User login
How to manage depression in overweight or obese patients
Discuss this article at www.facebook.com/CurrentPsychiatry
Mrs. G is a 52-year-old mother and teacher with a 20-year history of recurrent depressive episodes for which she has been treated with various antidepressants, including sertraline, fluoxetine, and citalopram. For some of her depressive recurrences, she also received adjunctive second-generation antipsychotics (SGAs), including quetiapine and olanzapine.
She describes feelings of “being defeated,” hopelessness, and boredom and frustration with her teaching. It takes her approximately 30 minutes to go to sleep each night, but she wakes up after 2 to 3 hours, and the remainder of her night’s sleep is markedly disrupted. Because of her hopeless feelings, she has given up on dieting and going to the gym. When feeling down she has donuts and coffee. She has gained 45 lbs over the past 10 years and now weighs 175 lbs. In addition to her disrupted mood, she complains of frequent headaches and sore muscles.
Mrs. G’s psychiatrist refers her to her primary care physician for evaluation of her physical complaints and recommendations regarding her weight gain. Her waistline measures 90 cm and her body mass index (BMI) is 29.1 kg/m2; a BMI of ≥30 is considered obese. Her blood pressure is 145/85 mmHg. Laboratory work reveals a total cholesterol level of 235 mg/dL, low-density lipoprotein of 146 mg/dL, and fasting blood sugar, 135 mg/dL.
Mrs. G’s case illustrates many of the issues psychiatrists face when caring for overweight or obese patients with depression (OW/OB-D). Both conditions can be challenging to manage, and may be especially difficult to treat when they co-occur. When depression and obesity co-occur, their capacity to inflict psychological and physical harm likely is greater than either condition alone. Data point to a “2-way street” of mutually destructive effects of being overweight/obese on depression and vice versa.1
This article summarizes ways that depression and obesity aggravate each other, and highlights research that suggests depression and obesity are manifestations of inflammatory processes. It also suggests a stepwise approach to treating OW/OB-D patients.
Mutually destructive processes
Self-esteem and body image. Lowered self-esteem is a hallmark of depression. In popular culture, “you can’t be too rich or too thin,” and the pressure to be slim is great. Therefore, OW/OB-D patients have 2 reasons to feel a depleted sense of self-worth: their psychiatric illness and their weight. Observant clinicians will recognize these dual sources of self-deprecation and tailor treatment to address both.
Increasing numbers of celebrities, performers, and prominent politicians are overweight or obese. Increased social acceptance of OW/OB individuals in our culture may be legitimizing weight gain and obesity. When OW/OB-D patients justify their weight by pointing to overweight celebrities, clinicians can counter this argument with data on the hazards of obesity on health and well-being, such as premature death, coronary artery disease, diabetes, arthritis, and some forms of cancer.
OW/OB patients tend to interact with other OW/OB individuals. Christakis et al2 reported that adults with obese friends were more likely to become obese than individuals without obese friends. Valente et al3 found that overweight teens were twice as likely to have overweight friends as non-overweight teens. This power of social connectedness can be harnessed when treating OW/OB-D patients, where therapeutic groups can help patients address both depression and weight gain.
Inactivity. OW/OB-D patients with psychomotor retardation or reduced activity may gain weight because they consume more calories than their body requires. Depressed patients may say they “have no energy” to participate in a clinician-recommended exercise program or that “it won’t do any good anyway.”
These tendencies are best dealt with by incorporating an exercise program into the comprehensive plan for OW/OB-D patients from the start of treatment. Several studies suggest that in addition to helping manage weight, exercise may have antidepressant effects. In a large, well-controlled trial of patients with major depressive disorder (MDD), Blumenthal et al4 found that an exercise program was as effective as fluoxetine, 20 mg/d, and the antidepressant effects persisted at 10-month follow-up for patients who continued to exercise.5 In a review of studies of exercise in depressed patients, Helmich et al6 concluded that in most studies exercise was beneficial. However, Mead et al7 found that nearly all trials of exercise and depression had substantial design flaws. Based on the 3 well-designed studies they reviewed, Mead et al concluded that the efficacy of exercise was comparable to that of cognitive therapy.
Although the evidence on exercise for treating depression is inconclusive, an exercise program is essential for OW/OB-D patients because it can help manage weight and improve cardiovascular fitness. Motivation is a key ingredient of successful programs.8 Encourage patients to make exercise enjoyable, perhaps by using video games or other interactive computer-based programs.9
Sleep disturbances. Disrupted sleep— another hallmark of depression—appears to be a risk factor for weight gain.10 Although the basis for this relationship is still under investigation, one possibility is that some patients with insomnia get up to eat more often than those without sleep disturbances. Research has shown that when sleep is curtailed in a sleep laboratory, patients consume approximately 20% more calories from snacks (1,086 calories) than non-sleep-deprived patients (866 calories).11 Although this 220-calorie increase may seem small, it would amount to approximately 2 lbs of additional weight per month.
Appetite. Although weight loss is a cardinal sign of MDD, increased appetite and weight gain can be seen in many depressed patients who do not meet diagnostic criteria for MDD as well as those with seasonal affective disorder and metabolic syndrome, a condition characterized by insulin resistance, glucose intolerance, atherogenic dyslipidemia, visceral adiposity, hypercoagulation, chronic inflammation, oxidative stress, and hypertension.12
Emerging information about the neuroendocrinology of appetite regulation may lead to a better understanding of weight management in OW/OB-D patients. Leptin, a hormone released by adipose tissue, increases when fat stores are high, leading to reduced appetite and fat stores. Conversely, when fat stores are low, plasma leptin levels decrease, producing increased appetite and reduced energy expenditure.13
Researchers have suggested that leptin insufficiency and/or leptin resistance may contribute to vulnerability to depression, and leptin may have antidepressant effects.14 Lawson et al15 found that leptin levels were inversely associated with Hamilton Depression Rating Scale scores in normal-weight (BMI ≤25) women.
Leptin levels also are significantly associated with comorbid depressed mood and sleep disturbance.16 In healthy volunteers, shortening sleep duration to 4 hours produced an approximately 20% reduction in leptin release compared with normal sleep duration.17 Because of the relationship between sleep disorders and depression, leptin may act on sleep regulatory mechanisms, depressogenic pathways, or both. But studies of leptin’s role in obesity, depression, and sleep have not yet found a single role for leptin that ties all 3 conditions to this hormone’s known physiological functions.
Nonadherence. Compared with non-depressed patients, depressed patients are 76% more likely to not adhere to treatment.18 Patients may report that they are not interested in the treatment program or lack hope that it will be successful. Furthermore, OW/OB-D patients may consider exercise programs to be too strenuous and diet programs too depriving.19
OW/OB-D patients may require special care in monitoring adherence. The presence of depression in patients enrolled in weight loss programs may prompt the treatment staff to modify the usual protocol by including the patient in an active depression treatment module.20
Effects of pharmacologic agents
Many antidepressant agents are associated with weight gain.21Tables 1 and 2 summarize the effects antidepressants and adjunctive medications used to treat depression have on weight.22,23 SGAs such as clozapine and olanzapine, which frequently are used as augmenting agents in patients with treatment-resistant depression (TRD), are associated with weight gain.22 Lamotrigine also is an effective adjunctive medication for TRD and is not associated with significant weight gain.24
Bupropion has antidepressant and weight-loss effects and may be a suitable primary medication for OW/OB-D patients.
Early weight gain with olanzapine/fluoxetine combination may be a strong indicator of substantial weight gain with longer-term treatment. A weight gain of >2 kg (4.4 lbs) during the first 2 weeks of treatment is a strong predictor of weight gain of ≥10 kg (22 lbs) at 26 weeks.25
Antidepressants may be associated with an increased risk of obesity, and strategies to offset this risk may be useful in clinical practice, particularly patient education on the risks of weight gain and early introduction of a diet and exercise program.
Evidence suggests that depression and obesity are associated with alterations in immune activity (Box). This suggests that anti-inflammatory agents might have a role in treating depression by reducing the release of cytokines that may lead to depressive symptoms.
Table 1
Pharmacotherapy and weight gain: Antidepressants
| Agent | Effect on weight |
|---|---|
| SSRIs | |
| Paroxetine | Moderate gain |
| Fluoxetine | Early: weight loss Long-term: moderate gain |
| SNRIs | |
| Duloxetine | Minimal gain |
| Escitalopram | Moderate gain |
| Other agents | |
| Imipramine (TCA) | Moderate gain |
| Selegiline (MAOI) | Moderate gain |
| Trazodone (tetracyclic) | Moderate gain |
| Bupropion (atypical) | Moderate loss |
| MAOI: monoamine oxidase inhibitor; SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCA: tricyclic antidepressant Source: References 22,23 | |
Table 2
Pharmacotherapy and weight gain: Adjunctive agents
| Agent | Use in depression | Effect on weight |
|---|---|---|
| SGAs | ||
| Olanzapine | Psychotic depression | Large gain |
| Clozapine | Adjunct; psychotic depression | Large gain |
| Quetiapine | Primary; adjunct | Large gain |
| Aripiprazole | Adjunct | Small gain |
| Risperidone | Psychotic depression | Small gain |
| Ziprasidone | Psychotic depression | Small loss |
| Mood stabilizers | ||
| Divalproex | Treatment resistance, bipolar disorder | Moderate to large gain |
| Lamotrigine | Treatment resistance | Neutral |
| SGAs: second-generation antipsychotics Source: References 22,23 | ||
Research suggests that both depression and obesity are associated with immune dysregulation and inflammation.a-d Although the complexities of these interactions are beyond the scope of this article, having a model for understanding the role of inflammation in overweight or obese patients with depression (OW/OB-D) may be useful. Data supporting a role for immune dysregulation in OW/OB-D patients rests on the following findings:
Fat and muscle are endocrine organs: Fat is not just a storage organ for energy-rich lipids but also a rich source of cytokines, including monocyte chemotactic protein-1 (MCP-1), interleukin-2, and tumor necrosis factor-α (TNF-α). The increase in MCP-1 in fat tissue triggers a cascade of events that leads to chronic inflammation in adipose tissue. These substances can be released into circulation, stimulating inflammatory responses in other tissues. Data suggest that obesity’s effects on cardiovascular disease are mediated by these adipose-derived inflammatory hormones. There is a strong relationship between the volume of adipose tissue and the amount of pro-inflammatory hormones released; therefore, reducing weight reduces inflammatory burden on the body.
Pedersene pointed out that muscle also is an endocrine organ. Among the cytokines (or “myokines”) muscle produces are interleukin-6 (IL-6), interleukin-8, and brain-derived neurotrophic factor. During exercise, the amount of IL-6 released from muscles may increase by 100-fold. Although IL-6 usually is considered a pro-inflammatory regulator, it—or other muscle-derived myokines—may be responsible for some of exercise’s beneficial effects.e
If this hypothesis is correct, patients whose exercise includes resistance training—which increases muscle mass—are not just getting stronger or burning calories but may be facilitating release of hormones that could counteract obesity’s inflammatory effects.
Cytokine levels are elevated in depression and obesity: A substantial body of evidence shows that depressed patients have elevated circulating levels of inflammation markers. In particular, the proinflammatory cytokines IL-6 and interleukin-1β and the acute phase reactant C-reactive protein (CRP) are elevated in depressed patients.f Studies also show that blood levels of IL-6, TNF-α, and CRP are elevated in obese patients.g
Fat-derived cytokines alter metabolic pathways related to mood and inflammation: Among the many possible pathways linking cytokine actions and depression, the effects of TNF-α on serotonin metabolism have been studied extensively.h,i TNF-α activates brain indoleamine 2,3-dioxygenase, leading to rapid depletion of serotonin and exacerbation of depressive symptoms.j
Regarding physical problems, evidence suggests adipose-tissue-derived pro-inflammatory agents are involved in development of metabolic syndrome, a condition characterized by insulin resistance, glucose intolerance, atherogenic dyslipidemia, visceral adiposity, hypercoagulation, chronic inflammation, oxidative stress, and hypertension.k These conditions are strong risk factors for type II diabetes, coronary artery disease, hypertension, and stroke.
Anti-inflammatory agents for depression
Data suggest a model in which weight gain leads to an increase in pro-inflammatory cytokines. When released into the circulation, these cytokines produce a variety of deleterious effects, including blockade of serotonin synthesis in the brain that leads to depressive symptoms. Evidence suggests that anti-inflammatory agents might disrupt this process.
Celecoxib. The anti-inflammatory agent celecoxib acts by inhibiting cyclooxygenase-2, the rate-limiting enzyme in the synthesis of prostaglandin, a powerful inflammation mediator. Three double-blind, placebo-controlled trials have compared groups of:
- depressed patients receiving reboxetine with and without celecoxibl or fluoxetine, 40 mg/d, with and without celecoxibm
- bipolar disorder patients taking mood stabilizers or atypical antipsychotics with and without celecoxib, 400 mg/d.n
These studies suggest that celecoxib may accelerate improvement in depressive symptoms. Celecoxib’s potential for increased cardiovascular risk may limit its use.
Aspirin. Mendlewicz et alo conducted an open-label study in which 24 depressed patients who failed to respond to 4 weeks of antidepressant treatment received adjunctive acetylsalicylic acid, 160 mg/d, for another 4 weeks. They found that 52% of patients responded when aspirin was added to their regimen, and the improvement was seen during the first week of treatment.
References
- Shelton RC, Miller AH. Inflammation in depression: is adiposity a cause? Dialogues Clin Neurosci. 2011;13(1):41-53.
- Shelton RC, Miller AH. Eating ourselves to death (and despair): the contribution of adiposity and inflammation to depression. Prog Neurobiol. 2010;91(4):275-299.
- Soczynska JK, Kennedy SH, Woldeyohannes HO, et al. Mood disorders and obesity: understanding inflammation as a pathophysiological nexus. Neuromolecular Med. 2011;13(2):93-116.
- Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121(6):2111-2117.
- Pedersen BK. Muscles and their myokines. J Exp Biol. 2011;214(Pt 2):337-346.
- Maes M, Kubera M, Obuchowiczwa E, et al. Depression’s multiple comorbidities explained by (neuro)inflammatory and oxidative & nitrosative stress pathways. Neuro Endocrinol Lett. 2011;32(1):7-24.
- Khaodhiar L, Ling PR, Blackburn GL, et al. Serum levels of interleukin-6 and C-reactive protein correlate with body mass index across the broad range of obesity. JPEN J Parenter Enteral Nutr. 2004;28(6):410-415.
- Capuron L, Miller AH. Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol Ther. 2011;130(2):226-238.
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732-741.
- O’Connor JC, André C, Wang Y, et al. Interferon-gamma and tumor necrosis factor-alpha mediate the upregulation of indoleamine 2,3-dioxygenase and the induction of depressive-like behavior in mice in response to bacillus Calmette-Guerin. J Neurosci. 2009;29(13):4200-4209.
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356-359.
- Müller N, Schwarz MJ, Dehning S, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. 2006;11(7):680-684.
- Akhondzadeh S, Jafari S, Raisi F, et al. Clinical trial of adjunctive celecoxib treatment in patients with major depression: a double blind and placebo controlled trial. Depress Anxiety. 2009;26(7):607-611.
- Nery FG, Monkul ES, Hatch JP, et al. Celecoxib as an adjunct in the treatment of depressive or mixed episodes of bipolar disorder: a double-blind, randomized, placebo-controlled study. Hum Psychopharmacol. 2008;23(2):87-94.
- Mendlewicz J, Kriwin P, Oswald P, et al. Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int Clin Psychopharmacol. 2006;21(4):227-231.
Cognitive/behavioral approaches
Although large, well-designed studies of OW/OB-D patients are in the planning or pilot phases,26-28 a substantial database supports incorporating behavioral or cognitive-behavioral therapies when treating these patients.29 Patients in programs that combine behavioral approaches with diet and exercise achieve the greatest weight loss, and frequently show improved depression scores.30-32
In a randomized trial, 203 obese women with moderate to severe depression showed significant weight loss and decreased depression scores whether they were in a behavioral weight-loss program or one that combined behavioral weigh loss with cognitive-behavioral depression management.33 This study raises important questions: Did the behavioral weight-loss program effectively treat depression? Did patients’ depressive symptoms improve because of their improved sense of well-being as they lost weight? Did a putative reduction in cytokine production by fat cells improve their mood?
Treatment implications
Mrs. G has TRD, a BMI that borders on obesity, sleep problems, and lab values that suggest she may have metabolic syndrome. To best manage patients such as Mrs. G, consider the following steps:
- Select an antidepressant that is unlikely to cause further weight gain, such as bupropion, duloxetine, or fluoxetine.
- If necessary, add an augmenting agent that is not associated with weight gain, such as bupropion, aripiprazole, or lamotrigine.
- Verify that your patient is getting adequate sleep. Begin by reviewing the principles of sleep hygiene and, if necessary, prescribe a sedative or hypnotic medication.
- Although controlled clinical trials are lacking, consider including an anti-inflammatory agent such as aspirin to the pharmacologic armamentarium.
- Institute an exercise and diet program at the beginning of treatment. Exercise can begin with 20 to 30 minutes a day of walking. Tell patients that exercising in groups is a good way to address nonadherence and social isolation and reinforce positive lifestyle changes. Recommend that patients combine aerobic exercise to burn calories with resistance training to build muscle. Suggest that patients try to make exercising fun using video games or interactive computer-based programs.
- Encourage your patient to keep a journal to record his or her weight, amount and type of exercise, medication taken, and dietary intake. Review this information at every session to reinforce the importance of this integrated exercise and diet program.
Related Resources
- Markowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clinical Psychology: Science and Practice. 2008:15(1):1-20.
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011;111(1):92-102.
Drug Brand Names
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Zyban
- Celecoxib • Celebrex
- Citalopram • Celexa
- Clozapine • Clozaril
- Divalproex • Depakote
- Duloxetine • Cymbalta
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Selegiline • Emsam
- Sertraline • Zoloft
- Trazodone • Desyrel, Oleptro
- Ziprasidone • Geodon
Disclosure
Dr. Crayton reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220-229.
2. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370-379.
3. Valente TW, Fujimoto K, Chou CP, et al. Adolescent affiliations and adiposity: a social network analysis of friendships and obesity. J Adolesc Health. 2009;45(2):202-204.
4. Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69(7):587-596.
5. Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62(5):633-638.
6. Helmich I, Latini A, Sigwalt A, et al. Neurobiological alterations induced by exercise and their impact on depressive disorders [corrected]. Clin Pract Epidemiol Ment Health. 2010;6:115-125.
7. Mead GE, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database Syst Rev. 2009;(3):CD004366.
8. Tse J, Chow E, Sultana-Cordero R, et al. Motivation-based interventions for obesity in serious mental illness. Psychiatric Ann. 2011;41(10):473-477.
9. Rosenberg D, Depp CA, Vahia IV, et al. Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. Am J Geriatr Psychiatry. 2010;18(3):221-226.
10. Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287-304.
11. Nedeltcheva AV, Kilkus JM, Imperial J, et al. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89(1):126-133.
12. Isomaa B. A major health hazard: the metabolic syndrome. Life Sci. 2003;73(19):2395-2411.
13. Friedman JM. Leptin at 14 y of age: an ongoing story. Am J Clin Nutr. 2009;89(3):973S-979S.
14. Lu XY. The leptin hypothesis of depression: a potential link between mood disorders and obesity? Curr Opin Pharmacol. 2007;7(6):648-652.
15. Lawson EA, Miller KK, Blum JI, et al. Leptin levels are associated with decreased depressive symptoms in women across the weight spectrum, independent of body fat. Clin Endocrinol (Oxf). 2012;76(4):520-525.
16. Häfner S, Baumert J, Emeny RT, et al. Sleep disturbances and depressed mood: a harmful combination associated with increased leptin levels in women with normal weight. Biol Psychol. 2012;89(1):163-169.
17. Spiegel K, Leproult R, L’hermite-Balériaux M, et al. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89(11):5762-5771.
18. Grenard JL, Munjas BA, Adams JL, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med. 2011;26(10):1175-1182.
19. Gonzalez JS, Safren SA, Delahanty LM, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med. 2008;25(9):1102-1107.
20. Somerset SM, Graham L, Markwell K. Depression scores predict adherence in a dietary weight loss intervention trial. Clin Nutr. 2011;30(5):593-598.
21. Patten SB, Williams JV, Lavorato DH, et al. Major depression, antidepressant medication and the risk of obesity. Psychother Psychosom. 2009;78(3):182-186.
22. Nihalani N, Schwartz TL, Siddiqui UA, et al. Weight gain, obesity, and psychotropic prescribing. J Obes. 2011;2011:893629.
23. Serretti A, Mandelli L. Antidepressants and body weight: a comprehensive review and meta-analysis. J Clin Psychiatry. 2010;71(10):1259-1272.
24. Gabriel A. Lamotrigine adjunctive treatment in resistant unipolar depression: an open, descriptive study. Depress Anxiety. 2006;23(8):485-488.
25. Degenhardt EK, Jamal HH, Tormey S, et al. Early weight gain as a predictor of substantial weight gain with olanzapine/fluoxetine combination: an analysis of 2 adult studies in treatment-resistant depression. J Clin Psychopharmacol. 2011;31(3):337-340.
26. Faulconbridge LF, Wadden TA, Berkowitz RI, et al. Treatment of comorbid obesity and major depressive disorder: a prospective pilot study for their combined treatment. J Obes. 2011;2011:870385.
27. Schneider KL, Bodenlos JS, Ma Y, et al. Design and methods for a randomized clinical trial treating comorbid obesity and major depressive disorder. BMC Psychiatry. 2008;8:77.
28. Pagoto S, Bodenlos JS, Schneider KL, et al. Initial investigation of behavioral activation therapy for co-morbid major depressive disorder and obesity. Psychotherapy (Chic). 2008;45(3):410-415.
29. Shaw K, O’Rourke P, Del Mar C, et al. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005;(2):CD003818.
30. Thieszen CL, Merrill RM, Aldana SG, et al. The Coronary Health Improvement Project (CHIP) for lowering weight and improving psychosocial health. Psychol Rep. 2011;109(1):338-352.
31. Fabricatore AN, Wadden TA, Higginbotham AJ, et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes (Lond). 2011;35(11):1363-1376.
32. Simon GE, Rohde P, Ludman EJ, et al. Association between change in depression and change in weight among women enrolled in weight loss treatment. Gen Hosp Psychiatry. 2010;32(6):583-589.
33. Linde JA, Simon GE, Ludman EJ, et al. A randomized controlled trial of behavioral weight loss treatment versus combined weight loss/depression treatment among women with comorbid obesity and depression. Ann Behav Med. 2011;41(1):119-130.
Discuss this article at www.facebook.com/CurrentPsychiatry
Mrs. G is a 52-year-old mother and teacher with a 20-year history of recurrent depressive episodes for which she has been treated with various antidepressants, including sertraline, fluoxetine, and citalopram. For some of her depressive recurrences, she also received adjunctive second-generation antipsychotics (SGAs), including quetiapine and olanzapine.
She describes feelings of “being defeated,” hopelessness, and boredom and frustration with her teaching. It takes her approximately 30 minutes to go to sleep each night, but she wakes up after 2 to 3 hours, and the remainder of her night’s sleep is markedly disrupted. Because of her hopeless feelings, she has given up on dieting and going to the gym. When feeling down she has donuts and coffee. She has gained 45 lbs over the past 10 years and now weighs 175 lbs. In addition to her disrupted mood, she complains of frequent headaches and sore muscles.
Mrs. G’s psychiatrist refers her to her primary care physician for evaluation of her physical complaints and recommendations regarding her weight gain. Her waistline measures 90 cm and her body mass index (BMI) is 29.1 kg/m2; a BMI of ≥30 is considered obese. Her blood pressure is 145/85 mmHg. Laboratory work reveals a total cholesterol level of 235 mg/dL, low-density lipoprotein of 146 mg/dL, and fasting blood sugar, 135 mg/dL.
Mrs. G’s case illustrates many of the issues psychiatrists face when caring for overweight or obese patients with depression (OW/OB-D). Both conditions can be challenging to manage, and may be especially difficult to treat when they co-occur. When depression and obesity co-occur, their capacity to inflict psychological and physical harm likely is greater than either condition alone. Data point to a “2-way street” of mutually destructive effects of being overweight/obese on depression and vice versa.1
This article summarizes ways that depression and obesity aggravate each other, and highlights research that suggests depression and obesity are manifestations of inflammatory processes. It also suggests a stepwise approach to treating OW/OB-D patients.
Mutually destructive processes
Self-esteem and body image. Lowered self-esteem is a hallmark of depression. In popular culture, “you can’t be too rich or too thin,” and the pressure to be slim is great. Therefore, OW/OB-D patients have 2 reasons to feel a depleted sense of self-worth: their psychiatric illness and their weight. Observant clinicians will recognize these dual sources of self-deprecation and tailor treatment to address both.
Increasing numbers of celebrities, performers, and prominent politicians are overweight or obese. Increased social acceptance of OW/OB individuals in our culture may be legitimizing weight gain and obesity. When OW/OB-D patients justify their weight by pointing to overweight celebrities, clinicians can counter this argument with data on the hazards of obesity on health and well-being, such as premature death, coronary artery disease, diabetes, arthritis, and some forms of cancer.
OW/OB patients tend to interact with other OW/OB individuals. Christakis et al2 reported that adults with obese friends were more likely to become obese than individuals without obese friends. Valente et al3 found that overweight teens were twice as likely to have overweight friends as non-overweight teens. This power of social connectedness can be harnessed when treating OW/OB-D patients, where therapeutic groups can help patients address both depression and weight gain.
Inactivity. OW/OB-D patients with psychomotor retardation or reduced activity may gain weight because they consume more calories than their body requires. Depressed patients may say they “have no energy” to participate in a clinician-recommended exercise program or that “it won’t do any good anyway.”
These tendencies are best dealt with by incorporating an exercise program into the comprehensive plan for OW/OB-D patients from the start of treatment. Several studies suggest that in addition to helping manage weight, exercise may have antidepressant effects. In a large, well-controlled trial of patients with major depressive disorder (MDD), Blumenthal et al4 found that an exercise program was as effective as fluoxetine, 20 mg/d, and the antidepressant effects persisted at 10-month follow-up for patients who continued to exercise.5 In a review of studies of exercise in depressed patients, Helmich et al6 concluded that in most studies exercise was beneficial. However, Mead et al7 found that nearly all trials of exercise and depression had substantial design flaws. Based on the 3 well-designed studies they reviewed, Mead et al concluded that the efficacy of exercise was comparable to that of cognitive therapy.
Although the evidence on exercise for treating depression is inconclusive, an exercise program is essential for OW/OB-D patients because it can help manage weight and improve cardiovascular fitness. Motivation is a key ingredient of successful programs.8 Encourage patients to make exercise enjoyable, perhaps by using video games or other interactive computer-based programs.9
Sleep disturbances. Disrupted sleep— another hallmark of depression—appears to be a risk factor for weight gain.10 Although the basis for this relationship is still under investigation, one possibility is that some patients with insomnia get up to eat more often than those without sleep disturbances. Research has shown that when sleep is curtailed in a sleep laboratory, patients consume approximately 20% more calories from snacks (1,086 calories) than non-sleep-deprived patients (866 calories).11 Although this 220-calorie increase may seem small, it would amount to approximately 2 lbs of additional weight per month.
Appetite. Although weight loss is a cardinal sign of MDD, increased appetite and weight gain can be seen in many depressed patients who do not meet diagnostic criteria for MDD as well as those with seasonal affective disorder and metabolic syndrome, a condition characterized by insulin resistance, glucose intolerance, atherogenic dyslipidemia, visceral adiposity, hypercoagulation, chronic inflammation, oxidative stress, and hypertension.12
Emerging information about the neuroendocrinology of appetite regulation may lead to a better understanding of weight management in OW/OB-D patients. Leptin, a hormone released by adipose tissue, increases when fat stores are high, leading to reduced appetite and fat stores. Conversely, when fat stores are low, plasma leptin levels decrease, producing increased appetite and reduced energy expenditure.13
Researchers have suggested that leptin insufficiency and/or leptin resistance may contribute to vulnerability to depression, and leptin may have antidepressant effects.14 Lawson et al15 found that leptin levels were inversely associated with Hamilton Depression Rating Scale scores in normal-weight (BMI ≤25) women.
Leptin levels also are significantly associated with comorbid depressed mood and sleep disturbance.16 In healthy volunteers, shortening sleep duration to 4 hours produced an approximately 20% reduction in leptin release compared with normal sleep duration.17 Because of the relationship between sleep disorders and depression, leptin may act on sleep regulatory mechanisms, depressogenic pathways, or both. But studies of leptin’s role in obesity, depression, and sleep have not yet found a single role for leptin that ties all 3 conditions to this hormone’s known physiological functions.
Nonadherence. Compared with non-depressed patients, depressed patients are 76% more likely to not adhere to treatment.18 Patients may report that they are not interested in the treatment program or lack hope that it will be successful. Furthermore, OW/OB-D patients may consider exercise programs to be too strenuous and diet programs too depriving.19
OW/OB-D patients may require special care in monitoring adherence. The presence of depression in patients enrolled in weight loss programs may prompt the treatment staff to modify the usual protocol by including the patient in an active depression treatment module.20
Effects of pharmacologic agents
Many antidepressant agents are associated with weight gain.21Tables 1 and 2 summarize the effects antidepressants and adjunctive medications used to treat depression have on weight.22,23 SGAs such as clozapine and olanzapine, which frequently are used as augmenting agents in patients with treatment-resistant depression (TRD), are associated with weight gain.22 Lamotrigine also is an effective adjunctive medication for TRD and is not associated with significant weight gain.24
Bupropion has antidepressant and weight-loss effects and may be a suitable primary medication for OW/OB-D patients.
Early weight gain with olanzapine/fluoxetine combination may be a strong indicator of substantial weight gain with longer-term treatment. A weight gain of >2 kg (4.4 lbs) during the first 2 weeks of treatment is a strong predictor of weight gain of ≥10 kg (22 lbs) at 26 weeks.25
Antidepressants may be associated with an increased risk of obesity, and strategies to offset this risk may be useful in clinical practice, particularly patient education on the risks of weight gain and early introduction of a diet and exercise program.
Evidence suggests that depression and obesity are associated with alterations in immune activity (Box). This suggests that anti-inflammatory agents might have a role in treating depression by reducing the release of cytokines that may lead to depressive symptoms.
Table 1
Pharmacotherapy and weight gain: Antidepressants
| Agent | Effect on weight |
|---|---|
| SSRIs | |
| Paroxetine | Moderate gain |
| Fluoxetine | Early: weight loss Long-term: moderate gain |
| SNRIs | |
| Duloxetine | Minimal gain |
| Escitalopram | Moderate gain |
| Other agents | |
| Imipramine (TCA) | Moderate gain |
| Selegiline (MAOI) | Moderate gain |
| Trazodone (tetracyclic) | Moderate gain |
| Bupropion (atypical) | Moderate loss |
| MAOI: monoamine oxidase inhibitor; SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCA: tricyclic antidepressant Source: References 22,23 | |
Table 2
Pharmacotherapy and weight gain: Adjunctive agents
| Agent | Use in depression | Effect on weight |
|---|---|---|
| SGAs | ||
| Olanzapine | Psychotic depression | Large gain |
| Clozapine | Adjunct; psychotic depression | Large gain |
| Quetiapine | Primary; adjunct | Large gain |
| Aripiprazole | Adjunct | Small gain |
| Risperidone | Psychotic depression | Small gain |
| Ziprasidone | Psychotic depression | Small loss |
| Mood stabilizers | ||
| Divalproex | Treatment resistance, bipolar disorder | Moderate to large gain |
| Lamotrigine | Treatment resistance | Neutral |
| SGAs: second-generation antipsychotics Source: References 22,23 | ||
Research suggests that both depression and obesity are associated with immune dysregulation and inflammation.a-d Although the complexities of these interactions are beyond the scope of this article, having a model for understanding the role of inflammation in overweight or obese patients with depression (OW/OB-D) may be useful. Data supporting a role for immune dysregulation in OW/OB-D patients rests on the following findings:
Fat and muscle are endocrine organs: Fat is not just a storage organ for energy-rich lipids but also a rich source of cytokines, including monocyte chemotactic protein-1 (MCP-1), interleukin-2, and tumor necrosis factor-α (TNF-α). The increase in MCP-1 in fat tissue triggers a cascade of events that leads to chronic inflammation in adipose tissue. These substances can be released into circulation, stimulating inflammatory responses in other tissues. Data suggest that obesity’s effects on cardiovascular disease are mediated by these adipose-derived inflammatory hormones. There is a strong relationship between the volume of adipose tissue and the amount of pro-inflammatory hormones released; therefore, reducing weight reduces inflammatory burden on the body.
Pedersene pointed out that muscle also is an endocrine organ. Among the cytokines (or “myokines”) muscle produces are interleukin-6 (IL-6), interleukin-8, and brain-derived neurotrophic factor. During exercise, the amount of IL-6 released from muscles may increase by 100-fold. Although IL-6 usually is considered a pro-inflammatory regulator, it—or other muscle-derived myokines—may be responsible for some of exercise’s beneficial effects.e
If this hypothesis is correct, patients whose exercise includes resistance training—which increases muscle mass—are not just getting stronger or burning calories but may be facilitating release of hormones that could counteract obesity’s inflammatory effects.
Cytokine levels are elevated in depression and obesity: A substantial body of evidence shows that depressed patients have elevated circulating levels of inflammation markers. In particular, the proinflammatory cytokines IL-6 and interleukin-1β and the acute phase reactant C-reactive protein (CRP) are elevated in depressed patients.f Studies also show that blood levels of IL-6, TNF-α, and CRP are elevated in obese patients.g
Fat-derived cytokines alter metabolic pathways related to mood and inflammation: Among the many possible pathways linking cytokine actions and depression, the effects of TNF-α on serotonin metabolism have been studied extensively.h,i TNF-α activates brain indoleamine 2,3-dioxygenase, leading to rapid depletion of serotonin and exacerbation of depressive symptoms.j
Regarding physical problems, evidence suggests adipose-tissue-derived pro-inflammatory agents are involved in development of metabolic syndrome, a condition characterized by insulin resistance, glucose intolerance, atherogenic dyslipidemia, visceral adiposity, hypercoagulation, chronic inflammation, oxidative stress, and hypertension.k These conditions are strong risk factors for type II diabetes, coronary artery disease, hypertension, and stroke.
Anti-inflammatory agents for depression
Data suggest a model in which weight gain leads to an increase in pro-inflammatory cytokines. When released into the circulation, these cytokines produce a variety of deleterious effects, including blockade of serotonin synthesis in the brain that leads to depressive symptoms. Evidence suggests that anti-inflammatory agents might disrupt this process.
Celecoxib. The anti-inflammatory agent celecoxib acts by inhibiting cyclooxygenase-2, the rate-limiting enzyme in the synthesis of prostaglandin, a powerful inflammation mediator. Three double-blind, placebo-controlled trials have compared groups of:
- depressed patients receiving reboxetine with and without celecoxibl or fluoxetine, 40 mg/d, with and without celecoxibm
- bipolar disorder patients taking mood stabilizers or atypical antipsychotics with and without celecoxib, 400 mg/d.n
These studies suggest that celecoxib may accelerate improvement in depressive symptoms. Celecoxib’s potential for increased cardiovascular risk may limit its use.
Aspirin. Mendlewicz et alo conducted an open-label study in which 24 depressed patients who failed to respond to 4 weeks of antidepressant treatment received adjunctive acetylsalicylic acid, 160 mg/d, for another 4 weeks. They found that 52% of patients responded when aspirin was added to their regimen, and the improvement was seen during the first week of treatment.
References
- Shelton RC, Miller AH. Inflammation in depression: is adiposity a cause? Dialogues Clin Neurosci. 2011;13(1):41-53.
- Shelton RC, Miller AH. Eating ourselves to death (and despair): the contribution of adiposity and inflammation to depression. Prog Neurobiol. 2010;91(4):275-299.
- Soczynska JK, Kennedy SH, Woldeyohannes HO, et al. Mood disorders and obesity: understanding inflammation as a pathophysiological nexus. Neuromolecular Med. 2011;13(2):93-116.
- Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121(6):2111-2117.
- Pedersen BK. Muscles and their myokines. J Exp Biol. 2011;214(Pt 2):337-346.
- Maes M, Kubera M, Obuchowiczwa E, et al. Depression’s multiple comorbidities explained by (neuro)inflammatory and oxidative & nitrosative stress pathways. Neuro Endocrinol Lett. 2011;32(1):7-24.
- Khaodhiar L, Ling PR, Blackburn GL, et al. Serum levels of interleukin-6 and C-reactive protein correlate with body mass index across the broad range of obesity. JPEN J Parenter Enteral Nutr. 2004;28(6):410-415.
- Capuron L, Miller AH. Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol Ther. 2011;130(2):226-238.
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732-741.
- O’Connor JC, André C, Wang Y, et al. Interferon-gamma and tumor necrosis factor-alpha mediate the upregulation of indoleamine 2,3-dioxygenase and the induction of depressive-like behavior in mice in response to bacillus Calmette-Guerin. J Neurosci. 2009;29(13):4200-4209.
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356-359.
- Müller N, Schwarz MJ, Dehning S, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. 2006;11(7):680-684.
- Akhondzadeh S, Jafari S, Raisi F, et al. Clinical trial of adjunctive celecoxib treatment in patients with major depression: a double blind and placebo controlled trial. Depress Anxiety. 2009;26(7):607-611.
- Nery FG, Monkul ES, Hatch JP, et al. Celecoxib as an adjunct in the treatment of depressive or mixed episodes of bipolar disorder: a double-blind, randomized, placebo-controlled study. Hum Psychopharmacol. 2008;23(2):87-94.
- Mendlewicz J, Kriwin P, Oswald P, et al. Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int Clin Psychopharmacol. 2006;21(4):227-231.
Cognitive/behavioral approaches
Although large, well-designed studies of OW/OB-D patients are in the planning or pilot phases,26-28 a substantial database supports incorporating behavioral or cognitive-behavioral therapies when treating these patients.29 Patients in programs that combine behavioral approaches with diet and exercise achieve the greatest weight loss, and frequently show improved depression scores.30-32
In a randomized trial, 203 obese women with moderate to severe depression showed significant weight loss and decreased depression scores whether they were in a behavioral weight-loss program or one that combined behavioral weigh loss with cognitive-behavioral depression management.33 This study raises important questions: Did the behavioral weight-loss program effectively treat depression? Did patients’ depressive symptoms improve because of their improved sense of well-being as they lost weight? Did a putative reduction in cytokine production by fat cells improve their mood?
Treatment implications
Mrs. G has TRD, a BMI that borders on obesity, sleep problems, and lab values that suggest she may have metabolic syndrome. To best manage patients such as Mrs. G, consider the following steps:
- Select an antidepressant that is unlikely to cause further weight gain, such as bupropion, duloxetine, or fluoxetine.
- If necessary, add an augmenting agent that is not associated with weight gain, such as bupropion, aripiprazole, or lamotrigine.
- Verify that your patient is getting adequate sleep. Begin by reviewing the principles of sleep hygiene and, if necessary, prescribe a sedative or hypnotic medication.
- Although controlled clinical trials are lacking, consider including an anti-inflammatory agent such as aspirin to the pharmacologic armamentarium.
- Institute an exercise and diet program at the beginning of treatment. Exercise can begin with 20 to 30 minutes a day of walking. Tell patients that exercising in groups is a good way to address nonadherence and social isolation and reinforce positive lifestyle changes. Recommend that patients combine aerobic exercise to burn calories with resistance training to build muscle. Suggest that patients try to make exercising fun using video games or interactive computer-based programs.
- Encourage your patient to keep a journal to record his or her weight, amount and type of exercise, medication taken, and dietary intake. Review this information at every session to reinforce the importance of this integrated exercise and diet program.
Related Resources
- Markowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clinical Psychology: Science and Practice. 2008:15(1):1-20.
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011;111(1):92-102.
Drug Brand Names
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Zyban
- Celecoxib • Celebrex
- Citalopram • Celexa
- Clozapine • Clozaril
- Divalproex • Depakote
- Duloxetine • Cymbalta
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Selegiline • Emsam
- Sertraline • Zoloft
- Trazodone • Desyrel, Oleptro
- Ziprasidone • Geodon
Disclosure
Dr. Crayton reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Mrs. G is a 52-year-old mother and teacher with a 20-year history of recurrent depressive episodes for which she has been treated with various antidepressants, including sertraline, fluoxetine, and citalopram. For some of her depressive recurrences, she also received adjunctive second-generation antipsychotics (SGAs), including quetiapine and olanzapine.
She describes feelings of “being defeated,” hopelessness, and boredom and frustration with her teaching. It takes her approximately 30 minutes to go to sleep each night, but she wakes up after 2 to 3 hours, and the remainder of her night’s sleep is markedly disrupted. Because of her hopeless feelings, she has given up on dieting and going to the gym. When feeling down she has donuts and coffee. She has gained 45 lbs over the past 10 years and now weighs 175 lbs. In addition to her disrupted mood, she complains of frequent headaches and sore muscles.
Mrs. G’s psychiatrist refers her to her primary care physician for evaluation of her physical complaints and recommendations regarding her weight gain. Her waistline measures 90 cm and her body mass index (BMI) is 29.1 kg/m2; a BMI of ≥30 is considered obese. Her blood pressure is 145/85 mmHg. Laboratory work reveals a total cholesterol level of 235 mg/dL, low-density lipoprotein of 146 mg/dL, and fasting blood sugar, 135 mg/dL.
Mrs. G’s case illustrates many of the issues psychiatrists face when caring for overweight or obese patients with depression (OW/OB-D). Both conditions can be challenging to manage, and may be especially difficult to treat when they co-occur. When depression and obesity co-occur, their capacity to inflict psychological and physical harm likely is greater than either condition alone. Data point to a “2-way street” of mutually destructive effects of being overweight/obese on depression and vice versa.1
This article summarizes ways that depression and obesity aggravate each other, and highlights research that suggests depression and obesity are manifestations of inflammatory processes. It also suggests a stepwise approach to treating OW/OB-D patients.
Mutually destructive processes
Self-esteem and body image. Lowered self-esteem is a hallmark of depression. In popular culture, “you can’t be too rich or too thin,” and the pressure to be slim is great. Therefore, OW/OB-D patients have 2 reasons to feel a depleted sense of self-worth: their psychiatric illness and their weight. Observant clinicians will recognize these dual sources of self-deprecation and tailor treatment to address both.
Increasing numbers of celebrities, performers, and prominent politicians are overweight or obese. Increased social acceptance of OW/OB individuals in our culture may be legitimizing weight gain and obesity. When OW/OB-D patients justify their weight by pointing to overweight celebrities, clinicians can counter this argument with data on the hazards of obesity on health and well-being, such as premature death, coronary artery disease, diabetes, arthritis, and some forms of cancer.
OW/OB patients tend to interact with other OW/OB individuals. Christakis et al2 reported that adults with obese friends were more likely to become obese than individuals without obese friends. Valente et al3 found that overweight teens were twice as likely to have overweight friends as non-overweight teens. This power of social connectedness can be harnessed when treating OW/OB-D patients, where therapeutic groups can help patients address both depression and weight gain.
Inactivity. OW/OB-D patients with psychomotor retardation or reduced activity may gain weight because they consume more calories than their body requires. Depressed patients may say they “have no energy” to participate in a clinician-recommended exercise program or that “it won’t do any good anyway.”
These tendencies are best dealt with by incorporating an exercise program into the comprehensive plan for OW/OB-D patients from the start of treatment. Several studies suggest that in addition to helping manage weight, exercise may have antidepressant effects. In a large, well-controlled trial of patients with major depressive disorder (MDD), Blumenthal et al4 found that an exercise program was as effective as fluoxetine, 20 mg/d, and the antidepressant effects persisted at 10-month follow-up for patients who continued to exercise.5 In a review of studies of exercise in depressed patients, Helmich et al6 concluded that in most studies exercise was beneficial. However, Mead et al7 found that nearly all trials of exercise and depression had substantial design flaws. Based on the 3 well-designed studies they reviewed, Mead et al concluded that the efficacy of exercise was comparable to that of cognitive therapy.
Although the evidence on exercise for treating depression is inconclusive, an exercise program is essential for OW/OB-D patients because it can help manage weight and improve cardiovascular fitness. Motivation is a key ingredient of successful programs.8 Encourage patients to make exercise enjoyable, perhaps by using video games or other interactive computer-based programs.9
Sleep disturbances. Disrupted sleep— another hallmark of depression—appears to be a risk factor for weight gain.10 Although the basis for this relationship is still under investigation, one possibility is that some patients with insomnia get up to eat more often than those without sleep disturbances. Research has shown that when sleep is curtailed in a sleep laboratory, patients consume approximately 20% more calories from snacks (1,086 calories) than non-sleep-deprived patients (866 calories).11 Although this 220-calorie increase may seem small, it would amount to approximately 2 lbs of additional weight per month.
Appetite. Although weight loss is a cardinal sign of MDD, increased appetite and weight gain can be seen in many depressed patients who do not meet diagnostic criteria for MDD as well as those with seasonal affective disorder and metabolic syndrome, a condition characterized by insulin resistance, glucose intolerance, atherogenic dyslipidemia, visceral adiposity, hypercoagulation, chronic inflammation, oxidative stress, and hypertension.12
Emerging information about the neuroendocrinology of appetite regulation may lead to a better understanding of weight management in OW/OB-D patients. Leptin, a hormone released by adipose tissue, increases when fat stores are high, leading to reduced appetite and fat stores. Conversely, when fat stores are low, plasma leptin levels decrease, producing increased appetite and reduced energy expenditure.13
Researchers have suggested that leptin insufficiency and/or leptin resistance may contribute to vulnerability to depression, and leptin may have antidepressant effects.14 Lawson et al15 found that leptin levels were inversely associated with Hamilton Depression Rating Scale scores in normal-weight (BMI ≤25) women.
Leptin levels also are significantly associated with comorbid depressed mood and sleep disturbance.16 In healthy volunteers, shortening sleep duration to 4 hours produced an approximately 20% reduction in leptin release compared with normal sleep duration.17 Because of the relationship between sleep disorders and depression, leptin may act on sleep regulatory mechanisms, depressogenic pathways, or both. But studies of leptin’s role in obesity, depression, and sleep have not yet found a single role for leptin that ties all 3 conditions to this hormone’s known physiological functions.
Nonadherence. Compared with non-depressed patients, depressed patients are 76% more likely to not adhere to treatment.18 Patients may report that they are not interested in the treatment program or lack hope that it will be successful. Furthermore, OW/OB-D patients may consider exercise programs to be too strenuous and diet programs too depriving.19
OW/OB-D patients may require special care in monitoring adherence. The presence of depression in patients enrolled in weight loss programs may prompt the treatment staff to modify the usual protocol by including the patient in an active depression treatment module.20
Effects of pharmacologic agents
Many antidepressant agents are associated with weight gain.21Tables 1 and 2 summarize the effects antidepressants and adjunctive medications used to treat depression have on weight.22,23 SGAs such as clozapine and olanzapine, which frequently are used as augmenting agents in patients with treatment-resistant depression (TRD), are associated with weight gain.22 Lamotrigine also is an effective adjunctive medication for TRD and is not associated with significant weight gain.24
Bupropion has antidepressant and weight-loss effects and may be a suitable primary medication for OW/OB-D patients.
Early weight gain with olanzapine/fluoxetine combination may be a strong indicator of substantial weight gain with longer-term treatment. A weight gain of >2 kg (4.4 lbs) during the first 2 weeks of treatment is a strong predictor of weight gain of ≥10 kg (22 lbs) at 26 weeks.25
Antidepressants may be associated with an increased risk of obesity, and strategies to offset this risk may be useful in clinical practice, particularly patient education on the risks of weight gain and early introduction of a diet and exercise program.
Evidence suggests that depression and obesity are associated with alterations in immune activity (Box). This suggests that anti-inflammatory agents might have a role in treating depression by reducing the release of cytokines that may lead to depressive symptoms.
Table 1
Pharmacotherapy and weight gain: Antidepressants
| Agent | Effect on weight |
|---|---|
| SSRIs | |
| Paroxetine | Moderate gain |
| Fluoxetine | Early: weight loss Long-term: moderate gain |
| SNRIs | |
| Duloxetine | Minimal gain |
| Escitalopram | Moderate gain |
| Other agents | |
| Imipramine (TCA) | Moderate gain |
| Selegiline (MAOI) | Moderate gain |
| Trazodone (tetracyclic) | Moderate gain |
| Bupropion (atypical) | Moderate loss |
| MAOI: monoamine oxidase inhibitor; SNRIs: serotonin-norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCA: tricyclic antidepressant Source: References 22,23 | |
Table 2
Pharmacotherapy and weight gain: Adjunctive agents
| Agent | Use in depression | Effect on weight |
|---|---|---|
| SGAs | ||
| Olanzapine | Psychotic depression | Large gain |
| Clozapine | Adjunct; psychotic depression | Large gain |
| Quetiapine | Primary; adjunct | Large gain |
| Aripiprazole | Adjunct | Small gain |
| Risperidone | Psychotic depression | Small gain |
| Ziprasidone | Psychotic depression | Small loss |
| Mood stabilizers | ||
| Divalproex | Treatment resistance, bipolar disorder | Moderate to large gain |
| Lamotrigine | Treatment resistance | Neutral |
| SGAs: second-generation antipsychotics Source: References 22,23 | ||
Research suggests that both depression and obesity are associated with immune dysregulation and inflammation.a-d Although the complexities of these interactions are beyond the scope of this article, having a model for understanding the role of inflammation in overweight or obese patients with depression (OW/OB-D) may be useful. Data supporting a role for immune dysregulation in OW/OB-D patients rests on the following findings:
Fat and muscle are endocrine organs: Fat is not just a storage organ for energy-rich lipids but also a rich source of cytokines, including monocyte chemotactic protein-1 (MCP-1), interleukin-2, and tumor necrosis factor-α (TNF-α). The increase in MCP-1 in fat tissue triggers a cascade of events that leads to chronic inflammation in adipose tissue. These substances can be released into circulation, stimulating inflammatory responses in other tissues. Data suggest that obesity’s effects on cardiovascular disease are mediated by these adipose-derived inflammatory hormones. There is a strong relationship between the volume of adipose tissue and the amount of pro-inflammatory hormones released; therefore, reducing weight reduces inflammatory burden on the body.
Pedersene pointed out that muscle also is an endocrine organ. Among the cytokines (or “myokines”) muscle produces are interleukin-6 (IL-6), interleukin-8, and brain-derived neurotrophic factor. During exercise, the amount of IL-6 released from muscles may increase by 100-fold. Although IL-6 usually is considered a pro-inflammatory regulator, it—or other muscle-derived myokines—may be responsible for some of exercise’s beneficial effects.e
If this hypothesis is correct, patients whose exercise includes resistance training—which increases muscle mass—are not just getting stronger or burning calories but may be facilitating release of hormones that could counteract obesity’s inflammatory effects.
Cytokine levels are elevated in depression and obesity: A substantial body of evidence shows that depressed patients have elevated circulating levels of inflammation markers. In particular, the proinflammatory cytokines IL-6 and interleukin-1β and the acute phase reactant C-reactive protein (CRP) are elevated in depressed patients.f Studies also show that blood levels of IL-6, TNF-α, and CRP are elevated in obese patients.g
Fat-derived cytokines alter metabolic pathways related to mood and inflammation: Among the many possible pathways linking cytokine actions and depression, the effects of TNF-α on serotonin metabolism have been studied extensively.h,i TNF-α activates brain indoleamine 2,3-dioxygenase, leading to rapid depletion of serotonin and exacerbation of depressive symptoms.j
Regarding physical problems, evidence suggests adipose-tissue-derived pro-inflammatory agents are involved in development of metabolic syndrome, a condition characterized by insulin resistance, glucose intolerance, atherogenic dyslipidemia, visceral adiposity, hypercoagulation, chronic inflammation, oxidative stress, and hypertension.k These conditions are strong risk factors for type II diabetes, coronary artery disease, hypertension, and stroke.
Anti-inflammatory agents for depression
Data suggest a model in which weight gain leads to an increase in pro-inflammatory cytokines. When released into the circulation, these cytokines produce a variety of deleterious effects, including blockade of serotonin synthesis in the brain that leads to depressive symptoms. Evidence suggests that anti-inflammatory agents might disrupt this process.
Celecoxib. The anti-inflammatory agent celecoxib acts by inhibiting cyclooxygenase-2, the rate-limiting enzyme in the synthesis of prostaglandin, a powerful inflammation mediator. Three double-blind, placebo-controlled trials have compared groups of:
- depressed patients receiving reboxetine with and without celecoxibl or fluoxetine, 40 mg/d, with and without celecoxibm
- bipolar disorder patients taking mood stabilizers or atypical antipsychotics with and without celecoxib, 400 mg/d.n
These studies suggest that celecoxib may accelerate improvement in depressive symptoms. Celecoxib’s potential for increased cardiovascular risk may limit its use.
Aspirin. Mendlewicz et alo conducted an open-label study in which 24 depressed patients who failed to respond to 4 weeks of antidepressant treatment received adjunctive acetylsalicylic acid, 160 mg/d, for another 4 weeks. They found that 52% of patients responded when aspirin was added to their regimen, and the improvement was seen during the first week of treatment.
References
- Shelton RC, Miller AH. Inflammation in depression: is adiposity a cause? Dialogues Clin Neurosci. 2011;13(1):41-53.
- Shelton RC, Miller AH. Eating ourselves to death (and despair): the contribution of adiposity and inflammation to depression. Prog Neurobiol. 2010;91(4):275-299.
- Soczynska JK, Kennedy SH, Woldeyohannes HO, et al. Mood disorders and obesity: understanding inflammation as a pathophysiological nexus. Neuromolecular Med. 2011;13(2):93-116.
- Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011;121(6):2111-2117.
- Pedersen BK. Muscles and their myokines. J Exp Biol. 2011;214(Pt 2):337-346.
- Maes M, Kubera M, Obuchowiczwa E, et al. Depression’s multiple comorbidities explained by (neuro)inflammatory and oxidative & nitrosative stress pathways. Neuro Endocrinol Lett. 2011;32(1):7-24.
- Khaodhiar L, Ling PR, Blackburn GL, et al. Serum levels of interleukin-6 and C-reactive protein correlate with body mass index across the broad range of obesity. JPEN J Parenter Enteral Nutr. 2004;28(6):410-415.
- Capuron L, Miller AH. Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol Ther. 2011;130(2):226-238.
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65(9):732-741.
- O’Connor JC, André C, Wang Y, et al. Interferon-gamma and tumor necrosis factor-alpha mediate the upregulation of indoleamine 2,3-dioxygenase and the induction of depressive-like behavior in mice in response to bacillus Calmette-Guerin. J Neurosci. 2009;29(13):4200-4209.
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356-359.
- Müller N, Schwarz MJ, Dehning S, et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol Psychiatry. 2006;11(7):680-684.
- Akhondzadeh S, Jafari S, Raisi F, et al. Clinical trial of adjunctive celecoxib treatment in patients with major depression: a double blind and placebo controlled trial. Depress Anxiety. 2009;26(7):607-611.
- Nery FG, Monkul ES, Hatch JP, et al. Celecoxib as an adjunct in the treatment of depressive or mixed episodes of bipolar disorder: a double-blind, randomized, placebo-controlled study. Hum Psychopharmacol. 2008;23(2):87-94.
- Mendlewicz J, Kriwin P, Oswald P, et al. Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int Clin Psychopharmacol. 2006;21(4):227-231.
Cognitive/behavioral approaches
Although large, well-designed studies of OW/OB-D patients are in the planning or pilot phases,26-28 a substantial database supports incorporating behavioral or cognitive-behavioral therapies when treating these patients.29 Patients in programs that combine behavioral approaches with diet and exercise achieve the greatest weight loss, and frequently show improved depression scores.30-32
In a randomized trial, 203 obese women with moderate to severe depression showed significant weight loss and decreased depression scores whether they were in a behavioral weight-loss program or one that combined behavioral weigh loss with cognitive-behavioral depression management.33 This study raises important questions: Did the behavioral weight-loss program effectively treat depression? Did patients’ depressive symptoms improve because of their improved sense of well-being as they lost weight? Did a putative reduction in cytokine production by fat cells improve their mood?
Treatment implications
Mrs. G has TRD, a BMI that borders on obesity, sleep problems, and lab values that suggest she may have metabolic syndrome. To best manage patients such as Mrs. G, consider the following steps:
- Select an antidepressant that is unlikely to cause further weight gain, such as bupropion, duloxetine, or fluoxetine.
- If necessary, add an augmenting agent that is not associated with weight gain, such as bupropion, aripiprazole, or lamotrigine.
- Verify that your patient is getting adequate sleep. Begin by reviewing the principles of sleep hygiene and, if necessary, prescribe a sedative or hypnotic medication.
- Although controlled clinical trials are lacking, consider including an anti-inflammatory agent such as aspirin to the pharmacologic armamentarium.
- Institute an exercise and diet program at the beginning of treatment. Exercise can begin with 20 to 30 minutes a day of walking. Tell patients that exercising in groups is a good way to address nonadherence and social isolation and reinforce positive lifestyle changes. Recommend that patients combine aerobic exercise to burn calories with resistance training to build muscle. Suggest that patients try to make exercising fun using video games or interactive computer-based programs.
- Encourage your patient to keep a journal to record his or her weight, amount and type of exercise, medication taken, and dietary intake. Review this information at every session to reinforce the importance of this integrated exercise and diet program.
Related Resources
- Markowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clinical Psychology: Science and Practice. 2008:15(1):1-20.
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011;111(1):92-102.
Drug Brand Names
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Zyban
- Celecoxib • Celebrex
- Citalopram • Celexa
- Clozapine • Clozaril
- Divalproex • Depakote
- Duloxetine • Cymbalta
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Imipramine • Tofranil
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Selegiline • Emsam
- Sertraline • Zoloft
- Trazodone • Desyrel, Oleptro
- Ziprasidone • Geodon
Disclosure
Dr. Crayton reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220-229.
2. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370-379.
3. Valente TW, Fujimoto K, Chou CP, et al. Adolescent affiliations and adiposity: a social network analysis of friendships and obesity. J Adolesc Health. 2009;45(2):202-204.
4. Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69(7):587-596.
5. Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62(5):633-638.
6. Helmich I, Latini A, Sigwalt A, et al. Neurobiological alterations induced by exercise and their impact on depressive disorders [corrected]. Clin Pract Epidemiol Ment Health. 2010;6:115-125.
7. Mead GE, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database Syst Rev. 2009;(3):CD004366.
8. Tse J, Chow E, Sultana-Cordero R, et al. Motivation-based interventions for obesity in serious mental illness. Psychiatric Ann. 2011;41(10):473-477.
9. Rosenberg D, Depp CA, Vahia IV, et al. Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. Am J Geriatr Psychiatry. 2010;18(3):221-226.
10. Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287-304.
11. Nedeltcheva AV, Kilkus JM, Imperial J, et al. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89(1):126-133.
12. Isomaa B. A major health hazard: the metabolic syndrome. Life Sci. 2003;73(19):2395-2411.
13. Friedman JM. Leptin at 14 y of age: an ongoing story. Am J Clin Nutr. 2009;89(3):973S-979S.
14. Lu XY. The leptin hypothesis of depression: a potential link between mood disorders and obesity? Curr Opin Pharmacol. 2007;7(6):648-652.
15. Lawson EA, Miller KK, Blum JI, et al. Leptin levels are associated with decreased depressive symptoms in women across the weight spectrum, independent of body fat. Clin Endocrinol (Oxf). 2012;76(4):520-525.
16. Häfner S, Baumert J, Emeny RT, et al. Sleep disturbances and depressed mood: a harmful combination associated with increased leptin levels in women with normal weight. Biol Psychol. 2012;89(1):163-169.
17. Spiegel K, Leproult R, L’hermite-Balériaux M, et al. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89(11):5762-5771.
18. Grenard JL, Munjas BA, Adams JL, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med. 2011;26(10):1175-1182.
19. Gonzalez JS, Safren SA, Delahanty LM, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med. 2008;25(9):1102-1107.
20. Somerset SM, Graham L, Markwell K. Depression scores predict adherence in a dietary weight loss intervention trial. Clin Nutr. 2011;30(5):593-598.
21. Patten SB, Williams JV, Lavorato DH, et al. Major depression, antidepressant medication and the risk of obesity. Psychother Psychosom. 2009;78(3):182-186.
22. Nihalani N, Schwartz TL, Siddiqui UA, et al. Weight gain, obesity, and psychotropic prescribing. J Obes. 2011;2011:893629.
23. Serretti A, Mandelli L. Antidepressants and body weight: a comprehensive review and meta-analysis. J Clin Psychiatry. 2010;71(10):1259-1272.
24. Gabriel A. Lamotrigine adjunctive treatment in resistant unipolar depression: an open, descriptive study. Depress Anxiety. 2006;23(8):485-488.
25. Degenhardt EK, Jamal HH, Tormey S, et al. Early weight gain as a predictor of substantial weight gain with olanzapine/fluoxetine combination: an analysis of 2 adult studies in treatment-resistant depression. J Clin Psychopharmacol. 2011;31(3):337-340.
26. Faulconbridge LF, Wadden TA, Berkowitz RI, et al. Treatment of comorbid obesity and major depressive disorder: a prospective pilot study for their combined treatment. J Obes. 2011;2011:870385.
27. Schneider KL, Bodenlos JS, Ma Y, et al. Design and methods for a randomized clinical trial treating comorbid obesity and major depressive disorder. BMC Psychiatry. 2008;8:77.
28. Pagoto S, Bodenlos JS, Schneider KL, et al. Initial investigation of behavioral activation therapy for co-morbid major depressive disorder and obesity. Psychotherapy (Chic). 2008;45(3):410-415.
29. Shaw K, O’Rourke P, Del Mar C, et al. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005;(2):CD003818.
30. Thieszen CL, Merrill RM, Aldana SG, et al. The Coronary Health Improvement Project (CHIP) for lowering weight and improving psychosocial health. Psychol Rep. 2011;109(1):338-352.
31. Fabricatore AN, Wadden TA, Higginbotham AJ, et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes (Lond). 2011;35(11):1363-1376.
32. Simon GE, Rohde P, Ludman EJ, et al. Association between change in depression and change in weight among women enrolled in weight loss treatment. Gen Hosp Psychiatry. 2010;32(6):583-589.
33. Linde JA, Simon GE, Ludman EJ, et al. A randomized controlled trial of behavioral weight loss treatment versus combined weight loss/depression treatment among women with comorbid obesity and depression. Ann Behav Med. 2011;41(1):119-130.
1. Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220-229.
2. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370-379.
3. Valente TW, Fujimoto K, Chou CP, et al. Adolescent affiliations and adiposity: a social network analysis of friendships and obesity. J Adolesc Health. 2009;45(2):202-204.
4. Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69(7):587-596.
5. Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62(5):633-638.
6. Helmich I, Latini A, Sigwalt A, et al. Neurobiological alterations induced by exercise and their impact on depressive disorders [corrected]. Clin Pract Epidemiol Ment Health. 2010;6:115-125.
7. Mead GE, Morley W, Campbell P, et al. Exercise for depression. Cochrane Database Syst Rev. 2009;(3):CD004366.
8. Tse J, Chow E, Sultana-Cordero R, et al. Motivation-based interventions for obesity in serious mental illness. Psychiatric Ann. 2011;41(10):473-477.
9. Rosenberg D, Depp CA, Vahia IV, et al. Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. Am J Geriatr Psychiatry. 2010;18(3):221-226.
10. Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287-304.
11. Nedeltcheva AV, Kilkus JM, Imperial J, et al. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89(1):126-133.
12. Isomaa B. A major health hazard: the metabolic syndrome. Life Sci. 2003;73(19):2395-2411.
13. Friedman JM. Leptin at 14 y of age: an ongoing story. Am J Clin Nutr. 2009;89(3):973S-979S.
14. Lu XY. The leptin hypothesis of depression: a potential link between mood disorders and obesity? Curr Opin Pharmacol. 2007;7(6):648-652.
15. Lawson EA, Miller KK, Blum JI, et al. Leptin levels are associated with decreased depressive symptoms in women across the weight spectrum, independent of body fat. Clin Endocrinol (Oxf). 2012;76(4):520-525.
16. Häfner S, Baumert J, Emeny RT, et al. Sleep disturbances and depressed mood: a harmful combination associated with increased leptin levels in women with normal weight. Biol Psychol. 2012;89(1):163-169.
17. Spiegel K, Leproult R, L’hermite-Balériaux M, et al. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89(11):5762-5771.
18. Grenard JL, Munjas BA, Adams JL, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med. 2011;26(10):1175-1182.
19. Gonzalez JS, Safren SA, Delahanty LM, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med. 2008;25(9):1102-1107.
20. Somerset SM, Graham L, Markwell K. Depression scores predict adherence in a dietary weight loss intervention trial. Clin Nutr. 2011;30(5):593-598.
21. Patten SB, Williams JV, Lavorato DH, et al. Major depression, antidepressant medication and the risk of obesity. Psychother Psychosom. 2009;78(3):182-186.
22. Nihalani N, Schwartz TL, Siddiqui UA, et al. Weight gain, obesity, and psychotropic prescribing. J Obes. 2011;2011:893629.
23. Serretti A, Mandelli L. Antidepressants and body weight: a comprehensive review and meta-analysis. J Clin Psychiatry. 2010;71(10):1259-1272.
24. Gabriel A. Lamotrigine adjunctive treatment in resistant unipolar depression: an open, descriptive study. Depress Anxiety. 2006;23(8):485-488.
25. Degenhardt EK, Jamal HH, Tormey S, et al. Early weight gain as a predictor of substantial weight gain with olanzapine/fluoxetine combination: an analysis of 2 adult studies in treatment-resistant depression. J Clin Psychopharmacol. 2011;31(3):337-340.
26. Faulconbridge LF, Wadden TA, Berkowitz RI, et al. Treatment of comorbid obesity and major depressive disorder: a prospective pilot study for their combined treatment. J Obes. 2011;2011:870385.
27. Schneider KL, Bodenlos JS, Ma Y, et al. Design and methods for a randomized clinical trial treating comorbid obesity and major depressive disorder. BMC Psychiatry. 2008;8:77.
28. Pagoto S, Bodenlos JS, Schneider KL, et al. Initial investigation of behavioral activation therapy for co-morbid major depressive disorder and obesity. Psychotherapy (Chic). 2008;45(3):410-415.
29. Shaw K, O’Rourke P, Del Mar C, et al. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005;(2):CD003818.
30. Thieszen CL, Merrill RM, Aldana SG, et al. The Coronary Health Improvement Project (CHIP) for lowering weight and improving psychosocial health. Psychol Rep. 2011;109(1):338-352.
31. Fabricatore AN, Wadden TA, Higginbotham AJ, et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes (Lond). 2011;35(11):1363-1376.
32. Simon GE, Rohde P, Ludman EJ, et al. Association between change in depression and change in weight among women enrolled in weight loss treatment. Gen Hosp Psychiatry. 2010;32(6):583-589.
33. Linde JA, Simon GE, Ludman EJ, et al. A randomized controlled trial of behavioral weight loss treatment versus combined weight loss/depression treatment among women with comorbid obesity and depression. Ann Behav Med. 2011;41(1):119-130.
New mother dies from PE; 7 cases of bowel injury … and more

A 39-YEAR-OLD WOMAN’S SECOND CHILD WAS BORN by cesarean delivery. The mother died the next day from a pulmonary embolism.
ESTATE’S CLAIM Physicians and nurses at the hospital were negligent in failing to recognize the mother’s risk factors for pulmonary embolism, including obesity, being over age 35, and hypertension. They failed to ensure that compression boots were in place and working prior to delivery. Although orders had been given for the woman to walk within 8 hours of delivery, she did not get out of bed and walk for 24 hours after delivery.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $3.5 million Illinois settlement was reached.
Woman told “Biopsy isn’t urgent”
TWO MONTHS AFTER HER INITIAL VISIT, a 58-year-old woman returned to the gynecologist with vaginal bleeding. In March 2004, ultrasonography (US) showed slight thickening of the endometrial lining and a “pin dot” described as being a prepolyp. Vaginal bleeding was determined to be due to thinning of the vaginal wall with menopause.
The patient reported daily vaginal bleeding when she saw the gynecologist in January 2005. A new, large, rounded, solid mass within the endometrial cavity consistent with a large endometrial polyp was seen on US. The radiologist recommended hysteroscopic biopsy with excision, but the gynecologist told the patient it was not urgent.
In March 2005, hysteroscopy confirmed carcinosarcoma of the uterus. The patient underwent a hysterectomy followed by pelvic radiation and brachytherapy.
Eight months later, metastasis was found in the lungs; she died in October 2006.
ESTATE’S CLAIM The gynecologist failed to react when the patient first reported vaginal bleeding. An earlier diagnosis could have prevented her death.
PHYSICIAN’S DEFENSE The case was settled before trial.
VERDICT An $820,000 Massachusetts settlement was reached.
US report misses fetal abnormalities
A PREGNANT WOMAN UNDERWENT US. The preliminary report indicated echogenic cardiac focus and unilateral pyelectasis. Twenty-five days later, the mother underwent a level II US. A radiologist wrote that fetal anatomy was normal in both reports. The mother had two additional sonograms, with no reported abnormality.
The baby was born with aplasia and hypoplasia with both arms absent below a short humerus, an absent left leg, and a shortened right leg with a remnant foot and three small toes.
PARENTS’ CLAIM The radiologist’s US reports failed to accurately describe the fetal anatomy, depriving the parents of the chance to terminate the pregnancy.
DEFENDANTS’ DEFENSE Proper treatment was given.
VERDICT A $4.5 million Florida verdict was returned. Fault was assigned to the radiologist (85%) and the level II technologist (15%).
Forceps delivery injures mother’s pelvic floor
DURING A TRIAL OF LABOR, a 34-year-old woman experienced deep transverse arrest and lack of progress due to pelvic restriction. The ObGyn proceeded to deliver the baby vaginally using forceps, which caused pelvic floor injuries to the mother.
Several months later, she underwent corrective repair surgery for pelvic floor prolapse. She has continuing vaginal and rectal pain and dysfunction.
PATIENT’S CLAIM A cesarean delivery should have been performed as soon as pelvic restriction was found. The injuries reduce the woman’s chances of having another child.
PHYSICIAN’S DEFENSE A trial of labor was proper. The patient’s continuing fertility problems are related to chronic yeast infections and prescription birth control.
VERDICT A $1,716,469 Illinois verdict was returned, which included $484,000 to the patient’s husband for loss of consortium.
7 CASES OF INJURED BOWEL
1 Woman dies from bowel injury
DURING A SLING PROCEDURE for vaginal prolapse, a 50-year-old woman required a transfusion. The next day, she was nauseated and constipated. A day later, she went to the ED with shortness of breath and chest and abdominal pain. Her symptoms persisted for 8 days before an injury to her transverse colon was found during exploratory surgery. She suffered massive organ failure caused by sepsis and died 3 weeks after the initial surgery.
ESTATE’S CLAIM The gynecologist should have investigated why she needed a transfusion during surgery. He should have reacted earlier to her postsurgical complaints.
PHYSICIAN’S DEFENSE Bowel injury is a known risk of the procedure. The patient suffered multiple strokes after being readmitted to the hospital.
VERDICT A $2.4 million South Carolina verdict was returned.
2 Colostomy, coma after hysterectomy
DUE TO FIBROID TUMORS and pelvic pain, a 39-year-old woman’s ObGyn suggested laparoscopic-assisted vaginal hysterectomy. A third-year resident performed most of the procedure. The ObGyn’s associate covered postsurgical care.
When the patient reported increasing pain and rectal bleeding, an exploratory laparotomy was performed 3 days after surgery. Bowel and ureter injuries were repaired and a permanent colostomy was created. The patient developed septic shock with multiple organ failure, and was placed in a chemically induced coma for 3 weeks, after which she had to relearn to walk, talk, and care for herself.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery. He failed to obtain consent for the resident’s participation. The associate failed to respond to her declining postoperative condition in a timely manner.
DEFENDANTS’ DEFENSE Surgery was properly performed and postoperative care was appropriate. The bowel injury was a thermal or pressure necrosis that occurred 3 days after surgery. Two different consent forms signed by the patient included notification that a resident might assist; the resident was introduced to the patient prior to surgery. The patient’s injury claims were exaggerated; her future medical bills would be limited to colostomy supplies.
VERDICT A $1,926,069 Texas verdict was returned.
3 Were physicians qualified on robot?
A 48-YEAR-OLD WOMAN UNDERWENT robotic-assisted total hysterectomy and oophorectomy for uterine fibroids and cysts. During surgery, the physicians realized that the sigmoid colon had been perforated. A general surgeon repaired the injury with a loop ileostomy, which was successfully reversed 3 months later. The patient continues to have constipation, with occasional bleeding, pain, and burning.
PATIENT’S CLAIM The risks of robotic surgery were never fully explained to her. Failure to properly visualize her internal organs led to the injury; the extent of damage exceeded what is considered “acceptable risk” of the procedure. The physicians had little experience and training in robotic surgery.
PHYSICIANS’ DEFENSE The case was settled before trial.
VERDICT A $350,000 Massachusetts settlement was reached.
4 Adhesions limit view of bowel
A 76-YEAR-OLD WOMAN UNDERWENT surgical removal of an ovarian cyst. The ObGyn attempted a laparoscopic procedure but converted to laparotomy when extensive adhesions were encountered. The next morning, the patient discovered that her navel was discharging fecal matter. Exploratory surgery determined that the bowel had been perforated. She required additional surgery and had a long recovery.
PATIENT’S CLAIM The ObGyn was negligent in failing to diagnose and treat bowel perforation in a timely manner. An intraoperative bowel inspection should have occurred due to the likelihood of a bowel injury related to the adhesions.
PHYSICIAN’S DEFENSE Adhesions restricted inspection of every area.
VERDICT A $225,000 New York settlement was reached.
5 Skydiver’s ongoing postop pain
AFTER REPORTING DYSMENORRHEA and menometrorrhagia, a 34-year-old woman underwent dilatation and curettage, thermal endometrial ablation, and diagnostic laparoscopy. A day later, she reported increasing pain. The ObGyn’s examination revealed minimal abdominal distension, sluggish bowel sounds, and some guarding, with no rebound tenderness or acute distress. US showed a 3-cm pocket of fluid in the abdomen. Two hours later, an exam revealed a soft abdomen and normal bowel sounds. She was sent home with instructions to return the next day or, if her condition worsened, to go to the ED.
Her husband called the next day to report she was feeling better. The patient woke the following morning with massive distension, worse pain, and severe shortness of breath. At the ED, a CT scan revealed a large amount of abdominal fluid. During emergency laparotomy, an injury was found in the jejunum, necessitating a 3-inch resection.
PATIENT’S CLAIM The ObGyn was negligent in not treating her postoperative symptoms in a more proactive manner. Adhesions developed from peritonitis, leading to chronic abdominal pain. Several operations were required.
PHYSICIAN’S DEFENSE Bowel injury is a known complication of the procedure. There was no indication during surgery or at the office visit that the jejunum was injured. Adhesions were not the cause of the patient’s ongoing pain; very few adhesions were found during subsequent operations. The woman was an avid skydiver who had completed 200 jumps since her initial surgery.
VERDICT An Illinois defense verdict was returned.
6 Bowel injury at laparoscopy
WHEN THE GYNECOLOGIST recognized a bowel injury during laparoscopic salpingectomy, he called a general surgeon, who repaired three areas of bowel. The patient was released 2 days after surgery. She called the gynecologist 2 days later to report fever and vaginal bleeding. She was told to come to the office, but she cancelled when the fever subsided. The next day, she went to the ED, where sepsis was diagnosed. She was flown to another hospital for surgery. A 1-cm small-bowel perforation was found in an area of earlier repair because a suture had been disrupted. A temporary colostomy was reversed 3 months later.
PATIENT’S CLAIM The gynecologist was negligent in performing laparoscopic salpingectomy. The patient should not have been discharged because her white blood cell count and heart rate were elevated.
DEFENDANTS’ DEFENSE Performance of a laparoscopic procedure was proper. Discharge was reasonable, as there was only a potential for complications with no evident problems.
VERDICT An Missouri defense verdict was returned.
7 Was treatment of abscess delayed?
A 49-YEAR-OLD WOMAN with menorrhagia underwent cryoablation. Two weeks later, she went to the ED with pain and constipation. Following CT scans and US, she was found to have a tubo-ovarian abscess. After an enema and subsequent bowel movement, her pain improved. She was discharged with instructions to follow-up with her gynecologist. Six days later, the gynecologist prescribed triple antibiotics, analgesics, and weekly visits for the abscess. Two weeks later, she reported unbearable pain and was sent to the ED. She was found to have a microperforation of the sigmoid colon and multiple gynecologic pathologies, including myomata, right serous cystadenoma, and left tubo-ovarian complex suggestive of endometriosis. Hysterectomy and colostomy were performed; the colostomy was reversed several months later.
PATIENT’S CLAIM She should have been hospitalized when the abscess was found so that the infection could be treated properly. She alleged lack of informed consent for the cryoablation.
PHYSICIAN’S DEFENSE Hospitalization was unnecessary; the patient had initially improved, and the outcome would not have changed with intravenous antibiotics. The patient was fully informed of the risks of the procedure.
VERDICT A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.

A 39-YEAR-OLD WOMAN’S SECOND CHILD WAS BORN by cesarean delivery. The mother died the next day from a pulmonary embolism.
ESTATE’S CLAIM Physicians and nurses at the hospital were negligent in failing to recognize the mother’s risk factors for pulmonary embolism, including obesity, being over age 35, and hypertension. They failed to ensure that compression boots were in place and working prior to delivery. Although orders had been given for the woman to walk within 8 hours of delivery, she did not get out of bed and walk for 24 hours after delivery.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $3.5 million Illinois settlement was reached.
Woman told “Biopsy isn’t urgent”
TWO MONTHS AFTER HER INITIAL VISIT, a 58-year-old woman returned to the gynecologist with vaginal bleeding. In March 2004, ultrasonography (US) showed slight thickening of the endometrial lining and a “pin dot” described as being a prepolyp. Vaginal bleeding was determined to be due to thinning of the vaginal wall with menopause.
The patient reported daily vaginal bleeding when she saw the gynecologist in January 2005. A new, large, rounded, solid mass within the endometrial cavity consistent with a large endometrial polyp was seen on US. The radiologist recommended hysteroscopic biopsy with excision, but the gynecologist told the patient it was not urgent.
In March 2005, hysteroscopy confirmed carcinosarcoma of the uterus. The patient underwent a hysterectomy followed by pelvic radiation and brachytherapy.
Eight months later, metastasis was found in the lungs; she died in October 2006.
ESTATE’S CLAIM The gynecologist failed to react when the patient first reported vaginal bleeding. An earlier diagnosis could have prevented her death.
PHYSICIAN’S DEFENSE The case was settled before trial.
VERDICT An $820,000 Massachusetts settlement was reached.
US report misses fetal abnormalities
A PREGNANT WOMAN UNDERWENT US. The preliminary report indicated echogenic cardiac focus and unilateral pyelectasis. Twenty-five days later, the mother underwent a level II US. A radiologist wrote that fetal anatomy was normal in both reports. The mother had two additional sonograms, with no reported abnormality.
The baby was born with aplasia and hypoplasia with both arms absent below a short humerus, an absent left leg, and a shortened right leg with a remnant foot and three small toes.
PARENTS’ CLAIM The radiologist’s US reports failed to accurately describe the fetal anatomy, depriving the parents of the chance to terminate the pregnancy.
DEFENDANTS’ DEFENSE Proper treatment was given.
VERDICT A $4.5 million Florida verdict was returned. Fault was assigned to the radiologist (85%) and the level II technologist (15%).
Forceps delivery injures mother’s pelvic floor
DURING A TRIAL OF LABOR, a 34-year-old woman experienced deep transverse arrest and lack of progress due to pelvic restriction. The ObGyn proceeded to deliver the baby vaginally using forceps, which caused pelvic floor injuries to the mother.
Several months later, she underwent corrective repair surgery for pelvic floor prolapse. She has continuing vaginal and rectal pain and dysfunction.
PATIENT’S CLAIM A cesarean delivery should have been performed as soon as pelvic restriction was found. The injuries reduce the woman’s chances of having another child.
PHYSICIAN’S DEFENSE A trial of labor was proper. The patient’s continuing fertility problems are related to chronic yeast infections and prescription birth control.
VERDICT A $1,716,469 Illinois verdict was returned, which included $484,000 to the patient’s husband for loss of consortium.
7 CASES OF INJURED BOWEL
1 Woman dies from bowel injury
DURING A SLING PROCEDURE for vaginal prolapse, a 50-year-old woman required a transfusion. The next day, she was nauseated and constipated. A day later, she went to the ED with shortness of breath and chest and abdominal pain. Her symptoms persisted for 8 days before an injury to her transverse colon was found during exploratory surgery. She suffered massive organ failure caused by sepsis and died 3 weeks after the initial surgery.
ESTATE’S CLAIM The gynecologist should have investigated why she needed a transfusion during surgery. He should have reacted earlier to her postsurgical complaints.
PHYSICIAN’S DEFENSE Bowel injury is a known risk of the procedure. The patient suffered multiple strokes after being readmitted to the hospital.
VERDICT A $2.4 million South Carolina verdict was returned.
2 Colostomy, coma after hysterectomy
DUE TO FIBROID TUMORS and pelvic pain, a 39-year-old woman’s ObGyn suggested laparoscopic-assisted vaginal hysterectomy. A third-year resident performed most of the procedure. The ObGyn’s associate covered postsurgical care.
When the patient reported increasing pain and rectal bleeding, an exploratory laparotomy was performed 3 days after surgery. Bowel and ureter injuries were repaired and a permanent colostomy was created. The patient developed septic shock with multiple organ failure, and was placed in a chemically induced coma for 3 weeks, after which she had to relearn to walk, talk, and care for herself.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery. He failed to obtain consent for the resident’s participation. The associate failed to respond to her declining postoperative condition in a timely manner.
DEFENDANTS’ DEFENSE Surgery was properly performed and postoperative care was appropriate. The bowel injury was a thermal or pressure necrosis that occurred 3 days after surgery. Two different consent forms signed by the patient included notification that a resident might assist; the resident was introduced to the patient prior to surgery. The patient’s injury claims were exaggerated; her future medical bills would be limited to colostomy supplies.
VERDICT A $1,926,069 Texas verdict was returned.
3 Were physicians qualified on robot?
A 48-YEAR-OLD WOMAN UNDERWENT robotic-assisted total hysterectomy and oophorectomy for uterine fibroids and cysts. During surgery, the physicians realized that the sigmoid colon had been perforated. A general surgeon repaired the injury with a loop ileostomy, which was successfully reversed 3 months later. The patient continues to have constipation, with occasional bleeding, pain, and burning.
PATIENT’S CLAIM The risks of robotic surgery were never fully explained to her. Failure to properly visualize her internal organs led to the injury; the extent of damage exceeded what is considered “acceptable risk” of the procedure. The physicians had little experience and training in robotic surgery.
PHYSICIANS’ DEFENSE The case was settled before trial.
VERDICT A $350,000 Massachusetts settlement was reached.
4 Adhesions limit view of bowel
A 76-YEAR-OLD WOMAN UNDERWENT surgical removal of an ovarian cyst. The ObGyn attempted a laparoscopic procedure but converted to laparotomy when extensive adhesions were encountered. The next morning, the patient discovered that her navel was discharging fecal matter. Exploratory surgery determined that the bowel had been perforated. She required additional surgery and had a long recovery.
PATIENT’S CLAIM The ObGyn was negligent in failing to diagnose and treat bowel perforation in a timely manner. An intraoperative bowel inspection should have occurred due to the likelihood of a bowel injury related to the adhesions.
PHYSICIAN’S DEFENSE Adhesions restricted inspection of every area.
VERDICT A $225,000 New York settlement was reached.
5 Skydiver’s ongoing postop pain
AFTER REPORTING DYSMENORRHEA and menometrorrhagia, a 34-year-old woman underwent dilatation and curettage, thermal endometrial ablation, and diagnostic laparoscopy. A day later, she reported increasing pain. The ObGyn’s examination revealed minimal abdominal distension, sluggish bowel sounds, and some guarding, with no rebound tenderness or acute distress. US showed a 3-cm pocket of fluid in the abdomen. Two hours later, an exam revealed a soft abdomen and normal bowel sounds. She was sent home with instructions to return the next day or, if her condition worsened, to go to the ED.
Her husband called the next day to report she was feeling better. The patient woke the following morning with massive distension, worse pain, and severe shortness of breath. At the ED, a CT scan revealed a large amount of abdominal fluid. During emergency laparotomy, an injury was found in the jejunum, necessitating a 3-inch resection.
PATIENT’S CLAIM The ObGyn was negligent in not treating her postoperative symptoms in a more proactive manner. Adhesions developed from peritonitis, leading to chronic abdominal pain. Several operations were required.
PHYSICIAN’S DEFENSE Bowel injury is a known complication of the procedure. There was no indication during surgery or at the office visit that the jejunum was injured. Adhesions were not the cause of the patient’s ongoing pain; very few adhesions were found during subsequent operations. The woman was an avid skydiver who had completed 200 jumps since her initial surgery.
VERDICT An Illinois defense verdict was returned.
6 Bowel injury at laparoscopy
WHEN THE GYNECOLOGIST recognized a bowel injury during laparoscopic salpingectomy, he called a general surgeon, who repaired three areas of bowel. The patient was released 2 days after surgery. She called the gynecologist 2 days later to report fever and vaginal bleeding. She was told to come to the office, but she cancelled when the fever subsided. The next day, she went to the ED, where sepsis was diagnosed. She was flown to another hospital for surgery. A 1-cm small-bowel perforation was found in an area of earlier repair because a suture had been disrupted. A temporary colostomy was reversed 3 months later.
PATIENT’S CLAIM The gynecologist was negligent in performing laparoscopic salpingectomy. The patient should not have been discharged because her white blood cell count and heart rate were elevated.
DEFENDANTS’ DEFENSE Performance of a laparoscopic procedure was proper. Discharge was reasonable, as there was only a potential for complications with no evident problems.
VERDICT An Missouri defense verdict was returned.
7 Was treatment of abscess delayed?
A 49-YEAR-OLD WOMAN with menorrhagia underwent cryoablation. Two weeks later, she went to the ED with pain and constipation. Following CT scans and US, she was found to have a tubo-ovarian abscess. After an enema and subsequent bowel movement, her pain improved. She was discharged with instructions to follow-up with her gynecologist. Six days later, the gynecologist prescribed triple antibiotics, analgesics, and weekly visits for the abscess. Two weeks later, she reported unbearable pain and was sent to the ED. She was found to have a microperforation of the sigmoid colon and multiple gynecologic pathologies, including myomata, right serous cystadenoma, and left tubo-ovarian complex suggestive of endometriosis. Hysterectomy and colostomy were performed; the colostomy was reversed several months later.
PATIENT’S CLAIM She should have been hospitalized when the abscess was found so that the infection could be treated properly. She alleged lack of informed consent for the cryoablation.
PHYSICIAN’S DEFENSE Hospitalization was unnecessary; the patient had initially improved, and the outcome would not have changed with intravenous antibiotics. The patient was fully informed of the risks of the procedure.
VERDICT A Pennsylvania defense verdict was returned.

A 39-YEAR-OLD WOMAN’S SECOND CHILD WAS BORN by cesarean delivery. The mother died the next day from a pulmonary embolism.
ESTATE’S CLAIM Physicians and nurses at the hospital were negligent in failing to recognize the mother’s risk factors for pulmonary embolism, including obesity, being over age 35, and hypertension. They failed to ensure that compression boots were in place and working prior to delivery. Although orders had been given for the woman to walk within 8 hours of delivery, she did not get out of bed and walk for 24 hours after delivery.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $3.5 million Illinois settlement was reached.
Woman told “Biopsy isn’t urgent”
TWO MONTHS AFTER HER INITIAL VISIT, a 58-year-old woman returned to the gynecologist with vaginal bleeding. In March 2004, ultrasonography (US) showed slight thickening of the endometrial lining and a “pin dot” described as being a prepolyp. Vaginal bleeding was determined to be due to thinning of the vaginal wall with menopause.
The patient reported daily vaginal bleeding when she saw the gynecologist in January 2005. A new, large, rounded, solid mass within the endometrial cavity consistent with a large endometrial polyp was seen on US. The radiologist recommended hysteroscopic biopsy with excision, but the gynecologist told the patient it was not urgent.
In March 2005, hysteroscopy confirmed carcinosarcoma of the uterus. The patient underwent a hysterectomy followed by pelvic radiation and brachytherapy.
Eight months later, metastasis was found in the lungs; she died in October 2006.
ESTATE’S CLAIM The gynecologist failed to react when the patient first reported vaginal bleeding. An earlier diagnosis could have prevented her death.
PHYSICIAN’S DEFENSE The case was settled before trial.
VERDICT An $820,000 Massachusetts settlement was reached.
US report misses fetal abnormalities
A PREGNANT WOMAN UNDERWENT US. The preliminary report indicated echogenic cardiac focus and unilateral pyelectasis. Twenty-five days later, the mother underwent a level II US. A radiologist wrote that fetal anatomy was normal in both reports. The mother had two additional sonograms, with no reported abnormality.
The baby was born with aplasia and hypoplasia with both arms absent below a short humerus, an absent left leg, and a shortened right leg with a remnant foot and three small toes.
PARENTS’ CLAIM The radiologist’s US reports failed to accurately describe the fetal anatomy, depriving the parents of the chance to terminate the pregnancy.
DEFENDANTS’ DEFENSE Proper treatment was given.
VERDICT A $4.5 million Florida verdict was returned. Fault was assigned to the radiologist (85%) and the level II technologist (15%).
Forceps delivery injures mother’s pelvic floor
DURING A TRIAL OF LABOR, a 34-year-old woman experienced deep transverse arrest and lack of progress due to pelvic restriction. The ObGyn proceeded to deliver the baby vaginally using forceps, which caused pelvic floor injuries to the mother.
Several months later, she underwent corrective repair surgery for pelvic floor prolapse. She has continuing vaginal and rectal pain and dysfunction.
PATIENT’S CLAIM A cesarean delivery should have been performed as soon as pelvic restriction was found. The injuries reduce the woman’s chances of having another child.
PHYSICIAN’S DEFENSE A trial of labor was proper. The patient’s continuing fertility problems are related to chronic yeast infections and prescription birth control.
VERDICT A $1,716,469 Illinois verdict was returned, which included $484,000 to the patient’s husband for loss of consortium.
7 CASES OF INJURED BOWEL
1 Woman dies from bowel injury
DURING A SLING PROCEDURE for vaginal prolapse, a 50-year-old woman required a transfusion. The next day, she was nauseated and constipated. A day later, she went to the ED with shortness of breath and chest and abdominal pain. Her symptoms persisted for 8 days before an injury to her transverse colon was found during exploratory surgery. She suffered massive organ failure caused by sepsis and died 3 weeks after the initial surgery.
ESTATE’S CLAIM The gynecologist should have investigated why she needed a transfusion during surgery. He should have reacted earlier to her postsurgical complaints.
PHYSICIAN’S DEFENSE Bowel injury is a known risk of the procedure. The patient suffered multiple strokes after being readmitted to the hospital.
VERDICT A $2.4 million South Carolina verdict was returned.
2 Colostomy, coma after hysterectomy
DUE TO FIBROID TUMORS and pelvic pain, a 39-year-old woman’s ObGyn suggested laparoscopic-assisted vaginal hysterectomy. A third-year resident performed most of the procedure. The ObGyn’s associate covered postsurgical care.
When the patient reported increasing pain and rectal bleeding, an exploratory laparotomy was performed 3 days after surgery. Bowel and ureter injuries were repaired and a permanent colostomy was created. The patient developed septic shock with multiple organ failure, and was placed in a chemically induced coma for 3 weeks, after which she had to relearn to walk, talk, and care for herself.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery. He failed to obtain consent for the resident’s participation. The associate failed to respond to her declining postoperative condition in a timely manner.
DEFENDANTS’ DEFENSE Surgery was properly performed and postoperative care was appropriate. The bowel injury was a thermal or pressure necrosis that occurred 3 days after surgery. Two different consent forms signed by the patient included notification that a resident might assist; the resident was introduced to the patient prior to surgery. The patient’s injury claims were exaggerated; her future medical bills would be limited to colostomy supplies.
VERDICT A $1,926,069 Texas verdict was returned.
3 Were physicians qualified on robot?
A 48-YEAR-OLD WOMAN UNDERWENT robotic-assisted total hysterectomy and oophorectomy for uterine fibroids and cysts. During surgery, the physicians realized that the sigmoid colon had been perforated. A general surgeon repaired the injury with a loop ileostomy, which was successfully reversed 3 months later. The patient continues to have constipation, with occasional bleeding, pain, and burning.
PATIENT’S CLAIM The risks of robotic surgery were never fully explained to her. Failure to properly visualize her internal organs led to the injury; the extent of damage exceeded what is considered “acceptable risk” of the procedure. The physicians had little experience and training in robotic surgery.
PHYSICIANS’ DEFENSE The case was settled before trial.
VERDICT A $350,000 Massachusetts settlement was reached.
4 Adhesions limit view of bowel
A 76-YEAR-OLD WOMAN UNDERWENT surgical removal of an ovarian cyst. The ObGyn attempted a laparoscopic procedure but converted to laparotomy when extensive adhesions were encountered. The next morning, the patient discovered that her navel was discharging fecal matter. Exploratory surgery determined that the bowel had been perforated. She required additional surgery and had a long recovery.
PATIENT’S CLAIM The ObGyn was negligent in failing to diagnose and treat bowel perforation in a timely manner. An intraoperative bowel inspection should have occurred due to the likelihood of a bowel injury related to the adhesions.
PHYSICIAN’S DEFENSE Adhesions restricted inspection of every area.
VERDICT A $225,000 New York settlement was reached.
5 Skydiver’s ongoing postop pain
AFTER REPORTING DYSMENORRHEA and menometrorrhagia, a 34-year-old woman underwent dilatation and curettage, thermal endometrial ablation, and diagnostic laparoscopy. A day later, she reported increasing pain. The ObGyn’s examination revealed minimal abdominal distension, sluggish bowel sounds, and some guarding, with no rebound tenderness or acute distress. US showed a 3-cm pocket of fluid in the abdomen. Two hours later, an exam revealed a soft abdomen and normal bowel sounds. She was sent home with instructions to return the next day or, if her condition worsened, to go to the ED.
Her husband called the next day to report she was feeling better. The patient woke the following morning with massive distension, worse pain, and severe shortness of breath. At the ED, a CT scan revealed a large amount of abdominal fluid. During emergency laparotomy, an injury was found in the jejunum, necessitating a 3-inch resection.
PATIENT’S CLAIM The ObGyn was negligent in not treating her postoperative symptoms in a more proactive manner. Adhesions developed from peritonitis, leading to chronic abdominal pain. Several operations were required.
PHYSICIAN’S DEFENSE Bowel injury is a known complication of the procedure. There was no indication during surgery or at the office visit that the jejunum was injured. Adhesions were not the cause of the patient’s ongoing pain; very few adhesions were found during subsequent operations. The woman was an avid skydiver who had completed 200 jumps since her initial surgery.
VERDICT An Illinois defense verdict was returned.
6 Bowel injury at laparoscopy
WHEN THE GYNECOLOGIST recognized a bowel injury during laparoscopic salpingectomy, he called a general surgeon, who repaired three areas of bowel. The patient was released 2 days after surgery. She called the gynecologist 2 days later to report fever and vaginal bleeding. She was told to come to the office, but she cancelled when the fever subsided. The next day, she went to the ED, where sepsis was diagnosed. She was flown to another hospital for surgery. A 1-cm small-bowel perforation was found in an area of earlier repair because a suture had been disrupted. A temporary colostomy was reversed 3 months later.
PATIENT’S CLAIM The gynecologist was negligent in performing laparoscopic salpingectomy. The patient should not have been discharged because her white blood cell count and heart rate were elevated.
DEFENDANTS’ DEFENSE Performance of a laparoscopic procedure was proper. Discharge was reasonable, as there was only a potential for complications with no evident problems.
VERDICT An Missouri defense verdict was returned.
7 Was treatment of abscess delayed?
A 49-YEAR-OLD WOMAN with menorrhagia underwent cryoablation. Two weeks later, she went to the ED with pain and constipation. Following CT scans and US, she was found to have a tubo-ovarian abscess. After an enema and subsequent bowel movement, her pain improved. She was discharged with instructions to follow-up with her gynecologist. Six days later, the gynecologist prescribed triple antibiotics, analgesics, and weekly visits for the abscess. Two weeks later, she reported unbearable pain and was sent to the ED. She was found to have a microperforation of the sigmoid colon and multiple gynecologic pathologies, including myomata, right serous cystadenoma, and left tubo-ovarian complex suggestive of endometriosis. Hysterectomy and colostomy were performed; the colostomy was reversed several months later.
PATIENT’S CLAIM She should have been hospitalized when the abscess was found so that the infection could be treated properly. She alleged lack of informed consent for the cryoablation.
PHYSICIAN’S DEFENSE Hospitalization was unnecessary; the patient had initially improved, and the outcome would not have changed with intravenous antibiotics. The patient was fully informed of the risks of the procedure.
VERDICT A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
Suicide rehearsals: A high-risk psychiatric emergency
A suicide rehearsal is a behavioral enactment of a suicide method, usually as part of a suicide plan. A mental suicide rehearsal is a process that evolves over time into a plan. Patients who are intent on attempting suicide usually do not reveal their plans. However, behavioral rehearsals display specific clinical characteristics that speak louder than the guarded patient’s denials, revealing the patient’s suicide plan (Table).
Suicide rehearsals may precede suicide attempts or suicide completions. The percentage of patients who stage suicide rehearsals before attempting or completing suicide is unknown; however, in my experience, suicide rehearsals are relatively common. This article describes suicide rehearsals, and offers 4 cases that illustrate what clinicians can learn from rehearsals to improve their patients’ safety.
Table
Clinical characteristics of suicide rehearsals
| Guarded patient |
| Behavioral enactment of a suicide method |
| Lethal means |
| Presumptive acute, high risk of suicide |
| Severe mental illness |
| Suicide attempt often within hours or days |
| Rehearsal usually covert |
| Rehearsal event or multiple events |
The psychology behind suicide rehearsals
Rehearsing suicidal behavior can lower the barrier to a suicide plan, thereby increasing a patient’s resolve and risk. Joiner1 notes that engaging in behavioral or mental suicide rehearsals increases the risk of suicide. Moreover, rehearsals diminish the prohibition against suicidal behavior and the fear of pain and dying. Examples of rehearsal psychology include:
- overcoming ambivalence about dying
- desensitizing anxiety about performing the suicide act
- testing or “perfecting” the method of a planned suicide
- firming one’s resolve to complete suicide.
Other non-lethal motivations include “a cry for help” and self-injurious behaviors motivated by external gains. Patients who do not intend to attempt suicide may openly rehearse low-risk methods, such as superficial cutting.
Rehearsal characteristics
Suicide rehearsals can be confused with aborted, interrupted, or failed suicide attempts. Suicide rehearsals usually are associated with severe psychiatric illness and high-risk lethal methods of attempting suicide. My experience is that suicide attempts or suicide completions often follow a rehearsal within a few hours or days. However, no short-term suicide risk factors—within hours, days, or weeks—can predict when or if a rehearsed suicide will proceed to a suicide attempt.2
A suicide rehearsal is presumptive evidence that the patient is at acute, high risk for suicide and immediate clinical intervention is necessary. A rehearsal allows the clinician to explore the various methods of suicide that the patient has considered, including prior rehearsals. Knowledge of prior rehearsals can inform the clinician’s management of the current suicide rehearsal.
Suicide rehearsals often are conducted covertly. On inpatient psychiatric units, the rehearsal usually is discovered by staff members or reported by other patients. In outpatient settings, the patient or a significant other may report a rehearsal.
The suicide method displayed in a rehearsal may change. A patient who is rehearsing a hanging may attempt suicide by overdose or a firearm. In a systematic review of prior suicide attempts (N = 1,397), Isometsä et al3 found that 82% of patients used 2 or more different methods in suicide attempts, including the completed suicide. However, in a cohort study of 48,649 individuals admitted to a hospital after an attempted suicide, Runeson et al4 found that patients who attempt suicide often used the same method in completed suicide (ie, >90% by hanging for both men and women). Therefore, when taking measures to restrict the patient’s access to lethal means, safety efforts should not be limited to the method used in the suicide rehearsal. Patients can always substitute methods.
Making overall preparations for suicide—for example, making a will, giving away valuable possessions, or putting financial affairs in order—could be confused with a suicide rehearsal, which displays the lethal method to be used in a suicide attempt, often after preparations are made. Suicide rehearsals tend to occur much closer in time to the suicide attempt than preparations for suicide. Similarly, a patient’s plan to hoard drugs for a suicide attempt is not the same as ingesting a sub-lethal dose of a drug to test his or her resolve to die.
By definition, impulsive suicide attempts are not rehearsed. However, an individual’s suicide rehearsal can impulsively segue into a suicide attempt. In a case control study (N = 153) Simon et al5 found that 24% of patients spent 6 found that 26% of individuals with lifetime suicide ideation transitioned from suicide ideation to an unplanned suicide attempt. In my experience, a suicide rehearsal before a suicide completion is presumptive evidence against an impulsive suicide.
Patients contemplating suicide may visit Web sites with instructions on “how to suicide,” providing “virtual” opportunities to rehearse suicide.7 Patients who are at risk for suicide should be asked if they have searched the Internet for suicide methodology.
What we can learn from rehearsals
Although the following case examples are fictional, they illustrate suicide rehearsals encountered in my clinical and forensic practice.
CASE 1: Looking for a location
Ms. B, a 28-year-old divorced mother of 2, is observed tarrying at the high point of a bridge on successive days. When police arrive and question her, she becomes agitated and distraught. Ms. B admits to “scoping out” the bridge and is taken to a hospital emergency room (ER). In the ER, Ms. B discloses, “I was looking for a good spot to jump.” She tells the triage nurse that she is very depressed but, “I couldn’t do it to my children.” Ms. B is placed in an unlocked room while she waits to be assessed by a psychiatrist. She leaves the ER, runs to a nearby parking garage, and jumps from the top level to her death.
Comment: A patient’s denial of suicide intent following a suicide rehearsal cannot be relied upon. Ms. B’s rehearsal revealed a plan with high-risk suicide intent and a lethal suicide method. Systematic suicide assessment that informs immediate clinical intervention is required.
CASE 2: Changing lethal means
Mr. N, a 43-year-old chief executive officer of a large company, is observed by an assistant loading and unloading a revolver at his desk. Alarmed, the assistant calls the company physician. Mr. N refuses psychiatric treatment, saying, “I’ll be all right; this is just a passing thing.” His wife tells the physician that her husband has a history of bipolar disorder but no prior suicide attempts. Guns and ammunition are removed from the home. One week later, Mr. N is found hanging in his garage. A loaded pistol is discovered in the glove compartment of his car.
Comment: There is no certainty that a subsequent suicide attempt will replicate the rehearsed method. A psychological autopsy was conducted, but no explanation was found for why Mr. N chose hanging after having rehearsed suicide with a loaded handgun. His wife thought that her husband, a very tidy person, did not want to leave a mess.
CASE 3: Grieving and depressed
Mr. O, age 67, is depressed after recently losing his wife. He considers a number of suicide methods. Mr. O decides to use a plastic bag to suffocate himself because he believes that this method will allow him to change his mind. Mr. O practices tying the bag tight around his neck. During this rehearsal, he realizes that he does not want to die. Instead, he pursues grief counseling.
Comment: For some patients, the act of rehearsing suicide can help them resolve ambivalent feelings about wanting to die in favor of wanting to live.
CASE 4: Suicide method and the Internet
Ms. S, a 22-year-old college student, is undergoing outpatient treatment for depression. She is accumulating prescription drugs to take as an overdose. Ms. S also searches the Internet for information about other suicide methods. Because she wants a “sure” method of suicide, she persuades an acquaintance to purchase a handgun. In private, Ms. S places the unloaded gun to her head and plays “Russian roulette,” pulling the trigger several times. Her mother discovers the gun and confronts her daughter. Ms. S is hospitalized on a closed psychiatric unit and tells a staff member, “I was practicing suicide with the gun.” Before Ms. S is discharged from the hospital, her parents are advised to watch for suicidal behaviors, especially the recurrence of rehearsals that indicate an acute, high suicide risk. Ms. S’s Internet use is restricted and monitored.
Comment: Suicide rehearsal with a gun reinforces the belief that a firearm death is quick and easy.8 Reaching for a loaded gun takes less time than most other methods of suicide. Patients who rehearse suicide with a gun should be prevented from having access to any firearms, weapons, or other highly lethal means of suicide.
Recognition and intervention
A guarded psychiatric inpatient who is intent on attempting suicide is unmasked when the discovery of a suicidal rehearsal reveals a suicide plan. This creates an opportunity for clinicians to intervene. The patient may attempt to cover up suicidal intent by stating, “I was just playing around” or “I just wanted to get attention.” Recognizing the emergency posed by a suicide rehearsal informs treatment. Safety measures—including 1-to-1 supervision—may be necessary during a period of acute, high suicide risk. The patient’s diagnosis, severity of illness, and treatment require reevaluation.
An outpatient who performs a suicide rehearsal should be considered at acute, high risk for suicide, and immediate psychiatric hospitalization may be necessary. Whether as an inpatient or outpatient, the patient’s suicide intent and plan require careful exploration. The information gained will guide treatment and management decisions. Continuing systematic suicide risk assessment is essential.
Related Resources
- American Association of Suicidology. www.suicidology.org.
- Joiner T. Why people die by suicide. Cambridge, MA: Harvard University Press; 2007.
- American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Washington, DC: American Psychiatric Publishing, Inc. 2003.
- Simon RI. Preventing patient suicide: clinical assessment and management. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
Disclosure
Dr. Simon reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Joiner TE, Jr. The trajectory of suicidal behavior over time. Suicide Life Threat Behav. 2002;32(1):33-41.
2. Simon RI. Imminent suicide: the illusion of short-term prediction. Suicide Life Threat Behav. 2006;36(3):296-301.
3. Isometsä ET, Lönnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
4. Runeson B, Tidemalm D, Dahlin M, et al. Method of attempted suicide as a predictor of subsequent successful suicide: national long-term cohort study. BMJ. 2010;341:c3222. doi:10.1136/bmj.63222.
5. Simon TR, Swann AC, Powell KE, et al. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32(suppl):49-59.
6. Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Study. Arch Gen Psychiatry. 1999;56(7):617-626.
7. Recupero PR. Suicide and the Internet. In: Simon RI Hales RE, eds. The American Psychiatric Publishing textbook of suicide assessment and management. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2012:515–538.
8. Simon RI. Gun safety management with patients at risk for suicide. Suicide Life Threat Behav. 2007;37(5):518-526.
A suicide rehearsal is a behavioral enactment of a suicide method, usually as part of a suicide plan. A mental suicide rehearsal is a process that evolves over time into a plan. Patients who are intent on attempting suicide usually do not reveal their plans. However, behavioral rehearsals display specific clinical characteristics that speak louder than the guarded patient’s denials, revealing the patient’s suicide plan (Table).
Suicide rehearsals may precede suicide attempts or suicide completions. The percentage of patients who stage suicide rehearsals before attempting or completing suicide is unknown; however, in my experience, suicide rehearsals are relatively common. This article describes suicide rehearsals, and offers 4 cases that illustrate what clinicians can learn from rehearsals to improve their patients’ safety.
Table
Clinical characteristics of suicide rehearsals
| Guarded patient |
| Behavioral enactment of a suicide method |
| Lethal means |
| Presumptive acute, high risk of suicide |
| Severe mental illness |
| Suicide attempt often within hours or days |
| Rehearsal usually covert |
| Rehearsal event or multiple events |
The psychology behind suicide rehearsals
Rehearsing suicidal behavior can lower the barrier to a suicide plan, thereby increasing a patient’s resolve and risk. Joiner1 notes that engaging in behavioral or mental suicide rehearsals increases the risk of suicide. Moreover, rehearsals diminish the prohibition against suicidal behavior and the fear of pain and dying. Examples of rehearsal psychology include:
- overcoming ambivalence about dying
- desensitizing anxiety about performing the suicide act
- testing or “perfecting” the method of a planned suicide
- firming one’s resolve to complete suicide.
Other non-lethal motivations include “a cry for help” and self-injurious behaviors motivated by external gains. Patients who do not intend to attempt suicide may openly rehearse low-risk methods, such as superficial cutting.
Rehearsal characteristics
Suicide rehearsals can be confused with aborted, interrupted, or failed suicide attempts. Suicide rehearsals usually are associated with severe psychiatric illness and high-risk lethal methods of attempting suicide. My experience is that suicide attempts or suicide completions often follow a rehearsal within a few hours or days. However, no short-term suicide risk factors—within hours, days, or weeks—can predict when or if a rehearsed suicide will proceed to a suicide attempt.2
A suicide rehearsal is presumptive evidence that the patient is at acute, high risk for suicide and immediate clinical intervention is necessary. A rehearsal allows the clinician to explore the various methods of suicide that the patient has considered, including prior rehearsals. Knowledge of prior rehearsals can inform the clinician’s management of the current suicide rehearsal.
Suicide rehearsals often are conducted covertly. On inpatient psychiatric units, the rehearsal usually is discovered by staff members or reported by other patients. In outpatient settings, the patient or a significant other may report a rehearsal.
The suicide method displayed in a rehearsal may change. A patient who is rehearsing a hanging may attempt suicide by overdose or a firearm. In a systematic review of prior suicide attempts (N = 1,397), Isometsä et al3 found that 82% of patients used 2 or more different methods in suicide attempts, including the completed suicide. However, in a cohort study of 48,649 individuals admitted to a hospital after an attempted suicide, Runeson et al4 found that patients who attempt suicide often used the same method in completed suicide (ie, >90% by hanging for both men and women). Therefore, when taking measures to restrict the patient’s access to lethal means, safety efforts should not be limited to the method used in the suicide rehearsal. Patients can always substitute methods.
Making overall preparations for suicide—for example, making a will, giving away valuable possessions, or putting financial affairs in order—could be confused with a suicide rehearsal, which displays the lethal method to be used in a suicide attempt, often after preparations are made. Suicide rehearsals tend to occur much closer in time to the suicide attempt than preparations for suicide. Similarly, a patient’s plan to hoard drugs for a suicide attempt is not the same as ingesting a sub-lethal dose of a drug to test his or her resolve to die.
By definition, impulsive suicide attempts are not rehearsed. However, an individual’s suicide rehearsal can impulsively segue into a suicide attempt. In a case control study (N = 153) Simon et al5 found that 24% of patients spent 6 found that 26% of individuals with lifetime suicide ideation transitioned from suicide ideation to an unplanned suicide attempt. In my experience, a suicide rehearsal before a suicide completion is presumptive evidence against an impulsive suicide.
Patients contemplating suicide may visit Web sites with instructions on “how to suicide,” providing “virtual” opportunities to rehearse suicide.7 Patients who are at risk for suicide should be asked if they have searched the Internet for suicide methodology.
What we can learn from rehearsals
Although the following case examples are fictional, they illustrate suicide rehearsals encountered in my clinical and forensic practice.
CASE 1: Looking for a location
Ms. B, a 28-year-old divorced mother of 2, is observed tarrying at the high point of a bridge on successive days. When police arrive and question her, she becomes agitated and distraught. Ms. B admits to “scoping out” the bridge and is taken to a hospital emergency room (ER). In the ER, Ms. B discloses, “I was looking for a good spot to jump.” She tells the triage nurse that she is very depressed but, “I couldn’t do it to my children.” Ms. B is placed in an unlocked room while she waits to be assessed by a psychiatrist. She leaves the ER, runs to a nearby parking garage, and jumps from the top level to her death.
Comment: A patient’s denial of suicide intent following a suicide rehearsal cannot be relied upon. Ms. B’s rehearsal revealed a plan with high-risk suicide intent and a lethal suicide method. Systematic suicide assessment that informs immediate clinical intervention is required.
CASE 2: Changing lethal means
Mr. N, a 43-year-old chief executive officer of a large company, is observed by an assistant loading and unloading a revolver at his desk. Alarmed, the assistant calls the company physician. Mr. N refuses psychiatric treatment, saying, “I’ll be all right; this is just a passing thing.” His wife tells the physician that her husband has a history of bipolar disorder but no prior suicide attempts. Guns and ammunition are removed from the home. One week later, Mr. N is found hanging in his garage. A loaded pistol is discovered in the glove compartment of his car.
Comment: There is no certainty that a subsequent suicide attempt will replicate the rehearsed method. A psychological autopsy was conducted, but no explanation was found for why Mr. N chose hanging after having rehearsed suicide with a loaded handgun. His wife thought that her husband, a very tidy person, did not want to leave a mess.
CASE 3: Grieving and depressed
Mr. O, age 67, is depressed after recently losing his wife. He considers a number of suicide methods. Mr. O decides to use a plastic bag to suffocate himself because he believes that this method will allow him to change his mind. Mr. O practices tying the bag tight around his neck. During this rehearsal, he realizes that he does not want to die. Instead, he pursues grief counseling.
Comment: For some patients, the act of rehearsing suicide can help them resolve ambivalent feelings about wanting to die in favor of wanting to live.
CASE 4: Suicide method and the Internet
Ms. S, a 22-year-old college student, is undergoing outpatient treatment for depression. She is accumulating prescription drugs to take as an overdose. Ms. S also searches the Internet for information about other suicide methods. Because she wants a “sure” method of suicide, she persuades an acquaintance to purchase a handgun. In private, Ms. S places the unloaded gun to her head and plays “Russian roulette,” pulling the trigger several times. Her mother discovers the gun and confronts her daughter. Ms. S is hospitalized on a closed psychiatric unit and tells a staff member, “I was practicing suicide with the gun.” Before Ms. S is discharged from the hospital, her parents are advised to watch for suicidal behaviors, especially the recurrence of rehearsals that indicate an acute, high suicide risk. Ms. S’s Internet use is restricted and monitored.
Comment: Suicide rehearsal with a gun reinforces the belief that a firearm death is quick and easy.8 Reaching for a loaded gun takes less time than most other methods of suicide. Patients who rehearse suicide with a gun should be prevented from having access to any firearms, weapons, or other highly lethal means of suicide.
Recognition and intervention
A guarded psychiatric inpatient who is intent on attempting suicide is unmasked when the discovery of a suicidal rehearsal reveals a suicide plan. This creates an opportunity for clinicians to intervene. The patient may attempt to cover up suicidal intent by stating, “I was just playing around” or “I just wanted to get attention.” Recognizing the emergency posed by a suicide rehearsal informs treatment. Safety measures—including 1-to-1 supervision—may be necessary during a period of acute, high suicide risk. The patient’s diagnosis, severity of illness, and treatment require reevaluation.
An outpatient who performs a suicide rehearsal should be considered at acute, high risk for suicide, and immediate psychiatric hospitalization may be necessary. Whether as an inpatient or outpatient, the patient’s suicide intent and plan require careful exploration. The information gained will guide treatment and management decisions. Continuing systematic suicide risk assessment is essential.
Related Resources
- American Association of Suicidology. www.suicidology.org.
- Joiner T. Why people die by suicide. Cambridge, MA: Harvard University Press; 2007.
- American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Washington, DC: American Psychiatric Publishing, Inc. 2003.
- Simon RI. Preventing patient suicide: clinical assessment and management. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
Disclosure
Dr. Simon reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
A suicide rehearsal is a behavioral enactment of a suicide method, usually as part of a suicide plan. A mental suicide rehearsal is a process that evolves over time into a plan. Patients who are intent on attempting suicide usually do not reveal their plans. However, behavioral rehearsals display specific clinical characteristics that speak louder than the guarded patient’s denials, revealing the patient’s suicide plan (Table).
Suicide rehearsals may precede suicide attempts or suicide completions. The percentage of patients who stage suicide rehearsals before attempting or completing suicide is unknown; however, in my experience, suicide rehearsals are relatively common. This article describes suicide rehearsals, and offers 4 cases that illustrate what clinicians can learn from rehearsals to improve their patients’ safety.
Table
Clinical characteristics of suicide rehearsals
| Guarded patient |
| Behavioral enactment of a suicide method |
| Lethal means |
| Presumptive acute, high risk of suicide |
| Severe mental illness |
| Suicide attempt often within hours or days |
| Rehearsal usually covert |
| Rehearsal event or multiple events |
The psychology behind suicide rehearsals
Rehearsing suicidal behavior can lower the barrier to a suicide plan, thereby increasing a patient’s resolve and risk. Joiner1 notes that engaging in behavioral or mental suicide rehearsals increases the risk of suicide. Moreover, rehearsals diminish the prohibition against suicidal behavior and the fear of pain and dying. Examples of rehearsal psychology include:
- overcoming ambivalence about dying
- desensitizing anxiety about performing the suicide act
- testing or “perfecting” the method of a planned suicide
- firming one’s resolve to complete suicide.
Other non-lethal motivations include “a cry for help” and self-injurious behaviors motivated by external gains. Patients who do not intend to attempt suicide may openly rehearse low-risk methods, such as superficial cutting.
Rehearsal characteristics
Suicide rehearsals can be confused with aborted, interrupted, or failed suicide attempts. Suicide rehearsals usually are associated with severe psychiatric illness and high-risk lethal methods of attempting suicide. My experience is that suicide attempts or suicide completions often follow a rehearsal within a few hours or days. However, no short-term suicide risk factors—within hours, days, or weeks—can predict when or if a rehearsed suicide will proceed to a suicide attempt.2
A suicide rehearsal is presumptive evidence that the patient is at acute, high risk for suicide and immediate clinical intervention is necessary. A rehearsal allows the clinician to explore the various methods of suicide that the patient has considered, including prior rehearsals. Knowledge of prior rehearsals can inform the clinician’s management of the current suicide rehearsal.
Suicide rehearsals often are conducted covertly. On inpatient psychiatric units, the rehearsal usually is discovered by staff members or reported by other patients. In outpatient settings, the patient or a significant other may report a rehearsal.
The suicide method displayed in a rehearsal may change. A patient who is rehearsing a hanging may attempt suicide by overdose or a firearm. In a systematic review of prior suicide attempts (N = 1,397), Isometsä et al3 found that 82% of patients used 2 or more different methods in suicide attempts, including the completed suicide. However, in a cohort study of 48,649 individuals admitted to a hospital after an attempted suicide, Runeson et al4 found that patients who attempt suicide often used the same method in completed suicide (ie, >90% by hanging for both men and women). Therefore, when taking measures to restrict the patient’s access to lethal means, safety efforts should not be limited to the method used in the suicide rehearsal. Patients can always substitute methods.
Making overall preparations for suicide—for example, making a will, giving away valuable possessions, or putting financial affairs in order—could be confused with a suicide rehearsal, which displays the lethal method to be used in a suicide attempt, often after preparations are made. Suicide rehearsals tend to occur much closer in time to the suicide attempt than preparations for suicide. Similarly, a patient’s plan to hoard drugs for a suicide attempt is not the same as ingesting a sub-lethal dose of a drug to test his or her resolve to die.
By definition, impulsive suicide attempts are not rehearsed. However, an individual’s suicide rehearsal can impulsively segue into a suicide attempt. In a case control study (N = 153) Simon et al5 found that 24% of patients spent 6 found that 26% of individuals with lifetime suicide ideation transitioned from suicide ideation to an unplanned suicide attempt. In my experience, a suicide rehearsal before a suicide completion is presumptive evidence against an impulsive suicide.
Patients contemplating suicide may visit Web sites with instructions on “how to suicide,” providing “virtual” opportunities to rehearse suicide.7 Patients who are at risk for suicide should be asked if they have searched the Internet for suicide methodology.
What we can learn from rehearsals
Although the following case examples are fictional, they illustrate suicide rehearsals encountered in my clinical and forensic practice.
CASE 1: Looking for a location
Ms. B, a 28-year-old divorced mother of 2, is observed tarrying at the high point of a bridge on successive days. When police arrive and question her, she becomes agitated and distraught. Ms. B admits to “scoping out” the bridge and is taken to a hospital emergency room (ER). In the ER, Ms. B discloses, “I was looking for a good spot to jump.” She tells the triage nurse that she is very depressed but, “I couldn’t do it to my children.” Ms. B is placed in an unlocked room while she waits to be assessed by a psychiatrist. She leaves the ER, runs to a nearby parking garage, and jumps from the top level to her death.
Comment: A patient’s denial of suicide intent following a suicide rehearsal cannot be relied upon. Ms. B’s rehearsal revealed a plan with high-risk suicide intent and a lethal suicide method. Systematic suicide assessment that informs immediate clinical intervention is required.
CASE 2: Changing lethal means
Mr. N, a 43-year-old chief executive officer of a large company, is observed by an assistant loading and unloading a revolver at his desk. Alarmed, the assistant calls the company physician. Mr. N refuses psychiatric treatment, saying, “I’ll be all right; this is just a passing thing.” His wife tells the physician that her husband has a history of bipolar disorder but no prior suicide attempts. Guns and ammunition are removed from the home. One week later, Mr. N is found hanging in his garage. A loaded pistol is discovered in the glove compartment of his car.
Comment: There is no certainty that a subsequent suicide attempt will replicate the rehearsed method. A psychological autopsy was conducted, but no explanation was found for why Mr. N chose hanging after having rehearsed suicide with a loaded handgun. His wife thought that her husband, a very tidy person, did not want to leave a mess.
CASE 3: Grieving and depressed
Mr. O, age 67, is depressed after recently losing his wife. He considers a number of suicide methods. Mr. O decides to use a plastic bag to suffocate himself because he believes that this method will allow him to change his mind. Mr. O practices tying the bag tight around his neck. During this rehearsal, he realizes that he does not want to die. Instead, he pursues grief counseling.
Comment: For some patients, the act of rehearsing suicide can help them resolve ambivalent feelings about wanting to die in favor of wanting to live.
CASE 4: Suicide method and the Internet
Ms. S, a 22-year-old college student, is undergoing outpatient treatment for depression. She is accumulating prescription drugs to take as an overdose. Ms. S also searches the Internet for information about other suicide methods. Because she wants a “sure” method of suicide, she persuades an acquaintance to purchase a handgun. In private, Ms. S places the unloaded gun to her head and plays “Russian roulette,” pulling the trigger several times. Her mother discovers the gun and confronts her daughter. Ms. S is hospitalized on a closed psychiatric unit and tells a staff member, “I was practicing suicide with the gun.” Before Ms. S is discharged from the hospital, her parents are advised to watch for suicidal behaviors, especially the recurrence of rehearsals that indicate an acute, high suicide risk. Ms. S’s Internet use is restricted and monitored.
Comment: Suicide rehearsal with a gun reinforces the belief that a firearm death is quick and easy.8 Reaching for a loaded gun takes less time than most other methods of suicide. Patients who rehearse suicide with a gun should be prevented from having access to any firearms, weapons, or other highly lethal means of suicide.
Recognition and intervention
A guarded psychiatric inpatient who is intent on attempting suicide is unmasked when the discovery of a suicidal rehearsal reveals a suicide plan. This creates an opportunity for clinicians to intervene. The patient may attempt to cover up suicidal intent by stating, “I was just playing around” or “I just wanted to get attention.” Recognizing the emergency posed by a suicide rehearsal informs treatment. Safety measures—including 1-to-1 supervision—may be necessary during a period of acute, high suicide risk. The patient’s diagnosis, severity of illness, and treatment require reevaluation.
An outpatient who performs a suicide rehearsal should be considered at acute, high risk for suicide, and immediate psychiatric hospitalization may be necessary. Whether as an inpatient or outpatient, the patient’s suicide intent and plan require careful exploration. The information gained will guide treatment and management decisions. Continuing systematic suicide risk assessment is essential.
Related Resources
- American Association of Suicidology. www.suicidology.org.
- Joiner T. Why people die by suicide. Cambridge, MA: Harvard University Press; 2007.
- American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Washington, DC: American Psychiatric Publishing, Inc. 2003.
- Simon RI. Preventing patient suicide: clinical assessment and management. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
Disclosure
Dr. Simon reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Joiner TE, Jr. The trajectory of suicidal behavior over time. Suicide Life Threat Behav. 2002;32(1):33-41.
2. Simon RI. Imminent suicide: the illusion of short-term prediction. Suicide Life Threat Behav. 2006;36(3):296-301.
3. Isometsä ET, Lönnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
4. Runeson B, Tidemalm D, Dahlin M, et al. Method of attempted suicide as a predictor of subsequent successful suicide: national long-term cohort study. BMJ. 2010;341:c3222. doi:10.1136/bmj.63222.
5. Simon TR, Swann AC, Powell KE, et al. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32(suppl):49-59.
6. Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Study. Arch Gen Psychiatry. 1999;56(7):617-626.
7. Recupero PR. Suicide and the Internet. In: Simon RI Hales RE, eds. The American Psychiatric Publishing textbook of suicide assessment and management. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2012:515–538.
8. Simon RI. Gun safety management with patients at risk for suicide. Suicide Life Threat Behav. 2007;37(5):518-526.
1. Joiner TE, Jr. The trajectory of suicidal behavior over time. Suicide Life Threat Behav. 2002;32(1):33-41.
2. Simon RI. Imminent suicide: the illusion of short-term prediction. Suicide Life Threat Behav. 2006;36(3):296-301.
3. Isometsä ET, Lönnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
4. Runeson B, Tidemalm D, Dahlin M, et al. Method of attempted suicide as a predictor of subsequent successful suicide: national long-term cohort study. BMJ. 2010;341:c3222. doi:10.1136/bmj.63222.
5. Simon TR, Swann AC, Powell KE, et al. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32(suppl):49-59.
6. Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Study. Arch Gen Psychiatry. 1999;56(7):617-626.
7. Recupero PR. Suicide and the Internet. In: Simon RI Hales RE, eds. The American Psychiatric Publishing textbook of suicide assessment and management. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2012:515–538.
8. Simon RI. Gun safety management with patients at risk for suicide. Suicide Life Threat Behav. 2007;37(5):518-526.
Trichotillomania: Targeting the root of the disorder
An estimated 1% of Americans have trichotillomania (TTM), an impulse-control disorder in which patients experience pleasure or gratification from recurrently pulling out their own hair, resulting in noticeable hair loss.1,2 This disorder is more commonly diagnosed in women, likely reflecting treatment-seeking bias; women may be more likely to seek care for TTM because of social stigma associated with hair loss.2 Avulsion of hair usually occurs at the scalp, but also can be seen in multiple sites, including eyebrows, eyelashes, beards, and pubic regions; the number of sites typically increases with the patient’s age.3
The lifetime prevalence of comorbid axis I disorders in patients with TTM is 82%.3 Because of this, TTM often is first encountered in a psychiatric setting. Psychiatrists should have knowledge of TTM diagnosis and treatment because they may be the only point of care for TTM patients. When considering a TTM diagnosis, be aware that in some cultures rending hair is a mourning ritual or a rite of passage.3
Evidence for cognitive therapies
Behavioral models suggest TTM behaviors are learned and maintained by both classical and operant conditioning. Therapies that target the cognitive processes that trigger urges to pull, the avulsion of hair, and recognizing the consequences have the best empirical support.3
Habit reversal training (HRT) is considered the most effective treatment for TTM.3 One trial found a single 2-hour HRT intervention resulted in greater reductions in hair pulling episodes and higher remission rates compared with placebo.3 HRT trains patients to create a competing response, such as fist clenching, that is incompatible and blocks the undesired response.
Other therapeutic approaches to TTM include acceptance and commitment therapy, cognitive-behavioral therapy (CBT), and dialectical behavioral therapy-enhanced HRT. Evidence is most robust for CBT-HRT; randomized controlled trials found a statistically significant reduction in TTM in patients receiving CBT-HRT.3 One review suggests CBT-HRT should be considered first-line therapy for TTM.3
Pharmacologic options
Although no medications are FDA-approved for treating TTM, options include clomipramine, olanzapine, fluoxetine, pimozide, inositol, naltrexone, and N-acetylcysteine.2,3 The most robust trials of pharmacotherapy monotherapy were for N-acetylcysteine and naltrexone; both medications had significantly greater reduction in hair-pulling symptoms compared with placebo.3 Some evidence suggests combined pharmacotherapy and psychotherapy might be an effective approach.2,3
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Woods DW, Flessner C, Franklin ME, et al. Understanding and treating trichotillomania: what we know and what we don’t know. Psychiatr Clin North Am. 2006;29(2):487-501, ix.
3. Duke DC, Keeley ML, Geffken GR, et al. Trichotillomania: a current review. Clin Psychol Rev. 2010;30(2):181-193.
An estimated 1% of Americans have trichotillomania (TTM), an impulse-control disorder in which patients experience pleasure or gratification from recurrently pulling out their own hair, resulting in noticeable hair loss.1,2 This disorder is more commonly diagnosed in women, likely reflecting treatment-seeking bias; women may be more likely to seek care for TTM because of social stigma associated with hair loss.2 Avulsion of hair usually occurs at the scalp, but also can be seen in multiple sites, including eyebrows, eyelashes, beards, and pubic regions; the number of sites typically increases with the patient’s age.3
The lifetime prevalence of comorbid axis I disorders in patients with TTM is 82%.3 Because of this, TTM often is first encountered in a psychiatric setting. Psychiatrists should have knowledge of TTM diagnosis and treatment because they may be the only point of care for TTM patients. When considering a TTM diagnosis, be aware that in some cultures rending hair is a mourning ritual or a rite of passage.3
Evidence for cognitive therapies
Behavioral models suggest TTM behaviors are learned and maintained by both classical and operant conditioning. Therapies that target the cognitive processes that trigger urges to pull, the avulsion of hair, and recognizing the consequences have the best empirical support.3
Habit reversal training (HRT) is considered the most effective treatment for TTM.3 One trial found a single 2-hour HRT intervention resulted in greater reductions in hair pulling episodes and higher remission rates compared with placebo.3 HRT trains patients to create a competing response, such as fist clenching, that is incompatible and blocks the undesired response.
Other therapeutic approaches to TTM include acceptance and commitment therapy, cognitive-behavioral therapy (CBT), and dialectical behavioral therapy-enhanced HRT. Evidence is most robust for CBT-HRT; randomized controlled trials found a statistically significant reduction in TTM in patients receiving CBT-HRT.3 One review suggests CBT-HRT should be considered first-line therapy for TTM.3
Pharmacologic options
Although no medications are FDA-approved for treating TTM, options include clomipramine, olanzapine, fluoxetine, pimozide, inositol, naltrexone, and N-acetylcysteine.2,3 The most robust trials of pharmacotherapy monotherapy were for N-acetylcysteine and naltrexone; both medications had significantly greater reduction in hair-pulling symptoms compared with placebo.3 Some evidence suggests combined pharmacotherapy and psychotherapy might be an effective approach.2,3
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
An estimated 1% of Americans have trichotillomania (TTM), an impulse-control disorder in which patients experience pleasure or gratification from recurrently pulling out their own hair, resulting in noticeable hair loss.1,2 This disorder is more commonly diagnosed in women, likely reflecting treatment-seeking bias; women may be more likely to seek care for TTM because of social stigma associated with hair loss.2 Avulsion of hair usually occurs at the scalp, but also can be seen in multiple sites, including eyebrows, eyelashes, beards, and pubic regions; the number of sites typically increases with the patient’s age.3
The lifetime prevalence of comorbid axis I disorders in patients with TTM is 82%.3 Because of this, TTM often is first encountered in a psychiatric setting. Psychiatrists should have knowledge of TTM diagnosis and treatment because they may be the only point of care for TTM patients. When considering a TTM diagnosis, be aware that in some cultures rending hair is a mourning ritual or a rite of passage.3
Evidence for cognitive therapies
Behavioral models suggest TTM behaviors are learned and maintained by both classical and operant conditioning. Therapies that target the cognitive processes that trigger urges to pull, the avulsion of hair, and recognizing the consequences have the best empirical support.3
Habit reversal training (HRT) is considered the most effective treatment for TTM.3 One trial found a single 2-hour HRT intervention resulted in greater reductions in hair pulling episodes and higher remission rates compared with placebo.3 HRT trains patients to create a competing response, such as fist clenching, that is incompatible and blocks the undesired response.
Other therapeutic approaches to TTM include acceptance and commitment therapy, cognitive-behavioral therapy (CBT), and dialectical behavioral therapy-enhanced HRT. Evidence is most robust for CBT-HRT; randomized controlled trials found a statistically significant reduction in TTM in patients receiving CBT-HRT.3 One review suggests CBT-HRT should be considered first-line therapy for TTM.3
Pharmacologic options
Although no medications are FDA-approved for treating TTM, options include clomipramine, olanzapine, fluoxetine, pimozide, inositol, naltrexone, and N-acetylcysteine.2,3 The most robust trials of pharmacotherapy monotherapy were for N-acetylcysteine and naltrexone; both medications had significantly greater reduction in hair-pulling symptoms compared with placebo.3 Some evidence suggests combined pharmacotherapy and psychotherapy might be an effective approach.2,3
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Woods DW, Flessner C, Franklin ME, et al. Understanding and treating trichotillomania: what we know and what we don’t know. Psychiatr Clin North Am. 2006;29(2):487-501, ix.
3. Duke DC, Keeley ML, Geffken GR, et al. Trichotillomania: a current review. Clin Psychol Rev. 2010;30(2):181-193.
1. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Woods DW, Flessner C, Franklin ME, et al. Understanding and treating trichotillomania: what we know and what we don’t know. Psychiatr Clin North Am. 2006;29(2):487-501, ix.
3. Duke DC, Keeley ML, Geffken GR, et al. Trichotillomania: a current review. Clin Psychol Rev. 2010;30(2):181-193.
‘Bugs in my skin’: What you should know about delusional infestation
Patients with delusional infestation (DI) falsely believe that they are infested with tiny infectious agents—typically vermin, insects, or small animals—that crawl on, in, or under their skin, leaving marks and building nests.1 Patients often describe the pathogens on the skin of hands, arms, feet, lower legs, scalp, or genital areas. They state the pathogen is difficult to diagnose and usually is contracted by human contact. Most patients with DI engage in intensive, repetitive, and often dangerous self-cleansing to get rid of the pathogens, which results in skin lesions.1 Less often, patients believe they are infested with bacteria or viruses.1
The typical DI patient is a middle age or older female with few social contacts, no psychiatric history, and normal cognitive and social function.1 Geriatric patients with dementia and vision or hearing impairment who live in a nursing home may develop DI; it also may be seen in geriatric patients with vascular encephalopathy.
What to consider
First rule out a genuine infestation by referring your patient for dermatologic and microbiologic testing. Order basic laboratory tests to assess inflammation markers—complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, electrolytes, liver function, thyroid-stimulating hormone, and fasting glucose.1 Suggest a cranial MRI to rule out a brain disorder. Also, perform a urinalysis for cocaine, amphetamines, or cannabinoids, which can cause DI.1 Rule out medical conditions that are associated with pruritus and psychiatric symptoms, including endocrine, renal, hepatic, rheumatoid, and nutritional conditions.
Treating DI patients
Collaborate with a dermatologist, microbiologist, and primary care physician because these clinicians can deliver medical interventions, such as treating skin lesions and prescribing non-sedating antihistamines to alleviate pruritus. The Table1 offers other suggestions for managing DI patients.
Pharmacotherapy. Although high-quality evidence supporting antipsychotics for treating DI is lacking, olanzapine and risperidone are considered first-line agents; haloperidol and perphenazine also are recommended.1 Response and remission rates are similar with typical and atypical antipsychotics and the median onset of efficacy with antipsychotics is approximately 1.5 weeks.1,2 Antidepressants—including escitalopram, sertraline, mirtazapine, and venlafaxine—have been shown to effectively treat DI.3 In treatment-resistant cases, pimozide and electroconvulsive therapy have been used.1
Psychotherapy is effective for only 10% of DI patients.4
Table
Treating patients with DI: What to do and what to avoid
| Do’s | Don’t |
|---|---|
| Do acknowledge and empathize with your patient’s concerns | Don’t try to convince your patient he or she is wrong about the self-diagnosis |
| Do perform a thorough physical exam and diagnostic investigation | Don’t use words such as “delusional” or “psychotic” |
| Do paraphrase symptoms as “sensations” or “crawling” instead of reinforcing or questioning them | Don’t start psychopharmacology until you establish rapport with your patient |
| Do indicate that symptoms could be secondary to overactivity of the nervous system or “unexplained dermopathy” | |
| Do suggest that antipsychotics may help reduce your patient’s distress and itching | |
| DI: delusional infestation Source: Adapted from reference 1 | |
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
2. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28(5):500-508.
3. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
4. Wykoff RF. Delusions of parasitosis: a review. Rev Infect Dis. 1987;9(3):433-437.
Patients with delusional infestation (DI) falsely believe that they are infested with tiny infectious agents—typically vermin, insects, or small animals—that crawl on, in, or under their skin, leaving marks and building nests.1 Patients often describe the pathogens on the skin of hands, arms, feet, lower legs, scalp, or genital areas. They state the pathogen is difficult to diagnose and usually is contracted by human contact. Most patients with DI engage in intensive, repetitive, and often dangerous self-cleansing to get rid of the pathogens, which results in skin lesions.1 Less often, patients believe they are infested with bacteria or viruses.1
The typical DI patient is a middle age or older female with few social contacts, no psychiatric history, and normal cognitive and social function.1 Geriatric patients with dementia and vision or hearing impairment who live in a nursing home may develop DI; it also may be seen in geriatric patients with vascular encephalopathy.
What to consider
First rule out a genuine infestation by referring your patient for dermatologic and microbiologic testing. Order basic laboratory tests to assess inflammation markers—complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, electrolytes, liver function, thyroid-stimulating hormone, and fasting glucose.1 Suggest a cranial MRI to rule out a brain disorder. Also, perform a urinalysis for cocaine, amphetamines, or cannabinoids, which can cause DI.1 Rule out medical conditions that are associated with pruritus and psychiatric symptoms, including endocrine, renal, hepatic, rheumatoid, and nutritional conditions.
Treating DI patients
Collaborate with a dermatologist, microbiologist, and primary care physician because these clinicians can deliver medical interventions, such as treating skin lesions and prescribing non-sedating antihistamines to alleviate pruritus. The Table1 offers other suggestions for managing DI patients.
Pharmacotherapy. Although high-quality evidence supporting antipsychotics for treating DI is lacking, olanzapine and risperidone are considered first-line agents; haloperidol and perphenazine also are recommended.1 Response and remission rates are similar with typical and atypical antipsychotics and the median onset of efficacy with antipsychotics is approximately 1.5 weeks.1,2 Antidepressants—including escitalopram, sertraline, mirtazapine, and venlafaxine—have been shown to effectively treat DI.3 In treatment-resistant cases, pimozide and electroconvulsive therapy have been used.1
Psychotherapy is effective for only 10% of DI patients.4
Table
Treating patients with DI: What to do and what to avoid
| Do’s | Don’t |
|---|---|
| Do acknowledge and empathize with your patient’s concerns | Don’t try to convince your patient he or she is wrong about the self-diagnosis |
| Do perform a thorough physical exam and diagnostic investigation | Don’t use words such as “delusional” or “psychotic” |
| Do paraphrase symptoms as “sensations” or “crawling” instead of reinforcing or questioning them | Don’t start psychopharmacology until you establish rapport with your patient |
| Do indicate that symptoms could be secondary to overactivity of the nervous system or “unexplained dermopathy” | |
| Do suggest that antipsychotics may help reduce your patient’s distress and itching | |
| DI: delusional infestation Source: Adapted from reference 1 | |
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Patients with delusional infestation (DI) falsely believe that they are infested with tiny infectious agents—typically vermin, insects, or small animals—that crawl on, in, or under their skin, leaving marks and building nests.1 Patients often describe the pathogens on the skin of hands, arms, feet, lower legs, scalp, or genital areas. They state the pathogen is difficult to diagnose and usually is contracted by human contact. Most patients with DI engage in intensive, repetitive, and often dangerous self-cleansing to get rid of the pathogens, which results in skin lesions.1 Less often, patients believe they are infested with bacteria or viruses.1
The typical DI patient is a middle age or older female with few social contacts, no psychiatric history, and normal cognitive and social function.1 Geriatric patients with dementia and vision or hearing impairment who live in a nursing home may develop DI; it also may be seen in geriatric patients with vascular encephalopathy.
What to consider
First rule out a genuine infestation by referring your patient for dermatologic and microbiologic testing. Order basic laboratory tests to assess inflammation markers—complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, electrolytes, liver function, thyroid-stimulating hormone, and fasting glucose.1 Suggest a cranial MRI to rule out a brain disorder. Also, perform a urinalysis for cocaine, amphetamines, or cannabinoids, which can cause DI.1 Rule out medical conditions that are associated with pruritus and psychiatric symptoms, including endocrine, renal, hepatic, rheumatoid, and nutritional conditions.
Treating DI patients
Collaborate with a dermatologist, microbiologist, and primary care physician because these clinicians can deliver medical interventions, such as treating skin lesions and prescribing non-sedating antihistamines to alleviate pruritus. The Table1 offers other suggestions for managing DI patients.
Pharmacotherapy. Although high-quality evidence supporting antipsychotics for treating DI is lacking, olanzapine and risperidone are considered first-line agents; haloperidol and perphenazine also are recommended.1 Response and remission rates are similar with typical and atypical antipsychotics and the median onset of efficacy with antipsychotics is approximately 1.5 weeks.1,2 Antidepressants—including escitalopram, sertraline, mirtazapine, and venlafaxine—have been shown to effectively treat DI.3 In treatment-resistant cases, pimozide and electroconvulsive therapy have been used.1
Psychotherapy is effective for only 10% of DI patients.4
Table
Treating patients with DI: What to do and what to avoid
| Do’s | Don’t |
|---|---|
| Do acknowledge and empathize with your patient’s concerns | Don’t try to convince your patient he or she is wrong about the self-diagnosis |
| Do perform a thorough physical exam and diagnostic investigation | Don’t use words such as “delusional” or “psychotic” |
| Do paraphrase symptoms as “sensations” or “crawling” instead of reinforcing or questioning them | Don’t start psychopharmacology until you establish rapport with your patient |
| Do indicate that symptoms could be secondary to overactivity of the nervous system or “unexplained dermopathy” | |
| Do suggest that antipsychotics may help reduce your patient’s distress and itching | |
| DI: delusional infestation Source: Adapted from reference 1 | |
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
2. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28(5):500-508.
3. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
4. Wykoff RF. Delusions of parasitosis: a review. Rev Infect Dis. 1987;9(3):433-437.
1. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
2. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28(5):500-508.
3. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
4. Wykoff RF. Delusions of parasitosis: a review. Rev Infect Dis. 1987;9(3):433-437.
Playing through the pain: Psychiatric risks among athletes
Discuss this article at www.facebook.com/CurrentPsychiatry
Suck it up. Tough it out. There is no “I” in team. These are a few of the messages athletes receive from coaches, teammates, and fans. There are norms, values, and expectations in every culture, including sports, that affect behavior and emotional expression. When taking a patient’s history, clinicians may ask about participation in sports because it provides health and lifestyle information. However, many clinicians fail to consider the extent to which sport participation can influence a person’s explanatory style, experience of injury, and attitude toward medications. Whether your patient is an elite athlete or someone who participates in sports solely for exercise, the extent to which he or she identifies as an athlete is worth exploring.
Research on athletes has focused on physical aspects of injury, but this may be just a small component of an athlete’s devastation after serious injury. In this article, we discuss athletes’:
- psychiatric risks after injury
- expression of pain
- risks of having an identity driven solely by sports
- distress tolerance.
We also provide tips for making a differential diagnosis and providing treatment. This information is based on our experience treating athletes, supplemented by relevant literature.
Psychiatric risks after injury
Research has explored eating disorders and substance use among athletes, but clinicians generally are less aware of the prevalence of mood and anxiety disorders in this population. Although participating in sports can protect against emotional distress, athletes who sustain an injury are at risk for major depressive disorder, posttraumatic stress disorder (PTSD), or an adjustment disorder.1 Only about 10% of injured athletes have severe, long-term psychological consequences,2 but the prevalence of anger and depression after an injury is well documented.3,4 Researchers have found that injured athletes experience clinically significant depression 6 times as often as non-injured athletes.5 Injured athletes also exhibit significantly greater anxiety and lower self-esteem than non-injured controls immediately after injury and at 2-month follow-up; those with more severe injuries are more likely to become depressed.6 Non-injured athletes seem to experience depression at the same rate as the general population.7
Injury and expression of pain
Psychiatric illnesses often are underreported and undertreated in athletes.8 This may be because athletes feel that admitting they have a psychiatric illness or symptoms could threaten their status with their team. One professional figure skater we treated failed to seek recommended treatment for a psychiatric disorder because she feared she would be asked to leave her skating company. Her symptoms dangerously escalated before she was hospitalized.
Based on our clinical experience, many athletes feel acute pressure to play through psychological and physical pain. Some athletes continue to play with an injury to hold on to a paycheck or scholarship. Some continue to play even though they no longer enjoy the sport to prevent letting down parents or coaches; others know no other way but to “tough it out.” Supporters such as coaches, parents, or teammates may encourage athletes to play with injury, and sometimes provide medication to do so.
Mostly, however, the pressure to continue to play despite injury comes from athletes themselves. The culture of sport may lead athletes to minimize pain, fear, and self doubt.9 Athletes who fuse the culture of sport with their own being may underreport physical and psychiatric symptoms. In a survey of National Collegiate Athletic Association Division I athletes, Nixon9 found that 70% of respondents reported having been injured at least once, and more than one-half felt pressure to play while injured. Feeling pressure to perform with injury was affected by “starter” status, and whites and men scored highest on pressure scales, although women showed a roughly equal probability of playing through injury. Students who received an athletic scholarship experienced more injuries that required surgery. There was no difference in pain expression between players of contact and non-contact sports. Finally, athletes may be less likely to seek pharmacologic treatments because of cultural messages that emphasize ideas such as “the body is a temple.”
Loss of identity
An athlete’s injury should be analyzed for meaning; what may seem insignificant to one person may be quite different for another. When injury makes athletic activity impossible, an athlete may suffer more distress than someone who does not exercise regularly. Understanding the significance of the experience for an athlete is crucial to achieving recovery.10 For example, to a non-athlete a fractured wrist may be an annoyance, but it may be disastrous to a collegiate pitcher who is forced to be inactive when scouts for Major League Baseball teams search for prospects.
To an athlete, injury can mean loss of identity. Whereas most people become competent in many aspects of life, and develop support systems across multiple contexts, an athlete—particularly an extraordinarily talented one—may have focused only on his or her sport. Although athletics can help young people develop confidence, participation also can be a trap. Individuals with strong athletic identities are less likely to explore other career, educational, and lifestyle options.11 In the context of team sports, an athlete may feel less emotionally supported if an injury results in the loss of his or her central role with the team. Helping athletes form an identity that is not based solely on sports is ideal because subsequent injuries could lead to recurrent struggles with loss of identity.
Athletes who achieve higher levels of success have higher levels of depression and higher suicidal ideation after injury.12 An athlete may attempt or complete suicide, particularly those who are injured (Box).13-16
Student athletes. When working with student athletes, it is crucial to understand the lifestyle that promotes forming a single-factor identity. Student athletes may be required to train 2 or 3 times a day, rarely spend their school breaks in tropical locations, often miss social events, and may forgo commencement ceremonies. When an injury suddenly makes these perpetual sacrifices seem to be in vain, the risk of psychiatric illness may increase.
Suicides by several high-profile athletes have called attention to the severity of psychiatric risks among athletes. In June 2002, 20-year-old Nathan Eisert died of a self-inflicted gunshot wound 5 weeks after being released from the Western Kentucky University basketball team for academic reasons; the year before, he had suffered a serious ankle injury.13 Former National Football League (NFL) player Kenny McKinley committed suicide in September 2010, after a knee injury sidelined him.14 In May 2012, former NFL star Junior Seau, who had retired in 2011, fatally shot himself.15
For some athletes, career-ending injuries lead to suicidal behaviors. A study of 5 athletes who attempted suicide after sustaining an injury found 5 common characteristics:
- all were successful in their sport before getting injured
- all sustained an injury severe enough to warrant surgery
- all endured a lengthy rehabilitation
- all were not as successful at their sport when they returned to play
- all were replaced by a teammate.16
Tolerating distress
Athletes often use their sport as an outlet for emotional expression. When an injury removes that outlet, an athlete may develop anxiety and disappointment. Left alone to manage these emotions, an athlete may become irritable, passive, socially isolated, depressed, or suicidal.17 Trying but failing to find socially acceptable ways to express these feelings may intensify depression or anger. Difficult life issues, such as avoided losses, relationship issues, or various insecurities, may come to the surface when an athlete’s primary coping skill is lost. In addition, without the support of the athletic “family” (eg, teammates, coaches, staff) many athletes turn to alcohol or drugs unless they have alternate coping strategies and social supports.18
Overtraining and stress
The differential diagnosis for athletes who present with psychiatric symptoms includes several mood and anxiety disorders and other conditions (Table). When evaluating athletes who have depressive symptoms, it is essential to rule out overtraining syndrome (OTS). A common phenomenon among athletes, OTS is characterized by athletic “staleness” and chronic fatigue.19 Although there are no official OTS diagnostic criteria, characteristic symptoms include decreased physical performance or stamina, fatigue, insomnia, change in appetite, irritability, restlessness, excitability, anxiety, weight loss, loss of motivation, and poor concentration.19 The primary distinction between OTS and depression is that OTS results from athletic endeavors and can be reversed by reducing activity.
Experiencing an injury—or even a near-miss—can be terrifying to a person who derives his or her identity from a fully functioning body and feels that a perfectly working body is essential to an acceptable life. Such athletes may develop acute stress disorder or PTSD.20,21 We treated a hockey player who just missed being involved in a serious incident on the ice. “I watched my whole athletic career up to that point flash before my eyes.… I keep getting flashes of that,” he said. After the incident, he experienced hypervigilance, avoidance, and anxiety—both on and off the ice—and was diagnosed with acute stress disorder. Similarly, we cared for a young running back whose physical symptoms had abated after experiencing a concussion. He developed an irrational fear that he would become injured again. Neither athlete had a history of psychiatric illness or serious injury, and both were paralyzed by the idea of returning to play. One of these athletes successfully engaged in exposure therapy, and the other experienced severe avoidance, hopelessness, depression, nightmares, and flashbacks before seeking treatment.
Table
Differential diagnosis of conditions associated with athletic injury
| Acute stress disorder |
| Adjustment disorder |
| Anxiety disorder NOS |
| Depressive disorder NOS |
| Major depressive disorder |
| Overtraining syndrome |
| Postconcussion syndrome |
| Posttraumatic stress disorder |
| NOS: Not otherwise specified |
Substance use: Common and risky
Anecdotal and clinical evidence suggests that athletes in different sports engage in different substance abuse patterns. Studies show that college athletes use alcohol at higher rates than non-athletes.22,23 In 2000, the American College of Sports Medicine reported that athletes’ abuse of recreational drugs far surpasses their abuse of performance-enhancing drugs.24 Some athletes may use prescription pain medications recreationally or to self-medicate emotional pain as a result of injury. Athletes may not understand the risks of recreational use of prescription medications or illicit substances—such as cocaine’s deleterious cardiovascular effects—and may hesitate to discuss their self-medicating with physicians.
Some athletes abuse performance-enhancing drugs, such as anabolic steroids, androstenedione, stimulants, diuretics, and creatine.25 Side effects of these substances include liver disease, brain hemorrhage, weight loss, and depression.25
Our recommendations
Working with athletes—particularly injured athletes who have internalized sports culture—requires informed clinical effort, whether your patient is a student athlete, elite athlete, leisure athlete, or former athlete. Successful diagnosis and treatment requires understanding the meaning of athletics in your patient’s life and the extent to which he or she has “back-up” stress relievers and support systems, and assessing for cognitive dysfunction that may contribute to mood or anxiety symptoms. During evaluation, take a careful history to distinguish major depression or adjustment disorders from OTS, and assess for PTSD symptoms. When treating an injured athlete, help the patient determine whether he or she can find another outlet—preferably more than one—to replace athletics.
For an athlete who has depressive symptoms, we recommend determining whether the patient’s symptoms remit after a brief period of rest before initiating pharmacotherapy. For patients who exhibit minimal neurovegetative features, we recommend psychotherapy as a first-line treatment. Many athletes are reluctant to take medication and would be more likely to follow through with cognitive-behavioral and biofeedback interventions.
If a patient requires pharmacotherapy, ask about his or her feelings toward medications that may impact adherence. For example, is a gymnast worried about weight gain? Is a sprinter concerned with lethargy? When prescribing, be aware of the prevalence of drug and alcohol problems among athletes, understand how habits and temptations differ among sports cultures, and provide patients with psychoeducation about substance abuse when appropriate.
Related Resources
- International Society for Sports Psychiatry. http://sportspsychiatry.org.
- Sabo D, Miller KE, Melnick MJ, et al. High school athletic participation and adolescent suicide: a nationwide U.S. study. Int Rev Sociol Sport. 2005;40(1):5-23. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563797. Accessed June 7, 2012.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brewer BW, Linder DE, Phelps CM. Situational correlates of emotional adjustment to athletic injury. Clin J Sport Med. 1995;5(4):241-245.
2. Brewer BW, Petrie TA. Psychopathology in sport and exercise. In: Van Raalte JL Brewer BW, eds. Exploring sport and exercise psychology. Washington, DC: American Psychological Association; 1996:257–274.
3. May J, Sieb G. Athletic injuries: psychosocial factors in the onset sequelae, rehabilitation and prevention. In: May JR, Asken MJ, eds. Sport psychology: the psychological health of the athlete. New York, NY: PMA Publishing; 1987: 157–185.
4. Quackenbush N, Crossman J. Injured athletes: a study of emotional responses. J Sport Behav. 1994;17:178-187.
5. Perna F, Roh J, Newcomer R, et al. Clinical depression among injured athletes: an empirical assessment. Presented at: Association for the Advancement of Applied Sport Psychology annual convention; September 1998; Hyannis, MA.
6. Leddy MH, Lambert MJ, Ogles BM. Psychological consequences of athletic injury among high-level competitors. Res Q Exerc Sport. 1994;65(4):347-354.
7. Schwenk TL. The stigmatisation and denial of mental illness in athletes. Br J Sports Med. 2000;34(1):4-5.
8. Rotella RJ, Heyman SR. Stress injury, and the psychological rehabilitation of athletes. In: Williams HR, ed. Applied sports psychology: personal growth to peak performance. 2nd ed. Mountain View, CA: Mayfield Publishing; 1993: 338–355.
9. Nixon HL, II. Explaining pain and injury attitudes and experiences in sport in terms of gender race, and sports status factors. Journal of Sport Social Issues. 1996;20(1):33-44.
10. Harris LL. Integrating and analyzing psychosocial and stage theories to challenge the development of the injured collegiate athlete. J Athl Train. 2003;38(1):75-82.
11. Brown C, Hartley DL. Athletic identity and career maturation of male college student athletes. International Journal of Sport Psychology. 1998;29(1):17-26.
12. Baum AL. Suicide in athletes: a review and commentary. Clin Sports Med. 2005;24(4):853-859, ix.
13. Ho J. Suicide on campus. CBS News. http://www.cbsnews.com/2100-500195_162-654130.html. Published February 11 2009. Accessed June 7, 2012.
14. Bunch J, Jones LH. Broncos WR Kenny McKinley found dead in apparent suicide. Denver Post. http://www.denverpost.com/sports/ci_16127852. Published September 20 2010. Accessed June 7, 2012.
15. Saraceno J. Junior Seau’s death came with ‘zero warning.’ USA Today. http://www.usatoday.com/sports/football/nfl/story/2012-05-02/junior-seau-dead-gunshot/54712488/1. Published May 3 2012. Accessed June 7, 2012.
16. Smith AM, Milliner EK. Injured athletes and the risk of suicide. J Athl Train. 1994;29(4):337-341.
17. Putukian M, Wilfert M. National Collegiate Athletic Association. Student-athletes also face dangers from depression. http://fs.ncaa.org/Docs/NCAANewsArchive/2004/Association-Wide/student-athletes+also+face+dangers+from+depression+-+4-12-04.html. Published April 12 2004. Accessed June 6, 2012.
18. Perna FM, Antoni MH, Baum A, et al. Cognitive behavioral stress management effects on injury and illness among competitive athletes: a randomized clinical trial. Ann Behav Med. 2003;25(1):66-73.
19. Armstrong LE, VanHeest JL. The unknown mechanism of the overtraining syndrome: clues from depression and psychoneuroimmunology. Sports Med. 2002;32(3):185-209.
20. Newcomer RR, Perna FM. Features of posttraumatic distress among adolescent athletes. J Athl Train. 2003;38(2):163-166.
21. Newcomer R, Roh J, Perna F, et al. Injury as a traumatic experience: Intrusive thoughts and avoidance behavior associated with injury among college student-athletes. J Appl Sport Psychol. 1998;10(suppl):S54.
22. Hildebrand KM, Johnson DJ, Bogle K. Comparison of patterns of alcohol use between high school and college athletes and non-athletes. College Student Journal. 2001;35:358-365.
23. Wilson GS, Pritchard ME, Schaffer J. Athletic status and drinking behavior in college students: the influence of gender and coping styles. J Am Coll Health. 2004;52(6):269-273.
24. Wadler GI. American College of Sports Medicine. Cocaine abuse in sports. http://www.acsm.org/docs/current-comments/cocainabuse.pdf. Accessed June 6, 2012.
25. Mayo Clinic. Performance-enhancing drugs: know the risks. http://www.mayoclinic.com/health/performance-enhancing-drugs/hq01105. Published December 23, 2010.
Discuss this article at www.facebook.com/CurrentPsychiatry
Suck it up. Tough it out. There is no “I” in team. These are a few of the messages athletes receive from coaches, teammates, and fans. There are norms, values, and expectations in every culture, including sports, that affect behavior and emotional expression. When taking a patient’s history, clinicians may ask about participation in sports because it provides health and lifestyle information. However, many clinicians fail to consider the extent to which sport participation can influence a person’s explanatory style, experience of injury, and attitude toward medications. Whether your patient is an elite athlete or someone who participates in sports solely for exercise, the extent to which he or she identifies as an athlete is worth exploring.
Research on athletes has focused on physical aspects of injury, but this may be just a small component of an athlete’s devastation after serious injury. In this article, we discuss athletes’:
- psychiatric risks after injury
- expression of pain
- risks of having an identity driven solely by sports
- distress tolerance.
We also provide tips for making a differential diagnosis and providing treatment. This information is based on our experience treating athletes, supplemented by relevant literature.
Psychiatric risks after injury
Research has explored eating disorders and substance use among athletes, but clinicians generally are less aware of the prevalence of mood and anxiety disorders in this population. Although participating in sports can protect against emotional distress, athletes who sustain an injury are at risk for major depressive disorder, posttraumatic stress disorder (PTSD), or an adjustment disorder.1 Only about 10% of injured athletes have severe, long-term psychological consequences,2 but the prevalence of anger and depression after an injury is well documented.3,4 Researchers have found that injured athletes experience clinically significant depression 6 times as often as non-injured athletes.5 Injured athletes also exhibit significantly greater anxiety and lower self-esteem than non-injured controls immediately after injury and at 2-month follow-up; those with more severe injuries are more likely to become depressed.6 Non-injured athletes seem to experience depression at the same rate as the general population.7
Injury and expression of pain
Psychiatric illnesses often are underreported and undertreated in athletes.8 This may be because athletes feel that admitting they have a psychiatric illness or symptoms could threaten their status with their team. One professional figure skater we treated failed to seek recommended treatment for a psychiatric disorder because she feared she would be asked to leave her skating company. Her symptoms dangerously escalated before she was hospitalized.
Based on our clinical experience, many athletes feel acute pressure to play through psychological and physical pain. Some athletes continue to play with an injury to hold on to a paycheck or scholarship. Some continue to play even though they no longer enjoy the sport to prevent letting down parents or coaches; others know no other way but to “tough it out.” Supporters such as coaches, parents, or teammates may encourage athletes to play with injury, and sometimes provide medication to do so.
Mostly, however, the pressure to continue to play despite injury comes from athletes themselves. The culture of sport may lead athletes to minimize pain, fear, and self doubt.9 Athletes who fuse the culture of sport with their own being may underreport physical and psychiatric symptoms. In a survey of National Collegiate Athletic Association Division I athletes, Nixon9 found that 70% of respondents reported having been injured at least once, and more than one-half felt pressure to play while injured. Feeling pressure to perform with injury was affected by “starter” status, and whites and men scored highest on pressure scales, although women showed a roughly equal probability of playing through injury. Students who received an athletic scholarship experienced more injuries that required surgery. There was no difference in pain expression between players of contact and non-contact sports. Finally, athletes may be less likely to seek pharmacologic treatments because of cultural messages that emphasize ideas such as “the body is a temple.”
Loss of identity
An athlete’s injury should be analyzed for meaning; what may seem insignificant to one person may be quite different for another. When injury makes athletic activity impossible, an athlete may suffer more distress than someone who does not exercise regularly. Understanding the significance of the experience for an athlete is crucial to achieving recovery.10 For example, to a non-athlete a fractured wrist may be an annoyance, but it may be disastrous to a collegiate pitcher who is forced to be inactive when scouts for Major League Baseball teams search for prospects.
To an athlete, injury can mean loss of identity. Whereas most people become competent in many aspects of life, and develop support systems across multiple contexts, an athlete—particularly an extraordinarily talented one—may have focused only on his or her sport. Although athletics can help young people develop confidence, participation also can be a trap. Individuals with strong athletic identities are less likely to explore other career, educational, and lifestyle options.11 In the context of team sports, an athlete may feel less emotionally supported if an injury results in the loss of his or her central role with the team. Helping athletes form an identity that is not based solely on sports is ideal because subsequent injuries could lead to recurrent struggles with loss of identity.
Athletes who achieve higher levels of success have higher levels of depression and higher suicidal ideation after injury.12 An athlete may attempt or complete suicide, particularly those who are injured (Box).13-16
Student athletes. When working with student athletes, it is crucial to understand the lifestyle that promotes forming a single-factor identity. Student athletes may be required to train 2 or 3 times a day, rarely spend their school breaks in tropical locations, often miss social events, and may forgo commencement ceremonies. When an injury suddenly makes these perpetual sacrifices seem to be in vain, the risk of psychiatric illness may increase.
Suicides by several high-profile athletes have called attention to the severity of psychiatric risks among athletes. In June 2002, 20-year-old Nathan Eisert died of a self-inflicted gunshot wound 5 weeks after being released from the Western Kentucky University basketball team for academic reasons; the year before, he had suffered a serious ankle injury.13 Former National Football League (NFL) player Kenny McKinley committed suicide in September 2010, after a knee injury sidelined him.14 In May 2012, former NFL star Junior Seau, who had retired in 2011, fatally shot himself.15
For some athletes, career-ending injuries lead to suicidal behaviors. A study of 5 athletes who attempted suicide after sustaining an injury found 5 common characteristics:
- all were successful in their sport before getting injured
- all sustained an injury severe enough to warrant surgery
- all endured a lengthy rehabilitation
- all were not as successful at their sport when they returned to play
- all were replaced by a teammate.16
Tolerating distress
Athletes often use their sport as an outlet for emotional expression. When an injury removes that outlet, an athlete may develop anxiety and disappointment. Left alone to manage these emotions, an athlete may become irritable, passive, socially isolated, depressed, or suicidal.17 Trying but failing to find socially acceptable ways to express these feelings may intensify depression or anger. Difficult life issues, such as avoided losses, relationship issues, or various insecurities, may come to the surface when an athlete’s primary coping skill is lost. In addition, without the support of the athletic “family” (eg, teammates, coaches, staff) many athletes turn to alcohol or drugs unless they have alternate coping strategies and social supports.18
Overtraining and stress
The differential diagnosis for athletes who present with psychiatric symptoms includes several mood and anxiety disorders and other conditions (Table). When evaluating athletes who have depressive symptoms, it is essential to rule out overtraining syndrome (OTS). A common phenomenon among athletes, OTS is characterized by athletic “staleness” and chronic fatigue.19 Although there are no official OTS diagnostic criteria, characteristic symptoms include decreased physical performance or stamina, fatigue, insomnia, change in appetite, irritability, restlessness, excitability, anxiety, weight loss, loss of motivation, and poor concentration.19 The primary distinction between OTS and depression is that OTS results from athletic endeavors and can be reversed by reducing activity.
Experiencing an injury—or even a near-miss—can be terrifying to a person who derives his or her identity from a fully functioning body and feels that a perfectly working body is essential to an acceptable life. Such athletes may develop acute stress disorder or PTSD.20,21 We treated a hockey player who just missed being involved in a serious incident on the ice. “I watched my whole athletic career up to that point flash before my eyes.… I keep getting flashes of that,” he said. After the incident, he experienced hypervigilance, avoidance, and anxiety—both on and off the ice—and was diagnosed with acute stress disorder. Similarly, we cared for a young running back whose physical symptoms had abated after experiencing a concussion. He developed an irrational fear that he would become injured again. Neither athlete had a history of psychiatric illness or serious injury, and both were paralyzed by the idea of returning to play. One of these athletes successfully engaged in exposure therapy, and the other experienced severe avoidance, hopelessness, depression, nightmares, and flashbacks before seeking treatment.
Table
Differential diagnosis of conditions associated with athletic injury
| Acute stress disorder |
| Adjustment disorder |
| Anxiety disorder NOS |
| Depressive disorder NOS |
| Major depressive disorder |
| Overtraining syndrome |
| Postconcussion syndrome |
| Posttraumatic stress disorder |
| NOS: Not otherwise specified |
Substance use: Common and risky
Anecdotal and clinical evidence suggests that athletes in different sports engage in different substance abuse patterns. Studies show that college athletes use alcohol at higher rates than non-athletes.22,23 In 2000, the American College of Sports Medicine reported that athletes’ abuse of recreational drugs far surpasses their abuse of performance-enhancing drugs.24 Some athletes may use prescription pain medications recreationally or to self-medicate emotional pain as a result of injury. Athletes may not understand the risks of recreational use of prescription medications or illicit substances—such as cocaine’s deleterious cardiovascular effects—and may hesitate to discuss their self-medicating with physicians.
Some athletes abuse performance-enhancing drugs, such as anabolic steroids, androstenedione, stimulants, diuretics, and creatine.25 Side effects of these substances include liver disease, brain hemorrhage, weight loss, and depression.25
Our recommendations
Working with athletes—particularly injured athletes who have internalized sports culture—requires informed clinical effort, whether your patient is a student athlete, elite athlete, leisure athlete, or former athlete. Successful diagnosis and treatment requires understanding the meaning of athletics in your patient’s life and the extent to which he or she has “back-up” stress relievers and support systems, and assessing for cognitive dysfunction that may contribute to mood or anxiety symptoms. During evaluation, take a careful history to distinguish major depression or adjustment disorders from OTS, and assess for PTSD symptoms. When treating an injured athlete, help the patient determine whether he or she can find another outlet—preferably more than one—to replace athletics.
For an athlete who has depressive symptoms, we recommend determining whether the patient’s symptoms remit after a brief period of rest before initiating pharmacotherapy. For patients who exhibit minimal neurovegetative features, we recommend psychotherapy as a first-line treatment. Many athletes are reluctant to take medication and would be more likely to follow through with cognitive-behavioral and biofeedback interventions.
If a patient requires pharmacotherapy, ask about his or her feelings toward medications that may impact adherence. For example, is a gymnast worried about weight gain? Is a sprinter concerned with lethargy? When prescribing, be aware of the prevalence of drug and alcohol problems among athletes, understand how habits and temptations differ among sports cultures, and provide patients with psychoeducation about substance abuse when appropriate.
Related Resources
- International Society for Sports Psychiatry. http://sportspsychiatry.org.
- Sabo D, Miller KE, Melnick MJ, et al. High school athletic participation and adolescent suicide: a nationwide U.S. study. Int Rev Sociol Sport. 2005;40(1):5-23. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563797. Accessed June 7, 2012.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Suck it up. Tough it out. There is no “I” in team. These are a few of the messages athletes receive from coaches, teammates, and fans. There are norms, values, and expectations in every culture, including sports, that affect behavior and emotional expression. When taking a patient’s history, clinicians may ask about participation in sports because it provides health and lifestyle information. However, many clinicians fail to consider the extent to which sport participation can influence a person’s explanatory style, experience of injury, and attitude toward medications. Whether your patient is an elite athlete or someone who participates in sports solely for exercise, the extent to which he or she identifies as an athlete is worth exploring.
Research on athletes has focused on physical aspects of injury, but this may be just a small component of an athlete’s devastation after serious injury. In this article, we discuss athletes’:
- psychiatric risks after injury
- expression of pain
- risks of having an identity driven solely by sports
- distress tolerance.
We also provide tips for making a differential diagnosis and providing treatment. This information is based on our experience treating athletes, supplemented by relevant literature.
Psychiatric risks after injury
Research has explored eating disorders and substance use among athletes, but clinicians generally are less aware of the prevalence of mood and anxiety disorders in this population. Although participating in sports can protect against emotional distress, athletes who sustain an injury are at risk for major depressive disorder, posttraumatic stress disorder (PTSD), or an adjustment disorder.1 Only about 10% of injured athletes have severe, long-term psychological consequences,2 but the prevalence of anger and depression after an injury is well documented.3,4 Researchers have found that injured athletes experience clinically significant depression 6 times as often as non-injured athletes.5 Injured athletes also exhibit significantly greater anxiety and lower self-esteem than non-injured controls immediately after injury and at 2-month follow-up; those with more severe injuries are more likely to become depressed.6 Non-injured athletes seem to experience depression at the same rate as the general population.7
Injury and expression of pain
Psychiatric illnesses often are underreported and undertreated in athletes.8 This may be because athletes feel that admitting they have a psychiatric illness or symptoms could threaten their status with their team. One professional figure skater we treated failed to seek recommended treatment for a psychiatric disorder because she feared she would be asked to leave her skating company. Her symptoms dangerously escalated before she was hospitalized.
Based on our clinical experience, many athletes feel acute pressure to play through psychological and physical pain. Some athletes continue to play with an injury to hold on to a paycheck or scholarship. Some continue to play even though they no longer enjoy the sport to prevent letting down parents or coaches; others know no other way but to “tough it out.” Supporters such as coaches, parents, or teammates may encourage athletes to play with injury, and sometimes provide medication to do so.
Mostly, however, the pressure to continue to play despite injury comes from athletes themselves. The culture of sport may lead athletes to minimize pain, fear, and self doubt.9 Athletes who fuse the culture of sport with their own being may underreport physical and psychiatric symptoms. In a survey of National Collegiate Athletic Association Division I athletes, Nixon9 found that 70% of respondents reported having been injured at least once, and more than one-half felt pressure to play while injured. Feeling pressure to perform with injury was affected by “starter” status, and whites and men scored highest on pressure scales, although women showed a roughly equal probability of playing through injury. Students who received an athletic scholarship experienced more injuries that required surgery. There was no difference in pain expression between players of contact and non-contact sports. Finally, athletes may be less likely to seek pharmacologic treatments because of cultural messages that emphasize ideas such as “the body is a temple.”
Loss of identity
An athlete’s injury should be analyzed for meaning; what may seem insignificant to one person may be quite different for another. When injury makes athletic activity impossible, an athlete may suffer more distress than someone who does not exercise regularly. Understanding the significance of the experience for an athlete is crucial to achieving recovery.10 For example, to a non-athlete a fractured wrist may be an annoyance, but it may be disastrous to a collegiate pitcher who is forced to be inactive when scouts for Major League Baseball teams search for prospects.
To an athlete, injury can mean loss of identity. Whereas most people become competent in many aspects of life, and develop support systems across multiple contexts, an athlete—particularly an extraordinarily talented one—may have focused only on his or her sport. Although athletics can help young people develop confidence, participation also can be a trap. Individuals with strong athletic identities are less likely to explore other career, educational, and lifestyle options.11 In the context of team sports, an athlete may feel less emotionally supported if an injury results in the loss of his or her central role with the team. Helping athletes form an identity that is not based solely on sports is ideal because subsequent injuries could lead to recurrent struggles with loss of identity.
Athletes who achieve higher levels of success have higher levels of depression and higher suicidal ideation after injury.12 An athlete may attempt or complete suicide, particularly those who are injured (Box).13-16
Student athletes. When working with student athletes, it is crucial to understand the lifestyle that promotes forming a single-factor identity. Student athletes may be required to train 2 or 3 times a day, rarely spend their school breaks in tropical locations, often miss social events, and may forgo commencement ceremonies. When an injury suddenly makes these perpetual sacrifices seem to be in vain, the risk of psychiatric illness may increase.
Suicides by several high-profile athletes have called attention to the severity of psychiatric risks among athletes. In June 2002, 20-year-old Nathan Eisert died of a self-inflicted gunshot wound 5 weeks after being released from the Western Kentucky University basketball team for academic reasons; the year before, he had suffered a serious ankle injury.13 Former National Football League (NFL) player Kenny McKinley committed suicide in September 2010, after a knee injury sidelined him.14 In May 2012, former NFL star Junior Seau, who had retired in 2011, fatally shot himself.15
For some athletes, career-ending injuries lead to suicidal behaviors. A study of 5 athletes who attempted suicide after sustaining an injury found 5 common characteristics:
- all were successful in their sport before getting injured
- all sustained an injury severe enough to warrant surgery
- all endured a lengthy rehabilitation
- all were not as successful at their sport when they returned to play
- all were replaced by a teammate.16
Tolerating distress
Athletes often use their sport as an outlet for emotional expression. When an injury removes that outlet, an athlete may develop anxiety and disappointment. Left alone to manage these emotions, an athlete may become irritable, passive, socially isolated, depressed, or suicidal.17 Trying but failing to find socially acceptable ways to express these feelings may intensify depression or anger. Difficult life issues, such as avoided losses, relationship issues, or various insecurities, may come to the surface when an athlete’s primary coping skill is lost. In addition, without the support of the athletic “family” (eg, teammates, coaches, staff) many athletes turn to alcohol or drugs unless they have alternate coping strategies and social supports.18
Overtraining and stress
The differential diagnosis for athletes who present with psychiatric symptoms includes several mood and anxiety disorders and other conditions (Table). When evaluating athletes who have depressive symptoms, it is essential to rule out overtraining syndrome (OTS). A common phenomenon among athletes, OTS is characterized by athletic “staleness” and chronic fatigue.19 Although there are no official OTS diagnostic criteria, characteristic symptoms include decreased physical performance or stamina, fatigue, insomnia, change in appetite, irritability, restlessness, excitability, anxiety, weight loss, loss of motivation, and poor concentration.19 The primary distinction between OTS and depression is that OTS results from athletic endeavors and can be reversed by reducing activity.
Experiencing an injury—or even a near-miss—can be terrifying to a person who derives his or her identity from a fully functioning body and feels that a perfectly working body is essential to an acceptable life. Such athletes may develop acute stress disorder or PTSD.20,21 We treated a hockey player who just missed being involved in a serious incident on the ice. “I watched my whole athletic career up to that point flash before my eyes.… I keep getting flashes of that,” he said. After the incident, he experienced hypervigilance, avoidance, and anxiety—both on and off the ice—and was diagnosed with acute stress disorder. Similarly, we cared for a young running back whose physical symptoms had abated after experiencing a concussion. He developed an irrational fear that he would become injured again. Neither athlete had a history of psychiatric illness or serious injury, and both were paralyzed by the idea of returning to play. One of these athletes successfully engaged in exposure therapy, and the other experienced severe avoidance, hopelessness, depression, nightmares, and flashbacks before seeking treatment.
Table
Differential diagnosis of conditions associated with athletic injury
| Acute stress disorder |
| Adjustment disorder |
| Anxiety disorder NOS |
| Depressive disorder NOS |
| Major depressive disorder |
| Overtraining syndrome |
| Postconcussion syndrome |
| Posttraumatic stress disorder |
| NOS: Not otherwise specified |
Substance use: Common and risky
Anecdotal and clinical evidence suggests that athletes in different sports engage in different substance abuse patterns. Studies show that college athletes use alcohol at higher rates than non-athletes.22,23 In 2000, the American College of Sports Medicine reported that athletes’ abuse of recreational drugs far surpasses their abuse of performance-enhancing drugs.24 Some athletes may use prescription pain medications recreationally or to self-medicate emotional pain as a result of injury. Athletes may not understand the risks of recreational use of prescription medications or illicit substances—such as cocaine’s deleterious cardiovascular effects—and may hesitate to discuss their self-medicating with physicians.
Some athletes abuse performance-enhancing drugs, such as anabolic steroids, androstenedione, stimulants, diuretics, and creatine.25 Side effects of these substances include liver disease, brain hemorrhage, weight loss, and depression.25
Our recommendations
Working with athletes—particularly injured athletes who have internalized sports culture—requires informed clinical effort, whether your patient is a student athlete, elite athlete, leisure athlete, or former athlete. Successful diagnosis and treatment requires understanding the meaning of athletics in your patient’s life and the extent to which he or she has “back-up” stress relievers and support systems, and assessing for cognitive dysfunction that may contribute to mood or anxiety symptoms. During evaluation, take a careful history to distinguish major depression or adjustment disorders from OTS, and assess for PTSD symptoms. When treating an injured athlete, help the patient determine whether he or she can find another outlet—preferably more than one—to replace athletics.
For an athlete who has depressive symptoms, we recommend determining whether the patient’s symptoms remit after a brief period of rest before initiating pharmacotherapy. For patients who exhibit minimal neurovegetative features, we recommend psychotherapy as a first-line treatment. Many athletes are reluctant to take medication and would be more likely to follow through with cognitive-behavioral and biofeedback interventions.
If a patient requires pharmacotherapy, ask about his or her feelings toward medications that may impact adherence. For example, is a gymnast worried about weight gain? Is a sprinter concerned with lethargy? When prescribing, be aware of the prevalence of drug and alcohol problems among athletes, understand how habits and temptations differ among sports cultures, and provide patients with psychoeducation about substance abuse when appropriate.
Related Resources
- International Society for Sports Psychiatry. http://sportspsychiatry.org.
- Sabo D, Miller KE, Melnick MJ, et al. High school athletic participation and adolescent suicide: a nationwide U.S. study. Int Rev Sociol Sport. 2005;40(1):5-23. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563797. Accessed June 7, 2012.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brewer BW, Linder DE, Phelps CM. Situational correlates of emotional adjustment to athletic injury. Clin J Sport Med. 1995;5(4):241-245.
2. Brewer BW, Petrie TA. Psychopathology in sport and exercise. In: Van Raalte JL Brewer BW, eds. Exploring sport and exercise psychology. Washington, DC: American Psychological Association; 1996:257–274.
3. May J, Sieb G. Athletic injuries: psychosocial factors in the onset sequelae, rehabilitation and prevention. In: May JR, Asken MJ, eds. Sport psychology: the psychological health of the athlete. New York, NY: PMA Publishing; 1987: 157–185.
4. Quackenbush N, Crossman J. Injured athletes: a study of emotional responses. J Sport Behav. 1994;17:178-187.
5. Perna F, Roh J, Newcomer R, et al. Clinical depression among injured athletes: an empirical assessment. Presented at: Association for the Advancement of Applied Sport Psychology annual convention; September 1998; Hyannis, MA.
6. Leddy MH, Lambert MJ, Ogles BM. Psychological consequences of athletic injury among high-level competitors. Res Q Exerc Sport. 1994;65(4):347-354.
7. Schwenk TL. The stigmatisation and denial of mental illness in athletes. Br J Sports Med. 2000;34(1):4-5.
8. Rotella RJ, Heyman SR. Stress injury, and the psychological rehabilitation of athletes. In: Williams HR, ed. Applied sports psychology: personal growth to peak performance. 2nd ed. Mountain View, CA: Mayfield Publishing; 1993: 338–355.
9. Nixon HL, II. Explaining pain and injury attitudes and experiences in sport in terms of gender race, and sports status factors. Journal of Sport Social Issues. 1996;20(1):33-44.
10. Harris LL. Integrating and analyzing psychosocial and stage theories to challenge the development of the injured collegiate athlete. J Athl Train. 2003;38(1):75-82.
11. Brown C, Hartley DL. Athletic identity and career maturation of male college student athletes. International Journal of Sport Psychology. 1998;29(1):17-26.
12. Baum AL. Suicide in athletes: a review and commentary. Clin Sports Med. 2005;24(4):853-859, ix.
13. Ho J. Suicide on campus. CBS News. http://www.cbsnews.com/2100-500195_162-654130.html. Published February 11 2009. Accessed June 7, 2012.
14. Bunch J, Jones LH. Broncos WR Kenny McKinley found dead in apparent suicide. Denver Post. http://www.denverpost.com/sports/ci_16127852. Published September 20 2010. Accessed June 7, 2012.
15. Saraceno J. Junior Seau’s death came with ‘zero warning.’ USA Today. http://www.usatoday.com/sports/football/nfl/story/2012-05-02/junior-seau-dead-gunshot/54712488/1. Published May 3 2012. Accessed June 7, 2012.
16. Smith AM, Milliner EK. Injured athletes and the risk of suicide. J Athl Train. 1994;29(4):337-341.
17. Putukian M, Wilfert M. National Collegiate Athletic Association. Student-athletes also face dangers from depression. http://fs.ncaa.org/Docs/NCAANewsArchive/2004/Association-Wide/student-athletes+also+face+dangers+from+depression+-+4-12-04.html. Published April 12 2004. Accessed June 6, 2012.
18. Perna FM, Antoni MH, Baum A, et al. Cognitive behavioral stress management effects on injury and illness among competitive athletes: a randomized clinical trial. Ann Behav Med. 2003;25(1):66-73.
19. Armstrong LE, VanHeest JL. The unknown mechanism of the overtraining syndrome: clues from depression and psychoneuroimmunology. Sports Med. 2002;32(3):185-209.
20. Newcomer RR, Perna FM. Features of posttraumatic distress among adolescent athletes. J Athl Train. 2003;38(2):163-166.
21. Newcomer R, Roh J, Perna F, et al. Injury as a traumatic experience: Intrusive thoughts and avoidance behavior associated with injury among college student-athletes. J Appl Sport Psychol. 1998;10(suppl):S54.
22. Hildebrand KM, Johnson DJ, Bogle K. Comparison of patterns of alcohol use between high school and college athletes and non-athletes. College Student Journal. 2001;35:358-365.
23. Wilson GS, Pritchard ME, Schaffer J. Athletic status and drinking behavior in college students: the influence of gender and coping styles. J Am Coll Health. 2004;52(6):269-273.
24. Wadler GI. American College of Sports Medicine. Cocaine abuse in sports. http://www.acsm.org/docs/current-comments/cocainabuse.pdf. Accessed June 6, 2012.
25. Mayo Clinic. Performance-enhancing drugs: know the risks. http://www.mayoclinic.com/health/performance-enhancing-drugs/hq01105. Published December 23, 2010.
1. Brewer BW, Linder DE, Phelps CM. Situational correlates of emotional adjustment to athletic injury. Clin J Sport Med. 1995;5(4):241-245.
2. Brewer BW, Petrie TA. Psychopathology in sport and exercise. In: Van Raalte JL Brewer BW, eds. Exploring sport and exercise psychology. Washington, DC: American Psychological Association; 1996:257–274.
3. May J, Sieb G. Athletic injuries: psychosocial factors in the onset sequelae, rehabilitation and prevention. In: May JR, Asken MJ, eds. Sport psychology: the psychological health of the athlete. New York, NY: PMA Publishing; 1987: 157–185.
4. Quackenbush N, Crossman J. Injured athletes: a study of emotional responses. J Sport Behav. 1994;17:178-187.
5. Perna F, Roh J, Newcomer R, et al. Clinical depression among injured athletes: an empirical assessment. Presented at: Association for the Advancement of Applied Sport Psychology annual convention; September 1998; Hyannis, MA.
6. Leddy MH, Lambert MJ, Ogles BM. Psychological consequences of athletic injury among high-level competitors. Res Q Exerc Sport. 1994;65(4):347-354.
7. Schwenk TL. The stigmatisation and denial of mental illness in athletes. Br J Sports Med. 2000;34(1):4-5.
8. Rotella RJ, Heyman SR. Stress injury, and the psychological rehabilitation of athletes. In: Williams HR, ed. Applied sports psychology: personal growth to peak performance. 2nd ed. Mountain View, CA: Mayfield Publishing; 1993: 338–355.
9. Nixon HL, II. Explaining pain and injury attitudes and experiences in sport in terms of gender race, and sports status factors. Journal of Sport Social Issues. 1996;20(1):33-44.
10. Harris LL. Integrating and analyzing psychosocial and stage theories to challenge the development of the injured collegiate athlete. J Athl Train. 2003;38(1):75-82.
11. Brown C, Hartley DL. Athletic identity and career maturation of male college student athletes. International Journal of Sport Psychology. 1998;29(1):17-26.
12. Baum AL. Suicide in athletes: a review and commentary. Clin Sports Med. 2005;24(4):853-859, ix.
13. Ho J. Suicide on campus. CBS News. http://www.cbsnews.com/2100-500195_162-654130.html. Published February 11 2009. Accessed June 7, 2012.
14. Bunch J, Jones LH. Broncos WR Kenny McKinley found dead in apparent suicide. Denver Post. http://www.denverpost.com/sports/ci_16127852. Published September 20 2010. Accessed June 7, 2012.
15. Saraceno J. Junior Seau’s death came with ‘zero warning.’ USA Today. http://www.usatoday.com/sports/football/nfl/story/2012-05-02/junior-seau-dead-gunshot/54712488/1. Published May 3 2012. Accessed June 7, 2012.
16. Smith AM, Milliner EK. Injured athletes and the risk of suicide. J Athl Train. 1994;29(4):337-341.
17. Putukian M, Wilfert M. National Collegiate Athletic Association. Student-athletes also face dangers from depression. http://fs.ncaa.org/Docs/NCAANewsArchive/2004/Association-Wide/student-athletes+also+face+dangers+from+depression+-+4-12-04.html. Published April 12 2004. Accessed June 6, 2012.
18. Perna FM, Antoni MH, Baum A, et al. Cognitive behavioral stress management effects on injury and illness among competitive athletes: a randomized clinical trial. Ann Behav Med. 2003;25(1):66-73.
19. Armstrong LE, VanHeest JL. The unknown mechanism of the overtraining syndrome: clues from depression and psychoneuroimmunology. Sports Med. 2002;32(3):185-209.
20. Newcomer RR, Perna FM. Features of posttraumatic distress among adolescent athletes. J Athl Train. 2003;38(2):163-166.
21. Newcomer R, Roh J, Perna F, et al. Injury as a traumatic experience: Intrusive thoughts and avoidance behavior associated with injury among college student-athletes. J Appl Sport Psychol. 1998;10(suppl):S54.
22. Hildebrand KM, Johnson DJ, Bogle K. Comparison of patterns of alcohol use between high school and college athletes and non-athletes. College Student Journal. 2001;35:358-365.
23. Wilson GS, Pritchard ME, Schaffer J. Athletic status and drinking behavior in college students: the influence of gender and coping styles. J Am Coll Health. 2004;52(6):269-273.
24. Wadler GI. American College of Sports Medicine. Cocaine abuse in sports. http://www.acsm.org/docs/current-comments/cocainabuse.pdf. Accessed June 6, 2012.
25. Mayo Clinic. Performance-enhancing drugs: know the risks. http://www.mayoclinic.com/health/performance-enhancing-drugs/hq01105. Published December 23, 2010.
Strategies for managing patients with chronic subjective dizziness
Discuss this article at www.facebook.com/CurrentPsychiatry
Chronic subjective dizziness (CSD) is characterized by persistent (>3 months) dizziness, lightheadedness, or unsteadiness, without vertigo or ataxia. Symptoms often are worse in highly stimulating visual environments (eg, busy malls or grocery stores) or settings with indistinct visual orientation cues (eg, large open areas, heavy fog). Neuro-otologic examination and laboratory testing reveal no active vestibular deficits.1
CSD is not a psychiatric illness, but exists at the interface of psychiatry and neuro-otology. For example, anxiety and depressive disorders often accompany CSD, but are not an integral part of it. Treatment outcomes are good and prognosis for full function is high.
Conditions that cause dizziness
Vertigo—a sensation of rotation or linear movement of self or surroundings—occurs in discrete attacks that typically have an acute onset and are caused by neuro-otologic conditions.2 Symptoms may last for seconds (benign paroxysmal positional vertigo [BPPV]), hours (Meniere’s disease), minutes to days (vestibular migraine), or weeks (vestibular neuronitis). Unsteadiness, a swaying or rocking sensation, dizziness, and a disturbed sense of spatial orientation without illusory movement may be acute, subacute, or chronic. These symptoms may accompany vertigo or occur independently.2 Psychiatric disorders (panic), dysautonomias (vasovagal spells), and cardiovascular conditions (dysrhythmias) may cause episodic unsteadiness and dizziness, but not vertigo. Several illnesses can cause persistent unsteadiness and dizziness, including bilateral peripheral vestibular deficits, central vestibular lesions (strokes), proprioceptive or visual loss (neuropathies), and generalized anxiety disorder.
Up to 30% of patients who experience episodic balance problems develop persistent unsteadiness or dizziness (ie, CSD).3 Clinical history, exam, and laboratory tests may be normal or identify previous triggering events (eg, past vestibular insults), but transient conditions cannot explain patients’ persistent symptoms. Often, patients describe a transition from episodic vertigo and ataxia to chronic, often daily unsteadiness and dizziness. In this situation, the illness that started the problem often is not the one that continues to be distressing. Rather, patients develop hypersensitivity to motion stimuli (visual, vestibular, and proprioceptive inputs) and hypervigilance about motion environments that last long after the trigger event has resolved. These CSD features are thought to arise from threat-related failure of postural control systems to return to normal functioning after shifting into high-risk strategies during the acute events that disrupted balance.
5 strategies for managing CSD
1. Develop a common language among other clinicians you work with. The concept of CSD will be new to most patients and their referring clinicians, so they will need to hear about it more than once. From a neuro-otologic standpoint, make a point of separating past and present problems (ie, not the vestibular neuronitis, BPPV, etc., that the patient previously had, but the CSD they presently have). From a psychological standpoint, talk in behavioral terms—hypersensitivity to motion, hypervigilance about motion environments, use of safety maneuvers (eg, touching a wall when walking), and avoiding situations that provoke dizziness. These are reflexive, fear-driven symptoms, but patients understand them better in terms of dizziness and unsteadiness.
2. Keep in mind that dizziness is the chief complaint. As patients go from primary care to otolaryngology, audiology, vestibular rehabilitation, and psychiatry, the problem is dizziness. You may find anxiety or depression along the way, but dizziness comes first for these patients.
3. Educate patients and referring physicians. Give patients and their referring physicians materials that define CSD and its differential diagnosis.3 Check off patients’ symptoms in the diagnostic list and circle their medical comorbidities, if present. For psychiatrists, this is a good point to start discussing behavioral morbidity and treatment.
4. Screen for coexisting medical-psychiatric diagnoses (eg, Meniere’s disease, panic disorder) or primarily psychiatric problems (conversion disorder). In addition to the otologic exam for vestibular diseases, patients should be screened for migraine, traumatic brain injury, dysautonomia, and dysrhythmias. Ask patients to complete symptom self-reports, including the Patient Health Questionnaire-9 (for depression) and Generalized Anxiety Disorder-7 (for anxiety).
5. Treat the patient’s primary problem (eg, CSD, vertigo, ataxia, or headache) first. If headache and balance symptoms are intertwined, use venlafaxine or combine a selective serotonin reuptake inhibitor (SSRI) with a separate migraine prophylactic agent.
Treatment options
Pharmacotherapy. Five open-label studies found SSRIs are effective for CSD even for patients without psychiatric comorbidity.3 Use a “start low, go slow” strategy to avoid aggravating symptoms. Final doses usually are in the lower half of the therapeutic range. Full treatment response may take 8 to 12 weeks. Vestibular suppressants such as meclizine work reasonably well for acute vertigo, but have no role in treating CSD.
Vestibular and balance rehabilitation therapy (VBRT) is an exercise program performed at home by patients but overseen by specially trained physical therapists. It is an excellent habituation/desensitization program that can be integrated with medication and psychotherapy. All patients with CSD should undergo VBRT.
Cognitive-behavioral therapy may be helpful for treating psychiatric morbidity (anxiety, depression, phobic avoidance) in patients with CSD, but it appears to be less effective for physical symptoms of dizziness.3
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Staab JP, Ruckenstein MJ. Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg. 2007;133(2):170-176.
2. Bisdorff A, Von Brevern M, Lempert T, et al. Classification of vestibular symptoms: towards an international classification of vestibular disorders. J Vestib Res. 2009;19(1-2):1-13.
3. Staab JP. Psychological aspects of vestibular disorders. In: Eggers SD Zee DS, eds Vertigo and imbalance: clinical neurophysiology of the vestibular system. Boston, MA: Elsevier. 2010;502-522.
Discuss this article at www.facebook.com/CurrentPsychiatry
Chronic subjective dizziness (CSD) is characterized by persistent (>3 months) dizziness, lightheadedness, or unsteadiness, without vertigo or ataxia. Symptoms often are worse in highly stimulating visual environments (eg, busy malls or grocery stores) or settings with indistinct visual orientation cues (eg, large open areas, heavy fog). Neuro-otologic examination and laboratory testing reveal no active vestibular deficits.1
CSD is not a psychiatric illness, but exists at the interface of psychiatry and neuro-otology. For example, anxiety and depressive disorders often accompany CSD, but are not an integral part of it. Treatment outcomes are good and prognosis for full function is high.
Conditions that cause dizziness
Vertigo—a sensation of rotation or linear movement of self or surroundings—occurs in discrete attacks that typically have an acute onset and are caused by neuro-otologic conditions.2 Symptoms may last for seconds (benign paroxysmal positional vertigo [BPPV]), hours (Meniere’s disease), minutes to days (vestibular migraine), or weeks (vestibular neuronitis). Unsteadiness, a swaying or rocking sensation, dizziness, and a disturbed sense of spatial orientation without illusory movement may be acute, subacute, or chronic. These symptoms may accompany vertigo or occur independently.2 Psychiatric disorders (panic), dysautonomias (vasovagal spells), and cardiovascular conditions (dysrhythmias) may cause episodic unsteadiness and dizziness, but not vertigo. Several illnesses can cause persistent unsteadiness and dizziness, including bilateral peripheral vestibular deficits, central vestibular lesions (strokes), proprioceptive or visual loss (neuropathies), and generalized anxiety disorder.
Up to 30% of patients who experience episodic balance problems develop persistent unsteadiness or dizziness (ie, CSD).3 Clinical history, exam, and laboratory tests may be normal or identify previous triggering events (eg, past vestibular insults), but transient conditions cannot explain patients’ persistent symptoms. Often, patients describe a transition from episodic vertigo and ataxia to chronic, often daily unsteadiness and dizziness. In this situation, the illness that started the problem often is not the one that continues to be distressing. Rather, patients develop hypersensitivity to motion stimuli (visual, vestibular, and proprioceptive inputs) and hypervigilance about motion environments that last long after the trigger event has resolved. These CSD features are thought to arise from threat-related failure of postural control systems to return to normal functioning after shifting into high-risk strategies during the acute events that disrupted balance.
5 strategies for managing CSD
1. Develop a common language among other clinicians you work with. The concept of CSD will be new to most patients and their referring clinicians, so they will need to hear about it more than once. From a neuro-otologic standpoint, make a point of separating past and present problems (ie, not the vestibular neuronitis, BPPV, etc., that the patient previously had, but the CSD they presently have). From a psychological standpoint, talk in behavioral terms—hypersensitivity to motion, hypervigilance about motion environments, use of safety maneuvers (eg, touching a wall when walking), and avoiding situations that provoke dizziness. These are reflexive, fear-driven symptoms, but patients understand them better in terms of dizziness and unsteadiness.
2. Keep in mind that dizziness is the chief complaint. As patients go from primary care to otolaryngology, audiology, vestibular rehabilitation, and psychiatry, the problem is dizziness. You may find anxiety or depression along the way, but dizziness comes first for these patients.
3. Educate patients and referring physicians. Give patients and their referring physicians materials that define CSD and its differential diagnosis.3 Check off patients’ symptoms in the diagnostic list and circle their medical comorbidities, if present. For psychiatrists, this is a good point to start discussing behavioral morbidity and treatment.
4. Screen for coexisting medical-psychiatric diagnoses (eg, Meniere’s disease, panic disorder) or primarily psychiatric problems (conversion disorder). In addition to the otologic exam for vestibular diseases, patients should be screened for migraine, traumatic brain injury, dysautonomia, and dysrhythmias. Ask patients to complete symptom self-reports, including the Patient Health Questionnaire-9 (for depression) and Generalized Anxiety Disorder-7 (for anxiety).
5. Treat the patient’s primary problem (eg, CSD, vertigo, ataxia, or headache) first. If headache and balance symptoms are intertwined, use venlafaxine or combine a selective serotonin reuptake inhibitor (SSRI) with a separate migraine prophylactic agent.
Treatment options
Pharmacotherapy. Five open-label studies found SSRIs are effective for CSD even for patients without psychiatric comorbidity.3 Use a “start low, go slow” strategy to avoid aggravating symptoms. Final doses usually are in the lower half of the therapeutic range. Full treatment response may take 8 to 12 weeks. Vestibular suppressants such as meclizine work reasonably well for acute vertigo, but have no role in treating CSD.
Vestibular and balance rehabilitation therapy (VBRT) is an exercise program performed at home by patients but overseen by specially trained physical therapists. It is an excellent habituation/desensitization program that can be integrated with medication and psychotherapy. All patients with CSD should undergo VBRT.
Cognitive-behavioral therapy may be helpful for treating psychiatric morbidity (anxiety, depression, phobic avoidance) in patients with CSD, but it appears to be less effective for physical symptoms of dizziness.3
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Chronic subjective dizziness (CSD) is characterized by persistent (>3 months) dizziness, lightheadedness, or unsteadiness, without vertigo or ataxia. Symptoms often are worse in highly stimulating visual environments (eg, busy malls or grocery stores) or settings with indistinct visual orientation cues (eg, large open areas, heavy fog). Neuro-otologic examination and laboratory testing reveal no active vestibular deficits.1
CSD is not a psychiatric illness, but exists at the interface of psychiatry and neuro-otology. For example, anxiety and depressive disorders often accompany CSD, but are not an integral part of it. Treatment outcomes are good and prognosis for full function is high.
Conditions that cause dizziness
Vertigo—a sensation of rotation or linear movement of self or surroundings—occurs in discrete attacks that typically have an acute onset and are caused by neuro-otologic conditions.2 Symptoms may last for seconds (benign paroxysmal positional vertigo [BPPV]), hours (Meniere’s disease), minutes to days (vestibular migraine), or weeks (vestibular neuronitis). Unsteadiness, a swaying or rocking sensation, dizziness, and a disturbed sense of spatial orientation without illusory movement may be acute, subacute, or chronic. These symptoms may accompany vertigo or occur independently.2 Psychiatric disorders (panic), dysautonomias (vasovagal spells), and cardiovascular conditions (dysrhythmias) may cause episodic unsteadiness and dizziness, but not vertigo. Several illnesses can cause persistent unsteadiness and dizziness, including bilateral peripheral vestibular deficits, central vestibular lesions (strokes), proprioceptive or visual loss (neuropathies), and generalized anxiety disorder.
Up to 30% of patients who experience episodic balance problems develop persistent unsteadiness or dizziness (ie, CSD).3 Clinical history, exam, and laboratory tests may be normal or identify previous triggering events (eg, past vestibular insults), but transient conditions cannot explain patients’ persistent symptoms. Often, patients describe a transition from episodic vertigo and ataxia to chronic, often daily unsteadiness and dizziness. In this situation, the illness that started the problem often is not the one that continues to be distressing. Rather, patients develop hypersensitivity to motion stimuli (visual, vestibular, and proprioceptive inputs) and hypervigilance about motion environments that last long after the trigger event has resolved. These CSD features are thought to arise from threat-related failure of postural control systems to return to normal functioning after shifting into high-risk strategies during the acute events that disrupted balance.
5 strategies for managing CSD
1. Develop a common language among other clinicians you work with. The concept of CSD will be new to most patients and their referring clinicians, so they will need to hear about it more than once. From a neuro-otologic standpoint, make a point of separating past and present problems (ie, not the vestibular neuronitis, BPPV, etc., that the patient previously had, but the CSD they presently have). From a psychological standpoint, talk in behavioral terms—hypersensitivity to motion, hypervigilance about motion environments, use of safety maneuvers (eg, touching a wall when walking), and avoiding situations that provoke dizziness. These are reflexive, fear-driven symptoms, but patients understand them better in terms of dizziness and unsteadiness.
2. Keep in mind that dizziness is the chief complaint. As patients go from primary care to otolaryngology, audiology, vestibular rehabilitation, and psychiatry, the problem is dizziness. You may find anxiety or depression along the way, but dizziness comes first for these patients.
3. Educate patients and referring physicians. Give patients and their referring physicians materials that define CSD and its differential diagnosis.3 Check off patients’ symptoms in the diagnostic list and circle their medical comorbidities, if present. For psychiatrists, this is a good point to start discussing behavioral morbidity and treatment.
4. Screen for coexisting medical-psychiatric diagnoses (eg, Meniere’s disease, panic disorder) or primarily psychiatric problems (conversion disorder). In addition to the otologic exam for vestibular diseases, patients should be screened for migraine, traumatic brain injury, dysautonomia, and dysrhythmias. Ask patients to complete symptom self-reports, including the Patient Health Questionnaire-9 (for depression) and Generalized Anxiety Disorder-7 (for anxiety).
5. Treat the patient’s primary problem (eg, CSD, vertigo, ataxia, or headache) first. If headache and balance symptoms are intertwined, use venlafaxine or combine a selective serotonin reuptake inhibitor (SSRI) with a separate migraine prophylactic agent.
Treatment options
Pharmacotherapy. Five open-label studies found SSRIs are effective for CSD even for patients without psychiatric comorbidity.3 Use a “start low, go slow” strategy to avoid aggravating symptoms. Final doses usually are in the lower half of the therapeutic range. Full treatment response may take 8 to 12 weeks. Vestibular suppressants such as meclizine work reasonably well for acute vertigo, but have no role in treating CSD.
Vestibular and balance rehabilitation therapy (VBRT) is an exercise program performed at home by patients but overseen by specially trained physical therapists. It is an excellent habituation/desensitization program that can be integrated with medication and psychotherapy. All patients with CSD should undergo VBRT.
Cognitive-behavioral therapy may be helpful for treating psychiatric morbidity (anxiety, depression, phobic avoidance) in patients with CSD, but it appears to be less effective for physical symptoms of dizziness.3
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Staab JP, Ruckenstein MJ. Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg. 2007;133(2):170-176.
2. Bisdorff A, Von Brevern M, Lempert T, et al. Classification of vestibular symptoms: towards an international classification of vestibular disorders. J Vestib Res. 2009;19(1-2):1-13.
3. Staab JP. Psychological aspects of vestibular disorders. In: Eggers SD Zee DS, eds Vertigo and imbalance: clinical neurophysiology of the vestibular system. Boston, MA: Elsevier. 2010;502-522.
1. Staab JP, Ruckenstein MJ. Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg. 2007;133(2):170-176.
2. Bisdorff A, Von Brevern M, Lempert T, et al. Classification of vestibular symptoms: towards an international classification of vestibular disorders. J Vestib Res. 2009;19(1-2):1-13.
3. Staab JP. Psychological aspects of vestibular disorders. In: Eggers SD Zee DS, eds Vertigo and imbalance: clinical neurophysiology of the vestibular system. Boston, MA: Elsevier. 2010;502-522.
When is off-label prescribing appropriate?
Discuss this article at www.facebook.com/CurrentPsychiatry
Off-label prescribing (OLP)—prescribing a medication in a manner different from that approved by the FDA—is common and can be clinically beneficial. A survey of 200 British psychiatrists found that 65% had prescribed a medication off-label within the previous month.1 However, OLP often is not supported by strong evidence and carries clinical risks, such as adverse effects and unproven efficacy. A 2006 study found that only 4% of off-label prescriptions of psychiatric medications were supported by strong scientific evidence.2
OLP may become unavoidable for several reasons, including:
- lack of data from quality trials on a specific indication or patient population
- patients seen in clinical practice vary from those evaluated in clinical trials (Figure 1)
- the need to treat patients who do not respond to first-line therapies or have treatment-resistant conditions.
At times, OLP may be a psychiatrist’s only option: >80% of DSM-IV-TR diagnoses have no FDA-approved medication.3
No practice guidelines are available to help clinicians decide when OLP is appropriate. Psychiatrists must rely on multiple, sometimes-conflicting sources to determine whether evidence is sufficient to support off-label use in a specific clinical scenario. This article looks at types of OLP and offers suggestions for clinicians who are considering prescribing a medication outside of its approved use.
Figure 1: Clinical trial patients vs ‘real world’ patients
The FDA’s role
Once the FDA approves a medication for a specific indication, physicians legally are permitted to prescribe that drug for indications, patient populations, or dosages not included on the FDA-approved label.2,4 The FDA oversees and regulates pharmaceutical companies, not physicians.4 Currently, pharmaceutical companies cannot market a drug for an indication not included on the label, but physicians are free to use the drug for any condition or disease.5
When is OLP used?
According to Baldwin et al,6 prescribing that is considered off-label generally falls into 1 of the following 4 categories:
Indication. This type of OLP is prescribing a medication for an indication other than those included on the FDA-approved label. The off-label indication may be a logical extension of an approved indication. For example, a medication approved for treating erectile dysfunction might be prescribed to a patient who is experiencing antidepressant-induced sexual dysfunction.
If a pharmaceutical company wishes to expand the indications of a medication they must seek supplemental approval from the FDA. This is a long, expensive process. In certain situations, it may be in the patient’s best interest to prescribe a medication off-label until that indication becomes approved. When clinicians identify new uses for existing medications while they care for patients, it is considered field discovery, and this innovative process may occur years before such indications receive FDA approval.
Dosage. The most common example of this type of OLP in psychiatry is prescribing higher-than-approved dosages of antidepressants or antipsychotics for patients who do not respond to the maximum approved dosages. The effectiveness of this strategy is unknown.6
Duration. This typically entails prescribing a medication for a period of time longer than specified on the label. For example, many antidepressants are approved only for treating depressive illness. Therefore, continuing an antidepressant as maintenance therapy for a patient who is in remission could be considered off-label. Benzodiazepines are approved primarily for short-term management of anxiety, but commonly are prescribed for patients with chronic, disabling anxiety disorders who do not respond to other medications.6
Patient age. The FDA approves medications for use in patients within a specified age range based on patients evaluated in clinical trials, and most trials of psychotropics include patients age 18 to 65. However, it is highly unlikely that a 17-year-old patient’s drug metabolism changes substantially when he or she reaches age 18, or when a 65-year-old turns 66. Research has demonstrated that medications can be effective outside of strict age ranges. For example, randomized controlled trials (RCTs) have shown that antidepressants are efficacious in treating depression in geriatric patients, and selective serotonin reuptake inhibitors are efficacious in treating obsessive-compulsive disorder (OCD) in children and adolescents.6
Few medications have been approved for treating geriatric patients with psychiatric illness. For example, no drugs are approved for treating psychotic, behavioral, and mood symptoms that may accompany dementia. For this reason, clinicians often prescribe psychotropics off-label to these patients.
The rate of psychotropic prescriptions to children and adolescents—particularly antidepressants and antipsychotics—has been increasing.7-9 The British Association for Psychopharmacology suggested that it may be reasonable to apply what we know regarding adults’ responses to drug treatment to children and adolescents with schizophrenia or OCD, but more caution is required in young patients with mood or anxiety disorders.10
Combination therapy is another type of OLP. Often a disease state consists of multiple underlying syndromes, and treating individual syndromes is a common strategy. For example, in addition to depressed mood, a patient with major depressive disorder also may have insomnia and poor concentration. A medication approved for treating depressed mood may not improve insomnia or poor concentration. Therefore, combination therapy may be necessary, but likely would be off-label. Combination therapy also may be tried when a patient does not respond to monotherapy. For example, although the evidence supporting the practice is inconclusive, clinicians commonly prescribe >1 antipsychotic to patients with schizophrenia or other psychotic disorders.
Help for making OLP decisions
Position statements/policies. The American Psychiatric Association (APA) and the American Medical Association support OLP when the practice is based on sound scientific evidence and medical opinion.11 The APA position statement encourages clinicians to use various compendia, including the American Hospital Formulary Service (AHFS) Drug Information, in conjunction with peer-reviewed literature to determine the medical acceptability of off-label uses.11
Evidence-based medicine includes a hierarchy of scientific and clinical evidence that can justify medical decisions. At the top of this hierarchy are large RCTs and smaller RCTs; cohort studies, case-control studies, poorly controlled or uncontrolled studies, case reports, and expert opinion are less valuable (Figure 2).4
Searching through all available resources for evidence supporting a specific off-label use is a cumbersome, time-consuming process. For this reason, clinicians may refer to compendia that evaluate and rate the available evidence supporting off-label use of medication, such as the AHFS Drug Information and DrugDex. Other resources include peer-reviewed medical journals. Physicians can contribute to knowledge of off-label uses by sharing their experiences, both good and bad, with their colleagues via presentations, publications, and/or initiating a study.
Other resources. Gazarian et al12 delineated 3 situations where OLP might be considered appropriate: use justified by high-quality evidence, use in research trials, and exceptional use justified by individual clinical circumstances. Exceptional use would require all of the following:
- the patient has a serious disease or condition
- evidence supports a potential beneficial effect of the off-label treatment
- potential benefits outweigh potential risks
- standard therapy has failed or is inappropriate
- an institutional drug committee approved the off-label use
- the patient provides written informed consent.12
Other authors13,14 have offered recommendations for psychiatrists considering OLP:
- Study available literature and assess whether sufficient evidence supports the proposed off-label use.
- If evidence is lacking, learn about the medication and its potential risks (interactions, adverse effects, and FDA “black-box” warnings). Also consult other resources for additional information and research, including peers and experts in the field.
- Consider and document risks and benefits of the proposed off-label use. Explain these, as well as uncertainties and potential costs, to patients and/or their families, and obtain and document informed consent.
- Cautiously initiate the off-label therapy, monitor patients closely, and meticulously document efficacy and tolerance.
Prescribing medications on-label does not guarantee safety or efficacy. Likewise, OLP does not imply a safety hazard or lack of efficacy. OLP may be in the best interest of the patient. Nonetheless, the practice must be carried out responsibly with utmost caution and consideration of acute and long-term burdens to patients, along with an assessment of the risk vs benefit of the proposed therapy.
Figure 2: The hierarchy of sources for evidence-based medicine
RCTs: randomized controlled trials
Source: Reference 4Related Resource
- Mossman D. Why off-label isn’t off base. Current Psychiatry. 2009;8(2):19-22.
Disclosures
Dr. Ali receives research/grant support from Cyberonics and is a speaker for Merck.
Dr Ajmal reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Lowe-Ponsford F, Baldwin D. Off-label prescribing by psychiatrists. Psychiatric Bulletin. 2000;24:415-417.
2. Radley DC, Finkelstein SN, Stafford RS. Off-label prescribing among office-based physicians. Arch Intern Med. 2006;166(9):1021-1026.
3. Devulapalli K, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian Journal of Psychiatry. 2009;2(1):29-36.
4. Dresser R, Frader J. Off-label prescribing: a call for heightened professional and government oversight. J Law Med Ethics. 2009;37(3):476-486, 396.
5. Food, Drug, and Cosmetic Act, 21 USC §396 (2010).
6. Baldwin DS, Kosky N. Off-label prescribing in psychiatric practice. Advances in Psychiatric Treatment. 2007;13:414-422.
7. Zito JM, Safer DJ, dosReis S, et al. Trends in the prescribing of psychotropic medications to preschoolers. JAMA. 2000;283(8):1025-1030.
8. Tournier M, Greenfield B, Galbaud du Fort G, et al. Patterns of antidepressant use in Quebec children and adolescents: trends and predictors. Psychiatry Res. 2010;179(1):57-63.
9. Cooper WO, Arbogast PG, Ding H, et al. Trends in prescribing of antipsychotic medications for US children. Ambul Pediatr. 2006;6(2):79-83.
10. Child and learning disability psychopharmacology. J Psychopharmacol. 1997;11(4):291-294.
11. American Psychiatric Association. Position statement on patient access to treatments prescribed by their physicians. 2007. http://www.psychiatry.org/advocacy—newsroom/position-statements/apa-position-statements. Accessed May 24 2012.
12. Gazarian M, Kelly M, McPhee JR, et al. Off-label use of medicines: consensus recommendations for evaluating appropriateness. Med J Aust. 2006;185(10):544-548.
13. Kramer SI, McCall WV. Off-label prescribing: 7 steps for safer more effective prescribing. Current Psychiatry. 2006;5(4):14-28.
14. Royal College of Psychiatrists. Use of licensed medicines for unlicensed applications in psychiatric practice. College report CR142. http://www.rcpsych.ac.uk/files/pdfversion/cr142.pdf. Accessed May 24 2012.
Discuss this article at www.facebook.com/CurrentPsychiatry
Off-label prescribing (OLP)—prescribing a medication in a manner different from that approved by the FDA—is common and can be clinically beneficial. A survey of 200 British psychiatrists found that 65% had prescribed a medication off-label within the previous month.1 However, OLP often is not supported by strong evidence and carries clinical risks, such as adverse effects and unproven efficacy. A 2006 study found that only 4% of off-label prescriptions of psychiatric medications were supported by strong scientific evidence.2
OLP may become unavoidable for several reasons, including:
- lack of data from quality trials on a specific indication or patient population
- patients seen in clinical practice vary from those evaluated in clinical trials (Figure 1)
- the need to treat patients who do not respond to first-line therapies or have treatment-resistant conditions.
At times, OLP may be a psychiatrist’s only option: >80% of DSM-IV-TR diagnoses have no FDA-approved medication.3
No practice guidelines are available to help clinicians decide when OLP is appropriate. Psychiatrists must rely on multiple, sometimes-conflicting sources to determine whether evidence is sufficient to support off-label use in a specific clinical scenario. This article looks at types of OLP and offers suggestions for clinicians who are considering prescribing a medication outside of its approved use.
Figure 1: Clinical trial patients vs ‘real world’ patients
The FDA’s role
Once the FDA approves a medication for a specific indication, physicians legally are permitted to prescribe that drug for indications, patient populations, or dosages not included on the FDA-approved label.2,4 The FDA oversees and regulates pharmaceutical companies, not physicians.4 Currently, pharmaceutical companies cannot market a drug for an indication not included on the label, but physicians are free to use the drug for any condition or disease.5
When is OLP used?
According to Baldwin et al,6 prescribing that is considered off-label generally falls into 1 of the following 4 categories:
Indication. This type of OLP is prescribing a medication for an indication other than those included on the FDA-approved label. The off-label indication may be a logical extension of an approved indication. For example, a medication approved for treating erectile dysfunction might be prescribed to a patient who is experiencing antidepressant-induced sexual dysfunction.
If a pharmaceutical company wishes to expand the indications of a medication they must seek supplemental approval from the FDA. This is a long, expensive process. In certain situations, it may be in the patient’s best interest to prescribe a medication off-label until that indication becomes approved. When clinicians identify new uses for existing medications while they care for patients, it is considered field discovery, and this innovative process may occur years before such indications receive FDA approval.
Dosage. The most common example of this type of OLP in psychiatry is prescribing higher-than-approved dosages of antidepressants or antipsychotics for patients who do not respond to the maximum approved dosages. The effectiveness of this strategy is unknown.6
Duration. This typically entails prescribing a medication for a period of time longer than specified on the label. For example, many antidepressants are approved only for treating depressive illness. Therefore, continuing an antidepressant as maintenance therapy for a patient who is in remission could be considered off-label. Benzodiazepines are approved primarily for short-term management of anxiety, but commonly are prescribed for patients with chronic, disabling anxiety disorders who do not respond to other medications.6
Patient age. The FDA approves medications for use in patients within a specified age range based on patients evaluated in clinical trials, and most trials of psychotropics include patients age 18 to 65. However, it is highly unlikely that a 17-year-old patient’s drug metabolism changes substantially when he or she reaches age 18, or when a 65-year-old turns 66. Research has demonstrated that medications can be effective outside of strict age ranges. For example, randomized controlled trials (RCTs) have shown that antidepressants are efficacious in treating depression in geriatric patients, and selective serotonin reuptake inhibitors are efficacious in treating obsessive-compulsive disorder (OCD) in children and adolescents.6
Few medications have been approved for treating geriatric patients with psychiatric illness. For example, no drugs are approved for treating psychotic, behavioral, and mood symptoms that may accompany dementia. For this reason, clinicians often prescribe psychotropics off-label to these patients.
The rate of psychotropic prescriptions to children and adolescents—particularly antidepressants and antipsychotics—has been increasing.7-9 The British Association for Psychopharmacology suggested that it may be reasonable to apply what we know regarding adults’ responses to drug treatment to children and adolescents with schizophrenia or OCD, but more caution is required in young patients with mood or anxiety disorders.10
Combination therapy is another type of OLP. Often a disease state consists of multiple underlying syndromes, and treating individual syndromes is a common strategy. For example, in addition to depressed mood, a patient with major depressive disorder also may have insomnia and poor concentration. A medication approved for treating depressed mood may not improve insomnia or poor concentration. Therefore, combination therapy may be necessary, but likely would be off-label. Combination therapy also may be tried when a patient does not respond to monotherapy. For example, although the evidence supporting the practice is inconclusive, clinicians commonly prescribe >1 antipsychotic to patients with schizophrenia or other psychotic disorders.
Help for making OLP decisions
Position statements/policies. The American Psychiatric Association (APA) and the American Medical Association support OLP when the practice is based on sound scientific evidence and medical opinion.11 The APA position statement encourages clinicians to use various compendia, including the American Hospital Formulary Service (AHFS) Drug Information, in conjunction with peer-reviewed literature to determine the medical acceptability of off-label uses.11
Evidence-based medicine includes a hierarchy of scientific and clinical evidence that can justify medical decisions. At the top of this hierarchy are large RCTs and smaller RCTs; cohort studies, case-control studies, poorly controlled or uncontrolled studies, case reports, and expert opinion are less valuable (Figure 2).4
Searching through all available resources for evidence supporting a specific off-label use is a cumbersome, time-consuming process. For this reason, clinicians may refer to compendia that evaluate and rate the available evidence supporting off-label use of medication, such as the AHFS Drug Information and DrugDex. Other resources include peer-reviewed medical journals. Physicians can contribute to knowledge of off-label uses by sharing their experiences, both good and bad, with their colleagues via presentations, publications, and/or initiating a study.
Other resources. Gazarian et al12 delineated 3 situations where OLP might be considered appropriate: use justified by high-quality evidence, use in research trials, and exceptional use justified by individual clinical circumstances. Exceptional use would require all of the following:
- the patient has a serious disease or condition
- evidence supports a potential beneficial effect of the off-label treatment
- potential benefits outweigh potential risks
- standard therapy has failed or is inappropriate
- an institutional drug committee approved the off-label use
- the patient provides written informed consent.12
Other authors13,14 have offered recommendations for psychiatrists considering OLP:
- Study available literature and assess whether sufficient evidence supports the proposed off-label use.
- If evidence is lacking, learn about the medication and its potential risks (interactions, adverse effects, and FDA “black-box” warnings). Also consult other resources for additional information and research, including peers and experts in the field.
- Consider and document risks and benefits of the proposed off-label use. Explain these, as well as uncertainties and potential costs, to patients and/or their families, and obtain and document informed consent.
- Cautiously initiate the off-label therapy, monitor patients closely, and meticulously document efficacy and tolerance.
Prescribing medications on-label does not guarantee safety or efficacy. Likewise, OLP does not imply a safety hazard or lack of efficacy. OLP may be in the best interest of the patient. Nonetheless, the practice must be carried out responsibly with utmost caution and consideration of acute and long-term burdens to patients, along with an assessment of the risk vs benefit of the proposed therapy.
Figure 2: The hierarchy of sources for evidence-based medicine
RCTs: randomized controlled trials
Source: Reference 4Related Resource
- Mossman D. Why off-label isn’t off base. Current Psychiatry. 2009;8(2):19-22.
Disclosures
Dr. Ali receives research/grant support from Cyberonics and is a speaker for Merck.
Dr Ajmal reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Off-label prescribing (OLP)—prescribing a medication in a manner different from that approved by the FDA—is common and can be clinically beneficial. A survey of 200 British psychiatrists found that 65% had prescribed a medication off-label within the previous month.1 However, OLP often is not supported by strong evidence and carries clinical risks, such as adverse effects and unproven efficacy. A 2006 study found that only 4% of off-label prescriptions of psychiatric medications were supported by strong scientific evidence.2
OLP may become unavoidable for several reasons, including:
- lack of data from quality trials on a specific indication or patient population
- patients seen in clinical practice vary from those evaluated in clinical trials (Figure 1)
- the need to treat patients who do not respond to first-line therapies or have treatment-resistant conditions.
At times, OLP may be a psychiatrist’s only option: >80% of DSM-IV-TR diagnoses have no FDA-approved medication.3
No practice guidelines are available to help clinicians decide when OLP is appropriate. Psychiatrists must rely on multiple, sometimes-conflicting sources to determine whether evidence is sufficient to support off-label use in a specific clinical scenario. This article looks at types of OLP and offers suggestions for clinicians who are considering prescribing a medication outside of its approved use.
Figure 1: Clinical trial patients vs ‘real world’ patients
The FDA’s role
Once the FDA approves a medication for a specific indication, physicians legally are permitted to prescribe that drug for indications, patient populations, or dosages not included on the FDA-approved label.2,4 The FDA oversees and regulates pharmaceutical companies, not physicians.4 Currently, pharmaceutical companies cannot market a drug for an indication not included on the label, but physicians are free to use the drug for any condition or disease.5
When is OLP used?
According to Baldwin et al,6 prescribing that is considered off-label generally falls into 1 of the following 4 categories:
Indication. This type of OLP is prescribing a medication for an indication other than those included on the FDA-approved label. The off-label indication may be a logical extension of an approved indication. For example, a medication approved for treating erectile dysfunction might be prescribed to a patient who is experiencing antidepressant-induced sexual dysfunction.
If a pharmaceutical company wishes to expand the indications of a medication they must seek supplemental approval from the FDA. This is a long, expensive process. In certain situations, it may be in the patient’s best interest to prescribe a medication off-label until that indication becomes approved. When clinicians identify new uses for existing medications while they care for patients, it is considered field discovery, and this innovative process may occur years before such indications receive FDA approval.
Dosage. The most common example of this type of OLP in psychiatry is prescribing higher-than-approved dosages of antidepressants or antipsychotics for patients who do not respond to the maximum approved dosages. The effectiveness of this strategy is unknown.6
Duration. This typically entails prescribing a medication for a period of time longer than specified on the label. For example, many antidepressants are approved only for treating depressive illness. Therefore, continuing an antidepressant as maintenance therapy for a patient who is in remission could be considered off-label. Benzodiazepines are approved primarily for short-term management of anxiety, but commonly are prescribed for patients with chronic, disabling anxiety disorders who do not respond to other medications.6
Patient age. The FDA approves medications for use in patients within a specified age range based on patients evaluated in clinical trials, and most trials of psychotropics include patients age 18 to 65. However, it is highly unlikely that a 17-year-old patient’s drug metabolism changes substantially when he or she reaches age 18, or when a 65-year-old turns 66. Research has demonstrated that medications can be effective outside of strict age ranges. For example, randomized controlled trials (RCTs) have shown that antidepressants are efficacious in treating depression in geriatric patients, and selective serotonin reuptake inhibitors are efficacious in treating obsessive-compulsive disorder (OCD) in children and adolescents.6
Few medications have been approved for treating geriatric patients with psychiatric illness. For example, no drugs are approved for treating psychotic, behavioral, and mood symptoms that may accompany dementia. For this reason, clinicians often prescribe psychotropics off-label to these patients.
The rate of psychotropic prescriptions to children and adolescents—particularly antidepressants and antipsychotics—has been increasing.7-9 The British Association for Psychopharmacology suggested that it may be reasonable to apply what we know regarding adults’ responses to drug treatment to children and adolescents with schizophrenia or OCD, but more caution is required in young patients with mood or anxiety disorders.10
Combination therapy is another type of OLP. Often a disease state consists of multiple underlying syndromes, and treating individual syndromes is a common strategy. For example, in addition to depressed mood, a patient with major depressive disorder also may have insomnia and poor concentration. A medication approved for treating depressed mood may not improve insomnia or poor concentration. Therefore, combination therapy may be necessary, but likely would be off-label. Combination therapy also may be tried when a patient does not respond to monotherapy. For example, although the evidence supporting the practice is inconclusive, clinicians commonly prescribe >1 antipsychotic to patients with schizophrenia or other psychotic disorders.
Help for making OLP decisions
Position statements/policies. The American Psychiatric Association (APA) and the American Medical Association support OLP when the practice is based on sound scientific evidence and medical opinion.11 The APA position statement encourages clinicians to use various compendia, including the American Hospital Formulary Service (AHFS) Drug Information, in conjunction with peer-reviewed literature to determine the medical acceptability of off-label uses.11
Evidence-based medicine includes a hierarchy of scientific and clinical evidence that can justify medical decisions. At the top of this hierarchy are large RCTs and smaller RCTs; cohort studies, case-control studies, poorly controlled or uncontrolled studies, case reports, and expert opinion are less valuable (Figure 2).4
Searching through all available resources for evidence supporting a specific off-label use is a cumbersome, time-consuming process. For this reason, clinicians may refer to compendia that evaluate and rate the available evidence supporting off-label use of medication, such as the AHFS Drug Information and DrugDex. Other resources include peer-reviewed medical journals. Physicians can contribute to knowledge of off-label uses by sharing their experiences, both good and bad, with their colleagues via presentations, publications, and/or initiating a study.
Other resources. Gazarian et al12 delineated 3 situations where OLP might be considered appropriate: use justified by high-quality evidence, use in research trials, and exceptional use justified by individual clinical circumstances. Exceptional use would require all of the following:
- the patient has a serious disease or condition
- evidence supports a potential beneficial effect of the off-label treatment
- potential benefits outweigh potential risks
- standard therapy has failed or is inappropriate
- an institutional drug committee approved the off-label use
- the patient provides written informed consent.12
Other authors13,14 have offered recommendations for psychiatrists considering OLP:
- Study available literature and assess whether sufficient evidence supports the proposed off-label use.
- If evidence is lacking, learn about the medication and its potential risks (interactions, adverse effects, and FDA “black-box” warnings). Also consult other resources for additional information and research, including peers and experts in the field.
- Consider and document risks and benefits of the proposed off-label use. Explain these, as well as uncertainties and potential costs, to patients and/or their families, and obtain and document informed consent.
- Cautiously initiate the off-label therapy, monitor patients closely, and meticulously document efficacy and tolerance.
Prescribing medications on-label does not guarantee safety or efficacy. Likewise, OLP does not imply a safety hazard or lack of efficacy. OLP may be in the best interest of the patient. Nonetheless, the practice must be carried out responsibly with utmost caution and consideration of acute and long-term burdens to patients, along with an assessment of the risk vs benefit of the proposed therapy.
Figure 2: The hierarchy of sources for evidence-based medicine
RCTs: randomized controlled trials
Source: Reference 4Related Resource
- Mossman D. Why off-label isn’t off base. Current Psychiatry. 2009;8(2):19-22.
Disclosures
Dr. Ali receives research/grant support from Cyberonics and is a speaker for Merck.
Dr Ajmal reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Lowe-Ponsford F, Baldwin D. Off-label prescribing by psychiatrists. Psychiatric Bulletin. 2000;24:415-417.
2. Radley DC, Finkelstein SN, Stafford RS. Off-label prescribing among office-based physicians. Arch Intern Med. 2006;166(9):1021-1026.
3. Devulapalli K, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian Journal of Psychiatry. 2009;2(1):29-36.
4. Dresser R, Frader J. Off-label prescribing: a call for heightened professional and government oversight. J Law Med Ethics. 2009;37(3):476-486, 396.
5. Food, Drug, and Cosmetic Act, 21 USC §396 (2010).
6. Baldwin DS, Kosky N. Off-label prescribing in psychiatric practice. Advances in Psychiatric Treatment. 2007;13:414-422.
7. Zito JM, Safer DJ, dosReis S, et al. Trends in the prescribing of psychotropic medications to preschoolers. JAMA. 2000;283(8):1025-1030.
8. Tournier M, Greenfield B, Galbaud du Fort G, et al. Patterns of antidepressant use in Quebec children and adolescents: trends and predictors. Psychiatry Res. 2010;179(1):57-63.
9. Cooper WO, Arbogast PG, Ding H, et al. Trends in prescribing of antipsychotic medications for US children. Ambul Pediatr. 2006;6(2):79-83.
10. Child and learning disability psychopharmacology. J Psychopharmacol. 1997;11(4):291-294.
11. American Psychiatric Association. Position statement on patient access to treatments prescribed by their physicians. 2007. http://www.psychiatry.org/advocacy—newsroom/position-statements/apa-position-statements. Accessed May 24 2012.
12. Gazarian M, Kelly M, McPhee JR, et al. Off-label use of medicines: consensus recommendations for evaluating appropriateness. Med J Aust. 2006;185(10):544-548.
13. Kramer SI, McCall WV. Off-label prescribing: 7 steps for safer more effective prescribing. Current Psychiatry. 2006;5(4):14-28.
14. Royal College of Psychiatrists. Use of licensed medicines for unlicensed applications in psychiatric practice. College report CR142. http://www.rcpsych.ac.uk/files/pdfversion/cr142.pdf. Accessed May 24 2012.
1. Lowe-Ponsford F, Baldwin D. Off-label prescribing by psychiatrists. Psychiatric Bulletin. 2000;24:415-417.
2. Radley DC, Finkelstein SN, Stafford RS. Off-label prescribing among office-based physicians. Arch Intern Med. 2006;166(9):1021-1026.
3. Devulapalli K, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian Journal of Psychiatry. 2009;2(1):29-36.
4. Dresser R, Frader J. Off-label prescribing: a call for heightened professional and government oversight. J Law Med Ethics. 2009;37(3):476-486, 396.
5. Food, Drug, and Cosmetic Act, 21 USC §396 (2010).
6. Baldwin DS, Kosky N. Off-label prescribing in psychiatric practice. Advances in Psychiatric Treatment. 2007;13:414-422.
7. Zito JM, Safer DJ, dosReis S, et al. Trends in the prescribing of psychotropic medications to preschoolers. JAMA. 2000;283(8):1025-1030.
8. Tournier M, Greenfield B, Galbaud du Fort G, et al. Patterns of antidepressant use in Quebec children and adolescents: trends and predictors. Psychiatry Res. 2010;179(1):57-63.
9. Cooper WO, Arbogast PG, Ding H, et al. Trends in prescribing of antipsychotic medications for US children. Ambul Pediatr. 2006;6(2):79-83.
10. Child and learning disability psychopharmacology. J Psychopharmacol. 1997;11(4):291-294.
11. American Psychiatric Association. Position statement on patient access to treatments prescribed by their physicians. 2007. http://www.psychiatry.org/advocacy—newsroom/position-statements/apa-position-statements. Accessed May 24 2012.
12. Gazarian M, Kelly M, McPhee JR, et al. Off-label use of medicines: consensus recommendations for evaluating appropriateness. Med J Aust. 2006;185(10):544-548.
13. Kramer SI, McCall WV. Off-label prescribing: 7 steps for safer more effective prescribing. Current Psychiatry. 2006;5(4):14-28.
14. Royal College of Psychiatrists. Use of licensed medicines for unlicensed applications in psychiatric practice. College report CR142. http://www.rcpsych.ac.uk/files/pdfversion/cr142.pdf. Accessed May 24 2012.
Statin Withdrawal After Major Surgery
Accumulating evidence suggests that perioperative treatment with 3‐hydroxy‐3‐methylglutaryl coenzyme‐A (HMG‐CoA) reductase inhibitors (or, statins) reduces the incidence of cardiovascular events during noncardiac surgery.16 This evidence has lead the European Society of Cardiology (ESC) and American College of Cardiology Foundation/American Heart Association (ACCF/AHA) to endorse the use of perioperative statins in patients already on this treatment or those at high‐risk of cardiovascular events.7, 8
However, statins are available only in oral formulation. Consequently, prolonged bowel recovery or clinical instability may interfere with use during surgery. Furthermore, many clinicians may not recognize the imperative of postoperative statin resumption, viewing them principally as lipid‐lowering entities and not as agents of perioperative benefit. Failure to resume statins postoperatively can be catastrophic, as the ensuing inflammation and thrombosis frequently culminates in myocardial infarction (MI) or death.9, 10
In this article, we review the potent anti‐inflammatory properties of statins and their role in preventing perioperative cardiac events. We outline the biochemical basis for perioperative statin benefit, summarizing the basic, clinical, and experimental evidence regarding statin withdrawal. We conclude by presenting strategies to avert postoperative statin cessation and outline a research agenda dedicated to informing this practice.
METHODS
We performed a literature search using MEDLINE via Ovid (1946present), EMBASE (1946present), Biosis (1926present), and Cochrane CENTRAL (1960present). We used Boolean logic to search for key terms including statins, 3‐hydroxy‐3‐methylglutaryl CoA reductase inhibitors, death, MI, stroke, acute coronary syndrome (ACS), and statin withdrawal or cessation. All studies published in full‐text or abstract form were included. A total of 489 articles were retrieved by this search (last updated March 15, 2012). For this narrative review, we focused on studies that examined adverse outcomes associated with statin withdrawal.
BIOCHEMICAL BASIS OF STATIN PLEIOTROPICITY
The nonlipid‐lowering or pleiotropic properties of statins are especially valuable in the perioperative setting.16, 11 Perioperative cardiac complications occur due to oxygen supply:demand mismatch, vascular inflammation, or a combination of these states. A significant perisurgical catecholamine surge produces unopposed sympathetic effects,12 increasing the risk of rupture of vulnerable coronary plaques, thrombus formation, and adverse cardiac events.13, 14 Similarly, augmented inflammatory responses and increased circulating coagulation factors further predispose to a hazardous perioperative milieu.15 Statins attenuate this vascular inflammatory response by suppressing the synthesis of mevalonate by inhibiting HMG‐CoA reductase. Suppression of mevalonate synthesis reduces the bioavailability of 2 important isoprenoid molecules: farnesyl‐pyrophosphate and geranylgeranyl‐pyrophosphate.16 Diminution of these isoprenoid intermediaries leads to reductions in the active intracellular signaling molecules Ras, Rho, and Rac, which play critical roles in vascular reactivity, endothelial function, and coagulation and inflammatory pathways.1723 The cumulative effect of these cellular changes is diminished inflammation during periods of surgical stress (Figure 1).
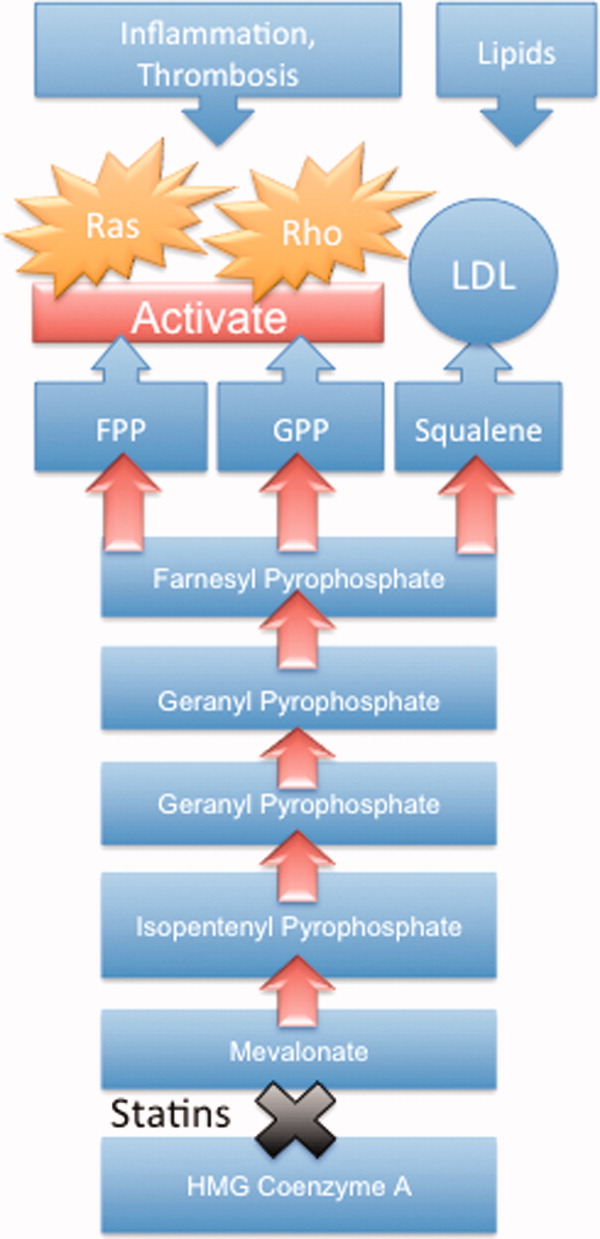
While the perioperative pleiotropicity of statins is of inherent clinical value, several studies have shown that these effects are lost and even reversed when statins are withdrawn.2428 During statin treatment, absence of isoprenoid intermediaries induces cytosolic accumulation of nonactivated Rho and Rac proteins. Abrupt cessation of statins activates Rho/Rac‐kinase pathways, leading to unregulated inflammation, platelet hyper‐activation, and endothelial dysfunction.24, 25, 28, 29 For instance, statin withdrawal in mice‐models leads to an overshoot activation of Rho, resulting in down‐regulation of endothelial nitric oxide production,25 activation of nicotinamide adenine dinucleotide phosphate (NAD[P]H)‐oxidase, and increased superoxide production.29 In another mouse‐model, statin withdrawal was associated with up‐regulation of key pro‐thrombotic molecules including platelet factor 4 and beta‐thromboglobulin.24 In human studies, a platelet hyper‐activation state (manifested by increased platelet P‐selectin expression and enhanced platelet aggregation) occurs after statin discontinuation.27 Furthermore, withdrawal of statins in patients with hyperlipidemia increases inflammatory markers such as C‐reactive protein and interleukin‐6.26 In the perioperative context, absence of these important anti‐inflammatory properties increases the risk of cardiac events.9, 10
EVIDENCE SUGGESTING BENEFIT FROM PERIOPERATIVE STATIN TREATMENT
Retrospective studies first suggested clinical benefit from perioperative statin treatment. In a case‐control study involving 2816 patients undergoing vascular surgery at Erasmus Medical Center, statin use was associated with substantially decreased postoperative mortality (adjusted odd ratio [OR] 0.22, 95% confidence interval [CI] 0.100.47).5 In a subsequent retrospective cohort study of 780,591 patients who underwent major noncardiac surgery, the risk of postoperative mortality was considerably lower among statin users (unadjusted OR 0.68, 95% CI 0.640.72) compared to patients who did not receive, or received delayed treatment with statins.3 A third retrospective study of 1163 vascular surgery patients found that statins prevented perioperative cardiac complications including death, MI, congestive heart failure, and ventricular tachyarrhythmias (OR 0.52, 95% CI 0.350.76).4
The benefit from statin treatment found in retrospective studies prompted the first double‐blinded, randomized controlled trial (RCT) of perioperative statin use. In 2004, Durazzo and colleagues1 randomized 100 statin‐naive patients scheduled to undergo elective aortic, femoro‐popliteal, or carotid surgery to receive either 20 mg of atorvastatin or placebo for 45 days. Vascular surgery was performed, on average, 31 days after randomization. Atorvastatin therapy reduced the incidence of death from cardiac causes, nonfatal acute MI, ischemic stroke, and unstable angina (26% in the placebo group vs 8% in the atorvastatin group; P = 0.031).1 Although the small size of the trial rendered it underpowered to show a mortality benefit, this remains the first RCT to demonstrate a protective perioperative effect of statins.
In the 2009 Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography (DECREASE)‐III trial, Schouten and colleagues6 randomized 497 high‐risk, statin‐naive patients undergoing vascular surgery to receive, in addition to a beta‐blocker, either fluvastatin or placebo before surgery (median of 37 days). Postoperative myocardial ischemia (hazard ratio [HR] 0.55, 95% CI 0.340.88), and combined death from cardiovascular causes or nonfatal MI (HR 0.47, 95% CI 0.240.94), occurred less frequently in the treatment group.6 In 2009, the same group published DECREASE‐IV, a multicenter, prospective, open‐label, 2 2 factorial design trial of 1066 intermediate‐risk patients, scheduled to undergo elective, noncardiac surgery. Patients were assigned to bisoprolol, fluvastatin, combination treatment, or control therapy before surgery (median of 34 days). Although those randomized to fluvastatin demonstrated lower incidence of 30‐day cardiac death and MI than control (HR 0.65, 95% CI 0.351.10), these outcomes failed to reach statistical significance as the trial was principally powered to examine the effects of perioperative beta‐blockade.30
Using this pool of data, a meta‐analysis of 15 studies (223,010 patients) found a substantial 38% reduction in the risk of mortality after cardiac surgery (1.9% vs 3.1%; P = 0.0001) and an even greater 59% reduction in the risk of mortality following vascular surgery (1.7% vs 6.1%; P = 0.0001) with perioperative statin therapy. When including noncardiac surgery, a 44% reduction in mortality was observed (2.2% vs 3.2%; P 0.01).2 We performed a similar meta‐analysis of 15 RCTs involving 2292 patients to determine whether perioperative statin treatment in statin‐naive patients, undergoing either cardiac or noncardiac surgery, improved clinical outcomes. Our analysis also found statistically significant reductions in the risk of MI associated with perioperative statin use in both cardiac and noncardiac surgery (risk reduction [RR] 0.53, 95% CI 0.380.74) and atrial fibrillation in statin‐naive patients undergoing cardiac surgery (RR 0.56, 95% CI 0.450.69).31 Taken together, a large volume of evidence supports the use of statins in surgical settings.
In view of this evidence, the ACCF/AHA perioperative guidelines for noncardiac surgery endorsed statins as an important risk‐reducing intervention in those undergoing noncardiac surgery, and recommended continued use in patients on chronic statin treatment scheduled for noncardiac surgery (Level of Evidence B, Class I; Benefits >>> Risk). Initiating statins in patients undergoing vascular surgery, with or without risk factors, was considered reasonable (Level of Evidence B, Class IIa; Benefits >> Risk).7 Current ESC perioperative guidelines in noncardiac surgery offer similar recommendations to those of ACCF/AHA, but differ by categorizing the recommendation to initiate statins in patients at high cardiovascular risk as a Class I recommendation.8
CLINICAL CONSEQUENCES OF STATIN WITHDRAWAL
Although statins provide important cardiac benefits, an important limitation to their perioperative use remains their oral‐only formulation. Thus, patients who are unable to resume oral intake may fail to resume treatment. Perioperative statin cessation has been hypothesized to lead to a statin withdrawal phenomenon. The evidence that supports the existence of this phenomenon comes from 3 distinct populations: ACS, ischemic stroke, and perioperative patients (Table 1).
| Author (ref) Year | Design | Study Population | Sample Size (N) (Total/ Continuation/Discontinuation) | Clinical Setting and Context | Timing of Statin Discontinuation | Study Outcome | Results (Withdrawal vs Continuation) |
|---|---|---|---|---|---|---|---|
| |||||||
| Heeschen et al33 2002 | Retrospective cohort | Mostly men (68%) in early 60s | 1616/379/86 | Chest pain in ACS | During or after admission | Incidence of death and nonfatal MI | OR (95% CI) |
| 2.93 (1.646.27) | |||||||
| Spencer et al32 2004 | Retrospective cohort | Mostly men (62%) in late 60s | 68,506/9001/487 | NonST‐segment elevation MI | During the first 24 hr of hospitalization | In‐hospital death | HR (95% CI) |
| 1.83 (1.582.13) | |||||||
| Daskalopoulou et al34 2008 | Retrospective cohort | 60% men in late 60s | 9939/2026/137 Non‐users 2124 (reference group) | Acute MI | Within 1 yr of the coronary event | 1‐yr all‐cause mortality | HR (95% CI) |
| 1.88 (1.133.07)* | |||||||
| Colivicchi et al36 2007 | Prospective cohort | 51% men in early 70s | 631/385/246 | Ischemic stroke | Mean 48.6 days | 1‐yr all‐cause mortality | HR (95% CI) |
| 2.78 (1.963.72) | |||||||
| Blanco et al37 2007 | RCT | 51% men in mid‐60s | 215/46/43 | Ischemic stroke | N/A | Risk of death or dependency at 3 mo | OR (95% CI) |
| 4.66 (1.4614.91) | |||||||
| Early neurologic deterioration | OR (95% CI) | ||||||
| 7.08 (2.7318.37) | |||||||
| Le Manach et al9 2007 | Quasi‐experimental (prepost) | Mostly men (89%) in late‐60s | 669/178/491 | Infra‐renal aortic surgery | Median of 4 days off statins | Postoperative troponin release, MI | OR (95% CI) |
| 2.9 (1.65.5) | |||||||
| Schouten et al10 2007 | Prospective cohort | Mostly men (75%) in mid‐60s | 298/228/70 | Aortic and lower extremity vascular surgery | Median of 3 days off statins | Postoperative troponin release | HR (95% CI) |
| 4.6 (2.29.6) | |||||||
| Combination of postoperative MI and CV death | HR (95% CI) | ||||||
| 7.5 (2.820.1) | |||||||
| Schouten et al6 2009 | RCT | Mostly men (75%) in mid‐60s | 250/189/61 | Vascular surgery (carotid, abdominal aortic, endovascular, and lower extremity arterial) | Median of 2 days off statins | Postoperative myocardial ischemia and combined death from cardiovascular causes or nonfatal MI | OR (95% CI) |
| 1.1 (0.482.52) | |||||||
Statin Withdrawal in Acute Coronary Syndromes
Several studies have demonstrated an association between statin withdrawal and heightened risk of cardiovascular events in ACS.3234 In a retrospective analysis of 1616 patients presenting with ACS, withdrawal of statins during or after admission was associated with more frequent death and nonfatal MI compared to those who continued therapy (OR 2.93, 95% CI 1.646.27).33 In another retrospective observational study of 68,606 nonST‐segment elevation MI patients, statin cessation during the first 24 hours of hospitalization was independently associated with adverse outcomes including in‐hospital death (adjusted HR 1.83; 95% CI 1.582.13), cardiac arrest, and cardiogenic shock.32 In a population‐based, cohort study in the United Kingdom, statin cessation following an acute MI was independently associated with greater all‐cause mortality at 1‐year (adjusted HR 1.88, 95% CI 1.133.07).34
The significantly increased risk of adverse outcomes associated with the interruption of statins in ACS may be moderated by vascular inflammation related to the inciting coronary event, as statin discontinuation in patients with stable cardiac conditions was not associated with increased risk of cardiovascular events in a large‐scale, double‐blind, parallel‐group study.35
Statin Withdrawal in Ischemic Stroke
Adverse events associated with statin withdrawal have also been reported in patients with cerebrovascular disease. In a prospective observational study of 631 consecutive stroke survivors, those who discontinued statins (owing to mild adverse effects or unclear reasons) experienced increased mortality during the first year after the event (adjusted HR 2.78, 95% CI 1.963.72).36 Using a controversial study design aimed at evaluating the effects of stopping oral intake (including chronic medications) during the first days of acute stroke, Blanco and colleagues37 randomized 89 stroke victims on chronic statins to either continue medications or experience statin withdrawal following admission. Statin withdrawal was independently associated with increased risk of mortality and dependency at 3 months (OR 4.66, 95% CI 1.4614.91).37
Perioperative Statin Withdrawal
In the perioperative setting, statin withdrawal has also been associated with adverse outcomes. Using a quasi‐experimental design, Le Manach et al.9 evaluated the risk of cardiac complications after infra‐renal aortic surgery when immediate, postoperative resumption of statins was adopted at their institution. The investigators compared the risk of developing MI, cardiac death, or abnormal troponin release in 491 patients who did not get early postoperative statin resumption (pre‐intervention group) to 178 patients who did. Statin withdrawal for 4 days was demonstrated to be an independent predictor of postoperative troponin leak and MI (OR 2.9, 95% CI 1.65.5). Similarly, Schouten et al.10 investigated the risk of adverse events related to interruption of long‐term statins by examining cardiac outcomes in 298 statin users undergoing major vascular surgery. Among the 70 patients who experienced statin withdrawal, an increased risk of postoperative troponin release (HR 4.6, 95% CI 2.29.6), and the composite endpoint of MI and cardiovascular death (HR 7.5, 95% CI 2.820.1), was observed compared to those who resumed treatment. Not unexpectedly, the most common reason for statin cessation was inability to take oral medications after surgery. However, even in patients who discontinued statins, the use of extended‐release fluvastatin was associated with fewer perioperative cardiac events than other statins. Furthermore, extended‐release fluvastatin was also held for 2 days following surgery (owing to inability to take the drug orally), in 25% of patients in the DECREASE‐III study. However, no impact in the rate of adverse outcomes was noted despite this interruption (OR 1.1, 95% CI 0.482.52).6 Although the authors surmised that the extended formulation of fluvastatin had provided sustained levels of statin activity despite lack of timely oral intake, it is important to note that this theory may not be generalizable to chronic statin users, as they were not enrolled in this study. Conversely, some patients may have experienced postoperative ileus for longer than 2 days, perhaps resulting in confounding or attenuation of the effect noted in the study.
CLINICAL INSIGHTS INTO FAILURE OF POSTOPERATIVE STATIN RESUMPTION
We hypothesize that failure to resume perioperative statins may occur for 4 cardinal reasons. First, resumption of an oral agent frequently proves clinically challenging when complications such as postoperative ileus, nausea, and vomiting peak. To date, no intravenous statin formulations are available, although phase‐I studies are currently underway.38 Second, it is not inconceivable that perioperative clinical instability may overshadow the resumption of statin treatment. Third, clinicians may also remain concerned regarding adverse effects of statins, a thought compounded by US Food and Drug Administration statin package inserts that specifically advocate for statins to be withheld during surgery. However, although the occurrence of elevated liver function tests and myopathy are theoretically important, the overwhelming majority of perioperative statin studies in noncardiac surgery have not found this to be a major occurrence.39 Nonetheless, a lack of uniform definitions and appropriate surveillance for adverse events are important limitations to this finding. In our recent systematic review, we were unable to provide refined estimates of these important side effects owing to differences in definition, variations in screening, and absence of standardized cutoffs used in studies.31 Finally, an important reason for failing to resume postoperative statins is that many physicians simply fail to recognize the perioperative importance of these agents.
STRATEGIES TO IMPROVE PERIOPERATIVE STATIN RESUMPTION
Using the existing evidence, we propose the following 4 clinical strategies to assist in avoiding a statin withdrawal state.
Nasogastric Administration
Utilizing a post‐pyloric nasogastric tube is a straightforward solution to provide statins in those who cannot otherwise tolerate oral intake due to nausea or emesis. Although this solution is hardly innovative, it is relevant as it forces consideration of the need to resume postoperative statins by available means. While the development of a high nasogastric output or a prolonged ileus may limit the applicability of this intervention, it is important that this option be considered as opposed to expectant watching for the clinical return of bowel function. Simvastatin, atorvastatin, rosuvastatin, and pravastatin can be crushed and delivered through this route.40
Development of Reminder Systems
Computerized reminder systems have proved important in ensuring the resumption of deep venous thrombosis prophylaxis and other preventative care compliance in hospitalized patients.41, 42 Using this process, pharmacist‐ or electronic health record‐based reminder systems could be implemented to ensure that statins are restarted when clinically feasible. Further studies are needed to test whether this approach can lead to improved outcomes.
Medication Reconciliation Prior to Hospital Discharge
Statin withdrawal highlights the pertinence of a robust, medical reconciliation process prior to the patient's departure from the hospital. In this context, the development of policies using single‐ or multi‐faceted interventions that promote cooperation between inpatient physicians, surgeons, and pharmacists with outpatient primary care providers are necessary.43
Preoperative Transition to Extended Release Statin Formulations
An innovative approach to minimizing statin withdrawal involves preoperative transition to an extended‐release statin formulation. This strategy may be of particular value in patients where prolonged bowel nonavailability is likely, such as those undergoing gastrointestinal surgery, or when prolonged postoperative dietary restriction (eg, NPO [nil per os]: nothing by mouth) status is expected (Figure 2).
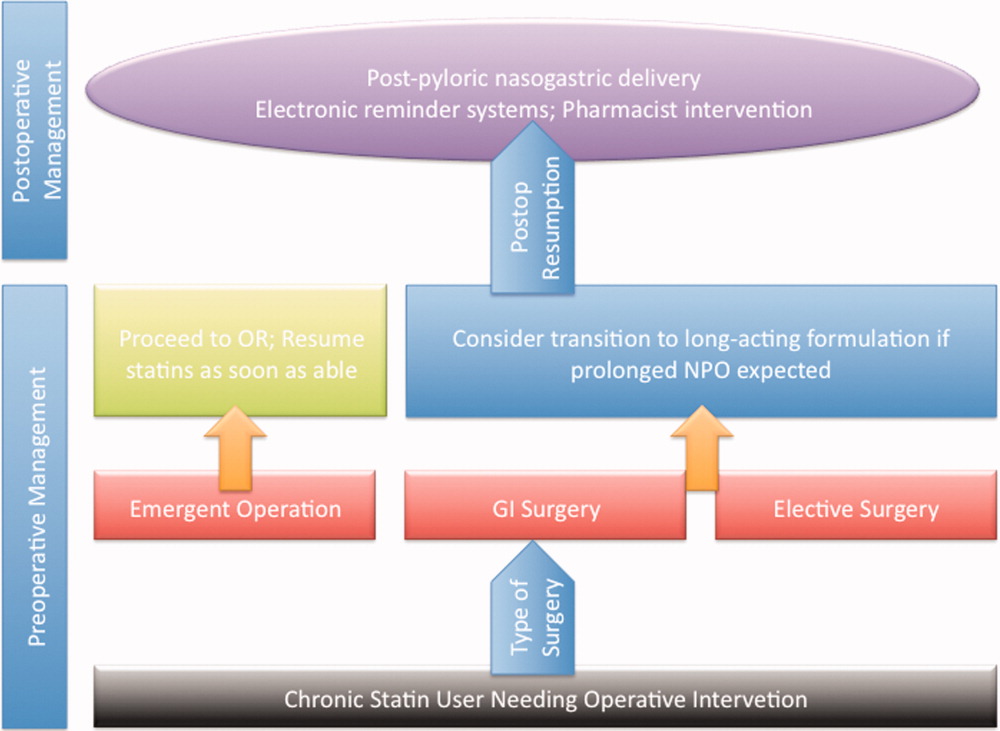
CONCLUSIONS AND FUTURE DIRECTIONS
Sudden withdrawal of perioperative statins results in adverse clinical outcomes. Individuals engaged in the care of patients during surgery such as hospitalists, anesthesiologists, and surgeons must become more cognizant of a statin withdrawal state.
An important limitation associated with the study of perioperative statin withdrawal remains the ambiguity regarding the extent of the problem in the United States. Therefore, a logical first step could be the use of infrastructure within the National Surgical Quality Improvement Program (NSQIP) to understand the epidemiology of perioperative statin use and consequences associated with statin discontinuation.44 Mandating such quality reporting could easily be built into current NSQIP performance metrics. These data would help inform a research agenda targeting patients that experience statin withdrawal and strategies most likely to prevent it.
Note Added in Proof
Disclosure: Nothing to report.
- , , , et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39(5):967–975.
- , , , , , . Improved postoperative outcomes associated with preoperative statin therapy. Anesthesiology. 2006;105(6):1260–1272; quiz 1289–1290.
- , , , , . Lipid‐lowering therapy and in‐hospital mortality following major noncardiac surgery. JAMA. 2004;291(17):2092–2099.
- , , , et al. Statins decrease perioperative cardiac complications in patients undergoing noncardiac vascular surgery: the Statins for Risk Reduction in Surgery (StaRRS) study. J Am Coll Cardiol. 2005;45(3):336–342.
- , , , et al. Statins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgery. Circulation. 2003;107(14):1848–1851.
- , , , et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361(10):980–989.
- , , , et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116(17):e418–e499.
- , , , et al. Guidelines for pre‐operative cardiac risk assessment and perioperative cardiac management in non‐cardiac surgery. Eur Heart J. 2009;30(22):2769–2812.
- , , , et al. The impact of postoperative discontinuation or continuation of chronic statin therapy on cardiac outcome after major vascular surgery. Anesth Analg. 2007;104(6):1326–1333.
- , , , et al. Effect of statin withdrawal on frequency of cardiac events after vascular surgery. Am J Cardiol. 2007;100(2):316–320.
- . Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004;109(23 suppl 1):III39–III43.
- , , , , , . Persistent endocrine stress response in patients undergoing cardiac surgery. J Endocrinol Invest. 1998;21(1):12–19.
- , , , , , . Pathology of fatal perioperative myocardial infarction: implications regarding pathophysiology and prevention. Int J Cardiol. 1996;57(1):37–44.
- , , , , , . Perioperative cardiac events in patients undergoing noncardiac surgery: a review of the magnitude of the problem, the pathophysiology of the events and methods to estimate and communicate risk. Can Med Assoc J. 2005;173(6):627–634.
- . Perioperative cardiac morbidity. Anesthesiology. 1990;72(1):153–184.
- , . Isoprenoid metabolism and the pleiotropic effects of statins. Curr Atheroscler Rep. 2003;5(5):372–378.
- , , , . Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97(12):1129–1135.
- , , , et al. Roles of rho‐associated kinase and oxidative stress in the pathogenesis of aortic stiffness. J Am Coll Cardiol. 2007;49(6):698–705.
- , , , et al. Inhibition of rho‐associated kinase results in suppression of neointimal formation of balloon‐injured arteries. Circulation. 2000;101(17):2030–2033.
- , , , . Reduced expression of endothelial cell markers after 1 year treatment with simvastatin and atorvastatin in patients with coronary heart disease. Atherosclerosis. 2002;162(1):179–185.
- , , , et al. Statins as antioxidant therapy for preventing cardiac myocyte hypertrophy. J Clin Invest. 2001;108(10):1429–1437.
- , , . Pleiotropic effects of statin therapy: molecular mechanisms and clinical results. Trends Mol Med. 2008;14(1):37–44.
- , , , et al. Inhibition of geranylgeranylation reduces angiotensin II‐mediated free radical production in vascular smooth muscle cells: involvement of angiotensin AT1 receptor expression and Rac1 GTPase. Mol Pharmacol. 2001;59(3):646–654.
- , , , et al. Withdrawal of statin treatment abrogates stroke protection in mice. Stroke. 2003;34(2):551–557.
- , , , et al. Suppression of endothelial nitric oxide production after withdrawal of statin treatment is mediated by negative feedback regulation of rho GTPase gene transcription. Circulation. 2000;102(25):3104–3110.
- , , , et al. Changes of plasma inflammatory markers after withdrawal of statin therapy in patients with hyperlipidemia. Clin Chim Acta. 2006;366(1–2):269–273.
- , , , et al. Platelet hyperactivity after statin treatment discontinuation. Thromb Haemost. 2003;90(3):476–482.
- , , , et al. Rebound inflammatory response during the acute phase of myocardial infarction after simvastatin withdrawal. Atherosclerosis. 2009;207(1):191–194.
- , . Effects of statins on endothelium and signaling mechanisms. Stroke. 2004;35(11 suppl 1):2708–2711.
- , , , et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate‐risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE‐IV). Ann Surg. 2009;249(6):921–926.
- , , , et al. Effect of perioperative statins on death, myocardial infarction, atrial fibrillation, and length of stay: a systematic review and meta‐analysis. Arch Surg. 2012;147(2):181–189.
- , , , et al. Early withdrawal of statin therapy in patients with non‐ST‐segment elevation myocardial infarction: National Registry of Myocardial Infarction. Arch Intern Med. 2004;164(19):2162–2168.
- , , , , , . Withdrawal of statins increases event rates in patients with acute coronary syndromes. Circulation. 2002;105(12):1446–1452.
- , , , , , . Discontinuation of statin therapy following an acute myocardial infarction: a population‐based study. Eur Heart J. 2008;29(17):2083–2091.
- . There is no evidence for an increase in acute coronary syndromes after short‐term abrupt discontinuation of statins in stable cardiac patients. Circulation. 2004;110(16):2333–2335.
- , , , . Discontinuation of statin therapy and clinical outcome after ischemic stroke. Stroke. 2007;38(10):2652–2657.
- , , , et al. Statin treatment withdrawal in ischemic stroke: a controlled randomized study. Neurology. 2007;69(9):904–910.
- , , , et al. Intravenous rosuvastatin for acute stroke treatment: an animal study. Stroke. 2008;39(2):433–438.
- , , , et al. Safety of perioperative statin use in high‐risk patients undergoing major vascular surgery. Am J Cardiol. 2005;95(5):658–660.
- Lexi‐Comp Online™, Lexi‐Drugs™, Hudson, OH: Lexi‐Comp, Inc; December 7, 2011.
- , , , , , . A computerized reminder system to increase the use of preventive care for hospitalized patients. N Engl J Med. 2001;345(13):965–970.
- , , , et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352(10):969–977.
- , , , . Medication review and reconciliation with cooperation between pharmacist and general practitioner and the benefit for the patient: a systematic review. Br J Clin Pharmacol. January 13, 2012. doi: 10.1111/j.1365–2125.2012.04178.x.
- American College of Surgeons National Surgical Quality Improvement Program. Available at: http://www.acsnsqip.org. Accessed December 15, 2012.
Accumulating evidence suggests that perioperative treatment with 3‐hydroxy‐3‐methylglutaryl coenzyme‐A (HMG‐CoA) reductase inhibitors (or, statins) reduces the incidence of cardiovascular events during noncardiac surgery.16 This evidence has lead the European Society of Cardiology (ESC) and American College of Cardiology Foundation/American Heart Association (ACCF/AHA) to endorse the use of perioperative statins in patients already on this treatment or those at high‐risk of cardiovascular events.7, 8
However, statins are available only in oral formulation. Consequently, prolonged bowel recovery or clinical instability may interfere with use during surgery. Furthermore, many clinicians may not recognize the imperative of postoperative statin resumption, viewing them principally as lipid‐lowering entities and not as agents of perioperative benefit. Failure to resume statins postoperatively can be catastrophic, as the ensuing inflammation and thrombosis frequently culminates in myocardial infarction (MI) or death.9, 10
In this article, we review the potent anti‐inflammatory properties of statins and their role in preventing perioperative cardiac events. We outline the biochemical basis for perioperative statin benefit, summarizing the basic, clinical, and experimental evidence regarding statin withdrawal. We conclude by presenting strategies to avert postoperative statin cessation and outline a research agenda dedicated to informing this practice.
METHODS
We performed a literature search using MEDLINE via Ovid (1946present), EMBASE (1946present), Biosis (1926present), and Cochrane CENTRAL (1960present). We used Boolean logic to search for key terms including statins, 3‐hydroxy‐3‐methylglutaryl CoA reductase inhibitors, death, MI, stroke, acute coronary syndrome (ACS), and statin withdrawal or cessation. All studies published in full‐text or abstract form were included. A total of 489 articles were retrieved by this search (last updated March 15, 2012). For this narrative review, we focused on studies that examined adverse outcomes associated with statin withdrawal.
BIOCHEMICAL BASIS OF STATIN PLEIOTROPICITY
The nonlipid‐lowering or pleiotropic properties of statins are especially valuable in the perioperative setting.16, 11 Perioperative cardiac complications occur due to oxygen supply:demand mismatch, vascular inflammation, or a combination of these states. A significant perisurgical catecholamine surge produces unopposed sympathetic effects,12 increasing the risk of rupture of vulnerable coronary plaques, thrombus formation, and adverse cardiac events.13, 14 Similarly, augmented inflammatory responses and increased circulating coagulation factors further predispose to a hazardous perioperative milieu.15 Statins attenuate this vascular inflammatory response by suppressing the synthesis of mevalonate by inhibiting HMG‐CoA reductase. Suppression of mevalonate synthesis reduces the bioavailability of 2 important isoprenoid molecules: farnesyl‐pyrophosphate and geranylgeranyl‐pyrophosphate.16 Diminution of these isoprenoid intermediaries leads to reductions in the active intracellular signaling molecules Ras, Rho, and Rac, which play critical roles in vascular reactivity, endothelial function, and coagulation and inflammatory pathways.1723 The cumulative effect of these cellular changes is diminished inflammation during periods of surgical stress (Figure 1).
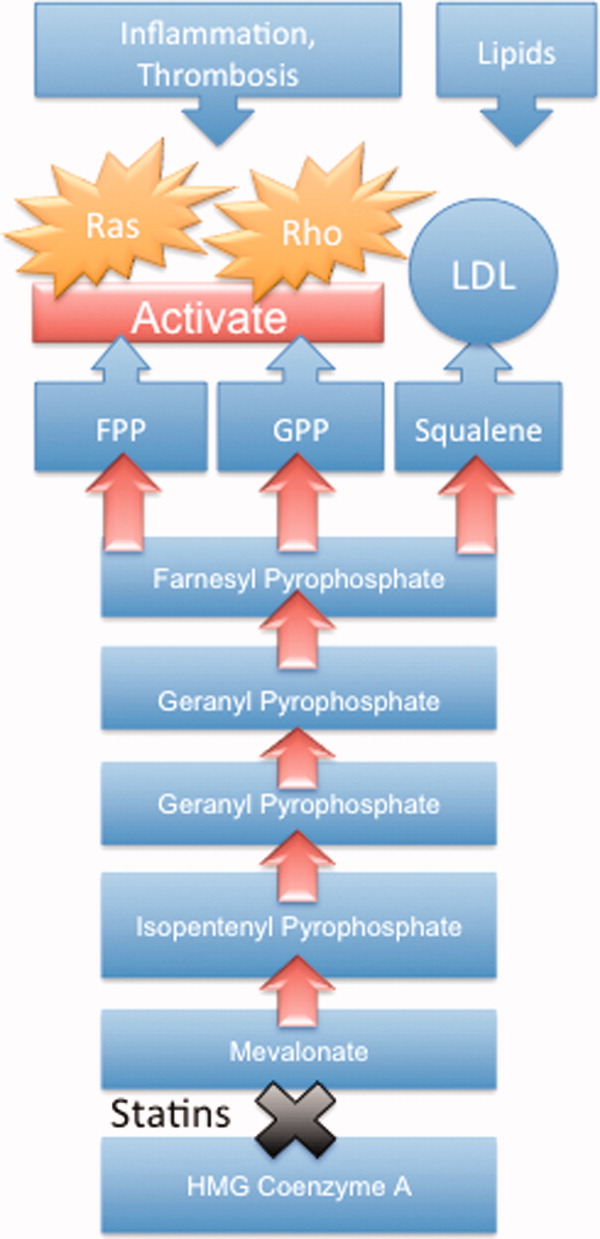
While the perioperative pleiotropicity of statins is of inherent clinical value, several studies have shown that these effects are lost and even reversed when statins are withdrawn.2428 During statin treatment, absence of isoprenoid intermediaries induces cytosolic accumulation of nonactivated Rho and Rac proteins. Abrupt cessation of statins activates Rho/Rac‐kinase pathways, leading to unregulated inflammation, platelet hyper‐activation, and endothelial dysfunction.24, 25, 28, 29 For instance, statin withdrawal in mice‐models leads to an overshoot activation of Rho, resulting in down‐regulation of endothelial nitric oxide production,25 activation of nicotinamide adenine dinucleotide phosphate (NAD[P]H)‐oxidase, and increased superoxide production.29 In another mouse‐model, statin withdrawal was associated with up‐regulation of key pro‐thrombotic molecules including platelet factor 4 and beta‐thromboglobulin.24 In human studies, a platelet hyper‐activation state (manifested by increased platelet P‐selectin expression and enhanced platelet aggregation) occurs after statin discontinuation.27 Furthermore, withdrawal of statins in patients with hyperlipidemia increases inflammatory markers such as C‐reactive protein and interleukin‐6.26 In the perioperative context, absence of these important anti‐inflammatory properties increases the risk of cardiac events.9, 10
EVIDENCE SUGGESTING BENEFIT FROM PERIOPERATIVE STATIN TREATMENT
Retrospective studies first suggested clinical benefit from perioperative statin treatment. In a case‐control study involving 2816 patients undergoing vascular surgery at Erasmus Medical Center, statin use was associated with substantially decreased postoperative mortality (adjusted odd ratio [OR] 0.22, 95% confidence interval [CI] 0.100.47).5 In a subsequent retrospective cohort study of 780,591 patients who underwent major noncardiac surgery, the risk of postoperative mortality was considerably lower among statin users (unadjusted OR 0.68, 95% CI 0.640.72) compared to patients who did not receive, or received delayed treatment with statins.3 A third retrospective study of 1163 vascular surgery patients found that statins prevented perioperative cardiac complications including death, MI, congestive heart failure, and ventricular tachyarrhythmias (OR 0.52, 95% CI 0.350.76).4
The benefit from statin treatment found in retrospective studies prompted the first double‐blinded, randomized controlled trial (RCT) of perioperative statin use. In 2004, Durazzo and colleagues1 randomized 100 statin‐naive patients scheduled to undergo elective aortic, femoro‐popliteal, or carotid surgery to receive either 20 mg of atorvastatin or placebo for 45 days. Vascular surgery was performed, on average, 31 days after randomization. Atorvastatin therapy reduced the incidence of death from cardiac causes, nonfatal acute MI, ischemic stroke, and unstable angina (26% in the placebo group vs 8% in the atorvastatin group; P = 0.031).1 Although the small size of the trial rendered it underpowered to show a mortality benefit, this remains the first RCT to demonstrate a protective perioperative effect of statins.
In the 2009 Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography (DECREASE)‐III trial, Schouten and colleagues6 randomized 497 high‐risk, statin‐naive patients undergoing vascular surgery to receive, in addition to a beta‐blocker, either fluvastatin or placebo before surgery (median of 37 days). Postoperative myocardial ischemia (hazard ratio [HR] 0.55, 95% CI 0.340.88), and combined death from cardiovascular causes or nonfatal MI (HR 0.47, 95% CI 0.240.94), occurred less frequently in the treatment group.6 In 2009, the same group published DECREASE‐IV, a multicenter, prospective, open‐label, 2 2 factorial design trial of 1066 intermediate‐risk patients, scheduled to undergo elective, noncardiac surgery. Patients were assigned to bisoprolol, fluvastatin, combination treatment, or control therapy before surgery (median of 34 days). Although those randomized to fluvastatin demonstrated lower incidence of 30‐day cardiac death and MI than control (HR 0.65, 95% CI 0.351.10), these outcomes failed to reach statistical significance as the trial was principally powered to examine the effects of perioperative beta‐blockade.30
Using this pool of data, a meta‐analysis of 15 studies (223,010 patients) found a substantial 38% reduction in the risk of mortality after cardiac surgery (1.9% vs 3.1%; P = 0.0001) and an even greater 59% reduction in the risk of mortality following vascular surgery (1.7% vs 6.1%; P = 0.0001) with perioperative statin therapy. When including noncardiac surgery, a 44% reduction in mortality was observed (2.2% vs 3.2%; P 0.01).2 We performed a similar meta‐analysis of 15 RCTs involving 2292 patients to determine whether perioperative statin treatment in statin‐naive patients, undergoing either cardiac or noncardiac surgery, improved clinical outcomes. Our analysis also found statistically significant reductions in the risk of MI associated with perioperative statin use in both cardiac and noncardiac surgery (risk reduction [RR] 0.53, 95% CI 0.380.74) and atrial fibrillation in statin‐naive patients undergoing cardiac surgery (RR 0.56, 95% CI 0.450.69).31 Taken together, a large volume of evidence supports the use of statins in surgical settings.
In view of this evidence, the ACCF/AHA perioperative guidelines for noncardiac surgery endorsed statins as an important risk‐reducing intervention in those undergoing noncardiac surgery, and recommended continued use in patients on chronic statin treatment scheduled for noncardiac surgery (Level of Evidence B, Class I; Benefits >>> Risk). Initiating statins in patients undergoing vascular surgery, with or without risk factors, was considered reasonable (Level of Evidence B, Class IIa; Benefits >> Risk).7 Current ESC perioperative guidelines in noncardiac surgery offer similar recommendations to those of ACCF/AHA, but differ by categorizing the recommendation to initiate statins in patients at high cardiovascular risk as a Class I recommendation.8
CLINICAL CONSEQUENCES OF STATIN WITHDRAWAL
Although statins provide important cardiac benefits, an important limitation to their perioperative use remains their oral‐only formulation. Thus, patients who are unable to resume oral intake may fail to resume treatment. Perioperative statin cessation has been hypothesized to lead to a statin withdrawal phenomenon. The evidence that supports the existence of this phenomenon comes from 3 distinct populations: ACS, ischemic stroke, and perioperative patients (Table 1).
| Author (ref) Year | Design | Study Population | Sample Size (N) (Total/ Continuation/Discontinuation) | Clinical Setting and Context | Timing of Statin Discontinuation | Study Outcome | Results (Withdrawal vs Continuation) |
|---|---|---|---|---|---|---|---|
| |||||||
| Heeschen et al33 2002 | Retrospective cohort | Mostly men (68%) in early 60s | 1616/379/86 | Chest pain in ACS | During or after admission | Incidence of death and nonfatal MI | OR (95% CI) |
| 2.93 (1.646.27) | |||||||
| Spencer et al32 2004 | Retrospective cohort | Mostly men (62%) in late 60s | 68,506/9001/487 | NonST‐segment elevation MI | During the first 24 hr of hospitalization | In‐hospital death | HR (95% CI) |
| 1.83 (1.582.13) | |||||||
| Daskalopoulou et al34 2008 | Retrospective cohort | 60% men in late 60s | 9939/2026/137 Non‐users 2124 (reference group) | Acute MI | Within 1 yr of the coronary event | 1‐yr all‐cause mortality | HR (95% CI) |
| 1.88 (1.133.07)* | |||||||
| Colivicchi et al36 2007 | Prospective cohort | 51% men in early 70s | 631/385/246 | Ischemic stroke | Mean 48.6 days | 1‐yr all‐cause mortality | HR (95% CI) |
| 2.78 (1.963.72) | |||||||
| Blanco et al37 2007 | RCT | 51% men in mid‐60s | 215/46/43 | Ischemic stroke | N/A | Risk of death or dependency at 3 mo | OR (95% CI) |
| 4.66 (1.4614.91) | |||||||
| Early neurologic deterioration | OR (95% CI) | ||||||
| 7.08 (2.7318.37) | |||||||
| Le Manach et al9 2007 | Quasi‐experimental (prepost) | Mostly men (89%) in late‐60s | 669/178/491 | Infra‐renal aortic surgery | Median of 4 days off statins | Postoperative troponin release, MI | OR (95% CI) |
| 2.9 (1.65.5) | |||||||
| Schouten et al10 2007 | Prospective cohort | Mostly men (75%) in mid‐60s | 298/228/70 | Aortic and lower extremity vascular surgery | Median of 3 days off statins | Postoperative troponin release | HR (95% CI) |
| 4.6 (2.29.6) | |||||||
| Combination of postoperative MI and CV death | HR (95% CI) | ||||||
| 7.5 (2.820.1) | |||||||
| Schouten et al6 2009 | RCT | Mostly men (75%) in mid‐60s | 250/189/61 | Vascular surgery (carotid, abdominal aortic, endovascular, and lower extremity arterial) | Median of 2 days off statins | Postoperative myocardial ischemia and combined death from cardiovascular causes or nonfatal MI | OR (95% CI) |
| 1.1 (0.482.52) | |||||||
Statin Withdrawal in Acute Coronary Syndromes
Several studies have demonstrated an association between statin withdrawal and heightened risk of cardiovascular events in ACS.3234 In a retrospective analysis of 1616 patients presenting with ACS, withdrawal of statins during or after admission was associated with more frequent death and nonfatal MI compared to those who continued therapy (OR 2.93, 95% CI 1.646.27).33 In another retrospective observational study of 68,606 nonST‐segment elevation MI patients, statin cessation during the first 24 hours of hospitalization was independently associated with adverse outcomes including in‐hospital death (adjusted HR 1.83; 95% CI 1.582.13), cardiac arrest, and cardiogenic shock.32 In a population‐based, cohort study in the United Kingdom, statin cessation following an acute MI was independently associated with greater all‐cause mortality at 1‐year (adjusted HR 1.88, 95% CI 1.133.07).34
The significantly increased risk of adverse outcomes associated with the interruption of statins in ACS may be moderated by vascular inflammation related to the inciting coronary event, as statin discontinuation in patients with stable cardiac conditions was not associated with increased risk of cardiovascular events in a large‐scale, double‐blind, parallel‐group study.35
Statin Withdrawal in Ischemic Stroke
Adverse events associated with statin withdrawal have also been reported in patients with cerebrovascular disease. In a prospective observational study of 631 consecutive stroke survivors, those who discontinued statins (owing to mild adverse effects or unclear reasons) experienced increased mortality during the first year after the event (adjusted HR 2.78, 95% CI 1.963.72).36 Using a controversial study design aimed at evaluating the effects of stopping oral intake (including chronic medications) during the first days of acute stroke, Blanco and colleagues37 randomized 89 stroke victims on chronic statins to either continue medications or experience statin withdrawal following admission. Statin withdrawal was independently associated with increased risk of mortality and dependency at 3 months (OR 4.66, 95% CI 1.4614.91).37
Perioperative Statin Withdrawal
In the perioperative setting, statin withdrawal has also been associated with adverse outcomes. Using a quasi‐experimental design, Le Manach et al.9 evaluated the risk of cardiac complications after infra‐renal aortic surgery when immediate, postoperative resumption of statins was adopted at their institution. The investigators compared the risk of developing MI, cardiac death, or abnormal troponin release in 491 patients who did not get early postoperative statin resumption (pre‐intervention group) to 178 patients who did. Statin withdrawal for 4 days was demonstrated to be an independent predictor of postoperative troponin leak and MI (OR 2.9, 95% CI 1.65.5). Similarly, Schouten et al.10 investigated the risk of adverse events related to interruption of long‐term statins by examining cardiac outcomes in 298 statin users undergoing major vascular surgery. Among the 70 patients who experienced statin withdrawal, an increased risk of postoperative troponin release (HR 4.6, 95% CI 2.29.6), and the composite endpoint of MI and cardiovascular death (HR 7.5, 95% CI 2.820.1), was observed compared to those who resumed treatment. Not unexpectedly, the most common reason for statin cessation was inability to take oral medications after surgery. However, even in patients who discontinued statins, the use of extended‐release fluvastatin was associated with fewer perioperative cardiac events than other statins. Furthermore, extended‐release fluvastatin was also held for 2 days following surgery (owing to inability to take the drug orally), in 25% of patients in the DECREASE‐III study. However, no impact in the rate of adverse outcomes was noted despite this interruption (OR 1.1, 95% CI 0.482.52).6 Although the authors surmised that the extended formulation of fluvastatin had provided sustained levels of statin activity despite lack of timely oral intake, it is important to note that this theory may not be generalizable to chronic statin users, as they were not enrolled in this study. Conversely, some patients may have experienced postoperative ileus for longer than 2 days, perhaps resulting in confounding or attenuation of the effect noted in the study.
CLINICAL INSIGHTS INTO FAILURE OF POSTOPERATIVE STATIN RESUMPTION
We hypothesize that failure to resume perioperative statins may occur for 4 cardinal reasons. First, resumption of an oral agent frequently proves clinically challenging when complications such as postoperative ileus, nausea, and vomiting peak. To date, no intravenous statin formulations are available, although phase‐I studies are currently underway.38 Second, it is not inconceivable that perioperative clinical instability may overshadow the resumption of statin treatment. Third, clinicians may also remain concerned regarding adverse effects of statins, a thought compounded by US Food and Drug Administration statin package inserts that specifically advocate for statins to be withheld during surgery. However, although the occurrence of elevated liver function tests and myopathy are theoretically important, the overwhelming majority of perioperative statin studies in noncardiac surgery have not found this to be a major occurrence.39 Nonetheless, a lack of uniform definitions and appropriate surveillance for adverse events are important limitations to this finding. In our recent systematic review, we were unable to provide refined estimates of these important side effects owing to differences in definition, variations in screening, and absence of standardized cutoffs used in studies.31 Finally, an important reason for failing to resume postoperative statins is that many physicians simply fail to recognize the perioperative importance of these agents.
STRATEGIES TO IMPROVE PERIOPERATIVE STATIN RESUMPTION
Using the existing evidence, we propose the following 4 clinical strategies to assist in avoiding a statin withdrawal state.
Nasogastric Administration
Utilizing a post‐pyloric nasogastric tube is a straightforward solution to provide statins in those who cannot otherwise tolerate oral intake due to nausea or emesis. Although this solution is hardly innovative, it is relevant as it forces consideration of the need to resume postoperative statins by available means. While the development of a high nasogastric output or a prolonged ileus may limit the applicability of this intervention, it is important that this option be considered as opposed to expectant watching for the clinical return of bowel function. Simvastatin, atorvastatin, rosuvastatin, and pravastatin can be crushed and delivered through this route.40
Development of Reminder Systems
Computerized reminder systems have proved important in ensuring the resumption of deep venous thrombosis prophylaxis and other preventative care compliance in hospitalized patients.41, 42 Using this process, pharmacist‐ or electronic health record‐based reminder systems could be implemented to ensure that statins are restarted when clinically feasible. Further studies are needed to test whether this approach can lead to improved outcomes.
Medication Reconciliation Prior to Hospital Discharge
Statin withdrawal highlights the pertinence of a robust, medical reconciliation process prior to the patient's departure from the hospital. In this context, the development of policies using single‐ or multi‐faceted interventions that promote cooperation between inpatient physicians, surgeons, and pharmacists with outpatient primary care providers are necessary.43
Preoperative Transition to Extended Release Statin Formulations
An innovative approach to minimizing statin withdrawal involves preoperative transition to an extended‐release statin formulation. This strategy may be of particular value in patients where prolonged bowel nonavailability is likely, such as those undergoing gastrointestinal surgery, or when prolonged postoperative dietary restriction (eg, NPO [nil per os]: nothing by mouth) status is expected (Figure 2).
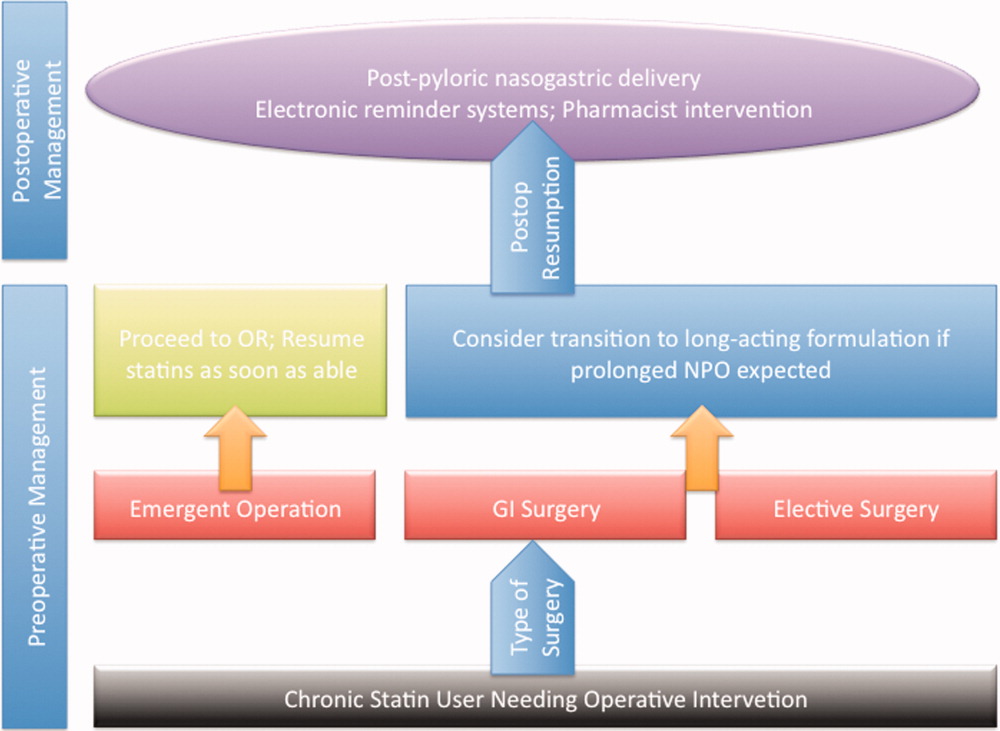
CONCLUSIONS AND FUTURE DIRECTIONS
Sudden withdrawal of perioperative statins results in adverse clinical outcomes. Individuals engaged in the care of patients during surgery such as hospitalists, anesthesiologists, and surgeons must become more cognizant of a statin withdrawal state.
An important limitation associated with the study of perioperative statin withdrawal remains the ambiguity regarding the extent of the problem in the United States. Therefore, a logical first step could be the use of infrastructure within the National Surgical Quality Improvement Program (NSQIP) to understand the epidemiology of perioperative statin use and consequences associated with statin discontinuation.44 Mandating such quality reporting could easily be built into current NSQIP performance metrics. These data would help inform a research agenda targeting patients that experience statin withdrawal and strategies most likely to prevent it.
Note Added in Proof
Disclosure: Nothing to report.
Accumulating evidence suggests that perioperative treatment with 3‐hydroxy‐3‐methylglutaryl coenzyme‐A (HMG‐CoA) reductase inhibitors (or, statins) reduces the incidence of cardiovascular events during noncardiac surgery.16 This evidence has lead the European Society of Cardiology (ESC) and American College of Cardiology Foundation/American Heart Association (ACCF/AHA) to endorse the use of perioperative statins in patients already on this treatment or those at high‐risk of cardiovascular events.7, 8
However, statins are available only in oral formulation. Consequently, prolonged bowel recovery or clinical instability may interfere with use during surgery. Furthermore, many clinicians may not recognize the imperative of postoperative statin resumption, viewing them principally as lipid‐lowering entities and not as agents of perioperative benefit. Failure to resume statins postoperatively can be catastrophic, as the ensuing inflammation and thrombosis frequently culminates in myocardial infarction (MI) or death.9, 10
In this article, we review the potent anti‐inflammatory properties of statins and their role in preventing perioperative cardiac events. We outline the biochemical basis for perioperative statin benefit, summarizing the basic, clinical, and experimental evidence regarding statin withdrawal. We conclude by presenting strategies to avert postoperative statin cessation and outline a research agenda dedicated to informing this practice.
METHODS
We performed a literature search using MEDLINE via Ovid (1946present), EMBASE (1946present), Biosis (1926present), and Cochrane CENTRAL (1960present). We used Boolean logic to search for key terms including statins, 3‐hydroxy‐3‐methylglutaryl CoA reductase inhibitors, death, MI, stroke, acute coronary syndrome (ACS), and statin withdrawal or cessation. All studies published in full‐text or abstract form were included. A total of 489 articles were retrieved by this search (last updated March 15, 2012). For this narrative review, we focused on studies that examined adverse outcomes associated with statin withdrawal.
BIOCHEMICAL BASIS OF STATIN PLEIOTROPICITY
The nonlipid‐lowering or pleiotropic properties of statins are especially valuable in the perioperative setting.16, 11 Perioperative cardiac complications occur due to oxygen supply:demand mismatch, vascular inflammation, or a combination of these states. A significant perisurgical catecholamine surge produces unopposed sympathetic effects,12 increasing the risk of rupture of vulnerable coronary plaques, thrombus formation, and adverse cardiac events.13, 14 Similarly, augmented inflammatory responses and increased circulating coagulation factors further predispose to a hazardous perioperative milieu.15 Statins attenuate this vascular inflammatory response by suppressing the synthesis of mevalonate by inhibiting HMG‐CoA reductase. Suppression of mevalonate synthesis reduces the bioavailability of 2 important isoprenoid molecules: farnesyl‐pyrophosphate and geranylgeranyl‐pyrophosphate.16 Diminution of these isoprenoid intermediaries leads to reductions in the active intracellular signaling molecules Ras, Rho, and Rac, which play critical roles in vascular reactivity, endothelial function, and coagulation and inflammatory pathways.1723 The cumulative effect of these cellular changes is diminished inflammation during periods of surgical stress (Figure 1).
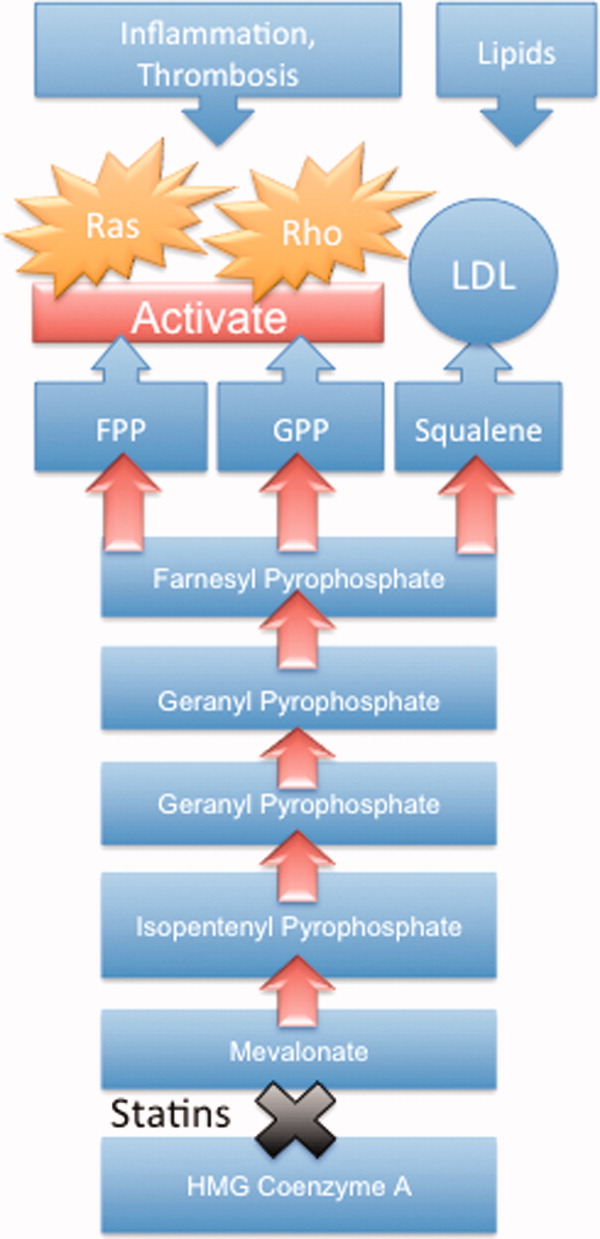
While the perioperative pleiotropicity of statins is of inherent clinical value, several studies have shown that these effects are lost and even reversed when statins are withdrawn.2428 During statin treatment, absence of isoprenoid intermediaries induces cytosolic accumulation of nonactivated Rho and Rac proteins. Abrupt cessation of statins activates Rho/Rac‐kinase pathways, leading to unregulated inflammation, platelet hyper‐activation, and endothelial dysfunction.24, 25, 28, 29 For instance, statin withdrawal in mice‐models leads to an overshoot activation of Rho, resulting in down‐regulation of endothelial nitric oxide production,25 activation of nicotinamide adenine dinucleotide phosphate (NAD[P]H)‐oxidase, and increased superoxide production.29 In another mouse‐model, statin withdrawal was associated with up‐regulation of key pro‐thrombotic molecules including platelet factor 4 and beta‐thromboglobulin.24 In human studies, a platelet hyper‐activation state (manifested by increased platelet P‐selectin expression and enhanced platelet aggregation) occurs after statin discontinuation.27 Furthermore, withdrawal of statins in patients with hyperlipidemia increases inflammatory markers such as C‐reactive protein and interleukin‐6.26 In the perioperative context, absence of these important anti‐inflammatory properties increases the risk of cardiac events.9, 10
EVIDENCE SUGGESTING BENEFIT FROM PERIOPERATIVE STATIN TREATMENT
Retrospective studies first suggested clinical benefit from perioperative statin treatment. In a case‐control study involving 2816 patients undergoing vascular surgery at Erasmus Medical Center, statin use was associated with substantially decreased postoperative mortality (adjusted odd ratio [OR] 0.22, 95% confidence interval [CI] 0.100.47).5 In a subsequent retrospective cohort study of 780,591 patients who underwent major noncardiac surgery, the risk of postoperative mortality was considerably lower among statin users (unadjusted OR 0.68, 95% CI 0.640.72) compared to patients who did not receive, or received delayed treatment with statins.3 A third retrospective study of 1163 vascular surgery patients found that statins prevented perioperative cardiac complications including death, MI, congestive heart failure, and ventricular tachyarrhythmias (OR 0.52, 95% CI 0.350.76).4
The benefit from statin treatment found in retrospective studies prompted the first double‐blinded, randomized controlled trial (RCT) of perioperative statin use. In 2004, Durazzo and colleagues1 randomized 100 statin‐naive patients scheduled to undergo elective aortic, femoro‐popliteal, or carotid surgery to receive either 20 mg of atorvastatin or placebo for 45 days. Vascular surgery was performed, on average, 31 days after randomization. Atorvastatin therapy reduced the incidence of death from cardiac causes, nonfatal acute MI, ischemic stroke, and unstable angina (26% in the placebo group vs 8% in the atorvastatin group; P = 0.031).1 Although the small size of the trial rendered it underpowered to show a mortality benefit, this remains the first RCT to demonstrate a protective perioperative effect of statins.
In the 2009 Dutch Echocardiographic Cardiac Risk Evaluation Applying Stress Echocardiography (DECREASE)‐III trial, Schouten and colleagues6 randomized 497 high‐risk, statin‐naive patients undergoing vascular surgery to receive, in addition to a beta‐blocker, either fluvastatin or placebo before surgery (median of 37 days). Postoperative myocardial ischemia (hazard ratio [HR] 0.55, 95% CI 0.340.88), and combined death from cardiovascular causes or nonfatal MI (HR 0.47, 95% CI 0.240.94), occurred less frequently in the treatment group.6 In 2009, the same group published DECREASE‐IV, a multicenter, prospective, open‐label, 2 2 factorial design trial of 1066 intermediate‐risk patients, scheduled to undergo elective, noncardiac surgery. Patients were assigned to bisoprolol, fluvastatin, combination treatment, or control therapy before surgery (median of 34 days). Although those randomized to fluvastatin demonstrated lower incidence of 30‐day cardiac death and MI than control (HR 0.65, 95% CI 0.351.10), these outcomes failed to reach statistical significance as the trial was principally powered to examine the effects of perioperative beta‐blockade.30
Using this pool of data, a meta‐analysis of 15 studies (223,010 patients) found a substantial 38% reduction in the risk of mortality after cardiac surgery (1.9% vs 3.1%; P = 0.0001) and an even greater 59% reduction in the risk of mortality following vascular surgery (1.7% vs 6.1%; P = 0.0001) with perioperative statin therapy. When including noncardiac surgery, a 44% reduction in mortality was observed (2.2% vs 3.2%; P 0.01).2 We performed a similar meta‐analysis of 15 RCTs involving 2292 patients to determine whether perioperative statin treatment in statin‐naive patients, undergoing either cardiac or noncardiac surgery, improved clinical outcomes. Our analysis also found statistically significant reductions in the risk of MI associated with perioperative statin use in both cardiac and noncardiac surgery (risk reduction [RR] 0.53, 95% CI 0.380.74) and atrial fibrillation in statin‐naive patients undergoing cardiac surgery (RR 0.56, 95% CI 0.450.69).31 Taken together, a large volume of evidence supports the use of statins in surgical settings.
In view of this evidence, the ACCF/AHA perioperative guidelines for noncardiac surgery endorsed statins as an important risk‐reducing intervention in those undergoing noncardiac surgery, and recommended continued use in patients on chronic statin treatment scheduled for noncardiac surgery (Level of Evidence B, Class I; Benefits >>> Risk). Initiating statins in patients undergoing vascular surgery, with or without risk factors, was considered reasonable (Level of Evidence B, Class IIa; Benefits >> Risk).7 Current ESC perioperative guidelines in noncardiac surgery offer similar recommendations to those of ACCF/AHA, but differ by categorizing the recommendation to initiate statins in patients at high cardiovascular risk as a Class I recommendation.8
CLINICAL CONSEQUENCES OF STATIN WITHDRAWAL
Although statins provide important cardiac benefits, an important limitation to their perioperative use remains their oral‐only formulation. Thus, patients who are unable to resume oral intake may fail to resume treatment. Perioperative statin cessation has been hypothesized to lead to a statin withdrawal phenomenon. The evidence that supports the existence of this phenomenon comes from 3 distinct populations: ACS, ischemic stroke, and perioperative patients (Table 1).
| Author (ref) Year | Design | Study Population | Sample Size (N) (Total/ Continuation/Discontinuation) | Clinical Setting and Context | Timing of Statin Discontinuation | Study Outcome | Results (Withdrawal vs Continuation) |
|---|---|---|---|---|---|---|---|
| |||||||
| Heeschen et al33 2002 | Retrospective cohort | Mostly men (68%) in early 60s | 1616/379/86 | Chest pain in ACS | During or after admission | Incidence of death and nonfatal MI | OR (95% CI) |
| 2.93 (1.646.27) | |||||||
| Spencer et al32 2004 | Retrospective cohort | Mostly men (62%) in late 60s | 68,506/9001/487 | NonST‐segment elevation MI | During the first 24 hr of hospitalization | In‐hospital death | HR (95% CI) |
| 1.83 (1.582.13) | |||||||
| Daskalopoulou et al34 2008 | Retrospective cohort | 60% men in late 60s | 9939/2026/137 Non‐users 2124 (reference group) | Acute MI | Within 1 yr of the coronary event | 1‐yr all‐cause mortality | HR (95% CI) |
| 1.88 (1.133.07)* | |||||||
| Colivicchi et al36 2007 | Prospective cohort | 51% men in early 70s | 631/385/246 | Ischemic stroke | Mean 48.6 days | 1‐yr all‐cause mortality | HR (95% CI) |
| 2.78 (1.963.72) | |||||||
| Blanco et al37 2007 | RCT | 51% men in mid‐60s | 215/46/43 | Ischemic stroke | N/A | Risk of death or dependency at 3 mo | OR (95% CI) |
| 4.66 (1.4614.91) | |||||||
| Early neurologic deterioration | OR (95% CI) | ||||||
| 7.08 (2.7318.37) | |||||||
| Le Manach et al9 2007 | Quasi‐experimental (prepost) | Mostly men (89%) in late‐60s | 669/178/491 | Infra‐renal aortic surgery | Median of 4 days off statins | Postoperative troponin release, MI | OR (95% CI) |
| 2.9 (1.65.5) | |||||||
| Schouten et al10 2007 | Prospective cohort | Mostly men (75%) in mid‐60s | 298/228/70 | Aortic and lower extremity vascular surgery | Median of 3 days off statins | Postoperative troponin release | HR (95% CI) |
| 4.6 (2.29.6) | |||||||
| Combination of postoperative MI and CV death | HR (95% CI) | ||||||
| 7.5 (2.820.1) | |||||||
| Schouten et al6 2009 | RCT | Mostly men (75%) in mid‐60s | 250/189/61 | Vascular surgery (carotid, abdominal aortic, endovascular, and lower extremity arterial) | Median of 2 days off statins | Postoperative myocardial ischemia and combined death from cardiovascular causes or nonfatal MI | OR (95% CI) |
| 1.1 (0.482.52) | |||||||
Statin Withdrawal in Acute Coronary Syndromes
Several studies have demonstrated an association between statin withdrawal and heightened risk of cardiovascular events in ACS.3234 In a retrospective analysis of 1616 patients presenting with ACS, withdrawal of statins during or after admission was associated with more frequent death and nonfatal MI compared to those who continued therapy (OR 2.93, 95% CI 1.646.27).33 In another retrospective observational study of 68,606 nonST‐segment elevation MI patients, statin cessation during the first 24 hours of hospitalization was independently associated with adverse outcomes including in‐hospital death (adjusted HR 1.83; 95% CI 1.582.13), cardiac arrest, and cardiogenic shock.32 In a population‐based, cohort study in the United Kingdom, statin cessation following an acute MI was independently associated with greater all‐cause mortality at 1‐year (adjusted HR 1.88, 95% CI 1.133.07).34
The significantly increased risk of adverse outcomes associated with the interruption of statins in ACS may be moderated by vascular inflammation related to the inciting coronary event, as statin discontinuation in patients with stable cardiac conditions was not associated with increased risk of cardiovascular events in a large‐scale, double‐blind, parallel‐group study.35
Statin Withdrawal in Ischemic Stroke
Adverse events associated with statin withdrawal have also been reported in patients with cerebrovascular disease. In a prospective observational study of 631 consecutive stroke survivors, those who discontinued statins (owing to mild adverse effects or unclear reasons) experienced increased mortality during the first year after the event (adjusted HR 2.78, 95% CI 1.963.72).36 Using a controversial study design aimed at evaluating the effects of stopping oral intake (including chronic medications) during the first days of acute stroke, Blanco and colleagues37 randomized 89 stroke victims on chronic statins to either continue medications or experience statin withdrawal following admission. Statin withdrawal was independently associated with increased risk of mortality and dependency at 3 months (OR 4.66, 95% CI 1.4614.91).37
Perioperative Statin Withdrawal
In the perioperative setting, statin withdrawal has also been associated with adverse outcomes. Using a quasi‐experimental design, Le Manach et al.9 evaluated the risk of cardiac complications after infra‐renal aortic surgery when immediate, postoperative resumption of statins was adopted at their institution. The investigators compared the risk of developing MI, cardiac death, or abnormal troponin release in 491 patients who did not get early postoperative statin resumption (pre‐intervention group) to 178 patients who did. Statin withdrawal for 4 days was demonstrated to be an independent predictor of postoperative troponin leak and MI (OR 2.9, 95% CI 1.65.5). Similarly, Schouten et al.10 investigated the risk of adverse events related to interruption of long‐term statins by examining cardiac outcomes in 298 statin users undergoing major vascular surgery. Among the 70 patients who experienced statin withdrawal, an increased risk of postoperative troponin release (HR 4.6, 95% CI 2.29.6), and the composite endpoint of MI and cardiovascular death (HR 7.5, 95% CI 2.820.1), was observed compared to those who resumed treatment. Not unexpectedly, the most common reason for statin cessation was inability to take oral medications after surgery. However, even in patients who discontinued statins, the use of extended‐release fluvastatin was associated with fewer perioperative cardiac events than other statins. Furthermore, extended‐release fluvastatin was also held for 2 days following surgery (owing to inability to take the drug orally), in 25% of patients in the DECREASE‐III study. However, no impact in the rate of adverse outcomes was noted despite this interruption (OR 1.1, 95% CI 0.482.52).6 Although the authors surmised that the extended formulation of fluvastatin had provided sustained levels of statin activity despite lack of timely oral intake, it is important to note that this theory may not be generalizable to chronic statin users, as they were not enrolled in this study. Conversely, some patients may have experienced postoperative ileus for longer than 2 days, perhaps resulting in confounding or attenuation of the effect noted in the study.
CLINICAL INSIGHTS INTO FAILURE OF POSTOPERATIVE STATIN RESUMPTION
We hypothesize that failure to resume perioperative statins may occur for 4 cardinal reasons. First, resumption of an oral agent frequently proves clinically challenging when complications such as postoperative ileus, nausea, and vomiting peak. To date, no intravenous statin formulations are available, although phase‐I studies are currently underway.38 Second, it is not inconceivable that perioperative clinical instability may overshadow the resumption of statin treatment. Third, clinicians may also remain concerned regarding adverse effects of statins, a thought compounded by US Food and Drug Administration statin package inserts that specifically advocate for statins to be withheld during surgery. However, although the occurrence of elevated liver function tests and myopathy are theoretically important, the overwhelming majority of perioperative statin studies in noncardiac surgery have not found this to be a major occurrence.39 Nonetheless, a lack of uniform definitions and appropriate surveillance for adverse events are important limitations to this finding. In our recent systematic review, we were unable to provide refined estimates of these important side effects owing to differences in definition, variations in screening, and absence of standardized cutoffs used in studies.31 Finally, an important reason for failing to resume postoperative statins is that many physicians simply fail to recognize the perioperative importance of these agents.
STRATEGIES TO IMPROVE PERIOPERATIVE STATIN RESUMPTION
Using the existing evidence, we propose the following 4 clinical strategies to assist in avoiding a statin withdrawal state.
Nasogastric Administration
Utilizing a post‐pyloric nasogastric tube is a straightforward solution to provide statins in those who cannot otherwise tolerate oral intake due to nausea or emesis. Although this solution is hardly innovative, it is relevant as it forces consideration of the need to resume postoperative statins by available means. While the development of a high nasogastric output or a prolonged ileus may limit the applicability of this intervention, it is important that this option be considered as opposed to expectant watching for the clinical return of bowel function. Simvastatin, atorvastatin, rosuvastatin, and pravastatin can be crushed and delivered through this route.40
Development of Reminder Systems
Computerized reminder systems have proved important in ensuring the resumption of deep venous thrombosis prophylaxis and other preventative care compliance in hospitalized patients.41, 42 Using this process, pharmacist‐ or electronic health record‐based reminder systems could be implemented to ensure that statins are restarted when clinically feasible. Further studies are needed to test whether this approach can lead to improved outcomes.
Medication Reconciliation Prior to Hospital Discharge
Statin withdrawal highlights the pertinence of a robust, medical reconciliation process prior to the patient's departure from the hospital. In this context, the development of policies using single‐ or multi‐faceted interventions that promote cooperation between inpatient physicians, surgeons, and pharmacists with outpatient primary care providers are necessary.43
Preoperative Transition to Extended Release Statin Formulations
An innovative approach to minimizing statin withdrawal involves preoperative transition to an extended‐release statin formulation. This strategy may be of particular value in patients where prolonged bowel nonavailability is likely, such as those undergoing gastrointestinal surgery, or when prolonged postoperative dietary restriction (eg, NPO [nil per os]: nothing by mouth) status is expected (Figure 2).
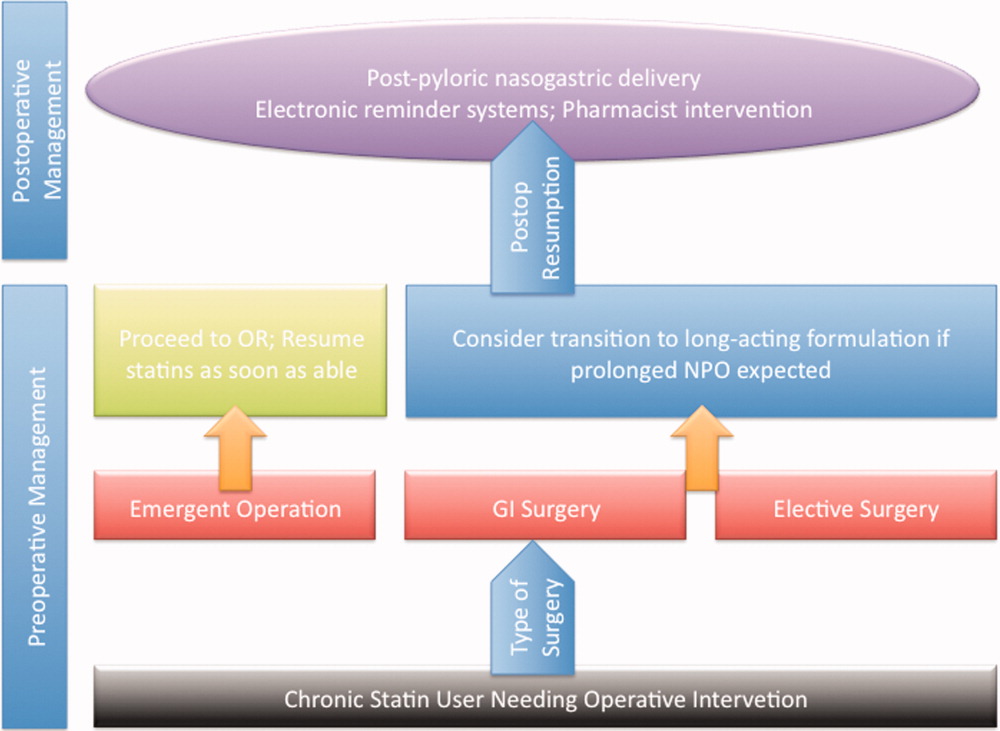
CONCLUSIONS AND FUTURE DIRECTIONS
Sudden withdrawal of perioperative statins results in adverse clinical outcomes. Individuals engaged in the care of patients during surgery such as hospitalists, anesthesiologists, and surgeons must become more cognizant of a statin withdrawal state.
An important limitation associated with the study of perioperative statin withdrawal remains the ambiguity regarding the extent of the problem in the United States. Therefore, a logical first step could be the use of infrastructure within the National Surgical Quality Improvement Program (NSQIP) to understand the epidemiology of perioperative statin use and consequences associated with statin discontinuation.44 Mandating such quality reporting could easily be built into current NSQIP performance metrics. These data would help inform a research agenda targeting patients that experience statin withdrawal and strategies most likely to prevent it.
Note Added in Proof
Disclosure: Nothing to report.
- , , , et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39(5):967–975.
- , , , , , . Improved postoperative outcomes associated with preoperative statin therapy. Anesthesiology. 2006;105(6):1260–1272; quiz 1289–1290.
- , , , , . Lipid‐lowering therapy and in‐hospital mortality following major noncardiac surgery. JAMA. 2004;291(17):2092–2099.
- , , , et al. Statins decrease perioperative cardiac complications in patients undergoing noncardiac vascular surgery: the Statins for Risk Reduction in Surgery (StaRRS) study. J Am Coll Cardiol. 2005;45(3):336–342.
- , , , et al. Statins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgery. Circulation. 2003;107(14):1848–1851.
- , , , et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361(10):980–989.
- , , , et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116(17):e418–e499.
- , , , et al. Guidelines for pre‐operative cardiac risk assessment and perioperative cardiac management in non‐cardiac surgery. Eur Heart J. 2009;30(22):2769–2812.
- , , , et al. The impact of postoperative discontinuation or continuation of chronic statin therapy on cardiac outcome after major vascular surgery. Anesth Analg. 2007;104(6):1326–1333.
- , , , et al. Effect of statin withdrawal on frequency of cardiac events after vascular surgery. Am J Cardiol. 2007;100(2):316–320.
- . Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004;109(23 suppl 1):III39–III43.
- , , , , , . Persistent endocrine stress response in patients undergoing cardiac surgery. J Endocrinol Invest. 1998;21(1):12–19.
- , , , , , . Pathology of fatal perioperative myocardial infarction: implications regarding pathophysiology and prevention. Int J Cardiol. 1996;57(1):37–44.
- , , , , , . Perioperative cardiac events in patients undergoing noncardiac surgery: a review of the magnitude of the problem, the pathophysiology of the events and methods to estimate and communicate risk. Can Med Assoc J. 2005;173(6):627–634.
- . Perioperative cardiac morbidity. Anesthesiology. 1990;72(1):153–184.
- , . Isoprenoid metabolism and the pleiotropic effects of statins. Curr Atheroscler Rep. 2003;5(5):372–378.
- , , , . Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97(12):1129–1135.
- , , , et al. Roles of rho‐associated kinase and oxidative stress in the pathogenesis of aortic stiffness. J Am Coll Cardiol. 2007;49(6):698–705.
- , , , et al. Inhibition of rho‐associated kinase results in suppression of neointimal formation of balloon‐injured arteries. Circulation. 2000;101(17):2030–2033.
- , , , . Reduced expression of endothelial cell markers after 1 year treatment with simvastatin and atorvastatin in patients with coronary heart disease. Atherosclerosis. 2002;162(1):179–185.
- , , , et al. Statins as antioxidant therapy for preventing cardiac myocyte hypertrophy. J Clin Invest. 2001;108(10):1429–1437.
- , , . Pleiotropic effects of statin therapy: molecular mechanisms and clinical results. Trends Mol Med. 2008;14(1):37–44.
- , , , et al. Inhibition of geranylgeranylation reduces angiotensin II‐mediated free radical production in vascular smooth muscle cells: involvement of angiotensin AT1 receptor expression and Rac1 GTPase. Mol Pharmacol. 2001;59(3):646–654.
- , , , et al. Withdrawal of statin treatment abrogates stroke protection in mice. Stroke. 2003;34(2):551–557.
- , , , et al. Suppression of endothelial nitric oxide production after withdrawal of statin treatment is mediated by negative feedback regulation of rho GTPase gene transcription. Circulation. 2000;102(25):3104–3110.
- , , , et al. Changes of plasma inflammatory markers after withdrawal of statin therapy in patients with hyperlipidemia. Clin Chim Acta. 2006;366(1–2):269–273.
- , , , et al. Platelet hyperactivity after statin treatment discontinuation. Thromb Haemost. 2003;90(3):476–482.
- , , , et al. Rebound inflammatory response during the acute phase of myocardial infarction after simvastatin withdrawal. Atherosclerosis. 2009;207(1):191–194.
- , . Effects of statins on endothelium and signaling mechanisms. Stroke. 2004;35(11 suppl 1):2708–2711.
- , , , et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate‐risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE‐IV). Ann Surg. 2009;249(6):921–926.
- , , , et al. Effect of perioperative statins on death, myocardial infarction, atrial fibrillation, and length of stay: a systematic review and meta‐analysis. Arch Surg. 2012;147(2):181–189.
- , , , et al. Early withdrawal of statin therapy in patients with non‐ST‐segment elevation myocardial infarction: National Registry of Myocardial Infarction. Arch Intern Med. 2004;164(19):2162–2168.
- , , , , , . Withdrawal of statins increases event rates in patients with acute coronary syndromes. Circulation. 2002;105(12):1446–1452.
- , , , , , . Discontinuation of statin therapy following an acute myocardial infarction: a population‐based study. Eur Heart J. 2008;29(17):2083–2091.
- . There is no evidence for an increase in acute coronary syndromes after short‐term abrupt discontinuation of statins in stable cardiac patients. Circulation. 2004;110(16):2333–2335.
- , , , . Discontinuation of statin therapy and clinical outcome after ischemic stroke. Stroke. 2007;38(10):2652–2657.
- , , , et al. Statin treatment withdrawal in ischemic stroke: a controlled randomized study. Neurology. 2007;69(9):904–910.
- , , , et al. Intravenous rosuvastatin for acute stroke treatment: an animal study. Stroke. 2008;39(2):433–438.
- , , , et al. Safety of perioperative statin use in high‐risk patients undergoing major vascular surgery. Am J Cardiol. 2005;95(5):658–660.
- Lexi‐Comp Online™, Lexi‐Drugs™, Hudson, OH: Lexi‐Comp, Inc; December 7, 2011.
- , , , , , . A computerized reminder system to increase the use of preventive care for hospitalized patients. N Engl J Med. 2001;345(13):965–970.
- , , , et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352(10):969–977.
- , , , . Medication review and reconciliation with cooperation between pharmacist and general practitioner and the benefit for the patient: a systematic review. Br J Clin Pharmacol. January 13, 2012. doi: 10.1111/j.1365–2125.2012.04178.x.
- American College of Surgeons National Surgical Quality Improvement Program. Available at: http://www.acsnsqip.org. Accessed December 15, 2012.
- , , , et al. Reduction in cardiovascular events after vascular surgery with atorvastatin: a randomized trial. J Vasc Surg. 2004;39(5):967–975.
- , , , , , . Improved postoperative outcomes associated with preoperative statin therapy. Anesthesiology. 2006;105(6):1260–1272; quiz 1289–1290.
- , , , , . Lipid‐lowering therapy and in‐hospital mortality following major noncardiac surgery. JAMA. 2004;291(17):2092–2099.
- , , , et al. Statins decrease perioperative cardiac complications in patients undergoing noncardiac vascular surgery: the Statins for Risk Reduction in Surgery (StaRRS) study. J Am Coll Cardiol. 2005;45(3):336–342.
- , , , et al. Statins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgery. Circulation. 2003;107(14):1848–1851.
- , , , et al. Fluvastatin and perioperative events in patients undergoing vascular surgery. N Engl J Med. 2009;361(10):980–989.
- , , , et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116(17):e418–e499.
- , , , et al. Guidelines for pre‐operative cardiac risk assessment and perioperative cardiac management in non‐cardiac surgery. Eur Heart J. 2009;30(22):2769–2812.
- , , , et al. The impact of postoperative discontinuation or continuation of chronic statin therapy on cardiac outcome after major vascular surgery. Anesth Analg. 2007;104(6):1326–1333.
- , , , et al. Effect of statin withdrawal on frequency of cardiac events after vascular surgery. Am J Cardiol. 2007;100(2):316–320.
- . Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004;109(23 suppl 1):III39–III43.
- , , , , , . Persistent endocrine stress response in patients undergoing cardiac surgery. J Endocrinol Invest. 1998;21(1):12–19.
- , , , , , . Pathology of fatal perioperative myocardial infarction: implications regarding pathophysiology and prevention. Int J Cardiol. 1996;57(1):37–44.
- , , , , , . Perioperative cardiac events in patients undergoing noncardiac surgery: a review of the magnitude of the problem, the pathophysiology of the events and methods to estimate and communicate risk. Can Med Assoc J. 2005;173(6):627–634.
- . Perioperative cardiac morbidity. Anesthesiology. 1990;72(1):153–184.
- , . Isoprenoid metabolism and the pleiotropic effects of statins. Curr Atheroscler Rep. 2003;5(5):372–378.
- , , , . Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97(12):1129–1135.
- , , , et al. Roles of rho‐associated kinase and oxidative stress in the pathogenesis of aortic stiffness. J Am Coll Cardiol. 2007;49(6):698–705.
- , , , et al. Inhibition of rho‐associated kinase results in suppression of neointimal formation of balloon‐injured arteries. Circulation. 2000;101(17):2030–2033.
- , , , . Reduced expression of endothelial cell markers after 1 year treatment with simvastatin and atorvastatin in patients with coronary heart disease. Atherosclerosis. 2002;162(1):179–185.
- , , , et al. Statins as antioxidant therapy for preventing cardiac myocyte hypertrophy. J Clin Invest. 2001;108(10):1429–1437.
- , , . Pleiotropic effects of statin therapy: molecular mechanisms and clinical results. Trends Mol Med. 2008;14(1):37–44.
- , , , et al. Inhibition of geranylgeranylation reduces angiotensin II‐mediated free radical production in vascular smooth muscle cells: involvement of angiotensin AT1 receptor expression and Rac1 GTPase. Mol Pharmacol. 2001;59(3):646–654.
- , , , et al. Withdrawal of statin treatment abrogates stroke protection in mice. Stroke. 2003;34(2):551–557.
- , , , et al. Suppression of endothelial nitric oxide production after withdrawal of statin treatment is mediated by negative feedback regulation of rho GTPase gene transcription. Circulation. 2000;102(25):3104–3110.
- , , , et al. Changes of plasma inflammatory markers after withdrawal of statin therapy in patients with hyperlipidemia. Clin Chim Acta. 2006;366(1–2):269–273.
- , , , et al. Platelet hyperactivity after statin treatment discontinuation. Thromb Haemost. 2003;90(3):476–482.
- , , , et al. Rebound inflammatory response during the acute phase of myocardial infarction after simvastatin withdrawal. Atherosclerosis. 2009;207(1):191–194.
- , . Effects of statins on endothelium and signaling mechanisms. Stroke. 2004;35(11 suppl 1):2708–2711.
- , , , et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate‐risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE‐IV). Ann Surg. 2009;249(6):921–926.
- , , , et al. Effect of perioperative statins on death, myocardial infarction, atrial fibrillation, and length of stay: a systematic review and meta‐analysis. Arch Surg. 2012;147(2):181–189.
- , , , et al. Early withdrawal of statin therapy in patients with non‐ST‐segment elevation myocardial infarction: National Registry of Myocardial Infarction. Arch Intern Med. 2004;164(19):2162–2168.
- , , , , , . Withdrawal of statins increases event rates in patients with acute coronary syndromes. Circulation. 2002;105(12):1446–1452.
- , , , , , . Discontinuation of statin therapy following an acute myocardial infarction: a population‐based study. Eur Heart J. 2008;29(17):2083–2091.
- . There is no evidence for an increase in acute coronary syndromes after short‐term abrupt discontinuation of statins in stable cardiac patients. Circulation. 2004;110(16):2333–2335.
- , , , . Discontinuation of statin therapy and clinical outcome after ischemic stroke. Stroke. 2007;38(10):2652–2657.
- , , , et al. Statin treatment withdrawal in ischemic stroke: a controlled randomized study. Neurology. 2007;69(9):904–910.
- , , , et al. Intravenous rosuvastatin for acute stroke treatment: an animal study. Stroke. 2008;39(2):433–438.
- , , , et al. Safety of perioperative statin use in high‐risk patients undergoing major vascular surgery. Am J Cardiol. 2005;95(5):658–660.
- Lexi‐Comp Online™, Lexi‐Drugs™, Hudson, OH: Lexi‐Comp, Inc; December 7, 2011.
- , , , , , . A computerized reminder system to increase the use of preventive care for hospitalized patients. N Engl J Med. 2001;345(13):965–970.
- , , , et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352(10):969–977.
- , , , . Medication review and reconciliation with cooperation between pharmacist and general practitioner and the benefit for the patient: a systematic review. Br J Clin Pharmacol. January 13, 2012. doi: 10.1111/j.1365–2125.2012.04178.x.
- American College of Surgeons National Surgical Quality Improvement Program. Available at: http://www.acsnsqip.org. Accessed December 15, 2012.
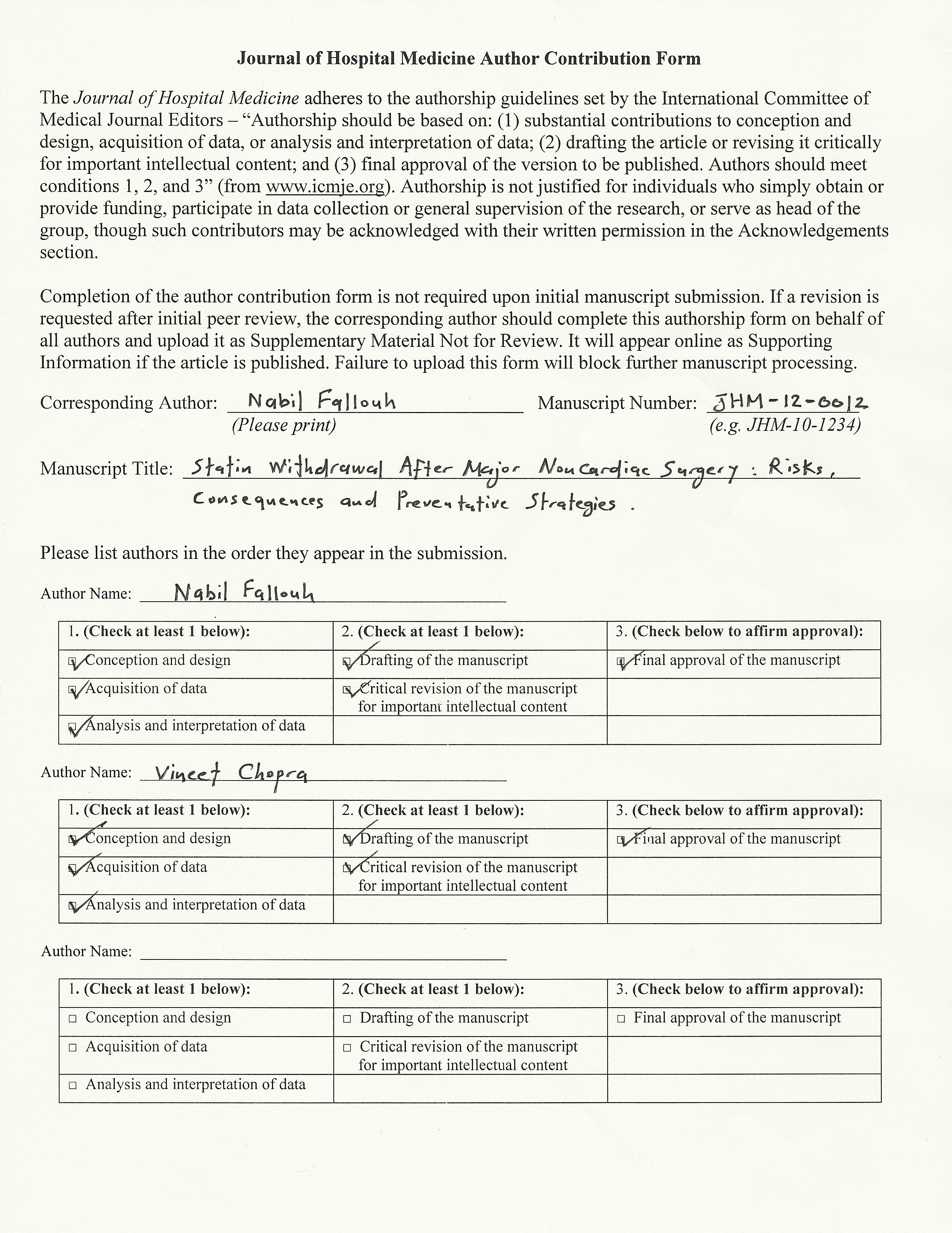
Central Nervous System Complications of Cancer Therapy
Central Nervous System Complications of Cancer Therapy
- Received 16 July 2011. Accepted 15 November 2011. Available online 26 April 2012.
Abstract
As more effective therapies prolong the survival of patients with cancer, therapy-related toxicities, particularly those affecting the central nervous system (CNS) become increasingly important. CNS complications can cause significant morbidity and can limit the dose or duration of otherwise effective treatments. Because effects on the CNS are disabling and often permanent and treatments remain limited, it is important that clinicians recognize the effects of cancer therapy on the CNS. Cytotoxic chemotherapy and radiation are well-known causes of neurotoxicity, but there is increasing recognition that novel therapies are also sources of adverse effects on the CNS. This review highlights the CNS complications that result from radiation, chemotherapy, and novel therapeutics.
Central nervous system (CNS) toxicity is a significant source of morbidity in the treatment of patients with cancer. Radiation, traditional cytotoxic chemotherapy, and novel biologic and targeted therapies all have recognized CNS side effects; and the risks of neurotoxicity can increase with combination therapy.1 Some CNS complications appear during treatment, while others present months or even years later. When patients present with neurologic deficits, practitioners need to recognize the signs and symptoms of treatment-related toxicity in order to intervene early and minimize neurologic damage. Treatment-related CNS toxicity needs to be distinguished from other direct or indirect effects of cancer, including tumor invasion, metastasis, metabolic derangements, infections, and paraneoplastic neurologic syndromes.
*For a PDF of the full article and accompanying viewpoint by Ivo Tremont-Lukats, click in the links to the left of this introduction.
Central Nervous System Complications of Cancer Therapy
- Received 16 July 2011. Accepted 15 November 2011. Available online 26 April 2012.
Abstract
As more effective therapies prolong the survival of patients with cancer, therapy-related toxicities, particularly those affecting the central nervous system (CNS) become increasingly important. CNS complications can cause significant morbidity and can limit the dose or duration of otherwise effective treatments. Because effects on the CNS are disabling and often permanent and treatments remain limited, it is important that clinicians recognize the effects of cancer therapy on the CNS. Cytotoxic chemotherapy and radiation are well-known causes of neurotoxicity, but there is increasing recognition that novel therapies are also sources of adverse effects on the CNS. This review highlights the CNS complications that result from radiation, chemotherapy, and novel therapeutics.
Central nervous system (CNS) toxicity is a significant source of morbidity in the treatment of patients with cancer. Radiation, traditional cytotoxic chemotherapy, and novel biologic and targeted therapies all have recognized CNS side effects; and the risks of neurotoxicity can increase with combination therapy.1 Some CNS complications appear during treatment, while others present months or even years later. When patients present with neurologic deficits, practitioners need to recognize the signs and symptoms of treatment-related toxicity in order to intervene early and minimize neurologic damage. Treatment-related CNS toxicity needs to be distinguished from other direct or indirect effects of cancer, including tumor invasion, metastasis, metabolic derangements, infections, and paraneoplastic neurologic syndromes.
*For a PDF of the full article and accompanying viewpoint by Ivo Tremont-Lukats, click in the links to the left of this introduction.
Central Nervous System Complications of Cancer Therapy
- Received 16 July 2011. Accepted 15 November 2011. Available online 26 April 2012.
Abstract
As more effective therapies prolong the survival of patients with cancer, therapy-related toxicities, particularly those affecting the central nervous system (CNS) become increasingly important. CNS complications can cause significant morbidity and can limit the dose or duration of otherwise effective treatments. Because effects on the CNS are disabling and often permanent and treatments remain limited, it is important that clinicians recognize the effects of cancer therapy on the CNS. Cytotoxic chemotherapy and radiation are well-known causes of neurotoxicity, but there is increasing recognition that novel therapies are also sources of adverse effects on the CNS. This review highlights the CNS complications that result from radiation, chemotherapy, and novel therapeutics.
Central nervous system (CNS) toxicity is a significant source of morbidity in the treatment of patients with cancer. Radiation, traditional cytotoxic chemotherapy, and novel biologic and targeted therapies all have recognized CNS side effects; and the risks of neurotoxicity can increase with combination therapy.1 Some CNS complications appear during treatment, while others present months or even years later. When patients present with neurologic deficits, practitioners need to recognize the signs and symptoms of treatment-related toxicity in order to intervene early and minimize neurologic damage. Treatment-related CNS toxicity needs to be distinguished from other direct or indirect effects of cancer, including tumor invasion, metastasis, metabolic derangements, infections, and paraneoplastic neurologic syndromes.
*For a PDF of the full article and accompanying viewpoint by Ivo Tremont-Lukats, click in the links to the left of this introduction.