User login
Sessions at DDW® 2018 designed for trainees and early career GIs
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Better manage acute pancreatitis to improve patient outcomes
AGA has a new clinical guideline on the initial management of acute pancreatitis, published in Gastroenterology. In the U.S., acute pancreatitis (AP) is a leading cause of inpatient care among gastrointestinal conditions with more than 275,000 patients hospitalized annually, at an aggregate cost of over $2.6 billion per year. The guideline focuses on patient care within the first 48-72 hours of admission when management decisions can alter the course of disease and duration of hospitalization.
Guideline recommendations
AGA’s new guideline aims to reduce practice variation and promote high-quality and high-value care for patients suffering from acute pancreatitis. It addresses questions on the benefits of goal-directed fluid resuscitation, early oral feeding, enteral vs. parenteral nutrition, the routine use of prophylactic antibiotics, and routine ERCP in all patients with AP.
The guideline is accompanied by a technical review, a new spotlight (infographic) and a patient companion infographic, which provides key points and important information directly to patients.
AGA has a new clinical guideline on the initial management of acute pancreatitis, published in Gastroenterology. In the U.S., acute pancreatitis (AP) is a leading cause of inpatient care among gastrointestinal conditions with more than 275,000 patients hospitalized annually, at an aggregate cost of over $2.6 billion per year. The guideline focuses on patient care within the first 48-72 hours of admission when management decisions can alter the course of disease and duration of hospitalization.
Guideline recommendations
AGA’s new guideline aims to reduce practice variation and promote high-quality and high-value care for patients suffering from acute pancreatitis. It addresses questions on the benefits of goal-directed fluid resuscitation, early oral feeding, enteral vs. parenteral nutrition, the routine use of prophylactic antibiotics, and routine ERCP in all patients with AP.
The guideline is accompanied by a technical review, a new spotlight (infographic) and a patient companion infographic, which provides key points and important information directly to patients.
AGA has a new clinical guideline on the initial management of acute pancreatitis, published in Gastroenterology. In the U.S., acute pancreatitis (AP) is a leading cause of inpatient care among gastrointestinal conditions with more than 275,000 patients hospitalized annually, at an aggregate cost of over $2.6 billion per year. The guideline focuses on patient care within the first 48-72 hours of admission when management decisions can alter the course of disease and duration of hospitalization.
Guideline recommendations
AGA’s new guideline aims to reduce practice variation and promote high-quality and high-value care for patients suffering from acute pancreatitis. It addresses questions on the benefits of goal-directed fluid resuscitation, early oral feeding, enteral vs. parenteral nutrition, the routine use of prophylactic antibiotics, and routine ERCP in all patients with AP.
The guideline is accompanied by a technical review, a new spotlight (infographic) and a patient companion infographic, which provides key points and important information directly to patients.
How to talk with your patients about PPIs and cognitive decline
A 2018 study published in Clinical Gastroenterology and Hepatology, “Lack of association between proton pump inhibitor use and cognitive decline,” found no association between PPI use and cognitive decline in analyzing data from two large population-based studies in Denmark. While this data is reassuring, clinicians should continue to anticipate questions from their patients about the risks associated with PPI therapy.
- Reassure patients that you prescribed a PPI for a clear-cut indication, in the lowest possible dose, and for an appropriate period of time (lowest dose, shortest time). This advice echoes that offered by AGA and ABIM in the Choosing Wisely campaign.
- Educate patients not to ask “what side effects do PPIs have?” but rather “is it really indicated?” Reassure patients that, when PPIs are indicated, benefits outweigh risks.
- Keep conversation channels open with patients. When patients require long-term use of PPIs, the medication should not be stopped without a discussion with you about the risks and benefits.
- Recommend that patients also consider life-style modifications that may reduce or eliminate the need for PPIs for long-term use.
A 2018 study published in Clinical Gastroenterology and Hepatology, “Lack of association between proton pump inhibitor use and cognitive decline,” found no association between PPI use and cognitive decline in analyzing data from two large population-based studies in Denmark. While this data is reassuring, clinicians should continue to anticipate questions from their patients about the risks associated with PPI therapy.
- Reassure patients that you prescribed a PPI for a clear-cut indication, in the lowest possible dose, and for an appropriate period of time (lowest dose, shortest time). This advice echoes that offered by AGA and ABIM in the Choosing Wisely campaign.
- Educate patients not to ask “what side effects do PPIs have?” but rather “is it really indicated?” Reassure patients that, when PPIs are indicated, benefits outweigh risks.
- Keep conversation channels open with patients. When patients require long-term use of PPIs, the medication should not be stopped without a discussion with you about the risks and benefits.
- Recommend that patients also consider life-style modifications that may reduce or eliminate the need for PPIs for long-term use.
A 2018 study published in Clinical Gastroenterology and Hepatology, “Lack of association between proton pump inhibitor use and cognitive decline,” found no association between PPI use and cognitive decline in analyzing data from two large population-based studies in Denmark. While this data is reassuring, clinicians should continue to anticipate questions from their patients about the risks associated with PPI therapy.
- Reassure patients that you prescribed a PPI for a clear-cut indication, in the lowest possible dose, and for an appropriate period of time (lowest dose, shortest time). This advice echoes that offered by AGA and ABIM in the Choosing Wisely campaign.
- Educate patients not to ask “what side effects do PPIs have?” but rather “is it really indicated?” Reassure patients that, when PPIs are indicated, benefits outweigh risks.
- Keep conversation channels open with patients. When patients require long-term use of PPIs, the medication should not be stopped without a discussion with you about the risks and benefits.
- Recommend that patients also consider life-style modifications that may reduce or eliminate the need for PPIs for long-term use.
Four new and noteworthy IBD drug studies
Inflammatory bowel disease (IBD) is a vibrant area of clinical research. Many of the 250+ abstracts presented at the inaugural Crohn’s & Colitis Congress — a partnership of the Crohn’s & Colitis Foundation and AGA — looked at the efficacy and safety of IBD therapies. You can review all abstracts presented at the Crohn’s & Colitis Congress in Gastroenterology.
Double-blind, randomized, placebo-controlled, crossover trial to evaluate induction of clinical response in patients with moderate-severe Crohn’s disease treated with rifaximin
By Scott D. Lee, University of Washington Medicine, et al.
Significance: It is now known that the intestinal microbiome is integral to the pathogenesis of IBD. However, antibiotic treatments for IBD have previously shown limited effectiveness. In this 8-week clinical trial, there was a fourfold greater response to the antibiotic rifaximin in Crohn’s disease treatment, compared with placebo. The positive impact on clinical disease activity was seen even in patients with a significant disease burden and prior exposure to one or more biologic therapies. Quality of life and laboratory measurements were numerically improved. No new safety concerns were identified. These results offer renewed hope for the use of antibiotics in treating Crohn’s disease.
Post-hoc analysis of tofacitinib Crohn’s disease phase 2 induction efficacy in subgroups with baseline endoscopic or biomarker evidence of inflammation
By Bruce E. Sands, Icahn School of Medicine at Mount Sinai, et al.
Significance: Tofacitinib, a Janus kinase (JAK) inhibitor, is under investigation for treatment of ulcerative colitis and Crohn’s disease. To date, response rates in ulcerative colitis have been higher than for Crohn’s disease. In this report, investigators performed post-hoc analysis studies using objective baseline criteria of disease activity. Their findings showed a greater proportion of patients with moderate to severe Crohn’s disease were in remission with tofacitinib compared to placebo. These results provide evidence of JAK inhibition for the treatment of Crohn’s disease and support further investigation.
Refined population pharmacokinetic model for infliximab precision dosing in pediatric inflammatory bowel disease
By Laura E. Bauman, Cincinnati Children’s Hospital Medical Center, et al.
Significance: Long-term clinical remission from IBD with anti-TNF therapies has generally been limited to less than half of the treated patients. Improved outcomes are seen with optimal pre-infusion trough drug levels, a measurement of the level of drugs in the patient’s bloodstream. However, standard weight-based dosing for pediatric patients has provided widely varying trough drug levels. The investigators report the development of a multifactorial pharmacokinetic model for predicting infliximab trough levels during maintenance therapy for IBD. Such dynamic approaches to treatment address a specific gap in pediatric IBD therapeutic strategies.
Primary nonresponse to tumor necrosis factor antagonists is associated with inferior response to second-line biologics in patients with inflammatory bowel diseases: A systematic review and meta-analysis
By Siddharth Singh, University of California San Diego Health, et al.
Significance: Primary nonresponse to anti-TNF therapy is seen in 35%-65% of IBD patients and another 40%-60% lose responsiveness during the first year of treatment. Physicians struggle with what treatments to recommend for these patients. The investigators in this study performed a literature search and identified eight randomized controlled trials of biologics in patients with prior exposure to anti-TNF and compared outcomes based on their prior responses to anti-TNF. The analysis reveals a 24% decrease in likelihood to achieve remission in patients who changed medications because of immediate nonresponse compared to loss of responsiveness or intolerance during the treatment. These findings raise important questions about the biology of IBD, including the pharmacology of anti-TNF in a subset of patients.
Inflammatory bowel disease (IBD) is a vibrant area of clinical research. Many of the 250+ abstracts presented at the inaugural Crohn’s & Colitis Congress — a partnership of the Crohn’s & Colitis Foundation and AGA — looked at the efficacy and safety of IBD therapies. You can review all abstracts presented at the Crohn’s & Colitis Congress in Gastroenterology.
Double-blind, randomized, placebo-controlled, crossover trial to evaluate induction of clinical response in patients with moderate-severe Crohn’s disease treated with rifaximin
By Scott D. Lee, University of Washington Medicine, et al.
Significance: It is now known that the intestinal microbiome is integral to the pathogenesis of IBD. However, antibiotic treatments for IBD have previously shown limited effectiveness. In this 8-week clinical trial, there was a fourfold greater response to the antibiotic rifaximin in Crohn’s disease treatment, compared with placebo. The positive impact on clinical disease activity was seen even in patients with a significant disease burden and prior exposure to one or more biologic therapies. Quality of life and laboratory measurements were numerically improved. No new safety concerns were identified. These results offer renewed hope for the use of antibiotics in treating Crohn’s disease.
Post-hoc analysis of tofacitinib Crohn’s disease phase 2 induction efficacy in subgroups with baseline endoscopic or biomarker evidence of inflammation
By Bruce E. Sands, Icahn School of Medicine at Mount Sinai, et al.
Significance: Tofacitinib, a Janus kinase (JAK) inhibitor, is under investigation for treatment of ulcerative colitis and Crohn’s disease. To date, response rates in ulcerative colitis have been higher than for Crohn’s disease. In this report, investigators performed post-hoc analysis studies using objective baseline criteria of disease activity. Their findings showed a greater proportion of patients with moderate to severe Crohn’s disease were in remission with tofacitinib compared to placebo. These results provide evidence of JAK inhibition for the treatment of Crohn’s disease and support further investigation.
Refined population pharmacokinetic model for infliximab precision dosing in pediatric inflammatory bowel disease
By Laura E. Bauman, Cincinnati Children’s Hospital Medical Center, et al.
Significance: Long-term clinical remission from IBD with anti-TNF therapies has generally been limited to less than half of the treated patients. Improved outcomes are seen with optimal pre-infusion trough drug levels, a measurement of the level of drugs in the patient’s bloodstream. However, standard weight-based dosing for pediatric patients has provided widely varying trough drug levels. The investigators report the development of a multifactorial pharmacokinetic model for predicting infliximab trough levels during maintenance therapy for IBD. Such dynamic approaches to treatment address a specific gap in pediatric IBD therapeutic strategies.
Primary nonresponse to tumor necrosis factor antagonists is associated with inferior response to second-line biologics in patients with inflammatory bowel diseases: A systematic review and meta-analysis
By Siddharth Singh, University of California San Diego Health, et al.
Significance: Primary nonresponse to anti-TNF therapy is seen in 35%-65% of IBD patients and another 40%-60% lose responsiveness during the first year of treatment. Physicians struggle with what treatments to recommend for these patients. The investigators in this study performed a literature search and identified eight randomized controlled trials of biologics in patients with prior exposure to anti-TNF and compared outcomes based on their prior responses to anti-TNF. The analysis reveals a 24% decrease in likelihood to achieve remission in patients who changed medications because of immediate nonresponse compared to loss of responsiveness or intolerance during the treatment. These findings raise important questions about the biology of IBD, including the pharmacology of anti-TNF in a subset of patients.
Inflammatory bowel disease (IBD) is a vibrant area of clinical research. Many of the 250+ abstracts presented at the inaugural Crohn’s & Colitis Congress — a partnership of the Crohn’s & Colitis Foundation and AGA — looked at the efficacy and safety of IBD therapies. You can review all abstracts presented at the Crohn’s & Colitis Congress in Gastroenterology.
Double-blind, randomized, placebo-controlled, crossover trial to evaluate induction of clinical response in patients with moderate-severe Crohn’s disease treated with rifaximin
By Scott D. Lee, University of Washington Medicine, et al.
Significance: It is now known that the intestinal microbiome is integral to the pathogenesis of IBD. However, antibiotic treatments for IBD have previously shown limited effectiveness. In this 8-week clinical trial, there was a fourfold greater response to the antibiotic rifaximin in Crohn’s disease treatment, compared with placebo. The positive impact on clinical disease activity was seen even in patients with a significant disease burden and prior exposure to one or more biologic therapies. Quality of life and laboratory measurements were numerically improved. No new safety concerns were identified. These results offer renewed hope for the use of antibiotics in treating Crohn’s disease.
Post-hoc analysis of tofacitinib Crohn’s disease phase 2 induction efficacy in subgroups with baseline endoscopic or biomarker evidence of inflammation
By Bruce E. Sands, Icahn School of Medicine at Mount Sinai, et al.
Significance: Tofacitinib, a Janus kinase (JAK) inhibitor, is under investigation for treatment of ulcerative colitis and Crohn’s disease. To date, response rates in ulcerative colitis have been higher than for Crohn’s disease. In this report, investigators performed post-hoc analysis studies using objective baseline criteria of disease activity. Their findings showed a greater proportion of patients with moderate to severe Crohn’s disease were in remission with tofacitinib compared to placebo. These results provide evidence of JAK inhibition for the treatment of Crohn’s disease and support further investigation.
Refined population pharmacokinetic model for infliximab precision dosing in pediatric inflammatory bowel disease
By Laura E. Bauman, Cincinnati Children’s Hospital Medical Center, et al.
Significance: Long-term clinical remission from IBD with anti-TNF therapies has generally been limited to less than half of the treated patients. Improved outcomes are seen with optimal pre-infusion trough drug levels, a measurement of the level of drugs in the patient’s bloodstream. However, standard weight-based dosing for pediatric patients has provided widely varying trough drug levels. The investigators report the development of a multifactorial pharmacokinetic model for predicting infliximab trough levels during maintenance therapy for IBD. Such dynamic approaches to treatment address a specific gap in pediatric IBD therapeutic strategies.
Primary nonresponse to tumor necrosis factor antagonists is associated with inferior response to second-line biologics in patients with inflammatory bowel diseases: A systematic review and meta-analysis
By Siddharth Singh, University of California San Diego Health, et al.
Significance: Primary nonresponse to anti-TNF therapy is seen in 35%-65% of IBD patients and another 40%-60% lose responsiveness during the first year of treatment. Physicians struggle with what treatments to recommend for these patients. The investigators in this study performed a literature search and identified eight randomized controlled trials of biologics in patients with prior exposure to anti-TNF and compared outcomes based on their prior responses to anti-TNF. The analysis reveals a 24% decrease in likelihood to achieve remission in patients who changed medications because of immediate nonresponse compared to loss of responsiveness or intolerance during the treatment. These findings raise important questions about the biology of IBD, including the pharmacology of anti-TNF in a subset of patients.
Remember the AGA Research Foundation in your will or living trust
What if all you had to do to ensure that the AGA Research Foundation can have an impact for years to come is to write a simple sentence? Sound impossible?
The AGA Research Foundation provides a key source of funding at a critical juncture in a young investigators’ career. Securing the future of the talented investigators we serve really is as simple as one sentence.
Including the AGA Research Foundation in your will is a popular gift to give because it is:
- • Affordable. The actual giving of your gift occurs after your lifetime, so your current income is not affected.
- • Flexible. Until your will goes into effect, you are free to alter your plans or change your mind.
- • Versatile. You can give a specific item, a set amount of money, or a percentage of your estate. You can also make your gift contingent upon certain events.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
Join others in donating to the AGA Research Foundation and help fill the funding gap and protect the next generation of investigators.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
What if all you had to do to ensure that the AGA Research Foundation can have an impact for years to come is to write a simple sentence? Sound impossible?
The AGA Research Foundation provides a key source of funding at a critical juncture in a young investigators’ career. Securing the future of the talented investigators we serve really is as simple as one sentence.
Including the AGA Research Foundation in your will is a popular gift to give because it is:
- • Affordable. The actual giving of your gift occurs after your lifetime, so your current income is not affected.
- • Flexible. Until your will goes into effect, you are free to alter your plans or change your mind.
- • Versatile. You can give a specific item, a set amount of money, or a percentage of your estate. You can also make your gift contingent upon certain events.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
Join others in donating to the AGA Research Foundation and help fill the funding gap and protect the next generation of investigators.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
What if all you had to do to ensure that the AGA Research Foundation can have an impact for years to come is to write a simple sentence? Sound impossible?
The AGA Research Foundation provides a key source of funding at a critical juncture in a young investigators’ career. Securing the future of the talented investigators we serve really is as simple as one sentence.
Including the AGA Research Foundation in your will is a popular gift to give because it is:
- • Affordable. The actual giving of your gift occurs after your lifetime, so your current income is not affected.
- • Flexible. Until your will goes into effect, you are free to alter your plans or change your mind.
- • Versatile. You can give a specific item, a set amount of money, or a percentage of your estate. You can also make your gift contingent upon certain events.
We hope you’ll consider including a gift to the AGA Research Foundation in your will or living trust. It’s simple – just a few sentences in your will or trust are all that is needed. The official bequest language for the AGA Research Foundation is: “I, [name], of [city, state, ZIP], give, devise and bequeath to the AGA Research Foundation [written amount or percentage of the estate or description of property] for its unrestricted use and purpose.”
Join others in donating to the AGA Research Foundation and help fill the funding gap and protect the next generation of investigators.
Please contact us for more information at [email protected] or visit http://gastro.planmylegacy.org/.
Congressional budget includes AGA wins
AGA spends a lot of time on Capitol Hill advocating to help gastroenterologists in practice better care for their patients and receive fair reimbursement. Therefore, we were pleased that the budget deal passed by Congress and signed by the president in February included several policy victories that AGA has been working diligently on for many years.
IPAB repeal
AGA, and all of organized medicine, have long opposed the Independent Payment Advisory Board (IPAB) that was created as part of the Affordable Care Act. IPAB is an unelected, unaccountable board whose sole purpose is to cut Medicare spending from providers should Medicare reach a certain threshold of spending. Since hospitals are exempt from their purview, physicians would be particularly vulnerable to cuts. However, repealing IPAB has had bipartisan support over the years, and we applaud Congress for listening to us and the medical community and taking action.
Misvalued codes
AGA and the physician community were also successful in removing a provision that would have extended the misvalued codes initiative for the next two years to reallocate savings from potentially overvalued codes. AGA, the Alliance of Specialty Medicine and the AMA opposed the original provision expanding the misvalued codes initiative and have argued that virtually all codes under the fee schedule, including gastroenterology, have been reevaluated and have already faced significant cuts. In the final agreement, Congress eliminated recapturing savings from the misvalued codes initiative and instead lowered overall updates for physician reimbursement under Medicare by .25 percent for 1 year. Although AGA would prefer this reduction not be included, it is much better than the misvalued codes provision, which disproportionately impacts specialties, like gastroenterology.
Geographic Practice Cost Index
The budget agreement extends the work for the Geographic Practice Cost Index (GPCI) floor for two additional years, which avoids a decrease in Medicare reimbursement for physicians that practice in rural areas. The work GPCI is a variable that Medicare uses to adjust the work component of physician payment based on where they live. A work GPCI floor of 1.0 protects physicians in low-cost, often rural areas, from being paid less for the work they do.
Meaningful use standards
The package addresses electronic health record (EHR) standards and eases requirements for physicians. The language removes the mandate that meaningful use standards become more stringent over time, which is a major financial burden for physician practices. The language also gives physicians more time to submit and receive a hardship exemption from the current EHR standards that would apply to meaningful use and the Quality Payment Program’s advancing care information performance category.
Biosimilars coverage under Medicare Part D
The agreement also levels the playing field between biologics and biosimilars by adding biosimilars to the Medicare Coverage Gap Discount Program. Additionally, by providing the 50 percent discount equally, beneficiary out-of-pocket costs will be reduced and the Medicare program will save money as a result of covering the less expensive medication.
AGA and the medical community have fought long and hard for these provisions and are happy to see them finally being implemented. We thank all of our members who have worked along with us to ensure that the voice of gastroenterology continues to be heard on Capitol Hill.
AGA spends a lot of time on Capitol Hill advocating to help gastroenterologists in practice better care for their patients and receive fair reimbursement. Therefore, we were pleased that the budget deal passed by Congress and signed by the president in February included several policy victories that AGA has been working diligently on for many years.
IPAB repeal
AGA, and all of organized medicine, have long opposed the Independent Payment Advisory Board (IPAB) that was created as part of the Affordable Care Act. IPAB is an unelected, unaccountable board whose sole purpose is to cut Medicare spending from providers should Medicare reach a certain threshold of spending. Since hospitals are exempt from their purview, physicians would be particularly vulnerable to cuts. However, repealing IPAB has had bipartisan support over the years, and we applaud Congress for listening to us and the medical community and taking action.
Misvalued codes
AGA and the physician community were also successful in removing a provision that would have extended the misvalued codes initiative for the next two years to reallocate savings from potentially overvalued codes. AGA, the Alliance of Specialty Medicine and the AMA opposed the original provision expanding the misvalued codes initiative and have argued that virtually all codes under the fee schedule, including gastroenterology, have been reevaluated and have already faced significant cuts. In the final agreement, Congress eliminated recapturing savings from the misvalued codes initiative and instead lowered overall updates for physician reimbursement under Medicare by .25 percent for 1 year. Although AGA would prefer this reduction not be included, it is much better than the misvalued codes provision, which disproportionately impacts specialties, like gastroenterology.
Geographic Practice Cost Index
The budget agreement extends the work for the Geographic Practice Cost Index (GPCI) floor for two additional years, which avoids a decrease in Medicare reimbursement for physicians that practice in rural areas. The work GPCI is a variable that Medicare uses to adjust the work component of physician payment based on where they live. A work GPCI floor of 1.0 protects physicians in low-cost, often rural areas, from being paid less for the work they do.
Meaningful use standards
The package addresses electronic health record (EHR) standards and eases requirements for physicians. The language removes the mandate that meaningful use standards become more stringent over time, which is a major financial burden for physician practices. The language also gives physicians more time to submit and receive a hardship exemption from the current EHR standards that would apply to meaningful use and the Quality Payment Program’s advancing care information performance category.
Biosimilars coverage under Medicare Part D
The agreement also levels the playing field between biologics and biosimilars by adding biosimilars to the Medicare Coverage Gap Discount Program. Additionally, by providing the 50 percent discount equally, beneficiary out-of-pocket costs will be reduced and the Medicare program will save money as a result of covering the less expensive medication.
AGA and the medical community have fought long and hard for these provisions and are happy to see them finally being implemented. We thank all of our members who have worked along with us to ensure that the voice of gastroenterology continues to be heard on Capitol Hill.
AGA spends a lot of time on Capitol Hill advocating to help gastroenterologists in practice better care for their patients and receive fair reimbursement. Therefore, we were pleased that the budget deal passed by Congress and signed by the president in February included several policy victories that AGA has been working diligently on for many years.
IPAB repeal
AGA, and all of organized medicine, have long opposed the Independent Payment Advisory Board (IPAB) that was created as part of the Affordable Care Act. IPAB is an unelected, unaccountable board whose sole purpose is to cut Medicare spending from providers should Medicare reach a certain threshold of spending. Since hospitals are exempt from their purview, physicians would be particularly vulnerable to cuts. However, repealing IPAB has had bipartisan support over the years, and we applaud Congress for listening to us and the medical community and taking action.
Misvalued codes
AGA and the physician community were also successful in removing a provision that would have extended the misvalued codes initiative for the next two years to reallocate savings from potentially overvalued codes. AGA, the Alliance of Specialty Medicine and the AMA opposed the original provision expanding the misvalued codes initiative and have argued that virtually all codes under the fee schedule, including gastroenterology, have been reevaluated and have already faced significant cuts. In the final agreement, Congress eliminated recapturing savings from the misvalued codes initiative and instead lowered overall updates for physician reimbursement under Medicare by .25 percent for 1 year. Although AGA would prefer this reduction not be included, it is much better than the misvalued codes provision, which disproportionately impacts specialties, like gastroenterology.
Geographic Practice Cost Index
The budget agreement extends the work for the Geographic Practice Cost Index (GPCI) floor for two additional years, which avoids a decrease in Medicare reimbursement for physicians that practice in rural areas. The work GPCI is a variable that Medicare uses to adjust the work component of physician payment based on where they live. A work GPCI floor of 1.0 protects physicians in low-cost, often rural areas, from being paid less for the work they do.
Meaningful use standards
The package addresses electronic health record (EHR) standards and eases requirements for physicians. The language removes the mandate that meaningful use standards become more stringent over time, which is a major financial burden for physician practices. The language also gives physicians more time to submit and receive a hardship exemption from the current EHR standards that would apply to meaningful use and the Quality Payment Program’s advancing care information performance category.
Biosimilars coverage under Medicare Part D
The agreement also levels the playing field between biologics and biosimilars by adding biosimilars to the Medicare Coverage Gap Discount Program. Additionally, by providing the 50 percent discount equally, beneficiary out-of-pocket costs will be reduced and the Medicare program will save money as a result of covering the less expensive medication.
AGA and the medical community have fought long and hard for these provisions and are happy to see them finally being implemented. We thank all of our members who have worked along with us to ensure that the voice of gastroenterology continues to be heard on Capitol Hill.
Legacy Society members sustain research
AGA Legacy Society members share a desire to guarantee long-term support for digestive disease research. Through their foresight and generosity, they help ensure the continued momentum of discovery and patient education that has characterized GI medicine in recent decades. Legacy Society member donations directly support young GI investigators as they establish independent research careers.
Legacy Society members are the most generous individual donors to the AGA Research Foundation. Members of the AGA Legacy Society provide tax-deductible gifts to the AGA Research Foundation of $5,000 or more per year for 5 years ($25,000 total) or $50,000 or more in a planned gift, such as a bequest. All Legacy Society contributions go directly to support research awards.
AGA members support young researchers at a critical decision point in their lives – when many consider giving up their research careers due to a lack of funding. “I am honored to be a recipient of the Research Scholar Award. I would like to thank the foundation for their generous contribution that will fund a crucial transition in my career,” said Jose Saenz, MD, PhD, Washington University School of Medicine and 2017 AGA – Gastric Cancer Foundation Research Scholar Award recipient.
The AGA Research Foundation’s mission is to raise funds to support young researchers in gastroenterology and hepatology. Gifts to the foundation support researchers working towards developing new treatments and diagnostics for patients with GI conditions.
“I am extremely grateful to be selected for this award. I would like to thank the foundation donors for their generous support. This award will me build a research program to better understand mechanisms that promote growth of cholangiocarcinoma,” remarks Silvia Affe, PhD, Columbia University, 2017 AGA Research Scholar recipient.
Donors who make gifts at the Legacy Society level before DDW will receive an invitation to the annual Benefactors’ Dinner at the Folger Shakespeare Library in Washington, DC. Individuals interested in learning more about Legacy Society membership may contact Stacey Hinton Tuneski, Senior Director of Development at [email protected] or via phone (301) 222-4005. More information on the AGA Legacy Society including the current roster and acceptance form is available on the foundation’s website at www.gastro.org/legacysociety.
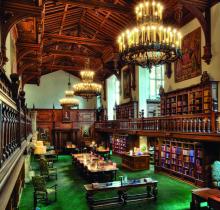
The makings of a grand celebration
Beginning with a memorable gathering at the United States Library of Congress in 2007, the AGA Benefactors’ Dinner has welcomed members of the AGA Legacy Society and other AGA dignitaries to special locations nationwide. The Folger Shakespeare Library will be the location of the 2018 AGA Research Foundation Benefactors Dinner during DDW in Washington, DC. Just steps from the Capitol, the Great Hall and Pastor Reading room are a spectacular setting for an enjoyable evening with friends. Members of the AGA Legacy Society will be among the distinguished honorees at the annual event.
AGA Legacy Society members share a desire to guarantee long-term support for digestive disease research. Through their foresight and generosity, they help ensure the continued momentum of discovery and patient education that has characterized GI medicine in recent decades. Legacy Society member donations directly support young GI investigators as they establish independent research careers.
Legacy Society members are the most generous individual donors to the AGA Research Foundation. Members of the AGA Legacy Society provide tax-deductible gifts to the AGA Research Foundation of $5,000 or more per year for 5 years ($25,000 total) or $50,000 or more in a planned gift, such as a bequest. All Legacy Society contributions go directly to support research awards.
AGA members support young researchers at a critical decision point in their lives – when many consider giving up their research careers due to a lack of funding. “I am honored to be a recipient of the Research Scholar Award. I would like to thank the foundation for their generous contribution that will fund a crucial transition in my career,” said Jose Saenz, MD, PhD, Washington University School of Medicine and 2017 AGA – Gastric Cancer Foundation Research Scholar Award recipient.
The AGA Research Foundation’s mission is to raise funds to support young researchers in gastroenterology and hepatology. Gifts to the foundation support researchers working towards developing new treatments and diagnostics for patients with GI conditions.
“I am extremely grateful to be selected for this award. I would like to thank the foundation donors for their generous support. This award will me build a research program to better understand mechanisms that promote growth of cholangiocarcinoma,” remarks Silvia Affe, PhD, Columbia University, 2017 AGA Research Scholar recipient.
Donors who make gifts at the Legacy Society level before DDW will receive an invitation to the annual Benefactors’ Dinner at the Folger Shakespeare Library in Washington, DC. Individuals interested in learning more about Legacy Society membership may contact Stacey Hinton Tuneski, Senior Director of Development at [email protected] or via phone (301) 222-4005. More information on the AGA Legacy Society including the current roster and acceptance form is available on the foundation’s website at www.gastro.org/legacysociety.
The makings of a grand celebration
Beginning with a memorable gathering at the United States Library of Congress in 2007, the AGA Benefactors’ Dinner has welcomed members of the AGA Legacy Society and other AGA dignitaries to special locations nationwide. The Folger Shakespeare Library will be the location of the 2018 AGA Research Foundation Benefactors Dinner during DDW in Washington, DC. Just steps from the Capitol, the Great Hall and Pastor Reading room are a spectacular setting for an enjoyable evening with friends. Members of the AGA Legacy Society will be among the distinguished honorees at the annual event.
AGA Legacy Society members share a desire to guarantee long-term support for digestive disease research. Through their foresight and generosity, they help ensure the continued momentum of discovery and patient education that has characterized GI medicine in recent decades. Legacy Society member donations directly support young GI investigators as they establish independent research careers.
Legacy Society members are the most generous individual donors to the AGA Research Foundation. Members of the AGA Legacy Society provide tax-deductible gifts to the AGA Research Foundation of $5,000 or more per year for 5 years ($25,000 total) or $50,000 or more in a planned gift, such as a bequest. All Legacy Society contributions go directly to support research awards.
AGA members support young researchers at a critical decision point in their lives – when many consider giving up their research careers due to a lack of funding. “I am honored to be a recipient of the Research Scholar Award. I would like to thank the foundation for their generous contribution that will fund a crucial transition in my career,” said Jose Saenz, MD, PhD, Washington University School of Medicine and 2017 AGA – Gastric Cancer Foundation Research Scholar Award recipient.
The AGA Research Foundation’s mission is to raise funds to support young researchers in gastroenterology and hepatology. Gifts to the foundation support researchers working towards developing new treatments and diagnostics for patients with GI conditions.
“I am extremely grateful to be selected for this award. I would like to thank the foundation donors for their generous support. This award will me build a research program to better understand mechanisms that promote growth of cholangiocarcinoma,” remarks Silvia Affe, PhD, Columbia University, 2017 AGA Research Scholar recipient.
Donors who make gifts at the Legacy Society level before DDW will receive an invitation to the annual Benefactors’ Dinner at the Folger Shakespeare Library in Washington, DC. Individuals interested in learning more about Legacy Society membership may contact Stacey Hinton Tuneski, Senior Director of Development at [email protected] or via phone (301) 222-4005. More information on the AGA Legacy Society including the current roster and acceptance form is available on the foundation’s website at www.gastro.org/legacysociety.
The makings of a grand celebration
Beginning with a memorable gathering at the United States Library of Congress in 2007, the AGA Benefactors’ Dinner has welcomed members of the AGA Legacy Society and other AGA dignitaries to special locations nationwide. The Folger Shakespeare Library will be the location of the 2018 AGA Research Foundation Benefactors Dinner during DDW in Washington, DC. Just steps from the Capitol, the Great Hall and Pastor Reading room are a spectacular setting for an enjoyable evening with friends. Members of the AGA Legacy Society will be among the distinguished honorees at the annual event.
AGA Pres. Sheila Crowe Spends the Day on Capitol Hill
AGA President Sheila Crowe, MD, FRCPC, FACP, FACG, AGAF, recently spent the day on Capitol Hill meeting with lawmakers to advocate for AGA legislative priorities including increasing funding for NIH and biomedical research, support for the Removing Barriers to Colorectal Cancer Screening Act, and support for the Restoring the Patient’s Voice Act. Dr. Crowe met with eight congressional offices and received helpful feedback on the upcoming agenda in Congress and how it impacts AGA’s priorities.
NIH funding
Removing Barriers to Colorectal Cancer Screening Act
Fixing the current coinsurance problem for Medicare beneficiaries who undergo a screening colonoscopy that becomes therapeutic remains a top AGA priority. Most of the offices that Dr. Crowe met with were cosponsors of the legislation, the Removing Barriers to Colorectal Cancer Screening Act (HR 1017/S.479), that would waive coinsurance payment regardless of the screening outcome. Dr. Crowe shared her experience with patients and the financial burden this places on beneficiaries who need to be screened. Rep. Raul Ruiz, D-CA, and Rep. Scott Peters, D-CA, both members of the House Energy and Commerce Committee and supporters of the bill, will continue to advocate that the bill receive a hearing this year to help move it through Congress. The bill continues to have wide bipartisan support. Read more about the issue and how you can explain it to your patients.
Step therapy
More and more patients are being subject to step therapy protocols, also known as “fail first” under which they are required to try and fail sometimes two or three therapies before receiving coverage of the initial therapy recommended by their physician. With the emergence of new biologics to treat diseases like inflammatory bowel disease, more and more digestive disease patients are being subject to these protocols, which can have adverse effects on their health. Restoring the Patient’s Voice Act (HR 2077) would provide patients and providers with a fair and equitable appeals process when step therapy has been imposed and provides common sense exceptions for the provider to appeal. Dr. Crowe spoke of the impact this policy is having on digestive disease patients and the burden it puts on physician practices that have to take time away from patients to navigate the convoluted insurance appeals process. We are hopeful that many of the offices that we met with will support HR 2077. Read more about the issue.
Food is Medicine Working Group
Dr. Crowe also had a productive meeting with Rep. Jim McGovern’s, D-MA, office and learned more about the recently created Food is Medicine Working Group that he has initiated. McGovern is the Ranking Member of the Agriculture Committee’s Subcommittee on Nutrition which is responsible for our nation’s nutrition guidelines and the Supplemental Nutrition Assistance Program. The Working Group will focus on costs related to hunger and the importance of nutrition in treating chronic illness and disease. AGA looks forward to working with McGovern and members of the Working Group on this bipartisan initiative.
Capitol Hill needs to hear the voice of GI
In conjunction with Dr. Crowe’s visit, AGA launched a Virtual Advocacy Day to encourage members to contact their legislators in support of the issues that Dr. Crowe was advocating during her meetings. We thank those members who took time out of their schedules to take action.
AGA President Sheila Crowe, MD, FRCPC, FACP, FACG, AGAF, recently spent the day on Capitol Hill meeting with lawmakers to advocate for AGA legislative priorities including increasing funding for NIH and biomedical research, support for the Removing Barriers to Colorectal Cancer Screening Act, and support for the Restoring the Patient’s Voice Act. Dr. Crowe met with eight congressional offices and received helpful feedback on the upcoming agenda in Congress and how it impacts AGA’s priorities.
NIH funding
Removing Barriers to Colorectal Cancer Screening Act
Fixing the current coinsurance problem for Medicare beneficiaries who undergo a screening colonoscopy that becomes therapeutic remains a top AGA priority. Most of the offices that Dr. Crowe met with were cosponsors of the legislation, the Removing Barriers to Colorectal Cancer Screening Act (HR 1017/S.479), that would waive coinsurance payment regardless of the screening outcome. Dr. Crowe shared her experience with patients and the financial burden this places on beneficiaries who need to be screened. Rep. Raul Ruiz, D-CA, and Rep. Scott Peters, D-CA, both members of the House Energy and Commerce Committee and supporters of the bill, will continue to advocate that the bill receive a hearing this year to help move it through Congress. The bill continues to have wide bipartisan support. Read more about the issue and how you can explain it to your patients.
Step therapy
More and more patients are being subject to step therapy protocols, also known as “fail first” under which they are required to try and fail sometimes two or three therapies before receiving coverage of the initial therapy recommended by their physician. With the emergence of new biologics to treat diseases like inflammatory bowel disease, more and more digestive disease patients are being subject to these protocols, which can have adverse effects on their health. Restoring the Patient’s Voice Act (HR 2077) would provide patients and providers with a fair and equitable appeals process when step therapy has been imposed and provides common sense exceptions for the provider to appeal. Dr. Crowe spoke of the impact this policy is having on digestive disease patients and the burden it puts on physician practices that have to take time away from patients to navigate the convoluted insurance appeals process. We are hopeful that many of the offices that we met with will support HR 2077. Read more about the issue.
Food is Medicine Working Group
Dr. Crowe also had a productive meeting with Rep. Jim McGovern’s, D-MA, office and learned more about the recently created Food is Medicine Working Group that he has initiated. McGovern is the Ranking Member of the Agriculture Committee’s Subcommittee on Nutrition which is responsible for our nation’s nutrition guidelines and the Supplemental Nutrition Assistance Program. The Working Group will focus on costs related to hunger and the importance of nutrition in treating chronic illness and disease. AGA looks forward to working with McGovern and members of the Working Group on this bipartisan initiative.
Capitol Hill needs to hear the voice of GI
In conjunction with Dr. Crowe’s visit, AGA launched a Virtual Advocacy Day to encourage members to contact their legislators in support of the issues that Dr. Crowe was advocating during her meetings. We thank those members who took time out of their schedules to take action.
AGA President Sheila Crowe, MD, FRCPC, FACP, FACG, AGAF, recently spent the day on Capitol Hill meeting with lawmakers to advocate for AGA legislative priorities including increasing funding for NIH and biomedical research, support for the Removing Barriers to Colorectal Cancer Screening Act, and support for the Restoring the Patient’s Voice Act. Dr. Crowe met with eight congressional offices and received helpful feedback on the upcoming agenda in Congress and how it impacts AGA’s priorities.
NIH funding
Removing Barriers to Colorectal Cancer Screening Act
Fixing the current coinsurance problem for Medicare beneficiaries who undergo a screening colonoscopy that becomes therapeutic remains a top AGA priority. Most of the offices that Dr. Crowe met with were cosponsors of the legislation, the Removing Barriers to Colorectal Cancer Screening Act (HR 1017/S.479), that would waive coinsurance payment regardless of the screening outcome. Dr. Crowe shared her experience with patients and the financial burden this places on beneficiaries who need to be screened. Rep. Raul Ruiz, D-CA, and Rep. Scott Peters, D-CA, both members of the House Energy and Commerce Committee and supporters of the bill, will continue to advocate that the bill receive a hearing this year to help move it through Congress. The bill continues to have wide bipartisan support. Read more about the issue and how you can explain it to your patients.
Step therapy
More and more patients are being subject to step therapy protocols, also known as “fail first” under which they are required to try and fail sometimes two or three therapies before receiving coverage of the initial therapy recommended by their physician. With the emergence of new biologics to treat diseases like inflammatory bowel disease, more and more digestive disease patients are being subject to these protocols, which can have adverse effects on their health. Restoring the Patient’s Voice Act (HR 2077) would provide patients and providers with a fair and equitable appeals process when step therapy has been imposed and provides common sense exceptions for the provider to appeal. Dr. Crowe spoke of the impact this policy is having on digestive disease patients and the burden it puts on physician practices that have to take time away from patients to navigate the convoluted insurance appeals process. We are hopeful that many of the offices that we met with will support HR 2077. Read more about the issue.
Food is Medicine Working Group
Dr. Crowe also had a productive meeting with Rep. Jim McGovern’s, D-MA, office and learned more about the recently created Food is Medicine Working Group that he has initiated. McGovern is the Ranking Member of the Agriculture Committee’s Subcommittee on Nutrition which is responsible for our nation’s nutrition guidelines and the Supplemental Nutrition Assistance Program. The Working Group will focus on costs related to hunger and the importance of nutrition in treating chronic illness and disease. AGA looks forward to working with McGovern and members of the Working Group on this bipartisan initiative.
Capitol Hill needs to hear the voice of GI
In conjunction with Dr. Crowe’s visit, AGA launched a Virtual Advocacy Day to encourage members to contact their legislators in support of the issues that Dr. Crowe was advocating during her meetings. We thank those members who took time out of their schedules to take action.
Headlines from the 2018 Gastrointestinal Cancers Symposium
The 2018 Gastrointestinal Cancers Symposium took place Jan. 18-20, 2018, in San Francisco. During the meeting, investigators presented groundbreaking research designed to improve the diagnosis and treatment of GI cancers. Here are some of the most noteworthy headlines from the 2018 meeting.
Promising Results Using Liquid Biopsy to Improve CRC Early Detection
Researchers in Taiwan developed a screening test for early colorectal cancer (CRC) detection that requires a simple blood draw to assess for circulating tumor cells in the blood. The test demonstrates 88% accuracy to detect all stages of colorectal illness, including precancerous lesions. If validated and made commercially available, this test could be readily integrated into a patient’s routine physical exam, thereby increasing CRC screening compliance.
CELESTIAL Results May Lead to Cabozantinib Approval in Second-Line HCC
The phase III CELESTIAL trial met its primary endpoint by demonstrating a survival advantage with cabozantinib in patients with advanced hepatocellular carcinoma (HCC) that progressed following prior systemic therapy. Other outcomes included improvements in progression-free survival and objective response rate, as well as an acceptable safety profile, thus positioning cabozantinib for potential approval in the second-line setting in HCC.
RAINFALL Meets Primary Endpoint, But Ramucirumab Will Not Be Pursued for a First-Line Indication in G-GEJ Cancer
Results of the global, randomized, double-blind, placebo-controlled, phase III RAINFALL trial established the statistical benefit of ramucirumab, a monoclonal antibody targeting VEGFR-2, added to standard chemotherapy for patients with previously untreated metastatic gastric or gastroesophageal junction (G-GEJ) adenocarcinoma. The findings revealed a significant 25% reduction in the risk of disease progression or death for the primary endpoint of progression-free survival (PFS). However, the reduction corresponded to only a 9-day improvement in median PFS, so the clinical benefit of frontline ramucirumab is debatable.
The Gastrointestinal Cancers Symposium is cosponsored by AGA, the American Society of Clinical Oncology (ASCO), the American Society for Radiation Oncology (ASTRO) and the Society of Surgical Oncology (SSO).
More news from the 2018 Gastrointestinal Cancers Symposium is available at gicasym.org/daily-news.
The 2018 Gastrointestinal Cancers Symposium took place Jan. 18-20, 2018, in San Francisco. During the meeting, investigators presented groundbreaking research designed to improve the diagnosis and treatment of GI cancers. Here are some of the most noteworthy headlines from the 2018 meeting.
Promising Results Using Liquid Biopsy to Improve CRC Early Detection
Researchers in Taiwan developed a screening test for early colorectal cancer (CRC) detection that requires a simple blood draw to assess for circulating tumor cells in the blood. The test demonstrates 88% accuracy to detect all stages of colorectal illness, including precancerous lesions. If validated and made commercially available, this test could be readily integrated into a patient’s routine physical exam, thereby increasing CRC screening compliance.
CELESTIAL Results May Lead to Cabozantinib Approval in Second-Line HCC
The phase III CELESTIAL trial met its primary endpoint by demonstrating a survival advantage with cabozantinib in patients with advanced hepatocellular carcinoma (HCC) that progressed following prior systemic therapy. Other outcomes included improvements in progression-free survival and objective response rate, as well as an acceptable safety profile, thus positioning cabozantinib for potential approval in the second-line setting in HCC.
RAINFALL Meets Primary Endpoint, But Ramucirumab Will Not Be Pursued for a First-Line Indication in G-GEJ Cancer
Results of the global, randomized, double-blind, placebo-controlled, phase III RAINFALL trial established the statistical benefit of ramucirumab, a monoclonal antibody targeting VEGFR-2, added to standard chemotherapy for patients with previously untreated metastatic gastric or gastroesophageal junction (G-GEJ) adenocarcinoma. The findings revealed a significant 25% reduction in the risk of disease progression or death for the primary endpoint of progression-free survival (PFS). However, the reduction corresponded to only a 9-day improvement in median PFS, so the clinical benefit of frontline ramucirumab is debatable.
The Gastrointestinal Cancers Symposium is cosponsored by AGA, the American Society of Clinical Oncology (ASCO), the American Society for Radiation Oncology (ASTRO) and the Society of Surgical Oncology (SSO).
More news from the 2018 Gastrointestinal Cancers Symposium is available at gicasym.org/daily-news.
The 2018 Gastrointestinal Cancers Symposium took place Jan. 18-20, 2018, in San Francisco. During the meeting, investigators presented groundbreaking research designed to improve the diagnosis and treatment of GI cancers. Here are some of the most noteworthy headlines from the 2018 meeting.
Promising Results Using Liquid Biopsy to Improve CRC Early Detection
Researchers in Taiwan developed a screening test for early colorectal cancer (CRC) detection that requires a simple blood draw to assess for circulating tumor cells in the blood. The test demonstrates 88% accuracy to detect all stages of colorectal illness, including precancerous lesions. If validated and made commercially available, this test could be readily integrated into a patient’s routine physical exam, thereby increasing CRC screening compliance.
CELESTIAL Results May Lead to Cabozantinib Approval in Second-Line HCC
The phase III CELESTIAL trial met its primary endpoint by demonstrating a survival advantage with cabozantinib in patients with advanced hepatocellular carcinoma (HCC) that progressed following prior systemic therapy. Other outcomes included improvements in progression-free survival and objective response rate, as well as an acceptable safety profile, thus positioning cabozantinib for potential approval in the second-line setting in HCC.
RAINFALL Meets Primary Endpoint, But Ramucirumab Will Not Be Pursued for a First-Line Indication in G-GEJ Cancer
Results of the global, randomized, double-blind, placebo-controlled, phase III RAINFALL trial established the statistical benefit of ramucirumab, a monoclonal antibody targeting VEGFR-2, added to standard chemotherapy for patients with previously untreated metastatic gastric or gastroesophageal junction (G-GEJ) adenocarcinoma. The findings revealed a significant 25% reduction in the risk of disease progression or death for the primary endpoint of progression-free survival (PFS). However, the reduction corresponded to only a 9-day improvement in median PFS, so the clinical benefit of frontline ramucirumab is debatable.
The Gastrointestinal Cancers Symposium is cosponsored by AGA, the American Society of Clinical Oncology (ASCO), the American Society for Radiation Oncology (ASTRO) and the Society of Surgical Oncology (SSO).
More news from the 2018 Gastrointestinal Cancers Symposium is available at gicasym.org/daily-news.
Thank you to our top Community contributors
2017 was a busy year in the AGA Community, our member-only discussion forum. Some of our favorite discussions included challenging clinical cases you shared, remembering your colleague Dr. Marv Sleisenger and first-hand recaps of AGA’s Advocacy Day experiences.
Thank you to everyone who contributed to the conversations in 2017, making the AGA Community a hub for collaboration to ever-expand the field of GI.
Tied for the title of top contributor in 2017 were Dmitriy Kedrin, MD, PhD, of Elliot Hospital in Manchester, N.H., and Sunanda Kane, MD, MSPH, AGAF, of Mayo Clinic in Rochester, MN.
Both are key influencers in the forum, especially with helping colleagues manage challenging patient cases. Learn more about each contributor and why keeping up with the Community is an important part of their regular routines in this brief Q&A.
Thanks for being such an active member of the AGA Community! Why do you contribute?
Dr. Kane: “You are welcome! I contribute because I feel I have helpful suggestions and recommendations for managing difficult patient scenarios as well as for professional issues.”
Dr. Kedrin: “I think it is important for GI docs to be a part of a larger community, stay informed on latest guidelines, research publications and approaches to difficult cases, where more than one road can be taken. I feel that it is a great forum for someone like me, relatively junior gastroenterologist.”
Why do you enjoy being part of the AGA Community?
Kane: “I feel engaged with my colleagues who I otherwise do not see on a regular basis, and get to ‘meet’ new ones.”
Kedrin: “I find the case discussions informative. I learn a great deal about current trends and opinions on important topics in the GI world.”
What do you like to do in your free time?
Kane: “I enjoy cooking and binge-watching Netflix.”
Kedrin: “I bake bread and run a gastroenterology literature review podcast called ‘GI Pearls.’”
What’s your approach to handling a difficult patient case you come across in your practice?
Kane: “I reach out to as many of my colleagues as I think appropriate who may have some experience or thoughts about how to help a difficult patient.”
Kedrin: “I often seek advice of other clinicians, some with more expertise in a particular area. I also go to the literature and try to learn more that way, help expand my differential as well as figure out the best therapeutic approach.”
Was there a conversation in the AGA Community in 2017 that was your favorite?
Kane: “All conversations have merit, none stick out as a favorite.”
Kedrin: “Oh, there are several. I recall a patient case where there were several thought leaders in the field who had a disagreement about the best approach to treatment. The work-life balance conversation [Early Career Group members only] was also very good. I also enjoyed reading about different opinions regarding the values of randomized versus observational trials that happened a while back.”
View the top discussions and contributors from 2017 on the AGA Community homepage, for a limited time.
2017 was a busy year in the AGA Community, our member-only discussion forum. Some of our favorite discussions included challenging clinical cases you shared, remembering your colleague Dr. Marv Sleisenger and first-hand recaps of AGA’s Advocacy Day experiences.
Thank you to everyone who contributed to the conversations in 2017, making the AGA Community a hub for collaboration to ever-expand the field of GI.
Tied for the title of top contributor in 2017 were Dmitriy Kedrin, MD, PhD, of Elliot Hospital in Manchester, N.H., and Sunanda Kane, MD, MSPH, AGAF, of Mayo Clinic in Rochester, MN.
Both are key influencers in the forum, especially with helping colleagues manage challenging patient cases. Learn more about each contributor and why keeping up with the Community is an important part of their regular routines in this brief Q&A.
Thanks for being such an active member of the AGA Community! Why do you contribute?
Dr. Kane: “You are welcome! I contribute because I feel I have helpful suggestions and recommendations for managing difficult patient scenarios as well as for professional issues.”
Dr. Kedrin: “I think it is important for GI docs to be a part of a larger community, stay informed on latest guidelines, research publications and approaches to difficult cases, where more than one road can be taken. I feel that it is a great forum for someone like me, relatively junior gastroenterologist.”
Why do you enjoy being part of the AGA Community?
Kane: “I feel engaged with my colleagues who I otherwise do not see on a regular basis, and get to ‘meet’ new ones.”
Kedrin: “I find the case discussions informative. I learn a great deal about current trends and opinions on important topics in the GI world.”
What do you like to do in your free time?
Kane: “I enjoy cooking and binge-watching Netflix.”
Kedrin: “I bake bread and run a gastroenterology literature review podcast called ‘GI Pearls.’”
What’s your approach to handling a difficult patient case you come across in your practice?
Kane: “I reach out to as many of my colleagues as I think appropriate who may have some experience or thoughts about how to help a difficult patient.”
Kedrin: “I often seek advice of other clinicians, some with more expertise in a particular area. I also go to the literature and try to learn more that way, help expand my differential as well as figure out the best therapeutic approach.”
Was there a conversation in the AGA Community in 2017 that was your favorite?
Kane: “All conversations have merit, none stick out as a favorite.”
Kedrin: “Oh, there are several. I recall a patient case where there were several thought leaders in the field who had a disagreement about the best approach to treatment. The work-life balance conversation [Early Career Group members only] was also very good. I also enjoyed reading about different opinions regarding the values of randomized versus observational trials that happened a while back.”
View the top discussions and contributors from 2017 on the AGA Community homepage, for a limited time.
2017 was a busy year in the AGA Community, our member-only discussion forum. Some of our favorite discussions included challenging clinical cases you shared, remembering your colleague Dr. Marv Sleisenger and first-hand recaps of AGA’s Advocacy Day experiences.
Thank you to everyone who contributed to the conversations in 2017, making the AGA Community a hub for collaboration to ever-expand the field of GI.
Tied for the title of top contributor in 2017 were Dmitriy Kedrin, MD, PhD, of Elliot Hospital in Manchester, N.H., and Sunanda Kane, MD, MSPH, AGAF, of Mayo Clinic in Rochester, MN.
Both are key influencers in the forum, especially with helping colleagues manage challenging patient cases. Learn more about each contributor and why keeping up with the Community is an important part of their regular routines in this brief Q&A.
Thanks for being such an active member of the AGA Community! Why do you contribute?
Dr. Kane: “You are welcome! I contribute because I feel I have helpful suggestions and recommendations for managing difficult patient scenarios as well as for professional issues.”
Dr. Kedrin: “I think it is important for GI docs to be a part of a larger community, stay informed on latest guidelines, research publications and approaches to difficult cases, where more than one road can be taken. I feel that it is a great forum for someone like me, relatively junior gastroenterologist.”
Why do you enjoy being part of the AGA Community?
Kane: “I feel engaged with my colleagues who I otherwise do not see on a regular basis, and get to ‘meet’ new ones.”
Kedrin: “I find the case discussions informative. I learn a great deal about current trends and opinions on important topics in the GI world.”
What do you like to do in your free time?
Kane: “I enjoy cooking and binge-watching Netflix.”
Kedrin: “I bake bread and run a gastroenterology literature review podcast called ‘GI Pearls.’”
What’s your approach to handling a difficult patient case you come across in your practice?
Kane: “I reach out to as many of my colleagues as I think appropriate who may have some experience or thoughts about how to help a difficult patient.”
Kedrin: “I often seek advice of other clinicians, some with more expertise in a particular area. I also go to the literature and try to learn more that way, help expand my differential as well as figure out the best therapeutic approach.”
Was there a conversation in the AGA Community in 2017 that was your favorite?
Kane: “All conversations have merit, none stick out as a favorite.”
Kedrin: “Oh, there are several. I recall a patient case where there were several thought leaders in the field who had a disagreement about the best approach to treatment. The work-life balance conversation [Early Career Group members only] was also very good. I also enjoyed reading about different opinions regarding the values of randomized versus observational trials that happened a while back.”
View the top discussions and contributors from 2017 on the AGA Community homepage, for a limited time.