User login
The enemy of carcinogenic fumes is my friendly begonia
Sowing the seeds of cancer prevention
Are you looking to add to your quality of life, even though pets are not your speed? Might we suggest something with lower maintenance? Something a little greener?
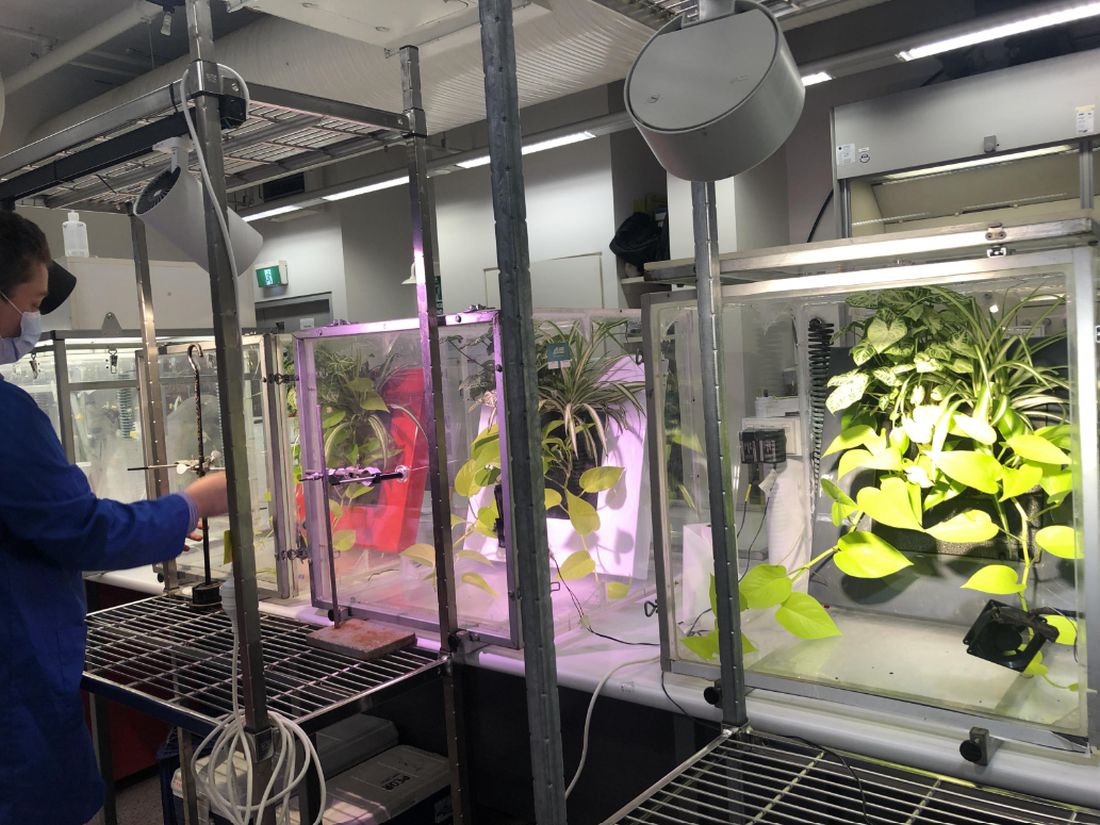
Indoor plants can purify the air that comes from outside. Researchers at the University of Technology Sydney, in partnership with the plantscaping company Ambius, showed that a “green wall” made up of mixed indoor plants was able to suck up 97% of “the most toxic compounds” from the air in just 8 hours. We’re talking about lung-irritating, headache-inducing, cancer risk–boosting compounds from gasoline fumes, including benzene.
Public health initiatives often strive to reduce cardiovascular and obesity risks, but breathing seems pretty important too. According to the World Health Organization, household air pollution is responsible for about 2.5 million global premature deaths each year. And since 2020 we’ve become accustomed to spending more time inside and at home.
“This new research proves that plants should not just be seen as ‘nice to have,’ but rather a crucial part of every workplace wellness plan,” Ambius General Manager Johan Hodgson said in statement released by the university.
So don’t spend hundreds of dollars on a fancy air filtration system when a wall of plants can do that for next to nothing. Find what works for you and your space and become a plant parent today! Your lungs will thank you.
But officer, I had to swerve to miss the duodenal ampulla
Tiny video capsule endoscopes have been around for many years, but they have one big weakness: The ingestible cameras’ journey through the GI tract is passively driven by gravity and the natural movement of the body, so they often miss potential problem areas.
Not anymore. That flaw has been addressed by medical technology company AnX Robotica, which has taken endoscopy to the next level by adding that wondrous directional control device of the modern electronic age, a joystick.
The new system “uses an external magnet and hand-held video game style joysticks to move the capsule in three dimensions,” which allows physicians to “remotely drive a miniature video capsule to all regions of the stomach to visualize and photograph potential problem areas,” according to Andrew C. Meltzer, MD, of George Washington University and associates, who conducted a pilot study funded by AnX Robotica.
The video capsule provided a 95% rate of visualization in the stomachs of 40 patients who were examined at a medical office building by an emergency medicine physician who had no previous specialty training in endoscopy. “Capsules were driven by the ER physician and then the study reports were reviewed by an attending gastroenterologist who was physically off site,” the investigators said in a written statement.
The capsule operator did receive some additional training, and development of artificial intelligence to self-drive the capsule is in the works, but for now, we’re talking about a device controlled by a human using a joystick. And we all know that 50-year-olds are not especially known for their joystick skills. For that we need real experts. Yup, we need to put those joystick-controlled capsule endoscopes in the hands of teenage gamers. Who wants to go first?
Maybe AI isn’t ready for the big time after all
“How long before some intrepid stockholder says: ‘Hey, instead of paying doctors, why don’t we just use the free robot instead?’ ” Those words appeared on LOTME but a month ago. After all, the AI is supposed to be smarter and more empathetic than a doctor. And did we mention it’s free? Or at least extremely cheap. Cheaper than, say, a group of recently unionized health care workers.
In early May, the paid employees manning the National Eating Disorders Association emergency hotline voted to unionize, as they felt overwhelmed and underpaid. Apparently, paying six people an extra few thousand a year was too much for NEDA’s leadership, as they decided a few weeks later to fire those workers, fully closing down the hotline. Instead of talking to a real person, people “calling in” for support would be met with Tessa, a wellness chatbot that would hopefully guide them through their crisis. Key word, hopefully.
In perhaps the least surprising twist of the year, NEDA was forced to walk back its decision about a week after its initial announcement. It all started with a viral Instagram post from a woman who called in and received the following advice from Tessa: Lose 1-2 pounds a week, count calories and work for a 500- to 1,000-calorie deficit, weigh herself weekly, and restrict her diet. Unfortunately, all of these suggestions were things that led to the development of the woman’s eating disorder.
Naturally, NEDA responded in good grace, accusing the woman of lying. A NEDA vice president even left some nasty comments on the post, but hastily deleted them a day later when NEDA announced it was shutting down Tessa “until further notice for a complete investigation.” NEDA’s CEO insisted they hadn’t seen that behavior from Tessa before, calling it a “bug” and insisting the bot would only be down temporarily until the triggers causing the bug were fixed.
In the aftermath, several doctors and psychologists chimed in, terming the rush to automate human roles dangerous and risky. After all, much of what makes these hotlines effective is the volunteers speaking from their own experience. An unsupervised bot doesn’t seem to have what it takes to deal with a mental health crisis, but we’re betting that Tessa will be back. As a wise cephalopod once said: Nobody gives a care about the fate of labor as long as they can get their instant gratification.
You can’t spell existential without s-t-e-n-t
This week, we’re including a special “bonus” item that, to be honest, has nothing to do with stents. That’s why our editor is making us call this a “bonus” (and making us use quote marks, too): It doesn’t really have anything to do with stents or health care or those who practice health care. Actually, his exact words were, “You can’t just give the readers someone else’s ****ing list and expect to get paid for it.” Did we mention that he looks like Jack Nicklaus but acts like BoJack Horseman?
Anywaaay, we’re pretty sure that the list in question – “America’s Top 10 Most Googled Existential Questions” – says something about the human condition, just not about stents:
1. Why is the sky blue?
2. What do dreams mean?
3. What is the meaning of life?
4. Why am I so tired?
5. Who am I?
6. What is love?
7. Is a hot dog a sandwich?
8. What came first, the chicken or the egg?
9. What should I do?
10. Do animals have souls?
Sowing the seeds of cancer prevention
Are you looking to add to your quality of life, even though pets are not your speed? Might we suggest something with lower maintenance? Something a little greener?
Indoor plants can purify the air that comes from outside. Researchers at the University of Technology Sydney, in partnership with the plantscaping company Ambius, showed that a “green wall” made up of mixed indoor plants was able to suck up 97% of “the most toxic compounds” from the air in just 8 hours. We’re talking about lung-irritating, headache-inducing, cancer risk–boosting compounds from gasoline fumes, including benzene.
Public health initiatives often strive to reduce cardiovascular and obesity risks, but breathing seems pretty important too. According to the World Health Organization, household air pollution is responsible for about 2.5 million global premature deaths each year. And since 2020 we’ve become accustomed to spending more time inside and at home.
“This new research proves that plants should not just be seen as ‘nice to have,’ but rather a crucial part of every workplace wellness plan,” Ambius General Manager Johan Hodgson said in statement released by the university.
So don’t spend hundreds of dollars on a fancy air filtration system when a wall of plants can do that for next to nothing. Find what works for you and your space and become a plant parent today! Your lungs will thank you.
But officer, I had to swerve to miss the duodenal ampulla
Tiny video capsule endoscopes have been around for many years, but they have one big weakness: The ingestible cameras’ journey through the GI tract is passively driven by gravity and the natural movement of the body, so they often miss potential problem areas.
Not anymore. That flaw has been addressed by medical technology company AnX Robotica, which has taken endoscopy to the next level by adding that wondrous directional control device of the modern electronic age, a joystick.
The new system “uses an external magnet and hand-held video game style joysticks to move the capsule in three dimensions,” which allows physicians to “remotely drive a miniature video capsule to all regions of the stomach to visualize and photograph potential problem areas,” according to Andrew C. Meltzer, MD, of George Washington University and associates, who conducted a pilot study funded by AnX Robotica.
The video capsule provided a 95% rate of visualization in the stomachs of 40 patients who were examined at a medical office building by an emergency medicine physician who had no previous specialty training in endoscopy. “Capsules were driven by the ER physician and then the study reports were reviewed by an attending gastroenterologist who was physically off site,” the investigators said in a written statement.
The capsule operator did receive some additional training, and development of artificial intelligence to self-drive the capsule is in the works, but for now, we’re talking about a device controlled by a human using a joystick. And we all know that 50-year-olds are not especially known for their joystick skills. For that we need real experts. Yup, we need to put those joystick-controlled capsule endoscopes in the hands of teenage gamers. Who wants to go first?
Maybe AI isn’t ready for the big time after all
“How long before some intrepid stockholder says: ‘Hey, instead of paying doctors, why don’t we just use the free robot instead?’ ” Those words appeared on LOTME but a month ago. After all, the AI is supposed to be smarter and more empathetic than a doctor. And did we mention it’s free? Or at least extremely cheap. Cheaper than, say, a group of recently unionized health care workers.
In early May, the paid employees manning the National Eating Disorders Association emergency hotline voted to unionize, as they felt overwhelmed and underpaid. Apparently, paying six people an extra few thousand a year was too much for NEDA’s leadership, as they decided a few weeks later to fire those workers, fully closing down the hotline. Instead of talking to a real person, people “calling in” for support would be met with Tessa, a wellness chatbot that would hopefully guide them through their crisis. Key word, hopefully.
In perhaps the least surprising twist of the year, NEDA was forced to walk back its decision about a week after its initial announcement. It all started with a viral Instagram post from a woman who called in and received the following advice from Tessa: Lose 1-2 pounds a week, count calories and work for a 500- to 1,000-calorie deficit, weigh herself weekly, and restrict her diet. Unfortunately, all of these suggestions were things that led to the development of the woman’s eating disorder.
Naturally, NEDA responded in good grace, accusing the woman of lying. A NEDA vice president even left some nasty comments on the post, but hastily deleted them a day later when NEDA announced it was shutting down Tessa “until further notice for a complete investigation.” NEDA’s CEO insisted they hadn’t seen that behavior from Tessa before, calling it a “bug” and insisting the bot would only be down temporarily until the triggers causing the bug were fixed.
In the aftermath, several doctors and psychologists chimed in, terming the rush to automate human roles dangerous and risky. After all, much of what makes these hotlines effective is the volunteers speaking from their own experience. An unsupervised bot doesn’t seem to have what it takes to deal with a mental health crisis, but we’re betting that Tessa will be back. As a wise cephalopod once said: Nobody gives a care about the fate of labor as long as they can get their instant gratification.
You can’t spell existential without s-t-e-n-t
This week, we’re including a special “bonus” item that, to be honest, has nothing to do with stents. That’s why our editor is making us call this a “bonus” (and making us use quote marks, too): It doesn’t really have anything to do with stents or health care or those who practice health care. Actually, his exact words were, “You can’t just give the readers someone else’s ****ing list and expect to get paid for it.” Did we mention that he looks like Jack Nicklaus but acts like BoJack Horseman?
Anywaaay, we’re pretty sure that the list in question – “America’s Top 10 Most Googled Existential Questions” – says something about the human condition, just not about stents:
1. Why is the sky blue?
2. What do dreams mean?
3. What is the meaning of life?
4. Why am I so tired?
5. Who am I?
6. What is love?
7. Is a hot dog a sandwich?
8. What came first, the chicken or the egg?
9. What should I do?
10. Do animals have souls?
Sowing the seeds of cancer prevention
Are you looking to add to your quality of life, even though pets are not your speed? Might we suggest something with lower maintenance? Something a little greener?
Indoor plants can purify the air that comes from outside. Researchers at the University of Technology Sydney, in partnership with the plantscaping company Ambius, showed that a “green wall” made up of mixed indoor plants was able to suck up 97% of “the most toxic compounds” from the air in just 8 hours. We’re talking about lung-irritating, headache-inducing, cancer risk–boosting compounds from gasoline fumes, including benzene.
Public health initiatives often strive to reduce cardiovascular and obesity risks, but breathing seems pretty important too. According to the World Health Organization, household air pollution is responsible for about 2.5 million global premature deaths each year. And since 2020 we’ve become accustomed to spending more time inside and at home.
“This new research proves that plants should not just be seen as ‘nice to have,’ but rather a crucial part of every workplace wellness plan,” Ambius General Manager Johan Hodgson said in statement released by the university.
So don’t spend hundreds of dollars on a fancy air filtration system when a wall of plants can do that for next to nothing. Find what works for you and your space and become a plant parent today! Your lungs will thank you.
But officer, I had to swerve to miss the duodenal ampulla
Tiny video capsule endoscopes have been around for many years, but they have one big weakness: The ingestible cameras’ journey through the GI tract is passively driven by gravity and the natural movement of the body, so they often miss potential problem areas.
Not anymore. That flaw has been addressed by medical technology company AnX Robotica, which has taken endoscopy to the next level by adding that wondrous directional control device of the modern electronic age, a joystick.
The new system “uses an external magnet and hand-held video game style joysticks to move the capsule in three dimensions,” which allows physicians to “remotely drive a miniature video capsule to all regions of the stomach to visualize and photograph potential problem areas,” according to Andrew C. Meltzer, MD, of George Washington University and associates, who conducted a pilot study funded by AnX Robotica.
The video capsule provided a 95% rate of visualization in the stomachs of 40 patients who were examined at a medical office building by an emergency medicine physician who had no previous specialty training in endoscopy. “Capsules were driven by the ER physician and then the study reports were reviewed by an attending gastroenterologist who was physically off site,” the investigators said in a written statement.
The capsule operator did receive some additional training, and development of artificial intelligence to self-drive the capsule is in the works, but for now, we’re talking about a device controlled by a human using a joystick. And we all know that 50-year-olds are not especially known for their joystick skills. For that we need real experts. Yup, we need to put those joystick-controlled capsule endoscopes in the hands of teenage gamers. Who wants to go first?
Maybe AI isn’t ready for the big time after all
“How long before some intrepid stockholder says: ‘Hey, instead of paying doctors, why don’t we just use the free robot instead?’ ” Those words appeared on LOTME but a month ago. After all, the AI is supposed to be smarter and more empathetic than a doctor. And did we mention it’s free? Or at least extremely cheap. Cheaper than, say, a group of recently unionized health care workers.
In early May, the paid employees manning the National Eating Disorders Association emergency hotline voted to unionize, as they felt overwhelmed and underpaid. Apparently, paying six people an extra few thousand a year was too much for NEDA’s leadership, as they decided a few weeks later to fire those workers, fully closing down the hotline. Instead of talking to a real person, people “calling in” for support would be met with Tessa, a wellness chatbot that would hopefully guide them through their crisis. Key word, hopefully.
In perhaps the least surprising twist of the year, NEDA was forced to walk back its decision about a week after its initial announcement. It all started with a viral Instagram post from a woman who called in and received the following advice from Tessa: Lose 1-2 pounds a week, count calories and work for a 500- to 1,000-calorie deficit, weigh herself weekly, and restrict her diet. Unfortunately, all of these suggestions were things that led to the development of the woman’s eating disorder.
Naturally, NEDA responded in good grace, accusing the woman of lying. A NEDA vice president even left some nasty comments on the post, but hastily deleted them a day later when NEDA announced it was shutting down Tessa “until further notice for a complete investigation.” NEDA’s CEO insisted they hadn’t seen that behavior from Tessa before, calling it a “bug” and insisting the bot would only be down temporarily until the triggers causing the bug were fixed.
In the aftermath, several doctors and psychologists chimed in, terming the rush to automate human roles dangerous and risky. After all, much of what makes these hotlines effective is the volunteers speaking from their own experience. An unsupervised bot doesn’t seem to have what it takes to deal with a mental health crisis, but we’re betting that Tessa will be back. As a wise cephalopod once said: Nobody gives a care about the fate of labor as long as they can get their instant gratification.
You can’t spell existential without s-t-e-n-t
This week, we’re including a special “bonus” item that, to be honest, has nothing to do with stents. That’s why our editor is making us call this a “bonus” (and making us use quote marks, too): It doesn’t really have anything to do with stents or health care or those who practice health care. Actually, his exact words were, “You can’t just give the readers someone else’s ****ing list and expect to get paid for it.” Did we mention that he looks like Jack Nicklaus but acts like BoJack Horseman?
Anywaaay, we’re pretty sure that the list in question – “America’s Top 10 Most Googled Existential Questions” – says something about the human condition, just not about stents:
1. Why is the sky blue?
2. What do dreams mean?
3. What is the meaning of life?
4. Why am I so tired?
5. Who am I?
6. What is love?
7. Is a hot dog a sandwich?
8. What came first, the chicken or the egg?
9. What should I do?
10. Do animals have souls?
Menopause and long COVID: What women should know
British researchers have noted that women at midlife who have long COVID seem to get specific, and severe, symptoms, including brain fog, fatigue, new-onset dizziness, and difficulty sleeping through the night.
Doctors also think it’s possible that long COVID worsens the symptoms of perimenopause and menopause. Lower levels of estrogen and testosterone appear to be the reason.
“A long COVID theory is that there is a temporary disruption to physiological ovarian steroid hormone production, which could [worsen] symptoms of perimenopause and menopause,” said JoAnn V. Pinkerton, MD, professor of obstetrics at the University of Virginia, Charlottesville, and executive director of the North American Menopause Society.
Long COVID symptoms and menopause symptoms can also be very hard to tell apart.
Another U.K. study cautions that because of this kind of symptom overlap, women at midlife may be misdiagnosed. Research from the North American Menopause Society shows that many women may have trouble recovering from long COVID unless their hormone deficiency is treated.
What are the symptoms of long COVID?
There are over 200 symptoms that have been associated with long COVID, according to the American Medical Association. Some common symptoms are currently defined as the following: feeling extremely tired, feeling depleted after exertion, cognitive issues such as brain fog, heart beating over 100 times a minute, and a loss of sense of smell and taste.
Long COVID symptoms begin a few weeks to a few months after a COVID infection. They can last an indefinite amount of time, but “the hope is that long COVID will not be lifelong,” said Clare Flannery, MD, an endocrinologist and associate professor in the departments of obstetrics, gynecology and reproductive sciences and internal medicine at Yale University, New Haven, Conn.
What are the symptoms of menopause?
Some symptoms of menopause include vaginal infections, irregular bleeding, urinary problems, and sexual problems.
Women in their middle years have other symptoms that can be the same as perimenopause/menopause symptoms.
“Common symptoms of perimenopause and menopause which may also be symptoms ascribed to long COVID include hot flashes, night sweats, disrupted sleep, low mood, depression or anxiety, decreased concentration, memory problems, joint and muscle pains, and headaches,” Dr. Pinkerton said.
Can long COVID actually bring on menopause?
In short: Possibly.
A new study from the Massachusetts Institute of Technology/Patient-Led Research Collaborative/University of California, San Francisco, found that long COVID can cause disruptions to a woman’s menstrual cycle, ovaries, fertility, and menopause itself.
This could be caused by chronic inflammation caused by long COVID on hormones as well. This kind of inflammatory response could explain irregularities in a woman’s menstrual cycle, according to the Newson Health Research and Education study. For instance, “when the body has inflammation, ovulation can happen,” Dr. Flannery said.
The mechanism for how long COVID could spur menopause can also involve a woman’s ovaries.
“Since the theory is that COVID affects the ovary with declines in ovarian reserve and ovarian function, it makes sense that long COVID could bring on symptoms of perimenopause or menopause more acutely or more severely and lengthen the symptoms of the perimenopause and menopausal transition,” Dr. Pinkerton said.
How can hormone replacement therapy benefit women dealing with long COVID during menopause?
Estradiol, the strongest estrogen hormone in a woman’s body, has already been shown to have a positive effect against COVID.
“Estradiol therapy treats symptoms more aggressively in the setting of long COVID,” said Dr. Flannery.
Estradiol is also a form of hormone therapy for menopause symptoms.
“Estradiol has been shown to help hot flashes, night sweats, and sleep and improve mood during perimenopause,” said Dr. Pinkerton. “So it’s likely that perimenopausal or menopausal women with long COVID would see improvements both due to the action of estradiol on the ovary seen during COVID and the improvements in symptoms.”
Estrogen-based hormone therapy has been linked to an increased risk for endometrial, breast, and ovarian cancer, according to the American Cancer Society. This means you should carefully consider how comfortable you are with those additional risks before starting this kind of therapy.
“Which of your symptoms are the most difficult to manage? You may see if you can navigate one to three of them. What are you willing to do for your symptoms? If a woman is willing to favor her sleep for the next 6 months to a year, she may be willing to change how she perceives her risk for cancer,” Dr. Flannery said. “What risk is a woman willing to take? I think if someone has a very low concern about a risk of cancer, and she’s suffering a disrupted life, then taking estradiol in a 1- to 2-year trial period could be critical to help.”
What else can help ease long COVID during menopause?
Getting the COVID vaccine, as well as getting a booster, could help. Not only will this help prevent people from being reinfected with COVID, which can worsen symptoms, but a new Swedish study says there is no evidence that it will cause postmenopausal problems like irregular bleeding.
“Weak and inconsistent associations were observed between SARS-CoV-2 vaccination and healthcare contacts for bleeding in women who are postmenopausal, and even less evidence was recorded of an association for menstrual disturbance or bleeding in women who were premenopausal,” said study coauthor Rickard Ljung, MD, PhD, MPH, professor and acting head of the pharmacoepidemiology and analysis department in the division of use and information of the Swedish Medical Products Agency in Uppsala.
A version of this article first appeared on WebMD.com.
British researchers have noted that women at midlife who have long COVID seem to get specific, and severe, symptoms, including brain fog, fatigue, new-onset dizziness, and difficulty sleeping through the night.
Doctors also think it’s possible that long COVID worsens the symptoms of perimenopause and menopause. Lower levels of estrogen and testosterone appear to be the reason.
“A long COVID theory is that there is a temporary disruption to physiological ovarian steroid hormone production, which could [worsen] symptoms of perimenopause and menopause,” said JoAnn V. Pinkerton, MD, professor of obstetrics at the University of Virginia, Charlottesville, and executive director of the North American Menopause Society.
Long COVID symptoms and menopause symptoms can also be very hard to tell apart.
Another U.K. study cautions that because of this kind of symptom overlap, women at midlife may be misdiagnosed. Research from the North American Menopause Society shows that many women may have trouble recovering from long COVID unless their hormone deficiency is treated.
What are the symptoms of long COVID?
There are over 200 symptoms that have been associated with long COVID, according to the American Medical Association. Some common symptoms are currently defined as the following: feeling extremely tired, feeling depleted after exertion, cognitive issues such as brain fog, heart beating over 100 times a minute, and a loss of sense of smell and taste.
Long COVID symptoms begin a few weeks to a few months after a COVID infection. They can last an indefinite amount of time, but “the hope is that long COVID will not be lifelong,” said Clare Flannery, MD, an endocrinologist and associate professor in the departments of obstetrics, gynecology and reproductive sciences and internal medicine at Yale University, New Haven, Conn.
What are the symptoms of menopause?
Some symptoms of menopause include vaginal infections, irregular bleeding, urinary problems, and sexual problems.
Women in their middle years have other symptoms that can be the same as perimenopause/menopause symptoms.
“Common symptoms of perimenopause and menopause which may also be symptoms ascribed to long COVID include hot flashes, night sweats, disrupted sleep, low mood, depression or anxiety, decreased concentration, memory problems, joint and muscle pains, and headaches,” Dr. Pinkerton said.
Can long COVID actually bring on menopause?
In short: Possibly.
A new study from the Massachusetts Institute of Technology/Patient-Led Research Collaborative/University of California, San Francisco, found that long COVID can cause disruptions to a woman’s menstrual cycle, ovaries, fertility, and menopause itself.
This could be caused by chronic inflammation caused by long COVID on hormones as well. This kind of inflammatory response could explain irregularities in a woman’s menstrual cycle, according to the Newson Health Research and Education study. For instance, “when the body has inflammation, ovulation can happen,” Dr. Flannery said.
The mechanism for how long COVID could spur menopause can also involve a woman’s ovaries.
“Since the theory is that COVID affects the ovary with declines in ovarian reserve and ovarian function, it makes sense that long COVID could bring on symptoms of perimenopause or menopause more acutely or more severely and lengthen the symptoms of the perimenopause and menopausal transition,” Dr. Pinkerton said.
How can hormone replacement therapy benefit women dealing with long COVID during menopause?
Estradiol, the strongest estrogen hormone in a woman’s body, has already been shown to have a positive effect against COVID.
“Estradiol therapy treats symptoms more aggressively in the setting of long COVID,” said Dr. Flannery.
Estradiol is also a form of hormone therapy for menopause symptoms.
“Estradiol has been shown to help hot flashes, night sweats, and sleep and improve mood during perimenopause,” said Dr. Pinkerton. “So it’s likely that perimenopausal or menopausal women with long COVID would see improvements both due to the action of estradiol on the ovary seen during COVID and the improvements in symptoms.”
Estrogen-based hormone therapy has been linked to an increased risk for endometrial, breast, and ovarian cancer, according to the American Cancer Society. This means you should carefully consider how comfortable you are with those additional risks before starting this kind of therapy.
“Which of your symptoms are the most difficult to manage? You may see if you can navigate one to three of them. What are you willing to do for your symptoms? If a woman is willing to favor her sleep for the next 6 months to a year, she may be willing to change how she perceives her risk for cancer,” Dr. Flannery said. “What risk is a woman willing to take? I think if someone has a very low concern about a risk of cancer, and she’s suffering a disrupted life, then taking estradiol in a 1- to 2-year trial period could be critical to help.”
What else can help ease long COVID during menopause?
Getting the COVID vaccine, as well as getting a booster, could help. Not only will this help prevent people from being reinfected with COVID, which can worsen symptoms, but a new Swedish study says there is no evidence that it will cause postmenopausal problems like irregular bleeding.
“Weak and inconsistent associations were observed between SARS-CoV-2 vaccination and healthcare contacts for bleeding in women who are postmenopausal, and even less evidence was recorded of an association for menstrual disturbance or bleeding in women who were premenopausal,” said study coauthor Rickard Ljung, MD, PhD, MPH, professor and acting head of the pharmacoepidemiology and analysis department in the division of use and information of the Swedish Medical Products Agency in Uppsala.
A version of this article first appeared on WebMD.com.
British researchers have noted that women at midlife who have long COVID seem to get specific, and severe, symptoms, including brain fog, fatigue, new-onset dizziness, and difficulty sleeping through the night.
Doctors also think it’s possible that long COVID worsens the symptoms of perimenopause and menopause. Lower levels of estrogen and testosterone appear to be the reason.
“A long COVID theory is that there is a temporary disruption to physiological ovarian steroid hormone production, which could [worsen] symptoms of perimenopause and menopause,” said JoAnn V. Pinkerton, MD, professor of obstetrics at the University of Virginia, Charlottesville, and executive director of the North American Menopause Society.
Long COVID symptoms and menopause symptoms can also be very hard to tell apart.
Another U.K. study cautions that because of this kind of symptom overlap, women at midlife may be misdiagnosed. Research from the North American Menopause Society shows that many women may have trouble recovering from long COVID unless their hormone deficiency is treated.
What are the symptoms of long COVID?
There are over 200 symptoms that have been associated with long COVID, according to the American Medical Association. Some common symptoms are currently defined as the following: feeling extremely tired, feeling depleted after exertion, cognitive issues such as brain fog, heart beating over 100 times a minute, and a loss of sense of smell and taste.
Long COVID symptoms begin a few weeks to a few months after a COVID infection. They can last an indefinite amount of time, but “the hope is that long COVID will not be lifelong,” said Clare Flannery, MD, an endocrinologist and associate professor in the departments of obstetrics, gynecology and reproductive sciences and internal medicine at Yale University, New Haven, Conn.
What are the symptoms of menopause?
Some symptoms of menopause include vaginal infections, irregular bleeding, urinary problems, and sexual problems.
Women in their middle years have other symptoms that can be the same as perimenopause/menopause symptoms.
“Common symptoms of perimenopause and menopause which may also be symptoms ascribed to long COVID include hot flashes, night sweats, disrupted sleep, low mood, depression or anxiety, decreased concentration, memory problems, joint and muscle pains, and headaches,” Dr. Pinkerton said.
Can long COVID actually bring on menopause?
In short: Possibly.
A new study from the Massachusetts Institute of Technology/Patient-Led Research Collaborative/University of California, San Francisco, found that long COVID can cause disruptions to a woman’s menstrual cycle, ovaries, fertility, and menopause itself.
This could be caused by chronic inflammation caused by long COVID on hormones as well. This kind of inflammatory response could explain irregularities in a woman’s menstrual cycle, according to the Newson Health Research and Education study. For instance, “when the body has inflammation, ovulation can happen,” Dr. Flannery said.
The mechanism for how long COVID could spur menopause can also involve a woman’s ovaries.
“Since the theory is that COVID affects the ovary with declines in ovarian reserve and ovarian function, it makes sense that long COVID could bring on symptoms of perimenopause or menopause more acutely or more severely and lengthen the symptoms of the perimenopause and menopausal transition,” Dr. Pinkerton said.
How can hormone replacement therapy benefit women dealing with long COVID during menopause?
Estradiol, the strongest estrogen hormone in a woman’s body, has already been shown to have a positive effect against COVID.
“Estradiol therapy treats symptoms more aggressively in the setting of long COVID,” said Dr. Flannery.
Estradiol is also a form of hormone therapy for menopause symptoms.
“Estradiol has been shown to help hot flashes, night sweats, and sleep and improve mood during perimenopause,” said Dr. Pinkerton. “So it’s likely that perimenopausal or menopausal women with long COVID would see improvements both due to the action of estradiol on the ovary seen during COVID and the improvements in symptoms.”
Estrogen-based hormone therapy has been linked to an increased risk for endometrial, breast, and ovarian cancer, according to the American Cancer Society. This means you should carefully consider how comfortable you are with those additional risks before starting this kind of therapy.
“Which of your symptoms are the most difficult to manage? You may see if you can navigate one to three of them. What are you willing to do for your symptoms? If a woman is willing to favor her sleep for the next 6 months to a year, she may be willing to change how she perceives her risk for cancer,” Dr. Flannery said. “What risk is a woman willing to take? I think if someone has a very low concern about a risk of cancer, and she’s suffering a disrupted life, then taking estradiol in a 1- to 2-year trial period could be critical to help.”
What else can help ease long COVID during menopause?
Getting the COVID vaccine, as well as getting a booster, could help. Not only will this help prevent people from being reinfected with COVID, which can worsen symptoms, but a new Swedish study says there is no evidence that it will cause postmenopausal problems like irregular bleeding.
“Weak and inconsistent associations were observed between SARS-CoV-2 vaccination and healthcare contacts for bleeding in women who are postmenopausal, and even less evidence was recorded of an association for menstrual disturbance or bleeding in women who were premenopausal,” said study coauthor Rickard Ljung, MD, PhD, MPH, professor and acting head of the pharmacoepidemiology and analysis department in the division of use and information of the Swedish Medical Products Agency in Uppsala.
A version of this article first appeared on WebMD.com.
Game-changing Alzheimer’s research: The latest on biomarkers
The field of neurodegenerative dementias, particularly Alzheimer’s disease (AD), has been revolutionized by the development of imaging and cerebrospinal fluid biomarkers and is on the brink of a new development: emerging plasma biomarkers. Research now recognizes the relationship between the cognitive-behavioral syndromic diagnosis (that is, the illness) and the etiologic diagnosis (the disease) – and the need to consider each separately when developing a diagnostic formulation. The National Institute on Aging and Alzheimer’s Association Research Framework uses the amyloid, tau, and neurodegeneration system to define AD biologically in living patients. Here is an overview of the framework, which requires biomarker evidence of amyloid plaques (amyloid positivity) and neurofibrillary tangles (tau positivity), with evidence of neurodegeneration (neurodegeneration positivity) to support the diagnosis.
The diagnostic approach for symptomatic patients
The differential diagnosis in symptomatic patients with mild cognitive impairment (MCI), mild behavioral impairment, or dementia is broad and includes multiple neurodegenerative diseases (for example, AD, frontotemporal lobar degeneration, dementia with Lewy bodies, argyrophilic grain disease, hippocampal sclerosis); vascular ischemic brain injury (for example, stroke); tumors; infectious, inflammatory, paraneoplastic, or demyelinating diseases; trauma; hydrocephalus; toxic/metabolic insults; and other rare diseases. The patient’s clinical syndrome narrows the differential diagnosis.
Once the clinician has a prioritized differential diagnosis of the brain disease or condition that is probably causing or contributing to the patient’s signs and symptoms, they can then select appropriate assessments and tests, typically starting with a laboratory panel and brain MRI. Strong evidence backed by practice recommendations also supports the use of fluorodeoxyglucose PET as a marker of functional brain abnormalities associated with dementia. Although molecular biomarkers are typically considered at the later stage of the clinical workup, the anticipated future availability of plasma biomarkers will probably change the timing of molecular biomarker assessment in patients with suspected cognitive impairment owing to AD.
Molecular PET biomarkers
Three PET tracers approved by the U.S. Food and Drug Administration for the detection of cerebral amyloid plaques have high sensitivity (89%-98%) and specificity (88%-100%), compared with autopsy, the gold standard diagnostic tool. However, these scans are costly and are not reimbursed by Medicare and Medicaid. Because all amyloid PET scans are covered by the Veterans Administration, this test is more readily accessible for patients receiving VA benefits.
The appropriate-use criteria developed by the Amyloid Imaging Task Force recommends amyloid PET for patients with persistent or progressive MCI or dementia. In such patients, a negative amyloid PET scan would strongly weigh against AD, supporting a differential diagnosis of other etiologies. Although a positive amyloid PET scan in patients with MCI or dementia indicates the presence of amyloid plaques, it does not necessarily confirm AD as the cause. Cerebral amyloid plaques may coexist with other pathologies and increase with age, even in cognitively normal individuals.
The IDEAS study looked at the clinical utility of amyloid PET in a real-world dementia specialist setting. In the study, dementia subspecialists documented their presumed etiologic diagnosis (and level of confidence) before and after amyloid PET. Of the 11,409 patients who completed the study, the etiologic diagnosis changed from AD to non-AD in just over 25% of cases and from non-AD to AD in 10.5%. Clinical management changed in about 60% of patients with MCI and 63.5% of patients with dementia.
In May 2020, the FDA approved flortaucipir F-18, the first diagnostic tau radiotracer for use with PET to estimate the density and distribution of aggregated tau neurofibrillary tangles in adults with cognitive impairment undergoing evaluation for AD. Regulatory approval of flortaucipir F-18 was based on findings from two clinical trials of terminally ill patients who were followed to autopsy. The studies included patients with a spectrum of clinically diagnosed dementias and those with normal cognition. The primary outcome of the studies was accurate visual interpretation of the images in detecting advanced AD tau neurofibrillary tangle pathology (Braak stage V or VI tau pathology). Sensitivity of five trained readers ranged from 68% to 86%, and specificity ranged from 63% to 100%; interrater agreement was 0.87. Tau PET is not yet reimbursed and is therefore not yet readily available in the clinical setting. Moreover, appropriate use criteria have not yet been published.
Molecular fluid biomarkers
Cerebrospinal fluid (CSF) analysis is currently the most readily available and reimbursed test to aid in diagnosing AD, with appropriate-use criteria for patients with suspected AD. CSF biomarkers for AD are useful in cognitively impaired patients when the etiologic diagnosis is equivocal, there is only an intermediate level of diagnostic confidence, or there is very high confidence in the etiologic diagnosis. Testing for CSF biomarkers is also recommended for patients at very early clinical stages (for example, early MCI) or with atypical clinical presentations.
A decreased concentration of amyloid-beta 42 in CSF is a marker of amyloid neuritic plaques in the brain. An increased concentration of total tau in CSF reflects injury to neurons, and an increased concentration of specific isoforms of hyperphosphorylated tau reflects neurofibrillary tangles. Presently, the ratios of t-tau to amyloid-beta 42, amyloid-beta 42 to amyloid-beta 40, and phosphorylated-tau 181 to amyloid-beta 42 are the best-performing markers of AD neuropathologic changes and are more accurate than assessing individual biomarkers. These CSF biomarkers of AD have been validated against autopsy, and ratio values of CSF amyloid-beta 42 have been further validated against amyloid PET, with overall sensitivity and specificity of approximately 90% and 84%, respectively.
Some of the most exciting recent advances in AD center around the measurement of these proteins and others in plasma. Appropriate-use criteria for plasma biomarkers in the evaluation of patients with cognitive impairment were published in 2022. In addition to their use in clinical trials, these criteria cautiously recommend using these biomarkers in specialized memory clinics in the diagnostic workup of patients with cognitive symptoms, along with confirmatory CSF markers or PET. Additional data are needed before plasma biomarkers of AD are used as standalone diagnostic markers or considered in the primary care setting.
We have made remarkable progress toward more precise molecular diagnosis of brain diseases underlying cognitive impairment and dementia. Ongoing efforts to evaluate the utility of these measures in clinical practice include the need to increase diversity of patients and providers. Ultimately, the tremendous progress in molecular biomarkers for the diseases causing dementia will help the field work toward our common goal of early and accurate diagnosis, better management, and hope for people living with these diseases.
Bradford C. Dickerson, MD, MMSc, is a professor, department of neurology, Harvard Medical School, and director, Frontotemporal Disorders Unit, department of neurology, at Massachusetts General Hospital, both in Boston.
A version of this article first appeared on Medscape.com.
The field of neurodegenerative dementias, particularly Alzheimer’s disease (AD), has been revolutionized by the development of imaging and cerebrospinal fluid biomarkers and is on the brink of a new development: emerging plasma biomarkers. Research now recognizes the relationship between the cognitive-behavioral syndromic diagnosis (that is, the illness) and the etiologic diagnosis (the disease) – and the need to consider each separately when developing a diagnostic formulation. The National Institute on Aging and Alzheimer’s Association Research Framework uses the amyloid, tau, and neurodegeneration system to define AD biologically in living patients. Here is an overview of the framework, which requires biomarker evidence of amyloid plaques (amyloid positivity) and neurofibrillary tangles (tau positivity), with evidence of neurodegeneration (neurodegeneration positivity) to support the diagnosis.
The diagnostic approach for symptomatic patients
The differential diagnosis in symptomatic patients with mild cognitive impairment (MCI), mild behavioral impairment, or dementia is broad and includes multiple neurodegenerative diseases (for example, AD, frontotemporal lobar degeneration, dementia with Lewy bodies, argyrophilic grain disease, hippocampal sclerosis); vascular ischemic brain injury (for example, stroke); tumors; infectious, inflammatory, paraneoplastic, or demyelinating diseases; trauma; hydrocephalus; toxic/metabolic insults; and other rare diseases. The patient’s clinical syndrome narrows the differential diagnosis.
Once the clinician has a prioritized differential diagnosis of the brain disease or condition that is probably causing or contributing to the patient’s signs and symptoms, they can then select appropriate assessments and tests, typically starting with a laboratory panel and brain MRI. Strong evidence backed by practice recommendations also supports the use of fluorodeoxyglucose PET as a marker of functional brain abnormalities associated with dementia. Although molecular biomarkers are typically considered at the later stage of the clinical workup, the anticipated future availability of plasma biomarkers will probably change the timing of molecular biomarker assessment in patients with suspected cognitive impairment owing to AD.
Molecular PET biomarkers
Three PET tracers approved by the U.S. Food and Drug Administration for the detection of cerebral amyloid plaques have high sensitivity (89%-98%) and specificity (88%-100%), compared with autopsy, the gold standard diagnostic tool. However, these scans are costly and are not reimbursed by Medicare and Medicaid. Because all amyloid PET scans are covered by the Veterans Administration, this test is more readily accessible for patients receiving VA benefits.
The appropriate-use criteria developed by the Amyloid Imaging Task Force recommends amyloid PET for patients with persistent or progressive MCI or dementia. In such patients, a negative amyloid PET scan would strongly weigh against AD, supporting a differential diagnosis of other etiologies. Although a positive amyloid PET scan in patients with MCI or dementia indicates the presence of amyloid plaques, it does not necessarily confirm AD as the cause. Cerebral amyloid plaques may coexist with other pathologies and increase with age, even in cognitively normal individuals.
The IDEAS study looked at the clinical utility of amyloid PET in a real-world dementia specialist setting. In the study, dementia subspecialists documented their presumed etiologic diagnosis (and level of confidence) before and after amyloid PET. Of the 11,409 patients who completed the study, the etiologic diagnosis changed from AD to non-AD in just over 25% of cases and from non-AD to AD in 10.5%. Clinical management changed in about 60% of patients with MCI and 63.5% of patients with dementia.
In May 2020, the FDA approved flortaucipir F-18, the first diagnostic tau radiotracer for use with PET to estimate the density and distribution of aggregated tau neurofibrillary tangles in adults with cognitive impairment undergoing evaluation for AD. Regulatory approval of flortaucipir F-18 was based on findings from two clinical trials of terminally ill patients who were followed to autopsy. The studies included patients with a spectrum of clinically diagnosed dementias and those with normal cognition. The primary outcome of the studies was accurate visual interpretation of the images in detecting advanced AD tau neurofibrillary tangle pathology (Braak stage V or VI tau pathology). Sensitivity of five trained readers ranged from 68% to 86%, and specificity ranged from 63% to 100%; interrater agreement was 0.87. Tau PET is not yet reimbursed and is therefore not yet readily available in the clinical setting. Moreover, appropriate use criteria have not yet been published.
Molecular fluid biomarkers
Cerebrospinal fluid (CSF) analysis is currently the most readily available and reimbursed test to aid in diagnosing AD, with appropriate-use criteria for patients with suspected AD. CSF biomarkers for AD are useful in cognitively impaired patients when the etiologic diagnosis is equivocal, there is only an intermediate level of diagnostic confidence, or there is very high confidence in the etiologic diagnosis. Testing for CSF biomarkers is also recommended for patients at very early clinical stages (for example, early MCI) or with atypical clinical presentations.
A decreased concentration of amyloid-beta 42 in CSF is a marker of amyloid neuritic plaques in the brain. An increased concentration of total tau in CSF reflects injury to neurons, and an increased concentration of specific isoforms of hyperphosphorylated tau reflects neurofibrillary tangles. Presently, the ratios of t-tau to amyloid-beta 42, amyloid-beta 42 to amyloid-beta 40, and phosphorylated-tau 181 to amyloid-beta 42 are the best-performing markers of AD neuropathologic changes and are more accurate than assessing individual biomarkers. These CSF biomarkers of AD have been validated against autopsy, and ratio values of CSF amyloid-beta 42 have been further validated against amyloid PET, with overall sensitivity and specificity of approximately 90% and 84%, respectively.
Some of the most exciting recent advances in AD center around the measurement of these proteins and others in plasma. Appropriate-use criteria for plasma biomarkers in the evaluation of patients with cognitive impairment were published in 2022. In addition to their use in clinical trials, these criteria cautiously recommend using these biomarkers in specialized memory clinics in the diagnostic workup of patients with cognitive symptoms, along with confirmatory CSF markers or PET. Additional data are needed before plasma biomarkers of AD are used as standalone diagnostic markers or considered in the primary care setting.
We have made remarkable progress toward more precise molecular diagnosis of brain diseases underlying cognitive impairment and dementia. Ongoing efforts to evaluate the utility of these measures in clinical practice include the need to increase diversity of patients and providers. Ultimately, the tremendous progress in molecular biomarkers for the diseases causing dementia will help the field work toward our common goal of early and accurate diagnosis, better management, and hope for people living with these diseases.
Bradford C. Dickerson, MD, MMSc, is a professor, department of neurology, Harvard Medical School, and director, Frontotemporal Disorders Unit, department of neurology, at Massachusetts General Hospital, both in Boston.
A version of this article first appeared on Medscape.com.
The field of neurodegenerative dementias, particularly Alzheimer’s disease (AD), has been revolutionized by the development of imaging and cerebrospinal fluid biomarkers and is on the brink of a new development: emerging plasma biomarkers. Research now recognizes the relationship between the cognitive-behavioral syndromic diagnosis (that is, the illness) and the etiologic diagnosis (the disease) – and the need to consider each separately when developing a diagnostic formulation. The National Institute on Aging and Alzheimer’s Association Research Framework uses the amyloid, tau, and neurodegeneration system to define AD biologically in living patients. Here is an overview of the framework, which requires biomarker evidence of amyloid plaques (amyloid positivity) and neurofibrillary tangles (tau positivity), with evidence of neurodegeneration (neurodegeneration positivity) to support the diagnosis.
The diagnostic approach for symptomatic patients
The differential diagnosis in symptomatic patients with mild cognitive impairment (MCI), mild behavioral impairment, or dementia is broad and includes multiple neurodegenerative diseases (for example, AD, frontotemporal lobar degeneration, dementia with Lewy bodies, argyrophilic grain disease, hippocampal sclerosis); vascular ischemic brain injury (for example, stroke); tumors; infectious, inflammatory, paraneoplastic, or demyelinating diseases; trauma; hydrocephalus; toxic/metabolic insults; and other rare diseases. The patient’s clinical syndrome narrows the differential diagnosis.
Once the clinician has a prioritized differential diagnosis of the brain disease or condition that is probably causing or contributing to the patient’s signs and symptoms, they can then select appropriate assessments and tests, typically starting with a laboratory panel and brain MRI. Strong evidence backed by practice recommendations also supports the use of fluorodeoxyglucose PET as a marker of functional brain abnormalities associated with dementia. Although molecular biomarkers are typically considered at the later stage of the clinical workup, the anticipated future availability of plasma biomarkers will probably change the timing of molecular biomarker assessment in patients with suspected cognitive impairment owing to AD.
Molecular PET biomarkers
Three PET tracers approved by the U.S. Food and Drug Administration for the detection of cerebral amyloid plaques have high sensitivity (89%-98%) and specificity (88%-100%), compared with autopsy, the gold standard diagnostic tool. However, these scans are costly and are not reimbursed by Medicare and Medicaid. Because all amyloid PET scans are covered by the Veterans Administration, this test is more readily accessible for patients receiving VA benefits.
The appropriate-use criteria developed by the Amyloid Imaging Task Force recommends amyloid PET for patients with persistent or progressive MCI or dementia. In such patients, a negative amyloid PET scan would strongly weigh against AD, supporting a differential diagnosis of other etiologies. Although a positive amyloid PET scan in patients with MCI or dementia indicates the presence of amyloid plaques, it does not necessarily confirm AD as the cause. Cerebral amyloid plaques may coexist with other pathologies and increase with age, even in cognitively normal individuals.
The IDEAS study looked at the clinical utility of amyloid PET in a real-world dementia specialist setting. In the study, dementia subspecialists documented their presumed etiologic diagnosis (and level of confidence) before and after amyloid PET. Of the 11,409 patients who completed the study, the etiologic diagnosis changed from AD to non-AD in just over 25% of cases and from non-AD to AD in 10.5%. Clinical management changed in about 60% of patients with MCI and 63.5% of patients with dementia.
In May 2020, the FDA approved flortaucipir F-18, the first diagnostic tau radiotracer for use with PET to estimate the density and distribution of aggregated tau neurofibrillary tangles in adults with cognitive impairment undergoing evaluation for AD. Regulatory approval of flortaucipir F-18 was based on findings from two clinical trials of terminally ill patients who were followed to autopsy. The studies included patients with a spectrum of clinically diagnosed dementias and those with normal cognition. The primary outcome of the studies was accurate visual interpretation of the images in detecting advanced AD tau neurofibrillary tangle pathology (Braak stage V or VI tau pathology). Sensitivity of five trained readers ranged from 68% to 86%, and specificity ranged from 63% to 100%; interrater agreement was 0.87. Tau PET is not yet reimbursed and is therefore not yet readily available in the clinical setting. Moreover, appropriate use criteria have not yet been published.
Molecular fluid biomarkers
Cerebrospinal fluid (CSF) analysis is currently the most readily available and reimbursed test to aid in diagnosing AD, with appropriate-use criteria for patients with suspected AD. CSF biomarkers for AD are useful in cognitively impaired patients when the etiologic diagnosis is equivocal, there is only an intermediate level of diagnostic confidence, or there is very high confidence in the etiologic diagnosis. Testing for CSF biomarkers is also recommended for patients at very early clinical stages (for example, early MCI) or with atypical clinical presentations.
A decreased concentration of amyloid-beta 42 in CSF is a marker of amyloid neuritic plaques in the brain. An increased concentration of total tau in CSF reflects injury to neurons, and an increased concentration of specific isoforms of hyperphosphorylated tau reflects neurofibrillary tangles. Presently, the ratios of t-tau to amyloid-beta 42, amyloid-beta 42 to amyloid-beta 40, and phosphorylated-tau 181 to amyloid-beta 42 are the best-performing markers of AD neuropathologic changes and are more accurate than assessing individual biomarkers. These CSF biomarkers of AD have been validated against autopsy, and ratio values of CSF amyloid-beta 42 have been further validated against amyloid PET, with overall sensitivity and specificity of approximately 90% and 84%, respectively.
Some of the most exciting recent advances in AD center around the measurement of these proteins and others in plasma. Appropriate-use criteria for plasma biomarkers in the evaluation of patients with cognitive impairment were published in 2022. In addition to their use in clinical trials, these criteria cautiously recommend using these biomarkers in specialized memory clinics in the diagnostic workup of patients with cognitive symptoms, along with confirmatory CSF markers or PET. Additional data are needed before plasma biomarkers of AD are used as standalone diagnostic markers or considered in the primary care setting.
We have made remarkable progress toward more precise molecular diagnosis of brain diseases underlying cognitive impairment and dementia. Ongoing efforts to evaluate the utility of these measures in clinical practice include the need to increase diversity of patients and providers. Ultimately, the tremendous progress in molecular biomarkers for the diseases causing dementia will help the field work toward our common goal of early and accurate diagnosis, better management, and hope for people living with these diseases.
Bradford C. Dickerson, MD, MMSc, is a professor, department of neurology, Harvard Medical School, and director, Frontotemporal Disorders Unit, department of neurology, at Massachusetts General Hospital, both in Boston.
A version of this article first appeared on Medscape.com.
Unlocking the riddle of REM sleep
Eugene Aserinsky, PhD, never wanted to study sleep. He tried being a social worker, a dental student, and even did a stint in the army as an explosives handler. He enrolled at the University of Chicago to pursue organ physiology, but all potential supervisors were too busy to take him on. His only choice was Nathaniel Kleitman, PhD, a middle-aged professor whom Dr. Aserinsky described as “always serious.” Dr. Kleitman was doing research on sleep and so, grudgingly, Dr. Aserinsky had followed suit.
Two years later, in 1953, the duo published a paper that shattered the way we saw sleep. They described a weird phenomenon Dr. Aserinsky later called REM sleep: periods of rapid eye movements paired with wakefulness-like activity in the brain. “We are still at the very beginning of understanding this phenomenon,” Mark Blumberg, PhD, professor of psychological and brain sciences at University of Iowa, Iowa City, said in an interview.
Before Dr. Aserinsky had walked into Dr. Kleitman’s lab, the widespread belief held that sleep was “the antithesis of wakefulness,” as Dr. Kleitman wrote in his seminal 1939 book, “Sleep and Wakefulness.” Others saw it as a kind of a coma, a passive state. Another theory, developed in the early 20th century by French psychologist Henri Piéron, PhD, held that sleepiness is caused by an accumulation of ‘hypnotoxins’ in the brain.
In his 1913 study that would likely fail a contemporary ethics review, Dr. Piéron drew fluid from the brains of sleep-deprived dogs and injected it into other dogs to induce sleep. As he explained in an interview with The Washington Times in 1933, he said he believed that fatigue toxins accumulate in the brain throughout the wakeful hours, then slowly seep into the spinal column, promoting drowsiness. Once we fall asleep, Dr. Piéron claimed, the hypnotoxins burn away.
From blinking to rapid eye movement
In 1925 when Dr. Kleitman established the world’s first sleep laboratory at the University of Chicago, sleep was a fringe science that most researchers avoided with a wide berth. Yet Dr. Kleitman was obsessed. The Moldova-born scientist famously worked 24/7 – literally. He not only stayed long hours in his lab, but also slept attached to a plethora of instruments to measure his brain waves, breathing, and heartbeat. At one point, Dr. Kleitman stayed awake for 180 hours (more than a week), to check how forced sleeplessness would affect his body (he later compared it to torture). He also lived 2 weeks aboard a submarine, moved his family north of the Arctic Circle, and spent over a month 119 feet below the surface in a cave in Kentucky, fighting rats, cold, and humidity to study circadian rhythms.
Dr. Kleitman was intrigued by an article in Nature in which the author asserted that he could detect the approach of slumber in train passengers by observing their blink frequencies. He instructed Dr. Aserinsky to observe sleeping infants (being monitored for a different study), to see how their blinking related to sleep. Yet Dr. Aserinsky was not amused. The project, he later wrote, “seemed about as exciting as warm milk.”
Dr. Aserinsky was uncertain whether eyelid movement with the eyes closed constituted a blink, then he noticed a 20-minute span in each hour when eye movement ceased entirely. Still short of getting his degree, Dr. Aserinsky decided to observe sleeping adults. He hauled a dusty clanker of a brain-wave machine out of the university’s basement, and started registering the electrical activity of the brain of his dozing subjects. Soon, he noticed something weird.
As he kept staring at the sleeping adults, he noticed that at times they’d have saccadic-like eye movements, just as the EEG machine would register a wake-like state of the brain. At first, he thought the machine was broken (it was ancient, after all). Then, that the subjects were awake and just keeping their eyes shut. Yet after conducting several sessions and tinkering with the EEG machine, Dr. Aserinsky finally concluded that the recordings and observations were correct: Something was indeed happening during sleep that kept the cortex activated and made the subjects’ eyes move in a jerky manner.
Dreams, memory, and thermoregulation
After studying dozens of subjects, including his son and Dr. Kleitman’s daughter, and using miles of polygraph paper, the two scientists published their findings in September 1953 in the journal Science. Dr. Kleitman didn’t expect the discovery to be particularly earth-shattering. When asked in a later interview how much research and excitement he thought the paper would generate, he replied: “none whatsoever.” That’s not how things went, though. “They completely changed the way people think,” Dr. Blumberg said. Once and for all, the REM discovery put to rest the idea that sleep was a passive state where nothing interesting happens.
Dr. Aserinsky soon left the University of Chicago, while Dr. Kleitman continued research on rapid eye movements in sleep with his new student, William Dement, MD. Together, they published studies suggesting that REM periods were when dreaming occurred – they reported that people who were awakened during REM sleep were far more likely to recall dreams than were those awakened outside of that period. “REM sleep = dreams” became established dogma for decades, even though first reports of dreams during non-REM sleep came as early as Dr. Kleitman’s and Dr. Dement’s original research (they assumed these were recollections from the preceding REM episodes).
“It turns out that you can have a perfectly good dream when you haven’t had a previous REM sleep period,” said Jerome Siegel, PhD, professor of psychiatry and biobehavioral sciences at UCLA’s Center for Sleep Research, pointing out that equating REM sleep with dreams is still “a common misconception.”
By the 1960s, REM sleep seemed to be well defined as the combination of rapid eye movement with EEG showing brain activation, first noted by Dr. Aserinsky, as well as muscle atonia – a state of near-total muscle relaxation or paralysis. Today, however, Dr. Blumberg said, things are considerably less clear cut. In one recent paper, Dr. Blumberg and his colleagues went as far as to question whether REM sleep is even “a thing.” REM sleep is prevalent across terrestrial vertebrates, but they found that it is also highly nuanced, messing up old definitions.
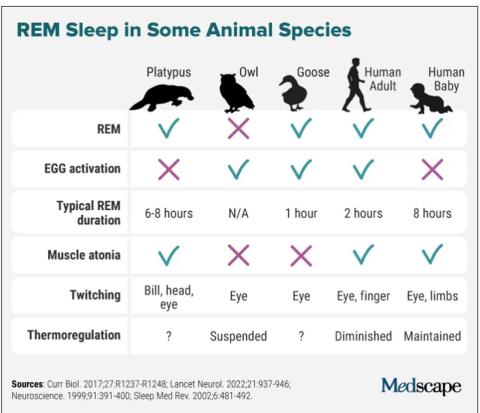
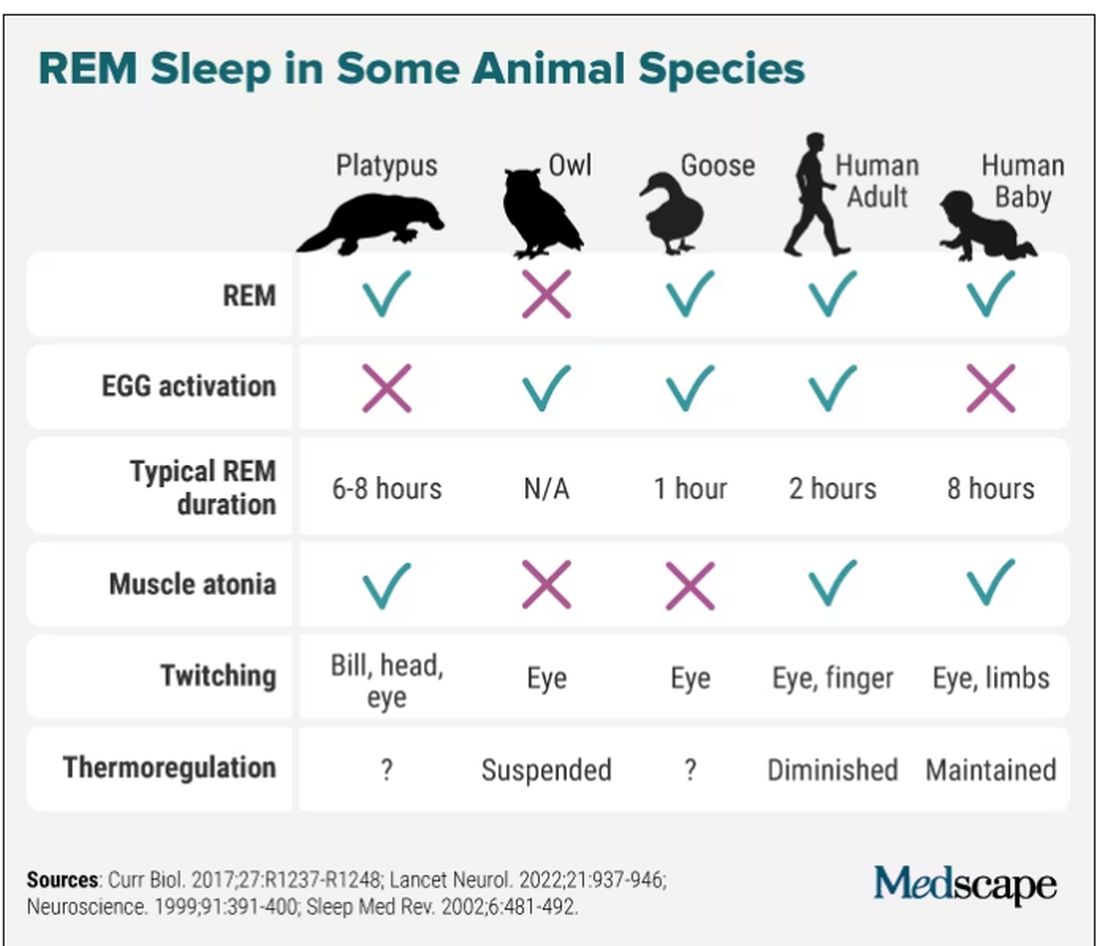
Take the platypus, for example, the animal with the most REM sleep (as far as we know): They have rapid eye movements and their bills twitch during REM (stillness punctuated by sudden twitches is typical of that period of sleep), but they don’t have the classic brain activation on EEG. Owls have EEG activation and twitching, but no rapid eye movements, since their eyes are largely immobile. Geese, meanwhile, are missing muscle atonia – that’s why they can sleep standing. And new studies are still coming in, showing, for instance, that even jumping spiders may have REM sleep, complete with jerky eye movements and limb twitching.
For Dr. Siegel, the findings on REM sleep in animals point to the potential explanation of what that bizarre stage of sleep may be all about: thermoregulation. “When you look at differences in sleep among the groups of warm-blooded animals, the correlation is almost perfect, and inverse. The colder they are, the more REM sleep they get,” Dr. Siegel said. During REM sleep, body thermoregulation is basically suspended, and so, as Dr. Siegel argued in The Lancet Neurology last fall, REM sleep could be a vital player in managing our brain’s temperature and metabolic activity during sleep.
Wallace B. Mendelson, MD, professor emeritus of psychiatry at the University of Chicago, said it’s likely, however, that REM sleep has more than one function. “There is no reason why one single theory has to be an answer. Most important physiological functions have multiple functions,” he said. The ideas are many, including that REM sleep helps consolidate our memories and plays an important role in emotion regulation But it’s not that simple. A Swiss study of nearly 1,000 healthy participants did not show any correlation between sleep stage and memory consolidation. Sleep disruption of any stage can prevent memory consolidation and quiet wakefulness with closed eyes can be as effective as sleep for memory recall.
In 1971, researchers from the National Institute of Mental Health published results of their study on total suppression of REM sleep. For as long as 40 days, they administered the monoamine oxidase inhibitor (MAOI) phenelzine, a type of drug that can completely eliminate REM sleep, to six patients with anxiety and depression. They showed that suppression of REM sleep could improve symptoms of depression, seemingly without impairing the patients’ cognitive function. Modern antidepressants, too, can greatly diminish REM sleep, Dr. Siegel said. “I’m not aware that there is any dramatic downside in having REM sleep reduced,” he said.
So do we even need REM sleep for optimal performance? Dr. Siegel said that there is a lot of exaggeration about how great REM sleep is for our health. “People just indulge their imaginations,” he said.
Dr. Blumberg pointed out that, in general, as long as you get enough sleep in the first place, you will get enough REM. “You can’t control the amount of REM sleep you have,” he explained.
REM sleep behavior disorder
Even though we may not need REM sleep to function well, REM sleep behavior disorder (RBD) is a sign that our health may be in trouble. In 1986, scientists from the University of Minnesota reported a bizarre REM sleep pathology in four men and one woman who would act out their dreams. One 67-year-old man, for example, reportedly punched and kicked his wife at night for years. One time he found himself kneeling alongside the bed with his arms extended as if he were holding a rifle (he dreamt he was in a shootout). His overall health, however, seemed unaffected apart from self-injury during some episodes.
However, in 1996 the same group of researchers reported that 11 of 29 men originally diagnosed with RBD went on to develop a parkinsonian disorder. Combined data from 24 centers of the International RBD Study Group puts that number as high as 74% at 12-year follow-up. These patients get diagnosed with Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy. Scientists believe that the protein alpha-synuclein forms toxic clumps in the brain, which are responsible both for malfunctioning of muscle atonia during REM sleep and subsequent neurodegenerative disorders.
While some researchers say that RBD may offer a unique window into better understanding REM sleep, we’re still a long way off from fully figuring out this biological phenomenon. According to Dr. Blumberg, the story of REM sleep has arguably become more muddled in the 7 decades since Dr. Aserinsky and Dr. Kleitman published their original findings, dispelling myths about ‘fatigue toxins’ and sleep as a passive, coma-like state. Dr. Mendelson concurred: “It truly remains a mystery.”
Dr. Blumberg, Dr. Mendelson, and Dr. Siegel reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Eugene Aserinsky, PhD, never wanted to study sleep. He tried being a social worker, a dental student, and even did a stint in the army as an explosives handler. He enrolled at the University of Chicago to pursue organ physiology, but all potential supervisors were too busy to take him on. His only choice was Nathaniel Kleitman, PhD, a middle-aged professor whom Dr. Aserinsky described as “always serious.” Dr. Kleitman was doing research on sleep and so, grudgingly, Dr. Aserinsky had followed suit.
Two years later, in 1953, the duo published a paper that shattered the way we saw sleep. They described a weird phenomenon Dr. Aserinsky later called REM sleep: periods of rapid eye movements paired with wakefulness-like activity in the brain. “We are still at the very beginning of understanding this phenomenon,” Mark Blumberg, PhD, professor of psychological and brain sciences at University of Iowa, Iowa City, said in an interview.
Before Dr. Aserinsky had walked into Dr. Kleitman’s lab, the widespread belief held that sleep was “the antithesis of wakefulness,” as Dr. Kleitman wrote in his seminal 1939 book, “Sleep and Wakefulness.” Others saw it as a kind of a coma, a passive state. Another theory, developed in the early 20th century by French psychologist Henri Piéron, PhD, held that sleepiness is caused by an accumulation of ‘hypnotoxins’ in the brain.
In his 1913 study that would likely fail a contemporary ethics review, Dr. Piéron drew fluid from the brains of sleep-deprived dogs and injected it into other dogs to induce sleep. As he explained in an interview with The Washington Times in 1933, he said he believed that fatigue toxins accumulate in the brain throughout the wakeful hours, then slowly seep into the spinal column, promoting drowsiness. Once we fall asleep, Dr. Piéron claimed, the hypnotoxins burn away.
From blinking to rapid eye movement
In 1925 when Dr. Kleitman established the world’s first sleep laboratory at the University of Chicago, sleep was a fringe science that most researchers avoided with a wide berth. Yet Dr. Kleitman was obsessed. The Moldova-born scientist famously worked 24/7 – literally. He not only stayed long hours in his lab, but also slept attached to a plethora of instruments to measure his brain waves, breathing, and heartbeat. At one point, Dr. Kleitman stayed awake for 180 hours (more than a week), to check how forced sleeplessness would affect his body (he later compared it to torture). He also lived 2 weeks aboard a submarine, moved his family north of the Arctic Circle, and spent over a month 119 feet below the surface in a cave in Kentucky, fighting rats, cold, and humidity to study circadian rhythms.
Dr. Kleitman was intrigued by an article in Nature in which the author asserted that he could detect the approach of slumber in train passengers by observing their blink frequencies. He instructed Dr. Aserinsky to observe sleeping infants (being monitored for a different study), to see how their blinking related to sleep. Yet Dr. Aserinsky was not amused. The project, he later wrote, “seemed about as exciting as warm milk.”
Dr. Aserinsky was uncertain whether eyelid movement with the eyes closed constituted a blink, then he noticed a 20-minute span in each hour when eye movement ceased entirely. Still short of getting his degree, Dr. Aserinsky decided to observe sleeping adults. He hauled a dusty clanker of a brain-wave machine out of the university’s basement, and started registering the electrical activity of the brain of his dozing subjects. Soon, he noticed something weird.
As he kept staring at the sleeping adults, he noticed that at times they’d have saccadic-like eye movements, just as the EEG machine would register a wake-like state of the brain. At first, he thought the machine was broken (it was ancient, after all). Then, that the subjects were awake and just keeping their eyes shut. Yet after conducting several sessions and tinkering with the EEG machine, Dr. Aserinsky finally concluded that the recordings and observations were correct: Something was indeed happening during sleep that kept the cortex activated and made the subjects’ eyes move in a jerky manner.
Dreams, memory, and thermoregulation
After studying dozens of subjects, including his son and Dr. Kleitman’s daughter, and using miles of polygraph paper, the two scientists published their findings in September 1953 in the journal Science. Dr. Kleitman didn’t expect the discovery to be particularly earth-shattering. When asked in a later interview how much research and excitement he thought the paper would generate, he replied: “none whatsoever.” That’s not how things went, though. “They completely changed the way people think,” Dr. Blumberg said. Once and for all, the REM discovery put to rest the idea that sleep was a passive state where nothing interesting happens.
Dr. Aserinsky soon left the University of Chicago, while Dr. Kleitman continued research on rapid eye movements in sleep with his new student, William Dement, MD. Together, they published studies suggesting that REM periods were when dreaming occurred – they reported that people who were awakened during REM sleep were far more likely to recall dreams than were those awakened outside of that period. “REM sleep = dreams” became established dogma for decades, even though first reports of dreams during non-REM sleep came as early as Dr. Kleitman’s and Dr. Dement’s original research (they assumed these were recollections from the preceding REM episodes).
“It turns out that you can have a perfectly good dream when you haven’t had a previous REM sleep period,” said Jerome Siegel, PhD, professor of psychiatry and biobehavioral sciences at UCLA’s Center for Sleep Research, pointing out that equating REM sleep with dreams is still “a common misconception.”
By the 1960s, REM sleep seemed to be well defined as the combination of rapid eye movement with EEG showing brain activation, first noted by Dr. Aserinsky, as well as muscle atonia – a state of near-total muscle relaxation or paralysis. Today, however, Dr. Blumberg said, things are considerably less clear cut. In one recent paper, Dr. Blumberg and his colleagues went as far as to question whether REM sleep is even “a thing.” REM sleep is prevalent across terrestrial vertebrates, but they found that it is also highly nuanced, messing up old definitions.
Take the platypus, for example, the animal with the most REM sleep (as far as we know): They have rapid eye movements and their bills twitch during REM (stillness punctuated by sudden twitches is typical of that period of sleep), but they don’t have the classic brain activation on EEG. Owls have EEG activation and twitching, but no rapid eye movements, since their eyes are largely immobile. Geese, meanwhile, are missing muscle atonia – that’s why they can sleep standing. And new studies are still coming in, showing, for instance, that even jumping spiders may have REM sleep, complete with jerky eye movements and limb twitching.
For Dr. Siegel, the findings on REM sleep in animals point to the potential explanation of what that bizarre stage of sleep may be all about: thermoregulation. “When you look at differences in sleep among the groups of warm-blooded animals, the correlation is almost perfect, and inverse. The colder they are, the more REM sleep they get,” Dr. Siegel said. During REM sleep, body thermoregulation is basically suspended, and so, as Dr. Siegel argued in The Lancet Neurology last fall, REM sleep could be a vital player in managing our brain’s temperature and metabolic activity during sleep.
Wallace B. Mendelson, MD, professor emeritus of psychiatry at the University of Chicago, said it’s likely, however, that REM sleep has more than one function. “There is no reason why one single theory has to be an answer. Most important physiological functions have multiple functions,” he said. The ideas are many, including that REM sleep helps consolidate our memories and plays an important role in emotion regulation But it’s not that simple. A Swiss study of nearly 1,000 healthy participants did not show any correlation between sleep stage and memory consolidation. Sleep disruption of any stage can prevent memory consolidation and quiet wakefulness with closed eyes can be as effective as sleep for memory recall.
In 1971, researchers from the National Institute of Mental Health published results of their study on total suppression of REM sleep. For as long as 40 days, they administered the monoamine oxidase inhibitor (MAOI) phenelzine, a type of drug that can completely eliminate REM sleep, to six patients with anxiety and depression. They showed that suppression of REM sleep could improve symptoms of depression, seemingly without impairing the patients’ cognitive function. Modern antidepressants, too, can greatly diminish REM sleep, Dr. Siegel said. “I’m not aware that there is any dramatic downside in having REM sleep reduced,” he said.
So do we even need REM sleep for optimal performance? Dr. Siegel said that there is a lot of exaggeration about how great REM sleep is for our health. “People just indulge their imaginations,” he said.
Dr. Blumberg pointed out that, in general, as long as you get enough sleep in the first place, you will get enough REM. “You can’t control the amount of REM sleep you have,” he explained.
REM sleep behavior disorder
Even though we may not need REM sleep to function well, REM sleep behavior disorder (RBD) is a sign that our health may be in trouble. In 1986, scientists from the University of Minnesota reported a bizarre REM sleep pathology in four men and one woman who would act out their dreams. One 67-year-old man, for example, reportedly punched and kicked his wife at night for years. One time he found himself kneeling alongside the bed with his arms extended as if he were holding a rifle (he dreamt he was in a shootout). His overall health, however, seemed unaffected apart from self-injury during some episodes.
However, in 1996 the same group of researchers reported that 11 of 29 men originally diagnosed with RBD went on to develop a parkinsonian disorder. Combined data from 24 centers of the International RBD Study Group puts that number as high as 74% at 12-year follow-up. These patients get diagnosed with Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy. Scientists believe that the protein alpha-synuclein forms toxic clumps in the brain, which are responsible both for malfunctioning of muscle atonia during REM sleep and subsequent neurodegenerative disorders.
While some researchers say that RBD may offer a unique window into better understanding REM sleep, we’re still a long way off from fully figuring out this biological phenomenon. According to Dr. Blumberg, the story of REM sleep has arguably become more muddled in the 7 decades since Dr. Aserinsky and Dr. Kleitman published their original findings, dispelling myths about ‘fatigue toxins’ and sleep as a passive, coma-like state. Dr. Mendelson concurred: “It truly remains a mystery.”
Dr. Blumberg, Dr. Mendelson, and Dr. Siegel reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Eugene Aserinsky, PhD, never wanted to study sleep. He tried being a social worker, a dental student, and even did a stint in the army as an explosives handler. He enrolled at the University of Chicago to pursue organ physiology, but all potential supervisors were too busy to take him on. His only choice was Nathaniel Kleitman, PhD, a middle-aged professor whom Dr. Aserinsky described as “always serious.” Dr. Kleitman was doing research on sleep and so, grudgingly, Dr. Aserinsky had followed suit.
Two years later, in 1953, the duo published a paper that shattered the way we saw sleep. They described a weird phenomenon Dr. Aserinsky later called REM sleep: periods of rapid eye movements paired with wakefulness-like activity in the brain. “We are still at the very beginning of understanding this phenomenon,” Mark Blumberg, PhD, professor of psychological and brain sciences at University of Iowa, Iowa City, said in an interview.
Before Dr. Aserinsky had walked into Dr. Kleitman’s lab, the widespread belief held that sleep was “the antithesis of wakefulness,” as Dr. Kleitman wrote in his seminal 1939 book, “Sleep and Wakefulness.” Others saw it as a kind of a coma, a passive state. Another theory, developed in the early 20th century by French psychologist Henri Piéron, PhD, held that sleepiness is caused by an accumulation of ‘hypnotoxins’ in the brain.
In his 1913 study that would likely fail a contemporary ethics review, Dr. Piéron drew fluid from the brains of sleep-deprived dogs and injected it into other dogs to induce sleep. As he explained in an interview with The Washington Times in 1933, he said he believed that fatigue toxins accumulate in the brain throughout the wakeful hours, then slowly seep into the spinal column, promoting drowsiness. Once we fall asleep, Dr. Piéron claimed, the hypnotoxins burn away.
From blinking to rapid eye movement
In 1925 when Dr. Kleitman established the world’s first sleep laboratory at the University of Chicago, sleep was a fringe science that most researchers avoided with a wide berth. Yet Dr. Kleitman was obsessed. The Moldova-born scientist famously worked 24/7 – literally. He not only stayed long hours in his lab, but also slept attached to a plethora of instruments to measure his brain waves, breathing, and heartbeat. At one point, Dr. Kleitman stayed awake for 180 hours (more than a week), to check how forced sleeplessness would affect his body (he later compared it to torture). He also lived 2 weeks aboard a submarine, moved his family north of the Arctic Circle, and spent over a month 119 feet below the surface in a cave in Kentucky, fighting rats, cold, and humidity to study circadian rhythms.
Dr. Kleitman was intrigued by an article in Nature in which the author asserted that he could detect the approach of slumber in train passengers by observing their blink frequencies. He instructed Dr. Aserinsky to observe sleeping infants (being monitored for a different study), to see how their blinking related to sleep. Yet Dr. Aserinsky was not amused. The project, he later wrote, “seemed about as exciting as warm milk.”
Dr. Aserinsky was uncertain whether eyelid movement with the eyes closed constituted a blink, then he noticed a 20-minute span in each hour when eye movement ceased entirely. Still short of getting his degree, Dr. Aserinsky decided to observe sleeping adults. He hauled a dusty clanker of a brain-wave machine out of the university’s basement, and started registering the electrical activity of the brain of his dozing subjects. Soon, he noticed something weird.
As he kept staring at the sleeping adults, he noticed that at times they’d have saccadic-like eye movements, just as the EEG machine would register a wake-like state of the brain. At first, he thought the machine was broken (it was ancient, after all). Then, that the subjects were awake and just keeping their eyes shut. Yet after conducting several sessions and tinkering with the EEG machine, Dr. Aserinsky finally concluded that the recordings and observations were correct: Something was indeed happening during sleep that kept the cortex activated and made the subjects’ eyes move in a jerky manner.
Dreams, memory, and thermoregulation
After studying dozens of subjects, including his son and Dr. Kleitman’s daughter, and using miles of polygraph paper, the two scientists published their findings in September 1953 in the journal Science. Dr. Kleitman didn’t expect the discovery to be particularly earth-shattering. When asked in a later interview how much research and excitement he thought the paper would generate, he replied: “none whatsoever.” That’s not how things went, though. “They completely changed the way people think,” Dr. Blumberg said. Once and for all, the REM discovery put to rest the idea that sleep was a passive state where nothing interesting happens.
Dr. Aserinsky soon left the University of Chicago, while Dr. Kleitman continued research on rapid eye movements in sleep with his new student, William Dement, MD. Together, they published studies suggesting that REM periods were when dreaming occurred – they reported that people who were awakened during REM sleep were far more likely to recall dreams than were those awakened outside of that period. “REM sleep = dreams” became established dogma for decades, even though first reports of dreams during non-REM sleep came as early as Dr. Kleitman’s and Dr. Dement’s original research (they assumed these were recollections from the preceding REM episodes).
“It turns out that you can have a perfectly good dream when you haven’t had a previous REM sleep period,” said Jerome Siegel, PhD, professor of psychiatry and biobehavioral sciences at UCLA’s Center for Sleep Research, pointing out that equating REM sleep with dreams is still “a common misconception.”
By the 1960s, REM sleep seemed to be well defined as the combination of rapid eye movement with EEG showing brain activation, first noted by Dr. Aserinsky, as well as muscle atonia – a state of near-total muscle relaxation or paralysis. Today, however, Dr. Blumberg said, things are considerably less clear cut. In one recent paper, Dr. Blumberg and his colleagues went as far as to question whether REM sleep is even “a thing.” REM sleep is prevalent across terrestrial vertebrates, but they found that it is also highly nuanced, messing up old definitions.
Take the platypus, for example, the animal with the most REM sleep (as far as we know): They have rapid eye movements and their bills twitch during REM (stillness punctuated by sudden twitches is typical of that period of sleep), but they don’t have the classic brain activation on EEG. Owls have EEG activation and twitching, but no rapid eye movements, since their eyes are largely immobile. Geese, meanwhile, are missing muscle atonia – that’s why they can sleep standing. And new studies are still coming in, showing, for instance, that even jumping spiders may have REM sleep, complete with jerky eye movements and limb twitching.
For Dr. Siegel, the findings on REM sleep in animals point to the potential explanation of what that bizarre stage of sleep may be all about: thermoregulation. “When you look at differences in sleep among the groups of warm-blooded animals, the correlation is almost perfect, and inverse. The colder they are, the more REM sleep they get,” Dr. Siegel said. During REM sleep, body thermoregulation is basically suspended, and so, as Dr. Siegel argued in The Lancet Neurology last fall, REM sleep could be a vital player in managing our brain’s temperature and metabolic activity during sleep.
Wallace B. Mendelson, MD, professor emeritus of psychiatry at the University of Chicago, said it’s likely, however, that REM sleep has more than one function. “There is no reason why one single theory has to be an answer. Most important physiological functions have multiple functions,” he said. The ideas are many, including that REM sleep helps consolidate our memories and plays an important role in emotion regulation But it’s not that simple. A Swiss study of nearly 1,000 healthy participants did not show any correlation between sleep stage and memory consolidation. Sleep disruption of any stage can prevent memory consolidation and quiet wakefulness with closed eyes can be as effective as sleep for memory recall.
In 1971, researchers from the National Institute of Mental Health published results of their study on total suppression of REM sleep. For as long as 40 days, they administered the monoamine oxidase inhibitor (MAOI) phenelzine, a type of drug that can completely eliminate REM sleep, to six patients with anxiety and depression. They showed that suppression of REM sleep could improve symptoms of depression, seemingly without impairing the patients’ cognitive function. Modern antidepressants, too, can greatly diminish REM sleep, Dr. Siegel said. “I’m not aware that there is any dramatic downside in having REM sleep reduced,” he said.
So do we even need REM sleep for optimal performance? Dr. Siegel said that there is a lot of exaggeration about how great REM sleep is for our health. “People just indulge their imaginations,” he said.
Dr. Blumberg pointed out that, in general, as long as you get enough sleep in the first place, you will get enough REM. “You can’t control the amount of REM sleep you have,” he explained.
REM sleep behavior disorder
Even though we may not need REM sleep to function well, REM sleep behavior disorder (RBD) is a sign that our health may be in trouble. In 1986, scientists from the University of Minnesota reported a bizarre REM sleep pathology in four men and one woman who would act out their dreams. One 67-year-old man, for example, reportedly punched and kicked his wife at night for years. One time he found himself kneeling alongside the bed with his arms extended as if he were holding a rifle (he dreamt he was in a shootout). His overall health, however, seemed unaffected apart from self-injury during some episodes.
However, in 1996 the same group of researchers reported that 11 of 29 men originally diagnosed with RBD went on to develop a parkinsonian disorder. Combined data from 24 centers of the International RBD Study Group puts that number as high as 74% at 12-year follow-up. These patients get diagnosed with Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy. Scientists believe that the protein alpha-synuclein forms toxic clumps in the brain, which are responsible both for malfunctioning of muscle atonia during REM sleep and subsequent neurodegenerative disorders.
While some researchers say that RBD may offer a unique window into better understanding REM sleep, we’re still a long way off from fully figuring out this biological phenomenon. According to Dr. Blumberg, the story of REM sleep has arguably become more muddled in the 7 decades since Dr. Aserinsky and Dr. Kleitman published their original findings, dispelling myths about ‘fatigue toxins’ and sleep as a passive, coma-like state. Dr. Mendelson concurred: “It truly remains a mystery.”
Dr. Blumberg, Dr. Mendelson, and Dr. Siegel reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Continuous glucose monitors come to hospitals
But that technological future will require ensuring that the monitoring devices are as accurate as the conventional method, experts told this news organization.
In 2020, the U.S. Food and Drug Administration enabled in-hospital use of CGMs to reduce contact between patients and health care providers during the COVID-19 pandemic. Diabetes is a risk factor for more severe COVID, meaning that many patients with the infection also required ongoing care for their blood sugar problems.
Prior to the pandemic, in-person finger-stick tests were the primary means of measuring glucose for hospitalized patients with diabetes.
The trouble is that finger-stick measurements quickly become inaccurate.
“Glucose is a measurement that changes pretty rapidly,” said Eileen Faulds, RN, PhD, an endocrinology nurse and health services researcher at the Ohio State University, Columbus. Finger sticks might occur only four or five times per day, Dr. Faulds noted, or as often as every hour for people who receive insulin intravenously. But even that more frequent pace is far from continuous.
“With CGM we can get the glucose level in real time,” Dr. Faulds said.
Dr. Faulds is lead author of a new study in the Journal of Diabetes Science and Technology, which shows that nurses in the ICU believe that using continuous monitors, subcutaneous filaments connected to sensors that regularly report glucose levels, enables better patient care than does relying on periodic glucose tests alone. Nurses still used traditional finger sticks, which Dr. Faulds notes are highly accurate at the time of the reading.
In a 2022 study, glucose levels generated by CGM and those measured by finger sticks varied by up to 14%. A hybrid care model combining CGMs and finger stick tests may emerge, Dr. Faulds said.
A gusher of glucose data
People with diabetes have long been able to use CGMs in their daily lives, which typically report the glucose value to a smartphone or watch. The devices are now part of hospital care as well. In 2022, the Food and Drug Administration granted a breakthrough therapy designation to the company Dexcom for use of its CGMs to manage care of people with diabetes in hospitals.
One open question is how often CGMs should report glucose readings for optimum patient health. Dexcom’s G6 CGM reports glucose levels every five minutes, for example, whereas Abbott’s FreeStyle Libre 2 delivers glucose values every minute.
“We wouldn’t look at each value, we would look at the big picture,” to determine if a patient is at risk of becoming hyper- or hypoglycemic, said Lizda Guerrero-Arroyo, MD, a postdoctoral fellow in endocrinology at the Emory University School of Medicine, Atlanta. Dr. Guerrero-Arroyo recently reported that clinicians in multiple ICUs began to use CGMs in conjunction with finger sticks during the pandemic and felt the devices could reduce patient discomfort.
“A finger stick is very painful,” Dr. Guerrero-Arroyo said, and a bottleneck for nursing staff who administer these tests. In contrast, Dr. Faulds said, CGM placement is essentially painless and requires less labor on the ward to manage.
Beyond use in the ICU, clinicians are also experimenting with use of CGMs to monitor blood sugar levels in people with diabetes who are undergoing general surgery. And other researchers are describing how to integrate data from CGMs into patient care tools such as the electronic health record, although a standard way to do this does not yet exist.
Assuming CGMs remain part of the mix for in-hospital care of people with diabetes, clinicians may mainly need trend summaries of how glucose levels rise and fall over time, said data scientist Samantha Spierling Bagsic, PhD, of the Scripps Whittier Diabetes Institute, San Diego. Dr. Guerrero-Arroyo said that she shares that vision. But a minute-by-minute analysis of glucose levels also may be necessary to get a granular sense of how changing a patient’s insulin level affects their blood sugar, Dr. Spierling Bagsic said.
“We need to figure out what data different audiences need, how often we need to measure glucose, and how to present that information to different audiences in different ways,” said Dr. Spierling Bagsic, a co-author of the study about integrating CGM data into patient care tools.
The wider use of CGMs in hospitals may be one silver lining of the COVID-19 pandemic. As an inpatient endocrinology nurse, Dr. Faulds said that she wanted to use CGMs prior to the outbreak, but at that point, a critical mass of studies about their benefits was missing.
“We all know the terrible things that happened during the pandemic,” Dr. Faulds said. “But it gave us the allowance to use CGMs, and we saw that nurses loved them.”
Dr. Faulds reports relationships with Dexcom and Insulet and has received an honorarium from Medscape. Dr. Guerrero-Arroyo and Dr. Spierling Bagsic reported no financial conflicts of interest.
A version of this article originally appeared on Medscape.com.
But that technological future will require ensuring that the monitoring devices are as accurate as the conventional method, experts told this news organization.
In 2020, the U.S. Food and Drug Administration enabled in-hospital use of CGMs to reduce contact between patients and health care providers during the COVID-19 pandemic. Diabetes is a risk factor for more severe COVID, meaning that many patients with the infection also required ongoing care for their blood sugar problems.
Prior to the pandemic, in-person finger-stick tests were the primary means of measuring glucose for hospitalized patients with diabetes.
The trouble is that finger-stick measurements quickly become inaccurate.
“Glucose is a measurement that changes pretty rapidly,” said Eileen Faulds, RN, PhD, an endocrinology nurse and health services researcher at the Ohio State University, Columbus. Finger sticks might occur only four or five times per day, Dr. Faulds noted, or as often as every hour for people who receive insulin intravenously. But even that more frequent pace is far from continuous.
“With CGM we can get the glucose level in real time,” Dr. Faulds said.
Dr. Faulds is lead author of a new study in the Journal of Diabetes Science and Technology, which shows that nurses in the ICU believe that using continuous monitors, subcutaneous filaments connected to sensors that regularly report glucose levels, enables better patient care than does relying on periodic glucose tests alone. Nurses still used traditional finger sticks, which Dr. Faulds notes are highly accurate at the time of the reading.
In a 2022 study, glucose levels generated by CGM and those measured by finger sticks varied by up to 14%. A hybrid care model combining CGMs and finger stick tests may emerge, Dr. Faulds said.
A gusher of glucose data
People with diabetes have long been able to use CGMs in their daily lives, which typically report the glucose value to a smartphone or watch. The devices are now part of hospital care as well. In 2022, the Food and Drug Administration granted a breakthrough therapy designation to the company Dexcom for use of its CGMs to manage care of people with diabetes in hospitals.
One open question is how often CGMs should report glucose readings for optimum patient health. Dexcom’s G6 CGM reports glucose levels every five minutes, for example, whereas Abbott’s FreeStyle Libre 2 delivers glucose values every minute.
“We wouldn’t look at each value, we would look at the big picture,” to determine if a patient is at risk of becoming hyper- or hypoglycemic, said Lizda Guerrero-Arroyo, MD, a postdoctoral fellow in endocrinology at the Emory University School of Medicine, Atlanta. Dr. Guerrero-Arroyo recently reported that clinicians in multiple ICUs began to use CGMs in conjunction with finger sticks during the pandemic and felt the devices could reduce patient discomfort.
“A finger stick is very painful,” Dr. Guerrero-Arroyo said, and a bottleneck for nursing staff who administer these tests. In contrast, Dr. Faulds said, CGM placement is essentially painless and requires less labor on the ward to manage.
Beyond use in the ICU, clinicians are also experimenting with use of CGMs to monitor blood sugar levels in people with diabetes who are undergoing general surgery. And other researchers are describing how to integrate data from CGMs into patient care tools such as the electronic health record, although a standard way to do this does not yet exist.
Assuming CGMs remain part of the mix for in-hospital care of people with diabetes, clinicians may mainly need trend summaries of how glucose levels rise and fall over time, said data scientist Samantha Spierling Bagsic, PhD, of the Scripps Whittier Diabetes Institute, San Diego. Dr. Guerrero-Arroyo said that she shares that vision. But a minute-by-minute analysis of glucose levels also may be necessary to get a granular sense of how changing a patient’s insulin level affects their blood sugar, Dr. Spierling Bagsic said.
“We need to figure out what data different audiences need, how often we need to measure glucose, and how to present that information to different audiences in different ways,” said Dr. Spierling Bagsic, a co-author of the study about integrating CGM data into patient care tools.
The wider use of CGMs in hospitals may be one silver lining of the COVID-19 pandemic. As an inpatient endocrinology nurse, Dr. Faulds said that she wanted to use CGMs prior to the outbreak, but at that point, a critical mass of studies about their benefits was missing.
“We all know the terrible things that happened during the pandemic,” Dr. Faulds said. “But it gave us the allowance to use CGMs, and we saw that nurses loved them.”
Dr. Faulds reports relationships with Dexcom and Insulet and has received an honorarium from Medscape. Dr. Guerrero-Arroyo and Dr. Spierling Bagsic reported no financial conflicts of interest.
A version of this article originally appeared on Medscape.com.
But that technological future will require ensuring that the monitoring devices are as accurate as the conventional method, experts told this news organization.
In 2020, the U.S. Food and Drug Administration enabled in-hospital use of CGMs to reduce contact between patients and health care providers during the COVID-19 pandemic. Diabetes is a risk factor for more severe COVID, meaning that many patients with the infection also required ongoing care for their blood sugar problems.
Prior to the pandemic, in-person finger-stick tests were the primary means of measuring glucose for hospitalized patients with diabetes.
The trouble is that finger-stick measurements quickly become inaccurate.
“Glucose is a measurement that changes pretty rapidly,” said Eileen Faulds, RN, PhD, an endocrinology nurse and health services researcher at the Ohio State University, Columbus. Finger sticks might occur only four or five times per day, Dr. Faulds noted, or as often as every hour for people who receive insulin intravenously. But even that more frequent pace is far from continuous.
“With CGM we can get the glucose level in real time,” Dr. Faulds said.
Dr. Faulds is lead author of a new study in the Journal of Diabetes Science and Technology, which shows that nurses in the ICU believe that using continuous monitors, subcutaneous filaments connected to sensors that regularly report glucose levels, enables better patient care than does relying on periodic glucose tests alone. Nurses still used traditional finger sticks, which Dr. Faulds notes are highly accurate at the time of the reading.
In a 2022 study, glucose levels generated by CGM and those measured by finger sticks varied by up to 14%. A hybrid care model combining CGMs and finger stick tests may emerge, Dr. Faulds said.
A gusher of glucose data
People with diabetes have long been able to use CGMs in their daily lives, which typically report the glucose value to a smartphone or watch. The devices are now part of hospital care as well. In 2022, the Food and Drug Administration granted a breakthrough therapy designation to the company Dexcom for use of its CGMs to manage care of people with diabetes in hospitals.
One open question is how often CGMs should report glucose readings for optimum patient health. Dexcom’s G6 CGM reports glucose levels every five minutes, for example, whereas Abbott’s FreeStyle Libre 2 delivers glucose values every minute.
“We wouldn’t look at each value, we would look at the big picture,” to determine if a patient is at risk of becoming hyper- or hypoglycemic, said Lizda Guerrero-Arroyo, MD, a postdoctoral fellow in endocrinology at the Emory University School of Medicine, Atlanta. Dr. Guerrero-Arroyo recently reported that clinicians in multiple ICUs began to use CGMs in conjunction with finger sticks during the pandemic and felt the devices could reduce patient discomfort.
“A finger stick is very painful,” Dr. Guerrero-Arroyo said, and a bottleneck for nursing staff who administer these tests. In contrast, Dr. Faulds said, CGM placement is essentially painless and requires less labor on the ward to manage.
Beyond use in the ICU, clinicians are also experimenting with use of CGMs to monitor blood sugar levels in people with diabetes who are undergoing general surgery. And other researchers are describing how to integrate data from CGMs into patient care tools such as the electronic health record, although a standard way to do this does not yet exist.
Assuming CGMs remain part of the mix for in-hospital care of people with diabetes, clinicians may mainly need trend summaries of how glucose levels rise and fall over time, said data scientist Samantha Spierling Bagsic, PhD, of the Scripps Whittier Diabetes Institute, San Diego. Dr. Guerrero-Arroyo said that she shares that vision. But a minute-by-minute analysis of glucose levels also may be necessary to get a granular sense of how changing a patient’s insulin level affects their blood sugar, Dr. Spierling Bagsic said.
“We need to figure out what data different audiences need, how often we need to measure glucose, and how to present that information to different audiences in different ways,” said Dr. Spierling Bagsic, a co-author of the study about integrating CGM data into patient care tools.
The wider use of CGMs in hospitals may be one silver lining of the COVID-19 pandemic. As an inpatient endocrinology nurse, Dr. Faulds said that she wanted to use CGMs prior to the outbreak, but at that point, a critical mass of studies about their benefits was missing.
“We all know the terrible things that happened during the pandemic,” Dr. Faulds said. “But it gave us the allowance to use CGMs, and we saw that nurses loved them.”
Dr. Faulds reports relationships with Dexcom and Insulet and has received an honorarium from Medscape. Dr. Guerrero-Arroyo and Dr. Spierling Bagsic reported no financial conflicts of interest.
A version of this article originally appeared on Medscape.com.
MDs with chronic illness live in a different medical world
Linda Bluestein remembers all the doctors who missed, ignored, or incompletely diagnosed her chronic illness.
There was the orthopedic surgeon who noted her hyperextended elbows but failed to check any of her other joints. The gastroenterologist who insisted on performing multiple scoping procedures but wouldn’t discuss how to manage her symptoms. The other surgeon who, after performing arthroscopy on her injured knee, yelled at her: “There is nothing wrong with your knee! You’re fine!” in a room full of people.
And then there was the rheumatologist who said: “Oh, you want something to be wrong with you?”
“No,” she replied, “I want an explanation. I want to keep working. I just want to know why these things keep happening to me.”
The medical frustration she experienced was especially difficult because, like her health care providers, Linda Bluestein has an MD after her name. She is a board-certified anesthesiologist and integrative medicine physician.
Along with the physically demanding schedule of medical practice, they must cope with what many call a “culture of invincibility” within medicine. Doctors are not supposed to get sick. In fact, the unwritten rule is presenteeism – to function without adequate food or sleep and to never prioritize their own self-care over their dedication to their patients.
Whether their conditions are visible, such as muscular dystrophy and multiple sclerosis, or invisible, such as fibromyalgia and mental illnesses – and now, long COVID – these doctors often meet significant stigma. They fight the assumption that they are less capable than their colleagues.
But they also experience an invaluable benefit: They gain firsthand knowledge of the patient experience, a profound understanding which, they say, enhances how they care for their own patients.
What it takes to become a doctor when you have a chronic condition
In short, it’s not easy.
Data from the 2018 National Health Interview Survey show that more than half of U.S. adults had at least one of several chronic conditions, including rheumatoid arthritis, asthma, diabetes, hypertension, and kidney problems. Nearly a third of respondents had more than one condition. But fewer than 5% of medical students and 3% of practicing physicians report having a chronic illness or disability, according to studies from 2019 and 2021.
While that could mean that fewer people with chronic illness enter medicine, cases also exist in which aspiring physicians with conditions were dissuaded from pursuing a career in medicine at all.
Amy Stenehjem, MD, a physical medicine and rehabilitation physician, is one of the exceptions. Diagnosed with several autoimmune-related conditions as a teenager and young adult, Dr. Stenehjem was determined to become a doctor. In her 20s, her health was relatively stable, and she was able to manage medical school and residency. Her training institutions agreed to provide some accommodations that helped her succeed.
“They let me build some flexibility into the training,” Dr. Stenehjem said. “In medical school, when I knew I wasn’t going to be able to do a particular specialty as a career, they let me work with an attending doctor that did not require a lot of on-call time during that particular rotation.”
Dr. Stenehjem specialized in chronic neck and back disorders, fibromyalgia, chronic fatigue syndrome (myalgic encephalomyelitis), and autoimmune-related diseases. She practiced for more than a decade. But in 2011, her condition spiraled. She couldn’t walk a few steps or even sit upright without experiencing dizziness and shortness of breath. She had debilitating fatigue and episodes of fever, rash, headaches, and joint pain.
It would take 7 years and more than 20 doctors to determine Dr. Stenehjem’s multiple diagnoses. In addition to her autoimmune diseases, she was diagnosed with postural orthostatic tachycardia syndrome, autoinflammatory periodic fever syndrome, Lyme disease, and reactivated Epstein-Barr infection.
While she suspects that her providers gave her more “leeway” because she was a physician, many did not show a deep understanding of the severity of her symptoms and the impact those symptoms had.
“When I was practicing, I really didn’t fully understand the impact chronic illness had on my patients,” Dr. Stenehjem said. “Things like chronic dizziness, headaches, fatigue, pain, or brain fog can be really hard to understand unless you’ve experienced these symptoms. When I got sick, I finally realized, ‘Oh my goodness, when a patient says they’re dealing with fatigue, this is not your normal, I’m-super-tired-from-being-on-call fatigue. This is I-can’t-get-out-of-bed fatigue.’ That’s what people with chronic illness often deal with on a daily basis.”
Treating the individual
Dr. Stenehjem was aware that her chronic illness would affect her medical career. For Jason Baker, MD, an endocrinologist at Weill Cornell Medicine, New York, it came as a shock. Dr. Baker was a third-year medical student when he experienced increased urination and rapid weight loss. It was only when friends pressed him to visit student health that a blood test revealed type 1 diabetes. Dr. Baker suddenly found himself lying in a hospital bed.
He remembers an attending physician who simply handed him a textbook on diabetic ketoacidosis (DKA) and a resident who informed him that he had kidney damage, which turned out to be untrue. Neither discussed the psychological issues from a frightening diagnosis that would require lifelong, daily management.
“There certainly could have been a bit more empathy from some of the people I dealt with early on,” he said.
Although his training gave him a stark picture of worst-case scenarios, Dr. Baker found that knowledge motivating. “I’d already seen patients come in who had diabetes complications,” Dr. Baker says. “I vowed to never ever get those complications. It was a good balance of fear and motivation.”
Dr. Baker had not planned to specialize in endocrinology, but he quickly realized that his personal diagnosis could help others. Now he often shares his experience with his patients who have diabetes, which he says makes them more comfortable discussing their own problems.
His approach, Dr. Baker explained, is to treat everyone as an individual. Trying to neatly classify patients with chronic illness is a common mistake he notices among physicians.
“There’s a lot of misunderstanding about type 1 versus type 2 [diabetes],” Dr. Baker said, “and trying to categorize people when sometimes people can’t be categorized. That’s really with any chronic condition; there’s no one size fits all.”
Managing his health is still a time-consuming task. At work, he needs breaks to eat, check his blood sugar, or take insulin. “During the workday seeing patients, I have to also remember that I’m a patient,” Dr. Baker said. “I have to be okay with prioritizing my own health. Otherwise I can’t help anybody.”
‘I am not the doctor for you’
Chronic diseases such as diabetes or hypertension are familiar to most doctors, and with good management, patients can usually function normally. When chronic conditions become disabling, however, attitudes in the medical field can change.
According to data from the Centers for Disease Control and Prevention and from studies, people with disabilities experience significant disparities and barriers to care. Some of this can be linked to social determinants of health. People with disabilities are more likely to be poor and to rely on Medicare and Medicaid for insurance coverage. But lack of training, unwillingness to provide accommodations, ignorance of legal requirements, and inaccurate assumptions among physicians also play a role.
These are themes that Lisa Iezzoni, MD, a professor of medicine at Harvard Medical School, Boston, has heard from hundreds of patients with disabilities during the more than 25 years that she has conducted research.
In late 2019, Dr. Iezzoni and coinvestigators fielded a national survey of 714 practicing physicians. Only 40.7% reported they were “very confident” that they could provide the same quality of care to patients with disabilities as they do for other patients. And only 56.5% “strongly agreed” that they welcomed these patients into their practices.
The survey was conducted through a series of small focus groups that Dr. Iezzoni held with physicians in 2018. These yielded views that were startling, and in some cases, overtly discriminatory:
- Doctors complained about the “burden” of caring for a patient with a disability.
- They lacked the time or equipment, such as accessible exam tables or weight scales.
- They admitted to inventing excuses for why appointments were not available or routine diagnostic tests were not performed.
- They described being fearful of lawsuits under the Americans with Disabilities Act.
The overall message was summed up in one doctor’s statement: “I am not the doctor for you.”
“Doctors are people too,” Dr. Iezzoni pointed out. “And so they reflect the same prejudices and stigmatized attitudes of the rest of the population. It might be implicit, so they might not be aware of it. [But] it might be explicit.”
Ableism in the medical field is all too familiar to Dr. Iezzoni. She was diagnosed with multiple sclerosis at age 26 during her first year at Harvard Medical School in the early 1980s. Despite symptom flare-ups, Dr. Iezzoni was able to graduate with her class, but many instructors and administrators had little interest in accommodating her physical limitations. In fact, several physicians discouraged her from continuing to train.
Unable to take call, run up flights of stairs, or stand for hours at a time, Dr. Iezzoni remembers being told by a senior surgeon that she shouldn’t become a doctor since she lacked the “most important quality,” which was “24/7 availability.” A hospital CEO informed her: “There are too many doctors in the country right now for us to worry about training a handicapped physician. If that means that some people get left by the wayside, so be it.”
Ultimately, Harvard Medical School declined to write Dr. Iezzoni a letter of recommendation for an internship. She would never practice medicine. “My career was just truncated from the start,” Dr. Iezzoni said. “It never happened because of discrimination.”
She later learned the legal term for her treatment: constructive dismissal.
“The medical school didn’t outright say, ‘Go away. We’re not allowing you to graduate.’ ” Dr. Iezzoni explained. “But they made my life so difficult that I did so voluntarily.”
Dr. Iezzoni graduated in 1984, before the passage of the ADA in 1990, and she refers to her experience as a “ghost from the past,” a historical reminder of how the legal landscape has changed – even though the tendency toward bias may not have.
The fight for inclusion
Zainub Dhanani, a fifth-year medical student at Stanford (Calif.) University, won’t forget an interview at one of the other schools to which she applied. The interviewer asked how she expected to be in a hospital all day if she had a chronic illness.
“Does it really make sense?” he wanted to know.
The question shocked her in the moment, but now she sees this type of bias as linked to the inequalities that many marginalized groups face in health care and beyond. That’s also why she believes physician-patients are crucial to improve the quality of care for people with chronic illness and other groups that face discrimination.
Who else, she wonders, could provide that “reaffirming” experience for patients or have that “unique edge” other than a provider who has navigated the same world?
Ms. Dhanani is the executive director and founder of Medical Students With Disability and Chronic Illness, an organization dedicated to empowering these students through advocacy, education, accessibility, and community. The group now has 19 chapters at medical schools across the country.
Ms. Dhanani said she has received excellent accommodations from Stanford for her own condition (which she prefers not to disclose), but all medical schools are not as responsive to students with various physical needs. Her organization offers support and resources to inform these future physicians about their options and rights.
“Disability justice is also racial justice,” Ms. Dhanani stressed. “It’s also environmental justice. It’s also gender and sexuality-based justice. Those compounded layers of biases lead to worse and worse levels of care. As a patient, it’s terrifying. And as a future physician, it’s tragic to know that this is something so pervasive and yet so under-addressed in medicine.”
Soldiering on
Unfortunately, for some physicians with chronic illness, there are no practical accommodations that could save their careers in clinical practice.
Dr. Stenehjem now works part-time as a health consultant, helping those with chronic illnesses navigate their health care systems.
Dr. Bluestein offers a similar coaching service to patients with Ehlers-Danlos syndrome (EDS) and other connective tissue and hypermobility disorders. Because of her own EDS, she can no longer practice as an anesthesiologist but instead opened an integrative pain management practice for patients with complex pain conditions..
She believes the idea that doctors are “invincible” needs to change. She recalls the time her former group practice told her in no uncertain terms to “never call in sick.”
The stories she hears from her current clients are similar to her own. She can empathize, knowing firsthand the physical and psychological damage these attitudes can cause.
“When I was at my worst physically, I was also at my worst psychologically,” said Dr. Bluestein. “We tend to think of them as separate, but they go hand in hand. If we can validate people’s experiences rather than disregard them, it has a positive forward cycle, as opposed to the reverse, which is what usually happens.”
A version of this article first appeared on Medscape.com.
Linda Bluestein remembers all the doctors who missed, ignored, or incompletely diagnosed her chronic illness.
There was the orthopedic surgeon who noted her hyperextended elbows but failed to check any of her other joints. The gastroenterologist who insisted on performing multiple scoping procedures but wouldn’t discuss how to manage her symptoms. The other surgeon who, after performing arthroscopy on her injured knee, yelled at her: “There is nothing wrong with your knee! You’re fine!” in a room full of people.
And then there was the rheumatologist who said: “Oh, you want something to be wrong with you?”
“No,” she replied, “I want an explanation. I want to keep working. I just want to know why these things keep happening to me.”
The medical frustration she experienced was especially difficult because, like her health care providers, Linda Bluestein has an MD after her name. She is a board-certified anesthesiologist and integrative medicine physician.
Along with the physically demanding schedule of medical practice, they must cope with what many call a “culture of invincibility” within medicine. Doctors are not supposed to get sick. In fact, the unwritten rule is presenteeism – to function without adequate food or sleep and to never prioritize their own self-care over their dedication to their patients.
Whether their conditions are visible, such as muscular dystrophy and multiple sclerosis, or invisible, such as fibromyalgia and mental illnesses – and now, long COVID – these doctors often meet significant stigma. They fight the assumption that they are less capable than their colleagues.
But they also experience an invaluable benefit: They gain firsthand knowledge of the patient experience, a profound understanding which, they say, enhances how they care for their own patients.
What it takes to become a doctor when you have a chronic condition
In short, it’s not easy.
Data from the 2018 National Health Interview Survey show that more than half of U.S. adults had at least one of several chronic conditions, including rheumatoid arthritis, asthma, diabetes, hypertension, and kidney problems. Nearly a third of respondents had more than one condition. But fewer than 5% of medical students and 3% of practicing physicians report having a chronic illness or disability, according to studies from 2019 and 2021.
While that could mean that fewer people with chronic illness enter medicine, cases also exist in which aspiring physicians with conditions were dissuaded from pursuing a career in medicine at all.
Amy Stenehjem, MD, a physical medicine and rehabilitation physician, is one of the exceptions. Diagnosed with several autoimmune-related conditions as a teenager and young adult, Dr. Stenehjem was determined to become a doctor. In her 20s, her health was relatively stable, and she was able to manage medical school and residency. Her training institutions agreed to provide some accommodations that helped her succeed.
“They let me build some flexibility into the training,” Dr. Stenehjem said. “In medical school, when I knew I wasn’t going to be able to do a particular specialty as a career, they let me work with an attending doctor that did not require a lot of on-call time during that particular rotation.”
Dr. Stenehjem specialized in chronic neck and back disorders, fibromyalgia, chronic fatigue syndrome (myalgic encephalomyelitis), and autoimmune-related diseases. She practiced for more than a decade. But in 2011, her condition spiraled. She couldn’t walk a few steps or even sit upright without experiencing dizziness and shortness of breath. She had debilitating fatigue and episodes of fever, rash, headaches, and joint pain.
It would take 7 years and more than 20 doctors to determine Dr. Stenehjem’s multiple diagnoses. In addition to her autoimmune diseases, she was diagnosed with postural orthostatic tachycardia syndrome, autoinflammatory periodic fever syndrome, Lyme disease, and reactivated Epstein-Barr infection.
While she suspects that her providers gave her more “leeway” because she was a physician, many did not show a deep understanding of the severity of her symptoms and the impact those symptoms had.
“When I was practicing, I really didn’t fully understand the impact chronic illness had on my patients,” Dr. Stenehjem said. “Things like chronic dizziness, headaches, fatigue, pain, or brain fog can be really hard to understand unless you’ve experienced these symptoms. When I got sick, I finally realized, ‘Oh my goodness, when a patient says they’re dealing with fatigue, this is not your normal, I’m-super-tired-from-being-on-call fatigue. This is I-can’t-get-out-of-bed fatigue.’ That’s what people with chronic illness often deal with on a daily basis.”
Treating the individual
Dr. Stenehjem was aware that her chronic illness would affect her medical career. For Jason Baker, MD, an endocrinologist at Weill Cornell Medicine, New York, it came as a shock. Dr. Baker was a third-year medical student when he experienced increased urination and rapid weight loss. It was only when friends pressed him to visit student health that a blood test revealed type 1 diabetes. Dr. Baker suddenly found himself lying in a hospital bed.
He remembers an attending physician who simply handed him a textbook on diabetic ketoacidosis (DKA) and a resident who informed him that he had kidney damage, which turned out to be untrue. Neither discussed the psychological issues from a frightening diagnosis that would require lifelong, daily management.
“There certainly could have been a bit more empathy from some of the people I dealt with early on,” he said.
Although his training gave him a stark picture of worst-case scenarios, Dr. Baker found that knowledge motivating. “I’d already seen patients come in who had diabetes complications,” Dr. Baker says. “I vowed to never ever get those complications. It was a good balance of fear and motivation.”
Dr. Baker had not planned to specialize in endocrinology, but he quickly realized that his personal diagnosis could help others. Now he often shares his experience with his patients who have diabetes, which he says makes them more comfortable discussing their own problems.
His approach, Dr. Baker explained, is to treat everyone as an individual. Trying to neatly classify patients with chronic illness is a common mistake he notices among physicians.
“There’s a lot of misunderstanding about type 1 versus type 2 [diabetes],” Dr. Baker said, “and trying to categorize people when sometimes people can’t be categorized. That’s really with any chronic condition; there’s no one size fits all.”
Managing his health is still a time-consuming task. At work, he needs breaks to eat, check his blood sugar, or take insulin. “During the workday seeing patients, I have to also remember that I’m a patient,” Dr. Baker said. “I have to be okay with prioritizing my own health. Otherwise I can’t help anybody.”
‘I am not the doctor for you’
Chronic diseases such as diabetes or hypertension are familiar to most doctors, and with good management, patients can usually function normally. When chronic conditions become disabling, however, attitudes in the medical field can change.
According to data from the Centers for Disease Control and Prevention and from studies, people with disabilities experience significant disparities and barriers to care. Some of this can be linked to social determinants of health. People with disabilities are more likely to be poor and to rely on Medicare and Medicaid for insurance coverage. But lack of training, unwillingness to provide accommodations, ignorance of legal requirements, and inaccurate assumptions among physicians also play a role.
These are themes that Lisa Iezzoni, MD, a professor of medicine at Harvard Medical School, Boston, has heard from hundreds of patients with disabilities during the more than 25 years that she has conducted research.
In late 2019, Dr. Iezzoni and coinvestigators fielded a national survey of 714 practicing physicians. Only 40.7% reported they were “very confident” that they could provide the same quality of care to patients with disabilities as they do for other patients. And only 56.5% “strongly agreed” that they welcomed these patients into their practices.
The survey was conducted through a series of small focus groups that Dr. Iezzoni held with physicians in 2018. These yielded views that were startling, and in some cases, overtly discriminatory:
- Doctors complained about the “burden” of caring for a patient with a disability.
- They lacked the time or equipment, such as accessible exam tables or weight scales.
- They admitted to inventing excuses for why appointments were not available or routine diagnostic tests were not performed.
- They described being fearful of lawsuits under the Americans with Disabilities Act.
The overall message was summed up in one doctor’s statement: “I am not the doctor for you.”
“Doctors are people too,” Dr. Iezzoni pointed out. “And so they reflect the same prejudices and stigmatized attitudes of the rest of the population. It might be implicit, so they might not be aware of it. [But] it might be explicit.”
Ableism in the medical field is all too familiar to Dr. Iezzoni. She was diagnosed with multiple sclerosis at age 26 during her first year at Harvard Medical School in the early 1980s. Despite symptom flare-ups, Dr. Iezzoni was able to graduate with her class, but many instructors and administrators had little interest in accommodating her physical limitations. In fact, several physicians discouraged her from continuing to train.
Unable to take call, run up flights of stairs, or stand for hours at a time, Dr. Iezzoni remembers being told by a senior surgeon that she shouldn’t become a doctor since she lacked the “most important quality,” which was “24/7 availability.” A hospital CEO informed her: “There are too many doctors in the country right now for us to worry about training a handicapped physician. If that means that some people get left by the wayside, so be it.”
Ultimately, Harvard Medical School declined to write Dr. Iezzoni a letter of recommendation for an internship. She would never practice medicine. “My career was just truncated from the start,” Dr. Iezzoni said. “It never happened because of discrimination.”
She later learned the legal term for her treatment: constructive dismissal.
“The medical school didn’t outright say, ‘Go away. We’re not allowing you to graduate.’ ” Dr. Iezzoni explained. “But they made my life so difficult that I did so voluntarily.”
Dr. Iezzoni graduated in 1984, before the passage of the ADA in 1990, and she refers to her experience as a “ghost from the past,” a historical reminder of how the legal landscape has changed – even though the tendency toward bias may not have.
The fight for inclusion
Zainub Dhanani, a fifth-year medical student at Stanford (Calif.) University, won’t forget an interview at one of the other schools to which she applied. The interviewer asked how she expected to be in a hospital all day if she had a chronic illness.
“Does it really make sense?” he wanted to know.
The question shocked her in the moment, but now she sees this type of bias as linked to the inequalities that many marginalized groups face in health care and beyond. That’s also why she believes physician-patients are crucial to improve the quality of care for people with chronic illness and other groups that face discrimination.
Who else, she wonders, could provide that “reaffirming” experience for patients or have that “unique edge” other than a provider who has navigated the same world?
Ms. Dhanani is the executive director and founder of Medical Students With Disability and Chronic Illness, an organization dedicated to empowering these students through advocacy, education, accessibility, and community. The group now has 19 chapters at medical schools across the country.
Ms. Dhanani said she has received excellent accommodations from Stanford for her own condition (which she prefers not to disclose), but all medical schools are not as responsive to students with various physical needs. Her organization offers support and resources to inform these future physicians about their options and rights.
“Disability justice is also racial justice,” Ms. Dhanani stressed. “It’s also environmental justice. It’s also gender and sexuality-based justice. Those compounded layers of biases lead to worse and worse levels of care. As a patient, it’s terrifying. And as a future physician, it’s tragic to know that this is something so pervasive and yet so under-addressed in medicine.”
Soldiering on
Unfortunately, for some physicians with chronic illness, there are no practical accommodations that could save their careers in clinical practice.
Dr. Stenehjem now works part-time as a health consultant, helping those with chronic illnesses navigate their health care systems.
Dr. Bluestein offers a similar coaching service to patients with Ehlers-Danlos syndrome (EDS) and other connective tissue and hypermobility disorders. Because of her own EDS, she can no longer practice as an anesthesiologist but instead opened an integrative pain management practice for patients with complex pain conditions..
She believes the idea that doctors are “invincible” needs to change. She recalls the time her former group practice told her in no uncertain terms to “never call in sick.”
The stories she hears from her current clients are similar to her own. She can empathize, knowing firsthand the physical and psychological damage these attitudes can cause.
“When I was at my worst physically, I was also at my worst psychologically,” said Dr. Bluestein. “We tend to think of them as separate, but they go hand in hand. If we can validate people’s experiences rather than disregard them, it has a positive forward cycle, as opposed to the reverse, which is what usually happens.”
A version of this article first appeared on Medscape.com.
Linda Bluestein remembers all the doctors who missed, ignored, or incompletely diagnosed her chronic illness.
There was the orthopedic surgeon who noted her hyperextended elbows but failed to check any of her other joints. The gastroenterologist who insisted on performing multiple scoping procedures but wouldn’t discuss how to manage her symptoms. The other surgeon who, after performing arthroscopy on her injured knee, yelled at her: “There is nothing wrong with your knee! You’re fine!” in a room full of people.
And then there was the rheumatologist who said: “Oh, you want something to be wrong with you?”
“No,” she replied, “I want an explanation. I want to keep working. I just want to know why these things keep happening to me.”
The medical frustration she experienced was especially difficult because, like her health care providers, Linda Bluestein has an MD after her name. She is a board-certified anesthesiologist and integrative medicine physician.
Along with the physically demanding schedule of medical practice, they must cope with what many call a “culture of invincibility” within medicine. Doctors are not supposed to get sick. In fact, the unwritten rule is presenteeism – to function without adequate food or sleep and to never prioritize their own self-care over their dedication to their patients.
Whether their conditions are visible, such as muscular dystrophy and multiple sclerosis, or invisible, such as fibromyalgia and mental illnesses – and now, long COVID – these doctors often meet significant stigma. They fight the assumption that they are less capable than their colleagues.
But they also experience an invaluable benefit: They gain firsthand knowledge of the patient experience, a profound understanding which, they say, enhances how they care for their own patients.
What it takes to become a doctor when you have a chronic condition
In short, it’s not easy.
Data from the 2018 National Health Interview Survey show that more than half of U.S. adults had at least one of several chronic conditions, including rheumatoid arthritis, asthma, diabetes, hypertension, and kidney problems. Nearly a third of respondents had more than one condition. But fewer than 5% of medical students and 3% of practicing physicians report having a chronic illness or disability, according to studies from 2019 and 2021.
While that could mean that fewer people with chronic illness enter medicine, cases also exist in which aspiring physicians with conditions were dissuaded from pursuing a career in medicine at all.
Amy Stenehjem, MD, a physical medicine and rehabilitation physician, is one of the exceptions. Diagnosed with several autoimmune-related conditions as a teenager and young adult, Dr. Stenehjem was determined to become a doctor. In her 20s, her health was relatively stable, and she was able to manage medical school and residency. Her training institutions agreed to provide some accommodations that helped her succeed.
“They let me build some flexibility into the training,” Dr. Stenehjem said. “In medical school, when I knew I wasn’t going to be able to do a particular specialty as a career, they let me work with an attending doctor that did not require a lot of on-call time during that particular rotation.”
Dr. Stenehjem specialized in chronic neck and back disorders, fibromyalgia, chronic fatigue syndrome (myalgic encephalomyelitis), and autoimmune-related diseases. She practiced for more than a decade. But in 2011, her condition spiraled. She couldn’t walk a few steps or even sit upright without experiencing dizziness and shortness of breath. She had debilitating fatigue and episodes of fever, rash, headaches, and joint pain.
It would take 7 years and more than 20 doctors to determine Dr. Stenehjem’s multiple diagnoses. In addition to her autoimmune diseases, she was diagnosed with postural orthostatic tachycardia syndrome, autoinflammatory periodic fever syndrome, Lyme disease, and reactivated Epstein-Barr infection.
While she suspects that her providers gave her more “leeway” because she was a physician, many did not show a deep understanding of the severity of her symptoms and the impact those symptoms had.
“When I was practicing, I really didn’t fully understand the impact chronic illness had on my patients,” Dr. Stenehjem said. “Things like chronic dizziness, headaches, fatigue, pain, or brain fog can be really hard to understand unless you’ve experienced these symptoms. When I got sick, I finally realized, ‘Oh my goodness, when a patient says they’re dealing with fatigue, this is not your normal, I’m-super-tired-from-being-on-call fatigue. This is I-can’t-get-out-of-bed fatigue.’ That’s what people with chronic illness often deal with on a daily basis.”
Treating the individual
Dr. Stenehjem was aware that her chronic illness would affect her medical career. For Jason Baker, MD, an endocrinologist at Weill Cornell Medicine, New York, it came as a shock. Dr. Baker was a third-year medical student when he experienced increased urination and rapid weight loss. It was only when friends pressed him to visit student health that a blood test revealed type 1 diabetes. Dr. Baker suddenly found himself lying in a hospital bed.
He remembers an attending physician who simply handed him a textbook on diabetic ketoacidosis (DKA) and a resident who informed him that he had kidney damage, which turned out to be untrue. Neither discussed the psychological issues from a frightening diagnosis that would require lifelong, daily management.
“There certainly could have been a bit more empathy from some of the people I dealt with early on,” he said.
Although his training gave him a stark picture of worst-case scenarios, Dr. Baker found that knowledge motivating. “I’d already seen patients come in who had diabetes complications,” Dr. Baker says. “I vowed to never ever get those complications. It was a good balance of fear and motivation.”
Dr. Baker had not planned to specialize in endocrinology, but he quickly realized that his personal diagnosis could help others. Now he often shares his experience with his patients who have diabetes, which he says makes them more comfortable discussing their own problems.
His approach, Dr. Baker explained, is to treat everyone as an individual. Trying to neatly classify patients with chronic illness is a common mistake he notices among physicians.
“There’s a lot of misunderstanding about type 1 versus type 2 [diabetes],” Dr. Baker said, “and trying to categorize people when sometimes people can’t be categorized. That’s really with any chronic condition; there’s no one size fits all.”
Managing his health is still a time-consuming task. At work, he needs breaks to eat, check his blood sugar, or take insulin. “During the workday seeing patients, I have to also remember that I’m a patient,” Dr. Baker said. “I have to be okay with prioritizing my own health. Otherwise I can’t help anybody.”
‘I am not the doctor for you’
Chronic diseases such as diabetes or hypertension are familiar to most doctors, and with good management, patients can usually function normally. When chronic conditions become disabling, however, attitudes in the medical field can change.
According to data from the Centers for Disease Control and Prevention and from studies, people with disabilities experience significant disparities and barriers to care. Some of this can be linked to social determinants of health. People with disabilities are more likely to be poor and to rely on Medicare and Medicaid for insurance coverage. But lack of training, unwillingness to provide accommodations, ignorance of legal requirements, and inaccurate assumptions among physicians also play a role.
These are themes that Lisa Iezzoni, MD, a professor of medicine at Harvard Medical School, Boston, has heard from hundreds of patients with disabilities during the more than 25 years that she has conducted research.
In late 2019, Dr. Iezzoni and coinvestigators fielded a national survey of 714 practicing physicians. Only 40.7% reported they were “very confident” that they could provide the same quality of care to patients with disabilities as they do for other patients. And only 56.5% “strongly agreed” that they welcomed these patients into their practices.
The survey was conducted through a series of small focus groups that Dr. Iezzoni held with physicians in 2018. These yielded views that were startling, and in some cases, overtly discriminatory:
- Doctors complained about the “burden” of caring for a patient with a disability.
- They lacked the time or equipment, such as accessible exam tables or weight scales.
- They admitted to inventing excuses for why appointments were not available or routine diagnostic tests were not performed.
- They described being fearful of lawsuits under the Americans with Disabilities Act.
The overall message was summed up in one doctor’s statement: “I am not the doctor for you.”
“Doctors are people too,” Dr. Iezzoni pointed out. “And so they reflect the same prejudices and stigmatized attitudes of the rest of the population. It might be implicit, so they might not be aware of it. [But] it might be explicit.”
Ableism in the medical field is all too familiar to Dr. Iezzoni. She was diagnosed with multiple sclerosis at age 26 during her first year at Harvard Medical School in the early 1980s. Despite symptom flare-ups, Dr. Iezzoni was able to graduate with her class, but many instructors and administrators had little interest in accommodating her physical limitations. In fact, several physicians discouraged her from continuing to train.
Unable to take call, run up flights of stairs, or stand for hours at a time, Dr. Iezzoni remembers being told by a senior surgeon that she shouldn’t become a doctor since she lacked the “most important quality,” which was “24/7 availability.” A hospital CEO informed her: “There are too many doctors in the country right now for us to worry about training a handicapped physician. If that means that some people get left by the wayside, so be it.”
Ultimately, Harvard Medical School declined to write Dr. Iezzoni a letter of recommendation for an internship. She would never practice medicine. “My career was just truncated from the start,” Dr. Iezzoni said. “It never happened because of discrimination.”
She later learned the legal term for her treatment: constructive dismissal.
“The medical school didn’t outright say, ‘Go away. We’re not allowing you to graduate.’ ” Dr. Iezzoni explained. “But they made my life so difficult that I did so voluntarily.”
Dr. Iezzoni graduated in 1984, before the passage of the ADA in 1990, and she refers to her experience as a “ghost from the past,” a historical reminder of how the legal landscape has changed – even though the tendency toward bias may not have.
The fight for inclusion
Zainub Dhanani, a fifth-year medical student at Stanford (Calif.) University, won’t forget an interview at one of the other schools to which she applied. The interviewer asked how she expected to be in a hospital all day if she had a chronic illness.
“Does it really make sense?” he wanted to know.
The question shocked her in the moment, but now she sees this type of bias as linked to the inequalities that many marginalized groups face in health care and beyond. That’s also why she believes physician-patients are crucial to improve the quality of care for people with chronic illness and other groups that face discrimination.
Who else, she wonders, could provide that “reaffirming” experience for patients or have that “unique edge” other than a provider who has navigated the same world?
Ms. Dhanani is the executive director and founder of Medical Students With Disability and Chronic Illness, an organization dedicated to empowering these students through advocacy, education, accessibility, and community. The group now has 19 chapters at medical schools across the country.
Ms. Dhanani said she has received excellent accommodations from Stanford for her own condition (which she prefers not to disclose), but all medical schools are not as responsive to students with various physical needs. Her organization offers support and resources to inform these future physicians about their options and rights.
“Disability justice is also racial justice,” Ms. Dhanani stressed. “It’s also environmental justice. It’s also gender and sexuality-based justice. Those compounded layers of biases lead to worse and worse levels of care. As a patient, it’s terrifying. And as a future physician, it’s tragic to know that this is something so pervasive and yet so under-addressed in medicine.”
Soldiering on
Unfortunately, for some physicians with chronic illness, there are no practical accommodations that could save their careers in clinical practice.
Dr. Stenehjem now works part-time as a health consultant, helping those with chronic illnesses navigate their health care systems.
Dr. Bluestein offers a similar coaching service to patients with Ehlers-Danlos syndrome (EDS) and other connective tissue and hypermobility disorders. Because of her own EDS, she can no longer practice as an anesthesiologist but instead opened an integrative pain management practice for patients with complex pain conditions..
She believes the idea that doctors are “invincible” needs to change. She recalls the time her former group practice told her in no uncertain terms to “never call in sick.”
The stories she hears from her current clients are similar to her own. She can empathize, knowing firsthand the physical and psychological damage these attitudes can cause.
“When I was at my worst physically, I was also at my worst psychologically,” said Dr. Bluestein. “We tend to think of them as separate, but they go hand in hand. If we can validate people’s experiences rather than disregard them, it has a positive forward cycle, as opposed to the reverse, which is what usually happens.”
A version of this article first appeared on Medscape.com.
We may need a new defense against new COVID variants
At the end of 2022, the European Medicines Agency’s Emergency Task Force warned European regulatory bodies, governments, and doctors that Antiviral drugs remain available but have many limitations. And, of course, there are still vaccines, which can significantly reduce (but not remove) the risk of severe cases and decrease the number of deaths, although they have lost the efficacy that they once had in countering the original virus.
Research therefore continues. Immunologists continue to search for new targets to synthesize broadly neutralizing monoclonal antibodies for treating or preventing the infection. These results could also lead to new vaccines that induce longer-lasting immunity not only against the thousands of subvariants and recombinant versions of SARS-CoV-2 being identified around the world, but also possibly against other coronaviruses that could emerge in the coming years. A study conducted at Stanford (Calif.) University and published in the journal Science Translational Medicine has afforded a glimmer of hope by discovering the broadly neutralizing efficacy of some antibodies produced by macaque monkeys in response to vaccination with AS03 (squalene) adjuvanted monovalent subunit vaccines.
The speed with which the virus continues to evolve has rendered the plan for annual vaccine updates, which initially was envisioned early in the pandemic, unfeasible for the time being. In 2020, scientists were considering updating vaccines annually based on the prevalent variants of the disease, similar to the approach to the flu. Perhaps that day will come, but in the meantime, laboratories are pursuing other routes: finding spike epitopes that are preserved more than others each time the virus evolves or focusing on other virus proteins that still manage to induce a neutralizing antibody response.
Eventually, artificial intelligence might be able to custom design monoclonal antibodies that are even more effective than natural ones. Or researchers could completely change tack and shift their attention to the host, rather than the virus itself.
This is the approach taken by one study published in Nature Microbiology, which starts from a simple assumption: SARS-CoV-2 continues to modify its spike protein because of the evolutionary pressure of the antibodies produced by millions of infected people, but all these variants and subvariants, both present and future, enter cells by binding – not solely, but mostly – to the ACE2 receptor. Instead of neutralizing the virus, why not try to block its access to the cells occupying its route in? In this way, we could also be ready for future emerging sarbecoviruses that will have a spike sequence that cannot yet be predicted.
Researchers at Rockefeller University, New York, have generated six human monoclonal antibodies that bind to the ACE2 receptor, rather than to the spike, preventing infection by all sarbecoviruses tested, even at low concentrations, including the virus that originated in Wuhan, China; the aggressive Delta variant; and various forms of Omicron.
The monoclonal antibodies bind to the ACE2 receptor at a part of the protein that is distal to the active enzyme portion that converts angiotensin and does not modify its expression on the cell surface. Therefore, no adverse effects are expected at this level. In animal models, these monoclonal antibodies succeed in stopping the infection. Moving into the clinical phase will be needed to find out if it will be possible to create products adapted to preventing and treating all SARS-CoV-2 variants, and perhaps also the next coronavirus large enough to spill over into a new epidemic that threatens the human race.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
At the end of 2022, the European Medicines Agency’s Emergency Task Force warned European regulatory bodies, governments, and doctors that Antiviral drugs remain available but have many limitations. And, of course, there are still vaccines, which can significantly reduce (but not remove) the risk of severe cases and decrease the number of deaths, although they have lost the efficacy that they once had in countering the original virus.
Research therefore continues. Immunologists continue to search for new targets to synthesize broadly neutralizing monoclonal antibodies for treating or preventing the infection. These results could also lead to new vaccines that induce longer-lasting immunity not only against the thousands of subvariants and recombinant versions of SARS-CoV-2 being identified around the world, but also possibly against other coronaviruses that could emerge in the coming years. A study conducted at Stanford (Calif.) University and published in the journal Science Translational Medicine has afforded a glimmer of hope by discovering the broadly neutralizing efficacy of some antibodies produced by macaque monkeys in response to vaccination with AS03 (squalene) adjuvanted monovalent subunit vaccines.
The speed with which the virus continues to evolve has rendered the plan for annual vaccine updates, which initially was envisioned early in the pandemic, unfeasible for the time being. In 2020, scientists were considering updating vaccines annually based on the prevalent variants of the disease, similar to the approach to the flu. Perhaps that day will come, but in the meantime, laboratories are pursuing other routes: finding spike epitopes that are preserved more than others each time the virus evolves or focusing on other virus proteins that still manage to induce a neutralizing antibody response.
Eventually, artificial intelligence might be able to custom design monoclonal antibodies that are even more effective than natural ones. Or researchers could completely change tack and shift their attention to the host, rather than the virus itself.
This is the approach taken by one study published in Nature Microbiology, which starts from a simple assumption: SARS-CoV-2 continues to modify its spike protein because of the evolutionary pressure of the antibodies produced by millions of infected people, but all these variants and subvariants, both present and future, enter cells by binding – not solely, but mostly – to the ACE2 receptor. Instead of neutralizing the virus, why not try to block its access to the cells occupying its route in? In this way, we could also be ready for future emerging sarbecoviruses that will have a spike sequence that cannot yet be predicted.
Researchers at Rockefeller University, New York, have generated six human monoclonal antibodies that bind to the ACE2 receptor, rather than to the spike, preventing infection by all sarbecoviruses tested, even at low concentrations, including the virus that originated in Wuhan, China; the aggressive Delta variant; and various forms of Omicron.
The monoclonal antibodies bind to the ACE2 receptor at a part of the protein that is distal to the active enzyme portion that converts angiotensin and does not modify its expression on the cell surface. Therefore, no adverse effects are expected at this level. In animal models, these monoclonal antibodies succeed in stopping the infection. Moving into the clinical phase will be needed to find out if it will be possible to create products adapted to preventing and treating all SARS-CoV-2 variants, and perhaps also the next coronavirus large enough to spill over into a new epidemic that threatens the human race.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
At the end of 2022, the European Medicines Agency’s Emergency Task Force warned European regulatory bodies, governments, and doctors that Antiviral drugs remain available but have many limitations. And, of course, there are still vaccines, which can significantly reduce (but not remove) the risk of severe cases and decrease the number of deaths, although they have lost the efficacy that they once had in countering the original virus.
Research therefore continues. Immunologists continue to search for new targets to synthesize broadly neutralizing monoclonal antibodies for treating or preventing the infection. These results could also lead to new vaccines that induce longer-lasting immunity not only against the thousands of subvariants and recombinant versions of SARS-CoV-2 being identified around the world, but also possibly against other coronaviruses that could emerge in the coming years. A study conducted at Stanford (Calif.) University and published in the journal Science Translational Medicine has afforded a glimmer of hope by discovering the broadly neutralizing efficacy of some antibodies produced by macaque monkeys in response to vaccination with AS03 (squalene) adjuvanted monovalent subunit vaccines.
The speed with which the virus continues to evolve has rendered the plan for annual vaccine updates, which initially was envisioned early in the pandemic, unfeasible for the time being. In 2020, scientists were considering updating vaccines annually based on the prevalent variants of the disease, similar to the approach to the flu. Perhaps that day will come, but in the meantime, laboratories are pursuing other routes: finding spike epitopes that are preserved more than others each time the virus evolves or focusing on other virus proteins that still manage to induce a neutralizing antibody response.
Eventually, artificial intelligence might be able to custom design monoclonal antibodies that are even more effective than natural ones. Or researchers could completely change tack and shift their attention to the host, rather than the virus itself.
This is the approach taken by one study published in Nature Microbiology, which starts from a simple assumption: SARS-CoV-2 continues to modify its spike protein because of the evolutionary pressure of the antibodies produced by millions of infected people, but all these variants and subvariants, both present and future, enter cells by binding – not solely, but mostly – to the ACE2 receptor. Instead of neutralizing the virus, why not try to block its access to the cells occupying its route in? In this way, we could also be ready for future emerging sarbecoviruses that will have a spike sequence that cannot yet be predicted.
Researchers at Rockefeller University, New York, have generated six human monoclonal antibodies that bind to the ACE2 receptor, rather than to the spike, preventing infection by all sarbecoviruses tested, even at low concentrations, including the virus that originated in Wuhan, China; the aggressive Delta variant; and various forms of Omicron.
The monoclonal antibodies bind to the ACE2 receptor at a part of the protein that is distal to the active enzyme portion that converts angiotensin and does not modify its expression on the cell surface. Therefore, no adverse effects are expected at this level. In animal models, these monoclonal antibodies succeed in stopping the infection. Moving into the clinical phase will be needed to find out if it will be possible to create products adapted to preventing and treating all SARS-CoV-2 variants, and perhaps also the next coronavirus large enough to spill over into a new epidemic that threatens the human race.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
Why doctors are disenchanted with Medicare
While physicians are getting less of a Medicare pay cut than they thought this year (Congress voted to cut Medicare payments by 2%, which was less than the expected 8.5%), Medicare still pays physicians only 80% of what many third-party insurers pay.
Moreover, those reimbursements are often slow to arrive, and the paperwork is burdensome. In fact, about 65% of doctors won’t accept new Medicare patients, down from 71% just 5 years ago, according to the Medscape Physician Compensation Report 2023.
Worse, inflation makes continuous cuts feel even steeper and trickles down to physicians and their patients as more and more doctors become disenchanted and consider dropping Medicare.
Medicare at a glance
Medicare pays physicians about 80% of the “reasonable charge” for covered services. At the same time, private insurers pay nearly double Medicare rates for hospital services.
The Medicare fee schedule is released each year. Physicians who accept Medicare can choose to be a “participating provider” by agreeing to the fee schedule and to not charging more than this amount. “Nonparticipating” providers can charge up to 15% more. Physicians can also opt out of Medicare entirely.
The earliest that physicians receive their payment is 14 days after electronic filing to 28 days after paper filing, but it often can take months.
Physicians lose an estimated 7.3% of Medicare claims to billing problems. With private insurers, an estimated 4.8% is lost.
In 2000, there were 50 million Medicare enrollees; it is projected that by 2050, there will be 87 million enrollees.
Why are doctors disenchanted?
“When Medicare started, the concept of the program was good,” said Rahul Gupta, MD, a geriatrician in Westport, Conn., and chief of internal medicine at St. Vincent’s Medical Center, Bridgeport, Conn. “However, over the years, with new developments in medicine and the explosion of the Medicare-eligible population, the program hasn’t kept up with coverages.” In addition, Medicare’s behemoth power as a government-run agency has ramifications that trickle down irrespective of a patient’s insurance carrier.
“Medicare sets the tone on price and reimbursement, and everyone follows suit,” Dr. Gupta said. “It’s a race to the bottom.”
“The program is great for patients when people need hospitalizations, skilled nursing, and physical therapy,” Dr. Gupta said. “But it’s not great about keeping people healthier and maintaining function via preventive treatments.” Many private insurers must become more adept at that too.
For instance, Dr. Gupta laments the lack of coverage for hearing aids, something his patients could greatly benefit from. Thanks to the Build Back Better bill, coverage of hearing aids will begin in 2024. But, again, most private insurers don’t cover hearing aids either. Some Medicare Advantage plans do.
Medicare doesn’t cover eye health (except for eye exams for diabetes patients), which is an issue for Daniel Laroche, MD, a glaucoma specialist and clinical associate professor of ophthalmology at Mount Sinai Medical Center, New York.
“I get paid less for Medicare patients by about 20% because of ‘lesser-of’ payments,” said Dr. Laroche. For example, as per Medicare, after patients meet their Part B deductible, they pay 20% of the Medicare-approved amount for glaucoma testing. “It would be nice to get the full amount for Medicare patients.”
“In addition, getting approvals for testing takes time and exhaustive amounts of paperwork, says Adeeti Gupta, MD, a gynecologist and founder of Walk In GYN Care in New York.
“Medicare only covers gynecologist visits every 2 years after the age of 65,” she said. “Any additional testing requires authorization, and Medicare doesn’t cover hormone replacement at all, which really makes me crazy. They will cover Viagra for men, but they won’t cover HRT, which prolongs life, reduces dementia, and prevents bone loss.”
While these three doctors find Medicare lacking in its coverage of their specialty, and their reimbursements are too low, many physicians also find fault regarding Medicare billing, which can put their patients at risk.
The problem with Medicare billing
Because claims are processed by Medicare administrative contractors, it can take about a month for the approval or denial process and for doctors to receive reimbursement.
Prior authorizations, especially with Medicare Advantage plans, are also problematic. For example, one 2022 study found that 18% of payment denials were for services that met coverage and billing rules.
Worse, all of this jockeying for coverage takes time. The average health care provider spends 16.4 hours a week on paperwork and on securing prior authorizations to cover services, according to the American Medical Association.
“A good 40% of my time is exclusively Medicare red tape paperwork,” Rahul Gupta says. “There’s a reason I spend 2-3 hours a night catching up on that stuff.”
Not only does this lead to burnout, but it also means that most physicians must hire an administrator to help with the paperwork.
In comparison, industry averages put the denial rate for all Medicare and private insurance claims at 20%.
“Excessive authorization controls required by health insurers are persistently responsible for serious harm to physician practices and patients when necessary medical care is delayed, denied, or disrupted in an attempt to increase profits,” Dr. Laroche said.
“Our office spends nearly 2 days per week on prior authorizations, creating costly administrative burdens.”
For Adeeti Gupta, the frustrations with Medicare have continued to mount. “We’re just at a dead end,” she said. “Authorizations keep getting denied, and the back-end paperwork is only increasing for us.”
Will more doctors opt out of Medicare?
When doctors don’t accept Medicare, it hurts the patients using it, especially patients who have selected either a Medicare Advantage plan or who become eligible for Medicare at age 65 only to find that fewer doctors take the government-sponsored insurance than in the past.
As of 2020, only 1% of nonpediatric physicians had formally opted out, per the Centers for Medicare & Medicaid Services. Psychiatrists account for the largest share of opt-outs (7.2%).
“Unfortunately, most doctors outside of hospital-based practices will reach a point when they can’t deal with Medicare paperwork, so they’ll stop taking it,” Rahul Gupta says.
A coalition of 120 physicians’ groups, including the American Medical Association, disputes that Medicare is paying a fair reimbursement rate to physicians and calls for an overhaul in how they adjust physician pay.
“Nothing much changes no matter how much the AMA shouts,” Rahul Gupta said in an interview.
What can doctors do
Prescription prices are another example of the challenges posed by Medicare. When prescriptions are denied because of Medicare’s medigap (or donut hole) program, which puts a cap on medication coverage, which was $4,660 in 2023, Dr. Gupta says she turns to alternative ways to fill them.
“I’ve been telling patients to pay out of pocket and use GoodRx, or we get medications compounded,” she said. “That’s cheaper. For example, for HRT, GoodRx can bring down the cost 40% to 50%.”
The American Medical Association as well as 150 other medical advocacy groups continue to urge Congress to work with the physician community to address the systematic problems within Medicare, especially reimbursement.
Despite the daily challenges, Rahul Gupta says he remains committed to caring for his patients.
“I want to care for the elderly, especially because they already have very few physicians to take care of them, and fortunately, I have a good practice with other coverages,” he said. “I can’t give up.”
A version of this article first appeared on Medscape.com.
While physicians are getting less of a Medicare pay cut than they thought this year (Congress voted to cut Medicare payments by 2%, which was less than the expected 8.5%), Medicare still pays physicians only 80% of what many third-party insurers pay.
Moreover, those reimbursements are often slow to arrive, and the paperwork is burdensome. In fact, about 65% of doctors won’t accept new Medicare patients, down from 71% just 5 years ago, according to the Medscape Physician Compensation Report 2023.
Worse, inflation makes continuous cuts feel even steeper and trickles down to physicians and their patients as more and more doctors become disenchanted and consider dropping Medicare.
Medicare at a glance
Medicare pays physicians about 80% of the “reasonable charge” for covered services. At the same time, private insurers pay nearly double Medicare rates for hospital services.
The Medicare fee schedule is released each year. Physicians who accept Medicare can choose to be a “participating provider” by agreeing to the fee schedule and to not charging more than this amount. “Nonparticipating” providers can charge up to 15% more. Physicians can also opt out of Medicare entirely.
The earliest that physicians receive their payment is 14 days after electronic filing to 28 days after paper filing, but it often can take months.
Physicians lose an estimated 7.3% of Medicare claims to billing problems. With private insurers, an estimated 4.8% is lost.
In 2000, there were 50 million Medicare enrollees; it is projected that by 2050, there will be 87 million enrollees.
Why are doctors disenchanted?
“When Medicare started, the concept of the program was good,” said Rahul Gupta, MD, a geriatrician in Westport, Conn., and chief of internal medicine at St. Vincent’s Medical Center, Bridgeport, Conn. “However, over the years, with new developments in medicine and the explosion of the Medicare-eligible population, the program hasn’t kept up with coverages.” In addition, Medicare’s behemoth power as a government-run agency has ramifications that trickle down irrespective of a patient’s insurance carrier.
“Medicare sets the tone on price and reimbursement, and everyone follows suit,” Dr. Gupta said. “It’s a race to the bottom.”
“The program is great for patients when people need hospitalizations, skilled nursing, and physical therapy,” Dr. Gupta said. “But it’s not great about keeping people healthier and maintaining function via preventive treatments.” Many private insurers must become more adept at that too.
For instance, Dr. Gupta laments the lack of coverage for hearing aids, something his patients could greatly benefit from. Thanks to the Build Back Better bill, coverage of hearing aids will begin in 2024. But, again, most private insurers don’t cover hearing aids either. Some Medicare Advantage plans do.
Medicare doesn’t cover eye health (except for eye exams for diabetes patients), which is an issue for Daniel Laroche, MD, a glaucoma specialist and clinical associate professor of ophthalmology at Mount Sinai Medical Center, New York.
“I get paid less for Medicare patients by about 20% because of ‘lesser-of’ payments,” said Dr. Laroche. For example, as per Medicare, after patients meet their Part B deductible, they pay 20% of the Medicare-approved amount for glaucoma testing. “It would be nice to get the full amount for Medicare patients.”
“In addition, getting approvals for testing takes time and exhaustive amounts of paperwork, says Adeeti Gupta, MD, a gynecologist and founder of Walk In GYN Care in New York.
“Medicare only covers gynecologist visits every 2 years after the age of 65,” she said. “Any additional testing requires authorization, and Medicare doesn’t cover hormone replacement at all, which really makes me crazy. They will cover Viagra for men, but they won’t cover HRT, which prolongs life, reduces dementia, and prevents bone loss.”
While these three doctors find Medicare lacking in its coverage of their specialty, and their reimbursements are too low, many physicians also find fault regarding Medicare billing, which can put their patients at risk.
The problem with Medicare billing
Because claims are processed by Medicare administrative contractors, it can take about a month for the approval or denial process and for doctors to receive reimbursement.
Prior authorizations, especially with Medicare Advantage plans, are also problematic. For example, one 2022 study found that 18% of payment denials were for services that met coverage and billing rules.
Worse, all of this jockeying for coverage takes time. The average health care provider spends 16.4 hours a week on paperwork and on securing prior authorizations to cover services, according to the American Medical Association.
“A good 40% of my time is exclusively Medicare red tape paperwork,” Rahul Gupta says. “There’s a reason I spend 2-3 hours a night catching up on that stuff.”
Not only does this lead to burnout, but it also means that most physicians must hire an administrator to help with the paperwork.
In comparison, industry averages put the denial rate for all Medicare and private insurance claims at 20%.
“Excessive authorization controls required by health insurers are persistently responsible for serious harm to physician practices and patients when necessary medical care is delayed, denied, or disrupted in an attempt to increase profits,” Dr. Laroche said.
“Our office spends nearly 2 days per week on prior authorizations, creating costly administrative burdens.”
For Adeeti Gupta, the frustrations with Medicare have continued to mount. “We’re just at a dead end,” she said. “Authorizations keep getting denied, and the back-end paperwork is only increasing for us.”
Will more doctors opt out of Medicare?
When doctors don’t accept Medicare, it hurts the patients using it, especially patients who have selected either a Medicare Advantage plan or who become eligible for Medicare at age 65 only to find that fewer doctors take the government-sponsored insurance than in the past.
As of 2020, only 1% of nonpediatric physicians had formally opted out, per the Centers for Medicare & Medicaid Services. Psychiatrists account for the largest share of opt-outs (7.2%).
“Unfortunately, most doctors outside of hospital-based practices will reach a point when they can’t deal with Medicare paperwork, so they’ll stop taking it,” Rahul Gupta says.
A coalition of 120 physicians’ groups, including the American Medical Association, disputes that Medicare is paying a fair reimbursement rate to physicians and calls for an overhaul in how they adjust physician pay.
“Nothing much changes no matter how much the AMA shouts,” Rahul Gupta said in an interview.
What can doctors do
Prescription prices are another example of the challenges posed by Medicare. When prescriptions are denied because of Medicare’s medigap (or donut hole) program, which puts a cap on medication coverage, which was $4,660 in 2023, Dr. Gupta says she turns to alternative ways to fill them.
“I’ve been telling patients to pay out of pocket and use GoodRx, or we get medications compounded,” she said. “That’s cheaper. For example, for HRT, GoodRx can bring down the cost 40% to 50%.”
The American Medical Association as well as 150 other medical advocacy groups continue to urge Congress to work with the physician community to address the systematic problems within Medicare, especially reimbursement.
Despite the daily challenges, Rahul Gupta says he remains committed to caring for his patients.
“I want to care for the elderly, especially because they already have very few physicians to take care of them, and fortunately, I have a good practice with other coverages,” he said. “I can’t give up.”
A version of this article first appeared on Medscape.com.
While physicians are getting less of a Medicare pay cut than they thought this year (Congress voted to cut Medicare payments by 2%, which was less than the expected 8.5%), Medicare still pays physicians only 80% of what many third-party insurers pay.
Moreover, those reimbursements are often slow to arrive, and the paperwork is burdensome. In fact, about 65% of doctors won’t accept new Medicare patients, down from 71% just 5 years ago, according to the Medscape Physician Compensation Report 2023.
Worse, inflation makes continuous cuts feel even steeper and trickles down to physicians and their patients as more and more doctors become disenchanted and consider dropping Medicare.
Medicare at a glance
Medicare pays physicians about 80% of the “reasonable charge” for covered services. At the same time, private insurers pay nearly double Medicare rates for hospital services.
The Medicare fee schedule is released each year. Physicians who accept Medicare can choose to be a “participating provider” by agreeing to the fee schedule and to not charging more than this amount. “Nonparticipating” providers can charge up to 15% more. Physicians can also opt out of Medicare entirely.
The earliest that physicians receive their payment is 14 days after electronic filing to 28 days after paper filing, but it often can take months.
Physicians lose an estimated 7.3% of Medicare claims to billing problems. With private insurers, an estimated 4.8% is lost.
In 2000, there were 50 million Medicare enrollees; it is projected that by 2050, there will be 87 million enrollees.
Why are doctors disenchanted?
“When Medicare started, the concept of the program was good,” said Rahul Gupta, MD, a geriatrician in Westport, Conn., and chief of internal medicine at St. Vincent’s Medical Center, Bridgeport, Conn. “However, over the years, with new developments in medicine and the explosion of the Medicare-eligible population, the program hasn’t kept up with coverages.” In addition, Medicare’s behemoth power as a government-run agency has ramifications that trickle down irrespective of a patient’s insurance carrier.
“Medicare sets the tone on price and reimbursement, and everyone follows suit,” Dr. Gupta said. “It’s a race to the bottom.”
“The program is great for patients when people need hospitalizations, skilled nursing, and physical therapy,” Dr. Gupta said. “But it’s not great about keeping people healthier and maintaining function via preventive treatments.” Many private insurers must become more adept at that too.
For instance, Dr. Gupta laments the lack of coverage for hearing aids, something his patients could greatly benefit from. Thanks to the Build Back Better bill, coverage of hearing aids will begin in 2024. But, again, most private insurers don’t cover hearing aids either. Some Medicare Advantage plans do.
Medicare doesn’t cover eye health (except for eye exams for diabetes patients), which is an issue for Daniel Laroche, MD, a glaucoma specialist and clinical associate professor of ophthalmology at Mount Sinai Medical Center, New York.
“I get paid less for Medicare patients by about 20% because of ‘lesser-of’ payments,” said Dr. Laroche. For example, as per Medicare, after patients meet their Part B deductible, they pay 20% of the Medicare-approved amount for glaucoma testing. “It would be nice to get the full amount for Medicare patients.”
“In addition, getting approvals for testing takes time and exhaustive amounts of paperwork, says Adeeti Gupta, MD, a gynecologist and founder of Walk In GYN Care in New York.
“Medicare only covers gynecologist visits every 2 years after the age of 65,” she said. “Any additional testing requires authorization, and Medicare doesn’t cover hormone replacement at all, which really makes me crazy. They will cover Viagra for men, but they won’t cover HRT, which prolongs life, reduces dementia, and prevents bone loss.”
While these three doctors find Medicare lacking in its coverage of their specialty, and their reimbursements are too low, many physicians also find fault regarding Medicare billing, which can put their patients at risk.
The problem with Medicare billing
Because claims are processed by Medicare administrative contractors, it can take about a month for the approval or denial process and for doctors to receive reimbursement.
Prior authorizations, especially with Medicare Advantage plans, are also problematic. For example, one 2022 study found that 18% of payment denials were for services that met coverage and billing rules.
Worse, all of this jockeying for coverage takes time. The average health care provider spends 16.4 hours a week on paperwork and on securing prior authorizations to cover services, according to the American Medical Association.
“A good 40% of my time is exclusively Medicare red tape paperwork,” Rahul Gupta says. “There’s a reason I spend 2-3 hours a night catching up on that stuff.”
Not only does this lead to burnout, but it also means that most physicians must hire an administrator to help with the paperwork.
In comparison, industry averages put the denial rate for all Medicare and private insurance claims at 20%.
“Excessive authorization controls required by health insurers are persistently responsible for serious harm to physician practices and patients when necessary medical care is delayed, denied, or disrupted in an attempt to increase profits,” Dr. Laroche said.
“Our office spends nearly 2 days per week on prior authorizations, creating costly administrative burdens.”
For Adeeti Gupta, the frustrations with Medicare have continued to mount. “We’re just at a dead end,” she said. “Authorizations keep getting denied, and the back-end paperwork is only increasing for us.”
Will more doctors opt out of Medicare?
When doctors don’t accept Medicare, it hurts the patients using it, especially patients who have selected either a Medicare Advantage plan or who become eligible for Medicare at age 65 only to find that fewer doctors take the government-sponsored insurance than in the past.
As of 2020, only 1% of nonpediatric physicians had formally opted out, per the Centers for Medicare & Medicaid Services. Psychiatrists account for the largest share of opt-outs (7.2%).
“Unfortunately, most doctors outside of hospital-based practices will reach a point when they can’t deal with Medicare paperwork, so they’ll stop taking it,” Rahul Gupta says.
A coalition of 120 physicians’ groups, including the American Medical Association, disputes that Medicare is paying a fair reimbursement rate to physicians and calls for an overhaul in how they adjust physician pay.
“Nothing much changes no matter how much the AMA shouts,” Rahul Gupta said in an interview.
What can doctors do
Prescription prices are another example of the challenges posed by Medicare. When prescriptions are denied because of Medicare’s medigap (or donut hole) program, which puts a cap on medication coverage, which was $4,660 in 2023, Dr. Gupta says she turns to alternative ways to fill them.
“I’ve been telling patients to pay out of pocket and use GoodRx, or we get medications compounded,” she said. “That’s cheaper. For example, for HRT, GoodRx can bring down the cost 40% to 50%.”
The American Medical Association as well as 150 other medical advocacy groups continue to urge Congress to work with the physician community to address the systematic problems within Medicare, especially reimbursement.
Despite the daily challenges, Rahul Gupta says he remains committed to caring for his patients.
“I want to care for the elderly, especially because they already have very few physicians to take care of them, and fortunately, I have a good practice with other coverages,” he said. “I can’t give up.”
A version of this article first appeared on Medscape.com.
Primary care’s per-person costs for addressing social needs not covered by federal funding
The costs of providing evidence-based interventions in primary care to address social needs far exceed current federal funding streams, say the authors of a new analysis.
A microsimulation analysis by Sanjay Basu, MD, PhD, with Clinical Product Development, Waymark Care, San Francisco, and colleagues found that, as primary care practices are being asked to screen for social needs, the cost of providing evidence-based interventions for these needs averaged $60 per member/person per month (PMPM) (95% confidence interval, $55-$65).
However, less than half ($27) of the $60 cost had existing federal financing in place to pay for it. Of the $60, $5 was for screening and referral.
The study results were published in JAMA Internal Medicine.
The researchers looked at key social needs areas and found major gaps between what interventions cost and what’s covered by federal payers. They demonstrate the gaps in four key areas. Many people in the analysis have more than one need:
- Food insecurity: Cost was $23 PMPM and the proportion borne by existing federal payers was 61.6%.
- Housing insecurity: Cost was $3 PMPM; proportion borne by federal payers was 45.6%.
- Transportation insecurity: Cost was $0.1 PMPM; proportion borne by federal payers was 27.8%.
- Community-based care coordination: Cost was $0.6 PMPM; proportion borne by federal payers is 6.4%.
Gaps varied by type of center
Primary care practices were grouped into federally qualified health centers; non-FQHC urban practices in high-poverty areas; non-FQHC rural practices in high-poverty areas; and practices in lower-poverty areas. Gaps varied among the groups.
While disproportionate funding was available to populations seen at FQHCs, populations seen at non-FQHC practices in high-poverty areas had larger funding gaps.
The study population consisted of 19,225 patients seen in primary care practices; data on social needs were pulled from the National Center for Health Statistics from 2015 to 2018.
Dr. Basu said in an interview with the journal’s deputy editor, Mitchell Katz, MD, that new sustainable revenue streams need to be identified to close the gap. Primary care physicians should not be charged with tasks such as researching the best housing programs and food benefits.
“I can’t imagine fitting this into my primary care appointments,” he said.
Is primary care the best setting for addressing these needs?
In an accompanying comment, Jenifer Clapp, MPA, with the Office of Ambulatory Care and Population Health, NYC Health + Hospitals, New York, and colleagues wrote that the study raises the question of whether the health care setting is the right place for addressing social needs. Some aspects have to be addressed in health care, such as asking about the home environment for a patient with environmentally triggered asthma.
“But how involved should health care professionals be in identifying needs unrelated to illness and solving those needs?” Ms. Clapp and colleagues asked.
They wrote that the health care sector in the United States must address these needs because in the United States, unlike in many European countries, “there is an insufficient social service sector to address the basic human needs of children and working-age adults.”
Eligible but not enrolled
Importantly, both the study authors and editorialists pointed out, in many cases, intervening doesn’t mean paying for the social services, but helping patients enroll in the services for which they already qualify.
The study authors wrote that among people who had food and housing needs, most met the criteria for federally funded programs, but had low enrollment for reasons including inadequate program capacity.
For example, 78% of people with housing needs were eligible for federal programs but only 24% were enrolled, and 95.6% of people with food needs were eligible for programs but only 70.2% were enrolled in programs like the Supplemental Nutrition and Assistance Program and Women, Infants and Children.
Commentary coauthor Nichola Davis, MD, also with NYC Health + Hospitals, said one thing they’ve done at NYC Health + Hospitals is partner with community-based organizations that provide food navigators so when patients screen positive for food insecurity they can then be seen by a food navigator to pinpoint appropriate programs.
The referral for those who indicate food insecurity is automatically generated by the electronic health system and appears on the after-visit summary.
“At the bare minimum, the patient would leave with a list of resources,” Dr. Davis said.
One place primary care providers can make a difference
Dr. Katz said that the $60 cost per person is much lower than that for a service such as an MRI.
“We should be able to achieve that,” he said.
Will Bleser, PhD, MSPH, assistant research director of health care transformation for social needs and health equity at the Duke-Margolis Center for Health Policy, Washington, said it’s exciting to see the per-person cost for social needs quantified.
He pointed to existing revenue options that have been underutilized.
Through Medicare, he noted, if you are part of a Medicare Advantage plan, there is a program implemented in 2020 called Special Supplemental Benefits for the Chronically Ill. “That authorizes Medicare Advantage plans to offer non–primarily health-related services through Medicare Advantage to individuals who meet certain chronic illness conditions.”
Non–primarily health-related services may include meals, transportation, and pest control, for example, the Centers for Medicare & Medicaid Services notes.
Also, within the shared-savings program of traditional Medicare, if an accountable care organization is providing quality care under the cost target and is reaping the savings, “you could use those bonuses to do things that you couldn’t do under the normal Medicare fee schedule like address social needs,” Dr. Bleser said.
Medicaid, he said, offers the most opportunities to address social needs through the health system. One policy mechanism within Medicaid is the Section 1115 Waiver, where states can propose to provide new services as long as they comply with the core rules of Medicaid and meet certain qualifications.
Avoiding checking boxes with no benefit to patients
Ms. Clapp and colleagues noted that whether health care professionals agree that social needs can or should be addressed in primary care, CMS will mandate social needs screening and reporting for all hospitalized adults starting in 2024. Additionally, the Joint Commission will require health care systems to gauge social needs and report on resources.
“We need to ensure that these mandates do not become administrative checkboxes that frustrate clinical staff and ratchet up health care costs with no benefit to patients,” they wrote.
Dr. Basu reported receiving personal fees from the University of California, Healthright360, Waymark and Collective Health outside the submitted work; he has a patent issued for a multimodel member outreach system; and a patent pending for operationalizing predicted changes in risk based on interventions. A coauthor reported grants from the North Carolina Department of Health and Human Services, Blue Cross Blue Shield of North Carolina, and personal fees from several nonprofit organizations outside the submitted work. Another coauthor reported personal fees from ZealCare outside the submitted work.
The costs of providing evidence-based interventions in primary care to address social needs far exceed current federal funding streams, say the authors of a new analysis.
A microsimulation analysis by Sanjay Basu, MD, PhD, with Clinical Product Development, Waymark Care, San Francisco, and colleagues found that, as primary care practices are being asked to screen for social needs, the cost of providing evidence-based interventions for these needs averaged $60 per member/person per month (PMPM) (95% confidence interval, $55-$65).
However, less than half ($27) of the $60 cost had existing federal financing in place to pay for it. Of the $60, $5 was for screening and referral.
The study results were published in JAMA Internal Medicine.
The researchers looked at key social needs areas and found major gaps between what interventions cost and what’s covered by federal payers. They demonstrate the gaps in four key areas. Many people in the analysis have more than one need:
- Food insecurity: Cost was $23 PMPM and the proportion borne by existing federal payers was 61.6%.
- Housing insecurity: Cost was $3 PMPM; proportion borne by federal payers was 45.6%.
- Transportation insecurity: Cost was $0.1 PMPM; proportion borne by federal payers was 27.8%.
- Community-based care coordination: Cost was $0.6 PMPM; proportion borne by federal payers is 6.4%.
Gaps varied by type of center
Primary care practices were grouped into federally qualified health centers; non-FQHC urban practices in high-poverty areas; non-FQHC rural practices in high-poverty areas; and practices in lower-poverty areas. Gaps varied among the groups.
While disproportionate funding was available to populations seen at FQHCs, populations seen at non-FQHC practices in high-poverty areas had larger funding gaps.
The study population consisted of 19,225 patients seen in primary care practices; data on social needs were pulled from the National Center for Health Statistics from 2015 to 2018.
Dr. Basu said in an interview with the journal’s deputy editor, Mitchell Katz, MD, that new sustainable revenue streams need to be identified to close the gap. Primary care physicians should not be charged with tasks such as researching the best housing programs and food benefits.
“I can’t imagine fitting this into my primary care appointments,” he said.
Is primary care the best setting for addressing these needs?
In an accompanying comment, Jenifer Clapp, MPA, with the Office of Ambulatory Care and Population Health, NYC Health + Hospitals, New York, and colleagues wrote that the study raises the question of whether the health care setting is the right place for addressing social needs. Some aspects have to be addressed in health care, such as asking about the home environment for a patient with environmentally triggered asthma.
“But how involved should health care professionals be in identifying needs unrelated to illness and solving those needs?” Ms. Clapp and colleagues asked.
They wrote that the health care sector in the United States must address these needs because in the United States, unlike in many European countries, “there is an insufficient social service sector to address the basic human needs of children and working-age adults.”
Eligible but not enrolled
Importantly, both the study authors and editorialists pointed out, in many cases, intervening doesn’t mean paying for the social services, but helping patients enroll in the services for which they already qualify.
The study authors wrote that among people who had food and housing needs, most met the criteria for federally funded programs, but had low enrollment for reasons including inadequate program capacity.
For example, 78% of people with housing needs were eligible for federal programs but only 24% were enrolled, and 95.6% of people with food needs were eligible for programs but only 70.2% were enrolled in programs like the Supplemental Nutrition and Assistance Program and Women, Infants and Children.
Commentary coauthor Nichola Davis, MD, also with NYC Health + Hospitals, said one thing they’ve done at NYC Health + Hospitals is partner with community-based organizations that provide food navigators so when patients screen positive for food insecurity they can then be seen by a food navigator to pinpoint appropriate programs.
The referral for those who indicate food insecurity is automatically generated by the electronic health system and appears on the after-visit summary.
“At the bare minimum, the patient would leave with a list of resources,” Dr. Davis said.
One place primary care providers can make a difference
Dr. Katz said that the $60 cost per person is much lower than that for a service such as an MRI.
“We should be able to achieve that,” he said.
Will Bleser, PhD, MSPH, assistant research director of health care transformation for social needs and health equity at the Duke-Margolis Center for Health Policy, Washington, said it’s exciting to see the per-person cost for social needs quantified.
He pointed to existing revenue options that have been underutilized.
Through Medicare, he noted, if you are part of a Medicare Advantage plan, there is a program implemented in 2020 called Special Supplemental Benefits for the Chronically Ill. “That authorizes Medicare Advantage plans to offer non–primarily health-related services through Medicare Advantage to individuals who meet certain chronic illness conditions.”
Non–primarily health-related services may include meals, transportation, and pest control, for example, the Centers for Medicare & Medicaid Services notes.
Also, within the shared-savings program of traditional Medicare, if an accountable care organization is providing quality care under the cost target and is reaping the savings, “you could use those bonuses to do things that you couldn’t do under the normal Medicare fee schedule like address social needs,” Dr. Bleser said.
Medicaid, he said, offers the most opportunities to address social needs through the health system. One policy mechanism within Medicaid is the Section 1115 Waiver, where states can propose to provide new services as long as they comply with the core rules of Medicaid and meet certain qualifications.
Avoiding checking boxes with no benefit to patients
Ms. Clapp and colleagues noted that whether health care professionals agree that social needs can or should be addressed in primary care, CMS will mandate social needs screening and reporting for all hospitalized adults starting in 2024. Additionally, the Joint Commission will require health care systems to gauge social needs and report on resources.
“We need to ensure that these mandates do not become administrative checkboxes that frustrate clinical staff and ratchet up health care costs with no benefit to patients,” they wrote.
Dr. Basu reported receiving personal fees from the University of California, Healthright360, Waymark and Collective Health outside the submitted work; he has a patent issued for a multimodel member outreach system; and a patent pending for operationalizing predicted changes in risk based on interventions. A coauthor reported grants from the North Carolina Department of Health and Human Services, Blue Cross Blue Shield of North Carolina, and personal fees from several nonprofit organizations outside the submitted work. Another coauthor reported personal fees from ZealCare outside the submitted work.
The costs of providing evidence-based interventions in primary care to address social needs far exceed current federal funding streams, say the authors of a new analysis.
A microsimulation analysis by Sanjay Basu, MD, PhD, with Clinical Product Development, Waymark Care, San Francisco, and colleagues found that, as primary care practices are being asked to screen for social needs, the cost of providing evidence-based interventions for these needs averaged $60 per member/person per month (PMPM) (95% confidence interval, $55-$65).
However, less than half ($27) of the $60 cost had existing federal financing in place to pay for it. Of the $60, $5 was for screening and referral.
The study results were published in JAMA Internal Medicine.
The researchers looked at key social needs areas and found major gaps between what interventions cost and what’s covered by federal payers. They demonstrate the gaps in four key areas. Many people in the analysis have more than one need:
- Food insecurity: Cost was $23 PMPM and the proportion borne by existing federal payers was 61.6%.
- Housing insecurity: Cost was $3 PMPM; proportion borne by federal payers was 45.6%.
- Transportation insecurity: Cost was $0.1 PMPM; proportion borne by federal payers was 27.8%.
- Community-based care coordination: Cost was $0.6 PMPM; proportion borne by federal payers is 6.4%.
Gaps varied by type of center
Primary care practices were grouped into federally qualified health centers; non-FQHC urban practices in high-poverty areas; non-FQHC rural practices in high-poverty areas; and practices in lower-poverty areas. Gaps varied among the groups.
While disproportionate funding was available to populations seen at FQHCs, populations seen at non-FQHC practices in high-poverty areas had larger funding gaps.
The study population consisted of 19,225 patients seen in primary care practices; data on social needs were pulled from the National Center for Health Statistics from 2015 to 2018.
Dr. Basu said in an interview with the journal’s deputy editor, Mitchell Katz, MD, that new sustainable revenue streams need to be identified to close the gap. Primary care physicians should not be charged with tasks such as researching the best housing programs and food benefits.
“I can’t imagine fitting this into my primary care appointments,” he said.
Is primary care the best setting for addressing these needs?
In an accompanying comment, Jenifer Clapp, MPA, with the Office of Ambulatory Care and Population Health, NYC Health + Hospitals, New York, and colleagues wrote that the study raises the question of whether the health care setting is the right place for addressing social needs. Some aspects have to be addressed in health care, such as asking about the home environment for a patient with environmentally triggered asthma.
“But how involved should health care professionals be in identifying needs unrelated to illness and solving those needs?” Ms. Clapp and colleagues asked.
They wrote that the health care sector in the United States must address these needs because in the United States, unlike in many European countries, “there is an insufficient social service sector to address the basic human needs of children and working-age adults.”
Eligible but not enrolled
Importantly, both the study authors and editorialists pointed out, in many cases, intervening doesn’t mean paying for the social services, but helping patients enroll in the services for which they already qualify.
The study authors wrote that among people who had food and housing needs, most met the criteria for federally funded programs, but had low enrollment for reasons including inadequate program capacity.
For example, 78% of people with housing needs were eligible for federal programs but only 24% were enrolled, and 95.6% of people with food needs were eligible for programs but only 70.2% were enrolled in programs like the Supplemental Nutrition and Assistance Program and Women, Infants and Children.
Commentary coauthor Nichola Davis, MD, also with NYC Health + Hospitals, said one thing they’ve done at NYC Health + Hospitals is partner with community-based organizations that provide food navigators so when patients screen positive for food insecurity they can then be seen by a food navigator to pinpoint appropriate programs.
The referral for those who indicate food insecurity is automatically generated by the electronic health system and appears on the after-visit summary.
“At the bare minimum, the patient would leave with a list of resources,” Dr. Davis said.
One place primary care providers can make a difference
Dr. Katz said that the $60 cost per person is much lower than that for a service such as an MRI.
“We should be able to achieve that,” he said.
Will Bleser, PhD, MSPH, assistant research director of health care transformation for social needs and health equity at the Duke-Margolis Center for Health Policy, Washington, said it’s exciting to see the per-person cost for social needs quantified.
He pointed to existing revenue options that have been underutilized.
Through Medicare, he noted, if you are part of a Medicare Advantage plan, there is a program implemented in 2020 called Special Supplemental Benefits for the Chronically Ill. “That authorizes Medicare Advantage plans to offer non–primarily health-related services through Medicare Advantage to individuals who meet certain chronic illness conditions.”
Non–primarily health-related services may include meals, transportation, and pest control, for example, the Centers for Medicare & Medicaid Services notes.
Also, within the shared-savings program of traditional Medicare, if an accountable care organization is providing quality care under the cost target and is reaping the savings, “you could use those bonuses to do things that you couldn’t do under the normal Medicare fee schedule like address social needs,” Dr. Bleser said.
Medicaid, he said, offers the most opportunities to address social needs through the health system. One policy mechanism within Medicaid is the Section 1115 Waiver, where states can propose to provide new services as long as they comply with the core rules of Medicaid and meet certain qualifications.
Avoiding checking boxes with no benefit to patients
Ms. Clapp and colleagues noted that whether health care professionals agree that social needs can or should be addressed in primary care, CMS will mandate social needs screening and reporting for all hospitalized adults starting in 2024. Additionally, the Joint Commission will require health care systems to gauge social needs and report on resources.
“We need to ensure that these mandates do not become administrative checkboxes that frustrate clinical staff and ratchet up health care costs with no benefit to patients,” they wrote.
Dr. Basu reported receiving personal fees from the University of California, Healthright360, Waymark and Collective Health outside the submitted work; he has a patent issued for a multimodel member outreach system; and a patent pending for operationalizing predicted changes in risk based on interventions. A coauthor reported grants from the North Carolina Department of Health and Human Services, Blue Cross Blue Shield of North Carolina, and personal fees from several nonprofit organizations outside the submitted work. Another coauthor reported personal fees from ZealCare outside the submitted work.
FROM JAMA INTERNAL MEDICINE
Enthesitis, arthritis, tenosynovitis linked to dupilumab use for atopic dermatitis
Around 5% of patients treated with dupilumab (Dupixent) for moderate-to-severe atopic dermatitis experience musculoskeletal (MSK) symptoms, according to the results of a descriptive study.
The main MSK symptom seen in the observational cohort was enthesitis, but some patients also experienced arthritis and tenosynovitis a median of 17 weeks after starting dupilumab treatment. Together these symptoms represent a new MSK syndrome, say researchers from the United Kingdom.
“The pattern of MSK symptoms and signs is characteristic of psoriatic arthritis/peripheral spondyloarthritis,” Bruce Kirkham, MD, and collaborators report in Arthritis & Rheumatology.
“We started a few years ago and have been following the patients for quite a long time,” Dr. Kirkham, a consultant rheumatologist at Guy’s and St. Thomas’ NHS Foundation Trust, London, told this news organization.
“We’re still seeing patients with the same type of syndrome presenting occasionally. It’s not a very common adverse event, but we think it continues,” he observed.
“Most of them don’t have very severe problems, and a lot of them can be treated with quite simple drugs or, alternatively, reducing the frequency of the injection,” Dr. Kirkham added.
Characterizing the MSK symptoms
Of 470 patients with atopic dermatitis who started treatment with dupilumab at Guy’s and St. Thomas’ NHS Foundation Trust between October 2018 and February 2021, 36 (7.65%) developed rheumatic symptoms and were referred to the rheumatology department. These individuals had their family history assessed and thorough MSK evaluations, which included antibody and inflammatory markers, ultrasound of the peripheral small joints, and MRI of the large joints and spine.
A total of 26 (5.5%) patients – 14 of whom were male – had inflammatory enthesitis, arthritis, and/or tenosynovitis. Of the others, seven had osteoarthritis and three had degenerative spine disease.
Enthesitis was the most common finding in those with rheumatic symptoms, occurring on its own in 11 patients, with arthritis in three patients, and tenosynovitis in two patients.
These symptoms appeared 2-48 weeks after starting dupilumab treatment and were categorized as mild in 16 (61%) cases, moderate in six cases, and severe in four cases.
No specific predictors of the MSK symptoms seen were noted. Patient age, sex, duration of their atopic dermatitis, or how their skin condition had been previously treated did not help identify those who might develop rheumatic problems.
Conservative management approach
All patients had “outstanding” responses to treatment, Dr. Kirkham noted: The mean Eczema Area and Severity Index score before dupilumab treatment was 21, falling to 4.2 with treatment, indicating a mean 80% improvement.
Co-author Joseph Nathan, MBChB, of London North West Healthcare NHS Trust, who collaborated on the research while working within Dr. Kirkham’s group, said separately: “The concern that patients have is that when they start a medication and develop a side effect is that the medication is going to be stopped.”
Clinicians treating the patients took a conservative approach, prescribing NSAIDs such as cyclooxygenase-2 inhibitors or altering the frequency with which dupilumab was given.
With this approach, MSK symptoms resolved in 15 patients who remained on treatment and in seven who had to stop dupilumab. There were four patients, however, who had unresolved symptoms even once dupilumab treatment had been stopped.
Altering the local cytokine balance
Dupilumab is a monoclonal antibody that binds to the alpha subunit of the interleukin-4 receptor. This results in blocking the function of not only IL-4 but also IL-13.
Dr. Kirkham and colleagues think this might not only alter the balance of cytokines in the skin but also in the joints and entheses with IL-17, IL-23, or even tumor necrosis factor playing a possible role. Another thought is that many circulating T-cells in the skin move to the joints and entheses to trigger symptoms.
IL-13 inhibition does seem to be important, as another British research team, from the Centre for Epidemiology Versus Arthritis at the University of Manchester (England), has found.
At the recent annual meeting of the British Society for Rheumatology, Sizheng Steven Zhao, MBChB, PhD, and colleagues reported that among people who carried a genetic variant predisposing them to having low IL-13 function, there was a higher risk for inflammatory diseases such as psoriatic arthritis and other spondyloarthropathy-related diseases.
Indeed, when the single nucleotide polymorphism rs20541 was present, the odds for having psoriatic arthritis and psoriasis were higher than when it was not.
The findings are consistent with the idea that IL-4 and IL-13 may be acting as a restraint towards MSK diseases in some patients, Dr. Zhao and co-authors suggest.
“The genetic data supports what [Dr. Kirkham and team] have said from a mechanistic point of view,” Dr. Zhao said in an interview. “What you’re observing has a genetic basis.”
Dermatology perspective
Approved by the U.S. Food and Drug Administration in 2017, dupilumab has since been hailed as a “breakthrough” in atopic dermatitis treatment. Given as a subcutaneous injection every 2 weeks, it provides a much-needed option for people who have moderate-to-severe disease and have tried other available treatments, including corticosteroids.
Dupilumab has since also been approved for asthma, chronic sinusitis with nasal polyposis, eosinophilic esophagitis, and prurigo nodularis and is used off-label for other skin conditions such as contact dermatitis, chronic spontaneous urticaria, and alopecia areata.
“Dupilumab, like a lot of medications for atopic dermatitis, is a relatively new drug, and we are still learning about its safety,” Joel M. Gelfand, MD, MSCE, of the University of Pennsylvania Perelman School of Medicine, Philadelphia, told this news organization.
“Inflammatory arthritis has been reported in patients treated with dupilumab, and this new study provides some useful estimates,” added Dr. Gelfand, who is a professor of dermatology and epidemiology and directs the Psoriasis and Phototherapy Treatment Center, Philadelphia.
“There was no control group,” Dr. Gelfand said, so “a causal relationship cannot be well established based on these data alone. The mechanism is not known but may result from a shifting of the immune system.”
Dr. Zhao observed: “We don’t know what the natural history of these adverse events is. We don’t know if stopping the drug early will prevent long-term adverse events. So, we don’t know if people will ultimately develop permanent psoriatic arthritis if we don’t intervene quick enough when we observe an adverse event.”
Being aware of the possibility of rheumatic side effects occurring with dupilumab and similar agents is key, Dr. Gelfand and Dr. Kirkham both said independently.
“I have personally seen this entity in my practice,” Dr. Gelfand said. “It is important to clinicians prescribing dupilumab to alert patients about this potential side effect and ask about joint symptoms in follow-up.”
Dr. Kirkham said: “Prescribers need to be aware of it, because up until now it’s been just very vaguely discussed as sort of aches and pains, arthralgias, and it’s a much more specific of a kind of syndrome of enthesitis, arthritis, tenosynovitis – a little like psoriatic arthritis.”
Not everyone has come across these side effects, however, as Steven Daveluy, MD, associate professor and dermatology program director at Wayne State University, Detroit, said in an interview.
“This article and the other case series both noted the musculoskeletal symptoms occurred in about 5% of patients, which surprised me since I haven’t seen it in my practice and have enough patients being treated with dupilumab that I would expect to see a case at that rate,” Dr. Daveluy said.
“The majority of cases are mild and respond to treatment with anti-inflammatories like naproxen, which is available over the counter. It’s likely that patients with a mild case could simply treat their pain with naproxen that’s already in their medicine cabinet until it resolves, never bringing it to the doctor’s attention,” he suggested.
“Dupilumab is still a safe and effective medication that can change the lives of patients suffering from atopic dermatitis,” he said.
“Awareness of this potential side effect can help dermatologists recognize it early and work together with patients to determine the best course of action.”
All research mentioned in this article was independently supported. Dr. Kirkham, Mr. Nathan, Dr. Zhao, and Dr. Daveluy report no relevant financial relationships. Dr. Gelfand has served as a consultant for numerous pharmaceutical companies and receives research grants from Amgen, Boehringer Ingelheim, and Pfizer. He is a co-patent holder of resiquimod for treatment of cutaneous T-cell lymphoma.
A version of this article first appeared on Medscape.com.
Around 5% of patients treated with dupilumab (Dupixent) for moderate-to-severe atopic dermatitis experience musculoskeletal (MSK) symptoms, according to the results of a descriptive study.
The main MSK symptom seen in the observational cohort was enthesitis, but some patients also experienced arthritis and tenosynovitis a median of 17 weeks after starting dupilumab treatment. Together these symptoms represent a new MSK syndrome, say researchers from the United Kingdom.
“The pattern of MSK symptoms and signs is characteristic of psoriatic arthritis/peripheral spondyloarthritis,” Bruce Kirkham, MD, and collaborators report in Arthritis & Rheumatology.
“We started a few years ago and have been following the patients for quite a long time,” Dr. Kirkham, a consultant rheumatologist at Guy’s and St. Thomas’ NHS Foundation Trust, London, told this news organization.
“We’re still seeing patients with the same type of syndrome presenting occasionally. It’s not a very common adverse event, but we think it continues,” he observed.
“Most of them don’t have very severe problems, and a lot of them can be treated with quite simple drugs or, alternatively, reducing the frequency of the injection,” Dr. Kirkham added.
Characterizing the MSK symptoms
Of 470 patients with atopic dermatitis who started treatment with dupilumab at Guy’s and St. Thomas’ NHS Foundation Trust between October 2018 and February 2021, 36 (7.65%) developed rheumatic symptoms and were referred to the rheumatology department. These individuals had their family history assessed and thorough MSK evaluations, which included antibody and inflammatory markers, ultrasound of the peripheral small joints, and MRI of the large joints and spine.
A total of 26 (5.5%) patients – 14 of whom were male – had inflammatory enthesitis, arthritis, and/or tenosynovitis. Of the others, seven had osteoarthritis and three had degenerative spine disease.
Enthesitis was the most common finding in those with rheumatic symptoms, occurring on its own in 11 patients, with arthritis in three patients, and tenosynovitis in two patients.
These symptoms appeared 2-48 weeks after starting dupilumab treatment and were categorized as mild in 16 (61%) cases, moderate in six cases, and severe in four cases.
No specific predictors of the MSK symptoms seen were noted. Patient age, sex, duration of their atopic dermatitis, or how their skin condition had been previously treated did not help identify those who might develop rheumatic problems.
Conservative management approach
All patients had “outstanding” responses to treatment, Dr. Kirkham noted: The mean Eczema Area and Severity Index score before dupilumab treatment was 21, falling to 4.2 with treatment, indicating a mean 80% improvement.
Co-author Joseph Nathan, MBChB, of London North West Healthcare NHS Trust, who collaborated on the research while working within Dr. Kirkham’s group, said separately: “The concern that patients have is that when they start a medication and develop a side effect is that the medication is going to be stopped.”
Clinicians treating the patients took a conservative approach, prescribing NSAIDs such as cyclooxygenase-2 inhibitors or altering the frequency with which dupilumab was given.
With this approach, MSK symptoms resolved in 15 patients who remained on treatment and in seven who had to stop dupilumab. There were four patients, however, who had unresolved symptoms even once dupilumab treatment had been stopped.
Altering the local cytokine balance
Dupilumab is a monoclonal antibody that binds to the alpha subunit of the interleukin-4 receptor. This results in blocking the function of not only IL-4 but also IL-13.
Dr. Kirkham and colleagues think this might not only alter the balance of cytokines in the skin but also in the joints and entheses with IL-17, IL-23, or even tumor necrosis factor playing a possible role. Another thought is that many circulating T-cells in the skin move to the joints and entheses to trigger symptoms.
IL-13 inhibition does seem to be important, as another British research team, from the Centre for Epidemiology Versus Arthritis at the University of Manchester (England), has found.
At the recent annual meeting of the British Society for Rheumatology, Sizheng Steven Zhao, MBChB, PhD, and colleagues reported that among people who carried a genetic variant predisposing them to having low IL-13 function, there was a higher risk for inflammatory diseases such as psoriatic arthritis and other spondyloarthropathy-related diseases.
Indeed, when the single nucleotide polymorphism rs20541 was present, the odds for having psoriatic arthritis and psoriasis were higher than when it was not.
The findings are consistent with the idea that IL-4 and IL-13 may be acting as a restraint towards MSK diseases in some patients, Dr. Zhao and co-authors suggest.
“The genetic data supports what [Dr. Kirkham and team] have said from a mechanistic point of view,” Dr. Zhao said in an interview. “What you’re observing has a genetic basis.”
Dermatology perspective
Approved by the U.S. Food and Drug Administration in 2017, dupilumab has since been hailed as a “breakthrough” in atopic dermatitis treatment. Given as a subcutaneous injection every 2 weeks, it provides a much-needed option for people who have moderate-to-severe disease and have tried other available treatments, including corticosteroids.
Dupilumab has since also been approved for asthma, chronic sinusitis with nasal polyposis, eosinophilic esophagitis, and prurigo nodularis and is used off-label for other skin conditions such as contact dermatitis, chronic spontaneous urticaria, and alopecia areata.
“Dupilumab, like a lot of medications for atopic dermatitis, is a relatively new drug, and we are still learning about its safety,” Joel M. Gelfand, MD, MSCE, of the University of Pennsylvania Perelman School of Medicine, Philadelphia, told this news organization.
“Inflammatory arthritis has been reported in patients treated with dupilumab, and this new study provides some useful estimates,” added Dr. Gelfand, who is a professor of dermatology and epidemiology and directs the Psoriasis and Phototherapy Treatment Center, Philadelphia.
“There was no control group,” Dr. Gelfand said, so “a causal relationship cannot be well established based on these data alone. The mechanism is not known but may result from a shifting of the immune system.”
Dr. Zhao observed: “We don’t know what the natural history of these adverse events is. We don’t know if stopping the drug early will prevent long-term adverse events. So, we don’t know if people will ultimately develop permanent psoriatic arthritis if we don’t intervene quick enough when we observe an adverse event.”
Being aware of the possibility of rheumatic side effects occurring with dupilumab and similar agents is key, Dr. Gelfand and Dr. Kirkham both said independently.
“I have personally seen this entity in my practice,” Dr. Gelfand said. “It is important to clinicians prescribing dupilumab to alert patients about this potential side effect and ask about joint symptoms in follow-up.”
Dr. Kirkham said: “Prescribers need to be aware of it, because up until now it’s been just very vaguely discussed as sort of aches and pains, arthralgias, and it’s a much more specific of a kind of syndrome of enthesitis, arthritis, tenosynovitis – a little like psoriatic arthritis.”
Not everyone has come across these side effects, however, as Steven Daveluy, MD, associate professor and dermatology program director at Wayne State University, Detroit, said in an interview.
“This article and the other case series both noted the musculoskeletal symptoms occurred in about 5% of patients, which surprised me since I haven’t seen it in my practice and have enough patients being treated with dupilumab that I would expect to see a case at that rate,” Dr. Daveluy said.
“The majority of cases are mild and respond to treatment with anti-inflammatories like naproxen, which is available over the counter. It’s likely that patients with a mild case could simply treat their pain with naproxen that’s already in their medicine cabinet until it resolves, never bringing it to the doctor’s attention,” he suggested.
“Dupilumab is still a safe and effective medication that can change the lives of patients suffering from atopic dermatitis,” he said.
“Awareness of this potential side effect can help dermatologists recognize it early and work together with patients to determine the best course of action.”
All research mentioned in this article was independently supported. Dr. Kirkham, Mr. Nathan, Dr. Zhao, and Dr. Daveluy report no relevant financial relationships. Dr. Gelfand has served as a consultant for numerous pharmaceutical companies and receives research grants from Amgen, Boehringer Ingelheim, and Pfizer. He is a co-patent holder of resiquimod for treatment of cutaneous T-cell lymphoma.
A version of this article first appeared on Medscape.com.
Around 5% of patients treated with dupilumab (Dupixent) for moderate-to-severe atopic dermatitis experience musculoskeletal (MSK) symptoms, according to the results of a descriptive study.
The main MSK symptom seen in the observational cohort was enthesitis, but some patients also experienced arthritis and tenosynovitis a median of 17 weeks after starting dupilumab treatment. Together these symptoms represent a new MSK syndrome, say researchers from the United Kingdom.
“The pattern of MSK symptoms and signs is characteristic of psoriatic arthritis/peripheral spondyloarthritis,” Bruce Kirkham, MD, and collaborators report in Arthritis & Rheumatology.
“We started a few years ago and have been following the patients for quite a long time,” Dr. Kirkham, a consultant rheumatologist at Guy’s and St. Thomas’ NHS Foundation Trust, London, told this news organization.
“We’re still seeing patients with the same type of syndrome presenting occasionally. It’s not a very common adverse event, but we think it continues,” he observed.
“Most of them don’t have very severe problems, and a lot of them can be treated with quite simple drugs or, alternatively, reducing the frequency of the injection,” Dr. Kirkham added.
Characterizing the MSK symptoms
Of 470 patients with atopic dermatitis who started treatment with dupilumab at Guy’s and St. Thomas’ NHS Foundation Trust between October 2018 and February 2021, 36 (7.65%) developed rheumatic symptoms and were referred to the rheumatology department. These individuals had their family history assessed and thorough MSK evaluations, which included antibody and inflammatory markers, ultrasound of the peripheral small joints, and MRI of the large joints and spine.
A total of 26 (5.5%) patients – 14 of whom were male – had inflammatory enthesitis, arthritis, and/or tenosynovitis. Of the others, seven had osteoarthritis and three had degenerative spine disease.
Enthesitis was the most common finding in those with rheumatic symptoms, occurring on its own in 11 patients, with arthritis in three patients, and tenosynovitis in two patients.
These symptoms appeared 2-48 weeks after starting dupilumab treatment and were categorized as mild in 16 (61%) cases, moderate in six cases, and severe in four cases.
No specific predictors of the MSK symptoms seen were noted. Patient age, sex, duration of their atopic dermatitis, or how their skin condition had been previously treated did not help identify those who might develop rheumatic problems.
Conservative management approach
All patients had “outstanding” responses to treatment, Dr. Kirkham noted: The mean Eczema Area and Severity Index score before dupilumab treatment was 21, falling to 4.2 with treatment, indicating a mean 80% improvement.
Co-author Joseph Nathan, MBChB, of London North West Healthcare NHS Trust, who collaborated on the research while working within Dr. Kirkham’s group, said separately: “The concern that patients have is that when they start a medication and develop a side effect is that the medication is going to be stopped.”
Clinicians treating the patients took a conservative approach, prescribing NSAIDs such as cyclooxygenase-2 inhibitors or altering the frequency with which dupilumab was given.
With this approach, MSK symptoms resolved in 15 patients who remained on treatment and in seven who had to stop dupilumab. There were four patients, however, who had unresolved symptoms even once dupilumab treatment had been stopped.
Altering the local cytokine balance
Dupilumab is a monoclonal antibody that binds to the alpha subunit of the interleukin-4 receptor. This results in blocking the function of not only IL-4 but also IL-13.
Dr. Kirkham and colleagues think this might not only alter the balance of cytokines in the skin but also in the joints and entheses with IL-17, IL-23, or even tumor necrosis factor playing a possible role. Another thought is that many circulating T-cells in the skin move to the joints and entheses to trigger symptoms.
IL-13 inhibition does seem to be important, as another British research team, from the Centre for Epidemiology Versus Arthritis at the University of Manchester (England), has found.
At the recent annual meeting of the British Society for Rheumatology, Sizheng Steven Zhao, MBChB, PhD, and colleagues reported that among people who carried a genetic variant predisposing them to having low IL-13 function, there was a higher risk for inflammatory diseases such as psoriatic arthritis and other spondyloarthropathy-related diseases.
Indeed, when the single nucleotide polymorphism rs20541 was present, the odds for having psoriatic arthritis and psoriasis were higher than when it was not.
The findings are consistent with the idea that IL-4 and IL-13 may be acting as a restraint towards MSK diseases in some patients, Dr. Zhao and co-authors suggest.
“The genetic data supports what [Dr. Kirkham and team] have said from a mechanistic point of view,” Dr. Zhao said in an interview. “What you’re observing has a genetic basis.”
Dermatology perspective
Approved by the U.S. Food and Drug Administration in 2017, dupilumab has since been hailed as a “breakthrough” in atopic dermatitis treatment. Given as a subcutaneous injection every 2 weeks, it provides a much-needed option for people who have moderate-to-severe disease and have tried other available treatments, including corticosteroids.
Dupilumab has since also been approved for asthma, chronic sinusitis with nasal polyposis, eosinophilic esophagitis, and prurigo nodularis and is used off-label for other skin conditions such as contact dermatitis, chronic spontaneous urticaria, and alopecia areata.
“Dupilumab, like a lot of medications for atopic dermatitis, is a relatively new drug, and we are still learning about its safety,” Joel M. Gelfand, MD, MSCE, of the University of Pennsylvania Perelman School of Medicine, Philadelphia, told this news organization.
“Inflammatory arthritis has been reported in patients treated with dupilumab, and this new study provides some useful estimates,” added Dr. Gelfand, who is a professor of dermatology and epidemiology and directs the Psoriasis and Phototherapy Treatment Center, Philadelphia.
“There was no control group,” Dr. Gelfand said, so “a causal relationship cannot be well established based on these data alone. The mechanism is not known but may result from a shifting of the immune system.”
Dr. Zhao observed: “We don’t know what the natural history of these adverse events is. We don’t know if stopping the drug early will prevent long-term adverse events. So, we don’t know if people will ultimately develop permanent psoriatic arthritis if we don’t intervene quick enough when we observe an adverse event.”
Being aware of the possibility of rheumatic side effects occurring with dupilumab and similar agents is key, Dr. Gelfand and Dr. Kirkham both said independently.
“I have personally seen this entity in my practice,” Dr. Gelfand said. “It is important to clinicians prescribing dupilumab to alert patients about this potential side effect and ask about joint symptoms in follow-up.”
Dr. Kirkham said: “Prescribers need to be aware of it, because up until now it’s been just very vaguely discussed as sort of aches and pains, arthralgias, and it’s a much more specific of a kind of syndrome of enthesitis, arthritis, tenosynovitis – a little like psoriatic arthritis.”
Not everyone has come across these side effects, however, as Steven Daveluy, MD, associate professor and dermatology program director at Wayne State University, Detroit, said in an interview.
“This article and the other case series both noted the musculoskeletal symptoms occurred in about 5% of patients, which surprised me since I haven’t seen it in my practice and have enough patients being treated with dupilumab that I would expect to see a case at that rate,” Dr. Daveluy said.
“The majority of cases are mild and respond to treatment with anti-inflammatories like naproxen, which is available over the counter. It’s likely that patients with a mild case could simply treat their pain with naproxen that’s already in their medicine cabinet until it resolves, never bringing it to the doctor’s attention,” he suggested.
“Dupilumab is still a safe and effective medication that can change the lives of patients suffering from atopic dermatitis,” he said.
“Awareness of this potential side effect can help dermatologists recognize it early and work together with patients to determine the best course of action.”
All research mentioned in this article was independently supported. Dr. Kirkham, Mr. Nathan, Dr. Zhao, and Dr. Daveluy report no relevant financial relationships. Dr. Gelfand has served as a consultant for numerous pharmaceutical companies and receives research grants from Amgen, Boehringer Ingelheim, and Pfizer. He is a co-patent holder of resiquimod for treatment of cutaneous T-cell lymphoma.
A version of this article first appeared on Medscape.com.
FROM ARTHRITIS & RHEUMATOLOGY