User login
Diminished hearing
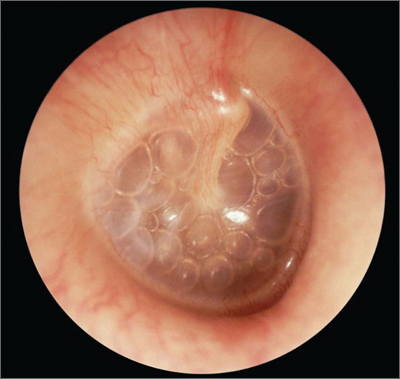
The patient had a cholesteatoma.
A cholesteatoma is similar to an epidermal inclusion cyst in the skin and causes the production of keratinaceous material that fills the middle ear, causing hearing loss and otorrhea. Oral and/or topical antibiotics are not effective at treating a cholesteatoma. The cholesteatoma often destroys the ossicles, which contributes to conductive hearing loss. A computed tomography scan can determine the extent of involvement and help the physician plan for surgery. Surgery is the definitive treatment to remove all of the abnormal tissue and prevent recurrence.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Vladimir Zlinsky, MD, in Roy F. Sullivan, PhD. Audiology Forum: video otoscopy, www.rcsullivan.com.
This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The patient had a cholesteatoma.
A cholesteatoma is similar to an epidermal inclusion cyst in the skin and causes the production of keratinaceous material that fills the middle ear, causing hearing loss and otorrhea. Oral and/or topical antibiotics are not effective at treating a cholesteatoma. The cholesteatoma often destroys the ossicles, which contributes to conductive hearing loss. A computed tomography scan can determine the extent of involvement and help the physician plan for surgery. Surgery is the definitive treatment to remove all of the abnormal tissue and prevent recurrence.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Vladimir Zlinsky, MD, in Roy F. Sullivan, PhD. Audiology Forum: video otoscopy, www.rcsullivan.com.
This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The patient had a cholesteatoma.
A cholesteatoma is similar to an epidermal inclusion cyst in the skin and causes the production of keratinaceous material that fills the middle ear, causing hearing loss and otorrhea. Oral and/or topical antibiotics are not effective at treating a cholesteatoma. The cholesteatoma often destroys the ossicles, which contributes to conductive hearing loss. A computed tomography scan can determine the extent of involvement and help the physician plan for surgery. Surgery is the definitive treatment to remove all of the abnormal tissue and prevent recurrence.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Vladimir Zlinsky, MD, in Roy F. Sullivan, PhD. Audiology Forum: video otoscopy, www.rcsullivan.com.
This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
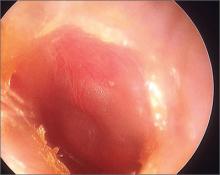
Air-fluid levels in ear
The family physician (FP) diagnosed otitis media with effusion (OME) in this patient.
OME is a characterized by fluid in the middle ear in a patient without signs or symptoms of an acute ear infection. The most common problem, present in more than half of patients, is mild hearing loss. This is usually identified when parents express concern regarding their child’s behavior, performance at school, or language development. The absence of signs and symptoms of acute illness assists in differentiating OME from AOM.
Common otoscopic findings for OME include: air–fluid level or bubbles or a cloudy tympanic membrane (TM). Redness of the TM may also be present. Physicians should use pneumatic otoscopy as the primary diagnostic method for OME. Impaired mobility of the TM is the hallmark.
Management of OME primarily consists of watchful waiting. Most cases resolve spontaneously within 3 months; only 5% to 10% last a year or longer. Treatment depends on duration and associated conditions.
Document the laterality, duration of effusion, and presence and severity of associated symptoms at each assessment of the child with OME. Distinguish the child with OME who is at risk for speech, language, or learning problems from other children with OME and more promptly evaluate hearing, speech, language, and need for intervention in those at risk. Hearing testing is recommended when OME persists for 3 months or longer or at any time if language delay, learning problems, or significant hearing loss is suspected in a child with OME.
In this particular case, the FP explained to the parents that watchful waiting was acceptable since the child was asymptomatic. At a follow-up appointment 3 months later, the effusion was completely resolved.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Frank Miller, MD. This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The family physician (FP) diagnosed otitis media with effusion (OME) in this patient.
OME is a characterized by fluid in the middle ear in a patient without signs or symptoms of an acute ear infection. The most common problem, present in more than half of patients, is mild hearing loss. This is usually identified when parents express concern regarding their child’s behavior, performance at school, or language development. The absence of signs and symptoms of acute illness assists in differentiating OME from AOM.
Common otoscopic findings for OME include: air–fluid level or bubbles or a cloudy tympanic membrane (TM). Redness of the TM may also be present. Physicians should use pneumatic otoscopy as the primary diagnostic method for OME. Impaired mobility of the TM is the hallmark.
Management of OME primarily consists of watchful waiting. Most cases resolve spontaneously within 3 months; only 5% to 10% last a year or longer. Treatment depends on duration and associated conditions.
Document the laterality, duration of effusion, and presence and severity of associated symptoms at each assessment of the child with OME. Distinguish the child with OME who is at risk for speech, language, or learning problems from other children with OME and more promptly evaluate hearing, speech, language, and need for intervention in those at risk. Hearing testing is recommended when OME persists for 3 months or longer or at any time if language delay, learning problems, or significant hearing loss is suspected in a child with OME.
In this particular case, the FP explained to the parents that watchful waiting was acceptable since the child was asymptomatic. At a follow-up appointment 3 months later, the effusion was completely resolved.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Frank Miller, MD. This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The family physician (FP) diagnosed otitis media with effusion (OME) in this patient.
OME is a characterized by fluid in the middle ear in a patient without signs or symptoms of an acute ear infection. The most common problem, present in more than half of patients, is mild hearing loss. This is usually identified when parents express concern regarding their child’s behavior, performance at school, or language development. The absence of signs and symptoms of acute illness assists in differentiating OME from AOM.
Common otoscopic findings for OME include: air–fluid level or bubbles or a cloudy tympanic membrane (TM). Redness of the TM may also be present. Physicians should use pneumatic otoscopy as the primary diagnostic method for OME. Impaired mobility of the TM is the hallmark.
Management of OME primarily consists of watchful waiting. Most cases resolve spontaneously within 3 months; only 5% to 10% last a year or longer. Treatment depends on duration and associated conditions.
Document the laterality, duration of effusion, and presence and severity of associated symptoms at each assessment of the child with OME. Distinguish the child with OME who is at risk for speech, language, or learning problems from other children with OME and more promptly evaluate hearing, speech, language, and need for intervention in those at risk. Hearing testing is recommended when OME persists for 3 months or longer or at any time if language delay, learning problems, or significant hearing loss is suspected in a child with OME.
In this particular case, the FP explained to the parents that watchful waiting was acceptable since the child was asymptomatic. At a follow-up appointment 3 months later, the effusion was completely resolved.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Frank Miller, MD. This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
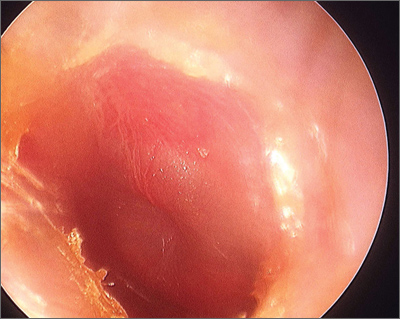
Ear pain in baby
The FP diagnosed acute otitis media (AOM) in this patient. AOM is characterized by middle-ear effusion in a patient with signs and symptoms of acute illness (eg, fever, irritability, otalgia).
Oral acetaminophen and ibuprofen may reduce earache when given with antibiotics. Antibiotics seem to be most beneficial in children younger than 2 years of age with bilateral AOM, high fever, or vomiting, and in children with both AOM and otorrhea. For most other children with mild disease, an observational policy is acceptable.
Antibiotics may lead to more rapid reduction in symptoms of AOM, but increase the risk of adverse effects including diarrhea, vomiting, and rash. Antibiotics seem to reduce pain at 2 to 7 days, and may prevent development of contralateral AOM, but increase the risk of adverse effects compared with placebo. Antibiotics found to be effective in AOM include amoxicillin, amoxicillin/clavulanic acid, ampicillin, penicillin, erythromycin, azithromycin, trimethoprim-sulfamethoxazole, and cephalosporins. Amoxicillin is a good first-line treatment because it is inexpensive and children tolerate the bubblegum taste well.
Longer (8- to 10-day) courses of antibiotics reduce short-term treatment failure but have no long-term benefits compared with shorter regimens (5-day courses). An observational approach substantially reduces the unnecessary use of antibiotics in children with AOM and may be an alternative to routinely treating them with antimicrobials.
In this case, the FP prescribed a 10-day course of amoxicillin and the child recovered uneventfully.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of William Clark, MD. This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP diagnosed acute otitis media (AOM) in this patient. AOM is characterized by middle-ear effusion in a patient with signs and symptoms of acute illness (eg, fever, irritability, otalgia).
Oral acetaminophen and ibuprofen may reduce earache when given with antibiotics. Antibiotics seem to be most beneficial in children younger than 2 years of age with bilateral AOM, high fever, or vomiting, and in children with both AOM and otorrhea. For most other children with mild disease, an observational policy is acceptable.
Antibiotics may lead to more rapid reduction in symptoms of AOM, but increase the risk of adverse effects including diarrhea, vomiting, and rash. Antibiotics seem to reduce pain at 2 to 7 days, and may prevent development of contralateral AOM, but increase the risk of adverse effects compared with placebo. Antibiotics found to be effective in AOM include amoxicillin, amoxicillin/clavulanic acid, ampicillin, penicillin, erythromycin, azithromycin, trimethoprim-sulfamethoxazole, and cephalosporins. Amoxicillin is a good first-line treatment because it is inexpensive and children tolerate the bubblegum taste well.
Longer (8- to 10-day) courses of antibiotics reduce short-term treatment failure but have no long-term benefits compared with shorter regimens (5-day courses). An observational approach substantially reduces the unnecessary use of antibiotics in children with AOM and may be an alternative to routinely treating them with antimicrobials.
In this case, the FP prescribed a 10-day course of amoxicillin and the child recovered uneventfully.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of William Clark, MD. This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP diagnosed acute otitis media (AOM) in this patient. AOM is characterized by middle-ear effusion in a patient with signs and symptoms of acute illness (eg, fever, irritability, otalgia).
Oral acetaminophen and ibuprofen may reduce earache when given with antibiotics. Antibiotics seem to be most beneficial in children younger than 2 years of age with bilateral AOM, high fever, or vomiting, and in children with both AOM and otorrhea. For most other children with mild disease, an observational policy is acceptable.
Antibiotics may lead to more rapid reduction in symptoms of AOM, but increase the risk of adverse effects including diarrhea, vomiting, and rash. Antibiotics seem to reduce pain at 2 to 7 days, and may prevent development of contralateral AOM, but increase the risk of adverse effects compared with placebo. Antibiotics found to be effective in AOM include amoxicillin, amoxicillin/clavulanic acid, ampicillin, penicillin, erythromycin, azithromycin, trimethoprim-sulfamethoxazole, and cephalosporins. Amoxicillin is a good first-line treatment because it is inexpensive and children tolerate the bubblegum taste well.
Longer (8- to 10-day) courses of antibiotics reduce short-term treatment failure but have no long-term benefits compared with shorter regimens (5-day courses). An observational approach substantially reduces the unnecessary use of antibiotics in children with AOM and may be an alternative to routinely treating them with antimicrobials.
In this case, the FP prescribed a 10-day course of amoxicillin and the child recovered uneventfully.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of William Clark, MD. This case was adapted from: Rayala B. Otitis media: acute otitis and otitis media with effusion. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:170-179.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
Rash on hand
The patient was given a diagnosis of tinea manuum on one hand and tinea pedis on both feet. Tinea manuum is known as two feet-one hand syndrome and is caused by a dermatophyte infection. The patient was initially treating his rash appropriately with the topical antifungal, but failed to treat his concomitant tinea pedis.
The infection may be spread from the feet to the hand by scratching, as tinea pedis or onychomycosis of the toenails precede infection of the hand. The hand that is used to scratch or pick at the feet may be the hand that becomes involved (but this is not always the case).
Topical antifungals such as terbinafine, clotrimazole, or ketoconazole are first-line therapy for the feet and hand.Consider oral antifungals if the affected area is large, the patient doesn’t respond to topical therapy, or the patient is immunocompromised.
In light of the patient’s previous failure with topical therapy, he was reluctant to try this approach again. After a normal hepatic panel, his physician started him on a 2-week course of oral terbinafine 250 mg daily. Follow-up at one month showed no sign of previous infection.
Adapted from: Crandall ML. Photo Rounds: Stubborn hand rash. J Fam Pract. 2012:61:421-424.
The patient was given a diagnosis of tinea manuum on one hand and tinea pedis on both feet. Tinea manuum is known as two feet-one hand syndrome and is caused by a dermatophyte infection. The patient was initially treating his rash appropriately with the topical antifungal, but failed to treat his concomitant tinea pedis.
The infection may be spread from the feet to the hand by scratching, as tinea pedis or onychomycosis of the toenails precede infection of the hand. The hand that is used to scratch or pick at the feet may be the hand that becomes involved (but this is not always the case).
Topical antifungals such as terbinafine, clotrimazole, or ketoconazole are first-line therapy for the feet and hand.Consider oral antifungals if the affected area is large, the patient doesn’t respond to topical therapy, or the patient is immunocompromised.
In light of the patient’s previous failure with topical therapy, he was reluctant to try this approach again. After a normal hepatic panel, his physician started him on a 2-week course of oral terbinafine 250 mg daily. Follow-up at one month showed no sign of previous infection.
Adapted from: Crandall ML. Photo Rounds: Stubborn hand rash. J Fam Pract. 2012:61:421-424.
The patient was given a diagnosis of tinea manuum on one hand and tinea pedis on both feet. Tinea manuum is known as two feet-one hand syndrome and is caused by a dermatophyte infection. The patient was initially treating his rash appropriately with the topical antifungal, but failed to treat his concomitant tinea pedis.
The infection may be spread from the feet to the hand by scratching, as tinea pedis or onychomycosis of the toenails precede infection of the hand. The hand that is used to scratch or pick at the feet may be the hand that becomes involved (but this is not always the case).
Topical antifungals such as terbinafine, clotrimazole, or ketoconazole are first-line therapy for the feet and hand.Consider oral antifungals if the affected area is large, the patient doesn’t respond to topical therapy, or the patient is immunocompromised.
In light of the patient’s previous failure with topical therapy, he was reluctant to try this approach again. After a normal hepatic panel, his physician started him on a 2-week course of oral terbinafine 250 mg daily. Follow-up at one month showed no sign of previous infection.
Adapted from: Crandall ML. Photo Rounds: Stubborn hand rash. J Fam Pract. 2012:61:421-424.
Painful ear nodules
A. Good-quality patient-oriented evidence
B. Inconsistent or limited-quality patient-oriented evidence
C. Consensus, usual practice, opinion, disease-oriented evidence, case series
A 49-year-old man with a history of hypertension, hypercholesterolemia, polysubstance use, recurrent methicillin-resistant Staphylococcus aureus skin infections, and chronic hepatitis C infection sought care at our emergency department (ED) because parts of his ears had started turning black 3 days earlier. They were also painful to the touch. He denied fever, any similar skin lesions, injury to his ears, or a history of easy bleeding or bruising. A recovering alcoholic, he admitted to regular marijuana use and twice-weekly cocaine use. He had last used cocaine 3 days ago.
The patient was thin and in no acute distress. His vital signs and cardiopulmonary exams were normal. Examination of his ears revealed bilateral violaceous firm, tender purpura on the pinnae (FIGURE).
A complete blood count (CBC) revealed mild leukopenia (white blood cell [WBC] count, 2.0 × 109/L), neutropenia (0.9 × 109/L), and a normal platelet count (264 × 109/L). A chemistry panel, liver function tests, and prothrombin time were normal. Erythrocyte sedimentation rate (ESR) was elevated to 69 mm/h. The patient’s cholesterol level was not elevated. Urine toxicology was positive for cocaine and opioids. A human immunodeficiency virus test was negative.
Figure
Tender purpura on the pinnae
What is your diagnosis?
How would you treat this patient?
Diagnosis: Levamisole toxicity
The patient was diagnosed with levamisole toxicity based on his clinical presentation and the fact that he had used cocaine around the time his ear lesions appeared.
Levamisole—primarily a veterinary antihelmintic medication—is used on rare occasions to treat nephrotic syndrome in children.1 Levamisole is frequently added to cocaine or heroin to increase the street drug’s potency. The Drug Enforcement Administration reports that 69% of seized cocaine lots in the United States contain levamisole.2
The compound is thought to cause a vasculitis and bone marrow suppression resulting in neutropenia. The vasculitis targets small vessels, resulting in thrombosis, which can lead to tissue necrosis.1
Other possibilities in the differential Dx
The differential diagnosis includes a variety of vasculitides and other microvascular pathologies.
Cholesterol emboli arise when cholesterol crystals are released from atherosclerotic plaques, typically after invasive cardiac procedures. In addition, anticoagulants can cause the release of these crystals by inhibiting the formation of protective clots around unstable plaques.3 These emboli can seed the microvasculature anywhere, but the kidneys and skin are most frequently affected. These crystals not only clog the vasculature, causing tissue ischemia, but also activate the complement cascade, triggering a series of inflammatory responses that can lead to luminal fibrosis and narrowing.3
Affected patients have a history of atherosclerotic disease or predisposing factors such as hypertension or diabetes. Ulcerations or frank cyanosis may be found at the tips of the fingers or toes. In severe cases, gangrene will form in these regions. Patients may also have livido reticularis, a lace-like hyperpigmented rash over the lower extremities. Laboratory analysis may indicate acute renal failure or eosinophilia.3
Bacterial endocarditis results from the seeding of bacterial emboli primarily from the mitral or tricuspid valves.4 Streptococci are the primary infectious agent, with staphylococci being more common among intravenous drug users. High-risk populations include patients with artificial valves, the elderly, and the immunocompromised.4
Clinical manifestations include Janeway lesions (asymptomatic hemorrhagic papules on the palms) and Osler’s nodes (tender nodules on the fingertips). Splinter hemorrhages, or linear nonblanching lesions, may be present within the nail beds. Palpable purpura and petechiae may also be found.
Patients may have positive blood cultures, leukocytosis, an elevated ESR, or vegetations on a transesophageal echocardiogram.4 The physical exam may reveal a new cardiac murmur.
High circulating levels of cryoglobulins can arise in the setting of hepatitis C infection, but can also be seen in a number of autoimmune disorders and other infectious diseases.5 Cryoglobulins are immune complexes that are deposited into the lumen of microvasculature. In cold temperatures, these cryoglobulins precipitate, resulting in vasculitis. While most patients are asymptomatic, cutaneous findings in the distal extremities can include palpable purpura, ulcerations, and livido reticularis.5 Patients may complain of arthritis or symptoms consistent with Raynaud’s phenomenon.
Detection of specific serum cryoprecipitates isolated by immunofixation is pathognomonic for this condition, provided the sample is collected in a warm tube. Elevated rheumatoid factor and decreased complement levels may also be seen.5
Henoch-Schönlein purpura (HSP) is a small vessel vasculitis caused by IgA deposition that predominantly affects children. HSP has a host of systemic symptoms, often preceded by a benign upper respiratory infection, consisting of palpable purpura, arthritis, abdominal pain, and glomerulonephritis.6 Palpable purpura will generally be found in dependent portions of the body—especially the buttocks and lower legs.
While the diagnosis is primarily clinical, serum IgA levels and ESR can be elevated, urinalysis may demonstrate hematuria or proteinuria, and a CBC may reveal a leukocytosis with normal platelets.6
Suspect levamisole toxicity in patients using cocaine
Patients with levamisole toxicity present with sudden-onset tender plaques or bullae with necrotic centers within days of cocaine use. Case reports cite lesions primarily on the ears and cheeks. However, they can appear almost anywhere on the body.2,7-9 Physicians should have a high index of suspicion for levamisole toxicity in patients using cocaine who present with unexplained neutropenia or vasculitis.
Laboratory tests. If needed, tissue biopsy and urine detection of levamisole can be used to confirm the diagnosis.1
Management is straight-forward, but not simple
Skin lesions have been reported to improve several weeks after discontinuing use of contaminated cocaine1 (strength of recommendation [SOR]: C). Known users should be referred to drug treatment centers and counseled on the risks of use.
Our patient required hospitalization
When our patient came into the ED, he also complained of left thigh pain and swelling. A computed tomography scan revealed a deep sartorius abscess. The patient was admitted for ultrasound-guided aspiration of the abscess and IV antibiotics. His bilateral painful ear nodules persisted throughout his hospitalization, although his neutropenia resolved after 3 days.
Correspondence: Katherine Winter, MD, 101 Manning Drive, Chapel Hill, NC 27514; [email protected]
1. Lee KC, Culpepper K, Kessler M. Levamisole-induced thrombosis: literature review and pertinent laboratory findings. J Am Acad Dermatol. 2011;65:e128-e129.
2. CDC. Agranulocytosis associated with cocaine use - four States, March 2008-November 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1381-1385.
3. Kronzon I, Saric M. Cholesterol embolization syndrome. Circulation. 2010;122:631-641.
4. Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001;345:1318-1330.
5. Tedeschi A, Barate C, Minola E, et al. Cryoglobulinemia. Blood Rev. 2007;21:183-200.
6. Trapani S, Micheli A, Grisolia F, et al. Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005;35:143-153.
7. Muirhead TT, Eide MJ. Images in clinical medicine. Toxic effects of levamisole in a cocaine user. N Engl J Med. 2011;364:e52.
8. Bradford M, Rosenberg B, Moreno J, et al. Bilateral necrosis of earlobes and cheeks: another complication of cocaine contaminated with levamisole. Ann Intern Med. 2010;152: 758-759.
9. Chung C, Tumeh P, Birnbaum R. Characteristic purpura of the ears, vasculitis, and neutropenia—a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65:722-725.
A. Good-quality patient-oriented evidence
B. Inconsistent or limited-quality patient-oriented evidence
C. Consensus, usual practice, opinion, disease-oriented evidence, case series
A 49-year-old man with a history of hypertension, hypercholesterolemia, polysubstance use, recurrent methicillin-resistant Staphylococcus aureus skin infections, and chronic hepatitis C infection sought care at our emergency department (ED) because parts of his ears had started turning black 3 days earlier. They were also painful to the touch. He denied fever, any similar skin lesions, injury to his ears, or a history of easy bleeding or bruising. A recovering alcoholic, he admitted to regular marijuana use and twice-weekly cocaine use. He had last used cocaine 3 days ago.
The patient was thin and in no acute distress. His vital signs and cardiopulmonary exams were normal. Examination of his ears revealed bilateral violaceous firm, tender purpura on the pinnae (FIGURE).
A complete blood count (CBC) revealed mild leukopenia (white blood cell [WBC] count, 2.0 × 109/L), neutropenia (0.9 × 109/L), and a normal platelet count (264 × 109/L). A chemistry panel, liver function tests, and prothrombin time were normal. Erythrocyte sedimentation rate (ESR) was elevated to 69 mm/h. The patient’s cholesterol level was not elevated. Urine toxicology was positive for cocaine and opioids. A human immunodeficiency virus test was negative.
Figure
Tender purpura on the pinnae
What is your diagnosis?
How would you treat this patient?
Diagnosis: Levamisole toxicity
The patient was diagnosed with levamisole toxicity based on his clinical presentation and the fact that he had used cocaine around the time his ear lesions appeared.
Levamisole—primarily a veterinary antihelmintic medication—is used on rare occasions to treat nephrotic syndrome in children.1 Levamisole is frequently added to cocaine or heroin to increase the street drug’s potency. The Drug Enforcement Administration reports that 69% of seized cocaine lots in the United States contain levamisole.2
The compound is thought to cause a vasculitis and bone marrow suppression resulting in neutropenia. The vasculitis targets small vessels, resulting in thrombosis, which can lead to tissue necrosis.1
Other possibilities in the differential Dx
The differential diagnosis includes a variety of vasculitides and other microvascular pathologies.
Cholesterol emboli arise when cholesterol crystals are released from atherosclerotic plaques, typically after invasive cardiac procedures. In addition, anticoagulants can cause the release of these crystals by inhibiting the formation of protective clots around unstable plaques.3 These emboli can seed the microvasculature anywhere, but the kidneys and skin are most frequently affected. These crystals not only clog the vasculature, causing tissue ischemia, but also activate the complement cascade, triggering a series of inflammatory responses that can lead to luminal fibrosis and narrowing.3
Affected patients have a history of atherosclerotic disease or predisposing factors such as hypertension or diabetes. Ulcerations or frank cyanosis may be found at the tips of the fingers or toes. In severe cases, gangrene will form in these regions. Patients may also have livido reticularis, a lace-like hyperpigmented rash over the lower extremities. Laboratory analysis may indicate acute renal failure or eosinophilia.3
Bacterial endocarditis results from the seeding of bacterial emboli primarily from the mitral or tricuspid valves.4 Streptococci are the primary infectious agent, with staphylococci being more common among intravenous drug users. High-risk populations include patients with artificial valves, the elderly, and the immunocompromised.4
Clinical manifestations include Janeway lesions (asymptomatic hemorrhagic papules on the palms) and Osler’s nodes (tender nodules on the fingertips). Splinter hemorrhages, or linear nonblanching lesions, may be present within the nail beds. Palpable purpura and petechiae may also be found.
Patients may have positive blood cultures, leukocytosis, an elevated ESR, or vegetations on a transesophageal echocardiogram.4 The physical exam may reveal a new cardiac murmur.
High circulating levels of cryoglobulins can arise in the setting of hepatitis C infection, but can also be seen in a number of autoimmune disorders and other infectious diseases.5 Cryoglobulins are immune complexes that are deposited into the lumen of microvasculature. In cold temperatures, these cryoglobulins precipitate, resulting in vasculitis. While most patients are asymptomatic, cutaneous findings in the distal extremities can include palpable purpura, ulcerations, and livido reticularis.5 Patients may complain of arthritis or symptoms consistent with Raynaud’s phenomenon.
Detection of specific serum cryoprecipitates isolated by immunofixation is pathognomonic for this condition, provided the sample is collected in a warm tube. Elevated rheumatoid factor and decreased complement levels may also be seen.5
Henoch-Schönlein purpura (HSP) is a small vessel vasculitis caused by IgA deposition that predominantly affects children. HSP has a host of systemic symptoms, often preceded by a benign upper respiratory infection, consisting of palpable purpura, arthritis, abdominal pain, and glomerulonephritis.6 Palpable purpura will generally be found in dependent portions of the body—especially the buttocks and lower legs.
While the diagnosis is primarily clinical, serum IgA levels and ESR can be elevated, urinalysis may demonstrate hematuria or proteinuria, and a CBC may reveal a leukocytosis with normal platelets.6
Suspect levamisole toxicity in patients using cocaine
Patients with levamisole toxicity present with sudden-onset tender plaques or bullae with necrotic centers within days of cocaine use. Case reports cite lesions primarily on the ears and cheeks. However, they can appear almost anywhere on the body.2,7-9 Physicians should have a high index of suspicion for levamisole toxicity in patients using cocaine who present with unexplained neutropenia or vasculitis.
Laboratory tests. If needed, tissue biopsy and urine detection of levamisole can be used to confirm the diagnosis.1
Management is straight-forward, but not simple
Skin lesions have been reported to improve several weeks after discontinuing use of contaminated cocaine1 (strength of recommendation [SOR]: C). Known users should be referred to drug treatment centers and counseled on the risks of use.
Our patient required hospitalization
When our patient came into the ED, he also complained of left thigh pain and swelling. A computed tomography scan revealed a deep sartorius abscess. The patient was admitted for ultrasound-guided aspiration of the abscess and IV antibiotics. His bilateral painful ear nodules persisted throughout his hospitalization, although his neutropenia resolved after 3 days.
Correspondence: Katherine Winter, MD, 101 Manning Drive, Chapel Hill, NC 27514; [email protected]
A. Good-quality patient-oriented evidence
B. Inconsistent or limited-quality patient-oriented evidence
C. Consensus, usual practice, opinion, disease-oriented evidence, case series
A 49-year-old man with a history of hypertension, hypercholesterolemia, polysubstance use, recurrent methicillin-resistant Staphylococcus aureus skin infections, and chronic hepatitis C infection sought care at our emergency department (ED) because parts of his ears had started turning black 3 days earlier. They were also painful to the touch. He denied fever, any similar skin lesions, injury to his ears, or a history of easy bleeding or bruising. A recovering alcoholic, he admitted to regular marijuana use and twice-weekly cocaine use. He had last used cocaine 3 days ago.
The patient was thin and in no acute distress. His vital signs and cardiopulmonary exams were normal. Examination of his ears revealed bilateral violaceous firm, tender purpura on the pinnae (FIGURE).
A complete blood count (CBC) revealed mild leukopenia (white blood cell [WBC] count, 2.0 × 109/L), neutropenia (0.9 × 109/L), and a normal platelet count (264 × 109/L). A chemistry panel, liver function tests, and prothrombin time were normal. Erythrocyte sedimentation rate (ESR) was elevated to 69 mm/h. The patient’s cholesterol level was not elevated. Urine toxicology was positive for cocaine and opioids. A human immunodeficiency virus test was negative.
Figure
Tender purpura on the pinnae
What is your diagnosis?
How would you treat this patient?
Diagnosis: Levamisole toxicity
The patient was diagnosed with levamisole toxicity based on his clinical presentation and the fact that he had used cocaine around the time his ear lesions appeared.
Levamisole—primarily a veterinary antihelmintic medication—is used on rare occasions to treat nephrotic syndrome in children.1 Levamisole is frequently added to cocaine or heroin to increase the street drug’s potency. The Drug Enforcement Administration reports that 69% of seized cocaine lots in the United States contain levamisole.2
The compound is thought to cause a vasculitis and bone marrow suppression resulting in neutropenia. The vasculitis targets small vessels, resulting in thrombosis, which can lead to tissue necrosis.1
Other possibilities in the differential Dx
The differential diagnosis includes a variety of vasculitides and other microvascular pathologies.
Cholesterol emboli arise when cholesterol crystals are released from atherosclerotic plaques, typically after invasive cardiac procedures. In addition, anticoagulants can cause the release of these crystals by inhibiting the formation of protective clots around unstable plaques.3 These emboli can seed the microvasculature anywhere, but the kidneys and skin are most frequently affected. These crystals not only clog the vasculature, causing tissue ischemia, but also activate the complement cascade, triggering a series of inflammatory responses that can lead to luminal fibrosis and narrowing.3
Affected patients have a history of atherosclerotic disease or predisposing factors such as hypertension or diabetes. Ulcerations or frank cyanosis may be found at the tips of the fingers or toes. In severe cases, gangrene will form in these regions. Patients may also have livido reticularis, a lace-like hyperpigmented rash over the lower extremities. Laboratory analysis may indicate acute renal failure or eosinophilia.3
Bacterial endocarditis results from the seeding of bacterial emboli primarily from the mitral or tricuspid valves.4 Streptococci are the primary infectious agent, with staphylococci being more common among intravenous drug users. High-risk populations include patients with artificial valves, the elderly, and the immunocompromised.4
Clinical manifestations include Janeway lesions (asymptomatic hemorrhagic papules on the palms) and Osler’s nodes (tender nodules on the fingertips). Splinter hemorrhages, or linear nonblanching lesions, may be present within the nail beds. Palpable purpura and petechiae may also be found.
Patients may have positive blood cultures, leukocytosis, an elevated ESR, or vegetations on a transesophageal echocardiogram.4 The physical exam may reveal a new cardiac murmur.
High circulating levels of cryoglobulins can arise in the setting of hepatitis C infection, but can also be seen in a number of autoimmune disorders and other infectious diseases.5 Cryoglobulins are immune complexes that are deposited into the lumen of microvasculature. In cold temperatures, these cryoglobulins precipitate, resulting in vasculitis. While most patients are asymptomatic, cutaneous findings in the distal extremities can include palpable purpura, ulcerations, and livido reticularis.5 Patients may complain of arthritis or symptoms consistent with Raynaud’s phenomenon.
Detection of specific serum cryoprecipitates isolated by immunofixation is pathognomonic for this condition, provided the sample is collected in a warm tube. Elevated rheumatoid factor and decreased complement levels may also be seen.5
Henoch-Schönlein purpura (HSP) is a small vessel vasculitis caused by IgA deposition that predominantly affects children. HSP has a host of systemic symptoms, often preceded by a benign upper respiratory infection, consisting of palpable purpura, arthritis, abdominal pain, and glomerulonephritis.6 Palpable purpura will generally be found in dependent portions of the body—especially the buttocks and lower legs.
While the diagnosis is primarily clinical, serum IgA levels and ESR can be elevated, urinalysis may demonstrate hematuria or proteinuria, and a CBC may reveal a leukocytosis with normal platelets.6
Suspect levamisole toxicity in patients using cocaine
Patients with levamisole toxicity present with sudden-onset tender plaques or bullae with necrotic centers within days of cocaine use. Case reports cite lesions primarily on the ears and cheeks. However, they can appear almost anywhere on the body.2,7-9 Physicians should have a high index of suspicion for levamisole toxicity in patients using cocaine who present with unexplained neutropenia or vasculitis.
Laboratory tests. If needed, tissue biopsy and urine detection of levamisole can be used to confirm the diagnosis.1
Management is straight-forward, but not simple
Skin lesions have been reported to improve several weeks after discontinuing use of contaminated cocaine1 (strength of recommendation [SOR]: C). Known users should be referred to drug treatment centers and counseled on the risks of use.
Our patient required hospitalization
When our patient came into the ED, he also complained of left thigh pain and swelling. A computed tomography scan revealed a deep sartorius abscess. The patient was admitted for ultrasound-guided aspiration of the abscess and IV antibiotics. His bilateral painful ear nodules persisted throughout his hospitalization, although his neutropenia resolved after 3 days.
Correspondence: Katherine Winter, MD, 101 Manning Drive, Chapel Hill, NC 27514; [email protected]
1. Lee KC, Culpepper K, Kessler M. Levamisole-induced thrombosis: literature review and pertinent laboratory findings. J Am Acad Dermatol. 2011;65:e128-e129.
2. CDC. Agranulocytosis associated with cocaine use - four States, March 2008-November 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1381-1385.
3. Kronzon I, Saric M. Cholesterol embolization syndrome. Circulation. 2010;122:631-641.
4. Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001;345:1318-1330.
5. Tedeschi A, Barate C, Minola E, et al. Cryoglobulinemia. Blood Rev. 2007;21:183-200.
6. Trapani S, Micheli A, Grisolia F, et al. Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005;35:143-153.
7. Muirhead TT, Eide MJ. Images in clinical medicine. Toxic effects of levamisole in a cocaine user. N Engl J Med. 2011;364:e52.
8. Bradford M, Rosenberg B, Moreno J, et al. Bilateral necrosis of earlobes and cheeks: another complication of cocaine contaminated with levamisole. Ann Intern Med. 2010;152: 758-759.
9. Chung C, Tumeh P, Birnbaum R. Characteristic purpura of the ears, vasculitis, and neutropenia—a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65:722-725.
1. Lee KC, Culpepper K, Kessler M. Levamisole-induced thrombosis: literature review and pertinent laboratory findings. J Am Acad Dermatol. 2011;65:e128-e129.
2. CDC. Agranulocytosis associated with cocaine use - four States, March 2008-November 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1381-1385.
3. Kronzon I, Saric M. Cholesterol embolization syndrome. Circulation. 2010;122:631-641.
4. Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001;345:1318-1330.
5. Tedeschi A, Barate C, Minola E, et al. Cryoglobulinemia. Blood Rev. 2007;21:183-200.
6. Trapani S, Micheli A, Grisolia F, et al. Henoch Schonlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005;35:143-153.
7. Muirhead TT, Eide MJ. Images in clinical medicine. Toxic effects of levamisole in a cocaine user. N Engl J Med. 2011;364:e52.
8. Bradford M, Rosenberg B, Moreno J, et al. Bilateral necrosis of earlobes and cheeks: another complication of cocaine contaminated with levamisole. Ann Intern Med. 2010;152: 758-759.
9. Chung C, Tumeh P, Birnbaum R. Characteristic purpura of the ears, vasculitis, and neutropenia—a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol. 2011;65:722-725.
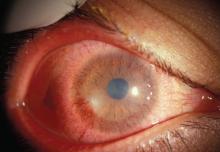
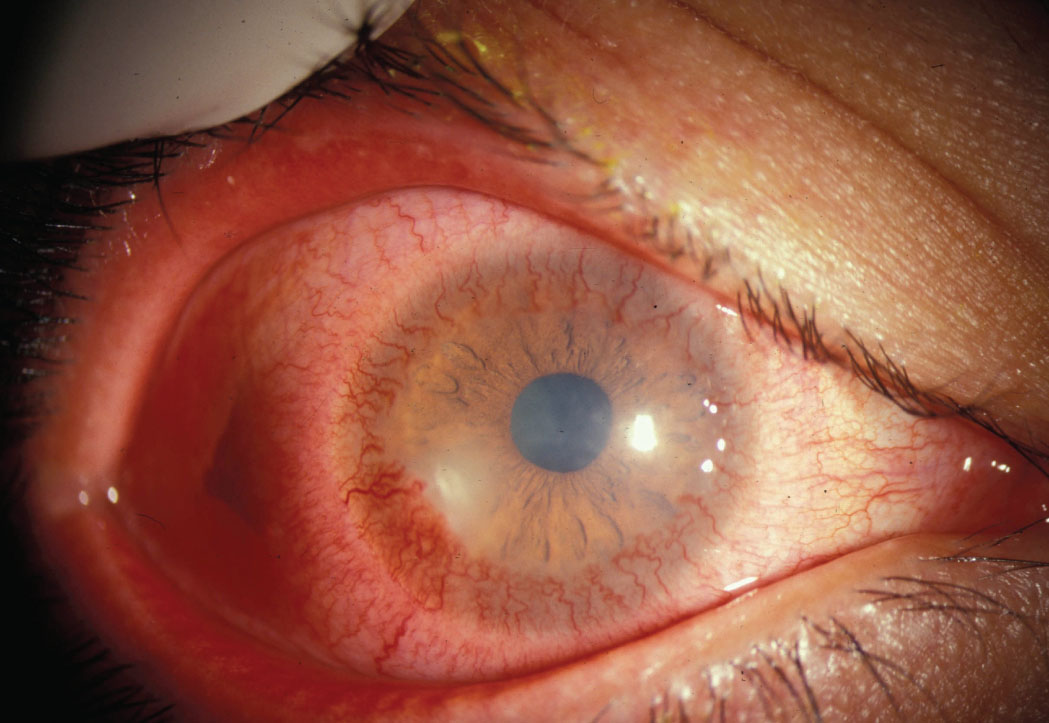
Blurred vision and red eyes
The FP recognized neovascularization growing onto both corneas. He had heard that this could occur with rosacea, but had never seen anything like it before. The FP called an ophthalmology colleague, who agreed to see the patient the next day.
Weeks later, the FP got a letter from the ophthalmologist thanking him for the referral and confirming that this was a severe type of ocular rosacea. It was so advanced that the patient was going to need a corneal transplant to restore normal vision.
The ophthalmologist placed the patient on oral doxycycline 100 mg twice daily and topical ophthalmic cyclosporin to control the inflammatory process until a corneal transplant could be arranged. (Getting inflammation under control is essential before a transplant can be performed.)
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP recognized neovascularization growing onto both corneas. He had heard that this could occur with rosacea, but had never seen anything like it before. The FP called an ophthalmology colleague, who agreed to see the patient the next day.
Weeks later, the FP got a letter from the ophthalmologist thanking him for the referral and confirming that this was a severe type of ocular rosacea. It was so advanced that the patient was going to need a corneal transplant to restore normal vision.
The ophthalmologist placed the patient on oral doxycycline 100 mg twice daily and topical ophthalmic cyclosporin to control the inflammatory process until a corneal transplant could be arranged. (Getting inflammation under control is essential before a transplant can be performed.)
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP recognized neovascularization growing onto both corneas. He had heard that this could occur with rosacea, but had never seen anything like it before. The FP called an ophthalmology colleague, who agreed to see the patient the next day.
Weeks later, the FP got a letter from the ophthalmologist thanking him for the referral and confirming that this was a severe type of ocular rosacea. It was so advanced that the patient was going to need a corneal transplant to restore normal vision.
The ophthalmologist placed the patient on oral doxycycline 100 mg twice daily and topical ophthalmic cyclosporin to control the inflammatory process until a corneal transplant could be arranged. (Getting inflammation under control is essential before a transplant can be performed.)
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
Red eyes following sneezing episode
The FP diagnosed bilateral subconjunctival hemorrhages. The bright red color that goes up to the cornea but leaves a small white ring of uninvolved tissue at the limbus is a classic finding for subconjunctival hemorrhage. While a subconjunctival hemorrhage appears concerning, it is not dangerous to the eye.
When caring for a patient who presents in this manner, it’s important to check for uncontrolled hypertension. You’ll also need to ask about other bleeding so that you can rule out clotting problems.
In most cases, the subconjunctival hemorrhage is caused by mild trauma including sneezing and coughing. In this case, the FP reassured the patient that his subconjunctival hemorrhages would resolve spontaneously. She also suggested that the patient take antihistamines prophylactically before being exposed to a cat.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP diagnosed bilateral subconjunctival hemorrhages. The bright red color that goes up to the cornea but leaves a small white ring of uninvolved tissue at the limbus is a classic finding for subconjunctival hemorrhage. While a subconjunctival hemorrhage appears concerning, it is not dangerous to the eye.
When caring for a patient who presents in this manner, it’s important to check for uncontrolled hypertension. You’ll also need to ask about other bleeding so that you can rule out clotting problems.
In most cases, the subconjunctival hemorrhage is caused by mild trauma including sneezing and coughing. In this case, the FP reassured the patient that his subconjunctival hemorrhages would resolve spontaneously. She also suggested that the patient take antihistamines prophylactically before being exposed to a cat.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP diagnosed bilateral subconjunctival hemorrhages. The bright red color that goes up to the cornea but leaves a small white ring of uninvolved tissue at the limbus is a classic finding for subconjunctival hemorrhage. While a subconjunctival hemorrhage appears concerning, it is not dangerous to the eye.
When caring for a patient who presents in this manner, it’s important to check for uncontrolled hypertension. You’ll also need to ask about other bleeding so that you can rule out clotting problems.
In most cases, the subconjunctival hemorrhage is caused by mild trauma including sneezing and coughing. In this case, the FP reassured the patient that his subconjunctival hemorrhages would resolve spontaneously. She also suggested that the patient take antihistamines prophylactically before being exposed to a cat.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
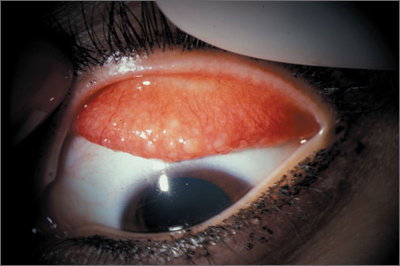
Eye irritation
The FP recognized the follicular pattern as giant papillary conjunctivitis, secondary to contact lens use. This is an allergic phenomenon involving mast cells.
While there are many topical ophthalmic medications that can be used to treat this condition, the FP preferred to have an ophthalmologist evaluate the patient. In the meantime, he advised the patient to stop wearing his contact lenses.
Meticulous attention to contact lens cleaning and hygiene is important to prevent the development of giant papillary conjunctivitis.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP recognized the follicular pattern as giant papillary conjunctivitis, secondary to contact lens use. This is an allergic phenomenon involving mast cells.
While there are many topical ophthalmic medications that can be used to treat this condition, the FP preferred to have an ophthalmologist evaluate the patient. In the meantime, he advised the patient to stop wearing his contact lenses.
Meticulous attention to contact lens cleaning and hygiene is important to prevent the development of giant papillary conjunctivitis.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The FP recognized the follicular pattern as giant papillary conjunctivitis, secondary to contact lens use. This is an allergic phenomenon involving mast cells.
While there are many topical ophthalmic medications that can be used to treat this condition, the FP preferred to have an ophthalmologist evaluate the patient. In the meantime, he advised the patient to stop wearing his contact lenses.
Meticulous attention to contact lens cleaning and hygiene is important to prevent the development of giant papillary conjunctivitis.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H, Usatine R. Differential diagnosis of the red eye. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:163-168.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
Eye pain and redness
The physician diagnosed hyphema—blood in the anterior chamber—which can be seen following eye trauma or as the result of clotting disturbances, vascular abnormalities, or mass effects from neoplasms. Traumatic hyphema occurs more often in boys and men and is often related to work or sports. In fact, 60% of hyphemas result from sports injuries.
Direct force to the eye (blunt trauma) forces the globe inward, distorting the normal architecture. Intraocular pressure rises instantaneously, causing the lens, iris, and ciliary body to move posteriorly. This disrupts the vascularization and results in bleeding.
Intraocular pressure continues to rise and bleeding stops when this pressure is high enough to compress the bleeding vessels. A fibrin-platelet clot forms and stabilizes in 4 to 7 days; this is eventually broken down by the fibrinolytic system and cleared through the trabecular meshwork.
An urgent referral is needed if there are concerns about globe rupture, elevated intraocular pressure, or other associated injuries.
A recent Cochrane review evaluated interventions that included antifibrinolytic agents, corticosteroids, cycloplegics, miotics, aspirin, conjugated estrogens, eye patching, head elevation, and bed rest. None of these significantly improves a patient’s visual acuity.
The patient in this case was referred urgently to ophthalmology and his eye was found to be otherwise healthy. He was given an eye shield for protection, advised to take acetaminophen for pain, and counseled not to engage in sporting activities until the hyphema resolved. In his case, it took 5 days.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H. Eye trauma--hyphema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:159-162.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The physician diagnosed hyphema—blood in the anterior chamber—which can be seen following eye trauma or as the result of clotting disturbances, vascular abnormalities, or mass effects from neoplasms. Traumatic hyphema occurs more often in boys and men and is often related to work or sports. In fact, 60% of hyphemas result from sports injuries.
Direct force to the eye (blunt trauma) forces the globe inward, distorting the normal architecture. Intraocular pressure rises instantaneously, causing the lens, iris, and ciliary body to move posteriorly. This disrupts the vascularization and results in bleeding.
Intraocular pressure continues to rise and bleeding stops when this pressure is high enough to compress the bleeding vessels. A fibrin-platelet clot forms and stabilizes in 4 to 7 days; this is eventually broken down by the fibrinolytic system and cleared through the trabecular meshwork.
An urgent referral is needed if there are concerns about globe rupture, elevated intraocular pressure, or other associated injuries.
A recent Cochrane review evaluated interventions that included antifibrinolytic agents, corticosteroids, cycloplegics, miotics, aspirin, conjugated estrogens, eye patching, head elevation, and bed rest. None of these significantly improves a patient’s visual acuity.
The patient in this case was referred urgently to ophthalmology and his eye was found to be otherwise healthy. He was given an eye shield for protection, advised to take acetaminophen for pain, and counseled not to engage in sporting activities until the hyphema resolved. In his case, it took 5 days.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H. Eye trauma--hyphema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:159-162.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
The physician diagnosed hyphema—blood in the anterior chamber—which can be seen following eye trauma or as the result of clotting disturbances, vascular abnormalities, or mass effects from neoplasms. Traumatic hyphema occurs more often in boys and men and is often related to work or sports. In fact, 60% of hyphemas result from sports injuries.
Direct force to the eye (blunt trauma) forces the globe inward, distorting the normal architecture. Intraocular pressure rises instantaneously, causing the lens, iris, and ciliary body to move posteriorly. This disrupts the vascularization and results in bleeding.
Intraocular pressure continues to rise and bleeding stops when this pressure is high enough to compress the bleeding vessels. A fibrin-platelet clot forms and stabilizes in 4 to 7 days; this is eventually broken down by the fibrinolytic system and cleared through the trabecular meshwork.
An urgent referral is needed if there are concerns about globe rupture, elevated intraocular pressure, or other associated injuries.
A recent Cochrane review evaluated interventions that included antifibrinolytic agents, corticosteroids, cycloplegics, miotics, aspirin, conjugated estrogens, eye patching, head elevation, and bed rest. None of these significantly improves a patient’s visual acuity.
The patient in this case was referred urgently to ophthalmology and his eye was found to be otherwise healthy. He was given an eye shield for protection, advised to take acetaminophen for pain, and counseled not to engage in sporting activities until the hyphema resolved. In his case, it took 5 days.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul Comeau. This case was adapted from: Chumley H. Eye trauma--hyphema. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:159-162.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can now get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: http://usatinemedia.com/
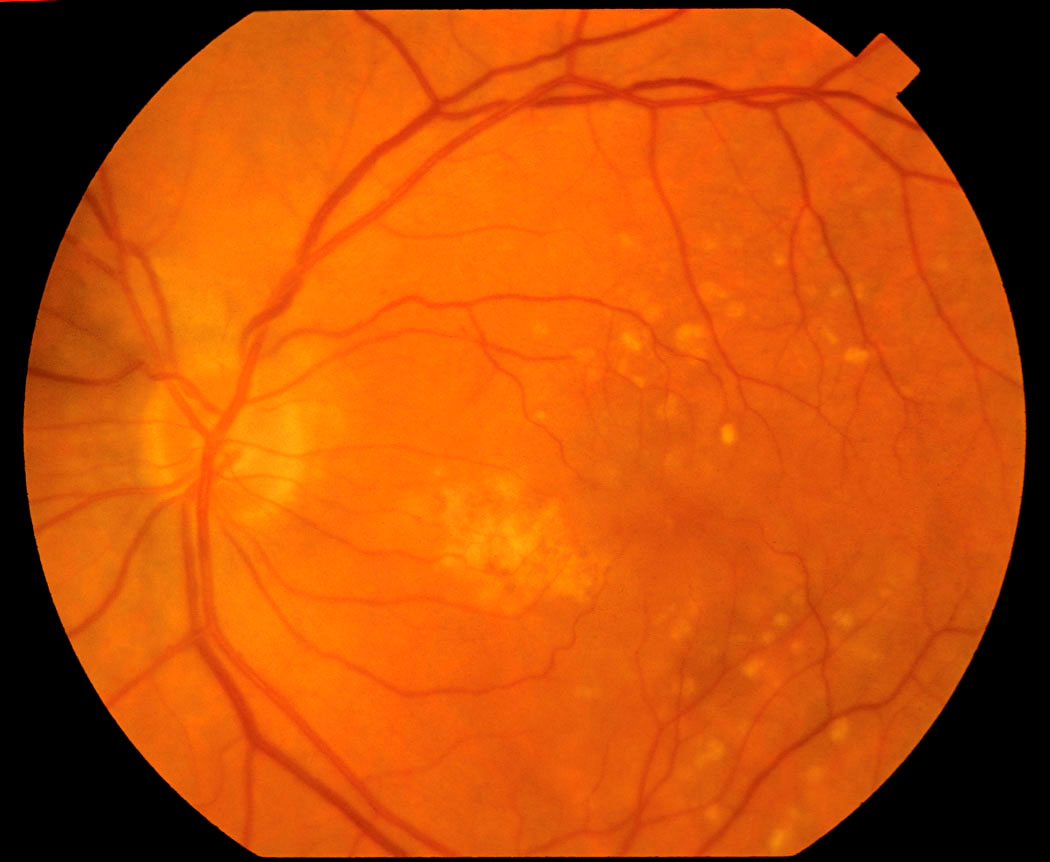
Loss of central vision
The physician referred the patient to an ophthalmologist, who noted macular depigmentation and drusen (yellowish-colored subretinal deposits on the macula) during the fundoscopic exam. The ophthalmologist diagnosed dry, age-related macular degeneration (AMD).
AMD causes central vision loss in elderly patients. The pathophysiology of AMD is not completely understood, but it involves chronic changes in the retina and retinal pigment epithelium mediated by environmental and genetic factors. AMD is diagnosed by ophthalmoscopic detection of drusen. A healthy lifestyle decreases the risk of development and progression of AMD.
AMD is the leading cause of irreversible vision loss in the industrialized world. Prevalence of advanced AMD is 1.4% in patients older than 40 years of age and 15% in white women older than 80 years of age. AMD that causes significant vision loss is more common in whites than blacks or Hispanics. Smoking increases the risk in women.
If you are caring for a patient with AMD, it’s wise to refer him or her to an ophthalmologist to evaluate for treatments such as intravitreal injections, laser photocoagulation, photodynamic therapy, or surgery.
Intraocular injections of pegaptanib and ranibizumab (anti-VEGFs) reduce the risk of visual acuity loss in patients with advanced neovascular AMD. Bevacizumab performs similarly to ranibizumab. Consider antioxidants (vitamin C, 500 mg; vitamin E, 400 IU; and beta-carotene, 15 mg) plus 80 mg zinc per day to decrease the risk of worsening vision loss in patients with intermediate to advanced AMD.
It is best, however, to avoid beta-carotene for smokers or people who have smoked in the last 10 years because in this population, the beta-carotene might increase the risk of lung and prostate cancer.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul D. Comeau. This case was adapted from: Chumley H. Age-related macular degeneration. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:155-157.
To learn more about the Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: • http://usatinemedia.com/
The physician referred the patient to an ophthalmologist, who noted macular depigmentation and drusen (yellowish-colored subretinal deposits on the macula) during the fundoscopic exam. The ophthalmologist diagnosed dry, age-related macular degeneration (AMD).
AMD causes central vision loss in elderly patients. The pathophysiology of AMD is not completely understood, but it involves chronic changes in the retina and retinal pigment epithelium mediated by environmental and genetic factors. AMD is diagnosed by ophthalmoscopic detection of drusen. A healthy lifestyle decreases the risk of development and progression of AMD.
AMD is the leading cause of irreversible vision loss in the industrialized world. Prevalence of advanced AMD is 1.4% in patients older than 40 years of age and 15% in white women older than 80 years of age. AMD that causes significant vision loss is more common in whites than blacks or Hispanics. Smoking increases the risk in women.
If you are caring for a patient with AMD, it’s wise to refer him or her to an ophthalmologist to evaluate for treatments such as intravitreal injections, laser photocoagulation, photodynamic therapy, or surgery.
Intraocular injections of pegaptanib and ranibizumab (anti-VEGFs) reduce the risk of visual acuity loss in patients with advanced neovascular AMD. Bevacizumab performs similarly to ranibizumab. Consider antioxidants (vitamin C, 500 mg; vitamin E, 400 IU; and beta-carotene, 15 mg) plus 80 mg zinc per day to decrease the risk of worsening vision loss in patients with intermediate to advanced AMD.
It is best, however, to avoid beta-carotene for smokers or people who have smoked in the last 10 years because in this population, the beta-carotene might increase the risk of lung and prostate cancer.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul D. Comeau. This case was adapted from: Chumley H. Age-related macular degeneration. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:155-157.
To learn more about the Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: • http://usatinemedia.com/
The physician referred the patient to an ophthalmologist, who noted macular depigmentation and drusen (yellowish-colored subretinal deposits on the macula) during the fundoscopic exam. The ophthalmologist diagnosed dry, age-related macular degeneration (AMD).
AMD causes central vision loss in elderly patients. The pathophysiology of AMD is not completely understood, but it involves chronic changes in the retina and retinal pigment epithelium mediated by environmental and genetic factors. AMD is diagnosed by ophthalmoscopic detection of drusen. A healthy lifestyle decreases the risk of development and progression of AMD.
AMD is the leading cause of irreversible vision loss in the industrialized world. Prevalence of advanced AMD is 1.4% in patients older than 40 years of age and 15% in white women older than 80 years of age. AMD that causes significant vision loss is more common in whites than blacks or Hispanics. Smoking increases the risk in women.
If you are caring for a patient with AMD, it’s wise to refer him or her to an ophthalmologist to evaluate for treatments such as intravitreal injections, laser photocoagulation, photodynamic therapy, or surgery.
Intraocular injections of pegaptanib and ranibizumab (anti-VEGFs) reduce the risk of visual acuity loss in patients with advanced neovascular AMD. Bevacizumab performs similarly to ranibizumab. Consider antioxidants (vitamin C, 500 mg; vitamin E, 400 IU; and beta-carotene, 15 mg) plus 80 mg zinc per day to decrease the risk of worsening vision loss in patients with intermediate to advanced AMD.
It is best, however, to avoid beta-carotene for smokers or people who have smoked in the last 10 years because in this population, the beta-carotene might increase the risk of lung and prostate cancer.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of Paul D. Comeau. This case was adapted from: Chumley H. Age-related macular degeneration. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:155-157.
To learn more about the Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/ref=dp_ob_title_bk
You can get the second edition of the Color Atlas of Family Medicine as an app for mobile devices by clicking this link: • http://usatinemedia.com/