User login
The Hospitalist only
Surgeries account for almost half of hospital costs
according to the Agency for Healthcare Research and Quality (AHRQ).
Of the 35.4 million inpatient stays in 2014 – the last full year of ICD-9-CM coding – 10.1 million (28.6%) involved at least one any-listed surgical procedure, and 25.2 million (71.4%) did not. The total cost of all admissions was $386.2 billion, of which $187.1 billion (48.4%) went for stays with surgeries and $199.1 billion (51.6%) went for nonsurgical stays, the AHRQ reported in a statistical brief.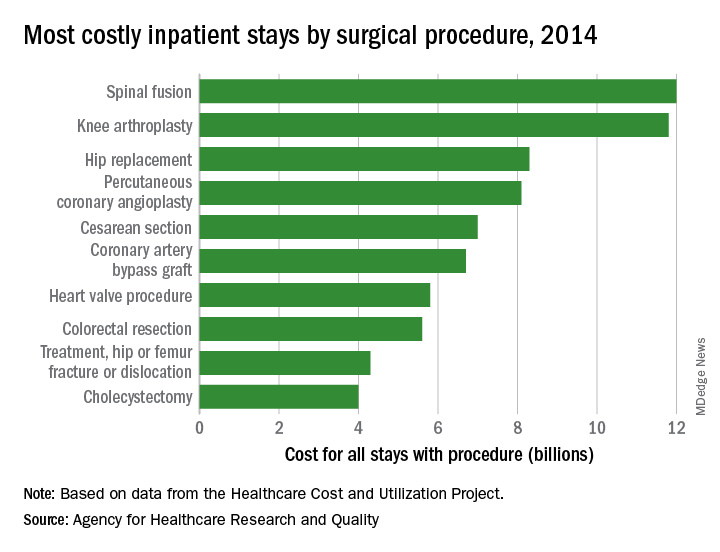
There were five other musculoskeletal procedures among the 20 most costly surgery-related admissions: knee arthroplasty was second at $11.8 billion, hip replacement was third at $8.3 billion, treatment of hip and femur fracture/dislocation was ninth at $4.3 billion, amputation of lower extremity was 13th at $2.5 billion, and treatment of lower extremity (other than hip or femur) fracture/dislocation was 14th at $2.4 billion. Those six procedures combined were $41.2 billion in hospital costs, which was a quarter of the total for all stays with a first-listed OR procedure, the AHRQ said.
The nonmusculoskeletal procedures in the top five were percutaneous coronary angioplasty in fourth, with an aggregate cost of $8.1 billion, and cesarean section in fifth at an even $7 billion. Coronary artery bypass graft, the most expensive procedure per stay ($52,000) among the top 20 procedures, was sixth in aggregate cost at $6.7 billion, according to the AHRQ researchers.
according to the Agency for Healthcare Research and Quality (AHRQ).
Of the 35.4 million inpatient stays in 2014 – the last full year of ICD-9-CM coding – 10.1 million (28.6%) involved at least one any-listed surgical procedure, and 25.2 million (71.4%) did not. The total cost of all admissions was $386.2 billion, of which $187.1 billion (48.4%) went for stays with surgeries and $199.1 billion (51.6%) went for nonsurgical stays, the AHRQ reported in a statistical brief.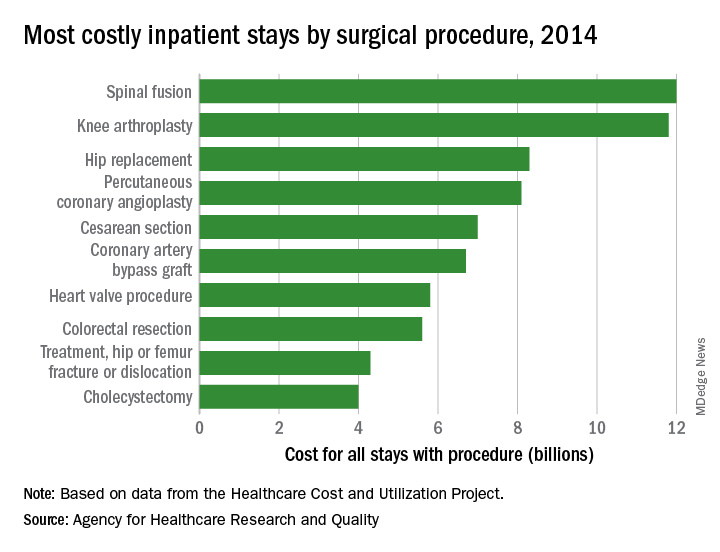
There were five other musculoskeletal procedures among the 20 most costly surgery-related admissions: knee arthroplasty was second at $11.8 billion, hip replacement was third at $8.3 billion, treatment of hip and femur fracture/dislocation was ninth at $4.3 billion, amputation of lower extremity was 13th at $2.5 billion, and treatment of lower extremity (other than hip or femur) fracture/dislocation was 14th at $2.4 billion. Those six procedures combined were $41.2 billion in hospital costs, which was a quarter of the total for all stays with a first-listed OR procedure, the AHRQ said.
The nonmusculoskeletal procedures in the top five were percutaneous coronary angioplasty in fourth, with an aggregate cost of $8.1 billion, and cesarean section in fifth at an even $7 billion. Coronary artery bypass graft, the most expensive procedure per stay ($52,000) among the top 20 procedures, was sixth in aggregate cost at $6.7 billion, according to the AHRQ researchers.
according to the Agency for Healthcare Research and Quality (AHRQ).
Of the 35.4 million inpatient stays in 2014 – the last full year of ICD-9-CM coding – 10.1 million (28.6%) involved at least one any-listed surgical procedure, and 25.2 million (71.4%) did not. The total cost of all admissions was $386.2 billion, of which $187.1 billion (48.4%) went for stays with surgeries and $199.1 billion (51.6%) went for nonsurgical stays, the AHRQ reported in a statistical brief.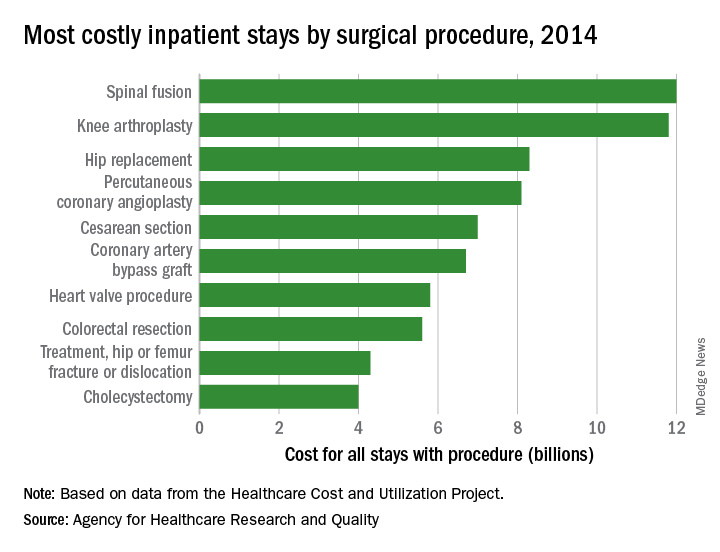
There were five other musculoskeletal procedures among the 20 most costly surgery-related admissions: knee arthroplasty was second at $11.8 billion, hip replacement was third at $8.3 billion, treatment of hip and femur fracture/dislocation was ninth at $4.3 billion, amputation of lower extremity was 13th at $2.5 billion, and treatment of lower extremity (other than hip or femur) fracture/dislocation was 14th at $2.4 billion. Those six procedures combined were $41.2 billion in hospital costs, which was a quarter of the total for all stays with a first-listed OR procedure, the AHRQ said.
The nonmusculoskeletal procedures in the top five were percutaneous coronary angioplasty in fourth, with an aggregate cost of $8.1 billion, and cesarean section in fifth at an even $7 billion. Coronary artery bypass graft, the most expensive procedure per stay ($52,000) among the top 20 procedures, was sixth in aggregate cost at $6.7 billion, according to the AHRQ researchers.
Do hospitalists improve inpatient outcomes?
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
Long continues the debate on what impact hospitalists have on inpatient outcomes. This issue has been playing out in the medical literature for 20 years, since the coining of the term in 1997. In a recent iteration of the debate, a study was published in JAMA Internal Medicine entitled “Comparison of Hospital Resource Use and Outcomes Among Hospitalists, Primary Care Physicians, and Other Generalists.”
The study retrospectively evaluated health care resources and outcomes from over a half-million Medicare beneficiaries hospitalized in 2013 for 20 common diagnosis-related groups, by type of physician provider (hospitalist, their primary care physician, or other generalist). The study found that nonhospitalists used more consultations and had longer lengths of stays, compared with hospitalists. In addition, relative to hospitalists, PCPs were more likely to discharge patients to home, had similar readmission rates, and lower 30-day mortality rates, but generalists were less likely to discharge patients home, had higher readmission rates, and higher mortality rates.
As hospitalists, we need to understand and acknowledge that most of our patients are “brand new” to us, and it is paramount that we use all available resources to gain a deep understanding of the patient in as short a time as possible. For example, ensuring all medical records available are reviewed, at least as much as possible, including a medical list (including a medication reconciliation). Interviewing family members or caregivers is also obviously a “best practice.” As well, having the insight of the PCP in these patients’ care is unquestionably good for us, for the PCP, and for the patient.
With good communication processes and an eye for excellence in care transitions, hospitalists can and should achieve the best outcomes for all of their patients. I look forward to more research in this arena, including a better understanding of the mechanisms by which we can all reliably produce excellent outcomes for the patients we serve.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
• Locums vs. F/T Hospitalists: Do Temps Stack Up? by Brad Flansbaum, DO, MPH, MHM
• Rounds: Are We Spinning Our Wheels? by Vineet Arora, MD, MPP, MHM
• Up Your Game in APP Integration by Tracy Cardin, ACNP-BC, SFHM
MedPAC urges CMS to curb low-value care
according to a staff presentation at a meeting of the Medicare Payment Advisory Commission.
At the commission’s April meeting, MedPAC staff presented data from various literature searches, noting a “substantial use of low-value services in Medicare.” For example, they found that about 20% of Virginians, across all payers, received a low-value service in 2014, while 15% of Medicaid patients and 11% of commercially insured patients in Oregon received a low-value service in 2013.
“It is very hard to know at the beginning of coverage that something is going to be low value,” MedPAC commission member Kathy Buto, former vice president of global health policy at Johnson & Johnson, noted. “It may be covered for something narrow for which it is high value and then spreads. It’s important to have those kinds of tools once technologies and procedures are covered to be able to actually monitor what is going on and assess.”
But, she added, the Centers for Medicare & Medicaid Services needs to do more to routinely reexamine its coverage decisions.
Ms. Buto noted that noncoverage decisions are rarely issued and suggested that “there is an opportunity for us to take a look at whether we would advise CMS to take a look at using more of those tools more aggressively.”
Paul Ginsburg, PhD, commissioner and senior fellow in economic studies at the Brookings Institution, Washington, suggested that, for any new procedure or drug, initial coverage is always provisional for a certain length of time, which would force CMS to revisit coverage decisions.
“If there is no evidence, the coverage ends,” Dr Ginsburg said. “If there is positive evidence, the coverage proceeds.”
However, as commissioner Rita Redberg, MD, of the University of California, San Francisco, said of CMS, even with tools to cut coverage, its hands may be tied by outside forces. “CMS needs a lot more political cover.”
Dr. Redberg noted that there was extensive lobbying of local carriers, and within 6 months, despite the lack of evidence, everyone was covering cardiac CT.
“A few years later, CMS tried to walk back the coverage because it was just hemorrhaging money for cardiac CT, but there was no chance because it was a capital investment,” she added. “Even when there are restrictions on coverage, CMS doesn’t enforce them.”
Ms. Buto also raised the issue of how much influence CMS has over Medicare Part D prescription drug plan sponsors’ coverage decision policies, but suggested CMS could play a larger role in that.
Commissioner Amy Bricker, vice president of supply chain strategy at Express Scripts, St. Louis, suggested that, “We need to do more from a Part D perspective to allow plans to manage drug coverage more aggressively and in line with the commercial space. CMS has handcuffed them,” noting that FDA approval, regardless of value, generally means Medicare coverage.
Commissioner Jack Hoadley, PhD, of Georgetown University in Washington, cautioned that any discussion on these or possibly other tools needs to take into account the needs of those who will legitimately benefit from some of the low-value services so they do not inadvertently prevent access for those patients.
At press time, MedPAC had not scheduled a vote on specific recommendations to address low-value care.
according to a staff presentation at a meeting of the Medicare Payment Advisory Commission.
At the commission’s April meeting, MedPAC staff presented data from various literature searches, noting a “substantial use of low-value services in Medicare.” For example, they found that about 20% of Virginians, across all payers, received a low-value service in 2014, while 15% of Medicaid patients and 11% of commercially insured patients in Oregon received a low-value service in 2013.
“It is very hard to know at the beginning of coverage that something is going to be low value,” MedPAC commission member Kathy Buto, former vice president of global health policy at Johnson & Johnson, noted. “It may be covered for something narrow for which it is high value and then spreads. It’s important to have those kinds of tools once technologies and procedures are covered to be able to actually monitor what is going on and assess.”
But, she added, the Centers for Medicare & Medicaid Services needs to do more to routinely reexamine its coverage decisions.
Ms. Buto noted that noncoverage decisions are rarely issued and suggested that “there is an opportunity for us to take a look at whether we would advise CMS to take a look at using more of those tools more aggressively.”
Paul Ginsburg, PhD, commissioner and senior fellow in economic studies at the Brookings Institution, Washington, suggested that, for any new procedure or drug, initial coverage is always provisional for a certain length of time, which would force CMS to revisit coverage decisions.
“If there is no evidence, the coverage ends,” Dr Ginsburg said. “If there is positive evidence, the coverage proceeds.”
However, as commissioner Rita Redberg, MD, of the University of California, San Francisco, said of CMS, even with tools to cut coverage, its hands may be tied by outside forces. “CMS needs a lot more political cover.”
Dr. Redberg noted that there was extensive lobbying of local carriers, and within 6 months, despite the lack of evidence, everyone was covering cardiac CT.
“A few years later, CMS tried to walk back the coverage because it was just hemorrhaging money for cardiac CT, but there was no chance because it was a capital investment,” she added. “Even when there are restrictions on coverage, CMS doesn’t enforce them.”
Ms. Buto also raised the issue of how much influence CMS has over Medicare Part D prescription drug plan sponsors’ coverage decision policies, but suggested CMS could play a larger role in that.
Commissioner Amy Bricker, vice president of supply chain strategy at Express Scripts, St. Louis, suggested that, “We need to do more from a Part D perspective to allow plans to manage drug coverage more aggressively and in line with the commercial space. CMS has handcuffed them,” noting that FDA approval, regardless of value, generally means Medicare coverage.
Commissioner Jack Hoadley, PhD, of Georgetown University in Washington, cautioned that any discussion on these or possibly other tools needs to take into account the needs of those who will legitimately benefit from some of the low-value services so they do not inadvertently prevent access for those patients.
At press time, MedPAC had not scheduled a vote on specific recommendations to address low-value care.
according to a staff presentation at a meeting of the Medicare Payment Advisory Commission.
At the commission’s April meeting, MedPAC staff presented data from various literature searches, noting a “substantial use of low-value services in Medicare.” For example, they found that about 20% of Virginians, across all payers, received a low-value service in 2014, while 15% of Medicaid patients and 11% of commercially insured patients in Oregon received a low-value service in 2013.
“It is very hard to know at the beginning of coverage that something is going to be low value,” MedPAC commission member Kathy Buto, former vice president of global health policy at Johnson & Johnson, noted. “It may be covered for something narrow for which it is high value and then spreads. It’s important to have those kinds of tools once technologies and procedures are covered to be able to actually monitor what is going on and assess.”
But, she added, the Centers for Medicare & Medicaid Services needs to do more to routinely reexamine its coverage decisions.
Ms. Buto noted that noncoverage decisions are rarely issued and suggested that “there is an opportunity for us to take a look at whether we would advise CMS to take a look at using more of those tools more aggressively.”
Paul Ginsburg, PhD, commissioner and senior fellow in economic studies at the Brookings Institution, Washington, suggested that, for any new procedure or drug, initial coverage is always provisional for a certain length of time, which would force CMS to revisit coverage decisions.
“If there is no evidence, the coverage ends,” Dr Ginsburg said. “If there is positive evidence, the coverage proceeds.”
However, as commissioner Rita Redberg, MD, of the University of California, San Francisco, said of CMS, even with tools to cut coverage, its hands may be tied by outside forces. “CMS needs a lot more political cover.”
Dr. Redberg noted that there was extensive lobbying of local carriers, and within 6 months, despite the lack of evidence, everyone was covering cardiac CT.
“A few years later, CMS tried to walk back the coverage because it was just hemorrhaging money for cardiac CT, but there was no chance because it was a capital investment,” she added. “Even when there are restrictions on coverage, CMS doesn’t enforce them.”
Ms. Buto also raised the issue of how much influence CMS has over Medicare Part D prescription drug plan sponsors’ coverage decision policies, but suggested CMS could play a larger role in that.
Commissioner Amy Bricker, vice president of supply chain strategy at Express Scripts, St. Louis, suggested that, “We need to do more from a Part D perspective to allow plans to manage drug coverage more aggressively and in line with the commercial space. CMS has handcuffed them,” noting that FDA approval, regardless of value, generally means Medicare coverage.
Commissioner Jack Hoadley, PhD, of Georgetown University in Washington, cautioned that any discussion on these or possibly other tools needs to take into account the needs of those who will legitimately benefit from some of the low-value services so they do not inadvertently prevent access for those patients.
At press time, MedPAC had not scheduled a vote on specific recommendations to address low-value care.
REPORTING FROM MEDPAC
Understanding the new CMS bundle model
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
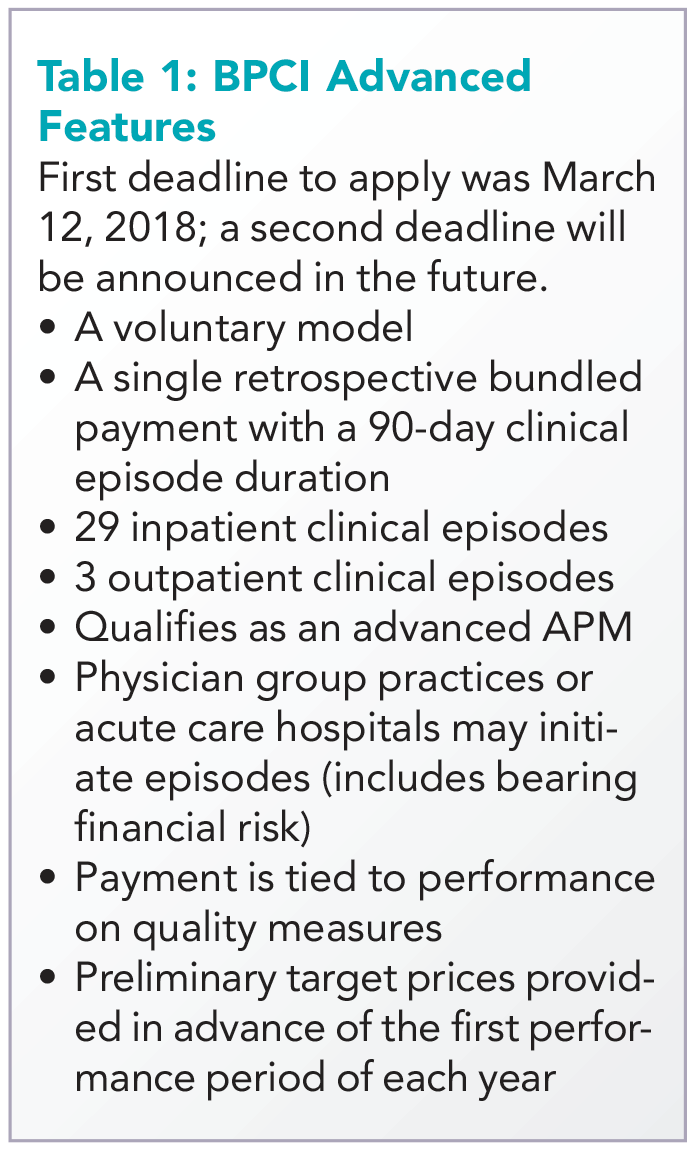
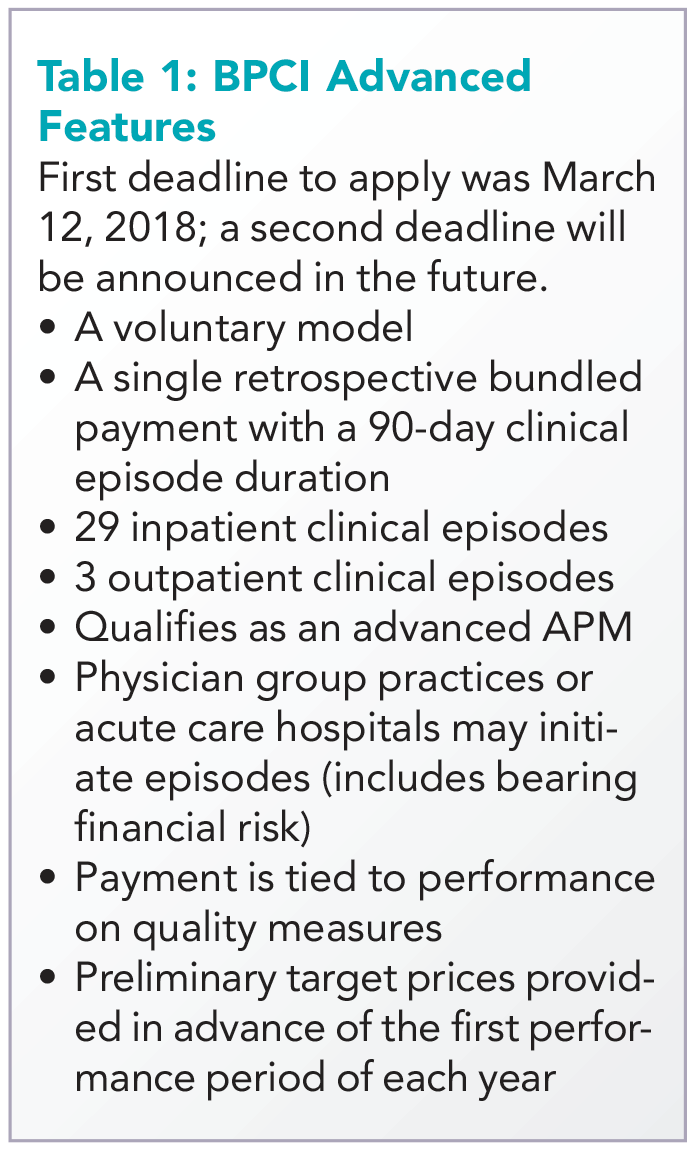
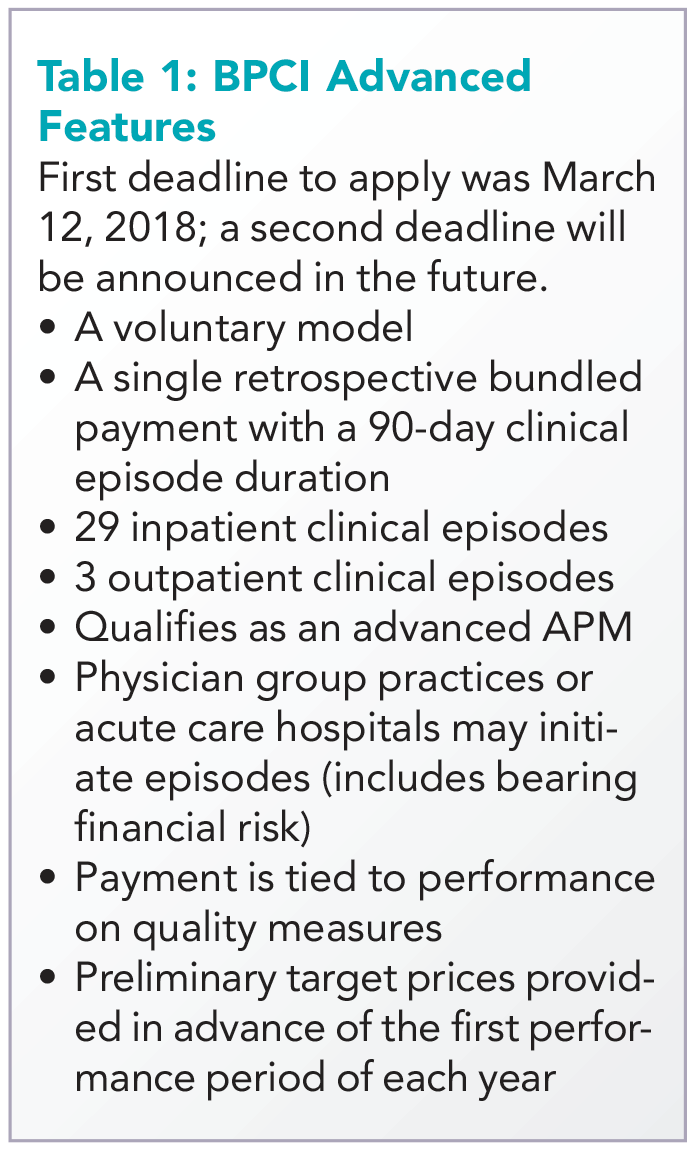
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
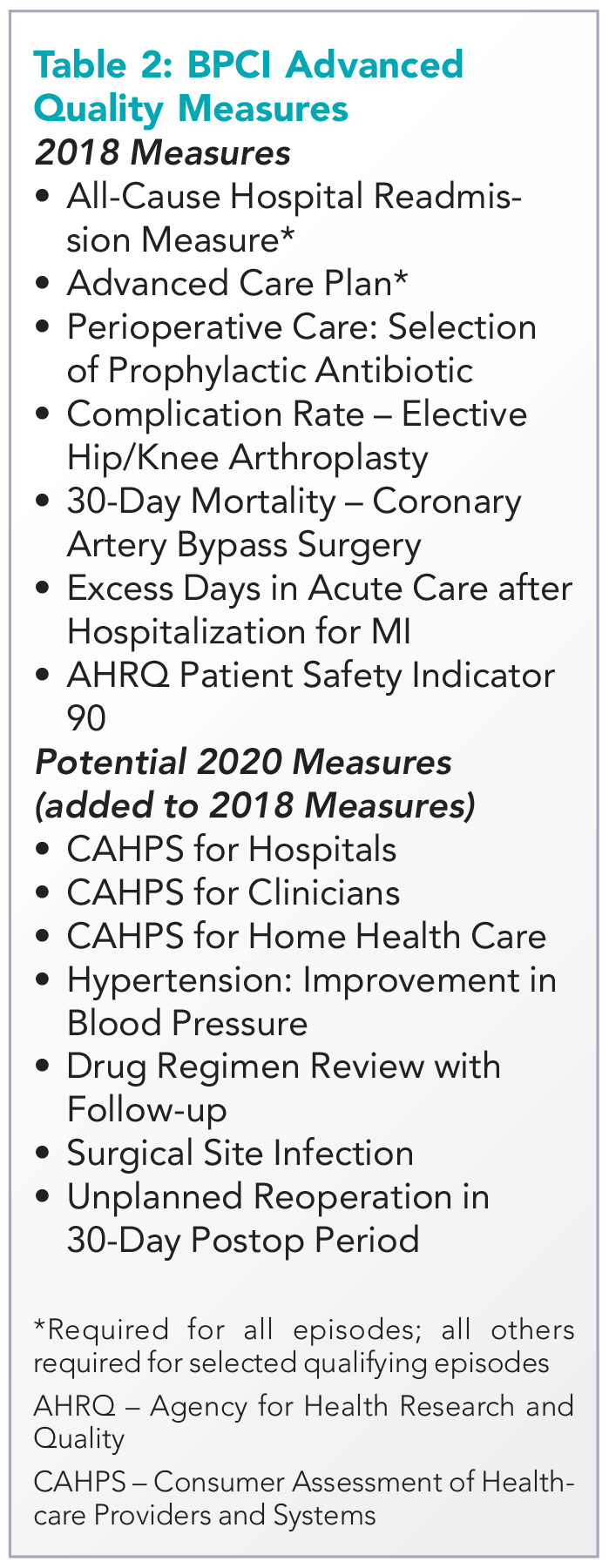
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
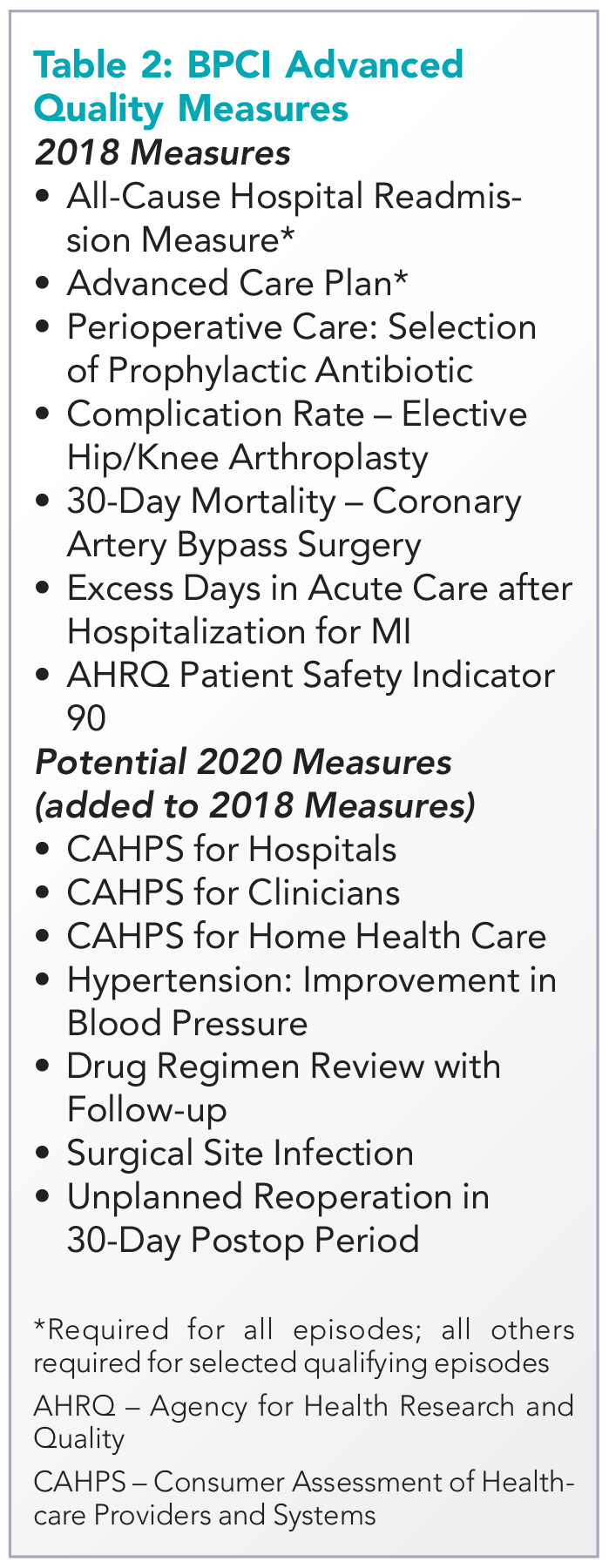
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Hospitalists have been among the highest-volume participants in Medicare’s Bundled Payments for Care Improvement (BPCI) demonstration model, initiating over 200,000 episodes representing $4.7 billion in spending since the model began.1 On Jan. 9, the Centers for Medicare & Medicaid Services announced BPCI’s follow-on model, “BPCI Advanced.”2
BPCI launched in October 2013 and sunsets at the end of Q3 2018. BPCI Advanced starts immediately upon conclusion of BPCI (Q4 2018) and is slated to finish at year-end 2023.
CMS intends for the program to qualify as an Advanced Alternative Payment Model (APM). As BPCI Advanced focuses on episodes of care involving an inpatient stay (It also includes three outpatient episodes.) and the subsequent 90-day recovery period, it represents the first large-scale opportunity for hospitalists to meet criteria for Advanced APM participation. Qualifying for the Advanced APM track of the Quality Payment Program – which involves meeting patient volume or payment thresholds3 – comes with a 5% lump-sum bonus based on Medicare Part B fees and avoids exposure to penalties and reporting requirements of the Merit-based Incentive Payment System (MIPS).
Key program features
Acute care hospitals and physician groups may initiate episodes under BPCI Advanced, assuming financial risk under the model. Similar to its predecessor, BPCI Advanced assigns a target price based on past claims payments associated with the “episode initiator.”
During the performance period, if the initiator can beat the price in the aggregate for its bundles, it can keep the difference, and if it comes in over the price, it must pay the difference back to Medicare. Medicare discounts the target price by 3%, effectively paying itself that amount. After that, there is no sharing of savings with Medicare, as opposed to the permanent ACO programs, where there is sharing after the ACO meets the minimum savings rate.
The program allows physician groups and hospital initiators to go it alone or to work with a “convener,” which may share risk and reward with initiators, and may provide software, analytics, networks of high-performing providers like nursing facilities, and knowledge of specific care redesign approaches to enable program success. See Table 1 for a listing of other notable features of BPCI Advanced.
Quality measures
BPCI Advanced qualifies as an Advanced APM in part because payment is tied to performance on a set of quality measures (see Table 2). There are two measures applied to all episodes: all-cause hospital readmissions and advance care plan. These are notable because hospitalists may be especially focused on improvement activities in these areas.
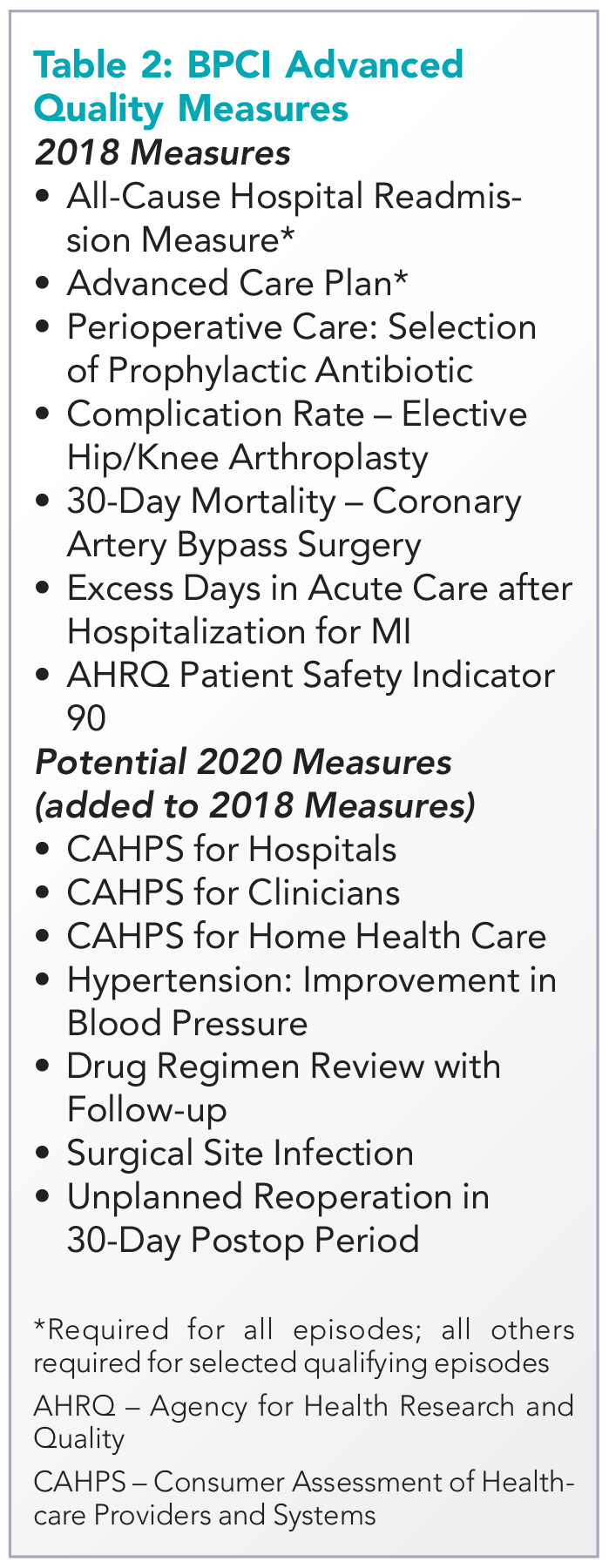
While the advance care plan measure refers to a process reflected by record documentation and is therefore directly under the control of hospitalists, readmissions – and most of the other measures – require a team approach. Because the outcome measures are risk adjusted, accurate and complete clinical documentation is crucial, as it drives how risk is adjusted. Of note, all the 2018 measures, collected directly through claims, will place no additional administrative burden for collection on providers.
Two ways for hospitalists to participate
Hospitalist groups – whether independent or employed – may be episode initiators in BPCI Advanced. In this case, any episodes in which the group participates that carry the name of a member of the hospitalist group in the “Attending Provider” field on the hospital bill claim form to Medicare (and the associated carrier claim) are attributed to that member’s physician group.
For example, if the group has chosen heart failure as an episode in which to participate at the program’s outset, a hospitalization is assigned the heart failure DRG (diagnosis-related group) and a group member is the Attending Provider on the claim form (and submits a claim for the physician services), then the episode is attributed to that group. This means that the group is responsible for payments represented by Medicare Part A and Part B claims (with a few exclusions like trauma and cancer) against the target price for the initial hospitalization and subsequent 90-day period. In practice, hospitalists are rewarded for actions aimed at optimizing location after discharge,4 avoiding readmissions, choosing efficient nursing facilities, and helping patients to maximize functional status.
The other way hospitalists may participate is through an agreement to share in savings with a hospital or physician group episode initiator. This requires hospitalist individuals or groups to enter into a contract with the initiator that meets certain program requirements – for example, report quality measures, engage in care redesign, use certified EHR technology (hospital-based clinicians automatically fulfill this criterion).
If there is broad participation, BPCI Advanced could represent a key milestone for hospitalists, as they seek to be recognized for the value they confer to the system as a whole instead of simply their professional billings. While there are legitimate concerns about the effect MIPS may have on health care value and the complexity of participation in APMs, barring a repeal of the law that created them, hospitalists now have the chance to extend their influence within and outside the hospital’s four walls and be more fairly rewarded for it.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of the Society of Hospital Medicine. Contact him at [email protected]. Disclosure: The author’s employer, Remedy Partners, is an Awardee Convener for the BPCI initiative and intends to apply as a Convener in BPCI Advanced.
References
1. Based on BPCI awardee convener Remedy Partners claims analysis.
2. https://innovation.cms.gov/initiatives/bpci-advanced.
3. https://qpp.cms.gov/apms/overview.
4. Whitcomb W. Choosing location after discharge wisely. The-hospitalist.org. 2018 Jan 3. Digital edition. Accessed Jan 13, 2018.
Embracing constant change in a growing practice
Although many physicians resist change, learning how to embrace change and making it work for you are keys to a long, successful practice in hospital medicine, said Thomas McIlraith, MD, SFHM, CLHM, immediate past chairman, department of hospital medicine, and immediate past treasurer of the board of directors of Mercy Medical Group in Sacramento, Calif.
During his Monday, April 9, session, “Scaling Up Your Hospital Medicine Group,” he will share what it was like to work through significant changes as the chair of a department that grew in 12 years from 12 hospitalists – averaging fewer than 100 patients per day – to 84 hospitalists averaging more than 500 patients per day.
“I will be discussing my experiences but relating some universal truths about leadership in hospital medicine that can be applied to all areas of hospital medicine and how to manage change in an environment where change is constant,” said Dr. McIlraith, who will share key lessons that he learned. “I will break it down into the cultural, personal, and structural aspects of thriving in this dynamic environment.”
Dr. McIlraith hopes that attendees will come away with a good understanding of what he dubs the “authority/accountability” equation in physician leadership. “This is a principle that is used to assess what is expected of you in order to be successful as a leader, and if your ‘authority’ is commensurate with your ‘accountability,’ ” he said. “The authority piece of the equation takes many forms: resources, personnel, reporting structure, clerical support, and so forth. The key is to make sure that the authority/accountably equation is balanced not only for you but also for your subordinates.”
One example of an imbalanced authority/accountability equation that he’ll discuss in some detail is becoming a figurehead, in which accountability exists without the necessary authority. “If you end up in that position, get out,” Dr. McIlraith said. He will also discuss an example of where the authority/accountability equation is tipped in the opposite direction, with disastrous consequences.
Dr. McIlraith and Kimberly Bell, MD, who will also present at this session, aim to make it interactive. Dr. Bell currently serves as the divisional director of the CHI Franciscan Inpatient Team located in Tacoma, Wash. “We both have a wealth of experience to offer, but we are not the only ones in attendance who have wisdom to share,” Dr. McIlraith said.
Another goal of this session is to help attendees identify other hospital medicine leaders in comparable situations for the purpose of networking outside of the meeting. The session, although aimed at physician leaders, will be relevant to all hospitalists.
Scaling Up Your Hospital Medicine Group
Monday, 1:35-2:35 p.m.
Grand Ballroom 7B
Although many physicians resist change, learning how to embrace change and making it work for you are keys to a long, successful practice in hospital medicine, said Thomas McIlraith, MD, SFHM, CLHM, immediate past chairman, department of hospital medicine, and immediate past treasurer of the board of directors of Mercy Medical Group in Sacramento, Calif.
During his Monday, April 9, session, “Scaling Up Your Hospital Medicine Group,” he will share what it was like to work through significant changes as the chair of a department that grew in 12 years from 12 hospitalists – averaging fewer than 100 patients per day – to 84 hospitalists averaging more than 500 patients per day.
“I will be discussing my experiences but relating some universal truths about leadership in hospital medicine that can be applied to all areas of hospital medicine and how to manage change in an environment where change is constant,” said Dr. McIlraith, who will share key lessons that he learned. “I will break it down into the cultural, personal, and structural aspects of thriving in this dynamic environment.”
Dr. McIlraith hopes that attendees will come away with a good understanding of what he dubs the “authority/accountability” equation in physician leadership. “This is a principle that is used to assess what is expected of you in order to be successful as a leader, and if your ‘authority’ is commensurate with your ‘accountability,’ ” he said. “The authority piece of the equation takes many forms: resources, personnel, reporting structure, clerical support, and so forth. The key is to make sure that the authority/accountably equation is balanced not only for you but also for your subordinates.”
One example of an imbalanced authority/accountability equation that he’ll discuss in some detail is becoming a figurehead, in which accountability exists without the necessary authority. “If you end up in that position, get out,” Dr. McIlraith said. He will also discuss an example of where the authority/accountability equation is tipped in the opposite direction, with disastrous consequences.
Dr. McIlraith and Kimberly Bell, MD, who will also present at this session, aim to make it interactive. Dr. Bell currently serves as the divisional director of the CHI Franciscan Inpatient Team located in Tacoma, Wash. “We both have a wealth of experience to offer, but we are not the only ones in attendance who have wisdom to share,” Dr. McIlraith said.
Another goal of this session is to help attendees identify other hospital medicine leaders in comparable situations for the purpose of networking outside of the meeting. The session, although aimed at physician leaders, will be relevant to all hospitalists.
Scaling Up Your Hospital Medicine Group
Monday, 1:35-2:35 p.m.
Grand Ballroom 7B
Although many physicians resist change, learning how to embrace change and making it work for you are keys to a long, successful practice in hospital medicine, said Thomas McIlraith, MD, SFHM, CLHM, immediate past chairman, department of hospital medicine, and immediate past treasurer of the board of directors of Mercy Medical Group in Sacramento, Calif.
During his Monday, April 9, session, “Scaling Up Your Hospital Medicine Group,” he will share what it was like to work through significant changes as the chair of a department that grew in 12 years from 12 hospitalists – averaging fewer than 100 patients per day – to 84 hospitalists averaging more than 500 patients per day.
“I will be discussing my experiences but relating some universal truths about leadership in hospital medicine that can be applied to all areas of hospital medicine and how to manage change in an environment where change is constant,” said Dr. McIlraith, who will share key lessons that he learned. “I will break it down into the cultural, personal, and structural aspects of thriving in this dynamic environment.”
Dr. McIlraith hopes that attendees will come away with a good understanding of what he dubs the “authority/accountability” equation in physician leadership. “This is a principle that is used to assess what is expected of you in order to be successful as a leader, and if your ‘authority’ is commensurate with your ‘accountability,’ ” he said. “The authority piece of the equation takes many forms: resources, personnel, reporting structure, clerical support, and so forth. The key is to make sure that the authority/accountably equation is balanced not only for you but also for your subordinates.”
One example of an imbalanced authority/accountability equation that he’ll discuss in some detail is becoming a figurehead, in which accountability exists without the necessary authority. “If you end up in that position, get out,” Dr. McIlraith said. He will also discuss an example of where the authority/accountability equation is tipped in the opposite direction, with disastrous consequences.
Dr. McIlraith and Kimberly Bell, MD, who will also present at this session, aim to make it interactive. Dr. Bell currently serves as the divisional director of the CHI Franciscan Inpatient Team located in Tacoma, Wash. “We both have a wealth of experience to offer, but we are not the only ones in attendance who have wisdom to share,” Dr. McIlraith said.
Another goal of this session is to help attendees identify other hospital medicine leaders in comparable situations for the purpose of networking outside of the meeting. The session, although aimed at physician leaders, will be relevant to all hospitalists.
Scaling Up Your Hospital Medicine Group
Monday, 1:35-2:35 p.m.
Grand Ballroom 7B
Engaging skeptical parents
While every day seems to bring extraordinary new advances in science – robotic surgery, individually targeted medications, and even gene therapy – there are many people who currently approach the science of medicine with skepticism.
While it is the right of legally competent adults in a free society to chose how best to care for their own health, to explore holistic or alternative therapies, or avoid medicine altogether, it is more complex when they are skeptical of accepted medical practice in managing the health of their children. For those parents who trust you enough to bring their children to you for care but remain skeptical of vaccines or other treatments, you have an opportunity to work with that trust and engage in a discussion so that they might reconsider their position on valuable and even life-saving treatments for their children.
In each of these cases, launching into an enthusiastic explanation of the advanced statistics that underpin your recommendation is unlikely to bridge the gap. Instead, you want to start with these parents by being curious. Resist the urge to tell, and listen instead. What is their understanding of the problem you are treating or preventing? What have they heard or read about the treatment or test in question? What do they most fear is going to happen to their child if they do or do not accept your recommendation? Are there specific events (with their child or with the health care system) that have informed this fear?
Respectfully listening to their experiences, thoughts, and feelings goes a long way toward building a trusting alliance. It can help overcome feelings of distrust or defensiveness around authority figures. And it models the thoughtful, respectful give and take that are essential to a healthy collaboration between pediatrician and parents.
Once you have information about what they think and some about how they think and make decisions, you then can offer your perspective. “You are the expert on your child, what I bring to this equation is experience with (this problem) and with assessing the scientific evidence that guides treatments in medicine. It is true that treatments often change as we learn more, but here is what the evidence currently supports.”
After learning something about how they think, you might offer more data or more warm acknowledgment of how difficult it can be to make medical decisions for your children with imperfect information. Be humble while also being accurate about your level of confidence in a recommendation. Humility is important because it is easy for parents to feel insecure and condescended to. You understand their greatest fear, now let them know what your greatest worry is for their child should they forgo a recommended treatment. Explaining all of this with humility and warmth makes it more likely that the parents will take in the facts you are trying to share with them and not be derailed by suspicion, defensiveness, or insecurity.
Make building an alliance with the parents your top priority. This does not mean that you do not offer your best recommendation for their child. Rather, it means that, if they still decline recommended treatment, you treat them with respect and invest your time in explaining what they should be watching or monitoring their child for without recommended treatment. Building trust is a long game. If you patiently stick with parents even when it’s not easy, they may be ready to trust you with a subsequent decision when the stakes are even higher.
Of course, all this thoughtful communication takes a lot of time! You may learn to block off more time for certain families. It also can be helpful to have these conversations as a team. If you and your nurse or social worker can meet with parents together, then some of the listening and learning can be done by the nurse or social worker alone, so that everyone’s time might be managed more efficiently. And managing skeptical parents as a team also can help to prevent frustration or burnout. It will not always succeed, but in some cases, your investment will pay off in a trusting alliance, mutual respect, and healthy patients.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at [email protected].
While every day seems to bring extraordinary new advances in science – robotic surgery, individually targeted medications, and even gene therapy – there are many people who currently approach the science of medicine with skepticism.
While it is the right of legally competent adults in a free society to chose how best to care for their own health, to explore holistic or alternative therapies, or avoid medicine altogether, it is more complex when they are skeptical of accepted medical practice in managing the health of their children. For those parents who trust you enough to bring their children to you for care but remain skeptical of vaccines or other treatments, you have an opportunity to work with that trust and engage in a discussion so that they might reconsider their position on valuable and even life-saving treatments for their children.
In each of these cases, launching into an enthusiastic explanation of the advanced statistics that underpin your recommendation is unlikely to bridge the gap. Instead, you want to start with these parents by being curious. Resist the urge to tell, and listen instead. What is their understanding of the problem you are treating or preventing? What have they heard or read about the treatment or test in question? What do they most fear is going to happen to their child if they do or do not accept your recommendation? Are there specific events (with their child or with the health care system) that have informed this fear?
Respectfully listening to their experiences, thoughts, and feelings goes a long way toward building a trusting alliance. It can help overcome feelings of distrust or defensiveness around authority figures. And it models the thoughtful, respectful give and take that are essential to a healthy collaboration between pediatrician and parents.
Once you have information about what they think and some about how they think and make decisions, you then can offer your perspective. “You are the expert on your child, what I bring to this equation is experience with (this problem) and with assessing the scientific evidence that guides treatments in medicine. It is true that treatments often change as we learn more, but here is what the evidence currently supports.”
After learning something about how they think, you might offer more data or more warm acknowledgment of how difficult it can be to make medical decisions for your children with imperfect information. Be humble while also being accurate about your level of confidence in a recommendation. Humility is important because it is easy for parents to feel insecure and condescended to. You understand their greatest fear, now let them know what your greatest worry is for their child should they forgo a recommended treatment. Explaining all of this with humility and warmth makes it more likely that the parents will take in the facts you are trying to share with them and not be derailed by suspicion, defensiveness, or insecurity.
Make building an alliance with the parents your top priority. This does not mean that you do not offer your best recommendation for their child. Rather, it means that, if they still decline recommended treatment, you treat them with respect and invest your time in explaining what they should be watching or monitoring their child for without recommended treatment. Building trust is a long game. If you patiently stick with parents even when it’s not easy, they may be ready to trust you with a subsequent decision when the stakes are even higher.
Of course, all this thoughtful communication takes a lot of time! You may learn to block off more time for certain families. It also can be helpful to have these conversations as a team. If you and your nurse or social worker can meet with parents together, then some of the listening and learning can be done by the nurse or social worker alone, so that everyone’s time might be managed more efficiently. And managing skeptical parents as a team also can help to prevent frustration or burnout. It will not always succeed, but in some cases, your investment will pay off in a trusting alliance, mutual respect, and healthy patients.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at [email protected].
While every day seems to bring extraordinary new advances in science – robotic surgery, individually targeted medications, and even gene therapy – there are many people who currently approach the science of medicine with skepticism.
While it is the right of legally competent adults in a free society to chose how best to care for their own health, to explore holistic or alternative therapies, or avoid medicine altogether, it is more complex when they are skeptical of accepted medical practice in managing the health of their children. For those parents who trust you enough to bring their children to you for care but remain skeptical of vaccines or other treatments, you have an opportunity to work with that trust and engage in a discussion so that they might reconsider their position on valuable and even life-saving treatments for their children.
In each of these cases, launching into an enthusiastic explanation of the advanced statistics that underpin your recommendation is unlikely to bridge the gap. Instead, you want to start with these parents by being curious. Resist the urge to tell, and listen instead. What is their understanding of the problem you are treating or preventing? What have they heard or read about the treatment or test in question? What do they most fear is going to happen to their child if they do or do not accept your recommendation? Are there specific events (with their child or with the health care system) that have informed this fear?
Respectfully listening to their experiences, thoughts, and feelings goes a long way toward building a trusting alliance. It can help overcome feelings of distrust or defensiveness around authority figures. And it models the thoughtful, respectful give and take that are essential to a healthy collaboration between pediatrician and parents.
Once you have information about what they think and some about how they think and make decisions, you then can offer your perspective. “You are the expert on your child, what I bring to this equation is experience with (this problem) and with assessing the scientific evidence that guides treatments in medicine. It is true that treatments often change as we learn more, but here is what the evidence currently supports.”
After learning something about how they think, you might offer more data or more warm acknowledgment of how difficult it can be to make medical decisions for your children with imperfect information. Be humble while also being accurate about your level of confidence in a recommendation. Humility is important because it is easy for parents to feel insecure and condescended to. You understand their greatest fear, now let them know what your greatest worry is for their child should they forgo a recommended treatment. Explaining all of this with humility and warmth makes it more likely that the parents will take in the facts you are trying to share with them and not be derailed by suspicion, defensiveness, or insecurity.
Make building an alliance with the parents your top priority. This does not mean that you do not offer your best recommendation for their child. Rather, it means that, if they still decline recommended treatment, you treat them with respect and invest your time in explaining what they should be watching or monitoring their child for without recommended treatment. Building trust is a long game. If you patiently stick with parents even when it’s not easy, they may be ready to trust you with a subsequent decision when the stakes are even higher.
Of course, all this thoughtful communication takes a lot of time! You may learn to block off more time for certain families. It also can be helpful to have these conversations as a team. If you and your nurse or social worker can meet with parents together, then some of the listening and learning can be done by the nurse or social worker alone, so that everyone’s time might be managed more efficiently. And managing skeptical parents as a team also can help to prevent frustration or burnout. It will not always succeed, but in some cases, your investment will pay off in a trusting alliance, mutual respect, and healthy patients.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics at Harvard Medical School, Boston. Email them at [email protected].
Teleconference is effective in assessing penicillin allergy
ORLANDO – and resulted in almost every patient having their allergy label removed, researchers reported.
In what the researchers said was the first study showing the utility of telemedicine in evaluating patient-reported penicillin allergies, allergy and immunology physicians did a secure telemedicine consultation with patients after they underwent penicillin skin testing with a physician assistant; an approach which, on average, took 123 minutes fewer each time than if the physician had done the consultation face-to-face. The teleconference can be done on a laptop or smartphone.
She said the approach is sensible and effective, and it is a good alternative to the traditional way of doing these tests. “What this takes out of that is the travel part. Someone else is doing the travel and the technique of testing,” added that people often are labeled in childhood after getting a rash that was thought to be related to penicillin, but actually was just a coincidence that was unrelated. Then the false allergy label is attached to them for life.
“This is so overlabeled,” Dr. Ramsey said. “Ten percent of the population thinks they’re allergic to penicillin, and 90% of them are not.”
A stark difference was found in the types of medicines administered before and after the evaluations, with aminopenicillin therapy jumping from 0 days of use to 188 days, and vancomycin – a more potent, but more costly alternative – dropping from 130 days of use to 16 days (P less than .05 for both).
Dr. Ramsey noted that, in part because of the time-consuming nature of the penicillin skin tests, they often are simply not done, so the false allergy labels are not caught, leading to pointless costs and exposure to more potent and potentially harmful forms of antibiotic therapy.
“Some hospitals don’t have allergists who will come in to do testing,” she said. “Sometimes patients are on medications that may interfere. And then a lot of times it’s just underrecognized – the implications of a penicillin allergy label. That is a very hot topic in our field and also in infectious disease.”
She hopes the telemedicine approach catches on more widely, which would help minimize the multitude of problems linked to penicillin allergy labels.
“Patients that avoid penicillin, they’re on more costly second-line antibiotics that are, in general, less effective, depending on which infection you’re talking about,” Dr. Ramsey said. “The [second-line antibiotics] have more side effects. And there’s data to show that patients with [a] penicillin allergy label have longer hospital stays, more costly hospital stays, are at risk for more resistant infections. And it breeds antimicrobial resistance in the long-term.”
Dr. Ramsey had no relevant financial disclosures.
SOURCE: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
ORLANDO – and resulted in almost every patient having their allergy label removed, researchers reported.
In what the researchers said was the first study showing the utility of telemedicine in evaluating patient-reported penicillin allergies, allergy and immunology physicians did a secure telemedicine consultation with patients after they underwent penicillin skin testing with a physician assistant; an approach which, on average, took 123 minutes fewer each time than if the physician had done the consultation face-to-face. The teleconference can be done on a laptop or smartphone.
She said the approach is sensible and effective, and it is a good alternative to the traditional way of doing these tests. “What this takes out of that is the travel part. Someone else is doing the travel and the technique of testing,” added that people often are labeled in childhood after getting a rash that was thought to be related to penicillin, but actually was just a coincidence that was unrelated. Then the false allergy label is attached to them for life.
“This is so overlabeled,” Dr. Ramsey said. “Ten percent of the population thinks they’re allergic to penicillin, and 90% of them are not.”
A stark difference was found in the types of medicines administered before and after the evaluations, with aminopenicillin therapy jumping from 0 days of use to 188 days, and vancomycin – a more potent, but more costly alternative – dropping from 130 days of use to 16 days (P less than .05 for both).
Dr. Ramsey noted that, in part because of the time-consuming nature of the penicillin skin tests, they often are simply not done, so the false allergy labels are not caught, leading to pointless costs and exposure to more potent and potentially harmful forms of antibiotic therapy.
“Some hospitals don’t have allergists who will come in to do testing,” she said. “Sometimes patients are on medications that may interfere. And then a lot of times it’s just underrecognized – the implications of a penicillin allergy label. That is a very hot topic in our field and also in infectious disease.”
She hopes the telemedicine approach catches on more widely, which would help minimize the multitude of problems linked to penicillin allergy labels.
“Patients that avoid penicillin, they’re on more costly second-line antibiotics that are, in general, less effective, depending on which infection you’re talking about,” Dr. Ramsey said. “The [second-line antibiotics] have more side effects. And there’s data to show that patients with [a] penicillin allergy label have longer hospital stays, more costly hospital stays, are at risk for more resistant infections. And it breeds antimicrobial resistance in the long-term.”
Dr. Ramsey had no relevant financial disclosures.
SOURCE: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
ORLANDO – and resulted in almost every patient having their allergy label removed, researchers reported.
In what the researchers said was the first study showing the utility of telemedicine in evaluating patient-reported penicillin allergies, allergy and immunology physicians did a secure telemedicine consultation with patients after they underwent penicillin skin testing with a physician assistant; an approach which, on average, took 123 minutes fewer each time than if the physician had done the consultation face-to-face. The teleconference can be done on a laptop or smartphone.
She said the approach is sensible and effective, and it is a good alternative to the traditional way of doing these tests. “What this takes out of that is the travel part. Someone else is doing the travel and the technique of testing,” added that people often are labeled in childhood after getting a rash that was thought to be related to penicillin, but actually was just a coincidence that was unrelated. Then the false allergy label is attached to them for life.
“This is so overlabeled,” Dr. Ramsey said. “Ten percent of the population thinks they’re allergic to penicillin, and 90% of them are not.”
A stark difference was found in the types of medicines administered before and after the evaluations, with aminopenicillin therapy jumping from 0 days of use to 188 days, and vancomycin – a more potent, but more costly alternative – dropping from 130 days of use to 16 days (P less than .05 for both).
Dr. Ramsey noted that, in part because of the time-consuming nature of the penicillin skin tests, they often are simply not done, so the false allergy labels are not caught, leading to pointless costs and exposure to more potent and potentially harmful forms of antibiotic therapy.
“Some hospitals don’t have allergists who will come in to do testing,” she said. “Sometimes patients are on medications that may interfere. And then a lot of times it’s just underrecognized – the implications of a penicillin allergy label. That is a very hot topic in our field and also in infectious disease.”
She hopes the telemedicine approach catches on more widely, which would help minimize the multitude of problems linked to penicillin allergy labels.
“Patients that avoid penicillin, they’re on more costly second-line antibiotics that are, in general, less effective, depending on which infection you’re talking about,” Dr. Ramsey said. “The [second-line antibiotics] have more side effects. And there’s data to show that patients with [a] penicillin allergy label have longer hospital stays, more costly hospital stays, are at risk for more resistant infections. And it breeds antimicrobial resistance in the long-term.”
Dr. Ramsey had no relevant financial disclosures.
SOURCE: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
REPORTING FROM AAAAI/WAO JOINT CONGRESS
Key clinical point: Teleconferencing to assess patient-reported penicillin allergies saves time and results in 9 out of 10 patients being delabeled.
Major finding: Of 50 patients prospectively assessed with this approach over a 4-month period last year, 46 were delabeled, with $23,000 in direct antibiotic cost savings, or $360 per patient.
Study details: A prospective study conducted over 4 months in 2017.
Disclosures: Dr. Ramsey had no relevant financial disclosures.
Source: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
Preparing to respond to workplace violence
SAN ANTONIO – , Lewis J. Kaplan, MD, said in a late-breaking session at the Critical Care Congress.
“Workplace violence is not just active shooter – it’s ubiquitous, and we only know a little bit about it,” noted Dr. Kaplan, section chief, surgical critical care, Corporal Michael J. Crescenz VA Medical Center, Philadelphia. “The facility and everyone in the health care team have a role in being an active participant, rather than a passive one.”
To actively prepare for premeditated events, Dr. Kaplan recommended that clinicians develop partnerships with local law enforcement officials and initiate active training that involves anyone who could come into contact with an active shooter.
There are many steps that can be taken to protect the facility, including visitor screening and management, security that extends to the perimeter of the facility, building design that limits access to specific places in the facility, and deployment of firearm detection canines, Dr. Kaplan said, during the session at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
In all, Dr. Kaplan listed 19 steps that facilities could take to avert a planned attack, drawing in part on recommendations from the FBI publication, Workplace violence: Issues in response.
“This is a lot, and you don’t need to do all of it,” Dr. Kaplan said. “But you need to have an internally consistent plan for how you will do this at your facility, and it must involve everyone. They all need to be able to be part of your team.”
Recent data on workplace violence
The latest data show that the great majority of workplace violence is perpetrated by individuals outside the organization. According to the IAHSS Foundation 2017 Healthcare Crime Survey, 89% of events involved a customer or patient of the workplace or employees.
In-hospital violence is prevalent, according to 2016 data from Occupational Safety and Health Administration that identified 24,000 workplace assaults in a 3-year span covering 2013-2015, including 33 homicides, 30 assaults, and 74 rapes.
Many in-hospital incidents are marked by failures in communication, patient observation, noncompliance with workplace violence policies or lack of such policies, and perhaps most importantly, an inadequate assessment for the violent potential of the perpetrator, according to Dr. Kaplan.
In a 2017 survey of 150 trauma nurses, 67% said they had been the victim of physical violence at work, though many did not report the incidents, Dr. Kaplan noted. Some reasons nurses gave for not reporting violence included the feeling that it was “just part of the job” in 27% of cases, and concerns about patient satisfaction scores in 10% of the cases.
Active shooter events in the workplace are of particular concern, though they are relatively rare; one recent report identified 160 events that occurred during 2000-2013 in which 1,043 individuals were injured, according to Dr. Kaplan.
Other presentations in the late-breaking session covered issues related to disaster preparedness and the Charlie Gard case.
“We picked these three topics to be in a late-breaker session not only because of the recent events that had happened, but because they have a common thread – it’s not a matter of if it will happen, but when will it happen, and are you ready and how do we prepare,” said session chair Gloria M. Rodriguez Vega, MD.
“One of the things I learned as a fellow was that part of the success in critical care was attention to detail and layers of safety,” said Dr. Rodriguez Vega, an intensivist in Bayamon, Puerto Rico. “I think you can apply that to all these situations.”
Dr. Kaplan had no industry disclosures related to his presentation.
SAN ANTONIO – , Lewis J. Kaplan, MD, said in a late-breaking session at the Critical Care Congress.
“Workplace violence is not just active shooter – it’s ubiquitous, and we only know a little bit about it,” noted Dr. Kaplan, section chief, surgical critical care, Corporal Michael J. Crescenz VA Medical Center, Philadelphia. “The facility and everyone in the health care team have a role in being an active participant, rather than a passive one.”
To actively prepare for premeditated events, Dr. Kaplan recommended that clinicians develop partnerships with local law enforcement officials and initiate active training that involves anyone who could come into contact with an active shooter.
There are many steps that can be taken to protect the facility, including visitor screening and management, security that extends to the perimeter of the facility, building design that limits access to specific places in the facility, and deployment of firearm detection canines, Dr. Kaplan said, during the session at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
In all, Dr. Kaplan listed 19 steps that facilities could take to avert a planned attack, drawing in part on recommendations from the FBI publication, Workplace violence: Issues in response.
“This is a lot, and you don’t need to do all of it,” Dr. Kaplan said. “But you need to have an internally consistent plan for how you will do this at your facility, and it must involve everyone. They all need to be able to be part of your team.”
Recent data on workplace violence
The latest data show that the great majority of workplace violence is perpetrated by individuals outside the organization. According to the IAHSS Foundation 2017 Healthcare Crime Survey, 89% of events involved a customer or patient of the workplace or employees.
In-hospital violence is prevalent, according to 2016 data from Occupational Safety and Health Administration that identified 24,000 workplace assaults in a 3-year span covering 2013-2015, including 33 homicides, 30 assaults, and 74 rapes.
Many in-hospital incidents are marked by failures in communication, patient observation, noncompliance with workplace violence policies or lack of such policies, and perhaps most importantly, an inadequate assessment for the violent potential of the perpetrator, according to Dr. Kaplan.
In a 2017 survey of 150 trauma nurses, 67% said they had been the victim of physical violence at work, though many did not report the incidents, Dr. Kaplan noted. Some reasons nurses gave for not reporting violence included the feeling that it was “just part of the job” in 27% of cases, and concerns about patient satisfaction scores in 10% of the cases.
Active shooter events in the workplace are of particular concern, though they are relatively rare; one recent report identified 160 events that occurred during 2000-2013 in which 1,043 individuals were injured, according to Dr. Kaplan.
Other presentations in the late-breaking session covered issues related to disaster preparedness and the Charlie Gard case.
“We picked these three topics to be in a late-breaker session not only because of the recent events that had happened, but because they have a common thread – it’s not a matter of if it will happen, but when will it happen, and are you ready and how do we prepare,” said session chair Gloria M. Rodriguez Vega, MD.
“One of the things I learned as a fellow was that part of the success in critical care was attention to detail and layers of safety,” said Dr. Rodriguez Vega, an intensivist in Bayamon, Puerto Rico. “I think you can apply that to all these situations.”
Dr. Kaplan had no industry disclosures related to his presentation.
SAN ANTONIO – , Lewis J. Kaplan, MD, said in a late-breaking session at the Critical Care Congress.
“Workplace violence is not just active shooter – it’s ubiquitous, and we only know a little bit about it,” noted Dr. Kaplan, section chief, surgical critical care, Corporal Michael J. Crescenz VA Medical Center, Philadelphia. “The facility and everyone in the health care team have a role in being an active participant, rather than a passive one.”
To actively prepare for premeditated events, Dr. Kaplan recommended that clinicians develop partnerships with local law enforcement officials and initiate active training that involves anyone who could come into contact with an active shooter.
There are many steps that can be taken to protect the facility, including visitor screening and management, security that extends to the perimeter of the facility, building design that limits access to specific places in the facility, and deployment of firearm detection canines, Dr. Kaplan said, during the session at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
In all, Dr. Kaplan listed 19 steps that facilities could take to avert a planned attack, drawing in part on recommendations from the FBI publication, Workplace violence: Issues in response.
“This is a lot, and you don’t need to do all of it,” Dr. Kaplan said. “But you need to have an internally consistent plan for how you will do this at your facility, and it must involve everyone. They all need to be able to be part of your team.”
Recent data on workplace violence
The latest data show that the great majority of workplace violence is perpetrated by individuals outside the organization. According to the IAHSS Foundation 2017 Healthcare Crime Survey, 89% of events involved a customer or patient of the workplace or employees.
In-hospital violence is prevalent, according to 2016 data from Occupational Safety and Health Administration that identified 24,000 workplace assaults in a 3-year span covering 2013-2015, including 33 homicides, 30 assaults, and 74 rapes.
Many in-hospital incidents are marked by failures in communication, patient observation, noncompliance with workplace violence policies or lack of such policies, and perhaps most importantly, an inadequate assessment for the violent potential of the perpetrator, according to Dr. Kaplan.
In a 2017 survey of 150 trauma nurses, 67% said they had been the victim of physical violence at work, though many did not report the incidents, Dr. Kaplan noted. Some reasons nurses gave for not reporting violence included the feeling that it was “just part of the job” in 27% of cases, and concerns about patient satisfaction scores in 10% of the cases.
Active shooter events in the workplace are of particular concern, though they are relatively rare; one recent report identified 160 events that occurred during 2000-2013 in which 1,043 individuals were injured, according to Dr. Kaplan.
Other presentations in the late-breaking session covered issues related to disaster preparedness and the Charlie Gard case.
“We picked these three topics to be in a late-breaker session not only because of the recent events that had happened, but because they have a common thread – it’s not a matter of if it will happen, but when will it happen, and are you ready and how do we prepare,” said session chair Gloria M. Rodriguez Vega, MD.
“One of the things I learned as a fellow was that part of the success in critical care was attention to detail and layers of safety,” said Dr. Rodriguez Vega, an intensivist in Bayamon, Puerto Rico. “I think you can apply that to all these situations.”
Dr. Kaplan had no industry disclosures related to his presentation.
REPORTING FROM CCC47