User login
DDW® 2018 general registration is now open
General registration and housing for Digestive Disease Week® (DDW) 2018 are now open. Registering during the early-bird period (until April 18) guarantees a savings of at least $80 on your registration.
Why DDW?
Just as monumental as this year’s host city, Washington, D.C., DDW is the premier meeting for GI professionals. Come to DDW 2018, taking place June 2-5, to:
- • Choose from an extensive program of high-quality education presented in a variety of learning formats.
- • Explore research unveiled in more than 4,000 poster presentations and over 1,000 abstract presentations.
- • Network and share capital ideas with more than 14,000 other attendees from around the world.
- • Browse an extensive Exhibit Hall featuring the latest products and services in gastroenterology and related fields.
Whether your area of expertise is in patient care, research, education, or administration, DDW has something for you. Register today
General registration and housing for Digestive Disease Week® (DDW) 2018 are now open. Registering during the early-bird period (until April 18) guarantees a savings of at least $80 on your registration.
Why DDW?
Just as monumental as this year’s host city, Washington, D.C., DDW is the premier meeting for GI professionals. Come to DDW 2018, taking place June 2-5, to:
- • Choose from an extensive program of high-quality education presented in a variety of learning formats.
- • Explore research unveiled in more than 4,000 poster presentations and over 1,000 abstract presentations.
- • Network and share capital ideas with more than 14,000 other attendees from around the world.
- • Browse an extensive Exhibit Hall featuring the latest products and services in gastroenterology and related fields.
Whether your area of expertise is in patient care, research, education, or administration, DDW has something for you. Register today
General registration and housing for Digestive Disease Week® (DDW) 2018 are now open. Registering during the early-bird period (until April 18) guarantees a savings of at least $80 on your registration.
Why DDW?
Just as monumental as this year’s host city, Washington, D.C., DDW is the premier meeting for GI professionals. Come to DDW 2018, taking place June 2-5, to:
- • Choose from an extensive program of high-quality education presented in a variety of learning formats.
- • Explore research unveiled in more than 4,000 poster presentations and over 1,000 abstract presentations.
- • Network and share capital ideas with more than 14,000 other attendees from around the world.
- • Browse an extensive Exhibit Hall featuring the latest products and services in gastroenterology and related fields.
Whether your area of expertise is in patient care, research, education, or administration, DDW has something for you. Register today
AGA’s Fecal Microbiota Transplantation National Registry enrolls first patient
The AGA Fecal Microbiota Transplantation (FMT) National Registry is officially underway! The first patient enrolled in the FMT National Registry received a fecal transplant through the Gastroenterology Center of Connecticut/Medical Research Center of Connecticut by Paul Feuerstadt, MD. The patient being treated had experienced multiple recurrences of C. difficile infection. As part of the registry, Dr. Feuerstadt will follow up with the patient four times over the next 2 years and report back on the patient’s health post-FMT. The patient will also provide yearly reports for up to 10 years.
The AGA FMT National Registry, a program of the AGA Center for Gut Microbiome Research and Education, was established in August 2016 after receiving funding from the National Institute of Allergy and Infectious Diseases (NIAID) of the NIH (award number R24AI118629). The registry aims to enroll 75 sites and track 4,000 patients for 5-10 years after their FMT procedure. The data collected from this registry will guide physicians in determining when to use FMT on their patients and will provide much-needed information on the potential risks associated with stool transplants.
If you’re interested in participating in the registry, email [email protected].
New registry collaborators
AGA will collaborate with the American Gut Project – an academic effort run by the laboratory of Rob Knight, PhD, professor and director of the Center for Microbiome Innovation at the University of California, San Diego – to build a biobank of stool samples from participants in the FMT National Registry. American Gut will receive stool samples from registry participants before and after their FMT. The microbiota will be sequenced in each sample, and remaining material will be frozen to be made available for future research. Eventually, this information could help doctors screen and select the best donor samples for individual patients.
AGA will also collaborate with OpenBiome, a public stool bank and nonprofit research organization that provides clinicians with rigorously screened, ready-to-use stool preparations for fecal transplant procedures. As the only public stool bank in the country, OpenBiome serves as the source of stool preparations for nearly 1,000 clinical partners performing FMT across the U.S. For patients enrolled in the registry who receive OpenBiome FMT material, OpenBiome will provide screening information and samples to support the registry’s research analyses. Learn more at www.gastro.org/FMTRegistry.
The AGA Fecal Microbiota Transplantation (FMT) National Registry is officially underway! The first patient enrolled in the FMT National Registry received a fecal transplant through the Gastroenterology Center of Connecticut/Medical Research Center of Connecticut by Paul Feuerstadt, MD. The patient being treated had experienced multiple recurrences of C. difficile infection. As part of the registry, Dr. Feuerstadt will follow up with the patient four times over the next 2 years and report back on the patient’s health post-FMT. The patient will also provide yearly reports for up to 10 years.
The AGA FMT National Registry, a program of the AGA Center for Gut Microbiome Research and Education, was established in August 2016 after receiving funding from the National Institute of Allergy and Infectious Diseases (NIAID) of the NIH (award number R24AI118629). The registry aims to enroll 75 sites and track 4,000 patients for 5-10 years after their FMT procedure. The data collected from this registry will guide physicians in determining when to use FMT on their patients and will provide much-needed information on the potential risks associated with stool transplants.
If you’re interested in participating in the registry, email [email protected].
New registry collaborators
AGA will collaborate with the American Gut Project – an academic effort run by the laboratory of Rob Knight, PhD, professor and director of the Center for Microbiome Innovation at the University of California, San Diego – to build a biobank of stool samples from participants in the FMT National Registry. American Gut will receive stool samples from registry participants before and after their FMT. The microbiota will be sequenced in each sample, and remaining material will be frozen to be made available for future research. Eventually, this information could help doctors screen and select the best donor samples for individual patients.
AGA will also collaborate with OpenBiome, a public stool bank and nonprofit research organization that provides clinicians with rigorously screened, ready-to-use stool preparations for fecal transplant procedures. As the only public stool bank in the country, OpenBiome serves as the source of stool preparations for nearly 1,000 clinical partners performing FMT across the U.S. For patients enrolled in the registry who receive OpenBiome FMT material, OpenBiome will provide screening information and samples to support the registry’s research analyses. Learn more at www.gastro.org/FMTRegistry.
The AGA Fecal Microbiota Transplantation (FMT) National Registry is officially underway! The first patient enrolled in the FMT National Registry received a fecal transplant through the Gastroenterology Center of Connecticut/Medical Research Center of Connecticut by Paul Feuerstadt, MD. The patient being treated had experienced multiple recurrences of C. difficile infection. As part of the registry, Dr. Feuerstadt will follow up with the patient four times over the next 2 years and report back on the patient’s health post-FMT. The patient will also provide yearly reports for up to 10 years.
The AGA FMT National Registry, a program of the AGA Center for Gut Microbiome Research and Education, was established in August 2016 after receiving funding from the National Institute of Allergy and Infectious Diseases (NIAID) of the NIH (award number R24AI118629). The registry aims to enroll 75 sites and track 4,000 patients for 5-10 years after their FMT procedure. The data collected from this registry will guide physicians in determining when to use FMT on their patients and will provide much-needed information on the potential risks associated with stool transplants.
If you’re interested in participating in the registry, email [email protected].
New registry collaborators
AGA will collaborate with the American Gut Project – an academic effort run by the laboratory of Rob Knight, PhD, professor and director of the Center for Microbiome Innovation at the University of California, San Diego – to build a biobank of stool samples from participants in the FMT National Registry. American Gut will receive stool samples from registry participants before and after their FMT. The microbiota will be sequenced in each sample, and remaining material will be frozen to be made available for future research. Eventually, this information could help doctors screen and select the best donor samples for individual patients.
AGA will also collaborate with OpenBiome, a public stool bank and nonprofit research organization that provides clinicians with rigorously screened, ready-to-use stool preparations for fecal transplant procedures. As the only public stool bank in the country, OpenBiome serves as the source of stool preparations for nearly 1,000 clinical partners performing FMT across the U.S. For patients enrolled in the registry who receive OpenBiome FMT material, OpenBiome will provide screening information and samples to support the registry’s research analyses. Learn more at www.gastro.org/FMTRegistry.
Support GI Research through the AGA Research Foundation
The way we diagnose and treat patients is thanks to years of research. Decades of research and discoveries by dedicated investigators have revolutionized the care of many digestive disease patients. As the charitable arm of the American Gastroenterological Association (AGA), the AGA Research Foundation contributes to this tradition of discovery.
Federal research funding is at risk. Promising early-stage investigators find it increasingly difficult to secure funding and many leave the field because they are unable to sustain a research career. The foundation provides a key source of funding at a critical juncture in a young investigator’s career.
“As a clinical researcher, funding for investigation is critical in scientific breakthroughs to promote more efficient and robust patient care. My project will provide novel insights into the role of distensibility in the treatment of patients with esophageal eosinophilia, potentially resulting in more efficient treatment selection and disease management.”
By joining others in donating to the AGA Research Foundation, you can help fill the funding gap and protect the next generation of investigators.
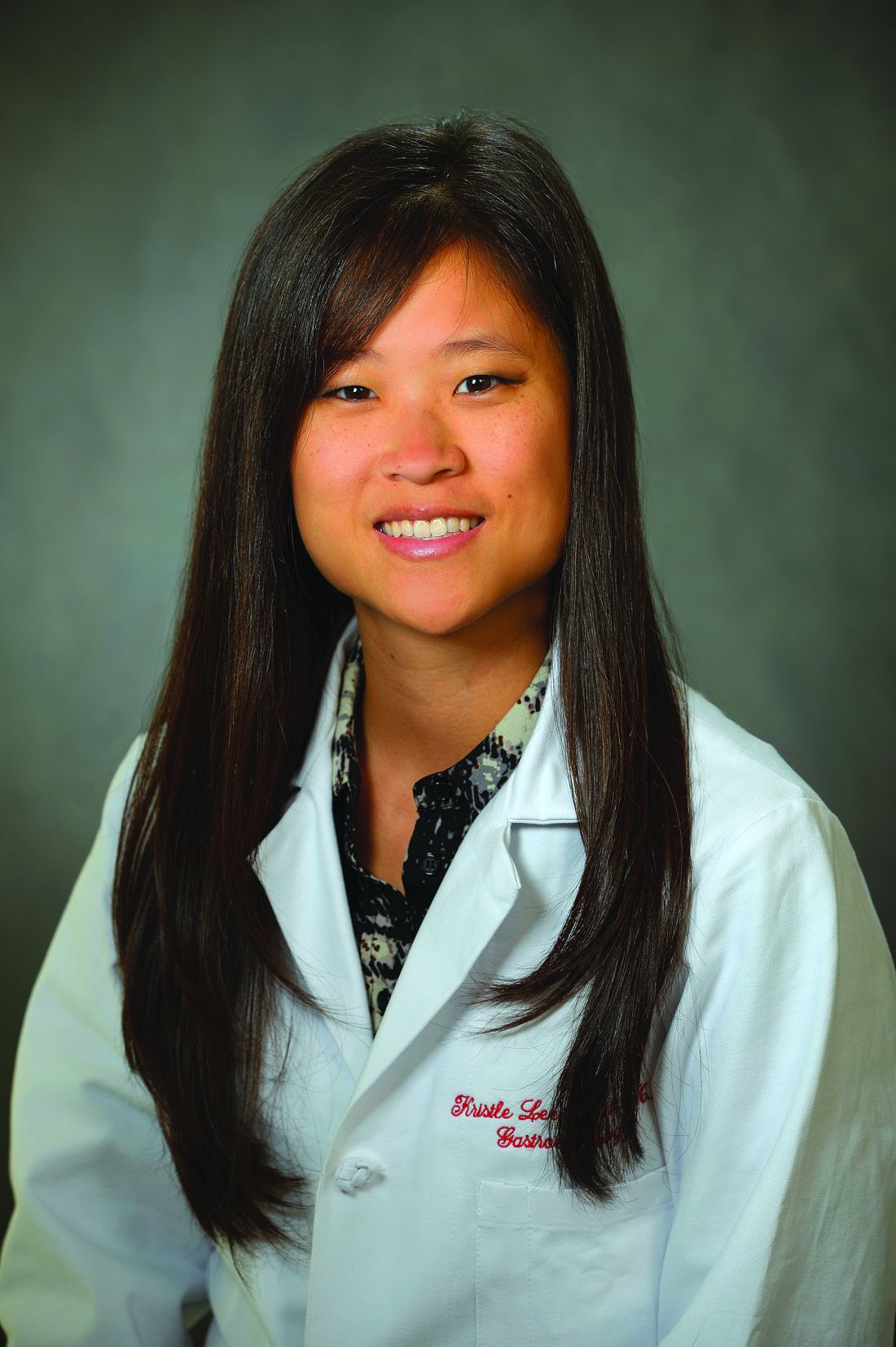
Your tax-deductible donation will make a critical difference in retaining talented GI scientists, like Dr. Kristle Lynch, whose research will impact the future care of patients.
Donate on the foundation’s website at www.gastro.org/donateonline or by mail to 4930 Del Ray Avenue, Bethesda, MD 20814.
The way we diagnose and treat patients is thanks to years of research. Decades of research and discoveries by dedicated investigators have revolutionized the care of many digestive disease patients. As the charitable arm of the American Gastroenterological Association (AGA), the AGA Research Foundation contributes to this tradition of discovery.
Federal research funding is at risk. Promising early-stage investigators find it increasingly difficult to secure funding and many leave the field because they are unable to sustain a research career. The foundation provides a key source of funding at a critical juncture in a young investigator’s career.
“As a clinical researcher, funding for investigation is critical in scientific breakthroughs to promote more efficient and robust patient care. My project will provide novel insights into the role of distensibility in the treatment of patients with esophageal eosinophilia, potentially resulting in more efficient treatment selection and disease management.”
By joining others in donating to the AGA Research Foundation, you can help fill the funding gap and protect the next generation of investigators.
Your tax-deductible donation will make a critical difference in retaining talented GI scientists, like Dr. Kristle Lynch, whose research will impact the future care of patients.
Donate on the foundation’s website at www.gastro.org/donateonline or by mail to 4930 Del Ray Avenue, Bethesda, MD 20814.
The way we diagnose and treat patients is thanks to years of research. Decades of research and discoveries by dedicated investigators have revolutionized the care of many digestive disease patients. As the charitable arm of the American Gastroenterological Association (AGA), the AGA Research Foundation contributes to this tradition of discovery.
Federal research funding is at risk. Promising early-stage investigators find it increasingly difficult to secure funding and many leave the field because they are unable to sustain a research career. The foundation provides a key source of funding at a critical juncture in a young investigator’s career.
“As a clinical researcher, funding for investigation is critical in scientific breakthroughs to promote more efficient and robust patient care. My project will provide novel insights into the role of distensibility in the treatment of patients with esophageal eosinophilia, potentially resulting in more efficient treatment selection and disease management.”
By joining others in donating to the AGA Research Foundation, you can help fill the funding gap and protect the next generation of investigators.
Your tax-deductible donation will make a critical difference in retaining talented GI scientists, like Dr. Kristle Lynch, whose research will impact the future care of patients.
Donate on the foundation’s website at www.gastro.org/donateonline or by mail to 4930 Del Ray Avenue, Bethesda, MD 20814.
Tough patient cases from 2017
AGA’s member-only online networking platform, the AGA Community, was the hub for clinical case scenarios in 2017. About 100 deidentified patient cases were submitted to the forum, generating over 475 private and public responses from your peers.
Here is a summary of the three cases that sparked the most discussion among AGA members. You can view all discussions in the forum at community.gastro.org/discussions.
#3 “Esophageal hyperkeratosis” (February 2017)
Patient scenario: Patient was having dysphagia. EGD showed circumferential thickening of esophageal lining in the lower half of the esophagus causing partial obstruction; lumen diameter was 7 mm (scope was able to pass with mild resistance). Human papillomavirus (HPV) stain was negative. Multiple biopsies were negative for malignancy, so the practice did not recommend esophagectomy and believed the symptoms were consistent with hyperkeratosis of esophagus. Endoscopic cryotherapy was being considered.
Question: Has anyone come across a case like this?
#2 Thickened stomach (May 2017)
Patient scenario: A 74-year-old male presented early satiety, anemia, and dyspepsia. EGD showed diffuse moderate erythema of the stomach sparing the antrum, and two small superficial duodenal ulcers. Biopsies showed mild chronic inflammation, duodenitis, and negative for H. pylori. The patient was started on a proton pump inhibitor (PPI).
One month later, patient reported early satiety, a 40-pound weight loss over last few months, nausea and vomiting, with minimal improvement while using the PPI. A CT scan of the abdomen and pelvis showed diffuse thickening of the stomach, but was otherwise unremarkable.
One month after that, a repeated EGD showed moderate erythema with enlarged gastric folds, cobblestone of mucosa, again all sparing the antrum. The colonoscopy results were unremarkable. Gastric biopsies showed mild chronic inflammation. Endoscopic ultrasound showed a thickened gastric wall to 14 mm (normal 5 mm) and fine needle aspiration showed normal gastric foveolar epithelium. The patient received a PEG-J tube to maintain nutrition, and then had a laparoscopic assisted full thickness gastric biopsy, which showed benign hypertrophic gastric smooth muscle tissue.
Serum protein electrophoresis and urine protein electrophoresis test results were normal, with total IgG and IgA normal, total IgM low at 31 (normal 60-265), albumin low, other proteins normal, and immunofixation negative. Prealbumin was low at 5 (normal 15-45). Albumin initially normal and over a couple of days low at 2.6 (normal 3.4-5.0). Total protein initially normal and over a couple of days was low at 6.3 (normal 6.8-8.8). Gastrin level was insignificant on the PPI, in the 400s. Zollinger Ellison gastrin not impressive, and the patient is HIV negative.
Question: With a negative biopsy and other test results, Menetrier’s, malignancy, sarcoidosis, eosinophilic gastroenteritis, and amyloidosis can be ruled out. What could the diagnosis be?
#1 IBD and prior hep B (July 2017)
Patient scenario: A 53-year-old male diagnosed with ulcerative colitis (UC) at outside hospital after presenting with abdominal pain, perforation of sigmoid colon. He underwent total colectomy with ileostomy, which showed he has remnant rectum, and the path of colon showed UC with sigmoid stricture. There is no malignancy or dysplasia, and the terminal ileum included in the resection was normal. He had complicated post-op course with enterocutaneous fistula.
He underwent takedown of ileostomy, small bowel resection and ileostomy revision. Path showed segmental small bowel showing viable mucosa with acute serositis and serial adhesions. Ileal mucosa was normal. Rectum has inflammation, and he has symptoms of mucus, urgency, and blood. He had rectal burning and did not tolerate CANASA® suppository. He did not seem to improve with hydrocortisone suppository either.
In trying to decipher next treatment step, hepatitis panel was done, which showed positive hepatitis B core antibody (IgM). Hepatitis B viral load was undetectable. Hepatitis B surface antibody test (HBsAb) quantitative was 6 (not quite the range for immunity of greater than 10). Hepatitis B “e” antigen (HBeAg) negative and hepatitis B “e” antibody (HBeAb) positive. This patient’s hep B core total was positive and hep B surface antigen was negative.
Question: How would you treat this patient? Would you use Imuran?
Share your difficult patient case for the GI community to help you solve at community.gastro.org/quickpost.
AGA’s member-only online networking platform, the AGA Community, was the hub for clinical case scenarios in 2017. About 100 deidentified patient cases were submitted to the forum, generating over 475 private and public responses from your peers.
Here is a summary of the three cases that sparked the most discussion among AGA members. You can view all discussions in the forum at community.gastro.org/discussions.
#3 “Esophageal hyperkeratosis” (February 2017)
Patient scenario: Patient was having dysphagia. EGD showed circumferential thickening of esophageal lining in the lower half of the esophagus causing partial obstruction; lumen diameter was 7 mm (scope was able to pass with mild resistance). Human papillomavirus (HPV) stain was negative. Multiple biopsies were negative for malignancy, so the practice did not recommend esophagectomy and believed the symptoms were consistent with hyperkeratosis of esophagus. Endoscopic cryotherapy was being considered.
Question: Has anyone come across a case like this?
#2 Thickened stomach (May 2017)
Patient scenario: A 74-year-old male presented early satiety, anemia, and dyspepsia. EGD showed diffuse moderate erythema of the stomach sparing the antrum, and two small superficial duodenal ulcers. Biopsies showed mild chronic inflammation, duodenitis, and negative for H. pylori. The patient was started on a proton pump inhibitor (PPI).
One month later, patient reported early satiety, a 40-pound weight loss over last few months, nausea and vomiting, with minimal improvement while using the PPI. A CT scan of the abdomen and pelvis showed diffuse thickening of the stomach, but was otherwise unremarkable.
One month after that, a repeated EGD showed moderate erythema with enlarged gastric folds, cobblestone of mucosa, again all sparing the antrum. The colonoscopy results were unremarkable. Gastric biopsies showed mild chronic inflammation. Endoscopic ultrasound showed a thickened gastric wall to 14 mm (normal 5 mm) and fine needle aspiration showed normal gastric foveolar epithelium. The patient received a PEG-J tube to maintain nutrition, and then had a laparoscopic assisted full thickness gastric biopsy, which showed benign hypertrophic gastric smooth muscle tissue.
Serum protein electrophoresis and urine protein electrophoresis test results were normal, with total IgG and IgA normal, total IgM low at 31 (normal 60-265), albumin low, other proteins normal, and immunofixation negative. Prealbumin was low at 5 (normal 15-45). Albumin initially normal and over a couple of days low at 2.6 (normal 3.4-5.0). Total protein initially normal and over a couple of days was low at 6.3 (normal 6.8-8.8). Gastrin level was insignificant on the PPI, in the 400s. Zollinger Ellison gastrin not impressive, and the patient is HIV negative.
Question: With a negative biopsy and other test results, Menetrier’s, malignancy, sarcoidosis, eosinophilic gastroenteritis, and amyloidosis can be ruled out. What could the diagnosis be?
#1 IBD and prior hep B (July 2017)
Patient scenario: A 53-year-old male diagnosed with ulcerative colitis (UC) at outside hospital after presenting with abdominal pain, perforation of sigmoid colon. He underwent total colectomy with ileostomy, which showed he has remnant rectum, and the path of colon showed UC with sigmoid stricture. There is no malignancy or dysplasia, and the terminal ileum included in the resection was normal. He had complicated post-op course with enterocutaneous fistula.
He underwent takedown of ileostomy, small bowel resection and ileostomy revision. Path showed segmental small bowel showing viable mucosa with acute serositis and serial adhesions. Ileal mucosa was normal. Rectum has inflammation, and he has symptoms of mucus, urgency, and blood. He had rectal burning and did not tolerate CANASA® suppository. He did not seem to improve with hydrocortisone suppository either.
In trying to decipher next treatment step, hepatitis panel was done, which showed positive hepatitis B core antibody (IgM). Hepatitis B viral load was undetectable. Hepatitis B surface antibody test (HBsAb) quantitative was 6 (not quite the range for immunity of greater than 10). Hepatitis B “e” antigen (HBeAg) negative and hepatitis B “e” antibody (HBeAb) positive. This patient’s hep B core total was positive and hep B surface antigen was negative.
Question: How would you treat this patient? Would you use Imuran?
Share your difficult patient case for the GI community to help you solve at community.gastro.org/quickpost.
AGA’s member-only online networking platform, the AGA Community, was the hub for clinical case scenarios in 2017. About 100 deidentified patient cases were submitted to the forum, generating over 475 private and public responses from your peers.
Here is a summary of the three cases that sparked the most discussion among AGA members. You can view all discussions in the forum at community.gastro.org/discussions.
#3 “Esophageal hyperkeratosis” (February 2017)
Patient scenario: Patient was having dysphagia. EGD showed circumferential thickening of esophageal lining in the lower half of the esophagus causing partial obstruction; lumen diameter was 7 mm (scope was able to pass with mild resistance). Human papillomavirus (HPV) stain was negative. Multiple biopsies were negative for malignancy, so the practice did not recommend esophagectomy and believed the symptoms were consistent with hyperkeratosis of esophagus. Endoscopic cryotherapy was being considered.
Question: Has anyone come across a case like this?
#2 Thickened stomach (May 2017)
Patient scenario: A 74-year-old male presented early satiety, anemia, and dyspepsia. EGD showed diffuse moderate erythema of the stomach sparing the antrum, and two small superficial duodenal ulcers. Biopsies showed mild chronic inflammation, duodenitis, and negative for H. pylori. The patient was started on a proton pump inhibitor (PPI).
One month later, patient reported early satiety, a 40-pound weight loss over last few months, nausea and vomiting, with minimal improvement while using the PPI. A CT scan of the abdomen and pelvis showed diffuse thickening of the stomach, but was otherwise unremarkable.
One month after that, a repeated EGD showed moderate erythema with enlarged gastric folds, cobblestone of mucosa, again all sparing the antrum. The colonoscopy results were unremarkable. Gastric biopsies showed mild chronic inflammation. Endoscopic ultrasound showed a thickened gastric wall to 14 mm (normal 5 mm) and fine needle aspiration showed normal gastric foveolar epithelium. The patient received a PEG-J tube to maintain nutrition, and then had a laparoscopic assisted full thickness gastric biopsy, which showed benign hypertrophic gastric smooth muscle tissue.
Serum protein electrophoresis and urine protein electrophoresis test results were normal, with total IgG and IgA normal, total IgM low at 31 (normal 60-265), albumin low, other proteins normal, and immunofixation negative. Prealbumin was low at 5 (normal 15-45). Albumin initially normal and over a couple of days low at 2.6 (normal 3.4-5.0). Total protein initially normal and over a couple of days was low at 6.3 (normal 6.8-8.8). Gastrin level was insignificant on the PPI, in the 400s. Zollinger Ellison gastrin not impressive, and the patient is HIV negative.
Question: With a negative biopsy and other test results, Menetrier’s, malignancy, sarcoidosis, eosinophilic gastroenteritis, and amyloidosis can be ruled out. What could the diagnosis be?
#1 IBD and prior hep B (July 2017)
Patient scenario: A 53-year-old male diagnosed with ulcerative colitis (UC) at outside hospital after presenting with abdominal pain, perforation of sigmoid colon. He underwent total colectomy with ileostomy, which showed he has remnant rectum, and the path of colon showed UC with sigmoid stricture. There is no malignancy or dysplasia, and the terminal ileum included in the resection was normal. He had complicated post-op course with enterocutaneous fistula.
He underwent takedown of ileostomy, small bowel resection and ileostomy revision. Path showed segmental small bowel showing viable mucosa with acute serositis and serial adhesions. Ileal mucosa was normal. Rectum has inflammation, and he has symptoms of mucus, urgency, and blood. He had rectal burning and did not tolerate CANASA® suppository. He did not seem to improve with hydrocortisone suppository either.
In trying to decipher next treatment step, hepatitis panel was done, which showed positive hepatitis B core antibody (IgM). Hepatitis B viral load was undetectable. Hepatitis B surface antibody test (HBsAb) quantitative was 6 (not quite the range for immunity of greater than 10). Hepatitis B “e” antigen (HBeAg) negative and hepatitis B “e” antibody (HBeAb) positive. This patient’s hep B core total was positive and hep B surface antigen was negative.
Question: How would you treat this patient? Would you use Imuran?
Share your difficult patient case for the GI community to help you solve at community.gastro.org/quickpost.
Insurance barriers should not hinder step therapy treatment for IBD
As part of Crohn’s and Colitis Awareness Week 2017 (Dec. 1-7), AGA participated in a congressional briefing sponsored by Takeda and the California Life Sciences Association highlighting advances in inflammatory bowel disease (IBD) therapies, as well as the barriers that patients face in receiving proper treatment for managing their disease.
Physician perspective
Michael Weinstein, MD, representing AGA and the Digestive Health Physicians Association, discussed how treatment options have changed considerably since he began practicing in the 1980s when the only treatment options were immunosuppressive drugs or high-dose steroids that led to dangerous side effects. He highlighted the burden that physicians face with prior authorization practices, especially step therapy in which a patient is required to fail several therapies before being granted coverage to the preferred, physician-prescribed therapy. These insurance protocols can have dire effects on patient care and can be very disruptive to patients who may be so ill that they cannot work or go to school. Dr. Weinstein stated that the burden step therapy places on his practice requires him to have a full-time employee just to navigate the various insurance policies. Many small practices do not have the resources to handle these burdens. Read more from Dr. Weinstein in his op-ed from The Hill.
Patient perspective
Members of Congress and congressional staff heard compelling testimony from Kate Detwiler, an IBD patient who spoke of her family history of IBD, her experience with the disease, and how disruptive it has been to find the best provider and treatments to manage her disease. She and Dr. Weinstein both stressed the financial burdens that the disease puts on families and how limiting it can be to patients who are starting out in their careers or school.
Legislator perspective
Rep. Brad Weinstrup, R-OH, and Rep. Raul Ruiz, D-CA, addressed the briefing as the lead sponsors of HR 2077, the Restoring Patient’s Voice Act, which would provide patients and providers with a clear, equitable, and transparent appeals process when subject to step therapy protocols. Both Rep. Wenstrup and Rep. Ruiz are physicians and have seen the real-life consequences of these policies and their impact on patient care. Both representatives stressed that this is a bipartisan, commonsense solution to ensuring that patients have access to the care that they need when they need it.
AGA continues to advocate for support and passage of HR 2077 and thanks those members who have contacted their members of Congress to request their support. If you haven’t already, please call on your legislator to support this legislation. We will continue to work to garner additional support for the bill in this Congress.
As part of Crohn’s and Colitis Awareness Week 2017 (Dec. 1-7), AGA participated in a congressional briefing sponsored by Takeda and the California Life Sciences Association highlighting advances in inflammatory bowel disease (IBD) therapies, as well as the barriers that patients face in receiving proper treatment for managing their disease.
Physician perspective
Michael Weinstein, MD, representing AGA and the Digestive Health Physicians Association, discussed how treatment options have changed considerably since he began practicing in the 1980s when the only treatment options were immunosuppressive drugs or high-dose steroids that led to dangerous side effects. He highlighted the burden that physicians face with prior authorization practices, especially step therapy in which a patient is required to fail several therapies before being granted coverage to the preferred, physician-prescribed therapy. These insurance protocols can have dire effects on patient care and can be very disruptive to patients who may be so ill that they cannot work or go to school. Dr. Weinstein stated that the burden step therapy places on his practice requires him to have a full-time employee just to navigate the various insurance policies. Many small practices do not have the resources to handle these burdens. Read more from Dr. Weinstein in his op-ed from The Hill.
Patient perspective
Members of Congress and congressional staff heard compelling testimony from Kate Detwiler, an IBD patient who spoke of her family history of IBD, her experience with the disease, and how disruptive it has been to find the best provider and treatments to manage her disease. She and Dr. Weinstein both stressed the financial burdens that the disease puts on families and how limiting it can be to patients who are starting out in their careers or school.
Legislator perspective
Rep. Brad Weinstrup, R-OH, and Rep. Raul Ruiz, D-CA, addressed the briefing as the lead sponsors of HR 2077, the Restoring Patient’s Voice Act, which would provide patients and providers with a clear, equitable, and transparent appeals process when subject to step therapy protocols. Both Rep. Wenstrup and Rep. Ruiz are physicians and have seen the real-life consequences of these policies and their impact on patient care. Both representatives stressed that this is a bipartisan, commonsense solution to ensuring that patients have access to the care that they need when they need it.
AGA continues to advocate for support and passage of HR 2077 and thanks those members who have contacted their members of Congress to request their support. If you haven’t already, please call on your legislator to support this legislation. We will continue to work to garner additional support for the bill in this Congress.
As part of Crohn’s and Colitis Awareness Week 2017 (Dec. 1-7), AGA participated in a congressional briefing sponsored by Takeda and the California Life Sciences Association highlighting advances in inflammatory bowel disease (IBD) therapies, as well as the barriers that patients face in receiving proper treatment for managing their disease.
Physician perspective
Michael Weinstein, MD, representing AGA and the Digestive Health Physicians Association, discussed how treatment options have changed considerably since he began practicing in the 1980s when the only treatment options were immunosuppressive drugs or high-dose steroids that led to dangerous side effects. He highlighted the burden that physicians face with prior authorization practices, especially step therapy in which a patient is required to fail several therapies before being granted coverage to the preferred, physician-prescribed therapy. These insurance protocols can have dire effects on patient care and can be very disruptive to patients who may be so ill that they cannot work or go to school. Dr. Weinstein stated that the burden step therapy places on his practice requires him to have a full-time employee just to navigate the various insurance policies. Many small practices do not have the resources to handle these burdens. Read more from Dr. Weinstein in his op-ed from The Hill.
Patient perspective
Members of Congress and congressional staff heard compelling testimony from Kate Detwiler, an IBD patient who spoke of her family history of IBD, her experience with the disease, and how disruptive it has been to find the best provider and treatments to manage her disease. She and Dr. Weinstein both stressed the financial burdens that the disease puts on families and how limiting it can be to patients who are starting out in their careers or school.
Legislator perspective
Rep. Brad Weinstrup, R-OH, and Rep. Raul Ruiz, D-CA, addressed the briefing as the lead sponsors of HR 2077, the Restoring Patient’s Voice Act, which would provide patients and providers with a clear, equitable, and transparent appeals process when subject to step therapy protocols. Both Rep. Wenstrup and Rep. Ruiz are physicians and have seen the real-life consequences of these policies and their impact on patient care. Both representatives stressed that this is a bipartisan, commonsense solution to ensuring that patients have access to the care that they need when they need it.
AGA continues to advocate for support and passage of HR 2077 and thanks those members who have contacted their members of Congress to request their support. If you haven’t already, please call on your legislator to support this legislation. We will continue to work to garner additional support for the bill in this Congress.
Registration open for DDW® 2018 and 2018 AGA Postgraduate Course
Digestive Disease Week® (DDW), taking place in Washington, D.C., June 2-5, is the gold standard digestive disease meeting. Attend to learn monumental developments in science and medicine, meet leaders in the field, network with colleagues, and attain practical takeaways that you can implement in your career. Visit www.ddw.org to register, for general meeting information, details about the host city, and much more.
On the DDW website, you can also register for the AGA Postgraduate Course taking place during DDW, June 2-3. The 2018 AGA Postgraduate Course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. At the end of the course, the take-home points will be compiled and distributed with the eSyllabus.
Digestive Disease Week® (DDW), taking place in Washington, D.C., June 2-5, is the gold standard digestive disease meeting. Attend to learn monumental developments in science and medicine, meet leaders in the field, network with colleagues, and attain practical takeaways that you can implement in your career. Visit www.ddw.org to register, for general meeting information, details about the host city, and much more.
On the DDW website, you can also register for the AGA Postgraduate Course taking place during DDW, June 2-3. The 2018 AGA Postgraduate Course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. At the end of the course, the take-home points will be compiled and distributed with the eSyllabus.
Digestive Disease Week® (DDW), taking place in Washington, D.C., June 2-5, is the gold standard digestive disease meeting. Attend to learn monumental developments in science and medicine, meet leaders in the field, network with colleagues, and attain practical takeaways that you can implement in your career. Visit www.ddw.org to register, for general meeting information, details about the host city, and much more.
On the DDW website, you can also register for the AGA Postgraduate Course taking place during DDW, June 2-3. The 2018 AGA Postgraduate Course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. At the end of the course, the take-home points will be compiled and distributed with the eSyllabus.
Memorial and honorary gifts: a special tribute
Make a tribute gift to honor someone whose life has been touched by GI research or celebrate a special occasion such as a birthday while supporting the AGA Research Awards Program through the AGA Research Foundation. A tribute gift will make your loved one feel special because it honors their passion, and also provides us with needed support in furthering basic digestive disease research.
- Giving a gift to the AGA Research Foundation in memory of a loved one. A memorial gift is a meaningful way to celebrate the legacy of a family member, friend, or colleague.
- Telling your friends and family members to donate to the AGA Research Foundation in YOUR honor.
Your next step
An honorary gift is a wonderful way to acknowledge someone’s vision for the future. To learn more about ways to recognize your honoree, visit our website at www.gastro.org/contribute or contact Harmony Excellent at 301-272-1602 or [email protected].
Make a tribute gift to honor someone whose life has been touched by GI research or celebrate a special occasion such as a birthday while supporting the AGA Research Awards Program through the AGA Research Foundation. A tribute gift will make your loved one feel special because it honors their passion, and also provides us with needed support in furthering basic digestive disease research.
- Giving a gift to the AGA Research Foundation in memory of a loved one. A memorial gift is a meaningful way to celebrate the legacy of a family member, friend, or colleague.
- Telling your friends and family members to donate to the AGA Research Foundation in YOUR honor.
Your next step
An honorary gift is a wonderful way to acknowledge someone’s vision for the future. To learn more about ways to recognize your honoree, visit our website at www.gastro.org/contribute or contact Harmony Excellent at 301-272-1602 or [email protected].
Make a tribute gift to honor someone whose life has been touched by GI research or celebrate a special occasion such as a birthday while supporting the AGA Research Awards Program through the AGA Research Foundation. A tribute gift will make your loved one feel special because it honors their passion, and also provides us with needed support in furthering basic digestive disease research.
- Giving a gift to the AGA Research Foundation in memory of a loved one. A memorial gift is a meaningful way to celebrate the legacy of a family member, friend, or colleague.
- Telling your friends and family members to donate to the AGA Research Foundation in YOUR honor.
Your next step
An honorary gift is a wonderful way to acknowledge someone’s vision for the future. To learn more about ways to recognize your honoree, visit our website at www.gastro.org/contribute or contact Harmony Excellent at 301-272-1602 or [email protected].
The New Gastroenterologist goes digital
Beginning in February 2018, The New Gastroenterologist (TNG) – a supplement to GI & Hepatology News that addresses issues pertinent to trainees and early-career GIs – will switch to a primarily digital format. We are excited about this change and confident that it will allow for a more effective and widespread dissemination of content that is valuable to both AGA members and our readership more broadly.
If you have any questions about these changes, or if there are any topics you’d be interested in writing or reading about in The New Gastroenterologist, please contact Editor in Chief Bryson Katona, MD, PhD ([email protected]) or Managing Editor Ryan Farrell ([email protected]).
Beginning in February 2018, The New Gastroenterologist (TNG) – a supplement to GI & Hepatology News that addresses issues pertinent to trainees and early-career GIs – will switch to a primarily digital format. We are excited about this change and confident that it will allow for a more effective and widespread dissemination of content that is valuable to both AGA members and our readership more broadly.
If you have any questions about these changes, or if there are any topics you’d be interested in writing or reading about in The New Gastroenterologist, please contact Editor in Chief Bryson Katona, MD, PhD ([email protected]) or Managing Editor Ryan Farrell ([email protected]).
Beginning in February 2018, The New Gastroenterologist (TNG) – a supplement to GI & Hepatology News that addresses issues pertinent to trainees and early-career GIs – will switch to a primarily digital format. We are excited about this change and confident that it will allow for a more effective and widespread dissemination of content that is valuable to both AGA members and our readership more broadly.
If you have any questions about these changes, or if there are any topics you’d be interested in writing or reading about in The New Gastroenterologist, please contact Editor in Chief Bryson Katona, MD, PhD ([email protected]) or Managing Editor Ryan Farrell ([email protected]).
AGA’s investment in the future of GI
What will the practice of gastroenterology look like in 20 years? It is our hope that physicians will have an abundance of new tools and treatments to care for their patients suffering from digestive disorders.
How will we get there? New treatments and devices are the result of years of research.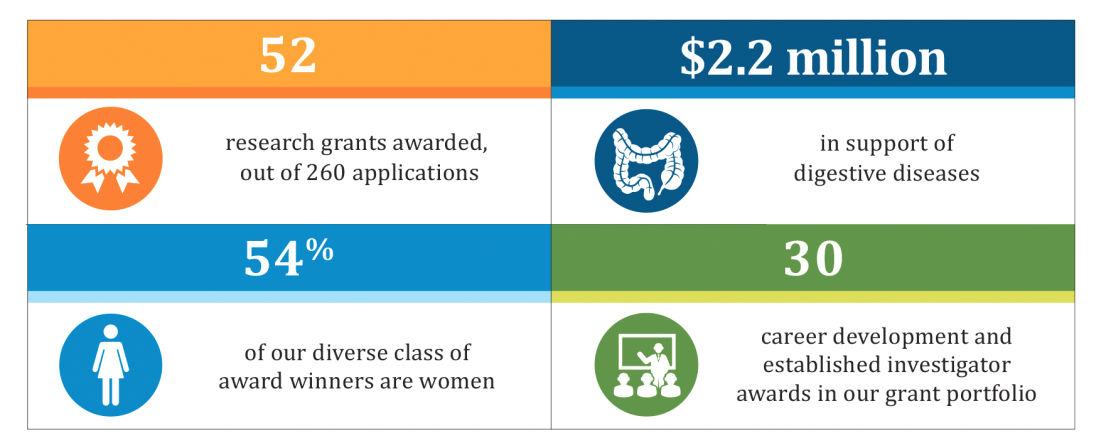
A snapshot of the foundation’s impact this year is highlighted in the chart below. The AGA Research Foundation sincerely thanks all of its donors – without your gifts, this work wouldn’t be possible. Please join us in advancing GI research with a tax-deductible gift to the AGA Research Foundation at www.gastro.org/about/aga-research-foundation.
What will the practice of gastroenterology look like in 20 years? It is our hope that physicians will have an abundance of new tools and treatments to care for their patients suffering from digestive disorders.
How will we get there? New treatments and devices are the result of years of research.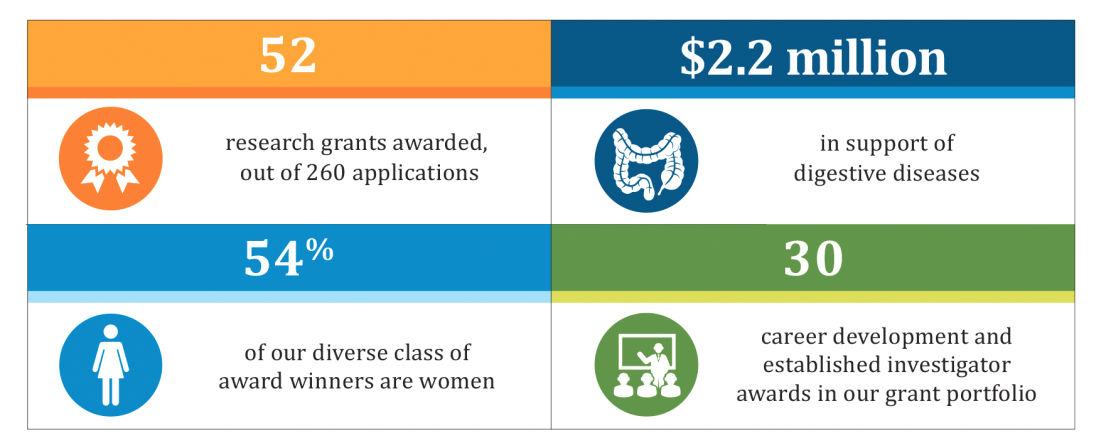
A snapshot of the foundation’s impact this year is highlighted in the chart below. The AGA Research Foundation sincerely thanks all of its donors – without your gifts, this work wouldn’t be possible. Please join us in advancing GI research with a tax-deductible gift to the AGA Research Foundation at www.gastro.org/about/aga-research-foundation.
What will the practice of gastroenterology look like in 20 years? It is our hope that physicians will have an abundance of new tools and treatments to care for their patients suffering from digestive disorders.
How will we get there? New treatments and devices are the result of years of research.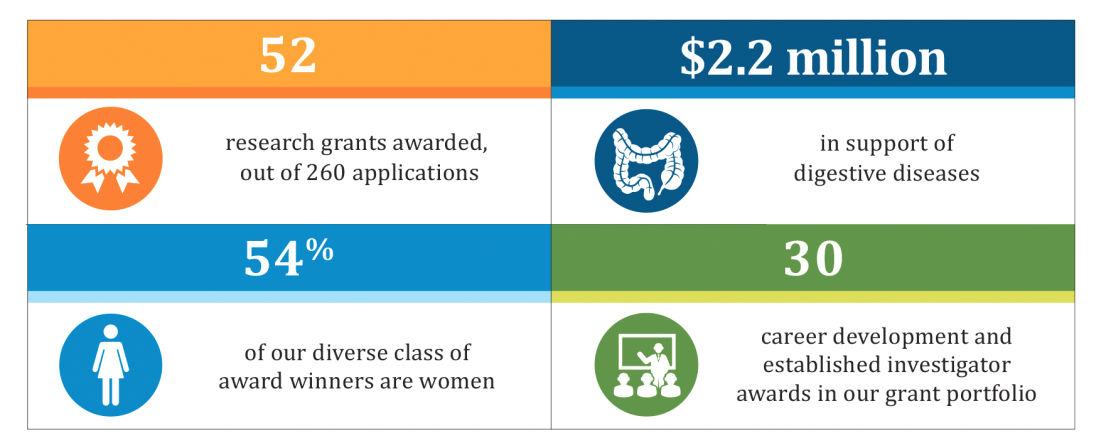
A snapshot of the foundation’s impact this year is highlighted in the chart below. The AGA Research Foundation sincerely thanks all of its donors – without your gifts, this work wouldn’t be possible. Please join us in advancing GI research with a tax-deductible gift to the AGA Research Foundation at www.gastro.org/about/aga-research-foundation.
GIs should be able to prescribe the most beneficial treatments
Appealing step therapy protocols can be time consuming and burdensome for physicians and patients, and can takes months to resolve. The Restoring the Patient’s Voice Act (HR 2077), introduced by physicians Reps. Brad Wenstrup, R-OH, and Raul Ruiz, D-CA, would provide a clear and timely appeals process when a patient has been subjected to step therapy by their insurance provider.
AGA endorsed this legislation to provide patients with a clear, equitable and fair appeals process when subjected to step therapy protocols. AGA is working with patient advocacy groups, like the Crohn’s and Colitis Foundation, provider, and professional societies to educate members of Congress on this issue and the implications it has for patients being able to access the right treatment at the right time.
Appealing step therapy protocols can be time consuming and burdensome for physicians and patients, and can takes months to resolve. The Restoring the Patient’s Voice Act (HR 2077), introduced by physicians Reps. Brad Wenstrup, R-OH, and Raul Ruiz, D-CA, would provide a clear and timely appeals process when a patient has been subjected to step therapy by their insurance provider.
AGA endorsed this legislation to provide patients with a clear, equitable and fair appeals process when subjected to step therapy protocols. AGA is working with patient advocacy groups, like the Crohn’s and Colitis Foundation, provider, and professional societies to educate members of Congress on this issue and the implications it has for patients being able to access the right treatment at the right time.
Appealing step therapy protocols can be time consuming and burdensome for physicians and patients, and can takes months to resolve. The Restoring the Patient’s Voice Act (HR 2077), introduced by physicians Reps. Brad Wenstrup, R-OH, and Raul Ruiz, D-CA, would provide a clear and timely appeals process when a patient has been subjected to step therapy by their insurance provider.
AGA endorsed this legislation to provide patients with a clear, equitable and fair appeals process when subjected to step therapy protocols. AGA is working with patient advocacy groups, like the Crohn’s and Colitis Foundation, provider, and professional societies to educate members of Congress on this issue and the implications it has for patients being able to access the right treatment at the right time.