User login
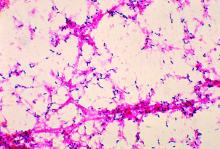
Streptococcal pneumonia’s resistance to macrolides increasing
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
FROM IDWEEK 2016
Key clinical point:
Major finding: S. pneumoniae isolates’ average resistance to the macrolide azithromycin was 48.4% in 2014.
Data source: A prospective collection and investigation of 4,567 non-replicative community-acquired bacterial pneumonia isolates.
Disclosures: The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
Surgical discharge data highlight stewardship need at transition
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
AT IDWEEK 2016
Key clinical point:
Major finding: 70% of prescriptions had at least one error in drug choice, dose, indication, or duration.
Data source: A review of discharge data for 150 patients at an academic hospital.
Disclosures: Dr. Scarpato reported having no conflicts of interest.
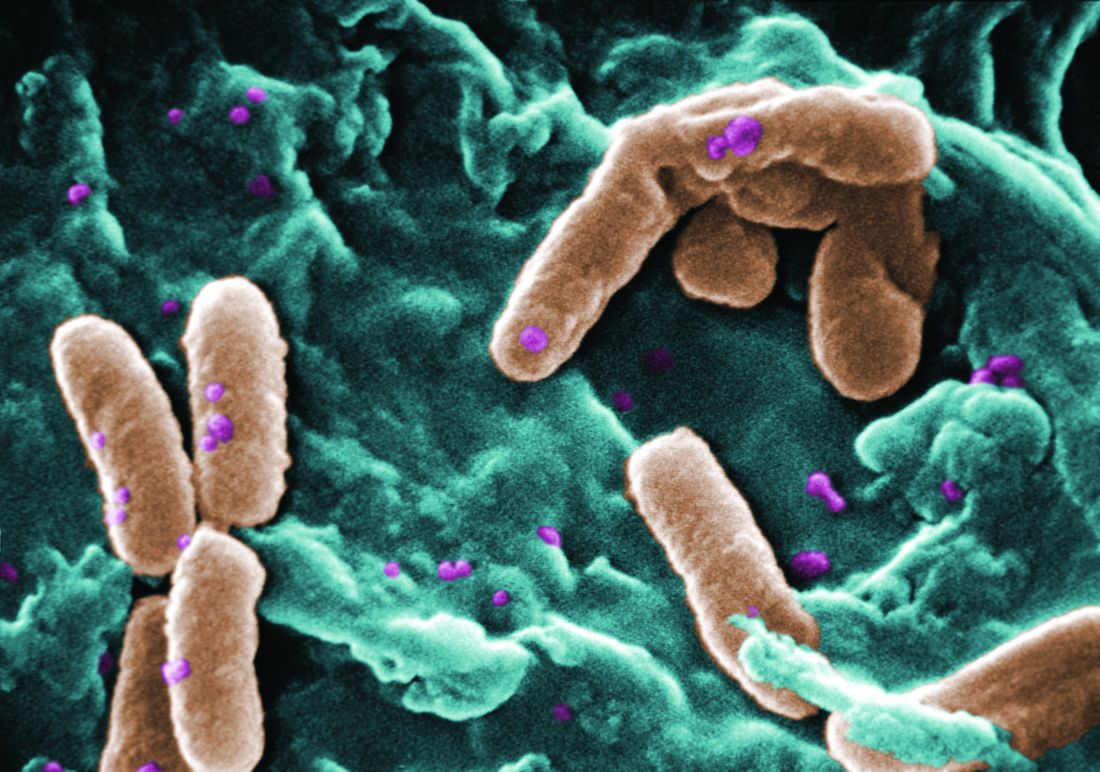
When to discontinue contact precautions for patients with MRSA
Methicillin-resistant Staphylococcus aureus (MRSA) is a common hospital-acquired infection with significant morbidity and mortality. The CDC currently recommends contact precautions as a mainstay to prevent transmission of MRSA in health care settings. Most hospitals routinely screen patients for MRSA and use contact precautions for those who screen positive. The duration of these precautions vary across hospitals and no standard recommendation exists.
A recent study of members of the Society for Healthcare Epidemiology of America (SHEA) research network indicated that the majority of physicians (94%) and nurses (76%) dislike contact precautions (CP) and most (63%) were in favor of implementing CP in a different way than current practice.1 Patients also report less satisfaction and increased isolation.1
My colleagues and I recently published a study2 in the American Journal of Infection Control to explore the necessary duration of contact precautions for hospitalized patients with MRSA. Our goal was to maintain contact precautions as long as necessary to prevent undesired MRSA infections and colonization but minimize unnecessary days in contact isolation. We also sought to figure out whether patients with positive MRSA surveillance cultures should always remain in isolation and, if not, at what point they could be considered for rescreening and removal of precautions if culture negative.
Our hospital has been performing active surveillance cultures weekly to screen for MRSA among our hospitalized patients for many years; however from 2010 to 2014, we began screening patients who were previously known to be positive for MRSA colonization or infection for at least 1 year. We then assessed medical and demographic factors associated with persistent carriage of MRSA.
In our study, more than 400 patients with known MRSA were rescreened with an active surveillance culture at a subsequent hospital admission. Ultimately 20% of the patients remained MRSA positive on the active surveillance culture. Most patients who were culture positive for MRSA were found on the first active surveillance culture (16.4%) but the remaining positive cultures were found on a second active surveillance culture or a clinical culture.
The amount of time that passed since the patient was culture positive was significantly associated with a lower risk of a positive culture at screening. This continued to drop over time with only 12.5% of patients remaining active surveillance culture positive for MRSA at 5 years after the original positive culture.
Two factors were found to significantly impact the MRSA culture on the multivariate analysis: (1) Female sex reduced the risk of positivity, and (2) Presence of a foreign body increased the risk of positivity.
Most patients who remained positive for an MRSA culture were found with the first active surveillance culture, less than 4% were detected subsequently with a repeat surveillance or clinical culture and this percentage also decreased over time. This indicates that in the absence of a positive active surveillance culture it may be reasonable to discontinue contact precautions, which could result in a substantial cost savings for the hospital and improved patient and provider satisfaction without increasing the risk of MRSA transmission.
We concluded that in the absence of a foreign body and with at least a year from the last known positive culture, patients with known MRSA should be rescreened and, if negative on an active surveillance culture, should be removed from contact precautions.
Lauren Richey, MD, MPH, is assistant professor in the infectious diseases division at the Medical University of South Carolina.
References
1. Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: A review of the literature. Am J Infect Control. 2009 Mar;37(2):85-93. doi: 10.1016/j.ajic.2008.04.257.
2. Richey LE, Oh Y, Tchamba DM, Engle M, Formby L, Salgado CD. When should contact precautions be discontinued for patients with Methicillin-resistant Staphylococcus aureus? Am J Infect Control. 2016 Aug 30. doi: 10.1016/j.ajic.2016.05.030.
Methicillin-resistant Staphylococcus aureus (MRSA) is a common hospital-acquired infection with significant morbidity and mortality. The CDC currently recommends contact precautions as a mainstay to prevent transmission of MRSA in health care settings. Most hospitals routinely screen patients for MRSA and use contact precautions for those who screen positive. The duration of these precautions vary across hospitals and no standard recommendation exists.
A recent study of members of the Society for Healthcare Epidemiology of America (SHEA) research network indicated that the majority of physicians (94%) and nurses (76%) dislike contact precautions (CP) and most (63%) were in favor of implementing CP in a different way than current practice.1 Patients also report less satisfaction and increased isolation.1
My colleagues and I recently published a study2 in the American Journal of Infection Control to explore the necessary duration of contact precautions for hospitalized patients with MRSA. Our goal was to maintain contact precautions as long as necessary to prevent undesired MRSA infections and colonization but minimize unnecessary days in contact isolation. We also sought to figure out whether patients with positive MRSA surveillance cultures should always remain in isolation and, if not, at what point they could be considered for rescreening and removal of precautions if culture negative.
Our hospital has been performing active surveillance cultures weekly to screen for MRSA among our hospitalized patients for many years; however from 2010 to 2014, we began screening patients who were previously known to be positive for MRSA colonization or infection for at least 1 year. We then assessed medical and demographic factors associated with persistent carriage of MRSA.
In our study, more than 400 patients with known MRSA were rescreened with an active surveillance culture at a subsequent hospital admission. Ultimately 20% of the patients remained MRSA positive on the active surveillance culture. Most patients who were culture positive for MRSA were found on the first active surveillance culture (16.4%) but the remaining positive cultures were found on a second active surveillance culture or a clinical culture.
The amount of time that passed since the patient was culture positive was significantly associated with a lower risk of a positive culture at screening. This continued to drop over time with only 12.5% of patients remaining active surveillance culture positive for MRSA at 5 years after the original positive culture.
Two factors were found to significantly impact the MRSA culture on the multivariate analysis: (1) Female sex reduced the risk of positivity, and (2) Presence of a foreign body increased the risk of positivity.
Most patients who remained positive for an MRSA culture were found with the first active surveillance culture, less than 4% were detected subsequently with a repeat surveillance or clinical culture and this percentage also decreased over time. This indicates that in the absence of a positive active surveillance culture it may be reasonable to discontinue contact precautions, which could result in a substantial cost savings for the hospital and improved patient and provider satisfaction without increasing the risk of MRSA transmission.
We concluded that in the absence of a foreign body and with at least a year from the last known positive culture, patients with known MRSA should be rescreened and, if negative on an active surveillance culture, should be removed from contact precautions.
Lauren Richey, MD, MPH, is assistant professor in the infectious diseases division at the Medical University of South Carolina.
References
1. Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: A review of the literature. Am J Infect Control. 2009 Mar;37(2):85-93. doi: 10.1016/j.ajic.2008.04.257.
2. Richey LE, Oh Y, Tchamba DM, Engle M, Formby L, Salgado CD. When should contact precautions be discontinued for patients with Methicillin-resistant Staphylococcus aureus? Am J Infect Control. 2016 Aug 30. doi: 10.1016/j.ajic.2016.05.030.
Methicillin-resistant Staphylococcus aureus (MRSA) is a common hospital-acquired infection with significant morbidity and mortality. The CDC currently recommends contact precautions as a mainstay to prevent transmission of MRSA in health care settings. Most hospitals routinely screen patients for MRSA and use contact precautions for those who screen positive. The duration of these precautions vary across hospitals and no standard recommendation exists.
A recent study of members of the Society for Healthcare Epidemiology of America (SHEA) research network indicated that the majority of physicians (94%) and nurses (76%) dislike contact precautions (CP) and most (63%) were in favor of implementing CP in a different way than current practice.1 Patients also report less satisfaction and increased isolation.1
My colleagues and I recently published a study2 in the American Journal of Infection Control to explore the necessary duration of contact precautions for hospitalized patients with MRSA. Our goal was to maintain contact precautions as long as necessary to prevent undesired MRSA infections and colonization but minimize unnecessary days in contact isolation. We also sought to figure out whether patients with positive MRSA surveillance cultures should always remain in isolation and, if not, at what point they could be considered for rescreening and removal of precautions if culture negative.
Our hospital has been performing active surveillance cultures weekly to screen for MRSA among our hospitalized patients for many years; however from 2010 to 2014, we began screening patients who were previously known to be positive for MRSA colonization or infection for at least 1 year. We then assessed medical and demographic factors associated with persistent carriage of MRSA.
In our study, more than 400 patients with known MRSA were rescreened with an active surveillance culture at a subsequent hospital admission. Ultimately 20% of the patients remained MRSA positive on the active surveillance culture. Most patients who were culture positive for MRSA were found on the first active surveillance culture (16.4%) but the remaining positive cultures were found on a second active surveillance culture or a clinical culture.
The amount of time that passed since the patient was culture positive was significantly associated with a lower risk of a positive culture at screening. This continued to drop over time with only 12.5% of patients remaining active surveillance culture positive for MRSA at 5 years after the original positive culture.
Two factors were found to significantly impact the MRSA culture on the multivariate analysis: (1) Female sex reduced the risk of positivity, and (2) Presence of a foreign body increased the risk of positivity.
Most patients who remained positive for an MRSA culture were found with the first active surveillance culture, less than 4% were detected subsequently with a repeat surveillance or clinical culture and this percentage also decreased over time. This indicates that in the absence of a positive active surveillance culture it may be reasonable to discontinue contact precautions, which could result in a substantial cost savings for the hospital and improved patient and provider satisfaction without increasing the risk of MRSA transmission.
We concluded that in the absence of a foreign body and with at least a year from the last known positive culture, patients with known MRSA should be rescreened and, if negative on an active surveillance culture, should be removed from contact precautions.
Lauren Richey, MD, MPH, is assistant professor in the infectious diseases division at the Medical University of South Carolina.
References
1. Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: A review of the literature. Am J Infect Control. 2009 Mar;37(2):85-93. doi: 10.1016/j.ajic.2008.04.257.
2. Richey LE, Oh Y, Tchamba DM, Engle M, Formby L, Salgado CD. When should contact precautions be discontinued for patients with Methicillin-resistant Staphylococcus aureus? Am J Infect Control. 2016 Aug 30. doi: 10.1016/j.ajic.2016.05.030.
Inpatient antibiotic use has not declined
Clinical question: How has inpatient antibiotic use changed in the United States in recent years?
Study design: Retrospective analysis.
Setting: Adult and pediatric data from 300 acute-care hospitals, 2006-2012.
Synopsis: Weighted extrapolation of data from a database was used to estimate national antibiotic use. Overall, 55.1% of discharged patients received antibiotics. The rate of antibiotic use was 755/1,000 patient-days over the study period. The small increase in antibiotic use over the years (5.6 days of therapy/1,000 patient-days increase; 95% CI, –18.9 to 30.1; P = .65) was not statistically significant. There was a significant decrease in the use of aminoglycosides, first- and second-generation cephalosporins, fluoroquinolones, sulfonamide, metronidazole, and penicillins. The use of third- and fourth-generation cephalosporins, macrolides, glycopeptides, beta-lactam/beta-lactamase inhibitor, carbapenems, and tetracyclines has increased significantly.
Limitations of the study include underrepresentation of pediatric hospitals and certain geographic regions.
Bottom line: Antibiotic-use rates have not changed during 2006-2012. However, broad-spectrum antibiotic use has increased significantly.
Citation: Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA. Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Intern Med. 2016;176(11):1639-1648.
Dr. Menon is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: How has inpatient antibiotic use changed in the United States in recent years?
Study design: Retrospective analysis.
Setting: Adult and pediatric data from 300 acute-care hospitals, 2006-2012.
Synopsis: Weighted extrapolation of data from a database was used to estimate national antibiotic use. Overall, 55.1% of discharged patients received antibiotics. The rate of antibiotic use was 755/1,000 patient-days over the study period. The small increase in antibiotic use over the years (5.6 days of therapy/1,000 patient-days increase; 95% CI, –18.9 to 30.1; P = .65) was not statistically significant. There was a significant decrease in the use of aminoglycosides, first- and second-generation cephalosporins, fluoroquinolones, sulfonamide, metronidazole, and penicillins. The use of third- and fourth-generation cephalosporins, macrolides, glycopeptides, beta-lactam/beta-lactamase inhibitor, carbapenems, and tetracyclines has increased significantly.
Limitations of the study include underrepresentation of pediatric hospitals and certain geographic regions.
Bottom line: Antibiotic-use rates have not changed during 2006-2012. However, broad-spectrum antibiotic use has increased significantly.
Citation: Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA. Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Intern Med. 2016;176(11):1639-1648.
Dr. Menon is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Clinical question: How has inpatient antibiotic use changed in the United States in recent years?
Study design: Retrospective analysis.
Setting: Adult and pediatric data from 300 acute-care hospitals, 2006-2012.
Synopsis: Weighted extrapolation of data from a database was used to estimate national antibiotic use. Overall, 55.1% of discharged patients received antibiotics. The rate of antibiotic use was 755/1,000 patient-days over the study period. The small increase in antibiotic use over the years (5.6 days of therapy/1,000 patient-days increase; 95% CI, –18.9 to 30.1; P = .65) was not statistically significant. There was a significant decrease in the use of aminoglycosides, first- and second-generation cephalosporins, fluoroquinolones, sulfonamide, metronidazole, and penicillins. The use of third- and fourth-generation cephalosporins, macrolides, glycopeptides, beta-lactam/beta-lactamase inhibitor, carbapenems, and tetracyclines has increased significantly.
Limitations of the study include underrepresentation of pediatric hospitals and certain geographic regions.
Bottom line: Antibiotic-use rates have not changed during 2006-2012. However, broad-spectrum antibiotic use has increased significantly.
Citation: Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA. Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Intern Med. 2016;176(11):1639-1648.
Dr. Menon is an assistant professor at the University of Miami Miller School of Medicine and a hospitalist at University of Miami Hospital and Jackson Memorial Hospital.
Shorter-course antimicrobials do not reduce antimicrobial resistance in AOM
A shorter duration of antimicrobial therapy for acute otitis media (AOM) in children is associated with higher rates of clinical failure and higher symptom scores but without any associated reduction in the rates of antimicrobial resistance or adverse events.
Alejandro Hoberman, MD, of the Children’s Hospital of Pittsburgh at the University of Pittsburgh Medical Center, and his coauthors report the results of a study in which 520 children aged 6-23 months were randomized to either 10 days of amoxicillin-clavulanate therapy, or 5 days of therapy followed by 5 days of placebo.
The children who received the full 10-day course also had lower mean symptom scores in the 6-14 days after initiation of therapy, compared with those who received 5 days of treatment (1.34 vs. 1.61; P = 0.07), while the number of children whose symptom scores decreased by 50% from baseline to the end of treatment was significantly lower in the 5-day group.
However, there were no significant differences between the two groups in the rate of nasopharyngeal colonization pathogens not susceptible to penicillin: 47% in the 10-day group, compared with 44% in the 5-day group (N Engl J Med. 2016 Dec 22;375[25]:2446-56).
Similarly, the rates of recurrence and adverse events were not significantly different between the two groups.
A shorter duration of treatment has been considered as a strategy for reducing the risk of antimicrobial resistance, but clinical trials so far have showed either modest difference favoring the standard duration of treatment, or no difference at all.
“The outcome differences we found were larger than the differences that have been reported previously, mainly because the rates of clinical failure among children who received reduced duration treatment were higher in our trial than in previous trials,” Dr. Hoberman and his associates wrote.
The researchers did note that clinical failure rates were higher among children with greater exposure to other children, and those with infection in both ears rather than a single ear.
The study was supported by the National Institute of Allergy and Infectious Diseases and the National Institutes of Health. Dr. Hoberman and Dr. Judith M. Martin declared consulting fees from Genocea Biosciences, and Dr. Hoberman declared grant support from Ricoh Innovations and holding pending patents for a reduced clavulanate concentration version of amoxicillin–clavulanate potassium, and a method and device for aiding in the diagnosis of otitis media. No other conflicts of interest were declared.
The study of acute otitis media is challenging owing to antibiotic pharmacokinetics, age of the patients, variation in regional pathogens, polymicrobial infection, viral cofactors, antibiotic resistance, status of patients with regard to receipt of PCV7 or PCV13, and a high rate of spontaneous resolution.
The study was not designed to address outcomes in older children, children with less severe acute otitis media or with acute otitis media in one ear, or children with additional risk factors such as cleft palate or trisomy 21. In addition, there is a paucity of studies from resource-poor and low income countries.
But for now, 10 days of amoxicillin-clavulanate for children younger than 2 years of age who have a definite diagnosis of acute otitis media seems to be a reasonable option.
Margaret A. Kenna, MD, MPH, is from the department of otolaryngology and communication enhancement at the Boston Children’s Hospital. These comments are excerpted from an accompanying editorial (N Engl J Med. 2016 Dec 22;375[25]:2492-93). Dr. Kenna declared a grant from Agilis outside the submitted work.
The study of acute otitis media is challenging owing to antibiotic pharmacokinetics, age of the patients, variation in regional pathogens, polymicrobial infection, viral cofactors, antibiotic resistance, status of patients with regard to receipt of PCV7 or PCV13, and a high rate of spontaneous resolution.
The study was not designed to address outcomes in older children, children with less severe acute otitis media or with acute otitis media in one ear, or children with additional risk factors such as cleft palate or trisomy 21. In addition, there is a paucity of studies from resource-poor and low income countries.
But for now, 10 days of amoxicillin-clavulanate for children younger than 2 years of age who have a definite diagnosis of acute otitis media seems to be a reasonable option.
Margaret A. Kenna, MD, MPH, is from the department of otolaryngology and communication enhancement at the Boston Children’s Hospital. These comments are excerpted from an accompanying editorial (N Engl J Med. 2016 Dec 22;375[25]:2492-93). Dr. Kenna declared a grant from Agilis outside the submitted work.
The study of acute otitis media is challenging owing to antibiotic pharmacokinetics, age of the patients, variation in regional pathogens, polymicrobial infection, viral cofactors, antibiotic resistance, status of patients with regard to receipt of PCV7 or PCV13, and a high rate of spontaneous resolution.
The study was not designed to address outcomes in older children, children with less severe acute otitis media or with acute otitis media in one ear, or children with additional risk factors such as cleft palate or trisomy 21. In addition, there is a paucity of studies from resource-poor and low income countries.
But for now, 10 days of amoxicillin-clavulanate for children younger than 2 years of age who have a definite diagnosis of acute otitis media seems to be a reasonable option.
Margaret A. Kenna, MD, MPH, is from the department of otolaryngology and communication enhancement at the Boston Children’s Hospital. These comments are excerpted from an accompanying editorial (N Engl J Med. 2016 Dec 22;375[25]:2492-93). Dr. Kenna declared a grant from Agilis outside the submitted work.
A shorter duration of antimicrobial therapy for acute otitis media (AOM) in children is associated with higher rates of clinical failure and higher symptom scores but without any associated reduction in the rates of antimicrobial resistance or adverse events.
Alejandro Hoberman, MD, of the Children’s Hospital of Pittsburgh at the University of Pittsburgh Medical Center, and his coauthors report the results of a study in which 520 children aged 6-23 months were randomized to either 10 days of amoxicillin-clavulanate therapy, or 5 days of therapy followed by 5 days of placebo.
The children who received the full 10-day course also had lower mean symptom scores in the 6-14 days after initiation of therapy, compared with those who received 5 days of treatment (1.34 vs. 1.61; P = 0.07), while the number of children whose symptom scores decreased by 50% from baseline to the end of treatment was significantly lower in the 5-day group.
However, there were no significant differences between the two groups in the rate of nasopharyngeal colonization pathogens not susceptible to penicillin: 47% in the 10-day group, compared with 44% in the 5-day group (N Engl J Med. 2016 Dec 22;375[25]:2446-56).
Similarly, the rates of recurrence and adverse events were not significantly different between the two groups.
A shorter duration of treatment has been considered as a strategy for reducing the risk of antimicrobial resistance, but clinical trials so far have showed either modest difference favoring the standard duration of treatment, or no difference at all.
“The outcome differences we found were larger than the differences that have been reported previously, mainly because the rates of clinical failure among children who received reduced duration treatment were higher in our trial than in previous trials,” Dr. Hoberman and his associates wrote.
The researchers did note that clinical failure rates were higher among children with greater exposure to other children, and those with infection in both ears rather than a single ear.
The study was supported by the National Institute of Allergy and Infectious Diseases and the National Institutes of Health. Dr. Hoberman and Dr. Judith M. Martin declared consulting fees from Genocea Biosciences, and Dr. Hoberman declared grant support from Ricoh Innovations and holding pending patents for a reduced clavulanate concentration version of amoxicillin–clavulanate potassium, and a method and device for aiding in the diagnosis of otitis media. No other conflicts of interest were declared.
A shorter duration of antimicrobial therapy for acute otitis media (AOM) in children is associated with higher rates of clinical failure and higher symptom scores but without any associated reduction in the rates of antimicrobial resistance or adverse events.
Alejandro Hoberman, MD, of the Children’s Hospital of Pittsburgh at the University of Pittsburgh Medical Center, and his coauthors report the results of a study in which 520 children aged 6-23 months were randomized to either 10 days of amoxicillin-clavulanate therapy, or 5 days of therapy followed by 5 days of placebo.
The children who received the full 10-day course also had lower mean symptom scores in the 6-14 days after initiation of therapy, compared with those who received 5 days of treatment (1.34 vs. 1.61; P = 0.07), while the number of children whose symptom scores decreased by 50% from baseline to the end of treatment was significantly lower in the 5-day group.
However, there were no significant differences between the two groups in the rate of nasopharyngeal colonization pathogens not susceptible to penicillin: 47% in the 10-day group, compared with 44% in the 5-day group (N Engl J Med. 2016 Dec 22;375[25]:2446-56).
Similarly, the rates of recurrence and adverse events were not significantly different between the two groups.
A shorter duration of treatment has been considered as a strategy for reducing the risk of antimicrobial resistance, but clinical trials so far have showed either modest difference favoring the standard duration of treatment, or no difference at all.
“The outcome differences we found were larger than the differences that have been reported previously, mainly because the rates of clinical failure among children who received reduced duration treatment were higher in our trial than in previous trials,” Dr. Hoberman and his associates wrote.
The researchers did note that clinical failure rates were higher among children with greater exposure to other children, and those with infection in both ears rather than a single ear.
The study was supported by the National Institute of Allergy and Infectious Diseases and the National Institutes of Health. Dr. Hoberman and Dr. Judith M. Martin declared consulting fees from Genocea Biosciences, and Dr. Hoberman declared grant support from Ricoh Innovations and holding pending patents for a reduced clavulanate concentration version of amoxicillin–clavulanate potassium, and a method and device for aiding in the diagnosis of otitis media. No other conflicts of interest were declared.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A shorter duration of antimicrobial therapy for acute otitis media (AOM) in children is associated with higher rates of clinical failure without a reduction in the rates of antimicrobial resistance.
Major finding: Children who received 5 days of antimicrobial experienced clinical failure rates of 35%, compared with 16% in those who received a full 10-day course.
Data source: Randomized controlled trial in 520 children aged 6-23 months with AOM.
Disclosures: The study was supported by the National Institute of Allergy and Infectious Diseases and the National Institutes of Health. Dr. Hoberman and Dr. Judith M. Martin declared consulting fees from Genocea Biosciences, and Dr. Hoberman declared grant support from Ricoh Innovations and holding pending patents for a reduced clavulanate concentration version of amoxicillin–clavulanate potassium, and a method and device for aiding in the diagnosis of otitis media. No other conflicts of interest were declared.
Antibiotic resistance remains a challenge for hospitals
The Centers for Disease Control and Prevention just released a surveillance report describing national estimates of antimicrobial resistance among health care–associated infections (HAIs) in hospitals. The report compiles HAI data submitted to the CDC’s National Healthcare Safety Network (NHSN) from almost all short-term acute care hospitals, inpatient rehabilitation facilities, and long-term acute care hospitals in the country.
These data highlight the broad reach and urgent nature of the drug resistance problem challenging clinicians today; resistance is occurring across different types of infections and patient populations, and dangerous resistance profiles such as carbapenem-resistant Enterobacteriaceae, or CRE, are not going away.
The report highlights the percentage of HAI organisms that were resistant to select antibiotics for 21 different bug-drug combinations from 2011 to 2014. Most noticeable across this time period was an increase in the percentage of Escherichia coli that tested resistant to extended-spectrum cephalosporins, fluoroquinolones, and were identified as multidrug resistant (Infect Control Hosp Epidemiol. 2016 Aug 30. doi: 10.1017/ice.2016.174).
In 2011, 41.1% of E. coli central line–associated bloodstream infections (CLABSIs) were resistant to fluoroquinolones; this percentage increased to 49.3% by 2014. And, among catheter-associated UTIs (CAUTIs), 8% of E. coli were identified as multidrug resistant in 2014, an increase from 5.5% in 2011.
Hospitals continue to report CRE infections, which are often untreatable and represent a serious public health threat. Across the major HAI types analyzed in this report, CRE were found in CLABSIs (7.1% of Enterobacteriaceae were resistant to carbapenems), CAUTIs (4.0% resistant), and surgical site infections (1.8% resistant). After taking a closer look at individual species of bacteria, we found that almost 11% of CLABSIs caused by Klebsiella species were resistant to carbapenems, which was the highest resistance among all Enterobacteriaceae species. Furthermore, Enterobacter species showed increasing resistance to carbapenems, as the percentage resistant in CLABSIs increased from 3.0% in 2011 to 6.6% in 2014.
These data underscore the urgent nature of CRE prevention efforts, and fighting back against these deadly bacteria will require collaborative efforts from the entire health care community including health care facility leaders, health care providers, and state and local health departments.
Antibiotic-resistant infections are an important patient safety issue and continue to pose a threat to modern medicine. There are small improvements in some phenotypes such as multidrug-resistant Acinetobacter, in which the percentage resistant in CLABSIs decreased from 60.9% in 2011 to 43.7% in 2014. Multidrug-resistant Klebsiella appears to be declining as well, from 20.9% resistant to 17.2%. Despite some improvements, the data in this report support the conclusion that much more work is needed to combat antibiotic resistance. The CDC has identified three critical efforts to slow the spread of resistant HAIs:
• Prevent infections related to devices and surgeries.
• Prevent the spread of bacteria between patients and between facilities.
• Improve antibiotic use in health care settings.
In addition to drug resistance, this report looked at the frequency of pathogens causing HAIs. The No. 1 and No. 3 most common pathogens among all HAIs were E.coli and Klebsiella, both of which are gram-negative bacteria with the propensity to develop antibiotic resistance.
The data also help identify important differences in the causes of HAIs across each of the infection types. For example, CLABSIs were more commonly due to gram positive organisms and Candida (a fungus), while surgical site infections (SSIs) were most frequently caused by Staph aureus. NHSN tracks SSIs following 39 different types of procedures, and while Staph aureus was the most common pathogen reported overall, the pathogen distributions did vary by surgery site. For example, almost 30% of SSIs following transplant procedures were caused by a species of Enterococcus.
Obviously, there’s far more data in the report than we can discuss here. Fortunately, the CDC’s new Antibiotic Resistance Patient Safety Atlas gives everyone an opportunity to explore these resistance patterns further; color-coded maps and charts included within the Atlas can help you identify common resistance phenotypes in your state and region. While these data give us a national snapshot of resistance profiles, we know there is wide variation among individual health care settings. It is important for providers to become familiar with the common pathogens and resistance profiles in their hospitals and recognize that common infecting organisms vary across different types of infections.
This report underscores the important challenges posed by resistant organisms in hospitals. Combating antibiotic resistance is a top public health priority in the United States and around the world, and having data to direct action is a key part of tackling the problem.
The CDC will continue to use and expand its efforts to monitor antibiotic resistance through surveillance systems such as NHSN, and will remain committed to providing data to support the health care community in efforts to reduce the spread of resistance and improve antibiotic use.
Lindsey Weiner, MPH, is an epidemiologist and associate service fellow in the Surveillance Branch, Division of Healthcare Quality Promotion, at the Centers for Disease Control and Prevention.
The Centers for Disease Control and Prevention just released a surveillance report describing national estimates of antimicrobial resistance among health care–associated infections (HAIs) in hospitals. The report compiles HAI data submitted to the CDC’s National Healthcare Safety Network (NHSN) from almost all short-term acute care hospitals, inpatient rehabilitation facilities, and long-term acute care hospitals in the country.
These data highlight the broad reach and urgent nature of the drug resistance problem challenging clinicians today; resistance is occurring across different types of infections and patient populations, and dangerous resistance profiles such as carbapenem-resistant Enterobacteriaceae, or CRE, are not going away.
The report highlights the percentage of HAI organisms that were resistant to select antibiotics for 21 different bug-drug combinations from 2011 to 2014. Most noticeable across this time period was an increase in the percentage of Escherichia coli that tested resistant to extended-spectrum cephalosporins, fluoroquinolones, and were identified as multidrug resistant (Infect Control Hosp Epidemiol. 2016 Aug 30. doi: 10.1017/ice.2016.174).
In 2011, 41.1% of E. coli central line–associated bloodstream infections (CLABSIs) were resistant to fluoroquinolones; this percentage increased to 49.3% by 2014. And, among catheter-associated UTIs (CAUTIs), 8% of E. coli were identified as multidrug resistant in 2014, an increase from 5.5% in 2011.
Hospitals continue to report CRE infections, which are often untreatable and represent a serious public health threat. Across the major HAI types analyzed in this report, CRE were found in CLABSIs (7.1% of Enterobacteriaceae were resistant to carbapenems), CAUTIs (4.0% resistant), and surgical site infections (1.8% resistant). After taking a closer look at individual species of bacteria, we found that almost 11% of CLABSIs caused by Klebsiella species were resistant to carbapenems, which was the highest resistance among all Enterobacteriaceae species. Furthermore, Enterobacter species showed increasing resistance to carbapenems, as the percentage resistant in CLABSIs increased from 3.0% in 2011 to 6.6% in 2014.
These data underscore the urgent nature of CRE prevention efforts, and fighting back against these deadly bacteria will require collaborative efforts from the entire health care community including health care facility leaders, health care providers, and state and local health departments.
Antibiotic-resistant infections are an important patient safety issue and continue to pose a threat to modern medicine. There are small improvements in some phenotypes such as multidrug-resistant Acinetobacter, in which the percentage resistant in CLABSIs decreased from 60.9% in 2011 to 43.7% in 2014. Multidrug-resistant Klebsiella appears to be declining as well, from 20.9% resistant to 17.2%. Despite some improvements, the data in this report support the conclusion that much more work is needed to combat antibiotic resistance. The CDC has identified three critical efforts to slow the spread of resistant HAIs:
• Prevent infections related to devices and surgeries.
• Prevent the spread of bacteria between patients and between facilities.
• Improve antibiotic use in health care settings.
In addition to drug resistance, this report looked at the frequency of pathogens causing HAIs. The No. 1 and No. 3 most common pathogens among all HAIs were E.coli and Klebsiella, both of which are gram-negative bacteria with the propensity to develop antibiotic resistance.
The data also help identify important differences in the causes of HAIs across each of the infection types. For example, CLABSIs were more commonly due to gram positive organisms and Candida (a fungus), while surgical site infections (SSIs) were most frequently caused by Staph aureus. NHSN tracks SSIs following 39 different types of procedures, and while Staph aureus was the most common pathogen reported overall, the pathogen distributions did vary by surgery site. For example, almost 30% of SSIs following transplant procedures were caused by a species of Enterococcus.
Obviously, there’s far more data in the report than we can discuss here. Fortunately, the CDC’s new Antibiotic Resistance Patient Safety Atlas gives everyone an opportunity to explore these resistance patterns further; color-coded maps and charts included within the Atlas can help you identify common resistance phenotypes in your state and region. While these data give us a national snapshot of resistance profiles, we know there is wide variation among individual health care settings. It is important for providers to become familiar with the common pathogens and resistance profiles in their hospitals and recognize that common infecting organisms vary across different types of infections.
This report underscores the important challenges posed by resistant organisms in hospitals. Combating antibiotic resistance is a top public health priority in the United States and around the world, and having data to direct action is a key part of tackling the problem.
The CDC will continue to use and expand its efforts to monitor antibiotic resistance through surveillance systems such as NHSN, and will remain committed to providing data to support the health care community in efforts to reduce the spread of resistance and improve antibiotic use.
Lindsey Weiner, MPH, is an epidemiologist and associate service fellow in the Surveillance Branch, Division of Healthcare Quality Promotion, at the Centers for Disease Control and Prevention.
The Centers for Disease Control and Prevention just released a surveillance report describing national estimates of antimicrobial resistance among health care–associated infections (HAIs) in hospitals. The report compiles HAI data submitted to the CDC’s National Healthcare Safety Network (NHSN) from almost all short-term acute care hospitals, inpatient rehabilitation facilities, and long-term acute care hospitals in the country.
These data highlight the broad reach and urgent nature of the drug resistance problem challenging clinicians today; resistance is occurring across different types of infections and patient populations, and dangerous resistance profiles such as carbapenem-resistant Enterobacteriaceae, or CRE, are not going away.
The report highlights the percentage of HAI organisms that were resistant to select antibiotics for 21 different bug-drug combinations from 2011 to 2014. Most noticeable across this time period was an increase in the percentage of Escherichia coli that tested resistant to extended-spectrum cephalosporins, fluoroquinolones, and were identified as multidrug resistant (Infect Control Hosp Epidemiol. 2016 Aug 30. doi: 10.1017/ice.2016.174).
In 2011, 41.1% of E. coli central line–associated bloodstream infections (CLABSIs) were resistant to fluoroquinolones; this percentage increased to 49.3% by 2014. And, among catheter-associated UTIs (CAUTIs), 8% of E. coli were identified as multidrug resistant in 2014, an increase from 5.5% in 2011.
Hospitals continue to report CRE infections, which are often untreatable and represent a serious public health threat. Across the major HAI types analyzed in this report, CRE were found in CLABSIs (7.1% of Enterobacteriaceae were resistant to carbapenems), CAUTIs (4.0% resistant), and surgical site infections (1.8% resistant). After taking a closer look at individual species of bacteria, we found that almost 11% of CLABSIs caused by Klebsiella species were resistant to carbapenems, which was the highest resistance among all Enterobacteriaceae species. Furthermore, Enterobacter species showed increasing resistance to carbapenems, as the percentage resistant in CLABSIs increased from 3.0% in 2011 to 6.6% in 2014.
These data underscore the urgent nature of CRE prevention efforts, and fighting back against these deadly bacteria will require collaborative efforts from the entire health care community including health care facility leaders, health care providers, and state and local health departments.
Antibiotic-resistant infections are an important patient safety issue and continue to pose a threat to modern medicine. There are small improvements in some phenotypes such as multidrug-resistant Acinetobacter, in which the percentage resistant in CLABSIs decreased from 60.9% in 2011 to 43.7% in 2014. Multidrug-resistant Klebsiella appears to be declining as well, from 20.9% resistant to 17.2%. Despite some improvements, the data in this report support the conclusion that much more work is needed to combat antibiotic resistance. The CDC has identified three critical efforts to slow the spread of resistant HAIs:
• Prevent infections related to devices and surgeries.
• Prevent the spread of bacteria between patients and between facilities.
• Improve antibiotic use in health care settings.
In addition to drug resistance, this report looked at the frequency of pathogens causing HAIs. The No. 1 and No. 3 most common pathogens among all HAIs were E.coli and Klebsiella, both of which are gram-negative bacteria with the propensity to develop antibiotic resistance.
The data also help identify important differences in the causes of HAIs across each of the infection types. For example, CLABSIs were more commonly due to gram positive organisms and Candida (a fungus), while surgical site infections (SSIs) were most frequently caused by Staph aureus. NHSN tracks SSIs following 39 different types of procedures, and while Staph aureus was the most common pathogen reported overall, the pathogen distributions did vary by surgery site. For example, almost 30% of SSIs following transplant procedures were caused by a species of Enterococcus.
Obviously, there’s far more data in the report than we can discuss here. Fortunately, the CDC’s new Antibiotic Resistance Patient Safety Atlas gives everyone an opportunity to explore these resistance patterns further; color-coded maps and charts included within the Atlas can help you identify common resistance phenotypes in your state and region. While these data give us a national snapshot of resistance profiles, we know there is wide variation among individual health care settings. It is important for providers to become familiar with the common pathogens and resistance profiles in their hospitals and recognize that common infecting organisms vary across different types of infections.
This report underscores the important challenges posed by resistant organisms in hospitals. Combating antibiotic resistance is a top public health priority in the United States and around the world, and having data to direct action is a key part of tackling the problem.
The CDC will continue to use and expand its efforts to monitor antibiotic resistance through surveillance systems such as NHSN, and will remain committed to providing data to support the health care community in efforts to reduce the spread of resistance and improve antibiotic use.
Lindsey Weiner, MPH, is an epidemiologist and associate service fellow in the Surveillance Branch, Division of Healthcare Quality Promotion, at the Centers for Disease Control and Prevention.
Macrolide monotherapy works in some NTM lung disease
Patients with cystic fibrosis or bronchiectasis and one form of Mycobacterium abscessus disease can be successfully treated with long-term oral macrolide monotherapy following short-term intravenous combination antibiotic therapy, a Korean research team has shown.
The M. abscessus complex is implicated in between a fifth and half of all cases of lung disease caused by nontuberculous mycobacteria (NTM). Though treatment is notoriously difficult and prolonged in all NTM lung disease, one subspecies of M. abscessus – M. massiliense – lacks the active gene needed for developing resistance to macrolide-based antibiotics, making it potentially more readily treated.
In research published in CHEST, Won-Jung Koh, MD, of Samsung Medical Center and Sungkyunkwan University in Seoul, South Korea, and colleagues, sought to determine the optimal treatment protocol for patients with massiliense disease (Chest. 2016 Dec;150[6]:1211-21). They identified 71 patients with massiliense disease who had initiated antibiotic treatment between January 2007 and December 2012. These patients were part of an ongoing prospective cohort study on NTM lung disease. The first 28 patients in the study were hospitalized for 4 weeks and treated with intravenous amikacin and cefoxitin along with oral clarithromycin and a fluoroquinolone. Following discharge these patients remained on the oral agents for 24 months.
Two years into the study, the protocol changed, and the next 43 patients were treated with a 2-week course of intravenous amikacin and cefoxitin along with the oral agents. In some patients, azithromycin, which came into use in Korea for NTM lung disease in 2011, replaced a fluoroquinolone. After discharge, all patients stayed on the oral macrolides (with seven also taking a fluoroquinolone) until their sputum cultures were negative for 12 months.
For the patients treated for 4 weeks, the response rates after 12 months of treatment were 89% for symptoms, 79% for computed tomography, and 100% for negative sputum cultures. In the patients treated for 2 weeks, they were 100%, 91%, and 91%, respectively. None of these differences between the two groups were statistically significant. Median total treatment duration, however, was significantly shorter – by nearly a year – in the 2-week plus macrolide monotherapy group than in the other group of patients (15.2 months vs. 23.9 months, P less than .001).
Acquired macrolide resistance developed in two patients in the group who received a 2-week course of intravenous amikacin and cefoxitin along with the oral agents, including one case of high-level clarithromycin resistance. Genotyping revealed reinfection with different strains of M. massiliense.
“[Oral] macrolide therapy after an initial 2-week course of combination antibiotics, rather than long-term parenteral antibiotics, might be effective in most patients with M. massiliense lung disease,” Dr. Koh and colleagues wrote, noting that their study’s nonrandomized single-site design was a limitation, and that multicenter randomized trials would be needed “to assess the efficacy” of the findings.
The Korean government funded Dr. Koh and colleagues’ study. None of the authors disclosed conflicts of interest.
“In this study by Koh et al., it is gratifying that most patients had a favorable microbiologic outcome. It is also somewhat surprising that only two patients developed acquired macrolide resistant M. abscessus subsp massiliense isolates. While the absolute number is low, for those two individuals, the consequences of developing macrolide resistance are far from trivial. They have transitioned from having a mycobacterial infection that is relatively easy to treat effectively to a mycobacterial infection that is not,” David E. Griffith, MD, FCCP, and Timothy R. Aksamit, MD, FCCP, wrote in an editorial published in the December issue of CHEST (Chest. 2016 Dec;150[6];1177-8).
The authors noted that they “enthusiastically applaud and acknowledge the prolific and consistently excellent work done by the group in South Korea, but we cannot endorse the widespread adoption of macrolide monotherapy for” this patient group. “In our view, the risk/benefit balance of this approach does not favor macrolide monotherapy even though the majority of patients in this study were adequately treated.”
Dr. Griffith is professor of medicine at University of Texas Health Science Center, Tyler, and Dr. Aksamit is a consultant on pulmonary disease and critical care medicine at the Mayo Clinic, Rochester, Minn. They disclosed no conflicts of interest.
“In this study by Koh et al., it is gratifying that most patients had a favorable microbiologic outcome. It is also somewhat surprising that only two patients developed acquired macrolide resistant M. abscessus subsp massiliense isolates. While the absolute number is low, for those two individuals, the consequences of developing macrolide resistance are far from trivial. They have transitioned from having a mycobacterial infection that is relatively easy to treat effectively to a mycobacterial infection that is not,” David E. Griffith, MD, FCCP, and Timothy R. Aksamit, MD, FCCP, wrote in an editorial published in the December issue of CHEST (Chest. 2016 Dec;150[6];1177-8).
The authors noted that they “enthusiastically applaud and acknowledge the prolific and consistently excellent work done by the group in South Korea, but we cannot endorse the widespread adoption of macrolide monotherapy for” this patient group. “In our view, the risk/benefit balance of this approach does not favor macrolide monotherapy even though the majority of patients in this study were adequately treated.”
Dr. Griffith is professor of medicine at University of Texas Health Science Center, Tyler, and Dr. Aksamit is a consultant on pulmonary disease and critical care medicine at the Mayo Clinic, Rochester, Minn. They disclosed no conflicts of interest.
“In this study by Koh et al., it is gratifying that most patients had a favorable microbiologic outcome. It is also somewhat surprising that only two patients developed acquired macrolide resistant M. abscessus subsp massiliense isolates. While the absolute number is low, for those two individuals, the consequences of developing macrolide resistance are far from trivial. They have transitioned from having a mycobacterial infection that is relatively easy to treat effectively to a mycobacterial infection that is not,” David E. Griffith, MD, FCCP, and Timothy R. Aksamit, MD, FCCP, wrote in an editorial published in the December issue of CHEST (Chest. 2016 Dec;150[6];1177-8).
The authors noted that they “enthusiastically applaud and acknowledge the prolific and consistently excellent work done by the group in South Korea, but we cannot endorse the widespread adoption of macrolide monotherapy for” this patient group. “In our view, the risk/benefit balance of this approach does not favor macrolide monotherapy even though the majority of patients in this study were adequately treated.”
Dr. Griffith is professor of medicine at University of Texas Health Science Center, Tyler, and Dr. Aksamit is a consultant on pulmonary disease and critical care medicine at the Mayo Clinic, Rochester, Minn. They disclosed no conflicts of interest.
Patients with cystic fibrosis or bronchiectasis and one form of Mycobacterium abscessus disease can be successfully treated with long-term oral macrolide monotherapy following short-term intravenous combination antibiotic therapy, a Korean research team has shown.
The M. abscessus complex is implicated in between a fifth and half of all cases of lung disease caused by nontuberculous mycobacteria (NTM). Though treatment is notoriously difficult and prolonged in all NTM lung disease, one subspecies of M. abscessus – M. massiliense – lacks the active gene needed for developing resistance to macrolide-based antibiotics, making it potentially more readily treated.
In research published in CHEST, Won-Jung Koh, MD, of Samsung Medical Center and Sungkyunkwan University in Seoul, South Korea, and colleagues, sought to determine the optimal treatment protocol for patients with massiliense disease (Chest. 2016 Dec;150[6]:1211-21). They identified 71 patients with massiliense disease who had initiated antibiotic treatment between January 2007 and December 2012. These patients were part of an ongoing prospective cohort study on NTM lung disease. The first 28 patients in the study were hospitalized for 4 weeks and treated with intravenous amikacin and cefoxitin along with oral clarithromycin and a fluoroquinolone. Following discharge these patients remained on the oral agents for 24 months.
Two years into the study, the protocol changed, and the next 43 patients were treated with a 2-week course of intravenous amikacin and cefoxitin along with the oral agents. In some patients, azithromycin, which came into use in Korea for NTM lung disease in 2011, replaced a fluoroquinolone. After discharge, all patients stayed on the oral macrolides (with seven also taking a fluoroquinolone) until their sputum cultures were negative for 12 months.
For the patients treated for 4 weeks, the response rates after 12 months of treatment were 89% for symptoms, 79% for computed tomography, and 100% for negative sputum cultures. In the patients treated for 2 weeks, they were 100%, 91%, and 91%, respectively. None of these differences between the two groups were statistically significant. Median total treatment duration, however, was significantly shorter – by nearly a year – in the 2-week plus macrolide monotherapy group than in the other group of patients (15.2 months vs. 23.9 months, P less than .001).
Acquired macrolide resistance developed in two patients in the group who received a 2-week course of intravenous amikacin and cefoxitin along with the oral agents, including one case of high-level clarithromycin resistance. Genotyping revealed reinfection with different strains of M. massiliense.
“[Oral] macrolide therapy after an initial 2-week course of combination antibiotics, rather than long-term parenteral antibiotics, might be effective in most patients with M. massiliense lung disease,” Dr. Koh and colleagues wrote, noting that their study’s nonrandomized single-site design was a limitation, and that multicenter randomized trials would be needed “to assess the efficacy” of the findings.
The Korean government funded Dr. Koh and colleagues’ study. None of the authors disclosed conflicts of interest.
Patients with cystic fibrosis or bronchiectasis and one form of Mycobacterium abscessus disease can be successfully treated with long-term oral macrolide monotherapy following short-term intravenous combination antibiotic therapy, a Korean research team has shown.
The M. abscessus complex is implicated in between a fifth and half of all cases of lung disease caused by nontuberculous mycobacteria (NTM). Though treatment is notoriously difficult and prolonged in all NTM lung disease, one subspecies of M. abscessus – M. massiliense – lacks the active gene needed for developing resistance to macrolide-based antibiotics, making it potentially more readily treated.
In research published in CHEST, Won-Jung Koh, MD, of Samsung Medical Center and Sungkyunkwan University in Seoul, South Korea, and colleagues, sought to determine the optimal treatment protocol for patients with massiliense disease (Chest. 2016 Dec;150[6]:1211-21). They identified 71 patients with massiliense disease who had initiated antibiotic treatment between January 2007 and December 2012. These patients were part of an ongoing prospective cohort study on NTM lung disease. The first 28 patients in the study were hospitalized for 4 weeks and treated with intravenous amikacin and cefoxitin along with oral clarithromycin and a fluoroquinolone. Following discharge these patients remained on the oral agents for 24 months.
Two years into the study, the protocol changed, and the next 43 patients were treated with a 2-week course of intravenous amikacin and cefoxitin along with the oral agents. In some patients, azithromycin, which came into use in Korea for NTM lung disease in 2011, replaced a fluoroquinolone. After discharge, all patients stayed on the oral macrolides (with seven also taking a fluoroquinolone) until their sputum cultures were negative for 12 months.
For the patients treated for 4 weeks, the response rates after 12 months of treatment were 89% for symptoms, 79% for computed tomography, and 100% for negative sputum cultures. In the patients treated for 2 weeks, they were 100%, 91%, and 91%, respectively. None of these differences between the two groups were statistically significant. Median total treatment duration, however, was significantly shorter – by nearly a year – in the 2-week plus macrolide monotherapy group than in the other group of patients (15.2 months vs. 23.9 months, P less than .001).
Acquired macrolide resistance developed in two patients in the group who received a 2-week course of intravenous amikacin and cefoxitin along with the oral agents, including one case of high-level clarithromycin resistance. Genotyping revealed reinfection with different strains of M. massiliense.
“[Oral] macrolide therapy after an initial 2-week course of combination antibiotics, rather than long-term parenteral antibiotics, might be effective in most patients with M. massiliense lung disease,” Dr. Koh and colleagues wrote, noting that their study’s nonrandomized single-site design was a limitation, and that multicenter randomized trials would be needed “to assess the efficacy” of the findings.
The Korean government funded Dr. Koh and colleagues’ study. None of the authors disclosed conflicts of interest.
FROM CHEST
Key clinical point: A short course of intravenous antibiotics followed by oral macrolides may be effective at treating lung disease caused by the massiliense subspecies of M. abscessus.
Major finding: Of 43 patients receiving 2 weeks of combination antibiotics followed by a year of oral macrolides, 39 (91%) converted to negative sputum cultures before 12 months.
Data source: A prospective cohort study enrolling 71 patients at a single treatment center in Korea.
Disclosures: The Korean government sponsored the study and investigators disclosed no conflicts of interest.
Rate of resistant P. aeruginosa in children rising steadily
The rate of infection with resistant Pseudomonas aeruginosa among children has risen steadily about 4% per year since 1999, according to a report.
Infections with P aeruginosa in children occur most often associated with pulmonary disease in patients with cystic fibrosis, but healthy children also can experience a variety of P aeruginosa infection types.
They focused on 77,349 P. aeruginosa isolates that were tested for resistance for all five antibiotic classes: cephalosporins, beta-lactam and beta-lactamase inhibitors, carbapenems, fluoroquinolones, and aminoglycosides. The investigators were specifically interested in multidrug- and carbapenem-resistant P. aeruginosa. They described the organism as “arguably the most resistance-prone health care–related pathogen.”
The study samples were obtained from the respiratory tract, urinary tract, ear, sinuses, wounds, skin, and connective tissues of children aged 1-17 years who were treated in 1999-2012; 2012 was the last year for which this information was collected in this database. Patients were treated in ambulatory, inpatient, ICU, and long-term-care settings. The study excluded children with cystic fibrosis and children under 1 year of age, so as to improve the applicability of the results to the general pediatric population.
The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%. This represents an average annual increase of approximately 4% for both types of resistance, Dr. Logan and her associates said (J Ped Infect Dis. 2016 Nov 16. doi: 10.1093/jpids/piw064).
These increases were consistent across all but one age group and all but one treatment setting, the exception being inpatients aged 13-17 years. The prevalence of resistant P. aeruginosa was highest among adolescents in ambulatory, ICU, or long-term-care settings; their rates were three times higher than those in children aged 1 year and two times higher than those in children aged 5 years. It is possible that this pattern reflects “an increasing number of older children with a medically complex condition who have frequent exposure to the health care environment,” the investigators noted.
“The results of our study highlight the need for bacterial surveillance, strategies for implementing effective infection prevention, and antimicrobial stewardship programs.” In addition, all health care facilities should consider using rapid molecular diagnostic platforms to guide antibiotic treatment decisions, “to reduce the burden of the persistent and continually evolving global threat of extensively drug-resistant organisms,” Dr. Logan and her associates added.
This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
The rate of infection with resistant Pseudomonas aeruginosa among children has risen steadily about 4% per year since 1999, according to a report.
Infections with P aeruginosa in children occur most often associated with pulmonary disease in patients with cystic fibrosis, but healthy children also can experience a variety of P aeruginosa infection types.
They focused on 77,349 P. aeruginosa isolates that were tested for resistance for all five antibiotic classes: cephalosporins, beta-lactam and beta-lactamase inhibitors, carbapenems, fluoroquinolones, and aminoglycosides. The investigators were specifically interested in multidrug- and carbapenem-resistant P. aeruginosa. They described the organism as “arguably the most resistance-prone health care–related pathogen.”
The study samples were obtained from the respiratory tract, urinary tract, ear, sinuses, wounds, skin, and connective tissues of children aged 1-17 years who were treated in 1999-2012; 2012 was the last year for which this information was collected in this database. Patients were treated in ambulatory, inpatient, ICU, and long-term-care settings. The study excluded children with cystic fibrosis and children under 1 year of age, so as to improve the applicability of the results to the general pediatric population.
The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%. This represents an average annual increase of approximately 4% for both types of resistance, Dr. Logan and her associates said (J Ped Infect Dis. 2016 Nov 16. doi: 10.1093/jpids/piw064).
These increases were consistent across all but one age group and all but one treatment setting, the exception being inpatients aged 13-17 years. The prevalence of resistant P. aeruginosa was highest among adolescents in ambulatory, ICU, or long-term-care settings; their rates were three times higher than those in children aged 1 year and two times higher than those in children aged 5 years. It is possible that this pattern reflects “an increasing number of older children with a medically complex condition who have frequent exposure to the health care environment,” the investigators noted.
“The results of our study highlight the need for bacterial surveillance, strategies for implementing effective infection prevention, and antimicrobial stewardship programs.” In addition, all health care facilities should consider using rapid molecular diagnostic platforms to guide antibiotic treatment decisions, “to reduce the burden of the persistent and continually evolving global threat of extensively drug-resistant organisms,” Dr. Logan and her associates added.
This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
The rate of infection with resistant Pseudomonas aeruginosa among children has risen steadily about 4% per year since 1999, according to a report.
Infections with P aeruginosa in children occur most often associated with pulmonary disease in patients with cystic fibrosis, but healthy children also can experience a variety of P aeruginosa infection types.
They focused on 77,349 P. aeruginosa isolates that were tested for resistance for all five antibiotic classes: cephalosporins, beta-lactam and beta-lactamase inhibitors, carbapenems, fluoroquinolones, and aminoglycosides. The investigators were specifically interested in multidrug- and carbapenem-resistant P. aeruginosa. They described the organism as “arguably the most resistance-prone health care–related pathogen.”
The study samples were obtained from the respiratory tract, urinary tract, ear, sinuses, wounds, skin, and connective tissues of children aged 1-17 years who were treated in 1999-2012; 2012 was the last year for which this information was collected in this database. Patients were treated in ambulatory, inpatient, ICU, and long-term-care settings. The study excluded children with cystic fibrosis and children under 1 year of age, so as to improve the applicability of the results to the general pediatric population.
The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%. This represents an average annual increase of approximately 4% for both types of resistance, Dr. Logan and her associates said (J Ped Infect Dis. 2016 Nov 16. doi: 10.1093/jpids/piw064).
These increases were consistent across all but one age group and all but one treatment setting, the exception being inpatients aged 13-17 years. The prevalence of resistant P. aeruginosa was highest among adolescents in ambulatory, ICU, or long-term-care settings; their rates were three times higher than those in children aged 1 year and two times higher than those in children aged 5 years. It is possible that this pattern reflects “an increasing number of older children with a medically complex condition who have frequent exposure to the health care environment,” the investigators noted.
“The results of our study highlight the need for bacterial surveillance, strategies for implementing effective infection prevention, and antimicrobial stewardship programs.” In addition, all health care facilities should consider using rapid molecular diagnostic platforms to guide antibiotic treatment decisions, “to reduce the burden of the persistent and continually evolving global threat of extensively drug-resistant organisms,” Dr. Logan and her associates added.
This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
FROM THE JOURNAL OF PEDIATRIC INFECTIOUS DISEASES
Key clinical point:
Major finding: The proportion of multidrug-resistant P. aeruginosa samples rose from 15% to 26% during the 13-year study period, and the proportion of carbapenem-resistant P. aeruginosa samples rose from 9% to 20%.
Data source: A longitudinal analysis of information in a nationally representative database of microbiology laboratories serving approximately 300 U.S. hospitals.
Disclosures: This study was supported by the National Institute of Allergy and Infectious Diseases; the Global Antibiotic Resistance Partnership, funded by the Bill and Melinda Gates Foundation; and the Health Grand Challenges Program at Princeton University. Dr. Logan and her associates reported having no relevant financial disclosures.
‘Skip phenomenon’ could explain fluctuating positivity for S. aureus bacteremia
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
‘Fight the Resistance’ with Antibiotic Stewardship Mentored Implementation
In conjunction with the Centers for Disease Control & Prevention’s Get Smart about Antibiotics Week, SHM is committed to promoting improved antibiotic-prescribing behaviors among the nation’s hospitalists through its “Fight the Resistance” awareness campaign.
Display SHM’s three downloadable “Fight the Resistance” posters, available at www.fighttheresistance.org. Hang them in your break rooms, hallways, or other high-profile locations to help remind your colleagues about the dangers of antibiotic resistance. SHM will be launching a mentored implementation program on antibiotics in early 2017. To be notified when the program becomes available, visit www.hospitalmedicine.org/ABX16.
In conjunction with the Centers for Disease Control & Prevention’s Get Smart about Antibiotics Week, SHM is committed to promoting improved antibiotic-prescribing behaviors among the nation’s hospitalists through its “Fight the Resistance” awareness campaign.
Display SHM’s three downloadable “Fight the Resistance” posters, available at www.fighttheresistance.org. Hang them in your break rooms, hallways, or other high-profile locations to help remind your colleagues about the dangers of antibiotic resistance. SHM will be launching a mentored implementation program on antibiotics in early 2017. To be notified when the program becomes available, visit www.hospitalmedicine.org/ABX16.
In conjunction with the Centers for Disease Control & Prevention’s Get Smart about Antibiotics Week, SHM is committed to promoting improved antibiotic-prescribing behaviors among the nation’s hospitalists through its “Fight the Resistance” awareness campaign.
Display SHM’s three downloadable “Fight the Resistance” posters, available at www.fighttheresistance.org. Hang them in your break rooms, hallways, or other high-profile locations to help remind your colleagues about the dangers of antibiotic resistance. SHM will be launching a mentored implementation program on antibiotics in early 2017. To be notified when the program becomes available, visit www.hospitalmedicine.org/ABX16.