User login
The hunt for N-acetylcysteine: Medicine or dietary supplement?
Medicine or dietary supplement? N-acetylcysteine (NAC) is marketed as both and in 2021, the supplement abruptly became difficult to find, causing distress to people who had been using it for a variety of conditions. The story behind its disappearance is one of a cat-and-mouse chase between manufacturers, advocacy agencies, and the Food and Drug Administration.
NAC is a medication that was approved by the FDA in 1963. It has two FDA-approved uses: To prevent hepatotoxicity after overdose with acetaminophen, administered intravenously or by mouth, and as a mucolytic agent – previously available as Mucomyst, now available only as a generic – given by inhaler or nebulizer for pulmonary illnesses. Since the 1990s, NAC has been labeled by manufacturers as a dietary supplement. It is a derivative of the amino acid L-cysteine and a precursor to glutathione, an antioxidant.
Studies have had small sample sizes, and the supplement has not been considered an “off label” use of an already available medication. People have purchased NAC from retail drug and big box stores, Amazon, and online companies. So what’s the problem?
In July 2020, the FDA issued a warning letter to Purple Biosciences LLC, because of claims on the company’s website that the product “Purple Tree,” sold by Amazon, could cure hangovers that result from alcohol intoxication. The letter discussed justification for why a hangover is a disease, and goes on to note:
Based on the product label on your website, it appears that you intend to market your Purple Tree® product, which contains N-acetyl-L-cysteine (NAC), as a dietary supplement. However, even if your product labeling did not have therapeutic claims that make your product an unapproved new drug, your product could not be a dietary supplement, because it does not meet the definition of dietary supplement ... products containing that article are outside the definition of a dietary supplement, unless before such approval that article was marketed as a dietary supplement or as a food. NAC was approved as a new drug under section 505 of the Act [21 U.S.C. § 355] on September 14, 1963.
The issue here is that because NAC was first approved as a drug in 1963, it cannot be marketed as a supplement. If it had been marketed as a supplement before it was approved as a drug by the FDA, then it could remain on the market. The fact that it had been sold as a supplement since the 1990s and could be classified as an “old dietary ingredient” according to the Dietary Supplement Health and Education Act of 1994 did not seem to matter. Following the warning letter, NAC was pulled from shelves and websites.
Citizen petitions allow people and organizations to request that the FDA change their policy. During summer 2021, there were two citizen petitions – one from the Council for Responsible Nutrition (CRN) and another from the Natural Products Association (NPA) – asking that the FDA look at policy around NAC. In response, in November 2021, the FDA put out a request for more information about how long NAC had been used and if there were safety concerns, to determine if making it a lawful supplement would be appropriate. CRN promptly released a response that they were “extremely dissatisfied” and felt this was an unnecessary tactic to delay a decision. Two members of Congress wrote letters to the FDA in support of leaving NAC as an available supplement. Congressman Jeff Duncan noted that there were over 1,170 products containing NAC.
The FDA continued to issue responses. On March 31, 2022, the agency formally denied the requests of the two citizen petitions, and 3 weeks later the Guidance for Industry: Policy Regarding N-acetyl-L-cysteine was released, saying that the FDA would “... exercise enforcement discretion with respect to the sale and distribution of certain products that contain NAC.” While NAC was still not considered a supplement, no safety issues had been identified to date. Thus, while the FDA investigation continues, the agency will essentially look the other way.
The agency will consider rulemaking to include NAC as a supplement, a process that may take years. In a notice of final guidance released in August 2022, the FDA reiterated, “unless we identify safety-related concerns during our ongoing review, FDA intends to exercise enforcement discretion until either of the following occurs: we complete notice-and-comment rulemaking to allow the use of NAC in or as a dietary supplement (should we move forward with such proceedings) or we deny the NPA citizen petition’s request for rulemaking.”
It’s a win for the consumer who wants the supplement, and a half-win for the supplement manufacturers and their advocacy organizations who would like NAC to be an official dietary supplement. But just to be clear, the issue is one of a technicality: If NAC had been marketed as a supplement before it was a drug, it would just be a dietary supplement without all the controversy and scrutiny. It was not pulled because of a clinical concern.
For now, NAC is again readily available.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
Medicine or dietary supplement? N-acetylcysteine (NAC) is marketed as both and in 2021, the supplement abruptly became difficult to find, causing distress to people who had been using it for a variety of conditions. The story behind its disappearance is one of a cat-and-mouse chase between manufacturers, advocacy agencies, and the Food and Drug Administration.
NAC is a medication that was approved by the FDA in 1963. It has two FDA-approved uses: To prevent hepatotoxicity after overdose with acetaminophen, administered intravenously or by mouth, and as a mucolytic agent – previously available as Mucomyst, now available only as a generic – given by inhaler or nebulizer for pulmonary illnesses. Since the 1990s, NAC has been labeled by manufacturers as a dietary supplement. It is a derivative of the amino acid L-cysteine and a precursor to glutathione, an antioxidant.
Studies have had small sample sizes, and the supplement has not been considered an “off label” use of an already available medication. People have purchased NAC from retail drug and big box stores, Amazon, and online companies. So what’s the problem?
In July 2020, the FDA issued a warning letter to Purple Biosciences LLC, because of claims on the company’s website that the product “Purple Tree,” sold by Amazon, could cure hangovers that result from alcohol intoxication. The letter discussed justification for why a hangover is a disease, and goes on to note:
Based on the product label on your website, it appears that you intend to market your Purple Tree® product, which contains N-acetyl-L-cysteine (NAC), as a dietary supplement. However, even if your product labeling did not have therapeutic claims that make your product an unapproved new drug, your product could not be a dietary supplement, because it does not meet the definition of dietary supplement ... products containing that article are outside the definition of a dietary supplement, unless before such approval that article was marketed as a dietary supplement or as a food. NAC was approved as a new drug under section 505 of the Act [21 U.S.C. § 355] on September 14, 1963.
The issue here is that because NAC was first approved as a drug in 1963, it cannot be marketed as a supplement. If it had been marketed as a supplement before it was approved as a drug by the FDA, then it could remain on the market. The fact that it had been sold as a supplement since the 1990s and could be classified as an “old dietary ingredient” according to the Dietary Supplement Health and Education Act of 1994 did not seem to matter. Following the warning letter, NAC was pulled from shelves and websites.
Citizen petitions allow people and organizations to request that the FDA change their policy. During summer 2021, there were two citizen petitions – one from the Council for Responsible Nutrition (CRN) and another from the Natural Products Association (NPA) – asking that the FDA look at policy around NAC. In response, in November 2021, the FDA put out a request for more information about how long NAC had been used and if there were safety concerns, to determine if making it a lawful supplement would be appropriate. CRN promptly released a response that they were “extremely dissatisfied” and felt this was an unnecessary tactic to delay a decision. Two members of Congress wrote letters to the FDA in support of leaving NAC as an available supplement. Congressman Jeff Duncan noted that there were over 1,170 products containing NAC.
The FDA continued to issue responses. On March 31, 2022, the agency formally denied the requests of the two citizen petitions, and 3 weeks later the Guidance for Industry: Policy Regarding N-acetyl-L-cysteine was released, saying that the FDA would “... exercise enforcement discretion with respect to the sale and distribution of certain products that contain NAC.” While NAC was still not considered a supplement, no safety issues had been identified to date. Thus, while the FDA investigation continues, the agency will essentially look the other way.
The agency will consider rulemaking to include NAC as a supplement, a process that may take years. In a notice of final guidance released in August 2022, the FDA reiterated, “unless we identify safety-related concerns during our ongoing review, FDA intends to exercise enforcement discretion until either of the following occurs: we complete notice-and-comment rulemaking to allow the use of NAC in or as a dietary supplement (should we move forward with such proceedings) or we deny the NPA citizen petition’s request for rulemaking.”
It’s a win for the consumer who wants the supplement, and a half-win for the supplement manufacturers and their advocacy organizations who would like NAC to be an official dietary supplement. But just to be clear, the issue is one of a technicality: If NAC had been marketed as a supplement before it was a drug, it would just be a dietary supplement without all the controversy and scrutiny. It was not pulled because of a clinical concern.
For now, NAC is again readily available.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
Medicine or dietary supplement? N-acetylcysteine (NAC) is marketed as both and in 2021, the supplement abruptly became difficult to find, causing distress to people who had been using it for a variety of conditions. The story behind its disappearance is one of a cat-and-mouse chase between manufacturers, advocacy agencies, and the Food and Drug Administration.
NAC is a medication that was approved by the FDA in 1963. It has two FDA-approved uses: To prevent hepatotoxicity after overdose with acetaminophen, administered intravenously or by mouth, and as a mucolytic agent – previously available as Mucomyst, now available only as a generic – given by inhaler or nebulizer for pulmonary illnesses. Since the 1990s, NAC has been labeled by manufacturers as a dietary supplement. It is a derivative of the amino acid L-cysteine and a precursor to glutathione, an antioxidant.
Studies have had small sample sizes, and the supplement has not been considered an “off label” use of an already available medication. People have purchased NAC from retail drug and big box stores, Amazon, and online companies. So what’s the problem?
In July 2020, the FDA issued a warning letter to Purple Biosciences LLC, because of claims on the company’s website that the product “Purple Tree,” sold by Amazon, could cure hangovers that result from alcohol intoxication. The letter discussed justification for why a hangover is a disease, and goes on to note:
Based on the product label on your website, it appears that you intend to market your Purple Tree® product, which contains N-acetyl-L-cysteine (NAC), as a dietary supplement. However, even if your product labeling did not have therapeutic claims that make your product an unapproved new drug, your product could not be a dietary supplement, because it does not meet the definition of dietary supplement ... products containing that article are outside the definition of a dietary supplement, unless before such approval that article was marketed as a dietary supplement or as a food. NAC was approved as a new drug under section 505 of the Act [21 U.S.C. § 355] on September 14, 1963.
The issue here is that because NAC was first approved as a drug in 1963, it cannot be marketed as a supplement. If it had been marketed as a supplement before it was approved as a drug by the FDA, then it could remain on the market. The fact that it had been sold as a supplement since the 1990s and could be classified as an “old dietary ingredient” according to the Dietary Supplement Health and Education Act of 1994 did not seem to matter. Following the warning letter, NAC was pulled from shelves and websites.
Citizen petitions allow people and organizations to request that the FDA change their policy. During summer 2021, there were two citizen petitions – one from the Council for Responsible Nutrition (CRN) and another from the Natural Products Association (NPA) – asking that the FDA look at policy around NAC. In response, in November 2021, the FDA put out a request for more information about how long NAC had been used and if there were safety concerns, to determine if making it a lawful supplement would be appropriate. CRN promptly released a response that they were “extremely dissatisfied” and felt this was an unnecessary tactic to delay a decision. Two members of Congress wrote letters to the FDA in support of leaving NAC as an available supplement. Congressman Jeff Duncan noted that there were over 1,170 products containing NAC.
The FDA continued to issue responses. On March 31, 2022, the agency formally denied the requests of the two citizen petitions, and 3 weeks later the Guidance for Industry: Policy Regarding N-acetyl-L-cysteine was released, saying that the FDA would “... exercise enforcement discretion with respect to the sale and distribution of certain products that contain NAC.” While NAC was still not considered a supplement, no safety issues had been identified to date. Thus, while the FDA investigation continues, the agency will essentially look the other way.
The agency will consider rulemaking to include NAC as a supplement, a process that may take years. In a notice of final guidance released in August 2022, the FDA reiterated, “unless we identify safety-related concerns during our ongoing review, FDA intends to exercise enforcement discretion until either of the following occurs: we complete notice-and-comment rulemaking to allow the use of NAC in or as a dietary supplement (should we move forward with such proceedings) or we deny the NPA citizen petition’s request for rulemaking.”
It’s a win for the consumer who wants the supplement, and a half-win for the supplement manufacturers and their advocacy organizations who would like NAC to be an official dietary supplement. But just to be clear, the issue is one of a technicality: If NAC had been marketed as a supplement before it was a drug, it would just be a dietary supplement without all the controversy and scrutiny. It was not pulled because of a clinical concern.
For now, NAC is again readily available.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
Had my patient come in today, we may have had other options
Decades ago I saw a patient with non–small cell lung cancer (NSCLC) whose tumor was sent out for next-generation sequencing only to find a HER2 mutation. What to do? Had my patient come in today, we may have had other options.
Multiple studies have shown that trastuzumab (Herceptin, Genentech), as assessed by HER2 overexpression or amplification, has been shown to have essentially no efficacy benefit in NSCLC alone or in combination with chemotherapy. In fact, a randomized, phase 2 study of gemcitabine-cisplatin with or without trastuzumab in HER2 mutation–positive NSCLC essentially showed no difference between gemcitabine-cisplatin or gemcitabine-cisplatin with trastuzumab.
NSCLC has become the poster child for targeted therapies. After all, NSCLC makes up about 85% of all lung cancer cases, some of which are driven by gene mutations or other genetic abnormalities like translocation, fusion, or amplification. Seven of these genetic alterations have Food and Drug Administration–approved targeted drugs: EGFR, ALK, ROS1, BRAF V6006, RET, KRAS, MET, and NTRK fusions. And, now we have a new one: HER2.
In August, the FDA granted accelerated approval of trastuzumab deruxtecan (T-DXd) (Enhertu, Daiichi Sankyo) for the second-line treatment of NSCLC patients with HER alterations. T-DXd is a humanized anti-HER antibody linked to a topoisomerase 1 inhibitor. When given intravenously, the antibody portion of the molecule binds to cells with a mutated HER2 on the surface. The molecule is taken up by the cancer cell and the linker between the antibody and the chemotherapy drug is broken, so the drug will be delivered very specifically only to cancer cells that have a mutated HER2. In theory, they will only target cells with HER alterations and thus should have less toxicity.
Unlike other driver mutations, HER mutations are relatively rare. Roughly 3% of nonsquamous NSCLC tumors carry mutations in the HER2 gene, and they are associated with female sex, never-smokers, and a poor prognosis. Accelerated approved by the FDA was based on data from the DESTINY-Lung 02 phase 2 trial. An interim efficacy analysis of this trial reported an overall response rate to trastuzumab deruxtecan (at 5.4 mg/kg every 3 weeks) of 57.7% in 52 patients. Median duration of response was 8.7 months. Data are also available from the DESTINY-Lung-01 clinical trial, published in the New England Journal of Medicine, in which 91 patients with metastatic HER2-mutant NSCLC that was refractory to standard treatment were treated with T-DXd (at 6.4 mg/kg every 3 weeks). The investigators reported a 55% objective response rate, a median duration of response of 9.3 months, a median progression-free survival (PFS) of 8.2 months, and a median overall survival of almost 18 months.
Companion tests
Biomarker testing is obviously a must in these cases. The FDA-approved companion diagnostic tests to detect HER2 mutations: Life Companion tests, Technologies Corporation’s Oncomine Dx Target Test for use in lung tissue, and Guardant Health’s Guardant360 CDx for use on plasma samples. The agency notes that, if no mutation is detected in a plasma specimen, the tumor tissue should be tested.
Other approvals
T-DXd is also approved for advanced breast and gastric patients who are HER-2 positive. Of note, the majority of HER2-positive NSCLC have HER2 mutations, whereas the majority of HER2-positive breast and gastric cancers have HER2 amplification (increased copy number) or overexpression (increased protein expression).
T-DXd is approved for unresectable or metastatic HER2-positive breast cancer patients who have received a prior anti-HER2–based regimen in the metastatic setting, or in the neoadjuvant or adjuvant setting and have developed disease recurrence during or within 6 months of completing therapy. DESTINY-Breast01 enrolled breast cancer patients who had received two or more prior anti-HER2 therapies in the metastatic setting, and reported a response rate of 60.3% with a median duration of response of 14.8 months.
For patients with locally advanced or metastatic HER2-positive gastric cancer who have received two or more prior therapies, including a trastuzumab-based regimen, approval was based on a randomized, phase 3 study comparing 6.4 mg/kg of T-DXd with physician’s choice – either irinotecan or paclitaxel. Overall survival was 12.5 months in the T-DXd arm, compared with 8.4 months in the irinotecan or paclitaxel arm (hazard ratio, 0.59). Response rates were 40.5% and 11.3%, respectively. Median PFS was 5.6 months in the T-DXd arm, compared with a median PFS of 3.5 months in the chemotherapy arm.
Trastuzumab emtansine vs. trastuzumab deruxtecan
Trastuzumab emtansine (T-DM1, ado-trastuzumab emtansine, Kadcyla) is another antibody-drug conjugate consisting of the humanized monoclonal antibody trastuzumab covalently linked to the antimicrotubule agent DM1. It is also approved for advanced breast cancer patients with HER2-positive disease. Although no studies comparing T-DXd with trastuzumab emtansine have been conducted in lung cancer patients, a randomized, phase 3 trial in patients with HER2-positive advanced breast cancer comparing the two reported an overall response rate of 79.7% of the patients who received trastuzumab deruxtecan and 34.2% of those who received trastuzumab emtansine. Drug-related interstitial lung disease (ILD) occurred in 10.5% of the patients in the trastuzumab deruxtecan group and in 1.9% of those in the trastuzumab emtansine group; at 12 months, 75.8% of the patients in the trastuzumab deruxtecan were alive without progression, compared with 34.1% of those receiving trastuzumab emtansine.
ILDs
In DESTINY-Lung01, ILD occurred in 26% of patients and resulted in death in two patients. Increased rates of ILD were more commonly observed at higher dose levels. Of 491 patients with unresectable or metastatic HER2-positive breast cancer treated with 5.4 mg/kg of T-TDx, ILD occurred in 13% of patients. Fatal outcomes caused by ILD and/or pneumonitis occurred in 1.4% of patients. Median time to first onset was 5.5 months (range, 1.1-20.8 months). In DESTINY-Gastric01, of the 125 patients with locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma treated with 6.4 mg/kg, T-DXd ILD occurred in 10% of patients. Median time to first onset was 2.8 months (range, 1.2-21.0 months).
Chemotherapy-like adverse effects
Other adverse events are more typically seen with cytotoxic agents and are presumably related to the release of the topoisomerase inhibitor into the blood stream. Although common (occurring in 97% of patients), these adverse events are generally mild (grade 1 or 2). Nausea was reported in about two-thirds of patients. Other side effects occurring in 20% or more of patients included vomiting, decreased appetite, alopecia, and constipation and diarrhea, musculoskeletal pain, and respiratory infections. Laboratory abnormalities occurred in 20% or more of patients included myelosuppression, increased AST, ALT, alkaline phosphatase, and hypokalemia (28%). Grade 3 or higher drug-related adverse events were observed in 46% of patients, with the most common being neutropenia and anemia which was observed in 19% and 10% of patients in the DESTINY-LUNG-01 trial.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Decades ago I saw a patient with non–small cell lung cancer (NSCLC) whose tumor was sent out for next-generation sequencing only to find a HER2 mutation. What to do? Had my patient come in today, we may have had other options.
Multiple studies have shown that trastuzumab (Herceptin, Genentech), as assessed by HER2 overexpression or amplification, has been shown to have essentially no efficacy benefit in NSCLC alone or in combination with chemotherapy. In fact, a randomized, phase 2 study of gemcitabine-cisplatin with or without trastuzumab in HER2 mutation–positive NSCLC essentially showed no difference between gemcitabine-cisplatin or gemcitabine-cisplatin with trastuzumab.
NSCLC has become the poster child for targeted therapies. After all, NSCLC makes up about 85% of all lung cancer cases, some of which are driven by gene mutations or other genetic abnormalities like translocation, fusion, or amplification. Seven of these genetic alterations have Food and Drug Administration–approved targeted drugs: EGFR, ALK, ROS1, BRAF V6006, RET, KRAS, MET, and NTRK fusions. And, now we have a new one: HER2.
In August, the FDA granted accelerated approval of trastuzumab deruxtecan (T-DXd) (Enhertu, Daiichi Sankyo) for the second-line treatment of NSCLC patients with HER alterations. T-DXd is a humanized anti-HER antibody linked to a topoisomerase 1 inhibitor. When given intravenously, the antibody portion of the molecule binds to cells with a mutated HER2 on the surface. The molecule is taken up by the cancer cell and the linker between the antibody and the chemotherapy drug is broken, so the drug will be delivered very specifically only to cancer cells that have a mutated HER2. In theory, they will only target cells with HER alterations and thus should have less toxicity.
Unlike other driver mutations, HER mutations are relatively rare. Roughly 3% of nonsquamous NSCLC tumors carry mutations in the HER2 gene, and they are associated with female sex, never-smokers, and a poor prognosis. Accelerated approved by the FDA was based on data from the DESTINY-Lung 02 phase 2 trial. An interim efficacy analysis of this trial reported an overall response rate to trastuzumab deruxtecan (at 5.4 mg/kg every 3 weeks) of 57.7% in 52 patients. Median duration of response was 8.7 months. Data are also available from the DESTINY-Lung-01 clinical trial, published in the New England Journal of Medicine, in which 91 patients with metastatic HER2-mutant NSCLC that was refractory to standard treatment were treated with T-DXd (at 6.4 mg/kg every 3 weeks). The investigators reported a 55% objective response rate, a median duration of response of 9.3 months, a median progression-free survival (PFS) of 8.2 months, and a median overall survival of almost 18 months.
Companion tests
Biomarker testing is obviously a must in these cases. The FDA-approved companion diagnostic tests to detect HER2 mutations: Life Companion tests, Technologies Corporation’s Oncomine Dx Target Test for use in lung tissue, and Guardant Health’s Guardant360 CDx for use on plasma samples. The agency notes that, if no mutation is detected in a plasma specimen, the tumor tissue should be tested.
Other approvals
T-DXd is also approved for advanced breast and gastric patients who are HER-2 positive. Of note, the majority of HER2-positive NSCLC have HER2 mutations, whereas the majority of HER2-positive breast and gastric cancers have HER2 amplification (increased copy number) or overexpression (increased protein expression).
T-DXd is approved for unresectable or metastatic HER2-positive breast cancer patients who have received a prior anti-HER2–based regimen in the metastatic setting, or in the neoadjuvant or adjuvant setting and have developed disease recurrence during or within 6 months of completing therapy. DESTINY-Breast01 enrolled breast cancer patients who had received two or more prior anti-HER2 therapies in the metastatic setting, and reported a response rate of 60.3% with a median duration of response of 14.8 months.
For patients with locally advanced or metastatic HER2-positive gastric cancer who have received two or more prior therapies, including a trastuzumab-based regimen, approval was based on a randomized, phase 3 study comparing 6.4 mg/kg of T-DXd with physician’s choice – either irinotecan or paclitaxel. Overall survival was 12.5 months in the T-DXd arm, compared with 8.4 months in the irinotecan or paclitaxel arm (hazard ratio, 0.59). Response rates were 40.5% and 11.3%, respectively. Median PFS was 5.6 months in the T-DXd arm, compared with a median PFS of 3.5 months in the chemotherapy arm.
Trastuzumab emtansine vs. trastuzumab deruxtecan
Trastuzumab emtansine (T-DM1, ado-trastuzumab emtansine, Kadcyla) is another antibody-drug conjugate consisting of the humanized monoclonal antibody trastuzumab covalently linked to the antimicrotubule agent DM1. It is also approved for advanced breast cancer patients with HER2-positive disease. Although no studies comparing T-DXd with trastuzumab emtansine have been conducted in lung cancer patients, a randomized, phase 3 trial in patients with HER2-positive advanced breast cancer comparing the two reported an overall response rate of 79.7% of the patients who received trastuzumab deruxtecan and 34.2% of those who received trastuzumab emtansine. Drug-related interstitial lung disease (ILD) occurred in 10.5% of the patients in the trastuzumab deruxtecan group and in 1.9% of those in the trastuzumab emtansine group; at 12 months, 75.8% of the patients in the trastuzumab deruxtecan were alive without progression, compared with 34.1% of those receiving trastuzumab emtansine.
ILDs
In DESTINY-Lung01, ILD occurred in 26% of patients and resulted in death in two patients. Increased rates of ILD were more commonly observed at higher dose levels. Of 491 patients with unresectable or metastatic HER2-positive breast cancer treated with 5.4 mg/kg of T-TDx, ILD occurred in 13% of patients. Fatal outcomes caused by ILD and/or pneumonitis occurred in 1.4% of patients. Median time to first onset was 5.5 months (range, 1.1-20.8 months). In DESTINY-Gastric01, of the 125 patients with locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma treated with 6.4 mg/kg, T-DXd ILD occurred in 10% of patients. Median time to first onset was 2.8 months (range, 1.2-21.0 months).
Chemotherapy-like adverse effects
Other adverse events are more typically seen with cytotoxic agents and are presumably related to the release of the topoisomerase inhibitor into the blood stream. Although common (occurring in 97% of patients), these adverse events are generally mild (grade 1 or 2). Nausea was reported in about two-thirds of patients. Other side effects occurring in 20% or more of patients included vomiting, decreased appetite, alopecia, and constipation and diarrhea, musculoskeletal pain, and respiratory infections. Laboratory abnormalities occurred in 20% or more of patients included myelosuppression, increased AST, ALT, alkaline phosphatase, and hypokalemia (28%). Grade 3 or higher drug-related adverse events were observed in 46% of patients, with the most common being neutropenia and anemia which was observed in 19% and 10% of patients in the DESTINY-LUNG-01 trial.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Decades ago I saw a patient with non–small cell lung cancer (NSCLC) whose tumor was sent out for next-generation sequencing only to find a HER2 mutation. What to do? Had my patient come in today, we may have had other options.
Multiple studies have shown that trastuzumab (Herceptin, Genentech), as assessed by HER2 overexpression or amplification, has been shown to have essentially no efficacy benefit in NSCLC alone or in combination with chemotherapy. In fact, a randomized, phase 2 study of gemcitabine-cisplatin with or without trastuzumab in HER2 mutation–positive NSCLC essentially showed no difference between gemcitabine-cisplatin or gemcitabine-cisplatin with trastuzumab.
NSCLC has become the poster child for targeted therapies. After all, NSCLC makes up about 85% of all lung cancer cases, some of which are driven by gene mutations or other genetic abnormalities like translocation, fusion, or amplification. Seven of these genetic alterations have Food and Drug Administration–approved targeted drugs: EGFR, ALK, ROS1, BRAF V6006, RET, KRAS, MET, and NTRK fusions. And, now we have a new one: HER2.
In August, the FDA granted accelerated approval of trastuzumab deruxtecan (T-DXd) (Enhertu, Daiichi Sankyo) for the second-line treatment of NSCLC patients with HER alterations. T-DXd is a humanized anti-HER antibody linked to a topoisomerase 1 inhibitor. When given intravenously, the antibody portion of the molecule binds to cells with a mutated HER2 on the surface. The molecule is taken up by the cancer cell and the linker between the antibody and the chemotherapy drug is broken, so the drug will be delivered very specifically only to cancer cells that have a mutated HER2. In theory, they will only target cells with HER alterations and thus should have less toxicity.
Unlike other driver mutations, HER mutations are relatively rare. Roughly 3% of nonsquamous NSCLC tumors carry mutations in the HER2 gene, and they are associated with female sex, never-smokers, and a poor prognosis. Accelerated approved by the FDA was based on data from the DESTINY-Lung 02 phase 2 trial. An interim efficacy analysis of this trial reported an overall response rate to trastuzumab deruxtecan (at 5.4 mg/kg every 3 weeks) of 57.7% in 52 patients. Median duration of response was 8.7 months. Data are also available from the DESTINY-Lung-01 clinical trial, published in the New England Journal of Medicine, in which 91 patients with metastatic HER2-mutant NSCLC that was refractory to standard treatment were treated with T-DXd (at 6.4 mg/kg every 3 weeks). The investigators reported a 55% objective response rate, a median duration of response of 9.3 months, a median progression-free survival (PFS) of 8.2 months, and a median overall survival of almost 18 months.
Companion tests
Biomarker testing is obviously a must in these cases. The FDA-approved companion diagnostic tests to detect HER2 mutations: Life Companion tests, Technologies Corporation’s Oncomine Dx Target Test for use in lung tissue, and Guardant Health’s Guardant360 CDx for use on plasma samples. The agency notes that, if no mutation is detected in a plasma specimen, the tumor tissue should be tested.
Other approvals
T-DXd is also approved for advanced breast and gastric patients who are HER-2 positive. Of note, the majority of HER2-positive NSCLC have HER2 mutations, whereas the majority of HER2-positive breast and gastric cancers have HER2 amplification (increased copy number) or overexpression (increased protein expression).
T-DXd is approved for unresectable or metastatic HER2-positive breast cancer patients who have received a prior anti-HER2–based regimen in the metastatic setting, or in the neoadjuvant or adjuvant setting and have developed disease recurrence during or within 6 months of completing therapy. DESTINY-Breast01 enrolled breast cancer patients who had received two or more prior anti-HER2 therapies in the metastatic setting, and reported a response rate of 60.3% with a median duration of response of 14.8 months.
For patients with locally advanced or metastatic HER2-positive gastric cancer who have received two or more prior therapies, including a trastuzumab-based regimen, approval was based on a randomized, phase 3 study comparing 6.4 mg/kg of T-DXd with physician’s choice – either irinotecan or paclitaxel. Overall survival was 12.5 months in the T-DXd arm, compared with 8.4 months in the irinotecan or paclitaxel arm (hazard ratio, 0.59). Response rates were 40.5% and 11.3%, respectively. Median PFS was 5.6 months in the T-DXd arm, compared with a median PFS of 3.5 months in the chemotherapy arm.
Trastuzumab emtansine vs. trastuzumab deruxtecan
Trastuzumab emtansine (T-DM1, ado-trastuzumab emtansine, Kadcyla) is another antibody-drug conjugate consisting of the humanized monoclonal antibody trastuzumab covalently linked to the antimicrotubule agent DM1. It is also approved for advanced breast cancer patients with HER2-positive disease. Although no studies comparing T-DXd with trastuzumab emtansine have been conducted in lung cancer patients, a randomized, phase 3 trial in patients with HER2-positive advanced breast cancer comparing the two reported an overall response rate of 79.7% of the patients who received trastuzumab deruxtecan and 34.2% of those who received trastuzumab emtansine. Drug-related interstitial lung disease (ILD) occurred in 10.5% of the patients in the trastuzumab deruxtecan group and in 1.9% of those in the trastuzumab emtansine group; at 12 months, 75.8% of the patients in the trastuzumab deruxtecan were alive without progression, compared with 34.1% of those receiving trastuzumab emtansine.
ILDs
In DESTINY-Lung01, ILD occurred in 26% of patients and resulted in death in two patients. Increased rates of ILD were more commonly observed at higher dose levels. Of 491 patients with unresectable or metastatic HER2-positive breast cancer treated with 5.4 mg/kg of T-TDx, ILD occurred in 13% of patients. Fatal outcomes caused by ILD and/or pneumonitis occurred in 1.4% of patients. Median time to first onset was 5.5 months (range, 1.1-20.8 months). In DESTINY-Gastric01, of the 125 patients with locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma treated with 6.4 mg/kg, T-DXd ILD occurred in 10% of patients. Median time to first onset was 2.8 months (range, 1.2-21.0 months).
Chemotherapy-like adverse effects
Other adverse events are more typically seen with cytotoxic agents and are presumably related to the release of the topoisomerase inhibitor into the blood stream. Although common (occurring in 97% of patients), these adverse events are generally mild (grade 1 or 2). Nausea was reported in about two-thirds of patients. Other side effects occurring in 20% or more of patients included vomiting, decreased appetite, alopecia, and constipation and diarrhea, musculoskeletal pain, and respiratory infections. Laboratory abnormalities occurred in 20% or more of patients included myelosuppression, increased AST, ALT, alkaline phosphatase, and hypokalemia (28%). Grade 3 or higher drug-related adverse events were observed in 46% of patients, with the most common being neutropenia and anemia which was observed in 19% and 10% of patients in the DESTINY-LUNG-01 trial.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Cancer as a full contact sport
John worked as a handyman and lived on a small sailboat in a marina. When he was diagnosed with metastatic kidney cancer at age 48, he quickly fell through the cracks. He failed to show to appointments and took oral anticancer treatments, but just sporadically. He had Medicaid, so insurance wasn’t the issue. It was everything else.
John was behind on his slip fees; he hadn’t been able to work for some time because of his progressive weakness and pain. He was chronically in danger of getting kicked out of his makeshift home aboard the boat. He had no reliable transportation to the clinic and so he didn’t come to appointments regularly. The specialty pharmacy refused to deliver his expensive oral chemotherapy to his address at the marina. He went days without eating full meals because he was too weak to cook for himself. Plus, he was estranged from his family who were unaware of his illness. His oncologist was overwhelmed trying to take care of him. He had a reasonable chance of achieving disease control on first-line oral therapy, but his problems seemed to hinder these chances at every turn. She was distraught – what could she do?
Enter the team approach. John’s oncologist reached out to our palliative care program for help. We recognized that this was a job too big for us alone so we connected John with the Extensivist Medicine program at UCLA Health, a high-intensity primary care program led by a physician specializing in primary care for high-risk individuals. The program provides wraparound outpatient services for chronically and seriously ill patients, like John, who are at risk for falling through the cracks. John went from receiving very little support to now having an entire team of caring professionals focused on helping him achieve his best possible outcome despite the seriousness of his disease.
He now had the support of a high-functioning team with clearly defined roles. Social work connected him with housing, food, and transportation resources. A nurse called him every day to check in and make sure he was taking medications and reminded him about his upcoming appointments. Case management helped him get needed equipment, such as grab bars and a walker. As his palliative care nurse practitioner, I counseled him on understanding his prognosis and planning ahead for medical emergencies. Our psycho-oncology clinicians helped John reconcile with his family, who were more than willing to take him in once they realized how ill he was. Once these social factors were addressed, John could more easily stay current with his oral chemotherapy, giving him the best chance possible to achieve a robust treatment response that could buy him more time.
And, John did get that time – he got 6 months of improved quality of life, during which he reconnected with his family, including his children, and rebuilt these important relationships. Eventually treatment failed him. His disease, already widely metastatic, became more active and painful. He accepted hospice care at his sister’s house and we transitioned him from our team to the hospice team. He died peacefully surrounded by family.
Interprofessional teamwork is fundamental to treat ‘total pain’
None of this would have been possible without the work of high-functioning teams. It is a commonly held belief that interprofessional teamwork is fundamental to the care of patients and families living with serious illness. But why? How did this idea come about? And what evidence is there to support teamwork?
Dame Cicely Saunders, who founded the modern hospice movement in mid-20th century England, embodied the interdisciplinary team by working first as a nurse, then a social worker, and finally as a physician. She wrote about patients’ “total pain,” the crisis of physical, spiritual, social, and emotional distress that many people have at the end of life. She understood that no single health care discipline was adequate to the task of addressing each of these domains equally well. Thus, hospice became synonymous with care provided by a quartet of specialists – physicians, nurses, social workers, and chaplains. Nowadays, there are other specialists that are added to the mix – home health aides, pharmacists, physical and occupational therapists, music and pet therapists, and so on.
But in medicine, like all areas of science, convention and tradition only go so far. What evidence is there to support the work of an interdisciplinary team in managing the distress of patients and families living with advanced illnesses? It turns out that there is good evidence to support the use of high-functioning interdisciplinary teams in the care of the seriously ill. Palliative care is associated with improved patient outcomes, including improvements in symptom control, quality of life, and end of life care, when it is delivered by an interdisciplinary team rather than by a solo practitioner.
You may think that teamwork is most useful for patients like John who have seemingly intractable social barriers. But it is also true that for even patients with many more social advantages teamwork improves quality of life. I got to see this up close recently in my own life.
Teamwork improves quality of life
My father recently passed away after a 9-month battle with advanced cancer. He had every advantage possible – financial stability, high health literacy, an incredibly devoted spouse who happens to be an RN, good insurance, and access to top-notch medical care. Yet, even he benefited from a team approach. It started small, with the oncologist and oncology NP providing excellent, patient-centered care. Then it grew to include myself as the daughter/palliative care nurse practitioner who made recommendations for treating his nausea and ensured that his advance directive was completed and uploaded to his chart. When my dad needed physical therapy, the home health agency sent a wonderful physical therapist, who brought all sorts of equipment that kept him more functional than he would have been otherwise. Other family members helped out – my sisters helped connect my dad with a priest who came to the home to provide spiritual care, which was crucial to ensuring that he was at peace. And, in his final days, my dad had the hospice team to help manage his symptoms and his family members to provide hands-on care.
The complexity of cancer care has long necessitated a team approach to planning cancer treatment – known as a tumor board – with medical oncology, radiation oncology, surgery, and pathology all weighing in. It makes sense that patients and their families would also need a team of clinicians representing different specialty areas to assist with the wide array of physical, psychosocial, practical, and spiritual concerns that arise throughout the cancer disease trajectory.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
John worked as a handyman and lived on a small sailboat in a marina. When he was diagnosed with metastatic kidney cancer at age 48, he quickly fell through the cracks. He failed to show to appointments and took oral anticancer treatments, but just sporadically. He had Medicaid, so insurance wasn’t the issue. It was everything else.
John was behind on his slip fees; he hadn’t been able to work for some time because of his progressive weakness and pain. He was chronically in danger of getting kicked out of his makeshift home aboard the boat. He had no reliable transportation to the clinic and so he didn’t come to appointments regularly. The specialty pharmacy refused to deliver his expensive oral chemotherapy to his address at the marina. He went days without eating full meals because he was too weak to cook for himself. Plus, he was estranged from his family who were unaware of his illness. His oncologist was overwhelmed trying to take care of him. He had a reasonable chance of achieving disease control on first-line oral therapy, but his problems seemed to hinder these chances at every turn. She was distraught – what could she do?
Enter the team approach. John’s oncologist reached out to our palliative care program for help. We recognized that this was a job too big for us alone so we connected John with the Extensivist Medicine program at UCLA Health, a high-intensity primary care program led by a physician specializing in primary care for high-risk individuals. The program provides wraparound outpatient services for chronically and seriously ill patients, like John, who are at risk for falling through the cracks. John went from receiving very little support to now having an entire team of caring professionals focused on helping him achieve his best possible outcome despite the seriousness of his disease.
He now had the support of a high-functioning team with clearly defined roles. Social work connected him with housing, food, and transportation resources. A nurse called him every day to check in and make sure he was taking medications and reminded him about his upcoming appointments. Case management helped him get needed equipment, such as grab bars and a walker. As his palliative care nurse practitioner, I counseled him on understanding his prognosis and planning ahead for medical emergencies. Our psycho-oncology clinicians helped John reconcile with his family, who were more than willing to take him in once they realized how ill he was. Once these social factors were addressed, John could more easily stay current with his oral chemotherapy, giving him the best chance possible to achieve a robust treatment response that could buy him more time.
And, John did get that time – he got 6 months of improved quality of life, during which he reconnected with his family, including his children, and rebuilt these important relationships. Eventually treatment failed him. His disease, already widely metastatic, became more active and painful. He accepted hospice care at his sister’s house and we transitioned him from our team to the hospice team. He died peacefully surrounded by family.
Interprofessional teamwork is fundamental to treat ‘total pain’
None of this would have been possible without the work of high-functioning teams. It is a commonly held belief that interprofessional teamwork is fundamental to the care of patients and families living with serious illness. But why? How did this idea come about? And what evidence is there to support teamwork?
Dame Cicely Saunders, who founded the modern hospice movement in mid-20th century England, embodied the interdisciplinary team by working first as a nurse, then a social worker, and finally as a physician. She wrote about patients’ “total pain,” the crisis of physical, spiritual, social, and emotional distress that many people have at the end of life. She understood that no single health care discipline was adequate to the task of addressing each of these domains equally well. Thus, hospice became synonymous with care provided by a quartet of specialists – physicians, nurses, social workers, and chaplains. Nowadays, there are other specialists that are added to the mix – home health aides, pharmacists, physical and occupational therapists, music and pet therapists, and so on.
But in medicine, like all areas of science, convention and tradition only go so far. What evidence is there to support the work of an interdisciplinary team in managing the distress of patients and families living with advanced illnesses? It turns out that there is good evidence to support the use of high-functioning interdisciplinary teams in the care of the seriously ill. Palliative care is associated with improved patient outcomes, including improvements in symptom control, quality of life, and end of life care, when it is delivered by an interdisciplinary team rather than by a solo practitioner.
You may think that teamwork is most useful for patients like John who have seemingly intractable social barriers. But it is also true that for even patients with many more social advantages teamwork improves quality of life. I got to see this up close recently in my own life.
Teamwork improves quality of life
My father recently passed away after a 9-month battle with advanced cancer. He had every advantage possible – financial stability, high health literacy, an incredibly devoted spouse who happens to be an RN, good insurance, and access to top-notch medical care. Yet, even he benefited from a team approach. It started small, with the oncologist and oncology NP providing excellent, patient-centered care. Then it grew to include myself as the daughter/palliative care nurse practitioner who made recommendations for treating his nausea and ensured that his advance directive was completed and uploaded to his chart. When my dad needed physical therapy, the home health agency sent a wonderful physical therapist, who brought all sorts of equipment that kept him more functional than he would have been otherwise. Other family members helped out – my sisters helped connect my dad with a priest who came to the home to provide spiritual care, which was crucial to ensuring that he was at peace. And, in his final days, my dad had the hospice team to help manage his symptoms and his family members to provide hands-on care.
The complexity of cancer care has long necessitated a team approach to planning cancer treatment – known as a tumor board – with medical oncology, radiation oncology, surgery, and pathology all weighing in. It makes sense that patients and their families would also need a team of clinicians representing different specialty areas to assist with the wide array of physical, psychosocial, practical, and spiritual concerns that arise throughout the cancer disease trajectory.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
John worked as a handyman and lived on a small sailboat in a marina. When he was diagnosed with metastatic kidney cancer at age 48, he quickly fell through the cracks. He failed to show to appointments and took oral anticancer treatments, but just sporadically. He had Medicaid, so insurance wasn’t the issue. It was everything else.
John was behind on his slip fees; he hadn’t been able to work for some time because of his progressive weakness and pain. He was chronically in danger of getting kicked out of his makeshift home aboard the boat. He had no reliable transportation to the clinic and so he didn’t come to appointments regularly. The specialty pharmacy refused to deliver his expensive oral chemotherapy to his address at the marina. He went days without eating full meals because he was too weak to cook for himself. Plus, he was estranged from his family who were unaware of his illness. His oncologist was overwhelmed trying to take care of him. He had a reasonable chance of achieving disease control on first-line oral therapy, but his problems seemed to hinder these chances at every turn. She was distraught – what could she do?
Enter the team approach. John’s oncologist reached out to our palliative care program for help. We recognized that this was a job too big for us alone so we connected John with the Extensivist Medicine program at UCLA Health, a high-intensity primary care program led by a physician specializing in primary care for high-risk individuals. The program provides wraparound outpatient services for chronically and seriously ill patients, like John, who are at risk for falling through the cracks. John went from receiving very little support to now having an entire team of caring professionals focused on helping him achieve his best possible outcome despite the seriousness of his disease.
He now had the support of a high-functioning team with clearly defined roles. Social work connected him with housing, food, and transportation resources. A nurse called him every day to check in and make sure he was taking medications and reminded him about his upcoming appointments. Case management helped him get needed equipment, such as grab bars and a walker. As his palliative care nurse practitioner, I counseled him on understanding his prognosis and planning ahead for medical emergencies. Our psycho-oncology clinicians helped John reconcile with his family, who were more than willing to take him in once they realized how ill he was. Once these social factors were addressed, John could more easily stay current with his oral chemotherapy, giving him the best chance possible to achieve a robust treatment response that could buy him more time.
And, John did get that time – he got 6 months of improved quality of life, during which he reconnected with his family, including his children, and rebuilt these important relationships. Eventually treatment failed him. His disease, already widely metastatic, became more active and painful. He accepted hospice care at his sister’s house and we transitioned him from our team to the hospice team. He died peacefully surrounded by family.
Interprofessional teamwork is fundamental to treat ‘total pain’
None of this would have been possible without the work of high-functioning teams. It is a commonly held belief that interprofessional teamwork is fundamental to the care of patients and families living with serious illness. But why? How did this idea come about? And what evidence is there to support teamwork?
Dame Cicely Saunders, who founded the modern hospice movement in mid-20th century England, embodied the interdisciplinary team by working first as a nurse, then a social worker, and finally as a physician. She wrote about patients’ “total pain,” the crisis of physical, spiritual, social, and emotional distress that many people have at the end of life. She understood that no single health care discipline was adequate to the task of addressing each of these domains equally well. Thus, hospice became synonymous with care provided by a quartet of specialists – physicians, nurses, social workers, and chaplains. Nowadays, there are other specialists that are added to the mix – home health aides, pharmacists, physical and occupational therapists, music and pet therapists, and so on.
But in medicine, like all areas of science, convention and tradition only go so far. What evidence is there to support the work of an interdisciplinary team in managing the distress of patients and families living with advanced illnesses? It turns out that there is good evidence to support the use of high-functioning interdisciplinary teams in the care of the seriously ill. Palliative care is associated with improved patient outcomes, including improvements in symptom control, quality of life, and end of life care, when it is delivered by an interdisciplinary team rather than by a solo practitioner.
You may think that teamwork is most useful for patients like John who have seemingly intractable social barriers. But it is also true that for even patients with many more social advantages teamwork improves quality of life. I got to see this up close recently in my own life.
Teamwork improves quality of life
My father recently passed away after a 9-month battle with advanced cancer. He had every advantage possible – financial stability, high health literacy, an incredibly devoted spouse who happens to be an RN, good insurance, and access to top-notch medical care. Yet, even he benefited from a team approach. It started small, with the oncologist and oncology NP providing excellent, patient-centered care. Then it grew to include myself as the daughter/palliative care nurse practitioner who made recommendations for treating his nausea and ensured that his advance directive was completed and uploaded to his chart. When my dad needed physical therapy, the home health agency sent a wonderful physical therapist, who brought all sorts of equipment that kept him more functional than he would have been otherwise. Other family members helped out – my sisters helped connect my dad with a priest who came to the home to provide spiritual care, which was crucial to ensuring that he was at peace. And, in his final days, my dad had the hospice team to help manage his symptoms and his family members to provide hands-on care.
The complexity of cancer care has long necessitated a team approach to planning cancer treatment – known as a tumor board – with medical oncology, radiation oncology, surgery, and pathology all weighing in. It makes sense that patients and their families would also need a team of clinicians representing different specialty areas to assist with the wide array of physical, psychosocial, practical, and spiritual concerns that arise throughout the cancer disease trajectory.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
The accelerating societal entropy undermines mental health
According to the second law of thermodynamics, it is inevitable that entropy will continue to increase over time.1 Entropy is a measure of disorder, which can eventuate in chaos and lead to profound uncertainty, with serious psychological consequences.
The increase in entropy is usually gradual. It took hundreds of years for powerful empires and civilizations to collapse and disappear. Inanimate objects such as a house, a piece of furniture, or a piece of equipment eventually deteriorate and break down over time. Tidy offices will become messy, cluttered, and dirty unless attended to regularly. Living organisms, including humans, inevitably undergo an aging process with cellular senescence, atrophy, and loss of cerebral, muscle, and bone tissue, ending in death. Even human relationships will eventually fracture, wither, and end. The passage of time ruthlessly increases the entropy of everything in life. Even the 13-billion-year-old universe, which currently looks formidable and permanent to us, is inexorably expanding and hurtling towards a calamitous end a few billion years from now.
To slow down, halt, or reverse entropy, work and energy must be invested. A house requires regular maintenance for all its components to avoid deteriorating and becoming uninhabitable (very high entropy). Humans require massive amounts of work during fetal life, infancy, childhood, adolescence, adulthood, and throughout old age. This includes work by parents, teachers, friends, physicians, farmers, and manufacturers of food, clothing, and sundry supplies, all targeted to maintain an individual and slow the rate of entropy. But death is inevitable as the final stage of human entropy.
The brain is an entropic organ.2 Psychiatric disorders can be conceptualized as a neurobiologic consequence of a major rise in brain entropy. The chaos created by high brain entropy will lead to a disruption of basic mental functions such as thought, mood, affect, impulses, behavior, and cognition. Brain entropy increases can be due to genetics or the environment, but most often are due an interaction of both (G x E).
Societal entropy and our patients
Psychiatric patients are deeply influenced by the context in which they live (society). The entropy of contemporary society is rising at an alarming rate, which means that order is rapidly degenerating into disorder at an unprecedented pace. When the COVID-19 pandemic abruptly emerged in early 2020, it was a major public health shock that drastically changed the lives of all citizens and dramatically increased societal entropy. The pandemic led to lockdowns, fear of death, gut-wrenching uncertainty (especially for a whole year before vaccines were developed, but even after), loss of socialization and sexual intimacy, loss of employment, financial straits, and an inability to access routine medical or surgical procedures. Everyone in society developed anxiety and acute stress reaction, but those with pre-existing psychiatric disorders suffered the most with an intensification of their symptoms.
The unforeseen, sudden, and traumatically life-altering pandemic triggered various degrees of posttraumatic stress disorder across all age groups, and painful death in medically compromised individuals and older adults. Both physical and psychological entropy skyrocketed and the “order” of life as we knew it rapidly disintegrated into shambles and disorder. The abrupt traumatic jolt triggered various degrees of deleterious impacts on the brains of all who experienced it in real time. The rise in the psychobiological entropy was unprecedented across the structures of society, especially the population, its vulnerable human component.
But even as the worst of the pandemic is in our rearview mirror and life again has a semblance of normality, the rise of entropy continues to accelerate because we continue to be surrounded and engulfed by countless stressful events in contemporary society. Those nagging stresses continue to transmute order to chaos and metamorphose comforting predictability to entrenched uncertainty:
- Toxic political hyperpartisanship, with intense animus and visceral bidirectional hatred
- Racial tensions, with overt bias across groups
- Economic turmoil, with inflation and threats of recession
- Actual wars and threats of war
- Social media that spreads bad news and distorts facts
- An opioid crisis, with hundreds of thousands of deaths
- Skyrocketing crime, with a decline in policing and quick release of criminals without bail
- A ruthless and arbitrary “cancel culture” that doesn’t even spare the previously revered founders of the republic
- Cognitive dissonance of disparaging Abraham Lincoln despite his major achievement of eliminating slavery by waging a civil war
- The social and medical strife regarding access to abortion.
Continue to: I also would include...
(I also would include some “entropy pet peeves” of mine: Torn clothes as a fashion statement, transforming tattoos from an oddity to a fad, nose rings that disfigure pretty faces, and banishing neckties for men.)
Our role in this scenario
As psychiatrists, we must step up to intensify the work needed to slow down and even reverse the dangerously rising brain entropy in our patients. But that is not an easy task given the implosion of societal norms and traditional values, along with the radicalization of beliefs, with utter intolerance of others’ beliefs. We also face the challenge of maintaining a modicum of resilience and wellness in ourselves, which can be antidotes to entropy.
It’s impossible to stop the inevitability of rising entropy, both physical and psychological, but psychiatrists and other mental health professionals must invest their skills and talents now more than ever to at least slow down the pace of entropy among our patients. Otherwise, psychological chaos and disorder will be quite damaging to their lives, and worsen their outcomes.
1. Ben-Naim A. Entropy Demystified. World Scientific; 2007.
2. Carhart-Harris RL. The entropic brain - revisited. Neuropharmacology. 2018;142:167-178. doi: 10.1016/j.neuropharm.2018.03.010
According to the second law of thermodynamics, it is inevitable that entropy will continue to increase over time.1 Entropy is a measure of disorder, which can eventuate in chaos and lead to profound uncertainty, with serious psychological consequences.
The increase in entropy is usually gradual. It took hundreds of years for powerful empires and civilizations to collapse and disappear. Inanimate objects such as a house, a piece of furniture, or a piece of equipment eventually deteriorate and break down over time. Tidy offices will become messy, cluttered, and dirty unless attended to regularly. Living organisms, including humans, inevitably undergo an aging process with cellular senescence, atrophy, and loss of cerebral, muscle, and bone tissue, ending in death. Even human relationships will eventually fracture, wither, and end. The passage of time ruthlessly increases the entropy of everything in life. Even the 13-billion-year-old universe, which currently looks formidable and permanent to us, is inexorably expanding and hurtling towards a calamitous end a few billion years from now.
To slow down, halt, or reverse entropy, work and energy must be invested. A house requires regular maintenance for all its components to avoid deteriorating and becoming uninhabitable (very high entropy). Humans require massive amounts of work during fetal life, infancy, childhood, adolescence, adulthood, and throughout old age. This includes work by parents, teachers, friends, physicians, farmers, and manufacturers of food, clothing, and sundry supplies, all targeted to maintain an individual and slow the rate of entropy. But death is inevitable as the final stage of human entropy.
The brain is an entropic organ.2 Psychiatric disorders can be conceptualized as a neurobiologic consequence of a major rise in brain entropy. The chaos created by high brain entropy will lead to a disruption of basic mental functions such as thought, mood, affect, impulses, behavior, and cognition. Brain entropy increases can be due to genetics or the environment, but most often are due an interaction of both (G x E).
Societal entropy and our patients
Psychiatric patients are deeply influenced by the context in which they live (society). The entropy of contemporary society is rising at an alarming rate, which means that order is rapidly degenerating into disorder at an unprecedented pace. When the COVID-19 pandemic abruptly emerged in early 2020, it was a major public health shock that drastically changed the lives of all citizens and dramatically increased societal entropy. The pandemic led to lockdowns, fear of death, gut-wrenching uncertainty (especially for a whole year before vaccines were developed, but even after), loss of socialization and sexual intimacy, loss of employment, financial straits, and an inability to access routine medical or surgical procedures. Everyone in society developed anxiety and acute stress reaction, but those with pre-existing psychiatric disorders suffered the most with an intensification of their symptoms.
The unforeseen, sudden, and traumatically life-altering pandemic triggered various degrees of posttraumatic stress disorder across all age groups, and painful death in medically compromised individuals and older adults. Both physical and psychological entropy skyrocketed and the “order” of life as we knew it rapidly disintegrated into shambles and disorder. The abrupt traumatic jolt triggered various degrees of deleterious impacts on the brains of all who experienced it in real time. The rise in the psychobiological entropy was unprecedented across the structures of society, especially the population, its vulnerable human component.
But even as the worst of the pandemic is in our rearview mirror and life again has a semblance of normality, the rise of entropy continues to accelerate because we continue to be surrounded and engulfed by countless stressful events in contemporary society. Those nagging stresses continue to transmute order to chaos and metamorphose comforting predictability to entrenched uncertainty:
- Toxic political hyperpartisanship, with intense animus and visceral bidirectional hatred
- Racial tensions, with overt bias across groups
- Economic turmoil, with inflation and threats of recession
- Actual wars and threats of war
- Social media that spreads bad news and distorts facts
- An opioid crisis, with hundreds of thousands of deaths
- Skyrocketing crime, with a decline in policing and quick release of criminals without bail
- A ruthless and arbitrary “cancel culture” that doesn’t even spare the previously revered founders of the republic
- Cognitive dissonance of disparaging Abraham Lincoln despite his major achievement of eliminating slavery by waging a civil war
- The social and medical strife regarding access to abortion.
Continue to: I also would include...
(I also would include some “entropy pet peeves” of mine: Torn clothes as a fashion statement, transforming tattoos from an oddity to a fad, nose rings that disfigure pretty faces, and banishing neckties for men.)
Our role in this scenario
As psychiatrists, we must step up to intensify the work needed to slow down and even reverse the dangerously rising brain entropy in our patients. But that is not an easy task given the implosion of societal norms and traditional values, along with the radicalization of beliefs, with utter intolerance of others’ beliefs. We also face the challenge of maintaining a modicum of resilience and wellness in ourselves, which can be antidotes to entropy.
It’s impossible to stop the inevitability of rising entropy, both physical and psychological, but psychiatrists and other mental health professionals must invest their skills and talents now more than ever to at least slow down the pace of entropy among our patients. Otherwise, psychological chaos and disorder will be quite damaging to their lives, and worsen their outcomes.
According to the second law of thermodynamics, it is inevitable that entropy will continue to increase over time.1 Entropy is a measure of disorder, which can eventuate in chaos and lead to profound uncertainty, with serious psychological consequences.
The increase in entropy is usually gradual. It took hundreds of years for powerful empires and civilizations to collapse and disappear. Inanimate objects such as a house, a piece of furniture, or a piece of equipment eventually deteriorate and break down over time. Tidy offices will become messy, cluttered, and dirty unless attended to regularly. Living organisms, including humans, inevitably undergo an aging process with cellular senescence, atrophy, and loss of cerebral, muscle, and bone tissue, ending in death. Even human relationships will eventually fracture, wither, and end. The passage of time ruthlessly increases the entropy of everything in life. Even the 13-billion-year-old universe, which currently looks formidable and permanent to us, is inexorably expanding and hurtling towards a calamitous end a few billion years from now.
To slow down, halt, or reverse entropy, work and energy must be invested. A house requires regular maintenance for all its components to avoid deteriorating and becoming uninhabitable (very high entropy). Humans require massive amounts of work during fetal life, infancy, childhood, adolescence, adulthood, and throughout old age. This includes work by parents, teachers, friends, physicians, farmers, and manufacturers of food, clothing, and sundry supplies, all targeted to maintain an individual and slow the rate of entropy. But death is inevitable as the final stage of human entropy.
The brain is an entropic organ.2 Psychiatric disorders can be conceptualized as a neurobiologic consequence of a major rise in brain entropy. The chaos created by high brain entropy will lead to a disruption of basic mental functions such as thought, mood, affect, impulses, behavior, and cognition. Brain entropy increases can be due to genetics or the environment, but most often are due an interaction of both (G x E).
Societal entropy and our patients
Psychiatric patients are deeply influenced by the context in which they live (society). The entropy of contemporary society is rising at an alarming rate, which means that order is rapidly degenerating into disorder at an unprecedented pace. When the COVID-19 pandemic abruptly emerged in early 2020, it was a major public health shock that drastically changed the lives of all citizens and dramatically increased societal entropy. The pandemic led to lockdowns, fear of death, gut-wrenching uncertainty (especially for a whole year before vaccines were developed, but even after), loss of socialization and sexual intimacy, loss of employment, financial straits, and an inability to access routine medical or surgical procedures. Everyone in society developed anxiety and acute stress reaction, but those with pre-existing psychiatric disorders suffered the most with an intensification of their symptoms.
The unforeseen, sudden, and traumatically life-altering pandemic triggered various degrees of posttraumatic stress disorder across all age groups, and painful death in medically compromised individuals and older adults. Both physical and psychological entropy skyrocketed and the “order” of life as we knew it rapidly disintegrated into shambles and disorder. The abrupt traumatic jolt triggered various degrees of deleterious impacts on the brains of all who experienced it in real time. The rise in the psychobiological entropy was unprecedented across the structures of society, especially the population, its vulnerable human component.
But even as the worst of the pandemic is in our rearview mirror and life again has a semblance of normality, the rise of entropy continues to accelerate because we continue to be surrounded and engulfed by countless stressful events in contemporary society. Those nagging stresses continue to transmute order to chaos and metamorphose comforting predictability to entrenched uncertainty:
- Toxic political hyperpartisanship, with intense animus and visceral bidirectional hatred
- Racial tensions, with overt bias across groups
- Economic turmoil, with inflation and threats of recession
- Actual wars and threats of war
- Social media that spreads bad news and distorts facts
- An opioid crisis, with hundreds of thousands of deaths
- Skyrocketing crime, with a decline in policing and quick release of criminals without bail
- A ruthless and arbitrary “cancel culture” that doesn’t even spare the previously revered founders of the republic
- Cognitive dissonance of disparaging Abraham Lincoln despite his major achievement of eliminating slavery by waging a civil war
- The social and medical strife regarding access to abortion.
Continue to: I also would include...
(I also would include some “entropy pet peeves” of mine: Torn clothes as a fashion statement, transforming tattoos from an oddity to a fad, nose rings that disfigure pretty faces, and banishing neckties for men.)
Our role in this scenario
As psychiatrists, we must step up to intensify the work needed to slow down and even reverse the dangerously rising brain entropy in our patients. But that is not an easy task given the implosion of societal norms and traditional values, along with the radicalization of beliefs, with utter intolerance of others’ beliefs. We also face the challenge of maintaining a modicum of resilience and wellness in ourselves, which can be antidotes to entropy.
It’s impossible to stop the inevitability of rising entropy, both physical and psychological, but psychiatrists and other mental health professionals must invest their skills and talents now more than ever to at least slow down the pace of entropy among our patients. Otherwise, psychological chaos and disorder will be quite damaging to their lives, and worsen their outcomes.
1. Ben-Naim A. Entropy Demystified. World Scientific; 2007.
2. Carhart-Harris RL. The entropic brain - revisited. Neuropharmacology. 2018;142:167-178. doi: 10.1016/j.neuropharm.2018.03.010
1. Ben-Naim A. Entropy Demystified. World Scientific; 2007.
2. Carhart-Harris RL. The entropic brain - revisited. Neuropharmacology. 2018;142:167-178. doi: 10.1016/j.neuropharm.2018.03.010
More on varenicline
Murray et al have written a timely, thoughtful, and useful article (“Smoking cessation: Varenicline and the risk of neuropsychiatric adverse events,”
Just a few caveats regarding Murray et al’s excellent summary:
• The article did not address that nicotine is consumed in multiple ways, such as vaping, snuff, chewing tobacco, and hookah
• The safety of varenicline appears fair when psychiatric illness is well controlled but can be problematic (and even severely detrimental) when mental illness is not well controlled. This should not be glossed over, especially since it was the reason for the original black-box warning (for risks including behavioral impulsivity, suicidality, severe insomnia, and nightmares) that was removed in 2016
• Patients with severe mental illness may not fully understand the risks, benefits, and priorities of the treatment intervention. The importance of psychiatric and internal medicine in addition to pharmacy follow-up is critical and needs to be documented.
Varenicline has been contextualized in its current role as a first-line treatment for smoking cessation. By bypassing a sizeable population of patients who have unstable psychiatric illness (especially bipolar I disorder), the path has been opened for risky “off-label” varenicline prescribing to this population by internists, who should be very cautious and prudent about prescribing for such patients. This alone is probably a good reason to reinstate the black-box warning.
Interestingly, one review found that only 1 of 11 patients receiving varenicline stopped smoking.1 Not dramatically beneficial for a first-line treatment! Decreasing smoking occurs as well and is more robust with combinational use with bupropion, nicotine replacement therapy, and cognitive-behavioral therapy.
If we are focusing on patients with unstable mental illness—who are seen primarily by psychiatrists—adherence, urgency of intervention, and context regarding acute safety for this population must be seen as top priorities.
So-called “second-line” treatment options must also be considered. Sandiego et al3 make excellent points regarding the role of alpha-adrenergic agonists such as guanfacine, which have been shown to be helpful in smoking cessation. They work by decreasing cortical dopamine release and their calming effects on the noradrenergic system, which may decrease smoking precipitated by stress. For the particularly challenging subpopulation of unstable smokers, the combination of varenicline plus guanfacine ER may turn out to be a game-changer.
Varenicline has not proven itself to be useful in patients who are severely mentally ill, and due to its low success rate, expectations should remain tempered, pragmatically realistic, and safety-based.4,5 The bottom line is that in an unstable psychiatrically ill patient, interventions other than varenicline should be first-line.
1. Crawford P, Cieslak D. Varenicline for smoking cessation. Am Fam Physician. 2017;96(5).
2. Beard E, Jackson SE, Anthenelli RM, et al. Estimation of risk of neuropsychiatric adverse events from varenicline, bupropion and nicotine patch versus placebo: secondary analysis of results from the EAGLES trial using Bayes factors. Addiction. 2021;116(10):2816-2824.
3. Sandiego CM, Matuskey D, Lavery M, et al. The effect of treatment with guanfacine, an alpha2 adrenergic agonist, on dopaminergic tone in tobacco smokers: an [11C]FLB457 PET study. Neuropsychopharmacology. 2018;43(5):1052-1058.
4. Sharma R, Alla K, Pfeffer D, et al. An appraisal of practice guidelines for smoking cessation in people with severe mental illness. Aust N Z J Psychiatry. 2017;51(11):1106-1120.
5. Tofler IR. Varenicline for smoking cessation in the bipolar patient. J Clin Psychiatry. 2015;76(5):625.
Murray et al have written a timely, thoughtful, and useful article (“Smoking cessation: Varenicline and the risk of neuropsychiatric adverse events,”
Just a few caveats regarding Murray et al’s excellent summary:
• The article did not address that nicotine is consumed in multiple ways, such as vaping, snuff, chewing tobacco, and hookah
• The safety of varenicline appears fair when psychiatric illness is well controlled but can be problematic (and even severely detrimental) when mental illness is not well controlled. This should not be glossed over, especially since it was the reason for the original black-box warning (for risks including behavioral impulsivity, suicidality, severe insomnia, and nightmares) that was removed in 2016
• Patients with severe mental illness may not fully understand the risks, benefits, and priorities of the treatment intervention. The importance of psychiatric and internal medicine in addition to pharmacy follow-up is critical and needs to be documented.
Varenicline has been contextualized in its current role as a first-line treatment for smoking cessation. By bypassing a sizeable population of patients who have unstable psychiatric illness (especially bipolar I disorder), the path has been opened for risky “off-label” varenicline prescribing to this population by internists, who should be very cautious and prudent about prescribing for such patients. This alone is probably a good reason to reinstate the black-box warning.
Interestingly, one review found that only 1 of 11 patients receiving varenicline stopped smoking.1 Not dramatically beneficial for a first-line treatment! Decreasing smoking occurs as well and is more robust with combinational use with bupropion, nicotine replacement therapy, and cognitive-behavioral therapy.
If we are focusing on patients with unstable mental illness—who are seen primarily by psychiatrists—adherence, urgency of intervention, and context regarding acute safety for this population must be seen as top priorities.
So-called “second-line” treatment options must also be considered. Sandiego et al3 make excellent points regarding the role of alpha-adrenergic agonists such as guanfacine, which have been shown to be helpful in smoking cessation. They work by decreasing cortical dopamine release and their calming effects on the noradrenergic system, which may decrease smoking precipitated by stress. For the particularly challenging subpopulation of unstable smokers, the combination of varenicline plus guanfacine ER may turn out to be a game-changer.
Varenicline has not proven itself to be useful in patients who are severely mentally ill, and due to its low success rate, expectations should remain tempered, pragmatically realistic, and safety-based.4,5 The bottom line is that in an unstable psychiatrically ill patient, interventions other than varenicline should be first-line.
Murray et al have written a timely, thoughtful, and useful article (“Smoking cessation: Varenicline and the risk of neuropsychiatric adverse events,”
Just a few caveats regarding Murray et al’s excellent summary:
• The article did not address that nicotine is consumed in multiple ways, such as vaping, snuff, chewing tobacco, and hookah
• The safety of varenicline appears fair when psychiatric illness is well controlled but can be problematic (and even severely detrimental) when mental illness is not well controlled. This should not be glossed over, especially since it was the reason for the original black-box warning (for risks including behavioral impulsivity, suicidality, severe insomnia, and nightmares) that was removed in 2016
• Patients with severe mental illness may not fully understand the risks, benefits, and priorities of the treatment intervention. The importance of psychiatric and internal medicine in addition to pharmacy follow-up is critical and needs to be documented.
Varenicline has been contextualized in its current role as a first-line treatment for smoking cessation. By bypassing a sizeable population of patients who have unstable psychiatric illness (especially bipolar I disorder), the path has been opened for risky “off-label” varenicline prescribing to this population by internists, who should be very cautious and prudent about prescribing for such patients. This alone is probably a good reason to reinstate the black-box warning.
Interestingly, one review found that only 1 of 11 patients receiving varenicline stopped smoking.1 Not dramatically beneficial for a first-line treatment! Decreasing smoking occurs as well and is more robust with combinational use with bupropion, nicotine replacement therapy, and cognitive-behavioral therapy.
If we are focusing on patients with unstable mental illness—who are seen primarily by psychiatrists—adherence, urgency of intervention, and context regarding acute safety for this population must be seen as top priorities.
So-called “second-line” treatment options must also be considered. Sandiego et al3 make excellent points regarding the role of alpha-adrenergic agonists such as guanfacine, which have been shown to be helpful in smoking cessation. They work by decreasing cortical dopamine release and their calming effects on the noradrenergic system, which may decrease smoking precipitated by stress. For the particularly challenging subpopulation of unstable smokers, the combination of varenicline plus guanfacine ER may turn out to be a game-changer.
Varenicline has not proven itself to be useful in patients who are severely mentally ill, and due to its low success rate, expectations should remain tempered, pragmatically realistic, and safety-based.4,5 The bottom line is that in an unstable psychiatrically ill patient, interventions other than varenicline should be first-line.
1. Crawford P, Cieslak D. Varenicline for smoking cessation. Am Fam Physician. 2017;96(5).
2. Beard E, Jackson SE, Anthenelli RM, et al. Estimation of risk of neuropsychiatric adverse events from varenicline, bupropion and nicotine patch versus placebo: secondary analysis of results from the EAGLES trial using Bayes factors. Addiction. 2021;116(10):2816-2824.
3. Sandiego CM, Matuskey D, Lavery M, et al. The effect of treatment with guanfacine, an alpha2 adrenergic agonist, on dopaminergic tone in tobacco smokers: an [11C]FLB457 PET study. Neuropsychopharmacology. 2018;43(5):1052-1058.
4. Sharma R, Alla K, Pfeffer D, et al. An appraisal of practice guidelines for smoking cessation in people with severe mental illness. Aust N Z J Psychiatry. 2017;51(11):1106-1120.
5. Tofler IR. Varenicline for smoking cessation in the bipolar patient. J Clin Psychiatry. 2015;76(5):625.
1. Crawford P, Cieslak D. Varenicline for smoking cessation. Am Fam Physician. 2017;96(5).
2. Beard E, Jackson SE, Anthenelli RM, et al. Estimation of risk of neuropsychiatric adverse events from varenicline, bupropion and nicotine patch versus placebo: secondary analysis of results from the EAGLES trial using Bayes factors. Addiction. 2021;116(10):2816-2824.
3. Sandiego CM, Matuskey D, Lavery M, et al. The effect of treatment with guanfacine, an alpha2 adrenergic agonist, on dopaminergic tone in tobacco smokers: an [11C]FLB457 PET study. Neuropsychopharmacology. 2018;43(5):1052-1058.
4. Sharma R, Alla K, Pfeffer D, et al. An appraisal of practice guidelines for smoking cessation in people with severe mental illness. Aust N Z J Psychiatry. 2017;51(11):1106-1120.
5. Tofler IR. Varenicline for smoking cessation in the bipolar patient. J Clin Psychiatry. 2015;76(5):625.
The winding road that leads to optimal temperature management after cardiac arrest
In 2002, two landmark trials found that targeted temperature management (TTM) after out-of-hospital cardiac arrest led to improvements in neurologic outcomes. The larger of the two trials found a reduction in mortality. Such treatment benefits are hard to come by in critical care in general and in out-of-hospital cardiac arrest in particular. With the therapeutic overconfidence typical of our profession, my institution embraced TTM quickly and completely soon after these trials were published. Remember, this was “back in the day” when sepsis management included drotrecogin alfa, Cortrosyn stim tests, tight glucose control (90-120 mg/dL), and horrible over-resuscitation via the early goal-directed therapy paradigm.
If you’ve been practicing critical care medicine for more than a few years, you already know where I’m going. Most of the interventions in the preceding paragraph were adopted but discarded before 2010. Hypothermia – temperature management with a goal of 32-36° C – has been struggling to stay relevant ever since the publication of the TTM randomized controlled trial (RCT) in 2013. Then came the HYPERION trial, which brought the 32-36° C target back from the dead (pun definitely intended) in 2019. This is critical care medicine: Today’s life-saving intervention proves harmful tomorrow, but withholding it may constitute malpractice a few months down the road.
So where are we now? Good question. I’ve had seasoned neurointensivists insist that 33° C remains the standard of care and others who’ve endorsed normothermia. So much for finding an answer via my more specialized colleagues.
Let’s go to the guidelines then. Prompted largely by HYPERION, a temperature target of 32-36° C was endorsed in 2020 and 2021. Then came publication of the TTM2 trial, the largest temperature management RCT to date, which found no benefit to targeting 33° C. A network meta-analysis published in 2021 reached a similar conclusion. A recently released update by the same international guideline group now recommends targeting normothermia (< 37.7° C) and avoiding fever, and it specifically says that there is insufficient evidence to support a 32-36° C target. Okay, everyone tracking all that?
Lest I sound overly catty and nihilistic, I see all this in a positive light. Huge credit goes to the critical care medicine academic community for putting together so many RCTs. The scientific reality is that it takes “a lotta” sample size to clarify the effects of an intervention. Throw in the inevitable bevy of confounders (in- vs. out-of-hospital cardiac arrest, resuscitation time, initial rhythm, and so on), and you get a feel for the work required to understand a treatment’s true effects.
Advances in guideline science and the hard, often unpaid work of panels are also important. The guideline panel I’ve been citing came out for aggressive temperature control (32-36° C) a few months before the TTM2 RCT was published. In the past, they updated their recommendations every 5 years, but this time, they were out with a new manuscript that incorporated TTM2 in less than a year. If you’ve been involved at any level with producing guidelines, you can appreciate this achievement. Assuming that aggressive hypothermia is truly harmful, waiting 5 years to incorporate TTM2 could have led to significant morbidity.
I do take issue with you early adopters, though. Given the litany of failed therapies that have shown initial promise, and the well-documented human tendency to underestimate the impact of sample size, your rapid implementation of major interventions is puzzling. One might think you’d learned your lessons after seeing drotrecogin alfa, Cortrosyn stim tests, tight glucose control, early goal-directed therapy, and aggressive TTM come and go. Your recent enthusiasm for vitamin C after publication of a single before-after study suggests that you haven’t.
Aaron B. Holley, MD, is an associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center, Bethesda, Md. He has received a research grant from Fisher-Paykel.
A version of this article first appeared on Medscape.com.
In 2002, two landmark trials found that targeted temperature management (TTM) after out-of-hospital cardiac arrest led to improvements in neurologic outcomes. The larger of the two trials found a reduction in mortality. Such treatment benefits are hard to come by in critical care in general and in out-of-hospital cardiac arrest in particular. With the therapeutic overconfidence typical of our profession, my institution embraced TTM quickly and completely soon after these trials were published. Remember, this was “back in the day” when sepsis management included drotrecogin alfa, Cortrosyn stim tests, tight glucose control (90-120 mg/dL), and horrible over-resuscitation via the early goal-directed therapy paradigm.
If you’ve been practicing critical care medicine for more than a few years, you already know where I’m going. Most of the interventions in the preceding paragraph were adopted but discarded before 2010. Hypothermia – temperature management with a goal of 32-36° C – has been struggling to stay relevant ever since the publication of the TTM randomized controlled trial (RCT) in 2013. Then came the HYPERION trial, which brought the 32-36° C target back from the dead (pun definitely intended) in 2019. This is critical care medicine: Today’s life-saving intervention proves harmful tomorrow, but withholding it may constitute malpractice a few months down the road.
So where are we now? Good question. I’ve had seasoned neurointensivists insist that 33° C remains the standard of care and others who’ve endorsed normothermia. So much for finding an answer via my more specialized colleagues.
Let’s go to the guidelines then. Prompted largely by HYPERION, a temperature target of 32-36° C was endorsed in 2020 and 2021. Then came publication of the TTM2 trial, the largest temperature management RCT to date, which found no benefit to targeting 33° C. A network meta-analysis published in 2021 reached a similar conclusion. A recently released update by the same international guideline group now recommends targeting normothermia (< 37.7° C) and avoiding fever, and it specifically says that there is insufficient evidence to support a 32-36° C target. Okay, everyone tracking all that?
Lest I sound overly catty and nihilistic, I see all this in a positive light. Huge credit goes to the critical care medicine academic community for putting together so many RCTs. The scientific reality is that it takes “a lotta” sample size to clarify the effects of an intervention. Throw in the inevitable bevy of confounders (in- vs. out-of-hospital cardiac arrest, resuscitation time, initial rhythm, and so on), and you get a feel for the work required to understand a treatment’s true effects.
Advances in guideline science and the hard, often unpaid work of panels are also important. The guideline panel I’ve been citing came out for aggressive temperature control (32-36° C) a few months before the TTM2 RCT was published. In the past, they updated their recommendations every 5 years, but this time, they were out with a new manuscript that incorporated TTM2 in less than a year. If you’ve been involved at any level with producing guidelines, you can appreciate this achievement. Assuming that aggressive hypothermia is truly harmful, waiting 5 years to incorporate TTM2 could have led to significant morbidity.
I do take issue with you early adopters, though. Given the litany of failed therapies that have shown initial promise, and the well-documented human tendency to underestimate the impact of sample size, your rapid implementation of major interventions is puzzling. One might think you’d learned your lessons after seeing drotrecogin alfa, Cortrosyn stim tests, tight glucose control, early goal-directed therapy, and aggressive TTM come and go. Your recent enthusiasm for vitamin C after publication of a single before-after study suggests that you haven’t.
Aaron B. Holley, MD, is an associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center, Bethesda, Md. He has received a research grant from Fisher-Paykel.
A version of this article first appeared on Medscape.com.
In 2002, two landmark trials found that targeted temperature management (TTM) after out-of-hospital cardiac arrest led to improvements in neurologic outcomes. The larger of the two trials found a reduction in mortality. Such treatment benefits are hard to come by in critical care in general and in out-of-hospital cardiac arrest in particular. With the therapeutic overconfidence typical of our profession, my institution embraced TTM quickly and completely soon after these trials were published. Remember, this was “back in the day” when sepsis management included drotrecogin alfa, Cortrosyn stim tests, tight glucose control (90-120 mg/dL), and horrible over-resuscitation via the early goal-directed therapy paradigm.
If you’ve been practicing critical care medicine for more than a few years, you already know where I’m going. Most of the interventions in the preceding paragraph were adopted but discarded before 2010. Hypothermia – temperature management with a goal of 32-36° C – has been struggling to stay relevant ever since the publication of the TTM randomized controlled trial (RCT) in 2013. Then came the HYPERION trial, which brought the 32-36° C target back from the dead (pun definitely intended) in 2019. This is critical care medicine: Today’s life-saving intervention proves harmful tomorrow, but withholding it may constitute malpractice a few months down the road.
So where are we now? Good question. I’ve had seasoned neurointensivists insist that 33° C remains the standard of care and others who’ve endorsed normothermia. So much for finding an answer via my more specialized colleagues.
Let’s go to the guidelines then. Prompted largely by HYPERION, a temperature target of 32-36° C was endorsed in 2020 and 2021. Then came publication of the TTM2 trial, the largest temperature management RCT to date, which found no benefit to targeting 33° C. A network meta-analysis published in 2021 reached a similar conclusion. A recently released update by the same international guideline group now recommends targeting normothermia (< 37.7° C) and avoiding fever, and it specifically says that there is insufficient evidence to support a 32-36° C target. Okay, everyone tracking all that?
Lest I sound overly catty and nihilistic, I see all this in a positive light. Huge credit goes to the critical care medicine academic community for putting together so many RCTs. The scientific reality is that it takes “a lotta” sample size to clarify the effects of an intervention. Throw in the inevitable bevy of confounders (in- vs. out-of-hospital cardiac arrest, resuscitation time, initial rhythm, and so on), and you get a feel for the work required to understand a treatment’s true effects.
Advances in guideline science and the hard, often unpaid work of panels are also important. The guideline panel I’ve been citing came out for aggressive temperature control (32-36° C) a few months before the TTM2 RCT was published. In the past, they updated their recommendations every 5 years, but this time, they were out with a new manuscript that incorporated TTM2 in less than a year. If you’ve been involved at any level with producing guidelines, you can appreciate this achievement. Assuming that aggressive hypothermia is truly harmful, waiting 5 years to incorporate TTM2 could have led to significant morbidity.
I do take issue with you early adopters, though. Given the litany of failed therapies that have shown initial promise, and the well-documented human tendency to underestimate the impact of sample size, your rapid implementation of major interventions is puzzling. One might think you’d learned your lessons after seeing drotrecogin alfa, Cortrosyn stim tests, tight glucose control, early goal-directed therapy, and aggressive TTM come and go. Your recent enthusiasm for vitamin C after publication of a single before-after study suggests that you haven’t.
Aaron B. Holley, MD, is an associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center, Bethesda, Md. He has received a research grant from Fisher-Paykel.
A version of this article first appeared on Medscape.com.
In progressive lung cancer second biopsies may be the norm now
Shortly after osimertinib was approved for patients with non–small cell lung cancer in 2020 by the Food and Drug Administration, a patient came to me with increasing shortness of breath. He had been on erlotinib (Tarceva) for about 2 years and had done well. Nearly all of his pulmonary lesions had resolved and he was feeling well. He enjoyed boating in the summer and visiting grandkids in California in the winter. However, on this day, it was different. He was losing weight; he was tired and didn’t feel strong enough to put his boat in the water that spring. Long story short: We ordered a CT scan and all of his lesions were progressing. Since osimertinib had just been approved, we got a second biopsy, hoping that his insurance would pay for it. It did and sure enough, a new T790M mutation was present. He was on osimertinib for another 2 years before progressing and starting chemotherapy.
Second biopsies increasingly routine
The practice of ordering a second biopsy for patients with non–small cell lung carcinoma (NSCLC) was not common practice until after 2015 when the Food and Drug Administration approved gefitinib, a tyrosine kinase inhibitor (TKI) for patients whose tumors have epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations.
Up until then, second biopsies were not routinely done for lung cancers. But with the advent of targeted therapy and new drugs designed specifically to tackle first- and second-line treatment resistance mutations, rebiopsies have become a necessity for patients with progressive disease.
Epidermal growth factors, including HER2, ErbB2, and MET, are receptors of tyrosine kinases that control cell growth, but when in overdrive, they can lead to the development of cancers, including lung adenocarcinoma, conventional glioblastoma multiforme, glioblastoma, colon adenocarcinoma, and NSCLC.
EGFRs date back to 1962 with their discovery by Stanley Cohen. The discovery was so important that in 1986, Mr. Cohen was awarded the Nobel Prize in physiology or medicine for the discovery along with Rita Levi-Montalcini.
Now, many years later, we finally have a string of new approvals for mutations in the EGF family of receptors and several under study.
Sensitizing mutations
The more commonly used strategy for blocking EGFR signaling in lung cancer is the use of tyrosine kinase inhibitors, which compete with adenosine triphosphate (ATP) for binding to the tyrosine kinase portion of the receptor. They are located at chromosome 7p11.2. The most frequent mutations that sensitize patients to EGFR inhibitors include exon 19 deletions and L858R point mutation in exon 21, although multiple other driver mutations also exist.
The first-generation of EGFR TKIs include gefitinib and erlotinib, which bind reversibly to the EGF receptor. Second-generation inhibitors afatinib and dacomitinib bind irreversibly. Osimertinib, a third-generation EGFR TKI, which also binds irreversibly, was approved in 2020 for adjuvant therapy, and first- and second-line treatment in patients with NSCLC who have EGFR mutation–positive disease.
First-generation EGFR tyrosine kinase inhibitors
Four randomized, first-line, placebo-controlled phase 3 trials conducted with EGFR TKIs in combination with platinum-based doublet chemotherapy in an EGFR nonselected patient population failed to show a survival benefit with erlotinib or gefitinib (TRIBUTE, Tarceva Lung Cancer Investigation Trial, INTACT 1, INTACT 2).
However, a first-line study randomized patients to gefitinib or chemotherapy with carboplatin-paclitaxel, and included patients with or without an EGFR mutations. In the subgroup of patients with an EGFR mutation, progression-free survival (PFS) was significantly longer among those who received gefitinib than among those who received carboplatin–paclitaxel (hazard ratio for progression or death, 0.48), whereas in the subgroup of patients who were negative for the mutation, PFS was significantly longer among those who received chemotherapy (HR for progression or death with gefitinib, 2.85).
Numerous studies have shown that EGFR TKIs used in the first-line setting improved progression free survival, response rates, and quality of life while reducing toxicity. A recent meta-analysis of randomized clinical trials involving EGFR TKIs showed that EGFR TKI improved PFS with a HR of 0.40, compared with standard chemotherapy with fewer serious adverse events, although no benefit on overall survival was observed (HR, 0.96; 95% confidence interval, 0.83-1.10; P = .556).
T790M: The most common resistance mutation
T790M is the most common resistance mechanism to develop in patients with EGFR mutations being treated with EGFR TKIs. A randomized phase 3 trial of osimertinib vs. chemotherapy in patients with T790M-positive advanced NSCLC who had disease progression after first-line EGFR-TKI therapy, reported a median duration of progression-free survival that was significantly longer with osimertinib than with platinum therapy plus pemetrexed (10.1 months vs. 4.4 months; HR, 0.30). In addition, among 144 patients with metastases to the central nervous system, the median duration of PFS was longer among patients receiving osimertinib than among those receiving platinum therapy plus pemetrexed (8.5 months vs. 4.2 months; HR, 0.32). However, now that osimertinib has moved into the front-line setting, it has left a void for the treatment of patients with advanced disease who have failed osimertinib.
New resistance mechanisms continue to be identified
One of the most common sets of resistance mutations are insertions in exon 20 of the EGF receptor gene. These are a heterogenous group of mutations, many of which do not respond to first-, second-, or third-generation TKIs. Some, such as EGFR-A763_Y764insFQEA, may be sensitive to first- and third-generation EGFR TKIs. Other drugs targeting exon 20 insertion mutations are under development.
Newly approved by the FDA within the last year are mobocertinib and CLN-081 for adult patients with locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations.
Savolitinib is a receptor tyrosine kinase (MET) inhibitor currently under development for NSCLC and other cancers. Amivantamab-vmjw was approved by the FDA last year for metastatic NSCLC. It targets EGF and MET receptors in patients with EGFR exon 20 insertion mutations.
We finally have approved drugs for exon 20 insertions and c-Met amplification, even though their approvals are based on small, single arm studies with no definitive claims of improved efficacy over older therapies. as in my patient described in this article.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Shortly after osimertinib was approved for patients with non–small cell lung cancer in 2020 by the Food and Drug Administration, a patient came to me with increasing shortness of breath. He had been on erlotinib (Tarceva) for about 2 years and had done well. Nearly all of his pulmonary lesions had resolved and he was feeling well. He enjoyed boating in the summer and visiting grandkids in California in the winter. However, on this day, it was different. He was losing weight; he was tired and didn’t feel strong enough to put his boat in the water that spring. Long story short: We ordered a CT scan and all of his lesions were progressing. Since osimertinib had just been approved, we got a second biopsy, hoping that his insurance would pay for it. It did and sure enough, a new T790M mutation was present. He was on osimertinib for another 2 years before progressing and starting chemotherapy.
Second biopsies increasingly routine
The practice of ordering a second biopsy for patients with non–small cell lung carcinoma (NSCLC) was not common practice until after 2015 when the Food and Drug Administration approved gefitinib, a tyrosine kinase inhibitor (TKI) for patients whose tumors have epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations.
Up until then, second biopsies were not routinely done for lung cancers. But with the advent of targeted therapy and new drugs designed specifically to tackle first- and second-line treatment resistance mutations, rebiopsies have become a necessity for patients with progressive disease.
Epidermal growth factors, including HER2, ErbB2, and MET, are receptors of tyrosine kinases that control cell growth, but when in overdrive, they can lead to the development of cancers, including lung adenocarcinoma, conventional glioblastoma multiforme, glioblastoma, colon adenocarcinoma, and NSCLC.
EGFRs date back to 1962 with their discovery by Stanley Cohen. The discovery was so important that in 1986, Mr. Cohen was awarded the Nobel Prize in physiology or medicine for the discovery along with Rita Levi-Montalcini.
Now, many years later, we finally have a string of new approvals for mutations in the EGF family of receptors and several under study.
Sensitizing mutations
The more commonly used strategy for blocking EGFR signaling in lung cancer is the use of tyrosine kinase inhibitors, which compete with adenosine triphosphate (ATP) for binding to the tyrosine kinase portion of the receptor. They are located at chromosome 7p11.2. The most frequent mutations that sensitize patients to EGFR inhibitors include exon 19 deletions and L858R point mutation in exon 21, although multiple other driver mutations also exist.
The first-generation of EGFR TKIs include gefitinib and erlotinib, which bind reversibly to the EGF receptor. Second-generation inhibitors afatinib and dacomitinib bind irreversibly. Osimertinib, a third-generation EGFR TKI, which also binds irreversibly, was approved in 2020 for adjuvant therapy, and first- and second-line treatment in patients with NSCLC who have EGFR mutation–positive disease.
First-generation EGFR tyrosine kinase inhibitors
Four randomized, first-line, placebo-controlled phase 3 trials conducted with EGFR TKIs in combination with platinum-based doublet chemotherapy in an EGFR nonselected patient population failed to show a survival benefit with erlotinib or gefitinib (TRIBUTE, Tarceva Lung Cancer Investigation Trial, INTACT 1, INTACT 2).
However, a first-line study randomized patients to gefitinib or chemotherapy with carboplatin-paclitaxel, and included patients with or without an EGFR mutations. In the subgroup of patients with an EGFR mutation, progression-free survival (PFS) was significantly longer among those who received gefitinib than among those who received carboplatin–paclitaxel (hazard ratio for progression or death, 0.48), whereas in the subgroup of patients who were negative for the mutation, PFS was significantly longer among those who received chemotherapy (HR for progression or death with gefitinib, 2.85).
Numerous studies have shown that EGFR TKIs used in the first-line setting improved progression free survival, response rates, and quality of life while reducing toxicity. A recent meta-analysis of randomized clinical trials involving EGFR TKIs showed that EGFR TKI improved PFS with a HR of 0.40, compared with standard chemotherapy with fewer serious adverse events, although no benefit on overall survival was observed (HR, 0.96; 95% confidence interval, 0.83-1.10; P = .556).
T790M: The most common resistance mutation
T790M is the most common resistance mechanism to develop in patients with EGFR mutations being treated with EGFR TKIs. A randomized phase 3 trial of osimertinib vs. chemotherapy in patients with T790M-positive advanced NSCLC who had disease progression after first-line EGFR-TKI therapy, reported a median duration of progression-free survival that was significantly longer with osimertinib than with platinum therapy plus pemetrexed (10.1 months vs. 4.4 months; HR, 0.30). In addition, among 144 patients with metastases to the central nervous system, the median duration of PFS was longer among patients receiving osimertinib than among those receiving platinum therapy plus pemetrexed (8.5 months vs. 4.2 months; HR, 0.32). However, now that osimertinib has moved into the front-line setting, it has left a void for the treatment of patients with advanced disease who have failed osimertinib.
New resistance mechanisms continue to be identified
One of the most common sets of resistance mutations are insertions in exon 20 of the EGF receptor gene. These are a heterogenous group of mutations, many of which do not respond to first-, second-, or third-generation TKIs. Some, such as EGFR-A763_Y764insFQEA, may be sensitive to first- and third-generation EGFR TKIs. Other drugs targeting exon 20 insertion mutations are under development.
Newly approved by the FDA within the last year are mobocertinib and CLN-081 for adult patients with locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations.
Savolitinib is a receptor tyrosine kinase (MET) inhibitor currently under development for NSCLC and other cancers. Amivantamab-vmjw was approved by the FDA last year for metastatic NSCLC. It targets EGF and MET receptors in patients with EGFR exon 20 insertion mutations.
We finally have approved drugs for exon 20 insertions and c-Met amplification, even though their approvals are based on small, single arm studies with no definitive claims of improved efficacy over older therapies. as in my patient described in this article.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Shortly after osimertinib was approved for patients with non–small cell lung cancer in 2020 by the Food and Drug Administration, a patient came to me with increasing shortness of breath. He had been on erlotinib (Tarceva) for about 2 years and had done well. Nearly all of his pulmonary lesions had resolved and he was feeling well. He enjoyed boating in the summer and visiting grandkids in California in the winter. However, on this day, it was different. He was losing weight; he was tired and didn’t feel strong enough to put his boat in the water that spring. Long story short: We ordered a CT scan and all of his lesions were progressing. Since osimertinib had just been approved, we got a second biopsy, hoping that his insurance would pay for it. It did and sure enough, a new T790M mutation was present. He was on osimertinib for another 2 years before progressing and starting chemotherapy.
Second biopsies increasingly routine
The practice of ordering a second biopsy for patients with non–small cell lung carcinoma (NSCLC) was not common practice until after 2015 when the Food and Drug Administration approved gefitinib, a tyrosine kinase inhibitor (TKI) for patients whose tumors have epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations.
Up until then, second biopsies were not routinely done for lung cancers. But with the advent of targeted therapy and new drugs designed specifically to tackle first- and second-line treatment resistance mutations, rebiopsies have become a necessity for patients with progressive disease.
Epidermal growth factors, including HER2, ErbB2, and MET, are receptors of tyrosine kinases that control cell growth, but when in overdrive, they can lead to the development of cancers, including lung adenocarcinoma, conventional glioblastoma multiforme, glioblastoma, colon adenocarcinoma, and NSCLC.
EGFRs date back to 1962 with their discovery by Stanley Cohen. The discovery was so important that in 1986, Mr. Cohen was awarded the Nobel Prize in physiology or medicine for the discovery along with Rita Levi-Montalcini.
Now, many years later, we finally have a string of new approvals for mutations in the EGF family of receptors and several under study.
Sensitizing mutations
The more commonly used strategy for blocking EGFR signaling in lung cancer is the use of tyrosine kinase inhibitors, which compete with adenosine triphosphate (ATP) for binding to the tyrosine kinase portion of the receptor. They are located at chromosome 7p11.2. The most frequent mutations that sensitize patients to EGFR inhibitors include exon 19 deletions and L858R point mutation in exon 21, although multiple other driver mutations also exist.
The first-generation of EGFR TKIs include gefitinib and erlotinib, which bind reversibly to the EGF receptor. Second-generation inhibitors afatinib and dacomitinib bind irreversibly. Osimertinib, a third-generation EGFR TKI, which also binds irreversibly, was approved in 2020 for adjuvant therapy, and first- and second-line treatment in patients with NSCLC who have EGFR mutation–positive disease.
First-generation EGFR tyrosine kinase inhibitors
Four randomized, first-line, placebo-controlled phase 3 trials conducted with EGFR TKIs in combination with platinum-based doublet chemotherapy in an EGFR nonselected patient population failed to show a survival benefit with erlotinib or gefitinib (TRIBUTE, Tarceva Lung Cancer Investigation Trial, INTACT 1, INTACT 2).
However, a first-line study randomized patients to gefitinib or chemotherapy with carboplatin-paclitaxel, and included patients with or without an EGFR mutations. In the subgroup of patients with an EGFR mutation, progression-free survival (PFS) was significantly longer among those who received gefitinib than among those who received carboplatin–paclitaxel (hazard ratio for progression or death, 0.48), whereas in the subgroup of patients who were negative for the mutation, PFS was significantly longer among those who received chemotherapy (HR for progression or death with gefitinib, 2.85).
Numerous studies have shown that EGFR TKIs used in the first-line setting improved progression free survival, response rates, and quality of life while reducing toxicity. A recent meta-analysis of randomized clinical trials involving EGFR TKIs showed that EGFR TKI improved PFS with a HR of 0.40, compared with standard chemotherapy with fewer serious adverse events, although no benefit on overall survival was observed (HR, 0.96; 95% confidence interval, 0.83-1.10; P = .556).
T790M: The most common resistance mutation
T790M is the most common resistance mechanism to develop in patients with EGFR mutations being treated with EGFR TKIs. A randomized phase 3 trial of osimertinib vs. chemotherapy in patients with T790M-positive advanced NSCLC who had disease progression after first-line EGFR-TKI therapy, reported a median duration of progression-free survival that was significantly longer with osimertinib than with platinum therapy plus pemetrexed (10.1 months vs. 4.4 months; HR, 0.30). In addition, among 144 patients with metastases to the central nervous system, the median duration of PFS was longer among patients receiving osimertinib than among those receiving platinum therapy plus pemetrexed (8.5 months vs. 4.2 months; HR, 0.32). However, now that osimertinib has moved into the front-line setting, it has left a void for the treatment of patients with advanced disease who have failed osimertinib.
New resistance mechanisms continue to be identified
One of the most common sets of resistance mutations are insertions in exon 20 of the EGF receptor gene. These are a heterogenous group of mutations, many of which do not respond to first-, second-, or third-generation TKIs. Some, such as EGFR-A763_Y764insFQEA, may be sensitive to first- and third-generation EGFR TKIs. Other drugs targeting exon 20 insertion mutations are under development.
Newly approved by the FDA within the last year are mobocertinib and CLN-081 for adult patients with locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations.
Savolitinib is a receptor tyrosine kinase (MET) inhibitor currently under development for NSCLC and other cancers. Amivantamab-vmjw was approved by the FDA last year for metastatic NSCLC. It targets EGF and MET receptors in patients with EGFR exon 20 insertion mutations.
We finally have approved drugs for exon 20 insertions and c-Met amplification, even though their approvals are based on small, single arm studies with no definitive claims of improved efficacy over older therapies. as in my patient described in this article.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Could a vaccine (and more) fix the fentanyl crisis?
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
Is exercise effective for constipation?
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
The role of repeat uterine curettage in postmolar gestational trophoblastic neoplasia
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
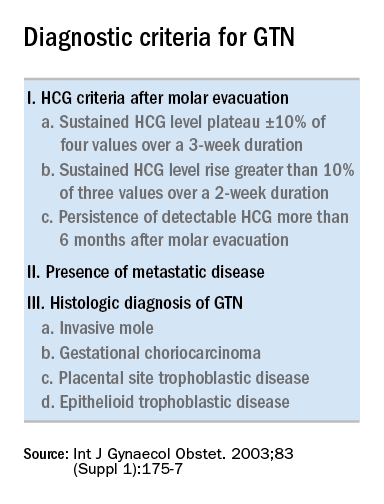
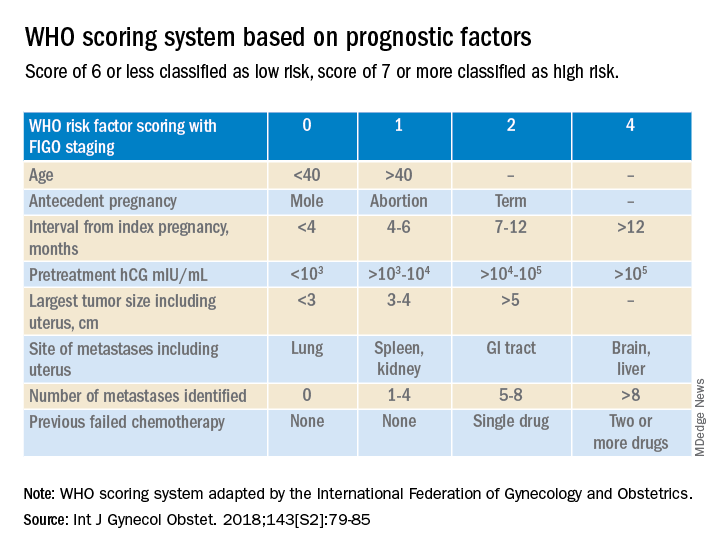
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
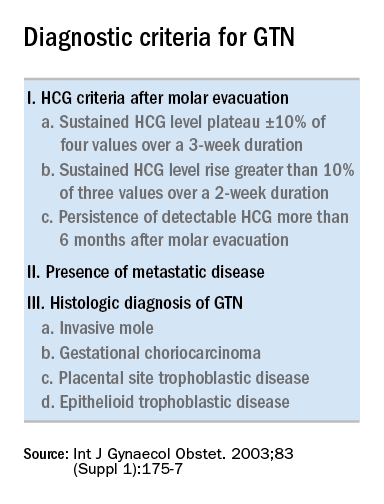
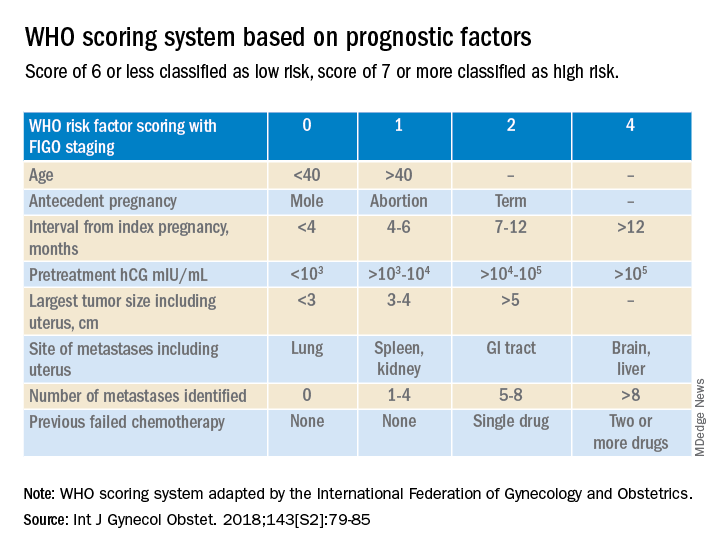
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
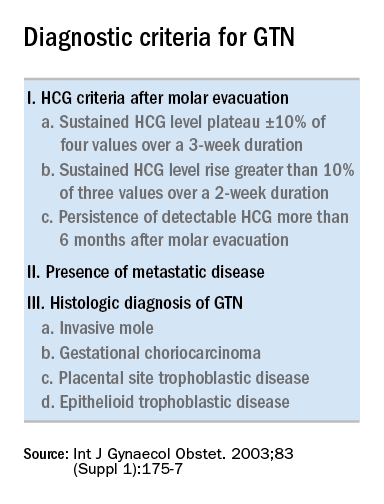
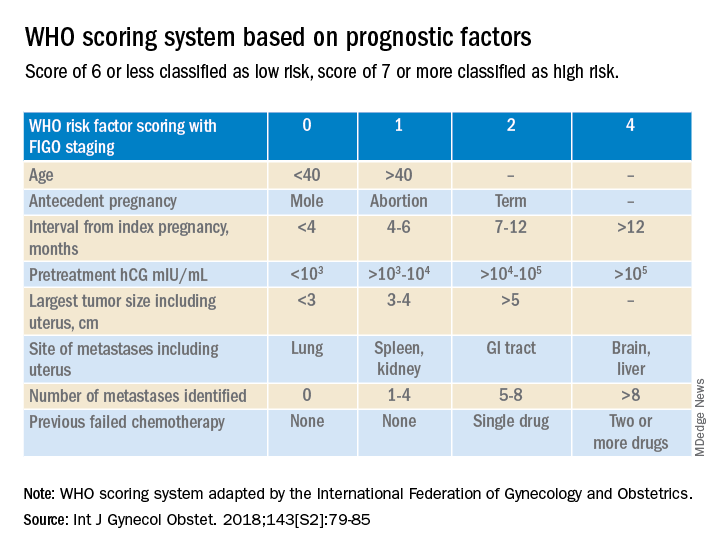
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.







