User login
The Hospitalist only
CMS pushes ACOs to take on more risk
Accountable care organizations (ACOs) are playing it too safe, according to the Centers for Medicare & Medicaid Services, which wants to change the rules and push more ACOs into taking on more financial risk – with a little flexibility added in.
“ACOs were designed to move Medicare away from fee for service by encouraging providers to find efficiencies and innovative ways to deliver high-quality care to their patients while reducing costs, giving them the flexibility they need to focus on health outcomes over process,” CMS Administrator Seema Verma said during an Aug. 9 press conference.
That’s not what is happening now, Ms. Verma said. Under the current program, physicians and other health care professionals can participate in an ACO that takes on upside risk only – that is, to share in any of the savings it is able to generate – for up to 6 years before having to take on downside risk to return payment to the government if the ACO fails to hit spending targets.
“This environment has created a perverse incentive leading to the shocking present day reality that, after 6 years, over 82% of shared saving program ACOs are in an upside-only track, meaning that these ACOs have no incentive at all to reduce health care cost while improving outcomes as they were intended,” she said. “The program has not lived up to the accountability part of their name.”
In the aggregate, ACOs that only take on upside risk generally are spending more money and not generating the savings that ACOs in a two-sided risk arrangement are, she added.
To get more health care professionals into two-sided risk arrangements, the CMS released a proposed rule Aug. 9 that caps ACO participation in an upside risk–only arrangement for 2 years before having to migrate to a two-sided risk arrangement. To sweeten the pot, the CMS proposes to allow more flexibility for innovation and encouraging patients to maintain their health.
“On top of [antikickback law] waivers they already receive, we are proposing to allow ACOs that are taking risk to give incentive payments in order to reward patients for taking steps to achieve good health, such as gift cards for patients who receive necessary primary and preventive care,” she said, adding that ACOs who take on downside risk also will be eligible to receive payments for providing telehealth services.
ACOs also will need to adopt the 2015 edition of certified EHR technology and the CMS also will be looking to streamline quality measures, according to the proposal.
The CMS is extending current ACO contracts for 6 months, with the new rules, if finalized, going into effect in the middle of 2019.
The proposal also simplifies the ACO program by offering two tracks, as detailed in a blog post penned by Administrator Verma that appeared Aug. 9 in Health Affairs.
The Basic track “would feature a glide path for taking risk,” she wrote. “It would begin with up to 2 years of upside-only risk and then gradually transition in years 3, 4, and 5 to increasing levels of performance risk, concluding in year 5 at a level of risk that meets the standard to qualify as an advanced alternative payment model [APM]” under the Quality Payment Program. Those entering the enhanced track, taking on two-sided risk immediately, would need to meet the standard of an APM immediately.
The proposal also calls for more transparency and would require providers to alert Medicare beneficiaries that services are being provided in the context of an ACO and to explain what that means for their care.
Spending benchmarks would continue to be calculated using both regional and national spending trends. Program integrity also will be enhanced “by holding ACOs in two-sided models accountable for losses even if they exit midway through a performance year, and by authorizing termination of ACOs with multiple years of poor financial performance,” Ms. Verma wrote.
The Pathways to Success proposed rule was slated to be published in the Federal Register on Aug. 17. Comments are being accepted at regulations.gov until Oct. 16.
Accountable care organizations (ACOs) are playing it too safe, according to the Centers for Medicare & Medicaid Services, which wants to change the rules and push more ACOs into taking on more financial risk – with a little flexibility added in.
“ACOs were designed to move Medicare away from fee for service by encouraging providers to find efficiencies and innovative ways to deliver high-quality care to their patients while reducing costs, giving them the flexibility they need to focus on health outcomes over process,” CMS Administrator Seema Verma said during an Aug. 9 press conference.
That’s not what is happening now, Ms. Verma said. Under the current program, physicians and other health care professionals can participate in an ACO that takes on upside risk only – that is, to share in any of the savings it is able to generate – for up to 6 years before having to take on downside risk to return payment to the government if the ACO fails to hit spending targets.
“This environment has created a perverse incentive leading to the shocking present day reality that, after 6 years, over 82% of shared saving program ACOs are in an upside-only track, meaning that these ACOs have no incentive at all to reduce health care cost while improving outcomes as they were intended,” she said. “The program has not lived up to the accountability part of their name.”
In the aggregate, ACOs that only take on upside risk generally are spending more money and not generating the savings that ACOs in a two-sided risk arrangement are, she added.
To get more health care professionals into two-sided risk arrangements, the CMS released a proposed rule Aug. 9 that caps ACO participation in an upside risk–only arrangement for 2 years before having to migrate to a two-sided risk arrangement. To sweeten the pot, the CMS proposes to allow more flexibility for innovation and encouraging patients to maintain their health.
“On top of [antikickback law] waivers they already receive, we are proposing to allow ACOs that are taking risk to give incentive payments in order to reward patients for taking steps to achieve good health, such as gift cards for patients who receive necessary primary and preventive care,” she said, adding that ACOs who take on downside risk also will be eligible to receive payments for providing telehealth services.
ACOs also will need to adopt the 2015 edition of certified EHR technology and the CMS also will be looking to streamline quality measures, according to the proposal.
The CMS is extending current ACO contracts for 6 months, with the new rules, if finalized, going into effect in the middle of 2019.
The proposal also simplifies the ACO program by offering two tracks, as detailed in a blog post penned by Administrator Verma that appeared Aug. 9 in Health Affairs.
The Basic track “would feature a glide path for taking risk,” she wrote. “It would begin with up to 2 years of upside-only risk and then gradually transition in years 3, 4, and 5 to increasing levels of performance risk, concluding in year 5 at a level of risk that meets the standard to qualify as an advanced alternative payment model [APM]” under the Quality Payment Program. Those entering the enhanced track, taking on two-sided risk immediately, would need to meet the standard of an APM immediately.
The proposal also calls for more transparency and would require providers to alert Medicare beneficiaries that services are being provided in the context of an ACO and to explain what that means for their care.
Spending benchmarks would continue to be calculated using both regional and national spending trends. Program integrity also will be enhanced “by holding ACOs in two-sided models accountable for losses even if they exit midway through a performance year, and by authorizing termination of ACOs with multiple years of poor financial performance,” Ms. Verma wrote.
The Pathways to Success proposed rule was slated to be published in the Federal Register on Aug. 17. Comments are being accepted at regulations.gov until Oct. 16.
Accountable care organizations (ACOs) are playing it too safe, according to the Centers for Medicare & Medicaid Services, which wants to change the rules and push more ACOs into taking on more financial risk – with a little flexibility added in.
“ACOs were designed to move Medicare away from fee for service by encouraging providers to find efficiencies and innovative ways to deliver high-quality care to their patients while reducing costs, giving them the flexibility they need to focus on health outcomes over process,” CMS Administrator Seema Verma said during an Aug. 9 press conference.
That’s not what is happening now, Ms. Verma said. Under the current program, physicians and other health care professionals can participate in an ACO that takes on upside risk only – that is, to share in any of the savings it is able to generate – for up to 6 years before having to take on downside risk to return payment to the government if the ACO fails to hit spending targets.
“This environment has created a perverse incentive leading to the shocking present day reality that, after 6 years, over 82% of shared saving program ACOs are in an upside-only track, meaning that these ACOs have no incentive at all to reduce health care cost while improving outcomes as they were intended,” she said. “The program has not lived up to the accountability part of their name.”
In the aggregate, ACOs that only take on upside risk generally are spending more money and not generating the savings that ACOs in a two-sided risk arrangement are, she added.
To get more health care professionals into two-sided risk arrangements, the CMS released a proposed rule Aug. 9 that caps ACO participation in an upside risk–only arrangement for 2 years before having to migrate to a two-sided risk arrangement. To sweeten the pot, the CMS proposes to allow more flexibility for innovation and encouraging patients to maintain their health.
“On top of [antikickback law] waivers they already receive, we are proposing to allow ACOs that are taking risk to give incentive payments in order to reward patients for taking steps to achieve good health, such as gift cards for patients who receive necessary primary and preventive care,” she said, adding that ACOs who take on downside risk also will be eligible to receive payments for providing telehealth services.
ACOs also will need to adopt the 2015 edition of certified EHR technology and the CMS also will be looking to streamline quality measures, according to the proposal.
The CMS is extending current ACO contracts for 6 months, with the new rules, if finalized, going into effect in the middle of 2019.
The proposal also simplifies the ACO program by offering two tracks, as detailed in a blog post penned by Administrator Verma that appeared Aug. 9 in Health Affairs.
The Basic track “would feature a glide path for taking risk,” she wrote. “It would begin with up to 2 years of upside-only risk and then gradually transition in years 3, 4, and 5 to increasing levels of performance risk, concluding in year 5 at a level of risk that meets the standard to qualify as an advanced alternative payment model [APM]” under the Quality Payment Program. Those entering the enhanced track, taking on two-sided risk immediately, would need to meet the standard of an APM immediately.
The proposal also calls for more transparency and would require providers to alert Medicare beneficiaries that services are being provided in the context of an ACO and to explain what that means for their care.
Spending benchmarks would continue to be calculated using both regional and national spending trends. Program integrity also will be enhanced “by holding ACOs in two-sided models accountable for losses even if they exit midway through a performance year, and by authorizing termination of ACOs with multiple years of poor financial performance,” Ms. Verma wrote.
The Pathways to Success proposed rule was slated to be published in the Federal Register on Aug. 17. Comments are being accepted at regulations.gov until Oct. 16.
Ranked: State of the states’ health care
In the wild world of health care rankings, a year can make a big difference … or not.
Iowa fell from second to ninth over the course of the last year while Connecticut and South Dakota moved out of the top 10 to make way for Colorado and Maryland, according to WalletHub.
There was less movement at the other end of the rankings, however, with no change at all in the bottom five: Louisiana finished 51st again (the rankings include the District of Columbia), preceded by fellow repeaters Mississippi (50), Alaska (49), Arkansas (48), and North Carolina (47). Texas and Nevada did manage to move on up out of the bottom 11 – to 38th and 40th, respectively – at the expense of Oklahoma and Tennessee, WalletHub reported.
For 2018, the company compared the states and D.C. “across 40 measures of cost, accessibility and outcome,” which is five more measures than last year and a possible explanation for the changes at the top. The cost dimension’s five metrics included cost of medical visits and share of high out-of-pocket medical spending. The accessibility dimension consisted of 21 metrics, including average emergency department wait time and share of insured children. The outcomes dimension included 14 metrics, among them maternal mortality rate and share of adults with type 2 diabetes.
Vermont did well in both the outcomes (first) and cost (third) dimensions but only middle of the pack (23rd) in access. The District of Columbia was ranked first in cost and Maine was the leader in access. The lowest-ranked states in each category were Alaska (cost), Texas (access), and Mississippi (outcomes), according to the WalletHub analysis, which was based on data from such sources as the Centers for Disease Control and Prevention, the Health Resources & Services Administration, and the United Health Foundation.
In the wild world of health care rankings, a year can make a big difference … or not.
Iowa fell from second to ninth over the course of the last year while Connecticut and South Dakota moved out of the top 10 to make way for Colorado and Maryland, according to WalletHub.
There was less movement at the other end of the rankings, however, with no change at all in the bottom five: Louisiana finished 51st again (the rankings include the District of Columbia), preceded by fellow repeaters Mississippi (50), Alaska (49), Arkansas (48), and North Carolina (47). Texas and Nevada did manage to move on up out of the bottom 11 – to 38th and 40th, respectively – at the expense of Oklahoma and Tennessee, WalletHub reported.
For 2018, the company compared the states and D.C. “across 40 measures of cost, accessibility and outcome,” which is five more measures than last year and a possible explanation for the changes at the top. The cost dimension’s five metrics included cost of medical visits and share of high out-of-pocket medical spending. The accessibility dimension consisted of 21 metrics, including average emergency department wait time and share of insured children. The outcomes dimension included 14 metrics, among them maternal mortality rate and share of adults with type 2 diabetes.
Vermont did well in both the outcomes (first) and cost (third) dimensions but only middle of the pack (23rd) in access. The District of Columbia was ranked first in cost and Maine was the leader in access. The lowest-ranked states in each category were Alaska (cost), Texas (access), and Mississippi (outcomes), according to the WalletHub analysis, which was based on data from such sources as the Centers for Disease Control and Prevention, the Health Resources & Services Administration, and the United Health Foundation.
In the wild world of health care rankings, a year can make a big difference … or not.
Iowa fell from second to ninth over the course of the last year while Connecticut and South Dakota moved out of the top 10 to make way for Colorado and Maryland, according to WalletHub.
There was less movement at the other end of the rankings, however, with no change at all in the bottom five: Louisiana finished 51st again (the rankings include the District of Columbia), preceded by fellow repeaters Mississippi (50), Alaska (49), Arkansas (48), and North Carolina (47). Texas and Nevada did manage to move on up out of the bottom 11 – to 38th and 40th, respectively – at the expense of Oklahoma and Tennessee, WalletHub reported.
For 2018, the company compared the states and D.C. “across 40 measures of cost, accessibility and outcome,” which is five more measures than last year and a possible explanation for the changes at the top. The cost dimension’s five metrics included cost of medical visits and share of high out-of-pocket medical spending. The accessibility dimension consisted of 21 metrics, including average emergency department wait time and share of insured children. The outcomes dimension included 14 metrics, among them maternal mortality rate and share of adults with type 2 diabetes.
Vermont did well in both the outcomes (first) and cost (third) dimensions but only middle of the pack (23rd) in access. The District of Columbia was ranked first in cost and Maine was the leader in access. The lowest-ranked states in each category were Alaska (cost), Texas (access), and Mississippi (outcomes), according to the WalletHub analysis, which was based on data from such sources as the Centers for Disease Control and Prevention, the Health Resources & Services Administration, and the United Health Foundation.
Documentation and billing: Tips for hospitalists
Is it AMS, Delirium, or Encephalopathy?
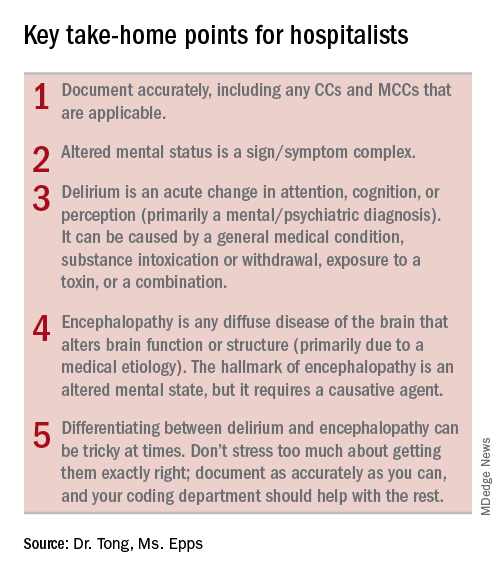
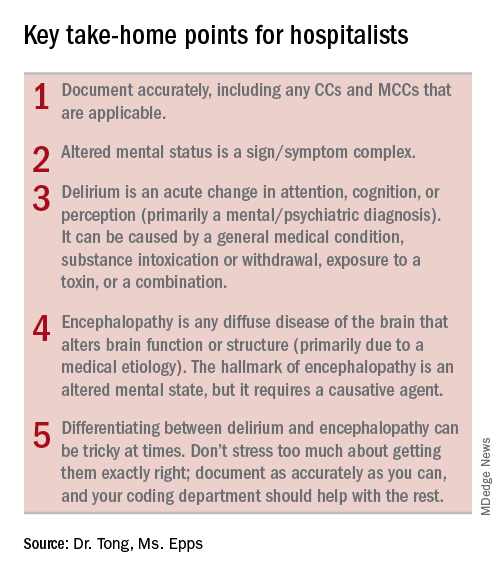
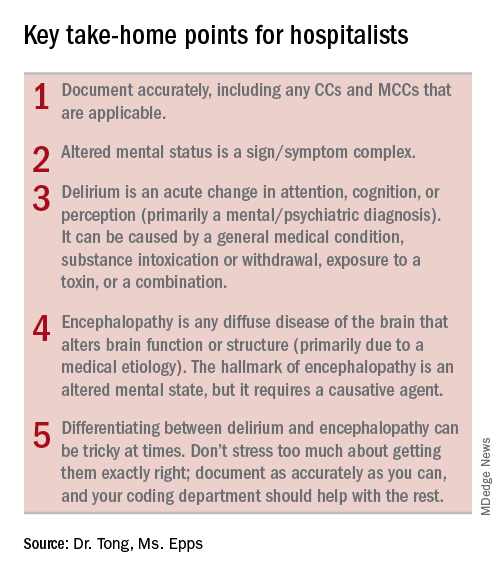
During residency, physicians are trained to care for patients and write notes that are clinically useful. However, physicians are often not taught about how documentation affects reimbursement and quality measures. Our purpose here, and in articles to follow, is to give readers tools to enable them to more accurately reflect the complexity and work that is done for accurate reimbursements.
If you were to get in a car accident, the body shop would document the damage done and submit it to the insurance company. It’s the body shop’s responsibility to record the damage, not the insurance company’s. So while documentation can seem onerous, the insurance company is not going to scour the chart to find diagnoses missed in the note. That would be like the body shop doing repair work without documenting the damage but then somehow expecting to get paid.
For the insurance company, “If you didn’t document it, it didn’t happen.” The body shop should not underdocument and say there were only a few scratches on the right rear panel if it was severely damaged. Likewise, it should not overbill and say the front bumper was damaged if it was not. The goal is not to bill as much as possible but rather to document appropriately.
Terminology
The expected length of stay (LOS) and the expected mortality for a particular patient is determined by how sick the patient appears to be based on the medical record documentation. So documenting all the appropriate diagnoses makes the LOS index (actual LOS divided by expected LOS) and mortality index more accurate as well. It is particularly important to document when a condition is (or is not) “present on admission”.
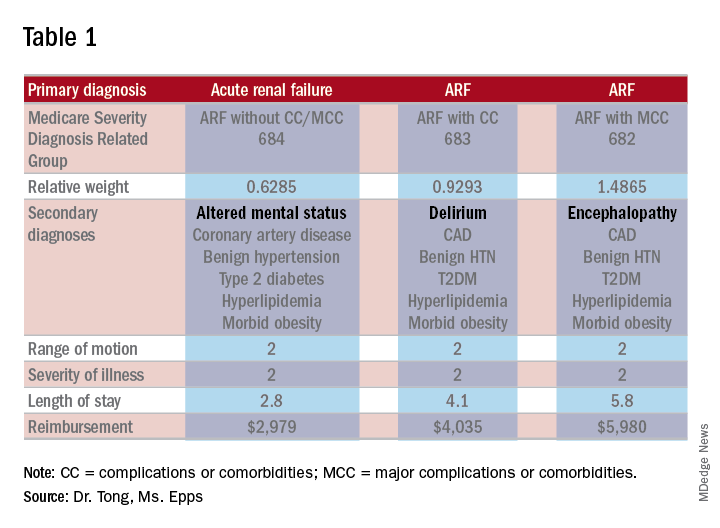
While physician payments can be based on evaluation and management coding, the hospital’s reimbursement is largely determined by physician documentation. Hospitals are paid by Medicare on a capitated basis according to the Acute Inpatient Prospective Payment System. The amount paid is determined by the base rate of the hospital multiplied by the relative weight (RW) of the Medicare Severity Diagnosis Related Group (MS-DRG).
The base rate is adjusted by the wage index of the hospital location. Hospitals that serve a high proportion of low income patients receive a Disproportionate Share Hospital adjustment. The base rate is not something hospitalists have control over.
The RW, however, is determined by the primary diagnosis (reason for admission) and whether or not there are complications or comorbidities (CCs) or major complications or comorbidities (MCCs). The more CCs and MCCs a patient has, the higher the severity of illness and expected increased resources needed to care for that patient.
Diagnoses are currently coded using ICD-10 used by the World Health Organization. The ICD-10 of the primary diagnosis is mapped to an MS-DRG. Many, but not all, MS-DRGs have increasing reimbursements for CCs and MCCs. Coders map the ICD-10 of the principal diagnosis along with any associated CCs or MCCs to the MS-DRG code. The relative weights for different DRGs can found on table 5 of the Medicare website (see reference 1).
Altered mental status versus delirium versus encephalopathy
As an example, let’s look at the difference in RW, LOS, and reimbursement in an otherwise identical patient based on documenting altered mental status (AMS), delirium, or encephalopathy. (see Table 1)
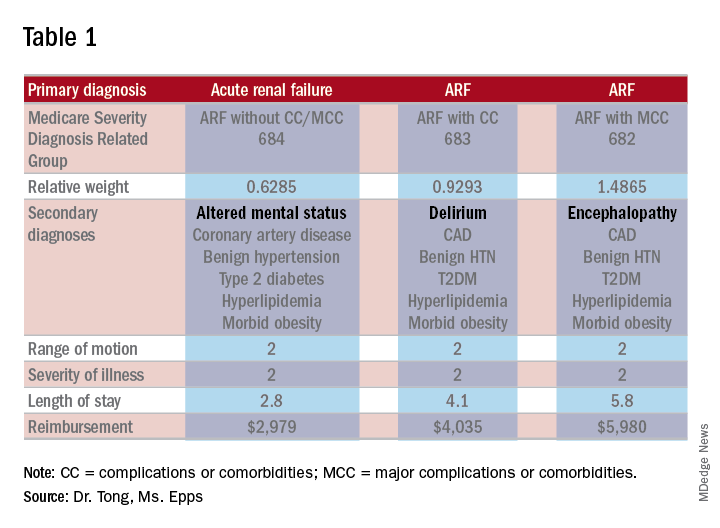
As one can see, RW, estimated LOS, and reimbursement would significantly increase for the patient with delirium (CC) or encephalopathy (MCC) versus AMS (no CC/MCC). A list of which diagnoses are considered CC’s versus MCC’s are on tables 6J and 6I, respectively, on the same Medicare website as table 5.
The difference between AMS, delirium, and encephalopathy
AMS is a sign/symptom complex similar to shortness of breath before an etiology is found. AMS can be the presenting symptom; when a specific etiology is found, however, a more specific diagnosis should be used such as delirium or encephalopathy.
Delirium, according to the DSM-5, is an acute change in the level of attention, cognition, or perception from baseline that developed over hours or days and tends to fluctuate during the course of a day. The change described is not better explained by a preexisting or evolving neurocognitive disorder and does not occur in the context of a severely reduced level of arousal, such as coma. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct consequence of a general medical condition, substance intoxication or withdrawal, exposure to a toxin, or more than one cause.
The National Institute of Neurological Diseases and Stroke defines encephalopathy as “any diffuse disease of the brain that alters brain function or structure. Encephalopathy may be caused by an infectious agent, metabolic or mitochondrial dysfunction, brain tumor or increased intracranial pressure, prolonged exposure to toxic elements, chronic progressive trauma, poor nutrition, or lack of oxygen or blood flow to the brain. The hallmark of encephalopathy is an altered mental state.”
It is confusing since there is a lot of overlap in the definitions of delirium and encephalopathy. One way to tease this out conceptually is noting that delirium is listed under mental, behavioral, and neurodevelopmental disorders, while encephalopathy appears under disorders of the nervous system. One can think of delirium as more of a “mental/psychiatric” diagnosis, while encephalopathy is caused by more “medical” causes.
If a patient who is normally not altered presents with confusion because of an infection or metabolic derangement, one can diagnose and document the cause of an acute encephalopathy. However, let’s say a patient is admitted in the morning with an infection, is started on treatment, but is not initially confused. If he/she later becomes confused at night, one could err conservatively and document delirium caused by sundowning.
Differentiating delirium and encephalopathy can be especially difficult in patients who have dementia with episodic confusion when they present with an infection and confusion. If the confusion is within what family members/caretakers say is “normal,” then one shouldn’t document encephalopathy. As a provider, one shouldn’t focus on all the rules and exceptions, just document as specifically and accurately as possible and the coders should take care of the rest.
Dr. Tong is an assistant professor of hospital medicine and an assistant director of the clinical research program at Emory University, Atlanta. Ms. Epps is director of clinical documentation improvement at Emory Healthcare, Atlanta.
References
1. “Acute Inpatient PPS.” Centers for Medicare and Medicaid Services. Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013.
3. “Details for title: FY 2018 Final Rule and Correction Notice Tables.” Centers for Medicare and Medicaid Services Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2018-IPPS-Final-Rule-Home-Page-Items/FY2018-IPPS-Final-Rule-Tables.html.
4. “Encephalopathy Information Page.” National Institute of Neurologic Disorders and Stroke. Accessed on 2/17/18. https://www.ninds.nih.gov/Disorders/All-Disorders/Encephalopathy-Information-Page.
5. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. http://apps.who.int/iris/handle/10665/37958.
Is it AMS, Delirium, or Encephalopathy?
Is it AMS, Delirium, or Encephalopathy?
During residency, physicians are trained to care for patients and write notes that are clinically useful. However, physicians are often not taught about how documentation affects reimbursement and quality measures. Our purpose here, and in articles to follow, is to give readers tools to enable them to more accurately reflect the complexity and work that is done for accurate reimbursements.
If you were to get in a car accident, the body shop would document the damage done and submit it to the insurance company. It’s the body shop’s responsibility to record the damage, not the insurance company’s. So while documentation can seem onerous, the insurance company is not going to scour the chart to find diagnoses missed in the note. That would be like the body shop doing repair work without documenting the damage but then somehow expecting to get paid.
For the insurance company, “If you didn’t document it, it didn’t happen.” The body shop should not underdocument and say there were only a few scratches on the right rear panel if it was severely damaged. Likewise, it should not overbill and say the front bumper was damaged if it was not. The goal is not to bill as much as possible but rather to document appropriately.
Terminology
The expected length of stay (LOS) and the expected mortality for a particular patient is determined by how sick the patient appears to be based on the medical record documentation. So documenting all the appropriate diagnoses makes the LOS index (actual LOS divided by expected LOS) and mortality index more accurate as well. It is particularly important to document when a condition is (or is not) “present on admission”.
While physician payments can be based on evaluation and management coding, the hospital’s reimbursement is largely determined by physician documentation. Hospitals are paid by Medicare on a capitated basis according to the Acute Inpatient Prospective Payment System. The amount paid is determined by the base rate of the hospital multiplied by the relative weight (RW) of the Medicare Severity Diagnosis Related Group (MS-DRG).
The base rate is adjusted by the wage index of the hospital location. Hospitals that serve a high proportion of low income patients receive a Disproportionate Share Hospital adjustment. The base rate is not something hospitalists have control over.
The RW, however, is determined by the primary diagnosis (reason for admission) and whether or not there are complications or comorbidities (CCs) or major complications or comorbidities (MCCs). The more CCs and MCCs a patient has, the higher the severity of illness and expected increased resources needed to care for that patient.
Diagnoses are currently coded using ICD-10 used by the World Health Organization. The ICD-10 of the primary diagnosis is mapped to an MS-DRG. Many, but not all, MS-DRGs have increasing reimbursements for CCs and MCCs. Coders map the ICD-10 of the principal diagnosis along with any associated CCs or MCCs to the MS-DRG code. The relative weights for different DRGs can found on table 5 of the Medicare website (see reference 1).
Altered mental status versus delirium versus encephalopathy
As an example, let’s look at the difference in RW, LOS, and reimbursement in an otherwise identical patient based on documenting altered mental status (AMS), delirium, or encephalopathy. (see Table 1)
As one can see, RW, estimated LOS, and reimbursement would significantly increase for the patient with delirium (CC) or encephalopathy (MCC) versus AMS (no CC/MCC). A list of which diagnoses are considered CC’s versus MCC’s are on tables 6J and 6I, respectively, on the same Medicare website as table 5.
The difference between AMS, delirium, and encephalopathy
AMS is a sign/symptom complex similar to shortness of breath before an etiology is found. AMS can be the presenting symptom; when a specific etiology is found, however, a more specific diagnosis should be used such as delirium or encephalopathy.
Delirium, according to the DSM-5, is an acute change in the level of attention, cognition, or perception from baseline that developed over hours or days and tends to fluctuate during the course of a day. The change described is not better explained by a preexisting or evolving neurocognitive disorder and does not occur in the context of a severely reduced level of arousal, such as coma. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct consequence of a general medical condition, substance intoxication or withdrawal, exposure to a toxin, or more than one cause.
The National Institute of Neurological Diseases and Stroke defines encephalopathy as “any diffuse disease of the brain that alters brain function or structure. Encephalopathy may be caused by an infectious agent, metabolic or mitochondrial dysfunction, brain tumor or increased intracranial pressure, prolonged exposure to toxic elements, chronic progressive trauma, poor nutrition, or lack of oxygen or blood flow to the brain. The hallmark of encephalopathy is an altered mental state.”
It is confusing since there is a lot of overlap in the definitions of delirium and encephalopathy. One way to tease this out conceptually is noting that delirium is listed under mental, behavioral, and neurodevelopmental disorders, while encephalopathy appears under disorders of the nervous system. One can think of delirium as more of a “mental/psychiatric” diagnosis, while encephalopathy is caused by more “medical” causes.
If a patient who is normally not altered presents with confusion because of an infection or metabolic derangement, one can diagnose and document the cause of an acute encephalopathy. However, let’s say a patient is admitted in the morning with an infection, is started on treatment, but is not initially confused. If he/she later becomes confused at night, one could err conservatively and document delirium caused by sundowning.
Differentiating delirium and encephalopathy can be especially difficult in patients who have dementia with episodic confusion when they present with an infection and confusion. If the confusion is within what family members/caretakers say is “normal,” then one shouldn’t document encephalopathy. As a provider, one shouldn’t focus on all the rules and exceptions, just document as specifically and accurately as possible and the coders should take care of the rest.
Dr. Tong is an assistant professor of hospital medicine and an assistant director of the clinical research program at Emory University, Atlanta. Ms. Epps is director of clinical documentation improvement at Emory Healthcare, Atlanta.
References
1. “Acute Inpatient PPS.” Centers for Medicare and Medicaid Services. Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013.
3. “Details for title: FY 2018 Final Rule and Correction Notice Tables.” Centers for Medicare and Medicaid Services Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2018-IPPS-Final-Rule-Home-Page-Items/FY2018-IPPS-Final-Rule-Tables.html.
4. “Encephalopathy Information Page.” National Institute of Neurologic Disorders and Stroke. Accessed on 2/17/18. https://www.ninds.nih.gov/Disorders/All-Disorders/Encephalopathy-Information-Page.
5. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. http://apps.who.int/iris/handle/10665/37958.
During residency, physicians are trained to care for patients and write notes that are clinically useful. However, physicians are often not taught about how documentation affects reimbursement and quality measures. Our purpose here, and in articles to follow, is to give readers tools to enable them to more accurately reflect the complexity and work that is done for accurate reimbursements.
If you were to get in a car accident, the body shop would document the damage done and submit it to the insurance company. It’s the body shop’s responsibility to record the damage, not the insurance company’s. So while documentation can seem onerous, the insurance company is not going to scour the chart to find diagnoses missed in the note. That would be like the body shop doing repair work without documenting the damage but then somehow expecting to get paid.
For the insurance company, “If you didn’t document it, it didn’t happen.” The body shop should not underdocument and say there were only a few scratches on the right rear panel if it was severely damaged. Likewise, it should not overbill and say the front bumper was damaged if it was not. The goal is not to bill as much as possible but rather to document appropriately.
Terminology
The expected length of stay (LOS) and the expected mortality for a particular patient is determined by how sick the patient appears to be based on the medical record documentation. So documenting all the appropriate diagnoses makes the LOS index (actual LOS divided by expected LOS) and mortality index more accurate as well. It is particularly important to document when a condition is (or is not) “present on admission”.
While physician payments can be based on evaluation and management coding, the hospital’s reimbursement is largely determined by physician documentation. Hospitals are paid by Medicare on a capitated basis according to the Acute Inpatient Prospective Payment System. The amount paid is determined by the base rate of the hospital multiplied by the relative weight (RW) of the Medicare Severity Diagnosis Related Group (MS-DRG).
The base rate is adjusted by the wage index of the hospital location. Hospitals that serve a high proportion of low income patients receive a Disproportionate Share Hospital adjustment. The base rate is not something hospitalists have control over.
The RW, however, is determined by the primary diagnosis (reason for admission) and whether or not there are complications or comorbidities (CCs) or major complications or comorbidities (MCCs). The more CCs and MCCs a patient has, the higher the severity of illness and expected increased resources needed to care for that patient.
Diagnoses are currently coded using ICD-10 used by the World Health Organization. The ICD-10 of the primary diagnosis is mapped to an MS-DRG. Many, but not all, MS-DRGs have increasing reimbursements for CCs and MCCs. Coders map the ICD-10 of the principal diagnosis along with any associated CCs or MCCs to the MS-DRG code. The relative weights for different DRGs can found on table 5 of the Medicare website (see reference 1).
Altered mental status versus delirium versus encephalopathy
As an example, let’s look at the difference in RW, LOS, and reimbursement in an otherwise identical patient based on documenting altered mental status (AMS), delirium, or encephalopathy. (see Table 1)
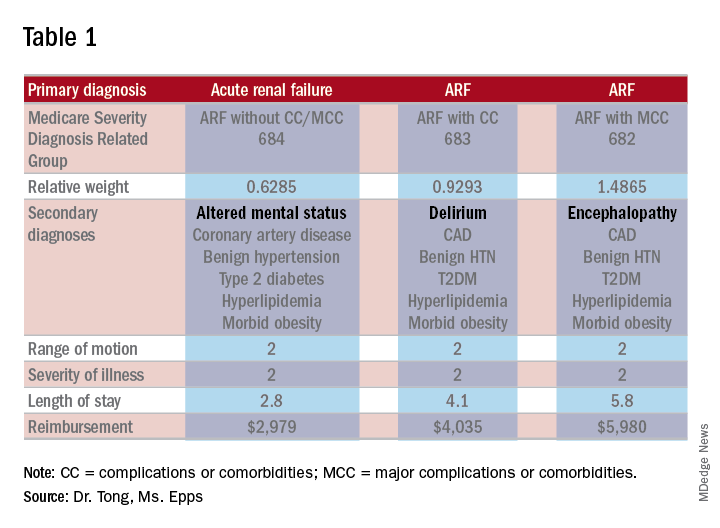
As one can see, RW, estimated LOS, and reimbursement would significantly increase for the patient with delirium (CC) or encephalopathy (MCC) versus AMS (no CC/MCC). A list of which diagnoses are considered CC’s versus MCC’s are on tables 6J and 6I, respectively, on the same Medicare website as table 5.
The difference between AMS, delirium, and encephalopathy
AMS is a sign/symptom complex similar to shortness of breath before an etiology is found. AMS can be the presenting symptom; when a specific etiology is found, however, a more specific diagnosis should be used such as delirium or encephalopathy.
Delirium, according to the DSM-5, is an acute change in the level of attention, cognition, or perception from baseline that developed over hours or days and tends to fluctuate during the course of a day. The change described is not better explained by a preexisting or evolving neurocognitive disorder and does not occur in the context of a severely reduced level of arousal, such as coma. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct consequence of a general medical condition, substance intoxication or withdrawal, exposure to a toxin, or more than one cause.
The National Institute of Neurological Diseases and Stroke defines encephalopathy as “any diffuse disease of the brain that alters brain function or structure. Encephalopathy may be caused by an infectious agent, metabolic or mitochondrial dysfunction, brain tumor or increased intracranial pressure, prolonged exposure to toxic elements, chronic progressive trauma, poor nutrition, or lack of oxygen or blood flow to the brain. The hallmark of encephalopathy is an altered mental state.”
It is confusing since there is a lot of overlap in the definitions of delirium and encephalopathy. One way to tease this out conceptually is noting that delirium is listed under mental, behavioral, and neurodevelopmental disorders, while encephalopathy appears under disorders of the nervous system. One can think of delirium as more of a “mental/psychiatric” diagnosis, while encephalopathy is caused by more “medical” causes.
If a patient who is normally not altered presents with confusion because of an infection or metabolic derangement, one can diagnose and document the cause of an acute encephalopathy. However, let’s say a patient is admitted in the morning with an infection, is started on treatment, but is not initially confused. If he/she later becomes confused at night, one could err conservatively and document delirium caused by sundowning.
Differentiating delirium and encephalopathy can be especially difficult in patients who have dementia with episodic confusion when they present with an infection and confusion. If the confusion is within what family members/caretakers say is “normal,” then one shouldn’t document encephalopathy. As a provider, one shouldn’t focus on all the rules and exceptions, just document as specifically and accurately as possible and the coders should take care of the rest.
Dr. Tong is an assistant professor of hospital medicine and an assistant director of the clinical research program at Emory University, Atlanta. Ms. Epps is director of clinical documentation improvement at Emory Healthcare, Atlanta.
References
1. “Acute Inpatient PPS.” Centers for Medicare and Medicaid Services. Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013.
3. “Details for title: FY 2018 Final Rule and Correction Notice Tables.” Centers for Medicare and Medicaid Services Accessed 2/17/18. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2018-IPPS-Final-Rule-Home-Page-Items/FY2018-IPPS-Final-Rule-Tables.html.
4. “Encephalopathy Information Page.” National Institute of Neurologic Disorders and Stroke. Accessed on 2/17/18. https://www.ninds.nih.gov/Disorders/All-Disorders/Encephalopathy-Information-Page.
5. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. http://apps.who.int/iris/handle/10665/37958.
Who are the 'high-need, high-cost' patients?
Among patients hospitalized with gastrointestinal and liver diseases, a clearly identifiable subset uses significantly more health care resources, which incurs significantly greater costs, according to the results of a national database analysis published in the August issue of Clinical Gastroenterology and Hepatology.
Compared with otherwise similar inpatients, these “high-need, high-cost” individuals are significantly more likely to be enrolled in Medicare or Medicaid, to have lower income, to initially be admitted to a large, rural hospital, to have multiple comorbidities, to be obese, or to be hospitalized for infection, said Nghia Nguyen, MD, and his associates. “[A] small fraction of high-need, high-cost patients contribute disproportionately to hospitalization costs,” they wrote. “Population health management directed toward these patients would facilitate high-value care.”
Gastrointestinal and liver diseases incur more than $100 billion in health care expenses annually in the United States, of which more than 60% is related to inpatient care, the researchers noted. However, few studies have comprehensively evaluated the annual burden and costs of hospitalization in patients with chronic gastrointestinal and liver diseases. Therefore, using the Nationwide Readmissions Database, the investigators studied patients with inflammatory bowel disease (IBD), chronic liver disease, functional gastrointestinal disorders, gastrointestinal hemorrhage, or pancreatic diseases who were hospitalized at least once during the first 6 months of 2013. All patients were diagnosed with IBD, chronic liver diseases, functional gastrointestinal disorders, gastrointestinal hemorrhage, or pancreatic diseases and followed for at least 6 months. The researchers stratified hospital days and costs and characterized the subset of patients who fell into the highest decile of days spent in the hospital per month.
The most common reason for hospitalization was chronic liver disease (nearly 377,000 patients), followed by functional gastrointestinal disorders (more than 351,000 patients), gastrointestinal hemorrhage (nearly 191,000 patients), pancreatic diseases (more than 98,000 patients), and IBD (more than 47,000 patients). Patients spent a median of 6-7 days in the hospital per year, with an interquartile range of 3-14 days. Compared with patients in the lowest decile for annual hospital stay (median, 0.13-0.14 days per month), patients in the highest decile spent a median of 3.7-5.1 days in the hospital per month. In this high-cost, high-need subset of patients, the costs of each hospitalization ranged from $7,438 per month to $11,425 per month, and they were typically hospitalized once every 2 months.
“Gastrointestinal diseases, infections, and cardiopulmonary causes were leading reasons for hospitalization of these patients,” the researchers wrote. “At a patient level, modifiable risk factors may include tackling the obesity epidemic and mental health issues and minimizing risk of iatrogenic or health care–associated infections, whereas at a health system level, interventions may include better access to care and connectivity between rural and specialty hospitals.”
Funders included the American College of Gastroenterology, the Crohn’s and Colitis Foundation, and the National Institutes of Health. Senior author Siddharth Singh disclosed unrelated grant funding from Pifzer and AbbVie. The other investigators reported having no conflicts of interest.
SOURCE: Nguyen NH et al. Clin Gastroenterol Hepatol. 2018 Feb 20. doi: 10.1016/j.cgh.2018.02.015.
Understanding the reasons underlying variations in health care utilization is central to any plan to reduce costs at the population level. To this end, Nguyen et al. provide crucial data for the patients for whom we care as gastroenterologists. Studying a longitudinal database of hospitalizations in 2013, the authors provide comprehensive demographic data for the top decile of inpatient health care utilizers (defined by hospital-days/month) with inflammatory bowel disease, chronic liver disease, functional gastrointestinal disorders, gastrointestinal hemorrhage, and pancreatic diseases. Although constrained by the limits of administrative data and the lack of outpatient/pharmaceutical data linkage, these findings are strengthened by their consistency across conditions. Indeed, despite the heterogeneous disorders surveyed, a remarkably consistent high-need/high-cost "phenotype" emerges: publicly insured, low-income, rural, obese but malnourished, and beset by infections and the complications of diabetes.
What are the next steps?
When a minority of the patients are responsible for a substantial portion of the costs (i.e., the 80/20 rule), one strategy for cost containment is "hot-spotting." Hot-spotting is a two-step process: Identify high-need, high-cost patients, and then deploy interventions tailored to their needs. Nguyen and colleague's work is a landmark for the first step. However, before these findings may be translated into policy or intervention, we need granular data to explain these associations and suggest clear action items. Solutions will likely be multifactorial including early, intensified care for obesity and diabetes (before end-stage complications arise), novel care delivery methods for gastroenterology specialty care in rural hospitals, and intensified outpatient resources for high-need patients in order to coordinate alternatives to hospitalization.
Elliot B. Tapper, MD, is assistant professor, division of gastroenterology and hepatology, University of Michigan, Ann Arbor. He reports consulting for Novartis and receiving unrestricted research grants from Valeant and Gilead, all unrelated to this work.
Understanding the reasons underlying variations in health care utilization is central to any plan to reduce costs at the population level. To this end, Nguyen et al. provide crucial data for the patients for whom we care as gastroenterologists. Studying a longitudinal database of hospitalizations in 2013, the authors provide comprehensive demographic data for the top decile of inpatient health care utilizers (defined by hospital-days/month) with inflammatory bowel disease, chronic liver disease, functional gastrointestinal disorders, gastrointestinal hemorrhage, and pancreatic diseases. Although constrained by the limits of administrative data and the lack of outpatient/pharmaceutical data linkage, these findings are strengthened by their consistency across conditions. Indeed, despite the heterogeneous disorders surveyed, a remarkably consistent high-need/high-cost "phenotype" emerges: publicly insured, low-income, rural, obese but malnourished, and beset by infections and the complications of diabetes.
What are the next steps?
When a minority of the patients are responsible for a substantial portion of the costs (i.e., the 80/20 rule), one strategy for cost containment is "hot-spotting." Hot-spotting is a two-step process: Identify high-need, high-cost patients, and then deploy interventions tailored to their needs. Nguyen and colleague's work is a landmark for the first step. However, before these findings may be translated into policy or intervention, we need granular data to explain these associations and suggest clear action items. Solutions will likely be multifactorial including early, intensified care for obesity and diabetes (before end-stage complications arise), novel care delivery methods for gastroenterology specialty care in rural hospitals, and intensified outpatient resources for high-need patients in order to coordinate alternatives to hospitalization.
Elliot B. Tapper, MD, is assistant professor, division of gastroenterology and hepatology, University of Michigan, Ann Arbor. He reports consulting for Novartis and receiving unrestricted research grants from Valeant and Gilead, all unrelated to this work.
Understanding the reasons underlying variations in health care utilization is central to any plan to reduce costs at the population level. To this end, Nguyen et al. provide crucial data for the patients for whom we care as gastroenterologists. Studying a longitudinal database of hospitalizations in 2013, the authors provide comprehensive demographic data for the top decile of inpatient health care utilizers (defined by hospital-days/month) with inflammatory bowel disease, chronic liver disease, functional gastrointestinal disorders, gastrointestinal hemorrhage, and pancreatic diseases. Although constrained by the limits of administrative data and the lack of outpatient/pharmaceutical data linkage, these findings are strengthened by their consistency across conditions. Indeed, despite the heterogeneous disorders surveyed, a remarkably consistent high-need/high-cost "phenotype" emerges: publicly insured, low-income, rural, obese but malnourished, and beset by infections and the complications of diabetes.
What are the next steps?
When a minority of the patients are responsible for a substantial portion of the costs (i.e., the 80/20 rule), one strategy for cost containment is "hot-spotting." Hot-spotting is a two-step process: Identify high-need, high-cost patients, and then deploy interventions tailored to their needs. Nguyen and colleague's work is a landmark for the first step. However, before these findings may be translated into policy or intervention, we need granular data to explain these associations and suggest clear action items. Solutions will likely be multifactorial including early, intensified care for obesity and diabetes (before end-stage complications arise), novel care delivery methods for gastroenterology specialty care in rural hospitals, and intensified outpatient resources for high-need patients in order to coordinate alternatives to hospitalization.
Elliot B. Tapper, MD, is assistant professor, division of gastroenterology and hepatology, University of Michigan, Ann Arbor. He reports consulting for Novartis and receiving unrestricted research grants from Valeant and Gilead, all unrelated to this work.
Among patients hospitalized with gastrointestinal and liver diseases, a clearly identifiable subset uses significantly more health care resources, which incurs significantly greater costs, according to the results of a national database analysis published in the August issue of Clinical Gastroenterology and Hepatology.
Compared with otherwise similar inpatients, these “high-need, high-cost” individuals are significantly more likely to be enrolled in Medicare or Medicaid, to have lower income, to initially be admitted to a large, rural hospital, to have multiple comorbidities, to be obese, or to be hospitalized for infection, said Nghia Nguyen, MD, and his associates. “[A] small fraction of high-need, high-cost patients contribute disproportionately to hospitalization costs,” they wrote. “Population health management directed toward these patients would facilitate high-value care.”
Gastrointestinal and liver diseases incur more than $100 billion in health care expenses annually in the United States, of which more than 60% is related to inpatient care, the researchers noted. However, few studies have comprehensively evaluated the annual burden and costs of hospitalization in patients with chronic gastrointestinal and liver diseases. Therefore, using the Nationwide Readmissions Database, the investigators studied patients with inflammatory bowel disease (IBD), chronic liver disease, functional gastrointestinal disorders, gastrointestinal hemorrhage, or pancreatic diseases who were hospitalized at least once during the first 6 months of 2013. All patients were diagnosed with IBD, chronic liver diseases, functional gastrointestinal disorders, gastrointestinal hemorrhage, or pancreatic diseases and followed for at least 6 months. The researchers stratified hospital days and costs and characterized the subset of patients who fell into the highest decile of days spent in the hospital per month.
The most common reason for hospitalization was chronic liver disease (nearly 377,000 patients), followed by functional gastrointestinal disorders (more than 351,000 patients), gastrointestinal hemorrhage (nearly 191,000 patients), pancreatic diseases (more than 98,000 patients), and IBD (more than 47,000 patients). Patients spent a median of 6-7 days in the hospital per year, with an interquartile range of 3-14 days. Compared with patients in the lowest decile for annual hospital stay (median, 0.13-0.14 days per month), patients in the highest decile spent a median of 3.7-5.1 days in the hospital per month. In this high-cost, high-need subset of patients, the costs of each hospitalization ranged from $7,438 per month to $11,425 per month, and they were typically hospitalized once every 2 months.
“Gastrointestinal diseases, infections, and cardiopulmonary causes were leading reasons for hospitalization of these patients,” the researchers wrote. “At a patient level, modifiable risk factors may include tackling the obesity epidemic and mental health issues and minimizing risk of iatrogenic or health care–associated infections, whereas at a health system level, interventions may include better access to care and connectivity between rural and specialty hospitals.”
Funders included the American College of Gastroenterology, the Crohn’s and Colitis Foundation, and the National Institutes of Health. Senior author Siddharth Singh disclosed unrelated grant funding from Pifzer and AbbVie. The other investigators reported having no conflicts of interest.
SOURCE: Nguyen NH et al. Clin Gastroenterol Hepatol. 2018 Feb 20. doi: 10.1016/j.cgh.2018.02.015.
Among patients hospitalized with gastrointestinal and liver diseases, a clearly identifiable subset uses significantly more health care resources, which incurs significantly greater costs, according to the results of a national database analysis published in the August issue of Clinical Gastroenterology and Hepatology.
Compared with otherwise similar inpatients, these “high-need, high-cost” individuals are significantly more likely to be enrolled in Medicare or Medicaid, to have lower income, to initially be admitted to a large, rural hospital, to have multiple comorbidities, to be obese, or to be hospitalized for infection, said Nghia Nguyen, MD, and his associates. “[A] small fraction of high-need, high-cost patients contribute disproportionately to hospitalization costs,” they wrote. “Population health management directed toward these patients would facilitate high-value care.”
Gastrointestinal and liver diseases incur more than $100 billion in health care expenses annually in the United States, of which more than 60% is related to inpatient care, the researchers noted. However, few studies have comprehensively evaluated the annual burden and costs of hospitalization in patients with chronic gastrointestinal and liver diseases. Therefore, using the Nationwide Readmissions Database, the investigators studied patients with inflammatory bowel disease (IBD), chronic liver disease, functional gastrointestinal disorders, gastrointestinal hemorrhage, or pancreatic diseases who were hospitalized at least once during the first 6 months of 2013. All patients were diagnosed with IBD, chronic liver diseases, functional gastrointestinal disorders, gastrointestinal hemorrhage, or pancreatic diseases and followed for at least 6 months. The researchers stratified hospital days and costs and characterized the subset of patients who fell into the highest decile of days spent in the hospital per month.
The most common reason for hospitalization was chronic liver disease (nearly 377,000 patients), followed by functional gastrointestinal disorders (more than 351,000 patients), gastrointestinal hemorrhage (nearly 191,000 patients), pancreatic diseases (more than 98,000 patients), and IBD (more than 47,000 patients). Patients spent a median of 6-7 days in the hospital per year, with an interquartile range of 3-14 days. Compared with patients in the lowest decile for annual hospital stay (median, 0.13-0.14 days per month), patients in the highest decile spent a median of 3.7-5.1 days in the hospital per month. In this high-cost, high-need subset of patients, the costs of each hospitalization ranged from $7,438 per month to $11,425 per month, and they were typically hospitalized once every 2 months.
“Gastrointestinal diseases, infections, and cardiopulmonary causes were leading reasons for hospitalization of these patients,” the researchers wrote. “At a patient level, modifiable risk factors may include tackling the obesity epidemic and mental health issues and minimizing risk of iatrogenic or health care–associated infections, whereas at a health system level, interventions may include better access to care and connectivity between rural and specialty hospitals.”
Funders included the American College of Gastroenterology, the Crohn’s and Colitis Foundation, and the National Institutes of Health. Senior author Siddharth Singh disclosed unrelated grant funding from Pifzer and AbbVie. The other investigators reported having no conflicts of interest.
SOURCE: Nguyen NH et al. Clin Gastroenterol Hepatol. 2018 Feb 20. doi: 10.1016/j.cgh.2018.02.015.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: For patients with gastrointestinal or liver disease, significant predictors of high need and cost during hospitalization included Medicare or Medicaid insurance, lower income, first hospitalization in a large rural hospital, high comorbidity burden, obesity, and hospitalization for infection.
Major finding: Patients in the highest decile spent a median of 3.7-4.1 days in the hospital per month for all causes. Gastrointestinal disease, infections, and cardiopulmonary morbidity were the most common reasons for hospitalization.
Study details: Analysis of patients with inflammatory bowel disease, chronic liver disease, functional gastrointestinal disorders, gastrointestinal hemorrhage, or pancreatic diseases hospitalized at least once during 2013.
Disclosures: Funders included the American College of Gastroenterology, the Crohn’s and Colitis Foundation, and the National Institutes of Health. Senior author Siddharth Singh disclosed unrelated grant funding from Pifzer and AbbVie. The other investigators reported having no conflicts of interest.
Source: Nguyen NH et al. Clin Gastroenterol Hepatol. 2018 Feb 20. doi: 10.1016/j.cgh.2018.02.015.
CMS proposes site-neutral payments for hospital outpatient setting
In the proposed update to the Outpatient Prospective Payment System (OPPS) for 2019, released July 27 and scheduled to be published July 31 in the Federal Register, the CMS is proposing to apply a physician fee schedule–equivalent for the clinic visit service when provided at an off-campus, provider-based department that is paid under the OPPS.
“The clinic visit is the most common service billed under the OPPS and is often furnished in the physician office setting,” the CMS said in a fact sheet detailing its proposal.
According to the CMS, the average current clinical visit paid by the CMS is $116 with $23 being the average copay by the patient. If the proposal is finalized, the payment would drop to about $46 with an average patient copay of $9.
“This is intended to address concerns about recent consolidations in the market that reduce competition,” CMS Administrator Seema Verma said during a July 25 press conference.
The American Hospital Association already is pushing back on this proposal.
“With today’s proposed rule, CMS has once again showed a lack of understanding about the reality in which hospitals and health systems operate daily to serve the needs of their communities,” AHA Executive Vice President Tom Nickels said in a statement. “In 2015, Congress clearly intended to provide current off-campus hospital clinics with the existing outpatient payment rate in recognition of the critical role they play in their communities. But CMS’s proposal runs counter to this and will instead impede access to care for the most vulnerable patients.”
However, Farzad Mostashari, MD, founder of the health care technology company Aledade and National Coordinator for Health IT under President Obama, suggested that this could actually be a good thing for hospitals.
“The truth is that this proposal could help hospitals be more competitive in value-based contracts/alternative-payment models, and they should embrace the changes,” he said in a tweet.
The OPPS update also includes proposals to expand the list of covered surgical procedures that can be performed in an ambulatory surgical center, a move that Ms. Verma said would “provide patients with more choices and options for lower-priced care.”
“For CY 2019, CMS is proposing to allow certain CPT codes outside of the surgical code range that directly crosswalk or are clinically similar to procedures within the CPT surgical code range to be included on the [covered procedure list] and is proposing to add certain cardiovascular codes to the ASC [covered procedure list] as a result,” the CMS fact sheet notes.
The CMS also will review all procedures added to the covered procedure list in the past 3 years to determine whether such procedures should continue to be covered.
In addition, the OPPS is seeking feedback on a number of topics.
One is related to price transparency. The agency is asking “whether providers and suppliers can and should be required to inform patients about charges and payment information for healthcare services and out-of-pocket costs, what data elements the public would find most useful, and what other charges are needed to empower patients,” according to the fact sheet.
The CMS also is seeking information about relaunching a revamped competitive acquisition program that would have private vendors administer payment arrangements for Part B drugs. The agency is soliciting feedback on ways to design a model for testing.
Finally, the agency is seeking more information on solutions to better promote interoperability.
In the proposed update to the Outpatient Prospective Payment System (OPPS) for 2019, released July 27 and scheduled to be published July 31 in the Federal Register, the CMS is proposing to apply a physician fee schedule–equivalent for the clinic visit service when provided at an off-campus, provider-based department that is paid under the OPPS.
“The clinic visit is the most common service billed under the OPPS and is often furnished in the physician office setting,” the CMS said in a fact sheet detailing its proposal.
According to the CMS, the average current clinical visit paid by the CMS is $116 with $23 being the average copay by the patient. If the proposal is finalized, the payment would drop to about $46 with an average patient copay of $9.
“This is intended to address concerns about recent consolidations in the market that reduce competition,” CMS Administrator Seema Verma said during a July 25 press conference.
The American Hospital Association already is pushing back on this proposal.
“With today’s proposed rule, CMS has once again showed a lack of understanding about the reality in which hospitals and health systems operate daily to serve the needs of their communities,” AHA Executive Vice President Tom Nickels said in a statement. “In 2015, Congress clearly intended to provide current off-campus hospital clinics with the existing outpatient payment rate in recognition of the critical role they play in their communities. But CMS’s proposal runs counter to this and will instead impede access to care for the most vulnerable patients.”
However, Farzad Mostashari, MD, founder of the health care technology company Aledade and National Coordinator for Health IT under President Obama, suggested that this could actually be a good thing for hospitals.
“The truth is that this proposal could help hospitals be more competitive in value-based contracts/alternative-payment models, and they should embrace the changes,” he said in a tweet.
The OPPS update also includes proposals to expand the list of covered surgical procedures that can be performed in an ambulatory surgical center, a move that Ms. Verma said would “provide patients with more choices and options for lower-priced care.”
“For CY 2019, CMS is proposing to allow certain CPT codes outside of the surgical code range that directly crosswalk or are clinically similar to procedures within the CPT surgical code range to be included on the [covered procedure list] and is proposing to add certain cardiovascular codes to the ASC [covered procedure list] as a result,” the CMS fact sheet notes.
The CMS also will review all procedures added to the covered procedure list in the past 3 years to determine whether such procedures should continue to be covered.
In addition, the OPPS is seeking feedback on a number of topics.
One is related to price transparency. The agency is asking “whether providers and suppliers can and should be required to inform patients about charges and payment information for healthcare services and out-of-pocket costs, what data elements the public would find most useful, and what other charges are needed to empower patients,” according to the fact sheet.
The CMS also is seeking information about relaunching a revamped competitive acquisition program that would have private vendors administer payment arrangements for Part B drugs. The agency is soliciting feedback on ways to design a model for testing.
Finally, the agency is seeking more information on solutions to better promote interoperability.
In the proposed update to the Outpatient Prospective Payment System (OPPS) for 2019, released July 27 and scheduled to be published July 31 in the Federal Register, the CMS is proposing to apply a physician fee schedule–equivalent for the clinic visit service when provided at an off-campus, provider-based department that is paid under the OPPS.
“The clinic visit is the most common service billed under the OPPS and is often furnished in the physician office setting,” the CMS said in a fact sheet detailing its proposal.
According to the CMS, the average current clinical visit paid by the CMS is $116 with $23 being the average copay by the patient. If the proposal is finalized, the payment would drop to about $46 with an average patient copay of $9.
“This is intended to address concerns about recent consolidations in the market that reduce competition,” CMS Administrator Seema Verma said during a July 25 press conference.
The American Hospital Association already is pushing back on this proposal.
“With today’s proposed rule, CMS has once again showed a lack of understanding about the reality in which hospitals and health systems operate daily to serve the needs of their communities,” AHA Executive Vice President Tom Nickels said in a statement. “In 2015, Congress clearly intended to provide current off-campus hospital clinics with the existing outpatient payment rate in recognition of the critical role they play in their communities. But CMS’s proposal runs counter to this and will instead impede access to care for the most vulnerable patients.”
However, Farzad Mostashari, MD, founder of the health care technology company Aledade and National Coordinator for Health IT under President Obama, suggested that this could actually be a good thing for hospitals.
“The truth is that this proposal could help hospitals be more competitive in value-based contracts/alternative-payment models, and they should embrace the changes,” he said in a tweet.
The OPPS update also includes proposals to expand the list of covered surgical procedures that can be performed in an ambulatory surgical center, a move that Ms. Verma said would “provide patients with more choices and options for lower-priced care.”
“For CY 2019, CMS is proposing to allow certain CPT codes outside of the surgical code range that directly crosswalk or are clinically similar to procedures within the CPT surgical code range to be included on the [covered procedure list] and is proposing to add certain cardiovascular codes to the ASC [covered procedure list] as a result,” the CMS fact sheet notes.
The CMS also will review all procedures added to the covered procedure list in the past 3 years to determine whether such procedures should continue to be covered.
In addition, the OPPS is seeking feedback on a number of topics.
One is related to price transparency. The agency is asking “whether providers and suppliers can and should be required to inform patients about charges and payment information for healthcare services and out-of-pocket costs, what data elements the public would find most useful, and what other charges are needed to empower patients,” according to the fact sheet.
The CMS also is seeking information about relaunching a revamped competitive acquisition program that would have private vendors administer payment arrangements for Part B drugs. The agency is soliciting feedback on ways to design a model for testing.
Finally, the agency is seeking more information on solutions to better promote interoperability.
CMS considers expanding telemedicine payments
Payment for more telemedicine services could be in store for physicians and other health providers if new proposals in the latest fee schedule from the Centers for Medicare & Medicaid Services are finalized.
Under the proposed physician fee schedule, announced July 12, the CMS would expand services that qualify for telemedicine payments and add reimbursement for virtual check-ins by phone or other technologies, such as Skype. Telemedicine clinicians would also be paid for time spent reviewing patient photos sent by text or e-mail under the suggested changes.
Such telehealth services would aid patients who have transportation difficulties by creating more opportunities for them to access personalized care, said CMS Administrator Seema Verma.
“CMS is committed to modernizing the Medicare program by leveraging technologies, such as audio/video applications or patient-facing health portals, that will help beneficiaries access high-quality services in a convenient manner,” Ms. Verma said in a statement.
Under the proposal, physicians could bill separately for brief, non–face-to-face patient check-ins with patients via communication technology beginning January 2019. In addition, the proposed rule carves out payments for the remote professional evaluation of patient-transmitted information conducted via prerecorded “store and forward” video or image technology. Doctors could use both services to determine whether an office visit or other service is warranted, according to the proposed rule.
The services would have limitations on when they could be separately billed. In cases where the brief communication technology–based service originated from a related evaluation and management (E/M) service provided within the previous 7 days by the same physician or other qualified health care professional, the service would be considered “bundled” into that previous E/M service and could not be billed separately. Similarly, a photo evaluation could not be separately billed if it stemmed from a related E/M service provided within the previous 7 days by the same physician, or if the evaluation results in an in-person E/M office visit with the same doctor.
Under the proposal, health providers could perform the newly covered telehealth services only with established patients, but the CMS is seeking comments as to whether in certain cases, such as dermatological or ophthalmological instances, it might be appropriate for a new patient to receive the services. Agency officials also want to know what types of communication technology are used by physicians in furnishing check-in services, including whether audio-only telephone interactions are sufficient, compared with interactions that are enhanced with video. The CMS is asking physicians whether it would be clinically appropriate to apply a frequency limitation on the use of the proposed telehealth services by the same physician.
Latoya Thomas, director of the American Telemedicine Association’s State Policy Resource Center, said the proposal is exciting because it acknowledges the pervasive growth, accessibility, and acceptance of technology advances.
“In expanding reimbursement to providers for more modality-neutral and site-neutral virtual care, such as store-and-forward and remote patient monitoring, [the rules] address longstanding barriers to broader dissemination of telehealth,” Ms. Thomas said in an interview. “By making available ‘virtual check ins’ to every Medicare beneficiary, it can improve patient engagement and reduce unnecessary trips back to their provider’s office.”
James P. Marcin, MD, a telemedicine physician and director of the Center for Health and Technology at UC Davis Children’s Hospital in Sacramento, Calif., said he was pleased with the proposed telehealth changes, but he noted that more work remains to address further telemedicine challenges.
“The needle is finally moving, albeit too slowly for some of us,” Dr. Marcin said in an interview. “There are still some areas users of telemedicine and organizations supporting the use of telemedicine want to address, including the need for verbal informed consent, the requirements for established relationships with patients, and of course, rate valuations for the remote patient monitoring and professional codes. But again, this is good news for patients.”
Public comments on the proposed rule are due by Sept. 10, 2018. Comments can be submitted to regulations.gov.
Payment for more telemedicine services could be in store for physicians and other health providers if new proposals in the latest fee schedule from the Centers for Medicare & Medicaid Services are finalized.
Under the proposed physician fee schedule, announced July 12, the CMS would expand services that qualify for telemedicine payments and add reimbursement for virtual check-ins by phone or other technologies, such as Skype. Telemedicine clinicians would also be paid for time spent reviewing patient photos sent by text or e-mail under the suggested changes.
Such telehealth services would aid patients who have transportation difficulties by creating more opportunities for them to access personalized care, said CMS Administrator Seema Verma.
“CMS is committed to modernizing the Medicare program by leveraging technologies, such as audio/video applications or patient-facing health portals, that will help beneficiaries access high-quality services in a convenient manner,” Ms. Verma said in a statement.
Under the proposal, physicians could bill separately for brief, non–face-to-face patient check-ins with patients via communication technology beginning January 2019. In addition, the proposed rule carves out payments for the remote professional evaluation of patient-transmitted information conducted via prerecorded “store and forward” video or image technology. Doctors could use both services to determine whether an office visit or other service is warranted, according to the proposed rule.
The services would have limitations on when they could be separately billed. In cases where the brief communication technology–based service originated from a related evaluation and management (E/M) service provided within the previous 7 days by the same physician or other qualified health care professional, the service would be considered “bundled” into that previous E/M service and could not be billed separately. Similarly, a photo evaluation could not be separately billed if it stemmed from a related E/M service provided within the previous 7 days by the same physician, or if the evaluation results in an in-person E/M office visit with the same doctor.
Under the proposal, health providers could perform the newly covered telehealth services only with established patients, but the CMS is seeking comments as to whether in certain cases, such as dermatological or ophthalmological instances, it might be appropriate for a new patient to receive the services. Agency officials also want to know what types of communication technology are used by physicians in furnishing check-in services, including whether audio-only telephone interactions are sufficient, compared with interactions that are enhanced with video. The CMS is asking physicians whether it would be clinically appropriate to apply a frequency limitation on the use of the proposed telehealth services by the same physician.
Latoya Thomas, director of the American Telemedicine Association’s State Policy Resource Center, said the proposal is exciting because it acknowledges the pervasive growth, accessibility, and acceptance of technology advances.
“In expanding reimbursement to providers for more modality-neutral and site-neutral virtual care, such as store-and-forward and remote patient monitoring, [the rules] address longstanding barriers to broader dissemination of telehealth,” Ms. Thomas said in an interview. “By making available ‘virtual check ins’ to every Medicare beneficiary, it can improve patient engagement and reduce unnecessary trips back to their provider’s office.”
James P. Marcin, MD, a telemedicine physician and director of the Center for Health and Technology at UC Davis Children’s Hospital in Sacramento, Calif., said he was pleased with the proposed telehealth changes, but he noted that more work remains to address further telemedicine challenges.
“The needle is finally moving, albeit too slowly for some of us,” Dr. Marcin said in an interview. “There are still some areas users of telemedicine and organizations supporting the use of telemedicine want to address, including the need for verbal informed consent, the requirements for established relationships with patients, and of course, rate valuations for the remote patient monitoring and professional codes. But again, this is good news for patients.”
Public comments on the proposed rule are due by Sept. 10, 2018. Comments can be submitted to regulations.gov.
Payment for more telemedicine services could be in store for physicians and other health providers if new proposals in the latest fee schedule from the Centers for Medicare & Medicaid Services are finalized.
Under the proposed physician fee schedule, announced July 12, the CMS would expand services that qualify for telemedicine payments and add reimbursement for virtual check-ins by phone or other technologies, such as Skype. Telemedicine clinicians would also be paid for time spent reviewing patient photos sent by text or e-mail under the suggested changes.
Such telehealth services would aid patients who have transportation difficulties by creating more opportunities for them to access personalized care, said CMS Administrator Seema Verma.
“CMS is committed to modernizing the Medicare program by leveraging technologies, such as audio/video applications or patient-facing health portals, that will help beneficiaries access high-quality services in a convenient manner,” Ms. Verma said in a statement.
Under the proposal, physicians could bill separately for brief, non–face-to-face patient check-ins with patients via communication technology beginning January 2019. In addition, the proposed rule carves out payments for the remote professional evaluation of patient-transmitted information conducted via prerecorded “store and forward” video or image technology. Doctors could use both services to determine whether an office visit or other service is warranted, according to the proposed rule.
The services would have limitations on when they could be separately billed. In cases where the brief communication technology–based service originated from a related evaluation and management (E/M) service provided within the previous 7 days by the same physician or other qualified health care professional, the service would be considered “bundled” into that previous E/M service and could not be billed separately. Similarly, a photo evaluation could not be separately billed if it stemmed from a related E/M service provided within the previous 7 days by the same physician, or if the evaluation results in an in-person E/M office visit with the same doctor.
Under the proposal, health providers could perform the newly covered telehealth services only with established patients, but the CMS is seeking comments as to whether in certain cases, such as dermatological or ophthalmological instances, it might be appropriate for a new patient to receive the services. Agency officials also want to know what types of communication technology are used by physicians in furnishing check-in services, including whether audio-only telephone interactions are sufficient, compared with interactions that are enhanced with video. The CMS is asking physicians whether it would be clinically appropriate to apply a frequency limitation on the use of the proposed telehealth services by the same physician.
Latoya Thomas, director of the American Telemedicine Association’s State Policy Resource Center, said the proposal is exciting because it acknowledges the pervasive growth, accessibility, and acceptance of technology advances.
“In expanding reimbursement to providers for more modality-neutral and site-neutral virtual care, such as store-and-forward and remote patient monitoring, [the rules] address longstanding barriers to broader dissemination of telehealth,” Ms. Thomas said in an interview. “By making available ‘virtual check ins’ to every Medicare beneficiary, it can improve patient engagement and reduce unnecessary trips back to their provider’s office.”
James P. Marcin, MD, a telemedicine physician and director of the Center for Health and Technology at UC Davis Children’s Hospital in Sacramento, Calif., said he was pleased with the proposed telehealth changes, but he noted that more work remains to address further telemedicine challenges.
“The needle is finally moving, albeit too slowly for some of us,” Dr. Marcin said in an interview. “There are still some areas users of telemedicine and organizations supporting the use of telemedicine want to address, including the need for verbal informed consent, the requirements for established relationships with patients, and of course, rate valuations for the remote patient monitoring and professional codes. But again, this is good news for patients.”
Public comments on the proposed rule are due by Sept. 10, 2018. Comments can be submitted to regulations.gov.
Benefits, drawbacks when hospitalists expand roles
Hospitalists can’t ‘fill all the cracks’ in primary care
As vice chair of the hospital medicine service at Northwell Health, Nick Fitterman, MD, FACP, SFHM, oversees 16 HM groups at 15 hospitals in New York. He says the duties of his hospitalist staff, like those of most U.S. hospitalists, are similar to what they have traditionally been – clinical care on the wards, teaching, comanagement of surgery, quality improvement, committee work, and research. But he has noticed a trend of late: rapid expansion of the hospitalist’s role.
Speaking at an education session at HM18 in Orlando, Dr. Fitterman said the role of the hospitalist is growing to include tasks that might not be as common, but are becoming more familiar all the time: working at infusion centers, caring for patients in skilled nursing facilities, specializing in electronic health record use, colocating in psychiatric hospitals, even being deployed to natural disasters. His list went on, and it was much longer than the list of traditional hospitalist responsibilities.
“Where do we draw the line and say, ‘Wait a minute, our primary site is going to suffer if we continue to get spread this thin. Can we really do it all?” Dr. Fitterman said. As the number of hats hospitalists wear grows ever bigger, he said more thought must be placed into how expansion happens.
The preop clinic
Efren Manjarrez, MD, SFHM, former chief of hospital medicine at the University of Miami, told a cautionary tale about a preoperative clinic staffed by hospitalists that appeared to provide a financial benefit to a hospital – helping to avoid costly last-minute cancellations of surgeries – but that ultimately was shuttered. The hospital, he said, loses $8,000-$10,000 for each case that gets canceled on the same day.
“Think about that just for a minute,” Dr. Manjarrez said. “If 100 cases are canceled during the year at the last minute, that’s a lot of money.”
A preoperative clinic seemed like a worthwhile role for hospitalists – the program was started in Miami by the same doctor who initiated a similar program at Cleveland Clinic. “Surgical cases are what support the hospital [financially], and we’re here to help them along,” Dr. Manjarrez said. “The purpose of hospitalists is to make sure that patients are medically optimized.”
The preop program concept, used in U.S. medicine since the 1990s, was originally started by anesthesiologists, but they may not always be the best fit to staff such programs.
“Anesthesiologists do not manage all beta blockers,” Dr. Manjarrez said. “They don’t manage ACE inhibitors by mouth. They don’t manage all oral diabetes agents, and they sure as heck don’t manage pills that are anticoagulants. That’s the domain of internal medicine. And as patients have become more complex, that’s where hospitalists who [work in] preop clinics have stepped in.”
Studies have found that hospitalists staffing preop clinics have improved quality metrics and some clinical outcomes, including lowering cancellation rates and more appropriate use of beta blockers, he said.
In the Miami program described by Dr. Manjarrez, hospitalists in the preop clinic at first saw only patients who’d been financially cleared as able to pay. But ultimately, a tiered system was developed, and hospitalists saw only patients who were higher risk – those with COPD or stroke patients, for example – without regard to ability to pay.
“The hospital would have to make up any financial deficit at the very end,” Dr. Manjarrez said. This meant there were no longer efficient 5-minute encounters with patients. Instead, visits lasted about 45 minutes, so fewer patients were seen.
The program was successful, in that the same-day cancellation rate for surgeries dropped to less than 0.1% – fewer than 1 in 1,000 – with the preop clinic up and running, Dr. Manjarrez. Still, the hospital decided to end the program. “The hospital no longer wanted to reimburse us,” he said.
A takeaway from this experience for Dr. Manjarrez was that hospitalists need to do a better job of showing the financial benefits in their expanding roles, if they want them to endure.
“At the end of the day, hospitalists do provide value in preoperative clinics,” he said. “But unfortunately, we’re not doing a great job of publishing our data and showing our value.”
At-home care
At Brigham and Women’s Hospital in Boston, hospitalists have demonstrated good results with a program to provide care at home rather than in the hospital.
David Levine, MD, MPH, MA, clinician and investigator at Brigham and Women’s and an instructor in medicine at Harvard Medical School, said that the structure of inpatient care has generally not changed much over decades, despite advances in technology.
“We round on them once a day – if they’re lucky, twice,” he said. “The medicines have changed and imaging has changed, but we really haven’t changed the structure of how we take care of acutely ill adults for almost a hundred years.”
Hospitalizing patients brings unintended consequences. Twenty percent of older adults will become delirious during their stay, 1 out of 3 will lose a level of functional status in the hospital that they’ll never regain, and 1 out of 10 hospitalized patients will experience an adverse event, like an infection or a medication error.
Brigham and Women’s program of at-home care involves “admitting” patients to their homes after being treated in the emergency department. The goal is to reduce costs by 20%, while maintaining quality and safety and improving patients’ quality of life and experience.
Researchers are studying their results. They randomized patients, after the ED determined they required admission, either to admission to the hospital or to their home. The decision on whether to admit was made before the study investigators became involved with the patients, Dr. Levine said.
The program is also intended to improve access to hospitals. Brigham and Women’s is often over 100% capacity in the general medical ward.
Patients in the study needed to live within a 5-mile radius of either Brigham and Women’s Hospital, or Brigham and Women’s Faulkner Hospital, a nearby community hospital. A physician and a registered nurse form the core team; they assess patient needs and ratchet care either up or down, perhaps adding a home health aide or social worker.
The home care team takes advantage of technology: Portable equipment allows a basic metabolic panel to be performed on the spot – for example, a hemoglobin and hematocrit can be produced within 2 minutes. Also, portable ultrasounds and x-rays are used. Doctors keep a “tackle box” of urgent medications such as antibiotics and diuretics.
“We showed a direct cost reduction taking care of patients at home,” Dr. Levine said. There was also a reduction in utilization of care, and an increase in patient activity, with patients taking about 1,800 steps at home, compared with 180 in the hospital. There were no significant changes in safety, quality, or patient experience, he said.
Postdischarge clinics
Lauren Doctoroff, MD, FHM – a hospitalist at Beth Israel Deaconness Medical Center in Boston and assistant professor of medicine at Harvard Medical School – explained another hospitalist-staffed project meant to improve access to care: her center’s postdischarge clinic, which was started in 2009 but is no longer operating.
The clinic tackled the problem of what to do with patients when you discharge them, Dr. Doctoroff said, and its goal was to foster more cooperation between hospitalists and the faculty primary care practice, as well as to improve postdischarge access for patients from that practice.
A dedicated group of hospitalists staffed the clinics, handling medication reconciliation, symptom management, pending tests, and other services the patients were supposed to be getting after discharge, Dr. Doctoroff said.
“We greatly improved access so that when you came to see us you generally saw a hospitalist a week before you would have seen your primary care doctor,” she said. “And that was mostly because we created open access in a clinic that did not have open access. So if a doctor discharging a patient really thought that the patient needed to be seen after discharge, they would often see us.”
Hospitalists considering starting such a clinic have several key questions to consider, Dr. Doctoroff said.
“You need to focus on who the patient population is, the clinic structure, how you plan to staff the clinic, and what your outcomes are – mainly how you will measure performance,” she said.
Dr. Doctoroff said hospitalists are good for this role because “we’re very comfortable with patients who are complicated, and we are very adept at accessing information from the hospitalization. I think, as a hospitalist who spent 5 years seeing patients in a discharge clinic, it greatly enhances my understanding of patients and their challenges at discharge.”
The clinic was closed, she said, in part because it was largely an extension of primary care, and the patient volume wasn’t big enough to justify continuing it.
“Postdischarge clinics are, in a very narrow sense, a bit of a Band-Aid for a really dysfunctional primary care system,” Dr. Doctoroff said. “Ideally, if all you’re doing is providing a postdischarge physician visit, then you really want primary care to be able to do that in order to reengage with their patient. I think this is because postdischarge clinics are construed in a very narrow way to address the simple need to see a patient after discharge. And this may lead to the failure of these clinics, or make them easy to replace. Also, often what patients really need is more than just a physician visit, so a discharge clinic may need to be designed to provide an enhanced array of services.”
Dr. Fitterman said that these stories show that not all role expansion in hospital medicine is good role expansion. The experiences described by Dr. Manjarrez, Dr. Levine, and Dr. Doctoroff demonstrate the challenges hospitalists face as they attempt expansions into new roles, he said.
“We can’t be expected to fill all the cracks in primary care,” Dr. Fitterman said. “As a country we need to really prop up primary care. This all can’t come under the roof of hospital medicine. We need to be part of a patient-centered medical home – but we are not the patient-centered medical home.”
He said the experience with the preop clinic described by Dr. Manjarrez also shows the need for buy-in from hospital or health system administration.
“While most of us are employed by hospitals and want to help meet their needs, we have to be more cautious. We have to look, I think, with a more critical eye, for the value; it may not always be in the dollars coming back in,” he said. “It might be in cost avoidance, such as reducing readmissions, or reducing same-day cancellations in an OR. Unless the C-suite appreciates that value, such programs will be short-lived.”
Hospitalists can’t ‘fill all the cracks’ in primary care
Hospitalists can’t ‘fill all the cracks’ in primary care
As vice chair of the hospital medicine service at Northwell Health, Nick Fitterman, MD, FACP, SFHM, oversees 16 HM groups at 15 hospitals in New York. He says the duties of his hospitalist staff, like those of most U.S. hospitalists, are similar to what they have traditionally been – clinical care on the wards, teaching, comanagement of surgery, quality improvement, committee work, and research. But he has noticed a trend of late: rapid expansion of the hospitalist’s role.
Speaking at an education session at HM18 in Orlando, Dr. Fitterman said the role of the hospitalist is growing to include tasks that might not be as common, but are becoming more familiar all the time: working at infusion centers, caring for patients in skilled nursing facilities, specializing in electronic health record use, colocating in psychiatric hospitals, even being deployed to natural disasters. His list went on, and it was much longer than the list of traditional hospitalist responsibilities.
“Where do we draw the line and say, ‘Wait a minute, our primary site is going to suffer if we continue to get spread this thin. Can we really do it all?” Dr. Fitterman said. As the number of hats hospitalists wear grows ever bigger, he said more thought must be placed into how expansion happens.
The preop clinic
Efren Manjarrez, MD, SFHM, former chief of hospital medicine at the University of Miami, told a cautionary tale about a preoperative clinic staffed by hospitalists that appeared to provide a financial benefit to a hospital – helping to avoid costly last-minute cancellations of surgeries – but that ultimately was shuttered. The hospital, he said, loses $8,000-$10,000 for each case that gets canceled on the same day.
“Think about that just for a minute,” Dr. Manjarrez said. “If 100 cases are canceled during the year at the last minute, that’s a lot of money.”
A preoperative clinic seemed like a worthwhile role for hospitalists – the program was started in Miami by the same doctor who initiated a similar program at Cleveland Clinic. “Surgical cases are what support the hospital [financially], and we’re here to help them along,” Dr. Manjarrez said. “The purpose of hospitalists is to make sure that patients are medically optimized.”
The preop program concept, used in U.S. medicine since the 1990s, was originally started by anesthesiologists, but they may not always be the best fit to staff such programs.
“Anesthesiologists do not manage all beta blockers,” Dr. Manjarrez said. “They don’t manage ACE inhibitors by mouth. They don’t manage all oral diabetes agents, and they sure as heck don’t manage pills that are anticoagulants. That’s the domain of internal medicine. And as patients have become more complex, that’s where hospitalists who [work in] preop clinics have stepped in.”
Studies have found that hospitalists staffing preop clinics have improved quality metrics and some clinical outcomes, including lowering cancellation rates and more appropriate use of beta blockers, he said.
In the Miami program described by Dr. Manjarrez, hospitalists in the preop clinic at first saw only patients who’d been financially cleared as able to pay. But ultimately, a tiered system was developed, and hospitalists saw only patients who were higher risk – those with COPD or stroke patients, for example – without regard to ability to pay.
“The hospital would have to make up any financial deficit at the very end,” Dr. Manjarrez said. This meant there were no longer efficient 5-minute encounters with patients. Instead, visits lasted about 45 minutes, so fewer patients were seen.
The program was successful, in that the same-day cancellation rate for surgeries dropped to less than 0.1% – fewer than 1 in 1,000 – with the preop clinic up and running, Dr. Manjarrez. Still, the hospital decided to end the program. “The hospital no longer wanted to reimburse us,” he said.
A takeaway from this experience for Dr. Manjarrez was that hospitalists need to do a better job of showing the financial benefits in their expanding roles, if they want them to endure.
“At the end of the day, hospitalists do provide value in preoperative clinics,” he said. “But unfortunately, we’re not doing a great job of publishing our data and showing our value.”
At-home care
At Brigham and Women’s Hospital in Boston, hospitalists have demonstrated good results with a program to provide care at home rather than in the hospital.
David Levine, MD, MPH, MA, clinician and investigator at Brigham and Women’s and an instructor in medicine at Harvard Medical School, said that the structure of inpatient care has generally not changed much over decades, despite advances in technology.
“We round on them once a day – if they’re lucky, twice,” he said. “The medicines have changed and imaging has changed, but we really haven’t changed the structure of how we take care of acutely ill adults for almost a hundred years.”
Hospitalizing patients brings unintended consequences. Twenty percent of older adults will become delirious during their stay, 1 out of 3 will lose a level of functional status in the hospital that they’ll never regain, and 1 out of 10 hospitalized patients will experience an adverse event, like an infection or a medication error.
Brigham and Women’s program of at-home care involves “admitting” patients to their homes after being treated in the emergency department. The goal is to reduce costs by 20%, while maintaining quality and safety and improving patients’ quality of life and experience.
Researchers are studying their results. They randomized patients, after the ED determined they required admission, either to admission to the hospital or to their home. The decision on whether to admit was made before the study investigators became involved with the patients, Dr. Levine said.
The program is also intended to improve access to hospitals. Brigham and Women’s is often over 100% capacity in the general medical ward.
Patients in the study needed to live within a 5-mile radius of either Brigham and Women’s Hospital, or Brigham and Women’s Faulkner Hospital, a nearby community hospital. A physician and a registered nurse form the core team; they assess patient needs and ratchet care either up or down, perhaps adding a home health aide or social worker.
The home care team takes advantage of technology: Portable equipment allows a basic metabolic panel to be performed on the spot – for example, a hemoglobin and hematocrit can be produced within 2 minutes. Also, portable ultrasounds and x-rays are used. Doctors keep a “tackle box” of urgent medications such as antibiotics and diuretics.
“We showed a direct cost reduction taking care of patients at home,” Dr. Levine said. There was also a reduction in utilization of care, and an increase in patient activity, with patients taking about 1,800 steps at home, compared with 180 in the hospital. There were no significant changes in safety, quality, or patient experience, he said.
Postdischarge clinics
Lauren Doctoroff, MD, FHM – a hospitalist at Beth Israel Deaconness Medical Center in Boston and assistant professor of medicine at Harvard Medical School – explained another hospitalist-staffed project meant to improve access to care: her center’s postdischarge clinic, which was started in 2009 but is no longer operating.
The clinic tackled the problem of what to do with patients when you discharge them, Dr. Doctoroff said, and its goal was to foster more cooperation between hospitalists and the faculty primary care practice, as well as to improve postdischarge access for patients from that practice.
A dedicated group of hospitalists staffed the clinics, handling medication reconciliation, symptom management, pending tests, and other services the patients were supposed to be getting after discharge, Dr. Doctoroff said.
“We greatly improved access so that when you came to see us you generally saw a hospitalist a week before you would have seen your primary care doctor,” she said. “And that was mostly because we created open access in a clinic that did not have open access. So if a doctor discharging a patient really thought that the patient needed to be seen after discharge, they would often see us.”
Hospitalists considering starting such a clinic have several key questions to consider, Dr. Doctoroff said.
“You need to focus on who the patient population is, the clinic structure, how you plan to staff the clinic, and what your outcomes are – mainly how you will measure performance,” she said.
Dr. Doctoroff said hospitalists are good for this role because “we’re very comfortable with patients who are complicated, and we are very adept at accessing information from the hospitalization. I think, as a hospitalist who spent 5 years seeing patients in a discharge clinic, it greatly enhances my understanding of patients and their challenges at discharge.”
The clinic was closed, she said, in part because it was largely an extension of primary care, and the patient volume wasn’t big enough to justify continuing it.
“Postdischarge clinics are, in a very narrow sense, a bit of a Band-Aid for a really dysfunctional primary care system,” Dr. Doctoroff said. “Ideally, if all you’re doing is providing a postdischarge physician visit, then you really want primary care to be able to do that in order to reengage with their patient. I think this is because postdischarge clinics are construed in a very narrow way to address the simple need to see a patient after discharge. And this may lead to the failure of these clinics, or make them easy to replace. Also, often what patients really need is more than just a physician visit, so a discharge clinic may need to be designed to provide an enhanced array of services.”
Dr. Fitterman said that these stories show that not all role expansion in hospital medicine is good role expansion. The experiences described by Dr. Manjarrez, Dr. Levine, and Dr. Doctoroff demonstrate the challenges hospitalists face as they attempt expansions into new roles, he said.
“We can’t be expected to fill all the cracks in primary care,” Dr. Fitterman said. “As a country we need to really prop up primary care. This all can’t come under the roof of hospital medicine. We need to be part of a patient-centered medical home – but we are not the patient-centered medical home.”
He said the experience with the preop clinic described by Dr. Manjarrez also shows the need for buy-in from hospital or health system administration.
“While most of us are employed by hospitals and want to help meet their needs, we have to be more cautious. We have to look, I think, with a more critical eye, for the value; it may not always be in the dollars coming back in,” he said. “It might be in cost avoidance, such as reducing readmissions, or reducing same-day cancellations in an OR. Unless the C-suite appreciates that value, such programs will be short-lived.”
As vice chair of the hospital medicine service at Northwell Health, Nick Fitterman, MD, FACP, SFHM, oversees 16 HM groups at 15 hospitals in New York. He says the duties of his hospitalist staff, like those of most U.S. hospitalists, are similar to what they have traditionally been – clinical care on the wards, teaching, comanagement of surgery, quality improvement, committee work, and research. But he has noticed a trend of late: rapid expansion of the hospitalist’s role.
Speaking at an education session at HM18 in Orlando, Dr. Fitterman said the role of the hospitalist is growing to include tasks that might not be as common, but are becoming more familiar all the time: working at infusion centers, caring for patients in skilled nursing facilities, specializing in electronic health record use, colocating in psychiatric hospitals, even being deployed to natural disasters. His list went on, and it was much longer than the list of traditional hospitalist responsibilities.
“Where do we draw the line and say, ‘Wait a minute, our primary site is going to suffer if we continue to get spread this thin. Can we really do it all?” Dr. Fitterman said. As the number of hats hospitalists wear grows ever bigger, he said more thought must be placed into how expansion happens.
The preop clinic
Efren Manjarrez, MD, SFHM, former chief of hospital medicine at the University of Miami, told a cautionary tale about a preoperative clinic staffed by hospitalists that appeared to provide a financial benefit to a hospital – helping to avoid costly last-minute cancellations of surgeries – but that ultimately was shuttered. The hospital, he said, loses $8,000-$10,000 for each case that gets canceled on the same day.
“Think about that just for a minute,” Dr. Manjarrez said. “If 100 cases are canceled during the year at the last minute, that’s a lot of money.”
A preoperative clinic seemed like a worthwhile role for hospitalists – the program was started in Miami by the same doctor who initiated a similar program at Cleveland Clinic. “Surgical cases are what support the hospital [financially], and we’re here to help them along,” Dr. Manjarrez said. “The purpose of hospitalists is to make sure that patients are medically optimized.”
The preop program concept, used in U.S. medicine since the 1990s, was originally started by anesthesiologists, but they may not always be the best fit to staff such programs.
“Anesthesiologists do not manage all beta blockers,” Dr. Manjarrez said. “They don’t manage ACE inhibitors by mouth. They don’t manage all oral diabetes agents, and they sure as heck don’t manage pills that are anticoagulants. That’s the domain of internal medicine. And as patients have become more complex, that’s where hospitalists who [work in] preop clinics have stepped in.”
Studies have found that hospitalists staffing preop clinics have improved quality metrics and some clinical outcomes, including lowering cancellation rates and more appropriate use of beta blockers, he said.
In the Miami program described by Dr. Manjarrez, hospitalists in the preop clinic at first saw only patients who’d been financially cleared as able to pay. But ultimately, a tiered system was developed, and hospitalists saw only patients who were higher risk – those with COPD or stroke patients, for example – without regard to ability to pay.
“The hospital would have to make up any financial deficit at the very end,” Dr. Manjarrez said. This meant there were no longer efficient 5-minute encounters with patients. Instead, visits lasted about 45 minutes, so fewer patients were seen.
The program was successful, in that the same-day cancellation rate for surgeries dropped to less than 0.1% – fewer than 1 in 1,000 – with the preop clinic up and running, Dr. Manjarrez. Still, the hospital decided to end the program. “The hospital no longer wanted to reimburse us,” he said.
A takeaway from this experience for Dr. Manjarrez was that hospitalists need to do a better job of showing the financial benefits in their expanding roles, if they want them to endure.
“At the end of the day, hospitalists do provide value in preoperative clinics,” he said. “But unfortunately, we’re not doing a great job of publishing our data and showing our value.”
At-home care
At Brigham and Women’s Hospital in Boston, hospitalists have demonstrated good results with a program to provide care at home rather than in the hospital.
David Levine, MD, MPH, MA, clinician and investigator at Brigham and Women’s and an instructor in medicine at Harvard Medical School, said that the structure of inpatient care has generally not changed much over decades, despite advances in technology.
“We round on them once a day – if they’re lucky, twice,” he said. “The medicines have changed and imaging has changed, but we really haven’t changed the structure of how we take care of acutely ill adults for almost a hundred years.”
Hospitalizing patients brings unintended consequences. Twenty percent of older adults will become delirious during their stay, 1 out of 3 will lose a level of functional status in the hospital that they’ll never regain, and 1 out of 10 hospitalized patients will experience an adverse event, like an infection or a medication error.
Brigham and Women’s program of at-home care involves “admitting” patients to their homes after being treated in the emergency department. The goal is to reduce costs by 20%, while maintaining quality and safety and improving patients’ quality of life and experience.
Researchers are studying their results. They randomized patients, after the ED determined they required admission, either to admission to the hospital or to their home. The decision on whether to admit was made before the study investigators became involved with the patients, Dr. Levine said.
The program is also intended to improve access to hospitals. Brigham and Women’s is often over 100% capacity in the general medical ward.
Patients in the study needed to live within a 5-mile radius of either Brigham and Women’s Hospital, or Brigham and Women’s Faulkner Hospital, a nearby community hospital. A physician and a registered nurse form the core team; they assess patient needs and ratchet care either up or down, perhaps adding a home health aide or social worker.
The home care team takes advantage of technology: Portable equipment allows a basic metabolic panel to be performed on the spot – for example, a hemoglobin and hematocrit can be produced within 2 minutes. Also, portable ultrasounds and x-rays are used. Doctors keep a “tackle box” of urgent medications such as antibiotics and diuretics.
“We showed a direct cost reduction taking care of patients at home,” Dr. Levine said. There was also a reduction in utilization of care, and an increase in patient activity, with patients taking about 1,800 steps at home, compared with 180 in the hospital. There were no significant changes in safety, quality, or patient experience, he said.
Postdischarge clinics
Lauren Doctoroff, MD, FHM – a hospitalist at Beth Israel Deaconness Medical Center in Boston and assistant professor of medicine at Harvard Medical School – explained another hospitalist-staffed project meant to improve access to care: her center’s postdischarge clinic, which was started in 2009 but is no longer operating.
The clinic tackled the problem of what to do with patients when you discharge them, Dr. Doctoroff said, and its goal was to foster more cooperation between hospitalists and the faculty primary care practice, as well as to improve postdischarge access for patients from that practice.
A dedicated group of hospitalists staffed the clinics, handling medication reconciliation, symptom management, pending tests, and other services the patients were supposed to be getting after discharge, Dr. Doctoroff said.
“We greatly improved access so that when you came to see us you generally saw a hospitalist a week before you would have seen your primary care doctor,” she said. “And that was mostly because we created open access in a clinic that did not have open access. So if a doctor discharging a patient really thought that the patient needed to be seen after discharge, they would often see us.”
Hospitalists considering starting such a clinic have several key questions to consider, Dr. Doctoroff said.
“You need to focus on who the patient population is, the clinic structure, how you plan to staff the clinic, and what your outcomes are – mainly how you will measure performance,” she said.
Dr. Doctoroff said hospitalists are good for this role because “we’re very comfortable with patients who are complicated, and we are very adept at accessing information from the hospitalization. I think, as a hospitalist who spent 5 years seeing patients in a discharge clinic, it greatly enhances my understanding of patients and their challenges at discharge.”
The clinic was closed, she said, in part because it was largely an extension of primary care, and the patient volume wasn’t big enough to justify continuing it.
“Postdischarge clinics are, in a very narrow sense, a bit of a Band-Aid for a really dysfunctional primary care system,” Dr. Doctoroff said. “Ideally, if all you’re doing is providing a postdischarge physician visit, then you really want primary care to be able to do that in order to reengage with their patient. I think this is because postdischarge clinics are construed in a very narrow way to address the simple need to see a patient after discharge. And this may lead to the failure of these clinics, or make them easy to replace. Also, often what patients really need is more than just a physician visit, so a discharge clinic may need to be designed to provide an enhanced array of services.”
Dr. Fitterman said that these stories show that not all role expansion in hospital medicine is good role expansion. The experiences described by Dr. Manjarrez, Dr. Levine, and Dr. Doctoroff demonstrate the challenges hospitalists face as they attempt expansions into new roles, he said.
“We can’t be expected to fill all the cracks in primary care,” Dr. Fitterman said. “As a country we need to really prop up primary care. This all can’t come under the roof of hospital medicine. We need to be part of a patient-centered medical home – but we are not the patient-centered medical home.”
He said the experience with the preop clinic described by Dr. Manjarrez also shows the need for buy-in from hospital or health system administration.
“While most of us are employed by hospitals and want to help meet their needs, we have to be more cautious. We have to look, I think, with a more critical eye, for the value; it may not always be in the dollars coming back in,” he said. “It might be in cost avoidance, such as reducing readmissions, or reducing same-day cancellations in an OR. Unless the C-suite appreciates that value, such programs will be short-lived.”
The rapidly disappearing community pediatric inpatient unit
Greed kills babies. Children’s lives matter. Children over profit.
These were the slogans proclaimed by signs carried by protesters outside of MedStar Franklin Square Medical Center in Baltimore in early May of 2018 to protest the closure of the dedicated pediatric emergency department and inpatient pediatric unit.
But administrators at Franklin Square Medical Center had made their decision long before the glue had dried on the signs, and the protests of patients and community officials fell on deaf ears. Eight doctors and 30 other staff had already lost their jobs, including the chair of pediatrics, Scott Krugman, MD.1
And this was just another drop in a slow ooze of pediatric inpatient units based in community hospitals that have seen the ax fall on what was thought to be a vital medical resource for their communities – yet not vital enough to survive its lack of profitability. From Taunton, Mass., to Chicago, Ill., to rural Tennessee, pediatric inpatient units in community hospitals have failed to even flirt with breaking even, let alone show profitability. Many community pediatric inpatient units are saddled with rock-bottom reimbursements offered by state Medicaid programs, the overwhelmingly prevalent payer for pediatric hospitalizations, which is compounded by the seasonality and unpredictability of pediatric inpatient volumes, so many have seen a glowing red bottom line lead to their demise.
What does this mean for pediatric health in underserved and rural communities? The closure of the pediatric inpatient unit at MedStar Franklin Square Medical Center meant the loss of physicians and nurses staffing the child protection team helping to assist the local district attorney in child abuse cases. Sometimes described as “secondary care,” community pediatric hospitalists also serve as a link between primary care providers and tertiary care subspecialists; they can serve as pediatric generalists throughout a hospital and provide newborn nursery care, delivery room resuscitations, ED consultations, procedural sedations, psychiatric unit support, surgical comanagement, and informal or formal outpatient consultations.2 Losing even a small inpatient pediatric unit can have a ripple effect on inpatient and outpatient pediatric services in a health system and community.
For patients and their caregivers, the loss of pediatric inpatient services in their community hospital can erect additional hurdles to appropriate health care. The need to travel longer distances to urban centers or even the other side of town can be challenging given the difficulties posed by long distances, traffic congestion, public transportation, or just parking.3 For patients suffering from longer hospitalizations caused by medical complexity or chronic illnesses, traveling long distances can exacerbate the caregiver stress from attempting to care for a family at home while participating in the care of a hospitalized child. Longer travel times can also worsen family stress by increasing a caregiver’s absence from home and increased nonmedical expenses, not to mention loss of wages.4 Comfort levels with inpatient providers can also suffer because most pediatric units in community hospitals are staffed by either community general pediatricians or very small pediatric hospitalist groups, which breeds familiarity with frequently admitted patients and their caregivers. This familiarity can be lacking in large academic centers, with confusing and ever-rotating teams of academic hospitalists, residents, and medical students.5
What is driving the slow drumbeat of pediatric inpatient unit closures? On a macroeconomic scale, pediatric hospitalizations have been dropping yearly, driven down by immunizations (despite the best efforts of certain celebrities), antibiotic stewardship, and improved access to outpatient care. In 2006, there were 6.6 million hospitalizations for children aged 17 years and younger,6 but by 2012 this had dropped to 5.9 million hospitalizations.7 In the same age group, the rate of hospitalization from the ED dropped from 4.4% in 2006 to 3.2% in 2015.8
On a hospital level, the presence of multiple small pediatric units in a region may not make sense from a cost standpoint, and a larger, merged unit may provide higher quality because of its higher volumes. On a state and local level, alternative payment models have been implemented with the best of intentions but have led administrators at community general hospitals to look at pediatric units as the lowest hanging money-losing fruit in their efforts to survive a brave new world of hospital payment.
The most extreme (or advanced, depending on your viewpoint) model is in Maryland: Since 2014, acute care hospitals have been only able to receive a fixed amount of revenue from all payers, including Medicare, Medicaid, and commercial insurers.9 Known as an all-payer global budget, it incentivizes lowering unnecessary costs of care, such as readmissions, but also encourages cauterization of cost centers hemorrhaging money – such as inpatient pediatrics. Even the venerable Johns Hopkins Children’s Center has seen its profitability pale in comparison to the expansion team Johns Hopkins All Children’s Hospital in St. Petersburg, Fla., which is the second-most profitable hospital in the Hopkins system, only edged out by Sibley Memorial Hospital – which also sports an out-of-state location in the District of Columbia.10
But all hope is not lost for your comfy local pediatric inpatient unit. In other states and regions where a more favorable (to hospitals) payer mix exists, large pediatric hospitals are still engaged in turf battles with other local competitors to grab market share. In these regions, community pediatric units have survived by partnering with large pediatric institutions, either through affiliations or wholesale transplantation of the larger pediatric institution’s providers, nurses, and EHRs into essentially what is a leased floor. In addition, large pediatric institutions that participate in capitated models such as accountable care organizations have paradoxically found it financially favorable to direct “bread-and-butter” pediatric hospitalizations to community pediatric units, which often provide the same care at a lower cost.
Utilizing community inpatient pediatric units was “initially … a means of expanding their market share and ‘downstream’ revenue from transfers, but more commonly now [is] a way of alleviating the costs associated with admitting low to moderate acuity patients to the main tertiary sites,” said Francisco Alvarez, MD, associate chief of Regional Pediatric Hospital Medicine Programs at Lucile Packard Children’s Hospital in Palo Alto, Calif. “The cost of care provided by pediatric hospitals has always been higher than the average cost for nonpediatric hospitals in regard to caring for pediatric patients due to their highly skilled specialties and services. These have become more scrutinized by private and government insurance plans and, in some cases, have led to lower reimbursements and therefore a lower or deficient net revenue for certain patient populations.”
For community pediatric hospitalists, the shifting sands of reimbursement on which pediatric inpatient care is built can be a motion illness–inducing experience. In addition to concerns over community health care, job security, and population health, care provided in community hospitals can often be subtly undercut by tertiary and quaternary care pediatric hospitals.
“The focus of pediatric residency programs in freestanding children’s hospitals has created a situation where new pediatricians have less opportunity to develop respect for community pediatric hospital medicine,” said Beth Natt, MD, director of pediatric hospital medicine in the Regional Programs at Connecticut Children’s Medical Center, Hartford. “We are the nameless ‘OSH,’ the place that gets ‘Monday-morning quarterbacked’ in resident morning reports without having a voice at the table. Add this to residents learning ‘only’ protocolized care as opposed to a spectrum of appropriate care, and we create a culture of ‘wrong and right’ with the backward nonprotocol driven community docs looking like they are practicing medicine in the Wild West.”
What’s a community pediatric hospitalist to do, faced with an uncertain future and diminishing respect? Continuing to partner with local pediatric providers, community leaders, and local health care advocacy groups will help to enmesh inpatient providers in the fabric of a community’s health care. But making the value case to hospital administrators is critical for community pediatric hospitalists, as adult hospitalists realized soon after the inception of the hospitalist field.
Goals valued by hospital administrators are pursued on a daily basis by community pediatric hospitalists, and these successes need to be brought to light. Achieving value and quality metrics, pursuing high-value care, reducing readmission rates, championing EHRs, and improving documentation are goals that community pediatric hospitalists and hospital administrators can work toward together.11 By pursuing and sharing success in meeting these shared goals, perhaps the local community pediatric inpatient unit can survive – and thrive.
As for Dr. Krugman, he has moved on and is soon to be gainfully employed again. But he continues to be focused, as always, on the health of his patients.
“What are we going to do to take care of kids in their own communities?” Dr. Krugman asked. “It’s going to be an increasing challenge over the next decade due to the consolidation of children’s hospitals and low payments, especially for hospitals that are adult-focused. Unless we find a way to pay for pediatric care as a country.”
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
References
1. McDaniels A. (2018). Protesters denounce reduction in pediatric services at Baltimore’s MedStar Franklin Square hospital. Baltimore Sun. Available at: http://www.baltimoresun.com/health/health-care/bs-hs-franklin-square-hospital-protest-20180508-story.html.
2. Roberts KB. Pediatric hospitalists in community hospitals: Hospital-based generalists with expanded roles. Hosp Pediatr. 2015 May;5(5):290-2.
3. Georgia Health News. (2018). A hospital crisis is killing rural communities. This state is ‘Ground Zero’. Available at: http://www.georgiahealthnews.com/2017/09/hospital-crisis-killing-rural-communities-state-ground-zero/.
4. DiFazio RL et al. Non-medical out-of-pocket expenses incurred by families during their child’s hospitalization. J Child Health Care. 2013 Sep;17(3):230-41.
5. Gunderman R. Hospitalist and the decline of comprehensive care. N Engl J Med. 2016 Sep 15; 375(11):1011-3.
6. Statistical Brief #56. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb56.jsp.
7. Overview of Hospital Stays for Children in the United States, 2012 #187. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb187-Hospital-Stays-Children-2012.jsp.
8. Trends in Hospital Inpatient Stays by Age and Payer, 2000-2015 #235. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb235-Inpatient-Stays-Age-Payer-Trends.jsp.
9. Maryland All-Payer Model | Center for Medicare & Medicaid Innovation. (2018). Retrieved from https://innovation.cms.gov/initiatives/Maryland-All-Payer-Model/.
10. The effects of Maryland’s unique health care system. (2018). Retrieved from https://www.axios.com/johns-hopkins-finances-maryland-1518553853-722c2195-731e-4e02-ab1e-94e4211ba945.html.
11. The Increasing Need for Hospitalist Programs to Demonstrate Value | SCP. (2018). Retrieved from https://www.schumacherclinical.com/providers/blog/the-increasing-need-for-hospitalist-programs-to-demonstrate-value.
Greed kills babies. Children’s lives matter. Children over profit.
These were the slogans proclaimed by signs carried by protesters outside of MedStar Franklin Square Medical Center in Baltimore in early May of 2018 to protest the closure of the dedicated pediatric emergency department and inpatient pediatric unit.
But administrators at Franklin Square Medical Center had made their decision long before the glue had dried on the signs, and the protests of patients and community officials fell on deaf ears. Eight doctors and 30 other staff had already lost their jobs, including the chair of pediatrics, Scott Krugman, MD.1
And this was just another drop in a slow ooze of pediatric inpatient units based in community hospitals that have seen the ax fall on what was thought to be a vital medical resource for their communities – yet not vital enough to survive its lack of profitability. From Taunton, Mass., to Chicago, Ill., to rural Tennessee, pediatric inpatient units in community hospitals have failed to even flirt with breaking even, let alone show profitability. Many community pediatric inpatient units are saddled with rock-bottom reimbursements offered by state Medicaid programs, the overwhelmingly prevalent payer for pediatric hospitalizations, which is compounded by the seasonality and unpredictability of pediatric inpatient volumes, so many have seen a glowing red bottom line lead to their demise.
What does this mean for pediatric health in underserved and rural communities? The closure of the pediatric inpatient unit at MedStar Franklin Square Medical Center meant the loss of physicians and nurses staffing the child protection team helping to assist the local district attorney in child abuse cases. Sometimes described as “secondary care,” community pediatric hospitalists also serve as a link between primary care providers and tertiary care subspecialists; they can serve as pediatric generalists throughout a hospital and provide newborn nursery care, delivery room resuscitations, ED consultations, procedural sedations, psychiatric unit support, surgical comanagement, and informal or formal outpatient consultations.2 Losing even a small inpatient pediatric unit can have a ripple effect on inpatient and outpatient pediatric services in a health system and community.
For patients and their caregivers, the loss of pediatric inpatient services in their community hospital can erect additional hurdles to appropriate health care. The need to travel longer distances to urban centers or even the other side of town can be challenging given the difficulties posed by long distances, traffic congestion, public transportation, or just parking.3 For patients suffering from longer hospitalizations caused by medical complexity or chronic illnesses, traveling long distances can exacerbate the caregiver stress from attempting to care for a family at home while participating in the care of a hospitalized child. Longer travel times can also worsen family stress by increasing a caregiver’s absence from home and increased nonmedical expenses, not to mention loss of wages.4 Comfort levels with inpatient providers can also suffer because most pediatric units in community hospitals are staffed by either community general pediatricians or very small pediatric hospitalist groups, which breeds familiarity with frequently admitted patients and their caregivers. This familiarity can be lacking in large academic centers, with confusing and ever-rotating teams of academic hospitalists, residents, and medical students.5
What is driving the slow drumbeat of pediatric inpatient unit closures? On a macroeconomic scale, pediatric hospitalizations have been dropping yearly, driven down by immunizations (despite the best efforts of certain celebrities), antibiotic stewardship, and improved access to outpatient care. In 2006, there were 6.6 million hospitalizations for children aged 17 years and younger,6 but by 2012 this had dropped to 5.9 million hospitalizations.7 In the same age group, the rate of hospitalization from the ED dropped from 4.4% in 2006 to 3.2% in 2015.8
On a hospital level, the presence of multiple small pediatric units in a region may not make sense from a cost standpoint, and a larger, merged unit may provide higher quality because of its higher volumes. On a state and local level, alternative payment models have been implemented with the best of intentions but have led administrators at community general hospitals to look at pediatric units as the lowest hanging money-losing fruit in their efforts to survive a brave new world of hospital payment.
The most extreme (or advanced, depending on your viewpoint) model is in Maryland: Since 2014, acute care hospitals have been only able to receive a fixed amount of revenue from all payers, including Medicare, Medicaid, and commercial insurers.9 Known as an all-payer global budget, it incentivizes lowering unnecessary costs of care, such as readmissions, but also encourages cauterization of cost centers hemorrhaging money – such as inpatient pediatrics. Even the venerable Johns Hopkins Children’s Center has seen its profitability pale in comparison to the expansion team Johns Hopkins All Children’s Hospital in St. Petersburg, Fla., which is the second-most profitable hospital in the Hopkins system, only edged out by Sibley Memorial Hospital – which also sports an out-of-state location in the District of Columbia.10
But all hope is not lost for your comfy local pediatric inpatient unit. In other states and regions where a more favorable (to hospitals) payer mix exists, large pediatric hospitals are still engaged in turf battles with other local competitors to grab market share. In these regions, community pediatric units have survived by partnering with large pediatric institutions, either through affiliations or wholesale transplantation of the larger pediatric institution’s providers, nurses, and EHRs into essentially what is a leased floor. In addition, large pediatric institutions that participate in capitated models such as accountable care organizations have paradoxically found it financially favorable to direct “bread-and-butter” pediatric hospitalizations to community pediatric units, which often provide the same care at a lower cost.
Utilizing community inpatient pediatric units was “initially … a means of expanding their market share and ‘downstream’ revenue from transfers, but more commonly now [is] a way of alleviating the costs associated with admitting low to moderate acuity patients to the main tertiary sites,” said Francisco Alvarez, MD, associate chief of Regional Pediatric Hospital Medicine Programs at Lucile Packard Children’s Hospital in Palo Alto, Calif. “The cost of care provided by pediatric hospitals has always been higher than the average cost for nonpediatric hospitals in regard to caring for pediatric patients due to their highly skilled specialties and services. These have become more scrutinized by private and government insurance plans and, in some cases, have led to lower reimbursements and therefore a lower or deficient net revenue for certain patient populations.”
For community pediatric hospitalists, the shifting sands of reimbursement on which pediatric inpatient care is built can be a motion illness–inducing experience. In addition to concerns over community health care, job security, and population health, care provided in community hospitals can often be subtly undercut by tertiary and quaternary care pediatric hospitals.
“The focus of pediatric residency programs in freestanding children’s hospitals has created a situation where new pediatricians have less opportunity to develop respect for community pediatric hospital medicine,” said Beth Natt, MD, director of pediatric hospital medicine in the Regional Programs at Connecticut Children’s Medical Center, Hartford. “We are the nameless ‘OSH,’ the place that gets ‘Monday-morning quarterbacked’ in resident morning reports without having a voice at the table. Add this to residents learning ‘only’ protocolized care as opposed to a spectrum of appropriate care, and we create a culture of ‘wrong and right’ with the backward nonprotocol driven community docs looking like they are practicing medicine in the Wild West.”
What’s a community pediatric hospitalist to do, faced with an uncertain future and diminishing respect? Continuing to partner with local pediatric providers, community leaders, and local health care advocacy groups will help to enmesh inpatient providers in the fabric of a community’s health care. But making the value case to hospital administrators is critical for community pediatric hospitalists, as adult hospitalists realized soon after the inception of the hospitalist field.
Goals valued by hospital administrators are pursued on a daily basis by community pediatric hospitalists, and these successes need to be brought to light. Achieving value and quality metrics, pursuing high-value care, reducing readmission rates, championing EHRs, and improving documentation are goals that community pediatric hospitalists and hospital administrators can work toward together.11 By pursuing and sharing success in meeting these shared goals, perhaps the local community pediatric inpatient unit can survive – and thrive.
As for Dr. Krugman, he has moved on and is soon to be gainfully employed again. But he continues to be focused, as always, on the health of his patients.
“What are we going to do to take care of kids in their own communities?” Dr. Krugman asked. “It’s going to be an increasing challenge over the next decade due to the consolidation of children’s hospitals and low payments, especially for hospitals that are adult-focused. Unless we find a way to pay for pediatric care as a country.”
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
References
1. McDaniels A. (2018). Protesters denounce reduction in pediatric services at Baltimore’s MedStar Franklin Square hospital. Baltimore Sun. Available at: http://www.baltimoresun.com/health/health-care/bs-hs-franklin-square-hospital-protest-20180508-story.html.
2. Roberts KB. Pediatric hospitalists in community hospitals: Hospital-based generalists with expanded roles. Hosp Pediatr. 2015 May;5(5):290-2.
3. Georgia Health News. (2018). A hospital crisis is killing rural communities. This state is ‘Ground Zero’. Available at: http://www.georgiahealthnews.com/2017/09/hospital-crisis-killing-rural-communities-state-ground-zero/.
4. DiFazio RL et al. Non-medical out-of-pocket expenses incurred by families during their child’s hospitalization. J Child Health Care. 2013 Sep;17(3):230-41.
5. Gunderman R. Hospitalist and the decline of comprehensive care. N Engl J Med. 2016 Sep 15; 375(11):1011-3.
6. Statistical Brief #56. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb56.jsp.
7. Overview of Hospital Stays for Children in the United States, 2012 #187. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb187-Hospital-Stays-Children-2012.jsp.
8. Trends in Hospital Inpatient Stays by Age and Payer, 2000-2015 #235. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb235-Inpatient-Stays-Age-Payer-Trends.jsp.
9. Maryland All-Payer Model | Center for Medicare & Medicaid Innovation. (2018). Retrieved from https://innovation.cms.gov/initiatives/Maryland-All-Payer-Model/.
10. The effects of Maryland’s unique health care system. (2018). Retrieved from https://www.axios.com/johns-hopkins-finances-maryland-1518553853-722c2195-731e-4e02-ab1e-94e4211ba945.html.
11. The Increasing Need for Hospitalist Programs to Demonstrate Value | SCP. (2018). Retrieved from https://www.schumacherclinical.com/providers/blog/the-increasing-need-for-hospitalist-programs-to-demonstrate-value.
Greed kills babies. Children’s lives matter. Children over profit.
These were the slogans proclaimed by signs carried by protesters outside of MedStar Franklin Square Medical Center in Baltimore in early May of 2018 to protest the closure of the dedicated pediatric emergency department and inpatient pediatric unit.
But administrators at Franklin Square Medical Center had made their decision long before the glue had dried on the signs, and the protests of patients and community officials fell on deaf ears. Eight doctors and 30 other staff had already lost their jobs, including the chair of pediatrics, Scott Krugman, MD.1
And this was just another drop in a slow ooze of pediatric inpatient units based in community hospitals that have seen the ax fall on what was thought to be a vital medical resource for their communities – yet not vital enough to survive its lack of profitability. From Taunton, Mass., to Chicago, Ill., to rural Tennessee, pediatric inpatient units in community hospitals have failed to even flirt with breaking even, let alone show profitability. Many community pediatric inpatient units are saddled with rock-bottom reimbursements offered by state Medicaid programs, the overwhelmingly prevalent payer for pediatric hospitalizations, which is compounded by the seasonality and unpredictability of pediatric inpatient volumes, so many have seen a glowing red bottom line lead to their demise.
What does this mean for pediatric health in underserved and rural communities? The closure of the pediatric inpatient unit at MedStar Franklin Square Medical Center meant the loss of physicians and nurses staffing the child protection team helping to assist the local district attorney in child abuse cases. Sometimes described as “secondary care,” community pediatric hospitalists also serve as a link between primary care providers and tertiary care subspecialists; they can serve as pediatric generalists throughout a hospital and provide newborn nursery care, delivery room resuscitations, ED consultations, procedural sedations, psychiatric unit support, surgical comanagement, and informal or formal outpatient consultations.2 Losing even a small inpatient pediatric unit can have a ripple effect on inpatient and outpatient pediatric services in a health system and community.
For patients and their caregivers, the loss of pediatric inpatient services in their community hospital can erect additional hurdles to appropriate health care. The need to travel longer distances to urban centers or even the other side of town can be challenging given the difficulties posed by long distances, traffic congestion, public transportation, or just parking.3 For patients suffering from longer hospitalizations caused by medical complexity or chronic illnesses, traveling long distances can exacerbate the caregiver stress from attempting to care for a family at home while participating in the care of a hospitalized child. Longer travel times can also worsen family stress by increasing a caregiver’s absence from home and increased nonmedical expenses, not to mention loss of wages.4 Comfort levels with inpatient providers can also suffer because most pediatric units in community hospitals are staffed by either community general pediatricians or very small pediatric hospitalist groups, which breeds familiarity with frequently admitted patients and their caregivers. This familiarity can be lacking in large academic centers, with confusing and ever-rotating teams of academic hospitalists, residents, and medical students.5
What is driving the slow drumbeat of pediatric inpatient unit closures? On a macroeconomic scale, pediatric hospitalizations have been dropping yearly, driven down by immunizations (despite the best efforts of certain celebrities), antibiotic stewardship, and improved access to outpatient care. In 2006, there were 6.6 million hospitalizations for children aged 17 years and younger,6 but by 2012 this had dropped to 5.9 million hospitalizations.7 In the same age group, the rate of hospitalization from the ED dropped from 4.4% in 2006 to 3.2% in 2015.8
On a hospital level, the presence of multiple small pediatric units in a region may not make sense from a cost standpoint, and a larger, merged unit may provide higher quality because of its higher volumes. On a state and local level, alternative payment models have been implemented with the best of intentions but have led administrators at community general hospitals to look at pediatric units as the lowest hanging money-losing fruit in their efforts to survive a brave new world of hospital payment.
The most extreme (or advanced, depending on your viewpoint) model is in Maryland: Since 2014, acute care hospitals have been only able to receive a fixed amount of revenue from all payers, including Medicare, Medicaid, and commercial insurers.9 Known as an all-payer global budget, it incentivizes lowering unnecessary costs of care, such as readmissions, but also encourages cauterization of cost centers hemorrhaging money – such as inpatient pediatrics. Even the venerable Johns Hopkins Children’s Center has seen its profitability pale in comparison to the expansion team Johns Hopkins All Children’s Hospital in St. Petersburg, Fla., which is the second-most profitable hospital in the Hopkins system, only edged out by Sibley Memorial Hospital – which also sports an out-of-state location in the District of Columbia.10
But all hope is not lost for your comfy local pediatric inpatient unit. In other states and regions where a more favorable (to hospitals) payer mix exists, large pediatric hospitals are still engaged in turf battles with other local competitors to grab market share. In these regions, community pediatric units have survived by partnering with large pediatric institutions, either through affiliations or wholesale transplantation of the larger pediatric institution’s providers, nurses, and EHRs into essentially what is a leased floor. In addition, large pediatric institutions that participate in capitated models such as accountable care organizations have paradoxically found it financially favorable to direct “bread-and-butter” pediatric hospitalizations to community pediatric units, which often provide the same care at a lower cost.
Utilizing community inpatient pediatric units was “initially … a means of expanding their market share and ‘downstream’ revenue from transfers, but more commonly now [is] a way of alleviating the costs associated with admitting low to moderate acuity patients to the main tertiary sites,” said Francisco Alvarez, MD, associate chief of Regional Pediatric Hospital Medicine Programs at Lucile Packard Children’s Hospital in Palo Alto, Calif. “The cost of care provided by pediatric hospitals has always been higher than the average cost for nonpediatric hospitals in regard to caring for pediatric patients due to their highly skilled specialties and services. These have become more scrutinized by private and government insurance plans and, in some cases, have led to lower reimbursements and therefore a lower or deficient net revenue for certain patient populations.”
For community pediatric hospitalists, the shifting sands of reimbursement on which pediatric inpatient care is built can be a motion illness–inducing experience. In addition to concerns over community health care, job security, and population health, care provided in community hospitals can often be subtly undercut by tertiary and quaternary care pediatric hospitals.
“The focus of pediatric residency programs in freestanding children’s hospitals has created a situation where new pediatricians have less opportunity to develop respect for community pediatric hospital medicine,” said Beth Natt, MD, director of pediatric hospital medicine in the Regional Programs at Connecticut Children’s Medical Center, Hartford. “We are the nameless ‘OSH,’ the place that gets ‘Monday-morning quarterbacked’ in resident morning reports without having a voice at the table. Add this to residents learning ‘only’ protocolized care as opposed to a spectrum of appropriate care, and we create a culture of ‘wrong and right’ with the backward nonprotocol driven community docs looking like they are practicing medicine in the Wild West.”
What’s a community pediatric hospitalist to do, faced with an uncertain future and diminishing respect? Continuing to partner with local pediatric providers, community leaders, and local health care advocacy groups will help to enmesh inpatient providers in the fabric of a community’s health care. But making the value case to hospital administrators is critical for community pediatric hospitalists, as adult hospitalists realized soon after the inception of the hospitalist field.
Goals valued by hospital administrators are pursued on a daily basis by community pediatric hospitalists, and these successes need to be brought to light. Achieving value and quality metrics, pursuing high-value care, reducing readmission rates, championing EHRs, and improving documentation are goals that community pediatric hospitalists and hospital administrators can work toward together.11 By pursuing and sharing success in meeting these shared goals, perhaps the local community pediatric inpatient unit can survive – and thrive.
As for Dr. Krugman, he has moved on and is soon to be gainfully employed again. But he continues to be focused, as always, on the health of his patients.
“What are we going to do to take care of kids in their own communities?” Dr. Krugman asked. “It’s going to be an increasing challenge over the next decade due to the consolidation of children’s hospitals and low payments, especially for hospitals that are adult-focused. Unless we find a way to pay for pediatric care as a country.”
Dr. Chang is a pediatric hospitalist at Baystate Children’s Hospital in Springfield, Mass., and is the pediatric editor of The Hospitalist.
References
1. McDaniels A. (2018). Protesters denounce reduction in pediatric services at Baltimore’s MedStar Franklin Square hospital. Baltimore Sun. Available at: http://www.baltimoresun.com/health/health-care/bs-hs-franklin-square-hospital-protest-20180508-story.html.
2. Roberts KB. Pediatric hospitalists in community hospitals: Hospital-based generalists with expanded roles. Hosp Pediatr. 2015 May;5(5):290-2.
3. Georgia Health News. (2018). A hospital crisis is killing rural communities. This state is ‘Ground Zero’. Available at: http://www.georgiahealthnews.com/2017/09/hospital-crisis-killing-rural-communities-state-ground-zero/.
4. DiFazio RL et al. Non-medical out-of-pocket expenses incurred by families during their child’s hospitalization. J Child Health Care. 2013 Sep;17(3):230-41.
5. Gunderman R. Hospitalist and the decline of comprehensive care. N Engl J Med. 2016 Sep 15; 375(11):1011-3.
6. Statistical Brief #56. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb56.jsp.
7. Overview of Hospital Stays for Children in the United States, 2012 #187. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb187-Hospital-Stays-Children-2012.jsp.
8. Trends in Hospital Inpatient Stays by Age and Payer, 2000-2015 #235. (2018). Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb235-Inpatient-Stays-Age-Payer-Trends.jsp.
9. Maryland All-Payer Model | Center for Medicare & Medicaid Innovation. (2018). Retrieved from https://innovation.cms.gov/initiatives/Maryland-All-Payer-Model/.
10. The effects of Maryland’s unique health care system. (2018). Retrieved from https://www.axios.com/johns-hopkins-finances-maryland-1518553853-722c2195-731e-4e02-ab1e-94e4211ba945.html.
11. The Increasing Need for Hospitalist Programs to Demonstrate Value | SCP. (2018). Retrieved from https://www.schumacherclinical.com/providers/blog/the-increasing-need-for-hospitalist-programs-to-demonstrate-value.
Health care, technology, and the future
Major forces combining to reshape care delivery
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Major forces combining to reshape care delivery
Major forces combining to reshape care delivery
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Do free meals to physicians affect opioid prescribing?
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
REPORTING FROM CPDD 2018
Key clinical point: Opioid marketing appears to affect physician prescribing practices.
Major finding: Physicians who received opioid marketing payments and meals in 2014 prescribed an adjusted 9% more opioids in 2015 than did their opioid-prescribing colleagues.
Study details: Retrospective 2014-2015 analysis of 369,139 opioid-prescribing physicians in a Medicare Part D database.
Disclosures: Dr. Hadland reported funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reported funding from NIDA. No additional relevant disclosures were reported.
Source: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.