User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Does new heart transplant method challenge definition of death?
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
Nurse makes millions selling her licensing exam study sheets
Ms. Beggs, 28, sells one-page study sheets or bundles of sheets, sometimes with colorful drawings, conversation bubbles and underlining, that boil down concepts for particular conditions into easy-to-understand language.
The biggest seller on Ms. Beggs’ online marketplace Etsy site, RNExplained, is a bundle of study guides covering eight core nursing classes. The notes range in price from $2 to $150. More than 70,000 customers have bought the $60 bundle, according to the website.
Ms. Beggs’ business developed in a “very unintentional” way when COVID hit with just months left in her nursing program at Mount Saint Mary’s University, Los Angeles, she told this news organization.
Classes had switched to Zoom, and she had no one to study with as she prepared to take her board exams.
“The best way I know how to study is to teach things out loud. But because I had nobody to teach out loud to, I would literally teach them to the wall,” Ms. Beggs said. “I would record myself so I could play it back and teach myself these topics that were hard for me to understand.”
Just for fun, she says, she posted them on TikTok and the responses started flowing in, with followers asking where she was selling the sheets. She now has more than 660,000 TikTok followers and 9 million likes.
Ms. Beggs said that every sheet highlights a condition, and she has made 308 of them.
Traditional classroom lessons typically teach one medical condition in 5-6 pages, Ms. Beggs said. “I go straight to the point.”
One reviewer on Ms. Beggs’ Etsy site appreciated the handwritten notes, calling them “simplified and concise.” Another commented: “Definitely helped me pass my last exam.”
Ms. Beggs says that her notes may seem simple, but each page represents comprehensive research.
“I have to go through not just one source of information to make sure my information is factual,” Ms. Beggs says. “What you teach in California might be a little different than what you teach in Florida. It’s very meticulous. The lab values will be a little different everywhere you go.”
She acknowledges her competition, noting that there are many other study guides for the NCLEX and nursing courses.
Nursing groups weigh in
Dawn Kappel, spokesperson for the National Council of State Boards of Nursing, which oversees NCLEX, said in an interview that “NCSBN has no issue with the current content of Stephanee Beggs’ business venture.”
For many students, the study guides will be helpful, especially for visual learners, said Carole Kenner, PhD, RN, dean and professor in the School of Nursing and Health Sciences at The College of New Jersey.
But for students “who are less confident in their knowledge, I would want to see a lot more in-depth explanation and rationale,” Dr. Kenner said.
“Since the NCLEX is moving to more cased-based scenarios, the next-gen unfolding cases, you really have to understand a lot of the rationale.”
The notes remind Dr. Kenner of traditional flash cards. “I don’t think it will work for all students, but even the fanciest of onsite review courses are useful to everyone,” she said.
‘Not cutting corners’
As an emergency nurse, Ms. Beggs said, “I have the experience as a nurse to show people that what you are learning will be seen in real life.”
“The way I teach my brand is not to take shortcuts. I love to teach to understand rather than teaching to memorize for an exam.”
She said she sees her guides as a supplement to learning, not a replacement.
“It’s not cutting corners,” she says. “I condense a medical condition that could take a very long time to understand and break it into layman’s terms.”
Ms. Beggs said when people hear about the $2 million, they often ask her whether she plans to give up her shifts in the emergency department for the more lucrative venture.
The answer is no, at least not yet.
“Aside from teaching, I genuinely love being at the bedside,” Ms. Beggs said. “I don’t foresee myself leaving that for good for as long as I can handle both.” She acknowledged, though, that her business now takes up most of her time.
“I love everything about both aspects, so it’s hard for me to choose.”
A version of this article first appeared on Medscape.com.
Ms. Beggs, 28, sells one-page study sheets or bundles of sheets, sometimes with colorful drawings, conversation bubbles and underlining, that boil down concepts for particular conditions into easy-to-understand language.
The biggest seller on Ms. Beggs’ online marketplace Etsy site, RNExplained, is a bundle of study guides covering eight core nursing classes. The notes range in price from $2 to $150. More than 70,000 customers have bought the $60 bundle, according to the website.
Ms. Beggs’ business developed in a “very unintentional” way when COVID hit with just months left in her nursing program at Mount Saint Mary’s University, Los Angeles, she told this news organization.
Classes had switched to Zoom, and she had no one to study with as she prepared to take her board exams.
“The best way I know how to study is to teach things out loud. But because I had nobody to teach out loud to, I would literally teach them to the wall,” Ms. Beggs said. “I would record myself so I could play it back and teach myself these topics that were hard for me to understand.”
Just for fun, she says, she posted them on TikTok and the responses started flowing in, with followers asking where she was selling the sheets. She now has more than 660,000 TikTok followers and 9 million likes.
Ms. Beggs said that every sheet highlights a condition, and she has made 308 of them.
Traditional classroom lessons typically teach one medical condition in 5-6 pages, Ms. Beggs said. “I go straight to the point.”
One reviewer on Ms. Beggs’ Etsy site appreciated the handwritten notes, calling them “simplified and concise.” Another commented: “Definitely helped me pass my last exam.”
Ms. Beggs says that her notes may seem simple, but each page represents comprehensive research.
“I have to go through not just one source of information to make sure my information is factual,” Ms. Beggs says. “What you teach in California might be a little different than what you teach in Florida. It’s very meticulous. The lab values will be a little different everywhere you go.”
She acknowledges her competition, noting that there are many other study guides for the NCLEX and nursing courses.
Nursing groups weigh in
Dawn Kappel, spokesperson for the National Council of State Boards of Nursing, which oversees NCLEX, said in an interview that “NCSBN has no issue with the current content of Stephanee Beggs’ business venture.”
For many students, the study guides will be helpful, especially for visual learners, said Carole Kenner, PhD, RN, dean and professor in the School of Nursing and Health Sciences at The College of New Jersey.
But for students “who are less confident in their knowledge, I would want to see a lot more in-depth explanation and rationale,” Dr. Kenner said.
“Since the NCLEX is moving to more cased-based scenarios, the next-gen unfolding cases, you really have to understand a lot of the rationale.”
The notes remind Dr. Kenner of traditional flash cards. “I don’t think it will work for all students, but even the fanciest of onsite review courses are useful to everyone,” she said.
‘Not cutting corners’
As an emergency nurse, Ms. Beggs said, “I have the experience as a nurse to show people that what you are learning will be seen in real life.”
“The way I teach my brand is not to take shortcuts. I love to teach to understand rather than teaching to memorize for an exam.”
She said she sees her guides as a supplement to learning, not a replacement.
“It’s not cutting corners,” she says. “I condense a medical condition that could take a very long time to understand and break it into layman’s terms.”
Ms. Beggs said when people hear about the $2 million, they often ask her whether she plans to give up her shifts in the emergency department for the more lucrative venture.
The answer is no, at least not yet.
“Aside from teaching, I genuinely love being at the bedside,” Ms. Beggs said. “I don’t foresee myself leaving that for good for as long as I can handle both.” She acknowledged, though, that her business now takes up most of her time.
“I love everything about both aspects, so it’s hard for me to choose.”
A version of this article first appeared on Medscape.com.
Ms. Beggs, 28, sells one-page study sheets or bundles of sheets, sometimes with colorful drawings, conversation bubbles and underlining, that boil down concepts for particular conditions into easy-to-understand language.
The biggest seller on Ms. Beggs’ online marketplace Etsy site, RNExplained, is a bundle of study guides covering eight core nursing classes. The notes range in price from $2 to $150. More than 70,000 customers have bought the $60 bundle, according to the website.
Ms. Beggs’ business developed in a “very unintentional” way when COVID hit with just months left in her nursing program at Mount Saint Mary’s University, Los Angeles, she told this news organization.
Classes had switched to Zoom, and she had no one to study with as she prepared to take her board exams.
“The best way I know how to study is to teach things out loud. But because I had nobody to teach out loud to, I would literally teach them to the wall,” Ms. Beggs said. “I would record myself so I could play it back and teach myself these topics that were hard for me to understand.”
Just for fun, she says, she posted them on TikTok and the responses started flowing in, with followers asking where she was selling the sheets. She now has more than 660,000 TikTok followers and 9 million likes.
Ms. Beggs said that every sheet highlights a condition, and she has made 308 of them.
Traditional classroom lessons typically teach one medical condition in 5-6 pages, Ms. Beggs said. “I go straight to the point.”
One reviewer on Ms. Beggs’ Etsy site appreciated the handwritten notes, calling them “simplified and concise.” Another commented: “Definitely helped me pass my last exam.”
Ms. Beggs says that her notes may seem simple, but each page represents comprehensive research.
“I have to go through not just one source of information to make sure my information is factual,” Ms. Beggs says. “What you teach in California might be a little different than what you teach in Florida. It’s very meticulous. The lab values will be a little different everywhere you go.”
She acknowledges her competition, noting that there are many other study guides for the NCLEX and nursing courses.
Nursing groups weigh in
Dawn Kappel, spokesperson for the National Council of State Boards of Nursing, which oversees NCLEX, said in an interview that “NCSBN has no issue with the current content of Stephanee Beggs’ business venture.”
For many students, the study guides will be helpful, especially for visual learners, said Carole Kenner, PhD, RN, dean and professor in the School of Nursing and Health Sciences at The College of New Jersey.
But for students “who are less confident in their knowledge, I would want to see a lot more in-depth explanation and rationale,” Dr. Kenner said.
“Since the NCLEX is moving to more cased-based scenarios, the next-gen unfolding cases, you really have to understand a lot of the rationale.”
The notes remind Dr. Kenner of traditional flash cards. “I don’t think it will work for all students, but even the fanciest of onsite review courses are useful to everyone,” she said.
‘Not cutting corners’
As an emergency nurse, Ms. Beggs said, “I have the experience as a nurse to show people that what you are learning will be seen in real life.”
“The way I teach my brand is not to take shortcuts. I love to teach to understand rather than teaching to memorize for an exam.”
She said she sees her guides as a supplement to learning, not a replacement.
“It’s not cutting corners,” she says. “I condense a medical condition that could take a very long time to understand and break it into layman’s terms.”
Ms. Beggs said when people hear about the $2 million, they often ask her whether she plans to give up her shifts in the emergency department for the more lucrative venture.
The answer is no, at least not yet.
“Aside from teaching, I genuinely love being at the bedside,” Ms. Beggs said. “I don’t foresee myself leaving that for good for as long as I can handle both.” She acknowledged, though, that her business now takes up most of her time.
“I love everything about both aspects, so it’s hard for me to choose.”
A version of this article first appeared on Medscape.com.
The air up there: Oxygen could be a bit overrated
Into thin, but healthy, air
Human civilization has essentially been built on proximity to water. Ancient civilizations in Mesopotamia, Egypt, Greece, China, and India were all intimately connected to either rivers or the ocean. Even today, with all our technology, about a third of Earth’s 8 billion people live within 100 vertical meters of sea level, and the median person lives at an elevation of just 200 meters.
All things considered, one might imagine life is pretty tough for the 2 million people living at an elevation of 4,500 meters (nearly 15,000 feet). Not too many Wal-Marts or McDonalds up there. Oh, and not much air either. And for most of us not named Spongebob, air is good.
Or is it? That’s the question posed by a new study. After all, the researchers said, people living at high altitudes, where the air has only 11% effective oxygen instead of the 21% we have at low altitude, have significantly lower rates of metabolic disorders such as diabetes and heart diseases. Maybe breathing isn’t all it’s cracked up to be.
To find out, the researchers placed a group of mice in environments with either 11% oxygen or 8% oxygen. This netted them a bunch of very tired mice. Hey, sudden altitude gain doesn’t go too well for us either, but after 3 weeks, all the mice in the hypoxic environments had regained their normal movement and were behaving as any mouse would.
While the critters seemed normal on the outside, a closer examination found the truth. Their metabolism had been permanently altered, and their blood sugar and weight went down and never bounced back up. Further examination through PET scans showed that the hypoxic mice’s organs showed an increase in glucose metabolism and that brown fat and skeletal muscles reduced the amount of sugar they used.
This goes against the prevailing assumption about hypoxic conditions, the researchers said, since it was previously theorized that the body simply burned more glucose in response to having less oxygen. And while that’s true, our organs also conspicuously use less glucose. Currently, many athletes use hypoxic environments to train, but these new data suggest that people with metabolic disorders also would see benefits from living in low-oxygen environments.
Do you know what this means? All we have to do to stop diabetes is take civilization and push it somewhere else. This can’t possibly end badly.
Sleep survey: The restless majority
Newsflash! This just in: Nobody is sleeping well.
When we go to bed, our goal is to get rest, right? Sorry America, but you’re falling short. In a recent survey conducted by OnePoll for Purple Mattress, almost two-thirds of the 2,011 participants considered themselves restless sleepers.
Not surprised. So what’s keeping us up?
Snoring partners (20%) and anxiety (26%) made the list, but the award for top complaint goes to body pain. Back pain was most prevalent, reported by 36% of respondents, followed by neck pain (33%) and shoulder pain (24%). No wonder, then, that only 10% of the group reported feeling well rested when they woke up.
Do you ever blame your tiredness on sleeping funny? Well, we all kind of sleep funny, and yet we’re still not sleeping well.
The largest proportion of people like to sleep on their side (48%), compared with 18% on their back and 17% on their stomach. The main reasons to choose certain positions were to ease soreness or sleep better, both at 28%. The largest share of participants (47%) reported sleeping in a “yearner” position, while 40% lay on their stomachs in the “free faller” position, and 39% reported using the “soldier” position.
Regardless of the method people use to get to sleep or the position they’re in, the goal is always the same. We’re all just trying to figure out what’s the right one for us.
Seen a UFO recently? Don’t blame COVID
First of all, because we know you’re going to be thinking it in a minute, no, we did not make this up. With COVID-19 still hanging around, there’s no need for fabrication on our part.
The pandemic, clearly, has caused humans to do some strange things over the last 3 years, but what about some of the more, shall we say … eccentric behavior that people were already exhibiting before COVID found its way into our lives?
If, like R. Chase Cockrell, PhD, of the University of Vermont and associates at the Center for UFO Studies, you were wondering if the pandemic affected UFO reporting, then wonder no more. After all, with all that extra time being spent outdoors back in 2020 and all the additional anxiety, surely somebody must have seen something.
The investigators started with the basics by analyzing data from the National UFO Reporting Center and the Mutual UFO Network. Sightings did increase by about 600 in each database during 2020, compared with 2018 and 2019, but not because of the pandemic.
That’s right, we can’t pin this one on our good friend SARS-CoV-2. Further analysis showed that the launches of SpaceX Starlink satellites – sometimes as many as 60 at a time – probably caused the increase in UFO sightings, which means that our favorite billionaire, Elon Musk, is to blame. Yup, the genial Mr. Muskellunge did something that even a global pandemic couldn’t, and yet we vaccinate for COVID.
Next week on tenuous connections: A new study links the 2020 presidential election to increased emergency department visits for external hemorrhoids.
See? That’s fabrication. We made that up.
This article was updated 5/15/23.
Into thin, but healthy, air
Human civilization has essentially been built on proximity to water. Ancient civilizations in Mesopotamia, Egypt, Greece, China, and India were all intimately connected to either rivers or the ocean. Even today, with all our technology, about a third of Earth’s 8 billion people live within 100 vertical meters of sea level, and the median person lives at an elevation of just 200 meters.
All things considered, one might imagine life is pretty tough for the 2 million people living at an elevation of 4,500 meters (nearly 15,000 feet). Not too many Wal-Marts or McDonalds up there. Oh, and not much air either. And for most of us not named Spongebob, air is good.
Or is it? That’s the question posed by a new study. After all, the researchers said, people living at high altitudes, where the air has only 11% effective oxygen instead of the 21% we have at low altitude, have significantly lower rates of metabolic disorders such as diabetes and heart diseases. Maybe breathing isn’t all it’s cracked up to be.
To find out, the researchers placed a group of mice in environments with either 11% oxygen or 8% oxygen. This netted them a bunch of very tired mice. Hey, sudden altitude gain doesn’t go too well for us either, but after 3 weeks, all the mice in the hypoxic environments had regained their normal movement and were behaving as any mouse would.
While the critters seemed normal on the outside, a closer examination found the truth. Their metabolism had been permanently altered, and their blood sugar and weight went down and never bounced back up. Further examination through PET scans showed that the hypoxic mice’s organs showed an increase in glucose metabolism and that brown fat and skeletal muscles reduced the amount of sugar they used.
This goes against the prevailing assumption about hypoxic conditions, the researchers said, since it was previously theorized that the body simply burned more glucose in response to having less oxygen. And while that’s true, our organs also conspicuously use less glucose. Currently, many athletes use hypoxic environments to train, but these new data suggest that people with metabolic disorders also would see benefits from living in low-oxygen environments.
Do you know what this means? All we have to do to stop diabetes is take civilization and push it somewhere else. This can’t possibly end badly.
Sleep survey: The restless majority
Newsflash! This just in: Nobody is sleeping well.
When we go to bed, our goal is to get rest, right? Sorry America, but you’re falling short. In a recent survey conducted by OnePoll for Purple Mattress, almost two-thirds of the 2,011 participants considered themselves restless sleepers.
Not surprised. So what’s keeping us up?
Snoring partners (20%) and anxiety (26%) made the list, but the award for top complaint goes to body pain. Back pain was most prevalent, reported by 36% of respondents, followed by neck pain (33%) and shoulder pain (24%). No wonder, then, that only 10% of the group reported feeling well rested when they woke up.
Do you ever blame your tiredness on sleeping funny? Well, we all kind of sleep funny, and yet we’re still not sleeping well.
The largest proportion of people like to sleep on their side (48%), compared with 18% on their back and 17% on their stomach. The main reasons to choose certain positions were to ease soreness or sleep better, both at 28%. The largest share of participants (47%) reported sleeping in a “yearner” position, while 40% lay on their stomachs in the “free faller” position, and 39% reported using the “soldier” position.
Regardless of the method people use to get to sleep or the position they’re in, the goal is always the same. We’re all just trying to figure out what’s the right one for us.
Seen a UFO recently? Don’t blame COVID
First of all, because we know you’re going to be thinking it in a minute, no, we did not make this up. With COVID-19 still hanging around, there’s no need for fabrication on our part.
The pandemic, clearly, has caused humans to do some strange things over the last 3 years, but what about some of the more, shall we say … eccentric behavior that people were already exhibiting before COVID found its way into our lives?
If, like R. Chase Cockrell, PhD, of the University of Vermont and associates at the Center for UFO Studies, you were wondering if the pandemic affected UFO reporting, then wonder no more. After all, with all that extra time being spent outdoors back in 2020 and all the additional anxiety, surely somebody must have seen something.
The investigators started with the basics by analyzing data from the National UFO Reporting Center and the Mutual UFO Network. Sightings did increase by about 600 in each database during 2020, compared with 2018 and 2019, but not because of the pandemic.
That’s right, we can’t pin this one on our good friend SARS-CoV-2. Further analysis showed that the launches of SpaceX Starlink satellites – sometimes as many as 60 at a time – probably caused the increase in UFO sightings, which means that our favorite billionaire, Elon Musk, is to blame. Yup, the genial Mr. Muskellunge did something that even a global pandemic couldn’t, and yet we vaccinate for COVID.
Next week on tenuous connections: A new study links the 2020 presidential election to increased emergency department visits for external hemorrhoids.
See? That’s fabrication. We made that up.
This article was updated 5/15/23.
Into thin, but healthy, air
Human civilization has essentially been built on proximity to water. Ancient civilizations in Mesopotamia, Egypt, Greece, China, and India were all intimately connected to either rivers or the ocean. Even today, with all our technology, about a third of Earth’s 8 billion people live within 100 vertical meters of sea level, and the median person lives at an elevation of just 200 meters.
All things considered, one might imagine life is pretty tough for the 2 million people living at an elevation of 4,500 meters (nearly 15,000 feet). Not too many Wal-Marts or McDonalds up there. Oh, and not much air either. And for most of us not named Spongebob, air is good.
Or is it? That’s the question posed by a new study. After all, the researchers said, people living at high altitudes, where the air has only 11% effective oxygen instead of the 21% we have at low altitude, have significantly lower rates of metabolic disorders such as diabetes and heart diseases. Maybe breathing isn’t all it’s cracked up to be.
To find out, the researchers placed a group of mice in environments with either 11% oxygen or 8% oxygen. This netted them a bunch of very tired mice. Hey, sudden altitude gain doesn’t go too well for us either, but after 3 weeks, all the mice in the hypoxic environments had regained their normal movement and were behaving as any mouse would.
While the critters seemed normal on the outside, a closer examination found the truth. Their metabolism had been permanently altered, and their blood sugar and weight went down and never bounced back up. Further examination through PET scans showed that the hypoxic mice’s organs showed an increase in glucose metabolism and that brown fat and skeletal muscles reduced the amount of sugar they used.
This goes against the prevailing assumption about hypoxic conditions, the researchers said, since it was previously theorized that the body simply burned more glucose in response to having less oxygen. And while that’s true, our organs also conspicuously use less glucose. Currently, many athletes use hypoxic environments to train, but these new data suggest that people with metabolic disorders also would see benefits from living in low-oxygen environments.
Do you know what this means? All we have to do to stop diabetes is take civilization and push it somewhere else. This can’t possibly end badly.
Sleep survey: The restless majority
Newsflash! This just in: Nobody is sleeping well.
When we go to bed, our goal is to get rest, right? Sorry America, but you’re falling short. In a recent survey conducted by OnePoll for Purple Mattress, almost two-thirds of the 2,011 participants considered themselves restless sleepers.
Not surprised. So what’s keeping us up?
Snoring partners (20%) and anxiety (26%) made the list, but the award for top complaint goes to body pain. Back pain was most prevalent, reported by 36% of respondents, followed by neck pain (33%) and shoulder pain (24%). No wonder, then, that only 10% of the group reported feeling well rested when they woke up.
Do you ever blame your tiredness on sleeping funny? Well, we all kind of sleep funny, and yet we’re still not sleeping well.
The largest proportion of people like to sleep on their side (48%), compared with 18% on their back and 17% on their stomach. The main reasons to choose certain positions were to ease soreness or sleep better, both at 28%. The largest share of participants (47%) reported sleeping in a “yearner” position, while 40% lay on their stomachs in the “free faller” position, and 39% reported using the “soldier” position.
Regardless of the method people use to get to sleep or the position they’re in, the goal is always the same. We’re all just trying to figure out what’s the right one for us.
Seen a UFO recently? Don’t blame COVID
First of all, because we know you’re going to be thinking it in a minute, no, we did not make this up. With COVID-19 still hanging around, there’s no need for fabrication on our part.
The pandemic, clearly, has caused humans to do some strange things over the last 3 years, but what about some of the more, shall we say … eccentric behavior that people were already exhibiting before COVID found its way into our lives?
If, like R. Chase Cockrell, PhD, of the University of Vermont and associates at the Center for UFO Studies, you were wondering if the pandemic affected UFO reporting, then wonder no more. After all, with all that extra time being spent outdoors back in 2020 and all the additional anxiety, surely somebody must have seen something.
The investigators started with the basics by analyzing data from the National UFO Reporting Center and the Mutual UFO Network. Sightings did increase by about 600 in each database during 2020, compared with 2018 and 2019, but not because of the pandemic.
That’s right, we can’t pin this one on our good friend SARS-CoV-2. Further analysis showed that the launches of SpaceX Starlink satellites – sometimes as many as 60 at a time – probably caused the increase in UFO sightings, which means that our favorite billionaire, Elon Musk, is to blame. Yup, the genial Mr. Muskellunge did something that even a global pandemic couldn’t, and yet we vaccinate for COVID.
Next week on tenuous connections: A new study links the 2020 presidential election to increased emergency department visits for external hemorrhoids.
See? That’s fabrication. We made that up.
This article was updated 5/15/23.
Surgery for early breast cancer can worsen frailty in older women
according to a new study.
About 1 in 5 experienced clinically significant deterioration in frailty status after treatment, the study team found. Women at highest risk for declines in frailty following treatment had “robust” baseline frailty status at diagnosis and underwent more invasive mastectomy compared with lumpectomy.
The fact that “robust” older women were more likely to become frail after locoregional therapy suggests that “thoughtful treatment decisions should be undertaken in all older women, not simply those who have frailty at diagnosis,” said the investigators, led by Christina Minami, MD, of Dana-Farber/Brigham and Women’s Cancer Center in Boston.
The study findings emphasize that there is no one-size-fits-all approach to breast cancer treatment in the elderly, said Sarah P. Cate, MD, director, Breast Surgery Quality Program, Mount Sinai Health System, New York, who wasn’t involved in the research. “Some patients will sail through a surgery, and others are severely affected by it.”
The study was published online in JAMA Surgery.
Given the growing number of older adults with breast cancer, understanding how age-related syndromes, such as frailty, may alter cancer outcomes and how cancer treatments change aging trajectories remains important.
To investigate, Dr. Minami and colleagues used Surveillance, Epidemiology, and End Results Medicare data to identify 31,084 women (mean age, 73) who had been diagnosed with ductal carcinoma in situ (DCIS) or stage I HR-positive, ERBB2-positive breast cancer and who underwent surgery (23% mastectomy, 77% lumpectomy) and radiation therapy.
Worsening frailty status was defined as a decline of 0.03 or greater in a validated frailty index from the time of diagnosis to 1 year. This level of change has been linked to greater mortality risk and greater cost of care.
Frailty status at diagnosis was “robust” in 56% of the women, prefrail in 40%, mildly frail in 4%, and moderately to severely frail in 0.3%.
According to the researchers, 21.4% of the women experienced clinically significant declines in their frailty status after treatment. These declines occurred in 25% of women who underwent mastectomy and 20% of those who underwent lumpectomy.
After adjusting for covariates, there was a higher likelihood of worsening frailty among women who were robustly frail at baseline, in comparison with those who were moderately to severely frail at baseline (odds ratio, 6.12), and in those who underwent mastectomy vs. lumpectomy (OR, 1.31).
Older age and race were also linked to worsening frailty status following treatment. Compared with younger women (aged 65-74 years), older women were more likely to experience worsening frailty (OR, 1.21 for women aged 75-79; OR, 1.53 for those aged 80-84; OR, 1.94 for those aged 85 and older). In addition, Black women were more likely than non-Hispanic White women to experience worsening frailty after treatment (OR, 1.12).
“Previous studies have documented lasting declines in functional status after surgery in older patients with breast cancer, but breast cancer treatment has not been implicated in worsening frailty to date,” Dr. Minami and colleagues explain. But “given the substantial proportion of women experiencing worsening frailty and the significant difference by breast surgery type, frailty status as a cancer therapy outcome should be further explored.” In addition, “tailoring locoregional therapy intensity in this population is important,” they write.
Dr. Cate explained that randomized clinical trials such as COMET and LORIS, which explore the monitoring of patients with DCIS in lieu of active treatment, “will likely make a big impact on this population, as we currently do not have randomized controlled data for observation of breast cancer.”
Dr. Cate added as well that assessing a patient’s ECOG [Eastern Cooperative Oncology Group] performance status is vital “to determine who can really tolerate a breast cancer surgery” and that opting for antiestrogens, such as aromatase inhibitors, which can keep cancer at bay for years, “may be preferable for many older patients.”
The study was funded by Brigham and Women’s Hospital’s Department of Surgery’s Beal Fellowship. Dr. Minami and Dr. Cate have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
About 1 in 5 experienced clinically significant deterioration in frailty status after treatment, the study team found. Women at highest risk for declines in frailty following treatment had “robust” baseline frailty status at diagnosis and underwent more invasive mastectomy compared with lumpectomy.
The fact that “robust” older women were more likely to become frail after locoregional therapy suggests that “thoughtful treatment decisions should be undertaken in all older women, not simply those who have frailty at diagnosis,” said the investigators, led by Christina Minami, MD, of Dana-Farber/Brigham and Women’s Cancer Center in Boston.
The study findings emphasize that there is no one-size-fits-all approach to breast cancer treatment in the elderly, said Sarah P. Cate, MD, director, Breast Surgery Quality Program, Mount Sinai Health System, New York, who wasn’t involved in the research. “Some patients will sail through a surgery, and others are severely affected by it.”
The study was published online in JAMA Surgery.
Given the growing number of older adults with breast cancer, understanding how age-related syndromes, such as frailty, may alter cancer outcomes and how cancer treatments change aging trajectories remains important.
To investigate, Dr. Minami and colleagues used Surveillance, Epidemiology, and End Results Medicare data to identify 31,084 women (mean age, 73) who had been diagnosed with ductal carcinoma in situ (DCIS) or stage I HR-positive, ERBB2-positive breast cancer and who underwent surgery (23% mastectomy, 77% lumpectomy) and radiation therapy.
Worsening frailty status was defined as a decline of 0.03 or greater in a validated frailty index from the time of diagnosis to 1 year. This level of change has been linked to greater mortality risk and greater cost of care.
Frailty status at diagnosis was “robust” in 56% of the women, prefrail in 40%, mildly frail in 4%, and moderately to severely frail in 0.3%.
According to the researchers, 21.4% of the women experienced clinically significant declines in their frailty status after treatment. These declines occurred in 25% of women who underwent mastectomy and 20% of those who underwent lumpectomy.
After adjusting for covariates, there was a higher likelihood of worsening frailty among women who were robustly frail at baseline, in comparison with those who were moderately to severely frail at baseline (odds ratio, 6.12), and in those who underwent mastectomy vs. lumpectomy (OR, 1.31).
Older age and race were also linked to worsening frailty status following treatment. Compared with younger women (aged 65-74 years), older women were more likely to experience worsening frailty (OR, 1.21 for women aged 75-79; OR, 1.53 for those aged 80-84; OR, 1.94 for those aged 85 and older). In addition, Black women were more likely than non-Hispanic White women to experience worsening frailty after treatment (OR, 1.12).
“Previous studies have documented lasting declines in functional status after surgery in older patients with breast cancer, but breast cancer treatment has not been implicated in worsening frailty to date,” Dr. Minami and colleagues explain. But “given the substantial proportion of women experiencing worsening frailty and the significant difference by breast surgery type, frailty status as a cancer therapy outcome should be further explored.” In addition, “tailoring locoregional therapy intensity in this population is important,” they write.
Dr. Cate explained that randomized clinical trials such as COMET and LORIS, which explore the monitoring of patients with DCIS in lieu of active treatment, “will likely make a big impact on this population, as we currently do not have randomized controlled data for observation of breast cancer.”
Dr. Cate added as well that assessing a patient’s ECOG [Eastern Cooperative Oncology Group] performance status is vital “to determine who can really tolerate a breast cancer surgery” and that opting for antiestrogens, such as aromatase inhibitors, which can keep cancer at bay for years, “may be preferable for many older patients.”
The study was funded by Brigham and Women’s Hospital’s Department of Surgery’s Beal Fellowship. Dr. Minami and Dr. Cate have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
About 1 in 5 experienced clinically significant deterioration in frailty status after treatment, the study team found. Women at highest risk for declines in frailty following treatment had “robust” baseline frailty status at diagnosis and underwent more invasive mastectomy compared with lumpectomy.
The fact that “robust” older women were more likely to become frail after locoregional therapy suggests that “thoughtful treatment decisions should be undertaken in all older women, not simply those who have frailty at diagnosis,” said the investigators, led by Christina Minami, MD, of Dana-Farber/Brigham and Women’s Cancer Center in Boston.
The study findings emphasize that there is no one-size-fits-all approach to breast cancer treatment in the elderly, said Sarah P. Cate, MD, director, Breast Surgery Quality Program, Mount Sinai Health System, New York, who wasn’t involved in the research. “Some patients will sail through a surgery, and others are severely affected by it.”
The study was published online in JAMA Surgery.
Given the growing number of older adults with breast cancer, understanding how age-related syndromes, such as frailty, may alter cancer outcomes and how cancer treatments change aging trajectories remains important.
To investigate, Dr. Minami and colleagues used Surveillance, Epidemiology, and End Results Medicare data to identify 31,084 women (mean age, 73) who had been diagnosed with ductal carcinoma in situ (DCIS) or stage I HR-positive, ERBB2-positive breast cancer and who underwent surgery (23% mastectomy, 77% lumpectomy) and radiation therapy.
Worsening frailty status was defined as a decline of 0.03 or greater in a validated frailty index from the time of diagnosis to 1 year. This level of change has been linked to greater mortality risk and greater cost of care.
Frailty status at diagnosis was “robust” in 56% of the women, prefrail in 40%, mildly frail in 4%, and moderately to severely frail in 0.3%.
According to the researchers, 21.4% of the women experienced clinically significant declines in their frailty status after treatment. These declines occurred in 25% of women who underwent mastectomy and 20% of those who underwent lumpectomy.
After adjusting for covariates, there was a higher likelihood of worsening frailty among women who were robustly frail at baseline, in comparison with those who were moderately to severely frail at baseline (odds ratio, 6.12), and in those who underwent mastectomy vs. lumpectomy (OR, 1.31).
Older age and race were also linked to worsening frailty status following treatment. Compared with younger women (aged 65-74 years), older women were more likely to experience worsening frailty (OR, 1.21 for women aged 75-79; OR, 1.53 for those aged 80-84; OR, 1.94 for those aged 85 and older). In addition, Black women were more likely than non-Hispanic White women to experience worsening frailty after treatment (OR, 1.12).
“Previous studies have documented lasting declines in functional status after surgery in older patients with breast cancer, but breast cancer treatment has not been implicated in worsening frailty to date,” Dr. Minami and colleagues explain. But “given the substantial proportion of women experiencing worsening frailty and the significant difference by breast surgery type, frailty status as a cancer therapy outcome should be further explored.” In addition, “tailoring locoregional therapy intensity in this population is important,” they write.
Dr. Cate explained that randomized clinical trials such as COMET and LORIS, which explore the monitoring of patients with DCIS in lieu of active treatment, “will likely make a big impact on this population, as we currently do not have randomized controlled data for observation of breast cancer.”
Dr. Cate added as well that assessing a patient’s ECOG [Eastern Cooperative Oncology Group] performance status is vital “to determine who can really tolerate a breast cancer surgery” and that opting for antiestrogens, such as aromatase inhibitors, which can keep cancer at bay for years, “may be preferable for many older patients.”
The study was funded by Brigham and Women’s Hospital’s Department of Surgery’s Beal Fellowship. Dr. Minami and Dr. Cate have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
After the Match: Next steps for new residents, unmatched
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.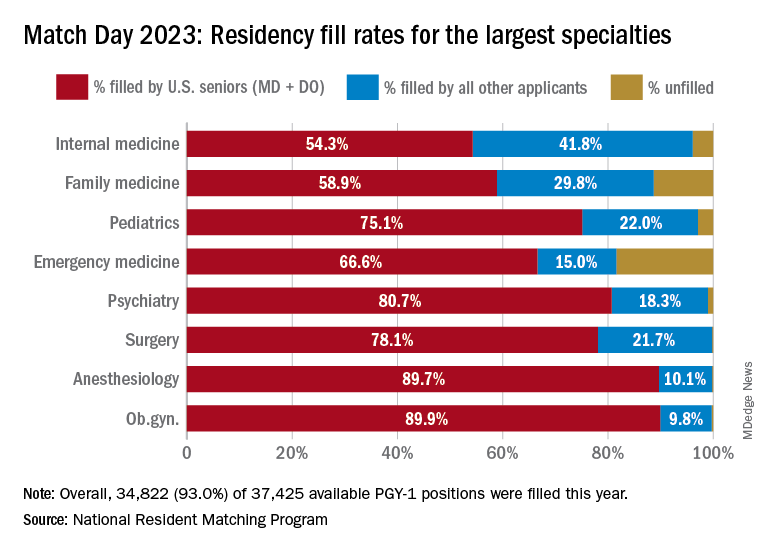
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.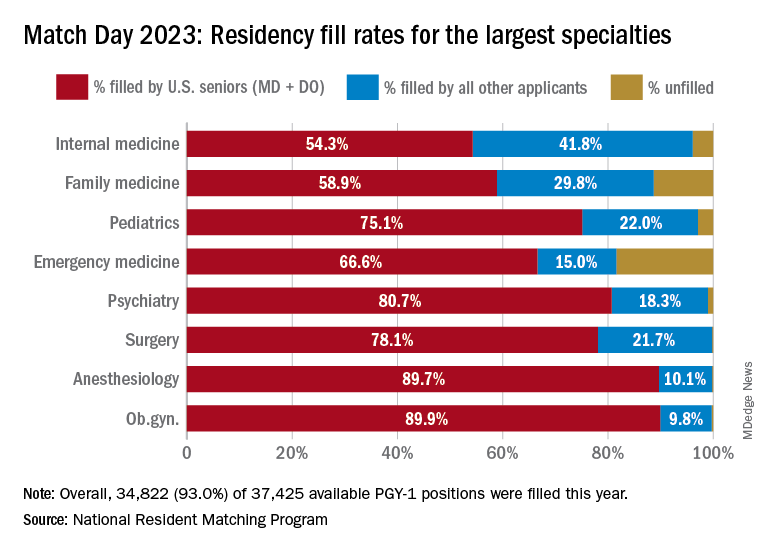
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Medical school graduates around the US took to social media after last week's Match Day to share their joy ― or explore their options if they did not match.
Take this post March 19 on Twitter: “I went unmatched this year; looking for research position at any institute for internal medicine.”
including an international medical graduate who matched into his chosen specialty after multiple disappointments.
“I’ve waited for this email for 8 years,” Sahil Bawa, MD, posted on Twitter on March 13. A few days later, when he learned about his residency position, he posted: “I’m beyond grateful. Will be moving to Alabama soon #familymedicine.”
Dr. Bawa, who matched into UAB Medicine Selma (Ala.), graduated from medical school in India in 2014. He said in an interview that he has visited the United States periodically since then to pass medical tests, obtain letters of recommendation, and participate in research.
Over the years he watched his Indian colleagues give up on becoming American doctors, find alternative careers, or resolve to practice in their native country. But he held onto the few success stories he saw on social media. “There were always one to two every year. It kept me going. If they can do it, I can do it.”
International medical graduates (IMGs) like Dr. Bawa applied in record numbers to Match2023, according to the National Resident Matching Program (NRMP), which announced the results on March 13 of its main residency match and the Supplemental Offer and Acceptance Program (SOAP) for unfilled positions or unmatched applicants.
Overall, 48,156 total applicants registered for the match, which was driven by the increase of non-U.S. IMG applicants and U.S. DO seniors over the past year, NRMP stated in its release. U.S. MD seniors had a match rate of nearly 94%, and U.S. DO seniors, nearly 92%. U.S. IMGs had a match rate of nearly 68%, an “all-time high,” and non-U.S. IMGs, nearly 60%, NRMP stated.
Three specialties that filled all of their 30 or more available positions were orthopedic surgery, plastic surgery (integrated), radiology – diagnostic, and thoracic surgery. Specialties with 30 or more positions that filled with the highest percentage of U.S. MD and DO seniors were plastic surgery (integrated), internal medicine-pediatrics, ob.gyn., and orthopedic surgery.
The number of available primary care positions increased slightly, NRMP reported. Considering “a serious and growing shortage of primary care physicians across the U.S.,” there were 571 more primary care positions than 2022. That’s an increase of about 3% over last year and 17% over the past 5 years. Primary care positions filled at a rate of 94%, which remained steady from 2022.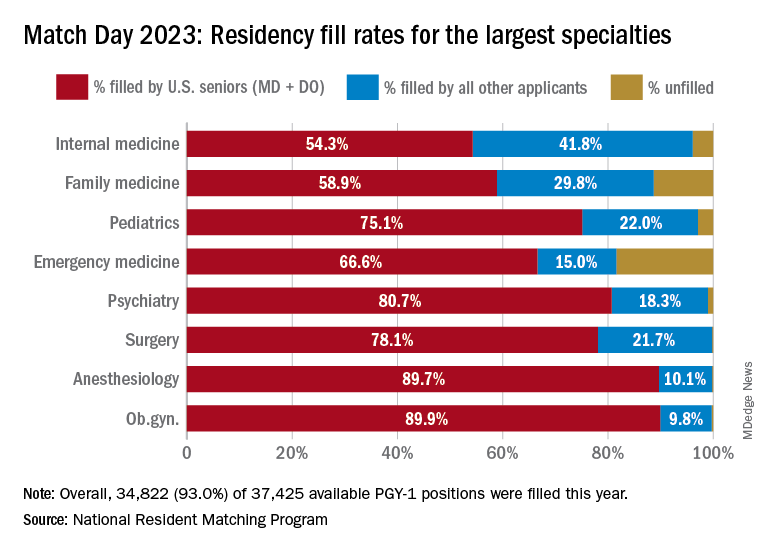
NRMP also pointed out specialties with increases in the number of positions filled by U.S. MD seniors of more than 10% and 10 positions in the past 5 years: anesthesiology, child neurology, interventional radiology, neurology, pathology, physical medicine and rehabilitation, plastic surgery (integrated), psychiatry, radiology-diagnostic, transitional year, and vascular surgery.
Bryan Carmody, MD, MPH, a pediatric nephrologist known for his medical school commentaries, said in an interview that the most competitive specialties he noted in 2023 were radiology, pathology, and neurology.
“The surgical specialties are always competitive, so it wasn’t a surprise that orthopedics, plastic surgery, and thoracic surgery filled all of their positions. But I was surprised to see diagnostic radiology fill every single one of their positions in the match. And although pathology and neurology aren’t typically considered extremely competitive specialties, they filled over 99% of their positions in the Match this year.”
On Dr. Carmody’s blog about the winners and losers of Match Day, he said that despite the record number of primary care positions offered, family medicine programs suffered. “Only 89% of family medicine programs filled in the Match, and graduating U.S. MD and DO students only filled a little more than half of all the available positions,” he wrote.
For a record number of applicants that match each year, and “the most favorable ratio in the past 2 decades” of applicants-to-positions in 2023, there are still a lot unmatched, Dr. Carmody said. “It’s a tough thing to talk about. The reality is the number of residency positions should be determined by the number of physicians needed.”
One student, Asim Ansari, didn’t match into a traditional residency or through SOAP. It was his fifth attempt. He was serving a transitional-year residency at Merit Health Wesley in Hattiesburg, Miss., and when he didn’t match, he accepted a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City.
He said he was “relieved and excited” to have found a program in his chosen specialty. Still, in 2 years, Mr. Ansari must again try to match into a traditional psychiatry residency.
Meanwhile, Dr. Bawa will prepare for his 3-year residency in Alabama after completing his interim research year in the surgery department at Wayne State University, Detroit, in May.
Despite his years in limbo, Dr. Bawa said, “I have no regrets, no complaints. I am still very happy.”
A version of this article originally appeared on Medscape.com.
Living kidney donors should receive money for their costs of donating
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University’s Grossman School of Medicine in New York City.
We try very hard to get organ donation from those who die. That’s a commendable thing to do. I think doctors should always be discussing the opportunity to donate organs upon death, even in primary care settings.
It’s good to find out what people’s attitudes are. Let them learn about organ donation as something they can think about. Let them talk about it with family and friends and partners so that they know their wishes.
However, despite these efforts to encourage organ donation, we still have far fewer organs than we could use to transplant people, many people die on waiting lists because there are no organs to give them, and we’re in a situation where demand for organ transplant is actually increasing.
There is more capacity to do transplants both in the United States and elsewhere, and more people are living longer, so organ failure starts to become more common before, let’s say, terminal illness is really there. Now, we have more people who might benefit from organ transplant in an aging population.
One place to turn to help reduce the shortage of organs is to living donation. At least insofar as kidneys go, kidney donation from living persons has become a prominent source of organs for those who need kidneys – most of whom are surviving on dialysis, by the way, at a very high cost and often with a quality of life that they don’t find particularly easy to accept.
Transplant is far preferred, even though they have to take immunosuppression to keep those organ transplants going, and that has its own risks and side effects. They still get more mobility. They still are able to have a broader diet. They enjoy life far more than they do having to show up for dialysis three times a week for a couple of hours, every week, for every week that they live.
There is an interest in living kidney donation. One battle has been that, well, maybe we could get more kidneys if we just paid people to sell us their kidneys. That has been resisted, and I’ve been resistant to that idea, too, because I worry that it leads to exploitation.
The people who sell their kidneys are poor. They’re often in debt. They feel coerced by their circumstances, so they make a kidney sale. This happens in countries like India, where there are markets underground, and you see that it’s the poorest of the poor who do this, and they don’t really work their way out of debt. They just wind up without a kidney, help relieve their debt a little bit, and pretty soon, because they don’t have a job or an income except that sale of a kidney, they’re not much better off than they were before they started.
Also, people who sell kidneys for money are more likely not to admit to their own health problems, raising risks about the quality of organs. Then, of course, it puts doctors in a position to take out an organ for pay, even though it doesn’t benefit you, so that you can sell it. This raises some questions about whether that’s consistent with medical ethics.
A different idea has emerged. New York State Governor Kathy Hochul just signed legislation that allows living donors to be compensated for legitimate costs. That’s a little different matter. You’re not buying the organ, but you’re saying that if you experience health care problems due to complications from a donation, if you need money for transportation, if you lost money because you did this altruistically and you had to take time off from work and had expenses for a babysitter, restaurants, or other things, the state is going to try to create funds that will compensate you.
That, I think we should agree, is not a bad idea. You’re in a situation there where you don’t want to make people who are heroic, altruistic, and trying to help others by donating a kidney end up financially worse off.
I think there’s a difference between making someone financially whole after the decision to make a kidney available and creating a market where the poorest of the poor come forward to just sell because they see no other choice in terms of how to get rid of debts. I see these situations as not ethically equivalent, so I support efforts to try to compensate people who are our heroes. I don’t think we should ask them to financially suffer.
We’ll watch to see what happens as the New York state law comes into effect. By the way, New York is one of the states that really lags in the supply of organs for transplant, so this measure is particularly important for that state. Many other states should be considering this legislation as well.
It’s one thing to reward, if you will, donors by making sure they don’t suffer financial loss. It’s a very different thing to say, let’s have a free market and we’ll pay whoever it is that’s willing to sell us a kidney to do so. The former seems to me to be humane and just, whereas the latter risks exploitation.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University’s Grossman School of Medicine in New York City.
We try very hard to get organ donation from those who die. That’s a commendable thing to do. I think doctors should always be discussing the opportunity to donate organs upon death, even in primary care settings.
It’s good to find out what people’s attitudes are. Let them learn about organ donation as something they can think about. Let them talk about it with family and friends and partners so that they know their wishes.
However, despite these efforts to encourage organ donation, we still have far fewer organs than we could use to transplant people, many people die on waiting lists because there are no organs to give them, and we’re in a situation where demand for organ transplant is actually increasing.
There is more capacity to do transplants both in the United States and elsewhere, and more people are living longer, so organ failure starts to become more common before, let’s say, terminal illness is really there. Now, we have more people who might benefit from organ transplant in an aging population.
One place to turn to help reduce the shortage of organs is to living donation. At least insofar as kidneys go, kidney donation from living persons has become a prominent source of organs for those who need kidneys – most of whom are surviving on dialysis, by the way, at a very high cost and often with a quality of life that they don’t find particularly easy to accept.
Transplant is far preferred, even though they have to take immunosuppression to keep those organ transplants going, and that has its own risks and side effects. They still get more mobility. They still are able to have a broader diet. They enjoy life far more than they do having to show up for dialysis three times a week for a couple of hours, every week, for every week that they live.
There is an interest in living kidney donation. One battle has been that, well, maybe we could get more kidneys if we just paid people to sell us their kidneys. That has been resisted, and I’ve been resistant to that idea, too, because I worry that it leads to exploitation.
The people who sell their kidneys are poor. They’re often in debt. They feel coerced by their circumstances, so they make a kidney sale. This happens in countries like India, where there are markets underground, and you see that it’s the poorest of the poor who do this, and they don’t really work their way out of debt. They just wind up without a kidney, help relieve their debt a little bit, and pretty soon, because they don’t have a job or an income except that sale of a kidney, they’re not much better off than they were before they started.
Also, people who sell kidneys for money are more likely not to admit to their own health problems, raising risks about the quality of organs. Then, of course, it puts doctors in a position to take out an organ for pay, even though it doesn’t benefit you, so that you can sell it. This raises some questions about whether that’s consistent with medical ethics.
A different idea has emerged. New York State Governor Kathy Hochul just signed legislation that allows living donors to be compensated for legitimate costs. That’s a little different matter. You’re not buying the organ, but you’re saying that if you experience health care problems due to complications from a donation, if you need money for transportation, if you lost money because you did this altruistically and you had to take time off from work and had expenses for a babysitter, restaurants, or other things, the state is going to try to create funds that will compensate you.
That, I think we should agree, is not a bad idea. You’re in a situation there where you don’t want to make people who are heroic, altruistic, and trying to help others by donating a kidney end up financially worse off.
I think there’s a difference between making someone financially whole after the decision to make a kidney available and creating a market where the poorest of the poor come forward to just sell because they see no other choice in terms of how to get rid of debts. I see these situations as not ethically equivalent, so I support efforts to try to compensate people who are our heroes. I don’t think we should ask them to financially suffer.
We’ll watch to see what happens as the New York state law comes into effect. By the way, New York is one of the states that really lags in the supply of organs for transplant, so this measure is particularly important for that state. Many other states should be considering this legislation as well.
It’s one thing to reward, if you will, donors by making sure they don’t suffer financial loss. It’s a very different thing to say, let’s have a free market and we’ll pay whoever it is that’s willing to sell us a kidney to do so. The former seems to me to be humane and just, whereas the latter risks exploitation.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University’s Grossman School of Medicine in New York City.
We try very hard to get organ donation from those who die. That’s a commendable thing to do. I think doctors should always be discussing the opportunity to donate organs upon death, even in primary care settings.
It’s good to find out what people’s attitudes are. Let them learn about organ donation as something they can think about. Let them talk about it with family and friends and partners so that they know their wishes.
However, despite these efforts to encourage organ donation, we still have far fewer organs than we could use to transplant people, many people die on waiting lists because there are no organs to give them, and we’re in a situation where demand for organ transplant is actually increasing.
There is more capacity to do transplants both in the United States and elsewhere, and more people are living longer, so organ failure starts to become more common before, let’s say, terminal illness is really there. Now, we have more people who might benefit from organ transplant in an aging population.
One place to turn to help reduce the shortage of organs is to living donation. At least insofar as kidneys go, kidney donation from living persons has become a prominent source of organs for those who need kidneys – most of whom are surviving on dialysis, by the way, at a very high cost and often with a quality of life that they don’t find particularly easy to accept.
Transplant is far preferred, even though they have to take immunosuppression to keep those organ transplants going, and that has its own risks and side effects. They still get more mobility. They still are able to have a broader diet. They enjoy life far more than they do having to show up for dialysis three times a week for a couple of hours, every week, for every week that they live.
There is an interest in living kidney donation. One battle has been that, well, maybe we could get more kidneys if we just paid people to sell us their kidneys. That has been resisted, and I’ve been resistant to that idea, too, because I worry that it leads to exploitation.
The people who sell their kidneys are poor. They’re often in debt. They feel coerced by their circumstances, so they make a kidney sale. This happens in countries like India, where there are markets underground, and you see that it’s the poorest of the poor who do this, and they don’t really work their way out of debt. They just wind up without a kidney, help relieve their debt a little bit, and pretty soon, because they don’t have a job or an income except that sale of a kidney, they’re not much better off than they were before they started.
Also, people who sell kidneys for money are more likely not to admit to their own health problems, raising risks about the quality of organs. Then, of course, it puts doctors in a position to take out an organ for pay, even though it doesn’t benefit you, so that you can sell it. This raises some questions about whether that’s consistent with medical ethics.
A different idea has emerged. New York State Governor Kathy Hochul just signed legislation that allows living donors to be compensated for legitimate costs. That’s a little different matter. You’re not buying the organ, but you’re saying that if you experience health care problems due to complications from a donation, if you need money for transportation, if you lost money because you did this altruistically and you had to take time off from work and had expenses for a babysitter, restaurants, or other things, the state is going to try to create funds that will compensate you.
That, I think we should agree, is not a bad idea. You’re in a situation there where you don’t want to make people who are heroic, altruistic, and trying to help others by donating a kidney end up financially worse off.
I think there’s a difference between making someone financially whole after the decision to make a kidney available and creating a market where the poorest of the poor come forward to just sell because they see no other choice in terms of how to get rid of debts. I see these situations as not ethically equivalent, so I support efforts to try to compensate people who are our heroes. I don’t think we should ask them to financially suffer.
We’ll watch to see what happens as the New York state law comes into effect. By the way, New York is one of the states that really lags in the supply of organs for transplant, so this measure is particularly important for that state. Many other states should be considering this legislation as well.
It’s one thing to reward, if you will, donors by making sure they don’t suffer financial loss. It’s a very different thing to say, let’s have a free market and we’ll pay whoever it is that’s willing to sell us a kidney to do so. The former seems to me to be humane and just, whereas the latter risks exploitation.
A version of this article first appeared on Medscape.com.
State medical board chair steps down amid Medicaid fraud accusations
He has stepped down as board chair, and state officials have suspended all Medicaid payments to Dr. Hyatt and his practice, Pinnacle Premier Psychiatry in Rogers, Arkansas.
Dr. Hyatt billed 99.95% of the claims for his patients’ hospital care to Medicaid at the highest severity level, according to an affidavit filed by an investigator with the Medicaid Fraud Control Unit, Arkansas Attorney General’s Office. Other Arkansas psychiatrists billed that same level in only about 39% of claims, the affidavit states.
The possible upcoding alleged in the affidavit was a red flag that prompted the state to temporarily suspend Dr. Hyatt’s Medicaid payments.
Dr. Hyatt has until this Friday to file an appeal. He did not respond to requests from this news organization for comment.
The affidavit pointed to other concerns. For example, a whistleblower who worked at the Northwest Medical Center where Dr. Hyatt admitted patients claimed that Dr. Hyatt was only on the floor a few minutes a day and that he had no contact with patients. A review of hundreds of hours of video by state investigators revealed that Dr. Hyatt did not enter patients’ rooms, nor did he have any contact with patients, according to the affidavit. Dr. Hyatt served as the hospital’s behavioral unit director from 2018 until his contract was abruptly terminated in May 2022, according to the affidavit.
However, Dr. Hyatt claimed to have conducted daily face-to-face evaluation and management with patients, according to the affidavit. In addition, the whistleblower claimed that Dr. Hyatt did not want patients to know his name and instructed staff to cover up his name on patient armbands.
Detaining patients
Dr. Hyatt also faces accusations that he held patients against their will, according to civil lawsuits filed in Washington County, Ark., reports the Arkansas Advocate.
Karla Adrian-Caceres filed suit on Jan. 17. Ms. Adrian-Caceres also named Brooke Green, Northwest Arkansas Hospitals, and 25 unidentified hospital employees as defendants.
According to the complaint, Ms. Adrian-Caceres, an engineering student at the University of Arkansas, arrived at the Northwest Medical Emergency Department after accidentally taking too many Tylenol on Jan. 18, 2022. She was then taken by ambulance to a Northwest psychiatric facility in Springdale, court records show.
According to the complaint, Ms. Adrian-Caceres said that she was given a sedative and asked to sign consent for admission while on the way to Northwest. She said that she “signed some documents without being able to read or understand them at the time.”
When she asked when she could go home, Ms. Adrian-Caceres said, “more than one employee told her there was a minimum stay and that if she asked to leave, they would take her to court where a judge would give her a longer stay because the judge always sides with Dr. Hyatt and Northwest,” according to court documents. Northwest employees stripped Ms. Adrian-Caceres, searched her body, took all of her possessions from her and issued underwear and a uniform, according to the lawsuit.
Ms. Adrian-Caceres’ mother, Katty Caceres, claimed in the lawsuit that she was prohibited from seeing her daughter. Ms. Caceres spoke with five different employees, four of whom had only their first names on their badges. Each of them reportedly said that they could not help, or that the plaintiff “would be in there for some time” and that it was Dr. Hyatt’s decision regarding how long that would be, according to court documents.
Katty Caceres hired a local attorney named Aaron Cash to represent her daughter. On Jan. 20, 2022, Mr. Cash faxed a letter to the hospital demanding her release. When Ms. Caceres arrived to pick up her daughter, she claimed that staff members indicated that the daughter was there voluntarily and refused to release her “at the direction of Dr Hyatt.” During a phone call later that day, the plaintiff told her mother that her status was being changed to an involuntary hold, court documents show.
“At one point she was threatened with the longer time in there if she kept asking to leave,” Mr. Cash told this news organization. In addition, staff members reportedly told Ms. Adrian-Caceres that the “judge always sided with Dr Hyatt” and she “would get way longer there, 30-45 days if [she] went before the judge,” according to Mr. Cash.
Mr. Cash said nine other patients have contacted his firm with similar allegations against Dr. Hyatt.
“We’ve talked to many people that have experienced the same threats,” Mr. Cash said. “When they’re asking to leave, they get these threats, they get coerced … and they’re never taken to court. They’re never given opportunity to talk to a judge or to have a public defender appointed.”
A version of this article first appeared on Medscape.com.
He has stepped down as board chair, and state officials have suspended all Medicaid payments to Dr. Hyatt and his practice, Pinnacle Premier Psychiatry in Rogers, Arkansas.
Dr. Hyatt billed 99.95% of the claims for his patients’ hospital care to Medicaid at the highest severity level, according to an affidavit filed by an investigator with the Medicaid Fraud Control Unit, Arkansas Attorney General’s Office. Other Arkansas psychiatrists billed that same level in only about 39% of claims, the affidavit states.
The possible upcoding alleged in the affidavit was a red flag that prompted the state to temporarily suspend Dr. Hyatt’s Medicaid payments.
Dr. Hyatt has until this Friday to file an appeal. He did not respond to requests from this news organization for comment.
The affidavit pointed to other concerns. For example, a whistleblower who worked at the Northwest Medical Center where Dr. Hyatt admitted patients claimed that Dr. Hyatt was only on the floor a few minutes a day and that he had no contact with patients. A review of hundreds of hours of video by state investigators revealed that Dr. Hyatt did not enter patients’ rooms, nor did he have any contact with patients, according to the affidavit. Dr. Hyatt served as the hospital’s behavioral unit director from 2018 until his contract was abruptly terminated in May 2022, according to the affidavit.
However, Dr. Hyatt claimed to have conducted daily face-to-face evaluation and management with patients, according to the affidavit. In addition, the whistleblower claimed that Dr. Hyatt did not want patients to know his name and instructed staff to cover up his name on patient armbands.
Detaining patients
Dr. Hyatt also faces accusations that he held patients against their will, according to civil lawsuits filed in Washington County, Ark., reports the Arkansas Advocate.
Karla Adrian-Caceres filed suit on Jan. 17. Ms. Adrian-Caceres also named Brooke Green, Northwest Arkansas Hospitals, and 25 unidentified hospital employees as defendants.
According to the complaint, Ms. Adrian-Caceres, an engineering student at the University of Arkansas, arrived at the Northwest Medical Emergency Department after accidentally taking too many Tylenol on Jan. 18, 2022. She was then taken by ambulance to a Northwest psychiatric facility in Springdale, court records show.
According to the complaint, Ms. Adrian-Caceres said that she was given a sedative and asked to sign consent for admission while on the way to Northwest. She said that she “signed some documents without being able to read or understand them at the time.”
When she asked when she could go home, Ms. Adrian-Caceres said, “more than one employee told her there was a minimum stay and that if she asked to leave, they would take her to court where a judge would give her a longer stay because the judge always sides with Dr. Hyatt and Northwest,” according to court documents. Northwest employees stripped Ms. Adrian-Caceres, searched her body, took all of her possessions from her and issued underwear and a uniform, according to the lawsuit.
Ms. Adrian-Caceres’ mother, Katty Caceres, claimed in the lawsuit that she was prohibited from seeing her daughter. Ms. Caceres spoke with five different employees, four of whom had only their first names on their badges. Each of them reportedly said that they could not help, or that the plaintiff “would be in there for some time” and that it was Dr. Hyatt’s decision regarding how long that would be, according to court documents.
Katty Caceres hired a local attorney named Aaron Cash to represent her daughter. On Jan. 20, 2022, Mr. Cash faxed a letter to the hospital demanding her release. When Ms. Caceres arrived to pick up her daughter, she claimed that staff members indicated that the daughter was there voluntarily and refused to release her “at the direction of Dr Hyatt.” During a phone call later that day, the plaintiff told her mother that her status was being changed to an involuntary hold, court documents show.
“At one point she was threatened with the longer time in there if she kept asking to leave,” Mr. Cash told this news organization. In addition, staff members reportedly told Ms. Adrian-Caceres that the “judge always sided with Dr Hyatt” and she “would get way longer there, 30-45 days if [she] went before the judge,” according to Mr. Cash.
Mr. Cash said nine other patients have contacted his firm with similar allegations against Dr. Hyatt.
“We’ve talked to many people that have experienced the same threats,” Mr. Cash said. “When they’re asking to leave, they get these threats, they get coerced … and they’re never taken to court. They’re never given opportunity to talk to a judge or to have a public defender appointed.”
A version of this article first appeared on Medscape.com.
He has stepped down as board chair, and state officials have suspended all Medicaid payments to Dr. Hyatt and his practice, Pinnacle Premier Psychiatry in Rogers, Arkansas.
Dr. Hyatt billed 99.95% of the claims for his patients’ hospital care to Medicaid at the highest severity level, according to an affidavit filed by an investigator with the Medicaid Fraud Control Unit, Arkansas Attorney General’s Office. Other Arkansas psychiatrists billed that same level in only about 39% of claims, the affidavit states.
The possible upcoding alleged in the affidavit was a red flag that prompted the state to temporarily suspend Dr. Hyatt’s Medicaid payments.
Dr. Hyatt has until this Friday to file an appeal. He did not respond to requests from this news organization for comment.
The affidavit pointed to other concerns. For example, a whistleblower who worked at the Northwest Medical Center where Dr. Hyatt admitted patients claimed that Dr. Hyatt was only on the floor a few minutes a day and that he had no contact with patients. A review of hundreds of hours of video by state investigators revealed that Dr. Hyatt did not enter patients’ rooms, nor did he have any contact with patients, according to the affidavit. Dr. Hyatt served as the hospital’s behavioral unit director from 2018 until his contract was abruptly terminated in May 2022, according to the affidavit.
However, Dr. Hyatt claimed to have conducted daily face-to-face evaluation and management with patients, according to the affidavit. In addition, the whistleblower claimed that Dr. Hyatt did not want patients to know his name and instructed staff to cover up his name on patient armbands.
Detaining patients
Dr. Hyatt also faces accusations that he held patients against their will, according to civil lawsuits filed in Washington County, Ark., reports the Arkansas Advocate.
Karla Adrian-Caceres filed suit on Jan. 17. Ms. Adrian-Caceres also named Brooke Green, Northwest Arkansas Hospitals, and 25 unidentified hospital employees as defendants.
According to the complaint, Ms. Adrian-Caceres, an engineering student at the University of Arkansas, arrived at the Northwest Medical Emergency Department after accidentally taking too many Tylenol on Jan. 18, 2022. She was then taken by ambulance to a Northwest psychiatric facility in Springdale, court records show.
According to the complaint, Ms. Adrian-Caceres said that she was given a sedative and asked to sign consent for admission while on the way to Northwest. She said that she “signed some documents without being able to read or understand them at the time.”
When she asked when she could go home, Ms. Adrian-Caceres said, “more than one employee told her there was a minimum stay and that if she asked to leave, they would take her to court where a judge would give her a longer stay because the judge always sides with Dr. Hyatt and Northwest,” according to court documents. Northwest employees stripped Ms. Adrian-Caceres, searched her body, took all of her possessions from her and issued underwear and a uniform, according to the lawsuit.
Ms. Adrian-Caceres’ mother, Katty Caceres, claimed in the lawsuit that she was prohibited from seeing her daughter. Ms. Caceres spoke with five different employees, four of whom had only their first names on their badges. Each of them reportedly said that they could not help, or that the plaintiff “would be in there for some time” and that it was Dr. Hyatt’s decision regarding how long that would be, according to court documents.
Katty Caceres hired a local attorney named Aaron Cash to represent her daughter. On Jan. 20, 2022, Mr. Cash faxed a letter to the hospital demanding her release. When Ms. Caceres arrived to pick up her daughter, she claimed that staff members indicated that the daughter was there voluntarily and refused to release her “at the direction of Dr Hyatt.” During a phone call later that day, the plaintiff told her mother that her status was being changed to an involuntary hold, court documents show.
“At one point she was threatened with the longer time in there if she kept asking to leave,” Mr. Cash told this news organization. In addition, staff members reportedly told Ms. Adrian-Caceres that the “judge always sided with Dr Hyatt” and she “would get way longer there, 30-45 days if [she] went before the judge,” according to Mr. Cash.
Mr. Cash said nine other patients have contacted his firm with similar allegations against Dr. Hyatt.
“We’ve talked to many people that have experienced the same threats,” Mr. Cash said. “When they’re asking to leave, they get these threats, they get coerced … and they’re never taken to court. They’re never given opportunity to talk to a judge or to have a public defender appointed.”
A version of this article first appeared on Medscape.com.
Presurgical expectations may influence patients’ attitudes, experiences after knee replacement
DENVER – People with lower expectations of how they would be able to use their knees during work activities after a total knee arthroplasty were more dissatisfied with their knee abilities 6 months after their surgery, according to a study presented at the OARSI 2023 World Congress.
Two out of 10 patients are dissatisfied after total knee arthroplasty, which is increasingly performed in younger and working patients who may have higher demands, presenter Yvonne van Zaanen, a physiotherapist in occupational health and ergonomics and a PhD candidate at Amsterdam University Medical Center, told attendees.
The findings suggest a correlation between patients’ low presurgical expectations of their ability to use their knees and having more difficulty with their knees postoperatively, she said. “We should take better care of working patients with low expectations by managing their preoperative expectations and improving their ability to perform work-related knee-straining activities in rehabilitation,” Ms. van Zaanen told attendees.
The researchers conducted a multicenter, prospective cohort study involving seven hospitals. They surveyed 175 employed individuals aged 18-65 years who were scheduled for a total knee arthroplasty and intended to return to work after their surgery. The first survey occurred before the operation, and the follow-up occurred 6 months after the surgery.
Just over half the participants were women (53%), and the average participant age was 59. Respondents had a mean body mass index (BMI) of 29 kg/m2, and had a Knee injury and Osteoarthritis Outcome Score (KOOS) pain score of 42 (on a 0-to-100 scale in which lower scores are worse). About half the respondents (51%) had a job that involved knee-straining activities.
The researchers assessed participants’ ability to perform work-related, knee-straining activities using the Work, Osteoarthritis, or joint-Replacement Questionnaire (WORQ) tool, which considers the following activities: kneeling, crouching, clambering, taking the stairs, walking on rough terrain, working with hands below knee height, standing, lifting or carrying, pushing or pulling, walking on ground level, operating a vehicle, operating foot pedals, and sitting. The 0-to-100 scale rates the difficulty of using knees for each particular activity, with higher scores indicating greater ease and less pain in doing that activity.
Among the 107 patients who expected to be satisfied after their surgery, half (n = 53) were satisfied, compared with 12% (n = 13) who were unsatisfied; the remaining participants (n = 41, 38%) were neither satisfied nor dissatisfied. Among the 24 patients who expected to be dissatisfied after their surgery, one-third (n = 8) were satisfied and 42% (n = 10) were dissatisfied. The remaining 44 patients didn’t expect to be satisfied or dissatisfied before their surgery, and 41% of them were satisfied while 23% were dissatisfied.
The researchers found that patients’ expectation of their satisfaction level going into the surgery was the only preoperative factor to be prognostic for dissatisfaction 6 months after surgery, based on their WORQ score. That is, patients who expected to be dissatisfied before their surgery had approximately five times greater odds of being dissatisfied after their surgery than did those who expected to be satisfied with their ability to do knee-straining activities at work (odds ratio, 5.1; 95% confidence interval, 1.7-15.5). Among those with a WORQ score of 40, indicating a greater expectation of difficulty using their knees postoperatively, 55% were dissatisfied after their surgery, compared with 19% of those with a WORQ score of 85, who expected greater knee ability after their surgery.
The other factors that the researchers examined, which had no effect on WORQ scores, included age, sex, BMI, education, comorbidities, KOOS pain subscale, having a knee-straining job, having needed surgery because of work, or having preoperative sick leave.
One discussion prompted by the presentation focused specifically on individuals’ ability to kneel without much difficulty after their surgery, an activity that’s not typically considered likely, Ms. van Zaanen noted. One audience member, Gillian Hawker, MD, MSc, a professor of medicine in the division of rheumatology at the University of Toronto, questioned whether the field should accept that current reality from surgical intervention. Dr. Hawker described a cohort she had analyzed in which two-thirds of the participants had expected they would be able to kneel after their surgery, regardless of whether it was related to work or other activities.
“Kneeling is important, not just for work; it’s important for culture and religion and lots of other things,” Dr. Hawker said. “How will you help these people to kneel after knee replacement when the surgery isn’t really performed to enable people to do that?” In response, Ms. van Zaanen noted it might not be achievable, as the research literature demonstrates, but Dr. Hawker suggested that is itself problematic.
“I guess what I’m asking is, why are we settling for that? If it’s important to so many people, and an expectation of so many people, why don’t we technologically improve such that, post arthroplasty, people can kneel?”
Another commenter suggested that the study’s findings may not indicate a need to manage patients’ expectations prior to surgery so much as showing that some patients simply have realistic expectations of what they will and will not be able to do after knee replacement.
“Is it possible that people who had low expectations – those who expected to be dissatisfied afterwards – were appropriately understanding that they were likely to be dissatisfied afterwards, in which case, managing their expectations might do nothing for their dissatisfaction afterwards?” the commenter asked. It is likely necessary to conduct additional research about expectations before surgery and experiences after surgery to address that question, Ms. van Zaanen suggested.
Ms. van Zaanen and Dr. Hawker reported having no relevant financial relationships. The presentation did not note any external funding. The Congress was sponsored by the Osteoarthritis Research Society International.
DENVER – People with lower expectations of how they would be able to use their knees during work activities after a total knee arthroplasty were more dissatisfied with their knee abilities 6 months after their surgery, according to a study presented at the OARSI 2023 World Congress.
Two out of 10 patients are dissatisfied after total knee arthroplasty, which is increasingly performed in younger and working patients who may have higher demands, presenter Yvonne van Zaanen, a physiotherapist in occupational health and ergonomics and a PhD candidate at Amsterdam University Medical Center, told attendees.
The findings suggest a correlation between patients’ low presurgical expectations of their ability to use their knees and having more difficulty with their knees postoperatively, she said. “We should take better care of working patients with low expectations by managing their preoperative expectations and improving their ability to perform work-related knee-straining activities in rehabilitation,” Ms. van Zaanen told attendees.
The researchers conducted a multicenter, prospective cohort study involving seven hospitals. They surveyed 175 employed individuals aged 18-65 years who were scheduled for a total knee arthroplasty and intended to return to work after their surgery. The first survey occurred before the operation, and the follow-up occurred 6 months after the surgery.
Just over half the participants were women (53%), and the average participant age was 59. Respondents had a mean body mass index (BMI) of 29 kg/m2, and had a Knee injury and Osteoarthritis Outcome Score (KOOS) pain score of 42 (on a 0-to-100 scale in which lower scores are worse). About half the respondents (51%) had a job that involved knee-straining activities.
The researchers assessed participants’ ability to perform work-related, knee-straining activities using the Work, Osteoarthritis, or joint-Replacement Questionnaire (WORQ) tool, which considers the following activities: kneeling, crouching, clambering, taking the stairs, walking on rough terrain, working with hands below knee height, standing, lifting or carrying, pushing or pulling, walking on ground level, operating a vehicle, operating foot pedals, and sitting. The 0-to-100 scale rates the difficulty of using knees for each particular activity, with higher scores indicating greater ease and less pain in doing that activity.
Among the 107 patients who expected to be satisfied after their surgery, half (n = 53) were satisfied, compared with 12% (n = 13) who were unsatisfied; the remaining participants (n = 41, 38%) were neither satisfied nor dissatisfied. Among the 24 patients who expected to be dissatisfied after their surgery, one-third (n = 8) were satisfied and 42% (n = 10) were dissatisfied. The remaining 44 patients didn’t expect to be satisfied or dissatisfied before their surgery, and 41% of them were satisfied while 23% were dissatisfied.
The researchers found that patients’ expectation of their satisfaction level going into the surgery was the only preoperative factor to be prognostic for dissatisfaction 6 months after surgery, based on their WORQ score. That is, patients who expected to be dissatisfied before their surgery had approximately five times greater odds of being dissatisfied after their surgery than did those who expected to be satisfied with their ability to do knee-straining activities at work (odds ratio, 5.1; 95% confidence interval, 1.7-15.5). Among those with a WORQ score of 40, indicating a greater expectation of difficulty using their knees postoperatively, 55% were dissatisfied after their surgery, compared with 19% of those with a WORQ score of 85, who expected greater knee ability after their surgery.
The other factors that the researchers examined, which had no effect on WORQ scores, included age, sex, BMI, education, comorbidities, KOOS pain subscale, having a knee-straining job, having needed surgery because of work, or having preoperative sick leave.
One discussion prompted by the presentation focused specifically on individuals’ ability to kneel without much difficulty after their surgery, an activity that’s not typically considered likely, Ms. van Zaanen noted. One audience member, Gillian Hawker, MD, MSc, a professor of medicine in the division of rheumatology at the University of Toronto, questioned whether the field should accept that current reality from surgical intervention. Dr. Hawker described a cohort she had analyzed in which two-thirds of the participants had expected they would be able to kneel after their surgery, regardless of whether it was related to work or other activities.
“Kneeling is important, not just for work; it’s important for culture and religion and lots of other things,” Dr. Hawker said. “How will you help these people to kneel after knee replacement when the surgery isn’t really performed to enable people to do that?” In response, Ms. van Zaanen noted it might not be achievable, as the research literature demonstrates, but Dr. Hawker suggested that is itself problematic.
“I guess what I’m asking is, why are we settling for that? If it’s important to so many people, and an expectation of so many people, why don’t we technologically improve such that, post arthroplasty, people can kneel?”
Another commenter suggested that the study’s findings may not indicate a need to manage patients’ expectations prior to surgery so much as showing that some patients simply have realistic expectations of what they will and will not be able to do after knee replacement.
“Is it possible that people who had low expectations – those who expected to be dissatisfied afterwards – were appropriately understanding that they were likely to be dissatisfied afterwards, in which case, managing their expectations might do nothing for their dissatisfaction afterwards?” the commenter asked. It is likely necessary to conduct additional research about expectations before surgery and experiences after surgery to address that question, Ms. van Zaanen suggested.
Ms. van Zaanen and Dr. Hawker reported having no relevant financial relationships. The presentation did not note any external funding. The Congress was sponsored by the Osteoarthritis Research Society International.
DENVER – People with lower expectations of how they would be able to use their knees during work activities after a total knee arthroplasty were more dissatisfied with their knee abilities 6 months after their surgery, according to a study presented at the OARSI 2023 World Congress.
Two out of 10 patients are dissatisfied after total knee arthroplasty, which is increasingly performed in younger and working patients who may have higher demands, presenter Yvonne van Zaanen, a physiotherapist in occupational health and ergonomics and a PhD candidate at Amsterdam University Medical Center, told attendees.
The findings suggest a correlation between patients’ low presurgical expectations of their ability to use their knees and having more difficulty with their knees postoperatively, she said. “We should take better care of working patients with low expectations by managing their preoperative expectations and improving their ability to perform work-related knee-straining activities in rehabilitation,” Ms. van Zaanen told attendees.
The researchers conducted a multicenter, prospective cohort study involving seven hospitals. They surveyed 175 employed individuals aged 18-65 years who were scheduled for a total knee arthroplasty and intended to return to work after their surgery. The first survey occurred before the operation, and the follow-up occurred 6 months after the surgery.
Just over half the participants were women (53%), and the average participant age was 59. Respondents had a mean body mass index (BMI) of 29 kg/m2, and had a Knee injury and Osteoarthritis Outcome Score (KOOS) pain score of 42 (on a 0-to-100 scale in which lower scores are worse). About half the respondents (51%) had a job that involved knee-straining activities.
The researchers assessed participants’ ability to perform work-related, knee-straining activities using the Work, Osteoarthritis, or joint-Replacement Questionnaire (WORQ) tool, which considers the following activities: kneeling, crouching, clambering, taking the stairs, walking on rough terrain, working with hands below knee height, standing, lifting or carrying, pushing or pulling, walking on ground level, operating a vehicle, operating foot pedals, and sitting. The 0-to-100 scale rates the difficulty of using knees for each particular activity, with higher scores indicating greater ease and less pain in doing that activity.
Among the 107 patients who expected to be satisfied after their surgery, half (n = 53) were satisfied, compared with 12% (n = 13) who were unsatisfied; the remaining participants (n = 41, 38%) were neither satisfied nor dissatisfied. Among the 24 patients who expected to be dissatisfied after their surgery, one-third (n = 8) were satisfied and 42% (n = 10) were dissatisfied. The remaining 44 patients didn’t expect to be satisfied or dissatisfied before their surgery, and 41% of them were satisfied while 23% were dissatisfied.
The researchers found that patients’ expectation of their satisfaction level going into the surgery was the only preoperative factor to be prognostic for dissatisfaction 6 months after surgery, based on their WORQ score. That is, patients who expected to be dissatisfied before their surgery had approximately five times greater odds of being dissatisfied after their surgery than did those who expected to be satisfied with their ability to do knee-straining activities at work (odds ratio, 5.1; 95% confidence interval, 1.7-15.5). Among those with a WORQ score of 40, indicating a greater expectation of difficulty using their knees postoperatively, 55% were dissatisfied after their surgery, compared with 19% of those with a WORQ score of 85, who expected greater knee ability after their surgery.
The other factors that the researchers examined, which had no effect on WORQ scores, included age, sex, BMI, education, comorbidities, KOOS pain subscale, having a knee-straining job, having needed surgery because of work, or having preoperative sick leave.
One discussion prompted by the presentation focused specifically on individuals’ ability to kneel without much difficulty after their surgery, an activity that’s not typically considered likely, Ms. van Zaanen noted. One audience member, Gillian Hawker, MD, MSc, a professor of medicine in the division of rheumatology at the University of Toronto, questioned whether the field should accept that current reality from surgical intervention. Dr. Hawker described a cohort she had analyzed in which two-thirds of the participants had expected they would be able to kneel after their surgery, regardless of whether it was related to work or other activities.
“Kneeling is important, not just for work; it’s important for culture and religion and lots of other things,” Dr. Hawker said. “How will you help these people to kneel after knee replacement when the surgery isn’t really performed to enable people to do that?” In response, Ms. van Zaanen noted it might not be achievable, as the research literature demonstrates, but Dr. Hawker suggested that is itself problematic.
“I guess what I’m asking is, why are we settling for that? If it’s important to so many people, and an expectation of so many people, why don’t we technologically improve such that, post arthroplasty, people can kneel?”
Another commenter suggested that the study’s findings may not indicate a need to manage patients’ expectations prior to surgery so much as showing that some patients simply have realistic expectations of what they will and will not be able to do after knee replacement.
“Is it possible that people who had low expectations – those who expected to be dissatisfied afterwards – were appropriately understanding that they were likely to be dissatisfied afterwards, in which case, managing their expectations might do nothing for their dissatisfaction afterwards?” the commenter asked. It is likely necessary to conduct additional research about expectations before surgery and experiences after surgery to address that question, Ms. van Zaanen suggested.
Ms. van Zaanen and Dr. Hawker reported having no relevant financial relationships. The presentation did not note any external funding. The Congress was sponsored by the Osteoarthritis Research Society International.
AT OARSI 2023
Another FDA class I recall of Cardiosave Hybrid/Rescue IABPs
Datascope/Getinge is recalling certain Cardiosave Hybrid and Cardiosave Rescue Intra-Aortic Balloon Pumps (IABPs) because the coiled cable connecting the display and base on some units may fail, causing an unexpected shutdown without warnings or alarms to alert the user.
The U.S. Food and Drug Administration has identified this as a class I recall, the most serious type of recall, because of the risk for serious injury or death.
The FDA warns that an unexpected pump shutdown and any interruption to therapy that occurs can lead to hemodynamic instability, organ damage, and/or death, especially in patients who are critically ill and most likely to receive therapy using these devices.
The devices are indicated for acute coronary syndrome, cardiac and noncardiac surgery, and complications of heart failure in adults.
From June 2019 to August 2022, Datascope/Getinge reported 44 complaints about damaged coiled cords resulting in unexpected shutdowns. There have been no reports of injuries or deaths related to this issue, according to the recall notice posted on the FDA’s website.
The recall includes a total of 2,300 CardioSave Hybrid or Rescue IABP units distributed prior to July 24, 2017, and/or coiled cord part number 0012-00-1801. Product model numbers for the recalled Cardiosave Hybrid and Cardiosave Rescue are available online.
The Cardiosave IABPs have previously been flagged by the FDA for subpar battery performance and fluid leaks.
To address the cable issue, Datascope/Getinge sent an urgent medical device correction letter to customers recommending that the coiled cable cord of the Cardiosave IABP be inspected for visible damage prior to use.
If an unexpected shutdown occurs, an attempt should be made to restart the Cardiosave IABP until an alternative pump is available. If the restart attempt is unsuccessful, an alternative IABP should be used. Any device that remains inoperable after a shutdown should be removed from patient care.
Customers should inspect their inventory to identify any Cardiosave Hybrid and/or Rescue IABPs that have the recalled coiled cord.
The company also asks customers to complete and sign the Medical Device Correction-Response form included with the letter and return it to Datascope/Getinge by emailing a scanned copy to [email protected] or by faxing the form to 1-877-660-5841.
Customers with questions about this recall should contact their Datascope/Getinge representative or call Datascope/Getinge technical support at 1-888-943-8872, Monday through Friday, between 8:00 AM and 6:00 PM ET.
The company has developed a hardware correction to address this issue and says a service representative will contact customers to schedule installation of the correction when the correction kit is available.
Any adverse events or suspected adverse events related to the recalled CardioSave Hybrid/Rescue IABPs should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article first appeared on Medscape.com.
Datascope/Getinge is recalling certain Cardiosave Hybrid and Cardiosave Rescue Intra-Aortic Balloon Pumps (IABPs) because the coiled cable connecting the display and base on some units may fail, causing an unexpected shutdown without warnings or alarms to alert the user.
The U.S. Food and Drug Administration has identified this as a class I recall, the most serious type of recall, because of the risk for serious injury or death.
The FDA warns that an unexpected pump shutdown and any interruption to therapy that occurs can lead to hemodynamic instability, organ damage, and/or death, especially in patients who are critically ill and most likely to receive therapy using these devices.
The devices are indicated for acute coronary syndrome, cardiac and noncardiac surgery, and complications of heart failure in adults.
From June 2019 to August 2022, Datascope/Getinge reported 44 complaints about damaged coiled cords resulting in unexpected shutdowns. There have been no reports of injuries or deaths related to this issue, according to the recall notice posted on the FDA’s website.
The recall includes a total of 2,300 CardioSave Hybrid or Rescue IABP units distributed prior to July 24, 2017, and/or coiled cord part number 0012-00-1801. Product model numbers for the recalled Cardiosave Hybrid and Cardiosave Rescue are available online.
The Cardiosave IABPs have previously been flagged by the FDA for subpar battery performance and fluid leaks.
To address the cable issue, Datascope/Getinge sent an urgent medical device correction letter to customers recommending that the coiled cable cord of the Cardiosave IABP be inspected for visible damage prior to use.
If an unexpected shutdown occurs, an attempt should be made to restart the Cardiosave IABP until an alternative pump is available. If the restart attempt is unsuccessful, an alternative IABP should be used. Any device that remains inoperable after a shutdown should be removed from patient care.
Customers should inspect their inventory to identify any Cardiosave Hybrid and/or Rescue IABPs that have the recalled coiled cord.
The company also asks customers to complete and sign the Medical Device Correction-Response form included with the letter and return it to Datascope/Getinge by emailing a scanned copy to [email protected] or by faxing the form to 1-877-660-5841.
Customers with questions about this recall should contact their Datascope/Getinge representative or call Datascope/Getinge technical support at 1-888-943-8872, Monday through Friday, between 8:00 AM and 6:00 PM ET.
The company has developed a hardware correction to address this issue and says a service representative will contact customers to schedule installation of the correction when the correction kit is available.
Any adverse events or suspected adverse events related to the recalled CardioSave Hybrid/Rescue IABPs should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article first appeared on Medscape.com.
Datascope/Getinge is recalling certain Cardiosave Hybrid and Cardiosave Rescue Intra-Aortic Balloon Pumps (IABPs) because the coiled cable connecting the display and base on some units may fail, causing an unexpected shutdown without warnings or alarms to alert the user.
The U.S. Food and Drug Administration has identified this as a class I recall, the most serious type of recall, because of the risk for serious injury or death.
The FDA warns that an unexpected pump shutdown and any interruption to therapy that occurs can lead to hemodynamic instability, organ damage, and/or death, especially in patients who are critically ill and most likely to receive therapy using these devices.
The devices are indicated for acute coronary syndrome, cardiac and noncardiac surgery, and complications of heart failure in adults.
From June 2019 to August 2022, Datascope/Getinge reported 44 complaints about damaged coiled cords resulting in unexpected shutdowns. There have been no reports of injuries or deaths related to this issue, according to the recall notice posted on the FDA’s website.
The recall includes a total of 2,300 CardioSave Hybrid or Rescue IABP units distributed prior to July 24, 2017, and/or coiled cord part number 0012-00-1801. Product model numbers for the recalled Cardiosave Hybrid and Cardiosave Rescue are available online.
The Cardiosave IABPs have previously been flagged by the FDA for subpar battery performance and fluid leaks.
To address the cable issue, Datascope/Getinge sent an urgent medical device correction letter to customers recommending that the coiled cable cord of the Cardiosave IABP be inspected for visible damage prior to use.
If an unexpected shutdown occurs, an attempt should be made to restart the Cardiosave IABP until an alternative pump is available. If the restart attempt is unsuccessful, an alternative IABP should be used. Any device that remains inoperable after a shutdown should be removed from patient care.
Customers should inspect their inventory to identify any Cardiosave Hybrid and/or Rescue IABPs that have the recalled coiled cord.
The company also asks customers to complete and sign the Medical Device Correction-Response form included with the letter and return it to Datascope/Getinge by emailing a scanned copy to [email protected] or by faxing the form to 1-877-660-5841.
Customers with questions about this recall should contact their Datascope/Getinge representative or call Datascope/Getinge technical support at 1-888-943-8872, Monday through Friday, between 8:00 AM and 6:00 PM ET.
The company has developed a hardware correction to address this issue and says a service representative will contact customers to schedule installation of the correction when the correction kit is available.
Any adverse events or suspected adverse events related to the recalled CardioSave Hybrid/Rescue IABPs should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article first appeared on Medscape.com.
Marathon running does not increase arthritis risk: Survey
Runners who had undergone knee or hip surgery or had a previous hip or knee injury that prevented running were most likely to have arthritis, researchers found. Family history of arthritis, higher body mass index (BMI), and older age were also associated with increased risk of the condition.
The study was presented at the American Academy of Orthopaedic Surgeons 2023 Annual Meeting.
It has generally been thought that running may increase risk of osteoarthritis because it puts more load on joints than walking or standing, noted Grace Hsiao-Wei Lo, MD, an assistant professor of immunology, allergy, and rheumatology at the Baylor College of Medicine, Houston, who was not involved with the work. Research in this area has yielded mixed results: A 2017 analysis of multiple studies found that competitive runners did have higher rates of arthritis than recreational runners, while another study conducted by Dr. Lo found that runners did not have an increased risk of knee osteoarthritis, compared with nonrunners. A 2018 study showed that marathon runners had lower instances of arthritis, compared with the general population.
In this new study, researchers surveyed 3,804 runners who participated in the 2019 or 2021 Chicago Marathon about their running history, average mileage per week, and average running pace. The survey also asked about known risk factors for osteoarthritis, including BMI, family history of arthritis, and past knee and hip injuries that prevented running.
Runners, on average, were about 44 years old and ran 27.9 miles per week. The largest proportion of respondents had completed 2-5 marathons (37.3%), around 21% of respondents had finished 6-10 marathons, and 17% were running their first marathon. Study participants had an average of 15 years of running experience, 1,892 reported a previous hip or knee injury, and 413 had undergone knee or hip surgery. Overall, 36.4% reported experiencing hip or knee pain in the past year, and 7.3% had been diagnosed with arthritis.
Researchers found that there was no association between the risk of osteoarthritis and weekly mileage, years spent running, number of marathons completed, or running pace. Respondents who had undergone knee or hip surgery had the highest risk of osteoarthritis (odds ratio, 5.85; P < .0001), followed by those with a history of knee or hip injuries that prevented running (OR, 5.04; P < .0001). Other identified risk factors were family history of arthritis (OR, 3.47; P < .0001), BMI (OR, 1.10; P < .0001), and older age (OR, 1.08; P < .0001).
The news should be encouraging for runners, said Matthew Hartwell, MD, an orthopedic surgeon at the University of California, San Francisco, who led the research. If someone does not have injuries or surgeries that keep them from running, “you can still continue to run,” he said. “There may not necessarily be this dose-response relationship where the more you run, the more you break down your knee or your hip.”
Still, 24.2% of runners reported that their physician had advised them to reduce their mileage or stop running altogether. Most runners (94.2%) said they planned to run another marathon.
“The results of this study are consistent with the experiences of many lifelong runners and observations of sports medicine professionals that osteoarthritis is not an inevitable consequence of distance running,” said Brett Toresdahl, MD, a sports medicine physician at the Hospital for Special Surgery in New York, who was not involved with the study.
Still, he emphasized that more research is necessary to understand whether running contributes to the risk of developing osteoarthritis. The participants in the study were current marathoners, he noted, so it is likely they have healthy joints that can tolerate running longer distances. “If there is a subset of people who have joints that are negatively affected by running, they wouldn’t likely be registering for a marathon,” he said in an email interview.
Dr. Lo added that comparing these marathoners to a group who did not run would help assess whether running can be harmful to joints. “To be fair, this is a challenging subject to study,” she said. “Osteoarthritis has a long natural history, and so it is difficult to evaluate this kind of question over many years of running and many years of evaluation of arthritis.”
While the research does not answer the question of whether running can lead to osteoarthritis, it helps show the need for long-term research on how running affects joints over time as well as one’s general health, Dr. Toresdahl noted. “I would not be surprised if future longitudinal research will come to the same conclusion that running for the majority of patients is a net benefit for overall health and at least net neutral for joint health when done in moderation,” he said.
Dr. Hartwell, Dr. Lo, and Dr. Toresdahl report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Runners who had undergone knee or hip surgery or had a previous hip or knee injury that prevented running were most likely to have arthritis, researchers found. Family history of arthritis, higher body mass index (BMI), and older age were also associated with increased risk of the condition.
The study was presented at the American Academy of Orthopaedic Surgeons 2023 Annual Meeting.
It has generally been thought that running may increase risk of osteoarthritis because it puts more load on joints than walking or standing, noted Grace Hsiao-Wei Lo, MD, an assistant professor of immunology, allergy, and rheumatology at the Baylor College of Medicine, Houston, who was not involved with the work. Research in this area has yielded mixed results: A 2017 analysis of multiple studies found that competitive runners did have higher rates of arthritis than recreational runners, while another study conducted by Dr. Lo found that runners did not have an increased risk of knee osteoarthritis, compared with nonrunners. A 2018 study showed that marathon runners had lower instances of arthritis, compared with the general population.
In this new study, researchers surveyed 3,804 runners who participated in the 2019 or 2021 Chicago Marathon about their running history, average mileage per week, and average running pace. The survey also asked about known risk factors for osteoarthritis, including BMI, family history of arthritis, and past knee and hip injuries that prevented running.
Runners, on average, were about 44 years old and ran 27.9 miles per week. The largest proportion of respondents had completed 2-5 marathons (37.3%), around 21% of respondents had finished 6-10 marathons, and 17% were running their first marathon. Study participants had an average of 15 years of running experience, 1,892 reported a previous hip or knee injury, and 413 had undergone knee or hip surgery. Overall, 36.4% reported experiencing hip or knee pain in the past year, and 7.3% had been diagnosed with arthritis.
Researchers found that there was no association between the risk of osteoarthritis and weekly mileage, years spent running, number of marathons completed, or running pace. Respondents who had undergone knee or hip surgery had the highest risk of osteoarthritis (odds ratio, 5.85; P < .0001), followed by those with a history of knee or hip injuries that prevented running (OR, 5.04; P < .0001). Other identified risk factors were family history of arthritis (OR, 3.47; P < .0001), BMI (OR, 1.10; P < .0001), and older age (OR, 1.08; P < .0001).
The news should be encouraging for runners, said Matthew Hartwell, MD, an orthopedic surgeon at the University of California, San Francisco, who led the research. If someone does not have injuries or surgeries that keep them from running, “you can still continue to run,” he said. “There may not necessarily be this dose-response relationship where the more you run, the more you break down your knee or your hip.”
Still, 24.2% of runners reported that their physician had advised them to reduce their mileage or stop running altogether. Most runners (94.2%) said they planned to run another marathon.
“The results of this study are consistent with the experiences of many lifelong runners and observations of sports medicine professionals that osteoarthritis is not an inevitable consequence of distance running,” said Brett Toresdahl, MD, a sports medicine physician at the Hospital for Special Surgery in New York, who was not involved with the study.
Still, he emphasized that more research is necessary to understand whether running contributes to the risk of developing osteoarthritis. The participants in the study were current marathoners, he noted, so it is likely they have healthy joints that can tolerate running longer distances. “If there is a subset of people who have joints that are negatively affected by running, they wouldn’t likely be registering for a marathon,” he said in an email interview.
Dr. Lo added that comparing these marathoners to a group who did not run would help assess whether running can be harmful to joints. “To be fair, this is a challenging subject to study,” she said. “Osteoarthritis has a long natural history, and so it is difficult to evaluate this kind of question over many years of running and many years of evaluation of arthritis.”
While the research does not answer the question of whether running can lead to osteoarthritis, it helps show the need for long-term research on how running affects joints over time as well as one’s general health, Dr. Toresdahl noted. “I would not be surprised if future longitudinal research will come to the same conclusion that running for the majority of patients is a net benefit for overall health and at least net neutral for joint health when done in moderation,” he said.
Dr. Hartwell, Dr. Lo, and Dr. Toresdahl report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Runners who had undergone knee or hip surgery or had a previous hip or knee injury that prevented running were most likely to have arthritis, researchers found. Family history of arthritis, higher body mass index (BMI), and older age were also associated with increased risk of the condition.
The study was presented at the American Academy of Orthopaedic Surgeons 2023 Annual Meeting.
It has generally been thought that running may increase risk of osteoarthritis because it puts more load on joints than walking or standing, noted Grace Hsiao-Wei Lo, MD, an assistant professor of immunology, allergy, and rheumatology at the Baylor College of Medicine, Houston, who was not involved with the work. Research in this area has yielded mixed results: A 2017 analysis of multiple studies found that competitive runners did have higher rates of arthritis than recreational runners, while another study conducted by Dr. Lo found that runners did not have an increased risk of knee osteoarthritis, compared with nonrunners. A 2018 study showed that marathon runners had lower instances of arthritis, compared with the general population.
In this new study, researchers surveyed 3,804 runners who participated in the 2019 or 2021 Chicago Marathon about their running history, average mileage per week, and average running pace. The survey also asked about known risk factors for osteoarthritis, including BMI, family history of arthritis, and past knee and hip injuries that prevented running.
Runners, on average, were about 44 years old and ran 27.9 miles per week. The largest proportion of respondents had completed 2-5 marathons (37.3%), around 21% of respondents had finished 6-10 marathons, and 17% were running their first marathon. Study participants had an average of 15 years of running experience, 1,892 reported a previous hip or knee injury, and 413 had undergone knee or hip surgery. Overall, 36.4% reported experiencing hip or knee pain in the past year, and 7.3% had been diagnosed with arthritis.
Researchers found that there was no association between the risk of osteoarthritis and weekly mileage, years spent running, number of marathons completed, or running pace. Respondents who had undergone knee or hip surgery had the highest risk of osteoarthritis (odds ratio, 5.85; P < .0001), followed by those with a history of knee or hip injuries that prevented running (OR, 5.04; P < .0001). Other identified risk factors were family history of arthritis (OR, 3.47; P < .0001), BMI (OR, 1.10; P < .0001), and older age (OR, 1.08; P < .0001).
The news should be encouraging for runners, said Matthew Hartwell, MD, an orthopedic surgeon at the University of California, San Francisco, who led the research. If someone does not have injuries or surgeries that keep them from running, “you can still continue to run,” he said. “There may not necessarily be this dose-response relationship where the more you run, the more you break down your knee or your hip.”
Still, 24.2% of runners reported that their physician had advised them to reduce their mileage or stop running altogether. Most runners (94.2%) said they planned to run another marathon.
“The results of this study are consistent with the experiences of many lifelong runners and observations of sports medicine professionals that osteoarthritis is not an inevitable consequence of distance running,” said Brett Toresdahl, MD, a sports medicine physician at the Hospital for Special Surgery in New York, who was not involved with the study.
Still, he emphasized that more research is necessary to understand whether running contributes to the risk of developing osteoarthritis. The participants in the study were current marathoners, he noted, so it is likely they have healthy joints that can tolerate running longer distances. “If there is a subset of people who have joints that are negatively affected by running, they wouldn’t likely be registering for a marathon,” he said in an email interview.
Dr. Lo added that comparing these marathoners to a group who did not run would help assess whether running can be harmful to joints. “To be fair, this is a challenging subject to study,” she said. “Osteoarthritis has a long natural history, and so it is difficult to evaluate this kind of question over many years of running and many years of evaluation of arthritis.”
While the research does not answer the question of whether running can lead to osteoarthritis, it helps show the need for long-term research on how running affects joints over time as well as one’s general health, Dr. Toresdahl noted. “I would not be surprised if future longitudinal research will come to the same conclusion that running for the majority of patients is a net benefit for overall health and at least net neutral for joint health when done in moderation,” he said.
Dr. Hartwell, Dr. Lo, and Dr. Toresdahl report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM AAOS 2023





