User login
Red wine’s potential benefits for cardiovascular health
In recent weeks, you may have noticed some familiar headlines about red wine and cardiovascular health. Why the sudden return of these stories? Because of an article recently published in the American Journal of Clinical Nutrition.
Funded in part by a grant from the São Paulo Research Foundation (FAPESP), the “Wine Flora Study” was carried out by prominent researchers from institutions in South America, Europe, and the United States: University of São Paulo; State University of Campinas, São Paulo; University of Brasília; University of Verona (Italy); Austrian Institute of Technology, Tulln; and Harvard Medical School, Boston. The team looked into the effects of red wine on gut flora and plasma levels of trimethylamine-N-oxide (TMAO). And what they found was quite interesting.
The study
Previous results have pointed to the beneficial effect that red wine has on the gut microbiome.
The Wine Flora Study involved 42 men (average age, 60 years) with documented coronary artery disease. The trial encompassed two 3-week interventions. In one, the participants consumed 250 mL of red wine per day; the red wine sample had an alcohol content (% v) of 12.75. The Brazilian Wine Institute produced and supplied the red wine: a 2014 Merlot bottled in August 2016 and customized for the study. The second intervention involved alcohol abstention.
Each intervention was preceded by a 2-week washout period. Because certain foods and drinks could interfere with the results, the participants were instructed not to consume alcoholic beverages, fermented foods (yogurt, kombucha, soy lecithin, kefir, sauerkraut, and other fermented vegetables), synthetic prebiotics (insulin, fructooligosaccharides), fiber, dairy, food polyphenols (grapes, grape juice, cranberries, strawberries), and probiotics.
At each intervention, the gut microbiota was analyzed via 16S ribosomal RNA highthroughput sequencing. This method makes it possible to identify bacterial species. The plasma metabolome of 20 randomly selected participants was evaluated by ultra–high-performance liquid chromatography with tandem mass spectrometry. In this method, liquid chromatography separates the compounds, and a mass spectrometer is used to analyze them.
One of the metabolites of interest was TMAO, which is produced from the trimethylamine released when gut bacteria process protein-rich foods. TMAO has been identified as playing a role in the development of atherosclerosis.
Results
with a difference in beta diversity and predominance of Parasutterella, Ruminococcaceae, several Bacteroides species, and Prevotella.
Plasma metabolomic analysis revealed significant changes in metabolites after red wine consumption, consistent with improved redox homeostasis, which is involved in the oxidative stress that promotes atherosclerosis.
Plasma TMAO, however, did not differ between red wine intervention and alcohol abstention.
Implications
The researchers concluded that modulation of the gut microbiota may contribute to the putative cardiovascular benefits of moderate red wine consumption. But, as they were careful to point out in the very title of the study, a red wine intervention does not modify plasma TMAO. They also mentioned that the 3-week period may have been too short for the findings to serve as the basis for promoting any meaningful modification. In addition, the team emphasized that these data remain hypothesisgenerating and pave the way for future research.
In an interview with FAPESP, the study’s corresponding author, Protásio Lemos da Luz, MD, PhD, warned about the risks associated with drinking too much alcohol (> 8.5 oz., or 250 mL, of wine daily).
It should be kept in mind that, in Brazil, people do not drink nearly as much wine as they do beer or liquor. Furthermore, the evidence that is available does not provide confirmation of the existence or the extent of the protective health effects associated with light or moderate alcohol intake.
This article was translated from the Medscape Portuguese edition. A version appeared on Medscape.com.
In recent weeks, you may have noticed some familiar headlines about red wine and cardiovascular health. Why the sudden return of these stories? Because of an article recently published in the American Journal of Clinical Nutrition.
Funded in part by a grant from the São Paulo Research Foundation (FAPESP), the “Wine Flora Study” was carried out by prominent researchers from institutions in South America, Europe, and the United States: University of São Paulo; State University of Campinas, São Paulo; University of Brasília; University of Verona (Italy); Austrian Institute of Technology, Tulln; and Harvard Medical School, Boston. The team looked into the effects of red wine on gut flora and plasma levels of trimethylamine-N-oxide (TMAO). And what they found was quite interesting.
The study
Previous results have pointed to the beneficial effect that red wine has on the gut microbiome.
The Wine Flora Study involved 42 men (average age, 60 years) with documented coronary artery disease. The trial encompassed two 3-week interventions. In one, the participants consumed 250 mL of red wine per day; the red wine sample had an alcohol content (% v) of 12.75. The Brazilian Wine Institute produced and supplied the red wine: a 2014 Merlot bottled in August 2016 and customized for the study. The second intervention involved alcohol abstention.
Each intervention was preceded by a 2-week washout period. Because certain foods and drinks could interfere with the results, the participants were instructed not to consume alcoholic beverages, fermented foods (yogurt, kombucha, soy lecithin, kefir, sauerkraut, and other fermented vegetables), synthetic prebiotics (insulin, fructooligosaccharides), fiber, dairy, food polyphenols (grapes, grape juice, cranberries, strawberries), and probiotics.
At each intervention, the gut microbiota was analyzed via 16S ribosomal RNA highthroughput sequencing. This method makes it possible to identify bacterial species. The plasma metabolome of 20 randomly selected participants was evaluated by ultra–high-performance liquid chromatography with tandem mass spectrometry. In this method, liquid chromatography separates the compounds, and a mass spectrometer is used to analyze them.
One of the metabolites of interest was TMAO, which is produced from the trimethylamine released when gut bacteria process protein-rich foods. TMAO has been identified as playing a role in the development of atherosclerosis.
Results
with a difference in beta diversity and predominance of Parasutterella, Ruminococcaceae, several Bacteroides species, and Prevotella.
Plasma metabolomic analysis revealed significant changes in metabolites after red wine consumption, consistent with improved redox homeostasis, which is involved in the oxidative stress that promotes atherosclerosis.
Plasma TMAO, however, did not differ between red wine intervention and alcohol abstention.
Implications
The researchers concluded that modulation of the gut microbiota may contribute to the putative cardiovascular benefits of moderate red wine consumption. But, as they were careful to point out in the very title of the study, a red wine intervention does not modify plasma TMAO. They also mentioned that the 3-week period may have been too short for the findings to serve as the basis for promoting any meaningful modification. In addition, the team emphasized that these data remain hypothesisgenerating and pave the way for future research.
In an interview with FAPESP, the study’s corresponding author, Protásio Lemos da Luz, MD, PhD, warned about the risks associated with drinking too much alcohol (> 8.5 oz., or 250 mL, of wine daily).
It should be kept in mind that, in Brazil, people do not drink nearly as much wine as they do beer or liquor. Furthermore, the evidence that is available does not provide confirmation of the existence or the extent of the protective health effects associated with light or moderate alcohol intake.
This article was translated from the Medscape Portuguese edition. A version appeared on Medscape.com.
In recent weeks, you may have noticed some familiar headlines about red wine and cardiovascular health. Why the sudden return of these stories? Because of an article recently published in the American Journal of Clinical Nutrition.
Funded in part by a grant from the São Paulo Research Foundation (FAPESP), the “Wine Flora Study” was carried out by prominent researchers from institutions in South America, Europe, and the United States: University of São Paulo; State University of Campinas, São Paulo; University of Brasília; University of Verona (Italy); Austrian Institute of Technology, Tulln; and Harvard Medical School, Boston. The team looked into the effects of red wine on gut flora and plasma levels of trimethylamine-N-oxide (TMAO). And what they found was quite interesting.
The study
Previous results have pointed to the beneficial effect that red wine has on the gut microbiome.
The Wine Flora Study involved 42 men (average age, 60 years) with documented coronary artery disease. The trial encompassed two 3-week interventions. In one, the participants consumed 250 mL of red wine per day; the red wine sample had an alcohol content (% v) of 12.75. The Brazilian Wine Institute produced and supplied the red wine: a 2014 Merlot bottled in August 2016 and customized for the study. The second intervention involved alcohol abstention.
Each intervention was preceded by a 2-week washout period. Because certain foods and drinks could interfere with the results, the participants were instructed not to consume alcoholic beverages, fermented foods (yogurt, kombucha, soy lecithin, kefir, sauerkraut, and other fermented vegetables), synthetic prebiotics (insulin, fructooligosaccharides), fiber, dairy, food polyphenols (grapes, grape juice, cranberries, strawberries), and probiotics.
At each intervention, the gut microbiota was analyzed via 16S ribosomal RNA highthroughput sequencing. This method makes it possible to identify bacterial species. The plasma metabolome of 20 randomly selected participants was evaluated by ultra–high-performance liquid chromatography with tandem mass spectrometry. In this method, liquid chromatography separates the compounds, and a mass spectrometer is used to analyze them.
One of the metabolites of interest was TMAO, which is produced from the trimethylamine released when gut bacteria process protein-rich foods. TMAO has been identified as playing a role in the development of atherosclerosis.
Results
with a difference in beta diversity and predominance of Parasutterella, Ruminococcaceae, several Bacteroides species, and Prevotella.
Plasma metabolomic analysis revealed significant changes in metabolites after red wine consumption, consistent with improved redox homeostasis, which is involved in the oxidative stress that promotes atherosclerosis.
Plasma TMAO, however, did not differ between red wine intervention and alcohol abstention.
Implications
The researchers concluded that modulation of the gut microbiota may contribute to the putative cardiovascular benefits of moderate red wine consumption. But, as they were careful to point out in the very title of the study, a red wine intervention does not modify plasma TMAO. They also mentioned that the 3-week period may have been too short for the findings to serve as the basis for promoting any meaningful modification. In addition, the team emphasized that these data remain hypothesisgenerating and pave the way for future research.
In an interview with FAPESP, the study’s corresponding author, Protásio Lemos da Luz, MD, PhD, warned about the risks associated with drinking too much alcohol (> 8.5 oz., or 250 mL, of wine daily).
It should be kept in mind that, in Brazil, people do not drink nearly as much wine as they do beer or liquor. Furthermore, the evidence that is available does not provide confirmation of the existence or the extent of the protective health effects associated with light or moderate alcohol intake.
This article was translated from the Medscape Portuguese edition. A version appeared on Medscape.com.
In weighing PCI vs. CABG for left main disease, diabetes matters
WASHINGTON – For patients with diabetes, there are trade-offs for selecting a percutaneous intervention (PCI) over coronary artery bypass grafting (CABG) for left main artery disease when either can be considered, according to a hypothesis-generating pooled analysis.
The pooled data from four trials indicate that either method of revascularization is “reasonable,” but risk of myocardial infarction and revascularization is higher and risk of stroke is lower in patients with diabetes following PCI relative to CABG, Prakriti Gaba, MD, said in presenting the analysis at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
Despite decades of advances in both PCI and CABG, the findings are remarkably similar to those of Emory Angioplasty Versus Surgery Trial (EAST), the first major study to compare PCI to CABG, which were published almost 30 years ago. In the new analysis, like in EAST, PCI and CABG were comparable for a primary composite endpoint overall, but patients with diabetes were the exception. In those, outcomes were modestly better after CABG, said Dr. Gaba, a cardiology fellow at Brigham and Women’s Hospital, Harvard Medical School, both in Boston.
“More and more I am hearing from practitioners that diabetes does not matter, but what I get from your data is that diabetes still matters,” said Spencer B. King, MD, a pioneer of PCI affiliated with Emory University, Atlanta.
Dr. King, the first author of the 1994 paper and a panelist in the late-breaking trial session where the new data were presented, pointed out that a relatively limited proportion of patients with diabetes are equally suitable for PCI and CABG because of other considerations. However, he said an updated look once again suggesting that PCI and CABG are not equivalent for left main lesions in patients with diabetes “is helpful to see.”
CABG traditionally preferred for left main revascularization
The issue was revisited because CABG has been preferred traditionally for left main disease, but there was increasing evidence that PCI is associated with similar survival, according to Dr. Gaba. These new data support that contention, even if it shows that outcomes are not the same in those with diabetes relative to those without.
In this pooled analysis, data were drawn from four trials. Each compared PCI with drug-eluting stents with CABG in patients that were considered suitable for either. From the four trials, the numbers in this analysis included 705 patients from SYNTAX, 600 patients from PRECOMBAT, 1,184 patients from NOBLE, and 1,905 patients from EXCEL.
The focus was on the 1,104 patients with diabetes relative to the 3,289 without. The primary endpoint was all-cause death at 5 years. The multiple secondary endpoints included cardiovascular (CV) death, MI, stroke, and revascularization.
Overall, the 5-year mortality, independent of revascularization procedure, was 14.8% for those with diabetes and 9.3% for those without (P < .001). For this endpoint, the rates were numerically lower but not statistically different for CABG whether patients had diabetes (14.1% vs. 15.3%) or no diabetes (8.9% vs. 9.7%).
However, the rate of spontaneous MI was twice as great with PCI than with CABG for those with diabetes (8.9% vs. 4.4%), which doubled the hazard ratio within significant confidence intervals (HR, 2.01; 95% CI, 1.21-3.35). The rates of revascularization were also about twice as great with PCI than with CABG (24.5% vs. 12.4%), again producing a twofold increase in risk (HR, 2.12; 95% CI, 1.56-2.87).
For stroke in patients with diabetes, there was no difference in events at 5 years for PCI relative to CABG (2.1% in both groups). However, in those without diabetes, a trend approaching significance favored CABG over PCI (1.2% vs. 2.1%; HR, 0.177; 95% CI, 0.99-1.77). This difference was concentrated in the first year, when stroke rates among those treated with CABG were more than double the rates among those treated with PCI. Over time, this difference dissipated so that the difference was reduced to a trend at the end of follow-up.
Data considered hypothesis generating
Although patients with diabetes were prespecified as a subgroup of interest in these studies, Dr. Gaba said that the data can only be considered hypothesis generating and pointed out several limitations, including the fact that these studies preceded some therapies, such as sodium-glucose cotransporter 2 inhibitors, that are known to affect CV outcomes.
However, Dr. King was not alone in suggesting that these data once again show that diabetes matters. Several panelists agreed, including the moderator of the session, Robert A Byrne, MBBcH, PhD, director of cardiology, Mater Private Hospital, Dublin.
“Of course, there has been a lot of discussion over the last 4 or 5 years about this issue since the long-term EXCEL data were presented,” Dr. Byrne said. He added that the team of investigators who put this together “have done a great service to the community” by providing a detailed combined analysis to explore the interaction between diabetes and outcomes relative to method of revascularization. Although PCI and CABG are not always equivalent choices for reasons other than diabetes, he echoed the sentiment that diabetes likely remains a variable to consider when considering revascularization of left main artery disease.
Dr. Gabi, Dr. Spencer, and Dr. Byrne report no potential conflicts of interest.
WASHINGTON – For patients with diabetes, there are trade-offs for selecting a percutaneous intervention (PCI) over coronary artery bypass grafting (CABG) for left main artery disease when either can be considered, according to a hypothesis-generating pooled analysis.
The pooled data from four trials indicate that either method of revascularization is “reasonable,” but risk of myocardial infarction and revascularization is higher and risk of stroke is lower in patients with diabetes following PCI relative to CABG, Prakriti Gaba, MD, said in presenting the analysis at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
Despite decades of advances in both PCI and CABG, the findings are remarkably similar to those of Emory Angioplasty Versus Surgery Trial (EAST), the first major study to compare PCI to CABG, which were published almost 30 years ago. In the new analysis, like in EAST, PCI and CABG were comparable for a primary composite endpoint overall, but patients with diabetes were the exception. In those, outcomes were modestly better after CABG, said Dr. Gaba, a cardiology fellow at Brigham and Women’s Hospital, Harvard Medical School, both in Boston.
“More and more I am hearing from practitioners that diabetes does not matter, but what I get from your data is that diabetes still matters,” said Spencer B. King, MD, a pioneer of PCI affiliated with Emory University, Atlanta.
Dr. King, the first author of the 1994 paper and a panelist in the late-breaking trial session where the new data were presented, pointed out that a relatively limited proportion of patients with diabetes are equally suitable for PCI and CABG because of other considerations. However, he said an updated look once again suggesting that PCI and CABG are not equivalent for left main lesions in patients with diabetes “is helpful to see.”
CABG traditionally preferred for left main revascularization
The issue was revisited because CABG has been preferred traditionally for left main disease, but there was increasing evidence that PCI is associated with similar survival, according to Dr. Gaba. These new data support that contention, even if it shows that outcomes are not the same in those with diabetes relative to those without.
In this pooled analysis, data were drawn from four trials. Each compared PCI with drug-eluting stents with CABG in patients that were considered suitable for either. From the four trials, the numbers in this analysis included 705 patients from SYNTAX, 600 patients from PRECOMBAT, 1,184 patients from NOBLE, and 1,905 patients from EXCEL.
The focus was on the 1,104 patients with diabetes relative to the 3,289 without. The primary endpoint was all-cause death at 5 years. The multiple secondary endpoints included cardiovascular (CV) death, MI, stroke, and revascularization.
Overall, the 5-year mortality, independent of revascularization procedure, was 14.8% for those with diabetes and 9.3% for those without (P < .001). For this endpoint, the rates were numerically lower but not statistically different for CABG whether patients had diabetes (14.1% vs. 15.3%) or no diabetes (8.9% vs. 9.7%).
However, the rate of spontaneous MI was twice as great with PCI than with CABG for those with diabetes (8.9% vs. 4.4%), which doubled the hazard ratio within significant confidence intervals (HR, 2.01; 95% CI, 1.21-3.35). The rates of revascularization were also about twice as great with PCI than with CABG (24.5% vs. 12.4%), again producing a twofold increase in risk (HR, 2.12; 95% CI, 1.56-2.87).
For stroke in patients with diabetes, there was no difference in events at 5 years for PCI relative to CABG (2.1% in both groups). However, in those without diabetes, a trend approaching significance favored CABG over PCI (1.2% vs. 2.1%; HR, 0.177; 95% CI, 0.99-1.77). This difference was concentrated in the first year, when stroke rates among those treated with CABG were more than double the rates among those treated with PCI. Over time, this difference dissipated so that the difference was reduced to a trend at the end of follow-up.
Data considered hypothesis generating
Although patients with diabetes were prespecified as a subgroup of interest in these studies, Dr. Gaba said that the data can only be considered hypothesis generating and pointed out several limitations, including the fact that these studies preceded some therapies, such as sodium-glucose cotransporter 2 inhibitors, that are known to affect CV outcomes.
However, Dr. King was not alone in suggesting that these data once again show that diabetes matters. Several panelists agreed, including the moderator of the session, Robert A Byrne, MBBcH, PhD, director of cardiology, Mater Private Hospital, Dublin.
“Of course, there has been a lot of discussion over the last 4 or 5 years about this issue since the long-term EXCEL data were presented,” Dr. Byrne said. He added that the team of investigators who put this together “have done a great service to the community” by providing a detailed combined analysis to explore the interaction between diabetes and outcomes relative to method of revascularization. Although PCI and CABG are not always equivalent choices for reasons other than diabetes, he echoed the sentiment that diabetes likely remains a variable to consider when considering revascularization of left main artery disease.
Dr. Gabi, Dr. Spencer, and Dr. Byrne report no potential conflicts of interest.
WASHINGTON – For patients with diabetes, there are trade-offs for selecting a percutaneous intervention (PCI) over coronary artery bypass grafting (CABG) for left main artery disease when either can be considered, according to a hypothesis-generating pooled analysis.
The pooled data from four trials indicate that either method of revascularization is “reasonable,” but risk of myocardial infarction and revascularization is higher and risk of stroke is lower in patients with diabetes following PCI relative to CABG, Prakriti Gaba, MD, said in presenting the analysis at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
Despite decades of advances in both PCI and CABG, the findings are remarkably similar to those of Emory Angioplasty Versus Surgery Trial (EAST), the first major study to compare PCI to CABG, which were published almost 30 years ago. In the new analysis, like in EAST, PCI and CABG were comparable for a primary composite endpoint overall, but patients with diabetes were the exception. In those, outcomes were modestly better after CABG, said Dr. Gaba, a cardiology fellow at Brigham and Women’s Hospital, Harvard Medical School, both in Boston.
“More and more I am hearing from practitioners that diabetes does not matter, but what I get from your data is that diabetes still matters,” said Spencer B. King, MD, a pioneer of PCI affiliated with Emory University, Atlanta.
Dr. King, the first author of the 1994 paper and a panelist in the late-breaking trial session where the new data were presented, pointed out that a relatively limited proportion of patients with diabetes are equally suitable for PCI and CABG because of other considerations. However, he said an updated look once again suggesting that PCI and CABG are not equivalent for left main lesions in patients with diabetes “is helpful to see.”
CABG traditionally preferred for left main revascularization
The issue was revisited because CABG has been preferred traditionally for left main disease, but there was increasing evidence that PCI is associated with similar survival, according to Dr. Gaba. These new data support that contention, even if it shows that outcomes are not the same in those with diabetes relative to those without.
In this pooled analysis, data were drawn from four trials. Each compared PCI with drug-eluting stents with CABG in patients that were considered suitable for either. From the four trials, the numbers in this analysis included 705 patients from SYNTAX, 600 patients from PRECOMBAT, 1,184 patients from NOBLE, and 1,905 patients from EXCEL.
The focus was on the 1,104 patients with diabetes relative to the 3,289 without. The primary endpoint was all-cause death at 5 years. The multiple secondary endpoints included cardiovascular (CV) death, MI, stroke, and revascularization.
Overall, the 5-year mortality, independent of revascularization procedure, was 14.8% for those with diabetes and 9.3% for those without (P < .001). For this endpoint, the rates were numerically lower but not statistically different for CABG whether patients had diabetes (14.1% vs. 15.3%) or no diabetes (8.9% vs. 9.7%).
However, the rate of spontaneous MI was twice as great with PCI than with CABG for those with diabetes (8.9% vs. 4.4%), which doubled the hazard ratio within significant confidence intervals (HR, 2.01; 95% CI, 1.21-3.35). The rates of revascularization were also about twice as great with PCI than with CABG (24.5% vs. 12.4%), again producing a twofold increase in risk (HR, 2.12; 95% CI, 1.56-2.87).
For stroke in patients with diabetes, there was no difference in events at 5 years for PCI relative to CABG (2.1% in both groups). However, in those without diabetes, a trend approaching significance favored CABG over PCI (1.2% vs. 2.1%; HR, 0.177; 95% CI, 0.99-1.77). This difference was concentrated in the first year, when stroke rates among those treated with CABG were more than double the rates among those treated with PCI. Over time, this difference dissipated so that the difference was reduced to a trend at the end of follow-up.
Data considered hypothesis generating
Although patients with diabetes were prespecified as a subgroup of interest in these studies, Dr. Gaba said that the data can only be considered hypothesis generating and pointed out several limitations, including the fact that these studies preceded some therapies, such as sodium-glucose cotransporter 2 inhibitors, that are known to affect CV outcomes.
However, Dr. King was not alone in suggesting that these data once again show that diabetes matters. Several panelists agreed, including the moderator of the session, Robert A Byrne, MBBcH, PhD, director of cardiology, Mater Private Hospital, Dublin.
“Of course, there has been a lot of discussion over the last 4 or 5 years about this issue since the long-term EXCEL data were presented,” Dr. Byrne said. He added that the team of investigators who put this together “have done a great service to the community” by providing a detailed combined analysis to explore the interaction between diabetes and outcomes relative to method of revascularization. Although PCI and CABG are not always equivalent choices for reasons other than diabetes, he echoed the sentiment that diabetes likely remains a variable to consider when considering revascularization of left main artery disease.
Dr. Gabi, Dr. Spencer, and Dr. Byrne report no potential conflicts of interest.
AT CRT 2023
Drinking beet juice tied to reduced post-PCI restenosis
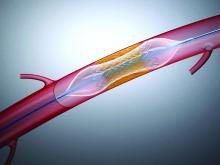
WASHINGTON – Late lumen loss (LLL) after percutaneous interventions (PCI) can be reduced significantly by a daily glass of beet juice, according to a phase 2 randomized trial.
The protection against LLL, attributed to the nitrate contained in beet juice, was accompanied by a trend for a reduced risk of major adverse cardiovascular events (MACE), according to Krishnaraj Rathod, MBBS, BMedSci, PhD, who presented results at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
The study grew out of relatively recent evidence that ingestion of nitrate-rich foods, such as beets, can trigger noncanonical pathways for nitric oxide generation, sometimes referred to as the nitrate-nitrite-nitric oxide sequence. Dr. Rathod cited experimental evidence associating this pathway with the traditional benefits of NO generation, such as anti-inflammatory and antithrombotic effects.
In this study, 300 patients scheduled for PCI to treat stable angina were randomized to the experimental arm of nitrate-rich beetroot juice or the control arm of nitrate-depleted beetroot juice. Each had a 70-mL glass of juice once daily. Dr. Rathod, a senior interventional cardiology registrar, Barts Heart Centre, London, described this as the equivalent of about four beets.
The primary endpoint of the study was in-stent LLL assessed by quantitative coronary angiography (QCA) at 6 months.
MACE, defined as death, MI, need for revascularization, and in-stent thrombosis, was assessed at 3, 9, 12, and 24 months. In addition, markers of NO activation, platelet reactivity, and inflammation were monitored.
Lumen loss reduced less than 50%
On OCA, the median stent LLL at 6 months was 0.244 mm in the nitrate-depleted beet juice group and 0.117 mm (P = .0165) in the group that received natural beet juice. The mean segment LLL similarly favored the natural beet juice (0.269 vs. 0.050 mm; P = .0011).
The same effect was reflected in the measurement of mean change in minimum lumen diameter at 6 months. From baseline, this in-stent measure was reduced at 6 months by 0.244 mm in the control group, but by only 0.117 mm in the group receiving the dietary nitrate (P = .0154 for two-way analysis of variance).
Over 24 months of follow-up, there were 18 MACE events in the control arm versus 9 in the arm randomized to dietary nitrate (P = .0718). There were no in-stent thromboses observed in either group, but death (two vs. five), MI (one vs. six), and target-vessel revascularization (six vs. seven) were all numerically lower in the group receiving dietary nitrate.
“Once-a-day oral dietary nitrate for 6 months was well tolerated and safe,” Dr. Rathod reported at the meeting.
Asked specifically about the taste of the daily glass of beet juice, Dr. Rathod acknowledged that some patients were not enamored, but many had no objections or even liked the taste.
The patients were reasonably representative of a PCI population. The mean age in both groups was 61 years. There were no significant differences in body mass index (approximately 29 kg/m2) or proportion with diabetes (22%), hypertension, or hypercholesterolemia (about 70% in both groups) and other comorbidities.
More PCI was performed in the left anterior descending artery (36.7% vs. 44.0%) in the control group, while less PCI was performed in the right coronary (27.3% vs. 30.7%). Neither difference was significant. The vast majority (~90%) of patients received drug-eluting stents with a mean of 1.4 implanted. Procedural success was 100% in both groups.
Discharge medications, including antiplatelet and antithrombotic therapies, were similar in the two groups.
Results characterized as highly positive
Based on the 53% reduction in LLL at 6 months and the trend for a MACE reduction, Dr. Rathod concluded that the results were highly positive.
“These results suggest that dietary nitrate may have a therapeutic role in reducing restenosis following PCI for stable angina,” he said.
In the discussion, several panelists pointed out that nearly one-third of patients were not available for evaluation at 6 months (41 of 150 in the experimental group and 51 of 150 in the control group) with further attrition at 1 and 2 years of follow-up. Of these about half were lost to follow-up and the other half withdrew.
The lack of follow-up on such a high proportion of participants is one weakness of this study,” acknowledged Hector M. Garcia-Garcia, MD, PhD, a cardiovascular researcher at MedStar Washington Hospital Center. However, he remains enthusiastic about the premise.
“It was encouraging to see every signal moving in the right direction,” said Dr. Garcia, who consulted with Dr. Rathod’s group on the design of the study. He called these data “promising,” and said they provide support for larger trial for a treatment with potential benefits at low cost.
George Dangas, MD, PhD, professor of medicine at the Icahn School of Medicine at Mount Sinai, New York, was among panelists who seemed surprised by such positive findings from a simple but novel concept. However, he remains open to further evaluations.
“As with any surprising result, further confirmation in a large and multicenter trial should be anticipated,” he said in an interview. If, as this study suggests, dietary changes are capable of providing therapeutic NO at the vascular level, he suggested studies to demonstrate anti-inflammatory effects or other mechanistic benefits would be helpful.
“Other sources of oral nitrate would also be a worthwhile investigation,” he said.
Dr. Rathod reports no potential conflicts of interest. Dr. Garcia-Garcia reports ties to Abbott, Biotronik, Boston Scientific, CorFlow, Medtronic, Neovasc, Phillips, and Shockwave. Dr. Dangas reports financial relationships with Abbott Vascular, AstraZeneca, Boston Scientific, Daiichi-Sankyo, and Medtronic.
WASHINGTON – Late lumen loss (LLL) after percutaneous interventions (PCI) can be reduced significantly by a daily glass of beet juice, according to a phase 2 randomized trial.
The protection against LLL, attributed to the nitrate contained in beet juice, was accompanied by a trend for a reduced risk of major adverse cardiovascular events (MACE), according to Krishnaraj Rathod, MBBS, BMedSci, PhD, who presented results at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
The study grew out of relatively recent evidence that ingestion of nitrate-rich foods, such as beets, can trigger noncanonical pathways for nitric oxide generation, sometimes referred to as the nitrate-nitrite-nitric oxide sequence. Dr. Rathod cited experimental evidence associating this pathway with the traditional benefits of NO generation, such as anti-inflammatory and antithrombotic effects.
In this study, 300 patients scheduled for PCI to treat stable angina were randomized to the experimental arm of nitrate-rich beetroot juice or the control arm of nitrate-depleted beetroot juice. Each had a 70-mL glass of juice once daily. Dr. Rathod, a senior interventional cardiology registrar, Barts Heart Centre, London, described this as the equivalent of about four beets.
The primary endpoint of the study was in-stent LLL assessed by quantitative coronary angiography (QCA) at 6 months.
MACE, defined as death, MI, need for revascularization, and in-stent thrombosis, was assessed at 3, 9, 12, and 24 months. In addition, markers of NO activation, platelet reactivity, and inflammation were monitored.
Lumen loss reduced less than 50%
On OCA, the median stent LLL at 6 months was 0.244 mm in the nitrate-depleted beet juice group and 0.117 mm (P = .0165) in the group that received natural beet juice. The mean segment LLL similarly favored the natural beet juice (0.269 vs. 0.050 mm; P = .0011).
The same effect was reflected in the measurement of mean change in minimum lumen diameter at 6 months. From baseline, this in-stent measure was reduced at 6 months by 0.244 mm in the control group, but by only 0.117 mm in the group receiving the dietary nitrate (P = .0154 for two-way analysis of variance).
Over 24 months of follow-up, there were 18 MACE events in the control arm versus 9 in the arm randomized to dietary nitrate (P = .0718). There were no in-stent thromboses observed in either group, but death (two vs. five), MI (one vs. six), and target-vessel revascularization (six vs. seven) were all numerically lower in the group receiving dietary nitrate.
“Once-a-day oral dietary nitrate for 6 months was well tolerated and safe,” Dr. Rathod reported at the meeting.
Asked specifically about the taste of the daily glass of beet juice, Dr. Rathod acknowledged that some patients were not enamored, but many had no objections or even liked the taste.
The patients were reasonably representative of a PCI population. The mean age in both groups was 61 years. There were no significant differences in body mass index (approximately 29 kg/m2) or proportion with diabetes (22%), hypertension, or hypercholesterolemia (about 70% in both groups) and other comorbidities.
More PCI was performed in the left anterior descending artery (36.7% vs. 44.0%) in the control group, while less PCI was performed in the right coronary (27.3% vs. 30.7%). Neither difference was significant. The vast majority (~90%) of patients received drug-eluting stents with a mean of 1.4 implanted. Procedural success was 100% in both groups.
Discharge medications, including antiplatelet and antithrombotic therapies, were similar in the two groups.
Results characterized as highly positive
Based on the 53% reduction in LLL at 6 months and the trend for a MACE reduction, Dr. Rathod concluded that the results were highly positive.
“These results suggest that dietary nitrate may have a therapeutic role in reducing restenosis following PCI for stable angina,” he said.
In the discussion, several panelists pointed out that nearly one-third of patients were not available for evaluation at 6 months (41 of 150 in the experimental group and 51 of 150 in the control group) with further attrition at 1 and 2 years of follow-up. Of these about half were lost to follow-up and the other half withdrew.
The lack of follow-up on such a high proportion of participants is one weakness of this study,” acknowledged Hector M. Garcia-Garcia, MD, PhD, a cardiovascular researcher at MedStar Washington Hospital Center. However, he remains enthusiastic about the premise.
“It was encouraging to see every signal moving in the right direction,” said Dr. Garcia, who consulted with Dr. Rathod’s group on the design of the study. He called these data “promising,” and said they provide support for larger trial for a treatment with potential benefits at low cost.
George Dangas, MD, PhD, professor of medicine at the Icahn School of Medicine at Mount Sinai, New York, was among panelists who seemed surprised by such positive findings from a simple but novel concept. However, he remains open to further evaluations.
“As with any surprising result, further confirmation in a large and multicenter trial should be anticipated,” he said in an interview. If, as this study suggests, dietary changes are capable of providing therapeutic NO at the vascular level, he suggested studies to demonstrate anti-inflammatory effects or other mechanistic benefits would be helpful.
“Other sources of oral nitrate would also be a worthwhile investigation,” he said.
Dr. Rathod reports no potential conflicts of interest. Dr. Garcia-Garcia reports ties to Abbott, Biotronik, Boston Scientific, CorFlow, Medtronic, Neovasc, Phillips, and Shockwave. Dr. Dangas reports financial relationships with Abbott Vascular, AstraZeneca, Boston Scientific, Daiichi-Sankyo, and Medtronic.
WASHINGTON – Late lumen loss (LLL) after percutaneous interventions (PCI) can be reduced significantly by a daily glass of beet juice, according to a phase 2 randomized trial.
The protection against LLL, attributed to the nitrate contained in beet juice, was accompanied by a trend for a reduced risk of major adverse cardiovascular events (MACE), according to Krishnaraj Rathod, MBBS, BMedSci, PhD, who presented results at the Cardiovascular Research Technologies conference, sponsored by MedStar Heart & Vascular Institute.
The study grew out of relatively recent evidence that ingestion of nitrate-rich foods, such as beets, can trigger noncanonical pathways for nitric oxide generation, sometimes referred to as the nitrate-nitrite-nitric oxide sequence. Dr. Rathod cited experimental evidence associating this pathway with the traditional benefits of NO generation, such as anti-inflammatory and antithrombotic effects.
In this study, 300 patients scheduled for PCI to treat stable angina were randomized to the experimental arm of nitrate-rich beetroot juice or the control arm of nitrate-depleted beetroot juice. Each had a 70-mL glass of juice once daily. Dr. Rathod, a senior interventional cardiology registrar, Barts Heart Centre, London, described this as the equivalent of about four beets.
The primary endpoint of the study was in-stent LLL assessed by quantitative coronary angiography (QCA) at 6 months.
MACE, defined as death, MI, need for revascularization, and in-stent thrombosis, was assessed at 3, 9, 12, and 24 months. In addition, markers of NO activation, platelet reactivity, and inflammation were monitored.
Lumen loss reduced less than 50%
On OCA, the median stent LLL at 6 months was 0.244 mm in the nitrate-depleted beet juice group and 0.117 mm (P = .0165) in the group that received natural beet juice. The mean segment LLL similarly favored the natural beet juice (0.269 vs. 0.050 mm; P = .0011).
The same effect was reflected in the measurement of mean change in minimum lumen diameter at 6 months. From baseline, this in-stent measure was reduced at 6 months by 0.244 mm in the control group, but by only 0.117 mm in the group receiving the dietary nitrate (P = .0154 for two-way analysis of variance).
Over 24 months of follow-up, there were 18 MACE events in the control arm versus 9 in the arm randomized to dietary nitrate (P = .0718). There were no in-stent thromboses observed in either group, but death (two vs. five), MI (one vs. six), and target-vessel revascularization (six vs. seven) were all numerically lower in the group receiving dietary nitrate.
“Once-a-day oral dietary nitrate for 6 months was well tolerated and safe,” Dr. Rathod reported at the meeting.
Asked specifically about the taste of the daily glass of beet juice, Dr. Rathod acknowledged that some patients were not enamored, but many had no objections or even liked the taste.
The patients were reasonably representative of a PCI population. The mean age in both groups was 61 years. There were no significant differences in body mass index (approximately 29 kg/m2) or proportion with diabetes (22%), hypertension, or hypercholesterolemia (about 70% in both groups) and other comorbidities.
More PCI was performed in the left anterior descending artery (36.7% vs. 44.0%) in the control group, while less PCI was performed in the right coronary (27.3% vs. 30.7%). Neither difference was significant. The vast majority (~90%) of patients received drug-eluting stents with a mean of 1.4 implanted. Procedural success was 100% in both groups.
Discharge medications, including antiplatelet and antithrombotic therapies, were similar in the two groups.
Results characterized as highly positive
Based on the 53% reduction in LLL at 6 months and the trend for a MACE reduction, Dr. Rathod concluded that the results were highly positive.
“These results suggest that dietary nitrate may have a therapeutic role in reducing restenosis following PCI for stable angina,” he said.
In the discussion, several panelists pointed out that nearly one-third of patients were not available for evaluation at 6 months (41 of 150 in the experimental group and 51 of 150 in the control group) with further attrition at 1 and 2 years of follow-up. Of these about half were lost to follow-up and the other half withdrew.
The lack of follow-up on such a high proportion of participants is one weakness of this study,” acknowledged Hector M. Garcia-Garcia, MD, PhD, a cardiovascular researcher at MedStar Washington Hospital Center. However, he remains enthusiastic about the premise.
“It was encouraging to see every signal moving in the right direction,” said Dr. Garcia, who consulted with Dr. Rathod’s group on the design of the study. He called these data “promising,” and said they provide support for larger trial for a treatment with potential benefits at low cost.
George Dangas, MD, PhD, professor of medicine at the Icahn School of Medicine at Mount Sinai, New York, was among panelists who seemed surprised by such positive findings from a simple but novel concept. However, he remains open to further evaluations.
“As with any surprising result, further confirmation in a large and multicenter trial should be anticipated,” he said in an interview. If, as this study suggests, dietary changes are capable of providing therapeutic NO at the vascular level, he suggested studies to demonstrate anti-inflammatory effects or other mechanistic benefits would be helpful.
“Other sources of oral nitrate would also be a worthwhile investigation,” he said.
Dr. Rathod reports no potential conflicts of interest. Dr. Garcia-Garcia reports ties to Abbott, Biotronik, Boston Scientific, CorFlow, Medtronic, Neovasc, Phillips, and Shockwave. Dr. Dangas reports financial relationships with Abbott Vascular, AstraZeneca, Boston Scientific, Daiichi-Sankyo, and Medtronic.
AT CRT 2023
Irregular sleep tied to markers of atherosclerosis
a new report suggests.
In particular, variation in sleep duration of more than 2 hours per night in the same week was tied to higher rates of atherosclerosis.
“Poor sleep is linked with several cardiovascular conditions, including heart disease, hypertension, and type 2 diabetes,” lead author Kelsie M. Full, PhD, MPH, assistant professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
“Overall, we found that participants who slept varying amounts of hours throughout the week (meaning that one night they slept less, one night they slept more) were more likely to have atherosclerosis than participants who slept about the same amount of time each night,” she said.
The study was published online in the Journal of the American Heart Association.
Analyzing associations
Dr. Full and colleagues examined data from 2032 participants in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study, which included adults aged between 45 and 84 years in six U.S. communities who completed 7-day wrist actigraphy assessment and kept a sleep diary between 2010 and 2013.
For subclinical markers of cardiovascular disease, participants underwent assessments of coronary artery calcium, carotid plaque presence, carotid intima-media thickness, and ankle-brachial index.
The research team assessed sleep duration, or the total number of minutes of sleep in a night, and sleep timing regularity, which was determined on the basis of the time someone initially fell asleep each night. They adjusted for cardiovascular disease risk factors and sleep characteristics, such as obstructive sleep apnea, sleep duration, and sleep fragmentation.
The average age of the participants was 68.6 years, and 53.6% were women. About 37.9% identified as White, 27.6% as Black or African American, 23.4% as Hispanic American, and 11.1% as Chinese American.
During the 7-day period, about 38% of participants experienced a change in sleep duration of more than 90 minutes, and 18% experienced a sleep duration change of more than 120 minutes. Those who had irregular sleep were more likely to be non-White, current smokers, have lower average annual incomes, have work shift schedules or did not work, and have a higher average body mass index.
For the study, sleep duration irregularity was defined as a standard deviation of more than 120 minutes. Those participants who had a greater degree of sleep irregularity were more likely to have high coronary artery calcium burden than those whose sleep duration was more more regular, defined as an SD of 60 minutes or less (> 300; prevalence ratio, 1.33; 95% confidence interval, 1.03-1.71), as well as abnormal ankle-brachial index (< 0.9, prevalence ratio, 1.75;95% CI, 1.03-2.95).
Further, those with irregular sleep timing (SD > 90 minutes) were more likely to have a high coronary artery calcium burden (prevalence ratio, 1.39; 95% CI, 1.07-1.82) in comparison with those with more regular sleep timing (SD < 30 minutes).
“The biggest surprise to me was that 30% of the participants in the study had total sleep times that varied by more than 90 minutes over the course of the week,” Dr. Full said. “This is consistent with prior studies that suggest that a large proportion of the general public have irregular sleep patterns, not just shift workers.”
Investigating next steps
In additional analyses, Dr. Full and colleagues found that sleep duration regularity continued to be associated with high coronary artery calcium burden and abnormal ankle-brachial index when accounting for severe obstructive sleep apnea, average nightly sleep duration, and average sleep fragmentation.
Notably, when sleep duration was added, all participants with more irregular sleep durations (SD > 60 minutes) were more likely to have a high coronary artery calcium burden, compared with those with regular sleep durations (SD < 60 minutes). The results remained when participants who reported shift work, including night shift work, were excluded.
Additional studies are needed to understand the mechanisms, the study authors wrote. Night-to-night variability in sleep duration and sleep timing can cause desynchronization in the sleep-wake timing and circadian disruption.
“A key issue highlighted in this study is that sleep irregularity itself, independent of how much sleep people were getting, was related to heart health. Sleep is a naturally recurring phenomenon, and maintaining regularity helps provide stability and predictability to the body,” Michael Grandner, PhD, associate professor of psychiatry and director of the sleep and health research program at the University of Arizona, Tucson, said in an interview.
Dr. Grandner, who wasn’t involved with this study, has researched sleep irregularity and associations with cardiovascular disease, diabetes, obesity, and many other adverse outcomes.
“When people have very irregular sleep schedules, it may make it harder for the body to optimally make good use of the sleep it is getting, since it such a moving target,” he said. “The unique angle here is the ability to focus on regularity of sleep.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences of the National Institutes of Health. One author received grants and consulting fees from pharmaceutical companies unrelated to the research. The other authors and Dr. Grandner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
a new report suggests.
In particular, variation in sleep duration of more than 2 hours per night in the same week was tied to higher rates of atherosclerosis.
“Poor sleep is linked with several cardiovascular conditions, including heart disease, hypertension, and type 2 diabetes,” lead author Kelsie M. Full, PhD, MPH, assistant professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
“Overall, we found that participants who slept varying amounts of hours throughout the week (meaning that one night they slept less, one night they slept more) were more likely to have atherosclerosis than participants who slept about the same amount of time each night,” she said.
The study was published online in the Journal of the American Heart Association.
Analyzing associations
Dr. Full and colleagues examined data from 2032 participants in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study, which included adults aged between 45 and 84 years in six U.S. communities who completed 7-day wrist actigraphy assessment and kept a sleep diary between 2010 and 2013.
For subclinical markers of cardiovascular disease, participants underwent assessments of coronary artery calcium, carotid plaque presence, carotid intima-media thickness, and ankle-brachial index.
The research team assessed sleep duration, or the total number of minutes of sleep in a night, and sleep timing regularity, which was determined on the basis of the time someone initially fell asleep each night. They adjusted for cardiovascular disease risk factors and sleep characteristics, such as obstructive sleep apnea, sleep duration, and sleep fragmentation.
The average age of the participants was 68.6 years, and 53.6% were women. About 37.9% identified as White, 27.6% as Black or African American, 23.4% as Hispanic American, and 11.1% as Chinese American.
During the 7-day period, about 38% of participants experienced a change in sleep duration of more than 90 minutes, and 18% experienced a sleep duration change of more than 120 minutes. Those who had irregular sleep were more likely to be non-White, current smokers, have lower average annual incomes, have work shift schedules or did not work, and have a higher average body mass index.
For the study, sleep duration irregularity was defined as a standard deviation of more than 120 minutes. Those participants who had a greater degree of sleep irregularity were more likely to have high coronary artery calcium burden than those whose sleep duration was more more regular, defined as an SD of 60 minutes or less (> 300; prevalence ratio, 1.33; 95% confidence interval, 1.03-1.71), as well as abnormal ankle-brachial index (< 0.9, prevalence ratio, 1.75;95% CI, 1.03-2.95).
Further, those with irregular sleep timing (SD > 90 minutes) were more likely to have a high coronary artery calcium burden (prevalence ratio, 1.39; 95% CI, 1.07-1.82) in comparison with those with more regular sleep timing (SD < 30 minutes).
“The biggest surprise to me was that 30% of the participants in the study had total sleep times that varied by more than 90 minutes over the course of the week,” Dr. Full said. “This is consistent with prior studies that suggest that a large proportion of the general public have irregular sleep patterns, not just shift workers.”
Investigating next steps
In additional analyses, Dr. Full and colleagues found that sleep duration regularity continued to be associated with high coronary artery calcium burden and abnormal ankle-brachial index when accounting for severe obstructive sleep apnea, average nightly sleep duration, and average sleep fragmentation.
Notably, when sleep duration was added, all participants with more irregular sleep durations (SD > 60 minutes) were more likely to have a high coronary artery calcium burden, compared with those with regular sleep durations (SD < 60 minutes). The results remained when participants who reported shift work, including night shift work, were excluded.
Additional studies are needed to understand the mechanisms, the study authors wrote. Night-to-night variability in sleep duration and sleep timing can cause desynchronization in the sleep-wake timing and circadian disruption.
“A key issue highlighted in this study is that sleep irregularity itself, independent of how much sleep people were getting, was related to heart health. Sleep is a naturally recurring phenomenon, and maintaining regularity helps provide stability and predictability to the body,” Michael Grandner, PhD, associate professor of psychiatry and director of the sleep and health research program at the University of Arizona, Tucson, said in an interview.
Dr. Grandner, who wasn’t involved with this study, has researched sleep irregularity and associations with cardiovascular disease, diabetes, obesity, and many other adverse outcomes.
“When people have very irregular sleep schedules, it may make it harder for the body to optimally make good use of the sleep it is getting, since it such a moving target,” he said. “The unique angle here is the ability to focus on regularity of sleep.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences of the National Institutes of Health. One author received grants and consulting fees from pharmaceutical companies unrelated to the research. The other authors and Dr. Grandner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
a new report suggests.
In particular, variation in sleep duration of more than 2 hours per night in the same week was tied to higher rates of atherosclerosis.
“Poor sleep is linked with several cardiovascular conditions, including heart disease, hypertension, and type 2 diabetes,” lead author Kelsie M. Full, PhD, MPH, assistant professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
“Overall, we found that participants who slept varying amounts of hours throughout the week (meaning that one night they slept less, one night they slept more) were more likely to have atherosclerosis than participants who slept about the same amount of time each night,” she said.
The study was published online in the Journal of the American Heart Association.
Analyzing associations
Dr. Full and colleagues examined data from 2032 participants in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study, which included adults aged between 45 and 84 years in six U.S. communities who completed 7-day wrist actigraphy assessment and kept a sleep diary between 2010 and 2013.
For subclinical markers of cardiovascular disease, participants underwent assessments of coronary artery calcium, carotid plaque presence, carotid intima-media thickness, and ankle-brachial index.
The research team assessed sleep duration, or the total number of minutes of sleep in a night, and sleep timing regularity, which was determined on the basis of the time someone initially fell asleep each night. They adjusted for cardiovascular disease risk factors and sleep characteristics, such as obstructive sleep apnea, sleep duration, and sleep fragmentation.
The average age of the participants was 68.6 years, and 53.6% were women. About 37.9% identified as White, 27.6% as Black or African American, 23.4% as Hispanic American, and 11.1% as Chinese American.
During the 7-day period, about 38% of participants experienced a change in sleep duration of more than 90 minutes, and 18% experienced a sleep duration change of more than 120 minutes. Those who had irregular sleep were more likely to be non-White, current smokers, have lower average annual incomes, have work shift schedules or did not work, and have a higher average body mass index.
For the study, sleep duration irregularity was defined as a standard deviation of more than 120 minutes. Those participants who had a greater degree of sleep irregularity were more likely to have high coronary artery calcium burden than those whose sleep duration was more more regular, defined as an SD of 60 minutes or less (> 300; prevalence ratio, 1.33; 95% confidence interval, 1.03-1.71), as well as abnormal ankle-brachial index (< 0.9, prevalence ratio, 1.75;95% CI, 1.03-2.95).
Further, those with irregular sleep timing (SD > 90 minutes) were more likely to have a high coronary artery calcium burden (prevalence ratio, 1.39; 95% CI, 1.07-1.82) in comparison with those with more regular sleep timing (SD < 30 minutes).
“The biggest surprise to me was that 30% of the participants in the study had total sleep times that varied by more than 90 minutes over the course of the week,” Dr. Full said. “This is consistent with prior studies that suggest that a large proportion of the general public have irregular sleep patterns, not just shift workers.”
Investigating next steps
In additional analyses, Dr. Full and colleagues found that sleep duration regularity continued to be associated with high coronary artery calcium burden and abnormal ankle-brachial index when accounting for severe obstructive sleep apnea, average nightly sleep duration, and average sleep fragmentation.
Notably, when sleep duration was added, all participants with more irregular sleep durations (SD > 60 minutes) were more likely to have a high coronary artery calcium burden, compared with those with regular sleep durations (SD < 60 minutes). The results remained when participants who reported shift work, including night shift work, were excluded.
Additional studies are needed to understand the mechanisms, the study authors wrote. Night-to-night variability in sleep duration and sleep timing can cause desynchronization in the sleep-wake timing and circadian disruption.
“A key issue highlighted in this study is that sleep irregularity itself, independent of how much sleep people were getting, was related to heart health. Sleep is a naturally recurring phenomenon, and maintaining regularity helps provide stability and predictability to the body,” Michael Grandner, PhD, associate professor of psychiatry and director of the sleep and health research program at the University of Arizona, Tucson, said in an interview.
Dr. Grandner, who wasn’t involved with this study, has researched sleep irregularity and associations with cardiovascular disease, diabetes, obesity, and many other adverse outcomes.
“When people have very irregular sleep schedules, it may make it harder for the body to optimally make good use of the sleep it is getting, since it such a moving target,” he said. “The unique angle here is the ability to focus on regularity of sleep.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences of the National Institutes of Health. One author received grants and consulting fees from pharmaceutical companies unrelated to the research. The other authors and Dr. Grandner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Concussion burden tied to later hypertension in football players
a new study suggests.
Among more than 4,000 participants, 37% had hypertension at a median of 24 years post career and reported a median concussion symptom score (CSS) of 23 on a scale of 0 to 130.
“We have long seen an incompletely explained link between football participation and later-life cardiovascular disease,” Aaron L. Baggish, MD, of Massachusetts Hospital and Harvard Medical School, Boston, told this news organization.
“This study tested [whether] concussion burden during years of active play would be a determinant of later-life hypertension, the most common cause of cardiovascular disease, and indeed found this relationship to be a strong one.”
The study was published online in Circulation.
Link to cognitive decline?
Dr. Baggish and colleagues recruited former professional American-style football (ASF) players to participate in a survey administered by the Football Players Health Study at Harvard University.
Concussion burden was quantified with respect to the occurrence and severity of common concussion symptoms – e.g., headaches, nausea, dizziness, confusion, loss of consciousness (LOC), disorientation, and feeling unsteady on one’s feet – over years of active participation.
Prevalent hypertension was determined either by the participants’ previously receiving from a clinician a recommendation for medication for “high blood pressure” or by the participants’ taking such medication at the time of survey completion. Diabetes status was determined by the participants’ receiving a prior recommendation for or prescription for “diabetes or high blood sugar” medication.
Of 15,070 invited to participate in the study, 4,168 did so. The mean age of the participants was 51.8 years; 39.4% were Black; the mean body mass index was 31.3; and 33.9% were linemen. Participants played for a mean of 6.9 seasons and were surveyed at a median 24.1 years post ASF career completion. The median CSS was 23.
A total of 1,542 participants (37.3%) had hypertension, and 8.8% had diabetes.
After adjustment for established hypertension risk factors, including smoking, race, diabetes, age, and BMI, there was a graded association between CSS category and odds of later-life hypertension and between high CSS exposure and prevalent hypertension.
Results persisted when LOC, a single highly specific severe concussion symptom, was used in isolation as a surrogate for CSS, the investigators noted.
“These results suggest that repetitive early-life brain injury may have later-life implications for cardiovascular health,” they wrote. They also noted that hypertension has been shown to independently increase the risk of cognitive decline.
While premature cognitive decline among ASF players is generally attributed to chronic traumatic encephalopathy, “data from the current study raise the possibility that some element of cognitive decline among former ASF players may be attributable to hypertension,” which is potentially treatable.
“Future studies clarifying associations and causal pathways between brain injury, hypertension, and brain health are warranted,” they concluded.
Dr. Baggish added, “We hope that clinicians will now understand that head injury is an independent risk factor for high blood pressure and will screen vulnerable populations accordingly, as this may lead to better recognition of previously underdiagnosed hypertension with subsequent opportunities for intervention.”
Close monitoring
Commenting on the study, Jonathan Kim, MD, chair-elect of the American College of Cardiology’s Sports–Cardiology Section and chief of sports cardiology at Emory University in Atlanta, said, “They clearly show an independent association, which is not causality but is a new finding that requires more research. To me, it really emphasizes that cardiovascular risk is the most important health consequence that we should be worried about in retired NFL [National Football League] players.
“There are multifactorial reasons – not just repetitive head trauma – why this athletic population is at risk for the development of high blood pressure, even among college players,” he said.
Dr. Kim’s team has shown in studies conducted in collaboration with Dr. Baggish and others that collegiate football players who gain weight and develop increased systolic blood pressure are at risk of developing a “pathologic” cardiovascular phenotype.
Other research from this group showed links between nonsteroidal anti-inflammatory drug use among high school and collegiate ASF players and increased cardiovascular risk, as well as ASF-associated hypertension and ventricular-arterial coupling.
The suggestion that late-life hypertension could play a role in premature cognitive decline among ASF players “warrants further study,” Dr. Kim said, “because we do know that hypertension in the general population can be associated with cognitive decline. So that’s an important future direction.”
He concluded: “It’s a matter of focusing on cardiac prevention.” After their careers, players should be counseled on the importance of losing weight and adopting heart-healthy habits. In addition to some of the traditional concerns that might lead to closer follow-up of these patients, “having a lot of concussions in the history could potentially be another risk factor that should warrant close monitoring of blood pressure and, of course, treatment if necessary.”
The study was supported by Harvard Catalyst/the Harvard Clinical and Translational Science Center and the NFL Players Association. Dr. Baggish and several coauthors have received funding from the NFL Players Association.
A version of this article originally appeared on Medscape.com.
a new study suggests.
Among more than 4,000 participants, 37% had hypertension at a median of 24 years post career and reported a median concussion symptom score (CSS) of 23 on a scale of 0 to 130.
“We have long seen an incompletely explained link between football participation and later-life cardiovascular disease,” Aaron L. Baggish, MD, of Massachusetts Hospital and Harvard Medical School, Boston, told this news organization.
“This study tested [whether] concussion burden during years of active play would be a determinant of later-life hypertension, the most common cause of cardiovascular disease, and indeed found this relationship to be a strong one.”
The study was published online in Circulation.
Link to cognitive decline?
Dr. Baggish and colleagues recruited former professional American-style football (ASF) players to participate in a survey administered by the Football Players Health Study at Harvard University.
Concussion burden was quantified with respect to the occurrence and severity of common concussion symptoms – e.g., headaches, nausea, dizziness, confusion, loss of consciousness (LOC), disorientation, and feeling unsteady on one’s feet – over years of active participation.
Prevalent hypertension was determined either by the participants’ previously receiving from a clinician a recommendation for medication for “high blood pressure” or by the participants’ taking such medication at the time of survey completion. Diabetes status was determined by the participants’ receiving a prior recommendation for or prescription for “diabetes or high blood sugar” medication.
Of 15,070 invited to participate in the study, 4,168 did so. The mean age of the participants was 51.8 years; 39.4% were Black; the mean body mass index was 31.3; and 33.9% were linemen. Participants played for a mean of 6.9 seasons and were surveyed at a median 24.1 years post ASF career completion. The median CSS was 23.
A total of 1,542 participants (37.3%) had hypertension, and 8.8% had diabetes.
After adjustment for established hypertension risk factors, including smoking, race, diabetes, age, and BMI, there was a graded association between CSS category and odds of later-life hypertension and between high CSS exposure and prevalent hypertension.
Results persisted when LOC, a single highly specific severe concussion symptom, was used in isolation as a surrogate for CSS, the investigators noted.
“These results suggest that repetitive early-life brain injury may have later-life implications for cardiovascular health,” they wrote. They also noted that hypertension has been shown to independently increase the risk of cognitive decline.
While premature cognitive decline among ASF players is generally attributed to chronic traumatic encephalopathy, “data from the current study raise the possibility that some element of cognitive decline among former ASF players may be attributable to hypertension,” which is potentially treatable.
“Future studies clarifying associations and causal pathways between brain injury, hypertension, and brain health are warranted,” they concluded.
Dr. Baggish added, “We hope that clinicians will now understand that head injury is an independent risk factor for high blood pressure and will screen vulnerable populations accordingly, as this may lead to better recognition of previously underdiagnosed hypertension with subsequent opportunities for intervention.”
Close monitoring
Commenting on the study, Jonathan Kim, MD, chair-elect of the American College of Cardiology’s Sports–Cardiology Section and chief of sports cardiology at Emory University in Atlanta, said, “They clearly show an independent association, which is not causality but is a new finding that requires more research. To me, it really emphasizes that cardiovascular risk is the most important health consequence that we should be worried about in retired NFL [National Football League] players.
“There are multifactorial reasons – not just repetitive head trauma – why this athletic population is at risk for the development of high blood pressure, even among college players,” he said.
Dr. Kim’s team has shown in studies conducted in collaboration with Dr. Baggish and others that collegiate football players who gain weight and develop increased systolic blood pressure are at risk of developing a “pathologic” cardiovascular phenotype.
Other research from this group showed links between nonsteroidal anti-inflammatory drug use among high school and collegiate ASF players and increased cardiovascular risk, as well as ASF-associated hypertension and ventricular-arterial coupling.
The suggestion that late-life hypertension could play a role in premature cognitive decline among ASF players “warrants further study,” Dr. Kim said, “because we do know that hypertension in the general population can be associated with cognitive decline. So that’s an important future direction.”
He concluded: “It’s a matter of focusing on cardiac prevention.” After their careers, players should be counseled on the importance of losing weight and adopting heart-healthy habits. In addition to some of the traditional concerns that might lead to closer follow-up of these patients, “having a lot of concussions in the history could potentially be another risk factor that should warrant close monitoring of blood pressure and, of course, treatment if necessary.”
The study was supported by Harvard Catalyst/the Harvard Clinical and Translational Science Center and the NFL Players Association. Dr. Baggish and several coauthors have received funding from the NFL Players Association.
A version of this article originally appeared on Medscape.com.
a new study suggests.
Among more than 4,000 participants, 37% had hypertension at a median of 24 years post career and reported a median concussion symptom score (CSS) of 23 on a scale of 0 to 130.
“We have long seen an incompletely explained link between football participation and later-life cardiovascular disease,” Aaron L. Baggish, MD, of Massachusetts Hospital and Harvard Medical School, Boston, told this news organization.
“This study tested [whether] concussion burden during years of active play would be a determinant of later-life hypertension, the most common cause of cardiovascular disease, and indeed found this relationship to be a strong one.”
The study was published online in Circulation.
Link to cognitive decline?
Dr. Baggish and colleagues recruited former professional American-style football (ASF) players to participate in a survey administered by the Football Players Health Study at Harvard University.
Concussion burden was quantified with respect to the occurrence and severity of common concussion symptoms – e.g., headaches, nausea, dizziness, confusion, loss of consciousness (LOC), disorientation, and feeling unsteady on one’s feet – over years of active participation.
Prevalent hypertension was determined either by the participants’ previously receiving from a clinician a recommendation for medication for “high blood pressure” or by the participants’ taking such medication at the time of survey completion. Diabetes status was determined by the participants’ receiving a prior recommendation for or prescription for “diabetes or high blood sugar” medication.
Of 15,070 invited to participate in the study, 4,168 did so. The mean age of the participants was 51.8 years; 39.4% were Black; the mean body mass index was 31.3; and 33.9% were linemen. Participants played for a mean of 6.9 seasons and were surveyed at a median 24.1 years post ASF career completion. The median CSS was 23.
A total of 1,542 participants (37.3%) had hypertension, and 8.8% had diabetes.
After adjustment for established hypertension risk factors, including smoking, race, diabetes, age, and BMI, there was a graded association between CSS category and odds of later-life hypertension and between high CSS exposure and prevalent hypertension.
Results persisted when LOC, a single highly specific severe concussion symptom, was used in isolation as a surrogate for CSS, the investigators noted.
“These results suggest that repetitive early-life brain injury may have later-life implications for cardiovascular health,” they wrote. They also noted that hypertension has been shown to independently increase the risk of cognitive decline.
While premature cognitive decline among ASF players is generally attributed to chronic traumatic encephalopathy, “data from the current study raise the possibility that some element of cognitive decline among former ASF players may be attributable to hypertension,” which is potentially treatable.
“Future studies clarifying associations and causal pathways between brain injury, hypertension, and brain health are warranted,” they concluded.
Dr. Baggish added, “We hope that clinicians will now understand that head injury is an independent risk factor for high blood pressure and will screen vulnerable populations accordingly, as this may lead to better recognition of previously underdiagnosed hypertension with subsequent opportunities for intervention.”
Close monitoring
Commenting on the study, Jonathan Kim, MD, chair-elect of the American College of Cardiology’s Sports–Cardiology Section and chief of sports cardiology at Emory University in Atlanta, said, “They clearly show an independent association, which is not causality but is a new finding that requires more research. To me, it really emphasizes that cardiovascular risk is the most important health consequence that we should be worried about in retired NFL [National Football League] players.
“There are multifactorial reasons – not just repetitive head trauma – why this athletic population is at risk for the development of high blood pressure, even among college players,” he said.
Dr. Kim’s team has shown in studies conducted in collaboration with Dr. Baggish and others that collegiate football players who gain weight and develop increased systolic blood pressure are at risk of developing a “pathologic” cardiovascular phenotype.
Other research from this group showed links between nonsteroidal anti-inflammatory drug use among high school and collegiate ASF players and increased cardiovascular risk, as well as ASF-associated hypertension and ventricular-arterial coupling.
The suggestion that late-life hypertension could play a role in premature cognitive decline among ASF players “warrants further study,” Dr. Kim said, “because we do know that hypertension in the general population can be associated with cognitive decline. So that’s an important future direction.”
He concluded: “It’s a matter of focusing on cardiac prevention.” After their careers, players should be counseled on the importance of losing weight and adopting heart-healthy habits. In addition to some of the traditional concerns that might lead to closer follow-up of these patients, “having a lot of concussions in the history could potentially be another risk factor that should warrant close monitoring of blood pressure and, of course, treatment if necessary.”
The study was supported by Harvard Catalyst/the Harvard Clinical and Translational Science Center and the NFL Players Association. Dr. Baggish and several coauthors have received funding from the NFL Players Association.
A version of this article originally appeared on Medscape.com.
FROM CIRCULATION
Two cups of coffee increase heart dangers with hypertension
according to researchers at Institute for Global Health Policy Research, Bureau of International Health Cooperation, National Center for Global Health and Medicine, Tokyo.
What to know
People with severely high blood pressure who drink two or more cups of caffeinated coffee each day could double their risk of dying from a heart attack, stroke, or any type of cardiovascular disease.
Too much coffee may raise blood pressure and lead to anxiety, heart palpitations, and difficulty sleeping.
An 8-ounce cup of coffee has 80-100 mg of caffeine, while an 8-ounce cup of green or black tea has 30-50 mg.
Drinking one cup of coffee a day or any amount of green tea was not associated with risk of death across any blood pressure categories, and drinking green tea was not associated with increased risk of death related to cardiovascular disease at any blood pressure level.
Frequent consumers of coffee were more likely to be younger, current smokers, current drinkers, to eat fewer vegetables, and to have higher total cholesterol levels and lower systolic blood pressure regardless of their blood pressure category.
This is a summary of the article “Coffee and Green Tea Consumption and Cardiovascular Disease Mortality Among People With and Without Hypertension,” published in the Journal of the American Heart Association.
A version of this article first appeared on Medscape.com.
according to researchers at Institute for Global Health Policy Research, Bureau of International Health Cooperation, National Center for Global Health and Medicine, Tokyo.
What to know
People with severely high blood pressure who drink two or more cups of caffeinated coffee each day could double their risk of dying from a heart attack, stroke, or any type of cardiovascular disease.
Too much coffee may raise blood pressure and lead to anxiety, heart palpitations, and difficulty sleeping.
An 8-ounce cup of coffee has 80-100 mg of caffeine, while an 8-ounce cup of green or black tea has 30-50 mg.
Drinking one cup of coffee a day or any amount of green tea was not associated with risk of death across any blood pressure categories, and drinking green tea was not associated with increased risk of death related to cardiovascular disease at any blood pressure level.
Frequent consumers of coffee were more likely to be younger, current smokers, current drinkers, to eat fewer vegetables, and to have higher total cholesterol levels and lower systolic blood pressure regardless of their blood pressure category.
This is a summary of the article “Coffee and Green Tea Consumption and Cardiovascular Disease Mortality Among People With and Without Hypertension,” published in the Journal of the American Heart Association.
A version of this article first appeared on Medscape.com.
according to researchers at Institute for Global Health Policy Research, Bureau of International Health Cooperation, National Center for Global Health and Medicine, Tokyo.
What to know
People with severely high blood pressure who drink two or more cups of caffeinated coffee each day could double their risk of dying from a heart attack, stroke, or any type of cardiovascular disease.
Too much coffee may raise blood pressure and lead to anxiety, heart palpitations, and difficulty sleeping.
An 8-ounce cup of coffee has 80-100 mg of caffeine, while an 8-ounce cup of green or black tea has 30-50 mg.
Drinking one cup of coffee a day or any amount of green tea was not associated with risk of death across any blood pressure categories, and drinking green tea was not associated with increased risk of death related to cardiovascular disease at any blood pressure level.
Frequent consumers of coffee were more likely to be younger, current smokers, current drinkers, to eat fewer vegetables, and to have higher total cholesterol levels and lower systolic blood pressure regardless of their blood pressure category.
This is a summary of the article “Coffee and Green Tea Consumption and Cardiovascular Disease Mortality Among People With and Without Hypertension,” published in the Journal of the American Heart Association.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF AMERICAN HEART ASSOCIATION
New ACC, AHA, SCAI interventional cardiology training guidance
The American College of Cardiology, the American Heart Association, and the Society for Cardiovascular Angiography and Interventions (SCAI) have jointly issued new guidance outlining competency-based advanced training requirements for interventional cardiology trainees.
It’s the first document of its kind to define the training requirements for the full breadth of interventional cardiology for adults, including coronary interventions, peripheral vascular interventions (PVIs), and structural heart interventions (SHIs), the organizations say.
“With this groundbreaking document, the writing committee provides a roadmap for both program directors and interventional cardiology trainees to help them progress through important training milestones,” Theodore A. Bass, MD, chair of the statement writing committee, says in a news release.
“The document defines the required competencies for the full scope of interventional cardiology, providing trainees for the first time with the information to support training across all these areas,” Dr. Bass adds.
Minimum of 250 procedures
To gain the necessary experience in interventional cardiology, cardiovascular fellows are advised to complete the following:
- A 3-year general cardiovascular disease fellowship (successful completion consists of Level I competency in all aspects of cardiovascular medicine and Level II competency in diagnostic cardiac catheterization to pursue interventional cardiology training);
- A 1-year accredited interventional cardiology fellowship, the focus of which is coronary intervention with the opportunity to gain procedural experience in various aspects of PVI or SHI (Level III competency);
- An option for additional post-fellowship training based on the trainee’s career goals.
The goal of Level III training is to provide the interventional cardiology trainees with a “well-rounded, competency-based education,” including didactic instruction, clinical experience in the diagnosis and care of patients, and hands-on procedural experience, the writing group says.
Competency requirements are defined using the Accreditation Council for Graduate Medical Education’s six “essential” competency domains: medical knowledge; patient care and procedural skills; practice-based learning and improvement; systems-based practice; interpersonal and communication skills; and professionalism.
To support attaining these competencies, the writing committee recommends a minimum of 250 interventional cardiology procedures. Of these, 200 should be coronary procedures, with the remaining 50 specialized in coronary, PVI, or SHI, which allows the fellows to customize training on the basis of their career goals.
Adjunctive procedures related to physiologic assessment and intracoronary imaging are also required (25 of each). “These minimum numbers are meant to provide trainees with exposure to a variety and spectrum of complexity of clinical case material and give supervising faculty sufficient opportunity to evaluate trainees’ competency,” the writing group says.
In addition to their procedural skills, evaluation of interventional cardiology trainee proficiency should include regular assessment of a trainee’s ability to clinically diagnose and manage patients across the broad spectrum of diseases.
Assessment of trainees should involve multiple components, including direct observation by instructors, case logs, chart reviews (including adherence to guideline recommendations, appropriate use criteria, and patient outcomes), simulation training, and assessment of leadership skills.
Trainees must also acquire experience working as part of a multidisciplinary team to provide a holistic approach to patient care. The document also highlights the importance of leadership skills, mentorship and lifelong learning beyond initial training.
The 2023 ACC/AHA/SCAI Advanced Training Statement on Interventional Cardiology (Coronary, Peripheral Vascular, and Structural Heart Interventions) was published online in the Journal of the American College of Cardiology.
The statement was developed in collaboration with and endorsed by the American Association for Thoracic Surgery, the American Society of Echocardiography, the Heart Failure Society of America, the Heart Rhythm Society, the Society of Cardiovascular Anesthesiologists, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, the Society of Thoracic Surgeons, and the Society for Vascular Medicine.
A version of this article first appeared on Medscape.com.
The American College of Cardiology, the American Heart Association, and the Society for Cardiovascular Angiography and Interventions (SCAI) have jointly issued new guidance outlining competency-based advanced training requirements for interventional cardiology trainees.
It’s the first document of its kind to define the training requirements for the full breadth of interventional cardiology for adults, including coronary interventions, peripheral vascular interventions (PVIs), and structural heart interventions (SHIs), the organizations say.
“With this groundbreaking document, the writing committee provides a roadmap for both program directors and interventional cardiology trainees to help them progress through important training milestones,” Theodore A. Bass, MD, chair of the statement writing committee, says in a news release.
“The document defines the required competencies for the full scope of interventional cardiology, providing trainees for the first time with the information to support training across all these areas,” Dr. Bass adds.
Minimum of 250 procedures
To gain the necessary experience in interventional cardiology, cardiovascular fellows are advised to complete the following:
- A 3-year general cardiovascular disease fellowship (successful completion consists of Level I competency in all aspects of cardiovascular medicine and Level II competency in diagnostic cardiac catheterization to pursue interventional cardiology training);
- A 1-year accredited interventional cardiology fellowship, the focus of which is coronary intervention with the opportunity to gain procedural experience in various aspects of PVI or SHI (Level III competency);
- An option for additional post-fellowship training based on the trainee’s career goals.
The goal of Level III training is to provide the interventional cardiology trainees with a “well-rounded, competency-based education,” including didactic instruction, clinical experience in the diagnosis and care of patients, and hands-on procedural experience, the writing group says.
Competency requirements are defined using the Accreditation Council for Graduate Medical Education’s six “essential” competency domains: medical knowledge; patient care and procedural skills; practice-based learning and improvement; systems-based practice; interpersonal and communication skills; and professionalism.
To support attaining these competencies, the writing committee recommends a minimum of 250 interventional cardiology procedures. Of these, 200 should be coronary procedures, with the remaining 50 specialized in coronary, PVI, or SHI, which allows the fellows to customize training on the basis of their career goals.
Adjunctive procedures related to physiologic assessment and intracoronary imaging are also required (25 of each). “These minimum numbers are meant to provide trainees with exposure to a variety and spectrum of complexity of clinical case material and give supervising faculty sufficient opportunity to evaluate trainees’ competency,” the writing group says.
In addition to their procedural skills, evaluation of interventional cardiology trainee proficiency should include regular assessment of a trainee’s ability to clinically diagnose and manage patients across the broad spectrum of diseases.
Assessment of trainees should involve multiple components, including direct observation by instructors, case logs, chart reviews (including adherence to guideline recommendations, appropriate use criteria, and patient outcomes), simulation training, and assessment of leadership skills.
Trainees must also acquire experience working as part of a multidisciplinary team to provide a holistic approach to patient care. The document also highlights the importance of leadership skills, mentorship and lifelong learning beyond initial training.
The 2023 ACC/AHA/SCAI Advanced Training Statement on Interventional Cardiology (Coronary, Peripheral Vascular, and Structural Heart Interventions) was published online in the Journal of the American College of Cardiology.
The statement was developed in collaboration with and endorsed by the American Association for Thoracic Surgery, the American Society of Echocardiography, the Heart Failure Society of America, the Heart Rhythm Society, the Society of Cardiovascular Anesthesiologists, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, the Society of Thoracic Surgeons, and the Society for Vascular Medicine.
A version of this article first appeared on Medscape.com.
The American College of Cardiology, the American Heart Association, and the Society for Cardiovascular Angiography and Interventions (SCAI) have jointly issued new guidance outlining competency-based advanced training requirements for interventional cardiology trainees.
It’s the first document of its kind to define the training requirements for the full breadth of interventional cardiology for adults, including coronary interventions, peripheral vascular interventions (PVIs), and structural heart interventions (SHIs), the organizations say.
“With this groundbreaking document, the writing committee provides a roadmap for both program directors and interventional cardiology trainees to help them progress through important training milestones,” Theodore A. Bass, MD, chair of the statement writing committee, says in a news release.
“The document defines the required competencies for the full scope of interventional cardiology, providing trainees for the first time with the information to support training across all these areas,” Dr. Bass adds.
Minimum of 250 procedures
To gain the necessary experience in interventional cardiology, cardiovascular fellows are advised to complete the following:
- A 3-year general cardiovascular disease fellowship (successful completion consists of Level I competency in all aspects of cardiovascular medicine and Level II competency in diagnostic cardiac catheterization to pursue interventional cardiology training);
- A 1-year accredited interventional cardiology fellowship, the focus of which is coronary intervention with the opportunity to gain procedural experience in various aspects of PVI or SHI (Level III competency);
- An option for additional post-fellowship training based on the trainee’s career goals.
The goal of Level III training is to provide the interventional cardiology trainees with a “well-rounded, competency-based education,” including didactic instruction, clinical experience in the diagnosis and care of patients, and hands-on procedural experience, the writing group says.
Competency requirements are defined using the Accreditation Council for Graduate Medical Education’s six “essential” competency domains: medical knowledge; patient care and procedural skills; practice-based learning and improvement; systems-based practice; interpersonal and communication skills; and professionalism.
To support attaining these competencies, the writing committee recommends a minimum of 250 interventional cardiology procedures. Of these, 200 should be coronary procedures, with the remaining 50 specialized in coronary, PVI, or SHI, which allows the fellows to customize training on the basis of their career goals.
Adjunctive procedures related to physiologic assessment and intracoronary imaging are also required (25 of each). “These minimum numbers are meant to provide trainees with exposure to a variety and spectrum of complexity of clinical case material and give supervising faculty sufficient opportunity to evaluate trainees’ competency,” the writing group says.
In addition to their procedural skills, evaluation of interventional cardiology trainee proficiency should include regular assessment of a trainee’s ability to clinically diagnose and manage patients across the broad spectrum of diseases.
Assessment of trainees should involve multiple components, including direct observation by instructors, case logs, chart reviews (including adherence to guideline recommendations, appropriate use criteria, and patient outcomes), simulation training, and assessment of leadership skills.
Trainees must also acquire experience working as part of a multidisciplinary team to provide a holistic approach to patient care. The document also highlights the importance of leadership skills, mentorship and lifelong learning beyond initial training.
The 2023 ACC/AHA/SCAI Advanced Training Statement on Interventional Cardiology (Coronary, Peripheral Vascular, and Structural Heart Interventions) was published online in the Journal of the American College of Cardiology.
The statement was developed in collaboration with and endorsed by the American Association for Thoracic Surgery, the American Society of Echocardiography, the Heart Failure Society of America, the Heart Rhythm Society, the Society of Cardiovascular Anesthesiologists, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, the Society of Thoracic Surgeons, and the Society for Vascular Medicine.
A version of this article first appeared on Medscape.com.
Steak dinners, sales reps, and risky procedures: Inside the big business of clogged arteries
On June 14, 2017, just before noon, a doctor made an incision near a patient’s groin. Kari Kirk, a representative for the world’s largest medical device company, Medtronic, looked on and began texting her colleague a play-by-play.
“Fixing both legs from the ankles,” she wrote.
It was a fairly common procedure at the Robert J. Dole Veterans Affairs Medical Center in Wichita, Kansas, performed to treat blockages in the leg vessels.
Within reach were an array of Medtronic products: tubes with blades attached to shave hardened deposits off of artery walls; stents to widen blood vessels; balloons coated with therapeutic drugs.
Each time a doctor puts a foreign device in someone’s body, it carries a risk of complication, which can include clots or even require amputation. So medical experts, research and even Medtronic’s own device instructions urge doctors to use as few as are necessary.
“Just used 12 [drug-coated balloons]!!” Kirk texted her colleague.
“Does that mean I owe u $$,” he responded.
“Thats what I’m thinking!!!” she said. “And now 14 balloons?!”
“but only one stent so far??”
“So far!”
As the texting continued, her colleague replied, “U are going to want to start going to the VA all the time.”
The messages, recently unsealed in an ongoing whistleblower lawsuit, give a window into the way money and medicine mingle in the booming business of peripheral artery disease, a condition that afflicts 6.5 million Americans over age 40 and is caused when fatty plaque builds up in arteries, blocking blood flow to the legs.
Representatives from companies are often present during vascular procedures to guide doctors on how to use their complex devices. This kind of access has the potential to influence treatment plans, as companies and their representatives profit when more of their product is used.
The suit, filed in 2017 by a sales representative for a competing medical device firm, alleges an illegal kickback scheme between Medtronic and hospital employees. According to the complaint and documents released in the suit, between 2011 and 2018, VA health care workers received steakhouse dinners, Apple electronics, and NASCAR tickets, and in turn, Medtronic secured a lucrative contract with the hospital. Meanwhile, the company’s representatives allegedly “groomed and trained” physicians at the facility, who then deployed the company’s devices even when it was not medically indicated.
Independently from the whistleblower suit, internal investigators at the Wichita facility have also examined the treatment patterns of its vascular patients in recent years and found numerous cases where medical devices were used excessively. While it’s not uncommon to deploy several devices, a medical expert on the investigation team found that the VA doctors sometimes used more than 15 at a time – one used 33 – deviating from the standard of care.
“It is unconscionable – there can be no valid medically acceptable basis to cram so many devices into a human being,” wrote attorneys representing the whistleblower in legal filings from January 2023. “This is not medical treatment. This is abuse.”
Dr. Kim Hodgson, former president of the Society for Vascular Surgery and an expert retained by the plaintiff, said the findings of the internal review of patient data raise “a high level of concern regarding necessity of treatment provided,” according to case documents.
Medtronic declined to respond to ProPublica’s questions, citing the ongoing litigation. “These allegations are false and Medtronic is defending against these claims in court,” said Boua Xiong, a spokesperson for the company. Medtronic representative Kirk declined to respond to ProPublica’s request for comment.
The hospital investigation found that amputations increased sixfold in the same time frame as the procedures in question, according to internal emails, but made no conclusion about whether those two things were connected. ProPublica reached out to the VA to ask whether any patients had been harmed.
The VA is “conducting an extensive review of patient care” at the Kansas hospital, “including the number of devices used on patients – to make sure that Veterans were not harmed by any procedures,” press secretary Terrence Hayes said in a statement. So far, the VA’s investigation has found no “quality of care issues,” he said, and the investigation will continue “until every Veteran’s case has been reviewed.” (Read the full statement here.) Neither the department nor the hospital has taken formal action against the medical providers, Hayes said.
The medical group that had a contract with the VA for vascular interventions, Wichita Radiological Group, did not respond to ProPublica’s requests for comment, nor did the doctors named in the suit: Dr. Shaun Gonda, Dr. Bret Winblad, and Dr. Kermit Rust. It is unclear from the case documents which doctors conducted which procedures. Eric Barth, an attorney for the medical group, denied the allegations in recent legal filings, calling the claims “baseless” and the lawsuit a “witch hunt.”
The lawsuit comes amid growing concern about one of these procedures – atherectomies – after researchers and doctors have uncovered patterns of excessive and inappropriate use. Recent research has found that this procedure, a common but costly treatment to shave or laser plaque from blood vessels, is not more effective than cheaper alternatives and may even be associated with a higher risk of complications including amputation. In recent years, several doctors and clinics have been investigated for allegedly taking advantage of Medicare’s reimbursement rates, and one study found that many doctors are resorting to atherectomies in the earliest stages of peripheral artery disease, against best practices that urge noninvasive treatment.
“Atherectomy is important in certain settings. But it’s being used in a way that is entirely inappropriate and it’s largely driven by the incentive structure,” said Dr. Caitlin Hicks, the lead author of the study and an associate professor of surgery at Johns Hopkins University School of Medicine.
Although different payment structures govern the care of veterans, the whistleblower lawsuit alleges that outside physicians, paid hourly by the Dole VA, were motivated to conduct longer and more complex procedures that would earn them higher payment.
Under different circumstances, the patient in the procedure room on that summer day could have been done after 2 hours.
But, 150 minutes in, those Medtronic representatives were still texting. At that point, more than 15 of their vascular devices had been used, including stents, balloons, and those for atherectomy.
“Long case!” Kirk’s colleague texted. “Is it looking ok??”
“It is,” she said. “Thought we were done a few times! Now he’s going back in to cut again!”
A little while later, she texted: “....17!”
He texted back [with laughing emoticons].
Hospital leaders had been scrutinizing the use of these procedures at the Dole VA for years.
In 2017, shortly after Rick Ament was hired to lead the facility, he noticed something was amiss. While the longtime hospital administrator was poring over the finances, he was alarmed to discover that the relatively small Dole VA had one of the most expensive cardiac programs in the country. As Ament dug deeper, he realized vascular interventions were the reason.
“It just did not make sense that the acuity level of our patients would generate such extreme cost variances from the norm,” he testified in December, in a deposition for the whistleblower case. “It was so significant, we needed to get to the bottom of it.”
Ament, a second generation Air Force veteran, quietly assembled a task force to investigate why the facility had purchased so many medical devices for these procedures. After they examined inventory records, calculating the total number of medical devices and the cost of devices per patient, they grew concerned.
“We were more expensive than, I believe it was, the top 10 hospitals in the VA combined,” he said. “My feeling was that we either had very, very bad providers or we had product walking out the door.”
Ament enlisted experts from other VA hospitals to help his team investigate, including an administrative officer who could understand finances and a respected interventional radiologist who could examine records. The task force gathered a list of patients from 2016 to 2018, according to internal emails, and analyzed their medical charts.
According to internal VA documents released through the whistleblower suit, the review found a number of clinical failings: Evidence-based medicine had not been followed in the majority of cases reviewed. Procedures were over-aggressive, treating lesions that should have been left alone. And there was a total disregard for established best practices for treating peripheral artery disease.
One of the experts on the investigative team explained to Ament that while it was not uncommon for doctors to use a couple of devices in one intervention, the total number of devices in many of the procedures at his facility went into the double digits, sometimes five times the expected amount.
In one encounter, a doctor deployed 33 devices in one procedure – 3 atherectomy devices, 9 stents, and 21 balloons.
This use of devices was exorbitant, Ament came to understand. “I want to say the term ‘egregious’ was used,” he testified. “It was kind of like validation, but I really wish I was wrong.”
“Did it make you concerned for patient care?” a lawyer asked during the deposition.
“It did,” Ament replied.
A member of his task force pulled data for veterans who had leg amputations due to vascular disease. Over 5 years, the number of veterans who had amputations increased, from about 6 in 2013 to 38 in 2018, according to internal emails released in the suit. The VA did not respond to ProPublica’s questions about the rise in amputations or whether it was due to complications from the procedures.
Even though Ament testified in December 2022 that he became aware of the excessive use of devices during his investigation that began about 5 years ago, neither he nor the VA have publicly acknowledged these findings outside of the lawsuit. It is unclear whether VA representatives informed the patients whose records were reviewed about their findings. ProPublica reached out to more than half a dozen veteran community groups in the Wichita area and none were aware of the investigation nor the allegations of overuse of vascular procedures at the facility.
The VA says that if its ongoing review finds instances of substandard care, it will reach out to affected patients and inform them about possible complications and benefits they may be entitled to. The press secretary said the review will take several months. Ament declined to respond to ProPublica’s questions, citing the ongoing case.
In 2018, Ament turned over his findings to the criminal division of the VA’s Office of Inspector General. He also shut down interventional radiology procedures at the facility’s catheter lab.
Federal agents separately opened an investigation into the same unit in the facility, looking into allegations of kickbacks.
More than 40 pages of expense reports from Medtronic, revealed in the whistleblower case, show sales representatives treating Dole health care workers to hundreds of meals over several years – lunches at Dempsey’s Biscuit Co.; business meals at the Scotch & Sirloin steakhouse; dinner at Chester’s Chophouse & Wine Bar, price per attendee: $122.39.
Federal agents obtained the receipts.
“Robert J. Dole VAMC employees may have received improper gratuities, in the forms of paid lunches, dinners, etc., from sales representatives from Medtronic,” Nathen Howard, a special agent in the VA OIG, wrote in an investigation memo from February 2019.
This kind of relationship could violate VA policy, which forbids federal employees from receiving any gifts, including meals, from people who do business or seek to do business with a federal institution. For health care workers, violating this policy could have serious implications for patients. Numerous studies have shown that even modest industry-sponsored gifts, including meals, may influence prescribing or treatment behavior of health care professionals.
The agents opened their investigation into kickbacks at the Wichita facility in response to the whistleblower lawsuit, which was filed by Thomas Schroeder in 2017. The VA OIG would not confirm or deny whether it was continuing to investigate kickbacks at the facility. The VA did not directly answer ProPublica’s questions about kickbacks at the Dole VA, but it said that every employee must complete an annual ethics training, which covers gift rules.
In recent years, Medtronic has settled a handful of other cases that have alleged kickbacks between company representatives and health care professionals.
In 2018, Medtronic’s subsidiary Covidien paid $13 million to settle claims with the U.S. Department of Justice that it paid kickbacks to health care institutions that used its mechanical blood clot devices. In 2019, the same subsidiary paid $17 million to resolve allegations that it provided in-kind marketing support to doctors using its vein products. And in 2020, Medtronic paid more than $8 million to settle claims that representatives had paid kickbacks to a neurosurgeon, including scores of lavish meals at a restaurant that the doctor owned, to induce him to purchase the company’s medication pumps.
Schroeder’s lawsuit is not the first time Medtronic’s vascular devices were named in an alleged kickback scheme. In early 2015, Medtronic acquired Covidien, and shortly after the merger, its subsidiary ev3 Inc. agreed to pay $1.25 million to resolve allegations that it had paid doctors who were “high volume users” of its atherectomy devices to act as evangelists for the company, and had provided physicians with company shares to participate in clinical trials for their tools.
The whistleblower in this earlier case, a former sales representative for the company, also alleged that the subsidiary was gaming Medicare’s payment system. Hospitals were often hesitant to conduct atherectomy procedures because of the low reimbursement rates. According to the suit, sales representatives encouraged doctors to admit patients for longer stays to reap greater reimbursements and make a profit, even though such stays were often not medically indicated.
“Medical device makers that try to boost their profits by causing patients to be admitted for unnecessary and expensive inpatient hospital stays will be held accountable,” special agent Thomas O’Donnell, from the Office of Inspector General at the U.S. Department of Health and Human Services, said in a press release for the settlement. “Both patients and taxpayers deserve to have medical decisions made based on what is medically appropriate.”
Medtronic spokesperson Xiong said that in each case, the company “cooperated fully with the DOJ to resolve its concerns and, where wrongdoing was found, took appropriate remedial action.”
Seton Hall Law School professor Jacob Elberg, a former assistant U.S. attorney for the District of New Jersey who led its health care and government fraud unit, is concerned by the frequency of such settlements in the last 2 decades. “There are, at this point, real questions as to whether the sanctions imposed by DOJ are sufficient to deter wrongdoing and to lead to meaningful change, especially within the medical device industry.”
Although the Department of Justice has declined to intervene in the lawsuit involving the Dole VA at this time, the case is ongoing and further depositions with Medtronic sales representatives and a former VA employee are scheduled for this month.
VA employees and doctors named in the suit declined to comment or did not respond to ProPublica’s questions about the alleged kickbacks and whether sales representatives may have influenced veterans’ treatment plans. In interviews with federal investigators, according to released transcripts, several of the employees who were questioned denied receiving frequent meals from sales representatives, contradicting Medtronic’s expense reports.
Their statements also stand in contrast to Medtronic representative Kari Kirk’s final text messages during that procedure in June 2017, which ultimately lasted more than 3 hours.
“Now u done??” her colleague asked.
“Just finished,” she texted. “Running to get them lunch!”
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
On June 14, 2017, just before noon, a doctor made an incision near a patient’s groin. Kari Kirk, a representative for the world’s largest medical device company, Medtronic, looked on and began texting her colleague a play-by-play.
“Fixing both legs from the ankles,” she wrote.
It was a fairly common procedure at the Robert J. Dole Veterans Affairs Medical Center in Wichita, Kansas, performed to treat blockages in the leg vessels.
Within reach were an array of Medtronic products: tubes with blades attached to shave hardened deposits off of artery walls; stents to widen blood vessels; balloons coated with therapeutic drugs.
Each time a doctor puts a foreign device in someone’s body, it carries a risk of complication, which can include clots or even require amputation. So medical experts, research and even Medtronic’s own device instructions urge doctors to use as few as are necessary.
“Just used 12 [drug-coated balloons]!!” Kirk texted her colleague.
“Does that mean I owe u $$,” he responded.
“Thats what I’m thinking!!!” she said. “And now 14 balloons?!”
“but only one stent so far??”
“So far!”
As the texting continued, her colleague replied, “U are going to want to start going to the VA all the time.”
The messages, recently unsealed in an ongoing whistleblower lawsuit, give a window into the way money and medicine mingle in the booming business of peripheral artery disease, a condition that afflicts 6.5 million Americans over age 40 and is caused when fatty plaque builds up in arteries, blocking blood flow to the legs.
Representatives from companies are often present during vascular procedures to guide doctors on how to use their complex devices. This kind of access has the potential to influence treatment plans, as companies and their representatives profit when more of their product is used.
The suit, filed in 2017 by a sales representative for a competing medical device firm, alleges an illegal kickback scheme between Medtronic and hospital employees. According to the complaint and documents released in the suit, between 2011 and 2018, VA health care workers received steakhouse dinners, Apple electronics, and NASCAR tickets, and in turn, Medtronic secured a lucrative contract with the hospital. Meanwhile, the company’s representatives allegedly “groomed and trained” physicians at the facility, who then deployed the company’s devices even when it was not medically indicated.
Independently from the whistleblower suit, internal investigators at the Wichita facility have also examined the treatment patterns of its vascular patients in recent years and found numerous cases where medical devices were used excessively. While it’s not uncommon to deploy several devices, a medical expert on the investigation team found that the VA doctors sometimes used more than 15 at a time – one used 33 – deviating from the standard of care.
“It is unconscionable – there can be no valid medically acceptable basis to cram so many devices into a human being,” wrote attorneys representing the whistleblower in legal filings from January 2023. “This is not medical treatment. This is abuse.”
Dr. Kim Hodgson, former president of the Society for Vascular Surgery and an expert retained by the plaintiff, said the findings of the internal review of patient data raise “a high level of concern regarding necessity of treatment provided,” according to case documents.
Medtronic declined to respond to ProPublica’s questions, citing the ongoing litigation. “These allegations are false and Medtronic is defending against these claims in court,” said Boua Xiong, a spokesperson for the company. Medtronic representative Kirk declined to respond to ProPublica’s request for comment.
The hospital investigation found that amputations increased sixfold in the same time frame as the procedures in question, according to internal emails, but made no conclusion about whether those two things were connected. ProPublica reached out to the VA to ask whether any patients had been harmed.
The VA is “conducting an extensive review of patient care” at the Kansas hospital, “including the number of devices used on patients – to make sure that Veterans were not harmed by any procedures,” press secretary Terrence Hayes said in a statement. So far, the VA’s investigation has found no “quality of care issues,” he said, and the investigation will continue “until every Veteran’s case has been reviewed.” (Read the full statement here.) Neither the department nor the hospital has taken formal action against the medical providers, Hayes said.
The medical group that had a contract with the VA for vascular interventions, Wichita Radiological Group, did not respond to ProPublica’s requests for comment, nor did the doctors named in the suit: Dr. Shaun Gonda, Dr. Bret Winblad, and Dr. Kermit Rust. It is unclear from the case documents which doctors conducted which procedures. Eric Barth, an attorney for the medical group, denied the allegations in recent legal filings, calling the claims “baseless” and the lawsuit a “witch hunt.”
The lawsuit comes amid growing concern about one of these procedures – atherectomies – after researchers and doctors have uncovered patterns of excessive and inappropriate use. Recent research has found that this procedure, a common but costly treatment to shave or laser plaque from blood vessels, is not more effective than cheaper alternatives and may even be associated with a higher risk of complications including amputation. In recent years, several doctors and clinics have been investigated for allegedly taking advantage of Medicare’s reimbursement rates, and one study found that many doctors are resorting to atherectomies in the earliest stages of peripheral artery disease, against best practices that urge noninvasive treatment.
“Atherectomy is important in certain settings. But it’s being used in a way that is entirely inappropriate and it’s largely driven by the incentive structure,” said Dr. Caitlin Hicks, the lead author of the study and an associate professor of surgery at Johns Hopkins University School of Medicine.
Although different payment structures govern the care of veterans, the whistleblower lawsuit alleges that outside physicians, paid hourly by the Dole VA, were motivated to conduct longer and more complex procedures that would earn them higher payment.
Under different circumstances, the patient in the procedure room on that summer day could have been done after 2 hours.
But, 150 minutes in, those Medtronic representatives were still texting. At that point, more than 15 of their vascular devices had been used, including stents, balloons, and those for atherectomy.
“Long case!” Kirk’s colleague texted. “Is it looking ok??”
“It is,” she said. “Thought we were done a few times! Now he’s going back in to cut again!”
A little while later, she texted: “....17!”
He texted back [with laughing emoticons].
Hospital leaders had been scrutinizing the use of these procedures at the Dole VA for years.
In 2017, shortly after Rick Ament was hired to lead the facility, he noticed something was amiss. While the longtime hospital administrator was poring over the finances, he was alarmed to discover that the relatively small Dole VA had one of the most expensive cardiac programs in the country. As Ament dug deeper, he realized vascular interventions were the reason.
“It just did not make sense that the acuity level of our patients would generate such extreme cost variances from the norm,” he testified in December, in a deposition for the whistleblower case. “It was so significant, we needed to get to the bottom of it.”
Ament, a second generation Air Force veteran, quietly assembled a task force to investigate why the facility had purchased so many medical devices for these procedures. After they examined inventory records, calculating the total number of medical devices and the cost of devices per patient, they grew concerned.
“We were more expensive than, I believe it was, the top 10 hospitals in the VA combined,” he said. “My feeling was that we either had very, very bad providers or we had product walking out the door.”
Ament enlisted experts from other VA hospitals to help his team investigate, including an administrative officer who could understand finances and a respected interventional radiologist who could examine records. The task force gathered a list of patients from 2016 to 2018, according to internal emails, and analyzed their medical charts.
According to internal VA documents released through the whistleblower suit, the review found a number of clinical failings: Evidence-based medicine had not been followed in the majority of cases reviewed. Procedures were over-aggressive, treating lesions that should have been left alone. And there was a total disregard for established best practices for treating peripheral artery disease.
One of the experts on the investigative team explained to Ament that while it was not uncommon for doctors to use a couple of devices in one intervention, the total number of devices in many of the procedures at his facility went into the double digits, sometimes five times the expected amount.
In one encounter, a doctor deployed 33 devices in one procedure – 3 atherectomy devices, 9 stents, and 21 balloons.
This use of devices was exorbitant, Ament came to understand. “I want to say the term ‘egregious’ was used,” he testified. “It was kind of like validation, but I really wish I was wrong.”
“Did it make you concerned for patient care?” a lawyer asked during the deposition.
“It did,” Ament replied.
A member of his task force pulled data for veterans who had leg amputations due to vascular disease. Over 5 years, the number of veterans who had amputations increased, from about 6 in 2013 to 38 in 2018, according to internal emails released in the suit. The VA did not respond to ProPublica’s questions about the rise in amputations or whether it was due to complications from the procedures.
Even though Ament testified in December 2022 that he became aware of the excessive use of devices during his investigation that began about 5 years ago, neither he nor the VA have publicly acknowledged these findings outside of the lawsuit. It is unclear whether VA representatives informed the patients whose records were reviewed about their findings. ProPublica reached out to more than half a dozen veteran community groups in the Wichita area and none were aware of the investigation nor the allegations of overuse of vascular procedures at the facility.
The VA says that if its ongoing review finds instances of substandard care, it will reach out to affected patients and inform them about possible complications and benefits they may be entitled to. The press secretary said the review will take several months. Ament declined to respond to ProPublica’s questions, citing the ongoing case.
In 2018, Ament turned over his findings to the criminal division of the VA’s Office of Inspector General. He also shut down interventional radiology procedures at the facility’s catheter lab.
Federal agents separately opened an investigation into the same unit in the facility, looking into allegations of kickbacks.
More than 40 pages of expense reports from Medtronic, revealed in the whistleblower case, show sales representatives treating Dole health care workers to hundreds of meals over several years – lunches at Dempsey’s Biscuit Co.; business meals at the Scotch & Sirloin steakhouse; dinner at Chester’s Chophouse & Wine Bar, price per attendee: $122.39.
Federal agents obtained the receipts.
“Robert J. Dole VAMC employees may have received improper gratuities, in the forms of paid lunches, dinners, etc., from sales representatives from Medtronic,” Nathen Howard, a special agent in the VA OIG, wrote in an investigation memo from February 2019.
This kind of relationship could violate VA policy, which forbids federal employees from receiving any gifts, including meals, from people who do business or seek to do business with a federal institution. For health care workers, violating this policy could have serious implications for patients. Numerous studies have shown that even modest industry-sponsored gifts, including meals, may influence prescribing or treatment behavior of health care professionals.
The agents opened their investigation into kickbacks at the Wichita facility in response to the whistleblower lawsuit, which was filed by Thomas Schroeder in 2017. The VA OIG would not confirm or deny whether it was continuing to investigate kickbacks at the facility. The VA did not directly answer ProPublica’s questions about kickbacks at the Dole VA, but it said that every employee must complete an annual ethics training, which covers gift rules.
In recent years, Medtronic has settled a handful of other cases that have alleged kickbacks between company representatives and health care professionals.
In 2018, Medtronic’s subsidiary Covidien paid $13 million to settle claims with the U.S. Department of Justice that it paid kickbacks to health care institutions that used its mechanical blood clot devices. In 2019, the same subsidiary paid $17 million to resolve allegations that it provided in-kind marketing support to doctors using its vein products. And in 2020, Medtronic paid more than $8 million to settle claims that representatives had paid kickbacks to a neurosurgeon, including scores of lavish meals at a restaurant that the doctor owned, to induce him to purchase the company’s medication pumps.
Schroeder’s lawsuit is not the first time Medtronic’s vascular devices were named in an alleged kickback scheme. In early 2015, Medtronic acquired Covidien, and shortly after the merger, its subsidiary ev3 Inc. agreed to pay $1.25 million to resolve allegations that it had paid doctors who were “high volume users” of its atherectomy devices to act as evangelists for the company, and had provided physicians with company shares to participate in clinical trials for their tools.
The whistleblower in this earlier case, a former sales representative for the company, also alleged that the subsidiary was gaming Medicare’s payment system. Hospitals were often hesitant to conduct atherectomy procedures because of the low reimbursement rates. According to the suit, sales representatives encouraged doctors to admit patients for longer stays to reap greater reimbursements and make a profit, even though such stays were often not medically indicated.
“Medical device makers that try to boost their profits by causing patients to be admitted for unnecessary and expensive inpatient hospital stays will be held accountable,” special agent Thomas O’Donnell, from the Office of Inspector General at the U.S. Department of Health and Human Services, said in a press release for the settlement. “Both patients and taxpayers deserve to have medical decisions made based on what is medically appropriate.”
Medtronic spokesperson Xiong said that in each case, the company “cooperated fully with the DOJ to resolve its concerns and, where wrongdoing was found, took appropriate remedial action.”
Seton Hall Law School professor Jacob Elberg, a former assistant U.S. attorney for the District of New Jersey who led its health care and government fraud unit, is concerned by the frequency of such settlements in the last 2 decades. “There are, at this point, real questions as to whether the sanctions imposed by DOJ are sufficient to deter wrongdoing and to lead to meaningful change, especially within the medical device industry.”
Although the Department of Justice has declined to intervene in the lawsuit involving the Dole VA at this time, the case is ongoing and further depositions with Medtronic sales representatives and a former VA employee are scheduled for this month.
VA employees and doctors named in the suit declined to comment or did not respond to ProPublica’s questions about the alleged kickbacks and whether sales representatives may have influenced veterans’ treatment plans. In interviews with federal investigators, according to released transcripts, several of the employees who were questioned denied receiving frequent meals from sales representatives, contradicting Medtronic’s expense reports.
Their statements also stand in contrast to Medtronic representative Kari Kirk’s final text messages during that procedure in June 2017, which ultimately lasted more than 3 hours.
“Now u done??” her colleague asked.
“Just finished,” she texted. “Running to get them lunch!”
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
On June 14, 2017, just before noon, a doctor made an incision near a patient’s groin. Kari Kirk, a representative for the world’s largest medical device company, Medtronic, looked on and began texting her colleague a play-by-play.
“Fixing both legs from the ankles,” she wrote.
It was a fairly common procedure at the Robert J. Dole Veterans Affairs Medical Center in Wichita, Kansas, performed to treat blockages in the leg vessels.
Within reach were an array of Medtronic products: tubes with blades attached to shave hardened deposits off of artery walls; stents to widen blood vessels; balloons coated with therapeutic drugs.
Each time a doctor puts a foreign device in someone’s body, it carries a risk of complication, which can include clots or even require amputation. So medical experts, research and even Medtronic’s own device instructions urge doctors to use as few as are necessary.
“Just used 12 [drug-coated balloons]!!” Kirk texted her colleague.
“Does that mean I owe u $$,” he responded.
“Thats what I’m thinking!!!” she said. “And now 14 balloons?!”
“but only one stent so far??”
“So far!”
As the texting continued, her colleague replied, “U are going to want to start going to the VA all the time.”
The messages, recently unsealed in an ongoing whistleblower lawsuit, give a window into the way money and medicine mingle in the booming business of peripheral artery disease, a condition that afflicts 6.5 million Americans over age 40 and is caused when fatty plaque builds up in arteries, blocking blood flow to the legs.
Representatives from companies are often present during vascular procedures to guide doctors on how to use their complex devices. This kind of access has the potential to influence treatment plans, as companies and their representatives profit when more of their product is used.
The suit, filed in 2017 by a sales representative for a competing medical device firm, alleges an illegal kickback scheme between Medtronic and hospital employees. According to the complaint and documents released in the suit, between 2011 and 2018, VA health care workers received steakhouse dinners, Apple electronics, and NASCAR tickets, and in turn, Medtronic secured a lucrative contract with the hospital. Meanwhile, the company’s representatives allegedly “groomed and trained” physicians at the facility, who then deployed the company’s devices even when it was not medically indicated.
Independently from the whistleblower suit, internal investigators at the Wichita facility have also examined the treatment patterns of its vascular patients in recent years and found numerous cases where medical devices were used excessively. While it’s not uncommon to deploy several devices, a medical expert on the investigation team found that the VA doctors sometimes used more than 15 at a time – one used 33 – deviating from the standard of care.
“It is unconscionable – there can be no valid medically acceptable basis to cram so many devices into a human being,” wrote attorneys representing the whistleblower in legal filings from January 2023. “This is not medical treatment. This is abuse.”
Dr. Kim Hodgson, former president of the Society for Vascular Surgery and an expert retained by the plaintiff, said the findings of the internal review of patient data raise “a high level of concern regarding necessity of treatment provided,” according to case documents.
Medtronic declined to respond to ProPublica’s questions, citing the ongoing litigation. “These allegations are false and Medtronic is defending against these claims in court,” said Boua Xiong, a spokesperson for the company. Medtronic representative Kirk declined to respond to ProPublica’s request for comment.
The hospital investigation found that amputations increased sixfold in the same time frame as the procedures in question, according to internal emails, but made no conclusion about whether those two things were connected. ProPublica reached out to the VA to ask whether any patients had been harmed.
The VA is “conducting an extensive review of patient care” at the Kansas hospital, “including the number of devices used on patients – to make sure that Veterans were not harmed by any procedures,” press secretary Terrence Hayes said in a statement. So far, the VA’s investigation has found no “quality of care issues,” he said, and the investigation will continue “until every Veteran’s case has been reviewed.” (Read the full statement here.) Neither the department nor the hospital has taken formal action against the medical providers, Hayes said.
The medical group that had a contract with the VA for vascular interventions, Wichita Radiological Group, did not respond to ProPublica’s requests for comment, nor did the doctors named in the suit: Dr. Shaun Gonda, Dr. Bret Winblad, and Dr. Kermit Rust. It is unclear from the case documents which doctors conducted which procedures. Eric Barth, an attorney for the medical group, denied the allegations in recent legal filings, calling the claims “baseless” and the lawsuit a “witch hunt.”
The lawsuit comes amid growing concern about one of these procedures – atherectomies – after researchers and doctors have uncovered patterns of excessive and inappropriate use. Recent research has found that this procedure, a common but costly treatment to shave or laser plaque from blood vessels, is not more effective than cheaper alternatives and may even be associated with a higher risk of complications including amputation. In recent years, several doctors and clinics have been investigated for allegedly taking advantage of Medicare’s reimbursement rates, and one study found that many doctors are resorting to atherectomies in the earliest stages of peripheral artery disease, against best practices that urge noninvasive treatment.
“Atherectomy is important in certain settings. But it’s being used in a way that is entirely inappropriate and it’s largely driven by the incentive structure,” said Dr. Caitlin Hicks, the lead author of the study and an associate professor of surgery at Johns Hopkins University School of Medicine.
Although different payment structures govern the care of veterans, the whistleblower lawsuit alleges that outside physicians, paid hourly by the Dole VA, were motivated to conduct longer and more complex procedures that would earn them higher payment.
Under different circumstances, the patient in the procedure room on that summer day could have been done after 2 hours.
But, 150 minutes in, those Medtronic representatives were still texting. At that point, more than 15 of their vascular devices had been used, including stents, balloons, and those for atherectomy.
“Long case!” Kirk’s colleague texted. “Is it looking ok??”
“It is,” she said. “Thought we were done a few times! Now he’s going back in to cut again!”
A little while later, she texted: “....17!”
He texted back [with laughing emoticons].
Hospital leaders had been scrutinizing the use of these procedures at the Dole VA for years.
In 2017, shortly after Rick Ament was hired to lead the facility, he noticed something was amiss. While the longtime hospital administrator was poring over the finances, he was alarmed to discover that the relatively small Dole VA had one of the most expensive cardiac programs in the country. As Ament dug deeper, he realized vascular interventions were the reason.
“It just did not make sense that the acuity level of our patients would generate such extreme cost variances from the norm,” he testified in December, in a deposition for the whistleblower case. “It was so significant, we needed to get to the bottom of it.”
Ament, a second generation Air Force veteran, quietly assembled a task force to investigate why the facility had purchased so many medical devices for these procedures. After they examined inventory records, calculating the total number of medical devices and the cost of devices per patient, they grew concerned.
“We were more expensive than, I believe it was, the top 10 hospitals in the VA combined,” he said. “My feeling was that we either had very, very bad providers or we had product walking out the door.”
Ament enlisted experts from other VA hospitals to help his team investigate, including an administrative officer who could understand finances and a respected interventional radiologist who could examine records. The task force gathered a list of patients from 2016 to 2018, according to internal emails, and analyzed their medical charts.
According to internal VA documents released through the whistleblower suit, the review found a number of clinical failings: Evidence-based medicine had not been followed in the majority of cases reviewed. Procedures were over-aggressive, treating lesions that should have been left alone. And there was a total disregard for established best practices for treating peripheral artery disease.
One of the experts on the investigative team explained to Ament that while it was not uncommon for doctors to use a couple of devices in one intervention, the total number of devices in many of the procedures at his facility went into the double digits, sometimes five times the expected amount.
In one encounter, a doctor deployed 33 devices in one procedure – 3 atherectomy devices, 9 stents, and 21 balloons.
This use of devices was exorbitant, Ament came to understand. “I want to say the term ‘egregious’ was used,” he testified. “It was kind of like validation, but I really wish I was wrong.”
“Did it make you concerned for patient care?” a lawyer asked during the deposition.
“It did,” Ament replied.
A member of his task force pulled data for veterans who had leg amputations due to vascular disease. Over 5 years, the number of veterans who had amputations increased, from about 6 in 2013 to 38 in 2018, according to internal emails released in the suit. The VA did not respond to ProPublica’s questions about the rise in amputations or whether it was due to complications from the procedures.
Even though Ament testified in December 2022 that he became aware of the excessive use of devices during his investigation that began about 5 years ago, neither he nor the VA have publicly acknowledged these findings outside of the lawsuit. It is unclear whether VA representatives informed the patients whose records were reviewed about their findings. ProPublica reached out to more than half a dozen veteran community groups in the Wichita area and none were aware of the investigation nor the allegations of overuse of vascular procedures at the facility.
The VA says that if its ongoing review finds instances of substandard care, it will reach out to affected patients and inform them about possible complications and benefits they may be entitled to. The press secretary said the review will take several months. Ament declined to respond to ProPublica’s questions, citing the ongoing case.
In 2018, Ament turned over his findings to the criminal division of the VA’s Office of Inspector General. He also shut down interventional radiology procedures at the facility’s catheter lab.
Federal agents separately opened an investigation into the same unit in the facility, looking into allegations of kickbacks.
More than 40 pages of expense reports from Medtronic, revealed in the whistleblower case, show sales representatives treating Dole health care workers to hundreds of meals over several years – lunches at Dempsey’s Biscuit Co.; business meals at the Scotch & Sirloin steakhouse; dinner at Chester’s Chophouse & Wine Bar, price per attendee: $122.39.
Federal agents obtained the receipts.
“Robert J. Dole VAMC employees may have received improper gratuities, in the forms of paid lunches, dinners, etc., from sales representatives from Medtronic,” Nathen Howard, a special agent in the VA OIG, wrote in an investigation memo from February 2019.
This kind of relationship could violate VA policy, which forbids federal employees from receiving any gifts, including meals, from people who do business or seek to do business with a federal institution. For health care workers, violating this policy could have serious implications for patients. Numerous studies have shown that even modest industry-sponsored gifts, including meals, may influence prescribing or treatment behavior of health care professionals.
The agents opened their investigation into kickbacks at the Wichita facility in response to the whistleblower lawsuit, which was filed by Thomas Schroeder in 2017. The VA OIG would not confirm or deny whether it was continuing to investigate kickbacks at the facility. The VA did not directly answer ProPublica’s questions about kickbacks at the Dole VA, but it said that every employee must complete an annual ethics training, which covers gift rules.
In recent years, Medtronic has settled a handful of other cases that have alleged kickbacks between company representatives and health care professionals.
In 2018, Medtronic’s subsidiary Covidien paid $13 million to settle claims with the U.S. Department of Justice that it paid kickbacks to health care institutions that used its mechanical blood clot devices. In 2019, the same subsidiary paid $17 million to resolve allegations that it provided in-kind marketing support to doctors using its vein products. And in 2020, Medtronic paid more than $8 million to settle claims that representatives had paid kickbacks to a neurosurgeon, including scores of lavish meals at a restaurant that the doctor owned, to induce him to purchase the company’s medication pumps.
Schroeder’s lawsuit is not the first time Medtronic’s vascular devices were named in an alleged kickback scheme. In early 2015, Medtronic acquired Covidien, and shortly after the merger, its subsidiary ev3 Inc. agreed to pay $1.25 million to resolve allegations that it had paid doctors who were “high volume users” of its atherectomy devices to act as evangelists for the company, and had provided physicians with company shares to participate in clinical trials for their tools.
The whistleblower in this earlier case, a former sales representative for the company, also alleged that the subsidiary was gaming Medicare’s payment system. Hospitals were often hesitant to conduct atherectomy procedures because of the low reimbursement rates. According to the suit, sales representatives encouraged doctors to admit patients for longer stays to reap greater reimbursements and make a profit, even though such stays were often not medically indicated.
“Medical device makers that try to boost their profits by causing patients to be admitted for unnecessary and expensive inpatient hospital stays will be held accountable,” special agent Thomas O’Donnell, from the Office of Inspector General at the U.S. Department of Health and Human Services, said in a press release for the settlement. “Both patients and taxpayers deserve to have medical decisions made based on what is medically appropriate.”
Medtronic spokesperson Xiong said that in each case, the company “cooperated fully with the DOJ to resolve its concerns and, where wrongdoing was found, took appropriate remedial action.”
Seton Hall Law School professor Jacob Elberg, a former assistant U.S. attorney for the District of New Jersey who led its health care and government fraud unit, is concerned by the frequency of such settlements in the last 2 decades. “There are, at this point, real questions as to whether the sanctions imposed by DOJ are sufficient to deter wrongdoing and to lead to meaningful change, especially within the medical device industry.”
Although the Department of Justice has declined to intervene in the lawsuit involving the Dole VA at this time, the case is ongoing and further depositions with Medtronic sales representatives and a former VA employee are scheduled for this month.
VA employees and doctors named in the suit declined to comment or did not respond to ProPublica’s questions about the alleged kickbacks and whether sales representatives may have influenced veterans’ treatment plans. In interviews with federal investigators, according to released transcripts, several of the employees who were questioned denied receiving frequent meals from sales representatives, contradicting Medtronic’s expense reports.
Their statements also stand in contrast to Medtronic representative Kari Kirk’s final text messages during that procedure in June 2017, which ultimately lasted more than 3 hours.
“Now u done??” her colleague asked.
“Just finished,” she texted. “Running to get them lunch!”
This story was originally published on ProPublica. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
Diabetes drug tied to lower dementia risk
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Overall, in a large cohort study from South Korea, patients who took pioglitazone were 16% less likely to develop dementia over an average of 10 years than peers who did not take the drug.
However, the dementia risk reduction was 54% among those with ischemic heart disease and 43% among those with a history of stroke.
“Our study was to see the association between pioglitazone use and incidence of dementia, not how (with what mechanisms) this drug can suppress dementia pathology,” coinvestigator Eosu Kim, MD, PhD, Yonsei University, Seoul, South Korea, said in an interview.
However, “as we found this drug is more effective in diabetic patients who have blood circulation problems in the heart or brain than in those without such problems, we speculate that pioglitazone’s antidementia action may be related to improving blood vessel’s health,” Dr. Kim said.
This finding suggests that pioglitazone could be used as a personalized treatment approach for dementia prevention in this subgroup of patients with diabetes, the researchers noted.
The results were published online in Neurology.
Dose-response relationship
Risk for dementia is doubled in adults with T2DM, the investigators wrote. Prior studies have suggested that pioglitazone may protect against dementia, as well as a first or recurrent stroke, in patients with T2DM.
This led Dr. Kim and colleagues to examine the effects of pioglitazone on dementia risk overall and in relation to stroke and ischemic heart disease.
Using the national Korean health database, the researchers identified 91,218 adults aged 50 and older with new-onset T2DM who did not have dementia. A total of 3,467 were treated with pioglitazone.
Pioglitazone exposure was defined as a total cumulative daily dose of 90 or more calculated from all dispensations during 4 years after T2DM diagnosis, with outcomes assessed after this period.
Over an average of 10 years, 8.3% of pioglitazone users developed dementia, compared with 10.0% of nonusers.
There was a statistically significant 16% lower risk for developing all-cause dementia among pioglitazone users than among nonusers (adjusted hazard ratio, 0.84; 95% confidence interval, 0.75-0.95).
A dose-response relationship was evident; pioglitazone users who received the highest cumulative daily dose were at lower risk for dementia (aHR, 0.72; 95% CI, 0.55-0.94).
Several limitations
The reduced risk for dementia was more pronounced among patients who used pioglitazone for 4 years in comparison with patients who did not use the drug (aHR, 0.63; 95% CI, 0.44-0.90).
The apparent protective effect of pioglitazone with regard to dementia was greater among those with a history of ischemic heart disease (aHR, 0.46; 95% CI, 0.24-0.90) or stroke (aHR, 0.57; 95% CI, 0.38-0.86) before diabetes diagnosis.
The incidence of stroke was also reduced with pioglitazone use (aHR, 0.81; 95% CI, 0.66-1.0).
“These results provide valuable information on who could potentially benefit from pioglitazone use for prevention of dementia,” Dr. Kim said in a news release.
However, “the risk and benefit balance of long-term use of this drug to prevent dementia should be prospectively assessed,” he said in an interview.
The researchers cautioned that the study was observational; hence, the reported associations cannot address causal relationships. Also, because of the use of claims data, drug compliance could not be guaranteed, and exposure may have been overestimated.
There is also the potential for selection bias, and no information on apolipoprotein E was available, they noted.
More data needed
In an accompanying editorial, Colleen J. Maxwell, PhD, University of Waterloo (Ont.), and colleagues wrote that the results “not only support previous studies showing the potential cognitive benefit of pioglitazone but also extend our understanding of this benefit through the mediating effect of reducing ischemic stroke.”
However, because of their associated risks, which include fractures, weight gain, heart failure, and bladder cancer, thiazolidinediones are not currently favored in diabetes management guidelines – and their use has significantly declined since the mid to late 2000s, the editorialists noted.
They agreed that it will be important to reassess the risk-benefit profile of pioglitazone in T2DM as additional findings emerge.
They also noted that sodium-glucose cotransporter-2 inhibitors, which have significant cardiovascular and renal benefits and minimal side effects, may also lower the risk for dementia.
“As both pioglitazone and SGLT-2 inhibitors are second-line options for physicians, the current decision would easily be in favor of SGLT-2 inhibitors given their safety profile,” Dr. Maxwell and colleagues wrote.
For now, pioglitazone “should not be used to prevent dementia in patients with T2DM,” they concluded.
The study was supported by grants from the National Research Foundation of Korea funded by the Korean government and the Ministry of Health and Welfare. The investigators and editorialists report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY
New tool better estimates cardiovascular risk in people with lupus
Current risk estimators are inaccurate
A tool that incorporates lupus-related variables with traditional risk factors provides a much more accurate assessment of cardiovascular (CV) risk in patients with systemic lupus erythematosus (SLE), according to data presented at the annual meeting of the Canadian Rheumatology Association.
In the initial clinical assessment of this tool, called the SLECRISK, “it identified high-risk lupus patients who would otherwise be missed by traditional methods of CV risk assessment,” reported May Y. Choi, MD, associate director of translational research at the University of Calgary’s (Alta.) Lupus Centre of Excellence.
It is well known that patients with SLE face an increased risk of CV events starting at an age long before risk begins climbing in the general population, according to Dr. Choi. She cited one study that showed women aged 35-44 years have a 50-fold greater risk of myocardial infarction than healthy individuals.
All major guidelines recognize this increased risk and recommend CV risk assessment in patients with SLE, even though Dr. Choi pointed out that traditional tools, such as the American College of Cardiology atherosclerotic cardiovascular disease (ASCVD) risk calculator or the Framingham Risk Score (FRS) have a limited ability to detect the patients with SLE who are most likely to have an event.
In SLE, current tools are inadequate
“These risk assessment tools perform poorly in SLE patients because they do not capture SLE-related inflammation,” Dr. Choi said. Of several examples, Dr. Choi cited a study showing “seven times more MIs and strokes observed than expected in SLE patients on the basis of the FRS.”
The disparity between expected and observed MIs and strokes is worse with increasing severity of SLE. In a study she presented 3 years ago, rates of CV events were 12 times higher in those with inactive or mild SLE, rising to a 16-fold increase among those with moderate disease and jumping to a 32-fold increase in those with severe SLE.
The SLECRISK tool was developed from the Brigham and Women’s Hospital SLE Registry, which was initiated in 1992. Patients without a history of CV disease were evaluated for traditional CV risk factors and for SLE-specific characteristics such as disease activity, levels of the complement proteins C3 and C4, kidney function, the presence of nephritis, and SLE duration. The value of these characteristics as predictors of CV events were then assessed over a 10-year follow-up period before being assembled into the SLECRISK tool.
In an example of the risk equation, Dr. Choi described a 50-year-old patient with SLE and a 5% 10-year ASCVD risk score, which is low. After adjustment for SLE risks, which included 10 years disease duration, high disease activity, elevated creatinine, and positive anti–double stranded DNA status, the 10-year CV risk score climbed to 16.2%, which is moderate.
The performance of the SLECRISK was evaluated in 1,243 patients providing 8,946.51 person-years of follow-up. During this period, there were 90 major adverse cardiac events (MACE), of which 82% were adjudicated by cardiologists, and 211 secondary events.
Relative to the ASCVD risk score, the SLECRISK identified about twice as many patients with SLE as having moderate risk and 3.5-fold more patients as having high risk. Among patients who experienced CV events, traditional CV risk factors were more common but so were SLE-specific risk factors, including greater disease severity, a greater likelihood of lupus nephritis, increased complement levels, and greater exposure to glucocorticoids, according to Dr. Choi.
Specificities for CV events higher on SLECRISK
In predicting CV events, the differences in specificities were in the same general range, although somewhat higher for the ASCVD risk score in regard to predicting MACE (83% vs. 72%) and MACE plus secondary events (90% vs. 79%). However, the sensitivities were much higher for SLECRISK relative to the ASCVD risk score for MACE alone (64% vs. 41%) and for MACE plus secondary events (58% vs. 35%).
When comparing those who had an MI or stroke, the ASCVD risk score identified 8 (7%) patients missed by SLECRISK, whereas SLECRISK identified 89 (73%) missed by the ASCVD risk score. The remaining 25 patients (20%) were identified by both. The advantage of SLECRISK was similar for MACE plus secondary outcomes.
Dr. Choi noted that all of the SLE-specific variables in SLECRISK are readily obtained and often already available in patient charts. She said that there is a plan to validate the tool in larger groups, but with a goal of creating a tool available online for clinicians and their patients to use. There is also an even more ambitious plan for the future.
“We have funding to look at machine learning to evaluate predictive variables in SLE patients,” Dr. Choi said. Rather than adding SLE-specific variables to traditional risks, the plan is to “start from scratch,” letting artificial intelligence assemble predictors without prejudice to what might or might not be relevant.
A SLE-specific tool for evaluating CV risk is an important “unmet need,” according to Karen H. Costenbader, MD, professor in the division of rheumatology, inflammation, and immunity at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. In an interview, she reiterated that measuring CV risk in SLE is already guideline recommended, but conventional tools have been shown to be inaccurate.
“I can envision it being used in clinical encounters to help guide shared decision-making with patients,” explained Dr. Costenbader, who was not involved in the presentation at the CRA meeting but worked with Dr. Choi in developing SLECRISK. “It would give us more precise estimates, allowing us to risk stratify our patients and informing us as to which modifiable SLE-specific and nonspecific factors are contributing most to CV risk.’
The problem of using conventional risk assessments in SLE has been well recognized. Of those who have written on this subject, Maureen McMahon, MD, site director of the Lupus Clinical Trials Network at the University of California, Los Angeles, said: “There is a critical need for the development of SLE-specific risk assessment tools like SLECRISK.”
Author of several studies looking at alternatives for CV risk assessment in SLE, including a study looking at a panel of biomarkers that was published in ACR Open Rheumatology, Dr. McMahon said in an interview that CV risk in SLE is high but conventional risk assessments are flawed.
“Multiple previous studies have demonstrated that these currently available calculators are not adequate for identifying risk in the lupus patient population,” she said. According to Dr. McMahon, the fact that rheumatologists remain “dependent upon [these conventional] cardiovascular risk calculators” is a well-recognized problem that needs resolution.
Dr. Choi has financial relationships with AstraZeneca, GlaxoSmithKline, Mallinckrodt. MitogenDx, Organon, and Werfen International. Dr. Costenbader reports no potential conflicts of interest. Dr. McMahon has financial relationships with AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, and GlaxoSmithKline.
Current risk estimators are inaccurate
Current risk estimators are inaccurate
A tool that incorporates lupus-related variables with traditional risk factors provides a much more accurate assessment of cardiovascular (CV) risk in patients with systemic lupus erythematosus (SLE), according to data presented at the annual meeting of the Canadian Rheumatology Association.
In the initial clinical assessment of this tool, called the SLECRISK, “it identified high-risk lupus patients who would otherwise be missed by traditional methods of CV risk assessment,” reported May Y. Choi, MD, associate director of translational research at the University of Calgary’s (Alta.) Lupus Centre of Excellence.
It is well known that patients with SLE face an increased risk of CV events starting at an age long before risk begins climbing in the general population, according to Dr. Choi. She cited one study that showed women aged 35-44 years have a 50-fold greater risk of myocardial infarction than healthy individuals.
All major guidelines recognize this increased risk and recommend CV risk assessment in patients with SLE, even though Dr. Choi pointed out that traditional tools, such as the American College of Cardiology atherosclerotic cardiovascular disease (ASCVD) risk calculator or the Framingham Risk Score (FRS) have a limited ability to detect the patients with SLE who are most likely to have an event.
In SLE, current tools are inadequate
“These risk assessment tools perform poorly in SLE patients because they do not capture SLE-related inflammation,” Dr. Choi said. Of several examples, Dr. Choi cited a study showing “seven times more MIs and strokes observed than expected in SLE patients on the basis of the FRS.”
The disparity between expected and observed MIs and strokes is worse with increasing severity of SLE. In a study she presented 3 years ago, rates of CV events were 12 times higher in those with inactive or mild SLE, rising to a 16-fold increase among those with moderate disease and jumping to a 32-fold increase in those with severe SLE.
The SLECRISK tool was developed from the Brigham and Women’s Hospital SLE Registry, which was initiated in 1992. Patients without a history of CV disease were evaluated for traditional CV risk factors and for SLE-specific characteristics such as disease activity, levels of the complement proteins C3 and C4, kidney function, the presence of nephritis, and SLE duration. The value of these characteristics as predictors of CV events were then assessed over a 10-year follow-up period before being assembled into the SLECRISK tool.
In an example of the risk equation, Dr. Choi described a 50-year-old patient with SLE and a 5% 10-year ASCVD risk score, which is low. After adjustment for SLE risks, which included 10 years disease duration, high disease activity, elevated creatinine, and positive anti–double stranded DNA status, the 10-year CV risk score climbed to 16.2%, which is moderate.
The performance of the SLECRISK was evaluated in 1,243 patients providing 8,946.51 person-years of follow-up. During this period, there were 90 major adverse cardiac events (MACE), of which 82% were adjudicated by cardiologists, and 211 secondary events.
Relative to the ASCVD risk score, the SLECRISK identified about twice as many patients with SLE as having moderate risk and 3.5-fold more patients as having high risk. Among patients who experienced CV events, traditional CV risk factors were more common but so were SLE-specific risk factors, including greater disease severity, a greater likelihood of lupus nephritis, increased complement levels, and greater exposure to glucocorticoids, according to Dr. Choi.
Specificities for CV events higher on SLECRISK
In predicting CV events, the differences in specificities were in the same general range, although somewhat higher for the ASCVD risk score in regard to predicting MACE (83% vs. 72%) and MACE plus secondary events (90% vs. 79%). However, the sensitivities were much higher for SLECRISK relative to the ASCVD risk score for MACE alone (64% vs. 41%) and for MACE plus secondary events (58% vs. 35%).
When comparing those who had an MI or stroke, the ASCVD risk score identified 8 (7%) patients missed by SLECRISK, whereas SLECRISK identified 89 (73%) missed by the ASCVD risk score. The remaining 25 patients (20%) were identified by both. The advantage of SLECRISK was similar for MACE plus secondary outcomes.
Dr. Choi noted that all of the SLE-specific variables in SLECRISK are readily obtained and often already available in patient charts. She said that there is a plan to validate the tool in larger groups, but with a goal of creating a tool available online for clinicians and their patients to use. There is also an even more ambitious plan for the future.
“We have funding to look at machine learning to evaluate predictive variables in SLE patients,” Dr. Choi said. Rather than adding SLE-specific variables to traditional risks, the plan is to “start from scratch,” letting artificial intelligence assemble predictors without prejudice to what might or might not be relevant.
A SLE-specific tool for evaluating CV risk is an important “unmet need,” according to Karen H. Costenbader, MD, professor in the division of rheumatology, inflammation, and immunity at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. In an interview, she reiterated that measuring CV risk in SLE is already guideline recommended, but conventional tools have been shown to be inaccurate.
“I can envision it being used in clinical encounters to help guide shared decision-making with patients,” explained Dr. Costenbader, who was not involved in the presentation at the CRA meeting but worked with Dr. Choi in developing SLECRISK. “It would give us more precise estimates, allowing us to risk stratify our patients and informing us as to which modifiable SLE-specific and nonspecific factors are contributing most to CV risk.’
The problem of using conventional risk assessments in SLE has been well recognized. Of those who have written on this subject, Maureen McMahon, MD, site director of the Lupus Clinical Trials Network at the University of California, Los Angeles, said: “There is a critical need for the development of SLE-specific risk assessment tools like SLECRISK.”
Author of several studies looking at alternatives for CV risk assessment in SLE, including a study looking at a panel of biomarkers that was published in ACR Open Rheumatology, Dr. McMahon said in an interview that CV risk in SLE is high but conventional risk assessments are flawed.
“Multiple previous studies have demonstrated that these currently available calculators are not adequate for identifying risk in the lupus patient population,” she said. According to Dr. McMahon, the fact that rheumatologists remain “dependent upon [these conventional] cardiovascular risk calculators” is a well-recognized problem that needs resolution.
Dr. Choi has financial relationships with AstraZeneca, GlaxoSmithKline, Mallinckrodt. MitogenDx, Organon, and Werfen International. Dr. Costenbader reports no potential conflicts of interest. Dr. McMahon has financial relationships with AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, and GlaxoSmithKline.
A tool that incorporates lupus-related variables with traditional risk factors provides a much more accurate assessment of cardiovascular (CV) risk in patients with systemic lupus erythematosus (SLE), according to data presented at the annual meeting of the Canadian Rheumatology Association.
In the initial clinical assessment of this tool, called the SLECRISK, “it identified high-risk lupus patients who would otherwise be missed by traditional methods of CV risk assessment,” reported May Y. Choi, MD, associate director of translational research at the University of Calgary’s (Alta.) Lupus Centre of Excellence.
It is well known that patients with SLE face an increased risk of CV events starting at an age long before risk begins climbing in the general population, according to Dr. Choi. She cited one study that showed women aged 35-44 years have a 50-fold greater risk of myocardial infarction than healthy individuals.
All major guidelines recognize this increased risk and recommend CV risk assessment in patients with SLE, even though Dr. Choi pointed out that traditional tools, such as the American College of Cardiology atherosclerotic cardiovascular disease (ASCVD) risk calculator or the Framingham Risk Score (FRS) have a limited ability to detect the patients with SLE who are most likely to have an event.
In SLE, current tools are inadequate
“These risk assessment tools perform poorly in SLE patients because they do not capture SLE-related inflammation,” Dr. Choi said. Of several examples, Dr. Choi cited a study showing “seven times more MIs and strokes observed than expected in SLE patients on the basis of the FRS.”
The disparity between expected and observed MIs and strokes is worse with increasing severity of SLE. In a study she presented 3 years ago, rates of CV events were 12 times higher in those with inactive or mild SLE, rising to a 16-fold increase among those with moderate disease and jumping to a 32-fold increase in those with severe SLE.
The SLECRISK tool was developed from the Brigham and Women’s Hospital SLE Registry, which was initiated in 1992. Patients without a history of CV disease were evaluated for traditional CV risk factors and for SLE-specific characteristics such as disease activity, levels of the complement proteins C3 and C4, kidney function, the presence of nephritis, and SLE duration. The value of these characteristics as predictors of CV events were then assessed over a 10-year follow-up period before being assembled into the SLECRISK tool.
In an example of the risk equation, Dr. Choi described a 50-year-old patient with SLE and a 5% 10-year ASCVD risk score, which is low. After adjustment for SLE risks, which included 10 years disease duration, high disease activity, elevated creatinine, and positive anti–double stranded DNA status, the 10-year CV risk score climbed to 16.2%, which is moderate.
The performance of the SLECRISK was evaluated in 1,243 patients providing 8,946.51 person-years of follow-up. During this period, there were 90 major adverse cardiac events (MACE), of which 82% were adjudicated by cardiologists, and 211 secondary events.
Relative to the ASCVD risk score, the SLECRISK identified about twice as many patients with SLE as having moderate risk and 3.5-fold more patients as having high risk. Among patients who experienced CV events, traditional CV risk factors were more common but so were SLE-specific risk factors, including greater disease severity, a greater likelihood of lupus nephritis, increased complement levels, and greater exposure to glucocorticoids, according to Dr. Choi.
Specificities for CV events higher on SLECRISK
In predicting CV events, the differences in specificities were in the same general range, although somewhat higher for the ASCVD risk score in regard to predicting MACE (83% vs. 72%) and MACE plus secondary events (90% vs. 79%). However, the sensitivities were much higher for SLECRISK relative to the ASCVD risk score for MACE alone (64% vs. 41%) and for MACE plus secondary events (58% vs. 35%).
When comparing those who had an MI or stroke, the ASCVD risk score identified 8 (7%) patients missed by SLECRISK, whereas SLECRISK identified 89 (73%) missed by the ASCVD risk score. The remaining 25 patients (20%) were identified by both. The advantage of SLECRISK was similar for MACE plus secondary outcomes.
Dr. Choi noted that all of the SLE-specific variables in SLECRISK are readily obtained and often already available in patient charts. She said that there is a plan to validate the tool in larger groups, but with a goal of creating a tool available online for clinicians and their patients to use. There is also an even more ambitious plan for the future.
“We have funding to look at machine learning to evaluate predictive variables in SLE patients,” Dr. Choi said. Rather than adding SLE-specific variables to traditional risks, the plan is to “start from scratch,” letting artificial intelligence assemble predictors without prejudice to what might or might not be relevant.
A SLE-specific tool for evaluating CV risk is an important “unmet need,” according to Karen H. Costenbader, MD, professor in the division of rheumatology, inflammation, and immunity at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. In an interview, she reiterated that measuring CV risk in SLE is already guideline recommended, but conventional tools have been shown to be inaccurate.
“I can envision it being used in clinical encounters to help guide shared decision-making with patients,” explained Dr. Costenbader, who was not involved in the presentation at the CRA meeting but worked with Dr. Choi in developing SLECRISK. “It would give us more precise estimates, allowing us to risk stratify our patients and informing us as to which modifiable SLE-specific and nonspecific factors are contributing most to CV risk.’
The problem of using conventional risk assessments in SLE has been well recognized. Of those who have written on this subject, Maureen McMahon, MD, site director of the Lupus Clinical Trials Network at the University of California, Los Angeles, said: “There is a critical need for the development of SLE-specific risk assessment tools like SLECRISK.”
Author of several studies looking at alternatives for CV risk assessment in SLE, including a study looking at a panel of biomarkers that was published in ACR Open Rheumatology, Dr. McMahon said in an interview that CV risk in SLE is high but conventional risk assessments are flawed.
“Multiple previous studies have demonstrated that these currently available calculators are not adequate for identifying risk in the lupus patient population,” she said. According to Dr. McMahon, the fact that rheumatologists remain “dependent upon [these conventional] cardiovascular risk calculators” is a well-recognized problem that needs resolution.
Dr. Choi has financial relationships with AstraZeneca, GlaxoSmithKline, Mallinckrodt. MitogenDx, Organon, and Werfen International. Dr. Costenbader reports no potential conflicts of interest. Dr. McMahon has financial relationships with AstraZeneca, Aurinia Pharmaceuticals, Eli Lilly, and GlaxoSmithKline.
FROM CRA 2023