User login
Shaun Frost: Call for Transparency in Healthcare Performance Results to Impact Hospitalists
Policymakers believe that publicly reporting healthcare performance results is essential to improving care delivery. In order to achieve a healthcare system that is consistently reliable, the Institute of Medicine (IOM) recently recommended that performance transparency be considered a foundational feature of healthcare systems that seek to constantly, systematically, and seamlessly improve.1 The IOM has suggested strategies (see Table 1, right) for producing readily available information on safety, quality, prices and cost, and health outcomes. As these strategies are being deployed, it is essential that hospitalists consider the impact they will have on their personal practice, key stakeholders, and the patients that they serve.
Performance Data Sources
The accessibility of publicly reported healthcare performance information is increasing rapidly. Among HM practitioners, perhaps the most widely recognized data source is the Centers for Medicare & Medicaid Services’ (CMS) Hospital Compare website (www.hospitalcompare.hhs.gov). According to CMS, its performance information on more than 4,000 hospitals is intended to help patients make decisions about where to seek healthcare, as well as encourage hospitals to improve the quality of care they provide.
The information currently reported is extensive and comprehensive (see Table 2, right). Furthermore, CMS continually adds data as new performance measures are created and validated.
Beyond the federal government, private health insurance companies, consortiums of employer purchasers of healthcare (e.g. the Leapfrog Group), and community collaboratives (e.g. Minnesota Community Measurement in the state of Minnesota) are reporting care provider performance information.
In addition, consumer advocacy groups have entered the picture. Earlier this year, Consumer Reports magazine launched an initiative to rate the quality of hospitals (and cardiac surgery groups) through the publication of patient outcomes (central-line-associated bloodstream infections, surgical site infections, readmissions, complications, mortality), patient experience (communications about medications and discharge, and other markers of satisfaction), and hospital best practices (use of EHR, and the appropriate use of abdominal and chest CT scanning). Consumer Reports also provides a composite hospital safety score, and a 36-page technical manual explaining the strategy and methodology behind their ratings.
Public performance reporting is furthermore becoming big business for healthcare entrepreneurs. Castlight Health, with its $181 million in private capital backing, is viewed by some as the “Travelocity of healthcare.” Castlight calls its searchable databases “transparency portals” that allow consumers to understand, before they visit a care provider, what they will be paying and how the care provider ranks on quality and outcomes.
Finally, numerous unregulated Internet sites that employ methodologically questionable practices are reporting on healthcare performance. Many of these sources collect and publish subjective reports of care experiences, with little or no requirement that the reporter confirm the nature of the relationship that they have with the care provider.
Transparency and Key Stakeholders
The hospital that you work in expects you to know how it performs, and to help it improve in the areas over which you have influence. Hospitals monitor publicly reported data because their futures depend on strong performance. As of October 2012, hospital Medicare reimbursement is linked to publicly reported performance measures that were incorporated into CMS’ value-based purchasing (VBP) initiative. Furthermore, hospital market share will be increasingly dependent on performance transparency as consumers and patients utilize these data to make informed decisions about where to seek high-value healthcare.
Patients have a vested interest in knowing how their care providers perform. A recent study by PricewaterhouseCoopers reported that 72% of consumers ranked provider reputation and personal experience as the top drivers of provider choice.2 Furthermore, employers and patients increasingly are demanding access to care affordability information—an interest driven in large part by the increasing popularity of consumer-directed health insurance plans (CDHPs). Under CDHPs, patients save money on premiums in exchange for higher deductibles that are typically paired with healthcare spending accounts. The intent is to increase consumer engagement and awareness of the cost of routine healthcare expenses while protecting against the cost of catastrophic events. It is estimated that 15% to 20% of people with employer-sponsored health insurance are in high-deductible plans, and many believe CDHPs will soon make up the majority of employer-provided coverage.
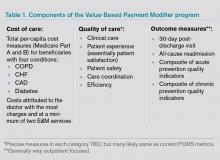
Patients interested in knowing how individual doctors perform will soon have increased access to this type of information as well. For example, CMS also produces a Physician Compare website (www.medicare.gov/find-a-doctor) that offers performance information on individual doctors. Currently, Physician Compare has little detailed information. Expect this to change, however, as Medicare moves forward with developing valid and reliable individual physician performance metrics for its Physician Value-Based Payment Modifier (VBPM) program (see “A New Measuring Stick,”).
Under VBPM, doctors will have payment modifiers assigned to their Medicare professional fee claims that will adjust payments based on the value of care that they have delivered historically. For example, it is possible in the future that physicians failing to prescribe ace inhibitors to heart failure patients will be paid less than physicians who universally provide evidence-based, best-practice heart failure care. The measurement period for the calculation of these modifiers begins this year, and hospitalists need to be aware that their performance after this time period might affect the amount of Medicare professional fee reimbursement they receive in the future.
Conclusions
Public performance reporting is a keystone healthcare reform strategy that will influence the behavior and practice patterns of hospitals and hospitalists. Hospitalists should regularly review publicly reported healthcare performance data, and commit to working collaboratively with colleagues to capitalize on improvement opportunities suggested by these data.
Dr. Frost is president of SHM.
References
- Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Institute of Medicine website. Available at: http://www.iom.edu/bestcare. Accessed Nov. 24, 2012.
- PricewaterhouseCoopers’ Health Research Institute. Customer experience in healthcare: the moment of truth. PricewaterhouseCoopers website. Available at: http://www.pwc.com/es_MX/mx/publicaciones/archivo/2012-09-customer-experience-healthcare.pdf. Accessed Nov. 25, 2012.
Policymakers believe that publicly reporting healthcare performance results is essential to improving care delivery. In order to achieve a healthcare system that is consistently reliable, the Institute of Medicine (IOM) recently recommended that performance transparency be considered a foundational feature of healthcare systems that seek to constantly, systematically, and seamlessly improve.1 The IOM has suggested strategies (see Table 1, right) for producing readily available information on safety, quality, prices and cost, and health outcomes. As these strategies are being deployed, it is essential that hospitalists consider the impact they will have on their personal practice, key stakeholders, and the patients that they serve.
Performance Data Sources
The accessibility of publicly reported healthcare performance information is increasing rapidly. Among HM practitioners, perhaps the most widely recognized data source is the Centers for Medicare & Medicaid Services’ (CMS) Hospital Compare website (www.hospitalcompare.hhs.gov). According to CMS, its performance information on more than 4,000 hospitals is intended to help patients make decisions about where to seek healthcare, as well as encourage hospitals to improve the quality of care they provide.
The information currently reported is extensive and comprehensive (see Table 2, right). Furthermore, CMS continually adds data as new performance measures are created and validated.
Beyond the federal government, private health insurance companies, consortiums of employer purchasers of healthcare (e.g. the Leapfrog Group), and community collaboratives (e.g. Minnesota Community Measurement in the state of Minnesota) are reporting care provider performance information.
In addition, consumer advocacy groups have entered the picture. Earlier this year, Consumer Reports magazine launched an initiative to rate the quality of hospitals (and cardiac surgery groups) through the publication of patient outcomes (central-line-associated bloodstream infections, surgical site infections, readmissions, complications, mortality), patient experience (communications about medications and discharge, and other markers of satisfaction), and hospital best practices (use of EHR, and the appropriate use of abdominal and chest CT scanning). Consumer Reports also provides a composite hospital safety score, and a 36-page technical manual explaining the strategy and methodology behind their ratings.
Public performance reporting is furthermore becoming big business for healthcare entrepreneurs. Castlight Health, with its $181 million in private capital backing, is viewed by some as the “Travelocity of healthcare.” Castlight calls its searchable databases “transparency portals” that allow consumers to understand, before they visit a care provider, what they will be paying and how the care provider ranks on quality and outcomes.
Finally, numerous unregulated Internet sites that employ methodologically questionable practices are reporting on healthcare performance. Many of these sources collect and publish subjective reports of care experiences, with little or no requirement that the reporter confirm the nature of the relationship that they have with the care provider.
Transparency and Key Stakeholders
The hospital that you work in expects you to know how it performs, and to help it improve in the areas over which you have influence. Hospitals monitor publicly reported data because their futures depend on strong performance. As of October 2012, hospital Medicare reimbursement is linked to publicly reported performance measures that were incorporated into CMS’ value-based purchasing (VBP) initiative. Furthermore, hospital market share will be increasingly dependent on performance transparency as consumers and patients utilize these data to make informed decisions about where to seek high-value healthcare.
Patients have a vested interest in knowing how their care providers perform. A recent study by PricewaterhouseCoopers reported that 72% of consumers ranked provider reputation and personal experience as the top drivers of provider choice.2 Furthermore, employers and patients increasingly are demanding access to care affordability information—an interest driven in large part by the increasing popularity of consumer-directed health insurance plans (CDHPs). Under CDHPs, patients save money on premiums in exchange for higher deductibles that are typically paired with healthcare spending accounts. The intent is to increase consumer engagement and awareness of the cost of routine healthcare expenses while protecting against the cost of catastrophic events. It is estimated that 15% to 20% of people with employer-sponsored health insurance are in high-deductible plans, and many believe CDHPs will soon make up the majority of employer-provided coverage.
Patients interested in knowing how individual doctors perform will soon have increased access to this type of information as well. For example, CMS also produces a Physician Compare website (www.medicare.gov/find-a-doctor) that offers performance information on individual doctors. Currently, Physician Compare has little detailed information. Expect this to change, however, as Medicare moves forward with developing valid and reliable individual physician performance metrics for its Physician Value-Based Payment Modifier (VBPM) program (see “A New Measuring Stick,”).
Under VBPM, doctors will have payment modifiers assigned to their Medicare professional fee claims that will adjust payments based on the value of care that they have delivered historically. For example, it is possible in the future that physicians failing to prescribe ace inhibitors to heart failure patients will be paid less than physicians who universally provide evidence-based, best-practice heart failure care. The measurement period for the calculation of these modifiers begins this year, and hospitalists need to be aware that their performance after this time period might affect the amount of Medicare professional fee reimbursement they receive in the future.
Conclusions
Public performance reporting is a keystone healthcare reform strategy that will influence the behavior and practice patterns of hospitals and hospitalists. Hospitalists should regularly review publicly reported healthcare performance data, and commit to working collaboratively with colleagues to capitalize on improvement opportunities suggested by these data.
Dr. Frost is president of SHM.
References
- Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Institute of Medicine website. Available at: http://www.iom.edu/bestcare. Accessed Nov. 24, 2012.
- PricewaterhouseCoopers’ Health Research Institute. Customer experience in healthcare: the moment of truth. PricewaterhouseCoopers website. Available at: http://www.pwc.com/es_MX/mx/publicaciones/archivo/2012-09-customer-experience-healthcare.pdf. Accessed Nov. 25, 2012.
Policymakers believe that publicly reporting healthcare performance results is essential to improving care delivery. In order to achieve a healthcare system that is consistently reliable, the Institute of Medicine (IOM) recently recommended that performance transparency be considered a foundational feature of healthcare systems that seek to constantly, systematically, and seamlessly improve.1 The IOM has suggested strategies (see Table 1, right) for producing readily available information on safety, quality, prices and cost, and health outcomes. As these strategies are being deployed, it is essential that hospitalists consider the impact they will have on their personal practice, key stakeholders, and the patients that they serve.
Performance Data Sources
The accessibility of publicly reported healthcare performance information is increasing rapidly. Among HM practitioners, perhaps the most widely recognized data source is the Centers for Medicare & Medicaid Services’ (CMS) Hospital Compare website (www.hospitalcompare.hhs.gov). According to CMS, its performance information on more than 4,000 hospitals is intended to help patients make decisions about where to seek healthcare, as well as encourage hospitals to improve the quality of care they provide.
The information currently reported is extensive and comprehensive (see Table 2, right). Furthermore, CMS continually adds data as new performance measures are created and validated.
Beyond the federal government, private health insurance companies, consortiums of employer purchasers of healthcare (e.g. the Leapfrog Group), and community collaboratives (e.g. Minnesota Community Measurement in the state of Minnesota) are reporting care provider performance information.
In addition, consumer advocacy groups have entered the picture. Earlier this year, Consumer Reports magazine launched an initiative to rate the quality of hospitals (and cardiac surgery groups) through the publication of patient outcomes (central-line-associated bloodstream infections, surgical site infections, readmissions, complications, mortality), patient experience (communications about medications and discharge, and other markers of satisfaction), and hospital best practices (use of EHR, and the appropriate use of abdominal and chest CT scanning). Consumer Reports also provides a composite hospital safety score, and a 36-page technical manual explaining the strategy and methodology behind their ratings.
Public performance reporting is furthermore becoming big business for healthcare entrepreneurs. Castlight Health, with its $181 million in private capital backing, is viewed by some as the “Travelocity of healthcare.” Castlight calls its searchable databases “transparency portals” that allow consumers to understand, before they visit a care provider, what they will be paying and how the care provider ranks on quality and outcomes.
Finally, numerous unregulated Internet sites that employ methodologically questionable practices are reporting on healthcare performance. Many of these sources collect and publish subjective reports of care experiences, with little or no requirement that the reporter confirm the nature of the relationship that they have with the care provider.
Transparency and Key Stakeholders
The hospital that you work in expects you to know how it performs, and to help it improve in the areas over which you have influence. Hospitals monitor publicly reported data because their futures depend on strong performance. As of October 2012, hospital Medicare reimbursement is linked to publicly reported performance measures that were incorporated into CMS’ value-based purchasing (VBP) initiative. Furthermore, hospital market share will be increasingly dependent on performance transparency as consumers and patients utilize these data to make informed decisions about where to seek high-value healthcare.
Patients have a vested interest in knowing how their care providers perform. A recent study by PricewaterhouseCoopers reported that 72% of consumers ranked provider reputation and personal experience as the top drivers of provider choice.2 Furthermore, employers and patients increasingly are demanding access to care affordability information—an interest driven in large part by the increasing popularity of consumer-directed health insurance plans (CDHPs). Under CDHPs, patients save money on premiums in exchange for higher deductibles that are typically paired with healthcare spending accounts. The intent is to increase consumer engagement and awareness of the cost of routine healthcare expenses while protecting against the cost of catastrophic events. It is estimated that 15% to 20% of people with employer-sponsored health insurance are in high-deductible plans, and many believe CDHPs will soon make up the majority of employer-provided coverage.
Patients interested in knowing how individual doctors perform will soon have increased access to this type of information as well. For example, CMS also produces a Physician Compare website (www.medicare.gov/find-a-doctor) that offers performance information on individual doctors. Currently, Physician Compare has little detailed information. Expect this to change, however, as Medicare moves forward with developing valid and reliable individual physician performance metrics for its Physician Value-Based Payment Modifier (VBPM) program (see “A New Measuring Stick,”).
Under VBPM, doctors will have payment modifiers assigned to their Medicare professional fee claims that will adjust payments based on the value of care that they have delivered historically. For example, it is possible in the future that physicians failing to prescribe ace inhibitors to heart failure patients will be paid less than physicians who universally provide evidence-based, best-practice heart failure care. The measurement period for the calculation of these modifiers begins this year, and hospitalists need to be aware that their performance after this time period might affect the amount of Medicare professional fee reimbursement they receive in the future.
Conclusions
Public performance reporting is a keystone healthcare reform strategy that will influence the behavior and practice patterns of hospitals and hospitalists. Hospitalists should regularly review publicly reported healthcare performance data, and commit to working collaboratively with colleagues to capitalize on improvement opportunities suggested by these data.
Dr. Frost is president of SHM.
References
- Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America. Institute of Medicine website. Available at: http://www.iom.edu/bestcare. Accessed Nov. 24, 2012.
- PricewaterhouseCoopers’ Health Research Institute. Customer experience in healthcare: the moment of truth. PricewaterhouseCoopers website. Available at: http://www.pwc.com/es_MX/mx/publicaciones/archivo/2012-09-customer-experience-healthcare.pdf. Accessed Nov. 25, 2012.
Bipartisan Proposal to Repeal SGR Plan Likely to be Reintroduced
As the Obama administration begins its second term, a great deal of attention is being paid to the advance of its healthcare reform agenda. Long overdue for reform is the sustainable growth rate (SGR) formula—an ill-fated attempt to provide predictable control for federal spending on Medicare by providing yearly updates (i.e. reductions) to Medicare’s physician reimbursement rates.
By adjusting the payment rates, the SGR was supposed to help control the cost of healthcare by linking it more closely with national growth and changes in the Medicare-eligible population. With each passing year, however, bipartisan consensus has grown stronger, the message being that a straight, fee-for-service system that is updated annually based on an expenditure target cannot substitute for fundamental delivery system reforms.
Congress has acted to override the SGR’s implementation every year since 2003, with the latest round being a potential 27% gutting of Medicare reimbursement rates. This cycle is not only tiresome, but threatens a massive disruption to physician practices and to seniors’ access to the Medicare program.
“The SGR, while well-intentioned, is flawed, and Congress can provide its temporary override for only so long, while Medicare spending continues to grow,” says Ryan Genzink, PA-C, an SHM Public Policy Committee member and a physician assistant with IPC: The Hospitalist Co. in Grand Rapids, Mich.
Repeal and Reform
Although various SGR repeal bills have been introduced over the years, only one—the Medicare Physician Payment Innovation Act of 2012 (H.R. 5707)—supplements repeal with a realistic plan to move away from the current fee-for-service payment system (and its inherent inefficiencies) toward more cost-effective reimbursement models that are designed to promote quality and value through coordinated patient care.
This bipartisan bill, introduced by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck, DO (R-Nev.), would repeal the SGR, stabilize payments at current rates for 2013, replace scheduled reductions with positive and predictable updates from 2014 to 2017, and set an aggressive timetable for testing and evaluating new payment systems focused on improving quality and reducing costs (see “Specific Components of the Schwartz-Heck Proposal,” left). The bill is expected to be reintroduced in 2013.
“SHM agrees that it is time finally to eliminate the SGR and move away from the prevailing fee-for-service payment system, which rewards physicians for simply providing more services, to one that provides incentives to deliver higher-quality, cost-effective care to our nation’s seniors,” wrote SHM President Shaun Frost, MD, SFHM, in a letter of support last year to Schwartz and Heck, commending them for introducing their bill.
“By providing a menu of options for physician participation, including an alternative, value-driven fee-for-service system for physicians who are not able to participate in one of the new payment and delivery models, the legislation does not force all providers into a ‘one size fits all’ solution, allowing for broader support, innovation, and flexibility,” Dr. Frost said.
Advancing New Reimbursement Models
The Schwartz-Heck bill “gives a timeline for CMS to test and adopt different reimbursement models, which presents advantageous options for hospitalists,” says Lauren Doctoroff, MD, an SHM Public Policy Committee member, hospitalist, and medical director of the post-discharge clinic at Beth Israel Deaconess Medical Center in Boston. “Hospitalists already focus on providing higher-quality, lower-cost care to hospitalized patients in their daily practice. We build effective care transitions to the outpatient and extended care settings. Our strengths are perfectly aligned to help these new, value-based payment models succeed.”
In fact, Dr. Doctoroff notes, Beth Israel is a participant in CMS’ Medicare Pioneer Accountable Care Organization project as well as Massachusetts Blue Cross Blue Shield’s Alternative Quality Contract, both of which use a risk-sharing global payment model in which the hospital and its physician network agree to provide for the healthcare needs of a defined population for a pre-arranged reimbursement amount.
“The global payment model is an attractive one for hospitalists because we play a key role in managing hospitalized patients efficiently and well, while also encouraging collaboration between inpatient and outpatient providers to avoid duplication of services,” Dr. Doctoroff says. “Some bundled payment models, which tie reimbursement to a defined episode of care, also could be advantageous for hospitalists, who coordinate the patient’s care throughout their entire healthcare episode, from inpatient diagnosis through post-discharge.”
Alternative Fee-for-Service System
For physicians who choose not to adopt one of the new reimbursement models, the bill directs CMS to offer an alternative fee-for-service system with incentives for improved quality and lower cost. This alternative would be available to physicians (including hospitalists) who participate in approved quality-reporting options, including the Physician Quality Reporting System (PQRS) or an approved Maintenance of Certification (MOC) program with quality registries. It also would apply to physicians who fall into the top 25% of CMS’ Value-Based Payment Modifier program (VBPM).
Boosting Primary Care
In addition to expediting the rollout of CMS-endorsed alternate payment models, the Schwartz bill recognizes the importance of primary care as the foundation of an effective healthcare delivery system and redresses its undervaluation with a 2.5% reimbursement update for physicians and other healthcare professionals for whom 60% of their Medicare physician fee schedule allowable charges are from a designated set of primary-care, preventive, and care-coordination codes.
“SHM specifically advocated for the inclusion of primary-care billing codes that hospitalists use,” Dr. Doctoroff says, “including hospital inpatient visits and observational services.”
“Of all the attempts to deal with the SGR over the past several years, Rep. Schwartz’s bill makes the most sense,” Genzink says. “While it doesn’t answer all of the healthcare system’s problems, it encapsulates many of the goals of reform—especially the shift from fee-for-service toward a payment system based on quality and outcomes. It recognizes that no one model will work for all physicians and offers the flexibility of multiple pathways. And it has bipartisan support, which seems to be a rarity these days.”
Chris Guadagnino is a freelance medical writer in Philadelphia.
As the Obama administration begins its second term, a great deal of attention is being paid to the advance of its healthcare reform agenda. Long overdue for reform is the sustainable growth rate (SGR) formula—an ill-fated attempt to provide predictable control for federal spending on Medicare by providing yearly updates (i.e. reductions) to Medicare’s physician reimbursement rates.
By adjusting the payment rates, the SGR was supposed to help control the cost of healthcare by linking it more closely with national growth and changes in the Medicare-eligible population. With each passing year, however, bipartisan consensus has grown stronger, the message being that a straight, fee-for-service system that is updated annually based on an expenditure target cannot substitute for fundamental delivery system reforms.
Congress has acted to override the SGR’s implementation every year since 2003, with the latest round being a potential 27% gutting of Medicare reimbursement rates. This cycle is not only tiresome, but threatens a massive disruption to physician practices and to seniors’ access to the Medicare program.
“The SGR, while well-intentioned, is flawed, and Congress can provide its temporary override for only so long, while Medicare spending continues to grow,” says Ryan Genzink, PA-C, an SHM Public Policy Committee member and a physician assistant with IPC: The Hospitalist Co. in Grand Rapids, Mich.
Repeal and Reform
Although various SGR repeal bills have been introduced over the years, only one—the Medicare Physician Payment Innovation Act of 2012 (H.R. 5707)—supplements repeal with a realistic plan to move away from the current fee-for-service payment system (and its inherent inefficiencies) toward more cost-effective reimbursement models that are designed to promote quality and value through coordinated patient care.
This bipartisan bill, introduced by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck, DO (R-Nev.), would repeal the SGR, stabilize payments at current rates for 2013, replace scheduled reductions with positive and predictable updates from 2014 to 2017, and set an aggressive timetable for testing and evaluating new payment systems focused on improving quality and reducing costs (see “Specific Components of the Schwartz-Heck Proposal,” left). The bill is expected to be reintroduced in 2013.
“SHM agrees that it is time finally to eliminate the SGR and move away from the prevailing fee-for-service payment system, which rewards physicians for simply providing more services, to one that provides incentives to deliver higher-quality, cost-effective care to our nation’s seniors,” wrote SHM President Shaun Frost, MD, SFHM, in a letter of support last year to Schwartz and Heck, commending them for introducing their bill.
“By providing a menu of options for physician participation, including an alternative, value-driven fee-for-service system for physicians who are not able to participate in one of the new payment and delivery models, the legislation does not force all providers into a ‘one size fits all’ solution, allowing for broader support, innovation, and flexibility,” Dr. Frost said.
Advancing New Reimbursement Models
The Schwartz-Heck bill “gives a timeline for CMS to test and adopt different reimbursement models, which presents advantageous options for hospitalists,” says Lauren Doctoroff, MD, an SHM Public Policy Committee member, hospitalist, and medical director of the post-discharge clinic at Beth Israel Deaconess Medical Center in Boston. “Hospitalists already focus on providing higher-quality, lower-cost care to hospitalized patients in their daily practice. We build effective care transitions to the outpatient and extended care settings. Our strengths are perfectly aligned to help these new, value-based payment models succeed.”
In fact, Dr. Doctoroff notes, Beth Israel is a participant in CMS’ Medicare Pioneer Accountable Care Organization project as well as Massachusetts Blue Cross Blue Shield’s Alternative Quality Contract, both of which use a risk-sharing global payment model in which the hospital and its physician network agree to provide for the healthcare needs of a defined population for a pre-arranged reimbursement amount.
“The global payment model is an attractive one for hospitalists because we play a key role in managing hospitalized patients efficiently and well, while also encouraging collaboration between inpatient and outpatient providers to avoid duplication of services,” Dr. Doctoroff says. “Some bundled payment models, which tie reimbursement to a defined episode of care, also could be advantageous for hospitalists, who coordinate the patient’s care throughout their entire healthcare episode, from inpatient diagnosis through post-discharge.”
Alternative Fee-for-Service System
For physicians who choose not to adopt one of the new reimbursement models, the bill directs CMS to offer an alternative fee-for-service system with incentives for improved quality and lower cost. This alternative would be available to physicians (including hospitalists) who participate in approved quality-reporting options, including the Physician Quality Reporting System (PQRS) or an approved Maintenance of Certification (MOC) program with quality registries. It also would apply to physicians who fall into the top 25% of CMS’ Value-Based Payment Modifier program (VBPM).
Boosting Primary Care
In addition to expediting the rollout of CMS-endorsed alternate payment models, the Schwartz bill recognizes the importance of primary care as the foundation of an effective healthcare delivery system and redresses its undervaluation with a 2.5% reimbursement update for physicians and other healthcare professionals for whom 60% of their Medicare physician fee schedule allowable charges are from a designated set of primary-care, preventive, and care-coordination codes.
“SHM specifically advocated for the inclusion of primary-care billing codes that hospitalists use,” Dr. Doctoroff says, “including hospital inpatient visits and observational services.”
“Of all the attempts to deal with the SGR over the past several years, Rep. Schwartz’s bill makes the most sense,” Genzink says. “While it doesn’t answer all of the healthcare system’s problems, it encapsulates many of the goals of reform—especially the shift from fee-for-service toward a payment system based on quality and outcomes. It recognizes that no one model will work for all physicians and offers the flexibility of multiple pathways. And it has bipartisan support, which seems to be a rarity these days.”
Chris Guadagnino is a freelance medical writer in Philadelphia.
As the Obama administration begins its second term, a great deal of attention is being paid to the advance of its healthcare reform agenda. Long overdue for reform is the sustainable growth rate (SGR) formula—an ill-fated attempt to provide predictable control for federal spending on Medicare by providing yearly updates (i.e. reductions) to Medicare’s physician reimbursement rates.
By adjusting the payment rates, the SGR was supposed to help control the cost of healthcare by linking it more closely with national growth and changes in the Medicare-eligible population. With each passing year, however, bipartisan consensus has grown stronger, the message being that a straight, fee-for-service system that is updated annually based on an expenditure target cannot substitute for fundamental delivery system reforms.
Congress has acted to override the SGR’s implementation every year since 2003, with the latest round being a potential 27% gutting of Medicare reimbursement rates. This cycle is not only tiresome, but threatens a massive disruption to physician practices and to seniors’ access to the Medicare program.
“The SGR, while well-intentioned, is flawed, and Congress can provide its temporary override for only so long, while Medicare spending continues to grow,” says Ryan Genzink, PA-C, an SHM Public Policy Committee member and a physician assistant with IPC: The Hospitalist Co. in Grand Rapids, Mich.
Repeal and Reform
Although various SGR repeal bills have been introduced over the years, only one—the Medicare Physician Payment Innovation Act of 2012 (H.R. 5707)—supplements repeal with a realistic plan to move away from the current fee-for-service payment system (and its inherent inefficiencies) toward more cost-effective reimbursement models that are designed to promote quality and value through coordinated patient care.
This bipartisan bill, introduced by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck, DO (R-Nev.), would repeal the SGR, stabilize payments at current rates for 2013, replace scheduled reductions with positive and predictable updates from 2014 to 2017, and set an aggressive timetable for testing and evaluating new payment systems focused on improving quality and reducing costs (see “Specific Components of the Schwartz-Heck Proposal,” left). The bill is expected to be reintroduced in 2013.
“SHM agrees that it is time finally to eliminate the SGR and move away from the prevailing fee-for-service payment system, which rewards physicians for simply providing more services, to one that provides incentives to deliver higher-quality, cost-effective care to our nation’s seniors,” wrote SHM President Shaun Frost, MD, SFHM, in a letter of support last year to Schwartz and Heck, commending them for introducing their bill.
“By providing a menu of options for physician participation, including an alternative, value-driven fee-for-service system for physicians who are not able to participate in one of the new payment and delivery models, the legislation does not force all providers into a ‘one size fits all’ solution, allowing for broader support, innovation, and flexibility,” Dr. Frost said.
Advancing New Reimbursement Models
The Schwartz-Heck bill “gives a timeline for CMS to test and adopt different reimbursement models, which presents advantageous options for hospitalists,” says Lauren Doctoroff, MD, an SHM Public Policy Committee member, hospitalist, and medical director of the post-discharge clinic at Beth Israel Deaconess Medical Center in Boston. “Hospitalists already focus on providing higher-quality, lower-cost care to hospitalized patients in their daily practice. We build effective care transitions to the outpatient and extended care settings. Our strengths are perfectly aligned to help these new, value-based payment models succeed.”
In fact, Dr. Doctoroff notes, Beth Israel is a participant in CMS’ Medicare Pioneer Accountable Care Organization project as well as Massachusetts Blue Cross Blue Shield’s Alternative Quality Contract, both of which use a risk-sharing global payment model in which the hospital and its physician network agree to provide for the healthcare needs of a defined population for a pre-arranged reimbursement amount.
“The global payment model is an attractive one for hospitalists because we play a key role in managing hospitalized patients efficiently and well, while also encouraging collaboration between inpatient and outpatient providers to avoid duplication of services,” Dr. Doctoroff says. “Some bundled payment models, which tie reimbursement to a defined episode of care, also could be advantageous for hospitalists, who coordinate the patient’s care throughout their entire healthcare episode, from inpatient diagnosis through post-discharge.”
Alternative Fee-for-Service System
For physicians who choose not to adopt one of the new reimbursement models, the bill directs CMS to offer an alternative fee-for-service system with incentives for improved quality and lower cost. This alternative would be available to physicians (including hospitalists) who participate in approved quality-reporting options, including the Physician Quality Reporting System (PQRS) or an approved Maintenance of Certification (MOC) program with quality registries. It also would apply to physicians who fall into the top 25% of CMS’ Value-Based Payment Modifier program (VBPM).
Boosting Primary Care
In addition to expediting the rollout of CMS-endorsed alternate payment models, the Schwartz bill recognizes the importance of primary care as the foundation of an effective healthcare delivery system and redresses its undervaluation with a 2.5% reimbursement update for physicians and other healthcare professionals for whom 60% of their Medicare physician fee schedule allowable charges are from a designated set of primary-care, preventive, and care-coordination codes.
“SHM specifically advocated for the inclusion of primary-care billing codes that hospitalists use,” Dr. Doctoroff says, “including hospital inpatient visits and observational services.”
“Of all the attempts to deal with the SGR over the past several years, Rep. Schwartz’s bill makes the most sense,” Genzink says. “While it doesn’t answer all of the healthcare system’s problems, it encapsulates many of the goals of reform—especially the shift from fee-for-service toward a payment system based on quality and outcomes. It recognizes that no one model will work for all physicians and offers the flexibility of multiple pathways. And it has bipartisan support, which seems to be a rarity these days.”
Chris Guadagnino is a freelance medical writer in Philadelphia.
Performance Disconnect: Measures Don’t Improve Hospitals’ Readmissions Experience
Two recent studies have reached the same surprising conclusion: Adherence to national quality and performance guidelines does not translate into reduced readmissions rates.
Sula Mazimba, MD, MPH, and colleagues at Kettering Medical Center in Kettering, Ohio, focused on congestive heart failure (CHF) patients, documenting compliance with four core CHF performance measures at discharge and subsequent 30-day readmissions. Only one measure-assessment of left ventricular function-had a significant association with readmissions.
A second study published the same month looked at a wider range of diagnoses in a Medicare population at more than 2,000 hospitals nationwide. That study reached similar conclusions about the disconnect between hospitals that followed Hospital Compare process quality measures and their readmission rates.
Dr. Mazimba says hospitalists and other physicians involved in quality improvement (QI) should be more involved in defining quality measures that reflect quality of care for their patients.
“We should be looking for parameters that have a higher yield for outcomes, such as preventing readmissions,” he says, encouraging better symptom management before the CHF patient is hospitalized and enhanced coordination of care after discharge.
Alpesh Amin, MD, MBA, SFHM, professor and chair of the department of medicine and executive director of the hospitalist program at the University of California at Irvine, says the findings are important, but he adds that the core quality measures studied were never designed to address readmissions.
“The challenge is to find a way to connect the dots between the core measures and readmissions,” he says.
Learn more about the four "core" heart failure quality measures for hospitals by visiting the Resource Rooms on the SHM website, or check out this 80-page implementation guide, “Improving Heart Failure Care for Hospitalized Patients [PDF],” also available on SHM’s website.
Read The Hospitalist columnist Win Whitcomb’s take on readmissions penalty programs.
Two recent studies have reached the same surprising conclusion: Adherence to national quality and performance guidelines does not translate into reduced readmissions rates.
Sula Mazimba, MD, MPH, and colleagues at Kettering Medical Center in Kettering, Ohio, focused on congestive heart failure (CHF) patients, documenting compliance with four core CHF performance measures at discharge and subsequent 30-day readmissions. Only one measure-assessment of left ventricular function-had a significant association with readmissions.
A second study published the same month looked at a wider range of diagnoses in a Medicare population at more than 2,000 hospitals nationwide. That study reached similar conclusions about the disconnect between hospitals that followed Hospital Compare process quality measures and their readmission rates.
Dr. Mazimba says hospitalists and other physicians involved in quality improvement (QI) should be more involved in defining quality measures that reflect quality of care for their patients.
“We should be looking for parameters that have a higher yield for outcomes, such as preventing readmissions,” he says, encouraging better symptom management before the CHF patient is hospitalized and enhanced coordination of care after discharge.
Alpesh Amin, MD, MBA, SFHM, professor and chair of the department of medicine and executive director of the hospitalist program at the University of California at Irvine, says the findings are important, but he adds that the core quality measures studied were never designed to address readmissions.
“The challenge is to find a way to connect the dots between the core measures and readmissions,” he says.
Learn more about the four "core" heart failure quality measures for hospitals by visiting the Resource Rooms on the SHM website, or check out this 80-page implementation guide, “Improving Heart Failure Care for Hospitalized Patients [PDF],” also available on SHM’s website.
Read The Hospitalist columnist Win Whitcomb’s take on readmissions penalty programs.
Two recent studies have reached the same surprising conclusion: Adherence to national quality and performance guidelines does not translate into reduced readmissions rates.
Sula Mazimba, MD, MPH, and colleagues at Kettering Medical Center in Kettering, Ohio, focused on congestive heart failure (CHF) patients, documenting compliance with four core CHF performance measures at discharge and subsequent 30-day readmissions. Only one measure-assessment of left ventricular function-had a significant association with readmissions.
A second study published the same month looked at a wider range of diagnoses in a Medicare population at more than 2,000 hospitals nationwide. That study reached similar conclusions about the disconnect between hospitals that followed Hospital Compare process quality measures and their readmission rates.
Dr. Mazimba says hospitalists and other physicians involved in quality improvement (QI) should be more involved in defining quality measures that reflect quality of care for their patients.
“We should be looking for parameters that have a higher yield for outcomes, such as preventing readmissions,” he says, encouraging better symptom management before the CHF patient is hospitalized and enhanced coordination of care after discharge.
Alpesh Amin, MD, MBA, SFHM, professor and chair of the department of medicine and executive director of the hospitalist program at the University of California at Irvine, says the findings are important, but he adds that the core quality measures studied were never designed to address readmissions.
“The challenge is to find a way to connect the dots between the core measures and readmissions,” he says.
Learn more about the four "core" heart failure quality measures for hospitals by visiting the Resource Rooms on the SHM website, or check out this 80-page implementation guide, “Improving Heart Failure Care for Hospitalized Patients [PDF],” also available on SHM’s website.
Read The Hospitalist columnist Win Whitcomb’s take on readmissions penalty programs.
Report Outlines Ways Hospital Medicine Can Redefine Healthcare Delivery
There are 10 industry-changing recommendations in the recent Institute of Medicine (IOM) report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Suggestions include reforming payment, adopting digital infrastructure, and improving the continuity of care. And to Brent James, MD, all of those recommendations are areas in which hospitalists can help lead healthcare from fee-for-service to an organized-care model.
Dr. James, executive director of the Institute for Health Care Delivery Research and chief quality officer at Intermountain Healthcare in Salt Lake City, says hospitalists can be linchpins to that hoped-for sea change because the specialty’s growth the past 15 years shows that physicians taking a collaborative, evidence-based approach to patient care can improve outcomes and lower costs.
“In some sense, the hospitalist movement triggered [the move to organized care],” says Dr. James, one of the IOM report’s authors. “You started to have teams caring for inpatients in a coordinated way. Pieces started to kind of fall into place underneath it. So I regard this as … [hospitalists] coming into their own, their vision of the future starting to really take hold.”
The report estimates the national cost of unnecessary or wasteful healthcare at $750 billion per year. Published in September, the report was crafted by a nationwide committee of healthcare leaders, including hospitalist and medical researcher David Meltzer, MD, PhD, chief of University of Chicago’s Division of Hospital Medicine and director of the Center for Health and Social Sciences in Chicago.
Dr. Meltzer says that for a relatively young specialty, hospitalists have been “remarkably forward-looking.” The specialty, in his view, has embraced teamwork, digital infrastructure, and quality initiatives. As the U.S. healthcare system evolves, he notes, HM leaders need to keep that mentality. Hospitalists are confronted daily with a combination of sicker patients and more treatment options, and making the right decisions is paramount to a “learning healthcare system,” Dr. Meltzer adds.
“As the database of options grows, decision-making becomes more difficult,” he says. “We have an important role to play in how to think about trying to control costs.”
Gary Kaplan, MD, FACP, FACMPE, FACPE, chairman and chief executive officer of Virginia Mason Health System in Seattle, agrees that HM’s priorities dovetail nicely with reform efforts. He hopes the IOM report’s findings will serve as a springboard for hospitalists to further spearhead improvements.
In particular, Dr. Kaplan notes that healthcare delivery organizations should develop, implement, and fine-tune their “systems, engineering tools, and process-improvement methods.” Such changes would help “eliminate inefficiencies, remove unnecessary burdens on clinicians and staff, enhance patient experience, and improve patient health outcomes,” he says.
“The hospitalists and the care teams with which the hospitalist connects are very critical to streamlining operations,” Dr. Kaplan adds.
Dr. James, who has long championed process improvement as the key to improved clinical outcomes, says that extending the hospitalist model throughout healthcare can only have good results. He preaches the implementation of standardized protocols and sees hospitalists as natural torchbearers for the cause.
“When you start to focus on process—our old jargon for it was ‘continuum of care’—it forces you to patient-centered care,” he says. “Instead of building your care around the physicians, or around the hospital, or around the technology, you build the care around the patient.”
Dr. James has heard physicians say protocols are too rigid and do not improve patient care. He disagrees—vehemently.

—Brent James, MD, executive director of the Institute for Health Care Delivery Research and chief quality officer, Intermountain Healthcare, Salt Lake City
“It’s not just that we allow, or even that we encourage, we demand that you modify [the protocol] for individual patient needs,” he says. “What I have is a standard process of care. That means that you don’t have to bird-dog every little step. I take my most important resource—a trained, expert mind—and focus it on that relatively small set of problems that need to be modified. We’ve found that it massively improves patient outcomes.”
Many of the IOM report’s complaints about unnecessary testing, poor communication, and inefficient care delivery connect with the quality, patient-safety, and practice-management improvements HM groups already push, Dr. Kaplan adds. To advance healthcare delivery’s evolution, hospitalists should view the task of reform as an opportunity, not a challenge.
“There are very powerful opportunities for the hospitalist now to have great impact,” he says. “To not just be the passive participants in a broken and dysfunctional system, but in many ways, [to be] one of the architects of an improved care system going forward.”
Richard Quinn is a freelance writer in New Jersey.
There are 10 industry-changing recommendations in the recent Institute of Medicine (IOM) report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Suggestions include reforming payment, adopting digital infrastructure, and improving the continuity of care. And to Brent James, MD, all of those recommendations are areas in which hospitalists can help lead healthcare from fee-for-service to an organized-care model.
Dr. James, executive director of the Institute for Health Care Delivery Research and chief quality officer at Intermountain Healthcare in Salt Lake City, says hospitalists can be linchpins to that hoped-for sea change because the specialty’s growth the past 15 years shows that physicians taking a collaborative, evidence-based approach to patient care can improve outcomes and lower costs.
“In some sense, the hospitalist movement triggered [the move to organized care],” says Dr. James, one of the IOM report’s authors. “You started to have teams caring for inpatients in a coordinated way. Pieces started to kind of fall into place underneath it. So I regard this as … [hospitalists] coming into their own, their vision of the future starting to really take hold.”
The report estimates the national cost of unnecessary or wasteful healthcare at $750 billion per year. Published in September, the report was crafted by a nationwide committee of healthcare leaders, including hospitalist and medical researcher David Meltzer, MD, PhD, chief of University of Chicago’s Division of Hospital Medicine and director of the Center for Health and Social Sciences in Chicago.
Dr. Meltzer says that for a relatively young specialty, hospitalists have been “remarkably forward-looking.” The specialty, in his view, has embraced teamwork, digital infrastructure, and quality initiatives. As the U.S. healthcare system evolves, he notes, HM leaders need to keep that mentality. Hospitalists are confronted daily with a combination of sicker patients and more treatment options, and making the right decisions is paramount to a “learning healthcare system,” Dr. Meltzer adds.
“As the database of options grows, decision-making becomes more difficult,” he says. “We have an important role to play in how to think about trying to control costs.”
Gary Kaplan, MD, FACP, FACMPE, FACPE, chairman and chief executive officer of Virginia Mason Health System in Seattle, agrees that HM’s priorities dovetail nicely with reform efforts. He hopes the IOM report’s findings will serve as a springboard for hospitalists to further spearhead improvements.
In particular, Dr. Kaplan notes that healthcare delivery organizations should develop, implement, and fine-tune their “systems, engineering tools, and process-improvement methods.” Such changes would help “eliminate inefficiencies, remove unnecessary burdens on clinicians and staff, enhance patient experience, and improve patient health outcomes,” he says.
“The hospitalists and the care teams with which the hospitalist connects are very critical to streamlining operations,” Dr. Kaplan adds.
Dr. James, who has long championed process improvement as the key to improved clinical outcomes, says that extending the hospitalist model throughout healthcare can only have good results. He preaches the implementation of standardized protocols and sees hospitalists as natural torchbearers for the cause.
“When you start to focus on process—our old jargon for it was ‘continuum of care’—it forces you to patient-centered care,” he says. “Instead of building your care around the physicians, or around the hospital, or around the technology, you build the care around the patient.”
Dr. James has heard physicians say protocols are too rigid and do not improve patient care. He disagrees—vehemently.

—Brent James, MD, executive director of the Institute for Health Care Delivery Research and chief quality officer, Intermountain Healthcare, Salt Lake City
“It’s not just that we allow, or even that we encourage, we demand that you modify [the protocol] for individual patient needs,” he says. “What I have is a standard process of care. That means that you don’t have to bird-dog every little step. I take my most important resource—a trained, expert mind—and focus it on that relatively small set of problems that need to be modified. We’ve found that it massively improves patient outcomes.”
Many of the IOM report’s complaints about unnecessary testing, poor communication, and inefficient care delivery connect with the quality, patient-safety, and practice-management improvements HM groups already push, Dr. Kaplan adds. To advance healthcare delivery’s evolution, hospitalists should view the task of reform as an opportunity, not a challenge.
“There are very powerful opportunities for the hospitalist now to have great impact,” he says. “To not just be the passive participants in a broken and dysfunctional system, but in many ways, [to be] one of the architects of an improved care system going forward.”
Richard Quinn is a freelance writer in New Jersey.
There are 10 industry-changing recommendations in the recent Institute of Medicine (IOM) report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Suggestions include reforming payment, adopting digital infrastructure, and improving the continuity of care. And to Brent James, MD, all of those recommendations are areas in which hospitalists can help lead healthcare from fee-for-service to an organized-care model.
Dr. James, executive director of the Institute for Health Care Delivery Research and chief quality officer at Intermountain Healthcare in Salt Lake City, says hospitalists can be linchpins to that hoped-for sea change because the specialty’s growth the past 15 years shows that physicians taking a collaborative, evidence-based approach to patient care can improve outcomes and lower costs.
“In some sense, the hospitalist movement triggered [the move to organized care],” says Dr. James, one of the IOM report’s authors. “You started to have teams caring for inpatients in a coordinated way. Pieces started to kind of fall into place underneath it. So I regard this as … [hospitalists] coming into their own, their vision of the future starting to really take hold.”
The report estimates the national cost of unnecessary or wasteful healthcare at $750 billion per year. Published in September, the report was crafted by a nationwide committee of healthcare leaders, including hospitalist and medical researcher David Meltzer, MD, PhD, chief of University of Chicago’s Division of Hospital Medicine and director of the Center for Health and Social Sciences in Chicago.
Dr. Meltzer says that for a relatively young specialty, hospitalists have been “remarkably forward-looking.” The specialty, in his view, has embraced teamwork, digital infrastructure, and quality initiatives. As the U.S. healthcare system evolves, he notes, HM leaders need to keep that mentality. Hospitalists are confronted daily with a combination of sicker patients and more treatment options, and making the right decisions is paramount to a “learning healthcare system,” Dr. Meltzer adds.
“As the database of options grows, decision-making becomes more difficult,” he says. “We have an important role to play in how to think about trying to control costs.”
Gary Kaplan, MD, FACP, FACMPE, FACPE, chairman and chief executive officer of Virginia Mason Health System in Seattle, agrees that HM’s priorities dovetail nicely with reform efforts. He hopes the IOM report’s findings will serve as a springboard for hospitalists to further spearhead improvements.
In particular, Dr. Kaplan notes that healthcare delivery organizations should develop, implement, and fine-tune their “systems, engineering tools, and process-improvement methods.” Such changes would help “eliminate inefficiencies, remove unnecessary burdens on clinicians and staff, enhance patient experience, and improve patient health outcomes,” he says.
“The hospitalists and the care teams with which the hospitalist connects are very critical to streamlining operations,” Dr. Kaplan adds.
Dr. James, who has long championed process improvement as the key to improved clinical outcomes, says that extending the hospitalist model throughout healthcare can only have good results. He preaches the implementation of standardized protocols and sees hospitalists as natural torchbearers for the cause.
“When you start to focus on process—our old jargon for it was ‘continuum of care’—it forces you to patient-centered care,” he says. “Instead of building your care around the physicians, or around the hospital, or around the technology, you build the care around the patient.”
Dr. James has heard physicians say protocols are too rigid and do not improve patient care. He disagrees—vehemently.

—Brent James, MD, executive director of the Institute for Health Care Delivery Research and chief quality officer, Intermountain Healthcare, Salt Lake City
“It’s not just that we allow, or even that we encourage, we demand that you modify [the protocol] for individual patient needs,” he says. “What I have is a standard process of care. That means that you don’t have to bird-dog every little step. I take my most important resource—a trained, expert mind—and focus it on that relatively small set of problems that need to be modified. We’ve found that it massively improves patient outcomes.”
Many of the IOM report’s complaints about unnecessary testing, poor communication, and inefficient care delivery connect with the quality, patient-safety, and practice-management improvements HM groups already push, Dr. Kaplan adds. To advance healthcare delivery’s evolution, hospitalists should view the task of reform as an opportunity, not a challenge.
“There are very powerful opportunities for the hospitalist now to have great impact,” he says. “To not just be the passive participants in a broken and dysfunctional system, but in many ways, [to be] one of the architects of an improved care system going forward.”
Richard Quinn is a freelance writer in New Jersey.
Soaring Healthcare Expenses Draw Attention to Price Transparency As Cost Control
As efforts intensify to rein in the soaring cost of healthcare, greater attention is being paid to the cost-control potential of price transparency. Initially envisioned as a consumer-driven dynamic, price transparency beckons physicians to consider much more seriously the cost impacts of their diagnostic and treatment decisions.
Consumer-Driven Approach
The U.S. Department of Health and Human Services (HHS) regards price transparency as an important weapon in its armamentarium of “value-driven” approaches to drive down the cost of healthcare. By unleashing the energy of the savvy shopper and empowering consumers with the ability to compare the price and quality of healthcare services, they can make informed choices of their doctors and hospitals. In turn, HHS hopes to motivate the entire system to provide better care for less money.
That “empowered consumerism” principle is the guiding impetus for the Affordable Care Act’s state-regulated health insurance exchange apparatus, which, beginning in 2014, will present a side-by-side comparison of health plan choices, premium costs, and out-of-pocket copays in a way that is designed to help consumers shop for better-value health plans.
Some health plans are using price transparency to nudge consumers to choose lower-cost healthcare service options. Anthem BlueCross BlueShield, for example, has launched the Compass SmartShopper program (www.compasssmartshopper.com), which gives members in New Hampshire, Connecticut, and Indiana $50 to $200 if they get a diagnostic test or surgical procedure at a less expensive facility. Anthem notes that the cost for the same service can vary greatly. For example, hernia repairs range in price from $4,026 to $7,498, and colonoscopies range from $1,450 to $2,973.
New price transparency tools also are available (HealthCareBlueBook.com and FairHealthConsumer.org, for example) to help consumers who face high deductibles or out-of-pocket costs to find “fair prices” for surgeries, hospital stays, doctor visits, and medical tests—and shop accordingly.
Despite these developments, however, there is limited evidence that the “empowered consumerism” approach to price transparency will spur consumers to choose lower-cost providers. Some experts note that many consumers equate higher-cost providers with higher quality, and caution that healthcare cost-profiling initiatives might even have the perverse effect of deterring them from seeking these providers.1 Cost measures, they argue, must be tied to quality information in order to neutralize the typical association of high costs with higher quality.1
Provider-Driven Approach
There are healthcare price transparency initiatives that address the supply side of the healthcare cost equation. These initiatives seek to educate physicians about the ways in which their clinical decisions drive cost and affect what patients pay for care. Some believe that this approach has the potential to make a much bigger dent in cost containment than the empowered-consumerism approach.
“Ninety percent of healthcare cost comes from a physician’s pen, but a lot of that spending doesn’t help patients get better,” says Neel Shah, MD, a Harvard-affiliated OBGYN and executive director of Costs of Care (www.costsofcare.org), a nonprofit aimed at empowering both patients and their caregivers to deflate medical bills. The challenge, he adds, is making physicians aware of how their decisions can inflate costs unnecessarily, and giving them the training and tools they need to take appropriate action.
“Just as the patient-safety movement helped caregivers think about how to prevent unintended harm, a new movement is needed to educate doctors, nurses, and other caregivers about the cost and value of their decisions, so they can avoid waste and protect patients from unintended financial harms as well,” Dr. Shah says.
Costs of Care recently launched its Teaching Value Project, which employs Web-based video education modules to help medical students and residents learn to optimize both quality and cost in clinical decision-making.
“We’re also developing an iPhone app to put cost and quality information at physicians’ fingertips at the critical moment when medical decisions are made,” Dr. Shah adds. “Just being able to see the price variation—an ultrasound versus a CT scan, a generic versus a brand-name medication, or the cost of a marginally valuable test—can help drive physician ordering behavior.”
Hospitalist Impacts
Robert A. Bessler, MD, CEO of Tacoma, Wash.-based hospitalist management firm Sound Physicians, says his hospitalists spend about $2 million a year “with their pen or computerized physician order entry.” A quarter of the cost is pharmacy-related, and the “majority of the rest is from bed-days.”
“The most expensive thing we do is make the decision to admit,” Dr. Bessler notes. “With hospitals switching from revenue centers to cost centers in a population health/ACO [accountable-care organization] environment, an increasingly important part of the hospitalist’s job will be asking
questions, such as, ‘Could this patient go to a nursing home tonight from the ER?’ and ‘Can my colleague in the post-acute environment take care of this patient, with the same effective outcome, if we provide more intense services in the nursing home, going forward?’”
Because most diagnostic testing is done on the front end of an inpatient’s stay, the hospitalist’s main contribution to cost control is to get that diagnosis right and use consults to answer specific questions, Dr. Bessler explains. “There is a direct correlation between the number of consults and the volume of procedures which lead to higher inpatient costs,” he adds.
As hospitals convert to value-based care models, and pressure increases on hospitalists to ramp up their analysis and sharing of cost data and resource utilization, not all physicians will find that conversion easy.

—Neel Shah, MD, executive director, Costs of Care
“We are trained to take good care of our patients, not to be financial stewards of the healthcare system,” says SHM Public Policy Committee member Bradley Flansbaum, DO, MPH, SFHM. “Now, physicians are being asked to do both—to watch our resource use without looking like we’re selling out to payors. You’re putting physicians in a difficult position. Will they say to patients, ‘You can’t have this service’? When does being pragmatic stewards of resources become rationing?” he cautions.
Dr. Shah concedes that there is a perceived tension between “what’s best” for my patient and “what’s best” for society. “We, as a profession, haven’t given serious attention to how to navigate those tensions,” he says.
Dr. Flansbaum, a hospitalist at Lenox Hill Hospital in New York City, says it’s time to start down the transparency road.
“Otherwise, we will have a centralized body making these decisions for us,” he says.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
As efforts intensify to rein in the soaring cost of healthcare, greater attention is being paid to the cost-control potential of price transparency. Initially envisioned as a consumer-driven dynamic, price transparency beckons physicians to consider much more seriously the cost impacts of their diagnostic and treatment decisions.
Consumer-Driven Approach
The U.S. Department of Health and Human Services (HHS) regards price transparency as an important weapon in its armamentarium of “value-driven” approaches to drive down the cost of healthcare. By unleashing the energy of the savvy shopper and empowering consumers with the ability to compare the price and quality of healthcare services, they can make informed choices of their doctors and hospitals. In turn, HHS hopes to motivate the entire system to provide better care for less money.
That “empowered consumerism” principle is the guiding impetus for the Affordable Care Act’s state-regulated health insurance exchange apparatus, which, beginning in 2014, will present a side-by-side comparison of health plan choices, premium costs, and out-of-pocket copays in a way that is designed to help consumers shop for better-value health plans.
Some health plans are using price transparency to nudge consumers to choose lower-cost healthcare service options. Anthem BlueCross BlueShield, for example, has launched the Compass SmartShopper program (www.compasssmartshopper.com), which gives members in New Hampshire, Connecticut, and Indiana $50 to $200 if they get a diagnostic test or surgical procedure at a less expensive facility. Anthem notes that the cost for the same service can vary greatly. For example, hernia repairs range in price from $4,026 to $7,498, and colonoscopies range from $1,450 to $2,973.
New price transparency tools also are available (HealthCareBlueBook.com and FairHealthConsumer.org, for example) to help consumers who face high deductibles or out-of-pocket costs to find “fair prices” for surgeries, hospital stays, doctor visits, and medical tests—and shop accordingly.
Despite these developments, however, there is limited evidence that the “empowered consumerism” approach to price transparency will spur consumers to choose lower-cost providers. Some experts note that many consumers equate higher-cost providers with higher quality, and caution that healthcare cost-profiling initiatives might even have the perverse effect of deterring them from seeking these providers.1 Cost measures, they argue, must be tied to quality information in order to neutralize the typical association of high costs with higher quality.1
Provider-Driven Approach
There are healthcare price transparency initiatives that address the supply side of the healthcare cost equation. These initiatives seek to educate physicians about the ways in which their clinical decisions drive cost and affect what patients pay for care. Some believe that this approach has the potential to make a much bigger dent in cost containment than the empowered-consumerism approach.
“Ninety percent of healthcare cost comes from a physician’s pen, but a lot of that spending doesn’t help patients get better,” says Neel Shah, MD, a Harvard-affiliated OBGYN and executive director of Costs of Care (www.costsofcare.org), a nonprofit aimed at empowering both patients and their caregivers to deflate medical bills. The challenge, he adds, is making physicians aware of how their decisions can inflate costs unnecessarily, and giving them the training and tools they need to take appropriate action.
“Just as the patient-safety movement helped caregivers think about how to prevent unintended harm, a new movement is needed to educate doctors, nurses, and other caregivers about the cost and value of their decisions, so they can avoid waste and protect patients from unintended financial harms as well,” Dr. Shah says.
Costs of Care recently launched its Teaching Value Project, which employs Web-based video education modules to help medical students and residents learn to optimize both quality and cost in clinical decision-making.
“We’re also developing an iPhone app to put cost and quality information at physicians’ fingertips at the critical moment when medical decisions are made,” Dr. Shah adds. “Just being able to see the price variation—an ultrasound versus a CT scan, a generic versus a brand-name medication, or the cost of a marginally valuable test—can help drive physician ordering behavior.”
Hospitalist Impacts
Robert A. Bessler, MD, CEO of Tacoma, Wash.-based hospitalist management firm Sound Physicians, says his hospitalists spend about $2 million a year “with their pen or computerized physician order entry.” A quarter of the cost is pharmacy-related, and the “majority of the rest is from bed-days.”
“The most expensive thing we do is make the decision to admit,” Dr. Bessler notes. “With hospitals switching from revenue centers to cost centers in a population health/ACO [accountable-care organization] environment, an increasingly important part of the hospitalist’s job will be asking
questions, such as, ‘Could this patient go to a nursing home tonight from the ER?’ and ‘Can my colleague in the post-acute environment take care of this patient, with the same effective outcome, if we provide more intense services in the nursing home, going forward?’”
Because most diagnostic testing is done on the front end of an inpatient’s stay, the hospitalist’s main contribution to cost control is to get that diagnosis right and use consults to answer specific questions, Dr. Bessler explains. “There is a direct correlation between the number of consults and the volume of procedures which lead to higher inpatient costs,” he adds.
As hospitals convert to value-based care models, and pressure increases on hospitalists to ramp up their analysis and sharing of cost data and resource utilization, not all physicians will find that conversion easy.

—Neel Shah, MD, executive director, Costs of Care
“We are trained to take good care of our patients, not to be financial stewards of the healthcare system,” says SHM Public Policy Committee member Bradley Flansbaum, DO, MPH, SFHM. “Now, physicians are being asked to do both—to watch our resource use without looking like we’re selling out to payors. You’re putting physicians in a difficult position. Will they say to patients, ‘You can’t have this service’? When does being pragmatic stewards of resources become rationing?” he cautions.
Dr. Shah concedes that there is a perceived tension between “what’s best” for my patient and “what’s best” for society. “We, as a profession, haven’t given serious attention to how to navigate those tensions,” he says.
Dr. Flansbaum, a hospitalist at Lenox Hill Hospital in New York City, says it’s time to start down the transparency road.
“Otherwise, we will have a centralized body making these decisions for us,” he says.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
As efforts intensify to rein in the soaring cost of healthcare, greater attention is being paid to the cost-control potential of price transparency. Initially envisioned as a consumer-driven dynamic, price transparency beckons physicians to consider much more seriously the cost impacts of their diagnostic and treatment decisions.
Consumer-Driven Approach
The U.S. Department of Health and Human Services (HHS) regards price transparency as an important weapon in its armamentarium of “value-driven” approaches to drive down the cost of healthcare. By unleashing the energy of the savvy shopper and empowering consumers with the ability to compare the price and quality of healthcare services, they can make informed choices of their doctors and hospitals. In turn, HHS hopes to motivate the entire system to provide better care for less money.
That “empowered consumerism” principle is the guiding impetus for the Affordable Care Act’s state-regulated health insurance exchange apparatus, which, beginning in 2014, will present a side-by-side comparison of health plan choices, premium costs, and out-of-pocket copays in a way that is designed to help consumers shop for better-value health plans.
Some health plans are using price transparency to nudge consumers to choose lower-cost healthcare service options. Anthem BlueCross BlueShield, for example, has launched the Compass SmartShopper program (www.compasssmartshopper.com), which gives members in New Hampshire, Connecticut, and Indiana $50 to $200 if they get a diagnostic test or surgical procedure at a less expensive facility. Anthem notes that the cost for the same service can vary greatly. For example, hernia repairs range in price from $4,026 to $7,498, and colonoscopies range from $1,450 to $2,973.
New price transparency tools also are available (HealthCareBlueBook.com and FairHealthConsumer.org, for example) to help consumers who face high deductibles or out-of-pocket costs to find “fair prices” for surgeries, hospital stays, doctor visits, and medical tests—and shop accordingly.
Despite these developments, however, there is limited evidence that the “empowered consumerism” approach to price transparency will spur consumers to choose lower-cost providers. Some experts note that many consumers equate higher-cost providers with higher quality, and caution that healthcare cost-profiling initiatives might even have the perverse effect of deterring them from seeking these providers.1 Cost measures, they argue, must be tied to quality information in order to neutralize the typical association of high costs with higher quality.1
Provider-Driven Approach
There are healthcare price transparency initiatives that address the supply side of the healthcare cost equation. These initiatives seek to educate physicians about the ways in which their clinical decisions drive cost and affect what patients pay for care. Some believe that this approach has the potential to make a much bigger dent in cost containment than the empowered-consumerism approach.
“Ninety percent of healthcare cost comes from a physician’s pen, but a lot of that spending doesn’t help patients get better,” says Neel Shah, MD, a Harvard-affiliated OBGYN and executive director of Costs of Care (www.costsofcare.org), a nonprofit aimed at empowering both patients and their caregivers to deflate medical bills. The challenge, he adds, is making physicians aware of how their decisions can inflate costs unnecessarily, and giving them the training and tools they need to take appropriate action.
“Just as the patient-safety movement helped caregivers think about how to prevent unintended harm, a new movement is needed to educate doctors, nurses, and other caregivers about the cost and value of their decisions, so they can avoid waste and protect patients from unintended financial harms as well,” Dr. Shah says.
Costs of Care recently launched its Teaching Value Project, which employs Web-based video education modules to help medical students and residents learn to optimize both quality and cost in clinical decision-making.
“We’re also developing an iPhone app to put cost and quality information at physicians’ fingertips at the critical moment when medical decisions are made,” Dr. Shah adds. “Just being able to see the price variation—an ultrasound versus a CT scan, a generic versus a brand-name medication, or the cost of a marginally valuable test—can help drive physician ordering behavior.”
Hospitalist Impacts
Robert A. Bessler, MD, CEO of Tacoma, Wash.-based hospitalist management firm Sound Physicians, says his hospitalists spend about $2 million a year “with their pen or computerized physician order entry.” A quarter of the cost is pharmacy-related, and the “majority of the rest is from bed-days.”
“The most expensive thing we do is make the decision to admit,” Dr. Bessler notes. “With hospitals switching from revenue centers to cost centers in a population health/ACO [accountable-care organization] environment, an increasingly important part of the hospitalist’s job will be asking
questions, such as, ‘Could this patient go to a nursing home tonight from the ER?’ and ‘Can my colleague in the post-acute environment take care of this patient, with the same effective outcome, if we provide more intense services in the nursing home, going forward?’”
Because most diagnostic testing is done on the front end of an inpatient’s stay, the hospitalist’s main contribution to cost control is to get that diagnosis right and use consults to answer specific questions, Dr. Bessler explains. “There is a direct correlation between the number of consults and the volume of procedures which lead to higher inpatient costs,” he adds.
As hospitals convert to value-based care models, and pressure increases on hospitalists to ramp up their analysis and sharing of cost data and resource utilization, not all physicians will find that conversion easy.

—Neel Shah, MD, executive director, Costs of Care
“We are trained to take good care of our patients, not to be financial stewards of the healthcare system,” says SHM Public Policy Committee member Bradley Flansbaum, DO, MPH, SFHM. “Now, physicians are being asked to do both—to watch our resource use without looking like we’re selling out to payors. You’re putting physicians in a difficult position. Will they say to patients, ‘You can’t have this service’? When does being pragmatic stewards of resources become rationing?” he cautions.
Dr. Shah concedes that there is a perceived tension between “what’s best” for my patient and “what’s best” for society. “We, as a profession, haven’t given serious attention to how to navigate those tensions,” he says.
Dr. Flansbaum, a hospitalist at Lenox Hill Hospital in New York City, says it’s time to start down the transparency road.
“Otherwise, we will have a centralized body making these decisions for us,” he says.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
iPad Rollout at UC-Irvine Medical Center Prompts Security Measures
The University of California’s Irvine Medical Center has been issuing iPads to its incoming class of 100 medical students and to all 18 resident physicians in its department of emergency medicine.1 The entire medical curriculum is on the iPad and employs document sharing via the SharePoint collaborative software platform, says Adam Gold, the medical center’s director of emerging technologies.
But the use of these new technologies and subsequent clamoring by students, professors, physicians, and other staff to connect their own mobile devices to the network have led to the establishment of security and management guidelines for monitoring technology use, now spelled out in the new “Bring Your Own Device” policy, Gold explains.
Reference
The University of California’s Irvine Medical Center has been issuing iPads to its incoming class of 100 medical students and to all 18 resident physicians in its department of emergency medicine.1 The entire medical curriculum is on the iPad and employs document sharing via the SharePoint collaborative software platform, says Adam Gold, the medical center’s director of emerging technologies.
But the use of these new technologies and subsequent clamoring by students, professors, physicians, and other staff to connect their own mobile devices to the network have led to the establishment of security and management guidelines for monitoring technology use, now spelled out in the new “Bring Your Own Device” policy, Gold explains.
Reference
The University of California’s Irvine Medical Center has been issuing iPads to its incoming class of 100 medical students and to all 18 resident physicians in its department of emergency medicine.1 The entire medical curriculum is on the iPad and employs document sharing via the SharePoint collaborative software platform, says Adam Gold, the medical center’s director of emerging technologies.
But the use of these new technologies and subsequent clamoring by students, professors, physicians, and other staff to connect their own mobile devices to the network have led to the establishment of security and management guidelines for monitoring technology use, now spelled out in the new “Bring Your Own Device” policy, Gold explains.
Reference
Guidelines Help Hospitalists Manage Acute Coronary Syndrome Patients
Acute coronary syndrome (ACS) accounts for more than 1.4 million hospital admissions per year, and as many as 1 in 5 ACS patients die in the first six months after diagnosis, according to the American Academy of Family Physicians. With that in mind, Bruce Darrow, MD, PhD, presented the seminar “Acute Coronary Syndrome (ACS): Keys to Treatment and New Advances” for more than 150 hospitalists at the seventh annual Mid-Atlantic Hospital Medicine Symposium in October at Mount Sinai Medical Center in New York City.
“ACS patients are being admitted to a hospitalist’s care, although these physicians are not coronary service-line providers,” said Dr. Darrow, Mount Sinai’s director of telemetry services. “Often they work with cardiologists, but there are things hospitalists should be comfortable doing without consulting a specialist.”
Dr. Darrow spent the majority of his presentation reviewing the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) 2012 update of the 2007 guidelines for managing patients with myocardial infarction (MI).
Three Phases of Treatment
To achieve the comfort level he believes hospitalists require, Dr. Darrow explained three phases of ACS care: initial medical treatment, reperfusion therapy, and transitional management.1,2 Hospitalists who see patients within the first 24 hours of their hospital stay are providing
initial treatment.
Once the physician determines that the patient is experiencing an acute myocardial infarction, treatment should begin with:
- Aspirin;
- Low-molecular-weight heparin (or heparin if the patient will be heading to the cath lab); and
- Antiplatelet agents (clopidogrel or ticagrelor for this “upstream” portion of therapy).
—Bruce Darrow, MD, PhD, director of telemetry services, Mount Sinai Medical Center, New York
Other medications to consider are intravenous IIb/IIIa inhibitors, such as abciximab, that often were used for patients going to the cath lab. Beta-blockers, although no longer required, can be included in the arsenal. Similarly, anti-ischemics may be employed, despite a lack of evidence to support their use (e.g. oxygen can be a good idea, and morphine will certainly benefit someone in pain).
In cases with ST elevation, after initial treatment, the patient is generally sent to reperfusion therapy, unless it is contraindicated. Primary percutaneous coronary intervention (PCI) is recommended in facilities with a 24/7 cath lab, or in cases for which the patient can be transferred to a hospital with an available cath lab within three hours. Otherwise, thrombolysis is the route to take, and all hospitals should be capable of that procedure, Dr. Darrow said.
After reperfusion or conservative management measures are taken, the patient is transitioned to post-MI care, which includes:
- Aspirin (except where contraindicated);
- Antiplatelet agents (clopidogrel, ticagrelor, and prasugruel, depending on patient risk factors; see Figure 1, right);
- Beta-blockers;
- Statins;
- ACE inhibitors (for patients with systolic dysfunction); and
- Eplerenone/spironolactone (for patients with systolic dysfunction and respiratory conditions).
Core Measures
Dr. Darrow also addressed the ACS Core Measures, performance measurement, and improvement initiatives set by The Joint Commission and the Centers for Medicare & Medicaid Services (CMS).3
Upon arrival, patients should be given:
- Aspirin (Joint Commission-required; voluntary according to CMS);
- Thrombolyis within 30 minutes (if applicable); and
- Primary PCI within 90 minutes (if applicable).
At discharge, patients should be given:
- Aspirin;
- Beta-blockers (Joint Commission-required; voluntary according to CMS);
- ACE/ARB for systolic heart failure (Joint Commission-required;
- voluntary according to CMS); and
- Statins.
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update). a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2012;60(7):645-681.
- Darrow B. Acute coronary syndrome (ACS): Keys to treatment and new advances. Paper presented at the seventh annual Mid-Atlantic Hospital Medicine Symposium; Oct. 19, 2012; New York, NY.
- Joint Commission and the Centers for Medicare & Medicaid Services. Specifications Manual for National Hospital Inpatient Quality Measures. The Joint Commission website. Available at: http://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx. Accessed Oct. 22, 2012.
Acute coronary syndrome (ACS) accounts for more than 1.4 million hospital admissions per year, and as many as 1 in 5 ACS patients die in the first six months after diagnosis, according to the American Academy of Family Physicians. With that in mind, Bruce Darrow, MD, PhD, presented the seminar “Acute Coronary Syndrome (ACS): Keys to Treatment and New Advances” for more than 150 hospitalists at the seventh annual Mid-Atlantic Hospital Medicine Symposium in October at Mount Sinai Medical Center in New York City.
“ACS patients are being admitted to a hospitalist’s care, although these physicians are not coronary service-line providers,” said Dr. Darrow, Mount Sinai’s director of telemetry services. “Often they work with cardiologists, but there are things hospitalists should be comfortable doing without consulting a specialist.”
Dr. Darrow spent the majority of his presentation reviewing the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) 2012 update of the 2007 guidelines for managing patients with myocardial infarction (MI).
Three Phases of Treatment
To achieve the comfort level he believes hospitalists require, Dr. Darrow explained three phases of ACS care: initial medical treatment, reperfusion therapy, and transitional management.1,2 Hospitalists who see patients within the first 24 hours of their hospital stay are providing
initial treatment.
Once the physician determines that the patient is experiencing an acute myocardial infarction, treatment should begin with:
- Aspirin;
- Low-molecular-weight heparin (or heparin if the patient will be heading to the cath lab); and
- Antiplatelet agents (clopidogrel or ticagrelor for this “upstream” portion of therapy).
—Bruce Darrow, MD, PhD, director of telemetry services, Mount Sinai Medical Center, New York
Other medications to consider are intravenous IIb/IIIa inhibitors, such as abciximab, that often were used for patients going to the cath lab. Beta-blockers, although no longer required, can be included in the arsenal. Similarly, anti-ischemics may be employed, despite a lack of evidence to support their use (e.g. oxygen can be a good idea, and morphine will certainly benefit someone in pain).
In cases with ST elevation, after initial treatment, the patient is generally sent to reperfusion therapy, unless it is contraindicated. Primary percutaneous coronary intervention (PCI) is recommended in facilities with a 24/7 cath lab, or in cases for which the patient can be transferred to a hospital with an available cath lab within three hours. Otherwise, thrombolysis is the route to take, and all hospitals should be capable of that procedure, Dr. Darrow said.
After reperfusion or conservative management measures are taken, the patient is transitioned to post-MI care, which includes:
- Aspirin (except where contraindicated);
- Antiplatelet agents (clopidogrel, ticagrelor, and prasugruel, depending on patient risk factors; see Figure 1, right);
- Beta-blockers;
- Statins;
- ACE inhibitors (for patients with systolic dysfunction); and
- Eplerenone/spironolactone (for patients with systolic dysfunction and respiratory conditions).
Core Measures
Dr. Darrow also addressed the ACS Core Measures, performance measurement, and improvement initiatives set by The Joint Commission and the Centers for Medicare & Medicaid Services (CMS).3
Upon arrival, patients should be given:
- Aspirin (Joint Commission-required; voluntary according to CMS);
- Thrombolyis within 30 minutes (if applicable); and
- Primary PCI within 90 minutes (if applicable).
At discharge, patients should be given:
- Aspirin;
- Beta-blockers (Joint Commission-required; voluntary according to CMS);
- ACE/ARB for systolic heart failure (Joint Commission-required;
- voluntary according to CMS); and
- Statins.
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update). a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2012;60(7):645-681.
- Darrow B. Acute coronary syndrome (ACS): Keys to treatment and new advances. Paper presented at the seventh annual Mid-Atlantic Hospital Medicine Symposium; Oct. 19, 2012; New York, NY.
- Joint Commission and the Centers for Medicare & Medicaid Services. Specifications Manual for National Hospital Inpatient Quality Measures. The Joint Commission website. Available at: http://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx. Accessed Oct. 22, 2012.
Acute coronary syndrome (ACS) accounts for more than 1.4 million hospital admissions per year, and as many as 1 in 5 ACS patients die in the first six months after diagnosis, according to the American Academy of Family Physicians. With that in mind, Bruce Darrow, MD, PhD, presented the seminar “Acute Coronary Syndrome (ACS): Keys to Treatment and New Advances” for more than 150 hospitalists at the seventh annual Mid-Atlantic Hospital Medicine Symposium in October at Mount Sinai Medical Center in New York City.
“ACS patients are being admitted to a hospitalist’s care, although these physicians are not coronary service-line providers,” said Dr. Darrow, Mount Sinai’s director of telemetry services. “Often they work with cardiologists, but there are things hospitalists should be comfortable doing without consulting a specialist.”
Dr. Darrow spent the majority of his presentation reviewing the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) 2012 update of the 2007 guidelines for managing patients with myocardial infarction (MI).
Three Phases of Treatment
To achieve the comfort level he believes hospitalists require, Dr. Darrow explained three phases of ACS care: initial medical treatment, reperfusion therapy, and transitional management.1,2 Hospitalists who see patients within the first 24 hours of their hospital stay are providing
initial treatment.
Once the physician determines that the patient is experiencing an acute myocardial infarction, treatment should begin with:
- Aspirin;
- Low-molecular-weight heparin (or heparin if the patient will be heading to the cath lab); and
- Antiplatelet agents (clopidogrel or ticagrelor for this “upstream” portion of therapy).
—Bruce Darrow, MD, PhD, director of telemetry services, Mount Sinai Medical Center, New York
Other medications to consider are intravenous IIb/IIIa inhibitors, such as abciximab, that often were used for patients going to the cath lab. Beta-blockers, although no longer required, can be included in the arsenal. Similarly, anti-ischemics may be employed, despite a lack of evidence to support their use (e.g. oxygen can be a good idea, and morphine will certainly benefit someone in pain).
In cases with ST elevation, after initial treatment, the patient is generally sent to reperfusion therapy, unless it is contraindicated. Primary percutaneous coronary intervention (PCI) is recommended in facilities with a 24/7 cath lab, or in cases for which the patient can be transferred to a hospital with an available cath lab within three hours. Otherwise, thrombolysis is the route to take, and all hospitals should be capable of that procedure, Dr. Darrow said.
After reperfusion or conservative management measures are taken, the patient is transitioned to post-MI care, which includes:
- Aspirin (except where contraindicated);
- Antiplatelet agents (clopidogrel, ticagrelor, and prasugruel, depending on patient risk factors; see Figure 1, right);
- Beta-blockers;
- Statins;
- ACE inhibitors (for patients with systolic dysfunction); and
- Eplerenone/spironolactone (for patients with systolic dysfunction and respiratory conditions).
Core Measures
Dr. Darrow also addressed the ACS Core Measures, performance measurement, and improvement initiatives set by The Joint Commission and the Centers for Medicare & Medicaid Services (CMS).3
Upon arrival, patients should be given:
- Aspirin (Joint Commission-required; voluntary according to CMS);
- Thrombolyis within 30 minutes (if applicable); and
- Primary PCI within 90 minutes (if applicable).
At discharge, patients should be given:
- Aspirin;
- Beta-blockers (Joint Commission-required; voluntary according to CMS);
- ACE/ARB for systolic heart failure (Joint Commission-required;
- voluntary according to CMS); and
- Statins.
Maybelle Cowan-Lincoln is a freelance writer in New Jersey.
References
- Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update). a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2012;60(7):645-681.
- Darrow B. Acute coronary syndrome (ACS): Keys to treatment and new advances. Paper presented at the seventh annual Mid-Atlantic Hospital Medicine Symposium; Oct. 19, 2012; New York, NY.
- Joint Commission and the Centers for Medicare & Medicaid Services. Specifications Manual for National Hospital Inpatient Quality Measures. The Joint Commission website. Available at: http://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx. Accessed Oct. 22, 2012.
The Numerators: Treating Noncompliant, Medically Complicated Hospital Patients
We hospitalists are scientifically minded. We understand basic statistics, including percentages, percentiles, numerators, denominators (see Figure 1, right). In healthcare, we see a lot of patients we call denominators; these denominators are generally the types of patients to whom not much happens. They come in “pre-” and they leave “post-.” They generally pass through our walls, and our lives, according to plan, without leaving an impenetrable memory of who they were or what they experienced.
The numerators, on the other hand, do have something happen to them—something unexpected, untoward, unanticipated, unlikely. Sometimes we describe numerators as “noncompliant” or “medically complicated” or “refractory to treatment.” We often find ways to rationalize and explain how the patient turned from a denominator into a numerator—something they did, or didn’t do, to nudge them above the line. They smoked, they ate too much, they didn’t take their medications “as prescribed.” Often there is a less robust discussion about what we could have done to reduce the nudge: understand their background, their literacy, their finances, their physical/cognitive limitations, their understanding of risks and benefits.
I read a powerful piece about “numerators” written by Kerry O’Connell. In this piece, she describes what it was like to cross over the line into being a numerator after acquiring a hospital-acquired infection:
Five years ago this summer while under deep anesthesia for arm surgery number 3, I drifted above the line and joined the group called Numerators. … Numerators have lost a lot to join this group; many have lost organs, and some have lost all their limbs, all have many kinds of scars from their journey. It was not our choice to leave the world of Denominators … and many will struggle the rest of their lives to understand why...
There are lots of silly rules for not counting some infected souls, as if by not counting us we might not exist. Numerators that are identified are then divided by the Denominators to create a nameless, faceless, mysteriously small number called infection rates. “Rates,” like their cousin “odds,” claim to portray hope while predicting doom for some of us. Denominators are in love with rates, for no matter how many Numerators they have sired, someone else has sired more. Rates soothe the Denominator conscious and allow them to sleep peacefully at night ...
Numerators don’t ask for much from the world. We ask that Denominators look behind the numbers to see the people, to love us, count us, respect our suffering, and help keep us out of bankruptcy, for once we were Denominators just like you. Our greatest dream is that you find the daily strength to truly care. To care enough to follow the checklists, to care enough to wash your hands, to care enough to only use virgin needles, for the saddest day for all Numerators is when another unsuspecting Denominator rises above the line to join our group.1
CB’s Story
Now think of all the numerators you have met. I am going to repeat that phrase. Think of all the numerators you have met. I have met quite a few. Now I am going to tell you about my most memorable numerator.
CB was a 36-year-old white female admitted to the hospital with a recent diagnosis of ulcerative colitis. She had a protracted hospital course on various immunosuppressant drugs, none of which relieved her symptoms. During her hospital stay, her family, including her 2-year-old twins, visited every single day. After several weeks with no improvement, the decision was made to proceed to a colectomy. The surgical procedure itself was uncomplicated, a true denominator.
Then, on post-op Day 5, the day of her anticipated discharge, a pulmonary embolus thrust her into the numerator position. A preventable, eventually fatal numerator—a numerator who “just would not keep her compression devices on” and whom the staff tried to get out of bed, “but she just wouldn’t do it.” A numerator who just so happened to be my sister.
Every year on April 2, when I call my niece and nephew to wish them a happy birthday, I think about numerators. And I think about how incredibly different life would be for those 10-year-old twins, had their mom just stayed a denominator. And every day, when I sit in conference rooms and hear from countless people about how difficult it is to prevent this and reduce that, and how zero is not feasible, I think about numerators. I don’t look at their bar chart, or their run chart, or their red line, or their blue line, or whether their line is within the control limits, or what their P-value is. I think about who represents that black dot, and about how we are going to actually convince ourselves to “First, do no harm.”
When I find myself amongst a crowd quibbling about finances, lunch breaks, workflows, accountability, and about who is going to check the box or fill out the form, I think about the numerators, and how we are truly wasting their time, their livelihood, and their ability to stay below the line.
And someday, when my niece and nephew are old enough to understand, I will try to help them tolerate and accept the fact that “preventable” and “prevented” are not interchangeable. At least not in the medical industry. At least not yet.
In memory of Colleen Conlin Bowen, May 14, 2004
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Reference
We hospitalists are scientifically minded. We understand basic statistics, including percentages, percentiles, numerators, denominators (see Figure 1, right). In healthcare, we see a lot of patients we call denominators; these denominators are generally the types of patients to whom not much happens. They come in “pre-” and they leave “post-.” They generally pass through our walls, and our lives, according to plan, without leaving an impenetrable memory of who they were or what they experienced.
The numerators, on the other hand, do have something happen to them—something unexpected, untoward, unanticipated, unlikely. Sometimes we describe numerators as “noncompliant” or “medically complicated” or “refractory to treatment.” We often find ways to rationalize and explain how the patient turned from a denominator into a numerator—something they did, or didn’t do, to nudge them above the line. They smoked, they ate too much, they didn’t take their medications “as prescribed.” Often there is a less robust discussion about what we could have done to reduce the nudge: understand their background, their literacy, their finances, their physical/cognitive limitations, their understanding of risks and benefits.
I read a powerful piece about “numerators” written by Kerry O’Connell. In this piece, she describes what it was like to cross over the line into being a numerator after acquiring a hospital-acquired infection:
Five years ago this summer while under deep anesthesia for arm surgery number 3, I drifted above the line and joined the group called Numerators. … Numerators have lost a lot to join this group; many have lost organs, and some have lost all their limbs, all have many kinds of scars from their journey. It was not our choice to leave the world of Denominators … and many will struggle the rest of their lives to understand why...
There are lots of silly rules for not counting some infected souls, as if by not counting us we might not exist. Numerators that are identified are then divided by the Denominators to create a nameless, faceless, mysteriously small number called infection rates. “Rates,” like their cousin “odds,” claim to portray hope while predicting doom for some of us. Denominators are in love with rates, for no matter how many Numerators they have sired, someone else has sired more. Rates soothe the Denominator conscious and allow them to sleep peacefully at night ...
Numerators don’t ask for much from the world. We ask that Denominators look behind the numbers to see the people, to love us, count us, respect our suffering, and help keep us out of bankruptcy, for once we were Denominators just like you. Our greatest dream is that you find the daily strength to truly care. To care enough to follow the checklists, to care enough to wash your hands, to care enough to only use virgin needles, for the saddest day for all Numerators is when another unsuspecting Denominator rises above the line to join our group.1
CB’s Story
Now think of all the numerators you have met. I am going to repeat that phrase. Think of all the numerators you have met. I have met quite a few. Now I am going to tell you about my most memorable numerator.
CB was a 36-year-old white female admitted to the hospital with a recent diagnosis of ulcerative colitis. She had a protracted hospital course on various immunosuppressant drugs, none of which relieved her symptoms. During her hospital stay, her family, including her 2-year-old twins, visited every single day. After several weeks with no improvement, the decision was made to proceed to a colectomy. The surgical procedure itself was uncomplicated, a true denominator.
Then, on post-op Day 5, the day of her anticipated discharge, a pulmonary embolus thrust her into the numerator position. A preventable, eventually fatal numerator—a numerator who “just would not keep her compression devices on” and whom the staff tried to get out of bed, “but she just wouldn’t do it.” A numerator who just so happened to be my sister.
Every year on April 2, when I call my niece and nephew to wish them a happy birthday, I think about numerators. And I think about how incredibly different life would be for those 10-year-old twins, had their mom just stayed a denominator. And every day, when I sit in conference rooms and hear from countless people about how difficult it is to prevent this and reduce that, and how zero is not feasible, I think about numerators. I don’t look at their bar chart, or their run chart, or their red line, or their blue line, or whether their line is within the control limits, or what their P-value is. I think about who represents that black dot, and about how we are going to actually convince ourselves to “First, do no harm.”
When I find myself amongst a crowd quibbling about finances, lunch breaks, workflows, accountability, and about who is going to check the box or fill out the form, I think about the numerators, and how we are truly wasting their time, their livelihood, and their ability to stay below the line.
And someday, when my niece and nephew are old enough to understand, I will try to help them tolerate and accept the fact that “preventable” and “prevented” are not interchangeable. At least not in the medical industry. At least not yet.
In memory of Colleen Conlin Bowen, May 14, 2004
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Reference
We hospitalists are scientifically minded. We understand basic statistics, including percentages, percentiles, numerators, denominators (see Figure 1, right). In healthcare, we see a lot of patients we call denominators; these denominators are generally the types of patients to whom not much happens. They come in “pre-” and they leave “post-.” They generally pass through our walls, and our lives, according to plan, without leaving an impenetrable memory of who they were or what they experienced.
The numerators, on the other hand, do have something happen to them—something unexpected, untoward, unanticipated, unlikely. Sometimes we describe numerators as “noncompliant” or “medically complicated” or “refractory to treatment.” We often find ways to rationalize and explain how the patient turned from a denominator into a numerator—something they did, or didn’t do, to nudge them above the line. They smoked, they ate too much, they didn’t take their medications “as prescribed.” Often there is a less robust discussion about what we could have done to reduce the nudge: understand their background, their literacy, their finances, their physical/cognitive limitations, their understanding of risks and benefits.
I read a powerful piece about “numerators” written by Kerry O’Connell. In this piece, she describes what it was like to cross over the line into being a numerator after acquiring a hospital-acquired infection:
Five years ago this summer while under deep anesthesia for arm surgery number 3, I drifted above the line and joined the group called Numerators. … Numerators have lost a lot to join this group; many have lost organs, and some have lost all their limbs, all have many kinds of scars from their journey. It was not our choice to leave the world of Denominators … and many will struggle the rest of their lives to understand why...
There are lots of silly rules for not counting some infected souls, as if by not counting us we might not exist. Numerators that are identified are then divided by the Denominators to create a nameless, faceless, mysteriously small number called infection rates. “Rates,” like their cousin “odds,” claim to portray hope while predicting doom for some of us. Denominators are in love with rates, for no matter how many Numerators they have sired, someone else has sired more. Rates soothe the Denominator conscious and allow them to sleep peacefully at night ...
Numerators don’t ask for much from the world. We ask that Denominators look behind the numbers to see the people, to love us, count us, respect our suffering, and help keep us out of bankruptcy, for once we were Denominators just like you. Our greatest dream is that you find the daily strength to truly care. To care enough to follow the checklists, to care enough to wash your hands, to care enough to only use virgin needles, for the saddest day for all Numerators is when another unsuspecting Denominator rises above the line to join our group.1
CB’s Story
Now think of all the numerators you have met. I am going to repeat that phrase. Think of all the numerators you have met. I have met quite a few. Now I am going to tell you about my most memorable numerator.
CB was a 36-year-old white female admitted to the hospital with a recent diagnosis of ulcerative colitis. She had a protracted hospital course on various immunosuppressant drugs, none of which relieved her symptoms. During her hospital stay, her family, including her 2-year-old twins, visited every single day. After several weeks with no improvement, the decision was made to proceed to a colectomy. The surgical procedure itself was uncomplicated, a true denominator.
Then, on post-op Day 5, the day of her anticipated discharge, a pulmonary embolus thrust her into the numerator position. A preventable, eventually fatal numerator—a numerator who “just would not keep her compression devices on” and whom the staff tried to get out of bed, “but she just wouldn’t do it.” A numerator who just so happened to be my sister.
Every year on April 2, when I call my niece and nephew to wish them a happy birthday, I think about numerators. And I think about how incredibly different life would be for those 10-year-old twins, had their mom just stayed a denominator. And every day, when I sit in conference rooms and hear from countless people about how difficult it is to prevent this and reduce that, and how zero is not feasible, I think about numerators. I don’t look at their bar chart, or their run chart, or their red line, or their blue line, or whether their line is within the control limits, or what their P-value is. I think about who represents that black dot, and about how we are going to actually convince ourselves to “First, do no harm.”
When I find myself amongst a crowd quibbling about finances, lunch breaks, workflows, accountability, and about who is going to check the box or fill out the form, I think about the numerators, and how we are truly wasting their time, their livelihood, and their ability to stay below the line.
And someday, when my niece and nephew are old enough to understand, I will try to help them tolerate and accept the fact that “preventable” and “prevented” are not interchangeable. At least not in the medical industry. At least not yet.
In memory of Colleen Conlin Bowen, May 14, 2004
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Reference
Recommendations for Antithrombotic and Thrombolytic Therapy
Background
Each year, 1 million people are hospitalized with a diagnosis of stroke; it was the fourth-leading cause of death in the U.S. in 2009 and 2010.1 The majority of strokes (80%) are caused by focal cerebral ischemia, and the remainder are caused by hemorrhage.1 In 2008, the direct medical costs of stroke were approximately $18.8 billion, with almost half of this amount directed toward hospitalization.1 Although stroke inpatients make up only 3% of total hospitalizations, the mortality rate is more than twice that of other patients’.1
Over the past several decades, much has been learned about the pathophysiology and treatment for ischemic stroke. The mainstays of therapies include restoring perfusion in a timely manner and targeting both clot formation and hemostasis. These therapies improve patient outcomes and reduce the risk of recurrence in appropriately selected populations.
Guideline Update
In February, the American College of Chest Physicians (ACCP) published new practice guidelines for medical patients regarding antithrombotic and thrombolytic therapy in acute ischemic stroke.2 These evidence-based guidelines are the result of new clinical trial data and a review of previous studies. They address three aspects of management decisions for stroke, including acute treatment, VTE prevention, and secondary prevention, as well as specifically address the treatment of cerebral venous sinus thrombosis.
In the management of acute ischemic stroke, several recommendations were made. In terms of IV recombinant tissue plasminogen activator (r-tPA) administration, the guidelines were expanded and allow for a less restrictive time threshold for administration. Previous recommendations limited the usage of IV r-tPA to within three hours of symptom onset in acute ischemic stroke. A science advisory from the American Heart Association/American Stroke Association (AHA/ASA) from 2009 extended that window to 4.5 hours. The 2012 ACCP guidelines have followed suit to extend this time to 4.5 hours from symptom onset as well.
In addition, intrarterial r-tPA can be given in patients not eligible for IV r-tPA within six hours of presentation of acute ischemic stroke due to proximal cerebral artery occlusion.
These updated acute stroke guidelines recommend against the use of mechanical thrombectomy based mostly on lack of data rather than lack of benefit.2
The new guidelines continue to recommend early aspirin therapy at a dosage of 160 mg to 325 mg within the first 48 hours of acute ischemic stroke. Therapeutic parenteral anticoagulation with heparin or related drugs was not recommended in patients with noncardioembolic stroke due to atrial fibrillation (afib) or in patients with stroke due to large artery stenosis or arterial dissection. In this updated analysis, there was no benefit of anticoagulation compared with antiplatelet therapy, and the risk for extracranial hemorrhage was increased. No specific recommendation regarding anticoagulation was made in patients with mechanical heart valves or intracardiac thrombus.
Updates have been made for VTE prophylaxis in patients hospitalized for acute stroke. In stroke patients with restricted mobility, prophylactic unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) and/or intermittent pneumatic compression devices should be initiated as early as possible. The panel is no longer recommending elastic compression stockings as VTE prevention given the risk of skin damage and no clear benefit in symptomatic VTE prevention. For patients with hemorrhagic stroke and restricted mobility, similar recommendations were made for VTE prevention, except to start pharmacologic treatment between days 2 and 4 of the hospital stay. However, if there is a bleeding concern, intermittent pneumatic compression devices are favored over pharmacologic prophylaxis. In all patients for whom pharmacologic prevention is utilized, prophylactic LMWH is preferred over UFH.
Secondary stroke prevention is addressed, with 2012 guidelines outlining a preference for clopidogrel or aspirin/extended-release dipyridamole rather than aspirin or cilostazol in patients with a history of noncardioembolic ischemic stroke or TIA. Oral anticoagulation is preferred in patients with a history of stroke or TIA with afib over aspirin alone, aspirin plus clopidogrel, or no antithrombotic therapy. Of the available anticoagulants, the panel recommended dabigatran 150 mg twice daily over adjusted-dose warfarin.2 This recommendation is based on results from the RE-LY trial, which showed dabigatran as noninferior to warfarin in patients with nonvalvular afib without severe renal failure or advanced liver disease.3
For patients who have contraindications or choose not to initiate anticoagulation, the combination of aspirin (ASA) and clopidogrel is a reasonable alternative. Timing of the initiation of oral anticoagulation should be between one and two weeks after the stroke. Patients with extensive infarction or hemorrhagic transformation should delay starting oral anticoagulation, with no exact timeline. Long-term antithrombotic therapy is contraindicated in patients with history of a symptomatic primary intracerebral hemorrhage.2 New guidelines also recommend full anticoagulation for patients with symptomatic cerebral venous sinus thrombosis.
The panel did not make any recommendations regarding statin usage. In several studies, findings showed that statins reduced infarct size and had improved outcome in all stroke types.4
Analysis
Prior to the 2012 update, the last guideline for antithrombotic and thrombolytic therapy for ischemic stroke was published by the ACCP in the June 2008 issue of Chest.5 Dating back to 2001, medications included r-tPA administration within three hours of stroke symptom onset, and aspirin, clopidogrel, or a com bination of aspirin and extended-release dipyridamole for stroke prophylaxis.
The management of stroke continues to focus on early intervention and secondary prevention. Thrombolytic therapy is an effective treatment of acute ischemic stroke if given within the narrow window from onset of stroke symptoms up to 4.5 hours, with the goal of treatment within a three-hour window. Beyond this time constraint, the risk outweighs the benefit of using r-tPA except in the case of intra-arterial r-tPA administration for proximal cerebral artery occlusion.
In 2010, a meta-analysis supported this by showing that the risk of death increased significantly in patients receiving r-tPA beyond 4.5 hours. Therefore, antiplatelet therapy is the best alternative for patients ineligible for thrombolytic therapy.6 Even so, that study offered little data for patients with mechanical heart valves or intracardiac thrombi. Thus, the choice for acute anticoagulation therapy is variable and uncertain. If the hemorrhagic risk is low, anticoagulation can be considered in this subgroup, but no specific guideline endorsement was made.
In 2011, the AHA/ASA published an updated treatment guideline for patients with stroke or TIA. This was an update to 2007 guidelines that outlined the early management of ischemic stroke and affirmed the benefit of IV r-tPA at 4.5 hours for the treatment of stroke.7 Of note, IV r-tPA is only FDA-approved for treatment of acute ischemic stroke within the previously recommended three-hour period from symptom onset.
Aspirin has been found to be effective in both early treatment of acute ischemic stroke and secondary prevention. The CAST trial showed a statistically significant rate of reduction of nonfatal strokes with the use of aspirin. Other antiplatelet agents, including clopidogrel and dipyridamole, can be used. The FASTER trial compared aspirin alone versus aspirin plus clopidogrel, with no difference in outcome measures, although the MATCH trial found a larger risk of hemorrhagic and bleeding complications in the acetylsalicylic acid (ASA)-plus-clopidogrel group.6,7
In TIA or stroke patients, clopidogrel is not superior to ASA in preventing recurrent stroke. However, patients who have peripheral artery disease (PAD), previous coronary artery bypass grafting (CABG), insulin dependent diabetes mellitus (IDDM), or recurrent vascular events show a benefit of transitioning from ASA to clopidogrel for secondary long-term prevention. Clopidogrel or aspirin/extended-release dipyridamole is preferred over aspirin alone or cilostazol for long-term treatment in patients with a history of noncardioembolic ischemic stroke or TIA based on the PROFESS trial.2,7
HM Takeaways
The 2012 guidelines are a resource available to hospitalists for treating acute ischemic stroke either alone or with neurology consultation. These guidelines further define the timing of r-tPA and the use of both anticoagulation and antiplatelet therapy in the proper clinical settings.
In terms of VTE prevention, the guidelines recommend using LMWH preferentially over UH, except in patients at risk for rebleeding. The clinician should be aware of the treatment considerations for secondary prevention, noting the primary role of aspirin therapy in ischemic stroke with consideration of other agents (i.e. clopidogrel) in select populations.
Drs. Barr and Schumacher are hospitalists and assistant professors in the division of hospital medicine at The Ohio State University College of Medicine in Columbus.
References
Available at the-hospitalist.org.
Background
Each year, 1 million people are hospitalized with a diagnosis of stroke; it was the fourth-leading cause of death in the U.S. in 2009 and 2010.1 The majority of strokes (80%) are caused by focal cerebral ischemia, and the remainder are caused by hemorrhage.1 In 2008, the direct medical costs of stroke were approximately $18.8 billion, with almost half of this amount directed toward hospitalization.1 Although stroke inpatients make up only 3% of total hospitalizations, the mortality rate is more than twice that of other patients’.1
Over the past several decades, much has been learned about the pathophysiology and treatment for ischemic stroke. The mainstays of therapies include restoring perfusion in a timely manner and targeting both clot formation and hemostasis. These therapies improve patient outcomes and reduce the risk of recurrence in appropriately selected populations.
Guideline Update
In February, the American College of Chest Physicians (ACCP) published new practice guidelines for medical patients regarding antithrombotic and thrombolytic therapy in acute ischemic stroke.2 These evidence-based guidelines are the result of new clinical trial data and a review of previous studies. They address three aspects of management decisions for stroke, including acute treatment, VTE prevention, and secondary prevention, as well as specifically address the treatment of cerebral venous sinus thrombosis.
In the management of acute ischemic stroke, several recommendations were made. In terms of IV recombinant tissue plasminogen activator (r-tPA) administration, the guidelines were expanded and allow for a less restrictive time threshold for administration. Previous recommendations limited the usage of IV r-tPA to within three hours of symptom onset in acute ischemic stroke. A science advisory from the American Heart Association/American Stroke Association (AHA/ASA) from 2009 extended that window to 4.5 hours. The 2012 ACCP guidelines have followed suit to extend this time to 4.5 hours from symptom onset as well.
In addition, intrarterial r-tPA can be given in patients not eligible for IV r-tPA within six hours of presentation of acute ischemic stroke due to proximal cerebral artery occlusion.
These updated acute stroke guidelines recommend against the use of mechanical thrombectomy based mostly on lack of data rather than lack of benefit.2
The new guidelines continue to recommend early aspirin therapy at a dosage of 160 mg to 325 mg within the first 48 hours of acute ischemic stroke. Therapeutic parenteral anticoagulation with heparin or related drugs was not recommended in patients with noncardioembolic stroke due to atrial fibrillation (afib) or in patients with stroke due to large artery stenosis or arterial dissection. In this updated analysis, there was no benefit of anticoagulation compared with antiplatelet therapy, and the risk for extracranial hemorrhage was increased. No specific recommendation regarding anticoagulation was made in patients with mechanical heart valves or intracardiac thrombus.
Updates have been made for VTE prophylaxis in patients hospitalized for acute stroke. In stroke patients with restricted mobility, prophylactic unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) and/or intermittent pneumatic compression devices should be initiated as early as possible. The panel is no longer recommending elastic compression stockings as VTE prevention given the risk of skin damage and no clear benefit in symptomatic VTE prevention. For patients with hemorrhagic stroke and restricted mobility, similar recommendations were made for VTE prevention, except to start pharmacologic treatment between days 2 and 4 of the hospital stay. However, if there is a bleeding concern, intermittent pneumatic compression devices are favored over pharmacologic prophylaxis. In all patients for whom pharmacologic prevention is utilized, prophylactic LMWH is preferred over UFH.
Secondary stroke prevention is addressed, with 2012 guidelines outlining a preference for clopidogrel or aspirin/extended-release dipyridamole rather than aspirin or cilostazol in patients with a history of noncardioembolic ischemic stroke or TIA. Oral anticoagulation is preferred in patients with a history of stroke or TIA with afib over aspirin alone, aspirin plus clopidogrel, or no antithrombotic therapy. Of the available anticoagulants, the panel recommended dabigatran 150 mg twice daily over adjusted-dose warfarin.2 This recommendation is based on results from the RE-LY trial, which showed dabigatran as noninferior to warfarin in patients with nonvalvular afib without severe renal failure or advanced liver disease.3
For patients who have contraindications or choose not to initiate anticoagulation, the combination of aspirin (ASA) and clopidogrel is a reasonable alternative. Timing of the initiation of oral anticoagulation should be between one and two weeks after the stroke. Patients with extensive infarction or hemorrhagic transformation should delay starting oral anticoagulation, with no exact timeline. Long-term antithrombotic therapy is contraindicated in patients with history of a symptomatic primary intracerebral hemorrhage.2 New guidelines also recommend full anticoagulation for patients with symptomatic cerebral venous sinus thrombosis.
The panel did not make any recommendations regarding statin usage. In several studies, findings showed that statins reduced infarct size and had improved outcome in all stroke types.4
Analysis
Prior to the 2012 update, the last guideline for antithrombotic and thrombolytic therapy for ischemic stroke was published by the ACCP in the June 2008 issue of Chest.5 Dating back to 2001, medications included r-tPA administration within three hours of stroke symptom onset, and aspirin, clopidogrel, or a com bination of aspirin and extended-release dipyridamole for stroke prophylaxis.
The management of stroke continues to focus on early intervention and secondary prevention. Thrombolytic therapy is an effective treatment of acute ischemic stroke if given within the narrow window from onset of stroke symptoms up to 4.5 hours, with the goal of treatment within a three-hour window. Beyond this time constraint, the risk outweighs the benefit of using r-tPA except in the case of intra-arterial r-tPA administration for proximal cerebral artery occlusion.
In 2010, a meta-analysis supported this by showing that the risk of death increased significantly in patients receiving r-tPA beyond 4.5 hours. Therefore, antiplatelet therapy is the best alternative for patients ineligible for thrombolytic therapy.6 Even so, that study offered little data for patients with mechanical heart valves or intracardiac thrombi. Thus, the choice for acute anticoagulation therapy is variable and uncertain. If the hemorrhagic risk is low, anticoagulation can be considered in this subgroup, but no specific guideline endorsement was made.
In 2011, the AHA/ASA published an updated treatment guideline for patients with stroke or TIA. This was an update to 2007 guidelines that outlined the early management of ischemic stroke and affirmed the benefit of IV r-tPA at 4.5 hours for the treatment of stroke.7 Of note, IV r-tPA is only FDA-approved for treatment of acute ischemic stroke within the previously recommended three-hour period from symptom onset.
Aspirin has been found to be effective in both early treatment of acute ischemic stroke and secondary prevention. The CAST trial showed a statistically significant rate of reduction of nonfatal strokes with the use of aspirin. Other antiplatelet agents, including clopidogrel and dipyridamole, can be used. The FASTER trial compared aspirin alone versus aspirin plus clopidogrel, with no difference in outcome measures, although the MATCH trial found a larger risk of hemorrhagic and bleeding complications in the acetylsalicylic acid (ASA)-plus-clopidogrel group.6,7
In TIA or stroke patients, clopidogrel is not superior to ASA in preventing recurrent stroke. However, patients who have peripheral artery disease (PAD), previous coronary artery bypass grafting (CABG), insulin dependent diabetes mellitus (IDDM), or recurrent vascular events show a benefit of transitioning from ASA to clopidogrel for secondary long-term prevention. Clopidogrel or aspirin/extended-release dipyridamole is preferred over aspirin alone or cilostazol for long-term treatment in patients with a history of noncardioembolic ischemic stroke or TIA based on the PROFESS trial.2,7
HM Takeaways
The 2012 guidelines are a resource available to hospitalists for treating acute ischemic stroke either alone or with neurology consultation. These guidelines further define the timing of r-tPA and the use of both anticoagulation and antiplatelet therapy in the proper clinical settings.
In terms of VTE prevention, the guidelines recommend using LMWH preferentially over UH, except in patients at risk for rebleeding. The clinician should be aware of the treatment considerations for secondary prevention, noting the primary role of aspirin therapy in ischemic stroke with consideration of other agents (i.e. clopidogrel) in select populations.
Drs. Barr and Schumacher are hospitalists and assistant professors in the division of hospital medicine at The Ohio State University College of Medicine in Columbus.
References
Available at the-hospitalist.org.
Background
Each year, 1 million people are hospitalized with a diagnosis of stroke; it was the fourth-leading cause of death in the U.S. in 2009 and 2010.1 The majority of strokes (80%) are caused by focal cerebral ischemia, and the remainder are caused by hemorrhage.1 In 2008, the direct medical costs of stroke were approximately $18.8 billion, with almost half of this amount directed toward hospitalization.1 Although stroke inpatients make up only 3% of total hospitalizations, the mortality rate is more than twice that of other patients’.1
Over the past several decades, much has been learned about the pathophysiology and treatment for ischemic stroke. The mainstays of therapies include restoring perfusion in a timely manner and targeting both clot formation and hemostasis. These therapies improve patient outcomes and reduce the risk of recurrence in appropriately selected populations.
Guideline Update
In February, the American College of Chest Physicians (ACCP) published new practice guidelines for medical patients regarding antithrombotic and thrombolytic therapy in acute ischemic stroke.2 These evidence-based guidelines are the result of new clinical trial data and a review of previous studies. They address three aspects of management decisions for stroke, including acute treatment, VTE prevention, and secondary prevention, as well as specifically address the treatment of cerebral venous sinus thrombosis.
In the management of acute ischemic stroke, several recommendations were made. In terms of IV recombinant tissue plasminogen activator (r-tPA) administration, the guidelines were expanded and allow for a less restrictive time threshold for administration. Previous recommendations limited the usage of IV r-tPA to within three hours of symptom onset in acute ischemic stroke. A science advisory from the American Heart Association/American Stroke Association (AHA/ASA) from 2009 extended that window to 4.5 hours. The 2012 ACCP guidelines have followed suit to extend this time to 4.5 hours from symptom onset as well.
In addition, intrarterial r-tPA can be given in patients not eligible for IV r-tPA within six hours of presentation of acute ischemic stroke due to proximal cerebral artery occlusion.
These updated acute stroke guidelines recommend against the use of mechanical thrombectomy based mostly on lack of data rather than lack of benefit.2
The new guidelines continue to recommend early aspirin therapy at a dosage of 160 mg to 325 mg within the first 48 hours of acute ischemic stroke. Therapeutic parenteral anticoagulation with heparin or related drugs was not recommended in patients with noncardioembolic stroke due to atrial fibrillation (afib) or in patients with stroke due to large artery stenosis or arterial dissection. In this updated analysis, there was no benefit of anticoagulation compared with antiplatelet therapy, and the risk for extracranial hemorrhage was increased. No specific recommendation regarding anticoagulation was made in patients with mechanical heart valves or intracardiac thrombus.
Updates have been made for VTE prophylaxis in patients hospitalized for acute stroke. In stroke patients with restricted mobility, prophylactic unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) and/or intermittent pneumatic compression devices should be initiated as early as possible. The panel is no longer recommending elastic compression stockings as VTE prevention given the risk of skin damage and no clear benefit in symptomatic VTE prevention. For patients with hemorrhagic stroke and restricted mobility, similar recommendations were made for VTE prevention, except to start pharmacologic treatment between days 2 and 4 of the hospital stay. However, if there is a bleeding concern, intermittent pneumatic compression devices are favored over pharmacologic prophylaxis. In all patients for whom pharmacologic prevention is utilized, prophylactic LMWH is preferred over UFH.
Secondary stroke prevention is addressed, with 2012 guidelines outlining a preference for clopidogrel or aspirin/extended-release dipyridamole rather than aspirin or cilostazol in patients with a history of noncardioembolic ischemic stroke or TIA. Oral anticoagulation is preferred in patients with a history of stroke or TIA with afib over aspirin alone, aspirin plus clopidogrel, or no antithrombotic therapy. Of the available anticoagulants, the panel recommended dabigatran 150 mg twice daily over adjusted-dose warfarin.2 This recommendation is based on results from the RE-LY trial, which showed dabigatran as noninferior to warfarin in patients with nonvalvular afib without severe renal failure or advanced liver disease.3
For patients who have contraindications or choose not to initiate anticoagulation, the combination of aspirin (ASA) and clopidogrel is a reasonable alternative. Timing of the initiation of oral anticoagulation should be between one and two weeks after the stroke. Patients with extensive infarction or hemorrhagic transformation should delay starting oral anticoagulation, with no exact timeline. Long-term antithrombotic therapy is contraindicated in patients with history of a symptomatic primary intracerebral hemorrhage.2 New guidelines also recommend full anticoagulation for patients with symptomatic cerebral venous sinus thrombosis.
The panel did not make any recommendations regarding statin usage. In several studies, findings showed that statins reduced infarct size and had improved outcome in all stroke types.4
Analysis
Prior to the 2012 update, the last guideline for antithrombotic and thrombolytic therapy for ischemic stroke was published by the ACCP in the June 2008 issue of Chest.5 Dating back to 2001, medications included r-tPA administration within three hours of stroke symptom onset, and aspirin, clopidogrel, or a com bination of aspirin and extended-release dipyridamole for stroke prophylaxis.
The management of stroke continues to focus on early intervention and secondary prevention. Thrombolytic therapy is an effective treatment of acute ischemic stroke if given within the narrow window from onset of stroke symptoms up to 4.5 hours, with the goal of treatment within a three-hour window. Beyond this time constraint, the risk outweighs the benefit of using r-tPA except in the case of intra-arterial r-tPA administration for proximal cerebral artery occlusion.
In 2010, a meta-analysis supported this by showing that the risk of death increased significantly in patients receiving r-tPA beyond 4.5 hours. Therefore, antiplatelet therapy is the best alternative for patients ineligible for thrombolytic therapy.6 Even so, that study offered little data for patients with mechanical heart valves or intracardiac thrombi. Thus, the choice for acute anticoagulation therapy is variable and uncertain. If the hemorrhagic risk is low, anticoagulation can be considered in this subgroup, but no specific guideline endorsement was made.
In 2011, the AHA/ASA published an updated treatment guideline for patients with stroke or TIA. This was an update to 2007 guidelines that outlined the early management of ischemic stroke and affirmed the benefit of IV r-tPA at 4.5 hours for the treatment of stroke.7 Of note, IV r-tPA is only FDA-approved for treatment of acute ischemic stroke within the previously recommended three-hour period from symptom onset.
Aspirin has been found to be effective in both early treatment of acute ischemic stroke and secondary prevention. The CAST trial showed a statistically significant rate of reduction of nonfatal strokes with the use of aspirin. Other antiplatelet agents, including clopidogrel and dipyridamole, can be used. The FASTER trial compared aspirin alone versus aspirin plus clopidogrel, with no difference in outcome measures, although the MATCH trial found a larger risk of hemorrhagic and bleeding complications in the acetylsalicylic acid (ASA)-plus-clopidogrel group.6,7
In TIA or stroke patients, clopidogrel is not superior to ASA in preventing recurrent stroke. However, patients who have peripheral artery disease (PAD), previous coronary artery bypass grafting (CABG), insulin dependent diabetes mellitus (IDDM), or recurrent vascular events show a benefit of transitioning from ASA to clopidogrel for secondary long-term prevention. Clopidogrel or aspirin/extended-release dipyridamole is preferred over aspirin alone or cilostazol for long-term treatment in patients with a history of noncardioembolic ischemic stroke or TIA based on the PROFESS trial.2,7
HM Takeaways
The 2012 guidelines are a resource available to hospitalists for treating acute ischemic stroke either alone or with neurology consultation. These guidelines further define the timing of r-tPA and the use of both anticoagulation and antiplatelet therapy in the proper clinical settings.
In terms of VTE prevention, the guidelines recommend using LMWH preferentially over UH, except in patients at risk for rebleeding. The clinician should be aware of the treatment considerations for secondary prevention, noting the primary role of aspirin therapy in ischemic stroke with consideration of other agents (i.e. clopidogrel) in select populations.
Drs. Barr and Schumacher are hospitalists and assistant professors in the division of hospital medicine at The Ohio State University College of Medicine in Columbus.
References
Available at the-hospitalist.org.
John Nelson: Peformance Key to Federal Value-Based Payment Modifier Plan
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.