User login
Consider Patient Safety, Outcomes Risk before Prescribing Off-Label Drugs
Consider Patient Safety, Outcomes Risk before Prescribing “Off-Label”
What is the story with off-label drug use? I have seen some other physicians in my group use dabigatran for VTE prophylaxis, which I know it is not an approved indication. Am I taking on risk by continuing this treatment?
—Fabian Harris, Tuscaloosa, Ala.
Dr. Hospitalist responds:
Our friends at the FDA are in the business of approving drugs for use, but they do not regulate medical practice. So the short answer to your question is that off-label drug use is perfectly acceptable. Once a drug has been approved for use, if, in your clinical judgment, there are other indications for which it could be beneficial, then you are well within your rights to prescribe it. The FDA does not dictate how you practice medicine.
However, you will still be held to the community standard when it comes to your medical practice. As an example, gabapentin is used all the time for neuropathic pain syndromes, though technically it is only approved for seizures and post-herpetic neuralgia. Although the FDA won’t restrict your prescribing, it does prohibit pharmaceutical companies from marketing their drugs for anything other than their approved indications. In fact, Pfizer settled a case in 2004 on this very drug due to the promotion of prescribing it for nonapproved indications. I think at this point it’s fairly well accepted that lots of physicians use gabapentin for neuropathic pain, so you would not be too far out on a limb in prescribing it yourself in this manner.
For newer drugs, I might proceed with a little more caution. Anyone out there remember trovofloxacin (Trovan)? It was a new antibiotic approved in the late 1990s, with a coverage spectrum similar to levofloxacin, but with even more weight toward the gram positives. A wonder drug! Oral! As a result, it got prescribed like water, but not for the serious infections it was designed for: It got prescribed “off label” for common URIs and sinusitis. Unfortunately, it also caused a fair amount of liver failure and was summarily pulled from the market.
Does this mean dabigatran is a bad drug? No, but we don’t have much history with it, either. So while it might seem to be an innocuous extension to prescribe it for VTE prevention when it has already been approved for stroke prevention in afib, I think you carry some risk by doing this. In addition, some insurers will not cover a drug being prescribed in this manner, so you might be exposing your patient to added costs as well. Additionally, there’s nothing about off-label prescribing that says you have to tell the patient that’s what you’re doing. However, if you put together the factors of not informing a patient about an off-label use, and a patient having to pay out of pocket for that medicine, with an adverse outcome ... well, let’s just say that might not end too well.
Ultimately, I think you will need to consider the safety profile of the drug, the risk for an adverse outcome, your own risk tolerance, and the current state of medical practice before you consistently agree to use a drug “off label.” Given the slow-moving jungle of FDA approval, I can understand the desire to use a newer drug in an off-label manner, but it’s probably best to stop and think about the alternatives before proceeding. If you’re practicing in a group, then it’s just as important to come to a consensus with your partners about which drugs you will comfortably use off-label and which ones you won’t, especially as newer drugs come into the marketplace.
Consider Patient Safety, Outcomes Risk before Prescribing “Off-Label”
What is the story with off-label drug use? I have seen some other physicians in my group use dabigatran for VTE prophylaxis, which I know it is not an approved indication. Am I taking on risk by continuing this treatment?
—Fabian Harris, Tuscaloosa, Ala.
Dr. Hospitalist responds:
Our friends at the FDA are in the business of approving drugs for use, but they do not regulate medical practice. So the short answer to your question is that off-label drug use is perfectly acceptable. Once a drug has been approved for use, if, in your clinical judgment, there are other indications for which it could be beneficial, then you are well within your rights to prescribe it. The FDA does not dictate how you practice medicine.
However, you will still be held to the community standard when it comes to your medical practice. As an example, gabapentin is used all the time for neuropathic pain syndromes, though technically it is only approved for seizures and post-herpetic neuralgia. Although the FDA won’t restrict your prescribing, it does prohibit pharmaceutical companies from marketing their drugs for anything other than their approved indications. In fact, Pfizer settled a case in 2004 on this very drug due to the promotion of prescribing it for nonapproved indications. I think at this point it’s fairly well accepted that lots of physicians use gabapentin for neuropathic pain, so you would not be too far out on a limb in prescribing it yourself in this manner.
For newer drugs, I might proceed with a little more caution. Anyone out there remember trovofloxacin (Trovan)? It was a new antibiotic approved in the late 1990s, with a coverage spectrum similar to levofloxacin, but with even more weight toward the gram positives. A wonder drug! Oral! As a result, it got prescribed like water, but not for the serious infections it was designed for: It got prescribed “off label” for common URIs and sinusitis. Unfortunately, it also caused a fair amount of liver failure and was summarily pulled from the market.
Does this mean dabigatran is a bad drug? No, but we don’t have much history with it, either. So while it might seem to be an innocuous extension to prescribe it for VTE prevention when it has already been approved for stroke prevention in afib, I think you carry some risk by doing this. In addition, some insurers will not cover a drug being prescribed in this manner, so you might be exposing your patient to added costs as well. Additionally, there’s nothing about off-label prescribing that says you have to tell the patient that’s what you’re doing. However, if you put together the factors of not informing a patient about an off-label use, and a patient having to pay out of pocket for that medicine, with an adverse outcome ... well, let’s just say that might not end too well.
Ultimately, I think you will need to consider the safety profile of the drug, the risk for an adverse outcome, your own risk tolerance, and the current state of medical practice before you consistently agree to use a drug “off label.” Given the slow-moving jungle of FDA approval, I can understand the desire to use a newer drug in an off-label manner, but it’s probably best to stop and think about the alternatives before proceeding. If you’re practicing in a group, then it’s just as important to come to a consensus with your partners about which drugs you will comfortably use off-label and which ones you won’t, especially as newer drugs come into the marketplace.
Consider Patient Safety, Outcomes Risk before Prescribing “Off-Label”
What is the story with off-label drug use? I have seen some other physicians in my group use dabigatran for VTE prophylaxis, which I know it is not an approved indication. Am I taking on risk by continuing this treatment?
—Fabian Harris, Tuscaloosa, Ala.
Dr. Hospitalist responds:
Our friends at the FDA are in the business of approving drugs for use, but they do not regulate medical practice. So the short answer to your question is that off-label drug use is perfectly acceptable. Once a drug has been approved for use, if, in your clinical judgment, there are other indications for which it could be beneficial, then you are well within your rights to prescribe it. The FDA does not dictate how you practice medicine.
However, you will still be held to the community standard when it comes to your medical practice. As an example, gabapentin is used all the time for neuropathic pain syndromes, though technically it is only approved for seizures and post-herpetic neuralgia. Although the FDA won’t restrict your prescribing, it does prohibit pharmaceutical companies from marketing their drugs for anything other than their approved indications. In fact, Pfizer settled a case in 2004 on this very drug due to the promotion of prescribing it for nonapproved indications. I think at this point it’s fairly well accepted that lots of physicians use gabapentin for neuropathic pain, so you would not be too far out on a limb in prescribing it yourself in this manner.
For newer drugs, I might proceed with a little more caution. Anyone out there remember trovofloxacin (Trovan)? It was a new antibiotic approved in the late 1990s, with a coverage spectrum similar to levofloxacin, but with even more weight toward the gram positives. A wonder drug! Oral! As a result, it got prescribed like water, but not for the serious infections it was designed for: It got prescribed “off label” for common URIs and sinusitis. Unfortunately, it also caused a fair amount of liver failure and was summarily pulled from the market.
Does this mean dabigatran is a bad drug? No, but we don’t have much history with it, either. So while it might seem to be an innocuous extension to prescribe it for VTE prevention when it has already been approved for stroke prevention in afib, I think you carry some risk by doing this. In addition, some insurers will not cover a drug being prescribed in this manner, so you might be exposing your patient to added costs as well. Additionally, there’s nothing about off-label prescribing that says you have to tell the patient that’s what you’re doing. However, if you put together the factors of not informing a patient about an off-label use, and a patient having to pay out of pocket for that medicine, with an adverse outcome ... well, let’s just say that might not end too well.
Ultimately, I think you will need to consider the safety profile of the drug, the risk for an adverse outcome, your own risk tolerance, and the current state of medical practice before you consistently agree to use a drug “off label.” Given the slow-moving jungle of FDA approval, I can understand the desire to use a newer drug in an off-label manner, but it’s probably best to stop and think about the alternatives before proceeding. If you’re practicing in a group, then it’s just as important to come to a consensus with your partners about which drugs you will comfortably use off-label and which ones you won’t, especially as newer drugs come into the marketplace.
Defining a Safe Workload for Pediatric Hospitalists
As I write this column, I am on the second leg of an overnight flight back home to Austin, Texas. I think it actually went pretty well, considering my 2-year-old daughter was wide awake after sleeping for the first three hours of this 14-hour odyssey. The remainder of the trip is a blur of awkward sleep positions interspersed with brief periods of semilucidity. Those of you with first-hand knowledge of what this experience is like might be feeling sorry for me, but you shouldn’t. I am returning from a “why don’t I live here” kind of vacation week in Hawaii. The rest of you are probably wondering how anyone could write a coherent column at this point, which is fair, but to which I would reply: Aren’t all hospitalists expected to function at high levels during periods of sleep deprivation?
While the issue of resident duty-hours has been discussed endlessly and studied increasingly, in terms of effects on outcomes, I am surprised there has not been more discussion surrounding the concept of attending duty-hours. The subject might not always be phrased to include the term “duty-hours,” but it seems that when it comes to scheduling, strong opinions come out in my group when the duration of, frequency of, or time off between night shifts are brought up. And when it comes to safety, I am certain sleep deprivation and sleep inertia (that period of haziness immediately after being awakened in the middle of the night) have led to questionable decisions on my part.
Why? Well...
So why do pediatric hospitalists avoid the issue of sleep hygiene, work schedules, and clinical impact? I think the reasons are multifactorial.
First, there are definitely individual variations in how all of us tolerate this work, and I suspect some of this is based on such traits as age and general ability to adapt to uncomfortable circadian flip-flops. I will admit that every time I wake up achy after a call night, I begin to wonder if I will be able to handle this in 10 to 15 years.
Second, I think pediatric HM as a field has not yet explored this topic fully because we are young both in terms of chronological age as well as nocturnal work-years. The work has not yet aged us to the point of making this a critical issue. We’re also somewhat behind our adult-hospitalist colleagues in terms of the volume of nocturnal work. Adult HM groups have long explored different shift schedules (seven-on/seven-off, day/evening/overnight distribution, etc.) because they routinely cover large services of more than 100 patients in large hospitals with more than 500 beds. In pediatrics, most of us operate in small community hospital settings or large academic centers where the nightly in-house quantity of work is relatively low, mitigated by the smaller size of most community programs and the presence of residents in most large children’s hospitals.
But I see this as an important issue for us to define: the imperative to define safe, round-the-clock clinical care and sustainable careers. Although we will need to learn from other fields, HM is somewhat different from other types of 24/7 medicine in that we require more continuity in our daytime work, which also carries over to night shifts both in terms of how the schedule is made as well as the benefit on the clinical side. The need for continuity adds an extra degree of difficulty in creating and studying different schedules that try to optimize nocturnal functioning.
Clarity, Please
Unfortunately, those looking for evidence-based, or even consensus-based, solutions might have to wait. A recent article in the Journal of Hospital Medicine does a nice job of synthesizing the literature and highlights the lack of clear answers for what kind of shift schedules work best.1
In the absence of scientific solutions, it might be too easy to say that we need “more research,” because what doesn’t need more research? (OK, we don’t need more research on interventions for bronchiolitis.) But in the same manner in which pediatric hospitalists have taken the lead in defining a night curriculum for residents (congratulations, Becky Blankenburg, on winning the Ray E. Helfer award in pediatric education), I believe there is an opportunity to improve circadian functioning for all hospital-based physicians, but more specifically attendings. This is even more important as residents work less and a 24/7 attending presence becomes the norm in teaching facilities. While the link between safety and fatigue may have been seen as a nonissue in past decades, I think that in our current era, this is something that we own and/or will be asked to define in the near future.
In the meantime, I think we’re left to our own schedules. And in defense of all schedulers like me out there, I will say that there are no proven solutions, so local culture will predominate. Different groups with different personalities and family makeups will have varying preferences. Smaller groups will tend to have longer shift times with less flexibility in “swing”-type midday or evening shifts, while larger groups might have increased flexibility in defining different shifts at the expense of added complexity in terms of creating a schedule with no gaps.
As we come up with more rules about night shifts, such as “clockwise” scheduling of day-evening-overnight shifts, single versus clustered nights based on frequency, and days off after night shifts, the more complex and awkward our Tetris-like schedule will become. I predict that this is something hospitalists will begin to think about more, with a necessary push for safe and sustainable schedules. In the short-term, allowing for financial and structural wiggle room in the scheduling process (i.e. adjusting shift patterns and differential pay for night work) might be the most balanced approach for the immediate future.
Dr. Shen is pediatric editor of The Hospitalist. Write to him at [email protected].
Reference
As I write this column, I am on the second leg of an overnight flight back home to Austin, Texas. I think it actually went pretty well, considering my 2-year-old daughter was wide awake after sleeping for the first three hours of this 14-hour odyssey. The remainder of the trip is a blur of awkward sleep positions interspersed with brief periods of semilucidity. Those of you with first-hand knowledge of what this experience is like might be feeling sorry for me, but you shouldn’t. I am returning from a “why don’t I live here” kind of vacation week in Hawaii. The rest of you are probably wondering how anyone could write a coherent column at this point, which is fair, but to which I would reply: Aren’t all hospitalists expected to function at high levels during periods of sleep deprivation?
While the issue of resident duty-hours has been discussed endlessly and studied increasingly, in terms of effects on outcomes, I am surprised there has not been more discussion surrounding the concept of attending duty-hours. The subject might not always be phrased to include the term “duty-hours,” but it seems that when it comes to scheduling, strong opinions come out in my group when the duration of, frequency of, or time off between night shifts are brought up. And when it comes to safety, I am certain sleep deprivation and sleep inertia (that period of haziness immediately after being awakened in the middle of the night) have led to questionable decisions on my part.
Why? Well...
So why do pediatric hospitalists avoid the issue of sleep hygiene, work schedules, and clinical impact? I think the reasons are multifactorial.
First, there are definitely individual variations in how all of us tolerate this work, and I suspect some of this is based on such traits as age and general ability to adapt to uncomfortable circadian flip-flops. I will admit that every time I wake up achy after a call night, I begin to wonder if I will be able to handle this in 10 to 15 years.
Second, I think pediatric HM as a field has not yet explored this topic fully because we are young both in terms of chronological age as well as nocturnal work-years. The work has not yet aged us to the point of making this a critical issue. We’re also somewhat behind our adult-hospitalist colleagues in terms of the volume of nocturnal work. Adult HM groups have long explored different shift schedules (seven-on/seven-off, day/evening/overnight distribution, etc.) because they routinely cover large services of more than 100 patients in large hospitals with more than 500 beds. In pediatrics, most of us operate in small community hospital settings or large academic centers where the nightly in-house quantity of work is relatively low, mitigated by the smaller size of most community programs and the presence of residents in most large children’s hospitals.
But I see this as an important issue for us to define: the imperative to define safe, round-the-clock clinical care and sustainable careers. Although we will need to learn from other fields, HM is somewhat different from other types of 24/7 medicine in that we require more continuity in our daytime work, which also carries over to night shifts both in terms of how the schedule is made as well as the benefit on the clinical side. The need for continuity adds an extra degree of difficulty in creating and studying different schedules that try to optimize nocturnal functioning.
Clarity, Please
Unfortunately, those looking for evidence-based, or even consensus-based, solutions might have to wait. A recent article in the Journal of Hospital Medicine does a nice job of synthesizing the literature and highlights the lack of clear answers for what kind of shift schedules work best.1
In the absence of scientific solutions, it might be too easy to say that we need “more research,” because what doesn’t need more research? (OK, we don’t need more research on interventions for bronchiolitis.) But in the same manner in which pediatric hospitalists have taken the lead in defining a night curriculum for residents (congratulations, Becky Blankenburg, on winning the Ray E. Helfer award in pediatric education), I believe there is an opportunity to improve circadian functioning for all hospital-based physicians, but more specifically attendings. This is even more important as residents work less and a 24/7 attending presence becomes the norm in teaching facilities. While the link between safety and fatigue may have been seen as a nonissue in past decades, I think that in our current era, this is something that we own and/or will be asked to define in the near future.
In the meantime, I think we’re left to our own schedules. And in defense of all schedulers like me out there, I will say that there are no proven solutions, so local culture will predominate. Different groups with different personalities and family makeups will have varying preferences. Smaller groups will tend to have longer shift times with less flexibility in “swing”-type midday or evening shifts, while larger groups might have increased flexibility in defining different shifts at the expense of added complexity in terms of creating a schedule with no gaps.
As we come up with more rules about night shifts, such as “clockwise” scheduling of day-evening-overnight shifts, single versus clustered nights based on frequency, and days off after night shifts, the more complex and awkward our Tetris-like schedule will become. I predict that this is something hospitalists will begin to think about more, with a necessary push for safe and sustainable schedules. In the short-term, allowing for financial and structural wiggle room in the scheduling process (i.e. adjusting shift patterns and differential pay for night work) might be the most balanced approach for the immediate future.
Dr. Shen is pediatric editor of The Hospitalist. Write to him at [email protected].
Reference
As I write this column, I am on the second leg of an overnight flight back home to Austin, Texas. I think it actually went pretty well, considering my 2-year-old daughter was wide awake after sleeping for the first three hours of this 14-hour odyssey. The remainder of the trip is a blur of awkward sleep positions interspersed with brief periods of semilucidity. Those of you with first-hand knowledge of what this experience is like might be feeling sorry for me, but you shouldn’t. I am returning from a “why don’t I live here” kind of vacation week in Hawaii. The rest of you are probably wondering how anyone could write a coherent column at this point, which is fair, but to which I would reply: Aren’t all hospitalists expected to function at high levels during periods of sleep deprivation?
While the issue of resident duty-hours has been discussed endlessly and studied increasingly, in terms of effects on outcomes, I am surprised there has not been more discussion surrounding the concept of attending duty-hours. The subject might not always be phrased to include the term “duty-hours,” but it seems that when it comes to scheduling, strong opinions come out in my group when the duration of, frequency of, or time off between night shifts are brought up. And when it comes to safety, I am certain sleep deprivation and sleep inertia (that period of haziness immediately after being awakened in the middle of the night) have led to questionable decisions on my part.
Why? Well...
So why do pediatric hospitalists avoid the issue of sleep hygiene, work schedules, and clinical impact? I think the reasons are multifactorial.
First, there are definitely individual variations in how all of us tolerate this work, and I suspect some of this is based on such traits as age and general ability to adapt to uncomfortable circadian flip-flops. I will admit that every time I wake up achy after a call night, I begin to wonder if I will be able to handle this in 10 to 15 years.
Second, I think pediatric HM as a field has not yet explored this topic fully because we are young both in terms of chronological age as well as nocturnal work-years. The work has not yet aged us to the point of making this a critical issue. We’re also somewhat behind our adult-hospitalist colleagues in terms of the volume of nocturnal work. Adult HM groups have long explored different shift schedules (seven-on/seven-off, day/evening/overnight distribution, etc.) because they routinely cover large services of more than 100 patients in large hospitals with more than 500 beds. In pediatrics, most of us operate in small community hospital settings or large academic centers where the nightly in-house quantity of work is relatively low, mitigated by the smaller size of most community programs and the presence of residents in most large children’s hospitals.
But I see this as an important issue for us to define: the imperative to define safe, round-the-clock clinical care and sustainable careers. Although we will need to learn from other fields, HM is somewhat different from other types of 24/7 medicine in that we require more continuity in our daytime work, which also carries over to night shifts both in terms of how the schedule is made as well as the benefit on the clinical side. The need for continuity adds an extra degree of difficulty in creating and studying different schedules that try to optimize nocturnal functioning.
Clarity, Please
Unfortunately, those looking for evidence-based, or even consensus-based, solutions might have to wait. A recent article in the Journal of Hospital Medicine does a nice job of synthesizing the literature and highlights the lack of clear answers for what kind of shift schedules work best.1
In the absence of scientific solutions, it might be too easy to say that we need “more research,” because what doesn’t need more research? (OK, we don’t need more research on interventions for bronchiolitis.) But in the same manner in which pediatric hospitalists have taken the lead in defining a night curriculum for residents (congratulations, Becky Blankenburg, on winning the Ray E. Helfer award in pediatric education), I believe there is an opportunity to improve circadian functioning for all hospital-based physicians, but more specifically attendings. This is even more important as residents work less and a 24/7 attending presence becomes the norm in teaching facilities. While the link between safety and fatigue may have been seen as a nonissue in past decades, I think that in our current era, this is something that we own and/or will be asked to define in the near future.
In the meantime, I think we’re left to our own schedules. And in defense of all schedulers like me out there, I will say that there are no proven solutions, so local culture will predominate. Different groups with different personalities and family makeups will have varying preferences. Smaller groups will tend to have longer shift times with less flexibility in “swing”-type midday or evening shifts, while larger groups might have increased flexibility in defining different shifts at the expense of added complexity in terms of creating a schedule with no gaps.
As we come up with more rules about night shifts, such as “clockwise” scheduling of day-evening-overnight shifts, single versus clustered nights based on frequency, and days off after night shifts, the more complex and awkward our Tetris-like schedule will become. I predict that this is something hospitalists will begin to think about more, with a necessary push for safe and sustainable schedules. In the short-term, allowing for financial and structural wiggle room in the scheduling process (i.e. adjusting shift patterns and differential pay for night work) might be the most balanced approach for the immediate future.
Dr. Shen is pediatric editor of The Hospitalist. Write to him at [email protected].
Reference
Pay-for-Performance Challenged as Best Model for Healthcare
Pushing healthcare toward pay-for-performance models that provide financial rewards for patient outcomes might not be the best direction for healthcare, according to an article published by a duo of doctors and a behavioral economist.
“Will Pay for Performance Backfire? Insights from Behavioral Economics” posted at Healthaffairs.org, questions the validity of paying for outcomes, particularly as there is no evidence yet that the model improves patient outcomes.
“You’re not actually paying for quality,” says David Himmelstein, MD, a professor at City University of New York School of Public Health at Hunter College, New York. “What you’re paying for is some very gameable measurement that doctors will find a way to cheat.”
The blog post notes that monetary rewards can actually undermine motivation for tasks that are intrinsically interesting or rewarding, a phenomenon known as “motivational crowd-out.” Dr. Himmelstein says it could focus attention on coding, rather than patients, or encourage providers to avoid noncompliant patients who will make their measured performances look bad.
“Injecting different monetary incentives into healthcare can certainly change it,” according to the article, “but not necessarily in the ways that policy makers would plan, much less hope for.”
Dr. Himmelstein says that without evidence for, or against, pay for performance, it’s difficult to say whether it will improve outcomes over the long term. Given the government push toward pay-for-performance programs—such as value-based purchasing (VBP)—he suggests physicians prepare themselves to comply. Accordingly, SHM supports policies that link "quality measurement to performance-based payment” and has created a toolkit to help hospitalists prepare for VBP, one of the most targeted pay-for-performance programs.
Even as HM moves toward adopting pay for performance as a mantra, Dr. Himmelstein believes hospitalists are in a good position to lead discussions on whether pay for performance is the only way to move forward.
“It can feel like a fait d’accompli, but things can change, and they can change rapidly,” Dr. Himmelstein adds. “The first step is to have real discussions about it. Up to now, much of the medical literature is saying, ‘It’s not working. We must have the wrong incentives.’ What if there are no right incentives?”
Visit our website for more information about pay-for-performance programs.
Pushing healthcare toward pay-for-performance models that provide financial rewards for patient outcomes might not be the best direction for healthcare, according to an article published by a duo of doctors and a behavioral economist.
“Will Pay for Performance Backfire? Insights from Behavioral Economics” posted at Healthaffairs.org, questions the validity of paying for outcomes, particularly as there is no evidence yet that the model improves patient outcomes.
“You’re not actually paying for quality,” says David Himmelstein, MD, a professor at City University of New York School of Public Health at Hunter College, New York. “What you’re paying for is some very gameable measurement that doctors will find a way to cheat.”
The blog post notes that monetary rewards can actually undermine motivation for tasks that are intrinsically interesting or rewarding, a phenomenon known as “motivational crowd-out.” Dr. Himmelstein says it could focus attention on coding, rather than patients, or encourage providers to avoid noncompliant patients who will make their measured performances look bad.
“Injecting different monetary incentives into healthcare can certainly change it,” according to the article, “but not necessarily in the ways that policy makers would plan, much less hope for.”
Dr. Himmelstein says that without evidence for, or against, pay for performance, it’s difficult to say whether it will improve outcomes over the long term. Given the government push toward pay-for-performance programs—such as value-based purchasing (VBP)—he suggests physicians prepare themselves to comply. Accordingly, SHM supports policies that link "quality measurement to performance-based payment” and has created a toolkit to help hospitalists prepare for VBP, one of the most targeted pay-for-performance programs.
Even as HM moves toward adopting pay for performance as a mantra, Dr. Himmelstein believes hospitalists are in a good position to lead discussions on whether pay for performance is the only way to move forward.
“It can feel like a fait d’accompli, but things can change, and they can change rapidly,” Dr. Himmelstein adds. “The first step is to have real discussions about it. Up to now, much of the medical literature is saying, ‘It’s not working. We must have the wrong incentives.’ What if there are no right incentives?”
Visit our website for more information about pay-for-performance programs.
Pushing healthcare toward pay-for-performance models that provide financial rewards for patient outcomes might not be the best direction for healthcare, according to an article published by a duo of doctors and a behavioral economist.
“Will Pay for Performance Backfire? Insights from Behavioral Economics” posted at Healthaffairs.org, questions the validity of paying for outcomes, particularly as there is no evidence yet that the model improves patient outcomes.
“You’re not actually paying for quality,” says David Himmelstein, MD, a professor at City University of New York School of Public Health at Hunter College, New York. “What you’re paying for is some very gameable measurement that doctors will find a way to cheat.”
The blog post notes that monetary rewards can actually undermine motivation for tasks that are intrinsically interesting or rewarding, a phenomenon known as “motivational crowd-out.” Dr. Himmelstein says it could focus attention on coding, rather than patients, or encourage providers to avoid noncompliant patients who will make their measured performances look bad.
“Injecting different monetary incentives into healthcare can certainly change it,” according to the article, “but not necessarily in the ways that policy makers would plan, much less hope for.”
Dr. Himmelstein says that without evidence for, or against, pay for performance, it’s difficult to say whether it will improve outcomes over the long term. Given the government push toward pay-for-performance programs—such as value-based purchasing (VBP)—he suggests physicians prepare themselves to comply. Accordingly, SHM supports policies that link "quality measurement to performance-based payment” and has created a toolkit to help hospitalists prepare for VBP, one of the most targeted pay-for-performance programs.
Even as HM moves toward adopting pay for performance as a mantra, Dr. Himmelstein believes hospitalists are in a good position to lead discussions on whether pay for performance is the only way to move forward.
“It can feel like a fait d’accompli, but things can change, and they can change rapidly,” Dr. Himmelstein adds. “The first step is to have real discussions about it. Up to now, much of the medical literature is saying, ‘It’s not working. We must have the wrong incentives.’ What if there are no right incentives?”
Visit our website for more information about pay-for-performance programs.
Accountable-Care Organizations on the Horizon for Hospitalists
Every HM group should look into transitioning from a fee-for-service model to an accountable-care organization (ACO), a leading hospitalist told conference attendees recently at the Third National Accountable Care Organization Congress.
"You need to be tackling it now, but that doesn't mean you need to be aggressively doing it now," Edward Murphy, MD, chairman of Sound Physicians, told eWire days before he spoke at the ACO Congress on Oct. 31 in Los Angeles. "By tackling it, you need to be doing a hard-nosed assessment of what's best for your group and your patients."
Question: Why is the ACO model so difficult in some instances?
Answer: The problem with the healthcare system today is we’ve spent 100 years building up a system that is designed around, and competent at, delivering services for fees. We're really not set up to manage care.
Q: What is the No. 1 thing you want hospitalists to know about ACOs today?
A: Figure out every single day how to improve the care of your patients at a lower cost. And then, how you can demonstrate it in a quantitative and clear way. ACO-style payments are really only a value proposition centered on providing superior outcomes for patients at higher satisfaction for lower cost. That’s a fundamental value that will always be noteworthy.
Q: Is a hospitalist's job to lead the charge toward ACOs, or support those who do?
A: That's the sort of thing that people on the ground don't have to be told. They just know. If I were the leader of a hospitalist group someplace and really thought the smart thing to do was to think about how to move to an accountable-care model … I would know from my discussions with my colleagues, my discussions with hospital executives where everybody was.
Visit our website for more information about ACOs.
Every HM group should look into transitioning from a fee-for-service model to an accountable-care organization (ACO), a leading hospitalist told conference attendees recently at the Third National Accountable Care Organization Congress.
"You need to be tackling it now, but that doesn't mean you need to be aggressively doing it now," Edward Murphy, MD, chairman of Sound Physicians, told eWire days before he spoke at the ACO Congress on Oct. 31 in Los Angeles. "By tackling it, you need to be doing a hard-nosed assessment of what's best for your group and your patients."
Question: Why is the ACO model so difficult in some instances?
Answer: The problem with the healthcare system today is we’ve spent 100 years building up a system that is designed around, and competent at, delivering services for fees. We're really not set up to manage care.
Q: What is the No. 1 thing you want hospitalists to know about ACOs today?
A: Figure out every single day how to improve the care of your patients at a lower cost. And then, how you can demonstrate it in a quantitative and clear way. ACO-style payments are really only a value proposition centered on providing superior outcomes for patients at higher satisfaction for lower cost. That’s a fundamental value that will always be noteworthy.
Q: Is a hospitalist's job to lead the charge toward ACOs, or support those who do?
A: That's the sort of thing that people on the ground don't have to be told. They just know. If I were the leader of a hospitalist group someplace and really thought the smart thing to do was to think about how to move to an accountable-care model … I would know from my discussions with my colleagues, my discussions with hospital executives where everybody was.
Visit our website for more information about ACOs.
Every HM group should look into transitioning from a fee-for-service model to an accountable-care organization (ACO), a leading hospitalist told conference attendees recently at the Third National Accountable Care Organization Congress.
"You need to be tackling it now, but that doesn't mean you need to be aggressively doing it now," Edward Murphy, MD, chairman of Sound Physicians, told eWire days before he spoke at the ACO Congress on Oct. 31 in Los Angeles. "By tackling it, you need to be doing a hard-nosed assessment of what's best for your group and your patients."
Question: Why is the ACO model so difficult in some instances?
Answer: The problem with the healthcare system today is we’ve spent 100 years building up a system that is designed around, and competent at, delivering services for fees. We're really not set up to manage care.
Q: What is the No. 1 thing you want hospitalists to know about ACOs today?
A: Figure out every single day how to improve the care of your patients at a lower cost. And then, how you can demonstrate it in a quantitative and clear way. ACO-style payments are really only a value proposition centered on providing superior outcomes for patients at higher satisfaction for lower cost. That’s a fundamental value that will always be noteworthy.
Q: Is a hospitalist's job to lead the charge toward ACOs, or support those who do?
A: That's the sort of thing that people on the ground don't have to be told. They just know. If I were the leader of a hospitalist group someplace and really thought the smart thing to do was to think about how to move to an accountable-care model … I would know from my discussions with my colleagues, my discussions with hospital executives where everybody was.
Visit our website for more information about ACOs.
ONLINE EXCLUSIVE: Anticoagulant's Receives FDA Approval to Treat Deep Vein Thrombosis, Pulmonary Embolism
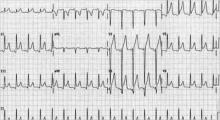
Rivaroxaban (Xarelto) has won another approval from the U.S. Food and Drug Administration (FDA). Already green-lighted for use to reduce the risk of DVT and pulmonary embolism (PE) after knee or hip replacement surgery—and reduce the risk of stroke in non-valvular atrial fibrillation patients—the anticoagulant therapy has been approved for use in the treatment of acute DVT and PE, and to reduce the risk of recurrent DVT and PE after initial treatment. It’s a landmark step that will likely have big implications for hospitalists.
“Xarelto is the first oral anti-clotting drug approved to treat and reduce the recurrence of blood clots since the approval of warfarin nearly 60 years ago,” Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a news release.
—Hiren Shah, MD, assistant professor of medicine, Northwestern University Feinberg School of Medicine, medical director, hospital medicine, Northwestern Memorial Hospital, Chicago
“Single-drug therapy without the need for parental bridging treatment, or drug-level monitoring, is a breakthrough in the treatment of VTE, and represents a paradigm shift that we have not seen in a long time for a very common emergency room and hospital-based medical condition,” says Hiren Shah, MD, assistant professor of medicine at Northwestern University’s Feinberg School of Medicine and medical director of hospital medicine at Northwestern Memorial Hospital in Chicago.
Ian Jenkins, assistant professor in the Division of Hospital Medicine at the University of California at San Diego, says factors that will help determine whether a patient is a candidate for rivaroxaban include the ability to pay for it; compliance, because the duration of effect is shorter than it is for warfarin; and good and stable renal function.
“We now have the first approved oral warfarin alternative for VTE, and for appropriate candidates, it's a more convenient if not better treatment,” Dr. Jenkins says. “The main downside is that warfarin remains reversible, and the new drugs are minimally so.”
Dr. Shah predicts a more efficient discharge process, which, for rivaroxaban patients, will no longer include arranging for international normalized ratio (INR) monitoring or time-consuming counseling on taking injections and drug interactions with vitamin-K antagonists.
“That’s a very complex, 30-minute process,” says Dr. Shah, who also who runs Northwestern’s VTE-prevention program. “With a single agent, I think the value here is you don’t need that complex care coordination anymore, and that’s time-saving for a hospitalist.”
Dr. Shah notes coordination of care will still be very important with this indication, especially because the dose for rivaroxaban in the treatment of acute DVT changes from twice a day to once a day starting at Day 21. “Whatever education initiatives we undertake, they have to extend that entire spectrum,” he adds.
Visit our website for more information about treating acute DVT.
Rivaroxaban (Xarelto) has won another approval from the U.S. Food and Drug Administration (FDA). Already green-lighted for use to reduce the risk of DVT and pulmonary embolism (PE) after knee or hip replacement surgery—and reduce the risk of stroke in non-valvular atrial fibrillation patients—the anticoagulant therapy has been approved for use in the treatment of acute DVT and PE, and to reduce the risk of recurrent DVT and PE after initial treatment. It’s a landmark step that will likely have big implications for hospitalists.
“Xarelto is the first oral anti-clotting drug approved to treat and reduce the recurrence of blood clots since the approval of warfarin nearly 60 years ago,” Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a news release.
—Hiren Shah, MD, assistant professor of medicine, Northwestern University Feinberg School of Medicine, medical director, hospital medicine, Northwestern Memorial Hospital, Chicago
“Single-drug therapy without the need for parental bridging treatment, or drug-level monitoring, is a breakthrough in the treatment of VTE, and represents a paradigm shift that we have not seen in a long time for a very common emergency room and hospital-based medical condition,” says Hiren Shah, MD, assistant professor of medicine at Northwestern University’s Feinberg School of Medicine and medical director of hospital medicine at Northwestern Memorial Hospital in Chicago.
Ian Jenkins, assistant professor in the Division of Hospital Medicine at the University of California at San Diego, says factors that will help determine whether a patient is a candidate for rivaroxaban include the ability to pay for it; compliance, because the duration of effect is shorter than it is for warfarin; and good and stable renal function.
“We now have the first approved oral warfarin alternative for VTE, and for appropriate candidates, it's a more convenient if not better treatment,” Dr. Jenkins says. “The main downside is that warfarin remains reversible, and the new drugs are minimally so.”
Dr. Shah predicts a more efficient discharge process, which, for rivaroxaban patients, will no longer include arranging for international normalized ratio (INR) monitoring or time-consuming counseling on taking injections and drug interactions with vitamin-K antagonists.
“That’s a very complex, 30-minute process,” says Dr. Shah, who also who runs Northwestern’s VTE-prevention program. “With a single agent, I think the value here is you don’t need that complex care coordination anymore, and that’s time-saving for a hospitalist.”
Dr. Shah notes coordination of care will still be very important with this indication, especially because the dose for rivaroxaban in the treatment of acute DVT changes from twice a day to once a day starting at Day 21. “Whatever education initiatives we undertake, they have to extend that entire spectrum,” he adds.
Visit our website for more information about treating acute DVT.
Rivaroxaban (Xarelto) has won another approval from the U.S. Food and Drug Administration (FDA). Already green-lighted for use to reduce the risk of DVT and pulmonary embolism (PE) after knee or hip replacement surgery—and reduce the risk of stroke in non-valvular atrial fibrillation patients—the anticoagulant therapy has been approved for use in the treatment of acute DVT and PE, and to reduce the risk of recurrent DVT and PE after initial treatment. It’s a landmark step that will likely have big implications for hospitalists.
“Xarelto is the first oral anti-clotting drug approved to treat and reduce the recurrence of blood clots since the approval of warfarin nearly 60 years ago,” Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, said in a news release.
—Hiren Shah, MD, assistant professor of medicine, Northwestern University Feinberg School of Medicine, medical director, hospital medicine, Northwestern Memorial Hospital, Chicago
“Single-drug therapy without the need for parental bridging treatment, or drug-level monitoring, is a breakthrough in the treatment of VTE, and represents a paradigm shift that we have not seen in a long time for a very common emergency room and hospital-based medical condition,” says Hiren Shah, MD, assistant professor of medicine at Northwestern University’s Feinberg School of Medicine and medical director of hospital medicine at Northwestern Memorial Hospital in Chicago.
Ian Jenkins, assistant professor in the Division of Hospital Medicine at the University of California at San Diego, says factors that will help determine whether a patient is a candidate for rivaroxaban include the ability to pay for it; compliance, because the duration of effect is shorter than it is for warfarin; and good and stable renal function.
“We now have the first approved oral warfarin alternative for VTE, and for appropriate candidates, it's a more convenient if not better treatment,” Dr. Jenkins says. “The main downside is that warfarin remains reversible, and the new drugs are minimally so.”
Dr. Shah predicts a more efficient discharge process, which, for rivaroxaban patients, will no longer include arranging for international normalized ratio (INR) monitoring or time-consuming counseling on taking injections and drug interactions with vitamin-K antagonists.
“That’s a very complex, 30-minute process,” says Dr. Shah, who also who runs Northwestern’s VTE-prevention program. “With a single agent, I think the value here is you don’t need that complex care coordination anymore, and that’s time-saving for a hospitalist.”
Dr. Shah notes coordination of care will still be very important with this indication, especially because the dose for rivaroxaban in the treatment of acute DVT changes from twice a day to once a day starting at Day 21. “Whatever education initiatives we undertake, they have to extend that entire spectrum,” he adds.
Visit our website for more information about treating acute DVT.
Win Whitcomb: Hospitalists Must Grin and Bear the Hospital-Acquired Conditions Program
The Inpatient Prospective Payment System FY2013 Final Rule charts a different future: By fiscal-year 2015 (October 2014), it will morph into a set of measures that are vetted by the National Quality Forum. Hopefully, this will be an improvement.
In recent years, hospitalists have been deluged with rules about documentation, being asked to use medical vocabulary in ways that were foreign to many of us during our training years. Much of the focus on documentation has been propelled by hospitals’ quest to optimize (“maximize” is a forbidden term) reimbursement, which is purely a function of what is written by “licensed providers” (doctors, physician assistants, and nurse practitioners) in the medical chart.
But another powerful driver of documentation practices of late is the hospital-acquired conditions (HAC) program developed by the Centers for Medicare & Medicaid Services (CMS) and enacted in 2009.
Origins of the HAC List
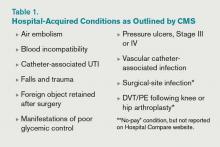
CMS disliked the fact that they were paying for conditions acquired in the hospital that were “reasonably preventable” if evidence-based—or at least “best”—practice was applied. After all, who likes to pay for a punctured gas tank when you brought the minivan in for an oil change? CMS worked with stakeholder groups, including SHM, to create a list of conditions known as hospital-acquired conditions (see Table 1, right).
(As an aside, SHM was supportive of CMS. In fact, we provided direct input into the final rule, recognizing some of the drawbacks of the CMS approach but understanding the larger objective of reengineering a flawed incentive system.)
The idea was that if a hospital submitted a bill to CMS that contained one of these conditions, the hospital would not be paid the amount by which that condition increased total reimbursement for that hospitalization. Note that if you’ve been told your hospital isn’t getting paid at all for patients with one of these conditions, that is not quite correct. Instead, your hospital may not get paid the added amount that is derived from having one of the diagnoses on the list submitted in your hospital’s bill to CMS for a given patient. At the end of the day, this might be a few hundred dollars each time one of these is documented—or $0, if your hospital biller can add another diagnosis in its place to capture the higher payment.
How big a hit to a hospital’s bottom line is this? Meddings and colleagues recently reported that a measly 0.003% of all hospitalizations in Michigan in 2009 saw payments lowered as a result of hospital-acquired catheter-associated UTI, one of the list’s HACs (Ann Int Med. 2012;157:305-312). When all the HACs are added together, one can extrapolate that they haven’t exactly had a big impact on hospital payments.
If the specter of nonpayment for one of these is not enough of a motivator (and it shouldn’t be, given the paltry financial stakes), the rate of HACs are now reported for all hospitals on the Hospital Compare website (www.hospitalcompare.hhs.gov). If a small poke to the pocketbook doesn’t work, maybe public humiliation will.
The Problem with HACs
Although CMS’ intent in creating the HAC program—to eliminate payment for “reasonably preventable” hospital-acquired conditions, thereby improving patient safety—was good, in practice, the program has turned out to be as much about documentation as it is about providing good care. For example, if I forget to write that a Stage III pressure ulcer was present on admission, it gets coded as hospital-acquired and my hospital gets dinged.
It’s important to note that HACs as quality measures were never endorsed by the National Quality Forum (NQF), and without such an endorsement, a quality measure suffers from Rodney Dangerfield syndrome: It don’t get no respect.
Finally, it is disquieting that Meddings et al showed that hospital-acquired catheter-associated UTI rates derived from chart documentation for HACs were but a small fraction of rates determined from rigorous epidemiologic studies, demonstrating that using claims data for determining rates for that specific HAC is flawed. We can only wonder how divergent reported vs. actual rates for the other HACs are.
The Future of the HAC Program
The Affordable Care Act specifies that the lowest-performing quartile of U.S. hospitals for HAC rates will see a 1% Medicare reimbursement reduction beginning in fiscal-year 2015. That’s right: Hospitals facing possible readmissions penalties and losses under value-based purchasing also will face a HAC penalty.
Thankfully, the recently released Inpatient Prospective Payment System FY2013 Final Rule, CMS’ annual update of how hospitals are paid, specifies that the HAC measures are to be removed from public reporting on the Hospital Compare website effective Oct. 1, 2014. They will be replaced by a new set of measures that will (hopefully) be more methodologically sound, because they will require the scrutiny required for endorsement by the NQF. Exactly how these measures will look is not certain, as the rule-making has not yet occurred.
We do know that the three infection measures—catheter-associated UTI, surgical-site infection, and vascular catheter infection—will be generated from clinical data and, therefore, more methodologically sound under the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network. The derivation of the other measures will have to wait until the rule is written next year.
So, until further notice, pay attention to the queries of your hospital’s documentation experts when they approach you about a potential HAC!
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The Inpatient Prospective Payment System FY2013 Final Rule charts a different future: By fiscal-year 2015 (October 2014), it will morph into a set of measures that are vetted by the National Quality Forum. Hopefully, this will be an improvement.
In recent years, hospitalists have been deluged with rules about documentation, being asked to use medical vocabulary in ways that were foreign to many of us during our training years. Much of the focus on documentation has been propelled by hospitals’ quest to optimize (“maximize” is a forbidden term) reimbursement, which is purely a function of what is written by “licensed providers” (doctors, physician assistants, and nurse practitioners) in the medical chart.
But another powerful driver of documentation practices of late is the hospital-acquired conditions (HAC) program developed by the Centers for Medicare & Medicaid Services (CMS) and enacted in 2009.
Origins of the HAC List
CMS disliked the fact that they were paying for conditions acquired in the hospital that were “reasonably preventable” if evidence-based—or at least “best”—practice was applied. After all, who likes to pay for a punctured gas tank when you brought the minivan in for an oil change? CMS worked with stakeholder groups, including SHM, to create a list of conditions known as hospital-acquired conditions (see Table 1, right).
(As an aside, SHM was supportive of CMS. In fact, we provided direct input into the final rule, recognizing some of the drawbacks of the CMS approach but understanding the larger objective of reengineering a flawed incentive system.)
The idea was that if a hospital submitted a bill to CMS that contained one of these conditions, the hospital would not be paid the amount by which that condition increased total reimbursement for that hospitalization. Note that if you’ve been told your hospital isn’t getting paid at all for patients with one of these conditions, that is not quite correct. Instead, your hospital may not get paid the added amount that is derived from having one of the diagnoses on the list submitted in your hospital’s bill to CMS for a given patient. At the end of the day, this might be a few hundred dollars each time one of these is documented—or $0, if your hospital biller can add another diagnosis in its place to capture the higher payment.
How big a hit to a hospital’s bottom line is this? Meddings and colleagues recently reported that a measly 0.003% of all hospitalizations in Michigan in 2009 saw payments lowered as a result of hospital-acquired catheter-associated UTI, one of the list’s HACs (Ann Int Med. 2012;157:305-312). When all the HACs are added together, one can extrapolate that they haven’t exactly had a big impact on hospital payments.
If the specter of nonpayment for one of these is not enough of a motivator (and it shouldn’t be, given the paltry financial stakes), the rate of HACs are now reported for all hospitals on the Hospital Compare website (www.hospitalcompare.hhs.gov). If a small poke to the pocketbook doesn’t work, maybe public humiliation will.
The Problem with HACs
Although CMS’ intent in creating the HAC program—to eliminate payment for “reasonably preventable” hospital-acquired conditions, thereby improving patient safety—was good, in practice, the program has turned out to be as much about documentation as it is about providing good care. For example, if I forget to write that a Stage III pressure ulcer was present on admission, it gets coded as hospital-acquired and my hospital gets dinged.
It’s important to note that HACs as quality measures were never endorsed by the National Quality Forum (NQF), and without such an endorsement, a quality measure suffers from Rodney Dangerfield syndrome: It don’t get no respect.
Finally, it is disquieting that Meddings et al showed that hospital-acquired catheter-associated UTI rates derived from chart documentation for HACs were but a small fraction of rates determined from rigorous epidemiologic studies, demonstrating that using claims data for determining rates for that specific HAC is flawed. We can only wonder how divergent reported vs. actual rates for the other HACs are.
The Future of the HAC Program
The Affordable Care Act specifies that the lowest-performing quartile of U.S. hospitals for HAC rates will see a 1% Medicare reimbursement reduction beginning in fiscal-year 2015. That’s right: Hospitals facing possible readmissions penalties and losses under value-based purchasing also will face a HAC penalty.
Thankfully, the recently released Inpatient Prospective Payment System FY2013 Final Rule, CMS’ annual update of how hospitals are paid, specifies that the HAC measures are to be removed from public reporting on the Hospital Compare website effective Oct. 1, 2014. They will be replaced by a new set of measures that will (hopefully) be more methodologically sound, because they will require the scrutiny required for endorsement by the NQF. Exactly how these measures will look is not certain, as the rule-making has not yet occurred.
We do know that the three infection measures—catheter-associated UTI, surgical-site infection, and vascular catheter infection—will be generated from clinical data and, therefore, more methodologically sound under the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network. The derivation of the other measures will have to wait until the rule is written next year.
So, until further notice, pay attention to the queries of your hospital’s documentation experts when they approach you about a potential HAC!
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The Inpatient Prospective Payment System FY2013 Final Rule charts a different future: By fiscal-year 2015 (October 2014), it will morph into a set of measures that are vetted by the National Quality Forum. Hopefully, this will be an improvement.
In recent years, hospitalists have been deluged with rules about documentation, being asked to use medical vocabulary in ways that were foreign to many of us during our training years. Much of the focus on documentation has been propelled by hospitals’ quest to optimize (“maximize” is a forbidden term) reimbursement, which is purely a function of what is written by “licensed providers” (doctors, physician assistants, and nurse practitioners) in the medical chart.
But another powerful driver of documentation practices of late is the hospital-acquired conditions (HAC) program developed by the Centers for Medicare & Medicaid Services (CMS) and enacted in 2009.
Origins of the HAC List
CMS disliked the fact that they were paying for conditions acquired in the hospital that were “reasonably preventable” if evidence-based—or at least “best”—practice was applied. After all, who likes to pay for a punctured gas tank when you brought the minivan in for an oil change? CMS worked with stakeholder groups, including SHM, to create a list of conditions known as hospital-acquired conditions (see Table 1, right).
(As an aside, SHM was supportive of CMS. In fact, we provided direct input into the final rule, recognizing some of the drawbacks of the CMS approach but understanding the larger objective of reengineering a flawed incentive system.)
The idea was that if a hospital submitted a bill to CMS that contained one of these conditions, the hospital would not be paid the amount by which that condition increased total reimbursement for that hospitalization. Note that if you’ve been told your hospital isn’t getting paid at all for patients with one of these conditions, that is not quite correct. Instead, your hospital may not get paid the added amount that is derived from having one of the diagnoses on the list submitted in your hospital’s bill to CMS for a given patient. At the end of the day, this might be a few hundred dollars each time one of these is documented—or $0, if your hospital biller can add another diagnosis in its place to capture the higher payment.
How big a hit to a hospital’s bottom line is this? Meddings and colleagues recently reported that a measly 0.003% of all hospitalizations in Michigan in 2009 saw payments lowered as a result of hospital-acquired catheter-associated UTI, one of the list’s HACs (Ann Int Med. 2012;157:305-312). When all the HACs are added together, one can extrapolate that they haven’t exactly had a big impact on hospital payments.
If the specter of nonpayment for one of these is not enough of a motivator (and it shouldn’t be, given the paltry financial stakes), the rate of HACs are now reported for all hospitals on the Hospital Compare website (www.hospitalcompare.hhs.gov). If a small poke to the pocketbook doesn’t work, maybe public humiliation will.
The Problem with HACs
Although CMS’ intent in creating the HAC program—to eliminate payment for “reasonably preventable” hospital-acquired conditions, thereby improving patient safety—was good, in practice, the program has turned out to be as much about documentation as it is about providing good care. For example, if I forget to write that a Stage III pressure ulcer was present on admission, it gets coded as hospital-acquired and my hospital gets dinged.
It’s important to note that HACs as quality measures were never endorsed by the National Quality Forum (NQF), and without such an endorsement, a quality measure suffers from Rodney Dangerfield syndrome: It don’t get no respect.
Finally, it is disquieting that Meddings et al showed that hospital-acquired catheter-associated UTI rates derived from chart documentation for HACs were but a small fraction of rates determined from rigorous epidemiologic studies, demonstrating that using claims data for determining rates for that specific HAC is flawed. We can only wonder how divergent reported vs. actual rates for the other HACs are.
The Future of the HAC Program
The Affordable Care Act specifies that the lowest-performing quartile of U.S. hospitals for HAC rates will see a 1% Medicare reimbursement reduction beginning in fiscal-year 2015. That’s right: Hospitals facing possible readmissions penalties and losses under value-based purchasing also will face a HAC penalty.
Thankfully, the recently released Inpatient Prospective Payment System FY2013 Final Rule, CMS’ annual update of how hospitals are paid, specifies that the HAC measures are to be removed from public reporting on the Hospital Compare website effective Oct. 1, 2014. They will be replaced by a new set of measures that will (hopefully) be more methodologically sound, because they will require the scrutiny required for endorsement by the NQF. Exactly how these measures will look is not certain, as the rule-making has not yet occurred.
We do know that the three infection measures—catheter-associated UTI, surgical-site infection, and vascular catheter infection—will be generated from clinical data and, therefore, more methodologically sound under the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network. The derivation of the other measures will have to wait until the rule is written next year.
So, until further notice, pay attention to the queries of your hospital’s documentation experts when they approach you about a potential HAC!
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Hospitalists' Voices to be Heard on Capitol Hill
Every year, hundreds of thousands of people from all parts of the country travel to Washington, D.C., and visit Congress. Regardless of the organizations they represent, almost all of them have one thing in common: They go to Capitol Hill with an “ask.”
Some ask for a vote on a particular piece of legislation; some request funding for their projects. Regardless, there is almost always an ask.
But hospitalists are different, according to SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, and committee member Brad Flansbaum, DO, MPH, SFHM. They are featured in a new video about “Hospitalists on the Hill,” SHM’s day to meet with members of Congress.
Rather than lobbying or asking for assistance, hospitalists bring solutions to the healthcare problems currently vexing communities throughout the country. By introducing the hospitalist model and its role in quality improvement (QI) to some of the most influential government figures in public health, hospitalists who make the visit to Capitol Hill help to spread some of the best practices in hospital-based healthcare and share their personal experiences at the same time.
“Every constituency that comes in is asking them for something,” Dr. Greeno says in one of the SHM-produced videos. “We don’t ask for anything. We offer. We offer our expertise. We offer to help them make better decisions than they would make otherwise.”
That contribution matters to members of Congress and their healthcare staff. Drs. Greeno and Flansbaum are “Hill Day” veterans who have seen firsthand how legislators and their staff absorb SHM’s message and materials.
“I thought that if we are leaving materials behind, that the minute we walk out of the office, it was going in the trash,” Dr. Greeno says. “That’s not what happens. They read this stuff.”
In 2013, Hospitalists on the Hill will take place May 16, the day before the official start of HM’s annual meeting at the Gaylord National Resort & Convention Center in National Harbor, Md., just a few minutes south of Washington, D.C. The agenda is ambitious, starting with a briefing about what to expect when meeting Congress members on Capitol Hill, followed by a full day of meetings with policymakers, regulators, and their staff.
“We spend our day going back and forth, from the Senate side of the Capitol to the House side of the Capitol, in and out of the office buildings, walking the halls of Congress,” Dr. Greeno says. “It’s a blast. It’s so interesting. And we’re getting a chance to sit down and deliver our message.”
For Dr. Flansbaum, it’s an opportunity to promote action in Washington.
“It really brings government to life,” he says. “You realize that, as bottlenecked as things might be sometimes, things have to get done.”
HM13 attendees can sign-up for Hospitalists on the Hill during annual-meeing registration. For more information, visit www.hospitalmedicine2013.org/onthehill.
Brendon Shank is SHM’s associate vice president of communications.
Every year, hundreds of thousands of people from all parts of the country travel to Washington, D.C., and visit Congress. Regardless of the organizations they represent, almost all of them have one thing in common: They go to Capitol Hill with an “ask.”
Some ask for a vote on a particular piece of legislation; some request funding for their projects. Regardless, there is almost always an ask.
But hospitalists are different, according to SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, and committee member Brad Flansbaum, DO, MPH, SFHM. They are featured in a new video about “Hospitalists on the Hill,” SHM’s day to meet with members of Congress.
Rather than lobbying or asking for assistance, hospitalists bring solutions to the healthcare problems currently vexing communities throughout the country. By introducing the hospitalist model and its role in quality improvement (QI) to some of the most influential government figures in public health, hospitalists who make the visit to Capitol Hill help to spread some of the best practices in hospital-based healthcare and share their personal experiences at the same time.
“Every constituency that comes in is asking them for something,” Dr. Greeno says in one of the SHM-produced videos. “We don’t ask for anything. We offer. We offer our expertise. We offer to help them make better decisions than they would make otherwise.”
That contribution matters to members of Congress and their healthcare staff. Drs. Greeno and Flansbaum are “Hill Day” veterans who have seen firsthand how legislators and their staff absorb SHM’s message and materials.
“I thought that if we are leaving materials behind, that the minute we walk out of the office, it was going in the trash,” Dr. Greeno says. “That’s not what happens. They read this stuff.”
In 2013, Hospitalists on the Hill will take place May 16, the day before the official start of HM’s annual meeting at the Gaylord National Resort & Convention Center in National Harbor, Md., just a few minutes south of Washington, D.C. The agenda is ambitious, starting with a briefing about what to expect when meeting Congress members on Capitol Hill, followed by a full day of meetings with policymakers, regulators, and their staff.
“We spend our day going back and forth, from the Senate side of the Capitol to the House side of the Capitol, in and out of the office buildings, walking the halls of Congress,” Dr. Greeno says. “It’s a blast. It’s so interesting. And we’re getting a chance to sit down and deliver our message.”
For Dr. Flansbaum, it’s an opportunity to promote action in Washington.
“It really brings government to life,” he says. “You realize that, as bottlenecked as things might be sometimes, things have to get done.”
HM13 attendees can sign-up for Hospitalists on the Hill during annual-meeing registration. For more information, visit www.hospitalmedicine2013.org/onthehill.
Brendon Shank is SHM’s associate vice president of communications.
Every year, hundreds of thousands of people from all parts of the country travel to Washington, D.C., and visit Congress. Regardless of the organizations they represent, almost all of them have one thing in common: They go to Capitol Hill with an “ask.”
Some ask for a vote on a particular piece of legislation; some request funding for their projects. Regardless, there is almost always an ask.
But hospitalists are different, according to SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, and committee member Brad Flansbaum, DO, MPH, SFHM. They are featured in a new video about “Hospitalists on the Hill,” SHM’s day to meet with members of Congress.
Rather than lobbying or asking for assistance, hospitalists bring solutions to the healthcare problems currently vexing communities throughout the country. By introducing the hospitalist model and its role in quality improvement (QI) to some of the most influential government figures in public health, hospitalists who make the visit to Capitol Hill help to spread some of the best practices in hospital-based healthcare and share their personal experiences at the same time.
“Every constituency that comes in is asking them for something,” Dr. Greeno says in one of the SHM-produced videos. “We don’t ask for anything. We offer. We offer our expertise. We offer to help them make better decisions than they would make otherwise.”
That contribution matters to members of Congress and their healthcare staff. Drs. Greeno and Flansbaum are “Hill Day” veterans who have seen firsthand how legislators and their staff absorb SHM’s message and materials.
“I thought that if we are leaving materials behind, that the minute we walk out of the office, it was going in the trash,” Dr. Greeno says. “That’s not what happens. They read this stuff.”
In 2013, Hospitalists on the Hill will take place May 16, the day before the official start of HM’s annual meeting at the Gaylord National Resort & Convention Center in National Harbor, Md., just a few minutes south of Washington, D.C. The agenda is ambitious, starting with a briefing about what to expect when meeting Congress members on Capitol Hill, followed by a full day of meetings with policymakers, regulators, and their staff.
“We spend our day going back and forth, from the Senate side of the Capitol to the House side of the Capitol, in and out of the office buildings, walking the halls of Congress,” Dr. Greeno says. “It’s a blast. It’s so interesting. And we’re getting a chance to sit down and deliver our message.”
For Dr. Flansbaum, it’s an opportunity to promote action in Washington.
“It really brings government to life,” he says. “You realize that, as bottlenecked as things might be sometimes, things have to get done.”
HM13 attendees can sign-up for Hospitalists on the Hill during annual-meeing registration. For more information, visit www.hospitalmedicine2013.org/onthehill.
Brendon Shank is SHM’s associate vice president of communications.
New 'Meaningful Use' Exemption is Valuable Option for Growing Number of Hospitalists
Hospital-based eligible professionals do not qualify for the Medicare or Medicaid electronic health record (EHR) incentive program or the impending payment penalties for not being “meaningful users” of EHR technology.
A hospital-based “eligible professional” (EP) is defined by the Centers for Medicare & Medicaid Services (CMS) as an EP who furnishes 90% or more of their covered professional services in either the inpatient or emergency departments of a hospital. This exemption applies to most hospitalists and recognizes they have very little control over whether their respective institutions invest in this technology.
Although this 90% threshold should qualify most hospitalists for the exemption, it does not tell the entire story. A growing number of hospitalists are spending time rounding in skilled nursing or other post-acute facilities, and some are focusing the entirety of their practice in the post-acute setting. Under the current CMS definition, these hospitalists are not hospital-based and will, therefore, be subject to the upcoming penalties for not being meaningful users of EHR technology.
Contrary to the 90% threshold, the reality for post-acute hospitalists is that when it comes to EHRs, they are no different than their hospital-based colleagues. A hospitalist, irrespective of setting, has very little control over what kind of technology, if any, a facility invests in.
For hospitalists who are rounding or spending more of their practice time in post-acute facilities, this mechanical classification based on practice location alone is problematic. A physician-implemented EHR is not practical and does not make sense given the unique practice patterns of hospitalists. Although SHM remains strongly committed to the promise represented by health information technology (HIT), SHM consistently has noted to CMS that hospitalist practice does not always fit the confines of their rulemaking.
Hospitalists should not be penalized for failure to implement their own HIT, because they already use facility EHRs or lack control over the availability of EHR systems. It is for these reasons that SHM has been a strong advocate for an additional exemption that works for hospitalists—an exemption that recognizes lack of control of availability.
In August, CMS released the final rule for Stage 2 of Meaningful Use, and the voice of hospitalists was clearly heard. The rule includes an SHM advanced-hardship exemption acknowledging that EPs who practice in multiple locations, such as nursing homes, could face a significant hardship as they would have no way to control the use of Certified EHR Technology (CEHRT). In promulgating the exemption, CMS specifically states that a “physician merely sees patients at the center or home, and does not have any other interest in the facility; they would exert little to no influence over whether the nursing home, center, or other similar outpatient site adopts and implements CEHRT.” Hospitalists seeking this exemption would need to apply annually for up to five years.
This hardship exemption could apply to hospitalists who work in multiple facilities outside of hospitals, such as nursing homes. Although imperfect due to the time-limited nature, the exemption represents a victory in the effort to differentiate HM from traditional practice patterns. It is precisely this difference that makes HM uniquely positioned to lead changes in the healthcare system.
Josh Boswell is SHM’s interim senior manager of government relations.
Hospital-based eligible professionals do not qualify for the Medicare or Medicaid electronic health record (EHR) incentive program or the impending payment penalties for not being “meaningful users” of EHR technology.
A hospital-based “eligible professional” (EP) is defined by the Centers for Medicare & Medicaid Services (CMS) as an EP who furnishes 90% or more of their covered professional services in either the inpatient or emergency departments of a hospital. This exemption applies to most hospitalists and recognizes they have very little control over whether their respective institutions invest in this technology.
Although this 90% threshold should qualify most hospitalists for the exemption, it does not tell the entire story. A growing number of hospitalists are spending time rounding in skilled nursing or other post-acute facilities, and some are focusing the entirety of their practice in the post-acute setting. Under the current CMS definition, these hospitalists are not hospital-based and will, therefore, be subject to the upcoming penalties for not being meaningful users of EHR technology.
Contrary to the 90% threshold, the reality for post-acute hospitalists is that when it comes to EHRs, they are no different than their hospital-based colleagues. A hospitalist, irrespective of setting, has very little control over what kind of technology, if any, a facility invests in.
For hospitalists who are rounding or spending more of their practice time in post-acute facilities, this mechanical classification based on practice location alone is problematic. A physician-implemented EHR is not practical and does not make sense given the unique practice patterns of hospitalists. Although SHM remains strongly committed to the promise represented by health information technology (HIT), SHM consistently has noted to CMS that hospitalist practice does not always fit the confines of their rulemaking.
Hospitalists should not be penalized for failure to implement their own HIT, because they already use facility EHRs or lack control over the availability of EHR systems. It is for these reasons that SHM has been a strong advocate for an additional exemption that works for hospitalists—an exemption that recognizes lack of control of availability.
In August, CMS released the final rule for Stage 2 of Meaningful Use, and the voice of hospitalists was clearly heard. The rule includes an SHM advanced-hardship exemption acknowledging that EPs who practice in multiple locations, such as nursing homes, could face a significant hardship as they would have no way to control the use of Certified EHR Technology (CEHRT). In promulgating the exemption, CMS specifically states that a “physician merely sees patients at the center or home, and does not have any other interest in the facility; they would exert little to no influence over whether the nursing home, center, or other similar outpatient site adopts and implements CEHRT.” Hospitalists seeking this exemption would need to apply annually for up to five years.
This hardship exemption could apply to hospitalists who work in multiple facilities outside of hospitals, such as nursing homes. Although imperfect due to the time-limited nature, the exemption represents a victory in the effort to differentiate HM from traditional practice patterns. It is precisely this difference that makes HM uniquely positioned to lead changes in the healthcare system.
Josh Boswell is SHM’s interim senior manager of government relations.
Hospital-based eligible professionals do not qualify for the Medicare or Medicaid electronic health record (EHR) incentive program or the impending payment penalties for not being “meaningful users” of EHR technology.
A hospital-based “eligible professional” (EP) is defined by the Centers for Medicare & Medicaid Services (CMS) as an EP who furnishes 90% or more of their covered professional services in either the inpatient or emergency departments of a hospital. This exemption applies to most hospitalists and recognizes they have very little control over whether their respective institutions invest in this technology.
Although this 90% threshold should qualify most hospitalists for the exemption, it does not tell the entire story. A growing number of hospitalists are spending time rounding in skilled nursing or other post-acute facilities, and some are focusing the entirety of their practice in the post-acute setting. Under the current CMS definition, these hospitalists are not hospital-based and will, therefore, be subject to the upcoming penalties for not being meaningful users of EHR technology.
Contrary to the 90% threshold, the reality for post-acute hospitalists is that when it comes to EHRs, they are no different than their hospital-based colleagues. A hospitalist, irrespective of setting, has very little control over what kind of technology, if any, a facility invests in.
For hospitalists who are rounding or spending more of their practice time in post-acute facilities, this mechanical classification based on practice location alone is problematic. A physician-implemented EHR is not practical and does not make sense given the unique practice patterns of hospitalists. Although SHM remains strongly committed to the promise represented by health information technology (HIT), SHM consistently has noted to CMS that hospitalist practice does not always fit the confines of their rulemaking.
Hospitalists should not be penalized for failure to implement their own HIT, because they already use facility EHRs or lack control over the availability of EHR systems. It is for these reasons that SHM has been a strong advocate for an additional exemption that works for hospitalists—an exemption that recognizes lack of control of availability.
In August, CMS released the final rule for Stage 2 of Meaningful Use, and the voice of hospitalists was clearly heard. The rule includes an SHM advanced-hardship exemption acknowledging that EPs who practice in multiple locations, such as nursing homes, could face a significant hardship as they would have no way to control the use of Certified EHR Technology (CEHRT). In promulgating the exemption, CMS specifically states that a “physician merely sees patients at the center or home, and does not have any other interest in the facility; they would exert little to no influence over whether the nursing home, center, or other similar outpatient site adopts and implements CEHRT.” Hospitalists seeking this exemption would need to apply annually for up to five years.
This hardship exemption could apply to hospitalists who work in multiple facilities outside of hospitals, such as nursing homes. Although imperfect due to the time-limited nature, the exemption represents a victory in the effort to differentiate HM from traditional practice patterns. It is precisely this difference that makes HM uniquely positioned to lead changes in the healthcare system.
Josh Boswell is SHM’s interim senior manager of government relations.
Off-Label Use of Antipsychotics for Dementia Patients Discouraged
Hospitalists can play a major role in reducing deaths that come as a result of off-label prescriptions for antipsychotic drugs being given to dementia patients, according to the Centers for Medicare & Medicaid Services (CMS) and SHM.
In a letter to hospitalist leaders, SHM encouraged hospitalists to “partner with others in your clinical work environment to reduce the use of antipsychotics for treating behavioral problems in patients with dementia. We believe that hospitalists have an important role to play in this initiative; hospital-based clinicians frequently care for patients with dementia and are responsible for medications prescribed during a patient’s hospitalization and at discharge.”
The joint education effort by CMS and SHM is based on an April 2011 report from the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) that found that antipsychotic medications sometimes are used to treat patients with dementia for off-label reasons (e.g. “behaviors”) or against black-box warnings despite potential dangers to patients’ health.
An earlier warning from the FDA in 2008 outlined the potential dangers as:
- Increased risk (60% to 70%) of death in older adults with dementia;
- Prolongation of the QT interval on electrocardiogram, particularly with intravenous haloperidol use;
- Increased risk of stroke and TIAs; and
- Worsening cognitive function.
The letter to hospitalists noted the necessary changes and the need for collaboration between SHM, its members, and hospital leaders. “Increased prescriber training and system practice changes will help reduce unnecessary antipsychotic drug prescribing,” the letter stated. “SHM looks forward to an ongoing collaboration with members and hospital leaders on this important patient safety concern.”
Hospitalists can play a major role in reducing deaths that come as a result of off-label prescriptions for antipsychotic drugs being given to dementia patients, according to the Centers for Medicare & Medicaid Services (CMS) and SHM.
In a letter to hospitalist leaders, SHM encouraged hospitalists to “partner with others in your clinical work environment to reduce the use of antipsychotics for treating behavioral problems in patients with dementia. We believe that hospitalists have an important role to play in this initiative; hospital-based clinicians frequently care for patients with dementia and are responsible for medications prescribed during a patient’s hospitalization and at discharge.”
The joint education effort by CMS and SHM is based on an April 2011 report from the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) that found that antipsychotic medications sometimes are used to treat patients with dementia for off-label reasons (e.g. “behaviors”) or against black-box warnings despite potential dangers to patients’ health.
An earlier warning from the FDA in 2008 outlined the potential dangers as:
- Increased risk (60% to 70%) of death in older adults with dementia;
- Prolongation of the QT interval on electrocardiogram, particularly with intravenous haloperidol use;
- Increased risk of stroke and TIAs; and
- Worsening cognitive function.
The letter to hospitalists noted the necessary changes and the need for collaboration between SHM, its members, and hospital leaders. “Increased prescriber training and system practice changes will help reduce unnecessary antipsychotic drug prescribing,” the letter stated. “SHM looks forward to an ongoing collaboration with members and hospital leaders on this important patient safety concern.”
Hospitalists can play a major role in reducing deaths that come as a result of off-label prescriptions for antipsychotic drugs being given to dementia patients, according to the Centers for Medicare & Medicaid Services (CMS) and SHM.
In a letter to hospitalist leaders, SHM encouraged hospitalists to “partner with others in your clinical work environment to reduce the use of antipsychotics for treating behavioral problems in patients with dementia. We believe that hospitalists have an important role to play in this initiative; hospital-based clinicians frequently care for patients with dementia and are responsible for medications prescribed during a patient’s hospitalization and at discharge.”
The joint education effort by CMS and SHM is based on an April 2011 report from the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) that found that antipsychotic medications sometimes are used to treat patients with dementia for off-label reasons (e.g. “behaviors”) or against black-box warnings despite potential dangers to patients’ health.
An earlier warning from the FDA in 2008 outlined the potential dangers as:
- Increased risk (60% to 70%) of death in older adults with dementia;
- Prolongation of the QT interval on electrocardiogram, particularly with intravenous haloperidol use;
- Increased risk of stroke and TIAs; and
- Worsening cognitive function.
The letter to hospitalists noted the necessary changes and the need for collaboration between SHM, its members, and hospital leaders. “Increased prescriber training and system practice changes will help reduce unnecessary antipsychotic drug prescribing,” the letter stated. “SHM looks forward to an ongoing collaboration with members and hospital leaders on this important patient safety concern.”
How is Acute Pericarditis Diagnosed and Treated?
Case
A 32-year-old female with no significant past medical history is evaluated for sharp, left-sided chest pain for five days. Her pain is intermittent, worse with deep inspiration and in the supine position. She denies any shortness of breath. Her temperature is 100.8ºF, but otherwise her vital signs are normal. The physical exam and chest radiograph are unremarkable, but an electrocardiogram shows diffuse ST-segment elevations. The initial troponin is mildly elevated at 0.35 ng/ml.
Could this patient have acute pericarditis? If so, how should she be managed?
Background
Pericarditis is the most common pericardial disease encountered by hospitalists. As many as 5% of chest pain cases unattributable to myocardial infarction (MI) are diagnosed with pericarditis.1 In immunocompetent individuals, as many as 90% of acute pericarditis cases are viral or idiopathic in etiology.1,2 Human immunodeficiency virus (HIV) and tuberculosis are common culprits in developing countries and immunocompromised hosts.3 Other specific etiologies of acute pericarditis include autoimmune diseases, neoplasms, chest irradiation, trauma, and metabolic disturbances (e.g. uremia). An etiologic classification of acute pericarditis is shown in Table 2 (p. 16).
Pericarditis primarily is a clinical diagnosis. Most patients present with chest pain.4 A pericardial friction rub may or may not be heard (sensitivity 16% to 85%), but when present is nearly 100% specific for pericarditis.2,5 Diffuse ST-segment elevation on electrocardiogram (EKG) is present in 60% to 90% of cases, but it can be difficult to differentiate from ST-segment elevations in acute MI.4,6
Uncomplicated acute pericarditis often is treated successfully as an outpatient.4 However, patients with high-risk features (see Table 1, right) should be hospitalized for identification and treatment of specific underlying etiology and for monitoring of complications, such as tamponade.7
Our patient has features consistent with pericarditis. In the following sections, we will review the diagnosis and treatment of acute pericarditis.
Review of the Data
How is acute pericarditis diagnosed?
Acute pericarditis is a clinical diagnosis supported by EKG and echocardiogram. At least two of the following four criteria must be present for the diagnosis: pleuritic chest pain, pericardial rub, diffuse ST-segment elevation on EKG, and pericardial effusion.8
History. Patients may report fever (46% in one small study of 69 patients) or a recent history of respiratory or gastrointestinal infection (40%).5 Most patients will report pleuritic chest pain. Typically, the pain is improved when sitting up and leaning forward, and gets worse when lying supine.4 Pain might radiate to the trapezius muscle ridge due to the common phrenic nerve innervation of pericardium and trapezius.9 However, pain might be minimal or absent in patients with uremic, neoplastic, tuberculous, or post-irradiation pericarditis.
Physical exam. A pericardial friction rub is nearly 100% specific for a pericarditis diagnosis, but sensitivity can vary (16% to 85%) depending on the frequency of auscultation and underlying etiology.2,5 It is thought to be caused by friction between the parietal and visceral layers of inflamed pericardium. A pericardial rub classically is described as a superficial, high-pitched, scratchy, or squeaking sound best heard with the diaphragm of the stethoscope at the lower left sternal border with the patient leaning forward.
Laboratory data. A complete blood count, metabolic panel, and cardiac enzymes should be checked in all patients with suspected acute pericarditis. Troponin values are elevated in up to one-third of patients, indicating cardiac muscle injury or myopericarditis, but have not been shown to adversely impact hospital length of stay, readmission, or complication rates.5,10 Markers of inflammation (e.g. erythrocyte sedimentation rate or C-reactive protein) are frequently elevated but do not point to a specific underlying etiology. Routine viral cultures and antibody titers are not useful.11
Most cases of pericarditis are presumed idiopathic (viral); however, finding a specific etiology should be considered in patients who do not respond after one week of therapy. Anti-nuclear antibody, complement levels, and rheumatoid factor can serve as screening tests for autoimmune disease. Purified protein derivative or quantiferon testing and HIV testing might be indicated in patients with appropriate risk factors. In cases of suspected tuberculous or neoplastic pericarditis, pericardial fluid analysis and biopsy could be warranted.
Electrocardiography. The EKG is the most useful test in diagnosing acute pericarditis. EKG changes in acute pericarditis can progress over four stages:
- Stage 1: diffuse ST elevations with or without PR depressions, initially;
- Stage 2: normalization of ST and PR segments, typically after several days;
- Stage 3: diffuse T-wave inversions; and
- Stage 4: normalization of T-waves, typically after weeks or months.
While all four stages are unlikely to be present in a given case, 80% of patients with pericarditis will demonstrate diffuse ST-segment elevations and PR-segment depression (see Figure 2, above).12
Table 3 lists EKG features helpful in differentiating acute pericarditis from acute myocardial infarction.
Chest radiography. Because a pericardial effusion often accompanies pericarditis, a chest radiograph (CXR) should be performed in all suspected cases. The CXR might show enlargement of the cardiac silhouette if more than 250 ml of pericardial fluid is present.3 A CXR also is helpful to diagnose concomitant pulmonary infection, pleural effusion, or mediastinal mass—all findings that could point to an underlying specific etiology of pericarditis and/or pericardial effusion.
Echocardiography. An echocardiogram should be performed in all patients with suspected pericarditis to detect effusion, associated myocardial, or paracardial disease.13 The echocardiogram frequently is normal but could show an effusion in 60%, and tamponade (see Figure 1, p. 15) in 5%, of cases.4
Computed tomography (CT) and cardiac magnetic resonance imaging (CMR).CT or CMR are the imaging modalities of choice when an echocardiogram is inconclusive or in cases of pericarditis complicated by a hemorrhagic or localized effusion, pericardial thickening, or pericardial mass.14 They also help in precise imaging of neighboring structures, such as lungs or mediastinum.
Pericardial fluid analysis and pericardial biopsy. In cases of refractory pericarditis with effusion, pericardial fluid analysis might provide clues to the underlying etiology. Routine chemistry, cell count, gram and acid fast staining, culture, and cytology should be sent. In addition, acid-fast bacillus staining and culture, adenosine deaminase, and interferon-gamma testing should be ordered when tuberculous pericarditis is suspected. A pericardial biopsy may show granulomas or neoplastic cells. Overall, pericardial fluid analysis and biopsy reveal a diagnosis in roughly 20% of cases.11
How is acute pericarditis treated?
Most cases of uncomplicated acute pericarditis are viral and respond well to NSAID plus colchicine therapy.2,4 Failure to respond to NSAIDs plus colchicine—evidenced by persistent fever, pericardial chest pain, new pericardial effusion, or worsening of general illness—within a week of treatment should prompt a search for an underlying systemic illness. If found, treatment should be aimed at the causative illness.
Bacterial pericarditis usually requires surgical drainage in addition to treatment with appropriate antibiotics.11 Tuberculous pericarditis is treated with multidrug therapy; when underlying HIV is present, patients should receive highly active anti-retroviral therapy as well. Steroids and immunosuppressants should be considered in addition to NSAIDs and colchicine in autoimmune pericarditis.10 Neoplastic pericarditis may resolve with chemotherapy but it has a high recurrence rate.13 Uremic pericarditis requires intensified dialysis.
Treatment options for uncomplicated idiopathic or viral pericarditis include:
NSAIDs. It is important to adequately dose NSAIDs when treating acute pericarditis. Initial treatment options include ibuprofen (1,600 to 3,200 mg daily), indomethacin (75 to 150 mg daily) or aspirin (2 to 4 gm daily) for one week.11,15 Aspirin is preferred in patients with ischemic heart disease. For patients with symptoms that persist longer than a week, NSAIDS may be continued, but investigation for an underlying etiology is indicated. Concomitant proton-pump-inhibitor therapy should be considered in patients at high risk for peptic ulcer disease to minimize gastric side effects.
Colchicine. Colchicine has a favorable risk-benefit profile as an adjunct treatment for acute and recurrent pericarditis. Patients experience better symptom relief when treated with both colchicine and an NSAID, compared with NSAIDs alone (88% versus 63%). Recurrence rates are lower with combined therapy (11% versus 32%).16 Colchicine treatment (0.6 mg twice daily after a loading dose of up to 2 mg) is recommended for several months to greater than one year.13,16,17
Glucocorticoids. Routine glucocorticoid use should be avoided in the treatment of acute pericarditis, as it has been associated with an increased risk for recurrence (OR 4.3).16,18 Glucocorticoid use should be considered in cases of pericarditis refractory to NSAIDs and colchicine, cases in which NSAIDs and or colchicine are contraindicated, and in autoimmune or connective-tissue-disease-related pericarditis. Prednisone should be dosed up to 1 mg/kg/day for at least one month, depending on symptom resolution, then tapered after either NSAIDs or colchicine have been started.13 Smaller prednisone doses of up to 0.5 mg/kg/day could be as effective, with the added benefit of reduced side effects and recurrences.19
Invasive treatment. Pericardiocentesis and/or pericardiectomy should be considered when pericarditis is complicated by a large effusion or tamponade, constrictive physiology, or recurrent effusion.11 Pericardiocentesis is the least invasive option and helps provide immediate relief in cases of tamponade or large symptomatic effusions. It is the preferred modality for obtaining pericardial fluid for diagnostic analysis. However, effusions can recur and in those cases pericardial window is preferred, as it provides continued outflow of pericardial fluid. Pericardiectomy is recommended in cases of symptomatic constrictive pericarditis unresponsive to medical therapy.15
Back to the Case
The patient’s presentation—prodrome followed by fever and pleuritic chest pain—is characteristic of acute idiopathic pericarditis. No pericardial rub was heard, but EKG findings were typical. Troponin I elevation suggested underlying myopericarditis. An echocardiogram was unremarkable. Given the likely viral or idiopathic etiology, no further diagnostic tests were ordered to explore the possibility of an underlying systemic illness.
The patient was started on ibuprofen 600 mg every eight hours. She had significant relief of her symptoms within two days. A routine fever workup was negative. She was discharged the following day.
The patient was readmitted three months later with recurrent pleuritic chest pain, which did not improve with resumption of NSAID therapy. Initial troponin I was 0.22 ng/ml, electrocardiogram was unchanged, and an echocardiogram showed small effusion. She was started on ibuprofen 800 mg every eight hours, as well as colchicine 0.6 mg twice daily. Her symptoms resolved the next day and she was discharged with prescriptions for ibuprofen and colchicine. She was instructed to follow up with a primary-care doctor in one week.
At the clinic visit, ibuprofen was tapered but colchicine was continued for another six months. She remained asymptomatic at her six-month clinic follow-up.
Bottom Line
Acute pericarditis is a clinical diagnosis supported by EKG findings. Most cases are idiopathic or viral, and can be treated successfully with NSAIDs and colchicine. For cases that do not respond to initial therapy, or cases that present with high-risk features, a specific etiology should be sought.
Dr. Southern is chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y. Dr. Galhorta is an instructor and Drs. Martin, Korcak, and Stehlihova are assistant professors in the department of medicine at Albert Einstein.
References
- Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004;351:2195-2202.
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378-382.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717-727.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042-1046.
- Bonnefoy E, Godon P, Kirkorian G, et al. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832-836.
- Salisbury AC, Olalla-Gomez C, Rihal CS, et al. Frequency and predictors of urgent coronary angiography in patients with acute pericarditis. Mayo Clin Proc. 2009;84(1):11-15.
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115:2739-2744.
- Imazio M, Spodick DH, Brucato A, et al. Diagnostic issues in the clinical management of pericarditis. Int J Clin Pract. 2010;64(10):1384-1392.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150-1153.
- Imazio M, Demichelis B, Cecchi E. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42(12):2144-2148.
- Sagristà Sauleda J, Permanyer Miralda G, Soler Soler J. Diagnosis and management of pericardial syndromes. Rev Esp Cardiol. 2005;58(7):830-841.
- Bruce MA, Spodick DH. Atypical electrocardiogram in acute pericarditis: characteristics and prevalence. J Electrocardiol. 1980;13:61-66.
- Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 2004; 25(7):587-610.
- Verhaert D, Gabriel RS, Johnston D, et al. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3:333-343.
- Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010;121:916-928.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the colchicine for acute pericarditis (COPE) trial. Circulation. 2005;112(13):2012-2016.
- Adler Y, Finkelstein Y, Guindo J, et al. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183-185.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the colchicine for recurrent pericarditis (CORE) trial. Arch Intern Med. 2005;165:1987-1991.
- Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation. 2008;118:667-771.
Case
A 32-year-old female with no significant past medical history is evaluated for sharp, left-sided chest pain for five days. Her pain is intermittent, worse with deep inspiration and in the supine position. She denies any shortness of breath. Her temperature is 100.8ºF, but otherwise her vital signs are normal. The physical exam and chest radiograph are unremarkable, but an electrocardiogram shows diffuse ST-segment elevations. The initial troponin is mildly elevated at 0.35 ng/ml.
Could this patient have acute pericarditis? If so, how should she be managed?
Background
Pericarditis is the most common pericardial disease encountered by hospitalists. As many as 5% of chest pain cases unattributable to myocardial infarction (MI) are diagnosed with pericarditis.1 In immunocompetent individuals, as many as 90% of acute pericarditis cases are viral or idiopathic in etiology.1,2 Human immunodeficiency virus (HIV) and tuberculosis are common culprits in developing countries and immunocompromised hosts.3 Other specific etiologies of acute pericarditis include autoimmune diseases, neoplasms, chest irradiation, trauma, and metabolic disturbances (e.g. uremia). An etiologic classification of acute pericarditis is shown in Table 2 (p. 16).
Pericarditis primarily is a clinical diagnosis. Most patients present with chest pain.4 A pericardial friction rub may or may not be heard (sensitivity 16% to 85%), but when present is nearly 100% specific for pericarditis.2,5 Diffuse ST-segment elevation on electrocardiogram (EKG) is present in 60% to 90% of cases, but it can be difficult to differentiate from ST-segment elevations in acute MI.4,6
Uncomplicated acute pericarditis often is treated successfully as an outpatient.4 However, patients with high-risk features (see Table 1, right) should be hospitalized for identification and treatment of specific underlying etiology and for monitoring of complications, such as tamponade.7
Our patient has features consistent with pericarditis. In the following sections, we will review the diagnosis and treatment of acute pericarditis.
Review of the Data
How is acute pericarditis diagnosed?
Acute pericarditis is a clinical diagnosis supported by EKG and echocardiogram. At least two of the following four criteria must be present for the diagnosis: pleuritic chest pain, pericardial rub, diffuse ST-segment elevation on EKG, and pericardial effusion.8
History. Patients may report fever (46% in one small study of 69 patients) or a recent history of respiratory or gastrointestinal infection (40%).5 Most patients will report pleuritic chest pain. Typically, the pain is improved when sitting up and leaning forward, and gets worse when lying supine.4 Pain might radiate to the trapezius muscle ridge due to the common phrenic nerve innervation of pericardium and trapezius.9 However, pain might be minimal or absent in patients with uremic, neoplastic, tuberculous, or post-irradiation pericarditis.
Physical exam. A pericardial friction rub is nearly 100% specific for a pericarditis diagnosis, but sensitivity can vary (16% to 85%) depending on the frequency of auscultation and underlying etiology.2,5 It is thought to be caused by friction between the parietal and visceral layers of inflamed pericardium. A pericardial rub classically is described as a superficial, high-pitched, scratchy, or squeaking sound best heard with the diaphragm of the stethoscope at the lower left sternal border with the patient leaning forward.
Laboratory data. A complete blood count, metabolic panel, and cardiac enzymes should be checked in all patients with suspected acute pericarditis. Troponin values are elevated in up to one-third of patients, indicating cardiac muscle injury or myopericarditis, but have not been shown to adversely impact hospital length of stay, readmission, or complication rates.5,10 Markers of inflammation (e.g. erythrocyte sedimentation rate or C-reactive protein) are frequently elevated but do not point to a specific underlying etiology. Routine viral cultures and antibody titers are not useful.11
Most cases of pericarditis are presumed idiopathic (viral); however, finding a specific etiology should be considered in patients who do not respond after one week of therapy. Anti-nuclear antibody, complement levels, and rheumatoid factor can serve as screening tests for autoimmune disease. Purified protein derivative or quantiferon testing and HIV testing might be indicated in patients with appropriate risk factors. In cases of suspected tuberculous or neoplastic pericarditis, pericardial fluid analysis and biopsy could be warranted.
Electrocardiography. The EKG is the most useful test in diagnosing acute pericarditis. EKG changes in acute pericarditis can progress over four stages:
- Stage 1: diffuse ST elevations with or without PR depressions, initially;
- Stage 2: normalization of ST and PR segments, typically after several days;
- Stage 3: diffuse T-wave inversions; and
- Stage 4: normalization of T-waves, typically after weeks or months.
While all four stages are unlikely to be present in a given case, 80% of patients with pericarditis will demonstrate diffuse ST-segment elevations and PR-segment depression (see Figure 2, above).12
Table 3 lists EKG features helpful in differentiating acute pericarditis from acute myocardial infarction.
Chest radiography. Because a pericardial effusion often accompanies pericarditis, a chest radiograph (CXR) should be performed in all suspected cases. The CXR might show enlargement of the cardiac silhouette if more than 250 ml of pericardial fluid is present.3 A CXR also is helpful to diagnose concomitant pulmonary infection, pleural effusion, or mediastinal mass—all findings that could point to an underlying specific etiology of pericarditis and/or pericardial effusion.
Echocardiography. An echocardiogram should be performed in all patients with suspected pericarditis to detect effusion, associated myocardial, or paracardial disease.13 The echocardiogram frequently is normal but could show an effusion in 60%, and tamponade (see Figure 1, p. 15) in 5%, of cases.4
Computed tomography (CT) and cardiac magnetic resonance imaging (CMR).CT or CMR are the imaging modalities of choice when an echocardiogram is inconclusive or in cases of pericarditis complicated by a hemorrhagic or localized effusion, pericardial thickening, or pericardial mass.14 They also help in precise imaging of neighboring structures, such as lungs or mediastinum.
Pericardial fluid analysis and pericardial biopsy. In cases of refractory pericarditis with effusion, pericardial fluid analysis might provide clues to the underlying etiology. Routine chemistry, cell count, gram and acid fast staining, culture, and cytology should be sent. In addition, acid-fast bacillus staining and culture, adenosine deaminase, and interferon-gamma testing should be ordered when tuberculous pericarditis is suspected. A pericardial biopsy may show granulomas or neoplastic cells. Overall, pericardial fluid analysis and biopsy reveal a diagnosis in roughly 20% of cases.11
How is acute pericarditis treated?
Most cases of uncomplicated acute pericarditis are viral and respond well to NSAID plus colchicine therapy.2,4 Failure to respond to NSAIDs plus colchicine—evidenced by persistent fever, pericardial chest pain, new pericardial effusion, or worsening of general illness—within a week of treatment should prompt a search for an underlying systemic illness. If found, treatment should be aimed at the causative illness.
Bacterial pericarditis usually requires surgical drainage in addition to treatment with appropriate antibiotics.11 Tuberculous pericarditis is treated with multidrug therapy; when underlying HIV is present, patients should receive highly active anti-retroviral therapy as well. Steroids and immunosuppressants should be considered in addition to NSAIDs and colchicine in autoimmune pericarditis.10 Neoplastic pericarditis may resolve with chemotherapy but it has a high recurrence rate.13 Uremic pericarditis requires intensified dialysis.
Treatment options for uncomplicated idiopathic or viral pericarditis include:
NSAIDs. It is important to adequately dose NSAIDs when treating acute pericarditis. Initial treatment options include ibuprofen (1,600 to 3,200 mg daily), indomethacin (75 to 150 mg daily) or aspirin (2 to 4 gm daily) for one week.11,15 Aspirin is preferred in patients with ischemic heart disease. For patients with symptoms that persist longer than a week, NSAIDS may be continued, but investigation for an underlying etiology is indicated. Concomitant proton-pump-inhibitor therapy should be considered in patients at high risk for peptic ulcer disease to minimize gastric side effects.
Colchicine. Colchicine has a favorable risk-benefit profile as an adjunct treatment for acute and recurrent pericarditis. Patients experience better symptom relief when treated with both colchicine and an NSAID, compared with NSAIDs alone (88% versus 63%). Recurrence rates are lower with combined therapy (11% versus 32%).16 Colchicine treatment (0.6 mg twice daily after a loading dose of up to 2 mg) is recommended for several months to greater than one year.13,16,17
Glucocorticoids. Routine glucocorticoid use should be avoided in the treatment of acute pericarditis, as it has been associated with an increased risk for recurrence (OR 4.3).16,18 Glucocorticoid use should be considered in cases of pericarditis refractory to NSAIDs and colchicine, cases in which NSAIDs and or colchicine are contraindicated, and in autoimmune or connective-tissue-disease-related pericarditis. Prednisone should be dosed up to 1 mg/kg/day for at least one month, depending on symptom resolution, then tapered after either NSAIDs or colchicine have been started.13 Smaller prednisone doses of up to 0.5 mg/kg/day could be as effective, with the added benefit of reduced side effects and recurrences.19
Invasive treatment. Pericardiocentesis and/or pericardiectomy should be considered when pericarditis is complicated by a large effusion or tamponade, constrictive physiology, or recurrent effusion.11 Pericardiocentesis is the least invasive option and helps provide immediate relief in cases of tamponade or large symptomatic effusions. It is the preferred modality for obtaining pericardial fluid for diagnostic analysis. However, effusions can recur and in those cases pericardial window is preferred, as it provides continued outflow of pericardial fluid. Pericardiectomy is recommended in cases of symptomatic constrictive pericarditis unresponsive to medical therapy.15
Back to the Case
The patient’s presentation—prodrome followed by fever and pleuritic chest pain—is characteristic of acute idiopathic pericarditis. No pericardial rub was heard, but EKG findings were typical. Troponin I elevation suggested underlying myopericarditis. An echocardiogram was unremarkable. Given the likely viral or idiopathic etiology, no further diagnostic tests were ordered to explore the possibility of an underlying systemic illness.
The patient was started on ibuprofen 600 mg every eight hours. She had significant relief of her symptoms within two days. A routine fever workup was negative. She was discharged the following day.
The patient was readmitted three months later with recurrent pleuritic chest pain, which did not improve with resumption of NSAID therapy. Initial troponin I was 0.22 ng/ml, electrocardiogram was unchanged, and an echocardiogram showed small effusion. She was started on ibuprofen 800 mg every eight hours, as well as colchicine 0.6 mg twice daily. Her symptoms resolved the next day and she was discharged with prescriptions for ibuprofen and colchicine. She was instructed to follow up with a primary-care doctor in one week.
At the clinic visit, ibuprofen was tapered but colchicine was continued for another six months. She remained asymptomatic at her six-month clinic follow-up.
Bottom Line
Acute pericarditis is a clinical diagnosis supported by EKG findings. Most cases are idiopathic or viral, and can be treated successfully with NSAIDs and colchicine. For cases that do not respond to initial therapy, or cases that present with high-risk features, a specific etiology should be sought.
Dr. Southern is chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y. Dr. Galhorta is an instructor and Drs. Martin, Korcak, and Stehlihova are assistant professors in the department of medicine at Albert Einstein.
References
- Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004;351:2195-2202.
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378-382.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717-727.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042-1046.
- Bonnefoy E, Godon P, Kirkorian G, et al. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832-836.
- Salisbury AC, Olalla-Gomez C, Rihal CS, et al. Frequency and predictors of urgent coronary angiography in patients with acute pericarditis. Mayo Clin Proc. 2009;84(1):11-15.
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115:2739-2744.
- Imazio M, Spodick DH, Brucato A, et al. Diagnostic issues in the clinical management of pericarditis. Int J Clin Pract. 2010;64(10):1384-1392.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150-1153.
- Imazio M, Demichelis B, Cecchi E. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42(12):2144-2148.
- Sagristà Sauleda J, Permanyer Miralda G, Soler Soler J. Diagnosis and management of pericardial syndromes. Rev Esp Cardiol. 2005;58(7):830-841.
- Bruce MA, Spodick DH. Atypical electrocardiogram in acute pericarditis: characteristics and prevalence. J Electrocardiol. 1980;13:61-66.
- Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 2004; 25(7):587-610.
- Verhaert D, Gabriel RS, Johnston D, et al. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3:333-343.
- Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010;121:916-928.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the colchicine for acute pericarditis (COPE) trial. Circulation. 2005;112(13):2012-2016.
- Adler Y, Finkelstein Y, Guindo J, et al. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183-185.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the colchicine for recurrent pericarditis (CORE) trial. Arch Intern Med. 2005;165:1987-1991.
- Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation. 2008;118:667-771.
Case
A 32-year-old female with no significant past medical history is evaluated for sharp, left-sided chest pain for five days. Her pain is intermittent, worse with deep inspiration and in the supine position. She denies any shortness of breath. Her temperature is 100.8ºF, but otherwise her vital signs are normal. The physical exam and chest radiograph are unremarkable, but an electrocardiogram shows diffuse ST-segment elevations. The initial troponin is mildly elevated at 0.35 ng/ml.
Could this patient have acute pericarditis? If so, how should she be managed?
Background
Pericarditis is the most common pericardial disease encountered by hospitalists. As many as 5% of chest pain cases unattributable to myocardial infarction (MI) are diagnosed with pericarditis.1 In immunocompetent individuals, as many as 90% of acute pericarditis cases are viral or idiopathic in etiology.1,2 Human immunodeficiency virus (HIV) and tuberculosis are common culprits in developing countries and immunocompromised hosts.3 Other specific etiologies of acute pericarditis include autoimmune diseases, neoplasms, chest irradiation, trauma, and metabolic disturbances (e.g. uremia). An etiologic classification of acute pericarditis is shown in Table 2 (p. 16).
Pericarditis primarily is a clinical diagnosis. Most patients present with chest pain.4 A pericardial friction rub may or may not be heard (sensitivity 16% to 85%), but when present is nearly 100% specific for pericarditis.2,5 Diffuse ST-segment elevation on electrocardiogram (EKG) is present in 60% to 90% of cases, but it can be difficult to differentiate from ST-segment elevations in acute MI.4,6
Uncomplicated acute pericarditis often is treated successfully as an outpatient.4 However, patients with high-risk features (see Table 1, right) should be hospitalized for identification and treatment of specific underlying etiology and for monitoring of complications, such as tamponade.7
Our patient has features consistent with pericarditis. In the following sections, we will review the diagnosis and treatment of acute pericarditis.
Review of the Data
How is acute pericarditis diagnosed?
Acute pericarditis is a clinical diagnosis supported by EKG and echocardiogram. At least two of the following four criteria must be present for the diagnosis: pleuritic chest pain, pericardial rub, diffuse ST-segment elevation on EKG, and pericardial effusion.8
History. Patients may report fever (46% in one small study of 69 patients) or a recent history of respiratory or gastrointestinal infection (40%).5 Most patients will report pleuritic chest pain. Typically, the pain is improved when sitting up and leaning forward, and gets worse when lying supine.4 Pain might radiate to the trapezius muscle ridge due to the common phrenic nerve innervation of pericardium and trapezius.9 However, pain might be minimal or absent in patients with uremic, neoplastic, tuberculous, or post-irradiation pericarditis.
Physical exam. A pericardial friction rub is nearly 100% specific for a pericarditis diagnosis, but sensitivity can vary (16% to 85%) depending on the frequency of auscultation and underlying etiology.2,5 It is thought to be caused by friction between the parietal and visceral layers of inflamed pericardium. A pericardial rub classically is described as a superficial, high-pitched, scratchy, or squeaking sound best heard with the diaphragm of the stethoscope at the lower left sternal border with the patient leaning forward.
Laboratory data. A complete blood count, metabolic panel, and cardiac enzymes should be checked in all patients with suspected acute pericarditis. Troponin values are elevated in up to one-third of patients, indicating cardiac muscle injury or myopericarditis, but have not been shown to adversely impact hospital length of stay, readmission, or complication rates.5,10 Markers of inflammation (e.g. erythrocyte sedimentation rate or C-reactive protein) are frequently elevated but do not point to a specific underlying etiology. Routine viral cultures and antibody titers are not useful.11
Most cases of pericarditis are presumed idiopathic (viral); however, finding a specific etiology should be considered in patients who do not respond after one week of therapy. Anti-nuclear antibody, complement levels, and rheumatoid factor can serve as screening tests for autoimmune disease. Purified protein derivative or quantiferon testing and HIV testing might be indicated in patients with appropriate risk factors. In cases of suspected tuberculous or neoplastic pericarditis, pericardial fluid analysis and biopsy could be warranted.
Electrocardiography. The EKG is the most useful test in diagnosing acute pericarditis. EKG changes in acute pericarditis can progress over four stages:
- Stage 1: diffuse ST elevations with or without PR depressions, initially;
- Stage 2: normalization of ST and PR segments, typically after several days;
- Stage 3: diffuse T-wave inversions; and
- Stage 4: normalization of T-waves, typically after weeks or months.
While all four stages are unlikely to be present in a given case, 80% of patients with pericarditis will demonstrate diffuse ST-segment elevations and PR-segment depression (see Figure 2, above).12
Table 3 lists EKG features helpful in differentiating acute pericarditis from acute myocardial infarction.
Chest radiography. Because a pericardial effusion often accompanies pericarditis, a chest radiograph (CXR) should be performed in all suspected cases. The CXR might show enlargement of the cardiac silhouette if more than 250 ml of pericardial fluid is present.3 A CXR also is helpful to diagnose concomitant pulmonary infection, pleural effusion, or mediastinal mass—all findings that could point to an underlying specific etiology of pericarditis and/or pericardial effusion.
Echocardiography. An echocardiogram should be performed in all patients with suspected pericarditis to detect effusion, associated myocardial, or paracardial disease.13 The echocardiogram frequently is normal but could show an effusion in 60%, and tamponade (see Figure 1, p. 15) in 5%, of cases.4
Computed tomography (CT) and cardiac magnetic resonance imaging (CMR).CT or CMR are the imaging modalities of choice when an echocardiogram is inconclusive or in cases of pericarditis complicated by a hemorrhagic or localized effusion, pericardial thickening, or pericardial mass.14 They also help in precise imaging of neighboring structures, such as lungs or mediastinum.
Pericardial fluid analysis and pericardial biopsy. In cases of refractory pericarditis with effusion, pericardial fluid analysis might provide clues to the underlying etiology. Routine chemistry, cell count, gram and acid fast staining, culture, and cytology should be sent. In addition, acid-fast bacillus staining and culture, adenosine deaminase, and interferon-gamma testing should be ordered when tuberculous pericarditis is suspected. A pericardial biopsy may show granulomas or neoplastic cells. Overall, pericardial fluid analysis and biopsy reveal a diagnosis in roughly 20% of cases.11
How is acute pericarditis treated?
Most cases of uncomplicated acute pericarditis are viral and respond well to NSAID plus colchicine therapy.2,4 Failure to respond to NSAIDs plus colchicine—evidenced by persistent fever, pericardial chest pain, new pericardial effusion, or worsening of general illness—within a week of treatment should prompt a search for an underlying systemic illness. If found, treatment should be aimed at the causative illness.
Bacterial pericarditis usually requires surgical drainage in addition to treatment with appropriate antibiotics.11 Tuberculous pericarditis is treated with multidrug therapy; when underlying HIV is present, patients should receive highly active anti-retroviral therapy as well. Steroids and immunosuppressants should be considered in addition to NSAIDs and colchicine in autoimmune pericarditis.10 Neoplastic pericarditis may resolve with chemotherapy but it has a high recurrence rate.13 Uremic pericarditis requires intensified dialysis.
Treatment options for uncomplicated idiopathic or viral pericarditis include:
NSAIDs. It is important to adequately dose NSAIDs when treating acute pericarditis. Initial treatment options include ibuprofen (1,600 to 3,200 mg daily), indomethacin (75 to 150 mg daily) or aspirin (2 to 4 gm daily) for one week.11,15 Aspirin is preferred in patients with ischemic heart disease. For patients with symptoms that persist longer than a week, NSAIDS may be continued, but investigation for an underlying etiology is indicated. Concomitant proton-pump-inhibitor therapy should be considered in patients at high risk for peptic ulcer disease to minimize gastric side effects.
Colchicine. Colchicine has a favorable risk-benefit profile as an adjunct treatment for acute and recurrent pericarditis. Patients experience better symptom relief when treated with both colchicine and an NSAID, compared with NSAIDs alone (88% versus 63%). Recurrence rates are lower with combined therapy (11% versus 32%).16 Colchicine treatment (0.6 mg twice daily after a loading dose of up to 2 mg) is recommended for several months to greater than one year.13,16,17
Glucocorticoids. Routine glucocorticoid use should be avoided in the treatment of acute pericarditis, as it has been associated with an increased risk for recurrence (OR 4.3).16,18 Glucocorticoid use should be considered in cases of pericarditis refractory to NSAIDs and colchicine, cases in which NSAIDs and or colchicine are contraindicated, and in autoimmune or connective-tissue-disease-related pericarditis. Prednisone should be dosed up to 1 mg/kg/day for at least one month, depending on symptom resolution, then tapered after either NSAIDs or colchicine have been started.13 Smaller prednisone doses of up to 0.5 mg/kg/day could be as effective, with the added benefit of reduced side effects and recurrences.19
Invasive treatment. Pericardiocentesis and/or pericardiectomy should be considered when pericarditis is complicated by a large effusion or tamponade, constrictive physiology, or recurrent effusion.11 Pericardiocentesis is the least invasive option and helps provide immediate relief in cases of tamponade or large symptomatic effusions. It is the preferred modality for obtaining pericardial fluid for diagnostic analysis. However, effusions can recur and in those cases pericardial window is preferred, as it provides continued outflow of pericardial fluid. Pericardiectomy is recommended in cases of symptomatic constrictive pericarditis unresponsive to medical therapy.15
Back to the Case
The patient’s presentation—prodrome followed by fever and pleuritic chest pain—is characteristic of acute idiopathic pericarditis. No pericardial rub was heard, but EKG findings were typical. Troponin I elevation suggested underlying myopericarditis. An echocardiogram was unremarkable. Given the likely viral or idiopathic etiology, no further diagnostic tests were ordered to explore the possibility of an underlying systemic illness.
The patient was started on ibuprofen 600 mg every eight hours. She had significant relief of her symptoms within two days. A routine fever workup was negative. She was discharged the following day.
The patient was readmitted three months later with recurrent pleuritic chest pain, which did not improve with resumption of NSAID therapy. Initial troponin I was 0.22 ng/ml, electrocardiogram was unchanged, and an echocardiogram showed small effusion. She was started on ibuprofen 800 mg every eight hours, as well as colchicine 0.6 mg twice daily. Her symptoms resolved the next day and she was discharged with prescriptions for ibuprofen and colchicine. She was instructed to follow up with a primary-care doctor in one week.
At the clinic visit, ibuprofen was tapered but colchicine was continued for another six months. She remained asymptomatic at her six-month clinic follow-up.
Bottom Line
Acute pericarditis is a clinical diagnosis supported by EKG findings. Most cases are idiopathic or viral, and can be treated successfully with NSAIDs and colchicine. For cases that do not respond to initial therapy, or cases that present with high-risk features, a specific etiology should be sought.
Dr. Southern is chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y. Dr. Galhorta is an instructor and Drs. Martin, Korcak, and Stehlihova are assistant professors in the department of medicine at Albert Einstein.
References
- Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004;351:2195-2202.
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378-382.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717-727.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042-1046.
- Bonnefoy E, Godon P, Kirkorian G, et al. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832-836.
- Salisbury AC, Olalla-Gomez C, Rihal CS, et al. Frequency and predictors of urgent coronary angiography in patients with acute pericarditis. Mayo Clin Proc. 2009;84(1):11-15.
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115:2739-2744.
- Imazio M, Spodick DH, Brucato A, et al. Diagnostic issues in the clinical management of pericarditis. Int J Clin Pract. 2010;64(10):1384-1392.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150-1153.
- Imazio M, Demichelis B, Cecchi E. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42(12):2144-2148.
- Sagristà Sauleda J, Permanyer Miralda G, Soler Soler J. Diagnosis and management of pericardial syndromes. Rev Esp Cardiol. 2005;58(7):830-841.
- Bruce MA, Spodick DH. Atypical electrocardiogram in acute pericarditis: characteristics and prevalence. J Electrocardiol. 1980;13:61-66.
- Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 2004; 25(7):587-610.
- Verhaert D, Gabriel RS, Johnston D, et al. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3:333-343.
- Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010;121:916-928.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the colchicine for acute pericarditis (COPE) trial. Circulation. 2005;112(13):2012-2016.
- Adler Y, Finkelstein Y, Guindo J, et al. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183-185.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the colchicine for recurrent pericarditis (CORE) trial. Arch Intern Med. 2005;165:1987-1991.
- Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation. 2008;118:667-771.