User login
The Next Frontier of Antibiotic Discovery: Inside Your Gut
Scientists at Stanford University and the University of Pennsylvania have discovered a new antibiotic candidate in a surprising place: the human gut.
In mice, the antibiotic — a peptide known as prevotellin-2 — showed antimicrobial potency on par with polymyxin B, an antibiotic medication used to treat multidrug-resistant infections. Meanwhile, the peptide mainly left commensal, or beneficial, bacteria alone. The study, published in Cell, also identified several other potent antibiotic peptides with the potential to combat antimicrobial-resistant infections.
The research is part of a larger quest to find new antibiotics that can fight drug-resistant infections, a critical public health threat with more than 2.8 million cases and 35,000 deaths annually in the United States. That quest is urgent, said study author César de la Fuente, PhD, professor of bioengineering at the University of Pennsylvania, Philadelphia.
“The main pillars that have enabled us to almost double our lifespan in the last 100 years or so have been antibiotics, vaccines, and clean water,” said Dr. de la Fuente. “Imagine taking out one of those. I think it would be pretty dramatic.” (Dr. De la Fuente’s lab has become known for finding antibiotic candidates in unusual places, like ancient genetic information of Neanderthals and woolly mammoths.)
The first widely used antibiotic, penicillin, was discovered in 1928, when a physician studying Staphylococcus bacteria returned to his lab after summer break to find mold growing in one of his petri dishes. But many other antibiotics — like streptomycin, tetracycline, and erythromycin — were discovered from soil bacteria, which produce variations of these substances to compete with other microorganisms.
By looking in the gut microbiome, the researchers hoped to identify peptides that the trillions of microbes use against each other in the fight for limited resources — ideally, peptides that wouldn’t broadly kill off the entire microbiome.
Kill the Bad, Spare the Good
Many traditional antibiotics are small molecules. This means they can wipe out the good bacteria in your body, and because each targets a specific bacterial function, bad bacteria can become resistant to them.
Peptide antibiotics, on the other hand, don’t diffuse into the whole body. If taken orally, they stay in the gut; if taken intravenously, they generally stay in the blood. And because of how they kill bacteria, targeting the membrane, they’re also less prone to bacterial resistance.
The microbiome is like a big reservoir of pathogens, said Ami Bhatt, MD, PhD, hematologist at Stanford University in California and one of the study’s authors. Because many antibiotics kill healthy gut bacteria, “what you have left over,” Dr. Bhatt said, “is this big open niche that gets filled up with multidrug-resistant organisms like E coli [Escherichia coli] or vancomycin-resistant Enterococcus.”
Dr. Bhatt has seen cancer patients undergo successful treatment only to die of a multidrug-resistant infection, because current antibiotics fail against those pathogens. “That’s like winning the battle to lose the war.”
By investigating the microbiome, “we wanted to see if we could identify antimicrobial peptides that might spare key members of our regular microbiome, so that we wouldn’t totally disrupt the microbiome the way we do when we use broad-spectrum, small molecule–based antibiotics,” Dr. Bhatt said.
The researchers used artificial intelligence to sift through 400,000 proteins to predict, based on known antibiotics, which peptide sequences might have antimicrobial properties. From the results, they chose 78 peptides to synthesize and test.
“The application of computational approaches combined with experimental validation is very powerful and exciting,” said Jennifer Geddes-McAlister, PhD, professor of cell biology at the University of Guelph in Ontario, Canada, who was not involved in the study. “The study is robust in its approach to microbiome sampling.”
The Long Journey from Lab to Clinic
More than half of the peptides the team tested effectively inhibited the growth of harmful bacteria, and prevotellin-2 (derived from the bacteria Prevotella copri)stood out as the most powerful.
“The study validates experimental data from the lab using animal models, which moves discoveries closer to the clinic,” said Dr. Geddes-McAlister. “Further testing with clinical trials is needed, but the potential for clinical application is promising.”
Unfortunately, that’s not likely to happen anytime soon, said Dr. de la Fuente. “There is not enough economic incentive” for companies to develop new antibiotics. Ten years is his most hopeful guess for when we might see prevotellin-2, or a similar antibiotic, complete clinical trials.
A version of this article first appeared on Medscape.com.
Scientists at Stanford University and the University of Pennsylvania have discovered a new antibiotic candidate in a surprising place: the human gut.
In mice, the antibiotic — a peptide known as prevotellin-2 — showed antimicrobial potency on par with polymyxin B, an antibiotic medication used to treat multidrug-resistant infections. Meanwhile, the peptide mainly left commensal, or beneficial, bacteria alone. The study, published in Cell, also identified several other potent antibiotic peptides with the potential to combat antimicrobial-resistant infections.
The research is part of a larger quest to find new antibiotics that can fight drug-resistant infections, a critical public health threat with more than 2.8 million cases and 35,000 deaths annually in the United States. That quest is urgent, said study author César de la Fuente, PhD, professor of bioengineering at the University of Pennsylvania, Philadelphia.
“The main pillars that have enabled us to almost double our lifespan in the last 100 years or so have been antibiotics, vaccines, and clean water,” said Dr. de la Fuente. “Imagine taking out one of those. I think it would be pretty dramatic.” (Dr. De la Fuente’s lab has become known for finding antibiotic candidates in unusual places, like ancient genetic information of Neanderthals and woolly mammoths.)
The first widely used antibiotic, penicillin, was discovered in 1928, when a physician studying Staphylococcus bacteria returned to his lab after summer break to find mold growing in one of his petri dishes. But many other antibiotics — like streptomycin, tetracycline, and erythromycin — were discovered from soil bacteria, which produce variations of these substances to compete with other microorganisms.
By looking in the gut microbiome, the researchers hoped to identify peptides that the trillions of microbes use against each other in the fight for limited resources — ideally, peptides that wouldn’t broadly kill off the entire microbiome.
Kill the Bad, Spare the Good
Many traditional antibiotics are small molecules. This means they can wipe out the good bacteria in your body, and because each targets a specific bacterial function, bad bacteria can become resistant to them.
Peptide antibiotics, on the other hand, don’t diffuse into the whole body. If taken orally, they stay in the gut; if taken intravenously, they generally stay in the blood. And because of how they kill bacteria, targeting the membrane, they’re also less prone to bacterial resistance.
The microbiome is like a big reservoir of pathogens, said Ami Bhatt, MD, PhD, hematologist at Stanford University in California and one of the study’s authors. Because many antibiotics kill healthy gut bacteria, “what you have left over,” Dr. Bhatt said, “is this big open niche that gets filled up with multidrug-resistant organisms like E coli [Escherichia coli] or vancomycin-resistant Enterococcus.”
Dr. Bhatt has seen cancer patients undergo successful treatment only to die of a multidrug-resistant infection, because current antibiotics fail against those pathogens. “That’s like winning the battle to lose the war.”
By investigating the microbiome, “we wanted to see if we could identify antimicrobial peptides that might spare key members of our regular microbiome, so that we wouldn’t totally disrupt the microbiome the way we do when we use broad-spectrum, small molecule–based antibiotics,” Dr. Bhatt said.
The researchers used artificial intelligence to sift through 400,000 proteins to predict, based on known antibiotics, which peptide sequences might have antimicrobial properties. From the results, they chose 78 peptides to synthesize and test.
“The application of computational approaches combined with experimental validation is very powerful and exciting,” said Jennifer Geddes-McAlister, PhD, professor of cell biology at the University of Guelph in Ontario, Canada, who was not involved in the study. “The study is robust in its approach to microbiome sampling.”
The Long Journey from Lab to Clinic
More than half of the peptides the team tested effectively inhibited the growth of harmful bacteria, and prevotellin-2 (derived from the bacteria Prevotella copri)stood out as the most powerful.
“The study validates experimental data from the lab using animal models, which moves discoveries closer to the clinic,” said Dr. Geddes-McAlister. “Further testing with clinical trials is needed, but the potential for clinical application is promising.”
Unfortunately, that’s not likely to happen anytime soon, said Dr. de la Fuente. “There is not enough economic incentive” for companies to develop new antibiotics. Ten years is his most hopeful guess for when we might see prevotellin-2, or a similar antibiotic, complete clinical trials.
A version of this article first appeared on Medscape.com.
Scientists at Stanford University and the University of Pennsylvania have discovered a new antibiotic candidate in a surprising place: the human gut.
In mice, the antibiotic — a peptide known as prevotellin-2 — showed antimicrobial potency on par with polymyxin B, an antibiotic medication used to treat multidrug-resistant infections. Meanwhile, the peptide mainly left commensal, or beneficial, bacteria alone. The study, published in Cell, also identified several other potent antibiotic peptides with the potential to combat antimicrobial-resistant infections.
The research is part of a larger quest to find new antibiotics that can fight drug-resistant infections, a critical public health threat with more than 2.8 million cases and 35,000 deaths annually in the United States. That quest is urgent, said study author César de la Fuente, PhD, professor of bioengineering at the University of Pennsylvania, Philadelphia.
“The main pillars that have enabled us to almost double our lifespan in the last 100 years or so have been antibiotics, vaccines, and clean water,” said Dr. de la Fuente. “Imagine taking out one of those. I think it would be pretty dramatic.” (Dr. De la Fuente’s lab has become known for finding antibiotic candidates in unusual places, like ancient genetic information of Neanderthals and woolly mammoths.)
The first widely used antibiotic, penicillin, was discovered in 1928, when a physician studying Staphylococcus bacteria returned to his lab after summer break to find mold growing in one of his petri dishes. But many other antibiotics — like streptomycin, tetracycline, and erythromycin — were discovered from soil bacteria, which produce variations of these substances to compete with other microorganisms.
By looking in the gut microbiome, the researchers hoped to identify peptides that the trillions of microbes use against each other in the fight for limited resources — ideally, peptides that wouldn’t broadly kill off the entire microbiome.
Kill the Bad, Spare the Good
Many traditional antibiotics are small molecules. This means they can wipe out the good bacteria in your body, and because each targets a specific bacterial function, bad bacteria can become resistant to them.
Peptide antibiotics, on the other hand, don’t diffuse into the whole body. If taken orally, they stay in the gut; if taken intravenously, they generally stay in the blood. And because of how they kill bacteria, targeting the membrane, they’re also less prone to bacterial resistance.
The microbiome is like a big reservoir of pathogens, said Ami Bhatt, MD, PhD, hematologist at Stanford University in California and one of the study’s authors. Because many antibiotics kill healthy gut bacteria, “what you have left over,” Dr. Bhatt said, “is this big open niche that gets filled up with multidrug-resistant organisms like E coli [Escherichia coli] or vancomycin-resistant Enterococcus.”
Dr. Bhatt has seen cancer patients undergo successful treatment only to die of a multidrug-resistant infection, because current antibiotics fail against those pathogens. “That’s like winning the battle to lose the war.”
By investigating the microbiome, “we wanted to see if we could identify antimicrobial peptides that might spare key members of our regular microbiome, so that we wouldn’t totally disrupt the microbiome the way we do when we use broad-spectrum, small molecule–based antibiotics,” Dr. Bhatt said.
The researchers used artificial intelligence to sift through 400,000 proteins to predict, based on known antibiotics, which peptide sequences might have antimicrobial properties. From the results, they chose 78 peptides to synthesize and test.
“The application of computational approaches combined with experimental validation is very powerful and exciting,” said Jennifer Geddes-McAlister, PhD, professor of cell biology at the University of Guelph in Ontario, Canada, who was not involved in the study. “The study is robust in its approach to microbiome sampling.”
The Long Journey from Lab to Clinic
More than half of the peptides the team tested effectively inhibited the growth of harmful bacteria, and prevotellin-2 (derived from the bacteria Prevotella copri)stood out as the most powerful.
“The study validates experimental data from the lab using animal models, which moves discoveries closer to the clinic,” said Dr. Geddes-McAlister. “Further testing with clinical trials is needed, but the potential for clinical application is promising.”
Unfortunately, that’s not likely to happen anytime soon, said Dr. de la Fuente. “There is not enough economic incentive” for companies to develop new antibiotics. Ten years is his most hopeful guess for when we might see prevotellin-2, or a similar antibiotic, complete clinical trials.
A version of this article first appeared on Medscape.com.
FROM CELL
Cancer Treatment 101: A Primer for Non-Oncologists
The remaining 700,000 or so often proceed to chemotherapy either immediately or upon cancer recurrence, spread, or newly recognized metastases. “Cures” after that point are rare.
I’m speaking in generalities, understanding that each cancer and each patient is unique.
Chemotherapy
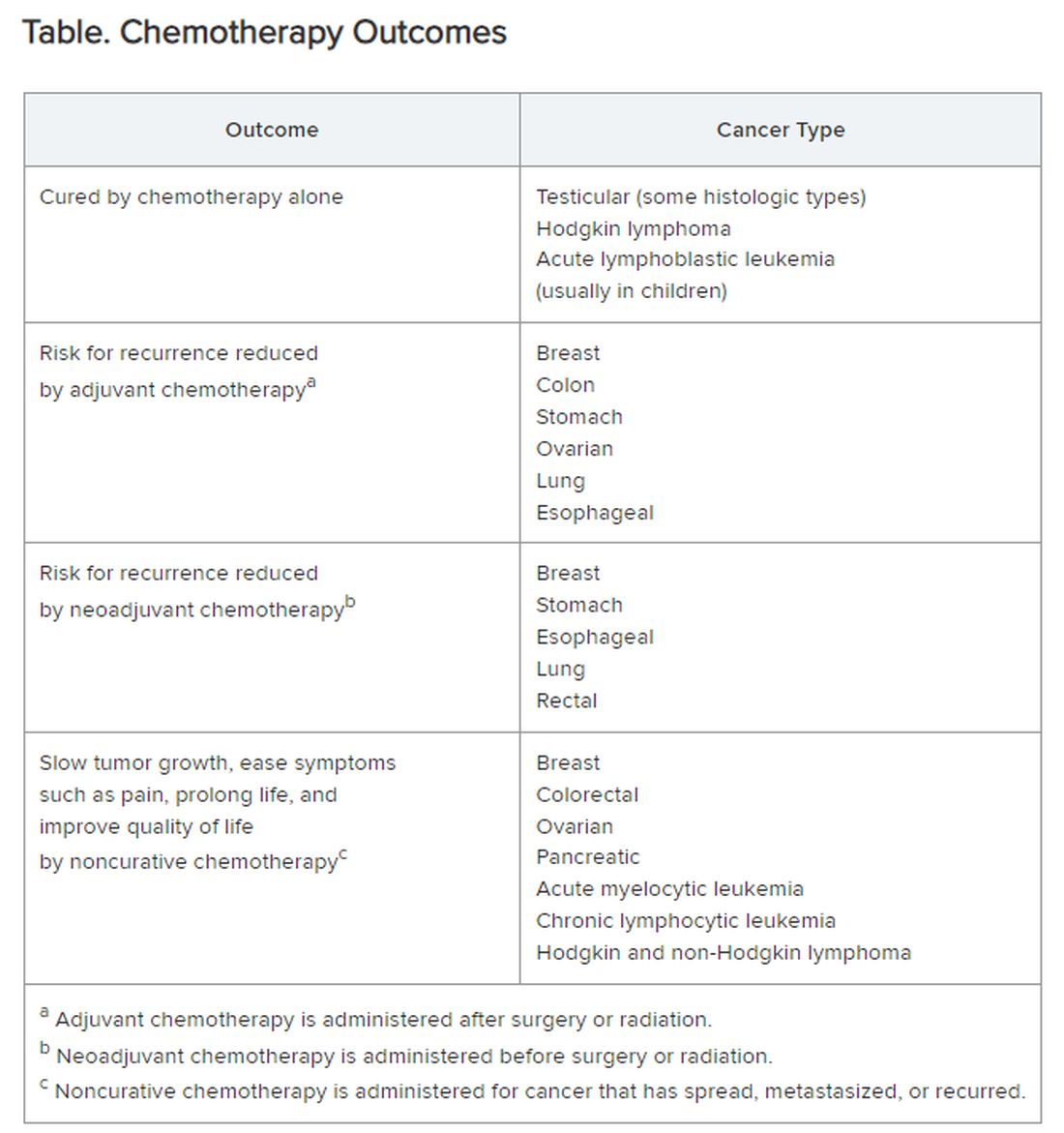
Chemotherapy alone can cure a small number of cancer types. When added to radiation or surgery, chemotherapy can help to cure a wider range of cancer types. As an add-on, chemotherapy can extend the length and quality of life for many patients with cancer. Since chemotherapy is by definition “toxic,” it can also shorten the duration or harm the quality of life and provide false hope. The Table summarizes what chemotherapy can and cannot achieve in selected cancer types.
Careful, compassionate communication between patient and physician is key. Goals and expectations must be clearly understood.
Organized chemotherapeutic efforts are further categorized as first line, second line, and third line.
First-line treatment. The initial round of recommended chemotherapy for a specific cancer. It is typically considered the most effective treatment for that type and stage of cancer on the basis of current research and clinical trials.
Second-line treatment. This is the treatment used if the first-line chemotherapy doesn’t work as desired. Reasons to switch to second-line chemo include:
- Lack of response (the tumor failed to shrink).
- Progression (the cancer may have grown or spread further).
- Adverse side effects were too severe to continue.
The drugs used in second-line chemo will typically be different from those used in first line, sometimes because cancer cells can develop resistance to chemotherapy drugs over time. Moreover, the goal of second-line chemo may differ from that of first-line therapy. Rather than chiefly aiming for a cure, second-line treatment might focus on slowing cancer growth, managing symptoms, or improving quality of life. Unfortunately, not every type of cancer has a readily available second-line option.
Third-line treatment. Third-line options come into play when both the initial course of chemo (first line) and the subsequent treatment (second line) have failed to achieve remission or control the cancer’s spread. Owing to the progressive nature of advanced cancers, patients might not be eligible or healthy enough for third-line therapy. Depending on cancer type, the patient’s general health, and response to previous treatments, third-line options could include:
- New or different chemotherapy drugs compared with prior lines.
- Surgery to debulk the tumor.
- Radiation for symptom control.
- Targeted therapy: drugs designed to target specific vulnerabilities in cancer cells.
- Immunotherapy: agents that help the body’s immune system fight cancer cells.
- Clinical trials testing new or investigational treatments, which may be applicable at any time, depending on the questions being addressed.
The goals of third-line therapy may shift from aiming for a cure to managing symptoms, improving quality of life, and potentially slowing cancer growth. The decision to pursue third-line therapy involves careful consideration by the doctor and patient, weighing the potential benefits and risks of treatment considering the individual’s overall health and specific situation.
It’s important to have realistic expectations about the potential outcomes of third-line therapy. Although remission may be unlikely, third-line therapy can still play a role in managing the disease.
Navigating advanced cancer treatment is very complex. The patient and physician must together consider detailed explanations and clarifications to set expectations and make informed decisions about care.
Interventions to Consider Earlier
In traditional clinical oncology practice, other interventions are possible, but these may not be offered until treatment has reached the third line:
- Molecular testing.
- Palliation.
- Clinical trials.
- Innovative testing to guide targeted therapy by ascertaining which agents are most likely (or not likely at all) to be effective.
I would argue that the patient’s interests are better served by considering and offering these other interventions much earlier, even before starting first-line chemotherapy.
Molecular testing. The best time for molecular testing of a new malignant tumor is typically at the time of diagnosis. Here’s why:
- Molecular testing helps identify specific genetic mutations in the cancer cells. This information can be crucial for selecting targeted therapies that are most effective against those specific mutations. Early detection allows for the most treatment options. For example, for non–small cell lung cancer, early is best because treatment and outcomes may well be changed by test results.
- Knowing the tumor’s molecular makeup can help determine whether a patient qualifies for clinical trials of new drugs designed for specific mutations.
- Some molecular markers can offer information about the tumor’s aggressiveness and potential for metastasis so that prognosis can be informed.
Molecular testing can be a valuable tool throughout a cancer patient’s journey. With genetically diverse tumors, the initial biopsy might not capture the full picture. Molecular testing of circulating tumor DNA can be used to monitor a patient’s response to treatment and detect potential mutations that might arise during treatment resistance. Retesting after metastasis can provide additional information that can aid in treatment decisions.
Palliative care. The ideal time to discuss palliative care with a patient with cancer is early in the diagnosis and treatment process. Palliative care is not the same as hospice care; it isn’t just about end-of-life. Palliative care focuses on improving a patient’s quality of life throughout cancer treatment. Palliative care specialists can address a wide range of symptoms a patient might experience from cancer or its treatment, including pain, fatigue, nausea, and anxiety.
Early discussions allow for a more comprehensive care plan. Open communication about all treatment options, including palliative care, empowers patients to make informed decisions about their care goals and preferences.
Specific situations where discussing palliative care might be appropriate are:
- Soon after a cancer diagnosis.
- If the patient experiences significant side effects from cancer treatment.
- When considering different treatment options, palliative care can complement those treatments.
- In advanced stages of cancer, to focus on comfort and quality of life.
Clinical trials. Participation in a clinical trial to explore new or investigational treatments should always be considered.
In theory, clinical trials should be an option at any time in the patient’s course. But the organized clinical trial experience may not be available or appropriate. Then, the individual becomes a de facto “clinical trial with an n of 1.” Read this brief open-access blog post at Cancer Commons to learn more about that circumstance.
Innovative testing. The best choice of chemotherapeutic or targeted therapies is often unclear. The clinician is likely to follow published guidelines, often from the National Comprehensive Cancer Network.
These are evidence based and driven by consensus of experts. But guideline-recommended therapy is not always effective, and weeks or months can pass before this ineffectiveness becomes apparent. Thus, many researchers and companies are seeking methods of testing each patient’s specific cancer to determine in advance, or very quickly, whether a particular drug is likely to be effective.
Read more about these leading innovations:
SAGE Oncotest: Entering the Next Generation of Tailored Cancer Treatment
Alibrex: A New Blood Test to Reveal Whether a Cancer Treatment is Working
PARIS Test Uses Lab-Grown Mini-Tumors to Find a Patient’s Best Treatment
Using Live Cells from Patients to Find the Right Cancer Drug
Other innovative therapies under investigation could even be agnostic to cancer type:
Treating Pancreatic Cancer: Could Metabolism — Not Genomics — Be the Key?
High-Energy Blue Light Powers a Promising New Treatment to Destroy Cancer Cells
All-Clear Follow-Up: Hydrogen Peroxide Appears to Treat Oral and Skin Lesions
Cancer is a tough nut to crack. Many people and organizations are trying very hard. So much is being learned. Some approaches will be effective. We can all hope.
Dr. Lundberg, editor in chief, Cancer Commons, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The remaining 700,000 or so often proceed to chemotherapy either immediately or upon cancer recurrence, spread, or newly recognized metastases. “Cures” after that point are rare.
I’m speaking in generalities, understanding that each cancer and each patient is unique.
Chemotherapy
Chemotherapy alone can cure a small number of cancer types. When added to radiation or surgery, chemotherapy can help to cure a wider range of cancer types. As an add-on, chemotherapy can extend the length and quality of life for many patients with cancer. Since chemotherapy is by definition “toxic,” it can also shorten the duration or harm the quality of life and provide false hope. The Table summarizes what chemotherapy can and cannot achieve in selected cancer types.
Careful, compassionate communication between patient and physician is key. Goals and expectations must be clearly understood.
Organized chemotherapeutic efforts are further categorized as first line, second line, and third line.
First-line treatment. The initial round of recommended chemotherapy for a specific cancer. It is typically considered the most effective treatment for that type and stage of cancer on the basis of current research and clinical trials.
Second-line treatment. This is the treatment used if the first-line chemotherapy doesn’t work as desired. Reasons to switch to second-line chemo include:
- Lack of response (the tumor failed to shrink).
- Progression (the cancer may have grown or spread further).
- Adverse side effects were too severe to continue.
The drugs used in second-line chemo will typically be different from those used in first line, sometimes because cancer cells can develop resistance to chemotherapy drugs over time. Moreover, the goal of second-line chemo may differ from that of first-line therapy. Rather than chiefly aiming for a cure, second-line treatment might focus on slowing cancer growth, managing symptoms, or improving quality of life. Unfortunately, not every type of cancer has a readily available second-line option.
Third-line treatment. Third-line options come into play when both the initial course of chemo (first line) and the subsequent treatment (second line) have failed to achieve remission or control the cancer’s spread. Owing to the progressive nature of advanced cancers, patients might not be eligible or healthy enough for third-line therapy. Depending on cancer type, the patient’s general health, and response to previous treatments, third-line options could include:
- New or different chemotherapy drugs compared with prior lines.
- Surgery to debulk the tumor.
- Radiation for symptom control.
- Targeted therapy: drugs designed to target specific vulnerabilities in cancer cells.
- Immunotherapy: agents that help the body’s immune system fight cancer cells.
- Clinical trials testing new or investigational treatments, which may be applicable at any time, depending on the questions being addressed.
The goals of third-line therapy may shift from aiming for a cure to managing symptoms, improving quality of life, and potentially slowing cancer growth. The decision to pursue third-line therapy involves careful consideration by the doctor and patient, weighing the potential benefits and risks of treatment considering the individual’s overall health and specific situation.
It’s important to have realistic expectations about the potential outcomes of third-line therapy. Although remission may be unlikely, third-line therapy can still play a role in managing the disease.
Navigating advanced cancer treatment is very complex. The patient and physician must together consider detailed explanations and clarifications to set expectations and make informed decisions about care.
Interventions to Consider Earlier
In traditional clinical oncology practice, other interventions are possible, but these may not be offered until treatment has reached the third line:
- Molecular testing.
- Palliation.
- Clinical trials.
- Innovative testing to guide targeted therapy by ascertaining which agents are most likely (or not likely at all) to be effective.
I would argue that the patient’s interests are better served by considering and offering these other interventions much earlier, even before starting first-line chemotherapy.
Molecular testing. The best time for molecular testing of a new malignant tumor is typically at the time of diagnosis. Here’s why:
- Molecular testing helps identify specific genetic mutations in the cancer cells. This information can be crucial for selecting targeted therapies that are most effective against those specific mutations. Early detection allows for the most treatment options. For example, for non–small cell lung cancer, early is best because treatment and outcomes may well be changed by test results.
- Knowing the tumor’s molecular makeup can help determine whether a patient qualifies for clinical trials of new drugs designed for specific mutations.
- Some molecular markers can offer information about the tumor’s aggressiveness and potential for metastasis so that prognosis can be informed.
Molecular testing can be a valuable tool throughout a cancer patient’s journey. With genetically diverse tumors, the initial biopsy might not capture the full picture. Molecular testing of circulating tumor DNA can be used to monitor a patient’s response to treatment and detect potential mutations that might arise during treatment resistance. Retesting after metastasis can provide additional information that can aid in treatment decisions.
Palliative care. The ideal time to discuss palliative care with a patient with cancer is early in the diagnosis and treatment process. Palliative care is not the same as hospice care; it isn’t just about end-of-life. Palliative care focuses on improving a patient’s quality of life throughout cancer treatment. Palliative care specialists can address a wide range of symptoms a patient might experience from cancer or its treatment, including pain, fatigue, nausea, and anxiety.
Early discussions allow for a more comprehensive care plan. Open communication about all treatment options, including palliative care, empowers patients to make informed decisions about their care goals and preferences.
Specific situations where discussing palliative care might be appropriate are:
- Soon after a cancer diagnosis.
- If the patient experiences significant side effects from cancer treatment.
- When considering different treatment options, palliative care can complement those treatments.
- In advanced stages of cancer, to focus on comfort and quality of life.
Clinical trials. Participation in a clinical trial to explore new or investigational treatments should always be considered.
In theory, clinical trials should be an option at any time in the patient’s course. But the organized clinical trial experience may not be available or appropriate. Then, the individual becomes a de facto “clinical trial with an n of 1.” Read this brief open-access blog post at Cancer Commons to learn more about that circumstance.
Innovative testing. The best choice of chemotherapeutic or targeted therapies is often unclear. The clinician is likely to follow published guidelines, often from the National Comprehensive Cancer Network.
These are evidence based and driven by consensus of experts. But guideline-recommended therapy is not always effective, and weeks or months can pass before this ineffectiveness becomes apparent. Thus, many researchers and companies are seeking methods of testing each patient’s specific cancer to determine in advance, or very quickly, whether a particular drug is likely to be effective.
Read more about these leading innovations:
SAGE Oncotest: Entering the Next Generation of Tailored Cancer Treatment
Alibrex: A New Blood Test to Reveal Whether a Cancer Treatment is Working
PARIS Test Uses Lab-Grown Mini-Tumors to Find a Patient’s Best Treatment
Using Live Cells from Patients to Find the Right Cancer Drug
Other innovative therapies under investigation could even be agnostic to cancer type:
Treating Pancreatic Cancer: Could Metabolism — Not Genomics — Be the Key?
High-Energy Blue Light Powers a Promising New Treatment to Destroy Cancer Cells
All-Clear Follow-Up: Hydrogen Peroxide Appears to Treat Oral and Skin Lesions
Cancer is a tough nut to crack. Many people and organizations are trying very hard. So much is being learned. Some approaches will be effective. We can all hope.
Dr. Lundberg, editor in chief, Cancer Commons, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
The remaining 700,000 or so often proceed to chemotherapy either immediately or upon cancer recurrence, spread, or newly recognized metastases. “Cures” after that point are rare.
I’m speaking in generalities, understanding that each cancer and each patient is unique.
Chemotherapy
Chemotherapy alone can cure a small number of cancer types. When added to radiation or surgery, chemotherapy can help to cure a wider range of cancer types. As an add-on, chemotherapy can extend the length and quality of life for many patients with cancer. Since chemotherapy is by definition “toxic,” it can also shorten the duration or harm the quality of life and provide false hope. The Table summarizes what chemotherapy can and cannot achieve in selected cancer types.
Careful, compassionate communication between patient and physician is key. Goals and expectations must be clearly understood.
Organized chemotherapeutic efforts are further categorized as first line, second line, and third line.
First-line treatment. The initial round of recommended chemotherapy for a specific cancer. It is typically considered the most effective treatment for that type and stage of cancer on the basis of current research and clinical trials.
Second-line treatment. This is the treatment used if the first-line chemotherapy doesn’t work as desired. Reasons to switch to second-line chemo include:
- Lack of response (the tumor failed to shrink).
- Progression (the cancer may have grown or spread further).
- Adverse side effects were too severe to continue.
The drugs used in second-line chemo will typically be different from those used in first line, sometimes because cancer cells can develop resistance to chemotherapy drugs over time. Moreover, the goal of second-line chemo may differ from that of first-line therapy. Rather than chiefly aiming for a cure, second-line treatment might focus on slowing cancer growth, managing symptoms, or improving quality of life. Unfortunately, not every type of cancer has a readily available second-line option.
Third-line treatment. Third-line options come into play when both the initial course of chemo (first line) and the subsequent treatment (second line) have failed to achieve remission or control the cancer’s spread. Owing to the progressive nature of advanced cancers, patients might not be eligible or healthy enough for third-line therapy. Depending on cancer type, the patient’s general health, and response to previous treatments, third-line options could include:
- New or different chemotherapy drugs compared with prior lines.
- Surgery to debulk the tumor.
- Radiation for symptom control.
- Targeted therapy: drugs designed to target specific vulnerabilities in cancer cells.
- Immunotherapy: agents that help the body’s immune system fight cancer cells.
- Clinical trials testing new or investigational treatments, which may be applicable at any time, depending on the questions being addressed.
The goals of third-line therapy may shift from aiming for a cure to managing symptoms, improving quality of life, and potentially slowing cancer growth. The decision to pursue third-line therapy involves careful consideration by the doctor and patient, weighing the potential benefits and risks of treatment considering the individual’s overall health and specific situation.
It’s important to have realistic expectations about the potential outcomes of third-line therapy. Although remission may be unlikely, third-line therapy can still play a role in managing the disease.
Navigating advanced cancer treatment is very complex. The patient and physician must together consider detailed explanations and clarifications to set expectations and make informed decisions about care.
Interventions to Consider Earlier
In traditional clinical oncology practice, other interventions are possible, but these may not be offered until treatment has reached the third line:
- Molecular testing.
- Palliation.
- Clinical trials.
- Innovative testing to guide targeted therapy by ascertaining which agents are most likely (or not likely at all) to be effective.
I would argue that the patient’s interests are better served by considering and offering these other interventions much earlier, even before starting first-line chemotherapy.
Molecular testing. The best time for molecular testing of a new malignant tumor is typically at the time of diagnosis. Here’s why:
- Molecular testing helps identify specific genetic mutations in the cancer cells. This information can be crucial for selecting targeted therapies that are most effective against those specific mutations. Early detection allows for the most treatment options. For example, for non–small cell lung cancer, early is best because treatment and outcomes may well be changed by test results.
- Knowing the tumor’s molecular makeup can help determine whether a patient qualifies for clinical trials of new drugs designed for specific mutations.
- Some molecular markers can offer information about the tumor’s aggressiveness and potential for metastasis so that prognosis can be informed.
Molecular testing can be a valuable tool throughout a cancer patient’s journey. With genetically diverse tumors, the initial biopsy might not capture the full picture. Molecular testing of circulating tumor DNA can be used to monitor a patient’s response to treatment and detect potential mutations that might arise during treatment resistance. Retesting after metastasis can provide additional information that can aid in treatment decisions.
Palliative care. The ideal time to discuss palliative care with a patient with cancer is early in the diagnosis and treatment process. Palliative care is not the same as hospice care; it isn’t just about end-of-life. Palliative care focuses on improving a patient’s quality of life throughout cancer treatment. Palliative care specialists can address a wide range of symptoms a patient might experience from cancer or its treatment, including pain, fatigue, nausea, and anxiety.
Early discussions allow for a more comprehensive care plan. Open communication about all treatment options, including palliative care, empowers patients to make informed decisions about their care goals and preferences.
Specific situations where discussing palliative care might be appropriate are:
- Soon after a cancer diagnosis.
- If the patient experiences significant side effects from cancer treatment.
- When considering different treatment options, palliative care can complement those treatments.
- In advanced stages of cancer, to focus on comfort and quality of life.
Clinical trials. Participation in a clinical trial to explore new or investigational treatments should always be considered.
In theory, clinical trials should be an option at any time in the patient’s course. But the organized clinical trial experience may not be available or appropriate. Then, the individual becomes a de facto “clinical trial with an n of 1.” Read this brief open-access blog post at Cancer Commons to learn more about that circumstance.
Innovative testing. The best choice of chemotherapeutic or targeted therapies is often unclear. The clinician is likely to follow published guidelines, often from the National Comprehensive Cancer Network.
These are evidence based and driven by consensus of experts. But guideline-recommended therapy is not always effective, and weeks or months can pass before this ineffectiveness becomes apparent. Thus, many researchers and companies are seeking methods of testing each patient’s specific cancer to determine in advance, or very quickly, whether a particular drug is likely to be effective.
Read more about these leading innovations:
SAGE Oncotest: Entering the Next Generation of Tailored Cancer Treatment
Alibrex: A New Blood Test to Reveal Whether a Cancer Treatment is Working
PARIS Test Uses Lab-Grown Mini-Tumors to Find a Patient’s Best Treatment
Using Live Cells from Patients to Find the Right Cancer Drug
Other innovative therapies under investigation could even be agnostic to cancer type:
Treating Pancreatic Cancer: Could Metabolism — Not Genomics — Be the Key?
High-Energy Blue Light Powers a Promising New Treatment to Destroy Cancer Cells
All-Clear Follow-Up: Hydrogen Peroxide Appears to Treat Oral and Skin Lesions
Cancer is a tough nut to crack. Many people and organizations are trying very hard. So much is being learned. Some approaches will be effective. We can all hope.
Dr. Lundberg, editor in chief, Cancer Commons, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Physicians Lament Over Reliance on Relative Value Units: Survey
Most physicians oppose the way standardized relative value units (RVUs) are used to determine performance and compensation, according to Medscape’s 2024 Physicians and RVUs Report. About 6 in 10 survey respondents were unhappy with how RVUs affected them financially, while 7 in 10 said RVUs were poor measures of productivity.
The report analyzed 2024 survey data from 1005 practicing physicians who earn RVUs.
“I’m already mad that the medical field is controlled by health insurers and what they pay and authorize,” said an anesthesiologist in New York. “Then [that approach] is transferred to medical offices and hospitals, where physicians are paid by RVUs.”
Most physicians surveyed produced between 4000 and 8000 RVUs per year. Roughly one in six were high RVU generators, generating more than 10,000 annually.
In most cases, the metric influences earning potential — 42% of doctors surveyed said RVUs affect their salaries to some degree. One quarter said their salary was based entirely on RVUs. More than three fourths of physicians who received performance bonuses said they must meet RVU targets to do so.
“The current RVU system encourages unnecessary procedures, hurting patients,” said an orthopedic surgeon in Maine.
Nearly three fourths of practitioners surveyed said they occasionally to frequently felt pressure to take on more patients as a result of this system.
“I know numerous primary care doctors and specialists who have been forced to increase patient volume to meet RVU goals, and none is happy about it,” said Alok Patel, MD, a pediatric hospitalist with Stanford Hospital in Palo Alto, California. “Plus, patients are definitely not happy about being rushed.”
More than half of respondents said they occasionally or frequently felt compelled by their employer to use higher-level coding, which interferes with a physician’s ethical responsibility to the patient, said Arthur L. Caplan, PhD, a bioethicist at NYU Langone Medical Center in New York City.
“Rather than rewarding excellence or good outcomes, you’re kind of rewarding procedures and volume,” said Dr. Caplan. “It’s more than pressure; it’s expected.”
Nearly 6 in 10 physicians said that the method for calculating reimbursements was unfair. Almost half said that they weren’t happy with how their workplace uses RVUs.
A few respondents said that their RVU model, which is often based on what Dr. Patel called an “overly complicated algorithm,” did not account for the time spent on tasks or the fact that some patients miss appointments. RVUs also rely on factors outside the control of a physician, such as location and patient volume, said one doctor.
The model can also lower the level of care patients receive, Dr. Patel said.
“I know primary care doctors who work in RVU-based systems and simply cannot take the necessary time — even if it’s 30-45 minutes — to thoroughly assess a patient, when the model forces them to take on 15-minute encounters.”
Finally, over half of clinicians said alternatives to the RVU system would be more effective, and 77% suggested including qualitative data. One respondent recommended incorporating time spent doing paperwork and communicating with patients, complexity of conditions, and medication management.
A version of this article first appeared on Medscape.com.
Most physicians oppose the way standardized relative value units (RVUs) are used to determine performance and compensation, according to Medscape’s 2024 Physicians and RVUs Report. About 6 in 10 survey respondents were unhappy with how RVUs affected them financially, while 7 in 10 said RVUs were poor measures of productivity.
The report analyzed 2024 survey data from 1005 practicing physicians who earn RVUs.
“I’m already mad that the medical field is controlled by health insurers and what they pay and authorize,” said an anesthesiologist in New York. “Then [that approach] is transferred to medical offices and hospitals, where physicians are paid by RVUs.”
Most physicians surveyed produced between 4000 and 8000 RVUs per year. Roughly one in six were high RVU generators, generating more than 10,000 annually.
In most cases, the metric influences earning potential — 42% of doctors surveyed said RVUs affect their salaries to some degree. One quarter said their salary was based entirely on RVUs. More than three fourths of physicians who received performance bonuses said they must meet RVU targets to do so.
“The current RVU system encourages unnecessary procedures, hurting patients,” said an orthopedic surgeon in Maine.
Nearly three fourths of practitioners surveyed said they occasionally to frequently felt pressure to take on more patients as a result of this system.
“I know numerous primary care doctors and specialists who have been forced to increase patient volume to meet RVU goals, and none is happy about it,” said Alok Patel, MD, a pediatric hospitalist with Stanford Hospital in Palo Alto, California. “Plus, patients are definitely not happy about being rushed.”
More than half of respondents said they occasionally or frequently felt compelled by their employer to use higher-level coding, which interferes with a physician’s ethical responsibility to the patient, said Arthur L. Caplan, PhD, a bioethicist at NYU Langone Medical Center in New York City.
“Rather than rewarding excellence or good outcomes, you’re kind of rewarding procedures and volume,” said Dr. Caplan. “It’s more than pressure; it’s expected.”
Nearly 6 in 10 physicians said that the method for calculating reimbursements was unfair. Almost half said that they weren’t happy with how their workplace uses RVUs.
A few respondents said that their RVU model, which is often based on what Dr. Patel called an “overly complicated algorithm,” did not account for the time spent on tasks or the fact that some patients miss appointments. RVUs also rely on factors outside the control of a physician, such as location and patient volume, said one doctor.
The model can also lower the level of care patients receive, Dr. Patel said.
“I know primary care doctors who work in RVU-based systems and simply cannot take the necessary time — even if it’s 30-45 minutes — to thoroughly assess a patient, when the model forces them to take on 15-minute encounters.”
Finally, over half of clinicians said alternatives to the RVU system would be more effective, and 77% suggested including qualitative data. One respondent recommended incorporating time spent doing paperwork and communicating with patients, complexity of conditions, and medication management.
A version of this article first appeared on Medscape.com.
Most physicians oppose the way standardized relative value units (RVUs) are used to determine performance and compensation, according to Medscape’s 2024 Physicians and RVUs Report. About 6 in 10 survey respondents were unhappy with how RVUs affected them financially, while 7 in 10 said RVUs were poor measures of productivity.
The report analyzed 2024 survey data from 1005 practicing physicians who earn RVUs.
“I’m already mad that the medical field is controlled by health insurers and what they pay and authorize,” said an anesthesiologist in New York. “Then [that approach] is transferred to medical offices and hospitals, where physicians are paid by RVUs.”
Most physicians surveyed produced between 4000 and 8000 RVUs per year. Roughly one in six were high RVU generators, generating more than 10,000 annually.
In most cases, the metric influences earning potential — 42% of doctors surveyed said RVUs affect their salaries to some degree. One quarter said their salary was based entirely on RVUs. More than three fourths of physicians who received performance bonuses said they must meet RVU targets to do so.
“The current RVU system encourages unnecessary procedures, hurting patients,” said an orthopedic surgeon in Maine.
Nearly three fourths of practitioners surveyed said they occasionally to frequently felt pressure to take on more patients as a result of this system.
“I know numerous primary care doctors and specialists who have been forced to increase patient volume to meet RVU goals, and none is happy about it,” said Alok Patel, MD, a pediatric hospitalist with Stanford Hospital in Palo Alto, California. “Plus, patients are definitely not happy about being rushed.”
More than half of respondents said they occasionally or frequently felt compelled by their employer to use higher-level coding, which interferes with a physician’s ethical responsibility to the patient, said Arthur L. Caplan, PhD, a bioethicist at NYU Langone Medical Center in New York City.
“Rather than rewarding excellence or good outcomes, you’re kind of rewarding procedures and volume,” said Dr. Caplan. “It’s more than pressure; it’s expected.”
Nearly 6 in 10 physicians said that the method for calculating reimbursements was unfair. Almost half said that they weren’t happy with how their workplace uses RVUs.
A few respondents said that their RVU model, which is often based on what Dr. Patel called an “overly complicated algorithm,” did not account for the time spent on tasks or the fact that some patients miss appointments. RVUs also rely on factors outside the control of a physician, such as location and patient volume, said one doctor.
The model can also lower the level of care patients receive, Dr. Patel said.
“I know primary care doctors who work in RVU-based systems and simply cannot take the necessary time — even if it’s 30-45 minutes — to thoroughly assess a patient, when the model forces them to take on 15-minute encounters.”
Finally, over half of clinicians said alternatives to the RVU system would be more effective, and 77% suggested including qualitative data. One respondent recommended incorporating time spent doing paperwork and communicating with patients, complexity of conditions, and medication management.
A version of this article first appeared on Medscape.com.
Will Compounding ‘Best Practices’ Guide Reassure Clinicians?
A new “best practices” guide released by the Alliance for Pharmacy Compounding (APC) aims to educate compounding pharmacists and reassure prescribers about the ethical, legal, and practical considerations that must be addressed to ensure quality standards and protect patients’ health.
Endocrinologists have expressed skepticism about the quality of compounded drugs, particularly the popular glucagon-like peptide 1 (GLP-1) semaglutide. The Food and Drug Administration (FDA) recently issued an alert linking hospitalizations to overdoses of compounded semaglutide.
“This document goes beyond today’s media-grabbing shortages,” APC Board Chair-Elect Gina Besteman, RPh, of Belmar Pharma Solutions told this news organization. “We developed these best practices to apply to all shortage drug compounding, and especially in this moment when so many are compounding GLP-1s. These serve as a reminder about what compliance and care look like.”
Prescribers determine whether a patient needs a compounded medication, not pharmacists, Ms. Besteman noted. “A patient-specific prescription order must be authorized for a compounded medication to be dispensed. Prescribers should ensure pharmacies they work with regularly check the FDA Drug Shortage List, as compounding of ‘essential copies’ of FDA-approved drugs is only allowed when a drug is listed as ‘currently in shortage.’ ”
Framework for Compounding
“With fake and illegal online stores popping up, it’s critical for legitimate, state-licensed compounding pharmacies to maintain the profession’s high standards,” the APC said in a media communication.
Highlights of its best practices, which are directed toward 503A state-licensed compounding pharmacies, include the following, among others:
- Pharmacies should check the FDA drug shortage list prior to preparing a copy of an FDA-approved drug and maintain documentation to demonstrate to regulators that the drug was in shortage at the time it was compounded.
- Pharmacies may only source active pharmaceutical ingredients (APIs) from state-licensed wholesalers who purchase from FDA-registered manufacturers or order directly from FDA-registered manufacturers.
- Verify from the wholesaler that the manufacturer is registered with the FDA and the API meets all the requirements of section 503A, and that both hold the appropriate permits or licenses in their home state and the shipped to state.
- Adhere to USP Chapter <797> testing requirements for sterility, endotoxin, stability, particulate, antimicrobial effectiveness, and container closure integrity studies.
- Counseling must be offered to the patient or the patient’s agent/caregiver. Providing written information that assists in the understanding of how to properly use the compounded medication is advised.
- Instructions should be written in a way that a layperson can understand (especially directions including dosage titrations and conversions between milligrams and milliliters or units).
- Like all medications, compounded drugs can only be prescribed in the presence of a valid patient-practitioner relationship and can only be dispensed by a pharmacy after receipt of a valid patient-specific prescription order.
- When marketing, never make claims of safety or efficacy of the compounded product.
- Advertising that patients will/may save money using compounded medications, compared with manufactured products is not allowed.
“Compounding FDA-approved drugs during shortages is nothing new — pharmacies have been doing it well before GLP-1s came on the scene, and they’ll continue long after this current shortage ends,” Ms. Besteman said. “Prescribers should be aware of APC’s guidelines because they provide a framework for ethically and legally compounding medications during drug shortages.
“To paraphrase The Police,” she concluded, “every move you make, every step you take, they’ll be watching you. Make sure they see those best practices in action.”
‘Reduces the Risks’
Commenting on the best practices guidance, Ivania Rizo, MD, director of Obesity Medicine and Diabetes and clinical colead at Boston Medical Center’s Health Equity Accelerator in Massachusetts, said: “These best practices will hopefully make a difference in the quality of compounded drugs.”
“The emphasis on rigorous testing of APIs and adherence to USP standards is particularly important for maintaining drug quality,” she noted. “This structured approach reduces the risk of variability and ensures that compounded drugs meet high-quality standards, thus enhancing their reliability.”
“Knowing that compounding pharmacies are adhering to rigorous standards for sourcing, testing, and compounding can at least reassure clinicians that specific steps are being taken for the safety and efficacy of these medications,” she said. “The transparency in documenting compliance with FDA guidelines and maintaining high-quality control measures can enhance trust among healthcare providers.”
Although clinicians are likely to have more confidence in compounded drugs when these best practices are followed, she said, “overall, we all hope that the shortages of medications such as tirzepatide are resolved promptly, allowing patients to access FDA-approved drugs without the need for compounding.”
“While the implementation of best practices for compounding during shortages is a positive and necessary step, our ultimate goal remains to address and resolve these shortages in the near future,” she concluded.
Dr. Rizo declared no competing interests.
A version of this article first appeared on Medscape.com.
A new “best practices” guide released by the Alliance for Pharmacy Compounding (APC) aims to educate compounding pharmacists and reassure prescribers about the ethical, legal, and practical considerations that must be addressed to ensure quality standards and protect patients’ health.
Endocrinologists have expressed skepticism about the quality of compounded drugs, particularly the popular glucagon-like peptide 1 (GLP-1) semaglutide. The Food and Drug Administration (FDA) recently issued an alert linking hospitalizations to overdoses of compounded semaglutide.
“This document goes beyond today’s media-grabbing shortages,” APC Board Chair-Elect Gina Besteman, RPh, of Belmar Pharma Solutions told this news organization. “We developed these best practices to apply to all shortage drug compounding, and especially in this moment when so many are compounding GLP-1s. These serve as a reminder about what compliance and care look like.”
Prescribers determine whether a patient needs a compounded medication, not pharmacists, Ms. Besteman noted. “A patient-specific prescription order must be authorized for a compounded medication to be dispensed. Prescribers should ensure pharmacies they work with regularly check the FDA Drug Shortage List, as compounding of ‘essential copies’ of FDA-approved drugs is only allowed when a drug is listed as ‘currently in shortage.’ ”
Framework for Compounding
“With fake and illegal online stores popping up, it’s critical for legitimate, state-licensed compounding pharmacies to maintain the profession’s high standards,” the APC said in a media communication.
Highlights of its best practices, which are directed toward 503A state-licensed compounding pharmacies, include the following, among others:
- Pharmacies should check the FDA drug shortage list prior to preparing a copy of an FDA-approved drug and maintain documentation to demonstrate to regulators that the drug was in shortage at the time it was compounded.
- Pharmacies may only source active pharmaceutical ingredients (APIs) from state-licensed wholesalers who purchase from FDA-registered manufacturers or order directly from FDA-registered manufacturers.
- Verify from the wholesaler that the manufacturer is registered with the FDA and the API meets all the requirements of section 503A, and that both hold the appropriate permits or licenses in their home state and the shipped to state.
- Adhere to USP Chapter <797> testing requirements for sterility, endotoxin, stability, particulate, antimicrobial effectiveness, and container closure integrity studies.
- Counseling must be offered to the patient or the patient’s agent/caregiver. Providing written information that assists in the understanding of how to properly use the compounded medication is advised.
- Instructions should be written in a way that a layperson can understand (especially directions including dosage titrations and conversions between milligrams and milliliters or units).
- Like all medications, compounded drugs can only be prescribed in the presence of a valid patient-practitioner relationship and can only be dispensed by a pharmacy after receipt of a valid patient-specific prescription order.
- When marketing, never make claims of safety or efficacy of the compounded product.
- Advertising that patients will/may save money using compounded medications, compared with manufactured products is not allowed.
“Compounding FDA-approved drugs during shortages is nothing new — pharmacies have been doing it well before GLP-1s came on the scene, and they’ll continue long after this current shortage ends,” Ms. Besteman said. “Prescribers should be aware of APC’s guidelines because they provide a framework for ethically and legally compounding medications during drug shortages.
“To paraphrase The Police,” she concluded, “every move you make, every step you take, they’ll be watching you. Make sure they see those best practices in action.”
‘Reduces the Risks’
Commenting on the best practices guidance, Ivania Rizo, MD, director of Obesity Medicine and Diabetes and clinical colead at Boston Medical Center’s Health Equity Accelerator in Massachusetts, said: “These best practices will hopefully make a difference in the quality of compounded drugs.”
“The emphasis on rigorous testing of APIs and adherence to USP standards is particularly important for maintaining drug quality,” she noted. “This structured approach reduces the risk of variability and ensures that compounded drugs meet high-quality standards, thus enhancing their reliability.”
“Knowing that compounding pharmacies are adhering to rigorous standards for sourcing, testing, and compounding can at least reassure clinicians that specific steps are being taken for the safety and efficacy of these medications,” she said. “The transparency in documenting compliance with FDA guidelines and maintaining high-quality control measures can enhance trust among healthcare providers.”
Although clinicians are likely to have more confidence in compounded drugs when these best practices are followed, she said, “overall, we all hope that the shortages of medications such as tirzepatide are resolved promptly, allowing patients to access FDA-approved drugs without the need for compounding.”
“While the implementation of best practices for compounding during shortages is a positive and necessary step, our ultimate goal remains to address and resolve these shortages in the near future,” she concluded.
Dr. Rizo declared no competing interests.
A version of this article first appeared on Medscape.com.
A new “best practices” guide released by the Alliance for Pharmacy Compounding (APC) aims to educate compounding pharmacists and reassure prescribers about the ethical, legal, and practical considerations that must be addressed to ensure quality standards and protect patients’ health.
Endocrinologists have expressed skepticism about the quality of compounded drugs, particularly the popular glucagon-like peptide 1 (GLP-1) semaglutide. The Food and Drug Administration (FDA) recently issued an alert linking hospitalizations to overdoses of compounded semaglutide.
“This document goes beyond today’s media-grabbing shortages,” APC Board Chair-Elect Gina Besteman, RPh, of Belmar Pharma Solutions told this news organization. “We developed these best practices to apply to all shortage drug compounding, and especially in this moment when so many are compounding GLP-1s. These serve as a reminder about what compliance and care look like.”
Prescribers determine whether a patient needs a compounded medication, not pharmacists, Ms. Besteman noted. “A patient-specific prescription order must be authorized for a compounded medication to be dispensed. Prescribers should ensure pharmacies they work with regularly check the FDA Drug Shortage List, as compounding of ‘essential copies’ of FDA-approved drugs is only allowed when a drug is listed as ‘currently in shortage.’ ”
Framework for Compounding
“With fake and illegal online stores popping up, it’s critical for legitimate, state-licensed compounding pharmacies to maintain the profession’s high standards,” the APC said in a media communication.
Highlights of its best practices, which are directed toward 503A state-licensed compounding pharmacies, include the following, among others:
- Pharmacies should check the FDA drug shortage list prior to preparing a copy of an FDA-approved drug and maintain documentation to demonstrate to regulators that the drug was in shortage at the time it was compounded.
- Pharmacies may only source active pharmaceutical ingredients (APIs) from state-licensed wholesalers who purchase from FDA-registered manufacturers or order directly from FDA-registered manufacturers.
- Verify from the wholesaler that the manufacturer is registered with the FDA and the API meets all the requirements of section 503A, and that both hold the appropriate permits or licenses in their home state and the shipped to state.
- Adhere to USP Chapter <797> testing requirements for sterility, endotoxin, stability, particulate, antimicrobial effectiveness, and container closure integrity studies.
- Counseling must be offered to the patient or the patient’s agent/caregiver. Providing written information that assists in the understanding of how to properly use the compounded medication is advised.
- Instructions should be written in a way that a layperson can understand (especially directions including dosage titrations and conversions between milligrams and milliliters or units).
- Like all medications, compounded drugs can only be prescribed in the presence of a valid patient-practitioner relationship and can only be dispensed by a pharmacy after receipt of a valid patient-specific prescription order.
- When marketing, never make claims of safety or efficacy of the compounded product.
- Advertising that patients will/may save money using compounded medications, compared with manufactured products is not allowed.
“Compounding FDA-approved drugs during shortages is nothing new — pharmacies have been doing it well before GLP-1s came on the scene, and they’ll continue long after this current shortage ends,” Ms. Besteman said. “Prescribers should be aware of APC’s guidelines because they provide a framework for ethically and legally compounding medications during drug shortages.
“To paraphrase The Police,” she concluded, “every move you make, every step you take, they’ll be watching you. Make sure they see those best practices in action.”
‘Reduces the Risks’
Commenting on the best practices guidance, Ivania Rizo, MD, director of Obesity Medicine and Diabetes and clinical colead at Boston Medical Center’s Health Equity Accelerator in Massachusetts, said: “These best practices will hopefully make a difference in the quality of compounded drugs.”
“The emphasis on rigorous testing of APIs and adherence to USP standards is particularly important for maintaining drug quality,” she noted. “This structured approach reduces the risk of variability and ensures that compounded drugs meet high-quality standards, thus enhancing their reliability.”
“Knowing that compounding pharmacies are adhering to rigorous standards for sourcing, testing, and compounding can at least reassure clinicians that specific steps are being taken for the safety and efficacy of these medications,” she said. “The transparency in documenting compliance with FDA guidelines and maintaining high-quality control measures can enhance trust among healthcare providers.”
Although clinicians are likely to have more confidence in compounded drugs when these best practices are followed, she said, “overall, we all hope that the shortages of medications such as tirzepatide are resolved promptly, allowing patients to access FDA-approved drugs without the need for compounding.”
“While the implementation of best practices for compounding during shortages is a positive and necessary step, our ultimate goal remains to address and resolve these shortages in the near future,” she concluded.
Dr. Rizo declared no competing interests.
A version of this article first appeared on Medscape.com.
Do New Blood Tests for Cancer Meet the Right Standards?
Biotech startups worldwide are rushing to market screening tests that they claim can detect various cancers in early stages with just a few drops of blood. The tests allegedly will simplify cancer care by eliminating tedious scans, scopes, and swabs at the doctor’s office.
The promise of these early detection tests is truly “enticing,” Hilary A. Robbins, PhD, from the International Agency for Research on Cancer of the World Health Organization in Lyon, France, said in an interview.
In an opinion article in The New England Journal of Medicine, she emphasized that the new cancer tests are much less cumbersome than traditional screening strategies for individual cancers. Moreover, they could enable the early detection of dozens of cancer types for which no screening has been available so far.
Meeting the Criteria
The problem is that these tests have not met the strict criteria typically required for traditional cancer screening tests. To be considered for introduction as a screening procedure, a test usually needs to meet the following four minimum requirements:
- The disease that the test screens for must have a presymptomatic form.
- The screening test must be able to identify this presymptomatic disease.
- Treating the disease in the presymptomatic phase improves prognosis (specifically, it affects cancer-specific mortality in a randomized controlled trial).
- The screening test is feasible, and the benefits outweigh potential risks.
“The new blood tests for multiple cancers have so far only met the second criteria, showing they can detect presymptomatic cancer,” Dr. Robbins wrote.
The next step would be to demonstrate that they affect cancer-specific mortality. “But currently, commercial interests seem to be influencing the evidence standards for these cancer tests,” said Dr. Robbins.
Inappropriate Endpoints?
Some proponents of such tests argue that, unlike for previous cancer screening procedures, initial approval should not depend on the endpoint of cancer-specific mortality. It would take too long to gather sufficient outcome data, and in the meantime, people would die, they argue.
Eric A. Klein, MD, from the Glickman Urological and Kidney Institute in Cleveland, Ohio, and colleagues advocate for alternative endpoints such as the incidence of late-stage cancer in an article published in Cancer Epidemiology, Biomarkers & Prevention.
“The concept would be,” they wrote, “that a negative signal would not indicate a mortality benefit, leading to the study being stopped. A positive signal, on the other hand, could result in provisional approval until mortality data and real-world evidence of effectiveness are available. This would resemble the accelerated approval of new cancer drugs, which often is based on progression-free survival until there postmarketing data on overall survival emerge.”
Dr. Klein is also employed at the US biotech start-up Grail, which developed the Galleri test, which is one of the best-known and most advanced cancer screening tests. The Galleri test uses cell-free DNA and machine learning to detect a common cancer signal in more than 50 cancer types and predict the origin of the cancer signal. Consumers in the United States can already order and perform the test.
An NHS Study
Arguments for different endpoints apparently resonated with the United Kingdom’s National Health Service (NHS). Three years ago, they initiated the Galleri study, a large randomized controlled trial to assess the effectiveness of Grail’s cancer test. The primary endpoint was not cancer-specific mortality, but the incidence of stage III or IV cancer.
The results are expected in 2026. But recruitment was stopped after 140,000 participants were enrolled. The NHS reported that the initial results were not convincing enough to continue the trial. Exact numbers were not disclosed.
The Galleri study deviates from the standard randomized controlled trial design for cancer screening procedures not only in terms of the primary endpoint, but also in blinding. The only participants who were unblinded and informed of their test results are those in the intervention group with a positive cancer test.
False Security
This trial design encourages participants to undergo blood tests once per year. But according to Dr. Robbins, it prevents the exploration of the phenomenon of “false security,” which is a potential drawback of the new cancer tests.
“Women with a negative mammogram can reasonably assume that they probably do not have breast cancer. But individuals with a negative cancer blood test could mistakenly believe they cannot have any cancer at all. As a result, they may not undergo standard early detection screenings or seek medical help early enough for potential cancer symptoms,” said Dr. Robbins.
To assess the actual risk-benefit ratio of the Galleri test, participants must receive their test results, she said. “Under real-world conditions, benefits and risks can come from positive and negative results.”
Upcoming Trial
More illuminating results may come from a large trial planned by the National Cancer Institute in the United States. Several new cancer tests will be evaluated for their ability to reduce cancer-specific mortality. A pilot phase will start later in 2024. “This study may be the only one with sufficient statistical power to determine whether an approach based on these cancer tests can reduce cancer-specific mortality,” said Dr. Robbins.
For the new blood tests for multiple cancers, it is crucial that health authorities “set a high bar for a benefit,” she said. This, according to her, also means that they must show an effect on cancer-specific mortality before being introduced. “This evidence must come from studies in which commercial interests do not influence the design, execution, data management, or data analysis.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version appeared on Medscape.com.
Biotech startups worldwide are rushing to market screening tests that they claim can detect various cancers in early stages with just a few drops of blood. The tests allegedly will simplify cancer care by eliminating tedious scans, scopes, and swabs at the doctor’s office.
The promise of these early detection tests is truly “enticing,” Hilary A. Robbins, PhD, from the International Agency for Research on Cancer of the World Health Organization in Lyon, France, said in an interview.
In an opinion article in The New England Journal of Medicine, she emphasized that the new cancer tests are much less cumbersome than traditional screening strategies for individual cancers. Moreover, they could enable the early detection of dozens of cancer types for which no screening has been available so far.
Meeting the Criteria
The problem is that these tests have not met the strict criteria typically required for traditional cancer screening tests. To be considered for introduction as a screening procedure, a test usually needs to meet the following four minimum requirements:
- The disease that the test screens for must have a presymptomatic form.
- The screening test must be able to identify this presymptomatic disease.
- Treating the disease in the presymptomatic phase improves prognosis (specifically, it affects cancer-specific mortality in a randomized controlled trial).
- The screening test is feasible, and the benefits outweigh potential risks.
“The new blood tests for multiple cancers have so far only met the second criteria, showing they can detect presymptomatic cancer,” Dr. Robbins wrote.
The next step would be to demonstrate that they affect cancer-specific mortality. “But currently, commercial interests seem to be influencing the evidence standards for these cancer tests,” said Dr. Robbins.
Inappropriate Endpoints?
Some proponents of such tests argue that, unlike for previous cancer screening procedures, initial approval should not depend on the endpoint of cancer-specific mortality. It would take too long to gather sufficient outcome data, and in the meantime, people would die, they argue.
Eric A. Klein, MD, from the Glickman Urological and Kidney Institute in Cleveland, Ohio, and colleagues advocate for alternative endpoints such as the incidence of late-stage cancer in an article published in Cancer Epidemiology, Biomarkers & Prevention.
“The concept would be,” they wrote, “that a negative signal would not indicate a mortality benefit, leading to the study being stopped. A positive signal, on the other hand, could result in provisional approval until mortality data and real-world evidence of effectiveness are available. This would resemble the accelerated approval of new cancer drugs, which often is based on progression-free survival until there postmarketing data on overall survival emerge.”
Dr. Klein is also employed at the US biotech start-up Grail, which developed the Galleri test, which is one of the best-known and most advanced cancer screening tests. The Galleri test uses cell-free DNA and machine learning to detect a common cancer signal in more than 50 cancer types and predict the origin of the cancer signal. Consumers in the United States can already order and perform the test.
An NHS Study
Arguments for different endpoints apparently resonated with the United Kingdom’s National Health Service (NHS). Three years ago, they initiated the Galleri study, a large randomized controlled trial to assess the effectiveness of Grail’s cancer test. The primary endpoint was not cancer-specific mortality, but the incidence of stage III or IV cancer.
The results are expected in 2026. But recruitment was stopped after 140,000 participants were enrolled. The NHS reported that the initial results were not convincing enough to continue the trial. Exact numbers were not disclosed.
The Galleri study deviates from the standard randomized controlled trial design for cancer screening procedures not only in terms of the primary endpoint, but also in blinding. The only participants who were unblinded and informed of their test results are those in the intervention group with a positive cancer test.
False Security
This trial design encourages participants to undergo blood tests once per year. But according to Dr. Robbins, it prevents the exploration of the phenomenon of “false security,” which is a potential drawback of the new cancer tests.
“Women with a negative mammogram can reasonably assume that they probably do not have breast cancer. But individuals with a negative cancer blood test could mistakenly believe they cannot have any cancer at all. As a result, they may not undergo standard early detection screenings or seek medical help early enough for potential cancer symptoms,” said Dr. Robbins.
To assess the actual risk-benefit ratio of the Galleri test, participants must receive their test results, she said. “Under real-world conditions, benefits and risks can come from positive and negative results.”
Upcoming Trial
More illuminating results may come from a large trial planned by the National Cancer Institute in the United States. Several new cancer tests will be evaluated for their ability to reduce cancer-specific mortality. A pilot phase will start later in 2024. “This study may be the only one with sufficient statistical power to determine whether an approach based on these cancer tests can reduce cancer-specific mortality,” said Dr. Robbins.
For the new blood tests for multiple cancers, it is crucial that health authorities “set a high bar for a benefit,” she said. This, according to her, also means that they must show an effect on cancer-specific mortality before being introduced. “This evidence must come from studies in which commercial interests do not influence the design, execution, data management, or data analysis.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version appeared on Medscape.com.
Biotech startups worldwide are rushing to market screening tests that they claim can detect various cancers in early stages with just a few drops of blood. The tests allegedly will simplify cancer care by eliminating tedious scans, scopes, and swabs at the doctor’s office.
The promise of these early detection tests is truly “enticing,” Hilary A. Robbins, PhD, from the International Agency for Research on Cancer of the World Health Organization in Lyon, France, said in an interview.
In an opinion article in The New England Journal of Medicine, she emphasized that the new cancer tests are much less cumbersome than traditional screening strategies for individual cancers. Moreover, they could enable the early detection of dozens of cancer types for which no screening has been available so far.
Meeting the Criteria
The problem is that these tests have not met the strict criteria typically required for traditional cancer screening tests. To be considered for introduction as a screening procedure, a test usually needs to meet the following four minimum requirements:
- The disease that the test screens for must have a presymptomatic form.
- The screening test must be able to identify this presymptomatic disease.
- Treating the disease in the presymptomatic phase improves prognosis (specifically, it affects cancer-specific mortality in a randomized controlled trial).
- The screening test is feasible, and the benefits outweigh potential risks.
“The new blood tests for multiple cancers have so far only met the second criteria, showing they can detect presymptomatic cancer,” Dr. Robbins wrote.
The next step would be to demonstrate that they affect cancer-specific mortality. “But currently, commercial interests seem to be influencing the evidence standards for these cancer tests,” said Dr. Robbins.
Inappropriate Endpoints?
Some proponents of such tests argue that, unlike for previous cancer screening procedures, initial approval should not depend on the endpoint of cancer-specific mortality. It would take too long to gather sufficient outcome data, and in the meantime, people would die, they argue.
Eric A. Klein, MD, from the Glickman Urological and Kidney Institute in Cleveland, Ohio, and colleagues advocate for alternative endpoints such as the incidence of late-stage cancer in an article published in Cancer Epidemiology, Biomarkers & Prevention.
“The concept would be,” they wrote, “that a negative signal would not indicate a mortality benefit, leading to the study being stopped. A positive signal, on the other hand, could result in provisional approval until mortality data and real-world evidence of effectiveness are available. This would resemble the accelerated approval of new cancer drugs, which often is based on progression-free survival until there postmarketing data on overall survival emerge.”
Dr. Klein is also employed at the US biotech start-up Grail, which developed the Galleri test, which is one of the best-known and most advanced cancer screening tests. The Galleri test uses cell-free DNA and machine learning to detect a common cancer signal in more than 50 cancer types and predict the origin of the cancer signal. Consumers in the United States can already order and perform the test.
An NHS Study
Arguments for different endpoints apparently resonated with the United Kingdom’s National Health Service (NHS). Three years ago, they initiated the Galleri study, a large randomized controlled trial to assess the effectiveness of Grail’s cancer test. The primary endpoint was not cancer-specific mortality, but the incidence of stage III or IV cancer.
The results are expected in 2026. But recruitment was stopped after 140,000 participants were enrolled. The NHS reported that the initial results were not convincing enough to continue the trial. Exact numbers were not disclosed.
The Galleri study deviates from the standard randomized controlled trial design for cancer screening procedures not only in terms of the primary endpoint, but also in blinding. The only participants who were unblinded and informed of their test results are those in the intervention group with a positive cancer test.
False Security
This trial design encourages participants to undergo blood tests once per year. But according to Dr. Robbins, it prevents the exploration of the phenomenon of “false security,” which is a potential drawback of the new cancer tests.
“Women with a negative mammogram can reasonably assume that they probably do not have breast cancer. But individuals with a negative cancer blood test could mistakenly believe they cannot have any cancer at all. As a result, they may not undergo standard early detection screenings or seek medical help early enough for potential cancer symptoms,” said Dr. Robbins.
To assess the actual risk-benefit ratio of the Galleri test, participants must receive their test results, she said. “Under real-world conditions, benefits and risks can come from positive and negative results.”
Upcoming Trial
More illuminating results may come from a large trial planned by the National Cancer Institute in the United States. Several new cancer tests will be evaluated for their ability to reduce cancer-specific mortality. A pilot phase will start later in 2024. “This study may be the only one with sufficient statistical power to determine whether an approach based on these cancer tests can reduce cancer-specific mortality,” said Dr. Robbins.
For the new blood tests for multiple cancers, it is crucial that health authorities “set a high bar for a benefit,” she said. This, according to her, also means that they must show an effect on cancer-specific mortality before being introduced. “This evidence must come from studies in which commercial interests do not influence the design, execution, data management, or data analysis.”
This story was translated from the Medscape German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version appeared on Medscape.com.
Jeffrey Weber, MD, PhD, Giant of Cancer Care, Dies
Dr. Weber, a melanoma and cancer immunotherapy specialist, served as deputy director of the Laura and Isaac Perlmutter Cancer Center at New York University (NYU) Langone Medical Center in New York City. He also held positions as the Laura and Isaac Perlmutter Professor of Oncology in the Department of Medicine at the NYU Grossman School of Medicine, director of the Experimental Therapeutics Program, and co-leader of the Clinical Melanoma Program Board at NYU Langone Health.
Dr. Weber was a principal investigator on many studies, including pivotal clinical drug trials in melanoma and trials focused on managing autoimmune side effects from immunotherapy. He published more than 150 articles in top peer-reviewed journals.
For many years, Dr. Weber hosted the popular “Weber on Oncology” series of video contributions for Medscape Oncology, sharing updates and insights on noteworthy research and breakthroughs in melanoma.
“The Melanoma Research Alliance mourns the passing of Dr. Jeffrey S. Weber, a true pioneer in the field of cancer immunotherapy and an extraordinary leader in melanoma research. His contributions have forever changed the landscape of melanoma treatment, bringing groundbreaking advances from the lab into clinical practice and offering hope to countless patients,” the Melanoma Research Alliance posted on LinkedIn.
Many X users also shared condolences and memories of Dr. Weber, praising his numerous contributions and accomplishments.
“[Cancer Research Institute] mourns the loss of Dr. Jeffrey S. Weber ... [a]s an accomplished physician scientist, Dr. Weber drove advances in melanoma research, and played an active role in educating patients about the lifesaving power of immunotherapy,” the Cancer Research Institute posted.
A colleague noted that “[h]e was involved in the early days of cytokine and cell therapy and most recently led studies of personalized vaccines for melanoma patients. ... He was a great friend and colleague to many of us in the melanoma and immunotherapy field and we will remember him as a pioneer, thought leader and compassionate physician.”
A version of this article first appeared on Medscape.com.
Dr. Weber, a melanoma and cancer immunotherapy specialist, served as deputy director of the Laura and Isaac Perlmutter Cancer Center at New York University (NYU) Langone Medical Center in New York City. He also held positions as the Laura and Isaac Perlmutter Professor of Oncology in the Department of Medicine at the NYU Grossman School of Medicine, director of the Experimental Therapeutics Program, and co-leader of the Clinical Melanoma Program Board at NYU Langone Health.
Dr. Weber was a principal investigator on many studies, including pivotal clinical drug trials in melanoma and trials focused on managing autoimmune side effects from immunotherapy. He published more than 150 articles in top peer-reviewed journals.
For many years, Dr. Weber hosted the popular “Weber on Oncology” series of video contributions for Medscape Oncology, sharing updates and insights on noteworthy research and breakthroughs in melanoma.
“The Melanoma Research Alliance mourns the passing of Dr. Jeffrey S. Weber, a true pioneer in the field of cancer immunotherapy and an extraordinary leader in melanoma research. His contributions have forever changed the landscape of melanoma treatment, bringing groundbreaking advances from the lab into clinical practice and offering hope to countless patients,” the Melanoma Research Alliance posted on LinkedIn.
Many X users also shared condolences and memories of Dr. Weber, praising his numerous contributions and accomplishments.
“[Cancer Research Institute] mourns the loss of Dr. Jeffrey S. Weber ... [a]s an accomplished physician scientist, Dr. Weber drove advances in melanoma research, and played an active role in educating patients about the lifesaving power of immunotherapy,” the Cancer Research Institute posted.
A colleague noted that “[h]e was involved in the early days of cytokine and cell therapy and most recently led studies of personalized vaccines for melanoma patients. ... He was a great friend and colleague to many of us in the melanoma and immunotherapy field and we will remember him as a pioneer, thought leader and compassionate physician.”
A version of this article first appeared on Medscape.com.
Dr. Weber, a melanoma and cancer immunotherapy specialist, served as deputy director of the Laura and Isaac Perlmutter Cancer Center at New York University (NYU) Langone Medical Center in New York City. He also held positions as the Laura and Isaac Perlmutter Professor of Oncology in the Department of Medicine at the NYU Grossman School of Medicine, director of the Experimental Therapeutics Program, and co-leader of the Clinical Melanoma Program Board at NYU Langone Health.
Dr. Weber was a principal investigator on many studies, including pivotal clinical drug trials in melanoma and trials focused on managing autoimmune side effects from immunotherapy. He published more than 150 articles in top peer-reviewed journals.
For many years, Dr. Weber hosted the popular “Weber on Oncology” series of video contributions for Medscape Oncology, sharing updates and insights on noteworthy research and breakthroughs in melanoma.
“The Melanoma Research Alliance mourns the passing of Dr. Jeffrey S. Weber, a true pioneer in the field of cancer immunotherapy and an extraordinary leader in melanoma research. His contributions have forever changed the landscape of melanoma treatment, bringing groundbreaking advances from the lab into clinical practice and offering hope to countless patients,” the Melanoma Research Alliance posted on LinkedIn.
Many X users also shared condolences and memories of Dr. Weber, praising his numerous contributions and accomplishments.
“[Cancer Research Institute] mourns the loss of Dr. Jeffrey S. Weber ... [a]s an accomplished physician scientist, Dr. Weber drove advances in melanoma research, and played an active role in educating patients about the lifesaving power of immunotherapy,” the Cancer Research Institute posted.
A colleague noted that “[h]e was involved in the early days of cytokine and cell therapy and most recently led studies of personalized vaccines for melanoma patients. ... He was a great friend and colleague to many of us in the melanoma and immunotherapy field and we will remember him as a pioneer, thought leader and compassionate physician.”
A version of this article first appeared on Medscape.com.
Alert System Could Warn of Impact of Severe Weather on Health
As more data show potentially dangerous effects of climate and weather on individuals with chronic medical conditions, CVS Health has introduced an initiative that uses technology to provide weather alerts and targeted outreach to those at increased risk, according to a press release from the company. Ultimately, the goals of the initiative are to improve health, reduce emergency department visits, hospital stays, and medical costs, according to the press release.
Extreme weather events such as heat waves are becoming more frequent and severe, but most heat-related deaths are preventable with outreach and intervention, Dan Knecht, MD, vice president and chief clinical innovation officer for CVS Caremark, a division of CVS Health, said in an interview. The approach will combine the company’s services, including care managers, health centers, and data, to aid patients vulnerable to severe weather.
The initiative is starting with a focus on extreme heat events and will expand this fall with alerts about high levels of air pollution for individuals with vulnerability to reduced lung function, asthma, and cardiac problems as a result of exposure to high air-pollution levels, according to Dr. Knecht.
For now, the initiative is available to members of Aetna Medicare, according to Dr. Knecht. “Our goal is to expand to other consumers, including those who visit MinuteClinic and CVS Pharmacy locations, where we can provide timely environment-related recommendations at time of care,” he said.
The alert system uses environmental data analytics to pair highly localized forecasts and real-time insights about air quality, wildfires, and high heat with medical and pharmacy data for high-risk patients in areas affected by extreme weather.
For example, for individuals who are at risk and living in areas facing extreme heat, “registered nurse care managers proactively reach out to vulnerable patients up to several days in advance of an extreme weather event and provide them personalized tips and resources,” said Dr. Knecht.
In addition, he added, “we talk to patients about how to manage their medications during periods of extreme heat and, when delivering medications, take weather data into account to determine appropriate packaging materials for shipments.”
These interventions direct patients to CVS Health–linked resources, such as Oak Street Health clinics available as cooling centers, health services provided at MinuteClinic locations, and medication management at CVS pharmacies. Other interventions include virtual or in-person mental health counseling through MinuteClinic.
Dr. Knecht offered additional guidance for clinicians and patients to help manage heat waves. “Heat and certain medications can impair heat tolerance and the ability to regulate body temperature,” he told this news organization. Extreme heat may affect the performance of some medications and their devices, such as inhalers and diabetes supplies, he added.
Health Alerts Have Potential, But Comprehensive Approach is Needed
“Patients with chronic lung conditions are highly susceptible to the impact of climate change,” MeiLan K. Han, MD, a pulmonologist and professor of internal medicine at the University of Michigan, Ann Arbor, said in an interview. “Increasing dust, hotter temperatures, and higher levels of air pollution make it more difficult for patients to breathe,” she said. Data also suggest that higher levels of air pollution may not only cause chronic lung disease but also cause worsening symptoms among those with existing disease, she added.
A weather-related health alert could be useful for patients so they can be prepared, Dr. Han told this news organization.
“For a patient with chronic lung disease, a hot weather alert may mean that it will be harder for patients to breathe, and [they] may [be] more susceptible to heat stroke and dehydration if they do not have access to air conditioning,” she said. “At a minimum, patients should ensure they are on their controller medications, which often means a daily inhaler for patients with conditions such as asthma and chronic obstructive pulmonary disease (COPD). However, patients also should have access to their short-term reliever medications so they can be prepared for increased shortness of breath that may accompany a hot weather day,” Dr. Han explained.
However, not all patients have access to technology such as smartphones or other devices that will alert them to impending weather events, such as heat waves, said Dr. Han. “For these patients, a standard phone call may be beneficial,” she said.
Looking ahead, “programs for weather-related health alerts will need to be comprehensive, focusing not only on access to needed medications but also climate-controlled settings for temporary relief of heat,” said Dr. Han. “For some of our most vulnerable patients, while they may have air conditioning, they may not be able to afford to run it, so this needs to be considered in developing a comprehensive program,” she emphasized.
Dr. Knecht had no financial conflicts to disclose. Dr. Han disclosed ties with Aerogen, Altesa BioSciences, American Lung Association, Amgen, Apreo Health, AstraZeneca, Biodesix, Boehringer Ingelheim, Chiesi, Cipla, COPD Foundation, DevPro, Gala Therapeutics, Genentech, GlaxoSmithKline, Integrity, MDBriefcase, Medscape, Medtronic, Medwiz, Meissa Vaccines, Merck, Mylan, NACE, National Institutes of Health, Novartis, Nuvaira, Polarian, Pulmonx, Regeneron, Roche, RS Biotherapeutics, Sanofi, Sunovion, Teva, UpToDate, and Verona..
A version of this article first appeared on Medscape.com.
As more data show potentially dangerous effects of climate and weather on individuals with chronic medical conditions, CVS Health has introduced an initiative that uses technology to provide weather alerts and targeted outreach to those at increased risk, according to a press release from the company. Ultimately, the goals of the initiative are to improve health, reduce emergency department visits, hospital stays, and medical costs, according to the press release.
Extreme weather events such as heat waves are becoming more frequent and severe, but most heat-related deaths are preventable with outreach and intervention, Dan Knecht, MD, vice president and chief clinical innovation officer for CVS Caremark, a division of CVS Health, said in an interview. The approach will combine the company’s services, including care managers, health centers, and data, to aid patients vulnerable to severe weather.
The initiative is starting with a focus on extreme heat events and will expand this fall with alerts about high levels of air pollution for individuals with vulnerability to reduced lung function, asthma, and cardiac problems as a result of exposure to high air-pollution levels, according to Dr. Knecht.
For now, the initiative is available to members of Aetna Medicare, according to Dr. Knecht. “Our goal is to expand to other consumers, including those who visit MinuteClinic and CVS Pharmacy locations, where we can provide timely environment-related recommendations at time of care,” he said.
The alert system uses environmental data analytics to pair highly localized forecasts and real-time insights about air quality, wildfires, and high heat with medical and pharmacy data for high-risk patients in areas affected by extreme weather.
For example, for individuals who are at risk and living in areas facing extreme heat, “registered nurse care managers proactively reach out to vulnerable patients up to several days in advance of an extreme weather event and provide them personalized tips and resources,” said Dr. Knecht.
In addition, he added, “we talk to patients about how to manage their medications during periods of extreme heat and, when delivering medications, take weather data into account to determine appropriate packaging materials for shipments.”
These interventions direct patients to CVS Health–linked resources, such as Oak Street Health clinics available as cooling centers, health services provided at MinuteClinic locations, and medication management at CVS pharmacies. Other interventions include virtual or in-person mental health counseling through MinuteClinic.
Dr. Knecht offered additional guidance for clinicians and patients to help manage heat waves. “Heat and certain medications can impair heat tolerance and the ability to regulate body temperature,” he told this news organization. Extreme heat may affect the performance of some medications and their devices, such as inhalers and diabetes supplies, he added.
Health Alerts Have Potential, But Comprehensive Approach is Needed
“Patients with chronic lung conditions are highly susceptible to the impact of climate change,” MeiLan K. Han, MD, a pulmonologist and professor of internal medicine at the University of Michigan, Ann Arbor, said in an interview. “Increasing dust, hotter temperatures, and higher levels of air pollution make it more difficult for patients to breathe,” she said. Data also suggest that higher levels of air pollution may not only cause chronic lung disease but also cause worsening symptoms among those with existing disease, she added.
A weather-related health alert could be useful for patients so they can be prepared, Dr. Han told this news organization.
“For a patient with chronic lung disease, a hot weather alert may mean that it will be harder for patients to breathe, and [they] may [be] more susceptible to heat stroke and dehydration if they do not have access to air conditioning,” she said. “At a minimum, patients should ensure they are on their controller medications, which often means a daily inhaler for patients with conditions such as asthma and chronic obstructive pulmonary disease (COPD). However, patients also should have access to their short-term reliever medications so they can be prepared for increased shortness of breath that may accompany a hot weather day,” Dr. Han explained.
However, not all patients have access to technology such as smartphones or other devices that will alert them to impending weather events, such as heat waves, said Dr. Han. “For these patients, a standard phone call may be beneficial,” she said.
Looking ahead, “programs for weather-related health alerts will need to be comprehensive, focusing not only on access to needed medications but also climate-controlled settings for temporary relief of heat,” said Dr. Han. “For some of our most vulnerable patients, while they may have air conditioning, they may not be able to afford to run it, so this needs to be considered in developing a comprehensive program,” she emphasized.
Dr. Knecht had no financial conflicts to disclose. Dr. Han disclosed ties with Aerogen, Altesa BioSciences, American Lung Association, Amgen, Apreo Health, AstraZeneca, Biodesix, Boehringer Ingelheim, Chiesi, Cipla, COPD Foundation, DevPro, Gala Therapeutics, Genentech, GlaxoSmithKline, Integrity, MDBriefcase, Medscape, Medtronic, Medwiz, Meissa Vaccines, Merck, Mylan, NACE, National Institutes of Health, Novartis, Nuvaira, Polarian, Pulmonx, Regeneron, Roche, RS Biotherapeutics, Sanofi, Sunovion, Teva, UpToDate, and Verona..
A version of this article first appeared on Medscape.com.
As more data show potentially dangerous effects of climate and weather on individuals with chronic medical conditions, CVS Health has introduced an initiative that uses technology to provide weather alerts and targeted outreach to those at increased risk, according to a press release from the company. Ultimately, the goals of the initiative are to improve health, reduce emergency department visits, hospital stays, and medical costs, according to the press release.
Extreme weather events such as heat waves are becoming more frequent and severe, but most heat-related deaths are preventable with outreach and intervention, Dan Knecht, MD, vice president and chief clinical innovation officer for CVS Caremark, a division of CVS Health, said in an interview. The approach will combine the company’s services, including care managers, health centers, and data, to aid patients vulnerable to severe weather.
The initiative is starting with a focus on extreme heat events and will expand this fall with alerts about high levels of air pollution for individuals with vulnerability to reduced lung function, asthma, and cardiac problems as a result of exposure to high air-pollution levels, according to Dr. Knecht.
For now, the initiative is available to members of Aetna Medicare, according to Dr. Knecht. “Our goal is to expand to other consumers, including those who visit MinuteClinic and CVS Pharmacy locations, where we can provide timely environment-related recommendations at time of care,” he said.
The alert system uses environmental data analytics to pair highly localized forecasts and real-time insights about air quality, wildfires, and high heat with medical and pharmacy data for high-risk patients in areas affected by extreme weather.
For example, for individuals who are at risk and living in areas facing extreme heat, “registered nurse care managers proactively reach out to vulnerable patients up to several days in advance of an extreme weather event and provide them personalized tips and resources,” said Dr. Knecht.
In addition, he added, “we talk to patients about how to manage their medications during periods of extreme heat and, when delivering medications, take weather data into account to determine appropriate packaging materials for shipments.”
These interventions direct patients to CVS Health–linked resources, such as Oak Street Health clinics available as cooling centers, health services provided at MinuteClinic locations, and medication management at CVS pharmacies. Other interventions include virtual or in-person mental health counseling through MinuteClinic.
Dr. Knecht offered additional guidance for clinicians and patients to help manage heat waves. “Heat and certain medications can impair heat tolerance and the ability to regulate body temperature,” he told this news organization. Extreme heat may affect the performance of some medications and their devices, such as inhalers and diabetes supplies, he added.
Health Alerts Have Potential, But Comprehensive Approach is Needed
“Patients with chronic lung conditions are highly susceptible to the impact of climate change,” MeiLan K. Han, MD, a pulmonologist and professor of internal medicine at the University of Michigan, Ann Arbor, said in an interview. “Increasing dust, hotter temperatures, and higher levels of air pollution make it more difficult for patients to breathe,” she said. Data also suggest that higher levels of air pollution may not only cause chronic lung disease but also cause worsening symptoms among those with existing disease, she added.
A weather-related health alert could be useful for patients so they can be prepared, Dr. Han told this news organization.
“For a patient with chronic lung disease, a hot weather alert may mean that it will be harder for patients to breathe, and [they] may [be] more susceptible to heat stroke and dehydration if they do not have access to air conditioning,” she said. “At a minimum, patients should ensure they are on their controller medications, which often means a daily inhaler for patients with conditions such as asthma and chronic obstructive pulmonary disease (COPD). However, patients also should have access to their short-term reliever medications so they can be prepared for increased shortness of breath that may accompany a hot weather day,” Dr. Han explained.
However, not all patients have access to technology such as smartphones or other devices that will alert them to impending weather events, such as heat waves, said Dr. Han. “For these patients, a standard phone call may be beneficial,” she said.
Looking ahead, “programs for weather-related health alerts will need to be comprehensive, focusing not only on access to needed medications but also climate-controlled settings for temporary relief of heat,” said Dr. Han. “For some of our most vulnerable patients, while they may have air conditioning, they may not be able to afford to run it, so this needs to be considered in developing a comprehensive program,” she emphasized.
Dr. Knecht had no financial conflicts to disclose. Dr. Han disclosed ties with Aerogen, Altesa BioSciences, American Lung Association, Amgen, Apreo Health, AstraZeneca, Biodesix, Boehringer Ingelheim, Chiesi, Cipla, COPD Foundation, DevPro, Gala Therapeutics, Genentech, GlaxoSmithKline, Integrity, MDBriefcase, Medscape, Medtronic, Medwiz, Meissa Vaccines, Merck, Mylan, NACE, National Institutes of Health, Novartis, Nuvaira, Polarian, Pulmonx, Regeneron, Roche, RS Biotherapeutics, Sanofi, Sunovion, Teva, UpToDate, and Verona..
A version of this article first appeared on Medscape.com.
Private Equity in Medicine: Cardiology in the Crosshairs
This transcript has been edited for clarity.
Robert A. Harrington, MD: I’m continuing my series of conversations with leaders in the field of cardiovascular medicine who are working on interesting projects and making contributions in the science and policy space. We have three guests joining us today who have recently written two papers in the Journal of the American College of Cardiology. One is an original research paper dealing with the issue of private equity’s acquisition of outpatient cardiology practices. And the second is an editorial that really tries to get at why this is happening. Is it a problem? Is it a solution to a problem?
Fortunately, I have all three as guests to think about this important issue that has implications for clinical care, reimbursement, physician wellness, and clinician wellness, and it has implications regarding public policy and how we should be thinking about the practice of medicine in this country.
Dr. Victoria L. Bartlett is an internal medicine resident at Brigham and Women’s Hospital in Boston, and a research fellow in the Smith Center at the Beth Israel Lahey medical center in Boston. Dr Rishi K. Wadhera is the senior author of the paper written by Dr. Bartlett. Dr. Rishi is associate professor of medicine at Harvard Medical School, and he is the associate director of the Smith Center at Beth Israel Lahey.
Rishi K. Wadhera, MD, MPP, MPhil: Thanks for having us, Bob.
Dr. Harrington: The editorialist, Dr. Ed Fry, is the national service line leader for cardiovascular medicine, for Ascension Health. Dr. Frey is a recent past president of the American College of Cardiology (ACC).
Edward T. A. Fry, MD: Great to be here. Thanks.
What is private equity? Why the interest in medicine?
Dr. Harrington: I was intrigued by the papers and it caused me to do a deeper dive into some of the earlier works that you have referenced about this growing topic of private equity making its way into medical practice. Rishi, I’ll start with you. For the casual reader like myself, what is the business of private equity?
Dr. Wadhera: Private equity firms basically used pooled investments from multiple sources. These can be individual and institutional investors, pension funds, endowments, and they use those funds to invest in private companies that have the potential to return a profit. The goal really is to turn a profit for institutional investors over a shorter time horizon.
Dr. Harrington: How do they do that? I can understand, you buy a factory and you want to make the factory a little more efficient, and you think that perhaps, by combining some technologies, etc., that you might have in other factories, you can drive more value out of the one you just invested in in a short period of time. What’s the general business sense of how they’re going to do that in a cardiology practice? Is it all about making us more efficient?
Dr. Wadhera: Operational efficiency is the overarching theme here. One could argue that perhaps, private equity firms have the expertise to bring that kind of organizational know-how and operational efficiency to medicine. But there’s evidence that the way that private equity firms maximize their margin is maybe through mechanisms that aren’t necessarily good for patient care, such as reduced nursing staffing. When private equity acquires hospitals or practices in the same location, they have greater negotiating power at the payer table, to have higher prices for the services they deliver. There’s a lot of discussion about whether the sort of changes that private equity firms tend to implement are good or bad for patient care and also for clinicians.
Dr. Harrington: Great summary. Ed. Why is this happening in medicine? What did we do in medicine that made us ripe for investment by private equity? When you and I started out years ago, I don’t think we ever would have thought that this was in the future.
Dr. Fry: I think number one, as we know, is that medicine represents about 20% of our economy. There are huge amounts of money involved in these considerations. If players in this space can access even a small fraction of that money, it’s a lot of money and a lot of incentive for them.
In medicine in general, and then maybe more specifically, in cardiology, we’ve seen a shift away from private practice into employed practice. When people made those decisions over the past 10-15 years, there were certainly positives and risks that they took. I think for some, along the way, they realized that perhaps they gave up more than they thought in terms of control and running their own business and the opportunity to shape that themselves and be rewarded for that as they were in private practice. In cardiology, more specifically, we’ve seen this shift to the outpatient space: moving diagnostics and even therapeutics into ambulatory surgical centers and outpatient-based labs, and that is another potential source of revenue for these private equity companies.
As I wrote in the editorial, there are certainly a lot of pressures and frustrations that the day-to-day clinician feels, and maybe, this move to private equity is more of a symptom of those concerns and that this could be an opportunity to take the bull by the horns again in cardiology. We’ve evolved from a predominantly hospital-based acute care specialty into one of diagnosis, chronic disease management, and longitudinal care punctuated by diagnostics and therapeutics, which are, again, I think, attractive to private equity firms as potential sources for revenue.
Dr. Harrington: Ed, why cardiology? What’s happened over the years that has led to that appearance, if you will, of private equity and cardiovascular medicine?
Dr. Fry: Some of the earlier specialties were dermatology, ophthalmology, and gastroenterology, in particular. And interestingly, those tend to be specialties that have less chronic disease management and are more based on procedures and things like that. Within cardiology, obviously, the big driver is that our population is aging: 11,000 people turn 65 every day and become eligible for Medicare. With that, we see a rise in disease prevalence and then the rise in risk factors, obviously, with obesity and diabetes driving that, so there are more people who are going to have an illness that requires evaluation, diagnostics, and procedures. Because of that, it is a very target rich environment for private equity.
Dr. Harrington: That’s great background. Now, let’s dive into what you did, Victoria. What got you interested in the question? And give us some background on the literature that you were trying to build upon when you asked your series of questions.
Victoria L. Bartlett, MD: There’s been a lot of interest in private equity acquisitions and healthcare. A lot of the existing literature has been around hospital acquisitions and what happens there. There’s some literature, as you’ve mentioned, in outpatient practices, in certain specialties, where private equity has existed a little bit longer than in cardiology. They’ve been asking really similar questions to what we have been asking about cardiology, which is what happens when practices are acquired.
A kind of overview is that many of those studies have found increased costs to payers, to patients, and many have also found evidence of decreased quality. The evidence for the latter is honestly more difficult to figure out, but there has been evidence of decreased nursing ratios in nursing homes. There’s been evidence of changing the mix in clinics to more advanced practice providers than physicians. There’s been some evidence in hospitals that maybe quality doesn’t change too much. But the deeper layer under that is that these private equity–acquired hospitals may be selecting certain patients that are less sick, that are not going to negatively affect their metrics as much. That’s the environment that we had been reading about and starting to ask: Are we seeing that in cardiology too?
Dr. Harrington: Share with the audience what you did. You took what I would call a descriptive approach to try to understand the current landscape in cardiovascular medicine. As Ed already pointed out, a lot of the earlier data does not concern cardiology practices. My read of your paper is that you were trying to at least lay the groundwork for us to understand as a community what’s going on out there. Is that a fair interpretation?
Dr. Bartlett: Absolutely. Even that initial question of what’s happening is more challenging than it seems it might be to answer, partly because with private equity, these are private transactions. They don’t have to publicly report anything. So there’s a lot of manual work to gather these data. Our first questions were: What are these transactions? When are they happening? Where are they happening? What are the clinics that private equity is interested in? What are the community characteristics of those clinics? And what could that tell us about what’s going on?
Who Is Getting Acquired?
Dr. Harrington: Tell the audience broadly what you found. What are those clinics? And how often does this happen?
Dr. Bartlett: We looked at acquisitions between 2013 and 2023, and in that 10-year span, we found 41 acquisitions of outpatient cardiology practices, which corresponded to 342 acquisitions of clinics. The vast majority of these, pretty much 95%, occurred between 2021 and 2023. We calculated that about 3% of cardiology clinics in the US are owned by private equity. The states with the highest number of acquisitions were Florida, Texas, and Arizona, and particularly the urban areas in those states, ie, Jacksonville, Houston, Dallas. And interestingly, that mirrors what we’ve seen before in anesthesia and dermatology.
Our last question was around community characteristics, we looked at several that had a statistically significant association with private equity acquisition, and we found that private equity firms were less likely to acquire clinics in the highest poverty communities. Within the communities, we looked at the proportion of adults over 65, the proportion of racial and ethnic minorities, educational level, rurality, and didn’t find any significant associations between private equity acquisition and those characteristics.
Dr. Harrington: Thank you. Rishi, do you want to interpret why private equity was targeting certain areas?
Dr. Wadhera: Private equity goes where they can actually acquire practices. Those states, in particular, have more independent practices than, say, Massachusetts does. Then there’s the target population available in those states. Building on what Ed said earlier, why all of a sudden? Because Victoria just pointed out that the vast majority of these acquisitions happened between 2020 and 2023 and you see the surge, and I expect that surge to continue over the next several years. And the question is why?
We know with the rise in cardiometabolic risk factors at a population level, that the cardiovascular disease is only going to become more common. Cardiac procedures are very well reimbursed. There’s likely a lot of appeal in entering a specialty with a highly profitable service line. Over the past decade, federal policymakers very intentionally have created incentives to shift the delivery of cardiac procedures to nonhospital settings. We see that with the rise of ambulatory surgical centers and more cardiac procedures are being reimbursed in these types of settings. And I think that private equity firms may see this as an opportunity to maximize profits.
Victoria created this beautiful map in our study that showed how concentrated these acquisitions are. They really concentrated in specific markets. And I think that parallels what we’re seeing with health systems more broadly, this consolidation, and concentration is the ultimate goal. These different stakeholders, it’s not just private equity, have more market power, so that when they go to insurers, they can demand higher prices for procedures and services.
Dr. Harrington: It’s hard to look at the dates of 2021 or 2020 to 2023, and not wonder if there is a COVID effect. Victoria, do you think there’s a COVID effect, or is it just true, true, unrelated?
Dr. Bartlett: COVID definitely put a lot of financial pressure on providers, and particularly small independent practices. They would have felt that the most, and I certainly think is a piece of the picture but may not be all the picture.
Dr. Harrington: That’s what I would have guessed. We were all under financial pressures, but the small, independent practices didn’t have the big health system behind them to backstop things. Ed, as a former leader of the ACC, and the ACC very much works at the local level, are you hearing from the governors of these states that this is an issue, and not hearing from other states?
Dr. Fry: Certainly this activity is concentrated in the states that Victoria and Rishi described for the reasons that they outlined. This is still a very small number and probably will remain relatively small if we consider that 85% of cardiologists are employed, and the bar to exit an employment arrangement and enter into a private equity situation is pretty darn high. There’s a lot of costs associated with that. So it may have a finite cap to it, and that may be part of what buffers some of the response.
I would like to go back and address other reasons why this is happening. Particularly because of the aging population of cardiovascular patients, we’ve also seen the rise of Medicare Advantage, which is a type of value, if you consider it a type of value-based care. There are incentives built into Medicare Advantage to manage costs and to do various things so there is certainly a reward incentive. I am not wearing my hat as a representative of the ACC nor Ascension, and I will probably be a consumer of these services before I’m ever a participant, but I would say that private equity in some respects, is acting as a disruptor in this entire process. One of the positive outcomes from this is for a reevaluation of the role of clinicians in the overall delivery of care for health systems and academic medical centers. I think that can be a positive; I always try to look at the bright side of things too.
Patient and Clinician Satisfaction
Dr. Harrington: To your last comment. Ed, maybe I’ll ask you Rishi or Victoria, any insights into clinician wellness, how people feel when their practice has been bought by private equity? Are there any data out there?
Dr. Wadhera: Not that I know of. I will say that we have a study under review right now that doesn’t answer your question directly, Bob, but that looks at how private equity acquisitions of US hospitals affect the patient care experience. And what we found, using a rigorous, quasi experimental study design comparing private equity–acquired hospitals to neighboring control hospitals, is that private equity acquisition leads to a pretty marked decrease in patient care experience and satisfaction.
That’s capturing another dimension of quality that mortality and readmissions don’t necessarily reflect. It doesn’t answer your question directly, but I think an important area for future research is understanding the effects on the clinician experience as well as, most importantly, the patient experience.
Dr. Harrington: Nicely said, it seems like a good time to think about mixed qualitative methods such as focus groups, etc., coupled with the more quantitative research methods. Victoria, I suspect you talked to people in acquired practices. Any insight into whether it’s observational or rigorous data on the clinician experience?
Dr. Bartlett: Not that I have seen. I imagine it’s probably mixed because as we’ve been saying, there’s a lot of financial pressure on practices, small, independent practices, and it can become overwhelming to run them. Private equity firms offer a very attractive value proposition or can. But I think it’s a great point that should be highlighted.
Dr. Harrington: Ed, taking off your cardiovascular leadership hat, not representing any specific organization, what are the policy things that we should be thinking about?
Dr. Fry: There’s an opportunity to combine these conversations around research, collecting more data, and the advocacy issues related to that. One of the things that perhaps differentiates cardiology in this space from other specialties, or subspecialties, surgical subspecialties, is the plethora of data that we already have with well-established registry tools. We have good benchmarks. From a professional society standpoint, we have an obligation to make sure that the care that is provided in whatever environment meets the standards and is measurable, reportable, and provides a level of consumerism to patients and payers to be able to look at that. I think we have an obligation to advocate for the use of well-validated registry tools to track the data, to have objective data, to be able to demonstrate outcomes.
Interestingly, there’s an ACC/American Heart Association policy document from 2020 on professionalism and ethics in cardiology. And it calls for the obligation of the profession to make sure that in alternative sites of care, that we are achieving at least as good a result, if not better. We have to be true to that.
Dr. Harrington: I was actually a coauthor on that paper on professionalism and talking about some of the research and education issues within the academic medical centers. You’re spot on. And I love the comment about the importance of long-standing registries, whether maintained by the ACC, the Heart Association, or the Society of Thoracic Surgeons, where we can get insights into the quality issues.
We need more work done on the patient experience, the clinician experience, but I also take the positive, Ed, that this may be a disruptor that could lend itself to some positive change in other areas that need to change.
This has been a fantastic conversation on the appearance, if you will, of private equity in cardiovascular medicine and some of the observations made by colleagues at the Smith Center at the Beth Israel Lahey, with great commentary by Ed Fry on whether this is a symptom or a solution and what we should be thinking about from a broader societal perspective. I want to thank my three guests today, Victoria, Ed, and Rishi, for joining us here.
Dr. Harrington is the Stephen and Suzanne Weiss Dean of Weill Cornell Medicine and provost for medical affairs of Cornell University, as well as a former president of the American Heart Association. He disclosed ties with several companies. Dr. Bartlett is resident physician, Department of Internal Medicine, Brigham & women’s Hospital, Boston, and has disclosed no relevant financial relationships. Dr. Fry is chair, Ascension National Cardiovascular Service Line, Ascension St. Vincent Heart Center in Indianapolis, Indiana. Dr. Wadhera is associate professor, Harvard Medical School, and associate director, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center, both in Boston. Dr. Wadhera disclosed ties with Abbott, ChamberCardio, CVS Health, the National Institutes of Health, American Heart Association, and the Donaghue Foundation.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert A. Harrington, MD: I’m continuing my series of conversations with leaders in the field of cardiovascular medicine who are working on interesting projects and making contributions in the science and policy space. We have three guests joining us today who have recently written two papers in the Journal of the American College of Cardiology. One is an original research paper dealing with the issue of private equity’s acquisition of outpatient cardiology practices. And the second is an editorial that really tries to get at why this is happening. Is it a problem? Is it a solution to a problem?
Fortunately, I have all three as guests to think about this important issue that has implications for clinical care, reimbursement, physician wellness, and clinician wellness, and it has implications regarding public policy and how we should be thinking about the practice of medicine in this country.
Dr. Victoria L. Bartlett is an internal medicine resident at Brigham and Women’s Hospital in Boston, and a research fellow in the Smith Center at the Beth Israel Lahey medical center in Boston. Dr Rishi K. Wadhera is the senior author of the paper written by Dr. Bartlett. Dr. Rishi is associate professor of medicine at Harvard Medical School, and he is the associate director of the Smith Center at Beth Israel Lahey.
Rishi K. Wadhera, MD, MPP, MPhil: Thanks for having us, Bob.
Dr. Harrington: The editorialist, Dr. Ed Fry, is the national service line leader for cardiovascular medicine, for Ascension Health. Dr. Frey is a recent past president of the American College of Cardiology (ACC).
Edward T. A. Fry, MD: Great to be here. Thanks.
What is private equity? Why the interest in medicine?
Dr. Harrington: I was intrigued by the papers and it caused me to do a deeper dive into some of the earlier works that you have referenced about this growing topic of private equity making its way into medical practice. Rishi, I’ll start with you. For the casual reader like myself, what is the business of private equity?
Dr. Wadhera: Private equity firms basically used pooled investments from multiple sources. These can be individual and institutional investors, pension funds, endowments, and they use those funds to invest in private companies that have the potential to return a profit. The goal really is to turn a profit for institutional investors over a shorter time horizon.
Dr. Harrington: How do they do that? I can understand, you buy a factory and you want to make the factory a little more efficient, and you think that perhaps, by combining some technologies, etc., that you might have in other factories, you can drive more value out of the one you just invested in in a short period of time. What’s the general business sense of how they’re going to do that in a cardiology practice? Is it all about making us more efficient?
Dr. Wadhera: Operational efficiency is the overarching theme here. One could argue that perhaps, private equity firms have the expertise to bring that kind of organizational know-how and operational efficiency to medicine. But there’s evidence that the way that private equity firms maximize their margin is maybe through mechanisms that aren’t necessarily good for patient care, such as reduced nursing staffing. When private equity acquires hospitals or practices in the same location, they have greater negotiating power at the payer table, to have higher prices for the services they deliver. There’s a lot of discussion about whether the sort of changes that private equity firms tend to implement are good or bad for patient care and also for clinicians.
Dr. Harrington: Great summary. Ed. Why is this happening in medicine? What did we do in medicine that made us ripe for investment by private equity? When you and I started out years ago, I don’t think we ever would have thought that this was in the future.
Dr. Fry: I think number one, as we know, is that medicine represents about 20% of our economy. There are huge amounts of money involved in these considerations. If players in this space can access even a small fraction of that money, it’s a lot of money and a lot of incentive for them.
In medicine in general, and then maybe more specifically, in cardiology, we’ve seen a shift away from private practice into employed practice. When people made those decisions over the past 10-15 years, there were certainly positives and risks that they took. I think for some, along the way, they realized that perhaps they gave up more than they thought in terms of control and running their own business and the opportunity to shape that themselves and be rewarded for that as they were in private practice. In cardiology, more specifically, we’ve seen this shift to the outpatient space: moving diagnostics and even therapeutics into ambulatory surgical centers and outpatient-based labs, and that is another potential source of revenue for these private equity companies.
As I wrote in the editorial, there are certainly a lot of pressures and frustrations that the day-to-day clinician feels, and maybe, this move to private equity is more of a symptom of those concerns and that this could be an opportunity to take the bull by the horns again in cardiology. We’ve evolved from a predominantly hospital-based acute care specialty into one of diagnosis, chronic disease management, and longitudinal care punctuated by diagnostics and therapeutics, which are, again, I think, attractive to private equity firms as potential sources for revenue.
Dr. Harrington: Ed, why cardiology? What’s happened over the years that has led to that appearance, if you will, of private equity and cardiovascular medicine?
Dr. Fry: Some of the earlier specialties were dermatology, ophthalmology, and gastroenterology, in particular. And interestingly, those tend to be specialties that have less chronic disease management and are more based on procedures and things like that. Within cardiology, obviously, the big driver is that our population is aging: 11,000 people turn 65 every day and become eligible for Medicare. With that, we see a rise in disease prevalence and then the rise in risk factors, obviously, with obesity and diabetes driving that, so there are more people who are going to have an illness that requires evaluation, diagnostics, and procedures. Because of that, it is a very target rich environment for private equity.
Dr. Harrington: That’s great background. Now, let’s dive into what you did, Victoria. What got you interested in the question? And give us some background on the literature that you were trying to build upon when you asked your series of questions.
Victoria L. Bartlett, MD: There’s been a lot of interest in private equity acquisitions and healthcare. A lot of the existing literature has been around hospital acquisitions and what happens there. There’s some literature, as you’ve mentioned, in outpatient practices, in certain specialties, where private equity has existed a little bit longer than in cardiology. They’ve been asking really similar questions to what we have been asking about cardiology, which is what happens when practices are acquired.
A kind of overview is that many of those studies have found increased costs to payers, to patients, and many have also found evidence of decreased quality. The evidence for the latter is honestly more difficult to figure out, but there has been evidence of decreased nursing ratios in nursing homes. There’s been evidence of changing the mix in clinics to more advanced practice providers than physicians. There’s been some evidence in hospitals that maybe quality doesn’t change too much. But the deeper layer under that is that these private equity–acquired hospitals may be selecting certain patients that are less sick, that are not going to negatively affect their metrics as much. That’s the environment that we had been reading about and starting to ask: Are we seeing that in cardiology too?
Dr. Harrington: Share with the audience what you did. You took what I would call a descriptive approach to try to understand the current landscape in cardiovascular medicine. As Ed already pointed out, a lot of the earlier data does not concern cardiology practices. My read of your paper is that you were trying to at least lay the groundwork for us to understand as a community what’s going on out there. Is that a fair interpretation?
Dr. Bartlett: Absolutely. Even that initial question of what’s happening is more challenging than it seems it might be to answer, partly because with private equity, these are private transactions. They don’t have to publicly report anything. So there’s a lot of manual work to gather these data. Our first questions were: What are these transactions? When are they happening? Where are they happening? What are the clinics that private equity is interested in? What are the community characteristics of those clinics? And what could that tell us about what’s going on?
Who Is Getting Acquired?
Dr. Harrington: Tell the audience broadly what you found. What are those clinics? And how often does this happen?
Dr. Bartlett: We looked at acquisitions between 2013 and 2023, and in that 10-year span, we found 41 acquisitions of outpatient cardiology practices, which corresponded to 342 acquisitions of clinics. The vast majority of these, pretty much 95%, occurred between 2021 and 2023. We calculated that about 3% of cardiology clinics in the US are owned by private equity. The states with the highest number of acquisitions were Florida, Texas, and Arizona, and particularly the urban areas in those states, ie, Jacksonville, Houston, Dallas. And interestingly, that mirrors what we’ve seen before in anesthesia and dermatology.
Our last question was around community characteristics, we looked at several that had a statistically significant association with private equity acquisition, and we found that private equity firms were less likely to acquire clinics in the highest poverty communities. Within the communities, we looked at the proportion of adults over 65, the proportion of racial and ethnic minorities, educational level, rurality, and didn’t find any significant associations between private equity acquisition and those characteristics.
Dr. Harrington: Thank you. Rishi, do you want to interpret why private equity was targeting certain areas?
Dr. Wadhera: Private equity goes where they can actually acquire practices. Those states, in particular, have more independent practices than, say, Massachusetts does. Then there’s the target population available in those states. Building on what Ed said earlier, why all of a sudden? Because Victoria just pointed out that the vast majority of these acquisitions happened between 2020 and 2023 and you see the surge, and I expect that surge to continue over the next several years. And the question is why?
We know with the rise in cardiometabolic risk factors at a population level, that the cardiovascular disease is only going to become more common. Cardiac procedures are very well reimbursed. There’s likely a lot of appeal in entering a specialty with a highly profitable service line. Over the past decade, federal policymakers very intentionally have created incentives to shift the delivery of cardiac procedures to nonhospital settings. We see that with the rise of ambulatory surgical centers and more cardiac procedures are being reimbursed in these types of settings. And I think that private equity firms may see this as an opportunity to maximize profits.
Victoria created this beautiful map in our study that showed how concentrated these acquisitions are. They really concentrated in specific markets. And I think that parallels what we’re seeing with health systems more broadly, this consolidation, and concentration is the ultimate goal. These different stakeholders, it’s not just private equity, have more market power, so that when they go to insurers, they can demand higher prices for procedures and services.
Dr. Harrington: It’s hard to look at the dates of 2021 or 2020 to 2023, and not wonder if there is a COVID effect. Victoria, do you think there’s a COVID effect, or is it just true, true, unrelated?
Dr. Bartlett: COVID definitely put a lot of financial pressure on providers, and particularly small independent practices. They would have felt that the most, and I certainly think is a piece of the picture but may not be all the picture.
Dr. Harrington: That’s what I would have guessed. We were all under financial pressures, but the small, independent practices didn’t have the big health system behind them to backstop things. Ed, as a former leader of the ACC, and the ACC very much works at the local level, are you hearing from the governors of these states that this is an issue, and not hearing from other states?
Dr. Fry: Certainly this activity is concentrated in the states that Victoria and Rishi described for the reasons that they outlined. This is still a very small number and probably will remain relatively small if we consider that 85% of cardiologists are employed, and the bar to exit an employment arrangement and enter into a private equity situation is pretty darn high. There’s a lot of costs associated with that. So it may have a finite cap to it, and that may be part of what buffers some of the response.
I would like to go back and address other reasons why this is happening. Particularly because of the aging population of cardiovascular patients, we’ve also seen the rise of Medicare Advantage, which is a type of value, if you consider it a type of value-based care. There are incentives built into Medicare Advantage to manage costs and to do various things so there is certainly a reward incentive. I am not wearing my hat as a representative of the ACC nor Ascension, and I will probably be a consumer of these services before I’m ever a participant, but I would say that private equity in some respects, is acting as a disruptor in this entire process. One of the positive outcomes from this is for a reevaluation of the role of clinicians in the overall delivery of care for health systems and academic medical centers. I think that can be a positive; I always try to look at the bright side of things too.
Patient and Clinician Satisfaction
Dr. Harrington: To your last comment. Ed, maybe I’ll ask you Rishi or Victoria, any insights into clinician wellness, how people feel when their practice has been bought by private equity? Are there any data out there?
Dr. Wadhera: Not that I know of. I will say that we have a study under review right now that doesn’t answer your question directly, Bob, but that looks at how private equity acquisitions of US hospitals affect the patient care experience. And what we found, using a rigorous, quasi experimental study design comparing private equity–acquired hospitals to neighboring control hospitals, is that private equity acquisition leads to a pretty marked decrease in patient care experience and satisfaction.
That’s capturing another dimension of quality that mortality and readmissions don’t necessarily reflect. It doesn’t answer your question directly, but I think an important area for future research is understanding the effects on the clinician experience as well as, most importantly, the patient experience.
Dr. Harrington: Nicely said, it seems like a good time to think about mixed qualitative methods such as focus groups, etc., coupled with the more quantitative research methods. Victoria, I suspect you talked to people in acquired practices. Any insight into whether it’s observational or rigorous data on the clinician experience?
Dr. Bartlett: Not that I have seen. I imagine it’s probably mixed because as we’ve been saying, there’s a lot of financial pressure on practices, small, independent practices, and it can become overwhelming to run them. Private equity firms offer a very attractive value proposition or can. But I think it’s a great point that should be highlighted.
Dr. Harrington: Ed, taking off your cardiovascular leadership hat, not representing any specific organization, what are the policy things that we should be thinking about?
Dr. Fry: There’s an opportunity to combine these conversations around research, collecting more data, and the advocacy issues related to that. One of the things that perhaps differentiates cardiology in this space from other specialties, or subspecialties, surgical subspecialties, is the plethora of data that we already have with well-established registry tools. We have good benchmarks. From a professional society standpoint, we have an obligation to make sure that the care that is provided in whatever environment meets the standards and is measurable, reportable, and provides a level of consumerism to patients and payers to be able to look at that. I think we have an obligation to advocate for the use of well-validated registry tools to track the data, to have objective data, to be able to demonstrate outcomes.
Interestingly, there’s an ACC/American Heart Association policy document from 2020 on professionalism and ethics in cardiology. And it calls for the obligation of the profession to make sure that in alternative sites of care, that we are achieving at least as good a result, if not better. We have to be true to that.
Dr. Harrington: I was actually a coauthor on that paper on professionalism and talking about some of the research and education issues within the academic medical centers. You’re spot on. And I love the comment about the importance of long-standing registries, whether maintained by the ACC, the Heart Association, or the Society of Thoracic Surgeons, where we can get insights into the quality issues.
We need more work done on the patient experience, the clinician experience, but I also take the positive, Ed, that this may be a disruptor that could lend itself to some positive change in other areas that need to change.
This has been a fantastic conversation on the appearance, if you will, of private equity in cardiovascular medicine and some of the observations made by colleagues at the Smith Center at the Beth Israel Lahey, with great commentary by Ed Fry on whether this is a symptom or a solution and what we should be thinking about from a broader societal perspective. I want to thank my three guests today, Victoria, Ed, and Rishi, for joining us here.
Dr. Harrington is the Stephen and Suzanne Weiss Dean of Weill Cornell Medicine and provost for medical affairs of Cornell University, as well as a former president of the American Heart Association. He disclosed ties with several companies. Dr. Bartlett is resident physician, Department of Internal Medicine, Brigham & women’s Hospital, Boston, and has disclosed no relevant financial relationships. Dr. Fry is chair, Ascension National Cardiovascular Service Line, Ascension St. Vincent Heart Center in Indianapolis, Indiana. Dr. Wadhera is associate professor, Harvard Medical School, and associate director, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center, both in Boston. Dr. Wadhera disclosed ties with Abbott, ChamberCardio, CVS Health, the National Institutes of Health, American Heart Association, and the Donaghue Foundation.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert A. Harrington, MD: I’m continuing my series of conversations with leaders in the field of cardiovascular medicine who are working on interesting projects and making contributions in the science and policy space. We have three guests joining us today who have recently written two papers in the Journal of the American College of Cardiology. One is an original research paper dealing with the issue of private equity’s acquisition of outpatient cardiology practices. And the second is an editorial that really tries to get at why this is happening. Is it a problem? Is it a solution to a problem?
Fortunately, I have all three as guests to think about this important issue that has implications for clinical care, reimbursement, physician wellness, and clinician wellness, and it has implications regarding public policy and how we should be thinking about the practice of medicine in this country.
Dr. Victoria L. Bartlett is an internal medicine resident at Brigham and Women’s Hospital in Boston, and a research fellow in the Smith Center at the Beth Israel Lahey medical center in Boston. Dr Rishi K. Wadhera is the senior author of the paper written by Dr. Bartlett. Dr. Rishi is associate professor of medicine at Harvard Medical School, and he is the associate director of the Smith Center at Beth Israel Lahey.
Rishi K. Wadhera, MD, MPP, MPhil: Thanks for having us, Bob.
Dr. Harrington: The editorialist, Dr. Ed Fry, is the national service line leader for cardiovascular medicine, for Ascension Health. Dr. Frey is a recent past president of the American College of Cardiology (ACC).
Edward T. A. Fry, MD: Great to be here. Thanks.
What is private equity? Why the interest in medicine?
Dr. Harrington: I was intrigued by the papers and it caused me to do a deeper dive into some of the earlier works that you have referenced about this growing topic of private equity making its way into medical practice. Rishi, I’ll start with you. For the casual reader like myself, what is the business of private equity?
Dr. Wadhera: Private equity firms basically used pooled investments from multiple sources. These can be individual and institutional investors, pension funds, endowments, and they use those funds to invest in private companies that have the potential to return a profit. The goal really is to turn a profit for institutional investors over a shorter time horizon.
Dr. Harrington: How do they do that? I can understand, you buy a factory and you want to make the factory a little more efficient, and you think that perhaps, by combining some technologies, etc., that you might have in other factories, you can drive more value out of the one you just invested in in a short period of time. What’s the general business sense of how they’re going to do that in a cardiology practice? Is it all about making us more efficient?
Dr. Wadhera: Operational efficiency is the overarching theme here. One could argue that perhaps, private equity firms have the expertise to bring that kind of organizational know-how and operational efficiency to medicine. But there’s evidence that the way that private equity firms maximize their margin is maybe through mechanisms that aren’t necessarily good for patient care, such as reduced nursing staffing. When private equity acquires hospitals or practices in the same location, they have greater negotiating power at the payer table, to have higher prices for the services they deliver. There’s a lot of discussion about whether the sort of changes that private equity firms tend to implement are good or bad for patient care and also for clinicians.
Dr. Harrington: Great summary. Ed. Why is this happening in medicine? What did we do in medicine that made us ripe for investment by private equity? When you and I started out years ago, I don’t think we ever would have thought that this was in the future.
Dr. Fry: I think number one, as we know, is that medicine represents about 20% of our economy. There are huge amounts of money involved in these considerations. If players in this space can access even a small fraction of that money, it’s a lot of money and a lot of incentive for them.
In medicine in general, and then maybe more specifically, in cardiology, we’ve seen a shift away from private practice into employed practice. When people made those decisions over the past 10-15 years, there were certainly positives and risks that they took. I think for some, along the way, they realized that perhaps they gave up more than they thought in terms of control and running their own business and the opportunity to shape that themselves and be rewarded for that as they were in private practice. In cardiology, more specifically, we’ve seen this shift to the outpatient space: moving diagnostics and even therapeutics into ambulatory surgical centers and outpatient-based labs, and that is another potential source of revenue for these private equity companies.
As I wrote in the editorial, there are certainly a lot of pressures and frustrations that the day-to-day clinician feels, and maybe, this move to private equity is more of a symptom of those concerns and that this could be an opportunity to take the bull by the horns again in cardiology. We’ve evolved from a predominantly hospital-based acute care specialty into one of diagnosis, chronic disease management, and longitudinal care punctuated by diagnostics and therapeutics, which are, again, I think, attractive to private equity firms as potential sources for revenue.
Dr. Harrington: Ed, why cardiology? What’s happened over the years that has led to that appearance, if you will, of private equity and cardiovascular medicine?
Dr. Fry: Some of the earlier specialties were dermatology, ophthalmology, and gastroenterology, in particular. And interestingly, those tend to be specialties that have less chronic disease management and are more based on procedures and things like that. Within cardiology, obviously, the big driver is that our population is aging: 11,000 people turn 65 every day and become eligible for Medicare. With that, we see a rise in disease prevalence and then the rise in risk factors, obviously, with obesity and diabetes driving that, so there are more people who are going to have an illness that requires evaluation, diagnostics, and procedures. Because of that, it is a very target rich environment for private equity.
Dr. Harrington: That’s great background. Now, let’s dive into what you did, Victoria. What got you interested in the question? And give us some background on the literature that you were trying to build upon when you asked your series of questions.
Victoria L. Bartlett, MD: There’s been a lot of interest in private equity acquisitions and healthcare. A lot of the existing literature has been around hospital acquisitions and what happens there. There’s some literature, as you’ve mentioned, in outpatient practices, in certain specialties, where private equity has existed a little bit longer than in cardiology. They’ve been asking really similar questions to what we have been asking about cardiology, which is what happens when practices are acquired.
A kind of overview is that many of those studies have found increased costs to payers, to patients, and many have also found evidence of decreased quality. The evidence for the latter is honestly more difficult to figure out, but there has been evidence of decreased nursing ratios in nursing homes. There’s been evidence of changing the mix in clinics to more advanced practice providers than physicians. There’s been some evidence in hospitals that maybe quality doesn’t change too much. But the deeper layer under that is that these private equity–acquired hospitals may be selecting certain patients that are less sick, that are not going to negatively affect their metrics as much. That’s the environment that we had been reading about and starting to ask: Are we seeing that in cardiology too?
Dr. Harrington: Share with the audience what you did. You took what I would call a descriptive approach to try to understand the current landscape in cardiovascular medicine. As Ed already pointed out, a lot of the earlier data does not concern cardiology practices. My read of your paper is that you were trying to at least lay the groundwork for us to understand as a community what’s going on out there. Is that a fair interpretation?
Dr. Bartlett: Absolutely. Even that initial question of what’s happening is more challenging than it seems it might be to answer, partly because with private equity, these are private transactions. They don’t have to publicly report anything. So there’s a lot of manual work to gather these data. Our first questions were: What are these transactions? When are they happening? Where are they happening? What are the clinics that private equity is interested in? What are the community characteristics of those clinics? And what could that tell us about what’s going on?
Who Is Getting Acquired?
Dr. Harrington: Tell the audience broadly what you found. What are those clinics? And how often does this happen?
Dr. Bartlett: We looked at acquisitions between 2013 and 2023, and in that 10-year span, we found 41 acquisitions of outpatient cardiology practices, which corresponded to 342 acquisitions of clinics. The vast majority of these, pretty much 95%, occurred between 2021 and 2023. We calculated that about 3% of cardiology clinics in the US are owned by private equity. The states with the highest number of acquisitions were Florida, Texas, and Arizona, and particularly the urban areas in those states, ie, Jacksonville, Houston, Dallas. And interestingly, that mirrors what we’ve seen before in anesthesia and dermatology.
Our last question was around community characteristics, we looked at several that had a statistically significant association with private equity acquisition, and we found that private equity firms were less likely to acquire clinics in the highest poverty communities. Within the communities, we looked at the proportion of adults over 65, the proportion of racial and ethnic minorities, educational level, rurality, and didn’t find any significant associations between private equity acquisition and those characteristics.
Dr. Harrington: Thank you. Rishi, do you want to interpret why private equity was targeting certain areas?
Dr. Wadhera: Private equity goes where they can actually acquire practices. Those states, in particular, have more independent practices than, say, Massachusetts does. Then there’s the target population available in those states. Building on what Ed said earlier, why all of a sudden? Because Victoria just pointed out that the vast majority of these acquisitions happened between 2020 and 2023 and you see the surge, and I expect that surge to continue over the next several years. And the question is why?
We know with the rise in cardiometabolic risk factors at a population level, that the cardiovascular disease is only going to become more common. Cardiac procedures are very well reimbursed. There’s likely a lot of appeal in entering a specialty with a highly profitable service line. Over the past decade, federal policymakers very intentionally have created incentives to shift the delivery of cardiac procedures to nonhospital settings. We see that with the rise of ambulatory surgical centers and more cardiac procedures are being reimbursed in these types of settings. And I think that private equity firms may see this as an opportunity to maximize profits.
Victoria created this beautiful map in our study that showed how concentrated these acquisitions are. They really concentrated in specific markets. And I think that parallels what we’re seeing with health systems more broadly, this consolidation, and concentration is the ultimate goal. These different stakeholders, it’s not just private equity, have more market power, so that when they go to insurers, they can demand higher prices for procedures and services.
Dr. Harrington: It’s hard to look at the dates of 2021 or 2020 to 2023, and not wonder if there is a COVID effect. Victoria, do you think there’s a COVID effect, or is it just true, true, unrelated?
Dr. Bartlett: COVID definitely put a lot of financial pressure on providers, and particularly small independent practices. They would have felt that the most, and I certainly think is a piece of the picture but may not be all the picture.
Dr. Harrington: That’s what I would have guessed. We were all under financial pressures, but the small, independent practices didn’t have the big health system behind them to backstop things. Ed, as a former leader of the ACC, and the ACC very much works at the local level, are you hearing from the governors of these states that this is an issue, and not hearing from other states?
Dr. Fry: Certainly this activity is concentrated in the states that Victoria and Rishi described for the reasons that they outlined. This is still a very small number and probably will remain relatively small if we consider that 85% of cardiologists are employed, and the bar to exit an employment arrangement and enter into a private equity situation is pretty darn high. There’s a lot of costs associated with that. So it may have a finite cap to it, and that may be part of what buffers some of the response.
I would like to go back and address other reasons why this is happening. Particularly because of the aging population of cardiovascular patients, we’ve also seen the rise of Medicare Advantage, which is a type of value, if you consider it a type of value-based care. There are incentives built into Medicare Advantage to manage costs and to do various things so there is certainly a reward incentive. I am not wearing my hat as a representative of the ACC nor Ascension, and I will probably be a consumer of these services before I’m ever a participant, but I would say that private equity in some respects, is acting as a disruptor in this entire process. One of the positive outcomes from this is for a reevaluation of the role of clinicians in the overall delivery of care for health systems and academic medical centers. I think that can be a positive; I always try to look at the bright side of things too.
Patient and Clinician Satisfaction
Dr. Harrington: To your last comment. Ed, maybe I’ll ask you Rishi or Victoria, any insights into clinician wellness, how people feel when their practice has been bought by private equity? Are there any data out there?
Dr. Wadhera: Not that I know of. I will say that we have a study under review right now that doesn’t answer your question directly, Bob, but that looks at how private equity acquisitions of US hospitals affect the patient care experience. And what we found, using a rigorous, quasi experimental study design comparing private equity–acquired hospitals to neighboring control hospitals, is that private equity acquisition leads to a pretty marked decrease in patient care experience and satisfaction.
That’s capturing another dimension of quality that mortality and readmissions don’t necessarily reflect. It doesn’t answer your question directly, but I think an important area for future research is understanding the effects on the clinician experience as well as, most importantly, the patient experience.
Dr. Harrington: Nicely said, it seems like a good time to think about mixed qualitative methods such as focus groups, etc., coupled with the more quantitative research methods. Victoria, I suspect you talked to people in acquired practices. Any insight into whether it’s observational or rigorous data on the clinician experience?
Dr. Bartlett: Not that I have seen. I imagine it’s probably mixed because as we’ve been saying, there’s a lot of financial pressure on practices, small, independent practices, and it can become overwhelming to run them. Private equity firms offer a very attractive value proposition or can. But I think it’s a great point that should be highlighted.
Dr. Harrington: Ed, taking off your cardiovascular leadership hat, not representing any specific organization, what are the policy things that we should be thinking about?
Dr. Fry: There’s an opportunity to combine these conversations around research, collecting more data, and the advocacy issues related to that. One of the things that perhaps differentiates cardiology in this space from other specialties, or subspecialties, surgical subspecialties, is the plethora of data that we already have with well-established registry tools. We have good benchmarks. From a professional society standpoint, we have an obligation to make sure that the care that is provided in whatever environment meets the standards and is measurable, reportable, and provides a level of consumerism to patients and payers to be able to look at that. I think we have an obligation to advocate for the use of well-validated registry tools to track the data, to have objective data, to be able to demonstrate outcomes.
Interestingly, there’s an ACC/American Heart Association policy document from 2020 on professionalism and ethics in cardiology. And it calls for the obligation of the profession to make sure that in alternative sites of care, that we are achieving at least as good a result, if not better. We have to be true to that.
Dr. Harrington: I was actually a coauthor on that paper on professionalism and talking about some of the research and education issues within the academic medical centers. You’re spot on. And I love the comment about the importance of long-standing registries, whether maintained by the ACC, the Heart Association, or the Society of Thoracic Surgeons, where we can get insights into the quality issues.
We need more work done on the patient experience, the clinician experience, but I also take the positive, Ed, that this may be a disruptor that could lend itself to some positive change in other areas that need to change.
This has been a fantastic conversation on the appearance, if you will, of private equity in cardiovascular medicine and some of the observations made by colleagues at the Smith Center at the Beth Israel Lahey, with great commentary by Ed Fry on whether this is a symptom or a solution and what we should be thinking about from a broader societal perspective. I want to thank my three guests today, Victoria, Ed, and Rishi, for joining us here.
Dr. Harrington is the Stephen and Suzanne Weiss Dean of Weill Cornell Medicine and provost for medical affairs of Cornell University, as well as a former president of the American Heart Association. He disclosed ties with several companies. Dr. Bartlett is resident physician, Department of Internal Medicine, Brigham & women’s Hospital, Boston, and has disclosed no relevant financial relationships. Dr. Fry is chair, Ascension National Cardiovascular Service Line, Ascension St. Vincent Heart Center in Indianapolis, Indiana. Dr. Wadhera is associate professor, Harvard Medical School, and associate director, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center, both in Boston. Dr. Wadhera disclosed ties with Abbott, ChamberCardio, CVS Health, the National Institutes of Health, American Heart Association, and the Donaghue Foundation.
A version of this article first appeared on Medscape.com.
Who’s Behind Cosmetic Procedures at MedSpas?
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
Primary Care: Re Carpe Your Diem
William Fox, MD, a self-described “dinosaur,” works in an independent internal medicine practice with two other physicians in Charlottesville, Virginia. He is rarely able to accept new patients, and when he does see one, they often have to wait months for the appointment. He accepts the burden of many pent-up needs, along with the huge administrative chore of coordinating their care with subspecialists.
“I will probably have to make multiple visits in a quick succession in order to make sure that I stabilize all the various issues,” Dr. Fox said. Doing so for a complicated new patient is nearly impossible because of time pressures, especially as it has become increasingly difficult for his patients to access subspecialists.
Dr. Fox traced the roots of the problem to a shortage of primary care physicians.
“Primary care is a vital part of healthcare and infrastructure in the United States, and it is being eroded unfortunately, as fewer and fewer medical students and residents choose to go into the primary care field,” Fox said. “And the reason it’s being eroded partly is because it is undervalued” and under-reimbursed, he added.
A study published 2 years ago in the Journal of General Internal Medicine proved what every primary care clinician already knows: The 24-hour day simply isn’t long enough.
Assuming an average panel of 2500 patients, the authors estimated the average time needed to provide currently recommended preventive care services and vaccines, chronic disease care, and management of acute illnesses. The answer: 26.7 hours a day.
However, using a team-based approach in which the necessary care was divided between physicians, advanced practice providers, and medical assistants, the physician component could be whittled down to 9 hours.
As chair of the Board of Regents of the American College of Physicians (ACP), Dr. Fox champions the ACP’s endorsement of physician-led team-based care, which improves patient outcomes and increases well-being among health professionals. But practices like his rarely have the necessary resources to support advanced practice clinicians or social workers. “Team-based care can be achieved in larger healthcare systems that have the resources to do it,” said Dr. Fox. “We need to find a way for smaller independent practices to also participate in team-based care.”
The solution? Major reform in the current fee-for-service payment structure, which incentivizes patient volume over patient outcomes. Dr. Fox co-authored a 2022 position statement from ACP outlining strategies such as prospective payment models that could achieve high-quality care and address social inequities. “We need to evolve our payment system from a fee-for-service system into a blended system where you have some population-based payments along with fee-for-service, or a fully capitated system,” he said.
Advantages of Team-Based Care
When a patient wrote on a satisfaction survey “the doctor spent more time examining the computer than examining me,” Kevin Hopkins, MD, decided he needed to change some things. Now the vice chief of Cleveland Clinic’s Primary Care Institute in Cleveland, in 2010, he developed a rudimentary team-based care model consisting of himself and two medical assistants at Cleveland Clinic.
The assistants did much of the patient intake, served as scribes while Dr. Hopkins saw his patients, and completed most of the required documentation. “I was able to see 30% more patients in a day and still take great care of them,” Dr. Hopkins said.
The concept of team-based care has evolved since then, often including some combination of advanced practice providers such as physician assistants (PAs) or nurse practitioners (NPs), nurses or medical assistants, and social workers or case managers working under the leadership of a physician. According to Dr. Hopkins, the basic strategy should be that “the physician does what only the physician is uniquely trained and qualified to do.” All other tasks, such as data entry, handling refill requests and messages from the patient portal, scheduling, or patient education, can — and should — be done by someone else.
Dr. Hopkins also serves as a senior physician advisor to the American Medical Association (AMA) and an instructor for workshops like “Saving Time: Practice Innovation Boot Camp.” His advice for clinicians who would like to streamline their workflow is to start with small steps.
“You’re not going to be able to hire all the people that you’d like to have,” he said. “I encourage physicians to look around at the people that they have and what they are currently doing as a part of their roles and responsibilities.”
The AMA Team-Based Care and Workflow website provides brief continuing medical education activities on topics such as implementing lab testing prior to office visits or advanced protocols for rooming and discharge; adopting any of these strategies can help save steps during office visits.
Dr. Hopkins said the AMA is committed to reducing the regulatory burden on clinicians. Clinical compliance officers may misinterpret regulatory requirements, putting into place overly conservative internal policies and procedures. The AMA’s “Reducing Regulatory Burden Playbook” offers advice on practices that could be stopped, such as two-factor authentication for approving or signing orders unless they are for controlled substances, or started, such as writing prescriptions for chronic daily medications for the maximum allowed length. Reducing a few clicks with each log-on to the electronic health record or reducing the number of tasks physicians must complete to log on can dramatically reduce hours spent on the computer.
Telehealth Changes Everything
But it might be even more efficient to keep patients out of the office.
Initially piloted in Palo Alto, California, from 2018 to 2022, the Tera Practice adopted team-based care strategies in a practice that conducts most of its work virtually. Sutter Health has since expanded the concept to three “Connected Care Clinics” in the San Francisco area, which provide 80% of their care via secure messaging, telephone, or video visit. Staff work primarily from home, and patients do not need to take off work or spend time driving to in-person visits to access care.
Matthew Sakumoto, MD, is a virtualist primary care physician at Sutter Health’s San Francisco clinic and an adjunct assistant clinical professor at the University of California, San Francisco. He leads a three-person team, which typically has included either an NP or a PA, along with a licensed vocational nurse or medical assistant.
“I go into clinic once a week, but a lot of the visits are video visits, so I don’t feel the pressure to address everything all in one visit,” Dr. Sakumoto said. “It is really freeing for both me and the patient.”
For more complex patients, for example, he prioritizes one problem at a visit because his team will follow up virtually for administrative issues like refills or specialty referrals. He can easily find time to schedule a patient for a follow-up virtual visit in the next week or 2 weeks to address additional needs. And on days he and his staff work from home, patients who message with an urgent concern can often be seen by video that same day.
Dr. Sakumoto and his team have a traditional huddle in the office the morning of their clinic day to plan for the scheduled visits, but most of their days are less structured. On non-clinic days, their morning Zoom huddle has a much different focus.
“We’re saying, ‘Okay, who are our high-risk patients? Who haven’t we seen in a while?’ ” Dr. Sakumoto said. They group patients into tiers based on factors such as age, number of complex medical needs, and frequency of emergency visits or hospitalizations. They also check in with higher-risk patients who haven’t contacted the office or been seen recently.
Dr. Sakumoto noticed in medical school doctors take excellent care of the patients who show up to the clinic. “We don’t do quite as well for those that don’t show up,” he said. The hybrid-virtual model gives him time to think in a more population-based way about engaging his entire panel of patients. The majority have capitated or value-based insurance plans, providing a dedicated monthly revenue stream that funds his virtual practice.
More clinicians may be able to hire staff and adopt some of these innovative approaches if Congress approves proposed changes to Medicare and Medicaid increasing the use of value-based payment systems. Although these changes may not provide all the funding needed to reinvigorate the field of primary care medicine, Dr. Fox said, “at least some people in positions of power and responsibility are beginning to think more seriously about these issues.”
Dr. Sakumoto reported personal fees from the following companies within the past 24 months: Clearstep Health, Carbon Health, Matter Health, CareAlign, PlushCare, Teladoc, and Nabla Health. Dr. Fox and Dr. Hopkins reported no financial conflicts of interest.
A former pediatrician and disease detective, Ann Thomas, MD, MPH, is a freelance science writer living in Portland, Oregon.
A version of this article first appeared on Medscape.com.
William Fox, MD, a self-described “dinosaur,” works in an independent internal medicine practice with two other physicians in Charlottesville, Virginia. He is rarely able to accept new patients, and when he does see one, they often have to wait months for the appointment. He accepts the burden of many pent-up needs, along with the huge administrative chore of coordinating their care with subspecialists.
“I will probably have to make multiple visits in a quick succession in order to make sure that I stabilize all the various issues,” Dr. Fox said. Doing so for a complicated new patient is nearly impossible because of time pressures, especially as it has become increasingly difficult for his patients to access subspecialists.
Dr. Fox traced the roots of the problem to a shortage of primary care physicians.
“Primary care is a vital part of healthcare and infrastructure in the United States, and it is being eroded unfortunately, as fewer and fewer medical students and residents choose to go into the primary care field,” Fox said. “And the reason it’s being eroded partly is because it is undervalued” and under-reimbursed, he added.
A study published 2 years ago in the Journal of General Internal Medicine proved what every primary care clinician already knows: The 24-hour day simply isn’t long enough.
Assuming an average panel of 2500 patients, the authors estimated the average time needed to provide currently recommended preventive care services and vaccines, chronic disease care, and management of acute illnesses. The answer: 26.7 hours a day.
However, using a team-based approach in which the necessary care was divided between physicians, advanced practice providers, and medical assistants, the physician component could be whittled down to 9 hours.
As chair of the Board of Regents of the American College of Physicians (ACP), Dr. Fox champions the ACP’s endorsement of physician-led team-based care, which improves patient outcomes and increases well-being among health professionals. But practices like his rarely have the necessary resources to support advanced practice clinicians or social workers. “Team-based care can be achieved in larger healthcare systems that have the resources to do it,” said Dr. Fox. “We need to find a way for smaller independent practices to also participate in team-based care.”
The solution? Major reform in the current fee-for-service payment structure, which incentivizes patient volume over patient outcomes. Dr. Fox co-authored a 2022 position statement from ACP outlining strategies such as prospective payment models that could achieve high-quality care and address social inequities. “We need to evolve our payment system from a fee-for-service system into a blended system where you have some population-based payments along with fee-for-service, or a fully capitated system,” he said.
Advantages of Team-Based Care
When a patient wrote on a satisfaction survey “the doctor spent more time examining the computer than examining me,” Kevin Hopkins, MD, decided he needed to change some things. Now the vice chief of Cleveland Clinic’s Primary Care Institute in Cleveland, in 2010, he developed a rudimentary team-based care model consisting of himself and two medical assistants at Cleveland Clinic.
The assistants did much of the patient intake, served as scribes while Dr. Hopkins saw his patients, and completed most of the required documentation. “I was able to see 30% more patients in a day and still take great care of them,” Dr. Hopkins said.
The concept of team-based care has evolved since then, often including some combination of advanced practice providers such as physician assistants (PAs) or nurse practitioners (NPs), nurses or medical assistants, and social workers or case managers working under the leadership of a physician. According to Dr. Hopkins, the basic strategy should be that “the physician does what only the physician is uniquely trained and qualified to do.” All other tasks, such as data entry, handling refill requests and messages from the patient portal, scheduling, or patient education, can — and should — be done by someone else.
Dr. Hopkins also serves as a senior physician advisor to the American Medical Association (AMA) and an instructor for workshops like “Saving Time: Practice Innovation Boot Camp.” His advice for clinicians who would like to streamline their workflow is to start with small steps.
“You’re not going to be able to hire all the people that you’d like to have,” he said. “I encourage physicians to look around at the people that they have and what they are currently doing as a part of their roles and responsibilities.”
The AMA Team-Based Care and Workflow website provides brief continuing medical education activities on topics such as implementing lab testing prior to office visits or advanced protocols for rooming and discharge; adopting any of these strategies can help save steps during office visits.
Dr. Hopkins said the AMA is committed to reducing the regulatory burden on clinicians. Clinical compliance officers may misinterpret regulatory requirements, putting into place overly conservative internal policies and procedures. The AMA’s “Reducing Regulatory Burden Playbook” offers advice on practices that could be stopped, such as two-factor authentication for approving or signing orders unless they are for controlled substances, or started, such as writing prescriptions for chronic daily medications for the maximum allowed length. Reducing a few clicks with each log-on to the electronic health record or reducing the number of tasks physicians must complete to log on can dramatically reduce hours spent on the computer.
Telehealth Changes Everything
But it might be even more efficient to keep patients out of the office.
Initially piloted in Palo Alto, California, from 2018 to 2022, the Tera Practice adopted team-based care strategies in a practice that conducts most of its work virtually. Sutter Health has since expanded the concept to three “Connected Care Clinics” in the San Francisco area, which provide 80% of their care via secure messaging, telephone, or video visit. Staff work primarily from home, and patients do not need to take off work or spend time driving to in-person visits to access care.
Matthew Sakumoto, MD, is a virtualist primary care physician at Sutter Health’s San Francisco clinic and an adjunct assistant clinical professor at the University of California, San Francisco. He leads a three-person team, which typically has included either an NP or a PA, along with a licensed vocational nurse or medical assistant.
“I go into clinic once a week, but a lot of the visits are video visits, so I don’t feel the pressure to address everything all in one visit,” Dr. Sakumoto said. “It is really freeing for both me and the patient.”
For more complex patients, for example, he prioritizes one problem at a visit because his team will follow up virtually for administrative issues like refills or specialty referrals. He can easily find time to schedule a patient for a follow-up virtual visit in the next week or 2 weeks to address additional needs. And on days he and his staff work from home, patients who message with an urgent concern can often be seen by video that same day.
Dr. Sakumoto and his team have a traditional huddle in the office the morning of their clinic day to plan for the scheduled visits, but most of their days are less structured. On non-clinic days, their morning Zoom huddle has a much different focus.
“We’re saying, ‘Okay, who are our high-risk patients? Who haven’t we seen in a while?’ ” Dr. Sakumoto said. They group patients into tiers based on factors such as age, number of complex medical needs, and frequency of emergency visits or hospitalizations. They also check in with higher-risk patients who haven’t contacted the office or been seen recently.
Dr. Sakumoto noticed in medical school doctors take excellent care of the patients who show up to the clinic. “We don’t do quite as well for those that don’t show up,” he said. The hybrid-virtual model gives him time to think in a more population-based way about engaging his entire panel of patients. The majority have capitated or value-based insurance plans, providing a dedicated monthly revenue stream that funds his virtual practice.
More clinicians may be able to hire staff and adopt some of these innovative approaches if Congress approves proposed changes to Medicare and Medicaid increasing the use of value-based payment systems. Although these changes may not provide all the funding needed to reinvigorate the field of primary care medicine, Dr. Fox said, “at least some people in positions of power and responsibility are beginning to think more seriously about these issues.”
Dr. Sakumoto reported personal fees from the following companies within the past 24 months: Clearstep Health, Carbon Health, Matter Health, CareAlign, PlushCare, Teladoc, and Nabla Health. Dr. Fox and Dr. Hopkins reported no financial conflicts of interest.
A former pediatrician and disease detective, Ann Thomas, MD, MPH, is a freelance science writer living in Portland, Oregon.
A version of this article first appeared on Medscape.com.
William Fox, MD, a self-described “dinosaur,” works in an independent internal medicine practice with two other physicians in Charlottesville, Virginia. He is rarely able to accept new patients, and when he does see one, they often have to wait months for the appointment. He accepts the burden of many pent-up needs, along with the huge administrative chore of coordinating their care with subspecialists.
“I will probably have to make multiple visits in a quick succession in order to make sure that I stabilize all the various issues,” Dr. Fox said. Doing so for a complicated new patient is nearly impossible because of time pressures, especially as it has become increasingly difficult for his patients to access subspecialists.
Dr. Fox traced the roots of the problem to a shortage of primary care physicians.
“Primary care is a vital part of healthcare and infrastructure in the United States, and it is being eroded unfortunately, as fewer and fewer medical students and residents choose to go into the primary care field,” Fox said. “And the reason it’s being eroded partly is because it is undervalued” and under-reimbursed, he added.
A study published 2 years ago in the Journal of General Internal Medicine proved what every primary care clinician already knows: The 24-hour day simply isn’t long enough.
Assuming an average panel of 2500 patients, the authors estimated the average time needed to provide currently recommended preventive care services and vaccines, chronic disease care, and management of acute illnesses. The answer: 26.7 hours a day.
However, using a team-based approach in which the necessary care was divided between physicians, advanced practice providers, and medical assistants, the physician component could be whittled down to 9 hours.
As chair of the Board of Regents of the American College of Physicians (ACP), Dr. Fox champions the ACP’s endorsement of physician-led team-based care, which improves patient outcomes and increases well-being among health professionals. But practices like his rarely have the necessary resources to support advanced practice clinicians or social workers. “Team-based care can be achieved in larger healthcare systems that have the resources to do it,” said Dr. Fox. “We need to find a way for smaller independent practices to also participate in team-based care.”
The solution? Major reform in the current fee-for-service payment structure, which incentivizes patient volume over patient outcomes. Dr. Fox co-authored a 2022 position statement from ACP outlining strategies such as prospective payment models that could achieve high-quality care and address social inequities. “We need to evolve our payment system from a fee-for-service system into a blended system where you have some population-based payments along with fee-for-service, or a fully capitated system,” he said.
Advantages of Team-Based Care
When a patient wrote on a satisfaction survey “the doctor spent more time examining the computer than examining me,” Kevin Hopkins, MD, decided he needed to change some things. Now the vice chief of Cleveland Clinic’s Primary Care Institute in Cleveland, in 2010, he developed a rudimentary team-based care model consisting of himself and two medical assistants at Cleveland Clinic.
The assistants did much of the patient intake, served as scribes while Dr. Hopkins saw his patients, and completed most of the required documentation. “I was able to see 30% more patients in a day and still take great care of them,” Dr. Hopkins said.
The concept of team-based care has evolved since then, often including some combination of advanced practice providers such as physician assistants (PAs) or nurse practitioners (NPs), nurses or medical assistants, and social workers or case managers working under the leadership of a physician. According to Dr. Hopkins, the basic strategy should be that “the physician does what only the physician is uniquely trained and qualified to do.” All other tasks, such as data entry, handling refill requests and messages from the patient portal, scheduling, or patient education, can — and should — be done by someone else.
Dr. Hopkins also serves as a senior physician advisor to the American Medical Association (AMA) and an instructor for workshops like “Saving Time: Practice Innovation Boot Camp.” His advice for clinicians who would like to streamline their workflow is to start with small steps.
“You’re not going to be able to hire all the people that you’d like to have,” he said. “I encourage physicians to look around at the people that they have and what they are currently doing as a part of their roles and responsibilities.”
The AMA Team-Based Care and Workflow website provides brief continuing medical education activities on topics such as implementing lab testing prior to office visits or advanced protocols for rooming and discharge; adopting any of these strategies can help save steps during office visits.
Dr. Hopkins said the AMA is committed to reducing the regulatory burden on clinicians. Clinical compliance officers may misinterpret regulatory requirements, putting into place overly conservative internal policies and procedures. The AMA’s “Reducing Regulatory Burden Playbook” offers advice on practices that could be stopped, such as two-factor authentication for approving or signing orders unless they are for controlled substances, or started, such as writing prescriptions for chronic daily medications for the maximum allowed length. Reducing a few clicks with each log-on to the electronic health record or reducing the number of tasks physicians must complete to log on can dramatically reduce hours spent on the computer.
Telehealth Changes Everything
But it might be even more efficient to keep patients out of the office.
Initially piloted in Palo Alto, California, from 2018 to 2022, the Tera Practice adopted team-based care strategies in a practice that conducts most of its work virtually. Sutter Health has since expanded the concept to three “Connected Care Clinics” in the San Francisco area, which provide 80% of their care via secure messaging, telephone, or video visit. Staff work primarily from home, and patients do not need to take off work or spend time driving to in-person visits to access care.
Matthew Sakumoto, MD, is a virtualist primary care physician at Sutter Health’s San Francisco clinic and an adjunct assistant clinical professor at the University of California, San Francisco. He leads a three-person team, which typically has included either an NP or a PA, along with a licensed vocational nurse or medical assistant.
“I go into clinic once a week, but a lot of the visits are video visits, so I don’t feel the pressure to address everything all in one visit,” Dr. Sakumoto said. “It is really freeing for both me and the patient.”
For more complex patients, for example, he prioritizes one problem at a visit because his team will follow up virtually for administrative issues like refills or specialty referrals. He can easily find time to schedule a patient for a follow-up virtual visit in the next week or 2 weeks to address additional needs. And on days he and his staff work from home, patients who message with an urgent concern can often be seen by video that same day.
Dr. Sakumoto and his team have a traditional huddle in the office the morning of their clinic day to plan for the scheduled visits, but most of their days are less structured. On non-clinic days, their morning Zoom huddle has a much different focus.
“We’re saying, ‘Okay, who are our high-risk patients? Who haven’t we seen in a while?’ ” Dr. Sakumoto said. They group patients into tiers based on factors such as age, number of complex medical needs, and frequency of emergency visits or hospitalizations. They also check in with higher-risk patients who haven’t contacted the office or been seen recently.
Dr. Sakumoto noticed in medical school doctors take excellent care of the patients who show up to the clinic. “We don’t do quite as well for those that don’t show up,” he said. The hybrid-virtual model gives him time to think in a more population-based way about engaging his entire panel of patients. The majority have capitated or value-based insurance plans, providing a dedicated monthly revenue stream that funds his virtual practice.
More clinicians may be able to hire staff and adopt some of these innovative approaches if Congress approves proposed changes to Medicare and Medicaid increasing the use of value-based payment systems. Although these changes may not provide all the funding needed to reinvigorate the field of primary care medicine, Dr. Fox said, “at least some people in positions of power and responsibility are beginning to think more seriously about these issues.”
Dr. Sakumoto reported personal fees from the following companies within the past 24 months: Clearstep Health, Carbon Health, Matter Health, CareAlign, PlushCare, Teladoc, and Nabla Health. Dr. Fox and Dr. Hopkins reported no financial conflicts of interest.
A former pediatrician and disease detective, Ann Thomas, MD, MPH, is a freelance science writer living in Portland, Oregon.
A version of this article first appeared on Medscape.com.