User login
Renal Function Caveats
Use of increased numbers of medications and age-related decline in renal function make older patients more susceptible to adverse medication effects. Drug pharmacokinetics change, and it’s important to remember that drug metabolism is affected by a number of processes.
Renal elimination of drugs is based on nephron and renal tubule capacity, which decrease with age.1 Older individuals will not metabolize and excrete drugs as efficiently as younger, healthier individuals.
According to the Centers for Disease Control and Prevention (CDC), there are more than 36 million adults in the United States older than 65, and overall U.S. healthcare costs related to them are projected to increase 25% by 2030.2
Preventing health problems, preserving patient function, and preventing patient injury that can lead to or prolong patient hospitalizations will help contain these costs.
Quartarolo, et al., recently reported that although physicians noted the estimated glomerular filtration rate (GFR) in elderly hospitalized patients, they didn’t modify their prescribing.3 They also noted that drug dose changes in these hospitalized patients are important to prevent dosing errors and adverse reactions.
There are four major age-related pharmacokinetic parameters:
- Usually decreased gastrointestinal absorption changes ;
- Increases or decreases of a drug’s volume of distribution leading to increased blood drug levels and/or plasma-protein-binding changes;
- Usually decreased clearance with increased drug half-life effect (hepatic metabolism changes); and/or
- Decreased clearance (and increased half-life) of renally eliminated drugs.4,5
Renal Effects
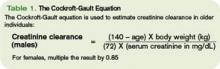
Renal excretion of drugs correlates with creatinine clearance. Because lean body mass decreases as people age, the serum creatinine level is a poor gauge of creatinine clearance in older individuals. Creatinine clearance decreases by 50% between age 25 and 85.6 The Cockroft-Gault equation is used to estimate creatinine clearance in older individuals to assist in renal dosing of drugs (See Table 1, above).
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative defines chronic kidney disease (CKD) as:
- Kidney damage for three or more months, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, marked by either pathological abnormalities or markers of kidney damage; or
- GFR of 60 mL/min/1.73 m2 or less for three or more months, with or without kidney damage.6
In these patients, adjustment of the drug dose or dosing interval is imperative to attain optimal drug effects and patient outcomes. The same is also true for older adults with decreased renal function, whether diagnosed with CKD or not.
In addition, patients with severe renal insufficiency, including those with CKD, may encounter accumulation of active metabolites, as well as accumulation of the parent drug compound. This can lead to significant toxicity in some cases. Examples of active metabolites include:
- Normeperidine, an active metabolite of meperidine that can lead to central nervous system stimulation including seizures;
- Morphine-6-glucuronide, an active metabolite of morphine and codeine with less analgesic effect. It can lead to a prolonged narcotic effect; or
- N-acetyl-p-benzoquinoneimine, a metabolite of acetaminophen responsible for hepatotoxicity.7
Doses of renally cleared drugs should be adjusted in patients with decreased renal function. Initial dosages can be determined using published guidelines.8 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Quartarolo JM, Thoelke M, Schafers SJ. Reporting of estimated glomerular filtration rate: effect on physician recognition of chronic kidney disease and prescribing practices for elderly hospitalized patients. J Hosp Med. 2007;2(2):74-78.
- Frye RF, Matzke GR. Drug therapy individualization for patients with renal insufficiency. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:939-952.
- Healthy Aging At-A-Glance 2007. Available at www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf. Last accessed Oct. 15, 2007.
- Hanlon JT, Ruby CM, Guay D, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:79-89.
- Williams CM. Using medications appropriately in older adults. Am Fam Physician. 2002;66(10):1917-1924.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Available at www.kidney.org/professionals/kdoqi/guidelines_ckd/p4_class_g1.htm. Last accessed Oct. 15, 2007.
- Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75(10):1487-1496.
- Brier ME, Aronoff GR. Drug Prescribing in Renal Failure: Dosing Guidelines for adults. 5th ed. Philadelphia, Pa : American College of Physicians; 2007.
Use of increased numbers of medications and age-related decline in renal function make older patients more susceptible to adverse medication effects. Drug pharmacokinetics change, and it’s important to remember that drug metabolism is affected by a number of processes.
Renal elimination of drugs is based on nephron and renal tubule capacity, which decrease with age.1 Older individuals will not metabolize and excrete drugs as efficiently as younger, healthier individuals.
According to the Centers for Disease Control and Prevention (CDC), there are more than 36 million adults in the United States older than 65, and overall U.S. healthcare costs related to them are projected to increase 25% by 2030.2
Preventing health problems, preserving patient function, and preventing patient injury that can lead to or prolong patient hospitalizations will help contain these costs.
Quartarolo, et al., recently reported that although physicians noted the estimated glomerular filtration rate (GFR) in elderly hospitalized patients, they didn’t modify their prescribing.3 They also noted that drug dose changes in these hospitalized patients are important to prevent dosing errors and adverse reactions.
There are four major age-related pharmacokinetic parameters:
- Usually decreased gastrointestinal absorption changes ;
- Increases or decreases of a drug’s volume of distribution leading to increased blood drug levels and/or plasma-protein-binding changes;
- Usually decreased clearance with increased drug half-life effect (hepatic metabolism changes); and/or
- Decreased clearance (and increased half-life) of renally eliminated drugs.4,5
Renal Effects
Renal excretion of drugs correlates with creatinine clearance. Because lean body mass decreases as people age, the serum creatinine level is a poor gauge of creatinine clearance in older individuals. Creatinine clearance decreases by 50% between age 25 and 85.6 The Cockroft-Gault equation is used to estimate creatinine clearance in older individuals to assist in renal dosing of drugs (See Table 1, above).
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative defines chronic kidney disease (CKD) as:
- Kidney damage for three or more months, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, marked by either pathological abnormalities or markers of kidney damage; or
- GFR of 60 mL/min/1.73 m2 or less for three or more months, with or without kidney damage.6
In these patients, adjustment of the drug dose or dosing interval is imperative to attain optimal drug effects and patient outcomes. The same is also true for older adults with decreased renal function, whether diagnosed with CKD or not.
In addition, patients with severe renal insufficiency, including those with CKD, may encounter accumulation of active metabolites, as well as accumulation of the parent drug compound. This can lead to significant toxicity in some cases. Examples of active metabolites include:
- Normeperidine, an active metabolite of meperidine that can lead to central nervous system stimulation including seizures;
- Morphine-6-glucuronide, an active metabolite of morphine and codeine with less analgesic effect. It can lead to a prolonged narcotic effect; or
- N-acetyl-p-benzoquinoneimine, a metabolite of acetaminophen responsible for hepatotoxicity.7
Doses of renally cleared drugs should be adjusted in patients with decreased renal function. Initial dosages can be determined using published guidelines.8 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Quartarolo JM, Thoelke M, Schafers SJ. Reporting of estimated glomerular filtration rate: effect on physician recognition of chronic kidney disease and prescribing practices for elderly hospitalized patients. J Hosp Med. 2007;2(2):74-78.
- Frye RF, Matzke GR. Drug therapy individualization for patients with renal insufficiency. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:939-952.
- Healthy Aging At-A-Glance 2007. Available at www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf. Last accessed Oct. 15, 2007.
- Hanlon JT, Ruby CM, Guay D, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:79-89.
- Williams CM. Using medications appropriately in older adults. Am Fam Physician. 2002;66(10):1917-1924.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Available at www.kidney.org/professionals/kdoqi/guidelines_ckd/p4_class_g1.htm. Last accessed Oct. 15, 2007.
- Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75(10):1487-1496.
- Brier ME, Aronoff GR. Drug Prescribing in Renal Failure: Dosing Guidelines for adults. 5th ed. Philadelphia, Pa : American College of Physicians; 2007.
Use of increased numbers of medications and age-related decline in renal function make older patients more susceptible to adverse medication effects. Drug pharmacokinetics change, and it’s important to remember that drug metabolism is affected by a number of processes.
Renal elimination of drugs is based on nephron and renal tubule capacity, which decrease with age.1 Older individuals will not metabolize and excrete drugs as efficiently as younger, healthier individuals.
According to the Centers for Disease Control and Prevention (CDC), there are more than 36 million adults in the United States older than 65, and overall U.S. healthcare costs related to them are projected to increase 25% by 2030.2
Preventing health problems, preserving patient function, and preventing patient injury that can lead to or prolong patient hospitalizations will help contain these costs.
Quartarolo, et al., recently reported that although physicians noted the estimated glomerular filtration rate (GFR) in elderly hospitalized patients, they didn’t modify their prescribing.3 They also noted that drug dose changes in these hospitalized patients are important to prevent dosing errors and adverse reactions.
There are four major age-related pharmacokinetic parameters:
- Usually decreased gastrointestinal absorption changes ;
- Increases or decreases of a drug’s volume of distribution leading to increased blood drug levels and/or plasma-protein-binding changes;
- Usually decreased clearance with increased drug half-life effect (hepatic metabolism changes); and/or
- Decreased clearance (and increased half-life) of renally eliminated drugs.4,5
Renal Effects
Renal excretion of drugs correlates with creatinine clearance. Because lean body mass decreases as people age, the serum creatinine level is a poor gauge of creatinine clearance in older individuals. Creatinine clearance decreases by 50% between age 25 and 85.6 The Cockroft-Gault equation is used to estimate creatinine clearance in older individuals to assist in renal dosing of drugs (See Table 1, above).
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative defines chronic kidney disease (CKD) as:
- Kidney damage for three or more months, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, marked by either pathological abnormalities or markers of kidney damage; or
- GFR of 60 mL/min/1.73 m2 or less for three or more months, with or without kidney damage.6
In these patients, adjustment of the drug dose or dosing interval is imperative to attain optimal drug effects and patient outcomes. The same is also true for older adults with decreased renal function, whether diagnosed with CKD or not.
In addition, patients with severe renal insufficiency, including those with CKD, may encounter accumulation of active metabolites, as well as accumulation of the parent drug compound. This can lead to significant toxicity in some cases. Examples of active metabolites include:
- Normeperidine, an active metabolite of meperidine that can lead to central nervous system stimulation including seizures;
- Morphine-6-glucuronide, an active metabolite of morphine and codeine with less analgesic effect. It can lead to a prolonged narcotic effect; or
- N-acetyl-p-benzoquinoneimine, a metabolite of acetaminophen responsible for hepatotoxicity.7
Doses of renally cleared drugs should be adjusted in patients with decreased renal function. Initial dosages can be determined using published guidelines.8 TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Quartarolo JM, Thoelke M, Schafers SJ. Reporting of estimated glomerular filtration rate: effect on physician recognition of chronic kidney disease and prescribing practices for elderly hospitalized patients. J Hosp Med. 2007;2(2):74-78.
- Frye RF, Matzke GR. Drug therapy individualization for patients with renal insufficiency. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:939-952.
- Healthy Aging At-A-Glance 2007. Available at www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf. Last accessed Oct. 15, 2007.
- Hanlon JT, Ruby CM, Guay D, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, eds. Pharmacotherapy A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:79-89.
- Williams CM. Using medications appropriately in older adults. Am Fam Physician. 2002;66(10):1917-1924.
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Available at www.kidney.org/professionals/kdoqi/guidelines_ckd/p4_class_g1.htm. Last accessed Oct. 15, 2007.
- Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75(10):1487-1496.
- Brier ME, Aronoff GR. Drug Prescribing in Renal Failure: Dosing Guidelines for adults. 5th ed. Philadelphia, Pa : American College of Physicians; 2007.
SHM Behind the Scenes
You may have noticed a new look to SHM’s Web site. To the naked eye, many of these changes might appear subtle. Behind the nuanced changes to the graphical interface, the content now resides in a completely different structure that allows users to more easily find information and resources.
Why the change? As SHM’s interactive services manager, I have spent a lot of time trying to find pages of content on the SHM Web site that need to be added, updated, or removed. This is not a task for the faint of heart, considering there are more than 10,000 active pages on the SHM Web site.
About a year ago, after a particularly head-splitting day of trying to find an obscure piece of information, I concluded: “There has got to be a better way to organize the information on this site!” After discussions with key stakeholders, we concluded it was time to completely reorganize our Web site. As a reward for bringing this to everyone’s attention, I was chosen to head the endeavor.
After a couple of minutes of pondering the sheer magnitude of the effort I thought for a moment about taking an extended leave of absence. It would have been easy to sit in my cubicle and pound out a new architecture I thought would work well for the organization’s needs. But the reality was that just about everybody would need a say in the process.
As one of the most prominent faces of the organization, the Web site projects the core of SHM. Its online presence is a major tool for finding and engaging members, promoting SHM’s major initiatives and letting the world know exactly what the hospital medicine movement is about. Because of this, it was imperative that all the individuals involved in making the Society what it is were involved in the process of creating an information architecture for the Web site that would best serve the needs of all our users.
Right from the beginning of the process, it was clear that in order to create an information structure that worked for the organization as a whole, everyone would need to understand the importance of each other’s stake in the content on the Web site. Once there was an across-the-board understanding of the key pieces and groups of information on the site, it would be easier to implement structural changes that made sense to the organization as a whole.
Buy-in needed to occur at a high level early on. From the beginning of this project, I saw an opportunity to use many of the teaching and group-participation skills I learned as a Peace Corp volunteer in Ukraine. Not surprisingly, much of what I used to engage individuals, generate discussions and create ideas actually worked better in a roomful of SHM staff than it did in a classroom packed with hormone driven teenagers who were more interested in knowing if I personally knew Britney Spears than speaking English.
The initial brainstorming and idea-gathering sessions we held laid a solid foundation for restructuring the site’s navigation and information architecture, making it easier to navigate and more engaging for the end-user.
In the end, brute force, hard work, and group collaboration got the job done. Without the contribution and dedication of countless members of the SHM staff and community, this project would not have become a reality.
SHM now boasts a site that is cleaner, easier to navigate, and better showcases SHM’s role as the heart of the hospital medicine movement. A Web site, like many other things in life, is always a work in progress. But we feel confident that what you see today is a significant improvement over its predecessor.
Stop by www.hospitalmedicine.org to check out the result of this organization-wide effort. Comments and suggestions are always welcome as we continue to strive to improve the user experience. E-mail me at [email protected].
You may have noticed a new look to SHM’s Web site. To the naked eye, many of these changes might appear subtle. Behind the nuanced changes to the graphical interface, the content now resides in a completely different structure that allows users to more easily find information and resources.
Why the change? As SHM’s interactive services manager, I have spent a lot of time trying to find pages of content on the SHM Web site that need to be added, updated, or removed. This is not a task for the faint of heart, considering there are more than 10,000 active pages on the SHM Web site.
About a year ago, after a particularly head-splitting day of trying to find an obscure piece of information, I concluded: “There has got to be a better way to organize the information on this site!” After discussions with key stakeholders, we concluded it was time to completely reorganize our Web site. As a reward for bringing this to everyone’s attention, I was chosen to head the endeavor.
After a couple of minutes of pondering the sheer magnitude of the effort I thought for a moment about taking an extended leave of absence. It would have been easy to sit in my cubicle and pound out a new architecture I thought would work well for the organization’s needs. But the reality was that just about everybody would need a say in the process.
As one of the most prominent faces of the organization, the Web site projects the core of SHM. Its online presence is a major tool for finding and engaging members, promoting SHM’s major initiatives and letting the world know exactly what the hospital medicine movement is about. Because of this, it was imperative that all the individuals involved in making the Society what it is were involved in the process of creating an information architecture for the Web site that would best serve the needs of all our users.
Right from the beginning of the process, it was clear that in order to create an information structure that worked for the organization as a whole, everyone would need to understand the importance of each other’s stake in the content on the Web site. Once there was an across-the-board understanding of the key pieces and groups of information on the site, it would be easier to implement structural changes that made sense to the organization as a whole.
Buy-in needed to occur at a high level early on. From the beginning of this project, I saw an opportunity to use many of the teaching and group-participation skills I learned as a Peace Corp volunteer in Ukraine. Not surprisingly, much of what I used to engage individuals, generate discussions and create ideas actually worked better in a roomful of SHM staff than it did in a classroom packed with hormone driven teenagers who were more interested in knowing if I personally knew Britney Spears than speaking English.
The initial brainstorming and idea-gathering sessions we held laid a solid foundation for restructuring the site’s navigation and information architecture, making it easier to navigate and more engaging for the end-user.
In the end, brute force, hard work, and group collaboration got the job done. Without the contribution and dedication of countless members of the SHM staff and community, this project would not have become a reality.
SHM now boasts a site that is cleaner, easier to navigate, and better showcases SHM’s role as the heart of the hospital medicine movement. A Web site, like many other things in life, is always a work in progress. But we feel confident that what you see today is a significant improvement over its predecessor.
Stop by www.hospitalmedicine.org to check out the result of this organization-wide effort. Comments and suggestions are always welcome as we continue to strive to improve the user experience. E-mail me at [email protected].
You may have noticed a new look to SHM’s Web site. To the naked eye, many of these changes might appear subtle. Behind the nuanced changes to the graphical interface, the content now resides in a completely different structure that allows users to more easily find information and resources.
Why the change? As SHM’s interactive services manager, I have spent a lot of time trying to find pages of content on the SHM Web site that need to be added, updated, or removed. This is not a task for the faint of heart, considering there are more than 10,000 active pages on the SHM Web site.
About a year ago, after a particularly head-splitting day of trying to find an obscure piece of information, I concluded: “There has got to be a better way to organize the information on this site!” After discussions with key stakeholders, we concluded it was time to completely reorganize our Web site. As a reward for bringing this to everyone’s attention, I was chosen to head the endeavor.
After a couple of minutes of pondering the sheer magnitude of the effort I thought for a moment about taking an extended leave of absence. It would have been easy to sit in my cubicle and pound out a new architecture I thought would work well for the organization’s needs. But the reality was that just about everybody would need a say in the process.
As one of the most prominent faces of the organization, the Web site projects the core of SHM. Its online presence is a major tool for finding and engaging members, promoting SHM’s major initiatives and letting the world know exactly what the hospital medicine movement is about. Because of this, it was imperative that all the individuals involved in making the Society what it is were involved in the process of creating an information architecture for the Web site that would best serve the needs of all our users.
Right from the beginning of the process, it was clear that in order to create an information structure that worked for the organization as a whole, everyone would need to understand the importance of each other’s stake in the content on the Web site. Once there was an across-the-board understanding of the key pieces and groups of information on the site, it would be easier to implement structural changes that made sense to the organization as a whole.
Buy-in needed to occur at a high level early on. From the beginning of this project, I saw an opportunity to use many of the teaching and group-participation skills I learned as a Peace Corp volunteer in Ukraine. Not surprisingly, much of what I used to engage individuals, generate discussions and create ideas actually worked better in a roomful of SHM staff than it did in a classroom packed with hormone driven teenagers who were more interested in knowing if I personally knew Britney Spears than speaking English.
The initial brainstorming and idea-gathering sessions we held laid a solid foundation for restructuring the site’s navigation and information architecture, making it easier to navigate and more engaging for the end-user.
In the end, brute force, hard work, and group collaboration got the job done. Without the contribution and dedication of countless members of the SHM staff and community, this project would not have become a reality.
SHM now boasts a site that is cleaner, easier to navigate, and better showcases SHM’s role as the heart of the hospital medicine movement. A Web site, like many other things in life, is always a work in progress. But we feel confident that what you see today is a significant improvement over its predecessor.
Stop by www.hospitalmedicine.org to check out the result of this organization-wide effort. Comments and suggestions are always welcome as we continue to strive to improve the user experience. E-mail me at [email protected].
All Eyes on San Diego
SHM’s Annual Meeting highlights hospital medicine as a distinct field within internal medicine. Being able to, year after year, incorporate core clinical topics, evidence-based practice, quality-related content, and career development into three days is only possible because of the foundation laid from previous meetings over the past 10 years.
Expectations about the role of hospitalists have taken shape through recommendations from education summits and national experts on healthcare policy, and via publications like the Journal of Hospital Medicine and The Core Competencies in Hospital Medicine. The Annual Meeting Committee’s goal was to define a program that facilitates hospitalists in achieving that role.
The 2008 meeting April 3-5 in San Diego will feature:
- National leaders in hospital medicine and healthcare;
- Six precourses addressing timely and relevant topics; and
- Seven tracks addressing clinical, operational, quality, academic, and pediatric issues.
Issues that have broad appeal and present challenges for hospitalists will be addressed in three widely anticipated keynotes:
Quality: Don Berwick, MD, MPP, FRCP, president and CEO, Institute for Healthcare Improvement (IHI) and architect of both the 100,000 Lives and 5 Million Lives campaigns;
The future of healthcare: Ian Morrison, PhD, president emeritus and health advisory panel chair, Institute for the Future, and an internationally known author on long-term forecasting with particular emphasis on healthcare;
Thriving in the face of comanagement, non-teaching services, transparency, and the reality of perpetual change: Robert Wachter, MD, professor and chief of the division of hospital medicine, associate chairman of the department of medicine, University of California, San Francisco.
The future of hospital medicine: opportunities and challenges: A special plenary session presented by a panel of hospital medicine leaders who will share perspectives from:
- The large hospitalist company;
- The large hospital company as an employer;
- The hospital CEO; and
- The individual hospital employed/associated hospital medicine group.
The following program elements are only a few of the many highlights of “Hospital Medicine 2008”:
The Evidence-Based Rapid-Fire Track: This track was developed in response from last year’s attendees. It is designed to provide participants—new or old attendees, academic or community caregivers—with “rapid bursts” of content and to address specific questions framed by the committee, based on the highest level of medical evidence available.
Research, Innovations, and Clinical Vignettes (RIV) Competition: Building on a new feature from “Hospital Medicine 2007,” a nationally renowned professor will again tour the poster session and comment on the entries, meet with academic hospitalists, attend forums, and generally be a “visiting professor” for the duration of the meeting. Additionally, SHM’s RIV Committee, along with staff, are working on arrangements for junior faculty to interact with senior researchers during times that run concurrent with non-plenary sessions. Senior hospitalists with expertise in quality-improvement research will also provide individual feedback to authors at the poster sessions. Mini poster presentation sessions will provide a way for residents to highlight their work, and there will be new, separate receptions for the posters (April 3) and exhibits (April 4).
More networking: Networking provides a critical outlet to interact with senior hospitalists, find out what others are doing to advance their careers, and seek mentorship. In addition to the networking opportunities incorporated in the RIV Competition, other networking opportunities include the exhibits, President’s Luncheon and additional receptions, and two new special-interest forums on com-anagement and consultative medicine and international hospital medicine.
The Annual Meeting Committee sought improvements in developing and implementing this year’s program. Committee brainstorming sessions for this year’s meeting focused on:
- Balancing what works with innovation;
- Making the meeting more valuable to clinical educators and researchers, and more applicable to community hospitalists; and
- Showing national leaders the extraordinary talent behind and work of SHM.
A key innovation was a successful “call for speakers.” Submissions were sought for three breakout sessions to create additional opportunity for members to play an active role in “Hospital Medicine 2008.” Based on submissions, sessions were added on the following topics:
- “Prevention, Management, and Treatment of Acute Delirium”;
- “Designing Compensation and Bonus Plans to Drive Desired Behavior”; and
- “Acute Coronary Syndrome Trials and Tribulations.”
Changes for “Hospital Medicine 2008” reflect the volunteerism of many professionals and would not have been possible without the mentorship and expertise of seasoned veteran leaders in hospital medicine, as well as the feedback and participation of hospitalists providing daily inpatient care. As part of a continuous quality-improvement initiative, rules of engagement were developed so speakers would have useful information up front.
The success of the SHM Annual Meeting depends upon the participation and leadership of SHM members, staff, committees, and task forces, as well as the SHM Board. My thanks goes out to them all for their efforts in once again creating a top-flight program.
For more information on “Hospital Medicine 2008,” and to register, visit www.hospitalmedicine.org/hospitalmedicine2008.
SHM’s Annual Meeting highlights hospital medicine as a distinct field within internal medicine. Being able to, year after year, incorporate core clinical topics, evidence-based practice, quality-related content, and career development into three days is only possible because of the foundation laid from previous meetings over the past 10 years.
Expectations about the role of hospitalists have taken shape through recommendations from education summits and national experts on healthcare policy, and via publications like the Journal of Hospital Medicine and The Core Competencies in Hospital Medicine. The Annual Meeting Committee’s goal was to define a program that facilitates hospitalists in achieving that role.
The 2008 meeting April 3-5 in San Diego will feature:
- National leaders in hospital medicine and healthcare;
- Six precourses addressing timely and relevant topics; and
- Seven tracks addressing clinical, operational, quality, academic, and pediatric issues.
Issues that have broad appeal and present challenges for hospitalists will be addressed in three widely anticipated keynotes:
Quality: Don Berwick, MD, MPP, FRCP, president and CEO, Institute for Healthcare Improvement (IHI) and architect of both the 100,000 Lives and 5 Million Lives campaigns;
The future of healthcare: Ian Morrison, PhD, president emeritus and health advisory panel chair, Institute for the Future, and an internationally known author on long-term forecasting with particular emphasis on healthcare;
Thriving in the face of comanagement, non-teaching services, transparency, and the reality of perpetual change: Robert Wachter, MD, professor and chief of the division of hospital medicine, associate chairman of the department of medicine, University of California, San Francisco.
The future of hospital medicine: opportunities and challenges: A special plenary session presented by a panel of hospital medicine leaders who will share perspectives from:
- The large hospitalist company;
- The large hospital company as an employer;
- The hospital CEO; and
- The individual hospital employed/associated hospital medicine group.
The following program elements are only a few of the many highlights of “Hospital Medicine 2008”:
The Evidence-Based Rapid-Fire Track: This track was developed in response from last year’s attendees. It is designed to provide participants—new or old attendees, academic or community caregivers—with “rapid bursts” of content and to address specific questions framed by the committee, based on the highest level of medical evidence available.
Research, Innovations, and Clinical Vignettes (RIV) Competition: Building on a new feature from “Hospital Medicine 2007,” a nationally renowned professor will again tour the poster session and comment on the entries, meet with academic hospitalists, attend forums, and generally be a “visiting professor” for the duration of the meeting. Additionally, SHM’s RIV Committee, along with staff, are working on arrangements for junior faculty to interact with senior researchers during times that run concurrent with non-plenary sessions. Senior hospitalists with expertise in quality-improvement research will also provide individual feedback to authors at the poster sessions. Mini poster presentation sessions will provide a way for residents to highlight their work, and there will be new, separate receptions for the posters (April 3) and exhibits (April 4).
More networking: Networking provides a critical outlet to interact with senior hospitalists, find out what others are doing to advance their careers, and seek mentorship. In addition to the networking opportunities incorporated in the RIV Competition, other networking opportunities include the exhibits, President’s Luncheon and additional receptions, and two new special-interest forums on com-anagement and consultative medicine and international hospital medicine.
The Annual Meeting Committee sought improvements in developing and implementing this year’s program. Committee brainstorming sessions for this year’s meeting focused on:
- Balancing what works with innovation;
- Making the meeting more valuable to clinical educators and researchers, and more applicable to community hospitalists; and
- Showing national leaders the extraordinary talent behind and work of SHM.
A key innovation was a successful “call for speakers.” Submissions were sought for three breakout sessions to create additional opportunity for members to play an active role in “Hospital Medicine 2008.” Based on submissions, sessions were added on the following topics:
- “Prevention, Management, and Treatment of Acute Delirium”;
- “Designing Compensation and Bonus Plans to Drive Desired Behavior”; and
- “Acute Coronary Syndrome Trials and Tribulations.”
Changes for “Hospital Medicine 2008” reflect the volunteerism of many professionals and would not have been possible without the mentorship and expertise of seasoned veteran leaders in hospital medicine, as well as the feedback and participation of hospitalists providing daily inpatient care. As part of a continuous quality-improvement initiative, rules of engagement were developed so speakers would have useful information up front.
The success of the SHM Annual Meeting depends upon the participation and leadership of SHM members, staff, committees, and task forces, as well as the SHM Board. My thanks goes out to them all for their efforts in once again creating a top-flight program.
For more information on “Hospital Medicine 2008,” and to register, visit www.hospitalmedicine.org/hospitalmedicine2008.
SHM’s Annual Meeting highlights hospital medicine as a distinct field within internal medicine. Being able to, year after year, incorporate core clinical topics, evidence-based practice, quality-related content, and career development into three days is only possible because of the foundation laid from previous meetings over the past 10 years.
Expectations about the role of hospitalists have taken shape through recommendations from education summits and national experts on healthcare policy, and via publications like the Journal of Hospital Medicine and The Core Competencies in Hospital Medicine. The Annual Meeting Committee’s goal was to define a program that facilitates hospitalists in achieving that role.
The 2008 meeting April 3-5 in San Diego will feature:
- National leaders in hospital medicine and healthcare;
- Six precourses addressing timely and relevant topics; and
- Seven tracks addressing clinical, operational, quality, academic, and pediatric issues.
Issues that have broad appeal and present challenges for hospitalists will be addressed in three widely anticipated keynotes:
Quality: Don Berwick, MD, MPP, FRCP, president and CEO, Institute for Healthcare Improvement (IHI) and architect of both the 100,000 Lives and 5 Million Lives campaigns;
The future of healthcare: Ian Morrison, PhD, president emeritus and health advisory panel chair, Institute for the Future, and an internationally known author on long-term forecasting with particular emphasis on healthcare;
Thriving in the face of comanagement, non-teaching services, transparency, and the reality of perpetual change: Robert Wachter, MD, professor and chief of the division of hospital medicine, associate chairman of the department of medicine, University of California, San Francisco.
The future of hospital medicine: opportunities and challenges: A special plenary session presented by a panel of hospital medicine leaders who will share perspectives from:
- The large hospitalist company;
- The large hospital company as an employer;
- The hospital CEO; and
- The individual hospital employed/associated hospital medicine group.
The following program elements are only a few of the many highlights of “Hospital Medicine 2008”:
The Evidence-Based Rapid-Fire Track: This track was developed in response from last year’s attendees. It is designed to provide participants—new or old attendees, academic or community caregivers—with “rapid bursts” of content and to address specific questions framed by the committee, based on the highest level of medical evidence available.
Research, Innovations, and Clinical Vignettes (RIV) Competition: Building on a new feature from “Hospital Medicine 2007,” a nationally renowned professor will again tour the poster session and comment on the entries, meet with academic hospitalists, attend forums, and generally be a “visiting professor” for the duration of the meeting. Additionally, SHM’s RIV Committee, along with staff, are working on arrangements for junior faculty to interact with senior researchers during times that run concurrent with non-plenary sessions. Senior hospitalists with expertise in quality-improvement research will also provide individual feedback to authors at the poster sessions. Mini poster presentation sessions will provide a way for residents to highlight their work, and there will be new, separate receptions for the posters (April 3) and exhibits (April 4).
More networking: Networking provides a critical outlet to interact with senior hospitalists, find out what others are doing to advance their careers, and seek mentorship. In addition to the networking opportunities incorporated in the RIV Competition, other networking opportunities include the exhibits, President’s Luncheon and additional receptions, and two new special-interest forums on com-anagement and consultative medicine and international hospital medicine.
The Annual Meeting Committee sought improvements in developing and implementing this year’s program. Committee brainstorming sessions for this year’s meeting focused on:
- Balancing what works with innovation;
- Making the meeting more valuable to clinical educators and researchers, and more applicable to community hospitalists; and
- Showing national leaders the extraordinary talent behind and work of SHM.
A key innovation was a successful “call for speakers.” Submissions were sought for three breakout sessions to create additional opportunity for members to play an active role in “Hospital Medicine 2008.” Based on submissions, sessions were added on the following topics:
- “Prevention, Management, and Treatment of Acute Delirium”;
- “Designing Compensation and Bonus Plans to Drive Desired Behavior”; and
- “Acute Coronary Syndrome Trials and Tribulations.”
Changes for “Hospital Medicine 2008” reflect the volunteerism of many professionals and would not have been possible without the mentorship and expertise of seasoned veteran leaders in hospital medicine, as well as the feedback and participation of hospitalists providing daily inpatient care. As part of a continuous quality-improvement initiative, rules of engagement were developed so speakers would have useful information up front.
The success of the SHM Annual Meeting depends upon the participation and leadership of SHM members, staff, committees, and task forces, as well as the SHM Board. My thanks goes out to them all for their efforts in once again creating a top-flight program.
For more information on “Hospital Medicine 2008,” and to register, visit www.hospitalmedicine.org/hospitalmedicine2008.
Malpractice Chronicle
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Who Was to Blame for Hyponatremia Death?
At age 63, a man visited the defendant family physician with complaints of fever and productive cough; he also needed a change in his blood pressure medication.
Chest x-ray results were negative, and the defendant prescribed an antibiotic. Six days later, the patient returned to the defendant’s office with similar but waning symptoms and new complaints consistent with anxiety and depression.
Over the following four days, the patient’s wife placed two documented calls to the defendant’s office to update him regarding the patient’s condition. The patient was subsequently taken to a hospital emergency department, where a sodium level of 101 mEq/L was detected on blood chemistry. A diagnosis of hyponatremia was made and an isotonic saline solution started.
The patient was then transferred to another hospital, where a hypertonic saline solution was ordered. Because his sodium level was replenished too quickly, the man developed central pontine myelinolysis (CPM). Three weeks later, he died of CPM-related aspiration pneumonia.
The plaintiff claimed that the defendant physician failed to diagnose hyponatremia and to give the patient proper treatment, which led to his death.
The defendant contended that there was no way to diagnose hyponatremia, based on the decedent’s signs and symptoms. The defendant also charged that death was caused by mistreatment at the hospital where the patient died.
According to a published account, a defense verdict was returned.
Pneumonia Patient Sent Home Too Soon
Complaints of upper back pain, evidently exacerbated by respiration, took a 44-year-old woman to a hospital emergency department. Tests revealed an elevated white blood cell count, but a chest x-ray was clear. A diagnosis of a pulled muscle was made; the patient was sent home with prescriptions for naproxen and hydrocodone with acetaminophen.
Four days later, the patient went to a clinic complaining of back pain. A second chest x-ray showed extensive right-sided pneumonia, for which she was hospitalized. Test results revealed that the patient was hypoxic, that her band cells were elevated to 65%, and that her white blood cell count was 5,000/mL. An additional chest x-ray was ordered, which the plaintiffs later claimed showed worsening pneumonia in the right lung.
When the patient complained of severely increased pain, her medications were discontinued and IV morphine was initiated. On day 5 of the patient’s hospital stay, her case was transferred to a different physician, and she was discharged two days later.
When the patient’s condition had not improved five days after her discharge, she placed a call to her physician, which was not returned. Very early the next morning, the woman was taken to the hospital. An hour later, she was pronounced dead as a result of cardiopulmonary arrest secondary to pneumonia.
Plaintiffs claimed that the decedent was prematurely discharged and that the defendant was negligent in failing to return her phone call. The defendant argued that the test results and x-rays that the plaintiffs claimed contraindicated discharge were not available when the decision was made to discharge the decedent. The defendant also claimed that, according to the office telephone record, the decedent had failed to convey any urgency when she called; thus, there was no negligence in failing to return the call that day. The plaintiffs maintained that the call had described the patient’s situation as urgent.
According to a published account, an $864,000 arbitration award was given.
Was Surgery for Hydrocephalus Delayed?
A 53-year-old man presented to a hospital emergency department (ED) after experiencing headaches, dizziness, nausea, vomiting, and a temperature as high as 101.9°F for several days. After the initial physical examination, nystagmus was diagnosed; meningitis was not considered. The patient was sent home with medication.
The next day, he returned to the same ED. MRI and CT of the brain revealed a 1.0-in brain tumor and hydrocephalus. The man was admitted for neurosurgical evaluation and treatment. During his examination, he was somewhat disoriented but could carry on a conversation. He was also able to stand, and his reflexes (including the pupillary reflexes) were normal. When increased hydrocephalus and intracranial pressure became evident, he was given steroids and mannitol.
The next day, the patient was lethargic, and his pupillary reflexes were slowly reactive. He responded to voice commands, but there were signs of increasing intracranial pressure.
That evening, the man ceased responding to voice commands and appeared increasingly confused. The following day, he was more lethargic. He made no spontaneous movements and no response to commands, although he did withdraw from painful stimuli. A repeat MRI showed the tumor and hydrocephalus.
Surgery was performed for removal of the tumor, which was identified as a T-cell lymphoma. The patient did not regain consciousness after the surgery. CT performed shortly thereafter showed herniation of the brain and diffuse hypoxic damage of a duration to suggest that it had occurred before the surgery.
The family refused a do-not-resuscitate (DNR) order and discontinuation of life support. For nine days after the surgery, the medical staff tried to persuade the family that the patient was dead; they then wrote a DNR order in the chart. When the family protested, doctors transferred the decedent out of the ICU and discontinued all medical support; they also clamped the ventriculostomy tube that had been placed after surgery. The decedent’s blood pressure and pulse remained normal, and his only requirements for life were IV fluids and a respirator.
After continued protest, the family was told that DNR orders are within the doctor’s decision. Consent was then sought to harvest the decedent’s organs for transplantation. Some 25 family members were present when a nurse discontinued the ventilator, and the man died.
Twenty-one family members sued for intentional infliction of emotional distress. Plaintiffs claimed that the decedent was in a coma that was caused not by the tumor but by hydrocephalus and increased intracranial pressure that accompanied the tumor. The plaintiffs claimed that a decompressing ventriculostomy would have prevented the herniation and hypoxic brain damage; this developed either before or during the surgery, which they charged was delayed. The plaintiffs also claimed that the decedent was not dead when life support was discontinued. The last electroencephalogram showed brain activity, they claimed, and the decedent’s blood pressure and pulse remained normal without any medical support. The plaintiffs also claimed that the decedent made respiratory movements for five minutes after the respirator was discontinued.
The defendants argued that the delay in performing surgery was necessary and that the decedent’s deterioration resulted from administration of sedatives to obtain a clear MRI. The defendants also claimed that the decedent was brain-dead after the surgery and that malpractice and wrongful death claims could not be applied to a person who was already dead.
According to a published report, a $425,000 settlement was reached.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Who Was to Blame for Hyponatremia Death?
At age 63, a man visited the defendant family physician with complaints of fever and productive cough; he also needed a change in his blood pressure medication.
Chest x-ray results were negative, and the defendant prescribed an antibiotic. Six days later, the patient returned to the defendant’s office with similar but waning symptoms and new complaints consistent with anxiety and depression.
Over the following four days, the patient’s wife placed two documented calls to the defendant’s office to update him regarding the patient’s condition. The patient was subsequently taken to a hospital emergency department, where a sodium level of 101 mEq/L was detected on blood chemistry. A diagnosis of hyponatremia was made and an isotonic saline solution started.
The patient was then transferred to another hospital, where a hypertonic saline solution was ordered. Because his sodium level was replenished too quickly, the man developed central pontine myelinolysis (CPM). Three weeks later, he died of CPM-related aspiration pneumonia.
The plaintiff claimed that the defendant physician failed to diagnose hyponatremia and to give the patient proper treatment, which led to his death.
The defendant contended that there was no way to diagnose hyponatremia, based on the decedent’s signs and symptoms. The defendant also charged that death was caused by mistreatment at the hospital where the patient died.
According to a published account, a defense verdict was returned.
Pneumonia Patient Sent Home Too Soon
Complaints of upper back pain, evidently exacerbated by respiration, took a 44-year-old woman to a hospital emergency department. Tests revealed an elevated white blood cell count, but a chest x-ray was clear. A diagnosis of a pulled muscle was made; the patient was sent home with prescriptions for naproxen and hydrocodone with acetaminophen.
Four days later, the patient went to a clinic complaining of back pain. A second chest x-ray showed extensive right-sided pneumonia, for which she was hospitalized. Test results revealed that the patient was hypoxic, that her band cells were elevated to 65%, and that her white blood cell count was 5,000/mL. An additional chest x-ray was ordered, which the plaintiffs later claimed showed worsening pneumonia in the right lung.
When the patient complained of severely increased pain, her medications were discontinued and IV morphine was initiated. On day 5 of the patient’s hospital stay, her case was transferred to a different physician, and she was discharged two days later.
When the patient’s condition had not improved five days after her discharge, she placed a call to her physician, which was not returned. Very early the next morning, the woman was taken to the hospital. An hour later, she was pronounced dead as a result of cardiopulmonary arrest secondary to pneumonia.
Plaintiffs claimed that the decedent was prematurely discharged and that the defendant was negligent in failing to return her phone call. The defendant argued that the test results and x-rays that the plaintiffs claimed contraindicated discharge were not available when the decision was made to discharge the decedent. The defendant also claimed that, according to the office telephone record, the decedent had failed to convey any urgency when she called; thus, there was no negligence in failing to return the call that day. The plaintiffs maintained that the call had described the patient’s situation as urgent.
According to a published account, an $864,000 arbitration award was given.
Was Surgery for Hydrocephalus Delayed?
A 53-year-old man presented to a hospital emergency department (ED) after experiencing headaches, dizziness, nausea, vomiting, and a temperature as high as 101.9°F for several days. After the initial physical examination, nystagmus was diagnosed; meningitis was not considered. The patient was sent home with medication.
The next day, he returned to the same ED. MRI and CT of the brain revealed a 1.0-in brain tumor and hydrocephalus. The man was admitted for neurosurgical evaluation and treatment. During his examination, he was somewhat disoriented but could carry on a conversation. He was also able to stand, and his reflexes (including the pupillary reflexes) were normal. When increased hydrocephalus and intracranial pressure became evident, he was given steroids and mannitol.
The next day, the patient was lethargic, and his pupillary reflexes were slowly reactive. He responded to voice commands, but there were signs of increasing intracranial pressure.
That evening, the man ceased responding to voice commands and appeared increasingly confused. The following day, he was more lethargic. He made no spontaneous movements and no response to commands, although he did withdraw from painful stimuli. A repeat MRI showed the tumor and hydrocephalus.
Surgery was performed for removal of the tumor, which was identified as a T-cell lymphoma. The patient did not regain consciousness after the surgery. CT performed shortly thereafter showed herniation of the brain and diffuse hypoxic damage of a duration to suggest that it had occurred before the surgery.
The family refused a do-not-resuscitate (DNR) order and discontinuation of life support. For nine days after the surgery, the medical staff tried to persuade the family that the patient was dead; they then wrote a DNR order in the chart. When the family protested, doctors transferred the decedent out of the ICU and discontinued all medical support; they also clamped the ventriculostomy tube that had been placed after surgery. The decedent’s blood pressure and pulse remained normal, and his only requirements for life were IV fluids and a respirator.
After continued protest, the family was told that DNR orders are within the doctor’s decision. Consent was then sought to harvest the decedent’s organs for transplantation. Some 25 family members were present when a nurse discontinued the ventilator, and the man died.
Twenty-one family members sued for intentional infliction of emotional distress. Plaintiffs claimed that the decedent was in a coma that was caused not by the tumor but by hydrocephalus and increased intracranial pressure that accompanied the tumor. The plaintiffs claimed that a decompressing ventriculostomy would have prevented the herniation and hypoxic brain damage; this developed either before or during the surgery, which they charged was delayed. The plaintiffs also claimed that the decedent was not dead when life support was discontinued. The last electroencephalogram showed brain activity, they claimed, and the decedent’s blood pressure and pulse remained normal without any medical support. The plaintiffs also claimed that the decedent made respiratory movements for five minutes after the respirator was discontinued.
The defendants argued that the delay in performing surgery was necessary and that the decedent’s deterioration resulted from administration of sedatives to obtain a clear MRI. The defendants also claimed that the decedent was brain-dead after the surgery and that malpractice and wrongful death claims could not be applied to a person who was already dead.
According to a published report, a $425,000 settlement was reached.
Reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Who Was to Blame for Hyponatremia Death?
At age 63, a man visited the defendant family physician with complaints of fever and productive cough; he also needed a change in his blood pressure medication.
Chest x-ray results were negative, and the defendant prescribed an antibiotic. Six days later, the patient returned to the defendant’s office with similar but waning symptoms and new complaints consistent with anxiety and depression.
Over the following four days, the patient’s wife placed two documented calls to the defendant’s office to update him regarding the patient’s condition. The patient was subsequently taken to a hospital emergency department, where a sodium level of 101 mEq/L was detected on blood chemistry. A diagnosis of hyponatremia was made and an isotonic saline solution started.
The patient was then transferred to another hospital, where a hypertonic saline solution was ordered. Because his sodium level was replenished too quickly, the man developed central pontine myelinolysis (CPM). Three weeks later, he died of CPM-related aspiration pneumonia.
The plaintiff claimed that the defendant physician failed to diagnose hyponatremia and to give the patient proper treatment, which led to his death.
The defendant contended that there was no way to diagnose hyponatremia, based on the decedent’s signs and symptoms. The defendant also charged that death was caused by mistreatment at the hospital where the patient died.
According to a published account, a defense verdict was returned.
Pneumonia Patient Sent Home Too Soon
Complaints of upper back pain, evidently exacerbated by respiration, took a 44-year-old woman to a hospital emergency department. Tests revealed an elevated white blood cell count, but a chest x-ray was clear. A diagnosis of a pulled muscle was made; the patient was sent home with prescriptions for naproxen and hydrocodone with acetaminophen.
Four days later, the patient went to a clinic complaining of back pain. A second chest x-ray showed extensive right-sided pneumonia, for which she was hospitalized. Test results revealed that the patient was hypoxic, that her band cells were elevated to 65%, and that her white blood cell count was 5,000/mL. An additional chest x-ray was ordered, which the plaintiffs later claimed showed worsening pneumonia in the right lung.
When the patient complained of severely increased pain, her medications were discontinued and IV morphine was initiated. On day 5 of the patient’s hospital stay, her case was transferred to a different physician, and she was discharged two days later.
When the patient’s condition had not improved five days after her discharge, she placed a call to her physician, which was not returned. Very early the next morning, the woman was taken to the hospital. An hour later, she was pronounced dead as a result of cardiopulmonary arrest secondary to pneumonia.
Plaintiffs claimed that the decedent was prematurely discharged and that the defendant was negligent in failing to return her phone call. The defendant argued that the test results and x-rays that the plaintiffs claimed contraindicated discharge were not available when the decision was made to discharge the decedent. The defendant also claimed that, according to the office telephone record, the decedent had failed to convey any urgency when she called; thus, there was no negligence in failing to return the call that day. The plaintiffs maintained that the call had described the patient’s situation as urgent.
According to a published account, an $864,000 arbitration award was given.
Was Surgery for Hydrocephalus Delayed?
A 53-year-old man presented to a hospital emergency department (ED) after experiencing headaches, dizziness, nausea, vomiting, and a temperature as high as 101.9°F for several days. After the initial physical examination, nystagmus was diagnosed; meningitis was not considered. The patient was sent home with medication.
The next day, he returned to the same ED. MRI and CT of the brain revealed a 1.0-in brain tumor and hydrocephalus. The man was admitted for neurosurgical evaluation and treatment. During his examination, he was somewhat disoriented but could carry on a conversation. He was also able to stand, and his reflexes (including the pupillary reflexes) were normal. When increased hydrocephalus and intracranial pressure became evident, he was given steroids and mannitol.
The next day, the patient was lethargic, and his pupillary reflexes were slowly reactive. He responded to voice commands, but there were signs of increasing intracranial pressure.
That evening, the man ceased responding to voice commands and appeared increasingly confused. The following day, he was more lethargic. He made no spontaneous movements and no response to commands, although he did withdraw from painful stimuli. A repeat MRI showed the tumor and hydrocephalus.
Surgery was performed for removal of the tumor, which was identified as a T-cell lymphoma. The patient did not regain consciousness after the surgery. CT performed shortly thereafter showed herniation of the brain and diffuse hypoxic damage of a duration to suggest that it had occurred before the surgery.
The family refused a do-not-resuscitate (DNR) order and discontinuation of life support. For nine days after the surgery, the medical staff tried to persuade the family that the patient was dead; they then wrote a DNR order in the chart. When the family protested, doctors transferred the decedent out of the ICU and discontinued all medical support; they also clamped the ventriculostomy tube that had been placed after surgery. The decedent’s blood pressure and pulse remained normal, and his only requirements for life were IV fluids and a respirator.
After continued protest, the family was told that DNR orders are within the doctor’s decision. Consent was then sought to harvest the decedent’s organs for transplantation. Some 25 family members were present when a nurse discontinued the ventilator, and the man died.
Twenty-one family members sued for intentional infliction of emotional distress. Plaintiffs claimed that the decedent was in a coma that was caused not by the tumor but by hydrocephalus and increased intracranial pressure that accompanied the tumor. The plaintiffs claimed that a decompressing ventriculostomy would have prevented the herniation and hypoxic brain damage; this developed either before or during the surgery, which they charged was delayed. The plaintiffs also claimed that the decedent was not dead when life support was discontinued. The last electroencephalogram showed brain activity, they claimed, and the decedent’s blood pressure and pulse remained normal without any medical support. The plaintiffs also claimed that the decedent made respiratory movements for five minutes after the respirator was discontinued.
The defendants argued that the delay in performing surgery was necessary and that the decedent’s deterioration resulted from administration of sedatives to obtain a clear MRI. The defendants also claimed that the decedent was brain-dead after the surgery and that malpractice and wrongful death claims could not be applied to a person who was already dead.
According to a published report, a $425,000 settlement was reached.
Do feeding tubes improve outcomes in patients with dementia?
Case
A 68-year-old cachectic female with a history of Alzheimer’s dementia presents with a slowly progressive decline in functional status. She is bed bound, minimally verbal, and has lost interest in eating.
Her problems with decreased oral intake started when her diet was changed to nectar-thickened liquids. This change was made after the patient was hospitalized multiple times for aspiration pneumonia and she underwent a fluoroscopic swallowing evaluation that revealed aspiration of thin liquids. The patient’s husband requests that a feeding tube be placed so his wife doesn’t “die of pneumonia or starve to death.”
Overview
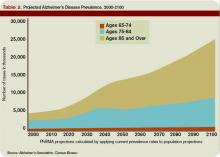
As the U.S. population ages, hospitalists are seeing a steady increase in the average patient age and the prevalence of dementia. Alzheimer’s dementia affects an estimated 4 million to 5 million Americans; this number expected to triple by the year 2050.1
As patients with dementia near the end of life, they often fail to thrive, with less oral intake and more swallowing disorders leading to aspiration. This is when physicians and patient family members must decide whether a feeding tube should be placed.
Placement of a nasogastric or percutaneous endogastric gastrostomy (PEG) feeding tube has become a relatively common medical intervention instituted to maintain or improve a patient’s nutritional status. Prior to 1980, permanent gastric or postpyloric feeding tubes were placed surgically by laparotomy, but the advent of endoscopy and computed tomography (CT) guided procedures offers a simplified procedure requiring only mild sedation and local anesthesia.2
Many patients who suffer multiple bouts of aspiration pneumonia and fail a swallowing evaluation because of an irreversible process are offered a percutaneous feeding tube to maintain nutrition. A feeding tube is also seen as a way to supply nutrition at the end of life in patients no longer able or willing to take food orally.
Although it seems logical that a feeding tube might improve the outcomes of these clinical scenarios, limited literature exists on the topic because of the legal, ethical, emotional, and religious implications a large, randomized, placebo-controlled trial would entail.
Review of the Data
Placement of a PEG has become accepted as a relatively benign procedure, although it is associated with significant morbidity and mortality. Minor complications including pain, abdominal wall ulcers, wound infections, peristomal leakage, and tube displacement occur in approximately 10% of cases.3 Major complications including hemorrhage, bowel or liver perforation, or aspiration occur in 3% of cases.4
These numbers do not account for long-term complications including peristomal infections, leakage problems, or the use of physical restraints to avoid self-extubation.
Aspiration Risk
A common indication for PEG placement is aspiration risk. PEG tubes are often placed in patients who fail swallowing evaluations in order to decrease their risk of aspiration and aspiration pneumonia.
True aspiration pneumonia is thought to originate from an inoculum of oral cavity or nasopharynx bacteria, which placement of a PEG tube would not prevent. Leibovitz, et al., showed that elderly patients with nasogastric or percutaneous feeding tubes are associated with colonization of the oropharynx with more pathogenic bacteria when compared with orally fed patients.5 Thus, the use of PEG tubes might put them at higher risk for pathogenic inoculation.
Aspiration pneumonia occurs in up to 50% of patients with feeding tubes. Studies have shown PEG tube placement decreases lower esophageal sphincter tone, potentially increasing regurgitation risk.6 It has also been shown that aspiration of gastric contents produces a pneumonitis with the resultant inflammatory response allowing for establishment of infection by smaller inoculums of or less virulent organisms.7
Small, randomized trials have shown no decrease in aspiration risk with post-pyloric versus gastric feeding tubes, nasogastric versus percutaneous feeding tubes, or continuous versus intermittent tube feeds.8 There have been no sizable randomized prospective trials to determine if feeding tube placement versus hand feeding patients with end-stage dementia alters aspiration pneumonia risk.
Pressure Ulcers
Patients with end-stage dementia often become bed bound as their disease progresses, and they commonly suffer from pressure ulcers. Pressure ulcers often coexist in patients with malnutrition, and it is well established that patients with biochemical markers of malnutrition are at higher risk for pressure ulcer formation.
Still, no studies show that improved nutrition prevents pressure ulcer formation. In a nursing home population of patients with dementia, a two-year follow-up study showed no significant improvement in pressure ulcer healing or decreased ulcer formation with nutrition by feeding tube.9 These studies are adjusted for independent risk factors for mortality and indication for PEG placement, but we can assume there are confounders that go into the decision for feeding tube placement that are not necessarily identifiable.
Nutritional Status
Family members are often concerned that if the patient is unable to take food by mouth and no feeding tube is placed, then the patient will suffer from the discomfort of starvation and dehydration.
As a patient with a severe dementing illness enters the end stage of his/her clinical course, practitioners frequently make a plan with families to change the goals of care toward keeping the patient comfortable. Comfort is a difficult clinical parameter to measure, but studies in the hospice population of patients with end-stage cancer and AIDS report that the hunger and thirst are transient and improve with ice chips and mouth swabs.10
Despite the lack of evidence of PEG tubes prolonging survival in patients with dementia who are no longer able or willing to take in food orally, it is logical that withholding all hydration or nutritional support will hasten death despite the risks associated with feeding tubes. This is where the ethical argument arises regarding prolonging life of decreasing quality.
In certain medical and legal sectors, artificial nutrition, and hydration are considered a medical intervention. Therefore, the ideals of patient autonomy dictate that the patient’s proxy should decide whether or not the patient would have wanted the intervention after weighing the risks and benefits.
If hospitalists view artificial nutrition as a medical intervention, our moral obligation is to instruct patients and their families about these risks and benefits.
Often, the patient will not clinically improve with artificial nutrition. But we can maintain physiologic processes or at least slow their decline.
Emerging research indicates the standard of care in how we present this information is changing to include presentation of data instead of only using a patient’s suspected beliefs about quality of life.
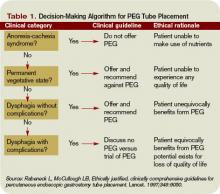
A useful algorithm proposed by Rabeneck, et al., provides comprehensive guidelines for PEG placement in all patient populations based on the reason for PEG consideration.11
Back to the Case
Our patient is likely nearing the end of her life because of end-stage dementia. There is no evidence to suggest placement of a feeding tube would extend her life more than hand feeding.
We know feeding-tube placement could increase aspiration pneumonia risk and significant short- and long-term morbidity and mortality. We can keep her comfortable with small amounts of water, wetting her lips with swabs. If a feeding tube is placed, its use should be evaluated based on the patient’s clinical course. TH
Dr. Pell is an instructor of medicine in the Section of Hospital Medicine at the University of Colorado, Denver.
References
- Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
- Hebert LE, Beckett LA, Scherr PA, and Evans DA. Annual incidence of Alzheimer disease in the United States projected to the years 2000 through 2050. Alzheimer Dis Assoc Disord. 2001;15:169-173.
- Grant MD, Rudberg MA, Brody JA. Gastrostomy placement and mortality among hospitalized Medicare beneficiaries. JAMA. 1998;279:1973-1976.
- Finocchiaro C, Galletti R, Rovera G, et al. Percutaneous endoscopic gastrostomy: a long-term follow-up. Nutrition. 1997;13(6):520-523.
- Leibovitz A, Plotnikov G, Habot B, et al. Pathogenic colonization of oral flora in frail elderly patients fed by nasogastric tube or percutaneous enterogastric tube. J Gerontol A Biol Sci Med. 2003;58(1):52-55.
- McCann R. Lack of evidence about tube feeding: food for thought. JAMA. 1999;282(14):1380-1381.
- Cameron JL, Caldini P, Toung J-K, et al. Aspiration pneumonia: physiologic data following experimental Aspiration. Surgery. 1972;72:238.
- Loeb MB, Becker M, Eady A, et al. Interventions to prevent aspiration pneumonia in older adults: a systematic review. JAGS. 2003;51(7):1018-1022.
- Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact on survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med. 1997;157:327-332.
- McCann RM, Hall WJ, Groth-Junker A. Comfort care for terminally ill patients: the appropriate use of nutrition and hydration. JAMA. 1994;272:1263-1266.
- Rabeneck L, McCullough LB. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349(9050):496-498.
Case
A 68-year-old cachectic female with a history of Alzheimer’s dementia presents with a slowly progressive decline in functional status. She is bed bound, minimally verbal, and has lost interest in eating.
Her problems with decreased oral intake started when her diet was changed to nectar-thickened liquids. This change was made after the patient was hospitalized multiple times for aspiration pneumonia and she underwent a fluoroscopic swallowing evaluation that revealed aspiration of thin liquids. The patient’s husband requests that a feeding tube be placed so his wife doesn’t “die of pneumonia or starve to death.”
Overview
As the U.S. population ages, hospitalists are seeing a steady increase in the average patient age and the prevalence of dementia. Alzheimer’s dementia affects an estimated 4 million to 5 million Americans; this number expected to triple by the year 2050.1
As patients with dementia near the end of life, they often fail to thrive, with less oral intake and more swallowing disorders leading to aspiration. This is when physicians and patient family members must decide whether a feeding tube should be placed.
Placement of a nasogastric or percutaneous endogastric gastrostomy (PEG) feeding tube has become a relatively common medical intervention instituted to maintain or improve a patient’s nutritional status. Prior to 1980, permanent gastric or postpyloric feeding tubes were placed surgically by laparotomy, but the advent of endoscopy and computed tomography (CT) guided procedures offers a simplified procedure requiring only mild sedation and local anesthesia.2
Many patients who suffer multiple bouts of aspiration pneumonia and fail a swallowing evaluation because of an irreversible process are offered a percutaneous feeding tube to maintain nutrition. A feeding tube is also seen as a way to supply nutrition at the end of life in patients no longer able or willing to take food orally.
Although it seems logical that a feeding tube might improve the outcomes of these clinical scenarios, limited literature exists on the topic because of the legal, ethical, emotional, and religious implications a large, randomized, placebo-controlled trial would entail.
Review of the Data
Placement of a PEG has become accepted as a relatively benign procedure, although it is associated with significant morbidity and mortality. Minor complications including pain, abdominal wall ulcers, wound infections, peristomal leakage, and tube displacement occur in approximately 10% of cases.3 Major complications including hemorrhage, bowel or liver perforation, or aspiration occur in 3% of cases.4
These numbers do not account for long-term complications including peristomal infections, leakage problems, or the use of physical restraints to avoid self-extubation.
Aspiration Risk
A common indication for PEG placement is aspiration risk. PEG tubes are often placed in patients who fail swallowing evaluations in order to decrease their risk of aspiration and aspiration pneumonia.
True aspiration pneumonia is thought to originate from an inoculum of oral cavity or nasopharynx bacteria, which placement of a PEG tube would not prevent. Leibovitz, et al., showed that elderly patients with nasogastric or percutaneous feeding tubes are associated with colonization of the oropharynx with more pathogenic bacteria when compared with orally fed patients.5 Thus, the use of PEG tubes might put them at higher risk for pathogenic inoculation.
Aspiration pneumonia occurs in up to 50% of patients with feeding tubes. Studies have shown PEG tube placement decreases lower esophageal sphincter tone, potentially increasing regurgitation risk.6 It has also been shown that aspiration of gastric contents produces a pneumonitis with the resultant inflammatory response allowing for establishment of infection by smaller inoculums of or less virulent organisms.7
Small, randomized trials have shown no decrease in aspiration risk with post-pyloric versus gastric feeding tubes, nasogastric versus percutaneous feeding tubes, or continuous versus intermittent tube feeds.8 There have been no sizable randomized prospective trials to determine if feeding tube placement versus hand feeding patients with end-stage dementia alters aspiration pneumonia risk.
Pressure Ulcers
Patients with end-stage dementia often become bed bound as their disease progresses, and they commonly suffer from pressure ulcers. Pressure ulcers often coexist in patients with malnutrition, and it is well established that patients with biochemical markers of malnutrition are at higher risk for pressure ulcer formation.
Still, no studies show that improved nutrition prevents pressure ulcer formation. In a nursing home population of patients with dementia, a two-year follow-up study showed no significant improvement in pressure ulcer healing or decreased ulcer formation with nutrition by feeding tube.9 These studies are adjusted for independent risk factors for mortality and indication for PEG placement, but we can assume there are confounders that go into the decision for feeding tube placement that are not necessarily identifiable.
Nutritional Status
Family members are often concerned that if the patient is unable to take food by mouth and no feeding tube is placed, then the patient will suffer from the discomfort of starvation and dehydration.
As a patient with a severe dementing illness enters the end stage of his/her clinical course, practitioners frequently make a plan with families to change the goals of care toward keeping the patient comfortable. Comfort is a difficult clinical parameter to measure, but studies in the hospice population of patients with end-stage cancer and AIDS report that the hunger and thirst are transient and improve with ice chips and mouth swabs.10
Despite the lack of evidence of PEG tubes prolonging survival in patients with dementia who are no longer able or willing to take in food orally, it is logical that withholding all hydration or nutritional support will hasten death despite the risks associated with feeding tubes. This is where the ethical argument arises regarding prolonging life of decreasing quality.
In certain medical and legal sectors, artificial nutrition, and hydration are considered a medical intervention. Therefore, the ideals of patient autonomy dictate that the patient’s proxy should decide whether or not the patient would have wanted the intervention after weighing the risks and benefits.
If hospitalists view artificial nutrition as a medical intervention, our moral obligation is to instruct patients and their families about these risks and benefits.
Often, the patient will not clinically improve with artificial nutrition. But we can maintain physiologic processes or at least slow their decline.
Emerging research indicates the standard of care in how we present this information is changing to include presentation of data instead of only using a patient’s suspected beliefs about quality of life.
A useful algorithm proposed by Rabeneck, et al., provides comprehensive guidelines for PEG placement in all patient populations based on the reason for PEG consideration.11
Back to the Case
Our patient is likely nearing the end of her life because of end-stage dementia. There is no evidence to suggest placement of a feeding tube would extend her life more than hand feeding.
We know feeding-tube placement could increase aspiration pneumonia risk and significant short- and long-term morbidity and mortality. We can keep her comfortable with small amounts of water, wetting her lips with swabs. If a feeding tube is placed, its use should be evaluated based on the patient’s clinical course. TH
Dr. Pell is an instructor of medicine in the Section of Hospital Medicine at the University of Colorado, Denver.
References
- Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
- Hebert LE, Beckett LA, Scherr PA, and Evans DA. Annual incidence of Alzheimer disease in the United States projected to the years 2000 through 2050. Alzheimer Dis Assoc Disord. 2001;15:169-173.
- Grant MD, Rudberg MA, Brody JA. Gastrostomy placement and mortality among hospitalized Medicare beneficiaries. JAMA. 1998;279:1973-1976.
- Finocchiaro C, Galletti R, Rovera G, et al. Percutaneous endoscopic gastrostomy: a long-term follow-up. Nutrition. 1997;13(6):520-523.
- Leibovitz A, Plotnikov G, Habot B, et al. Pathogenic colonization of oral flora in frail elderly patients fed by nasogastric tube or percutaneous enterogastric tube. J Gerontol A Biol Sci Med. 2003;58(1):52-55.
- McCann R. Lack of evidence about tube feeding: food for thought. JAMA. 1999;282(14):1380-1381.
- Cameron JL, Caldini P, Toung J-K, et al. Aspiration pneumonia: physiologic data following experimental Aspiration. Surgery. 1972;72:238.
- Loeb MB, Becker M, Eady A, et al. Interventions to prevent aspiration pneumonia in older adults: a systematic review. JAGS. 2003;51(7):1018-1022.
- Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact on survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med. 1997;157:327-332.
- McCann RM, Hall WJ, Groth-Junker A. Comfort care for terminally ill patients: the appropriate use of nutrition and hydration. JAMA. 1994;272:1263-1266.
- Rabeneck L, McCullough LB. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349(9050):496-498.
Case
A 68-year-old cachectic female with a history of Alzheimer’s dementia presents with a slowly progressive decline in functional status. She is bed bound, minimally verbal, and has lost interest in eating.
Her problems with decreased oral intake started when her diet was changed to nectar-thickened liquids. This change was made after the patient was hospitalized multiple times for aspiration pneumonia and she underwent a fluoroscopic swallowing evaluation that revealed aspiration of thin liquids. The patient’s husband requests that a feeding tube be placed so his wife doesn’t “die of pneumonia or starve to death.”
Overview
As the U.S. population ages, hospitalists are seeing a steady increase in the average patient age and the prevalence of dementia. Alzheimer’s dementia affects an estimated 4 million to 5 million Americans; this number expected to triple by the year 2050.1
As patients with dementia near the end of life, they often fail to thrive, with less oral intake and more swallowing disorders leading to aspiration. This is when physicians and patient family members must decide whether a feeding tube should be placed.
Placement of a nasogastric or percutaneous endogastric gastrostomy (PEG) feeding tube has become a relatively common medical intervention instituted to maintain or improve a patient’s nutritional status. Prior to 1980, permanent gastric or postpyloric feeding tubes were placed surgically by laparotomy, but the advent of endoscopy and computed tomography (CT) guided procedures offers a simplified procedure requiring only mild sedation and local anesthesia.2
Many patients who suffer multiple bouts of aspiration pneumonia and fail a swallowing evaluation because of an irreversible process are offered a percutaneous feeding tube to maintain nutrition. A feeding tube is also seen as a way to supply nutrition at the end of life in patients no longer able or willing to take food orally.
Although it seems logical that a feeding tube might improve the outcomes of these clinical scenarios, limited literature exists on the topic because of the legal, ethical, emotional, and religious implications a large, randomized, placebo-controlled trial would entail.
Review of the Data
Placement of a PEG has become accepted as a relatively benign procedure, although it is associated with significant morbidity and mortality. Minor complications including pain, abdominal wall ulcers, wound infections, peristomal leakage, and tube displacement occur in approximately 10% of cases.3 Major complications including hemorrhage, bowel or liver perforation, or aspiration occur in 3% of cases.4
These numbers do not account for long-term complications including peristomal infections, leakage problems, or the use of physical restraints to avoid self-extubation.
Aspiration Risk
A common indication for PEG placement is aspiration risk. PEG tubes are often placed in patients who fail swallowing evaluations in order to decrease their risk of aspiration and aspiration pneumonia.
True aspiration pneumonia is thought to originate from an inoculum of oral cavity or nasopharynx bacteria, which placement of a PEG tube would not prevent. Leibovitz, et al., showed that elderly patients with nasogastric or percutaneous feeding tubes are associated with colonization of the oropharynx with more pathogenic bacteria when compared with orally fed patients.5 Thus, the use of PEG tubes might put them at higher risk for pathogenic inoculation.
Aspiration pneumonia occurs in up to 50% of patients with feeding tubes. Studies have shown PEG tube placement decreases lower esophageal sphincter tone, potentially increasing regurgitation risk.6 It has also been shown that aspiration of gastric contents produces a pneumonitis with the resultant inflammatory response allowing for establishment of infection by smaller inoculums of or less virulent organisms.7
Small, randomized trials have shown no decrease in aspiration risk with post-pyloric versus gastric feeding tubes, nasogastric versus percutaneous feeding tubes, or continuous versus intermittent tube feeds.8 There have been no sizable randomized prospective trials to determine if feeding tube placement versus hand feeding patients with end-stage dementia alters aspiration pneumonia risk.
Pressure Ulcers
Patients with end-stage dementia often become bed bound as their disease progresses, and they commonly suffer from pressure ulcers. Pressure ulcers often coexist in patients with malnutrition, and it is well established that patients with biochemical markers of malnutrition are at higher risk for pressure ulcer formation.
Still, no studies show that improved nutrition prevents pressure ulcer formation. In a nursing home population of patients with dementia, a two-year follow-up study showed no significant improvement in pressure ulcer healing or decreased ulcer formation with nutrition by feeding tube.9 These studies are adjusted for independent risk factors for mortality and indication for PEG placement, but we can assume there are confounders that go into the decision for feeding tube placement that are not necessarily identifiable.
Nutritional Status
Family members are often concerned that if the patient is unable to take food by mouth and no feeding tube is placed, then the patient will suffer from the discomfort of starvation and dehydration.
As a patient with a severe dementing illness enters the end stage of his/her clinical course, practitioners frequently make a plan with families to change the goals of care toward keeping the patient comfortable. Comfort is a difficult clinical parameter to measure, but studies in the hospice population of patients with end-stage cancer and AIDS report that the hunger and thirst are transient and improve with ice chips and mouth swabs.10
Despite the lack of evidence of PEG tubes prolonging survival in patients with dementia who are no longer able or willing to take in food orally, it is logical that withholding all hydration or nutritional support will hasten death despite the risks associated with feeding tubes. This is where the ethical argument arises regarding prolonging life of decreasing quality.
In certain medical and legal sectors, artificial nutrition, and hydration are considered a medical intervention. Therefore, the ideals of patient autonomy dictate that the patient’s proxy should decide whether or not the patient would have wanted the intervention after weighing the risks and benefits.
If hospitalists view artificial nutrition as a medical intervention, our moral obligation is to instruct patients and their families about these risks and benefits.
Often, the patient will not clinically improve with artificial nutrition. But we can maintain physiologic processes or at least slow their decline.
Emerging research indicates the standard of care in how we present this information is changing to include presentation of data instead of only using a patient’s suspected beliefs about quality of life.
A useful algorithm proposed by Rabeneck, et al., provides comprehensive guidelines for PEG placement in all patient populations based on the reason for PEG consideration.11
Back to the Case
Our patient is likely nearing the end of her life because of end-stage dementia. There is no evidence to suggest placement of a feeding tube would extend her life more than hand feeding.
We know feeding-tube placement could increase aspiration pneumonia risk and significant short- and long-term morbidity and mortality. We can keep her comfortable with small amounts of water, wetting her lips with swabs. If a feeding tube is placed, its use should be evaluated based on the patient’s clinical course. TH
Dr. Pell is an instructor of medicine in the Section of Hospital Medicine at the University of Colorado, Denver.
References
- Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15(6):872-875.
- Hebert LE, Beckett LA, Scherr PA, and Evans DA. Annual incidence of Alzheimer disease in the United States projected to the years 2000 through 2050. Alzheimer Dis Assoc Disord. 2001;15:169-173.
- Grant MD, Rudberg MA, Brody JA. Gastrostomy placement and mortality among hospitalized Medicare beneficiaries. JAMA. 1998;279:1973-1976.
- Finocchiaro C, Galletti R, Rovera G, et al. Percutaneous endoscopic gastrostomy: a long-term follow-up. Nutrition. 1997;13(6):520-523.
- Leibovitz A, Plotnikov G, Habot B, et al. Pathogenic colonization of oral flora in frail elderly patients fed by nasogastric tube or percutaneous enterogastric tube. J Gerontol A Biol Sci Med. 2003;58(1):52-55.
- McCann R. Lack of evidence about tube feeding: food for thought. JAMA. 1999;282(14):1380-1381.
- Cameron JL, Caldini P, Toung J-K, et al. Aspiration pneumonia: physiologic data following experimental Aspiration. Surgery. 1972;72:238.
- Loeb MB, Becker M, Eady A, et al. Interventions to prevent aspiration pneumonia in older adults: a systematic review. JAGS. 2003;51(7):1018-1022.
- Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact on survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med. 1997;157:327-332.
- McCann RM, Hall WJ, Groth-Junker A. Comfort care for terminally ill patients: the appropriate use of nutrition and hydration. JAMA. 1994;272:1263-1266.
- Rabeneck L, McCullough LB. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349(9050):496-498.
Contract Caveats
It happens at least once a year. One of the physicians we represent calls and says, “I want you to look at a contract I signed.” It’s the equivalent of a patient coming to the emergency department to show the doctor the job he did with his own stitches. Although you can try to clean up trouble spots, you can’t achieve the best result.
Nonetheless, because we know some hospitalists will continue to enter employment contracts without consulting an attorney, we want to provide some basics for evaluating contracts. These can be agreements signed with a hospital or hospitalist group, or with a group practice that covers a hospital or healthcare system.
Appropriate Mindset
Parties enter contracts expecting a mutually beneficial relationship. But our job is to assume the relationship will not only fail, it will go down in flames. By assuming worst-case scenarios we can assess the risks and benefits of each contract provision.
Identify the Parties
Although this may seem self-evident, it’s not. A physician may think he’s contracting with another physician, but the agreement is with a corporation. There are various options for structuring healthcare entities, each with advantages and disadvantages. All are designed to limit liability. There are also legal limits on physician arrangements with certain types of entities. It’s important to understand how the entity with which you’re contracting is organized and operated.
The status of the contracting physician is equally important. A hospitalist can contract individually as an employee, independent contractor, member (full or limited), or through his/her own professional corporation. These options have significant implications for compensation, tax, insurance, and liability.
Define the Purpose
Many contracts begin with recitals, or introductory paragraphs that explain the reasons for the contract. Most people zoom past the recitals—but that’s a mistake. A court asked to resolve a contract dispute attempts to construe the contract in a manner that effectuates the parties’ intent. Make sure recitals accurately state the parties’ intent.
Know the Benefits
All contracts include “consideration,” which is something of value exchanged for contractual obligations. What constitutes fair consideration varies by contract. Important considerations include:
- Compensation (salaries, bonuses, payment formulas, and profit distributions);
- Insurance (health, dental, vision, life, and disability);
- Paid time off (illness, vacation, and professional meetings);
- Retirement plans (401k and profit-sharing plans);
- Professional fees (hospital privileges, professional organizations, medical license, drug enforcement, administration registration, continuing medical education, subscriptions);
- Malpractice insurance and tail coverage;
- Indemnity; and
- Services and equipment (billing, support staff, equipment, and other resources).
All benefits must be adequately described in a contract to be enforceable because most contracts include “integration” clauses stating that the written agreement is the entire agreement between the parties and “no other agreements, written or oral, exist.” Courts will not let parties claim benefits not reflected in the written contract.
Know the Obligations
For a legally binding contract, each party must incur an obligation in exchange for consideration. For example, in a services agreement, a physician can readily agree to provide medical services in exchange for compensation and other benefits. Most contracts fail to provide enough detail about how obligations must be performed. When a physician agrees to “devote their full professional attention and best efforts” to a practice, what does that mean? Who determines whether one has devoted his “best efforts?”
Provisions that impose duties or obligations as described in other documents are also troublesome. Courts enforce obligations imposed by other documents incorporated into a contract, even if a party did not possess the other document at the time he signed the contract. Never agree to obligations contained in a document you haven’t read.
Reasonable Termination
Except for duties imposed by law or contract, parties generally don’t have continuing obligations to each other. For example, most states presume employment is at-will: Either party can terminate the employment at any time, without notice, for any lawful reason. Thus, the manager at McDonald’s can terminate a cashier in the middle of a shift because he thinks the cashier is rude. The cashier can quit his position in the middle of a shift because he doesn’t like his job.
Contract obligations limiting the circumstances under which employment can terminate comprise a major exception to employment at will. For example, a physician might agree to provide 90 days’ notice before leaving his employment. While the physician might agree to this provision, certain circumstances should allow for immediate termination. This includes when the practice has financial issues (fails to pay the physician or enters bankruptcy), allows insurance to lapse, fails to provide adequate staff, improperly bills, or sells to another owner. A healthcare entity can also have legitimate reasons for immediately terminating a physician, such as loss or suspension of his medical license, hospital privileges, or DEA registration.
Provisions that allow termination for vague reasons such as “conduct detrimental to the practice” or “failure to provide services in a professional manner” are problematic. It wouldn’t be hard to manufacture an instance where a physician engaged in conduct detrimental to the practice. Being late for an appointment is detrimental to the practice but probably unavoidable in some circumstances.
Be wary of contractual provisions that give one party unilateral or unlimited discretion over a term.
Evaluate Survival Terms
Some relationships simply end, with the parties going their separate ways. But contracts often include obligations that survive termination. A party to a contract should always make sure to understand the scope and effect of any contractual provision that continues after the parties’ relationship has otherwise ended.
In physician contracts, the most prevalent survival provisions are non-compete clauses. Non-compete clauses provide a good model to discuss post-termination obligations. A standard non-compete clause might read like this:
Dr. Jones will not, in the three years immediately following termination of this agreement, practice medicine in any location within a three-mile radius of any location where he has provided services for P.C.
If Dr. Jones has performed surgery at both area hospitals while under contract, this clause could require him to pack up his stethoscope and leave town. When coupled with a provision allowing an injunction or liquidated damages, non-compete clauses are a big deal and give rise to lots of lawsuits. Even in circumstances where a non-compete clause is unenforceable, a party is unlikely to receive a favorable determination without substantial litigation. Negotiate a non-compete clause or other survival terms everyone can live with.
Understand Remedies
Lawyers use the term “remedy” to describe the recourse available when a party breaches an agreement. Remedies come in three basic forms:
- Compensatory damages;
- Liquidated damages; and
- Equitable relief.
Compensatory damages are monetary awards designed to compensate an injured party for actual loss. The party seeking compensatory damages must prove the nature of the injury and the amount of compensation that should be awarded.
Liquidated damages are monetary awards to compensate a party for an agreed-upon loss. So long as the parties agree it would be difficult to calculate an actual award of damages, that the amount of liquidated damages is reasonable, and that the award of liquidated damages is not punitive, a court would likely enforce the liquidated damages provision.
Because liquidated damage provisions relieve a party of the burden of proving actual damages, they should be carefully considered.
Equitable relief consists of non-monetary remedies, such as an injunction. If a party agrees to injunctive relief to enforce a contract term, a judge could order the party discontinue certain conduct. If the party disobeys, he/she could be held in contempt of court and jailed. Injunctive relief alters a legal presumption that breaches of contract can be remedied through monetary awards. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
It happens at least once a year. One of the physicians we represent calls and says, “I want you to look at a contract I signed.” It’s the equivalent of a patient coming to the emergency department to show the doctor the job he did with his own stitches. Although you can try to clean up trouble spots, you can’t achieve the best result.
Nonetheless, because we know some hospitalists will continue to enter employment contracts without consulting an attorney, we want to provide some basics for evaluating contracts. These can be agreements signed with a hospital or hospitalist group, or with a group practice that covers a hospital or healthcare system.
Appropriate Mindset
Parties enter contracts expecting a mutually beneficial relationship. But our job is to assume the relationship will not only fail, it will go down in flames. By assuming worst-case scenarios we can assess the risks and benefits of each contract provision.
Identify the Parties
Although this may seem self-evident, it’s not. A physician may think he’s contracting with another physician, but the agreement is with a corporation. There are various options for structuring healthcare entities, each with advantages and disadvantages. All are designed to limit liability. There are also legal limits on physician arrangements with certain types of entities. It’s important to understand how the entity with which you’re contracting is organized and operated.
The status of the contracting physician is equally important. A hospitalist can contract individually as an employee, independent contractor, member (full or limited), or through his/her own professional corporation. These options have significant implications for compensation, tax, insurance, and liability.
Define the Purpose
Many contracts begin with recitals, or introductory paragraphs that explain the reasons for the contract. Most people zoom past the recitals—but that’s a mistake. A court asked to resolve a contract dispute attempts to construe the contract in a manner that effectuates the parties’ intent. Make sure recitals accurately state the parties’ intent.
Know the Benefits
All contracts include “consideration,” which is something of value exchanged for contractual obligations. What constitutes fair consideration varies by contract. Important considerations include:
- Compensation (salaries, bonuses, payment formulas, and profit distributions);
- Insurance (health, dental, vision, life, and disability);
- Paid time off (illness, vacation, and professional meetings);
- Retirement plans (401k and profit-sharing plans);
- Professional fees (hospital privileges, professional organizations, medical license, drug enforcement, administration registration, continuing medical education, subscriptions);
- Malpractice insurance and tail coverage;
- Indemnity; and
- Services and equipment (billing, support staff, equipment, and other resources).
All benefits must be adequately described in a contract to be enforceable because most contracts include “integration” clauses stating that the written agreement is the entire agreement between the parties and “no other agreements, written or oral, exist.” Courts will not let parties claim benefits not reflected in the written contract.
Know the Obligations
For a legally binding contract, each party must incur an obligation in exchange for consideration. For example, in a services agreement, a physician can readily agree to provide medical services in exchange for compensation and other benefits. Most contracts fail to provide enough detail about how obligations must be performed. When a physician agrees to “devote their full professional attention and best efforts” to a practice, what does that mean? Who determines whether one has devoted his “best efforts?”
Provisions that impose duties or obligations as described in other documents are also troublesome. Courts enforce obligations imposed by other documents incorporated into a contract, even if a party did not possess the other document at the time he signed the contract. Never agree to obligations contained in a document you haven’t read.
Reasonable Termination
Except for duties imposed by law or contract, parties generally don’t have continuing obligations to each other. For example, most states presume employment is at-will: Either party can terminate the employment at any time, without notice, for any lawful reason. Thus, the manager at McDonald’s can terminate a cashier in the middle of a shift because he thinks the cashier is rude. The cashier can quit his position in the middle of a shift because he doesn’t like his job.
Contract obligations limiting the circumstances under which employment can terminate comprise a major exception to employment at will. For example, a physician might agree to provide 90 days’ notice before leaving his employment. While the physician might agree to this provision, certain circumstances should allow for immediate termination. This includes when the practice has financial issues (fails to pay the physician or enters bankruptcy), allows insurance to lapse, fails to provide adequate staff, improperly bills, or sells to another owner. A healthcare entity can also have legitimate reasons for immediately terminating a physician, such as loss or suspension of his medical license, hospital privileges, or DEA registration.
Provisions that allow termination for vague reasons such as “conduct detrimental to the practice” or “failure to provide services in a professional manner” are problematic. It wouldn’t be hard to manufacture an instance where a physician engaged in conduct detrimental to the practice. Being late for an appointment is detrimental to the practice but probably unavoidable in some circumstances.
Be wary of contractual provisions that give one party unilateral or unlimited discretion over a term.
Evaluate Survival Terms
Some relationships simply end, with the parties going their separate ways. But contracts often include obligations that survive termination. A party to a contract should always make sure to understand the scope and effect of any contractual provision that continues after the parties’ relationship has otherwise ended.
In physician contracts, the most prevalent survival provisions are non-compete clauses. Non-compete clauses provide a good model to discuss post-termination obligations. A standard non-compete clause might read like this:
Dr. Jones will not, in the three years immediately following termination of this agreement, practice medicine in any location within a three-mile radius of any location where he has provided services for P.C.
If Dr. Jones has performed surgery at both area hospitals while under contract, this clause could require him to pack up his stethoscope and leave town. When coupled with a provision allowing an injunction or liquidated damages, non-compete clauses are a big deal and give rise to lots of lawsuits. Even in circumstances where a non-compete clause is unenforceable, a party is unlikely to receive a favorable determination without substantial litigation. Negotiate a non-compete clause or other survival terms everyone can live with.
Understand Remedies
Lawyers use the term “remedy” to describe the recourse available when a party breaches an agreement. Remedies come in three basic forms:
- Compensatory damages;
- Liquidated damages; and
- Equitable relief.
Compensatory damages are monetary awards designed to compensate an injured party for actual loss. The party seeking compensatory damages must prove the nature of the injury and the amount of compensation that should be awarded.
Liquidated damages are monetary awards to compensate a party for an agreed-upon loss. So long as the parties agree it would be difficult to calculate an actual award of damages, that the amount of liquidated damages is reasonable, and that the award of liquidated damages is not punitive, a court would likely enforce the liquidated damages provision.
Because liquidated damage provisions relieve a party of the burden of proving actual damages, they should be carefully considered.
Equitable relief consists of non-monetary remedies, such as an injunction. If a party agrees to injunctive relief to enforce a contract term, a judge could order the party discontinue certain conduct. If the party disobeys, he/she could be held in contempt of court and jailed. Injunctive relief alters a legal presumption that breaches of contract can be remedied through monetary awards. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
It happens at least once a year. One of the physicians we represent calls and says, “I want you to look at a contract I signed.” It’s the equivalent of a patient coming to the emergency department to show the doctor the job he did with his own stitches. Although you can try to clean up trouble spots, you can’t achieve the best result.
Nonetheless, because we know some hospitalists will continue to enter employment contracts without consulting an attorney, we want to provide some basics for evaluating contracts. These can be agreements signed with a hospital or hospitalist group, or with a group practice that covers a hospital or healthcare system.
Appropriate Mindset
Parties enter contracts expecting a mutually beneficial relationship. But our job is to assume the relationship will not only fail, it will go down in flames. By assuming worst-case scenarios we can assess the risks and benefits of each contract provision.
Identify the Parties
Although this may seem self-evident, it’s not. A physician may think he’s contracting with another physician, but the agreement is with a corporation. There are various options for structuring healthcare entities, each with advantages and disadvantages. All are designed to limit liability. There are also legal limits on physician arrangements with certain types of entities. It’s important to understand how the entity with which you’re contracting is organized and operated.
The status of the contracting physician is equally important. A hospitalist can contract individually as an employee, independent contractor, member (full or limited), or through his/her own professional corporation. These options have significant implications for compensation, tax, insurance, and liability.
Define the Purpose
Many contracts begin with recitals, or introductory paragraphs that explain the reasons for the contract. Most people zoom past the recitals—but that’s a mistake. A court asked to resolve a contract dispute attempts to construe the contract in a manner that effectuates the parties’ intent. Make sure recitals accurately state the parties’ intent.
Know the Benefits
All contracts include “consideration,” which is something of value exchanged for contractual obligations. What constitutes fair consideration varies by contract. Important considerations include:
- Compensation (salaries, bonuses, payment formulas, and profit distributions);
- Insurance (health, dental, vision, life, and disability);
- Paid time off (illness, vacation, and professional meetings);
- Retirement plans (401k and profit-sharing plans);
- Professional fees (hospital privileges, professional organizations, medical license, drug enforcement, administration registration, continuing medical education, subscriptions);
- Malpractice insurance and tail coverage;
- Indemnity; and
- Services and equipment (billing, support staff, equipment, and other resources).
All benefits must be adequately described in a contract to be enforceable because most contracts include “integration” clauses stating that the written agreement is the entire agreement between the parties and “no other agreements, written or oral, exist.” Courts will not let parties claim benefits not reflected in the written contract.
Know the Obligations
For a legally binding contract, each party must incur an obligation in exchange for consideration. For example, in a services agreement, a physician can readily agree to provide medical services in exchange for compensation and other benefits. Most contracts fail to provide enough detail about how obligations must be performed. When a physician agrees to “devote their full professional attention and best efforts” to a practice, what does that mean? Who determines whether one has devoted his “best efforts?”
Provisions that impose duties or obligations as described in other documents are also troublesome. Courts enforce obligations imposed by other documents incorporated into a contract, even if a party did not possess the other document at the time he signed the contract. Never agree to obligations contained in a document you haven’t read.
Reasonable Termination
Except for duties imposed by law or contract, parties generally don’t have continuing obligations to each other. For example, most states presume employment is at-will: Either party can terminate the employment at any time, without notice, for any lawful reason. Thus, the manager at McDonald’s can terminate a cashier in the middle of a shift because he thinks the cashier is rude. The cashier can quit his position in the middle of a shift because he doesn’t like his job.
Contract obligations limiting the circumstances under which employment can terminate comprise a major exception to employment at will. For example, a physician might agree to provide 90 days’ notice before leaving his employment. While the physician might agree to this provision, certain circumstances should allow for immediate termination. This includes when the practice has financial issues (fails to pay the physician or enters bankruptcy), allows insurance to lapse, fails to provide adequate staff, improperly bills, or sells to another owner. A healthcare entity can also have legitimate reasons for immediately terminating a physician, such as loss or suspension of his medical license, hospital privileges, or DEA registration.
Provisions that allow termination for vague reasons such as “conduct detrimental to the practice” or “failure to provide services in a professional manner” are problematic. It wouldn’t be hard to manufacture an instance where a physician engaged in conduct detrimental to the practice. Being late for an appointment is detrimental to the practice but probably unavoidable in some circumstances.
Be wary of contractual provisions that give one party unilateral or unlimited discretion over a term.
Evaluate Survival Terms
Some relationships simply end, with the parties going their separate ways. But contracts often include obligations that survive termination. A party to a contract should always make sure to understand the scope and effect of any contractual provision that continues after the parties’ relationship has otherwise ended.
In physician contracts, the most prevalent survival provisions are non-compete clauses. Non-compete clauses provide a good model to discuss post-termination obligations. A standard non-compete clause might read like this:
Dr. Jones will not, in the three years immediately following termination of this agreement, practice medicine in any location within a three-mile radius of any location where he has provided services for P.C.
If Dr. Jones has performed surgery at both area hospitals while under contract, this clause could require him to pack up his stethoscope and leave town. When coupled with a provision allowing an injunction or liquidated damages, non-compete clauses are a big deal and give rise to lots of lawsuits. Even in circumstances where a non-compete clause is unenforceable, a party is unlikely to receive a favorable determination without substantial litigation. Negotiate a non-compete clause or other survival terms everyone can live with.
Understand Remedies
Lawyers use the term “remedy” to describe the recourse available when a party breaches an agreement. Remedies come in three basic forms:
- Compensatory damages;
- Liquidated damages; and
- Equitable relief.
Compensatory damages are monetary awards designed to compensate an injured party for actual loss. The party seeking compensatory damages must prove the nature of the injury and the amount of compensation that should be awarded.
Liquidated damages are monetary awards to compensate a party for an agreed-upon loss. So long as the parties agree it would be difficult to calculate an actual award of damages, that the amount of liquidated damages is reasonable, and that the award of liquidated damages is not punitive, a court would likely enforce the liquidated damages provision.
Because liquidated damage provisions relieve a party of the burden of proving actual damages, they should be carefully considered.
Equitable relief consists of non-monetary remedies, such as an injunction. If a party agrees to injunctive relief to enforce a contract term, a judge could order the party discontinue certain conduct. If the party disobeys, he/she could be held in contempt of court and jailed. Injunctive relief alters a legal presumption that breaches of contract can be remedied through monetary awards. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
Massachusetts Effect
With the first major statewide attempt at universal healthcare access under way in Massachusetts, everyone from presidential candidates to uninsured families on the other side of the U.S. is watching to see if the state’s plan will succeed. If so, it could become the basis of a national healthcare plan.
Massachusetts healthcare reform became law April 2006 as part of the Act Providing Access to Affordable, Quality, Accountable Health Care. It requires that virtually all state residents either purchase health insurance or get coverage through state-sponsored insurance for people with low incomes (May 2007 The Hospitalist, p. 1). The plan, based on insurance market reforms, merges the individual and small-group insurance market, allowing residents to get lower group insurance rates.
The law required coverage by July 1, and residents must show evidence of their coverage on their income tax return or face a substantial fine—up to 50% of the cost of a health insurance plan.
Many Massachusetts residents get healthcare coverage through their employers. The state plan requires companies with more than 10 employees to provide coverage or to pay a “Fair Share” contribution of up to $295 for each employee each year. Employers must also offer a “cafeteria plan” that allows workers to purchase healthcare with pre-tax income.
The bill created the Commonwealth Health Insurance Connector, which offers affordable, quality insurance to individuals and small businesses. The Connector board approved plans offered by seven insurers that include several options.
As for low-income residents, sliding-scale government-funded subsidies are provided by the Commonwealth Care Health Insurance Program (C-CHIP). As of June 1, nearly 80,000 low-income adults had enrolled in C-CHIP. In addition, the statute expanded MassHealth (Medicaid and SCHIP) coverage for children of low-income parents and restored MassHealth benefits such as dental and vision care.
The plan also includes a system for quality standards and for publicizing performance of providers.
The money for the plan comes from several sources. Gov. Deval Patrick has requested $1.725 billion to fund the program in the next fiscal year. This will supplement federal Medicaid payments, employer contributions, and general revenues.
What Hospitalists Face
How will universal healthcare coverage for state residents affect Massachusetts hospitalists and other physicians? Massachusetts resident Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, and co-founder of SHM, weighed the pros and cons.
“The first issue is the effect on primary care providers,” says Dr. Whitcomb. “A large number of patients will be steered into the system of primary care, which is already overwhelmed. A new [state] commission has been formed to address this shortage, but it’s too late—the system already lacks capacity.”
Soon-to-be-overwhelmed primary care physicians will take every step possible to share the workload: “I think [the plan] will be a new impetus for primary care providers to refer patients to hospitalists,” stresses Dr. Whitcomb. “Hospitalists may well see new demand from primary care providers.”
Will this trend mean more openings for hospitalists at Massachusetts institutions? “There are so many drivers behind [the growth of the hospital medicine]; this is just another driver,” says Dr. Whitcomb.
The second likely outcome of the plan will be a transformation of the types of patients treated by hospitalists. Hospitalists around the country are well aware of the problems of treating today’s uninsured patients. “The uninsured tend to show up in the ER in the middle of the night, with diseases in an advanced state” because they haven’t seen a doctor until the last minute, says Dr. Whitcomb. “That situation is not going to go away, but it might decrease” in Massachusetts under the new plan.
“The big question is, will the previously uninsured population, which hospitalists are all too familiar with, be a fundamentally different population?” muses Dr. Whitcomb. “In other words, if [patients] go through a primary care provider and have good management of their illness, will they become a different type of patient than hospitalists are seeing at present? This would be good for hospitalists; it will mean more control over chronic disease and illness.”
—Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., and co-founder of SHM
How Is It Working?
The plan is still in its infancy, but more than 150,000 of the state’s previously uninsured residents had coverage before the July deadline. However, the total estimated number of remaining uninsured is 250,000 to 375,000.
“The two roadblocks are the ability to enroll patients and finding primary care to handle everyone,” says Dr. Whitcomb. “It’s just one of those wait-and-see issues. I applaud the plan. It’s a sincere effort to deal with the uninsured. I think the primary care shortage is a major problem and will impact the success of the plan.”
Hospitalists around the country may want to keep an eye on developments in Massachusetts because the state’s healthcare system could affect their patient loads, daily work, and compensation. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
With the first major statewide attempt at universal healthcare access under way in Massachusetts, everyone from presidential candidates to uninsured families on the other side of the U.S. is watching to see if the state’s plan will succeed. If so, it could become the basis of a national healthcare plan.
Massachusetts healthcare reform became law April 2006 as part of the Act Providing Access to Affordable, Quality, Accountable Health Care. It requires that virtually all state residents either purchase health insurance or get coverage through state-sponsored insurance for people with low incomes (May 2007 The Hospitalist, p. 1). The plan, based on insurance market reforms, merges the individual and small-group insurance market, allowing residents to get lower group insurance rates.
The law required coverage by July 1, and residents must show evidence of their coverage on their income tax return or face a substantial fine—up to 50% of the cost of a health insurance plan.
Many Massachusetts residents get healthcare coverage through their employers. The state plan requires companies with more than 10 employees to provide coverage or to pay a “Fair Share” contribution of up to $295 for each employee each year. Employers must also offer a “cafeteria plan” that allows workers to purchase healthcare with pre-tax income.
The bill created the Commonwealth Health Insurance Connector, which offers affordable, quality insurance to individuals and small businesses. The Connector board approved plans offered by seven insurers that include several options.
As for low-income residents, sliding-scale government-funded subsidies are provided by the Commonwealth Care Health Insurance Program (C-CHIP). As of June 1, nearly 80,000 low-income adults had enrolled in C-CHIP. In addition, the statute expanded MassHealth (Medicaid and SCHIP) coverage for children of low-income parents and restored MassHealth benefits such as dental and vision care.
The plan also includes a system for quality standards and for publicizing performance of providers.
The money for the plan comes from several sources. Gov. Deval Patrick has requested $1.725 billion to fund the program in the next fiscal year. This will supplement federal Medicaid payments, employer contributions, and general revenues.
What Hospitalists Face
How will universal healthcare coverage for state residents affect Massachusetts hospitalists and other physicians? Massachusetts resident Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, and co-founder of SHM, weighed the pros and cons.
“The first issue is the effect on primary care providers,” says Dr. Whitcomb. “A large number of patients will be steered into the system of primary care, which is already overwhelmed. A new [state] commission has been formed to address this shortage, but it’s too late—the system already lacks capacity.”
Soon-to-be-overwhelmed primary care physicians will take every step possible to share the workload: “I think [the plan] will be a new impetus for primary care providers to refer patients to hospitalists,” stresses Dr. Whitcomb. “Hospitalists may well see new demand from primary care providers.”
Will this trend mean more openings for hospitalists at Massachusetts institutions? “There are so many drivers behind [the growth of the hospital medicine]; this is just another driver,” says Dr. Whitcomb.
The second likely outcome of the plan will be a transformation of the types of patients treated by hospitalists. Hospitalists around the country are well aware of the problems of treating today’s uninsured patients. “The uninsured tend to show up in the ER in the middle of the night, with diseases in an advanced state” because they haven’t seen a doctor until the last minute, says Dr. Whitcomb. “That situation is not going to go away, but it might decrease” in Massachusetts under the new plan.
“The big question is, will the previously uninsured population, which hospitalists are all too familiar with, be a fundamentally different population?” muses Dr. Whitcomb. “In other words, if [patients] go through a primary care provider and have good management of their illness, will they become a different type of patient than hospitalists are seeing at present? This would be good for hospitalists; it will mean more control over chronic disease and illness.”
—Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., and co-founder of SHM
How Is It Working?
The plan is still in its infancy, but more than 150,000 of the state’s previously uninsured residents had coverage before the July deadline. However, the total estimated number of remaining uninsured is 250,000 to 375,000.
“The two roadblocks are the ability to enroll patients and finding primary care to handle everyone,” says Dr. Whitcomb. “It’s just one of those wait-and-see issues. I applaud the plan. It’s a sincere effort to deal with the uninsured. I think the primary care shortage is a major problem and will impact the success of the plan.”
Hospitalists around the country may want to keep an eye on developments in Massachusetts because the state’s healthcare system could affect their patient loads, daily work, and compensation. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
With the first major statewide attempt at universal healthcare access under way in Massachusetts, everyone from presidential candidates to uninsured families on the other side of the U.S. is watching to see if the state’s plan will succeed. If so, it could become the basis of a national healthcare plan.
Massachusetts healthcare reform became law April 2006 as part of the Act Providing Access to Affordable, Quality, Accountable Health Care. It requires that virtually all state residents either purchase health insurance or get coverage through state-sponsored insurance for people with low incomes (May 2007 The Hospitalist, p. 1). The plan, based on insurance market reforms, merges the individual and small-group insurance market, allowing residents to get lower group insurance rates.
The law required coverage by July 1, and residents must show evidence of their coverage on their income tax return or face a substantial fine—up to 50% of the cost of a health insurance plan.
Many Massachusetts residents get healthcare coverage through their employers. The state plan requires companies with more than 10 employees to provide coverage or to pay a “Fair Share” contribution of up to $295 for each employee each year. Employers must also offer a “cafeteria plan” that allows workers to purchase healthcare with pre-tax income.
The bill created the Commonwealth Health Insurance Connector, which offers affordable, quality insurance to individuals and small businesses. The Connector board approved plans offered by seven insurers that include several options.
As for low-income residents, sliding-scale government-funded subsidies are provided by the Commonwealth Care Health Insurance Program (C-CHIP). As of June 1, nearly 80,000 low-income adults had enrolled in C-CHIP. In addition, the statute expanded MassHealth (Medicaid and SCHIP) coverage for children of low-income parents and restored MassHealth benefits such as dental and vision care.
The plan also includes a system for quality standards and for publicizing performance of providers.
The money for the plan comes from several sources. Gov. Deval Patrick has requested $1.725 billion to fund the program in the next fiscal year. This will supplement federal Medicaid payments, employer contributions, and general revenues.
What Hospitalists Face
How will universal healthcare coverage for state residents affect Massachusetts hospitalists and other physicians? Massachusetts resident Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, and co-founder of SHM, weighed the pros and cons.
“The first issue is the effect on primary care providers,” says Dr. Whitcomb. “A large number of patients will be steered into the system of primary care, which is already overwhelmed. A new [state] commission has been formed to address this shortage, but it’s too late—the system already lacks capacity.”
Soon-to-be-overwhelmed primary care physicians will take every step possible to share the workload: “I think [the plan] will be a new impetus for primary care providers to refer patients to hospitalists,” stresses Dr. Whitcomb. “Hospitalists may well see new demand from primary care providers.”
Will this trend mean more openings for hospitalists at Massachusetts institutions? “There are so many drivers behind [the growth of the hospital medicine]; this is just another driver,” says Dr. Whitcomb.
The second likely outcome of the plan will be a transformation of the types of patients treated by hospitalists. Hospitalists around the country are well aware of the problems of treating today’s uninsured patients. “The uninsured tend to show up in the ER in the middle of the night, with diseases in an advanced state” because they haven’t seen a doctor until the last minute, says Dr. Whitcomb. “That situation is not going to go away, but it might decrease” in Massachusetts under the new plan.
“The big question is, will the previously uninsured population, which hospitalists are all too familiar with, be a fundamentally different population?” muses Dr. Whitcomb. “In other words, if [patients] go through a primary care provider and have good management of their illness, will they become a different type of patient than hospitalists are seeing at present? This would be good for hospitalists; it will mean more control over chronic disease and illness.”
—Win Whitcomb, MD, director of clinical performance improvement at Mercy Medical Center in Springfield, Mass., and co-founder of SHM
How Is It Working?
The plan is still in its infancy, but more than 150,000 of the state’s previously uninsured residents had coverage before the July deadline. However, the total estimated number of remaining uninsured is 250,000 to 375,000.
“The two roadblocks are the ability to enroll patients and finding primary care to handle everyone,” says Dr. Whitcomb. “It’s just one of those wait-and-see issues. I applaud the plan. It’s a sincere effort to deal with the uninsured. I think the primary care shortage is a major problem and will impact the success of the plan.”
Hospitalists around the country may want to keep an eye on developments in Massachusetts because the state’s healthcare system could affect their patient loads, daily work, and compensation. TH
Jane Jerrard has been writing for The Hospitalist since 2005.
Succeed in Business
You may have an idea for a business you’d like to start, perhaps attracted by the prospect of controlling your time and work, chasing extra income, or fulfilling the dream of having an alternate career. Should you try turning your dream into reality—and if so, how?
Philippa Kennealy, MD, MPH, has guided hospitalists and other physicians along this path. She heads The Entrepreneurial MD, a Los Angeles-based coaching service for physicians who want to become more entrepreneurial with their practices or start a side business. She has a unique perspective on how physicians can add a satisfying second career to their practice of medicine. “I myself am a physician-entrepreneur,” says Dr. Kennealy.
Why Increase Workloads?
What makes busy hospitalists seek a side business? Why overload your schedule with the extra hours and responsibilities of running a business?
“It’s an opportunity to do something that feels creative, that gives you control,” explains Dr. Kennealy. “I feel that physicians don’t get to use creativity, and they don’t have much control. Their daily actions and decisions are quite regulated. Owning their own time is attractive to physicians. Hospitalists in particular are at it all day in the hospital.”
Is it really possible to continue to work as a hospitalist while shaping a second business? Yes—and others have done it.
“A lot of physicians dream of [entrepreneurship] but feel trapped by their existing time commitments,” says Dr. Kennealy. “But there are some who take the necessary steps, who carve out the time to do it. Many of them hook up with someone to form a partnership—often this is with a non-physician.”
Types of Endeavors
Some physicians are interested in a start-up business that goes hand in hand with their patient care; others may go in a completely different direction.
“There’s an enormous array of [physician-owned businesses] out there,” says Dr. Kennealy. “Many of my clients go into consulting, mostly within healthcare. Some have developed a software application that supports some aspect of healthcare.” Other physicians open health and wellness centers. One of Dr. Kennealy’s clients has developed a sculpting business and is ready to open her own gallery.
Lucia Ferreras-Cox, MD, works as an independent contractor in urgent care and hospital medicine while she runs her company, Ejerce Medecina USA, in Gilbert, Ariz. Ejerce offers Web-based training for Spanish-speaking physicians in other countries to help them pass the U.S. medical board review, then serves as a recruiting firm for those physicians once they get their U.S. licenses.
“I went back to business school for three months to refresh my skills,” says Dr. Ferreras-Cox, who previously had a pediatric practice. “I had to relearn—to learn that I was not a not-for-profit anymore.”
Marica Pook, MD, is a full-time hospitalist in Superior, Colo., and president of ExtraMD PC, a company that provides short-term physician staffing. Her start-up was quite simple. “I’ve been a hospitalist for seven years now, and of course part of my job is to call primary care physicians about patients,” Dr. Pook says. “I started thinking about what it’s like for those physicians and how they can get some help when they’re at their busiest.”
She decided to provide that help. In 2004 she used her contacts to start a kind of mini locum tenens job, working for different physician groups and hospitals. “Nine months into it, I started bringing in other physicians,” she says. Today, the business is thriving, with a growing number of local physicians involved, as well as some much-needed staff.
“I have an excellent bookkeeper, who does all the financials, invoicing, and budgeting—almost like a controller,” says Dr. Pook. “And I just hired a virtual assistant last week. I’ve found that it works best when I farm out the calling and scheduling and I just focus on the marketing. And I include talking to the physicians in that.”
Get Started
So how do you begin your transformation from hospitalist to hospitalist-entrepreneur?
“The basic steps begin with identifying whether this is an escapist fantasy or a deep, abiding interest,” stresses Dr. Kennealy. “It will take a deep interest to get you through the difficult times—it’s a real commitment.”
Once you determine you’re willing to invest time and expense in your own business, Dr. Kennealy advises you to assess your skills and acquire any new ones you’ll need. One way is to meet businesspeople, learn how they think, and understand the language of business. You can also study business and marketing books and journals or take business courses.
“I think physicians don’t know how to run a business,” says Dr. Pook. “We’re not trained to do this. What really helped me was a business coach. I’d advise others to either get a coach or get hooked up with someone who knows a lot about business.”
Before you make too deep a commitment, consider an important component. “You need some sense of the marketplace,” says Dr. Kennealy. Who will buy your product or service? Is there enough interest to support your efforts? What is the competition like in your area?
The next step, she says, is to develop a business plan. “There are free resources available at SCORE.org [the Web site of SCORE, Counselors to America’s Small Business],” she says. “As you start on your plan, you may see that you require further analysis. You need to close those knowledge gaps before you start the business.”
And finally, you have to have marketing savvy to make it work. “Wrap it all up in a sound marketing plan,” concludes Dr. Kennealy. “How will you reach your target audience, and how will you do it efficiently? You must learn the art of marketing, and most physicians don’t have a clue. You have to shift your thinking from a physician whose patients basically come flocking to someone who has to attract and keep customers.” TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
You may have an idea for a business you’d like to start, perhaps attracted by the prospect of controlling your time and work, chasing extra income, or fulfilling the dream of having an alternate career. Should you try turning your dream into reality—and if so, how?
Philippa Kennealy, MD, MPH, has guided hospitalists and other physicians along this path. She heads The Entrepreneurial MD, a Los Angeles-based coaching service for physicians who want to become more entrepreneurial with their practices or start a side business. She has a unique perspective on how physicians can add a satisfying second career to their practice of medicine. “I myself am a physician-entrepreneur,” says Dr. Kennealy.
Why Increase Workloads?
What makes busy hospitalists seek a side business? Why overload your schedule with the extra hours and responsibilities of running a business?
“It’s an opportunity to do something that feels creative, that gives you control,” explains Dr. Kennealy. “I feel that physicians don’t get to use creativity, and they don’t have much control. Their daily actions and decisions are quite regulated. Owning their own time is attractive to physicians. Hospitalists in particular are at it all day in the hospital.”
Is it really possible to continue to work as a hospitalist while shaping a second business? Yes—and others have done it.
“A lot of physicians dream of [entrepreneurship] but feel trapped by their existing time commitments,” says Dr. Kennealy. “But there are some who take the necessary steps, who carve out the time to do it. Many of them hook up with someone to form a partnership—often this is with a non-physician.”
Types of Endeavors
Some physicians are interested in a start-up business that goes hand in hand with their patient care; others may go in a completely different direction.
“There’s an enormous array of [physician-owned businesses] out there,” says Dr. Kennealy. “Many of my clients go into consulting, mostly within healthcare. Some have developed a software application that supports some aspect of healthcare.” Other physicians open health and wellness centers. One of Dr. Kennealy’s clients has developed a sculpting business and is ready to open her own gallery.
Lucia Ferreras-Cox, MD, works as an independent contractor in urgent care and hospital medicine while she runs her company, Ejerce Medecina USA, in Gilbert, Ariz. Ejerce offers Web-based training for Spanish-speaking physicians in other countries to help them pass the U.S. medical board review, then serves as a recruiting firm for those physicians once they get their U.S. licenses.
“I went back to business school for three months to refresh my skills,” says Dr. Ferreras-Cox, who previously had a pediatric practice. “I had to relearn—to learn that I was not a not-for-profit anymore.”
Marica Pook, MD, is a full-time hospitalist in Superior, Colo., and president of ExtraMD PC, a company that provides short-term physician staffing. Her start-up was quite simple. “I’ve been a hospitalist for seven years now, and of course part of my job is to call primary care physicians about patients,” Dr. Pook says. “I started thinking about what it’s like for those physicians and how they can get some help when they’re at their busiest.”
She decided to provide that help. In 2004 she used her contacts to start a kind of mini locum tenens job, working for different physician groups and hospitals. “Nine months into it, I started bringing in other physicians,” she says. Today, the business is thriving, with a growing number of local physicians involved, as well as some much-needed staff.
“I have an excellent bookkeeper, who does all the financials, invoicing, and budgeting—almost like a controller,” says Dr. Pook. “And I just hired a virtual assistant last week. I’ve found that it works best when I farm out the calling and scheduling and I just focus on the marketing. And I include talking to the physicians in that.”
Get Started
So how do you begin your transformation from hospitalist to hospitalist-entrepreneur?
“The basic steps begin with identifying whether this is an escapist fantasy or a deep, abiding interest,” stresses Dr. Kennealy. “It will take a deep interest to get you through the difficult times—it’s a real commitment.”
Once you determine you’re willing to invest time and expense in your own business, Dr. Kennealy advises you to assess your skills and acquire any new ones you’ll need. One way is to meet businesspeople, learn how they think, and understand the language of business. You can also study business and marketing books and journals or take business courses.
“I think physicians don’t know how to run a business,” says Dr. Pook. “We’re not trained to do this. What really helped me was a business coach. I’d advise others to either get a coach or get hooked up with someone who knows a lot about business.”
Before you make too deep a commitment, consider an important component. “You need some sense of the marketplace,” says Dr. Kennealy. Who will buy your product or service? Is there enough interest to support your efforts? What is the competition like in your area?
The next step, she says, is to develop a business plan. “There are free resources available at SCORE.org [the Web site of SCORE, Counselors to America’s Small Business],” she says. “As you start on your plan, you may see that you require further analysis. You need to close those knowledge gaps before you start the business.”
And finally, you have to have marketing savvy to make it work. “Wrap it all up in a sound marketing plan,” concludes Dr. Kennealy. “How will you reach your target audience, and how will you do it efficiently? You must learn the art of marketing, and most physicians don’t have a clue. You have to shift your thinking from a physician whose patients basically come flocking to someone who has to attract and keep customers.” TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
You may have an idea for a business you’d like to start, perhaps attracted by the prospect of controlling your time and work, chasing extra income, or fulfilling the dream of having an alternate career. Should you try turning your dream into reality—and if so, how?
Philippa Kennealy, MD, MPH, has guided hospitalists and other physicians along this path. She heads The Entrepreneurial MD, a Los Angeles-based coaching service for physicians who want to become more entrepreneurial with their practices or start a side business. She has a unique perspective on how physicians can add a satisfying second career to their practice of medicine. “I myself am a physician-entrepreneur,” says Dr. Kennealy.
Why Increase Workloads?
What makes busy hospitalists seek a side business? Why overload your schedule with the extra hours and responsibilities of running a business?
“It’s an opportunity to do something that feels creative, that gives you control,” explains Dr. Kennealy. “I feel that physicians don’t get to use creativity, and they don’t have much control. Their daily actions and decisions are quite regulated. Owning their own time is attractive to physicians. Hospitalists in particular are at it all day in the hospital.”
Is it really possible to continue to work as a hospitalist while shaping a second business? Yes—and others have done it.
“A lot of physicians dream of [entrepreneurship] but feel trapped by their existing time commitments,” says Dr. Kennealy. “But there are some who take the necessary steps, who carve out the time to do it. Many of them hook up with someone to form a partnership—often this is with a non-physician.”
Types of Endeavors
Some physicians are interested in a start-up business that goes hand in hand with their patient care; others may go in a completely different direction.
“There’s an enormous array of [physician-owned businesses] out there,” says Dr. Kennealy. “Many of my clients go into consulting, mostly within healthcare. Some have developed a software application that supports some aspect of healthcare.” Other physicians open health and wellness centers. One of Dr. Kennealy’s clients has developed a sculpting business and is ready to open her own gallery.
Lucia Ferreras-Cox, MD, works as an independent contractor in urgent care and hospital medicine while she runs her company, Ejerce Medecina USA, in Gilbert, Ariz. Ejerce offers Web-based training for Spanish-speaking physicians in other countries to help them pass the U.S. medical board review, then serves as a recruiting firm for those physicians once they get their U.S. licenses.
“I went back to business school for three months to refresh my skills,” says Dr. Ferreras-Cox, who previously had a pediatric practice. “I had to relearn—to learn that I was not a not-for-profit anymore.”
Marica Pook, MD, is a full-time hospitalist in Superior, Colo., and president of ExtraMD PC, a company that provides short-term physician staffing. Her start-up was quite simple. “I’ve been a hospitalist for seven years now, and of course part of my job is to call primary care physicians about patients,” Dr. Pook says. “I started thinking about what it’s like for those physicians and how they can get some help when they’re at their busiest.”
She decided to provide that help. In 2004 she used her contacts to start a kind of mini locum tenens job, working for different physician groups and hospitals. “Nine months into it, I started bringing in other physicians,” she says. Today, the business is thriving, with a growing number of local physicians involved, as well as some much-needed staff.
“I have an excellent bookkeeper, who does all the financials, invoicing, and budgeting—almost like a controller,” says Dr. Pook. “And I just hired a virtual assistant last week. I’ve found that it works best when I farm out the calling and scheduling and I just focus on the marketing. And I include talking to the physicians in that.”
Get Started
So how do you begin your transformation from hospitalist to hospitalist-entrepreneur?
“The basic steps begin with identifying whether this is an escapist fantasy or a deep, abiding interest,” stresses Dr. Kennealy. “It will take a deep interest to get you through the difficult times—it’s a real commitment.”
Once you determine you’re willing to invest time and expense in your own business, Dr. Kennealy advises you to assess your skills and acquire any new ones you’ll need. One way is to meet businesspeople, learn how they think, and understand the language of business. You can also study business and marketing books and journals or take business courses.
“I think physicians don’t know how to run a business,” says Dr. Pook. “We’re not trained to do this. What really helped me was a business coach. I’d advise others to either get a coach or get hooked up with someone who knows a lot about business.”
Before you make too deep a commitment, consider an important component. “You need some sense of the marketplace,” says Dr. Kennealy. Who will buy your product or service? Is there enough interest to support your efforts? What is the competition like in your area?
The next step, she says, is to develop a business plan. “There are free resources available at SCORE.org [the Web site of SCORE, Counselors to America’s Small Business],” she says. “As you start on your plan, you may see that you require further analysis. You need to close those knowledge gaps before you start the business.”
And finally, you have to have marketing savvy to make it work. “Wrap it all up in a sound marketing plan,” concludes Dr. Kennealy. “How will you reach your target audience, and how will you do it efficiently? You must learn the art of marketing, and most physicians don’t have a clue. You have to shift your thinking from a physician whose patients basically come flocking to someone who has to attract and keep customers.” TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
The DNR Dilemma
When it comes to communicating do-not-resuscitate (DNR) orders, hospitals rely on a bewildering array of paper documentation, electronic records, and colored wristbands that can easily be misinterpreted.
These are the findings reported in the November-December issue of the Journal of Hospital Medicine by Niraj Sehgal, MD, and Robert Wachter, MD. Dr. Wachter is associate chair of the department of medicine at the University of California, San Francisco. Dr. Sehgal is an assistant clinical professor of medicine at the school.
In a survey of 69 nursing executives representing hospitals in a consortium of academic medical centers, “More than 70% of respondents recalled situations when confusion around a DNR order led to problems in patient care,” the authors say.
Everyone has a “near-miss” story, says Dr. Sehgal.
In one budget-minded hospital where materials were recycled, someone forgot to remove a DNR sticker from a previous patient’s folder before the folder was assigned to someone else. Several nurses told of instances in which patients were resuscitated inappropriately because hospital staff members did not see DNR stickers in the patient’s chart, the patient was off the unit for a procedure without a complete chart, or the DNR order was buried under other materials.
Much of the problem stems from the lack of a standardized method for making a patient’s DNR wishes known, Dr. Sehgal explains.
For example, in 2004 Dr. Sehgal saw a newspaper report that BayCare Health hospitals, in and around Tampa, Fla., were covering yellow “Livestrong” bracelets issued by the Lance Armstrong Foundation and worn by some patients to support those living with cancer. BayCare uses yellow bracelets for DNR patients. Nearly 20% of Americans wear “Livestrong” bracelets, posing a challenge for any hospital that also uses yellow bracelets to indicate DNR.
The newspaper story was the impetus for this study, Dr. Sehgal recalls. “I saw that article and thought, ‘What a great metaphor for the need for standardization.’”
He and Dr. Wachter designed a brief survey and distributed it via an e-mail listserve to senior nursing staff members of the University HealthSystem Consortium, an alliance of 97 academic medical centers and their affiliated hospitals. Those institutions represent 90% of the nation’s nonprofit academic medical centers.
Of the 127 nursing executives who received survey announcements, 69 (54%) returned completed questionnaires. Of those, 39 (56%) reported that their hospitals documented patients’ DNR preferences only in the charts, while 11 (16%) used only electronic health records (EHRs). Seventeen (25%) augmented the paper charts or EHRs with color-coded wristbands in eight colors.
“We expected variability, but even so we were struck by how much variability existed in our findings,” Dr. Sehgal says.
Hospitals use wristbands in a rainbow of colors to convey many messages. Of the hospitals represented in this survey, 55% used them to warn of allergies, fall risks, and even same last names. The authors found “12 different indications were depicted by various colors, with variations in both the color choice for a given indication (e.g., red and yellow used for allergy wristbands at different hospitals) and across indications (e.g., red for allergy at one hospital and red for bleeding risk at another).”
A national, standardized system for conveying patients’ DNR wishes would seem logical, but no system is in place, Dr. Sehgal says. Hospitals cannot even agree on which method to use. While some use wristbands, others use notices or stickers incorporated into the chart. Still others use EHRs.
A few states, including Arizona, Pennsylvania, and Colorado have established statewide standards for using wristbands—but each state chose a different color. “I suspect that many physicians don’t know the meaning of many of the wristbands used in their hospitals, especially if those doctors rotate among different hospitals or hospital systems,” Dr. Sehgal says.
Developing a system for making a patient’s wishes known to hospital staff is one of two challenges reflected in this study, he adds. The second is to use what might be perfunctory questions about advance directives as an opening for a deeper discussion about the patient’s thoughts on end-of-life care. Right now, those questions are just another process measure hospitals must document. “It becomes just another box to check instead of a tool for opening a conversation about what the patient’s wishes are,” he says.
Hospitalists should embrace the opportunity to involve the patient, the patient’s family members, and the primary care provider in an ongoing discussion about the patient’s desires over the course of the hospital stay. “This can give patients a mechanism for thinking about what they’d want under certain circumstances,” Dr. Sehgal explains.
From this study’s findings emerge two take-home messages for hospitalists, he maintains. The first is to remember that “we in inpatient settings spend a lot of time taking care of patients, and we must be aware of what those patients’ wishes are with respect to DNR.” The second is to step back and take an even broader view by remaining alert to processes other than DNR that might benefit from a standardized approach. “Maybe we should think about that, particularly when there is the potential to significantly harm patients,” he says. TH
Norra MacReady is a medical writer based in California.
When it comes to communicating do-not-resuscitate (DNR) orders, hospitals rely on a bewildering array of paper documentation, electronic records, and colored wristbands that can easily be misinterpreted.
These are the findings reported in the November-December issue of the Journal of Hospital Medicine by Niraj Sehgal, MD, and Robert Wachter, MD. Dr. Wachter is associate chair of the department of medicine at the University of California, San Francisco. Dr. Sehgal is an assistant clinical professor of medicine at the school.
In a survey of 69 nursing executives representing hospitals in a consortium of academic medical centers, “More than 70% of respondents recalled situations when confusion around a DNR order led to problems in patient care,” the authors say.
Everyone has a “near-miss” story, says Dr. Sehgal.
In one budget-minded hospital where materials were recycled, someone forgot to remove a DNR sticker from a previous patient’s folder before the folder was assigned to someone else. Several nurses told of instances in which patients were resuscitated inappropriately because hospital staff members did not see DNR stickers in the patient’s chart, the patient was off the unit for a procedure without a complete chart, or the DNR order was buried under other materials.
Much of the problem stems from the lack of a standardized method for making a patient’s DNR wishes known, Dr. Sehgal explains.
For example, in 2004 Dr. Sehgal saw a newspaper report that BayCare Health hospitals, in and around Tampa, Fla., were covering yellow “Livestrong” bracelets issued by the Lance Armstrong Foundation and worn by some patients to support those living with cancer. BayCare uses yellow bracelets for DNR patients. Nearly 20% of Americans wear “Livestrong” bracelets, posing a challenge for any hospital that also uses yellow bracelets to indicate DNR.
The newspaper story was the impetus for this study, Dr. Sehgal recalls. “I saw that article and thought, ‘What a great metaphor for the need for standardization.’”
He and Dr. Wachter designed a brief survey and distributed it via an e-mail listserve to senior nursing staff members of the University HealthSystem Consortium, an alliance of 97 academic medical centers and their affiliated hospitals. Those institutions represent 90% of the nation’s nonprofit academic medical centers.
Of the 127 nursing executives who received survey announcements, 69 (54%) returned completed questionnaires. Of those, 39 (56%) reported that their hospitals documented patients’ DNR preferences only in the charts, while 11 (16%) used only electronic health records (EHRs). Seventeen (25%) augmented the paper charts or EHRs with color-coded wristbands in eight colors.
“We expected variability, but even so we were struck by how much variability existed in our findings,” Dr. Sehgal says.
Hospitals use wristbands in a rainbow of colors to convey many messages. Of the hospitals represented in this survey, 55% used them to warn of allergies, fall risks, and even same last names. The authors found “12 different indications were depicted by various colors, with variations in both the color choice for a given indication (e.g., red and yellow used for allergy wristbands at different hospitals) and across indications (e.g., red for allergy at one hospital and red for bleeding risk at another).”
A national, standardized system for conveying patients’ DNR wishes would seem logical, but no system is in place, Dr. Sehgal says. Hospitals cannot even agree on which method to use. While some use wristbands, others use notices or stickers incorporated into the chart. Still others use EHRs.
A few states, including Arizona, Pennsylvania, and Colorado have established statewide standards for using wristbands—but each state chose a different color. “I suspect that many physicians don’t know the meaning of many of the wristbands used in their hospitals, especially if those doctors rotate among different hospitals or hospital systems,” Dr. Sehgal says.
Developing a system for making a patient’s wishes known to hospital staff is one of two challenges reflected in this study, he adds. The second is to use what might be perfunctory questions about advance directives as an opening for a deeper discussion about the patient’s thoughts on end-of-life care. Right now, those questions are just another process measure hospitals must document. “It becomes just another box to check instead of a tool for opening a conversation about what the patient’s wishes are,” he says.
Hospitalists should embrace the opportunity to involve the patient, the patient’s family members, and the primary care provider in an ongoing discussion about the patient’s desires over the course of the hospital stay. “This can give patients a mechanism for thinking about what they’d want under certain circumstances,” Dr. Sehgal explains.
From this study’s findings emerge two take-home messages for hospitalists, he maintains. The first is to remember that “we in inpatient settings spend a lot of time taking care of patients, and we must be aware of what those patients’ wishes are with respect to DNR.” The second is to step back and take an even broader view by remaining alert to processes other than DNR that might benefit from a standardized approach. “Maybe we should think about that, particularly when there is the potential to significantly harm patients,” he says. TH
Norra MacReady is a medical writer based in California.
When it comes to communicating do-not-resuscitate (DNR) orders, hospitals rely on a bewildering array of paper documentation, electronic records, and colored wristbands that can easily be misinterpreted.
These are the findings reported in the November-December issue of the Journal of Hospital Medicine by Niraj Sehgal, MD, and Robert Wachter, MD. Dr. Wachter is associate chair of the department of medicine at the University of California, San Francisco. Dr. Sehgal is an assistant clinical professor of medicine at the school.
In a survey of 69 nursing executives representing hospitals in a consortium of academic medical centers, “More than 70% of respondents recalled situations when confusion around a DNR order led to problems in patient care,” the authors say.
Everyone has a “near-miss” story, says Dr. Sehgal.
In one budget-minded hospital where materials were recycled, someone forgot to remove a DNR sticker from a previous patient’s folder before the folder was assigned to someone else. Several nurses told of instances in which patients were resuscitated inappropriately because hospital staff members did not see DNR stickers in the patient’s chart, the patient was off the unit for a procedure without a complete chart, or the DNR order was buried under other materials.
Much of the problem stems from the lack of a standardized method for making a patient’s DNR wishes known, Dr. Sehgal explains.
For example, in 2004 Dr. Sehgal saw a newspaper report that BayCare Health hospitals, in and around Tampa, Fla., were covering yellow “Livestrong” bracelets issued by the Lance Armstrong Foundation and worn by some patients to support those living with cancer. BayCare uses yellow bracelets for DNR patients. Nearly 20% of Americans wear “Livestrong” bracelets, posing a challenge for any hospital that also uses yellow bracelets to indicate DNR.
The newspaper story was the impetus for this study, Dr. Sehgal recalls. “I saw that article and thought, ‘What a great metaphor for the need for standardization.’”
He and Dr. Wachter designed a brief survey and distributed it via an e-mail listserve to senior nursing staff members of the University HealthSystem Consortium, an alliance of 97 academic medical centers and their affiliated hospitals. Those institutions represent 90% of the nation’s nonprofit academic medical centers.
Of the 127 nursing executives who received survey announcements, 69 (54%) returned completed questionnaires. Of those, 39 (56%) reported that their hospitals documented patients’ DNR preferences only in the charts, while 11 (16%) used only electronic health records (EHRs). Seventeen (25%) augmented the paper charts or EHRs with color-coded wristbands in eight colors.
“We expected variability, but even so we were struck by how much variability existed in our findings,” Dr. Sehgal says.
Hospitals use wristbands in a rainbow of colors to convey many messages. Of the hospitals represented in this survey, 55% used them to warn of allergies, fall risks, and even same last names. The authors found “12 different indications were depicted by various colors, with variations in both the color choice for a given indication (e.g., red and yellow used for allergy wristbands at different hospitals) and across indications (e.g., red for allergy at one hospital and red for bleeding risk at another).”
A national, standardized system for conveying patients’ DNR wishes would seem logical, but no system is in place, Dr. Sehgal says. Hospitals cannot even agree on which method to use. While some use wristbands, others use notices or stickers incorporated into the chart. Still others use EHRs.
A few states, including Arizona, Pennsylvania, and Colorado have established statewide standards for using wristbands—but each state chose a different color. “I suspect that many physicians don’t know the meaning of many of the wristbands used in their hospitals, especially if those doctors rotate among different hospitals or hospital systems,” Dr. Sehgal says.
Developing a system for making a patient’s wishes known to hospital staff is one of two challenges reflected in this study, he adds. The second is to use what might be perfunctory questions about advance directives as an opening for a deeper discussion about the patient’s thoughts on end-of-life care. Right now, those questions are just another process measure hospitals must document. “It becomes just another box to check instead of a tool for opening a conversation about what the patient’s wishes are,” he says.
Hospitalists should embrace the opportunity to involve the patient, the patient’s family members, and the primary care provider in an ongoing discussion about the patient’s desires over the course of the hospital stay. “This can give patients a mechanism for thinking about what they’d want under certain circumstances,” Dr. Sehgal explains.
From this study’s findings emerge two take-home messages for hospitalists, he maintains. The first is to remember that “we in inpatient settings spend a lot of time taking care of patients, and we must be aware of what those patients’ wishes are with respect to DNR.” The second is to step back and take an even broader view by remaining alert to processes other than DNR that might benefit from a standardized approach. “Maybe we should think about that, particularly when there is the potential to significantly harm patients,” he says. TH
Norra MacReady is a medical writer based in California.
Avoid Pancreatitis Risk
Drugs are an often-overlooked cause of pancreatitis in hospitalized patients.1,2 Knowing which drugs are associated with acute pancreatic inflammation can help the hospitalist consider specific drugs as the cause within their differential diagnosis.
The two most common causes of acute pancreatitis are biliary disease (30%-60%) and chronic alcohol use (15%-30%). Drug-induced pancreatitis (DIP) has occurred with more than 100 prescribed medications.3,4
Most cases of acute pancreatitis are reversible and resolve on their own within three to seven days after treatment begins. A small number of patients develop severe complications, and their mortality rate nears 30%. Symptoms may last a few days and can include mild to severe epigastric pain that can radiate to the back, chest, flank, or lower abdomen.
Other symptoms can include nausea, vomiting, fever, abdominal tenderness, jaundice, or hypotension. Serum amylase and lipase levels usually rise to three times the upper limit of normal. Use of computerized tomography (CT) or ultrasound can help the diagnosis.
The mechanism of DIP is not known, but is thought to be predominantly due to an idiosyncratic reaction, and for a few agents/classes, to intrinsic drug toxicity.5 The incidence of DIP is approximately 1.4%-5%. Not knowing the exact number of prescriptions for each medication and the cases of pancreatitis from each impedes the determination of incidence.
Most data on DIP are from case reports or reviews of compiled cases. The validity and severity of DIP is unknown mostly because cases are underreported to MedWatch. Reasons for underreporting include:
- Low index of suspicion for DIP compared with drug- induced hepatotoxicity;
- Milder cases due to missed lower enzyme levels (not routinely ascertained in a metabolic panel);
- Missed latency of exposure; and
- Erroneous classification as alcoholic or biliary disease by default.
Drug-induced pancreatitis is more common in patients who have inflammatory bowel disease, AIDS, cancer, or gastrointestinal disease. It is also common in those who are geriatric, HIV positive, or who are on immunomodulating agents.6
An early compilation of DIP reports was published by Lankisch, et al. This was a retrospective evaluation that excluded all other pancreatitis etiologies (e.g., post-endoscopic retrograde cholangiopancreatography (ERCP), post-traumatic, post-operative, viral), except drugs. Out of 1,613 patients with acute pancreatitis, there were 22 cases of DIP due to the following agents: azathioprine (n=6), mesalamine/sulfasalazine (n=5) didanosine (ddI, n=4), estrogens (n=3), furosemide (n=2), hydrochlorothiazide (HCTZ, n=1), and rifampicin (n=1). Rechallenge was not attempted for ethical reasons. The mean hospital stay was 25.5 days (range two to 78 days), with an incidence of 1.2%. Two patients died (from AIDS and tuberculosis). The authors noted that other studies show a high fatality rate from azathioprine, ddI, furosemide, and HCTZ.
Additionally, Triveldi, et al., evaluated cases reported in the literature or unpublished cases from 1966 through 2004. They then classified the drugs into one of three categories based on strength of evidence of DIP association.
Class I included medications causing more than 20 reported cases with at least one case following rechallenge. Class II were medications causing more than 10 but fewer than 20 reported cases with/without a positive rechallenge, and Class III were all medications in 10 or fewer cases or unpublished reports (FDA or pharmaceutical company records). Following are some of the most common reports from drugs available in the U.S.:
- Class I: ddI (n=883), asparaginase (n=177), azathioprine (n=86), valproic acid (n=80), pentavalent antimonials (parenterals to treat leishmaniasis, n=80), pentamidine (n=79), mercaptopurine (n=69), mesalamine (n=59), estrogens (n=42), opiates (n=42), tetracycline (n=34), cytarabine (n=26), steroids (n=25), sulfamethoxazole/trimethoprim (SMZ-TMP, n=24), sulfasalazine (n=23), furosemide (n=21), sulindac (n=21);
- Class II: rifampin, lamivudine, octreotide, carbamazepine, acetaminophen, interferon alfa-2b, enalapril, HCTZ, cisplatin, erythromycin; and
- Class III (numerous agents, including the following classes): quinolones, macrolides, angiotensin-converting enzyme inhibitors (ACEIs), statins, and others.
Most recently Badalov, et al., evaluated cases from Medline (through July 1, 2006) and classified them based on levels of evidence. These levels were:
- Definite (imaging study or autopsy confirmed diagnosis);
- Probable (typical symptoms present and threefold increase in amylase and/or lipase); or
- Possible (all others, not included in the final analysis).
Cases were further subclassified into four classes:
- Class Ia (1 or more cases with positive rechallenge, excluding all other causes): codeine, conjugated estrogens, enalapril, isoniazid, metronidazole, mesalamine, pravastatin (other statins), procainamide, simvastatin, sulindac, sulfa drugs, tetracycline, and valproic acid;
- Class Ib (1 or more cases with positive rechallenge, not excluding all other causes): amiodarone, azathioprine, clomiphene, cytosine arabinoside, dapsone, dexamethasone (other steroids), estrogens, furosemide, ifosfamide, lamivudine, losartan, 6-MP, methimazole, methyldopa, nelfinavir, omeprazole, pentamidine, SMZ-TMP, and trans-retinoic acid (not topical);
- Class II (four or more cases, consistent latency in 75% of cases): acetaminophen, clozapine, ddI, erythromycin, l-asparaginase/peg-asparaginase, pentamidine, propofol, and tamoxifen;
- Class III (two or more cases, no consistent latency, no rechallenge): alendronate, captopril, carbamazepine, ceftriaxone, HCTZ, interferon, lisinopril, metformin, mirtazapine, naproxen, and others; and
- Class IV (one case, no other class, without rechallenge): too numerous.
Additionally, the Australian Adverse Drug Reactions Advisory Committee reported on the top 12 DIP-associated medications (n=414 reports implicating 695 drugs). The most commonly reported drugs included azathioprine, ddI, valproate, stavudine, simvastatin, clozapine, lamivudine, ezetimibe, prednisolone, olanzapine, celecoxib and 6-MP, which are listed in each medication’s Australian product information.
The following drugs/classes have been implicated in causing DIP:
- AIDS therapies: ddI, pentamidine;
- Antimicrobials: metronidazole, sulfonamides, tetracyclines;
- Diuretics: furosemide, HCTZ;
- Anti-inflammatories: mesalamine, salicylates, sulindac, sulfasalazine;
- Immunosuppressives: asparaginase, azathioprine, mercaptopurine; and
- Neuropsychiatric agents: valproic acid.
The American Gastroenterologic Association Institute has developed a guide for managing acute pancreatitis. Additionally, they note that when assessing DIP, consider prescription, over-the-counter, and herbal products, too.7 Pancreatitis can occur with certain drugs or medication classes, some more often than others.
Consider DIP in the differential diagnosis of patients who present with or develop epigastric pain. Question all patients with acute pancreatitis about their medication use as a possible cause for the disease. Assessment of amylase/lipase will aid in the diagnosis. To prevent further compromise in cases where DIP is suspected, hold the offending agent (and substitute if possible) to decrease further episodes. TH
Michele B Kaufman is a freelance medical writer based in New York City.
References
- Lankisch PG, Dröge M, Gottesleben F. Drug-induced acute pancreatitis: incidence and severity. Gut. 1995 Oct;37(4):565-567.
- Eltookhy A, Pearson NL. Drug-induced pancreatitis. Can Pharm J. 2006;139(6):58-60.
- Trivedi CD, Pitchumoni CS. Drug-induced pancreatitis: an update. J Clin Gastroenterol. 2005 Sept;39(8):709-716.
- Badalov N, Baradarian R, Iswara K, et al. Drug-induced pancreatitis: an evidence-based review. Clin Gastroenterol Hepatol. 2007 Jun;5(6):648-661.
- Vege SS, Chari ST. Etiology of acute pancreatitis. In: UpToDate, Rose, BD (Ed), UpToDate, Waltham, Mass., 2007.
- Skirvin A. Drug-induced pancreatitis. Aust Adv Drug Reactions Bull. 2006 Dec;25(6):22.
- American Gastroenterological Association Institute Medical Position Statement on Acute Pancreatitis. Gastroenterology. 1998 Sep;115(3):763-764.
Drugs are an often-overlooked cause of pancreatitis in hospitalized patients.1,2 Knowing which drugs are associated with acute pancreatic inflammation can help the hospitalist consider specific drugs as the cause within their differential diagnosis.
The two most common causes of acute pancreatitis are biliary disease (30%-60%) and chronic alcohol use (15%-30%). Drug-induced pancreatitis (DIP) has occurred with more than 100 prescribed medications.3,4
Most cases of acute pancreatitis are reversible and resolve on their own within three to seven days after treatment begins. A small number of patients develop severe complications, and their mortality rate nears 30%. Symptoms may last a few days and can include mild to severe epigastric pain that can radiate to the back, chest, flank, or lower abdomen.
Other symptoms can include nausea, vomiting, fever, abdominal tenderness, jaundice, or hypotension. Serum amylase and lipase levels usually rise to three times the upper limit of normal. Use of computerized tomography (CT) or ultrasound can help the diagnosis.
The mechanism of DIP is not known, but is thought to be predominantly due to an idiosyncratic reaction, and for a few agents/classes, to intrinsic drug toxicity.5 The incidence of DIP is approximately 1.4%-5%. Not knowing the exact number of prescriptions for each medication and the cases of pancreatitis from each impedes the determination of incidence.
Most data on DIP are from case reports or reviews of compiled cases. The validity and severity of DIP is unknown mostly because cases are underreported to MedWatch. Reasons for underreporting include:
- Low index of suspicion for DIP compared with drug- induced hepatotoxicity;
- Milder cases due to missed lower enzyme levels (not routinely ascertained in a metabolic panel);
- Missed latency of exposure; and
- Erroneous classification as alcoholic or biliary disease by default.
Drug-induced pancreatitis is more common in patients who have inflammatory bowel disease, AIDS, cancer, or gastrointestinal disease. It is also common in those who are geriatric, HIV positive, or who are on immunomodulating agents.6
An early compilation of DIP reports was published by Lankisch, et al. This was a retrospective evaluation that excluded all other pancreatitis etiologies (e.g., post-endoscopic retrograde cholangiopancreatography (ERCP), post-traumatic, post-operative, viral), except drugs. Out of 1,613 patients with acute pancreatitis, there were 22 cases of DIP due to the following agents: azathioprine (n=6), mesalamine/sulfasalazine (n=5) didanosine (ddI, n=4), estrogens (n=3), furosemide (n=2), hydrochlorothiazide (HCTZ, n=1), and rifampicin (n=1). Rechallenge was not attempted for ethical reasons. The mean hospital stay was 25.5 days (range two to 78 days), with an incidence of 1.2%. Two patients died (from AIDS and tuberculosis). The authors noted that other studies show a high fatality rate from azathioprine, ddI, furosemide, and HCTZ.
Additionally, Triveldi, et al., evaluated cases reported in the literature or unpublished cases from 1966 through 2004. They then classified the drugs into one of three categories based on strength of evidence of DIP association.
Class I included medications causing more than 20 reported cases with at least one case following rechallenge. Class II were medications causing more than 10 but fewer than 20 reported cases with/without a positive rechallenge, and Class III were all medications in 10 or fewer cases or unpublished reports (FDA or pharmaceutical company records). Following are some of the most common reports from drugs available in the U.S.:
- Class I: ddI (n=883), asparaginase (n=177), azathioprine (n=86), valproic acid (n=80), pentavalent antimonials (parenterals to treat leishmaniasis, n=80), pentamidine (n=79), mercaptopurine (n=69), mesalamine (n=59), estrogens (n=42), opiates (n=42), tetracycline (n=34), cytarabine (n=26), steroids (n=25), sulfamethoxazole/trimethoprim (SMZ-TMP, n=24), sulfasalazine (n=23), furosemide (n=21), sulindac (n=21);
- Class II: rifampin, lamivudine, octreotide, carbamazepine, acetaminophen, interferon alfa-2b, enalapril, HCTZ, cisplatin, erythromycin; and
- Class III (numerous agents, including the following classes): quinolones, macrolides, angiotensin-converting enzyme inhibitors (ACEIs), statins, and others.
Most recently Badalov, et al., evaluated cases from Medline (through July 1, 2006) and classified them based on levels of evidence. These levels were:
- Definite (imaging study or autopsy confirmed diagnosis);
- Probable (typical symptoms present and threefold increase in amylase and/or lipase); or
- Possible (all others, not included in the final analysis).
Cases were further subclassified into four classes:
- Class Ia (1 or more cases with positive rechallenge, excluding all other causes): codeine, conjugated estrogens, enalapril, isoniazid, metronidazole, mesalamine, pravastatin (other statins), procainamide, simvastatin, sulindac, sulfa drugs, tetracycline, and valproic acid;
- Class Ib (1 or more cases with positive rechallenge, not excluding all other causes): amiodarone, azathioprine, clomiphene, cytosine arabinoside, dapsone, dexamethasone (other steroids), estrogens, furosemide, ifosfamide, lamivudine, losartan, 6-MP, methimazole, methyldopa, nelfinavir, omeprazole, pentamidine, SMZ-TMP, and trans-retinoic acid (not topical);
- Class II (four or more cases, consistent latency in 75% of cases): acetaminophen, clozapine, ddI, erythromycin, l-asparaginase/peg-asparaginase, pentamidine, propofol, and tamoxifen;
- Class III (two or more cases, no consistent latency, no rechallenge): alendronate, captopril, carbamazepine, ceftriaxone, HCTZ, interferon, lisinopril, metformin, mirtazapine, naproxen, and others; and
- Class IV (one case, no other class, without rechallenge): too numerous.
Additionally, the Australian Adverse Drug Reactions Advisory Committee reported on the top 12 DIP-associated medications (n=414 reports implicating 695 drugs). The most commonly reported drugs included azathioprine, ddI, valproate, stavudine, simvastatin, clozapine, lamivudine, ezetimibe, prednisolone, olanzapine, celecoxib and 6-MP, which are listed in each medication’s Australian product information.
The following drugs/classes have been implicated in causing DIP:
- AIDS therapies: ddI, pentamidine;
- Antimicrobials: metronidazole, sulfonamides, tetracyclines;
- Diuretics: furosemide, HCTZ;
- Anti-inflammatories: mesalamine, salicylates, sulindac, sulfasalazine;
- Immunosuppressives: asparaginase, azathioprine, mercaptopurine; and
- Neuropsychiatric agents: valproic acid.
The American Gastroenterologic Association Institute has developed a guide for managing acute pancreatitis. Additionally, they note that when assessing DIP, consider prescription, over-the-counter, and herbal products, too.7 Pancreatitis can occur with certain drugs or medication classes, some more often than others.
Consider DIP in the differential diagnosis of patients who present with or develop epigastric pain. Question all patients with acute pancreatitis about their medication use as a possible cause for the disease. Assessment of amylase/lipase will aid in the diagnosis. To prevent further compromise in cases where DIP is suspected, hold the offending agent (and substitute if possible) to decrease further episodes. TH
Michele B Kaufman is a freelance medical writer based in New York City.
References
- Lankisch PG, Dröge M, Gottesleben F. Drug-induced acute pancreatitis: incidence and severity. Gut. 1995 Oct;37(4):565-567.
- Eltookhy A, Pearson NL. Drug-induced pancreatitis. Can Pharm J. 2006;139(6):58-60.
- Trivedi CD, Pitchumoni CS. Drug-induced pancreatitis: an update. J Clin Gastroenterol. 2005 Sept;39(8):709-716.
- Badalov N, Baradarian R, Iswara K, et al. Drug-induced pancreatitis: an evidence-based review. Clin Gastroenterol Hepatol. 2007 Jun;5(6):648-661.
- Vege SS, Chari ST. Etiology of acute pancreatitis. In: UpToDate, Rose, BD (Ed), UpToDate, Waltham, Mass., 2007.
- Skirvin A. Drug-induced pancreatitis. Aust Adv Drug Reactions Bull. 2006 Dec;25(6):22.
- American Gastroenterological Association Institute Medical Position Statement on Acute Pancreatitis. Gastroenterology. 1998 Sep;115(3):763-764.
Drugs are an often-overlooked cause of pancreatitis in hospitalized patients.1,2 Knowing which drugs are associated with acute pancreatic inflammation can help the hospitalist consider specific drugs as the cause within their differential diagnosis.
The two most common causes of acute pancreatitis are biliary disease (30%-60%) and chronic alcohol use (15%-30%). Drug-induced pancreatitis (DIP) has occurred with more than 100 prescribed medications.3,4
Most cases of acute pancreatitis are reversible and resolve on their own within three to seven days after treatment begins. A small number of patients develop severe complications, and their mortality rate nears 30%. Symptoms may last a few days and can include mild to severe epigastric pain that can radiate to the back, chest, flank, or lower abdomen.
Other symptoms can include nausea, vomiting, fever, abdominal tenderness, jaundice, or hypotension. Serum amylase and lipase levels usually rise to three times the upper limit of normal. Use of computerized tomography (CT) or ultrasound can help the diagnosis.
The mechanism of DIP is not known, but is thought to be predominantly due to an idiosyncratic reaction, and for a few agents/classes, to intrinsic drug toxicity.5 The incidence of DIP is approximately 1.4%-5%. Not knowing the exact number of prescriptions for each medication and the cases of pancreatitis from each impedes the determination of incidence.
Most data on DIP are from case reports or reviews of compiled cases. The validity and severity of DIP is unknown mostly because cases are underreported to MedWatch. Reasons for underreporting include:
- Low index of suspicion for DIP compared with drug- induced hepatotoxicity;
- Milder cases due to missed lower enzyme levels (not routinely ascertained in a metabolic panel);
- Missed latency of exposure; and
- Erroneous classification as alcoholic or biliary disease by default.
Drug-induced pancreatitis is more common in patients who have inflammatory bowel disease, AIDS, cancer, or gastrointestinal disease. It is also common in those who are geriatric, HIV positive, or who are on immunomodulating agents.6
An early compilation of DIP reports was published by Lankisch, et al. This was a retrospective evaluation that excluded all other pancreatitis etiologies (e.g., post-endoscopic retrograde cholangiopancreatography (ERCP), post-traumatic, post-operative, viral), except drugs. Out of 1,613 patients with acute pancreatitis, there were 22 cases of DIP due to the following agents: azathioprine (n=6), mesalamine/sulfasalazine (n=5) didanosine (ddI, n=4), estrogens (n=3), furosemide (n=2), hydrochlorothiazide (HCTZ, n=1), and rifampicin (n=1). Rechallenge was not attempted for ethical reasons. The mean hospital stay was 25.5 days (range two to 78 days), with an incidence of 1.2%. Two patients died (from AIDS and tuberculosis). The authors noted that other studies show a high fatality rate from azathioprine, ddI, furosemide, and HCTZ.
Additionally, Triveldi, et al., evaluated cases reported in the literature or unpublished cases from 1966 through 2004. They then classified the drugs into one of three categories based on strength of evidence of DIP association.
Class I included medications causing more than 20 reported cases with at least one case following rechallenge. Class II were medications causing more than 10 but fewer than 20 reported cases with/without a positive rechallenge, and Class III were all medications in 10 or fewer cases or unpublished reports (FDA or pharmaceutical company records). Following are some of the most common reports from drugs available in the U.S.:
- Class I: ddI (n=883), asparaginase (n=177), azathioprine (n=86), valproic acid (n=80), pentavalent antimonials (parenterals to treat leishmaniasis, n=80), pentamidine (n=79), mercaptopurine (n=69), mesalamine (n=59), estrogens (n=42), opiates (n=42), tetracycline (n=34), cytarabine (n=26), steroids (n=25), sulfamethoxazole/trimethoprim (SMZ-TMP, n=24), sulfasalazine (n=23), furosemide (n=21), sulindac (n=21);
- Class II: rifampin, lamivudine, octreotide, carbamazepine, acetaminophen, interferon alfa-2b, enalapril, HCTZ, cisplatin, erythromycin; and
- Class III (numerous agents, including the following classes): quinolones, macrolides, angiotensin-converting enzyme inhibitors (ACEIs), statins, and others.
Most recently Badalov, et al., evaluated cases from Medline (through July 1, 2006) and classified them based on levels of evidence. These levels were:
- Definite (imaging study or autopsy confirmed diagnosis);
- Probable (typical symptoms present and threefold increase in amylase and/or lipase); or
- Possible (all others, not included in the final analysis).
Cases were further subclassified into four classes:
- Class Ia (1 or more cases with positive rechallenge, excluding all other causes): codeine, conjugated estrogens, enalapril, isoniazid, metronidazole, mesalamine, pravastatin (other statins), procainamide, simvastatin, sulindac, sulfa drugs, tetracycline, and valproic acid;
- Class Ib (1 or more cases with positive rechallenge, not excluding all other causes): amiodarone, azathioprine, clomiphene, cytosine arabinoside, dapsone, dexamethasone (other steroids), estrogens, furosemide, ifosfamide, lamivudine, losartan, 6-MP, methimazole, methyldopa, nelfinavir, omeprazole, pentamidine, SMZ-TMP, and trans-retinoic acid (not topical);
- Class II (four or more cases, consistent latency in 75% of cases): acetaminophen, clozapine, ddI, erythromycin, l-asparaginase/peg-asparaginase, pentamidine, propofol, and tamoxifen;
- Class III (two or more cases, no consistent latency, no rechallenge): alendronate, captopril, carbamazepine, ceftriaxone, HCTZ, interferon, lisinopril, metformin, mirtazapine, naproxen, and others; and
- Class IV (one case, no other class, without rechallenge): too numerous.
Additionally, the Australian Adverse Drug Reactions Advisory Committee reported on the top 12 DIP-associated medications (n=414 reports implicating 695 drugs). The most commonly reported drugs included azathioprine, ddI, valproate, stavudine, simvastatin, clozapine, lamivudine, ezetimibe, prednisolone, olanzapine, celecoxib and 6-MP, which are listed in each medication’s Australian product information.
The following drugs/classes have been implicated in causing DIP:
- AIDS therapies: ddI, pentamidine;
- Antimicrobials: metronidazole, sulfonamides, tetracyclines;
- Diuretics: furosemide, HCTZ;
- Anti-inflammatories: mesalamine, salicylates, sulindac, sulfasalazine;
- Immunosuppressives: asparaginase, azathioprine, mercaptopurine; and
- Neuropsychiatric agents: valproic acid.
The American Gastroenterologic Association Institute has developed a guide for managing acute pancreatitis. Additionally, they note that when assessing DIP, consider prescription, over-the-counter, and herbal products, too.7 Pancreatitis can occur with certain drugs or medication classes, some more often than others.
Consider DIP in the differential diagnosis of patients who present with or develop epigastric pain. Question all patients with acute pancreatitis about their medication use as a possible cause for the disease. Assessment of amylase/lipase will aid in the diagnosis. To prevent further compromise in cases where DIP is suspected, hold the offending agent (and substitute if possible) to decrease further episodes. TH
Michele B Kaufman is a freelance medical writer based in New York City.
References
- Lankisch PG, Dröge M, Gottesleben F. Drug-induced acute pancreatitis: incidence and severity. Gut. 1995 Oct;37(4):565-567.
- Eltookhy A, Pearson NL. Drug-induced pancreatitis. Can Pharm J. 2006;139(6):58-60.
- Trivedi CD, Pitchumoni CS. Drug-induced pancreatitis: an update. J Clin Gastroenterol. 2005 Sept;39(8):709-716.
- Badalov N, Baradarian R, Iswara K, et al. Drug-induced pancreatitis: an evidence-based review. Clin Gastroenterol Hepatol. 2007 Jun;5(6):648-661.
- Vege SS, Chari ST. Etiology of acute pancreatitis. In: UpToDate, Rose, BD (Ed), UpToDate, Waltham, Mass., 2007.
- Skirvin A. Drug-induced pancreatitis. Aust Adv Drug Reactions Bull. 2006 Dec;25(6):22.
- American Gastroenterological Association Institute Medical Position Statement on Acute Pancreatitis. Gastroenterology. 1998 Sep;115(3):763-764.