User login
VIDEO: U.S. hypertension guidelines reset threshold to 130/80 mm Hg
ANAHEIM, CALIF. – Thirty million Americans became hypertensive overnight on Nov. 13 with the introduction of new high blood pressure guidelines from the American College of Cardiology and American Heart Association.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, a change that jumps the U.S. adult prevalence of hypertension from roughly 32% to 46%. Nearly half of all U.S. adults now have hypertension, bringing the total national hypertensive population to a staggering 103 million.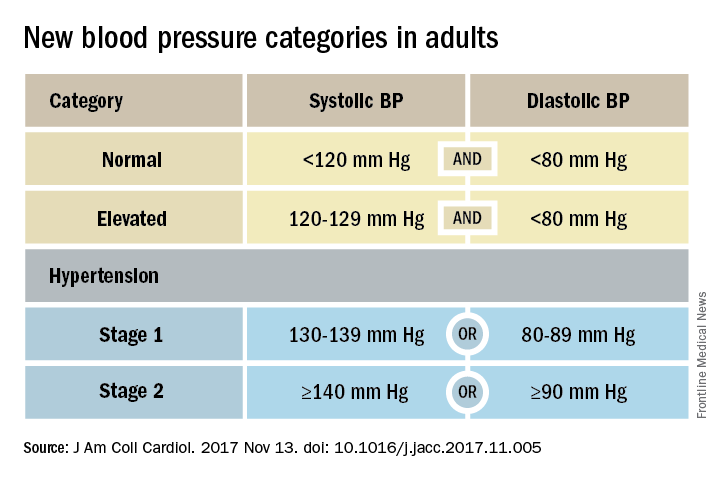
Goal is to transform care
But the new guidelines (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.005) for preventing, detecting, evaluating, and managing adult hypertension do lots more than just shake up the epidemiology of high blood pressure. With 106 total recommendations, the guidelines seek to transform every aspect of blood pressure in American medical practice, starting with how it’s measured and stretching to redefine applications of medical systems to try to ensure that every person with a blood pressure that truly falls outside the redefined limits gets a comprehensive package of interventions.
Many of these are “seismic changes,” said Lawrence J. Appel, MD. He particularly cited as seismic the new classification of stage 1 hypertension as a pressure at or above 130/80 mm Hg, the emphasis on using some form of out-of-office blood pressure measurement to confirm a diagnosis, the use of risk assessment when deciding whether to treat certain patients with drugs, and the same blood pressure goal of less than 130/80 mm Hg for all hypertensives, regardless of age, as long as they remain ambulatory and community dwelling.
One goal for all adults
“The systolic blood pressure goal for older people has gone from 140 mm Hg to 150 mm Hg and now to 130 mm Hg in the space of 2-3 years,” commented Dr. Appel, professor of epidemiology at Johns Hopkins University in Baltimore and not involved in the guideline-writing process.
In fact, the guidelines simplified the treatment goal all around, to less than 130/80 mm Hg for patients with diabetes, those with chronic kidney disease, and the elderly; that goal remains the same for all adults.
“It will be clearer and easier now that everyone should be less than 130/80 mm Hg. You won’t need to remember a second target,” said Sandra J. Taler, MD, a nephrologist and professor of medicine at the Mayo Clinic in Rochester, Minn., and a member of the guidelines task force.
“Some people may be upset that we changed the rules on them. They had normal blood pressure yesterday, and today it’s high. But it’s a good awakening, especially for using lifestyle interventions,” Dr. Taler said in an interview.
Preferred intervention: Lifestyle, not drugs
Lifestyle optimization is repeatedly cited as the cornerstone of intervention for everyone, including those with elevated blood pressure with a systolic pressure of 120-129 mm Hg, and as the only endorsed intervention for patients with hypertension of 130-139 mm Hg but below a 10% risk for a cardiovascular disease event during the next 10 years on the American College of Cardiology’s online risk calculator. The guidelines list six lifestyle goals: weight loss, following a DASH diet, reducing sodium, enhancing potassium, 90-150 min/wk of physical activity, and moderate alcohol intake.
Team-based care essential
The guidelines also put unprecedented emphasis on using a team-based management approach, which means having nurses, nurse practitioners, pharmacists, dietitians, and other clinicians, allowing for more frequent and focused care. Dr. Whelton and others cited in particular the VA Health System and Kaiser-Permanente as operating team-based and system-driven blood pressure management programs that have resulted in control rates for more than 90% of hypertensive patients. The team-based approach is also a key in the Target:BP program that the American Heart Association and American Medical Association founded. Target:BP will be instrumental in promoting implementation of the new guidelines, Dr. Carey said. Another systems recommendation is that every patient with hypertension should have a “clear, detailed, and current evidence-based plan of care.”
“Using nurse practitioners, physician assistants, and pharmacists has been shown to improve blood pressure levels,” and health systems that use this approach have had “great success,” commented Donald M. Lloyd-Jones, MD, professor and chairman of preventive medicine at Northwestern University in Chicago and not part of the guidelines task force. Some systems have used this approach to achieve high levels of blood pressure control. Now that financial penalties and incentives from payers also exist to push for higher levels of blood pressure control, the alignment of financial and health incentives should result in big changes, Dr. Lloyd-Jones predicted in a video interview.
[email protected]
On Twitter @mitchelzoler
ANAHEIM, CALIF. – Thirty million Americans became hypertensive overnight on Nov. 13 with the introduction of new high blood pressure guidelines from the American College of Cardiology and American Heart Association.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, a change that jumps the U.S. adult prevalence of hypertension from roughly 32% to 46%. Nearly half of all U.S. adults now have hypertension, bringing the total national hypertensive population to a staggering 103 million.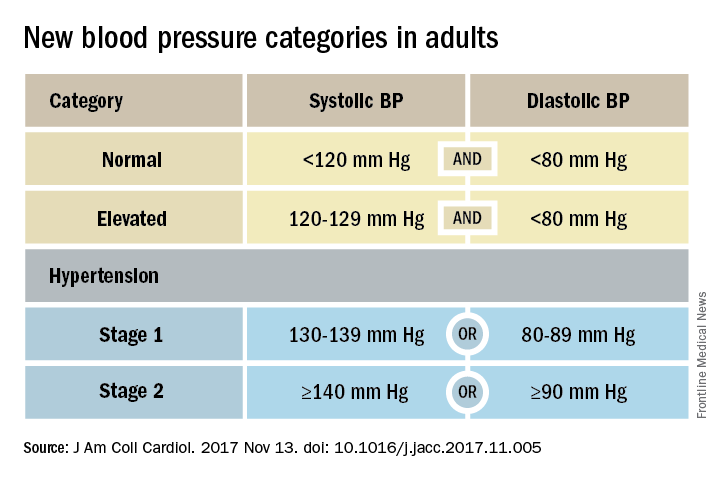
Goal is to transform care
But the new guidelines (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.005) for preventing, detecting, evaluating, and managing adult hypertension do lots more than just shake up the epidemiology of high blood pressure. With 106 total recommendations, the guidelines seek to transform every aspect of blood pressure in American medical practice, starting with how it’s measured and stretching to redefine applications of medical systems to try to ensure that every person with a blood pressure that truly falls outside the redefined limits gets a comprehensive package of interventions.
Many of these are “seismic changes,” said Lawrence J. Appel, MD. He particularly cited as seismic the new classification of stage 1 hypertension as a pressure at or above 130/80 mm Hg, the emphasis on using some form of out-of-office blood pressure measurement to confirm a diagnosis, the use of risk assessment when deciding whether to treat certain patients with drugs, and the same blood pressure goal of less than 130/80 mm Hg for all hypertensives, regardless of age, as long as they remain ambulatory and community dwelling.
One goal for all adults
“The systolic blood pressure goal for older people has gone from 140 mm Hg to 150 mm Hg and now to 130 mm Hg in the space of 2-3 years,” commented Dr. Appel, professor of epidemiology at Johns Hopkins University in Baltimore and not involved in the guideline-writing process.
In fact, the guidelines simplified the treatment goal all around, to less than 130/80 mm Hg for patients with diabetes, those with chronic kidney disease, and the elderly; that goal remains the same for all adults.
“It will be clearer and easier now that everyone should be less than 130/80 mm Hg. You won’t need to remember a second target,” said Sandra J. Taler, MD, a nephrologist and professor of medicine at the Mayo Clinic in Rochester, Minn., and a member of the guidelines task force.
“Some people may be upset that we changed the rules on them. They had normal blood pressure yesterday, and today it’s high. But it’s a good awakening, especially for using lifestyle interventions,” Dr. Taler said in an interview.
Preferred intervention: Lifestyle, not drugs
Lifestyle optimization is repeatedly cited as the cornerstone of intervention for everyone, including those with elevated blood pressure with a systolic pressure of 120-129 mm Hg, and as the only endorsed intervention for patients with hypertension of 130-139 mm Hg but below a 10% risk for a cardiovascular disease event during the next 10 years on the American College of Cardiology’s online risk calculator. The guidelines list six lifestyle goals: weight loss, following a DASH diet, reducing sodium, enhancing potassium, 90-150 min/wk of physical activity, and moderate alcohol intake.
Team-based care essential
The guidelines also put unprecedented emphasis on using a team-based management approach, which means having nurses, nurse practitioners, pharmacists, dietitians, and other clinicians, allowing for more frequent and focused care. Dr. Whelton and others cited in particular the VA Health System and Kaiser-Permanente as operating team-based and system-driven blood pressure management programs that have resulted in control rates for more than 90% of hypertensive patients. The team-based approach is also a key in the Target:BP program that the American Heart Association and American Medical Association founded. Target:BP will be instrumental in promoting implementation of the new guidelines, Dr. Carey said. Another systems recommendation is that every patient with hypertension should have a “clear, detailed, and current evidence-based plan of care.”
“Using nurse practitioners, physician assistants, and pharmacists has been shown to improve blood pressure levels,” and health systems that use this approach have had “great success,” commented Donald M. Lloyd-Jones, MD, professor and chairman of preventive medicine at Northwestern University in Chicago and not part of the guidelines task force. Some systems have used this approach to achieve high levels of blood pressure control. Now that financial penalties and incentives from payers also exist to push for higher levels of blood pressure control, the alignment of financial and health incentives should result in big changes, Dr. Lloyd-Jones predicted in a video interview.
[email protected]
On Twitter @mitchelzoler
ANAHEIM, CALIF. – Thirty million Americans became hypertensive overnight on Nov. 13 with the introduction of new high blood pressure guidelines from the American College of Cardiology and American Heart Association.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, a change that jumps the U.S. adult prevalence of hypertension from roughly 32% to 46%. Nearly half of all U.S. adults now have hypertension, bringing the total national hypertensive population to a staggering 103 million.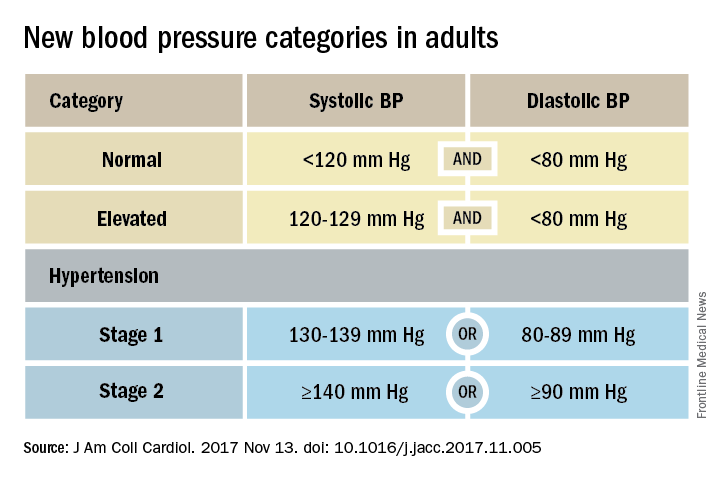
Goal is to transform care
But the new guidelines (J Am Coll Cardiol. 2017 Nov 13. doi: 10.1016/j.jacc.2017.11.005) for preventing, detecting, evaluating, and managing adult hypertension do lots more than just shake up the epidemiology of high blood pressure. With 106 total recommendations, the guidelines seek to transform every aspect of blood pressure in American medical practice, starting with how it’s measured and stretching to redefine applications of medical systems to try to ensure that every person with a blood pressure that truly falls outside the redefined limits gets a comprehensive package of interventions.
Many of these are “seismic changes,” said Lawrence J. Appel, MD. He particularly cited as seismic the new classification of stage 1 hypertension as a pressure at or above 130/80 mm Hg, the emphasis on using some form of out-of-office blood pressure measurement to confirm a diagnosis, the use of risk assessment when deciding whether to treat certain patients with drugs, and the same blood pressure goal of less than 130/80 mm Hg for all hypertensives, regardless of age, as long as they remain ambulatory and community dwelling.
One goal for all adults
“The systolic blood pressure goal for older people has gone from 140 mm Hg to 150 mm Hg and now to 130 mm Hg in the space of 2-3 years,” commented Dr. Appel, professor of epidemiology at Johns Hopkins University in Baltimore and not involved in the guideline-writing process.
In fact, the guidelines simplified the treatment goal all around, to less than 130/80 mm Hg for patients with diabetes, those with chronic kidney disease, and the elderly; that goal remains the same for all adults.
“It will be clearer and easier now that everyone should be less than 130/80 mm Hg. You won’t need to remember a second target,” said Sandra J. Taler, MD, a nephrologist and professor of medicine at the Mayo Clinic in Rochester, Minn., and a member of the guidelines task force.
“Some people may be upset that we changed the rules on them. They had normal blood pressure yesterday, and today it’s high. But it’s a good awakening, especially for using lifestyle interventions,” Dr. Taler said in an interview.
Preferred intervention: Lifestyle, not drugs
Lifestyle optimization is repeatedly cited as the cornerstone of intervention for everyone, including those with elevated blood pressure with a systolic pressure of 120-129 mm Hg, and as the only endorsed intervention for patients with hypertension of 130-139 mm Hg but below a 10% risk for a cardiovascular disease event during the next 10 years on the American College of Cardiology’s online risk calculator. The guidelines list six lifestyle goals: weight loss, following a DASH diet, reducing sodium, enhancing potassium, 90-150 min/wk of physical activity, and moderate alcohol intake.
Team-based care essential
The guidelines also put unprecedented emphasis on using a team-based management approach, which means having nurses, nurse practitioners, pharmacists, dietitians, and other clinicians, allowing for more frequent and focused care. Dr. Whelton and others cited in particular the VA Health System and Kaiser-Permanente as operating team-based and system-driven blood pressure management programs that have resulted in control rates for more than 90% of hypertensive patients. The team-based approach is also a key in the Target:BP program that the American Heart Association and American Medical Association founded. Target:BP will be instrumental in promoting implementation of the new guidelines, Dr. Carey said. Another systems recommendation is that every patient with hypertension should have a “clear, detailed, and current evidence-based plan of care.”
“Using nurse practitioners, physician assistants, and pharmacists has been shown to improve blood pressure levels,” and health systems that use this approach have had “great success,” commented Donald M. Lloyd-Jones, MD, professor and chairman of preventive medicine at Northwestern University in Chicago and not part of the guidelines task force. Some systems have used this approach to achieve high levels of blood pressure control. Now that financial penalties and incentives from payers also exist to push for higher levels of blood pressure control, the alignment of financial and health incentives should result in big changes, Dr. Lloyd-Jones predicted in a video interview.
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE AHA SCIENTIFIC SESSIONS
Doctors’ and nurses’ predictions of ICU outcomes have variable accuracy
Clinical question: How accurate are doctors and nurses at predicting survival and functional outcomes in critically ill patients?
Background: Doctors have been shown to have moderate accuracy at predicting in-hospital mortality in critically ill patients; however, little is known about their ability to predict longer-term outcomes.
Study design: Prospective cohort study.
Synopsis: Physicians and nurses predicted survival and functional outcomes for critically ill patients requiring mechanical ventilation or vasopressors. Outcomes predicted were in-hospital and 6-month mortality and ability to return to original residence, toilet independently, ambulate stairs, remember most things, think clearly, and solve problems.
Six-month follow-up was completed for 299 patients. Accuracy was highest when either physicians or nurses expressed confidence in their predictions; doctors confident in their predications of 6-month survival had a positive likelihood ratio of 33.00 (95% CI, 8.34-130.63). Both doctors and nurses least accurately predicted cognitive function (positive LR, 2.36; 95% CI, 1.36-4.12; negative LR, 0.75; 95% CI, 0.61-0.92 for doctors, positive LR, 1.50; 95% CI, 0.86-2.60; negative LR, 0.88; 95% CI, 0.73-1.06 for nurses), while doctors most accurately predicated 6-month mortality (positive LR, 5.91; 95% CI, 3.74-9.32; negative LR, 0.41; 95% CI, 0.33-0.52) and nurses most accurately predicted in-hospital mortality (positive LR, 4.71; 95% CI, 2.94-7.56; negative LR, 0.6; 95% CI,0.49-0.75).
Bottom line: Doctors and nurses were better at predicting mortality than they were at predicting cognition, and their predicted outcomes were most accurate when they expressed a high degree of confidence in the predictions.
Citation: Detsky ME, Harhay MO, Bayard DF, et al. Discriminative accuracy of physician and nurse predictions for survival and functional outcomes 6 months after an ICU admission. JAMA. 2017;317(21):2187-95.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: How accurate are doctors and nurses at predicting survival and functional outcomes in critically ill patients?
Background: Doctors have been shown to have moderate accuracy at predicting in-hospital mortality in critically ill patients; however, little is known about their ability to predict longer-term outcomes.
Study design: Prospective cohort study.
Synopsis: Physicians and nurses predicted survival and functional outcomes for critically ill patients requiring mechanical ventilation or vasopressors. Outcomes predicted were in-hospital and 6-month mortality and ability to return to original residence, toilet independently, ambulate stairs, remember most things, think clearly, and solve problems.
Six-month follow-up was completed for 299 patients. Accuracy was highest when either physicians or nurses expressed confidence in their predictions; doctors confident in their predications of 6-month survival had a positive likelihood ratio of 33.00 (95% CI, 8.34-130.63). Both doctors and nurses least accurately predicted cognitive function (positive LR, 2.36; 95% CI, 1.36-4.12; negative LR, 0.75; 95% CI, 0.61-0.92 for doctors, positive LR, 1.50; 95% CI, 0.86-2.60; negative LR, 0.88; 95% CI, 0.73-1.06 for nurses), while doctors most accurately predicated 6-month mortality (positive LR, 5.91; 95% CI, 3.74-9.32; negative LR, 0.41; 95% CI, 0.33-0.52) and nurses most accurately predicted in-hospital mortality (positive LR, 4.71; 95% CI, 2.94-7.56; negative LR, 0.6; 95% CI,0.49-0.75).
Bottom line: Doctors and nurses were better at predicting mortality than they were at predicting cognition, and their predicted outcomes were most accurate when they expressed a high degree of confidence in the predictions.
Citation: Detsky ME, Harhay MO, Bayard DF, et al. Discriminative accuracy of physician and nurse predictions for survival and functional outcomes 6 months after an ICU admission. JAMA. 2017;317(21):2187-95.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: How accurate are doctors and nurses at predicting survival and functional outcomes in critically ill patients?
Background: Doctors have been shown to have moderate accuracy at predicting in-hospital mortality in critically ill patients; however, little is known about their ability to predict longer-term outcomes.
Study design: Prospective cohort study.
Synopsis: Physicians and nurses predicted survival and functional outcomes for critically ill patients requiring mechanical ventilation or vasopressors. Outcomes predicted were in-hospital and 6-month mortality and ability to return to original residence, toilet independently, ambulate stairs, remember most things, think clearly, and solve problems.
Six-month follow-up was completed for 299 patients. Accuracy was highest when either physicians or nurses expressed confidence in their predictions; doctors confident in their predications of 6-month survival had a positive likelihood ratio of 33.00 (95% CI, 8.34-130.63). Both doctors and nurses least accurately predicted cognitive function (positive LR, 2.36; 95% CI, 1.36-4.12; negative LR, 0.75; 95% CI, 0.61-0.92 for doctors, positive LR, 1.50; 95% CI, 0.86-2.60; negative LR, 0.88; 95% CI, 0.73-1.06 for nurses), while doctors most accurately predicated 6-month mortality (positive LR, 5.91; 95% CI, 3.74-9.32; negative LR, 0.41; 95% CI, 0.33-0.52) and nurses most accurately predicted in-hospital mortality (positive LR, 4.71; 95% CI, 2.94-7.56; negative LR, 0.6; 95% CI,0.49-0.75).
Bottom line: Doctors and nurses were better at predicting mortality than they were at predicting cognition, and their predicted outcomes were most accurate when they expressed a high degree of confidence in the predictions.
Citation: Detsky ME, Harhay MO, Bayard DF, et al. Discriminative accuracy of physician and nurse predictions for survival and functional outcomes 6 months after an ICU admission. JAMA. 2017;317(21):2187-95.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
ARDS incidence is declining. Is it a preventable syndrome?
TORONTO – The incidence of acute respiratory distress syndrome (ARDS) is on the decline, according to a retrospective, population-based cohort study conducted at the Mayo Clinic in Rochester, Minn.
“This is very promising data in combating this syndrome,” reported Augustin Joseph of the Mayo Clinic, and “it suggests that ARDS may in part be a completely preventable disease.”
To see if ARDS incidence has continued to decline, Mr. Joseph’s group studied all patients admitted during 2009-2014 to the Mayo Clinic’s ICU, the only facility in the county that cares for ARDS patients. From 82,388 ICU admissions, they identified 505 patients with ARDS according to the Berlin definition of ARDS developed in 2012.
The number of annual cases dropped from 108 in 2009 to 59 in 2014, and the incidence steadily declined from 74.5 cases per 100,000 in 2009 to 39.3 per 100,000 in 2014.
Median age was 67 years in 2009 and 62 years in 2014. Hospital mortality ranged from 15% to 26% during the study period, while hospital length of stay ranged from 8 to 15 days, with no clear decline in either.
“For hospital and ICU mortality and hospital and ICU length of stay, we did not see much difference [from 2009 to 2014], so the overall picture between the Guangxi Li study and mine was that we did not see much of a difference in the patients who had ARDS, but [in terms of] preventing ARDS, the incidence has continued to decline,” Mr. Joseph reported.
While the earlier study used the American-European Consensus Conference (AECC) definition of ARDS, Mr. Joseph and his colleagues diagnosed ARDS according to the Berlin definition. One of the major changes seen in the new Berlin rules is that acute lung injury no longer exists and patients with a P/F ratio (PaO2/FiO2 ratio, or the ratio of arterial oxygen partial pressure to fractional inspired oxygen) between 200 and 300 are now considered to have “mild ARDS,” Mr. Joseph explained. With the AECC definition, a P/F ratio in this range was classified as acute lung injury and only one less than 200 was considered ARDS.
The researchers are now trying to parse out how changing ARDS diagnosis and management at their institution might be contributing to declining incidence, said Mr. Joseph.
TORONTO – The incidence of acute respiratory distress syndrome (ARDS) is on the decline, according to a retrospective, population-based cohort study conducted at the Mayo Clinic in Rochester, Minn.
“This is very promising data in combating this syndrome,” reported Augustin Joseph of the Mayo Clinic, and “it suggests that ARDS may in part be a completely preventable disease.”
To see if ARDS incidence has continued to decline, Mr. Joseph’s group studied all patients admitted during 2009-2014 to the Mayo Clinic’s ICU, the only facility in the county that cares for ARDS patients. From 82,388 ICU admissions, they identified 505 patients with ARDS according to the Berlin definition of ARDS developed in 2012.
The number of annual cases dropped from 108 in 2009 to 59 in 2014, and the incidence steadily declined from 74.5 cases per 100,000 in 2009 to 39.3 per 100,000 in 2014.
Median age was 67 years in 2009 and 62 years in 2014. Hospital mortality ranged from 15% to 26% during the study period, while hospital length of stay ranged from 8 to 15 days, with no clear decline in either.
“For hospital and ICU mortality and hospital and ICU length of stay, we did not see much difference [from 2009 to 2014], so the overall picture between the Guangxi Li study and mine was that we did not see much of a difference in the patients who had ARDS, but [in terms of] preventing ARDS, the incidence has continued to decline,” Mr. Joseph reported.
While the earlier study used the American-European Consensus Conference (AECC) definition of ARDS, Mr. Joseph and his colleagues diagnosed ARDS according to the Berlin definition. One of the major changes seen in the new Berlin rules is that acute lung injury no longer exists and patients with a P/F ratio (PaO2/FiO2 ratio, or the ratio of arterial oxygen partial pressure to fractional inspired oxygen) between 200 and 300 are now considered to have “mild ARDS,” Mr. Joseph explained. With the AECC definition, a P/F ratio in this range was classified as acute lung injury and only one less than 200 was considered ARDS.
The researchers are now trying to parse out how changing ARDS diagnosis and management at their institution might be contributing to declining incidence, said Mr. Joseph.
TORONTO – The incidence of acute respiratory distress syndrome (ARDS) is on the decline, according to a retrospective, population-based cohort study conducted at the Mayo Clinic in Rochester, Minn.
“This is very promising data in combating this syndrome,” reported Augustin Joseph of the Mayo Clinic, and “it suggests that ARDS may in part be a completely preventable disease.”
To see if ARDS incidence has continued to decline, Mr. Joseph’s group studied all patients admitted during 2009-2014 to the Mayo Clinic’s ICU, the only facility in the county that cares for ARDS patients. From 82,388 ICU admissions, they identified 505 patients with ARDS according to the Berlin definition of ARDS developed in 2012.
The number of annual cases dropped from 108 in 2009 to 59 in 2014, and the incidence steadily declined from 74.5 cases per 100,000 in 2009 to 39.3 per 100,000 in 2014.
Median age was 67 years in 2009 and 62 years in 2014. Hospital mortality ranged from 15% to 26% during the study period, while hospital length of stay ranged from 8 to 15 days, with no clear decline in either.
“For hospital and ICU mortality and hospital and ICU length of stay, we did not see much difference [from 2009 to 2014], so the overall picture between the Guangxi Li study and mine was that we did not see much of a difference in the patients who had ARDS, but [in terms of] preventing ARDS, the incidence has continued to decline,” Mr. Joseph reported.
While the earlier study used the American-European Consensus Conference (AECC) definition of ARDS, Mr. Joseph and his colleagues diagnosed ARDS according to the Berlin definition. One of the major changes seen in the new Berlin rules is that acute lung injury no longer exists and patients with a P/F ratio (PaO2/FiO2 ratio, or the ratio of arterial oxygen partial pressure to fractional inspired oxygen) between 200 and 300 are now considered to have “mild ARDS,” Mr. Joseph explained. With the AECC definition, a P/F ratio in this range was classified as acute lung injury and only one less than 200 was considered ARDS.
The researchers are now trying to parse out how changing ARDS diagnosis and management at their institution might be contributing to declining incidence, said Mr. Joseph.
AT CHEST 2017
Key clinical point: The incidence of acute respiratory distress syndrome is declining, an indication that it may be preventable, according to researchers.
Major finding: The number of annual cases dropped from 108 in 2009 to 59 in 2014, and the incidence steadily declined from 74.5 cases per 100,000 in 2009 to 39.3 per 100,000 in 2014.
Data source: Retrospective, population-based cohort study of all (505) patients admitted to the ICU for ARDS at a single center.
Disclosures: The authors reported having no relevant disclosures.
Incidental lung nodules are frequently not mentioned in hospital discharge summary
Clinical question: How often are incidentally found pulmonary nodules and instructions for follow-up included in the discharge summary?
Background: Lung nodules are frequent incidental findings on imaging, but it is unclear whether patients are subsequently receiving the recommended follow-up.
Study design: Retrospective cohort study.
Synopsis: The authors identified 7,173 patients who had undergone abdominal CT scans during their admission and reviewed charts of 402 patients who had incidentally found pulmonary nodules identified on the scans. For each of the patients, discharge summaries were evaluated to determine whether they made reference to the nodules and whether follow-up instructions were included. Of the 208 patients noted to have nodules requiring follow-up, only 48 (23%) had discharge summaries that mentioned the nodules. Factors associated with including the nodules in the discharge summary were the radiologist recommending further surveillance, radiologist including the nodule in the summary heading of the report, and being on a medical as opposed to a surgical service. The authors concluded that systems-based approaches to incidentally found lung nodules are needed to ensure adequate follow-up.
Bottom line: Incidentally found lung nodules are often not included in discharge documentation and therefore may not receive the recommended follow-up.
Citation: Bates R, Plooster C, Croghan I, et al. Incidental pulmonary nodules reported on CT abdominal imaging: Frequency and factors affecting inclusion in the hospital discharge summary. J Hosp Med. 2017;6:454-7.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: How often are incidentally found pulmonary nodules and instructions for follow-up included in the discharge summary?
Background: Lung nodules are frequent incidental findings on imaging, but it is unclear whether patients are subsequently receiving the recommended follow-up.
Study design: Retrospective cohort study.
Synopsis: The authors identified 7,173 patients who had undergone abdominal CT scans during their admission and reviewed charts of 402 patients who had incidentally found pulmonary nodules identified on the scans. For each of the patients, discharge summaries were evaluated to determine whether they made reference to the nodules and whether follow-up instructions were included. Of the 208 patients noted to have nodules requiring follow-up, only 48 (23%) had discharge summaries that mentioned the nodules. Factors associated with including the nodules in the discharge summary were the radiologist recommending further surveillance, radiologist including the nodule in the summary heading of the report, and being on a medical as opposed to a surgical service. The authors concluded that systems-based approaches to incidentally found lung nodules are needed to ensure adequate follow-up.
Bottom line: Incidentally found lung nodules are often not included in discharge documentation and therefore may not receive the recommended follow-up.
Citation: Bates R, Plooster C, Croghan I, et al. Incidental pulmonary nodules reported on CT abdominal imaging: Frequency and factors affecting inclusion in the hospital discharge summary. J Hosp Med. 2017;6:454-7.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: How often are incidentally found pulmonary nodules and instructions for follow-up included in the discharge summary?
Background: Lung nodules are frequent incidental findings on imaging, but it is unclear whether patients are subsequently receiving the recommended follow-up.
Study design: Retrospective cohort study.
Synopsis: The authors identified 7,173 patients who had undergone abdominal CT scans during their admission and reviewed charts of 402 patients who had incidentally found pulmonary nodules identified on the scans. For each of the patients, discharge summaries were evaluated to determine whether they made reference to the nodules and whether follow-up instructions were included. Of the 208 patients noted to have nodules requiring follow-up, only 48 (23%) had discharge summaries that mentioned the nodules. Factors associated with including the nodules in the discharge summary were the radiologist recommending further surveillance, radiologist including the nodule in the summary heading of the report, and being on a medical as opposed to a surgical service. The authors concluded that systems-based approaches to incidentally found lung nodules are needed to ensure adequate follow-up.
Bottom line: Incidentally found lung nodules are often not included in discharge documentation and therefore may not receive the recommended follow-up.
Citation: Bates R, Plooster C, Croghan I, et al. Incidental pulmonary nodules reported on CT abdominal imaging: Frequency and factors affecting inclusion in the hospital discharge summary. J Hosp Med. 2017;6:454-7.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Home noninvasive ventilation reduces COPD readmissions
Clinical question: Is there a benefit to home noninvasive ventilation (NIV) following a hospital admission for chronic obstructive pulmonary disease (COPD) exacerbation?
Background: Preventing hospital readmission following a COPD exacerbation is a priority; however, the role of NIV in this situation remains uncertain.
Setting: 13 medical centers in the United Kingdom.
Synopsis: Investigators randomized 116 patients with COPD and persistent hypercapnia (paCO2 less than 53) 2-4 weeks following a COPD exacerbation to either home oxygen therapy with NIV or to home oxygen therapy alone. The study’s primary endpoint was a composite of time to readmission or death within 12 months. They found that the median time to this endpoint was significantly longer in the intervention group (1.4 vs. 4.3 months; 95% CI, 0.31-0.77; P = .002) and that the absolute risk reduction was 17.0% (80.4% vs. 63.4%; 95% CI, 0.1%-34.0%). The differences were driven by readmissions, as the mortality rate did not differ significantly between groups, although the study was not powered to evaluate this. Of note, the median NIV settings were 24/4, which constitutes a “high-pressure strategy” which may account for the benefits seen in this study that have been absent in some other trials.
Bottom line: NIV reduced readmissions in patients with COPD and persistent hypercapnia several weeks following an acute exacerbation.
Citation: Murphy PB, Rehal S, Arbane G, et al. Effect of home noninvasive ventilation with oxygen therapy vs. oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation, a randomized clinical trial. JAMA. 2017;317(21):2177-86.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Is there a benefit to home noninvasive ventilation (NIV) following a hospital admission for chronic obstructive pulmonary disease (COPD) exacerbation?
Background: Preventing hospital readmission following a COPD exacerbation is a priority; however, the role of NIV in this situation remains uncertain.
Setting: 13 medical centers in the United Kingdom.
Synopsis: Investigators randomized 116 patients with COPD and persistent hypercapnia (paCO2 less than 53) 2-4 weeks following a COPD exacerbation to either home oxygen therapy with NIV or to home oxygen therapy alone. The study’s primary endpoint was a composite of time to readmission or death within 12 months. They found that the median time to this endpoint was significantly longer in the intervention group (1.4 vs. 4.3 months; 95% CI, 0.31-0.77; P = .002) and that the absolute risk reduction was 17.0% (80.4% vs. 63.4%; 95% CI, 0.1%-34.0%). The differences were driven by readmissions, as the mortality rate did not differ significantly between groups, although the study was not powered to evaluate this. Of note, the median NIV settings were 24/4, which constitutes a “high-pressure strategy” which may account for the benefits seen in this study that have been absent in some other trials.
Bottom line: NIV reduced readmissions in patients with COPD and persistent hypercapnia several weeks following an acute exacerbation.
Citation: Murphy PB, Rehal S, Arbane G, et al. Effect of home noninvasive ventilation with oxygen therapy vs. oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation, a randomized clinical trial. JAMA. 2017;317(21):2177-86.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Is there a benefit to home noninvasive ventilation (NIV) following a hospital admission for chronic obstructive pulmonary disease (COPD) exacerbation?
Background: Preventing hospital readmission following a COPD exacerbation is a priority; however, the role of NIV in this situation remains uncertain.
Setting: 13 medical centers in the United Kingdom.
Synopsis: Investigators randomized 116 patients with COPD and persistent hypercapnia (paCO2 less than 53) 2-4 weeks following a COPD exacerbation to either home oxygen therapy with NIV or to home oxygen therapy alone. The study’s primary endpoint was a composite of time to readmission or death within 12 months. They found that the median time to this endpoint was significantly longer in the intervention group (1.4 vs. 4.3 months; 95% CI, 0.31-0.77; P = .002) and that the absolute risk reduction was 17.0% (80.4% vs. 63.4%; 95% CI, 0.1%-34.0%). The differences were driven by readmissions, as the mortality rate did not differ significantly between groups, although the study was not powered to evaluate this. Of note, the median NIV settings were 24/4, which constitutes a “high-pressure strategy” which may account for the benefits seen in this study that have been absent in some other trials.
Bottom line: NIV reduced readmissions in patients with COPD and persistent hypercapnia several weeks following an acute exacerbation.
Citation: Murphy PB, Rehal S, Arbane G, et al. Effect of home noninvasive ventilation with oxygen therapy vs. oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation, a randomized clinical trial. JAMA. 2017;317(21):2177-86.
Dr. Herscher is assistant professor, division of hospital medicine, Icahn School of Medicine of the Mount Sinai Health System.
Renal dosing of non–vitamin K antagonist oral anticoagulants in atrial fibrillation is important in preventing thrombotic and bleeding complications
Clinical question: Does renal underdosing and overdosing of non–vitamin K antagonist oral anticoagulants (NOACs) impact the risk of thrombotic and bleeding complications?
Background: All of the NOACs have at least partial renal clearance, but compliance with Food and Drug Administration–labeled renal dosing recommendations is inconsistent. This study examines the risk of adverse thrombotic and bleeding events in patients with improper anticoagulant dosing.
Study design: Retrospective cohort study.
Setting: United States (OptumLabs data warehouse, a database of over 100 million patients hospitalized in the United States in the last 20 years).
Synopsis: With use of data from the OptumLabs data warehouse of privately insured and Medicare Advantage enrollees, 14,865 patients with nonvalvular atrial fibrillation who were started on NOACs (apixaban, dabigatran, or rivaroxaban) were identified. Creatinine values within the year before treatment were used to calculate an estimated glomerular filtration rate (eGFR).
Of patients qualifying for renal dose reduction, 43% received the standard dosing (overdose). Of patients not qualifying for renal dose reduction, 13% received a reduced dose (underdose). The overdosed group had a higher rate of bleeding events, compared with controls (hazard ratio, 2.19; 95% CI, 1.07-4.46). The underdosed group had a higher rate of stroke (HR, 4.87; 95% CI, 1.30-18.26).
Bottom line: Excessive dosing of NOACs in patients with renal insufficiency is common and is associated with bleeding.Citation: Yao X, Shah ND, Sangaralingham LR, Gersh BJ, and Noseworthy PA. Non–vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. JACC. 2017;69(23):2779-90.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does renal underdosing and overdosing of non–vitamin K antagonist oral anticoagulants (NOACs) impact the risk of thrombotic and bleeding complications?
Background: All of the NOACs have at least partial renal clearance, but compliance with Food and Drug Administration–labeled renal dosing recommendations is inconsistent. This study examines the risk of adverse thrombotic and bleeding events in patients with improper anticoagulant dosing.
Study design: Retrospective cohort study.
Setting: United States (OptumLabs data warehouse, a database of over 100 million patients hospitalized in the United States in the last 20 years).
Synopsis: With use of data from the OptumLabs data warehouse of privately insured and Medicare Advantage enrollees, 14,865 patients with nonvalvular atrial fibrillation who were started on NOACs (apixaban, dabigatran, or rivaroxaban) were identified. Creatinine values within the year before treatment were used to calculate an estimated glomerular filtration rate (eGFR).
Of patients qualifying for renal dose reduction, 43% received the standard dosing (overdose). Of patients not qualifying for renal dose reduction, 13% received a reduced dose (underdose). The overdosed group had a higher rate of bleeding events, compared with controls (hazard ratio, 2.19; 95% CI, 1.07-4.46). The underdosed group had a higher rate of stroke (HR, 4.87; 95% CI, 1.30-18.26).
Bottom line: Excessive dosing of NOACs in patients with renal insufficiency is common and is associated with bleeding.Citation: Yao X, Shah ND, Sangaralingham LR, Gersh BJ, and Noseworthy PA. Non–vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. JACC. 2017;69(23):2779-90.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does renal underdosing and overdosing of non–vitamin K antagonist oral anticoagulants (NOACs) impact the risk of thrombotic and bleeding complications?
Background: All of the NOACs have at least partial renal clearance, but compliance with Food and Drug Administration–labeled renal dosing recommendations is inconsistent. This study examines the risk of adverse thrombotic and bleeding events in patients with improper anticoagulant dosing.
Study design: Retrospective cohort study.
Setting: United States (OptumLabs data warehouse, a database of over 100 million patients hospitalized in the United States in the last 20 years).
Synopsis: With use of data from the OptumLabs data warehouse of privately insured and Medicare Advantage enrollees, 14,865 patients with nonvalvular atrial fibrillation who were started on NOACs (apixaban, dabigatran, or rivaroxaban) were identified. Creatinine values within the year before treatment were used to calculate an estimated glomerular filtration rate (eGFR).
Of patients qualifying for renal dose reduction, 43% received the standard dosing (overdose). Of patients not qualifying for renal dose reduction, 13% received a reduced dose (underdose). The overdosed group had a higher rate of bleeding events, compared with controls (hazard ratio, 2.19; 95% CI, 1.07-4.46). The underdosed group had a higher rate of stroke (HR, 4.87; 95% CI, 1.30-18.26).
Bottom line: Excessive dosing of NOACs in patients with renal insufficiency is common and is associated with bleeding.Citation: Yao X, Shah ND, Sangaralingham LR, Gersh BJ, and Noseworthy PA. Non–vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. JACC. 2017;69(23):2779-90.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
CABG and PCI with drug-eluting stents for left main coronary disease have superior outcomes to medical therapy alone
Clinical question: Does coronary artery bypass grafting (CABG) have superior mortality outcomes to percutaneous coronary intervention (PCI) for left main coronary disease, and how do these interventions compare with medical therapy alone?
Background: Optimal therapy for left main coronary disease is a highly researched topic with CABG having been standard therapy of choice for several decades. However, most studies have not included data comparing CABG to newer drug-eluting stent (DES) generations and no studies have directly compared PCI with DES to medical therapy alone (MTA).
Study design: Meta-analysis.
Setting: Largely European acute care hospitals as well as some VA hospitals.
Synopsis: With PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a review of PubMed and Cochrane databases was conducted, yielding eight RCTs, including a total of 4,850 patients. Six of the RCTs compared CABG with DES, while two compared CABG with MTA. Network meta-analysis was used to compare DES with MTA. At 5 years there were no differences in all-cause mortality between CABG and DES groups (RR, 0.94; 95% CI, 0.68-1.32), though both groups had lower mortality than MTA (RR, 0.21; 95% CI, 0.09-0.47 for CABG vs. MTA and RR, 0.20; 95% CI, 0.08-0.46 for DES vs MTA).
PCI did have higher risk of revascularization at 5 years (RR, 1.68; 95% CI, 1.36-2.08) and lower risk of stroke at 1 year (RR, 0.21; 95% CI, 0.07-0.63), compared with CABG, suggesting younger patients might prefer CABG to avoid revascularization, and older patients may prefer PCI to avoid postprocedural morbidity.
Bottom line: For patients with left main disease, CABG and PCI with DES appear equally effective with regards to prevention of all-cause mortality and both are superior to MTA.
Citation: Shah R, Morsy MS, Weiman DS, and Vetrovec GW. Meta-analysis comparing coronary artery bypass grafting to drug-eluting stents. Am J Cardiol. 2017;120:63-8.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does coronary artery bypass grafting (CABG) have superior mortality outcomes to percutaneous coronary intervention (PCI) for left main coronary disease, and how do these interventions compare with medical therapy alone?
Background: Optimal therapy for left main coronary disease is a highly researched topic with CABG having been standard therapy of choice for several decades. However, most studies have not included data comparing CABG to newer drug-eluting stent (DES) generations and no studies have directly compared PCI with DES to medical therapy alone (MTA).
Study design: Meta-analysis.
Setting: Largely European acute care hospitals as well as some VA hospitals.
Synopsis: With PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a review of PubMed and Cochrane databases was conducted, yielding eight RCTs, including a total of 4,850 patients. Six of the RCTs compared CABG with DES, while two compared CABG with MTA. Network meta-analysis was used to compare DES with MTA. At 5 years there were no differences in all-cause mortality between CABG and DES groups (RR, 0.94; 95% CI, 0.68-1.32), though both groups had lower mortality than MTA (RR, 0.21; 95% CI, 0.09-0.47 for CABG vs. MTA and RR, 0.20; 95% CI, 0.08-0.46 for DES vs MTA).
PCI did have higher risk of revascularization at 5 years (RR, 1.68; 95% CI, 1.36-2.08) and lower risk of stroke at 1 year (RR, 0.21; 95% CI, 0.07-0.63), compared with CABG, suggesting younger patients might prefer CABG to avoid revascularization, and older patients may prefer PCI to avoid postprocedural morbidity.
Bottom line: For patients with left main disease, CABG and PCI with DES appear equally effective with regards to prevention of all-cause mortality and both are superior to MTA.
Citation: Shah R, Morsy MS, Weiman DS, and Vetrovec GW. Meta-analysis comparing coronary artery bypass grafting to drug-eluting stents. Am J Cardiol. 2017;120:63-8.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does coronary artery bypass grafting (CABG) have superior mortality outcomes to percutaneous coronary intervention (PCI) for left main coronary disease, and how do these interventions compare with medical therapy alone?
Background: Optimal therapy for left main coronary disease is a highly researched topic with CABG having been standard therapy of choice for several decades. However, most studies have not included data comparing CABG to newer drug-eluting stent (DES) generations and no studies have directly compared PCI with DES to medical therapy alone (MTA).
Study design: Meta-analysis.
Setting: Largely European acute care hospitals as well as some VA hospitals.
Synopsis: With PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a review of PubMed and Cochrane databases was conducted, yielding eight RCTs, including a total of 4,850 patients. Six of the RCTs compared CABG with DES, while two compared CABG with MTA. Network meta-analysis was used to compare DES with MTA. At 5 years there were no differences in all-cause mortality between CABG and DES groups (RR, 0.94; 95% CI, 0.68-1.32), though both groups had lower mortality than MTA (RR, 0.21; 95% CI, 0.09-0.47 for CABG vs. MTA and RR, 0.20; 95% CI, 0.08-0.46 for DES vs MTA).
PCI did have higher risk of revascularization at 5 years (RR, 1.68; 95% CI, 1.36-2.08) and lower risk of stroke at 1 year (RR, 0.21; 95% CI, 0.07-0.63), compared with CABG, suggesting younger patients might prefer CABG to avoid revascularization, and older patients may prefer PCI to avoid postprocedural morbidity.
Bottom line: For patients with left main disease, CABG and PCI with DES appear equally effective with regards to prevention of all-cause mortality and both are superior to MTA.
Citation: Shah R, Morsy MS, Weiman DS, and Vetrovec GW. Meta-analysis comparing coronary artery bypass grafting to drug-eluting stents. Am J Cardiol. 2017;120:63-8.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Antiplatelet therapy can be continued through surgery without increased risk of reintervention for bleeding
Clinical question: Does continuing antiplatelet therapy through noncardiac surgery increase the risk of postoperative blood transfusion or surgical reintervention for bleeding?
Background: Many prior studies have analyzed the risks and benefits of holding versus continuing antiplatelet therapy in the perioperative setting, but heterogeneity in outcome reporting has limited the ability to compare and contrast studies.
Study design: Meta-analysis.
Setting: Both domestic and international studies were included in the meta-analysis.
Synopsis: With a MEDLINE search, 37 studies with over 30,000 patients total were identified and included in the meta-analysis. Studies compared outcomes of transfusion and surgical reintervention for bleeding in patients receiving noncardiac surgery. Patients were either on no antiplatelet therapy, single therapy, or dual-antiplatelet therapy (DAPT). Relative risk of transfusion escalated in proportion to the amount of antiplatelet therapy; there was a 14% increased risk (95% confidence interval, 1.03-1.26) with aspirin over control and a 33% (95% CI, 1.15-1.55) increased risk with DAPT over control.
Risk of surgical reintervention for bleeding, however, was not increased above control whether on aspirin (relative risk, 0.96; 95% CI, 0.76-1.22), clopidogrel (RR, 1.84; 95% CI, 0.87-3.87), or DAPT (RR, 1.51; (95% CI, 0.92-2.49).
Bottom line: In noncardiac surgery, continuing aspirin or DAPT perioperatively increases the need for transfusion, but not the need for surgical reintervention for bleeding.
Citation: Columbo JA, Lambour AJ, Sundling RA, et. al. A meta-analysis of the impact of aspirin, clopidogrel, and dual-antiplatelet therapy on bleeding complications in noncardiac surgery. Ann Surg. 2017;20(20):1-9.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does continuing antiplatelet therapy through noncardiac surgery increase the risk of postoperative blood transfusion or surgical reintervention for bleeding?
Background: Many prior studies have analyzed the risks and benefits of holding versus continuing antiplatelet therapy in the perioperative setting, but heterogeneity in outcome reporting has limited the ability to compare and contrast studies.
Study design: Meta-analysis.
Setting: Both domestic and international studies were included in the meta-analysis.
Synopsis: With a MEDLINE search, 37 studies with over 30,000 patients total were identified and included in the meta-analysis. Studies compared outcomes of transfusion and surgical reintervention for bleeding in patients receiving noncardiac surgery. Patients were either on no antiplatelet therapy, single therapy, or dual-antiplatelet therapy (DAPT). Relative risk of transfusion escalated in proportion to the amount of antiplatelet therapy; there was a 14% increased risk (95% confidence interval, 1.03-1.26) with aspirin over control and a 33% (95% CI, 1.15-1.55) increased risk with DAPT over control.
Risk of surgical reintervention for bleeding, however, was not increased above control whether on aspirin (relative risk, 0.96; 95% CI, 0.76-1.22), clopidogrel (RR, 1.84; 95% CI, 0.87-3.87), or DAPT (RR, 1.51; (95% CI, 0.92-2.49).
Bottom line: In noncardiac surgery, continuing aspirin or DAPT perioperatively increases the need for transfusion, but not the need for surgical reintervention for bleeding.
Citation: Columbo JA, Lambour AJ, Sundling RA, et. al. A meta-analysis of the impact of aspirin, clopidogrel, and dual-antiplatelet therapy on bleeding complications in noncardiac surgery. Ann Surg. 2017;20(20):1-9.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Clinical question: Does continuing antiplatelet therapy through noncardiac surgery increase the risk of postoperative blood transfusion or surgical reintervention for bleeding?
Background: Many prior studies have analyzed the risks and benefits of holding versus continuing antiplatelet therapy in the perioperative setting, but heterogeneity in outcome reporting has limited the ability to compare and contrast studies.
Study design: Meta-analysis.
Setting: Both domestic and international studies were included in the meta-analysis.
Synopsis: With a MEDLINE search, 37 studies with over 30,000 patients total were identified and included in the meta-analysis. Studies compared outcomes of transfusion and surgical reintervention for bleeding in patients receiving noncardiac surgery. Patients were either on no antiplatelet therapy, single therapy, or dual-antiplatelet therapy (DAPT). Relative risk of transfusion escalated in proportion to the amount of antiplatelet therapy; there was a 14% increased risk (95% confidence interval, 1.03-1.26) with aspirin over control and a 33% (95% CI, 1.15-1.55) increased risk with DAPT over control.
Risk of surgical reintervention for bleeding, however, was not increased above control whether on aspirin (relative risk, 0.96; 95% CI, 0.76-1.22), clopidogrel (RR, 1.84; 95% CI, 0.87-3.87), or DAPT (RR, 1.51; (95% CI, 0.92-2.49).
Bottom line: In noncardiac surgery, continuing aspirin or DAPT perioperatively increases the need for transfusion, but not the need for surgical reintervention for bleeding.
Citation: Columbo JA, Lambour AJ, Sundling RA, et. al. A meta-analysis of the impact of aspirin, clopidogrel, and dual-antiplatelet therapy on bleeding complications in noncardiac surgery. Ann Surg. 2017;20(20):1-9.
Dr. Portnoy is hospitalist and instructor of medicine, Icahn School of Medicine of the Mount Sinai Health System.
Public health hazard: Bring your flu to work day
Slightly more than 41% of health care personnel who had the flu during the 2014-2015 influenza season went to work while they were ill, according to an annual survey.
Physicians, however, were well above this average, with 63% reporting they had worked with an influenza-like illness (ILI); they were not quite as far above average as pharmacists, though, who had a 67% rate of “presenteeism” – the highest among all of the health care occupations included in the survey, said Sophia Chiu, MD, MPH, of the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health, and her associates.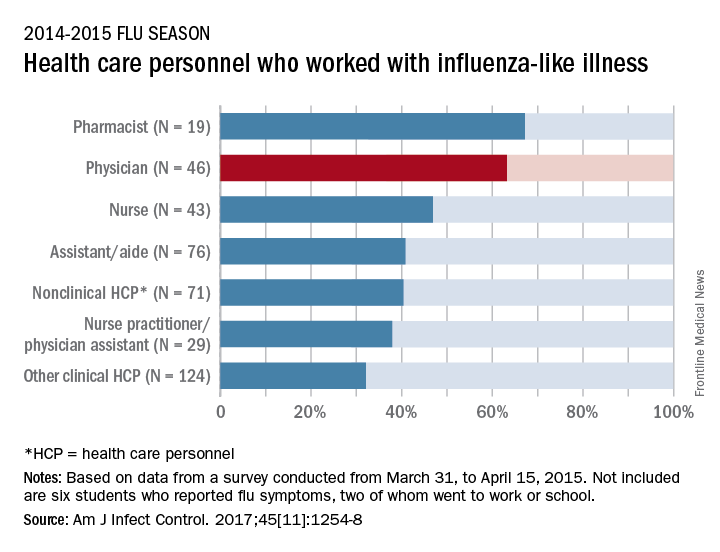
“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a health care worker who is sick are five times more likely to get a health care–associated infection,” Dr. Chiu said in a separate written statement.
For the study, ILI was defined as “fever (without a specified temperature cutoff) and sore throat or cough.” The “nonclinical personnel” category included managers, food service workers, and janitors, while the “other clinical personnel” category included technicians and technologists. The annual Internet panel survey was conducted from March 31, 2015, to April 15, 2015, and 414 of its 1,914 respondents self-reported having an ILI, of whom 183 said that they worked during their illness, Dr. Chiu and her associates said.
The investigators are all CDC employees. The respondents were recruited from Internet panels operated by Survey Sampling International through a contract with Abt Associates.
Slightly more than 41% of health care personnel who had the flu during the 2014-2015 influenza season went to work while they were ill, according to an annual survey.
Physicians, however, were well above this average, with 63% reporting they had worked with an influenza-like illness (ILI); they were not quite as far above average as pharmacists, though, who had a 67% rate of “presenteeism” – the highest among all of the health care occupations included in the survey, said Sophia Chiu, MD, MPH, of the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health, and her associates.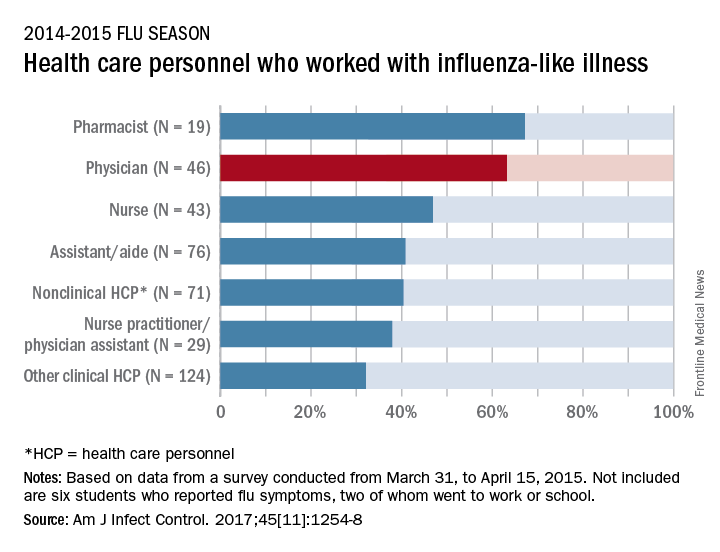
“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a health care worker who is sick are five times more likely to get a health care–associated infection,” Dr. Chiu said in a separate written statement.
For the study, ILI was defined as “fever (without a specified temperature cutoff) and sore throat or cough.” The “nonclinical personnel” category included managers, food service workers, and janitors, while the “other clinical personnel” category included technicians and technologists. The annual Internet panel survey was conducted from March 31, 2015, to April 15, 2015, and 414 of its 1,914 respondents self-reported having an ILI, of whom 183 said that they worked during their illness, Dr. Chiu and her associates said.
The investigators are all CDC employees. The respondents were recruited from Internet panels operated by Survey Sampling International through a contract with Abt Associates.
Slightly more than 41% of health care personnel who had the flu during the 2014-2015 influenza season went to work while they were ill, according to an annual survey.
Physicians, however, were well above this average, with 63% reporting they had worked with an influenza-like illness (ILI); they were not quite as far above average as pharmacists, though, who had a 67% rate of “presenteeism” – the highest among all of the health care occupations included in the survey, said Sophia Chiu, MD, MPH, of the Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health, and her associates.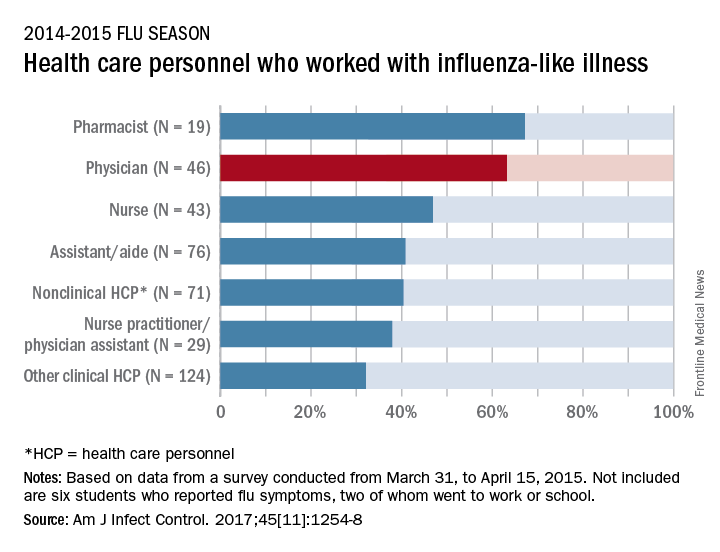
“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a health care worker who is sick are five times more likely to get a health care–associated infection,” Dr. Chiu said in a separate written statement.
For the study, ILI was defined as “fever (without a specified temperature cutoff) and sore throat or cough.” The “nonclinical personnel” category included managers, food service workers, and janitors, while the “other clinical personnel” category included technicians and technologists. The annual Internet panel survey was conducted from March 31, 2015, to April 15, 2015, and 414 of its 1,914 respondents self-reported having an ILI, of whom 183 said that they worked during their illness, Dr. Chiu and her associates said.
The investigators are all CDC employees. The respondents were recruited from Internet panels operated by Survey Sampling International through a contract with Abt Associates.
FROM THE AMERICAN JOURNAL OF INFECTION CONTROL
Identifying high-value care practices
A new tool can help where hospitalists need it most: at the bedside.
The focus on providing high-value care (HVC) continues to grow and expand in health care today. Still, most education around HVC currently happens in a formalized setting – lectures, modules, and so on, says Carolyn D. Sy, MD, interim director of the Hospital Medicine Service at the University of Washington, Seattle, and coauthor of a recent abstract about a new tool to address this shortcoming. “There are no instruments for measuring HVC discussions or practices at the bedside, confounding efforts to assess behavior changes associated with curricular interventions,” she said.
So she and other doctors undertook a study to identify 10 HVC topics in three domains (quality, cost, patient values), then measured their reliability with the goal of designing an HVC Rounding Tool and showing that it is an effective tool to measure observable markers of HVC at the bedside. “This is critical as it addresses an important educational gap in translating HVC from theoretical knowledge to bedside practice,” Dr. Sy said.
The tool is designed to capture multidisciplinary participation, she says, including involvement from not only faculty, fellows, or trainees, but also nursing, pharmacists, families, and other members of the health care team. The tool can be used as a peer feedback instrument to help physicians integrate HVC topics during bedside rounds or as a metric to assess the educational efficacy of future curriculum.
“The HVC Rounding Tool provides an opportunity for faculty development through peer observation and feedback on the integration and role modeling of HVC at the bedside,” Dr. Sy said. “It also is an instrument to help assess the educational efficacy of formal HVC curriculum and translation into bedside practice. Lastly, it is a tool that could be used to measure the relationship between HVC behaviors and actual patient outcomes such as length of stay, readmissions, cost of hospitalization – a feature with increasing importance given our move toward value-based health care.”
Reference
Sy CD, McDaniel C, Bradford M, et al. The Development and Validation of a High Value Care Rounding Tool Using the Delphi Method [abstract]. J Hosp Med. 2017; 12 (suppl 2). http://www.shmabstracts.com/abstract/the-development-and-validation-of-a-high-value-care-rounding-tool-using-the-delphi-method/. Accessed June 6, 2017.
A new tool can help where hospitalists need it most: at the bedside.
The focus on providing high-value care (HVC) continues to grow and expand in health care today. Still, most education around HVC currently happens in a formalized setting – lectures, modules, and so on, says Carolyn D. Sy, MD, interim director of the Hospital Medicine Service at the University of Washington, Seattle, and coauthor of a recent abstract about a new tool to address this shortcoming. “There are no instruments for measuring HVC discussions or practices at the bedside, confounding efforts to assess behavior changes associated with curricular interventions,” she said.
So she and other doctors undertook a study to identify 10 HVC topics in three domains (quality, cost, patient values), then measured their reliability with the goal of designing an HVC Rounding Tool and showing that it is an effective tool to measure observable markers of HVC at the bedside. “This is critical as it addresses an important educational gap in translating HVC from theoretical knowledge to bedside practice,” Dr. Sy said.
The tool is designed to capture multidisciplinary participation, she says, including involvement from not only faculty, fellows, or trainees, but also nursing, pharmacists, families, and other members of the health care team. The tool can be used as a peer feedback instrument to help physicians integrate HVC topics during bedside rounds or as a metric to assess the educational efficacy of future curriculum.
“The HVC Rounding Tool provides an opportunity for faculty development through peer observation and feedback on the integration and role modeling of HVC at the bedside,” Dr. Sy said. “It also is an instrument to help assess the educational efficacy of formal HVC curriculum and translation into bedside practice. Lastly, it is a tool that could be used to measure the relationship between HVC behaviors and actual patient outcomes such as length of stay, readmissions, cost of hospitalization – a feature with increasing importance given our move toward value-based health care.”
Reference
Sy CD, McDaniel C, Bradford M, et al. The Development and Validation of a High Value Care Rounding Tool Using the Delphi Method [abstract]. J Hosp Med. 2017; 12 (suppl 2). http://www.shmabstracts.com/abstract/the-development-and-validation-of-a-high-value-care-rounding-tool-using-the-delphi-method/. Accessed June 6, 2017.
A new tool can help where hospitalists need it most: at the bedside.
The focus on providing high-value care (HVC) continues to grow and expand in health care today. Still, most education around HVC currently happens in a formalized setting – lectures, modules, and so on, says Carolyn D. Sy, MD, interim director of the Hospital Medicine Service at the University of Washington, Seattle, and coauthor of a recent abstract about a new tool to address this shortcoming. “There are no instruments for measuring HVC discussions or practices at the bedside, confounding efforts to assess behavior changes associated with curricular interventions,” she said.
So she and other doctors undertook a study to identify 10 HVC topics in three domains (quality, cost, patient values), then measured their reliability with the goal of designing an HVC Rounding Tool and showing that it is an effective tool to measure observable markers of HVC at the bedside. “This is critical as it addresses an important educational gap in translating HVC from theoretical knowledge to bedside practice,” Dr. Sy said.
The tool is designed to capture multidisciplinary participation, she says, including involvement from not only faculty, fellows, or trainees, but also nursing, pharmacists, families, and other members of the health care team. The tool can be used as a peer feedback instrument to help physicians integrate HVC topics during bedside rounds or as a metric to assess the educational efficacy of future curriculum.
“The HVC Rounding Tool provides an opportunity for faculty development through peer observation and feedback on the integration and role modeling of HVC at the bedside,” Dr. Sy said. “It also is an instrument to help assess the educational efficacy of formal HVC curriculum and translation into bedside practice. Lastly, it is a tool that could be used to measure the relationship between HVC behaviors and actual patient outcomes such as length of stay, readmissions, cost of hospitalization – a feature with increasing importance given our move toward value-based health care.”
Reference
Sy CD, McDaniel C, Bradford M, et al. The Development and Validation of a High Value Care Rounding Tool Using the Delphi Method [abstract]. J Hosp Med. 2017; 12 (suppl 2). http://www.shmabstracts.com/abstract/the-development-and-validation-of-a-high-value-care-rounding-tool-using-the-delphi-method/. Accessed June 6, 2017.