User login
STS: Score stratifies risks for isolated tricuspid valve surgery patients
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
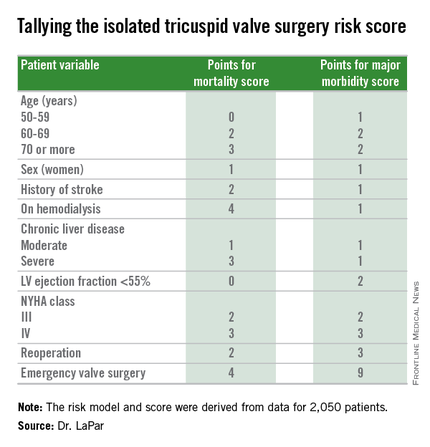
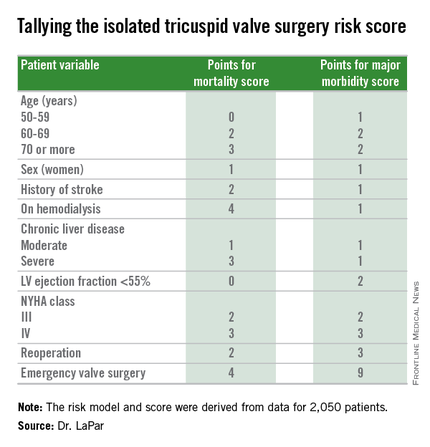
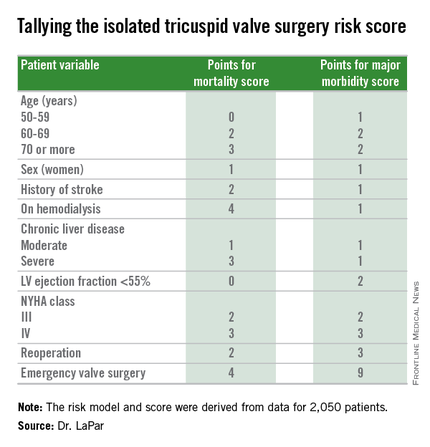
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
AT THE STS ANNUAL MEETING
Key clinical point: A risk-scoring system estimates a patient’s mortality and morbidity risk when undergoing isolated tricuspid valve surgery.
Major finding: The scoring system discriminated mortality risk from 2% to 34%, and major morbidity risk from 13% to 71%.
Data source: Analysis of 2,050 patients who underwent isolated tricuspid valve surgery in the STS Adult Cardiac Surgery Database.
Disclosures: Dr. LaPar had no disclosures.
VIDEO: Preventing healthcare acquired infections after CT surgery
PHOENIX – More and more attention is being paid to preventing healthcare acquired infections (HAIs) in the hospital setting, and the role of HAIs in cardiothoracic surgery is a particlularly important area of focus.
“The good news is that cardiothoracic surgeons are really good at preventing infections. There’s been a lot of pressure over the past many years to report infections after cardiothoracic surgery, and so they’ve gotten a lot of things right,” Dr. Emily Landon said in a video interview at the annual meeting of the Society of Thoracic Surgeons.
“However, patients that undergo cardiothoracic surgery are still at risk of the infections that plague everyone in hospitals ... all of these are a problem based on whatever the hospital’s current situation is.”
Dr. Landon, who is the medical director of antimicrobial stewardship and infection control at University of Chicago Medicine, Chicago, discussed how cardiothroacic surgeons can maintain their own good outcomes and how they can have a postive impact outside the OR on protecting their patients after surgery.
Dr. Landon reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – More and more attention is being paid to preventing healthcare acquired infections (HAIs) in the hospital setting, and the role of HAIs in cardiothoracic surgery is a particlularly important area of focus.
“The good news is that cardiothoracic surgeons are really good at preventing infections. There’s been a lot of pressure over the past many years to report infections after cardiothoracic surgery, and so they’ve gotten a lot of things right,” Dr. Emily Landon said in a video interview at the annual meeting of the Society of Thoracic Surgeons.
“However, patients that undergo cardiothoracic surgery are still at risk of the infections that plague everyone in hospitals ... all of these are a problem based on whatever the hospital’s current situation is.”
Dr. Landon, who is the medical director of antimicrobial stewardship and infection control at University of Chicago Medicine, Chicago, discussed how cardiothroacic surgeons can maintain their own good outcomes and how they can have a postive impact outside the OR on protecting their patients after surgery.
Dr. Landon reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – More and more attention is being paid to preventing healthcare acquired infections (HAIs) in the hospital setting, and the role of HAIs in cardiothoracic surgery is a particlularly important area of focus.
“The good news is that cardiothoracic surgeons are really good at preventing infections. There’s been a lot of pressure over the past many years to report infections after cardiothoracic surgery, and so they’ve gotten a lot of things right,” Dr. Emily Landon said in a video interview at the annual meeting of the Society of Thoracic Surgeons.
“However, patients that undergo cardiothoracic surgery are still at risk of the infections that plague everyone in hospitals ... all of these are a problem based on whatever the hospital’s current situation is.”
Dr. Landon, who is the medical director of antimicrobial stewardship and infection control at University of Chicago Medicine, Chicago, discussed how cardiothroacic surgeons can maintain their own good outcomes and how they can have a postive impact outside the OR on protecting their patients after surgery.
Dr. Landon reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE STS ANNUAL MEETING
STS: Hybrid thoracic suite leverages CT’s imaging sensitivity
PHOENIX – Using CT imaging to detect lung cancers in people at high risk for developing it has made it possible to find small tumors with substantially increased sensitivity than is possible with radiography, However, this approach has posed a new challenge to thoracic surgeons: How to visualize these nodules – subcentimeter and nonpalpable – for biopsy or for resection?
The answer may be the hybrid thoracic operating room developed by Dr. Kazuhiro Yasufuku and his associates at Toronto General Hospital, a novel surgical suite that he described at the annual meeting of the Society of Thoracic Surgeons.
Dr. Yasufuku and his team began using the hybrid operating room on an investigational basis in 2013 and have now done about 50 cases as part of several research protocols. The trials address the feasibility of resection, biopsy, and nodule localization, as well as whether the hybrid approach reduces the amount of radiation exposure to both patients and to the surgical team, he said. They plan to report some of their initial results later this year.
The Toronto group assembled the hybrid array of equipment into a single operating room that includes both a dual-source, dual-energy CT scanner and a robotic cone-beam CT scanner, equipment for minimally invasive procedures including video-assisted thoracoscopic and robotic surgery, and advanced endoscopic technology including endobronchial ultrasound and navigational bronchoscopy. “We use innovative methods that we already know about, but bring them all together” within a single space, Dr. Yasufuku explained. “Rather than having patients go to several locations, we can do everything at the same time in one room.”
Perhaps the most novel aspect of this operating room is inclusion of a robotic cone-beam CT scanner, which uses mobile, flat CT-imaging panels that overcome the limitations of a conventional, fixed CT scanner. “They scan the patient and then we can retract them and get them out of the way” to better facilitate surgery, he said in an interview.
“We do not have a culture in thoracic surgery of using imaging during surgery,” said Dr. Yasufuku, director of the interventional thoracic surgery program at the University of Toronto. Hybrid operating rooms using noninvasive or minimally invasive equipment and procedures have become commonplace for cardiovascular surgeons and cardiac interventionalists, but this approach has generally not yet been applied to thoracic surgery for cancer, in large part because of the imaging limitations, he said. “It is difficult to perform video-assisted thorascopic surgery using fixed CT.”
Bronchoscopic technologies provide additional, important tools for minimally invasive thoracic surgery. “We use the hybrid operating room to mark small [nonpalpable] lesions.” One approach to marking is to place a microcoil within the nodule with a percutaneous needle. Another approach is to tag the nodule with a fluorescent dye using navigational bronchoscopy.
Dr. Yasufuku also emphasized that the hybrid operating room will also be valuable when new, minimally invasive, nonsurgical therapeutic options for treatment of lung cancer become available in the near future.
Dr. Yasufuku said that he had no relevant disclosures.
On Twitter @mitchelzoler
PHOENIX – Using CT imaging to detect lung cancers in people at high risk for developing it has made it possible to find small tumors with substantially increased sensitivity than is possible with radiography, However, this approach has posed a new challenge to thoracic surgeons: How to visualize these nodules – subcentimeter and nonpalpable – for biopsy or for resection?
The answer may be the hybrid thoracic operating room developed by Dr. Kazuhiro Yasufuku and his associates at Toronto General Hospital, a novel surgical suite that he described at the annual meeting of the Society of Thoracic Surgeons.
Dr. Yasufuku and his team began using the hybrid operating room on an investigational basis in 2013 and have now done about 50 cases as part of several research protocols. The trials address the feasibility of resection, biopsy, and nodule localization, as well as whether the hybrid approach reduces the amount of radiation exposure to both patients and to the surgical team, he said. They plan to report some of their initial results later this year.
The Toronto group assembled the hybrid array of equipment into a single operating room that includes both a dual-source, dual-energy CT scanner and a robotic cone-beam CT scanner, equipment for minimally invasive procedures including video-assisted thoracoscopic and robotic surgery, and advanced endoscopic technology including endobronchial ultrasound and navigational bronchoscopy. “We use innovative methods that we already know about, but bring them all together” within a single space, Dr. Yasufuku explained. “Rather than having patients go to several locations, we can do everything at the same time in one room.”
Perhaps the most novel aspect of this operating room is inclusion of a robotic cone-beam CT scanner, which uses mobile, flat CT-imaging panels that overcome the limitations of a conventional, fixed CT scanner. “They scan the patient and then we can retract them and get them out of the way” to better facilitate surgery, he said in an interview.
“We do not have a culture in thoracic surgery of using imaging during surgery,” said Dr. Yasufuku, director of the interventional thoracic surgery program at the University of Toronto. Hybrid operating rooms using noninvasive or minimally invasive equipment and procedures have become commonplace for cardiovascular surgeons and cardiac interventionalists, but this approach has generally not yet been applied to thoracic surgery for cancer, in large part because of the imaging limitations, he said. “It is difficult to perform video-assisted thorascopic surgery using fixed CT.”
Bronchoscopic technologies provide additional, important tools for minimally invasive thoracic surgery. “We use the hybrid operating room to mark small [nonpalpable] lesions.” One approach to marking is to place a microcoil within the nodule with a percutaneous needle. Another approach is to tag the nodule with a fluorescent dye using navigational bronchoscopy.
Dr. Yasufuku also emphasized that the hybrid operating room will also be valuable when new, minimally invasive, nonsurgical therapeutic options for treatment of lung cancer become available in the near future.
Dr. Yasufuku said that he had no relevant disclosures.
On Twitter @mitchelzoler
PHOENIX – Using CT imaging to detect lung cancers in people at high risk for developing it has made it possible to find small tumors with substantially increased sensitivity than is possible with radiography, However, this approach has posed a new challenge to thoracic surgeons: How to visualize these nodules – subcentimeter and nonpalpable – for biopsy or for resection?
The answer may be the hybrid thoracic operating room developed by Dr. Kazuhiro Yasufuku and his associates at Toronto General Hospital, a novel surgical suite that he described at the annual meeting of the Society of Thoracic Surgeons.
Dr. Yasufuku and his team began using the hybrid operating room on an investigational basis in 2013 and have now done about 50 cases as part of several research protocols. The trials address the feasibility of resection, biopsy, and nodule localization, as well as whether the hybrid approach reduces the amount of radiation exposure to both patients and to the surgical team, he said. They plan to report some of their initial results later this year.
The Toronto group assembled the hybrid array of equipment into a single operating room that includes both a dual-source, dual-energy CT scanner and a robotic cone-beam CT scanner, equipment for minimally invasive procedures including video-assisted thoracoscopic and robotic surgery, and advanced endoscopic technology including endobronchial ultrasound and navigational bronchoscopy. “We use innovative methods that we already know about, but bring them all together” within a single space, Dr. Yasufuku explained. “Rather than having patients go to several locations, we can do everything at the same time in one room.”
Perhaps the most novel aspect of this operating room is inclusion of a robotic cone-beam CT scanner, which uses mobile, flat CT-imaging panels that overcome the limitations of a conventional, fixed CT scanner. “They scan the patient and then we can retract them and get them out of the way” to better facilitate surgery, he said in an interview.
“We do not have a culture in thoracic surgery of using imaging during surgery,” said Dr. Yasufuku, director of the interventional thoracic surgery program at the University of Toronto. Hybrid operating rooms using noninvasive or minimally invasive equipment and procedures have become commonplace for cardiovascular surgeons and cardiac interventionalists, but this approach has generally not yet been applied to thoracic surgery for cancer, in large part because of the imaging limitations, he said. “It is difficult to perform video-assisted thorascopic surgery using fixed CT.”
Bronchoscopic technologies provide additional, important tools for minimally invasive thoracic surgery. “We use the hybrid operating room to mark small [nonpalpable] lesions.” One approach to marking is to place a microcoil within the nodule with a percutaneous needle. Another approach is to tag the nodule with a fluorescent dye using navigational bronchoscopy.
Dr. Yasufuku also emphasized that the hybrid operating room will also be valuable when new, minimally invasive, nonsurgical therapeutic options for treatment of lung cancer become available in the near future.
Dr. Yasufuku said that he had no relevant disclosures.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE STS ANNUAL MEETING
Hypertrophic cardiomyopathy: Who should get an ICD?
SNOWMASS, COLO. – Since the 2011 release of the current American College of Cardiology/American Heart Association guidelines on hypertrophic cardiomyopathy, several new evidence-based tools have emerged as being helpful in decision making regarding which patients should receive an implantable cardioverter-defibrillator (ICD) for primary prevention of sudden cardiac death, Dr. Rick A. Nishimura said at the annual Cardiovascular Conference at Snowmass.
These three tools – gadolinium-enhanced cardiovascular magnetic resonance imaging, a novel European risk score calculator, and a new appreciation of the importance of age-related risk – are most useful in the many cases of hypertrophic cardiomyopathy (HCM) where the cardiologist is on the fence regarding ICD placement because the patient doesn’t clearly meet the conventional major criteria for an ICD, according to Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Nishimura, a member of the writing panel for the current guidelines (Circulation. 2011 Dec 13;124[24]:2761-96), predicted these tools will be incorporated into the next iteration of the HCM guidelines.
Notably absent from Dr. Nishimura’s list of useful tools was genetic testing for assessment of SCD risk in a patient with HCM.
“You should not spend $6,000 to do a genetic study to try to predict who’s at risk for sudden death. It turns out that most mutations are neither inherently benign nor malignant. High-risk mutations come from high-risk families, so you can do just as well by taking a family history,” according to the cardiologist.
Dr. Nishimura explained that the clinical dilemma in trying to evaluate SCD risk in a patient who presents with HCM is that the overall risk is quite low – probably 1% or less per year in the total HCM population – yet HCM is the number-one cause of SCD in younger patients. And it can occur unpredictably years or decades after diagnosis of HCM.
While ICDs are of proven effectiveness in preventing SCD in patients with HCM, reliance solely upon the conventional risk predictors to identify those who should get a device is clearly inadequate. Those criteria have a positive predictive accuracy of less than 15%; in other words, roughly 85% of HCM patients who get an ICD never receive an appropriate, life-saving shock, Dr. Nishimura said.
“We have a lot of work left to do in order to better identify these patients. In our own data from the Mayo Clinic, 20%-25% of patients have inappropriate ICD shocks despite efforts to program the device to prevent such shocks. That’s especially common in younger, active patients with HCM, and when it occurs patients find it absolutely devastating,” according to the cardiologist.
As stated in the current guidelines, the established SCD risk factors that provide a strong indication for an ICD in a patient with HCM are prior documented cardiac arrest, ventricular fibrillation, or hemodynamically significant ventricular tachycardia. Additionally, risk factors which, in Dr. Nishimura’s view, probably warrant insertion of an ICD and, at the very least should trigger a physician-patient discussion about the risks and benefits of preventive device therapy, include a family history of HCM-related sudden death in a first-degree relative, massive left ventricular (LV) hypertrophy as defined by a maximum wall thickness of at least 30 mm, and recent unexplained syncope inconsistent with neurocardiogenic origin.
Less potent risk predictors where savvy clinical judgment becomes imperative include nonsustained ventricular tachycardia on 24-hour Holter monitoring, a hypotensive blood pressure response to exercise, and an increased LV wall thickness in a younger patient that doesn’t rise to the 30-mm standard. These are situations where gadolinium-enhanced MRI, consideration of patient age, and the European risk scoring system can help in the decision-making process, he said.
Gadolinium-enhanced MRI: Contrast-enhanced cardiovascular MRI with late gadolinium enhancement has emerged as a reliable marker of the myocyte disarray and interstitial fibrosis which serves as a substrate for ventricular arrhythmias. In a recent study of 1,293 HCM patients followed for a median of 3.3 years, the incidence of SCD events increased progressively with the extent of late gadolinium enhancement. Extensive late gadolinium enhancement, defined as involving at least 15% of LV mass, was associated with a doubled risk of SCD events in patients otherwise considered at low risk (Circulation. 2014 Aug 5;130[6]:484-95).
“This is probably going to become one of the key markers that can help you when you’re on the fence as to whether or not to put in an ICD. We’re getting MRIs with gadolinium now in all of our HCM patients. What matters is not gadolinium enhancement at the insertion of the left ventricle into the septum – a lot of people have that – but diffuse gadolinium enhancement throughout the septum,” Dr. Nishimura said.
Because SCD risk increases linearly with greater maximal LV wall thickness, gadolinium-enhanced MRI is particularly helpful in assessing risk in a younger patient with a maximal LV wall thickness of, say, 26 mm, he added.
Age: A study by led by Dr. Barry J. Maron, the cochair of the 2011 guideline committee and director of the HCM center at the Minneapolis Heart Institute, provides a new understanding that prophylactic ICD implantation is not warranted in patients with HCM who present at age 60 or older. In their study of 428 consecutive patients presenting with HCM at age 60 or above, the investigators found during 5.8 years of follow-up that the incidence of arrhythmic sudden death events was just 0.2% per year (Circulation. 2013 Feb 5;127[5]:585-93).
“They’ve shown that if you look at patients age 60 or above who have HCM, the risk of sudden cardiac death is almost nonexistent. That’s incredibly important to remember. Sudden death is something that’s going to happen in the younger population, under age 30,” Dr. Nishimura emphasized.
European SCD risk prediction tool: This tool was hailed as a major advance in the current European Society of Cardiology guidelines on HCM (Eur Heart J. 2014;35:2733-2779). The tool was incorporated into the guidelines. It is also available as a smartphone app.
The risk prediction tool (Eur Heart J. 2014 Aug 7;35[30]:2010-20) is a complex equation that incorporates seven predictive factors: age, maximal LV wall thickness, left atrial diameter, LV outflow tract gradient, family history of SCD, nonsustained VT, and unexplained syncope. After input on these seven factors, the equation spits out an individual’s estimated 5-year SCD risk. Based on the study of 3,675 consecutive HCM patients with a median 5.7 years of follow-up that was used to develop the risk equation, the current ESC guidelines state that an ICD is not warranted in HCM patients with a 5-year risk below 4%, device implantation should be considered in those whose risk is 4%-6%, and an ICD should be even more strongly considered in patients with a 5-year risk in excess of 6%.
“A lot of people across the pond are using this risk score. But there are some problems with it,” according to Dr. Nishimura.
In his view, it “doesn’t make much sense” to include left ventricular outflow tract gradient or left atrial diameter in the risk equation. Nor is unexplained syncope carefully defined. Also, the equation would be improved by incorporation of late gadolinium enhancement on MRI, left ventricular dysfunction, and presence or absence of apical aneurysm as predictive variables. But on the plus side, the European equation treats maximal LV wall thickness as a continuous variable, which is more appropriate than the single 30-mm cutoff used in the ACC/AHA guidelines.
The biggest limitation of the European prognostic score, however, is that it hasn’t yet been validated in an independent patient cohort, Dr. Nishimura said. He noted that when Dr. Maron and coworkers recently applied the European SCD risk equation retrospectively to 1,629 consecutive U.S. patients with HCM, the investigators concluded that the risk equation proved unreliable for prediction of future SCD events. Fifty-nine percent of patients who got an appropriate ICD shock or experienced SCD were misclassified as low risk and hence would not have received an ICD under the European guidelines (Am J Cardiol. 2015 Sep 1;116[5]:757-64).
Nonetheless, because of the limited predictive accuracy of today’s standard methods of assessing SCD risk, Dr. Nishimura considers application of the European risk score to be “reasonable” in HCM patients who don’t have any of the strong indications for an ICD.
“If it comes up with an estimated 5-year risk greater than 6%, I think it’s very reasonable to consider implantation of an ICD,” he said.
Dr. Nishimura observed that in addition to assessing SCD risk, cardiologists have two other separate essential tasks when a patient presents with HCM. One is to screen and counsel the first-degree relatives. The other is to determine whether a left ventricular outflow tract obstruction is present in a symptomatic patient and, if so, to improve symptoms by treating the associated hemodynamic abnormalities medically and if need be by septal ablation or septal myectomy.
He reported having no financial conflicts of interest regarding his presentation.
SNOWMASS, COLO. – Since the 2011 release of the current American College of Cardiology/American Heart Association guidelines on hypertrophic cardiomyopathy, several new evidence-based tools have emerged as being helpful in decision making regarding which patients should receive an implantable cardioverter-defibrillator (ICD) for primary prevention of sudden cardiac death, Dr. Rick A. Nishimura said at the annual Cardiovascular Conference at Snowmass.
These three tools – gadolinium-enhanced cardiovascular magnetic resonance imaging, a novel European risk score calculator, and a new appreciation of the importance of age-related risk – are most useful in the many cases of hypertrophic cardiomyopathy (HCM) where the cardiologist is on the fence regarding ICD placement because the patient doesn’t clearly meet the conventional major criteria for an ICD, according to Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Nishimura, a member of the writing panel for the current guidelines (Circulation. 2011 Dec 13;124[24]:2761-96), predicted these tools will be incorporated into the next iteration of the HCM guidelines.
Notably absent from Dr. Nishimura’s list of useful tools was genetic testing for assessment of SCD risk in a patient with HCM.
“You should not spend $6,000 to do a genetic study to try to predict who’s at risk for sudden death. It turns out that most mutations are neither inherently benign nor malignant. High-risk mutations come from high-risk families, so you can do just as well by taking a family history,” according to the cardiologist.
Dr. Nishimura explained that the clinical dilemma in trying to evaluate SCD risk in a patient who presents with HCM is that the overall risk is quite low – probably 1% or less per year in the total HCM population – yet HCM is the number-one cause of SCD in younger patients. And it can occur unpredictably years or decades after diagnosis of HCM.
While ICDs are of proven effectiveness in preventing SCD in patients with HCM, reliance solely upon the conventional risk predictors to identify those who should get a device is clearly inadequate. Those criteria have a positive predictive accuracy of less than 15%; in other words, roughly 85% of HCM patients who get an ICD never receive an appropriate, life-saving shock, Dr. Nishimura said.
“We have a lot of work left to do in order to better identify these patients. In our own data from the Mayo Clinic, 20%-25% of patients have inappropriate ICD shocks despite efforts to program the device to prevent such shocks. That’s especially common in younger, active patients with HCM, and when it occurs patients find it absolutely devastating,” according to the cardiologist.
As stated in the current guidelines, the established SCD risk factors that provide a strong indication for an ICD in a patient with HCM are prior documented cardiac arrest, ventricular fibrillation, or hemodynamically significant ventricular tachycardia. Additionally, risk factors which, in Dr. Nishimura’s view, probably warrant insertion of an ICD and, at the very least should trigger a physician-patient discussion about the risks and benefits of preventive device therapy, include a family history of HCM-related sudden death in a first-degree relative, massive left ventricular (LV) hypertrophy as defined by a maximum wall thickness of at least 30 mm, and recent unexplained syncope inconsistent with neurocardiogenic origin.
Less potent risk predictors where savvy clinical judgment becomes imperative include nonsustained ventricular tachycardia on 24-hour Holter monitoring, a hypotensive blood pressure response to exercise, and an increased LV wall thickness in a younger patient that doesn’t rise to the 30-mm standard. These are situations where gadolinium-enhanced MRI, consideration of patient age, and the European risk scoring system can help in the decision-making process, he said.
Gadolinium-enhanced MRI: Contrast-enhanced cardiovascular MRI with late gadolinium enhancement has emerged as a reliable marker of the myocyte disarray and interstitial fibrosis which serves as a substrate for ventricular arrhythmias. In a recent study of 1,293 HCM patients followed for a median of 3.3 years, the incidence of SCD events increased progressively with the extent of late gadolinium enhancement. Extensive late gadolinium enhancement, defined as involving at least 15% of LV mass, was associated with a doubled risk of SCD events in patients otherwise considered at low risk (Circulation. 2014 Aug 5;130[6]:484-95).
“This is probably going to become one of the key markers that can help you when you’re on the fence as to whether or not to put in an ICD. We’re getting MRIs with gadolinium now in all of our HCM patients. What matters is not gadolinium enhancement at the insertion of the left ventricle into the septum – a lot of people have that – but diffuse gadolinium enhancement throughout the septum,” Dr. Nishimura said.
Because SCD risk increases linearly with greater maximal LV wall thickness, gadolinium-enhanced MRI is particularly helpful in assessing risk in a younger patient with a maximal LV wall thickness of, say, 26 mm, he added.
Age: A study by led by Dr. Barry J. Maron, the cochair of the 2011 guideline committee and director of the HCM center at the Minneapolis Heart Institute, provides a new understanding that prophylactic ICD implantation is not warranted in patients with HCM who present at age 60 or older. In their study of 428 consecutive patients presenting with HCM at age 60 or above, the investigators found during 5.8 years of follow-up that the incidence of arrhythmic sudden death events was just 0.2% per year (Circulation. 2013 Feb 5;127[5]:585-93).
“They’ve shown that if you look at patients age 60 or above who have HCM, the risk of sudden cardiac death is almost nonexistent. That’s incredibly important to remember. Sudden death is something that’s going to happen in the younger population, under age 30,” Dr. Nishimura emphasized.
European SCD risk prediction tool: This tool was hailed as a major advance in the current European Society of Cardiology guidelines on HCM (Eur Heart J. 2014;35:2733-2779). The tool was incorporated into the guidelines. It is also available as a smartphone app.
The risk prediction tool (Eur Heart J. 2014 Aug 7;35[30]:2010-20) is a complex equation that incorporates seven predictive factors: age, maximal LV wall thickness, left atrial diameter, LV outflow tract gradient, family history of SCD, nonsustained VT, and unexplained syncope. After input on these seven factors, the equation spits out an individual’s estimated 5-year SCD risk. Based on the study of 3,675 consecutive HCM patients with a median 5.7 years of follow-up that was used to develop the risk equation, the current ESC guidelines state that an ICD is not warranted in HCM patients with a 5-year risk below 4%, device implantation should be considered in those whose risk is 4%-6%, and an ICD should be even more strongly considered in patients with a 5-year risk in excess of 6%.
“A lot of people across the pond are using this risk score. But there are some problems with it,” according to Dr. Nishimura.
In his view, it “doesn’t make much sense” to include left ventricular outflow tract gradient or left atrial diameter in the risk equation. Nor is unexplained syncope carefully defined. Also, the equation would be improved by incorporation of late gadolinium enhancement on MRI, left ventricular dysfunction, and presence or absence of apical aneurysm as predictive variables. But on the plus side, the European equation treats maximal LV wall thickness as a continuous variable, which is more appropriate than the single 30-mm cutoff used in the ACC/AHA guidelines.
The biggest limitation of the European prognostic score, however, is that it hasn’t yet been validated in an independent patient cohort, Dr. Nishimura said. He noted that when Dr. Maron and coworkers recently applied the European SCD risk equation retrospectively to 1,629 consecutive U.S. patients with HCM, the investigators concluded that the risk equation proved unreliable for prediction of future SCD events. Fifty-nine percent of patients who got an appropriate ICD shock or experienced SCD were misclassified as low risk and hence would not have received an ICD under the European guidelines (Am J Cardiol. 2015 Sep 1;116[5]:757-64).
Nonetheless, because of the limited predictive accuracy of today’s standard methods of assessing SCD risk, Dr. Nishimura considers application of the European risk score to be “reasonable” in HCM patients who don’t have any of the strong indications for an ICD.
“If it comes up with an estimated 5-year risk greater than 6%, I think it’s very reasonable to consider implantation of an ICD,” he said.
Dr. Nishimura observed that in addition to assessing SCD risk, cardiologists have two other separate essential tasks when a patient presents with HCM. One is to screen and counsel the first-degree relatives. The other is to determine whether a left ventricular outflow tract obstruction is present in a symptomatic patient and, if so, to improve symptoms by treating the associated hemodynamic abnormalities medically and if need be by septal ablation or septal myectomy.
He reported having no financial conflicts of interest regarding his presentation.
SNOWMASS, COLO. – Since the 2011 release of the current American College of Cardiology/American Heart Association guidelines on hypertrophic cardiomyopathy, several new evidence-based tools have emerged as being helpful in decision making regarding which patients should receive an implantable cardioverter-defibrillator (ICD) for primary prevention of sudden cardiac death, Dr. Rick A. Nishimura said at the annual Cardiovascular Conference at Snowmass.
These three tools – gadolinium-enhanced cardiovascular magnetic resonance imaging, a novel European risk score calculator, and a new appreciation of the importance of age-related risk – are most useful in the many cases of hypertrophic cardiomyopathy (HCM) where the cardiologist is on the fence regarding ICD placement because the patient doesn’t clearly meet the conventional major criteria for an ICD, according to Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Nishimura, a member of the writing panel for the current guidelines (Circulation. 2011 Dec 13;124[24]:2761-96), predicted these tools will be incorporated into the next iteration of the HCM guidelines.
Notably absent from Dr. Nishimura’s list of useful tools was genetic testing for assessment of SCD risk in a patient with HCM.
“You should not spend $6,000 to do a genetic study to try to predict who’s at risk for sudden death. It turns out that most mutations are neither inherently benign nor malignant. High-risk mutations come from high-risk families, so you can do just as well by taking a family history,” according to the cardiologist.
Dr. Nishimura explained that the clinical dilemma in trying to evaluate SCD risk in a patient who presents with HCM is that the overall risk is quite low – probably 1% or less per year in the total HCM population – yet HCM is the number-one cause of SCD in younger patients. And it can occur unpredictably years or decades after diagnosis of HCM.
While ICDs are of proven effectiveness in preventing SCD in patients with HCM, reliance solely upon the conventional risk predictors to identify those who should get a device is clearly inadequate. Those criteria have a positive predictive accuracy of less than 15%; in other words, roughly 85% of HCM patients who get an ICD never receive an appropriate, life-saving shock, Dr. Nishimura said.
“We have a lot of work left to do in order to better identify these patients. In our own data from the Mayo Clinic, 20%-25% of patients have inappropriate ICD shocks despite efforts to program the device to prevent such shocks. That’s especially common in younger, active patients with HCM, and when it occurs patients find it absolutely devastating,” according to the cardiologist.
As stated in the current guidelines, the established SCD risk factors that provide a strong indication for an ICD in a patient with HCM are prior documented cardiac arrest, ventricular fibrillation, or hemodynamically significant ventricular tachycardia. Additionally, risk factors which, in Dr. Nishimura’s view, probably warrant insertion of an ICD and, at the very least should trigger a physician-patient discussion about the risks and benefits of preventive device therapy, include a family history of HCM-related sudden death in a first-degree relative, massive left ventricular (LV) hypertrophy as defined by a maximum wall thickness of at least 30 mm, and recent unexplained syncope inconsistent with neurocardiogenic origin.
Less potent risk predictors where savvy clinical judgment becomes imperative include nonsustained ventricular tachycardia on 24-hour Holter monitoring, a hypotensive blood pressure response to exercise, and an increased LV wall thickness in a younger patient that doesn’t rise to the 30-mm standard. These are situations where gadolinium-enhanced MRI, consideration of patient age, and the European risk scoring system can help in the decision-making process, he said.
Gadolinium-enhanced MRI: Contrast-enhanced cardiovascular MRI with late gadolinium enhancement has emerged as a reliable marker of the myocyte disarray and interstitial fibrosis which serves as a substrate for ventricular arrhythmias. In a recent study of 1,293 HCM patients followed for a median of 3.3 years, the incidence of SCD events increased progressively with the extent of late gadolinium enhancement. Extensive late gadolinium enhancement, defined as involving at least 15% of LV mass, was associated with a doubled risk of SCD events in patients otherwise considered at low risk (Circulation. 2014 Aug 5;130[6]:484-95).
“This is probably going to become one of the key markers that can help you when you’re on the fence as to whether or not to put in an ICD. We’re getting MRIs with gadolinium now in all of our HCM patients. What matters is not gadolinium enhancement at the insertion of the left ventricle into the septum – a lot of people have that – but diffuse gadolinium enhancement throughout the septum,” Dr. Nishimura said.
Because SCD risk increases linearly with greater maximal LV wall thickness, gadolinium-enhanced MRI is particularly helpful in assessing risk in a younger patient with a maximal LV wall thickness of, say, 26 mm, he added.
Age: A study by led by Dr. Barry J. Maron, the cochair of the 2011 guideline committee and director of the HCM center at the Minneapolis Heart Institute, provides a new understanding that prophylactic ICD implantation is not warranted in patients with HCM who present at age 60 or older. In their study of 428 consecutive patients presenting with HCM at age 60 or above, the investigators found during 5.8 years of follow-up that the incidence of arrhythmic sudden death events was just 0.2% per year (Circulation. 2013 Feb 5;127[5]:585-93).
“They’ve shown that if you look at patients age 60 or above who have HCM, the risk of sudden cardiac death is almost nonexistent. That’s incredibly important to remember. Sudden death is something that’s going to happen in the younger population, under age 30,” Dr. Nishimura emphasized.
European SCD risk prediction tool: This tool was hailed as a major advance in the current European Society of Cardiology guidelines on HCM (Eur Heart J. 2014;35:2733-2779). The tool was incorporated into the guidelines. It is also available as a smartphone app.
The risk prediction tool (Eur Heart J. 2014 Aug 7;35[30]:2010-20) is a complex equation that incorporates seven predictive factors: age, maximal LV wall thickness, left atrial diameter, LV outflow tract gradient, family history of SCD, nonsustained VT, and unexplained syncope. After input on these seven factors, the equation spits out an individual’s estimated 5-year SCD risk. Based on the study of 3,675 consecutive HCM patients with a median 5.7 years of follow-up that was used to develop the risk equation, the current ESC guidelines state that an ICD is not warranted in HCM patients with a 5-year risk below 4%, device implantation should be considered in those whose risk is 4%-6%, and an ICD should be even more strongly considered in patients with a 5-year risk in excess of 6%.
“A lot of people across the pond are using this risk score. But there are some problems with it,” according to Dr. Nishimura.
In his view, it “doesn’t make much sense” to include left ventricular outflow tract gradient or left atrial diameter in the risk equation. Nor is unexplained syncope carefully defined. Also, the equation would be improved by incorporation of late gadolinium enhancement on MRI, left ventricular dysfunction, and presence or absence of apical aneurysm as predictive variables. But on the plus side, the European equation treats maximal LV wall thickness as a continuous variable, which is more appropriate than the single 30-mm cutoff used in the ACC/AHA guidelines.
The biggest limitation of the European prognostic score, however, is that it hasn’t yet been validated in an independent patient cohort, Dr. Nishimura said. He noted that when Dr. Maron and coworkers recently applied the European SCD risk equation retrospectively to 1,629 consecutive U.S. patients with HCM, the investigators concluded that the risk equation proved unreliable for prediction of future SCD events. Fifty-nine percent of patients who got an appropriate ICD shock or experienced SCD were misclassified as low risk and hence would not have received an ICD under the European guidelines (Am J Cardiol. 2015 Sep 1;116[5]:757-64).
Nonetheless, because of the limited predictive accuracy of today’s standard methods of assessing SCD risk, Dr. Nishimura considers application of the European risk score to be “reasonable” in HCM patients who don’t have any of the strong indications for an ICD.
“If it comes up with an estimated 5-year risk greater than 6%, I think it’s very reasonable to consider implantation of an ICD,” he said.
Dr. Nishimura observed that in addition to assessing SCD risk, cardiologists have two other separate essential tasks when a patient presents with HCM. One is to screen and counsel the first-degree relatives. The other is to determine whether a left ventricular outflow tract obstruction is present in a symptomatic patient and, if so, to improve symptoms by treating the associated hemodynamic abnormalities medically and if need be by septal ablation or septal myectomy.
He reported having no financial conflicts of interest regarding his presentation.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
FDA approves marketing of sutureless aortic valve
LivaNova announced that the U.S. Food and Drug Administration has announced the approval of their Perceval Sutureless Heart Valve. The approval was issued Jan. 8 and is effective immediately, and LivaNova indicated that it will begin commercial distribution of the device in the United States over the coming quarter.
According to an FDA summary document, the Perceval Sutureless Heart Valve is a bioprosthetic valve designed to replace a diseased native or a malfunctioning prosthetic aortic valve via open heart surgery. The self-expanding stent frame consists of a tissue component made from bovine pericardium and a self-expandable nitinol stent, along with a dedicated delivery system that allows physicians to position and anchor the valve suturelessly.
The Perceval heart valve is supplied unmounted and must be loaded onto an accompanying holder by reducing the valve size using a supplied polycarbonate collapser. The holder is used for sternal approaches and includes a rigid shaft with an end section that houses the valve prosthesis during delivery. A separate holder, approximately 3 cm longer, is also available for minimally invasive procedures. After implantation, the physician uses the a post-dilation catheter to expand the valve in situ.
Perceval’s approval was based upon the results of a pivotal European study performed to assess the device, the CAVALIER (Safety and Effectiveness Study of Perceval S Valve for Extended CE Mark) trial. The prospective, multicenter, nonrandomized clinical study was conducted at 26 investigational sites in Austria, Belgium, England, France, Germany, and the Netherlands.
Patients were treated between Feb. 23, 2010, and Sept. 30, 2013, and the database for the PDA-assessed data collected through Nov. 5, 2014, and included 658 patients.
The differences between the New York Heart Association (NYHA) class at 12 months and the baseline were calculated. In total, 77.5% of patients showed a decrease of NYHA equal to at least one class, whereas 19.7% of patients remained stable over the time. Only 2.8% of patients showed a worsened clinical status.
Reduction in mean gradients and increase in effective orifice area were both observed at 1 year follow-up, according to the FDA report.
At the 1-, 2-, and 3-year follow-up time points, 75.1% or greater of the implanted patients with available data had improved by one to three classes and at the 4-year follow-up time point 72.6% of the patients had improved by one to three classes, according to the report. In addition, at the 1-, 2-, and 3-year follow-up time points, 92.9% or greater of the patients were in NYHA Class I and Class II, and at the 4-year follow-up time point, 86.3% of the patients were in NYHA Class I and Class II.
Although there was a predominance of women in the study population (64.4%), patients of both sexes demonstrated acceptable hemodynamic outcomes and significant improvement in functional status, according to the FDA summary.
Sutureless valves are considered to have a promising future according to a recent international consensus panel recommendationpublished online in the European Journal of Cardio-Thoracic Surgery (2015 Oct 29. doi: 10.1093/ejcts/ezv369). The report assessed various benefits of sutureless and rapid deployment technology, and concluded these devices “may represent a helpful tool in aortic valve replacement for patients requiring a biological valve.” However, further evidence will be needed to reaffirm the benefit of sutureless and rapid deployment valves, they concluded.
LivaNova announced that the U.S. Food and Drug Administration has announced the approval of their Perceval Sutureless Heart Valve. The approval was issued Jan. 8 and is effective immediately, and LivaNova indicated that it will begin commercial distribution of the device in the United States over the coming quarter.
According to an FDA summary document, the Perceval Sutureless Heart Valve is a bioprosthetic valve designed to replace a diseased native or a malfunctioning prosthetic aortic valve via open heart surgery. The self-expanding stent frame consists of a tissue component made from bovine pericardium and a self-expandable nitinol stent, along with a dedicated delivery system that allows physicians to position and anchor the valve suturelessly.
The Perceval heart valve is supplied unmounted and must be loaded onto an accompanying holder by reducing the valve size using a supplied polycarbonate collapser. The holder is used for sternal approaches and includes a rigid shaft with an end section that houses the valve prosthesis during delivery. A separate holder, approximately 3 cm longer, is also available for minimally invasive procedures. After implantation, the physician uses the a post-dilation catheter to expand the valve in situ.
Perceval’s approval was based upon the results of a pivotal European study performed to assess the device, the CAVALIER (Safety and Effectiveness Study of Perceval S Valve for Extended CE Mark) trial. The prospective, multicenter, nonrandomized clinical study was conducted at 26 investigational sites in Austria, Belgium, England, France, Germany, and the Netherlands.
Patients were treated between Feb. 23, 2010, and Sept. 30, 2013, and the database for the PDA-assessed data collected through Nov. 5, 2014, and included 658 patients.
The differences between the New York Heart Association (NYHA) class at 12 months and the baseline were calculated. In total, 77.5% of patients showed a decrease of NYHA equal to at least one class, whereas 19.7% of patients remained stable over the time. Only 2.8% of patients showed a worsened clinical status.
Reduction in mean gradients and increase in effective orifice area were both observed at 1 year follow-up, according to the FDA report.
At the 1-, 2-, and 3-year follow-up time points, 75.1% or greater of the implanted patients with available data had improved by one to three classes and at the 4-year follow-up time point 72.6% of the patients had improved by one to three classes, according to the report. In addition, at the 1-, 2-, and 3-year follow-up time points, 92.9% or greater of the patients were in NYHA Class I and Class II, and at the 4-year follow-up time point, 86.3% of the patients were in NYHA Class I and Class II.
Although there was a predominance of women in the study population (64.4%), patients of both sexes demonstrated acceptable hemodynamic outcomes and significant improvement in functional status, according to the FDA summary.
Sutureless valves are considered to have a promising future according to a recent international consensus panel recommendationpublished online in the European Journal of Cardio-Thoracic Surgery (2015 Oct 29. doi: 10.1093/ejcts/ezv369). The report assessed various benefits of sutureless and rapid deployment technology, and concluded these devices “may represent a helpful tool in aortic valve replacement for patients requiring a biological valve.” However, further evidence will be needed to reaffirm the benefit of sutureless and rapid deployment valves, they concluded.
LivaNova announced that the U.S. Food and Drug Administration has announced the approval of their Perceval Sutureless Heart Valve. The approval was issued Jan. 8 and is effective immediately, and LivaNova indicated that it will begin commercial distribution of the device in the United States over the coming quarter.
According to an FDA summary document, the Perceval Sutureless Heart Valve is a bioprosthetic valve designed to replace a diseased native or a malfunctioning prosthetic aortic valve via open heart surgery. The self-expanding stent frame consists of a tissue component made from bovine pericardium and a self-expandable nitinol stent, along with a dedicated delivery system that allows physicians to position and anchor the valve suturelessly.
The Perceval heart valve is supplied unmounted and must be loaded onto an accompanying holder by reducing the valve size using a supplied polycarbonate collapser. The holder is used for sternal approaches and includes a rigid shaft with an end section that houses the valve prosthesis during delivery. A separate holder, approximately 3 cm longer, is also available for minimally invasive procedures. After implantation, the physician uses the a post-dilation catheter to expand the valve in situ.
Perceval’s approval was based upon the results of a pivotal European study performed to assess the device, the CAVALIER (Safety and Effectiveness Study of Perceval S Valve for Extended CE Mark) trial. The prospective, multicenter, nonrandomized clinical study was conducted at 26 investigational sites in Austria, Belgium, England, France, Germany, and the Netherlands.
Patients were treated between Feb. 23, 2010, and Sept. 30, 2013, and the database for the PDA-assessed data collected through Nov. 5, 2014, and included 658 patients.
The differences between the New York Heart Association (NYHA) class at 12 months and the baseline were calculated. In total, 77.5% of patients showed a decrease of NYHA equal to at least one class, whereas 19.7% of patients remained stable over the time. Only 2.8% of patients showed a worsened clinical status.
Reduction in mean gradients and increase in effective orifice area were both observed at 1 year follow-up, according to the FDA report.
At the 1-, 2-, and 3-year follow-up time points, 75.1% or greater of the implanted patients with available data had improved by one to three classes and at the 4-year follow-up time point 72.6% of the patients had improved by one to three classes, according to the report. In addition, at the 1-, 2-, and 3-year follow-up time points, 92.9% or greater of the patients were in NYHA Class I and Class II, and at the 4-year follow-up time point, 86.3% of the patients were in NYHA Class I and Class II.
Although there was a predominance of women in the study population (64.4%), patients of both sexes demonstrated acceptable hemodynamic outcomes and significant improvement in functional status, according to the FDA summary.
Sutureless valves are considered to have a promising future according to a recent international consensus panel recommendationpublished online in the European Journal of Cardio-Thoracic Surgery (2015 Oct 29. doi: 10.1093/ejcts/ezv369). The report assessed various benefits of sutureless and rapid deployment technology, and concluded these devices “may represent a helpful tool in aortic valve replacement for patients requiring a biological valve.” However, further evidence will be needed to reaffirm the benefit of sutureless and rapid deployment valves, they concluded.
Finding more transplant hearts but not more donors
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
Key clinical point: A group approach to systematically review rejected donor organs has led to expanded donor criteria and resulted in improved donor organ utilization and transplant volume.
Major finding: Transplant utilization rate increased from 28% to 49% with no significant change in 30-day survival after implementation of a donor review protocol.
Data source: Retrospective review of 293 total donor heart offers at a single center from July 2012 to June 2013 compared with review of 279 heart offers from July 2013 to June 2014.
Disclosures: Lead author Dr. Jason Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia, and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
Presurgery radiation shows benefit in lung cancer
The popularity of extrapleural pneumonectomy to treat asbestos-related thoracic mesothelioma has yielded to extended pleurectomy/decortication in recent years, but a recent study suggests that the extrapleural pneumonectomy procedure can achieve good results in a new protocol that involves administering radiation therapy before surgery as opposed the more conventional approach of radiation after surgery.
Researchers at the University of Toronto reported on their protocol that uses accelerated intensity modulated radiation therapy (IMRT) for malignant pleural mesothelioma (MPM) (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.09.129). They call the protocol SMART, for Surgery for Mesothelioma After Radiation Therapy.
“The rationale to develop this protocol was to optimize the delivery of radiation to the whole tumor bed, sterilize the edges of the tumor to limit the risk of spillage at the time of surgery, develop a shorter treatment plan and potentiate the activation of the immune system by using a hypofractionated regimen,” wrote Dr. Marc de Perrot and colleagues.
The protocol involves delivering 25 Gy of radiation in five daily fractions over a week to the entire side of the thorax with 5 Gy boosts based on imaging, followed by extrapleural pneumonectomy (EPP) 4-6 days later. Patients with three or more positive lymph notes (ypN2 disease) also are offered adjuvant chemotherapy.
The researchers performed the protocol on 62 patients from November 2008 to October 2014, which represents 24% of all patients with MPM seen at the institution in that period. Fifty-two patients were men and ages ranged from 41 to 75 years. Clinical stage of cancer ranged from T1N0 in 10 patients, to T2N0 in 35 and T3N0 in 13 (two had T4N0 and two had T3N2). Forty-five had right-side cancers. Six patients received an extended protocol for various reasons, including tumor extending to the chest wall.
All 62 patients completed IMRT and EPP. All but one had resection and reconstruction of the diaphragm, and all but four had resection and reconstruction of the pericardium.
Overall death rate was 4.8% (three patients). Results were better in patients with epithelioid tumors, with a median survival of 51 months and disease-free survival of 47 months. Those with biphasic subtypes had median survival of 10 months and disease-free survival of 8 months. Eight patients had ipsilateral chest recurrence. “This analysis demonstrates that the SMART approach is particularly encouraging for patients with epithelial subtype,” Dr. de Perrot and coauthors said. They no longer perform the SMART protocol on patients with biphasic subtype.
The protocol was not without complications. Twenty-four patients, about 38%, had serious complications that required intervention or worse. Twelve had atrial fibrillation, but none advanced to life-threatening disease. Among other complications, four had empyema – one resulting in death – and three had pulmonary emboli. One other patient in the complications group died from pneumonia, and another died from a heart attack at home.
This is the Toronto researchers’ second attempt at studying the three-modality approach. In their first attempt, only half the patients who started with preoperative chemotherapy went onto complete the radiation after surgery because of difficulties administering it (J Thorac Cardiovasc Surg. 2007;133:111-6; J Clin Oncol. 2009;27:1413-8). Also, about 25% of patients had disease progression during induction chemotherapy and could not go onto surgery.
They designed the most recent trial to deliver radiation before surgery because of the excellent local control of cancer along with evidence that MPM tumors were radio-sensitive. “Considering the risk of disease progression on induction chemotherapy, we felt that switching the order of therapy was potentially a better option for patients with surgically resectable disease,” Dr. de Perrott and colleagues said.
The researchers cited the study’s single-center nature with a single treatment arm, and the lack of longer-term follow-up, as limitations. “However, in our own experience, this approach has been very encouraging and has become our primary option for patients with surgically resectable MPM,” they noted.
The study authors had no conflicts to disclose.
Implementing the treatment regimen for malignant pleural mesothelioma (MPM) that the Toronto researchers studied poses “several high stakes challenges,” Dr. Valerie Rusch and coauthors at Memorial Sloan-Kettering Cancer Center, New York, said in their invited commentary (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.10.038).

|
Dr. Valerie W. Rusch |
But they noted challenges involved with conventional multi-modality treatment for MPM, namely the 6 months of intensive treatment. However, the experience of the Toronto researchers will be difficult to replicate, they said. “Such outstanding results reflect the expertise of Dr. de Perrot and colleagues in the surgical care of MPM and the excellence of their multidisciplinary program,” Dr. Rusch and coauthors said.
The study results are among the best reported for MPM to date, they added, but they asked why. “Are they solely related to patient selection or do they reflect the true impact of a novel approach to treatment?”
Patients selected for the treatment need to be able to undergo the extrapleural pneumonectomy (EPP) and the surgeon has to be able to predict the resectability of the tumor. But limitations in existing staging methods for MPM make it difficult to predict tumor resectability. “To avoid bronchial stump leaks and other serious complications after EPP requires experience along with meticulous surgical technique and postoperative care,” Dr. Rusch and colleagues said. “Only high-volume centers of excellence could potentially reproduce these results.”
Despite the waning in popularity of EPP, the study results underscore its effectiveness in carefully selected patients – “those with epithelioid tumor histology and no tumor metastases.” To corroborate the findings, reports on other centers’ experience along with human and animal studies rather than a randomized clinical trial are needed. “Dr. de Perrot and colleagues may have been not only bold but SMART,” Dr. Rusch and colleagues said.
Implementing the treatment regimen for malignant pleural mesothelioma (MPM) that the Toronto researchers studied poses “several high stakes challenges,” Dr. Valerie Rusch and coauthors at Memorial Sloan-Kettering Cancer Center, New York, said in their invited commentary (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.10.038).

|
Dr. Valerie W. Rusch |
But they noted challenges involved with conventional multi-modality treatment for MPM, namely the 6 months of intensive treatment. However, the experience of the Toronto researchers will be difficult to replicate, they said. “Such outstanding results reflect the expertise of Dr. de Perrot and colleagues in the surgical care of MPM and the excellence of their multidisciplinary program,” Dr. Rusch and coauthors said.
The study results are among the best reported for MPM to date, they added, but they asked why. “Are they solely related to patient selection or do they reflect the true impact of a novel approach to treatment?”
Patients selected for the treatment need to be able to undergo the extrapleural pneumonectomy (EPP) and the surgeon has to be able to predict the resectability of the tumor. But limitations in existing staging methods for MPM make it difficult to predict tumor resectability. “To avoid bronchial stump leaks and other serious complications after EPP requires experience along with meticulous surgical technique and postoperative care,” Dr. Rusch and colleagues said. “Only high-volume centers of excellence could potentially reproduce these results.”
Despite the waning in popularity of EPP, the study results underscore its effectiveness in carefully selected patients – “those with epithelioid tumor histology and no tumor metastases.” To corroborate the findings, reports on other centers’ experience along with human and animal studies rather than a randomized clinical trial are needed. “Dr. de Perrot and colleagues may have been not only bold but SMART,” Dr. Rusch and colleagues said.
Implementing the treatment regimen for malignant pleural mesothelioma (MPM) that the Toronto researchers studied poses “several high stakes challenges,” Dr. Valerie Rusch and coauthors at Memorial Sloan-Kettering Cancer Center, New York, said in their invited commentary (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.10.038).

|
Dr. Valerie W. Rusch |
But they noted challenges involved with conventional multi-modality treatment for MPM, namely the 6 months of intensive treatment. However, the experience of the Toronto researchers will be difficult to replicate, they said. “Such outstanding results reflect the expertise of Dr. de Perrot and colleagues in the surgical care of MPM and the excellence of their multidisciplinary program,” Dr. Rusch and coauthors said.
The study results are among the best reported for MPM to date, they added, but they asked why. “Are they solely related to patient selection or do they reflect the true impact of a novel approach to treatment?”
Patients selected for the treatment need to be able to undergo the extrapleural pneumonectomy (EPP) and the surgeon has to be able to predict the resectability of the tumor. But limitations in existing staging methods for MPM make it difficult to predict tumor resectability. “To avoid bronchial stump leaks and other serious complications after EPP requires experience along with meticulous surgical technique and postoperative care,” Dr. Rusch and colleagues said. “Only high-volume centers of excellence could potentially reproduce these results.”
Despite the waning in popularity of EPP, the study results underscore its effectiveness in carefully selected patients – “those with epithelioid tumor histology and no tumor metastases.” To corroborate the findings, reports on other centers’ experience along with human and animal studies rather than a randomized clinical trial are needed. “Dr. de Perrot and colleagues may have been not only bold but SMART,” Dr. Rusch and colleagues said.
The popularity of extrapleural pneumonectomy to treat asbestos-related thoracic mesothelioma has yielded to extended pleurectomy/decortication in recent years, but a recent study suggests that the extrapleural pneumonectomy procedure can achieve good results in a new protocol that involves administering radiation therapy before surgery as opposed the more conventional approach of radiation after surgery.
Researchers at the University of Toronto reported on their protocol that uses accelerated intensity modulated radiation therapy (IMRT) for malignant pleural mesothelioma (MPM) (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.09.129). They call the protocol SMART, for Surgery for Mesothelioma After Radiation Therapy.
“The rationale to develop this protocol was to optimize the delivery of radiation to the whole tumor bed, sterilize the edges of the tumor to limit the risk of spillage at the time of surgery, develop a shorter treatment plan and potentiate the activation of the immune system by using a hypofractionated regimen,” wrote Dr. Marc de Perrot and colleagues.
The protocol involves delivering 25 Gy of radiation in five daily fractions over a week to the entire side of the thorax with 5 Gy boosts based on imaging, followed by extrapleural pneumonectomy (EPP) 4-6 days later. Patients with three or more positive lymph notes (ypN2 disease) also are offered adjuvant chemotherapy.
The researchers performed the protocol on 62 patients from November 2008 to October 2014, which represents 24% of all patients with MPM seen at the institution in that period. Fifty-two patients were men and ages ranged from 41 to 75 years. Clinical stage of cancer ranged from T1N0 in 10 patients, to T2N0 in 35 and T3N0 in 13 (two had T4N0 and two had T3N2). Forty-five had right-side cancers. Six patients received an extended protocol for various reasons, including tumor extending to the chest wall.
All 62 patients completed IMRT and EPP. All but one had resection and reconstruction of the diaphragm, and all but four had resection and reconstruction of the pericardium.
Overall death rate was 4.8% (three patients). Results were better in patients with epithelioid tumors, with a median survival of 51 months and disease-free survival of 47 months. Those with biphasic subtypes had median survival of 10 months and disease-free survival of 8 months. Eight patients had ipsilateral chest recurrence. “This analysis demonstrates that the SMART approach is particularly encouraging for patients with epithelial subtype,” Dr. de Perrot and coauthors said. They no longer perform the SMART protocol on patients with biphasic subtype.
The protocol was not without complications. Twenty-four patients, about 38%, had serious complications that required intervention or worse. Twelve had atrial fibrillation, but none advanced to life-threatening disease. Among other complications, four had empyema – one resulting in death – and three had pulmonary emboli. One other patient in the complications group died from pneumonia, and another died from a heart attack at home.
This is the Toronto researchers’ second attempt at studying the three-modality approach. In their first attempt, only half the patients who started with preoperative chemotherapy went onto complete the radiation after surgery because of difficulties administering it (J Thorac Cardiovasc Surg. 2007;133:111-6; J Clin Oncol. 2009;27:1413-8). Also, about 25% of patients had disease progression during induction chemotherapy and could not go onto surgery.
They designed the most recent trial to deliver radiation before surgery because of the excellent local control of cancer along with evidence that MPM tumors were radio-sensitive. “Considering the risk of disease progression on induction chemotherapy, we felt that switching the order of therapy was potentially a better option for patients with surgically resectable disease,” Dr. de Perrott and colleagues said.
The researchers cited the study’s single-center nature with a single treatment arm, and the lack of longer-term follow-up, as limitations. “However, in our own experience, this approach has been very encouraging and has become our primary option for patients with surgically resectable MPM,” they noted.
The study authors had no conflicts to disclose.
The popularity of extrapleural pneumonectomy to treat asbestos-related thoracic mesothelioma has yielded to extended pleurectomy/decortication in recent years, but a recent study suggests that the extrapleural pneumonectomy procedure can achieve good results in a new protocol that involves administering radiation therapy before surgery as opposed the more conventional approach of radiation after surgery.
Researchers at the University of Toronto reported on their protocol that uses accelerated intensity modulated radiation therapy (IMRT) for malignant pleural mesothelioma (MPM) (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.09.129). They call the protocol SMART, for Surgery for Mesothelioma After Radiation Therapy.
“The rationale to develop this protocol was to optimize the delivery of radiation to the whole tumor bed, sterilize the edges of the tumor to limit the risk of spillage at the time of surgery, develop a shorter treatment plan and potentiate the activation of the immune system by using a hypofractionated regimen,” wrote Dr. Marc de Perrot and colleagues.
The protocol involves delivering 25 Gy of radiation in five daily fractions over a week to the entire side of the thorax with 5 Gy boosts based on imaging, followed by extrapleural pneumonectomy (EPP) 4-6 days later. Patients with three or more positive lymph notes (ypN2 disease) also are offered adjuvant chemotherapy.
The researchers performed the protocol on 62 patients from November 2008 to October 2014, which represents 24% of all patients with MPM seen at the institution in that period. Fifty-two patients were men and ages ranged from 41 to 75 years. Clinical stage of cancer ranged from T1N0 in 10 patients, to T2N0 in 35 and T3N0 in 13 (two had T4N0 and two had T3N2). Forty-five had right-side cancers. Six patients received an extended protocol for various reasons, including tumor extending to the chest wall.
All 62 patients completed IMRT and EPP. All but one had resection and reconstruction of the diaphragm, and all but four had resection and reconstruction of the pericardium.
Overall death rate was 4.8% (three patients). Results were better in patients with epithelioid tumors, with a median survival of 51 months and disease-free survival of 47 months. Those with biphasic subtypes had median survival of 10 months and disease-free survival of 8 months. Eight patients had ipsilateral chest recurrence. “This analysis demonstrates that the SMART approach is particularly encouraging for patients with epithelial subtype,” Dr. de Perrot and coauthors said. They no longer perform the SMART protocol on patients with biphasic subtype.
The protocol was not without complications. Twenty-four patients, about 38%, had serious complications that required intervention or worse. Twelve had atrial fibrillation, but none advanced to life-threatening disease. Among other complications, four had empyema – one resulting in death – and three had pulmonary emboli. One other patient in the complications group died from pneumonia, and another died from a heart attack at home.
This is the Toronto researchers’ second attempt at studying the three-modality approach. In their first attempt, only half the patients who started with preoperative chemotherapy went onto complete the radiation after surgery because of difficulties administering it (J Thorac Cardiovasc Surg. 2007;133:111-6; J Clin Oncol. 2009;27:1413-8). Also, about 25% of patients had disease progression during induction chemotherapy and could not go onto surgery.
They designed the most recent trial to deliver radiation before surgery because of the excellent local control of cancer along with evidence that MPM tumors were radio-sensitive. “Considering the risk of disease progression on induction chemotherapy, we felt that switching the order of therapy was potentially a better option for patients with surgically resectable disease,” Dr. de Perrott and colleagues said.
The researchers cited the study’s single-center nature with a single treatment arm, and the lack of longer-term follow-up, as limitations. “However, in our own experience, this approach has been very encouraging and has become our primary option for patients with surgically resectable MPM,” they noted.
The study authors had no conflicts to disclose.
Key clinical point: A new protocol that involves accelerated hemithoracic intensity modulated radiation before surgery for lung mesothelioma delivered encouraging results in patients with epithelioid tumors.
Major finding: Disease-free survival was 47 months in epithelial subtypes compared with 8 months in biphasic subtypes.
Data source: A single-center population of 62 patients with malignant pleural mesothelioma treated between November 2008 and October 2014.
Disclosures: The study authors had no relationships to disclose.
Off-pump bypass may confer stroke benefit
Claims that off-pump coronary artery bypass (OPCAB) carries a lower risk of short-term stroke than conventional on-pump coronary artery bypass grafting (CABG) have been the subject of contradicting evidence, mostly because of the small size of the studies that showed a benefit, but European investigators published a meta-analysis involving more than 19,000 cases that showed what they called a “significant reduction” in the odds of a stroke.
“OPCAB was associated with a significant (28%) reduction in the odds of stroke compared with CABG,” said lead author Dr. Mariusz Kowalewski of Copernicus University in Bydgoszcz, Poland, and coauthors. The meta-analysis appeared in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:60-77).
The coauthors represent 10 different centers throughout Europe. Dr. Kowalewski and three other coauthors are also with the Systemic Investigation and Research on Interventions and Outcomes MEDICINE Research Network based in Düsseldorf, Germany.
Dr. Kowalewski and colleagues said this is the largest meta-analysis of randomized clinical trials comparing short-term outcomes of the two approaches to coronary bypass. “By its unique design, this analysis is the first report to investigate the causal relationship between underlying patient risk profile and the benefits of off-pump coronary revascularization,” they noted.
The meta-analysis looked at results of three primary outcomes: death within 30 days of the operation (2.25% overall, 2% in the OPCAB group and 2.04% in the CABG group); MI 30 days after surgery (4.49% overall, 4.3% for OPCAB and 4.67% for CABG); and 30-day occurrence of stroke (1.67% overall, 1.34% for OPCAB group and 2% for CABG).
In the meta-analysis, the researchers evaluated 100 studies for potential bias and conducted three separate analyses: one of all studies; and then separate analyses of studies of more than 50 and 100 subjects, respectively. Their goal was to check if small studies were driving the results.
Dr. Kowalewski and the study team acknowledged the conflicting science surrounding the benefits of the off-pump vs. conventional bypass. They pointed out that a host of randomized studies failed to show significant differences in stroke rates between the two approaches, and that conflicting European and American guidelines on the role of off-pump surgery to provide a better neurologic outcome do not help to clarify the relative risk.
“This apparent contradiction with the available registries’ data reporting a significantly decreased incidence of stroke with OPCAB may be explained by the fact that cerebral stroke represents a relatively rare entity after CABG, and thus even the largest randomized studies are underpowered to prove a possible advantage of one technique over the other,” Dr. Kowalewski and colleagues said.
They cited the CORONARY trial (N Engl J Med. 2012;366:1489-97), the largest trial to date, with 4,752 patients, which found no difference in the rate of stroke between the two groups. Three previous meta-analyses demonstrated 30%-50% reductions in stroke, but a systemic review called those results into question (Cochrane Database Syst. Rev. 2012;3:CD007224).
The “most important” finding of their study may be the confirmation of what large registries have reported: that OPCAB is safer and more effective than conventional bypass surgery in older and sicker patients. But they acknowledged that why this is the case “remains a subject of ongoing debate.”
Dr. Kowalewski and coresearchers acknowledged a number of limitations of their meta-analysis, namely that sensitivity analysis may have missed clinically important differences in patient results and broad patient inclusion criteria. However, the random-effects model they used accounted for study variations. “The findings on significant risk profile meta-regression are further corroborated in the analysis of MI and stroke,” they said.
Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other coauthors had no relationships to disclose.
That off-pump coronary artery bypass (OPCAB) grafting provides no benefit or, at best, a negligible benefit over conventional on-pump surgery in terms of 30-day death rates and risk of myocardial infarction is a question that can be laid “safely to bed,” Dr. Fraser Rubens of the University of Ottawa Heart Institute said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:78-9).
However, less clear cut is the meta-analysis researchers’ assertion that off-pump CABG can significantly reduce the risk of future stroke, and that requires a close examination of the structural shortcomings of any meta-analysis, Dr. Rubens said. He cited a report that stated meta-analyses may inaccurately predict the outcomes of subsequent large randomized clinical trials in about one-third of all cases (N Engl J Med 1997;337:536-42).
Smaller trials like those used in a meta-analysis are more likely to be flawed because of a lax peer review or compromised methodology, Dr. Rubens said. The largest randomized trial the authors used in the meta-analysis showed “certainly no difference in stroke,” and when all trials with 200 or fewer patients were excluded, the stroke rates were 1.4% in the off-pump group vs. 1.6% in the on-pump population, he said.
To validate that difference would require a number needed to treat of 500 patients to prevent one stroke, Dr. Rubens said, “and the sample size required to prove this difference would exceed 58,000 patients per group” – whereas the large-trial cohort in this meta-analysis population was about a tenth of that.
“One must therefore assimilate this information with the worrisome evidence that off-pump surgery is associated with an increased incidence of incomplete revascularization, which is likely related to the subsequent increased need for repeat revascularization,” Dr. Rubens said.
Dr. Rubens had no disclosures.
That off-pump coronary artery bypass (OPCAB) grafting provides no benefit or, at best, a negligible benefit over conventional on-pump surgery in terms of 30-day death rates and risk of myocardial infarction is a question that can be laid “safely to bed,” Dr. Fraser Rubens of the University of Ottawa Heart Institute said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:78-9).
However, less clear cut is the meta-analysis researchers’ assertion that off-pump CABG can significantly reduce the risk of future stroke, and that requires a close examination of the structural shortcomings of any meta-analysis, Dr. Rubens said. He cited a report that stated meta-analyses may inaccurately predict the outcomes of subsequent large randomized clinical trials in about one-third of all cases (N Engl J Med 1997;337:536-42).
Smaller trials like those used in a meta-analysis are more likely to be flawed because of a lax peer review or compromised methodology, Dr. Rubens said. The largest randomized trial the authors used in the meta-analysis showed “certainly no difference in stroke,” and when all trials with 200 or fewer patients were excluded, the stroke rates were 1.4% in the off-pump group vs. 1.6% in the on-pump population, he said.
To validate that difference would require a number needed to treat of 500 patients to prevent one stroke, Dr. Rubens said, “and the sample size required to prove this difference would exceed 58,000 patients per group” – whereas the large-trial cohort in this meta-analysis population was about a tenth of that.
“One must therefore assimilate this information with the worrisome evidence that off-pump surgery is associated with an increased incidence of incomplete revascularization, which is likely related to the subsequent increased need for repeat revascularization,” Dr. Rubens said.
Dr. Rubens had no disclosures.
That off-pump coronary artery bypass (OPCAB) grafting provides no benefit or, at best, a negligible benefit over conventional on-pump surgery in terms of 30-day death rates and risk of myocardial infarction is a question that can be laid “safely to bed,” Dr. Fraser Rubens of the University of Ottawa Heart Institute said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:78-9).
However, less clear cut is the meta-analysis researchers’ assertion that off-pump CABG can significantly reduce the risk of future stroke, and that requires a close examination of the structural shortcomings of any meta-analysis, Dr. Rubens said. He cited a report that stated meta-analyses may inaccurately predict the outcomes of subsequent large randomized clinical trials in about one-third of all cases (N Engl J Med 1997;337:536-42).
Smaller trials like those used in a meta-analysis are more likely to be flawed because of a lax peer review or compromised methodology, Dr. Rubens said. The largest randomized trial the authors used in the meta-analysis showed “certainly no difference in stroke,” and when all trials with 200 or fewer patients were excluded, the stroke rates were 1.4% in the off-pump group vs. 1.6% in the on-pump population, he said.
To validate that difference would require a number needed to treat of 500 patients to prevent one stroke, Dr. Rubens said, “and the sample size required to prove this difference would exceed 58,000 patients per group” – whereas the large-trial cohort in this meta-analysis population was about a tenth of that.
“One must therefore assimilate this information with the worrisome evidence that off-pump surgery is associated with an increased incidence of incomplete revascularization, which is likely related to the subsequent increased need for repeat revascularization,” Dr. Rubens said.
Dr. Rubens had no disclosures.
Claims that off-pump coronary artery bypass (OPCAB) carries a lower risk of short-term stroke than conventional on-pump coronary artery bypass grafting (CABG) have been the subject of contradicting evidence, mostly because of the small size of the studies that showed a benefit, but European investigators published a meta-analysis involving more than 19,000 cases that showed what they called a “significant reduction” in the odds of a stroke.
“OPCAB was associated with a significant (28%) reduction in the odds of stroke compared with CABG,” said lead author Dr. Mariusz Kowalewski of Copernicus University in Bydgoszcz, Poland, and coauthors. The meta-analysis appeared in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:60-77).
The coauthors represent 10 different centers throughout Europe. Dr. Kowalewski and three other coauthors are also with the Systemic Investigation and Research on Interventions and Outcomes MEDICINE Research Network based in Düsseldorf, Germany.
Dr. Kowalewski and colleagues said this is the largest meta-analysis of randomized clinical trials comparing short-term outcomes of the two approaches to coronary bypass. “By its unique design, this analysis is the first report to investigate the causal relationship between underlying patient risk profile and the benefits of off-pump coronary revascularization,” they noted.
The meta-analysis looked at results of three primary outcomes: death within 30 days of the operation (2.25% overall, 2% in the OPCAB group and 2.04% in the CABG group); MI 30 days after surgery (4.49% overall, 4.3% for OPCAB and 4.67% for CABG); and 30-day occurrence of stroke (1.67% overall, 1.34% for OPCAB group and 2% for CABG).
In the meta-analysis, the researchers evaluated 100 studies for potential bias and conducted three separate analyses: one of all studies; and then separate analyses of studies of more than 50 and 100 subjects, respectively. Their goal was to check if small studies were driving the results.
Dr. Kowalewski and the study team acknowledged the conflicting science surrounding the benefits of the off-pump vs. conventional bypass. They pointed out that a host of randomized studies failed to show significant differences in stroke rates between the two approaches, and that conflicting European and American guidelines on the role of off-pump surgery to provide a better neurologic outcome do not help to clarify the relative risk.
“This apparent contradiction with the available registries’ data reporting a significantly decreased incidence of stroke with OPCAB may be explained by the fact that cerebral stroke represents a relatively rare entity after CABG, and thus even the largest randomized studies are underpowered to prove a possible advantage of one technique over the other,” Dr. Kowalewski and colleagues said.
They cited the CORONARY trial (N Engl J Med. 2012;366:1489-97), the largest trial to date, with 4,752 patients, which found no difference in the rate of stroke between the two groups. Three previous meta-analyses demonstrated 30%-50% reductions in stroke, but a systemic review called those results into question (Cochrane Database Syst. Rev. 2012;3:CD007224).
The “most important” finding of their study may be the confirmation of what large registries have reported: that OPCAB is safer and more effective than conventional bypass surgery in older and sicker patients. But they acknowledged that why this is the case “remains a subject of ongoing debate.”
Dr. Kowalewski and coresearchers acknowledged a number of limitations of their meta-analysis, namely that sensitivity analysis may have missed clinically important differences in patient results and broad patient inclusion criteria. However, the random-effects model they used accounted for study variations. “The findings on significant risk profile meta-regression are further corroborated in the analysis of MI and stroke,” they said.
Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other coauthors had no relationships to disclose.
Claims that off-pump coronary artery bypass (OPCAB) carries a lower risk of short-term stroke than conventional on-pump coronary artery bypass grafting (CABG) have been the subject of contradicting evidence, mostly because of the small size of the studies that showed a benefit, but European investigators published a meta-analysis involving more than 19,000 cases that showed what they called a “significant reduction” in the odds of a stroke.
“OPCAB was associated with a significant (28%) reduction in the odds of stroke compared with CABG,” said lead author Dr. Mariusz Kowalewski of Copernicus University in Bydgoszcz, Poland, and coauthors. The meta-analysis appeared in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:60-77).
The coauthors represent 10 different centers throughout Europe. Dr. Kowalewski and three other coauthors are also with the Systemic Investigation and Research on Interventions and Outcomes MEDICINE Research Network based in Düsseldorf, Germany.
Dr. Kowalewski and colleagues said this is the largest meta-analysis of randomized clinical trials comparing short-term outcomes of the two approaches to coronary bypass. “By its unique design, this analysis is the first report to investigate the causal relationship between underlying patient risk profile and the benefits of off-pump coronary revascularization,” they noted.
The meta-analysis looked at results of three primary outcomes: death within 30 days of the operation (2.25% overall, 2% in the OPCAB group and 2.04% in the CABG group); MI 30 days after surgery (4.49% overall, 4.3% for OPCAB and 4.67% for CABG); and 30-day occurrence of stroke (1.67% overall, 1.34% for OPCAB group and 2% for CABG).
In the meta-analysis, the researchers evaluated 100 studies for potential bias and conducted three separate analyses: one of all studies; and then separate analyses of studies of more than 50 and 100 subjects, respectively. Their goal was to check if small studies were driving the results.
Dr. Kowalewski and the study team acknowledged the conflicting science surrounding the benefits of the off-pump vs. conventional bypass. They pointed out that a host of randomized studies failed to show significant differences in stroke rates between the two approaches, and that conflicting European and American guidelines on the role of off-pump surgery to provide a better neurologic outcome do not help to clarify the relative risk.
“This apparent contradiction with the available registries’ data reporting a significantly decreased incidence of stroke with OPCAB may be explained by the fact that cerebral stroke represents a relatively rare entity after CABG, and thus even the largest randomized studies are underpowered to prove a possible advantage of one technique over the other,” Dr. Kowalewski and colleagues said.
They cited the CORONARY trial (N Engl J Med. 2012;366:1489-97), the largest trial to date, with 4,752 patients, which found no difference in the rate of stroke between the two groups. Three previous meta-analyses demonstrated 30%-50% reductions in stroke, but a systemic review called those results into question (Cochrane Database Syst. Rev. 2012;3:CD007224).
The “most important” finding of their study may be the confirmation of what large registries have reported: that OPCAB is safer and more effective than conventional bypass surgery in older and sicker patients. But they acknowledged that why this is the case “remains a subject of ongoing debate.”
Dr. Kowalewski and coresearchers acknowledged a number of limitations of their meta-analysis, namely that sensitivity analysis may have missed clinically important differences in patient results and broad patient inclusion criteria. However, the random-effects model they used accounted for study variations. “The findings on significant risk profile meta-regression are further corroborated in the analysis of MI and stroke,” they said.
Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other coauthors had no relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Off-pump coronary artery bypass is associated with a significant reduction in the odds of stroke compared with conventional coronary artery bypass grafting and should be considered in high-risk patients.
Major finding: Off-pump coronary artery bypass was associated with a 28% reduction in the odds of patients having a cerebral stroke when compared with the conventional on-pump procedure.
Data source: Meta-analysis of 100 studies with a total of 19,192 patients.
Disclosures: Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other authors had no relationships to disclose.
Post-repair MR may be worse than thought
In patients who undergo transcatheter mitral valve repair for mitral valve regurgitation (MR), residual mild (+2) regurgitation has been considered procedural success, but a team of Italian investigators has provided evidence that such a result may actually foretell far worse long-term outcomes than residual trace (≤1) MR.
The investigators from San Raffaele Scientific Institute in Milan reported their findings in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg 2016;151:88-96). They compared follow-up outcomes of 223 consecutive patients with residual MR 2+ and MR ≤1 after implantation of the MitraClip system (Abbott Vascular). The procedures were performed between October 2008 and December 2014.
“In this study we found a clear unfavorable impact on follow-up outcomes of acute residual 2+ MR after MitraClip repair when compared to residual ≤1+ MR,” lead author Dr. Nicola Buzzatti and colleagues said.
The study cited a scarcity of data on the long-term impact of residual mild MR. “This topic is therefore particularly of interest, especially when assessing the convenience to expand transcatheter mitral repair procedures to intermediate or low-risk patients,” Dr. Buzzatti and coauthors said.
The study group all had moderate or greater (≥3+) MR when they underwent mitral valve repair (MVR). The post-MVR study cohort excluded patients who had residual MR of 3 or greater, which was considered a procedural failure. Four patients died within 30 days, each from a different cause: multi-organ failure, lung rupture, pneumonia with heart failure, and sudden death. The overall 30-day death rate was 1.8%.
Among the remainder of patients, the average follow-up was 20.5 months, with some follow-up extending to 75 months. The overall survival was 74.4% at 24 months and 63% at 48 months.
The study calculated the cumulative incidence function, or the probability of failure, of cardiac death in patients with residual MR ≤1 at 7.1% at 24 months and 10.9% at 48 months, compared with 26.9% at 24 months and 35.3% at 48 months in those with MR 2+. The probability of failure of recurrence of moderate or severe MR with residual MR ≤1 was 5.6% at 24 months and 13.3% at 48 months, compared with 45.2% at both 24 and 48 months with residual MR 2+. “The difference between MR ≤1 and MR=2 was significant,” Dr. Buzzatti and colleagues said.
The researchers separately evaluated outcomes among those who had functional MR (FMR) and degenerative MR (DMR). In FMR, patients with MR 2+ had a higher risk profile at baseline because of a slightly higher rate of advanced heart disease; they typically had larger ventricles with larger mitral valves and greater pulmonary pressure than the ≤1 MR patients. “Notably, these features could have impaired the surgeon’s ability to achieve acute optimal MR reduction during the MitraClip procedure,” Dr. Buzzatti and coauthors said. “For sure, advanced left ventricle remodeling was a strong independent predictor of increased cardiac death.” The study authors could not draw a similar conclusion with DMR because only three patients in the group died of cardiac causes.
MR recurrence was “remarkably higher” in MR 2+ patients, compared with the MR ≤1 group with FMR and DMR, and MR 2+ developed in 21.4% of the FMR group within 30 days of the procedure. “This poor efficacy results in a population of patients who were supposed to have had a ‘procedural success’ is striking,” Dr. Buzzatti and coauthors noted.
Dr. Buzzatti and coauthor Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Coauthor Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other coauthors had no relationships to disclose.
In interpreting the findings of the Italian study and applying them in the clinic, one must consider the etiology of mitral valve regurgitation (MR) because that can determine the outcome of transcatheter mitral valve repair, Dr. Vincent Chan and Dr. Marc Ruel of the University of Ottawa Heart Institute said in their invited commentary (J Thorac Cardiovasc Surg 2016;151:97-8).
“In patients with coronary artery disease, it is well known that the presence of moderate chronic ischemic MR is associated with worse survival and more congestive heart failure compared to patients without MR,” Dr. Chan and Dr. Ruel said.
In a series his group studied, they noted that recurrent moderate MR was more common after MV repair than replacement; the survival rates between the two groups were similar (Ann Thorac Surg. 2011;92:1358-1365). That may be because late left ventricle (LV) function was similar between patients who had recurrent moderate MR and those that did not, but the Italian study did not clarify difference in late LV function between functional MR patients. “Perhaps differences in clinical outcome between patients with MR 2+ and MR ≤1+ relate to differences in ventricular function that portend mortality?” they asked.
They also called the researchers’ assertion that moderate MR impacts outcomes after repair “interesting.” They cited studies that linked effective worse outcomes to effective regurgitant orifice area (EROA) of 20-39 mm2, but that the complexity of echocardiographic measurement raises challenges in calculating EROA (Circulation. 2001;103:1759-64; N Engl J Med. 2005;352:875-83). “Also residual prolapse following MitraClip, as with any prolapse, may be brief and therefore instantaneous measures or regurgitation with pulse wave Doppler may be limited,” they said.
While percutaneous approaches to treat MR have “revolutionized” the care of these patients, the technology has its limitations, Dr. Chan and Dr. Ruel said. “Although many patients benefit from this therapy, the understanding of incomplete MR reduction with this technology continues to evolve.”
They had no disclosures.
In interpreting the findings of the Italian study and applying them in the clinic, one must consider the etiology of mitral valve regurgitation (MR) because that can determine the outcome of transcatheter mitral valve repair, Dr. Vincent Chan and Dr. Marc Ruel of the University of Ottawa Heart Institute said in their invited commentary (J Thorac Cardiovasc Surg 2016;151:97-8).
“In patients with coronary artery disease, it is well known that the presence of moderate chronic ischemic MR is associated with worse survival and more congestive heart failure compared to patients without MR,” Dr. Chan and Dr. Ruel said.
In a series his group studied, they noted that recurrent moderate MR was more common after MV repair than replacement; the survival rates between the two groups were similar (Ann Thorac Surg. 2011;92:1358-1365). That may be because late left ventricle (LV) function was similar between patients who had recurrent moderate MR and those that did not, but the Italian study did not clarify difference in late LV function between functional MR patients. “Perhaps differences in clinical outcome between patients with MR 2+ and MR ≤1+ relate to differences in ventricular function that portend mortality?” they asked.
They also called the researchers’ assertion that moderate MR impacts outcomes after repair “interesting.” They cited studies that linked effective worse outcomes to effective regurgitant orifice area (EROA) of 20-39 mm2, but that the complexity of echocardiographic measurement raises challenges in calculating EROA (Circulation. 2001;103:1759-64; N Engl J Med. 2005;352:875-83). “Also residual prolapse following MitraClip, as with any prolapse, may be brief and therefore instantaneous measures or regurgitation with pulse wave Doppler may be limited,” they said.
While percutaneous approaches to treat MR have “revolutionized” the care of these patients, the technology has its limitations, Dr. Chan and Dr. Ruel said. “Although many patients benefit from this therapy, the understanding of incomplete MR reduction with this technology continues to evolve.”
They had no disclosures.
In interpreting the findings of the Italian study and applying them in the clinic, one must consider the etiology of mitral valve regurgitation (MR) because that can determine the outcome of transcatheter mitral valve repair, Dr. Vincent Chan and Dr. Marc Ruel of the University of Ottawa Heart Institute said in their invited commentary (J Thorac Cardiovasc Surg 2016;151:97-8).
“In patients with coronary artery disease, it is well known that the presence of moderate chronic ischemic MR is associated with worse survival and more congestive heart failure compared to patients without MR,” Dr. Chan and Dr. Ruel said.
In a series his group studied, they noted that recurrent moderate MR was more common after MV repair than replacement; the survival rates between the two groups were similar (Ann Thorac Surg. 2011;92:1358-1365). That may be because late left ventricle (LV) function was similar between patients who had recurrent moderate MR and those that did not, but the Italian study did not clarify difference in late LV function between functional MR patients. “Perhaps differences in clinical outcome between patients with MR 2+ and MR ≤1+ relate to differences in ventricular function that portend mortality?” they asked.
They also called the researchers’ assertion that moderate MR impacts outcomes after repair “interesting.” They cited studies that linked effective worse outcomes to effective regurgitant orifice area (EROA) of 20-39 mm2, but that the complexity of echocardiographic measurement raises challenges in calculating EROA (Circulation. 2001;103:1759-64; N Engl J Med. 2005;352:875-83). “Also residual prolapse following MitraClip, as with any prolapse, may be brief and therefore instantaneous measures or regurgitation with pulse wave Doppler may be limited,” they said.
While percutaneous approaches to treat MR have “revolutionized” the care of these patients, the technology has its limitations, Dr. Chan and Dr. Ruel said. “Although many patients benefit from this therapy, the understanding of incomplete MR reduction with this technology continues to evolve.”
They had no disclosures.
In patients who undergo transcatheter mitral valve repair for mitral valve regurgitation (MR), residual mild (+2) regurgitation has been considered procedural success, but a team of Italian investigators has provided evidence that such a result may actually foretell far worse long-term outcomes than residual trace (≤1) MR.
The investigators from San Raffaele Scientific Institute in Milan reported their findings in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg 2016;151:88-96). They compared follow-up outcomes of 223 consecutive patients with residual MR 2+ and MR ≤1 after implantation of the MitraClip system (Abbott Vascular). The procedures were performed between October 2008 and December 2014.
“In this study we found a clear unfavorable impact on follow-up outcomes of acute residual 2+ MR after MitraClip repair when compared to residual ≤1+ MR,” lead author Dr. Nicola Buzzatti and colleagues said.
The study cited a scarcity of data on the long-term impact of residual mild MR. “This topic is therefore particularly of interest, especially when assessing the convenience to expand transcatheter mitral repair procedures to intermediate or low-risk patients,” Dr. Buzzatti and coauthors said.
The study group all had moderate or greater (≥3+) MR when they underwent mitral valve repair (MVR). The post-MVR study cohort excluded patients who had residual MR of 3 or greater, which was considered a procedural failure. Four patients died within 30 days, each from a different cause: multi-organ failure, lung rupture, pneumonia with heart failure, and sudden death. The overall 30-day death rate was 1.8%.
Among the remainder of patients, the average follow-up was 20.5 months, with some follow-up extending to 75 months. The overall survival was 74.4% at 24 months and 63% at 48 months.
The study calculated the cumulative incidence function, or the probability of failure, of cardiac death in patients with residual MR ≤1 at 7.1% at 24 months and 10.9% at 48 months, compared with 26.9% at 24 months and 35.3% at 48 months in those with MR 2+. The probability of failure of recurrence of moderate or severe MR with residual MR ≤1 was 5.6% at 24 months and 13.3% at 48 months, compared with 45.2% at both 24 and 48 months with residual MR 2+. “The difference between MR ≤1 and MR=2 was significant,” Dr. Buzzatti and colleagues said.
The researchers separately evaluated outcomes among those who had functional MR (FMR) and degenerative MR (DMR). In FMR, patients with MR 2+ had a higher risk profile at baseline because of a slightly higher rate of advanced heart disease; they typically had larger ventricles with larger mitral valves and greater pulmonary pressure than the ≤1 MR patients. “Notably, these features could have impaired the surgeon’s ability to achieve acute optimal MR reduction during the MitraClip procedure,” Dr. Buzzatti and coauthors said. “For sure, advanced left ventricle remodeling was a strong independent predictor of increased cardiac death.” The study authors could not draw a similar conclusion with DMR because only three patients in the group died of cardiac causes.
MR recurrence was “remarkably higher” in MR 2+ patients, compared with the MR ≤1 group with FMR and DMR, and MR 2+ developed in 21.4% of the FMR group within 30 days of the procedure. “This poor efficacy results in a population of patients who were supposed to have had a ‘procedural success’ is striking,” Dr. Buzzatti and coauthors noted.
Dr. Buzzatti and coauthor Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Coauthor Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other coauthors had no relationships to disclose.
In patients who undergo transcatheter mitral valve repair for mitral valve regurgitation (MR), residual mild (+2) regurgitation has been considered procedural success, but a team of Italian investigators has provided evidence that such a result may actually foretell far worse long-term outcomes than residual trace (≤1) MR.
The investigators from San Raffaele Scientific Institute in Milan reported their findings in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg 2016;151:88-96). They compared follow-up outcomes of 223 consecutive patients with residual MR 2+ and MR ≤1 after implantation of the MitraClip system (Abbott Vascular). The procedures were performed between October 2008 and December 2014.
“In this study we found a clear unfavorable impact on follow-up outcomes of acute residual 2+ MR after MitraClip repair when compared to residual ≤1+ MR,” lead author Dr. Nicola Buzzatti and colleagues said.
The study cited a scarcity of data on the long-term impact of residual mild MR. “This topic is therefore particularly of interest, especially when assessing the convenience to expand transcatheter mitral repair procedures to intermediate or low-risk patients,” Dr. Buzzatti and coauthors said.
The study group all had moderate or greater (≥3+) MR when they underwent mitral valve repair (MVR). The post-MVR study cohort excluded patients who had residual MR of 3 or greater, which was considered a procedural failure. Four patients died within 30 days, each from a different cause: multi-organ failure, lung rupture, pneumonia with heart failure, and sudden death. The overall 30-day death rate was 1.8%.
Among the remainder of patients, the average follow-up was 20.5 months, with some follow-up extending to 75 months. The overall survival was 74.4% at 24 months and 63% at 48 months.
The study calculated the cumulative incidence function, or the probability of failure, of cardiac death in patients with residual MR ≤1 at 7.1% at 24 months and 10.9% at 48 months, compared with 26.9% at 24 months and 35.3% at 48 months in those with MR 2+. The probability of failure of recurrence of moderate or severe MR with residual MR ≤1 was 5.6% at 24 months and 13.3% at 48 months, compared with 45.2% at both 24 and 48 months with residual MR 2+. “The difference between MR ≤1 and MR=2 was significant,” Dr. Buzzatti and colleagues said.
The researchers separately evaluated outcomes among those who had functional MR (FMR) and degenerative MR (DMR). In FMR, patients with MR 2+ had a higher risk profile at baseline because of a slightly higher rate of advanced heart disease; they typically had larger ventricles with larger mitral valves and greater pulmonary pressure than the ≤1 MR patients. “Notably, these features could have impaired the surgeon’s ability to achieve acute optimal MR reduction during the MitraClip procedure,” Dr. Buzzatti and coauthors said. “For sure, advanced left ventricle remodeling was a strong independent predictor of increased cardiac death.” The study authors could not draw a similar conclusion with DMR because only three patients in the group died of cardiac causes.
MR recurrence was “remarkably higher” in MR 2+ patients, compared with the MR ≤1 group with FMR and DMR, and MR 2+ developed in 21.4% of the FMR group within 30 days of the procedure. “This poor efficacy results in a population of patients who were supposed to have had a ‘procedural success’ is striking,” Dr. Buzzatti and coauthors noted.
Dr. Buzzatti and coauthor Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Coauthor Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other coauthors had no relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Residual mild mitral valve regurgitation (MR) after implantation of the MitraClip device (Abbott Vascular) was associated with worse survival, symptom relief, and risk of moderate or severe MR than residual trace MR after implantation.
Major finding: Patients with residual mild MR after MitraClip implantation had a 45% probability of recurrence of moderate or severe MR within 4 years, more than three times that of those who had residual trace MR.
Data source: Population of 223 consecutive patients with acute residual trace or mild MR after MitraClip implantation between 2008 and 2014 at a single institution.
Disclosures: Dr. Nicola Buzzatti and Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other authors had no relationships to disclose.
No benefit in open massage over closed compressions in trauma cardiac arrest
SAN ANTONIO – Open-chest cardiac massage offers no benefit over closed-chest compressions in patients with traumatic cardiac arrest, according to a prospective observational study from the University of Maryland Shock Trauma Center in Baltimore.
The investigators compared 16 open-chest cardiac massage (OCCM) patients with 17 closed-chest compression (CCC) patients delivered directly to the level 1 trauma center in cardiac arrest. The open-massage group received closed compressions for a mean of 66 seconds before being converted to open massage for reasons that weren’t captured by the data.
End-tidal carbon dioxide (ETCO2) – the gold standard for determining the effectiveness of chest compressions and return of spontaneous circulation – was used as a surrogate for cardiac output and adequacy of resuscitation. Continuous high-resolution ETCO2 measurements were collected every 6 seconds in both groups.
When periods of OCCM were compared to equivalent periods of CCC, there were no differences in the initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
“Unless the patient has a thoracic injury that you need to get into the chest to fix, we didn’t see any benefit in opening the chest just to massage the heart. The data suggest that maybe we shouldn’t be so aggressive in doing open cardiac massage. There’s renewed interest in performing endovascular balloon occlusion techniques for the aorta to obtain hemorrhage control; if you do that and you do closed-chest compressions, it’s just as effective as opening up the chest and doing cardiac massage,” said investigator Dr. Matthew Bradley, a trauma surgeon at the Shock Trauma Center, at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
Most of the patients were men, and there was a higher percentage of penetrating trauma in the OCCM group (81% versus 47%; P = .04).
The results were the same, however, in subgroup analyses limited to blunt and penetrating trauma.
All of the open massage patients died, but there were a few survivors in the CCC group. Dr. Bradley didn’t think the closed versus open approach was the reason for the survival difference.
Resuscitative endovascular balloon occlusion of the aorta patients were excluded from the trial to prevent confounding.
The investigators have no relevant disclosures.
SAN ANTONIO – Open-chest cardiac massage offers no benefit over closed-chest compressions in patients with traumatic cardiac arrest, according to a prospective observational study from the University of Maryland Shock Trauma Center in Baltimore.
The investigators compared 16 open-chest cardiac massage (OCCM) patients with 17 closed-chest compression (CCC) patients delivered directly to the level 1 trauma center in cardiac arrest. The open-massage group received closed compressions for a mean of 66 seconds before being converted to open massage for reasons that weren’t captured by the data.
End-tidal carbon dioxide (ETCO2) – the gold standard for determining the effectiveness of chest compressions and return of spontaneous circulation – was used as a surrogate for cardiac output and adequacy of resuscitation. Continuous high-resolution ETCO2 measurements were collected every 6 seconds in both groups.
When periods of OCCM were compared to equivalent periods of CCC, there were no differences in the initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
“Unless the patient has a thoracic injury that you need to get into the chest to fix, we didn’t see any benefit in opening the chest just to massage the heart. The data suggest that maybe we shouldn’t be so aggressive in doing open cardiac massage. There’s renewed interest in performing endovascular balloon occlusion techniques for the aorta to obtain hemorrhage control; if you do that and you do closed-chest compressions, it’s just as effective as opening up the chest and doing cardiac massage,” said investigator Dr. Matthew Bradley, a trauma surgeon at the Shock Trauma Center, at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
Most of the patients were men, and there was a higher percentage of penetrating trauma in the OCCM group (81% versus 47%; P = .04).
The results were the same, however, in subgroup analyses limited to blunt and penetrating trauma.
All of the open massage patients died, but there were a few survivors in the CCC group. Dr. Bradley didn’t think the closed versus open approach was the reason for the survival difference.
Resuscitative endovascular balloon occlusion of the aorta patients were excluded from the trial to prevent confounding.
The investigators have no relevant disclosures.
SAN ANTONIO – Open-chest cardiac massage offers no benefit over closed-chest compressions in patients with traumatic cardiac arrest, according to a prospective observational study from the University of Maryland Shock Trauma Center in Baltimore.
The investigators compared 16 open-chest cardiac massage (OCCM) patients with 17 closed-chest compression (CCC) patients delivered directly to the level 1 trauma center in cardiac arrest. The open-massage group received closed compressions for a mean of 66 seconds before being converted to open massage for reasons that weren’t captured by the data.
End-tidal carbon dioxide (ETCO2) – the gold standard for determining the effectiveness of chest compressions and return of spontaneous circulation – was used as a surrogate for cardiac output and adequacy of resuscitation. Continuous high-resolution ETCO2 measurements were collected every 6 seconds in both groups.
When periods of OCCM were compared to equivalent periods of CCC, there were no differences in the initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
“Unless the patient has a thoracic injury that you need to get into the chest to fix, we didn’t see any benefit in opening the chest just to massage the heart. The data suggest that maybe we shouldn’t be so aggressive in doing open cardiac massage. There’s renewed interest in performing endovascular balloon occlusion techniques for the aorta to obtain hemorrhage control; if you do that and you do closed-chest compressions, it’s just as effective as opening up the chest and doing cardiac massage,” said investigator Dr. Matthew Bradley, a trauma surgeon at the Shock Trauma Center, at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
Most of the patients were men, and there was a higher percentage of penetrating trauma in the OCCM group (81% versus 47%; P = .04).
The results were the same, however, in subgroup analyses limited to blunt and penetrating trauma.
All of the open massage patients died, but there were a few survivors in the CCC group. Dr. Bradley didn’t think the closed versus open approach was the reason for the survival difference.
Resuscitative endovascular balloon occlusion of the aorta patients were excluded from the trial to prevent confounding.
The investigators have no relevant disclosures.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: There’s no benefit in opening the chest just to massage the heart.
Major finding: When periods of OCCM were compared to equivalent periods of CCC, there were no differences in initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
Data source: Prospective observational study in 33 patients
Disclosures: The investigators have no relevant disclosures.










