapiro GI, et al. A phase I open-label study evaluating the cardiovascular safety of sorafenib in patients with advanced cancer. Cancer Chemother Pharmacol. 2011;67(4):751-764.
3. Votrient [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2017.
4. Sutent [package insert]. New York, NY: Pfizer Labs; 2018.
5. Nexavar [package insert]. Wayne, NJ; Bayer HealthCare Pharmaceuticals Inc; 2018.
6. Ghatalia P, Morgan CJ, Je Y, et al. Congestive heart failure with vascular endothelial growth factor receptor tyrosine kinase inhibitors. Crit Rev Oncol Hematol 2015;94:228–237.
7. Hall PS, Harshman LC, Srinivas S, Witteles RM. The frequency and severity of cardiovascular toxicity from targeted therapy in advanced renal cell carcinoma patients. JACC Heart Fail. 2013;1(1):72-78.
8. Rini BI, Cohen DP, Lu DR, et al. Hypertension as a biomarker of efficacy in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst. 2011;103(9):763-773.
9. Richards CJ, Je Y, Schutz FA, et al. Incidence and risk of congestive heart failure in patients with renal and nonrenal cell carcinoma treated with sunitinib. J Clin Oncol. 2011;29(25):3450-3456.
10. Schmidinger M, Zielinski CC, Vogl UM, et al. Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2008;26(32):5204-5212.
11. Albiges L, Oudard S, Negrier S, et al. Complete remission with tyrosine kinase inhibitors in renal cell carcinoma. J Clin Oncol. 2012;30(5):482-487.
12. Jang S, Zheng C, Tsai HT, et al. Cardiovascular toxicity after antiangiogenic therapy in persons older than 65 years with advanced renal cell carcinoma. Cancer. 2016;122(1):124-130
13. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
14. Yancy CW, Jessup M, Bozkurt B, et al. ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. JACC. 2017;70(6):776-803.
15. Kernan WN, Ovbiagele B, Black HR, et al; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160-2236.
16. O’Gara PT, Kushner FG, Ascheim DD, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. JACC. 2013;61(4):e78-e140.
17. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228.
18. Galiè N, Humbert M, Vachiery JL, et al; ESC Scientific Document Group. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119.
1. Rini, BI, Escudier B, Tomczak P, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2011;378(9807):1931-1939.
2. Tolcher AW, Appleman LJ, Shapiro GI, et al. A phase I open-label study evaluating the cardiovascular safety of sorafenib in patients with advanced cancer. Cancer Chemother Pharmacol. 2011;67(4):751-764.
3. Votrient [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2017.
4. Sutent [package insert]. New York, NY: Pfizer Labs; 2018.
5. Nexavar [package insert]. Wayne, NJ; Bayer HealthCare Pharmaceuticals Inc; 2018.
6. Ghatalia P, Morgan CJ, Je Y, et al. Congestive heart failure with vascular endothelial growth factor receptor tyrosine kinase inhibitors. Crit Rev Oncol Hematol 2015;94:228–237.
7. Hall PS, Harshman LC, Srinivas S, Witteles RM. The frequency and severity of cardiovascular toxicity from targeted therapy in advanced renal cell carcinoma patients. JACC Heart Fail. 2013;1(1):72-78.
8. Rini BI, Cohen DP, Lu DR, et al. Hypertension as a biomarker of efficacy in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst. 2011;103(9):763-773.
9. Richards CJ, Je Y, Schutz FA, et al. Incidence and risk of congestive heart failure in patients with renal and nonrenal cell carcinoma treated with sunitinib. J Clin Oncol. 2011;29(25):3450-3456.
10. Schmidinger M, Zielinski CC, Vogl UM, et al. Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2008;26(32):5204-5212.
11. Albiges L, Oudard S, Negrier S, et al. Complete remission with tyrosine kinase inhibitors in renal cell carcinoma. J Clin Oncol. 2012;30(5):482-487.
12. Jang S, Zheng C, Tsai HT, et al. Cardiovascular toxicity after antiangiogenic therapy in persons older than 65 years with advanced renal cell carcinoma. Cancer. 2016;122(1):124-130
13. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
14. Yancy CW, Jessup M, Bozkurt B, et al. ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. JACC. 2017;70(6):776-803.
15. Kernan WN, Ovbiagele B, Black HR, et al; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160-2236.
16. O’Gara PT, Kushner FG, Ascheim DD, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. JACC. 2013;61(4):e78-e140.
17. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228.
18. Galiè N, Humbert M, Vachiery JL, et al; ESC Scientific Document Group. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119.
Treating rectal cancer in the COVID-19 era: Expert guidance
As the COVID-19 pandemic continues, minimizing risks of infection to patients with cancer while maintaining good outcomes remains a priority. An international panel of experts has now issued recommendations for treating patients with rectal cancer, which includes using a short pre-operative course of radiotherapy (SCRT) and then delaying surgery.
Using SCRT translates to fewer hospital appointments, which will keep patients safer and allow them to maintain social distancing. The panel also found that surgery can be safely delayed by up to 12 weeks, and thus will allow procedures to be rescheduled after the pandemic peaks.
“The COVID-19 pandemic is a global emergency and we needed to work very quickly to identify changes that would benefit patients,” said David Sebag-Montefiore, MD, a professor of clinical oncology at the University of Leeds and honorary clinical oncologist with the Leeds Teaching Hospitals NHS Trust, who led the 15 member panel. “Our recommendations were published 20 days after our first meeting.”
“This process normally takes many months, if not years,” he said in a statement.
The recommendations were published online April 2 in Radiotherapy and Oncology.
The panel used the European Society for Medical Oncology (ESMO) rectal cancer guidelines as a framework to describe these new recommendations.
Recommendations by Stage
The recommendations were categorized into four subgroups based on cancer stage.
Early stage
- The ESMO guidelines recommend total mesorectal excision (TME) surgery without pre-operative radiotherapy for most cases.
- Panel recommendation also strongly supports the use of TME without pre-operative radiotherapy.
Intermediate stage
- The ESMO guidelines recommend TME alone or combined with SCRT or conventional radiotherapy (CRT) if there is uncertainty that a good quality mesorectal excision can be achieved.
- The panel strongly recommends TME alone in regions where high quality surgery is performed. The use of radiotherapy in this subgroup requires careful discussion, as the benefits of preoperative radiotherapy are likely to be small. If radiotherapy is used, then the preferred option should be SCRT.
Locally advanced
- The ESMO guideline recommends either pre-operative SCRT or CRT.
- The panel strongly recommends the use of SCRT and notes two phase 3 trials have compared SCRT and CRT and showed comparable outcomes for local recurrence, disease-free survival, overall survival, and late toxicity. In the COVID-19 setting, the panel points out that SCRT has many advantages over CRT, namely that there is less acute toxicity, fewer treatments which translate to less travel and contact with other patients and staff, and a significantly reduced risk of COVID-19 infection during treatment.
Timing of surgery after SCRT
- The ESMO guideline does not have any recommendations as they were issued before the Stockholm III trial (Lancet Oncol. 2017;18:336-46).
- The panel notes that the use of SCRT and delaying surgery has advantages that can be beneficial in both routine clinical practice and the COVID-19 setting. Several clinical trials have recommended that surgery should be performed within 3-7 days of completing radiotherapy, but the Stockholm III trial reported no difference in outcomes when surgery was delayed. It compared surgery performed within 1 week versus 4-8 weeks following SCRT and there was no difference in any survival endpoints. In addition, a longer delay to surgery was associated with a reduction in post-operative and surgical morbidity although no differences in severe complications or re-operations.
Advanced subgroup
- The ESMO guidelines recommend the use of pre-operative CRT or SCRT followed by neoadjuvant chemotherapy. CRT should be given as a fluoropyrimidine (usually capecitabine) combined with radiotherapy of 45-50.4 Gy over 5-5.5 weeks. Adjuvant chemotherapy should be considered but there is wide international variation in its use.
- The panel recommends that two options be considered based on the current evidence. The first is pre-op CRT, which is the most established standard of care, with the duration of concurrent capecitabine chemotherapy limited to 5-5.5 weeks. The second option is SCRT with or without neoadjuvant chemotherapy. In this case, the duration of radiotherapy is substantially less and has advantages versus CRT. “We consider both options to be acceptable but note the advantages of using SCRT in the COVID-19 setting,” the authors write. “The decision to use neoadjuvant chemotherapy in option 2 will reflect the attitudes to neoadjuvant and adjuvant chemotherapy in each country, the assessment of the risk-benefit ratio, considering the risk factors for COVID-19 increased mortality, and the capacity and prioritization of chemotherapy delivery.”
Organ Preservation
Organ preservation is being increasingly considered when a complete clinical response is achieved after CRT or SCRT, the panel points out. “An organ preservation approach may be considered during the COVID-19 period providing that resources for an adequate surveillance including imaging and endoscopy are available to detect local failures that require salvage surgery,” they write.
This article first appeared on Medscape.com.
As the COVID-19 pandemic continues, minimizing risks of infection to patients with cancer while maintaining good outcomes remains a priority. An international panel of experts has now issued recommendations for treating patients with rectal cancer, which includes using a short pre-operative course of radiotherapy (SCRT) and then delaying surgery.
Using SCRT translates to fewer hospital appointments, which will keep patients safer and allow them to maintain social distancing. The panel also found that surgery can be safely delayed by up to 12 weeks, and thus will allow procedures to be rescheduled after the pandemic peaks.
“The COVID-19 pandemic is a global emergency and we needed to work very quickly to identify changes that would benefit patients,” said David Sebag-Montefiore, MD, a professor of clinical oncology at the University of Leeds and honorary clinical oncologist with the Leeds Teaching Hospitals NHS Trust, who led the 15 member panel. “Our recommendations were published 20 days after our first meeting.”
“This process normally takes many months, if not years,” he said in a statement.
The recommendations were published online April 2 in Radiotherapy and Oncology.
The panel used the European Society for Medical Oncology (ESMO) rectal cancer guidelines as a framework to describe these new recommendations.
Recommendations by Stage
The recommendations were categorized into four subgroups based on cancer stage.
Early stage
- The ESMO guidelines recommend total mesorectal excision (TME) surgery without pre-operative radiotherapy for most cases.
- Panel recommendation also strongly supports the use of TME without pre-operative radiotherapy.
Intermediate stage
- The ESMO guidelines recommend TME alone or combined with SCRT or conventional radiotherapy (CRT) if there is uncertainty that a good quality mesorectal excision can be achieved.
- The panel strongly recommends TME alone in regions where high quality surgery is performed. The use of radiotherapy in this subgroup requires careful discussion, as the benefits of preoperative radiotherapy are likely to be small. If radiotherapy is used, then the preferred option should be SCRT.
Locally advanced
- The ESMO guideline recommends either pre-operative SCRT or CRT.
- The panel strongly recommends the use of SCRT and notes two phase 3 trials have compared SCRT and CRT and showed comparable outcomes for local recurrence, disease-free survival, overall survival, and late toxicity. In the COVID-19 setting, the panel points out that SCRT has many advantages over CRT, namely that there is less acute toxicity, fewer treatments which translate to less travel and contact with other patients and staff, and a significantly reduced risk of COVID-19 infection during treatment.
Timing of surgery after SCRT
- The ESMO guideline does not have any recommendations as they were issued before the Stockholm III trial (Lancet Oncol. 2017;18:336-46).
- The panel notes that the use of SCRT and delaying surgery has advantages that can be beneficial in both routine clinical practice and the COVID-19 setting. Several clinical trials have recommended that surgery should be performed within 3-7 days of completing radiotherapy, but the Stockholm III trial reported no difference in outcomes when surgery was delayed. It compared surgery performed within 1 week versus 4-8 weeks following SCRT and there was no difference in any survival endpoints. In addition, a longer delay to surgery was associated with a reduction in post-operative and surgical morbidity although no differences in severe complications or re-operations.
Advanced subgroup
- The ESMO guidelines recommend the use of pre-operative CRT or SCRT followed by neoadjuvant chemotherapy. CRT should be given as a fluoropyrimidine (usually capecitabine) combined with radiotherapy of 45-50.4 Gy over 5-5.5 weeks. Adjuvant chemotherapy should be considered but there is wide international variation in its use.
- The panel recommends that two options be considered based on the current evidence. The first is pre-op CRT, which is the most established standard of care, with the duration of concurrent capecitabine chemotherapy limited to 5-5.5 weeks. The second option is SCRT with or without neoadjuvant chemotherapy. In this case, the duration of radiotherapy is substantially less and has advantages versus CRT. “We consider both options to be acceptable but note the advantages of using SCRT in the COVID-19 setting,” the authors write. “The decision to use neoadjuvant chemotherapy in option 2 will reflect the attitudes to neoadjuvant and adjuvant chemotherapy in each country, the assessment of the risk-benefit ratio, considering the risk factors for COVID-19 increased mortality, and the capacity and prioritization of chemotherapy delivery.”
Organ Preservation
Organ preservation is being increasingly considered when a complete clinical response is achieved after CRT or SCRT, the panel points out. “An organ preservation approach may be considered during the COVID-19 period providing that resources for an adequate surveillance including imaging and endoscopy are available to detect local failures that require salvage surgery,” they write.
This article first appeared on Medscape.com.
As the COVID-19 pandemic continues, minimizing risks of infection to patients with cancer while maintaining good outcomes remains a priority. An international panel of experts has now issued recommendations for treating patients with rectal cancer, which includes using a short pre-operative course of radiotherapy (SCRT) and then delaying surgery.
Using SCRT translates to fewer hospital appointments, which will keep patients safer and allow them to maintain social distancing. The panel also found that surgery can be safely delayed by up to 12 weeks, and thus will allow procedures to be rescheduled after the pandemic peaks.
“The COVID-19 pandemic is a global emergency and we needed to work very quickly to identify changes that would benefit patients,” said David Sebag-Montefiore, MD, a professor of clinical oncology at the University of Leeds and honorary clinical oncologist with the Leeds Teaching Hospitals NHS Trust, who led the 15 member panel. “Our recommendations were published 20 days after our first meeting.”
“This process normally takes many months, if not years,” he said in a statement.
The recommendations were published online April 2 in Radiotherapy and Oncology.
The panel used the European Society for Medical Oncology (ESMO) rectal cancer guidelines as a framework to describe these new recommendations.
Recommendations by Stage
The recommendations were categorized into four subgroups based on cancer stage.
Early stage
- The ESMO guidelines recommend total mesorectal excision (TME) surgery without pre-operative radiotherapy for most cases.
- Panel recommendation also strongly supports the use of TME without pre-operative radiotherapy.
Intermediate stage
- The ESMO guidelines recommend TME alone or combined with SCRT or conventional radiotherapy (CRT) if there is uncertainty that a good quality mesorectal excision can be achieved.
- The panel strongly recommends TME alone in regions where high quality surgery is performed. The use of radiotherapy in this subgroup requires careful discussion, as the benefits of preoperative radiotherapy are likely to be small. If radiotherapy is used, then the preferred option should be SCRT.
Locally advanced
- The ESMO guideline recommends either pre-operative SCRT or CRT.
- The panel strongly recommends the use of SCRT and notes two phase 3 trials have compared SCRT and CRT and showed comparable outcomes for local recurrence, disease-free survival, overall survival, and late toxicity. In the COVID-19 setting, the panel points out that SCRT has many advantages over CRT, namely that there is less acute toxicity, fewer treatments which translate to less travel and contact with other patients and staff, and a significantly reduced risk of COVID-19 infection during treatment.
Timing of surgery after SCRT
- The ESMO guideline does not have any recommendations as they were issued before the Stockholm III trial (Lancet Oncol. 2017;18:336-46).
- The panel notes that the use of SCRT and delaying surgery has advantages that can be beneficial in both routine clinical practice and the COVID-19 setting. Several clinical trials have recommended that surgery should be performed within 3-7 days of completing radiotherapy, but the Stockholm III trial reported no difference in outcomes when surgery was delayed. It compared surgery performed within 1 week versus 4-8 weeks following SCRT and there was no difference in any survival endpoints. In addition, a longer delay to surgery was associated with a reduction in post-operative and surgical morbidity although no differences in severe complications or re-operations.
Advanced subgroup
- The ESMO guidelines recommend the use of pre-operative CRT or SCRT followed by neoadjuvant chemotherapy. CRT should be given as a fluoropyrimidine (usually capecitabine) combined with radiotherapy of 45-50.4 Gy over 5-5.5 weeks. Adjuvant chemotherapy should be considered but there is wide international variation in its use.
- The panel recommends that two options be considered based on the current evidence. The first is pre-op CRT, which is the most established standard of care, with the duration of concurrent capecitabine chemotherapy limited to 5-5.5 weeks. The second option is SCRT with or without neoadjuvant chemotherapy. In this case, the duration of radiotherapy is substantially less and has advantages versus CRT. “We consider both options to be acceptable but note the advantages of using SCRT in the COVID-19 setting,” the authors write. “The decision to use neoadjuvant chemotherapy in option 2 will reflect the attitudes to neoadjuvant and adjuvant chemotherapy in each country, the assessment of the risk-benefit ratio, considering the risk factors for COVID-19 increased mortality, and the capacity and prioritization of chemotherapy delivery.”
Organ Preservation
Organ preservation is being increasingly considered when a complete clinical response is achieved after CRT or SCRT, the panel points out. “An organ preservation approach may be considered during the COVID-19 period providing that resources for an adequate surveillance including imaging and endoscopy are available to detect local failures that require salvage surgery,” they write.
This article first appeared on Medscape.com.
Colorectal cancer: Proposed treatment guidelines for the COVID-19 era
In light of the rapid changes affecting cancer clinics due to the COVID-19 pandemic, Dr. David Kerr and Dr. Rachel Kerr, both specialists in gastrointestinal cancers at the University of Oxford in Oxford, United Kingdom, drafted these guidelines for the use of chemotherapy in colorectal cancer patients. Dr. Kerr and Dr. Kerr are putting forth this guidance as a topic for discussion and debate.
Our aim in developing these recommendations for the care of colorectal cancer patients in areas affected by the COVID-19 outbreak is to reduce the comorbidity of chemotherapy and decrease the risk of patients dying from COVID-19, weighed against the potential benefits of receiving chemotherapy. These recommendations are also designed to reduce the burden on chemotherapy units during a time of great pressure.
We have modified the guidelines in such a way that, we believe, will decrease the total number of patients receiving chemotherapy – particularly in the adjuvant setting – and reduce the overall immune impact of chemotherapy on these patients. Specifically, we suggest changing doublet chemotherapy to single-agent chemotherapy for some groups; changing to combinations involving capecitabine rather than bolus and infusional 5-FU for other patients; and, finally, making reasonable dose reductions upfront to reduce the risk for cycle 1 complications.
By changing from push-and-pump 5-FU to capecitabine for the vast majority of patients, we will both reduce the rates of neutropenia and decrease throughput in chemotherapy outpatient units, reducing requirements for weekly line flushing, pump disconnections, and other routine maintenance.
We continue to recommend the use of ToxNav germline genetic testing as a genetic screen for DPYD/ENOSF1 single-nucleotide polymorphisms (SNPs) to identify patients at high risk for fluoropyrimidine toxicity.
Use of biomarkers to sharpen prognosis should also be considered to refine therapeutic decisions.
Recommendations for stage II-III colorectal cancer
Recommendations for advanced colorectal cancer
Which regimen? Capecitabine/oxaliplatin should be the default backbone chemotherapy (rather than FOLFOX) in order to decrease the stress on infusion units.
Capecitabine plus irinotecan should be considered rather than FOLFIRI. However, in order to increase safety, reduce the dose of the capecitabine and the irinotecan, both to 80%, in all patient groups; and perhaps reduce the capecitabine dose further to 60% in those over the age of 70 or with significant comorbid conditions.
Treatment breaks. Full treatment breaks should be considered after 3 months of treatment in most patients with lower-volume, more indolent disease.
Treatment deintensification to capecitabine alone should be used in those with higher-volume disease (for example, more than 50% of liver replaced by tumor) at the beginning of treatment.
Deferring the start of any chemotherapy. Some older patients, or those with significant other comorbidities (that is, those who will be at increased risk for COVID-19 complications and death); who have low-volume disease, such as a couple of small lung metastases or a single liver metastasis; or who were diagnosed more than 12 months since adjuvant chemotherapy may decide to defer any chemotherapy for a period of time.
In these cases, we suggest rescanning at 3 months and discussing further treatment at that point. Some of these patients will be eligible for other interventions, such as resection, ablation, or stereotactic body radiation therapy. However, it will be important to consider the pressures on these other services during this unprecedented time.
Chemotherapy after resection of metastases. Given the lack of evidence and the present extenuating circumstances, we would not recommend any chemotherapy in this setting.
David J. Kerr, MD, CBE, MD, DSc, is a professor of cancer medicine at the University of Oxford. He is recognized internationally for his work in the research and treatment of colorectal cancer, and has founded three university spin-out companies: COBRA Therapeutics, Celleron Therapeutics, and Oxford Cancer Biomarkers. In 2002, he was appointed Commander of the British Empire by Queen Elizabeth. Rachel S. Kerr, MBChB, is a medical oncologist and associate professor of gastrointestinal oncology at the University of Oxford. She holds a UK Department of Health Fellowship, where she is clinical director of phase 3 trials in the oncology clinical trials office.
This article first appeared on Medscape.com.
In light of the rapid changes affecting cancer clinics due to the COVID-19 pandemic, Dr. David Kerr and Dr. Rachel Kerr, both specialists in gastrointestinal cancers at the University of Oxford in Oxford, United Kingdom, drafted these guidelines for the use of chemotherapy in colorectal cancer patients. Dr. Kerr and Dr. Kerr are putting forth this guidance as a topic for discussion and debate.
Our aim in developing these recommendations for the care of colorectal cancer patients in areas affected by the COVID-19 outbreak is to reduce the comorbidity of chemotherapy and decrease the risk of patients dying from COVID-19, weighed against the potential benefits of receiving chemotherapy. These recommendations are also designed to reduce the burden on chemotherapy units during a time of great pressure.
We have modified the guidelines in such a way that, we believe, will decrease the total number of patients receiving chemotherapy – particularly in the adjuvant setting – and reduce the overall immune impact of chemotherapy on these patients. Specifically, we suggest changing doublet chemotherapy to single-agent chemotherapy for some groups; changing to combinations involving capecitabine rather than bolus and infusional 5-FU for other patients; and, finally, making reasonable dose reductions upfront to reduce the risk for cycle 1 complications.
By changing from push-and-pump 5-FU to capecitabine for the vast majority of patients, we will both reduce the rates of neutropenia and decrease throughput in chemotherapy outpatient units, reducing requirements for weekly line flushing, pump disconnections, and other routine maintenance.
We continue to recommend the use of ToxNav germline genetic testing as a genetic screen for DPYD/ENOSF1 single-nucleotide polymorphisms (SNPs) to identify patients at high risk for fluoropyrimidine toxicity.
Use of biomarkers to sharpen prognosis should also be considered to refine therapeutic decisions.
Recommendations for stage II-III colorectal cancer
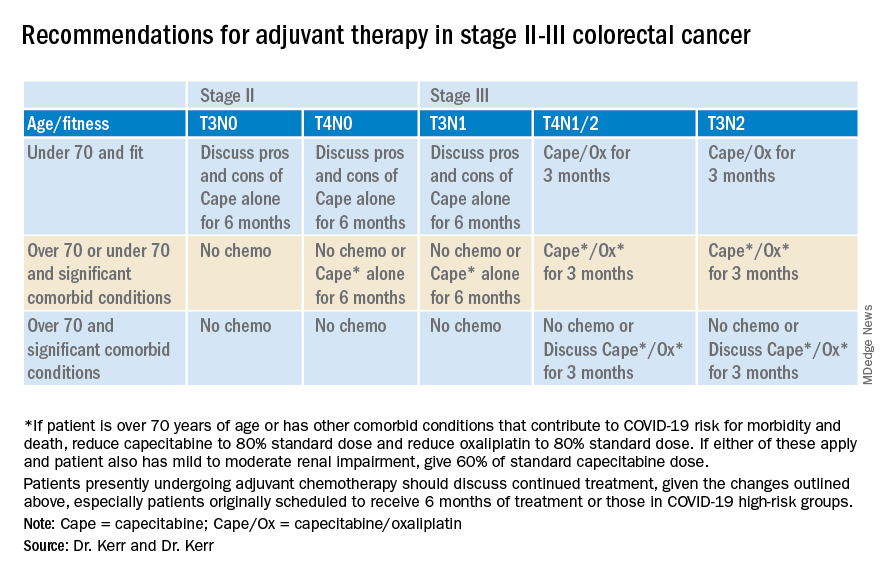
Recommendations for advanced colorectal cancer
Which regimen? Capecitabine/oxaliplatin should be the default backbone chemotherapy (rather than FOLFOX) in order to decrease the stress on infusion units.
Capecitabine plus irinotecan should be considered rather than FOLFIRI. However, in order to increase safety, reduce the dose of the capecitabine and the irinotecan, both to 80%, in all patient groups; and perhaps reduce the capecitabine dose further to 60% in those over the age of 70 or with significant comorbid conditions.
Treatment breaks. Full treatment breaks should be considered after 3 months of treatment in most patients with lower-volume, more indolent disease.
Treatment deintensification to capecitabine alone should be used in those with higher-volume disease (for example, more than 50% of liver replaced by tumor) at the beginning of treatment.
Deferring the start of any chemotherapy. Some older patients, or those with significant other comorbidities (that is, those who will be at increased risk for COVID-19 complications and death); who have low-volume disease, such as a couple of small lung metastases or a single liver metastasis; or who were diagnosed more than 12 months since adjuvant chemotherapy may decide to defer any chemotherapy for a period of time.
In these cases, we suggest rescanning at 3 months and discussing further treatment at that point. Some of these patients will be eligible for other interventions, such as resection, ablation, or stereotactic body radiation therapy. However, it will be important to consider the pressures on these other services during this unprecedented time.
Chemotherapy after resection of metastases. Given the lack of evidence and the present extenuating circumstances, we would not recommend any chemotherapy in this setting.
David J. Kerr, MD, CBE, MD, DSc, is a professor of cancer medicine at the University of Oxford. He is recognized internationally for his work in the research and treatment of colorectal cancer, and has founded three university spin-out companies: COBRA Therapeutics, Celleron Therapeutics, and Oxford Cancer Biomarkers. In 2002, he was appointed Commander of the British Empire by Queen Elizabeth. Rachel S. Kerr, MBChB, is a medical oncologist and associate professor of gastrointestinal oncology at the University of Oxford. She holds a UK Department of Health Fellowship, where she is clinical director of phase 3 trials in the oncology clinical trials office.
This article first appeared on Medscape.com.
In light of the rapid changes affecting cancer clinics due to the COVID-19 pandemic, Dr. David Kerr and Dr. Rachel Kerr, both specialists in gastrointestinal cancers at the University of Oxford in Oxford, United Kingdom, drafted these guidelines for the use of chemotherapy in colorectal cancer patients. Dr. Kerr and Dr. Kerr are putting forth this guidance as a topic for discussion and debate.
Our aim in developing these recommendations for the care of colorectal cancer patients in areas affected by the COVID-19 outbreak is to reduce the comorbidity of chemotherapy and decrease the risk of patients dying from COVID-19, weighed against the potential benefits of receiving chemotherapy. These recommendations are also designed to reduce the burden on chemotherapy units during a time of great pressure.
We have modified the guidelines in such a way that, we believe, will decrease the total number of patients receiving chemotherapy – particularly in the adjuvant setting – and reduce the overall immune impact of chemotherapy on these patients. Specifically, we suggest changing doublet chemotherapy to single-agent chemotherapy for some groups; changing to combinations involving capecitabine rather than bolus and infusional 5-FU for other patients; and, finally, making reasonable dose reductions upfront to reduce the risk for cycle 1 complications.
By changing from push-and-pump 5-FU to capecitabine for the vast majority of patients, we will both reduce the rates of neutropenia and decrease throughput in chemotherapy outpatient units, reducing requirements for weekly line flushing, pump disconnections, and other routine maintenance.
We continue to recommend the use of ToxNav germline genetic testing as a genetic screen for DPYD/ENOSF1 single-nucleotide polymorphisms (SNPs) to identify patients at high risk for fluoropyrimidine toxicity.
Use of biomarkers to sharpen prognosis should also be considered to refine therapeutic decisions.
Recommendations for stage II-III colorectal cancer
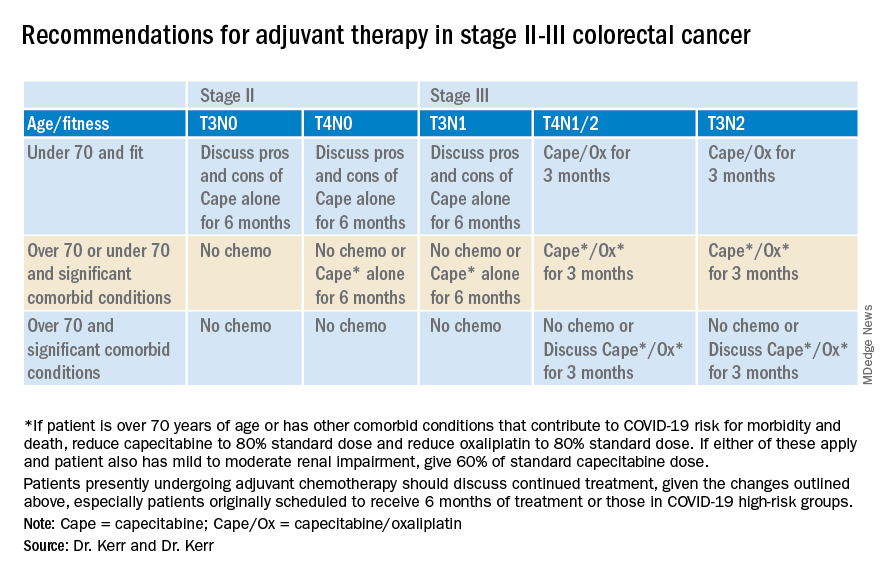
Recommendations for advanced colorectal cancer
Which regimen? Capecitabine/oxaliplatin should be the default backbone chemotherapy (rather than FOLFOX) in order to decrease the stress on infusion units.
Capecitabine plus irinotecan should be considered rather than FOLFIRI. However, in order to increase safety, reduce the dose of the capecitabine and the irinotecan, both to 80%, in all patient groups; and perhaps reduce the capecitabine dose further to 60% in those over the age of 70 or with significant comorbid conditions.
Treatment breaks. Full treatment breaks should be considered after 3 months of treatment in most patients with lower-volume, more indolent disease.
Treatment deintensification to capecitabine alone should be used in those with higher-volume disease (for example, more than 50% of liver replaced by tumor) at the beginning of treatment.
Deferring the start of any chemotherapy. Some older patients, or those with significant other comorbidities (that is, those who will be at increased risk for COVID-19 complications and death); who have low-volume disease, such as a couple of small lung metastases or a single liver metastasis; or who were diagnosed more than 12 months since adjuvant chemotherapy may decide to defer any chemotherapy for a period of time.
In these cases, we suggest rescanning at 3 months and discussing further treatment at that point. Some of these patients will be eligible for other interventions, such as resection, ablation, or stereotactic body radiation therapy. However, it will be important to consider the pressures on these other services during this unprecedented time.
Chemotherapy after resection of metastases. Given the lack of evidence and the present extenuating circumstances, we would not recommend any chemotherapy in this setting.
David J. Kerr, MD, CBE, MD, DSc, is a professor of cancer medicine at the University of Oxford. He is recognized internationally for his work in the research and treatment of colorectal cancer, and has founded three university spin-out companies: COBRA Therapeutics, Celleron Therapeutics, and Oxford Cancer Biomarkers. In 2002, he was appointed Commander of the British Empire by Queen Elizabeth. Rachel S. Kerr, MBChB, is a medical oncologist and associate professor of gastrointestinal oncology at the University of Oxford. She holds a UK Department of Health Fellowship, where she is clinical director of phase 3 trials in the oncology clinical trials office.
This article first appeared on Medscape.com.