User login
VIDEO: How to halve serious reportable events in the OR
SAN FRANCISCO– Little steps, when added together, lead to big reductions in serious reportable events in the operating room, according to investigators from the Phoenix-based Banner Health system.
After slight modifications to the count, timeout, and other OR procedures, Banner saw a 52% reduction in serious reportable events (SREs), including a 70% reduction in wrong-site surgeries, across its 22 hospitals and 8 ambulatory surgery centers (J. Am. Coll. Surg. 2014 Oct. 4 [doi:http://dx.doi.org/10.1016/j.jamcollsurg.2014.09.018]).
In an interview at the annual clinical congress of the American College of Surgeons, lead investigator Dr. Terrence Loftus, the health system’s medical director of surgery services and clinical resources, explained how they did it. He also explained why surgical SREs are seven times more common in the system’s robotic surgery program, despite overall improvements, and what Banner is planning to do about it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Little steps, when added together, lead to big reductions in serious reportable events in the operating room, according to investigators from the Phoenix-based Banner Health system.
After slight modifications to the count, timeout, and other OR procedures, Banner saw a 52% reduction in serious reportable events (SREs), including a 70% reduction in wrong-site surgeries, across its 22 hospitals and 8 ambulatory surgery centers (J. Am. Coll. Surg. 2014 Oct. 4 [doi:http://dx.doi.org/10.1016/j.jamcollsurg.2014.09.018]).
In an interview at the annual clinical congress of the American College of Surgeons, lead investigator Dr. Terrence Loftus, the health system’s medical director of surgery services and clinical resources, explained how they did it. He also explained why surgical SREs are seven times more common in the system’s robotic surgery program, despite overall improvements, and what Banner is planning to do about it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO– Little steps, when added together, lead to big reductions in serious reportable events in the operating room, according to investigators from the Phoenix-based Banner Health system.
After slight modifications to the count, timeout, and other OR procedures, Banner saw a 52% reduction in serious reportable events (SREs), including a 70% reduction in wrong-site surgeries, across its 22 hospitals and 8 ambulatory surgery centers (J. Am. Coll. Surg. 2014 Oct. 4 [doi:http://dx.doi.org/10.1016/j.jamcollsurg.2014.09.018]).
In an interview at the annual clinical congress of the American College of Surgeons, lead investigator Dr. Terrence Loftus, the health system’s medical director of surgery services and clinical resources, explained how they did it. He also explained why surgical SREs are seven times more common in the system’s robotic surgery program, despite overall improvements, and what Banner is planning to do about it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
VIDEO: EMR reminder reduces unnecessary transfusions
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
Spotlight falls on rising levels of tricuspid valve surgery
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
Dr. Hossein Almassi, FCCP,comments: Historically, cardiac surgeons have been reluctant to operate on the tricuspid valve, mainly because of poor outcome and a high mortality rate. The excellent results with mitral valve repair and the emerging experience on tricuspid valve surgery have led to a welcome shift in the attitude of cardiac surgeons and cardiologists in adopting an earlier and more proactive approach in treating patients with significant tricuspid valve regurgitation, either alone or in conjunction with other valvular operations, as evidenced by changes in the 2014 AHA/ACC guidelines.
Dr. Almassi is with the Cardiothoracic Surgery Division at the Medical College of Wisconsin in Milwaukee, WI.
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
CHICAGO – Ten times as many papers were published on the mitral valve as were published on the tricuspid valve during the 1990s, based on a literature review.
Things have picked up over the past decade, however, for the “forgotten,” little-respected “Rodney Dangerfield” valve, with surgeons writing more about tricuspid regurgitation and doing more tricuspid surgery than ever before, Dr. Patrick McCarthy said at Heart Valve Summit 2014.
Tricuspid interventions more than doubled from 1999 to 2008, although overall hospital mortality was substantial at 10.6%. (J. Thorac. Cardiovasc. Surg. 2012;143:1043-9).
A Society of Thoracic Surgeons risk model containing intraoperative variables showed that multiple-valve surgery mortality is more than twice that of single-valve surgery, but that performance of arrhythmia ablation and atrioventricular valve repair are protective for mortality (Ann. Thorac. Surg. 2013;95:1484-90).
“There isn’t any data that the tricuspid per se is actually the reason that the operation is higher risk,” said Dr. McCarthy, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, Northwestern University in Chicago.
The new American Heart Association/American College of Cardiology (AHA/ACC) guideline on valvular heart disease, published earlier this year, reflects the changing attitudes about mitral valve surgery and the need for earlier intervention.
A class I indication for surgery remains in place for severe tricuspid regurgitation (TR) with mitral valve disease. However, what had been a class IIb indication in the 2006 guidelines for primary TR with symptoms is now a class I indication in the 2014 guidelines.
“Don’t wait for right ventricular failure in primary TR. Plan for earlier intervention, and think of it more like we do mitral regurgitation,” Dr. McCarthy said.
The recommendation for more moderate TR has also changed. The class IIb recommendation for patients with less than severe TR during mitral valve repair with pulmonary hypertension, right heart failure, or tricuspid dilation is now class IIa, indicating a lower threshold for surgery for these patients, he said.
Asymptomatic primary TR with right ventricle dilation or reoperations for TR with symptoms and prior left heart surgery had been a class III indication against surgery in 2006, but are now in sync with the European valvular guidelines with a class IIb indication, suggesting surgery may be considered.
The move toward earlier surgery is supported by results showing that TR only gets worse if left untreated, Dr. McCarthy said. Among patients with annular dilation greater than 70 mm as the only criterion for tricuspid valve repair (TVR), TR was shown to increase by more than 2 grades after 2 years in just 2% of patients who underwent TVR during mitral valve repair (MVR), versus 48% without TVR (Ann. Thorac. Surg. 2005;79:127-32).
Another study showed that prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing MVR reduces the rate of TR progression, improves right ventricular remodeling, and improves functional outcomes on the 6-minute walk test (J. Thorac. Cardiovasc. Surg. 2012;143:632-8).
Not all data, however, have been viewed through the same lens, with the “Mayo Clinic and Cleveland Clinic finding the same thing but drawing different conclusions,” Dr. McCarthy observed.
A Cleveland Clinic analysis involving 1,833 patients with degenerative mitral valve disease reported that MVR alone improved TR and right ventricular function in patients with severe TR (grade 3+/4+), but that improvements were incomplete and temporary. In contrast, MVR with concomitant TVR eliminated severe TR and improved RV function toward normal, “supporting an aggressive approach to important functional tricuspid regurgitation” (J. Cardiovasc Surg. 2013;146:1126-32).
An 11-year review by the Mayo Clinic in Rochester, Minn., involving 699 patients with functional TR and degenerative mitral valve leaflet prolapse also showed that MVR alone significantly reduced TR within the first year in all patients and produced significant decreases until the third year in those with severe regurgitation. Only one patient required tricuspid reoperation 4.5 years after mitral repair. The authors argued for a selective approach to TR, concluding that “tricuspid valve surgery is rarely necessary for most patients undergoing repair of isolated mitral valve prolapse.”
“While both Cleveland and Mayo Clinic found that untreated TR persisted, Mayo interpreted the rare need for reoperation and no decrease in 5-year survival as evidence that it need not be repaired, while Cleveland suggested with the evidence of improved RV function that it should be repaired,” Dr. McCarthy said in an interview. “The European Society of Cardiology and AHA/ACC guidelines would support the approach from the Cleveland Clinic.”
Dr. McCarthy disclosed inventing the Edwards MC3 tricuspid valve repair ring.
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2014
Annual echo an option for cardiac allograft vasculopathy screening
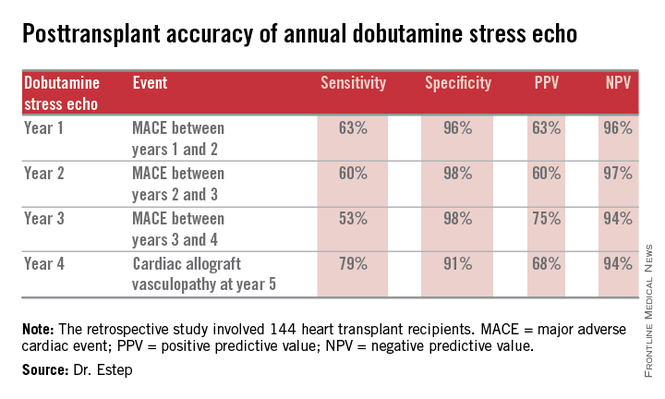
LAS VEGAS – The experience at one major heart transplantation center indicates that annual screening dobutamine stress echocardiography to detect cardiac allograft vasculopathy renders annual coronary angiography unnecessary.
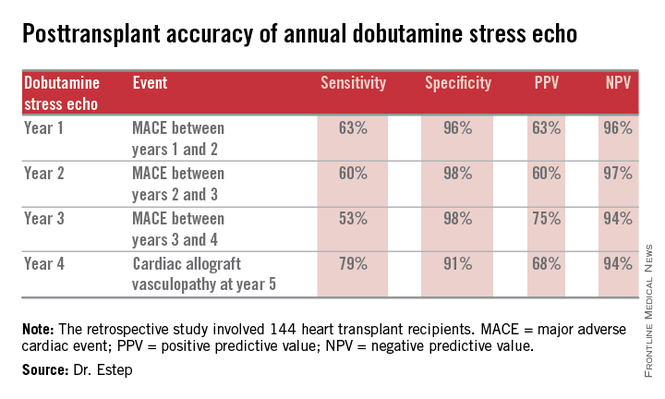
“This noninvasive method has very good specificity and is associated with a negative predictive value of 94%-97%. It can be used in our experience in lieu of annual invasive coronary angiography,” Dr. Jerry D. Estep declared at the annual meeting of the Heart Failure Society of America.
Cardiac allograft vasculopathy (CAV) is a unique, highly aggressive form of CAD. After 3 years post transplant it becomes the No. 1 cause of cardiac retransplantation and mortality. Guidelines recommend consideration of annual screening coronary angiography to detect it early to institute aggressive countermeasures. That’s the practice at most transplant centers.
However, at Houston Methodist Hospital, where Dr. Estep is medical director of the heart transplant and LVAD program, annual dobutamine stress echocardiography (DSE) is used instead. Because there is a scarcity of published data on this noninvasive alternative approach, he presented a retrospective study of the Houston transplant center’s experience over a recent 5-year period.
The study included 144 heart transplant recipients who underwent screening DSE for CAV annually for the first 4 years post transplant and coronary angiography at year 5.
During years 1-4, DSE detected CAV in 19% of patients. They didn’t differ in terms of baseline characteristics from those who remained free of this serious complication.
The good news: Ninety-four percent of patients with normal DSEs during years 1-4 had no CAV upon angiography at year 5. Moreover, the 5% who did have CAV at year 5 after earlier negative DSEs had mild to moderate disease.
The investigators documented the performance of annual screening DSE in predicting the development of major adverse cardiac events, defined as readmission for acute coronary syndrome, heart failure, revascularization, repeat heart transplantation, or cardiac death.
Dr. Estep reported having no financial conflicts regarding this study.
Dr. Hossein Almassi, FCCP, comments: Among solid organ transplants, cardiac transplant is rather unique in its need for invasive biopsy and angiography in following up the cardiac allograft. The search for noninvasive monitoring tools has been ongoing for a number of years. The report by the Houston group is a positive development in the right direction awaiting further confirmation by other cardiac transplant centers.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: Among solid organ transplants, cardiac transplant is rather unique in its need for invasive biopsy and angiography in following up the cardiac allograft. The search for noninvasive monitoring tools has been ongoing for a number of years. The report by the Houston group is a positive development in the right direction awaiting further confirmation by other cardiac transplant centers.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: Among solid organ transplants, cardiac transplant is rather unique in its need for invasive biopsy and angiography in following up the cardiac allograft. The search for noninvasive monitoring tools has been ongoing for a number of years. The report by the Houston group is a positive development in the right direction awaiting further confirmation by other cardiac transplant centers.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
LAS VEGAS – The experience at one major heart transplantation center indicates that annual screening dobutamine stress echocardiography to detect cardiac allograft vasculopathy renders annual coronary angiography unnecessary.
“This noninvasive method has very good specificity and is associated with a negative predictive value of 94%-97%. It can be used in our experience in lieu of annual invasive coronary angiography,” Dr. Jerry D. Estep declared at the annual meeting of the Heart Failure Society of America.
Cardiac allograft vasculopathy (CAV) is a unique, highly aggressive form of CAD. After 3 years post transplant it becomes the No. 1 cause of cardiac retransplantation and mortality. Guidelines recommend consideration of annual screening coronary angiography to detect it early to institute aggressive countermeasures. That’s the practice at most transplant centers.
However, at Houston Methodist Hospital, where Dr. Estep is medical director of the heart transplant and LVAD program, annual dobutamine stress echocardiography (DSE) is used instead. Because there is a scarcity of published data on this noninvasive alternative approach, he presented a retrospective study of the Houston transplant center’s experience over a recent 5-year period.
The study included 144 heart transplant recipients who underwent screening DSE for CAV annually for the first 4 years post transplant and coronary angiography at year 5.
During years 1-4, DSE detected CAV in 19% of patients. They didn’t differ in terms of baseline characteristics from those who remained free of this serious complication.
The good news: Ninety-four percent of patients with normal DSEs during years 1-4 had no CAV upon angiography at year 5. Moreover, the 5% who did have CAV at year 5 after earlier negative DSEs had mild to moderate disease.
The investigators documented the performance of annual screening DSE in predicting the development of major adverse cardiac events, defined as readmission for acute coronary syndrome, heart failure, revascularization, repeat heart transplantation, or cardiac death.
Dr. Estep reported having no financial conflicts regarding this study.
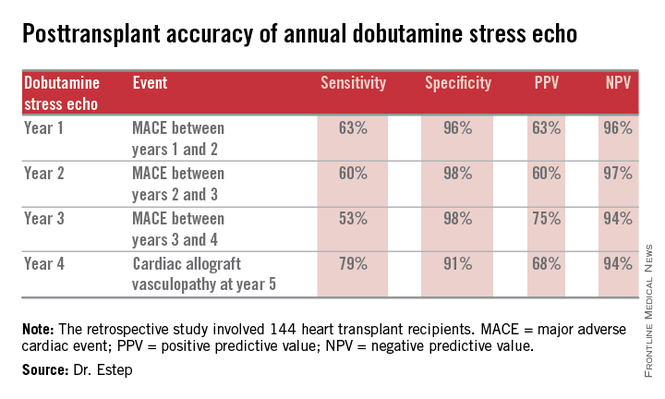
LAS VEGAS – The experience at one major heart transplantation center indicates that annual screening dobutamine stress echocardiography to detect cardiac allograft vasculopathy renders annual coronary angiography unnecessary.
“This noninvasive method has very good specificity and is associated with a negative predictive value of 94%-97%. It can be used in our experience in lieu of annual invasive coronary angiography,” Dr. Jerry D. Estep declared at the annual meeting of the Heart Failure Society of America.
Cardiac allograft vasculopathy (CAV) is a unique, highly aggressive form of CAD. After 3 years post transplant it becomes the No. 1 cause of cardiac retransplantation and mortality. Guidelines recommend consideration of annual screening coronary angiography to detect it early to institute aggressive countermeasures. That’s the practice at most transplant centers.
However, at Houston Methodist Hospital, where Dr. Estep is medical director of the heart transplant and LVAD program, annual dobutamine stress echocardiography (DSE) is used instead. Because there is a scarcity of published data on this noninvasive alternative approach, he presented a retrospective study of the Houston transplant center’s experience over a recent 5-year period.
The study included 144 heart transplant recipients who underwent screening DSE for CAV annually for the first 4 years post transplant and coronary angiography at year 5.
During years 1-4, DSE detected CAV in 19% of patients. They didn’t differ in terms of baseline characteristics from those who remained free of this serious complication.
The good news: Ninety-four percent of patients with normal DSEs during years 1-4 had no CAV upon angiography at year 5. Moreover, the 5% who did have CAV at year 5 after earlier negative DSEs had mild to moderate disease.
The investigators documented the performance of annual screening DSE in predicting the development of major adverse cardiac events, defined as readmission for acute coronary syndrome, heart failure, revascularization, repeat heart transplantation, or cardiac death.
Dr. Estep reported having no financial conflicts regarding this study.
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: Annual dobutamine stress echocardiography to screen heart transplant recipients for cardiac allograft vasculopathy is an excellent noninvasive alternative to the widely used practice of annual screening coronary angiography.
Major finding: Annual screening dobutamine stress echo during years 1-4 after heart transplant had a 94% negative predictive value for cardiac allograft vasculopathy at year 5.
Data source: A retrospective study of 144 heart transplant recipients at a major transplant center where screening for cardiac allograft vasculopathy is done noninvasively by annual dobutamine stress echocardiography rather than angiography, which is widely used elsewhere.
Disclosures: The presenter reported having no conflicts relevant to the study, which was free of commercial support.
VIDEO: Nonclinical factors affect lung resection survival
SAN FRANCISCO– A study of data from more than 200,000 patients identified several nonclinical factors ssociated with 30-day survival after lung resection for non–small cell lung cancer, Dr. Manu S. Sancheti reported at the annual clinical congress of the American College of Surgeons.
The analysis by Dr. Sancheti and his associates won the top prize for poster presentations at the congress.
In an interview at the award presentation, Dr. Sancheti of Emory University, Atlanta, described his results and ideas about how physicians and health care systems might use this information to improve care.
He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO– A study of data from more than 200,000 patients identified several nonclinical factors ssociated with 30-day survival after lung resection for non–small cell lung cancer, Dr. Manu S. Sancheti reported at the annual clinical congress of the American College of Surgeons.
The analysis by Dr. Sancheti and his associates won the top prize for poster presentations at the congress.
In an interview at the award presentation, Dr. Sancheti of Emory University, Atlanta, described his results and ideas about how physicians and health care systems might use this information to improve care.
He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
SAN FRANCISCO– A study of data from more than 200,000 patients identified several nonclinical factors ssociated with 30-day survival after lung resection for non–small cell lung cancer, Dr. Manu S. Sancheti reported at the annual clinical congress of the American College of Surgeons.
The analysis by Dr. Sancheti and his associates won the top prize for poster presentations at the congress.
In an interview at the award presentation, Dr. Sancheti of Emory University, Atlanta, described his results and ideas about how physicians and health care systems might use this information to improve care.
He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
AT THE ACS CLINICAL CONGRESS
Lungs donated after cardiac arrest, brain death yield similar survival rates
AUSTIN, TEX. – The risk of death at 1 year after lung transplantation with organs donated either after cardiac arrest or after brain death was virtually the same, an analysis of the literature has shown.
“Donation after cardiac death appears to be a safe and effective method to expand the donor pool,” said Dr. Dustin Krutsinger of the University of Iowa, Iowa City, who presented the findings during the Hot Topics in Pulmonary Critical Care session at the annual meeting of the American College of Chest Physicians.
Over the years, the demand for organ donations for lung transplant candidates has steadily increased while the number of available organs has remained static. This is due, in part, to physicians being concerned about injury to the organs during the ischemic period, as well as what can often be as much as an hour before organ procurement after withdrawal of life support. However, Dr. Krutsinger said the similarities between the two cohorts could result from the fact that before procurement, systemic circulation allows the lungs to oxygenate by perfusion, and so there is less impact during the ischemic period.
“There is also a thought that the ischemic period might actually protect the lungs and the liver from reperfusion injury. And we’re avoiding brain death, which is not a completely benign state,” he told the audience.
After conducting an extensive review of the literature for 1-year survival rates post lung transplantation, the investigators found 519 unique citations, including 58 citations selected for full text review, 10 observational cohort studies for systematic review, and another 5 such studies for meta-analysis.
Dr. Krutsinger and his colleagues found no significant difference in 1-year survival rates between the donation after cardiac death and the donation after brain death cohorts (P = .658). In a pooled analysis of the five studies, no significant difference in risk of death was found at 1 year after either transplantation procedure (relative risk, 0.66; 95% confidence interval, 0.38-1.15; P = .15). Although he thought the findings were limited by shortcomings in the data, such as the fact that the study was a retrospective analysis of unmatched cohorts and that the follow-up period was short, Dr. Krutsinger said in an interview that he thought the data were compelling enough for institutions to begin rethinking organ procurement and transplantation protocols. In addition to his own study, he cited a 2013 study which he said indicated that if lungs donated after cardiac arrest were included, the pool of available organs would increase by as much as 50% (Ann. Am. Thorac. Soc. 2013;10:73-80).
But challenges remain.
“There are some things you can do to the potential donors that are questionable ethicswise, such as administering heparin premortem, which would be beneficial to the actual recipients. But, up until they are pronounced dead, they are still a patient. You don’t really have that complication with a donation after brain death, since once brain death is determined, the person is officially dead. Things you then do to them to benefit the eventual recipients aren’t being done to a ‘patient.’ ”
Still, Dr. Krutsinger said that if organs procured after cardiac arrest were to become more common than after brain death, he would be “disappointed” since the data showed “the outcomes are similar, not inferior.”
Dr. Krutsinger said he had no relevant disclosures.
On Twitter @whitneymcknight
AUSTIN, TEX. – The risk of death at 1 year after lung transplantation with organs donated either after cardiac arrest or after brain death was virtually the same, an analysis of the literature has shown.
“Donation after cardiac death appears to be a safe and effective method to expand the donor pool,” said Dr. Dustin Krutsinger of the University of Iowa, Iowa City, who presented the findings during the Hot Topics in Pulmonary Critical Care session at the annual meeting of the American College of Chest Physicians.
Over the years, the demand for organ donations for lung transplant candidates has steadily increased while the number of available organs has remained static. This is due, in part, to physicians being concerned about injury to the organs during the ischemic period, as well as what can often be as much as an hour before organ procurement after withdrawal of life support. However, Dr. Krutsinger said the similarities between the two cohorts could result from the fact that before procurement, systemic circulation allows the lungs to oxygenate by perfusion, and so there is less impact during the ischemic period.
“There is also a thought that the ischemic period might actually protect the lungs and the liver from reperfusion injury. And we’re avoiding brain death, which is not a completely benign state,” he told the audience.
After conducting an extensive review of the literature for 1-year survival rates post lung transplantation, the investigators found 519 unique citations, including 58 citations selected for full text review, 10 observational cohort studies for systematic review, and another 5 such studies for meta-analysis.
Dr. Krutsinger and his colleagues found no significant difference in 1-year survival rates between the donation after cardiac death and the donation after brain death cohorts (P = .658). In a pooled analysis of the five studies, no significant difference in risk of death was found at 1 year after either transplantation procedure (relative risk, 0.66; 95% confidence interval, 0.38-1.15; P = .15). Although he thought the findings were limited by shortcomings in the data, such as the fact that the study was a retrospective analysis of unmatched cohorts and that the follow-up period was short, Dr. Krutsinger said in an interview that he thought the data were compelling enough for institutions to begin rethinking organ procurement and transplantation protocols. In addition to his own study, he cited a 2013 study which he said indicated that if lungs donated after cardiac arrest were included, the pool of available organs would increase by as much as 50% (Ann. Am. Thorac. Soc. 2013;10:73-80).
But challenges remain.
“There are some things you can do to the potential donors that are questionable ethicswise, such as administering heparin premortem, which would be beneficial to the actual recipients. But, up until they are pronounced dead, they are still a patient. You don’t really have that complication with a donation after brain death, since once brain death is determined, the person is officially dead. Things you then do to them to benefit the eventual recipients aren’t being done to a ‘patient.’ ”
Still, Dr. Krutsinger said that if organs procured after cardiac arrest were to become more common than after brain death, he would be “disappointed” since the data showed “the outcomes are similar, not inferior.”
Dr. Krutsinger said he had no relevant disclosures.
On Twitter @whitneymcknight
AUSTIN, TEX. – The risk of death at 1 year after lung transplantation with organs donated either after cardiac arrest or after brain death was virtually the same, an analysis of the literature has shown.
“Donation after cardiac death appears to be a safe and effective method to expand the donor pool,” said Dr. Dustin Krutsinger of the University of Iowa, Iowa City, who presented the findings during the Hot Topics in Pulmonary Critical Care session at the annual meeting of the American College of Chest Physicians.
Over the years, the demand for organ donations for lung transplant candidates has steadily increased while the number of available organs has remained static. This is due, in part, to physicians being concerned about injury to the organs during the ischemic period, as well as what can often be as much as an hour before organ procurement after withdrawal of life support. However, Dr. Krutsinger said the similarities between the two cohorts could result from the fact that before procurement, systemic circulation allows the lungs to oxygenate by perfusion, and so there is less impact during the ischemic period.
“There is also a thought that the ischemic period might actually protect the lungs and the liver from reperfusion injury. And we’re avoiding brain death, which is not a completely benign state,” he told the audience.
After conducting an extensive review of the literature for 1-year survival rates post lung transplantation, the investigators found 519 unique citations, including 58 citations selected for full text review, 10 observational cohort studies for systematic review, and another 5 such studies for meta-analysis.
Dr. Krutsinger and his colleagues found no significant difference in 1-year survival rates between the donation after cardiac death and the donation after brain death cohorts (P = .658). In a pooled analysis of the five studies, no significant difference in risk of death was found at 1 year after either transplantation procedure (relative risk, 0.66; 95% confidence interval, 0.38-1.15; P = .15). Although he thought the findings were limited by shortcomings in the data, such as the fact that the study was a retrospective analysis of unmatched cohorts and that the follow-up period was short, Dr. Krutsinger said in an interview that he thought the data were compelling enough for institutions to begin rethinking organ procurement and transplantation protocols. In addition to his own study, he cited a 2013 study which he said indicated that if lungs donated after cardiac arrest were included, the pool of available organs would increase by as much as 50% (Ann. Am. Thorac. Soc. 2013;10:73-80).
But challenges remain.
“There are some things you can do to the potential donors that are questionable ethicswise, such as administering heparin premortem, which would be beneficial to the actual recipients. But, up until they are pronounced dead, they are still a patient. You don’t really have that complication with a donation after brain death, since once brain death is determined, the person is officially dead. Things you then do to them to benefit the eventual recipients aren’t being done to a ‘patient.’ ”
Still, Dr. Krutsinger said that if organs procured after cardiac arrest were to become more common than after brain death, he would be “disappointed” since the data showed “the outcomes are similar, not inferior.”
Dr. Krutsinger said he had no relevant disclosures.
On Twitter @whitneymcknight
AT CHEST 2014
Key clinical point: Expansion of organ donation programs to include organs donated after cardiac death could help meet a growing demand for donated lungs.
Major finding: No significant difference was seen in lung transplantation 1-year survival rates between donation after cardiac arrest and donation after brain death.
Data source: A systematic review of 10 observational cohort studies and a meta-analysis of 5 studies, chosen from more than 500 citations that included 1-year survival data for lung transplantation occuring after either cardiac arrest or brain death.
Disclosures: Dr. Krutsinger said he had no relevant disclosures.
Lungs donated after asphyxiation, drowning found suitable for transplant
Patients who received lung transplants from donors who died of asphyxiation or drowning had similar survival rates and clinical outcomes as those whose donors died of other causes, according to a large registry analysis in the October issue of The Annals of Thoracic Surgery.
“Asphyxiation or drowning as a donor cause of death should not automatically exclude the organ from transplant consideration,” said Dr. Bryan A. Whitson of Ohio State University, Columbus, and his associates. Donor death from asphyxiation or drowning did not significantly affect rates of airway dehiscence, transplant rejection, posttransplant stroke or dialysis, or long-term survival.
Lungs donated after asphyxiation or drowning should be carefully evaluated for parenchymal injury, microbial contamination, and the possibility of primary graft dysfunction, the researchers cautioned. For example, asphyxiation and drowning can alter lung surfactant levels (Ann. Thorac. Surg. 2014;98:1145-51).
The analysis included 18,205 U.S. adults who underwent lung transplantation between 1987 and 2010, including 309 patients whose donors had reportedly died from drowning or asphyxiation. Patients were identified from the UNOS/OPTN STAR (United Network for Organ Sharing/Organ Procurement and Transplantation Network Standard Transplant Analysis and Research) database, which is overseen by the U.S. Department of Health & Human Services.
Ten-year survival curves did not vary based on donor cause of death, either when analyzed individually or when asphyxiation or drowning was compared with all other causes (P = .52), the researchers said. In fact, pulmonary deaths were significantly less common (5.8%) among recipients whose donors had died of asphyxiation or drowning compared with other causes (9.5%; P = .02).
Donor death from drowning and asphyxiation also did not significantly affect rates of treatment for transplant rejection within the first year after surgery (50.8% vs. 47.4% for all other causes of donor death), or posttransplant rates of stroke (0.7% vs. 2.1%) or dialysis (5.4% vs. 5.2%), the investigators said. However, hospital length of stay averaged 0.8 days longer when donors had died of asphyxiation or drowning compared with other causes (27.3 vs. 26.5 days; P < 0.001).
Dr. Jacques-Pierre Fontaine comments: The shortage of suitable donor lungs remains an important problem. Less than 20% of lungs being offered for donation are being used. The notion that asphyxiation or drowning excludes a patient from being a potential donor is widespread among some clinicians.
This extensive retrospective review of the robust UNOS Database demonstrates that recipients of lungs from donors who died from asphyxiation or drowning have similar 10-year survival and post-transplant complication rates. In carefully selected donors, these lungs may be successfully used. Furthermore, "optimization" of marginal donor lungs may become more prevalent as ex-vivo lung perfusion technology evolves.
Dr. Fontaine specializes in thoracic surgery at the Moffitt Cancer Center in Tampa, Florida.
Dr. Jacques-Pierre Fontaine comments: The shortage of suitable donor lungs remains an important problem. Less than 20% of lungs being offered for donation are being used. The notion that asphyxiation or drowning excludes a patient from being a potential donor is widespread among some clinicians.
This extensive retrospective review of the robust UNOS Database demonstrates that recipients of lungs from donors who died from asphyxiation or drowning have similar 10-year survival and post-transplant complication rates. In carefully selected donors, these lungs may be successfully used. Furthermore, "optimization" of marginal donor lungs may become more prevalent as ex-vivo lung perfusion technology evolves.
Dr. Fontaine specializes in thoracic surgery at the Moffitt Cancer Center in Tampa, Florida.
Dr. Jacques-Pierre Fontaine comments: The shortage of suitable donor lungs remains an important problem. Less than 20% of lungs being offered for donation are being used. The notion that asphyxiation or drowning excludes a patient from being a potential donor is widespread among some clinicians.
This extensive retrospective review of the robust UNOS Database demonstrates that recipients of lungs from donors who died from asphyxiation or drowning have similar 10-year survival and post-transplant complication rates. In carefully selected donors, these lungs may be successfully used. Furthermore, "optimization" of marginal donor lungs may become more prevalent as ex-vivo lung perfusion technology evolves.
Dr. Fontaine specializes in thoracic surgery at the Moffitt Cancer Center in Tampa, Florida.
Patients who received lung transplants from donors who died of asphyxiation or drowning had similar survival rates and clinical outcomes as those whose donors died of other causes, according to a large registry analysis in the October issue of The Annals of Thoracic Surgery.
“Asphyxiation or drowning as a donor cause of death should not automatically exclude the organ from transplant consideration,” said Dr. Bryan A. Whitson of Ohio State University, Columbus, and his associates. Donor death from asphyxiation or drowning did not significantly affect rates of airway dehiscence, transplant rejection, posttransplant stroke or dialysis, or long-term survival.
Lungs donated after asphyxiation or drowning should be carefully evaluated for parenchymal injury, microbial contamination, and the possibility of primary graft dysfunction, the researchers cautioned. For example, asphyxiation and drowning can alter lung surfactant levels (Ann. Thorac. Surg. 2014;98:1145-51).
The analysis included 18,205 U.S. adults who underwent lung transplantation between 1987 and 2010, including 309 patients whose donors had reportedly died from drowning or asphyxiation. Patients were identified from the UNOS/OPTN STAR (United Network for Organ Sharing/Organ Procurement and Transplantation Network Standard Transplant Analysis and Research) database, which is overseen by the U.S. Department of Health & Human Services.
Ten-year survival curves did not vary based on donor cause of death, either when analyzed individually or when asphyxiation or drowning was compared with all other causes (P = .52), the researchers said. In fact, pulmonary deaths were significantly less common (5.8%) among recipients whose donors had died of asphyxiation or drowning compared with other causes (9.5%; P = .02).
Donor death from drowning and asphyxiation also did not significantly affect rates of treatment for transplant rejection within the first year after surgery (50.8% vs. 47.4% for all other causes of donor death), or posttransplant rates of stroke (0.7% vs. 2.1%) or dialysis (5.4% vs. 5.2%), the investigators said. However, hospital length of stay averaged 0.8 days longer when donors had died of asphyxiation or drowning compared with other causes (27.3 vs. 26.5 days; P < 0.001).
Patients who received lung transplants from donors who died of asphyxiation or drowning had similar survival rates and clinical outcomes as those whose donors died of other causes, according to a large registry analysis in the October issue of The Annals of Thoracic Surgery.
“Asphyxiation or drowning as a donor cause of death should not automatically exclude the organ from transplant consideration,” said Dr. Bryan A. Whitson of Ohio State University, Columbus, and his associates. Donor death from asphyxiation or drowning did not significantly affect rates of airway dehiscence, transplant rejection, posttransplant stroke or dialysis, or long-term survival.
Lungs donated after asphyxiation or drowning should be carefully evaluated for parenchymal injury, microbial contamination, and the possibility of primary graft dysfunction, the researchers cautioned. For example, asphyxiation and drowning can alter lung surfactant levels (Ann. Thorac. Surg. 2014;98:1145-51).
The analysis included 18,205 U.S. adults who underwent lung transplantation between 1987 and 2010, including 309 patients whose donors had reportedly died from drowning or asphyxiation. Patients were identified from the UNOS/OPTN STAR (United Network for Organ Sharing/Organ Procurement and Transplantation Network Standard Transplant Analysis and Research) database, which is overseen by the U.S. Department of Health & Human Services.
Ten-year survival curves did not vary based on donor cause of death, either when analyzed individually or when asphyxiation or drowning was compared with all other causes (P = .52), the researchers said. In fact, pulmonary deaths were significantly less common (5.8%) among recipients whose donors had died of asphyxiation or drowning compared with other causes (9.5%; P = .02).
Donor death from drowning and asphyxiation also did not significantly affect rates of treatment for transplant rejection within the first year after surgery (50.8% vs. 47.4% for all other causes of donor death), or posttransplant rates of stroke (0.7% vs. 2.1%) or dialysis (5.4% vs. 5.2%), the investigators said. However, hospital length of stay averaged 0.8 days longer when donors had died of asphyxiation or drowning compared with other causes (27.3 vs. 26.5 days; P < 0.001).
Key clinical point: Lung transplant recipients had good outcomes and long-term survival in cases involving donors who died of asphyxiation or drowning.
Major finding: Pulmonary deaths were significantly less common (5.8%) among recipients whose donors had died of asphyxiation or drowning compared with other causes (9.5%; P = .02).
Data source: Retrospective registry analysis of 18,250 lung transplant recipients.
Disclosures: The authors did not report funding sources or conflicts of interest.
Meta-analysis: Transapical TAVR associated with higher mortality
BARCELONA – The transfemoral approach to aortic valve replacement is associated with lower risk of death, stroke, and bleeding, compared with the more invasive transapical approach, according to a meta-analysis of more than a dozen studies.
After adjustment for baseline characteristics, Italian researchers found that, compared with patients who underwent transapical transcatheter aortic valve replacement (TAVR), the transfemoral group was nearly 20% less likely to die within 30 days and during the first year after the procedure. The transfemoral group also was significantly less likely to have periprocedural bleeding or stroke.
Although the findings should be viewed as hypothesis generating, they suggest that “transapical access should be reserved as a last option in TAVR patients. This choice may guarantee less mortality, less stroke, and less bleeding in this frail and elderly population,” Dr. Federico Conrotto said at the annual congress of the European Society of Cardiology.
Although the transfemoral approach for aortic valve replacement is completely percutaneous, the transapical approach is more invasive and involves the direct puncture of the left ventricle. Also, the transapical approach is mostly reserved for patients in whom femoral vessels are unapproachable. These patients also turn out to be sicker, hence making it difficult to compare the two approaches, and there are no randomized trials comparing the two, said Dr. Conrotto of Città della Salute e della Scienza Hospital in Turin, Italy.
In the absence of randomized trials, Dr. Conrotto and his colleagues selected 13 studies that reported the adjustments for clinical baseline characteristics and reported the baseline, periprocedural, and midterm (median, 365 days) outcomes for patients who underwent transfemoral and transapical TAVR.
Their primary endpoint was all-cause mortality at 1-year follow-up. The secondary endpoint was 30-day mortality and in-hospital complications, including bleeding and stroke.
In total, the studies included 10,468 patients who underwent TAVR between 2005 and 2012. The patients’ median age was 82 years and half were men: one-fourth had diabetes, 18% had renal dysfunction, 61% had coronary artery disease, and the average ejection fraction was 50%. Almost 70% of the TAVR procedures were performed transfemorally.
Results showed that patients who underwent the transfemoral approach were 15% less likely to die at 365 days following TAVR and 20% less likely to die at 30 days, compared with those who underwent the transapical approach, Dr. Conrotto said. Both differences were statistically significant.
Those who underwent the transfemoral approach were almost 30% less likely to have periprocedural bleeding and 10% less likely to have a periprocedural stroke. Again, both differences were statistically significant, he noted.
“Not only does the transfemoral approach lead to longer life, but it’s safer,” said Dr. Conrotto.
But Dr. Michael A. Borger, director of the cardiovascular institute at Columbia University Medical Center, New York, had his reservations about drawing any practice-changing conclusion from the study. In many centers, the transfemoral approach is the preferred method, so naturally only sicker patients undergo transapical TAVR, “and those patients are going to have worse outcomes. So no matter how much they try with statistics, they will not be able to account for that selection bias. And really, the only way to know is with a randomized trial, but there’s no desire within the cardiology community for a randomized trial,” he said, citing the current widespread preference for the transfemoral approach.
Dr. Conrotto and Dr. Borger had no disclosures.
On Twitter @naseemmiller
BARCELONA – The transfemoral approach to aortic valve replacement is associated with lower risk of death, stroke, and bleeding, compared with the more invasive transapical approach, according to a meta-analysis of more than a dozen studies.
After adjustment for baseline characteristics, Italian researchers found that, compared with patients who underwent transapical transcatheter aortic valve replacement (TAVR), the transfemoral group was nearly 20% less likely to die within 30 days and during the first year after the procedure. The transfemoral group also was significantly less likely to have periprocedural bleeding or stroke.
Although the findings should be viewed as hypothesis generating, they suggest that “transapical access should be reserved as a last option in TAVR patients. This choice may guarantee less mortality, less stroke, and less bleeding in this frail and elderly population,” Dr. Federico Conrotto said at the annual congress of the European Society of Cardiology.
Although the transfemoral approach for aortic valve replacement is completely percutaneous, the transapical approach is more invasive and involves the direct puncture of the left ventricle. Also, the transapical approach is mostly reserved for patients in whom femoral vessels are unapproachable. These patients also turn out to be sicker, hence making it difficult to compare the two approaches, and there are no randomized trials comparing the two, said Dr. Conrotto of Città della Salute e della Scienza Hospital in Turin, Italy.
In the absence of randomized trials, Dr. Conrotto and his colleagues selected 13 studies that reported the adjustments for clinical baseline characteristics and reported the baseline, periprocedural, and midterm (median, 365 days) outcomes for patients who underwent transfemoral and transapical TAVR.
Their primary endpoint was all-cause mortality at 1-year follow-up. The secondary endpoint was 30-day mortality and in-hospital complications, including bleeding and stroke.
In total, the studies included 10,468 patients who underwent TAVR between 2005 and 2012. The patients’ median age was 82 years and half were men: one-fourth had diabetes, 18% had renal dysfunction, 61% had coronary artery disease, and the average ejection fraction was 50%. Almost 70% of the TAVR procedures were performed transfemorally.
Results showed that patients who underwent the transfemoral approach were 15% less likely to die at 365 days following TAVR and 20% less likely to die at 30 days, compared with those who underwent the transapical approach, Dr. Conrotto said. Both differences were statistically significant.
Those who underwent the transfemoral approach were almost 30% less likely to have periprocedural bleeding and 10% less likely to have a periprocedural stroke. Again, both differences were statistically significant, he noted.
“Not only does the transfemoral approach lead to longer life, but it’s safer,” said Dr. Conrotto.
But Dr. Michael A. Borger, director of the cardiovascular institute at Columbia University Medical Center, New York, had his reservations about drawing any practice-changing conclusion from the study. In many centers, the transfemoral approach is the preferred method, so naturally only sicker patients undergo transapical TAVR, “and those patients are going to have worse outcomes. So no matter how much they try with statistics, they will not be able to account for that selection bias. And really, the only way to know is with a randomized trial, but there’s no desire within the cardiology community for a randomized trial,” he said, citing the current widespread preference for the transfemoral approach.
Dr. Conrotto and Dr. Borger had no disclosures.
On Twitter @naseemmiller
BARCELONA – The transfemoral approach to aortic valve replacement is associated with lower risk of death, stroke, and bleeding, compared with the more invasive transapical approach, according to a meta-analysis of more than a dozen studies.
After adjustment for baseline characteristics, Italian researchers found that, compared with patients who underwent transapical transcatheter aortic valve replacement (TAVR), the transfemoral group was nearly 20% less likely to die within 30 days and during the first year after the procedure. The transfemoral group also was significantly less likely to have periprocedural bleeding or stroke.
Although the findings should be viewed as hypothesis generating, they suggest that “transapical access should be reserved as a last option in TAVR patients. This choice may guarantee less mortality, less stroke, and less bleeding in this frail and elderly population,” Dr. Federico Conrotto said at the annual congress of the European Society of Cardiology.
Although the transfemoral approach for aortic valve replacement is completely percutaneous, the transapical approach is more invasive and involves the direct puncture of the left ventricle. Also, the transapical approach is mostly reserved for patients in whom femoral vessels are unapproachable. These patients also turn out to be sicker, hence making it difficult to compare the two approaches, and there are no randomized trials comparing the two, said Dr. Conrotto of Città della Salute e della Scienza Hospital in Turin, Italy.
In the absence of randomized trials, Dr. Conrotto and his colleagues selected 13 studies that reported the adjustments for clinical baseline characteristics and reported the baseline, periprocedural, and midterm (median, 365 days) outcomes for patients who underwent transfemoral and transapical TAVR.
Their primary endpoint was all-cause mortality at 1-year follow-up. The secondary endpoint was 30-day mortality and in-hospital complications, including bleeding and stroke.
In total, the studies included 10,468 patients who underwent TAVR between 2005 and 2012. The patients’ median age was 82 years and half were men: one-fourth had diabetes, 18% had renal dysfunction, 61% had coronary artery disease, and the average ejection fraction was 50%. Almost 70% of the TAVR procedures were performed transfemorally.
Results showed that patients who underwent the transfemoral approach were 15% less likely to die at 365 days following TAVR and 20% less likely to die at 30 days, compared with those who underwent the transapical approach, Dr. Conrotto said. Both differences were statistically significant.
Those who underwent the transfemoral approach were almost 30% less likely to have periprocedural bleeding and 10% less likely to have a periprocedural stroke. Again, both differences were statistically significant, he noted.
“Not only does the transfemoral approach lead to longer life, but it’s safer,” said Dr. Conrotto.
But Dr. Michael A. Borger, director of the cardiovascular institute at Columbia University Medical Center, New York, had his reservations about drawing any practice-changing conclusion from the study. In many centers, the transfemoral approach is the preferred method, so naturally only sicker patients undergo transapical TAVR, “and those patients are going to have worse outcomes. So no matter how much they try with statistics, they will not be able to account for that selection bias. And really, the only way to know is with a randomized trial, but there’s no desire within the cardiology community for a randomized trial,” he said, citing the current widespread preference for the transfemoral approach.
Dr. Conrotto and Dr. Borger had no disclosures.
On Twitter @naseemmiller
AT THE ESC CONGRESS 2014
Key clinical finding:The improved outcomes with transfemoral TAVR may be a result of patient selection because transapical TAVR is used primarily in patients unsuitable for the transfemoral procedure.
Major finding:Compared with transapical approach, patients who underwent transfemoral TAVR were nearly 20% less likely to die within 30 days and during the first year after the procedure.
Data source: Meta-analysis of 13 studies involving almost 10,500 patients.
Disclosures:Dr. Conrotto and Dr. Borger had no disclosures.
ESC issues cascade of new cardiology practice guidelines
BARCELONA – Routine use of a new risk calculator tool to estimate the 5-year risk of sudden cardiac death is recommended in all patients with hypertrophic cardiomyopathy in updated guidelines launched at the annual congress of the European Society of Cardiology.
“Based on that estimate, you can now have an intelligent conversation with the patient about what the threshold is for implantable cardioverter-defibrillator placement given an individual’s risk/benefit ratio,” explained Dr. Perry M. Elliott, chair of the guidelines task force and professor of inherited cardiovascular disease at The Heart Hospital, London.
The hypertrophic cardiomyopathy guidelines were among five new practice guidelines introduced at the annual congress. Others addressed acute pulmonary embolism, noncardiac surgery, myocardial revascularization, and aortic diseases.
Here are selected highlights of the new guidelines:
• Hypertrophic cardiomyopathy. The novel sudden cardiac death risk prognostication tool, known as HCM Risk-SCD, is a major innovation in the new guidelines. The risk calculator grew out of a recent multicenter study of nearly 3,700 patients conducted by Dr. Elliott and his coinvestigators (Eur. Heart J. 2014;35:2010-20).
Now physicians can plug a series of validated risk factors into an online calculator and receive an estimated 5-year risk figure. The input factors include maximal wall thickness, left atrial diameter, family history of sudden cardiac death, unexplained syncope, and maximal left ventricular outflow gradient. If the estimated 5-year risk is 6% or more and the patient has a life expectancy of more than a year, implantation of a cardioverter-defibrillator should be seriously considered, according to the guidelines.
“What we’re trying to do in these guidelines is to change a mind-set, because hypertrophic cardiomyopathy is not really a diagnosis; it actually represents a family of diseases. Running throughout this entire document is an emphasis on individualization, from diagnosis all the way through treatment,” Dr. Elliott said. “There’s a strong emphasis on making a specific diagnosis if you possibly can, because these subtypes of cardiomyopathy have totally different natural histories and in the future will have very different treatments.”
Other highlights of the new guidelines include a stepwise approach to management of left ventricular outflow tract obstruction and heart failure, advice on reproduction, suggestions regarding simple laboratory tests with diagnostic utility, and guidance on the effective utilization of ECG, echocardiography, and cardiac magnetic resonance imaging.
“We show a number of echocardiographic red flags, some of which are perhaps not readily appreciated in everyday practice,” Dr. Elliott said. “For example, the presence of hypertrophy with impaired systolic function immediately narrows down your diagnosis to one of five or six different conditions.”
• Pulmonary embolism. The new guidelines place the novel oral anticoagulants rivaroxaban (Xarelto), apixaban (Eliquis), dabigatran (Pradaxa), and edoxaban (Savaysa) on equal footing with once-standard warfarin.
Task force chair Dr. Stavros Konstantinides highlighted as new in the 2014 guidelines a strong recommendation that patients who do not have a high-risk pulmonary embolism – that is, those who are not in shock or hypotensive – should be scored using the Pulmonary Embolism Severity Index or another validated clinical risk prediction score. The purpose is to distinguish between those at low versus intermediate risk.
Those at intermediate risk should undergo right ventricular imaging via CT or echocardiography, along with a biomarker test for myocardial injury. If both the imaging study and biomarker are positive, the patient is classified as being at intermediate-high risk; if not, intermediate-low. This has treatment implications, since it’s recommended that systemic thrombolysis be considered only in those with intermediate-high-risk pulmonary embolism and clinical signs of hemodynamic decompensation, explained Dr. Konstantinides of University Medical Center in Mainz (Germany).
• Noncardiac surgery. Perioperative initiation of beta-blocker therapy is no longer recommended routinely, but may be considered in patients scheduled for high-risk noncardiac surgery who also have two or more cardiovascular risk factors or known ischemic heart disease. Atenolol and bisoprolol are recommended as the perioperative beta-blockers of choice. If a patient is already on a beta-blocker prior to surgery, the drug can be continued perioperatively, according to task force cochair Dr. Juhani Knuuti of the University of Turku (Finland).
The guidelines emphasize that prophylactic coronary revascularization is seldom indicated in patients undergoing noncardiac surgery that has a low or intermediate cardiovascular risk.
• Myocardial revascularization. These guidelines, with more than 300 recommendations, are the lengthiest of the five new sets of guidelines. The myocardial revascularization guidelines rely heavily upon the findings of a recent meta-analysis conducted by task force cochairs Dr. Stephan Windecker of Bern (Switzerland) University and Dr. Philippe Kohl of the University of Liege (Belgium) and their coinvestigators. The meta-analysis encompassed 100 randomized controlled trials with nearly 94,000 randomized patients and more than 262,000 patient-years of follow-u p (BMJ 2014 June 23 [doi: 10.1136.bmj.g3859]).
The guidelines introduce substantial changes in the recommended method of revascularization in various situations. There is a strong emphasis on risk stratification using the SYNTAX score; in fact, the guidelines include a primer on how to calculate it.
Based largely on the results of the meta-analysis as well as 5-year follow-up in the SYNTAX trial (Lancet 2013;381:629-38), the guidelines now regard percutaneous coronary intervention as equivalent to coronary artery bypass graft surgery in several patient subsets where CABG was previously preferred. These include patients with left main or triple-vessel disease and a SYNTAX score below 22. In patients with one- or two-vessel disease and proximal left anterior descending coronary artery stenosis, both PCI and CABG get a Class I recommendation.
The new guidelines emphasize the value of intracoronary fractional flow reserve measurement to identify hemodynamically relevant lesions warranting revascularization in patients with stable coronary artery disease lacking noninvasive evidence of ischemia.
• Aortic diseases. Routine screening for abdominal aortic aneurysm via ultrasound is recommended in all men over age 65 and “may be considered” in women over 65 with a history of smoking, according to the new guidelines. That’s a much stronger proscreening stance than has been taken by the U.S. Preventive Services Task Force.
Former ESC guidelines were confined to aortic dissection and focused on the thoracic aorta. The new guidelines expand in scope to include intramural hematomas, thoracic and abdominal aneurysms, aortic valve lesions, and penetrating ulcers.
“We are not only dealing with the thoracic aorta, but are taking the holistic view of the aorta as one organ,” according to guidelines task force cochair Dr. Raimund Erbel, professor of medicine at the University of Essen (Germany).
“When an aortic aneurysm is identified at any location, assessment of the entire aorta and aortic valve is recommended at baseline and during follow-up,” he added.
All of the new guidelines can be downloaded in their entirely at the ESC website (escardio.org/guidelines).
BARCELONA – Routine use of a new risk calculator tool to estimate the 5-year risk of sudden cardiac death is recommended in all patients with hypertrophic cardiomyopathy in updated guidelines launched at the annual congress of the European Society of Cardiology.
“Based on that estimate, you can now have an intelligent conversation with the patient about what the threshold is for implantable cardioverter-defibrillator placement given an individual’s risk/benefit ratio,” explained Dr. Perry M. Elliott, chair of the guidelines task force and professor of inherited cardiovascular disease at The Heart Hospital, London.
The hypertrophic cardiomyopathy guidelines were among five new practice guidelines introduced at the annual congress. Others addressed acute pulmonary embolism, noncardiac surgery, myocardial revascularization, and aortic diseases.
Here are selected highlights of the new guidelines:
• Hypertrophic cardiomyopathy. The novel sudden cardiac death risk prognostication tool, known as HCM Risk-SCD, is a major innovation in the new guidelines. The risk calculator grew out of a recent multicenter study of nearly 3,700 patients conducted by Dr. Elliott and his coinvestigators (Eur. Heart J. 2014;35:2010-20).
Now physicians can plug a series of validated risk factors into an online calculator and receive an estimated 5-year risk figure. The input factors include maximal wall thickness, left atrial diameter, family history of sudden cardiac death, unexplained syncope, and maximal left ventricular outflow gradient. If the estimated 5-year risk is 6% or more and the patient has a life expectancy of more than a year, implantation of a cardioverter-defibrillator should be seriously considered, according to the guidelines.
“What we’re trying to do in these guidelines is to change a mind-set, because hypertrophic cardiomyopathy is not really a diagnosis; it actually represents a family of diseases. Running throughout this entire document is an emphasis on individualization, from diagnosis all the way through treatment,” Dr. Elliott said. “There’s a strong emphasis on making a specific diagnosis if you possibly can, because these subtypes of cardiomyopathy have totally different natural histories and in the future will have very different treatments.”
Other highlights of the new guidelines include a stepwise approach to management of left ventricular outflow tract obstruction and heart failure, advice on reproduction, suggestions regarding simple laboratory tests with diagnostic utility, and guidance on the effective utilization of ECG, echocardiography, and cardiac magnetic resonance imaging.
“We show a number of echocardiographic red flags, some of which are perhaps not readily appreciated in everyday practice,” Dr. Elliott said. “For example, the presence of hypertrophy with impaired systolic function immediately narrows down your diagnosis to one of five or six different conditions.”
• Pulmonary embolism. The new guidelines place the novel oral anticoagulants rivaroxaban (Xarelto), apixaban (Eliquis), dabigatran (Pradaxa), and edoxaban (Savaysa) on equal footing with once-standard warfarin.
Task force chair Dr. Stavros Konstantinides highlighted as new in the 2014 guidelines a strong recommendation that patients who do not have a high-risk pulmonary embolism – that is, those who are not in shock or hypotensive – should be scored using the Pulmonary Embolism Severity Index or another validated clinical risk prediction score. The purpose is to distinguish between those at low versus intermediate risk.
Those at intermediate risk should undergo right ventricular imaging via CT or echocardiography, along with a biomarker test for myocardial injury. If both the imaging study and biomarker are positive, the patient is classified as being at intermediate-high risk; if not, intermediate-low. This has treatment implications, since it’s recommended that systemic thrombolysis be considered only in those with intermediate-high-risk pulmonary embolism and clinical signs of hemodynamic decompensation, explained Dr. Konstantinides of University Medical Center in Mainz (Germany).
• Noncardiac surgery. Perioperative initiation of beta-blocker therapy is no longer recommended routinely, but may be considered in patients scheduled for high-risk noncardiac surgery who also have two or more cardiovascular risk factors or known ischemic heart disease. Atenolol and bisoprolol are recommended as the perioperative beta-blockers of choice. If a patient is already on a beta-blocker prior to surgery, the drug can be continued perioperatively, according to task force cochair Dr. Juhani Knuuti of the University of Turku (Finland).
The guidelines emphasize that prophylactic coronary revascularization is seldom indicated in patients undergoing noncardiac surgery that has a low or intermediate cardiovascular risk.
• Myocardial revascularization. These guidelines, with more than 300 recommendations, are the lengthiest of the five new sets of guidelines. The myocardial revascularization guidelines rely heavily upon the findings of a recent meta-analysis conducted by task force cochairs Dr. Stephan Windecker of Bern (Switzerland) University and Dr. Philippe Kohl of the University of Liege (Belgium) and their coinvestigators. The meta-analysis encompassed 100 randomized controlled trials with nearly 94,000 randomized patients and more than 262,000 patient-years of follow-u p (BMJ 2014 June 23 [doi: 10.1136.bmj.g3859]).
The guidelines introduce substantial changes in the recommended method of revascularization in various situations. There is a strong emphasis on risk stratification using the SYNTAX score; in fact, the guidelines include a primer on how to calculate it.
Based largely on the results of the meta-analysis as well as 5-year follow-up in the SYNTAX trial (Lancet 2013;381:629-38), the guidelines now regard percutaneous coronary intervention as equivalent to coronary artery bypass graft surgery in several patient subsets where CABG was previously preferred. These include patients with left main or triple-vessel disease and a SYNTAX score below 22. In patients with one- or two-vessel disease and proximal left anterior descending coronary artery stenosis, both PCI and CABG get a Class I recommendation.
The new guidelines emphasize the value of intracoronary fractional flow reserve measurement to identify hemodynamically relevant lesions warranting revascularization in patients with stable coronary artery disease lacking noninvasive evidence of ischemia.
• Aortic diseases. Routine screening for abdominal aortic aneurysm via ultrasound is recommended in all men over age 65 and “may be considered” in women over 65 with a history of smoking, according to the new guidelines. That’s a much stronger proscreening stance than has been taken by the U.S. Preventive Services Task Force.
Former ESC guidelines were confined to aortic dissection and focused on the thoracic aorta. The new guidelines expand in scope to include intramural hematomas, thoracic and abdominal aneurysms, aortic valve lesions, and penetrating ulcers.
“We are not only dealing with the thoracic aorta, but are taking the holistic view of the aorta as one organ,” according to guidelines task force cochair Dr. Raimund Erbel, professor of medicine at the University of Essen (Germany).
“When an aortic aneurysm is identified at any location, assessment of the entire aorta and aortic valve is recommended at baseline and during follow-up,” he added.
All of the new guidelines can be downloaded in their entirely at the ESC website (escardio.org/guidelines).
BARCELONA – Routine use of a new risk calculator tool to estimate the 5-year risk of sudden cardiac death is recommended in all patients with hypertrophic cardiomyopathy in updated guidelines launched at the annual congress of the European Society of Cardiology.
“Based on that estimate, you can now have an intelligent conversation with the patient about what the threshold is for implantable cardioverter-defibrillator placement given an individual’s risk/benefit ratio,” explained Dr. Perry M. Elliott, chair of the guidelines task force and professor of inherited cardiovascular disease at The Heart Hospital, London.
The hypertrophic cardiomyopathy guidelines were among five new practice guidelines introduced at the annual congress. Others addressed acute pulmonary embolism, noncardiac surgery, myocardial revascularization, and aortic diseases.
Here are selected highlights of the new guidelines:
• Hypertrophic cardiomyopathy. The novel sudden cardiac death risk prognostication tool, known as HCM Risk-SCD, is a major innovation in the new guidelines. The risk calculator grew out of a recent multicenter study of nearly 3,700 patients conducted by Dr. Elliott and his coinvestigators (Eur. Heart J. 2014;35:2010-20).
Now physicians can plug a series of validated risk factors into an online calculator and receive an estimated 5-year risk figure. The input factors include maximal wall thickness, left atrial diameter, family history of sudden cardiac death, unexplained syncope, and maximal left ventricular outflow gradient. If the estimated 5-year risk is 6% or more and the patient has a life expectancy of more than a year, implantation of a cardioverter-defibrillator should be seriously considered, according to the guidelines.
“What we’re trying to do in these guidelines is to change a mind-set, because hypertrophic cardiomyopathy is not really a diagnosis; it actually represents a family of diseases. Running throughout this entire document is an emphasis on individualization, from diagnosis all the way through treatment,” Dr. Elliott said. “There’s a strong emphasis on making a specific diagnosis if you possibly can, because these subtypes of cardiomyopathy have totally different natural histories and in the future will have very different treatments.”
Other highlights of the new guidelines include a stepwise approach to management of left ventricular outflow tract obstruction and heart failure, advice on reproduction, suggestions regarding simple laboratory tests with diagnostic utility, and guidance on the effective utilization of ECG, echocardiography, and cardiac magnetic resonance imaging.
“We show a number of echocardiographic red flags, some of which are perhaps not readily appreciated in everyday practice,” Dr. Elliott said. “For example, the presence of hypertrophy with impaired systolic function immediately narrows down your diagnosis to one of five or six different conditions.”
• Pulmonary embolism. The new guidelines place the novel oral anticoagulants rivaroxaban (Xarelto), apixaban (Eliquis), dabigatran (Pradaxa), and edoxaban (Savaysa) on equal footing with once-standard warfarin.
Task force chair Dr. Stavros Konstantinides highlighted as new in the 2014 guidelines a strong recommendation that patients who do not have a high-risk pulmonary embolism – that is, those who are not in shock or hypotensive – should be scored using the Pulmonary Embolism Severity Index or another validated clinical risk prediction score. The purpose is to distinguish between those at low versus intermediate risk.
Those at intermediate risk should undergo right ventricular imaging via CT or echocardiography, along with a biomarker test for myocardial injury. If both the imaging study and biomarker are positive, the patient is classified as being at intermediate-high risk; if not, intermediate-low. This has treatment implications, since it’s recommended that systemic thrombolysis be considered only in those with intermediate-high-risk pulmonary embolism and clinical signs of hemodynamic decompensation, explained Dr. Konstantinides of University Medical Center in Mainz (Germany).
• Noncardiac surgery. Perioperative initiation of beta-blocker therapy is no longer recommended routinely, but may be considered in patients scheduled for high-risk noncardiac surgery who also have two or more cardiovascular risk factors or known ischemic heart disease. Atenolol and bisoprolol are recommended as the perioperative beta-blockers of choice. If a patient is already on a beta-blocker prior to surgery, the drug can be continued perioperatively, according to task force cochair Dr. Juhani Knuuti of the University of Turku (Finland).
The guidelines emphasize that prophylactic coronary revascularization is seldom indicated in patients undergoing noncardiac surgery that has a low or intermediate cardiovascular risk.
• Myocardial revascularization. These guidelines, with more than 300 recommendations, are the lengthiest of the five new sets of guidelines. The myocardial revascularization guidelines rely heavily upon the findings of a recent meta-analysis conducted by task force cochairs Dr. Stephan Windecker of Bern (Switzerland) University and Dr. Philippe Kohl of the University of Liege (Belgium) and their coinvestigators. The meta-analysis encompassed 100 randomized controlled trials with nearly 94,000 randomized patients and more than 262,000 patient-years of follow-u p (BMJ 2014 June 23 [doi: 10.1136.bmj.g3859]).
The guidelines introduce substantial changes in the recommended method of revascularization in various situations. There is a strong emphasis on risk stratification using the SYNTAX score; in fact, the guidelines include a primer on how to calculate it.
Based largely on the results of the meta-analysis as well as 5-year follow-up in the SYNTAX trial (Lancet 2013;381:629-38), the guidelines now regard percutaneous coronary intervention as equivalent to coronary artery bypass graft surgery in several patient subsets where CABG was previously preferred. These include patients with left main or triple-vessel disease and a SYNTAX score below 22. In patients with one- or two-vessel disease and proximal left anterior descending coronary artery stenosis, both PCI and CABG get a Class I recommendation.
The new guidelines emphasize the value of intracoronary fractional flow reserve measurement to identify hemodynamically relevant lesions warranting revascularization in patients with stable coronary artery disease lacking noninvasive evidence of ischemia.
• Aortic diseases. Routine screening for abdominal aortic aneurysm via ultrasound is recommended in all men over age 65 and “may be considered” in women over 65 with a history of smoking, according to the new guidelines. That’s a much stronger proscreening stance than has been taken by the U.S. Preventive Services Task Force.
Former ESC guidelines were confined to aortic dissection and focused on the thoracic aorta. The new guidelines expand in scope to include intramural hematomas, thoracic and abdominal aneurysms, aortic valve lesions, and penetrating ulcers.
“We are not only dealing with the thoracic aorta, but are taking the holistic view of the aorta as one organ,” according to guidelines task force cochair Dr. Raimund Erbel, professor of medicine at the University of Essen (Germany).
“When an aortic aneurysm is identified at any location, assessment of the entire aorta and aortic valve is recommended at baseline and during follow-up,” he added.
All of the new guidelines can be downloaded in their entirely at the ESC website (escardio.org/guidelines).
AT THE ESC CONGRESS 2014
Mechanical heart valves create high pregnancy risk
BARCELONA – Women with mechanical heart valves who become pregnant face a very-high-risk pregnancy, with a 58% rate of an uncomplicated pregnancy resulting in a live birth, according to international registry data collected since 2007.
Pregnant women at high risk because of a mechanical heart valve need management by a multidisciplinary team at a referral center that focuses on these cases, a type of care that many of these women do not receive today, Dr. Jolien W. Roos-Hesselink said at the annual congress of the European Society of Cardiology.
“We believe management of these women needs to be better structured and organized,” said Dr. Roos-Hesselink, professor and head of the department of congenital cardiology at Erasmus Medical Center in Rotterdam, the Netherlands. “Pregnancy is a time of risk for any woman with structural heart disease, but for those with a mechanical valve are really high-risk patients,” she said in an interview.
“Most of these women are now cared for by a general cardiologist. They need a specialist in obstetric cardiology,” as well as care from other experts with experience in the types of complications these woman develop, said Dr. Roger J.C. Hall, professor of cardiology at Norfolk and Norwich (U.K.) University Hospital.
The data also showed that physicians around the world used any one of seven different anticoagulant regimens during these pregnancies, a strikingly high number that highlights uncertainty about which regimen is best, although heparin use during the first trimester was linked with a higher rate of valve thrombosis. The various regimens use different combinations of periods of treatment with unfractionated heparin, low-molecular-weight heparin, or a vitamin K antagonist drug during the first trimester, during weeks 14-36, and during the last weeks of pregnancy.
“We found large differences in management among different countries, physicians, and among individual patients. All the regimens have advantages and disadvantages” and are based on expert opinion with no prospect for a randomized, controlled trial, said Dr. Roos-Hesselink. For now, the numbers of women receiving each of the seven regimens remains too small for statistical analysis, but the researchers hope that eventually larger numbers may start to reveal which regimens work best, said Dr. Hall.
However, the available data showed two clear trends: Treatment with vitamin K antagonists was tied to an increased rate of miscarriages, and treatment with heparin during the first trimester was associated with an increased rate of valve thrombosis, noted Dr. Roos-Hesselink.
One other notable finding was that the risks faced by women with mechanical heart valves far exceeded the risk seen in women with tissue valves, and in women with other forms of mechanical heart disease but no valve prostheses. Adolescents and young women who need a heart valve should be part of a shared decision process that reviews the pros and cons of a mechanical and tissue valve, said Dr. Roos-Hesselink and Dr. Hall. A tissue valve is less durable, and so typically requires replacement sooner than does a mechanical valve. But in the current study, the pregnancy loss and complication rates among the 134 women with a tissue valve roughly matched the rates among the 2,620 women with no valve prosthesis, while the rates among 212 women with a mechanical valve ran much higher.
The Registry of Pregnancy and Cardiac Diseases began in 2007 through an initiative of two interest groups of the European Society of Cardiology, the valve group and the congenital heart disease group (Eur. Heart J. 2013;34:657-65). By September 2014, the registry had enrolled more than 3,600 pregnancies. The current report focused on the first 2,966 women enrolled, with an average age of 29 years. Slightly more than half the enrolled women had congenital heart disease, slightly fewer than a third had valvular heart disease (usually because of rheumatic heart disease), 7% had cardiomyopathy, and smaller number of women had other etiologies.
Maternal mortality averaged 1.4% for women with mechanical valves, 1.5% for those with tissue valves, and 0.2% for everyone else. Miscarriage rates were 16% for mothers with mechanical valves and 2% for everyone else, including those with tissues valves. Fetal mortality was 3% among women with mechanical valves and less than 1% for everyone else. Thrombotic and hemorrhagic events occurred in about 29% of women with mechanical valves, compared with less than 6% in everyone else. Ten of the women with mechanical valves (5%) developed valve thrombosis. The live birth rate was 80% for women with mechanical valves and 95% or better for everyone else.
Dr. Roos-Hesselink and Dr. Hall had no disclosures.
On Twitter @mitchelzoler
Dr. Hossein Almassi, FCCP, comments: One of the toughest decisions in valvular heart surgery is the selection of a valve prosthesis for a young female. Historically, age has been the major deciding factor in selecting a mechanical valve over a tissue valve. The current report is a testament to this difficulty, showing a lack of a standardized anticoagulation regimen and a much higher rate of pregnancy loss and complications with mechanical heart valves. Availability of transcatheter valve technology may make the tissue valves more attractive for this group of patients. Clearly, the care for these women would be best provided by a multidisciplinary team of specialists.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: One of the toughest decisions in valvular heart surgery is the selection of a valve prosthesis for a young female. Historically, age has been the major deciding factor in selecting a mechanical valve over a tissue valve. The current report is a testament to this difficulty, showing a lack of a standardized anticoagulation regimen and a much higher rate of pregnancy loss and complications with mechanical heart valves. Availability of transcatheter valve technology may make the tissue valves more attractive for this group of patients. Clearly, the care for these women would be best provided by a multidisciplinary team of specialists.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: One of the toughest decisions in valvular heart surgery is the selection of a valve prosthesis for a young female. Historically, age has been the major deciding factor in selecting a mechanical valve over a tissue valve. The current report is a testament to this difficulty, showing a lack of a standardized anticoagulation regimen and a much higher rate of pregnancy loss and complications with mechanical heart valves. Availability of transcatheter valve technology may make the tissue valves more attractive for this group of patients. Clearly, the care for these women would be best provided by a multidisciplinary team of specialists.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
BARCELONA – Women with mechanical heart valves who become pregnant face a very-high-risk pregnancy, with a 58% rate of an uncomplicated pregnancy resulting in a live birth, according to international registry data collected since 2007.
Pregnant women at high risk because of a mechanical heart valve need management by a multidisciplinary team at a referral center that focuses on these cases, a type of care that many of these women do not receive today, Dr. Jolien W. Roos-Hesselink said at the annual congress of the European Society of Cardiology.
“We believe management of these women needs to be better structured and organized,” said Dr. Roos-Hesselink, professor and head of the department of congenital cardiology at Erasmus Medical Center in Rotterdam, the Netherlands. “Pregnancy is a time of risk for any woman with structural heart disease, but for those with a mechanical valve are really high-risk patients,” she said in an interview.
“Most of these women are now cared for by a general cardiologist. They need a specialist in obstetric cardiology,” as well as care from other experts with experience in the types of complications these woman develop, said Dr. Roger J.C. Hall, professor of cardiology at Norfolk and Norwich (U.K.) University Hospital.
The data also showed that physicians around the world used any one of seven different anticoagulant regimens during these pregnancies, a strikingly high number that highlights uncertainty about which regimen is best, although heparin use during the first trimester was linked with a higher rate of valve thrombosis. The various regimens use different combinations of periods of treatment with unfractionated heparin, low-molecular-weight heparin, or a vitamin K antagonist drug during the first trimester, during weeks 14-36, and during the last weeks of pregnancy.
“We found large differences in management among different countries, physicians, and among individual patients. All the regimens have advantages and disadvantages” and are based on expert opinion with no prospect for a randomized, controlled trial, said Dr. Roos-Hesselink. For now, the numbers of women receiving each of the seven regimens remains too small for statistical analysis, but the researchers hope that eventually larger numbers may start to reveal which regimens work best, said Dr. Hall.
However, the available data showed two clear trends: Treatment with vitamin K antagonists was tied to an increased rate of miscarriages, and treatment with heparin during the first trimester was associated with an increased rate of valve thrombosis, noted Dr. Roos-Hesselink.
One other notable finding was that the risks faced by women with mechanical heart valves far exceeded the risk seen in women with tissue valves, and in women with other forms of mechanical heart disease but no valve prostheses. Adolescents and young women who need a heart valve should be part of a shared decision process that reviews the pros and cons of a mechanical and tissue valve, said Dr. Roos-Hesselink and Dr. Hall. A tissue valve is less durable, and so typically requires replacement sooner than does a mechanical valve. But in the current study, the pregnancy loss and complication rates among the 134 women with a tissue valve roughly matched the rates among the 2,620 women with no valve prosthesis, while the rates among 212 women with a mechanical valve ran much higher.
The Registry of Pregnancy and Cardiac Diseases began in 2007 through an initiative of two interest groups of the European Society of Cardiology, the valve group and the congenital heart disease group (Eur. Heart J. 2013;34:657-65). By September 2014, the registry had enrolled more than 3,600 pregnancies. The current report focused on the first 2,966 women enrolled, with an average age of 29 years. Slightly more than half the enrolled women had congenital heart disease, slightly fewer than a third had valvular heart disease (usually because of rheumatic heart disease), 7% had cardiomyopathy, and smaller number of women had other etiologies.
Maternal mortality averaged 1.4% for women with mechanical valves, 1.5% for those with tissue valves, and 0.2% for everyone else. Miscarriage rates were 16% for mothers with mechanical valves and 2% for everyone else, including those with tissues valves. Fetal mortality was 3% among women with mechanical valves and less than 1% for everyone else. Thrombotic and hemorrhagic events occurred in about 29% of women with mechanical valves, compared with less than 6% in everyone else. Ten of the women with mechanical valves (5%) developed valve thrombosis. The live birth rate was 80% for women with mechanical valves and 95% or better for everyone else.
Dr. Roos-Hesselink and Dr. Hall had no disclosures.
On Twitter @mitchelzoler
BARCELONA – Women with mechanical heart valves who become pregnant face a very-high-risk pregnancy, with a 58% rate of an uncomplicated pregnancy resulting in a live birth, according to international registry data collected since 2007.
Pregnant women at high risk because of a mechanical heart valve need management by a multidisciplinary team at a referral center that focuses on these cases, a type of care that many of these women do not receive today, Dr. Jolien W. Roos-Hesselink said at the annual congress of the European Society of Cardiology.
“We believe management of these women needs to be better structured and organized,” said Dr. Roos-Hesselink, professor and head of the department of congenital cardiology at Erasmus Medical Center in Rotterdam, the Netherlands. “Pregnancy is a time of risk for any woman with structural heart disease, but for those with a mechanical valve are really high-risk patients,” she said in an interview.
“Most of these women are now cared for by a general cardiologist. They need a specialist in obstetric cardiology,” as well as care from other experts with experience in the types of complications these woman develop, said Dr. Roger J.C. Hall, professor of cardiology at Norfolk and Norwich (U.K.) University Hospital.
The data also showed that physicians around the world used any one of seven different anticoagulant regimens during these pregnancies, a strikingly high number that highlights uncertainty about which regimen is best, although heparin use during the first trimester was linked with a higher rate of valve thrombosis. The various regimens use different combinations of periods of treatment with unfractionated heparin, low-molecular-weight heparin, or a vitamin K antagonist drug during the first trimester, during weeks 14-36, and during the last weeks of pregnancy.
“We found large differences in management among different countries, physicians, and among individual patients. All the regimens have advantages and disadvantages” and are based on expert opinion with no prospect for a randomized, controlled trial, said Dr. Roos-Hesselink. For now, the numbers of women receiving each of the seven regimens remains too small for statistical analysis, but the researchers hope that eventually larger numbers may start to reveal which regimens work best, said Dr. Hall.
However, the available data showed two clear trends: Treatment with vitamin K antagonists was tied to an increased rate of miscarriages, and treatment with heparin during the first trimester was associated with an increased rate of valve thrombosis, noted Dr. Roos-Hesselink.
One other notable finding was that the risks faced by women with mechanical heart valves far exceeded the risk seen in women with tissue valves, and in women with other forms of mechanical heart disease but no valve prostheses. Adolescents and young women who need a heart valve should be part of a shared decision process that reviews the pros and cons of a mechanical and tissue valve, said Dr. Roos-Hesselink and Dr. Hall. A tissue valve is less durable, and so typically requires replacement sooner than does a mechanical valve. But in the current study, the pregnancy loss and complication rates among the 134 women with a tissue valve roughly matched the rates among the 2,620 women with no valve prosthesis, while the rates among 212 women with a mechanical valve ran much higher.
The Registry of Pregnancy and Cardiac Diseases began in 2007 through an initiative of two interest groups of the European Society of Cardiology, the valve group and the congenital heart disease group (Eur. Heart J. 2013;34:657-65). By September 2014, the registry had enrolled more than 3,600 pregnancies. The current report focused on the first 2,966 women enrolled, with an average age of 29 years. Slightly more than half the enrolled women had congenital heart disease, slightly fewer than a third had valvular heart disease (usually because of rheumatic heart disease), 7% had cardiomyopathy, and smaller number of women had other etiologies.
Maternal mortality averaged 1.4% for women with mechanical valves, 1.5% for those with tissue valves, and 0.2% for everyone else. Miscarriage rates were 16% for mothers with mechanical valves and 2% for everyone else, including those with tissues valves. Fetal mortality was 3% among women with mechanical valves and less than 1% for everyone else. Thrombotic and hemorrhagic events occurred in about 29% of women with mechanical valves, compared with less than 6% in everyone else. Ten of the women with mechanical valves (5%) developed valve thrombosis. The live birth rate was 80% for women with mechanical valves and 95% or better for everyone else.
Dr. Roos-Hesselink and Dr. Hall had no disclosures.
On Twitter @mitchelzoler
AT ESC 2014
Key clinical point: Pregnant women with mechanical heart valves have a very high rate of pregnancy complications and miscarriages.
Major finding: The rate of live births without complications was 58% in women with a mechanical heart valve.
Data source: ROPAC registry of 2,966 pregnant women with structural heart disease from 132 centers in 48 countries.
Disclosures: Dr. Roos-Hesselink and Dr. Hall had no disclosures.