User login
Updated ACCP Guideline for Antithrombotic Therapy for VTE Disease
Venous thromboembolism (VTE), which includes deep venous thrombosis (DVT) and pulmonary embolism (PE), continues to be a major cause of morbidity and mortality among hospitalized patients. Although it is well-known that anticoagulation therapy is effective in the prevention and treatment of VTE events, these agents are some of the highest-risk medications a hospitalist will prescribe given the danger of major bleeding. With the recent approval of several newer anticoagulants, it is important for the practicing hospitalist to be comfortable initiating, maintaining, and stopping these agents in a wide variety of patient populations.
Guideline Updates
In February 2016, an update to the ninth edition of the antithrombotic guideline from the American College of Chest Physician (ACCP) was published and included updated recommendations on 12 topics in addition to three new topics. This 10th-edition guideline update is referred to as AT10.1
One of the most notable changes in the updated guideline is the recommended choice of anticoagulant in patients with acute DVT or PE without cancer. Now, the direct oral anticoagulants (DOACs) dabigatran, rivaroxaban, apixaban, or edoxaban are recommended over warfarin. Although this is a weak recommendation based on moderate-quality evidence (grade 2B), this is the first time that warfarin is not considered first-line therapy. It should be emphasized that none of the four FDA-approved DOACs are preferred over another, and they should be avoided in patients who are pregnant or have severe renal disease. In patients with DVT or PE and cancer, low-molecular-weight heparin (LMWH) is still the preferred medication. If LMWH is not prescribed, AT10 does not have a preference for either a DOAC or warfarin for patients with cancer.
When it comes to duration of anticoagulation following a VTE event, the updated guideline continues to recommend three months for a provoked VTE event, with consideration for lifelong anticoagulation for an unprovoked event for patients at low or moderate bleeding risk. However, it now suggests that the recurrence risk factors of male sex and a positive D-dimer measured one month after stopping anticoagulant therapy should be taken into consideration when deciding whether extended anticoagulation is indicated.
AT10 also includes new recommendations concerning the role of aspirin for extended VTE treatment. Interestingly, the 2008 ACCP guideline gave a strong recommendation against the use of aspirin for VTE management in any patient population. In the 2012 guideline, the role of aspirin was not addressed for VTE treatment. Now, AT10 states that low-dose aspirin can be used in patients who stop anticoagulant therapy for treatment of an unprovoked proximal DVT or PE as an extended therapy (grade 2B). The significant change in this recommendation stems from two recent randomized trials that compared aspirin with placebo for the prevention of VTE recurrence in patients who have completed a course of anticoagulation for a first unprovoked proximal DVT or PE.2,3 Although the guideline doesn’t consider aspirin to be a reasonable alternative to anticoagulation for patients who require extended therapy and are agreeable to continue, for patients who have decided to stop anticoagulation, aspirin appears to reduce recurrent VTE by approximately one-third, with no significant increased risk of bleeding.
Another significant change in AT10 is the recommendation against the routine use of compression stockings to prevent postthrombotic syndrome (PTS). This change was influenced by a recent multicenter randomized trial showing that elastic compression stockings did not prevent PTS after an acute proximal DVT.4 The guideline authors remark that this recommendation focuses on the prevention of the chronic complications of PTS rather than treatment of the symptoms. Thus, for patients with acute or chronic leg pain or swelling from DVT, compression stockings may be justified.
A topic that was not addressed in the previous guideline was whether patients with a subsegmental PE should be treated. The guideline now suggests that patients with only subsegmental PE and no ultrasound-proven proximal DVT of the legs should undergo “clinical surveillance” rather than anticoagulation (grade 2C). Exceptions include patients at high risk for recurrent VTE (e.g., hospitalization, reduced mobility, active cancer, or irreversible VTE risk factors) and those with a low cardiopulmonary reserve or marked symptoms thought to be from PE. AT10 also states that patient preferences regarding anticoagulation treatment as well as the patient’s risk of bleeding should be taken into consideration. If the decision is made to not prescribe anticoagulation for subsegmental PE, patients should be advised to seek reevaluation if their symptoms persist or worsen.
The 2012 guideline included a new recommendation that patients with low-risk PE (typically defined by a low Pulmonary Embolism Severity Index [PESI] score) could be discharged “early” from the hospital. This recommendation has now been modified to state that patients with low-risk PE may be treated entirely at home. It is worth noting that outpatient management of low-risk PE has become much less complicated if using a DOAC, particularly rivaroxaban and apixaban as neither require initial treatment with parenteral anticoagulation.
AT10 has not changed the recommendation for which patients should receive thrombolytic therapy for treatment of PE. It recommends systemic thrombolytic therapy for patients with acute PE associated with hypotension (defined as systolic blood pressure less than 90 mmHg for 15 minutes) who are not at high risk for bleeding (grade 2B). Likewise, for patients with acute PE not associated with hypotension, the guideline recommends against systemic thrombolytics (grade 1B). If thrombolytics are implemented, AT10 favors systemic administration over catheter-directed thrombolysis (CDT) due to the higher-quality evidence available. However, the authors state that CDT may be preferred for patients at higher risk of bleeding and when local expertise is available. Lastly, catheter-assisted thrombus removal should be considered in patients with acute PE and hypotension who have a high bleeding risk, who have failed systemic thrombolytics, or who are in shock and likely to die before systemic thrombolytics become therapeutic.
Although no prospective trials have evaluated the management of patients with recurrent VTE events while on anticoagulation therapy, AT10 offers some guidance. After ensuring the patient truly had a recurrent VTE event while on therapeutic warfarin or compliant with a DOAC, the authors suggest switching to LMWH for at least one month (grade 2C). Furthermore, for patients who have a recurrent VTE event while compliant on long-term LMWH, the guideline suggests increasing the dose of LMWH by about one-quarter to one-third (grade 2C).
Guideline Analysis
It is important to note that of the 54 recommendations included in the complete guideline update, only 20 were strong recommendations (grade 1), and none were based on high-quality evidence (level A). It is obvious that more research is needed in this field. Regardless, the ACCP antithrombotic guideline remains the authoritative source in VTE management and has a strong influence on practice behavior. With the recent addition of several newer anticoagulants, AT10 is particularly useful in helping providers understand when and when not to use them. The authors indicate that future iterations will be continually updated, describing them as “living guidelines.” The format of AT10 was designed to facilitate this method with the goal of having discrete topics discussed as new evidence becomes available.
Hospital Medicine Takeaways
Despite the lack of randomized and prospective clinical trials, the updated recommendations from AT10 provide important information on challenging VTE issues that the hospitalist can apply to most patients most of the time. Important updates include:
- Prescribe DOACs as first-line agents for the treatment of acute VTE in patients without cancer.
- Use aspirin for the prevention of recurrent VTE in patients who stop anticoagulation for treatment of an unprovoked DVT or PE.
- Avoid compression stockings for the sole purpose of preventing postthrombotic syndrome.
- Do not admit patients with low-risk PE (as determined by the PESI score) to the hospital but rather treat them entirely at home.
Lastly, it is important to remember that VTE treatment decisions need to be individualized based on the clinical, imaging, and biochemical features of your patient.
Paul J. Grant, MD, SFHM, is assistant professor of medicine and director of perioperative and consultative medicine within the Department of Internal Medicine at the University of Michigan Health System in Ann Arbor.
References
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-352.
- Brighton TA, Eikelboom JW, Mann K, et al. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med. 2012;367(21):1979-1987.
- Becattini C, Agnelli G, Schenone A, et al. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med. 2012;366(21):1959-1967.
- Kahn SR, Shapiro S, Wells PS, et al. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo controlled trial. Lancet. 2014;383(9920):880-888.
Venous thromboembolism (VTE), which includes deep venous thrombosis (DVT) and pulmonary embolism (PE), continues to be a major cause of morbidity and mortality among hospitalized patients. Although it is well-known that anticoagulation therapy is effective in the prevention and treatment of VTE events, these agents are some of the highest-risk medications a hospitalist will prescribe given the danger of major bleeding. With the recent approval of several newer anticoagulants, it is important for the practicing hospitalist to be comfortable initiating, maintaining, and stopping these agents in a wide variety of patient populations.
Guideline Updates
In February 2016, an update to the ninth edition of the antithrombotic guideline from the American College of Chest Physician (ACCP) was published and included updated recommendations on 12 topics in addition to three new topics. This 10th-edition guideline update is referred to as AT10.1
One of the most notable changes in the updated guideline is the recommended choice of anticoagulant in patients with acute DVT or PE without cancer. Now, the direct oral anticoagulants (DOACs) dabigatran, rivaroxaban, apixaban, or edoxaban are recommended over warfarin. Although this is a weak recommendation based on moderate-quality evidence (grade 2B), this is the first time that warfarin is not considered first-line therapy. It should be emphasized that none of the four FDA-approved DOACs are preferred over another, and they should be avoided in patients who are pregnant or have severe renal disease. In patients with DVT or PE and cancer, low-molecular-weight heparin (LMWH) is still the preferred medication. If LMWH is not prescribed, AT10 does not have a preference for either a DOAC or warfarin for patients with cancer.
When it comes to duration of anticoagulation following a VTE event, the updated guideline continues to recommend three months for a provoked VTE event, with consideration for lifelong anticoagulation for an unprovoked event for patients at low or moderate bleeding risk. However, it now suggests that the recurrence risk factors of male sex and a positive D-dimer measured one month after stopping anticoagulant therapy should be taken into consideration when deciding whether extended anticoagulation is indicated.
AT10 also includes new recommendations concerning the role of aspirin for extended VTE treatment. Interestingly, the 2008 ACCP guideline gave a strong recommendation against the use of aspirin for VTE management in any patient population. In the 2012 guideline, the role of aspirin was not addressed for VTE treatment. Now, AT10 states that low-dose aspirin can be used in patients who stop anticoagulant therapy for treatment of an unprovoked proximal DVT or PE as an extended therapy (grade 2B). The significant change in this recommendation stems from two recent randomized trials that compared aspirin with placebo for the prevention of VTE recurrence in patients who have completed a course of anticoagulation for a first unprovoked proximal DVT or PE.2,3 Although the guideline doesn’t consider aspirin to be a reasonable alternative to anticoagulation for patients who require extended therapy and are agreeable to continue, for patients who have decided to stop anticoagulation, aspirin appears to reduce recurrent VTE by approximately one-third, with no significant increased risk of bleeding.
Another significant change in AT10 is the recommendation against the routine use of compression stockings to prevent postthrombotic syndrome (PTS). This change was influenced by a recent multicenter randomized trial showing that elastic compression stockings did not prevent PTS after an acute proximal DVT.4 The guideline authors remark that this recommendation focuses on the prevention of the chronic complications of PTS rather than treatment of the symptoms. Thus, for patients with acute or chronic leg pain or swelling from DVT, compression stockings may be justified.
A topic that was not addressed in the previous guideline was whether patients with a subsegmental PE should be treated. The guideline now suggests that patients with only subsegmental PE and no ultrasound-proven proximal DVT of the legs should undergo “clinical surveillance” rather than anticoagulation (grade 2C). Exceptions include patients at high risk for recurrent VTE (e.g., hospitalization, reduced mobility, active cancer, or irreversible VTE risk factors) and those with a low cardiopulmonary reserve or marked symptoms thought to be from PE. AT10 also states that patient preferences regarding anticoagulation treatment as well as the patient’s risk of bleeding should be taken into consideration. If the decision is made to not prescribe anticoagulation for subsegmental PE, patients should be advised to seek reevaluation if their symptoms persist or worsen.
The 2012 guideline included a new recommendation that patients with low-risk PE (typically defined by a low Pulmonary Embolism Severity Index [PESI] score) could be discharged “early” from the hospital. This recommendation has now been modified to state that patients with low-risk PE may be treated entirely at home. It is worth noting that outpatient management of low-risk PE has become much less complicated if using a DOAC, particularly rivaroxaban and apixaban as neither require initial treatment with parenteral anticoagulation.
AT10 has not changed the recommendation for which patients should receive thrombolytic therapy for treatment of PE. It recommends systemic thrombolytic therapy for patients with acute PE associated with hypotension (defined as systolic blood pressure less than 90 mmHg for 15 minutes) who are not at high risk for bleeding (grade 2B). Likewise, for patients with acute PE not associated with hypotension, the guideline recommends against systemic thrombolytics (grade 1B). If thrombolytics are implemented, AT10 favors systemic administration over catheter-directed thrombolysis (CDT) due to the higher-quality evidence available. However, the authors state that CDT may be preferred for patients at higher risk of bleeding and when local expertise is available. Lastly, catheter-assisted thrombus removal should be considered in patients with acute PE and hypotension who have a high bleeding risk, who have failed systemic thrombolytics, or who are in shock and likely to die before systemic thrombolytics become therapeutic.
Although no prospective trials have evaluated the management of patients with recurrent VTE events while on anticoagulation therapy, AT10 offers some guidance. After ensuring the patient truly had a recurrent VTE event while on therapeutic warfarin or compliant with a DOAC, the authors suggest switching to LMWH for at least one month (grade 2C). Furthermore, for patients who have a recurrent VTE event while compliant on long-term LMWH, the guideline suggests increasing the dose of LMWH by about one-quarter to one-third (grade 2C).
Guideline Analysis
It is important to note that of the 54 recommendations included in the complete guideline update, only 20 were strong recommendations (grade 1), and none were based on high-quality evidence (level A). It is obvious that more research is needed in this field. Regardless, the ACCP antithrombotic guideline remains the authoritative source in VTE management and has a strong influence on practice behavior. With the recent addition of several newer anticoagulants, AT10 is particularly useful in helping providers understand when and when not to use them. The authors indicate that future iterations will be continually updated, describing them as “living guidelines.” The format of AT10 was designed to facilitate this method with the goal of having discrete topics discussed as new evidence becomes available.
Hospital Medicine Takeaways
Despite the lack of randomized and prospective clinical trials, the updated recommendations from AT10 provide important information on challenging VTE issues that the hospitalist can apply to most patients most of the time. Important updates include:
- Prescribe DOACs as first-line agents for the treatment of acute VTE in patients without cancer.
- Use aspirin for the prevention of recurrent VTE in patients who stop anticoagulation for treatment of an unprovoked DVT or PE.
- Avoid compression stockings for the sole purpose of preventing postthrombotic syndrome.
- Do not admit patients with low-risk PE (as determined by the PESI score) to the hospital but rather treat them entirely at home.
Lastly, it is important to remember that VTE treatment decisions need to be individualized based on the clinical, imaging, and biochemical features of your patient.
Paul J. Grant, MD, SFHM, is assistant professor of medicine and director of perioperative and consultative medicine within the Department of Internal Medicine at the University of Michigan Health System in Ann Arbor.
References
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-352.
- Brighton TA, Eikelboom JW, Mann K, et al. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med. 2012;367(21):1979-1987.
- Becattini C, Agnelli G, Schenone A, et al. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med. 2012;366(21):1959-1967.
- Kahn SR, Shapiro S, Wells PS, et al. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo controlled trial. Lancet. 2014;383(9920):880-888.
Venous thromboembolism (VTE), which includes deep venous thrombosis (DVT) and pulmonary embolism (PE), continues to be a major cause of morbidity and mortality among hospitalized patients. Although it is well-known that anticoagulation therapy is effective in the prevention and treatment of VTE events, these agents are some of the highest-risk medications a hospitalist will prescribe given the danger of major bleeding. With the recent approval of several newer anticoagulants, it is important for the practicing hospitalist to be comfortable initiating, maintaining, and stopping these agents in a wide variety of patient populations.
Guideline Updates
In February 2016, an update to the ninth edition of the antithrombotic guideline from the American College of Chest Physician (ACCP) was published and included updated recommendations on 12 topics in addition to three new topics. This 10th-edition guideline update is referred to as AT10.1
One of the most notable changes in the updated guideline is the recommended choice of anticoagulant in patients with acute DVT or PE without cancer. Now, the direct oral anticoagulants (DOACs) dabigatran, rivaroxaban, apixaban, or edoxaban are recommended over warfarin. Although this is a weak recommendation based on moderate-quality evidence (grade 2B), this is the first time that warfarin is not considered first-line therapy. It should be emphasized that none of the four FDA-approved DOACs are preferred over another, and they should be avoided in patients who are pregnant or have severe renal disease. In patients with DVT or PE and cancer, low-molecular-weight heparin (LMWH) is still the preferred medication. If LMWH is not prescribed, AT10 does not have a preference for either a DOAC or warfarin for patients with cancer.
When it comes to duration of anticoagulation following a VTE event, the updated guideline continues to recommend three months for a provoked VTE event, with consideration for lifelong anticoagulation for an unprovoked event for patients at low or moderate bleeding risk. However, it now suggests that the recurrence risk factors of male sex and a positive D-dimer measured one month after stopping anticoagulant therapy should be taken into consideration when deciding whether extended anticoagulation is indicated.
AT10 also includes new recommendations concerning the role of aspirin for extended VTE treatment. Interestingly, the 2008 ACCP guideline gave a strong recommendation against the use of aspirin for VTE management in any patient population. In the 2012 guideline, the role of aspirin was not addressed for VTE treatment. Now, AT10 states that low-dose aspirin can be used in patients who stop anticoagulant therapy for treatment of an unprovoked proximal DVT or PE as an extended therapy (grade 2B). The significant change in this recommendation stems from two recent randomized trials that compared aspirin with placebo for the prevention of VTE recurrence in patients who have completed a course of anticoagulation for a first unprovoked proximal DVT or PE.2,3 Although the guideline doesn’t consider aspirin to be a reasonable alternative to anticoagulation for patients who require extended therapy and are agreeable to continue, for patients who have decided to stop anticoagulation, aspirin appears to reduce recurrent VTE by approximately one-third, with no significant increased risk of bleeding.
Another significant change in AT10 is the recommendation against the routine use of compression stockings to prevent postthrombotic syndrome (PTS). This change was influenced by a recent multicenter randomized trial showing that elastic compression stockings did not prevent PTS after an acute proximal DVT.4 The guideline authors remark that this recommendation focuses on the prevention of the chronic complications of PTS rather than treatment of the symptoms. Thus, for patients with acute or chronic leg pain or swelling from DVT, compression stockings may be justified.
A topic that was not addressed in the previous guideline was whether patients with a subsegmental PE should be treated. The guideline now suggests that patients with only subsegmental PE and no ultrasound-proven proximal DVT of the legs should undergo “clinical surveillance” rather than anticoagulation (grade 2C). Exceptions include patients at high risk for recurrent VTE (e.g., hospitalization, reduced mobility, active cancer, or irreversible VTE risk factors) and those with a low cardiopulmonary reserve or marked symptoms thought to be from PE. AT10 also states that patient preferences regarding anticoagulation treatment as well as the patient’s risk of bleeding should be taken into consideration. If the decision is made to not prescribe anticoagulation for subsegmental PE, patients should be advised to seek reevaluation if their symptoms persist or worsen.
The 2012 guideline included a new recommendation that patients with low-risk PE (typically defined by a low Pulmonary Embolism Severity Index [PESI] score) could be discharged “early” from the hospital. This recommendation has now been modified to state that patients with low-risk PE may be treated entirely at home. It is worth noting that outpatient management of low-risk PE has become much less complicated if using a DOAC, particularly rivaroxaban and apixaban as neither require initial treatment with parenteral anticoagulation.
AT10 has not changed the recommendation for which patients should receive thrombolytic therapy for treatment of PE. It recommends systemic thrombolytic therapy for patients with acute PE associated with hypotension (defined as systolic blood pressure less than 90 mmHg for 15 minutes) who are not at high risk for bleeding (grade 2B). Likewise, for patients with acute PE not associated with hypotension, the guideline recommends against systemic thrombolytics (grade 1B). If thrombolytics are implemented, AT10 favors systemic administration over catheter-directed thrombolysis (CDT) due to the higher-quality evidence available. However, the authors state that CDT may be preferred for patients at higher risk of bleeding and when local expertise is available. Lastly, catheter-assisted thrombus removal should be considered in patients with acute PE and hypotension who have a high bleeding risk, who have failed systemic thrombolytics, or who are in shock and likely to die before systemic thrombolytics become therapeutic.
Although no prospective trials have evaluated the management of patients with recurrent VTE events while on anticoagulation therapy, AT10 offers some guidance. After ensuring the patient truly had a recurrent VTE event while on therapeutic warfarin or compliant with a DOAC, the authors suggest switching to LMWH for at least one month (grade 2C). Furthermore, for patients who have a recurrent VTE event while compliant on long-term LMWH, the guideline suggests increasing the dose of LMWH by about one-quarter to one-third (grade 2C).
Guideline Analysis
It is important to note that of the 54 recommendations included in the complete guideline update, only 20 were strong recommendations (grade 1), and none were based on high-quality evidence (level A). It is obvious that more research is needed in this field. Regardless, the ACCP antithrombotic guideline remains the authoritative source in VTE management and has a strong influence on practice behavior. With the recent addition of several newer anticoagulants, AT10 is particularly useful in helping providers understand when and when not to use them. The authors indicate that future iterations will be continually updated, describing them as “living guidelines.” The format of AT10 was designed to facilitate this method with the goal of having discrete topics discussed as new evidence becomes available.
Hospital Medicine Takeaways
Despite the lack of randomized and prospective clinical trials, the updated recommendations from AT10 provide important information on challenging VTE issues that the hospitalist can apply to most patients most of the time. Important updates include:
- Prescribe DOACs as first-line agents for the treatment of acute VTE in patients without cancer.
- Use aspirin for the prevention of recurrent VTE in patients who stop anticoagulation for treatment of an unprovoked DVT or PE.
- Avoid compression stockings for the sole purpose of preventing postthrombotic syndrome.
- Do not admit patients with low-risk PE (as determined by the PESI score) to the hospital but rather treat them entirely at home.
Lastly, it is important to remember that VTE treatment decisions need to be individualized based on the clinical, imaging, and biochemical features of your patient.
Paul J. Grant, MD, SFHM, is assistant professor of medicine and director of perioperative and consultative medicine within the Department of Internal Medicine at the University of Michigan Health System in Ann Arbor.
References
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-352.
- Brighton TA, Eikelboom JW, Mann K, et al. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med. 2012;367(21):1979-1987.
- Becattini C, Agnelli G, Schenone A, et al. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med. 2012;366(21):1959-1967.
- Kahn SR, Shapiro S, Wells PS, et al. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo controlled trial. Lancet. 2014;383(9920):880-888.
ASTRO guidelines lower age thresholds for APBI
The American Society for Radiation Oncology has issued new guidelines recommending accelerated partial breast irradiation brachytherapy (APBI) as an alternative to whole breast irradiation (WBI) after surgery in early-stage breast cancer patients, and lowering the age range of patients considered suitable for the procedure to people 50 and older, from 60.
With APBI, localized radiation is delivered to the region around the excised tissue, reducing treatment time and sparing healthy tissue. APBI may also be considered for patients 40 and older, according to ASTRO, if they meet all of the pathologic criteria for suitability listed in the guidelines for patients 50 and above.
The guidelines represent the first ASTRO update on APBI since 2009. In addition to expanding the age range for APBI treatment, the guidelines add low-risk ductal carcinoma in situ as an indication. The guidelines also address intraoperative radiation therapy, or IORT, in which patients receive low-energy photon or electron radiation during surgery (Pract Rad Oncol. 2016 Nov. 17 doi: 10.1016/j.prro.2016.09.007).
While IORT is suitable for patients with invasive cancer eligible for APBI, the guidelines say, patients considering this option should be counseled about the risk of recurrence compared with standard treatment, and, with photon IORT, about potential toxicity risk requiring follow-up. Though more than 40 studies were considered by the ASTRO committee, including large randomized trials comparing APBI with WBI, the new recommendations represent “more of a tweak than a revolution,” said Jay Harris, MD, of Brigham and Women’s Hospital and Dana-Farber Cancer Institute, Boston, one of the guideline authors.
Dr. Harris noted in an interview that two important randomized controlled trials comparing APBI and WBI are still underway, with full follow-up results expected in 2-3 years, after which more definitive recommendations can be made. For the intraoperative radiation advice contained in the guidelines, “we had evidence from two trials looking at different approaches,” Dr. Harris said. “One has long-term data using an electron beam in the operating room – this group showed that that approach seems reasonable in patients that we at ASTRO considered suitable in general for APBI. The other approach is low-dose photon radiation, for which we have only short-term follow-up, making us more hesitant to endorse it.” As for the new recommendation sanctioning APBI for ductal carcinoma, “There’s a lot of variation [in protocols] across the country, compared with invasive cancer,” Dr. Harris said. “We’re kind of all over the map with DCIS. This guideline presents another option.”
The guidelines were sponsored by ASTRO; two authors disclosed financial relationships with firms that make radiologic technology.
The American Society for Radiation Oncology has issued new guidelines recommending accelerated partial breast irradiation brachytherapy (APBI) as an alternative to whole breast irradiation (WBI) after surgery in early-stage breast cancer patients, and lowering the age range of patients considered suitable for the procedure to people 50 and older, from 60.
With APBI, localized radiation is delivered to the region around the excised tissue, reducing treatment time and sparing healthy tissue. APBI may also be considered for patients 40 and older, according to ASTRO, if they meet all of the pathologic criteria for suitability listed in the guidelines for patients 50 and above.
The guidelines represent the first ASTRO update on APBI since 2009. In addition to expanding the age range for APBI treatment, the guidelines add low-risk ductal carcinoma in situ as an indication. The guidelines also address intraoperative radiation therapy, or IORT, in which patients receive low-energy photon or electron radiation during surgery (Pract Rad Oncol. 2016 Nov. 17 doi: 10.1016/j.prro.2016.09.007).
While IORT is suitable for patients with invasive cancer eligible for APBI, the guidelines say, patients considering this option should be counseled about the risk of recurrence compared with standard treatment, and, with photon IORT, about potential toxicity risk requiring follow-up. Though more than 40 studies were considered by the ASTRO committee, including large randomized trials comparing APBI with WBI, the new recommendations represent “more of a tweak than a revolution,” said Jay Harris, MD, of Brigham and Women’s Hospital and Dana-Farber Cancer Institute, Boston, one of the guideline authors.
Dr. Harris noted in an interview that two important randomized controlled trials comparing APBI and WBI are still underway, with full follow-up results expected in 2-3 years, after which more definitive recommendations can be made. For the intraoperative radiation advice contained in the guidelines, “we had evidence from two trials looking at different approaches,” Dr. Harris said. “One has long-term data using an electron beam in the operating room – this group showed that that approach seems reasonable in patients that we at ASTRO considered suitable in general for APBI. The other approach is low-dose photon radiation, for which we have only short-term follow-up, making us more hesitant to endorse it.” As for the new recommendation sanctioning APBI for ductal carcinoma, “There’s a lot of variation [in protocols] across the country, compared with invasive cancer,” Dr. Harris said. “We’re kind of all over the map with DCIS. This guideline presents another option.”
The guidelines were sponsored by ASTRO; two authors disclosed financial relationships with firms that make radiologic technology.
The American Society for Radiation Oncology has issued new guidelines recommending accelerated partial breast irradiation brachytherapy (APBI) as an alternative to whole breast irradiation (WBI) after surgery in early-stage breast cancer patients, and lowering the age range of patients considered suitable for the procedure to people 50 and older, from 60.
With APBI, localized radiation is delivered to the region around the excised tissue, reducing treatment time and sparing healthy tissue. APBI may also be considered for patients 40 and older, according to ASTRO, if they meet all of the pathologic criteria for suitability listed in the guidelines for patients 50 and above.
The guidelines represent the first ASTRO update on APBI since 2009. In addition to expanding the age range for APBI treatment, the guidelines add low-risk ductal carcinoma in situ as an indication. The guidelines also address intraoperative radiation therapy, or IORT, in which patients receive low-energy photon or electron radiation during surgery (Pract Rad Oncol. 2016 Nov. 17 doi: 10.1016/j.prro.2016.09.007).
While IORT is suitable for patients with invasive cancer eligible for APBI, the guidelines say, patients considering this option should be counseled about the risk of recurrence compared with standard treatment, and, with photon IORT, about potential toxicity risk requiring follow-up. Though more than 40 studies were considered by the ASTRO committee, including large randomized trials comparing APBI with WBI, the new recommendations represent “more of a tweak than a revolution,” said Jay Harris, MD, of Brigham and Women’s Hospital and Dana-Farber Cancer Institute, Boston, one of the guideline authors.
Dr. Harris noted in an interview that two important randomized controlled trials comparing APBI and WBI are still underway, with full follow-up results expected in 2-3 years, after which more definitive recommendations can be made. For the intraoperative radiation advice contained in the guidelines, “we had evidence from two trials looking at different approaches,” Dr. Harris said. “One has long-term data using an electron beam in the operating room – this group showed that that approach seems reasonable in patients that we at ASTRO considered suitable in general for APBI. The other approach is low-dose photon radiation, for which we have only short-term follow-up, making us more hesitant to endorse it.” As for the new recommendation sanctioning APBI for ductal carcinoma, “There’s a lot of variation [in protocols] across the country, compared with invasive cancer,” Dr. Harris said. “We’re kind of all over the map with DCIS. This guideline presents another option.”
The guidelines were sponsored by ASTRO; two authors disclosed financial relationships with firms that make radiologic technology.
FROM PRACTICAL RADIATION ONCOLOGY
NCCN: Deliver vincristine by mini IV drip bag
Always dilute chemotherapy agent vincristine and administer it by mini IV-drip bag, instead of syringe, urges the National Comprehensive Cancer Network in a new campaign.
The goal of “Just Bag It” is to prevent a rare but uniformly fatal medical error – administering vincristine to the spinal fluid. When syringes are side by side – one with vincristine for IV push, another with a chemotherapeutic agent meant for push into the spinal fluid – it is just too easy to make a mistake. When administered intrathecally, vincristine causes ascending paralysis, neurological defects, and eventually death.
Despite all the warning labels and checks, “this still happens,” Marc Stewart, MD, cochair of the National Comprehensive Cancer Network (NCCN) Best Practices Committee, as well as medical director of the Seattle Cancer Care Alliance and professor of medicine at the University of Washington, said at a press conference.
Mini IV-drip bag administration will make it “virtually impossible. No physician would hook the bag up to a needle in someone’s spine” and even if they did, there wouldn’t be enough pressure in the bag to push vincristine in, he said.
The group has encouraged drip-bag delivery of vincristine for years, but only about half of hospitals have adopted the policy. The mistake happens so rarely – about 125 cases since the 1960s – “that the motivation for change is just not there.” Until somebody like NCCN calls it out in a high-profile campaign, “it’s not high on the radar screen,” Dr. Stewart said. It should be a relatively easy fix because bagging vincristine is not more costly. In general, the cost difference versus syringe “is going to be pennies,” he said.
“We challenge all medical centers, hospitals, and oncology practices around the nation and the world to implement this medication safety policy so this error never occurs again,” NCCN Chief Executive Officer Robert Carlson, MD, said in a press release. A medical oncologist, he witnessed the death of a 21-year-old patient after an intrathecal vincristine injection in 2005.
“Some health care providers may associate the use of an IV bag with a heightened risk of extravasation, but research shows that the risk of extravasation is extremely low (less than 0.05%) regardless of how vincristine is administered,” the press release noted.
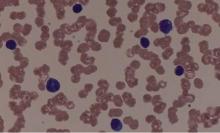
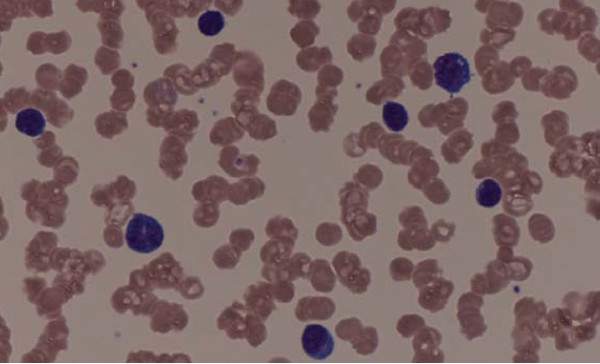
Vincristine is widely used in treating patients with leukemia or lymphoma.
The safety of intravenous administration of vincristine has been a long-standing concern for anyone who participates in the management of patients with hematologic malignancies. As we all know, accidental intrathecal administration of vincristine is uniformly fatal.
At many centers, including ours, policies related to intravenous infusion of vesicants via a peripheral line have made the implementation of the safety recommendations difficult. It is not surprising that only 50% of hospitals surveyed by NCCN have fully implemented the mini-bag recommendation given the concern for extravasation. However, the newest ONS guidelines for vesicant administration allow for short-term infusions via a peripheral line. For our center, this support has been instrumental in allowing us to move to a practice with the recommended mini-bags. The NCCN “Just Bag It” campaign will likely help to move institutions such as ours to be in compliance with this important safety initiative.
Donna Capozzi, PharmD, is associate director of ambulatory services in the department of pharmacy at the Hospital of the University of Pennsylvania Perelman Center for Advanced Medicine in Philadelphia. She is on the editorial advisory board of Hematology News, a publication of this news company.
The safety of intravenous administration of vincristine has been a long-standing concern for anyone who participates in the management of patients with hematologic malignancies. As we all know, accidental intrathecal administration of vincristine is uniformly fatal.
At many centers, including ours, policies related to intravenous infusion of vesicants via a peripheral line have made the implementation of the safety recommendations difficult. It is not surprising that only 50% of hospitals surveyed by NCCN have fully implemented the mini-bag recommendation given the concern for extravasation. However, the newest ONS guidelines for vesicant administration allow for short-term infusions via a peripheral line. For our center, this support has been instrumental in allowing us to move to a practice with the recommended mini-bags. The NCCN “Just Bag It” campaign will likely help to move institutions such as ours to be in compliance with this important safety initiative.
Donna Capozzi, PharmD, is associate director of ambulatory services in the department of pharmacy at the Hospital of the University of Pennsylvania Perelman Center for Advanced Medicine in Philadelphia. She is on the editorial advisory board of Hematology News, a publication of this news company.
The safety of intravenous administration of vincristine has been a long-standing concern for anyone who participates in the management of patients with hematologic malignancies. As we all know, accidental intrathecal administration of vincristine is uniformly fatal.
At many centers, including ours, policies related to intravenous infusion of vesicants via a peripheral line have made the implementation of the safety recommendations difficult. It is not surprising that only 50% of hospitals surveyed by NCCN have fully implemented the mini-bag recommendation given the concern for extravasation. However, the newest ONS guidelines for vesicant administration allow for short-term infusions via a peripheral line. For our center, this support has been instrumental in allowing us to move to a practice with the recommended mini-bags. The NCCN “Just Bag It” campaign will likely help to move institutions such as ours to be in compliance with this important safety initiative.
Donna Capozzi, PharmD, is associate director of ambulatory services in the department of pharmacy at the Hospital of the University of Pennsylvania Perelman Center for Advanced Medicine in Philadelphia. She is on the editorial advisory board of Hematology News, a publication of this news company.
Always dilute chemotherapy agent vincristine and administer it by mini IV-drip bag, instead of syringe, urges the National Comprehensive Cancer Network in a new campaign.
The goal of “Just Bag It” is to prevent a rare but uniformly fatal medical error – administering vincristine to the spinal fluid. When syringes are side by side – one with vincristine for IV push, another with a chemotherapeutic agent meant for push into the spinal fluid – it is just too easy to make a mistake. When administered intrathecally, vincristine causes ascending paralysis, neurological defects, and eventually death.
Despite all the warning labels and checks, “this still happens,” Marc Stewart, MD, cochair of the National Comprehensive Cancer Network (NCCN) Best Practices Committee, as well as medical director of the Seattle Cancer Care Alliance and professor of medicine at the University of Washington, said at a press conference.
Mini IV-drip bag administration will make it “virtually impossible. No physician would hook the bag up to a needle in someone’s spine” and even if they did, there wouldn’t be enough pressure in the bag to push vincristine in, he said.
The group has encouraged drip-bag delivery of vincristine for years, but only about half of hospitals have adopted the policy. The mistake happens so rarely – about 125 cases since the 1960s – “that the motivation for change is just not there.” Until somebody like NCCN calls it out in a high-profile campaign, “it’s not high on the radar screen,” Dr. Stewart said. It should be a relatively easy fix because bagging vincristine is not more costly. In general, the cost difference versus syringe “is going to be pennies,” he said.
“We challenge all medical centers, hospitals, and oncology practices around the nation and the world to implement this medication safety policy so this error never occurs again,” NCCN Chief Executive Officer Robert Carlson, MD, said in a press release. A medical oncologist, he witnessed the death of a 21-year-old patient after an intrathecal vincristine injection in 2005.
“Some health care providers may associate the use of an IV bag with a heightened risk of extravasation, but research shows that the risk of extravasation is extremely low (less than 0.05%) regardless of how vincristine is administered,” the press release noted.
Vincristine is widely used in treating patients with leukemia or lymphoma.
Always dilute chemotherapy agent vincristine and administer it by mini IV-drip bag, instead of syringe, urges the National Comprehensive Cancer Network in a new campaign.
The goal of “Just Bag It” is to prevent a rare but uniformly fatal medical error – administering vincristine to the spinal fluid. When syringes are side by side – one with vincristine for IV push, another with a chemotherapeutic agent meant for push into the spinal fluid – it is just too easy to make a mistake. When administered intrathecally, vincristine causes ascending paralysis, neurological defects, and eventually death.
Despite all the warning labels and checks, “this still happens,” Marc Stewart, MD, cochair of the National Comprehensive Cancer Network (NCCN) Best Practices Committee, as well as medical director of the Seattle Cancer Care Alliance and professor of medicine at the University of Washington, said at a press conference.
Mini IV-drip bag administration will make it “virtually impossible. No physician would hook the bag up to a needle in someone’s spine” and even if they did, there wouldn’t be enough pressure in the bag to push vincristine in, he said.
The group has encouraged drip-bag delivery of vincristine for years, but only about half of hospitals have adopted the policy. The mistake happens so rarely – about 125 cases since the 1960s – “that the motivation for change is just not there.” Until somebody like NCCN calls it out in a high-profile campaign, “it’s not high on the radar screen,” Dr. Stewart said. It should be a relatively easy fix because bagging vincristine is not more costly. In general, the cost difference versus syringe “is going to be pennies,” he said.
“We challenge all medical centers, hospitals, and oncology practices around the nation and the world to implement this medication safety policy so this error never occurs again,” NCCN Chief Executive Officer Robert Carlson, MD, said in a press release. A medical oncologist, he witnessed the death of a 21-year-old patient after an intrathecal vincristine injection in 2005.
“Some health care providers may associate the use of an IV bag with a heightened risk of extravasation, but research shows that the risk of extravasation is extremely low (less than 0.05%) regardless of how vincristine is administered,” the press release noted.
Vincristine is widely used in treating patients with leukemia or lymphoma.
Why Aren’t Doctors Following Guidelines?
One recent paper in Clinical Pediatrics, for example, chronicled low adherence to the 2011 National Heart, Lung, and Blood Institute lipid screening guidelines in primary-care settings.1 Another cautioned providers to “mind the (implementation) gap” in venous thromboembolism prevention guidelines for medical inpatients.2 A third found that lower adherence to guidelines issued by the American College of Cardiology/American Heart Association for acute coronary syndrome patients was significantly associated with higher bleeding and mortality rates.3
Both clinical trials and real-world studies have demonstrated that when guidelines are applied, patients do better, says William Lewis, MD, professor of medicine at Case Western Reserve University and director of the Heart & Vascular Center at MetroHealth in Cleveland. So why aren’t they followed more consistently?
Experts in both HM and other disciplines cite multiple obstacles. Lack of evidence, conflicting evidence, or lack of awareness about evidence can all conspire against the main goal of helping providers deliver consistent high-value care, says Christopher Moriates, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California, San Francisco.
“In our day-to-day lives as hospitalists, for the vast majority probably of what we do there’s no clear guideline or there’s a guideline that doesn’t necessarily apply to the patient standing in front of me,” he says.
Even when a guideline is clear and relevant, other doctors say inadequate dissemination and implementation can still derail quality improvement efforts.
“A lot of what we do as physicians is what we learned in residency, and to incorporate the new data is difficult,” says Leonard Feldman, MD, SFHM, a hospitalist and associate professor of internal medicine and pediatrics at Johns Hopkins School of Medicine in Baltimore.
Dr. Feldman believes many doctors have yet to integrate recently revised hypertension and cholesterol guidelines into their practice, for example. Some guidelines have proven more complex or controversial, limiting their adoption.
“I know I struggle to keep up with all of the guidelines, and I’m in a big academic center where people are talking about them all the time, and I’m working with residents who are talking about them all the time,” Dr. Feldman says.
Despite the remaining gaps, however, many researchers agree that momentum has built steadily over the past two decades toward a more systematic approach to creating solid evidence-based guidelines and integrating them into real-world decision making.
Emphasis on Evidence and Transparency
The term “evidence-based medicine” was coined in 1990 by Gordon Guyatt, MD, MSc, FRCPC, distinguished professor of medicine and clinical epidemiology at McMaster University in Hamilton, Ontario. It’s played an active role in formulating guidelines for multiple organizations. The guideline-writing process, Dr. Guyatt says, once consisted of little more than self-selected clinicians sitting around a table.
“It used to be that a bunch of experts got together and decided and made the recommendations with very little in the way of a systematic process and certainly not evidence based,” he says.
Cincinnati Children’s Hospital Medical Center was among the pioneers pushing for a more systematic approach; the hospital began working on its own guidelines in 1995 and published the first of many the following year.
“We started evidence-based guidelines when the docs were still saying, ‘This is cookbook medicine. I don’t know if I want to do this or not,’” says Wendy Gerhardt, MSN, director of evidence-based decision making in the James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s.
Some doctors also argued that clinical guidelines would stifle innovation, cramp their individual style, or intrude on their relationships with patients. Despite some lingering misgivings among clinicians, however, the process has gained considerable support. In 2000, an organization called the GRADE Working Group (Grading of Recommendations, Assessment, Development and Evaluation) began developing a new approach to raise the quality of evidence and strength of recommendations.
The group’s work led to a 2004 article in BMJ, and the journal subsequently published a six-part series about GRADE for clinicians.4 More recently, the Journal of Clinical Epidemiology also delved into the issue with a 15-part series detailing the GRADE methodology.5 Together, Dr. Guyatt says, the articles have become a go-to guide for guidelines and have helped solidify the focus on evidence.
Cincinnati Children’s and other institutions also have developed tools, and the Institute of Medicine has published guideline-writing standards.
“So it’s easier than it’s ever been to know whether or not you have a decent guideline in your hand,” Gerhardt says.
Likewise, medical organizations are more clearly explaining how they came up with different kinds of guidelines. Evidence-based and consensus guidelines aren’t necessarily mutually exclusive, though consensus building is often used in the absence of high-quality evidence. Some organizations have limited the pool of evidence for guidelines to randomized controlled trial data.
“Unfortunately, for us in the real world, we actually have to make decisions even when there’s not enough data,” Dr. Feldman says.
Sometimes, the best available evidence may be observational studies, and some committees still try to reach a consensus based on that evidence and on the panelists’ professional opinions.
Dr. Guyatt agrees that it’s “absolutely not” true that evidence-based guidelines require randomized controlled trials. “What you need for any recommendation is a thorough review and summary of the best available evidence,” he says.
As part of each final document, Cincinnati Children’s details how it created the guideline, when the literature searches occurred, how the committee reached a consensus, and which panelists participated in the deliberations. The information, Gerhardt says, allows anyone else to “make some sensible decisions about whether or not it’s a guideline you want to use.”
Guideline-crafting institutions are also focusing more on the proper makeup of their panels. In general, Dr. Guyatt says, a panel with more than 10 people can be unwieldy. Guidelines that include many specific recommendations, however, may require multiple subsections, each with its own committee.
Dr. Guyatt is careful to note that, like many other experts, he has multiple potential conflicts of interest, such as working on the anti-thrombotic guidelines issued by the American College of Chest Physicians. Committees, he says, have become increasingly aware of how properly handling conflicts (financial or otherwise) can be critical in building and maintaining trust among clinicians and patients. One technique is to ensure that a diversity of opinions is reflected among a committee whose experts have various conflicts. If one expert’s company makes drug A, for example, then the committee also includes experts involved with drugs B or C. As an alternative, some committees have explicitly barred anyone with a conflict of interest from participating at all.
But experts often provide crucial input, Dr. Guyatt says, and several committees have adopted variations of a middle-ground approach. In an approach that he favors, all guideline-formulating panelists are conflict-free but begin their work by meeting with a separate group of experts who may have some conflicts but can help point out the main issues. The panelists then deliberate and write a draft of the recommendations, after which they meet again with the experts to receive feedback before finalizing the draft.
In a related approach, experts sit on the panel and discuss the evidence, but those with conflicts recuse themselves before the group votes on any recommendations. Delineating between discussions of the evidence and discussions of recommendations can be tricky, though, increasing the risk that a conflict of interest may influence the outcome. Even so, Dr. Guyatt says the model is still preferable to other alternatives.
Getting the Word Out
Once guidelines have been crafted and vetted, how can hospitalists get up to speed on them? Dr. Feldman’s favorite go-to source is Guideline.gov, a national guideline clearinghouse that he calls one of the best compendiums of available information. Especially helpful, he adds, are details such as how the guidelines were created.
To help maximize his time, he also uses tools like NEJM Journal Watch, which sends daily emails on noteworthy articles and weekend roundups of the most important studies.
“It is a way of at least trying to keep up with what’s going on,” he says. Similarly, he adds, ACP Journal Club provides summaries of important new articles, The Hospitalist can help highlight important guidelines that affect HM, and CME meetings or online modules like SHMconsults.com can help doctors keep pace.
For the past decade, Dr. Guyatt has worked with another popular tool, a guideline-disseminating service called UpToDate. Many alternatives exist, such as DynaMed Plus.
“I think you just need to pick away,” Dr. Feldman says. “You need to decide that as a physician, as a lifelong learner, that you are going to do something that is going to keep you up-to-date. There are many ways of doing it. You just have to decide what you’re going to do and commit to it.”
Researchers are helping out by studying how to present new guidelines in ways that engage doctors and improve patient outcomes. Another trend is to make guidelines routinely accessible not only in electronic medical records but also on tablets and smartphones. Lisa Shieh, MD, PhD, FHM, a hospitalist and clinical professor of medicine at Stanford University Medical Center, has studied how best-practice alerts, or BPAs, impact adherence to guidelines covering the appropriate use of blood products. Dr. Shieh, who splits her time between quality improvement and hospital medicine, says getting new information and guidelines into clinicians’ hands can be a logistical challenge.
“At Stanford, we had a huge official campaign around the guidelines, and that did make some impact, but it wasn’t huge in improving appropriate blood use,” she says. When the medial center set up a BPA through the electronic medical record system, however, both overall and inappropriate blood use declined significantly. In fact, the percentage of providers ordering blood products for patients with a hemoglobin count above 8 g/dL dropped from 60% to 25%.6
One difference maker, Dr. Shieh says, was providing education at the moment a doctor actually ordered blood. To avoid alert fatigue, the “smart BPA” fires only if a doctor tries to order blood and the patient’s hemoglobin is greater than 7 or 8 g/dL, depending on the diagnosis. If the doctor still wants to transfuse, the system requests a clinical indication for the exception.
Despite the clear improvement in appropriate use, the team wanted to understand why 25% of providers were still ordering blood products for patients with a hemoglobin count greater than 8 despite the triggered BPA and whether additional interventions could yield further improvements. Through their study, the researchers documented several reasons for the continued ordering. In some cases, the system failed to properly document actual or potential bleeding as an indicator. In other cases, the ordering reflected a lack of consensus on the guidelines in fields like hematology and oncology.
One of the most intriguing reasons, though, was that residents often did the ordering at the behest of an attending who might have never seen the BPA.
“It’s not actually reaching the audience making the decision; it might be reaching the audience that’s just carrying out the order,” Dr. Shieh says.
The insight, she says, may provide an opportunity to talk with attending physicians who may not have completely bought into the guidelines and to involve the entire team in the decision-making process.
Hospitalists, she says, can play a vital role in guideline development and implementation, especially for strategies that include BPAs.
“I think they’re the perfect group to help use this technology wisely because they are at the front lines taking care of patients so they’ll know the best workflow of when these alerts fire and maybe which ones happen the most often,” Dr. Shieh says. “I think this is a fantastic opportunity to get more hospitalists involved in designing these alerts and collaborating with the IT folks.”
Even with widespread buy-in from providers, guidelines may not reach their full potential without a careful consideration of patients’ values and concerns. Experts say joint deliberations and discussions are especially important for guidelines that are complicated, controversial, or carrying potential risks that must be weighed against the benefits.
Some of the conversations are easy, with well-defined risks and benefits and clear patient preferences, but others must traverse vast tracts of gray area. Fortunately, Dr. Feldman says, more tools also are becoming available for this kind of shared decision making. Some use pictorial representations to help patients understand the potential outcomes of alternative courses of action or inaction.
“Sometimes, that pictorial representation is worth the 1,000 words that we wouldn’t be able to adequately describe otherwise,” he says.
Similarly, Cincinnati Children’s has developed tools to help to ease the shared decision-making process.
“We look where there’s equivocal evidence or no evidence and have developed tools that help the clinician have that conversation with the family and then have them informed enough that they can actually weigh in on what they want,” Gerhardt says. One end product is a card or trifold pamphlet that might help parents understand the benefits and side effects of alternate strategies.
“Typically, in medicine, we’re used to telling people what needs to be done,” she says. “So shared decision making is kind of a different thing for clinicians to engage in.” TH
Bryn Nelson, PhD, is a freelance writer in Seattle.
References
- Valle CW, Binns HJ, Quadri-Sheriff M, Benuck I, Patel A. Physicians’ lack of adherence to National Heart, Lung, and Blood Institute guidelines for pediatric lipid screening. Clin Pediatr. 2015;54(12):1200-1205.
- Maynard G, Jenkins IH, Merli GJ. Venous thromboembolism prevention guidelines for medical inpatients: mind the (implementation) gap. J Hosp Med. 2013;8(10):582-588.
- Mehta RH, Chen AY, Alexander KP, Ohman EM, Roe MT, Peterson ED. Doing the right things and doing them the right way: association between hospital guideline adherence, dosing safety, and outcomes among patients with acute coronary syndrome. Circulation. 2015;131(11):980-987.
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490
- Andrews JC, Schünemann HJ, Oxman AD, et al. GRADE guidelines: 15. Going from evidence to recommendation—determinants of a recommendation’s direction and strength. J Clin Epidemiol. 2013;66(7):726-735.
- 6. Chen JH, Fang DZ, Tim Goodnough L, Evans KH, Lee Porter M, Shieh L. Why providers transfuse blood products outside recommended guidelines in spite of integrated electronic best practice alerts. J Hosp Med. 2015;10(1):1-7.
One recent paper in Clinical Pediatrics, for example, chronicled low adherence to the 2011 National Heart, Lung, and Blood Institute lipid screening guidelines in primary-care settings.1 Another cautioned providers to “mind the (implementation) gap” in venous thromboembolism prevention guidelines for medical inpatients.2 A third found that lower adherence to guidelines issued by the American College of Cardiology/American Heart Association for acute coronary syndrome patients was significantly associated with higher bleeding and mortality rates.3
Both clinical trials and real-world studies have demonstrated that when guidelines are applied, patients do better, says William Lewis, MD, professor of medicine at Case Western Reserve University and director of the Heart & Vascular Center at MetroHealth in Cleveland. So why aren’t they followed more consistently?
Experts in both HM and other disciplines cite multiple obstacles. Lack of evidence, conflicting evidence, or lack of awareness about evidence can all conspire against the main goal of helping providers deliver consistent high-value care, says Christopher Moriates, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California, San Francisco.
“In our day-to-day lives as hospitalists, for the vast majority probably of what we do there’s no clear guideline or there’s a guideline that doesn’t necessarily apply to the patient standing in front of me,” he says.
Even when a guideline is clear and relevant, other doctors say inadequate dissemination and implementation can still derail quality improvement efforts.
“A lot of what we do as physicians is what we learned in residency, and to incorporate the new data is difficult,” says Leonard Feldman, MD, SFHM, a hospitalist and associate professor of internal medicine and pediatrics at Johns Hopkins School of Medicine in Baltimore.
Dr. Feldman believes many doctors have yet to integrate recently revised hypertension and cholesterol guidelines into their practice, for example. Some guidelines have proven more complex or controversial, limiting their adoption.
“I know I struggle to keep up with all of the guidelines, and I’m in a big academic center where people are talking about them all the time, and I’m working with residents who are talking about them all the time,” Dr. Feldman says.
Despite the remaining gaps, however, many researchers agree that momentum has built steadily over the past two decades toward a more systematic approach to creating solid evidence-based guidelines and integrating them into real-world decision making.
Emphasis on Evidence and Transparency
The term “evidence-based medicine” was coined in 1990 by Gordon Guyatt, MD, MSc, FRCPC, distinguished professor of medicine and clinical epidemiology at McMaster University in Hamilton, Ontario. It’s played an active role in formulating guidelines for multiple organizations. The guideline-writing process, Dr. Guyatt says, once consisted of little more than self-selected clinicians sitting around a table.
“It used to be that a bunch of experts got together and decided and made the recommendations with very little in the way of a systematic process and certainly not evidence based,” he says.
Cincinnati Children’s Hospital Medical Center was among the pioneers pushing for a more systematic approach; the hospital began working on its own guidelines in 1995 and published the first of many the following year.
“We started evidence-based guidelines when the docs were still saying, ‘This is cookbook medicine. I don’t know if I want to do this or not,’” says Wendy Gerhardt, MSN, director of evidence-based decision making in the James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s.
Some doctors also argued that clinical guidelines would stifle innovation, cramp their individual style, or intrude on their relationships with patients. Despite some lingering misgivings among clinicians, however, the process has gained considerable support. In 2000, an organization called the GRADE Working Group (Grading of Recommendations, Assessment, Development and Evaluation) began developing a new approach to raise the quality of evidence and strength of recommendations.
The group’s work led to a 2004 article in BMJ, and the journal subsequently published a six-part series about GRADE for clinicians.4 More recently, the Journal of Clinical Epidemiology also delved into the issue with a 15-part series detailing the GRADE methodology.5 Together, Dr. Guyatt says, the articles have become a go-to guide for guidelines and have helped solidify the focus on evidence.
Cincinnati Children’s and other institutions also have developed tools, and the Institute of Medicine has published guideline-writing standards.
“So it’s easier than it’s ever been to know whether or not you have a decent guideline in your hand,” Gerhardt says.
Likewise, medical organizations are more clearly explaining how they came up with different kinds of guidelines. Evidence-based and consensus guidelines aren’t necessarily mutually exclusive, though consensus building is often used in the absence of high-quality evidence. Some organizations have limited the pool of evidence for guidelines to randomized controlled trial data.
“Unfortunately, for us in the real world, we actually have to make decisions even when there’s not enough data,” Dr. Feldman says.
Sometimes, the best available evidence may be observational studies, and some committees still try to reach a consensus based on that evidence and on the panelists’ professional opinions.
Dr. Guyatt agrees that it’s “absolutely not” true that evidence-based guidelines require randomized controlled trials. “What you need for any recommendation is a thorough review and summary of the best available evidence,” he says.
As part of each final document, Cincinnati Children’s details how it created the guideline, when the literature searches occurred, how the committee reached a consensus, and which panelists participated in the deliberations. The information, Gerhardt says, allows anyone else to “make some sensible decisions about whether or not it’s a guideline you want to use.”
Guideline-crafting institutions are also focusing more on the proper makeup of their panels. In general, Dr. Guyatt says, a panel with more than 10 people can be unwieldy. Guidelines that include many specific recommendations, however, may require multiple subsections, each with its own committee.
Dr. Guyatt is careful to note that, like many other experts, he has multiple potential conflicts of interest, such as working on the anti-thrombotic guidelines issued by the American College of Chest Physicians. Committees, he says, have become increasingly aware of how properly handling conflicts (financial or otherwise) can be critical in building and maintaining trust among clinicians and patients. One technique is to ensure that a diversity of opinions is reflected among a committee whose experts have various conflicts. If one expert’s company makes drug A, for example, then the committee also includes experts involved with drugs B or C. As an alternative, some committees have explicitly barred anyone with a conflict of interest from participating at all.
But experts often provide crucial input, Dr. Guyatt says, and several committees have adopted variations of a middle-ground approach. In an approach that he favors, all guideline-formulating panelists are conflict-free but begin their work by meeting with a separate group of experts who may have some conflicts but can help point out the main issues. The panelists then deliberate and write a draft of the recommendations, after which they meet again with the experts to receive feedback before finalizing the draft.
In a related approach, experts sit on the panel and discuss the evidence, but those with conflicts recuse themselves before the group votes on any recommendations. Delineating between discussions of the evidence and discussions of recommendations can be tricky, though, increasing the risk that a conflict of interest may influence the outcome. Even so, Dr. Guyatt says the model is still preferable to other alternatives.
Getting the Word Out
Once guidelines have been crafted and vetted, how can hospitalists get up to speed on them? Dr. Feldman’s favorite go-to source is Guideline.gov, a national guideline clearinghouse that he calls one of the best compendiums of available information. Especially helpful, he adds, are details such as how the guidelines were created.
To help maximize his time, he also uses tools like NEJM Journal Watch, which sends daily emails on noteworthy articles and weekend roundups of the most important studies.
“It is a way of at least trying to keep up with what’s going on,” he says. Similarly, he adds, ACP Journal Club provides summaries of important new articles, The Hospitalist can help highlight important guidelines that affect HM, and CME meetings or online modules like SHMconsults.com can help doctors keep pace.
For the past decade, Dr. Guyatt has worked with another popular tool, a guideline-disseminating service called UpToDate. Many alternatives exist, such as DynaMed Plus.
“I think you just need to pick away,” Dr. Feldman says. “You need to decide that as a physician, as a lifelong learner, that you are going to do something that is going to keep you up-to-date. There are many ways of doing it. You just have to decide what you’re going to do and commit to it.”
Researchers are helping out by studying how to present new guidelines in ways that engage doctors and improve patient outcomes. Another trend is to make guidelines routinely accessible not only in electronic medical records but also on tablets and smartphones. Lisa Shieh, MD, PhD, FHM, a hospitalist and clinical professor of medicine at Stanford University Medical Center, has studied how best-practice alerts, or BPAs, impact adherence to guidelines covering the appropriate use of blood products. Dr. Shieh, who splits her time between quality improvement and hospital medicine, says getting new information and guidelines into clinicians’ hands can be a logistical challenge.
“At Stanford, we had a huge official campaign around the guidelines, and that did make some impact, but it wasn’t huge in improving appropriate blood use,” she says. When the medial center set up a BPA through the electronic medical record system, however, both overall and inappropriate blood use declined significantly. In fact, the percentage of providers ordering blood products for patients with a hemoglobin count above 8 g/dL dropped from 60% to 25%.6
One difference maker, Dr. Shieh says, was providing education at the moment a doctor actually ordered blood. To avoid alert fatigue, the “smart BPA” fires only if a doctor tries to order blood and the patient’s hemoglobin is greater than 7 or 8 g/dL, depending on the diagnosis. If the doctor still wants to transfuse, the system requests a clinical indication for the exception.
Despite the clear improvement in appropriate use, the team wanted to understand why 25% of providers were still ordering blood products for patients with a hemoglobin count greater than 8 despite the triggered BPA and whether additional interventions could yield further improvements. Through their study, the researchers documented several reasons for the continued ordering. In some cases, the system failed to properly document actual or potential bleeding as an indicator. In other cases, the ordering reflected a lack of consensus on the guidelines in fields like hematology and oncology.
One of the most intriguing reasons, though, was that residents often did the ordering at the behest of an attending who might have never seen the BPA.
“It’s not actually reaching the audience making the decision; it might be reaching the audience that’s just carrying out the order,” Dr. Shieh says.
The insight, she says, may provide an opportunity to talk with attending physicians who may not have completely bought into the guidelines and to involve the entire team in the decision-making process.
Hospitalists, she says, can play a vital role in guideline development and implementation, especially for strategies that include BPAs.
“I think they’re the perfect group to help use this technology wisely because they are at the front lines taking care of patients so they’ll know the best workflow of when these alerts fire and maybe which ones happen the most often,” Dr. Shieh says. “I think this is a fantastic opportunity to get more hospitalists involved in designing these alerts and collaborating with the IT folks.”
Even with widespread buy-in from providers, guidelines may not reach their full potential without a careful consideration of patients’ values and concerns. Experts say joint deliberations and discussions are especially important for guidelines that are complicated, controversial, or carrying potential risks that must be weighed against the benefits.
Some of the conversations are easy, with well-defined risks and benefits and clear patient preferences, but others must traverse vast tracts of gray area. Fortunately, Dr. Feldman says, more tools also are becoming available for this kind of shared decision making. Some use pictorial representations to help patients understand the potential outcomes of alternative courses of action or inaction.
“Sometimes, that pictorial representation is worth the 1,000 words that we wouldn’t be able to adequately describe otherwise,” he says.
Similarly, Cincinnati Children’s has developed tools to help to ease the shared decision-making process.
“We look where there’s equivocal evidence or no evidence and have developed tools that help the clinician have that conversation with the family and then have them informed enough that they can actually weigh in on what they want,” Gerhardt says. One end product is a card or trifold pamphlet that might help parents understand the benefits and side effects of alternate strategies.
“Typically, in medicine, we’re used to telling people what needs to be done,” she says. “So shared decision making is kind of a different thing for clinicians to engage in.” TH
Bryn Nelson, PhD, is a freelance writer in Seattle.
References
- Valle CW, Binns HJ, Quadri-Sheriff M, Benuck I, Patel A. Physicians’ lack of adherence to National Heart, Lung, and Blood Institute guidelines for pediatric lipid screening. Clin Pediatr. 2015;54(12):1200-1205.
- Maynard G, Jenkins IH, Merli GJ. Venous thromboembolism prevention guidelines for medical inpatients: mind the (implementation) gap. J Hosp Med. 2013;8(10):582-588.
- Mehta RH, Chen AY, Alexander KP, Ohman EM, Roe MT, Peterson ED. Doing the right things and doing them the right way: association between hospital guideline adherence, dosing safety, and outcomes among patients with acute coronary syndrome. Circulation. 2015;131(11):980-987.
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490
- Andrews JC, Schünemann HJ, Oxman AD, et al. GRADE guidelines: 15. Going from evidence to recommendation—determinants of a recommendation’s direction and strength. J Clin Epidemiol. 2013;66(7):726-735.
- 6. Chen JH, Fang DZ, Tim Goodnough L, Evans KH, Lee Porter M, Shieh L. Why providers transfuse blood products outside recommended guidelines in spite of integrated electronic best practice alerts. J Hosp Med. 2015;10(1):1-7.
One recent paper in Clinical Pediatrics, for example, chronicled low adherence to the 2011 National Heart, Lung, and Blood Institute lipid screening guidelines in primary-care settings.1 Another cautioned providers to “mind the (implementation) gap” in venous thromboembolism prevention guidelines for medical inpatients.2 A third found that lower adherence to guidelines issued by the American College of Cardiology/American Heart Association for acute coronary syndrome patients was significantly associated with higher bleeding and mortality rates.3
Both clinical trials and real-world studies have demonstrated that when guidelines are applied, patients do better, says William Lewis, MD, professor of medicine at Case Western Reserve University and director of the Heart & Vascular Center at MetroHealth in Cleveland. So why aren’t they followed more consistently?
Experts in both HM and other disciplines cite multiple obstacles. Lack of evidence, conflicting evidence, or lack of awareness about evidence can all conspire against the main goal of helping providers deliver consistent high-value care, says Christopher Moriates, MD, assistant clinical professor in the Division of Hospital Medicine at the University of California, San Francisco.
“In our day-to-day lives as hospitalists, for the vast majority probably of what we do there’s no clear guideline or there’s a guideline that doesn’t necessarily apply to the patient standing in front of me,” he says.
Even when a guideline is clear and relevant, other doctors say inadequate dissemination and implementation can still derail quality improvement efforts.
“A lot of what we do as physicians is what we learned in residency, and to incorporate the new data is difficult,” says Leonard Feldman, MD, SFHM, a hospitalist and associate professor of internal medicine and pediatrics at Johns Hopkins School of Medicine in Baltimore.
Dr. Feldman believes many doctors have yet to integrate recently revised hypertension and cholesterol guidelines into their practice, for example. Some guidelines have proven more complex or controversial, limiting their adoption.
“I know I struggle to keep up with all of the guidelines, and I’m in a big academic center where people are talking about them all the time, and I’m working with residents who are talking about them all the time,” Dr. Feldman says.
Despite the remaining gaps, however, many researchers agree that momentum has built steadily over the past two decades toward a more systematic approach to creating solid evidence-based guidelines and integrating them into real-world decision making.
Emphasis on Evidence and Transparency
The term “evidence-based medicine” was coined in 1990 by Gordon Guyatt, MD, MSc, FRCPC, distinguished professor of medicine and clinical epidemiology at McMaster University in Hamilton, Ontario. It’s played an active role in formulating guidelines for multiple organizations. The guideline-writing process, Dr. Guyatt says, once consisted of little more than self-selected clinicians sitting around a table.
“It used to be that a bunch of experts got together and decided and made the recommendations with very little in the way of a systematic process and certainly not evidence based,” he says.
Cincinnati Children’s Hospital Medical Center was among the pioneers pushing for a more systematic approach; the hospital began working on its own guidelines in 1995 and published the first of many the following year.
“We started evidence-based guidelines when the docs were still saying, ‘This is cookbook medicine. I don’t know if I want to do this or not,’” says Wendy Gerhardt, MSN, director of evidence-based decision making in the James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s.
Some doctors also argued that clinical guidelines would stifle innovation, cramp their individual style, or intrude on their relationships with patients. Despite some lingering misgivings among clinicians, however, the process has gained considerable support. In 2000, an organization called the GRADE Working Group (Grading of Recommendations, Assessment, Development and Evaluation) began developing a new approach to raise the quality of evidence and strength of recommendations.
The group’s work led to a 2004 article in BMJ, and the journal subsequently published a six-part series about GRADE for clinicians.4 More recently, the Journal of Clinical Epidemiology also delved into the issue with a 15-part series detailing the GRADE methodology.5 Together, Dr. Guyatt says, the articles have become a go-to guide for guidelines and have helped solidify the focus on evidence.
Cincinnati Children’s and other institutions also have developed tools, and the Institute of Medicine has published guideline-writing standards.
“So it’s easier than it’s ever been to know whether or not you have a decent guideline in your hand,” Gerhardt says.
Likewise, medical organizations are more clearly explaining how they came up with different kinds of guidelines. Evidence-based and consensus guidelines aren’t necessarily mutually exclusive, though consensus building is often used in the absence of high-quality evidence. Some organizations have limited the pool of evidence for guidelines to randomized controlled trial data.
“Unfortunately, for us in the real world, we actually have to make decisions even when there’s not enough data,” Dr. Feldman says.
Sometimes, the best available evidence may be observational studies, and some committees still try to reach a consensus based on that evidence and on the panelists’ professional opinions.
Dr. Guyatt agrees that it’s “absolutely not” true that evidence-based guidelines require randomized controlled trials. “What you need for any recommendation is a thorough review and summary of the best available evidence,” he says.
As part of each final document, Cincinnati Children’s details how it created the guideline, when the literature searches occurred, how the committee reached a consensus, and which panelists participated in the deliberations. The information, Gerhardt says, allows anyone else to “make some sensible decisions about whether or not it’s a guideline you want to use.”
Guideline-crafting institutions are also focusing more on the proper makeup of their panels. In general, Dr. Guyatt says, a panel with more than 10 people can be unwieldy. Guidelines that include many specific recommendations, however, may require multiple subsections, each with its own committee.
Dr. Guyatt is careful to note that, like many other experts, he has multiple potential conflicts of interest, such as working on the anti-thrombotic guidelines issued by the American College of Chest Physicians. Committees, he says, have become increasingly aware of how properly handling conflicts (financial or otherwise) can be critical in building and maintaining trust among clinicians and patients. One technique is to ensure that a diversity of opinions is reflected among a committee whose experts have various conflicts. If one expert’s company makes drug A, for example, then the committee also includes experts involved with drugs B or C. As an alternative, some committees have explicitly barred anyone with a conflict of interest from participating at all.
But experts often provide crucial input, Dr. Guyatt says, and several committees have adopted variations of a middle-ground approach. In an approach that he favors, all guideline-formulating panelists are conflict-free but begin their work by meeting with a separate group of experts who may have some conflicts but can help point out the main issues. The panelists then deliberate and write a draft of the recommendations, after which they meet again with the experts to receive feedback before finalizing the draft.
In a related approach, experts sit on the panel and discuss the evidence, but those with conflicts recuse themselves before the group votes on any recommendations. Delineating between discussions of the evidence and discussions of recommendations can be tricky, though, increasing the risk that a conflict of interest may influence the outcome. Even so, Dr. Guyatt says the model is still preferable to other alternatives.
Getting the Word Out
Once guidelines have been crafted and vetted, how can hospitalists get up to speed on them? Dr. Feldman’s favorite go-to source is Guideline.gov, a national guideline clearinghouse that he calls one of the best compendiums of available information. Especially helpful, he adds, are details such as how the guidelines were created.
To help maximize his time, he also uses tools like NEJM Journal Watch, which sends daily emails on noteworthy articles and weekend roundups of the most important studies.
“It is a way of at least trying to keep up with what’s going on,” he says. Similarly, he adds, ACP Journal Club provides summaries of important new articles, The Hospitalist can help highlight important guidelines that affect HM, and CME meetings or online modules like SHMconsults.com can help doctors keep pace.
For the past decade, Dr. Guyatt has worked with another popular tool, a guideline-disseminating service called UpToDate. Many alternatives exist, such as DynaMed Plus.
“I think you just need to pick away,” Dr. Feldman says. “You need to decide that as a physician, as a lifelong learner, that you are going to do something that is going to keep you up-to-date. There are many ways of doing it. You just have to decide what you’re going to do and commit to it.”
Researchers are helping out by studying how to present new guidelines in ways that engage doctors and improve patient outcomes. Another trend is to make guidelines routinely accessible not only in electronic medical records but also on tablets and smartphones. Lisa Shieh, MD, PhD, FHM, a hospitalist and clinical professor of medicine at Stanford University Medical Center, has studied how best-practice alerts, or BPAs, impact adherence to guidelines covering the appropriate use of blood products. Dr. Shieh, who splits her time between quality improvement and hospital medicine, says getting new information and guidelines into clinicians’ hands can be a logistical challenge.
“At Stanford, we had a huge official campaign around the guidelines, and that did make some impact, but it wasn’t huge in improving appropriate blood use,” she says. When the medial center set up a BPA through the electronic medical record system, however, both overall and inappropriate blood use declined significantly. In fact, the percentage of providers ordering blood products for patients with a hemoglobin count above 8 g/dL dropped from 60% to 25%.6
One difference maker, Dr. Shieh says, was providing education at the moment a doctor actually ordered blood. To avoid alert fatigue, the “smart BPA” fires only if a doctor tries to order blood and the patient’s hemoglobin is greater than 7 or 8 g/dL, depending on the diagnosis. If the doctor still wants to transfuse, the system requests a clinical indication for the exception.
Despite the clear improvement in appropriate use, the team wanted to understand why 25% of providers were still ordering blood products for patients with a hemoglobin count greater than 8 despite the triggered BPA and whether additional interventions could yield further improvements. Through their study, the researchers documented several reasons for the continued ordering. In some cases, the system failed to properly document actual or potential bleeding as an indicator. In other cases, the ordering reflected a lack of consensus on the guidelines in fields like hematology and oncology.
One of the most intriguing reasons, though, was that residents often did the ordering at the behest of an attending who might have never seen the BPA.
“It’s not actually reaching the audience making the decision; it might be reaching the audience that’s just carrying out the order,” Dr. Shieh says.
The insight, she says, may provide an opportunity to talk with attending physicians who may not have completely bought into the guidelines and to involve the entire team in the decision-making process.
Hospitalists, she says, can play a vital role in guideline development and implementation, especially for strategies that include BPAs.
“I think they’re the perfect group to help use this technology wisely because they are at the front lines taking care of patients so they’ll know the best workflow of when these alerts fire and maybe which ones happen the most often,” Dr. Shieh says. “I think this is a fantastic opportunity to get more hospitalists involved in designing these alerts and collaborating with the IT folks.”
Even with widespread buy-in from providers, guidelines may not reach their full potential without a careful consideration of patients’ values and concerns. Experts say joint deliberations and discussions are especially important for guidelines that are complicated, controversial, or carrying potential risks that must be weighed against the benefits.
Some of the conversations are easy, with well-defined risks and benefits and clear patient preferences, but others must traverse vast tracts of gray area. Fortunately, Dr. Feldman says, more tools also are becoming available for this kind of shared decision making. Some use pictorial representations to help patients understand the potential outcomes of alternative courses of action or inaction.
“Sometimes, that pictorial representation is worth the 1,000 words that we wouldn’t be able to adequately describe otherwise,” he says.
Similarly, Cincinnati Children’s has developed tools to help to ease the shared decision-making process.
“We look where there’s equivocal evidence or no evidence and have developed tools that help the clinician have that conversation with the family and then have them informed enough that they can actually weigh in on what they want,” Gerhardt says. One end product is a card or trifold pamphlet that might help parents understand the benefits and side effects of alternate strategies.
“Typically, in medicine, we’re used to telling people what needs to be done,” she says. “So shared decision making is kind of a different thing for clinicians to engage in.” TH
Bryn Nelson, PhD, is a freelance writer in Seattle.
References
- Valle CW, Binns HJ, Quadri-Sheriff M, Benuck I, Patel A. Physicians’ lack of adherence to National Heart, Lung, and Blood Institute guidelines for pediatric lipid screening. Clin Pediatr. 2015;54(12):1200-1205.
- Maynard G, Jenkins IH, Merli GJ. Venous thromboembolism prevention guidelines for medical inpatients: mind the (implementation) gap. J Hosp Med. 2013;8(10):582-588.
- Mehta RH, Chen AY, Alexander KP, Ohman EM, Roe MT, Peterson ED. Doing the right things and doing them the right way: association between hospital guideline adherence, dosing safety, and outcomes among patients with acute coronary syndrome. Circulation. 2015;131(11):980-987.
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490
- Andrews JC, Schünemann HJ, Oxman AD, et al. GRADE guidelines: 15. Going from evidence to recommendation—determinants of a recommendation’s direction and strength. J Clin Epidemiol. 2013;66(7):726-735.
- 6. Chen JH, Fang DZ, Tim Goodnough L, Evans KH, Lee Porter M, Shieh L. Why providers transfuse blood products outside recommended guidelines in spite of integrated electronic best practice alerts. J Hosp Med. 2015;10(1):1-7.
Guideline: Supplemental, dietary calcium both heart safe
Both dietary and supplemental calcium should be considered safe for the cardiovascular system as long as total intake doesn’t exceed 2,000-2,500 mg/day – the maximal tolerable level defined by the National Academy of Medicine, according to an updated Clinical Practice Guideline published online October 24 in Annals of Internal Medicine.
For generally healthy patients who don’t consume adequate calcium and take supplements, either alone or in combination with vitamin D, to prevent osteoporosis and related fractures, “discontinuation of supplemental calcium for safety reasons is not necessary and may be harmful to bone health,” said Stephen L. Kopecky, MD, of the Mayo Clinic, Rochester Minn., and his associates on the expert panel that wrote the new guideline.
The National Osteoporosis Foundation (NOF) and the American Society for Preventive Cardiology (ASPC) commissioned an independent review of the current evidence to update the Evidence Report and assembled the expert panel to write the guideline based on the new findings (Ann Intern Med. 2016 Oct 24. doi: 10.7326/M16-1743).
Separately, Mei Chung, PhD, of the department of public health and community medicine, and her associates at Tufts University, Boston, reviewed 4 recent randomized clinical trials, 1 nested case-control study, and 26 cohort studies that assessed the effects of calcium intake on 17 health outcomes in generally healthy adults of all ages. None of the studies evaluated cardiovascular disease risk as a primary outcome. “We conclude that calcium intake (from either food or supplement sources) at levels within the recommended tolerable upper intake range (2,000-2,500 mg/d) are not associated with CVD risks in generally healthy adults,” they said.
“Although a few trials and cohort studies reported increased risks with higher calcium intake, risk estimates in most of those studies were small (10% relative risk) and not considered clinically important, even if they were statistically significant,” Dr. Chung and her associates added (Ann Int Med. 2016 Oct 24. doi: 10.7326/M16-1165).
According to the guideline, “The NOF and the ASPC now adopt the position that there is moderate-quality evidence that calcium with or without vitamin D intake from food or supplements has no relationship (beneficial or harmful) with the risk for cardiovascular or cerebrovascular disease, mortality, or all-cause mortality in generally healthy adults at this time.”
In addition, “Currently, no established biological mechanism supports and association between calcium and cardiovascular disease,” Dr. Kopecky and his associates on the expert panel noted.
The volume of literature on the subject of calcium’s potential harmful cardiovascular disease effects appears to be robust, with the largest meta-analysis to date including 18 studies with 64,000 participants. But this evidence base has some limitations, chief among them the fact that none of the studies was designed to evaluate CVD as a primary outcome.
In addition, concerns about harmful cardiovascular effects arose after most of the trials had already been initiated, so unpublished data on those outcomes were collected and adjudicated retrospectively. In addition, many of the participants showed poor long-term treatment adherence, making it difficult to interpret the data.
Karen L. Margolis, MD, of HealthPartners Institute in Minneapolis and JoAnn E. Manson, MD, DrPH, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, made these remarks in an editorial accompanying the new Clinical Practice Guideline (Ann Intern Med. 2016 Oct 24. doi: 10.7326/M16-2193). Their financial disclosures are available at www.acponline.org.
The volume of literature on the subject of calcium’s potential harmful cardiovascular disease effects appears to be robust, with the largest meta-analysis to date including 18 studies with 64,000 participants. But this evidence base has some limitations, chief among them the fact that none of the studies was designed to evaluate CVD as a primary outcome.
In addition, concerns about harmful cardiovascular effects arose after most of the trials had already been initiated, so unpublished data on those outcomes were collected and adjudicated retrospectively. In addition, many of the participants showed poor long-term treatment adherence, making it difficult to interpret the data.
Karen L. Margolis, MD, of HealthPartners Institute in Minneapolis and JoAnn E. Manson, MD, DrPH, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, made these remarks in an editorial accompanying the new Clinical Practice Guideline (Ann Intern Med. 2016 Oct 24. doi: 10.7326/M16-2193). Their financial disclosures are available at www.acponline.org.
The volume of literature on the subject of calcium’s potential harmful cardiovascular disease effects appears to be robust, with the largest meta-analysis to date including 18 studies with 64,000 participants. But this evidence base has some limitations, chief among them the fact that none of the studies was designed to evaluate CVD as a primary outcome.
In addition, concerns about harmful cardiovascular effects arose after most of the trials had already been initiated, so unpublished data on those outcomes were collected and adjudicated retrospectively. In addition, many of the participants showed poor long-term treatment adherence, making it difficult to interpret the data.
Karen L. Margolis, MD, of HealthPartners Institute in Minneapolis and JoAnn E. Manson, MD, DrPH, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, made these remarks in an editorial accompanying the new Clinical Practice Guideline (Ann Intern Med. 2016 Oct 24. doi: 10.7326/M16-2193). Their financial disclosures are available at www.acponline.org.
Both dietary and supplemental calcium should be considered safe for the cardiovascular system as long as total intake doesn’t exceed 2,000-2,500 mg/day – the maximal tolerable level defined by the National Academy of Medicine, according to an updated Clinical Practice Guideline published online October 24 in Annals of Internal Medicine.
For generally healthy patients who don’t consume adequate calcium and take supplements, either alone or in combination with vitamin D, to prevent osteoporosis and related fractures, “discontinuation of supplemental calcium for safety reasons is not necessary and may be harmful to bone health,” said Stephen L. Kopecky, MD, of the Mayo Clinic, Rochester Minn., and his associates on the expert panel that wrote the new guideline.
The National Osteoporosis Foundation (NOF) and the American Society for Preventive Cardiology (ASPC) commissioned an independent review of the current evidence to update the Evidence Report and assembled the expert panel to write the guideline based on the new findings (Ann Intern Med. 2016 Oct 24. doi: 10.7326/M16-1743).
Separately, Mei Chung, PhD, of the department of public health and community medicine, and her associates at Tufts University, Boston, reviewed 4 recent randomized clinical trials, 1 nested case-control study, and 26 cohort studies that assessed the effects of calcium intake on 17 health outcomes in generally healthy adults of all ages. None of the studies evaluated cardiovascular disease risk as a primary outcome. “We conclude that calcium intake (from either food or supplement sources) at levels within the recommended tolerable upper intake range (2,000-2,500 mg/d) are not associated with CVD risks in generally healthy adults,” they said.
“Although a few trials and cohort studies reported increased risks with higher calcium intake, risk estimates in most of those studies were small (10% relative risk) and not considered clinically important, even if they were statistically significant,” Dr. Chung and her associates added (Ann Int Med. 2016 Oct 24. doi: 10.7326/M16-1165).
According to the guideline, “The NOF and the ASPC now adopt the position that there is moderate-quality evidence that calcium with or without vitamin D intake from food or supplements has no relationship (beneficial or harmful) with the risk for cardiovascular or cerebrovascular disease, mortality, or all-cause mortality in generally healthy adults at this time.”
In addition, “Currently, no established biological mechanism supports and association between calcium and cardiovascular disease,” Dr. Kopecky and his associates on the expert panel noted.
Both dietary and supplemental calcium should be considered safe for the cardiovascular system as long as total intake doesn’t exceed 2,000-2,500 mg/day – the maximal tolerable level defined by the National Academy of Medicine, according to an updated Clinical Practice Guideline published online October 24 in Annals of Internal Medicine.
For generally healthy patients who don’t consume adequate calcium and take supplements, either alone or in combination with vitamin D, to prevent osteoporosis and related fractures, “discontinuation of supplemental calcium for safety reasons is not necessary and may be harmful to bone health,” said Stephen L. Kopecky, MD, of the Mayo Clinic, Rochester Minn., and his associates on the expert panel that wrote the new guideline.
The National Osteoporosis Foundation (NOF) and the American Society for Preventive Cardiology (ASPC) commissioned an independent review of the current evidence to update the Evidence Report and assembled the expert panel to write the guideline based on the new findings (Ann Intern Med. 2016 Oct 24. doi: 10.7326/M16-1743).
Separately, Mei Chung, PhD, of the department of public health and community medicine, and her associates at Tufts University, Boston, reviewed 4 recent randomized clinical trials, 1 nested case-control study, and 26 cohort studies that assessed the effects of calcium intake on 17 health outcomes in generally healthy adults of all ages. None of the studies evaluated cardiovascular disease risk as a primary outcome. “We conclude that calcium intake (from either food or supplement sources) at levels within the recommended tolerable upper intake range (2,000-2,500 mg/d) are not associated with CVD risks in generally healthy adults,” they said.
“Although a few trials and cohort studies reported increased risks with higher calcium intake, risk estimates in most of those studies were small (10% relative risk) and not considered clinically important, even if they were statistically significant,” Dr. Chung and her associates added (Ann Int Med. 2016 Oct 24. doi: 10.7326/M16-1165).
According to the guideline, “The NOF and the ASPC now adopt the position that there is moderate-quality evidence that calcium with or without vitamin D intake from food or supplements has no relationship (beneficial or harmful) with the risk for cardiovascular or cerebrovascular disease, mortality, or all-cause mortality in generally healthy adults at this time.”
In addition, “Currently, no established biological mechanism supports and association between calcium and cardiovascular disease,” Dr. Kopecky and his associates on the expert panel noted.
CMS offering educational webinars on MACRA
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
The Centers for Medicare & Medicaid Services is offering a pair of webinars aimed at helping physicians navigate the new regulation that operationalizes the Medicare Access and CHIP Reauthorization Act (MACRA).
The first webinar, scheduled for Oct. 26, will provide an overview of the two components of the Quality Payment Program – the Merit-Based Incentive Payment System (MIPS) and advanced Alternative Payment Models (APMs).
The second webinar, scheduled for Nov. 15, is targeted to Medicare Part B fee-for-service clinicians, office managers and administrators, state and national associations that represent health care providers, and other stakeholders and will feature a question-and-answer session.
The webinars are part of the agency’s ongoing efforts to help educate practitioners on the provisions of the final MACRA regulation, which was issued on Oct. 14. CMS also recently launched a website to help in that regard.
What to Know about CMS’s New Emergency Preparedness Requirements
Are you ready?
The Centers for Medicare & Medicaid Services (CMS) recently released new emergency preparedness requirements to ensure that providers and suppliers are duly prepared to adequately serve their community during disasters or emergencies. These requirements were stimulated by unexpected and catastrophic events, such as the September 11 terrorist attacks, the 2009 H1N1 pandemic, and innumerable natural disasters (tornados, floods, and hurricanes, to name a few). The CMS final rule issued “requirements that establish a comprehensive, consistent, flexible, and dynamic regulatory approach to emergency preparedness and response that incorporates the lessons learned from the past, combined with the proven best practices of the present.” In the rule, CMS outlines three essential guiding principles that any healthcare facility or supplier would need to preserve in the event of a disaster:
- Safeguard human resources.
- Maintain business continuity.
- Protect physical resources.
4 Ways to Be Prepared
What does having a comprehensive disaster preparedness program mean for hospitalists, regardless of site of practice? CMS recommends having four key elements for an adequate program:
1. Perform a risk assessment that focuses on the capacities and capabilities that are critical for a full spectrum of types of emergencies or disasters. This risk assessment should take into consideration the type and location of the facility as well as the disasters that are most likely to occur in its area. It should include at a minimum “care-related emergencies; equipment and power failures; interruptions in communications, including cyber attacks; loss of a portion or all of a facility; and interruptions in the normal supply of essentials, such as water and food.”
2. Develop and implement policies and procedures that support the emergency plan. Hospitalists should know about organizational policies and procedures that support the implementation of the emergency plan and how their team is factored into that plan.
3. Develop and maintain a communication plan that also complies with state and federal law. All the preparations in the world can be crippled without a robust and clear communication plan. The facility must have primary and backup mechanisms to contact providers, staff, and personnel in a timely fashion; this should include mechanisms to repeatedly update providers as the event evolves so that everyone knows what they are supposed to be doing and when.
4. Develop and maintain a training and testing program for all personnel. This includes onboarding and annual refreshers, including drills and exercises that test the plan and identify any gaps in performance. Hospitalists will undoubtedly be key members in developing, implementing, and receiving such critical training.
Expectations
There isn’t a single U.S. healthcare facility or provider that will not be affected by these provisions. An estimated 72,000 healthcare providers and suppliers (from nursing homes to dialysis facilities to home health agencies) will be expected to comply with these requirements within about a year.
In addition to hospitals, CMS also extended the requirements to many types of facilities and suppliers so that such providers can more likely stay open and provide care during disasters and emergencies, or at least can resume operations as soon as possible, to provide the very best ongoing care to the affected community. In most of these scenarios, the need for complex and varied care goes up, not down, further exacerbating gaps in basic care if ambulatory facilities and home care providers are unavailable.
CMS does acknowledge that these requirements will be more difficult to execute in facilities that previously did not have requirements or in smaller facilities with more limited resources. It also acknowledges that the cost of implementation could reach up to $279 million, which some argue is actually an underestimation. Despite these challenges, it is hard to argue against basic disaster preparedness for any healthcare facility or provider as a standard and positive business practice. While most acute-care hospitals have long had disaster preparedness plans and programs, gaps in these programs have become readily apparent during natural disasters such as Hurricane Katrina and Superstorm Sandy. CMS also stresses the need for a community approach to planning and implementation and that there is no reason during planning, or during an actual event, that facilities should operate in isolation but rather train and respond together as a community.
As hospitalists, regardless of site of practice, we should all be involved in at least understanding, if not developing and implementing, these basic requirements in our facilities. It is without a doubt that hospitalists will be a core group of physicians who will be called upon to serve within or outside healthcare facilities in the event of a disaster or emergency. In fact, in most recent disasters, we already have. It is better, of course, to be prepared and ready to serve than unprepared and regretful.
Reference
- The Centers for Medicare and Medicaid Services. Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Federal Register website. Accessed October 6, 2016.

Are you ready?
The Centers for Medicare & Medicaid Services (CMS) recently released new emergency preparedness requirements to ensure that providers and suppliers are duly prepared to adequately serve their community during disasters or emergencies. These requirements were stimulated by unexpected and catastrophic events, such as the September 11 terrorist attacks, the 2009 H1N1 pandemic, and innumerable natural disasters (tornados, floods, and hurricanes, to name a few). The CMS final rule issued “requirements that establish a comprehensive, consistent, flexible, and dynamic regulatory approach to emergency preparedness and response that incorporates the lessons learned from the past, combined with the proven best practices of the present.” In the rule, CMS outlines three essential guiding principles that any healthcare facility or supplier would need to preserve in the event of a disaster:
- Safeguard human resources.
- Maintain business continuity.
- Protect physical resources.
4 Ways to Be Prepared
What does having a comprehensive disaster preparedness program mean for hospitalists, regardless of site of practice? CMS recommends having four key elements for an adequate program:
1. Perform a risk assessment that focuses on the capacities and capabilities that are critical for a full spectrum of types of emergencies or disasters. This risk assessment should take into consideration the type and location of the facility as well as the disasters that are most likely to occur in its area. It should include at a minimum “care-related emergencies; equipment and power failures; interruptions in communications, including cyber attacks; loss of a portion or all of a facility; and interruptions in the normal supply of essentials, such as water and food.”
2. Develop and implement policies and procedures that support the emergency plan. Hospitalists should know about organizational policies and procedures that support the implementation of the emergency plan and how their team is factored into that plan.
3. Develop and maintain a communication plan that also complies with state and federal law. All the preparations in the world can be crippled without a robust and clear communication plan. The facility must have primary and backup mechanisms to contact providers, staff, and personnel in a timely fashion; this should include mechanisms to repeatedly update providers as the event evolves so that everyone knows what they are supposed to be doing and when.
4. Develop and maintain a training and testing program for all personnel. This includes onboarding and annual refreshers, including drills and exercises that test the plan and identify any gaps in performance. Hospitalists will undoubtedly be key members in developing, implementing, and receiving such critical training.
Expectations
There isn’t a single U.S. healthcare facility or provider that will not be affected by these provisions. An estimated 72,000 healthcare providers and suppliers (from nursing homes to dialysis facilities to home health agencies) will be expected to comply with these requirements within about a year.
In addition to hospitals, CMS also extended the requirements to many types of facilities and suppliers so that such providers can more likely stay open and provide care during disasters and emergencies, or at least can resume operations as soon as possible, to provide the very best ongoing care to the affected community. In most of these scenarios, the need for complex and varied care goes up, not down, further exacerbating gaps in basic care if ambulatory facilities and home care providers are unavailable.
CMS does acknowledge that these requirements will be more difficult to execute in facilities that previously did not have requirements or in smaller facilities with more limited resources. It also acknowledges that the cost of implementation could reach up to $279 million, which some argue is actually an underestimation. Despite these challenges, it is hard to argue against basic disaster preparedness for any healthcare facility or provider as a standard and positive business practice. While most acute-care hospitals have long had disaster preparedness plans and programs, gaps in these programs have become readily apparent during natural disasters such as Hurricane Katrina and Superstorm Sandy. CMS also stresses the need for a community approach to planning and implementation and that there is no reason during planning, or during an actual event, that facilities should operate in isolation but rather train and respond together as a community.
As hospitalists, regardless of site of practice, we should all be involved in at least understanding, if not developing and implementing, these basic requirements in our facilities. It is without a doubt that hospitalists will be a core group of physicians who will be called upon to serve within or outside healthcare facilities in the event of a disaster or emergency. In fact, in most recent disasters, we already have. It is better, of course, to be prepared and ready to serve than unprepared and regretful.
Reference
- The Centers for Medicare and Medicaid Services. Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Federal Register website. Accessed October 6, 2016.

Are you ready?
The Centers for Medicare & Medicaid Services (CMS) recently released new emergency preparedness requirements to ensure that providers and suppliers are duly prepared to adequately serve their community during disasters or emergencies. These requirements were stimulated by unexpected and catastrophic events, such as the September 11 terrorist attacks, the 2009 H1N1 pandemic, and innumerable natural disasters (tornados, floods, and hurricanes, to name a few). The CMS final rule issued “requirements that establish a comprehensive, consistent, flexible, and dynamic regulatory approach to emergency preparedness and response that incorporates the lessons learned from the past, combined with the proven best practices of the present.” In the rule, CMS outlines three essential guiding principles that any healthcare facility or supplier would need to preserve in the event of a disaster:
- Safeguard human resources.
- Maintain business continuity.
- Protect physical resources.
4 Ways to Be Prepared
What does having a comprehensive disaster preparedness program mean for hospitalists, regardless of site of practice? CMS recommends having four key elements for an adequate program:
1. Perform a risk assessment that focuses on the capacities and capabilities that are critical for a full spectrum of types of emergencies or disasters. This risk assessment should take into consideration the type and location of the facility as well as the disasters that are most likely to occur in its area. It should include at a minimum “care-related emergencies; equipment and power failures; interruptions in communications, including cyber attacks; loss of a portion or all of a facility; and interruptions in the normal supply of essentials, such as water and food.”
2. Develop and implement policies and procedures that support the emergency plan. Hospitalists should know about organizational policies and procedures that support the implementation of the emergency plan and how their team is factored into that plan.
3. Develop and maintain a communication plan that also complies with state and federal law. All the preparations in the world can be crippled without a robust and clear communication plan. The facility must have primary and backup mechanisms to contact providers, staff, and personnel in a timely fashion; this should include mechanisms to repeatedly update providers as the event evolves so that everyone knows what they are supposed to be doing and when.
4. Develop and maintain a training and testing program for all personnel. This includes onboarding and annual refreshers, including drills and exercises that test the plan and identify any gaps in performance. Hospitalists will undoubtedly be key members in developing, implementing, and receiving such critical training.
Expectations
There isn’t a single U.S. healthcare facility or provider that will not be affected by these provisions. An estimated 72,000 healthcare providers and suppliers (from nursing homes to dialysis facilities to home health agencies) will be expected to comply with these requirements within about a year.
In addition to hospitals, CMS also extended the requirements to many types of facilities and suppliers so that such providers can more likely stay open and provide care during disasters and emergencies, or at least can resume operations as soon as possible, to provide the very best ongoing care to the affected community. In most of these scenarios, the need for complex and varied care goes up, not down, further exacerbating gaps in basic care if ambulatory facilities and home care providers are unavailable.
CMS does acknowledge that these requirements will be more difficult to execute in facilities that previously did not have requirements or in smaller facilities with more limited resources. It also acknowledges that the cost of implementation could reach up to $279 million, which some argue is actually an underestimation. Despite these challenges, it is hard to argue against basic disaster preparedness for any healthcare facility or provider as a standard and positive business practice. While most acute-care hospitals have long had disaster preparedness plans and programs, gaps in these programs have become readily apparent during natural disasters such as Hurricane Katrina and Superstorm Sandy. CMS also stresses the need for a community approach to planning and implementation and that there is no reason during planning, or during an actual event, that facilities should operate in isolation but rather train and respond together as a community.
As hospitalists, regardless of site of practice, we should all be involved in at least understanding, if not developing and implementing, these basic requirements in our facilities. It is without a doubt that hospitalists will be a core group of physicians who will be called upon to serve within or outside healthcare facilities in the event of a disaster or emergency. In fact, in most recent disasters, we already have. It is better, of course, to be prepared and ready to serve than unprepared and regretful.
Reference
- The Centers for Medicare and Medicaid Services. Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Federal Register website. Accessed October 6, 2016.

More restrictive hemoglobin threshold recommended for transfusion
New guidelines on red blood cell blood transfusion recommend a restrictive threshold in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL for most patients, finding that it is safe in most clinical settings.
The updated clinical practice guidelines on transfusion thresholds and storage from the AABB (formerly known as the American Association of Blood Banks), also note that red blood cell units can be used at any time within their licensed dating period, rather than a preference being given to fresher units less than 10 days old.
The guidelines, published online Oct. 12 in JAMA, are an update of the 2012 transfusion guidelines, and are a response to a more than doubling of the number of patients since enrolled in randomized controlled trials of red blood cell transfusions.
The AABB’s clinical transfusion medicine committee, led by Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School, New Brunswick, N.J., analyzed data from 31 randomized controlled trials of 12,587 participants, which compared restrictive transfusion thresholds of 7-8 g/dL to more liberal thresholds of 9-10 g/dL.
This analysis showed that the use of restrictive transfusion protocols was associated with an absolute difference in 30-day mortality of three fewer deaths compared to the more liberal thresholds. There was no significant difference in 30-day mortality in trials that compared a threshold of 8-9 g/dL to a threshold of less than 7 g/dL (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.9185).
“For all other outcomes evaluated, there was no evidence to suggest that patients were harmed by restrictive transfusion protocols, although the quality of the evidence was low for the outcomes of congestive heart failure and rebleeding,” the authors reported.
Based on these findings, they recommended a restrictive red blood cell transfusion threshold, in which transfusion is not indicated until the hemoglobin level is 7 g/dL for hospitalized adult patients who are hemodynamically stable, including critically ill patients.
However for patients undergoing orthopedic or cardiac surgery, or those with preexisting cardiovascular disease, they advised a threshold of 8 g/dL for initiating a red blood cell transfusion.
They also stressed that these recommendations did not apply to patients with acute coronary syndrome, those with severe thrombocytopenia, those treated for hematologic or oncologic disorders who at risk of bleeding, and those with chronic transfusion–dependent anemia, citing a lack of quality randomized controlled trial evidence.
The guideline authors examined the issue of the optimal length of time that red blood cell units should be stored, pointing out that there is currently no formal guidance on the optimal period of red blood cell storage prior to transfusion.
While units of red blood cells can be stored for up to 42 days, the committee said there was some evidence that longer storage may be associated with adverse transfusion outcomes.
“The RBCs stored for longer periods have decreased ability to deliver oxygen due to decreased levels of 2,3-diphsophoglycerate, decreased nitric oxide metabolism, alterations of the RBC membrane leading to increased rigidity, and increased RBC endothelial adherence,” they wrote.
Despite this, the review of 13 randomized controlled trials examining the effect of storage duration found no evidence that fresher units had any impact on mortality compared to standard issue units, nor were there any more adverse events with the standard issue units.
The absolute difference in 30-day mortality was four more deaths per 1,000 with fresher blood, and there was a higher risk of nosocomial infections among patients who received fresher red blood cell units although the authors said the quality of evidence was low.
They therefore recommended that no preference be given to fresher red blood cell units, and that all patients be treated with units chosen at any point within their licensed dating period.
Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies, but no other conflicts of interest were declared.
The two-tiered approach of this important update to the red blood cell transfusion guidelines acknowledges the current state of the evidence and also provides support for making more individualized transfusion decisions.
These new guidelines represent medicine at its best in that they are evidence based, derived from randomized controlled trials, reflect important clinical perspectives, and are definitive for conditions in which data are substantial, but provide greater flexibility for conditions in which data are less certain.
One major limitation of these guidelines is that they are based on hemoglobin level as the transfusion trigger, when good clinical practice dictates that the decision to transfuse should also be based on clinical factors, availability of alternative therapies, and patient preferences.
Mark H. Yazer, MD and Darrell J. Triulzi, MD, are in the division of transfusion medicine at the University of Pittsburgh Medical Center. These comments are adapted from an editorial (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.10887 ). Dr Triulzi reported receiving grants from the National Heart, Lung, and Blood Institute; and receiving personal fees for serving on an advisory board for Fresenius Kabi.
The two-tiered approach of this important update to the red blood cell transfusion guidelines acknowledges the current state of the evidence and also provides support for making more individualized transfusion decisions.
These new guidelines represent medicine at its best in that they are evidence based, derived from randomized controlled trials, reflect important clinical perspectives, and are definitive for conditions in which data are substantial, but provide greater flexibility for conditions in which data are less certain.
One major limitation of these guidelines is that they are based on hemoglobin level as the transfusion trigger, when good clinical practice dictates that the decision to transfuse should also be based on clinical factors, availability of alternative therapies, and patient preferences.
Mark H. Yazer, MD and Darrell J. Triulzi, MD, are in the division of transfusion medicine at the University of Pittsburgh Medical Center. These comments are adapted from an editorial (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.10887 ). Dr Triulzi reported receiving grants from the National Heart, Lung, and Blood Institute; and receiving personal fees for serving on an advisory board for Fresenius Kabi.
The two-tiered approach of this important update to the red blood cell transfusion guidelines acknowledges the current state of the evidence and also provides support for making more individualized transfusion decisions.
These new guidelines represent medicine at its best in that they are evidence based, derived from randomized controlled trials, reflect important clinical perspectives, and are definitive for conditions in which data are substantial, but provide greater flexibility for conditions in which data are less certain.
One major limitation of these guidelines is that they are based on hemoglobin level as the transfusion trigger, when good clinical practice dictates that the decision to transfuse should also be based on clinical factors, availability of alternative therapies, and patient preferences.
Mark H. Yazer, MD and Darrell J. Triulzi, MD, are in the division of transfusion medicine at the University of Pittsburgh Medical Center. These comments are adapted from an editorial (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.10887 ). Dr Triulzi reported receiving grants from the National Heart, Lung, and Blood Institute; and receiving personal fees for serving on an advisory board for Fresenius Kabi.
New guidelines on red blood cell blood transfusion recommend a restrictive threshold in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL for most patients, finding that it is safe in most clinical settings.
The updated clinical practice guidelines on transfusion thresholds and storage from the AABB (formerly known as the American Association of Blood Banks), also note that red blood cell units can be used at any time within their licensed dating period, rather than a preference being given to fresher units less than 10 days old.
The guidelines, published online Oct. 12 in JAMA, are an update of the 2012 transfusion guidelines, and are a response to a more than doubling of the number of patients since enrolled in randomized controlled trials of red blood cell transfusions.
The AABB’s clinical transfusion medicine committee, led by Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School, New Brunswick, N.J., analyzed data from 31 randomized controlled trials of 12,587 participants, which compared restrictive transfusion thresholds of 7-8 g/dL to more liberal thresholds of 9-10 g/dL.
This analysis showed that the use of restrictive transfusion protocols was associated with an absolute difference in 30-day mortality of three fewer deaths compared to the more liberal thresholds. There was no significant difference in 30-day mortality in trials that compared a threshold of 8-9 g/dL to a threshold of less than 7 g/dL (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.9185).
“For all other outcomes evaluated, there was no evidence to suggest that patients were harmed by restrictive transfusion protocols, although the quality of the evidence was low for the outcomes of congestive heart failure and rebleeding,” the authors reported.
Based on these findings, they recommended a restrictive red blood cell transfusion threshold, in which transfusion is not indicated until the hemoglobin level is 7 g/dL for hospitalized adult patients who are hemodynamically stable, including critically ill patients.
However for patients undergoing orthopedic or cardiac surgery, or those with preexisting cardiovascular disease, they advised a threshold of 8 g/dL for initiating a red blood cell transfusion.
They also stressed that these recommendations did not apply to patients with acute coronary syndrome, those with severe thrombocytopenia, those treated for hematologic or oncologic disorders who at risk of bleeding, and those with chronic transfusion–dependent anemia, citing a lack of quality randomized controlled trial evidence.
The guideline authors examined the issue of the optimal length of time that red blood cell units should be stored, pointing out that there is currently no formal guidance on the optimal period of red blood cell storage prior to transfusion.
While units of red blood cells can be stored for up to 42 days, the committee said there was some evidence that longer storage may be associated with adverse transfusion outcomes.
“The RBCs stored for longer periods have decreased ability to deliver oxygen due to decreased levels of 2,3-diphsophoglycerate, decreased nitric oxide metabolism, alterations of the RBC membrane leading to increased rigidity, and increased RBC endothelial adherence,” they wrote.
Despite this, the review of 13 randomized controlled trials examining the effect of storage duration found no evidence that fresher units had any impact on mortality compared to standard issue units, nor were there any more adverse events with the standard issue units.
The absolute difference in 30-day mortality was four more deaths per 1,000 with fresher blood, and there was a higher risk of nosocomial infections among patients who received fresher red blood cell units although the authors said the quality of evidence was low.
They therefore recommended that no preference be given to fresher red blood cell units, and that all patients be treated with units chosen at any point within their licensed dating period.
Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies, but no other conflicts of interest were declared.
New guidelines on red blood cell blood transfusion recommend a restrictive threshold in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL for most patients, finding that it is safe in most clinical settings.
The updated clinical practice guidelines on transfusion thresholds and storage from the AABB (formerly known as the American Association of Blood Banks), also note that red blood cell units can be used at any time within their licensed dating period, rather than a preference being given to fresher units less than 10 days old.
The guidelines, published online Oct. 12 in JAMA, are an update of the 2012 transfusion guidelines, and are a response to a more than doubling of the number of patients since enrolled in randomized controlled trials of red blood cell transfusions.
The AABB’s clinical transfusion medicine committee, led by Jeffrey L. Carson, MD, of Robert Wood Johnson Medical School, New Brunswick, N.J., analyzed data from 31 randomized controlled trials of 12,587 participants, which compared restrictive transfusion thresholds of 7-8 g/dL to more liberal thresholds of 9-10 g/dL.
This analysis showed that the use of restrictive transfusion protocols was associated with an absolute difference in 30-day mortality of three fewer deaths compared to the more liberal thresholds. There was no significant difference in 30-day mortality in trials that compared a threshold of 8-9 g/dL to a threshold of less than 7 g/dL (JAMA 2016, Oct 12. doi: 10.1001/jama.2016.9185).
“For all other outcomes evaluated, there was no evidence to suggest that patients were harmed by restrictive transfusion protocols, although the quality of the evidence was low for the outcomes of congestive heart failure and rebleeding,” the authors reported.
Based on these findings, they recommended a restrictive red blood cell transfusion threshold, in which transfusion is not indicated until the hemoglobin level is 7 g/dL for hospitalized adult patients who are hemodynamically stable, including critically ill patients.
However for patients undergoing orthopedic or cardiac surgery, or those with preexisting cardiovascular disease, they advised a threshold of 8 g/dL for initiating a red blood cell transfusion.
They also stressed that these recommendations did not apply to patients with acute coronary syndrome, those with severe thrombocytopenia, those treated for hematologic or oncologic disorders who at risk of bleeding, and those with chronic transfusion–dependent anemia, citing a lack of quality randomized controlled trial evidence.
The guideline authors examined the issue of the optimal length of time that red blood cell units should be stored, pointing out that there is currently no formal guidance on the optimal period of red blood cell storage prior to transfusion.
While units of red blood cells can be stored for up to 42 days, the committee said there was some evidence that longer storage may be associated with adverse transfusion outcomes.
“The RBCs stored for longer periods have decreased ability to deliver oxygen due to decreased levels of 2,3-diphsophoglycerate, decreased nitric oxide metabolism, alterations of the RBC membrane leading to increased rigidity, and increased RBC endothelial adherence,” they wrote.
Despite this, the review of 13 randomized controlled trials examining the effect of storage duration found no evidence that fresher units had any impact on mortality compared to standard issue units, nor were there any more adverse events with the standard issue units.
The absolute difference in 30-day mortality was four more deaths per 1,000 with fresher blood, and there was a higher risk of nosocomial infections among patients who received fresher red blood cell units although the authors said the quality of evidence was low.
They therefore recommended that no preference be given to fresher red blood cell units, and that all patients be treated with units chosen at any point within their licensed dating period.
Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies, but no other conflicts of interest were declared.
FROM JAMA
Key clinical point: A restrictive threshold for red blood cell transfusion, in which transfusion is not indicated until the hemoglobin level is 7-8 g/dL, is now recommended for most patients.
Major finding: A more restrictive threshold for red blood cell transfusion is not associated with an increased risk of mortality or other adverse outcomes from transfusion.
Data source: Updated guidelines from the AABB (formerly known as the American Association of Blood Banks).
Disclosures: Guideline development was supported by AABB. Four authors declared grants, fees, stock options or consultancies from pharmaceutical companies including CSL and Fresenius Kabi, but no other conflicts of interest were declared.
Expert panel offers treatment recommendations in Waldenström macroglobulinemia
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
FROM BLOOD
Opioids, Obesity among Topics in Newly Released AAP Clinical Reports
NEW YORK (Reuters Health) - The American Academy of Pediatrics (AAP) today released six clinical reports and one policy statement covering a range of timely topics relevant to the health and care of children. Here is a snapshot.
1) Evaluation and Management of Children and Adolescents With Acute Mental Health or Behavioral Problems. Part I: Common Clinical Challenges of Patients With Mental Health and/or Behavioral Emergencies.
This report focuses on the issues relevant to children and adolescents presenting to the emergency department (ED) or primary care clinic with a mental health condition or emergency and covers the following topics: medical clearance of pediatric psychiatric patients; suicidal ideation and suicide attempts; involuntary hospitalization; restraint of the agitated patient (verbal restraint, chemical restraint and physical restraint); coordination with the medical home.
2) Evaluation and Management of Children With Acute Mental Health or Behavioral Problems. Part II: Recognition of Clinically Challenging Mental Health Related Conditions Presenting With Medical or Uncertain Symptoms.
This clinical report focuses on the challenges a pediatrician may face when evaluating patients with a mental health condition, which may be contributing to or complicating a medical or indeterminate clinical presentation. Topics include somatic symptom and related disorders; adverse effects of psychiatric medications (antipsychotic adverse effects, neuroleptic malignant syndrome, serotonin syndrome); children with special needs in the ED (autism spectrum and developmental disorders); mental health screening in the ED.
Both reports are from the AAP Committee on Pediatric Emergency Medicine and the American College of Emergency Physicians Pediatric Emergency Medicine Committee and include an executive summary.
3) Mind-Body Therapies in Children and Youth
From the AAP Section on Integrative Medicine, this report notes that a "growing body of evidence supports the effectiveness and safety of mind-body therapies in pediatrics. This clinical report outlines popular mind-body therapies for children and youth and examines the best-available evidence for a variety of mind-body therapies and practices, including biofeedback, clinical hypnosis, guided imagery, meditation, and yoga. The report is intended to help health care professionals guide their patients to nonpharmacologic approaches to improve concentration, help decrease pain, control discomfort, or ease anxiety."
4) Preventing Obesity and Eating Disorders in Adolescents
This report, from the AAP Committee on Nutrition, Committee on Adolescence, Section on Obesity, notes that "messages from pediatricians addressing obesity and reviewing constructive ways to manage weight can be safely and supportively incorporated into health care visits. Avoiding certain weight-based language and using motivational interviewing (MI) techniques may improve communication and promote successful outcomes when providing weight-management counseling. This clinical report addresses the interaction between obesity prevention and eating disorders (EDs) in teenagers, provides the pediatrician with evidence-informed tools to identify behaviors that predispose to both obesity and EDs, and provides guidance about obesity and ED prevention messages. The focus should be on a healthy lifestyle rather than on weight. Evidence suggests that obesity prevention and treatment, if conducted correctly, do not predispose to EDs."
5) Parental Presence During Treatment of Ebola or Other Highly Consequential Infection
From the AAP Committee on Infectious Diseases, this report offers "guidance to health care providers and hospitals on options to consider regarding parental presence at the bedside while caring for a child with suspected or proven Ebola virus disease (Ebola) or other highly consequential infection. Options are presented to help meet the needs of the patient and the family while also posing the least risk to providers and health care organizations."
6) Safe Sleep and Skin-to-Skin Care in the Neonatal Period for Healthy Term Newborns
This report, from the Committee on Fetus and Newborn, Task Force on Sudden Infant Death Syndrome, notes that skin-to-skin care (SSC) and rooming-in are now common in the newborn period for healthy newborns with the implementation of maternity care practices that support breastfeeding as outlined in the World Health Organization's "Ten Steps to Successful Breastfeeding." The evidence indicates that implementation of these practices "increases overall and exclusive breastfeeding, safer and healthier transitions, and improved maternal-infant bonding. In some cases, however, the practice of SSC and rooming-in may pose safety concerns, particularly with regard to sleep. This clinical report is intended for birthing centers and delivery hospitals caring for healthy newborns to assist in the establishment of appropriate SSC and safe sleep policies."
The policy statement - Medication-Assisted Treatment of Adolescents With Opioid Use Disorders - is from the Committee on Substance Use and Prevention. It notes that opioid use disorder is "a leading cause of morbidity and mortality among US youth. Effective treatments, both medications and substance use disorder counseling, are available but underused, and access to developmentally appropriate treatment is severely restricted for adolescents and young adults. Resources to disseminate available therapies and to develop new treatments specifically for this age group are needed to save and improve lives of youth with opioid addiction."
"The AAP recommends that pediatricians consider offering medication-assisted treatment to their adolescent and young adult patients with severe opioid use disorders or discuss referrals to other providers for this service," the statement advises.
The six clinical reports and one policy statement are published in the September issue of Pediatrics and were released online August 22.
SOURCE: http://bit.ly/2bfNEj8
Pediatrics 2016.
(c) Copyright Thomson Reuters 2016.
NEW YORK (Reuters Health) - The American Academy of Pediatrics (AAP) today released six clinical reports and one policy statement covering a range of timely topics relevant to the health and care of children. Here is a snapshot.
1) Evaluation and Management of Children and Adolescents With Acute Mental Health or Behavioral Problems. Part I: Common Clinical Challenges of Patients With Mental Health and/or Behavioral Emergencies.
This report focuses on the issues relevant to children and adolescents presenting to the emergency department (ED) or primary care clinic with a mental health condition or emergency and covers the following topics: medical clearance of pediatric psychiatric patients; suicidal ideation and suicide attempts; involuntary hospitalization; restraint of the agitated patient (verbal restraint, chemical restraint and physical restraint); coordination with the medical home.
2) Evaluation and Management of Children With Acute Mental Health or Behavioral Problems. Part II: Recognition of Clinically Challenging Mental Health Related Conditions Presenting With Medical or Uncertain Symptoms.
This clinical report focuses on the challenges a pediatrician may face when evaluating patients with a mental health condition, which may be contributing to or complicating a medical or indeterminate clinical presentation. Topics include somatic symptom and related disorders; adverse effects of psychiatric medications (antipsychotic adverse effects, neuroleptic malignant syndrome, serotonin syndrome); children with special needs in the ED (autism spectrum and developmental disorders); mental health screening in the ED.
Both reports are from the AAP Committee on Pediatric Emergency Medicine and the American College of Emergency Physicians Pediatric Emergency Medicine Committee and include an executive summary.
3) Mind-Body Therapies in Children and Youth
From the AAP Section on Integrative Medicine, this report notes that a "growing body of evidence supports the effectiveness and safety of mind-body therapies in pediatrics. This clinical report outlines popular mind-body therapies for children and youth and examines the best-available evidence for a variety of mind-body therapies and practices, including biofeedback, clinical hypnosis, guided imagery, meditation, and yoga. The report is intended to help health care professionals guide their patients to nonpharmacologic approaches to improve concentration, help decrease pain, control discomfort, or ease anxiety."
4) Preventing Obesity and Eating Disorders in Adolescents
This report, from the AAP Committee on Nutrition, Committee on Adolescence, Section on Obesity, notes that "messages from pediatricians addressing obesity and reviewing constructive ways to manage weight can be safely and supportively incorporated into health care visits. Avoiding certain weight-based language and using motivational interviewing (MI) techniques may improve communication and promote successful outcomes when providing weight-management counseling. This clinical report addresses the interaction between obesity prevention and eating disorders (EDs) in teenagers, provides the pediatrician with evidence-informed tools to identify behaviors that predispose to both obesity and EDs, and provides guidance about obesity and ED prevention messages. The focus should be on a healthy lifestyle rather than on weight. Evidence suggests that obesity prevention and treatment, if conducted correctly, do not predispose to EDs."
5) Parental Presence During Treatment of Ebola or Other Highly Consequential Infection
From the AAP Committee on Infectious Diseases, this report offers "guidance to health care providers and hospitals on options to consider regarding parental presence at the bedside while caring for a child with suspected or proven Ebola virus disease (Ebola) or other highly consequential infection. Options are presented to help meet the needs of the patient and the family while also posing the least risk to providers and health care organizations."
6) Safe Sleep and Skin-to-Skin Care in the Neonatal Period for Healthy Term Newborns
This report, from the Committee on Fetus and Newborn, Task Force on Sudden Infant Death Syndrome, notes that skin-to-skin care (SSC) and rooming-in are now common in the newborn period for healthy newborns with the implementation of maternity care practices that support breastfeeding as outlined in the World Health Organization's "Ten Steps to Successful Breastfeeding." The evidence indicates that implementation of these practices "increases overall and exclusive breastfeeding, safer and healthier transitions, and improved maternal-infant bonding. In some cases, however, the practice of SSC and rooming-in may pose safety concerns, particularly with regard to sleep. This clinical report is intended for birthing centers and delivery hospitals caring for healthy newborns to assist in the establishment of appropriate SSC and safe sleep policies."
The policy statement - Medication-Assisted Treatment of Adolescents With Opioid Use Disorders - is from the Committee on Substance Use and Prevention. It notes that opioid use disorder is "a leading cause of morbidity and mortality among US youth. Effective treatments, both medications and substance use disorder counseling, are available but underused, and access to developmentally appropriate treatment is severely restricted for adolescents and young adults. Resources to disseminate available therapies and to develop new treatments specifically for this age group are needed to save and improve lives of youth with opioid addiction."
"The AAP recommends that pediatricians consider offering medication-assisted treatment to their adolescent and young adult patients with severe opioid use disorders or discuss referrals to other providers for this service," the statement advises.
The six clinical reports and one policy statement are published in the September issue of Pediatrics and were released online August 22.
SOURCE: http://bit.ly/2bfNEj8
Pediatrics 2016.
(c) Copyright Thomson Reuters 2016.
NEW YORK (Reuters Health) - The American Academy of Pediatrics (AAP) today released six clinical reports and one policy statement covering a range of timely topics relevant to the health and care of children. Here is a snapshot.
1) Evaluation and Management of Children and Adolescents With Acute Mental Health or Behavioral Problems. Part I: Common Clinical Challenges of Patients With Mental Health and/or Behavioral Emergencies.
This report focuses on the issues relevant to children and adolescents presenting to the emergency department (ED) or primary care clinic with a mental health condition or emergency and covers the following topics: medical clearance of pediatric psychiatric patients; suicidal ideation and suicide attempts; involuntary hospitalization; restraint of the agitated patient (verbal restraint, chemical restraint and physical restraint); coordination with the medical home.
2) Evaluation and Management of Children With Acute Mental Health or Behavioral Problems. Part II: Recognition of Clinically Challenging Mental Health Related Conditions Presenting With Medical or Uncertain Symptoms.
This clinical report focuses on the challenges a pediatrician may face when evaluating patients with a mental health condition, which may be contributing to or complicating a medical or indeterminate clinical presentation. Topics include somatic symptom and related disorders; adverse effects of psychiatric medications (antipsychotic adverse effects, neuroleptic malignant syndrome, serotonin syndrome); children with special needs in the ED (autism spectrum and developmental disorders); mental health screening in the ED.
Both reports are from the AAP Committee on Pediatric Emergency Medicine and the American College of Emergency Physicians Pediatric Emergency Medicine Committee and include an executive summary.
3) Mind-Body Therapies in Children and Youth
From the AAP Section on Integrative Medicine, this report notes that a "growing body of evidence supports the effectiveness and safety of mind-body therapies in pediatrics. This clinical report outlines popular mind-body therapies for children and youth and examines the best-available evidence for a variety of mind-body therapies and practices, including biofeedback, clinical hypnosis, guided imagery, meditation, and yoga. The report is intended to help health care professionals guide their patients to nonpharmacologic approaches to improve concentration, help decrease pain, control discomfort, or ease anxiety."
4) Preventing Obesity and Eating Disorders in Adolescents
This report, from the AAP Committee on Nutrition, Committee on Adolescence, Section on Obesity, notes that "messages from pediatricians addressing obesity and reviewing constructive ways to manage weight can be safely and supportively incorporated into health care visits. Avoiding certain weight-based language and using motivational interviewing (MI) techniques may improve communication and promote successful outcomes when providing weight-management counseling. This clinical report addresses the interaction between obesity prevention and eating disorders (EDs) in teenagers, provides the pediatrician with evidence-informed tools to identify behaviors that predispose to both obesity and EDs, and provides guidance about obesity and ED prevention messages. The focus should be on a healthy lifestyle rather than on weight. Evidence suggests that obesity prevention and treatment, if conducted correctly, do not predispose to EDs."
5) Parental Presence During Treatment of Ebola or Other Highly Consequential Infection
From the AAP Committee on Infectious Diseases, this report offers "guidance to health care providers and hospitals on options to consider regarding parental presence at the bedside while caring for a child with suspected or proven Ebola virus disease (Ebola) or other highly consequential infection. Options are presented to help meet the needs of the patient and the family while also posing the least risk to providers and health care organizations."
6) Safe Sleep and Skin-to-Skin Care in the Neonatal Period for Healthy Term Newborns
This report, from the Committee on Fetus and Newborn, Task Force on Sudden Infant Death Syndrome, notes that skin-to-skin care (SSC) and rooming-in are now common in the newborn period for healthy newborns with the implementation of maternity care practices that support breastfeeding as outlined in the World Health Organization's "Ten Steps to Successful Breastfeeding." The evidence indicates that implementation of these practices "increases overall and exclusive breastfeeding, safer and healthier transitions, and improved maternal-infant bonding. In some cases, however, the practice of SSC and rooming-in may pose safety concerns, particularly with regard to sleep. This clinical report is intended for birthing centers and delivery hospitals caring for healthy newborns to assist in the establishment of appropriate SSC and safe sleep policies."
The policy statement - Medication-Assisted Treatment of Adolescents With Opioid Use Disorders - is from the Committee on Substance Use and Prevention. It notes that opioid use disorder is "a leading cause of morbidity and mortality among US youth. Effective treatments, both medications and substance use disorder counseling, are available but underused, and access to developmentally appropriate treatment is severely restricted for adolescents and young adults. Resources to disseminate available therapies and to develop new treatments specifically for this age group are needed to save and improve lives of youth with opioid addiction."
"The AAP recommends that pediatricians consider offering medication-assisted treatment to their adolescent and young adult patients with severe opioid use disorders or discuss referrals to other providers for this service," the statement advises.
The six clinical reports and one policy statement are published in the September issue of Pediatrics and were released online August 22.
SOURCE: http://bit.ly/2bfNEj8
Pediatrics 2016.
(c) Copyright Thomson Reuters 2016.