User login
Revering Furry Valor
National K9 Veterans Day celebrates the loyalty, bravery, and sacrifice of canine warriors. On March 13, 1942, canines officially became members of the Armed Services, with the Army’s founding of its New War Dog Program, more popularly known as the K9 Corps. The dogs underwent basic training and then entered more specialized preparation just as human soldiers did.2 There had been unofficial dogs of war who served courageously and selflessly in almost all of our armed conflicts.3 Indeed, the title of this column is taken from a wonderful article of the same name narrating the heroism of dogs in the 2 world wars.4
The dedication of canines to those who serve is not confined to combat or even active duty. Thousands of military and veteran men and women have benefited immensely from their relationship with service and emotional support dogs.
Before I continue, let me state 2 important limitations of this column. First, I am a dog person. Of course, veterans have formed healing and caring relationships with many types of companions. Equine therapy is increasingly recognized as a powerful means of helping veterans reduce distress and find purpose.5 Nevertheless, for this column, I will focus exclusively on dogs. Second, there are many worthy organizations, projects, and programs that pair veterans with therapeutic dogs inside and outside the VA. I am in no way an expert and will invariably neglect many of these positive initiatives in this brief review.
The long, proud history of canines in the military and the many moving stories of men and women in and out of uniform for whom dogs have been life changing, if not life-saving, have created 2 ethical dilemmas for the VA that I examine here. Both dilemmas pivot on the terms of official recognition of service dogs, the benefits, and who can qualify for them in the VA.
Under VA regulation and VHA policy, a service companion only can be a dog that is individually trained to do work or perform tasks to assist a person with a disability; dogs whose sole function is to provide emotional support, well-being, comfort, or companionship are not considered service pets.6
Prior to the widespread implementation of VHA Directive 1188, some VA medical centers had, pardon the pun, “gone to the dogs,” in the sense that depending on the facility, emotional support companions were found in almost every area of hospitals and clinics. Their presence enabled many patients to feel comfortable enough to seek medical and mental health care, as the canine companion gave them a sense of security and calm. But some dogs had not received the extensive training that enables a service dog to follow commands and handle the stimulation of a large, busy hospital with all its sights, sounds, and smells. Infectious disease, police, and public health authorities raised legitimate public health and safety risks about the increasing number of dogs on VA grounds who were not formally certified as service dogs. In response to those concerns, in August 2015, VHA declared a uniform policy that restricted service dogs access to VA property.7 This was, as with most health policy, a necessary, albeit utilitarian decision, that the common good outweighed that of individual veterans. Unfortunately, some veterans experienced the decision as a form of psychological rejection, and others no longer felt able mentally or physically to master the stresses of seeking health care without a canine companion.
A valid question to ask is why couldn’t the most vulnerable of these veterans, for instance those with severe mental health conditions, have service dogs that could accompany them into at least most areas of the medical center? Part of the reason is cost: Some training organizations estimate it may cost as much as $27,000 to train service dogs.8 Though there are many wonderful volunteer and not-for-profit organizations that train mostly shelter dogs and their veteran handlers—a double rescue—the lengthy process and expense means that many veterans wait years for a companion.
Congressional representatives, ethicists, veterans advocates, and canine therapy groups claim that this was unjust discrimination against those suffering with the equally, if not more disabling, mental health conditions.9 For many years, the VA has done a very good deed: For those who qualify for a service dog, VA pays for veterinary care and the equipment to handle the dog, but not boarding, grooming, food, and other miscellaneous expenses.10 But until 2016, those veterans approved for service dogs in the main had sensory or physical disabilities.
A partial breakthrough emerged when the Center for Compassionate Care Innovation launched the Mental Health Mobility Service Dogs Program that expanded veterinary health benefits to veterans with a “substantial mobility limitation.” For example, veterans whose hypervigilance and hyperarousal are so severe that they cannot attend medical appointments.11
VA experts argue that at this time there is insufficient evidence to fund service dogs as even adjunctive PTSD therapy for the hundreds of veterans who might potentially qualify. It becomes an ethical question of prudent stewardship of public funds and trust. There is certainly plenty of compelling anecdotal testimony that companion canines are a high-benefit, relatively low-risk form of complementary and integrated therapy for the spectrum of trauma disorders that afflict many of the men and women who served in our conflicts. Demonstrating those positive effects scientifically may be more difficult than it seems, although early evidence is promising, and the VA is intensively researching the question.12 For some veterans and their legislators, the VA has not gone far enough, fast enough in mainstreaming therapy dogs, they are calling for VA to expand veterans’ benefits to include mental health service dogs and to define what benefits would be covered.
National K9 Veterans Day is an important step toward giving dogs of war the homage they have earned, as are increasing efforts to ensure care for military canines throughout their life cycle. But as the seventeenth century poet John Milton wrote when he reflected on his own worth despite his blindness, “Those also serve who only stand and wait.”13 The institutions charged to care for those the battle has most burdened are still trying to discover how to properly and proportionately revere that kind of furry valor.
1. Schweitzer A. Civilization and Ethics. Naish JP, trans. London, England: A. & C. Black; 1923.
2. Bergeron AW Jr. War dogs: the birth of the K-9 Corps. https://www.army.mil/article/7463/war_dogs_the_birth_of_the_k_9_corps. Published February 14, 2008. Accessed March 22, 2019.
3. Nye L. A brief history of dogs in warfare. https://www.military.com/undertheradar/2017/03/brief-history-dogs-warfare. Published March 20, 2017. Accessed March 24, 2019.
4. Liao S. Furry valor: The tactical dogs of WW I and II. Vet Herit. 2016;39(1):24-29.
5. Romaniuk M, Evans J, Kidd C. Evaluation of an equine-assisted therapy program for veterans who identify as ‘wounded, injured, or ill’ and their partners. PLoS One. 2018;13(9):e0203943.
6. US Department of Veterans Affairs. Frequently asked questions: service animals on VA property. https://www.blogs.va.gov/VAntage/wp-content/uploads/2015/08/FAQs_RegulationsAboutAnimalsonVAProperty.pdf. Published Accessed March 24, 2019.
7. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1188: animals on Veterans Health Administration (VHA) property. https://www.boise.va.gov/docs/Service_Animal_Policy.pdf August 26, 2015.
8. Brulliard K. For military veterans suffering from PTSD, are service dogs good therapy? Washington Post. March 27, 2018.
9. Weinmeyer R. Service dogs for veterans with post-traumatic stress disorder. AMA J Ethics. 2015;17(6):547-552.
10. US Department of Veterans Affairs, Veterans Health Administration, Office of Patient Care Services. Guide and service dogs. https://www.prosthetics.va.gov/serviceandguidedogs.asp. Updated August 18, 2016. Accessed March 24, 2019.
11. US Department of Veterans Affairs. VA pilots program to expand veterinary benefits for mental health mobility service dogs. https://www.blogs.va.gov/VAntage/33379/va-pilots-program-to-expand-veterinary-health-benefit-for-mental-health-mobility-service-dogs. Published Accessed March 24, 2019.
12. Yarborough BJH, Stumbo SP, Yarborough MT, Owen-Smith A, Green CA. Benefits and challenges of using service dogs for veterans with posttraumatic stress disorder. Psychiatr Rehabil J. 2018;41(2):118-124.
National K9 Veterans Day celebrates the loyalty, bravery, and sacrifice of canine warriors. On March 13, 1942, canines officially became members of the Armed Services, with the Army’s founding of its New War Dog Program, more popularly known as the K9 Corps. The dogs underwent basic training and then entered more specialized preparation just as human soldiers did.2 There had been unofficial dogs of war who served courageously and selflessly in almost all of our armed conflicts.3 Indeed, the title of this column is taken from a wonderful article of the same name narrating the heroism of dogs in the 2 world wars.4
The dedication of canines to those who serve is not confined to combat or even active duty. Thousands of military and veteran men and women have benefited immensely from their relationship with service and emotional support dogs.
Before I continue, let me state 2 important limitations of this column. First, I am a dog person. Of course, veterans have formed healing and caring relationships with many types of companions. Equine therapy is increasingly recognized as a powerful means of helping veterans reduce distress and find purpose.5 Nevertheless, for this column, I will focus exclusively on dogs. Second, there are many worthy organizations, projects, and programs that pair veterans with therapeutic dogs inside and outside the VA. I am in no way an expert and will invariably neglect many of these positive initiatives in this brief review.
The long, proud history of canines in the military and the many moving stories of men and women in and out of uniform for whom dogs have been life changing, if not life-saving, have created 2 ethical dilemmas for the VA that I examine here. Both dilemmas pivot on the terms of official recognition of service dogs, the benefits, and who can qualify for them in the VA.
Under VA regulation and VHA policy, a service companion only can be a dog that is individually trained to do work or perform tasks to assist a person with a disability; dogs whose sole function is to provide emotional support, well-being, comfort, or companionship are not considered service pets.6
Prior to the widespread implementation of VHA Directive 1188, some VA medical centers had, pardon the pun, “gone to the dogs,” in the sense that depending on the facility, emotional support companions were found in almost every area of hospitals and clinics. Their presence enabled many patients to feel comfortable enough to seek medical and mental health care, as the canine companion gave them a sense of security and calm. But some dogs had not received the extensive training that enables a service dog to follow commands and handle the stimulation of a large, busy hospital with all its sights, sounds, and smells. Infectious disease, police, and public health authorities raised legitimate public health and safety risks about the increasing number of dogs on VA grounds who were not formally certified as service dogs. In response to those concerns, in August 2015, VHA declared a uniform policy that restricted service dogs access to VA property.7 This was, as with most health policy, a necessary, albeit utilitarian decision, that the common good outweighed that of individual veterans. Unfortunately, some veterans experienced the decision as a form of psychological rejection, and others no longer felt able mentally or physically to master the stresses of seeking health care without a canine companion.
A valid question to ask is why couldn’t the most vulnerable of these veterans, for instance those with severe mental health conditions, have service dogs that could accompany them into at least most areas of the medical center? Part of the reason is cost: Some training organizations estimate it may cost as much as $27,000 to train service dogs.8 Though there are many wonderful volunteer and not-for-profit organizations that train mostly shelter dogs and their veteran handlers—a double rescue—the lengthy process and expense means that many veterans wait years for a companion.
Congressional representatives, ethicists, veterans advocates, and canine therapy groups claim that this was unjust discrimination against those suffering with the equally, if not more disabling, mental health conditions.9 For many years, the VA has done a very good deed: For those who qualify for a service dog, VA pays for veterinary care and the equipment to handle the dog, but not boarding, grooming, food, and other miscellaneous expenses.10 But until 2016, those veterans approved for service dogs in the main had sensory or physical disabilities.
A partial breakthrough emerged when the Center for Compassionate Care Innovation launched the Mental Health Mobility Service Dogs Program that expanded veterinary health benefits to veterans with a “substantial mobility limitation.” For example, veterans whose hypervigilance and hyperarousal are so severe that they cannot attend medical appointments.11
VA experts argue that at this time there is insufficient evidence to fund service dogs as even adjunctive PTSD therapy for the hundreds of veterans who might potentially qualify. It becomes an ethical question of prudent stewardship of public funds and trust. There is certainly plenty of compelling anecdotal testimony that companion canines are a high-benefit, relatively low-risk form of complementary and integrated therapy for the spectrum of trauma disorders that afflict many of the men and women who served in our conflicts. Demonstrating those positive effects scientifically may be more difficult than it seems, although early evidence is promising, and the VA is intensively researching the question.12 For some veterans and their legislators, the VA has not gone far enough, fast enough in mainstreaming therapy dogs, they are calling for VA to expand veterans’ benefits to include mental health service dogs and to define what benefits would be covered.
National K9 Veterans Day is an important step toward giving dogs of war the homage they have earned, as are increasing efforts to ensure care for military canines throughout their life cycle. But as the seventeenth century poet John Milton wrote when he reflected on his own worth despite his blindness, “Those also serve who only stand and wait.”13 The institutions charged to care for those the battle has most burdened are still trying to discover how to properly and proportionately revere that kind of furry valor.
National K9 Veterans Day celebrates the loyalty, bravery, and sacrifice of canine warriors. On March 13, 1942, canines officially became members of the Armed Services, with the Army’s founding of its New War Dog Program, more popularly known as the K9 Corps. The dogs underwent basic training and then entered more specialized preparation just as human soldiers did.2 There had been unofficial dogs of war who served courageously and selflessly in almost all of our armed conflicts.3 Indeed, the title of this column is taken from a wonderful article of the same name narrating the heroism of dogs in the 2 world wars.4
The dedication of canines to those who serve is not confined to combat or even active duty. Thousands of military and veteran men and women have benefited immensely from their relationship with service and emotional support dogs.
Before I continue, let me state 2 important limitations of this column. First, I am a dog person. Of course, veterans have formed healing and caring relationships with many types of companions. Equine therapy is increasingly recognized as a powerful means of helping veterans reduce distress and find purpose.5 Nevertheless, for this column, I will focus exclusively on dogs. Second, there are many worthy organizations, projects, and programs that pair veterans with therapeutic dogs inside and outside the VA. I am in no way an expert and will invariably neglect many of these positive initiatives in this brief review.
The long, proud history of canines in the military and the many moving stories of men and women in and out of uniform for whom dogs have been life changing, if not life-saving, have created 2 ethical dilemmas for the VA that I examine here. Both dilemmas pivot on the terms of official recognition of service dogs, the benefits, and who can qualify for them in the VA.
Under VA regulation and VHA policy, a service companion only can be a dog that is individually trained to do work or perform tasks to assist a person with a disability; dogs whose sole function is to provide emotional support, well-being, comfort, or companionship are not considered service pets.6
Prior to the widespread implementation of VHA Directive 1188, some VA medical centers had, pardon the pun, “gone to the dogs,” in the sense that depending on the facility, emotional support companions were found in almost every area of hospitals and clinics. Their presence enabled many patients to feel comfortable enough to seek medical and mental health care, as the canine companion gave them a sense of security and calm. But some dogs had not received the extensive training that enables a service dog to follow commands and handle the stimulation of a large, busy hospital with all its sights, sounds, and smells. Infectious disease, police, and public health authorities raised legitimate public health and safety risks about the increasing number of dogs on VA grounds who were not formally certified as service dogs. In response to those concerns, in August 2015, VHA declared a uniform policy that restricted service dogs access to VA property.7 This was, as with most health policy, a necessary, albeit utilitarian decision, that the common good outweighed that of individual veterans. Unfortunately, some veterans experienced the decision as a form of psychological rejection, and others no longer felt able mentally or physically to master the stresses of seeking health care without a canine companion.
A valid question to ask is why couldn’t the most vulnerable of these veterans, for instance those with severe mental health conditions, have service dogs that could accompany them into at least most areas of the medical center? Part of the reason is cost: Some training organizations estimate it may cost as much as $27,000 to train service dogs.8 Though there are many wonderful volunteer and not-for-profit organizations that train mostly shelter dogs and their veteran handlers—a double rescue—the lengthy process and expense means that many veterans wait years for a companion.
Congressional representatives, ethicists, veterans advocates, and canine therapy groups claim that this was unjust discrimination against those suffering with the equally, if not more disabling, mental health conditions.9 For many years, the VA has done a very good deed: For those who qualify for a service dog, VA pays for veterinary care and the equipment to handle the dog, but not boarding, grooming, food, and other miscellaneous expenses.10 But until 2016, those veterans approved for service dogs in the main had sensory or physical disabilities.
A partial breakthrough emerged when the Center for Compassionate Care Innovation launched the Mental Health Mobility Service Dogs Program that expanded veterinary health benefits to veterans with a “substantial mobility limitation.” For example, veterans whose hypervigilance and hyperarousal are so severe that they cannot attend medical appointments.11
VA experts argue that at this time there is insufficient evidence to fund service dogs as even adjunctive PTSD therapy for the hundreds of veterans who might potentially qualify. It becomes an ethical question of prudent stewardship of public funds and trust. There is certainly plenty of compelling anecdotal testimony that companion canines are a high-benefit, relatively low-risk form of complementary and integrated therapy for the spectrum of trauma disorders that afflict many of the men and women who served in our conflicts. Demonstrating those positive effects scientifically may be more difficult than it seems, although early evidence is promising, and the VA is intensively researching the question.12 For some veterans and their legislators, the VA has not gone far enough, fast enough in mainstreaming therapy dogs, they are calling for VA to expand veterans’ benefits to include mental health service dogs and to define what benefits would be covered.
National K9 Veterans Day is an important step toward giving dogs of war the homage they have earned, as are increasing efforts to ensure care for military canines throughout their life cycle. But as the seventeenth century poet John Milton wrote when he reflected on his own worth despite his blindness, “Those also serve who only stand and wait.”13 The institutions charged to care for those the battle has most burdened are still trying to discover how to properly and proportionately revere that kind of furry valor.
1. Schweitzer A. Civilization and Ethics. Naish JP, trans. London, England: A. & C. Black; 1923.
2. Bergeron AW Jr. War dogs: the birth of the K-9 Corps. https://www.army.mil/article/7463/war_dogs_the_birth_of_the_k_9_corps. Published February 14, 2008. Accessed March 22, 2019.
3. Nye L. A brief history of dogs in warfare. https://www.military.com/undertheradar/2017/03/brief-history-dogs-warfare. Published March 20, 2017. Accessed March 24, 2019.
4. Liao S. Furry valor: The tactical dogs of WW I and II. Vet Herit. 2016;39(1):24-29.
5. Romaniuk M, Evans J, Kidd C. Evaluation of an equine-assisted therapy program for veterans who identify as ‘wounded, injured, or ill’ and their partners. PLoS One. 2018;13(9):e0203943.
6. US Department of Veterans Affairs. Frequently asked questions: service animals on VA property. https://www.blogs.va.gov/VAntage/wp-content/uploads/2015/08/FAQs_RegulationsAboutAnimalsonVAProperty.pdf. Published Accessed March 24, 2019.
7. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1188: animals on Veterans Health Administration (VHA) property. https://www.boise.va.gov/docs/Service_Animal_Policy.pdf August 26, 2015.
8. Brulliard K. For military veterans suffering from PTSD, are service dogs good therapy? Washington Post. March 27, 2018.
9. Weinmeyer R. Service dogs for veterans with post-traumatic stress disorder. AMA J Ethics. 2015;17(6):547-552.
10. US Department of Veterans Affairs, Veterans Health Administration, Office of Patient Care Services. Guide and service dogs. https://www.prosthetics.va.gov/serviceandguidedogs.asp. Updated August 18, 2016. Accessed March 24, 2019.
11. US Department of Veterans Affairs. VA pilots program to expand veterinary benefits for mental health mobility service dogs. https://www.blogs.va.gov/VAntage/33379/va-pilots-program-to-expand-veterinary-health-benefit-for-mental-health-mobility-service-dogs. Published Accessed March 24, 2019.
12. Yarborough BJH, Stumbo SP, Yarborough MT, Owen-Smith A, Green CA. Benefits and challenges of using service dogs for veterans with posttraumatic stress disorder. Psychiatr Rehabil J. 2018;41(2):118-124.
1. Schweitzer A. Civilization and Ethics. Naish JP, trans. London, England: A. & C. Black; 1923.
2. Bergeron AW Jr. War dogs: the birth of the K-9 Corps. https://www.army.mil/article/7463/war_dogs_the_birth_of_the_k_9_corps. Published February 14, 2008. Accessed March 22, 2019.
3. Nye L. A brief history of dogs in warfare. https://www.military.com/undertheradar/2017/03/brief-history-dogs-warfare. Published March 20, 2017. Accessed March 24, 2019.
4. Liao S. Furry valor: The tactical dogs of WW I and II. Vet Herit. 2016;39(1):24-29.
5. Romaniuk M, Evans J, Kidd C. Evaluation of an equine-assisted therapy program for veterans who identify as ‘wounded, injured, or ill’ and their partners. PLoS One. 2018;13(9):e0203943.
6. US Department of Veterans Affairs. Frequently asked questions: service animals on VA property. https://www.blogs.va.gov/VAntage/wp-content/uploads/2015/08/FAQs_RegulationsAboutAnimalsonVAProperty.pdf. Published Accessed March 24, 2019.
7. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1188: animals on Veterans Health Administration (VHA) property. https://www.boise.va.gov/docs/Service_Animal_Policy.pdf August 26, 2015.
8. Brulliard K. For military veterans suffering from PTSD, are service dogs good therapy? Washington Post. March 27, 2018.
9. Weinmeyer R. Service dogs for veterans with post-traumatic stress disorder. AMA J Ethics. 2015;17(6):547-552.
10. US Department of Veterans Affairs, Veterans Health Administration, Office of Patient Care Services. Guide and service dogs. https://www.prosthetics.va.gov/serviceandguidedogs.asp. Updated August 18, 2016. Accessed March 24, 2019.
11. US Department of Veterans Affairs. VA pilots program to expand veterinary benefits for mental health mobility service dogs. https://www.blogs.va.gov/VAntage/33379/va-pilots-program-to-expand-veterinary-health-benefit-for-mental-health-mobility-service-dogs. Published Accessed March 24, 2019.
12. Yarborough BJH, Stumbo SP, Yarborough MT, Owen-Smith A, Green CA. Benefits and challenges of using service dogs for veterans with posttraumatic stress disorder. Psychiatr Rehabil J. 2018;41(2):118-124.
NIH Program Enhances Diversity Among Researchers
The NIH has chosen 13 researchers for the inaugural class of the Distinguished Scholars Program (DSP), launched earlier this year to build diversity within the NIH Intramural Research Program. “Nurturing diversity in the NIH Intramural Research Program is paramount to upholding our mission,” said NIH Director Francis Collins, MD, PhD. Research has shown that a “diversity of perspectives” is vital to the improved quality and number of discoveries, he adds.
The DSP aims to facilitate hiring and career progression of tenure-track investigators who have demonstrated commitment to promoting diversity and inclusion in the biomedical research workforce, according to the NIH. The DSP is unique in its focus on early-stage investigators, says Hannah A. Valantine, MD, NIH Chief Officer for Scientific Workforce Diversity. She says that is the “major point where we lose underrepresented groups from scientific careers.”
Dr. Collins says the DSP can serve as a model for universities to prevent the attrition of underrepresented groups, including women, blacks, Hispanics or Latinos, American Indians and Alaska Natives, Native Hawaiians and other Pacific Islanders, individuals with disabilities, and individuals from disadvantaged backgrounds.
The pilot program will fund 3 cohorts of up to 15 scholars each. Nominees are chosen for their scientific excellence and commitment to diversity and inclusion, shown through participation in activities, such as mentoring programs.
Scholars will receive 4 years of research support of up to $2.35 million from the DSP; their nominating institute or center will continue to fund their research throughout their tenure track. Each scholar also will be mentored by a highly experienced NIH senior investigator and receive professional leadership training, workshops on management skills, and networking opportunities with NIH leadership.
Source:
NIH selects first scholars in pioneering program to enhance diversity within inhouse research program [news release]. Bethesda, MD: National Institutes of Health; October 23, 2018. https://www.nih.gov/news-events/news-releases/nih-selects-first-scholars-pioneering-program-enhance-diversity-within-house-research-program . Accessed October 31, 2018.
The NIH has chosen 13 researchers for the inaugural class of the Distinguished Scholars Program (DSP), launched earlier this year to build diversity within the NIH Intramural Research Program. “Nurturing diversity in the NIH Intramural Research Program is paramount to upholding our mission,” said NIH Director Francis Collins, MD, PhD. Research has shown that a “diversity of perspectives” is vital to the improved quality and number of discoveries, he adds.
The DSP aims to facilitate hiring and career progression of tenure-track investigators who have demonstrated commitment to promoting diversity and inclusion in the biomedical research workforce, according to the NIH. The DSP is unique in its focus on early-stage investigators, says Hannah A. Valantine, MD, NIH Chief Officer for Scientific Workforce Diversity. She says that is the “major point where we lose underrepresented groups from scientific careers.”
Dr. Collins says the DSP can serve as a model for universities to prevent the attrition of underrepresented groups, including women, blacks, Hispanics or Latinos, American Indians and Alaska Natives, Native Hawaiians and other Pacific Islanders, individuals with disabilities, and individuals from disadvantaged backgrounds.
The pilot program will fund 3 cohorts of up to 15 scholars each. Nominees are chosen for their scientific excellence and commitment to diversity and inclusion, shown through participation in activities, such as mentoring programs.
Scholars will receive 4 years of research support of up to $2.35 million from the DSP; their nominating institute or center will continue to fund their research throughout their tenure track. Each scholar also will be mentored by a highly experienced NIH senior investigator and receive professional leadership training, workshops on management skills, and networking opportunities with NIH leadership.
Source:
NIH selects first scholars in pioneering program to enhance diversity within inhouse research program [news release]. Bethesda, MD: National Institutes of Health; October 23, 2018. https://www.nih.gov/news-events/news-releases/nih-selects-first-scholars-pioneering-program-enhance-diversity-within-house-research-program . Accessed October 31, 2018.
The NIH has chosen 13 researchers for the inaugural class of the Distinguished Scholars Program (DSP), launched earlier this year to build diversity within the NIH Intramural Research Program. “Nurturing diversity in the NIH Intramural Research Program is paramount to upholding our mission,” said NIH Director Francis Collins, MD, PhD. Research has shown that a “diversity of perspectives” is vital to the improved quality and number of discoveries, he adds.
The DSP aims to facilitate hiring and career progression of tenure-track investigators who have demonstrated commitment to promoting diversity and inclusion in the biomedical research workforce, according to the NIH. The DSP is unique in its focus on early-stage investigators, says Hannah A. Valantine, MD, NIH Chief Officer for Scientific Workforce Diversity. She says that is the “major point where we lose underrepresented groups from scientific careers.”
Dr. Collins says the DSP can serve as a model for universities to prevent the attrition of underrepresented groups, including women, blacks, Hispanics or Latinos, American Indians and Alaska Natives, Native Hawaiians and other Pacific Islanders, individuals with disabilities, and individuals from disadvantaged backgrounds.
The pilot program will fund 3 cohorts of up to 15 scholars each. Nominees are chosen for their scientific excellence and commitment to diversity and inclusion, shown through participation in activities, such as mentoring programs.
Scholars will receive 4 years of research support of up to $2.35 million from the DSP; their nominating institute or center will continue to fund their research throughout their tenure track. Each scholar also will be mentored by a highly experienced NIH senior investigator and receive professional leadership training, workshops on management skills, and networking opportunities with NIH leadership.
Source:
NIH selects first scholars in pioneering program to enhance diversity within inhouse research program [news release]. Bethesda, MD: National Institutes of Health; October 23, 2018. https://www.nih.gov/news-events/news-releases/nih-selects-first-scholars-pioneering-program-enhance-diversity-within-house-research-program . Accessed October 31, 2018.
VA Reaches Milestone in Digitizing Claims Process
In a “significant modernization effort,” the VA has removed nearly 8 million paper files from 60 locations in under 22 months. The files are scanned into the electronic claims process system, which means faster claims decisions, the VA says.
According to the VA, it is a milestone in a years-long project to improve the veteran experience and streamline claims processes. The project began in 2013 when the VA began removing paper records from its regional offices to save space and money. It then expanded in 2016 when the VA launched the File Bank Extraction initiative, which removed more than 1.7 million paper claims files. In 2017, the agency began extracting 6.1 million paper records held in the Records Control Division (RCD) in St. Louis.
The records are temporarily stored in a secure facility certified by the National Archives and Records Administration, where they are inventoried, prioritized, and sent to VA vendors for scanning into the VA’s Veterans Benefits Management System.
The VA is negotiating to return the RCD’s leased warehouse space to the General Services Administration, estimating the move will save roughly $1.8 million per year.
Source:
VA achieves major milestone in effort to modernize claims processing [news release]. Washington, DC: U.S. Department of Veteran Affairs Office of Public Affairs and Media Relations; October 23,2018. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5131. Accessed October 31, 2018.
In a “significant modernization effort,” the VA has removed nearly 8 million paper files from 60 locations in under 22 months. The files are scanned into the electronic claims process system, which means faster claims decisions, the VA says.
According to the VA, it is a milestone in a years-long project to improve the veteran experience and streamline claims processes. The project began in 2013 when the VA began removing paper records from its regional offices to save space and money. It then expanded in 2016 when the VA launched the File Bank Extraction initiative, which removed more than 1.7 million paper claims files. In 2017, the agency began extracting 6.1 million paper records held in the Records Control Division (RCD) in St. Louis.
The records are temporarily stored in a secure facility certified by the National Archives and Records Administration, where they are inventoried, prioritized, and sent to VA vendors for scanning into the VA’s Veterans Benefits Management System.
The VA is negotiating to return the RCD’s leased warehouse space to the General Services Administration, estimating the move will save roughly $1.8 million per year.
Source:
VA achieves major milestone in effort to modernize claims processing [news release]. Washington, DC: U.S. Department of Veteran Affairs Office of Public Affairs and Media Relations; October 23,2018. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5131. Accessed October 31, 2018.
In a “significant modernization effort,” the VA has removed nearly 8 million paper files from 60 locations in under 22 months. The files are scanned into the electronic claims process system, which means faster claims decisions, the VA says.
According to the VA, it is a milestone in a years-long project to improve the veteran experience and streamline claims processes. The project began in 2013 when the VA began removing paper records from its regional offices to save space and money. It then expanded in 2016 when the VA launched the File Bank Extraction initiative, which removed more than 1.7 million paper claims files. In 2017, the agency began extracting 6.1 million paper records held in the Records Control Division (RCD) in St. Louis.
The records are temporarily stored in a secure facility certified by the National Archives and Records Administration, where they are inventoried, prioritized, and sent to VA vendors for scanning into the VA’s Veterans Benefits Management System.
The VA is negotiating to return the RCD’s leased warehouse space to the General Services Administration, estimating the move will save roughly $1.8 million per year.
Source:
VA achieves major milestone in effort to modernize claims processing [news release]. Washington, DC: U.S. Department of Veteran Affairs Office of Public Affairs and Media Relations; October 23,2018. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5131. Accessed October 31, 2018.
DoD and VA Sign Commitment to “Seamlessly” Sharing EHRs
Compatible electronic health record (EHR) systems at the US Department of Veterans Affairs (VA) and US Department of Defense (DoD) will ensure quality health care as service members transition to veterans, according to Defense Secretary James Mattis. The VA signed a contract with Cerner Corp last May to replace the 40-year-old Veterans Integrated System Technology Architecture (VistA) records system over the next 10 years with the new Cerner systems, which is in the pilot phase at DoD.
Mattis and VA Secretary Robert Wilkie signed a joint statement reinforcing the departments’ commitment to ensuring a successful transition from a legacy patient-data system to a modernized one. The statement represents “tangible evidence of our commitment to change how we deliver veteran-focused, provider-friendly care,” Wilkie said.
Both departments say the new EHR will be fully interoperable. Among the benefits: The collaboration will ensure that the VA understands the challenges encountered as DoD deploys Military Health System Genesis, its EHR system, the DoD says. It also will allow the VA to apply lessons learned to anticipate and mitigate known issues and assess prospective efficiencies to help deploy faster.
“The EHR will give health care providers a full picture of patient medical history, driving better clinical outcomes,” Wilkie said. “It will also help us identify veterans proactively who are at higher risk for issues, such as opioid addiction and suicide, so health care providers can intervene earlier and save lives.”
Compatible electronic health record (EHR) systems at the US Department of Veterans Affairs (VA) and US Department of Defense (DoD) will ensure quality health care as service members transition to veterans, according to Defense Secretary James Mattis. The VA signed a contract with Cerner Corp last May to replace the 40-year-old Veterans Integrated System Technology Architecture (VistA) records system over the next 10 years with the new Cerner systems, which is in the pilot phase at DoD.
Mattis and VA Secretary Robert Wilkie signed a joint statement reinforcing the departments’ commitment to ensuring a successful transition from a legacy patient-data system to a modernized one. The statement represents “tangible evidence of our commitment to change how we deliver veteran-focused, provider-friendly care,” Wilkie said.
Both departments say the new EHR will be fully interoperable. Among the benefits: The collaboration will ensure that the VA understands the challenges encountered as DoD deploys Military Health System Genesis, its EHR system, the DoD says. It also will allow the VA to apply lessons learned to anticipate and mitigate known issues and assess prospective efficiencies to help deploy faster.
“The EHR will give health care providers a full picture of patient medical history, driving better clinical outcomes,” Wilkie said. “It will also help us identify veterans proactively who are at higher risk for issues, such as opioid addiction and suicide, so health care providers can intervene earlier and save lives.”
Compatible electronic health record (EHR) systems at the US Department of Veterans Affairs (VA) and US Department of Defense (DoD) will ensure quality health care as service members transition to veterans, according to Defense Secretary James Mattis. The VA signed a contract with Cerner Corp last May to replace the 40-year-old Veterans Integrated System Technology Architecture (VistA) records system over the next 10 years with the new Cerner systems, which is in the pilot phase at DoD.
Mattis and VA Secretary Robert Wilkie signed a joint statement reinforcing the departments’ commitment to ensuring a successful transition from a legacy patient-data system to a modernized one. The statement represents “tangible evidence of our commitment to change how we deliver veteran-focused, provider-friendly care,” Wilkie said.
Both departments say the new EHR will be fully interoperable. Among the benefits: The collaboration will ensure that the VA understands the challenges encountered as DoD deploys Military Health System Genesis, its EHR system, the DoD says. It also will allow the VA to apply lessons learned to anticipate and mitigate known issues and assess prospective efficiencies to help deploy faster.
“The EHR will give health care providers a full picture of patient medical history, driving better clinical outcomes,” Wilkie said. “It will also help us identify veterans proactively who are at higher risk for issues, such as opioid addiction and suicide, so health care providers can intervene earlier and save lives.”
Breaking News: Trump Upends Federal Pay for 2019
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
VA Nursing Homes Superior to Private-Sector
Data from a VA report on its nursing homesshow that the VA’s 132 community living centers compare closely with 15,487 private-sector nursing homes even though the VA on average cares for sicker patients, with a higher proportion of conditions such as spinal cord injury, PTSD, and combat injury: 25.6% of VA nursing homes rated 5 stars (the highest rating), as did 28.7% of private-sector facilities.
The VA report notes that VA nursing homes do not refuse service to any eligible veteran. The fact that they often house residents with more complex medical needs than private-sector facilities will accept “makes achieving good quality ratings more challenging,” the VA says. VA nursing homes at times rate lower than private-sector facilities on specific metrics such as pain and type of treatment.
But the VA has a significantly lower percentage of 1-star (lowest rated) facilities. Moreover, 60 of the VA’s nursing homes improved their quality score in the past year. The report also says VA nursing homes have a higher staff-to-resident ratio than private-sector facilities, meaning residents in VA facilities get more direct attention
Data from a VA report on its nursing homesshow that the VA’s 132 community living centers compare closely with 15,487 private-sector nursing homes even though the VA on average cares for sicker patients, with a higher proportion of conditions such as spinal cord injury, PTSD, and combat injury: 25.6% of VA nursing homes rated 5 stars (the highest rating), as did 28.7% of private-sector facilities.
The VA report notes that VA nursing homes do not refuse service to any eligible veteran. The fact that they often house residents with more complex medical needs than private-sector facilities will accept “makes achieving good quality ratings more challenging,” the VA says. VA nursing homes at times rate lower than private-sector facilities on specific metrics such as pain and type of treatment.
But the VA has a significantly lower percentage of 1-star (lowest rated) facilities. Moreover, 60 of the VA’s nursing homes improved their quality score in the past year. The report also says VA nursing homes have a higher staff-to-resident ratio than private-sector facilities, meaning residents in VA facilities get more direct attention
Data from a VA report on its nursing homesshow that the VA’s 132 community living centers compare closely with 15,487 private-sector nursing homes even though the VA on average cares for sicker patients, with a higher proportion of conditions such as spinal cord injury, PTSD, and combat injury: 25.6% of VA nursing homes rated 5 stars (the highest rating), as did 28.7% of private-sector facilities.
The VA report notes that VA nursing homes do not refuse service to any eligible veteran. The fact that they often house residents with more complex medical needs than private-sector facilities will accept “makes achieving good quality ratings more challenging,” the VA says. VA nursing homes at times rate lower than private-sector facilities on specific metrics such as pain and type of treatment.
But the VA has a significantly lower percentage of 1-star (lowest rated) facilities. Moreover, 60 of the VA’s nursing homes improved their quality score in the past year. The report also says VA nursing homes have a higher staff-to-resident ratio than private-sector facilities, meaning residents in VA facilities get more direct attention
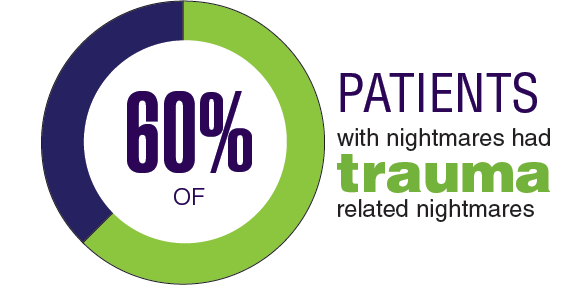
Federal Health Care Data Trends: Sleep Disorders
In 2017, the VA had more than 1 million health care visits related to sleep disorders.1 Although predominantly sleep apnea, other sleep disorders such as insomnia, hypersomnia, narcolepsy, sleep-related bruxism, nightmares, and poor sleep quality present significant health care burdens for both the VA and Military Health Systems.
Click here to continue reading.
In 2017, the VA had more than 1 million health care visits related to sleep disorders.1 Although predominantly sleep apnea, other sleep disorders such as insomnia, hypersomnia, narcolepsy, sleep-related bruxism, nightmares, and poor sleep quality present significant health care burdens for both the VA and Military Health Systems.
Click here to continue reading.
In 2017, the VA had more than 1 million health care visits related to sleep disorders.1 Although predominantly sleep apnea, other sleep disorders such as insomnia, hypersomnia, narcolepsy, sleep-related bruxism, nightmares, and poor sleep quality present significant health care burdens for both the VA and Military Health Systems.
Click here to continue reading.
VA Funds Intimate Partner Violence Programs
In the US, 36% of women and 29% of men have experienced rape, physical violence, or stalking by an intimate partner. Research suggests that veterans may be at greater risk for intimate partner violence than civilian counterparts, given the unique stressors posed by military life, such as military deployments that result in family separation, reintegration issues, and combat-related health issues, including PTSD and TBI. According to the VA’s Domestic Violence Task Force, the overall 12-month prevalence of inmate partner violence (IPV) perpetration among active duty service members was 22%, and victimization was 30%.
To help address this problem, the VA launched the IPV Assistance Program in 2014 and has since established coordinators at more than 115 facilities. The program coordinators use resources from mental health, primary care, women’s health, veterans’ justice outreach, and employee occupational health and assistance programs. The program also offers intervention through VA and community partnerships that address housing, education, and employment needs.
The program takes a holistic approach, focusing on developing a culture of safety, the VA says, with the goal of understanding, recognizing and responding to the effects of all types of trauma, including physical, sexual, and psychological. “We are giving careful attention to this program,” says Acting VA Secretary Peter O’Rourke, “ensuring it is integrated into clinical care and workplace safety.”
In the US, 36% of women and 29% of men have experienced rape, physical violence, or stalking by an intimate partner. Research suggests that veterans may be at greater risk for intimate partner violence than civilian counterparts, given the unique stressors posed by military life, such as military deployments that result in family separation, reintegration issues, and combat-related health issues, including PTSD and TBI. According to the VA’s Domestic Violence Task Force, the overall 12-month prevalence of inmate partner violence (IPV) perpetration among active duty service members was 22%, and victimization was 30%.
To help address this problem, the VA launched the IPV Assistance Program in 2014 and has since established coordinators at more than 115 facilities. The program coordinators use resources from mental health, primary care, women’s health, veterans’ justice outreach, and employee occupational health and assistance programs. The program also offers intervention through VA and community partnerships that address housing, education, and employment needs.
The program takes a holistic approach, focusing on developing a culture of safety, the VA says, with the goal of understanding, recognizing and responding to the effects of all types of trauma, including physical, sexual, and psychological. “We are giving careful attention to this program,” says Acting VA Secretary Peter O’Rourke, “ensuring it is integrated into clinical care and workplace safety.”
In the US, 36% of women and 29% of men have experienced rape, physical violence, or stalking by an intimate partner. Research suggests that veterans may be at greater risk for intimate partner violence than civilian counterparts, given the unique stressors posed by military life, such as military deployments that result in family separation, reintegration issues, and combat-related health issues, including PTSD and TBI. According to the VA’s Domestic Violence Task Force, the overall 12-month prevalence of inmate partner violence (IPV) perpetration among active duty service members was 22%, and victimization was 30%.
To help address this problem, the VA launched the IPV Assistance Program in 2014 and has since established coordinators at more than 115 facilities. The program coordinators use resources from mental health, primary care, women’s health, veterans’ justice outreach, and employee occupational health and assistance programs. The program also offers intervention through VA and community partnerships that address housing, education, and employment needs.
The program takes a holistic approach, focusing on developing a culture of safety, the VA says, with the goal of understanding, recognizing and responding to the effects of all types of trauma, including physical, sexual, and psychological. “We are giving careful attention to this program,” says Acting VA Secretary Peter O’Rourke, “ensuring it is integrated into clinical care and workplace safety.”
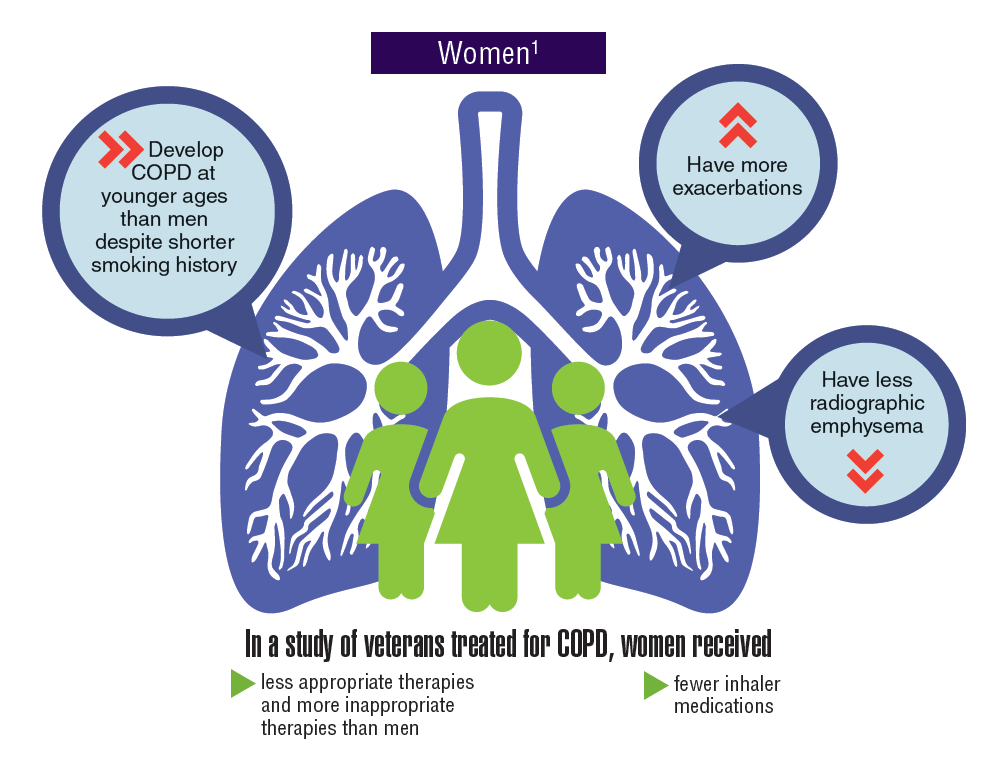
Federal Health Care Data Trends: Respiratory Disorders
Asthma and chronic obstructive pulmonary disease (COPD), which comprises a combination of chronic and slowly progressive respiratory disorders, including emphysema and chronic bronchitis, are prevalent respiratory disorders in the active-duty and veteran populations. Although chronic and manageable, asthma, COPD, and other respiratory diseases represent a significant disease burden. Women tend to develop COPD at younger ages, have more exacerbations, and yet received fewer inhaler medications and less appropriate therapies. Not only do many respiratory diseases present a risk of mortality, but evidence suggests that there is increased risk of developing lung cancer.
Click here to continue reading.
Asthma and chronic obstructive pulmonary disease (COPD), which comprises a combination of chronic and slowly progressive respiratory disorders, including emphysema and chronic bronchitis, are prevalent respiratory disorders in the active-duty and veteran populations. Although chronic and manageable, asthma, COPD, and other respiratory diseases represent a significant disease burden. Women tend to develop COPD at younger ages, have more exacerbations, and yet received fewer inhaler medications and less appropriate therapies. Not only do many respiratory diseases present a risk of mortality, but evidence suggests that there is increased risk of developing lung cancer.
Click here to continue reading.
Asthma and chronic obstructive pulmonary disease (COPD), which comprises a combination of chronic and slowly progressive respiratory disorders, including emphysema and chronic bronchitis, are prevalent respiratory disorders in the active-duty and veteran populations. Although chronic and manageable, asthma, COPD, and other respiratory diseases represent a significant disease burden. Women tend to develop COPD at younger ages, have more exacerbations, and yet received fewer inhaler medications and less appropriate therapies. Not only do many respiratory diseases present a risk of mortality, but evidence suggests that there is increased risk of developing lung cancer.
Click here to continue reading.
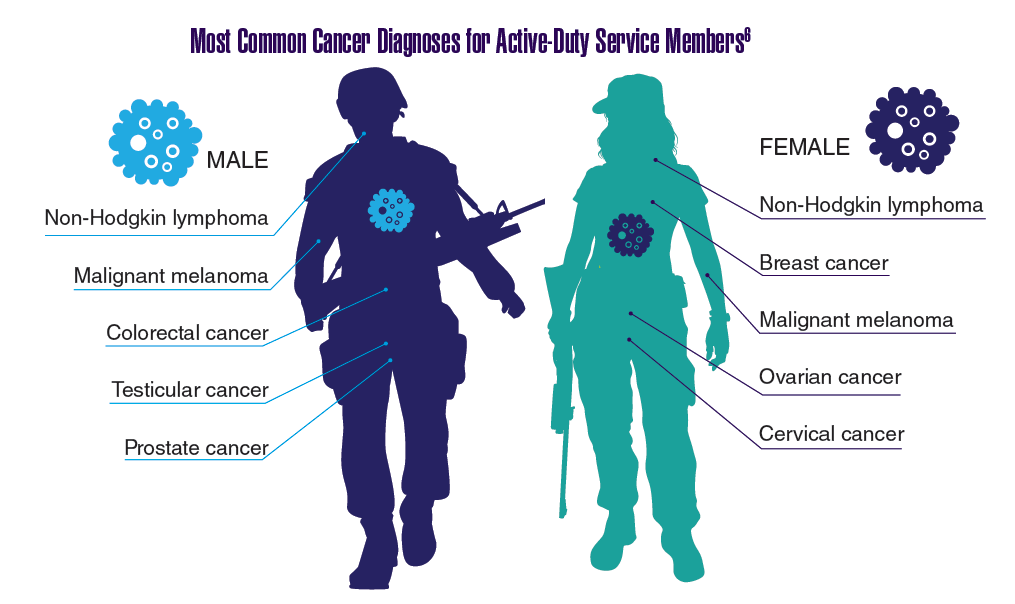
Federal Health Care Data Trends: Oncology
In 2012, a study conducted by Zullig and colleagues revealed that about 40,000 cancer cases are reported annually to the Veterans Affairs Central Cancer Registry.1 This represented about 3% of all cancer cases in the US. Within the VA patient population, the most commonly diagnosed cancers are prostate, lung and bronchial, colorectal, urinary and bladder cancers, and skin melanomas. This mirrors the commonly diagnosed cancers within the total US patient population.
Click here to continue reading.
In 2012, a study conducted by Zullig and colleagues revealed that about 40,000 cancer cases are reported annually to the Veterans Affairs Central Cancer Registry.1 This represented about 3% of all cancer cases in the US. Within the VA patient population, the most commonly diagnosed cancers are prostate, lung and bronchial, colorectal, urinary and bladder cancers, and skin melanomas. This mirrors the commonly diagnosed cancers within the total US patient population.
Click here to continue reading.
In 2012, a study conducted by Zullig and colleagues revealed that about 40,000 cancer cases are reported annually to the Veterans Affairs Central Cancer Registry.1 This represented about 3% of all cancer cases in the US. Within the VA patient population, the most commonly diagnosed cancers are prostate, lung and bronchial, colorectal, urinary and bladder cancers, and skin melanomas. This mirrors the commonly diagnosed cancers within the total US patient population.