User login
Society of Hospital Medicine Joins Fight to Delay Medicare Cuts that Reduce Pay for Hospitalists
SHM has joined scores of medical societies pushing Congress to stop pending cuts to Medicare that would directly impact hospitalists.
Scheduled to go into effect at the start of the New Year, the cuts include sequestration, which would reduce hospitalists' Medicare payments by 2%, and slash funding to the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC). This is in addition to a 27% cut to Medicare physician payment rates resulting from Medicare's sustainable growth rate (SGR) formula.
In a letter last month to congressional leaders [PDF], and an accompanying note to society members, SHM said hospitalists need to lobby legislators "to find a reasonable and measured solution to deficit reduction that does not include arbitrary across-the-board cuts to Medicare providers."
"Congress needs to know we're not happy," says SHM board member Eric Siegal, MD, SFHM, board liaison SHM's Public Policy Committee. "The only way that we are going to get them to change their behavior is if enough of us mobilize, and make enough noise to make it clear that we are not going to stand for this anymore."
Dr. Siegal says that because Congress has repeatedly delayed draconian cuts, there is a general consensus that another delay is likely. But Dr. Siegal also notes lobbying is still necessary to ensure that will happen. SHM has previously supported a meaningful replacement to the SGR, which has yet to receive significant action in Congress.
"What the entire healthcare community needs to push for is a solution," Dr. Siegal adds. "It's very hard to develop any kind of a strategy for how you're going to deliver care if every X number of months you have to worry [whether] you're going to take a massive cut in your compensation."
SHM has joined scores of medical societies pushing Congress to stop pending cuts to Medicare that would directly impact hospitalists.
Scheduled to go into effect at the start of the New Year, the cuts include sequestration, which would reduce hospitalists' Medicare payments by 2%, and slash funding to the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC). This is in addition to a 27% cut to Medicare physician payment rates resulting from Medicare's sustainable growth rate (SGR) formula.
In a letter last month to congressional leaders [PDF], and an accompanying note to society members, SHM said hospitalists need to lobby legislators "to find a reasonable and measured solution to deficit reduction that does not include arbitrary across-the-board cuts to Medicare providers."
"Congress needs to know we're not happy," says SHM board member Eric Siegal, MD, SFHM, board liaison SHM's Public Policy Committee. "The only way that we are going to get them to change their behavior is if enough of us mobilize, and make enough noise to make it clear that we are not going to stand for this anymore."
Dr. Siegal says that because Congress has repeatedly delayed draconian cuts, there is a general consensus that another delay is likely. But Dr. Siegal also notes lobbying is still necessary to ensure that will happen. SHM has previously supported a meaningful replacement to the SGR, which has yet to receive significant action in Congress.
"What the entire healthcare community needs to push for is a solution," Dr. Siegal adds. "It's very hard to develop any kind of a strategy for how you're going to deliver care if every X number of months you have to worry [whether] you're going to take a massive cut in your compensation."
SHM has joined scores of medical societies pushing Congress to stop pending cuts to Medicare that would directly impact hospitalists.
Scheduled to go into effect at the start of the New Year, the cuts include sequestration, which would reduce hospitalists' Medicare payments by 2%, and slash funding to the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC). This is in addition to a 27% cut to Medicare physician payment rates resulting from Medicare's sustainable growth rate (SGR) formula.
In a letter last month to congressional leaders [PDF], and an accompanying note to society members, SHM said hospitalists need to lobby legislators "to find a reasonable and measured solution to deficit reduction that does not include arbitrary across-the-board cuts to Medicare providers."
"Congress needs to know we're not happy," says SHM board member Eric Siegal, MD, SFHM, board liaison SHM's Public Policy Committee. "The only way that we are going to get them to change their behavior is if enough of us mobilize, and make enough noise to make it clear that we are not going to stand for this anymore."
Dr. Siegal says that because Congress has repeatedly delayed draconian cuts, there is a general consensus that another delay is likely. But Dr. Siegal also notes lobbying is still necessary to ensure that will happen. SHM has previously supported a meaningful replacement to the SGR, which has yet to receive significant action in Congress.
"What the entire healthcare community needs to push for is a solution," Dr. Siegal adds. "It's very hard to develop any kind of a strategy for how you're going to deliver care if every X number of months you have to worry [whether] you're going to take a massive cut in your compensation."
Penalties for Hospitals with Excessive Readmissions Take Effect
The new era of penalizing hospitals for higher-than-predicted 30-day avoidable readmissions rates has begun. Under the federal Hospital Readmissions Reduction Program, some calculate a hospital's excessive readmissions rate for each applicable condition.
Penalties for the current fiscal year—FY 2013, which began Oct. 1, 2012—will be based on discharges that occurred during the three-year period from July 1, 2008, to June 30, 2011, according to the program guidelines. For hospitals that don't improve, the penalty grows to a maximum 2% next year (FY14) and 3% in FY15.
Hospitalists are not penalized directly for readmissions, and many hospitalists are wondering about the extent to which they're responsible for a readmission after the patient leaves the hospital, notes Mark Williams, MD, FACP, MHM, chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. Williams is the principal investigator of SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions), one of several national quality initiatives that teach hospitals and other healthcare providers how to improve transitions of care through such techniques as patient coaching and community partnerships.
"These new penalties mean that hospitals will start talking to their physicians about readmissions, and looking for methods to incentivize the hospitalists to get involved in preventing them," Dr. Williams says.
The new era of penalizing hospitals for higher-than-predicted 30-day avoidable readmissions rates has begun. Under the federal Hospital Readmissions Reduction Program, some calculate a hospital's excessive readmissions rate for each applicable condition.
Penalties for the current fiscal year—FY 2013, which began Oct. 1, 2012—will be based on discharges that occurred during the three-year period from July 1, 2008, to June 30, 2011, according to the program guidelines. For hospitals that don't improve, the penalty grows to a maximum 2% next year (FY14) and 3% in FY15.
Hospitalists are not penalized directly for readmissions, and many hospitalists are wondering about the extent to which they're responsible for a readmission after the patient leaves the hospital, notes Mark Williams, MD, FACP, MHM, chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. Williams is the principal investigator of SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions), one of several national quality initiatives that teach hospitals and other healthcare providers how to improve transitions of care through such techniques as patient coaching and community partnerships.
"These new penalties mean that hospitals will start talking to their physicians about readmissions, and looking for methods to incentivize the hospitalists to get involved in preventing them," Dr. Williams says.
The new era of penalizing hospitals for higher-than-predicted 30-day avoidable readmissions rates has begun. Under the federal Hospital Readmissions Reduction Program, some calculate a hospital's excessive readmissions rate for each applicable condition.
Penalties for the current fiscal year—FY 2013, which began Oct. 1, 2012—will be based on discharges that occurred during the three-year period from July 1, 2008, to June 30, 2011, according to the program guidelines. For hospitals that don't improve, the penalty grows to a maximum 2% next year (FY14) and 3% in FY15.
Hospitalists are not penalized directly for readmissions, and many hospitalists are wondering about the extent to which they're responsible for a readmission after the patient leaves the hospital, notes Mark Williams, MD, FACP, MHM, chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago.
Dr. Williams is the principal investigator of SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions), one of several national quality initiatives that teach hospitals and other healthcare providers how to improve transitions of care through such techniques as patient coaching and community partnerships.
"These new penalties mean that hospitals will start talking to their physicians about readmissions, and looking for methods to incentivize the hospitalists to get involved in preventing them," Dr. Williams says.
Rules of Engagement Necessary for Comanagement of Orthopedic Patients
One of our providers wants to use adult hospitalists for coverage of inpatient orthopedic surgery patients. Is this acceptable practice? Are there qualifiers?
–Libby Gardner
Dr. Hospitalist responds:
Let’s see how far we can tackle this open-ended question. There has been lots of discussion on the topic of comanagement in the past by people eminently more qualified than I am. Still, it never hurts to take a fresh look at things.
For one, on the subject of admissions, I am a firm believer that hospitalists should admit all adult hip fractures. The overwhelming majority of the time, these patients are elderly with comorbid conditions. Sure, they are going to get their hip fixed, because the alternative is usually unacceptable, but some thought needs to go into the process. The orthopedic surgeon sees a hip that needs fixing and not much else. When issues like renal failure, afib, CHF, prior DVT, or dementia are present, hospitalists should take charge of the case. It is the best way to ensure that the patient receives optimal medical care and the documentation that goes along with it. I love our orthopedic surgeons, but I don’t want them primarily admitting, managing, and discharging my elderly patients. Let the surgeon do what they do best, which is operate, and leave the rest to us.
On the subject of orthopedic trauma, I take the exact opposite tack—this is not something for which I or most of my colleagues have expertise. A young, healthy patient with trauma should be admitted by the orthopedic service; that patient population’s complications are much more likely to be directly related to their trauma.
When it comes to elective surgery, when the admitting surgeon (orthopedic or otherwise) wants the help of a hospitalist, then I think it is of paramount importance to have clear “rules of engagement.” I think with good expectations, you can have a fantastic working relationship with your surgeons. Without them, it becomes a nightmare.
Here are my HM group’s rules for elective orthopedic surgery:
- Orthopedics handles all pain medications and VTE prophylaxis, including discharge prescriptions.
- Medicine handles all admit and discharge medication reconciliation (“med rec”).
- There is shared discussion on:
- Need for transfusion; and
- The VTE prophylaxis when a patient already is on chronic anticoagulation.
We do not vary from this protocol. I never adjust a patient’s pain medications. Even the floor nurses know this. Because I’m doing the admit med rec, it also means that the patient doesn’t have their HCTZ continued after 600cc of EBL and spinal anesthesia.
The system works because the rules are clear and the communication is consistent. This does not mean that we cover the orthopedic service at night. They are equally responsible for their patients under the items outlined above. In my view—and this might sound simplistic—the surgeon caused the post-op pain, so they should be responsible for managing it. On VTE prophylaxis, I might take a more nuanced view, but for our surgeons, they own the wound and the post-op follow-up, so they get the choice on what agent to use.
Would I accept an arrangement in which I covered all the orthopedic issues out of regular hours? Nope—not when they have primary responsibility for the case; they should always be directly available to the nurse. I think that anything else would be a system ripe for abuse.
Our exact rules will not work for every situation, but I would strongly encourage the two basic tenets from above: No. 1, the hospitalist should primarily admit and manage elderly hip fractures, and No. 2, clear rules of engagement should be established with your orthopedic or surgery group. It’s a discussion worth having during daylight hours, because trying to figure out the rules at 3 in the morning rarely ends well.
One of our providers wants to use adult hospitalists for coverage of inpatient orthopedic surgery patients. Is this acceptable practice? Are there qualifiers?
–Libby Gardner
Dr. Hospitalist responds:
Let’s see how far we can tackle this open-ended question. There has been lots of discussion on the topic of comanagement in the past by people eminently more qualified than I am. Still, it never hurts to take a fresh look at things.
For one, on the subject of admissions, I am a firm believer that hospitalists should admit all adult hip fractures. The overwhelming majority of the time, these patients are elderly with comorbid conditions. Sure, they are going to get their hip fixed, because the alternative is usually unacceptable, but some thought needs to go into the process. The orthopedic surgeon sees a hip that needs fixing and not much else. When issues like renal failure, afib, CHF, prior DVT, or dementia are present, hospitalists should take charge of the case. It is the best way to ensure that the patient receives optimal medical care and the documentation that goes along with it. I love our orthopedic surgeons, but I don’t want them primarily admitting, managing, and discharging my elderly patients. Let the surgeon do what they do best, which is operate, and leave the rest to us.
On the subject of orthopedic trauma, I take the exact opposite tack—this is not something for which I or most of my colleagues have expertise. A young, healthy patient with trauma should be admitted by the orthopedic service; that patient population’s complications are much more likely to be directly related to their trauma.
When it comes to elective surgery, when the admitting surgeon (orthopedic or otherwise) wants the help of a hospitalist, then I think it is of paramount importance to have clear “rules of engagement.” I think with good expectations, you can have a fantastic working relationship with your surgeons. Without them, it becomes a nightmare.
Here are my HM group’s rules for elective orthopedic surgery:
- Orthopedics handles all pain medications and VTE prophylaxis, including discharge prescriptions.
- Medicine handles all admit and discharge medication reconciliation (“med rec”).
- There is shared discussion on:
- Need for transfusion; and
- The VTE prophylaxis when a patient already is on chronic anticoagulation.
We do not vary from this protocol. I never adjust a patient’s pain medications. Even the floor nurses know this. Because I’m doing the admit med rec, it also means that the patient doesn’t have their HCTZ continued after 600cc of EBL and spinal anesthesia.
The system works because the rules are clear and the communication is consistent. This does not mean that we cover the orthopedic service at night. They are equally responsible for their patients under the items outlined above. In my view—and this might sound simplistic—the surgeon caused the post-op pain, so they should be responsible for managing it. On VTE prophylaxis, I might take a more nuanced view, but for our surgeons, they own the wound and the post-op follow-up, so they get the choice on what agent to use.
Would I accept an arrangement in which I covered all the orthopedic issues out of regular hours? Nope—not when they have primary responsibility for the case; they should always be directly available to the nurse. I think that anything else would be a system ripe for abuse.
Our exact rules will not work for every situation, but I would strongly encourage the two basic tenets from above: No. 1, the hospitalist should primarily admit and manage elderly hip fractures, and No. 2, clear rules of engagement should be established with your orthopedic or surgery group. It’s a discussion worth having during daylight hours, because trying to figure out the rules at 3 in the morning rarely ends well.
One of our providers wants to use adult hospitalists for coverage of inpatient orthopedic surgery patients. Is this acceptable practice? Are there qualifiers?
–Libby Gardner
Dr. Hospitalist responds:
Let’s see how far we can tackle this open-ended question. There has been lots of discussion on the topic of comanagement in the past by people eminently more qualified than I am. Still, it never hurts to take a fresh look at things.
For one, on the subject of admissions, I am a firm believer that hospitalists should admit all adult hip fractures. The overwhelming majority of the time, these patients are elderly with comorbid conditions. Sure, they are going to get their hip fixed, because the alternative is usually unacceptable, but some thought needs to go into the process. The orthopedic surgeon sees a hip that needs fixing and not much else. When issues like renal failure, afib, CHF, prior DVT, or dementia are present, hospitalists should take charge of the case. It is the best way to ensure that the patient receives optimal medical care and the documentation that goes along with it. I love our orthopedic surgeons, but I don’t want them primarily admitting, managing, and discharging my elderly patients. Let the surgeon do what they do best, which is operate, and leave the rest to us.
On the subject of orthopedic trauma, I take the exact opposite tack—this is not something for which I or most of my colleagues have expertise. A young, healthy patient with trauma should be admitted by the orthopedic service; that patient population’s complications are much more likely to be directly related to their trauma.
When it comes to elective surgery, when the admitting surgeon (orthopedic or otherwise) wants the help of a hospitalist, then I think it is of paramount importance to have clear “rules of engagement.” I think with good expectations, you can have a fantastic working relationship with your surgeons. Without them, it becomes a nightmare.
Here are my HM group’s rules for elective orthopedic surgery:
- Orthopedics handles all pain medications and VTE prophylaxis, including discharge prescriptions.
- Medicine handles all admit and discharge medication reconciliation (“med rec”).
- There is shared discussion on:
- Need for transfusion; and
- The VTE prophylaxis when a patient already is on chronic anticoagulation.
We do not vary from this protocol. I never adjust a patient’s pain medications. Even the floor nurses know this. Because I’m doing the admit med rec, it also means that the patient doesn’t have their HCTZ continued after 600cc of EBL and spinal anesthesia.
The system works because the rules are clear and the communication is consistent. This does not mean that we cover the orthopedic service at night. They are equally responsible for their patients under the items outlined above. In my view—and this might sound simplistic—the surgeon caused the post-op pain, so they should be responsible for managing it. On VTE prophylaxis, I might take a more nuanced view, but for our surgeons, they own the wound and the post-op follow-up, so they get the choice on what agent to use.
Would I accept an arrangement in which I covered all the orthopedic issues out of regular hours? Nope—not when they have primary responsibility for the case; they should always be directly available to the nurse. I think that anything else would be a system ripe for abuse.
Our exact rules will not work for every situation, but I would strongly encourage the two basic tenets from above: No. 1, the hospitalist should primarily admit and manage elderly hip fractures, and No. 2, clear rules of engagement should be established with your orthopedic or surgery group. It’s a discussion worth having during daylight hours, because trying to figure out the rules at 3 in the morning rarely ends well.
Physician Value-Based Payment Initiative Would Change Medicare Reimbursement
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
The healthcare market is saturated with fee-for-service reimbursement schemes. The Bureau of Labor Statistics estimates that 78% of employer-sponsored health insurance plans are some type of fee-for-service plan.1 In Medicare, about 75% of beneficiaries use the traditional fee-for-service program.2 Fee-for-service denotes that payments are made on individual services, billed separately, irrespective of outcome and, in some cases, necessity.
The physician value-based payment modifier (VBPM) is an initiative that will begin shifting Medicare reimbursement for physicians away from fee-for-service schemes and toward some type of pay-for-performance model.
For hospitalists, this will have a marked impact on HM practice and might have reverberating effects in the field itself.
Established under the 2008 Medicare Improvements for Patients and Providers Act (MIPPA) and expanded under the 2010 Affordable Care Act (ACA), the VBPM will be applied to all physicians by 2017.
The VBPM program is the physician version of hospital value-based purchasing; both are designed to move the basis of payment toward the quality of care delivered, not simply for the quantity of services rendered. By linking quality measurement with payment, the Centers for Medicare & Medicaid Services (CMS) hopes to start paying for value.
While legislation required the creation of pay-for-performance programs for physicians and hospitals, the design and implementation details have been delegated to CMS, part of the U.S. Department of Health and Human Services. Thus, CMS has oversight on the specifics of the program. These specifics are promulgated through the federal rulemaking process, which requires such agencies as CMS to seek input from the general public—as well as medical societies, including SHM—as rules are proposed and finalized. Generally, there is a 30- to 90-day period after a rule is proposed for public comment, after which a rule will be finalized.
For the VBPM and its performance period starting next year, the guidelines were published for public comment in a proposed rule for the fiscal-year 2013 Physician Fee Schedule. The final rule, which will provide more definitive guidance for hospitalists, is slated to come out in November.
Hospitalists should be cognizant of how quality measurements apply to their practice and find ways to participate in such quality measurement programs as the Physician Quality Reporting System (PQRS). PQRS will become the evaluative backbone of the VBPM. It is imperative that hospitalists stay abreast of these transformative changes in the healthcare system and work to ensure that their practice patterns, which fill critical gaps in patient care, are adequately represented in these changes.
Although legislation and legislative advocacy are undoubtedly important features of policymaking, participating in the federal rulemaking process is a vital tool for helping to shape healthcare. SHM actively pursues regulatory issues in order to advocate for hospitalists and their patients. The experiences and expertise of members are critical for SHM to be able to accurately represent the specialty.
By staying informed on health policy and being engaged with SHM, members can provide invaluable perspectives to help transform the field and revolutionize the healthcare system.
Josh Lapps is SHM's government relations specialist.
References
- U.S. Bureau of Labor Statistics. Program Perspectives: fee-for-service plans. U.S. Bureau of Labor Statistics website. Available at: http://www.bls.gov/opub/perspectives/program_perspectives_vol2_issue5.pdf. Accessed Aug. 15, 2012.
- The Henry J. Kaiser Family Foundation. Medicare at a glance. The Henry J. Kaiser Family Foundation website. Available at: http://www.kff.org/medicare/upload/1066_11.pdf. Accessed Aug. 29, 2012.
SHM's Quality and Safety Educators Academy: Preparing Successful Residents and Students
Tomorrow’s hospital will be increasingly oriented around quality and safety; today’s students must prepare to thrive in that environment.
That’s the philosophy behind SHM’s Quality and Safety Educators Academy (QSEA). Now in its second year, the two-and-a-half-day academy trains hospitalist educators to teach medical students and residents about quality and safety.
QSEA, co-hosted by SHM and the Alliance for Academic Internal Medicine, is March 7-9 at Tempe Mission Palms in Tempe, Ariz. Registration is now open at www.hospitalmedicine.org/qsea.
“In order to be successful, we must teach medical students and residents about these goals so that they incorporate them into their practice from day one,” says Jennifer S. Myers, MD, associate professor of clinical medicine, patient safety officer, and director of quality and safety education at the University of Pennsylvania’s Perelman School of Medicine in Philadelphia.
Progress in quality improvement (QI) and patient safety has been slow because many current physicians aren’t familiar with the materials, creating what Dr. Myers refers to as a “faculty development” gap. QSEA is the first and only academy designed to close that gap for hospitalist faculty by giving them specific knowledge, skills, a take-home toolkit, and a brand-new peer network of other quality-minded educators.
A major part of the academy is dedicated to the career trajectory of educators and, in Dr. Myers’ words, “how a hospitalist can be successful in making quality and safety education a career path.”
Despite the serious topics, she also is quick to point out that the academy is anything but dry.
“You have to experience it,” she says. “We have a ton of fun. You will leave with a new family.”
At the end of the inaugural QSEA, the faculty and course directors were so energized by the attendees that they formed a human pyramid. “It was a great moment,” she says.
Dr. Myers says she still enjoys receiving email from QSEA attendees about their new adventures in quality and safety education. “This makes it all worth it and why the QSEA team does this work,” she says.
Tomorrow’s hospital will be increasingly oriented around quality and safety; today’s students must prepare to thrive in that environment.
That’s the philosophy behind SHM’s Quality and Safety Educators Academy (QSEA). Now in its second year, the two-and-a-half-day academy trains hospitalist educators to teach medical students and residents about quality and safety.
QSEA, co-hosted by SHM and the Alliance for Academic Internal Medicine, is March 7-9 at Tempe Mission Palms in Tempe, Ariz. Registration is now open at www.hospitalmedicine.org/qsea.
“In order to be successful, we must teach medical students and residents about these goals so that they incorporate them into their practice from day one,” says Jennifer S. Myers, MD, associate professor of clinical medicine, patient safety officer, and director of quality and safety education at the University of Pennsylvania’s Perelman School of Medicine in Philadelphia.
Progress in quality improvement (QI) and patient safety has been slow because many current physicians aren’t familiar with the materials, creating what Dr. Myers refers to as a “faculty development” gap. QSEA is the first and only academy designed to close that gap for hospitalist faculty by giving them specific knowledge, skills, a take-home toolkit, and a brand-new peer network of other quality-minded educators.
A major part of the academy is dedicated to the career trajectory of educators and, in Dr. Myers’ words, “how a hospitalist can be successful in making quality and safety education a career path.”
Despite the serious topics, she also is quick to point out that the academy is anything but dry.
“You have to experience it,” she says. “We have a ton of fun. You will leave with a new family.”
At the end of the inaugural QSEA, the faculty and course directors were so energized by the attendees that they formed a human pyramid. “It was a great moment,” she says.
Dr. Myers says she still enjoys receiving email from QSEA attendees about their new adventures in quality and safety education. “This makes it all worth it and why the QSEA team does this work,” she says.
Tomorrow’s hospital will be increasingly oriented around quality and safety; today’s students must prepare to thrive in that environment.
That’s the philosophy behind SHM’s Quality and Safety Educators Academy (QSEA). Now in its second year, the two-and-a-half-day academy trains hospitalist educators to teach medical students and residents about quality and safety.
QSEA, co-hosted by SHM and the Alliance for Academic Internal Medicine, is March 7-9 at Tempe Mission Palms in Tempe, Ariz. Registration is now open at www.hospitalmedicine.org/qsea.
“In order to be successful, we must teach medical students and residents about these goals so that they incorporate them into their practice from day one,” says Jennifer S. Myers, MD, associate professor of clinical medicine, patient safety officer, and director of quality and safety education at the University of Pennsylvania’s Perelman School of Medicine in Philadelphia.
Progress in quality improvement (QI) and patient safety has been slow because many current physicians aren’t familiar with the materials, creating what Dr. Myers refers to as a “faculty development” gap. QSEA is the first and only academy designed to close that gap for hospitalist faculty by giving them specific knowledge, skills, a take-home toolkit, and a brand-new peer network of other quality-minded educators.
A major part of the academy is dedicated to the career trajectory of educators and, in Dr. Myers’ words, “how a hospitalist can be successful in making quality and safety education a career path.”
Despite the serious topics, she also is quick to point out that the academy is anything but dry.
“You have to experience it,” she says. “We have a ton of fun. You will leave with a new family.”
At the end of the inaugural QSEA, the faculty and course directors were so energized by the attendees that they formed a human pyramid. “It was a great moment,” she says.
Dr. Myers says she still enjoys receiving email from QSEA attendees about their new adventures in quality and safety education. “This makes it all worth it and why the QSEA team does this work,” she says.
Win Whitcomb: Hospital Readmissions Penalties Start Now
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
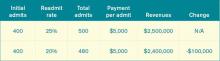
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Guidelines Drive Optimal Care for Heart Failure Patients
Cardiologists aren’t shy about repeating it: guidelines, guidelines, guidelines. That is, follow them.
“Evidence-based, guideline-driven optimal care for heart failure truly is beneficial,” Dr. Yancy says. “Every effort should be made to strive to achieve ideal thresholds and meeting best practices.”
There is now compelling evidence that, for patients with heart failure, the higher the degree of adherence to Class I-recommended therapies, the greater the reduction in 24-month mortality risk.5
“It would seem as if practicing best quality is almost a perfunctory statement, but consistently, when we look at surveys of quality improvement and adherence to evidence-based strategies, persistent gaps remain in the broader community,” Dr. Yancy says. “We know what we need to do. We’re still striving to get closer and closer to optimal care.”
Dr. Harold says the guidelines are there to make things simpler. So take advantage of them.
“If anything, hospitalists tend to be ahead of most other groups in terms of knowing evidence-based pathways and really tracking very specific protocols,” he says. “I think one of the advantages of hospitalist care is very often, it is guideline-driven. You have less variation in terms of care and quality outcomes.”
Cardiologists aren’t shy about repeating it: guidelines, guidelines, guidelines. That is, follow them.
“Evidence-based, guideline-driven optimal care for heart failure truly is beneficial,” Dr. Yancy says. “Every effort should be made to strive to achieve ideal thresholds and meeting best practices.”
There is now compelling evidence that, for patients with heart failure, the higher the degree of adherence to Class I-recommended therapies, the greater the reduction in 24-month mortality risk.5
“It would seem as if practicing best quality is almost a perfunctory statement, but consistently, when we look at surveys of quality improvement and adherence to evidence-based strategies, persistent gaps remain in the broader community,” Dr. Yancy says. “We know what we need to do. We’re still striving to get closer and closer to optimal care.”
Dr. Harold says the guidelines are there to make things simpler. So take advantage of them.
“If anything, hospitalists tend to be ahead of most other groups in terms of knowing evidence-based pathways and really tracking very specific protocols,” he says. “I think one of the advantages of hospitalist care is very often, it is guideline-driven. You have less variation in terms of care and quality outcomes.”
Cardiologists aren’t shy about repeating it: guidelines, guidelines, guidelines. That is, follow them.
“Evidence-based, guideline-driven optimal care for heart failure truly is beneficial,” Dr. Yancy says. “Every effort should be made to strive to achieve ideal thresholds and meeting best practices.”
There is now compelling evidence that, for patients with heart failure, the higher the degree of adherence to Class I-recommended therapies, the greater the reduction in 24-month mortality risk.5
“It would seem as if practicing best quality is almost a perfunctory statement, but consistently, when we look at surveys of quality improvement and adherence to evidence-based strategies, persistent gaps remain in the broader community,” Dr. Yancy says. “We know what we need to do. We’re still striving to get closer and closer to optimal care.”
Dr. Harold says the guidelines are there to make things simpler. So take advantage of them.
“If anything, hospitalists tend to be ahead of most other groups in terms of knowing evidence-based pathways and really tracking very specific protocols,” he says. “I think one of the advantages of hospitalist care is very often, it is guideline-driven. You have less variation in terms of care and quality outcomes.”
CMS Rule on Use of Electronic Health Records Gets Mixed Reviews
The Centers for Medicare & Medicaid Services' (CMS) recently announced final rule [PDF] on Stage 2 compliance for "meaningful use" of electronic health records (EHR) has been met with mixed reactions among most providers and trade groups, including SHM which voiced its concerns back in July.
"It's the classic government mixed bag," says Brenda Pawlak, director of Manatt Health Solutions, a division of New York City law firm Manatt, Phelps & Phillips.
Physician groups, including SHM and the Medical Group Management Association (MGMA), have lauded CMS for pushing back the implementation of Stage 2 meaningful-use requirements to 2014 from 2013. They also praised the agency for halving to 5% the percentage of a practice's patients who interact with an online portal. But for some providers, even the 5% threshold will be difficult to meet. And because physicians have to meet all requirements to qualify for incentive bonuses, the issue could loom large for specific groups.
"I don't think the 10% to 5% is a substantive change," Pawlak says.
Although most hospitalists are not directly subject to "meaningful use" requirements, many are heavily involved with assisting their institutions with implementation. SHM, which voiced its concerns in a July letter to CMS, is following this topic closely.
Some physician groups also lamented that the deadline for Stage 1 compliance remains unchanged at 2015. As physicians and provider groups attempt to comply with myriad rules, Pawlak says, meeting the 5% threshold will emerge as more burdensome as the deadline approaches. Still, CMS and federal officials say, the final rule will help nudge the healthcare system further into the digital age.
"The big message here is the push on standards-based interoperability of information," says Farzad Mostashari, MD, ScM, of the U.S. Department of Health and Human Services' Office of the National Coordinator for Health Information Technology. "We are staying on course with the road map that we set in Stage 1."
The Centers for Medicare & Medicaid Services' (CMS) recently announced final rule [PDF] on Stage 2 compliance for "meaningful use" of electronic health records (EHR) has been met with mixed reactions among most providers and trade groups, including SHM which voiced its concerns back in July.
"It's the classic government mixed bag," says Brenda Pawlak, director of Manatt Health Solutions, a division of New York City law firm Manatt, Phelps & Phillips.
Physician groups, including SHM and the Medical Group Management Association (MGMA), have lauded CMS for pushing back the implementation of Stage 2 meaningful-use requirements to 2014 from 2013. They also praised the agency for halving to 5% the percentage of a practice's patients who interact with an online portal. But for some providers, even the 5% threshold will be difficult to meet. And because physicians have to meet all requirements to qualify for incentive bonuses, the issue could loom large for specific groups.
"I don't think the 10% to 5% is a substantive change," Pawlak says.
Although most hospitalists are not directly subject to "meaningful use" requirements, many are heavily involved with assisting their institutions with implementation. SHM, which voiced its concerns in a July letter to CMS, is following this topic closely.
Some physician groups also lamented that the deadline for Stage 1 compliance remains unchanged at 2015. As physicians and provider groups attempt to comply with myriad rules, Pawlak says, meeting the 5% threshold will emerge as more burdensome as the deadline approaches. Still, CMS and federal officials say, the final rule will help nudge the healthcare system further into the digital age.
"The big message here is the push on standards-based interoperability of information," says Farzad Mostashari, MD, ScM, of the U.S. Department of Health and Human Services' Office of the National Coordinator for Health Information Technology. "We are staying on course with the road map that we set in Stage 1."
The Centers for Medicare & Medicaid Services' (CMS) recently announced final rule [PDF] on Stage 2 compliance for "meaningful use" of electronic health records (EHR) has been met with mixed reactions among most providers and trade groups, including SHM which voiced its concerns back in July.
"It's the classic government mixed bag," says Brenda Pawlak, director of Manatt Health Solutions, a division of New York City law firm Manatt, Phelps & Phillips.
Physician groups, including SHM and the Medical Group Management Association (MGMA), have lauded CMS for pushing back the implementation of Stage 2 meaningful-use requirements to 2014 from 2013. They also praised the agency for halving to 5% the percentage of a practice's patients who interact with an online portal. But for some providers, even the 5% threshold will be difficult to meet. And because physicians have to meet all requirements to qualify for incentive bonuses, the issue could loom large for specific groups.
"I don't think the 10% to 5% is a substantive change," Pawlak says.
Although most hospitalists are not directly subject to "meaningful use" requirements, many are heavily involved with assisting their institutions with implementation. SHM, which voiced its concerns in a July letter to CMS, is following this topic closely.
Some physician groups also lamented that the deadline for Stage 1 compliance remains unchanged at 2015. As physicians and provider groups attempt to comply with myriad rules, Pawlak says, meeting the 5% threshold will emerge as more burdensome as the deadline approaches. Still, CMS and federal officials say, the final rule will help nudge the healthcare system further into the digital age.
"The big message here is the push on standards-based interoperability of information," says Farzad Mostashari, MD, ScM, of the U.S. Department of Health and Human Services' Office of the National Coordinator for Health Information Technology. "We are staying on course with the road map that we set in Stage 1."
Hospitalists Play Integral Roles in HHS-Funded Innovation Projects
In May and June, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius in May and June announced 107 healthcare innovations grants to improve coordination of care and reduce costs. The grants, a provision of the Affordable Care Act (ACA), range from $1 million to $30 million. HHS anticipates that the projects will reduce healthcare spending by $254 million over the next three years and provide "new ideas on how to deliver better health, improved care, and lower costs to people enrolled in Medicare, Medicaid and [the] Children's Health Insurance Program (CHIP)."
Hospitalists played key roles in planning and developing several of the projects. Common themes include coordination and integration of services, promotion of community collaborations, integrating behavioral and physical care, and the use of telemedicine—many of the same approaches utilized by SHM's Project BOOST and other national initiatives for preventing unnecessary readmissions.
In Atlanta, Emory University's Center for Critical Care received a $10.7 million grant to deploy 40 nurse practitioners (NPs) and physician assistants (PAs) trained in critical care to underserved and rural ICUs in Georgia. In many of the targeted hospitals, hospitalists manage patients in the ICU, but this program brings an additional layer of staffing and expertise to the care, allowing patients to stay in their beds rather than having to be transferred, says Daniel Owens, MBA, the center’s director of operations and senior administrator of the division of hospital medicine at Emory.
The project will bring NPs and PAs from participating hospitals to Emory for an intensive, six-month, critical-care residency. "If they don't have these folks, we'll help to identify staff for the jobs," he adds.
At Vanderbilt University Medical Center in Nashville, Tenn., a $2.4 million project to reduce rehospitalizations for a high-risk geriatric patients aims to close the gaps in care transitions between hospital, outpatient, post-acute, and extended-care settings, says Vanderbilt hospitalist Eduard Vasilevskis, MD. The project will employ transition advocates or coordinators in the hospital to improve communication at both ends, with evidence-based protocols to improve discharge planning. Long-term care providers will be offered Web-based training and video conferencing.
"The goal is to break the cycle of rehospitalization," says Dr. Vasilevskis, "but if patients need to come back to the hospital, there will be someone involved in their care who is familiar with the settings where they’ve come from."
Beth Israel Deaconess Medical Center (BIDMC) in Boston received $4.9 million for its Post-Acute Care Transitions program (PACT), which links the hospital to six affiliated primary care practices using a bundle of post-acute care interventions, care-transition specialists, and dedicated clinical pharmacists. Nurses remain in contact with patients by telephone for 30 days post-hospital discharge and coordinate the services of extended-care facilities and visiting nurses. Pharmacists perform in-hospital medication reconciliation and patient education, says hospitalist Lauren Doctoroff, MD, FHM. She and Julius Yang, MD, BIDMC medical director of inpatient quality, helped develop the pilot program, which began in August 2011.
"These care-transitions specialists offer us an added level of patient support and a different level of integration focused on risk assessment of such issues as social supports and problems with medical compliance, which can be used by the inpatient team to come up with the most rational and ideal discharge plan," Dr. Doctoroff says. "One of my colleagues said to me, ‘I feel so much better knowing there is this added level of support for patients after discharge.'"
The HHS grants reflect an important recognition that what happens to patients following discharge partly reflects what happens in the hospital but also depends on collaborations with post-acute providers, Dr. Doctoroff says.
"Hospitalists can't do everything, but they need their eye out of the hospital on post-acute providers in order to deliver the best care," she adds.
In May and June, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius in May and June announced 107 healthcare innovations grants to improve coordination of care and reduce costs. The grants, a provision of the Affordable Care Act (ACA), range from $1 million to $30 million. HHS anticipates that the projects will reduce healthcare spending by $254 million over the next three years and provide "new ideas on how to deliver better health, improved care, and lower costs to people enrolled in Medicare, Medicaid and [the] Children's Health Insurance Program (CHIP)."
Hospitalists played key roles in planning and developing several of the projects. Common themes include coordination and integration of services, promotion of community collaborations, integrating behavioral and physical care, and the use of telemedicine—many of the same approaches utilized by SHM's Project BOOST and other national initiatives for preventing unnecessary readmissions.
In Atlanta, Emory University's Center for Critical Care received a $10.7 million grant to deploy 40 nurse practitioners (NPs) and physician assistants (PAs) trained in critical care to underserved and rural ICUs in Georgia. In many of the targeted hospitals, hospitalists manage patients in the ICU, but this program brings an additional layer of staffing and expertise to the care, allowing patients to stay in their beds rather than having to be transferred, says Daniel Owens, MBA, the center’s director of operations and senior administrator of the division of hospital medicine at Emory.
The project will bring NPs and PAs from participating hospitals to Emory for an intensive, six-month, critical-care residency. "If they don't have these folks, we'll help to identify staff for the jobs," he adds.
At Vanderbilt University Medical Center in Nashville, Tenn., a $2.4 million project to reduce rehospitalizations for a high-risk geriatric patients aims to close the gaps in care transitions between hospital, outpatient, post-acute, and extended-care settings, says Vanderbilt hospitalist Eduard Vasilevskis, MD. The project will employ transition advocates or coordinators in the hospital to improve communication at both ends, with evidence-based protocols to improve discharge planning. Long-term care providers will be offered Web-based training and video conferencing.
"The goal is to break the cycle of rehospitalization," says Dr. Vasilevskis, "but if patients need to come back to the hospital, there will be someone involved in their care who is familiar with the settings where they’ve come from."
Beth Israel Deaconess Medical Center (BIDMC) in Boston received $4.9 million for its Post-Acute Care Transitions program (PACT), which links the hospital to six affiliated primary care practices using a bundle of post-acute care interventions, care-transition specialists, and dedicated clinical pharmacists. Nurses remain in contact with patients by telephone for 30 days post-hospital discharge and coordinate the services of extended-care facilities and visiting nurses. Pharmacists perform in-hospital medication reconciliation and patient education, says hospitalist Lauren Doctoroff, MD, FHM. She and Julius Yang, MD, BIDMC medical director of inpatient quality, helped develop the pilot program, which began in August 2011.
"These care-transitions specialists offer us an added level of patient support and a different level of integration focused on risk assessment of such issues as social supports and problems with medical compliance, which can be used by the inpatient team to come up with the most rational and ideal discharge plan," Dr. Doctoroff says. "One of my colleagues said to me, ‘I feel so much better knowing there is this added level of support for patients after discharge.'"
The HHS grants reflect an important recognition that what happens to patients following discharge partly reflects what happens in the hospital but also depends on collaborations with post-acute providers, Dr. Doctoroff says.
"Hospitalists can't do everything, but they need their eye out of the hospital on post-acute providers in order to deliver the best care," she adds.
In May and June, U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius in May and June announced 107 healthcare innovations grants to improve coordination of care and reduce costs. The grants, a provision of the Affordable Care Act (ACA), range from $1 million to $30 million. HHS anticipates that the projects will reduce healthcare spending by $254 million over the next three years and provide "new ideas on how to deliver better health, improved care, and lower costs to people enrolled in Medicare, Medicaid and [the] Children's Health Insurance Program (CHIP)."
Hospitalists played key roles in planning and developing several of the projects. Common themes include coordination and integration of services, promotion of community collaborations, integrating behavioral and physical care, and the use of telemedicine—many of the same approaches utilized by SHM's Project BOOST and other national initiatives for preventing unnecessary readmissions.
In Atlanta, Emory University's Center for Critical Care received a $10.7 million grant to deploy 40 nurse practitioners (NPs) and physician assistants (PAs) trained in critical care to underserved and rural ICUs in Georgia. In many of the targeted hospitals, hospitalists manage patients in the ICU, but this program brings an additional layer of staffing and expertise to the care, allowing patients to stay in their beds rather than having to be transferred, says Daniel Owens, MBA, the center’s director of operations and senior administrator of the division of hospital medicine at Emory.
The project will bring NPs and PAs from participating hospitals to Emory for an intensive, six-month, critical-care residency. "If they don't have these folks, we'll help to identify staff for the jobs," he adds.
At Vanderbilt University Medical Center in Nashville, Tenn., a $2.4 million project to reduce rehospitalizations for a high-risk geriatric patients aims to close the gaps in care transitions between hospital, outpatient, post-acute, and extended-care settings, says Vanderbilt hospitalist Eduard Vasilevskis, MD. The project will employ transition advocates or coordinators in the hospital to improve communication at both ends, with evidence-based protocols to improve discharge planning. Long-term care providers will be offered Web-based training and video conferencing.
"The goal is to break the cycle of rehospitalization," says Dr. Vasilevskis, "but if patients need to come back to the hospital, there will be someone involved in their care who is familiar with the settings where they’ve come from."
Beth Israel Deaconess Medical Center (BIDMC) in Boston received $4.9 million for its Post-Acute Care Transitions program (PACT), which links the hospital to six affiliated primary care practices using a bundle of post-acute care interventions, care-transition specialists, and dedicated clinical pharmacists. Nurses remain in contact with patients by telephone for 30 days post-hospital discharge and coordinate the services of extended-care facilities and visiting nurses. Pharmacists perform in-hospital medication reconciliation and patient education, says hospitalist Lauren Doctoroff, MD, FHM. She and Julius Yang, MD, BIDMC medical director of inpatient quality, helped develop the pilot program, which began in August 2011.
"These care-transitions specialists offer us an added level of patient support and a different level of integration focused on risk assessment of such issues as social supports and problems with medical compliance, which can be used by the inpatient team to come up with the most rational and ideal discharge plan," Dr. Doctoroff says. "One of my colleagues said to me, ‘I feel so much better knowing there is this added level of support for patients after discharge.'"
The HHS grants reflect an important recognition that what happens to patients following discharge partly reflects what happens in the hospital but also depends on collaborations with post-acute providers, Dr. Doctoroff says.
"Hospitalists can't do everything, but they need their eye out of the hospital on post-acute providers in order to deliver the best care," she adds.
Is ‘Meaningful Use’ Safe?
Earlier this summer, the Centers for Medicare & Medicaid Services (CMS) announced that more than 100,000 healthcare providers and 48% of all eligible hospitals are using electronic health records (EHRs) that meet federal standards, and they have benefited from federal incentive programs to do so.1
According to CMS acting administrator Marilyn Tavenner, meeting that provider goal makes 2012 the “Year of Meaningful Use.” She also says healthcare providers have recognized the potential of EHRs to cut down on paperwork, eliminate duplicate screenings and tests, and facilitate better, safer, patient-centered care.2
Belying CMS’ celebratory declarations, however, are concerns among experts that health information technology’s (HIT) actual use falls short of its promise—and might even endanger patients—due to shortcomings in system interoperability, safety, accountability, and other issues.
“Federal funding of IT was a step in the right direction, but it has also created a guaranteed customer base for electronic medical records, so vendors have less incentive to improve their products to meet clinicians needs,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, chair of SHsM’s IT Executive Committee and chief of hospital medicine at the University of New Mexico Health Sciences Center School of Medicine in Albuquerque. “We want systems that help us make better clinical decisions and allow us to work more efficiently. Unfortunately, many hospitalists are frustrated with existing HIT systems, knowing how much better they need to be. It can be a dangerous gamble to push rapid adoption of potentially unsafe systems in hospitals.”
Questioning HIT Safety
Health IT experts affirm that potential danger. Jerry Osheroff, MD, FACP, FACMI, principal and founder of TMIT Consulting LLC and former chief clinical informatics officer for Thomson Reuters Healthcare, says HIT “is most effective when it gets the right information to the right people, through the right channels, in the right format, at the right point in the workflow. The danger comes when it gets one of those five ‘rights’ wrong; that can lead to distraction, confusion, wasted time, missed improvement opportunities, and safety concerns.”
Last November, the Institute of Medicine (IOM) released a scathing critique of HIT’s current ability to ensure patient safety.3 As the federal government invests billions of dollars to encourage hospitals and healthcare providers to adopt HIT, the IOM report said, improvements in care and safety are not yet established, and little evidence exists that quantifies the magnitude of the risk associated with HIT problems—partly because many HIT vendors discourage providers from sharing patient-safety concerns with nondisclosure and “hold harmless” provisions in contracts that shift the liability of unsafe HIT features to care providers.3
The report also cautioned that serious errors involving these technologies—including medication dosing errors, failure to detect fatal illnesses, and treatment delays due to complex data interfaces and poor human-computer interactions or loss of data—have led to several reported patient deaths and injuries. Furthermore, there is no way to publicly track adverse outcomes because there is no systematic regulation or authority to collect, analyze, and disseminate such information.
The report concluded that the current state of safety and health IT is not acceptable and that regulation of the industry might be necessary because the private sector to date has not taken sufficient action on its own to improve HIT safety.
SHM applauds the IOM report as an overdue and direly needed call to action, Dr. Rogers says. SHM sent a letter to the U.S. Department of Health and Human Services underscoring the importance of the IOM report.
“In our practices, we have experienced the threats to patient safety outlined in the report: poor user-interface design, poor workflow, complex data interfaces, lack of system interoperability, and lack of sufficient vendor action to build safer products,” Dr. Rogers says.
“Lack of interoperability—preventing access to patient data from previous physician or other hospital visits—makes a mockery of a coordinated, patient-centered healthcare system,” says HIT researcher Ross Koppel, PhD, faculty member of University of Pennsylvania’s Sociology Department and School of Medicine.
Although Dr. Rogers acknowledges that HIT has the potential to revolutionize healthcare systems, boost quality and safety, and lower cost, he maintains that current HIT products fall short of those ambitious goals. “Vendors typically regard usability of their products as a convenience request by clinicians; any errors are regarded as training issues for physicians,” Dr. Rogers says. “But the way that data is presented on a screen matters—if it is difficult to input or retrieve data and leads to cognitive or process errors, that’s a product redesign issue for which vendors should be held accountable.”
Dr. Koppel says many HIT systems originated from billing system applications “and were not initially designed with the clinical perspective in mind. Hospitalists have to be particularly focused on usability of HIT systems when it comes to patient-safety impacts. They’re not the canary in the coal mine, they’re the miners—often the teachers guiding other clinicians on HIT use.”
Improvement Agenda
SHM fully supports many of the IOM’s recommendations to improve the safety and functionality of HIT systems, including these as stated in an email to its members:
- Remove contractual restrictions, promote public reporting of safety issues, and put a system in place for independent investigations that drive patient-safety improvement.
- Establish standards and a common infrastructure for “interoperable” data exchange across systems.
- Create dual accountability between vendors and providers to address safety concerns that might require
- changes in an IT product’s functionality or design.
- Promote research on usability and human-factors design, safer implementation, and sociotechnical systems associated with HIT.
- Promote education of safety, quality, and reliability principles in design and implementation of HIT among all levels of the workforce, including frontline clinicians and staff, hospital IT, and quality teams—as well as IT vendors themselves.
There also are ongoing efforts in the private sector to improve HIT system functionality. For example, the HIMSS CDS Guidebook Series, of which Dr. Osheroff is lead editor and author and Dr. Rogers is a contributing author, is a respected repository of information synthesizing and vetting critical guidance for the effective implementation of clinical decision support (CDS).
“We’re also working with Greg Maynard [senior vice president of SHM’s Center for Hospital Innovation & Improvement] to use the collaborative’s tools to disseminate clinical-decision-support best practices for improving VTE prophylaxis rates,” Dr. Osheroff notes.
Hospitalists, as central players in quality improvement (QI), standardization, and care coordination, are natural choices as HIT champions, with valuable insight into how HIT systems should be customized to accommodate workflows and order sets in an optimal fashion, Dr. Rogers says.
“As critical as we are about the status of current HIT systems, we believe that systems can be designed more effectively to meet our needs,” he says. “By adopting many of the improvements enumerated in the IOM report, hospitalists are uniquely positioned to advance HIT to help achieve the goals of safer, higher-quality, and more efficient care.”
Christopher Guadagnino is a freelance writer based in Philadelphia.
References
- Centers for Medicare & Medicaid Services. More than 100,000 health care providers paid for using electronic health records. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4383&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&sr. Accessed July 31, 2012.
- Centers for Medicare & Medicaid Services. 2012: the year of meaningful use. The CMS Blog website. Available at: http://blog.cms.gov/2012/03/23/2012-the-year-of-meaningful-use. Accessed July 18, 2012.
- Institute of Medicine of the National Academies. Health IT and patient safety: building safer systems for better care. Institute of Medicine of the National Academies website. Available at: http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx. Accessed July 14, 2012.
Earlier this summer, the Centers for Medicare & Medicaid Services (CMS) announced that more than 100,000 healthcare providers and 48% of all eligible hospitals are using electronic health records (EHRs) that meet federal standards, and they have benefited from federal incentive programs to do so.1
According to CMS acting administrator Marilyn Tavenner, meeting that provider goal makes 2012 the “Year of Meaningful Use.” She also says healthcare providers have recognized the potential of EHRs to cut down on paperwork, eliminate duplicate screenings and tests, and facilitate better, safer, patient-centered care.2
Belying CMS’ celebratory declarations, however, are concerns among experts that health information technology’s (HIT) actual use falls short of its promise—and might even endanger patients—due to shortcomings in system interoperability, safety, accountability, and other issues.
“Federal funding of IT was a step in the right direction, but it has also created a guaranteed customer base for electronic medical records, so vendors have less incentive to improve their products to meet clinicians needs,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, chair of SHsM’s IT Executive Committee and chief of hospital medicine at the University of New Mexico Health Sciences Center School of Medicine in Albuquerque. “We want systems that help us make better clinical decisions and allow us to work more efficiently. Unfortunately, many hospitalists are frustrated with existing HIT systems, knowing how much better they need to be. It can be a dangerous gamble to push rapid adoption of potentially unsafe systems in hospitals.”
Questioning HIT Safety
Health IT experts affirm that potential danger. Jerry Osheroff, MD, FACP, FACMI, principal and founder of TMIT Consulting LLC and former chief clinical informatics officer for Thomson Reuters Healthcare, says HIT “is most effective when it gets the right information to the right people, through the right channels, in the right format, at the right point in the workflow. The danger comes when it gets one of those five ‘rights’ wrong; that can lead to distraction, confusion, wasted time, missed improvement opportunities, and safety concerns.”
Last November, the Institute of Medicine (IOM) released a scathing critique of HIT’s current ability to ensure patient safety.3 As the federal government invests billions of dollars to encourage hospitals and healthcare providers to adopt HIT, the IOM report said, improvements in care and safety are not yet established, and little evidence exists that quantifies the magnitude of the risk associated with HIT problems—partly because many HIT vendors discourage providers from sharing patient-safety concerns with nondisclosure and “hold harmless” provisions in contracts that shift the liability of unsafe HIT features to care providers.3
The report also cautioned that serious errors involving these technologies—including medication dosing errors, failure to detect fatal illnesses, and treatment delays due to complex data interfaces and poor human-computer interactions or loss of data—have led to several reported patient deaths and injuries. Furthermore, there is no way to publicly track adverse outcomes because there is no systematic regulation or authority to collect, analyze, and disseminate such information.
The report concluded that the current state of safety and health IT is not acceptable and that regulation of the industry might be necessary because the private sector to date has not taken sufficient action on its own to improve HIT safety.
SHM applauds the IOM report as an overdue and direly needed call to action, Dr. Rogers says. SHM sent a letter to the U.S. Department of Health and Human Services underscoring the importance of the IOM report.
“In our practices, we have experienced the threats to patient safety outlined in the report: poor user-interface design, poor workflow, complex data interfaces, lack of system interoperability, and lack of sufficient vendor action to build safer products,” Dr. Rogers says.
“Lack of interoperability—preventing access to patient data from previous physician or other hospital visits—makes a mockery of a coordinated, patient-centered healthcare system,” says HIT researcher Ross Koppel, PhD, faculty member of University of Pennsylvania’s Sociology Department and School of Medicine.
Although Dr. Rogers acknowledges that HIT has the potential to revolutionize healthcare systems, boost quality and safety, and lower cost, he maintains that current HIT products fall short of those ambitious goals. “Vendors typically regard usability of their products as a convenience request by clinicians; any errors are regarded as training issues for physicians,” Dr. Rogers says. “But the way that data is presented on a screen matters—if it is difficult to input or retrieve data and leads to cognitive or process errors, that’s a product redesign issue for which vendors should be held accountable.”
Dr. Koppel says many HIT systems originated from billing system applications “and were not initially designed with the clinical perspective in mind. Hospitalists have to be particularly focused on usability of HIT systems when it comes to patient-safety impacts. They’re not the canary in the coal mine, they’re the miners—often the teachers guiding other clinicians on HIT use.”
Improvement Agenda
SHM fully supports many of the IOM’s recommendations to improve the safety and functionality of HIT systems, including these as stated in an email to its members:
- Remove contractual restrictions, promote public reporting of safety issues, and put a system in place for independent investigations that drive patient-safety improvement.
- Establish standards and a common infrastructure for “interoperable” data exchange across systems.
- Create dual accountability between vendors and providers to address safety concerns that might require
- changes in an IT product’s functionality or design.
- Promote research on usability and human-factors design, safer implementation, and sociotechnical systems associated with HIT.
- Promote education of safety, quality, and reliability principles in design and implementation of HIT among all levels of the workforce, including frontline clinicians and staff, hospital IT, and quality teams—as well as IT vendors themselves.
There also are ongoing efforts in the private sector to improve HIT system functionality. For example, the HIMSS CDS Guidebook Series, of which Dr. Osheroff is lead editor and author and Dr. Rogers is a contributing author, is a respected repository of information synthesizing and vetting critical guidance for the effective implementation of clinical decision support (CDS).
“We’re also working with Greg Maynard [senior vice president of SHM’s Center for Hospital Innovation & Improvement] to use the collaborative’s tools to disseminate clinical-decision-support best practices for improving VTE prophylaxis rates,” Dr. Osheroff notes.
Hospitalists, as central players in quality improvement (QI), standardization, and care coordination, are natural choices as HIT champions, with valuable insight into how HIT systems should be customized to accommodate workflows and order sets in an optimal fashion, Dr. Rogers says.
“As critical as we are about the status of current HIT systems, we believe that systems can be designed more effectively to meet our needs,” he says. “By adopting many of the improvements enumerated in the IOM report, hospitalists are uniquely positioned to advance HIT to help achieve the goals of safer, higher-quality, and more efficient care.”
Christopher Guadagnino is a freelance writer based in Philadelphia.
References
- Centers for Medicare & Medicaid Services. More than 100,000 health care providers paid for using electronic health records. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4383&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&sr. Accessed July 31, 2012.
- Centers for Medicare & Medicaid Services. 2012: the year of meaningful use. The CMS Blog website. Available at: http://blog.cms.gov/2012/03/23/2012-the-year-of-meaningful-use. Accessed July 18, 2012.
- Institute of Medicine of the National Academies. Health IT and patient safety: building safer systems for better care. Institute of Medicine of the National Academies website. Available at: http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx. Accessed July 14, 2012.
Earlier this summer, the Centers for Medicare & Medicaid Services (CMS) announced that more than 100,000 healthcare providers and 48% of all eligible hospitals are using electronic health records (EHRs) that meet federal standards, and they have benefited from federal incentive programs to do so.1
According to CMS acting administrator Marilyn Tavenner, meeting that provider goal makes 2012 the “Year of Meaningful Use.” She also says healthcare providers have recognized the potential of EHRs to cut down on paperwork, eliminate duplicate screenings and tests, and facilitate better, safer, patient-centered care.2
Belying CMS’ celebratory declarations, however, are concerns among experts that health information technology’s (HIT) actual use falls short of its promise—and might even endanger patients—due to shortcomings in system interoperability, safety, accountability, and other issues.
“Federal funding of IT was a step in the right direction, but it has also created a guaranteed customer base for electronic medical records, so vendors have less incentive to improve their products to meet clinicians needs,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, chair of SHsM’s IT Executive Committee and chief of hospital medicine at the University of New Mexico Health Sciences Center School of Medicine in Albuquerque. “We want systems that help us make better clinical decisions and allow us to work more efficiently. Unfortunately, many hospitalists are frustrated with existing HIT systems, knowing how much better they need to be. It can be a dangerous gamble to push rapid adoption of potentially unsafe systems in hospitals.”
Questioning HIT Safety
Health IT experts affirm that potential danger. Jerry Osheroff, MD, FACP, FACMI, principal and founder of TMIT Consulting LLC and former chief clinical informatics officer for Thomson Reuters Healthcare, says HIT “is most effective when it gets the right information to the right people, through the right channels, in the right format, at the right point in the workflow. The danger comes when it gets one of those five ‘rights’ wrong; that can lead to distraction, confusion, wasted time, missed improvement opportunities, and safety concerns.”
Last November, the Institute of Medicine (IOM) released a scathing critique of HIT’s current ability to ensure patient safety.3 As the federal government invests billions of dollars to encourage hospitals and healthcare providers to adopt HIT, the IOM report said, improvements in care and safety are not yet established, and little evidence exists that quantifies the magnitude of the risk associated with HIT problems—partly because many HIT vendors discourage providers from sharing patient-safety concerns with nondisclosure and “hold harmless” provisions in contracts that shift the liability of unsafe HIT features to care providers.3
The report also cautioned that serious errors involving these technologies—including medication dosing errors, failure to detect fatal illnesses, and treatment delays due to complex data interfaces and poor human-computer interactions or loss of data—have led to several reported patient deaths and injuries. Furthermore, there is no way to publicly track adverse outcomes because there is no systematic regulation or authority to collect, analyze, and disseminate such information.
The report concluded that the current state of safety and health IT is not acceptable and that regulation of the industry might be necessary because the private sector to date has not taken sufficient action on its own to improve HIT safety.
SHM applauds the IOM report as an overdue and direly needed call to action, Dr. Rogers says. SHM sent a letter to the U.S. Department of Health and Human Services underscoring the importance of the IOM report.
“In our practices, we have experienced the threats to patient safety outlined in the report: poor user-interface design, poor workflow, complex data interfaces, lack of system interoperability, and lack of sufficient vendor action to build safer products,” Dr. Rogers says.
“Lack of interoperability—preventing access to patient data from previous physician or other hospital visits—makes a mockery of a coordinated, patient-centered healthcare system,” says HIT researcher Ross Koppel, PhD, faculty member of University of Pennsylvania’s Sociology Department and School of Medicine.
Although Dr. Rogers acknowledges that HIT has the potential to revolutionize healthcare systems, boost quality and safety, and lower cost, he maintains that current HIT products fall short of those ambitious goals. “Vendors typically regard usability of their products as a convenience request by clinicians; any errors are regarded as training issues for physicians,” Dr. Rogers says. “But the way that data is presented on a screen matters—if it is difficult to input or retrieve data and leads to cognitive or process errors, that’s a product redesign issue for which vendors should be held accountable.”
Dr. Koppel says many HIT systems originated from billing system applications “and were not initially designed with the clinical perspective in mind. Hospitalists have to be particularly focused on usability of HIT systems when it comes to patient-safety impacts. They’re not the canary in the coal mine, they’re the miners—often the teachers guiding other clinicians on HIT use.”
Improvement Agenda
SHM fully supports many of the IOM’s recommendations to improve the safety and functionality of HIT systems, including these as stated in an email to its members:
- Remove contractual restrictions, promote public reporting of safety issues, and put a system in place for independent investigations that drive patient-safety improvement.
- Establish standards and a common infrastructure for “interoperable” data exchange across systems.
- Create dual accountability between vendors and providers to address safety concerns that might require
- changes in an IT product’s functionality or design.
- Promote research on usability and human-factors design, safer implementation, and sociotechnical systems associated with HIT.
- Promote education of safety, quality, and reliability principles in design and implementation of HIT among all levels of the workforce, including frontline clinicians and staff, hospital IT, and quality teams—as well as IT vendors themselves.
There also are ongoing efforts in the private sector to improve HIT system functionality. For example, the HIMSS CDS Guidebook Series, of which Dr. Osheroff is lead editor and author and Dr. Rogers is a contributing author, is a respected repository of information synthesizing and vetting critical guidance for the effective implementation of clinical decision support (CDS).
“We’re also working with Greg Maynard [senior vice president of SHM’s Center for Hospital Innovation & Improvement] to use the collaborative’s tools to disseminate clinical-decision-support best practices for improving VTE prophylaxis rates,” Dr. Osheroff notes.
Hospitalists, as central players in quality improvement (QI), standardization, and care coordination, are natural choices as HIT champions, with valuable insight into how HIT systems should be customized to accommodate workflows and order sets in an optimal fashion, Dr. Rogers says.
“As critical as we are about the status of current HIT systems, we believe that systems can be designed more effectively to meet our needs,” he says. “By adopting many of the improvements enumerated in the IOM report, hospitalists are uniquely positioned to advance HIT to help achieve the goals of safer, higher-quality, and more efficient care.”
Christopher Guadagnino is a freelance writer based in Philadelphia.
References
- Centers for Medicare & Medicaid Services. More than 100,000 health care providers paid for using electronic health records. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4383&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&sr. Accessed July 31, 2012.
- Centers for Medicare & Medicaid Services. 2012: the year of meaningful use. The CMS Blog website. Available at: http://blog.cms.gov/2012/03/23/2012-the-year-of-meaningful-use. Accessed July 18, 2012.
- Institute of Medicine of the National Academies. Health IT and patient safety: building safer systems for better care. Institute of Medicine of the National Academies website. Available at: http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx. Accessed July 14, 2012.